User login
Oncologists may be too quick to refer patients to palliative care
I recently met Jane, a 53-year-old woman with metastatic breast cancer. She was referred to me by the breast oncology team, which routinely refers all metastatic patients to our palliative care clinic.
Clocking in at under 20 minutes, my consultation with Jane might have been one of my shortest on record. Not only had the breast oncology team already addressed Jane’s symptoms, which mainly consisted of hot flashes and joint pain attributable to treatment with an aromatase inhibitor, but they had already started planning ahead for the future of her illness. Jane had completed an advance directive and had a realistic and hopeful perspective on how her illness would progress. She understood the goal of her treatment was to “keep the cancer asleep,” as she put it, and she was very clear about her own goals: to live long enough to see her granddaughter graduate from high school in 2 years and to take a long-awaited trip to Australia later in 2023.
There wasn’t much for me to do. In fact, I daresay that Jane really did not need to see a palliative care specialist because the primary palliative care she was receiving from the breast oncology team was superb. Jane was receiving excellent symptom management from a nurse practitioner and oncologist, plus a social worker provided her with coping strategies. She was already having conversations with her primary medical team and her family about what to expect in the future and how to plan ahead for all possible outcomes.
When should a patient be referred to palliative care?
Integrating palliative care into routine oncologic care need not always require the time and skill of a palliative care team for every patient. Oncology providers can provide basic palliative care services without consulting a palliative care specialist.
For example, if a primary care doctor tried to refer every patient with hypertension to cardiology, the cardiologist would probably say that primary care should be able to handle basic hypertension management. In my experience from working in an oncology clinic for the past 9 years, I’ve found that oncology providers don’t need to refer every advanced cancer patient to our palliative care program. Most oncologists have good communication skills and are more than capable of managing symptoms for patients.
But don’t get me wrong.
Palliative care for all?
In 2010, Jennifer S. Temel MD, published a landmark study in the New England Journal of Medicine that demonstrated significant improvements in quality of life and mood in patients with metastatic lung cancer who received concurrent palliative care. After the study was published many voices inside oncology and palliative care began to advocate for a “palliative care for all” approach to patients with metastatic disease. But this is often interpreted as “specialty palliative care for all,” rather than its original intended meaning that all patients with metastatic disease receive the essential elements of palliative care (biopsychosocial symptom support and conversations about goals of care) either through their primary oncology teams or, if needed, specialty palliative care teams.
The fact is that most specialty palliative care clinics do not have the manpower to meet the needs of all patients with advanced cancers, much less all patients living with serious illness. A main goal of integrating palliative care into routine outpatient health care has always been (and in my opinion, should continue to be) to enhance the primary palliative care skills of specialists, such as oncologists and cardiologists, who care for some of our sickest patients.
This could take many forms. For one, it can be helpful to screen patients for palliative care needs. The American College of Surgeons Commission on Cancer mandates distress screening for all patients as a condition of accreditation. Distress screening using a validated tool such as the National Comprehensive Cancer Network Distress Thermometer can differentiate patients who have minimal distress and may not need much additional support beyond what is provided by their oncology team from those whose distress feels unmanageable and overwhelming.
In terms of primary palliative care symptom management, most oncology teams I work with are comfortable prescribing basic medications for pain, nausea, constipation, and anxiety. They’re also comfortable referring oncology patients for nutrition needs while undergoing chemotherapy as well as to social work and spiritual care for emotional support and counseling.
Oncology teams should continually work on communications skills. They should use “Ask, Tell, Ask” to elicit prognostic awareness, convey critical information, and assess for recall and understanding at pivotal points in the cancer journey, such as when the disease progresses or the patient’s clinical condition changes. They should practice a normalizing script they can use to introduce advance care planning to their patients in the first few visits. When I meet with a patient for the first time, I usually begin by asking if they have prepared an advanced directive. If not, I ask if they’ve thought about who will make medical decisions for them should the need arise. If the patient has documented in writing their preference for care in an emergency situation, I ask for a copy for their chart.
When should patients be referred to a specialty palliative care program?
I tell our oncology teams to involve me after they have tried to intervene, but unsuccessfully because of the patient having intractable symptoms, such as pain, or the disease is not responding to treatments. Or, because there are significant communication or health literacy barriers. Or, because there are challenging family dynamics that are impeding progress in establishing goals of care.
A physician should refer to specialty palliative care when there are multiple comorbid conditions that impact a patient’s prognosis and ability to tolerate treatments. These patients will need detailed symptom management and nuanced conversations about the delicate balance of maintaining quality of life and trying to address their malignancy while also avoiding treatments that may do more harm than good.
At the end of the day, all patients with serious illnesses deserve a palliative care approach to their care from all of their clinicians, not just from the palliative care team. By continuously honing and implementing primary palliative care skills, oncology teams can feel empowered to meet the needs of their patients themselves, strengthening their bond with their patients making truly patient-centered care much more likely.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
I recently met Jane, a 53-year-old woman with metastatic breast cancer. She was referred to me by the breast oncology team, which routinely refers all metastatic patients to our palliative care clinic.
Clocking in at under 20 minutes, my consultation with Jane might have been one of my shortest on record. Not only had the breast oncology team already addressed Jane’s symptoms, which mainly consisted of hot flashes and joint pain attributable to treatment with an aromatase inhibitor, but they had already started planning ahead for the future of her illness. Jane had completed an advance directive and had a realistic and hopeful perspective on how her illness would progress. She understood the goal of her treatment was to “keep the cancer asleep,” as she put it, and she was very clear about her own goals: to live long enough to see her granddaughter graduate from high school in 2 years and to take a long-awaited trip to Australia later in 2023.
There wasn’t much for me to do. In fact, I daresay that Jane really did not need to see a palliative care specialist because the primary palliative care she was receiving from the breast oncology team was superb. Jane was receiving excellent symptom management from a nurse practitioner and oncologist, plus a social worker provided her with coping strategies. She was already having conversations with her primary medical team and her family about what to expect in the future and how to plan ahead for all possible outcomes.
When should a patient be referred to palliative care?
Integrating palliative care into routine oncologic care need not always require the time and skill of a palliative care team for every patient. Oncology providers can provide basic palliative care services without consulting a palliative care specialist.
For example, if a primary care doctor tried to refer every patient with hypertension to cardiology, the cardiologist would probably say that primary care should be able to handle basic hypertension management. In my experience from working in an oncology clinic for the past 9 years, I’ve found that oncology providers don’t need to refer every advanced cancer patient to our palliative care program. Most oncologists have good communication skills and are more than capable of managing symptoms for patients.
But don’t get me wrong.
Palliative care for all?
In 2010, Jennifer S. Temel MD, published a landmark study in the New England Journal of Medicine that demonstrated significant improvements in quality of life and mood in patients with metastatic lung cancer who received concurrent palliative care. After the study was published many voices inside oncology and palliative care began to advocate for a “palliative care for all” approach to patients with metastatic disease. But this is often interpreted as “specialty palliative care for all,” rather than its original intended meaning that all patients with metastatic disease receive the essential elements of palliative care (biopsychosocial symptom support and conversations about goals of care) either through their primary oncology teams or, if needed, specialty palliative care teams.
The fact is that most specialty palliative care clinics do not have the manpower to meet the needs of all patients with advanced cancers, much less all patients living with serious illness. A main goal of integrating palliative care into routine outpatient health care has always been (and in my opinion, should continue to be) to enhance the primary palliative care skills of specialists, such as oncologists and cardiologists, who care for some of our sickest patients.
This could take many forms. For one, it can be helpful to screen patients for palliative care needs. The American College of Surgeons Commission on Cancer mandates distress screening for all patients as a condition of accreditation. Distress screening using a validated tool such as the National Comprehensive Cancer Network Distress Thermometer can differentiate patients who have minimal distress and may not need much additional support beyond what is provided by their oncology team from those whose distress feels unmanageable and overwhelming.
In terms of primary palliative care symptom management, most oncology teams I work with are comfortable prescribing basic medications for pain, nausea, constipation, and anxiety. They’re also comfortable referring oncology patients for nutrition needs while undergoing chemotherapy as well as to social work and spiritual care for emotional support and counseling.
Oncology teams should continually work on communications skills. They should use “Ask, Tell, Ask” to elicit prognostic awareness, convey critical information, and assess for recall and understanding at pivotal points in the cancer journey, such as when the disease progresses or the patient’s clinical condition changes. They should practice a normalizing script they can use to introduce advance care planning to their patients in the first few visits. When I meet with a patient for the first time, I usually begin by asking if they have prepared an advanced directive. If not, I ask if they’ve thought about who will make medical decisions for them should the need arise. If the patient has documented in writing their preference for care in an emergency situation, I ask for a copy for their chart.
When should patients be referred to a specialty palliative care program?
I tell our oncology teams to involve me after they have tried to intervene, but unsuccessfully because of the patient having intractable symptoms, such as pain, or the disease is not responding to treatments. Or, because there are significant communication or health literacy barriers. Or, because there are challenging family dynamics that are impeding progress in establishing goals of care.
A physician should refer to specialty palliative care when there are multiple comorbid conditions that impact a patient’s prognosis and ability to tolerate treatments. These patients will need detailed symptom management and nuanced conversations about the delicate balance of maintaining quality of life and trying to address their malignancy while also avoiding treatments that may do more harm than good.
At the end of the day, all patients with serious illnesses deserve a palliative care approach to their care from all of their clinicians, not just from the palliative care team. By continuously honing and implementing primary palliative care skills, oncology teams can feel empowered to meet the needs of their patients themselves, strengthening their bond with their patients making truly patient-centered care much more likely.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
I recently met Jane, a 53-year-old woman with metastatic breast cancer. She was referred to me by the breast oncology team, which routinely refers all metastatic patients to our palliative care clinic.
Clocking in at under 20 minutes, my consultation with Jane might have been one of my shortest on record. Not only had the breast oncology team already addressed Jane’s symptoms, which mainly consisted of hot flashes and joint pain attributable to treatment with an aromatase inhibitor, but they had already started planning ahead for the future of her illness. Jane had completed an advance directive and had a realistic and hopeful perspective on how her illness would progress. She understood the goal of her treatment was to “keep the cancer asleep,” as she put it, and she was very clear about her own goals: to live long enough to see her granddaughter graduate from high school in 2 years and to take a long-awaited trip to Australia later in 2023.
There wasn’t much for me to do. In fact, I daresay that Jane really did not need to see a palliative care specialist because the primary palliative care she was receiving from the breast oncology team was superb. Jane was receiving excellent symptom management from a nurse practitioner and oncologist, plus a social worker provided her with coping strategies. She was already having conversations with her primary medical team and her family about what to expect in the future and how to plan ahead for all possible outcomes.
When should a patient be referred to palliative care?
Integrating palliative care into routine oncologic care need not always require the time and skill of a palliative care team for every patient. Oncology providers can provide basic palliative care services without consulting a palliative care specialist.
For example, if a primary care doctor tried to refer every patient with hypertension to cardiology, the cardiologist would probably say that primary care should be able to handle basic hypertension management. In my experience from working in an oncology clinic for the past 9 years, I’ve found that oncology providers don’t need to refer every advanced cancer patient to our palliative care program. Most oncologists have good communication skills and are more than capable of managing symptoms for patients.
But don’t get me wrong.
Palliative care for all?
In 2010, Jennifer S. Temel MD, published a landmark study in the New England Journal of Medicine that demonstrated significant improvements in quality of life and mood in patients with metastatic lung cancer who received concurrent palliative care. After the study was published many voices inside oncology and palliative care began to advocate for a “palliative care for all” approach to patients with metastatic disease. But this is often interpreted as “specialty palliative care for all,” rather than its original intended meaning that all patients with metastatic disease receive the essential elements of palliative care (biopsychosocial symptom support and conversations about goals of care) either through their primary oncology teams or, if needed, specialty palliative care teams.
The fact is that most specialty palliative care clinics do not have the manpower to meet the needs of all patients with advanced cancers, much less all patients living with serious illness. A main goal of integrating palliative care into routine outpatient health care has always been (and in my opinion, should continue to be) to enhance the primary palliative care skills of specialists, such as oncologists and cardiologists, who care for some of our sickest patients.
This could take many forms. For one, it can be helpful to screen patients for palliative care needs. The American College of Surgeons Commission on Cancer mandates distress screening for all patients as a condition of accreditation. Distress screening using a validated tool such as the National Comprehensive Cancer Network Distress Thermometer can differentiate patients who have minimal distress and may not need much additional support beyond what is provided by their oncology team from those whose distress feels unmanageable and overwhelming.
In terms of primary palliative care symptom management, most oncology teams I work with are comfortable prescribing basic medications for pain, nausea, constipation, and anxiety. They’re also comfortable referring oncology patients for nutrition needs while undergoing chemotherapy as well as to social work and spiritual care for emotional support and counseling.
Oncology teams should continually work on communications skills. They should use “Ask, Tell, Ask” to elicit prognostic awareness, convey critical information, and assess for recall and understanding at pivotal points in the cancer journey, such as when the disease progresses or the patient’s clinical condition changes. They should practice a normalizing script they can use to introduce advance care planning to their patients in the first few visits. When I meet with a patient for the first time, I usually begin by asking if they have prepared an advanced directive. If not, I ask if they’ve thought about who will make medical decisions for them should the need arise. If the patient has documented in writing their preference for care in an emergency situation, I ask for a copy for their chart.
When should patients be referred to a specialty palliative care program?
I tell our oncology teams to involve me after they have tried to intervene, but unsuccessfully because of the patient having intractable symptoms, such as pain, or the disease is not responding to treatments. Or, because there are significant communication or health literacy barriers. Or, because there are challenging family dynamics that are impeding progress in establishing goals of care.
A physician should refer to specialty palliative care when there are multiple comorbid conditions that impact a patient’s prognosis and ability to tolerate treatments. These patients will need detailed symptom management and nuanced conversations about the delicate balance of maintaining quality of life and trying to address their malignancy while also avoiding treatments that may do more harm than good.
At the end of the day, all patients with serious illnesses deserve a palliative care approach to their care from all of their clinicians, not just from the palliative care team. By continuously honing and implementing primary palliative care skills, oncology teams can feel empowered to meet the needs of their patients themselves, strengthening their bond with their patients making truly patient-centered care much more likely.
Ms. D’Ambruoso is a hospice and palliative care nurse practitioner for UCLA Health Cancer Care, Santa Monica, Calif.
Cancer clinics begin to accommodate patients demanding new cancer detection tests
Doug Flora, MD, knows the value of early cancer detection because it helped him survive kidney cancer 5 years ago. But as a medical oncologist and hematologist, and the executive medical director of oncology services at St. Elizabeth Healthcare in Edgewood, Ky., he also knows that a new era of early cancer detection testing poses big challenges for his network of six hospitals and 169 specialty and primary care offices throughout Kentucky, Ohio, and Indiana.
Multicancer early detection (MCED) tests are finally a reality and could be a potential game changer because they can screen for the possibility of up to 50 different cancers in asymptomatic individuals with one blood draw. They represent one of the fastest growing segments in medical diagnostics with a projected value of $2.77 billion by 2030, according to the market research firm Grand View Research.
These tests are different from traditional liquid biopsies, which are designed to identify actionable gene mutations to help inform treatment decisions of patients already diagnosed with cancer. Instead, MCED tests work to detect fragments of circulating free DNA that have been shed by tumors and released into the bloodstream. Detecting these cancer signals could indicate that an individual has cancer well before they ever develop symptoms.
For some cancer types, particularly those commonly diagnosed at advanced stages or those without general population screening tests, MCED testing could have a significant impact.
In its new report, Grand View Research highlights nine “prominent players” active in the MCED market; of these, two have been granted breakthrough device designation by the Food and Drug Administration: OverC MCDBT by Burning Rock on Jan. 3, 2023, and Galleri by Grail in 2019. Galleri was launched in June 2021 and can be obtained with a prescription at a cost of $949.
Yet, while patients are asking for these tests and primary care physicians are prescribing them, oncologists are grappling with how to manage the first patients whose tests tell them they may have cancer.
Ordering the tests may seem straightforward, but in reality, it is not. In fact, they are so new that most health systems have no internal guidelines for physicians. Guidelines would address when the tests should be prescribed, and whether a patient should undergo more testing or be referred to an oncologist.
Clinical trials underway
There are currently at least 17 clinical trials underway to investigate the performance and clinical utility of MCED tests. Six of these involve Grail, including NHS-Galleri, the largest study to date of 140,000 participants in the United Kingdom where participants will be followed for 3 years with annual visits at 12 and 24 months. And, the National Cancer Institute is spearheading a clinical trial of its own, according to a search of ClinicalTrials.gov.
In September 2022, Grail presented findings from its pivotal PATHFINDER study at the annual meeting of the European Society of Medical Oncology. Researchers reported that cancer signals were detected in 1.4% (92) of 6,621 participants enrolled in the study. Of the 92, 35 people were diagnosed with 36 cancers: 19 were solid tumors (2 oropharyngeal, 5 breast, l liver, 1 intrahepatic bile duct, 2 colon/rectum, 2 prostate, 1 lung, 1 pancreas, 1 small intestine, 1 uterus, 1 ovary and 1 bone) and 17 hematologic cancers (1 plasma cell myeloma/disorders, 2 lymphoid leukemia, 2 Waldenström’s macroglobulinemia, and 12 lymphoma).
Almost half of newly diagnosed cases were cancers in stage 1 or 2. Of stage 1 cancers, three were solid tumors and four were hematologic cancers. Of stage 2 cancers, three were solid tumors and four were hematologic cancers. All other cancers were in stage 3 and 4 or were listed as recurrent or no stage. Deb Schrag, MD, MPH, chair of the department of medicine at Memorial Sloan Kettering Cancer Center in New York, who presented the results from PATHFINDER at ESMO, reported that, of all diagnosed cancers, only breast, colon/rectum, prostate, and lung have established screening protocols.
The findings were so striking that the meeting scientific co-chair, Fabrice André, MD, PhD, told ESMO the oncology field must prepare for an onslaught of new patients.
“Within the next 5 years, we will need more doctors, surgeons and nurses with more diagnostic and treatment infrastructures to care for the rising number of people who will be identified by multicancer early detection tests,” said Dr. André, who is director of research at Gustave Roussy Cancer Center, Villejuif, France, and future president of ESMO (2025-2026). “We need to involve all stakeholders in deciding new pathways of care. We need to agree who will be tested and when and where tests will be carried out, and to anticipate the changes that will happen as a result of these tests.”
But first, he urged, the need for comparative trials “across all types of cancer to find out if having an early detection test affects morbidity and mortality. We also need to know how the tests benefit patients, and how to discuss the results with them,” Dr. André said.
Demand may burden health systems
Dr. Flora suggested that companies like Grail are rushing their product to market without conducting long-term sizable clinical trials.
“These diagnostic companies are a billion dollar publicly traded or venture capital-funded companies that are losing millions of dollars a quarter as they’re scaling up these tests. So, there is some pressure on the sales forces ... to start moving product long before the science has met our lowest areas for entry,” Dr. Flora said. “They are aggressively marketing to a primary care audience that knows nothing about MCEDs. It’s a sales-driven development solving a problem we all believe is real, but we don’t know if it actually solves the problem.”
There are many unanswered questions, he said. Among these include whether the tests do indeed extend survival. “What they’re suggesting – that is if the blood test detects it – that we’re going to save your life. That’s not yet been proven. This is where the providers are pushing back against these industry types to say: ‘This is the wild west right now.’ It’s very irresponsible to go out there and try to sell hundreds of millions of dollars of product to doctors who have never studied genetics,” Dr. Flora said.
