User login
Conservatism spreads in prostate cancer
, the United States now has more than 100 measles cases for the year, e-cigarette use reverses progress in reducing teens’ tobacco use, and consider adopting the MESA 10-year coronary heart disease risk calculator.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
, the United States now has more than 100 measles cases for the year, e-cigarette use reverses progress in reducing teens’ tobacco use, and consider adopting the MESA 10-year coronary heart disease risk calculator.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
, the United States now has more than 100 measles cases for the year, e-cigarette use reverses progress in reducing teens’ tobacco use, and consider adopting the MESA 10-year coronary heart disease risk calculator.
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
The Dyad Model for Interprofessional Academic Patient Aligned Care Teams
Background
In 2011, 5 US Department of Veterans Affairs (VA) medical centers were selected by the VA Office of Academic Affiliations (OAA) to establish Centers of Excellence in Primary Care Education (CoEPCE). As part of VA’s New Models of Care initiative, the 5 CoEPCEs are using VA primary care settings to develop and test innovative approaches to prepare physician residents and students, advanced practice nurses (APRNs), undergraduate nursing students, and other health professions trainees (such as pharmacy, social work, psychology, physician assistants) for primary care practice. The CoEPCE sites are developing, implementing, and evaluating curricula to prepare learners from relevant professions to practice in patientcentered, interprofessional team-based primary care settings. Patient aligned care teams (PACTs) that have 2 or more health professions trainees engaged in learning, working, and teaching are known as interprofessional academic PACTs (iAPACTs), which is the preferred model for the VA.
The Cleveland Transforming Outpatient Care (TOPC)-CoEPCE was designed for collaborative learning among nurse practitioner (NP) students and physician residents. Its robust curriculum consists of a dedicated half-day of didactics for all learners, interprofessional quality improvement projects, panel management sessions, and primary care clinical sessions for nursing and physician learners that include the dyad workplace learning model.
In 2015, the OAA lead evaluator observed the TOPC-CoEPCE dyad model process, reviewed background documents, and conducted 10 open-ended interviews with TOPC-CoEPCE staff, participating trainees, faculty, and affiliate leadership. Informants described their involvement, challenges encountered, and benefits of the TOPCCoEPC dyad model to participants, veterans, VA, and affiliates.
Lack of Interprofessional Learning Opportunities
Current health care professional education models typically do not have many workplace learning settings where physician and nursing trainees learn together and provide patient-centered care. Often in a shared clinical environment, trainees may engage in “parallel play,” which can result in physician trainees and NP students learning independently and being ill-prepared to practice effectively together.
Moreover, trainees from different professions have different learning needs. For example, less experienced NP students require greater time, supervision, and evaluation of their patient care skills. On the other hand, senior physician residents, who require less clinical instruction, need to be engaged in ways that provide opportunities to enhance their ambulatory teaching skills. Although enhancement of resident teaching skills occurs in the inpatient hospital setting, there have been limited teaching experiences for residents in a primary care setting where the instruction is traditionally faculty-based. The TOPCCoEPCE dyad model offers an opportunity to simultaneously provide trainees with a true interprofessional experience through advancement of skills in primary care, teamwork, and teaching, while addressing health care needs.
The Dyad Model
In 2011, the OAA directed COEPCE sites to develop innovative curriculum and workplace learning strategies to create more opportunities for physician and NP trainees to work as a team. There is evidence demonstrating that when students develop a shared understanding of each other’s skill set, care procedures, and values, patient care is improved.1 Further, training in pairs can be an effective strategy in education of preclerkship medical students.2 In April 2013, TOPC-CoEPCE staff asked representatives from the Student-Run Clinic at Case Western Reserve University (CWRU) in Cleveland, Ohio, to present their approach to pairing nursing and medical students in clinic under supervision by volunteer faculty. However, formal structure and curricular objectives were lacking. To address diverse TOPCCoEPCE trainee needs and create a team approach to patient care, the staff formalized and developed a workplace curriculum called the dyad model. Specifically, the model pairs 1 NP student with a senior (PGY2 or PGY3) physician resident to care for ambulatory patients as a dyad teaching/learning team. The dyad model has 3 goals: improving clinical performance, learning team dynamics, and improving the physician resident’s teaching skills in an ambulatory setting.
Planning and Implementation
Planning the dyad model took 4 months. Initial conceptualization of the model was discussed at TOPC-CoEPCE infrastructure meetings. Workgroups with representatives from medicine, nursing, evaluation and medical center administration were formed to finalize the model. The workgroups met weekly or biweekly to develop protocols for scheduling, ongoing monitoring and assessment, microteaching session curriculum development, and logistics. A pilot program was initiated for 1 month with 2 dyads to monitor learner progress and improve components, such as adjusting the patient exam start times and curriculum. In maintaining the program, the workgroups continue to meet monthly to check for areas for further improvement and maintain dissemination activities.
Curriculum
The dyad model is a novel opportunity to have trainees from different professions not only collaborate in the care of the same patient at the same time, but also negotiate their respective responsibilities preand postvisit. The experience focuses on interprofessional relationships and open communication. TOPC-CoEPCE used a modified version of the RIME (Reporter-Interpreter-Manager-Educator) model called the O-RIME model (Table 1), which includes an observer (O) phase as the first component for clarification about a beginners’ role.3,4
Four dyad pairs provide collaborative clinical care for veterans during one halfday session per week. The dyad conducts 4 hour-long patient visits per session. To be a dyad participant, the physician residents must be at least a PGY2, and their schedule must align with the NP student clinic schedule. Participation is mandatory for both NP students and physician residents. TOPC staff assemble the pairs.
The dyad model requires knowledge of the clinical and curricular interface and when to block the dyad team members’ schedules for 4 patients instead of 6. Physician residents are in the TOPC-CoEPCE for 12 weeks and then on inpatient for 12 weeks. Depending on the nursing school affiliate, NP student trainees are scheduled for either a 6- or 12-month TOPC-CoEPCE experience. For the 12-month NP students, they are paired with up to 4 internal medicine residents over the course of their dyad participation so they can experience different teaching styles of each resident while developing more varied interprofessional communication skills.
Faculty Roles and Development
The dyad model also seeks to address the paucity of deliberate interprofessional precepting in academic primary care settings. The TOPC-CoEPCE staff decided to use the existing primary care clinic faculty development series bimonthly for 1 hour each. The dyad model team members presented sessions covering foundational material in interprofessional teaching and precepting skills, which prepare faculty to precept for different professions and the dyad teams. It is important for preceptors to develop awareness of learners from different professions and the corresponding educational trajectories, so they can communicate with paired trainees of differing professions and academic levels who may require different levels of discussion.
Resources
By utilizing advanced residents as teachers, faculty were able to increase the number of learners in the clinic without increasing the number preceptors. For example, precepting a student typically requires more preceptor time, especially when we consider that the preceptor must also see the patient. The TOPC-CoEPCE faculty run the microteaching sessions, and an evaluator monitors and evaluates the program. The microteaching sessions were derived from several teaching resources.
Monitoring and Assessment
The Cleveland TOPC administered 2 different surveys developed by the Dyad Model Infrastructure and Evaluation workgroup. A 7-item survey assesses dyad team communication and interprofessional team functioning, and an 8-item survey assesses the teaching/mentoring of the resident as teacher. Both were collected from all participants to evaluate the residents’ and students’ point of view. Surveys are collected in the first and last weeks of the dyad experience. Feedback from participants has been used to make improvements to the program (eg, monitoring how the dyad teams are functioning, coaching individual learners).
Partnerships
In addition to TOPC staff and faculty support and engagement, the initiative has benefited from partnerships with VA clinic staff and with the associated academic affiliates. In particular, the Associate Chief of General Internal Medicine at the Cleveland VA medical center and interim clinic director helped institute changes to the primary care clinic structure. Additionally, buy-in from the clinic nurse manager was needed to make adjustments with staff schedules and clinic resources. To implement the dyad model, the clinic director had to approve reductions in the residents’ clinic loads for the mornings when they participated.
The NP affiliates’ faculty at the schools of nursing are integral partners who assist with student recruitment and participate in the planning and refinement of TOPCCoEPCE components. The Frances Payne Bolton School of Nursing at CWRU and the Breen School of Nursing of Ursuline College in Pepper Pike, Ohio, were involved in the planning stages and continue to receive monthly updates from TOPC-CoEPCE. Similarly, the CWRU School of Medicine and Cleveland Clinic Foundation affiliates contribute on an ongoing basis to the improvement and implementation process.
Discussion
One challenge has been advancing aspects of a nonhierarchical team approach while it is a teacher-student relationship. The dyad model is viewed as an opportunity to recognize nonhierarchical structures and teach negotiation and communication skills as well as increase interprofessional understanding of each other’s education, expertise, and scope of practice.
Another challenge is accommodating the diversity in NP training and clinical expertise. The NP student participants are in either the first or second year of their academic program. This is a challenge since both physician residents and physician faculty preceptors need to assess the NP students’ skills before providing opportunities to build on their skill level. Staff members have learned the value of checking in weekly on this issue.
Factors for Success
VA facility support and TOPC-CoEPCE leadership with the operations/academic partnership remain critical to integrating and sustaining the model into the Cleveland primary care clinic. The expertise of TOPC-CoEPCE dyad model faculty who serve as facilitators has been crucial, as they oversee team development concepts such as developing problem solving and negotiation skills. The workgroups ensured that faculty were skilled in understanding the different types of learners and provided guidance to dyad teams. Another success factor was the continual monitoring of the process and real-time evaluation of the program to adapt the model as needed.
Accomplishments and Benefits
There is evidence that the dyad model is achieving its goals: Trainees are using team skills during and outside formal dyad pairs; NP students report improvements in skill levels and comfort; and physician residents feel the teaching role in the dyad pair is an opportunity for them to improve their practice.
Interprofessional Educational Capacity
The dyad model complements the curriculum components and advances trainee understanding of 4 core domains: shared decision-making (SDM), sustained relationships (SR), interprofessional collaboration (IPC), and performance improvement (PI) (Table 2). The dyad model supports the other CoEPCE interprofessional education activities and is reinforced by these activities. The model is a learning laboratory for studying team dynamics and developing a curriculum that strengthens a team approach to patient-centered care.
Participants’ Knowledge, Attitudes, Skills, and Competencies
As of May 2015, 35 trainees (21 internal medicine physician residents and 14 NP students) have participated in dyads. Because physician residents participate over 2 years and may partner with more than 1 NP student, this has resulted in 27 dyad pairs in this time frame. Findings from an analysis of evaluations suggest that the dyad pair trainees learn from one another, and the model provides a safe space where trainees can practice and increase their confidence.1,6,7 The NP students seem to increase clinical skills quickly—expanding physical exam skills, building a differential diagnosis, and formulating therapeutic plans—and progressing to the Interpreter and Manager levels in the O-RIME model. The physician resident achieves the Educator level.
As of September 2015, the results from the pairs who completed beginning and end evaluations show that the physician residents increased the amount of feedback they provided about performance to the student, and likewise the student NPs also felt they received an increased amount of feedback about performance from the physician resident. In addition, physician residents reported improving the most in the following areas: allowing the student to make commitments in diagnoses and treatment plans and asking the student to provide supporting evidence for their commitment to the diagnoses. NP students reported the largest increases in receiving weekly feedback about their performance from the physician and their ability to listen to the patient.1,6,7
Interprofessional Collaboration
The TOPC-CoEPCE staff observed strengthened dyad pair relationships and mutual respect between the dyad partners. Trainees communicate with each other and work together to provide care of the patient. Second, dyad pair partners are learning about the other profession—their trajectory, their education model, and their differences. The physician resident develops an awareness of the partner NP student’s knowledge and expertise, such as their experience of social and psychological factors to become a more effective teacher, contributing to patient-centered care. The evaluation results illustrate increased ability of trainees to give and receive feedback and the change in roles for providing diagnosis and providing supporting evidence within the TOPCCoEPCE dyad team.6-8
The Future
The model has broad applicability for interprofessional education in the VA since it enhances skills that providers need to work in a PACT/PCMH model. Additionally, the TOPC-CoEPCE dyad model has proven to be an effective interprofessional training experience for its affiliates and may have applicability in other VA/affiliate training programs. The dyad model can be adapted to different trainee types in the ambulatory care setting. The TOPCCoEPCE is piloting a version of the dyad with NP residents (postgraduate) and first-year medical students. Additionally, the TOPCCoEPCE is paving the way for integrating improvement of physician resident teaching skills into the primary care setting and facilitating bidirectional teaching among different professions. TOPC-CoEPCE intends to develop additional resources to facilitate use of the model application in other settings such as the dyad implementation template.
1. Billett SR. Securing intersubjectivity through interprofessional workplace learning experiences. J Interprof Care. 2014;28(3):206-211.
2. Tolsgaard MG, Bjørck S, Rasmussen MB, Gustafsson A, Ringsted C. Improving efficiency of clinical skills training: a randomized trial. J Gen Intern Med. 2013;28(8);1072-1077.
3. Pangaro L. A new vocabulary and other innovations for improving descriptive in-training evaluations. Acad Med. 1999;74(11):1203-1207.
4. Tham KY. Observer-Reporter-Interpreter-Manager-Educator (O-RIME) framework to guide formative assessment of medical students. Ann Acad Med Singapore. 2013;42(11):603-607.
6. Clementz L, Dolansky MA, Lawrence RH, et al. Dyad teams: interprofessional collaboration and learning in ambulatory setting. Poster session presented: 38th Annual Meeting of the Society of General Internal Medicine; April 2015:Toronto, Canada. www.pcori.org/sites/default/files /SGIM-Conference-Program-2015.pdf. Accessed August 29, 2018.
7. Singh M, Clementz L, Dolansky MA, et al. MD-NP learning dyad model: an innovative approach to interprofessional teaching and learning. Workshop presented at: Annual Meeting of the Midwest Society of General Internal Medicine; August 27, 2015: Cleveland, Ohio.
8. Lawrence RH, Dolansky MA, Clementz L, et al. Dyad teams: collaboration and learning in the ambulatory care setting. Poster session presented at: AAMC meeting, Innovations in Academic Medicine; November 7-11, 2014: Chicago, IL.
Background
In 2011, 5 US Department of Veterans Affairs (VA) medical centers were selected by the VA Office of Academic Affiliations (OAA) to establish Centers of Excellence in Primary Care Education (CoEPCE). As part of VA’s New Models of Care initiative, the 5 CoEPCEs are using VA primary care settings to develop and test innovative approaches to prepare physician residents and students, advanced practice nurses (APRNs), undergraduate nursing students, and other health professions trainees (such as pharmacy, social work, psychology, physician assistants) for primary care practice. The CoEPCE sites are developing, implementing, and evaluating curricula to prepare learners from relevant professions to practice in patientcentered, interprofessional team-based primary care settings. Patient aligned care teams (PACTs) that have 2 or more health professions trainees engaged in learning, working, and teaching are known as interprofessional academic PACTs (iAPACTs), which is the preferred model for the VA.
The Cleveland Transforming Outpatient Care (TOPC)-CoEPCE was designed for collaborative learning among nurse practitioner (NP) students and physician residents. Its robust curriculum consists of a dedicated half-day of didactics for all learners, interprofessional quality improvement projects, panel management sessions, and primary care clinical sessions for nursing and physician learners that include the dyad workplace learning model.
In 2015, the OAA lead evaluator observed the TOPC-CoEPCE dyad model process, reviewed background documents, and conducted 10 open-ended interviews with TOPC-CoEPCE staff, participating trainees, faculty, and affiliate leadership. Informants described their involvement, challenges encountered, and benefits of the TOPCCoEPC dyad model to participants, veterans, VA, and affiliates.
Lack of Interprofessional Learning Opportunities
Current health care professional education models typically do not have many workplace learning settings where physician and nursing trainees learn together and provide patient-centered care. Often in a shared clinical environment, trainees may engage in “parallel play,” which can result in physician trainees and NP students learning independently and being ill-prepared to practice effectively together.
Moreover, trainees from different professions have different learning needs. For example, less experienced NP students require greater time, supervision, and evaluation of their patient care skills. On the other hand, senior physician residents, who require less clinical instruction, need to be engaged in ways that provide opportunities to enhance their ambulatory teaching skills. Although enhancement of resident teaching skills occurs in the inpatient hospital setting, there have been limited teaching experiences for residents in a primary care setting where the instruction is traditionally faculty-based. The TOPCCoEPCE dyad model offers an opportunity to simultaneously provide trainees with a true interprofessional experience through advancement of skills in primary care, teamwork, and teaching, while addressing health care needs.
The Dyad Model
In 2011, the OAA directed COEPCE sites to develop innovative curriculum and workplace learning strategies to create more opportunities for physician and NP trainees to work as a team. There is evidence demonstrating that when students develop a shared understanding of each other’s skill set, care procedures, and values, patient care is improved.1 Further, training in pairs can be an effective strategy in education of preclerkship medical students.2 In April 2013, TOPC-CoEPCE staff asked representatives from the Student-Run Clinic at Case Western Reserve University (CWRU) in Cleveland, Ohio, to present their approach to pairing nursing and medical students in clinic under supervision by volunteer faculty. However, formal structure and curricular objectives were lacking. To address diverse TOPCCoEPCE trainee needs and create a team approach to patient care, the staff formalized and developed a workplace curriculum called the dyad model. Specifically, the model pairs 1 NP student with a senior (PGY2 or PGY3) physician resident to care for ambulatory patients as a dyad teaching/learning team. The dyad model has 3 goals: improving clinical performance, learning team dynamics, and improving the physician resident’s teaching skills in an ambulatory setting.
Planning and Implementation
Planning the dyad model took 4 months. Initial conceptualization of the model was discussed at TOPC-CoEPCE infrastructure meetings. Workgroups with representatives from medicine, nursing, evaluation and medical center administration were formed to finalize the model. The workgroups met weekly or biweekly to develop protocols for scheduling, ongoing monitoring and assessment, microteaching session curriculum development, and logistics. A pilot program was initiated for 1 month with 2 dyads to monitor learner progress and improve components, such as adjusting the patient exam start times and curriculum. In maintaining the program, the workgroups continue to meet monthly to check for areas for further improvement and maintain dissemination activities.
Curriculum
The dyad model is a novel opportunity to have trainees from different professions not only collaborate in the care of the same patient at the same time, but also negotiate their respective responsibilities preand postvisit. The experience focuses on interprofessional relationships and open communication. TOPC-CoEPCE used a modified version of the RIME (Reporter-Interpreter-Manager-Educator) model called the O-RIME model (Table 1), which includes an observer (O) phase as the first component for clarification about a beginners’ role.3,4
Four dyad pairs provide collaborative clinical care for veterans during one halfday session per week. The dyad conducts 4 hour-long patient visits per session. To be a dyad participant, the physician residents must be at least a PGY2, and their schedule must align with the NP student clinic schedule. Participation is mandatory for both NP students and physician residents. TOPC staff assemble the pairs.
The dyad model requires knowledge of the clinical and curricular interface and when to block the dyad team members’ schedules for 4 patients instead of 6. Physician residents are in the TOPC-CoEPCE for 12 weeks and then on inpatient for 12 weeks. Depending on the nursing school affiliate, NP student trainees are scheduled for either a 6- or 12-month TOPC-CoEPCE experience. For the 12-month NP students, they are paired with up to 4 internal medicine residents over the course of their dyad participation so they can experience different teaching styles of each resident while developing more varied interprofessional communication skills.
Faculty Roles and Development
The dyad model also seeks to address the paucity of deliberate interprofessional precepting in academic primary care settings. The TOPC-CoEPCE staff decided to use the existing primary care clinic faculty development series bimonthly for 1 hour each. The dyad model team members presented sessions covering foundational material in interprofessional teaching and precepting skills, which prepare faculty to precept for different professions and the dyad teams. It is important for preceptors to develop awareness of learners from different professions and the corresponding educational trajectories, so they can communicate with paired trainees of differing professions and academic levels who may require different levels of discussion.
Resources
By utilizing advanced residents as teachers, faculty were able to increase the number of learners in the clinic without increasing the number preceptors. For example, precepting a student typically requires more preceptor time, especially when we consider that the preceptor must also see the patient. The TOPC-CoEPCE faculty run the microteaching sessions, and an evaluator monitors and evaluates the program. The microteaching sessions were derived from several teaching resources.
Monitoring and Assessment
The Cleveland TOPC administered 2 different surveys developed by the Dyad Model Infrastructure and Evaluation workgroup. A 7-item survey assesses dyad team communication and interprofessional team functioning, and an 8-item survey assesses the teaching/mentoring of the resident as teacher. Both were collected from all participants to evaluate the residents’ and students’ point of view. Surveys are collected in the first and last weeks of the dyad experience. Feedback from participants has been used to make improvements to the program (eg, monitoring how the dyad teams are functioning, coaching individual learners).
Partnerships
In addition to TOPC staff and faculty support and engagement, the initiative has benefited from partnerships with VA clinic staff and with the associated academic affiliates. In particular, the Associate Chief of General Internal Medicine at the Cleveland VA medical center and interim clinic director helped institute changes to the primary care clinic structure. Additionally, buy-in from the clinic nurse manager was needed to make adjustments with staff schedules and clinic resources. To implement the dyad model, the clinic director had to approve reductions in the residents’ clinic loads for the mornings when they participated.
The NP affiliates’ faculty at the schools of nursing are integral partners who assist with student recruitment and participate in the planning and refinement of TOPCCoEPCE components. The Frances Payne Bolton School of Nursing at CWRU and the Breen School of Nursing of Ursuline College in Pepper Pike, Ohio, were involved in the planning stages and continue to receive monthly updates from TOPC-CoEPCE. Similarly, the CWRU School of Medicine and Cleveland Clinic Foundation affiliates contribute on an ongoing basis to the improvement and implementation process.
Discussion
One challenge has been advancing aspects of a nonhierarchical team approach while it is a teacher-student relationship. The dyad model is viewed as an opportunity to recognize nonhierarchical structures and teach negotiation and communication skills as well as increase interprofessional understanding of each other’s education, expertise, and scope of practice.
Another challenge is accommodating the diversity in NP training and clinical expertise. The NP student participants are in either the first or second year of their academic program. This is a challenge since both physician residents and physician faculty preceptors need to assess the NP students’ skills before providing opportunities to build on their skill level. Staff members have learned the value of checking in weekly on this issue.
Factors for Success
VA facility support and TOPC-CoEPCE leadership with the operations/academic partnership remain critical to integrating and sustaining the model into the Cleveland primary care clinic. The expertise of TOPC-CoEPCE dyad model faculty who serve as facilitators has been crucial, as they oversee team development concepts such as developing problem solving and negotiation skills. The workgroups ensured that faculty were skilled in understanding the different types of learners and provided guidance to dyad teams. Another success factor was the continual monitoring of the process and real-time evaluation of the program to adapt the model as needed.
Accomplishments and Benefits
There is evidence that the dyad model is achieving its goals: Trainees are using team skills during and outside formal dyad pairs; NP students report improvements in skill levels and comfort; and physician residents feel the teaching role in the dyad pair is an opportunity for them to improve their practice.
Interprofessional Educational Capacity
The dyad model complements the curriculum components and advances trainee understanding of 4 core domains: shared decision-making (SDM), sustained relationships (SR), interprofessional collaboration (IPC), and performance improvement (PI) (Table 2). The dyad model supports the other CoEPCE interprofessional education activities and is reinforced by these activities. The model is a learning laboratory for studying team dynamics and developing a curriculum that strengthens a team approach to patient-centered care.
Participants’ Knowledge, Attitudes, Skills, and Competencies
As of May 2015, 35 trainees (21 internal medicine physician residents and 14 NP students) have participated in dyads. Because physician residents participate over 2 years and may partner with more than 1 NP student, this has resulted in 27 dyad pairs in this time frame. Findings from an analysis of evaluations suggest that the dyad pair trainees learn from one another, and the model provides a safe space where trainees can practice and increase their confidence.1,6,7 The NP students seem to increase clinical skills quickly—expanding physical exam skills, building a differential diagnosis, and formulating therapeutic plans—and progressing to the Interpreter and Manager levels in the O-RIME model. The physician resident achieves the Educator level.
As of September 2015, the results from the pairs who completed beginning and end evaluations show that the physician residents increased the amount of feedback they provided about performance to the student, and likewise the student NPs also felt they received an increased amount of feedback about performance from the physician resident. In addition, physician residents reported improving the most in the following areas: allowing the student to make commitments in diagnoses and treatment plans and asking the student to provide supporting evidence for their commitment to the diagnoses. NP students reported the largest increases in receiving weekly feedback about their performance from the physician and their ability to listen to the patient.1,6,7
Interprofessional Collaboration
The TOPC-CoEPCE staff observed strengthened dyad pair relationships and mutual respect between the dyad partners. Trainees communicate with each other and work together to provide care of the patient. Second, dyad pair partners are learning about the other profession—their trajectory, their education model, and their differences. The physician resident develops an awareness of the partner NP student’s knowledge and expertise, such as their experience of social and psychological factors to become a more effective teacher, contributing to patient-centered care. The evaluation results illustrate increased ability of trainees to give and receive feedback and the change in roles for providing diagnosis and providing supporting evidence within the TOPCCoEPCE dyad team.6-8
The Future
The model has broad applicability for interprofessional education in the VA since it enhances skills that providers need to work in a PACT/PCMH model. Additionally, the TOPC-CoEPCE dyad model has proven to be an effective interprofessional training experience for its affiliates and may have applicability in other VA/affiliate training programs. The dyad model can be adapted to different trainee types in the ambulatory care setting. The TOPCCoEPCE is piloting a version of the dyad with NP residents (postgraduate) and first-year medical students. Additionally, the TOPCCoEPCE is paving the way for integrating improvement of physician resident teaching skills into the primary care setting and facilitating bidirectional teaching among different professions. TOPC-CoEPCE intends to develop additional resources to facilitate use of the model application in other settings such as the dyad implementation template.
Background
In 2011, 5 US Department of Veterans Affairs (VA) medical centers were selected by the VA Office of Academic Affiliations (OAA) to establish Centers of Excellence in Primary Care Education (CoEPCE). As part of VA’s New Models of Care initiative, the 5 CoEPCEs are using VA primary care settings to develop and test innovative approaches to prepare physician residents and students, advanced practice nurses (APRNs), undergraduate nursing students, and other health professions trainees (such as pharmacy, social work, psychology, physician assistants) for primary care practice. The CoEPCE sites are developing, implementing, and evaluating curricula to prepare learners from relevant professions to practice in patientcentered, interprofessional team-based primary care settings. Patient aligned care teams (PACTs) that have 2 or more health professions trainees engaged in learning, working, and teaching are known as interprofessional academic PACTs (iAPACTs), which is the preferred model for the VA.
