User login
Dementia diagnosis a good time to reduce polypharmacy
Physicians may be missing opportunities to reduce harmful polypharmacy in elderly patients with newly diagnosed dementia, investigators for a large study of Medicare beneficiaries reported.
They found that those with an incident dementia diagnosis were somewhat more likely to initiate central nervous system–active medications and slightly more likely to discontinue cardiometabolic and anticholinergic medications, compared with controls.
According to the authors, time of diagnosis can be a potential inflexion point for deprescribing long-term medications with high safety risks, limited likelihood of benefit, or possible association with impaired cognition.
“Understanding the chronology of medication changes following a first dementia diagnosis may identify targets for deprescribing interventions to reduce preventable medication-related harms, said Timothy S. Anderson, MD, MAS, of the division of general medicine at Beth Israel Deaconess Medical Center, Boston, and colleagues in JAMA Internal Medicine.
“Our results provide a baseline to inform efforts to rethink the clinical approach to medication use at the time of a new dementia diagnosis.”
Hundreds of thousands of Americans are diagnosed annually with Alzheimer’s and related dementias, the authors pointed out, and the majority have multiple other chronic conditions. Worsening cognitive impairment may alter the risk-benefit balance of medications taken for these conditions.
Matched cohort study
The sample consisted of adults 67 years or older enrolled in traditional Medicare and Medicare Part D. Patients with an initial incident dementia diagnosis between January 2012 and December 2018 were matched with controls (as of last doctor’s office visit) based on demographics, geographic location, and baseline medication count. Data were analyzed from 2021 to June 2023.
The study included 266,675 adults with incident dementia and 266,675 controls. In both groups, 65.1% were 80 years or older (mean age, 82.2) and 67.8% were female. At baseline, patients with incident dementia were more likely than controls to use CNS-active medications (54.32% vs. 48.39%) and anticholinergic medications (17.79% vs. 15.96%) and less likely to use most cardiometabolic medications (for example, antidiabetics, 31.19% vs. 36.45%).
Immediately following the index diagnosis, the dementia cohort had greater increases in the mean number of medications used: 0.41 vs. –0.06 (95% confidence interval, 0.27-0.66) and in the proportion using CNS-active medications (absolute change, 3.44% vs. 0.79%; 95% CI, 0.85%-4.45%). The rise was because of an increased use of antipsychotics, antidepressants, and antiepileptics.
The affected cohort showed a modestly greater decline in anticholinergic medications: quarterly change in use: −0.53% vs. −0.21% (95% CI, −0.55% to −0.08%); and in most cardiometabolic medications: for example, quarterly change in antihypertensive use: –0.84% vs. –0.40% (95% CI, –0.64% to –0.25%). Still, a year post diagnosis, 75.2% of dementia patients were using five or more medications, for a 2.8% increase.
The drug classes with the steepest rate of discontinuation – such as lipid-lowering and antihypertensive medications – had low risks for adverse drug events, while higher-risk classes – such as insulins and antiplatelet and anticoagulant agents – had smaller or no reductions in use.
While the findings point to opportunities to reduce polypharmacy by deprescribing long-term medications of dubious benefit, interventions to reduce polypharmacy and inappropriate medications have been modestly successful for patients without dementia, the authors said. But the recent OPTIMIZE trial, an educational effort aimed at primary care clinicians and patients with cognitive impairment, reduced neither polypharmacy nor potentially inappropriate medications.
Luke D. Kim, MD, a geriatrician at the Cleveland Clinic in Ohio, agreed that seniors with dementia can benefit from reassessment of their pharmacologic therapies. “Older adults in general are more prone to have side effects from medications as their renal and hepatic clearance and metabolism are different and lower than those of younger individuals. But they tend to take multiple medications owing to more comorbidities,” said Dr. Kim, who was not involved in the study. “While all older adults need to be more careful about medication management, those with dementia need an even more careful approach as they have diminished cognitive reserve and risk more potential harm from medications.”
The authors noted that since decision-making models aligned with patient priorities for older adults without dementia led to reductions in overall medication use, that may be a path forward in populations with dementia.
The study was supported by grants from the National Institute on Aging, National Institutes of Health. The authors had no competing interests to disclose. Dr. Kim disclosed no competing interests relevant to his comments.
Physicians may be missing opportunities to reduce harmful polypharmacy in elderly patients with newly diagnosed dementia, investigators for a large study of Medicare beneficiaries reported.
They found that those with an incident dementia diagnosis were somewhat more likely to initiate central nervous system–active medications and slightly more likely to discontinue cardiometabolic and anticholinergic medications, compared with controls.
According to the authors, time of diagnosis can be a potential inflexion point for deprescribing long-term medications with high safety risks, limited likelihood of benefit, or possible association with impaired cognition.
“Understanding the chronology of medication changes following a first dementia diagnosis may identify targets for deprescribing interventions to reduce preventable medication-related harms, said Timothy S. Anderson, MD, MAS, of the division of general medicine at Beth Israel Deaconess Medical Center, Boston, and colleagues in JAMA Internal Medicine.
“Our results provide a baseline to inform efforts to rethink the clinical approach to medication use at the time of a new dementia diagnosis.”
Hundreds of thousands of Americans are diagnosed annually with Alzheimer’s and related dementias, the authors pointed out, and the majority have multiple other chronic conditions. Worsening cognitive impairment may alter the risk-benefit balance of medications taken for these conditions.
Matched cohort study
The sample consisted of adults 67 years or older enrolled in traditional Medicare and Medicare Part D. Patients with an initial incident dementia diagnosis between January 2012 and December 2018 were matched with controls (as of last doctor’s office visit) based on demographics, geographic location, and baseline medication count. Data were analyzed from 2021 to June 2023.
The study included 266,675 adults with incident dementia and 266,675 controls. In both groups, 65.1% were 80 years or older (mean age, 82.2) and 67.8% were female. At baseline, patients with incident dementia were more likely than controls to use CNS-active medications (54.32% vs. 48.39%) and anticholinergic medications (17.79% vs. 15.96%) and less likely to use most cardiometabolic medications (for example, antidiabetics, 31.19% vs. 36.45%).
Immediately following the index diagnosis, the dementia cohort had greater increases in the mean number of medications used: 0.41 vs. –0.06 (95% confidence interval, 0.27-0.66) and in the proportion using CNS-active medications (absolute change, 3.44% vs. 0.79%; 95% CI, 0.85%-4.45%). The rise was because of an increased use of antipsychotics, antidepressants, and antiepileptics.
The affected cohort showed a modestly greater decline in anticholinergic medications: quarterly change in use: −0.53% vs. −0.21% (95% CI, −0.55% to −0.08%); and in most cardiometabolic medications: for example, quarterly change in antihypertensive use: –0.84% vs. –0.40% (95% CI, –0.64% to –0.25%). Still, a year post diagnosis, 75.2% of dementia patients were using five or more medications, for a 2.8% increase.
The drug classes with the steepest rate of discontinuation – such as lipid-lowering and antihypertensive medications – had low risks for adverse drug events, while higher-risk classes – such as insulins and antiplatelet and anticoagulant agents – had smaller or no reductions in use.
While the findings point to opportunities to reduce polypharmacy by deprescribing long-term medications of dubious benefit, interventions to reduce polypharmacy and inappropriate medications have been modestly successful for patients without dementia, the authors said. But the recent OPTIMIZE trial, an educational effort aimed at primary care clinicians and patients with cognitive impairment, reduced neither polypharmacy nor potentially inappropriate medications.
Luke D. Kim, MD, a geriatrician at the Cleveland Clinic in Ohio, agreed that seniors with dementia can benefit from reassessment of their pharmacologic therapies. “Older adults in general are more prone to have side effects from medications as their renal and hepatic clearance and metabolism are different and lower than those of younger individuals. But they tend to take multiple medications owing to more comorbidities,” said Dr. Kim, who was not involved in the study. “While all older adults need to be more careful about medication management, those with dementia need an even more careful approach as they have diminished cognitive reserve and risk more potential harm from medications.”
The authors noted that since decision-making models aligned with patient priorities for older adults without dementia led to reductions in overall medication use, that may be a path forward in populations with dementia.
The study was supported by grants from the National Institute on Aging, National Institutes of Health. The authors had no competing interests to disclose. Dr. Kim disclosed no competing interests relevant to his comments.
Physicians may be missing opportunities to reduce harmful polypharmacy in elderly patients with newly diagnosed dementia, investigators for a large study of Medicare beneficiaries reported.
They found that those with an incident dementia diagnosis were somewhat more likely to initiate central nervous system–active medications and slightly more likely to discontinue cardiometabolic and anticholinergic medications, compared with controls.
According to the authors, time of diagnosis can be a potential inflexion point for deprescribing long-term medications with high safety risks, limited likelihood of benefit, or possible association with impaired cognition.
“Understanding the chronology of medication changes following a first dementia diagnosis may identify targets for deprescribing interventions to reduce preventable medication-related harms, said Timothy S. Anderson, MD, MAS, of the division of general medicine at Beth Israel Deaconess Medical Center, Boston, and colleagues in JAMA Internal Medicine.
“Our results provide a baseline to inform efforts to rethink the clinical approach to medication use at the time of a new dementia diagnosis.”
Hundreds of thousands of Americans are diagnosed annually with Alzheimer’s and related dementias, the authors pointed out, and the majority have multiple other chronic conditions. Worsening cognitive impairment may alter the risk-benefit balance of medications taken for these conditions.
Matched cohort study
The sample consisted of adults 67 years or older enrolled in traditional Medicare and Medicare Part D. Patients with an initial incident dementia diagnosis between January 2012 and December 2018 were matched with controls (as of last doctor’s office visit) based on demographics, geographic location, and baseline medication count. Data were analyzed from 2021 to June 2023.
The study included 266,675 adults with incident dementia and 266,675 controls. In both groups, 65.1% were 80 years or older (mean age, 82.2) and 67.8% were female. At baseline, patients with incident dementia were more likely than controls to use CNS-active medications (54.32% vs. 48.39%) and anticholinergic medications (17.79% vs. 15.96%) and less likely to use most cardiometabolic medications (for example, antidiabetics, 31.19% vs. 36.45%).
Immediately following the index diagnosis, the dementia cohort had greater increases in the mean number of medications used: 0.41 vs. –0.06 (95% confidence interval, 0.27-0.66) and in the proportion using CNS-active medications (absolute change, 3.44% vs. 0.79%; 95% CI, 0.85%-4.45%). The rise was because of an increased use of antipsychotics, antidepressants, and antiepileptics.
The affected cohort showed a modestly greater decline in anticholinergic medications: quarterly change in use: −0.53% vs. −0.21% (95% CI, −0.55% to −0.08%); and in most cardiometabolic medications: for example, quarterly change in antihypertensive use: –0.84% vs. –0.40% (95% CI, –0.64% to –0.25%). Still, a year post diagnosis, 75.2% of dementia patients were using five or more medications, for a 2.8% increase.
The drug classes with the steepest rate of discontinuation – such as lipid-lowering and antihypertensive medications – had low risks for adverse drug events, while higher-risk classes – such as insulins and antiplatelet and anticoagulant agents – had smaller or no reductions in use.
While the findings point to opportunities to reduce polypharmacy by deprescribing long-term medications of dubious benefit, interventions to reduce polypharmacy and inappropriate medications have been modestly successful for patients without dementia, the authors said. But the recent OPTIMIZE trial, an educational effort aimed at primary care clinicians and patients with cognitive impairment, reduced neither polypharmacy nor potentially inappropriate medications.
Luke D. Kim, MD, a geriatrician at the Cleveland Clinic in Ohio, agreed that seniors with dementia can benefit from reassessment of their pharmacologic therapies. “Older adults in general are more prone to have side effects from medications as their renal and hepatic clearance and metabolism are different and lower than those of younger individuals. But they tend to take multiple medications owing to more comorbidities,” said Dr. Kim, who was not involved in the study. “While all older adults need to be more careful about medication management, those with dementia need an even more careful approach as they have diminished cognitive reserve and risk more potential harm from medications.”
The authors noted that since decision-making models aligned with patient priorities for older adults without dementia led to reductions in overall medication use, that may be a path forward in populations with dementia.
The study was supported by grants from the National Institute on Aging, National Institutes of Health. The authors had no competing interests to disclose. Dr. Kim disclosed no competing interests relevant to his comments.
FROM JAMA INTERNAL MEDICINE
Low-dose oral minoxidil for female pattern hair loss: Benefits, impact on BP, heart rate evaluated
results from a small retrospective analysis showed.
“Additionally, few patients experienced hair loss progression while slightly over a third experienced hair regrowth,” the study’s first author, Reese Imhof, MD, a third-year resident in the department of dermatology at Mayo Clinic, Rochester, Minn., said in an interview. The results were published online in JAAD International.
At low doses, oral minoxidil, approved as an antihypertensive over 40 years ago, has become an increasingly popular treatment for hair loss, particularly since an article about its use for hair loss was published in the New York Times in August 2022. (Oral minoxidil is not approved for treating alopecia, and is used off label for this purpose.)
To evaluate the effects of LDOM in female patients with female pattern hair loss, Dr. Imhof, along with colleagues Beija Villalpando, MD, of the department of medicine and Rochelle R. Torgerson, MD, PhD, of the department of dermatology at the Mayo Clinic, reviewed the records of 25 adult women who were evaluated for female pattern hair loss at the Mayo Clinic over a 5-year period that ended on Nov. 27, 2022. Previous studies have looked at the cardiovascular effects of treatment with oral minoxidil and impact on BP in men, but “few studies have reported on female patients receiving LDOM as monotherapy for female pattern hair loss,” the authors noted.
The mean age of the women in their study was 61 years, and they took LDOM for a mean of 6.2 months. Slightly more than half (52%) took a dose of 1.25 mg daily, while 40% took 2.5 mg daily and 8% took 0.625 mg daily.
Of the 25 patients, 10 (40%) had previously tried topical minoxidil but had discontinued it because of local side effects or challenges with adherence. Also, three patients (12%) had previously tried finasteride and spironolactone but discontinued those medications because of adverse side effects.
The researchers noted disease improvement and hair regrowth was observed in nine patients who were treated with LDOM (36%), while three patients (12%) had “unaltered disease progression.” Adverse side effects observed in the cohort included four patients with facial hypertrichosis (16%) and one patient with fluid retention/lower limb edema (4%).
The patients who developed hypertrichosis did not discontinue LDOM, but the patient who developed edema did stop treatment.
At baseline, systolic BP (SBP) ranged from 107-161 mm Hg, diastolic BP (DBP) ranged from 58-88 mm Hg, and heart rate ranged from 54-114 beats per minute. Post treatment, SBP ranged from 102-152 mm Hg, DBP ranged from 63-90 mm Hg, and heart rate ranged from 56 to 105 bpm. “It was surprising how little ambulatory blood pressure and heart rate changed after an average of 6 months of treatment,” Dr. Imhof said in an interview. “On average, SBP decreased by 2.8 mm HG while DBP decreased by 1.4 mm Hg. Heart rate increased an average of 4.4 beats per minute.”
He acknowledged certain limitations of the study, including its small sample size and lack of inclusion of patients who were being treated for hypertension with concomitant antihypertensive medications. “Some unique aspects of our study are that we focused on women, and we had a slightly older cohort than prior studies (61 years old on average) as well as exposure to higher doses of LDOM, with most patients on either 1.25 mg daily or 2.5 mg daily,” Dr. Imhof said.
The researchers reported having no relevant disclosures, and there was no funding source for the study.
results from a small retrospective analysis showed.
“Additionally, few patients experienced hair loss progression while slightly over a third experienced hair regrowth,” the study’s first author, Reese Imhof, MD, a third-year resident in the department of dermatology at Mayo Clinic, Rochester, Minn., said in an interview. The results were published online in JAAD International.
At low doses, oral minoxidil, approved as an antihypertensive over 40 years ago, has become an increasingly popular treatment for hair loss, particularly since an article about its use for hair loss was published in the New York Times in August 2022. (Oral minoxidil is not approved for treating alopecia, and is used off label for this purpose.)
To evaluate the effects of LDOM in female patients with female pattern hair loss, Dr. Imhof, along with colleagues Beija Villalpando, MD, of the department of medicine and Rochelle R. Torgerson, MD, PhD, of the department of dermatology at the Mayo Clinic, reviewed the records of 25 adult women who were evaluated for female pattern hair loss at the Mayo Clinic over a 5-year period that ended on Nov. 27, 2022. Previous studies have looked at the cardiovascular effects of treatment with oral minoxidil and impact on BP in men, but “few studies have reported on female patients receiving LDOM as monotherapy for female pattern hair loss,” the authors noted.
The mean age of the women in their study was 61 years, and they took LDOM for a mean of 6.2 months. Slightly more than half (52%) took a dose of 1.25 mg daily, while 40% took 2.5 mg daily and 8% took 0.625 mg daily.
Of the 25 patients, 10 (40%) had previously tried topical minoxidil but had discontinued it because of local side effects or challenges with adherence. Also, three patients (12%) had previously tried finasteride and spironolactone but discontinued those medications because of adverse side effects.
The researchers noted disease improvement and hair regrowth was observed in nine patients who were treated with LDOM (36%), while three patients (12%) had “unaltered disease progression.” Adverse side effects observed in the cohort included four patients with facial hypertrichosis (16%) and one patient with fluid retention/lower limb edema (4%).
The patients who developed hypertrichosis did not discontinue LDOM, but the patient who developed edema did stop treatment.
At baseline, systolic BP (SBP) ranged from 107-161 mm Hg, diastolic BP (DBP) ranged from 58-88 mm Hg, and heart rate ranged from 54-114 beats per minute. Post treatment, SBP ranged from 102-152 mm Hg, DBP ranged from 63-90 mm Hg, and heart rate ranged from 56 to 105 bpm. “It was surprising how little ambulatory blood pressure and heart rate changed after an average of 6 months of treatment,” Dr. Imhof said in an interview. “On average, SBP decreased by 2.8 mm HG while DBP decreased by 1.4 mm Hg. Heart rate increased an average of 4.4 beats per minute.”
He acknowledged certain limitations of the study, including its small sample size and lack of inclusion of patients who were being treated for hypertension with concomitant antihypertensive medications. “Some unique aspects of our study are that we focused on women, and we had a slightly older cohort than prior studies (61 years old on average) as well as exposure to higher doses of LDOM, with most patients on either 1.25 mg daily or 2.5 mg daily,” Dr. Imhof said.
The researchers reported having no relevant disclosures, and there was no funding source for the study.
results from a small retrospective analysis showed.
“Additionally, few patients experienced hair loss progression while slightly over a third experienced hair regrowth,” the study’s first author, Reese Imhof, MD, a third-year resident in the department of dermatology at Mayo Clinic, Rochester, Minn., said in an interview. The results were published online in JAAD International.
At low doses, oral minoxidil, approved as an antihypertensive over 40 years ago, has become an increasingly popular treatment for hair loss, particularly since an article about its use for hair loss was published in the New York Times in August 2022. (Oral minoxidil is not approved for treating alopecia, and is used off label for this purpose.)
