User login
Prioritizing ambulatory gynecology care during COVID-19: The latest guidance
What exactly constitutes appropriate ambulatory gynecology during this time of social distancing?
On March 30, 2020, the American College of Obstetricians and Gynecologists (ACOG) weighed in, releasing COVID-19 FAQs for Obstetrician-Gynecologists. These recommendations, which include information about obstetric and gynecologic surgery, are available to everyone, including the general public. They are intended to supplement guidance from the Centers for Disease Control and Prevention, as well as previously released ACOG guidance.
The recommendations include examples of patients needing in-person appointments, telehealth visits, or visits that should be deferred.
In-person appointments. Examples of patients for whom in-person appointments are appropriate include those with suspected ectopic pregnancy or profuse vaginal bleeding. With respect to contraceptive services, ACOG suggests that placement of IUDs and implants should continue whenever possible. If placement of the contraceptive device is deferred, use of self-administered hormonal contraceptives (including subcutaneous injections, oral, transdermal patch, and vaginal ring) should be encouraged as a bridge to later initiation of long-acting methods.
Telehealth visits. Video or telephone visits are advised for women desiring counseling and prescribing for contraception or menopausal symptoms.
Deferred. Deferral of office visits until after COVID-19 lockdowns is advised for average-risk women wishing routine well-woman visits. Other situations in which deferral should be considered include the following:
- For patients with abnormal cervical cancer screening results, ACOG suggests that colposcopy with cervical biopsies could be deferred for 6-12 months for patients with low-grade test results. In contrast, for patients with high-grade results, ACOG recommends that evaluation be performed within 3 months.
- For women who wish to discontinue their contraceptive, ACOG advises that removal of IUDs and implants be postponed when possible. These women should be counseled regarding extended use of these devices.
ACOG emphasizes that decisions regarding ambulatory gynecology should be individualized and take into consideration such issues as availability of local and regional resources, staffing, personal protective equipment, and the local prevalence of COVID-19.
As a gynecologist focused on ambulatory care, I believe that many clinicians will welcome this guidance from ACOG, which helps us provide optimal care during these challenging times.
Dr. Kaunitz is professor and associate chairman in the department of obstetrics and gynecology at the University of Florida, Jacksonville. He has disclosed receiving royalties from UpToDate, serving on the safety monitoring board for Femasys, and serving as a consultant for AMAG Pharmaceuticals, Merck & Co, Mithra, and Pfizer. His institution has received funding from pharmaceutical companies and nonprofits.
A version of this article originally appeared on Medscape.com.
What exactly constitutes appropriate ambulatory gynecology during this time of social distancing?
On March 30, 2020, the American College of Obstetricians and Gynecologists (ACOG) weighed in, releasing COVID-19 FAQs for Obstetrician-Gynecologists. These recommendations, which include information about obstetric and gynecologic surgery, are available to everyone, including the general public. They are intended to supplement guidance from the Centers for Disease Control and Prevention, as well as previously released ACOG guidance.
The recommendations include examples of patients needing in-person appointments, telehealth visits, or visits that should be deferred.
In-person appointments. Examples of patients for whom in-person appointments are appropriate include those with suspected ectopic pregnancy or profuse vaginal bleeding. With respect to contraceptive services, ACOG suggests that placement of IUDs and implants should continue whenever possible. If placement of the contraceptive device is deferred, use of self-administered hormonal contraceptives (including subcutaneous injections, oral, transdermal patch, and vaginal ring) should be encouraged as a bridge to later initiation of long-acting methods.
Telehealth visits. Video or telephone visits are advised for women desiring counseling and prescribing for contraception or menopausal symptoms.
Deferred. Deferral of office visits until after COVID-19 lockdowns is advised for average-risk women wishing routine well-woman visits. Other situations in which deferral should be considered include the following:
- For patients with abnormal cervical cancer screening results, ACOG suggests that colposcopy with cervical biopsies could be deferred for 6-12 months for patients with low-grade test results. In contrast, for patients with high-grade results, ACOG recommends that evaluation be performed within 3 months.
- For women who wish to discontinue their contraceptive, ACOG advises that removal of IUDs and implants be postponed when possible. These women should be counseled regarding extended use of these devices.
ACOG emphasizes that decisions regarding ambulatory gynecology should be individualized and take into consideration such issues as availability of local and regional resources, staffing, personal protective equipment, and the local prevalence of COVID-19.
As a gynecologist focused on ambulatory care, I believe that many clinicians will welcome this guidance from ACOG, which helps us provide optimal care during these challenging times.
Dr. Kaunitz is professor and associate chairman in the department of obstetrics and gynecology at the University of Florida, Jacksonville. He has disclosed receiving royalties from UpToDate, serving on the safety monitoring board for Femasys, and serving as a consultant for AMAG Pharmaceuticals, Merck & Co, Mithra, and Pfizer. His institution has received funding from pharmaceutical companies and nonprofits.
A version of this article originally appeared on Medscape.com.
What exactly constitutes appropriate ambulatory gynecology during this time of social distancing?
On March 30, 2020, the American College of Obstetricians and Gynecologists (ACOG) weighed in, releasing COVID-19 FAQs for Obstetrician-Gynecologists. These recommendations, which include information about obstetric and gynecologic surgery, are available to everyone, including the general public. They are intended to supplement guidance from the Centers for Disease Control and Prevention, as well as previously released ACOG guidance.
The recommendations include examples of patients needing in-person appointments, telehealth visits, or visits that should be deferred.
In-person appointments. Examples of patients for whom in-person appointments are appropriate include those with suspected ectopic pregnancy or profuse vaginal bleeding. With respect to contraceptive services, ACOG suggests that placement of IUDs and implants should continue whenever possible. If placement of the contraceptive device is deferred, use of self-administered hormonal contraceptives (including subcutaneous injections, oral, transdermal patch, and vaginal ring) should be encouraged as a bridge to later initiation of long-acting methods.