The Cleveland Transforming Outpatient Care (TOPC)-CoEPCE was designed for collaborative learning among nurse practitioner (NP) students and physician residents. Its robust curriculum consists of a dedicated half-day of didactics for all learners, interprofessional quality improvement projects, panel management sessions, and primary care clinical sessions for nursing and physician learners that include the dyad workplace learning model.
In 2015, the OAA lead evaluator observed the TOPC-CoEPCE dyad model process, reviewed background documents, and conducted 10 open-ended interviews with TOPC-CoEPCE staff, participating trainees, faculty, and affiliate leadership. Informants described their involvement, challenges encountered, and benefits of the TOPCCoEPC dyad model to participants, veterans, VA, and affiliates.
Lack of Interprofessional Learning Opportunities
Current health care professional education models typically do not have many workplace learning settings where physician and nursing trainees learn together and provide patient-centered care. Often in a shared clinical environment, trainees may engage in “parallel play,” which can result in physician trainees and NP students learning independently and being ill-prepared to practice effectively together.
Moreover, trainees from different professions have different learning needs. For example, less experienced NP students require greater time, supervision, and evaluation of their patient care skills. On the other hand, senior physician residents, who require less clinical instruction, need to be engaged in ways that provide opportunities to enhance their ambulatory teaching skills. Although enhancement of resident teaching skills occurs in the inpatient hospital setting, there have been limited teaching experiences for residents in a primary care setting where the instruction is traditionally faculty-based. The TOPCCoEPCE dyad model offers an opportunity to simultaneously provide trainees with a true interprofessional experience through advancement of skills in primary care, teamwork, and teaching, while addressing health care needs.
The Dyad Model
In 2011, the OAA directed COEPCE sites to develop innovative curriculum and workplace learning strategies to create more opportunities for physician and NP trainees to work as a team. There is evidence demonstrating that when students develop a shared understanding of each other’s skill set, care procedures, and values, patient care is improved.1 Further, training in pairs can be an effective strategy in education of preclerkship medical students.2 In April 2013, TOPC-CoEPCE staff asked representatives from the Student-Run Clinic at Case Western Reserve University (CWRU) in Cleveland, Ohio, to present their approach to pairing nursing and medical students in clinic under supervision by volunteer faculty. However, formal structure and curricular objectives were lacking. To address diverse TOPCCoEPCE trainee needs and create a team approach to patient care, the staff formalized and developed a workplace curriculum called the dyad model. Specifically, the model pairs 1 NP student with a senior (PGY2 or PGY3) physician resident to care for ambulatory patients as a dyad teaching/learning team. The dyad model has 3 goals: improving clinical performance, learning team dynamics, and improving the physician resident’s teaching skills in an ambulatory setting.
Planning and Implementation
Planning the dyad model took 4 months. Initial conceptualization of the model was discussed at TOPC-CoEPCE infrastructure meetings. Workgroups with representatives from medicine, nursing, evaluation and medical center administration were formed to finalize the model. The workgroups met weekly or biweekly to develop protocols for scheduling, ongoing monitoring and assessment, microteaching session curriculum development, and logistics. A pilot program was initiated for 1 month with 2 dyads to monitor learner progress and improve components, such as adjusting the patient exam start times and curriculum. In maintaining the program, the workgroups continue to meet monthly to check for areas for further improvement and maintain dissemination activities.
Curriculum
The dyad model is a novel opportunity to have trainees from different professions not only collaborate in the care of the same patient at the same time, but also negotiate their respective responsibilities preand postvisit. The experience focuses on interprofessional relationships and open communication. TOPC-CoEPCE used a modified version of the RIME (Reporter-Interpreter-Manager-Educator) model called the O-RIME model (Table 1), which includes an observer (O) phase as the first component for clarification about a beginners’ role.3,4
Four dyad pairs provide collaborative clinical care for veterans during one halfday session per week. The dyad conducts 4 hour-long patient visits per session. To be a dyad participant, the physician residents must be at least a PGY2, and their schedule must align with the NP student clinic schedule. Participation is mandatory for both NP students and physician residents. TOPC staff assemble the pairs.
The dyad model requires knowledge of the clinical and curricular interface and when to block the dyad team members’ schedules for 4 patients instead of 6. Physician residents are in the TOPC-CoEPCE for 12 weeks and then on inpatient for 12 weeks. Depending on the nursing school affiliate, NP student trainees are scheduled for either a 6- or 12-month TOPC-CoEPCE experience. For the 12-month NP students, they are paired with up to 4 internal medicine residents over the course of their dyad participation so they can experience different teaching styles of each resident while developing more varied interprofessional communication skills.
Faculty Roles and Development
The dyad model also seeks to address the paucity of deliberate interprofessional precepting in academic primary care settings. The TOPC-CoEPCE staff decided to use the existing primary care clinic faculty development series bimonthly for 1 hour each. The dyad model team members presented sessions covering foundational material in interprofessional teaching and precepting skills, which prepare faculty to precept for different professions and the dyad teams. It is important for preceptors to develop awareness of learners from different professions and the corresponding educational trajectories, so they can communicate with paired trainees of differing professions and academic levels who may require different levels of discussion.
Resources
By utilizing advanced residents as teachers, faculty were able to increase the number of learners in the clinic without increasing the number preceptors. For example, precepting a student typically requires more preceptor time, especially when we consider that the preceptor must also see the patient. The TOPC-CoEPCE faculty run the microteaching sessions, and an evaluator monitors and evaluates the program. The microteaching sessions were derived from several teaching resources.
Monitoring and Assessment
The Cleveland TOPC administered 2 different surveys developed by the Dyad Model Infrastructure and Evaluation workgroup. A 7-item survey assesses dyad team communication and interprofessional team functioning, and an 8-item survey assesses the teaching/mentoring of the resident as teacher. Both were collected from all participants to evaluate the residents’ and students’ point of view. Surveys are collected in the first and last weeks of the dyad experience. Feedback from participants has been used to make improvements to the program (eg, monitoring how the dyad teams are functioning, coaching individual learners).
Partnerships
In addition to TOPC staff and faculty support and engagement, the initiative has benefited from partnerships with VA clinic staff and with the associated academic affiliates. In particular, the Associate Chief of General Internal Medicine at the Cleveland VA medical center and interim clinic director helped institute changes to the primary care clinic structure. Additionally, buy-in from the clinic nurse manager was needed to make adjustments with staff schedules and clinic resources. To implement the dyad model, the clinic director had to approve reductions in the residents’ clinic loads for the mornings when they participated.
The NP affiliates’ faculty at the schools of nursing are integral partners who assist with student recruitment and participate in the planning and refinement of TOPCCoEPCE components. The Frances Payne Bolton School of Nursing at CWRU and the Breen School of Nursing of Ursuline College in Pepper Pike, Ohio, were involved in the planning stages and continue to receive monthly updates from TOPC-CoEPCE. Similarly, the CWRU School of Medicine and Cleveland Clinic Foundation affiliates contribute on an ongoing basis to the improvement and implementation process.
Discussion
One challenge has been advancing aspects of a nonhierarchical team approach while it is a teacher-student relationship. The dyad model is viewed as an opportunity to recognize nonhierarchical structures and teach negotiation and communication skills as well as increase interprofessional understanding of each other’s education, expertise, and scope of practice.
Another challenge is accommodating the diversity in NP training and clinical expertise. The NP student participants are in either the first or second year of their academic program. This is a challenge since both physician residents and physician faculty preceptors need to assess the NP students’ skills before providing opportunities to build on their skill level. Staff members have learned the value of checking in weekly on this issue.
Factors for Success
VA facility support and TOPC-CoEPCE leadership with the operations/academic partnership remain critical to integrating and sustaining the model into the Cleveland primary care clinic. The expertise of TOPC-CoEPCE dyad model faculty who serve as facilitators has been crucial, as they oversee team development concepts such as developing problem solving and negotiation skills. The workgroups ensured that faculty were skilled in understanding the different types of learners and provided guidance to dyad teams. Another success factor was the continual monitoring of the process and real-time evaluation of the program to adapt the model as needed.
Accomplishments and Benefits
There is evidence that the dyad model is achieving its goals: Trainees are using team skills during and outside formal dyad pairs; NP students report improvements in skill levels and comfort; and physician residents feel the teaching role in the dyad pair is an opportunity for them to improve their practice.
Interprofessional Educational Capacity
The dyad model complements the curriculum components and advances trainee understanding of 4 core domains: shared decision-making (SDM), sustained relationships (SR), interprofessional collaboration (IPC), and performance improvement (PI) (Table 2). The dyad model supports the other CoEPCE interprofessional education activities and is reinforced by these activities. The model is a learning laboratory for studying team dynamics and developing a curriculum that strengthens a team approach to patient-centered care.
Participants’ Knowledge, Attitudes, Skills, and Competencies
As of May 2015, 35 trainees (21 internal medicine physician residents and 14 NP students) have participated in dyads. Because physician residents participate over 2 years and may partner with more than 1 NP student, this has resulted in 27 dyad pairs in this time frame. Findings from an analysis of evaluations suggest that the dyad pair trainees learn from one another, and the model provides a safe space where trainees can practice and increase their confidence.1,6,7 The NP students seem to increase clinical skills quickly—expanding physical exam skills, building a differential diagnosis, and formulating therapeutic plans—and progressing to the Interpreter and Manager levels in the O-RIME model. The physician resident achieves the Educator level.
As of September 2015, the results from the pairs who completed beginning and end evaluations show that the physician residents increased the amount of feedback they provided about performance to the student, and likewise the student NPs also felt they received an increased amount of feedback about performance from the physician resident. In addition, physician residents reported improving the most in the following areas: allowing the student to make commitments in diagnoses and treatment plans and asking the student to provide supporting evidence for their commitment to the diagnoses. NP students reported the largest increases in receiving weekly feedback about their performance from the physician and their ability to listen to the patient.1,6,7
Interprofessional Collaboration
The TOPC-CoEPCE staff observed strengthened dyad pair relationships and mutual respect between the dyad partners. Trainees communicate with each other and work together to provide care of the patient. Second, dyad pair partners are learning about the other profession—their trajectory, their education model, and their differences. The physician resident develops an awareness of the partner NP student’s knowledge and expertise, such as their experience of social and psychological factors to become a more effective teacher, contributing to patient-centered care. The evaluation results illustrate increased ability of trainees to give and receive feedback and the change in roles for providing diagnosis and providing supporting evidence within the TOPCCoEPCE dyad team.6-8
The Future
The model has broad applicability for interprofessional education in the VA since it enhances skills that providers need to work in a PACT/PCMH model. Additionally, the TOPC-CoEPCE dyad model has proven to be an effective interprofessional training experience for its affiliates and may have applicability in other VA/affiliate training programs. The dyad model can be adapted to different trainee types in the ambulatory care setting. The TOPCCoEPCE is piloting a version of the dyad with NP residents (postgraduate) and first-year medical students. Additionally, the TOPCCoEPCE is paving the way for integrating improvement of physician resident teaching skills into the primary care setting and facilitating bidirectional teaching among different professions. TOPC-CoEPCE intends to develop additional resources to facilitate use of the model application in other settings such as the dyad implementation template.
1. Billett SR. Securing intersubjectivity through interprofessional workplace learning experiences. J Interprof Care. 2014;28(3):206-211.
2. Tolsgaard MG, Bjørck S, Rasmussen MB, Gustafsson A, Ringsted C. Improving efficiency of clinical skills training: a randomized trial. J Gen Intern Med. 2013;28(8);1072-1077.
3. Pangaro L. A new vocabulary and other innovations for improving descriptive in-training evaluations. Acad Med. 1999;74(11):1203-1207.
4. Tham KY. Observer-Reporter-Interpreter-Manager-Educator (O-RIME) framework to guide formative assessment of medical students. Ann Acad Med Singapore. 2013;42(11):603-607.
6. Clementz L, Dolansky MA, Lawrence RH, et al. Dyad teams: interprofessional collaboration and learning in ambulatory setting. Poster session presented: 38th Annual Meeting of the Society of General Internal Medicine; April 2015:Toronto, Canada. www.pcori.org/sites/default/files /SGIM-Conference-Program-2015.pdf. Accessed August 29, 2018.
7. Singh M, Clementz L, Dolansky MA, et al. MD-NP learning dyad model: an innovative approach to interprofessional teaching and learning. Workshop presented at: Annual Meeting of the Midwest Society of General Internal Medicine; August 27, 2015: Cleveland, Ohio.
8. Lawrence RH, Dolansky MA, Clementz L, et al. Dyad teams: collaboration and learning in the ambulatory care setting. Poster session presented at: AAMC meeting, Innovations in Academic Medicine; November 7-11, 2014: Chicago, IL.
1. Billett SR. Securing intersubjectivity through interprofessional workplace learning experiences. J Interprof Care. 2014;28(3):206-211.
2. Tolsgaard MG, Bjørck S, Rasmussen MB, Gustafsson A, Ringsted C. Improving efficiency of clinical skills training: a randomized trial. J Gen Intern Med. 2013;28(8);1072-1077.
3. Pangaro L. A new vocabulary and other innovations for improving descriptive in-training evaluations. Acad Med. 1999;74(11):1203-1207.
4. Tham KY. Observer-Reporter-Interpreter-Manager-Educator (O-RIME) framework to guide formative assessment of medical students. Ann Acad Med Singapore. 2013;42(11):603-607.
6. Clementz L, Dolansky MA, Lawrence RH, et al. Dyad teams: interprofessional collaboration and learning in ambulatory setting. Poster session presented: 38th Annual Meeting of the Society of General Internal Medicine; April 2015:Toronto, Canada. www.pcori.org/sites/default/files /SGIM-Conference-Program-2015.pdf. Accessed August 29, 2018.
7. Singh M, Clementz L, Dolansky MA, et al. MD-NP learning dyad model: an innovative approach to interprofessional teaching and learning. Workshop presented at: Annual Meeting of the Midwest Society of General Internal Medicine; August 27, 2015: Cleveland, Ohio.
8. Lawrence RH, Dolansky MA, Clementz L, et al. Dyad teams: collaboration and learning in the ambulatory care setting. Poster session presented at: AAMC meeting, Innovations in Academic Medicine; November 7-11, 2014: Chicago, IL.
Population Management of Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease (NAFLD) is an umbrella term that covers a spectrum of phenotypes ranging from nonalcoholic fatty liver or simple hepatic steatosis to nonalcoholic steatohepatitis (NASH) defined by histologic findings of steatosis, lobular inflammation, cytologic ballooning, and some degree of fibrosis.1 While frequently observed in patients with at least 1 risk factor (eg, obesity, diabetes mellitus [DM], dyslipidemia, hypertension), NAFLD also is an independent risk factor for type 2 DM (T2DM), chronic kidney disease, and cardiovascular disease.2 At early disease stages with absence of liver fibrosis, mortality is linked to cardiovascular and not liver disease. However, in the presence of NASH, fibrosis progression to liver cirrhosis, or hepatocellular carcinoma (HCC) represent the most important liver-related outcomes that determine morbidity and mortality.3 Mirroring the obesity and T2DM epidemics, the health care burden is projected to dramatically rise.
In the following article, we will discuss how the Veterans Health Administration (VHA) is well positioned to implement an organizational strategy of comprehensive care for veterans with NAFLD. This comprehensive care strategy should include the development of a NAFLD clinic offering care for comorbid conditions frequently present in these patients, point-of-care testing, access to clinical trials, and outcomes monitoring as a key performance target for providers and the respective facility.
NAFLD disease burden
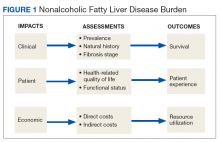
To fully appreciate the burden of a chronic disease like NAFLD, it is important to assess its long- and short-term consequences in a comprehensive manner with regard to its clinical impact, impact on the patient, and economic impact (Figure 1).
Clinical Impact
Clinical impact is assessed based on the prevalence and natural history of NAFLD and the liver fibrosis stage and determines patient survival. Coinciding with the epidemic of obesity and T2DM, the prevalence of NAFLD in the general population in North America is 24% and even higher with older age and higher body mass index (BMI).4,5 The prevalence for NAFLD is particularly high in patients with T2DM (47%). Of patients with T2DM and NAFLD, 65% have biopsy-proven NASH of which 15% have bridging fibrosis or liver cirrhosis.6
NAFLD is the fastest growing cause of cirrhosis in the US with a forecasted NAFLD population of 101 million by 2030.7 At the same time, the number of patients with NASH will rise to 27 million of which > 7 million will have bridging fibrosis or liver cirrhosis; hepatic decompensation events are estimated to occur in 105,430 patients with liver cirrhosis, posing a major public health threat related to organ availability for liver transplantation.8 Since 2013, NAFLD has been the second leading cause for liver transplantation and the top reason for transplantation in patients aged < 50 years.9,10 As many patients with NAFLD are diagnosed with HCC at stages where liver transplantation is not an option, mortality from HCC in NAFLD patients is higher than with other etiologies as treatment options are restricted.11,12
Compared with that of the general population, veterans seeking care are older and sicker with 43% of veterans taking > 5 prescribed medications.13 Of those receiving VHA care, 6.6 million veterans are either overweight or obese; 165,000 are morbidly obese with a BMI > 40.14 In addition, veterans are 2.5 times more likely to have T2DM compared with that of nonveterans. Because T2DM and obesity are the most common risk factors for NAFLD, it is not surprising that NAFLD prevalence among veterans rose 3-fold from 2003 to 2011.15 It is now estimated that 540,000 veterans will progress to NASH and 108,000 will develop bridging fibrosis or liver cirrhosis by 2030.8 Similar to that of the general population, liver cirrhosis is attributed to NAFLD in 15% of veterans.15,16 NAFLD is the third most common cause of cirrhosis and HCC, occurring at an average age of 66 years and 70 years, respectively.16,17 Shockingly, 20% of HCCs were not linked to liver cirrhosis and escaped recommended HCC screening for patients with cirrhosis.18,19
Patient Impact
Assessment of disease burden should not be restricted to clinical outcomes as patients can experience a range of symptoms that may have significant impact on their health-related quality of life (QOL) and functional status.20 Using general but not disease-specific instruments, NAFLD patients reported outcomes score low regarding fatigue, activity, and emotions.21 More disease-specific questionnaires may provide better and disease-specific insights as how NASH impacts patients’ QOL.22-24
Economic Impact
There is mounting evidence that the clinical implications of NAFLD directly influence the economic burden of NAFLD.25 The annual burden associated with all incident and prevalent NAFLD cases in the US has been estimated at $103 billion, and projections suggest that the expected 10-year burden of NAFLD may increase to $1.005 trillion.26 It is anticipated that increased NAFLD costs will affect the VHA with billions of dollars in annual expenditures in addition to the $1.5 billion already spent annually for T2DM care (4% of the VA pharmacy budget is spent on T2DM treatment).27-29
Current Patient Care
Obesity, DM, and dyslipidemia are common conditions managed by primary care providers (PCPs). Given the close association of these conditions with NAFLD, the PCP is often the first point of medical contact for patients with or at risk for NAFLD.30 For that reason, PCP awareness of NAFLD is critical for effective management of these patients. PCPs should be actively involved in the management of patients with NAFLD with pathways in place for identifying patients at high risk of liver disease for timely referral to a specialist and adequate education on the follow-up and treatment of low-risk patients. Instead, diagnosis of NAFLD is primarily triggered by either abnormal aminotransferases or detection of steatosis on imaging performed for other indications.
Barriers to optimal management of NAFLD by PCPs have been identified and occur at different levels of patient care. In the absence of clinical practice guidelines by the American Association of Family Practice covering NAFLD and a substantial latency period without signs of symptoms, NAFLD may not be perceived as a potentially serious condition by PCPs and their patients; interestingly this holds true even for some medical specialties.31-39 More than half of PCPs do not test their patients at highest risk for NAFLD (eg, patients with obesity or T2DM) and may be unaware of practice guidelines.40-42
Guidelines from Europe and the US are not completely in accordance. The US guidelines are vague regarding screening and are supported by only 1 medical society, due to the lack of NASH-specific drug therapies. The European guidelines are built on the support of 3 different stakeholders covering liver diseases, obesity, and DM and the experience using noninvasive liver fibrosis assessments for patients with NAFLD. To overcome this apparent conflict, a more practical and risk-stratified approach is warranted.41,42
Making the diagnosis can be challenging in cases with competing etiologies, such as T2DM and alcohol misuse. There also is an overreliance on aminotransferase levels to diagnose NAFLD. Significant liver disease can exist in the presence of normal aminotransferases, and this may be attributed to either spontaneous aminotransferase fluctuations or upper limits of normal that have been chosen too high.43-47 Often additional workup by PCPs depends on the magnitude of aminotransferase abnormalities.
Even if NAFLD has been diagnosed by PCPs, identifying those with NASH is hindered by the absence of an accurate noninvasive diagnostic method and the need to perform a liver biopsy. Liver biopsy is often not considered or delayed to monitor patients with serial aminotransferases, regardless of the patient’s metabolic comorbidity profile or baseline aminotransferases.32 As a result, referral to a specialist often depends on the magnitude of the aminotransferase abnormality,30,48 and often occurs when advanced liver disease is already present.49 Finally, providers may not be aware of beneficial effects of lifestyle interventions and certain medications, including statins on NASH and liver fibrosis.50-53 As NAFLD is associated with excess cardiovascular- and cancer-related morbidity and mortality, it is possible that regression of NAFLD may improve associated risk for these outcomes as well.
Framework for Comprehensive NAFLD Care
Chronic liver diseases and associated comorbidities have long been addressed by PCPs and specialty providers working in isolation and within the narrow focus of each discipline. Contrary to working in silos of the past, a coordinated management strategy with other disciplines that cover these comorbidities needs to be established, or alternatively the PCP must be aware of the management of comorbidities to execute them independently. Integration of hepatology-driven NAFLD care with other specialties involves communication, collaboration, and sharing of resources and expertise that will address patient care needs. Obviously, this cannot be undertaken in a single outpatient visit and requires vertical and longitudinal follow-up over time. One important aspect of comprehensive NAFLD care is the targeting of a particular patient population rather than being seen as a panacea for all; cost-utility analysis is hampered by uncertainties around accuracy of noninvasive biomarkers reflecting liver injury and a lack of effectiveness data for treatment. However, it seems reasonable to screen patients at high risk for NASH and adverse clinical outcomes. Such a risk stratification approach should be cost-effective.
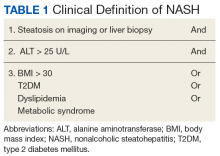
A first key step by the PCP is to identify whether a patient is at risk, especially patients with NASH. The majority of patients at risk are already seen by PCPs. While there is no consensus on ideal screening for NAFLD by PCPs, the use of ultrasound in the at-risk population is recommended in Europe.42 Although NASH remains a histopathologic diagnosis, a reasonable approach is to define NASH based on clinical criteria as done similarly in a real-world observational NAFLD cohort study.54 In the absence of chronic alcohol consumption and viral hepatitis and in a real-world scenario, NASH can be defined as steatosis shown on liver imaging or biopsy and alanine aminotransferase (ALT) levels of > 25 U/L. In addition, ≥ 1 of the following criteria must be met: BMI > 30, T2DM, dyslipidemia, or metabolic syndrome (Table 1).
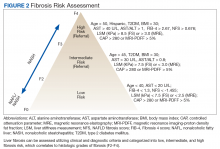
In the absence of easy-to-use validated tests, all patients with NAFLD need to be assessed with simple, noninvasive scores for the presence of clinically relevant liver fibrosis (F2-portal fibrosis with septa; F3-bridging fibrosis; F4-liver cirrhosis); those that meet the fibrosis criteria should receive further assessment usually only offered in a comprehensive NAFLD clinic.1 PCPs should focus on addressing 2 aspects related to NAFLD: (1) Does my patient have NASH based on clinical criteria; and (2) Is my patient at risk for clinically relevant liver fibrosis? PCPs are integral in optimal management of comorbidities and metabolic syndrome abnormalities with lifestyle and exercise interventions.
The care needs of a typical patient with NAFLD can be classified into 3 categories: liver disease (NAFLD) management, addressing NAFLD associated comorbidities, and attending to the personal care needs of the patient. With considerable interactions between these categories, interventions done within the framework of 1 category can influence the needs pertaining to another, requiring closer monitoring of the patient and potentially modifying care. For example, initiating a low carbohydrate diet in a patient with DM and NAFLD who is on antidiabetic medication may require adjusting the medication; disease progression or failure to achieve treatment goals may affect the emotional state of the patient, which can affect adherence.
Referrals to a comprehensive NAFLD clinic need to be standardized. Clearly, the referral process depends in part on local resources, comprehensiveness of available services, and patient characteristics, among others. Most often, PCPs refer patients with suspected diagnosis of NAFLD, with or without abnormal aminotransferases, to a hepatologist to confirm the diagnosis and for disease staging and liver disease management. This may have the advantage of greatest extent of access and should limit the number of patients with advanced liver fibrosis who otherwise may have been missed. On the other hand, different thresholds of PCPs for referrals may delay the patient’s access to comprehensive NAFLD care. Of those referred by primary care, the hepatologist identifies patients with NAFLD who benefit most from a comprehensive care approach. This automated referral process without predefined criteria remains more a vision than reality as it would require an infrastructure and resources that no health care system can provide currently.
The alternative approach of automatic referral may use predefined criteria related to patients’ diagnoses and prognoses (Figure 2).
Patient-Centered Care
At present the narrow focus of VHA specialty outpatient clinics associated with time constraints of providers and gaps in NAFLD awareness clearly does not address the complex metabolic needs of veterans with NAFLD. This is in striking contrast to the comprehensive care offered to patients with cancer. To overcome these limitations, new care delivery models need to be explored. At first it seems attractive to embed NAFLD patient care geographically into a hepatology clinic with the potential advantages of improving volume and timeliness of referral and reinforcing communication among specialty providers while maximizing convenience for patients. However, this is resource intensive not only concerning clinic space, but also in terms of staffing clinics with specialty providers.
