User login
Accelerated pacing a possible strategy for HFpEF?
Evidence supporting medications that slow the heart rate (HR), notably beta-blockers, is overwhelming in heart failure (HF) with reduced ejection fraction. Underwhelming, however, is clinical trial support for such agents in patients with HF with preserved ejection fraction (HFpEF).
Indeed, at least for some such patients, a treatment that modestly accelerates resting HR may be a more promising strategy, suggests an early line of research that challenges prevalent thinking about HFpEF therapy.
In a small, randomized test of the idea, patients with HFpEF and standard pacemakers set to a backup resting HR a bit higher than a standard of care 60 bpm, usually to about 75 bpm, reaped important quality of life benefits.
More strikingly, their natriuretic peptide levels and burden of atrial fibrillation (AFib) fell significantly, the latter by 27% over 1 year.
The trial enrolled only HFpEF patients with pacemakers previously implanted for sick sinus syndrome or atrioventricular block. But researchers say their 107-patient study called myPACE – if confirmed in larger, multicenter trials – lays the groundwork for a device therapy that is broadly useful, potentially, in patients with “preclinical or overt” HFpEF.
Indeed, some of the intervention’s “quite substantial” benefits rivaled or surpassed what his group has observed with available HFpEF drug therapies, including the sodium-glucose cotransporter 2 inhibitors, observed Markus Meyer, MD, PhD, University of Minnesota, Minneapolis.
Moreover, the study may be “the first to show that, with this approach, we can actually also reduce atrial fibrillation,” he said in an interview.
Dr. Meyer said his group is “confident” that the HR-modulation strategy will be successful in appropriate clinical trials and that “pacemakers, in the end, will become a treatment modality for HFpEF.”
Meyer is senior author on the trial’s publication in JAMA Cardiology in JAMA Cardiology (2023 Feb 1. doi: 10.1001/jamacardio.2022.5320), with lead author Margaret Infeld, MD, University of Vermont, Burlington.
The trial entered pacemaker patients with HFpEF of stage B or C – that is, either asymptomatic with structural disease or fully symptomatic. But, Dr. Meyer said, “we saw that the treatment effect was much more pronounced in the patients who had overt heart failure with preserved ejection fraction.”
Challenging beta-blocker dogma
The study, the report states, “contradicts canonical thinking” by suggesting HFpEF patients may benefit from a higher resting heart rate, which would presumably shorten diastolic filling time. It also “may help reduce the overprescription of beta-blockers to allow higher heart rates in this population.”
Indeed, Dr. Meyer observed, no one really knows whether beta-blockers work in HFpEF, “because they really have never been studied in a sufficiently powered randomized controlled trial.”
The current study “basically rewrites what we know about the pathophysiology of this form of clinical heart failure,” said Michael R. Zile, MD, Medical University of South Carolina and Veterans Affairs Medical Center, both in Charleston, who was not part of the trial or report.
Previously in HFpEF, Dr. Zile said in an interview, “everybody thought you needed to make diastole longer to give the ventricle a longer time to fill. And none of that really made any sense. It was just sort of accepted as dogma.”
The idea led to widespread use of beta-blockers in HFpEF but “turned out just not to be true.” Indeed, European and North American guidelines, Dr. Zile observed, “have all taken beta-blockers out of the equation for HFpEF” except for treating comorbidities that can be associated with HFpEF, like hypertension or AFib.
Many patients with HFpEF and chronotropic incompetence could be provided with standard pacemakers with primarily conduction-system pacing but are not getting them, he observed.
The current study might help change that. No one is suggesting, based on the current study, “that we start putting pacemakers in every single patient with HFpEF,” Dr. Zile said. Still, for HFpEF patients already with a pacemaker, the study provides “reasonable assurance” that its criteria for elevated resting HR may well improve symptoms.
Moreover, it suggests such pacemakers, programmed as in the study, might potentially give a boost to HFpEF patients without chronotropic incompetence but with persisting symptoms despite guideline-directed drug therapy. That’s certainly worth exploring in further trials, Dr. Zile said.
How the study worked
The single-center trial entered 107 participants with HFpEF and pacemakers set, at baseline, to a backup resting HR of 60 bpm; their age averaged 75 and 48% were women. Only patients with devices for atrial pacing, conduction-system pacing, or biventricular pacing – which are unlikely to promote ventricular dyssynchrony – were included.
They were randomly assigned, double-blind, to have their devices set to an accelerated backup rate or to be continued at 60 bpm. The backup resting rate set for the intervention group’s 50 patients was individualized based on height and other factors; the median was 75 bpm.
Scores on the Minnesota Living with Heart Failure Questionnaire, the primary endpoint, improved in the intervention group, compared with baseline, by about 11 points after 1 month and by 15 points after 1 year (P < .001).
The scores in the usual-care group deteriorated by half a point and by 3.5 points at 1 month and 1 year (P = .03), respectively.
Consistent advantages for the accelerated-HR strategy were evident throughout the major secondary endpoints. For example, levels of N-terminal pro-B-type natriuretic peptide fell an average 109 pg/dL after 1 month in the accelerated-HR group and rose a mean of 128 pg/dL in the usual-care group (P = .02).
Mean daily pacemaker-monitored activity level rose by 47 minutes by 1 year in the accelerated-HR group, compared with a drop of 22 minutes for those assigned to the standard-care rate (P < .001).
AFib was detected in 18% of intervention patients at the 1-year follow-up, down from 31% at baseline. Their risk ratio for AFib at 1 year was 0.73 (95% confidence interval, 0.55-0.99, P = .04), compared with the control group.
In other patients with HFpEF “we have done pacing studies where we just ramped up the pacing rate, and we see that these pressures in the left atrium actually drop immediately,” Dr. Meyer said. It’s that “unburdening of the atria,” he added, that probably leads to the reduction in AFib.
Dr. Meyer reported holding a patent for pacemakers for HFpEF licensed to Medtronic. Dr. Zile said he consults for Medtronic and has no other relevant financial relationships.
A version of this article first appeared on Medscape.com.
Evidence supporting medications that slow the heart rate (HR), notably beta-blockers, is overwhelming in heart failure (HF) with reduced ejection fraction. Underwhelming, however, is clinical trial support for such agents in patients with HF with preserved ejection fraction (HFpEF).
Indeed, at least for some such patients, a treatment that modestly accelerates resting HR may be a more promising strategy, suggests an early line of research that challenges prevalent thinking about HFpEF therapy.
In a small, randomized test of the idea, patients with HFpEF and standard pacemakers set to a backup resting HR a bit higher than a standard of care 60 bpm, usually to about 75 bpm, reaped important quality of life benefits.
More strikingly, their natriuretic peptide levels and burden of atrial fibrillation (AFib) fell significantly, the latter by 27% over 1 year.
The trial enrolled only HFpEF patients with pacemakers previously implanted for sick sinus syndrome or atrioventricular block. But researchers say their 107-patient study called myPACE – if confirmed in larger, multicenter trials – lays the groundwork for a device therapy that is broadly useful, potentially, in patients with “preclinical or overt” HFpEF.
Indeed, some of the intervention’s “quite substantial” benefits rivaled or surpassed what his group has observed with available HFpEF drug therapies, including the sodium-glucose cotransporter 2 inhibitors, observed Markus Meyer, MD, PhD, University of Minnesota, Minneapolis.
Moreover, the study may be “the first to show that, with this approach, we can actually also reduce atrial fibrillation,” he said in an interview.
Dr. Meyer said his group is “confident” that the HR-modulation strategy will be successful in appropriate clinical trials and that “pacemakers, in the end, will become a treatment modality for HFpEF.”
Meyer is senior author on the trial’s publication in JAMA Cardiology in JAMA Cardiology (2023 Feb 1. doi: 10.1001/jamacardio.2022.5320), with lead author Margaret Infeld, MD, University of Vermont, Burlington.
The trial entered pacemaker patients with HFpEF of stage B or C – that is, either asymptomatic with structural disease or fully symptomatic. But, Dr. Meyer said, “we saw that the treatment effect was much more pronounced in the patients who had overt heart failure with preserved ejection fraction.”
Challenging beta-blocker dogma
The study, the report states, “contradicts canonical thinking” by suggesting HFpEF patients may benefit from a higher resting heart rate, which would presumably shorten diastolic filling time. It also “may help reduce the overprescription of beta-blockers to allow higher heart rates in this population.”
Indeed, Dr. Meyer observed, no one really knows whether beta-blockers work in HFpEF, “because they really have never been studied in a sufficiently powered randomized controlled trial.”
The current study “basically rewrites what we know about the pathophysiology of this form of clinical heart failure,” said Michael R. Zile, MD, Medical University of South Carolina and Veterans Affairs Medical Center, both in Charleston, who was not part of the trial or report.
Previously in HFpEF, Dr. Zile said in an interview, “everybody thought you needed to make diastole longer to give the ventricle a longer time to fill. And none of that really made any sense. It was just sort of accepted as dogma.”
The idea led to widespread use of beta-blockers in HFpEF but “turned out just not to be true.” Indeed, European and North American guidelines, Dr. Zile observed, “have all taken beta-blockers out of the equation for HFpEF” except for treating comorbidities that can be associated with HFpEF, like hypertension or AFib.
Many patients with HFpEF and chronotropic incompetence could be provided with standard pacemakers with primarily conduction-system pacing but are not getting them, he observed.
The current study might help change that. No one is suggesting, based on the current study, “that we start putting pacemakers in every single patient with HFpEF,” Dr. Zile said. Still, for HFpEF patients already with a pacemaker, the study provides “reasonable assurance” that its criteria for elevated resting HR may well improve symptoms.
Moreover, it suggests such pacemakers, programmed as in the study, might potentially give a boost to HFpEF patients without chronotropic incompetence but with persisting symptoms despite guideline-directed drug therapy. That’s certainly worth exploring in further trials, Dr. Zile said.
How the study worked
The single-center trial entered 107 participants with HFpEF and pacemakers set, at baseline, to a backup resting HR of 60 bpm; their age averaged 75 and 48% were women. Only patients with devices for atrial pacing, conduction-system pacing, or biventricular pacing – which are unlikely to promote ventricular dyssynchrony – were included.
They were randomly assigned, double-blind, to have their devices set to an accelerated backup rate or to be continued at 60 bpm. The backup resting rate set for the intervention group’s 50 patients was individualized based on height and other factors; the median was 75 bpm.
Scores on the Minnesota Living with Heart Failure Questionnaire, the primary endpoint, improved in the intervention group, compared with baseline, by about 11 points after 1 month and by 15 points after 1 year (P < .001).
The scores in the usual-care group deteriorated by half a point and by 3.5 points at 1 month and 1 year (P = .03), respectively.
Consistent advantages for the accelerated-HR strategy were evident throughout the major secondary endpoints. For example, levels of N-terminal pro-B-type natriuretic peptide fell an average 109 pg/dL after 1 month in the accelerated-HR group and rose a mean of 128 pg/dL in the usual-care group (P = .02).
Mean daily pacemaker-monitored activity level rose by 47 minutes by 1 year in the accelerated-HR group, compared with a drop of 22 minutes for those assigned to the standard-care rate (P < .001).
AFib was detected in 18% of intervention patients at the 1-year follow-up, down from 31% at baseline. Their risk ratio for AFib at 1 year was 0.73 (95% confidence interval, 0.55-0.99, P = .04), compared with the control group.
In other patients with HFpEF “we have done pacing studies where we just ramped up the pacing rate, and we see that these pressures in the left atrium actually drop immediately,” Dr. Meyer said. It’s that “unburdening of the atria,” he added, that probably leads to the reduction in AFib.
Dr. Meyer reported holding a patent for pacemakers for HFpEF licensed to Medtronic. Dr. Zile said he consults for Medtronic and has no other relevant financial relationships.
A version of this article first appeared on Medscape.com.
Evidence supporting medications that slow the heart rate (HR), notably beta-blockers, is overwhelming in heart failure (HF) with reduced ejection fraction. Underwhelming, however, is clinical trial support for such agents in patients with HF with preserved ejection fraction (HFpEF).
Indeed, at least for some such patients, a treatment that modestly accelerates resting HR may be a more promising strategy, suggests an early line of research that challenges prevalent thinking about HFpEF therapy.
In a small, randomized test of the idea, patients with HFpEF and standard pacemakers set to a backup resting HR a bit higher than a standard of care 60 bpm, usually to about 75 bpm, reaped important quality of life benefits.
More strikingly, their natriuretic peptide levels and burden of atrial fibrillation (AFib) fell significantly, the latter by 27% over 1 year.
The trial enrolled only HFpEF patients with pacemakers previously implanted for sick sinus syndrome or atrioventricular block. But researchers say their 107-patient study called myPACE – if confirmed in larger, multicenter trials – lays the groundwork for a device therapy that is broadly useful, potentially, in patients with “preclinical or overt” HFpEF.
Indeed, some of the intervention’s “quite substantial” benefits rivaled or surpassed what his group has observed with available HFpEF drug therapies, including the sodium-glucose cotransporter 2 inhibitors, observed Markus Meyer, MD, PhD, University of Minnesota, Minneapolis.
Moreover, the study may be “the first to show that, with this approach, we can actually also reduce atrial fibrillation,” he said in an interview.
Dr. Meyer said his group is “confident” that the HR-modulation strategy will be successful in appropriate clinical trials and that “pacemakers, in the end, will become a treatment modality for HFpEF.”
Meyer is senior author on the trial’s publication in JAMA Cardiology in JAMA Cardiology (2023 Feb 1. doi: 10.1001/jamacardio.2022.5320), with lead author Margaret Infeld, MD, University of Vermont, Burlington.
The trial entered pacemaker patients with HFpEF of stage B or C – that is, either asymptomatic with structural disease or fully symptomatic. But, Dr. Meyer said, “we saw that the treatment effect was much more pronounced in the patients who had overt heart failure with preserved ejection fraction.”
Challenging beta-blocker dogma
The study, the report states, “contradicts canonical thinking” by suggesting HFpEF patients may benefit from a higher resting heart rate, which would presumably shorten diastolic filling time. It also “may help reduce the overprescription of beta-blockers to allow higher heart rates in this population.”
Indeed, Dr. Meyer observed, no one really knows whether beta-blockers work in HFpEF, “because they really have never been studied in a sufficiently powered randomized controlled trial.”
The current study “basically rewrites what we know about the pathophysiology of this form of clinical heart failure,” said Michael R. Zile, MD, Medical University of South Carolina and Veterans Affairs Medical Center, both in Charleston, who was not part of the trial or report.
Previously in HFpEF, Dr. Zile said in an interview, “everybody thought you needed to make diastole longer to give the ventricle a longer time to fill. And none of that really made any sense. It was just sort of accepted as dogma.”
The idea led to widespread use of beta-blockers in HFpEF but “turned out just not to be true.” Indeed, European and North American guidelines, Dr. Zile observed, “have all taken beta-blockers out of the equation for HFpEF” except for treating comorbidities that can be associated with HFpEF, like hypertension or AFib.
Many patients with HFpEF and chronotropic incompetence could be provided with standard pacemakers with primarily conduction-system pacing but are not getting them, he observed.
The current study might help change that. No one is suggesting, based on the current study, “that we start putting pacemakers in every single patient with HFpEF,” Dr. Zile said. Still, for HFpEF patients already with a pacemaker, the study provides “reasonable assurance” that its criteria for elevated resting HR may well improve symptoms.
Moreover, it suggests such pacemakers, programmed as in the study, might potentially give a boost to HFpEF patients without chronotropic incompetence but with persisting symptoms despite guideline-directed drug therapy. That’s certainly worth exploring in further trials, Dr. Zile said.
How the study worked
The single-center trial entered 107 participants with HFpEF and pacemakers set, at baseline, to a backup resting HR of 60 bpm; their age averaged 75 and 48% were women. Only patients with devices for atrial pacing, conduction-system pacing, or biventricular pacing – which are unlikely to promote ventricular dyssynchrony – were included.
They were randomly assigned, double-blind, to have their devices set to an accelerated backup rate or to be continued at 60 bpm. The backup resting rate set for the intervention group’s 50 patients was individualized based on height and other factors; the median was 75 bpm.
Scores on the Minnesota Living with Heart Failure Questionnaire, the primary endpoint, improved in the intervention group, compared with baseline, by about 11 points after 1 month and by 15 points after 1 year (P < .001).
The scores in the usual-care group deteriorated by half a point and by 3.5 points at 1 month and 1 year (P = .03), respectively.
Consistent advantages for the accelerated-HR strategy were evident throughout the major secondary endpoints. For example, levels of N-terminal pro-B-type natriuretic peptide fell an average 109 pg/dL after 1 month in the accelerated-HR group and rose a mean of 128 pg/dL in the usual-care group (P = .02).