Telehealth visits. Video or telephone visits are advised for women desiring counseling and prescribing for contraception or menopausal symptoms.
Deferred. Deferral of office visits until after COVID-19 lockdowns is advised for average-risk women wishing routine well-woman visits. Other situations in which deferral should be considered include the following:
- For patients with abnormal cervical cancer screening results, ACOG suggests that colposcopy with cervical biopsies could be deferred for 6-12 months for patients with low-grade test results. In contrast, for patients with high-grade results, ACOG recommends that evaluation be performed within 3 months.
- For women who wish to discontinue their contraceptive, ACOG advises that removal of IUDs and implants be postponed when possible. These women should be counseled regarding extended use of these devices.
ACOG emphasizes that decisions regarding ambulatory gynecology should be individualized and take into consideration such issues as availability of local and regional resources, staffing, personal protective equipment, and the local prevalence of COVID-19.
As a gynecologist focused on ambulatory care, I believe that many clinicians will welcome this guidance from ACOG, which helps us provide optimal care during these challenging times.
Dr. Kaunitz is professor and associate chairman in the department of obstetrics and gynecology at the University of Florida, Jacksonville. He has disclosed receiving royalties from UpToDate, serving on the safety monitoring board for Femasys, and serving as a consultant for AMAG Pharmaceuticals, Merck & Co, Mithra, and Pfizer. His institution has received funding from pharmaceutical companies and nonprofits.
A version of this article originally appeared on Medscape.com.
European COVID-19 insights: Try helmet CPAP
Noninvasive ventilation with helmet continuous positive air pressure (CPAP) deserves to be embraced as an effective strategy in preventing self-induced lung injury, often a key factor in progression from the early milder expression of COVID-19 disease to classic severe acute respiratory distress syndrome, according to European physicians who have been through what they hope are the worst days of the pandemic in the Lombardy region of Northern Italy.
Helmet CPAP is a relatively inexpensive, convenient, well-tolerated intervention. It allows patients to remain conscious and responsive to commands such as “Time to roll over,” which in turn frees up nursing staff. The purpose of helmet CPAP is to curb the huge inspiratory drive that’s a defining feature of this disease and which, unchecked, can lead to self-induced lung injury (SILI), Luciano Gattinoni, MD, explained at a webinar hosted by the European Society of Anaesthesiology.
“Paranoid attention to inspiratory effort – checking it and correcting it – is something where we can make the difference between death and life. It’s extremely important,” said Dr. Gattinoni, guest professor of anesthesiology and intensive care at the University of Gottingen (Germany).
He and his fellow panelists were in accord regarding the merits of helmet CPAP as the premier method of noninvasive ventilatory assistance. They also addressed the importance of monitoring for hypercoagulation, as well as what they’ve come to see as the essential role of pronation in what they define as Type H disease, and the need to have detailed respiratory physiotherapy protocols in place.
“COVID-19 doesn’t like physiotherapy,” explained Paolo Pelosi, MD, professor of anesthesiology and intensive care medicine at the University of Genoa (Italy).
Dr. Gattinoni is credited for identification of two polar phenotypes of what he considers to be a single COVID-19 disease. Early on, many patients present with an atypical form of acute respiratory distress syndrome (ARDS), distinguished by an often-unexpected degree of hypoxia accompanied by high pulmonary compliance and surprisingly little shortness of breath. Dr. Gattinoni and colleagues call this Type L disease, which stands for low elastane, low ventilation to perfusion ratio, low lung weight on CT, and low lung recruitability, which means the patient has a high proportion of aerated lung tissue. Over time, because of either the natural history of the disease or SILI, this may shift to Type H disease, marked by high elastane, high right-to-left shunt, high lung weight, and high recruitability.
“If the pulmonary compliance is above 60 [mL/cm H2O], I’m pretty sure it’s Type L. If it’s 30 [mL/cm H2O] or less, I’m pretty sure it’s Type H. Don’t ask me about 45-55 [mL/cm H2O]; it’s a grey zone,” Dr. Gattinoni said.
Giuseppe Foti, MD, said helmet CPAP in patients with COVID-19 should be free flow, not attached to a ventilator, and the gas flow should be set high – at least 50 L/min – in order to prevent CO2 rebreathing. Although noninvasive ventilation is well accepted for patients with chronic obstructive pulmonary disease or acute cardiogenic pulmonary edema, it hasn’t been extensively studied in the setting of ARDS. A notable exception is a single-center randomized trial in which 83 patients with ARDS at the University of Chicago were assigned to noninvasive ventilation delivered by helmet or face mask (JAMA. 2016 Jun 14;315[22]:2435-41). The endotracheal intubation rate was just 18% in the helmet group, compared with 62% in the face mask group. The 90-day mortality rate was significantly lower in the helmet group as well, noted Dr. Foti, director of the department of anesthesia and intensive care at Monza University Hospital in Milan.
Christian Putensen, MD, said he views intubation for mechanical ventilation as wise in moderate or severe ARDS with an arterial oxygen partial pressure/fraction of inspired oxygen (PaO2/FiO2) ratio below 150. But in milder, Type L COVID-19 disease, he also likes helmet CPAP. It spares the patient from the traumatic compressive stress to the lung induced by mechanical ventilation, which may cause alveolar edema and SILI.
There is, however, a caveat: “Watch carefully and do not delay intubation if you see helmet CPAP is not working; that is, if the blood gas analysis doesn’t improve, the respiratory rate increases, tidal volume increases, and there is still increased respiratory drive,” advised Dr. Putensen, an anesthesiologist at the University of Bonn (Germany).
