User login
One strikeout, one hit against low-grade serous carcinomas
Two MEK inhibitors were tested against recurrent low-grade serous carcinomas of the ovaries, fallopian tubes, or peritoneum, but only one inhibitor offered clinical benefit over standard care, investigators from two randomized trials reported.
Trametinib improved progression-free survival (PFS) when compared with standard care, while binimetinib conferred no PFS benefit.
In a phase 2/3 trial, the median PFS was 13 months for patients treated with trametinib and 7.2 months for patients who received an aromatase inhibitor or chemotherapy (P < .0001).
“Our findings suggest that trametinib represents a new standard-of-care treatment option for women with recurrent low-grade serous carcinoma,” said investigator David M. Gershenson, MD, of the University of Texas MD Anderson Cancer Center in Houston.
In contrast, in the phase 3 MILO/ENGOT-ov11 trial, there was no significant difference in PFS between patients treated with binimetinib and those who received physician’s choice of chemotherapy. The median PFS was 11.2 months with binimetinib and 14.1 months with chemotherapy (P = .752).
“Although this study did not meet its primary endpoint, binimetinib showed activity in low-grade serous ovarian cancer across the efficacy endpoints evaluated, with a response rate of 24% and a median PFS of 11.2 months on updated analysis. Chemotherapy responses were better than predicted, based on historical retrospective data,” said investigator Rachel N. Grisham, MD, of Memorial Sloan Kettering Cancer Center in New York.
The binimetinib trial and the trametinib trial were both discussed during a webinar on rare tumors covering research slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer. The meeting was canceled because of the COVID-19 pandemic.
Chemoresistant cancers
Low-grade serous ovarian or peritoneal cancers are rare, accounting for only 5% to 10% of all serous cancers, Dr. Gershenson noted.
“[Low-grade serous cancers are] characterized by alterations in the MAP kinase pathway, as well as relative chemoresistance, and prolonged overall survival compared to high-grade serous cancers. Because of this subtype’s relative chemoresistance, the search for novel therapeutics has predominated over the last decade or so,” he said.
MEK inhibitors interfere with the MEK1 and MEK2 enzymes in the MAPK pathway. Alterations in MAPK, especially in KRAS and BRAF proteins, are found in 30%-60% of low-grade serous carcinomas, providing the rationale for MEK inhibitors in these rare malignancies.
Trametinib study
In a phase 2/3 study, Dr. Gershenson and colleagues enrolled 260 patients with recurrent, low-grade serous carcinoma of the ovary or peritoneum. Patients were randomized to receive either trametinib at 2 mg daily continuously until progression (n = 130) or standard care (n = 130).
Standard care consisted of one of the following: letrozole at 2.5 mg daily; pegylated liposomal doxorubicin at 40-50 mg IV every 28 days; weekly paclitaxel at 80 mg/m2 for 3 out of 4 weeks; tamoxifen at 20 mg twice daily; or topotecan at 4 mg/m2 on days 1, 8, and 15 every 28 days. Patients randomized to standard care could be crossed over to trametinib at progression.
All patients had at least one prior line of platinum-based chemotherapy, and nearly half had three or more prior lines of therapy. The median age was 56.6 years in the trametinib arm and 55.3 years in the control arm.
At a median follow-up of 31.4 months, median PFS, the primary endpoint, was 13 months with trametinib vs. 7.2 months with standard care. The hazard ratio (HR) for progression on trametinib was 0.48 (P < .0001).
The overall response rates were 26.2% in the trametinib arm and 6.2% in the standard care arm. The odds ratio for response on trametinib was 5.4 (P < .0001).
For 88 patients who crossed over to trametinib, the median PFS was 10.8 months, and the overall response rate was 15%.
Trametinib was also associated with a significantly longer response duration, at a median of 13.6 months, compared with 5.9 months for standard care (P value not shown).
The median overall survival was 37 months with trametinib and 29.2 months with standard care, with an HR favoring trametinib of 0.75, although this just missed statistical significance (P = .054). Dr. Gershenson pointed out that the overall survival in the standard care arm included patients who had been crossed over to trametinib.
Grade 3 or greater adverse events included hematologic toxicities in 13.4% of patients on trametinib and 9.4% on standard care; gastrointestinal toxicity in 27.6% and 29%, respectively; skin toxicities in 15% and 3.9%, respectively; and vascular toxicities in 18.9% and 8.6%, respectively.
Binimetinib study
The phase 3 MILO/ENGOT-ov11 study enrolled 341 patients with low-grade serous carcinomas of the ovaries, fallopian tubes, or peritoneum. Patients were randomized on a 2:1 basis to receive either binimetinib at 45 mg twice daily (n = 228) or physician’s choice of chemotherapy (n = 113). Chemotherapy consisted of pegylated liposomal doxorubicin at 40 mg/m2 on day 1 of each 28-day cycle; paclitaxel at 80 mg/m2 on days 1, 8, and 15 of each 28-day cycle; or topotecan at 1.25 mg/m2 IV on days 1-5 of each 21-day cycle.
The efficacy analysis included 227 patients assigned to binimetinib and 106 assigned to chemotherapy.
A planned interim analysis was performed in 2016 after the first 303 patients were enrolled. At that time, the median PFS by blinded central review was 9.1 months in the binimetinib arm and 10.6 months in the physician’s choice arm (HR, 1.21; P = .807), so the trial was halted early for futility. Patients on active treatment at the time could continue until progression and were followed by local radiology.
At the interim analysis, secondary endpoints were also similar between the arms. The overall response rate was 16% in the binimetinib arm and 13% in the chemotherapy arm.
The most common grade 3 or greater adverse events with binimetinib were blood creatinine phosphokinase increase (26%) and vomiting (10%).
Dr. Grisham also reported updated follow-up results through January 2019.
The median PFS in the updated analysis was 11.2 months with the MEK inhibitor and 14.1 months with chemotherapy, a difference that was not statistically significant (HR, 1.12; P = .752). Updated overall response rates were the same in both arms, at 24%.
A post hoc molecular analysis of 215 patients suggested a possible association between KRAS mutation and response to binimetinib.
Two MEKs, one ‘meh’
Discussant Jubilee Brown, MD, of the Levine Cancer Institute at Atrium Health in Charlotte, N.C., said that “with a 2% to 5% chance of response in patients with low-grade serous ovarian cancer, there is a low bar for any compound to demonstrate success.”
Regarding the MILO/ENGOT-ov11 trial, she noted that “this study did not meet its primary endpoint, but perhaps the endpoint is not reflective of the importance of the study.”
A different outcome might have occurred had investigators stratified patients by KRAS status upfront, comparing patients with KRAS mutations treated with binimetinib to KRAS wild-type patients treated with either a MEK inhibitor or physician’s choice of care, Dr. Brown said.
She agreed with the assertion by Dr. Gershenson and colleagues that improved PFS qualifies trametinib to be considered a new option for standard care, ”especially in a rare tumor setting with limited options. This is a huge win for patients.”
The trametinib study was sponsored by NRG Oncology and the UK National Cancer Research Institute. Dr. Gershenson disclosed relationships with NRG Oncology, Genentech, Novartis, Elsevier, and UpToDate, as well as stock in several companies.
The binimetinib study was sponsored by Pfizer. Dr. Grisham disclosed relationships with Clovis, Regeneron, Mateon, Amgen, Abbvie, OncLive, PRIME, MCM, and Medscape. MDedge News and Medscape are owned by the same parent organization.
Dr. Brown disclosed consulting for Biodesix, Caris, Clovis, Genentech, Invitae, Janssen, Olympus, OncLive, and Tempus.
SOURCE: Gershenson DM et al. SGO 2020, Abstract 42; Grisham RN et al. SGO 2020, Abstract 41.
Two MEK inhibitors were tested against recurrent low-grade serous carcinomas of the ovaries, fallopian tubes, or peritoneum, but only one inhibitor offered clinical benefit over standard care, investigators from two randomized trials reported.
Trametinib improved progression-free survival (PFS) when compared with standard care, while binimetinib conferred no PFS benefit.
In a phase 2/3 trial, the median PFS was 13 months for patients treated with trametinib and 7.2 months for patients who received an aromatase inhibitor or chemotherapy (P < .0001).
“Our findings suggest that trametinib represents a new standard-of-care treatment option for women with recurrent low-grade serous carcinoma,” said investigator David M. Gershenson, MD, of the University of Texas MD Anderson Cancer Center in Houston.
In contrast, in the phase 3 MILO/ENGOT-ov11 trial, there was no significant difference in PFS between patients treated with binimetinib and those who received physician’s choice of chemotherapy. The median PFS was 11.2 months with binimetinib and 14.1 months with chemotherapy (P = .752).
“Although this study did not meet its primary endpoint, binimetinib showed activity in low-grade serous ovarian cancer across the efficacy endpoints evaluated, with a response rate of 24% and a median PFS of 11.2 months on updated analysis. Chemotherapy responses were better than predicted, based on historical retrospective data,” said investigator Rachel N. Grisham, MD, of Memorial Sloan Kettering Cancer Center in New York.
The binimetinib trial and the trametinib trial were both discussed during a webinar on rare tumors covering research slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer. The meeting was canceled because of the COVID-19 pandemic.
Chemoresistant cancers
Low-grade serous ovarian or peritoneal cancers are rare, accounting for only 5% to 10% of all serous cancers, Dr. Gershenson noted.
“[Low-grade serous cancers are] characterized by alterations in the MAP kinase pathway, as well as relative chemoresistance, and prolonged overall survival compared to high-grade serous cancers. Because of this subtype’s relative chemoresistance, the search for novel therapeutics has predominated over the last decade or so,” he said.
MEK inhibitors interfere with the MEK1 and MEK2 enzymes in the MAPK pathway. Alterations in MAPK, especially in KRAS and BRAF proteins, are found in 30%-60% of low-grade serous carcinomas, providing the rationale for MEK inhibitors in these rare malignancies.
Trametinib study
In a phase 2/3 study, Dr. Gershenson and colleagues enrolled 260 patients with recurrent, low-grade serous carcinoma of the ovary or peritoneum. Patients were randomized to receive either trametinib at 2 mg daily continuously until progression (n = 130) or standard care (n = 130).
Standard care consisted of one of the following: letrozole at 2.5 mg daily; pegylated liposomal doxorubicin at 40-50 mg IV every 28 days; weekly paclitaxel at 80 mg/m2 for 3 out of 4 weeks; tamoxifen at 20 mg twice daily; or topotecan at 4 mg/m2 on days 1, 8, and 15 every 28 days. Patients randomized to standard care could be crossed over to trametinib at progression.
All patients had at least one prior line of platinum-based chemotherapy, and nearly half had three or more prior lines of therapy. The median age was 56.6 years in the trametinib arm and 55.3 years in the control arm.
At a median follow-up of 31.4 months, median PFS, the primary endpoint, was 13 months with trametinib vs. 7.2 months with standard care. The hazard ratio (HR) for progression on trametinib was 0.48 (P < .0001).
The overall response rates were 26.2% in the trametinib arm and 6.2% in the standard care arm. The odds ratio for response on trametinib was 5.4 (P < .0001).
For 88 patients who crossed over to trametinib, the median PFS was 10.8 months, and the overall response rate was 15%.
Trametinib was also associated with a significantly longer response duration, at a median of 13.6 months, compared with 5.9 months for standard care (P value not shown).
The median overall survival was 37 months with trametinib and 29.2 months with standard care, with an HR favoring trametinib of 0.75, although this just missed statistical significance (P = .054). Dr. Gershenson pointed out that the overall survival in the standard care arm included patients who had been crossed over to trametinib.
Grade 3 or greater adverse events included hematologic toxicities in 13.4% of patients on trametinib and 9.4% on standard care; gastrointestinal toxicity in 27.6% and 29%, respectively; skin toxicities in 15% and 3.9%, respectively; and vascular toxicities in 18.9% and 8.6%, respectively.
Binimetinib study
The phase 3 MILO/ENGOT-ov11 study enrolled 341 patients with low-grade serous carcinomas of the ovaries, fallopian tubes, or peritoneum. Patients were randomized on a 2:1 basis to receive either binimetinib at 45 mg twice daily (n = 228) or physician’s choice of chemotherapy (n = 113). Chemotherapy consisted of pegylated liposomal doxorubicin at 40 mg/m2 on day 1 of each 28-day cycle; paclitaxel at 80 mg/m2 on days 1, 8, and 15 of each 28-day cycle; or topotecan at 1.25 mg/m2 IV on days 1-5 of each 21-day cycle.
The efficacy analysis included 227 patients assigned to binimetinib and 106 assigned to chemotherapy.
A planned interim analysis was performed in 2016 after the first 303 patients were enrolled. At that time, the median PFS by blinded central review was 9.1 months in the binimetinib arm and 10.6 months in the physician’s choice arm (HR, 1.21; P = .807), so the trial was halted early for futility. Patients on active treatment at the time could continue until progression and were followed by local radiology.
At the interim analysis, secondary endpoints were also similar between the arms. The overall response rate was 16% in the binimetinib arm and 13% in the chemotherapy arm.
The most common grade 3 or greater adverse events with binimetinib were blood creatinine phosphokinase increase (26%) and vomiting (10%).
Dr. Grisham also reported updated follow-up results through January 2019.
The median PFS in the updated analysis was 11.2 months with the MEK inhibitor and 14.1 months with chemotherapy, a difference that was not statistically significant (HR, 1.12; P = .752). Updated overall response rates were the same in both arms, at 24%.
A post hoc molecular analysis of 215 patients suggested a possible association between KRAS mutation and response to binimetinib.
Two MEKs, one ‘meh’
Discussant Jubilee Brown, MD, of the Levine Cancer Institute at Atrium Health in Charlotte, N.C., said that “with a 2% to 5% chance of response in patients with low-grade serous ovarian cancer, there is a low bar for any compound to demonstrate success.”
Regarding the MILO/ENGOT-ov11 trial, she noted that “this study did not meet its primary endpoint, but perhaps the endpoint is not reflective of the importance of the study.”
A different outcome might have occurred had investigators stratified patients by KRAS status upfront, comparing patients with KRAS mutations treated with binimetinib to KRAS wild-type patients treated with either a MEK inhibitor or physician’s choice of care, Dr. Brown said.
She agreed with the assertion by Dr. Gershenson and colleagues that improved PFS qualifies trametinib to be considered a new option for standard care, ”especially in a rare tumor setting with limited options. This is a huge win for patients.”
The trametinib study was sponsored by NRG Oncology and the UK National Cancer Research Institute. Dr. Gershenson disclosed relationships with NRG Oncology, Genentech, Novartis, Elsevier, and UpToDate, as well as stock in several companies.
The binimetinib study was sponsored by Pfizer. Dr. Grisham disclosed relationships with Clovis, Regeneron, Mateon, Amgen, Abbvie, OncLive, PRIME, MCM, and Medscape. MDedge News and Medscape are owned by the same parent organization.
Dr. Brown disclosed consulting for Biodesix, Caris, Clovis, Genentech, Invitae, Janssen, Olympus, OncLive, and Tempus.
SOURCE: Gershenson DM et al. SGO 2020, Abstract 42; Grisham RN et al. SGO 2020, Abstract 41.
Two MEK inhibitors were tested against recurrent low-grade serous carcinomas of the ovaries, fallopian tubes, or peritoneum, but only one inhibitor offered clinical benefit over standard care, investigators from two randomized trials reported.
Trametinib improved progression-free survival (PFS) when compared with standard care, while binimetinib conferred no PFS benefit.
In a phase 2/3 trial, the median PFS was 13 months for patients treated with trametinib and 7.2 months for patients who received an aromatase inhibitor or chemotherapy (P < .0001).