Mean daily pacemaker-monitored activity level rose by 47 minutes by 1 year in the accelerated-HR group, compared with a drop of 22 minutes for those assigned to the standard-care rate (P < .001).
AFib was detected in 18% of intervention patients at the 1-year follow-up, down from 31% at baseline. Their risk ratio for AFib at 1 year was 0.73 (95% confidence interval, 0.55-0.99, P = .04), compared with the control group.
In other patients with HFpEF “we have done pacing studies where we just ramped up the pacing rate, and we see that these pressures in the left atrium actually drop immediately,” Dr. Meyer said. It’s that “unburdening of the atria,” he added, that probably leads to the reduction in AFib.
Dr. Meyer reported holding a patent for pacemakers for HFpEF licensed to Medtronic. Dr. Zile said he consults for Medtronic and has no other relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA CARDIOLOGY
Longer diabetes duration links with increased heart failure
The longer people had diabetes, the greater their rate of incident heart failure, suggests a recently published review of prospectively collected observational data from nearly 24,000 people with diabetes in the UK Biobank.
The findings “add to the growing body of evidence suggesting that duration of diabetes is an important and independent determinant of heart failure among patients with diabetes,” comments Justin B. Echouffo-Tcheugui, MD, PhD, in an accompanying editorial.
Collectively, the new UK Biobank results and prior findings, “provide additional persuasive evidence that the link between duration of diabetes and heart failure is real,” although the physiological mechanisms behind the relationship remain incompletely understood, wrote Dr. Echouffo-Tcheugui, an endocrinologist at Johns Hopkins Medicine, Baltimore.
“The duration of diabetes may reflect cumulative effects of various adverse processes in the setting of diabetes” that result in “intrinsic myocardial lesions,” he suggested. These adverse processes might include not only hyperglycemia, but also glucotoxicity, lipotoxicity, hyperinsulinemia, advanced glycosylation end products, oxidative stress, mitochondrial dysfunction, cardiac autonomic neuropathy, and coronary microvascular dysfunction. Long-duration diabetes may also contribute to declining kidney function, which can further worsen heart failure risk.
The upshot is that clinicians may need to consider more systematically the duration of diabetes when assessing people with diabetes for heart failure.
Existing risk-assessment tools for predicting heart failure in people with diabetes “have not always accounted for diabetes duration,” Dr. Echouffo-Tcheugui noted.
Intensify heart failure detection with longer diabetes duration
“Active heart failure detection should perhaps be intensified with increased diabetes duration,” Dr. Echouffo-Tcheugui suggested in his editorial. He noted that a 2022 consensus report by the American Diabetes Association recommends clinicians measure natriuretic peptide or high-sensitivity cardiac troponin in all people with diabetes “on at least a yearly basis to identify the earliest heart failure stages and implement strategies to prevent transition to symptomatic heart failure.”
The UK Biobank study was run by investigators primarily based in China and included data from 23,754 people with type 1 or type 2 diabetes and no heart failure at baseline. The prospectively collected data allowed for a median follow-up of 11.7 years, during which time 2,081 people developed incident heart failure.
In an analysis that divided participants into four categories of diabetes duration (< 5 years, 5-9 years, 10-14 years, and ≥ 15 years) and adjusted for potential confounders, heart failure incidence showed a significant 32% increased incidence among those with diabetes for at least 15 years, compared with those with diabetes for less than 5 years. People with a diabetes duration of 5-14 years showed a trend toward having more incident heart failure, compared with those with diabetes for less than 5 years, but the difference was not significant.
An adjusted analysis also showed poor glycemic control at baseline (hemoglobin A1c ≥ 8.0%) significantly linked with a 46% increased incidence of heart failure, compared with those with baseline A1c less than 7.0%.
Additive effect?
When the authors analyzed the effect of both these variables, they saw a roughly additive effect.
Patients with diabetes for at least 15 years and a baseline A1c of at least 8.0% had a 98% increased incidence of heart failure, compared with those who had diabetes for less than 5 years and a baseline A1c less than 7.0%, after adjustment. This association was independent of age, sex, and race.
These findings “highlight the paramount role of the duration of diabetes and its interaction with glycemic control in the development of heart failure,” the authors concluded. “Long duration of diabetes and poor glycemic control may result in structural and functional changes in the myocardium, which is likely to underlie the pathogenesis of heart failure among individuals with diabetes.”
In his editorial, Dr. Echouffo-Tcheugui lauded the report for its “robust” analyses that included a large sample and accounted for key confounders, such as glycemic control. However, he also cited eight “shortcomings” of the study, including its sole reliance on A1c levels to identify diabetes, a likely underestimation of diabetes duration, the lumping together of people with type 1 and type 2 diabetes, and lack of a subanalysis of incident heart failure in those with preserved or reduced left ventricular ejection fraction.
Among prior reports of evidence also suggesting an effect of diabetes duration on incident heart failure, Dr. Echouffo-Tcheugui cited a study he led, published in 2021, that analyzed prospective, longitudinal, observational data from 9,734 adults enrolled in the Atherosclerosis Risk in Communities study. The results showed that, compared with those without diabetes, the incidence of heart failure rose with longer diabetes duration, with the highest risk among those with diabetes for at least 15 years, who had a 2.8-fold increase in heart failure versus the reference group. Each 5-year increase in diabetes duration was associated with a significant 17% relative increase in heart failure incidence.
The study received no commercial funding. The authors and editorialist reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The longer people had diabetes, the greater their rate of incident heart failure, suggests a recently published review of prospectively collected observational data from nearly 24,000 people with diabetes in the UK Biobank.
The findings “add to the growing body of evidence suggesting that duration of diabetes is an important and independent determinant of heart failure among patients with diabetes,” comments Justin B. Echouffo-Tcheugui, MD, PhD, in an accompanying editorial.
Collectively, the new UK Biobank results and prior findings, “provide additional persuasive evidence that the link between duration of diabetes and heart failure is real,” although the physiological mechanisms behind the relationship remain incompletely understood, wrote Dr. Echouffo-Tcheugui, an endocrinologist at Johns Hopkins Medicine, Baltimore.
“The duration of diabetes may reflect cumulative effects of various adverse processes in the setting of diabetes” that result in “intrinsic myocardial lesions,” he suggested. These adverse processes might include not only hyperglycemia, but also glucotoxicity, lipotoxicity, hyperinsulinemia, advanced glycosylation end products, oxidative stress, mitochondrial dysfunction, cardiac autonomic neuropathy, and coronary microvascular dysfunction. Long-duration diabetes may also contribute to declining kidney function, which can further worsen heart failure risk.
The upshot is that clinicians may need to consider more systematically the duration of diabetes when assessing people with diabetes for heart failure.
Existing risk-assessment tools for predicting heart failure in people with diabetes “have not always accounted for diabetes duration,” Dr. Echouffo-Tcheugui noted.
Intensify heart failure detection with longer diabetes duration
“Active heart failure detection should perhaps be intensified with increased diabetes duration,” Dr. Echouffo-Tcheugui suggested in his editorial. He noted that a 2022 consensus report by the American Diabetes Association recommends clinicians measure natriuretic peptide or high-sensitivity cardiac troponin in all people with diabetes “on at least a yearly basis to identify the earliest heart failure stages and implement strategies to prevent transition to symptomatic heart failure.”
The UK Biobank study was run by investigators primarily based in China and included data from 23,754 people with type 1 or type 2 diabetes and no heart failure at baseline. The prospectively collected data allowed for a median follow-up of 11.7 years, during which time 2,081 people developed incident heart failure.
In an analysis that divided participants into four categories of diabetes duration (< 5 years, 5-9 years, 10-14 years, and ≥ 15 years) and adjusted for potential confounders, heart failure incidence showed a significant 32% increased incidence among those with diabetes for at least 15 years, compared with those with diabetes for less than 5 years. People with a diabetes duration of 5-14 years showed a trend toward having more incident heart failure, compared with those with diabetes for less than 5 years, but the difference was not significant.
An adjusted analysis also showed poor glycemic control at baseline (hemoglobin A1c ≥ 8.0%) significantly linked with a 46% increased incidence of heart failure, compared with those with baseline A1c less than 7.0%.
Additive effect?
When the authors analyzed the effect of both these variables, they saw a roughly additive effect.
Patients with diabetes for at least 15 years and a baseline A1c of at least 8.0% had a 98% increased incidence of heart failure, compared with those who had diabetes for less than 5 years and a baseline A1c less than 7.0%, after adjustment. This association was independent of age, sex, and race.
These findings “highlight the paramount role of the duration of diabetes and its interaction with glycemic control in the development of heart failure,” the authors concluded. “Long duration of diabetes and poor glycemic control may result in structural and functional changes in the myocardium, which is likely to underlie the pathogenesis of heart failure among individuals with diabetes.”
In his editorial, Dr. Echouffo-Tcheugui lauded the report for its “robust” analyses that included a large sample and accounted for key confounders, such as glycemic control. However, he also cited eight “shortcomings” of the study, including its sole reliance on A1c levels to identify diabetes, a likely underestimation of diabetes duration, the lumping together of people with type 1 and type 2 diabetes, and lack of a subanalysis of incident heart failure in those with preserved or reduced left ventricular ejection fraction.
Among prior reports of evidence also suggesting an effect of diabetes duration on incident heart failure, Dr. Echouffo-Tcheugui cited a study he led, published in 2021, that analyzed prospective, longitudinal, observational data from 9,734 adults enrolled in the Atherosclerosis Risk in Communities study. The results showed that, compared with those without diabetes, the incidence of heart failure rose with longer diabetes duration, with the highest risk among those with diabetes for at least 15 years, who had a 2.8-fold increase in heart failure versus the reference group. Each 5-year increase in diabetes duration was associated with a significant 17% relative increase in heart failure incidence.
The study received no commercial funding. The authors and editorialist reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The longer people had diabetes, the greater their rate of incident heart failure, suggests a recently published review of prospectively collected observational data from nearly 24,000 people with diabetes in the UK Biobank.
The findings “add to the growing body of evidence suggesting that duration of diabetes is an important and independent determinant of heart failure among patients with diabetes,” comments Justin B. Echouffo-Tcheugui, MD, PhD, in an accompanying editorial.
Collectively, the new UK Biobank results and prior findings, “provide additional persuasive evidence that the link between duration of diabetes and heart failure is real,” although the physiological mechanisms behind the relationship remain incompletely understood, wrote Dr. Echouffo-Tcheugui, an endocrinologist at Johns Hopkins Medicine, Baltimore.
“The duration of diabetes may reflect cumulative effects of various adverse processes in the setting of diabetes” that result in “intrinsic myocardial lesions,” he suggested. These adverse processes might include not only hyperglycemia, but also glucotoxicity, lipotoxicity, hyperinsulinemia, advanced glycosylation end products, oxidative stress, mitochondrial dysfunction, cardiac autonomic neuropathy, and coronary microvascular dysfunction. Long-duration diabetes may also contribute to declining kidney function, which can further worsen heart failure risk.
The upshot is that clinicians may need to consider more systematically the duration of diabetes when assessing people with diabetes for heart failure.
Existing risk-assessment tools for predicting heart failure in people with diabetes “have not always accounted for diabetes duration,” Dr. Echouffo-Tcheugui noted.
Intensify heart failure detection with longer diabetes duration
“Active heart failure detection should perhaps be intensified with increased diabetes duration,” Dr. Echouffo-Tcheugui suggested in his editorial. He noted that a 2022 consensus report by the American Diabetes Association recommends clinicians measure natriuretic peptide or high-sensitivity cardiac troponin in all people with diabetes “on at least a yearly basis to identify the earliest heart failure stages and implement strategies to prevent transition to symptomatic heart failure.”
The UK Biobank study was run by investigators primarily based in China and included data from 23,754 people with type 1 or type 2 diabetes and no heart failure at baseline. The prospectively collected data allowed for a median follow-up of 11.7 years, during which time 2,081 people developed incident heart failure.
In an analysis that divided participants into four categories of diabetes duration (< 5 years, 5-9 years, 10-14 years, and ≥ 15 years) and adjusted for potential confounders, heart failure incidence showed a significant 32% increased incidence among those with diabetes for at least 15 years, compared with those with diabetes for less than 5 years. People with a diabetes duration of 5-14 years showed a trend toward having more incident heart failure, compared with those with diabetes for less than 5 years, but the difference was not significant.
An adjusted analysis also showed poor glycemic control at baseline (hemoglobin A1c ≥ 8.0%) significantly linked with a 46% increased incidence of heart failure, compared with those with baseline A1c less than 7.0%.
Additive effect?
When the authors analyzed the effect of both these variables, they saw a roughly additive effect.
Patients with diabetes for at least 15 years and a baseline A1c of at least 8.0% had a 98% increased incidence of heart failure, compared with those who had diabetes for less than 5 years and a baseline A1c less than 7.0%, after adjustment. This association was independent of age, sex, and race.
These findings “highlight the paramount role of the duration of diabetes and its interaction with glycemic control in the development of heart failure,” the authors concluded. “Long duration of diabetes and poor glycemic control may result in structural and functional changes in the myocardium, which is likely to underlie the pathogenesis of heart failure among individuals with diabetes.”
In his editorial, Dr. Echouffo-Tcheugui lauded the report for its “robust” analyses that included a large sample and accounted for key confounders, such as glycemic control. However, he also cited eight “shortcomings” of the study, including its sole reliance on A1c levels to identify diabetes, a likely underestimation of diabetes duration, the lumping together of people with type 1 and type 2 diabetes, and lack of a subanalysis of incident heart failure in those with preserved or reduced left ventricular ejection fraction.
Among prior reports of evidence also suggesting an effect of diabetes duration on incident heart failure, Dr. Echouffo-Tcheugui cited a study he led, published in 2021, that analyzed prospective, longitudinal, observational data from 9,734 adults enrolled in the Atherosclerosis Risk in Communities study. The results showed that, compared with those without diabetes, the incidence of heart failure rose with longer diabetes duration, with the highest risk among those with diabetes for at least 15 years, who had a 2.8-fold increase in heart failure versus the reference group. Each 5-year increase in diabetes duration was associated with a significant 17% relative increase in heart failure incidence.
The study received no commercial funding. The authors and editorialist reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
Legacy ICDs exposed to MRI still shock, pace as needed
Functions like sensing and pacing in implantable cardioverter defibrillators (ICDs) tend to resist interference from the energy fields generated by MRI, as long as device programming is properly adjusted before the scan.
That applies even to patients with older “legacy” devices implanted before the 2015 advent of MRI-conditional ICDs despite, in practice, prevalent but misguided resistance to obtaining MRI scans in such cases.
Less is known whether such non–MRI-conditional devices, once exposed to MRI, will then reliably deliver antiarrhythmic shocks or antitachycardia pacing (ATP) when needed.
A new cohort study has tried to fill in some of that knowledge gap. It showed no evidence of an excess risk for death or ICD failure to deliver therapy within about 2 years of clinically indicated MRI scans in 629 patients with non–MRI-conditional devices.
The findings, published online in the Annals of Internal Medicine, come with caveats. For example, they’re based on the experience of one, albeit major, center and on MRIs that were for varied indications using 1.5-tesla equipment only.
Despite such safety evidence for appropriately adjusted non–MRI-conditional ICDs, many patients with the devices don›t receive clinically indicated MRI scans due to “perceived risk” that the ICDs won’t then reliably deliver appropriate therapy, observe the authors, led by Joshua Ra, MD, University of California, San Francisco.
Any such risks are “largely theoretical,” but may still explain “why some institutions are shying away from offering MRI exams” to patients with non–MRI-conditional ICDs, Dr. Ra told this news organization.
Many such hospitals refer such patients to more experienced centers, creating “significant logistical barriers in terms of patient access to these MRIs,” he said. “That seems to still be prevalent, unfortunately.”
The current findings “provide another layer of reassurance” that MRI scans in patients with non–MRI-conditional ICDs don’t impair a device’s ability to deliver shocks or ATP, Dr. Ra said.
The cohort consisted of 629 patients with non–MRI-conditional ICDs who underwent 813 clinically indicated MRI exams from 2003 to early 2015 at Johns Hopkins University, Baltimore.
Scans performed within 4 weeks of device implantation were excluded because, the report notes, that’s when spontaneous lead dislodgements or changes to device parameters are most likely to occur. Also excluded were patients with permanent epicardial leads, abandoned leads, or subcutaneous ICD lead systems, the report states.
Still, Dr. Ra said, the cohort is fairly representative of “the modern patient population” of non–MRI-conditional ICD recipients.
A total of 4,177 arrhythmia episodes were documented during a median 2.2 years between scans and last device interrogation prior to pulse-generator change-out or lead exchange.
Of note, Dr. Ra observed, the arrhythmias were confirmed in only 85% of the cohort. Most of the remainder were referral patients who were lost to follow-up whose devices were unavailable for interrogation.