Grail’s chief medical officer Jeff Venstrom, MD, however, said physicians don’t need a background in genetic testing to order or interpret Galleri because it’s not a genetic test. Genetic tests look for genetic variants associated with cancer risk, which Galleri does not. MCED tests rely on genomic profiling to identify alterations in tumors.
“Maybe there’s still confusion in the market, which is common for new technologies when they’re initially launched. This is not a 23andMe test. We do not report germline mutations that have implications for cancer risk. We’re using this blood sample to test for the presence or absence of a cancer signal. The test result is very clear and simple: One area of the report says ‘yes’ or ‘no.’ It is a binary result that says if a signal is detected or not. The second provides additional information around where that signal could be coming from,” he said.
Galleri could fill a huge unmet need in cancer prevention, Dr. Venstrom said. Not only could it detect cancer at an earlier stage, but it could serve as a screening tool for cancers like pancreatic cancer in which screening is not available.
The test is not intended to replace standard of care screening, he said. The ordering provider should have a conversation with the patient about overall cancer risk. “Are you smoking? What’s your risk of obesity-associated cancers? Do you have a family history of cancer? I think this should all be in the context of a good conversation around preventative care,” he said.
Planning and prep in Boston
In Boston, Aparna Parikh, MD, an oncologist who specializes in gastrointestinal cancers, agreed that MCED testing has forced her team at the Mass General Cancer Center global cancer care program to think outside of the box.
“We’re a major academic center and it’s not easy [because] this is all uncharted territory,” she said. “We all recognize there are more tests coming, and they are here to stay. As a health system, we have to be ready to manage not only the tests, but patient anxieties, and all the complexities that come with it. We just don’t know yet how to best navigate.”
Although Dr. Parikh’s center has set up a working group tasked with organizing an outpatient clinic for patients with positive MCED tests, the current system is haphazard.
“Right now, it gets bounced around between people,” she explained. “Sometimes, patients are getting referred to the oncology team rather than the primary care team to try to sort out where the cancer signal is coming from, that is, if it’s not immediately obvious. No one really knows who should be the right person to own it,” Dr. Parikh said. While the test is supposed to give tissue-specific results, “it’s not perfect” and sometimes imaging and other work-ups are needed to locate the source of the signa.
“A group of four or five oncologists get looped in and then we’re trying to sort it out on a case-by-case basis, but understanding that with more and more tests coming, that kind of ad hoc approach isn’t going to be sufficient. We need a happy medium between the primary care and the disease specific oncologist, someone who can kind of help think through the diagnostic workup until they have a cancer diagnosis to get them to the right place,” Dr. Parikh said.
Dr. Venstrom said Grail is committed to providing support to clinicians in these situations. “We’re doing everything we can with our medical education forums. We have this pretty intense and extensive postpositive suite of resources,” he explained. “Some of our doctors on staff call the ordering provider within 24 hours just to clarify if there are any questions or confusion from the report. For example, if it suggests the signal is coming from the lung, we provide additional support around additional workups.”
Out-of-pocket test may widen disparities in care
With the exception of a few health insurance companies that have committed to covering some of the cost for the test, Galleri is an out-of-pocket expense.
Dr. Venstrom acknowledged that broad insurance coverage for the Galleri test remains a hurdle, although “we’ve secured coverage for a handful of companies of self-insured employers and forward-thinking insurers.” This includes partnerships with Point32Health, and Alignment Health, among others, he said.
There is also growing support among more than 400 cancer organizations for the Multi-Cancer Early Detection Screening Coverage Act to accelerate coverage for Medicare beneficiaries. “We are constantly trying to understand the evidence that’s needed for payors to make sure that we get the broadest access possible for this test,” he said.
The first positive test result
Back at St. Elizabeth Healthcare where they’ve only seen one positive MCED test result thus far, Dr. Flora is more concerned about patients giving informed consent before they even get the test. “When the reps started hammering our primary care doctors, we sent communiques throughout the system saying that we would very much like to regulate this to make sure that before our patients receive accidental harm, that they at least have a conversation with somebody who understands the test,” he explained.
All 15 patients who requested the test at the hospital were first required to discuss the implications with a genetic counselor who is part of the system. “We are really pro–cancer screening,” he said, but added his hospital is “not pumped” about the Galleri test. “We’re being very cautious about overstatements made by sales guys to our primary care doctors, so we’re letting our own precision medicine people handle it.”
There’s a similar system in place at Community Health Network, a nonprofit health system with nine hospitals and 1,300 employee providers throughout Central Indiana. Patrick McGill, MD, a primary care physician and chief analytics officer for the network says they have streamlined patients with positive tests through their high-risk oncology clinic. “They don’t go straight to a medical oncologist which I know some systems are struggling with,” he said. “They get additional testing, whether it’s imaging they might need or other lab testing. We’ve had a few lung positives, and a few leukemia positives which might go straight to medical oncology. I think we had one breast that was positive so she got additional breast imaging.”
Through its foundation, CHN will offer 2,000 tests free of charge. “We decided to take cost off the table with this funding,” Dr. McGill said. “A lot of health systems I talk to are always concerned that insurance doesn’t cover it and it’s cost prohibitive. Is it creating additional disparities because only people who can afford it can get the test?”
Dr. Schrag serves as an uncompensated advisor for Grail. Previously, while with the Dana-Farber Cancer Institute, she received research funding from Grail.
Doug Flora, MD, knows the value of early cancer detection because it helped him survive kidney cancer 5 years ago. But as a medical oncologist and hematologist, and the executive medical director of oncology services at St. Elizabeth Healthcare in Edgewood, Ky., he also knows that a new era of early cancer detection testing poses big challenges for his network of six hospitals and 169 specialty and primary care offices throughout Kentucky, Ohio, and Indiana.
Multicancer early detection (MCED) tests are finally a reality and could be a potential game changer because they can screen for the possibility of up to 50 different cancers in asymptomatic individuals with one blood draw. They represent one of the fastest growing segments in medical diagnostics with a projected value of $2.77 billion by 2030, according to the market research firm Grand View Research.
These tests are different from traditional liquid biopsies, which are designed to identify actionable gene mutations to help inform treatment decisions of patients already diagnosed with cancer. Instead, MCED tests work to detect fragments of circulating free DNA that have been shed by tumors and released into the bloodstream. Detecting these cancer signals could indicate that an individual has cancer well before they ever develop symptoms.
For some cancer types, particularly those commonly diagnosed at advanced stages or those without general population screening tests, MCED testing could have a significant impact.
In its new report, Grand View Research highlights nine “prominent players” active in the MCED market; of these, two have been granted breakthrough device designation by the Food and Drug Administration: OverC MCDBT by Burning Rock on Jan. 3, 2023, and Galleri by Grail in 2019. Galleri was launched in June 2021 and can be obtained with a prescription at a cost of $949.
Yet, while patients are asking for these tests and primary care physicians are prescribing them, oncologists are grappling with how to manage the first patients whose tests tell them they may have cancer.
Ordering the tests may seem straightforward, but in reality, it is not. In fact, they are so new that most health systems have no internal guidelines for physicians. Guidelines would address when the tests should be prescribed, and whether a patient should undergo more testing or be referred to an oncologist.
Clinical trials underway
There are currently at least 17 clinical trials underway to investigate the performance and clinical utility of MCED tests. Six of these involve Grail, including NHS-Galleri, the largest study to date of 140,000 participants in the United Kingdom where participants will be followed for 3 years with annual visits at 12 and 24 months. And, the National Cancer Institute is spearheading a clinical trial of its own, according to a search of ClinicalTrials.gov.
In September 2022, Grail presented findings from its pivotal PATHFINDER study at the annual meeting of the European Society of Medical Oncology. Researchers reported that cancer signals were detected in 1.4% (92) of 6,621 participants enrolled in the study. Of the 92, 35 people were diagnosed with 36 cancers: 19 were solid tumors (2 oropharyngeal, 5 breast, l liver, 1 intrahepatic bile duct, 2 colon/rectum, 2 prostate, 1 lung, 1 pancreas, 1 small intestine, 1 uterus, 1 ovary and 1 bone) and 17 hematologic cancers (1 plasma cell myeloma/disorders, 2 lymphoid leukemia, 2 Waldenström’s macroglobulinemia, and 12 lymphoma).
Almost half of newly diagnosed cases were cancers in stage 1 or 2. Of stage 1 cancers, three were solid tumors and four were hematologic cancers. Of stage 2 cancers, three were solid tumors and four were hematologic cancers. All other cancers were in stage 3 and 4 or were listed as recurrent or no stage. Deb Schrag, MD, MPH, chair of the department of medicine at Memorial Sloan Kettering Cancer Center in New York, who presented the results from PATHFINDER at ESMO, reported that, of all diagnosed cancers, only breast, colon/rectum, prostate, and lung have established screening protocols.
The findings were so striking that the meeting scientific co-chair, Fabrice André, MD, PhD, told ESMO the oncology field must prepare for an onslaught of new patients.
“Within the next 5 years, we will need more doctors, surgeons and nurses with more diagnostic and treatment infrastructures to care for the rising number of people who will be identified by multicancer early detection tests,” said Dr. André, who is director of research at Gustave Roussy Cancer Center, Villejuif, France, and future president of ESMO (2025-2026). “We need to involve all stakeholders in deciding new pathways of care. We need to agree who will be tested and when and where tests will be carried out, and to anticipate the changes that will happen as a result of these tests.”
But first, he urged, the need for comparative trials “across all types of cancer to find out if having an early detection test affects morbidity and mortality. We also need to know how the tests benefit patients, and how to discuss the results with them,” Dr. André said.
Demand may burden health systems
Dr. Flora suggested that companies like Grail are rushing their product to market without conducting long-term sizable clinical trials.
“These diagnostic companies are a billion dollar publicly traded or venture capital-funded companies that are losing millions of dollars a quarter as they’re scaling up these tests. So, there is some pressure on the sales forces ... to start moving product long before the science has met our lowest areas for entry,” Dr. Flora said. “They are aggressively marketing to a primary care audience that knows nothing about MCEDs. It’s a sales-driven development solving a problem we all believe is real, but we don’t know if it actually solves the problem.”
There are many unanswered questions, he said. Among these include whether the tests do indeed extend survival. “What they’re suggesting – that is if the blood test detects it – that we’re going to save your life. That’s not yet been proven. This is where the providers are pushing back against these industry types to say: ‘This is the wild west right now.’ It’s very irresponsible to go out there and try to sell hundreds of millions of dollars of product to doctors who have never studied genetics,” Dr. Flora said.
Grail’s chief medical officer Jeff Venstrom, MD, however, said physicians don’t need a background in genetic testing to order or interpret Galleri because it’s not a genetic test. Genetic tests look for genetic variants associated with cancer risk, which Galleri does not. MCED tests rely on genomic profiling to identify alterations in tumors.
“Maybe there’s still confusion in the market, which is common for new technologies when they’re initially launched. This is not a 23andMe test. We do not report germline mutations that have implications for cancer risk. We’re using this blood sample to test for the presence or absence of a cancer signal. The test result is very clear and simple: One area of the report says ‘yes’ or ‘no.’ It is a binary result that says if a signal is detected or not. The second provides additional information around where that signal could be coming from,” he said.
Galleri could fill a huge unmet need in cancer prevention, Dr. Venstrom said. Not only could it detect cancer at an earlier stage, but it could serve as a screening tool for cancers like pancreatic cancer in which screening is not available.
The test is not intended to replace standard of care screening, he said. The ordering provider should have a conversation with the patient about overall cancer risk. “Are you smoking? What’s your risk of obesity-associated cancers? Do you have a family history of cancer? I think this should all be in the context of a good conversation around preventative care,” he said.
Planning and prep in Boston
In Boston, Aparna Parikh, MD, an oncologist who specializes in gastrointestinal cancers, agreed that MCED testing has forced her team at the Mass General Cancer Center global cancer care program to think outside of the box.
“We’re a major academic center and it’s not easy [because] this is all uncharted territory,” she said. “We all recognize there are more tests coming, and they are here to stay. As a health system, we have to be ready to manage not only the tests, but patient anxieties, and all the complexities that come with it. We just don’t know yet how to best navigate.”
Although Dr. Parikh’s center has set up a working group tasked with organizing an outpatient clinic for patients with positive MCED tests, the current system is haphazard.
“Right now, it gets bounced around between people,” she explained. “Sometimes, patients are getting referred to the oncology team rather than the primary care team to try to sort out where the cancer signal is coming from, that is, if it’s not immediately obvious. No one really knows who should be the right person to own it,” Dr. Parikh said. While the test is supposed to give tissue-specific results, “it’s not perfect” and sometimes imaging and other work-ups are needed to locate the source of the signa.
“A group of four or five oncologists get looped in and then we’re trying to sort it out on a case-by-case basis, but understanding that with more and more tests coming, that kind of ad hoc approach isn’t going to be sufficient. We need a happy medium between the primary care and the disease specific oncologist, someone who can kind of help think through the diagnostic workup until they have a cancer diagnosis to get them to the right place,” Dr. Parikh said.
Dr. Venstrom said Grail is committed to providing support to clinicians in these situations. “We’re doing everything we can with our medical education forums. We have this pretty intense and extensive postpositive suite of resources,” he explained. “Some of our doctors on staff call the ordering provider within 24 hours just to clarify if there are any questions or confusion from the report. For example, if it suggests the signal is coming from the lung, we provide additional support around additional workups.”
Out-of-pocket test may widen disparities in care
With the exception of a few health insurance companies that have committed to covering some of the cost for the test, Galleri is an out-of-pocket expense.
Dr. Venstrom acknowledged that broad insurance coverage for the Galleri test remains a hurdle, although “we’ve secured coverage for a handful of companies of self-insured employers and forward-thinking insurers.” This includes partnerships with Point32Health, and Alignment Health, among others, he said.
There is also growing support among more than 400 cancer organizations for the Multi-Cancer Early Detection Screening Coverage Act to accelerate coverage for Medicare beneficiaries. “We are constantly trying to understand the evidence that’s needed for payors to make sure that we get the broadest access possible for this test,” he said.
The first positive test result
Back at St. Elizabeth Healthcare where they’ve only seen one positive MCED test result thus far, Dr. Flora is more concerned about patients giving informed consent before they even get the test. “When the reps started hammering our primary care doctors, we sent communiques throughout the system saying that we would very much like to regulate this to make sure that before our patients receive accidental harm, that they at least have a conversation with somebody who understands the test,” he explained.
All 15 patients who requested the test at the hospital were first required to discuss the implications with a genetic counselor who is part of the system. “We are really pro–cancer screening,” he said, but added his hospital is “not pumped” about the Galleri test. “We’re being very cautious about overstatements made by sales guys to our primary care doctors, so we’re letting our own precision medicine people handle it.”
There’s a similar system in place at Community Health Network, a nonprofit health system with nine hospitals and 1,300 employee providers throughout Central Indiana. Patrick McGill, MD, a primary care physician and chief analytics officer for the network says they have streamlined patients with positive tests through their high-risk oncology clinic. “They don’t go straight to a medical oncologist which I know some systems are struggling with,” he said. “They get additional testing, whether it’s imaging they might need or other lab testing. We’ve had a few lung positives, and a few leukemia positives which might go straight to medical oncology. I think we had one breast that was positive so she got additional breast imaging.”
Through its foundation, CHN will offer 2,000 tests free of charge. “We decided to take cost off the table with this funding,” Dr. McGill said. “A lot of health systems I talk to are always concerned that insurance doesn’t cover it and it’s cost prohibitive. Is it creating additional disparities because only people who can afford it can get the test?”
Dr. Schrag serves as an uncompensated advisor for Grail. Previously, while with the Dana-Farber Cancer Institute, she received research funding from Grail.
Doug Flora, MD, knows the value of early cancer detection because it helped him survive kidney cancer 5 years ago. But as a medical oncologist and hematologist, and the executive medical director of oncology services at St. Elizabeth Healthcare in Edgewood, Ky., he also knows that a new era of early cancer detection testing poses big challenges for his network of six hospitals and 169 specialty and primary care offices throughout Kentucky, Ohio, and Indiana.
Multicancer early detection (MCED) tests are finally a reality and could be a potential game changer because they can screen for the possibility of up to 50 different cancers in asymptomatic individuals with one blood draw. They represent one of the fastest growing segments in medical diagnostics with a projected value of $2.77 billion by 2030, according to the market research firm Grand View Research.
These tests are different from traditional liquid biopsies, which are designed to identify actionable gene mutations to help inform treatment decisions of patients already diagnosed with cancer. Instead, MCED tests work to detect fragments of circulating free DNA that have been shed by tumors and released into the bloodstream. Detecting these cancer signals could indicate that an individual has cancer well before they ever develop symptoms.
For some cancer types, particularly those commonly diagnosed at advanced stages or those without general population screening tests, MCED testing could have a significant impact.
In its new report, Grand View Research highlights nine “prominent players” active in the MCED market; of these, two have been granted breakthrough device designation by the Food and Drug Administration: OverC MCDBT by Burning Rock on Jan. 3, 2023, and Galleri by Grail in 2019. Galleri was launched in June 2021 and can be obtained with a prescription at a cost of $949.
Yet, while patients are asking for these tests and primary care physicians are prescribing them, oncologists are grappling with how to manage the first patients whose tests tell them they may have cancer.
Ordering the tests may seem straightforward, but in reality, it is not. In fact, they are so new that most health systems have no internal guidelines for physicians. Guidelines would address when the tests should be prescribed, and whether a patient should undergo more testing or be referred to an oncologist.
Clinical trials underway
There are currently at least 17 clinical trials underway to investigate the performance and clinical utility of MCED tests. Six of these involve Grail, including NHS-Galleri, the largest study to date of 140,000 participants in the United Kingdom where participants will be followed for 3 years with annual visits at 12 and 24 months. And, the National Cancer Institute is spearheading a clinical trial of its own, according to a search of ClinicalTrials.gov.
In September 2022, Grail presented findings from its pivotal PATHFINDER study at the annual meeting of the European Society of Medical Oncology. Researchers reported that cancer signals were detected in 1.4% (92) of 6,621 participants enrolled in the study. Of the 92, 35 people were diagnosed with 36 cancers: 19 were solid tumors (2 oropharyngeal, 5 breast, l liver, 1 intrahepatic bile duct, 2 colon/rectum, 2 prostate, 1 lung, 1 pancreas, 1 small intestine, 1 uterus, 1 ovary and 1 bone) and 17 hematologic cancers (1 plasma cell myeloma/disorders, 2 lymphoid leukemia, 2 Waldenström’s macroglobulinemia, and 12 lymphoma).
Almost half of newly diagnosed cases were cancers in stage 1 or 2. Of stage 1 cancers, three were solid tumors and four were hematologic cancers. Of stage 2 cancers, three were solid tumors and four were hematologic cancers. All other cancers were in stage 3 and 4 or were listed as recurrent or no stage. Deb Schrag, MD, MPH, chair of the department of medicine at Memorial Sloan Kettering Cancer Center in New York, who presented the results from PATHFINDER at ESMO, reported that, of all diagnosed cancers, only breast, colon/rectum, prostate, and lung have established screening protocols.
The findings were so striking that the meeting scientific co-chair, Fabrice André, MD, PhD, told ESMO the oncology field must prepare for an onslaught of new patients.
“Within the next 5 years, we will need more doctors, surgeons and nurses with more diagnostic and treatment infrastructures to care for the rising number of people who will be identified by multicancer early detection tests,” said Dr. André, who is director of research at Gustave Roussy Cancer Center, Villejuif, France, and future president of ESMO (2025-2026). “We need to involve all stakeholders in deciding new pathways of care. We need to agree who will be tested and when and where tests will be carried out, and to anticipate the changes that will happen as a result of these tests.”