To evaluate the effects of LDOM in female patients with female pattern hair loss, Dr. Imhof, along with colleagues Beija Villalpando, MD, of the department of medicine and Rochelle R. Torgerson, MD, PhD, of the department of dermatology at the Mayo Clinic, reviewed the records of 25 adult women who were evaluated for female pattern hair loss at the Mayo Clinic over a 5-year period that ended on Nov. 27, 2022. Previous studies have looked at the cardiovascular effects of treatment with oral minoxidil and impact on BP in men, but “few studies have reported on female patients receiving LDOM as monotherapy for female pattern hair loss,” the authors noted.
The mean age of the women in their study was 61 years, and they took LDOM for a mean of 6.2 months. Slightly more than half (52%) took a dose of 1.25 mg daily, while 40% took 2.5 mg daily and 8% took 0.625 mg daily.
Of the 25 patients, 10 (40%) had previously tried topical minoxidil but had discontinued it because of local side effects or challenges with adherence. Also, three patients (12%) had previously tried finasteride and spironolactone but discontinued those medications because of adverse side effects.
The researchers noted disease improvement and hair regrowth was observed in nine patients who were treated with LDOM (36%), while three patients (12%) had “unaltered disease progression.” Adverse side effects observed in the cohort included four patients with facial hypertrichosis (16%) and one patient with fluid retention/lower limb edema (4%).
The patients who developed hypertrichosis did not discontinue LDOM, but the patient who developed edema did stop treatment.
At baseline, systolic BP (SBP) ranged from 107-161 mm Hg, diastolic BP (DBP) ranged from 58-88 mm Hg, and heart rate ranged from 54-114 beats per minute. Post treatment, SBP ranged from 102-152 mm Hg, DBP ranged from 63-90 mm Hg, and heart rate ranged from 56 to 105 bpm. “It was surprising how little ambulatory blood pressure and heart rate changed after an average of 6 months of treatment,” Dr. Imhof said in an interview. “On average, SBP decreased by 2.8 mm HG while DBP decreased by 1.4 mm Hg. Heart rate increased an average of 4.4 beats per minute.”
He acknowledged certain limitations of the study, including its small sample size and lack of inclusion of patients who were being treated for hypertension with concomitant antihypertensive medications. “Some unique aspects of our study are that we focused on women, and we had a slightly older cohort than prior studies (61 years old on average) as well as exposure to higher doses of LDOM, with most patients on either 1.25 mg daily or 2.5 mg daily,” Dr. Imhof said.
The researchers reported having no relevant disclosures, and there was no funding source for the study.
FROM JAAD INTERNATIONAL
‘Water fasting’ benefits don’t last
Health benefits of prolonged “water fasting” (zero calories) or Buchinger fasting (200-300 calories/day) don’t last, according to authors of a review of eight studies.
Five days of fasting lowered weight by about 6%, but this weight was regained after 3 months of regular eating, the investigators found. The article was published in Nutrition Reviews.
“Water fasting led to improvements in blood pressure, cholesterol, and blood sugar levels, but these were short-lived,” senior author Krista A. Varady, PhD, told this news organization.
“Levels returned to baseline ... quickly after participants started eating. Most benefits disappeared in 3-4 months,” said Dr. Varady, professor of nutrition at the University of Illinois, Chicago.
“My overall conclusion,” she said, “is that I guess you could try it, but it just seems like a lot of work, and all those metabolic benefits disappear. I would encourage someone hoping to lose weight to try intermittent fasting instead of water fasting, because there’s a lot more data to show it can help with weight management.
“People should consult their doctor if they have diabetes or any other major obesity-related conditions before doing water fasting,” Dr. Varady cautioned.
“Healthy people with obesity can probably fast safely for 5 days on their own (if they don’t have any other conditions). However, no one should undertake one of these fasts for more than 5 days without medical supervision,” she stressed.
Eight studies of water and Buchinger fasting
Although several favorable effects of prolonged fasting have been observed, benefits must be weighed against risks, Dr. Varady and her coauthors wrote.
Most medically supervised fasting programs have reported only minor adverse events, which included hunger, headaches, nausea, vomiting, dry mouth, and fatigue. However, more severe events have been documented, including edema, abnormal results on liver function tests, decreased bone density, and metabolic acidosis.
The researchers aimed to determine the effect of prolonged fasting on weight, blood pressure, lipid levels, and glycemic control, as well as safety and the effects of refeeding.
They examined two types of prolonged fasting: water fasting and Buchinger fasting, which involves consuming 250 mL of fruit or vegetable juice for lunch and 250 mL of soup for dinner every day of the 5- to 20-day fast.
Buchinger fasting is popular in Central Europe. Water fasting “institutes” exist in the United States, such as one in California, Dr. Varady noted.
The researchers excluded fasting during Ramadan or fasting practiced by Seventh Day Adventists.
They identified four studies of water fasting and four studies of Buchinger fasting (of which one study of 1,422 participants assessed fasting for 5, 10, 15, and 20 days).
The review showed that prolonged fasting for 5-20 days produced large increases in circulating ketones, weight loss of 2%-10%, and decreases in systolic and diastolic blood pressure.
People who fasted 5 days typically lost 4%-6% of their weight; those who fasted 7-10 days lost 2%-10% of their weight; and those who fasted 15-20 days lost 7%-10% of their weight.
LDL cholesterol and triglyceride levels decreased in some trials.
Fasting glucose levels, fasting insulin levels, insulin resistance, and A1c decreased in adults without diabetes but remained unchanged in patients with type 1 or type 2 diabetes.
Some participants experienced metabolic acidosis, headaches, insomnia, or hunger.
About two-thirds of the weight lost was of lean mass, and one-third was of fat mass. The loss of lean mass loss suggests that prolonged fasting may increase the breakdown of muscle proteins, which is a concern, the researchers noted.
Few of the trials examined the effects of refeeding. In one study, normal-weight adults lost 6% of their weight after 5 days of water-only fasting but then gained it all back after 3 months of eating regularly.
In three trials, participants regained 1%-2% of their weight 2-4 months after fasting; however, those trials instructed participants to follow a calorie-restricted diet during the refeeding period.
Three to 4 months after the fast was completed, none of the metabolic benefits were maintained, even when weight loss was maintained.
The study did not receive external funding. Dr. Varady has received author fees from Hachette Book Group for “The Every Other Day Diet” and from Pan Macmillan Press for “The Fastest Diet.” The other authors have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Health benefits of prolonged “water fasting” (zero calories) or Buchinger fasting (200-300 calories/day) don’t last, according to authors of a review of eight studies.
Five days of fasting lowered weight by about 6%, but this weight was regained after 3 months of regular eating, the investigators found. The article was published in Nutrition Reviews.
“Water fasting led to improvements in blood pressure, cholesterol, and blood sugar levels, but these were short-lived,” senior author Krista A. Varady, PhD, told this news organization.
“Levels returned to baseline ... quickly after participants started eating. Most benefits disappeared in 3-4 months,” said Dr. Varady, professor of nutrition at the University of Illinois, Chicago.
“My overall conclusion,” she said, “is that I guess you could try it, but it just seems like a lot of work, and all those metabolic benefits disappear. I would encourage someone hoping to lose weight to try intermittent fasting instead of water fasting, because there’s a lot more data to show it can help with weight management.
“People should consult their doctor if they have diabetes or any other major obesity-related conditions before doing water fasting,” Dr. Varady cautioned.
“Healthy people with obesity can probably fast safely for 5 days on their own (if they don’t have any other conditions). However, no one should undertake one of these fasts for more than 5 days without medical supervision,” she stressed.
Eight studies of water and Buchinger fasting
Although several favorable effects of prolonged fasting have been observed, benefits must be weighed against risks, Dr. Varady and her coauthors wrote.
Most medically supervised fasting programs have reported only minor adverse events, which included hunger, headaches, nausea, vomiting, dry mouth, and fatigue. However, more severe events have been documented, including edema, abnormal results on liver function tests, decreased bone density, and metabolic acidosis.
The researchers aimed to determine the effect of prolonged fasting on weight, blood pressure, lipid levels, and glycemic control, as well as safety and the effects of refeeding.
They examined two types of prolonged fasting: water fasting and Buchinger fasting, which involves consuming 250 mL of fruit or vegetable juice for lunch and 250 mL of soup for dinner every day of the 5- to 20-day fast.
Buchinger fasting is popular in Central Europe. Water fasting “institutes” exist in the United States, such as one in California, Dr. Varady noted.
The researchers excluded fasting during Ramadan or fasting practiced by Seventh Day Adventists.
They identified four studies of water fasting and four studies of Buchinger fasting (of which one study of 1,422 participants assessed fasting for 5, 10, 15, and 20 days).
The review showed that prolonged fasting for 5-20 days produced large increases in circulating ketones, weight loss of 2%-10%, and decreases in systolic and diastolic blood pressure.
People who fasted 5 days typically lost 4%-6% of their weight; those who fasted 7-10 days lost 2%-10% of their weight; and those who fasted 15-20 days lost 7%-10% of their weight.
LDL cholesterol and triglyceride levels decreased in some trials.
Fasting glucose levels, fasting insulin levels, insulin resistance, and A1c decreased in adults without diabetes but remained unchanged in patients with type 1 or type 2 diabetes.
Some participants experienced metabolic acidosis, headaches, insomnia, or hunger.
About two-thirds of the weight lost was of lean mass, and one-third was of fat mass. The loss of lean mass loss suggests that prolonged fasting may increase the breakdown of muscle proteins, which is a concern, the researchers noted.
Few of the trials examined the effects of refeeding. In one study, normal-weight adults lost 6% of their weight after 5 days of water-only fasting but then gained it all back after 3 months of eating regularly.
In three trials, participants regained 1%-2% of their weight 2-4 months after fasting; however, those trials instructed participants to follow a calorie-restricted diet during the refeeding period.
Three to 4 months after the fast was completed, none of the metabolic benefits were maintained, even when weight loss was maintained.
The study did not receive external funding. Dr. Varady has received author fees from Hachette Book Group for “The Every Other Day Diet” and from Pan Macmillan Press for “The Fastest Diet.” The other authors have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Health benefits of prolonged “water fasting” (zero calories) or Buchinger fasting (200-300 calories/day) don’t last, according to authors of a review of eight studies.
Five days of fasting lowered weight by about 6%, but this weight was regained after 3 months of regular eating, the investigators found. The article was published in Nutrition Reviews.
“Water fasting led to improvements in blood pressure, cholesterol, and blood sugar levels, but these were short-lived,” senior author Krista A. Varady, PhD, told this news organization.
“Levels returned to baseline ... quickly after participants started eating. Most benefits disappeared in 3-4 months,” said Dr. Varady, professor of nutrition at the University of Illinois, Chicago.
“My overall conclusion,” she said, “is that I guess you could try it, but it just seems like a lot of work, and all those metabolic benefits disappear. I would encourage someone hoping to lose weight to try intermittent fasting instead of water fasting, because there’s a lot more data to show it can help with weight management.
“People should consult their doctor if they have diabetes or any other major obesity-related conditions before doing water fasting,” Dr. Varady cautioned.
“Healthy people with obesity can probably fast safely for 5 days on their own (if they don’t have any other conditions). However, no one should undertake one of these fasts for more than 5 days without medical supervision,” she stressed.
Eight studies of water and Buchinger fasting
Although several favorable effects of prolonged fasting have been observed, benefits must be weighed against risks, Dr. Varady and her coauthors wrote.
Most medically supervised fasting programs have reported only minor adverse events, which included hunger, headaches, nausea, vomiting, dry mouth, and fatigue. However, more severe events have been documented, including edema, abnormal results on liver function tests, decreased bone density, and metabolic acidosis.
The researchers aimed to determine the effect of prolonged fasting on weight, blood pressure, lipid levels, and glycemic control, as well as safety and the effects of refeeding.
They examined two types of prolonged fasting: water fasting and Buchinger fasting, which involves consuming 250 mL of fruit or vegetable juice for lunch and 250 mL of soup for dinner every day of the 5- to 20-day fast.
Buchinger fasting is popular in Central Europe. Water fasting “institutes” exist in the United States, such as one in California, Dr. Varady noted.
The researchers excluded fasting during Ramadan or fasting practiced by Seventh Day Adventists.
They identified four studies of water fasting and four studies of Buchinger fasting (of which one study of 1,422 participants assessed fasting for 5, 10, 15, and 20 days).
The review showed that prolonged fasting for 5-20 days produced large increases in circulating ketones, weight loss of 2%-10%, and decreases in systolic and diastolic blood pressure.
People who fasted 5 days typically lost 4%-6% of their weight; those who fasted 7-10 days lost 2%-10% of their weight; and those who fasted 15-20 days lost 7%-10% of their weight.
LDL cholesterol and triglyceride levels decreased in some trials.
Fasting glucose levels, fasting insulin levels, insulin resistance, and A1c decreased in adults without diabetes but remained unchanged in patients with type 1 or type 2 diabetes.
Some participants experienced metabolic acidosis, headaches, insomnia, or hunger.
About two-thirds of the weight lost was of lean mass, and one-third was of fat mass. The loss of lean mass loss suggests that prolonged fasting may increase the breakdown of muscle proteins, which is a concern, the researchers noted.
Few of the trials examined the effects of refeeding. In one study, normal-weight adults lost 6% of their weight after 5 days of water-only fasting but then gained it all back after 3 months of eating regularly.
In three trials, participants regained 1%-2% of their weight 2-4 months after fasting; however, those trials instructed participants to follow a calorie-restricted diet during the refeeding period.
Three to 4 months after the fast was completed, none of the metabolic benefits were maintained, even when weight loss was maintained.
The study did not receive external funding. Dr. Varady has received author fees from Hachette Book Group for “The Every Other Day Diet” and from Pan Macmillan Press for “The Fastest Diet.” The other authors have disclosed no relevant financial relationships.
A version of this article appeared on Medscape.com.
Isometric exercise found optimal for lowering blood pressure?
The findings support the development of new exercise guidelines for blood pressure control, the authors said.
Previous research, based on older data that excluded high-intensity interval training (HIIT) and isometric exercise training (IET), led to aerobic exercise training (AET) being recommended for managing blood pressure, according to the authors.
Although AET, HIIT, dynamic resistance training (RT), and combined training (CT) are also effective in reducing both systolic and diastolic blood pressure, the new analysis suggests that IET does it best.
The analysis showed reductions in blood pressure of 8.24/4 mm Hg after IET, compared with 4.49/2.53 mm Hg after AET; 4.55/3.04 mm Hg after RT; 6.04/2.54 mm Hg after CT; and 4.08/2.50 mm Hg after HIIT.
“These findings mirror our smaller-scale trials, and therefore we anticipated that isometrics would be largely effective,” Jamie O’Driscoll, PhD, of Canterbury (England) Christ Church University, said in an interview. However, “the magnitude of difference between isometrics and some other modes was surprising.”
The study was published online in the British Journal of Sports Medicine.
All modes effective
The investigators analyzed data from 270 randomized controlled trials including 15,827 people published between 1990 and February 2023. For consistency, the protocol/intensity of each included paper was screened against the Exercise Prescription in Everyday Practice and Rehabilitative Training tool to be defined and categorized.
All protocols were then stratified as AET, RT, CT, HIIT or IET.
As appropriate, protocols were then further stratified into subgroups: AET included walking, running, and cycling; HIIT included sprint interval training and aerobic interval training; and IET included isometric leg extension and isometric wall squat.
Healthy resting blood pressure was defined as a reading below 130/85 mm Hg, prehypertension as 130-139/85-89 mm Hg, and hypertension as 140/90 mm Hg or higher.
All exercise modes led to statistically significant reductions in systolic BP in normal blood pressure cohorts; however, all reductions were substantially larger in individuals with hypertension.
Pairwise analyses showed significant reductions in resting systolic BP and diastolic BP following AET (−4.49/–2.53 mm Hg); RT (–4.55/–3.04 mm Hg), CT (–6.04/–2.54 mm Hg), HIT (–4.08/–2.50 mm Hg); and IET (–8.24/–4.00 mm Hg).
In the network meta-analysis, the rank order of effectiveness for systolic BP based on surface under the cumulative ranking curve values were IET (SUCRA: 98.3%), CT (75.7%), RT (46.1%), AET (40.5%), and HIIT (39.4%).
Secondary network meta-analyses showed that isometric wall squat was the most effective submode for reducing systolic BP (90.4%), followed by isometric leg extension, isometric hand grip, cycling, running, CT, sprint interval training, other aerobic, RT, aerobic interval training, and walking.
Running was the most effective submode for lowering diastolic BP (91.3%), followed by isometric wall squat, isometric handgrip, isometric leg extension, cycling, sprint interval training, RT, AIT, other aerobic, CT, and walking.
The authors acknowledged limitations, including variability in exercise interventions, missing data, variable quality of exercise monitoring and analyses, lack of blinding to group allocation, varying participant populations, and publication bias.
Nevertheless, they concluded, “the results of this analysis should inform future exercise guideline recommendations for the prevention and treatment of arterial hypertension.”
Guideline changing?
“There are numerous organizations involved in providing and communicating population exercise guidelines,” including World Health Organization, American and European exercise guidelines, and the National Institute for Health and Care Excellence, Dr. O’Driscoll said. “We are currently developing an international collaborative project with other world leaders in the area to develop this line of enquiry.”
In addition, the team is exploring the prescription of IET within England’s National Health Service and extending the study to wider clinical populations.
In a comment, John A. Osborne, MD, PhD, founder and director of State of the Heart Cardiology in Southlake, Tex., said: “This study further lends credence that other forms of exercise, beyond the usually recommended aerobic exercise promulgated in prior guidelines, have significant value for blood pressure lowering, and, potentially, may offer even greater benefits for ... controlling hypertension.”
“This study should inform contemporary nonpharmacological approaches to blood pressure management and allows providers more flexibility in different strategies of exercise to combat high blood pressure,” said Dr. Osborne, a volunteer spokesperson for the American Heart Association.
That said, “while this study by itself is extremely provocative, thoughtful, and rigorously performed, it should be used as hypothesis generating and hopefully [will be followed by] head-to-head studies of aerobic exercise versus resistance training to confirm the findings.”
The study received no funding. Dr. O’Driscoll and Dr. Osborne reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The findings support the development of new exercise guidelines for blood pressure control, the authors said.
Previous research, based on older data that excluded high-intensity interval training (HIIT) and isometric exercise training (IET), led to aerobic exercise training (AET) being recommended for managing blood pressure, according to the authors.
Although AET, HIIT, dynamic resistance training (RT), and combined training (CT) are also effective in reducing both systolic and diastolic blood pressure, the new analysis suggests that IET does it best.
The analysis showed reductions in blood pressure of 8.24/4 mm Hg after IET, compared with 4.49/2.53 mm Hg after AET; 4.55/3.04 mm Hg after RT; 6.04/2.54 mm Hg after CT; and 4.08/2.50 mm Hg after HIIT.
“These findings mirror our smaller-scale trials, and therefore we anticipated that isometrics would be largely effective,” Jamie O’Driscoll, PhD, of Canterbury (England) Christ Church University, said in an interview. However, “the magnitude of difference between isometrics and some other modes was surprising.”