Device therapy terminated “nearly all” documented spontaneous arrhythmias in that 85% of patients, the report states. They included 757 episodes of ventricular tachycardia (VT) or ventricular fibrillation (VF), including 130 that were shocked and the remainder that were managed with ATP. There were also 105 supraventricular tachycardias, all successfully terminated with shocks.
There were no cases of VT or VF detection delay from undersensing or instances of syncope because of “abnormalities” in device detection of arrhythmias, the report states.
Of the 210 known deaths, which occurred a median 1.7 years after the scan, about half were noncardiac and more than a third were cardiac but nonarrhythmic.
Ten patients died from arrhythmia-related cardiac causes, representing 5% of deaths; but 7% of deaths were of undetermined cause.
“No direct relationship of deaths attributable to prior MRI exposure was found or reported,” the report states.
The researchers informally compared outcomes between older and more recently implanted non–MRI-conditional ICDs, the latter presumably with more modern design features. Their data, based on device interrogations, Dr. Ra said, “seem to suggest there were no differences.”
The study was supported by Johns Hopkins University and the National Institutes of Health. Author disclosures are available at apconline.org.
A version of this article first appeared on Medscape.com.
Functions like sensing and pacing in implantable cardioverter defibrillators (ICDs) tend to resist interference from the energy fields generated by MRI, as long as device programming is properly adjusted before the scan.
That applies even to patients with older “legacy” devices implanted before the 2015 advent of MRI-conditional ICDs despite, in practice, prevalent but misguided resistance to obtaining MRI scans in such cases.
Less is known whether such non–MRI-conditional devices, once exposed to MRI, will then reliably deliver antiarrhythmic shocks or antitachycardia pacing (ATP) when needed.
A new cohort study has tried to fill in some of that knowledge gap. It showed no evidence of an excess risk for death or ICD failure to deliver therapy within about 2 years of clinically indicated MRI scans in 629 patients with non–MRI-conditional devices.
The findings, published online in the Annals of Internal Medicine, come with caveats. For example, they’re based on the experience of one, albeit major, center and on MRIs that were for varied indications using 1.5-tesla equipment only.
Despite such safety evidence for appropriately adjusted non–MRI-conditional ICDs, many patients with the devices don›t receive clinically indicated MRI scans due to “perceived risk” that the ICDs won’t then reliably deliver appropriate therapy, observe the authors, led by Joshua Ra, MD, University of California, San Francisco.
Any such risks are “largely theoretical,” but may still explain “why some institutions are shying away from offering MRI exams” to patients with non–MRI-conditional ICDs, Dr. Ra told this news organization.
Many such hospitals refer such patients to more experienced centers, creating “significant logistical barriers in terms of patient access to these MRIs,” he said. “That seems to still be prevalent, unfortunately.”
The current findings “provide another layer of reassurance” that MRI scans in patients with non–MRI-conditional ICDs don’t impair a device’s ability to deliver shocks or ATP, Dr. Ra said.
The cohort consisted of 629 patients with non–MRI-conditional ICDs who underwent 813 clinically indicated MRI exams from 2003 to early 2015 at Johns Hopkins University, Baltimore.
Scans performed within 4 weeks of device implantation were excluded because, the report notes, that’s when spontaneous lead dislodgements or changes to device parameters are most likely to occur. Also excluded were patients with permanent epicardial leads, abandoned leads, or subcutaneous ICD lead systems, the report states.
Still, Dr. Ra said, the cohort is fairly representative of “the modern patient population” of non–MRI-conditional ICD recipients.
A total of 4,177 arrhythmia episodes were documented during a median 2.2 years between scans and last device interrogation prior to pulse-generator change-out or lead exchange.
Of note, Dr. Ra observed, the arrhythmias were confirmed in only 85% of the cohort. Most of the remainder were referral patients who were lost to follow-up whose devices were unavailable for interrogation.
Device therapy terminated “nearly all” documented spontaneous arrhythmias in that 85% of patients, the report states. They included 757 episodes of ventricular tachycardia (VT) or ventricular fibrillation (VF), including 130 that were shocked and the remainder that were managed with ATP. There were also 105 supraventricular tachycardias, all successfully terminated with shocks.
There were no cases of VT or VF detection delay from undersensing or instances of syncope because of “abnormalities” in device detection of arrhythmias, the report states.
Of the 210 known deaths, which occurred a median 1.7 years after the scan, about half were noncardiac and more than a third were cardiac but nonarrhythmic.
Ten patients died from arrhythmia-related cardiac causes, representing 5% of deaths; but 7% of deaths were of undetermined cause.
“No direct relationship of deaths attributable to prior MRI exposure was found or reported,” the report states.
The researchers informally compared outcomes between older and more recently implanted non–MRI-conditional ICDs, the latter presumably with more modern design features. Their data, based on device interrogations, Dr. Ra said, “seem to suggest there were no differences.”
The study was supported by Johns Hopkins University and the National Institutes of Health. Author disclosures are available at apconline.org.
A version of this article first appeared on Medscape.com.
Functions like sensing and pacing in implantable cardioverter defibrillators (ICDs) tend to resist interference from the energy fields generated by MRI, as long as device programming is properly adjusted before the scan.
That applies even to patients with older “legacy” devices implanted before the 2015 advent of MRI-conditional ICDs despite, in practice, prevalent but misguided resistance to obtaining MRI scans in such cases.
Less is known whether such non–MRI-conditional devices, once exposed to MRI, will then reliably deliver antiarrhythmic shocks or antitachycardia pacing (ATP) when needed.
A new cohort study has tried to fill in some of that knowledge gap. It showed no evidence of an excess risk for death or ICD failure to deliver therapy within about 2 years of clinically indicated MRI scans in 629 patients with non–MRI-conditional devices.
The findings, published online in the Annals of Internal Medicine, come with caveats. For example, they’re based on the experience of one, albeit major, center and on MRIs that were for varied indications using 1.5-tesla equipment only.
Despite such safety evidence for appropriately adjusted non–MRI-conditional ICDs, many patients with the devices don›t receive clinically indicated MRI scans due to “perceived risk” that the ICDs won’t then reliably deliver appropriate therapy, observe the authors, led by Joshua Ra, MD, University of California, San Francisco.
Any such risks are “largely theoretical,” but may still explain “why some institutions are shying away from offering MRI exams” to patients with non–MRI-conditional ICDs, Dr. Ra told this news organization.
Many such hospitals refer such patients to more experienced centers, creating “significant logistical barriers in terms of patient access to these MRIs,” he said. “That seems to still be prevalent, unfortunately.”
The current findings “provide another layer of reassurance” that MRI scans in patients with non–MRI-conditional ICDs don’t impair a device’s ability to deliver shocks or ATP, Dr. Ra said.
The cohort consisted of 629 patients with non–MRI-conditional ICDs who underwent 813 clinically indicated MRI exams from 2003 to early 2015 at Johns Hopkins University, Baltimore.
Scans performed within 4 weeks of device implantation were excluded because, the report notes, that’s when spontaneous lead dislodgements or changes to device parameters are most likely to occur. Also excluded were patients with permanent epicardial leads, abandoned leads, or subcutaneous ICD lead systems, the report states.
Still, Dr. Ra said, the cohort is fairly representative of “the modern patient population” of non–MRI-conditional ICD recipients.
A total of 4,177 arrhythmia episodes were documented during a median 2.2 years between scans and last device interrogation prior to pulse-generator change-out or lead exchange.
Of note, Dr. Ra observed, the arrhythmias were confirmed in only 85% of the cohort. Most of the remainder were referral patients who were lost to follow-up whose devices were unavailable for interrogation.
Device therapy terminated “nearly all” documented spontaneous arrhythmias in that 85% of patients, the report states. They included 757 episodes of ventricular tachycardia (VT) or ventricular fibrillation (VF), including 130 that were shocked and the remainder that were managed with ATP. There were also 105 supraventricular tachycardias, all successfully terminated with shocks.
There were no cases of VT or VF detection delay from undersensing or instances of syncope because of “abnormalities” in device detection of arrhythmias, the report states.
Of the 210 known deaths, which occurred a median 1.7 years after the scan, about half were noncardiac and more than a third were cardiac but nonarrhythmic.
Ten patients died from arrhythmia-related cardiac causes, representing 5% of deaths; but 7% of deaths were of undetermined cause.
“No direct relationship of deaths attributable to prior MRI exposure was found or reported,” the report states.
The researchers informally compared outcomes between older and more recently implanted non–MRI-conditional ICDs, the latter presumably with more modern design features. Their data, based on device interrogations, Dr. Ra said, “seem to suggest there were no differences.”
The study was supported by Johns Hopkins University and the National Institutes of Health. Author disclosures are available at apconline.org.
A version of this article first appeared on Medscape.com.
CV deaths jumped in 2020, reflecting pandemic toll
Cardiovascular-related deaths increased dramatically in 2020, marking the largest single-year increase since 2015 and surpassing the previous record from 2003, according to the American Heart Association’s 2023 Statistical Update.
During the first year of the COVID-19 pandemic, the largest increases in cardiovascular disease (CVD) deaths were seen among Asian, Black, and Hispanic people.
“We thought we had been improving as a country with respect to CVD deaths over the past few decades,” Connie Tsao, MD, chair of the AHA Statistical Update writing committee, told this news organization.
Since 2020, however, those trends have changed. Dr. Tsao, a staff cardiologist at Beth Israel Deaconess Medical Center and assistant professor of medicine at Harvard Medical School, both in Boston, noted the firsthand experience that many clinicians had in seeing the shift.
“We observed this sharp rise in age-adjusted CVD deaths, which corresponds to the COVID-19 pandemic,” she said. “Those of us health care providers knew from the overfull hospitals and ICUs that clearly COVID took a toll, particularly in those with cardiovascular risk factors.”
The AHA Statistical Update was published online in the journal Circulation.
Data on deaths
Each year, the American Heart Association and National Institutes of Health report the latest statistics related to heart disease, stroke, and cardiovascular risk factors. The 2023 update includes additional information about pandemic-related data.
Overall, the number of people who died from cardiovascular disease increased during the first year of the pandemic, rising from 876,613 in 2019 to 928,741 in 2020. This topped the previous high of 910,000 in 2003.
In addition, the age-adjusted mortality rate increased for the first time in several years, Dr. Tsao said, by a “fairly substantial” 4.6%. The age-adjusted mortality rate incorporates the variability in the aging population from year to year, accounting for higher death rates among older people.
“Even though our total number of deaths has been slowly increasing over the past decade, we have seen a decline each year in our age-adjusted rates – until 2020,” she said. “I think that is very indicative of what has been going on within our country – and the world – in light of people of all ages being impacted by the COVID-19 pandemic, especially before vaccines were available to slow the spread.”
The largest increases in CVD-related deaths occurred among Asian, Black, and Hispanic people, who were most heavily affected during the first year of the pandemic.
“People from communities of color were among those most highly impacted, especially early on, often due to a disproportionate burden of cardiovascular risk factors, such as hypertension and obesity,” Michelle Albert, MD, MPH, president of AHA and a professor of medicine at the University of California, San Francisco, said in a statement.
Dr. Albert, who is also the director of UCSF’s Center for the Study of Adversity and Cardiovascular Disease, does research on health equity and noted the disparities seen in the 2020 numbers. “Additionally, there are socioeconomic considerations, as well as the ongoing impact of structural racism on multiple factors, including limiting the ability to access quality health care,” she said.
Additional considerations
In a special commentary, the Statistical Update writing committee pointed to the need to track data for other underrepresented communities, including LGBTQ people and those living in rural or urban areas. The authors outlined several ways to better understand the effects of identity and social determinants of health, as well as strategies to reduce cardiovascular-related disparities.
“This year’s writing group made a concerted effort to gather information on specific social factors related to health risk and outcomes, including sexual orientation, gender identity, urbanization, and socioeconomic position,” Dr. Tsao said. “However, the data are lacking because these communities are grossly underrepresented in clinical and epidemiological research.”
For the next several years, the AHA Statistical Update will likely include more insights about the effects of the COVID-19 pandemic, as well as ongoing disparities.
“For sure, we will be continuing to see the effects of the pandemic for years to come,” Dr. Tsao said. “Recognition of the disparities in outcomes among vulnerable groups should be a call to action among health care providers and researchers, administration, and policy leaders to investigate the reasons and make changes to reverse these trends.”
The statistical update was prepared by a volunteer writing group on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee.
A version of this article first appeared on Medscape.com.
Cardiovascular-related deaths increased dramatically in 2020, marking the largest single-year increase since 2015 and surpassing the previous record from 2003, according to the American Heart Association’s 2023 Statistical Update.
During the first year of the COVID-19 pandemic, the largest increases in cardiovascular disease (CVD) deaths were seen among Asian, Black, and Hispanic people.
“We thought we had been improving as a country with respect to CVD deaths over the past few decades,” Connie Tsao, MD, chair of the AHA Statistical Update writing committee, told this news organization.
Since 2020, however, those trends have changed. Dr. Tsao, a staff cardiologist at Beth Israel Deaconess Medical Center and assistant professor of medicine at Harvard Medical School, both in Boston, noted the firsthand experience that many clinicians had in seeing the shift.
“We observed this sharp rise in age-adjusted CVD deaths, which corresponds to the COVID-19 pandemic,” she said. “Those of us health care providers knew from the overfull hospitals and ICUs that clearly COVID took a toll, particularly in those with cardiovascular risk factors.”
The AHA Statistical Update was published online in the journal Circulation.
Data on deaths
Each year, the American Heart Association and National Institutes of Health report the latest statistics related to heart disease, stroke, and cardiovascular risk factors. The 2023 update includes additional information about pandemic-related data.
Overall, the number of people who died from cardiovascular disease increased during the first year of the pandemic, rising from 876,613 in 2019 to 928,741 in 2020. This topped the previous high of 910,000 in 2003.
In addition, the age-adjusted mortality rate increased for the first time in several years, Dr. Tsao said, by a “fairly substantial” 4.6%. The age-adjusted mortality rate incorporates the variability in the aging population from year to year, accounting for higher death rates among older people.
“Even though our total number of deaths has been slowly increasing over the past decade, we have seen a decline each year in our age-adjusted rates – until 2020,” she said. “I think that is very indicative of what has been going on within our country – and the world – in light of people of all ages being impacted by the COVID-19 pandemic, especially before vaccines were available to slow the spread.”
The largest increases in CVD-related deaths occurred among Asian, Black, and Hispanic people, who were most heavily affected during the first year of the pandemic.
“People from communities of color were among those most highly impacted, especially early on, often due to a disproportionate burden of cardiovascular risk factors, such as hypertension and obesity,” Michelle Albert, MD, MPH, president of AHA and a professor of medicine at the University of California, San Francisco, said in a statement.
Dr. Albert, who is also the director of UCSF’s Center for the Study of Adversity and Cardiovascular Disease, does research on health equity and noted the disparities seen in the 2020 numbers. “Additionally, there are socioeconomic considerations, as well as the ongoing impact of structural racism on multiple factors, including limiting the ability to access quality health care,” she said.
Additional considerations
In a special commentary, the Statistical Update writing committee pointed to the need to track data for other underrepresented communities, including LGBTQ people and those living in rural or urban areas. The authors outlined several ways to better understand the effects of identity and social determinants of health, as well as strategies to reduce cardiovascular-related disparities.
“This year’s writing group made a concerted effort to gather information on specific social factors related to health risk and outcomes, including sexual orientation, gender identity, urbanization, and socioeconomic position,” Dr. Tsao said. “However, the data are lacking because these communities are grossly underrepresented in clinical and epidemiological research.”
For the next several years, the AHA Statistical Update will likely include more insights about the effects of the COVID-19 pandemic, as well as ongoing disparities.
“For sure, we will be continuing to see the effects of the pandemic for years to come,” Dr. Tsao said. “Recognition of the disparities in outcomes among vulnerable groups should be a call to action among health care providers and researchers, administration, and policy leaders to investigate the reasons and make changes to reverse these trends.”
The statistical update was prepared by a volunteer writing group on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee.
A version of this article first appeared on Medscape.com.
Cardiovascular-related deaths increased dramatically in 2020, marking the largest single-year increase since 2015 and surpassing the previous record from 2003, according to the American Heart Association’s 2023 Statistical Update.
During the first year of the COVID-19 pandemic, the largest increases in cardiovascular disease (CVD) deaths were seen among Asian, Black, and Hispanic people.
“We thought we had been improving as a country with respect to CVD deaths over the past few decades,” Connie Tsao, MD, chair of the AHA Statistical Update writing committee, told this news organization.
Since 2020, however, those trends have changed. Dr. Tsao, a staff cardiologist at Beth Israel Deaconess Medical Center and assistant professor of medicine at Harvard Medical School, both in Boston, noted the firsthand experience that many clinicians had in seeing the shift.