There is no agreed-upon practical quantitative measure of respiratory drive. A clinical evaluation of the patient’s depth of inspiration is the best guide, he added.
Dr. Gattinoni said that, when helmet CPAP can’t control respiratory drive in a patient with early-stage disease, he feels the only way to interrupt this destructive process is through early intubation and what he termed “gentle mechanical ventilation,” not with a positive end expiratory pressure of 20 cm H2O, but more like 4-5.
Watch for hypercoagulation
Thromboembolic complications are a common feature in COVID-19 disease.
“I’ve had occasion to see the autopsy results in more than 100 patients. It’s devastating to see the number of thromboses and microthromboses in the lungs, the liver, the kidney, and in the brain,” Dr. Gattinoni said.
“COVID-19 is a serial killer, no doubt,” Dr. Pelosi agreed. “He has no mercy for anyone. And he has two bullets: The first one is for the lung, the second is on the vascular side.”
Dr. Putensen is aggressive in utilizing prophylactic high-dose anticoagulation with heparin. He carefully monitors levels of fibrinogen, Factors V and VIII, and d-dimers. In the setting of COVID-19, he has found thromboelastography to be more reliable than partial thromboplastin time in guiding heparin titration.
Pronation
Panelists agreed that pronation is an especially valuable means of enhancing oxygenation in patients with Type H disease. Dr. Putensen tries for more than 16 hours per day. Dr. Foti is preparing a study of the impact of pronation in 50 awake, nonintubated patients, most of whom were on helmet CPAP. Seven of them couldn’t tolerate pronation for even an hour at a time; for the others, the median duration was 3.5 hours at a time.
“We saw a dramatic improvement, a nearly doubling in the PaO2/FiO2 ratio,” Dr. Foti said.
The helmet CPAP study was done outside of the ICU because, in March 2020, the Milan hospital was utterly overwhelmed by COVID-19. The university hospital ordinarily has 25 ICU beds. This was expanded to 100 ICU beds in an effort to meet the emergency, but that still wasn’t sufficient. Indeed, COVID-19 patients occupied 600 of the hospital’s 650 beds. Physicians were forced to do something formerly unthinkable: triage patients for intubation and mechanical ventilation based upon age, comorbidities, and survival prospects.
“We felt schizophrenic. I completely agree with Luciano’s idea to intubate early when we cannot control the respiratory drive that’s due to the disease. But we couldn’t do it because we had too many patients. So we had to triage,” Dr. Foti recalled, breaking off with a sob as other panelists wiped away their own tears during the webcast.
Respiratory physical therapy
Dr. Pelosi said he believes that optimal care of patients with COVID-19 disease requires a major commitment to physical therapy. He strongly recommends having thoughtfully designed separate written protocols in place for respiratory physiotherapy during mechanical ventilation, weaning, and postextubation. COVID-19 patients typically require 7-10 days of assisted ventilation before weaning, and weaning is a protracted process as well.
“I like to say COVID-19 always requires patience. You have to be very, very patient with this disease,” he emphasized. “These patients have a long and difficult weaning. If the patient isn’t improving during weaning, look at two issues: superinfection and thrombembolism, macro and micro.” The physical therapy measures routinely utilized at his hospital during mechanical ventilation include elevation of the bed head greater than 30 degrees, neuromuscular electrical stimulation, subglottic secretion suctioning, tracheal and oral aspiration, and cough assistance. Separate physical therapy menus are used during before and after extubation.
Dr. Gattinoni offered a final word: “We can do almost nothing with this disease. We try our best to keep the patient alive. What we can do is avoid excessive ventilation of the patient. Applying the typical treatment of ARDS in atypical [Type L] ARDS does not make sense and may be extremely harmful.”
Noninvasive ventilation with helmet continuous positive air pressure (CPAP) deserves to be embraced as an effective strategy in preventing self-induced lung injury, often a key factor in progression from the early milder expression of COVID-19 disease to classic severe acute respiratory distress syndrome, according to European physicians who have been through what they hope are the worst days of the pandemic in the Lombardy region of Northern Italy.
Helmet CPAP is a relatively inexpensive, convenient, well-tolerated intervention. It allows patients to remain conscious and responsive to commands such as “Time to roll over,” which in turn frees up nursing staff. The purpose of helmet CPAP is to curb the huge inspiratory drive that’s a defining feature of this disease and which, unchecked, can lead to self-induced lung injury (SILI), Luciano Gattinoni, MD, explained at a webinar hosted by the European Society of Anaesthesiology.
“Paranoid attention to inspiratory effort – checking it and correcting it – is something where we can make the difference between death and life. It’s extremely important,” said Dr. Gattinoni, guest professor of anesthesiology and intensive care at the University of Gottingen (Germany).
He and his fellow panelists were in accord regarding the merits of helmet CPAP as the premier method of noninvasive ventilatory assistance. They also addressed the importance of monitoring for hypercoagulation, as well as what they’ve come to see as the essential role of pronation in what they define as Type H disease, and the need to have detailed respiratory physiotherapy protocols in place.
“COVID-19 doesn’t like physiotherapy,” explained Paolo Pelosi, MD, professor of anesthesiology and intensive care medicine at the University of Genoa (Italy).
Dr. Gattinoni is credited for identification of two polar phenotypes of what he considers to be a single COVID-19 disease. Early on, many patients present with an atypical form of acute respiratory distress syndrome (ARDS), distinguished by an often-unexpected degree of hypoxia accompanied by high pulmonary compliance and surprisingly little shortness of breath. Dr. Gattinoni and colleagues call this Type L disease, which stands for low elastane, low ventilation to perfusion ratio, low lung weight on CT, and low lung recruitability, which means the patient has a high proportion of aerated lung tissue. Over time, because of either the natural history of the disease or SILI, this may shift to Type H disease, marked by high elastane, high right-to-left shunt, high lung weight, and high recruitability.
