User login
FDA tightens requirements for COVID-19 antibody tests
The U.S. Food and Drug Administration is tightening requirements for companies that develop COVID-19 antibody tests in an effort to combat fraud and better regulate the frenzy of tests coming to market.
The updated policy, announced May 4, requires commercial antibody test developers to apply for Emergency Use Authorization (EUA) from the FDA under a tight time frame and also provides specific performance threshold recommendations for test specificity and sensitivity. The revised requirements follow a March 16 policy that allowed developers to validate their own tests and bring them to market without an agency review. More than 100 coronavirus antibody tests have since entered the market, fueling a congressional investigation into the accuracy of tests.
When the March policy was issued, FDA Commissioner Stephen M. Hahn, MD, said it was critical for the FDA to provide regulatory flexibility for serology test developers, given the nature of the COVID-19 public health emergency and an understanding that the tests were not meant to be used as the sole basis for COVID-19 diagnosis.
“As FDA has authorized more antibody tests and validation data has become available, including through the capability at [the National Cancer Institute] the careful balancing of risks and benefits has shifted to the approach we have outlined today and our policy update,” Dr. Hahn said during a May 4 press conference.
The new approach requires all commercial manufacturers to submit EUA requests with their validation data within 10 business days from the date they notified the FDA of their validation testing or from the date of the May 4 policy, whichever is later. Additionally, the FDA has provided specific performance threshold recommendations for specificity and sensitivity for all serology test developers.
In a statement released May 4, FDA leaders acknowledged the widespread fraud that is occurring in connection to antibody tests entering the market.
“We unfortunately see unscrupulous actors marketing fraudulent test kits and using the pandemic as an opportunity to take advantage of Americans’ anxiety,” wrote Anand Shah, MD, FDA deputy commissioner for medical and scientific affairs in a joint statement with Jeff E. Shuren, MD, director for the FDA’s Center for Devices and Radiological Health. “Some test developers have falsely claimed their serological tests are FDA approved or authorized. Others have falsely claimed that their tests can diagnose COVID-19 or that they are for at-home testing, which would fall outside of the policies outlined in our March 16 guidance, as well as the updated guidance.”
At the same time, FDA officials said they are aware of a “concerning number” of commercial serology tests that are being inappropriately marketed, including for diagnostic use, or that are performing poorly based on an independent evaluation by the National Institutes of Health, according to the May 4 statement.
In addition to tightening its requirements for test developers, the FDA also is introducing a more streamlined process to support EUA submissions and review. Two voluntary EUA templates for antibody tests are now available – one for commercial manufacturers and one for Clinical Laboratory Improvement Amendments-certified high-complexity labs seeking FDA authorization. The templates will facilitate the preparation and submission of EUA requests and can be used by any interested developer, according to the FDA.
To date, 12 antibody tests have been authorized under an individual EUA, and more than 200 antibody tests are currently the subject of a pre-EUA or EUA review, according to the FDA.
Many unknowns remain about antibody tests and how they might help researchers and clinicians understand and/or potentially treat COVID-19. Antibody tests may be able to provide information on disease prevalence and frequency of asymptomatic infection, as well as identify potential donors of “convalescent plasma,” an approach in which blood plasma containing antibodies from a recovered individual serves as a therapy for an infected patient with severe disease, Dr. Shah wrote in the May 4 statement.
“There are a lot of unanswered questions about this particular issue,” Dr. Hahn said during the press conference. “We need the data because we need to understand this particular aspect of the disease and put it as part of the puzzle around COVID-19.”
The U.S. Food and Drug Administration is tightening requirements for companies that develop COVID-19 antibody tests in an effort to combat fraud and better regulate the frenzy of tests coming to market.
The updated policy, announced May 4, requires commercial antibody test developers to apply for Emergency Use Authorization (EUA) from the FDA under a tight time frame and also provides specific performance threshold recommendations for test specificity and sensitivity. The revised requirements follow a March 16 policy that allowed developers to validate their own tests and bring them to market without an agency review. More than 100 coronavirus antibody tests have since entered the market, fueling a congressional investigation into the accuracy of tests.
When the March policy was issued, FDA Commissioner Stephen M. Hahn, MD, said it was critical for the FDA to provide regulatory flexibility for serology test developers, given the nature of the COVID-19 public health emergency and an understanding that the tests were not meant to be used as the sole basis for COVID-19 diagnosis.
“As FDA has authorized more antibody tests and validation data has become available, including through the capability at [the National Cancer Institute] the careful balancing of risks and benefits has shifted to the approach we have outlined today and our policy update,” Dr. Hahn said during a May 4 press conference.
The new approach requires all commercial manufacturers to submit EUA requests with their validation data within 10 business days from the date they notified the FDA of their validation testing or from the date of the May 4 policy, whichever is later. Additionally, the FDA has provided specific performance threshold recommendations for specificity and sensitivity for all serology test developers.
In a statement released May 4, FDA leaders acknowledged the widespread fraud that is occurring in connection to antibody tests entering the market.
“We unfortunately see unscrupulous actors marketing fraudulent test kits and using the pandemic as an opportunity to take advantage of Americans’ anxiety,” wrote Anand Shah, MD, FDA deputy commissioner for medical and scientific affairs in a joint statement with Jeff E. Shuren, MD, director for the FDA’s Center for Devices and Radiological Health. “Some test developers have falsely claimed their serological tests are FDA approved or authorized. Others have falsely claimed that their tests can diagnose COVID-19 or that they are for at-home testing, which would fall outside of the policies outlined in our March 16 guidance, as well as the updated guidance.”
At the same time, FDA officials said they are aware of a “concerning number” of commercial serology tests that are being inappropriately marketed, including for diagnostic use, or that are performing poorly based on an independent evaluation by the National Institutes of Health, according to the May 4 statement.
In addition to tightening its requirements for test developers, the FDA also is introducing a more streamlined process to support EUA submissions and review. Two voluntary EUA templates for antibody tests are now available – one for commercial manufacturers and one for Clinical Laboratory Improvement Amendments-certified high-complexity labs seeking FDA authorization. The templates will facilitate the preparation and submission of EUA requests and can be used by any interested developer, according to the FDA.
To date, 12 antibody tests have been authorized under an individual EUA, and more than 200 antibody tests are currently the subject of a pre-EUA or EUA review, according to the FDA.
Many unknowns remain about antibody tests and how they might help researchers and clinicians understand and/or potentially treat COVID-19. Antibody tests may be able to provide information on disease prevalence and frequency of asymptomatic infection, as well as identify potential donors of “convalescent plasma,” an approach in which blood plasma containing antibodies from a recovered individual serves as a therapy for an infected patient with severe disease, Dr. Shah wrote in the May 4 statement.
“There are a lot of unanswered questions about this particular issue,” Dr. Hahn said during the press conference. “We need the data because we need to understand this particular aspect of the disease and put it as part of the puzzle around COVID-19.”
The U.S. Food and Drug Administration is tightening requirements for companies that develop COVID-19 antibody tests in an effort to combat fraud and better regulate the frenzy of tests coming to market.
The updated policy, announced May 4, requires commercial antibody test developers to apply for Emergency Use Authorization (EUA) from the FDA under a tight time frame and also provides specific performance threshold recommendations for test specificity and sensitivity. The revised requirements follow a March 16 policy that allowed developers to validate their own tests and bring them to market without an agency review. More than 100 coronavirus antibody tests have since entered the market, fueling a congressional investigation into the accuracy of tests.
When the March policy was issued, FDA Commissioner Stephen M. Hahn, MD, said it was critical for the FDA to provide regulatory flexibility for serology test developers, given the nature of the COVID-19 public health emergency and an understanding that the tests were not meant to be used as the sole basis for COVID-19 diagnosis.
“As FDA has authorized more antibody tests and validation data has become available, including through the capability at [the National Cancer Institute] the careful balancing of risks and benefits has shifted to the approach we have outlined today and our policy update,” Dr. Hahn said during a May 4 press conference.
The new approach requires all commercial manufacturers to submit EUA requests with their validation data within 10 business days from the date they notified the FDA of their validation testing or from the date of the May 4 policy, whichever is later. Additionally, the FDA has provided specific performance threshold recommendations for specificity and sensitivity for all serology test developers.
In a statement released May 4, FDA leaders acknowledged the widespread fraud that is occurring in connection to antibody tests entering the market.
“We unfortunately see unscrupulous actors marketing fraudulent test kits and using the pandemic as an opportunity to take advantage of Americans’ anxiety,” wrote Anand Shah, MD, FDA deputy commissioner for medical and scientific affairs in a joint statement with Jeff E. Shuren, MD, director for the FDA’s Center for Devices and Radiological Health. “Some test developers have falsely claimed their serological tests are FDA approved or authorized. Others have falsely claimed that their tests can diagnose COVID-19 or that they are for at-home testing, which would fall outside of the policies outlined in our March 16 guidance, as well as the updated guidance.”
At the same time, FDA officials said they are aware of a “concerning number” of commercial serology tests that are being inappropriately marketed, including for diagnostic use, or that are performing poorly based on an independent evaluation by the National Institutes of Health, according to the May 4 statement.
In addition to tightening its requirements for test developers, the FDA also is introducing a more streamlined process to support EUA submissions and review. Two voluntary EUA templates for antibody tests are now available – one for commercial manufacturers and one for Clinical Laboratory Improvement Amendments-certified high-complexity labs seeking FDA authorization. The templates will facilitate the preparation and submission of EUA requests and can be used by any interested developer, according to the FDA.
To date, 12 antibody tests have been authorized under an individual EUA, and more than 200 antibody tests are currently the subject of a pre-EUA or EUA review, according to the FDA.
Many unknowns remain about antibody tests and how they might help researchers and clinicians understand and/or potentially treat COVID-19. Antibody tests may be able to provide information on disease prevalence and frequency of asymptomatic infection, as well as identify potential donors of “convalescent plasma,” an approach in which blood plasma containing antibodies from a recovered individual serves as a therapy for an infected patient with severe disease, Dr. Shah wrote in the May 4 statement.
“There are a lot of unanswered questions about this particular issue,” Dr. Hahn said during the press conference. “We need the data because we need to understand this particular aspect of the disease and put it as part of the puzzle around COVID-19.”
COVID-19: To have and to hold ... in quarantine
Tips for marriage survival during a pandemic
Most married couples vowed to stay with their partners during sickness and health, but none of us vowed to remain trapped with our loved ones behind the same four walls, all day, every day, for an unknown period of time. We didn’t sign up for this! Some romantics may be titillated by the prospect, while more independent partners may panic at the mere thought of spending all day and night with their loved ones.
Because of the swift implementation of the lifestyle-altering restrictions, couples did not have ample time to mentally and physically prepare. A lack of preparation and loss of control heightens our emotions. It can make couples more susceptible to engage in unhealthy styles of communication and destructive behaviors that are harmful to their relationships.
There are psychological reasons that “absence makes the heart grow fonder.” Distance from your partner is not just a clever way to make your partner appreciate and desire you more. It is human nature to habituate to what is part of your daily life. For instance, when your partner is away from you while on a work trip, you may find the first night or two alone relaxing; but by day 3, you begin to miss your partner’s hugs and kisses, smell, and touch. And after many days apart, you may even miss the incessant nagging that secretly motivates you. Physical distance from our partners essentially gives us the ability to long for and appreciate each other. Our brains are wired to pay more attention to things that are novel and exciting and less interested in what is in our everyday lives.
Separation gives us the ability to miss our partners, while quarantine does the complete opposite.
To avoid contemplating how to murder one’s spouse before quarantine ends, partners can strengthen their relationships by using the strategies I’ve outlined below, which are loosely based on dialectical behavior therapy (DBT). These strategies can be useful for anyone – providers and patients alike – going through these struggles.
Dialectical behavior therapy was developed by psychologist Marsha Linehan PhD, to help regulate emotions for people diagnosed with borderline personality disorder. These skills help to identify thoughts and feelings, to accept one’s inner emotional world and outward behaviors. The idea is that, once you can recognize and accept, then change is possible. The “dialectic” in dialectical behavior therapy implies that one is attempting to find a balance between acceptance and change. All of us can benefit from these skills, especially emotionally volatile couples who are trapped together in quarantine.
Radically accept what is uncertain in your lives
Radical acceptance is a practice used in DBT in situations that are out of our control, such as the COVID-19 pandemic. Radically accept that you and your partner are trapped in quarantine without attempting to place blame on our government, your spouse, your boss, and even yourself. Radical acceptance is exactly what the name implies. Accept your current situation for what it is and not what you hoped it to be.
Accept the unknown and unanswered questions such as when will this quarantine end? Will there be a summer camp? Will I get back to my office this summer? Will my children even return to school in the fall? The acceptance of what is out of your control will ultimately decrease your mental time spent worrying and obsessing about the uncertainties of your post-quarantine life and instead provide you more time to be present with your spouse.
Remain mindful during all communication with your spouse. To stay in the moment, you need to be aware of your bodily reactions to distress and notice when your heart rate increases, breathing becomes more shallow, stomach muscles tighten, and when your thoughts become more negative. Mindfulness skills enable us to use physiological changes in our body to become aware of our emotions. You can use your partner’s nonverbal body language and tone of voice to gauge that person’s emotional reactivity.
The practice of mindfulness leads to an increased emotional intelligence. The goal is to have enough self-awareness and emotional understanding of your partner and enough empathy to know when a conversation is becoming too emotionally charged and to let it go and back off. Mindfulness is not nagging your partner to remember to change the heating unit filters with a reminder of what happened years ago when this wasn’t done promptly – without first checking in to make sure your partner is emotionally ready for this type of conversation.
When we have strong emotions, we are using the more primitive parts of our brain that induce a fight or flight reaction. These emotional reactions overshadow the more advanced prefrontal region of our brain that stores our rational thoughts and reasoning skills, a concept identified by psychologist Daniel Goleman as “emotional hijacking.”
Use distress tolerance skills to deal with negative emotions
Distress tolerance is an individual’s ability to manage feelings in response to stress. Distress tolerance skills are aimed at helping one manage intense emotions without worsening a situation by engaging in behaviors that are destructive and may exacerbate the problem. The goal is to tolerate the stress while with your partner and not respond negatively or in a way that is harmful to the integrity of your relationship.
To prioritize your relationship, this may mean that you choose not to react negatively when your partner makes a passive-aggressive comment on how you spent your day during quarantine since you still have a pile of laundry on your bedroom floor and overflowing dishes in the kitchen sink. A high level of distress tolerance will enable you to not overreact or withdraw from your spouse when flooded with emotions of anger or sadness.
Distraction techniques are a type of distress tolerance skill. You can engage in activities that keep you distracted and require your full attention. When things get heated between you and your spouse during quarantine, try to obtain some distance from each other to cool down and engage in an activity that involves your full concentration.
Many of us have been surprised by our hidden talents that were discovered during the quarantine. Use the time away from your partner to distract yourself with your new passion for writing, baking, organizing, and even your newfound love of balloon artistry. Do an activity that engages your mind and provides you the necessary physical and mental time away from your partner to deescalate. You can always revisit the initial cause of the conflict when both you and your partner are not emotionally charged. You can also distract yourself with self-soothing tactics such as taking a warm bath or a reading good book. Perhaps distract yourself by giving back to others and spending time planning a drive-by surprise party for your sister’s birthday next month. It can be helpful to distract yourself by comparing yourself to others less fortunate than you or a time in your life when you and your partner were struggling much worse than now, to provide perspective. The goal is not to add to your distress but instead, provide yourself a sense of perspective.
Use interpersonal effectiveness skills to establish a healthy relationship
Be gentle in all your communications with your partner, think about your spouse’s perspective, show empathy and interest in what your partner has to say by your verbal communication or body language, such as maintaining eye contact, and offer recognitional cues, such as “uh-huh” and “oh, really.” Avoid communication that is at all invalidating. Never start a sentence with “YOU” while having heated conversations with your spouse; instead, use “I feel” statements. This type of communication avoids the blame game that gets many couples into trouble.
Instead, communicate how you feel while not necessarily blaming your spouse but rather expressing your emotions. This will ultimately lead to less defensive communication from your partner. Remember that not all communication is for the sole purpose of communicating. Much of the time, communication is used as an attempt for one partner to connect with the other partner. Couples may say that they have difficulty with communication when it is not the communication that is the issue but instead the underlying disconnect of the couple.
This disconnect usually manifests while couples are communicating, and therefore, can be misconstrued as solely a communication issue by the couple. When your partner asks you to stop staring at your phone during dinner, it is not necessarily that your spouse is attempting to control you or wants to engage in some deep conversation, but more likely a bid to try to connect with you. Your partner is attempting to tell you that he or she feels disconnected, misses you, and wants to reconnect.
Provide validation and acceptance to your partner
Focus on your partner’s strengths and accept the weaknesses. Accept that your partner is scattered, disorganized, and takes at least 20 minutes to find the phone and keys every morning. Remember that during your courtship days, you found your partner’s flighty attributes to be endearing. Do the same for your strengths and weaknesses.
Accept that the pandemic is unpredictable and that you may need to strengthen your ability to be flexible and more adaptable. This will ultimately lead to feeling less disappointment by your partner and more accepting of shortcomings. Acceptance of your imperfections will improve your sense of worth and confidence and lessen negative emotions, such as guilt, regret, and shame.
Accept the fact that, as similar as we all are, we use different methods to recharge ourselves. In contrast, your spouse needs alone time without distractions to reboot mentally and prepare for the following day. In the pre-pandemic world, if there were a mismatch in what a couple needed to feel rejuvenated, they could independently compensate and search for fulfillment outside of the home. Before stay-at-home orders were rolled out throughout the country, spouses had ample opportunities to spend time away from their partners at work, dinner with friends, or while squeezing in a 7 p.m. yoga sculpt class – barely getting home in time to kiss our children goodnight – with a few minutes to spare to engage in mundane conversation with our partners before our nighttime routine of TV commenced. Unfortunately, COVID-19 has made it very hard for couples to carve out that time for compensatory activities outside of the home.
Remember that you are a team
Remind yourself of the reason why you initially fell in love with your partner. Teammates do not keep score or compete with one another. They support each other when one player is not feeling well, and they make sacrifices for the betterment of the team.
Your marriage vows included “through sickness and health” and now should include “through quarantine.”
Dr. Abraham is a psychiatrist in private practice in Philadelphia. She has no disclosures.
Tips for marriage survival during a pandemic
Tips for marriage survival during a pandemic
Most married couples vowed to stay with their partners during sickness and health, but none of us vowed to remain trapped with our loved ones behind the same four walls, all day, every day, for an unknown period of time. We didn’t sign up for this! Some romantics may be titillated by the prospect, while more independent partners may panic at the mere thought of spending all day and night with their loved ones.
Because of the swift implementation of the lifestyle-altering restrictions, couples did not have ample time to mentally and physically prepare. A lack of preparation and loss of control heightens our emotions. It can make couples more susceptible to engage in unhealthy styles of communication and destructive behaviors that are harmful to their relationships.
There are psychological reasons that “absence makes the heart grow fonder.” Distance from your partner is not just a clever way to make your partner appreciate and desire you more. It is human nature to habituate to what is part of your daily life. For instance, when your partner is away from you while on a work trip, you may find the first night or two alone relaxing; but by day 3, you begin to miss your partner’s hugs and kisses, smell, and touch. And after many days apart, you may even miss the incessant nagging that secretly motivates you. Physical distance from our partners essentially gives us the ability to long for and appreciate each other. Our brains are wired to pay more attention to things that are novel and exciting and less interested in what is in our everyday lives.
Separation gives us the ability to miss our partners, while quarantine does the complete opposite.
To avoid contemplating how to murder one’s spouse before quarantine ends, partners can strengthen their relationships by using the strategies I’ve outlined below, which are loosely based on dialectical behavior therapy (DBT). These strategies can be useful for anyone – providers and patients alike – going through these struggles.
Dialectical behavior therapy was developed by psychologist Marsha Linehan PhD, to help regulate emotions for people diagnosed with borderline personality disorder. These skills help to identify thoughts and feelings, to accept one’s inner emotional world and outward behaviors. The idea is that, once you can recognize and accept, then change is possible. The “dialectic” in dialectical behavior therapy implies that one is attempting to find a balance between acceptance and change. All of us can benefit from these skills, especially emotionally volatile couples who are trapped together in quarantine.
Radically accept what is uncertain in your lives
Radical acceptance is a practice used in DBT in situations that are out of our control, such as the COVID-19 pandemic. Radically accept that you and your partner are trapped in quarantine without attempting to place blame on our government, your spouse, your boss, and even yourself. Radical acceptance is exactly what the name implies. Accept your current situation for what it is and not what you hoped it to be.
Accept the unknown and unanswered questions such as when will this quarantine end? Will there be a summer camp? Will I get back to my office this summer? Will my children even return to school in the fall? The acceptance of what is out of your control will ultimately decrease your mental time spent worrying and obsessing about the uncertainties of your post-quarantine life and instead provide you more time to be present with your spouse.
Remain mindful during all communication with your spouse. To stay in the moment, you need to be aware of your bodily reactions to distress and notice when your heart rate increases, breathing becomes more shallow, stomach muscles tighten, and when your thoughts become more negative. Mindfulness skills enable us to use physiological changes in our body to become aware of our emotions. You can use your partner’s nonverbal body language and tone of voice to gauge that person’s emotional reactivity.