“We observed this sharp rise in age-adjusted CVD deaths, which corresponds to the COVID-19 pandemic,” she said. “Those of us health care providers knew from the overfull hospitals and ICUs that clearly COVID took a toll, particularly in those with cardiovascular risk factors.”
The AHA Statistical Update was published online in the journal Circulation.
Data on deaths
Each year, the American Heart Association and National Institutes of Health report the latest statistics related to heart disease, stroke, and cardiovascular risk factors. The 2023 update includes additional information about pandemic-related data.
Overall, the number of people who died from cardiovascular disease increased during the first year of the pandemic, rising from 876,613 in 2019 to 928,741 in 2020. This topped the previous high of 910,000 in 2003.
In addition, the age-adjusted mortality rate increased for the first time in several years, Dr. Tsao said, by a “fairly substantial” 4.6%. The age-adjusted mortality rate incorporates the variability in the aging population from year to year, accounting for higher death rates among older people.
“Even though our total number of deaths has been slowly increasing over the past decade, we have seen a decline each year in our age-adjusted rates – until 2020,” she said. “I think that is very indicative of what has been going on within our country – and the world – in light of people of all ages being impacted by the COVID-19 pandemic, especially before vaccines were available to slow the spread.”
The largest increases in CVD-related deaths occurred among Asian, Black, and Hispanic people, who were most heavily affected during the first year of the pandemic.
“People from communities of color were among those most highly impacted, especially early on, often due to a disproportionate burden of cardiovascular risk factors, such as hypertension and obesity,” Michelle Albert, MD, MPH, president of AHA and a professor of medicine at the University of California, San Francisco, said in a statement.
Dr. Albert, who is also the director of UCSF’s Center for the Study of Adversity and Cardiovascular Disease, does research on health equity and noted the disparities seen in the 2020 numbers. “Additionally, there are socioeconomic considerations, as well as the ongoing impact of structural racism on multiple factors, including limiting the ability to access quality health care,” she said.
Additional considerations
In a special commentary, the Statistical Update writing committee pointed to the need to track data for other underrepresented communities, including LGBTQ people and those living in rural or urban areas. The authors outlined several ways to better understand the effects of identity and social determinants of health, as well as strategies to reduce cardiovascular-related disparities.
“This year’s writing group made a concerted effort to gather information on specific social factors related to health risk and outcomes, including sexual orientation, gender identity, urbanization, and socioeconomic position,” Dr. Tsao said. “However, the data are lacking because these communities are grossly underrepresented in clinical and epidemiological research.”
For the next several years, the AHA Statistical Update will likely include more insights about the effects of the COVID-19 pandemic, as well as ongoing disparities.
“For sure, we will be continuing to see the effects of the pandemic for years to come,” Dr. Tsao said. “Recognition of the disparities in outcomes among vulnerable groups should be a call to action among health care providers and researchers, administration, and policy leaders to investigate the reasons and make changes to reverse these trends.”
The statistical update was prepared by a volunteer writing group on behalf of the American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
Angioedema risk jumps when switching HF meds
New renin-angiotensin-system (RAS) inhibitor therapy using sacubitril-valsartan (Entresto) is no more likely to cause angioedema than starting out with an ACE inhibitor or angiotensin receptor blocker (ARB).
But the risk climbs when such patients start on an ACE inhibitor or ARB and then switch to sacubitril-valsartan, compared with those prescribed the newer drug, the only available angiotensin receptor-neprilysin inhibitor (ARNI), in the first place.
Those findings and others from a large database analysis, by researchers at the Food and Drug Administration and Harvard Medical School, may clarify and help alleviate a residual safety concern about the ARNI – that it might promote angioedema – that persists after the drug’s major HF trials.
The angioedema risk increased the most right after the switch to the ARNI from one of the older RAS inhibitors. For example, the overall risk doubled for patients who started with an ARB then switched to sacubitril-valsartan, compared with those who started on the newer drug. But it went up about 2.5 times during the first 14 days after the switch.
A similar pattern emerged for ACE inhibitors, but the increased angioedema risk reached significance only within 2 weeks of the switch from an ACE inhibitor to sacubitril-valsartan compared to starting on the latter.
The analysis, based on data from the FDA’s Sentinel adverse event reporting system, was published in the Journal of the American College of Cardiology.
A rare complication, but ...
Angioedema was rare overall in the study, with an unadjusted rate of about 6.75 per 1,000 person-years for users of ACE inhibitors, less than half that rate for ARB users, and only one-fifth that rate for sacubitril-valsartan recipients.
But even a rare complication can be a worry for drugs as widely used as RAS inhibitors. And it’s not unusual for patients cautiously started on an ACE inhibitor or ARB to be switched to sacubitril-valsartan, which is only recently a core guideline–recommended therapy for HF with reduced ejection fraction.
Such patients transitioning to the ARNI, the current study suggests, should probably be watched closely for signs of angioedema for 2 weeks but especially during the first few days. Indeed, the study’s event curves show most of the extra risk “popping up” right after the switch to sacubitril-valsartan, lead author Efe Eworuke, PhD, told this news organization.
The ARNI’s labeling, which states the drug should follow ACE inhibitors only after 36-hour washout period, “has done justice to this issue,” she said. But “whether clinicians are adhering to that, we can’t tell.”
Potentially, patients who miss the 36-hour washout between ACE inhibitors or ARBs and sacubitril-valsartan may account for the excess angioedema risk seen in the analysis, said Dr. Eworuke, with the FDA’s Center for Drug Evaluation and Research, Silver Spring, Md.
But the analysis doesn’t nail down the window of excess risk to only 36 hours. It suggests that patients switching to the ARNI – even those pausing for 36 hours in between drugs – should probably be monitored “2 weeks or longer,” she said. “They could still have angioedema after the washout period.”
Indeed, the “timing of the switch may be critical,” according to an editorial accompanying the report. “Perhaps a longer initial exposure period of ACE inhibitor or ARB,” beyond 2 weeks, “should be considered before switching to an ARNI,” contended Robert L. Page II, PharmD, MSPH, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora.
Moreover, he wrote, the study suggests that “initiation of an ARNI de novo may be safer compared with trialing an ACE inhibitor or ARB then switching to an ARNI,” and “should be a consideration when beginning guideline-directed medical therapy for patients with HF.”
New RAS inhibition with ARNI ‘protective’
Compared with ARNI “new users” who had not received any RAS inhibitor in the prior 6 months, patients in the study who switched from an ACE inhibitor to ARNI (41,548 matched pairs) showed a hazard ratio (HR) for angioedema of 1.62 (95% confidence interval [CI], 0.91-2.89), that is, only a “trend,” the report states.
But that trend became significant when the analysis considered only angioedema cases in the first 14 days after the drug switch: HR, 1.98 (95% CI, 1.11-3.53).
Those switching from an ARB to ARNI, compared with ARNI new users (37,893 matched pairs), showed a significant HR for angioedema of 2.03 (95% CI, 1.16-3.54). The effect was more pronounced when considering only angioedema arising in the first 2 weeks: HR, 2.45 (95% CI, 1.36-4.43).
Compared with new use of ACE inhibitors, new ARNI use (41,998 matched pairs) was “protective,” the report states, with an HR for angioedema of 0.18 (95% CI, 0.11-0.29). So was a switch from ACE inhibitors to the ARNI (69,639 matched pairs), with an HR of 0.31 (95% CI, 0.23-0.43).
But compared with starting with an ARB, ARNI new use (43,755 matched pairs) had a null effect on angioedema risk, HR, 0.59 (95% CI, 0.35-1.01); as did switching from an ARB to ARNI (49,137 matched pairs), HR, 0.85 (95% CI, 0.58-1.26).
The analysis has limitations, Dr. Eworuke acknowledged. The comparator groups probably differed in unknown ways given the limits of propensity matching, for example, and because the FDA’s Sentinel system data can reflect only cases that are reported, the study probably underestimates the true prevalence of angioedema.
For example, a patient may see a clinician for a milder case that resolves without a significant intervention, she noted. But “those types of angioedema would not have been captured by our study.”
Dr. Eworuke disclosed that her comments reflect her views and are not those of the Food and Drug Administration; she and the other authors, as well as editorialist Dr. Page, report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New renin-angiotensin-system (RAS) inhibitor therapy using sacubitril-valsartan (Entresto) is no more likely to cause angioedema than starting out with an ACE inhibitor or angiotensin receptor blocker (ARB).
But the risk climbs when such patients start on an ACE inhibitor or ARB and then switch to sacubitril-valsartan, compared with those prescribed the newer drug, the only available angiotensin receptor-neprilysin inhibitor (ARNI), in the first place.
Those findings and others from a large database analysis, by researchers at the Food and Drug Administration and Harvard Medical School, may clarify and help alleviate a residual safety concern about the ARNI – that it might promote angioedema – that persists after the drug’s major HF trials.
The angioedema risk increased the most right after the switch to the ARNI from one of the older RAS inhibitors. For example, the overall risk doubled for patients who started with an ARB then switched to sacubitril-valsartan, compared with those who started on the newer drug. But it went up about 2.5 times during the first 14 days after the switch.
A similar pattern emerged for ACE inhibitors, but the increased angioedema risk reached significance only within 2 weeks of the switch from an ACE inhibitor to sacubitril-valsartan compared to starting on the latter.
The analysis, based on data from the FDA’s Sentinel adverse event reporting system, was published in the Journal of the American College of Cardiology.
A rare complication, but ...
Angioedema was rare overall in the study, with an unadjusted rate of about 6.75 per 1,000 person-years for users of ACE inhibitors, less than half that rate for ARB users, and only one-fifth that rate for sacubitril-valsartan recipients.
But even a rare complication can be a worry for drugs as widely used as RAS inhibitors. And it’s not unusual for patients cautiously started on an ACE inhibitor or ARB to be switched to sacubitril-valsartan, which is only recently a core guideline–recommended therapy for HF with reduced ejection fraction.
Such patients transitioning to the ARNI, the current study suggests, should probably be watched closely for signs of angioedema for 2 weeks but especially during the first few days. Indeed, the study’s event curves show most of the extra risk “popping up” right after the switch to sacubitril-valsartan, lead author Efe Eworuke, PhD, told this news organization.
The ARNI’s labeling, which states the drug should follow ACE inhibitors only after 36-hour washout period, “has done justice to this issue,” she said. But “whether clinicians are adhering to that, we can’t tell.”
Potentially, patients who miss the 36-hour washout between ACE inhibitors or ARBs and sacubitril-valsartan may account for the excess angioedema risk seen in the analysis, said Dr. Eworuke, with the FDA’s Center for Drug Evaluation and Research, Silver Spring, Md.
But the analysis doesn’t nail down the window of excess risk to only 36 hours. It suggests that patients switching to the ARNI – even those pausing for 36 hours in between drugs – should probably be monitored “2 weeks or longer,” she said. “They could still have angioedema after the washout period.”
Indeed, the “timing of the switch may be critical,” according to an editorial accompanying the report. “Perhaps a longer initial exposure period of ACE inhibitor or ARB,” beyond 2 weeks, “should be considered before switching to an ARNI,” contended Robert L. Page II, PharmD, MSPH, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora.
Moreover, he wrote, the study suggests that “initiation of an ARNI de novo may be safer compared with trialing an ACE inhibitor or ARB then switching to an ARNI,” and “should be a consideration when beginning guideline-directed medical therapy for patients with HF.”
New RAS inhibition with ARNI ‘protective’
Compared with ARNI “new users” who had not received any RAS inhibitor in the prior 6 months, patients in the study who switched from an ACE inhibitor to ARNI (41,548 matched pairs) showed a hazard ratio (HR) for angioedema of 1.62 (95% confidence interval [CI], 0.91-2.89), that is, only a “trend,” the report states.
But that trend became significant when the analysis considered only angioedema cases in the first 14 days after the drug switch: HR, 1.98 (95% CI, 1.11-3.53).
Those switching from an ARB to ARNI, compared with ARNI new users (37,893 matched pairs), showed a significant HR for angioedema of 2.03 (95% CI, 1.16-3.54). The effect was more pronounced when considering only angioedema arising in the first 2 weeks: HR, 2.45 (95% CI, 1.36-4.43).
Compared with new use of ACE inhibitors, new ARNI use (41,998 matched pairs) was “protective,” the report states, with an HR for angioedema of 0.18 (95% CI, 0.11-0.29). So was a switch from ACE inhibitors to the ARNI (69,639 matched pairs), with an HR of 0.31 (95% CI, 0.23-0.43).
But compared with starting with an ARB, ARNI new use (43,755 matched pairs) had a null effect on angioedema risk, HR, 0.59 (95% CI, 0.35-1.01); as did switching from an ARB to ARNI (49,137 matched pairs), HR, 0.85 (95% CI, 0.58-1.26).
The analysis has limitations, Dr. Eworuke acknowledged. The comparator groups probably differed in unknown ways given the limits of propensity matching, for example, and because the FDA’s Sentinel system data can reflect only cases that are reported, the study probably underestimates the true prevalence of angioedema.
For example, a patient may see a clinician for a milder case that resolves without a significant intervention, she noted. But “those types of angioedema would not have been captured by our study.”
Dr. Eworuke disclosed that her comments reflect her views and are not those of the Food and Drug Administration; she and the other authors, as well as editorialist Dr. Page, report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
New renin-angiotensin-system (RAS) inhibitor therapy using sacubitril-valsartan (Entresto) is no more likely to cause angioedema than starting out with an ACE inhibitor or angiotensin receptor blocker (ARB).
But the risk climbs when such patients start on an ACE inhibitor or ARB and then switch to sacubitril-valsartan, compared with those prescribed the newer drug, the only available angiotensin receptor-neprilysin inhibitor (ARNI), in the first place.
Those findings and others from a large database analysis, by researchers at the Food and Drug Administration and Harvard Medical School, may clarify and help alleviate a residual safety concern about the ARNI – that it might promote angioedema – that persists after the drug’s major HF trials.
The angioedema risk increased the most right after the switch to the ARNI from one of the older RAS inhibitors. For example, the overall risk doubled for patients who started with an ARB then switched to sacubitril-valsartan, compared with those who started on the newer drug. But it went up about 2.5 times during the first 14 days after the switch.
A similar pattern emerged for ACE inhibitors, but the increased angioedema risk reached significance only within 2 weeks of the switch from an ACE inhibitor to sacubitril-valsartan compared to starting on the latter.
The analysis, based on data from the FDA’s Sentinel adverse event reporting system, was published in the Journal of the American College of Cardiology.
A rare complication, but ...
Angioedema was rare overall in the study, with an unadjusted rate of about 6.75 per 1,000 person-years for users of ACE inhibitors, less than half that rate for ARB users, and only one-fifth that rate for sacubitril-valsartan recipients.
But even a rare complication can be a worry for drugs as widely used as RAS inhibitors. And it’s not unusual for patients cautiously started on an ACE inhibitor or ARB to be switched to sacubitril-valsartan, which is only recently a core guideline–recommended therapy for HF with reduced ejection fraction.
Such patients transitioning to the ARNI, the current study suggests, should probably be watched closely for signs of angioedema for 2 weeks but especially during the first few days. Indeed, the study’s event curves show most of the extra risk “popping up” right after the switch to sacubitril-valsartan, lead author Efe Eworuke, PhD, told this news organization.
The ARNI’s labeling, which states the drug should follow ACE inhibitors only after 36-hour washout period, “has done justice to this issue,” she said. But “whether clinicians are adhering to that, we can’t tell.”
Potentially, patients who miss the 36-hour washout between ACE inhibitors or ARBs and sacubitril-valsartan may account for the excess angioedema risk seen in the analysis, said Dr. Eworuke, with the FDA’s Center for Drug Evaluation and Research, Silver Spring, Md.
But the analysis doesn’t nail down the window of excess risk to only 36 hours. It suggests that patients switching to the ARNI – even those pausing for 36 hours in between drugs – should probably be monitored “2 weeks or longer,” she said. “They could still have angioedema after the washout period.”
Indeed, the “timing of the switch may be critical,” according to an editorial accompanying the report. “Perhaps a longer initial exposure period of ACE inhibitor or ARB,” beyond 2 weeks, “should be considered before switching to an ARNI,” contended Robert L. Page II, PharmD, MSPH, University of Colorado Skaggs School of Pharmacy and Pharmaceutical Sciences, Aurora.
Moreover, he wrote, the study suggests that “initiation of an ARNI de novo may be safer compared with trialing an ACE inhibitor or ARB then switching to an ARNI,” and “should be a consideration when beginning guideline-directed medical therapy for patients with HF.”
