User login
What does 'Medicare for all' mean?
Only about a fifth of Americans correctly identified the description of a Medicare-for-all system in a recent national tracking poll.
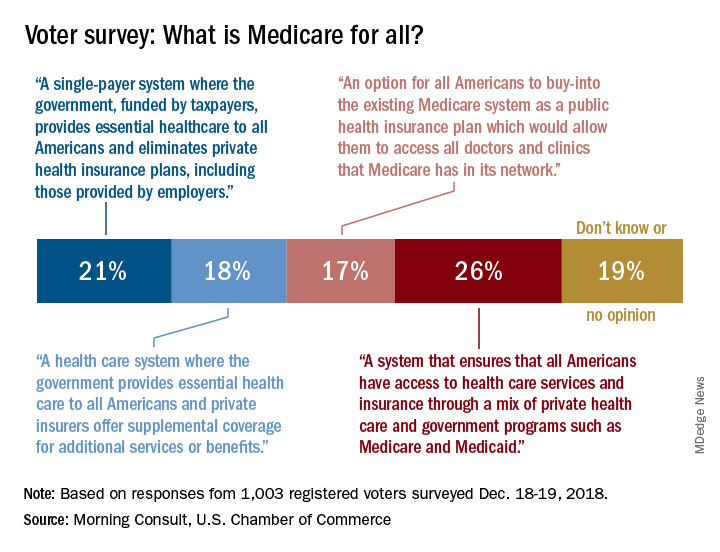
Four descriptions of a Medicare-for-all health care system were provided, and only 21% of respondents correctly selected “a single-payer system where the government, funded by taxpayers, provides essential health care to all Americans and eliminates private health insurance plans, including those provided by employers,” according to the tracking poll from the U.S. Chamber of Commerce and digital media company Morning Consult.
The most common selection – chosen by 26% of the 1,003 registered voters who answered the question (about half of all the respondents) – involved “a system that ensures that all Americans have access to health care services and insurance through a mix of private health care and government programs such as Medicare and Medicaid.”
The other choices covered a federal system with available private supplemental coverage and another with the option of buying in to the existing Medicare system, the report said. Another 19% of respondents to the survey, which was conducted Dec. 18-19, said that they didn’t know or had no opinion.
Questions covering other areas of possible future legislation, which were answered by all of the 2,000 respondents, showed strong support for protection against surprise hospital bills (90%), reforming the Affordable Care Act (73%), and protecting the Affordable Care Act (63%), the U.S. Chamber and Morning Consult reported. The survey’s margin of error was plus or minus two percentage points.
Only about a fifth of Americans correctly identified the description of a Medicare-for-all system in a recent national tracking poll.
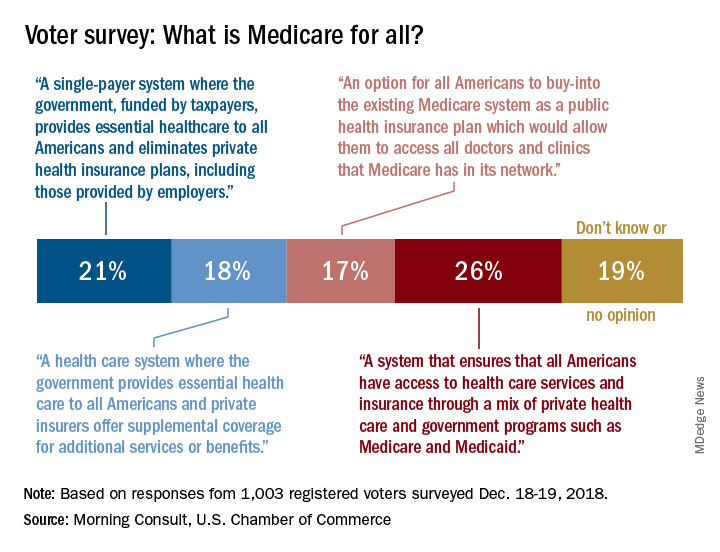
Four descriptions of a Medicare-for-all health care system were provided, and only 21% of respondents correctly selected “a single-payer system where the government, funded by taxpayers, provides essential health care to all Americans and eliminates private health insurance plans, including those provided by employers,” according to the tracking poll from the U.S. Chamber of Commerce and digital media company Morning Consult.
The most common selection – chosen by 26% of the 1,003 registered voters who answered the question (about half of all the respondents) – involved “a system that ensures that all Americans have access to health care services and insurance through a mix of private health care and government programs such as Medicare and Medicaid.”
The other choices covered a federal system with available private supplemental coverage and another with the option of buying in to the existing Medicare system, the report said. Another 19% of respondents to the survey, which was conducted Dec. 18-19, said that they didn’t know or had no opinion.
Questions covering other areas of possible future legislation, which were answered by all of the 2,000 respondents, showed strong support for protection against surprise hospital bills (90%), reforming the Affordable Care Act (73%), and protecting the Affordable Care Act (63%), the U.S. Chamber and Morning Consult reported. The survey’s margin of error was plus or minus two percentage points.
Only about a fifth of Americans correctly identified the description of a Medicare-for-all system in a recent national tracking poll.
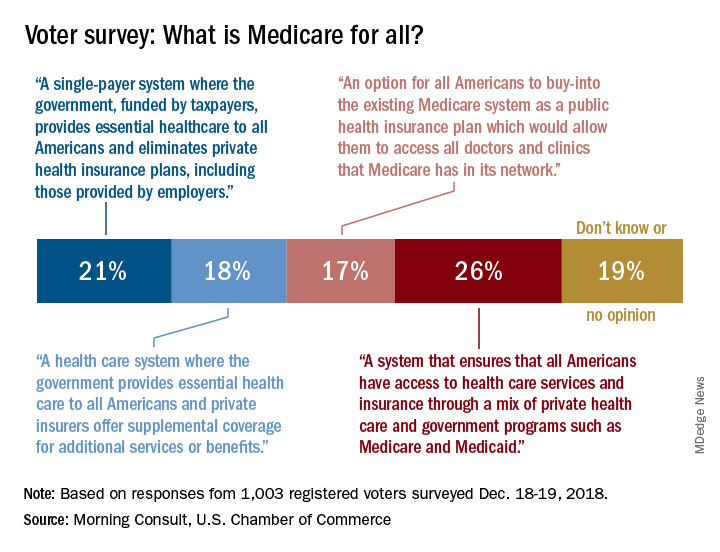
Four descriptions of a Medicare-for-all health care system were provided, and only 21% of respondents correctly selected “a single-payer system where the government, funded by taxpayers, provides essential health care to all Americans and eliminates private health insurance plans, including those provided by employers,” according to the tracking poll from the U.S. Chamber of Commerce and digital media company Morning Consult.
The most common selection – chosen by 26% of the 1,003 registered voters who answered the question (about half of all the respondents) – involved “a system that ensures that all Americans have access to health care services and insurance through a mix of private health care and government programs such as Medicare and Medicaid.”
The other choices covered a federal system with available private supplemental coverage and another with the option of buying in to the existing Medicare system, the report said. Another 19% of respondents to the survey, which was conducted Dec. 18-19, said that they didn’t know or had no opinion.
Questions covering other areas of possible future legislation, which were answered by all of the 2,000 respondents, showed strong support for protection against surprise hospital bills (90%), reforming the Affordable Care Act (73%), and protecting the Affordable Care Act (63%), the U.S. Chamber and Morning Consult reported. The survey’s margin of error was plus or minus two percentage points.
Medicine grapples with COI reporting
Conflict of interest (COI) reporting has moved center stage again in recent months, with some medical journals, professional societies, cancer centers, and academic medical institutions reviewing policies and practices in the wake of a highly publicized disclosure failure last fall at Memorial Sloan Kettering Cancer Center (MSK).
And in some settings, oncologists and other physician researchers are being encouraged to check what the federal Open Payments database says about their payments from industry.
The spotlight is on the field of cancer research and treatment, where MSK’s chief medical officer, José Baselga, MD, PhD, resigned in September 2018 after the New York Times and ProPublica reported that he’d failed to disclose millions of dollars of industry payments and ownership interests in the majority of journal articles he wrote or cowrote over a 4-year period.
COI disclosure issues have a broad reach, however, and the policy reviews, debates, and hashing out of responsibilities that are now taking place likely will have implications for all of medicine.
Among the questions: Who enforces disclosure rules and how should cases of incomplete or inconsistent disclosure be handled? How can COI declarations be made easier for researchers? Should disclosure be based on self-reported relevancy, or more comprehensive in nature?
Such questions are being debated nationally. On Feb. 12, 2019, leaders from academia, journals, and medical societies came together in Washington, D.C., at the offices of the Association of American Medical Colleges (AAMC) for a closed-door meeting focused on COI disclosures. MSK, the Journal of the American Medical Association (JAMA), the American Society of Clinical Oncology (ASCO), and the Council of Medical Specialty Societies led the charge as cosponsors of the meeting.
“We’ve been dealing with disclosure issues in a siloed way in exchanges [between journal editors and authors, for instance, or between speakers and CME providers]. And academic institutions have their own robust disclosure mechanisms that they use internally,” said Heather Pierce, JD, MPH, senior director of science policy and regulatory counsel for the AAMC. “There’s a growing understanding that these conversations need to be happening across these different sectors.”
Pleas for accuracy
At academic medical institutions, conflicts of interest are identified and then managed; it’s common for researchers’ COI management plans to include requirements for disclosure in all presentations and publications.
Journals and professional medical societies require authors and speakers to submit disclosure forms of varying lengths and with differing questions about relationships with industry, often based on the notion of relevancy to the subject at hand. Disclosure forms are reviewed, but editors and other reviewers rely largely – if not entirely – on the honor system.
Dr. Baselga’s disclosure lapses and his subsequent resignation have rattled leaders in each of these settings. Researchers at MSK were instructed to review their COI disclosures and submit corrections when necessary, and in December 2018 the hospital was reportedly evaluating its process for reviewing conflicts of interest, according to reports in the New York Times and ProPublica. (MSK did not respond to requests for comment about actions taken.)
The Dana Farber Cancer Institute in Boston similarly has “been reminding faculty and other researchers” of their disclosure responsibilities and is conducting a review of “all our policies in this area,” a spokeswoman said. And at Fred Hutchinson Cancer Research Center in Seattle, a spokesman said they have established an internal task force to review individual and institutional COI policies to ensure that COIs are “appropriately managed while also enabling research collaborations that bring scientific advances to our patients.”
Other centers contacted for this article, such as the Cleveland Clinic Cancer Center and the Mayo Clinic Cancer Center, said that they have no new reviews ongoing and no plans to change policies at this time.
The heightened attention to disclosure has, in turn, shone a spotlight on increasingly complex physician-industry relationships and on the Open Payments website run by the Centers for Medicare and Medicaid Services. Open Payments is a disclosure program and database that tracks payments made to physicians and teaching hospitals by drug and device companies.
Journalists, including those who reported on Dr. Baselga’s disclosures, have searched the public database for industry payment data. So have other researchers who have studied financial disclosure statements; a study reported in JAMA Oncology last year, for instance, concluded through the use of Open Payments data that about one-third of authors of cancer drug trial reports did not completely disclose payments from trial sponsors (JAMA Oncol. 2018;4[10]:1426-8
In a column published in December 2018 in AAMC News, AAMC President and CEO Darrell G. Kirch, MD, wrote that failures to disclose can raise questions about the integrity of research, whether or not there is an actual conflict. He advised institutions to “encourage faculty to review the information posted about them on the Open Payments website” of the CMS to “ensure it is accurate and consistent with disclosures related to all their professional responsibilities.”
ASCO issues similar advice, encouraging authors and CME speakers and participants of other ASCO activities to double-check their disclosures against other sources, including “publicly reported interactions with companies that may have been inadvertently omitted.”
In the world of journals, the New England Journal of Medicine (NEJM) began asking authors at the end of 2018 to “certify that they have reconciled their disclosures” with the Open Payments database, said Jennifer Zeis, a spokeswoman forthe journal.
Time may tell how well such requests work. When the Institute of Medicine (now called the National Academy of Medicine) called on Congress in 2009 to create a national program requiring pharmaceutical, device, and biotechnology companies to publicly report their payments, it envisioned universities, journals, and others using the program to verify disclosures made to them. But the resulting Open Payments database has limitations – for instance, it doesn’t include payments from companies without FDA-approved products, it is not necessarily up to date, and its payment categories do not necessarily match categories of disclosure.
“Some entries in the Open Payments database need further explanation,” said Ms. Zeis of NEJM. “Some authors, for example, have said that the database does not fully and accurately explain that the funds were disbursed not to them personally, but to their academic institutions.” While the database provides transparency, it also “needs context that’s not currently provided,” she said.