The practice of mindfulness leads to an increased emotional intelligence. The goal is to have enough self-awareness and emotional understanding of your partner and enough empathy to know when a conversation is becoming too emotionally charged and to let it go and back off. Mindfulness is not nagging your partner to remember to change the heating unit filters with a reminder of what happened years ago when this wasn’t done promptly – without first checking in to make sure your partner is emotionally ready for this type of conversation.
When we have strong emotions, we are using the more primitive parts of our brain that induce a fight or flight reaction. These emotional reactions overshadow the more advanced prefrontal region of our brain that stores our rational thoughts and reasoning skills, a concept identified by psychologist Daniel Goleman as “emotional hijacking.”
Use distress tolerance skills to deal with negative emotions
Distress tolerance is an individual’s ability to manage feelings in response to stress. Distress tolerance skills are aimed at helping one manage intense emotions without worsening a situation by engaging in behaviors that are destructive and may exacerbate the problem. The goal is to tolerate the stress while with your partner and not respond negatively or in a way that is harmful to the integrity of your relationship.
To prioritize your relationship, this may mean that you choose not to react negatively when your partner makes a passive-aggressive comment on how you spent your day during quarantine since you still have a pile of laundry on your bedroom floor and overflowing dishes in the kitchen sink. A high level of distress tolerance will enable you to not overreact or withdraw from your spouse when flooded with emotions of anger or sadness.
Distraction techniques are a type of distress tolerance skill. You can engage in activities that keep you distracted and require your full attention. When things get heated between you and your spouse during quarantine, try to obtain some distance from each other to cool down and engage in an activity that involves your full concentration.
Many of us have been surprised by our hidden talents that were discovered during the quarantine. Use the time away from your partner to distract yourself with your new passion for writing, baking, organizing, and even your newfound love of balloon artistry. Do an activity that engages your mind and provides you the necessary physical and mental time away from your partner to deescalate. You can always revisit the initial cause of the conflict when both you and your partner are not emotionally charged. You can also distract yourself with self-soothing tactics such as taking a warm bath or a reading good book. Perhaps distract yourself by giving back to others and spending time planning a drive-by surprise party for your sister’s birthday next month. It can be helpful to distract yourself by comparing yourself to others less fortunate than you or a time in your life when you and your partner were struggling much worse than now, to provide perspective. The goal is not to add to your distress but instead, provide yourself a sense of perspective.
Use interpersonal effectiveness skills to establish a healthy relationship
Be gentle in all your communications with your partner, think about your spouse’s perspective, show empathy and interest in what your partner has to say by your verbal communication or body language, such as maintaining eye contact, and offer recognitional cues, such as “uh-huh” and “oh, really.” Avoid communication that is at all invalidating. Never start a sentence with “YOU” while having heated conversations with your spouse; instead, use “I feel” statements. This type of communication avoids the blame game that gets many couples into trouble.
Instead, communicate how you feel while not necessarily blaming your spouse but rather expressing your emotions. This will ultimately lead to less defensive communication from your partner. Remember that not all communication is for the sole purpose of communicating. Much of the time, communication is used as an attempt for one partner to connect with the other partner. Couples may say that they have difficulty with communication when it is not the communication that is the issue but instead the underlying disconnect of the couple.
This disconnect usually manifests while couples are communicating, and therefore, can be misconstrued as solely a communication issue by the couple. When your partner asks you to stop staring at your phone during dinner, it is not necessarily that your spouse is attempting to control you or wants to engage in some deep conversation, but more likely a bid to try to connect with you. Your partner is attempting to tell you that he or she feels disconnected, misses you, and wants to reconnect.
Provide validation and acceptance to your partner
Focus on your partner’s strengths and accept the weaknesses. Accept that your partner is scattered, disorganized, and takes at least 20 minutes to find the phone and keys every morning. Remember that during your courtship days, you found your partner’s flighty attributes to be endearing. Do the same for your strengths and weaknesses.
Accept that the pandemic is unpredictable and that you may need to strengthen your ability to be flexible and more adaptable. This will ultimately lead to feeling less disappointment by your partner and more accepting of shortcomings. Acceptance of your imperfections will improve your sense of worth and confidence and lessen negative emotions, such as guilt, regret, and shame.
Accept the fact that, as similar as we all are, we use different methods to recharge ourselves. In contrast, your spouse needs alone time without distractions to reboot mentally and prepare for the following day. In the pre-pandemic world, if there were a mismatch in what a couple needed to feel rejuvenated, they could independently compensate and search for fulfillment outside of the home. Before stay-at-home orders were rolled out throughout the country, spouses had ample opportunities to spend time away from their partners at work, dinner with friends, or while squeezing in a 7 p.m. yoga sculpt class – barely getting home in time to kiss our children goodnight – with a few minutes to spare to engage in mundane conversation with our partners before our nighttime routine of TV commenced. Unfortunately, COVID-19 has made it very hard for couples to carve out that time for compensatory activities outside of the home.
Remember that you are a team
Remind yourself of the reason why you initially fell in love with your partner. Teammates do not keep score or compete with one another. They support each other when one player is not feeling well, and they make sacrifices for the betterment of the team.
Your marriage vows included “through sickness and health” and now should include “through quarantine.”
Dr. Abraham is a psychiatrist in private practice in Philadelphia. She has no disclosures.
Most married couples vowed to stay with their partners during sickness and health, but none of us vowed to remain trapped with our loved ones behind the same four walls, all day, every day, for an unknown period of time. We didn’t sign up for this! Some romantics may be titillated by the prospect, while more independent partners may panic at the mere thought of spending all day and night with their loved ones.
Because of the swift implementation of the lifestyle-altering restrictions, couples did not have ample time to mentally and physically prepare. A lack of preparation and loss of control heightens our emotions. It can make couples more susceptible to engage in unhealthy styles of communication and destructive behaviors that are harmful to their relationships.
There are psychological reasons that “absence makes the heart grow fonder.” Distance from your partner is not just a clever way to make your partner appreciate and desire you more. It is human nature to habituate to what is part of your daily life. For instance, when your partner is away from you while on a work trip, you may find the first night or two alone relaxing; but by day 3, you begin to miss your partner’s hugs and kisses, smell, and touch. And after many days apart, you may even miss the incessant nagging that secretly motivates you. Physical distance from our partners essentially gives us the ability to long for and appreciate each other. Our brains are wired to pay more attention to things that are novel and exciting and less interested in what is in our everyday lives.
Separation gives us the ability to miss our partners, while quarantine does the complete opposite.
To avoid contemplating how to murder one’s spouse before quarantine ends, partners can strengthen their relationships by using the strategies I’ve outlined below, which are loosely based on dialectical behavior therapy (DBT). These strategies can be useful for anyone – providers and patients alike – going through these struggles.
Dialectical behavior therapy was developed by psychologist Marsha Linehan PhD, to help regulate emotions for people diagnosed with borderline personality disorder. These skills help to identify thoughts and feelings, to accept one’s inner emotional world and outward behaviors. The idea is that, once you can recognize and accept, then change is possible. The “dialectic” in dialectical behavior therapy implies that one is attempting to find a balance between acceptance and change. All of us can benefit from these skills, especially emotionally volatile couples who are trapped together in quarantine.
Radically accept what is uncertain in your lives
Radical acceptance is a practice used in DBT in situations that are out of our control, such as the COVID-19 pandemic. Radically accept that you and your partner are trapped in quarantine without attempting to place blame on our government, your spouse, your boss, and even yourself. Radical acceptance is exactly what the name implies. Accept your current situation for what it is and not what you hoped it to be.
Accept the unknown and unanswered questions such as when will this quarantine end? Will there be a summer camp? Will I get back to my office this summer? Will my children even return to school in the fall? The acceptance of what is out of your control will ultimately decrease your mental time spent worrying and obsessing about the uncertainties of your post-quarantine life and instead provide you more time to be present with your spouse.
Remain mindful during all communication with your spouse. To stay in the moment, you need to be aware of your bodily reactions to distress and notice when your heart rate increases, breathing becomes more shallow, stomach muscles tighten, and when your thoughts become more negative. Mindfulness skills enable us to use physiological changes in our body to become aware of our emotions. You can use your partner’s nonverbal body language and tone of voice to gauge that person’s emotional reactivity.
The practice of mindfulness leads to an increased emotional intelligence. The goal is to have enough self-awareness and emotional understanding of your partner and enough empathy to know when a conversation is becoming too emotionally charged and to let it go and back off. Mindfulness is not nagging your partner to remember to change the heating unit filters with a reminder of what happened years ago when this wasn’t done promptly – without first checking in to make sure your partner is emotionally ready for this type of conversation.
When we have strong emotions, we are using the more primitive parts of our brain that induce a fight or flight reaction. These emotional reactions overshadow the more advanced prefrontal region of our brain that stores our rational thoughts and reasoning skills, a concept identified by psychologist Daniel Goleman as “emotional hijacking.”
Use distress tolerance skills to deal with negative emotions
Distress tolerance is an individual’s ability to manage feelings in response to stress. Distress tolerance skills are aimed at helping one manage intense emotions without worsening a situation by engaging in behaviors that are destructive and may exacerbate the problem. The goal is to tolerate the stress while with your partner and not respond negatively or in a way that is harmful to the integrity of your relationship.
To prioritize your relationship, this may mean that you choose not to react negatively when your partner makes a passive-aggressive comment on how you spent your day during quarantine since you still have a pile of laundry on your bedroom floor and overflowing dishes in the kitchen sink. A high level of distress tolerance will enable you to not overreact or withdraw from your spouse when flooded with emotions of anger or sadness.
Distraction techniques are a type of distress tolerance skill. You can engage in activities that keep you distracted and require your full attention. When things get heated between you and your spouse during quarantine, try to obtain some distance from each other to cool down and engage in an activity that involves your full concentration.
Many of us have been surprised by our hidden talents that were discovered during the quarantine. Use the time away from your partner to distract yourself with your new passion for writing, baking, organizing, and even your newfound love of balloon artistry. Do an activity that engages your mind and provides you the necessary physical and mental time away from your partner to deescalate. You can always revisit the initial cause of the conflict when both you and your partner are not emotionally charged. You can also distract yourself with self-soothing tactics such as taking a warm bath or a reading good book. Perhaps distract yourself by giving back to others and spending time planning a drive-by surprise party for your sister’s birthday next month. It can be helpful to distract yourself by comparing yourself to others less fortunate than you or a time in your life when you and your partner were struggling much worse than now, to provide perspective. The goal is not to add to your distress but instead, provide yourself a sense of perspective.
Use interpersonal effectiveness skills to establish a healthy relationship
Be gentle in all your communications with your partner, think about your spouse’s perspective, show empathy and interest in what your partner has to say by your verbal communication or body language, such as maintaining eye contact, and offer recognitional cues, such as “uh-huh” and “oh, really.” Avoid communication that is at all invalidating. Never start a sentence with “YOU” while having heated conversations with your spouse; instead, use “I feel” statements. This type of communication avoids the blame game that gets many couples into trouble.
Instead, communicate how you feel while not necessarily blaming your spouse but rather expressing your emotions. This will ultimately lead to less defensive communication from your partner. Remember that not all communication is for the sole purpose of communicating. Much of the time, communication is used as an attempt for one partner to connect with the other partner. Couples may say that they have difficulty with communication when it is not the communication that is the issue but instead the underlying disconnect of the couple.
This disconnect usually manifests while couples are communicating, and therefore, can be misconstrued as solely a communication issue by the couple. When your partner asks you to stop staring at your phone during dinner, it is not necessarily that your spouse is attempting to control you or wants to engage in some deep conversation, but more likely a bid to try to connect with you. Your partner is attempting to tell you that he or she feels disconnected, misses you, and wants to reconnect.
Provide validation and acceptance to your partner
Focus on your partner’s strengths and accept the weaknesses. Accept that your partner is scattered, disorganized, and takes at least 20 minutes to find the phone and keys every morning. Remember that during your courtship days, you found your partner’s flighty attributes to be endearing. Do the same for your strengths and weaknesses.
Accept that the pandemic is unpredictable and that you may need to strengthen your ability to be flexible and more adaptable. This will ultimately lead to feeling less disappointment by your partner and more accepting of shortcomings. Acceptance of your imperfections will improve your sense of worth and confidence and lessen negative emotions, such as guilt, regret, and shame.
Accept the fact that, as similar as we all are, we use different methods to recharge ourselves. In contrast, your spouse needs alone time without distractions to reboot mentally and prepare for the following day. In the pre-pandemic world, if there were a mismatch in what a couple needed to feel rejuvenated, they could independently compensate and search for fulfillment outside of the home. Before stay-at-home orders were rolled out throughout the country, spouses had ample opportunities to spend time away from their partners at work, dinner with friends, or while squeezing in a 7 p.m. yoga sculpt class – barely getting home in time to kiss our children goodnight – with a few minutes to spare to engage in mundane conversation with our partners before our nighttime routine of TV commenced. Unfortunately, COVID-19 has made it very hard for couples to carve out that time for compensatory activities outside of the home.
Remember that you are a team
Remind yourself of the reason why you initially fell in love with your partner. Teammates do not keep score or compete with one another. They support each other when one player is not feeling well, and they make sacrifices for the betterment of the team.
Your marriage vows included “through sickness and health” and now should include “through quarantine.”
Dr. Abraham is a psychiatrist in private practice in Philadelphia. She has no disclosures.
FDA authorizes emergency use of remdesivir for COVID-19
The investigational antiviral drug, manufactured by Gilead Sciences Inc., was shown in a preliminary analysis of a National Institutes of Health (NIH) clinical trial to shorten recovery time in some patients, according to information presented during a White House press conference earlier this week. However, the results of the trial have not been published and little is known about how safe and effective it is in treating people in the hospital with COVID-19.
The emergency use authorization (EUA) designation means remdesivir can be distributed in the United States and administered intravenously by healthcare providers, as appropriate to treat severe disease. Those with severe disease, the FDA said in a press release, are patients with low blood oxygen levels or those who need oxygen therapy or more intensive support such as a mechanical ventilator.
“There’s tremendous interest among all parties to identify and arm ourselves with medicines to combat COVID-19, and through our Coronavirus Treatment Acceleration Program, the FDA is working around-the-clock and using every tool at our disposal to speed these efforts,” FDA Commissioner Stephen M. Hahn, MD, said in a statement.
The FDA writes, “Based on evaluation of the emergency use authorization criteria and the scientific evidence available, it was determined that it is reasonable to believe that remdesivir may be effective in treating COVID-19, and that, given there are no adequate, approved, or available alternative treatments, the known and potential benefits to treat this serious or life-threatening virus currently outweigh the known and potential risks of the drug’s use.”
The drug must be administered intravenously and the optimal dosing and duration are not yet known, the company said in a press release issued May 1.
In addition, Gilead advises that infusion-related reactions and liver transaminase elevations have been seen in patients treated with the drug.
“If signs and symptoms of a clinically significant infusion reaction occur, immediately discontinue administration of remdesivir and initiate appropriate treatment. Patients should have appropriate clinical and laboratory monitoring to aid in early detection of any potential adverse events. Monitor renal and hepatic function prior to initiating and daily during therapy with remdesivir; additionally monitor serum chemistries and hematology daily during therapy,” the company said.
Before granting the emergency use authorization, the FDA had allowed for study of the drug in clinical trials, as well as expanded access use for individual patients and through a multipatient expanded access program coordinated by Gilead.
“The EUA will be effective until the declaration that circumstances exist justifying the authorization of the emergency use of drugs and biologics for prevention and treatment of COVID-19 is terminated and may be revised or revoked if it is determined the EUA no longer meets the statutory criteria for issuance,” the FDA said.
This article first appeared on Medscape.com.
The investigational antiviral drug, manufactured by Gilead Sciences Inc., was shown in a preliminary analysis of a National Institutes of Health (NIH) clinical trial to shorten recovery time in some patients, according to information presented during a White House press conference earlier this week. However, the results of the trial have not been published and little is known about how safe and effective it is in treating people in the hospital with COVID-19.
The emergency use authorization (EUA) designation means remdesivir can be distributed in the United States and administered intravenously by healthcare providers, as appropriate to treat severe disease. Those with severe disease, the FDA said in a press release, are patients with low blood oxygen levels or those who need oxygen therapy or more intensive support such as a mechanical ventilator.
“There’s tremendous interest among all parties to identify and arm ourselves with medicines to combat COVID-19, and through our Coronavirus Treatment Acceleration Program, the FDA is working around-the-clock and using every tool at our disposal to speed these efforts,” FDA Commissioner Stephen M. Hahn, MD, said in a statement.
The FDA writes, “Based on evaluation of the emergency use authorization criteria and the scientific evidence available, it was determined that it is reasonable to believe that remdesivir may be effective in treating COVID-19, and that, given there are no adequate, approved, or available alternative treatments, the known and potential benefits to treat this serious or life-threatening virus currently outweigh the known and potential risks of the drug’s use.”
The drug must be administered intravenously and the optimal dosing and duration are not yet known, the company said in a press release issued May 1.
In addition, Gilead advises that infusion-related reactions and liver transaminase elevations have been seen in patients treated with the drug.
“If signs and symptoms of a clinically significant infusion reaction occur, immediately discontinue administration of remdesivir and initiate appropriate treatment. Patients should have appropriate clinical and laboratory monitoring to aid in early detection of any potential adverse events. Monitor renal and hepatic function prior to initiating and daily during therapy with remdesivir; additionally monitor serum chemistries and hematology daily during therapy,” the company said.
Before granting the emergency use authorization, the FDA had allowed for study of the drug in clinical trials, as well as expanded access use for individual patients and through a multipatient expanded access program coordinated by Gilead.
“The EUA will be effective until the declaration that circumstances exist justifying the authorization of the emergency use of drugs and biologics for prevention and treatment of COVID-19 is terminated and may be revised or revoked if it is determined the EUA no longer meets the statutory criteria for issuance,” the FDA said.
This article first appeared on Medscape.com.
The investigational antiviral drug, manufactured by Gilead Sciences Inc., was shown in a preliminary analysis of a National Institutes of Health (NIH) clinical trial to shorten recovery time in some patients, according to information presented during a White House press conference earlier this week. However, the results of the trial have not been published and little is known about how safe and effective it is in treating people in the hospital with COVID-19.
The emergency use authorization (EUA) designation means remdesivir can be distributed in the United States and administered intravenously by healthcare providers, as appropriate to treat severe disease. Those with severe disease, the FDA said in a press release, are patients with low blood oxygen levels or those who need oxygen therapy or more intensive support such as a mechanical ventilator.
“There’s tremendous interest among all parties to identify and arm ourselves with medicines to combat COVID-19, and through our Coronavirus Treatment Acceleration Program, the FDA is working around-the-clock and using every tool at our disposal to speed these efforts,” FDA Commissioner Stephen M. Hahn, MD, said in a statement.
The FDA writes, “Based on evaluation of the emergency use authorization criteria and the scientific evidence available, it was determined that it is reasonable to believe that remdesivir may be effective in treating COVID-19, and that, given there are no adequate, approved, or available alternative treatments, the known and potential benefits to treat this serious or life-threatening virus currently outweigh the known and potential risks of the drug’s use.”
The drug must be administered intravenously and the optimal dosing and duration are not yet known, the company said in a press release issued May 1.
In addition, Gilead advises that infusion-related reactions and liver transaminase elevations have been seen in patients treated with the drug.
“If signs and symptoms of a clinically significant infusion reaction occur, immediately discontinue administration of remdesivir and initiate appropriate treatment. Patients should have appropriate clinical and laboratory monitoring to aid in early detection of any potential adverse events. Monitor renal and hepatic function prior to initiating and daily during therapy with remdesivir; additionally monitor serum chemistries and hematology daily during therapy,” the company said.
Before granting the emergency use authorization, the FDA had allowed for study of the drug in clinical trials, as well as expanded access use for individual patients and through a multipatient expanded access program coordinated by Gilead.
“The EUA will be effective until the declaration that circumstances exist justifying the authorization of the emergency use of drugs and biologics for prevention and treatment of COVID-19 is terminated and may be revised or revoked if it is determined the EUA no longer meets the statutory criteria for issuance,” the FDA said.
This article first appeared on Medscape.com.
Primary care physicians reshuffle their work, lives in a pandemic
During his shift at a COVID-19 drive-through triage screening area set up outside the University of Arkansas for Medical Sciences in Little Rock, Robert Hopkins Jr., MD, noticed a woman bowled over in the front seat of her car.
A nurse practitioner had just informed her that she had met the criteria for undergoing testing for the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
“She was very upset and was crying nearly inconsolably,” said Dr. Hopkins, who directs the division of general internal medicine at the University of Arkansas Medical Sciences College of Medicine. “I went over and visited with her for a few minutes. She was scared to death that we [had] told her she was going to die. In her mind, if she had COVID-19 that meant a death sentence, and if we were testing her that meant she was likely to not survive.”
Dr. Hopkins tried his best to put testing in perspective for the woman. “At least she came to a level of comfort and realized that we were doing this for her, that this was not a death sentence, that this was not her fault,” he said. “She was worried about infecting her kids and her grandkids and ending up in the hospital and being a burden. Being able to spend that few minutes with her and help to bring down her level of anxiety – I think that’s where we need to put our efforts as physicians right now, helping people understand, ‘Yes, this is serious. Yes, we need to continue to social distance. Yes, we need to be cautious. But, we will get through this if we all work together to do so.’ ”
Prior to the COVID-19 pandemic, Dr. Hopkins spent part of his time seeing patients in the university’s main hospital, but most of it in an outpatient clinic where he and about 20 other primary care physicians care for patients and precept medical residents. Now, medical residents have been deployed to other services, primarily in the hospital, and he and his physician colleagues are conducting 80%-90% of patient visits by video conferencing or by telephone. It’s a whole new world.