The study was published online in the British Journal of Sports Medicine.
All modes effective
The investigators analyzed data from 270 randomized controlled trials including 15,827 people published between 1990 and February 2023. For consistency, the protocol/intensity of each included paper was screened against the Exercise Prescription in Everyday Practice and Rehabilitative Training tool to be defined and categorized.
All protocols were then stratified as AET, RT, CT, HIIT or IET.
As appropriate, protocols were then further stratified into subgroups: AET included walking, running, and cycling; HIIT included sprint interval training and aerobic interval training; and IET included isometric leg extension and isometric wall squat.
Healthy resting blood pressure was defined as a reading below 130/85 mm Hg, prehypertension as 130-139/85-89 mm Hg, and hypertension as 140/90 mm Hg or higher.
All exercise modes led to statistically significant reductions in systolic BP in normal blood pressure cohorts; however, all reductions were substantially larger in individuals with hypertension.
Pairwise analyses showed significant reductions in resting systolic BP and diastolic BP following AET (−4.49/–2.53 mm Hg); RT (–4.55/–3.04 mm Hg), CT (–6.04/–2.54 mm Hg), HIT (–4.08/–2.50 mm Hg); and IET (–8.24/–4.00 mm Hg).
In the network meta-analysis, the rank order of effectiveness for systolic BP based on surface under the cumulative ranking curve values were IET (SUCRA: 98.3%), CT (75.7%), RT (46.1%), AET (40.5%), and HIIT (39.4%).
Secondary network meta-analyses showed that isometric wall squat was the most effective submode for reducing systolic BP (90.4%), followed by isometric leg extension, isometric hand grip, cycling, running, CT, sprint interval training, other aerobic, RT, aerobic interval training, and walking.
Running was the most effective submode for lowering diastolic BP (91.3%), followed by isometric wall squat, isometric handgrip, isometric leg extension, cycling, sprint interval training, RT, AIT, other aerobic, CT, and walking.
The authors acknowledged limitations, including variability in exercise interventions, missing data, variable quality of exercise monitoring and analyses, lack of blinding to group allocation, varying participant populations, and publication bias.
Nevertheless, they concluded, “the results of this analysis should inform future exercise guideline recommendations for the prevention and treatment of arterial hypertension.”
Guideline changing?
“There are numerous organizations involved in providing and communicating population exercise guidelines,” including World Health Organization, American and European exercise guidelines, and the National Institute for Health and Care Excellence, Dr. O’Driscoll said. “We are currently developing an international collaborative project with other world leaders in the area to develop this line of enquiry.”
In addition, the team is exploring the prescription of IET within England’s National Health Service and extending the study to wider clinical populations.
In a comment, John A. Osborne, MD, PhD, founder and director of State of the Heart Cardiology in Southlake, Tex., said: “This study further lends credence that other forms of exercise, beyond the usually recommended aerobic exercise promulgated in prior guidelines, have significant value for blood pressure lowering, and, potentially, may offer even greater benefits for ... controlling hypertension.”
“This study should inform contemporary nonpharmacological approaches to blood pressure management and allows providers more flexibility in different strategies of exercise to combat high blood pressure,” said Dr. Osborne, a volunteer spokesperson for the American Heart Association.
That said, “while this study by itself is extremely provocative, thoughtful, and rigorously performed, it should be used as hypothesis generating and hopefully [will be followed by] head-to-head studies of aerobic exercise versus resistance training to confirm the findings.”
The study received no funding. Dr. O’Driscoll and Dr. Osborne reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The findings support the development of new exercise guidelines for blood pressure control, the authors said.
Previous research, based on older data that excluded high-intensity interval training (HIIT) and isometric exercise training (IET), led to aerobic exercise training (AET) being recommended for managing blood pressure, according to the authors.
Although AET, HIIT, dynamic resistance training (RT), and combined training (CT) are also effective in reducing both systolic and diastolic blood pressure, the new analysis suggests that IET does it best.
The analysis showed reductions in blood pressure of 8.24/4 mm Hg after IET, compared with 4.49/2.53 mm Hg after AET; 4.55/3.04 mm Hg after RT; 6.04/2.54 mm Hg after CT; and 4.08/2.50 mm Hg after HIIT.
“These findings mirror our smaller-scale trials, and therefore we anticipated that isometrics would be largely effective,” Jamie O’Driscoll, PhD, of Canterbury (England) Christ Church University, said in an interview. However, “the magnitude of difference between isometrics and some other modes was surprising.”
The study was published online in the British Journal of Sports Medicine.
All modes effective
The investigators analyzed data from 270 randomized controlled trials including 15,827 people published between 1990 and February 2023. For consistency, the protocol/intensity of each included paper was screened against the Exercise Prescription in Everyday Practice and Rehabilitative Training tool to be defined and categorized.
All protocols were then stratified as AET, RT, CT, HIIT or IET.
As appropriate, protocols were then further stratified into subgroups: AET included walking, running, and cycling; HIIT included sprint interval training and aerobic interval training; and IET included isometric leg extension and isometric wall squat.
Healthy resting blood pressure was defined as a reading below 130/85 mm Hg, prehypertension as 130-139/85-89 mm Hg, and hypertension as 140/90 mm Hg or higher.
All exercise modes led to statistically significant reductions in systolic BP in normal blood pressure cohorts; however, all reductions were substantially larger in individuals with hypertension.
Pairwise analyses showed significant reductions in resting systolic BP and diastolic BP following AET (−4.49/–2.53 mm Hg); RT (–4.55/–3.04 mm Hg), CT (–6.04/–2.54 mm Hg), HIT (–4.08/–2.50 mm Hg); and IET (–8.24/–4.00 mm Hg).
In the network meta-analysis, the rank order of effectiveness for systolic BP based on surface under the cumulative ranking curve values were IET (SUCRA: 98.3%), CT (75.7%), RT (46.1%), AET (40.5%), and HIIT (39.4%).
Secondary network meta-analyses showed that isometric wall squat was the most effective submode for reducing systolic BP (90.4%), followed by isometric leg extension, isometric hand grip, cycling, running, CT, sprint interval training, other aerobic, RT, aerobic interval training, and walking.
Running was the most effective submode for lowering diastolic BP (91.3%), followed by isometric wall squat, isometric handgrip, isometric leg extension, cycling, sprint interval training, RT, AIT, other aerobic, CT, and walking.
The authors acknowledged limitations, including variability in exercise interventions, missing data, variable quality of exercise monitoring and analyses, lack of blinding to group allocation, varying participant populations, and publication bias.
Nevertheless, they concluded, “the results of this analysis should inform future exercise guideline recommendations for the prevention and treatment of arterial hypertension.”
Guideline changing?
“There are numerous organizations involved in providing and communicating population exercise guidelines,” including World Health Organization, American and European exercise guidelines, and the National Institute for Health and Care Excellence, Dr. O’Driscoll said. “We are currently developing an international collaborative project with other world leaders in the area to develop this line of enquiry.”
In addition, the team is exploring the prescription of IET within England’s National Health Service and extending the study to wider clinical populations.
In a comment, John A. Osborne, MD, PhD, founder and director of State of the Heart Cardiology in Southlake, Tex., said: “This study further lends credence that other forms of exercise, beyond the usually recommended aerobic exercise promulgated in prior guidelines, have significant value for blood pressure lowering, and, potentially, may offer even greater benefits for ... controlling hypertension.”
“This study should inform contemporary nonpharmacological approaches to blood pressure management and allows providers more flexibility in different strategies of exercise to combat high blood pressure,” said Dr. Osborne, a volunteer spokesperson for the American Heart Association.
That said, “while this study by itself is extremely provocative, thoughtful, and rigorously performed, it should be used as hypothesis generating and hopefully [will be followed by] head-to-head studies of aerobic exercise versus resistance training to confirm the findings.”
The study received no funding. Dr. O’Driscoll and Dr. Osborne reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF SPORTS MEDICINE
One size doesn’t fit all in blood pressure measurement
As with porridge, so with blood pressure: Just right makes all the difference.
according to research published in JAMA Internal Medicine.
People whose mid-upper arm circumference exceeds 32 cm require larger cuffs than the standard size, but in many cases the regular-sized cuff is used on everyone. As a result, patients with larger arms may be falsely diagnosed with high blood pressure because of a too-small cuff, leading to overprescribing of medications that could make their health worse, according to the researchers.
“A person whose blood pressure is 120/80, which is normal – if they’re using the wrong cuff, they could get a measurement that says 140/90, let’s say,” said study author Tammy M. Brady, MD, PhD, vice chair for clinical research in the department of pediatrics at Johns Hopkins University, Baltimore. “They might think they not only have hypertension, but stage 2 hypertension. Providers might give one or even two medicines to lower this, which could lead to hypotension,” Dr. Brady said.
Conversely, someone with smaller arms whose cuff is too big may present with an artificially low blood pressure. The implications of using ill-fitting cuffs are well known. Dr. Brady, among others, has studied the topic extensively. Even so, she said the measurement errors in the latest study were larger than expected.
The Goldilocks test
People with an arm circumference of 20-25 cm should use a smaller cuff than the regular size, Dr. Brady and colleagues reported. Circumferences of 25.1-32 cm require a regular-sized cuff; large cuffs are for circumferences of 32.1-40 cm; and extra-large cuffs should be used at 40.1-55 cm.
The study included 195 residents of Baltimore (128 women, 67 men; 132 Black, 58 White, 5 Hispanic) with an average age of 54 years. The researchers measured every participant’s blood pressure using an automated device on four occasions, taking three measurements each time.
The first three sets of measurements used, respectively, an appropriate cuff size for each person’s arm circumference; a cuff that was too big; and a cuff that was too small. This study design ensured that a regular-sized cuff would be used during one of the three measurements – sometimes that cuff was too small, sometimes it was appropriate, and other times it was too big.
The final set of three measurements used the appropriate cuff size for a person’s arm every time. Dr. Brady and colleagues then compared people’s blood pressure measurements when using the right-sized cuff to measurements with a regular-sized cuff that was not suited for them.
They found that using a cuff that was too large for the patient’s arm (i.e., using a regular cuff when a small cuff was the right choice) led to understating systolic blood pressure by –3.6 mm Hg (95% confidence interval [CI], –5.6 to –1.7). A cuff that was one size too small – using regular instead of a large – overestimated systolic blood pressure by 4.8 (3.0-6.6) mm Hg. And a cuff that was two sizes too small – someone who should have received an extra-large cuff but received the regular size – overestimated systolic blood pressure by 19.5 (16.1-22.9) mm Hg. All differences were statistically significant, the researchers reported.
“To our knowledge, this is the first randomized cross-over trial to examine the effect of miscuffing on automated blood pressure readings,” Mathias Lalika, MD, MPH, of the Mayo Clinic in Rochester, Minn.; Stephen P. Juraschek, MD, PhD, of Beth Israel Deaconess Medical Center in Boston; and LaPrincess C. Brewer, MD, MPH, of the Mayo Clinic, wrote in an editorial accompanying the journal article.
“Interestingly, the degree of underestimation or overestimation increased as the appropriate cuff size progressed from the regular to extra-large BP cuff. More importantly, the effect of miscuffing did not vary with BP or obesity status,” they wrote.
“This was more of a pragmatic trial to see real world, all comers,” Dr. Brady said, when regular-sized cuffs are used whether or not that made sense.
“This study reaffirms findings of previous studies and highlights a major source of error in blood pressure measurement,” Raj Padwal, MD, director of the University of Alberta Hypertension Clinic, Edmonton, Alta., said in an interview. Dr. Padwal, who was not involved in the study, said the findings highlight the importance of ensuring that technicians who typically measure blood pressure understand the value of using the right-sized cuff.
Dr. Brady noted that measuring arm circumference takes about 15 seconds. He advised health organizations and clinics to carry multiple cuffs sizes to avoid a scramble to find a right-sized cuff. In the editorial, Dr. Lalika, Dr. Juraschek, and Dr. Brewer call for particular attention to providing the right-sized cuffs to facilities that work with underserved populations, such as federally qualified health centers.
Dr. Padwal added that even a perfectly measured blood pressure test at a clinic indicates pressure at a moment in time. Ten minutes later the story could be different. For this reason, he and other clinicians recommend frequent home blood pressure measurements rather than relying solely on the sparse number of readings collected in the clinic setting.
“A properly educated patient can give many readings that are separated in space and time and, when averaged, can give a much better picture of overall blood pressure and future risk,” Dr. Padwal said.
Dr. Brady agreed with the value of home readings but said home-based readings also can be erroneous if the patient uses a cuff that is the wrong size. She cochairs a committee for the American Medical Association that recommends validated home blood pressure measurement devices on a periodically updated website called Validate BP. The details for each device listing show the cuff sizes available per device. Many devices provide only the standard cuff, Dr. Brady noted, but some offer multiple cuff sizes.
“One of the things that would be great if it came out of this paper is if patients were empowered to ask physicians to measure their arm” and then use that information to select the appropriate cuff for their home device, she said.
Dr. Brady and Dr. Padwal reported no relevant financial relationships. This study was supported by Resolve to Save Lives, which is funded by Bloomberg Philanthropies, the Bill & Melinda Gates Foundation, and Gates Philanthropy Partners, which is funded with support from the Chan Zuckerberg Foundation.
A version of this article appeared on Medscape.com.
As with porridge, so with blood pressure: Just right makes all the difference.
according to research published in JAMA Internal Medicine.
People whose mid-upper arm circumference exceeds 32 cm require larger cuffs than the standard size, but in many cases the regular-sized cuff is used on everyone. As a result, patients with larger arms may be falsely diagnosed with high blood pressure because of a too-small cuff, leading to overprescribing of medications that could make their health worse, according to the researchers.
“A person whose blood pressure is 120/80, which is normal – if they’re using the wrong cuff, they could get a measurement that says 140/90, let’s say,” said study author Tammy M. Brady, MD, PhD, vice chair for clinical research in the department of pediatrics at Johns Hopkins University, Baltimore. “They might think they not only have hypertension, but stage 2 hypertension. Providers might give one or even two medicines to lower this, which could lead to hypotension,” Dr. Brady said.
Conversely, someone with smaller arms whose cuff is too big may present with an artificially low blood pressure. The implications of using ill-fitting cuffs are well known. Dr. Brady, among others, has studied the topic extensively. Even so, she said the measurement errors in the latest study were larger than expected.
The Goldilocks test
People with an arm circumference of 20-25 cm should use a smaller cuff than the regular size, Dr. Brady and colleagues reported. Circumferences of 25.1-32 cm require a regular-sized cuff; large cuffs are for circumferences of 32.1-40 cm; and extra-large cuffs should be used at 40.1-55 cm.
The study included 195 residents of Baltimore (128 women, 67 men; 132 Black, 58 White, 5 Hispanic) with an average age of 54 years. The researchers measured every participant’s blood pressure using an automated device on four occasions, taking three measurements each time.
The first three sets of measurements used, respectively, an appropriate cuff size for each person’s arm circumference; a cuff that was too big; and a cuff that was too small. This study design ensured that a regular-sized cuff would be used during one of the three measurements – sometimes that cuff was too small, sometimes it was appropriate, and other times it was too big.
The final set of three measurements used the appropriate cuff size for a person’s arm every time. Dr. Brady and colleagues then compared people’s blood pressure measurements when using the right-sized cuff to measurements with a regular-sized cuff that was not suited for them.
They found that using a cuff that was too large for the patient’s arm (i.e., using a regular cuff when a small cuff was the right choice) led to understating systolic blood pressure by –3.6 mm Hg (95% confidence interval [CI], –5.6 to –1.7). A cuff that was one size too small – using regular instead of a large – overestimated systolic blood pressure by 4.8 (3.0-6.6) mm Hg. And a cuff that was two sizes too small – someone who should have received an extra-large cuff but received the regular size – overestimated systolic blood pressure by 19.5 (16.1-22.9) mm Hg. All differences were statistically significant, the researchers reported.
“To our knowledge, this is the first randomized cross-over trial to examine the effect of miscuffing on automated blood pressure readings,” Mathias Lalika, MD, MPH, of the Mayo Clinic in Rochester, Minn.; Stephen P. Juraschek, MD, PhD, of Beth Israel Deaconess Medical Center in Boston; and LaPrincess C. Brewer, MD, MPH, of the Mayo Clinic, wrote in an editorial accompanying the journal article.
“Interestingly, the degree of underestimation or overestimation increased as the appropriate cuff size progressed from the regular to extra-large BP cuff. More importantly, the effect of miscuffing did not vary with BP or obesity status,” they wrote.
“This was more of a pragmatic trial to see real world, all comers,” Dr. Brady said, when regular-sized cuffs are used whether or not that made sense.
“This study reaffirms findings of previous studies and highlights a major source of error in blood pressure measurement,” Raj Padwal, MD, director of the University of Alberta Hypertension Clinic, Edmonton, Alta., said in an interview. Dr. Padwal, who was not involved in the study, said the findings highlight the importance of ensuring that technicians who typically measure blood pressure understand the value of using the right-sized cuff.
Dr. Brady noted that measuring arm circumference takes about 15 seconds. He advised health organizations and clinics to carry multiple cuffs sizes to avoid a scramble to find a right-sized cuff. In the editorial, Dr. Lalika, Dr. Juraschek, and Dr. Brewer call for particular attention to providing the right-sized cuffs to facilities that work with underserved populations, such as federally qualified health centers.
Dr. Padwal added that even a perfectly measured blood pressure test at a clinic indicates pressure at a moment in time. Ten minutes later the story could be different. For this reason, he and other clinicians recommend frequent home blood pressure measurements rather than relying solely on the sparse number of readings collected in the clinic setting.
“A properly educated patient can give many readings that are separated in space and time and, when averaged, can give a much better picture of overall blood pressure and future risk,” Dr. Padwal said.
Dr. Brady agreed with the value of home readings but said home-based readings also can be erroneous if the patient uses a cuff that is the wrong size. She cochairs a committee for the American Medical Association that recommends validated home blood pressure measurement devices on a periodically updated website called Validate BP. The details for each device listing show the cuff sizes available per device. Many devices provide only the standard cuff, Dr. Brady noted, but some offer multiple cuff sizes.
“One of the things that would be great if it came out of this paper is if patients were empowered to ask physicians to measure their arm” and then use that information to select the appropriate cuff for their home device, she said.
Dr. Brady and Dr. Padwal reported no relevant financial relationships. This study was supported by Resolve to Save Lives, which is funded by Bloomberg Philanthropies, the Bill & Melinda Gates Foundation, and Gates Philanthropy Partners, which is funded with support from the Chan Zuckerberg Foundation.
A version of this article appeared on Medscape.com.
As with porridge, so with blood pressure: Just right makes all the difference.
according to research published in JAMA Internal Medicine.
People whose mid-upper arm circumference exceeds 32 cm require larger cuffs than the standard size, but in many cases the regular-sized cuff is used on everyone. As a result, patients with larger arms may be falsely diagnosed with high blood pressure because of a too-small cuff, leading to overprescribing of medications that could make their health worse, according to the researchers.