“If the pulmonary compliance is above 60 [mL/cm H2O], I’m pretty sure it’s Type L. If it’s 30 [mL/cm H2O] or less, I’m pretty sure it’s Type H. Don’t ask me about 45-55 [mL/cm H2O]; it’s a grey zone,” Dr. Gattinoni said.
Giuseppe Foti, MD, said helmet CPAP in patients with COVID-19 should be free flow, not attached to a ventilator, and the gas flow should be set high – at least 50 L/min – in order to prevent CO2 rebreathing. Although noninvasive ventilation is well accepted for patients with chronic obstructive pulmonary disease or acute cardiogenic pulmonary edema, it hasn’t been extensively studied in the setting of ARDS. A notable exception is a single-center randomized trial in which 83 patients with ARDS at the University of Chicago were assigned to noninvasive ventilation delivered by helmet or face mask (JAMA. 2016 Jun 14;315[22]:2435-41). The endotracheal intubation rate was just 18% in the helmet group, compared with 62% in the face mask group. The 90-day mortality rate was significantly lower in the helmet group as well, noted Dr. Foti, director of the department of anesthesia and intensive care at Monza University Hospital in Milan.
Christian Putensen, MD, said he views intubation for mechanical ventilation as wise in moderate or severe ARDS with an arterial oxygen partial pressure/fraction of inspired oxygen (PaO2/FiO2) ratio below 150. But in milder, Type L COVID-19 disease, he also likes helmet CPAP. It spares the patient from the traumatic compressive stress to the lung induced by mechanical ventilation, which may cause alveolar edema and SILI.
There is, however, a caveat: “Watch carefully and do not delay intubation if you see helmet CPAP is not working; that is, if the blood gas analysis doesn’t improve, the respiratory rate increases, tidal volume increases, and there is still increased respiratory drive,” advised Dr. Putensen, an anesthesiologist at the University of Bonn (Germany).
There is no agreed-upon practical quantitative measure of respiratory drive. A clinical evaluation of the patient’s depth of inspiration is the best guide, he added.
Dr. Gattinoni said that, when helmet CPAP can’t control respiratory drive in a patient with early-stage disease, he feels the only way to interrupt this destructive process is through early intubation and what he termed “gentle mechanical ventilation,” not with a positive end expiratory pressure of 20 cm H2O, but more like 4-5.
Watch for hypercoagulation
Thromboembolic complications are a common feature in COVID-19 disease.
“I’ve had occasion to see the autopsy results in more than 100 patients. It’s devastating to see the number of thromboses and microthromboses in the lungs, the liver, the kidney, and in the brain,” Dr. Gattinoni said.
“COVID-19 is a serial killer, no doubt,” Dr. Pelosi agreed. “He has no mercy for anyone. And he has two bullets: The first one is for the lung, the second is on the vascular side.”
Dr. Putensen is aggressive in utilizing prophylactic high-dose anticoagulation with heparin. He carefully monitors levels of fibrinogen, Factors V and VIII, and d-dimers. In the setting of COVID-19, he has found thromboelastography to be more reliable than partial thromboplastin time in guiding heparin titration.
Pronation
Panelists agreed that pronation is an especially valuable means of enhancing oxygenation in patients with Type H disease. Dr. Putensen tries for more than 16 hours per day. Dr. Foti is preparing a study of the impact of pronation in 50 awake, nonintubated patients, most of whom were on helmet CPAP. Seven of them couldn’t tolerate pronation for even an hour at a time; for the others, the median duration was 3.5 hours at a time.
“We saw a dramatic improvement, a nearly doubling in the PaO2/FiO2 ratio,” Dr. Foti said.
The helmet CPAP study was done outside of the ICU because, in March 2020, the Milan hospital was utterly overwhelmed by COVID-19. The university hospital ordinarily has 25 ICU beds. This was expanded to 100 ICU beds in an effort to meet the emergency, but that still wasn’t sufficient. Indeed, COVID-19 patients occupied 600 of the hospital’s 650 beds. Physicians were forced to do something formerly unthinkable: triage patients for intubation and mechanical ventilation based upon age, comorbidities, and survival prospects.
“We felt schizophrenic. I completely agree with Luciano’s idea to intubate early when we cannot control the respiratory drive that’s due to the disease. But we couldn’t do it because we had too many patients. So we had to triage,” Dr. Foti recalled, breaking off with a sob as other panelists wiped away their own tears during the webcast.
Respiratory physical therapy
Dr. Pelosi said he believes that optimal care of patients with COVID-19 disease requires a major commitment to physical therapy. He strongly recommends having thoughtfully designed separate written protocols in place for respiratory physiotherapy during mechanical ventilation, weaning, and postextubation. COVID-19 patients typically require 7-10 days of assisted ventilation before weaning, and weaning is a protracted process as well.
“I like to say COVID-19 always requires patience. You have to be very, very patient with this disease,” he emphasized. “These patients have a long and difficult weaning. If the patient isn’t improving during weaning, look at two issues: superinfection and thrombembolism, macro and micro.” The physical therapy measures routinely utilized at his hospital during mechanical ventilation include elevation of the bed head greater than 30 degrees, neuromuscular electrical stimulation, subglottic secretion suctioning, tracheal and oral aspiration, and cough assistance. Separate physical therapy menus are used during before and after extubation.
Dr. Gattinoni offered a final word: “We can do almost nothing with this disease. We try our best to keep the patient alive. What we can do is avoid excessive ventilation of the patient. Applying the typical treatment of ARDS in atypical [Type L] ARDS does not make sense and may be extremely harmful.”