But first, he urged, the need for comparative trials “across all types of cancer to find out if having an early detection test affects morbidity and mortality. We also need to know how the tests benefit patients, and how to discuss the results with them,” Dr. André said.
Demand may burden health systems
Dr. Flora suggested that companies like Grail are rushing their product to market without conducting long-term sizable clinical trials.
“These diagnostic companies are a billion dollar publicly traded or venture capital-funded companies that are losing millions of dollars a quarter as they’re scaling up these tests. So, there is some pressure on the sales forces ... to start moving product long before the science has met our lowest areas for entry,” Dr. Flora said. “They are aggressively marketing to a primary care audience that knows nothing about MCEDs. It’s a sales-driven development solving a problem we all believe is real, but we don’t know if it actually solves the problem.”
There are many unanswered questions, he said. Among these include whether the tests do indeed extend survival. “What they’re suggesting – that is if the blood test detects it – that we’re going to save your life. That’s not yet been proven. This is where the providers are pushing back against these industry types to say: ‘This is the wild west right now.’ It’s very irresponsible to go out there and try to sell hundreds of millions of dollars of product to doctors who have never studied genetics,” Dr. Flora said.
Grail’s chief medical officer Jeff Venstrom, MD, however, said physicians don’t need a background in genetic testing to order or interpret Galleri because it’s not a genetic test. Genetic tests look for genetic variants associated with cancer risk, which Galleri does not. MCED tests rely on genomic profiling to identify alterations in tumors.
“Maybe there’s still confusion in the market, which is common for new technologies when they’re initially launched. This is not a 23andMe test. We do not report germline mutations that have implications for cancer risk. We’re using this blood sample to test for the presence or absence of a cancer signal. The test result is very clear and simple: One area of the report says ‘yes’ or ‘no.’ It is a binary result that says if a signal is detected or not. The second provides additional information around where that signal could be coming from,” he said.
Galleri could fill a huge unmet need in cancer prevention, Dr. Venstrom said. Not only could it detect cancer at an earlier stage, but it could serve as a screening tool for cancers like pancreatic cancer in which screening is not available.
The test is not intended to replace standard of care screening, he said. The ordering provider should have a conversation with the patient about overall cancer risk. “Are you smoking? What’s your risk of obesity-associated cancers? Do you have a family history of cancer? I think this should all be in the context of a good conversation around preventative care,” he said.
Planning and prep in Boston
In Boston, Aparna Parikh, MD, an oncologist who specializes in gastrointestinal cancers, agreed that MCED testing has forced her team at the Mass General Cancer Center global cancer care program to think outside of the box.
“We’re a major academic center and it’s not easy [because] this is all uncharted territory,” she said. “We all recognize there are more tests coming, and they are here to stay. As a health system, we have to be ready to manage not only the tests, but patient anxieties, and all the complexities that come with it. We just don’t know yet how to best navigate.”
Although Dr. Parikh’s center has set up a working group tasked with organizing an outpatient clinic for patients with positive MCED tests, the current system is haphazard.
“Right now, it gets bounced around between people,” she explained. “Sometimes, patients are getting referred to the oncology team rather than the primary care team to try to sort out where the cancer signal is coming from, that is, if it’s not immediately obvious. No one really knows who should be the right person to own it,” Dr. Parikh said. While the test is supposed to give tissue-specific results, “it’s not perfect” and sometimes imaging and other work-ups are needed to locate the source of the signa.
“A group of four or five oncologists get looped in and then we’re trying to sort it out on a case-by-case basis, but understanding that with more and more tests coming, that kind of ad hoc approach isn’t going to be sufficient. We need a happy medium between the primary care and the disease specific oncologist, someone who can kind of help think through the diagnostic workup until they have a cancer diagnosis to get them to the right place,” Dr. Parikh said.
Dr. Venstrom said Grail is committed to providing support to clinicians in these situations. “We’re doing everything we can with our medical education forums. We have this pretty intense and extensive postpositive suite of resources,” he explained. “Some of our doctors on staff call the ordering provider within 24 hours just to clarify if there are any questions or confusion from the report. For example, if it suggests the signal is coming from the lung, we provide additional support around additional workups.”
Out-of-pocket test may widen disparities in care
With the exception of a few health insurance companies that have committed to covering some of the cost for the test, Galleri is an out-of-pocket expense.
Dr. Venstrom acknowledged that broad insurance coverage for the Galleri test remains a hurdle, although “we’ve secured coverage for a handful of companies of self-insured employers and forward-thinking insurers.” This includes partnerships with Point32Health, and Alignment Health, among others, he said.
There is also growing support among more than 400 cancer organizations for the Multi-Cancer Early Detection Screening Coverage Act to accelerate coverage for Medicare beneficiaries. “We are constantly trying to understand the evidence that’s needed for payors to make sure that we get the broadest access possible for this test,” he said.
The first positive test result
Back at St. Elizabeth Healthcare where they’ve only seen one positive MCED test result thus far, Dr. Flora is more concerned about patients giving informed consent before they even get the test. “When the reps started hammering our primary care doctors, we sent communiques throughout the system saying that we would very much like to regulate this to make sure that before our patients receive accidental harm, that they at least have a conversation with somebody who understands the test,” he explained.
All 15 patients who requested the test at the hospital were first required to discuss the implications with a genetic counselor who is part of the system. “We are really pro–cancer screening,” he said, but added his hospital is “not pumped” about the Galleri test. “We’re being very cautious about overstatements made by sales guys to our primary care doctors, so we’re letting our own precision medicine people handle it.”
There’s a similar system in place at Community Health Network, a nonprofit health system with nine hospitals and 1,300 employee providers throughout Central Indiana. Patrick McGill, MD, a primary care physician and chief analytics officer for the network says they have streamlined patients with positive tests through their high-risk oncology clinic. “They don’t go straight to a medical oncologist which I know some systems are struggling with,” he said. “They get additional testing, whether it’s imaging they might need or other lab testing. We’ve had a few lung positives, and a few leukemia positives which might go straight to medical oncology. I think we had one breast that was positive so she got additional breast imaging.”
Through its foundation, CHN will offer 2,000 tests free of charge. “We decided to take cost off the table with this funding,” Dr. McGill said. “A lot of health systems I talk to are always concerned that insurance doesn’t cover it and it’s cost prohibitive. Is it creating additional disparities because only people who can afford it can get the test?”
Dr. Schrag serves as an uncompensated advisor for Grail. Previously, while with the Dana-Farber Cancer Institute, she received research funding from Grail.
Cervical cancer rise in White women: A ‘canary in the coal mine’
Cervical cancer appears to be rising more rapidly in White women than in Black women in the United States, according to two independent studies. Researchers puzzling over this counterintuitive finding say that, if true, the findings may be a “canary in the coal mine,” signaling problems with U.S. health care that go way beyond women’s health.
Cervical cancer incidence in the United States has plateaued since 2010 and now stands at 7.5 per 100,000 people. Well-known disparities exist: Compared with White women, Black women are more likely to have distant-stage disease at diagnosis and more commonly die of their cancer.
However, two unconnected studies published in the past 5 months suggest that White women are catching up fast.
Cervical cancer rates in White women aged 30-34 are rising 2.8% a year, but holding steady for Black women, according to a recent study led by Ashish A. Deshmukh, PhD, of the Medical University of South Carolina, Charleston. His team analyzed the 2001-2019 National Program of Cancer Registries (NPCR) and Surveillance, Epidemiology, and End Results (SEER) dataset, which covers 98% of the U.S. population and 227,062 cervical cancer cases.
These findings were echoed by an analysis of the same database for 2001-2018 by the University of California, Los Angeles (UCLA), suggesting that distant-stage cervical cancer (defined as disease that has spread to the bladder and/or rectum at diagnosis) is climbing 1.69% a year in White people versus 0.67% in Black individuals.
The UCLA researchers, headed by Alex Francoeur, MD, a resident in the department of obstetrics and gynecology, found that disparities were most stark in adenocarcinoma, with an annual increase of 3.40% a year among White women and 1.71% in Black women.
Such findings have equity researchers scratching their heads. In cancer, it’s rare to see evidence that Black patients are doing better than their White counterparts.
One theoretical explanation is that the data are flawed, Ahmedin Jemal, DVM, PhD, senior vice president of surveillance and health equity science at the American Cancer Society, told this news organization. For example, the UCLA analysis may have been fogged by changes in staging definitions over time, Dr. Jemal said, although this would not explain the racial disparities per se.
Dr. Deshmukh stands by his data and said that, for him, the message is clear: “If rising incidence is not for localized-stage disease, but for advanced stages, that means it’s attributable to lack of screening,” he told this news organization.
However, this ‘simple’ explanation generates even more questions, Dr. Deshmukh said: “Screening is not a one-time procedure [but] a spectrum of timely cervical precancer treatment if [required]. We don’t know when exactly non-Hispanic White women are falling behind on that spectrum.”
The UCLA study supports Dr. Deshmukh’s conclusions. Using data from the Behavioral Risk Factor Surveillance System to calculate trends in “nonguideline screening,” the researchers found that White women were almost twice as likely to report that they were not following screening guidelines compared with Black women over the period of 2001-2016 (26.6% vs. 13.8%; P < .001).
“It’s not an artifact, it’s real,” said Timothy Rebbeck, PhD, the Vincent L. Gregory Jr. Professor of Cancer Prevention at Harvard TH Chan School of Public Health, Boston, who was not an author of either study and was approached for comment.
“The data are correct but there are so many things going on that might explain these patterns,” he told this news organization.
“This is a great example of complex changes in our social system, political system, health care system that are having really clear, measurable effects,” Dr. Rebbeck said. “Cervical cancer is almost a canary in the coal mine for some of this because it’s so preventable.”
(The saying “canary in a coal mine” is a warning of danger or trouble ahead. It comes from the time when coal miners would carry a caged canary down into the tunnels to warn them of noxious gases, which would kill the bird but give men time to escape.)
For example, Dr. Rebbeck said, recent turmoil in U.S. health care has left many people distrustful of the system. Although he acknowledged this was “high speculation,” he suggested that some women may have become less willing to participate in any mass health care intervention because of their political beliefs.
The UCLA study found that distant cervical cancer was rising fastest in middle-aged White women in the U.S. South, at a rate of 4.5% per year (P < .001).
Dr. Rebbeck also suggested that Medicaid expansion – the broadening of health insurance coverage in some states since the Affordable Care Act in 2014 – could be implicated. Of the 11 states that have not yet expanded Medicaid, eight are in the South.
“White populations who are in states that didn’t expand Medicaid are not getting a lot of the standard treatment and care that you would expect ...” Dr. Rebbeck said. “You could very well imagine that Medicaid nonexpanding states would have all kinds of patterns that would lead to more aggressive disease.”
In fact, there is already evidence that Medicaid expansion has affected racial disparities, disproportionately benefiting Black and Hispanic families, as for example, from an analysis of 65 studies by the Kaiser Family Foundation in 2020.
Commenting on these data, Dr. Rebbeck said, “Does that mean that the patterns of advanced cervical cancer had a smaller effect on Black women in this period because there was a greater shift in access to care? This is again a speculation, but it does fit with the ‘canary in a coal mine’ concept that advanced cervical cancer may be more rapidly influenced by health care access than other health conditions.”
The authors of the UCLA study suggested another explanation for their results: Differing enthusiasm for human papillomavirus (HPV) vaccination among White and Black families. The team also analyzed data on HPV vaccination, which offers protection against cervical cancer. The researchers found that vaccination rates were lowest, at 66.1%, among White teenagers aged 13-17 years, compared with Hispanics at 75.3%, Black teenagers at 74.6%, and Asians at 68.1%.
However, this theory was dismissed by both Dr. Jemal and Dr. Rebbeck due to timing. HPV vaccines have been around for approximately 15 years, so women who benefited (or didn’t benefit) from vaccination would be only in their late 20s today, they pointed out.
“Ninety-five percent of the cervical cancer cases we see now are in women who have not been vaccinated,” said Dr. Jemal, “So that’s out of the equation.”
Dr. Rebbeck agreed: “HPV may or may not be a thing here because it’s [got] such a latency.”
HPV vaccination may be out of the picture, but what about the epidemiology of HPV itself? Could the virus directly or indirectly be boosting advanced cervical cancer in White women?
Dr. Deshmukh thinks that it might be doing so.
He published an analysis of 2000-2018 SEER data showing that U.S. counties with the highest incidences of HPV-associated cancers also had the highest levels of smoking.
Other recent data suggest that middle-aged White women in the United States are more likely to reach for a smoke than are Black women.
Dr. Deshmukh acknowledges that the link is speculative but reasonable: “We don’t know exactly what the impact of smoking would be in terms of ... the ability to clear HPV infection. It may inhibit apoptosis, promoting tumor growth. There’s no causal association. It’s a cofactor risk.”
Dr. Rebbeck is also suspicious that smoking patterns might be a factor, pointing out that “smoking is certainly associated with both health behaviors and advanced cervical cancer.”
Both Dr. Rebbeck and Dr. Deshmukh concluded that, at this point, we can only speculate on what’s driving the puzzling acceleration of cervical cancer in White women in the United States.
However, whether it’s political aversion to screening, smoking-boosted HPV infection, Medicaid expansion or lack of it, or something else, they all agree that this canary in the coal mine clearly needs urgent medical attention.
Dr. Rebbeck and Dr. Jemal have declared no conflicts of interest. Dr. Deshmukh has declared consultant or advisory roles for Merck and Value Analytics Labs. None of the authors of the UCLA study have declared competing interests.
A version of this article first appeared on Medscape.com.
Cervical cancer appears to be rising more rapidly in White women than in Black women in the United States, according to two independent studies. Researchers puzzling over this counterintuitive finding say that, if true, the findings may be a “canary in the coal mine,” signaling problems with U.S. health care that go way beyond women’s health.
Cervical cancer incidence in the United States has plateaued since 2010 and now stands at 7.5 per 100,000 people. Well-known disparities exist: Compared with White women, Black women are more likely to have distant-stage disease at diagnosis and more commonly die of their cancer.
However, two unconnected studies published in the past 5 months suggest that White women are catching up fast.
Cervical cancer rates in White women aged 30-34 are rising 2.8% a year, but holding steady for Black women, according to a recent study led by Ashish A. Deshmukh, PhD, of the Medical University of South Carolina, Charleston. His team analyzed the 2001-2019 National Program of Cancer Registries (NPCR) and Surveillance, Epidemiology, and End Results (SEER) dataset, which covers 98% of the U.S. population and 227,062 cervical cancer cases.
These findings were echoed by an analysis of the same database for 2001-2018 by the University of California, Los Angeles (UCLA), suggesting that distant-stage cervical cancer (defined as disease that has spread to the bladder and/or rectum at diagnosis) is climbing 1.69% a year in White people versus 0.67% in Black individuals.
The UCLA researchers, headed by Alex Francoeur, MD, a resident in the department of obstetrics and gynecology, found that disparities were most stark in adenocarcinoma, with an annual increase of 3.40% a year among White women and 1.71% in Black women.
Such findings have equity researchers scratching their heads. In cancer, it’s rare to see evidence that Black patients are doing better than their White counterparts.
One theoretical explanation is that the data are flawed, Ahmedin Jemal, DVM, PhD, senior vice president of surveillance and health equity science at the American Cancer Society, told this news organization. For example, the UCLA analysis may have been fogged by changes in staging definitions over time, Dr. Jemal said, although this would not explain the racial disparities per se.
Dr. Deshmukh stands by his data and said that, for him, the message is clear: “If rising incidence is not for localized-stage disease, but for advanced stages, that means it’s attributable to lack of screening,” he told this news organization.
However, this ‘simple’ explanation generates even more questions, Dr. Deshmukh said: “Screening is not a one-time procedure [but] a spectrum of timely cervical precancer treatment if [required]. We don’t know when exactly non-Hispanic White women are falling behind on that spectrum.”
The UCLA study supports Dr. Deshmukh’s conclusions. Using data from the Behavioral Risk Factor Surveillance System to calculate trends in “nonguideline screening,” the researchers found that White women were almost twice as likely to report that they were not following screening guidelines compared with Black women over the period of 2001-2016 (26.6% vs. 13.8%; P < .001).
“It’s not an artifact, it’s real,” said Timothy Rebbeck, PhD, the Vincent L. Gregory Jr. Professor of Cancer Prevention at Harvard TH Chan School of Public Health, Boston, who was not an author of either study and was approached for comment.
“The data are correct but there are so many things going on that might explain these patterns,” he told this news organization.
“This is a great example of complex changes in our social system, political system, health care system that are having really clear, measurable effects,” Dr. Rebbeck said. “Cervical cancer is almost a canary in the coal mine for some of this because it’s so preventable.”
(The saying “canary in a coal mine” is a warning of danger or trouble ahead. It comes from the time when coal miners would carry a caged canary down into the tunnels to warn them of noxious gases, which would kill the bird but give men time to escape.)
For example, Dr. Rebbeck said, recent turmoil in U.S. health care has left many people distrustful of the system. Although he acknowledged this was “high speculation,” he suggested that some women may have become less willing to participate in any mass health care intervention because of their political beliefs.
The UCLA study found that distant cervical cancer was rising fastest in middle-aged White women in the U.S. South, at a rate of 4.5% per year (P < .001).
Dr. Rebbeck also suggested that Medicaid expansion – the broadening of health insurance coverage in some states since the Affordable Care Act in 2014 – could be implicated. Of the 11 states that have not yet expanded Medicaid, eight are in the South.
“White populations who are in states that didn’t expand Medicaid are not getting a lot of the standard treatment and care that you would expect ...” Dr. Rebbeck said. “You could very well imagine that Medicaid nonexpanding states would have all kinds of patterns that would lead to more aggressive disease.”
In fact, there is already evidence that Medicaid expansion has affected racial disparities, disproportionately benefiting Black and Hispanic families, as for example, from an analysis of 65 studies by the Kaiser Family Foundation in 2020.
Commenting on these data, Dr. Rebbeck said, “Does that mean that the patterns of advanced cervical cancer had a smaller effect on Black women in this period because there was a greater shift in access to care? This is again a speculation, but it does fit with the ‘canary in a coal mine’ concept that advanced cervical cancer may be more rapidly influenced by health care access than other health conditions.”
The authors of the UCLA study suggested another explanation for their results: Differing enthusiasm for human papillomavirus (HPV) vaccination among White and Black families. The team also analyzed data on HPV vaccination, which offers protection against cervical cancer. The researchers found that vaccination rates were lowest, at 66.1%, among White teenagers aged 13-17 years, compared with Hispanics at 75.3%, Black teenagers at 74.6%, and Asians at 68.1%.
However, this theory was dismissed by both Dr. Jemal and Dr. Rebbeck due to timing. HPV vaccines have been around for approximately 15 years, so women who benefited (or didn’t benefit) from vaccination would be only in their late 20s today, they pointed out.
“Ninety-five percent of the cervical cancer cases we see now are in women who have not been vaccinated,” said Dr. Jemal, “So that’s out of the equation.”
Dr. Rebbeck agreed: “HPV may or may not be a thing here because it’s [got] such a latency.”
HPV vaccination may be out of the picture, but what about the epidemiology of HPV itself? Could the virus directly or indirectly be boosting advanced cervical cancer in White women?
Dr. Deshmukh thinks that it might be doing so.
He published an analysis of 2000-2018 SEER data showing that U.S. counties with the highest incidences of HPV-associated cancers also had the highest levels of smoking.
Other recent data suggest that middle-aged White women in the United States are more likely to reach for a smoke than are Black women.