“A person whose blood pressure is 120/80, which is normal – if they’re using the wrong cuff, they could get a measurement that says 140/90, let’s say,” said study author Tammy M. Brady, MD, PhD, vice chair for clinical research in the department of pediatrics at Johns Hopkins University, Baltimore. “They might think they not only have hypertension, but stage 2 hypertension. Providers might give one or even two medicines to lower this, which could lead to hypotension,” Dr. Brady said.
Conversely, someone with smaller arms whose cuff is too big may present with an artificially low blood pressure. The implications of using ill-fitting cuffs are well known. Dr. Brady, among others, has studied the topic extensively. Even so, she said the measurement errors in the latest study were larger than expected.
The Goldilocks test
People with an arm circumference of 20-25 cm should use a smaller cuff than the regular size, Dr. Brady and colleagues reported. Circumferences of 25.1-32 cm require a regular-sized cuff; large cuffs are for circumferences of 32.1-40 cm; and extra-large cuffs should be used at 40.1-55 cm.
The study included 195 residents of Baltimore (128 women, 67 men; 132 Black, 58 White, 5 Hispanic) with an average age of 54 years. The researchers measured every participant’s blood pressure using an automated device on four occasions, taking three measurements each time.
The first three sets of measurements used, respectively, an appropriate cuff size for each person’s arm circumference; a cuff that was too big; and a cuff that was too small. This study design ensured that a regular-sized cuff would be used during one of the three measurements – sometimes that cuff was too small, sometimes it was appropriate, and other times it was too big.
The final set of three measurements used the appropriate cuff size for a person’s arm every time. Dr. Brady and colleagues then compared people’s blood pressure measurements when using the right-sized cuff to measurements with a regular-sized cuff that was not suited for them.
They found that using a cuff that was too large for the patient’s arm (i.e., using a regular cuff when a small cuff was the right choice) led to understating systolic blood pressure by –3.6 mm Hg (95% confidence interval [CI], –5.6 to –1.7). A cuff that was one size too small – using regular instead of a large – overestimated systolic blood pressure by 4.8 (3.0-6.6) mm Hg. And a cuff that was two sizes too small – someone who should have received an extra-large cuff but received the regular size – overestimated systolic blood pressure by 19.5 (16.1-22.9) mm Hg. All differences were statistically significant, the researchers reported.
“To our knowledge, this is the first randomized cross-over trial to examine the effect of miscuffing on automated blood pressure readings,” Mathias Lalika, MD, MPH, of the Mayo Clinic in Rochester, Minn.; Stephen P. Juraschek, MD, PhD, of Beth Israel Deaconess Medical Center in Boston; and LaPrincess C. Brewer, MD, MPH, of the Mayo Clinic, wrote in an editorial accompanying the journal article.
“Interestingly, the degree of underestimation or overestimation increased as the appropriate cuff size progressed from the regular to extra-large BP cuff. More importantly, the effect of miscuffing did not vary with BP or obesity status,” they wrote.
“This was more of a pragmatic trial to see real world, all comers,” Dr. Brady said, when regular-sized cuffs are used whether or not that made sense.
“This study reaffirms findings of previous studies and highlights a major source of error in blood pressure measurement,” Raj Padwal, MD, director of the University of Alberta Hypertension Clinic, Edmonton, Alta., said in an interview. Dr. Padwal, who was not involved in the study, said the findings highlight the importance of ensuring that technicians who typically measure blood pressure understand the value of using the right-sized cuff.
Dr. Brady noted that measuring arm circumference takes about 15 seconds. He advised health organizations and clinics to carry multiple cuffs sizes to avoid a scramble to find a right-sized cuff. In the editorial, Dr. Lalika, Dr. Juraschek, and Dr. Brewer call for particular attention to providing the right-sized cuffs to facilities that work with underserved populations, such as federally qualified health centers.
Dr. Padwal added that even a perfectly measured blood pressure test at a clinic indicates pressure at a moment in time. Ten minutes later the story could be different. For this reason, he and other clinicians recommend frequent home blood pressure measurements rather than relying solely on the sparse number of readings collected in the clinic setting.
“A properly educated patient can give many readings that are separated in space and time and, when averaged, can give a much better picture of overall blood pressure and future risk,” Dr. Padwal said.
Dr. Brady agreed with the value of home readings but said home-based readings also can be erroneous if the patient uses a cuff that is the wrong size. She cochairs a committee for the American Medical Association that recommends validated home blood pressure measurement devices on a periodically updated website called Validate BP. The details for each device listing show the cuff sizes available per device. Many devices provide only the standard cuff, Dr. Brady noted, but some offer multiple cuff sizes.
“One of the things that would be great if it came out of this paper is if patients were empowered to ask physicians to measure their arm” and then use that information to select the appropriate cuff for their home device, she said.
Dr. Brady and Dr. Padwal reported no relevant financial relationships. This study was supported by Resolve to Save Lives, which is funded by Bloomberg Philanthropies, the Bill & Melinda Gates Foundation, and Gates Philanthropy Partners, which is funded with support from the Chan Zuckerberg Foundation.
A version of this article appeared on Medscape.com.
FROM JAMA INTERNAL MEDICINE
Even one drink a day tied to increased BP in healthy adults
“A vexing question has been whether usual intake of small amounts of alcohol is associated with a higher level of BP. We identified a continuous, more or less linear association, with no evidence of a threshold for the association,” study coauthor Paul Whelton, MD, of Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
For systolic BP (SBP), “the most important BP risk indicator for CVD [cardiovascular disease], the association was robust, being present in both men and women and in both North America as well as Asia,” Dr. Whelton noted.
Based on the results, “the lower the better, and no consumption even better, as we did not find any indication that human health may benefit from consumption of very small amounts of alcohol,” senior author Marco Vinceti, MD, PhD, of University of Modena and Reggio Emilia University in Italy, told this news organization.
“Clearly, alcohol is not the only or necessarily the main determinant of high blood pressure, and the effects of small intakes of alcohol emerging from our pooled analysis were certainly not biologically as relevant and meaningful as those induced by high intakes,” Dr. Vinceti added.
The study was published online in Hypertension.
The researchers analyzed data from seven large, observational studies conducted in the United States, Korea, and Japan involving 19,548 adults (65% men).
Participants ranged in age from 20 years to the early 70s at baseline and were followed for a median of 5.3 years (range, 4-12 years). None of the participants had previously been diagnosed with hypertension or other CVD, diabetes, liver disease, alcoholism, or binge drinking.
Compared with nondrinkers, SBP was 1.25 mm Hg higher in adults who consumed an average of 12 grams of alcohol per day, rising to 4.90 mm Hg in adults consuming an average of 48 grams of alcohol per day.
For reference, in the United States, 12 ounces of regular beer, 5 ounces of wine, or a 1.5-ounce shot of distilled spirits contains about 14 grams of alcohol.
Diastolic BP (DBP) was 1.14 mm Hg higher in adults who consumed an average of 12 grams of alcohol per day, rising to 3.10 mm Hg in those who consumed an average of 48 grams of alcohol per day.
Subgroup analyses by gender showed an almost linear association between baseline alcohol intake and SBP changes in men and women and for DBP in men, while in women, there was an inverted U-shaped association.
No safe level
“From a BP perspective, it’s best to avoid alcohol intake. This is what the WHO [World Health Organization] recommends,” Dr. Whelton said.
“If someone is already drinking alcohol and does not want to stop doing so, minimizing alcohol consumption is desirable; many guidelines recommend not starting to drink alcohol but in those already drinking alcohol, consumption of two or less standard drinks per day for men and one or less standard drinks of alcohol per day for women,” Dr. Whelton noted.
Commenting on the study for this article, Alberto Ascherio, MD, of Harvard T. H. Chan School of Public Health, Boston, said it’s been known for more than 30 years that alcohol intake is associated with increased systolic and diastolic BP. The added value of this new study is a “refinement of the estimate of the dose response.”
Dr. Ascherio noted that “moderate alcohol consumption is associated with a modest increase in risk of cancer, but, in spite of the adverse association with BP, with a potentially beneficial effect on cardiovascular disease.” However, “the causality of the latter association has been questioned, but there is no consensus on this.”
Also weighing in, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York City, said this new study represents “yet another piece of evidence suggesting that there simply is no ‘healthy’ amount of alcohol use in humans.
“Even small amounts of alcohol intake can have negative health effects, as demonstrated in this study,” Dr. Brennan said. “There is still a widely held belief among people that drinking in moderation is good for you. It is becoming more and more clear that this is simply not the case. As health authorities grapple with drinking ‘recommendations,’ additional datasets like these will be helpful.”
The study had no specific funding. Dr. Whelton, Dr. Vinceti, Dr. Ascherio, and Dr. Brennan have no relevant disclosures.
A version of this article first appeared on Medscape.com.
“A vexing question has been whether usual intake of small amounts of alcohol is associated with a higher level of BP. We identified a continuous, more or less linear association, with no evidence of a threshold for the association,” study coauthor Paul Whelton, MD, of Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
For systolic BP (SBP), “the most important BP risk indicator for CVD [cardiovascular disease], the association was robust, being present in both men and women and in both North America as well as Asia,” Dr. Whelton noted.
Based on the results, “the lower the better, and no consumption even better, as we did not find any indication that human health may benefit from consumption of very small amounts of alcohol,” senior author Marco Vinceti, MD, PhD, of University of Modena and Reggio Emilia University in Italy, told this news organization.
“Clearly, alcohol is not the only or necessarily the main determinant of high blood pressure, and the effects of small intakes of alcohol emerging from our pooled analysis were certainly not biologically as relevant and meaningful as those induced by high intakes,” Dr. Vinceti added.
The study was published online in Hypertension.
The researchers analyzed data from seven large, observational studies conducted in the United States, Korea, and Japan involving 19,548 adults (65% men).
Participants ranged in age from 20 years to the early 70s at baseline and were followed for a median of 5.3 years (range, 4-12 years). None of the participants had previously been diagnosed with hypertension or other CVD, diabetes, liver disease, alcoholism, or binge drinking.
Compared with nondrinkers, SBP was 1.25 mm Hg higher in adults who consumed an average of 12 grams of alcohol per day, rising to 4.90 mm Hg in adults consuming an average of 48 grams of alcohol per day.
For reference, in the United States, 12 ounces of regular beer, 5 ounces of wine, or a 1.5-ounce shot of distilled spirits contains about 14 grams of alcohol.
Diastolic BP (DBP) was 1.14 mm Hg higher in adults who consumed an average of 12 grams of alcohol per day, rising to 3.10 mm Hg in those who consumed an average of 48 grams of alcohol per day.
Subgroup analyses by gender showed an almost linear association between baseline alcohol intake and SBP changes in men and women and for DBP in men, while in women, there was an inverted U-shaped association.
No safe level
“From a BP perspective, it’s best to avoid alcohol intake. This is what the WHO [World Health Organization] recommends,” Dr. Whelton said.
“If someone is already drinking alcohol and does not want to stop doing so, minimizing alcohol consumption is desirable; many guidelines recommend not starting to drink alcohol but in those already drinking alcohol, consumption of two or less standard drinks per day for men and one or less standard drinks of alcohol per day for women,” Dr. Whelton noted.
Commenting on the study for this article, Alberto Ascherio, MD, of Harvard T. H. Chan School of Public Health, Boston, said it’s been known for more than 30 years that alcohol intake is associated with increased systolic and diastolic BP. The added value of this new study is a “refinement of the estimate of the dose response.”
Dr. Ascherio noted that “moderate alcohol consumption is associated with a modest increase in risk of cancer, but, in spite of the adverse association with BP, with a potentially beneficial effect on cardiovascular disease.” However, “the causality of the latter association has been questioned, but there is no consensus on this.”
Also weighing in, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York City, said this new study represents “yet another piece of evidence suggesting that there simply is no ‘healthy’ amount of alcohol use in humans.
“Even small amounts of alcohol intake can have negative health effects, as demonstrated in this study,” Dr. Brennan said. “There is still a widely held belief among people that drinking in moderation is good for you. It is becoming more and more clear that this is simply not the case. As health authorities grapple with drinking ‘recommendations,’ additional datasets like these will be helpful.”
The study had no specific funding. Dr. Whelton, Dr. Vinceti, Dr. Ascherio, and Dr. Brennan have no relevant disclosures.
A version of this article first appeared on Medscape.com.
“A vexing question has been whether usual intake of small amounts of alcohol is associated with a higher level of BP. We identified a continuous, more or less linear association, with no evidence of a threshold for the association,” study coauthor Paul Whelton, MD, of Tulane University School of Public Health and Tropical Medicine, New Orleans, said in an interview.
For systolic BP (SBP), “the most important BP risk indicator for CVD [cardiovascular disease], the association was robust, being present in both men and women and in both North America as well as Asia,” Dr. Whelton noted.
Based on the results, “the lower the better, and no consumption even better, as we did not find any indication that human health may benefit from consumption of very small amounts of alcohol,” senior author Marco Vinceti, MD, PhD, of University of Modena and Reggio Emilia University in Italy, told this news organization.
“Clearly, alcohol is not the only or necessarily the main determinant of high blood pressure, and the effects of small intakes of alcohol emerging from our pooled analysis were certainly not biologically as relevant and meaningful as those induced by high intakes,” Dr. Vinceti added.
The study was published online in Hypertension.
The researchers analyzed data from seven large, observational studies conducted in the United States, Korea, and Japan involving 19,548 adults (65% men).
Participants ranged in age from 20 years to the early 70s at baseline and were followed for a median of 5.3 years (range, 4-12 years). None of the participants had previously been diagnosed with hypertension or other CVD, diabetes, liver disease, alcoholism, or binge drinking.
Compared with nondrinkers, SBP was 1.25 mm Hg higher in adults who consumed an average of 12 grams of alcohol per day, rising to 4.90 mm Hg in adults consuming an average of 48 grams of alcohol per day.
For reference, in the United States, 12 ounces of regular beer, 5 ounces of wine, or a 1.5-ounce shot of distilled spirits contains about 14 grams of alcohol.
Diastolic BP (DBP) was 1.14 mm Hg higher in adults who consumed an average of 12 grams of alcohol per day, rising to 3.10 mm Hg in those who consumed an average of 48 grams of alcohol per day.
Subgroup analyses by gender showed an almost linear association between baseline alcohol intake and SBP changes in men and women and for DBP in men, while in women, there was an inverted U-shaped association.
No safe level
“From a BP perspective, it’s best to avoid alcohol intake. This is what the WHO [World Health Organization] recommends,” Dr. Whelton said.
“If someone is already drinking alcohol and does not want to stop doing so, minimizing alcohol consumption is desirable; many guidelines recommend not starting to drink alcohol but in those already drinking alcohol, consumption of two or less standard drinks per day for men and one or less standard drinks of alcohol per day for women,” Dr. Whelton noted.
Commenting on the study for this article, Alberto Ascherio, MD, of Harvard T. H. Chan School of Public Health, Boston, said it’s been known for more than 30 years that alcohol intake is associated with increased systolic and diastolic BP. The added value of this new study is a “refinement of the estimate of the dose response.”
Dr. Ascherio noted that “moderate alcohol consumption is associated with a modest increase in risk of cancer, but, in spite of the adverse association with BP, with a potentially beneficial effect on cardiovascular disease.” However, “the causality of the latter association has been questioned, but there is no consensus on this.”
Also weighing in, Timothy Brennan, MD, MPH, chief of clinical services for the Addiction Institute of Mount Sinai Health System in New York City, said this new study represents “yet another piece of evidence suggesting that there simply is no ‘healthy’ amount of alcohol use in humans.
“Even small amounts of alcohol intake can have negative health effects, as demonstrated in this study,” Dr. Brennan said. “There is still a widely held belief among people that drinking in moderation is good for you. It is becoming more and more clear that this is simply not the case. As health authorities grapple with drinking ‘recommendations,’ additional datasets like these will be helpful.”
The study had no specific funding. Dr. Whelton, Dr. Vinceti, Dr. Ascherio, and Dr. Brennan have no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM HYPERTENSION
Experts call for early screening for chronic kidney disease
MADRID – A late diagnosis of chronic kidney disease is cause for concern. Scientific societies are therefore advocating for screening at younger ages to reverse this trend and slow the progression of the disease. Nearly all patients seen in primary care are candidates for screening because of their risk factors for kidney disease.
During the 29th National Conference of General and Family Medicine of the Spanish Society for General and Family Physicians, Teresa Benedito, MD, family doctor and member of the society’s cardiovascular group, and Roberto Alcázar, MD, nephrologist at the Infanta Leonor University Hospital, Madrid, presented a clinical case encountered in primary care. They used this case to frame a strong argument for the importance of early screening for chronic kidney disease, and they discussed how to properly manage such screening.
The presentation followed the guidelines in the SEMG publication regarding the management and referral of patients with type 2 diabetes. Dr. Benedito explained that the first thing to ask oneself during a patient visit is “whether they present risk factors for kidney disease. If so, we can’t let them leave before we do a kidney screening.” She then listed the factors in question: age older than 60 years, African heritage, family history of chronic kidney disease, decreased kidney mass, weight loss at birth, hypertension, diabetes, smoking, obesity, and low socioeconomic status.
For his part, Dr. Alcázar mentioned how these factors are similar to cardiovascular risk factors, because “the kidneys are a ball of vessels with double capillarization for purifying blood. They’re the organs with the most arteries per unit of weight, so anything that can damage the arteries can damage the kidneys.”
Candidates for screening
“Chronic kidney disease develops in 15% of the adult population in Spain. So, it’s worth asking how many patients have been diagnosed and who should we should be screening.” To the factors listed above, Dr. Alcázar added treatment with nephrotoxic drugs (including nonsteroidal anti-inflammatory drugs) for patients with obstructive urinary tract disease, and a history of acute kidney injury for patients with chronic autoimmune disease or neoplasms. “Thus, nearly all patients seen in primary care would need to be screened.”
Another fundamental question raised was whether patients should be screened before age 60 years. “As a nephrologist, I feel that we have been diagnosing chronic kidney disease late, even though we’ve been doing everything by the book,” said Dr. Alcázar. In his opinion, “the answer to whether we should be screening earlier ... is yes, for two reasons: first, because it’s cost-effective, and second, because it’s very inexpensive.”
Dr. Benedito explained in detail the process for diagnosing this disease. She began by defining the disease as changes in kidney structure and function that last longer than 3 months. These changes are identified by use of two criteria: glomerular filtration rate less than 60 mL/min and kidney injury or lesions with or without reduced filtration rate (renal biopsy, albumin/creatinine ratio greater than 30 mg/g, proteinuria, alterations in urinary sediment or in imaging tests). Thus, “if one of these two criteria persists for more than 3 months, the diagnosis is chronic kidney disease. Also, high creatinine levels are not diagnostic for the disease,” she emphasized.
Two related parameters
Glomerular filtration and albuminuria “are highly relevant, because screening for chronic kidney disease is based on these two parameters,” said Dr. Benedito. Glomerular filtration rate varies with age, sex, ethnicity, and body mass. It is useful for identifying the stage of the disease and for monitoring disease progression. Albuminuria, on the other hand, is an indication of the severity of the disease. It’s an early marker for kidney injury and systemic disease and is more sensitive than proteinuria. Therefore, “this factor, together with glomerular filtration rate, allows us to detect, classify, and monitor the progression of chronic kidney disease.”