Patient-centered care for veterans with NAFLD seems to be best organized around a comprehensive NAFLD clinic with access to specialized diagnostics and knowledge in day-to-day NAFLD management. This evolving care concept has been developed already for patients with liver cirrhosis and inflammatory bowel disease and considers NAFLD a chronic disease that cannot be addressed sufficiently by providing episodic care.55,56 The development of comprehensive NAFLD care can build on the great success of the Hepatitis Innovation Team Collaborative that employed lean management strategies with local and regional teams to facilitate efforts to make chronic hepatitis C virus a rare disease in the VHA.57
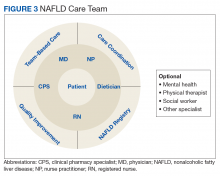
NAFLD Care Team
Given the central role of the liver and gastrointestinal tract in the field of nutrition, knowledge of the pathophysiology of the liver and digestive tract as well as emerging therapeutic options offered via metabolic endoscopy uniquely positions the hepatologist/gastroenterologist to take the lead in managing NAFLD. Treating NAFLD is best accomplished when the specialist partners with other health care providers who have expertise in the nutritional, behavioral, and physical activity aspects of treatment. The composition of the NAFLD care team and the roles that different providers fulfill can vary depending on the clinical setting; however, the hepatologist/gastroenterologist is best suited to lead the team, or alternatively, this role can be fulfilled by a provider with liver disease expertise.
Based on experiences from the United Kingdom, the minimum staffing of a NAFLD clinic should include a physician and nurse practitioner who has expertise in managing patients with chronic liver disease, a registered nurse, a dietitian, and a clinical pharmacy specialist (CPS).58 With coexistent diseases common and many veterans who have > 5 prescribed medications, risk of polypharmacy and adverse drug reactions are a concern, particularly since adherence in patients with chronic diseases has been reported to be as low as 43%.59-61 Risk of medication errors and serious adverse effects are magnified by difficulties with patient adherence, medication interactions, and potential need for frequent dose adjustments, particularly when on a weight-loss diet.
Without doubt, comprehensive medication management, offered by a highly trained CPS with independent prescriptive authority occurring while the veteran is in the NAFLD clinic, is highly desirable. Establishing a functional statement and care coordination agreement could describe the role of the CPS as a member of the NAFLD provider team.
Patient Evaluation
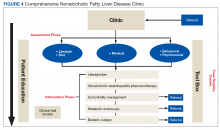
After being referred to the NAFLD clinic, the veteran should have a thorough assessment, including medical, nutritional, physical activity, exercise, and psychosocial evaluations (Figure 4).
The assessment also should include patient education to ensure that the patient has sufficient knowledge and skills to achieve the treatment goals. Educating on NAFLD is critical as most patients with NAFLD do not think of themselves as sick and have limited readiness for lifestyle changes.63,64 A better understanding of NAFLD combined with a higher self-efficacy seems to be positively linked to better nutritional habits.65
An online patient-reported outcomes measurement information system for a patient with NAFLD (eg, assessmentcenter.net) may be beneficial and can be applied within a routine NAFLD clinic visit because of its multidimensionality and compatibility with other chronic diseases.66-68 Other tools to assess health-related QOL include questionnaires, such as the functional assessment of chronic illness therapy-fatigue, work productivity and activity impairment questionnaire: specific health problem, Short Form-36, and chronic liver disease questionnaire-NAFLD.23,69
The medical evaluation includes assessment of secondary causes of NAFLD and identification of NAFLD-related comorbidities. Weight, height, blood pressure, waist circumference, and BMI should be recorded. The physical exam should focus on signs of chronic liver disease and include inspection for acanthosis nigricans, hirsutism, and large neck circumference, which are associated with insulin resistance, polycystic ovarian syndrome, and obstructive sleep apnea, respectively. NAFLD-associated comorbidities may contribute to frailty or physical limitations that affect treatment with diet and exercise and need to be assessed. A thorough medication reconciliation will reveal whether the patient is prescribed obesogenic medications and whether comorbidities (eg, DM and dyslipidemia) are being treated optimally and according to current society guidelines.
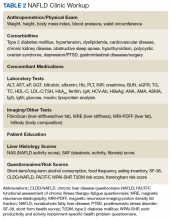
Making the diagnosis of NAFLD requires excluding other (concomitant) chronic liver diseases. While often this is done indirectly using order sets with a panoply of available serologic tests without accounting for risks for rare causes of liver injury, a more focused and cost-effective approach is warranted. As most patients will already have had imaging studies that show fatty liver, assessment of liver fibrosis is an important step for risk stratification. Noninvasive scores (eg, FIB-4) can be used by the PCP to identify high-risk patients requiring further workup and referral.1,70 More sophisticated tools, including transient elastography and/or magnetic resonance elastography are applied for more sophisticated risk stratification and liver disease management (Table 2).71
A nutritional evaluation includes information about eating behavior and food choices, body composition analysis, and an assessment of short- and long-term alcohol consumption. Presence of bilateral muscle wasting, subcutaneous fat loss, and signs of micronutrient deficiencies also should be explored. The lifestyle evaluation should include the patient’s typical physical activity and exercise as well as limiting factors.
Finally, and equally important, the patient’s psychosocial situation should be assessed, as motivation and accountability are key to success and may require behavioral modification. Assessing readiness is done best with motivational interviewing, the 5As counseling framework (Ask, Advise, Assess, Assist, Arrange) or using open-ended questions, affirmation, reflections, and summaries.72,73 Even if not personally delivering behavioral treatment, such an approach also can help move patients toward addressing important health-related behaviors.
Personalized Interventions
If available, patients should be offered participation in NAFLD clinical trials. A personalized treatment plan should be developed for each patient with input from all NAFLD care team members. The patient and providers should work together to make important decisions about the treatment plan and goals of care. Making the patient an active participant in their treatment rather than the passive recipient will lead to improvement in adherence and outcomes. Patients will engage when they are comfortable speaking with providers and are sufficiently educated about their disease.
Personalized interventions may be built by combining different strategies, such as lifestyle and dietary interventions, NASH-specific pharmacotherapy, comorbidity management, metabolic endoscopy, and bariatric surgery. Although NASH-specific medications are not currently available, approved medications, including pioglitazone or liraglutide, can be considered for therapy.74,75 Ideally, the NAFLD team CPS would manage comorbidities, such as T2DM and dyslipidemia, but this also can be done by a hepatologist or other specialist. Metabolic endoscopy (eg, intragastric balloons) or bariatric surgery would be done by referral.
Resource-Limited Settings
Although the VHA offers care at > 150 medical centers and > 1,000 outpatient clinics, specialty care such as hepatology and sophisticated and novel testing modalities are not available at many facilities. In 2011 VHA launched the Specialty Care Access Network Extension for Community Healthcare Outcomes to bring hepatitis C therapy and liver transplantation evaluations to rural areas without specialists.76-78 It is logical to explore how telehealth can be used for NAFLD care that requires complex management using new treatments and has a high societal impact, particularly when left untreated.
Telehealth must be easy to use and integrated into everyday routines to be useful for NAFLD management by addressing different aspects of promoting self-management, optimizing therapy, and care coordination. Participation in a structured face-to-face or group-based lifestyle program is often jeopardized by time and job constraints but can be successfully overcome using online approaches.79 The Internet-based VA Video Connect videoconferencing, which incorporates cell phone, laptop, or tablet use could help expand lifestyle interventions to a much larger community of patients with NAFLD and overcome local resource constraints. Finally, e-consultation also can be used in circumstances where synchronous communication with specialists may not be necessary.
Patient Monitoring and Quality Metrics
Monitoring of the patient after initiation of an intervention is variable but occurs more frequently at the beginning. For high-intensity dietary interventions, weekly monitoring for the first several weeks can ensure ongoing motivation, and accountability may increase the patient’s confidence and provide encouragement for further weight loss. It also is an opportunity to reestablish goals with patients with declining motivation. Long-term monitoring of patients may occur in 6- to 12-month intervals to document patient-reported outcomes, liver-related mortality, cardiovascular events, malignancies, and disease progression or regression.
While quality indicators have been proposed for cirrhosis care, such indicators have yet to be defined for NALD care.80 Such quality indicators assessed with validated questionnaires should include knowledge about NAFLD, satisfaction with care, perception of quality of care, and patient-reported outcomes. Other indicators may include use of therapies to treat dyslipidemia and T2DM. Last and likely the most important indicator of improved liver health in NAFLD will be either histologic improvement of NASH or improvement of the fibrosis risk category.
Outlook
With the enormous burden of NAFLD on the rise for many more years to come, quality care delivered to patients with NAFLD warrants resource-adaptive population health management strategies. With a limited number of providers specialized in liver disease, provider education assisted by clinical guidelines and decision support tools, development of referral and access to care mechanisms through integrated care, remote monitoring strategies as well as development of patient self-management and community resources will become more important. We have outlined essential components of an effective population health management strategy for NAFLD and actionable items for the VHA to consider when implementing these strategies. This is the time for the VHA to invest in efforts for NAFLD population care. Clearly, consideration must be given to local needs and resources and integration of technology platforms. Addressing NAFLD at a population level will provide yet another opportunity to demonstrate that VHA performs better on quality when compared with care systems in the private sector.81
1. Hunt CM, Turner MJ, Gifford EJ, Britt RB, Su GL. Identifying and treating nonalcoholic fatty liver disease. Fed Pract. 2019;36(1):20-29.
2. Glass LM, Hunt CM, Fuchs M, Su GL. Comorbidities and non-alcoholic fatty liver disease: the chicken, the egg, or both? Fed Pract. 2019;36(2):64-71.
3. Vilar-Gomez E, Calzadilla-Bertot L, Wai-Sun Wong V, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology. 2018;155(2):443-457.e17.
4. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73-84.
5. Yki-Järvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2(11):901-910.
6. Golabi P, Shahab O, Stepanova M, Sayiner M, Clement SC, Younossi ZM. Long-term outcomes of diabetic patients with non-alcoholic fatty liver disease (NAFLD) [abstract]. Hepatology. 2017;66(suppl 1):1142A-1143A.
7. Wong RJ, Cheung R, Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology. 2014;59(6):2188-2195.
8. Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67(1):123-133.
9. Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547-555.
10. Banini B, Mota M, Behnke M, Sharma A, Sanyal AJ. Nonalcoholic steatohepatitis (NASH) has surpassed hepatitis C as the leading cause for listing for liver transplant: implications for NASH in children and young adults. Presented at the American College of Gastroenterology Annual Scientific Meeting, Las Vegas, NV, October 18, 2016. Abstract 46. https://www.eventscribe.com/2016/ACG/QRcode.asp?Pres=199366. Accessed January 15, 2019.
11. Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020-1022.
12. Younossi ZM, Otgonsuren M, Henry L, et al. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004-2009. Hepatology. 2015;62(6):1723-1730.
13. Breland JY, Phibbs CS, Hoggatt KJ, et al. The obesity epidemic in the Veterans Health Administration: prevalence among key populations of women and men veterans. J Gen Intern Med. 2017;32(suppl 1):11-17.
14. Gunnar W. Bariatric surgery provided by the Veterans Health Administration: current state and a look to the future. J Gen Intern Med. 2017;32(suppl 1):4-5.
15. Kanwal F, Kramer JR, Duan Z, Yu X, White D, El-Seraq HB. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin Gastroenterol Hepatol. 2016;14(2):301-308.e1-2.
16. Goldberg D, Ditah IC, Saeian K, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the wait list for liver transplantation. Gastroenterology. 2017;152(5):1090-1099.e1.
17. Beste L, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001-2013. Gastroenterology. 2015;149(6):1471-1482.e5.
18. Mittal S, El-Seraq HB, Sada YH, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14(1):124-131.
19. Kanwal F, Kramer JR, Mapakshi S, et al. Risk of hepatocellular cancer in patients with nonalcoholic fatty liver disease. Gastroenterology. 2018;55(6):1828-1837.e2.
20. David K, Kowdley KV, Unalp A, Kanwal F, Brunt EM, Schwimmer JB; NASH CRN Research Group. Quality of life in adults with nonalcoholic fatty liver disease: baseline data from the nonalcoholic steatohepatitis clinical research network. Hepatology. 2009;49(6):1904-1912.
21. Younossi ZM, Stepanova M, Henry L. Performance and validation of Chronic Liver Disease Questionnaire-Hepatitis C Version (CLDQ-HCV) in clinical trials of patients with chronic hepatitis C. Value Health. 2016;19(5):544-551.
22. Younossi ZM, Henry L. Economic and quality-of-life implications of nonalcoholic fatty liver disease. Pharmacoeconomics. 2015;33(12):1245-1253.
23. Younossi ZM, Stepanova M, Henry L, et al. A disease-specific quality of life instrument for nonalcoholic fatty liver disease and non-alcoholic steatohepatitis: CLDQ-NAFLD. Liver Int. 2017;37(8):1209-1218.
24. Chawla KS, Talwalkar JA, Keach JC, Malinchoc M, Lindor KD, Jorgensen R. Reliability and validity of the chronic liver disease questionnaire (CLDQ) in adults with non-alcoholic steatohepatitis (NASH). BMJ Open Gastroenterol. 2016;3(1):e000069.
25. Shetty A, Syn WK. Health, and economic burden of nonalcoholic fatty liver disease in the United States and its impact on Veterans. Fed Pract. 2019;36(1):14-19.
26. Younossi ZM, Blissett D, Blissett R, et al. The economic and clinical burden of nonalcoholic liver disease in the United States and Europe. Hepatology. 2016;64(5):1577-1586.
27. Younossi ZM, Tampi R, Priyadarshini M, Nader F, Younossi IM, Racila A. Burden of illness and economic model for patients with non-alcoholic steatohepatitis (NASH) in the United States. Hepatology. 2018. [Epub ahead of print.]
28. Allen AM, van Houten HK, Sangaralingham LR, Talwalkar JA, McCoy RG. Healthcare cost and utilization in nonalcoholic fatty liver disease: real-world data from a large U.S. claims database. Hepatology. 2018;68(6):2230-2238.
29. Diabetes mellitus. http://www.fedprac-digital.com/federalpractitioner/data_trends_2017?pg=20#pg20. Published July 2017. Accessed January 15, 2019.
30. Grattagliano I, D’Ambrosio G, Palmieri VO, Moschetta A, Palasciano G, Portincasa P; “Steatostop Project” Group. Improving nonalcoholic fatty liver disease management by general practitioners: a critical evaluation and impact of an educational training program. J Gastrointestin Liver Dis. 2008;17(4):389-394.
31. Polanco-Briceno S, Glass D, Stuntz M, Caze A. Awareness of nonalcoholic steatohepatitis and associated practice patterns of primary care physicians and specialists. BMC Res Notes. 2016;9:157.
32. Patel PJ, Banh X, Horsfall LU, et al. Underappreciation of non-alcoholic fatty liver disease by primary care clinicians: limited awareness of surrogate markers of fibrosis. Intern Med. 2018;48(2):144-151.
33. Standing HC, Jarvis H, Orr J, et al. GPs’ experiences and perceptions of early detection of liver disease: a qualitative study in primary care. Br J Gen Pract. 2018;68(676):e743-e749.
34. Wieland AC, Quallick M, Truesdale A, Mettler P, Bambha KM. Identifying practice gaps to optimize medical care for patients with nonalcoholic fatty liver disease. Dig Dis Sci. 2013;58(10):2809-2816.
35. Alexander M, Loomis AK, Fairburn-Beech J, et al. Real-world data reveal a diagnostic gap in non-alcoholic fatty liver disease. BMC Med. 2018;16(1):130.
36. Ratziu V, Cadranel JF, Serfaty L, et al. A survey of patterns of practice and perception of NAFLD in a large sample of practicing gastroenterologists in France. J Hepatol. 2012;57(2):376-383.
37. Blais P, Husain N, Kramer JR, Kowalkowski M, El-Seraq H, Kanwal F. Nonalcoholic fatty liver disease is underrecognized in the primary care setting. Am J Gastroenterol. 2015;110(1):10-14.
38. Bergqvist CJ, Skoien R, Horsfall L, Clouston AD, Jonsson JR, Powell EE. Awareness and opinions of non-alcoholic fatty liver disease by hospital specialists. Intern Med J. 2013;43(3):247-253.
39. Said A, Gagovic V, Malecki K, Givens ML, Nieto FJ. Primary care practitioners survey of non-alcoholic fatty liver disease. Ann Hepatol. 2013;12(5):758-765.
40. Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328-357.
41. NICE National Institute for Health and Care Excellence. Non-alcoholic fatty liver disease (NAFLD): assessment and management. https://www.nice.org.uk/guidance/ng49. Published July 2016. Accessed January 15, 2019.
42. European Association for the Study of the Liver (EASL), European Association for the Study of diabetes (EASD), European Association for the study of obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388-1402.
43. Mofrad P, Contos MJ, Haque M, et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37(6):1286-1292.
44. Koehler EM, Plompen EP, Schouten JN, et al. Presence of diabetes mellitus and steatosis is associated with liver stiffness in a general population: the Rotterdam study. Hepatology. 2016;63(1):138-147.
45. Kwok R, Choi KC, Wong GL, et al. Screening diabetic patients for non-alcoholic fatty liver disease with controlled attenuation parameter and liver stiffness measurements: a prospective cohort study. Gut. 2016;65(8):1359-1368.
46. Harman DJ, Ryder SD, James MW, et al. Obesity and type 2 diabetes are important risk factors underlying previously undiagnosed cirrhosis in general practice: a cross-sectional study using transient elastography. Aliment Pharmacol Ther. 2018;47(4):504-515.
47. Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002;137(1):1-10.
48. Rinella ME, Lominadze Z, Loomba R, et al. Practice pattern in NAFLD and NASH: real life differs from published guidelines. Therap Adv Gastroenterol. 2016;9(1):4-12.
49. El-Atem NA, Wojcik K, Horsfall L, et al. Patterns of service utilization within Australian hepatology clinics: high prevalence of advanced liver disease. Intern Med. 2016;46(4):420-426.
50. Dongiovanni P, Petta S, Mannisto V, et al. Statin use and nonalcoholic steatohepatitis in at risk individuals. J Hepatol. 2015;63(3):705-712.
51. Nascimbeni F, Aron-Wisnewsky J, Pais R, et al; LIDO Study Group. Statins, antidiabetic medications and liver histology in patients with diabetes with non-alcoholic fatty liver disease. BMJ Open Gastroenterol. 2016;3(1):e000075.
52. Romero-Gomez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67(4):829-846.
53. Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149(2):367-378.
54. Barritt AS 4th, Gitlin N, Klein S, et al. Design and rationale for a real-world observational cohort of patients with nonalcoholic fatty liver disease: The TARGET-NASH study. Contemp Clin Trials. 2017;61:33-38.
55. Meier SK, Shah ND, Talwalkar JA. Adapting the patient-centered specialty practice model for populations with cirrhosis. Clin Gastroenterol Hepatol. 2016;14(4):492-496.
56. Dulai PS, Singh S, Ohno-Machado L, Sandborn WJ. Population health management for inflammatory bowel disease. Gastroenterology. 2018;154(1):37-45.
57. Park A, Gonzalez R, Chartier M, et al. Screening and treating hepatitis C in the VA: achieving excellence using lean and system redesign. Fed Pract. 2018;35(7):24-29.
58. Cobbold JFL, Raveendran S, Peake CM, Anstee QM, Yee MS, Thursz MR. Piloting a multidisciplinary clinic for the management of non-alcoholic fatty liver disease: initial 5-year experience. Frontline Gastroenterol. 2013;4(4):263-269.
59. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(3):487-497.
60. Harrison SA. NASH, from diagnosis to treatment: where do we stand? Hepatology. 2015;62(6):1652-1655.
61. Patel PJ, Hayward KL, Rudra R, et al. Multimorbidity and polypharmacy in diabetic patients with NAFLD: implications for disease severity and management. Medicine (Baltimore). 2017;96(26):e6761.
62. Kanwal F, Mapashki S, Smith D, et al. Implementation of a population-based cirrhosis identification and management system. Clin Gastroenterol Hepatol. 2018;16(8):1182-1186.e2.
63. Mlynarski L, Schlesinger D, Lotan R, et al. Non-alcoholic fatty liver disease is not associated with a lower health perception. World J Gastroenterol. 2016;22(17):4362-4372.
64. Centis E, Moscatiello S, Bugianesi E, et al. Stage of change and motivation to healthier lifestyle in non-alcoholic fatty liver disease. J Hepatol. 2013;58(4):771-777.
65. Zelber-Sagi S, Bord S, Dror-Lavi G, et al. Role of illness perception and self-efficacy in lifestyle modification among non-alcoholic fatty liver disease patients. World J Gastroenterol. 2017;23(10):1881-1890.
66. Bajaj JS, Thacker LR, Wade JB, et al. PROMIS computerized adaptive tests are dynamic instruments to measure health-related quality of life in patients with cirrhosis. Aliment Pharmacol Ther. 2011;34(9):1123-1132.
67. Verma M, Stites S, Navarro V. Bringing assessment of patient-reported outcomes to hepatology practice. Clin Gastroenterol Hepatol. 2018;16(3):447-448.
68. Ahmed S, Ware P, Gardner W, et al. Montreal Accord on patient-reported outcomes (PROs) use series – paper 8: patient-reported outcomes in electronic health records can inform clinical and policy decisions. J Clin Epidemiol. 2017;89:160-167.
69. Younossi ZM, Stepanova M, Lawitz E, et al. Improvement of hepatic fibrosis and patient-reported outcomes in non-alcoholic steatohepatitis treated with selonsertib. Liver Int. 2018;38(10):1849-1859.
70. Patel YA, Gifford EJ, Glass LM, et al. Identifying nonalcoholic fatty liver disease advanced fibrosis in the Veterans Health Administration. Dig Dis Sci. 2018;63(9):2259-2266.
71. Hsu C, Caussy C, Imajo K, et al. Magnetic resonance vs transient elastography analysis of patients with nonalcoholic fatty liver disease: a systematic review and pooled analysis of individual participants. Clin Gastroenterol Hepatol. 2018;pii:S1542-3565(18)30613-X. [Epub ahead of print.]
72. Searight R. Realistic approaches to counseling in the office setting. Am Fam Physician. 2009;79(4):277-284.
73. Vallis M, Piccinini-Vallis H, Sharma AM, Freedhoff Y. Clinical review: modified 5 As: minimal intervention for obesity counseling in primary care. Can Fam Physician. 2013:59(1):27-31.
74. Cusi K, Orsak B, Bril F, et al. Long-term pioglitazone treatment for patients with nonalcoholic steatohepatitis and prediabetes or type 2 diabetes mellitus: a randomized trial. Ann Intern Med. 2016;165(5):305-315.
75. Armstrong MJ, Gaunt P, Aithal GP, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387(10019):679-690.
76. Salgia RJ, Mullan PB, McCurdy H, Sales A, Moseley RH, Su GL. The educational impact of the specialty care access network-extension of community healthcare outcomes program. Telemed J E Health. 2014;20(11):1004-1008.
77. Konjeti VR, Heuman D, Bajaj J, et al. Telehealth-based evaluation identifies patients who are not candidates for liver transplantation. Clin Gastroenterol Hepatol. 2019;17(1):207-209.e1
78. Su GL, Glass L, Tapper EB, Van T, Waljee AK, Sales AE. Virtual consultations through the Veterans Administration SCAN-ECHO project improves survival for veterans with liver disease. Hepatology. 2018;68(6):2317-2324.
79. Mazzotti A, Caletti MT, Brodosi L, et al. An internet-based approach for lifestyle changes in patients with NAFLD: two-year effects on weight loss and surrogate markers. J Hepatol. 2018;69(5):1155-1163.
80. Kanwal F, Kramer J, Asch SM, et al. An explicit quality indicator set for measurement of quality of care in patients with cirrhosis. Clin Gastroenterol Hepatol. 2010,8(8):709-717.
81. Blay E Jr, DeLancey JO, Hewitt DB, Chung JW, Bilimoria KY. Initial public reporting of quality at Veterans Affairs vs Non-Veterans Affairs hospitals. JAMA Intern Med. 2017;177(6):882-885.
Nonalcoholic fatty liver disease (NAFLD) is an umbrella term that covers a spectrum of phenotypes ranging from nonalcoholic fatty liver or simple hepatic steatosis to nonalcoholic steatohepatitis (NASH) defined by histologic findings of steatosis, lobular inflammation, cytologic ballooning, and some degree of fibrosis.1 While frequently observed in patients with at least 1 risk factor (eg, obesity, diabetes mellitus [DM], dyslipidemia, hypertension), NAFLD also is an independent risk factor for type 2 DM (T2DM), chronic kidney disease, and cardiovascular disease.2 At early disease stages with absence of liver fibrosis, mortality is linked to cardiovascular and not liver disease. However, in the presence of NASH, fibrosis progression to liver cirrhosis, or hepatocellular carcinoma (HCC) represent the most important liver-related outcomes that determine morbidity and mortality.3 Mirroring the obesity and T2DM epidemics, the health care burden is projected to dramatically rise.
In the following article, we will discuss how the Veterans Health Administration (VHA) is well positioned to implement an organizational strategy of comprehensive care for veterans with NAFLD. This comprehensive care strategy should include the development of a NAFLD clinic offering care for comorbid conditions frequently present in these patients, point-of-care testing, access to clinical trials, and outcomes monitoring as a key performance target for providers and the respective facility.
NAFLD disease burden
To fully appreciate the burden of a chronic disease like NAFLD, it is important to assess its long- and short-term consequences in a comprehensive manner with regard to its clinical impact, impact on the patient, and economic impact (Figure 1).