New RAS inhibition with ARNI ‘protective’
Compared with ARNI “new users” who had not received any RAS inhibitor in the prior 6 months, patients in the study who switched from an ACE inhibitor to ARNI (41,548 matched pairs) showed a hazard ratio (HR) for angioedema of 1.62 (95% confidence interval [CI], 0.91-2.89), that is, only a “trend,” the report states.
But that trend became significant when the analysis considered only angioedema cases in the first 14 days after the drug switch: HR, 1.98 (95% CI, 1.11-3.53).
Those switching from an ARB to ARNI, compared with ARNI new users (37,893 matched pairs), showed a significant HR for angioedema of 2.03 (95% CI, 1.16-3.54). The effect was more pronounced when considering only angioedema arising in the first 2 weeks: HR, 2.45 (95% CI, 1.36-4.43).
Compared with new use of ACE inhibitors, new ARNI use (41,998 matched pairs) was “protective,” the report states, with an HR for angioedema of 0.18 (95% CI, 0.11-0.29). So was a switch from ACE inhibitors to the ARNI (69,639 matched pairs), with an HR of 0.31 (95% CI, 0.23-0.43).
But compared with starting with an ARB, ARNI new use (43,755 matched pairs) had a null effect on angioedema risk, HR, 0.59 (95% CI, 0.35-1.01); as did switching from an ARB to ARNI (49,137 matched pairs), HR, 0.85 (95% CI, 0.58-1.26).
The analysis has limitations, Dr. Eworuke acknowledged. The comparator groups probably differed in unknown ways given the limits of propensity matching, for example, and because the FDA’s Sentinel system data can reflect only cases that are reported, the study probably underestimates the true prevalence of angioedema.
For example, a patient may see a clinician for a milder case that resolves without a significant intervention, she noted. But “those types of angioedema would not have been captured by our study.”
Dr. Eworuke disclosed that her comments reflect her views and are not those of the Food and Drug Administration; she and the other authors, as well as editorialist Dr. Page, report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Noninvasive liver test may help select asymptomatic candidates for heart failure tests
A noninvasive test for liver disease may be a useful, low-cost screening tool to select asymptomatic candidates for a detailed examination of heart failure with preserved ejection fraction (HFpEF), say authors of a report published in Gastro Hep Advances.
The fibrosis-4 (FIB-4) index was a significant predictor of high HFpEF risk, wrote Chisato Okamoto, MD, of the department of medical biochemistry at Osaka University Graduate School of Medicine and the National Cerebral and Cardiovascular Center in Japan, and colleagues.
“Recognition of heart failure with preserved ejection fraction at an early stage in mass screening is desirable, but difficult to achieve,” the authors wrote. “The FIB-4 index is calculated using only four parameters that are routinely evaluated in general health check-up programs.”
HFpEF is an emerging disease in recent years with a poor prognosis, they wrote. Early diagnosis can be challenging for several reasons, particularly because HFpEF patients are often asymptomatic until late in the disease process and have normal left ventricular filling pressures at rest. By using a tool to select probable cases from subclinical participants in a health check-up program, clinicians can refer patients for a diastolic stress test, which is considered the gold standard for diagnosing HFpEF.
Previous studies have found that the FIB-4 index, a noninvasive tool to estimate liver stiffness and fibrosis, is associated with a higher risk of major adverse cardiovascular events (MACE) in patients with HFpEF. In addition, patients with nonalcoholic fatty liver disease (NAFLD) have a twofold higher prevalence of HFpEF than the general population.
Dr. Okamoto and colleagues examined the association between the FIB-4 index and HFpEF risk based on the Heart Failure Association’s diagnostic algorithm for HFpEF in patients with breathlessness (HFA-PEFF). The researchers looked at the prognostic impact of the FIB-4 index in 710 patients who participated in a health check-up program in the rural community of Arita-cho, Japan, between 2006 and 2007. They excluded participants with a history of cardiovascular disease or reduced left ventricular systolic function (LVEF < 50%). Researchers calculated the FIB-4 index and HFA-PEFF score for all participants.
First, using the HFA-PEFF scores, the researchers sorted participants into five groups by HFpEF risk: 215 (30%) with zero points, 100 (14%) with 1 point, 171 (24%) with 2 points, 163 (23%) with 3 points, and 61 (9%) with 4-6 points. Participants in the high-risk group (scores 4-6) were older, mostly men, and had higher blood pressure, alcohol intake, hypertension, dyslipidemia, and liver disease. The higher the HFpEF risk group, the higher the rates of all-cause mortality, hospitalization for heart failure, and MACE.
Overall, the FIB-4 index was correlated with the HFpEF risk groups and showed a stepwise increase across the groups, with .94 for the low-risk group, 1.45 for the intermediate-risk group, and 1.99 for the high-risk group, the authors wrote. The FIB-4 index also correlated with markers associated with components of the HFA-PEFF scoring system.
Using multivariate logistic regression analysis, the FIB-4 index was associated with a high HFpEF risk, and an increase in FIB-4 was associated with increased odds of high HFpEF risk. The association remained significant across four separate models that accounted for risk factors associated with lifestyle-related diseases, blood parameters associated with liver disease, and chronic conditions such as hypertension, dyslipidemia, diabetes mellitus, and liver disease.
In additional area under the curve (AUC) analyses, the FIB-4 index was a significant predictor of high HFpEF risk. At cutoff values typically used for advanced liver fibrosis in NAFLD, a FIB-4 cutoff of 1.3 or less had a sensitivity of 85.2%, while a FIB-4 cutoff of 2.67 or higher had a specificity of 94.8%. At alternate cutoff values typically used for patients with HIV/hepatitis C virus infection, a FIB-4 cutoff of less than 1.45 had a sensitivity of 75.4%, while a FIB-4 cutoff of greater than 3.25 had a specificity of 98%.
Using cutoffs of 1.3 and 2.67, a higher FIB-4 was associated with higher rates of clinical events and MACE, as well as a higher HFpEF risk. Using the alternate cutoffs of 1.45 and 3.25, prognostic stratification of clinical events and MACE was also possible.
When all variables were included in the multivariate model, the FIB-4 index remained a significant prognostic predictor. The FIB-4 index stratified clinical prognosis was also an independent predictor of all-cause mortality and hospitalization for heart failure.
Although additional studies are needed to reveal the interaction between liver and heart function, the study authors wrote, the findings provide valuable insights that can help discover the cardiohepatic interaction to reduce the development of HFpEF.
“Since it can be easily, quickly, and inexpensively measured, routine or repeated measurements of the FIB-4 index could help in selecting preferred candidates for detailed examination of HFpEF risk, which may improve clinical outcomes by diagnosing HFpEF at an early stage,” they wrote.
The study was supported by grants from the Osaka Medical Research Foundation for Intractable Disease, the Japan Arteriosclerosis Prevention Fund, the Japan Society for the Promotion of Science, and the Japan Heart Foundation. The authors disclosed no conflicts.
The 2021 NAFLD clinical care pathway is a shining example of how a simple score like the fibrosis-4 (FIB-4) index – paired sequentially with a second noninvasive test like vibration-controlled elastography – can provide an accurate, cost-effective screening tool and risk stratification and further limit invasive testing such as liver biopsy.
Broader use of FIB-4 by cardiovascular and hepatology providers may increase earlier identification of NAFLD or HFpEF or both.
Anand S. Shah, MD, is director of hepatology at Atlanta VA Healthcare and assistant professor of medicine, division of digestive disease, department of medicine, Emory University, Atlanta. He has no financial conflicts.
The 2021 NAFLD clinical care pathway is a shining example of how a simple score like the fibrosis-4 (FIB-4) index – paired sequentially with a second noninvasive test like vibration-controlled elastography – can provide an accurate, cost-effective screening tool and risk stratification and further limit invasive testing such as liver biopsy.
Broader use of FIB-4 by cardiovascular and hepatology providers may increase earlier identification of NAFLD or HFpEF or both.
Anand S. Shah, MD, is director of hepatology at Atlanta VA Healthcare and assistant professor of medicine, division of digestive disease, department of medicine, Emory University, Atlanta. He has no financial conflicts.
The 2021 NAFLD clinical care pathway is a shining example of how a simple score like the fibrosis-4 (FIB-4) index – paired sequentially with a second noninvasive test like vibration-controlled elastography – can provide an accurate, cost-effective screening tool and risk stratification and further limit invasive testing such as liver biopsy.
Broader use of FIB-4 by cardiovascular and hepatology providers may increase earlier identification of NAFLD or HFpEF or both.
Anand S. Shah, MD, is director of hepatology at Atlanta VA Healthcare and assistant professor of medicine, division of digestive disease, department of medicine, Emory University, Atlanta. He has no financial conflicts.
A noninvasive test for liver disease may be a useful, low-cost screening tool to select asymptomatic candidates for a detailed examination of heart failure with preserved ejection fraction (HFpEF), say authors of a report published in Gastro Hep Advances.
The fibrosis-4 (FIB-4) index was a significant predictor of high HFpEF risk, wrote Chisato Okamoto, MD, of the department of medical biochemistry at Osaka University Graduate School of Medicine and the National Cerebral and Cardiovascular Center in Japan, and colleagues.
“Recognition of heart failure with preserved ejection fraction at an early stage in mass screening is desirable, but difficult to achieve,” the authors wrote. “The FIB-4 index is calculated using only four parameters that are routinely evaluated in general health check-up programs.”
HFpEF is an emerging disease in recent years with a poor prognosis, they wrote. Early diagnosis can be challenging for several reasons, particularly because HFpEF patients are often asymptomatic until late in the disease process and have normal left ventricular filling pressures at rest. By using a tool to select probable cases from subclinical participants in a health check-up program, clinicians can refer patients for a diastolic stress test, which is considered the gold standard for diagnosing HFpEF.
Previous studies have found that the FIB-4 index, a noninvasive tool to estimate liver stiffness and fibrosis, is associated with a higher risk of major adverse cardiovascular events (MACE) in patients with HFpEF. In addition, patients with nonalcoholic fatty liver disease (NAFLD) have a twofold higher prevalence of HFpEF than the general population.
Dr. Okamoto and colleagues examined the association between the FIB-4 index and HFpEF risk based on the Heart Failure Association’s diagnostic algorithm for HFpEF in patients with breathlessness (HFA-PEFF). The researchers looked at the prognostic impact of the FIB-4 index in 710 patients who participated in a health check-up program in the rural community of Arita-cho, Japan, between 2006 and 2007. They excluded participants with a history of cardiovascular disease or reduced left ventricular systolic function (LVEF < 50%). Researchers calculated the FIB-4 index and HFA-PEFF score for all participants.
First, using the HFA-PEFF scores, the researchers sorted participants into five groups by HFpEF risk: 215 (30%) with zero points, 100 (14%) with 1 point, 171 (24%) with 2 points, 163 (23%) with 3 points, and 61 (9%) with 4-6 points. Participants in the high-risk group (scores 4-6) were older, mostly men, and had higher blood pressure, alcohol intake, hypertension, dyslipidemia, and liver disease. The higher the HFpEF risk group, the higher the rates of all-cause mortality, hospitalization for heart failure, and MACE.
Overall, the FIB-4 index was correlated with the HFpEF risk groups and showed a stepwise increase across the groups, with .94 for the low-risk group, 1.45 for the intermediate-risk group, and 1.99 for the high-risk group, the authors wrote. The FIB-4 index also correlated with markers associated with components of the HFA-PEFF scoring system.
Using multivariate logistic regression analysis, the FIB-4 index was associated with a high HFpEF risk, and an increase in FIB-4 was associated with increased odds of high HFpEF risk. The association remained significant across four separate models that accounted for risk factors associated with lifestyle-related diseases, blood parameters associated with liver disease, and chronic conditions such as hypertension, dyslipidemia, diabetes mellitus, and liver disease.
In additional area under the curve (AUC) analyses, the FIB-4 index was a significant predictor of high HFpEF risk. At cutoff values typically used for advanced liver fibrosis in NAFLD, a FIB-4 cutoff of 1.3 or less had a sensitivity of 85.2%, while a FIB-4 cutoff of 2.67 or higher had a specificity of 94.8%. At alternate cutoff values typically used for patients with HIV/hepatitis C virus infection, a FIB-4 cutoff of less than 1.45 had a sensitivity of 75.4%, while a FIB-4 cutoff of greater than 3.25 had a specificity of 98%.
Using cutoffs of 1.3 and 2.67, a higher FIB-4 was associated with higher rates of clinical events and MACE, as well as a higher HFpEF risk. Using the alternate cutoffs of 1.45 and 3.25, prognostic stratification of clinical events and MACE was also possible.
When all variables were included in the multivariate model, the FIB-4 index remained a significant prognostic predictor. The FIB-4 index stratified clinical prognosis was also an independent predictor of all-cause mortality and hospitalization for heart failure.
Although additional studies are needed to reveal the interaction between liver and heart function, the study authors wrote, the findings provide valuable insights that can help discover the cardiohepatic interaction to reduce the development of HFpEF.
“Since it can be easily, quickly, and inexpensively measured, routine or repeated measurements of the FIB-4 index could help in selecting preferred candidates for detailed examination of HFpEF risk, which may improve clinical outcomes by diagnosing HFpEF at an early stage,” they wrote.
The study was supported by grants from the Osaka Medical Research Foundation for Intractable Disease, the Japan Arteriosclerosis Prevention Fund, the Japan Society for the Promotion of Science, and the Japan Heart Foundation. The authors disclosed no conflicts.
A noninvasive test for liver disease may be a useful, low-cost screening tool to select asymptomatic candidates for a detailed examination of heart failure with preserved ejection fraction (HFpEF), say authors of a report published in Gastro Hep Advances.
The fibrosis-4 (FIB-4) index was a significant predictor of high HFpEF risk, wrote Chisato Okamoto, MD, of the department of medical biochemistry at Osaka University Graduate School of Medicine and the National Cerebral and Cardiovascular Center in Japan, and colleagues.
“Recognition of heart failure with preserved ejection fraction at an early stage in mass screening is desirable, but difficult to achieve,” the authors wrote. “The FIB-4 index is calculated using only four parameters that are routinely evaluated in general health check-up programs.”
HFpEF is an emerging disease in recent years with a poor prognosis, they wrote. Early diagnosis can be challenging for several reasons, particularly because HFpEF patients are often asymptomatic until late in the disease process and have normal left ventricular filling pressures at rest. By using a tool to select probable cases from subclinical participants in a health check-up program, clinicians can refer patients for a diastolic stress test, which is considered the gold standard for diagnosing HFpEF.
Previous studies have found that the FIB-4 index, a noninvasive tool to estimate liver stiffness and fibrosis, is associated with a higher risk of major adverse cardiovascular events (MACE) in patients with HFpEF. In addition, patients with nonalcoholic fatty liver disease (NAFLD) have a twofold higher prevalence of HFpEF than the general population.
Dr. Okamoto and colleagues examined the association between the FIB-4 index and HFpEF risk based on the Heart Failure Association’s diagnostic algorithm for HFpEF in patients with breathlessness (HFA-PEFF). The researchers looked at the prognostic impact of the FIB-4 index in 710 patients who participated in a health check-up program in the rural community of Arita-cho, Japan, between 2006 and 2007. They excluded participants with a history of cardiovascular disease or reduced left ventricular systolic function (LVEF < 50%). Researchers calculated the FIB-4 index and HFA-PEFF score for all participants.
First, using the HFA-PEFF scores, the researchers sorted participants into five groups by HFpEF risk: 215 (30%) with zero points, 100 (14%) with 1 point, 171 (24%) with 2 points, 163 (23%) with 3 points, and 61 (9%) with 4-6 points. Participants in the high-risk group (scores 4-6) were older, mostly men, and had higher blood pressure, alcohol intake, hypertension, dyslipidemia, and liver disease. The higher the HFpEF risk group, the higher the rates of all-cause mortality, hospitalization for heart failure, and MACE.
Overall, the FIB-4 index was correlated with the HFpEF risk groups and showed a stepwise increase across the groups, with .94 for the low-risk group, 1.45 for the intermediate-risk group, and 1.99 for the high-risk group, the authors wrote. The FIB-4 index also correlated with markers associated with components of the HFA-PEFF scoring system.
Using multivariate logistic regression analysis, the FIB-4 index was associated with a high HFpEF risk, and an increase in FIB-4 was associated with increased odds of high HFpEF risk. The association remained significant across four separate models that accounted for risk factors associated with lifestyle-related diseases, blood parameters associated with liver disease, and chronic conditions such as hypertension, dyslipidemia, diabetes mellitus, and liver disease.
In additional area under the curve (AUC) analyses, the FIB-4 index was a significant predictor of high HFpEF risk. At cutoff values typically used for advanced liver fibrosis in NAFLD, a FIB-4 cutoff of 1.3 or less had a sensitivity of 85.2%, while a FIB-4 cutoff of 2.67 or higher had a specificity of 94.8%. At alternate cutoff values typically used for patients with HIV/hepatitis C virus infection, a FIB-4 cutoff of less than 1.45 had a sensitivity of 75.4%, while a FIB-4 cutoff of greater than 3.25 had a specificity of 98%.