On this point, Dr. Alcázar emphasized the importance of trends, since variation in glomerular filtration depends on serum creatinine, which can vary by nearly 9%. He explained that glomerular filtration rate is related to the number of nephrons remaining. A glomerular filtration rate of less than 60 mL/min implies that more than half of the nephrons in each kidney have been lost. Albuminuria informs about structural damage (that is, the condition of the remaining nephrons). It’s therefore essential to test for both parameters. “We need to be actively monitoring and then making our decisions based on trends and not on isolated results. We need to be aware of albuminuria when we make our decisions,” said Dr. Alcázar. Some studies have shown the importance of testing for albuminuria whenever creatinine level is assessed. “We need to buy into this. If we don’t do this, we’ll only ever have half the information we need.”
Reducing late diagnosis
According to the IBERICAN study, 14% of patients seen in primary care in Spain have chronic kidney disease. “This statistic should make us stop and think, own our responsibility, and ask ourselves why this screening isn’t taking place [earlier],” said Dr. Benedito. She added, “We need to head off this trend toward late diagnosis. As the disease progresses, it significantly increases cardiovascular risk and leads to higher mortality, going on dialysis, transplants, et cetera.”
Dr. Alcázar noted that 80% of nephrology cases that are referred to him come from primary care. He explained the need to understand that “these patients have a sevenfold greater risk of suffering a serious cardiovascular event within the next year than people without kidney problems.” Most of these patients will experience an event, even if they don’t undergo dialysis (stage 3 and those near stage 4).
Correct staging
Also fundamental is having a detailed understanding of how staging is performed. Dr. Benedito explained that a chart that pairs glomerular filtration rate (six categories) with the level of albuminuria (three categories) should be used during the visit. For example, a case might be classified as G3a-A2. However, the simplified form of the chart may prove more practical. It classifies chronic kidney disease as being associated with mild, moderate, and severe risk, using different colors to aid comprehension.
Dr. Alcázar noted that the latest guidelines from the European Society of Hypertension for 2023 include albuminuria as an important parameter. The guidelines indicate that for a patient with moderate or severe risk, it is not necessary to calculate their score. “It’s considered high cardiovascular risk, and steps would need to be taken for intervention.”
He then listed the tools available for reversing albuminuria. The process begins by reducing salt consumption and involves the use of medications (angiotensin-converting enzyme inhibitors/angiotensin II receptor antagonists, aldosterone receptor antagonists, glucagon-like peptide-1 analogues, and sodium-glucose cotransporter-2 inhibitors, which slow kidney damage regardless of other measures) and strict management of cardiovascular risk factors (smoking, weight management, blood glucose, hypertension, and moderate physical activity).
Reducing cardiovascular risk
Dr. Alcázar highlighted important factors to keep in mind when managing each of the cardiovascular risk factors. For hypertension, the aim is to achieve levels less than 130/80 mm Hg, although recommendations vary, depending on the guidelines consulted. “KDIGO (Kidney Disease: Improving Global Outcomes) 2021 states that there is no evidence for monitoring diastolic blood pressure, only systolic blood pressure. If we measure it according to the standardized form, SBP should be less than 120 mm Hg, and if not, we would fall back on readings of 130/80 mm Hg.”
For lipid control (specifically, low-density lipoprotein cholesterol), the staging chart indicates that for patients at mild risk, levels should be less than 100 mg/dL; for those at moderate risk, less than 70 mg/dL; and for those at severe risk, less than 55 mg/dL. Hypertriglyceridemia “should only be treated with fibrates if it comes in over 1,000 mg/dL. Also, care must be taken, because these drugs interfere with creatinine excretion, increasing it,” said Dr. Alcázar.
Guidelines from the KDIGO and the American Diabetes Association state that anyone with diabetes and chronic kidney disease should receive a sodium-glucose cotransporter-2 inhibitor if their glomerular filtration rate exceeds 20 mL/min, “which may contradict slightly what it says on the label. Also, if they have hypertension, they should take an angiotensin-converting enzyme inhibitor,” said Dr. Alcázar. He added that “oral antidiabetics, including metformin, must be adjusted based on renal function if glomerular filtration rate is under 30 mL/min.”
Act immediately
When asked whether the course of chronic kidney disease can be changed, Dr. Alcázar responded with an emphatic yes and added that cardiovascular risk can also be substantially reduced. “As nephrologists, we don’t have access to patients in early stages. But family doctors do. Hence the importance of early screening, because going on dialysis at age 60 isn’t the same as at 80.” Currently, “scientific societies are encouraging authorities to screen for chronic kidney disease at earlier ages.”
Regarding drug-based therapy, Dr. Alcázar said that “empagliflozin is not currently indicated for chronic kidney disease in adults.” This sodium-glucose cotransporter-2 inhibitor delays kidney disease and reduces morbidity. Both benefits were highlighted in two recent studies (DAPA-CKD and CREDENCE). Published in January, EMPA-KIDNEY presents a new twist on nephroprotection for patients with chronic kidney disease (diabetic or not) whose glomerular filtration rates are between 20 and 40 mL/min without albuminuria or whose glomerular filtration rates are between 45 and 90 mL/min with albuminuria. For more than 6,000 patients, empagliflozin was observed “to clearly reduce kidney disease progression, cardiovascular mortality and all-cause mortality, and the need to go on dialysis,” stated Dr. Alcázar.
What professionals expect
Dr. Benedito also explained the criteria for referral to a specialist: glomerular filtration rate less than 30 mL/min (unless the patient is older than 80 years and does not have progressively worsening renal function), albumin/creatinine ratio greater than 300 mg/g, acute worsening of renal function, progressive worsening of renal function of greater than 5 mL/min/yr, chronic kidney disease, hypertension treated with triple therapy (including a diuretic) at maximum doses, anemia of less than 10 g/dL, and nonurologic hematuria, especially in combination with albuminuria.
Dr. Benedito explained what nephrologists expect from family doctors in the management of chronic kidney disease: “screening for early detection, identifying and treating risk factors for chronic kidney disease, detecting progression and complications, adjusting drugs based on glomerular filtration rate, and ensuring that our patients are benefiting from sodium-glucose cotransporter-2 inhibitors. These are among the most important steps to be taken.”
Dr. Alcázar mentioned what family doctors expect from nephrologists: “two-way communication, accessibility, coordination of actions to be taken, and using shared and mutually agreed-upon protocols.”
This article was translated from the Medscape Spanish Edition and a version appeared on Medscape.com.
MADRID – A late diagnosis of chronic kidney disease is cause for concern. Scientific societies are therefore advocating for screening at younger ages to reverse this trend and slow the progression of the disease. Nearly all patients seen in primary care are candidates for screening because of their risk factors for kidney disease.
During the 29th National Conference of General and Family Medicine of the Spanish Society for General and Family Physicians, Teresa Benedito, MD, family doctor and member of the society’s cardiovascular group, and Roberto Alcázar, MD, nephrologist at the Infanta Leonor University Hospital, Madrid, presented a clinical case encountered in primary care. They used this case to frame a strong argument for the importance of early screening for chronic kidney disease, and they discussed how to properly manage such screening.
The presentation followed the guidelines in the SEMG publication regarding the management and referral of patients with type 2 diabetes. Dr. Benedito explained that the first thing to ask oneself during a patient visit is “whether they present risk factors for kidney disease. If so, we can’t let them leave before we do a kidney screening.” She then listed the factors in question: age older than 60 years, African heritage, family history of chronic kidney disease, decreased kidney mass, weight loss at birth, hypertension, diabetes, smoking, obesity, and low socioeconomic status.
For his part, Dr. Alcázar mentioned how these factors are similar to cardiovascular risk factors, because “the kidneys are a ball of vessels with double capillarization for purifying blood. They’re the organs with the most arteries per unit of weight, so anything that can damage the arteries can damage the kidneys.”
Candidates for screening
“Chronic kidney disease develops in 15% of the adult population in Spain. So, it’s worth asking how many patients have been diagnosed and who should we should be screening.” To the factors listed above, Dr. Alcázar added treatment with nephrotoxic drugs (including nonsteroidal anti-inflammatory drugs) for patients with obstructive urinary tract disease, and a history of acute kidney injury for patients with chronic autoimmune disease or neoplasms. “Thus, nearly all patients seen in primary care would need to be screened.”
Another fundamental question raised was whether patients should be screened before age 60 years. “As a nephrologist, I feel that we have been diagnosing chronic kidney disease late, even though we’ve been doing everything by the book,” said Dr. Alcázar. In his opinion, “the answer to whether we should be screening earlier ... is yes, for two reasons: first, because it’s cost-effective, and second, because it’s very inexpensive.”
Dr. Benedito explained in detail the process for diagnosing this disease. She began by defining the disease as changes in kidney structure and function that last longer than 3 months. These changes are identified by use of two criteria: glomerular filtration rate less than 60 mL/min and kidney injury or lesions with or without reduced filtration rate (renal biopsy, albumin/creatinine ratio greater than 30 mg/g, proteinuria, alterations in urinary sediment or in imaging tests). Thus, “if one of these two criteria persists for more than 3 months, the diagnosis is chronic kidney disease. Also, high creatinine levels are not diagnostic for the disease,” she emphasized.
Two related parameters
Glomerular filtration and albuminuria “are highly relevant, because screening for chronic kidney disease is based on these two parameters,” said Dr. Benedito. Glomerular filtration rate varies with age, sex, ethnicity, and body mass. It is useful for identifying the stage of the disease and for monitoring disease progression. Albuminuria, on the other hand, is an indication of the severity of the disease. It’s an early marker for kidney injury and systemic disease and is more sensitive than proteinuria. Therefore, “this factor, together with glomerular filtration rate, allows us to detect, classify, and monitor the progression of chronic kidney disease.”
On this point, Dr. Alcázar emphasized the importance of trends, since variation in glomerular filtration depends on serum creatinine, which can vary by nearly 9%. He explained that glomerular filtration rate is related to the number of nephrons remaining. A glomerular filtration rate of less than 60 mL/min implies that more than half of the nephrons in each kidney have been lost. Albuminuria informs about structural damage (that is, the condition of the remaining nephrons). It’s therefore essential to test for both parameters. “We need to be actively monitoring and then making our decisions based on trends and not on isolated results. We need to be aware of albuminuria when we make our decisions,” said Dr. Alcázar. Some studies have shown the importance of testing for albuminuria whenever creatinine level is assessed. “We need to buy into this. If we don’t do this, we’ll only ever have half the information we need.”
Reducing late diagnosis
According to the IBERICAN study, 14% of patients seen in primary care in Spain have chronic kidney disease. “This statistic should make us stop and think, own our responsibility, and ask ourselves why this screening isn’t taking place [earlier],” said Dr. Benedito. She added, “We need to head off this trend toward late diagnosis. As the disease progresses, it significantly increases cardiovascular risk and leads to higher mortality, going on dialysis, transplants, et cetera.”
Dr. Alcázar noted that 80% of nephrology cases that are referred to him come from primary care. He explained the need to understand that “these patients have a sevenfold greater risk of suffering a serious cardiovascular event within the next year than people without kidney problems.” Most of these patients will experience an event, even if they don’t undergo dialysis (stage 3 and those near stage 4).
Correct staging
Also fundamental is having a detailed understanding of how staging is performed. Dr. Benedito explained that a chart that pairs glomerular filtration rate (six categories) with the level of albuminuria (three categories) should be used during the visit. For example, a case might be classified as G3a-A2. However, the simplified form of the chart may prove more practical. It classifies chronic kidney disease as being associated with mild, moderate, and severe risk, using different colors to aid comprehension.
Dr. Alcázar noted that the latest guidelines from the European Society of Hypertension for 2023 include albuminuria as an important parameter. The guidelines indicate that for a patient with moderate or severe risk, it is not necessary to calculate their score. “It’s considered high cardiovascular risk, and steps would need to be taken for intervention.”
He then listed the tools available for reversing albuminuria. The process begins by reducing salt consumption and involves the use of medications (angiotensin-converting enzyme inhibitors/angiotensin II receptor antagonists, aldosterone receptor antagonists, glucagon-like peptide-1 analogues, and sodium-glucose cotransporter-2 inhibitors, which slow kidney damage regardless of other measures) and strict management of cardiovascular risk factors (smoking, weight management, blood glucose, hypertension, and moderate physical activity).
Reducing cardiovascular risk
Dr. Alcázar highlighted important factors to keep in mind when managing each of the cardiovascular risk factors. For hypertension, the aim is to achieve levels less than 130/80 mm Hg, although recommendations vary, depending on the guidelines consulted. “KDIGO (Kidney Disease: Improving Global Outcomes) 2021 states that there is no evidence for monitoring diastolic blood pressure, only systolic blood pressure. If we measure it according to the standardized form, SBP should be less than 120 mm Hg, and if not, we would fall back on readings of 130/80 mm Hg.”
For lipid control (specifically, low-density lipoprotein cholesterol), the staging chart indicates that for patients at mild risk, levels should be less than 100 mg/dL; for those at moderate risk, less than 70 mg/dL; and for those at severe risk, less than 55 mg/dL. Hypertriglyceridemia “should only be treated with fibrates if it comes in over 1,000 mg/dL. Also, care must be taken, because these drugs interfere with creatinine excretion, increasing it,” said Dr. Alcázar.
Guidelines from the KDIGO and the American Diabetes Association state that anyone with diabetes and chronic kidney disease should receive a sodium-glucose cotransporter-2 inhibitor if their glomerular filtration rate exceeds 20 mL/min, “which may contradict slightly what it says on the label. Also, if they have hypertension, they should take an angiotensin-converting enzyme inhibitor,” said Dr. Alcázar. He added that “oral antidiabetics, including metformin, must be adjusted based on renal function if glomerular filtration rate is under 30 mL/min.”
Act immediately
When asked whether the course of chronic kidney disease can be changed, Dr. Alcázar responded with an emphatic yes and added that cardiovascular risk can also be substantially reduced. “As nephrologists, we don’t have access to patients in early stages. But family doctors do. Hence the importance of early screening, because going on dialysis at age 60 isn’t the same as at 80.” Currently, “scientific societies are encouraging authorities to screen for chronic kidney disease at earlier ages.”
Regarding drug-based therapy, Dr. Alcázar said that “empagliflozin is not currently indicated for chronic kidney disease in adults.” This sodium-glucose cotransporter-2 inhibitor delays kidney disease and reduces morbidity. Both benefits were highlighted in two recent studies (DAPA-CKD and CREDENCE). Published in January, EMPA-KIDNEY presents a new twist on nephroprotection for patients with chronic kidney disease (diabetic or not) whose glomerular filtration rates are between 20 and 40 mL/min without albuminuria or whose glomerular filtration rates are between 45 and 90 mL/min with albuminuria. For more than 6,000 patients, empagliflozin was observed “to clearly reduce kidney disease progression, cardiovascular mortality and all-cause mortality, and the need to go on dialysis,” stated Dr. Alcázar.
What professionals expect
Dr. Benedito also explained the criteria for referral to a specialist: glomerular filtration rate less than 30 mL/min (unless the patient is older than 80 years and does not have progressively worsening renal function), albumin/creatinine ratio greater than 300 mg/g, acute worsening of renal function, progressive worsening of renal function of greater than 5 mL/min/yr, chronic kidney disease, hypertension treated with triple therapy (including a diuretic) at maximum doses, anemia of less than 10 g/dL, and nonurologic hematuria, especially in combination with albuminuria.
Dr. Benedito explained what nephrologists expect from family doctors in the management of chronic kidney disease: “screening for early detection, identifying and treating risk factors for chronic kidney disease, detecting progression and complications, adjusting drugs based on glomerular filtration rate, and ensuring that our patients are benefiting from sodium-glucose cotransporter-2 inhibitors. These are among the most important steps to be taken.”
Dr. Alcázar mentioned what family doctors expect from nephrologists: “two-way communication, accessibility, coordination of actions to be taken, and using shared and mutually agreed-upon protocols.”
This article was translated from the Medscape Spanish Edition and a version appeared on Medscape.com.
MADRID – A late diagnosis of chronic kidney disease is cause for concern. Scientific societies are therefore advocating for screening at younger ages to reverse this trend and slow the progression of the disease. Nearly all patients seen in primary care are candidates for screening because of their risk factors for kidney disease.
During the 29th National Conference of General and Family Medicine of the Spanish Society for General and Family Physicians, Teresa Benedito, MD, family doctor and member of the society’s cardiovascular group, and Roberto Alcázar, MD, nephrologist at the Infanta Leonor University Hospital, Madrid, presented a clinical case encountered in primary care. They used this case to frame a strong argument for the importance of early screening for chronic kidney disease, and they discussed how to properly manage such screening.
The presentation followed the guidelines in the SEMG publication regarding the management and referral of patients with type 2 diabetes. Dr. Benedito explained that the first thing to ask oneself during a patient visit is “whether they present risk factors for kidney disease. If so, we can’t let them leave before we do a kidney screening.” She then listed the factors in question: age older than 60 years, African heritage, family history of chronic kidney disease, decreased kidney mass, weight loss at birth, hypertension, diabetes, smoking, obesity, and low socioeconomic status.
For his part, Dr. Alcázar mentioned how these factors are similar to cardiovascular risk factors, because “the kidneys are a ball of vessels with double capillarization for purifying blood. They’re the organs with the most arteries per unit of weight, so anything that can damage the arteries can damage the kidneys.”
Candidates for screening
“Chronic kidney disease develops in 15% of the adult population in Spain. So, it’s worth asking how many patients have been diagnosed and who should we should be screening.” To the factors listed above, Dr. Alcázar added treatment with nephrotoxic drugs (including nonsteroidal anti-inflammatory drugs) for patients with obstructive urinary tract disease, and a history of acute kidney injury for patients with chronic autoimmune disease or neoplasms. “Thus, nearly all patients seen in primary care would need to be screened.”
Another fundamental question raised was whether patients should be screened before age 60 years. “As a nephrologist, I feel that we have been diagnosing chronic kidney disease late, even though we’ve been doing everything by the book,” said Dr. Alcázar. In his opinion, “the answer to whether we should be screening earlier ... is yes, for two reasons: first, because it’s cost-effective, and second, because it’s very inexpensive.”
Dr. Benedito explained in detail the process for diagnosing this disease. She began by defining the disease as changes in kidney structure and function that last longer than 3 months. These changes are identified by use of two criteria: glomerular filtration rate less than 60 mL/min and kidney injury or lesions with or without reduced filtration rate (renal biopsy, albumin/creatinine ratio greater than 30 mg/g, proteinuria, alterations in urinary sediment or in imaging tests). Thus, “if one of these two criteria persists for more than 3 months, the diagnosis is chronic kidney disease. Also, high creatinine levels are not diagnostic for the disease,” she emphasized.