“We’ve gone from a relatively traditional inpatient/outpatient practice where we’re seeing patients face to face to doing some face-to-face visits, but an awful lot of what we do now is in the technology domain,” said Dr. Hopkins, who also assisted with health care relief efforts during hurricanes Rita and Katrina.
“A group of six of us has been redeployed to assist with the surge unit for the inpatient facility, so our outpatient duties are being taken on by some of our partners.”
He also pitches in at the drive-through COVID-19 screening clinic, which was set up on March 27 and operates between 8 a.m. and 8 p.m., 7 days a week. “We’re able to measure people’s temperature, take a quick screening history, decide whether their risk is such that we need to do a COVID-19 PCR [polymerase chain reaction] test,” he said. “Then we make a determination of whether they need to go home on quarantine awaiting those results, or if they don’t have anything that needs to be evaluated, or whether they need to be triaged to an urgent care setting or to the emergency department.”
To minimize his risk of acquiring COVID-19, he follows personal hygiene practices recommended by the Centers for Disease Control and Prevention. He also places his work shoes in a shoebox, which he keeps in his car. “I put them on when I get to the parking deck at work, do my work, and then I put them in the shoebox, slip on another pair of shoes and drive home so I’m not tracking in things I potentially had on me,” said Dr. Hopkins, who is married and a father to two college-aged sons and a daughter in fourth grade. “When I get home I immediately shower, and then I exercise or have dinner with my family.”
Despite the longer-than-usual work hours and upheaval to the traditional medical practice model brought on by the pandemic, Dr. Hopkins, a self-described “glass half full person,” said that he does his best to keep watch over his patients and colleagues. “I’m trying to keep an eye out on my team members – physicians, nurses, medical assistants, and folks at the front desk – trying to make sure that people are getting rest, trying to make sure that people are not overcommitting,” he said. “Because if we’re not all working together and working for the long term, we’re going to be in trouble. This is not going to be a sprint; this is going to be a marathon for us to get through.”
To keep mentally centered, he engages in at least 40 minutes of exercise each day on his bicycle or on the elliptical machine at home. Dr. Hopkins hopes that the current efforts to redeploy resources, expand clinician skill sets, and forge relationships with colleagues in other disciplines will carry over into the delivery of health care when COVID-19 is a distant memory. “I hope that some of those relationships are going to continue and result in better care for all of our patients,” he said.
"We are in dire need of hugs"
Typically, Dr. Dakkak, a family physician at Boston University, practices a mix of clinic-based family medicine and obstetrics, and works in inpatient medicine 6 weeks a year. Currently, she is leading a COVID-19 team full time at Boston Medical Center, a 300-bed safety-net hospital located on the campus of Boston University Medical Center.
COVID-19 has also shaken up her life at home.
When Dr. Dakkak volunteered to take on her new role, the first thing that came to her mind was how making the switch would affect the well-being of her 8-year-old son and 10-year-old daughter.
“I thought, ‘How do I get my children somewhere where I don’t have to worry about them?’ ” Dr. Dakkak said.
She floated the idea with her husband of flying their children out to stay with her recently retired parents, who live outside of Sacramento, Calif., until the pandemic eases up. “I was thinking to myself, ‘Am I overreacting? Is the pandemic not going to be that bad?’ because the rest of the country seemed to be in some amount of denial,” she said. “So, I called my dad, who’s a retired pediatric anesthesiologist. He’s from Egypt so he’s done crisis medicine in his time. He encouraged me to send the kids.”
On the same day that Dr. Dakkak began her first 12-hour COVID-19 shift at the hospital, her husband and children boarded a plane to California, where the kids remain in the care of her parents. Her husband returned after staying there for 2 weeks. “Every day when I’m working, I validate my decision,” she said. “When I first started, I worked 5 nights in a row, had 2 days off, and then worked 6 nights in a row. I was busy so I didn’t think about [being away from my kids], but at the same time I was grateful that I didn’t have to come home and worry about homeschooling the kids or infecting them.”
She checks in with them as she can via cell phone or FaceTime. “My son has been very honest,” Dr. Dakkak said. “He says, ‘FaceTime makes me miss you more, and I don’t like it,’ which I understand. I’ll call my mom, and if they want to talk to me, they’ll talk to me. If they don’t want to talk to me, I’m okay. This is about them being healthy and safe. I sent them a care package a few days ago with cards and some workbooks. I’m optimistic that in June I can at least see them if not bring them home.”
Dr. Dakkak describes leading a COVID-19 team as a grueling experience that challenges her medical know-how nearly every day, with seemingly ever-changing algorithms. “Our knowledge of this disease is five steps behind, and changing at lightning speed,” said Dr. Dakkak, who completed a fellowship in surgical and high-risk obstetrics. “It’s hard to balance continuing to teach evidence-based medicine for everything else in medicine [with continuing] to practice minimal and ever-changing evidence-based COVID medicine. We just don’t know enough [about the virus] yet. This is nothing like we were taught in medical school. Everyone has elevated d-dimers with COVID-19, and we don’t get CT pulmonary angiograms [CTPAs] on all of them; we wouldn’t physically be able to. Some patients have d-dimers in the thousands, and only some are stable to get CTPAs. We are also finding pulmonary embolisms. Now we’re basing our algorithm on anticoagulation due to d-dimers because sometimes you can’t always do a CTPA even if you want to. On the other hand, we have people who are coming into the hospital too late. We’ve had a few who have come in after having days of stroke symptoms. I worry about our patients at home who hesitate to come in when they really should.”
Sometimes she feels sad for the medical residents on her team because their instinct is to go in and check on each patient, “but I don’t want them to get exposed,” she said. “So, we check in by phone, or if they need a physical check-in, we minimize the check-ins; only one of us goes in. I’m more willing to put myself in the room than to put them in the room. I also feel for them because they came into medicine for the humanity of medicine – not the charting or the ordering of medicine. I also worry about the acuity and sadness they’re seeing. This is a rough introduction to medicine for them.”
When interviewed for this story in late April, Dr. Dakkak had kept track of her intubated COVID-19 patients. “Most of my patients get to go home without having been intubated, but those aren’t the ones I worry about,” she said. “I have two patients I have been watching. One of them has just been extubated and I’m still worried about him, but I’m hoping he’s going to be fine. The other one is the first pregnant woman we intubated. She is now extubated, doing really well, and went home. Her fetus is doing well, never had any issues while she was intubated. Those cases make me happy. They were both under the age of 35. It is nice to follow those intubations and find that the majority are doing okay.”
The first patient she had cared for who died was a young man “who was always in good spirits,” she recalled. “We called his brother right before intubating him. After intubation, his oxygen saturation didn’t jump up, which made me worry a bit.” About a week later, the young man died. “I kept thinking, ‘We intubated him when he was still comfortable talking. Should I have put it off and had him call more people to say goodbye? Should I have known that he wasn’t going to wake up?’ ” said Dr. Dakkak, who is also women’s health director at Manet Community Health Centers. “A lot of us have worked on our end-of-life discussions in the past month, just being able to tell somebody, ‘This might be your last time to call family. Call family and talk to whoever you want.’ Guilt isn’t the right word, but it’s unsettling if I’m the last person a patient talks to. I feel that, if that’s the case, then I didn’t do a good enough job trying to get them to their family or friends. If I am worried about a patient’s clinical status declining, I tell families now, when I call them, ‘I hope I’m wrong; I hope they don’t need to be intubated, but I think this is the time to talk.’ ”
To keep herself grounded during off hours, Dr. Dakkak spends time resting, checking in with her family, journaling “to get a lot of feelings out,” gardening, hiking, and joining Zoom chats with friends. Once recentered, she draws from a sense of obligation to others as she prepares for her next shift caring for COVID-19 patients.
“I have a lot of love for the world that I get to expend by doing this hard work,” she said. “I love humanity and I love humanity in times of crisis. The interactions I have with patients and their families are still central to why I do this work. I love my medical teams, and I would never want to let them down. It is nice to feel the sense of teamwork across the hospital. The nurses that I sit with and experience this with are amazing. I keep saying that the only thing I want to do when this pandemic is over is hug everyone. I think we are in dire need of hugs.”
Finding light in the darkness
Internist Katie Jobbins, DO, also has worked in a professional role that was created because of COVID-19.
Shortly before Dr. Jobbins was deployed to Baystate Medical Center in Springfield, Ma., for 2 weeks in April of 2020 to help clinicians with an anticipated surge of COVID-19 cases, she encountered a patient who walked into Baystate’s High Street Health Center.
“I think I have COVID-19,” the patient proclaimed to her, at the outpatient clinic that serves mostly inner-city, Medicaid patients.
Prior to becoming an ambulatory internist, Dr. Jobbins was a surgical resident. “So I went into that mode of ‘I need to do this, this, and this,’ ” she said. “I went through a checklist in my head to make sure I was prepared to take care of the patient.”
She applied that same systems approach during her redeployment assignment in the tertiary care hospital, which typically involved 10-hour shifts overseeing internal medicine residents in a medical telemetry unit. “We would take care of people under investigation for COVID-19, but we were not assigned to the actual COVID unit,” said Dr. Jobbins, who is also associate program director for the internal medicine residency program at the University of Massachusetts Medical School–Baystate Springfield. “They tried to redeploy other people to those units who had special training, and we were trying to back fill into where those people that got moved to the COVID units or the ICU units were actually working. We were taking more of the medical side of the floors.”
Even so, one patient on the unit was suspected of having COVID-19, so Dr. Jobbins suited up with personal protective equipment and conducted a thorough exam with residents waiting outside the patient’s room, a safe distance away. “I explained everything I found on the exam to the residents, trying to give them some educational benefit, even though they couldn’t physically examine the patient because we’re trying to protect them since they’re in training,” she said. “It was anxiety provoking, on some level, knowing that there’s a potential risk of exposure [to the virus], but knowing that Baystate Health has gone to extraordinary measures to make sure we have the correct PPE and support us is reassuring. I knew I had the right equipment and the right tools to take care of the patient, which calmed my nerves and made me feel like I could do the job. That’s the most important thing as a physician during this time: knowing that you have people supporting you who have your back at all times.”
Like Dr. Dakkak, Dr. Jobbins had to make some adjustments to her interaction with her family.
Before she began the deployment, Dr. Jobbins engaged in a frank discussion with her husband and her two young boys about the risks she faced working in a hospital caring for patients with COVID-19. “My husband and I made sure our wills were up to date, and we talked about what we would do if either of us got the virus,” she said. To minimize the potential risk of transmitting the virus to her loved ones during the two-week deployment, she considered living away from her family in a nearby home owned by her father, but decided against that and to “take it day by day.” Following her hospital shifts, Dr. Jobbins changed into a fresh set of clothes before leaving the hospital. Once she arrived home, she showered to reduce the risk of possibly becoming a vector to her family.
She had to tell her kids: “You can’t kiss me right now.”
“As much as it’s hard for them to understand, we had a conversation [in which I explained] ‘This is a virus. It will go away eventually, but it’s a virus we’re fighting.’ It’s interesting to watch a 3-year-old try to process that and take his play samurai sword or Marvel toys and decide he’s going to run around the neighborhood and try to kill the virus.”
At the High Street Health Center, Dr. Jobbins and her colleagues have transitioned to conducting most patient encounters via telephone or video appointments. “We have tried to maintain as much continuity for our patients to address their chronic medical needs through these visits, such as hypertension management and diabetes care,” she said. “We have begun a rigorous screening process to triage and treat patients suspicious for COVID-19 through telehealth in hopes of keeping them safe and in their own homes. We also continue to see patients for nonrespiratory urgent care needs in person once they have screened negative for COVID-19.”
“In terms of the inpatient setting, we’ve noticed that a lot of people are choosing not to go to the hospital now, unless they’re extremely ill,” Dr. Jobbins noted. “We’re going to need to find a balance with when do people truly need to go to the hospital and when do they not? What can we manage as an outpatient versus having someone go to the emergency department? That’s really the role of the primary care physician. We need to help people understand, ‘You don’t need to go to the ED for everything, but here are the things you really need to go for.’ ”
“It will be interesting to see what health care looks like in 6 months or a year. I’m excited to see where we land,” Dr. Jobbins added.
Hopes for the Future of Telemedicine
When the practice of medicine enters a post–COVID-19 era, Dr. Jobbins hopes that telemedicine will be incorporated more into the delivery of patient care. “I’ve found that many of my patients who often are no-shows to the inpatient version of their visits have had a higher success rate of follow-through when we do the telephone visits,” she said. “It’s been very successful. I hope that the insurance companies and [Centers for Medicare & Medicaid] will continue to reimburse this as they see this is a benefit to our patients.
Dr. Hopkins is also hopeful that physicians will be able to successfully see patients via telemedicine in the postpandemic world.
“For the ups and downs we’ve had with telemedicine, I’d love for us to be able to enhance the positives and incorporate that into our practice going forward. If we can reach our patients and help treat them where they are, rather than them having to come to us, that may be a plus,” he said.
In the meantime, Dr. Jobbins presses on as the curve of COVID-19 cases flattens in Western Massachusetts and remains grateful that she chose to practice medicine.
“The commitment I have to being an educator in addition to being a physician is part of why I keep doing this,” Dr. Jobbins said. “I find this to be one of the most fulfilling jobs and careers you could ever have: being there for people when they need you the most. That’s really what a physician’s job is: being there for people when a family member has passed away or when they just need to talk because they’re having anxiety. At the end of the day, if we can impart that to those we work with and bring in a positive attitude, it’s infectious and it makes people see this is a reason we keep doing what we’re doing.”
She’s also been heartened by the kindness of strangers during this pandemic, from those who made and donated face shields when they were in short supply, to those who delivered food to the hospital as a gesture of thanks.
“I had a patient who made homemade masks and sent them to my office,” she said. “There’s obviously good and bad during this time, but I get hope from seeing all of the good things that are coming out of this, the whole idea of finding the light in the darkness.”
During his shift at a COVID-19 drive-through triage screening area set up outside the University of Arkansas for Medical Sciences in Little Rock, Robert Hopkins Jr., MD, noticed a woman bowled over in the front seat of her car.
A nurse practitioner had just informed her that she had met the criteria for undergoing testing for the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
“She was very upset and was crying nearly inconsolably,” said Dr. Hopkins, who directs the division of general internal medicine at the University of Arkansas Medical Sciences College of Medicine. “I went over and visited with her for a few minutes. She was scared to death that we [had] told her she was going to die. In her mind, if she had COVID-19 that meant a death sentence, and if we were testing her that meant she was likely to not survive.”
Dr. Hopkins tried his best to put testing in perspective for the woman. “At least she came to a level of comfort and realized that we were doing this for her, that this was not a death sentence, that this was not her fault,” he said. “She was worried about infecting her kids and her grandkids and ending up in the hospital and being a burden. Being able to spend that few minutes with her and help to bring down her level of anxiety – I think that’s where we need to put our efforts as physicians right now, helping people understand, ‘Yes, this is serious. Yes, we need to continue to social distance. Yes, we need to be cautious. But, we will get through this if we all work together to do so.’ ”
Prior to the COVID-19 pandemic, Dr. Hopkins spent part of his time seeing patients in the university’s main hospital, but most of it in an outpatient clinic where he and about 20 other primary care physicians care for patients and precept medical residents. Now, medical residents have been deployed to other services, primarily in the hospital, and he and his physician colleagues are conducting 80%-90% of patient visits by video conferencing or by telephone. It’s a whole new world.
“We’ve gone from a relatively traditional inpatient/outpatient practice where we’re seeing patients face to face to doing some face-to-face visits, but an awful lot of what we do now is in the technology domain,” said Dr. Hopkins, who also assisted with health care relief efforts during hurricanes Rita and Katrina.
“A group of six of us has been redeployed to assist with the surge unit for the inpatient facility, so our outpatient duties are being taken on by some of our partners.”
He also pitches in at the drive-through COVID-19 screening clinic, which was set up on March 27 and operates between 8 a.m. and 8 p.m., 7 days a week. “We’re able to measure people’s temperature, take a quick screening history, decide whether their risk is such that we need to do a COVID-19 PCR [polymerase chain reaction] test,” he said. “Then we make a determination of whether they need to go home on quarantine awaiting those results, or if they don’t have anything that needs to be evaluated, or whether they need to be triaged to an urgent care setting or to the emergency department.”
To minimize his risk of acquiring COVID-19, he follows personal hygiene practices recommended by the Centers for Disease Control and Prevention. He also places his work shoes in a shoebox, which he keeps in his car. “I put them on when I get to the parking deck at work, do my work, and then I put them in the shoebox, slip on another pair of shoes and drive home so I’m not tracking in things I potentially had on me,” said Dr. Hopkins, who is married and a father to two college-aged sons and a daughter in fourth grade. “When I get home I immediately shower, and then I exercise or have dinner with my family.”
Despite the longer-than-usual work hours and upheaval to the traditional medical practice model brought on by the pandemic, Dr. Hopkins, a self-described “glass half full person,” said that he does his best to keep watch over his patients and colleagues. “I’m trying to keep an eye out on my team members – physicians, nurses, medical assistants, and folks at the front desk – trying to make sure that people are getting rest, trying to make sure that people are not overcommitting,” he said. “Because if we’re not all working together and working for the long term, we’re going to be in trouble. This is not going to be a sprint; this is going to be a marathon for us to get through.”
To keep mentally centered, he engages in at least 40 minutes of exercise each day on his bicycle or on the elliptical machine at home. Dr. Hopkins hopes that the current efforts to redeploy resources, expand clinician skill sets, and forge relationships with colleagues in other disciplines will carry over into the delivery of health care when COVID-19 is a distant memory. “I hope that some of those relationships are going to continue and result in better care for all of our patients,” he said.
"We are in dire need of hugs"
Typically, Dr. Dakkak, a family physician at Boston University, practices a mix of clinic-based family medicine and obstetrics, and works in inpatient medicine 6 weeks a year. Currently, she is leading a COVID-19 team full time at Boston Medical Center, a 300-bed safety-net hospital located on the campus of Boston University Medical Center.
COVID-19 has also shaken up her life at home.
When Dr. Dakkak volunteered to take on her new role, the first thing that came to her mind was how making the switch would affect the well-being of her 8-year-old son and 10-year-old daughter.
“I thought, ‘How do I get my children somewhere where I don’t have to worry about them?’ ” Dr. Dakkak said.
She floated the idea with her husband of flying their children out to stay with her recently retired parents, who live outside of Sacramento, Calif., until the pandemic eases up. “I was thinking to myself, ‘Am I overreacting? Is the pandemic not going to be that bad?’ because the rest of the country seemed to be in some amount of denial,” she said. “So, I called my dad, who’s a retired pediatric anesthesiologist. He’s from Egypt so he’s done crisis medicine in his time. He encouraged me to send the kids.”
On the same day that Dr. Dakkak began her first 12-hour COVID-19 shift at the hospital, her husband and children boarded a plane to California, where the kids remain in the care of her parents. Her husband returned after staying there for 2 weeks. “Every day when I’m working, I validate my decision,” she said. “When I first started, I worked 5 nights in a row, had 2 days off, and then worked 6 nights in a row. I was busy so I didn’t think about [being away from my kids], but at the same time I was grateful that I didn’t have to come home and worry about homeschooling the kids or infecting them.”
She checks in with them as she can via cell phone or FaceTime. “My son has been very honest,” Dr. Dakkak said. “He says, ‘FaceTime makes me miss you more, and I don’t like it,’ which I understand. I’ll call my mom, and if they want to talk to me, they’ll talk to me. If they don’t want to talk to me, I’m okay. This is about them being healthy and safe. I sent them a care package a few days ago with cards and some workbooks. I’m optimistic that in June I can at least see them if not bring them home.”
Dr. Dakkak describes leading a COVID-19 team as a grueling experience that challenges her medical know-how nearly every day, with seemingly ever-changing algorithms. “Our knowledge of this disease is five steps behind, and changing at lightning speed,” said Dr. Dakkak, who completed a fellowship in surgical and high-risk obstetrics. “It’s hard to balance continuing to teach evidence-based medicine for everything else in medicine [with continuing] to practice minimal and ever-changing evidence-based COVID medicine. We just don’t know enough [about the virus] yet. This is nothing like we were taught in medical school. Everyone has elevated d-dimers with COVID-19, and we don’t get CT pulmonary angiograms [CTPAs] on all of them; we wouldn’t physically be able to. Some patients have d-dimers in the thousands, and only some are stable to get CTPAs. We are also finding pulmonary embolisms. Now we’re basing our algorithm on anticoagulation due to d-dimers because sometimes you can’t always do a CTPA even if you want to. On the other hand, we have people who are coming into the hospital too late. We’ve had a few who have come in after having days of stroke symptoms. I worry about our patients at home who hesitate to come in when they really should.”
Sometimes she feels sad for the medical residents on her team because their instinct is to go in and check on each patient, “but I don’t want them to get exposed,” she said. “So, we check in by phone, or if they need a physical check-in, we minimize the check-ins; only one of us goes in. I’m more willing to put myself in the room than to put them in the room. I also feel for them because they came into medicine for the humanity of medicine – not the charting or the ordering of medicine. I also worry about the acuity and sadness they’re seeing. This is a rough introduction to medicine for them.”