Dr. Deshmukh acknowledges that the link is speculative but reasonable: “We don’t know exactly what the impact of smoking would be in terms of ... the ability to clear HPV infection. It may inhibit apoptosis, promoting tumor growth. There’s no causal association. It’s a cofactor risk.”
Dr. Rebbeck is also suspicious that smoking patterns might be a factor, pointing out that “smoking is certainly associated with both health behaviors and advanced cervical cancer.”
Both Dr. Rebbeck and Dr. Deshmukh concluded that, at this point, we can only speculate on what’s driving the puzzling acceleration of cervical cancer in White women in the United States.
However, whether it’s political aversion to screening, smoking-boosted HPV infection, Medicaid expansion or lack of it, or something else, they all agree that this canary in the coal mine clearly needs urgent medical attention.
Dr. Rebbeck and Dr. Jemal have declared no conflicts of interest. Dr. Deshmukh has declared consultant or advisory roles for Merck and Value Analytics Labs. None of the authors of the UCLA study have declared competing interests.
A version of this article first appeared on Medscape.com.
Cervical cancer appears to be rising more rapidly in White women than in Black women in the United States, according to two independent studies. Researchers puzzling over this counterintuitive finding say that, if true, the findings may be a “canary in the coal mine,” signaling problems with U.S. health care that go way beyond women’s health.
Cervical cancer incidence in the United States has plateaued since 2010 and now stands at 7.5 per 100,000 people. Well-known disparities exist: Compared with White women, Black women are more likely to have distant-stage disease at diagnosis and more commonly die of their cancer.
However, two unconnected studies published in the past 5 months suggest that White women are catching up fast.
Cervical cancer rates in White women aged 30-34 are rising 2.8% a year, but holding steady for Black women, according to a recent study led by Ashish A. Deshmukh, PhD, of the Medical University of South Carolina, Charleston. His team analyzed the 2001-2019 National Program of Cancer Registries (NPCR) and Surveillance, Epidemiology, and End Results (SEER) dataset, which covers 98% of the U.S. population and 227,062 cervical cancer cases.
These findings were echoed by an analysis of the same database for 2001-2018 by the University of California, Los Angeles (UCLA), suggesting that distant-stage cervical cancer (defined as disease that has spread to the bladder and/or rectum at diagnosis) is climbing 1.69% a year in White people versus 0.67% in Black individuals.
The UCLA researchers, headed by Alex Francoeur, MD, a resident in the department of obstetrics and gynecology, found that disparities were most stark in adenocarcinoma, with an annual increase of 3.40% a year among White women and 1.71% in Black women.
Such findings have equity researchers scratching their heads. In cancer, it’s rare to see evidence that Black patients are doing better than their White counterparts.
One theoretical explanation is that the data are flawed, Ahmedin Jemal, DVM, PhD, senior vice president of surveillance and health equity science at the American Cancer Society, told this news organization. For example, the UCLA analysis may have been fogged by changes in staging definitions over time, Dr. Jemal said, although this would not explain the racial disparities per se.
Dr. Deshmukh stands by his data and said that, for him, the message is clear: “If rising incidence is not for localized-stage disease, but for advanced stages, that means it’s attributable to lack of screening,” he told this news organization.
However, this ‘simple’ explanation generates even more questions, Dr. Deshmukh said: “Screening is not a one-time procedure [but] a spectrum of timely cervical precancer treatment if [required]. We don’t know when exactly non-Hispanic White women are falling behind on that spectrum.”
The UCLA study supports Dr. Deshmukh’s conclusions. Using data from the Behavioral Risk Factor Surveillance System to calculate trends in “nonguideline screening,” the researchers found that White women were almost twice as likely to report that they were not following screening guidelines compared with Black women over the period of 2001-2016 (26.6% vs. 13.8%; P < .001).
“It’s not an artifact, it’s real,” said Timothy Rebbeck, PhD, the Vincent L. Gregory Jr. Professor of Cancer Prevention at Harvard TH Chan School of Public Health, Boston, who was not an author of either study and was approached for comment.
“The data are correct but there are so many things going on that might explain these patterns,” he told this news organization.
“This is a great example of complex changes in our social system, political system, health care system that are having really clear, measurable effects,” Dr. Rebbeck said. “Cervical cancer is almost a canary in the coal mine for some of this because it’s so preventable.”
(The saying “canary in a coal mine” is a warning of danger or trouble ahead. It comes from the time when coal miners would carry a caged canary down into the tunnels to warn them of noxious gases, which would kill the bird but give men time to escape.)
For example, Dr. Rebbeck said, recent turmoil in U.S. health care has left many people distrustful of the system. Although he acknowledged this was “high speculation,” he suggested that some women may have become less willing to participate in any mass health care intervention because of their political beliefs.
The UCLA study found that distant cervical cancer was rising fastest in middle-aged White women in the U.S. South, at a rate of 4.5% per year (P < .001).
Dr. Rebbeck also suggested that Medicaid expansion – the broadening of health insurance coverage in some states since the Affordable Care Act in 2014 – could be implicated. Of the 11 states that have not yet expanded Medicaid, eight are in the South.
“White populations who are in states that didn’t expand Medicaid are not getting a lot of the standard treatment and care that you would expect ...” Dr. Rebbeck said. “You could very well imagine that Medicaid nonexpanding states would have all kinds of patterns that would lead to more aggressive disease.”
In fact, there is already evidence that Medicaid expansion has affected racial disparities, disproportionately benefiting Black and Hispanic families, as for example, from an analysis of 65 studies by the Kaiser Family Foundation in 2020.
Commenting on these data, Dr. Rebbeck said, “Does that mean that the patterns of advanced cervical cancer had a smaller effect on Black women in this period because there was a greater shift in access to care? This is again a speculation, but it does fit with the ‘canary in a coal mine’ concept that advanced cervical cancer may be more rapidly influenced by health care access than other health conditions.”
The authors of the UCLA study suggested another explanation for their results: Differing enthusiasm for human papillomavirus (HPV) vaccination among White and Black families. The team also analyzed data on HPV vaccination, which offers protection against cervical cancer. The researchers found that vaccination rates were lowest, at 66.1%, among White teenagers aged 13-17 years, compared with Hispanics at 75.3%, Black teenagers at 74.6%, and Asians at 68.1%.
However, this theory was dismissed by both Dr. Jemal and Dr. Rebbeck due to timing. HPV vaccines have been around for approximately 15 years, so women who benefited (or didn’t benefit) from vaccination would be only in their late 20s today, they pointed out.
“Ninety-five percent of the cervical cancer cases we see now are in women who have not been vaccinated,” said Dr. Jemal, “So that’s out of the equation.”
Dr. Rebbeck agreed: “HPV may or may not be a thing here because it’s [got] such a latency.”
HPV vaccination may be out of the picture, but what about the epidemiology of HPV itself? Could the virus directly or indirectly be boosting advanced cervical cancer in White women?
Dr. Deshmukh thinks that it might be doing so.
He published an analysis of 2000-2018 SEER data showing that U.S. counties with the highest incidences of HPV-associated cancers also had the highest levels of smoking.
Other recent data suggest that middle-aged White women in the United States are more likely to reach for a smoke than are Black women.
Dr. Deshmukh acknowledges that the link is speculative but reasonable: “We don’t know exactly what the impact of smoking would be in terms of ... the ability to clear HPV infection. It may inhibit apoptosis, promoting tumor growth. There’s no causal association. It’s a cofactor risk.”
Dr. Rebbeck is also suspicious that smoking patterns might be a factor, pointing out that “smoking is certainly associated with both health behaviors and advanced cervical cancer.”
Both Dr. Rebbeck and Dr. Deshmukh concluded that, at this point, we can only speculate on what’s driving the puzzling acceleration of cervical cancer in White women in the United States.
However, whether it’s political aversion to screening, smoking-boosted HPV infection, Medicaid expansion or lack of it, or something else, they all agree that this canary in the coal mine clearly needs urgent medical attention.
Dr. Rebbeck and Dr. Jemal have declared no conflicts of interest. Dr. Deshmukh has declared consultant or advisory roles for Merck and Value Analytics Labs. None of the authors of the UCLA study have declared competing interests.
A version of this article first appeared on Medscape.com.
Diagnosed too late
It had only been 3 weeks since I first met this patient. She presented with an advanced case of colon cancer, but instead of treatment,
Within the course of 2 weeks I saw another new patient, but this time with pancreatic cancer that metastasized to the liver. “When can we start treatment?” he asked. Like my female patient with colon cancer, he was diagnosed too late as he was already in an incurable stage. He was shocked to learn that his condition was in stage 4, that achieving remission would be difficult and a cure, not likely. Certainly, standard of care treatments and clinical trials offered him hope, but they were unlikely to change the outcome.
We take a course in this – that is, in giving bad news, but every doctor has his or her own approach. Some are so uncomfortable with the talk, they choose avoidance and adopt the “look like you gotta go approach.” Or, the doctor may schedule another treatment or another test with the intention of avoiding end-of-life discussions. Other doctors opt for straight talk: “I think you should get your affairs in order. You’ve got 3 months to live.” These are extreme behaviors I wouldn’t recommend.
In my practice, I sit with my patients and explain the diagnosis. After discussing all options and the advanced stage and diagnosis, it ultimately comes down to “Win or lose, I will be here to take care of you.” Sometimes there is therapy that may help, but either way, the patient understands that death is a real possibility.
I find that people just want to know if there is hope. A different treatment regimen or a clinical trial may (or may not) extend their life. And while we cannot predict outcomes, we can give them hope. You can’t shut down hope. True for some people the cup is always half empty, but most people want to live and are optimistic no matter how small the chances are.
These conversations are very difficult. I don’t like them, but then I don’t avoid them either. Fortunately, patients don’t usually come to my office for the first visit presenting with advanced disease. In the cases I described above, one patient had been experiencing unexplained weight loss, but didn’t share it with a physician. And, for the patient with pancreatic cancer, other than some discomfort in the last couple of weeks, the disease was not associated with other symptoms. But the absence of symptoms should not in any way rule out a malignant disease. A diagnosis should be based on a complete evaluation of signs and symptoms followed by testing.
We’ve got to be able to take the time to listen to our patients during these encounters. We may not spend as much time as we should because we’re so busy now and we’re slaves to EMRs. It helps if we take more time to probe symptoms a little longer, especially in the primary care setting.
It is possible for a patient with cancer to be asymptomatic up until the later stages of the disease. A study published in ESMO Open in 2020 found that fewer than half of patients with stage 4 non–small cell lung cancer have only one or two symptoms at diagnosis regardless of whether the patient was a smoker. In this study only 33% of patients reported having a cough and 25% had chest pain.
A study presented in October at the United European Gastroenterology Week found that of 600 pancreatic cancer cases, 46 of these were not detected by CT or MRI conducted 3-18 months prior to diagnosis. Of the 46 cases, 26% were not picked up by the radiologist and the rest were largely as a result of imaging changes over time. Radiology techniques are good, but they cannot pick up lesions that are too small. And some lesions, particularly in pancreatic cancer, can grow and metastasize rather quickly.
When a patient is diagnosed with advanced disease, it is most often simply because of the nature of the disease. But sometimes patients put off scheduling a doctor visit because of fear of the potential for bad news or fear of the doctor belittling their symptoms. Some tell me they were “just hoping the symptoms would disappear.” Waiting too long to see a doctor is never a good idea because timing is crucial. In many cases, there is a small window of opportunity to treat disease if remission is to be achieved.
Dr. Henry is a practicing clinical oncologist with PennMedicine in Philadelphia where he also serves as Vice Chair of the Department of Medicine at Pennsylvania Hospital.
This article was updated 12/7/22.
It had only been 3 weeks since I first met this patient. She presented with an advanced case of colon cancer, but instead of treatment,
Within the course of 2 weeks I saw another new patient, but this time with pancreatic cancer that metastasized to the liver. “When can we start treatment?” he asked. Like my female patient with colon cancer, he was diagnosed too late as he was already in an incurable stage. He was shocked to learn that his condition was in stage 4, that achieving remission would be difficult and a cure, not likely. Certainly, standard of care treatments and clinical trials offered him hope, but they were unlikely to change the outcome.
We take a course in this – that is, in giving bad news, but every doctor has his or her own approach. Some are so uncomfortable with the talk, they choose avoidance and adopt the “look like you gotta go approach.” Or, the doctor may schedule another treatment or another test with the intention of avoiding end-of-life discussions. Other doctors opt for straight talk: “I think you should get your affairs in order. You’ve got 3 months to live.” These are extreme behaviors I wouldn’t recommend.
In my practice, I sit with my patients and explain the diagnosis. After discussing all options and the advanced stage and diagnosis, it ultimately comes down to “Win or lose, I will be here to take care of you.” Sometimes there is therapy that may help, but either way, the patient understands that death is a real possibility.
I find that people just want to know if there is hope. A different treatment regimen or a clinical trial may (or may not) extend their life. And while we cannot predict outcomes, we can give them hope. You can’t shut down hope. True for some people the cup is always half empty, but most people want to live and are optimistic no matter how small the chances are.
These conversations are very difficult. I don’t like them, but then I don’t avoid them either. Fortunately, patients don’t usually come to my office for the first visit presenting with advanced disease. In the cases I described above, one patient had been experiencing unexplained weight loss, but didn’t share it with a physician. And, for the patient with pancreatic cancer, other than some discomfort in the last couple of weeks, the disease was not associated with other symptoms. But the absence of symptoms should not in any way rule out a malignant disease. A diagnosis should be based on a complete evaluation of signs and symptoms followed by testing.
We’ve got to be able to take the time to listen to our patients during these encounters. We may not spend as much time as we should because we’re so busy now and we’re slaves to EMRs. It helps if we take more time to probe symptoms a little longer, especially in the primary care setting.
It is possible for a patient with cancer to be asymptomatic up until the later stages of the disease. A study published in ESMO Open in 2020 found that fewer than half of patients with stage 4 non–small cell lung cancer have only one or two symptoms at diagnosis regardless of whether the patient was a smoker. In this study only 33% of patients reported having a cough and 25% had chest pain.
A study presented in October at the United European Gastroenterology Week found that of 600 pancreatic cancer cases, 46 of these were not detected by CT or MRI conducted 3-18 months prior to diagnosis. Of the 46 cases, 26% were not picked up by the radiologist and the rest were largely as a result of imaging changes over time. Radiology techniques are good, but they cannot pick up lesions that are too small. And some lesions, particularly in pancreatic cancer, can grow and metastasize rather quickly.
When a patient is diagnosed with advanced disease, it is most often simply because of the nature of the disease. But sometimes patients put off scheduling a doctor visit because of fear of the potential for bad news or fear of the doctor belittling their symptoms. Some tell me they were “just hoping the symptoms would disappear.” Waiting too long to see a doctor is never a good idea because timing is crucial. In many cases, there is a small window of opportunity to treat disease if remission is to be achieved.
Dr. Henry is a practicing clinical oncologist with PennMedicine in Philadelphia where he also serves as Vice Chair of the Department of Medicine at Pennsylvania Hospital.
This article was updated 12/7/22.
It had only been 3 weeks since I first met this patient. She presented with an advanced case of colon cancer, but instead of treatment,
Within the course of 2 weeks I saw another new patient, but this time with pancreatic cancer that metastasized to the liver. “When can we start treatment?” he asked. Like my female patient with colon cancer, he was diagnosed too late as he was already in an incurable stage. He was shocked to learn that his condition was in stage 4, that achieving remission would be difficult and a cure, not likely. Certainly, standard of care treatments and clinical trials offered him hope, but they were unlikely to change the outcome.
We take a course in this – that is, in giving bad news, but every doctor has his or her own approach. Some are so uncomfortable with the talk, they choose avoidance and adopt the “look like you gotta go approach.” Or, the doctor may schedule another treatment or another test with the intention of avoiding end-of-life discussions. Other doctors opt for straight talk: “I think you should get your affairs in order. You’ve got 3 months to live.” These are extreme behaviors I wouldn’t recommend.
In my practice, I sit with my patients and explain the diagnosis. After discussing all options and the advanced stage and diagnosis, it ultimately comes down to “Win or lose, I will be here to take care of you.” Sometimes there is therapy that may help, but either way, the patient understands that death is a real possibility.
I find that people just want to know if there is hope. A different treatment regimen or a clinical trial may (or may not) extend their life. And while we cannot predict outcomes, we can give them hope. You can’t shut down hope. True for some people the cup is always half empty, but most people want to live and are optimistic no matter how small the chances are.
These conversations are very difficult. I don’t like them, but then I don’t avoid them either. Fortunately, patients don’t usually come to my office for the first visit presenting with advanced disease. In the cases I described above, one patient had been experiencing unexplained weight loss, but didn’t share it with a physician. And, for the patient with pancreatic cancer, other than some discomfort in the last couple of weeks, the disease was not associated with other symptoms. But the absence of symptoms should not in any way rule out a malignant disease. A diagnosis should be based on a complete evaluation of signs and symptoms followed by testing.
We’ve got to be able to take the time to listen to our patients during these encounters. We may not spend as much time as we should because we’re so busy now and we’re slaves to EMRs. It helps if we take more time to probe symptoms a little longer, especially in the primary care setting.
It is possible for a patient with cancer to be asymptomatic up until the later stages of the disease. A study published in ESMO Open in 2020 found that fewer than half of patients with stage 4 non–small cell lung cancer have only one or two symptoms at diagnosis regardless of whether the patient was a smoker. In this study only 33% of patients reported having a cough and 25% had chest pain.
A study presented in October at the United European Gastroenterology Week found that of 600 pancreatic cancer cases, 46 of these were not detected by CT or MRI conducted 3-18 months prior to diagnosis. Of the 46 cases, 26% were not picked up by the radiologist and the rest were largely as a result of imaging changes over time. Radiology techniques are good, but they cannot pick up lesions that are too small. And some lesions, particularly in pancreatic cancer, can grow and metastasize rather quickly.
When a patient is diagnosed with advanced disease, it is most often simply because of the nature of the disease. But sometimes patients put off scheduling a doctor visit because of fear of the potential for bad news or fear of the doctor belittling their symptoms. Some tell me they were “just hoping the symptoms would disappear.” Waiting too long to see a doctor is never a good idea because timing is crucial. In many cases, there is a small window of opportunity to treat disease if remission is to be achieved.
Dr. Henry is a practicing clinical oncologist with PennMedicine in Philadelphia where he also serves as Vice Chair of the Department of Medicine at Pennsylvania Hospital.
This article was updated 12/7/22.
FDA requests more restrictions on ovarian cancer drugs
citing recent data showing an increased risk for death with the agents versus chemotherapy.
These restrictions could mean bankruptcy for one company.
Earlier this year, several companies voluntarily withdrew their respective PARP inhibitors for heavily pretreated patients with ovarian cancer in later-line indications.
Now, the FDA has asked GlaxoSmithKline and Clovis Oncology to restrict the second-line indications for their PARP inhibitors – niraparib (Zejula) for GSK and rucaparib (Rubraca) for Clovis.
The FDA’s requests are based on recent data showing an increased risk for death with the PARP inhibitors versus chemotherapy.
On Nov. 11, GSK announced that, at the FDA’s request, it will limit the second-line maintenance indication for its PARP inhibitor niraparib to patients with deleterious or suspected deleterious germline BRCA mutations.
The prescribing change was based on an FDA review of the final overall survival analysis of the NOVA phase 3 trial, which served as the basis for the approval of the second-line maintenance indication. The final overall survival data showed a hazard ratio of 1.06 (95% confidence interval, 0.81-1.37) in the cohort without germline BRCA mutations.