Clinical Impact
Clinical impact is assessed based on the prevalence and natural history of NAFLD and the liver fibrosis stage and determines patient survival. Coinciding with the epidemic of obesity and T2DM, the prevalence of NAFLD in the general population in North America is 24% and even higher with older age and higher body mass index (BMI).4,5 The prevalence for NAFLD is particularly high in patients with T2DM (47%). Of patients with T2DM and NAFLD, 65% have biopsy-proven NASH of which 15% have bridging fibrosis or liver cirrhosis.6
NAFLD is the fastest growing cause of cirrhosis in the US with a forecasted NAFLD population of 101 million by 2030.7 At the same time, the number of patients with NASH will rise to 27 million of which > 7 million will have bridging fibrosis or liver cirrhosis; hepatic decompensation events are estimated to occur in 105,430 patients with liver cirrhosis, posing a major public health threat related to organ availability for liver transplantation.8 Since 2013, NAFLD has been the second leading cause for liver transplantation and the top reason for transplantation in patients aged < 50 years.9,10 As many patients with NAFLD are diagnosed with HCC at stages where liver transplantation is not an option, mortality from HCC in NAFLD patients is higher than with other etiologies as treatment options are restricted.11,12
Compared with that of the general population, veterans seeking care are older and sicker with 43% of veterans taking > 5 prescribed medications.13 Of those receiving VHA care, 6.6 million veterans are either overweight or obese; 165,000 are morbidly obese with a BMI > 40.14 In addition, veterans are 2.5 times more likely to have T2DM compared with that of nonveterans. Because T2DM and obesity are the most common risk factors for NAFLD, it is not surprising that NAFLD prevalence among veterans rose 3-fold from 2003 to 2011.15 It is now estimated that 540,000 veterans will progress to NASH and 108,000 will develop bridging fibrosis or liver cirrhosis by 2030.8 Similar to that of the general population, liver cirrhosis is attributed to NAFLD in 15% of veterans.15,16 NAFLD is the third most common cause of cirrhosis and HCC, occurring at an average age of 66 years and 70 years, respectively.16,17 Shockingly, 20% of HCCs were not linked to liver cirrhosis and escaped recommended HCC screening for patients with cirrhosis.18,19
Patient Impact
Assessment of disease burden should not be restricted to clinical outcomes as patients can experience a range of symptoms that may have significant impact on their health-related quality of life (QOL) and functional status.20 Using general but not disease-specific instruments, NAFLD patients reported outcomes score low regarding fatigue, activity, and emotions.21 More disease-specific questionnaires may provide better and disease-specific insights as how NASH impacts patients’ QOL.22-24
Economic Impact
There is mounting evidence that the clinical implications of NAFLD directly influence the economic burden of NAFLD.25 The annual burden associated with all incident and prevalent NAFLD cases in the US has been estimated at $103 billion, and projections suggest that the expected 10-year burden of NAFLD may increase to $1.005 trillion.26 It is anticipated that increased NAFLD costs will affect the VHA with billions of dollars in annual expenditures in addition to the $1.5 billion already spent annually for T2DM care (4% of the VA pharmacy budget is spent on T2DM treatment).27-29
Current Patient Care
Obesity, DM, and dyslipidemia are common conditions managed by primary care providers (PCPs). Given the close association of these conditions with NAFLD, the PCP is often the first point of medical contact for patients with or at risk for NAFLD.30 For that reason, PCP awareness of NAFLD is critical for effective management of these patients. PCPs should be actively involved in the management of patients with NAFLD with pathways in place for identifying patients at high risk of liver disease for timely referral to a specialist and adequate education on the follow-up and treatment of low-risk patients. Instead, diagnosis of NAFLD is primarily triggered by either abnormal aminotransferases or detection of steatosis on imaging performed for other indications.
Barriers to optimal management of NAFLD by PCPs have been identified and occur at different levels of patient care. In the absence of clinical practice guidelines by the American Association of Family Practice covering NAFLD and a substantial latency period without signs of symptoms, NAFLD may not be perceived as a potentially serious condition by PCPs and their patients; interestingly this holds true even for some medical specialties.31-39 More than half of PCPs do not test their patients at highest risk for NAFLD (eg, patients with obesity or T2DM) and may be unaware of practice guidelines.40-42
Guidelines from Europe and the US are not completely in accordance. The US guidelines are vague regarding screening and are supported by only 1 medical society, due to the lack of NASH-specific drug therapies. The European guidelines are built on the support of 3 different stakeholders covering liver diseases, obesity, and DM and the experience using noninvasive liver fibrosis assessments for patients with NAFLD. To overcome this apparent conflict, a more practical and risk-stratified approach is warranted.41,42
Making the diagnosis can be challenging in cases with competing etiologies, such as T2DM and alcohol misuse. There also is an overreliance on aminotransferase levels to diagnose NAFLD. Significant liver disease can exist in the presence of normal aminotransferases, and this may be attributed to either spontaneous aminotransferase fluctuations or upper limits of normal that have been chosen too high.43-47 Often additional workup by PCPs depends on the magnitude of aminotransferase abnormalities.
Even if NAFLD has been diagnosed by PCPs, identifying those with NASH is hindered by the absence of an accurate noninvasive diagnostic method and the need to perform a liver biopsy. Liver biopsy is often not considered or delayed to monitor patients with serial aminotransferases, regardless of the patient’s metabolic comorbidity profile or baseline aminotransferases.32 As a result, referral to a specialist often depends on the magnitude of the aminotransferase abnormality,30,48 and often occurs when advanced liver disease is already present.49 Finally, providers may not be aware of beneficial effects of lifestyle interventions and certain medications, including statins on NASH and liver fibrosis.50-53 As NAFLD is associated with excess cardiovascular- and cancer-related morbidity and mortality, it is possible that regression of NAFLD may improve associated risk for these outcomes as well.
Framework for Comprehensive NAFLD Care
Chronic liver diseases and associated comorbidities have long been addressed by PCPs and specialty providers working in isolation and within the narrow focus of each discipline. Contrary to working in silos of the past, a coordinated management strategy with other disciplines that cover these comorbidities needs to be established, or alternatively the PCP must be aware of the management of comorbidities to execute them independently. Integration of hepatology-driven NAFLD care with other specialties involves communication, collaboration, and sharing of resources and expertise that will address patient care needs. Obviously, this cannot be undertaken in a single outpatient visit and requires vertical and longitudinal follow-up over time. One important aspect of comprehensive NAFLD care is the targeting of a particular patient population rather than being seen as a panacea for all; cost-utility analysis is hampered by uncertainties around accuracy of noninvasive biomarkers reflecting liver injury and a lack of effectiveness data for treatment. However, it seems reasonable to screen patients at high risk for NASH and adverse clinical outcomes. Such a risk stratification approach should be cost-effective.
A first key step by the PCP is to identify whether a patient is at risk, especially patients with NASH. The majority of patients at risk are already seen by PCPs. While there is no consensus on ideal screening for NAFLD by PCPs, the use of ultrasound in the at-risk population is recommended in Europe.42 Although NASH remains a histopathologic diagnosis, a reasonable approach is to define NASH based on clinical criteria as done similarly in a real-world observational NAFLD cohort study.54 In the absence of chronic alcohol consumption and viral hepatitis and in a real-world scenario, NASH can be defined as steatosis shown on liver imaging or biopsy and alanine aminotransferase (ALT) levels of > 25 U/L. In addition, ≥ 1 of the following criteria must be met: BMI > 30, T2DM, dyslipidemia, or metabolic syndrome (Table 1).
In the absence of easy-to-use validated tests, all patients with NAFLD need to be assessed with simple, noninvasive scores for the presence of clinically relevant liver fibrosis (F2-portal fibrosis with septa; F3-bridging fibrosis; F4-liver cirrhosis); those that meet the fibrosis criteria should receive further assessment usually only offered in a comprehensive NAFLD clinic.1 PCPs should focus on addressing 2 aspects related to NAFLD: (1) Does my patient have NASH based on clinical criteria; and (2) Is my patient at risk for clinically relevant liver fibrosis? PCPs are integral in optimal management of comorbidities and metabolic syndrome abnormalities with lifestyle and exercise interventions.
The care needs of a typical patient with NAFLD can be classified into 3 categories: liver disease (NAFLD) management, addressing NAFLD associated comorbidities, and attending to the personal care needs of the patient. With considerable interactions between these categories, interventions done within the framework of 1 category can influence the needs pertaining to another, requiring closer monitoring of the patient and potentially modifying care. For example, initiating a low carbohydrate diet in a patient with DM and NAFLD who is on antidiabetic medication may require adjusting the medication; disease progression or failure to achieve treatment goals may affect the emotional state of the patient, which can affect adherence.
Referrals to a comprehensive NAFLD clinic need to be standardized. Clearly, the referral process depends in part on local resources, comprehensiveness of available services, and patient characteristics, among others. Most often, PCPs refer patients with suspected diagnosis of NAFLD, with or without abnormal aminotransferases, to a hepatologist to confirm the diagnosis and for disease staging and liver disease management. This may have the advantage of greatest extent of access and should limit the number of patients with advanced liver fibrosis who otherwise may have been missed. On the other hand, different thresholds of PCPs for referrals may delay the patient’s access to comprehensive NAFLD care. Of those referred by primary care, the hepatologist identifies patients with NAFLD who benefit most from a comprehensive care approach. This automated referral process without predefined criteria remains more a vision than reality as it would require an infrastructure and resources that no health care system can provide currently.
The alternative approach of automatic referral may use predefined criteria related to patients’ diagnoses and prognoses (Figure 2).
Patient-Centered Care
At present the narrow focus of VHA specialty outpatient clinics associated with time constraints of providers and gaps in NAFLD awareness clearly does not address the complex metabolic needs of veterans with NAFLD. This is in striking contrast to the comprehensive care offered to patients with cancer. To overcome these limitations, new care delivery models need to be explored. At first it seems attractive to embed NAFLD patient care geographically into a hepatology clinic with the potential advantages of improving volume and timeliness of referral and reinforcing communication among specialty providers while maximizing convenience for patients. However, this is resource intensive not only concerning clinic space, but also in terms of staffing clinics with specialty providers.
Patient-centered care for veterans with NAFLD seems to be best organized around a comprehensive NAFLD clinic with access to specialized diagnostics and knowledge in day-to-day NAFLD management. This evolving care concept has been developed already for patients with liver cirrhosis and inflammatory bowel disease and considers NAFLD a chronic disease that cannot be addressed sufficiently by providing episodic care.55,56 The development of comprehensive NAFLD care can build on the great success of the Hepatitis Innovation Team Collaborative that employed lean management strategies with local and regional teams to facilitate efforts to make chronic hepatitis C virus a rare disease in the VHA.57
NAFLD Care Team
Given the central role of the liver and gastrointestinal tract in the field of nutrition, knowledge of the pathophysiology of the liver and digestive tract as well as emerging therapeutic options offered via metabolic endoscopy uniquely positions the hepatologist/gastroenterologist to take the lead in managing NAFLD. Treating NAFLD is best accomplished when the specialist partners with other health care providers who have expertise in the nutritional, behavioral, and physical activity aspects of treatment. The composition of the NAFLD care team and the roles that different providers fulfill can vary depending on the clinical setting; however, the hepatologist/gastroenterologist is best suited to lead the team, or alternatively, this role can be fulfilled by a provider with liver disease expertise.
Based on experiences from the United Kingdom, the minimum staffing of a NAFLD clinic should include a physician and nurse practitioner who has expertise in managing patients with chronic liver disease, a registered nurse, a dietitian, and a clinical pharmacy specialist (CPS).58 With coexistent diseases common and many veterans who have > 5 prescribed medications, risk of polypharmacy and adverse drug reactions are a concern, particularly since adherence in patients with chronic diseases has been reported to be as low as 43%.59-61 Risk of medication errors and serious adverse effects are magnified by difficulties with patient adherence, medication interactions, and potential need for frequent dose adjustments, particularly when on a weight-loss diet.
Without doubt, comprehensive medication management, offered by a highly trained CPS with independent prescriptive authority occurring while the veteran is in the NAFLD clinic, is highly desirable. Establishing a functional statement and care coordination agreement could describe the role of the CPS as a member of the NAFLD provider team.
Patient Evaluation
After being referred to the NAFLD clinic, the veteran should have a thorough assessment, including medical, nutritional, physical activity, exercise, and psychosocial evaluations (Figure 4).
The assessment also should include patient education to ensure that the patient has sufficient knowledge and skills to achieve the treatment goals. Educating on NAFLD is critical as most patients with NAFLD do not think of themselves as sick and have limited readiness for lifestyle changes.63,64 A better understanding of NAFLD combined with a higher self-efficacy seems to be positively linked to better nutritional habits.65
An online patient-reported outcomes measurement information system for a patient with NAFLD (eg, assessmentcenter.net) may be beneficial and can be applied within a routine NAFLD clinic visit because of its multidimensionality and compatibility with other chronic diseases.66-68 Other tools to assess health-related QOL include questionnaires, such as the functional assessment of chronic illness therapy-fatigue, work productivity and activity impairment questionnaire: specific health problem, Short Form-36, and chronic liver disease questionnaire-NAFLD.23,69
The medical evaluation includes assessment of secondary causes of NAFLD and identification of NAFLD-related comorbidities. Weight, height, blood pressure, waist circumference, and BMI should be recorded. The physical exam should focus on signs of chronic liver disease and include inspection for acanthosis nigricans, hirsutism, and large neck circumference, which are associated with insulin resistance, polycystic ovarian syndrome, and obstructive sleep apnea, respectively. NAFLD-associated comorbidities may contribute to frailty or physical limitations that affect treatment with diet and exercise and need to be assessed. A thorough medication reconciliation will reveal whether the patient is prescribed obesogenic medications and whether comorbidities (eg, DM and dyslipidemia) are being treated optimally and according to current society guidelines.
Making the diagnosis of NAFLD requires excluding other (concomitant) chronic liver diseases. While often this is done indirectly using order sets with a panoply of available serologic tests without accounting for risks for rare causes of liver injury, a more focused and cost-effective approach is warranted. As most patients will already have had imaging studies that show fatty liver, assessment of liver fibrosis is an important step for risk stratification. Noninvasive scores (eg, FIB-4) can be used by the PCP to identify high-risk patients requiring further workup and referral.1,70 More sophisticated tools, including transient elastography and/or magnetic resonance elastography are applied for more sophisticated risk stratification and liver disease management (Table 2).71
A nutritional evaluation includes information about eating behavior and food choices, body composition analysis, and an assessment of short- and long-term alcohol consumption. Presence of bilateral muscle wasting, subcutaneous fat loss, and signs of micronutrient deficiencies also should be explored. The lifestyle evaluation should include the patient’s typical physical activity and exercise as well as limiting factors.
Finally, and equally important, the patient’s psychosocial situation should be assessed, as motivation and accountability are key to success and may require behavioral modification. Assessing readiness is done best with motivational interviewing, the 5As counseling framework (Ask, Advise, Assess, Assist, Arrange) or using open-ended questions, affirmation, reflections, and summaries.72,73 Even if not personally delivering behavioral treatment, such an approach also can help move patients toward addressing important health-related behaviors.
Personalized Interventions
If available, patients should be offered participation in NAFLD clinical trials. A personalized treatment plan should be developed for each patient with input from all NAFLD care team members. The patient and providers should work together to make important decisions about the treatment plan and goals of care. Making the patient an active participant in their treatment rather than the passive recipient will lead to improvement in adherence and outcomes. Patients will engage when they are comfortable speaking with providers and are sufficiently educated about their disease.
Personalized interventions may be built by combining different strategies, such as lifestyle and dietary interventions, NASH-specific pharmacotherapy, comorbidity management, metabolic endoscopy, and bariatric surgery. Although NASH-specific medications are not currently available, approved medications, including pioglitazone or liraglutide, can be considered for therapy.74,75 Ideally, the NAFLD team CPS would manage comorbidities, such as T2DM and dyslipidemia, but this also can be done by a hepatologist or other specialist. Metabolic endoscopy (eg, intragastric balloons) or bariatric surgery would be done by referral.
Resource-Limited Settings
Although the VHA offers care at > 150 medical centers and > 1,000 outpatient clinics, specialty care such as hepatology and sophisticated and novel testing modalities are not available at many facilities. In 2011 VHA launched the Specialty Care Access Network Extension for Community Healthcare Outcomes to bring hepatitis C therapy and liver transplantation evaluations to rural areas without specialists.76-78 It is logical to explore how telehealth can be used for NAFLD care that requires complex management using new treatments and has a high societal impact, particularly when left untreated.
Telehealth must be easy to use and integrated into everyday routines to be useful for NAFLD management by addressing different aspects of promoting self-management, optimizing therapy, and care coordination. Participation in a structured face-to-face or group-based lifestyle program is often jeopardized by time and job constraints but can be successfully overcome using online approaches.79 The Internet-based VA Video Connect videoconferencing, which incorporates cell phone, laptop, or tablet use could help expand lifestyle interventions to a much larger community of patients with NAFLD and overcome local resource constraints. Finally, e-consultation also can be used in circumstances where synchronous communication with specialists may not be necessary.
Patient Monitoring and Quality Metrics
Monitoring of the patient after initiation of an intervention is variable but occurs more frequently at the beginning. For high-intensity dietary interventions, weekly monitoring for the first several weeks can ensure ongoing motivation, and accountability may increase the patient’s confidence and provide encouragement for further weight loss. It also is an opportunity to reestablish goals with patients with declining motivation. Long-term monitoring of patients may occur in 6- to 12-month intervals to document patient-reported outcomes, liver-related mortality, cardiovascular events, malignancies, and disease progression or regression.
While quality indicators have been proposed for cirrhosis care, such indicators have yet to be defined for NALD care.80 Such quality indicators assessed with validated questionnaires should include knowledge about NAFLD, satisfaction with care, perception of quality of care, and patient-reported outcomes. Other indicators may include use of therapies to treat dyslipidemia and T2DM. Last and likely the most important indicator of improved liver health in NAFLD will be either histologic improvement of NASH or improvement of the fibrosis risk category.
Outlook
With the enormous burden of NAFLD on the rise for many more years to come, quality care delivered to patients with NAFLD warrants resource-adaptive population health management strategies. With a limited number of providers specialized in liver disease, provider education assisted by clinical guidelines and decision support tools, development of referral and access to care mechanisms through integrated care, remote monitoring strategies as well as development of patient self-management and community resources will become more important. We have outlined essential components of an effective population health management strategy for NAFLD and actionable items for the VHA to consider when implementing these strategies. This is the time for the VHA to invest in efforts for NAFLD population care. Clearly, consideration must be given to local needs and resources and integration of technology platforms. Addressing NAFLD at a population level will provide yet another opportunity to demonstrate that VHA performs better on quality when compared with care systems in the private sector.81
Nonalcoholic fatty liver disease (NAFLD) is an umbrella term that covers a spectrum of phenotypes ranging from nonalcoholic fatty liver or simple hepatic steatosis to nonalcoholic steatohepatitis (NASH) defined by histologic findings of steatosis, lobular inflammation, cytologic ballooning, and some degree of fibrosis.1 While frequently observed in patients with at least 1 risk factor (eg, obesity, diabetes mellitus [DM], dyslipidemia, hypertension), NAFLD also is an independent risk factor for type 2 DM (T2DM), chronic kidney disease, and cardiovascular disease.2 At early disease stages with absence of liver fibrosis, mortality is linked to cardiovascular and not liver disease. However, in the presence of NASH, fibrosis progression to liver cirrhosis, or hepatocellular carcinoma (HCC) represent the most important liver-related outcomes that determine morbidity and mortality.3 Mirroring the obesity and T2DM epidemics, the health care burden is projected to dramatically rise.
In the following article, we will discuss how the Veterans Health Administration (VHA) is well positioned to implement an organizational strategy of comprehensive care for veterans with NAFLD. This comprehensive care strategy should include the development of a NAFLD clinic offering care for comorbid conditions frequently present in these patients, point-of-care testing, access to clinical trials, and outcomes monitoring as a key performance target for providers and the respective facility.
NAFLD disease burden
To fully appreciate the burden of a chronic disease like NAFLD, it is important to assess its long- and short-term consequences in a comprehensive manner with regard to its clinical impact, impact on the patient, and economic impact (Figure 1).
Clinical Impact
Clinical impact is assessed based on the prevalence and natural history of NAFLD and the liver fibrosis stage and determines patient survival. Coinciding with the epidemic of obesity and T2DM, the prevalence of NAFLD in the general population in North America is 24% and even higher with older age and higher body mass index (BMI).4,5 The prevalence for NAFLD is particularly high in patients with T2DM (47%). Of patients with T2DM and NAFLD, 65% have biopsy-proven NASH of which 15% have bridging fibrosis or liver cirrhosis.6
NAFLD is the fastest growing cause of cirrhosis in the US with a forecasted NAFLD population of 101 million by 2030.7 At the same time, the number of patients with NASH will rise to 27 million of which > 7 million will have bridging fibrosis or liver cirrhosis; hepatic decompensation events are estimated to occur in 105,430 patients with liver cirrhosis, posing a major public health threat related to organ availability for liver transplantation.8 Since 2013, NAFLD has been the second leading cause for liver transplantation and the top reason for transplantation in patients aged < 50 years.9,10 As many patients with NAFLD are diagnosed with HCC at stages where liver transplantation is not an option, mortality from HCC in NAFLD patients is higher than with other etiologies as treatment options are restricted.11,12
Compared with that of the general population, veterans seeking care are older and sicker with 43% of veterans taking > 5 prescribed medications.13 Of those receiving VHA care, 6.6 million veterans are either overweight or obese; 165,000 are morbidly obese with a BMI > 40.14 In addition, veterans are 2.5 times more likely to have T2DM compared with that of nonveterans. Because T2DM and obesity are the most common risk factors for NAFLD, it is not surprising that NAFLD prevalence among veterans rose 3-fold from 2003 to 2011.15 It is now estimated that 540,000 veterans will progress to NASH and 108,000 will develop bridging fibrosis or liver cirrhosis by 2030.8 Similar to that of the general population, liver cirrhosis is attributed to NAFLD in 15% of veterans.15,16 NAFLD is the third most common cause of cirrhosis and HCC, occurring at an average age of 66 years and 70 years, respectively.16,17 Shockingly, 20% of HCCs were not linked to liver cirrhosis and escaped recommended HCC screening for patients with cirrhosis.18,19
Patient Impact
Assessment of disease burden should not be restricted to clinical outcomes as patients can experience a range of symptoms that may have significant impact on their health-related quality of life (QOL) and functional status.20 Using general but not disease-specific instruments, NAFLD patients reported outcomes score low regarding fatigue, activity, and emotions.21 More disease-specific questionnaires may provide better and disease-specific insights as how NASH impacts patients’ QOL.22-24
Economic Impact
There is mounting evidence that the clinical implications of NAFLD directly influence the economic burden of NAFLD.25 The annual burden associated with all incident and prevalent NAFLD cases in the US has been estimated at $103 billion, and projections suggest that the expected 10-year burden of NAFLD may increase to $1.005 trillion.26 It is anticipated that increased NAFLD costs will affect the VHA with billions of dollars in annual expenditures in addition to the $1.5 billion already spent annually for T2DM care (4% of the VA pharmacy budget is spent on T2DM treatment).27-29
Current Patient Care
Obesity, DM, and dyslipidemia are common conditions managed by primary care providers (PCPs). Given the close association of these conditions with NAFLD, the PCP is often the first point of medical contact for patients with or at risk for NAFLD.30 For that reason, PCP awareness of NAFLD is critical for effective management of these patients. PCPs should be actively involved in the management of patients with NAFLD with pathways in place for identifying patients at high risk of liver disease for timely referral to a specialist and adequate education on the follow-up and treatment of low-risk patients. Instead, diagnosis of NAFLD is primarily triggered by either abnormal aminotransferases or detection of steatosis on imaging performed for other indications.
Barriers to optimal management of NAFLD by PCPs have been identified and occur at different levels of patient care. In the absence of clinical practice guidelines by the American Association of Family Practice covering NAFLD and a substantial latency period without signs of symptoms, NAFLD may not be perceived as a potentially serious condition by PCPs and their patients; interestingly this holds true even for some medical specialties.31-39 More than half of PCPs do not test their patients at highest risk for NAFLD (eg, patients with obesity or T2DM) and may be unaware of practice guidelines.40-42
Guidelines from Europe and the US are not completely in accordance. The US guidelines are vague regarding screening and are supported by only 1 medical society, due to the lack of NASH-specific drug therapies. The European guidelines are built on the support of 3 different stakeholders covering liver diseases, obesity, and DM and the experience using noninvasive liver fibrosis assessments for patients with NAFLD. To overcome this apparent conflict, a more practical and risk-stratified approach is warranted.41,42
Making the diagnosis can be challenging in cases with competing etiologies, such as T2DM and alcohol misuse. There also is an overreliance on aminotransferase levels to diagnose NAFLD. Significant liver disease can exist in the presence of normal aminotransferases, and this may be attributed to either spontaneous aminotransferase fluctuations or upper limits of normal that have been chosen too high.43-47 Often additional workup by PCPs depends on the magnitude of aminotransferase abnormalities.
Even if NAFLD has been diagnosed by PCPs, identifying those with NASH is hindered by the absence of an accurate noninvasive diagnostic method and the need to perform a liver biopsy. Liver biopsy is often not considered or delayed to monitor patients with serial aminotransferases, regardless of the patient’s metabolic comorbidity profile or baseline aminotransferases.32 As a result, referral to a specialist often depends on the magnitude of the aminotransferase abnormality,30,48 and often occurs when advanced liver disease is already present.49 Finally, providers may not be aware of beneficial effects of lifestyle interventions and certain medications, including statins on NASH and liver fibrosis.50-53 As NAFLD is associated with excess cardiovascular- and cancer-related morbidity and mortality, it is possible that regression of NAFLD may improve associated risk for these outcomes as well.
Framework for Comprehensive NAFLD Care
Chronic liver diseases and associated comorbidities have long been addressed by PCPs and specialty providers working in isolation and within the narrow focus of each discipline. Contrary to working in silos of the past, a coordinated management strategy with other disciplines that cover these comorbidities needs to be established, or alternatively the PCP must be aware of the management of comorbidities to execute them independently. Integration of hepatology-driven NAFLD care with other specialties involves communication, collaboration, and sharing of resources and expertise that will address patient care needs. Obviously, this cannot be undertaken in a single outpatient visit and requires vertical and longitudinal follow-up over time. One important aspect of comprehensive NAFLD care is the targeting of a particular patient population rather than being seen as a panacea for all; cost-utility analysis is hampered by uncertainties around accuracy of noninvasive biomarkers reflecting liver injury and a lack of effectiveness data for treatment. However, it seems reasonable to screen patients at high risk for NASH and adverse clinical outcomes. Such a risk stratification approach should be cost-effective.