When interviewed for this story in late April, Dr. Dakkak had kept track of her intubated COVID-19 patients. “Most of my patients get to go home without having been intubated, but those aren’t the ones I worry about,” she said. “I have two patients I have been watching. One of them has just been extubated and I’m still worried about him, but I’m hoping he’s going to be fine. The other one is the first pregnant woman we intubated. She is now extubated, doing really well, and went home. Her fetus is doing well, never had any issues while she was intubated. Those cases make me happy. They were both under the age of 35. It is nice to follow those intubations and find that the majority are doing okay.”
The first patient she had cared for who died was a young man “who was always in good spirits,” she recalled. “We called his brother right before intubating him. After intubation, his oxygen saturation didn’t jump up, which made me worry a bit.” About a week later, the young man died. “I kept thinking, ‘We intubated him when he was still comfortable talking. Should I have put it off and had him call more people to say goodbye? Should I have known that he wasn’t going to wake up?’ ” said Dr. Dakkak, who is also women’s health director at Manet Community Health Centers. “A lot of us have worked on our end-of-life discussions in the past month, just being able to tell somebody, ‘This might be your last time to call family. Call family and talk to whoever you want.’ Guilt isn’t the right word, but it’s unsettling if I’m the last person a patient talks to. I feel that, if that’s the case, then I didn’t do a good enough job trying to get them to their family or friends. If I am worried about a patient’s clinical status declining, I tell families now, when I call them, ‘I hope I’m wrong; I hope they don’t need to be intubated, but I think this is the time to talk.’ ”
To keep herself grounded during off hours, Dr. Dakkak spends time resting, checking in with her family, journaling “to get a lot of feelings out,” gardening, hiking, and joining Zoom chats with friends. Once recentered, she draws from a sense of obligation to others as she prepares for her next shift caring for COVID-19 patients.
“I have a lot of love for the world that I get to expend by doing this hard work,” she said. “I love humanity and I love humanity in times of crisis. The interactions I have with patients and their families are still central to why I do this work. I love my medical teams, and I would never want to let them down. It is nice to feel the sense of teamwork across the hospital. The nurses that I sit with and experience this with are amazing. I keep saying that the only thing I want to do when this pandemic is over is hug everyone. I think we are in dire need of hugs.”
Finding light in the darkness
Internist Katie Jobbins, DO, also has worked in a professional role that was created because of COVID-19.
Shortly before Dr. Jobbins was deployed to Baystate Medical Center in Springfield, Ma., for 2 weeks in April of 2020 to help clinicians with an anticipated surge of COVID-19 cases, she encountered a patient who walked into Baystate’s High Street Health Center.
“I think I have COVID-19,” the patient proclaimed to her, at the outpatient clinic that serves mostly inner-city, Medicaid patients.
Prior to becoming an ambulatory internist, Dr. Jobbins was a surgical resident. “So I went into that mode of ‘I need to do this, this, and this,’ ” she said. “I went through a checklist in my head to make sure I was prepared to take care of the patient.”
She applied that same systems approach during her redeployment assignment in the tertiary care hospital, which typically involved 10-hour shifts overseeing internal medicine residents in a medical telemetry unit. “We would take care of people under investigation for COVID-19, but we were not assigned to the actual COVID unit,” said Dr. Jobbins, who is also associate program director for the internal medicine residency program at the University of Massachusetts Medical School–Baystate Springfield. “They tried to redeploy other people to those units who had special training, and we were trying to back fill into where those people that got moved to the COVID units or the ICU units were actually working. We were taking more of the medical side of the floors.”
Even so, one patient on the unit was suspected of having COVID-19, so Dr. Jobbins suited up with personal protective equipment and conducted a thorough exam with residents waiting outside the patient’s room, a safe distance away. “I explained everything I found on the exam to the residents, trying to give them some educational benefit, even though they couldn’t physically examine the patient because we’re trying to protect them since they’re in training,” she said. “It was anxiety provoking, on some level, knowing that there’s a potential risk of exposure [to the virus], but knowing that Baystate Health has gone to extraordinary measures to make sure we have the correct PPE and support us is reassuring. I knew I had the right equipment and the right tools to take care of the patient, which calmed my nerves and made me feel like I could do the job. That’s the most important thing as a physician during this time: knowing that you have people supporting you who have your back at all times.”
Like Dr. Dakkak, Dr. Jobbins had to make some adjustments to her interaction with her family.
Before she began the deployment, Dr. Jobbins engaged in a frank discussion with her husband and her two young boys about the risks she faced working in a hospital caring for patients with COVID-19. “My husband and I made sure our wills were up to date, and we talked about what we would do if either of us got the virus,” she said. To minimize the potential risk of transmitting the virus to her loved ones during the two-week deployment, she considered living away from her family in a nearby home owned by her father, but decided against that and to “take it day by day.” Following her hospital shifts, Dr. Jobbins changed into a fresh set of clothes before leaving the hospital. Once she arrived home, she showered to reduce the risk of possibly becoming a vector to her family.
She had to tell her kids: “You can’t kiss me right now.”
“As much as it’s hard for them to understand, we had a conversation [in which I explained] ‘This is a virus. It will go away eventually, but it’s a virus we’re fighting.’ It’s interesting to watch a 3-year-old try to process that and take his play samurai sword or Marvel toys and decide he’s going to run around the neighborhood and try to kill the virus.”
At the High Street Health Center, Dr. Jobbins and her colleagues have transitioned to conducting most patient encounters via telephone or video appointments. “We have tried to maintain as much continuity for our patients to address their chronic medical needs through these visits, such as hypertension management and diabetes care,” she said. “We have begun a rigorous screening process to triage and treat patients suspicious for COVID-19 through telehealth in hopes of keeping them safe and in their own homes. We also continue to see patients for nonrespiratory urgent care needs in person once they have screened negative for COVID-19.”
“In terms of the inpatient setting, we’ve noticed that a lot of people are choosing not to go to the hospital now, unless they’re extremely ill,” Dr. Jobbins noted. “We’re going to need to find a balance with when do people truly need to go to the hospital and when do they not? What can we manage as an outpatient versus having someone go to the emergency department? That’s really the role of the primary care physician. We need to help people understand, ‘You don’t need to go to the ED for everything, but here are the things you really need to go for.’ ”
“It will be interesting to see what health care looks like in 6 months or a year. I’m excited to see where we land,” Dr. Jobbins added.
Hopes for the Future of Telemedicine
When the practice of medicine enters a post–COVID-19 era, Dr. Jobbins hopes that telemedicine will be incorporated more into the delivery of patient care. “I’ve found that many of my patients who often are no-shows to the inpatient version of their visits have had a higher success rate of follow-through when we do the telephone visits,” she said. “It’s been very successful. I hope that the insurance companies and [Centers for Medicare & Medicaid] will continue to reimburse this as they see this is a benefit to our patients.
Dr. Hopkins is also hopeful that physicians will be able to successfully see patients via telemedicine in the postpandemic world.
“For the ups and downs we’ve had with telemedicine, I’d love for us to be able to enhance the positives and incorporate that into our practice going forward. If we can reach our patients and help treat them where they are, rather than them having to come to us, that may be a plus,” he said.
In the meantime, Dr. Jobbins presses on as the curve of COVID-19 cases flattens in Western Massachusetts and remains grateful that she chose to practice medicine.
“The commitment I have to being an educator in addition to being a physician is part of why I keep doing this,” Dr. Jobbins said. “I find this to be one of the most fulfilling jobs and careers you could ever have: being there for people when they need you the most. That’s really what a physician’s job is: being there for people when a family member has passed away or when they just need to talk because they’re having anxiety. At the end of the day, if we can impart that to those we work with and bring in a positive attitude, it’s infectious and it makes people see this is a reason we keep doing what we’re doing.”
She’s also been heartened by the kindness of strangers during this pandemic, from those who made and donated face shields when they were in short supply, to those who delivered food to the hospital as a gesture of thanks.
“I had a patient who made homemade masks and sent them to my office,” she said. “There’s obviously good and bad during this time, but I get hope from seeing all of the good things that are coming out of this, the whole idea of finding the light in the darkness.”
During his shift at a COVID-19 drive-through triage screening area set up outside the University of Arkansas for Medical Sciences in Little Rock, Robert Hopkins Jr., MD, noticed a woman bowled over in the front seat of her car.
A nurse practitioner had just informed her that she had met the criteria for undergoing testing for the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
“She was very upset and was crying nearly inconsolably,” said Dr. Hopkins, who directs the division of general internal medicine at the University of Arkansas Medical Sciences College of Medicine. “I went over and visited with her for a few minutes. She was scared to death that we [had] told her she was going to die. In her mind, if she had COVID-19 that meant a death sentence, and if we were testing her that meant she was likely to not survive.”
Dr. Hopkins tried his best to put testing in perspective for the woman. “At least she came to a level of comfort and realized that we were doing this for her, that this was not a death sentence, that this was not her fault,” he said. “She was worried about infecting her kids and her grandkids and ending up in the hospital and being a burden. Being able to spend that few minutes with her and help to bring down her level of anxiety – I think that’s where we need to put our efforts as physicians right now, helping people understand, ‘Yes, this is serious. Yes, we need to continue to social distance. Yes, we need to be cautious. But, we will get through this if we all work together to do so.’ ”
Prior to the COVID-19 pandemic, Dr. Hopkins spent part of his time seeing patients in the university’s main hospital, but most of it in an outpatient clinic where he and about 20 other primary care physicians care for patients and precept medical residents. Now, medical residents have been deployed to other services, primarily in the hospital, and he and his physician colleagues are conducting 80%-90% of patient visits by video conferencing or by telephone. It’s a whole new world.
“We’ve gone from a relatively traditional inpatient/outpatient practice where we’re seeing patients face to face to doing some face-to-face visits, but an awful lot of what we do now is in the technology domain,” said Dr. Hopkins, who also assisted with health care relief efforts during hurricanes Rita and Katrina.
“A group of six of us has been redeployed to assist with the surge unit for the inpatient facility, so our outpatient duties are being taken on by some of our partners.”
He also pitches in at the drive-through COVID-19 screening clinic, which was set up on March 27 and operates between 8 a.m. and 8 p.m., 7 days a week. “We’re able to measure people’s temperature, take a quick screening history, decide whether their risk is such that we need to do a COVID-19 PCR [polymerase chain reaction] test,” he said. “Then we make a determination of whether they need to go home on quarantine awaiting those results, or if they don’t have anything that needs to be evaluated, or whether they need to be triaged to an urgent care setting or to the emergency department.”
To minimize his risk of acquiring COVID-19, he follows personal hygiene practices recommended by the Centers for Disease Control and Prevention. He also places his work shoes in a shoebox, which he keeps in his car. “I put them on when I get to the parking deck at work, do my work, and then I put them in the shoebox, slip on another pair of shoes and drive home so I’m not tracking in things I potentially had on me,” said Dr. Hopkins, who is married and a father to two college-aged sons and a daughter in fourth grade. “When I get home I immediately shower, and then I exercise or have dinner with my family.”
Despite the longer-than-usual work hours and upheaval to the traditional medical practice model brought on by the pandemic, Dr. Hopkins, a self-described “glass half full person,” said that he does his best to keep watch over his patients and colleagues. “I’m trying to keep an eye out on my team members – physicians, nurses, medical assistants, and folks at the front desk – trying to make sure that people are getting rest, trying to make sure that people are not overcommitting,” he said. “Because if we’re not all working together and working for the long term, we’re going to be in trouble. This is not going to be a sprint; this is going to be a marathon for us to get through.”
To keep mentally centered, he engages in at least 40 minutes of exercise each day on his bicycle or on the elliptical machine at home. Dr. Hopkins hopes that the current efforts to redeploy resources, expand clinician skill sets, and forge relationships with colleagues in other disciplines will carry over into the delivery of health care when COVID-19 is a distant memory. “I hope that some of those relationships are going to continue and result in better care for all of our patients,” he said.
"We are in dire need of hugs"
Typically, Dr. Dakkak, a family physician at Boston University, practices a mix of clinic-based family medicine and obstetrics, and works in inpatient medicine 6 weeks a year. Currently, she is leading a COVID-19 team full time at Boston Medical Center, a 300-bed safety-net hospital located on the campus of Boston University Medical Center.
COVID-19 has also shaken up her life at home.
When Dr. Dakkak volunteered to take on her new role, the first thing that came to her mind was how making the switch would affect the well-being of her 8-year-old son and 10-year-old daughter.
“I thought, ‘How do I get my children somewhere where I don’t have to worry about them?’ ” Dr. Dakkak said.
She floated the idea with her husband of flying their children out to stay with her recently retired parents, who live outside of Sacramento, Calif., until the pandemic eases up. “I was thinking to myself, ‘Am I overreacting? Is the pandemic not going to be that bad?’ because the rest of the country seemed to be in some amount of denial,” she said. “So, I called my dad, who’s a retired pediatric anesthesiologist. He’s from Egypt so he’s done crisis medicine in his time. He encouraged me to send the kids.”
On the same day that Dr. Dakkak began her first 12-hour COVID-19 shift at the hospital, her husband and children boarded a plane to California, where the kids remain in the care of her parents. Her husband returned after staying there for 2 weeks. “Every day when I’m working, I validate my decision,” she said. “When I first started, I worked 5 nights in a row, had 2 days off, and then worked 6 nights in a row. I was busy so I didn’t think about [being away from my kids], but at the same time I was grateful that I didn’t have to come home and worry about homeschooling the kids or infecting them.”
She checks in with them as she can via cell phone or FaceTime. “My son has been very honest,” Dr. Dakkak said. “He says, ‘FaceTime makes me miss you more, and I don’t like it,’ which I understand. I’ll call my mom, and if they want to talk to me, they’ll talk to me. If they don’t want to talk to me, I’m okay. This is about them being healthy and safe. I sent them a care package a few days ago with cards and some workbooks. I’m optimistic that in June I can at least see them if not bring them home.”
Dr. Dakkak describes leading a COVID-19 team as a grueling experience that challenges her medical know-how nearly every day, with seemingly ever-changing algorithms. “Our knowledge of this disease is five steps behind, and changing at lightning speed,” said Dr. Dakkak, who completed a fellowship in surgical and high-risk obstetrics. “It’s hard to balance continuing to teach evidence-based medicine for everything else in medicine [with continuing] to practice minimal and ever-changing evidence-based COVID medicine. We just don’t know enough [about the virus] yet. This is nothing like we were taught in medical school. Everyone has elevated d-dimers with COVID-19, and we don’t get CT pulmonary angiograms [CTPAs] on all of them; we wouldn’t physically be able to. Some patients have d-dimers in the thousands, and only some are stable to get CTPAs. We are also finding pulmonary embolisms. Now we’re basing our algorithm on anticoagulation due to d-dimers because sometimes you can’t always do a CTPA even if you want to. On the other hand, we have people who are coming into the hospital too late. We’ve had a few who have come in after having days of stroke symptoms. I worry about our patients at home who hesitate to come in when they really should.”
Sometimes she feels sad for the medical residents on her team because their instinct is to go in and check on each patient, “but I don’t want them to get exposed,” she said. “So, we check in by phone, or if they need a physical check-in, we minimize the check-ins; only one of us goes in. I’m more willing to put myself in the room than to put them in the room. I also feel for them because they came into medicine for the humanity of medicine – not the charting or the ordering of medicine. I also worry about the acuity and sadness they’re seeing. This is a rough introduction to medicine for them.”
When interviewed for this story in late April, Dr. Dakkak had kept track of her intubated COVID-19 patients. “Most of my patients get to go home without having been intubated, but those aren’t the ones I worry about,” she said. “I have two patients I have been watching. One of them has just been extubated and I’m still worried about him, but I’m hoping he’s going to be fine. The other one is the first pregnant woman we intubated. She is now extubated, doing really well, and went home. Her fetus is doing well, never had any issues while she was intubated. Those cases make me happy. They were both under the age of 35. It is nice to follow those intubations and find that the majority are doing okay.”
The first patient she had cared for who died was a young man “who was always in good spirits,” she recalled. “We called his brother right before intubating him. After intubation, his oxygen saturation didn’t jump up, which made me worry a bit.” About a week later, the young man died. “I kept thinking, ‘We intubated him when he was still comfortable talking. Should I have put it off and had him call more people to say goodbye? Should I have known that he wasn’t going to wake up?’ ” said Dr. Dakkak, who is also women’s health director at Manet Community Health Centers. “A lot of us have worked on our end-of-life discussions in the past month, just being able to tell somebody, ‘This might be your last time to call family. Call family and talk to whoever you want.’ Guilt isn’t the right word, but it’s unsettling if I’m the last person a patient talks to. I feel that, if that’s the case, then I didn’t do a good enough job trying to get them to their family or friends. If I am worried about a patient’s clinical status declining, I tell families now, when I call them, ‘I hope I’m wrong; I hope they don’t need to be intubated, but I think this is the time to talk.’ ”
To keep herself grounded during off hours, Dr. Dakkak spends time resting, checking in with her family, journaling “to get a lot of feelings out,” gardening, hiking, and joining Zoom chats with friends. Once recentered, she draws from a sense of obligation to others as she prepares for her next shift caring for COVID-19 patients.
“I have a lot of love for the world that I get to expend by doing this hard work,” she said. “I love humanity and I love humanity in times of crisis. The interactions I have with patients and their families are still central to why I do this work. I love my medical teams, and I would never want to let them down. It is nice to feel the sense of teamwork across the hospital. The nurses that I sit with and experience this with are amazing. I keep saying that the only thing I want to do when this pandemic is over is hug everyone. I think we are in dire need of hugs.”
Finding light in the darkness
Internist Katie Jobbins, DO, also has worked in a professional role that was created because of COVID-19.
Shortly before Dr. Jobbins was deployed to Baystate Medical Center in Springfield, Ma., for 2 weeks in April of 2020 to help clinicians with an anticipated surge of COVID-19 cases, she encountered a patient who walked into Baystate’s High Street Health Center.
“I think I have COVID-19,” the patient proclaimed to her, at the outpatient clinic that serves mostly inner-city, Medicaid patients.
Prior to becoming an ambulatory internist, Dr. Jobbins was a surgical resident. “So I went into that mode of ‘I need to do this, this, and this,’ ” she said. “I went through a checklist in my head to make sure I was prepared to take care of the patient.”
She applied that same systems approach during her redeployment assignment in the tertiary care hospital, which typically involved 10-hour shifts overseeing internal medicine residents in a medical telemetry unit. “We would take care of people under investigation for COVID-19, but we were not assigned to the actual COVID unit,” said Dr. Jobbins, who is also associate program director for the internal medicine residency program at the University of Massachusetts Medical School–Baystate Springfield. “They tried to redeploy other people to those units who had special training, and we were trying to back fill into where those people that got moved to the COVID units or the ICU units were actually working. We were taking more of the medical side of the floors.”
Even so, one patient on the unit was suspected of having COVID-19, so Dr. Jobbins suited up with personal protective equipment and conducted a thorough exam with residents waiting outside the patient’s room, a safe distance away. “I explained everything I found on the exam to the residents, trying to give them some educational benefit, even though they couldn’t physically examine the patient because we’re trying to protect them since they’re in training,” she said. “It was anxiety provoking, on some level, knowing that there’s a potential risk of exposure [to the virus], but knowing that Baystate Health has gone to extraordinary measures to make sure we have the correct PPE and support us is reassuring. I knew I had the right equipment and the right tools to take care of the patient, which calmed my nerves and made me feel like I could do the job. That’s the most important thing as a physician during this time: knowing that you have people supporting you who have your back at all times.”
Like Dr. Dakkak, Dr. Jobbins had to make some adjustments to her interaction with her family.
Before she began the deployment, Dr. Jobbins engaged in a frank discussion with her husband and her two young boys about the risks she faced working in a hospital caring for patients with COVID-19. “My husband and I made sure our wills were up to date, and we talked about what we would do if either of us got the virus,” she said. To minimize the potential risk of transmitting the virus to her loved ones during the two-week deployment, she considered living away from her family in a nearby home owned by her father, but decided against that and to “take it day by day.” Following her hospital shifts, Dr. Jobbins changed into a fresh set of clothes before leaving the hospital. Once she arrived home, she showered to reduce the risk of possibly becoming a vector to her family.
She had to tell her kids: “You can’t kiss me right now.”
“As much as it’s hard for them to understand, we had a conversation [in which I explained] ‘This is a virus. It will go away eventually, but it’s a virus we’re fighting.’ It’s interesting to watch a 3-year-old try to process that and take his play samurai sword or Marvel toys and decide he’s going to run around the neighborhood and try to kill the virus.”
At the High Street Health Center, Dr. Jobbins and her colleagues have transitioned to conducting most patient encounters via telephone or video appointments. “We have tried to maintain as much continuity for our patients to address their chronic medical needs through these visits, such as hypertension management and diabetes care,” she said. “We have begun a rigorous screening process to triage and treat patients suspicious for COVID-19 through telehealth in hopes of keeping them safe and in their own homes. We also continue to see patients for nonrespiratory urgent care needs in person once they have screened negative for COVID-19.”
“In terms of the inpatient setting, we’ve noticed that a lot of people are choosing not to go to the hospital now, unless they’re extremely ill,” Dr. Jobbins noted. “We’re going to need to find a balance with when do people truly need to go to the hospital and when do they not? What can we manage as an outpatient versus having someone go to the emergency department? That’s really the role of the primary care physician. We need to help people understand, ‘You don’t need to go to the ED for everything, but here are the things you really need to go for.’ ”
“It will be interesting to see what health care looks like in 6 months or a year. I’m excited to see where we land,” Dr. Jobbins added.