Noninvasive ventilation with helmet continuous positive air pressure (CPAP) deserves to be embraced as an effective strategy in preventing self-induced lung injury, often a key factor in progression from the early milder expression of COVID-19 disease to classic severe acute respiratory distress syndrome, according to European physicians who have been through what they hope are the worst days of the pandemic in the Lombardy region of Northern Italy.
Helmet CPAP is a relatively inexpensive, convenient, well-tolerated intervention. It allows patients to remain conscious and responsive to commands such as “Time to roll over,” which in turn frees up nursing staff. The purpose of helmet CPAP is to curb the huge inspiratory drive that’s a defining feature of this disease and which, unchecked, can lead to self-induced lung injury (SILI), Luciano Gattinoni, MD, explained at a webinar hosted by the European Society of Anaesthesiology.
“Paranoid attention to inspiratory effort – checking it and correcting it – is something where we can make the difference between death and life. It’s extremely important,” said Dr. Gattinoni, guest professor of anesthesiology and intensive care at the University of Gottingen (Germany).
He and his fellow panelists were in accord regarding the merits of helmet CPAP as the premier method of noninvasive ventilatory assistance. They also addressed the importance of monitoring for hypercoagulation, as well as what they’ve come to see as the essential role of pronation in what they define as Type H disease, and the need to have detailed respiratory physiotherapy protocols in place.
“COVID-19 doesn’t like physiotherapy,” explained Paolo Pelosi, MD, professor of anesthesiology and intensive care medicine at the University of Genoa (Italy).
Dr. Gattinoni is credited for identification of two polar phenotypes of what he considers to be a single COVID-19 disease. Early on, many patients present with an atypical form of acute respiratory distress syndrome (ARDS), distinguished by an often-unexpected degree of hypoxia accompanied by high pulmonary compliance and surprisingly little shortness of breath. Dr. Gattinoni and colleagues call this Type L disease, which stands for low elastane, low ventilation to perfusion ratio, low lung weight on CT, and low lung recruitability, which means the patient has a high proportion of aerated lung tissue. Over time, because of either the natural history of the disease or SILI, this may shift to Type H disease, marked by high elastane, high right-to-left shunt, high lung weight, and high recruitability.
“If the pulmonary compliance is above 60 [mL/cm H2O], I’m pretty sure it’s Type L. If it’s 30 [mL/cm H2O] or less, I’m pretty sure it’s Type H. Don’t ask me about 45-55 [mL/cm H2O]; it’s a grey zone,” Dr. Gattinoni said.
Giuseppe Foti, MD, said helmet CPAP in patients with COVID-19 should be free flow, not attached to a ventilator, and the gas flow should be set high – at least 50 L/min – in order to prevent CO2 rebreathing. Although noninvasive ventilation is well accepted for patients with chronic obstructive pulmonary disease or acute cardiogenic pulmonary edema, it hasn’t been extensively studied in the setting of ARDS. A notable exception is a single-center randomized trial in which 83 patients with ARDS at the University of Chicago were assigned to noninvasive ventilation delivered by helmet or face mask (JAMA. 2016 Jun 14;315[22]:2435-41). The endotracheal intubation rate was just 18% in the helmet group, compared with 62% in the face mask group. The 90-day mortality rate was significantly lower in the helmet group as well, noted Dr. Foti, director of the department of anesthesia and intensive care at Monza University Hospital in Milan.
Christian Putensen, MD, said he views intubation for mechanical ventilation as wise in moderate or severe ARDS with an arterial oxygen partial pressure/fraction of inspired oxygen (PaO2/FiO2) ratio below 150. But in milder, Type L COVID-19 disease, he also likes helmet CPAP. It spares the patient from the traumatic compressive stress to the lung induced by mechanical ventilation, which may cause alveolar edema and SILI.
There is, however, a caveat: “Watch carefully and do not delay intubation if you see helmet CPAP is not working; that is, if the blood gas analysis doesn’t improve, the respiratory rate increases, tidal volume increases, and there is still increased respiratory drive,” advised Dr. Putensen, an anesthesiologist at the University of Bonn (Germany).
There is no agreed-upon practical quantitative measure of respiratory drive. A clinical evaluation of the patient’s depth of inspiration is the best guide, he added.
Dr. Gattinoni said that, when helmet CPAP can’t control respiratory drive in a patient with early-stage disease, he feels the only way to interrupt this destructive process is through early intubation and what he termed “gentle mechanical ventilation,” not with a positive end expiratory pressure of 20 cm H2O, but more like 4-5.
Watch for hypercoagulation
Thromboembolic complications are a common feature in COVID-19 disease.
“I’ve had occasion to see the autopsy results in more than 100 patients. It’s devastating to see the number of thromboses and microthromboses in the lungs, the liver, the kidney, and in the brain,” Dr. Gattinoni said.
“COVID-19 is a serial killer, no doubt,” Dr. Pelosi agreed. “He has no mercy for anyone. And he has two bullets: The first one is for the lung, the second is on the vascular side.”
Dr. Putensen is aggressive in utilizing prophylactic high-dose anticoagulation with heparin. He carefully monitors levels of fibrinogen, Factors V and VIII, and d-dimers. In the setting of COVID-19, he has found thromboelastography to be more reliable than partial thromboplastin time in guiding heparin titration.
Pronation
Panelists agreed that pronation is an especially valuable means of enhancing oxygenation in patients with Type H disease. Dr. Putensen tries for more than 16 hours per day. Dr. Foti is preparing a study of the impact of pronation in 50 awake, nonintubated patients, most of whom were on helmet CPAP. Seven of them couldn’t tolerate pronation for even an hour at a time; for the others, the median duration was 3.5 hours at a time.
“We saw a dramatic improvement, a nearly doubling in the PaO2/FiO2 ratio,” Dr. Foti said.