Mistakes in the database can also be “very hard to challenge,” said Clifford A. Hudis, MD, CEO of the American Society of Clinical Oncology, which produces the Journal of Clinical Oncology (JCO).
All in all, he said, “there’s really no timely, comprehensive, and fully reliable source of information with which to verify an individual’s disclosures.”
Policies and practices are also under review at the American Association for Cancer Research (AACR) and the American Society of Hematology (ASH).
The AACR has appointed a panel of experts, including physicians, basic scientists, a patient advocate, and others to conduct “a comprehensive review of [its] disclosure policies and to explore whether any current policies need to be revised,” said Rachel Salis-Silverman, director of public relations. It also will convene a session on COI disclosures at its 2019 annual meeting at the end of March, she said.
ASH, which publishes the journal Blood, is exploring possible changes in its “internal processes with regards to ASH publications,” said Matt Gertzog, deputy executive director of the group. COI disclosure is “more of a journey than a destination,” he said. “We are continuously reflecting on and refining our processes.”
Moving away from ‘relevancy’
Physicians and others who have relationships with industry have long complained about a patchwork of disclosure requirements, and significant efforts have been made in the last decade to standardize forms and practices. However, the current system is still “a little bit of a Tower of Babel,” said Dr. Hudis of ASCO. “Every day, physicians have to complete from scratch similar, but not identical, disclosure forms that ask similar, but not identical, questions.”
A disclosable compensation amount “might be first dollar, or it might be over $10,000. [Time periods] might cover 1 year, or 3 years. ... Stock ownership might be dollar value, or a percentage of shares,” he explained. “If you want a system that would make it hard to be compliant and easy to mess up, that’s what we have.”
To standardize the COI disclosure process for all Society-related publications and activities – including CME, JCO, and practice guidelines – ASCO moved about 5 years ago to a system of general disclosure, asking physicians and others to disclose all financial interests and industry relationships rather than what they deem relevant.
The thinking was that general disclosure “would be easier for disclosers, and nobody would ever be accused of hiding anything,” Dr. Hudis said.
“We’d [also] recognized,” he explained, “that there was a risk to the relevancy approach in that it put the judgment for the potential conflict in the hands of the potentially conflicted, while others might have a different point of view about what is or isn’t relevant.”
Those concerned about general disclosure worry that it may “obscure [for the reader or listener] what’s really important or the most meaningful,” he said.
Some physicians have expressed in interviews for this article, moreover, the concern that too many disclosures – too long a list of financial relationships – will be viewed negatively. This is something ASCO aims to guard against as it strives to achieve full transparency, Dr. Hudis said. “If one were to suggest that engagement itself is automatically a negative, then you’re starting to put negative pressure on compliance with disclosure.”
And full disclosure matters, he said. “We have to err in the direction of believing that disclosure is good,” he said, “even if we can’t prove it has clear and measurable impact. That is why our goal is to make full disclosure easier. What potential conflicts are acceptable, or not, is an important but entirely separate matter.”
Howard Bauchner, MD, editor in chief of JAMA and the JAMA Network, frames the pros and cons of general and relevant disclosure similarly, and emphasizes that the relationships of authors with industry – particularly with private equity start-up companies – has changed dramatically over the past decade. Editors have “talked about complete versus [more narrowly] relevant disclosures at length,” he said, and have been moving overall “toward more complete disclosure where the reader can make a decision on their own.”
Other journals also are taking this approach. In 2009, in an effort to reduce variability in reporting processes and formats, the International Committee of Medical Journal Editors (ICMJE) developed a uniform electronic disclosure form that asks about financial relationships and interactions with any entity that could be considered “broadly relevant” to the submitted work. The group updated the form in December 2018.
As an example, the form reads, an article about testing an epidermal growth factor receptor (EGFR) antagonist in lung cancer requires the reporting of “all associations with entities pursuing diagnostic or therapeutic strategies in cancer in general, not just in the area of EGFR or lung cancer.” JAMA, NEJM, and The Lancet are among those journals that embrace the ICMJE’s policies and use its form.
To simplify its own disclosure process, JAMA and the network’s journals ended the practice in January 2019 of requiring both the ICMJE form and JAMA’s own separate disclosure form. The journals now use a single electronic form that includes questions from the ICMJE form. And to promote more consistent and complete reporting, the electronic form contains prompts that ask authors each time they answer “no” to one of four specific questions about potential COI whether they are certain of their answers and whether their answers are consistent with other disclosures they recently made.
While relevancy statements “create struggles for authors,” about two-thirds of the disclosure inaccuracies reported by readers and verified by JAMA’s editors (most often through editor-author discussions) involve a complete lack of disclosure rather than questions of relevancy, Dr. Bauchner noted. (JAMA and the network’s journals receive about 30,000 disclosure forms each year.)
The AAMC, in the meantime, has developed a central web-based repository for disclosures called Convey. Physicians and others can maintain secure records of financial interests in the repository, and these records can then be disclosed directly to any journal or organization that uses the system. The tool – born from discussions that followed the 2009 IOM report on COI – is “intended to facilitate more complete, more accurate, and more consistent” disclosures,” said Ms. Pierce of the AAMC. It is now live and in its early stages of use; NEJM assisted in its development and has been one of its pilot testers.
Enforcement questions
Some experts believe that institutions should maintain public databases of disclosures and/or that disclosure requirements should be better enforced in-house.
“There often are no clear guidelines in institutions about how to respond to people who are negligent in how they’re managing their disclosures,” said Jeffrey R. Botkin, MD, MPH, professor of pediatrics and associate vice president for research at the University of Utah, Salt Lake City, who has served on a variety of ethics committees and is an elected member of the Hastings Center. Dr. Botkin proposed in a Viewpoint published last October in JAMA that failure to disclose significant COIs should be considered research misconduct (JAMA 2018;320[22]:2307-8).
At the University of Utah, “we’re getting better at saying, ‘show us that you’ve disclosed,’ ” he said. “In some cases we’ll do spot checks of journal articles to make sure [researchers have] followed through with their disclosures.”
John Abramson, MD, a lecturer in the department of health care policy at Harvard Medical School, Boston, contends that incomplete declarations of COI have been shown to correlate with reporting of manufacturer-friendly research results. Journals should have “zero tolerance” standards for incomplete or inaccurate COI declarations and should, among other things, “inform academic institutions of breaches of integrity.”
At JAMA, which in 2017 published a theme issue on COI and COI declarations, editors have been discussing whether they will contact an author’s institution “if there’s a pattern involved [with disclosure problems] or if there’s a lack of declaration of multiple COIs,” Dr. Bauchner said.
Conflict of interest (COI) reporting has moved center stage again in recent months, with some medical journals, professional societies, cancer centers, and academic medical institutions reviewing policies and practices in the wake of a highly publicized disclosure failure last fall at Memorial Sloan Kettering Cancer Center (MSK).
And in some settings, oncologists and other physician researchers are being encouraged to check what the federal Open Payments database says about their payments from industry.
The spotlight is on the field of cancer research and treatment, where MSK’s chief medical officer, José Baselga, MD, PhD, resigned in September 2018 after the New York Times and ProPublica reported that he’d failed to disclose millions of dollars of industry payments and ownership interests in the majority of journal articles he wrote or cowrote over a 4-year period.
COI disclosure issues have a broad reach, however, and the policy reviews, debates, and hashing out of responsibilities that are now taking place likely will have implications for all of medicine.
Among the questions: Who enforces disclosure rules and how should cases of incomplete or inconsistent disclosure be handled? How can COI declarations be made easier for researchers? Should disclosure be based on self-reported relevancy, or more comprehensive in nature?
Such questions are being debated nationally. On Feb. 12, 2019, leaders from academia, journals, and medical societies came together in Washington, D.C., at the offices of the Association of American Medical Colleges (AAMC) for a closed-door meeting focused on COI disclosures. MSK, the Journal of the American Medical Association (JAMA), the American Society of Clinical Oncology (ASCO), and the Council of Medical Specialty Societies led the charge as cosponsors of the meeting.
“We’ve been dealing with disclosure issues in a siloed way in exchanges [between journal editors and authors, for instance, or between speakers and CME providers]. And academic institutions have their own robust disclosure mechanisms that they use internally,” said Heather Pierce, JD, MPH, senior director of science policy and regulatory counsel for the AAMC. “There’s a growing understanding that these conversations need to be happening across these different sectors.”
Pleas for accuracy
At academic medical institutions, conflicts of interest are identified and then managed; it’s common for researchers’ COI management plans to include requirements for disclosure in all presentations and publications.
Journals and professional medical societies require authors and speakers to submit disclosure forms of varying lengths and with differing questions about relationships with industry, often based on the notion of relevancy to the subject at hand. Disclosure forms are reviewed, but editors and other reviewers rely largely – if not entirely – on the honor system.
Dr. Baselga’s disclosure lapses and his subsequent resignation have rattled leaders in each of these settings. Researchers at MSK were instructed to review their COI disclosures and submit corrections when necessary, and in December 2018 the hospital was reportedly evaluating its process for reviewing conflicts of interest, according to reports in the New York Times and ProPublica. (MSK did not respond to requests for comment about actions taken.)
The Dana Farber Cancer Institute in Boston similarly has “been reminding faculty and other researchers” of their disclosure responsibilities and is conducting a review of “all our policies in this area,” a spokeswoman said. And at Fred Hutchinson Cancer Research Center in Seattle, a spokesman said they have established an internal task force to review individual and institutional COI policies to ensure that COIs are “appropriately managed while also enabling research collaborations that bring scientific advances to our patients.”
Other centers contacted for this article, such as the Cleveland Clinic Cancer Center and the Mayo Clinic Cancer Center, said that they have no new reviews ongoing and no plans to change policies at this time.
The heightened attention to disclosure has, in turn, shone a spotlight on increasingly complex physician-industry relationships and on the Open Payments website run by the Centers for Medicare and Medicaid Services. Open Payments is a disclosure program and database that tracks payments made to physicians and teaching hospitals by drug and device companies.
Journalists, including those who reported on Dr. Baselga’s disclosures, have searched the public database for industry payment data. So have other researchers who have studied financial disclosure statements; a study reported in JAMA Oncology last year, for instance, concluded through the use of Open Payments data that about one-third of authors of cancer drug trial reports did not completely disclose payments from trial sponsors (JAMA Oncol. 2018;4[10]:1426-8
In a column published in December 2018 in AAMC News, AAMC President and CEO Darrell G. Kirch, MD, wrote that failures to disclose can raise questions about the integrity of research, whether or not there is an actual conflict. He advised institutions to “encourage faculty to review the information posted about them on the Open Payments website” of the CMS to “ensure it is accurate and consistent with disclosures related to all their professional responsibilities.”
ASCO issues similar advice, encouraging authors and CME speakers and participants of other ASCO activities to double-check their disclosures against other sources, including “publicly reported interactions with companies that may have been inadvertently omitted.”
In the world of journals, the New England Journal of Medicine (NEJM) began asking authors at the end of 2018 to “certify that they have reconciled their disclosures” with the Open Payments database, said Jennifer Zeis, a spokeswoman forthe journal.
Time may tell how well such requests work. When the Institute of Medicine (now called the National Academy of Medicine) called on Congress in 2009 to create a national program requiring pharmaceutical, device, and biotechnology companies to publicly report their payments, it envisioned universities, journals, and others using the program to verify disclosures made to them. But the resulting Open Payments database has limitations – for instance, it doesn’t include payments from companies without FDA-approved products, it is not necessarily up to date, and its payment categories do not necessarily match categories of disclosure.
“Some entries in the Open Payments database need further explanation,” said Ms. Zeis of NEJM. “Some authors, for example, have said that the database does not fully and accurately explain that the funds were disbursed not to them personally, but to their academic institutions.” While the database provides transparency, it also “needs context that’s not currently provided,” she said.
Mistakes in the database can also be “very hard to challenge,” said Clifford A. Hudis, MD, CEO of the American Society of Clinical Oncology, which produces the Journal of Clinical Oncology (JCO).
All in all, he said, “there’s really no timely, comprehensive, and fully reliable source of information with which to verify an individual’s disclosures.”
Policies and practices are also under review at the American Association for Cancer Research (AACR) and the American Society of Hematology (ASH).
The AACR has appointed a panel of experts, including physicians, basic scientists, a patient advocate, and others to conduct “a comprehensive review of [its] disclosure policies and to explore whether any current policies need to be revised,” said Rachel Salis-Silverman, director of public relations. It also will convene a session on COI disclosures at its 2019 annual meeting at the end of March, she said.