Hopes for the Future of Telemedicine
When the practice of medicine enters a post–COVID-19 era, Dr. Jobbins hopes that telemedicine will be incorporated more into the delivery of patient care. “I’ve found that many of my patients who often are no-shows to the inpatient version of their visits have had a higher success rate of follow-through when we do the telephone visits,” she said. “It’s been very successful. I hope that the insurance companies and [Centers for Medicare & Medicaid] will continue to reimburse this as they see this is a benefit to our patients.
Dr. Hopkins is also hopeful that physicians will be able to successfully see patients via telemedicine in the postpandemic world.
“For the ups and downs we’ve had with telemedicine, I’d love for us to be able to enhance the positives and incorporate that into our practice going forward. If we can reach our patients and help treat them where they are, rather than them having to come to us, that may be a plus,” he said.
In the meantime, Dr. Jobbins presses on as the curve of COVID-19 cases flattens in Western Massachusetts and remains grateful that she chose to practice medicine.
“The commitment I have to being an educator in addition to being a physician is part of why I keep doing this,” Dr. Jobbins said. “I find this to be one of the most fulfilling jobs and careers you could ever have: being there for people when they need you the most. That’s really what a physician’s job is: being there for people when a family member has passed away or when they just need to talk because they’re having anxiety. At the end of the day, if we can impart that to those we work with and bring in a positive attitude, it’s infectious and it makes people see this is a reason we keep doing what we’re doing.”
She’s also been heartened by the kindness of strangers during this pandemic, from those who made and donated face shields when they were in short supply, to those who delivered food to the hospital as a gesture of thanks.
“I had a patient who made homemade masks and sent them to my office,” she said. “There’s obviously good and bad during this time, but I get hope from seeing all of the good things that are coming out of this, the whole idea of finding the light in the darkness.”
COVID-19: Addressing the mental health needs of clinicians
SARS-CoV-2 and the disease it causes, COVID-19, continues to spread around the world with a devastating social and economic impact. Undoubtedly, health care workers are essential to overcoming this crisis. If these issues are left unaddressed, low morale, burnout, or absenteeism could lead to the collapse of health care systems.
Historically, the health care industry has been one of the most hazardous environments in which to work. Employees in this industry are constantly exposed to a complex variety of health and safety hazards.
Particularly, risks from biological exposure to diseases such as tuberculosis, HIV, and currently COVID-19 are taking a considerable toll on health care workers’ health and well-being. Health care workers are leaving their families to work extra shifts, dealing with limited resources, and navigating the chaos. On top of all that, they are sacrificing their lives through these uncertain times.
Despite their resilience, health care workers – like the general population – can have strong psychological reactions of anxiety and fear during a pandemic. Still, they are required to continue their work amid uncertainty and danger.
Current research studies on COVID-19
Several studies have identified the impact of working in this type of environment during previous pandemics and disasters. In a study of hospital employees in China during the SARS epidemic (2002-2003), Ping Wu, PhD, and colleagues found that 10% of the participants experienced high levels of posttraumatic stress.1 In a similar study in Taiwan, researchers found that 17.3% of employees had developed significant mental health symptoms during the SARS outbreak.2
The impact of COVID-19 on health care workers seems to be much worse. A recent study from China indicates that 50.4% of hospital employees showed signs of depression, 44.6% had anxiety, and 34% had insomnia.3
Another recent cross-sectional study conducted by Lijun Kang, PhD, and associates evaluated the impact on mental health among health care workers in Wuhan, China, during the COVID-19 outbreak. This was the first study on the mental health of health care workers. This study recruited health care workers in Wuhan to participate in the survey from Jan. 29 to Feb. 4, 2020. The data were collected online with an anonymous, self-rated questionnaire that was distributed to all workstations. All subjects provided informed consent electronically prior to participating in the survey.
The survey questionnaire was made up of six components: primary demographic data, mental health assessment, risks of direct and indirect exposure to COVID-19, mental health care services accessed, psychological needs, and self-perceived health status, compared with that before the COVID-19 outbreak. A total of 994 health care workers responded to this survey, and the results are fascinating: 36.9% had subthreshold mental health distress (mean Patient Health Questionnaire–9 score, 2.4), 34.4% reported mild disturbances (mean PHQ-9, 5.4), 22.4% had moderate (mean PHQ-9, 9.0), and 6.2% reported severe disturbance (mean PHQ-9, 15.1). In this study, young women experienced more significant psychological distress. Regarding access to mental health services, 36.3% reported access to psychological materials, such as books on mental health; 50.4% used psychological resources available through media, such as online self-help coping methods; and 17.5% participated in counseling or psychotherapy.4
These findings emphasize the importance of being equipped to ensure the health and safety of health care workers through mental health interventions, both at work and in the community during this time of anxiety and uncertainty.
Future studies will become more critical in addressing this issue.
Risks to clinicians, families prevail
According to a recent report released by the Centers for Disease Control and Prevention, more than 9,000 health care workers across the United States had contracted COVID-19 as of mid-April, and 27 had died since the start of the pandemic.5
Health care workers are at risk around the globe, not only by the nature of their jobs but also by the shortage of personal protective equipment (PPE). In addition, the scarcity of N95 masks, respirators, and COVID-19 testing programs is causing the virus to spread among health care workers all over the world.
A study published recently by Celso Arango, MD, PhD, reported that 18% of staff at a hospital in Madrid had been infected with COVID-19. Dr. Arango speculated that transmission might be attributable to interactions with colleagues rather than with patients.6 We know, for example, that large proportions of people in China reportedly carried the virus while being asymptomatic.7 Those findings might not be generalizable, but they do suggest that an asymptomatic person could be a cause of contagion among professionals. Therefore, early screening and testing are critical – and should be priorities in health care settings.
Another problem clinicians can encounter is that, when they are called on to deal with very agitated patients, they might not get enough time to put on PPE. In addition, PPE can easily break and tear during the physical restraint process.
Working long hours is also putting a significant strain on health care workers and exposes them to the risk of infection. Also, health care workers not only worry about their safety but also fear bringing the virus to their families. They can also feel guilty about their conflicting feelings about exposing themselves and their families to risk. It is quite possible that, during this COVID-19 pandemic, health care workers will face a “care paradox,” in which they must choose between patients’ safety and their own. This care paradox can significantly contribute to a feeling of burnout, stress, and anxiety. Ultimately, this pandemic could lead to attrition from the field at a time when we most need all hands on deck.8
Further, according to a World Health Organization report on mental health and psychosocial consideration during the COVID-19 outbreak, some health care workers, unfortunately, experience avoidance by their family members or communities because of stigma, fear, and anxiety. This avoidance threatens to make an already challenging situation far worse for health care workers by increasing isolation.
Even after acute outbreak are over, the effects on health care workers can persist for years. In a follow-up study 13-26 months after the SARS outbreak, Robert G. Maunder, MD, and associates found that Toronto-area health care workers reported significantly higher levels of burnout, psychological distress, and posttraumatic stress. They were more likely to have reduced patient contact and work hours, and to have avoided behavioral consequences of stress.9 Exposure to stressful work conditions during a pandemic also might put hospital employees at a much higher risk of alcohol and substance use disorders.10
Potential solutions for improving care
COVID-19 has had a massive impact on the mental health of health care workers around the globe. Fortunately, there are evidence-based strategies aimed at mitigating the effects of this pandemic on health care workers. Fostering self-efficacy and optimism has been shown to improve coping and efficiency during disasters.9 Higher perceived workplace safety is associated with a lower risk of anxiety, depression, and posttraumatic stress among health care workers, while a lack of social support has been linked to adverse behavioral outcomes.10
A recent study found that, among Chinese physicians who cared for COVID-19 victims, more significant social support was associated with better sleep quality, greater self-effectiveness, and less psychological distress.11 Positive leadership and a professional culture of trust, and openness with unambiguous communication have been shown to improve the engagement of the medical workforce.12,13 Psychiatrists must advocate for the adoption of these practices in the workplace. Assessing and addressing mental health needs, in addition to the physical health of the health care workforce, is of utmost importance.
We can accomplish this in many ways, but we have to access our health care workers. Similar to our patient population, health care workers also experience stigma and anxiety tied to the disclosure of mental health challenges. This was reported in a study conducted in China, in which a specific psychological intervention using a hotline program was used for the medical team.14 This program provided psychological interventions/group activities aimed at releasing stress and anxiety. However, initially, the implementation of psychological interventions encountered obstacles.
For example, some members of the medical staff declined to participate in group or individual psychological interventions. Moreover, nurses showed irritability, unwillingness to join, and some staff refused, stating that “they did not have any problems.” Finally, psychological counselors regularly visited the facility to listen to difficulties or stories encountered by staff at work and provide support accordingly. More than 100 frontline medical staff participated and reported feeling better.15
Currently, several U.S. universities/institutes have implemented programs aimed at protecting the health and well-being of their staff during the COVID-19 pandemic. For instance, the department of psychiatry and behavioral health at Hackensack Meridian Health has put comprehensive system programs in place for at 16 affiliated medical centers and other patient care facilities to provide support during the COVID-19 crisis. A 24/7 team member support hotline connecting team members with a behavioral health specialist has become available when needed. This hotline is backed up by social workers, who provide mental health resources. In addition, another service called “Coping with COVID Talks” is available. This service is a virtual psychoeducational group facilitated by psychologists focusing on building coping skills and resilience.
Also, the consultation-liaison psychiatrists in the medical centers provide daily support to clinicians working in ICUs. These efforts have led to paradoxical benefits for employers, further leading to less commuting, more safety, and enhanced productivity for the clinician, according to Ramon Solhkhah, MD, MBA, chairman of the psychiatry department.16
Some universities, such as the University of North Carolina at Chapel Hill, have created mental health/telehealth support for health care workers, where they are conducting webinars on coping with uncertainty tied to COVID-19.17 The University of California, San Francisco, also has been a leader in this effort. That institution has employed its psychiatric workforce as volunteers – encouraging health care workers to use digital health apps and referral resources. Also, these volunteers provide peer counseling, phone support, and spiritual counseling to their health care workers.18
These approaches are crucial in this uncertain, challenging time. Our mental health system is deeply flawed, understaffed, and not well prepared to manage the mental health issues among health care workers. Psychiatric institutes/facilities should follow comprehensive and multifaceted approaches to combat the COVID-19 crisis. Several preventive measures can be considered in coping with this pandemic, such as stress reduction, mindfulness, and disseminating educational materials. Also, increased use of technology, such as in-the-moment measures, development of hotlines, crisis support, and treatment telepsychiatry for therapy and medication, should play a pivotal role in addressing the mental health needs of health care workers.
In addition, it is expected that, as a nation, we will see a surge of mental health needs for illnesses such as depression and PTSD, just as we do after “natural disasters” caused by a variety of reasons, including economic downturns. After the SARS outbreak in 2003, for example, health care workers showed symptoms of PTSD. The COVID-19 pandemic could have a similar impact.
The severity of mental health challenges among clinicians cannot be predicted at this time, but we can speculate that the traumatic impact of COVID-19 will prove long lasting, particularly among clinicians who served vulnerable populations and witnessed suffering, misery, and deaths. The long-term consequences might range from stress and anxiety to fear, depression, and PTSD. Implementation of mental health programs/psychological interventions/support will reduce the impact of mental health issues among these clinicians.
We must think about the best ways to optimize mental health among health care workers while also come up with innovative ways to target this at-risk group. The mental health of people who are saving lives – our frontline heroes – should be taken into consideration seriously around the globe. We also must prioritize the mental health of these workers during this unprecedented, challenging, and anxiety-provoking time.
Dr. Malik and Mr. Van Wert are affiliated with Johns Hopkins University, Baltimore. Dr. Kumari, Dr. Afzal, Dr. Doumas, and Dr. Solhkhah are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. All six authors disclosed having no conflicts of interest. The authors would like to thank Vinay Kumar for his assistance with the literature review and for proofreading and editing this article.
References
1. Wu P et al. Can J Psychiatry. 2009;54(5):302-11.
2. Lu YC et al. Psychother Psychosom. 2006;75(6):370-5.
3. Lai J et al. JAMA Netw Open. 2020;3(3):e203976.
4. Kang L et al. Brain Behav Immun. 2020 Mar 30. doi: 10.1016/j.bbi.2020.03.028.
5. Centers for Disease Control and Prevention COVID-19 Response Team. MMWR. 2020 Apr 17;69(15):477-81.
6. Arango C. Biol Psychiatry. 2020 Apr 8. doi: 10.1016/j.biopsych.2020.04.003.
7. Day M. BMJ. 2020 Apr 2. doi: 10.1136/bmj.m1375.
8. Kirsch T. “Coronavirus, COVID-19: What happens if health care workers stop showing up?” The Atlantic. 2020 Mar 24.
9. Maunder RG et al. Emerg Infect Dis. 2006;12(12):1924-32.
10. Wu P et al. Alcohol Alcohol. 2008;43(6):706-12.
11. Brooks SK et al. BMC Psychol. 2016 Apr 26;4:18.
12. Smith BW et al. Am J Infect Control. 2009; 37:371-80.
13. Chen Q et al. Lancet Psychiatry. 2020 Apr 1;7(14):PE15-6.
14. Xiao H et al. Med Sci Monit. 2020;26:e923549.
15. Bergus GR et al. Acad Med. 2001;76:1148-52.
16. Bergeron T. “Working from home will be stressful. Here’s how employees (and employers) can handle it.” roi-nj.com. 2020 Mar 23.
17. UNChealthcare.org. “Mental Health/Emotional Support Resources for Coworkers and Providers Coping with COVID-19.”
18. Psych.ucsf.edu/coronoavirus. “Resources to Support Your Mental Health During the COVID-19 Outbreak.”
SARS-CoV-2 and the disease it causes, COVID-19, continues to spread around the world with a devastating social and economic impact. Undoubtedly, health care workers are essential to overcoming this crisis. If these issues are left unaddressed, low morale, burnout, or absenteeism could lead to the collapse of health care systems.
Historically, the health care industry has been one of the most hazardous environments in which to work. Employees in this industry are constantly exposed to a complex variety of health and safety hazards.
Particularly, risks from biological exposure to diseases such as tuberculosis, HIV, and currently COVID-19 are taking a considerable toll on health care workers’ health and well-being. Health care workers are leaving their families to work extra shifts, dealing with limited resources, and navigating the chaos. On top of all that, they are sacrificing their lives through these uncertain times.
Despite their resilience, health care workers – like the general population – can have strong psychological reactions of anxiety and fear during a pandemic. Still, they are required to continue their work amid uncertainty and danger.
Current research studies on COVID-19
Several studies have identified the impact of working in this type of environment during previous pandemics and disasters. In a study of hospital employees in China during the SARS epidemic (2002-2003), Ping Wu, PhD, and colleagues found that 10% of the participants experienced high levels of posttraumatic stress.1 In a similar study in Taiwan, researchers found that 17.3% of employees had developed significant mental health symptoms during the SARS outbreak.2
The impact of COVID-19 on health care workers seems to be much worse. A recent study from China indicates that 50.4% of hospital employees showed signs of depression, 44.6% had anxiety, and 34% had insomnia.3
Another recent cross-sectional study conducted by Lijun Kang, PhD, and associates evaluated the impact on mental health among health care workers in Wuhan, China, during the COVID-19 outbreak. This was the first study on the mental health of health care workers. This study recruited health care workers in Wuhan to participate in the survey from Jan. 29 to Feb. 4, 2020. The data were collected online with an anonymous, self-rated questionnaire that was distributed to all workstations. All subjects provided informed consent electronically prior to participating in the survey.
The survey questionnaire was made up of six components: primary demographic data, mental health assessment, risks of direct and indirect exposure to COVID-19, mental health care services accessed, psychological needs, and self-perceived health status, compared with that before the COVID-19 outbreak. A total of 994 health care workers responded to this survey, and the results are fascinating: 36.9% had subthreshold mental health distress (mean Patient Health Questionnaire–9 score, 2.4), 34.4% reported mild disturbances (mean PHQ-9, 5.4), 22.4% had moderate (mean PHQ-9, 9.0), and 6.2% reported severe disturbance (mean PHQ-9, 15.1). In this study, young women experienced more significant psychological distress. Regarding access to mental health services, 36.3% reported access to psychological materials, such as books on mental health; 50.4% used psychological resources available through media, such as online self-help coping methods; and 17.5% participated in counseling or psychotherapy.4
These findings emphasize the importance of being equipped to ensure the health and safety of health care workers through mental health interventions, both at work and in the community during this time of anxiety and uncertainty.
Future studies will become more critical in addressing this issue.
Risks to clinicians, families prevail
According to a recent report released by the Centers for Disease Control and Prevention, more than 9,000 health care workers across the United States had contracted COVID-19 as of mid-April, and 27 had died since the start of the pandemic.5
Health care workers are at risk around the globe, not only by the nature of their jobs but also by the shortage of personal protective equipment (PPE). In addition, the scarcity of N95 masks, respirators, and COVID-19 testing programs is causing the virus to spread among health care workers all over the world.
A study published recently by Celso Arango, MD, PhD, reported that 18% of staff at a hospital in Madrid had been infected with COVID-19. Dr. Arango speculated that transmission might be attributable to interactions with colleagues rather than with patients.6 We know, for example, that large proportions of people in China reportedly carried the virus while being asymptomatic.7 Those findings might not be generalizable, but they do suggest that an asymptomatic person could be a cause of contagion among professionals. Therefore, early screening and testing are critical – and should be priorities in health care settings.
Another problem clinicians can encounter is that, when they are called on to deal with very agitated patients, they might not get enough time to put on PPE. In addition, PPE can easily break and tear during the physical restraint process.
Working long hours is also putting a significant strain on health care workers and exposes them to the risk of infection. Also, health care workers not only worry about their safety but also fear bringing the virus to their families. They can also feel guilty about their conflicting feelings about exposing themselves and their families to risk. It is quite possible that, during this COVID-19 pandemic, health care workers will face a “care paradox,” in which they must choose between patients’ safety and their own. This care paradox can significantly contribute to a feeling of burnout, stress, and anxiety. Ultimately, this pandemic could lead to attrition from the field at a time when we most need all hands on deck.8
Further, according to a World Health Organization report on mental health and psychosocial consideration during the COVID-19 outbreak, some health care workers, unfortunately, experience avoidance by their family members or communities because of stigma, fear, and anxiety. This avoidance threatens to make an already challenging situation far worse for health care workers by increasing isolation.
Even after acute outbreak are over, the effects on health care workers can persist for years. In a follow-up study 13-26 months after the SARS outbreak, Robert G. Maunder, MD, and associates found that Toronto-area health care workers reported significantly higher levels of burnout, psychological distress, and posttraumatic stress. They were more likely to have reduced patient contact and work hours, and to have avoided behavioral consequences of stress.9 Exposure to stressful work conditions during a pandemic also might put hospital employees at a much higher risk of alcohol and substance use disorders.10
Potential solutions for improving care
COVID-19 has had a massive impact on the mental health of health care workers around the globe. Fortunately, there are evidence-based strategies aimed at mitigating the effects of this pandemic on health care workers. Fostering self-efficacy and optimism has been shown to improve coping and efficiency during disasters.9 Higher perceived workplace safety is associated with a lower risk of anxiety, depression, and posttraumatic stress among health care workers, while a lack of social support has been linked to adverse behavioral outcomes.10
A recent study found that, among Chinese physicians who cared for COVID-19 victims, more significant social support was associated with better sleep quality, greater self-effectiveness, and less psychological distress.11 Positive leadership and a professional culture of trust, and openness with unambiguous communication have been shown to improve the engagement of the medical workforce.12,13 Psychiatrists must advocate for the adoption of these practices in the workplace. Assessing and addressing mental health needs, in addition to the physical health of the health care workforce, is of utmost importance.
We can accomplish this in many ways, but we have to access our health care workers. Similar to our patient population, health care workers also experience stigma and anxiety tied to the disclosure of mental health challenges. This was reported in a study conducted in China, in which a specific psychological intervention using a hotline program was used for the medical team.14 This program provided psychological interventions/group activities aimed at releasing stress and anxiety. However, initially, the implementation of psychological interventions encountered obstacles.
For example, some members of the medical staff declined to participate in group or individual psychological interventions. Moreover, nurses showed irritability, unwillingness to join, and some staff refused, stating that “they did not have any problems.” Finally, psychological counselors regularly visited the facility to listen to difficulties or stories encountered by staff at work and provide support accordingly. More than 100 frontline medical staff participated and reported feeling better.15
Currently, several U.S. universities/institutes have implemented programs aimed at protecting the health and well-being of their staff during the COVID-19 pandemic. For instance, the department of psychiatry and behavioral health at Hackensack Meridian Health has put comprehensive system programs in place for at 16 affiliated medical centers and other patient care facilities to provide support during the COVID-19 crisis. A 24/7 team member support hotline connecting team members with a behavioral health specialist has become available when needed. This hotline is backed up by social workers, who provide mental health resources. In addition, another service called “Coping with COVID Talks” is available. This service is a virtual psychoeducational group facilitated by psychologists focusing on building coping skills and resilience.