“Our findings suggest that trametinib represents a new standard-of-care treatment option for women with recurrent low-grade serous carcinoma,” said investigator David M. Gershenson, MD, of the University of Texas MD Anderson Cancer Center in Houston.
In contrast, in the phase 3 MILO/ENGOT-ov11 trial, there was no significant difference in PFS between patients treated with binimetinib and those who received physician’s choice of chemotherapy. The median PFS was 11.2 months with binimetinib and 14.1 months with chemotherapy (P = .752).
“Although this study did not meet its primary endpoint, binimetinib showed activity in low-grade serous ovarian cancer across the efficacy endpoints evaluated, with a response rate of 24% and a median PFS of 11.2 months on updated analysis. Chemotherapy responses were better than predicted, based on historical retrospective data,” said investigator Rachel N. Grisham, MD, of Memorial Sloan Kettering Cancer Center in New York.
The binimetinib trial and the trametinib trial were both discussed during a webinar on rare tumors covering research slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancer. The meeting was canceled because of the COVID-19 pandemic.
Chemoresistant cancers
Low-grade serous ovarian or peritoneal cancers are rare, accounting for only 5% to 10% of all serous cancers, Dr. Gershenson noted.
“[Low-grade serous cancers are] characterized by alterations in the MAP kinase pathway, as well as relative chemoresistance, and prolonged overall survival compared to high-grade serous cancers. Because of this subtype’s relative chemoresistance, the search for novel therapeutics has predominated over the last decade or so,” he said.
MEK inhibitors interfere with the MEK1 and MEK2 enzymes in the MAPK pathway. Alterations in MAPK, especially in KRAS and BRAF proteins, are found in 30%-60% of low-grade serous carcinomas, providing the rationale for MEK inhibitors in these rare malignancies.
Trametinib study
In a phase 2/3 study, Dr. Gershenson and colleagues enrolled 260 patients with recurrent, low-grade serous carcinoma of the ovary or peritoneum. Patients were randomized to receive either trametinib at 2 mg daily continuously until progression (n = 130) or standard care (n = 130).
Standard care consisted of one of the following: letrozole at 2.5 mg daily; pegylated liposomal doxorubicin at 40-50 mg IV every 28 days; weekly paclitaxel at 80 mg/m2 for 3 out of 4 weeks; tamoxifen at 20 mg twice daily; or topotecan at 4 mg/m2 on days 1, 8, and 15 every 28 days. Patients randomized to standard care could be crossed over to trametinib at progression.
All patients had at least one prior line of platinum-based chemotherapy, and nearly half had three or more prior lines of therapy. The median age was 56.6 years in the trametinib arm and 55.3 years in the control arm.
At a median follow-up of 31.4 months, median PFS, the primary endpoint, was 13 months with trametinib vs. 7.2 months with standard care. The hazard ratio (HR) for progression on trametinib was 0.48 (P < .0001).
The overall response rates were 26.2% in the trametinib arm and 6.2% in the standard care arm. The odds ratio for response on trametinib was 5.4 (P < .0001).
For 88 patients who crossed over to trametinib, the median PFS was 10.8 months, and the overall response rate was 15%.
Trametinib was also associated with a significantly longer response duration, at a median of 13.6 months, compared with 5.9 months for standard care (P value not shown).
The median overall survival was 37 months with trametinib and 29.2 months with standard care, with an HR favoring trametinib of 0.75, although this just missed statistical significance (P = .054). Dr. Gershenson pointed out that the overall survival in the standard care arm included patients who had been crossed over to trametinib.
Grade 3 or greater adverse events included hematologic toxicities in 13.4% of patients on trametinib and 9.4% on standard care; gastrointestinal toxicity in 27.6% and 29%, respectively; skin toxicities in 15% and 3.9%, respectively; and vascular toxicities in 18.9% and 8.6%, respectively.
Binimetinib study
The phase 3 MILO/ENGOT-ov11 study enrolled 341 patients with low-grade serous carcinomas of the ovaries, fallopian tubes, or peritoneum. Patients were randomized on a 2:1 basis to receive either binimetinib at 45 mg twice daily (n = 228) or physician’s choice of chemotherapy (n = 113). Chemotherapy consisted of pegylated liposomal doxorubicin at 40 mg/m2 on day 1 of each 28-day cycle; paclitaxel at 80 mg/m2 on days 1, 8, and 15 of each 28-day cycle; or topotecan at 1.25 mg/m2 IV on days 1-5 of each 21-day cycle.
The efficacy analysis included 227 patients assigned to binimetinib and 106 assigned to chemotherapy.
A planned interim analysis was performed in 2016 after the first 303 patients were enrolled. At that time, the median PFS by blinded central review was 9.1 months in the binimetinib arm and 10.6 months in the physician’s choice arm (HR, 1.21; P = .807), so the trial was halted early for futility. Patients on active treatment at the time could continue until progression and were followed by local radiology.
At the interim analysis, secondary endpoints were also similar between the arms. The overall response rate was 16% in the binimetinib arm and 13% in the chemotherapy arm.
The most common grade 3 or greater adverse events with binimetinib were blood creatinine phosphokinase increase (26%) and vomiting (10%).
Dr. Grisham also reported updated follow-up results through January 2019.
The median PFS in the updated analysis was 11.2 months with the MEK inhibitor and 14.1 months with chemotherapy, a difference that was not statistically significant (HR, 1.12; P = .752). Updated overall response rates were the same in both arms, at 24%.
A post hoc molecular analysis of 215 patients suggested a possible association between KRAS mutation and response to binimetinib.
Two MEKs, one ‘meh’
Discussant Jubilee Brown, MD, of the Levine Cancer Institute at Atrium Health in Charlotte, N.C., said that “with a 2% to 5% chance of response in patients with low-grade serous ovarian cancer, there is a low bar for any compound to demonstrate success.”
Regarding the MILO/ENGOT-ov11 trial, she noted that “this study did not meet its primary endpoint, but perhaps the endpoint is not reflective of the importance of the study.”
A different outcome might have occurred had investigators stratified patients by KRAS status upfront, comparing patients with KRAS mutations treated with binimetinib to KRAS wild-type patients treated with either a MEK inhibitor or physician’s choice of care, Dr. Brown said.
She agreed with the assertion by Dr. Gershenson and colleagues that improved PFS qualifies trametinib to be considered a new option for standard care, ”especially in a rare tumor setting with limited options. This is a huge win for patients.”
The trametinib study was sponsored by NRG Oncology and the UK National Cancer Research Institute. Dr. Gershenson disclosed relationships with NRG Oncology, Genentech, Novartis, Elsevier, and UpToDate, as well as stock in several companies.
The binimetinib study was sponsored by Pfizer. Dr. Grisham disclosed relationships with Clovis, Regeneron, Mateon, Amgen, Abbvie, OncLive, PRIME, MCM, and Medscape. MDedge News and Medscape are owned by the same parent organization.
Dr. Brown disclosed consulting for Biodesix, Caris, Clovis, Genentech, Invitae, Janssen, Olympus, OncLive, and Tempus.
SOURCE: Gershenson DM et al. SGO 2020, Abstract 42; Grisham RN et al. SGO 2020, Abstract 41.
FROM SGO 2020
FDA approves olaparib/bevacizumab maintenance
The Food and Drug Administration has announced a new approved indication for olaparib (Lynparza) in adults with advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer.
Olaparib is now FDA-approved for use in combination with bevacizumab as maintenance therapy in patients who responded to first-line platinum-based chemotherapy and whose cancer is homologous recombination deficiency positive, as defined by a deleterious or suspected deleterious BRCA mutation and/or genomic instability.
The FDA also approved the Myriad myChoice CDx test as a companion diagnostic for olaparib.
Trial results
The efficacy of olaparib and the myChoice CDx test were assessed in patients in the phase 3 PAOLA-1 trial (NCT02477644). The study enrolled patients with advanced high-grade epithelial ovarian, fallopian tube, or primary peritoneal cancer who had received first-line platinum-based chemotherapy and bevacizumab.
Patients were stratified by first-line treatment outcome and BRCA mutation status, as determined by prospective local testing. All available clinical samples were retrospectively tested with the Myriad myChoice CDx test.
The patients were randomized to receive olaparib at 300 mg orally twice daily in combination with bevacizumab at 15 mg/kg every 3 weeks (n = 537) or placebo plus bevacizumab (n = 269). Patients continued bevacizumab in the maintenance setting and started olaparib 3-9 weeks after their last chemotherapy dose. Olaparib could be continued for up to 2 years or until disease progression or unacceptable toxicity.
The median progression-free survival among the 387 patients with homologous recombination deficiency-positive tumors was 37.2 months in the olaparib arm and 17.7 months in the placebo arm (hazard ratio, 0.33), according to the prescribing information for olaparib.
Serious adverse events occurred in 31% of patients in the olaparib arm. The most common were hypertension (19%) and anemia (17%).
Dose interruptions from adverse events occurred in 54% of patients in the olaparib arm, and dose reductions from adverse events occurred in 41%.
The Food and Drug Administration has announced a new approved indication for olaparib (Lynparza) in adults with advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer.
Olaparib is now FDA-approved for use in combination with bevacizumab as maintenance therapy in patients who responded to first-line platinum-based chemotherapy and whose cancer is homologous recombination deficiency positive, as defined by a deleterious or suspected deleterious BRCA mutation and/or genomic instability.
The FDA also approved the Myriad myChoice CDx test as a companion diagnostic for olaparib.
Trial results
The efficacy of olaparib and the myChoice CDx test were assessed in patients in the phase 3 PAOLA-1 trial (NCT02477644). The study enrolled patients with advanced high-grade epithelial ovarian, fallopian tube, or primary peritoneal cancer who had received first-line platinum-based chemotherapy and bevacizumab.
Patients were stratified by first-line treatment outcome and BRCA mutation status, as determined by prospective local testing. All available clinical samples were retrospectively tested with the Myriad myChoice CDx test.
The patients were randomized to receive olaparib at 300 mg orally twice daily in combination with bevacizumab at 15 mg/kg every 3 weeks (n = 537) or placebo plus bevacizumab (n = 269). Patients continued bevacizumab in the maintenance setting and started olaparib 3-9 weeks after their last chemotherapy dose. Olaparib could be continued for up to 2 years or until disease progression or unacceptable toxicity.
The median progression-free survival among the 387 patients with homologous recombination deficiency-positive tumors was 37.2 months in the olaparib arm and 17.7 months in the placebo arm (hazard ratio, 0.33), according to the prescribing information for olaparib.
Serious adverse events occurred in 31% of patients in the olaparib arm. The most common were hypertension (19%) and anemia (17%).
Dose interruptions from adverse events occurred in 54% of patients in the olaparib arm, and dose reductions from adverse events occurred in 41%.
The Food and Drug Administration has announced a new approved indication for olaparib (Lynparza) in adults with advanced epithelial ovarian, fallopian tube, or primary peritoneal cancer.
Olaparib is now FDA-approved for use in combination with bevacizumab as maintenance therapy in patients who responded to first-line platinum-based chemotherapy and whose cancer is homologous recombination deficiency positive, as defined by a deleterious or suspected deleterious BRCA mutation and/or genomic instability.
The FDA also approved the Myriad myChoice CDx test as a companion diagnostic for olaparib.
Trial results
The efficacy of olaparib and the myChoice CDx test were assessed in patients in the phase 3 PAOLA-1 trial (NCT02477644). The study enrolled patients with advanced high-grade epithelial ovarian, fallopian tube, or primary peritoneal cancer who had received first-line platinum-based chemotherapy and bevacizumab.
Patients were stratified by first-line treatment outcome and BRCA mutation status, as determined by prospective local testing. All available clinical samples were retrospectively tested with the Myriad myChoice CDx test.
The patients were randomized to receive olaparib at 300 mg orally twice daily in combination with bevacizumab at 15 mg/kg every 3 weeks (n = 537) or placebo plus bevacizumab (n = 269). Patients continued bevacizumab in the maintenance setting and started olaparib 3-9 weeks after their last chemotherapy dose. Olaparib could be continued for up to 2 years or until disease progression or unacceptable toxicity.
The median progression-free survival among the 387 patients with homologous recombination deficiency-positive tumors was 37.2 months in the olaparib arm and 17.7 months in the placebo arm (hazard ratio, 0.33), according to the prescribing information for olaparib.
Serious adverse events occurred in 31% of patients in the olaparib arm. The most common were hypertension (19%) and anemia (17%).
Dose interruptions from adverse events occurred in 54% of patients in the olaparib arm, and dose reductions from adverse events occurred in 41%.
ASCO goes ahead online, as conference center is used as hospital
Traditionally at this time of year, everyone working in cancer turns their attention toward Chicago, and 40,000 or so travel to the city for the annual meeting of the American Society of Clinical Oncology (ASCO).
Not this year.
The McCormick Place convention center has been converted to a field hospital to cope with the ongoing COVID-19 pandemic. The cavernous meeting halls have been filled with makeshift wards with 750 acute care beds, as shown in a tweet from Toni Choueiri, MD, chief of genitourinary oncology at the Dana Farber Cancer Center in Boston.
But the annual meeting is still going ahead, having been transferred online.
“We have to remember that even though there’s a pandemic going on and people are dying every day from coronavirus, people are still dying every day from cancer,” Richard Schilsky, MD, PhD, chief medical officer at ASCO, told Medscape Medical News.
“This pandemic will end, but cancer will continue, and we need to be able to continue to get the most cutting edge scientific results out there to our members and our constituents so they can act on those results on behalf of their patients,” he said.
The ASCO Virtual Scientific Program will take place over the weekend of May 30-31.
“We’re certainly hoping that we’re going to deliver a program that features all of the most important science that would have been presented in person in Chicago,” Schilsky commented in an interview.
Most of the presentations will be prerecorded and then streamed, which “we hope will mitigate any of the technical glitches that could come from trying to do a live broadcast of the meeting,” he said.
There will be 250 oral and 2500 poster presentations in 24 disease-based and specialty tracks.
The majority of the abstracts will be released online on May 13. The majority of the on-demand content will be released on May 29. Some of the abstracts will be highlighted at ASCO press briefings and released on those two dates.
But some of the material will be made available only on the weekend of the meeting. The opening session, plenaries featuring late-breaking abstracts, special highlights sessions, and other clinical science symposia will be broadcast on Saturday, May 30, and Sunday, May 31 (the schedule for the weekend program is available on the ASCO meeting website).
Among the plenary presentations are some clinical results that are likely to change practice immediately, Schilsky predicted. These include data to be presented in the following abstracts:
- Abstract LBA4 on the KEYNOTE-177 study comparing immunotherapy using pembrolizumab (Keytruda, Merck & Co) with chemotherapy in patients with metastatic colorectal cancer whose tumors show microsatellite instability or mismatch repair deficiency;
- Abstract LBA5 on the ADAURA study exploring osimertinib (Tagrisso, AstraZeneca) as adjuvant therapy after complete tumor reseaction in patients with early-stage non–small cell lung cancer whose tumors are EGFR mutation positive;
- Abstract LBA1 on the JAVELIN Bladder 100 study exploring maintenance avelumab (Bavencio, Merck and Pfizer) with best supportive care after platinum-based first-line chemotherapy in patients with advanced urothelial carcinoma.
However, some of the material that would have been part of the annual meeting, which includes mostly educational sessions and invited talks, has been moved to another event, the ASCO Educational Program, to be held in August 2020.
“So I suppose, in the grand scheme of things, the meeting is going to be compressed a little bit,” Schilsky commented. “Obviously, we can’t deliver all the interactions that happen in the hallways and everywhere else at the meeting that really gives so much energy to the meeting, but, at this moment in our history, probably getting the science out there is what’s most important.”