Two related parameters
Glomerular filtration and albuminuria “are highly relevant, because screening for chronic kidney disease is based on these two parameters,” said Dr. Benedito. Glomerular filtration rate varies with age, sex, ethnicity, and body mass. It is useful for identifying the stage of the disease and for monitoring disease progression. Albuminuria, on the other hand, is an indication of the severity of the disease. It’s an early marker for kidney injury and systemic disease and is more sensitive than proteinuria. Therefore, “this factor, together with glomerular filtration rate, allows us to detect, classify, and monitor the progression of chronic kidney disease.”
On this point, Dr. Alcázar emphasized the importance of trends, since variation in glomerular filtration depends on serum creatinine, which can vary by nearly 9%. He explained that glomerular filtration rate is related to the number of nephrons remaining. A glomerular filtration rate of less than 60 mL/min implies that more than half of the nephrons in each kidney have been lost. Albuminuria informs about structural damage (that is, the condition of the remaining nephrons). It’s therefore essential to test for both parameters. “We need to be actively monitoring and then making our decisions based on trends and not on isolated results. We need to be aware of albuminuria when we make our decisions,” said Dr. Alcázar. Some studies have shown the importance of testing for albuminuria whenever creatinine level is assessed. “We need to buy into this. If we don’t do this, we’ll only ever have half the information we need.”
Reducing late diagnosis
According to the IBERICAN study, 14% of patients seen in primary care in Spain have chronic kidney disease. “This statistic should make us stop and think, own our responsibility, and ask ourselves why this screening isn’t taking place [earlier],” said Dr. Benedito. She added, “We need to head off this trend toward late diagnosis. As the disease progresses, it significantly increases cardiovascular risk and leads to higher mortality, going on dialysis, transplants, et cetera.”
Dr. Alcázar noted that 80% of nephrology cases that are referred to him come from primary care. He explained the need to understand that “these patients have a sevenfold greater risk of suffering a serious cardiovascular event within the next year than people without kidney problems.” Most of these patients will experience an event, even if they don’t undergo dialysis (stage 3 and those near stage 4).
Correct staging
Also fundamental is having a detailed understanding of how staging is performed. Dr. Benedito explained that a chart that pairs glomerular filtration rate (six categories) with the level of albuminuria (three categories) should be used during the visit. For example, a case might be classified as G3a-A2. However, the simplified form of the chart may prove more practical. It classifies chronic kidney disease as being associated with mild, moderate, and severe risk, using different colors to aid comprehension.
Dr. Alcázar noted that the latest guidelines from the European Society of Hypertension for 2023 include albuminuria as an important parameter. The guidelines indicate that for a patient with moderate or severe risk, it is not necessary to calculate their score. “It’s considered high cardiovascular risk, and steps would need to be taken for intervention.”
He then listed the tools available for reversing albuminuria. The process begins by reducing salt consumption and involves the use of medications (angiotensin-converting enzyme inhibitors/angiotensin II receptor antagonists, aldosterone receptor antagonists, glucagon-like peptide-1 analogues, and sodium-glucose cotransporter-2 inhibitors, which slow kidney damage regardless of other measures) and strict management of cardiovascular risk factors (smoking, weight management, blood glucose, hypertension, and moderate physical activity).
Reducing cardiovascular risk
Dr. Alcázar highlighted important factors to keep in mind when managing each of the cardiovascular risk factors. For hypertension, the aim is to achieve levels less than 130/80 mm Hg, although recommendations vary, depending on the guidelines consulted. “KDIGO (Kidney Disease: Improving Global Outcomes) 2021 states that there is no evidence for monitoring diastolic blood pressure, only systolic blood pressure. If we measure it according to the standardized form, SBP should be less than 120 mm Hg, and if not, we would fall back on readings of 130/80 mm Hg.”
For lipid control (specifically, low-density lipoprotein cholesterol), the staging chart indicates that for patients at mild risk, levels should be less than 100 mg/dL; for those at moderate risk, less than 70 mg/dL; and for those at severe risk, less than 55 mg/dL. Hypertriglyceridemia “should only be treated with fibrates if it comes in over 1,000 mg/dL. Also, care must be taken, because these drugs interfere with creatinine excretion, increasing it,” said Dr. Alcázar.
Guidelines from the KDIGO and the American Diabetes Association state that anyone with diabetes and chronic kidney disease should receive a sodium-glucose cotransporter-2 inhibitor if their glomerular filtration rate exceeds 20 mL/min, “which may contradict slightly what it says on the label. Also, if they have hypertension, they should take an angiotensin-converting enzyme inhibitor,” said Dr. Alcázar. He added that “oral antidiabetics, including metformin, must be adjusted based on renal function if glomerular filtration rate is under 30 mL/min.”
Act immediately
When asked whether the course of chronic kidney disease can be changed, Dr. Alcázar responded with an emphatic yes and added that cardiovascular risk can also be substantially reduced. “As nephrologists, we don’t have access to patients in early stages. But family doctors do. Hence the importance of early screening, because going on dialysis at age 60 isn’t the same as at 80.” Currently, “scientific societies are encouraging authorities to screen for chronic kidney disease at earlier ages.”
Regarding drug-based therapy, Dr. Alcázar said that “empagliflozin is not currently indicated for chronic kidney disease in adults.” This sodium-glucose cotransporter-2 inhibitor delays kidney disease and reduces morbidity. Both benefits were highlighted in two recent studies (DAPA-CKD and CREDENCE). Published in January, EMPA-KIDNEY presents a new twist on nephroprotection for patients with chronic kidney disease (diabetic or not) whose glomerular filtration rates are between 20 and 40 mL/min without albuminuria or whose glomerular filtration rates are between 45 and 90 mL/min with albuminuria. For more than 6,000 patients, empagliflozin was observed “to clearly reduce kidney disease progression, cardiovascular mortality and all-cause mortality, and the need to go on dialysis,” stated Dr. Alcázar.
What professionals expect
Dr. Benedito also explained the criteria for referral to a specialist: glomerular filtration rate less than 30 mL/min (unless the patient is older than 80 years and does not have progressively worsening renal function), albumin/creatinine ratio greater than 300 mg/g, acute worsening of renal function, progressive worsening of renal function of greater than 5 mL/min/yr, chronic kidney disease, hypertension treated with triple therapy (including a diuretic) at maximum doses, anemia of less than 10 g/dL, and nonurologic hematuria, especially in combination with albuminuria.
Dr. Benedito explained what nephrologists expect from family doctors in the management of chronic kidney disease: “screening for early detection, identifying and treating risk factors for chronic kidney disease, detecting progression and complications, adjusting drugs based on glomerular filtration rate, and ensuring that our patients are benefiting from sodium-glucose cotransporter-2 inhibitors. These are among the most important steps to be taken.”
Dr. Alcázar mentioned what family doctors expect from nephrologists: “two-way communication, accessibility, coordination of actions to be taken, and using shared and mutually agreed-upon protocols.”
This article was translated from the Medscape Spanish Edition and a version appeared on Medscape.com.
Conflicting blood pressure targets: Déjà vu all over again
Stop me if you’ve heard this before. There’s a controversy over blood pressure targets. Some argue for 140/90 mm Hg, others for 130/80 mm Hg, and some super ambitious folks think that we should aim for 120/80 mm Hg. If this sounds familiar, it should. We did it in 2017. It’s unclear what, if anything, we learned from the experience. On the upside, it’s not as bad as it was 100 years ago.
When high blood pressure was a ‘good’ thing
Back then, many believed that you needed higher blood pressure as you got older to push the blood through your progressively stiffened and hardened arteries. Hence the name “essential” hypertension. The concern was that lowering blood pressure would hypoperfuse your organs and be dangerous. In the 1930s, John Hay told an audience at a British Medical Association lecture: “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.”
The 1900s were a simpler time when people had fatal strokes in their 50s, and their families were consoled by the knowledge that they had lived a good life.
If our thinking around blood pressure had evolved slightly faster, perhaps President Roosevelt wouldn’t have died of a stroke during World War II as his doctors watched his systolic blood pressure climb above 200 mm Hg and suggested massages and barbiturates to take the edge off.
The current controversy
Not that long ago, 180 mm Hg was considered mild hypertension. Now, we are arguing about a systolic blood pressure of 140 versus 130 mm Hg.
The American Academy of Family Physicians takes the view that 140/90 mm Hg is good enough for most people. Their most recent clinical practice guideline, based primarily on two 2020 Cochrane Reviews of blood pressure targets in patients with and without cardiovascular disease, did not find any mortality benefit for a lower blood pressure threshold.
This puts the AAFP guideline in conflict with the 2017 guideline issued jointly by the American College of Cardiology, American Heart Association, and nine other groups, which recommended a target of 130/80 mm Hg for pretty much everyone. Though they say greater than 140/90 mm Hg should be the threshold for low-risk patients or for starting therapy post stroke, we often forget those nuances. The main point of contention is that the AAFP guideline was looking for a mortality benefit, whereas the ACC/AHA/everyone else guideline was looking at preventing cardiovascular events. The latter guideline was driven mainly by the results of the SPRINT trial. ACC/AHA argue for more aggressive targets to prevent the things that cardiologists care about, namely heart attacks.
The AAFP guideline conceded that more aggressive control will result in fewer myocardial infarctions but warn that it comes with more adverse events. Treating 1,000 patients to this lower target would theoretically prevent four MIs, possibly prevent three strokes, but result in 30 adverse events.
In the end, what we are seeing here is not so much a debate over the evidence as a debate over priorities. Interventions that don’t improve mortality can be questioned in terms of their cost effectiveness. But you probably don’t want to have a heart attack (even a nonfatal one). And you certainly don’t want to have a stroke. However, lower blood pressure targets inevitably require more medications. Notwithstanding the economic costs, the dangers of polypharmacy, medication interactions, side effects, and syncope leading to falls cannot be ignored. Falls are not benign adverse events, especially in older adults.
The counter argument is that physicians are human and often let things slide. Set the target at 140/90 mm Hg, and many physicians won’t jump on a systolic blood pressure of 144 mm Hg. Set the target at 130 mm Hg, and maybe they’ll be more likely to react. There’s a fine line between permissiveness and complacency.
If you zoom out and look at the multitude of blood pressure guidelines, you start to notice an important fact. There is not much daylight between them. There are subtle differences in what constitutes high risk and different definitions of older (older should be defined as 10 years older than the reader’s current age). But otherwise, the blood pressure targets are not that different.
Does that final 10 mm Hg really matter when barriers to care mean that tens of millions in the United States are unaware they have hypertension? Even among those diagnosed, many are either untreated or inadequately treated.
With this context, perhaps the most insightful thing that can be said about the blood pressure guideline controversy is that it’s not all that controversial. We can likely all agree that we need to be better at treating hypertension and that creative solutions to reach underserved communities are necessary.
Arguing about 140/90 mm Hg or 130/80 mm Hg is less important than acknowledging that we should be aggressive in screening for and treating hypertension. We should acknowledge that beyond a certain point any cardiovascular benefit comes at the cost of hypotension and side effects. That tipping point will be different for different groups, and probably at a higher set point in older patients.
Individualizing care isn’t difficult. We do it all the time. We just shouldn’t be letting people walk around with untreated hypertension. It’s not the 1900s anymore.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Stop me if you’ve heard this before. There’s a controversy over blood pressure targets. Some argue for 140/90 mm Hg, others for 130/80 mm Hg, and some super ambitious folks think that we should aim for 120/80 mm Hg. If this sounds familiar, it should. We did it in 2017. It’s unclear what, if anything, we learned from the experience. On the upside, it’s not as bad as it was 100 years ago.
When high blood pressure was a ‘good’ thing
Back then, many believed that you needed higher blood pressure as you got older to push the blood through your progressively stiffened and hardened arteries. Hence the name “essential” hypertension. The concern was that lowering blood pressure would hypoperfuse your organs and be dangerous. In the 1930s, John Hay told an audience at a British Medical Association lecture: “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.”
The 1900s were a simpler time when people had fatal strokes in their 50s, and their families were consoled by the knowledge that they had lived a good life.
If our thinking around blood pressure had evolved slightly faster, perhaps President Roosevelt wouldn’t have died of a stroke during World War II as his doctors watched his systolic blood pressure climb above 200 mm Hg and suggested massages and barbiturates to take the edge off.
The current controversy
Not that long ago, 180 mm Hg was considered mild hypertension. Now, we are arguing about a systolic blood pressure of 140 versus 130 mm Hg.
The American Academy of Family Physicians takes the view that 140/90 mm Hg is good enough for most people. Their most recent clinical practice guideline, based primarily on two 2020 Cochrane Reviews of blood pressure targets in patients with and without cardiovascular disease, did not find any mortality benefit for a lower blood pressure threshold.
This puts the AAFP guideline in conflict with the 2017 guideline issued jointly by the American College of Cardiology, American Heart Association, and nine other groups, which recommended a target of 130/80 mm Hg for pretty much everyone. Though they say greater than 140/90 mm Hg should be the threshold for low-risk patients or for starting therapy post stroke, we often forget those nuances. The main point of contention is that the AAFP guideline was looking for a mortality benefit, whereas the ACC/AHA/everyone else guideline was looking at preventing cardiovascular events. The latter guideline was driven mainly by the results of the SPRINT trial. ACC/AHA argue for more aggressive targets to prevent the things that cardiologists care about, namely heart attacks.
The AAFP guideline conceded that more aggressive control will result in fewer myocardial infarctions but warn that it comes with more adverse events. Treating 1,000 patients to this lower target would theoretically prevent four MIs, possibly prevent three strokes, but result in 30 adverse events.
In the end, what we are seeing here is not so much a debate over the evidence as a debate over priorities. Interventions that don’t improve mortality can be questioned in terms of their cost effectiveness. But you probably don’t want to have a heart attack (even a nonfatal one). And you certainly don’t want to have a stroke. However, lower blood pressure targets inevitably require more medications. Notwithstanding the economic costs, the dangers of polypharmacy, medication interactions, side effects, and syncope leading to falls cannot be ignored. Falls are not benign adverse events, especially in older adults.
The counter argument is that physicians are human and often let things slide. Set the target at 140/90 mm Hg, and many physicians won’t jump on a systolic blood pressure of 144 mm Hg. Set the target at 130 mm Hg, and maybe they’ll be more likely to react. There’s a fine line between permissiveness and complacency.
If you zoom out and look at the multitude of blood pressure guidelines, you start to notice an important fact. There is not much daylight between them. There are subtle differences in what constitutes high risk and different definitions of older (older should be defined as 10 years older than the reader’s current age). But otherwise, the blood pressure targets are not that different.
Does that final 10 mm Hg really matter when barriers to care mean that tens of millions in the United States are unaware they have hypertension? Even among those diagnosed, many are either untreated or inadequately treated.
With this context, perhaps the most insightful thing that can be said about the blood pressure guideline controversy is that it’s not all that controversial. We can likely all agree that we need to be better at treating hypertension and that creative solutions to reach underserved communities are necessary.
Arguing about 140/90 mm Hg or 130/80 mm Hg is less important than acknowledging that we should be aggressive in screening for and treating hypertension. We should acknowledge that beyond a certain point any cardiovascular benefit comes at the cost of hypotension and side effects. That tipping point will be different for different groups, and probably at a higher set point in older patients.
Individualizing care isn’t difficult. We do it all the time. We just shouldn’t be letting people walk around with untreated hypertension. It’s not the 1900s anymore.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
Stop me if you’ve heard this before. There’s a controversy over blood pressure targets. Some argue for 140/90 mm Hg, others for 130/80 mm Hg, and some super ambitious folks think that we should aim for 120/80 mm Hg. If this sounds familiar, it should. We did it in 2017. It’s unclear what, if anything, we learned from the experience. On the upside, it’s not as bad as it was 100 years ago.
When high blood pressure was a ‘good’ thing
Back then, many believed that you needed higher blood pressure as you got older to push the blood through your progressively stiffened and hardened arteries. Hence the name “essential” hypertension. The concern was that lowering blood pressure would hypoperfuse your organs and be dangerous. In the 1930s, John Hay told an audience at a British Medical Association lecture: “The greatest danger to a man with high blood pressure lies in its discovery, because then some fool is certain to try and reduce it.”
The 1900s were a simpler time when people had fatal strokes in their 50s, and their families were consoled by the knowledge that they had lived a good life.
If our thinking around blood pressure had evolved slightly faster, perhaps President Roosevelt wouldn’t have died of a stroke during World War II as his doctors watched his systolic blood pressure climb above 200 mm Hg and suggested massages and barbiturates to take the edge off.
The current controversy
Not that long ago, 180 mm Hg was considered mild hypertension. Now, we are arguing about a systolic blood pressure of 140 versus 130 mm Hg.
The American Academy of Family Physicians takes the view that 140/90 mm Hg is good enough for most people. Their most recent clinical practice guideline, based primarily on two 2020 Cochrane Reviews of blood pressure targets in patients with and without cardiovascular disease, did not find any mortality benefit for a lower blood pressure threshold.
This puts the AAFP guideline in conflict with the 2017 guideline issued jointly by the American College of Cardiology, American Heart Association, and nine other groups, which recommended a target of 130/80 mm Hg for pretty much everyone. Though they say greater than 140/90 mm Hg should be the threshold for low-risk patients or for starting therapy post stroke, we often forget those nuances. The main point of contention is that the AAFP guideline was looking for a mortality benefit, whereas the ACC/AHA/everyone else guideline was looking at preventing cardiovascular events. The latter guideline was driven mainly by the results of the SPRINT trial. ACC/AHA argue for more aggressive targets to prevent the things that cardiologists care about, namely heart attacks.
The AAFP guideline conceded that more aggressive control will result in fewer myocardial infarctions but warn that it comes with more adverse events. Treating 1,000 patients to this lower target would theoretically prevent four MIs, possibly prevent three strokes, but result in 30 adverse events.
In the end, what we are seeing here is not so much a debate over the evidence as a debate over priorities. Interventions that don’t improve mortality can be questioned in terms of their cost effectiveness. But you probably don’t want to have a heart attack (even a nonfatal one). And you certainly don’t want to have a stroke. However, lower blood pressure targets inevitably require more medications. Notwithstanding the economic costs, the dangers of polypharmacy, medication interactions, side effects, and syncope leading to falls cannot be ignored. Falls are not benign adverse events, especially in older adults.
The counter argument is that physicians are human and often let things slide. Set the target at 140/90 mm Hg, and many physicians won’t jump on a systolic blood pressure of 144 mm Hg. Set the target at 130 mm Hg, and maybe they’ll be more likely to react. There’s a fine line between permissiveness and complacency.
If you zoom out and look at the multitude of blood pressure guidelines, you start to notice an important fact. There is not much daylight between them. There are subtle differences in what constitutes high risk and different definitions of older (older should be defined as 10 years older than the reader’s current age). But otherwise, the blood pressure targets are not that different.
Does that final 10 mm Hg really matter when barriers to care mean that tens of millions in the United States are unaware they have hypertension? Even among those diagnosed, many are either untreated or inadequately treated.
With this context, perhaps the most insightful thing that can be said about the blood pressure guideline controversy is that it’s not all that controversial. We can likely all agree that we need to be better at treating hypertension and that creative solutions to reach underserved communities are necessary.