Also, the consultation-liaison psychiatrists in the medical centers provide daily support to clinicians working in ICUs. These efforts have led to paradoxical benefits for employers, further leading to less commuting, more safety, and enhanced productivity for the clinician, according to Ramon Solhkhah, MD, MBA, chairman of the psychiatry department.16
Some universities, such as the University of North Carolina at Chapel Hill, have created mental health/telehealth support for health care workers, where they are conducting webinars on coping with uncertainty tied to COVID-19.17 The University of California, San Francisco, also has been a leader in this effort. That institution has employed its psychiatric workforce as volunteers – encouraging health care workers to use digital health apps and referral resources. Also, these volunteers provide peer counseling, phone support, and spiritual counseling to their health care workers.18
These approaches are crucial in this uncertain, challenging time. Our mental health system is deeply flawed, understaffed, and not well prepared to manage the mental health issues among health care workers. Psychiatric institutes/facilities should follow comprehensive and multifaceted approaches to combat the COVID-19 crisis. Several preventive measures can be considered in coping with this pandemic, such as stress reduction, mindfulness, and disseminating educational materials. Also, increased use of technology, such as in-the-moment measures, development of hotlines, crisis support, and treatment telepsychiatry for therapy and medication, should play a pivotal role in addressing the mental health needs of health care workers.
In addition, it is expected that, as a nation, we will see a surge of mental health needs for illnesses such as depression and PTSD, just as we do after “natural disasters” caused by a variety of reasons, including economic downturns. After the SARS outbreak in 2003, for example, health care workers showed symptoms of PTSD. The COVID-19 pandemic could have a similar impact.
The severity of mental health challenges among clinicians cannot be predicted at this time, but we can speculate that the traumatic impact of COVID-19 will prove long lasting, particularly among clinicians who served vulnerable populations and witnessed suffering, misery, and deaths. The long-term consequences might range from stress and anxiety to fear, depression, and PTSD. Implementation of mental health programs/psychological interventions/support will reduce the impact of mental health issues among these clinicians.
We must think about the best ways to optimize mental health among health care workers while also come up with innovative ways to target this at-risk group. The mental health of people who are saving lives – our frontline heroes – should be taken into consideration seriously around the globe. We also must prioritize the mental health of these workers during this unprecedented, challenging, and anxiety-provoking time.
Dr. Malik and Mr. Van Wert are affiliated with Johns Hopkins University, Baltimore. Dr. Kumari, Dr. Afzal, Dr. Doumas, and Dr. Solhkhah are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. All six authors disclosed having no conflicts of interest. The authors would like to thank Vinay Kumar for his assistance with the literature review and for proofreading and editing this article.
References
1. Wu P et al. Can J Psychiatry. 2009;54(5):302-11.
2. Lu YC et al. Psychother Psychosom. 2006;75(6):370-5.
3. Lai J et al. JAMA Netw Open. 2020;3(3):e203976.
4. Kang L et al. Brain Behav Immun. 2020 Mar 30. doi: 10.1016/j.bbi.2020.03.028.
5. Centers for Disease Control and Prevention COVID-19 Response Team. MMWR. 2020 Apr 17;69(15):477-81.
6. Arango C. Biol Psychiatry. 2020 Apr 8. doi: 10.1016/j.biopsych.2020.04.003.
7. Day M. BMJ. 2020 Apr 2. doi: 10.1136/bmj.m1375.
8. Kirsch T. “Coronavirus, COVID-19: What happens if health care workers stop showing up?” The Atlantic. 2020 Mar 24.
9. Maunder RG et al. Emerg Infect Dis. 2006;12(12):1924-32.
10. Wu P et al. Alcohol Alcohol. 2008;43(6):706-12.
11. Brooks SK et al. BMC Psychol. 2016 Apr 26;4:18.
12. Smith BW et al. Am J Infect Control. 2009; 37:371-80.
13. Chen Q et al. Lancet Psychiatry. 2020 Apr 1;7(14):PE15-6.
14. Xiao H et al. Med Sci Monit. 2020;26:e923549.
15. Bergus GR et al. Acad Med. 2001;76:1148-52.
16. Bergeron T. “Working from home will be stressful. Here’s how employees (and employers) can handle it.” roi-nj.com. 2020 Mar 23.
17. UNChealthcare.org. “Mental Health/Emotional Support Resources for Coworkers and Providers Coping with COVID-19.”
18. Psych.ucsf.edu/coronoavirus. “Resources to Support Your Mental Health During the COVID-19 Outbreak.”
SARS-CoV-2 and the disease it causes, COVID-19, continues to spread around the world with a devastating social and economic impact. Undoubtedly, health care workers are essential to overcoming this crisis. If these issues are left unaddressed, low morale, burnout, or absenteeism could lead to the collapse of health care systems.
Historically, the health care industry has been one of the most hazardous environments in which to work. Employees in this industry are constantly exposed to a complex variety of health and safety hazards.
Particularly, risks from biological exposure to diseases such as tuberculosis, HIV, and currently COVID-19 are taking a considerable toll on health care workers’ health and well-being. Health care workers are leaving their families to work extra shifts, dealing with limited resources, and navigating the chaos. On top of all that, they are sacrificing their lives through these uncertain times.
Despite their resilience, health care workers – like the general population – can have strong psychological reactions of anxiety and fear during a pandemic. Still, they are required to continue their work amid uncertainty and danger.
Current research studies on COVID-19
Several studies have identified the impact of working in this type of environment during previous pandemics and disasters. In a study of hospital employees in China during the SARS epidemic (2002-2003), Ping Wu, PhD, and colleagues found that 10% of the participants experienced high levels of posttraumatic stress.1 In a similar study in Taiwan, researchers found that 17.3% of employees had developed significant mental health symptoms during the SARS outbreak.2
The impact of COVID-19 on health care workers seems to be much worse. A recent study from China indicates that 50.4% of hospital employees showed signs of depression, 44.6% had anxiety, and 34% had insomnia.3
Another recent cross-sectional study conducted by Lijun Kang, PhD, and associates evaluated the impact on mental health among health care workers in Wuhan, China, during the COVID-19 outbreak. This was the first study on the mental health of health care workers. This study recruited health care workers in Wuhan to participate in the survey from Jan. 29 to Feb. 4, 2020. The data were collected online with an anonymous, self-rated questionnaire that was distributed to all workstations. All subjects provided informed consent electronically prior to participating in the survey.
The survey questionnaire was made up of six components: primary demographic data, mental health assessment, risks of direct and indirect exposure to COVID-19, mental health care services accessed, psychological needs, and self-perceived health status, compared with that before the COVID-19 outbreak. A total of 994 health care workers responded to this survey, and the results are fascinating: 36.9% had subthreshold mental health distress (mean Patient Health Questionnaire–9 score, 2.4), 34.4% reported mild disturbances (mean PHQ-9, 5.4), 22.4% had moderate (mean PHQ-9, 9.0), and 6.2% reported severe disturbance (mean PHQ-9, 15.1). In this study, young women experienced more significant psychological distress. Regarding access to mental health services, 36.3% reported access to psychological materials, such as books on mental health; 50.4% used psychological resources available through media, such as online self-help coping methods; and 17.5% participated in counseling or psychotherapy.4
These findings emphasize the importance of being equipped to ensure the health and safety of health care workers through mental health interventions, both at work and in the community during this time of anxiety and uncertainty.
Future studies will become more critical in addressing this issue.
Risks to clinicians, families prevail
According to a recent report released by the Centers for Disease Control and Prevention, more than 9,000 health care workers across the United States had contracted COVID-19 as of mid-April, and 27 had died since the start of the pandemic.5
Health care workers are at risk around the globe, not only by the nature of their jobs but also by the shortage of personal protective equipment (PPE). In addition, the scarcity of N95 masks, respirators, and COVID-19 testing programs is causing the virus to spread among health care workers all over the world.
A study published recently by Celso Arango, MD, PhD, reported that 18% of staff at a hospital in Madrid had been infected with COVID-19. Dr. Arango speculated that transmission might be attributable to interactions with colleagues rather than with patients.6 We know, for example, that large proportions of people in China reportedly carried the virus while being asymptomatic.7 Those findings might not be generalizable, but they do suggest that an asymptomatic person could be a cause of contagion among professionals. Therefore, early screening and testing are critical – and should be priorities in health care settings.
Another problem clinicians can encounter is that, when they are called on to deal with very agitated patients, they might not get enough time to put on PPE. In addition, PPE can easily break and tear during the physical restraint process.
Working long hours is also putting a significant strain on health care workers and exposes them to the risk of infection. Also, health care workers not only worry about their safety but also fear bringing the virus to their families. They can also feel guilty about their conflicting feelings about exposing themselves and their families to risk. It is quite possible that, during this COVID-19 pandemic, health care workers will face a “care paradox,” in which they must choose between patients’ safety and their own. This care paradox can significantly contribute to a feeling of burnout, stress, and anxiety. Ultimately, this pandemic could lead to attrition from the field at a time when we most need all hands on deck.8
Further, according to a World Health Organization report on mental health and psychosocial consideration during the COVID-19 outbreak, some health care workers, unfortunately, experience avoidance by their family members or communities because of stigma, fear, and anxiety. This avoidance threatens to make an already challenging situation far worse for health care workers by increasing isolation.
Even after acute outbreak are over, the effects on health care workers can persist for years. In a follow-up study 13-26 months after the SARS outbreak, Robert G. Maunder, MD, and associates found that Toronto-area health care workers reported significantly higher levels of burnout, psychological distress, and posttraumatic stress. They were more likely to have reduced patient contact and work hours, and to have avoided behavioral consequences of stress.9 Exposure to stressful work conditions during a pandemic also might put hospital employees at a much higher risk of alcohol and substance use disorders.10
Potential solutions for improving care
COVID-19 has had a massive impact on the mental health of health care workers around the globe. Fortunately, there are evidence-based strategies aimed at mitigating the effects of this pandemic on health care workers. Fostering self-efficacy and optimism has been shown to improve coping and efficiency during disasters.9 Higher perceived workplace safety is associated with a lower risk of anxiety, depression, and posttraumatic stress among health care workers, while a lack of social support has been linked to adverse behavioral outcomes.10
A recent study found that, among Chinese physicians who cared for COVID-19 victims, more significant social support was associated with better sleep quality, greater self-effectiveness, and less psychological distress.11 Positive leadership and a professional culture of trust, and openness with unambiguous communication have been shown to improve the engagement of the medical workforce.12,13 Psychiatrists must advocate for the adoption of these practices in the workplace. Assessing and addressing mental health needs, in addition to the physical health of the health care workforce, is of utmost importance.
We can accomplish this in many ways, but we have to access our health care workers. Similar to our patient population, health care workers also experience stigma and anxiety tied to the disclosure of mental health challenges. This was reported in a study conducted in China, in which a specific psychological intervention using a hotline program was used for the medical team.14 This program provided psychological interventions/group activities aimed at releasing stress and anxiety. However, initially, the implementation of psychological interventions encountered obstacles.
For example, some members of the medical staff declined to participate in group or individual psychological interventions. Moreover, nurses showed irritability, unwillingness to join, and some staff refused, stating that “they did not have any problems.” Finally, psychological counselors regularly visited the facility to listen to difficulties or stories encountered by staff at work and provide support accordingly. More than 100 frontline medical staff participated and reported feeling better.15
Currently, several U.S. universities/institutes have implemented programs aimed at protecting the health and well-being of their staff during the COVID-19 pandemic. For instance, the department of psychiatry and behavioral health at Hackensack Meridian Health has put comprehensive system programs in place for at 16 affiliated medical centers and other patient care facilities to provide support during the COVID-19 crisis. A 24/7 team member support hotline connecting team members with a behavioral health specialist has become available when needed. This hotline is backed up by social workers, who provide mental health resources. In addition, another service called “Coping with COVID Talks” is available. This service is a virtual psychoeducational group facilitated by psychologists focusing on building coping skills and resilience.
Also, the consultation-liaison psychiatrists in the medical centers provide daily support to clinicians working in ICUs. These efforts have led to paradoxical benefits for employers, further leading to less commuting, more safety, and enhanced productivity for the clinician, according to Ramon Solhkhah, MD, MBA, chairman of the psychiatry department.16
Some universities, such as the University of North Carolina at Chapel Hill, have created mental health/telehealth support for health care workers, where they are conducting webinars on coping with uncertainty tied to COVID-19.17 The University of California, San Francisco, also has been a leader in this effort. That institution has employed its psychiatric workforce as volunteers – encouraging health care workers to use digital health apps and referral resources. Also, these volunteers provide peer counseling, phone support, and spiritual counseling to their health care workers.18
These approaches are crucial in this uncertain, challenging time. Our mental health system is deeply flawed, understaffed, and not well prepared to manage the mental health issues among health care workers. Psychiatric institutes/facilities should follow comprehensive and multifaceted approaches to combat the COVID-19 crisis. Several preventive measures can be considered in coping with this pandemic, such as stress reduction, mindfulness, and disseminating educational materials. Also, increased use of technology, such as in-the-moment measures, development of hotlines, crisis support, and treatment telepsychiatry for therapy and medication, should play a pivotal role in addressing the mental health needs of health care workers.
In addition, it is expected that, as a nation, we will see a surge of mental health needs for illnesses such as depression and PTSD, just as we do after “natural disasters” caused by a variety of reasons, including economic downturns. After the SARS outbreak in 2003, for example, health care workers showed symptoms of PTSD. The COVID-19 pandemic could have a similar impact.
The severity of mental health challenges among clinicians cannot be predicted at this time, but we can speculate that the traumatic impact of COVID-19 will prove long lasting, particularly among clinicians who served vulnerable populations and witnessed suffering, misery, and deaths. The long-term consequences might range from stress and anxiety to fear, depression, and PTSD. Implementation of mental health programs/psychological interventions/support will reduce the impact of mental health issues among these clinicians.
We must think about the best ways to optimize mental health among health care workers while also come up with innovative ways to target this at-risk group. The mental health of people who are saving lives – our frontline heroes – should be taken into consideration seriously around the globe. We also must prioritize the mental health of these workers during this unprecedented, challenging, and anxiety-provoking time.
Dr. Malik and Mr. Van Wert are affiliated with Johns Hopkins University, Baltimore. Dr. Kumari, Dr. Afzal, Dr. Doumas, and Dr. Solhkhah are affiliated with Hackensack Meridian Health at Ocean Medical Center, Brick, N.J. All six authors disclosed having no conflicts of interest. The authors would like to thank Vinay Kumar for his assistance with the literature review and for proofreading and editing this article.
References
1. Wu P et al. Can J Psychiatry. 2009;54(5):302-11.
2. Lu YC et al. Psychother Psychosom. 2006;75(6):370-5.
3. Lai J et al. JAMA Netw Open. 2020;3(3):e203976.
4. Kang L et al. Brain Behav Immun. 2020 Mar 30. doi: 10.1016/j.bbi.2020.03.028.
5. Centers for Disease Control and Prevention COVID-19 Response Team. MMWR. 2020 Apr 17;69(15):477-81.
6. Arango C. Biol Psychiatry. 2020 Apr 8. doi: 10.1016/j.biopsych.2020.04.003.
7. Day M. BMJ. 2020 Apr 2. doi: 10.1136/bmj.m1375.
8. Kirsch T. “Coronavirus, COVID-19: What happens if health care workers stop showing up?” The Atlantic. 2020 Mar 24.
9. Maunder RG et al. Emerg Infect Dis. 2006;12(12):1924-32.
10. Wu P et al. Alcohol Alcohol. 2008;43(6):706-12.
11. Brooks SK et al. BMC Psychol. 2016 Apr 26;4:18.
12. Smith BW et al. Am J Infect Control. 2009; 37:371-80.
13. Chen Q et al. Lancet Psychiatry. 2020 Apr 1;7(14):PE15-6.
14. Xiao H et al. Med Sci Monit. 2020;26:e923549.
15. Bergus GR et al. Acad Med. 2001;76:1148-52.
16. Bergeron T. “Working from home will be stressful. Here’s how employees (and employers) can handle it.” roi-nj.com. 2020 Mar 23.
17. UNChealthcare.org. “Mental Health/Emotional Support Resources for Coworkers and Providers Coping with COVID-19.”
18. Psych.ucsf.edu/coronoavirus. “Resources to Support Your Mental Health During the COVID-19 Outbreak.”
New tetracycline antibiotic effective in acute bacterial skin and skin-structure infections
Background: Acute bacterial skin and skin-structure infections (ABSSSIs) continue to account for substantial morbidity and health care burden, with the emergence of drug-resistant pathogens further complicating their management. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of causative agents of ABSSSI, including Streptococcus pyogenes, Staphylococcus aureus (including methicillin-resistant strains, or MRSA), and Enterococcus spp.
Study design: Phase 3, randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: A total of 55 sites in the United States, Peru, South Africa, and Europe.
Synopsis: The trial recruited 645 adults with a qualifying ABSSSI (such as wound infection, cellulitis or erysipelas, or major abscess) with evidence of an inflammatory response (white blood cell count at least 10,000 cells/mm3 or 4,000 cells/mm3 and below, immature neutrophils at least 15%, lymphatic involvement, or oral or rectal temperature greater than 38.0° C or less than 36.0° C). Exclusion criteria included infections associated with chronic skin lesions and clinically significant liver or renal insufficiency or immunocompromised state. All patients received either omadacycline or linezolid IV with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy.
Omadacycline was noninferior to moxifloxacin with respect to early clinical response (84.8% vs. 85.5%, respectively) and posttreatment clinical response rates (86.1% vs. 83.6%). Efficacy was similar for methicillin-susceptible or methicillin-resistant Staphylococcus aureus, the most common isolated pathogens. Frequency of adverse events (primarily gastrointestinal) was also similar in the two groups. Mean duration of IV therapy was 4.4 days, and mean duration of oral therapy was 5.5 days in the omadacycline group.
Bottom line: Omadacycline provides similar clinical benefit as linezolid in the treatment of ABSSSIs.
Citation: O’Riordan W et al. Omadacycline for acute bacterial skin and skin-structure infections. N Eng J Med. 2019;380:528-38.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Background: Acute bacterial skin and skin-structure infections (ABSSSIs) continue to account for substantial morbidity and health care burden, with the emergence of drug-resistant pathogens further complicating their management. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of causative agents of ABSSSI, including Streptococcus pyogenes, Staphylococcus aureus (including methicillin-resistant strains, or MRSA), and Enterococcus spp.
Study design: Phase 3, randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: A total of 55 sites in the United States, Peru, South Africa, and Europe.
Synopsis: The trial recruited 645 adults with a qualifying ABSSSI (such as wound infection, cellulitis or erysipelas, or major abscess) with evidence of an inflammatory response (white blood cell count at least 10,000 cells/mm3 or 4,000 cells/mm3 and below, immature neutrophils at least 15%, lymphatic involvement, or oral or rectal temperature greater than 38.0° C or less than 36.0° C). Exclusion criteria included infections associated with chronic skin lesions and clinically significant liver or renal insufficiency or immunocompromised state. All patients received either omadacycline or linezolid IV with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy.
Omadacycline was noninferior to moxifloxacin with respect to early clinical response (84.8% vs. 85.5%, respectively) and posttreatment clinical response rates (86.1% vs. 83.6%). Efficacy was similar for methicillin-susceptible or methicillin-resistant Staphylococcus aureus, the most common isolated pathogens. Frequency of adverse events (primarily gastrointestinal) was also similar in the two groups. Mean duration of IV therapy was 4.4 days, and mean duration of oral therapy was 5.5 days in the omadacycline group.
Bottom line: Omadacycline provides similar clinical benefit as linezolid in the treatment of ABSSSIs.
Citation: O’Riordan W et al. Omadacycline for acute bacterial skin and skin-structure infections. N Eng J Med. 2019;380:528-38.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Background: Acute bacterial skin and skin-structure infections (ABSSSIs) continue to account for substantial morbidity and health care burden, with the emergence of drug-resistant pathogens further complicating their management. Omadacycline is a new once-daily tetracycline with in vitro activity against a wide range of causative agents of ABSSSI, including Streptococcus pyogenes, Staphylococcus aureus (including methicillin-resistant strains, or MRSA), and Enterococcus spp.
Study design: Phase 3, randomized, double-blind, double-dummy, placebo-controlled trial.
Setting: A total of 55 sites in the United States, Peru, South Africa, and Europe.
Synopsis: The trial recruited 645 adults with a qualifying ABSSSI (such as wound infection, cellulitis or erysipelas, or major abscess) with evidence of an inflammatory response (white blood cell count at least 10,000 cells/mm3 or 4,000 cells/mm3 and below, immature neutrophils at least 15%, lymphatic involvement, or oral or rectal temperature greater than 38.0° C or less than 36.0° C). Exclusion criteria included infections associated with chronic skin lesions and clinically significant liver or renal insufficiency or immunocompromised state. All patients received either omadacycline or linezolid IV with the option to switch to the oral preparation of the respective drugs after at least 3 days of therapy.
Omadacycline was noninferior to moxifloxacin with respect to early clinical response (84.8% vs. 85.5%, respectively) and posttreatment clinical response rates (86.1% vs. 83.6%). Efficacy was similar for methicillin-susceptible or methicillin-resistant Staphylococcus aureus, the most common isolated pathogens. Frequency of adverse events (primarily gastrointestinal) was also similar in the two groups. Mean duration of IV therapy was 4.4 days, and mean duration of oral therapy was 5.5 days in the omadacycline group.
Bottom line: Omadacycline provides similar clinical benefit as linezolid in the treatment of ABSSSIs.
Citation: O’Riordan W et al. Omadacycline for acute bacterial skin and skin-structure infections. N Eng J Med. 2019;380:528-38.
Dr. Manian is a core educator faculty member in the department of medicine at Massachusetts General Hospital and an associate professor of medicine at Harvard Medical School, Boston.