ASH, which publishes the journal Blood, is exploring possible changes in its “internal processes with regards to ASH publications,” said Matt Gertzog, deputy executive director of the group. COI disclosure is “more of a journey than a destination,” he said. “We are continuously reflecting on and refining our processes.”
Moving away from ‘relevancy’
Physicians and others who have relationships with industry have long complained about a patchwork of disclosure requirements, and significant efforts have been made in the last decade to standardize forms and practices. However, the current system is still “a little bit of a Tower of Babel,” said Dr. Hudis of ASCO. “Every day, physicians have to complete from scratch similar, but not identical, disclosure forms that ask similar, but not identical, questions.”
A disclosable compensation amount “might be first dollar, or it might be over $10,000. [Time periods] might cover 1 year, or 3 years. ... Stock ownership might be dollar value, or a percentage of shares,” he explained. “If you want a system that would make it hard to be compliant and easy to mess up, that’s what we have.”
To standardize the COI disclosure process for all Society-related publications and activities – including CME, JCO, and practice guidelines – ASCO moved about 5 years ago to a system of general disclosure, asking physicians and others to disclose all financial interests and industry relationships rather than what they deem relevant.
The thinking was that general disclosure “would be easier for disclosers, and nobody would ever be accused of hiding anything,” Dr. Hudis said.
“We’d [also] recognized,” he explained, “that there was a risk to the relevancy approach in that it put the judgment for the potential conflict in the hands of the potentially conflicted, while others might have a different point of view about what is or isn’t relevant.”
Those concerned about general disclosure worry that it may “obscure [for the reader or listener] what’s really important or the most meaningful,” he said.
Some physicians have expressed in interviews for this article, moreover, the concern that too many disclosures – too long a list of financial relationships – will be viewed negatively. This is something ASCO aims to guard against as it strives to achieve full transparency, Dr. Hudis said. “If one were to suggest that engagement itself is automatically a negative, then you’re starting to put negative pressure on compliance with disclosure.”
And full disclosure matters, he said. “We have to err in the direction of believing that disclosure is good,” he said, “even if we can’t prove it has clear and measurable impact. That is why our goal is to make full disclosure easier. What potential conflicts are acceptable, or not, is an important but entirely separate matter.”
Howard Bauchner, MD, editor in chief of JAMA and the JAMA Network, frames the pros and cons of general and relevant disclosure similarly, and emphasizes that the relationships of authors with industry – particularly with private equity start-up companies – has changed dramatically over the past decade. Editors have “talked about complete versus [more narrowly] relevant disclosures at length,” he said, and have been moving overall “toward more complete disclosure where the reader can make a decision on their own.”
Other journals also are taking this approach. In 2009, in an effort to reduce variability in reporting processes and formats, the International Committee of Medical Journal Editors (ICMJE) developed a uniform electronic disclosure form that asks about financial relationships and interactions with any entity that could be considered “broadly relevant” to the submitted work. The group updated the form in December 2018.
As an example, the form reads, an article about testing an epidermal growth factor receptor (EGFR) antagonist in lung cancer requires the reporting of “all associations with entities pursuing diagnostic or therapeutic strategies in cancer in general, not just in the area of EGFR or lung cancer.” JAMA, NEJM, and The Lancet are among those journals that embrace the ICMJE’s policies and use its form.
To simplify its own disclosure process, JAMA and the network’s journals ended the practice in January 2019 of requiring both the ICMJE form and JAMA’s own separate disclosure form. The journals now use a single electronic form that includes questions from the ICMJE form. And to promote more consistent and complete reporting, the electronic form contains prompts that ask authors each time they answer “no” to one of four specific questions about potential COI whether they are certain of their answers and whether their answers are consistent with other disclosures they recently made.
While relevancy statements “create struggles for authors,” about two-thirds of the disclosure inaccuracies reported by readers and verified by JAMA’s editors (most often through editor-author discussions) involve a complete lack of disclosure rather than questions of relevancy, Dr. Bauchner noted. (JAMA and the network’s journals receive about 30,000 disclosure forms each year.)
The AAMC, in the meantime, has developed a central web-based repository for disclosures called Convey. Physicians and others can maintain secure records of financial interests in the repository, and these records can then be disclosed directly to any journal or organization that uses the system. The tool – born from discussions that followed the 2009 IOM report on COI – is “intended to facilitate more complete, more accurate, and more consistent” disclosures,” said Ms. Pierce of the AAMC. It is now live and in its early stages of use; NEJM assisted in its development and has been one of its pilot testers.
Enforcement questions
Some experts believe that institutions should maintain public databases of disclosures and/or that disclosure requirements should be better enforced in-house.
“There often are no clear guidelines in institutions about how to respond to people who are negligent in how they’re managing their disclosures,” said Jeffrey R. Botkin, MD, MPH, professor of pediatrics and associate vice president for research at the University of Utah, Salt Lake City, who has served on a variety of ethics committees and is an elected member of the Hastings Center. Dr. Botkin proposed in a Viewpoint published last October in JAMA that failure to disclose significant COIs should be considered research misconduct (JAMA 2018;320[22]:2307-8).
At the University of Utah, “we’re getting better at saying, ‘show us that you’ve disclosed,’ ” he said. “In some cases we’ll do spot checks of journal articles to make sure [researchers have] followed through with their disclosures.”
John Abramson, MD, a lecturer in the department of health care policy at Harvard Medical School, Boston, contends that incomplete declarations of COI have been shown to correlate with reporting of manufacturer-friendly research results. Journals should have “zero tolerance” standards for incomplete or inaccurate COI declarations and should, among other things, “inform academic institutions of breaches of integrity.”
At JAMA, which in 2017 published a theme issue on COI and COI declarations, editors have been discussing whether they will contact an author’s institution “if there’s a pattern involved [with disclosure problems] or if there’s a lack of declaration of multiple COIs,” Dr. Bauchner said.
Conflict of interest (COI) reporting has moved center stage again in recent months, with some medical journals, professional societies, cancer centers, and academic medical institutions reviewing policies and practices in the wake of a highly publicized disclosure failure last fall at Memorial Sloan Kettering Cancer Center (MSK).
And in some settings, oncologists and other physician researchers are being encouraged to check what the federal Open Payments database says about their payments from industry.
The spotlight is on the field of cancer research and treatment, where MSK’s chief medical officer, José Baselga, MD, PhD, resigned in September 2018 after the New York Times and ProPublica reported that he’d failed to disclose millions of dollars of industry payments and ownership interests in the majority of journal articles he wrote or cowrote over a 4-year period.
COI disclosure issues have a broad reach, however, and the policy reviews, debates, and hashing out of responsibilities that are now taking place likely will have implications for all of medicine.
Among the questions: Who enforces disclosure rules and how should cases of incomplete or inconsistent disclosure be handled? How can COI declarations be made easier for researchers? Should disclosure be based on self-reported relevancy, or more comprehensive in nature?
Such questions are being debated nationally. On Feb. 12, 2019, leaders from academia, journals, and medical societies came together in Washington, D.C., at the offices of the Association of American Medical Colleges (AAMC) for a closed-door meeting focused on COI disclosures. MSK, the Journal of the American Medical Association (JAMA), the American Society of Clinical Oncology (ASCO), and the Council of Medical Specialty Societies led the charge as cosponsors of the meeting.
“We’ve been dealing with disclosure issues in a siloed way in exchanges [between journal editors and authors, for instance, or between speakers and CME providers]. And academic institutions have their own robust disclosure mechanisms that they use internally,” said Heather Pierce, JD, MPH, senior director of science policy and regulatory counsel for the AAMC. “There’s a growing understanding that these conversations need to be happening across these different sectors.”
Pleas for accuracy
At academic medical institutions, conflicts of interest are identified and then managed; it’s common for researchers’ COI management plans to include requirements for disclosure in all presentations and publications.
Journals and professional medical societies require authors and speakers to submit disclosure forms of varying lengths and with differing questions about relationships with industry, often based on the notion of relevancy to the subject at hand. Disclosure forms are reviewed, but editors and other reviewers rely largely – if not entirely – on the honor system.
Dr. Baselga’s disclosure lapses and his subsequent resignation have rattled leaders in each of these settings. Researchers at MSK were instructed to review their COI disclosures and submit corrections when necessary, and in December 2018 the hospital was reportedly evaluating its process for reviewing conflicts of interest, according to reports in the New York Times and ProPublica. (MSK did not respond to requests for comment about actions taken.)
The Dana Farber Cancer Institute in Boston similarly has “been reminding faculty and other researchers” of their disclosure responsibilities and is conducting a review of “all our policies in this area,” a spokeswoman said. And at Fred Hutchinson Cancer Research Center in Seattle, a spokesman said they have established an internal task force to review individual and institutional COI policies to ensure that COIs are “appropriately managed while also enabling research collaborations that bring scientific advances to our patients.”
Other centers contacted for this article, such as the Cleveland Clinic Cancer Center and the Mayo Clinic Cancer Center, said that they have no new reviews ongoing and no plans to change policies at this time.
The heightened attention to disclosure has, in turn, shone a spotlight on increasingly complex physician-industry relationships and on the Open Payments website run by the Centers for Medicare and Medicaid Services. Open Payments is a disclosure program and database that tracks payments made to physicians and teaching hospitals by drug and device companies.
Journalists, including those who reported on Dr. Baselga’s disclosures, have searched the public database for industry payment data. So have other researchers who have studied financial disclosure statements; a study reported in JAMA Oncology last year, for instance, concluded through the use of Open Payments data that about one-third of authors of cancer drug trial reports did not completely disclose payments from trial sponsors (JAMA Oncol. 2018;4[10]:1426-8
In a column published in December 2018 in AAMC News, AAMC President and CEO Darrell G. Kirch, MD, wrote that failures to disclose can raise questions about the integrity of research, whether or not there is an actual conflict. He advised institutions to “encourage faculty to review the information posted about them on the Open Payments website” of the CMS to “ensure it is accurate and consistent with disclosures related to all their professional responsibilities.”
ASCO issues similar advice, encouraging authors and CME speakers and participants of other ASCO activities to double-check their disclosures against other sources, including “publicly reported interactions with companies that may have been inadvertently omitted.”
In the world of journals, the New England Journal of Medicine (NEJM) began asking authors at the end of 2018 to “certify that they have reconciled their disclosures” with the Open Payments database, said Jennifer Zeis, a spokeswoman forthe journal.
Time may tell how well such requests work. When the Institute of Medicine (now called the National Academy of Medicine) called on Congress in 2009 to create a national program requiring pharmaceutical, device, and biotechnology companies to publicly report their payments, it envisioned universities, journals, and others using the program to verify disclosures made to them. But the resulting Open Payments database has limitations – for instance, it doesn’t include payments from companies without FDA-approved products, it is not necessarily up to date, and its payment categories do not necessarily match categories of disclosure.
“Some entries in the Open Payments database need further explanation,” said Ms. Zeis of NEJM. “Some authors, for example, have said that the database does not fully and accurately explain that the funds were disbursed not to them personally, but to their academic institutions.” While the database provides transparency, it also “needs context that’s not currently provided,” she said.
Mistakes in the database can also be “very hard to challenge,” said Clifford A. Hudis, MD, CEO of the American Society of Clinical Oncology, which produces the Journal of Clinical Oncology (JCO).
All in all, he said, “there’s really no timely, comprehensive, and fully reliable source of information with which to verify an individual’s disclosures.”
Policies and practices are also under review at the American Association for Cancer Research (AACR) and the American Society of Hematology (ASH).
The AACR has appointed a panel of experts, including physicians, basic scientists, a patient advocate, and others to conduct “a comprehensive review of [its] disclosure policies and to explore whether any current policies need to be revised,” said Rachel Salis-Silverman, director of public relations. It also will convene a session on COI disclosures at its 2019 annual meeting at the end of March, she said.
ASH, which publishes the journal Blood, is exploring possible changes in its “internal processes with regards to ASH publications,” said Matt Gertzog, deputy executive director of the group. COI disclosure is “more of a journey than a destination,” he said. “We are continuously reflecting on and refining our processes.”
Moving away from ‘relevancy’
Physicians and others who have relationships with industry have long complained about a patchwork of disclosure requirements, and significant efforts have been made in the last decade to standardize forms and practices. However, the current system is still “a little bit of a Tower of Babel,” said Dr. Hudis of ASCO. “Every day, physicians have to complete from scratch similar, but not identical, disclosure forms that ask similar, but not identical, questions.”
A disclosable compensation amount “might be first dollar, or it might be over $10,000. [Time periods] might cover 1 year, or 3 years. ... Stock ownership might be dollar value, or a percentage of shares,” he explained. “If you want a system that would make it hard to be compliant and easy to mess up, that’s what we have.”