Using cutoffs of 1.3 and 2.67, a higher FIB-4 was associated with higher rates of clinical events and MACE, as well as a higher HFpEF risk. Using the alternate cutoffs of 1.45 and 3.25, prognostic stratification of clinical events and MACE was also possible.
When all variables were included in the multivariate model, the FIB-4 index remained a significant prognostic predictor. The FIB-4 index stratified clinical prognosis was also an independent predictor of all-cause mortality and hospitalization for heart failure.
Although additional studies are needed to reveal the interaction between liver and heart function, the study authors wrote, the findings provide valuable insights that can help discover the cardiohepatic interaction to reduce the development of HFpEF.
“Since it can be easily, quickly, and inexpensively measured, routine or repeated measurements of the FIB-4 index could help in selecting preferred candidates for detailed examination of HFpEF risk, which may improve clinical outcomes by diagnosing HFpEF at an early stage,” they wrote.
The study was supported by grants from the Osaka Medical Research Foundation for Intractable Disease, the Japan Arteriosclerosis Prevention Fund, the Japan Society for the Promotion of Science, and the Japan Heart Foundation. The authors disclosed no conflicts.
FROM GASTRO HEP ADVANCES
More type 2 diabetes deaths from cancer than heart disease
Cancer appears to have overtaken cardiovascular disease (CVD) as a leading cause of death in adults with type 2 diabetes, a 20-year population study in England suggests.
The researchers found that, from 1998 to 2018, in more than 130,000 adults aged 35 and older with type 2 diabetes, all-cause mortality declined for all ages, but cancer mortality increased for those aged 75 and older; people with type 2 diabetes who were smokers had higher and steadily increasing cancer mortality rates; and people with type 2 diabetes had more than twice the rate of colorectal, pancreatic, liver, and endometrial cancer mortality than age- and sex-matched individuals in the general population.
The findings suggest that “cancer prevention strategies therefore deserve at least a similar level of attention as cardiovascular disease prevention, particularly in older people and for some cancers such as liver, colorectal, and pancreatic cancer,” the researchers wrote.
Tailored cancer prevention and early-detection strategies are needed to address persistent inequalities in the older population, the most deprived, and smokers, they added.
Breast cancer rates in younger women with type 2 diabetes rising
According to the researchers, “early cancer detection through changes to existing screening [programs], or more in-depth investigations for suspected/nonspecific symptoms, may reduce the number of avoidable cancer deaths in people with type 2 diabetes.”
Moreover, breast cancer rates in younger women with type 2 diabetes are rising by 4.1% per year, they wrote, which suggests such women are high risk and should be screened at a younger age, but screening age would need to be determined in cost-effectiveness analyses.
The study by Suping Ling, PhD, and colleagues was published online in Diabetologia.
Results challenge belief that preventing CVD is priority in type 2 diabetes
“The prevention of cardiovascular disease has been, and is still considered, a priority in people with diabetes,” the researchers wrote.
“Our results challenge this view by showing that cancer may have overtaken cardiovascular disease as a leading cause of death in people with type 2 diabetes.”
“The proportion of cancer deaths out of all-cause deaths remains high (> 30%) in young ages, and it was steadily increasing in older ages,” Dr. Ling, from the department of noncommunicable disease epidemiology, London School of Hygiene & Tropical Medicine, said in a comment.
“Combined with previous studies reporting decreasing CVD mortality rates,” she said, “we concluded that cancer might have overtaken CVD as the leading cause of death in people with type 2 diabetes.”
Many evidence-based cancer-prevention strategies related to lifestyle (such as being physically active, being a healthy weight, eating a better diet, stopping smoking, as summarized by the World Cancer Research Fund), are helpful for preventing both cancer and CVD, Ling observed.
However, in the medical community, many additional efforts were made for monitoring, early detection, and innovating medications for CVD, she noted. “Therefore, we would like to propose a similar level of attention and effort for cancer in people with type 2 diabetes.”
Deaths from cancer vs. all causes in patients with diabetes
The researchers identified 137,804 patients aged 35 and older who were newly diagnosed with type 2 diabetes from 1998 to 2018 in general practices in the UK that were part of the Clinical Practice Research Datalink.
Patients were a median age of 64 years and 45% were women. Most (83%) were White, followed by South Asian (3.5%), Black (2.0%), and other (3%); 8.4% had missing information for race. Patients had a median body mass index (BMI) of 30.6 kg/m2.
Researchers divided patients into socioeconomic quintiles of most to least deprived based on income, employment, education, and other factors. During a median follow-up of 8.4 years, there were 39,212 deaths (28.5%).
Cancer mortality in subgroups of patients with type 2 diabetes
Researchers analyzed annual deaths from cancer and from all causes over 20 years in subgroups of patients with type 2 diabetes.
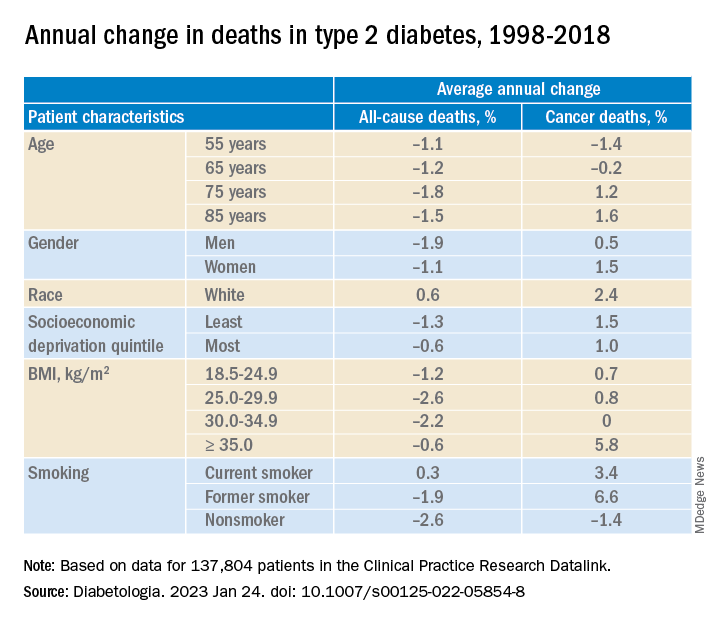
In adults with type 2 diabetes, the average percentage change in cancer mortality per year, from 1998 to 2018 decreased in people aged 55 and 65 (–1.4% and –0.2%, respectively), but increased in people aged 75 and 85 (1.2% and 1.6%, respectively); increased more in women than in men (1.5% vs 1.0%), although women had lower cancer mortality than men; and increased more in the least deprived (wealthiest) individuals than in the most deprived (1.5% vs 1.0%). Cancer mortality rates were consistently higher in the most deprived individuals, Dr. Ling noted.
Cancer mortality also increased more in people with class III obesity (BMI ≥ 35) versus normal weight (5.8% vs 0.7%) and versus other weights. In addition, there was an upward trend in cancer mortality in people who were White or former/current smokers.
Deaths from specific cancers in diabetes vs. general population
Next, researchers determined cancer mortality ratios – the cancer mortality of the patients with diabetes divided by the cancer mortality of the general population.
They determined this for all cancers, the four most common cancers in the United Kingdom (lung, colorectal, breast, and prostate), and cancers caused by type 2 diabetes (pancreatic, liver, gallbladder, and endometrial cancer), standardized by sex and age.
Mortality from all cancer was 18% higher in patients with type 2 diabetes, compared with the general population.
Overall, mortality from colorectal cancer, pancreatic cancer, and liver cancer was 2.4 times, 2.12 times, and 2.13 times higher, respectively, in patients with type 2 diabetes than in the general population.
Mortality from breast cancer was 9% higher and mortality from endometrial cancer was 2.08 times higher in women with type 2 diabetes than in women in the general population.
There was a constant upward trend for mortality rates for pancreatic, liver, and lung cancer at all ages, colorectal cancer at most ages, breast cancer at younger ages, and prostate and endometrial cancer at older ages.
The study was funded by Hope Against Cancer. Dr. Ling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cancer appears to have overtaken cardiovascular disease (CVD) as a leading cause of death in adults with type 2 diabetes, a 20-year population study in England suggests.
The researchers found that, from 1998 to 2018, in more than 130,000 adults aged 35 and older with type 2 diabetes, all-cause mortality declined for all ages, but cancer mortality increased for those aged 75 and older; people with type 2 diabetes who were smokers had higher and steadily increasing cancer mortality rates; and people with type 2 diabetes had more than twice the rate of colorectal, pancreatic, liver, and endometrial cancer mortality than age- and sex-matched individuals in the general population.
The findings suggest that “cancer prevention strategies therefore deserve at least a similar level of attention as cardiovascular disease prevention, particularly in older people and for some cancers such as liver, colorectal, and pancreatic cancer,” the researchers wrote.
Tailored cancer prevention and early-detection strategies are needed to address persistent inequalities in the older population, the most deprived, and smokers, they added.
Breast cancer rates in younger women with type 2 diabetes rising
According to the researchers, “early cancer detection through changes to existing screening [programs], or more in-depth investigations for suspected/nonspecific symptoms, may reduce the number of avoidable cancer deaths in people with type 2 diabetes.”
Moreover, breast cancer rates in younger women with type 2 diabetes are rising by 4.1% per year, they wrote, which suggests such women are high risk and should be screened at a younger age, but screening age would need to be determined in cost-effectiveness analyses.
The study by Suping Ling, PhD, and colleagues was published online in Diabetologia.
Results challenge belief that preventing CVD is priority in type 2 diabetes
“The prevention of cardiovascular disease has been, and is still considered, a priority in people with diabetes,” the researchers wrote.
“Our results challenge this view by showing that cancer may have overtaken cardiovascular disease as a leading cause of death in people with type 2 diabetes.”
“The proportion of cancer deaths out of all-cause deaths remains high (> 30%) in young ages, and it was steadily increasing in older ages,” Dr. Ling, from the department of noncommunicable disease epidemiology, London School of Hygiene & Tropical Medicine, said in a comment.
“Combined with previous studies reporting decreasing CVD mortality rates,” she said, “we concluded that cancer might have overtaken CVD as the leading cause of death in people with type 2 diabetes.”
Many evidence-based cancer-prevention strategies related to lifestyle (such as being physically active, being a healthy weight, eating a better diet, stopping smoking, as summarized by the World Cancer Research Fund), are helpful for preventing both cancer and CVD, Ling observed.
However, in the medical community, many additional efforts were made for monitoring, early detection, and innovating medications for CVD, she noted. “Therefore, we would like to propose a similar level of attention and effort for cancer in people with type 2 diabetes.”
Deaths from cancer vs. all causes in patients with diabetes
The researchers identified 137,804 patients aged 35 and older who were newly diagnosed with type 2 diabetes from 1998 to 2018 in general practices in the UK that were part of the Clinical Practice Research Datalink.
Patients were a median age of 64 years and 45% were women. Most (83%) were White, followed by South Asian (3.5%), Black (2.0%), and other (3%); 8.4% had missing information for race. Patients had a median body mass index (BMI) of 30.6 kg/m2.
Researchers divided patients into socioeconomic quintiles of most to least deprived based on income, employment, education, and other factors. During a median follow-up of 8.4 years, there were 39,212 deaths (28.5%).
Cancer mortality in subgroups of patients with type 2 diabetes
Researchers analyzed annual deaths from cancer and from all causes over 20 years in subgroups of patients with type 2 diabetes.
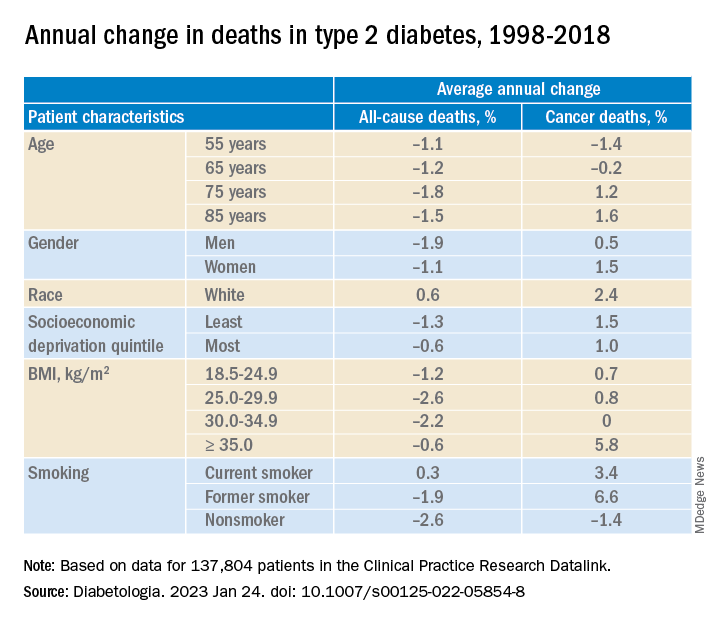
In adults with type 2 diabetes, the average percentage change in cancer mortality per year, from 1998 to 2018 decreased in people aged 55 and 65 (–1.4% and –0.2%, respectively), but increased in people aged 75 and 85 (1.2% and 1.6%, respectively); increased more in women than in men (1.5% vs 1.0%), although women had lower cancer mortality than men; and increased more in the least deprived (wealthiest) individuals than in the most deprived (1.5% vs 1.0%). Cancer mortality rates were consistently higher in the most deprived individuals, Dr. Ling noted.
Cancer mortality also increased more in people with class III obesity (BMI ≥ 35) versus normal weight (5.8% vs 0.7%) and versus other weights. In addition, there was an upward trend in cancer mortality in people who were White or former/current smokers.
Deaths from specific cancers in diabetes vs. general population
Next, researchers determined cancer mortality ratios – the cancer mortality of the patients with diabetes divided by the cancer mortality of the general population.
They determined this for all cancers, the four most common cancers in the United Kingdom (lung, colorectal, breast, and prostate), and cancers caused by type 2 diabetes (pancreatic, liver, gallbladder, and endometrial cancer), standardized by sex and age.
Mortality from all cancer was 18% higher in patients with type 2 diabetes, compared with the general population.
Overall, mortality from colorectal cancer, pancreatic cancer, and liver cancer was 2.4 times, 2.12 times, and 2.13 times higher, respectively, in patients with type 2 diabetes than in the general population.
Mortality from breast cancer was 9% higher and mortality from endometrial cancer was 2.08 times higher in women with type 2 diabetes than in women in the general population.
There was a constant upward trend for mortality rates for pancreatic, liver, and lung cancer at all ages, colorectal cancer at most ages, breast cancer at younger ages, and prostate and endometrial cancer at older ages.
The study was funded by Hope Against Cancer. Dr. Ling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Cancer appears to have overtaken cardiovascular disease (CVD) as a leading cause of death in adults with type 2 diabetes, a 20-year population study in England suggests.
The researchers found that, from 1998 to 2018, in more than 130,000 adults aged 35 and older with type 2 diabetes, all-cause mortality declined for all ages, but cancer mortality increased for those aged 75 and older; people with type 2 diabetes who were smokers had higher and steadily increasing cancer mortality rates; and people with type 2 diabetes had more than twice the rate of colorectal, pancreatic, liver, and endometrial cancer mortality than age- and sex-matched individuals in the general population.
The findings suggest that “cancer prevention strategies therefore deserve at least a similar level of attention as cardiovascular disease prevention, particularly in older people and for some cancers such as liver, colorectal, and pancreatic cancer,” the researchers wrote.
Tailored cancer prevention and early-detection strategies are needed to address persistent inequalities in the older population, the most deprived, and smokers, they added.
Breast cancer rates in younger women with type 2 diabetes rising
According to the researchers, “early cancer detection through changes to existing screening [programs], or more in-depth investigations for suspected/nonspecific symptoms, may reduce the number of avoidable cancer deaths in people with type 2 diabetes.”
Moreover, breast cancer rates in younger women with type 2 diabetes are rising by 4.1% per year, they wrote, which suggests such women are high risk and should be screened at a younger age, but screening age would need to be determined in cost-effectiveness analyses.
The study by Suping Ling, PhD, and colleagues was published online in Diabetologia.
Results challenge belief that preventing CVD is priority in type 2 diabetes
“The prevention of cardiovascular disease has been, and is still considered, a priority in people with diabetes,” the researchers wrote.
“Our results challenge this view by showing that cancer may have overtaken cardiovascular disease as a leading cause of death in people with type 2 diabetes.”