A first key step by the PCP is to identify whether a patient is at risk, especially patients with NASH. The majority of patients at risk are already seen by PCPs. While there is no consensus on ideal screening for NAFLD by PCPs, the use of ultrasound in the at-risk population is recommended in Europe.42 Although NASH remains a histopathologic diagnosis, a reasonable approach is to define NASH based on clinical criteria as done similarly in a real-world observational NAFLD cohort study.54 In the absence of chronic alcohol consumption and viral hepatitis and in a real-world scenario, NASH can be defined as steatosis shown on liver imaging or biopsy and alanine aminotransferase (ALT) levels of > 25 U/L. In addition, ≥ 1 of the following criteria must be met: BMI > 30, T2DM, dyslipidemia, or metabolic syndrome (Table 1).
In the absence of easy-to-use validated tests, all patients with NAFLD need to be assessed with simple, noninvasive scores for the presence of clinically relevant liver fibrosis (F2-portal fibrosis with septa; F3-bridging fibrosis; F4-liver cirrhosis); those that meet the fibrosis criteria should receive further assessment usually only offered in a comprehensive NAFLD clinic.1 PCPs should focus on addressing 2 aspects related to NAFLD: (1) Does my patient have NASH based on clinical criteria; and (2) Is my patient at risk for clinically relevant liver fibrosis? PCPs are integral in optimal management of comorbidities and metabolic syndrome abnormalities with lifestyle and exercise interventions.
The care needs of a typical patient with NAFLD can be classified into 3 categories: liver disease (NAFLD) management, addressing NAFLD associated comorbidities, and attending to the personal care needs of the patient. With considerable interactions between these categories, interventions done within the framework of 1 category can influence the needs pertaining to another, requiring closer monitoring of the patient and potentially modifying care. For example, initiating a low carbohydrate diet in a patient with DM and NAFLD who is on antidiabetic medication may require adjusting the medication; disease progression or failure to achieve treatment goals may affect the emotional state of the patient, which can affect adherence.
Referrals to a comprehensive NAFLD clinic need to be standardized. Clearly, the referral process depends in part on local resources, comprehensiveness of available services, and patient characteristics, among others. Most often, PCPs refer patients with suspected diagnosis of NAFLD, with or without abnormal aminotransferases, to a hepatologist to confirm the diagnosis and for disease staging and liver disease management. This may have the advantage of greatest extent of access and should limit the number of patients with advanced liver fibrosis who otherwise may have been missed. On the other hand, different thresholds of PCPs for referrals may delay the patient’s access to comprehensive NAFLD care. Of those referred by primary care, the hepatologist identifies patients with NAFLD who benefit most from a comprehensive care approach. This automated referral process without predefined criteria remains more a vision than reality as it would require an infrastructure and resources that no health care system can provide currently.
The alternative approach of automatic referral may use predefined criteria related to patients’ diagnoses and prognoses (Figure 2).
Patient-Centered Care
At present the narrow focus of VHA specialty outpatient clinics associated with time constraints of providers and gaps in NAFLD awareness clearly does not address the complex metabolic needs of veterans with NAFLD. This is in striking contrast to the comprehensive care offered to patients with cancer. To overcome these limitations, new care delivery models need to be explored. At first it seems attractive to embed NAFLD patient care geographically into a hepatology clinic with the potential advantages of improving volume and timeliness of referral and reinforcing communication among specialty providers while maximizing convenience for patients. However, this is resource intensive not only concerning clinic space, but also in terms of staffing clinics with specialty providers.
Patient-centered care for veterans with NAFLD seems to be best organized around a comprehensive NAFLD clinic with access to specialized diagnostics and knowledge in day-to-day NAFLD management. This evolving care concept has been developed already for patients with liver cirrhosis and inflammatory bowel disease and considers NAFLD a chronic disease that cannot be addressed sufficiently by providing episodic care.55,56 The development of comprehensive NAFLD care can build on the great success of the Hepatitis Innovation Team Collaborative that employed lean management strategies with local and regional teams to facilitate efforts to make chronic hepatitis C virus a rare disease in the VHA.57
NAFLD Care Team
Given the central role of the liver and gastrointestinal tract in the field of nutrition, knowledge of the pathophysiology of the liver and digestive tract as well as emerging therapeutic options offered via metabolic endoscopy uniquely positions the hepatologist/gastroenterologist to take the lead in managing NAFLD. Treating NAFLD is best accomplished when the specialist partners with other health care providers who have expertise in the nutritional, behavioral, and physical activity aspects of treatment. The composition of the NAFLD care team and the roles that different providers fulfill can vary depending on the clinical setting; however, the hepatologist/gastroenterologist is best suited to lead the team, or alternatively, this role can be fulfilled by a provider with liver disease expertise.
Based on experiences from the United Kingdom, the minimum staffing of a NAFLD clinic should include a physician and nurse practitioner who has expertise in managing patients with chronic liver disease, a registered nurse, a dietitian, and a clinical pharmacy specialist (CPS).58 With coexistent diseases common and many veterans who have > 5 prescribed medications, risk of polypharmacy and adverse drug reactions are a concern, particularly since adherence in patients with chronic diseases has been reported to be as low as 43%.59-61 Risk of medication errors and serious adverse effects are magnified by difficulties with patient adherence, medication interactions, and potential need for frequent dose adjustments, particularly when on a weight-loss diet.
Without doubt, comprehensive medication management, offered by a highly trained CPS with independent prescriptive authority occurring while the veteran is in the NAFLD clinic, is highly desirable. Establishing a functional statement and care coordination agreement could describe the role of the CPS as a member of the NAFLD provider team.
Patient Evaluation
After being referred to the NAFLD clinic, the veteran should have a thorough assessment, including medical, nutritional, physical activity, exercise, and psychosocial evaluations (Figure 4).
The assessment also should include patient education to ensure that the patient has sufficient knowledge and skills to achieve the treatment goals. Educating on NAFLD is critical as most patients with NAFLD do not think of themselves as sick and have limited readiness for lifestyle changes.63,64 A better understanding of NAFLD combined with a higher self-efficacy seems to be positively linked to better nutritional habits.65
An online patient-reported outcomes measurement information system for a patient with NAFLD (eg, assessmentcenter.net) may be beneficial and can be applied within a routine NAFLD clinic visit because of its multidimensionality and compatibility with other chronic diseases.66-68 Other tools to assess health-related QOL include questionnaires, such as the functional assessment of chronic illness therapy-fatigue, work productivity and activity impairment questionnaire: specific health problem, Short Form-36, and chronic liver disease questionnaire-NAFLD.23,69
The medical evaluation includes assessment of secondary causes of NAFLD and identification of NAFLD-related comorbidities. Weight, height, blood pressure, waist circumference, and BMI should be recorded. The physical exam should focus on signs of chronic liver disease and include inspection for acanthosis nigricans, hirsutism, and large neck circumference, which are associated with insulin resistance, polycystic ovarian syndrome, and obstructive sleep apnea, respectively. NAFLD-associated comorbidities may contribute to frailty or physical limitations that affect treatment with diet and exercise and need to be assessed. A thorough medication reconciliation will reveal whether the patient is prescribed obesogenic medications and whether comorbidities (eg, DM and dyslipidemia) are being treated optimally and according to current society guidelines.
Making the diagnosis of NAFLD requires excluding other (concomitant) chronic liver diseases. While often this is done indirectly using order sets with a panoply of available serologic tests without accounting for risks for rare causes of liver injury, a more focused and cost-effective approach is warranted. As most patients will already have had imaging studies that show fatty liver, assessment of liver fibrosis is an important step for risk stratification. Noninvasive scores (eg, FIB-4) can be used by the PCP to identify high-risk patients requiring further workup and referral.1,70 More sophisticated tools, including transient elastography and/or magnetic resonance elastography are applied for more sophisticated risk stratification and liver disease management (Table 2).71
A nutritional evaluation includes information about eating behavior and food choices, body composition analysis, and an assessment of short- and long-term alcohol consumption. Presence of bilateral muscle wasting, subcutaneous fat loss, and signs of micronutrient deficiencies also should be explored. The lifestyle evaluation should include the patient’s typical physical activity and exercise as well as limiting factors.
Finally, and equally important, the patient’s psychosocial situation should be assessed, as motivation and accountability are key to success and may require behavioral modification. Assessing readiness is done best with motivational interviewing, the 5As counseling framework (Ask, Advise, Assess, Assist, Arrange) or using open-ended questions, affirmation, reflections, and summaries.72,73 Even if not personally delivering behavioral treatment, such an approach also can help move patients toward addressing important health-related behaviors.
Personalized Interventions
If available, patients should be offered participation in NAFLD clinical trials. A personalized treatment plan should be developed for each patient with input from all NAFLD care team members. The patient and providers should work together to make important decisions about the treatment plan and goals of care. Making the patient an active participant in their treatment rather than the passive recipient will lead to improvement in adherence and outcomes. Patients will engage when they are comfortable speaking with providers and are sufficiently educated about their disease.
Personalized interventions may be built by combining different strategies, such as lifestyle and dietary interventions, NASH-specific pharmacotherapy, comorbidity management, metabolic endoscopy, and bariatric surgery. Although NASH-specific medications are not currently available, approved medications, including pioglitazone or liraglutide, can be considered for therapy.74,75 Ideally, the NAFLD team CPS would manage comorbidities, such as T2DM and dyslipidemia, but this also can be done by a hepatologist or other specialist. Metabolic endoscopy (eg, intragastric balloons) or bariatric surgery would be done by referral.
Resource-Limited Settings
Although the VHA offers care at > 150 medical centers and > 1,000 outpatient clinics, specialty care such as hepatology and sophisticated and novel testing modalities are not available at many facilities. In 2011 VHA launched the Specialty Care Access Network Extension for Community Healthcare Outcomes to bring hepatitis C therapy and liver transplantation evaluations to rural areas without specialists.76-78 It is logical to explore how telehealth can be used for NAFLD care that requires complex management using new treatments and has a high societal impact, particularly when left untreated.
Telehealth must be easy to use and integrated into everyday routines to be useful for NAFLD management by addressing different aspects of promoting self-management, optimizing therapy, and care coordination. Participation in a structured face-to-face or group-based lifestyle program is often jeopardized by time and job constraints but can be successfully overcome using online approaches.79 The Internet-based VA Video Connect videoconferencing, which incorporates cell phone, laptop, or tablet use could help expand lifestyle interventions to a much larger community of patients with NAFLD and overcome local resource constraints. Finally, e-consultation also can be used in circumstances where synchronous communication with specialists may not be necessary.
Patient Monitoring and Quality Metrics
Monitoring of the patient after initiation of an intervention is variable but occurs more frequently at the beginning. For high-intensity dietary interventions, weekly monitoring for the first several weeks can ensure ongoing motivation, and accountability may increase the patient’s confidence and provide encouragement for further weight loss. It also is an opportunity to reestablish goals with patients with declining motivation. Long-term monitoring of patients may occur in 6- to 12-month intervals to document patient-reported outcomes, liver-related mortality, cardiovascular events, malignancies, and disease progression or regression.
While quality indicators have been proposed for cirrhosis care, such indicators have yet to be defined for NALD care.80 Such quality indicators assessed with validated questionnaires should include knowledge about NAFLD, satisfaction with care, perception of quality of care, and patient-reported outcomes. Other indicators may include use of therapies to treat dyslipidemia and T2DM. Last and likely the most important indicator of improved liver health in NAFLD will be either histologic improvement of NASH or improvement of the fibrosis risk category.
Outlook
With the enormous burden of NAFLD on the rise for many more years to come, quality care delivered to patients with NAFLD warrants resource-adaptive population health management strategies. With a limited number of providers specialized in liver disease, provider education assisted by clinical guidelines and decision support tools, development of referral and access to care mechanisms through integrated care, remote monitoring strategies as well as development of patient self-management and community resources will become more important. We have outlined essential components of an effective population health management strategy for NAFLD and actionable items for the VHA to consider when implementing these strategies. This is the time for the VHA to invest in efforts for NAFLD population care. Clearly, consideration must be given to local needs and resources and integration of technology platforms. Addressing NAFLD at a population level will provide yet another opportunity to demonstrate that VHA performs better on quality when compared with care systems in the private sector.81
1. Hunt CM, Turner MJ, Gifford EJ, Britt RB, Su GL. Identifying and treating nonalcoholic fatty liver disease. Fed Pract. 2019;36(1):20-29.
2. Glass LM, Hunt CM, Fuchs M, Su GL. Comorbidities and non-alcoholic fatty liver disease: the chicken, the egg, or both? Fed Pract. 2019;36(2):64-71.
3. Vilar-Gomez E, Calzadilla-Bertot L, Wai-Sun Wong V, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology. 2018;155(2):443-457.e17.
4. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73-84.
5. Yki-Järvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2(11):901-910.
6. Golabi P, Shahab O, Stepanova M, Sayiner M, Clement SC, Younossi ZM. Long-term outcomes of diabetic patients with non-alcoholic fatty liver disease (NAFLD) [abstract]. Hepatology. 2017;66(suppl 1):1142A-1143A.
7. Wong RJ, Cheung R, Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology. 2014;59(6):2188-2195.
8. Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67(1):123-133.
9. Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547-555.
10. Banini B, Mota M, Behnke M, Sharma A, Sanyal AJ. Nonalcoholic steatohepatitis (NASH) has surpassed hepatitis C as the leading cause for listing for liver transplant: implications for NASH in children and young adults. Presented at the American College of Gastroenterology Annual Scientific Meeting, Las Vegas, NV, October 18, 2016. Abstract 46. https://www.eventscribe.com/2016/ACG/QRcode.asp?Pres=199366. Accessed January 15, 2019.
11. Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020-1022.
12. Younossi ZM, Otgonsuren M, Henry L, et al. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004-2009. Hepatology. 2015;62(6):1723-1730.
13. Breland JY, Phibbs CS, Hoggatt KJ, et al. The obesity epidemic in the Veterans Health Administration: prevalence among key populations of women and men veterans. J Gen Intern Med. 2017;32(suppl 1):11-17.
14. Gunnar W. Bariatric surgery provided by the Veterans Health Administration: current state and a look to the future. J Gen Intern Med. 2017;32(suppl 1):4-5.
15. Kanwal F, Kramer JR, Duan Z, Yu X, White D, El-Seraq HB. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin Gastroenterol Hepatol. 2016;14(2):301-308.e1-2.
16. Goldberg D, Ditah IC, Saeian K, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the wait list for liver transplantation. Gastroenterology. 2017;152(5):1090-1099.e1.
17. Beste L, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001-2013. Gastroenterology. 2015;149(6):1471-1482.e5.
18. Mittal S, El-Seraq HB, Sada YH, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14(1):124-131.
19. Kanwal F, Kramer JR, Mapakshi S, et al. Risk of hepatocellular cancer in patients with nonalcoholic fatty liver disease. Gastroenterology. 2018;55(6):1828-1837.e2.
20. David K, Kowdley KV, Unalp A, Kanwal F, Brunt EM, Schwimmer JB; NASH CRN Research Group. Quality of life in adults with nonalcoholic fatty liver disease: baseline data from the nonalcoholic steatohepatitis clinical research network. Hepatology. 2009;49(6):1904-1912.
21. Younossi ZM, Stepanova M, Henry L. Performance and validation of Chronic Liver Disease Questionnaire-Hepatitis C Version (CLDQ-HCV) in clinical trials of patients with chronic hepatitis C. Value Health. 2016;19(5):544-551.
22. Younossi ZM, Henry L. Economic and quality-of-life implications of nonalcoholic fatty liver disease. Pharmacoeconomics. 2015;33(12):1245-1253.
23. Younossi ZM, Stepanova M, Henry L, et al. A disease-specific quality of life instrument for nonalcoholic fatty liver disease and non-alcoholic steatohepatitis: CLDQ-NAFLD. Liver Int. 2017;37(8):1209-1218.
24. Chawla KS, Talwalkar JA, Keach JC, Malinchoc M, Lindor KD, Jorgensen R. Reliability and validity of the chronic liver disease questionnaire (CLDQ) in adults with non-alcoholic steatohepatitis (NASH). BMJ Open Gastroenterol. 2016;3(1):e000069.
25. Shetty A, Syn WK. Health, and economic burden of nonalcoholic fatty liver disease in the United States and its impact on Veterans. Fed Pract. 2019;36(1):14-19.
26. Younossi ZM, Blissett D, Blissett R, et al. The economic and clinical burden of nonalcoholic liver disease in the United States and Europe. Hepatology. 2016;64(5):1577-1586.
27. Younossi ZM, Tampi R, Priyadarshini M, Nader F, Younossi IM, Racila A. Burden of illness and economic model for patients with non-alcoholic steatohepatitis (NASH) in the United States. Hepatology. 2018. [Epub ahead of print.]
28. Allen AM, van Houten HK, Sangaralingham LR, Talwalkar JA, McCoy RG. Healthcare cost and utilization in nonalcoholic fatty liver disease: real-world data from a large U.S. claims database. Hepatology. 2018;68(6):2230-2238.
29. Diabetes mellitus. http://www.fedprac-digital.com/federalpractitioner/data_trends_2017?pg=20#pg20. Published July 2017. Accessed January 15, 2019.
30. Grattagliano I, D’Ambrosio G, Palmieri VO, Moschetta A, Palasciano G, Portincasa P; “Steatostop Project” Group. Improving nonalcoholic fatty liver disease management by general practitioners: a critical evaluation and impact of an educational training program. J Gastrointestin Liver Dis. 2008;17(4):389-394.
31. Polanco-Briceno S, Glass D, Stuntz M, Caze A. Awareness of nonalcoholic steatohepatitis and associated practice patterns of primary care physicians and specialists. BMC Res Notes. 2016;9:157.
32. Patel PJ, Banh X, Horsfall LU, et al. Underappreciation of non-alcoholic fatty liver disease by primary care clinicians: limited awareness of surrogate markers of fibrosis. Intern Med. 2018;48(2):144-151.
33. Standing HC, Jarvis H, Orr J, et al. GPs’ experiences and perceptions of early detection of liver disease: a qualitative study in primary care. Br J Gen Pract. 2018;68(676):e743-e749.
34. Wieland AC, Quallick M, Truesdale A, Mettler P, Bambha KM. Identifying practice gaps to optimize medical care for patients with nonalcoholic fatty liver disease. Dig Dis Sci. 2013;58(10):2809-2816.
35. Alexander M, Loomis AK, Fairburn-Beech J, et al. Real-world data reveal a diagnostic gap in non-alcoholic fatty liver disease. BMC Med. 2018;16(1):130.
36. Ratziu V, Cadranel JF, Serfaty L, et al. A survey of patterns of practice and perception of NAFLD in a large sample of practicing gastroenterologists in France. J Hepatol. 2012;57(2):376-383.
37. Blais P, Husain N, Kramer JR, Kowalkowski M, El-Seraq H, Kanwal F. Nonalcoholic fatty liver disease is underrecognized in the primary care setting. Am J Gastroenterol. 2015;110(1):10-14.
38. Bergqvist CJ, Skoien R, Horsfall L, Clouston AD, Jonsson JR, Powell EE. Awareness and opinions of non-alcoholic fatty liver disease by hospital specialists. Intern Med J. 2013;43(3):247-253.
39. Said A, Gagovic V, Malecki K, Givens ML, Nieto FJ. Primary care practitioners survey of non-alcoholic fatty liver disease. Ann Hepatol. 2013;12(5):758-765.
40. Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328-357.
41. NICE National Institute for Health and Care Excellence. Non-alcoholic fatty liver disease (NAFLD): assessment and management. https://www.nice.org.uk/guidance/ng49. Published July 2016. Accessed January 15, 2019.
42. European Association for the Study of the Liver (EASL), European Association for the Study of diabetes (EASD), European Association for the study of obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388-1402.
43. Mofrad P, Contos MJ, Haque M, et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37(6):1286-1292.
44. Koehler EM, Plompen EP, Schouten JN, et al. Presence of diabetes mellitus and steatosis is associated with liver stiffness in a general population: the Rotterdam study. Hepatology. 2016;63(1):138-147.
45. Kwok R, Choi KC, Wong GL, et al. Screening diabetic patients for non-alcoholic fatty liver disease with controlled attenuation parameter and liver stiffness measurements: a prospective cohort study. Gut. 2016;65(8):1359-1368.
46. Harman DJ, Ryder SD, James MW, et al. Obesity and type 2 diabetes are important risk factors underlying previously undiagnosed cirrhosis in general practice: a cross-sectional study using transient elastography. Aliment Pharmacol Ther. 2018;47(4):504-515.
47. Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002;137(1):1-10.
48. Rinella ME, Lominadze Z, Loomba R, et al. Practice pattern in NAFLD and NASH: real life differs from published guidelines. Therap Adv Gastroenterol. 2016;9(1):4-12.
49. El-Atem NA, Wojcik K, Horsfall L, et al. Patterns of service utilization within Australian hepatology clinics: high prevalence of advanced liver disease. Intern Med. 2016;46(4):420-426.
50. Dongiovanni P, Petta S, Mannisto V, et al. Statin use and nonalcoholic steatohepatitis in at risk individuals. J Hepatol. 2015;63(3):705-712.
51. Nascimbeni F, Aron-Wisnewsky J, Pais R, et al; LIDO Study Group. Statins, antidiabetic medications and liver histology in patients with diabetes with non-alcoholic fatty liver disease. BMJ Open Gastroenterol. 2016;3(1):e000075.
52. Romero-Gomez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67(4):829-846.
53. Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149(2):367-378.
54. Barritt AS 4th, Gitlin N, Klein S, et al. Design and rationale for a real-world observational cohort of patients with nonalcoholic fatty liver disease: The TARGET-NASH study. Contemp Clin Trials. 2017;61:33-38.
55. Meier SK, Shah ND, Talwalkar JA. Adapting the patient-centered specialty practice model for populations with cirrhosis. Clin Gastroenterol Hepatol. 2016;14(4):492-496.
56. Dulai PS, Singh S, Ohno-Machado L, Sandborn WJ. Population health management for inflammatory bowel disease. Gastroenterology. 2018;154(1):37-45.
57. Park A, Gonzalez R, Chartier M, et al. Screening and treating hepatitis C in the VA: achieving excellence using lean and system redesign. Fed Pract. 2018;35(7):24-29.
58. Cobbold JFL, Raveendran S, Peake CM, Anstee QM, Yee MS, Thursz MR. Piloting a multidisciplinary clinic for the management of non-alcoholic fatty liver disease: initial 5-year experience. Frontline Gastroenterol. 2013;4(4):263-269.
59. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(3):487-497.
60. Harrison SA. NASH, from diagnosis to treatment: where do we stand? Hepatology. 2015;62(6):1652-1655.
61. Patel PJ, Hayward KL, Rudra R, et al. Multimorbidity and polypharmacy in diabetic patients with NAFLD: implications for disease severity and management. Medicine (Baltimore). 2017;96(26):e6761.
62. Kanwal F, Mapashki S, Smith D, et al. Implementation of a population-based cirrhosis identification and management system. Clin Gastroenterol Hepatol. 2018;16(8):1182-1186.e2.
63. Mlynarski L, Schlesinger D, Lotan R, et al. Non-alcoholic fatty liver disease is not associated with a lower health perception. World J Gastroenterol. 2016;22(17):4362-4372.
64. Centis E, Moscatiello S, Bugianesi E, et al. Stage of change and motivation to healthier lifestyle in non-alcoholic fatty liver disease. J Hepatol. 2013;58(4):771-777.
65. Zelber-Sagi S, Bord S, Dror-Lavi G, et al. Role of illness perception and self-efficacy in lifestyle modification among non-alcoholic fatty liver disease patients. World J Gastroenterol. 2017;23(10):1881-1890.
66. Bajaj JS, Thacker LR, Wade JB, et al. PROMIS computerized adaptive tests are dynamic instruments to measure health-related quality of life in patients with cirrhosis. Aliment Pharmacol Ther. 2011;34(9):1123-1132.
67. Verma M, Stites S, Navarro V. Bringing assessment of patient-reported outcomes to hepatology practice. Clin Gastroenterol Hepatol. 2018;16(3):447-448.
68. Ahmed S, Ware P, Gardner W, et al. Montreal Accord on patient-reported outcomes (PROs) use series – paper 8: patient-reported outcomes in electronic health records can inform clinical and policy decisions. J Clin Epidemiol. 2017;89:160-167.
69. Younossi ZM, Stepanova M, Lawitz E, et al. Improvement of hepatic fibrosis and patient-reported outcomes in non-alcoholic steatohepatitis treated with selonsertib. Liver Int. 2018;38(10):1849-1859.
70. Patel YA, Gifford EJ, Glass LM, et al. Identifying nonalcoholic fatty liver disease advanced fibrosis in the Veterans Health Administration. Dig Dis Sci. 2018;63(9):2259-2266.
71. Hsu C, Caussy C, Imajo K, et al. Magnetic resonance vs transient elastography analysis of patients with nonalcoholic fatty liver disease: a systematic review and pooled analysis of individual participants. Clin Gastroenterol Hepatol. 2018;pii:S1542-3565(18)30613-X. [Epub ahead of print.]
72. Searight R. Realistic approaches to counseling in the office setting. Am Fam Physician. 2009;79(4):277-284.
73. Vallis M, Piccinini-Vallis H, Sharma AM, Freedhoff Y. Clinical review: modified 5 As: minimal intervention for obesity counseling in primary care. Can Fam Physician. 2013:59(1):27-31.
74. Cusi K, Orsak B, Bril F, et al. Long-term pioglitazone treatment for patients with nonalcoholic steatohepatitis and prediabetes or type 2 diabetes mellitus: a randomized trial. Ann Intern Med. 2016;165(5):305-315.
75. Armstrong MJ, Gaunt P, Aithal GP, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387(10019):679-690.
76. Salgia RJ, Mullan PB, McCurdy H, Sales A, Moseley RH, Su GL. The educational impact of the specialty care access network-extension of community healthcare outcomes program. Telemed J E Health. 2014;20(11):1004-1008.
77. Konjeti VR, Heuman D, Bajaj J, et al. Telehealth-based evaluation identifies patients who are not candidates for liver transplantation. Clin Gastroenterol Hepatol. 2019;17(1):207-209.e1
78. Su GL, Glass L, Tapper EB, Van T, Waljee AK, Sales AE. Virtual consultations through the Veterans Administration SCAN-ECHO project improves survival for veterans with liver disease. Hepatology. 2018;68(6):2317-2324.
79. Mazzotti A, Caletti MT, Brodosi L, et al. An internet-based approach for lifestyle changes in patients with NAFLD: two-year effects on weight loss and surrogate markers. J Hepatol. 2018;69(5):1155-1163.