Virtual exhibition hall
There will also be a virtual exhibition hall, which will open on May 29.
“Just as there is a typical exhibit hall in the convention center,” Schilsky commented, most of the companies that were planning to be in Chicago have “now transitioned to creating a virtual booth that people who are participating in the virtual meeting can visit.
“I don’t know exactly how each company is going to use their time and their virtual space, and that’s part of the whole learning process here to see how this whole experiment is going to work out,” he added.
Unlike some of the other conferences that have gone virtual, in which access has been made available to everyone for free, registration is still required for the ASCO meeting. But the society notes that the registration fee has been discounted for nonmembers and has been waived for ASCO members. Also, the fee covers both the Virtual Scientific Program in May and the ASCO Educational Program in August.
Registrants will have access to video and slide presentations, as well as discussant commentaries, for 180 days.
The article first appeared on Medscape.com.
Traditionally at this time of year, everyone working in cancer turns their attention toward Chicago, and 40,000 or so travel to the city for the annual meeting of the American Society of Clinical Oncology (ASCO).
Not this year.
The McCormick Place convention center has been converted to a field hospital to cope with the ongoing COVID-19 pandemic. The cavernous meeting halls have been filled with makeshift wards with 750 acute care beds, as shown in a tweet from Toni Choueiri, MD, chief of genitourinary oncology at the Dana Farber Cancer Center in Boston.
But the annual meeting is still going ahead, having been transferred online.
“We have to remember that even though there’s a pandemic going on and people are dying every day from coronavirus, people are still dying every day from cancer,” Richard Schilsky, MD, PhD, chief medical officer at ASCO, told Medscape Medical News.
“This pandemic will end, but cancer will continue, and we need to be able to continue to get the most cutting edge scientific results out there to our members and our constituents so they can act on those results on behalf of their patients,” he said.
The ASCO Virtual Scientific Program will take place over the weekend of May 30-31.
“We’re certainly hoping that we’re going to deliver a program that features all of the most important science that would have been presented in person in Chicago,” Schilsky commented in an interview.
Most of the presentations will be prerecorded and then streamed, which “we hope will mitigate any of the technical glitches that could come from trying to do a live broadcast of the meeting,” he said.
There will be 250 oral and 2500 poster presentations in 24 disease-based and specialty tracks.
The majority of the abstracts will be released online on May 13. The majority of the on-demand content will be released on May 29. Some of the abstracts will be highlighted at ASCO press briefings and released on those two dates.
But some of the material will be made available only on the weekend of the meeting. The opening session, plenaries featuring late-breaking abstracts, special highlights sessions, and other clinical science symposia will be broadcast on Saturday, May 30, and Sunday, May 31 (the schedule for the weekend program is available on the ASCO meeting website).
Among the plenary presentations are some clinical results that are likely to change practice immediately, Schilsky predicted. These include data to be presented in the following abstracts:
- Abstract LBA4 on the KEYNOTE-177 study comparing immunotherapy using pembrolizumab (Keytruda, Merck & Co) with chemotherapy in patients with metastatic colorectal cancer whose tumors show microsatellite instability or mismatch repair deficiency;
- Abstract LBA5 on the ADAURA study exploring osimertinib (Tagrisso, AstraZeneca) as adjuvant therapy after complete tumor reseaction in patients with early-stage non–small cell lung cancer whose tumors are EGFR mutation positive;
- Abstract LBA1 on the JAVELIN Bladder 100 study exploring maintenance avelumab (Bavencio, Merck and Pfizer) with best supportive care after platinum-based first-line chemotherapy in patients with advanced urothelial carcinoma.
However, some of the material that would have been part of the annual meeting, which includes mostly educational sessions and invited talks, has been moved to another event, the ASCO Educational Program, to be held in August 2020.
“So I suppose, in the grand scheme of things, the meeting is going to be compressed a little bit,” Schilsky commented. “Obviously, we can’t deliver all the interactions that happen in the hallways and everywhere else at the meeting that really gives so much energy to the meeting, but, at this moment in our history, probably getting the science out there is what’s most important.”
Virtual exhibition hall
There will also be a virtual exhibition hall, which will open on May 29.
“Just as there is a typical exhibit hall in the convention center,” Schilsky commented, most of the companies that were planning to be in Chicago have “now transitioned to creating a virtual booth that people who are participating in the virtual meeting can visit.
“I don’t know exactly how each company is going to use their time and their virtual space, and that’s part of the whole learning process here to see how this whole experiment is going to work out,” he added.
Unlike some of the other conferences that have gone virtual, in which access has been made available to everyone for free, registration is still required for the ASCO meeting. But the society notes that the registration fee has been discounted for nonmembers and has been waived for ASCO members. Also, the fee covers both the Virtual Scientific Program in May and the ASCO Educational Program in August.
Registrants will have access to video and slide presentations, as well as discussant commentaries, for 180 days.
The article first appeared on Medscape.com.
Traditionally at this time of year, everyone working in cancer turns their attention toward Chicago, and 40,000 or so travel to the city for the annual meeting of the American Society of Clinical Oncology (ASCO).
Not this year.
The McCormick Place convention center has been converted to a field hospital to cope with the ongoing COVID-19 pandemic. The cavernous meeting halls have been filled with makeshift wards with 750 acute care beds, as shown in a tweet from Toni Choueiri, MD, chief of genitourinary oncology at the Dana Farber Cancer Center in Boston.
But the annual meeting is still going ahead, having been transferred online.
“We have to remember that even though there’s a pandemic going on and people are dying every day from coronavirus, people are still dying every day from cancer,” Richard Schilsky, MD, PhD, chief medical officer at ASCO, told Medscape Medical News.
“This pandemic will end, but cancer will continue, and we need to be able to continue to get the most cutting edge scientific results out there to our members and our constituents so they can act on those results on behalf of their patients,” he said.
The ASCO Virtual Scientific Program will take place over the weekend of May 30-31.
“We’re certainly hoping that we’re going to deliver a program that features all of the most important science that would have been presented in person in Chicago,” Schilsky commented in an interview.
Most of the presentations will be prerecorded and then streamed, which “we hope will mitigate any of the technical glitches that could come from trying to do a live broadcast of the meeting,” he said.
There will be 250 oral and 2500 poster presentations in 24 disease-based and specialty tracks.
The majority of the abstracts will be released online on May 13. The majority of the on-demand content will be released on May 29. Some of the abstracts will be highlighted at ASCO press briefings and released on those two dates.
But some of the material will be made available only on the weekend of the meeting. The opening session, plenaries featuring late-breaking abstracts, special highlights sessions, and other clinical science symposia will be broadcast on Saturday, May 30, and Sunday, May 31 (the schedule for the weekend program is available on the ASCO meeting website).
Among the plenary presentations are some clinical results that are likely to change practice immediately, Schilsky predicted. These include data to be presented in the following abstracts:
- Abstract LBA4 on the KEYNOTE-177 study comparing immunotherapy using pembrolizumab (Keytruda, Merck & Co) with chemotherapy in patients with metastatic colorectal cancer whose tumors show microsatellite instability or mismatch repair deficiency;
- Abstract LBA5 on the ADAURA study exploring osimertinib (Tagrisso, AstraZeneca) as adjuvant therapy after complete tumor reseaction in patients with early-stage non–small cell lung cancer whose tumors are EGFR mutation positive;
- Abstract LBA1 on the JAVELIN Bladder 100 study exploring maintenance avelumab (Bavencio, Merck and Pfizer) with best supportive care after platinum-based first-line chemotherapy in patients with advanced urothelial carcinoma.
However, some of the material that would have been part of the annual meeting, which includes mostly educational sessions and invited talks, has been moved to another event, the ASCO Educational Program, to be held in August 2020.
“So I suppose, in the grand scheme of things, the meeting is going to be compressed a little bit,” Schilsky commented. “Obviously, we can’t deliver all the interactions that happen in the hallways and everywhere else at the meeting that really gives so much energy to the meeting, but, at this moment in our history, probably getting the science out there is what’s most important.”
Virtual exhibition hall
There will also be a virtual exhibition hall, which will open on May 29.
“Just as there is a typical exhibit hall in the convention center,” Schilsky commented, most of the companies that were planning to be in Chicago have “now transitioned to creating a virtual booth that people who are participating in the virtual meeting can visit.
“I don’t know exactly how each company is going to use their time and their virtual space, and that’s part of the whole learning process here to see how this whole experiment is going to work out,” he added.
Unlike some of the other conferences that have gone virtual, in which access has been made available to everyone for free, registration is still required for the ASCO meeting. But the society notes that the registration fee has been discounted for nonmembers and has been waived for ASCO members. Also, the fee covers both the Virtual Scientific Program in May and the ASCO Educational Program in August.
Registrants will have access to video and slide presentations, as well as discussant commentaries, for 180 days.
The article first appeared on Medscape.com.
Vaccine maintenance improves relapse-free survival in BRCA wild-type ovarian cancer
The autologous tumor cell vaccine gemogenovatucel-T (Vigil Ovarian) is well tolerated as maintenance therapy in stage III-IV ovarian cancer patients and may improve relapse-free survival, particularly in BRCA wild-type disease, according to findings from the ongoing VITAL study.
In patients with and without BRCA1/2 mutations, the median relapse-free survival was longer with gemogenovatucel-T maintenance than with placebo, but the difference did not reach statistical significance (P = .065).
However, among patients with wild-type BRCA, the median relapse-free survival was significantly longer with gemogenovatucel-T (P = .0007).
Rodney P. Rocconi, MD, of the Mitchell Cancer Institute at University of South Alabama, Mobile, reported these results in an abstract that was slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancers. The meeting was canceled because of the COVID-19 pandemic. Some data have been updated from the abstract.
Study rationale
Gemogenovatucel-T (formerly called FANG) is an autologous tumor cell vaccine transfected with a plasmid encoding granulocyte-macrophage colony–stimulating factor and a novel bifunctional short hairpin interfering RNA targeting furin convertase.
“In the era of personalized, targeted medicine, I think this is about as personalized as you can get, this type of vaccine,” Dr. Rocconi said. “Essentially, we harvest patients’ own cancer cells and create a vaccine that is targeted to the antigens on their cells so that it recognizes only that patient’s cancer.”
The vaccine also helps recruit immune cells to the area and has a very limited off-target effect, Dr. Rocconi added.
He noted that gemogenovatucel-T previously demonstrated promising efficacy and limited side effects in a phase 1 study that included patients with advanced ovarian cancer (Mol Ther. 2012 Mar;20[3]:679-86).
“So we thought that, in ovarian cancer, as a maintenance therapy, it made a lot of sense,” Dr. Rocconi said, noting that the overall prognosis for advanced epithelial ovarian cancer remains limited.
Treatment and toxicity
Dr. Rocconi and colleagues reported data on 91 patients in the VITAL study. The patients had achieved a complete response after frontline surgery and chemotherapy, and they were randomized to maintenance with gemogenovatucel-T or placebo.
Patients had a median time from surgery to randomization of 208.5 days in the gemogenovatucel-T group and 200 days in the control group. The patients were treated with 1 x 107 cells/mL of gemogenovatucel-T or placebo intradermally once a month for up to 12 doses.
Gemogenovatucel-T was well tolerated. No added overall toxicity was noted in the gemogenovatucel-T group versus the control group, and no grade 4/5 toxicities were observed, Dr. Rocconi said. Grade 2/3 toxic events were observed in 8% of patients in the gemogenovatucel-T group, compared with 18% in the control group. The most common events were nausea and musculoskeletal pain in the gemogenovatucel-T group, and were bone pain and fatigue in the control group.
Relapse-free and overall survival
In the entire cohort, the median relapse-free survival was longer with gemogenovatucel-T maintenance – 12.6 months versus 8.4 months with placebo (hazard ratio, 0.69) – but the difference did not reach statistical significance (P = .065).
However, in the 67 patients with wild-type BRCA, the median relapse-free survival was 19.4 months with gemogenovatucel-T and 14.8 months with placebo, a statistically significant difference (HR, 0.459; P = .0007).
The median overall survival was not reached in the BRCA wild-type patients treated with gemogenovatucel-T, and it was 41.4 months from the time of randomization in those who received placebo (HR, 0.417; P = .02).
No benefit was seen with gemogenovatucel-T in patients with known BRCA1/2 mutations, Dr. Rocconi said.
‘Encouraging’ results
The overall improvement in the gemogenovatucel-T group was encouraging, particularly in a maintenance-type trial, Dr. Rocconi said. He noted that prior treatments for maintenance have received approval based on shorter survival gains, and the finding of particular benefit in BRCA wild-type disease could have important implications for a population that usually has lesser benefit from treatments, compared with patients who have BRCA mutations.
“So this result is very unique,” Dr. Rocconi said, explaining that about 85% of ovarian cancer patients have BRCA wild-type disease; with this treatment, patients with wild-type BRCA may achieve similar survival rates as those seen in BRCA-mutant disease.
“I think, in general, immunotherapy has been somewhat disappointing in ovarian cancer, so to have a targeted vaccine work in ovarian cancer, just broadly ... is pretty noteworthy,” he said. “We’re really excited, obviously, about the overall success we’ve seen for all patients, but most importantly in those with BRCA wild type. This is a pretty marked significance in recurrence-free intervals and overall survival, and we’re definitely pleased with that.”
Next steps
The findings from this trial have been submitted for publication, and efforts are underway to determine next steps through communication with the Food and Drug Administration, Dr. Rocconi said.
Additionally, other studies are underway to assess gemogenovatucel-T in patients who fall in “the middle ground” – that is, patients who have BRCA wild-type disease but have “some homologous recombination deficiency where the tumor itself might be BRCA deficient or have some other type of deficiency,” Dr. Rocconi explained.
“So we’re trying to tease out specifically what is going on across all the different variations of ovarian cancer patients, and also looking for potential biomarkers for predicting response,” he said. “What we would like to see is a companion test where we’re able to predict which patients can really respond and do best with this technology, and, that way, we know how to stratify patients most appropriately.”
The current trial was sponsored by Gradalis. Dr. Rocconi disclosed relationships with Gradalis, Genentech, Clovis, and Johnson & Johnson.
SOURCE: Rocconi RP et al. SGO 2020, Abstract LBA7.
The autologous tumor cell vaccine gemogenovatucel-T (Vigil Ovarian) is well tolerated as maintenance therapy in stage III-IV ovarian cancer patients and may improve relapse-free survival, particularly in BRCA wild-type disease, according to findings from the ongoing VITAL study.
In patients with and without BRCA1/2 mutations, the median relapse-free survival was longer with gemogenovatucel-T maintenance than with placebo, but the difference did not reach statistical significance (P = .065).
However, among patients with wild-type BRCA, the median relapse-free survival was significantly longer with gemogenovatucel-T (P = .0007).
Rodney P. Rocconi, MD, of the Mitchell Cancer Institute at University of South Alabama, Mobile, reported these results in an abstract that was slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancers. The meeting was canceled because of the COVID-19 pandemic. Some data have been updated from the abstract.
Study rationale
Gemogenovatucel-T (formerly called FANG) is an autologous tumor cell vaccine transfected with a plasmid encoding granulocyte-macrophage colony–stimulating factor and a novel bifunctional short hairpin interfering RNA targeting furin convertase.
“In the era of personalized, targeted medicine, I think this is about as personalized as you can get, this type of vaccine,” Dr. Rocconi said. “Essentially, we harvest patients’ own cancer cells and create a vaccine that is targeted to the antigens on their cells so that it recognizes only that patient’s cancer.”
The vaccine also helps recruit immune cells to the area and has a very limited off-target effect, Dr. Rocconi added.