“The proportion of cancer deaths out of all-cause deaths remains high (> 30%) in young ages, and it was steadily increasing in older ages,” Dr. Ling, from the department of noncommunicable disease epidemiology, London School of Hygiene & Tropical Medicine, said in a comment.
“Combined with previous studies reporting decreasing CVD mortality rates,” she said, “we concluded that cancer might have overtaken CVD as the leading cause of death in people with type 2 diabetes.”
Many evidence-based cancer-prevention strategies related to lifestyle (such as being physically active, being a healthy weight, eating a better diet, stopping smoking, as summarized by the World Cancer Research Fund), are helpful for preventing both cancer and CVD, Ling observed.
However, in the medical community, many additional efforts were made for monitoring, early detection, and innovating medications for CVD, she noted. “Therefore, we would like to propose a similar level of attention and effort for cancer in people with type 2 diabetes.”
Deaths from cancer vs. all causes in patients with diabetes
The researchers identified 137,804 patients aged 35 and older who were newly diagnosed with type 2 diabetes from 1998 to 2018 in general practices in the UK that were part of the Clinical Practice Research Datalink.
Patients were a median age of 64 years and 45% were women. Most (83%) were White, followed by South Asian (3.5%), Black (2.0%), and other (3%); 8.4% had missing information for race. Patients had a median body mass index (BMI) of 30.6 kg/m2.
Researchers divided patients into socioeconomic quintiles of most to least deprived based on income, employment, education, and other factors. During a median follow-up of 8.4 years, there were 39,212 deaths (28.5%).
Cancer mortality in subgroups of patients with type 2 diabetes
Researchers analyzed annual deaths from cancer and from all causes over 20 years in subgroups of patients with type 2 diabetes.
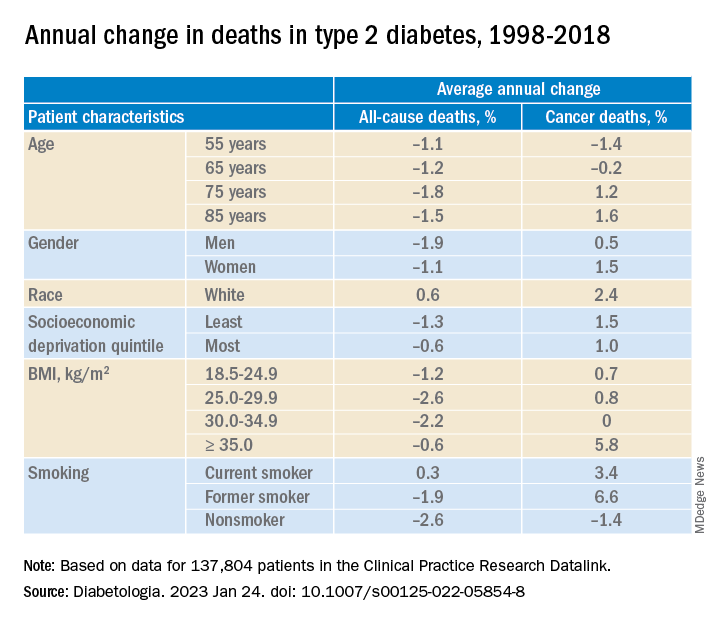
In adults with type 2 diabetes, the average percentage change in cancer mortality per year, from 1998 to 2018 decreased in people aged 55 and 65 (–1.4% and –0.2%, respectively), but increased in people aged 75 and 85 (1.2% and 1.6%, respectively); increased more in women than in men (1.5% vs 1.0%), although women had lower cancer mortality than men; and increased more in the least deprived (wealthiest) individuals than in the most deprived (1.5% vs 1.0%). Cancer mortality rates were consistently higher in the most deprived individuals, Dr. Ling noted.
Cancer mortality also increased more in people with class III obesity (BMI ≥ 35) versus normal weight (5.8% vs 0.7%) and versus other weights. In addition, there was an upward trend in cancer mortality in people who were White or former/current smokers.
Deaths from specific cancers in diabetes vs. general population
Next, researchers determined cancer mortality ratios – the cancer mortality of the patients with diabetes divided by the cancer mortality of the general population.
They determined this for all cancers, the four most common cancers in the United Kingdom (lung, colorectal, breast, and prostate), and cancers caused by type 2 diabetes (pancreatic, liver, gallbladder, and endometrial cancer), standardized by sex and age.
Mortality from all cancer was 18% higher in patients with type 2 diabetes, compared with the general population.
Overall, mortality from colorectal cancer, pancreatic cancer, and liver cancer was 2.4 times, 2.12 times, and 2.13 times higher, respectively, in patients with type 2 diabetes than in the general population.
Mortality from breast cancer was 9% higher and mortality from endometrial cancer was 2.08 times higher in women with type 2 diabetes than in women in the general population.
There was a constant upward trend for mortality rates for pancreatic, liver, and lung cancer at all ages, colorectal cancer at most ages, breast cancer at younger ages, and prostate and endometrial cancer at older ages.
The study was funded by Hope Against Cancer. Dr. Ling reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM DIABETOLOGIA
Medicare policy tweak on LVADs may reduce access to transplant
A recent change in Medicare policy designed to increase access to left ventricular assist devices (LVADs) may have had the unintended consequence of increasing inequalities in access to heart transplant for patients with advanced heart failure.
In December 2020, the Centers for Medicare & Medicaid Services relaxed restrictions on centers that implant LVADs but don’t perform heart transplants. Specifically, they dropped the requirement that LVAD-only centers obtain permission from a Medicare-approved heart transplant center authorizing LVAD implantation with “bridge-to-transplant” (BTT) intent, meaning the patient is a transplant candidate.
While the relaxed requirement has the potential to increase access to LVADs for appropriate patients, a look back at 22,221 LVAD recipients found that patients who received LVADs at transplant-capable centers had a 79% higher likelihood of receiving a BTT LVAD designation.
The 2-year heart transplant rate following LVAD implant was 25.6% for patients who received an LVAD at a heart transplant center, compared with 11.9% at LVAD-only centers.
Thomas Cascino, MD, with University of Michigan Health Frankel Cardiovascular Center, Ann Arbor, and colleagues reported their findings in JAMA Network Open.
Differential assessment?
Nontransplant LVAD centers are increasing in number in the United States now that the CMS has made establishing an LVAD-only center easier.
“Although there should be enthusiasm for the potential of LVAD-only centers to increase access to LVAD, it appears that receiving an LVAD at a center that does not perform transplants results in differential assessment of transplant eligibility at the time of LVAD implant and inequities in receipt of transplant,” Dr. Cascino and colleagues said.
“Being cared for at a center that does not perform heart transplant should not result in a lesser chance to receive a heart transplant,” Dr. Cascino added in a university news release. “Our study shows that this disparity existed before the policy change, and we think it will likely grow larger now that there is less collaboration.”
The CMS policy will likely “further challenge equity in access to transplant for patients seeking care at nontransplant centers and may have the unintended consequence of contributing to increasing inequities in access to transplants, as has been feared,” the researchers wrote.
They also note that recent changes in the adult heart allocation system under the United Network for Organ Sharing have significantly reduced the likelihood of transplant after durable LVAD implant unless candidates are listed as being at higher urgency status owing to an LVAD complication or clinical deterioration.
“The reality is that durable LVADs are much less likely to be a bridge to the best therapy (that is, transplant) in the current allocation system. As a result, there is a critical need to select appropriate durable LVAD and transplant candidates at the initial evaluation,” the authors said.
“This puts the onus on the transplant community to select appropriate LVAD and transplant candidates during the initial evaluation. We need a system in which any patient can walk into the same hospital and get the right therapy for them,” Dr. Cascino added in the news release.
The research was supported in part through funding from the University of Michigan Health department of cardiac surgery and the National Institutes of Health, National Heart, Lung, and Blood Institute. Dr. Cascino has received grants from Johnson & Johnson.
A version of this article first appeared on Medscape.com.
A recent change in Medicare policy designed to increase access to left ventricular assist devices (LVADs) may have had the unintended consequence of increasing inequalities in access to heart transplant for patients with advanced heart failure.
In December 2020, the Centers for Medicare & Medicaid Services relaxed restrictions on centers that implant LVADs but don’t perform heart transplants. Specifically, they dropped the requirement that LVAD-only centers obtain permission from a Medicare-approved heart transplant center authorizing LVAD implantation with “bridge-to-transplant” (BTT) intent, meaning the patient is a transplant candidate.
While the relaxed requirement has the potential to increase access to LVADs for appropriate patients, a look back at 22,221 LVAD recipients found that patients who received LVADs at transplant-capable centers had a 79% higher likelihood of receiving a BTT LVAD designation.
The 2-year heart transplant rate following LVAD implant was 25.6% for patients who received an LVAD at a heart transplant center, compared with 11.9% at LVAD-only centers.
Thomas Cascino, MD, with University of Michigan Health Frankel Cardiovascular Center, Ann Arbor, and colleagues reported their findings in JAMA Network Open.
Differential assessment?
Nontransplant LVAD centers are increasing in number in the United States now that the CMS has made establishing an LVAD-only center easier.
“Although there should be enthusiasm for the potential of LVAD-only centers to increase access to LVAD, it appears that receiving an LVAD at a center that does not perform transplants results in differential assessment of transplant eligibility at the time of LVAD implant and inequities in receipt of transplant,” Dr. Cascino and colleagues said.
“Being cared for at a center that does not perform heart transplant should not result in a lesser chance to receive a heart transplant,” Dr. Cascino added in a university news release. “Our study shows that this disparity existed before the policy change, and we think it will likely grow larger now that there is less collaboration.”
The CMS policy will likely “further challenge equity in access to transplant for patients seeking care at nontransplant centers and may have the unintended consequence of contributing to increasing inequities in access to transplants, as has been feared,” the researchers wrote.
They also note that recent changes in the adult heart allocation system under the United Network for Organ Sharing have significantly reduced the likelihood of transplant after durable LVAD implant unless candidates are listed as being at higher urgency status owing to an LVAD complication or clinical deterioration.
“The reality is that durable LVADs are much less likely to be a bridge to the best therapy (that is, transplant) in the current allocation system. As a result, there is a critical need to select appropriate durable LVAD and transplant candidates at the initial evaluation,” the authors said.
“This puts the onus on the transplant community to select appropriate LVAD and transplant candidates during the initial evaluation. We need a system in which any patient can walk into the same hospital and get the right therapy for them,” Dr. Cascino added in the news release.
The research was supported in part through funding from the University of Michigan Health department of cardiac surgery and the National Institutes of Health, National Heart, Lung, and Blood Institute. Dr. Cascino has received grants from Johnson & Johnson.
A version of this article first appeared on Medscape.com.
A recent change in Medicare policy designed to increase access to left ventricular assist devices (LVADs) may have had the unintended consequence of increasing inequalities in access to heart transplant for patients with advanced heart failure.
In December 2020, the Centers for Medicare & Medicaid Services relaxed restrictions on centers that implant LVADs but don’t perform heart transplants. Specifically, they dropped the requirement that LVAD-only centers obtain permission from a Medicare-approved heart transplant center authorizing LVAD implantation with “bridge-to-transplant” (BTT) intent, meaning the patient is a transplant candidate.
While the relaxed requirement has the potential to increase access to LVADs for appropriate patients, a look back at 22,221 LVAD recipients found that patients who received LVADs at transplant-capable centers had a 79% higher likelihood of receiving a BTT LVAD designation.
The 2-year heart transplant rate following LVAD implant was 25.6% for patients who received an LVAD at a heart transplant center, compared with 11.9% at LVAD-only centers.
Thomas Cascino, MD, with University of Michigan Health Frankel Cardiovascular Center, Ann Arbor, and colleagues reported their findings in JAMA Network Open.
Differential assessment?
Nontransplant LVAD centers are increasing in number in the United States now that the CMS has made establishing an LVAD-only center easier.
“Although there should be enthusiasm for the potential of LVAD-only centers to increase access to LVAD, it appears that receiving an LVAD at a center that does not perform transplants results in differential assessment of transplant eligibility at the time of LVAD implant and inequities in receipt of transplant,” Dr. Cascino and colleagues said.
“Being cared for at a center that does not perform heart transplant should not result in a lesser chance to receive a heart transplant,” Dr. Cascino added in a university news release. “Our study shows that this disparity existed before the policy change, and we think it will likely grow larger now that there is less collaboration.”
The CMS policy will likely “further challenge equity in access to transplant for patients seeking care at nontransplant centers and may have the unintended consequence of contributing to increasing inequities in access to transplants, as has been feared,” the researchers wrote.
They also note that recent changes in the adult heart allocation system under the United Network for Organ Sharing have significantly reduced the likelihood of transplant after durable LVAD implant unless candidates are listed as being at higher urgency status owing to an LVAD complication or clinical deterioration.
“The reality is that durable LVADs are much less likely to be a bridge to the best therapy (that is, transplant) in the current allocation system. As a result, there is a critical need to select appropriate durable LVAD and transplant candidates at the initial evaluation,” the authors said.
“This puts the onus on the transplant community to select appropriate LVAD and transplant candidates during the initial evaluation. We need a system in which any patient can walk into the same hospital and get the right therapy for them,” Dr. Cascino added in the news release.
The research was supported in part through funding from the University of Michigan Health department of cardiac surgery and the National Institutes of Health, National Heart, Lung, and Blood Institute. Dr. Cascino has received grants from Johnson & Johnson.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Clarity on torsemide vs. furosemide in HF: TRANSFORM-HF published
Survival and readmission risk were similar whether patients hospitalized with heart failure (HF) were discharged on furosemide or torsemide in a randomized trial.
The study, TRANSFORM-HF, helps fill a major gap in the sparse evidence base guiding diuretic therapy in patients with a history of HF hospitalization. In that setting, for example, results suggest that discharge on any appropriate loop diuretic is more important than which loop diuretic is chosen.
TRANSFORM-HF is no ordinary randomized trial. Designed as a pragmatic comparative effectiveness study, it featured a streamlined protocol and other adaptations that made it easier and cheaper to conduct but that have also complicated its interpretation, the trialists and some observers acknowledge.
Perceived torsemide advantages
Furosemide may be the most-prescribed loop diuretic in HF, but in practice – based on some limited evidence – clinicians often prefer torsemide for its perceived advantages that include greater bioavailability, potassium sparing, and potentially helpful pleiotropic effects.
TRANSFORM-HF, however, provides no evidence to support such a preference. The primary endpoint of all-cause mortality was about 26% over a median 17 months whether patients were assigned to an initial furosemide or torsemide-first strategy, regardless of ejection fraction. Composite rates of death or hospitalization at 12 months also weren’t significantly different, at about 49% and 47%, respectively.
The findings suggest that clinicians may safely continue to prescribe either loop diuretic at their discretion, now with the support of data from a randomized trial.
TRANSFORM-HF was published in the Journal of the American Medical Association, with lead author Robert J. Mentz, MD, Duke University School of Medicine, Durham, N.C.
Dr. Mentz had also presented the trial’s preliminary results at the November American Heart Association Scientific Sessions in Chicago. The findings unveiled at the meeting and those published in the journal are essentially the same.
Reflections of standard practice
With its pragmatic design, TRANSFORM-HF entered a diverse HF population broadly representative of actual clinical practice. Patients were managed with few restrictions in a protocol that allowed, for example, loop-diuretic crossovers and other discretionary diuretic changes.
Diuretic dosing also varied significantly between the groups, and there was an unexpectedly high prevalence of diuretic withdrawal, the published report notes. Those factors, it states, may have “diminished” the trial’s ability “to distinguish the hypothesized between-group differences.”
Still, the trial “should be celebrated for dispelling a long-standing myth, based on surrogate markers and small trials, of the superiority of torsemide over furosemide,” writes Michelle M. Kittleson, MD, PhD, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, in an accompanying editorial .
Now, she continues, “when faced with a patient with heart failure and congestive symptoms, clinicians can focus their energy on what really matters: Not the relative merits of different loop diuretics, but rather the initiation and optimization of evidence and guideline-based therapies to help their patients feel better and live longer.”
Trial design caveats
But that pragmatic design raises cautions, the editorial notes. “Pragmatic trials are more flexible and nimbler in design and execution, but this agility comes at a cost. An overly heterogeneous patient population can impact the trial’s ability to assess efficacy of therapies while minimally intensive follow-up precludes comprehensive outcome assessment.”
The study’s 2,859 patients hospitalized with HF were assigned to open-label treatment with furosemide or torsemide at more than 60 U.S. centers. Of the 1,428 and 1,431 patients, respectively, about 37% were women and 34% were African American.
The hazard ratio for all cause mortality across the 17.4-month follow-up, torsemide versus furosemide, was 1.02 (95% confidence interval, 0.89-1.18). The HR for death or hospitalization for any cause at 12 months was 0.92 (95% CI, 0.83-1.02). And the rate ratio for 12-month all-cause hospitalization was 0.94 (95% CI, 0.84-1.07).