Progress report: Elimination of neonatal tetanus
Worldwide cases of neonatal tetanus fell by 90% from 2000 to 2018, deaths dropped by 85%, and 45 countries achieved elimination of maternal and neonatal tetanus (MNT), according to the Centers for Disease Control and Prevention.
“Despite this progress, some countries that achieved elimination are still struggling to sustain performance indicators; war and insecurity pose challenges in countries that have not achieved MNT elimination,” Henry N. Njuguna, MD, of the CDC’s global immunization division, and associates wrote in the Morbidity and Mortality Weekly Report.
Other worldwide measures also improved from 2000 to 2018: and the percentage of deliveries attended by a skilled birth attendant increased from 62% during 2000-2005 to 81% in 2013-2018, they reported.
The MNT elimination initiative, which began in 1999 and targeted 59 priority countries, immunized approximately 154 million women of reproductive age with at least two doses of tetanus toxoid–containing vaccine from 2000 to 2018, the investigators wrote, based on data from the World Health Organization and the United Nations Children’s Fund.
With 14 of the priority countries – including Nigeria, Pakistan, and Yemen – still dealing with MNT, however, numerous challenges remain, they noted. About 47 million women and their babies are still unprotected, and 49 million women have not received tetanus toxoid–containing vaccine.
This lack of coverage “can be attributed to weak health systems, including conflict and security issues that limit access to vaccination services, competing priorities that limit the implementation of planned MNT elimination activities, and withdrawal of donor funding,” Dr. Njuguna and associates wrote.
SOURCE: Njuguna HN et al. MMWR. 2020 May 1;69(17):515-20.
Worldwide cases of neonatal tetanus fell by 90% from 2000 to 2018, deaths dropped by 85%, and 45 countries achieved elimination of maternal and neonatal tetanus (MNT), according to the Centers for Disease Control and Prevention.
“Despite this progress, some countries that achieved elimination are still struggling to sustain performance indicators; war and insecurity pose challenges in countries that have not achieved MNT elimination,” Henry N. Njuguna, MD, of the CDC’s global immunization division, and associates wrote in the Morbidity and Mortality Weekly Report.
Other worldwide measures also improved from 2000 to 2018: and the percentage of deliveries attended by a skilled birth attendant increased from 62% during 2000-2005 to 81% in 2013-2018, they reported.
The MNT elimination initiative, which began in 1999 and targeted 59 priority countries, immunized approximately 154 million women of reproductive age with at least two doses of tetanus toxoid–containing vaccine from 2000 to 2018, the investigators wrote, based on data from the World Health Organization and the United Nations Children’s Fund.
With 14 of the priority countries – including Nigeria, Pakistan, and Yemen – still dealing with MNT, however, numerous challenges remain, they noted. About 47 million women and their babies are still unprotected, and 49 million women have not received tetanus toxoid–containing vaccine.
This lack of coverage “can be attributed to weak health systems, including conflict and security issues that limit access to vaccination services, competing priorities that limit the implementation of planned MNT elimination activities, and withdrawal of donor funding,” Dr. Njuguna and associates wrote.
SOURCE: Njuguna HN et al. MMWR. 2020 May 1;69(17):515-20.
Worldwide cases of neonatal tetanus fell by 90% from 2000 to 2018, deaths dropped by 85%, and 45 countries achieved elimination of maternal and neonatal tetanus (MNT), according to the Centers for Disease Control and Prevention.
“Despite this progress, some countries that achieved elimination are still struggling to sustain performance indicators; war and insecurity pose challenges in countries that have not achieved MNT elimination,” Henry N. Njuguna, MD, of the CDC’s global immunization division, and associates wrote in the Morbidity and Mortality Weekly Report.
Other worldwide measures also improved from 2000 to 2018: and the percentage of deliveries attended by a skilled birth attendant increased from 62% during 2000-2005 to 81% in 2013-2018, they reported.
The MNT elimination initiative, which began in 1999 and targeted 59 priority countries, immunized approximately 154 million women of reproductive age with at least two doses of tetanus toxoid–containing vaccine from 2000 to 2018, the investigators wrote, based on data from the World Health Organization and the United Nations Children’s Fund.
With 14 of the priority countries – including Nigeria, Pakistan, and Yemen – still dealing with MNT, however, numerous challenges remain, they noted. About 47 million women and their babies are still unprotected, and 49 million women have not received tetanus toxoid–containing vaccine.
This lack of coverage “can be attributed to weak health systems, including conflict and security issues that limit access to vaccination services, competing priorities that limit the implementation of planned MNT elimination activities, and withdrawal of donor funding,” Dr. Njuguna and associates wrote.
SOURCE: Njuguna HN et al. MMWR. 2020 May 1;69(17):515-20.
FROM MMWR
Yale’s COVID-19 inpatient protocol: Hydroxychloroquine plus/minus tocilizumab
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
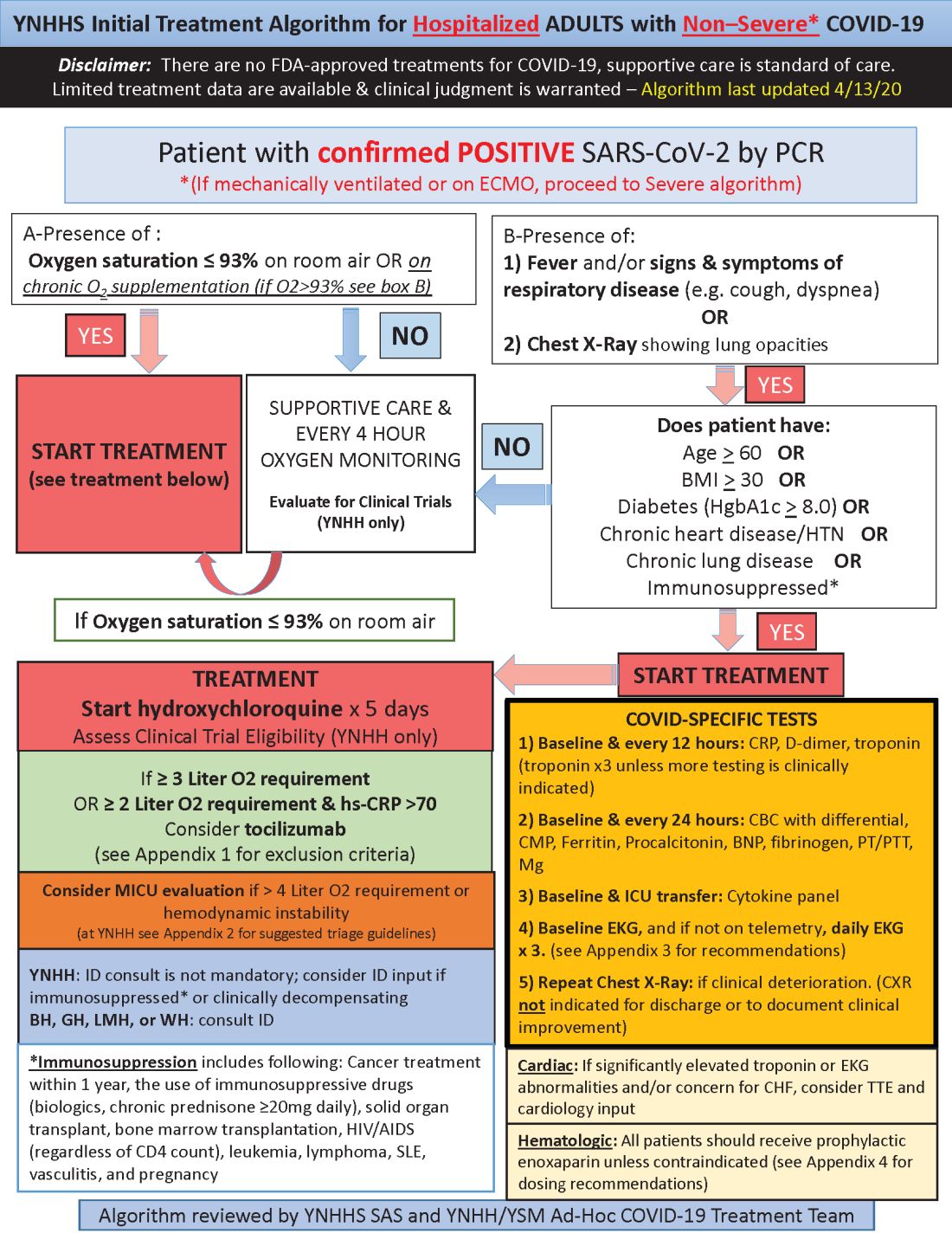
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
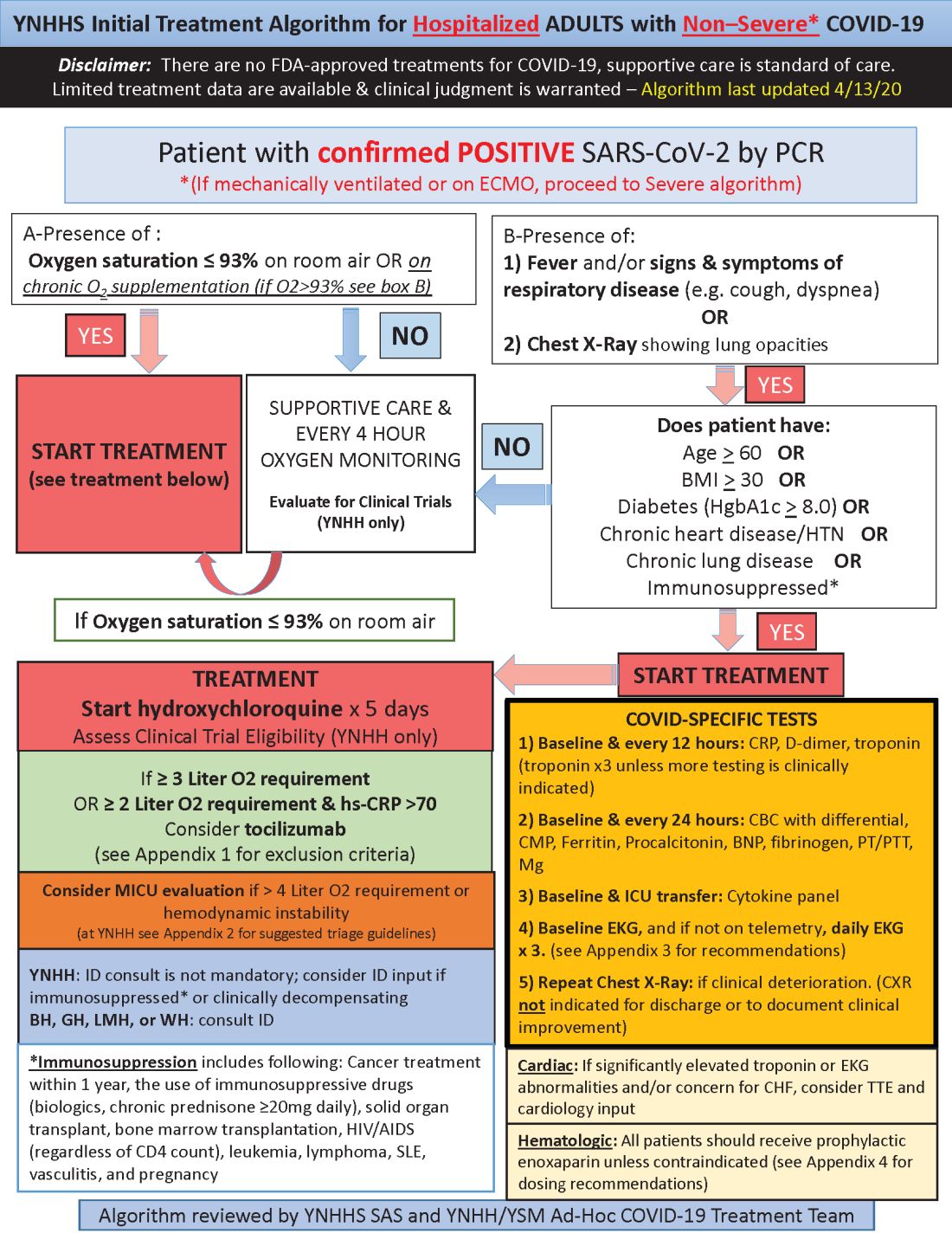
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.
Hydroxychloroquine is currently first-line, and tocilizumab second-line, for people hospitalized with polymerase chain reaction–confirmed COVID-19 in the Yale New Haven (Conn.) Health System, which operates hospitals across Connecticut, many of them hard hit by the pandemic.
Patients enter the treatment algorithm if they have an oxygen saturation at or below 93% on room air or chronic supplementation, or by being acutely ill with fever, respiratory signs, or opacities on chest x-ray, plus risk factors for severe illness such as age over 60 years, chronic heart or lung disease, immunosuppression, diabetes, hypertension, or obesity, which makes it harder to ventilate.
Physicians at Yale have seen both presentations – oxygen desaturation and frank illness – and “wanted to make sure we weren’t missing anyone,” said Nihar Desai, MD, a Yale cardiologist who is helping to coordinate the health system’s response to COVID-19.
In either case, the initial treatment is the same at Yale hospitals: hydroxychloroquine for 5 days, with tocilizumab (Actemra) considered when not contraindicated and oxygen requirements reach or pass 3 L, or 2 L with C-reactive protein levels above 70 mg/L.
Patients are put on prophylactic enoxaparin to thin the blood unless contraindicated; inflammatory, cardiac, kidney, and other markers are checked every 12 or 24 hours; and ECGs are taken daily if telemetry isn’t used. Chest x-rays are repeated if clinical signs worsen, and transthoracic echocardiograms are ordered for suspected heart problems.
ICUs are notified early if the clinical situation worsens because patients “can deteriorate very quickly; at the first sign of trouble, people are really aggressive,” said Dr. Desai, also the associate chief of clinical operations in the Section of Cardiovascular Medicine at the Yale University, New Haven.
The haze of battle
Yale has updated its algorithm several times since the virus first hit Connecticut weeks ago. A team including pulmonologists, critical care physicians, pharmacologists, infectious disease experts, and cardiologists, including Dr. Desai, are constantly monitoring the situation and making changes as new information comes in.
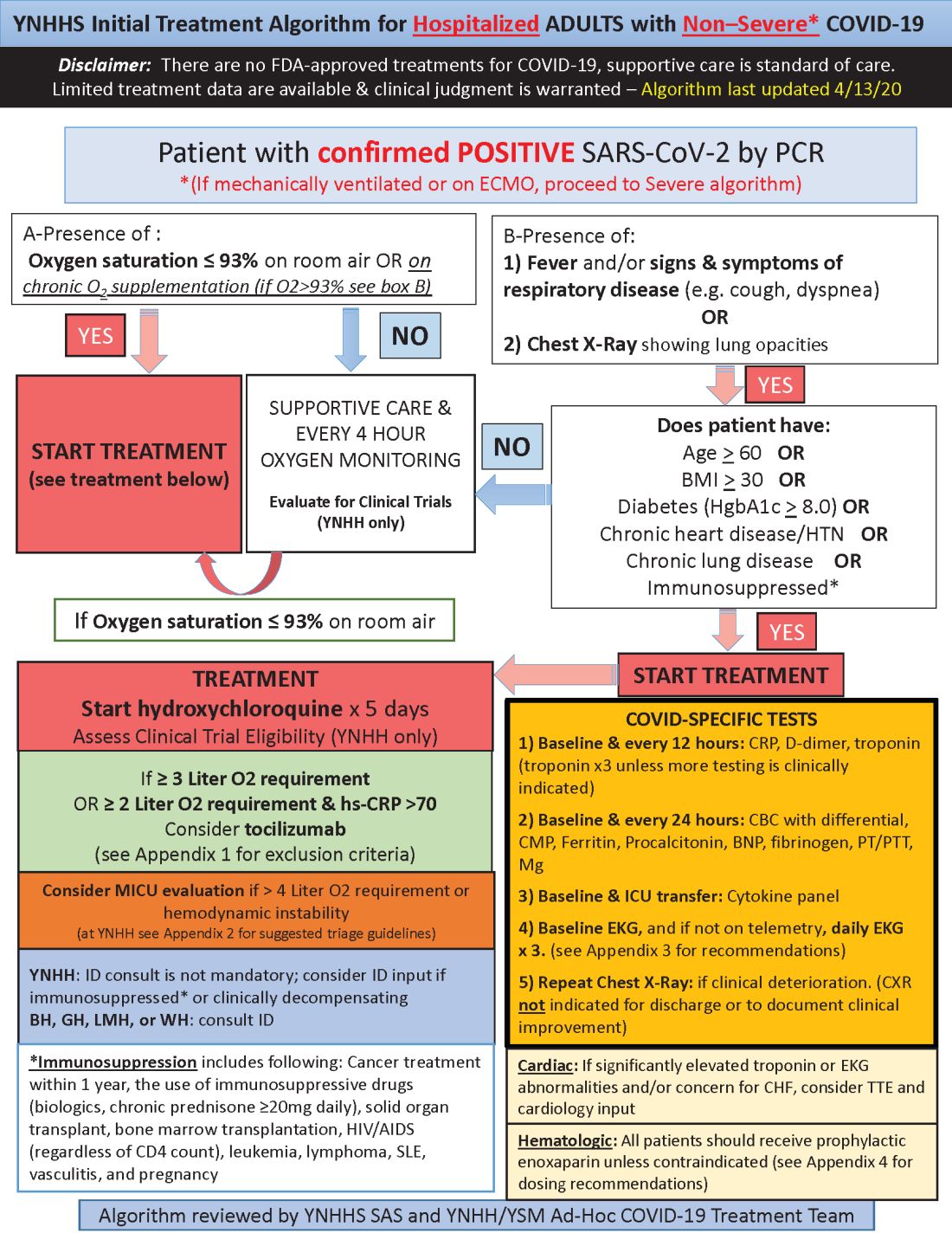
Much of what’s being done at Yale and elsewhere is empiric because there are simply not much data to go on. “We are trying to do the best we can” in “the haze of battle. People really came together quickly to develop this. One hopes we never have to go through anything like this again,” he said.
Hydroxychloroquine is first-line at Yale because in-vitro data show potent inhibition of the virus and possible clinical benefit, which is about as good as evidence gets at the moment. Also, “it’s cheap, it’s been used for decades, and people are relatively comfortable with it,” Dr. Desai said.
Tocilizumab, an interleukin-6 (IL-6) receptor antagonist, is second-line because it might counter the cytokine storm thought to be at least partly responsible for severe complications, and retrospective data suggest possible benefit. The antiviral remdesivir and IL-6 blocker sarulimab (Kevzara) are also potential candidates, available through clinical trials.
Dr. Desai wanted to share the algorithm with other providers because, he noted, “there are a lot of places that may not have all the resources we have.”
His home institution, Yale New Haven Hospital, is almost half full with COVID-19 patients, at more than 400.
A moving target
Yale’s approach is similar in confirmed COVID-19 cases already in respiratory failure, including those on mechanical ventilation and extracorporeal membrane oxygenation: hydroxychloroquine and possibly tocilizumab, but also methylprednisolone if clinical status worsens or inflammatory markers go up. The steroid is for additional help battling the cytokine storm, Dr. Desai said.
The degree of anticoagulation in the ICU is based on d-dimer levels or suspicion or confirmation of venous thromboembolism. Telemetry is monitored closely for QTc prolongation, and point of care ultrasound is considered to check left ventricular function in the setting of markedly increased cardiac troponin levels, ECG abnormalities, or hemodynamic instability.
Previous versions of Yale’s algorithm included HIV protease inhibitors, but they were pulled after a recent trial found no benefit. Frequency of monitoring was also reduced from every 8 hours because it didn’t improve decision making and put staff collecting specimens at risk (N Engl J Med. 2020 Mar 18. doi: 10.1056/NEJMoa2001282).
Anticoagulation was added to newer versions after it became clear that COVID-19 is prothrombotic. “We are still seeing thrombotic events that might warrant further intensification,” Dr. Desai said.
Newer algorithms also have Yale watching QTc intervals more closely. It’s unclear if the prolongation risk is caused by the infection or hydroxychloroquine.
On April 24, the Food and Drug Administration reiterated it’s concern about the arrhythmia risk with hydroxychloroquine and emphasized that it should only be used for COVID-19 patients when they are hospitalized and it is not feasible for them to participate in a clinical trial.
To help keep patients safe, ECGs from confirmed or suspected COVID-19 cases are now first in line to be reviewed by cardiologists across Yale hospitals to pick up prolongations and notify providers as soon as possible. Hydroxychloroquine is held if there are no other explanations.
Cardiologists are on the fontline at Yale and elsewhere, Dr. Desai said, because heart complications like myocarditis and arrhythmias emerged early as common problems in hospitalized patients.
[email protected]
This article was updated with the latest treatment algorithm on 5/6/2020.
POPCoRN network mobilizes pediatric capacity during pandemic
Med-Peds hospitalists were an organizing force
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
Med-Peds hospitalists were an organizing force
Med-Peds hospitalists were an organizing force
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
As U.S. health care systems prepare for inpatient surges linked to hospitalizations of critically ill COVID-19 patients, two hospitalists with med-peds training (combined training in internal medicine and pediatrics) have launched an innovative solution to help facilities deal with the challenge.