He noted that gemogenovatucel-T previously demonstrated promising efficacy and limited side effects in a phase 1 study that included patients with advanced ovarian cancer (Mol Ther. 2012 Mar;20[3]:679-86).
“So we thought that, in ovarian cancer, as a maintenance therapy, it made a lot of sense,” Dr. Rocconi said, noting that the overall prognosis for advanced epithelial ovarian cancer remains limited.
Treatment and toxicity
Dr. Rocconi and colleagues reported data on 91 patients in the VITAL study. The patients had achieved a complete response after frontline surgery and chemotherapy, and they were randomized to maintenance with gemogenovatucel-T or placebo.
Patients had a median time from surgery to randomization of 208.5 days in the gemogenovatucel-T group and 200 days in the control group. The patients were treated with 1 x 107 cells/mL of gemogenovatucel-T or placebo intradermally once a month for up to 12 doses.
Gemogenovatucel-T was well tolerated. No added overall toxicity was noted in the gemogenovatucel-T group versus the control group, and no grade 4/5 toxicities were observed, Dr. Rocconi said. Grade 2/3 toxic events were observed in 8% of patients in the gemogenovatucel-T group, compared with 18% in the control group. The most common events were nausea and musculoskeletal pain in the gemogenovatucel-T group, and were bone pain and fatigue in the control group.
Relapse-free and overall survival
In the entire cohort, the median relapse-free survival was longer with gemogenovatucel-T maintenance – 12.6 months versus 8.4 months with placebo (hazard ratio, 0.69) – but the difference did not reach statistical significance (P = .065).
However, in the 67 patients with wild-type BRCA, the median relapse-free survival was 19.4 months with gemogenovatucel-T and 14.8 months with placebo, a statistically significant difference (HR, 0.459; P = .0007).
The median overall survival was not reached in the BRCA wild-type patients treated with gemogenovatucel-T, and it was 41.4 months from the time of randomization in those who received placebo (HR, 0.417; P = .02).
No benefit was seen with gemogenovatucel-T in patients with known BRCA1/2 mutations, Dr. Rocconi said.
‘Encouraging’ results
The overall improvement in the gemogenovatucel-T group was encouraging, particularly in a maintenance-type trial, Dr. Rocconi said. He noted that prior treatments for maintenance have received approval based on shorter survival gains, and the finding of particular benefit in BRCA wild-type disease could have important implications for a population that usually has lesser benefit from treatments, compared with patients who have BRCA mutations.
“So this result is very unique,” Dr. Rocconi said, explaining that about 85% of ovarian cancer patients have BRCA wild-type disease; with this treatment, patients with wild-type BRCA may achieve similar survival rates as those seen in BRCA-mutant disease.
“I think, in general, immunotherapy has been somewhat disappointing in ovarian cancer, so to have a targeted vaccine work in ovarian cancer, just broadly ... is pretty noteworthy,” he said. “We’re really excited, obviously, about the overall success we’ve seen for all patients, but most importantly in those with BRCA wild type. This is a pretty marked significance in recurrence-free intervals and overall survival, and we’re definitely pleased with that.”
Next steps
The findings from this trial have been submitted for publication, and efforts are underway to determine next steps through communication with the Food and Drug Administration, Dr. Rocconi said.
Additionally, other studies are underway to assess gemogenovatucel-T in patients who fall in “the middle ground” – that is, patients who have BRCA wild-type disease but have “some homologous recombination deficiency where the tumor itself might be BRCA deficient or have some other type of deficiency,” Dr. Rocconi explained.
“So we’re trying to tease out specifically what is going on across all the different variations of ovarian cancer patients, and also looking for potential biomarkers for predicting response,” he said. “What we would like to see is a companion test where we’re able to predict which patients can really respond and do best with this technology, and, that way, we know how to stratify patients most appropriately.”
The current trial was sponsored by Gradalis. Dr. Rocconi disclosed relationships with Gradalis, Genentech, Clovis, and Johnson & Johnson.
SOURCE: Rocconi RP et al. SGO 2020, Abstract LBA7.
The autologous tumor cell vaccine gemogenovatucel-T (Vigil Ovarian) is well tolerated as maintenance therapy in stage III-IV ovarian cancer patients and may improve relapse-free survival, particularly in BRCA wild-type disease, according to findings from the ongoing VITAL study.
In patients with and without BRCA1/2 mutations, the median relapse-free survival was longer with gemogenovatucel-T maintenance than with placebo, but the difference did not reach statistical significance (P = .065).
However, among patients with wild-type BRCA, the median relapse-free survival was significantly longer with gemogenovatucel-T (P = .0007).
Rodney P. Rocconi, MD, of the Mitchell Cancer Institute at University of South Alabama, Mobile, reported these results in an abstract that was slated for presentation at the Society of Gynecologic Oncology’s Annual Meeting on Women’s Cancers. The meeting was canceled because of the COVID-19 pandemic. Some data have been updated from the abstract.
Study rationale
Gemogenovatucel-T (formerly called FANG) is an autologous tumor cell vaccine transfected with a plasmid encoding granulocyte-macrophage colony–stimulating factor and a novel bifunctional short hairpin interfering RNA targeting furin convertase.
“In the era of personalized, targeted medicine, I think this is about as personalized as you can get, this type of vaccine,” Dr. Rocconi said. “Essentially, we harvest patients’ own cancer cells and create a vaccine that is targeted to the antigens on their cells so that it recognizes only that patient’s cancer.”
The vaccine also helps recruit immune cells to the area and has a very limited off-target effect, Dr. Rocconi added.
He noted that gemogenovatucel-T previously demonstrated promising efficacy and limited side effects in a phase 1 study that included patients with advanced ovarian cancer (Mol Ther. 2012 Mar;20[3]:679-86).
“So we thought that, in ovarian cancer, as a maintenance therapy, it made a lot of sense,” Dr. Rocconi said, noting that the overall prognosis for advanced epithelial ovarian cancer remains limited.
Treatment and toxicity
Dr. Rocconi and colleagues reported data on 91 patients in the VITAL study. The patients had achieved a complete response after frontline surgery and chemotherapy, and they were randomized to maintenance with gemogenovatucel-T or placebo.
Patients had a median time from surgery to randomization of 208.5 days in the gemogenovatucel-T group and 200 days in the control group. The patients were treated with 1 x 107 cells/mL of gemogenovatucel-T or placebo intradermally once a month for up to 12 doses.
Gemogenovatucel-T was well tolerated. No added overall toxicity was noted in the gemogenovatucel-T group versus the control group, and no grade 4/5 toxicities were observed, Dr. Rocconi said. Grade 2/3 toxic events were observed in 8% of patients in the gemogenovatucel-T group, compared with 18% in the control group. The most common events were nausea and musculoskeletal pain in the gemogenovatucel-T group, and were bone pain and fatigue in the control group.
Relapse-free and overall survival
In the entire cohort, the median relapse-free survival was longer with gemogenovatucel-T maintenance – 12.6 months versus 8.4 months with placebo (hazard ratio, 0.69) – but the difference did not reach statistical significance (P = .065).
However, in the 67 patients with wild-type BRCA, the median relapse-free survival was 19.4 months with gemogenovatucel-T and 14.8 months with placebo, a statistically significant difference (HR, 0.459; P = .0007).
The median overall survival was not reached in the BRCA wild-type patients treated with gemogenovatucel-T, and it was 41.4 months from the time of randomization in those who received placebo (HR, 0.417; P = .02).
No benefit was seen with gemogenovatucel-T in patients with known BRCA1/2 mutations, Dr. Rocconi said.
‘Encouraging’ results
The overall improvement in the gemogenovatucel-T group was encouraging, particularly in a maintenance-type trial, Dr. Rocconi said. He noted that prior treatments for maintenance have received approval based on shorter survival gains, and the finding of particular benefit in BRCA wild-type disease could have important implications for a population that usually has lesser benefit from treatments, compared with patients who have BRCA mutations.
“So this result is very unique,” Dr. Rocconi said, explaining that about 85% of ovarian cancer patients have BRCA wild-type disease; with this treatment, patients with wild-type BRCA may achieve similar survival rates as those seen in BRCA-mutant disease.
“I think, in general, immunotherapy has been somewhat disappointing in ovarian cancer, so to have a targeted vaccine work in ovarian cancer, just broadly ... is pretty noteworthy,” he said. “We’re really excited, obviously, about the overall success we’ve seen for all patients, but most importantly in those with BRCA wild type. This is a pretty marked significance in recurrence-free intervals and overall survival, and we’re definitely pleased with that.”
Next steps
The findings from this trial have been submitted for publication, and efforts are underway to determine next steps through communication with the Food and Drug Administration, Dr. Rocconi said.
Additionally, other studies are underway to assess gemogenovatucel-T in patients who fall in “the middle ground” – that is, patients who have BRCA wild-type disease but have “some homologous recombination deficiency where the tumor itself might be BRCA deficient or have some other type of deficiency,” Dr. Rocconi explained.
“So we’re trying to tease out specifically what is going on across all the different variations of ovarian cancer patients, and also looking for potential biomarkers for predicting response,” he said. “What we would like to see is a companion test where we’re able to predict which patients can really respond and do best with this technology, and, that way, we know how to stratify patients most appropriately.”
The current trial was sponsored by Gradalis. Dr. Rocconi disclosed relationships with Gradalis, Genentech, Clovis, and Johnson & Johnson.
SOURCE: Rocconi RP et al. SGO 2020, Abstract LBA7.
FROM SGO 2020
COVID-19 death rate was twice as high in cancer patients in NYC study
COVID-19 patients with cancer had double the fatality rate of COVID-19 patients without cancer treated in an urban New York hospital system, according to data from a retrospective study.
with COVID-19 treated during the same time period in the same hospital system.
Vikas Mehta, MD, of Montefiore Medical Center, New York, and colleagues reported these results in Cancer Discovery.
“As New York has emerged as the current epicenter of the pandemic, we sought to investigate the risk posed by COVID-19 to our cancer population,” the authors wrote.
They identified 218 cancer patients treated for COVID-19 in the Montefiore Health System between March 18 and April 8, 2020. Three-quarters of patients had solid tumors, and 25% had hematologic malignancies. Most patients were adults (98.6%), their median age was 69 years (range, 10-92 years), and 58% were men.
In all, 28% of the cancer patients (61/218) died from COVID-19, including 25% (41/164) of those with solid tumors and 37% (20/54) of those with hematologic malignancies.
Deaths by cancer type
Among the 164 patients with solid tumors, case fatality rates were as follows:
- Pancreatic – 67% (2/3)
- Lung – 55% (6/11)
- Colorectal – 38% (8/21)
- Upper gastrointestinal – 38% (3/8)
- Gynecologic – 38% (5/13)
- Skin – 33% (1/3)
- Hepatobiliary – 29% (2/7)
- Bone/soft tissue – 20% (1/5)
- Genitourinary – 15% (7/46)
- Breast – 14% (4/28)
- Neurologic – 13% (1/8)
- Head and neck – 13% (1/8).
None of the three patients with neuroendocrine tumors died.
Among the 54 patients with hematologic malignancies, case fatality rates were as follows:
- Chronic myeloid leukemia – 100% (1/1)
- Hodgkin lymphoma – 60% (3/5)
- Myelodysplastic syndromes – 60% (3/5)
- Multiple myeloma – 38% (5/13)
- Non-Hodgkin lymphoma – 33% (5/15)
- Chronic lymphocytic leukemia – 33% (1/3)
- Myeloproliferative neoplasms – 29% (2/7).
None of the four patients with acute lymphoblastic leukemia died, and there was one patient with acute myeloid leukemia who did not die.
Factors associated with increased mortality
The researchers compared the 218 cancer patients with COVID-19 with 1,090 age- and sex-matched noncancer patients with COVID-19 treated in the Montefiore Health System between March 18 and April 8, 2020.
Case fatality rates in cancer patients with COVID-19 were significantly increased in all age groups, but older age was associated with higher mortality.
“We observed case fatality rates were elevated in all age cohorts in cancer patients and achieved statistical significance in the age groups 45-64 and in patients older than 75 years of age,” the authors reported.
Other factors significantly associated with higher mortality in a multivariable analysis included the presence of multiple comorbidities; the need for ICU support; and increased levels of d-dimer, lactate, and lactate dehydrogenase.
Additional factors, such as socioeconomic and health disparities, may also be significant predictors of mortality, according to the authors. They noted that this cohort largely consisted of patients from a socioeconomically underprivileged community where mortality because of COVID-19 is reportedly higher.
Proactive strategies moving forward
“We have been addressing the significant burden of the COVID-19 pandemic on our vulnerable cancer patients through a variety of ways,” said study author Balazs Halmos, MD, of Montefiore Medical Center.
The center set up a separate infusion unit exclusively for COVID-positive patients and established separate inpatient areas. Dr. Halmos and colleagues are also providing telemedicine, virtual supportive care services, telephonic counseling, and bilingual peer-support programs.
“Many questions remain as we continue to establish new practices for our cancer patients,” Dr. Halmos said. “We will find answers to these questions as we continue to focus on adaptation and not acceptance in response to the COVID crisis. Our patients deserve nothing less.”
The Albert Einstein Cancer Center supported this study. The authors reported having no conflicts of interest.
SOURCE: Mehta V et al. Cancer Discov. 2020 May 1. doi: 10.1158/2159-8290.CD-20-0516.
COVID-19 patients with cancer had double the fatality rate of COVID-19 patients without cancer treated in an urban New York hospital system, according to data from a retrospective study.
with COVID-19 treated during the same time period in the same hospital system.
Vikas Mehta, MD, of Montefiore Medical Center, New York, and colleagues reported these results in Cancer Discovery.
“As New York has emerged as the current epicenter of the pandemic, we sought to investigate the risk posed by COVID-19 to our cancer population,” the authors wrote.
They identified 218 cancer patients treated for COVID-19 in the Montefiore Health System between March 18 and April 8, 2020. Three-quarters of patients had solid tumors, and 25% had hematologic malignancies. Most patients were adults (98.6%), their median age was 69 years (range, 10-92 years), and 58% were men.
In all, 28% of the cancer patients (61/218) died from COVID-19, including 25% (41/164) of those with solid tumors and 37% (20/54) of those with hematologic malignancies.
Deaths by cancer type
Among the 164 patients with solid tumors, case fatality rates were as follows:
- Pancreatic – 67% (2/3)
- Lung – 55% (6/11)
- Colorectal – 38% (8/21)
- Upper gastrointestinal – 38% (3/8)
- Gynecologic – 38% (5/13)
- Skin – 33% (1/3)
- Hepatobiliary – 29% (2/7)
- Bone/soft tissue – 20% (1/5)
- Genitourinary – 15% (7/46)
- Breast – 14% (4/28)
- Neurologic – 13% (1/8)
- Head and neck – 13% (1/8).
None of the three patients with neuroendocrine tumors died.
Among the 54 patients with hematologic malignancies, case fatality rates were as follows:
- Chronic myeloid leukemia – 100% (1/1)
- Hodgkin lymphoma – 60% (3/5)
- Myelodysplastic syndromes – 60% (3/5)
- Multiple myeloma – 38% (5/13)
- Non-Hodgkin lymphoma – 33% (5/15)
- Chronic lymphocytic leukemia – 33% (1/3)
- Myeloproliferative neoplasms – 29% (2/7).
None of the four patients with acute lymphoblastic leukemia died, and there was one patient with acute myeloid leukemia who did not die.
Factors associated with increased mortality
The researchers compared the 218 cancer patients with COVID-19 with 1,090 age- and sex-matched noncancer patients with COVID-19 treated in the Montefiore Health System between March 18 and April 8, 2020.