The company noted, however, that its first-line indication remains unchanged.
The FDA has also asked Clovis Oncology to restrict its PARP inhibitor rucaparib in the second-line maintenance therapy setting, according to a Nov. 14 U.S. Securities and Exchange Commission filing from the company. Rucaparib is currently not approved to treat ovarian cancer in the first-line setting.
According to the filing, the FDA met with Clovis Oncology to discuss the overall survival data from the ARIEL3 clinical trial, which formed the basis for the drug’s approval in the United States as second-line maintenance for adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who had a complete or partial response to platinum-based chemotherapy.
In September 2022, Clovis Oncology submitted the final overall survival data from the ARIEL3 trial to FDA. According to the company, among all populations analyzed, the confidence intervals for all hazard ratios crossed 1, “indicating no difference between the treatment arms.”
Based on the overall survival data, the FDA requested that Clovis “voluntarily revise the label to limit the indication of Rubraca in this second-line maintenance treatment” to only patients with BRCA mutations.
Clovis said it is “currently evaluating FDA’s request.” If an agreement can’t be reached, the FDA said it would convene an advisory committee to review the matter.
However, further restricting the indication for rucaparib could put the company’s future in jeopardy. In an earlier report, Clovis Oncology foreshadowed a “potential bankruptcy filing in the very near term” as “increasingly probable.”
The company explained that, because “a substantial portion” of the drug’s revenue is attributable to its second-line indication, limiting that indication “could result in a significant impact on our revenue.”
The report continued: “Based on our current cash and cash equivalents, together with current estimates for revenues to be generated by sales of Rubraca, we will not have sufficient liquidity to maintain our operations beyond January 2023.”
A version of this article first appeared on Medscape.com.
citing recent data showing an increased risk for death with the agents versus chemotherapy.
These restrictions could mean bankruptcy for one company.
Earlier this year, several companies voluntarily withdrew their respective PARP inhibitors for heavily pretreated patients with ovarian cancer in later-line indications.
Now, the FDA has asked GlaxoSmithKline and Clovis Oncology to restrict the second-line indications for their PARP inhibitors – niraparib (Zejula) for GSK and rucaparib (Rubraca) for Clovis.
The FDA’s requests are based on recent data showing an increased risk for death with the PARP inhibitors versus chemotherapy.
On Nov. 11, GSK announced that, at the FDA’s request, it will limit the second-line maintenance indication for its PARP inhibitor niraparib to patients with deleterious or suspected deleterious germline BRCA mutations.
The prescribing change was based on an FDA review of the final overall survival analysis of the NOVA phase 3 trial, which served as the basis for the approval of the second-line maintenance indication. The final overall survival data showed a hazard ratio of 1.06 (95% confidence interval, 0.81-1.37) in the cohort without germline BRCA mutations.
The company noted, however, that its first-line indication remains unchanged.
The FDA has also asked Clovis Oncology to restrict its PARP inhibitor rucaparib in the second-line maintenance therapy setting, according to a Nov. 14 U.S. Securities and Exchange Commission filing from the company. Rucaparib is currently not approved to treat ovarian cancer in the first-line setting.
According to the filing, the FDA met with Clovis Oncology to discuss the overall survival data from the ARIEL3 clinical trial, which formed the basis for the drug’s approval in the United States as second-line maintenance for adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who had a complete or partial response to platinum-based chemotherapy.
In September 2022, Clovis Oncology submitted the final overall survival data from the ARIEL3 trial to FDA. According to the company, among all populations analyzed, the confidence intervals for all hazard ratios crossed 1, “indicating no difference between the treatment arms.”
Based on the overall survival data, the FDA requested that Clovis “voluntarily revise the label to limit the indication of Rubraca in this second-line maintenance treatment” to only patients with BRCA mutations.
Clovis said it is “currently evaluating FDA’s request.” If an agreement can’t be reached, the FDA said it would convene an advisory committee to review the matter.
However, further restricting the indication for rucaparib could put the company’s future in jeopardy. In an earlier report, Clovis Oncology foreshadowed a “potential bankruptcy filing in the very near term” as “increasingly probable.”
The company explained that, because “a substantial portion” of the drug’s revenue is attributable to its second-line indication, limiting that indication “could result in a significant impact on our revenue.”
The report continued: “Based on our current cash and cash equivalents, together with current estimates for revenues to be generated by sales of Rubraca, we will not have sufficient liquidity to maintain our operations beyond January 2023.”
A version of this article first appeared on Medscape.com.
citing recent data showing an increased risk for death with the agents versus chemotherapy.
These restrictions could mean bankruptcy for one company.
Earlier this year, several companies voluntarily withdrew their respective PARP inhibitors for heavily pretreated patients with ovarian cancer in later-line indications.
Now, the FDA has asked GlaxoSmithKline and Clovis Oncology to restrict the second-line indications for their PARP inhibitors – niraparib (Zejula) for GSK and rucaparib (Rubraca) for Clovis.
The FDA’s requests are based on recent data showing an increased risk for death with the PARP inhibitors versus chemotherapy.
On Nov. 11, GSK announced that, at the FDA’s request, it will limit the second-line maintenance indication for its PARP inhibitor niraparib to patients with deleterious or suspected deleterious germline BRCA mutations.
The prescribing change was based on an FDA review of the final overall survival analysis of the NOVA phase 3 trial, which served as the basis for the approval of the second-line maintenance indication. The final overall survival data showed a hazard ratio of 1.06 (95% confidence interval, 0.81-1.37) in the cohort without germline BRCA mutations.
The company noted, however, that its first-line indication remains unchanged.
The FDA has also asked Clovis Oncology to restrict its PARP inhibitor rucaparib in the second-line maintenance therapy setting, according to a Nov. 14 U.S. Securities and Exchange Commission filing from the company. Rucaparib is currently not approved to treat ovarian cancer in the first-line setting.
According to the filing, the FDA met with Clovis Oncology to discuss the overall survival data from the ARIEL3 clinical trial, which formed the basis for the drug’s approval in the United States as second-line maintenance for adult patients with recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who had a complete or partial response to platinum-based chemotherapy.
In September 2022, Clovis Oncology submitted the final overall survival data from the ARIEL3 trial to FDA. According to the company, among all populations analyzed, the confidence intervals for all hazard ratios crossed 1, “indicating no difference between the treatment arms.”
Based on the overall survival data, the FDA requested that Clovis “voluntarily revise the label to limit the indication of Rubraca in this second-line maintenance treatment” to only patients with BRCA mutations.
Clovis said it is “currently evaluating FDA’s request.” If an agreement can’t be reached, the FDA said it would convene an advisory committee to review the matter.
However, further restricting the indication for rucaparib could put the company’s future in jeopardy. In an earlier report, Clovis Oncology foreshadowed a “potential bankruptcy filing in the very near term” as “increasingly probable.”
The company explained that, because “a substantial portion” of the drug’s revenue is attributable to its second-line indication, limiting that indication “could result in a significant impact on our revenue.”
The report continued: “Based on our current cash and cash equivalents, together with current estimates for revenues to be generated by sales of Rubraca, we will not have sufficient liquidity to maintain our operations beyond January 2023.”
A version of this article first appeared on Medscape.com.
Transgender patients on hormone therapy require monitoring
PAU, France – Transgender patients on hormone therapy have an increased mortality risk and so must be closely monitored, especially in terms of cardiovascular health and oncology, reported Marie D’Assigny, MD, of the department of endocrinology, diabetes, and dietetics at Poitiers (France) University Hospital, at the Infogyn 2022 conference. Because transgender women (those assigned male at birth who have assumed a female gender identity) are at risk of breast cancer, they should also be recommended for breast cancer screening.
Transgender men and women, especially transgender women, “should be deemed high-risk cardiovascular patients, or even very high risk in some cases,” said Dr. D’Assigny. This means that they should be considered candidates for cholesterol-lowering medication earlier than their cisgender counterparts, and a target LDL cholesterol of less than 0.70 g/L (70 mg/dL) should be sought. Likewise, blood pressure must be strictly monitored, especially because it tends to rise when on hormone therapy.
Feminizing hormone therapy requires chemical castration with the use of anti-androgen drugs to achieve a blood testosterone level less than 0.5 ng/mL (1.73 nmol/L). Low-dose cyproterone acetate (< 25 to 50 mg/day) is usually used. Treatment is stopped if a patient undergoes an orchidectomy. For feminizing hormone therapy, administration of 17beta-estradiol transcutaneously (patch or gel) is recommended, because it is associated with a lower risk of thromboembolism than oral administration.
Masculinizing hormone therapy is based on administration of progestogens, then testosterone in the form of an injection (mostly testosterone enanthate via intramuscular injection every 10 days) or percutaneously (gel or patch). There are few contraindications, and treatment is generally well tolerated.
High mortality rate
A recent retrospective study highlighted the mortality and risk factors for death in transgender men and women receiving hormone therapy. More than 4,500 people, mostly male to female transgender women, were enrolled in this study, which was conducted over a 47-year period (1972-2018) at a specialist clinic at Amsterdam UMC.
Over the course of the study, the mortality rate in transgender men and women was twice that of the general population. The death rate was 10.8% in transgender women vs. 2.7% in transgender men, after a follow-up of 40,232 person-years and 17,285 person-years, respectively. In transgender women, mortality was nearly three times that of cisgender women in the general population.
Over the nearly 5 decades of study, there was no improvement in the mortality rate, even over the last 10 years when transgender issues started to be more recognized. The mortality trends are markedly distinct over the years from those observed in the cisgender population, and this is especially true for transgender women compared to transgender men. “Much is still to be done,” said Dr. D’Assigny.
According to the study, cause-specific mortality in transgender women was high for cardiovascular disease and lung cancer, possibly because of a higher smoking rate in this population. HIV-related disease and suicide remained very high in both transgender men and women.
People with gender dysphoria who do not receive treatment for gender reassignment have a suicide rate of 40%, reported François-Xavier Madec, MD, of Foch Hospital in Suresnes, France, at a previous presentation. For transgender men and women who receive care, this rate is lowered to 15%, which is still significantly higher than the rate of 1.6% observed in the general population.
“These causes of death don’t give any indication as to a specific effect of hormone treatment but show that monitoring and, if necessary, treatment of comorbidities and lifestyle-related factors are important in managing transgender patients,” said the study authors.
“Strengthening social acceptance and treating cardiovascular risk factors could also help to reduce mortality in transgender men and women,” they added.
Screening for osteoporosis
In addition to receiving cardiovascular risk factor assessment and monitoring, transgender men and women on hormone therapy should also undergo bone density testing “when risk factors for osteoporosis are present, especially in patients stopping hormone therapy after a gonadectomy,” said Dr. D’Assigny.
Calcium and vitamin D supplements are also recommended for all patients after a gonadectomy, especially in transgender men on testosterone. Osteoporosis screening is recommended for transgender men 10 years after starting treatment with testosterone, then every 10 years.
There is also the risk for breast cancer in transgender women, although the risk is lower than in cisgender women. This risk was highlighted in another study of more than 2,260 transgender women that was carried out by a team at Amsterdam UMC.
A total of 18 cases of breast cancer (15 invasive) were diagnosed after a median 18 years of hormone treatment. This represents an incidence of breast cancer that is 46 times higher than that expected in cisgender men of the same age but 3 times lower than in cisgender women.
The authors noted that “the risk of breast cancer in transgender women increases during a relatively short duration of hormone treatment,” going on to say that “these results suggest that breast cancer screening recommendations are relevant for transgender men and women on hormone therapy.”
Poorly attended screening
All of this means that transgender women older than age 50 years, as well as transgender men who have not had a mastectomy, should be offered a mammogram screening, taking into account the possible presence of implants in the former. Transgender women are also at risk for prostate cancer. Monitoring is personalized according to the individual risk of prostate disease, as it is for cisgender men.
There is no consensus on the monitoring of transgender men on hormone therapy for uterine cancer. Yet there is a risk. “Testosterone causes thinning of the endometrium, which may lead to dysplasia,” said Dr. D’Assigny. A physical examination once a year or a pelvic ultrasound scan every 2 years should form the basis of endometrial and ovarian appearance monitoring.
Transgender women are also at risk for prostate cancer. However, they are less likely to attend a prostate cancer screening test, said Dr. D’Assigny, which means “we need to raise awareness of their benefit in advance.” Vaginal swabs for transgender men and mammograms in transgender women “are resented, on both a physical and emotional level.” As a result, delays in diagnosis are common in transgender men and women.
Globally, access to care is still difficult for transgender patients because they don’t always receive appropriate gynecological monitoring, through fear of judgment or discrimination. Many transgender men and women are reluctant to see a gynecologist, even though they are at risk of gynecological cancers, as well as unwanted pregnancies in transgender men who have not undergone a hysterectomy.
In a demonstration of the collective desire to improve patient care for the transgender community, a literature review was recently published by a French team that analyzed gynecological monitoring methods in transgender patients. In September, the French National Authority for Health also issued a guidance memorandum on the transgender transition pathway, pending new recommendations scheduled for 2023.
A version of this article first appeared on Medscape.com.
This article was translated from the Medscape French edition.
PAU, France – Transgender patients on hormone therapy have an increased mortality risk and so must be closely monitored, especially in terms of cardiovascular health and oncology, reported Marie D’Assigny, MD, of the department of endocrinology, diabetes, and dietetics at Poitiers (France) University Hospital, at the Infogyn 2022 conference. Because transgender women (those assigned male at birth who have assumed a female gender identity) are at risk of breast cancer, they should also be recommended for breast cancer screening.
Transgender men and women, especially transgender women, “should be deemed high-risk cardiovascular patients, or even very high risk in some cases,” said Dr. D’Assigny. This means that they should be considered candidates for cholesterol-lowering medication earlier than their cisgender counterparts, and a target LDL cholesterol of less than 0.70 g/L (70 mg/dL) should be sought. Likewise, blood pressure must be strictly monitored, especially because it tends to rise when on hormone therapy.
Feminizing hormone therapy requires chemical castration with the use of anti-androgen drugs to achieve a blood testosterone level less than 0.5 ng/mL (1.73 nmol/L). Low-dose cyproterone acetate (< 25 to 50 mg/day) is usually used. Treatment is stopped if a patient undergoes an orchidectomy. For feminizing hormone therapy, administration of 17beta-estradiol transcutaneously (patch or gel) is recommended, because it is associated with a lower risk of thromboembolism than oral administration.
Masculinizing hormone therapy is based on administration of progestogens, then testosterone in the form of an injection (mostly testosterone enanthate via intramuscular injection every 10 days) or percutaneously (gel or patch). There are few contraindications, and treatment is generally well tolerated.
High mortality rate
A recent retrospective study highlighted the mortality and risk factors for death in transgender men and women receiving hormone therapy. More than 4,500 people, mostly male to female transgender women, were enrolled in this study, which was conducted over a 47-year period (1972-2018) at a specialist clinic at Amsterdam UMC.
Over the course of the study, the mortality rate in transgender men and women was twice that of the general population. The death rate was 10.8% in transgender women vs. 2.7% in transgender men, after a follow-up of 40,232 person-years and 17,285 person-years, respectively. In transgender women, mortality was nearly three times that of cisgender women in the general population.
Over the nearly 5 decades of study, there was no improvement in the mortality rate, even over the last 10 years when transgender issues started to be more recognized. The mortality trends are markedly distinct over the years from those observed in the cisgender population, and this is especially true for transgender women compared to transgender men. “Much is still to be done,” said Dr. D’Assigny.
According to the study, cause-specific mortality in transgender women was high for cardiovascular disease and lung cancer, possibly because of a higher smoking rate in this population. HIV-related disease and suicide remained very high in both transgender men and women.
People with gender dysphoria who do not receive treatment for gender reassignment have a suicide rate of 40%, reported François-Xavier Madec, MD, of Foch Hospital in Suresnes, France, at a previous presentation. For transgender men and women who receive care, this rate is lowered to 15%, which is still significantly higher than the rate of 1.6% observed in the general population.
“These causes of death don’t give any indication as to a specific effect of hormone treatment but show that monitoring and, if necessary, treatment of comorbidities and lifestyle-related factors are important in managing transgender patients,” said the study authors.
“Strengthening social acceptance and treating cardiovascular risk factors could also help to reduce mortality in transgender men and women,” they added.
Screening for osteoporosis
In addition to receiving cardiovascular risk factor assessment and monitoring, transgender men and women on hormone therapy should also undergo bone density testing “when risk factors for osteoporosis are present, especially in patients stopping hormone therapy after a gonadectomy,” said Dr. D’Assigny.
Calcium and vitamin D supplements are also recommended for all patients after a gonadectomy, especially in transgender men on testosterone. Osteoporosis screening is recommended for transgender men 10 years after starting treatment with testosterone, then every 10 years.
There is also the risk for breast cancer in transgender women, although the risk is lower than in cisgender women. This risk was highlighted in another study of more than 2,260 transgender women that was carried out by a team at Amsterdam UMC.
A total of 18 cases of breast cancer (15 invasive) were diagnosed after a median 18 years of hormone treatment. This represents an incidence of breast cancer that is 46 times higher than that expected in cisgender men of the same age but 3 times lower than in cisgender women.
The authors noted that “the risk of breast cancer in transgender women increases during a relatively short duration of hormone treatment,” going on to say that “these results suggest that breast cancer screening recommendations are relevant for transgender men and women on hormone therapy.”
Poorly attended screening
All of this means that transgender women older than age 50 years, as well as transgender men who have not had a mastectomy, should be offered a mammogram screening, taking into account the possible presence of implants in the former. Transgender women are also at risk for prostate cancer. Monitoring is personalized according to the individual risk of prostate disease, as it is for cisgender men.
There is no consensus on the monitoring of transgender men on hormone therapy for uterine cancer. Yet there is a risk. “Testosterone causes thinning of the endometrium, which may lead to dysplasia,” said Dr. D’Assigny. A physical examination once a year or a pelvic ultrasound scan every 2 years should form the basis of endometrial and ovarian appearance monitoring.
Transgender women are also at risk for prostate cancer. However, they are less likely to attend a prostate cancer screening test, said Dr. D’Assigny, which means “we need to raise awareness of their benefit in advance.” Vaginal swabs for transgender men and mammograms in transgender women “are resented, on both a physical and emotional level.” As a result, delays in diagnosis are common in transgender men and women.
Globally, access to care is still difficult for transgender patients because they don’t always receive appropriate gynecological monitoring, through fear of judgment or discrimination. Many transgender men and women are reluctant to see a gynecologist, even though they are at risk of gynecological cancers, as well as unwanted pregnancies in transgender men who have not undergone a hysterectomy.
In a demonstration of the collective desire to improve patient care for the transgender community, a literature review was recently published by a French team that analyzed gynecological monitoring methods in transgender patients. In September, the French National Authority for Health also issued a guidance memorandum on the transgender transition pathway, pending new recommendations scheduled for 2023.
A version of this article first appeared on Medscape.com.
This article was translated from the Medscape French edition.
PAU, France – Transgender patients on hormone therapy have an increased mortality risk and so must be closely monitored, especially in terms of cardiovascular health and oncology, reported Marie D’Assigny, MD, of the department of endocrinology, diabetes, and dietetics at Poitiers (France) University Hospital, at the Infogyn 2022 conference. Because transgender women (those assigned male at birth who have assumed a female gender identity) are at risk of breast cancer, they should also be recommended for breast cancer screening.
Transgender men and women, especially transgender women, “should be deemed high-risk cardiovascular patients, or even very high risk in some cases,” said Dr. D’Assigny. This means that they should be considered candidates for cholesterol-lowering medication earlier than their cisgender counterparts, and a target LDL cholesterol of less than 0.70 g/L (70 mg/dL) should be sought. Likewise, blood pressure must be strictly monitored, especially because it tends to rise when on hormone therapy.