Arguing about 140/90 mm Hg or 130/80 mm Hg is less important than acknowledging that we should be aggressive in screening for and treating hypertension. We should acknowledge that beyond a certain point any cardiovascular benefit comes at the cost of hypotension and side effects. That tipping point will be different for different groups, and probably at a higher set point in older patients.
Individualizing care isn’t difficult. We do it all the time. We just shouldn’t be letting people walk around with untreated hypertension. It’s not the 1900s anymore.
Dr. Labos is a cardiologist at Hôpital Notre-Dame, Montreal. He reported no conflicts of interest.
A version of this article first appeared on Medscape.com.
New ESH hypertension guidelines aim for simplified message
The guidelines, which are endorsed by the European Renal Association and the International Society of Hypertension, were presented during the annual European Meeting on Hypertension and Cardiovascular Protection Meeting in Milan, Italy.
The guidelines consensus document was also published online in the Journal of Hypertension. Giuseppe Mancia, MD, professor emeritus of medicine, University Milano-Bicocca, Italy, and Reinhold Kreutz, MD, PhD, Charité–University Medicine Berlin, were cochairs of the task force that created the document.
“We have tried to provide a simplified message to key topics with these new guidelines,” Dr. Kreutz said in an interview.
“We have confirmed the definition of hypertension and provide clear guidance for blood pressure monitoring and a simplified general strategy targeting similar blood pressure goals for most patients, although the treatment algorithms of how you get there may be different for different patient groups.”
Dr. Kreutz added: “Because hypertension is so prevalent and many patients have comorbidities, it is not easy to have one approach for all, but we have tried to simplify the key messages as much as possible, with a target that is more general to the whole population.”
While there are no major surprises in the guidelines, there are multiple advances and added-value changes, including clear advice on how to measure blood pressure, an upgrade for beta-blockers in the treatment algorithms, and a new definition and treatment recommendations for “true resistant hypertension.”
Definition remains unchanged
The definition of hypertension remains unchanged from the previous guidelines – repeated office systolic blood pressure values of ≥ 140 mm Hg and/or diastolic blood pressure values of ≥ 90 mm Hg.
“The definition and classification of hypertension has not changed in these new guidelines,” Dr. Kreutz said. “While there have been suggestions that the definition/target should be changed again, particularly about blood pressure lowering being beneficial at the very low pressure range, after reviewing all the evidence we do not agree with this, and we are standing with the definition of hypertension when intervention is beneficial rather than doing nothing or causing harm.”
Clear guidance on measurement
Dr. Kreutz points out that the correct measurement of blood pressure is of key importance, and the new guidelines include a detailed algorithm on how to measure blood pressure. The preferred method is automated cuff-based blood pressure measurement.
“There are still many variations in blood pressure measurement in clinical practice, so we now have clear guidance on how to measure blood pressure in the office but also at home,” he commented.
They have upgraded the use of out-of-office blood pressure measurement, particularly home measurement, as useful in long-term management. “In future, there should be more emphasis on follow-up using technology with remote control and virtual care.”
Thresholds for starting treatment
On thresholds for initiating antihypertensive therapy, the guidelines recommend that treatment be initiated for most patients when systolic blood pressure is ≥ 140 mm Hg or diastolic blood pressure is ≥ 90 mm Hg.
The same recommendation is given for patients with grade 1 hypertension (systolic, 140-159 mm Hg; and/or diastolic, 90-99 mm Hg) irrespective of cardiovascular risk, although they add that for patients in the lower blood pressure range who have no hypertension-mediated organ damage and who are at low cardiovascular risk, consideration may be given to starting treatment with lifestyle changes only. If, however, blood pressure control is not achieved within a few months of a lifestyle-based approach alone, drug treatment is necessary.
For older patients (aged 80 or older), the task force recommends initiation of drug treatment at 160 mm Hg systolic, although a lower systolic threshold of 140-160 mm Hg may be considered. The authors note that thresholds for the initiation of drug treatment for very frail patients should be individualized.
Blood pressure targets
In the new guidelines, the blood pressure target is the same as in the previous guidelines for the general population of patients with hypertension. The goal is < 140/80 mm Hg for most patients. This accounts for the major portion of the protective effect of blood pressure lowering.
However, the consensus document notes that despite the smaller incremental benefit, an effort should be made to reach a range of 120-129/70-79 mm Hg, but only if treatment is well tolerated to avoid the risk of treatment discontinuation because of adverse events, which might offset, in part or completely, the incremental reduction in cardiovascular outcomes.
Elaborating on this, Dr. Kreutz said, “We should aim for the systolic blood pressure to be within the range of below 140 mm Hg down to 120 mm Hg, with a specific target of around 130 mm Hg for most patients and lower in patients in whom drug treatments are well tolerated and who are at high risk.
“The problem is, if we go for a target of lower that 130 mm Hg, the evidence gets weaker, the benefits diminish, and we risk losing patients because of adverse effects from using so many drugs,” he added. “But in younger and fitter patients, we would recommend the lower the better, but not below 120 mm Hg.”
Dr. Kreutz noted that the new guidelines have tried to simplify recommendations on target pressures. “We have tried to simplify guidance to focus on a target of around 130 for almost all patients. Before, it wasn’t so clear. There were different targets for different groups of patients with various comorbidities or older patients. But now we are saying the range of 120 to 139 is suitable for the vast majority of patients.”
The guidelines do allow slightly higher targets for older and very frail patients.
Drug treatments
The guidelines advise that blood pressure lowering be prioritized over the selection of specific antihypertensive drug classes. The use of any of the five major drug classes – angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, calcium blockers, and thiazide/thiazidelike diuretics – and their combinations are recommended as the basis of antihypertensive treatment strategies.
They advise starting with a two-drug combination for most patients. The preferred combinations including a renin-angiotensin blocker (either an ACE inhibitor or an ARB) with a calcium blocker or a thiazide/thiazidelike diuretic, preferably in a single-pill combination to reduce pill burden and improve adherence and outcome.
If blood pressure is not controlled with the initial two-drug combination at the maximum recommended and tolerated dose of the respective components, treatment should be increased to a three-drug combination.
“We can control 60% of patients in the general hypertensive population with dual therapy, and up to 90% with triple therapy,” Dr. Kreutz said. “Only a small percentage need a fourth drug.”
A new feature of the guidelines is the upgrading of beta-blockers in the treatment algorithms.
“Beta-blockers may not have previously been considered as a first choice of antihypertensive medication, but we see that in clinical practice, many patients are actually treated with these drugs because there are so many conditions in which beta-blockers have a compelling evidence-based indication or are believed to be favorable,” he said. “So, we are now positioning beta-blockers as drugs that can be used at any step of the treatment algorithm if there is a guideline directed indication or other conditions for which they are thought to be beneficial.”
The guidelines also recommend that all drugs be given as once-daily preparations and that they be taken preferably in the morning.
“The new TIME study has established that there is no difference in outcome with morning or evening dosing, but we know that adherence is often better when drugs are taken in the morning, and it is not advisable to take diuretics in the evening,” Dr. Kreutz said.
‘True resistant hypertension’
The guidelines have introduced a new term, “true resistant hypertension,” defined as systolic blood pressure of ≥ 140 mm Hg or diastolic blood pressure of ≥ 90 mm Hg in the presence of the following conditions: the maximum recommended and tolerated doses of a three-drug combination comprising a renin-angiotensin system blocker (either an ACE inhibitor or an ARB), a calcium blocker, and a thiazide/thiazidelike diuretic were used; inadequate blood pressure control has been confirmed by ambulatory (preferable) or home blood pressure measurement; and various causes of pseudo-resistant hypertension (especially poor medication adherence) and secondary hypertension have been excluded.
“There are many patients who may appear to have resistant hypertension, but we need to screen them carefully to ensure they are adherent to treatment, and then most of these patients are found not to be truly resistant,” Dr. Kreutz explained. “We estimate that only about 5% of patients have true resistant hypertension.”
For these patients with true resistant hypertension, two treatment approaches are recommended.
For those who do not have advanced kidney disease (glomerular filtration rate > 40 mL/min), renal denervation can be considered. This is a new II B recommendation.
Dr. Kreutz noted that studies of renal denervation excluded patients with advanced kidney disease, so there are no data for this group. For these patients, the guidelines suggest that a combination diuretic approach (chlorthalidone with a loop diuretic) could be considered in light of the results of the recent CLICK study.
Differences from U.S. guidelines?
Commenting on the new European guidelines for this news organization, Paul Whelton, MD, chair of the most recent American College of Cardiology/American Heart Association hypertension guidelines committee, said: “Publication of these guidelines is important. I congratulate the European task force. It is an enormous amount of time and effort.”
Dr. Whelton, who is Show Chwan Chair in Global Public Health at Tulane University, New Orleans, and president of the World Hypertension League, added: “I would say the changes are incremental rather than major, but that is probably appropriate.”
He welcomed the greater emphasis on out-of-office blood pressure measurement, saying, “That’s where we should be headed.”
Asked how the European guidelines differ from the U.S. guidelines, Dr. Whelton commented: “There are differences, but they are not huge. The major hypertension guidelines across the world are much more alike than they are different.”
He pointed out that both the U.S. and European guidelines aim for a target blood pressure of 130/80 mm Hg for most patients but have different ways of issuing that advice.
“The Europeans recommend a minimum goal of 140/90 mm Hg, and if there are no issues, then press on to get to under 130/80 mm Hg. That’s kind of a two-step process,” he said. “In the U.S., we’ve gone for a more direct approach of just recommending less than 130/80 mm Hg.
“My fear with the European approach is that by saying, get to 140/90 mm Hg first, then move on to 130/80 mm Hg, is that you’re likely to lose people. And doctors could feel that 140/90 is fine.”
More effort needed on implementation
Dr. Whelton says that where all hypertension guidelines are lacking is in the implementation of the recommendations.
“We are all falling down on implementation,” he said. “We have a huge burden of illness, and it is a very cost-effective area for management, but still, rates of blood pressure control are very bad. Generally speaking, even with a very conservative target of 140/90, the best countries only have control rates of around 30%, and this can be as low as 8% in some low/middle-income countries.”
Dr. Whelton believes the approach to blood pressure management needs to change.
“We know that the current traditional model of care, where blood pressure is managed by your local doctor, is not working. It is hopeless,” he said. “That is not an indictment of these doctors. It’s just that they have more pressing issues to deal with, so we need to look at other models.”
He suggests that the way forward is through convenient, community-based care delivered by a team in which nonphysicians assist in much of the management and in which reliable, affordable medications are given at the point of care, with patients tracked with electronic health records so as to identify those who are not adhering to their medication regimens.
“We know that using simple protocols will work for the vast majority of people. We don’t need to individualize or complicate this too much. That tends to lose people in the process.”
Dr. Whelton makes the point that it is well known how to diagnose and treat hypertension, yet this is not being done well.
“We are doing these things really badly. In routine care, blood pressure is measured horribly. Nobody would accept a pilot of a plane saying he should be doing all these procedures but he’s too busy and it’s probably okay, but that’s the way blood pressure is often measured in clinical practice,” he added. “And we can’t really do a good job if were not measuring the key variable properly that the diagnosis is based on.”
Dr. Whelton also points out that the medical profession is not making enough effort to have patients reach target levels.
“If you’re in a country where very few people are being treated and very high pressures are common, then of course you have to focus on that group first. But in most of the Western world, we are long past that, so we can move on down the chain. We then get to a lot more people with moderately high blood pressure getting exposed to increases in risk, and while this is not quite as dramatic as those with very high pressures at the individual risk level, because there are so many of them, that’s where a lot of events are occurring,” he says.
“If we get everyone to 140/90 mm Hg, we can probably prevent 60% of blood pressure–related events. But if we can get them all down to 130 mm Hg systolic, then we can prevent 75%-80% of events. It’s often quite easy to get to that target, but patients need help and encouragement.”
Going forward, he concluded, guidelines should pivot to focus more on implementation.
“We all try to make the guidelines as approachable as possible, but they are encyclopedic, and many doctors just continue doing what they are doing. That is our big challenge.”
A version of this article first appeared on Medscape.com.
The guidelines, which are endorsed by the European Renal Association and the International Society of Hypertension, were presented during the annual European Meeting on Hypertension and Cardiovascular Protection Meeting in Milan, Italy.
The guidelines consensus document was also published online in the Journal of Hypertension. Giuseppe Mancia, MD, professor emeritus of medicine, University Milano-Bicocca, Italy, and Reinhold Kreutz, MD, PhD, Charité–University Medicine Berlin, were cochairs of the task force that created the document.
“We have tried to provide a simplified message to key topics with these new guidelines,” Dr. Kreutz said in an interview.
“We have confirmed the definition of hypertension and provide clear guidance for blood pressure monitoring and a simplified general strategy targeting similar blood pressure goals for most patients, although the treatment algorithms of how you get there may be different for different patient groups.”
Dr. Kreutz added: “Because hypertension is so prevalent and many patients have comorbidities, it is not easy to have one approach for all, but we have tried to simplify the key messages as much as possible, with a target that is more general to the whole population.”
While there are no major surprises in the guidelines, there are multiple advances and added-value changes, including clear advice on how to measure blood pressure, an upgrade for beta-blockers in the treatment algorithms, and a new definition and treatment recommendations for “true resistant hypertension.”
Definition remains unchanged
The definition of hypertension remains unchanged from the previous guidelines – repeated office systolic blood pressure values of ≥ 140 mm Hg and/or diastolic blood pressure values of ≥ 90 mm Hg.
“The definition and classification of hypertension has not changed in these new guidelines,” Dr. Kreutz said. “While there have been suggestions that the definition/target should be changed again, particularly about blood pressure lowering being beneficial at the very low pressure range, after reviewing all the evidence we do not agree with this, and we are standing with the definition of hypertension when intervention is beneficial rather than doing nothing or causing harm.”
Clear guidance on measurement
Dr. Kreutz points out that the correct measurement of blood pressure is of key importance, and the new guidelines include a detailed algorithm on how to measure blood pressure. The preferred method is automated cuff-based blood pressure measurement.
“There are still many variations in blood pressure measurement in clinical practice, so we now have clear guidance on how to measure blood pressure in the office but also at home,” he commented.
They have upgraded the use of out-of-office blood pressure measurement, particularly home measurement, as useful in long-term management. “In future, there should be more emphasis on follow-up using technology with remote control and virtual care.”
Thresholds for starting treatment
On thresholds for initiating antihypertensive therapy, the guidelines recommend that treatment be initiated for most patients when systolic blood pressure is ≥ 140 mm Hg or diastolic blood pressure is ≥ 90 mm Hg.
The same recommendation is given for patients with grade 1 hypertension (systolic, 140-159 mm Hg; and/or diastolic, 90-99 mm Hg) irrespective of cardiovascular risk, although they add that for patients in the lower blood pressure range who have no hypertension-mediated organ damage and who are at low cardiovascular risk, consideration may be given to starting treatment with lifestyle changes only. If, however, blood pressure control is not achieved within a few months of a lifestyle-based approach alone, drug treatment is necessary.
For older patients (aged 80 or older), the task force recommends initiation of drug treatment at 160 mm Hg systolic, although a lower systolic threshold of 140-160 mm Hg may be considered. The authors note that thresholds for the initiation of drug treatment for very frail patients should be individualized.
Blood pressure targets
In the new guidelines, the blood pressure target is the same as in the previous guidelines for the general population of patients with hypertension. The goal is < 140/80 mm Hg for most patients. This accounts for the major portion of the protective effect of blood pressure lowering.
However, the consensus document notes that despite the smaller incremental benefit, an effort should be made to reach a range of 120-129/70-79 mm Hg, but only if treatment is well tolerated to avoid the risk of treatment discontinuation because of adverse events, which might offset, in part or completely, the incremental reduction in cardiovascular outcomes.
Elaborating on this, Dr. Kreutz said, “We should aim for the systolic blood pressure to be within the range of below 140 mm Hg down to 120 mm Hg, with a specific target of around 130 mm Hg for most patients and lower in patients in whom drug treatments are well tolerated and who are at high risk.
“The problem is, if we go for a target of lower that 130 mm Hg, the evidence gets weaker, the benefits diminish, and we risk losing patients because of adverse effects from using so many drugs,” he added. “But in younger and fitter patients, we would recommend the lower the better, but not below 120 mm Hg.”
Dr. Kreutz noted that the new guidelines have tried to simplify recommendations on target pressures. “We have tried to simplify guidance to focus on a target of around 130 for almost all patients. Before, it wasn’t so clear. There were different targets for different groups of patients with various comorbidities or older patients. But now we are saying the range of 120 to 139 is suitable for the vast majority of patients.”
The guidelines do allow slightly higher targets for older and very frail patients.
Drug treatments
The guidelines advise that blood pressure lowering be prioritized over the selection of specific antihypertensive drug classes. The use of any of the five major drug classes – angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, calcium blockers, and thiazide/thiazidelike diuretics – and their combinations are recommended as the basis of antihypertensive treatment strategies.
They advise starting with a two-drug combination for most patients. The preferred combinations including a renin-angiotensin blocker (either an ACE inhibitor or an ARB) with a calcium blocker or a thiazide/thiazidelike diuretic, preferably in a single-pill combination to reduce pill burden and improve adherence and outcome.
If blood pressure is not controlled with the initial two-drug combination at the maximum recommended and tolerated dose of the respective components, treatment should be increased to a three-drug combination.
“We can control 60% of patients in the general hypertensive population with dual therapy, and up to 90% with triple therapy,” Dr. Kreutz said. “Only a small percentage need a fourth drug.”
A new feature of the guidelines is the upgrading of beta-blockers in the treatment algorithms.
“Beta-blockers may not have previously been considered as a first choice of antihypertensive medication, but we see that in clinical practice, many patients are actually treated with these drugs because there are so many conditions in which beta-blockers have a compelling evidence-based indication or are believed to be favorable,” he said. “So, we are now positioning beta-blockers as drugs that can be used at any step of the treatment algorithm if there is a guideline directed indication or other conditions for which they are thought to be beneficial.”
The guidelines also recommend that all drugs be given as once-daily preparations and that they be taken preferably in the morning.
“The new TIME study has established that there is no difference in outcome with morning or evening dosing, but we know that adherence is often better when drugs are taken in the morning, and it is not advisable to take diuretics in the evening,” Dr. Kreutz said.
‘True resistant hypertension’
The guidelines have introduced a new term, “true resistant hypertension,” defined as systolic blood pressure of ≥ 140 mm Hg or diastolic blood pressure of ≥ 90 mm Hg in the presence of the following conditions: the maximum recommended and tolerated doses of a three-drug combination comprising a renin-angiotensin system blocker (either an ACE inhibitor or an ARB), a calcium blocker, and a thiazide/thiazidelike diuretic were used; inadequate blood pressure control has been confirmed by ambulatory (preferable) or home blood pressure measurement; and various causes of pseudo-resistant hypertension (especially poor medication adherence) and secondary hypertension have been excluded.
“There are many patients who may appear to have resistant hypertension, but we need to screen them carefully to ensure they are adherent to treatment, and then most of these patients are found not to be truly resistant,” Dr. Kreutz explained. “We estimate that only about 5% of patients have true resistant hypertension.”