Case fatality rates in cancer patients with COVID-19 were significantly increased in all age groups, but older age was associated with higher mortality.
“We observed case fatality rates were elevated in all age cohorts in cancer patients and achieved statistical significance in the age groups 45-64 and in patients older than 75 years of age,” the authors reported.
Other factors significantly associated with higher mortality in a multivariable analysis included the presence of multiple comorbidities; the need for ICU support; and increased levels of d-dimer, lactate, and lactate dehydrogenase.
Additional factors, such as socioeconomic and health disparities, may also be significant predictors of mortality, according to the authors. They noted that this cohort largely consisted of patients from a socioeconomically underprivileged community where mortality because of COVID-19 is reportedly higher.
Proactive strategies moving forward
“We have been addressing the significant burden of the COVID-19 pandemic on our vulnerable cancer patients through a variety of ways,” said study author Balazs Halmos, MD, of Montefiore Medical Center.
The center set up a separate infusion unit exclusively for COVID-positive patients and established separate inpatient areas. Dr. Halmos and colleagues are also providing telemedicine, virtual supportive care services, telephonic counseling, and bilingual peer-support programs.
“Many questions remain as we continue to establish new practices for our cancer patients,” Dr. Halmos said. “We will find answers to these questions as we continue to focus on adaptation and not acceptance in response to the COVID crisis. Our patients deserve nothing less.”
The Albert Einstein Cancer Center supported this study. The authors reported having no conflicts of interest.
SOURCE: Mehta V et al. Cancer Discov. 2020 May 1. doi: 10.1158/2159-8290.CD-20-0516.
COVID-19 patients with cancer had double the fatality rate of COVID-19 patients without cancer treated in an urban New York hospital system, according to data from a retrospective study.
with COVID-19 treated during the same time period in the same hospital system.
Vikas Mehta, MD, of Montefiore Medical Center, New York, and colleagues reported these results in Cancer Discovery.
“As New York has emerged as the current epicenter of the pandemic, we sought to investigate the risk posed by COVID-19 to our cancer population,” the authors wrote.
They identified 218 cancer patients treated for COVID-19 in the Montefiore Health System between March 18 and April 8, 2020. Three-quarters of patients had solid tumors, and 25% had hematologic malignancies. Most patients were adults (98.6%), their median age was 69 years (range, 10-92 years), and 58% were men.
In all, 28% of the cancer patients (61/218) died from COVID-19, including 25% (41/164) of those with solid tumors and 37% (20/54) of those with hematologic malignancies.
Deaths by cancer type
Among the 164 patients with solid tumors, case fatality rates were as follows:
- Pancreatic – 67% (2/3)
- Lung – 55% (6/11)
- Colorectal – 38% (8/21)
- Upper gastrointestinal – 38% (3/8)
- Gynecologic – 38% (5/13)
- Skin – 33% (1/3)
- Hepatobiliary – 29% (2/7)
- Bone/soft tissue – 20% (1/5)
- Genitourinary – 15% (7/46)
- Breast – 14% (4/28)
- Neurologic – 13% (1/8)
- Head and neck – 13% (1/8).
None of the three patients with neuroendocrine tumors died.
Among the 54 patients with hematologic malignancies, case fatality rates were as follows:
- Chronic myeloid leukemia – 100% (1/1)
- Hodgkin lymphoma – 60% (3/5)
- Myelodysplastic syndromes – 60% (3/5)
- Multiple myeloma – 38% (5/13)
- Non-Hodgkin lymphoma – 33% (5/15)
- Chronic lymphocytic leukemia – 33% (1/3)
- Myeloproliferative neoplasms – 29% (2/7).
None of the four patients with acute lymphoblastic leukemia died, and there was one patient with acute myeloid leukemia who did not die.
Factors associated with increased mortality
The researchers compared the 218 cancer patients with COVID-19 with 1,090 age- and sex-matched noncancer patients with COVID-19 treated in the Montefiore Health System between March 18 and April 8, 2020.
Case fatality rates in cancer patients with COVID-19 were significantly increased in all age groups, but older age was associated with higher mortality.
“We observed case fatality rates were elevated in all age cohorts in cancer patients and achieved statistical significance in the age groups 45-64 and in patients older than 75 years of age,” the authors reported.
Other factors significantly associated with higher mortality in a multivariable analysis included the presence of multiple comorbidities; the need for ICU support; and increased levels of d-dimer, lactate, and lactate dehydrogenase.
Additional factors, such as socioeconomic and health disparities, may also be significant predictors of mortality, according to the authors. They noted that this cohort largely consisted of patients from a socioeconomically underprivileged community where mortality because of COVID-19 is reportedly higher.
Proactive strategies moving forward
“We have been addressing the significant burden of the COVID-19 pandemic on our vulnerable cancer patients through a variety of ways,” said study author Balazs Halmos, MD, of Montefiore Medical Center.
The center set up a separate infusion unit exclusively for COVID-positive patients and established separate inpatient areas. Dr. Halmos and colleagues are also providing telemedicine, virtual supportive care services, telephonic counseling, and bilingual peer-support programs.
“Many questions remain as we continue to establish new practices for our cancer patients,” Dr. Halmos said. “We will find answers to these questions as we continue to focus on adaptation and not acceptance in response to the COVID crisis. Our patients deserve nothing less.”
The Albert Einstein Cancer Center supported this study. The authors reported having no conflicts of interest.
SOURCE: Mehta V et al. Cancer Discov. 2020 May 1. doi: 10.1158/2159-8290.CD-20-0516.
FROM CANCER DISCOVERY
Three months of COVID-19 may mean 80,000 missed cancer diagnoses
, according to a report by the IQVIA Institute for Human Data Science looking at trends in the United States.
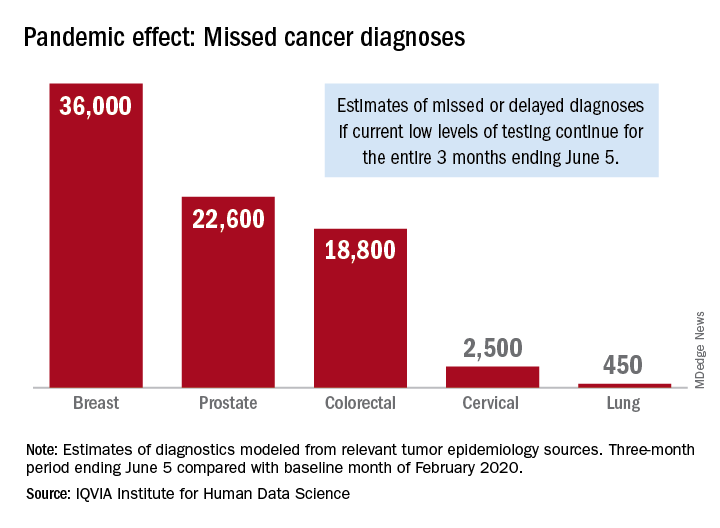
Screening and monitoring tests for breast, prostate, colorectal, cervical, and lung cancer were down 39%-90% in early April, compared with the baseline month of February, according to report authors Murray Aitken and Michael Kleinrock, both of IQVIA.
These findings are based on data from IQVIA’s medical claims database, which includes more than 205 million patients, over 1.7 billion claims, and 3 billion service records obtained annually.
The data suggest that, at current positivity rates, there could be 36,000 missed or delayed diagnoses of breast cancer during the 3-month period from early March through early June. Estimates for missed diagnoses of the four other cancers analyzed include 450 for lung cancer, 2,500 for cervical cancer, 18,800 for colorectal cancer, and 22,600 for prostate cancer.
The authors project a total of 22 million canceled or delayed tests for the five cancers over the 3-month period ending June 5, based on a comparison of claims data for early April with the February baseline. Catching up on this backlog will be problematic, according to the authors.
“Current excess health care capacity ... would require providers to shift priorities to make time and space in schedules and facilities as well as the cooperation of patients to return to health care providers,” the authors wrote. “Both of these could be further disrupted by economic factors or reintroduction of social distancing in a reemergence of the outbreak.”
The report was produced by the IQVIA Institute for Human Data Science without industry or government funding.
SOURCE: Murray A and Kleinrock M. Shifts in healthcare demand, delivery and care during the COVID-19 era. IQVIA Institute for Human Data Science. April 2020.
, according to a report by the IQVIA Institute for Human Data Science looking at trends in the United States.
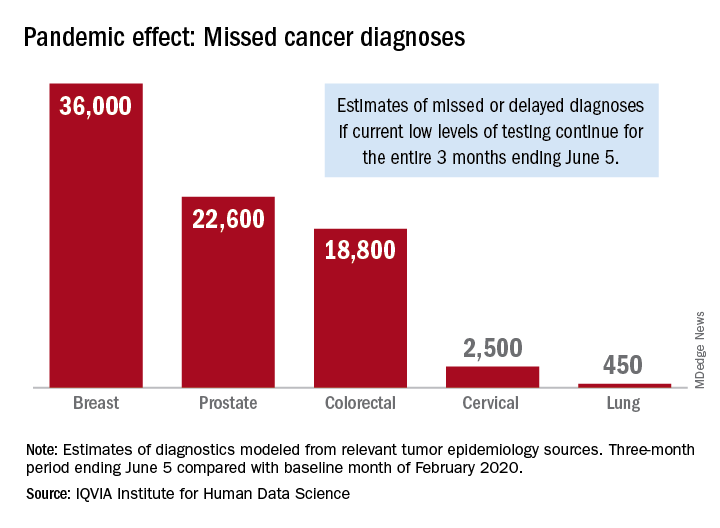
Screening and monitoring tests for breast, prostate, colorectal, cervical, and lung cancer were down 39%-90% in early April, compared with the baseline month of February, according to report authors Murray Aitken and Michael Kleinrock, both of IQVIA.
These findings are based on data from IQVIA’s medical claims database, which includes more than 205 million patients, over 1.7 billion claims, and 3 billion service records obtained annually.
The data suggest that, at current positivity rates, there could be 36,000 missed or delayed diagnoses of breast cancer during the 3-month period from early March through early June. Estimates for missed diagnoses of the four other cancers analyzed include 450 for lung cancer, 2,500 for cervical cancer, 18,800 for colorectal cancer, and 22,600 for prostate cancer.
The authors project a total of 22 million canceled or delayed tests for the five cancers over the 3-month period ending June 5, based on a comparison of claims data for early April with the February baseline. Catching up on this backlog will be problematic, according to the authors.
“Current excess health care capacity ... would require providers to shift priorities to make time and space in schedules and facilities as well as the cooperation of patients to return to health care providers,” the authors wrote. “Both of these could be further disrupted by economic factors or reintroduction of social distancing in a reemergence of the outbreak.”
The report was produced by the IQVIA Institute for Human Data Science without industry or government funding.
SOURCE: Murray A and Kleinrock M. Shifts in healthcare demand, delivery and care during the COVID-19 era. IQVIA Institute for Human Data Science. April 2020.
, according to a report by the IQVIA Institute for Human Data Science looking at trends in the United States.
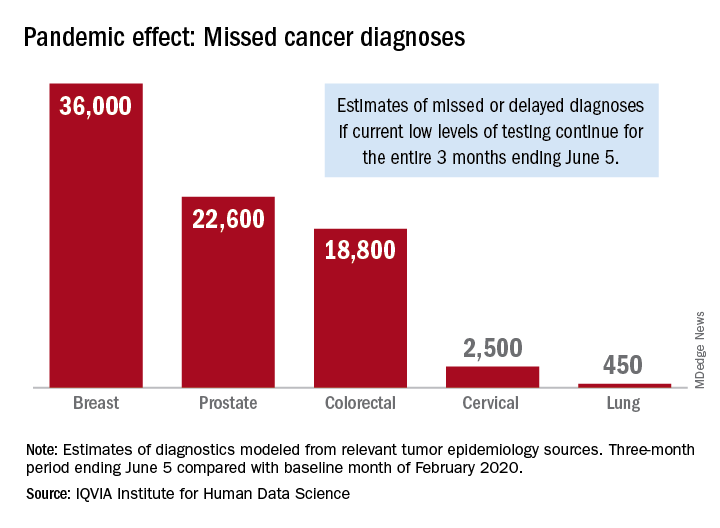
Screening and monitoring tests for breast, prostate, colorectal, cervical, and lung cancer were down 39%-90% in early April, compared with the baseline month of February, according to report authors Murray Aitken and Michael Kleinrock, both of IQVIA.
These findings are based on data from IQVIA’s medical claims database, which includes more than 205 million patients, over 1.7 billion claims, and 3 billion service records obtained annually.
The data suggest that, at current positivity rates, there could be 36,000 missed or delayed diagnoses of breast cancer during the 3-month period from early March through early June. Estimates for missed diagnoses of the four other cancers analyzed include 450 for lung cancer, 2,500 for cervical cancer, 18,800 for colorectal cancer, and 22,600 for prostate cancer.
The authors project a total of 22 million canceled or delayed tests for the five cancers over the 3-month period ending June 5, based on a comparison of claims data for early April with the February baseline. Catching up on this backlog will be problematic, according to the authors.
“Current excess health care capacity ... would require providers to shift priorities to make time and space in schedules and facilities as well as the cooperation of patients to return to health care providers,” the authors wrote. “Both of these could be further disrupted by economic factors or reintroduction of social distancing in a reemergence of the outbreak.”
The report was produced by the IQVIA Institute for Human Data Science without industry or government funding.
SOURCE: Murray A and Kleinrock M. Shifts in healthcare demand, delivery and care during the COVID-19 era. IQVIA Institute for Human Data Science. April 2020.
Cancer screening, monitoring down during pandemic
according to a report by the IQVIA Institute for Human Data Science.
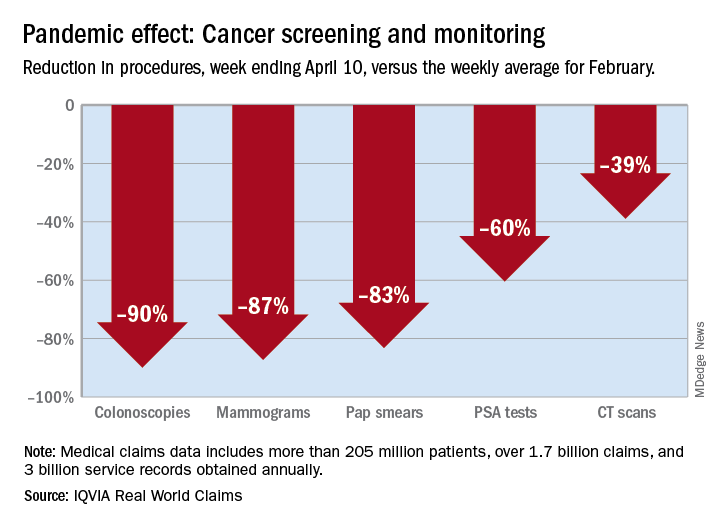
There were 90% fewer colonoscopies ordered during the week ending April 10, compared with the weekly average for Feb. 1-28, based on claims data analyzed by IQVIA.
IQVIA’s medical claims database includes more than 205 million patients, over 1.7 billion claims, and 3 billion service records obtained annually.
The data also showed an 87% reduction in mammograms and an 83% reduction in Pap smears during the week ending April 10. Prostate-specific antigen tests for prostate cancer decreased by 60%, and CT scans for lung cancer decreased by 39%.
The smaller decrease in CT scans for lung cancer “may reflect the generally more serious nature of those tumors or be due to concerns about ruling out COVID-related issues in some patients,” according to report authors Murray Aitken and Michael Kleinrock, both of IQVIA.
The report also showed that overall patient interactions with oncologists were down by 20% through April 3, based on medical and pharmacy claims processed since February, but there was variation by tumor type.