To standardize the COI disclosure process for all Society-related publications and activities – including CME, JCO, and practice guidelines – ASCO moved about 5 years ago to a system of general disclosure, asking physicians and others to disclose all financial interests and industry relationships rather than what they deem relevant.
The thinking was that general disclosure “would be easier for disclosers, and nobody would ever be accused of hiding anything,” Dr. Hudis said.
“We’d [also] recognized,” he explained, “that there was a risk to the relevancy approach in that it put the judgment for the potential conflict in the hands of the potentially conflicted, while others might have a different point of view about what is or isn’t relevant.”
Those concerned about general disclosure worry that it may “obscure [for the reader or listener] what’s really important or the most meaningful,” he said.
Some physicians have expressed in interviews for this article, moreover, the concern that too many disclosures – too long a list of financial relationships – will be viewed negatively. This is something ASCO aims to guard against as it strives to achieve full transparency, Dr. Hudis said. “If one were to suggest that engagement itself is automatically a negative, then you’re starting to put negative pressure on compliance with disclosure.”
And full disclosure matters, he said. “We have to err in the direction of believing that disclosure is good,” he said, “even if we can’t prove it has clear and measurable impact. That is why our goal is to make full disclosure easier. What potential conflicts are acceptable, or not, is an important but entirely separate matter.”
Howard Bauchner, MD, editor in chief of JAMA and the JAMA Network, frames the pros and cons of general and relevant disclosure similarly, and emphasizes that the relationships of authors with industry – particularly with private equity start-up companies – has changed dramatically over the past decade. Editors have “talked about complete versus [more narrowly] relevant disclosures at length,” he said, and have been moving overall “toward more complete disclosure where the reader can make a decision on their own.”
Other journals also are taking this approach. In 2009, in an effort to reduce variability in reporting processes and formats, the International Committee of Medical Journal Editors (ICMJE) developed a uniform electronic disclosure form that asks about financial relationships and interactions with any entity that could be considered “broadly relevant” to the submitted work. The group updated the form in December 2018.
As an example, the form reads, an article about testing an epidermal growth factor receptor (EGFR) antagonist in lung cancer requires the reporting of “all associations with entities pursuing diagnostic or therapeutic strategies in cancer in general, not just in the area of EGFR or lung cancer.” JAMA, NEJM, and The Lancet are among those journals that embrace the ICMJE’s policies and use its form.
To simplify its own disclosure process, JAMA and the network’s journals ended the practice in January 2019 of requiring both the ICMJE form and JAMA’s own separate disclosure form. The journals now use a single electronic form that includes questions from the ICMJE form. And to promote more consistent and complete reporting, the electronic form contains prompts that ask authors each time they answer “no” to one of four specific questions about potential COI whether they are certain of their answers and whether their answers are consistent with other disclosures they recently made.
While relevancy statements “create struggles for authors,” about two-thirds of the disclosure inaccuracies reported by readers and verified by JAMA’s editors (most often through editor-author discussions) involve a complete lack of disclosure rather than questions of relevancy, Dr. Bauchner noted. (JAMA and the network’s journals receive about 30,000 disclosure forms each year.)
The AAMC, in the meantime, has developed a central web-based repository for disclosures called Convey. Physicians and others can maintain secure records of financial interests in the repository, and these records can then be disclosed directly to any journal or organization that uses the system. The tool – born from discussions that followed the 2009 IOM report on COI – is “intended to facilitate more complete, more accurate, and more consistent” disclosures,” said Ms. Pierce of the AAMC. It is now live and in its early stages of use; NEJM assisted in its development and has been one of its pilot testers.
Enforcement questions
Some experts believe that institutions should maintain public databases of disclosures and/or that disclosure requirements should be better enforced in-house.
“There often are no clear guidelines in institutions about how to respond to people who are negligent in how they’re managing their disclosures,” said Jeffrey R. Botkin, MD, MPH, professor of pediatrics and associate vice president for research at the University of Utah, Salt Lake City, who has served on a variety of ethics committees and is an elected member of the Hastings Center. Dr. Botkin proposed in a Viewpoint published last October in JAMA that failure to disclose significant COIs should be considered research misconduct (JAMA 2018;320[22]:2307-8).
At the University of Utah, “we’re getting better at saying, ‘show us that you’ve disclosed,’ ” he said. “In some cases we’ll do spot checks of journal articles to make sure [researchers have] followed through with their disclosures.”
John Abramson, MD, a lecturer in the department of health care policy at Harvard Medical School, Boston, contends that incomplete declarations of COI have been shown to correlate with reporting of manufacturer-friendly research results. Journals should have “zero tolerance” standards for incomplete or inaccurate COI declarations and should, among other things, “inform academic institutions of breaches of integrity.”
At JAMA, which in 2017 published a theme issue on COI and COI declarations, editors have been discussing whether they will contact an author’s institution “if there’s a pattern involved [with disclosure problems] or if there’s a lack of declaration of multiple COIs,” Dr. Bauchner said.
Physician PAC dollars support candidates against gun regulation
Despite many physician professional organizations endorsing policies that support firearm regulation, more of their political donations go to candidates who oppose those policies, according to a study of political action committee (PAC) campaign contributions during the 2016 election cycle.
“Our analysis indicates that most of the largest physician organizations’ PACs contribute more to candidates whose stances on firearm policy are in direct opposition to evidence-based firearm policies and to their organization’s stances,” wrote lead author Jeremiah D. Schuur, MD, of Brown University, Providence, R.I., and his coauthors.
The study was published in JAMA Network Open.
This retrospective, cross sectional study examined contributions from the 25 largest physician organization–affiliated PACs during the 2016 election cycle and compared them to federal candidate support for firearm regulation.
Support for regulation was measured by voting history on U.S. House and Senate legislation proposing firearm background checks and their rating from the National Rifle Association Political Victory Fund (NRA-PVF).
Health care professional–related PACs in general contributed $23.7 million during the 2016 election cycle; 57% of that sum ($13.6 million) came from the 25 largest physician-affiliated PACs.
Of the 29 Senate incumbents running for reelection who voted on S.A. 4750, an amendment that would have expanded background checks, those who voted against it (n = 21) received $500,000 more in contributions than did those who voted for it (n = 8).
The findings were similar with H.R. 1217, a bill in the House of Representatives to expand background checks; the PACs contributed $2,878,675 more to candidates who did not cosponsor it (n = 227) than to cosponsors (n = 166).
In regard to ratings from the NRA-PVF, the 25 PACs gave $5.6 million to candidates with an A rating and $4.1 million to candidates with a rating other than A.
But the trend was somewhat different when it came to the 2015 call to action on firearm-related injury and death, endorsed by several physician groups. Among the nine PACs with affiliated organizations that had endorsed the call to action, eight contributed to more candidates who did not support firearm safety policies. But after adjustment for political factors, those nine PACs had a lower likelihood of donating to NRA-PVF A-rated candidates, compared with nonendorsing PACs (odds ratio, 0.76; 95% confidence interval, 0.58-0.99; P = .04).
“Although endorsement of firearm safety policies may reflect a small difference in political giving, it does not mean that a physicians’ organization has elevated firearm policy to the level of a contribution criteria for the PAC,” the researchers wrote.
The researchers noted that it is “unlikely that physician organization–affiliated PACs contribute to candidates because they are opposed to firearm regulation.” Rather, they said, these PACs consider a number of factors, including a candidates’ stance on malpractice reform, physician payment policies, and the Patient Protection and Affordable Care Act, as well as their chance of winning.
The authors reported having no conflicts of interest.
SOURCE: Schuur JD et al. JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7831.
Though national membership organizations have finally taken a lead in advocating for firearm safety, this study from Schuur et al. illustrates the disconnect between physician PACs and the physicians themselves, according to Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, of the University of Michigan, Ann Arbor.
The study comes in the wake of the NRA admonishing physicians to “stay in their lane,” which was met by a very vocal response via social and mass media. “Health care professionals demonstrated that, contrary to the NRA position, they have an undeniably central role and authority in addressing this public health problem through the direct care that they provide to patients and their families, prevention-based research, and advocacy for policy-level changes that make patients safer,” they wrote.
The coauthors noted the parallels to the American Medical Association previously calling for tobacco regulation while financially supporting politicians who felt otherwise. It’s a comparison that is meant as a cautionary tale; as more focus is placed on this particular issue, “medical PACs must consider the increasing physician voice on the need to address firearm-associated morbidity and mortality in the policy arena to reduce their experience with this issue in emergency bays, operating rooms, and clinics.”
Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, are with the University of Michigan, Ann Arbor. They reported having no conflicts of interest. Their comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7823 ).
Though national membership organizations have finally taken a lead in advocating for firearm safety, this study from Schuur et al. illustrates the disconnect between physician PACs and the physicians themselves, according to Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, of the University of Michigan, Ann Arbor.
The study comes in the wake of the NRA admonishing physicians to “stay in their lane,” which was met by a very vocal response via social and mass media. “Health care professionals demonstrated that, contrary to the NRA position, they have an undeniably central role and authority in addressing this public health problem through the direct care that they provide to patients and their families, prevention-based research, and advocacy for policy-level changes that make patients safer,” they wrote.
The coauthors noted the parallels to the American Medical Association previously calling for tobacco regulation while financially supporting politicians who felt otherwise. It’s a comparison that is meant as a cautionary tale; as more focus is placed on this particular issue, “medical PACs must consider the increasing physician voice on the need to address firearm-associated morbidity and mortality in the policy arena to reduce their experience with this issue in emergency bays, operating rooms, and clinics.”
Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, are with the University of Michigan, Ann Arbor. They reported having no conflicts of interest. Their comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7823 ).
Though national membership organizations have finally taken a lead in advocating for firearm safety, this study from Schuur et al. illustrates the disconnect between physician PACs and the physicians themselves, according to Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, of the University of Michigan, Ann Arbor.
The study comes in the wake of the NRA admonishing physicians to “stay in their lane,” which was met by a very vocal response via social and mass media. “Health care professionals demonstrated that, contrary to the NRA position, they have an undeniably central role and authority in addressing this public health problem through the direct care that they provide to patients and their families, prevention-based research, and advocacy for policy-level changes that make patients safer,” they wrote.
The coauthors noted the parallels to the American Medical Association previously calling for tobacco regulation while financially supporting politicians who felt otherwise. It’s a comparison that is meant as a cautionary tale; as more focus is placed on this particular issue, “medical PACs must consider the increasing physician voice on the need to address firearm-associated morbidity and mortality in the policy arena to reduce their experience with this issue in emergency bays, operating rooms, and clinics.”
Rebecca M. Cunningham, MD, Marc A. Zimmerman, PhD, and Patrick M. Carter, MD, are with the University of Michigan, Ann Arbor. They reported having no conflicts of interest. Their comments are adapted from an accompanying editorial (JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7823 ).
Despite many physician professional organizations endorsing policies that support firearm regulation, more of their political donations go to candidates who oppose those policies, according to a study of political action committee (PAC) campaign contributions during the 2016 election cycle.
“Our analysis indicates that most of the largest physician organizations’ PACs contribute more to candidates whose stances on firearm policy are in direct opposition to evidence-based firearm policies and to their organization’s stances,” wrote lead author Jeremiah D. Schuur, MD, of Brown University, Providence, R.I., and his coauthors.
The study was published in JAMA Network Open.
This retrospective, cross sectional study examined contributions from the 25 largest physician organization–affiliated PACs during the 2016 election cycle and compared them to federal candidate support for firearm regulation.
Support for regulation was measured by voting history on U.S. House and Senate legislation proposing firearm background checks and their rating from the National Rifle Association Political Victory Fund (NRA-PVF).
Health care professional–related PACs in general contributed $23.7 million during the 2016 election cycle; 57% of that sum ($13.6 million) came from the 25 largest physician-affiliated PACs.
Of the 29 Senate incumbents running for reelection who voted on S.A. 4750, an amendment that would have expanded background checks, those who voted against it (n = 21) received $500,000 more in contributions than did those who voted for it (n = 8).
The findings were similar with H.R. 1217, a bill in the House of Representatives to expand background checks; the PACs contributed $2,878,675 more to candidates who did not cosponsor it (n = 227) than to cosponsors (n = 166).
In regard to ratings from the NRA-PVF, the 25 PACs gave $5.6 million to candidates with an A rating and $4.1 million to candidates with a rating other than A.
But the trend was somewhat different when it came to the 2015 call to action on firearm-related injury and death, endorsed by several physician groups. Among the nine PACs with affiliated organizations that had endorsed the call to action, eight contributed to more candidates who did not support firearm safety policies. But after adjustment for political factors, those nine PACs had a lower likelihood of donating to NRA-PVF A-rated candidates, compared with nonendorsing PACs (odds ratio, 0.76; 95% confidence interval, 0.58-0.99; P = .04).