The helmet CPAP study was done outside of the ICU because, in March 2020, the Milan hospital was utterly overwhelmed by COVID-19. The university hospital ordinarily has 25 ICU beds. This was expanded to 100 ICU beds in an effort to meet the emergency, but that still wasn’t sufficient. Indeed, COVID-19 patients occupied 600 of the hospital’s 650 beds. Physicians were forced to do something formerly unthinkable: triage patients for intubation and mechanical ventilation based upon age, comorbidities, and survival prospects.
“We felt schizophrenic. I completely agree with Luciano’s idea to intubate early when we cannot control the respiratory drive that’s due to the disease. But we couldn’t do it because we had too many patients. So we had to triage,” Dr. Foti recalled, breaking off with a sob as other panelists wiped away their own tears during the webcast.
Respiratory physical therapy
Dr. Pelosi said he believes that optimal care of patients with COVID-19 disease requires a major commitment to physical therapy. He strongly recommends having thoughtfully designed separate written protocols in place for respiratory physiotherapy during mechanical ventilation, weaning, and postextubation. COVID-19 patients typically require 7-10 days of assisted ventilation before weaning, and weaning is a protracted process as well.
“I like to say COVID-19 always requires patience. You have to be very, very patient with this disease,” he emphasized. “These patients have a long and difficult weaning. If the patient isn’t improving during weaning, look at two issues: superinfection and thrombembolism, macro and micro.” The physical therapy measures routinely utilized at his hospital during mechanical ventilation include elevation of the bed head greater than 30 degrees, neuromuscular electrical stimulation, subglottic secretion suctioning, tracheal and oral aspiration, and cough assistance. Separate physical therapy menus are used during before and after extubation.
Dr. Gattinoni offered a final word: “We can do almost nothing with this disease. We try our best to keep the patient alive. What we can do is avoid excessive ventilation of the patient. Applying the typical treatment of ARDS in atypical [Type L] ARDS does not make sense and may be extremely harmful.”
Are patients with epilepsy at increased risk of COVID-19 infection?
Chronic conditions such as lung disease, diabetes, and heart disease frequently receive attention for increasing the risk of complications for people who contract the coronavirus. Meanwhile, many members of the epilepsy community continue to wonder how the virus affects them. To address these concerns, the Epilepsy Foundation has released information that answers many common questions that people with epilepsy have about how COVID-19 can impact their health.
Perhaps the most pressing of these questions is: Does epilepsy increase the risk or severity of the coronavirus?
“The most common thing we’re hearing from patients in my practice is their proactive concern for being at increased risk for getting the coronavirus,” confirmed Selim Benbadis, MD, division director, epilepsy, EEG, and sleep medicine at the University of South Florida in Tampa. “Epilepsy patients are not at increased risk for complications from the coronavirus because epilepsy does not affect the immune system.”
In other words, people who have epilepsy face the same health challenges as people who do not have the condition and are otherwise healthy. For this reason, people who have epilepsy should exercise the same habits and preventative measures that healthy people would typically take, such as social distancing; avoiding contact with sick people; washing hands regularly; disinfecting surfaces regularly; and avoiding touching hands, eyes, nose and mouth.
However, as Dr. Benbadis explained, the high fever associated with coronavirus can trigger seizures. The increased risk is another reason people who have epilepsy should do their best to avoid getting sick.
Seizure medications do not increase COVID-19 risk but other conditions can
Similarly, epilepsy medications do not increase the risk of contracting the disease.
“The medications patients take to treat their epilepsy do not affect their immune system,” said Andrew Wilner, MD, associate professor of neurology at the University of Tennessee Health Science Center, Memphis. There are a few exceptions – such as adrenocorticotropic hormone and everolimus – but doctors rarely use these drugs to treat epilepsy.
However, there are some situations and conditions that may pose a risk for people who contact the coronavirus. For instance, people who have problems swallowing their food and tend to suck food down their windpipes are more likely to develop pneumonia. Also, much like the general population, having diabetes, heart disease, or lung problems increase the chances of developing complications from the virus.
The best ways to avoid additional risks in epilepsy
Because of the pandemic, people who have epilepsy may have found that many of their doctors’ appointments have been canceled. Many clinics and medical practices have done this in order minimize exposing people who have acute illnesses to the virus. By focusing more on patients with acute conditions, doctors and nurses can better tend to patients with acute problems. As a result, practices have shifted to providing patient care using telemedicine as much as possible.
“Telemedicine services have surged, and I’ve been saying for years that telemedicine was going to grow,” Dr. Benbadis said. “It’s more convenient, and I believe that we’re going to see increased use of telemedicine long after the coronavirus pandemic is over.”
Aside from communicating with their doctors, the Epilepsy Foundation and Dr. Wilner stress that the best way for people who have epilepsy to stay healthy is by taking their medications on a regular basis exactly as prescribed.
“Taking mediation correctly and regularly is the best strategy for epilepsy patients to avoid unnecessary hospitalizations,” Dr. Wilner said. “If they have breakthrough seizures and get sent to the emergency room, then they risk being exposed to the virus in the ER.”
Also, because ERs are more crowded than usual, the Epilepsy Foundation encourages people who suspect they have the coronavirus to call their doctor’s office first. The goal is to try to make sure that people who have severe or life-threatening symptoms have access to treatment in the ER.
As with the general population, the first thing that epilepsy patients who suspect they have the coronavirus should do is call his or her doctor’s office. The health care professional taking the call will ask the patient a series of questions to determine whether the patient has COVID-19 or another condition or needs to seek emergency medical attention.
Fever, cough, and trouble breathing fall among the most commonly reported symptoms of the coronavirus. In many cases, health care providers recommend that people with mild versions of these symptoms stay at home.
Helpful tips
The Epilepsy Foundation offers tips on signs to look for when trying to figure out when a seizure requires an ER visit. These are:
- Seizures in which awareness is lost for more than 5 minutes and no reversal medications are available.