The authors noted “little or no disruption” in oncologist visits in March for patients with aggressive tumors or those diagnosed at advanced stages, compared with February. However, for patients with skin cancer or prostate cancer, visit rates were down by 20%-50% in March.
“This may reflect that oncologists who are providing care across multiple tumor types are prioritizing their time and efforts to those patients with more advanced or aggressive tumors,” the authors wrote.
This report was produced by the IQVIA Institute for Human Data Science without industry or government funding.
SOURCE: Murray A and Kleinrock M. Shifts in healthcare demand, delivery and care during the COVID-19 era. IQVIA Institute for Human Data Science. April 2020.
according to a report by the IQVIA Institute for Human Data Science.
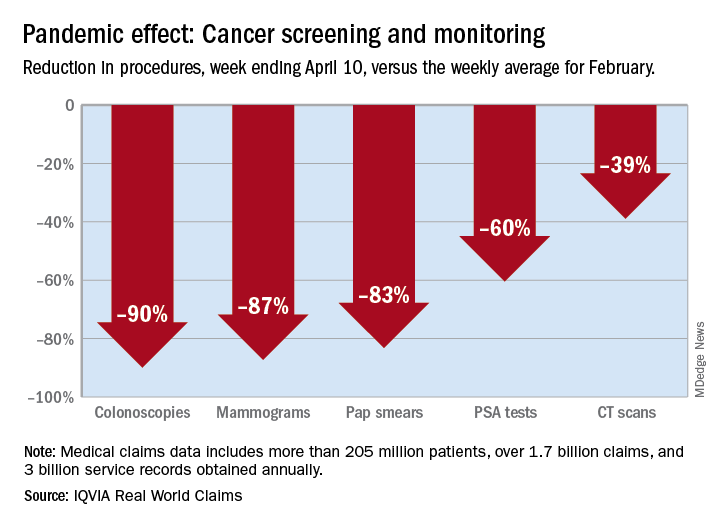
There were 90% fewer colonoscopies ordered during the week ending April 10, compared with the weekly average for Feb. 1-28, based on claims data analyzed by IQVIA.
IQVIA’s medical claims database includes more than 205 million patients, over 1.7 billion claims, and 3 billion service records obtained annually.
The data also showed an 87% reduction in mammograms and an 83% reduction in Pap smears during the week ending April 10. Prostate-specific antigen tests for prostate cancer decreased by 60%, and CT scans for lung cancer decreased by 39%.
The smaller decrease in CT scans for lung cancer “may reflect the generally more serious nature of those tumors or be due to concerns about ruling out COVID-related issues in some patients,” according to report authors Murray Aitken and Michael Kleinrock, both of IQVIA.
The report also showed that overall patient interactions with oncologists were down by 20% through April 3, based on medical and pharmacy claims processed since February, but there was variation by tumor type.
The authors noted “little or no disruption” in oncologist visits in March for patients with aggressive tumors or those diagnosed at advanced stages, compared with February. However, for patients with skin cancer or prostate cancer, visit rates were down by 20%-50% in March.
“This may reflect that oncologists who are providing care across multiple tumor types are prioritizing their time and efforts to those patients with more advanced or aggressive tumors,” the authors wrote.
This report was produced by the IQVIA Institute for Human Data Science without industry or government funding.
SOURCE: Murray A and Kleinrock M. Shifts in healthcare demand, delivery and care during the COVID-19 era. IQVIA Institute for Human Data Science. April 2020.
according to a report by the IQVIA Institute for Human Data Science.
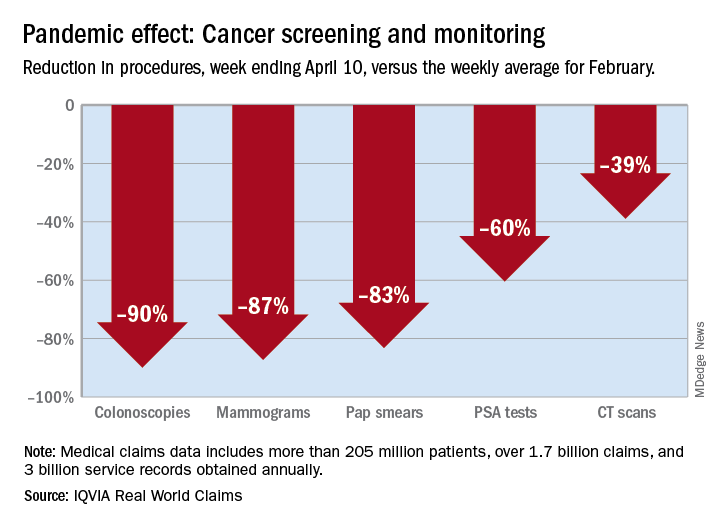
There were 90% fewer colonoscopies ordered during the week ending April 10, compared with the weekly average for Feb. 1-28, based on claims data analyzed by IQVIA.
IQVIA’s medical claims database includes more than 205 million patients, over 1.7 billion claims, and 3 billion service records obtained annually.
The data also showed an 87% reduction in mammograms and an 83% reduction in Pap smears during the week ending April 10. Prostate-specific antigen tests for prostate cancer decreased by 60%, and CT scans for lung cancer decreased by 39%.
The smaller decrease in CT scans for lung cancer “may reflect the generally more serious nature of those tumors or be due to concerns about ruling out COVID-related issues in some patients,” according to report authors Murray Aitken and Michael Kleinrock, both of IQVIA.
The report also showed that overall patient interactions with oncologists were down by 20% through April 3, based on medical and pharmacy claims processed since February, but there was variation by tumor type.
The authors noted “little or no disruption” in oncologist visits in March for patients with aggressive tumors or those diagnosed at advanced stages, compared with February. However, for patients with skin cancer or prostate cancer, visit rates were down by 20%-50% in March.
“This may reflect that oncologists who are providing care across multiple tumor types are prioritizing their time and efforts to those patients with more advanced or aggressive tumors,” the authors wrote.
This report was produced by the IQVIA Institute for Human Data Science without industry or government funding.
SOURCE: Murray A and Kleinrock M. Shifts in healthcare demand, delivery and care during the COVID-19 era. IQVIA Institute for Human Data Science. April 2020.
Adding a blood test to standard screening may improve early cancer detection
A minimally invasive multicancer blood test used with standard-of-care screening is safe, effective, and feasible for use in routine clinical care, according to interim findings from a large, prospective study.
The DETECT-A blood test, an early version of the CancerSEEK test currently in development, effectively guided patient management in real time, in some cases leading to diagnosis of early cancer and potentially curative surgery in asymptomatic women with no history of cancer.
Nickolas Papadopoulos, PhD, of Johns Hopkins Medicine in Baltimore, reported these findings at the AACR virtual meeting I. The findings were simultaneously published in Science.
The study enrolled 10,006 women, aged 65-75 years, with no prior cancer diagnosis. After exclusion and loss to follow-up, 9,911 women remained.
There were 26 patients who had cancer detected by the DETECT-A blood test, 15 of whom underwent follow-up PET-CT imaging and 9 of whom underwent surgical excision. An additional 24 cancers were detected by standard screening, and 46 were detected by other means.
The positive predictive value of the blood test was 19%. When the blood test was combined with imaging, the positive predictive value was 41%.
Improving upon standard screening
“Standard-of-care screening [was used] for three different organs: breast, lung, and colon. It was more sensitive for breast cancer,” Dr. Papadopoulos noted. “Blood testing, though, identified cancer in 10 different organs.”
In fact, the DETECT-A blood test detected 14 of 45 cancers in 7 organs for which no standard screening test is available.
In addition, 12 cancers in 3 organs (breast, lung, and colon) were first detected by DETECT-A rather than by standard screening. This increased the sensitivity of cancer detection from 47% with standard screening alone to 71% with standard screening plus blood testing.
“More important, 65% [of the cancers detected by blood test] were localized or regional, which have higher chance of successful treatment with intent to cure,” Dr. Papadopoulos said.
DETECT-A covers regions of 16 commonly mutated genes and 9 proteins known to be associated with cancer. In this study, 57% of cancers were detected by mutations.
Safety and additional screening
DETECT-A also proved safe, “without incurring a large number of futile invasive follow-up tests,” Dr. Papadopoulos said.
In fact, only 1% of patients without cancer underwent PET-CT imaging, and only 0.22% underwent a “futile” invasive follow-up procedure.
Three surgeries occurred in patients who were counted as false-positives, but the surgeries were determined to be indicated, Dr. Papadopoulos said. He explained that one was for large colonic polyps with high-grade dysplasia that could not be removed endoscopically, one was for an in situ carcinoma of the appendix, and one was for a 10-cm ovarian lesion that was found to be a mucinous cystadenoma.
The investigators also analyzed whether the availability of a “liquid biopsy” test like DETECT-A would inadvertently reduce patients’ use of standard screening and found that it did not. Mammography screening habits after receiving the baseline DETECT-A blood test did not differ significantly from those prior to study enrollment.
These findings are important because early detection is a key factor in reducing cancer-specific morbidity and mortality, and although minimally invasive screening tests, including liquid biopsies like DETECT-A, hold great promise, prospective clinical studies of these new methods are needed to ensure that the anticipated benefits outweigh the potential risks, Dr. Papadopoulos explained.
“The problem is that most cancers are detected at advanced stages when they are difficult to treat,” he said. “The earlier cancer is detected, the greater the chance of successful treatment.”
Unanswered questions and future studies
This study demonstrates that it is feasible for a minimally invasive blood test to safely detect multiple cancer types in patients without a history of cancer and to enable treatment with curative intent, at least in a subset of individuals, Dr. Papadopoulos said. He added that the findings also inform the design of future randomized trials “to establish clinical utility, cost-effectiveness, and benefit-to-risk ratio of future tests.”
Further studies will also be required to determine the clinical validity and utility of the strategy of using liquid biopsy as a complement to standard-of-care screening, Dr. Papadopoulos said.
Invited discussant David G. Huntsman, MD, of the University of British Columbia in Vancouver, applauded the investigators, saying this study serves to “move the field forward.” However, it still isn’t clear how sensitivity and negative predictive value will be determined and what the optimal testing schedule is.
“This is a prospective study that will provide the data on how this assay will be used [and] whether it should be used going forward,” Dr. Huntsman said, noting that the “much bigger and more important question” is whether it improves survival.
Cost-effectiveness will also be critical, he said.
This research was supported by The Marcus Foundation, Lustgarten Foundation for Pancreatic Cancer Research, The Virginia and D.K. Ludwig Fund for Cancer Research, The Sol Goldman Center for Pancreatic Cancer Research, Susan Wojcicki and Dennis Troper, the Rolfe Foundation, The Conrad R. Hilton Foundation, The John Templeton Foundation, Burroughs Wellcome Career Award For Medical Scientists, and grants/contracts from the National Institutes of Health.
Dr. Papadopoulos disclosed relationships with Thrive Earlier Detection Inc., PGDx Inc., NeoPhore, Cage Pharma, and other companies. Dr. Huntsman is a founder, shareholder, and chief medical officer for Contextual Genomics.
SOURCE: Papadopoulos N et al. AACR 2020, Abstract CT022; Lennon AM et al. Science. 2020 Apr 28. pii: eabb9601. doi: 10.1126/science.abb9601.
A minimally invasive multicancer blood test used with standard-of-care screening is safe, effective, and feasible for use in routine clinical care, according to interim findings from a large, prospective study.
The DETECT-A blood test, an early version of the CancerSEEK test currently in development, effectively guided patient management in real time, in some cases leading to diagnosis of early cancer and potentially curative surgery in asymptomatic women with no history of cancer.
Nickolas Papadopoulos, PhD, of Johns Hopkins Medicine in Baltimore, reported these findings at the AACR virtual meeting I. The findings were simultaneously published in Science.
The study enrolled 10,006 women, aged 65-75 years, with no prior cancer diagnosis. After exclusion and loss to follow-up, 9,911 women remained.
There were 26 patients who had cancer detected by the DETECT-A blood test, 15 of whom underwent follow-up PET-CT imaging and 9 of whom underwent surgical excision. An additional 24 cancers were detected by standard screening, and 46 were detected by other means.
The positive predictive value of the blood test was 19%. When the blood test was combined with imaging, the positive predictive value was 41%.
Improving upon standard screening
“Standard-of-care screening [was used] for three different organs: breast, lung, and colon. It was more sensitive for breast cancer,” Dr. Papadopoulos noted. “Blood testing, though, identified cancer in 10 different organs.”
In fact, the DETECT-A blood test detected 14 of 45 cancers in 7 organs for which no standard screening test is available.
In addition, 12 cancers in 3 organs (breast, lung, and colon) were first detected by DETECT-A rather than by standard screening. This increased the sensitivity of cancer detection from 47% with standard screening alone to 71% with standard screening plus blood testing.
“More important, 65% [of the cancers detected by blood test] were localized or regional, which have higher chance of successful treatment with intent to cure,” Dr. Papadopoulos said.
DETECT-A covers regions of 16 commonly mutated genes and 9 proteins known to be associated with cancer. In this study, 57% of cancers were detected by mutations.
Safety and additional screening
DETECT-A also proved safe, “without incurring a large number of futile invasive follow-up tests,” Dr. Papadopoulos said.
In fact, only 1% of patients without cancer underwent PET-CT imaging, and only 0.22% underwent a “futile” invasive follow-up procedure.
Three surgeries occurred in patients who were counted as false-positives, but the surgeries were determined to be indicated, Dr. Papadopoulos said. He explained that one was for large colonic polyps with high-grade dysplasia that could not be removed endoscopically, one was for an in situ carcinoma of the appendix, and one was for a 10-cm ovarian lesion that was found to be a mucinous cystadenoma.
The investigators also analyzed whether the availability of a “liquid biopsy” test like DETECT-A would inadvertently reduce patients’ use of standard screening and found that it did not. Mammography screening habits after receiving the baseline DETECT-A blood test did not differ significantly from those prior to study enrollment.
These findings are important because early detection is a key factor in reducing cancer-specific morbidity and mortality, and although minimally invasive screening tests, including liquid biopsies like DETECT-A, hold great promise, prospective clinical studies of these new methods are needed to ensure that the anticipated benefits outweigh the potential risks, Dr. Papadopoulos explained.
“The problem is that most cancers are detected at advanced stages when they are difficult to treat,” he said. “The earlier cancer is detected, the greater the chance of successful treatment.”
Unanswered questions and future studies
This study demonstrates that it is feasible for a minimally invasive blood test to safely detect multiple cancer types in patients without a history of cancer and to enable treatment with curative intent, at least in a subset of individuals, Dr. Papadopoulos said. He added that the findings also inform the design of future randomized trials “to establish clinical utility, cost-effectiveness, and benefit-to-risk ratio of future tests.”
Further studies will also be required to determine the clinical validity and utility of the strategy of using liquid biopsy as a complement to standard-of-care screening, Dr. Papadopoulos said.
Invited discussant David G. Huntsman, MD, of the University of British Columbia in Vancouver, applauded the investigators, saying this study serves to “move the field forward.” However, it still isn’t clear how sensitivity and negative predictive value will be determined and what the optimal testing schedule is.
“This is a prospective study that will provide the data on how this assay will be used [and] whether it should be used going forward,” Dr. Huntsman said, noting that the “much bigger and more important question” is whether it improves survival.
Cost-effectiveness will also be critical, he said.
This research was supported by The Marcus Foundation, Lustgarten Foundation for Pancreatic Cancer Research, The Virginia and D.K. Ludwig Fund for Cancer Research, The Sol Goldman Center for Pancreatic Cancer Research, Susan Wojcicki and Dennis Troper, the Rolfe Foundation, The Conrad R. Hilton Foundation, The John Templeton Foundation, Burroughs Wellcome Career Award For Medical Scientists, and grants/contracts from the National Institutes of Health.