“Although endorsement of firearm safety policies may reflect a small difference in political giving, it does not mean that a physicians’ organization has elevated firearm policy to the level of a contribution criteria for the PAC,” the researchers wrote.
The researchers noted that it is “unlikely that physician organization–affiliated PACs contribute to candidates because they are opposed to firearm regulation.” Rather, they said, these PACs consider a number of factors, including a candidates’ stance on malpractice reform, physician payment policies, and the Patient Protection and Affordable Care Act, as well as their chance of winning.
The authors reported having no conflicts of interest.
SOURCE: Schuur JD et al. JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7831.
Despite many physician professional organizations endorsing policies that support firearm regulation, more of their political donations go to candidates who oppose those policies, according to a study of political action committee (PAC) campaign contributions during the 2016 election cycle.
“Our analysis indicates that most of the largest physician organizations’ PACs contribute more to candidates whose stances on firearm policy are in direct opposition to evidence-based firearm policies and to their organization’s stances,” wrote lead author Jeremiah D. Schuur, MD, of Brown University, Providence, R.I., and his coauthors.
The study was published in JAMA Network Open.
This retrospective, cross sectional study examined contributions from the 25 largest physician organization–affiliated PACs during the 2016 election cycle and compared them to federal candidate support for firearm regulation.
Support for regulation was measured by voting history on U.S. House and Senate legislation proposing firearm background checks and their rating from the National Rifle Association Political Victory Fund (NRA-PVF).
Health care professional–related PACs in general contributed $23.7 million during the 2016 election cycle; 57% of that sum ($13.6 million) came from the 25 largest physician-affiliated PACs.
Of the 29 Senate incumbents running for reelection who voted on S.A. 4750, an amendment that would have expanded background checks, those who voted against it (n = 21) received $500,000 more in contributions than did those who voted for it (n = 8).
The findings were similar with H.R. 1217, a bill in the House of Representatives to expand background checks; the PACs contributed $2,878,675 more to candidates who did not cosponsor it (n = 227) than to cosponsors (n = 166).
In regard to ratings from the NRA-PVF, the 25 PACs gave $5.6 million to candidates with an A rating and $4.1 million to candidates with a rating other than A.
But the trend was somewhat different when it came to the 2015 call to action on firearm-related injury and death, endorsed by several physician groups. Among the nine PACs with affiliated organizations that had endorsed the call to action, eight contributed to more candidates who did not support firearm safety policies. But after adjustment for political factors, those nine PACs had a lower likelihood of donating to NRA-PVF A-rated candidates, compared with nonendorsing PACs (odds ratio, 0.76; 95% confidence interval, 0.58-0.99; P = .04).
“Although endorsement of firearm safety policies may reflect a small difference in political giving, it does not mean that a physicians’ organization has elevated firearm policy to the level of a contribution criteria for the PAC,” the researchers wrote.
The researchers noted that it is “unlikely that physician organization–affiliated PACs contribute to candidates because they are opposed to firearm regulation.” Rather, they said, these PACs consider a number of factors, including a candidates’ stance on malpractice reform, physician payment policies, and the Patient Protection and Affordable Care Act, as well as their chance of winning.
The authors reported having no conflicts of interest.
SOURCE: Schuur JD et al. JAMA Netw Open. 2019 Feb 22. doi: 10.1001/jamanetworkopen.2018.7831.
FROM JAMA NETWORK OPEN
Health spending: Boomers will spike costs, but growing uninsured will soften their impact
Spending on health care is projected to rise at a faster-than-average rate throughout the next decade, according to the Office of the Actuary at the Centers for Medicare & Medicaid Services.
“Overall, national health spending is projected to grow at 5.5% per year, on average, for 2018-27,” wrote Andrea Sisko, economist in the Office of the Actuary, and colleagues (Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499). “This is faster than the average growth rate experienced following the last recession (3.9% for 2008-2013) and the more recent period inclusive of the Affordable Care Act’s major coverage expansions (5.3% for 2014-16).”
Medicare is projected to see the fastest growth in spending at 7.4% per year “as the shift of the Baby Boom generation into the program continues to result in robust growth in enrollment,” according to the authors.
Private payers should see a corollary slower growth in spending (4.8% per year) over the same period, while Medicaid spending is projected at 5.5% per year.
Faster growth in Medicare spending is expected to come from higher spending on prescription drugs and hospital services, as well as higher fee-for-service payment updates.
Spending increases are projected to be mitigated somewhat by the end of the ACA penalty for not having insurance – which is projected to add 1.3 million people this year to the ranks of the uninsured, according to the report.
Half of the overall growth in health care spending is attributable to rising prices in personal health care prices, on average, Ms. Sisko and colleagues wrote. “Growth in use and intensity is expected to account for just under one-third of the average annual personal health care spending growth, with population growth and the changing age-sex mix of the population accounting for the remainder.”
For those with private insurance, out-of-pocket spending is projected to accelerate to a 3.6% growth rate in 2018 from 2.6% in 2017 “a rate that is consistent with faster income growth as well as with the higher average deductibles for employer-based private health insurance enrollees in 2018 compared to 2017,” the authors note.
“Growth in out-of-pocket spending, which is also primarily influenced by economic factors, is expected to be similar to that of private health insurance spending in 2020-27, at 5%,” they add.
Prescription drug spending also is expected to grow.
“Following growth of just 0.4% in 2017, prescription drug spending is expected to have grown 3.3% in 2018 but still be among the slowest-growing health care sectors,” according to the authors. “Higher utilization growth is anticipated, compared to the relatively low growth in 2016 and 2017, partially driven by an increase in the number of new drug introductions.”
Growth in prescription drug spending is expected to accelerate further to 4.6% in 2019, based on growth in utilization and a “modest increase in drug price growth.”
Starting in 2020, that growth rate is projected to increase, on average, by 6.1% per year, based on the expectation that employers and insurers will lower barriers to maintenance medications for chronic conditions.
In 2019, growth in spending for physician clinical services is projected to accelerate to 5.4% from 4.9% in 2018.
“An acceleration in Medicaid spending growth is the primary factor contributing to the trend, which is in part associated with program’s expansion by additional states,” the authors note.
From 2020 to 2027, growth in spending on physician and clinical services is expected to average 5.4% per year, driven in part by price growth for these services.
“Underlying this acceleration are projected rising costs related to the provision of care,” the report said. “In particular, wages are expected to increase as a result of the supply of physicians not being able to meet expected increases in demand for care connected with the aging population. Furthermore, some of the productivity gains that have been achieved through the use of lower-cost providers as a substitute for physician care within physician practices may be less pronounced in the future, because of limitations such as licensing restrictions on the scope of care that may be provided by nonphysician providers.”
SOURCE: Sisko A et al. Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499.
Spending on health care is projected to rise at a faster-than-average rate throughout the next decade, according to the Office of the Actuary at the Centers for Medicare & Medicaid Services.
“Overall, national health spending is projected to grow at 5.5% per year, on average, for 2018-27,” wrote Andrea Sisko, economist in the Office of the Actuary, and colleagues (Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499). “This is faster than the average growth rate experienced following the last recession (3.9% for 2008-2013) and the more recent period inclusive of the Affordable Care Act’s major coverage expansions (5.3% for 2014-16).”
Medicare is projected to see the fastest growth in spending at 7.4% per year “as the shift of the Baby Boom generation into the program continues to result in robust growth in enrollment,” according to the authors.
Private payers should see a corollary slower growth in spending (4.8% per year) over the same period, while Medicaid spending is projected at 5.5% per year.
Faster growth in Medicare spending is expected to come from higher spending on prescription drugs and hospital services, as well as higher fee-for-service payment updates.
Spending increases are projected to be mitigated somewhat by the end of the ACA penalty for not having insurance – which is projected to add 1.3 million people this year to the ranks of the uninsured, according to the report.
Half of the overall growth in health care spending is attributable to rising prices in personal health care prices, on average, Ms. Sisko and colleagues wrote. “Growth in use and intensity is expected to account for just under one-third of the average annual personal health care spending growth, with population growth and the changing age-sex mix of the population accounting for the remainder.”
For those with private insurance, out-of-pocket spending is projected to accelerate to a 3.6% growth rate in 2018 from 2.6% in 2017 “a rate that is consistent with faster income growth as well as with the higher average deductibles for employer-based private health insurance enrollees in 2018 compared to 2017,” the authors note.
“Growth in out-of-pocket spending, which is also primarily influenced by economic factors, is expected to be similar to that of private health insurance spending in 2020-27, at 5%,” they add.
Prescription drug spending also is expected to grow.
“Following growth of just 0.4% in 2017, prescription drug spending is expected to have grown 3.3% in 2018 but still be among the slowest-growing health care sectors,” according to the authors. “Higher utilization growth is anticipated, compared to the relatively low growth in 2016 and 2017, partially driven by an increase in the number of new drug introductions.”
Growth in prescription drug spending is expected to accelerate further to 4.6% in 2019, based on growth in utilization and a “modest increase in drug price growth.”
Starting in 2020, that growth rate is projected to increase, on average, by 6.1% per year, based on the expectation that employers and insurers will lower barriers to maintenance medications for chronic conditions.
In 2019, growth in spending for physician clinical services is projected to accelerate to 5.4% from 4.9% in 2018.
“An acceleration in Medicaid spending growth is the primary factor contributing to the trend, which is in part associated with program’s expansion by additional states,” the authors note.
From 2020 to 2027, growth in spending on physician and clinical services is expected to average 5.4% per year, driven in part by price growth for these services.
“Underlying this acceleration are projected rising costs related to the provision of care,” the report said. “In particular, wages are expected to increase as a result of the supply of physicians not being able to meet expected increases in demand for care connected with the aging population. Furthermore, some of the productivity gains that have been achieved through the use of lower-cost providers as a substitute for physician care within physician practices may be less pronounced in the future, because of limitations such as licensing restrictions on the scope of care that may be provided by nonphysician providers.”
SOURCE: Sisko A et al. Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499.
Spending on health care is projected to rise at a faster-than-average rate throughout the next decade, according to the Office of the Actuary at the Centers for Medicare & Medicaid Services.
“Overall, national health spending is projected to grow at 5.5% per year, on average, for 2018-27,” wrote Andrea Sisko, economist in the Office of the Actuary, and colleagues (Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499). “This is faster than the average growth rate experienced following the last recession (3.9% for 2008-2013) and the more recent period inclusive of the Affordable Care Act’s major coverage expansions (5.3% for 2014-16).”
Medicare is projected to see the fastest growth in spending at 7.4% per year “as the shift of the Baby Boom generation into the program continues to result in robust growth in enrollment,” according to the authors.
Private payers should see a corollary slower growth in spending (4.8% per year) over the same period, while Medicaid spending is projected at 5.5% per year.
Faster growth in Medicare spending is expected to come from higher spending on prescription drugs and hospital services, as well as higher fee-for-service payment updates.
Spending increases are projected to be mitigated somewhat by the end of the ACA penalty for not having insurance – which is projected to add 1.3 million people this year to the ranks of the uninsured, according to the report.
Half of the overall growth in health care spending is attributable to rising prices in personal health care prices, on average, Ms. Sisko and colleagues wrote. “Growth in use and intensity is expected to account for just under one-third of the average annual personal health care spending growth, with population growth and the changing age-sex mix of the population accounting for the remainder.”
For those with private insurance, out-of-pocket spending is projected to accelerate to a 3.6% growth rate in 2018 from 2.6% in 2017 “a rate that is consistent with faster income growth as well as with the higher average deductibles for employer-based private health insurance enrollees in 2018 compared to 2017,” the authors note.
“Growth in out-of-pocket spending, which is also primarily influenced by economic factors, is expected to be similar to that of private health insurance spending in 2020-27, at 5%,” they add.
Prescription drug spending also is expected to grow.
“Following growth of just 0.4% in 2017, prescription drug spending is expected to have grown 3.3% in 2018 but still be among the slowest-growing health care sectors,” according to the authors. “Higher utilization growth is anticipated, compared to the relatively low growth in 2016 and 2017, partially driven by an increase in the number of new drug introductions.”
Growth in prescription drug spending is expected to accelerate further to 4.6% in 2019, based on growth in utilization and a “modest increase in drug price growth.”
Starting in 2020, that growth rate is projected to increase, on average, by 6.1% per year, based on the expectation that employers and insurers will lower barriers to maintenance medications for chronic conditions.
In 2019, growth in spending for physician clinical services is projected to accelerate to 5.4% from 4.9% in 2018.