80. Kanwal F, Kramer J, Asch SM, et al. An explicit quality indicator set for measurement of quality of care in patients with cirrhosis. Clin Gastroenterol Hepatol. 2010,8(8):709-717.
81. Blay E Jr, DeLancey JO, Hewitt DB, Chung JW, Bilimoria KY. Initial public reporting of quality at Veterans Affairs vs Non-Veterans Affairs hospitals. JAMA Intern Med. 2017;177(6):882-885.
1. Hunt CM, Turner MJ, Gifford EJ, Britt RB, Su GL. Identifying and treating nonalcoholic fatty liver disease. Fed Pract. 2019;36(1):20-29.
2. Glass LM, Hunt CM, Fuchs M, Su GL. Comorbidities and non-alcoholic fatty liver disease: the chicken, the egg, or both? Fed Pract. 2019;36(2):64-71.
3. Vilar-Gomez E, Calzadilla-Bertot L, Wai-Sun Wong V, et al. Fibrosis severity as a determinant of cause-specific mortality in patients with advanced nonalcoholic fatty liver disease: a multi-national cohort study. Gastroenterology. 2018;155(2):443-457.e17.
4. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease—meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73-84.
5. Yki-Järvinen H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol. 2014;2(11):901-910.
6. Golabi P, Shahab O, Stepanova M, Sayiner M, Clement SC, Younossi ZM. Long-term outcomes of diabetic patients with non-alcoholic fatty liver disease (NAFLD) [abstract]. Hepatology. 2017;66(suppl 1):1142A-1143A.
7. Wong RJ, Cheung R, Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology. 2014;59(6):2188-2195.
8. Estes C, Razavi H, Loomba R, Younossi Z, Sanyal AJ. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2018;67(1):123-133.
9. Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547-555.
10. Banini B, Mota M, Behnke M, Sharma A, Sanyal AJ. Nonalcoholic steatohepatitis (NASH) has surpassed hepatitis C as the leading cause for listing for liver transplant: implications for NASH in children and young adults. Presented at the American College of Gastroenterology Annual Scientific Meeting, Las Vegas, NV, October 18, 2016. Abstract 46. https://www.eventscribe.com/2016/ACG/QRcode.asp?Pres=199366. Accessed January 15, 2019.
11. Bruix J, Sherman M; American Association for the Study of Liver Diseases. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020-1022.
12. Younossi ZM, Otgonsuren M, Henry L, et al. Association of nonalcoholic fatty liver disease (NAFLD) with hepatocellular carcinoma (HCC) in the United States from 2004-2009. Hepatology. 2015;62(6):1723-1730.
13. Breland JY, Phibbs CS, Hoggatt KJ, et al. The obesity epidemic in the Veterans Health Administration: prevalence among key populations of women and men veterans. J Gen Intern Med. 2017;32(suppl 1):11-17.
14. Gunnar W. Bariatric surgery provided by the Veterans Health Administration: current state and a look to the future. J Gen Intern Med. 2017;32(suppl 1):4-5.
15. Kanwal F, Kramer JR, Duan Z, Yu X, White D, El-Seraq HB. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin Gastroenterol Hepatol. 2016;14(2):301-308.e1-2.
16. Goldberg D, Ditah IC, Saeian K, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the wait list for liver transplantation. Gastroenterology. 2017;152(5):1090-1099.e1.
17. Beste L, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001-2013. Gastroenterology. 2015;149(6):1471-1482.e5.
18. Mittal S, El-Seraq HB, Sada YH, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14(1):124-131.
19. Kanwal F, Kramer JR, Mapakshi S, et al. Risk of hepatocellular cancer in patients with nonalcoholic fatty liver disease. Gastroenterology. 2018;55(6):1828-1837.e2.
20. David K, Kowdley KV, Unalp A, Kanwal F, Brunt EM, Schwimmer JB; NASH CRN Research Group. Quality of life in adults with nonalcoholic fatty liver disease: baseline data from the nonalcoholic steatohepatitis clinical research network. Hepatology. 2009;49(6):1904-1912.
21. Younossi ZM, Stepanova M, Henry L. Performance and validation of Chronic Liver Disease Questionnaire-Hepatitis C Version (CLDQ-HCV) in clinical trials of patients with chronic hepatitis C. Value Health. 2016;19(5):544-551.
22. Younossi ZM, Henry L. Economic and quality-of-life implications of nonalcoholic fatty liver disease. Pharmacoeconomics. 2015;33(12):1245-1253.
23. Younossi ZM, Stepanova M, Henry L, et al. A disease-specific quality of life instrument for nonalcoholic fatty liver disease and non-alcoholic steatohepatitis: CLDQ-NAFLD. Liver Int. 2017;37(8):1209-1218.
24. Chawla KS, Talwalkar JA, Keach JC, Malinchoc M, Lindor KD, Jorgensen R. Reliability and validity of the chronic liver disease questionnaire (CLDQ) in adults with non-alcoholic steatohepatitis (NASH). BMJ Open Gastroenterol. 2016;3(1):e000069.
25. Shetty A, Syn WK. Health, and economic burden of nonalcoholic fatty liver disease in the United States and its impact on Veterans. Fed Pract. 2019;36(1):14-19.
26. Younossi ZM, Blissett D, Blissett R, et al. The economic and clinical burden of nonalcoholic liver disease in the United States and Europe. Hepatology. 2016;64(5):1577-1586.
27. Younossi ZM, Tampi R, Priyadarshini M, Nader F, Younossi IM, Racila A. Burden of illness and economic model for patients with non-alcoholic steatohepatitis (NASH) in the United States. Hepatology. 2018. [Epub ahead of print.]
28. Allen AM, van Houten HK, Sangaralingham LR, Talwalkar JA, McCoy RG. Healthcare cost and utilization in nonalcoholic fatty liver disease: real-world data from a large U.S. claims database. Hepatology. 2018;68(6):2230-2238.
29. Diabetes mellitus. http://www.fedprac-digital.com/federalpractitioner/data_trends_2017?pg=20#pg20. Published July 2017. Accessed January 15, 2019.
30. Grattagliano I, D’Ambrosio G, Palmieri VO, Moschetta A, Palasciano G, Portincasa P; “Steatostop Project” Group. Improving nonalcoholic fatty liver disease management by general practitioners: a critical evaluation and impact of an educational training program. J Gastrointestin Liver Dis. 2008;17(4):389-394.
31. Polanco-Briceno S, Glass D, Stuntz M, Caze A. Awareness of nonalcoholic steatohepatitis and associated practice patterns of primary care physicians and specialists. BMC Res Notes. 2016;9:157.
32. Patel PJ, Banh X, Horsfall LU, et al. Underappreciation of non-alcoholic fatty liver disease by primary care clinicians: limited awareness of surrogate markers of fibrosis. Intern Med. 2018;48(2):144-151.
33. Standing HC, Jarvis H, Orr J, et al. GPs’ experiences and perceptions of early detection of liver disease: a qualitative study in primary care. Br J Gen Pract. 2018;68(676):e743-e749.
34. Wieland AC, Quallick M, Truesdale A, Mettler P, Bambha KM. Identifying practice gaps to optimize medical care for patients with nonalcoholic fatty liver disease. Dig Dis Sci. 2013;58(10):2809-2816.
35. Alexander M, Loomis AK, Fairburn-Beech J, et al. Real-world data reveal a diagnostic gap in non-alcoholic fatty liver disease. BMC Med. 2018;16(1):130.
36. Ratziu V, Cadranel JF, Serfaty L, et al. A survey of patterns of practice and perception of NAFLD in a large sample of practicing gastroenterologists in France. J Hepatol. 2012;57(2):376-383.
37. Blais P, Husain N, Kramer JR, Kowalkowski M, El-Seraq H, Kanwal F. Nonalcoholic fatty liver disease is underrecognized in the primary care setting. Am J Gastroenterol. 2015;110(1):10-14.
38. Bergqvist CJ, Skoien R, Horsfall L, Clouston AD, Jonsson JR, Powell EE. Awareness and opinions of non-alcoholic fatty liver disease by hospital specialists. Intern Med J. 2013;43(3):247-253.
39. Said A, Gagovic V, Malecki K, Givens ML, Nieto FJ. Primary care practitioners survey of non-alcoholic fatty liver disease. Ann Hepatol. 2013;12(5):758-765.
40. Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018;67(1):328-357.
41. NICE National Institute for Health and Care Excellence. Non-alcoholic fatty liver disease (NAFLD): assessment and management. https://www.nice.org.uk/guidance/ng49. Published July 2016. Accessed January 15, 2019.
42. European Association for the Study of the Liver (EASL), European Association for the Study of diabetes (EASD), European Association for the study of obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016;64(6):1388-1402.
43. Mofrad P, Contos MJ, Haque M, et al. Clinical and histologic spectrum of nonalcoholic fatty liver disease associated with normal ALT values. Hepatology. 2003;37(6):1286-1292.
44. Koehler EM, Plompen EP, Schouten JN, et al. Presence of diabetes mellitus and steatosis is associated with liver stiffness in a general population: the Rotterdam study. Hepatology. 2016;63(1):138-147.
45. Kwok R, Choi KC, Wong GL, et al. Screening diabetic patients for non-alcoholic fatty liver disease with controlled attenuation parameter and liver stiffness measurements: a prospective cohort study. Gut. 2016;65(8):1359-1368.
46. Harman DJ, Ryder SD, James MW, et al. Obesity and type 2 diabetes are important risk factors underlying previously undiagnosed cirrhosis in general practice: a cross-sectional study using transient elastography. Aliment Pharmacol Ther. 2018;47(4):504-515.
47. Prati D, Taioli E, Zanella A, et al. Updated definitions of healthy ranges for serum alanine aminotransferase levels. Ann Intern Med. 2002;137(1):1-10.
48. Rinella ME, Lominadze Z, Loomba R, et al. Practice pattern in NAFLD and NASH: real life differs from published guidelines. Therap Adv Gastroenterol. 2016;9(1):4-12.
49. El-Atem NA, Wojcik K, Horsfall L, et al. Patterns of service utilization within Australian hepatology clinics: high prevalence of advanced liver disease. Intern Med. 2016;46(4):420-426.
50. Dongiovanni P, Petta S, Mannisto V, et al. Statin use and nonalcoholic steatohepatitis in at risk individuals. J Hepatol. 2015;63(3):705-712.
51. Nascimbeni F, Aron-Wisnewsky J, Pais R, et al; LIDO Study Group. Statins, antidiabetic medications and liver histology in patients with diabetes with non-alcoholic fatty liver disease. BMJ Open Gastroenterol. 2016;3(1):e000075.
52. Romero-Gomez M, Zelber-Sagi S, Trenell M. Treatment of NAFLD with diet, physical activity and exercise. J Hepatol. 2017;67(4):829-846.
53. Vilar-Gomez E, Martinez-Perez Y, Calzadilla-Bertot L, et al. Weight loss through lifestyle modification significantly reduces features of nonalcoholic steatohepatitis. Gastroenterology. 2015;149(2):367-378.
54. Barritt AS 4th, Gitlin N, Klein S, et al. Design and rationale for a real-world observational cohort of patients with nonalcoholic fatty liver disease: The TARGET-NASH study. Contemp Clin Trials. 2017;61:33-38.
55. Meier SK, Shah ND, Talwalkar JA. Adapting the patient-centered specialty practice model for populations with cirrhosis. Clin Gastroenterol Hepatol. 2016;14(4):492-496.
56. Dulai PS, Singh S, Ohno-Machado L, Sandborn WJ. Population health management for inflammatory bowel disease. Gastroenterology. 2018;154(1):37-45.
57. Park A, Gonzalez R, Chartier M, et al. Screening and treating hepatitis C in the VA: achieving excellence using lean and system redesign. Fed Pract. 2018;35(7):24-29.
58. Cobbold JFL, Raveendran S, Peake CM, Anstee QM, Yee MS, Thursz MR. Piloting a multidisciplinary clinic for the management of non-alcoholic fatty liver disease: initial 5-year experience. Frontline Gastroenterol. 2013;4(4):263-269.
59. Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353(3):487-497.
60. Harrison SA. NASH, from diagnosis to treatment: where do we stand? Hepatology. 2015;62(6):1652-1655.
61. Patel PJ, Hayward KL, Rudra R, et al. Multimorbidity and polypharmacy in diabetic patients with NAFLD: implications for disease severity and management. Medicine (Baltimore). 2017;96(26):e6761.
62. Kanwal F, Mapashki S, Smith D, et al. Implementation of a population-based cirrhosis identification and management system. Clin Gastroenterol Hepatol. 2018;16(8):1182-1186.e2.
63. Mlynarski L, Schlesinger D, Lotan R, et al. Non-alcoholic fatty liver disease is not associated with a lower health perception. World J Gastroenterol. 2016;22(17):4362-4372.
64. Centis E, Moscatiello S, Bugianesi E, et al. Stage of change and motivation to healthier lifestyle in non-alcoholic fatty liver disease. J Hepatol. 2013;58(4):771-777.
65. Zelber-Sagi S, Bord S, Dror-Lavi G, et al. Role of illness perception and self-efficacy in lifestyle modification among non-alcoholic fatty liver disease patients. World J Gastroenterol. 2017;23(10):1881-1890.
66. Bajaj JS, Thacker LR, Wade JB, et al. PROMIS computerized adaptive tests are dynamic instruments to measure health-related quality of life in patients with cirrhosis. Aliment Pharmacol Ther. 2011;34(9):1123-1132.
67. Verma M, Stites S, Navarro V. Bringing assessment of patient-reported outcomes to hepatology practice. Clin Gastroenterol Hepatol. 2018;16(3):447-448.
68. Ahmed S, Ware P, Gardner W, et al. Montreal Accord on patient-reported outcomes (PROs) use series – paper 8: patient-reported outcomes in electronic health records can inform clinical and policy decisions. J Clin Epidemiol. 2017;89:160-167.
69. Younossi ZM, Stepanova M, Lawitz E, et al. Improvement of hepatic fibrosis and patient-reported outcomes in non-alcoholic steatohepatitis treated with selonsertib. Liver Int. 2018;38(10):1849-1859.
70. Patel YA, Gifford EJ, Glass LM, et al. Identifying nonalcoholic fatty liver disease advanced fibrosis in the Veterans Health Administration. Dig Dis Sci. 2018;63(9):2259-2266.
71. Hsu C, Caussy C, Imajo K, et al. Magnetic resonance vs transient elastography analysis of patients with nonalcoholic fatty liver disease: a systematic review and pooled analysis of individual participants. Clin Gastroenterol Hepatol. 2018;pii:S1542-3565(18)30613-X. [Epub ahead of print.]
72. Searight R. Realistic approaches to counseling in the office setting. Am Fam Physician. 2009;79(4):277-284.
73. Vallis M, Piccinini-Vallis H, Sharma AM, Freedhoff Y. Clinical review: modified 5 As: minimal intervention for obesity counseling in primary care. Can Fam Physician. 2013:59(1):27-31.
74. Cusi K, Orsak B, Bril F, et al. Long-term pioglitazone treatment for patients with nonalcoholic steatohepatitis and prediabetes or type 2 diabetes mellitus: a randomized trial. Ann Intern Med. 2016;165(5):305-315.
75. Armstrong MJ, Gaunt P, Aithal GP, et al. Liraglutide safety and efficacy in patients with non-alcoholic steatohepatitis (LEAN): a multicentre, double-blind, randomised, placebo-controlled phase 2 study. Lancet. 2016;387(10019):679-690.
76. Salgia RJ, Mullan PB, McCurdy H, Sales A, Moseley RH, Su GL. The educational impact of the specialty care access network-extension of community healthcare outcomes program. Telemed J E Health. 2014;20(11):1004-1008.
77. Konjeti VR, Heuman D, Bajaj J, et al. Telehealth-based evaluation identifies patients who are not candidates for liver transplantation. Clin Gastroenterol Hepatol. 2019;17(1):207-209.e1
78. Su GL, Glass L, Tapper EB, Van T, Waljee AK, Sales AE. Virtual consultations through the Veterans Administration SCAN-ECHO project improves survival for veterans with liver disease. Hepatology. 2018;68(6):2317-2324.
79. Mazzotti A, Caletti MT, Brodosi L, et al. An internet-based approach for lifestyle changes in patients with NAFLD: two-year effects on weight loss and surrogate markers. J Hepatol. 2018;69(5):1155-1163.
80. Kanwal F, Kramer J, Asch SM, et al. An explicit quality indicator set for measurement of quality of care in patients with cirrhosis. Clin Gastroenterol Hepatol. 2010,8(8):709-717.
81. Blay E Jr, DeLancey JO, Hewitt DB, Chung JW, Bilimoria KY. Initial public reporting of quality at Veterans Affairs vs Non-Veterans Affairs hospitals. JAMA Intern Med. 2017;177(6):882-885.
Treatment missing for U.S. children with mental illness
according to data from a national survey of parents.

Among the estimated 7.7 million children with a treatable mental illness, 49.4% did not receive needed treatment from a psychiatrist, psychologist, psychiatric nurse, or clinical social worker in the previous 12 months, Daniel G. Whitney, PhD, and Mark D. Peterson, PhD, of the University of Michigan, Ann Arbor, wrote in JAMA Pediatrics.
State-level data from the National Survey of Children’s Health show considerable variation from the national average. North Carolina had the highest prevalence of nontreatment at 72.2% and Washington, D.C., had the lowest rate at 29.5%. The prevalence of at least one mental health disorder was highest in Maine (27.2%) and lowest in Hawaii (7.6%), the investigators reported.
Four states – Alabama, Mississippi, Oklahoma, and Utah – were in the top quartile for both mental health disorder prevalence and prevalence of children with a disorder who did not receive treatment, they noted.
“State-level practices and policies play a role in health care needs and use, which may help to explain the state variability observed in this study. Nevertheless, initiatives that assist systems of care coordination have demonstrated a reduction of mental health–related burdens across multiple domains,” Dr. Whitney and Dr. Peterson wrote.
SOURCE: Whitney DG et al. JAMA Pediatr. 2019 Feb 11. doi: 10.1001/jamapediatrics.2018.5399.
according to data from a national survey of parents.

Among the estimated 7.7 million children with a treatable mental illness, 49.4% did not receive needed treatment from a psychiatrist, psychologist, psychiatric nurse, or clinical social worker in the previous 12 months, Daniel G. Whitney, PhD, and Mark D. Peterson, PhD, of the University of Michigan, Ann Arbor, wrote in JAMA Pediatrics.
State-level data from the National Survey of Children’s Health show considerable variation from the national average. North Carolina had the highest prevalence of nontreatment at 72.2% and Washington, D.C., had the lowest rate at 29.5%. The prevalence of at least one mental health disorder was highest in Maine (27.2%) and lowest in Hawaii (7.6%), the investigators reported.
Four states – Alabama, Mississippi, Oklahoma, and Utah – were in the top quartile for both mental health disorder prevalence and prevalence of children with a disorder who did not receive treatment, they noted.
“State-level practices and policies play a role in health care needs and use, which may help to explain the state variability observed in this study. Nevertheless, initiatives that assist systems of care coordination have demonstrated a reduction of mental health–related burdens across multiple domains,” Dr. Whitney and Dr. Peterson wrote.
SOURCE: Whitney DG et al. JAMA Pediatr. 2019 Feb 11. doi: 10.1001/jamapediatrics.2018.5399.
according to data from a national survey of parents.

Among the estimated 7.7 million children with a treatable mental illness, 49.4% did not receive needed treatment from a psychiatrist, psychologist, psychiatric nurse, or clinical social worker in the previous 12 months, Daniel G. Whitney, PhD, and Mark D. Peterson, PhD, of the University of Michigan, Ann Arbor, wrote in JAMA Pediatrics.
State-level data from the National Survey of Children’s Health show considerable variation from the national average. North Carolina had the highest prevalence of nontreatment at 72.2% and Washington, D.C., had the lowest rate at 29.5%. The prevalence of at least one mental health disorder was highest in Maine (27.2%) and lowest in Hawaii (7.6%), the investigators reported.
Four states – Alabama, Mississippi, Oklahoma, and Utah – were in the top quartile for both mental health disorder prevalence and prevalence of children with a disorder who did not receive treatment, they noted.
“State-level practices and policies play a role in health care needs and use, which may help to explain the state variability observed in this study. Nevertheless, initiatives that assist systems of care coordination have demonstrated a reduction of mental health–related burdens across multiple domains,” Dr. Whitney and Dr. Peterson wrote.
SOURCE: Whitney DG et al. JAMA Pediatr. 2019 Feb 11. doi: 10.1001/jamapediatrics.2018.5399.
FROM JAMA PEDIATRICS
ALA report: Federal and state actions to limit tobacco use fall short
Tobacco use is currently at an all-time low thanks to public and private efforts, but more aggressive action from federal, state, and local governments is needed to protect the public, according to a review of tobacco control trends in the United States.
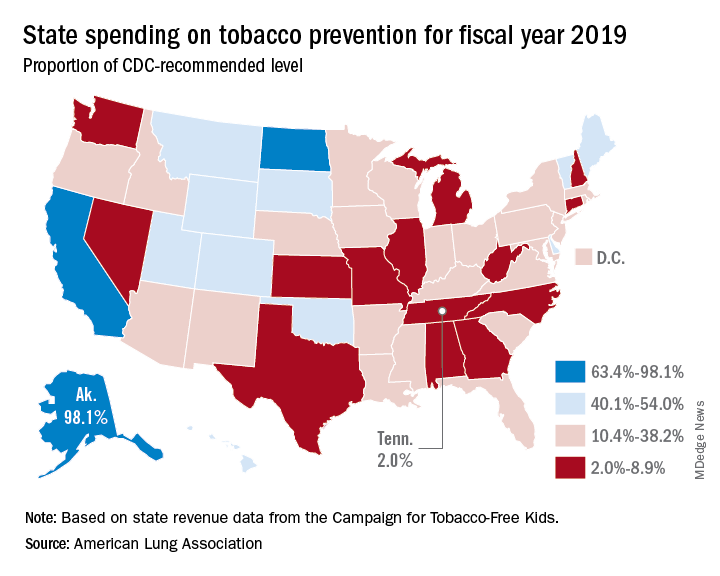
The American Lung Association (ALA) released “State of Tobacco Control” 2019, its 17th annual state-by-state analysis and list of recommended policy priorities to limit tobacco use. Although the report notes some positive steps taken by the federal and state governments, shortfalls in policy and legislation also are highlighted. The report states, “We know how and are ready to save more lives, but we need our elected officials to do much more. To many, solving America’s tobacco crisis might seem like a complex puzzle with no solution. And yet we have known for years what pieces are needed to reduce the disease and death caused by tobacco use.”
In this report, the federal government and each state are graded on a scale, A through F, for policy actions and laws to limit tobacco use. The grading methodology is based on a detailed point system cataloging the implementation and strength of specific actions and policies to limit tobacco use.
Areas of Impact
The report focused on six areas of public policy that affect exposure to and use of tobacco:
- Smoke-free air: Protecting the public from secondhand smoke should be a priority for policymakers, according the report, but 22 states have no smoke-free workplace laws in place. Laws restricting e-cigarettes in workplaces and public buildings have lagged behind tobacco laws in many states.
- Tobacco prevention funding: Dedicated funds to prevent tobacco addiction before it starts is a key element of a public health attack on tobacco use, but no U.S. state currently spends what the Centers for Disease Control and Prevention has recommended. Twenty years ago, the Master Settlement Agreement between the tobacco industry and 46 states and the District of Columbia guaranteed ongoing payments to the states to be used for tobacco prevention and control. Although those funds have been collected in the states to the tune of $27 billion since 1998, overall only 2.4% of those funds have been spent for this purpose, and the rest has been budgeted for other purposes.
- Tobacco taxes: Sales taxes on tobacco products have been highly effective in preventing young people from taking up tobacco use, but those taxation rates have remained unchanged in 2018 in all but the District of Columbia and Oklahoma. The tobacco industry spent $22 million in a successful effort to defeat ballot measures to increase sales taxes on tobacco in Montana and South Dakota.
- Tobacco 21: “Increasing the legal age of sale for tobacco products to 21 would decrease tobacco use by 12% and could prevent 223,000 deaths among those born between 2000 and 2019,” the report noted, citing a 2015 report by the Institute of Medicine. So far, the this restriction has been legislated in six states, the District of Columbia, and numerous local governments. The ALA considers increasing the age for tobacco sales to 21 to be a public health priority.
- Helping smokers quit: The addictive qualities of tobacco mean that many smokers struggle unsuccessfully to quit, and medical intervention is needed to help them. The report notes that current law requires that Medicaid expansion health plans and private insurance plans cover comprehensive smoking cessation treatment. However, not all states have the expanded Medicaid program, and many of those with Medicaid expansion don’t offer coverage of all Food and Drug–approved cessation treatments. Despite laws requiring smoking cessation coverage, many private insurance plans still do not include this coverage. The ALA recommends enforcement of the current law with regard to tobacco cessation insurance coverage.
- FDA regulation of tobacco products: The FDA has announced plans to make a major effort to reduce tobacco use in young people, decrease nicotine in cigarettes, and to restrict flavored tobacco products. But these plans fall short of the aggressive action needed to curb the tobacco “epidemic,” according to the report. Delayed action and timid policy have “resulted in tobacco companies becoming more emboldened to devise new and egregious ways to addict youth and sustain addiction among current users.” The ALA report points to the steep rise in e-cigarette use among youth with a 20.8% rise in high school students using these products in 2018, a rise from 11.7% in 2017. This trend is not likely to be reversed by the FDA proposals to date, which rely on voluntary action by the industry to curb youth use, sales restrictions to youth, and restrictions on some flavored tobacco products.
The report card
Federal government efforts in regulation of tobacco products, taxation, and health insurance coverage of cessation all received an F in this report, while mass media campaigns were given an A.
The states didn’t fare much better. They were graded on prevention and control funding, smoke-free air, taxation, access to cessation services, and minimum age for sales. A total of 19 states received a grade of F in four or five of these areas.
Funding for prevention and control was evaluated as the percentage of the amount recommended by the CDC, adjusted for a variety of state-specific factors such as prevalence of tobacco use, cost and complexity of conducting mass media campaigns, and proportion of the audience below 200% of the federal poverty level. A limitation of this methodology of grading funding is that it doesn’t evaluate effectiveness of the spending or the level of spending in different program categories. The higher spenders on prevention and control were Alaska at 98.1% and California at 74.5% of the CDC recommended level. The lowest spenders were Georgia at 2.8% and Missouri at 3.0%.