- Seizures with an unusual pattern or duration.
- Seizures that cannot be treated safely at home or are not responding to rescue medication even after the medication has had enough time to work.
- Seizures that occur after a severe blow to the head.
Additionally, while COVID-19 can cause death and sudden death in patients, the virus does not cause sudden unexpected death in epilepsy (SUDEP). Because SUDEP is extremely rare, Dr. Benbadis said that there is no information to suggest that contracting the coronavirus will increase the risk,
Finally, no shortages of seizures medications have been reported as a result of COVID-19. However, there were shortages of generic levetiracetam immediate-release and levetiracetam extended-release medications prior to and during COVID-19. Experts expect the shortage to continue.
Overall, people who have epilepsy should be able to stay healthy – provided they exercise healthy and preventative habits.
“The majority of epilepsy patients should be reassured that if they continue their usual care, take their meds as directed, get adequate sleep, nutritious diet, they’re not at any increased risk compared to the general population,” said Dr. Wilner.
Dr. Benbadis reported the following disclosures: consultant for Bioserenity (DigiTrace), Brain Sentinel, Cavion, Ceribell, Eisai, Greenwich, LivaNova, Neuropace, SK biopharmaceuticals, Sunovion; speakers bureau for Eisai, Greenwich, LivaNova, Sunovion; Florida Medical Director of Stratus/Alliance; Member: Epilepsy Study Consortium; grant support from Cavion, LivaNova, Greenwich, SK biopharmaceuticals, Sunovion, Takeda, UCB, Xenon; royalties as an author or editor for Emedicine-Medscape-WebMD, UpToDate; editorial board for the Epilepsy.com (Epilepsy Foundation) controversy section, Emedicine-Medscape-WebMD, Epileptic Disorders, Epilepsy and Behavior, and Expert Review of Neurotherapeutics. Dr. Wilner reports Medical Advisory Board of Accordant Health Services, Greensboro, S.C., and book royalties: “The Locum Life: A Physician’s Guide to Locum Tenens,” Lulu Press.
Chronic conditions such as lung disease, diabetes, and heart disease frequently receive attention for increasing the risk of complications for people who contract the coronavirus. Meanwhile, many members of the epilepsy community continue to wonder how the virus affects them. To address these concerns, the Epilepsy Foundation has released information that answers many common questions that people with epilepsy have about how COVID-19 can impact their health.
Perhaps the most pressing of these questions is: Does epilepsy increase the risk or severity of the coronavirus?
“The most common thing we’re hearing from patients in my practice is their proactive concern for being at increased risk for getting the coronavirus,” confirmed Selim Benbadis, MD, division director, epilepsy, EEG, and sleep medicine at the University of South Florida in Tampa. “Epilepsy patients are not at increased risk for complications from the coronavirus because epilepsy does not affect the immune system.”
In other words, people who have epilepsy face the same health challenges as people who do not have the condition and are otherwise healthy. For this reason, people who have epilepsy should exercise the same habits and preventative measures that healthy people would typically take, such as social distancing; avoiding contact with sick people; washing hands regularly; disinfecting surfaces regularly; and avoiding touching hands, eyes, nose and mouth.
However, as Dr. Benbadis explained, the high fever associated with coronavirus can trigger seizures. The increased risk is another reason people who have epilepsy should do their best to avoid getting sick.
Seizure medications do not increase COVID-19 risk but other conditions can
Similarly, epilepsy medications do not increase the risk of contracting the disease.
“The medications patients take to treat their epilepsy do not affect their immune system,” said Andrew Wilner, MD, associate professor of neurology at the University of Tennessee Health Science Center, Memphis. There are a few exceptions – such as adrenocorticotropic hormone and everolimus – but doctors rarely use these drugs to treat epilepsy.
However, there are some situations and conditions that may pose a risk for people who contact the coronavirus. For instance, people who have problems swallowing their food and tend to suck food down their windpipes are more likely to develop pneumonia. Also, much like the general population, having diabetes, heart disease, or lung problems increase the chances of developing complications from the virus.
The best ways to avoid additional risks in epilepsy
Because of the pandemic, people who have epilepsy may have found that many of their doctors’ appointments have been canceled. Many clinics and medical practices have done this in order minimize exposing people who have acute illnesses to the virus. By focusing more on patients with acute conditions, doctors and nurses can better tend to patients with acute problems. As a result, practices have shifted to providing patient care using telemedicine as much as possible.
“Telemedicine services have surged, and I’ve been saying for years that telemedicine was going to grow,” Dr. Benbadis said. “It’s more convenient, and I believe that we’re going to see increased use of telemedicine long after the coronavirus pandemic is over.”
Aside from communicating with their doctors, the Epilepsy Foundation and Dr. Wilner stress that the best way for people who have epilepsy to stay healthy is by taking their medications on a regular basis exactly as prescribed.
“Taking mediation correctly and regularly is the best strategy for epilepsy patients to avoid unnecessary hospitalizations,” Dr. Wilner said. “If they have breakthrough seizures and get sent to the emergency room, then they risk being exposed to the virus in the ER.”
Also, because ERs are more crowded than usual, the Epilepsy Foundation encourages people who suspect they have the coronavirus to call their doctor’s office first. The goal is to try to make sure that people who have severe or life-threatening symptoms have access to treatment in the ER.
As with the general population, the first thing that epilepsy patients who suspect they have the coronavirus should do is call his or her doctor’s office. The health care professional taking the call will ask the patient a series of questions to determine whether the patient has COVID-19 or another condition or needs to seek emergency medical attention.
Fever, cough, and trouble breathing fall among the most commonly reported symptoms of the coronavirus. In many cases, health care providers recommend that people with mild versions of these symptoms stay at home.