Feminizing hormone therapy requires chemical castration with the use of anti-androgen drugs to achieve a blood testosterone level less than 0.5 ng/mL (1.73 nmol/L). Low-dose cyproterone acetate (< 25 to 50 mg/day) is usually used. Treatment is stopped if a patient undergoes an orchidectomy. For feminizing hormone therapy, administration of 17beta-estradiol transcutaneously (patch or gel) is recommended, because it is associated with a lower risk of thromboembolism than oral administration.
Masculinizing hormone therapy is based on administration of progestogens, then testosterone in the form of an injection (mostly testosterone enanthate via intramuscular injection every 10 days) or percutaneously (gel or patch). There are few contraindications, and treatment is generally well tolerated.
High mortality rate
A recent retrospective study highlighted the mortality and risk factors for death in transgender men and women receiving hormone therapy. More than 4,500 people, mostly male to female transgender women, were enrolled in this study, which was conducted over a 47-year period (1972-2018) at a specialist clinic at Amsterdam UMC.
Over the course of the study, the mortality rate in transgender men and women was twice that of the general population. The death rate was 10.8% in transgender women vs. 2.7% in transgender men, after a follow-up of 40,232 person-years and 17,285 person-years, respectively. In transgender women, mortality was nearly three times that of cisgender women in the general population.
Over the nearly 5 decades of study, there was no improvement in the mortality rate, even over the last 10 years when transgender issues started to be more recognized. The mortality trends are markedly distinct over the years from those observed in the cisgender population, and this is especially true for transgender women compared to transgender men. “Much is still to be done,” said Dr. D’Assigny.
According to the study, cause-specific mortality in transgender women was high for cardiovascular disease and lung cancer, possibly because of a higher smoking rate in this population. HIV-related disease and suicide remained very high in both transgender men and women.
People with gender dysphoria who do not receive treatment for gender reassignment have a suicide rate of 40%, reported François-Xavier Madec, MD, of Foch Hospital in Suresnes, France, at a previous presentation. For transgender men and women who receive care, this rate is lowered to 15%, which is still significantly higher than the rate of 1.6% observed in the general population.
“These causes of death don’t give any indication as to a specific effect of hormone treatment but show that monitoring and, if necessary, treatment of comorbidities and lifestyle-related factors are important in managing transgender patients,” said the study authors.
“Strengthening social acceptance and treating cardiovascular risk factors could also help to reduce mortality in transgender men and women,” they added.
Screening for osteoporosis
In addition to receiving cardiovascular risk factor assessment and monitoring, transgender men and women on hormone therapy should also undergo bone density testing “when risk factors for osteoporosis are present, especially in patients stopping hormone therapy after a gonadectomy,” said Dr. D’Assigny.
Calcium and vitamin D supplements are also recommended for all patients after a gonadectomy, especially in transgender men on testosterone. Osteoporosis screening is recommended for transgender men 10 years after starting treatment with testosterone, then every 10 years.
There is also the risk for breast cancer in transgender women, although the risk is lower than in cisgender women. This risk was highlighted in another study of more than 2,260 transgender women that was carried out by a team at Amsterdam UMC.
A total of 18 cases of breast cancer (15 invasive) were diagnosed after a median 18 years of hormone treatment. This represents an incidence of breast cancer that is 46 times higher than that expected in cisgender men of the same age but 3 times lower than in cisgender women.
The authors noted that “the risk of breast cancer in transgender women increases during a relatively short duration of hormone treatment,” going on to say that “these results suggest that breast cancer screening recommendations are relevant for transgender men and women on hormone therapy.”
Poorly attended screening
All of this means that transgender women older than age 50 years, as well as transgender men who have not had a mastectomy, should be offered a mammogram screening, taking into account the possible presence of implants in the former. Transgender women are also at risk for prostate cancer. Monitoring is personalized according to the individual risk of prostate disease, as it is for cisgender men.
There is no consensus on the monitoring of transgender men on hormone therapy for uterine cancer. Yet there is a risk. “Testosterone causes thinning of the endometrium, which may lead to dysplasia,” said Dr. D’Assigny. A physical examination once a year or a pelvic ultrasound scan every 2 years should form the basis of endometrial and ovarian appearance monitoring.
Transgender women are also at risk for prostate cancer. However, they are less likely to attend a prostate cancer screening test, said Dr. D’Assigny, which means “we need to raise awareness of their benefit in advance.” Vaginal swabs for transgender men and mammograms in transgender women “are resented, on both a physical and emotional level.” As a result, delays in diagnosis are common in transgender men and women.
Globally, access to care is still difficult for transgender patients because they don’t always receive appropriate gynecological monitoring, through fear of judgment or discrimination. Many transgender men and women are reluctant to see a gynecologist, even though they are at risk of gynecological cancers, as well as unwanted pregnancies in transgender men who have not undergone a hysterectomy.
In a demonstration of the collective desire to improve patient care for the transgender community, a literature review was recently published by a French team that analyzed gynecological monitoring methods in transgender patients. In September, the French National Authority for Health also issued a guidance memorandum on the transgender transition pathway, pending new recommendations scheduled for 2023.
A version of this article first appeared on Medscape.com.
This article was translated from the Medscape French edition.
Discontinuing immunotherapy: Is the infusion bag half empty or half full?
It’s a “champagne problem” many of us have encountered over the past few years in the clinic.
A patient with advanced non–small cell lung cancer (NSCLC) is fortunate enough to continue to do well for 2 years on ongoing pembrolizumab or perhaps pemetrexed and pembrolizumab as maintenance therapy. The latest CT shows a residual but far smaller primary tumor than what she started with.
In this instance, you may be considering stopping treatment but are concerned about doing so with evidence of disease still present.
Clinical trials of immunotherapy or chemoimmunotherapy have generally terminated treatment in nonprogressing patients after 2 years. We also know that some patients in early trials of immunotherapy stopped treatment after a fixed period of 1 or 2 years and continued to show no evidence of progression many years later.
The reason some patients experience this kind of success: Unlike the mechanism of action of conventional chemotherapy or targeted therapies, where ongoing treatment would be important to continue to exert an inhibitory effect, the active substrate of immunotherapy is the patient’s immune system, which can potentially have a self-sustaining efficacy beyond the stimulatory effect of the checkpoint inhibitor.
One trial directly addressed this question of stopping vs. continuing treatment in patients on immunotherapy. The CheckMate 153 trial, published in 2020, randomly assigned 252 previously treated patients who hadn’t demonstrated progression after 1 year on nivolumab to either discontinue nivolumab or continue nivolumab on an ongoing basis. The results were strongly in favor of ongoing therapy. Both progression-free survival (PFS) and overall survival (OS) were significantly longer in patients who continued therapy: PFS of 24.7 months vs. 9.4 months and OS not reached vs. 32.5 months.
This finding is important, but there’s an important caveat. The study population included many heavily pretreated patients, but, in practice, immunotherapy has generally moved into the first-line setting, where we see dramatic responses in a significant subset of patients.
Even more recent data are emerging that may help us evaluate who will do well off therapy and who should continue treatment.
We now have a growing collection of long-term data on patients who are more likely to have good outcomes with immunotherapy, specifically those with high tumor programmed death-ligand 1 (PD-L1) expression (≥ 50%), from the KEYNOTE-024 trial. In this study, 39 of 151 (25.8%) patients assigned to pembrolizumab completed the planned maximum of 2 years of treatment, among whom 82.1% achieved an objective response; but, only 10% (4 patients) achieved a complete response. The proportion of patients without progression and remaining off therapy wasn’t reported, but the OS rate 3 years after completing treatment was 81.4%.
In addition, restarting immunotherapy after discontinuing appears to be a moderately effective strategy. In the KEYNOTE-024 trial, 12 patients received a second course of pembrolizumab because of disease progression a median of 15.2 months after discontinuing pembrolizumab. In this small cohort, eight of these patients (66.7%) were alive at the data cutoff, and six (50%) achieved stable disease.
Recently, we received additional insight in the follow-up from two chemoimmunotherapy trials that have most shaped my practice for patients with advanced NSCLC and any level of PD-L1 expression. These are the KEYNOTE-189 trial of platinum-pemetrexed with pembrolizumab vs. placebo in those with nonsquamous NSCLC, and the KEYNOTE-407 trial of carboplatin-taxane with pembrolizumab vs. placebo in patients with advanced squamous NSCLC. The National Comprehensive Cancer Network has designated each as a “preferred regimen” for patients with advanced NSCLC.
Both regimens have demonstrated sustained efficacy benefits with prolonged follow-up, including significantly superior objective response rate, PFS, and OS with the addition of pembrolizumab. These findings merely cemented the role of these regimens in our practice, but the trials also reported on the cohort of patients who completed 35 cycles of treatment over 2 years then discontinued therapy. In both, the majority of patients showed an objective response (86% in KEYNOTE-189 and 90% in KEYNOTE-407), with most patients alive at 3 years after 2 years of treatment (71.9% in KEYNOTE-189 and 69.5% in KEYNOTE-407). In addition, the proportion of patients alive without disease progression or subsequent therapy was notable – 40.4% in KEYNOTE-189 and 43.6% KEYNOTE-407.
How should we interpret these data for the patient who is in the exam room with us?
The short answer is that we don’t know. I see this as a half-empty, half-full conundrum.
I’m disappointed that more patients who responded for 2 years will experience disease progression in the 1-3 years that follow. This signals that their immune systems have not perpetuated their initial response over the long-term. But these patients may have demonstrated disease progression even if they had continued therapy.
We also know that some patients can be rechallenged and will respond again. Some of these patients will show stable disease, whereas others will progress with repeat treatment. I would love to be able to better predict which patients are destined to do well without treatment vs. those who benefit from treatment beyond 2 years.
Might the level of PD-L1 expression tell us? Can PET imaging discriminate those with residual hypermetabolism who may need continued treatment from those with no residual uptake who could be spared it? Would serial measurement of circulating tumor DNA (ctDNA) in responding patients identify when they have achieved a point of diminishing returns, potentially indicating that some can safely discontinue treatment after 2 years, whereas others need to continue to suppress on prolonged maintenance therapy?
These questions have yet to be studied systematically. In the meantime, I take an individualized approach with my patients facing this decision. Some have experienced escalating arthralgias and myalgias, cost concerns, or other issues related to immunotherapy that may dissuade us from continuing treatment. But several others have been grateful to continue with their treatment, hesitant to do anything that could change the path of their disease.
In my patients who tolerate therapy well, I’m more worried about potential undertreatment than overtreatment. I tend to favor having my patients continue therapy in the absence of problematic toxicity or practical challenges. There is certainly room for debate here while we await data to better guide these decisions. How do you approach these patients?
Dr. West is Clinical Associate Professor, Department of Medical Oncology, City of Hope Comprehensive Cancer Care, Duarte, Calif. He reported conflicts of interest with Ariad/Takeda, Bristol-Myers Squibb, Boehringer Ingelheim, Spectrum, AstraZeneca, Celgene, Genentech/Roche, Pfizer, Merck, and Eli Lilly.
A version of this article first appeared on Medscape.com.
It’s a “champagne problem” many of us have encountered over the past few years in the clinic.
A patient with advanced non–small cell lung cancer (NSCLC) is fortunate enough to continue to do well for 2 years on ongoing pembrolizumab or perhaps pemetrexed and pembrolizumab as maintenance therapy. The latest CT shows a residual but far smaller primary tumor than what she started with.
In this instance, you may be considering stopping treatment but are concerned about doing so with evidence of disease still present.
Clinical trials of immunotherapy or chemoimmunotherapy have generally terminated treatment in nonprogressing patients after 2 years. We also know that some patients in early trials of immunotherapy stopped treatment after a fixed period of 1 or 2 years and continued to show no evidence of progression many years later.
The reason some patients experience this kind of success: Unlike the mechanism of action of conventional chemotherapy or targeted therapies, where ongoing treatment would be important to continue to exert an inhibitory effect, the active substrate of immunotherapy is the patient’s immune system, which can potentially have a self-sustaining efficacy beyond the stimulatory effect of the checkpoint inhibitor.
One trial directly addressed this question of stopping vs. continuing treatment in patients on immunotherapy. The CheckMate 153 trial, published in 2020, randomly assigned 252 previously treated patients who hadn’t demonstrated progression after 1 year on nivolumab to either discontinue nivolumab or continue nivolumab on an ongoing basis. The results were strongly in favor of ongoing therapy. Both progression-free survival (PFS) and overall survival (OS) were significantly longer in patients who continued therapy: PFS of 24.7 months vs. 9.4 months and OS not reached vs. 32.5 months.
This finding is important, but there’s an important caveat. The study population included many heavily pretreated patients, but, in practice, immunotherapy has generally moved into the first-line setting, where we see dramatic responses in a significant subset of patients.
Even more recent data are emerging that may help us evaluate who will do well off therapy and who should continue treatment.
We now have a growing collection of long-term data on patients who are more likely to have good outcomes with immunotherapy, specifically those with high tumor programmed death-ligand 1 (PD-L1) expression (≥ 50%), from the KEYNOTE-024 trial. In this study, 39 of 151 (25.8%) patients assigned to pembrolizumab completed the planned maximum of 2 years of treatment, among whom 82.1% achieved an objective response; but, only 10% (4 patients) achieved a complete response. The proportion of patients without progression and remaining off therapy wasn’t reported, but the OS rate 3 years after completing treatment was 81.4%.
In addition, restarting immunotherapy after discontinuing appears to be a moderately effective strategy. In the KEYNOTE-024 trial, 12 patients received a second course of pembrolizumab because of disease progression a median of 15.2 months after discontinuing pembrolizumab. In this small cohort, eight of these patients (66.7%) were alive at the data cutoff, and six (50%) achieved stable disease.
Recently, we received additional insight in the follow-up from two chemoimmunotherapy trials that have most shaped my practice for patients with advanced NSCLC and any level of PD-L1 expression. These are the KEYNOTE-189 trial of platinum-pemetrexed with pembrolizumab vs. placebo in those with nonsquamous NSCLC, and the KEYNOTE-407 trial of carboplatin-taxane with pembrolizumab vs. placebo in patients with advanced squamous NSCLC. The National Comprehensive Cancer Network has designated each as a “preferred regimen” for patients with advanced NSCLC.
Both regimens have demonstrated sustained efficacy benefits with prolonged follow-up, including significantly superior objective response rate, PFS, and OS with the addition of pembrolizumab. These findings merely cemented the role of these regimens in our practice, but the trials also reported on the cohort of patients who completed 35 cycles of treatment over 2 years then discontinued therapy. In both, the majority of patients showed an objective response (86% in KEYNOTE-189 and 90% in KEYNOTE-407), with most patients alive at 3 years after 2 years of treatment (71.9% in KEYNOTE-189 and 69.5% in KEYNOTE-407). In addition, the proportion of patients alive without disease progression or subsequent therapy was notable – 40.4% in KEYNOTE-189 and 43.6% KEYNOTE-407.
How should we interpret these data for the patient who is in the exam room with us?
The short answer is that we don’t know. I see this as a half-empty, half-full conundrum.
I’m disappointed that more patients who responded for 2 years will experience disease progression in the 1-3 years that follow. This signals that their immune systems have not perpetuated their initial response over the long-term. But these patients may have demonstrated disease progression even if they had continued therapy.
We also know that some patients can be rechallenged and will respond again. Some of these patients will show stable disease, whereas others will progress with repeat treatment. I would love to be able to better predict which patients are destined to do well without treatment vs. those who benefit from treatment beyond 2 years.
Might the level of PD-L1 expression tell us? Can PET imaging discriminate those with residual hypermetabolism who may need continued treatment from those with no residual uptake who could be spared it? Would serial measurement of circulating tumor DNA (ctDNA) in responding patients identify when they have achieved a point of diminishing returns, potentially indicating that some can safely discontinue treatment after 2 years, whereas others need to continue to suppress on prolonged maintenance therapy?
These questions have yet to be studied systematically. In the meantime, I take an individualized approach with my patients facing this decision. Some have experienced escalating arthralgias and myalgias, cost concerns, or other issues related to immunotherapy that may dissuade us from continuing treatment. But several others have been grateful to continue with their treatment, hesitant to do anything that could change the path of their disease.
In my patients who tolerate therapy well, I’m more worried about potential undertreatment than overtreatment. I tend to favor having my patients continue therapy in the absence of problematic toxicity or practical challenges. There is certainly room for debate here while we await data to better guide these decisions. How do you approach these patients?
Dr. West is Clinical Associate Professor, Department of Medical Oncology, City of Hope Comprehensive Cancer Care, Duarte, Calif. He reported conflicts of interest with Ariad/Takeda, Bristol-Myers Squibb, Boehringer Ingelheim, Spectrum, AstraZeneca, Celgene, Genentech/Roche, Pfizer, Merck, and Eli Lilly.
A version of this article first appeared on Medscape.com.
It’s a “champagne problem” many of us have encountered over the past few years in the clinic.
A patient with advanced non–small cell lung cancer (NSCLC) is fortunate enough to continue to do well for 2 years on ongoing pembrolizumab or perhaps pemetrexed and pembrolizumab as maintenance therapy. The latest CT shows a residual but far smaller primary tumor than what she started with.
In this instance, you may be considering stopping treatment but are concerned about doing so with evidence of disease still present.
Clinical trials of immunotherapy or chemoimmunotherapy have generally terminated treatment in nonprogressing patients after 2 years. We also know that some patients in early trials of immunotherapy stopped treatment after a fixed period of 1 or 2 years and continued to show no evidence of progression many years later.
The reason some patients experience this kind of success: Unlike the mechanism of action of conventional chemotherapy or targeted therapies, where ongoing treatment would be important to continue to exert an inhibitory effect, the active substrate of immunotherapy is the patient’s immune system, which can potentially have a self-sustaining efficacy beyond the stimulatory effect of the checkpoint inhibitor.
One trial directly addressed this question of stopping vs. continuing treatment in patients on immunotherapy. The CheckMate 153 trial, published in 2020, randomly assigned 252 previously treated patients who hadn’t demonstrated progression after 1 year on nivolumab to either discontinue nivolumab or continue nivolumab on an ongoing basis. The results were strongly in favor of ongoing therapy. Both progression-free survival (PFS) and overall survival (OS) were significantly longer in patients who continued therapy: PFS of 24.7 months vs. 9.4 months and OS not reached vs. 32.5 months.
This finding is important, but there’s an important caveat. The study population included many heavily pretreated patients, but, in practice, immunotherapy has generally moved into the first-line setting, where we see dramatic responses in a significant subset of patients.
Even more recent data are emerging that may help us evaluate who will do well off therapy and who should continue treatment.
We now have a growing collection of long-term data on patients who are more likely to have good outcomes with immunotherapy, specifically those with high tumor programmed death-ligand 1 (PD-L1) expression (≥ 50%), from the KEYNOTE-024 trial. In this study, 39 of 151 (25.8%) patients assigned to pembrolizumab completed the planned maximum of 2 years of treatment, among whom 82.1% achieved an objective response; but, only 10% (4 patients) achieved a complete response. The proportion of patients without progression and remaining off therapy wasn’t reported, but the OS rate 3 years after completing treatment was 81.4%.
In addition, restarting immunotherapy after discontinuing appears to be a moderately effective strategy. In the KEYNOTE-024 trial, 12 patients received a second course of pembrolizumab because of disease progression a median of 15.2 months after discontinuing pembrolizumab. In this small cohort, eight of these patients (66.7%) were alive at the data cutoff, and six (50%) achieved stable disease.