All but eight states received an F on minimum age for tobacco sales because most have an age limit 18 instead of the ALA and CDC recommendation of age 21.
Harold Wimmer, the CEO of the American Lung Association, wrote, “Aggressive action by our country’s federal and state policymakers is urgently required. However, ‘State of Tobacco Control’ 2019 has found a disturbing failure by federal and state governments to take action to put in place meaningful and proven-effective policies that would have prevented, and reduced tobacco use during 2018. This failure to act places the lung health and lives of Americans at risk. We have also found that this lack of action has emboldened tobacco companies to be even more brazen in producing and marketing products squarely aimed at kids, such as the JUUL e-cigarettes that look like an easily concealed USB drive, which now dominate the market driven by youth use.”
The full report is available for download at the ALA website.
SOURCE: American Lung Association, “State of Tobacco Control 2019”.
Tobacco use is currently at an all-time low thanks to public and private efforts, but more aggressive action from federal, state, and local governments is needed to protect the public, according to a review of tobacco control trends in the United States.
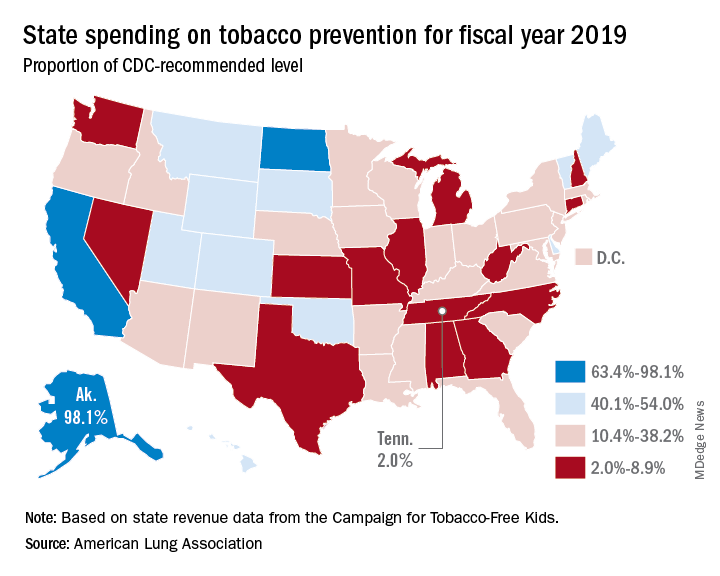
The American Lung Association (ALA) released “State of Tobacco Control” 2019, its 17th annual state-by-state analysis and list of recommended policy priorities to limit tobacco use. Although the report notes some positive steps taken by the federal and state governments, shortfalls in policy and legislation also are highlighted. The report states, “We know how and are ready to save more lives, but we need our elected officials to do much more. To many, solving America’s tobacco crisis might seem like a complex puzzle with no solution. And yet we have known for years what pieces are needed to reduce the disease and death caused by tobacco use.”
In this report, the federal government and each state are graded on a scale, A through F, for policy actions and laws to limit tobacco use. The grading methodology is based on a detailed point system cataloging the implementation and strength of specific actions and policies to limit tobacco use.
Areas of Impact
The report focused on six areas of public policy that affect exposure to and use of tobacco:
- Smoke-free air: Protecting the public from secondhand smoke should be a priority for policymakers, according the report, but 22 states have no smoke-free workplace laws in place. Laws restricting e-cigarettes in workplaces and public buildings have lagged behind tobacco laws in many states.
- Tobacco prevention funding: Dedicated funds to prevent tobacco addiction before it starts is a key element of a public health attack on tobacco use, but no U.S. state currently spends what the Centers for Disease Control and Prevention has recommended. Twenty years ago, the Master Settlement Agreement between the tobacco industry and 46 states and the District of Columbia guaranteed ongoing payments to the states to be used for tobacco prevention and control. Although those funds have been collected in the states to the tune of $27 billion since 1998, overall only 2.4% of those funds have been spent for this purpose, and the rest has been budgeted for other purposes.
- Tobacco taxes: Sales taxes on tobacco products have been highly effective in preventing young people from taking up tobacco use, but those taxation rates have remained unchanged in 2018 in all but the District of Columbia and Oklahoma. The tobacco industry spent $22 million in a successful effort to defeat ballot measures to increase sales taxes on tobacco in Montana and South Dakota.
- Tobacco 21: “Increasing the legal age of sale for tobacco products to 21 would decrease tobacco use by 12% and could prevent 223,000 deaths among those born between 2000 and 2019,” the report noted, citing a 2015 report by the Institute of Medicine. So far, the this restriction has been legislated in six states, the District of Columbia, and numerous local governments. The ALA considers increasing the age for tobacco sales to 21 to be a public health priority.
- Helping smokers quit: The addictive qualities of tobacco mean that many smokers struggle unsuccessfully to quit, and medical intervention is needed to help them. The report notes that current law requires that Medicaid expansion health plans and private insurance plans cover comprehensive smoking cessation treatment. However, not all states have the expanded Medicaid program, and many of those with Medicaid expansion don’t offer coverage of all Food and Drug–approved cessation treatments. Despite laws requiring smoking cessation coverage, many private insurance plans still do not include this coverage. The ALA recommends enforcement of the current law with regard to tobacco cessation insurance coverage.
- FDA regulation of tobacco products: The FDA has announced plans to make a major effort to reduce tobacco use in young people, decrease nicotine in cigarettes, and to restrict flavored tobacco products. But these plans fall short of the aggressive action needed to curb the tobacco “epidemic,” according to the report. Delayed action and timid policy have “resulted in tobacco companies becoming more emboldened to devise new and egregious ways to addict youth and sustain addiction among current users.” The ALA report points to the steep rise in e-cigarette use among youth with a 20.8% rise in high school students using these products in 2018, a rise from 11.7% in 2017. This trend is not likely to be reversed by the FDA proposals to date, which rely on voluntary action by the industry to curb youth use, sales restrictions to youth, and restrictions on some flavored tobacco products.
The report card
Federal government efforts in regulation of tobacco products, taxation, and health insurance coverage of cessation all received an F in this report, while mass media campaigns were given an A.
The states didn’t fare much better. They were graded on prevention and control funding, smoke-free air, taxation, access to cessation services, and minimum age for sales. A total of 19 states received a grade of F in four or five of these areas.
Funding for prevention and control was evaluated as the percentage of the amount recommended by the CDC, adjusted for a variety of state-specific factors such as prevalence of tobacco use, cost and complexity of conducting mass media campaigns, and proportion of the audience below 200% of the federal poverty level. A limitation of this methodology of grading funding is that it doesn’t evaluate effectiveness of the spending or the level of spending in different program categories. The higher spenders on prevention and control were Alaska at 98.1% and California at 74.5% of the CDC recommended level. The lowest spenders were Georgia at 2.8% and Missouri at 3.0%.
All but eight states received an F on minimum age for tobacco sales because most have an age limit 18 instead of the ALA and CDC recommendation of age 21.
Harold Wimmer, the CEO of the American Lung Association, wrote, “Aggressive action by our country’s federal and state policymakers is urgently required. However, ‘State of Tobacco Control’ 2019 has found a disturbing failure by federal and state governments to take action to put in place meaningful and proven-effective policies that would have prevented, and reduced tobacco use during 2018. This failure to act places the lung health and lives of Americans at risk. We have also found that this lack of action has emboldened tobacco companies to be even more brazen in producing and marketing products squarely aimed at kids, such as the JUUL e-cigarettes that look like an easily concealed USB drive, which now dominate the market driven by youth use.”
The full report is available for download at the ALA website.
SOURCE: American Lung Association, “State of Tobacco Control 2019”.
Tobacco use is currently at an all-time low thanks to public and private efforts, but more aggressive action from federal, state, and local governments is needed to protect the public, according to a review of tobacco control trends in the United States.
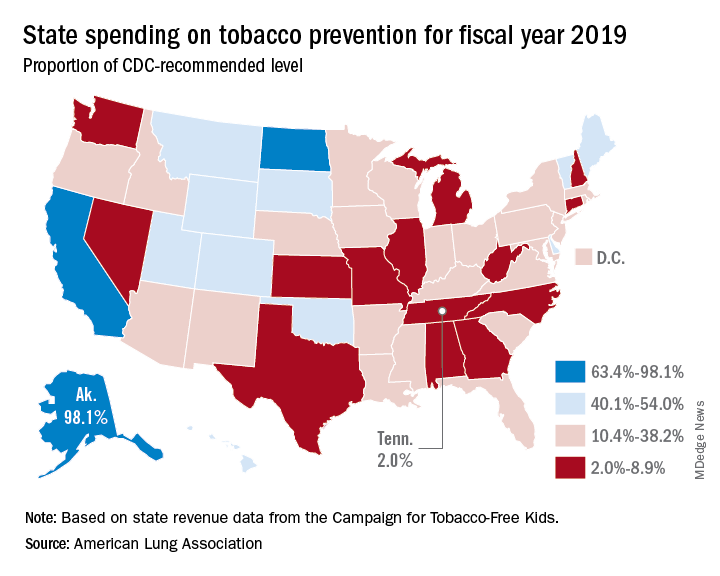
The American Lung Association (ALA) released “State of Tobacco Control” 2019, its 17th annual state-by-state analysis and list of recommended policy priorities to limit tobacco use. Although the report notes some positive steps taken by the federal and state governments, shortfalls in policy and legislation also are highlighted. The report states, “We know how and are ready to save more lives, but we need our elected officials to do much more. To many, solving America’s tobacco crisis might seem like a complex puzzle with no solution. And yet we have known for years what pieces are needed to reduce the disease and death caused by tobacco use.”
In this report, the federal government and each state are graded on a scale, A through F, for policy actions and laws to limit tobacco use. The grading methodology is based on a detailed point system cataloging the implementation and strength of specific actions and policies to limit tobacco use.
Areas of Impact
The report focused on six areas of public policy that affect exposure to and use of tobacco:
- Smoke-free air: Protecting the public from secondhand smoke should be a priority for policymakers, according the report, but 22 states have no smoke-free workplace laws in place. Laws restricting e-cigarettes in workplaces and public buildings have lagged behind tobacco laws in many states.
- Tobacco prevention funding: Dedicated funds to prevent tobacco addiction before it starts is a key element of a public health attack on tobacco use, but no U.S. state currently spends what the Centers for Disease Control and Prevention has recommended. Twenty years ago, the Master Settlement Agreement between the tobacco industry and 46 states and the District of Columbia guaranteed ongoing payments to the states to be used for tobacco prevention and control. Although those funds have been collected in the states to the tune of $27 billion since 1998, overall only 2.4% of those funds have been spent for this purpose, and the rest has been budgeted for other purposes.
- Tobacco taxes: Sales taxes on tobacco products have been highly effective in preventing young people from taking up tobacco use, but those taxation rates have remained unchanged in 2018 in all but the District of Columbia and Oklahoma. The tobacco industry spent $22 million in a successful effort to defeat ballot measures to increase sales taxes on tobacco in Montana and South Dakota.
- Tobacco 21: “Increasing the legal age of sale for tobacco products to 21 would decrease tobacco use by 12% and could prevent 223,000 deaths among those born between 2000 and 2019,” the report noted, citing a 2015 report by the Institute of Medicine. So far, the this restriction has been legislated in six states, the District of Columbia, and numerous local governments. The ALA considers increasing the age for tobacco sales to 21 to be a public health priority.
- Helping smokers quit: The addictive qualities of tobacco mean that many smokers struggle unsuccessfully to quit, and medical intervention is needed to help them. The report notes that current law requires that Medicaid expansion health plans and private insurance plans cover comprehensive smoking cessation treatment. However, not all states have the expanded Medicaid program, and many of those with Medicaid expansion don’t offer coverage of all Food and Drug–approved cessation treatments. Despite laws requiring smoking cessation coverage, many private insurance plans still do not include this coverage. The ALA recommends enforcement of the current law with regard to tobacco cessation insurance coverage.
- FDA regulation of tobacco products: The FDA has announced plans to make a major effort to reduce tobacco use in young people, decrease nicotine in cigarettes, and to restrict flavored tobacco products. But these plans fall short of the aggressive action needed to curb the tobacco “epidemic,” according to the report. Delayed action and timid policy have “resulted in tobacco companies becoming more emboldened to devise new and egregious ways to addict youth and sustain addiction among current users.” The ALA report points to the steep rise in e-cigarette use among youth with a 20.8% rise in high school students using these products in 2018, a rise from 11.7% in 2017. This trend is not likely to be reversed by the FDA proposals to date, which rely on voluntary action by the industry to curb youth use, sales restrictions to youth, and restrictions on some flavored tobacco products.
The report card
Federal government efforts in regulation of tobacco products, taxation, and health insurance coverage of cessation all received an F in this report, while mass media campaigns were given an A.
The states didn’t fare much better. They were graded on prevention and control funding, smoke-free air, taxation, access to cessation services, and minimum age for sales. A total of 19 states received a grade of F in four or five of these areas.
Funding for prevention and control was evaluated as the percentage of the amount recommended by the CDC, adjusted for a variety of state-specific factors such as prevalence of tobacco use, cost and complexity of conducting mass media campaigns, and proportion of the audience below 200% of the federal poverty level. A limitation of this methodology of grading funding is that it doesn’t evaluate effectiveness of the spending or the level of spending in different program categories. The higher spenders on prevention and control were Alaska at 98.1% and California at 74.5% of the CDC recommended level. The lowest spenders were Georgia at 2.8% and Missouri at 3.0%.
All but eight states received an F on minimum age for tobacco sales because most have an age limit 18 instead of the ALA and CDC recommendation of age 21.
Harold Wimmer, the CEO of the American Lung Association, wrote, “Aggressive action by our country’s federal and state policymakers is urgently required. However, ‘State of Tobacco Control’ 2019 has found a disturbing failure by federal and state governments to take action to put in place meaningful and proven-effective policies that would have prevented, and reduced tobacco use during 2018. This failure to act places the lung health and lives of Americans at risk. We have also found that this lack of action has emboldened tobacco companies to be even more brazen in producing and marketing products squarely aimed at kids, such as the JUUL e-cigarettes that look like an easily concealed USB drive, which now dominate the market driven by youth use.”
The full report is available for download at the ALA website.
SOURCE: American Lung Association, “State of Tobacco Control 2019”.
Loan Repayment Plan for Substance Use Clinicians
The opioid emergency claims > 130 lives every day, says Health Resources and Services Administration (HRSA) Administrator George Sigounas, MS, PhD. By strengthening the health workforce, HRSA hopes to ensure that there are enough clinicians to cope with the growing epidemic.
That is why, in December 2018, HRSA launched a program that Sigounas says is “critical to HHS’ response to the opioid crisis.” The new National Health Service Corps (NHSC) Substance Use Disorder (SUD) Workforce Loan Repayment Program (LRP) will provide eligible health care clinicians with student loan repayment assistance in exchange for service in underserved communities.
A clinician may be awarded up to $75,000 for 3 years of full-time service at an NHSC-approved SUD site and $37,500 for part-time. Eligible providers use evidence-based treatment models to treat SUDs and must be trained and licensed to provide SUD treatment at NHSC-approved facilities. Qualification criteria are available at https://nhsc.hrsa.gov/loan-repayment/nhsc-sud-workforce-loan-repayment-program.html.
Clinicians also can apply to the NHSC Loan Repayment Program for primary care, dental, and behavioral health professionals. If accepted, they may receive up to $50,000 for 2 years of full-time service, $25,000 for part-time.
Military reservists also are eligible to participate in either the NHSC LRP or the NHSC Students to Service Loan Repayment Program. (Military training or service will not satisfy the NHSC service commitment.) More information is available at https://nhsc.hrsa.gov/loan-repayment/military-reservists.html.
Clinicians can only apply for 1 program. Sigounas says, “I am grateful to the clinicians who will apply and are looking to make a positive impact on patients, caregivers, and hard-hit communities throughout the country.”
The opioid emergency claims > 130 lives every day, says Health Resources and Services Administration (HRSA) Administrator George Sigounas, MS, PhD. By strengthening the health workforce, HRSA hopes to ensure that there are enough clinicians to cope with the growing epidemic.
That is why, in December 2018, HRSA launched a program that Sigounas says is “critical to HHS’ response to the opioid crisis.” The new National Health Service Corps (NHSC) Substance Use Disorder (SUD) Workforce Loan Repayment Program (LRP) will provide eligible health care clinicians with student loan repayment assistance in exchange for service in underserved communities.
A clinician may be awarded up to $75,000 for 3 years of full-time service at an NHSC-approved SUD site and $37,500 for part-time. Eligible providers use evidence-based treatment models to treat SUDs and must be trained and licensed to provide SUD treatment at NHSC-approved facilities. Qualification criteria are available at https://nhsc.hrsa.gov/loan-repayment/nhsc-sud-workforce-loan-repayment-program.html.
Clinicians also can apply to the NHSC Loan Repayment Program for primary care, dental, and behavioral health professionals. If accepted, they may receive up to $50,000 for 2 years of full-time service, $25,000 for part-time.
Military reservists also are eligible to participate in either the NHSC LRP or the NHSC Students to Service Loan Repayment Program. (Military training or service will not satisfy the NHSC service commitment.) More information is available at https://nhsc.hrsa.gov/loan-repayment/military-reservists.html.
Clinicians can only apply for 1 program. Sigounas says, “I am grateful to the clinicians who will apply and are looking to make a positive impact on patients, caregivers, and hard-hit communities throughout the country.”
The opioid emergency claims > 130 lives every day, says Health Resources and Services Administration (HRSA) Administrator George Sigounas, MS, PhD. By strengthening the health workforce, HRSA hopes to ensure that there are enough clinicians to cope with the growing epidemic.
That is why, in December 2018, HRSA launched a program that Sigounas says is “critical to HHS’ response to the opioid crisis.” The new National Health Service Corps (NHSC) Substance Use Disorder (SUD) Workforce Loan Repayment Program (LRP) will provide eligible health care clinicians with student loan repayment assistance in exchange for service in underserved communities.
A clinician may be awarded up to $75,000 for 3 years of full-time service at an NHSC-approved SUD site and $37,500 for part-time. Eligible providers use evidence-based treatment models to treat SUDs and must be trained and licensed to provide SUD treatment at NHSC-approved facilities. Qualification criteria are available at https://nhsc.hrsa.gov/loan-repayment/nhsc-sud-workforce-loan-repayment-program.html.
Clinicians also can apply to the NHSC Loan Repayment Program for primary care, dental, and behavioral health professionals. If accepted, they may receive up to $50,000 for 2 years of full-time service, $25,000 for part-time.
Military reservists also are eligible to participate in either the NHSC LRP or the NHSC Students to Service Loan Repayment Program. (Military training or service will not satisfy the NHSC service commitment.) More information is available at https://nhsc.hrsa.gov/loan-repayment/military-reservists.html.
Clinicians can only apply for 1 program. Sigounas says, “I am grateful to the clinicians who will apply and are looking to make a positive impact on patients, caregivers, and hard-hit communities throughout the country.”
Cloud of inconsistency hangs over cannabis data
More people are using medical cannabis as it becomes legal in more states, but the lack of standardization in states’ data collection hindered investigators’ efforts to track that use.
Legalized medical cannabis is now available in 33 states and the District of Columbia, and the number of users has risen from just over 72,000 in 2009 to almost 814,000 in 2017. That 814,000, however, covers only 16 states and D.C., since 1 state (Connecticut) does not publish reports on medical cannabis use, 12 did not have statistics available, 2 (New York and Vermont) didn’t report data for 2017, and 2 (California and Maine) have voluntary registries that are unlikely to be accurate, according to Kevin F. Boehnke, PhD, of the University of Michigan, Ann Arbor, and his associates.
Michigan had the largest reported number of patients enrolled in its medical cannabis program in 2017, almost 270,000. California – the state with the oldest medical cannabis legislation (passed in 1996) and the largest overall population but a voluntary cannabis registry – reported its highest number of enrollees, 12,659, in 2009-2010, the investigators said. Colorado had more than 116,000 patients in its medical cannabis program in 2010 (Health Aff. 2019;38[2]:295-302).
The “many inconsistencies in data quality across states [suggest] the need for further standardization of data collection. Such standardization would add transparency to understanding how medical cannabis programs are used, which would help guide both research and policy needs,” Dr. Boehnke and his associates wrote.
More consistency was seen in the reasons for using medical cannabis. Chronic pain made up 62.2% of all qualifying conditions reported by patients during 1999-2016, with the annual average varying between 33.3% and 73%. Multiple sclerosis spasticity symptoms had the second-highest number of reports over the study period, followed by chemotherapy-induced nausea and vomiting, posttraumatic stress disorder, and cancer, they reported.
The investigators also looked at the appropriateness of cannabis and determined that its use in 85.5% of patient-reported conditions was “supported by conclusive or substantial evidence of therapeutic effectiveness, according to the 2017 National Academies report” on the health effects of cannabis.
“We believe not only that it is inappropriate for cannabis to remain a Schedule I substance, but also that state and federal policy makers should begin evaluating evidence-based ways for safely integrating cannabis research and products into the health care system,” they concluded.
SOURCE: Boehnke KF et al. Health Aff. 2019;38(2):295-302.
More people are using medical cannabis as it becomes legal in more states, but the lack of standardization in states’ data collection hindered investigators’ efforts to track that use.
Legalized medical cannabis is now available in 33 states and the District of Columbia, and the number of users has risen from just over 72,000 in 2009 to almost 814,000 in 2017. That 814,000, however, covers only 16 states and D.C., since 1 state (Connecticut) does not publish reports on medical cannabis use, 12 did not have statistics available, 2 (New York and Vermont) didn’t report data for 2017, and 2 (California and Maine) have voluntary registries that are unlikely to be accurate, according to Kevin F. Boehnke, PhD, of the University of Michigan, Ann Arbor, and his associates.
Michigan had the largest reported number of patients enrolled in its medical cannabis program in 2017, almost 270,000. California – the state with the oldest medical cannabis legislation (passed in 1996) and the largest overall population but a voluntary cannabis registry – reported its highest number of enrollees, 12,659, in 2009-2010, the investigators said. Colorado had more than 116,000 patients in its medical cannabis program in 2010 (Health Aff. 2019;38[2]:295-302).
The “many inconsistencies in data quality across states [suggest] the need for further standardization of data collection. Such standardization would add transparency to understanding how medical cannabis programs are used, which would help guide both research and policy needs,” Dr. Boehnke and his associates wrote.
More consistency was seen in the reasons for using medical cannabis. Chronic pain made up 62.2% of all qualifying conditions reported by patients during 1999-2016, with the annual average varying between 33.3% and 73%. Multiple sclerosis spasticity symptoms had the second-highest number of reports over the study period, followed by chemotherapy-induced nausea and vomiting, posttraumatic stress disorder, and cancer, they reported.
The investigators also looked at the appropriateness of cannabis and determined that its use in 85.5% of patient-reported conditions was “supported by conclusive or substantial evidence of therapeutic effectiveness, according to the 2017 National Academies report” on the health effects of cannabis.
“We believe not only that it is inappropriate for cannabis to remain a Schedule I substance, but also that state and federal policy makers should begin evaluating evidence-based ways for safely integrating cannabis research and products into the health care system,” they concluded.
SOURCE: Boehnke KF et al. Health Aff. 2019;38(2):295-302.
More people are using medical cannabis as it becomes legal in more states, but the lack of standardization in states’ data collection hindered investigators’ efforts to track that use.
Legalized medical cannabis is now available in 33 states and the District of Columbia, and the number of users has risen from just over 72,000 in 2009 to almost 814,000 in 2017. That 814,000, however, covers only 16 states and D.C., since 1 state (Connecticut) does not publish reports on medical cannabis use, 12 did not have statistics available, 2 (New York and Vermont) didn’t report data for 2017, and 2 (California and Maine) have voluntary registries that are unlikely to be accurate, according to Kevin F. Boehnke, PhD, of the University of Michigan, Ann Arbor, and his associates.
Michigan had the largest reported number of patients enrolled in its medical cannabis program in 2017, almost 270,000. California – the state with the oldest medical cannabis legislation (passed in 1996) and the largest overall population but a voluntary cannabis registry – reported its highest number of enrollees, 12,659, in 2009-2010, the investigators said. Colorado had more than 116,000 patients in its medical cannabis program in 2010 (Health Aff. 2019;38[2]:295-302).
The “many inconsistencies in data quality across states [suggest] the need for further standardization of data collection. Such standardization would add transparency to understanding how medical cannabis programs are used, which would help guide both research and policy needs,” Dr. Boehnke and his associates wrote.
More consistency was seen in the reasons for using medical cannabis. Chronic pain made up 62.2% of all qualifying conditions reported by patients during 1999-2016, with the annual average varying between 33.3% and 73%. Multiple sclerosis spasticity symptoms had the second-highest number of reports over the study period, followed by chemotherapy-induced nausea and vomiting, posttraumatic stress disorder, and cancer, they reported.
The investigators also looked at the appropriateness of cannabis and determined that its use in 85.5% of patient-reported conditions was “supported by conclusive or substantial evidence of therapeutic effectiveness, according to the 2017 National Academies report” on the health effects of cannabis.
“We believe not only that it is inappropriate for cannabis to remain a Schedule I substance, but also that state and federal policy makers should begin evaluating evidence-based ways for safely integrating cannabis research and products into the health care system,” they concluded.
SOURCE: Boehnke KF et al. Health Aff. 2019;38(2):295-302.
FROM HEALTH AFFAIRS
President Trump calls for end to HIV/AIDS, pediatric cancer
HIV/AIDS, pediatric cancer research, abortion, prescription drug prices, and preexisting conditions were among the health care highlights of President Donald Trump’s second State of the Union address Feb. 5.

Mr. Trump promised to push for funds to end HIV/AIDS and childhood cancer within in 10 years. “In recent years, we have made remarkable progress in the fight against HIV and AIDS. Scientific breakthroughs have brought a once-distant dream within reach,” he said to assembled members of Congress and leaders of the executive and judicial branches of government. “My budget will ask Democrats and Republicans to make the needed commitment to eliminate the HIV epidemic in the United States within 10 years.”
Following the speech, Alex Azar, secretary of the Department of Health and Human Services, offered more details in a blog post on the agency’s website.