“An acceleration in Medicaid spending growth is the primary factor contributing to the trend, which is in part associated with program’s expansion by additional states,” the authors note.
From 2020 to 2027, growth in spending on physician and clinical services is expected to average 5.4% per year, driven in part by price growth for these services.
“Underlying this acceleration are projected rising costs related to the provision of care,” the report said. “In particular, wages are expected to increase as a result of the supply of physicians not being able to meet expected increases in demand for care connected with the aging population. Furthermore, some of the productivity gains that have been achieved through the use of lower-cost providers as a substitute for physician care within physician practices may be less pronounced in the future, because of limitations such as licensing restrictions on the scope of care that may be provided by nonphysician providers.”
SOURCE: Sisko A et al. Health Aff. 2019 Feb 20. doi: 10.1377/hlthaff.2018.05499.
FROM HEALTH AFFAIRS
McAneny: Transparency needed for meaningful talk on drug pricing
WASHINGTON – As the rising cost of prescription drugs continues to garner heightened scrutiny from the federal government, one thing is missing from the conversation that would make any solution more effective, according to American Medical Association President Barbara L. McAneny, MD.
“We would like to see transparency from end to end in this pipeline because that is the way we will have the ability to look for savings,” she said in an interview at a national advocacy conference sponsored by the American Medical Association.
“I think we don’t have the information we need to make rational decisions,” she said. “I think the first thing we need to do is to understand the entire pipeline from the basic research that results in a drug’s clinical trials that results in a new drug to the pharmacy benefit managers and all of the ways that they have increased the cost of the drugs all the way to when the patient actually gets it.”
In particular, Dr. McAneny targeted the need for transparency in the role and financial impact pharmacy benefit managers have on the cost of prescription drugs.
“We were told at our state advocacy conference, which we held in January, by an expert who studied pharmacy benefit managers, that 42% of the cost of any drug is attributable to the profits of pharmacy benefit managers,” she said. “To me, that makes me wonder what value do they add that is worth 42% of these exorbitant costs and if they are not adding value, why do we have them in this process?”
She also called on the pharmaceutical manufacturers to be more forthcoming with their financial information regarding marketing and advertising, but she stressed that it needs to be done in a way that does not hinder future development of life-saving therapies.
“We do not want to stifle innovation.” Dr. McAneny said. “As a cancer doctor, I have seen diseases that I used to treat with morphine and sympathy now be diseases that I can treat, where I can restore people to good quality of life and buy them additional years of life because of these drugs. They are amazing and I don’t want to do without them and I want more of them. ... We want to support that research. That is probably worth a lot of the price tag. But how much of that goes to direct-to-consumer advertising? How much of that is the advertising budget? Where can we cut some of this out of the system so that we get the innovation, but we get innovation that all of our patients can afford?”
Another issue that is looming for physicians is a payment rate freeze from 2020-2025 under the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program, which was created under the Medicare Access and CHIP Reauthorization Act (MACRA).
“A 5-year freeze when my expenses do not freeze is a terrifying thing and could be a practice-ending expense for a lot of practices,” Dr. McAneny warned. “I will point out that independent practices, if they sell to a hospital, the cost of care immediately doubles. The amount that is paid for it, not the cost of delivering it. So that is not a great solution. But we also have this increasing practice expense and a flat rate is not going to help practices survive. So I am very concerned.”
Related to the QPP, Dr. McAneny also wants to see the Centers for Medicare & Medicaid Services do more with physician-developed alternative payment models. The Physician-Focused Payment Model Technical Advisory Committee (PTAC) continues to review and evaluate submissions, but to date, the CMS has yet to implement any of the committee’s recommendations.
“I read all of the PTAC submissions that went to CMS. Some of them I thought were a little on the weak side, but there are a lot of them that I thought were really good ideas. I do not know why CMS did not approve them and fund them and let them be tried,” she said, although she did offer an opinion on why the agency has yet to act on any of them.
“I read their paper saying why they didn’t approve [the recommended physician-developed alternative payment models]. It seemed to me they are waiting for one silver bullet that will fix all of health care. I don’t think a silver bullet is going to fix health care. It’s not an issue. It’s a complicated set of issues. You will not have a quick fix.”
WASHINGTON – As the rising cost of prescription drugs continues to garner heightened scrutiny from the federal government, one thing is missing from the conversation that would make any solution more effective, according to American Medical Association President Barbara L. McAneny, MD.
“We would like to see transparency from end to end in this pipeline because that is the way we will have the ability to look for savings,” she said in an interview at a national advocacy conference sponsored by the American Medical Association.
“I think we don’t have the information we need to make rational decisions,” she said. “I think the first thing we need to do is to understand the entire pipeline from the basic research that results in a drug’s clinical trials that results in a new drug to the pharmacy benefit managers and all of the ways that they have increased the cost of the drugs all the way to when the patient actually gets it.”
In particular, Dr. McAneny targeted the need for transparency in the role and financial impact pharmacy benefit managers have on the cost of prescription drugs.
“We were told at our state advocacy conference, which we held in January, by an expert who studied pharmacy benefit managers, that 42% of the cost of any drug is attributable to the profits of pharmacy benefit managers,” she said. “To me, that makes me wonder what value do they add that is worth 42% of these exorbitant costs and if they are not adding value, why do we have them in this process?”
She also called on the pharmaceutical manufacturers to be more forthcoming with their financial information regarding marketing and advertising, but she stressed that it needs to be done in a way that does not hinder future development of life-saving therapies.
“We do not want to stifle innovation.” Dr. McAneny said. “As a cancer doctor, I have seen diseases that I used to treat with morphine and sympathy now be diseases that I can treat, where I can restore people to good quality of life and buy them additional years of life because of these drugs. They are amazing and I don’t want to do without them and I want more of them. ... We want to support that research. That is probably worth a lot of the price tag. But how much of that goes to direct-to-consumer advertising? How much of that is the advertising budget? Where can we cut some of this out of the system so that we get the innovation, but we get innovation that all of our patients can afford?”
Another issue that is looming for physicians is a payment rate freeze from 2020-2025 under the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program, which was created under the Medicare Access and CHIP Reauthorization Act (MACRA).
“A 5-year freeze when my expenses do not freeze is a terrifying thing and could be a practice-ending expense for a lot of practices,” Dr. McAneny warned. “I will point out that independent practices, if they sell to a hospital, the cost of care immediately doubles. The amount that is paid for it, not the cost of delivering it. So that is not a great solution. But we also have this increasing practice expense and a flat rate is not going to help practices survive. So I am very concerned.”
Related to the QPP, Dr. McAneny also wants to see the Centers for Medicare & Medicaid Services do more with physician-developed alternative payment models. The Physician-Focused Payment Model Technical Advisory Committee (PTAC) continues to review and evaluate submissions, but to date, the CMS has yet to implement any of the committee’s recommendations.
“I read all of the PTAC submissions that went to CMS. Some of them I thought were a little on the weak side, but there are a lot of them that I thought were really good ideas. I do not know why CMS did not approve them and fund them and let them be tried,” she said, although she did offer an opinion on why the agency has yet to act on any of them.
“I read their paper saying why they didn’t approve [the recommended physician-developed alternative payment models]. It seemed to me they are waiting for one silver bullet that will fix all of health care. I don’t think a silver bullet is going to fix health care. It’s not an issue. It’s a complicated set of issues. You will not have a quick fix.”
WASHINGTON – As the rising cost of prescription drugs continues to garner heightened scrutiny from the federal government, one thing is missing from the conversation that would make any solution more effective, according to American Medical Association President Barbara L. McAneny, MD.
“We would like to see transparency from end to end in this pipeline because that is the way we will have the ability to look for savings,” she said in an interview at a national advocacy conference sponsored by the American Medical Association.
“I think we don’t have the information we need to make rational decisions,” she said. “I think the first thing we need to do is to understand the entire pipeline from the basic research that results in a drug’s clinical trials that results in a new drug to the pharmacy benefit managers and all of the ways that they have increased the cost of the drugs all the way to when the patient actually gets it.”
In particular, Dr. McAneny targeted the need for transparency in the role and financial impact pharmacy benefit managers have on the cost of prescription drugs.
“We were told at our state advocacy conference, which we held in January, by an expert who studied pharmacy benefit managers, that 42% of the cost of any drug is attributable to the profits of pharmacy benefit managers,” she said. “To me, that makes me wonder what value do they add that is worth 42% of these exorbitant costs and if they are not adding value, why do we have them in this process?”
She also called on the pharmaceutical manufacturers to be more forthcoming with their financial information regarding marketing and advertising, but she stressed that it needs to be done in a way that does not hinder future development of life-saving therapies.
“We do not want to stifle innovation.” Dr. McAneny said. “As a cancer doctor, I have seen diseases that I used to treat with morphine and sympathy now be diseases that I can treat, where I can restore people to good quality of life and buy them additional years of life because of these drugs. They are amazing and I don’t want to do without them and I want more of them. ... We want to support that research. That is probably worth a lot of the price tag. But how much of that goes to direct-to-consumer advertising? How much of that is the advertising budget? Where can we cut some of this out of the system so that we get the innovation, but we get innovation that all of our patients can afford?”
Another issue that is looming for physicians is a payment rate freeze from 2020-2025 under the Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program, which was created under the Medicare Access and CHIP Reauthorization Act (MACRA).
“A 5-year freeze when my expenses do not freeze is a terrifying thing and could be a practice-ending expense for a lot of practices,” Dr. McAneny warned. “I will point out that independent practices, if they sell to a hospital, the cost of care immediately doubles. The amount that is paid for it, not the cost of delivering it. So that is not a great solution. But we also have this increasing practice expense and a flat rate is not going to help practices survive. So I am very concerned.”
Related to the QPP, Dr. McAneny also wants to see the Centers for Medicare & Medicaid Services do more with physician-developed alternative payment models. The Physician-Focused Payment Model Technical Advisory Committee (PTAC) continues to review and evaluate submissions, but to date, the CMS has yet to implement any of the committee’s recommendations.
“I read all of the PTAC submissions that went to CMS. Some of them I thought were a little on the weak side, but there are a lot of them that I thought were really good ideas. I do not know why CMS did not approve them and fund them and let them be tried,” she said, although she did offer an opinion on why the agency has yet to act on any of them.
“I read their paper saying why they didn’t approve [the recommended physician-developed alternative payment models]. It seemed to me they are waiting for one silver bullet that will fix all of health care. I don’t think a silver bullet is going to fix health care. It’s not an issue. It’s a complicated set of issues. You will not have a quick fix.”
REPORTING FROM THE AMA NATIONAL ADVOCACY CONFERENCE
A prescription for medicine’s gender inequality
A small study identifies skin microbiome changes after UV exposure. Lower prices drive OTC insulin sales at Walmart. And early intensive treatment of multiple sclerosis may benefit patients.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
A small study identifies skin microbiome changes after UV exposure. Lower prices drive OTC insulin sales at Walmart. And early intensive treatment of multiple sclerosis may benefit patients.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
A small study identifies skin microbiome changes after UV exposure. Lower prices drive OTC insulin sales at Walmart. And early intensive treatment of multiple sclerosis may benefit patients.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Possible mechanism for fluoroquinolone-induced aortopathy uncovered
A new study finds that patients taking fluoroquinolone antibiotics may be at higher risk of aortopathy in part because of human aortic myofibroblast–mediated extracellular matrix (ECM) dysregulation.
“Emerging evidence supports pharmacologic-associated aortopathy in patients receiving fluoroquinolone [FQ] antibiotics,” said first author David G. Guzzardi, PhD, and his colleagues, citing previous research showing that, “compared with patients receiving amoxicillin antibiotics, those receiving FQ have a 66% higher risk of aneurysm or dissection within a 2-month period after commencing FQ use.”
Based upon such data, the Food and Drug Administration issued a December 2018 warning about the increased risk of ruptures or tears in the aorta with fluoroquinolone antibiotics in certain patients, updating their May 2017 warning regarding “disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient,” upon exposure to this class of antibiotics. Earlier in 2018, the FDA had reinforced their safety information about serious and potentially fatal low blood sugar levels and mental health side effects with fluoroquinolone antibiotics.
Dr. Guzzardi and his colleagues at the University of Calgary (Alta.) performed a study to attempt to determine the possible cellular mechanisms for the observed aortopathy. In their study published in the Journal of Thoracic and Cardiovascular Surgery, Dr. Guzzardi and his colleagues isolated human aortic myofibroblasts from nine patients with aortopathy who were undergoing elective ascending aortic resection.