Recently, we received additional insight in the follow-up from two chemoimmunotherapy trials that have most shaped my practice for patients with advanced NSCLC and any level of PD-L1 expression. These are the KEYNOTE-189 trial of platinum-pemetrexed with pembrolizumab vs. placebo in those with nonsquamous NSCLC, and the KEYNOTE-407 trial of carboplatin-taxane with pembrolizumab vs. placebo in patients with advanced squamous NSCLC. The National Comprehensive Cancer Network has designated each as a “preferred regimen” for patients with advanced NSCLC.
Both regimens have demonstrated sustained efficacy benefits with prolonged follow-up, including significantly superior objective response rate, PFS, and OS with the addition of pembrolizumab. These findings merely cemented the role of these regimens in our practice, but the trials also reported on the cohort of patients who completed 35 cycles of treatment over 2 years then discontinued therapy. In both, the majority of patients showed an objective response (86% in KEYNOTE-189 and 90% in KEYNOTE-407), with most patients alive at 3 years after 2 years of treatment (71.9% in KEYNOTE-189 and 69.5% in KEYNOTE-407). In addition, the proportion of patients alive without disease progression or subsequent therapy was notable – 40.4% in KEYNOTE-189 and 43.6% KEYNOTE-407.
How should we interpret these data for the patient who is in the exam room with us?
The short answer is that we don’t know. I see this as a half-empty, half-full conundrum.
I’m disappointed that more patients who responded for 2 years will experience disease progression in the 1-3 years that follow. This signals that their immune systems have not perpetuated their initial response over the long-term. But these patients may have demonstrated disease progression even if they had continued therapy.
We also know that some patients can be rechallenged and will respond again. Some of these patients will show stable disease, whereas others will progress with repeat treatment. I would love to be able to better predict which patients are destined to do well without treatment vs. those who benefit from treatment beyond 2 years.
Might the level of PD-L1 expression tell us? Can PET imaging discriminate those with residual hypermetabolism who may need continued treatment from those with no residual uptake who could be spared it? Would serial measurement of circulating tumor DNA (ctDNA) in responding patients identify when they have achieved a point of diminishing returns, potentially indicating that some can safely discontinue treatment after 2 years, whereas others need to continue to suppress on prolonged maintenance therapy?
These questions have yet to be studied systematically. In the meantime, I take an individualized approach with my patients facing this decision. Some have experienced escalating arthralgias and myalgias, cost concerns, or other issues related to immunotherapy that may dissuade us from continuing treatment. But several others have been grateful to continue with their treatment, hesitant to do anything that could change the path of their disease.
In my patients who tolerate therapy well, I’m more worried about potential undertreatment than overtreatment. I tend to favor having my patients continue therapy in the absence of problematic toxicity or practical challenges. There is certainly room for debate here while we await data to better guide these decisions. How do you approach these patients?
Dr. West is Clinical Associate Professor, Department of Medical Oncology, City of Hope Comprehensive Cancer Care, Duarte, Calif. He reported conflicts of interest with Ariad/Takeda, Bristol-Myers Squibb, Boehringer Ingelheim, Spectrum, AstraZeneca, Celgene, Genentech/Roche, Pfizer, Merck, and Eli Lilly.
A version of this article first appeared on Medscape.com.
Update on high-grade vulvar interepithelial neoplasia
Vulvar squamous cell carcinomas (VSCC) comprise approximately 90% of all vulvar malignancies. Unlike cervical SCC, which are predominantly human papilloma virus (HPV) positive, only a minority of VSCC are HPV positive – on the order of 15%-25% of cases. Most cases occur in the setting of lichen sclerosus and are HPV negative.
Lichen sclerosus is a chronic inflammatory dermatitis typically involving the anogenital area, which in some cases can become seriously distorted (e.g. atrophy of the labia minora, clitoral phimosis, and introital stenosis). Although most cases are diagnosed in postmenopausal women, LS can affect women of any age. The true prevalence of lichen sclerosus is unknown. Recent studies have shown a prevalence of 1 in 60; among older women, it can even be as high as 1 in 30. While lichen sclerosus is a pruriginous condition, it is often asymptomatic. It is not considered a premalignant condition. The diagnosis is clinical; however, suspicious lesions (erosions/ulcerations, hyperkeratosis, pigmented areas, ecchymosis, warty or papular lesions), particularly when recalcitrant to adequate first-line therapy, should be biopsied.
VSCC arises from precursor lesions or high-grade vulvar intraepithelial neoplasia (VIN). The 2015 International Society for the Study of Vulvovaginal Disease nomenclature classifies high-grade VIN into high-grade squamous intraepithelial lesion (HSIL) and differentiated VIN (dVIN). Most patients with high-grade VIN are diagnosed with HSIL or usual type VIN. A preponderance of these lesions (75%-85%) are HPV positive, predominantly HPV 16. Vulvar HSIL (vHSIL) lesions affect younger women. The lesions tend to be multifocal and extensive. On the other hand, dVIN typically affects older women and commonly develops as a solitary lesion. While dVIN accounts for only a small subset of patients with high-grade VIN, these lesions are HPV negative and associated with lichen sclerosus.
Both disease entities, vHSIL and dVIN, are increasing in incidence. There is a higher risk and shortened period of progression to cancer in patients with dVIN compared to HSIL. The cancer risk of vHSIL is relatively low. The 10-year cumulative VSCC risk reported in the literature is 10.3%; 9.7% for vHSIL and 50% for dVIN. Patients with vHSIL could benefit from less aggressive treatment modalities.
Patients present with a constellation of signs such as itching, pain, burning, bleeding, and discharge. Chronic symptoms portend HPV-independent lesions associated with lichen sclerosus while episodic signs are suggestive of HPV-positive lesions.
The recurrence risk of high-grade VIN is 46%-70%. Risk factors for recurrence include age greater than 50, immunosuppression, metasynchronous HSIL, and multifocal lesions. Recurrences occur in up to 50% of women who have undergone surgery. For those who undergo surgical treatment for high-grade VIN, recurrence is more common in the setting of positive margins, underlying lichen sclerosis, persistent HPV infection, and immunosuppression.
Management of high-grade VIN is determined by the lesion characteristics, patient characteristics, and medical expertise. Given the risk of progression of high-grade VIN to cancer and risk of underlying cancer, surgical therapy is typically recommended. The treatment of choice is surgical excision in cases of dVIN. Surgical treatments include CO2 laser ablation, wide local excision, and vulvectomy. Women who undergo surgical treatment for vHSIL have about a 50% chance of the condition recurring 1 year later, irrespective of whether treatment is by surgical excision or laser vaporization.
Since surgery can be associated with disfigurement and sexual dysfunction, alternatives to surgery should be considered in cases of vHSIL. The potential for effect on sexual function should be part of preoperative counseling and treatment. Women treated for VIN often experience increased inhibition of sexual excitement and increased inhibition of orgasm. One study found that in women undergoing vulvar excision for VIN, the impairment was found to be psychological in nature. Overall, the studies of sexual effect from treatment of VIN have found that women do not return to their pretreatment sexual function. However, the optimal management of vHSIL has not been determined. Nonsurgical options include topical therapies (imiquimod, 5-fluorouracil, cidofovir, and interferon) and nonpharmacologic treatments, such as photodynamic therapy.
Imiquimod, a topical immune modulator, is the most studied pharmacologic treatment of vHSIL. The drug induces secretion of cytokines, creating an immune response that clears the HPV infection. Imiquimod is safe and well tolerated. The clinical response rate varies between 35% and 81%. A recent study demonstrated the efficacy of imiquimod and the treatment was found to be noninferior to surgery. Adverse events differed, with local pain following surgical treatment and local pruritus and erythema associated with imiquimod use. Some patients did not respond to imiquimod; it was thought by the authors of the study that specific immunological factors affect the clinical response.
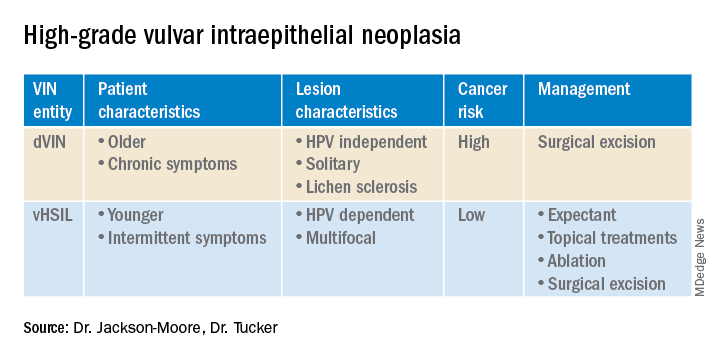
In conclusion, high-grade VIN is a heterogeneous disease made up of two distinct disease entities with rising incidence. In contrast to dVIN, the cancer risk is low for patients with vHSIL. Treatment should be driven by the clinical characteristics of the vulvar lesions, patients’ preferences, sexual activity, and compliance. Future directions include risk stratification of patients with vHSIL who are most likely to benefit from topical treatments, thus reducing overtreatment. Molecular biomarkers that could identify dVIN at an early stage are needed.
Dr. Jackson-Moore is associate professor in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Tucker is assistant professor of gynecologic oncology at the university.
References
Cendejas BR et al. Am J Obstet Gynecol. 2015 Mar;212(3):291-7.
Lebreton M et al. J Gynecol Obstet Hum Reprod. 2020 Nov;49(9):101801.
Thuijs NB et al. Int J Cancer. 2021 Jan 1;148(1):90-8. doi: 10.1002/ijc.33198. .
Trutnovsky G et al. Lancet. 2022 May 7;399(10337):1790-8. Erratum in: Lancet. 2022 Oct 8;400(10359):1194.
Vulvar squamous cell carcinomas (VSCC) comprise approximately 90% of all vulvar malignancies. Unlike cervical SCC, which are predominantly human papilloma virus (HPV) positive, only a minority of VSCC are HPV positive – on the order of 15%-25% of cases. Most cases occur in the setting of lichen sclerosus and are HPV negative.
Lichen sclerosus is a chronic inflammatory dermatitis typically involving the anogenital area, which in some cases can become seriously distorted (e.g. atrophy of the labia minora, clitoral phimosis, and introital stenosis). Although most cases are diagnosed in postmenopausal women, LS can affect women of any age. The true prevalence of lichen sclerosus is unknown. Recent studies have shown a prevalence of 1 in 60; among older women, it can even be as high as 1 in 30. While lichen sclerosus is a pruriginous condition, it is often asymptomatic. It is not considered a premalignant condition. The diagnosis is clinical; however, suspicious lesions (erosions/ulcerations, hyperkeratosis, pigmented areas, ecchymosis, warty or papular lesions), particularly when recalcitrant to adequate first-line therapy, should be biopsied.
VSCC arises from precursor lesions or high-grade vulvar intraepithelial neoplasia (VIN). The 2015 International Society for the Study of Vulvovaginal Disease nomenclature classifies high-grade VIN into high-grade squamous intraepithelial lesion (HSIL) and differentiated VIN (dVIN). Most patients with high-grade VIN are diagnosed with HSIL or usual type VIN. A preponderance of these lesions (75%-85%) are HPV positive, predominantly HPV 16. Vulvar HSIL (vHSIL) lesions affect younger women. The lesions tend to be multifocal and extensive. On the other hand, dVIN typically affects older women and commonly develops as a solitary lesion. While dVIN accounts for only a small subset of patients with high-grade VIN, these lesions are HPV negative and associated with lichen sclerosus.
Both disease entities, vHSIL and dVIN, are increasing in incidence. There is a higher risk and shortened period of progression to cancer in patients with dVIN compared to HSIL. The cancer risk of vHSIL is relatively low. The 10-year cumulative VSCC risk reported in the literature is 10.3%; 9.7% for vHSIL and 50% for dVIN. Patients with vHSIL could benefit from less aggressive treatment modalities.
Patients present with a constellation of signs such as itching, pain, burning, bleeding, and discharge. Chronic symptoms portend HPV-independent lesions associated with lichen sclerosus while episodic signs are suggestive of HPV-positive lesions.
The recurrence risk of high-grade VIN is 46%-70%. Risk factors for recurrence include age greater than 50, immunosuppression, metasynchronous HSIL, and multifocal lesions. Recurrences occur in up to 50% of women who have undergone surgery. For those who undergo surgical treatment for high-grade VIN, recurrence is more common in the setting of positive margins, underlying lichen sclerosis, persistent HPV infection, and immunosuppression.
Management of high-grade VIN is determined by the lesion characteristics, patient characteristics, and medical expertise. Given the risk of progression of high-grade VIN to cancer and risk of underlying cancer, surgical therapy is typically recommended. The treatment of choice is surgical excision in cases of dVIN. Surgical treatments include CO2 laser ablation, wide local excision, and vulvectomy. Women who undergo surgical treatment for vHSIL have about a 50% chance of the condition recurring 1 year later, irrespective of whether treatment is by surgical excision or laser vaporization.
Since surgery can be associated with disfigurement and sexual dysfunction, alternatives to surgery should be considered in cases of vHSIL. The potential for effect on sexual function should be part of preoperative counseling and treatment. Women treated for VIN often experience increased inhibition of sexual excitement and increased inhibition of orgasm. One study found that in women undergoing vulvar excision for VIN, the impairment was found to be psychological in nature. Overall, the studies of sexual effect from treatment of VIN have found that women do not return to their pretreatment sexual function. However, the optimal management of vHSIL has not been determined. Nonsurgical options include topical therapies (imiquimod, 5-fluorouracil, cidofovir, and interferon) and nonpharmacologic treatments, such as photodynamic therapy.
Imiquimod, a topical immune modulator, is the most studied pharmacologic treatment of vHSIL. The drug induces secretion of cytokines, creating an immune response that clears the HPV infection. Imiquimod is safe and well tolerated. The clinical response rate varies between 35% and 81%. A recent study demonstrated the efficacy of imiquimod and the treatment was found to be noninferior to surgery. Adverse events differed, with local pain following surgical treatment and local pruritus and erythema associated with imiquimod use. Some patients did not respond to imiquimod; it was thought by the authors of the study that specific immunological factors affect the clinical response.
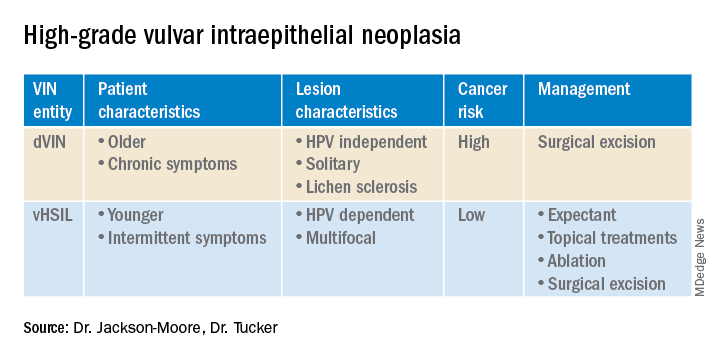
In conclusion, high-grade VIN is a heterogeneous disease made up of two distinct disease entities with rising incidence. In contrast to dVIN, the cancer risk is low for patients with vHSIL. Treatment should be driven by the clinical characteristics of the vulvar lesions, patients’ preferences, sexual activity, and compliance. Future directions include risk stratification of patients with vHSIL who are most likely to benefit from topical treatments, thus reducing overtreatment. Molecular biomarkers that could identify dVIN at an early stage are needed.
Dr. Jackson-Moore is associate professor in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Tucker is assistant professor of gynecologic oncology at the university.
References
Cendejas BR et al. Am J Obstet Gynecol. 2015 Mar;212(3):291-7.
Lebreton M et al. J Gynecol Obstet Hum Reprod. 2020 Nov;49(9):101801.
Thuijs NB et al. Int J Cancer. 2021 Jan 1;148(1):90-8. doi: 10.1002/ijc.33198. .
Trutnovsky G et al. Lancet. 2022 May 7;399(10337):1790-8. Erratum in: Lancet. 2022 Oct 8;400(10359):1194.
Vulvar squamous cell carcinomas (VSCC) comprise approximately 90% of all vulvar malignancies. Unlike cervical SCC, which are predominantly human papilloma virus (HPV) positive, only a minority of VSCC are HPV positive – on the order of 15%-25% of cases. Most cases occur in the setting of lichen sclerosus and are HPV negative.
Lichen sclerosus is a chronic inflammatory dermatitis typically involving the anogenital area, which in some cases can become seriously distorted (e.g. atrophy of the labia minora, clitoral phimosis, and introital stenosis). Although most cases are diagnosed in postmenopausal women, LS can affect women of any age. The true prevalence of lichen sclerosus is unknown. Recent studies have shown a prevalence of 1 in 60; among older women, it can even be as high as 1 in 30. While lichen sclerosus is a pruriginous condition, it is often asymptomatic. It is not considered a premalignant condition. The diagnosis is clinical; however, suspicious lesions (erosions/ulcerations, hyperkeratosis, pigmented areas, ecchymosis, warty or papular lesions), particularly when recalcitrant to adequate first-line therapy, should be biopsied.
VSCC arises from precursor lesions or high-grade vulvar intraepithelial neoplasia (VIN). The 2015 International Society for the Study of Vulvovaginal Disease nomenclature classifies high-grade VIN into high-grade squamous intraepithelial lesion (HSIL) and differentiated VIN (dVIN). Most patients with high-grade VIN are diagnosed with HSIL or usual type VIN. A preponderance of these lesions (75%-85%) are HPV positive, predominantly HPV 16. Vulvar HSIL (vHSIL) lesions affect younger women. The lesions tend to be multifocal and extensive. On the other hand, dVIN typically affects older women and commonly develops as a solitary lesion. While dVIN accounts for only a small subset of patients with high-grade VIN, these lesions are HPV negative and associated with lichen sclerosus.
Both disease entities, vHSIL and dVIN, are increasing in incidence. There is a higher risk and shortened period of progression to cancer in patients with dVIN compared to HSIL. The cancer risk of vHSIL is relatively low. The 10-year cumulative VSCC risk reported in the literature is 10.3%; 9.7% for vHSIL and 50% for dVIN. Patients with vHSIL could benefit from less aggressive treatment modalities.
Patients present with a constellation of signs such as itching, pain, burning, bleeding, and discharge. Chronic symptoms portend HPV-independent lesions associated with lichen sclerosus while episodic signs are suggestive of HPV-positive lesions.
The recurrence risk of high-grade VIN is 46%-70%. Risk factors for recurrence include age greater than 50, immunosuppression, metasynchronous HSIL, and multifocal lesions. Recurrences occur in up to 50% of women who have undergone surgery. For those who undergo surgical treatment for high-grade VIN, recurrence is more common in the setting of positive margins, underlying lichen sclerosis, persistent HPV infection, and immunosuppression.
Management of high-grade VIN is determined by the lesion characteristics, patient characteristics, and medical expertise. Given the risk of progression of high-grade VIN to cancer and risk of underlying cancer, surgical therapy is typically recommended. The treatment of choice is surgical excision in cases of dVIN. Surgical treatments include CO2 laser ablation, wide local excision, and vulvectomy. Women who undergo surgical treatment for vHSIL have about a 50% chance of the condition recurring 1 year later, irrespective of whether treatment is by surgical excision or laser vaporization.
Since surgery can be associated with disfigurement and sexual dysfunction, alternatives to surgery should be considered in cases of vHSIL. The potential for effect on sexual function should be part of preoperative counseling and treatment. Women treated for VIN often experience increased inhibition of sexual excitement and increased inhibition of orgasm. One study found that in women undergoing vulvar excision for VIN, the impairment was found to be psychological in nature. Overall, the studies of sexual effect from treatment of VIN have found that women do not return to their pretreatment sexual function. However, the optimal management of vHSIL has not been determined. Nonsurgical options include topical therapies (imiquimod, 5-fluorouracil, cidofovir, and interferon) and nonpharmacologic treatments, such as photodynamic therapy.