The Pediatric Overflow Planning Contingency Response Network (POPCoRN network) has quickly linked almost 400 physicians and other health professionals, including hospitalists, attending physicians, residents, medical students, and nurses. The network wants to help provide more information about how pediatric-focused institutions can safely gear up to admit adult patients in children’s hospitals, in order to offset the predicted demand for hospital beds for patients with COVID-19.
According to the POPCoRN network website (www.popcornetwork.org), the majority of providers who have contacted the network say they have already started or are committed to planning for their pediatric facilities to be used for adult overflow. The Children’s Hospital Association has issued a guidance on this kind of community collaboration for children’s hospitals partnering with adult hospitals in their community and with policy makers.
“We are a network of folks from different institutions, many med-peds–trained hospitalists but quickly growing,” said Leah Ratner, MD, a second-year fellow in the Global Pediatrics Program at Boston Children’s Hospital and cofounder of the POPCoRN network. “We came together to think about how to increase capacity – both in the work force and for actual hospital space – by helping to train pediatric hospitalists and pediatrics-trained nurses to care for adult patients.”
A web-based platform filled with a rapidly expanding list of resources, an active Twitter account, and utilization of Zoom networking software for webinars and working group meetings have facilitated the network’s growth. “Social media has helped us,” Dr. Ratner said. But equally important are personal connections.
“It all started just a few weeks ago,” added cofounder Ashley Jenkins, MD, a med-peds hospital medicine and general academics research fellow in the division of hospital medicine at Cincinnati Children’s Hospital Medical Center. “I sent out some emails in mid-March, asking what other people were doing about these issues. Leah and I met as a result of these initial emails. We immediately started connecting with other health systems and it just expanded from there. Once we knew that enough other systems were thinking about it and trying to build capacity, we started pulling the people and information together.”
High-yield one-pagers
A third or more of those on the POPCoRN contact list are also participating as volunteers on its varied working groups, including health system operation groups exploring the needs of three distinct hospital models: freestanding children’s hospitals; community hospitals, which may see small numbers of children; and integrated mixed hospitals, which often means a pediatric hospital or pediatric units located within an adult hospital.
An immediate goal is to develop high-yield informational “one-pagers,” culling essential clinical facts on a variety of topics in adult inpatient medicine that may no longer be familiar to working pediatric hospitalists. These one-pagers, designed with the help of network members with graphic design skills, address topics such as syncope or chest pain or managing exacerbation of COPD in adults. They draw upon existing informational sources, encapsulating practical information tips that can be used at the bedside, including test workups, differential diagnoses, treatment approaches, and other pearls for providers. Drafts are reviewed for content by specialists, and then by pediatricians to make sure the information covers what they need.
Also under development are educational materials for nurses trained in pediatrics, a section for outpatient providers redeployed to triage or telehealth, and information for other team members including occupational, physical, and respiratory therapists. Another section offers critical care lectures for the nonintensivist. A metrics and outcomes working group is looking for ways to evaluate how the network is doing and who is being reached without having to ask frontline providers to fill out surveys.
Dr. Ratner and Dr. Jenkins have created an intentional structure for encouraging mentoring. They also call on their own mentors – Ahmet Uluer, DO, director of Weitzman Family Bridges Adult Transition Program at Boston Children’s Hospital, and Brian Herbst Jr., MD, medical director of the Hospital Medicine Adult Care Service at Cincinnati Children’s – for advice.
Beyond the silos
Pediatric hospitalists may have been doing similar things, working on similar projects, but not necessarily reaching out to each other across a system that tends to promote staying within administrative silos, Dr. Uluer said. “Through our personal contacts in POPCoRN, we’ve been able to reach beyond the silos. This network has worked like medical crowd sourcing, and the founders have been inspirational.”
Dr. Herbst added, “How do we expand bandwidth and safely expand services to take young patients and adults from other hospitals? What other populations do we need to expand to take? This network is a workplace of ideas. It’s amazing to see what has been built in a few weeks and how useful it can be.”
Med-peds hospitalists are an important resource for bridging the two specialties. Their experience with transitioning young adults with long-standing chronic conditions of childhood, who have received most of their care at a children’s hospital before reaching adulthood, offers a helpful model. “We’ve also tried to target junior physicians who could step up into leadership roles and to pull in medical students – who are the backbone of this network through their administrative support,” Dr. Jenkins said.
Marie Pfarr, MD, also a med-peds trained hospital medicine fellow at Cincinnati Children’s, was contacted in March by Dr. Jenkins. “She said they had this brainstorm, and they were getting feedback that it would be helpful to provide educational materials for pediatric providers. Because I have an interest in medical education, she asked if I wanted to help. I was at home struggling with what I could contribute during this crazy time, so I said yes.”
Dr. Pfarr leads POPCoRN’s educational working group, which came up with a list of 50 topics in need of one-pagers and people willing to create them, mostly still under development. The aim for the one-pagers is to offer a good starting point for pediatricians, helping them, for example, to ask the right questions during history and physical exams. “We also want to offer additional resources for those who want to do a deeper dive.”
Dr. Pfarr said she has enjoyed working closely with medical students, who really want to help. “That’s been great to see. We are all working toward the same goal, and we help to keep each other in check. I think there’s a future for this kind of mobilization through collaborations to connect pediatric to adult providers. A lot of good things will come out of the network, which is an example of how folks can talk to each other. It’s very dynamic and changing every day.”
One of those medical students is Chinma Onyewuenyi, finishing her fourth year at Baylor College of Medicine. Scheduled to start a med-peds residency at Geisinger Health on July 1, she had completed all of her rotations and was looking for ways to get involved in the pandemic response while respecting the shelter-in-place order. “I had heard about the network, which was recruiting medical students to play administrative roles for the working groups. I said, ‘If you have anything else you need help with, I have time on my hands.’”
Ms. Onyewuenyi says she fell into the role of a lead administrative volunteer, and her responsibilities grew from there, eventually taking charge of all the medical students’ recruiting, screening, and assignments, freeing up the project’s physician leaders from administrative tasks. “I wanted something active to do to contribute, and I appreciate all that I’m learning. With a master’s degree in public health, I have researched how health care is delivered,” she said.
“This experience has really opened my eyes to what’s required to deliver care, and just the level of collaboration that needs to go on with something like this. Even as a medical student, I felt glad to have an opportunity to contribute beyond the administrative tasks. At meetings, they ask for my opinion.”
Equitable access to resources
Another major focus for the network is promoting health equity – giving pediatric providers and health systems equitable access to information that meets their needs, Dr. Ratner said. “We’ve made a particular effort to reach out to hospitals that are the most vulnerable, including rural hospitals, and to those serving the most vulnerable patients,” she noted. These also include the homeless and refugees.
“We’ve been trying to be mindful of avoiding the sometimes-intimidating power structure that has been traditional in medicine,” Dr. Ratner said. The network’s equity working group is trying to provide content with structural competency and cultural humility. “We’re learning a lot about the ways the health care system is broken,” she added. “We all agree that we have a fragmented health care system, but there are ways to make it less fragmented and learn from each other.”
In the tragedy of the COVID epidemic, there are also unique opportunities to learn to work collaboratively and make the health care system stronger for those in greatest need, Dr. Ratner added. “What we hope is that our network becomes an example of that, even as it is moving so quickly.”
Audrey Uong, MD, an attending physician in the division of hospital medicine at Children’s Hospital at Montefiore Medical Center in New York, connected with POPCoRN for an educational presentation reviewing resuscitation in adult patients. She wanted to talk with peers about what’s going on, so as not to feel alone in her practice. She has also found the network’s website useful for identifying educational resources.
“As pediatricians, we have been asked to care for adult patients. One of our units has been admitting mostly patients under age 30, and we are accepting older patients in another unit on the pediatric wing.” This kind of thing is also happening in a lot of other places, Dr. Uong said. Keeping up with these changes in her own practice has been challenging.
She tries to take one day at a time. “Everyone at this institution feels the same – that we’re locked in on meeting the need. Even our child life specialists, when they’re not working with younger patients, have created this amazing support room for staff, with snacks and soothing music. There’s been a lot of attention paid to making us feel supported in this work.”
AAP releases updated guidance on male teen sexual, reproductive health
The American Academy of Pediatrics’ Committee on Adolescence has updated its guidance on addressing sexual reproductive health in male adolescents.
Since the last guidance was published by AAP in 2011, new data have been released that focus on adolescent male sexual behavior, their use of media, sexually transmitted infections (STIs), vaccination for human papillomavirus (HPV), discussions surrounding consent, and information for LGBT individuals.
“Of all these recommendations, the most significant changes are to provide more STI screening for higher risk males and vaccinate all males for HPV starting as early as age 9 years old,” lead author Laura K. Grubb, MD, director of adolescent medicine at Floating Hospital for Children at Tufts Medical Center, Boston, said in an interview.
AAP recommends pediatricians consider the following when discussing sexuality and reproductive health with adolescent males:
- Discuss the topics of sex and sexuality during routine visits and appropriate opportunities, taking the time to screen for sexual activity and identifying who is at higher risk.
- Ask male adolescent patients about social media use, how often they view pornography, and how they perceive sexually explicit material. If there is a concern that sexually explicit content is having an adverse effect on the patient, pediatricians should counsel patients and their parents on how to safely and sensibly use the Internet and social media.
- Screen for nonconsensual sexual activity during well visits and other visits, as appropriate. The principles of consent and nonconsent in the context of sexual activity should be discussed.
- For patients who are sexually active, screen for sexual problems, including any mental health issues and sexual dysfunction, and initiate counseling or pharmacotherapy where warranted.
- Coach male adolescent patients on broaching discussions about sex and family planning with their partners, including joint decision making on sexual and reproductive health. Contraception and barrier methods should be discussed and encouraged as appropriate.
- Assess each patient for appropriate STI risk, testing, and treatment/prevention for HIV, syphilis, chlamydia, and gonorrhea.
- Consider HPV vaccination for children at least 9 years old and start administration starting at 11 years old. according to the guidance.
Dr. Grubb said she hopes this guidance helps start a conversation between pediatricians and their adolescent male patients. “Talk with your male adolescents about puberty, sexuality, and reproductive health! When pediatricians are informed about these issues and take the initiative to discuss these topics with adolescent males, they are uniquely situated to help them navigate this challenging time safely and confidently.”
“I am especially excited about the significant resources this report provides for pediatricians in the supplemental document,” Dr. Grubb added. “There are so many great resources out there, especially on the Internet, for adolescents, parents, and pediatricians.”
Kelly Curran, MD, adolescent medicine specialist and assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, said in an interview that the guidance information on sexting, “sextortion,” and sexual dysfunction are important updates for pediatricians. Sextortion is defined as the “threatened dissemination of explicit, intimate, or embarrassing images of a sexual nature without consent, usually for the purpose of procuring additional images, sexual acts, money, or something else.”
“We have all seen how social media and technology has transformed adolescence, especially with the rise of sexting. We must remember that males are often the victims of ‘sextortion’ and sexual assault, especially sexual minority youth, and men may not have the support and services to which female victims have access,” said Dr. Curran, who was not a member of the committee.
Another important area where pediatricians can help educate adolescent males and their parents is the concept of consent during sexual encounters.
“As we as a society are having more frank discussions around sexual assault and rape, I think it is essential there is a continued dialogue with young people about consent. Pediatricians have an important role to play in the discussion with their patients, especially in regard to paying attention to verbal and nonverbal cues, and recognizing that consent is an ongoing process, instead of a ‘one time thing,’ ” said Dr. Curran, who is a member of the Pediatric News editorial advisory board.
One area of the new AAP guidance that surprised Dr. Curran was the number of adolescent males reporting sexual dysfunction – 4%. “While it’s something I ask about periodically in young men, I haven’t been consistently asking in visits for those who are at risk,” she said. “This guideline reminds me to screen more frequently, especially as patients may be too embarrassed to ask.”
Concerning STI screening, Dr. Curran feels guidelines from the Centers for Disease Control and Prevention and the United States Preventive Services Task Force (USPSTF) don’t go far enough, and the AAP’s guidance to provide routine STI risk assessment for all patients is more appropriate.
“We know that STIs are on the rise and adolescents experience high rates of STI, yet there are only routine screening guidelines for adolescent and young adult women and ‘at-risk’ populations or in areas of higher prevalence,” she said. “In my experience, all sexually active adolescents are ‘at risk.’ I think there should be universal screening of all sexually active adolescents and young adults.”
The paper had no funding source, and the authors reported no relevant conflicts of interest. Dr. Curran also reported no relevant conflicts of interest.
SOURCE: Grubb L et al. Pediatrics. 2020 Apr 27;145(5):e20200627.
The American Academy of Pediatrics’ Committee on Adolescence has updated its guidance on addressing sexual reproductive health in male adolescents.
Since the last guidance was published by AAP in 2011, new data have been released that focus on adolescent male sexual behavior, their use of media, sexually transmitted infections (STIs), vaccination for human papillomavirus (HPV), discussions surrounding consent, and information for LGBT individuals.
“Of all these recommendations, the most significant changes are to provide more STI screening for higher risk males and vaccinate all males for HPV starting as early as age 9 years old,” lead author Laura K. Grubb, MD, director of adolescent medicine at Floating Hospital for Children at Tufts Medical Center, Boston, said in an interview.
AAP recommends pediatricians consider the following when discussing sexuality and reproductive health with adolescent males:
- Discuss the topics of sex and sexuality during routine visits and appropriate opportunities, taking the time to screen for sexual activity and identifying who is at higher risk.
- Ask male adolescent patients about social media use, how often they view pornography, and how they perceive sexually explicit material. If there is a concern that sexually explicit content is having an adverse effect on the patient, pediatricians should counsel patients and their parents on how to safely and sensibly use the Internet and social media.
- Screen for nonconsensual sexual activity during well visits and other visits, as appropriate. The principles of consent and nonconsent in the context of sexual activity should be discussed.
- For patients who are sexually active, screen for sexual problems, including any mental health issues and sexual dysfunction, and initiate counseling or pharmacotherapy where warranted.
- Coach male adolescent patients on broaching discussions about sex and family planning with their partners, including joint decision making on sexual and reproductive health. Contraception and barrier methods should be discussed and encouraged as appropriate.
- Assess each patient for appropriate STI risk, testing, and treatment/prevention for HIV, syphilis, chlamydia, and gonorrhea.
- Consider HPV vaccination for children at least 9 years old and start administration starting at 11 years old. according to the guidance.
Dr. Grubb said she hopes this guidance helps start a conversation between pediatricians and their adolescent male patients. “Talk with your male adolescents about puberty, sexuality, and reproductive health! When pediatricians are informed about these issues and take the initiative to discuss these topics with adolescent males, they are uniquely situated to help them navigate this challenging time safely and confidently.”
“I am especially excited about the significant resources this report provides for pediatricians in the supplemental document,” Dr. Grubb added. “There are so many great resources out there, especially on the Internet, for adolescents, parents, and pediatricians.”
Kelly Curran, MD, adolescent medicine specialist and assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, said in an interview that the guidance information on sexting, “sextortion,” and sexual dysfunction are important updates for pediatricians. Sextortion is defined as the “threatened dissemination of explicit, intimate, or embarrassing images of a sexual nature without consent, usually for the purpose of procuring additional images, sexual acts, money, or something else.”
“We have all seen how social media and technology has transformed adolescence, especially with the rise of sexting. We must remember that males are often the victims of ‘sextortion’ and sexual assault, especially sexual minority youth, and men may not have the support and services to which female victims have access,” said Dr. Curran, who was not a member of the committee.
Another important area where pediatricians can help educate adolescent males and their parents is the concept of consent during sexual encounters.
“As we as a society are having more frank discussions around sexual assault and rape, I think it is essential there is a continued dialogue with young people about consent. Pediatricians have an important role to play in the discussion with their patients, especially in regard to paying attention to verbal and nonverbal cues, and recognizing that consent is an ongoing process, instead of a ‘one time thing,’ ” said Dr. Curran, who is a member of the Pediatric News editorial advisory board.
One area of the new AAP guidance that surprised Dr. Curran was the number of adolescent males reporting sexual dysfunction – 4%. “While it’s something I ask about periodically in young men, I haven’t been consistently asking in visits for those who are at risk,” she said. “This guideline reminds me to screen more frequently, especially as patients may be too embarrassed to ask.”
Concerning STI screening, Dr. Curran feels guidelines from the Centers for Disease Control and Prevention and the United States Preventive Services Task Force (USPSTF) don’t go far enough, and the AAP’s guidance to provide routine STI risk assessment for all patients is more appropriate.
“We know that STIs are on the rise and adolescents experience high rates of STI, yet there are only routine screening guidelines for adolescent and young adult women and ‘at-risk’ populations or in areas of higher prevalence,” she said. “In my experience, all sexually active adolescents are ‘at risk.’ I think there should be universal screening of all sexually active adolescents and young adults.”
The paper had no funding source, and the authors reported no relevant conflicts of interest. Dr. Curran also reported no relevant conflicts of interest.
SOURCE: Grubb L et al. Pediatrics. 2020 Apr 27;145(5):e20200627.
The American Academy of Pediatrics’ Committee on Adolescence has updated its guidance on addressing sexual reproductive health in male adolescents.
Since the last guidance was published by AAP in 2011, new data have been released that focus on adolescent male sexual behavior, their use of media, sexually transmitted infections (STIs), vaccination for human papillomavirus (HPV), discussions surrounding consent, and information for LGBT individuals.
“Of all these recommendations, the most significant changes are to provide more STI screening for higher risk males and vaccinate all males for HPV starting as early as age 9 years old,” lead author Laura K. Grubb, MD, director of adolescent medicine at Floating Hospital for Children at Tufts Medical Center, Boston, said in an interview.
AAP recommends pediatricians consider the following when discussing sexuality and reproductive health with adolescent males:
- Discuss the topics of sex and sexuality during routine visits and appropriate opportunities, taking the time to screen for sexual activity and identifying who is at higher risk.
- Ask male adolescent patients about social media use, how often they view pornography, and how they perceive sexually explicit material. If there is a concern that sexually explicit content is having an adverse effect on the patient, pediatricians should counsel patients and their parents on how to safely and sensibly use the Internet and social media.
- Screen for nonconsensual sexual activity during well visits and other visits, as appropriate. The principles of consent and nonconsent in the context of sexual activity should be discussed.
- For patients who are sexually active, screen for sexual problems, including any mental health issues and sexual dysfunction, and initiate counseling or pharmacotherapy where warranted.
- Coach male adolescent patients on broaching discussions about sex and family planning with their partners, including joint decision making on sexual and reproductive health. Contraception and barrier methods should be discussed and encouraged as appropriate.
- Assess each patient for appropriate STI risk, testing, and treatment/prevention for HIV, syphilis, chlamydia, and gonorrhea.
- Consider HPV vaccination for children at least 9 years old and start administration starting at 11 years old. according to the guidance.
Dr. Grubb said she hopes this guidance helps start a conversation between pediatricians and their adolescent male patients. “Talk with your male adolescents about puberty, sexuality, and reproductive health! When pediatricians are informed about these issues and take the initiative to discuss these topics with adolescent males, they are uniquely situated to help them navigate this challenging time safely and confidently.”
“I am especially excited about the significant resources this report provides for pediatricians in the supplemental document,” Dr. Grubb added. “There are so many great resources out there, especially on the Internet, for adolescents, parents, and pediatricians.”
Kelly Curran, MD, adolescent medicine specialist and assistant professor of pediatrics at the University of Oklahoma Health Sciences Center, said in an interview that the guidance information on sexting, “sextortion,” and sexual dysfunction are important updates for pediatricians. Sextortion is defined as the “threatened dissemination of explicit, intimate, or embarrassing images of a sexual nature without consent, usually for the purpose of procuring additional images, sexual acts, money, or something else.”
“We have all seen how social media and technology has transformed adolescence, especially with the rise of sexting. We must remember that males are often the victims of ‘sextortion’ and sexual assault, especially sexual minority youth, and men may not have the support and services to which female victims have access,” said Dr. Curran, who was not a member of the committee.
Another important area where pediatricians can help educate adolescent males and their parents is the concept of consent during sexual encounters.
“As we as a society are having more frank discussions around sexual assault and rape, I think it is essential there is a continued dialogue with young people about consent. Pediatricians have an important role to play in the discussion with their patients, especially in regard to paying attention to verbal and nonverbal cues, and recognizing that consent is an ongoing process, instead of a ‘one time thing,’ ” said Dr. Curran, who is a member of the Pediatric News editorial advisory board.
One area of the new AAP guidance that surprised Dr. Curran was the number of adolescent males reporting sexual dysfunction – 4%. “While it’s something I ask about periodically in young men, I haven’t been consistently asking in visits for those who are at risk,” she said. “This guideline reminds me to screen more frequently, especially as patients may be too embarrassed to ask.”
Concerning STI screening, Dr. Curran feels guidelines from the Centers for Disease Control and Prevention and the United States Preventive Services Task Force (USPSTF) don’t go far enough, and the AAP’s guidance to provide routine STI risk assessment for all patients is more appropriate.
“We know that STIs are on the rise and adolescents experience high rates of STI, yet there are only routine screening guidelines for adolescent and young adult women and ‘at-risk’ populations or in areas of higher prevalence,” she said. “In my experience, all sexually active adolescents are ‘at risk.’ I think there should be universal screening of all sexually active adolescents and young adults.”
The paper had no funding source, and the authors reported no relevant conflicts of interest. Dr. Curran also reported no relevant conflicts of interest.
SOURCE: Grubb L et al. Pediatrics. 2020 Apr 27;145(5):e20200627.
FROM PEDIATRICS