For these patients with true resistant hypertension, two treatment approaches are recommended.
For those who do not have advanced kidney disease (glomerular filtration rate > 40 mL/min), renal denervation can be considered. This is a new II B recommendation.
Dr. Kreutz noted that studies of renal denervation excluded patients with advanced kidney disease, so there are no data for this group. For these patients, the guidelines suggest that a combination diuretic approach (chlorthalidone with a loop diuretic) could be considered in light of the results of the recent CLICK study.
Differences from U.S. guidelines?
Commenting on the new European guidelines for this news organization, Paul Whelton, MD, chair of the most recent American College of Cardiology/American Heart Association hypertension guidelines committee, said: “Publication of these guidelines is important. I congratulate the European task force. It is an enormous amount of time and effort.”
Dr. Whelton, who is Show Chwan Chair in Global Public Health at Tulane University, New Orleans, and president of the World Hypertension League, added: “I would say the changes are incremental rather than major, but that is probably appropriate.”
He welcomed the greater emphasis on out-of-office blood pressure measurement, saying, “That’s where we should be headed.”
Asked how the European guidelines differ from the U.S. guidelines, Dr. Whelton commented: “There are differences, but they are not huge. The major hypertension guidelines across the world are much more alike than they are different.”
He pointed out that both the U.S. and European guidelines aim for a target blood pressure of 130/80 mm Hg for most patients but have different ways of issuing that advice.
“The Europeans recommend a minimum goal of 140/90 mm Hg, and if there are no issues, then press on to get to under 130/80 mm Hg. That’s kind of a two-step process,” he said. “In the U.S., we’ve gone for a more direct approach of just recommending less than 130/80 mm Hg.
“My fear with the European approach is that by saying, get to 140/90 mm Hg first, then move on to 130/80 mm Hg, is that you’re likely to lose people. And doctors could feel that 140/90 is fine.”
More effort needed on implementation
Dr. Whelton says that where all hypertension guidelines are lacking is in the implementation of the recommendations.
“We are all falling down on implementation,” he said. “We have a huge burden of illness, and it is a very cost-effective area for management, but still, rates of blood pressure control are very bad. Generally speaking, even with a very conservative target of 140/90, the best countries only have control rates of around 30%, and this can be as low as 8% in some low/middle-income countries.”
Dr. Whelton believes the approach to blood pressure management needs to change.
“We know that the current traditional model of care, where blood pressure is managed by your local doctor, is not working. It is hopeless,” he said. “That is not an indictment of these doctors. It’s just that they have more pressing issues to deal with, so we need to look at other models.”
He suggests that the way forward is through convenient, community-based care delivered by a team in which nonphysicians assist in much of the management and in which reliable, affordable medications are given at the point of care, with patients tracked with electronic health records so as to identify those who are not adhering to their medication regimens.
“We know that using simple protocols will work for the vast majority of people. We don’t need to individualize or complicate this too much. That tends to lose people in the process.”
Dr. Whelton makes the point that it is well known how to diagnose and treat hypertension, yet this is not being done well.
“We are doing these things really badly. In routine care, blood pressure is measured horribly. Nobody would accept a pilot of a plane saying he should be doing all these procedures but he’s too busy and it’s probably okay, but that’s the way blood pressure is often measured in clinical practice,” he added. “And we can’t really do a good job if were not measuring the key variable properly that the diagnosis is based on.”
Dr. Whelton also points out that the medical profession is not making enough effort to have patients reach target levels.
“If you’re in a country where very few people are being treated and very high pressures are common, then of course you have to focus on that group first. But in most of the Western world, we are long past that, so we can move on down the chain. We then get to a lot more people with moderately high blood pressure getting exposed to increases in risk, and while this is not quite as dramatic as those with very high pressures at the individual risk level, because there are so many of them, that’s where a lot of events are occurring,” he says.
“If we get everyone to 140/90 mm Hg, we can probably prevent 60% of blood pressure–related events. But if we can get them all down to 130 mm Hg systolic, then we can prevent 75%-80% of events. It’s often quite easy to get to that target, but patients need help and encouragement.”
Going forward, he concluded, guidelines should pivot to focus more on implementation.
“We all try to make the guidelines as approachable as possible, but they are encyclopedic, and many doctors just continue doing what they are doing. That is our big challenge.”
A version of this article first appeared on Medscape.com.
The guidelines, which are endorsed by the European Renal Association and the International Society of Hypertension, were presented during the annual European Meeting on Hypertension and Cardiovascular Protection Meeting in Milan, Italy.
The guidelines consensus document was also published online in the Journal of Hypertension. Giuseppe Mancia, MD, professor emeritus of medicine, University Milano-Bicocca, Italy, and Reinhold Kreutz, MD, PhD, Charité–University Medicine Berlin, were cochairs of the task force that created the document.
“We have tried to provide a simplified message to key topics with these new guidelines,” Dr. Kreutz said in an interview.
“We have confirmed the definition of hypertension and provide clear guidance for blood pressure monitoring and a simplified general strategy targeting similar blood pressure goals for most patients, although the treatment algorithms of how you get there may be different for different patient groups.”
Dr. Kreutz added: “Because hypertension is so prevalent and many patients have comorbidities, it is not easy to have one approach for all, but we have tried to simplify the key messages as much as possible, with a target that is more general to the whole population.”
While there are no major surprises in the guidelines, there are multiple advances and added-value changes, including clear advice on how to measure blood pressure, an upgrade for beta-blockers in the treatment algorithms, and a new definition and treatment recommendations for “true resistant hypertension.”
Definition remains unchanged
The definition of hypertension remains unchanged from the previous guidelines – repeated office systolic blood pressure values of ≥ 140 mm Hg and/or diastolic blood pressure values of ≥ 90 mm Hg.
“The definition and classification of hypertension has not changed in these new guidelines,” Dr. Kreutz said. “While there have been suggestions that the definition/target should be changed again, particularly about blood pressure lowering being beneficial at the very low pressure range, after reviewing all the evidence we do not agree with this, and we are standing with the definition of hypertension when intervention is beneficial rather than doing nothing or causing harm.”
Clear guidance on measurement
Dr. Kreutz points out that the correct measurement of blood pressure is of key importance, and the new guidelines include a detailed algorithm on how to measure blood pressure. The preferred method is automated cuff-based blood pressure measurement.
“There are still many variations in blood pressure measurement in clinical practice, so we now have clear guidance on how to measure blood pressure in the office but also at home,” he commented.
They have upgraded the use of out-of-office blood pressure measurement, particularly home measurement, as useful in long-term management. “In future, there should be more emphasis on follow-up using technology with remote control and virtual care.”
Thresholds for starting treatment
On thresholds for initiating antihypertensive therapy, the guidelines recommend that treatment be initiated for most patients when systolic blood pressure is ≥ 140 mm Hg or diastolic blood pressure is ≥ 90 mm Hg.
The same recommendation is given for patients with grade 1 hypertension (systolic, 140-159 mm Hg; and/or diastolic, 90-99 mm Hg) irrespective of cardiovascular risk, although they add that for patients in the lower blood pressure range who have no hypertension-mediated organ damage and who are at low cardiovascular risk, consideration may be given to starting treatment with lifestyle changes only. If, however, blood pressure control is not achieved within a few months of a lifestyle-based approach alone, drug treatment is necessary.
For older patients (aged 80 or older), the task force recommends initiation of drug treatment at 160 mm Hg systolic, although a lower systolic threshold of 140-160 mm Hg may be considered. The authors note that thresholds for the initiation of drug treatment for very frail patients should be individualized.
Blood pressure targets
In the new guidelines, the blood pressure target is the same as in the previous guidelines for the general population of patients with hypertension. The goal is < 140/80 mm Hg for most patients. This accounts for the major portion of the protective effect of blood pressure lowering.
However, the consensus document notes that despite the smaller incremental benefit, an effort should be made to reach a range of 120-129/70-79 mm Hg, but only if treatment is well tolerated to avoid the risk of treatment discontinuation because of adverse events, which might offset, in part or completely, the incremental reduction in cardiovascular outcomes.
Elaborating on this, Dr. Kreutz said, “We should aim for the systolic blood pressure to be within the range of below 140 mm Hg down to 120 mm Hg, with a specific target of around 130 mm Hg for most patients and lower in patients in whom drug treatments are well tolerated and who are at high risk.
“The problem is, if we go for a target of lower that 130 mm Hg, the evidence gets weaker, the benefits diminish, and we risk losing patients because of adverse effects from using so many drugs,” he added. “But in younger and fitter patients, we would recommend the lower the better, but not below 120 mm Hg.”
Dr. Kreutz noted that the new guidelines have tried to simplify recommendations on target pressures. “We have tried to simplify guidance to focus on a target of around 130 for almost all patients. Before, it wasn’t so clear. There were different targets for different groups of patients with various comorbidities or older patients. But now we are saying the range of 120 to 139 is suitable for the vast majority of patients.”
The guidelines do allow slightly higher targets for older and very frail patients.
Drug treatments
The guidelines advise that blood pressure lowering be prioritized over the selection of specific antihypertensive drug classes. The use of any of the five major drug classes – angiotensin-converting enzyme (ACE) inhibitors, angiotensin receptor blockers (ARBs), beta-blockers, calcium blockers, and thiazide/thiazidelike diuretics – and their combinations are recommended as the basis of antihypertensive treatment strategies.
They advise starting with a two-drug combination for most patients. The preferred combinations including a renin-angiotensin blocker (either an ACE inhibitor or an ARB) with a calcium blocker or a thiazide/thiazidelike diuretic, preferably in a single-pill combination to reduce pill burden and improve adherence and outcome.
If blood pressure is not controlled with the initial two-drug combination at the maximum recommended and tolerated dose of the respective components, treatment should be increased to a three-drug combination.
“We can control 60% of patients in the general hypertensive population with dual therapy, and up to 90% with triple therapy,” Dr. Kreutz said. “Only a small percentage need a fourth drug.”
A new feature of the guidelines is the upgrading of beta-blockers in the treatment algorithms.
“Beta-blockers may not have previously been considered as a first choice of antihypertensive medication, but we see that in clinical practice, many patients are actually treated with these drugs because there are so many conditions in which beta-blockers have a compelling evidence-based indication or are believed to be favorable,” he said. “So, we are now positioning beta-blockers as drugs that can be used at any step of the treatment algorithm if there is a guideline directed indication or other conditions for which they are thought to be beneficial.”
The guidelines also recommend that all drugs be given as once-daily preparations and that they be taken preferably in the morning.
“The new TIME study has established that there is no difference in outcome with morning or evening dosing, but we know that adherence is often better when drugs are taken in the morning, and it is not advisable to take diuretics in the evening,” Dr. Kreutz said.
‘True resistant hypertension’
The guidelines have introduced a new term, “true resistant hypertension,” defined as systolic blood pressure of ≥ 140 mm Hg or diastolic blood pressure of ≥ 90 mm Hg in the presence of the following conditions: the maximum recommended and tolerated doses of a three-drug combination comprising a renin-angiotensin system blocker (either an ACE inhibitor or an ARB), a calcium blocker, and a thiazide/thiazidelike diuretic were used; inadequate blood pressure control has been confirmed by ambulatory (preferable) or home blood pressure measurement; and various causes of pseudo-resistant hypertension (especially poor medication adherence) and secondary hypertension have been excluded.
“There are many patients who may appear to have resistant hypertension, but we need to screen them carefully to ensure they are adherent to treatment, and then most of these patients are found not to be truly resistant,” Dr. Kreutz explained. “We estimate that only about 5% of patients have true resistant hypertension.”
For these patients with true resistant hypertension, two treatment approaches are recommended.
For those who do not have advanced kidney disease (glomerular filtration rate > 40 mL/min), renal denervation can be considered. This is a new II B recommendation.
Dr. Kreutz noted that studies of renal denervation excluded patients with advanced kidney disease, so there are no data for this group. For these patients, the guidelines suggest that a combination diuretic approach (chlorthalidone with a loop diuretic) could be considered in light of the results of the recent CLICK study.
Differences from U.S. guidelines?
Commenting on the new European guidelines for this news organization, Paul Whelton, MD, chair of the most recent American College of Cardiology/American Heart Association hypertension guidelines committee, said: “Publication of these guidelines is important. I congratulate the European task force. It is an enormous amount of time and effort.”
Dr. Whelton, who is Show Chwan Chair in Global Public Health at Tulane University, New Orleans, and president of the World Hypertension League, added: “I would say the changes are incremental rather than major, but that is probably appropriate.”
He welcomed the greater emphasis on out-of-office blood pressure measurement, saying, “That’s where we should be headed.”
Asked how the European guidelines differ from the U.S. guidelines, Dr. Whelton commented: “There are differences, but they are not huge. The major hypertension guidelines across the world are much more alike than they are different.”
He pointed out that both the U.S. and European guidelines aim for a target blood pressure of 130/80 mm Hg for most patients but have different ways of issuing that advice.
“The Europeans recommend a minimum goal of 140/90 mm Hg, and if there are no issues, then press on to get to under 130/80 mm Hg. That’s kind of a two-step process,” he said. “In the U.S., we’ve gone for a more direct approach of just recommending less than 130/80 mm Hg.
“My fear with the European approach is that by saying, get to 140/90 mm Hg first, then move on to 130/80 mm Hg, is that you’re likely to lose people. And doctors could feel that 140/90 is fine.”
More effort needed on implementation
Dr. Whelton says that where all hypertension guidelines are lacking is in the implementation of the recommendations.
“We are all falling down on implementation,” he said. “We have a huge burden of illness, and it is a very cost-effective area for management, but still, rates of blood pressure control are very bad. Generally speaking, even with a very conservative target of 140/90, the best countries only have control rates of around 30%, and this can be as low as 8% in some low/middle-income countries.”
Dr. Whelton believes the approach to blood pressure management needs to change.
“We know that the current traditional model of care, where blood pressure is managed by your local doctor, is not working. It is hopeless,” he said. “That is not an indictment of these doctors. It’s just that they have more pressing issues to deal with, so we need to look at other models.”
He suggests that the way forward is through convenient, community-based care delivered by a team in which nonphysicians assist in much of the management and in which reliable, affordable medications are given at the point of care, with patients tracked with electronic health records so as to identify those who are not adhering to their medication regimens.
“We know that using simple protocols will work for the vast majority of people. We don’t need to individualize or complicate this too much. That tends to lose people in the process.”
Dr. Whelton makes the point that it is well known how to diagnose and treat hypertension, yet this is not being done well.
“We are doing these things really badly. In routine care, blood pressure is measured horribly. Nobody would accept a pilot of a plane saying he should be doing all these procedures but he’s too busy and it’s probably okay, but that’s the way blood pressure is often measured in clinical practice,” he added. “And we can’t really do a good job if were not measuring the key variable properly that the diagnosis is based on.”
Dr. Whelton also points out that the medical profession is not making enough effort to have patients reach target levels.
“If you’re in a country where very few people are being treated and very high pressures are common, then of course you have to focus on that group first. But in most of the Western world, we are long past that, so we can move on down the chain. We then get to a lot more people with moderately high blood pressure getting exposed to increases in risk, and while this is not quite as dramatic as those with very high pressures at the individual risk level, because there are so many of them, that’s where a lot of events are occurring,” he says.
“If we get everyone to 140/90 mm Hg, we can probably prevent 60% of blood pressure–related events. But if we can get them all down to 130 mm Hg systolic, then we can prevent 75%-80% of events. It’s often quite easy to get to that target, but patients need help and encouragement.”
Going forward, he concluded, guidelines should pivot to focus more on implementation.
“We all try to make the guidelines as approachable as possible, but they are encyclopedic, and many doctors just continue doing what they are doing. That is our big challenge.”
A version of this article first appeared on Medscape.com.
New definition for iron deficiency in CV disease proposed
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.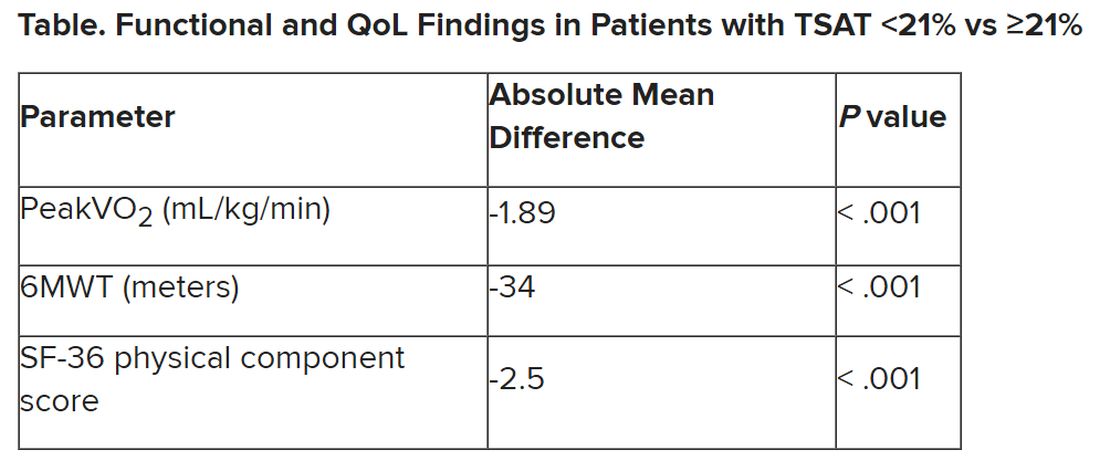
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.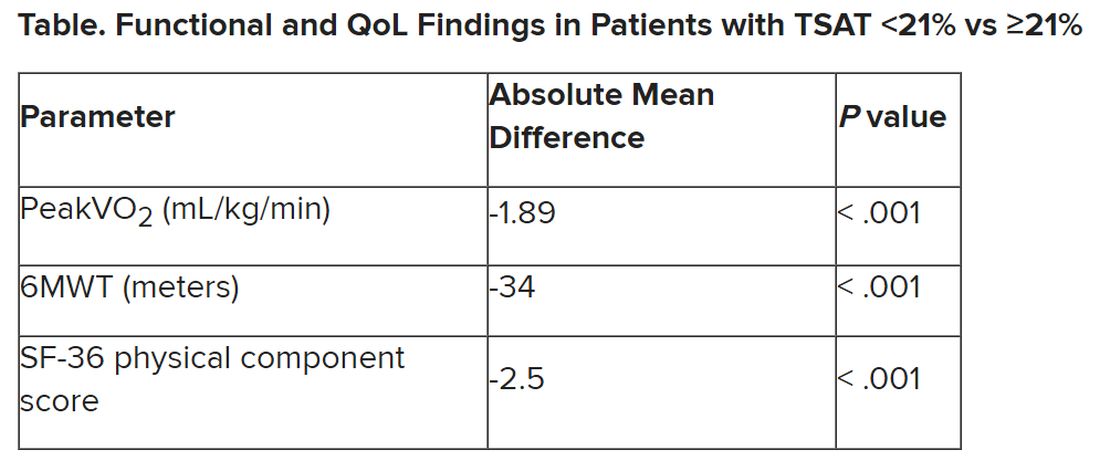
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
FROM EUROPEAN HEART JOURNAL