Dr. Papadopoulos disclosed relationships with Thrive Earlier Detection Inc., PGDx Inc., NeoPhore, Cage Pharma, and other companies. Dr. Huntsman is a founder, shareholder, and chief medical officer for Contextual Genomics.
SOURCE: Papadopoulos N et al. AACR 2020, Abstract CT022; Lennon AM et al. Science. 2020 Apr 28. pii: eabb9601. doi: 10.1126/science.abb9601.
A minimally invasive multicancer blood test used with standard-of-care screening is safe, effective, and feasible for use in routine clinical care, according to interim findings from a large, prospective study.
The DETECT-A blood test, an early version of the CancerSEEK test currently in development, effectively guided patient management in real time, in some cases leading to diagnosis of early cancer and potentially curative surgery in asymptomatic women with no history of cancer.
Nickolas Papadopoulos, PhD, of Johns Hopkins Medicine in Baltimore, reported these findings at the AACR virtual meeting I. The findings were simultaneously published in Science.
The study enrolled 10,006 women, aged 65-75 years, with no prior cancer diagnosis. After exclusion and loss to follow-up, 9,911 women remained.
There were 26 patients who had cancer detected by the DETECT-A blood test, 15 of whom underwent follow-up PET-CT imaging and 9 of whom underwent surgical excision. An additional 24 cancers were detected by standard screening, and 46 were detected by other means.
The positive predictive value of the blood test was 19%. When the blood test was combined with imaging, the positive predictive value was 41%.
Improving upon standard screening
“Standard-of-care screening [was used] for three different organs: breast, lung, and colon. It was more sensitive for breast cancer,” Dr. Papadopoulos noted. “Blood testing, though, identified cancer in 10 different organs.”
In fact, the DETECT-A blood test detected 14 of 45 cancers in 7 organs for which no standard screening test is available.
In addition, 12 cancers in 3 organs (breast, lung, and colon) were first detected by DETECT-A rather than by standard screening. This increased the sensitivity of cancer detection from 47% with standard screening alone to 71% with standard screening plus blood testing.
“More important, 65% [of the cancers detected by blood test] were localized or regional, which have higher chance of successful treatment with intent to cure,” Dr. Papadopoulos said.
DETECT-A covers regions of 16 commonly mutated genes and 9 proteins known to be associated with cancer. In this study, 57% of cancers were detected by mutations.
Safety and additional screening
DETECT-A also proved safe, “without incurring a large number of futile invasive follow-up tests,” Dr. Papadopoulos said.
In fact, only 1% of patients without cancer underwent PET-CT imaging, and only 0.22% underwent a “futile” invasive follow-up procedure.
Three surgeries occurred in patients who were counted as false-positives, but the surgeries were determined to be indicated, Dr. Papadopoulos said. He explained that one was for large colonic polyps with high-grade dysplasia that could not be removed endoscopically, one was for an in situ carcinoma of the appendix, and one was for a 10-cm ovarian lesion that was found to be a mucinous cystadenoma.
The investigators also analyzed whether the availability of a “liquid biopsy” test like DETECT-A would inadvertently reduce patients’ use of standard screening and found that it did not. Mammography screening habits after receiving the baseline DETECT-A blood test did not differ significantly from those prior to study enrollment.
These findings are important because early detection is a key factor in reducing cancer-specific morbidity and mortality, and although minimally invasive screening tests, including liquid biopsies like DETECT-A, hold great promise, prospective clinical studies of these new methods are needed to ensure that the anticipated benefits outweigh the potential risks, Dr. Papadopoulos explained.
“The problem is that most cancers are detected at advanced stages when they are difficult to treat,” he said. “The earlier cancer is detected, the greater the chance of successful treatment.”
Unanswered questions and future studies
This study demonstrates that it is feasible for a minimally invasive blood test to safely detect multiple cancer types in patients without a history of cancer and to enable treatment with curative intent, at least in a subset of individuals, Dr. Papadopoulos said. He added that the findings also inform the design of future randomized trials “to establish clinical utility, cost-effectiveness, and benefit-to-risk ratio of future tests.”
Further studies will also be required to determine the clinical validity and utility of the strategy of using liquid biopsy as a complement to standard-of-care screening, Dr. Papadopoulos said.
Invited discussant David G. Huntsman, MD, of the University of British Columbia in Vancouver, applauded the investigators, saying this study serves to “move the field forward.” However, it still isn’t clear how sensitivity and negative predictive value will be determined and what the optimal testing schedule is.
“This is a prospective study that will provide the data on how this assay will be used [and] whether it should be used going forward,” Dr. Huntsman said, noting that the “much bigger and more important question” is whether it improves survival.
Cost-effectiveness will also be critical, he said.
This research was supported by The Marcus Foundation, Lustgarten Foundation for Pancreatic Cancer Research, The Virginia and D.K. Ludwig Fund for Cancer Research, The Sol Goldman Center for Pancreatic Cancer Research, Susan Wojcicki and Dennis Troper, the Rolfe Foundation, The Conrad R. Hilton Foundation, The John Templeton Foundation, Burroughs Wellcome Career Award For Medical Scientists, and grants/contracts from the National Institutes of Health.
Dr. Papadopoulos disclosed relationships with Thrive Earlier Detection Inc., PGDx Inc., NeoPhore, Cage Pharma, and other companies. Dr. Huntsman is a founder, shareholder, and chief medical officer for Contextual Genomics.
SOURCE: Papadopoulos N et al. AACR 2020, Abstract CT022; Lennon AM et al. Science. 2020 Apr 28. pii: eabb9601. doi: 10.1126/science.abb9601.
FROM AACR 2020
Excess cancer deaths predicted as care is disrupted by COVID-19
The majority of patients who have cancer or are suspected of having cancer are not accessing healthcare services in the United Kingdom or the United States because of the COVID-19 pandemic, the first report of its kind estimates.
As a result, there will be an excess of deaths among patients who have cancer and multiple comorbidities in both countries during the current coronavirus emergency, the report warns.
The authors calculate that there will be 6,270 excess deaths among cancer patients 1 year from now in England and 33,890 excess deaths among cancer patients in the United States. (In the United States, the estimated excess number of deaths applies only to patients older than 40 years, they note.)
“The recorded underlying cause of these excess deaths may be cancer, COVID-19, or comorbidity (such as myocardial infarction),” Alvina Lai, PhD, University College London, United Kingdom, and colleagues observe.
“Our data have highlighted how cancer patients with multimorbidity are a particularly at-risk group during the current pandemic,” they emphasize.
The study was published on ResearchGate as a preprint and has not undergone peer review.
Commenting on the study on the UK Science Media Center, several experts emphasized the lack of peer review, noting that interpretation of these data needs to be further refined on the basis of that input. One expert suggested that there are “substantial uncertainties that this paper does not adequately communicate.” But others argued that this topic was important enough to warrant early release of the data.
Chris Bunce, PhD, University of Birmingham, United Kingdom, said this study represents “a highly valuable contribution.”
“It is universally accepted that early diagnosis and treatment and adherence to treatment regimens saves lives,” he pointed out.
“Therefore, these COVID-19-related impacts will cost lives,” Bunce said.
“And if this information is to influence cancer care and guide policy during the COVID-19 crisis, then it is important that the findings are disseminated and discussed immediately, warranting their release ahead of peer view,” he added.
In a Medscape UK commentary, oncologist Karol Sikora, MD, PhD, argues that “restarting cancer services can’t come soon enough.”
“Resonably Argued Numerical Estimate”
“It’s well known that there have been considerable changes in the provision of health care for many conditions, including cancers, as a result of all the measures to deal with the COVID-19 crisis,” said Kevin McConway, PhD, professor emeritus of applied statistics, the Open University, Milton Keynes, United Kingdom.
“It seems inevitable that there will be increased deaths in cancer patients if they are infected with the virus or because of changes in the health services available to them, and quite possibly also from socio-economic effects of the responses to the crisis,” he continued.
“This study is the first that I have seen that produces a reasonably argued numerical estimate of the number of excess deaths of people with cancer arising from these factors in the UK and the USA,” he added.
Declines in Urgent Referrals and Chemo Attendance
For the study, the team used DATA-CAN, the UK National Health Data Research Hub for Cancer, to assess weekly returns for urgent cancer referrals for early diagnosis and also chemotherapy attendances for hospitals in Leeds, London, and Northern Ireland going back to 2018.
The data revealed that there have been major declines in chemotherapy attendances. There has been, on average, a 60% decrease from prepandemic levels in eight hospitals in the three regions that were assessed.
Urgent cancer referrals have dropped by an average of 76% compared to prepandemic levels in the three regions.
On the conservative assumption that the COVID-19 pandemic will only affect patients with newly diagnosed cancer (incident cases), the researchers estimate that the proportion of the population affected by the emergency (PAE) is 40% and that the relative impact of the emergency (RIE) is 1.5.
PAE is a summary measure of exposure to the adverse health consequences of the emergency; RIE is a summary measure of the combined impact on mortality of infection, health service change, physical distancing, and economic downturn, the authors explain.
Comorbidities Common
“Comorbidities were common in people with cancer,” the study authors note. For example, more than one quarter of the study population had at least one comorbidity; more than 14% had two.
For incident cancers, the number of excess deaths steadily increased in conjunction with an increase in the number of comorbidities, such that more than 80% of deaths occurred in patients with one or more comorbidities.
“When considering both prevalent and incident cancers together with a COVID-19 PAE of 40%, we estimated 17,991 excess deaths at a RIE of 1.5; 78.1% of these deaths occur in patients with ≥1 comorbidities,” the authors report.
“The excess risk of death in people living with cancer during the COVID-19 emergency may be due not only to COVID-19 infection, but also to the unintended health consequences of changes in health service provision, the physical or psychological effects of social distancing, and economic upheaval,” they state.
“This is the first study demonstrating profound recent changes in cancer care delivery in multiple centers,” the authors observe.
Lai has disclosed no relevant financial relationships. Several coauthors have various relationships with industry, as listed in their article. The commentators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The majority of patients who have cancer or are suspected of having cancer are not accessing healthcare services in the United Kingdom or the United States because of the COVID-19 pandemic, the first report of its kind estimates.
As a result, there will be an excess of deaths among patients who have cancer and multiple comorbidities in both countries during the current coronavirus emergency, the report warns.
The authors calculate that there will be 6,270 excess deaths among cancer patients 1 year from now in England and 33,890 excess deaths among cancer patients in the United States. (In the United States, the estimated excess number of deaths applies only to patients older than 40 years, they note.)
“The recorded underlying cause of these excess deaths may be cancer, COVID-19, or comorbidity (such as myocardial infarction),” Alvina Lai, PhD, University College London, United Kingdom, and colleagues observe.
“Our data have highlighted how cancer patients with multimorbidity are a particularly at-risk group during the current pandemic,” they emphasize.
The study was published on ResearchGate as a preprint and has not undergone peer review.
Commenting on the study on the UK Science Media Center, several experts emphasized the lack of peer review, noting that interpretation of these data needs to be further refined on the basis of that input. One expert suggested that there are “substantial uncertainties that this paper does not adequately communicate.” But others argued that this topic was important enough to warrant early release of the data.
Chris Bunce, PhD, University of Birmingham, United Kingdom, said this study represents “a highly valuable contribution.”
“It is universally accepted that early diagnosis and treatment and adherence to treatment regimens saves lives,” he pointed out.
“Therefore, these COVID-19-related impacts will cost lives,” Bunce said.
“And if this information is to influence cancer care and guide policy during the COVID-19 crisis, then it is important that the findings are disseminated and discussed immediately, warranting their release ahead of peer view,” he added.
In a Medscape UK commentary, oncologist Karol Sikora, MD, PhD, argues that “restarting cancer services can’t come soon enough.”
“Resonably Argued Numerical Estimate”
“It’s well known that there have been considerable changes in the provision of health care for many conditions, including cancers, as a result of all the measures to deal with the COVID-19 crisis,” said Kevin McConway, PhD, professor emeritus of applied statistics, the Open University, Milton Keynes, United Kingdom.
“It seems inevitable that there will be increased deaths in cancer patients if they are infected with the virus or because of changes in the health services available to them, and quite possibly also from socio-economic effects of the responses to the crisis,” he continued.
“This study is the first that I have seen that produces a reasonably argued numerical estimate of the number of excess deaths of people with cancer arising from these factors in the UK and the USA,” he added.
Declines in Urgent Referrals and Chemo Attendance
For the study, the team used DATA-CAN, the UK National Health Data Research Hub for Cancer, to assess weekly returns for urgent cancer referrals for early diagnosis and also chemotherapy attendances for hospitals in Leeds, London, and Northern Ireland going back to 2018.
The data revealed that there have been major declines in chemotherapy attendances. There has been, on average, a 60% decrease from prepandemic levels in eight hospitals in the three regions that were assessed.
Urgent cancer referrals have dropped by an average of 76% compared to prepandemic levels in the three regions.
On the conservative assumption that the COVID-19 pandemic will only affect patients with newly diagnosed cancer (incident cases), the researchers estimate that the proportion of the population affected by the emergency (PAE) is 40% and that the relative impact of the emergency (RIE) is 1.5.
PAE is a summary measure of exposure to the adverse health consequences of the emergency; RIE is a summary measure of the combined impact on mortality of infection, health service change, physical distancing, and economic downturn, the authors explain.
Comorbidities Common
“Comorbidities were common in people with cancer,” the study authors note. For example, more than one quarter of the study population had at least one comorbidity; more than 14% had two.
For incident cancers, the number of excess deaths steadily increased in conjunction with an increase in the number of comorbidities, such that more than 80% of deaths occurred in patients with one or more comorbidities.
“When considering both prevalent and incident cancers together with a COVID-19 PAE of 40%, we estimated 17,991 excess deaths at a RIE of 1.5; 78.1% of these deaths occur in patients with ≥1 comorbidities,” the authors report.
“The excess risk of death in people living with cancer during the COVID-19 emergency may be due not only to COVID-19 infection, but also to the unintended health consequences of changes in health service provision, the physical or psychological effects of social distancing, and economic upheaval,” they state.
“This is the first study demonstrating profound recent changes in cancer care delivery in multiple centers,” the authors observe.
Lai has disclosed no relevant financial relationships. Several coauthors have various relationships with industry, as listed in their article. The commentators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
The majority of patients who have cancer or are suspected of having cancer are not accessing healthcare services in the United Kingdom or the United States because of the COVID-19 pandemic, the first report of its kind estimates.
As a result, there will be an excess of deaths among patients who have cancer and multiple comorbidities in both countries during the current coronavirus emergency, the report warns.
The authors calculate that there will be 6,270 excess deaths among cancer patients 1 year from now in England and 33,890 excess deaths among cancer patients in the United States. (In the United States, the estimated excess number of deaths applies only to patients older than 40 years, they note.)
“The recorded underlying cause of these excess deaths may be cancer, COVID-19, or comorbidity (such as myocardial infarction),” Alvina Lai, PhD, University College London, United Kingdom, and colleagues observe.
“Our data have highlighted how cancer patients with multimorbidity are a particularly at-risk group during the current pandemic,” they emphasize.
The study was published on ResearchGate as a preprint and has not undergone peer review.
Commenting on the study on the UK Science Media Center, several experts emphasized the lack of peer review, noting that interpretation of these data needs to be further refined on the basis of that input. One expert suggested that there are “substantial uncertainties that this paper does not adequately communicate.” But others argued that this topic was important enough to warrant early release of the data.
Chris Bunce, PhD, University of Birmingham, United Kingdom, said this study represents “a highly valuable contribution.”