Following exposure of cells to FQ, the researchers assessed secreted matrix metalloproteinases relative to tissue inhibitors of matrix metalloproteinases (TIMPs). In addition, they examined ECM degradation by using a three-dimensional gelatin-fluorescein isothiocyanate fluorescence microgel assay. Aortic cellular collagen type I expression following FQ exposure was determined by immunoblotting and immunofluorescent staining. Dr. Guzzardi and his colleagues also looked at cell apoptosis, necrosis, and metabolic viability using two versions of vital staining.
They found that FQ exposure significantly decreased aortic cell TIMP-1 (P less than .004) and TIMP-2 (P less than .0004) protein expression, compared with controls, and the ratio of matrix metalloproteinase 9/TIMP-2 was increased (P less than .01). This suggests an increased capacity for ECM degradation after FQ exposure, according to the researchers.
In addition, FQ exposure attenuated collagen type I expression as assessed by immunoblotting (P less than .002) and immunofluorescence (P less than .02).
“FQ induces human aortic myofibroblast–mediated ECM dysregulation by decreasing TIMP expression and preventing compensatory collagen deposition. These data provide novel insights into the mechanisms that may underlie the clinical association of FQ exposure and increased risk of acute aortic events in the community. Our data suggest cautious use of FQ in selected patient populations with preexistent aortopathy and connective tissue disorders,” the researchers concluded.
In an accompanying editorial, while warning that these are preliminary observations based upon a small number of patients with aortopathy, Ari A. Mennander, MD, PhD, of Tampere (Finland) University, wrote that, “for the first time, the wild theory of fluoroquinolone-associated aortopathy has a molecular hint that is based on collagen degeneration and progression of aortic disease. ... This theory is in line with previous observations revealing antifibrotic activity and decreased collagen-1 protein expression with fluoroquinolones. The enigmatic puzzle of the progression of some aortic events may alarmingly be iatrogenic, and the clinician may wisely consider a prudent use of fluoroquinolones in patients with aortic dilatation.”
The authors and commentators reported that they had no commercial conflicts to disclose.
SOURCE: Guzzardi DG et al. J Thorac Cardiovasc Surg. 2019;157:109-19.
The issue of fluoroquinolones is certainly of concern. I wonder how many of my patients who have suffered a ruptured aneurysm were on one of these drugs? In the last few years, Cipro (ciprofloxacin) and Levaquin (levofloxacin) were commonly used by our family practice and internal medicine colleagues for almost all outpatient infections. It was so common that even my wife, who is not a physician, would request Cipro whenever she had a sneeze. We would also bring large bottles of Cipro every time we went traveling to some exotic destination, reassuring ourselves that the only “runs” we would have would be in the airport trying to catch a flight. A cousin of mine, prescribed Levaquin by a well-meaning physician while he was cruising the Nile River, ruptured his Achilles tendon.
Russell H. Samson, MD, FACS, DFSVS , is a clinical professor of surgery at Florida State University, Sarasota, a senior surgeon at Sarasota Vascular Specialists, and President of the Mote Vascular Foundation.
The issue of fluoroquinolones is certainly of concern. I wonder how many of my patients who have suffered a ruptured aneurysm were on one of these drugs? In the last few years, Cipro (ciprofloxacin) and Levaquin (levofloxacin) were commonly used by our family practice and internal medicine colleagues for almost all outpatient infections. It was so common that even my wife, who is not a physician, would request Cipro whenever she had a sneeze. We would also bring large bottles of Cipro every time we went traveling to some exotic destination, reassuring ourselves that the only “runs” we would have would be in the airport trying to catch a flight. A cousin of mine, prescribed Levaquin by a well-meaning physician while he was cruising the Nile River, ruptured his Achilles tendon.
Russell H. Samson, MD, FACS, DFSVS , is a clinical professor of surgery at Florida State University, Sarasota, a senior surgeon at Sarasota Vascular Specialists, and President of the Mote Vascular Foundation.
The issue of fluoroquinolones is certainly of concern. I wonder how many of my patients who have suffered a ruptured aneurysm were on one of these drugs? In the last few years, Cipro (ciprofloxacin) and Levaquin (levofloxacin) were commonly used by our family practice and internal medicine colleagues for almost all outpatient infections. It was so common that even my wife, who is not a physician, would request Cipro whenever she had a sneeze. We would also bring large bottles of Cipro every time we went traveling to some exotic destination, reassuring ourselves that the only “runs” we would have would be in the airport trying to catch a flight. A cousin of mine, prescribed Levaquin by a well-meaning physician while he was cruising the Nile River, ruptured his Achilles tendon.
Russell H. Samson, MD, FACS, DFSVS , is a clinical professor of surgery at Florida State University, Sarasota, a senior surgeon at Sarasota Vascular Specialists, and President of the Mote Vascular Foundation.
A new study finds that patients taking fluoroquinolone antibiotics may be at higher risk of aortopathy in part because of human aortic myofibroblast–mediated extracellular matrix (ECM) dysregulation.
“Emerging evidence supports pharmacologic-associated aortopathy in patients receiving fluoroquinolone [FQ] antibiotics,” said first author David G. Guzzardi, PhD, and his colleagues, citing previous research showing that, “compared with patients receiving amoxicillin antibiotics, those receiving FQ have a 66% higher risk of aneurysm or dissection within a 2-month period after commencing FQ use.”
Based upon such data, the Food and Drug Administration issued a December 2018 warning about the increased risk of ruptures or tears in the aorta with fluoroquinolone antibiotics in certain patients, updating their May 2017 warning regarding “disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient,” upon exposure to this class of antibiotics. Earlier in 2018, the FDA had reinforced their safety information about serious and potentially fatal low blood sugar levels and mental health side effects with fluoroquinolone antibiotics.
Dr. Guzzardi and his colleagues at the University of Calgary (Alta.) performed a study to attempt to determine the possible cellular mechanisms for the observed aortopathy. In their study published in the Journal of Thoracic and Cardiovascular Surgery, Dr. Guzzardi and his colleagues isolated human aortic myofibroblasts from nine patients with aortopathy who were undergoing elective ascending aortic resection.
Following exposure of cells to FQ, the researchers assessed secreted matrix metalloproteinases relative to tissue inhibitors of matrix metalloproteinases (TIMPs). In addition, they examined ECM degradation by using a three-dimensional gelatin-fluorescein isothiocyanate fluorescence microgel assay. Aortic cellular collagen type I expression following FQ exposure was determined by immunoblotting and immunofluorescent staining. Dr. Guzzardi and his colleagues also looked at cell apoptosis, necrosis, and metabolic viability using two versions of vital staining.
They found that FQ exposure significantly decreased aortic cell TIMP-1 (P less than .004) and TIMP-2 (P less than .0004) protein expression, compared with controls, and the ratio of matrix metalloproteinase 9/TIMP-2 was increased (P less than .01). This suggests an increased capacity for ECM degradation after FQ exposure, according to the researchers.
In addition, FQ exposure attenuated collagen type I expression as assessed by immunoblotting (P less than .002) and immunofluorescence (P less than .02).
“FQ induces human aortic myofibroblast–mediated ECM dysregulation by decreasing TIMP expression and preventing compensatory collagen deposition. These data provide novel insights into the mechanisms that may underlie the clinical association of FQ exposure and increased risk of acute aortic events in the community. Our data suggest cautious use of FQ in selected patient populations with preexistent aortopathy and connective tissue disorders,” the researchers concluded.
In an accompanying editorial, while warning that these are preliminary observations based upon a small number of patients with aortopathy, Ari A. Mennander, MD, PhD, of Tampere (Finland) University, wrote that, “for the first time, the wild theory of fluoroquinolone-associated aortopathy has a molecular hint that is based on collagen degeneration and progression of aortic disease. ... This theory is in line with previous observations revealing antifibrotic activity and decreased collagen-1 protein expression with fluoroquinolones. The enigmatic puzzle of the progression of some aortic events may alarmingly be iatrogenic, and the clinician may wisely consider a prudent use of fluoroquinolones in patients with aortic dilatation.”
The authors and commentators reported that they had no commercial conflicts to disclose.
SOURCE: Guzzardi DG et al. J Thorac Cardiovasc Surg. 2019;157:109-19.
A new study finds that patients taking fluoroquinolone antibiotics may be at higher risk of aortopathy in part because of human aortic myofibroblast–mediated extracellular matrix (ECM) dysregulation.
“Emerging evidence supports pharmacologic-associated aortopathy in patients receiving fluoroquinolone [FQ] antibiotics,” said first author David G. Guzzardi, PhD, and his colleagues, citing previous research showing that, “compared with patients receiving amoxicillin antibiotics, those receiving FQ have a 66% higher risk of aneurysm or dissection within a 2-month period after commencing FQ use.”
Based upon such data, the Food and Drug Administration issued a December 2018 warning about the increased risk of ruptures or tears in the aorta with fluoroquinolone antibiotics in certain patients, updating their May 2017 warning regarding “disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient,” upon exposure to this class of antibiotics. Earlier in 2018, the FDA had reinforced their safety information about serious and potentially fatal low blood sugar levels and mental health side effects with fluoroquinolone antibiotics.
Dr. Guzzardi and his colleagues at the University of Calgary (Alta.) performed a study to attempt to determine the possible cellular mechanisms for the observed aortopathy. In their study published in the Journal of Thoracic and Cardiovascular Surgery, Dr. Guzzardi and his colleagues isolated human aortic myofibroblasts from nine patients with aortopathy who were undergoing elective ascending aortic resection.
Following exposure of cells to FQ, the researchers assessed secreted matrix metalloproteinases relative to tissue inhibitors of matrix metalloproteinases (TIMPs). In addition, they examined ECM degradation by using a three-dimensional gelatin-fluorescein isothiocyanate fluorescence microgel assay. Aortic cellular collagen type I expression following FQ exposure was determined by immunoblotting and immunofluorescent staining. Dr. Guzzardi and his colleagues also looked at cell apoptosis, necrosis, and metabolic viability using two versions of vital staining.
They found that FQ exposure significantly decreased aortic cell TIMP-1 (P less than .004) and TIMP-2 (P less than .0004) protein expression, compared with controls, and the ratio of matrix metalloproteinase 9/TIMP-2 was increased (P less than .01). This suggests an increased capacity for ECM degradation after FQ exposure, according to the researchers.
In addition, FQ exposure attenuated collagen type I expression as assessed by immunoblotting (P less than .002) and immunofluorescence (P less than .02).
“FQ induces human aortic myofibroblast–mediated ECM dysregulation by decreasing TIMP expression and preventing compensatory collagen deposition. These data provide novel insights into the mechanisms that may underlie the clinical association of FQ exposure and increased risk of acute aortic events in the community. Our data suggest cautious use of FQ in selected patient populations with preexistent aortopathy and connective tissue disorders,” the researchers concluded.
In an accompanying editorial, while warning that these are preliminary observations based upon a small number of patients with aortopathy, Ari A. Mennander, MD, PhD, of Tampere (Finland) University, wrote that, “for the first time, the wild theory of fluoroquinolone-associated aortopathy has a molecular hint that is based on collagen degeneration and progression of aortic disease. ... This theory is in line with previous observations revealing antifibrotic activity and decreased collagen-1 protein expression with fluoroquinolones. The enigmatic puzzle of the progression of some aortic events may alarmingly be iatrogenic, and the clinician may wisely consider a prudent use of fluoroquinolones in patients with aortic dilatation.”
The authors and commentators reported that they had no commercial conflicts to disclose.
SOURCE: Guzzardi DG et al. J Thorac Cardiovasc Surg. 2019;157:109-19.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
CMS proposes coverage of CAR T-cell therapy in trials
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
The Centers for Medicare & Medicaid Services has proposed to cover chimeric antigen receptor (CAR) T-cell therapy for cancer patients participating in clinical trials that study the treatment’s effectiveness, according to a Feb. 15 announcement.
The proposed national coverage determination would require CMS to cover CAR T-cell therapies nationwide when the treatment is offered in CMS-approved registries or clinical studies in which patients are monitored for 2 or more years following treatment.
Results from the studies would help CMS identify which patients benefit most from CAR T-cell therapies and inform future coverage decisions, CMS Administrator Seema Verma said.
“CAR T-cell therapy was the first FDA-approved gene therapy, marking the beginning of an entirely new approach to treating serious and even life-threatening diseases,” Ms. Verma said in a statement. “Today’s proposed coverage decision would improve access to this therapy while deepening CMS’s understanding of how patients in Medicare respond to it, so the agency can ensure that it is paying for CAR T-cell therapy for cases in which the benefits outweigh the risks.”
As part of the proposal, CMS would cover autologous treatment with T cells expressing at least one chimeric antigen receptor (CAR) through coverage with evidence development when prescribed by a treating oncologist and performed in a hospital, according to a summary of the proposal.