“TRANSFORM-HF joins a catalog of cautionary tales in cardiology, whereby carefully executed negative trials have refuted the misleading promise of plausible surrogate end points and preliminary data,” Dr. Kittleson writes.
“The lesson: Clinicians should have a healthy suspicion for plausible pathophysiology, surrogate end points, and nonrandomized data as the sole basis of defining superiority of an intervention.”
TRANSFORM-HF was funded by the National Institutes of Health. Dr. Mentz reports receiving grants from American Regent and Novartis; personal fees from AstraZeneca, Boehringer Ingelheim/Eli Lilly, Cytokinetics, Bayer, Merck, and Pharmacosmos; and research support from Abbott, Amgen, Bayer, Boston Scientific, Fast BioMedical, Gilead, Innolife, Medtronic, Relypsa, Respicardia, Roche, Sanofi, Vifor, Windtree Therapeutics, and Zoll. Disclosures for the other authors can be found with the original article. Dr. Kittleson reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Survival and readmission risk were similar whether patients hospitalized with heart failure (HF) were discharged on furosemide or torsemide in a randomized trial.
The study, TRANSFORM-HF, helps fill a major gap in the sparse evidence base guiding diuretic therapy in patients with a history of HF hospitalization. In that setting, for example, results suggest that discharge on any appropriate loop diuretic is more important than which loop diuretic is chosen.
TRANSFORM-HF is no ordinary randomized trial. Designed as a pragmatic comparative effectiveness study, it featured a streamlined protocol and other adaptations that made it easier and cheaper to conduct but that have also complicated its interpretation, the trialists and some observers acknowledge.
Perceived torsemide advantages
Furosemide may be the most-prescribed loop diuretic in HF, but in practice – based on some limited evidence – clinicians often prefer torsemide for its perceived advantages that include greater bioavailability, potassium sparing, and potentially helpful pleiotropic effects.
TRANSFORM-HF, however, provides no evidence to support such a preference. The primary endpoint of all-cause mortality was about 26% over a median 17 months whether patients were assigned to an initial furosemide or torsemide-first strategy, regardless of ejection fraction. Composite rates of death or hospitalization at 12 months also weren’t significantly different, at about 49% and 47%, respectively.
The findings suggest that clinicians may safely continue to prescribe either loop diuretic at their discretion, now with the support of data from a randomized trial.
TRANSFORM-HF was published in the Journal of the American Medical Association, with lead author Robert J. Mentz, MD, Duke University School of Medicine, Durham, N.C.
Dr. Mentz had also presented the trial’s preliminary results at the November American Heart Association Scientific Sessions in Chicago. The findings unveiled at the meeting and those published in the journal are essentially the same.
Reflections of standard practice
With its pragmatic design, TRANSFORM-HF entered a diverse HF population broadly representative of actual clinical practice. Patients were managed with few restrictions in a protocol that allowed, for example, loop-diuretic crossovers and other discretionary diuretic changes.
Diuretic dosing also varied significantly between the groups, and there was an unexpectedly high prevalence of diuretic withdrawal, the published report notes. Those factors, it states, may have “diminished” the trial’s ability “to distinguish the hypothesized between-group differences.”
Still, the trial “should be celebrated for dispelling a long-standing myth, based on surrogate markers and small trials, of the superiority of torsemide over furosemide,” writes Michelle M. Kittleson, MD, PhD, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, in an accompanying editorial .
Now, she continues, “when faced with a patient with heart failure and congestive symptoms, clinicians can focus their energy on what really matters: Not the relative merits of different loop diuretics, but rather the initiation and optimization of evidence and guideline-based therapies to help their patients feel better and live longer.”
Trial design caveats
But that pragmatic design raises cautions, the editorial notes. “Pragmatic trials are more flexible and nimbler in design and execution, but this agility comes at a cost. An overly heterogeneous patient population can impact the trial’s ability to assess efficacy of therapies while minimally intensive follow-up precludes comprehensive outcome assessment.”
The study’s 2,859 patients hospitalized with HF were assigned to open-label treatment with furosemide or torsemide at more than 60 U.S. centers. Of the 1,428 and 1,431 patients, respectively, about 37% were women and 34% were African American.
The hazard ratio for all cause mortality across the 17.4-month follow-up, torsemide versus furosemide, was 1.02 (95% confidence interval, 0.89-1.18). The HR for death or hospitalization for any cause at 12 months was 0.92 (95% CI, 0.83-1.02). And the rate ratio for 12-month all-cause hospitalization was 0.94 (95% CI, 0.84-1.07).
“TRANSFORM-HF joins a catalog of cautionary tales in cardiology, whereby carefully executed negative trials have refuted the misleading promise of plausible surrogate end points and preliminary data,” Dr. Kittleson writes.
“The lesson: Clinicians should have a healthy suspicion for plausible pathophysiology, surrogate end points, and nonrandomized data as the sole basis of defining superiority of an intervention.”
TRANSFORM-HF was funded by the National Institutes of Health. Dr. Mentz reports receiving grants from American Regent and Novartis; personal fees from AstraZeneca, Boehringer Ingelheim/Eli Lilly, Cytokinetics, Bayer, Merck, and Pharmacosmos; and research support from Abbott, Amgen, Bayer, Boston Scientific, Fast BioMedical, Gilead, Innolife, Medtronic, Relypsa, Respicardia, Roche, Sanofi, Vifor, Windtree Therapeutics, and Zoll. Disclosures for the other authors can be found with the original article. Dr. Kittleson reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Survival and readmission risk were similar whether patients hospitalized with heart failure (HF) were discharged on furosemide or torsemide in a randomized trial.
The study, TRANSFORM-HF, helps fill a major gap in the sparse evidence base guiding diuretic therapy in patients with a history of HF hospitalization. In that setting, for example, results suggest that discharge on any appropriate loop diuretic is more important than which loop diuretic is chosen.
TRANSFORM-HF is no ordinary randomized trial. Designed as a pragmatic comparative effectiveness study, it featured a streamlined protocol and other adaptations that made it easier and cheaper to conduct but that have also complicated its interpretation, the trialists and some observers acknowledge.
Perceived torsemide advantages
Furosemide may be the most-prescribed loop diuretic in HF, but in practice – based on some limited evidence – clinicians often prefer torsemide for its perceived advantages that include greater bioavailability, potassium sparing, and potentially helpful pleiotropic effects.
TRANSFORM-HF, however, provides no evidence to support such a preference. The primary endpoint of all-cause mortality was about 26% over a median 17 months whether patients were assigned to an initial furosemide or torsemide-first strategy, regardless of ejection fraction. Composite rates of death or hospitalization at 12 months also weren’t significantly different, at about 49% and 47%, respectively.
The findings suggest that clinicians may safely continue to prescribe either loop diuretic at their discretion, now with the support of data from a randomized trial.
TRANSFORM-HF was published in the Journal of the American Medical Association, with lead author Robert J. Mentz, MD, Duke University School of Medicine, Durham, N.C.
Dr. Mentz had also presented the trial’s preliminary results at the November American Heart Association Scientific Sessions in Chicago. The findings unveiled at the meeting and those published in the journal are essentially the same.
Reflections of standard practice
With its pragmatic design, TRANSFORM-HF entered a diverse HF population broadly representative of actual clinical practice. Patients were managed with few restrictions in a protocol that allowed, for example, loop-diuretic crossovers and other discretionary diuretic changes.
Diuretic dosing also varied significantly between the groups, and there was an unexpectedly high prevalence of diuretic withdrawal, the published report notes. Those factors, it states, may have “diminished” the trial’s ability “to distinguish the hypothesized between-group differences.”
Still, the trial “should be celebrated for dispelling a long-standing myth, based on surrogate markers and small trials, of the superiority of torsemide over furosemide,” writes Michelle M. Kittleson, MD, PhD, Smidt Heart Institute, Cedars-Sinai Medical Center, Los Angeles, in an accompanying editorial .
Now, she continues, “when faced with a patient with heart failure and congestive symptoms, clinicians can focus their energy on what really matters: Not the relative merits of different loop diuretics, but rather the initiation and optimization of evidence and guideline-based therapies to help their patients feel better and live longer.”
Trial design caveats
But that pragmatic design raises cautions, the editorial notes. “Pragmatic trials are more flexible and nimbler in design and execution, but this agility comes at a cost. An overly heterogeneous patient population can impact the trial’s ability to assess efficacy of therapies while minimally intensive follow-up precludes comprehensive outcome assessment.”
The study’s 2,859 patients hospitalized with HF were assigned to open-label treatment with furosemide or torsemide at more than 60 U.S. centers. Of the 1,428 and 1,431 patients, respectively, about 37% were women and 34% were African American.
The hazard ratio for all cause mortality across the 17.4-month follow-up, torsemide versus furosemide, was 1.02 (95% confidence interval, 0.89-1.18). The HR for death or hospitalization for any cause at 12 months was 0.92 (95% CI, 0.83-1.02). And the rate ratio for 12-month all-cause hospitalization was 0.94 (95% CI, 0.84-1.07).
“TRANSFORM-HF joins a catalog of cautionary tales in cardiology, whereby carefully executed negative trials have refuted the misleading promise of plausible surrogate end points and preliminary data,” Dr. Kittleson writes.
“The lesson: Clinicians should have a healthy suspicion for plausible pathophysiology, surrogate end points, and nonrandomized data as the sole basis of defining superiority of an intervention.”
TRANSFORM-HF was funded by the National Institutes of Health. Dr. Mentz reports receiving grants from American Regent and Novartis; personal fees from AstraZeneca, Boehringer Ingelheim/Eli Lilly, Cytokinetics, Bayer, Merck, and Pharmacosmos; and research support from Abbott, Amgen, Bayer, Boston Scientific, Fast BioMedical, Gilead, Innolife, Medtronic, Relypsa, Respicardia, Roche, Sanofi, Vifor, Windtree Therapeutics, and Zoll. Disclosures for the other authors can be found with the original article. Dr. Kittleson reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA
FDA approves new type 2 diabetes drug bexagliflozin
The U.S. Food and Drug Administration has approved bexagliflozin (Brenzavvy, TheracosBio) for the treatment of adults with type 2 diabetes.
The once-daily 20-mg oral sodium-glucose cotransporter 2 (SGLT2) inhibitor is indicated as an adjunct to diet and exercise to improve glycemic control for those with type 2 diabetes, but not type 1 diabetes. It can be used in adults with an estimated glomerular filtration rate (eGFR) > 30 mL/min per 1.73 m2.
Approval was based on results from 23 clinical trials with more than 5,000 participants, including more than 300 patients with stage 3 kidney disease (eGFR < 60 and > 30 mL/min per 1.73 m2).
In the phase 3 studies, bexagliflozin significantly reduced hemoglobin A1c and fasting blood glucose at 24 weeks as monotherapy or as add-on to metformin and other glucose-lowering drugs and combinations. It also produced modest reductions in body weight and systolic blood pressure.
In the phase 3 Bexagliflozin Efficacy and Safety Trial (BEST) cardiovascular outcomes trial, the drug met its efficacy and safety objectives in patients at high cardiovascular risk. Noninferiority was demonstrated for the composite outcome of cardiovascular death, myocardial infarction, stroke, or unstable angina.
“As a class of drugs, SGLT2 inhibitors have shown tremendous benefit in treating adults with type 2 diabetes,” said Mason Freeman, MD, director of the Translational Research Center at Massachusetts General Hospital, Boston, in a press release from TheracosBio.
“Being involved in all of the clinical trials for Brenzavvy, I am greatly impressed with the efficacy of the drug in reducing blood glucose levels and I believe it is an important addition to the SGLT2 inhibitor class of drugs.”
As with other SGLT2 inhibitors, adverse events seen in the trials include ketoacidosis, lower limb amputation, volume depletion, urosepsis, pyelonephritis, Fournier’s gangrene, genital mycotic infections, and hypoglycemia when used with insulin or insulin secretagogues.
Bexagliflozin joins an already crowded field of SGLT2 inhibitors, some of which have been approved for additional cardiovascular and kidney indications.
Of interest, bexagliflozin was approved by the FDA for diabetes in cats in December 2022, as the first oral new animal drug to improve glycemic control in otherwise healthy cats with diabetes not previously treated with insulin.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved bexagliflozin (Brenzavvy, TheracosBio) for the treatment of adults with type 2 diabetes.
The once-daily 20-mg oral sodium-glucose cotransporter 2 (SGLT2) inhibitor is indicated as an adjunct to diet and exercise to improve glycemic control for those with type 2 diabetes, but not type 1 diabetes. It can be used in adults with an estimated glomerular filtration rate (eGFR) > 30 mL/min per 1.73 m2.
Approval was based on results from 23 clinical trials with more than 5,000 participants, including more than 300 patients with stage 3 kidney disease (eGFR < 60 and > 30 mL/min per 1.73 m2).
In the phase 3 studies, bexagliflozin significantly reduced hemoglobin A1c and fasting blood glucose at 24 weeks as monotherapy or as add-on to metformin and other glucose-lowering drugs and combinations. It also produced modest reductions in body weight and systolic blood pressure.
In the phase 3 Bexagliflozin Efficacy and Safety Trial (BEST) cardiovascular outcomes trial, the drug met its efficacy and safety objectives in patients at high cardiovascular risk. Noninferiority was demonstrated for the composite outcome of cardiovascular death, myocardial infarction, stroke, or unstable angina.
“As a class of drugs, SGLT2 inhibitors have shown tremendous benefit in treating adults with type 2 diabetes,” said Mason Freeman, MD, director of the Translational Research Center at Massachusetts General Hospital, Boston, in a press release from TheracosBio.
“Being involved in all of the clinical trials for Brenzavvy, I am greatly impressed with the efficacy of the drug in reducing blood glucose levels and I believe it is an important addition to the SGLT2 inhibitor class of drugs.”
As with other SGLT2 inhibitors, adverse events seen in the trials include ketoacidosis, lower limb amputation, volume depletion, urosepsis, pyelonephritis, Fournier’s gangrene, genital mycotic infections, and hypoglycemia when used with insulin or insulin secretagogues.
Bexagliflozin joins an already crowded field of SGLT2 inhibitors, some of which have been approved for additional cardiovascular and kidney indications.
Of interest, bexagliflozin was approved by the FDA for diabetes in cats in December 2022, as the first oral new animal drug to improve glycemic control in otherwise healthy cats with diabetes not previously treated with insulin.
A version of this article first appeared on Medscape.com.
The U.S. Food and Drug Administration has approved bexagliflozin (Brenzavvy, TheracosBio) for the treatment of adults with type 2 diabetes.
The once-daily 20-mg oral sodium-glucose cotransporter 2 (SGLT2) inhibitor is indicated as an adjunct to diet and exercise to improve glycemic control for those with type 2 diabetes, but not type 1 diabetes. It can be used in adults with an estimated glomerular filtration rate (eGFR) > 30 mL/min per 1.73 m2.
Approval was based on results from 23 clinical trials with more than 5,000 participants, including more than 300 patients with stage 3 kidney disease (eGFR < 60 and > 30 mL/min per 1.73 m2).
In the phase 3 studies, bexagliflozin significantly reduced hemoglobin A1c and fasting blood glucose at 24 weeks as monotherapy or as add-on to metformin and other glucose-lowering drugs and combinations. It also produced modest reductions in body weight and systolic blood pressure.
In the phase 3 Bexagliflozin Efficacy and Safety Trial (BEST) cardiovascular outcomes trial, the drug met its efficacy and safety objectives in patients at high cardiovascular risk. Noninferiority was demonstrated for the composite outcome of cardiovascular death, myocardial infarction, stroke, or unstable angina.
“As a class of drugs, SGLT2 inhibitors have shown tremendous benefit in treating adults with type 2 diabetes,” said Mason Freeman, MD, director of the Translational Research Center at Massachusetts General Hospital, Boston, in a press release from TheracosBio.
“Being involved in all of the clinical trials for Brenzavvy, I am greatly impressed with the efficacy of the drug in reducing blood glucose levels and I believe it is an important addition to the SGLT2 inhibitor class of drugs.”
As with other SGLT2 inhibitors, adverse events seen in the trials include ketoacidosis, lower limb amputation, volume depletion, urosepsis, pyelonephritis, Fournier’s gangrene, genital mycotic infections, and hypoglycemia when used with insulin or insulin secretagogues.
Bexagliflozin joins an already crowded field of SGLT2 inhibitors, some of which have been approved for additional cardiovascular and kidney indications.
Of interest, bexagliflozin was approved by the FDA for diabetes in cats in December 2022, as the first oral new animal drug to improve glycemic control in otherwise healthy cats with diabetes not previously treated with insulin.
A version of this article first appeared on Medscape.com.