Imiquimod, a topical immune modulator, is the most studied pharmacologic treatment of vHSIL. The drug induces secretion of cytokines, creating an immune response that clears the HPV infection. Imiquimod is safe and well tolerated. The clinical response rate varies between 35% and 81%. A recent study demonstrated the efficacy of imiquimod and the treatment was found to be noninferior to surgery. Adverse events differed, with local pain following surgical treatment and local pruritus and erythema associated with imiquimod use. Some patients did not respond to imiquimod; it was thought by the authors of the study that specific immunological factors affect the clinical response.
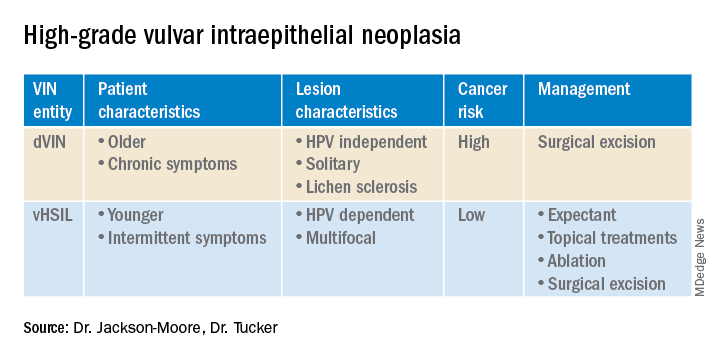
In conclusion, high-grade VIN is a heterogeneous disease made up of two distinct disease entities with rising incidence. In contrast to dVIN, the cancer risk is low for patients with vHSIL. Treatment should be driven by the clinical characteristics of the vulvar lesions, patients’ preferences, sexual activity, and compliance. Future directions include risk stratification of patients with vHSIL who are most likely to benefit from topical treatments, thus reducing overtreatment. Molecular biomarkers that could identify dVIN at an early stage are needed.
Dr. Jackson-Moore is associate professor in gynecologic oncology at the University of North Carolina at Chapel Hill. Dr. Tucker is assistant professor of gynecologic oncology at the university.
References
Cendejas BR et al. Am J Obstet Gynecol. 2015 Mar;212(3):291-7.
Lebreton M et al. J Gynecol Obstet Hum Reprod. 2020 Nov;49(9):101801.
Thuijs NB et al. Int J Cancer. 2021 Jan 1;148(1):90-8. doi: 10.1002/ijc.33198. .
Trutnovsky G et al. Lancet. 2022 May 7;399(10337):1790-8. Erratum in: Lancet. 2022 Oct 8;400(10359):1194.
FDA grants accelerated approval for new treatment of female cancers
The Food and Drug Administration has granted accelerated approval to mirvetuximab soravtansine (Elahere) for use in pretreated patients with folate receptor (FR) alpha–positive, platinum-resistant epithelial ovarian, fallopian tube, and primary peritoneal cancer. These patients can have received one to three prior lines of treatment.
“ according to labeling.
Mirvetuximab soravtansine is an antibody-drug conjugate (ADC) with an antibody directed against FR alpha that is linked to a microtubule inhibitor conjugate.
This product is a first-in-class ADC directed against FR alpha, a cell-surface protein highly expressed in ovarian cancer, and is the first FDA-approved ADC for platinum-resistant disease, said the manufacturer, ImmunoGen.
Patients are selected for treatment with this drug using a diagnostic test that the FDA approved along with the agent: the VENTANA FOLR1 (FOLR-2.1) RxDx Assay.
FR alpha–positive platinum-resistant ovarian cancer is characterized by limited treatment options and poor outcomes, commented Ursula Matulonis, MD, chief of the division of gynecologic oncology at the Dana-Farber Cancer Institute, Boston, and co–principal investigator of the SORAYA trial that led to the approval. In a company press release, she said results from this trial show that mirvetuximab soravtansine has “impressive antitumor activity, durability of response, and overall tolerability ... [which] demonstrate the benefit of this new therapeutic option.”
The SORAYA trial (also known as Study 0417 [NCT04296890]) was a single-arm trial of 106 patients with FR alpha–positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer.
These patients were identified as FR alpha positive by using the assay. They were permitted to receive up to three prior lines of systemic therapy, and all patients were required to have received bevacizumab.
All patients received mirvetuximab soravtansine-gynx 6 mg/kg (based on adjusted ideal body weight) as an intravenous infusion every 3 weeks until disease progression or unacceptable toxicity.
The approval was based on an investigator-assessed overall response rate of 31.7%, which included five complete responses, and a median duration of response of 6.9 months.
Safety was evaluated in a pooled analysis from three studies among a total of 464 patients with FR alpha–positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer who received at least one dose of the drug.
The most common adverse events, occurring in 20% or more of study participants, were vision impairment, fatigue, increased AST level, nausea, increased alanine aminotransferase level, keratopathy, abdominal pain, decreased lymphocytes, peripheral neuropathy, diarrhea, decreased albumin, constipation, increased alkaline phosphatase level, dry eye, decreased magnesium level, decreased leukocyte count, decreased neutrophil count, and decreased hemoglobin level.
Potential participants were excluded if they had corneal disorders, ocular conditions requiring ongoing treatment, peripheral neuropathy above grade 1, or noninfectious interstitial lung disease.
The product labeling contains a boxed warning of ocular toxicity. Full prescribing information is available.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has granted accelerated approval to mirvetuximab soravtansine (Elahere) for use in pretreated patients with folate receptor (FR) alpha–positive, platinum-resistant epithelial ovarian, fallopian tube, and primary peritoneal cancer. These patients can have received one to three prior lines of treatment.
“ according to labeling.
Mirvetuximab soravtansine is an antibody-drug conjugate (ADC) with an antibody directed against FR alpha that is linked to a microtubule inhibitor conjugate.
This product is a first-in-class ADC directed against FR alpha, a cell-surface protein highly expressed in ovarian cancer, and is the first FDA-approved ADC for platinum-resistant disease, said the manufacturer, ImmunoGen.
Patients are selected for treatment with this drug using a diagnostic test that the FDA approved along with the agent: the VENTANA FOLR1 (FOLR-2.1) RxDx Assay.
FR alpha–positive platinum-resistant ovarian cancer is characterized by limited treatment options and poor outcomes, commented Ursula Matulonis, MD, chief of the division of gynecologic oncology at the Dana-Farber Cancer Institute, Boston, and co–principal investigator of the SORAYA trial that led to the approval. In a company press release, she said results from this trial show that mirvetuximab soravtansine has “impressive antitumor activity, durability of response, and overall tolerability ... [which] demonstrate the benefit of this new therapeutic option.”
The SORAYA trial (also known as Study 0417 [NCT04296890]) was a single-arm trial of 106 patients with FR alpha–positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer.
These patients were identified as FR alpha positive by using the assay. They were permitted to receive up to three prior lines of systemic therapy, and all patients were required to have received bevacizumab.
All patients received mirvetuximab soravtansine-gynx 6 mg/kg (based on adjusted ideal body weight) as an intravenous infusion every 3 weeks until disease progression or unacceptable toxicity.
The approval was based on an investigator-assessed overall response rate of 31.7%, which included five complete responses, and a median duration of response of 6.9 months.
Safety was evaluated in a pooled analysis from three studies among a total of 464 patients with FR alpha–positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer who received at least one dose of the drug.
The most common adverse events, occurring in 20% or more of study participants, were vision impairment, fatigue, increased AST level, nausea, increased alanine aminotransferase level, keratopathy, abdominal pain, decreased lymphocytes, peripheral neuropathy, diarrhea, decreased albumin, constipation, increased alkaline phosphatase level, dry eye, decreased magnesium level, decreased leukocyte count, decreased neutrophil count, and decreased hemoglobin level.
Potential participants were excluded if they had corneal disorders, ocular conditions requiring ongoing treatment, peripheral neuropathy above grade 1, or noninfectious interstitial lung disease.
The product labeling contains a boxed warning of ocular toxicity. Full prescribing information is available.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has granted accelerated approval to mirvetuximab soravtansine (Elahere) for use in pretreated patients with folate receptor (FR) alpha–positive, platinum-resistant epithelial ovarian, fallopian tube, and primary peritoneal cancer. These patients can have received one to three prior lines of treatment.
“ according to labeling.
Mirvetuximab soravtansine is an antibody-drug conjugate (ADC) with an antibody directed against FR alpha that is linked to a microtubule inhibitor conjugate.
This product is a first-in-class ADC directed against FR alpha, a cell-surface protein highly expressed in ovarian cancer, and is the first FDA-approved ADC for platinum-resistant disease, said the manufacturer, ImmunoGen.
Patients are selected for treatment with this drug using a diagnostic test that the FDA approved along with the agent: the VENTANA FOLR1 (FOLR-2.1) RxDx Assay.
FR alpha–positive platinum-resistant ovarian cancer is characterized by limited treatment options and poor outcomes, commented Ursula Matulonis, MD, chief of the division of gynecologic oncology at the Dana-Farber Cancer Institute, Boston, and co–principal investigator of the SORAYA trial that led to the approval. In a company press release, she said results from this trial show that mirvetuximab soravtansine has “impressive antitumor activity, durability of response, and overall tolerability ... [which] demonstrate the benefit of this new therapeutic option.”
The SORAYA trial (also known as Study 0417 [NCT04296890]) was a single-arm trial of 106 patients with FR alpha–positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer.
These patients were identified as FR alpha positive by using the assay. They were permitted to receive up to three prior lines of systemic therapy, and all patients were required to have received bevacizumab.
All patients received mirvetuximab soravtansine-gynx 6 mg/kg (based on adjusted ideal body weight) as an intravenous infusion every 3 weeks until disease progression or unacceptable toxicity.
The approval was based on an investigator-assessed overall response rate of 31.7%, which included five complete responses, and a median duration of response of 6.9 months.
Safety was evaluated in a pooled analysis from three studies among a total of 464 patients with FR alpha–positive, platinum-resistant epithelial ovarian, fallopian tube, or primary peritoneal cancer who received at least one dose of the drug.
The most common adverse events, occurring in 20% or more of study participants, were vision impairment, fatigue, increased AST level, nausea, increased alanine aminotransferase level, keratopathy, abdominal pain, decreased lymphocytes, peripheral neuropathy, diarrhea, decreased albumin, constipation, increased alkaline phosphatase level, dry eye, decreased magnesium level, decreased leukocyte count, decreased neutrophil count, and decreased hemoglobin level.
Potential participants were excluded if they had corneal disorders, ocular conditions requiring ongoing treatment, peripheral neuropathy above grade 1, or noninfectious interstitial lung disease.
The product labeling contains a boxed warning of ocular toxicity. Full prescribing information is available.
A version of this article first appeared on Medscape.com.
Analysis affirms that giving birth protects against endometrial cancer
Compared with having no children, the risk reduction for endometrial cancer was 21% with having one child, 38% with having two, and 51% with having three, Gunn-Helen Moen, MSc, PhD, a research fellow at the University of Queensland Institute for Molecular Bioscience in St. Lucia, Australia, and the senior author of the study, said in an email.
In the United States, the prevalence of endometrial cancer is 25.7 per 100,000 women per year, with a lifetime risk of 2.8%.
Multiple observational studies have linked giving birth to risk of endometrial cancer. For the new study, Dr. Moen and her team assessed various risk factors related to ovulation and reproductive function using Mendelian randomization, an epidemiological technique that deploys genetic variants to detect cause-and-effect relationships between potentially modifiable risk factors and health outcomes in observational data.
The researcher published their findings in BMC Medicine.
Leverage genetic data
The study used detailed genetic and health data from the UK Biobank, a databank with more than half a million participants. Genetic variants related to some of the risk factors were used to assess whether the variants make people more likely to develop endometrial cancer.
Genomewide significant single-nucleotide polymorphisms (SNPs) related to number of live births, age at menopause and menarche, and body mass index (BMI) had been identified in previous studies, the researchers reported. They conducted genomewide association analyses of the databank to identify SNPs associated with years ovulating, years using the contraceptive pill, and age at last live birth.
The MR analysis showed a potential causal effect for the number of live births (inverse variance–weighted odds ratio, 0.537) and number of years ovulating (IVW OR, 1.051), in addition to known risk factors of BMI, age at menarche, and age at menopause.
A further multivariable MR analysis showed that number of births had a negative causal effect on endometrial cancer risk (OR, 0.783), independent of the causal effect of known risk factors such as BMI, age at menarche and age at menopause.
Reported limitations included being unable to perform MR analyses on some factors, such as oral contraceptive use, because of a lack of valid genetic instruments. The researchers could not perform an age adjustment at diagnosis because of a lack of data.
In addition, the genetic data came exclusively from White women of European ancestry.
‘A personal choice’
Other investigators have hypothesized that the protective effect of childbirth may be caused by shedding of malignant and premalignant endometrial cells during and after childbirth and exposure to high levels of progesterone in late stages of pregnancy, the research team noted.
Dr. Moen said, based on the results, physicians might consider number of childbirths in assessing a patient’s risk of endometrial cancer.
However, Britton Trabert, MSPH, MS, PhD, an epidemiologist and assistant professor of obstetrics and gynecology at the University of Utah, Salt Lake City, said it’s unlikely the findings will affect clinical practice given that they “largely replicate well-characterized endometrial cancer risk associations.”
“Pregnancy and childbirth are a personal choice and is not largely regarded as a modifiable factor for cancer prevention,” said Dr. Trabert, who was not involved in the study.
The study’s investigators reported funding from the governments of Australia, Norway and the United Kingdom and the British Heart Foundation. No financial conflicts of interest were reported. Dr. Trabert reported no relevant financial interests.
Compared with having no children, the risk reduction for endometrial cancer was 21% with having one child, 38% with having two, and 51% with having three, Gunn-Helen Moen, MSc, PhD, a research fellow at the University of Queensland Institute for Molecular Bioscience in St. Lucia, Australia, and the senior author of the study, said in an email.
In the United States, the prevalence of endometrial cancer is 25.7 per 100,000 women per year, with a lifetime risk of 2.8%.
Multiple observational studies have linked giving birth to risk of endometrial cancer. For the new study, Dr. Moen and her team assessed various risk factors related to ovulation and reproductive function using Mendelian randomization, an epidemiological technique that deploys genetic variants to detect cause-and-effect relationships between potentially modifiable risk factors and health outcomes in observational data.
The researcher published their findings in BMC Medicine.
Leverage genetic data
The study used detailed genetic and health data from the UK Biobank, a databank with more than half a million participants. Genetic variants related to some of the risk factors were used to assess whether the variants make people more likely to develop endometrial cancer.
Genomewide significant single-nucleotide polymorphisms (SNPs) related to number of live births, age at menopause and menarche, and body mass index (BMI) had been identified in previous studies, the researchers reported. They conducted genomewide association analyses of the databank to identify SNPs associated with years ovulating, years using the contraceptive pill, and age at last live birth.
The MR analysis showed a potential causal effect for the number of live births (inverse variance–weighted odds ratio, 0.537) and number of years ovulating (IVW OR, 1.051), in addition to known risk factors of BMI, age at menarche, and age at menopause.
A further multivariable MR analysis showed that number of births had a negative causal effect on endometrial cancer risk (OR, 0.783), independent of the causal effect of known risk factors such as BMI, age at menarche and age at menopause.
Reported limitations included being unable to perform MR analyses on some factors, such as oral contraceptive use, because of a lack of valid genetic instruments. The researchers could not perform an age adjustment at diagnosis because of a lack of data.
In addition, the genetic data came exclusively from White women of European ancestry.
‘A personal choice’
Other investigators have hypothesized that the protective effect of childbirth may be caused by shedding of malignant and premalignant endometrial cells during and after childbirth and exposure to high levels of progesterone in late stages of pregnancy, the research team noted.
Dr. Moen said, based on the results, physicians might consider number of childbirths in assessing a patient’s risk of endometrial cancer.
However, Britton Trabert, MSPH, MS, PhD, an epidemiologist and assistant professor of obstetrics and gynecology at the University of Utah, Salt Lake City, said it’s unlikely the findings will affect clinical practice given that they “largely replicate well-characterized endometrial cancer risk associations.”
“Pregnancy and childbirth are a personal choice and is not largely regarded as a modifiable factor for cancer prevention,” said Dr. Trabert, who was not involved in the study.
The study’s investigators reported funding from the governments of Australia, Norway and the United Kingdom and the British Heart Foundation. No financial conflicts of interest were reported. Dr. Trabert reported no relevant financial interests.
Compared with having no children, the risk reduction for endometrial cancer was 21% with having one child, 38% with having two, and 51% with having three, Gunn-Helen Moen, MSc, PhD, a research fellow at the University of Queensland Institute for Molecular Bioscience in St. Lucia, Australia, and the senior author of the study, said in an email.
In the United States, the prevalence of endometrial cancer is 25.7 per 100,000 women per year, with a lifetime risk of 2.8%.
Multiple observational studies have linked giving birth to risk of endometrial cancer. For the new study, Dr. Moen and her team assessed various risk factors related to ovulation and reproductive function using Mendelian randomization, an epidemiological technique that deploys genetic variants to detect cause-and-effect relationships between potentially modifiable risk factors and health outcomes in observational data.
The researcher published their findings in BMC Medicine.
Leverage genetic data
The study used detailed genetic and health data from the UK Biobank, a databank with more than half a million participants. Genetic variants related to some of the risk factors were used to assess whether the variants make people more likely to develop endometrial cancer.
Genomewide significant single-nucleotide polymorphisms (SNPs) related to number of live births, age at menopause and menarche, and body mass index (BMI) had been identified in previous studies, the researchers reported. They conducted genomewide association analyses of the databank to identify SNPs associated with years ovulating, years using the contraceptive pill, and age at last live birth.
The MR analysis showed a potential causal effect for the number of live births (inverse variance–weighted odds ratio, 0.537) and number of years ovulating (IVW OR, 1.051), in addition to known risk factors of BMI, age at menarche, and age at menopause.
A further multivariable MR analysis showed that number of births had a negative causal effect on endometrial cancer risk (OR, 0.783), independent of the causal effect of known risk factors such as BMI, age at menarche and age at menopause.
Reported limitations included being unable to perform MR analyses on some factors, such as oral contraceptive use, because of a lack of valid genetic instruments. The researchers could not perform an age adjustment at diagnosis because of a lack of data.
In addition, the genetic data came exclusively from White women of European ancestry.
‘A personal choice’
Other investigators have hypothesized that the protective effect of childbirth may be caused by shedding of malignant and premalignant endometrial cells during and after childbirth and exposure to high levels of progesterone in late stages of pregnancy, the research team noted.
Dr. Moen said, based on the results, physicians might consider number of childbirths in assessing a patient’s risk of endometrial cancer.
However, Britton Trabert, MSPH, MS, PhD, an epidemiologist and assistant professor of obstetrics and gynecology at the University of Utah, Salt Lake City, said it’s unlikely the findings will affect clinical practice given that they “largely replicate well-characterized endometrial cancer risk associations.”
“Pregnancy and childbirth are a personal choice and is not largely regarded as a modifiable factor for cancer prevention,” said Dr. Trabert, who was not involved in the study.
The study’s investigators reported funding from the governments of Australia, Norway and the United Kingdom and the British Heart Foundation. No financial conflicts of interest were reported. Dr. Trabert reported no relevant financial interests.
FROM BMC MEDICINE