The patient and hospital must meet specific criteria to be eligible for coverage, including that patients have relapsed or refractory cancer and do not have a comorbidity that would otherwise preclude patient benefit.
Hospitals, meanwhile, must have a cellular therapy program consisting of an integrated medical team that includes a clinical program director, a quality manager, and at least one physician experienced in cellular therapy, among other requirements.
CMS also would require that treatment is an FDA-approved biologic, providing targeted therapy for a known antigen expressed in the patient’s cancer according to an FDA indication. Repeat treatment would be covered only when a new primary cancer diagnosis is made by the treating oncologist and certain patient conditions are met.
Both inpatient and outpatient settings for the CAR T-cell therapy treatment are acceptable under the proposal. In either case, the patient and the hospital must be participating in a prospective, national, audited registry that consecutively enrolls patients, accepts all manufactured products, follows the patient for at least 2 years, and addresses a set of approved evidence-development questions. Additionally, all registries must be reviewed and approved by CMS.
The proposed national coverage determination was the result of an Aug. 22, 2018 meeting of the Medicare Evidence Development & Coverage Advisory Committee. The committee provides CMS with an external assessment of the appropriateness of therapies under review.
Public comments about the CAR T-cell therapy proposal will be accepted online here until March 15. A final decision on the proposal is expected by May 2019.
The agency’s proposal follows an Aug. 17 final rule by CMS that sets a new payment scheme for inpatient administration of two CAR T-cell therapies. The rule categorizes CAR T-cell therapies under the umbrella of the renamed Medicare Severity–Diagnosis Related Groups 016 – Autologous Bone Marrow Transplant with CC/MCC or T-cell Immunotherapy – and assigns ICD-10 PCS procedure codes XW033C3 and XW043C3 to the use of axicabtagene ciloleucel (Yescarta) and tisagenlecleucel (Kymriah) in the inpatient setting for fiscal year 2019, which began in October 2018. CMS also approved a temporary New Technology Add-On Payment for use of the therapies with a maximum threshold of $186,500.
In April 2018, CMS announced payment rates for outpatient administration of the two drugs, settling on $395,380 for axicabtagene ciloleucel and $500,839 for tisagenlecleucel. The two medications have list prices of $373,000 and $475,000, respectively.
Survey: Health care costs, access unlikely to improve in 2019
but most predict that the Affordable Care Act will make it through the year despite government efforts to defund it, according to a survey by health care market research company InCrowd.

Over 80% of the 200 physicians surveyed Dec. 20-22, 2018, said that it was somewhat or very unlikely that health care costs would improve over the course of this year, and almost 70% expressed those opinions regarding improved access to care. More than 70% said that the federal government will find ways to defund the ACA, but 60% believe that it will remain in place and almost 70% said that coverage for preexisting conditions will continue, InCrowd reported. A minority of respondents (45%) predicted that the quality of health care was very likely or somewhat likely to improve in 2019.
A number of other issues were covered in the survey: 71% of physicians predicted that children up to age 26 years will be able to stay on their parents’ coverage, 69% expect the insurance mandate to be eliminated, 58% believe that mental health coverage will be allowed, and 56% said that it is unlikely for more states to expand Medicaid, according to data from the 100 primary care physicians and 100 specialists who responded to the InCrowd MicroSurvey.
but most predict that the Affordable Care Act will make it through the year despite government efforts to defund it, according to a survey by health care market research company InCrowd.

Over 80% of the 200 physicians surveyed Dec. 20-22, 2018, said that it was somewhat or very unlikely that health care costs would improve over the course of this year, and almost 70% expressed those opinions regarding improved access to care. More than 70% said that the federal government will find ways to defund the ACA, but 60% believe that it will remain in place and almost 70% said that coverage for preexisting conditions will continue, InCrowd reported. A minority of respondents (45%) predicted that the quality of health care was very likely or somewhat likely to improve in 2019.
A number of other issues were covered in the survey: 71% of physicians predicted that children up to age 26 years will be able to stay on their parents’ coverage, 69% expect the insurance mandate to be eliminated, 58% believe that mental health coverage will be allowed, and 56% said that it is unlikely for more states to expand Medicaid, according to data from the 100 primary care physicians and 100 specialists who responded to the InCrowd MicroSurvey.
but most predict that the Affordable Care Act will make it through the year despite government efforts to defund it, according to a survey by health care market research company InCrowd.

Over 80% of the 200 physicians surveyed Dec. 20-22, 2018, said that it was somewhat or very unlikely that health care costs would improve over the course of this year, and almost 70% expressed those opinions regarding improved access to care. More than 70% said that the federal government will find ways to defund the ACA, but 60% believe that it will remain in place and almost 70% said that coverage for preexisting conditions will continue, InCrowd reported. A minority of respondents (45%) predicted that the quality of health care was very likely or somewhat likely to improve in 2019.
A number of other issues were covered in the survey: 71% of physicians predicted that children up to age 26 years will be able to stay on their parents’ coverage, 69% expect the insurance mandate to be eliminated, 58% believe that mental health coverage will be allowed, and 56% said that it is unlikely for more states to expand Medicaid, according to data from the 100 primary care physicians and 100 specialists who responded to the InCrowd MicroSurvey.
HHS to target step therapy, Stark Law in 2019
WASHINGTON –
Speaking Feb. 12 at the American Medical Association’s National Advocacy Conference, Secretary Azar said the agency will be looking into ensuring that patients on medical plans who have found a working drug after going through a step-therapy protocol will not have to restart on a drug that has already failed for them if they switch insurance providers.
“I was very disturbed to hear that stable patients switching among insurance plans, like switching among Medicare Advantage plans, can often be required to start over again on a step therapy regimen,” he said.
“This is not just potentially injurious to their health, it’s also penny-wise and pound-foolish,” Secretary Azar continued. “We know that getting a patient on the right drug, at the right time, is one of the best investments we can make in their health, and we do not want to impede physicians from making that happen. We’re looking at how we can address that issue now.”
The other area Secretary Azar highlighted that the agency is working on is making changes to the Stark Law.
“The Stark Law was written with noble purposes in mind, but it was designed for a fee-for-service system, not the kind of system we are moving toward today,” he said. “We’ve heard from many, many stakeholders, including the AMA, about the need to update the enumerated exceptions in the Stark Law to include value-based approaches to care.”
He added that how care coordination interacts with the antikickback statutes and HIPAA are also going to be examined.
Secretary Azar did not offer any timelines or other more specific details about how the agency plans to tackle these issues.
He used most of his speech to discuss recent regulatory actions around drug pricing and pushed for support for the Part B drug pricing model that the agency is preparing for a formal proposed rule, despite having received a critical reception from medical societies.
“If you have a small practice that uses infusions, and you don’t want to bear the risk of buy and bill, now you’re off the hook,” he said. “We’ll allow you to work with private vendors who can take the risk for buying the drugs in a way that isn’t possible today. But if you’re part of a much larger practice that’s able to drive a better deal than you could on your own, or want to band together with other practices to do the purchasing, then you can do that, too.”
He continued: “Next is the launch of the actual proposed rule, followed by the rule itself, which, I’ll remind you, is just a model.”
However, despite it being a model under test from the Center for Medicare & Medicaid Innovation, the advanced notice of proposed rule making that was issued in October 2018 suggested that participation in the so-called International Pricing Index model would be mandatory.
Secretary Azar did not acknowledge any mandatory participation in his pitch for support, noting that CMMI models “are carefully assessed. We will closely monitor how the model will affect clinical outcomes, including patients’ adherence to their drugs. We believe that the lower costs will, of course, mean better patient access to drugs, better adherence, and better outcomes for the care you provide. That is the goal.”
WASHINGTON –
Speaking Feb. 12 at the American Medical Association’s National Advocacy Conference, Secretary Azar said the agency will be looking into ensuring that patients on medical plans who have found a working drug after going through a step-therapy protocol will not have to restart on a drug that has already failed for them if they switch insurance providers.
“I was very disturbed to hear that stable patients switching among insurance plans, like switching among Medicare Advantage plans, can often be required to start over again on a step therapy regimen,” he said.
“This is not just potentially injurious to their health, it’s also penny-wise and pound-foolish,” Secretary Azar continued. “We know that getting a patient on the right drug, at the right time, is one of the best investments we can make in their health, and we do not want to impede physicians from making that happen. We’re looking at how we can address that issue now.”
The other area Secretary Azar highlighted that the agency is working on is making changes to the Stark Law.
“The Stark Law was written with noble purposes in mind, but it was designed for a fee-for-service system, not the kind of system we are moving toward today,” he said. “We’ve heard from many, many stakeholders, including the AMA, about the need to update the enumerated exceptions in the Stark Law to include value-based approaches to care.”
He added that how care coordination interacts with the antikickback statutes and HIPAA are also going to be examined.
Secretary Azar did not offer any timelines or other more specific details about how the agency plans to tackle these issues.
He used most of his speech to discuss recent regulatory actions around drug pricing and pushed for support for the Part B drug pricing model that the agency is preparing for a formal proposed rule, despite having received a critical reception from medical societies.
“If you have a small practice that uses infusions, and you don’t want to bear the risk of buy and bill, now you’re off the hook,” he said. “We’ll allow you to work with private vendors who can take the risk for buying the drugs in a way that isn’t possible today. But if you’re part of a much larger practice that’s able to drive a better deal than you could on your own, or want to band together with other practices to do the purchasing, then you can do that, too.”
He continued: “Next is the launch of the actual proposed rule, followed by the rule itself, which, I’ll remind you, is just a model.”
However, despite it being a model under test from the Center for Medicare & Medicaid Innovation, the advanced notice of proposed rule making that was issued in October 2018 suggested that participation in the so-called International Pricing Index model would be mandatory.
Secretary Azar did not acknowledge any mandatory participation in his pitch for support, noting that CMMI models “are carefully assessed. We will closely monitor how the model will affect clinical outcomes, including patients’ adherence to their drugs. We believe that the lower costs will, of course, mean better patient access to drugs, better adherence, and better outcomes for the care you provide. That is the goal.”
WASHINGTON –
Speaking Feb. 12 at the American Medical Association’s National Advocacy Conference, Secretary Azar said the agency will be looking into ensuring that patients on medical plans who have found a working drug after going through a step-therapy protocol will not have to restart on a drug that has already failed for them if they switch insurance providers.
“I was very disturbed to hear that stable patients switching among insurance plans, like switching among Medicare Advantage plans, can often be required to start over again on a step therapy regimen,” he said.
“This is not just potentially injurious to their health, it’s also penny-wise and pound-foolish,” Secretary Azar continued. “We know that getting a patient on the right drug, at the right time, is one of the best investments we can make in their health, and we do not want to impede physicians from making that happen. We’re looking at how we can address that issue now.”
The other area Secretary Azar highlighted that the agency is working on is making changes to the Stark Law.
“The Stark Law was written with noble purposes in mind, but it was designed for a fee-for-service system, not the kind of system we are moving toward today,” he said. “We’ve heard from many, many stakeholders, including the AMA, about the need to update the enumerated exceptions in the Stark Law to include value-based approaches to care.”
He added that how care coordination interacts with the antikickback statutes and HIPAA are also going to be examined.
Secretary Azar did not offer any timelines or other more specific details about how the agency plans to tackle these issues.
He used most of his speech to discuss recent regulatory actions around drug pricing and pushed for support for the Part B drug pricing model that the agency is preparing for a formal proposed rule, despite having received a critical reception from medical societies.
“If you have a small practice that uses infusions, and you don’t want to bear the risk of buy and bill, now you’re off the hook,” he said. “We’ll allow you to work with private vendors who can take the risk for buying the drugs in a way that isn’t possible today. But if you’re part of a much larger practice that’s able to drive a better deal than you could on your own, or want to band together with other practices to do the purchasing, then you can do that, too.”
He continued: “Next is the launch of the actual proposed rule, followed by the rule itself, which, I’ll remind you, is just a model.”
However, despite it being a model under test from the Center for Medicare & Medicaid Innovation, the advanced notice of proposed rule making that was issued in October 2018 suggested that participation in the so-called International Pricing Index model would be mandatory.
Secretary Azar did not acknowledge any mandatory participation in his pitch for support, noting that CMMI models “are carefully assessed. We will closely monitor how the model will affect clinical outcomes, including patients’ adherence to their drugs. We believe that the lower costs will, of course, mean better patient access to drugs, better adherence, and better outcomes for the care you provide. That is the goal.”
REPORTING FROM AMA NATIONAL ADVOCACY CONFERENCE

