Funding for the initiative, dubbed “Ending the HIV Epidemic: A Plan for America,” will have three components.
The first involves increasing investments in “geographic hotspots” though existing programs like the Ryan White HIV/AIDS Program and a new community health center–based program to provide antiretroviral therapy (ART) and preexposure prophylaxis (PrEP) to those at the highest risk of contracting the disease.
Second is the use of data to track where the disease is spreading most rapidly to help target prevention, care, and treatment at the local level. The third will provide funds for the creation of a local HIV HealthForce in these targeted areas to expand HIV prevention and treatment efforts.
A fact sheet on this initiative called for a 75% reduction in new cases of HIV infection in 5 years and at least a 90% reduction within 10 years.
President Trump called for similar efforts to address pediatric cancer.
“Tonight I am also asking you to join me in another fight that all American can get behind – the fight against childhood cancer,” he said, adding that his budget request will come with a line item of $500 million over 10 years to fund research. “Many childhood cancers have not seen new therapies in decades.”
President Trump also asked Congress to legislate a prohibition of late-term abortion.
“There could be no greater contrast to the beautiful image of a mother holding her infant child than the chilling displays our nation saw in recent days,” he said. “Lawmakers in New York cheered with delight upon the passage of legislation that would allow a baby to be ripped from the mother’s womb moments from birth. These are living, feeling beautiful babies who will never get the chance to share their love and their dreams with the world. ... Let us work together to build a culture that cherishes innocent life.”
He also touched on the recurring themes regarding lowering the cost of health care and prescription drugs, as well as protecting those with preexisting conditions, something he called a major priority.
“It’s unacceptable that Americans pay vastly more than people in other countries for the exact same drugs, often made in the exact same place. This is wrong. This is unfair and together we will stop it, and we will stop it fast,” he said.
He did not offer any specific policy recommendation on how to address prescription drug costs, other than a comment on the need for greater price transparency.
“I am asking Congress to pass legislation that finally takes on the problem of global freeloading and delivers fairness and price transparency for American patients,” he said.
“We should also require drug companies, insurance companies, and hospitals to disclose real prices to foster competition and bring costs way down.”
SOURCE: Trump D. State of the Union Address, Feb. 5, 2019.
HIV/AIDS, pediatric cancer research, abortion, prescription drug prices, and preexisting conditions were among the health care highlights of President Donald Trump’s second State of the Union address Feb. 5.

Mr. Trump promised to push for funds to end HIV/AIDS and childhood cancer within in 10 years. “In recent years, we have made remarkable progress in the fight against HIV and AIDS. Scientific breakthroughs have brought a once-distant dream within reach,” he said to assembled members of Congress and leaders of the executive and judicial branches of government. “My budget will ask Democrats and Republicans to make the needed commitment to eliminate the HIV epidemic in the United States within 10 years.”
Following the speech, Alex Azar, secretary of the Department of Health and Human Services, offered more details in a blog post on the agency’s website.
Funding for the initiative, dubbed “Ending the HIV Epidemic: A Plan for America,” will have three components.
The first involves increasing investments in “geographic hotspots” though existing programs like the Ryan White HIV/AIDS Program and a new community health center–based program to provide antiretroviral therapy (ART) and preexposure prophylaxis (PrEP) to those at the highest risk of contracting the disease.
Second is the use of data to track where the disease is spreading most rapidly to help target prevention, care, and treatment at the local level. The third will provide funds for the creation of a local HIV HealthForce in these targeted areas to expand HIV prevention and treatment efforts.
A fact sheet on this initiative called for a 75% reduction in new cases of HIV infection in 5 years and at least a 90% reduction within 10 years.
President Trump called for similar efforts to address pediatric cancer.
“Tonight I am also asking you to join me in another fight that all American can get behind – the fight against childhood cancer,” he said, adding that his budget request will come with a line item of $500 million over 10 years to fund research. “Many childhood cancers have not seen new therapies in decades.”
President Trump also asked Congress to legislate a prohibition of late-term abortion.
“There could be no greater contrast to the beautiful image of a mother holding her infant child than the chilling displays our nation saw in recent days,” he said. “Lawmakers in New York cheered with delight upon the passage of legislation that would allow a baby to be ripped from the mother’s womb moments from birth. These are living, feeling beautiful babies who will never get the chance to share their love and their dreams with the world. ... Let us work together to build a culture that cherishes innocent life.”
He also touched on the recurring themes regarding lowering the cost of health care and prescription drugs, as well as protecting those with preexisting conditions, something he called a major priority.
“It’s unacceptable that Americans pay vastly more than people in other countries for the exact same drugs, often made in the exact same place. This is wrong. This is unfair and together we will stop it, and we will stop it fast,” he said.
He did not offer any specific policy recommendation on how to address prescription drug costs, other than a comment on the need for greater price transparency.
“I am asking Congress to pass legislation that finally takes on the problem of global freeloading and delivers fairness and price transparency for American patients,” he said.
“We should also require drug companies, insurance companies, and hospitals to disclose real prices to foster competition and bring costs way down.”
SOURCE: Trump D. State of the Union Address, Feb. 5, 2019.
HIV/AIDS, pediatric cancer research, abortion, prescription drug prices, and preexisting conditions were among the health care highlights of President Donald Trump’s second State of the Union address Feb. 5.

Mr. Trump promised to push for funds to end HIV/AIDS and childhood cancer within in 10 years. “In recent years, we have made remarkable progress in the fight against HIV and AIDS. Scientific breakthroughs have brought a once-distant dream within reach,” he said to assembled members of Congress and leaders of the executive and judicial branches of government. “My budget will ask Democrats and Republicans to make the needed commitment to eliminate the HIV epidemic in the United States within 10 years.”
Following the speech, Alex Azar, secretary of the Department of Health and Human Services, offered more details in a blog post on the agency’s website.
Funding for the initiative, dubbed “Ending the HIV Epidemic: A Plan for America,” will have three components.
The first involves increasing investments in “geographic hotspots” though existing programs like the Ryan White HIV/AIDS Program and a new community health center–based program to provide antiretroviral therapy (ART) and preexposure prophylaxis (PrEP) to those at the highest risk of contracting the disease.
Second is the use of data to track where the disease is spreading most rapidly to help target prevention, care, and treatment at the local level. The third will provide funds for the creation of a local HIV HealthForce in these targeted areas to expand HIV prevention and treatment efforts.
A fact sheet on this initiative called for a 75% reduction in new cases of HIV infection in 5 years and at least a 90% reduction within 10 years.
President Trump called for similar efforts to address pediatric cancer.
“Tonight I am also asking you to join me in another fight that all American can get behind – the fight against childhood cancer,” he said, adding that his budget request will come with a line item of $500 million over 10 years to fund research. “Many childhood cancers have not seen new therapies in decades.”
President Trump also asked Congress to legislate a prohibition of late-term abortion.
“There could be no greater contrast to the beautiful image of a mother holding her infant child than the chilling displays our nation saw in recent days,” he said. “Lawmakers in New York cheered with delight upon the passage of legislation that would allow a baby to be ripped from the mother’s womb moments from birth. These are living, feeling beautiful babies who will never get the chance to share their love and their dreams with the world. ... Let us work together to build a culture that cherishes innocent life.”
He also touched on the recurring themes regarding lowering the cost of health care and prescription drugs, as well as protecting those with preexisting conditions, something he called a major priority.
“It’s unacceptable that Americans pay vastly more than people in other countries for the exact same drugs, often made in the exact same place. This is wrong. This is unfair and together we will stop it, and we will stop it fast,” he said.
He did not offer any specific policy recommendation on how to address prescription drug costs, other than a comment on the need for greater price transparency.
“I am asking Congress to pass legislation that finally takes on the problem of global freeloading and delivers fairness and price transparency for American patients,” he said.
“We should also require drug companies, insurance companies, and hospitals to disclose real prices to foster competition and bring costs way down.”
SOURCE: Trump D. State of the Union Address, Feb. 5, 2019.
Key clinical point: President Trump calls for an end to HIV/AIDS and pediatric cancer in 10 years.
Major finding: His budget will request $500 million for cancer research and as yet undisclosed amount for HIV/AIDS research.
Study details: More specific details on the proposals will likely come when the president makes his budget submission to Congress in the coming weeks.
Disclosures: There are no disclosures.
Source: Trump D. State of the Union Address, Feb. 5, 2019.
Winners and losers under bold Trump plan to slash drug rebate deals
Few consumers have heard of the secret, business-to-business payments that the Trump administration wants to ban in an attempt to control drug costs.
But the administration’s plan for drug rebates, announced Jan. 31, would end the pharmaceutical business as usual, shift billions in revenue and cause far-reaching, unforeseen change, say health policy authorities.
In pointed language sure to anger middlemen who benefit from the deals, administration officials proposed banning rebates paid by drug companies to ensure coverage for their products under Medicare and Medicaid plans.
“A shadowy system of kickbacks,” was how Health and Human Services Secretary Alex Azar described the current system in a speech on Feb. 1.
The proposal is a regulatory change applying only to Medicare plans for seniors and managed Medicaid plans for low-income people. But private insurers, who often take cues from government programs, might make a similar shift, administration officials said.
Drug rebates are essentially discounts off the list price. Outlawing them would divert $29 billion in rebates now paid to insurers and pharmacy benefit managers into “seniors’ pocketbooks at the pharmacy counter,” Azar said.
The measure already faces fierce opposition from some in the industry and is unlikely to be implemented as presented or by the proposed 2020 effective date, health policy analysts said.
In any event, it’s hardly a pure win for seniors or patients in general. Consumers are unlikely to collect the full benefit of eliminated rebates.
At the same time, the change would produce uncertain ricochets, including higher drug-plan premiums for consumers, that would produce new winners and losers across the economy.
“It is the most significant proposal that the administration has introduced so far” to try to control drug prices, said Rachel Sachs, a law professor at Washington University in St. Louis. “But I’m struck by the uncertainty that the administration has in what the effects would be.”
Chronically ill patients who take lots of expensive medicine
The list price for many brand-name medicines has doubled or tripled in recent years. But virtually the only ones affected by the full increases are the many patients who pay cash or whose out-of-pocket payments are based on the posted price.
By banning rebates, the administration says its intention is to ensure discounts are passed all the way to the patient instead of the middlemen, the so-called pharmacy benefit managers or PBMs. That means consumers using expensive drugs might see their out-of-pocket costs go down.
If rebates were eliminated for commercial insurance, where deductibles and out-of-pocket costs are generally much higher, chronically ill patients could benefit much more.
Drug companies
Ending rebates would give the administration a drug-policy “win” that doesn’t directly threaten pharmaceutical company profits.
“We applaud the administration for taking steps to reform the rebate system” Stephen Ubl, CEO of PhRMA, the main lobby for branded drugs, said after the proposal came out.
The change might also slow the soaring list-price increases that have become a publicity nightmare for the industry. When list prices pop by 5% or 10% each year, drugmakers pay part of the proceeds to insurers and PBMs in the form of rebates to guarantee health-plan coverage.
No one is claiming that eliminating rebates would stop escalating list prices, even if all insurers adopted the practice. But some believe it would remove an important factor.
Pharmacy benefit managers
PBMs reap billions of dollars in rebate revenue in return for putting particular products on lists of covered drugs. The administration is essentially proposing to make those payments illegal, at least for Medicare and Medicaid plans.
PBMs, which claim they control costs by negotiating with drugmakers, might have to go back to their roots – processing pharmacy claims for a fee. After recent industry consolidation into a few enormous companies, on the other hand, they might have the market power to charge very high fees, replacing much of the lost rebate revenue.
PBMs “are concerned” that the move “would increase drug costs and force Medicare beneficiaries to pay higher premiums and out-of-pocket expenses,” said JC Scott, CEO of the Pharmaceutical Care Management Association, the PBM lobby.
Insurance companies
Insurers, who often receive rebates directly, could also be hurt financially.
“From the start, the focus on rebates has been a distraction from the real issue – the problem is the price” of the drugs, said Matt Eyles, CEO of America’s Health Insurance Plans, a trade group. “We are not middlemen – we are your bargaining power, working hard to negotiate lower prices.”
Patients without chronic conditions and high drug costs
Lower out-of-pocket costs at the pharmacy counter would be financed, at least in part, by higher premiums for Medicare and Medicaid plans paid by consumers and the government. Premiums for Medicare Part D plans could rise from $3.20 to $5.64 per month, according to consultants hired by the Department of Health and Human Services.
“There is likely to be a wide variation in how much savings people see based on the drugs they take and the point-of-sale discounts that are negotiated,” said Elizabeth Carpenter, policy practice director at Avalere, a consultancy.
Consumers who don’t need expensive drugs every month could see insurance costs go up slightly without getting the benefits of lower out-of-pocket expense for purchased drugs.
Other policy changes giving health plans more negotiating power against drugmakers would keep a lid on premium increases, administration officials argue.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Few consumers have heard of the secret, business-to-business payments that the Trump administration wants to ban in an attempt to control drug costs.
But the administration’s plan for drug rebates, announced Jan. 31, would end the pharmaceutical business as usual, shift billions in revenue and cause far-reaching, unforeseen change, say health policy authorities.
In pointed language sure to anger middlemen who benefit from the deals, administration officials proposed banning rebates paid by drug companies to ensure coverage for their products under Medicare and Medicaid plans.
“A shadowy system of kickbacks,” was how Health and Human Services Secretary Alex Azar described the current system in a speech on Feb. 1.
The proposal is a regulatory change applying only to Medicare plans for seniors and managed Medicaid plans for low-income people. But private insurers, who often take cues from government programs, might make a similar shift, administration officials said.
Drug rebates are essentially discounts off the list price. Outlawing them would divert $29 billion in rebates now paid to insurers and pharmacy benefit managers into “seniors’ pocketbooks at the pharmacy counter,” Azar said.
The measure already faces fierce opposition from some in the industry and is unlikely to be implemented as presented or by the proposed 2020 effective date, health policy analysts said.
In any event, it’s hardly a pure win for seniors or patients in general. Consumers are unlikely to collect the full benefit of eliminated rebates.
At the same time, the change would produce uncertain ricochets, including higher drug-plan premiums for consumers, that would produce new winners and losers across the economy.
“It is the most significant proposal that the administration has introduced so far” to try to control drug prices, said Rachel Sachs, a law professor at Washington University in St. Louis. “But I’m struck by the uncertainty that the administration has in what the effects would be.”
Chronically ill patients who take lots of expensive medicine
The list price for many brand-name medicines has doubled or tripled in recent years. But virtually the only ones affected by the full increases are the many patients who pay cash or whose out-of-pocket payments are based on the posted price.
By banning rebates, the administration says its intention is to ensure discounts are passed all the way to the patient instead of the middlemen, the so-called pharmacy benefit managers or PBMs. That means consumers using expensive drugs might see their out-of-pocket costs go down.
If rebates were eliminated for commercial insurance, where deductibles and out-of-pocket costs are generally much higher, chronically ill patients could benefit much more.
Drug companies
Ending rebates would give the administration a drug-policy “win” that doesn’t directly threaten pharmaceutical company profits.
“We applaud the administration for taking steps to reform the rebate system” Stephen Ubl, CEO of PhRMA, the main lobby for branded drugs, said after the proposal came out.
The change might also slow the soaring list-price increases that have become a publicity nightmare for the industry. When list prices pop by 5% or 10% each year, drugmakers pay part of the proceeds to insurers and PBMs in the form of rebates to guarantee health-plan coverage.
No one is claiming that eliminating rebates would stop escalating list prices, even if all insurers adopted the practice. But some believe it would remove an important factor.
Pharmacy benefit managers
PBMs reap billions of dollars in rebate revenue in return for putting particular products on lists of covered drugs. The administration is essentially proposing to make those payments illegal, at least for Medicare and Medicaid plans.
PBMs, which claim they control costs by negotiating with drugmakers, might have to go back to their roots – processing pharmacy claims for a fee. After recent industry consolidation into a few enormous companies, on the other hand, they might have the market power to charge very high fees, replacing much of the lost rebate revenue.
PBMs “are concerned” that the move “would increase drug costs and force Medicare beneficiaries to pay higher premiums and out-of-pocket expenses,” said JC Scott, CEO of the Pharmaceutical Care Management Association, the PBM lobby.
Insurance companies
Insurers, who often receive rebates directly, could also be hurt financially.
“From the start, the focus on rebates has been a distraction from the real issue – the problem is the price” of the drugs, said Matt Eyles, CEO of America’s Health Insurance Plans, a trade group. “We are not middlemen – we are your bargaining power, working hard to negotiate lower prices.”
Patients without chronic conditions and high drug costs
Lower out-of-pocket costs at the pharmacy counter would be financed, at least in part, by higher premiums for Medicare and Medicaid plans paid by consumers and the government. Premiums for Medicare Part D plans could rise from $3.20 to $5.64 per month, according to consultants hired by the Department of Health and Human Services.
“There is likely to be a wide variation in how much savings people see based on the drugs they take and the point-of-sale discounts that are negotiated,” said Elizabeth Carpenter, policy practice director at Avalere, a consultancy.
Consumers who don’t need expensive drugs every month could see insurance costs go up slightly without getting the benefits of lower out-of-pocket expense for purchased drugs.
Other policy changes giving health plans more negotiating power against drugmakers would keep a lid on premium increases, administration officials argue.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
Few consumers have heard of the secret, business-to-business payments that the Trump administration wants to ban in an attempt to control drug costs.
But the administration’s plan for drug rebates, announced Jan. 31, would end the pharmaceutical business as usual, shift billions in revenue and cause far-reaching, unforeseen change, say health policy authorities.
In pointed language sure to anger middlemen who benefit from the deals, administration officials proposed banning rebates paid by drug companies to ensure coverage for their products under Medicare and Medicaid plans.
“A shadowy system of kickbacks,” was how Health and Human Services Secretary Alex Azar described the current system in a speech on Feb. 1.
The proposal is a regulatory change applying only to Medicare plans for seniors and managed Medicaid plans for low-income people. But private insurers, who often take cues from government programs, might make a similar shift, administration officials said.
Drug rebates are essentially discounts off the list price. Outlawing them would divert $29 billion in rebates now paid to insurers and pharmacy benefit managers into “seniors’ pocketbooks at the pharmacy counter,” Azar said.
The measure already faces fierce opposition from some in the industry and is unlikely to be implemented as presented or by the proposed 2020 effective date, health policy analysts said.
In any event, it’s hardly a pure win for seniors or patients in general. Consumers are unlikely to collect the full benefit of eliminated rebates.
At the same time, the change would produce uncertain ricochets, including higher drug-plan premiums for consumers, that would produce new winners and losers across the economy.
“It is the most significant proposal that the administration has introduced so far” to try to control drug prices, said Rachel Sachs, a law professor at Washington University in St. Louis. “But I’m struck by the uncertainty that the administration has in what the effects would be.”
Chronically ill patients who take lots of expensive medicine
The list price for many brand-name medicines has doubled or tripled in recent years. But virtually the only ones affected by the full increases are the many patients who pay cash or whose out-of-pocket payments are based on the posted price.
By banning rebates, the administration says its intention is to ensure discounts are passed all the way to the patient instead of the middlemen, the so-called pharmacy benefit managers or PBMs. That means consumers using expensive drugs might see their out-of-pocket costs go down.
If rebates were eliminated for commercial insurance, where deductibles and out-of-pocket costs are generally much higher, chronically ill patients could benefit much more.
Drug companies
Ending rebates would give the administration a drug-policy “win” that doesn’t directly threaten pharmaceutical company profits.
“We applaud the administration for taking steps to reform the rebate system” Stephen Ubl, CEO of PhRMA, the main lobby for branded drugs, said after the proposal came out.
The change might also slow the soaring list-price increases that have become a publicity nightmare for the industry. When list prices pop by 5% or 10% each year, drugmakers pay part of the proceeds to insurers and PBMs in the form of rebates to guarantee health-plan coverage.
No one is claiming that eliminating rebates would stop escalating list prices, even if all insurers adopted the practice. But some believe it would remove an important factor.
Pharmacy benefit managers
PBMs reap billions of dollars in rebate revenue in return for putting particular products on lists of covered drugs. The administration is essentially proposing to make those payments illegal, at least for Medicare and Medicaid plans.
PBMs, which claim they control costs by negotiating with drugmakers, might have to go back to their roots – processing pharmacy claims for a fee. After recent industry consolidation into a few enormous companies, on the other hand, they might have the market power to charge very high fees, replacing much of the lost rebate revenue.
PBMs “are concerned” that the move “would increase drug costs and force Medicare beneficiaries to pay higher premiums and out-of-pocket expenses,” said JC Scott, CEO of the Pharmaceutical Care Management Association, the PBM lobby.
Insurance companies
Insurers, who often receive rebates directly, could also be hurt financially.
“From the start, the focus on rebates has been a distraction from the real issue – the problem is the price” of the drugs, said Matt Eyles, CEO of America’s Health Insurance Plans, a trade group. “We are not middlemen – we are your bargaining power, working hard to negotiate lower prices.”
Patients without chronic conditions and high drug costs
Lower out-of-pocket costs at the pharmacy counter would be financed, at least in part, by higher premiums for Medicare and Medicaid plans paid by consumers and the government. Premiums for Medicare Part D plans could rise from $3.20 to $5.64 per month, according to consultants hired by the Department of Health and Human Services.
“There is likely to be a wide variation in how much savings people see based on the drugs they take and the point-of-sale discounts that are negotiated,” said Elizabeth Carpenter, policy practice director at Avalere, a consultancy.
Consumers who don’t need expensive drugs every month could see insurance costs go up slightly without getting the benefits of lower out-of-pocket expense for purchased drugs.
Other policy changes giving health plans more negotiating power against drugmakers would keep a lid on premium increases, administration officials argue.
Kaiser Health News is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
CMS proposing more flexibility in Medicare Advantage, Part D
More flexibility in benefits design could be coming to Medicare Advantage and the Part D prescription drug benefit if proposals offered by the Centers for Medicare & Medicaid Services are finalized.
The agency issued its proposed update for both programs for the 2020 plan year, which would allow Medicare Advantage plan sponsors to offer more specialized supplemental benefits for beneficiaries with chronic illnesses.
“For the 2020 plan year and beyond, Medicare Advantage plans will have greater flexibility to offer chronically ill patients any benefit that improves or maintains their health,” Demetrios Kouzoukas, CMS principal deputy administrator for Medicare and director of the Center for Medicare, said during a Jan. 30 press teleconference. “For example, plans could provide home-delivered or special meals in a far broader set of circumstances than what is allowed today.”
He noted that it would be up to the plans to determine what kinds of supplemental benefits would be offered and added that the offering of these benefits would not require a waiver, but would be evaluated as part of the plan’s overall bid submitted to the agency.
“We recognize that Medicare beneficiaries frequently have multiple chronic conditions,” Mr. Kouzoukas said. “We are excited that these changes will allow these beneficiaries to have new options for improving their health as a result of innovative health plan benefits.”
For Medicare Part D, the agency is specifically encouraging plan sponsors “to provide lower cost sharing for opioid reversal agents such as naloxone,” he added. The proposal also offers additional flexibility for plans to offer targeted benefits and cost sharing reductions to patients with chronic pain or those undergoing addiction treatment, according to a fact sheet highlighting key proposals.
Comments on the proposals are due by March 1. CMS expects to finalize the changes by the beginning of April.
More flexibility in benefits design could be coming to Medicare Advantage and the Part D prescription drug benefit if proposals offered by the Centers for Medicare & Medicaid Services are finalized.
The agency issued its proposed update for both programs for the 2020 plan year, which would allow Medicare Advantage plan sponsors to offer more specialized supplemental benefits for beneficiaries with chronic illnesses.
“For the 2020 plan year and beyond, Medicare Advantage plans will have greater flexibility to offer chronically ill patients any benefit that improves or maintains their health,” Demetrios Kouzoukas, CMS principal deputy administrator for Medicare and director of the Center for Medicare, said during a Jan. 30 press teleconference. “For example, plans could provide home-delivered or special meals in a far broader set of circumstances than what is allowed today.”
He noted that it would be up to the plans to determine what kinds of supplemental benefits would be offered and added that the offering of these benefits would not require a waiver, but would be evaluated as part of the plan’s overall bid submitted to the agency.
“We recognize that Medicare beneficiaries frequently have multiple chronic conditions,” Mr. Kouzoukas said. “We are excited that these changes will allow these beneficiaries to have new options for improving their health as a result of innovative health plan benefits.”
For Medicare Part D, the agency is specifically encouraging plan sponsors “to provide lower cost sharing for opioid reversal agents such as naloxone,” he added. The proposal also offers additional flexibility for plans to offer targeted benefits and cost sharing reductions to patients with chronic pain or those undergoing addiction treatment, according to a fact sheet highlighting key proposals.
Comments on the proposals are due by March 1. CMS expects to finalize the changes by the beginning of April.
More flexibility in benefits design could be coming to Medicare Advantage and the Part D prescription drug benefit if proposals offered by the Centers for Medicare & Medicaid Services are finalized.
The agency issued its proposed update for both programs for the 2020 plan year, which would allow Medicare Advantage plan sponsors to offer more specialized supplemental benefits for beneficiaries with chronic illnesses.
“For the 2020 plan year and beyond, Medicare Advantage plans will have greater flexibility to offer chronically ill patients any benefit that improves or maintains their health,” Demetrios Kouzoukas, CMS principal deputy administrator for Medicare and director of the Center for Medicare, said during a Jan. 30 press teleconference. “For example, plans could provide home-delivered or special meals in a far broader set of circumstances than what is allowed today.”
He noted that it would be up to the plans to determine what kinds of supplemental benefits would be offered and added that the offering of these benefits would not require a waiver, but would be evaluated as part of the plan’s overall bid submitted to the agency.
“We recognize that Medicare beneficiaries frequently have multiple chronic conditions,” Mr. Kouzoukas said. “We are excited that these changes will allow these beneficiaries to have new options for improving their health as a result of innovative health plan benefits.”
For Medicare Part D, the agency is specifically encouraging plan sponsors “to provide lower cost sharing for opioid reversal agents such as naloxone,” he added. The proposal also offers additional flexibility for plans to offer targeted benefits and cost sharing reductions to patients with chronic pain or those undergoing addiction treatment, according to a fact sheet highlighting key proposals.
Comments on the proposals are due by March 1. CMS expects to finalize the changes by the beginning of April.