“It is universally accepted that early diagnosis and treatment and adherence to treatment regimens saves lives,” he pointed out.
“Therefore, these COVID-19-related impacts will cost lives,” Bunce said.
“And if this information is to influence cancer care and guide policy during the COVID-19 crisis, then it is important that the findings are disseminated and discussed immediately, warranting their release ahead of peer view,” he added.
In a Medscape UK commentary, oncologist Karol Sikora, MD, PhD, argues that “restarting cancer services can’t come soon enough.”
“Resonably Argued Numerical Estimate”
“It’s well known that there have been considerable changes in the provision of health care for many conditions, including cancers, as a result of all the measures to deal with the COVID-19 crisis,” said Kevin McConway, PhD, professor emeritus of applied statistics, the Open University, Milton Keynes, United Kingdom.
“It seems inevitable that there will be increased deaths in cancer patients if they are infected with the virus or because of changes in the health services available to them, and quite possibly also from socio-economic effects of the responses to the crisis,” he continued.
“This study is the first that I have seen that produces a reasonably argued numerical estimate of the number of excess deaths of people with cancer arising from these factors in the UK and the USA,” he added.
Declines in Urgent Referrals and Chemo Attendance
For the study, the team used DATA-CAN, the UK National Health Data Research Hub for Cancer, to assess weekly returns for urgent cancer referrals for early diagnosis and also chemotherapy attendances for hospitals in Leeds, London, and Northern Ireland going back to 2018.
The data revealed that there have been major declines in chemotherapy attendances. There has been, on average, a 60% decrease from prepandemic levels in eight hospitals in the three regions that were assessed.
Urgent cancer referrals have dropped by an average of 76% compared to prepandemic levels in the three regions.
On the conservative assumption that the COVID-19 pandemic will only affect patients with newly diagnosed cancer (incident cases), the researchers estimate that the proportion of the population affected by the emergency (PAE) is 40% and that the relative impact of the emergency (RIE) is 1.5.
PAE is a summary measure of exposure to the adverse health consequences of the emergency; RIE is a summary measure of the combined impact on mortality of infection, health service change, physical distancing, and economic downturn, the authors explain.
Comorbidities Common
“Comorbidities were common in people with cancer,” the study authors note. For example, more than one quarter of the study population had at least one comorbidity; more than 14% had two.
For incident cancers, the number of excess deaths steadily increased in conjunction with an increase in the number of comorbidities, such that more than 80% of deaths occurred in patients with one or more comorbidities.
“When considering both prevalent and incident cancers together with a COVID-19 PAE of 40%, we estimated 17,991 excess deaths at a RIE of 1.5; 78.1% of these deaths occur in patients with ≥1 comorbidities,” the authors report.
“The excess risk of death in people living with cancer during the COVID-19 emergency may be due not only to COVID-19 infection, but also to the unintended health consequences of changes in health service provision, the physical or psychological effects of social distancing, and economic upheaval,” they state.
“This is the first study demonstrating profound recent changes in cancer care delivery in multiple centers,” the authors observe.
Lai has disclosed no relevant financial relationships. Several coauthors have various relationships with industry, as listed in their article. The commentators have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Antitumor treatment may increase risk of severe events in COVID-19 patients
Cancer patients who received antitumor treatment within 14 days of COVID-19 diagnosis had an increased risk of severe events, according to data from three hospitals in Wuhan.
Patients with patchy consolidation at hospital admission also had an increased risk of severe events, defined as ICU admission, mechanical ventilation, or death.
However, these findings are limited by the small number of patients studied and the retrospective nature of the analysis, according to researchers.
Li Zhang, MD, PhD, of Tongji Hospital in Wuhan, China, presented this research at the AACR virtual meeting I. Some of the data were previously published in Annals of Oncology.
The researchers studied 28 patients with cancer among 1,276 patients with COVID-19 treated at three hospitals in Wuhan. The most common cancer types were lung (n = 7), esophageal (n = 4), and breast (n = 3). Patients had other gastrointestinal, gynecologic, genitourinary, and head and neck cancers as well.
The patients’ median age was 65 years (range, 56-70 years), 60.9% were men, 35.7% had stage IV cancer, and 28.6% had hospital-acquired COVID-19. Antitumor treatments included chemotherapy (n = 22), surgery (n = 21), radiotherapy (n = 21), targeted therapy (n = 5), and immune checkpoint inhibitors (n = 2).
COVID-19 treatment
Most patients (n = 22) received oxygen as their only respiratory intervention, although 10 received mechanical ventilation.
For systemic therapy, patients received antibiotic treatment (n = 23), corticosteroids (n = 15), intravenous immunoglobulin (n = 10), and tocilizumab (n = 1).
Antiviral treatments included umifenovir (n = 14), lopinavir/ritonavir (n = 10), ganciclovir (n = 9), ribavirin (n = 1), or a combination of antiviral drugs (n = 9).
“No cancer patients were enrolled in clinical trials, so no one received hydroxychloroquine or remdesivir,” Dr. Zhang noted.
Outcomes
In all, 15 patients (53.6%) had severe events. The median time from COVID-19 diagnosis to severe events was 7 days (range, 5-15 days).
A total of eight patients (28.6%) died – three with lung cancer, two with prostate cancer, one with liver cancer, one with rectal cancer, and one with testicular cancer.
Causes of death were acute respiratory distress syndrome (n = 5), septic shock (n = 1), suspected pulmonary embolism (n = 1), and acute myocardial infarction (n = 1).
By April 4, 14 patients had been discharged from the hospital, and 6 were still hospitalized. The median duration of hospitalization was 18.4 days for discharged patients and 29.4 days for patients still in hospital.
Follow-up CT scans showed improvement in 13 patients, no changes in 5 patients, and deterioration in 6 patients.
Factors associated with severe events
In a multivariable analysis, receiving antitumor treatment within 14 days of COVID-19 diagnosis was associated with severe events (hazard ratio, 4.079; P = .037).
However, only seven patients received antitumor treatments within 14 days of COVID-19 diagnosis – three chemotherapy, two targeted therapy, one radiotherapy, and one immune checkpoint inhibitor. Five of these seven patients had severe events.
Another factor associated with severe events in multivariable analysis was patchy consolidation on CT scan at admission (HR, 5.438; P = .01). Age and gender were not significantly associated with severe events.
Immune checkpoint inhibitors
Dr. Zhang and colleagues also analyzed a second group of cancer patients and their family members to determine if patients on immune checkpoint inhibitors have an increased risk of COVID-19.
This group included 124 cancer patients treated with immune checkpoint inhibitors for at least 2 months. The patients had a median age of 59 years (range, 54-65 years), and 61.8% were men. Most patients (95.2%) had stage IV cancer, and the most common cancers were lung (54.0%), esophageal (18.6%), and head and neck (10.7%).
In this group, only one cancer patient developed COVID-19 (via nosocomial infection). In another case, a patient’s spouse developed COVID-19, but the patient did not.
Dr. Zhang said this “limited information did not suggest cancer patients treated with immune checkpoint inhibitors were more vulnerable to COVID infection.”
Dr. Zhang and colleagues reported no conflicts of interest. This research was funded by the National Natural Science Foundation of China and Huazhong University of Science and Technology COVID-19 Rapid Response Call China.
SOURCE: Zhang L et al. Ann Oncol. 2020 Mar 26. doi: 10.1016/j.annonc.2020.03.296.
Cancer patients who received antitumor treatment within 14 days of COVID-19 diagnosis had an increased risk of severe events, according to data from three hospitals in Wuhan.
Patients with patchy consolidation at hospital admission also had an increased risk of severe events, defined as ICU admission, mechanical ventilation, or death.
However, these findings are limited by the small number of patients studied and the retrospective nature of the analysis, according to researchers.
Li Zhang, MD, PhD, of Tongji Hospital in Wuhan, China, presented this research at the AACR virtual meeting I. Some of the data were previously published in Annals of Oncology.
The researchers studied 28 patients with cancer among 1,276 patients with COVID-19 treated at three hospitals in Wuhan. The most common cancer types were lung (n = 7), esophageal (n = 4), and breast (n = 3). Patients had other gastrointestinal, gynecologic, genitourinary, and head and neck cancers as well.
The patients’ median age was 65 years (range, 56-70 years), 60.9% were men, 35.7% had stage IV cancer, and 28.6% had hospital-acquired COVID-19. Antitumor treatments included chemotherapy (n = 22), surgery (n = 21), radiotherapy (n = 21), targeted therapy (n = 5), and immune checkpoint inhibitors (n = 2).
COVID-19 treatment
Most patients (n = 22) received oxygen as their only respiratory intervention, although 10 received mechanical ventilation.
For systemic therapy, patients received antibiotic treatment (n = 23), corticosteroids (n = 15), intravenous immunoglobulin (n = 10), and tocilizumab (n = 1).
Antiviral treatments included umifenovir (n = 14), lopinavir/ritonavir (n = 10), ganciclovir (n = 9), ribavirin (n = 1), or a combination of antiviral drugs (n = 9).
“No cancer patients were enrolled in clinical trials, so no one received hydroxychloroquine or remdesivir,” Dr. Zhang noted.
Outcomes
In all, 15 patients (53.6%) had severe events. The median time from COVID-19 diagnosis to severe events was 7 days (range, 5-15 days).
A total of eight patients (28.6%) died – three with lung cancer, two with prostate cancer, one with liver cancer, one with rectal cancer, and one with testicular cancer.
Causes of death were acute respiratory distress syndrome (n = 5), septic shock (n = 1), suspected pulmonary embolism (n = 1), and acute myocardial infarction (n = 1).
By April 4, 14 patients had been discharged from the hospital, and 6 were still hospitalized. The median duration of hospitalization was 18.4 days for discharged patients and 29.4 days for patients still in hospital.
Follow-up CT scans showed improvement in 13 patients, no changes in 5 patients, and deterioration in 6 patients.
Factors associated with severe events
In a multivariable analysis, receiving antitumor treatment within 14 days of COVID-19 diagnosis was associated with severe events (hazard ratio, 4.079; P = .037).
However, only seven patients received antitumor treatments within 14 days of COVID-19 diagnosis – three chemotherapy, two targeted therapy, one radiotherapy, and one immune checkpoint inhibitor. Five of these seven patients had severe events.
Another factor associated with severe events in multivariable analysis was patchy consolidation on CT scan at admission (HR, 5.438; P = .01). Age and gender were not significantly associated with severe events.
Immune checkpoint inhibitors
Dr. Zhang and colleagues also analyzed a second group of cancer patients and their family members to determine if patients on immune checkpoint inhibitors have an increased risk of COVID-19.
This group included 124 cancer patients treated with immune checkpoint inhibitors for at least 2 months. The patients had a median age of 59 years (range, 54-65 years), and 61.8% were men. Most patients (95.2%) had stage IV cancer, and the most common cancers were lung (54.0%), esophageal (18.6%), and head and neck (10.7%).
In this group, only one cancer patient developed COVID-19 (via nosocomial infection). In another case, a patient’s spouse developed COVID-19, but the patient did not.
Dr. Zhang said this “limited information did not suggest cancer patients treated with immune checkpoint inhibitors were more vulnerable to COVID infection.”
Dr. Zhang and colleagues reported no conflicts of interest. This research was funded by the National Natural Science Foundation of China and Huazhong University of Science and Technology COVID-19 Rapid Response Call China.
SOURCE: Zhang L et al. Ann Oncol. 2020 Mar 26. doi: 10.1016/j.annonc.2020.03.296.
Cancer patients who received antitumor treatment within 14 days of COVID-19 diagnosis had an increased risk of severe events, according to data from three hospitals in Wuhan.
Patients with patchy consolidation at hospital admission also had an increased risk of severe events, defined as ICU admission, mechanical ventilation, or death.
However, these findings are limited by the small number of patients studied and the retrospective nature of the analysis, according to researchers.
Li Zhang, MD, PhD, of Tongji Hospital in Wuhan, China, presented this research at the AACR virtual meeting I. Some of the data were previously published in Annals of Oncology.
The researchers studied 28 patients with cancer among 1,276 patients with COVID-19 treated at three hospitals in Wuhan. The most common cancer types were lung (n = 7), esophageal (n = 4), and breast (n = 3). Patients had other gastrointestinal, gynecologic, genitourinary, and head and neck cancers as well.
The patients’ median age was 65 years (range, 56-70 years), 60.9% were men, 35.7% had stage IV cancer, and 28.6% had hospital-acquired COVID-19. Antitumor treatments included chemotherapy (n = 22), surgery (n = 21), radiotherapy (n = 21), targeted therapy (n = 5), and immune checkpoint inhibitors (n = 2).
COVID-19 treatment
Most patients (n = 22) received oxygen as their only respiratory intervention, although 10 received mechanical ventilation.
For systemic therapy, patients received antibiotic treatment (n = 23), corticosteroids (n = 15), intravenous immunoglobulin (n = 10), and tocilizumab (n = 1).
Antiviral treatments included umifenovir (n = 14), lopinavir/ritonavir (n = 10), ganciclovir (n = 9), ribavirin (n = 1), or a combination of antiviral drugs (n = 9).
“No cancer patients were enrolled in clinical trials, so no one received hydroxychloroquine or remdesivir,” Dr. Zhang noted.
Outcomes
In all, 15 patients (53.6%) had severe events. The median time from COVID-19 diagnosis to severe events was 7 days (range, 5-15 days).
A total of eight patients (28.6%) died – three with lung cancer, two with prostate cancer, one with liver cancer, one with rectal cancer, and one with testicular cancer.
Causes of death were acute respiratory distress syndrome (n = 5), septic shock (n = 1), suspected pulmonary embolism (n = 1), and acute myocardial infarction (n = 1).
By April 4, 14 patients had been discharged from the hospital, and 6 were still hospitalized. The median duration of hospitalization was 18.4 days for discharged patients and 29.4 days for patients still in hospital.
Follow-up CT scans showed improvement in 13 patients, no changes in 5 patients, and deterioration in 6 patients.
Factors associated with severe events
In a multivariable analysis, receiving antitumor treatment within 14 days of COVID-19 diagnosis was associated with severe events (hazard ratio, 4.079; P = .037).
However, only seven patients received antitumor treatments within 14 days of COVID-19 diagnosis – three chemotherapy, two targeted therapy, one radiotherapy, and one immune checkpoint inhibitor. Five of these seven patients had severe events.
Another factor associated with severe events in multivariable analysis was patchy consolidation on CT scan at admission (HR, 5.438; P = .01). Age and gender were not significantly associated with severe events.
Immune checkpoint inhibitors
Dr. Zhang and colleagues also analyzed a second group of cancer patients and their family members to determine if patients on immune checkpoint inhibitors have an increased risk of COVID-19.
This group included 124 cancer patients treated with immune checkpoint inhibitors for at least 2 months. The patients had a median age of 59 years (range, 54-65 years), and 61.8% were men. Most patients (95.2%) had stage IV cancer, and the most common cancers were lung (54.0%), esophageal (18.6%), and head and neck (10.7%).
In this group, only one cancer patient developed COVID-19 (via nosocomial infection). In another case, a patient’s spouse developed COVID-19, but the patient did not.
Dr. Zhang said this “limited information did not suggest cancer patients treated with immune checkpoint inhibitors were more vulnerable to COVID infection.”
Dr. Zhang and colleagues reported no conflicts of interest. This research was funded by the National Natural Science Foundation of China and Huazhong University of Science and Technology COVID-19 Rapid Response Call China.
SOURCE: Zhang L et al. Ann Oncol. 2020 Mar 26. doi: 10.1016/j.annonc.2020.03.296.
FROM AACR 2020