Helpful tips
The Epilepsy Foundation offers tips on signs to look for when trying to figure out when a seizure requires an ER visit. These are:
- Seizures in which awareness is lost for more than 5 minutes and no reversal medications are available.
- Seizures with an unusual pattern or duration.
- Seizures that cannot be treated safely at home or are not responding to rescue medication even after the medication has had enough time to work.
- Seizures that occur after a severe blow to the head.
Additionally, while COVID-19 can cause death and sudden death in patients, the virus does not cause sudden unexpected death in epilepsy (SUDEP). Because SUDEP is extremely rare, Dr. Benbadis said that there is no information to suggest that contracting the coronavirus will increase the risk,
Finally, no shortages of seizures medications have been reported as a result of COVID-19. However, there were shortages of generic levetiracetam immediate-release and levetiracetam extended-release medications prior to and during COVID-19. Experts expect the shortage to continue.
Overall, people who have epilepsy should be able to stay healthy – provided they exercise healthy and preventative habits.
“The majority of epilepsy patients should be reassured that if they continue their usual care, take their meds as directed, get adequate sleep, nutritious diet, they’re not at any increased risk compared to the general population,” said Dr. Wilner.
Dr. Benbadis reported the following disclosures: consultant for Bioserenity (DigiTrace), Brain Sentinel, Cavion, Ceribell, Eisai, Greenwich, LivaNova, Neuropace, SK biopharmaceuticals, Sunovion; speakers bureau for Eisai, Greenwich, LivaNova, Sunovion; Florida Medical Director of Stratus/Alliance; Member: Epilepsy Study Consortium; grant support from Cavion, LivaNova, Greenwich, SK biopharmaceuticals, Sunovion, Takeda, UCB, Xenon; royalties as an author or editor for Emedicine-Medscape-WebMD, UpToDate; editorial board for the Epilepsy.com (Epilepsy Foundation) controversy section, Emedicine-Medscape-WebMD, Epileptic Disorders, Epilepsy and Behavior, and Expert Review of Neurotherapeutics. Dr. Wilner reports Medical Advisory Board of Accordant Health Services, Greensboro, S.C., and book royalties: “The Locum Life: A Physician’s Guide to Locum Tenens,” Lulu Press.
Chronic conditions such as lung disease, diabetes, and heart disease frequently receive attention for increasing the risk of complications for people who contract the coronavirus. Meanwhile, many members of the epilepsy community continue to wonder how the virus affects them. To address these concerns, the Epilepsy Foundation has released information that answers many common questions that people with epilepsy have about how COVID-19 can impact their health.
Perhaps the most pressing of these questions is: Does epilepsy increase the risk or severity of the coronavirus?
“The most common thing we’re hearing from patients in my practice is their proactive concern for being at increased risk for getting the coronavirus,” confirmed Selim Benbadis, MD, division director, epilepsy, EEG, and sleep medicine at the University of South Florida in Tampa. “Epilepsy patients are not at increased risk for complications from the coronavirus because epilepsy does not affect the immune system.”
In other words, people who have epilepsy face the same health challenges as people who do not have the condition and are otherwise healthy. For this reason, people who have epilepsy should exercise the same habits and preventative measures that healthy people would typically take, such as social distancing; avoiding contact with sick people; washing hands regularly; disinfecting surfaces regularly; and avoiding touching hands, eyes, nose and mouth.
However, as Dr. Benbadis explained, the high fever associated with coronavirus can trigger seizures. The increased risk is another reason people who have epilepsy should do their best to avoid getting sick.
Seizure medications do not increase COVID-19 risk but other conditions can
Similarly, epilepsy medications do not increase the risk of contracting the disease.
“The medications patients take to treat their epilepsy do not affect their immune system,” said Andrew Wilner, MD, associate professor of neurology at the University of Tennessee Health Science Center, Memphis. There are a few exceptions – such as adrenocorticotropic hormone and everolimus – but doctors rarely use these drugs to treat epilepsy.
However, there are some situations and conditions that may pose a risk for people who contact the coronavirus. For instance, people who have problems swallowing their food and tend to suck food down their windpipes are more likely to develop pneumonia. Also, much like the general population, having diabetes, heart disease, or lung problems increase the chances of developing complications from the virus.
The best ways to avoid additional risks in epilepsy
Because of the pandemic, people who have epilepsy may have found that many of their doctors’ appointments have been canceled. Many clinics and medical practices have done this in order minimize exposing people who have acute illnesses to the virus. By focusing more on patients with acute conditions, doctors and nurses can better tend to patients with acute problems. As a result, practices have shifted to providing patient care using telemedicine as much as possible.
“Telemedicine services have surged, and I’ve been saying for years that telemedicine was going to grow,” Dr. Benbadis said. “It’s more convenient, and I believe that we’re going to see increased use of telemedicine long after the coronavirus pandemic is over.”
Aside from communicating with their doctors, the Epilepsy Foundation and Dr. Wilner stress that the best way for people who have epilepsy to stay healthy is by taking their medications on a regular basis exactly as prescribed.
“Taking mediation correctly and regularly is the best strategy for epilepsy patients to avoid unnecessary hospitalizations,” Dr. Wilner said. “If they have breakthrough seizures and get sent to the emergency room, then they risk being exposed to the virus in the ER.”
Also, because ERs are more crowded than usual, the Epilepsy Foundation encourages people who suspect they have the coronavirus to call their doctor’s office first. The goal is to try to make sure that people who have severe or life-threatening symptoms have access to treatment in the ER.
As with the general population, the first thing that epilepsy patients who suspect they have the coronavirus should do is call his or her doctor’s office. The health care professional taking the call will ask the patient a series of questions to determine whether the patient has COVID-19 or another condition or needs to seek emergency medical attention.
Fever, cough, and trouble breathing fall among the most commonly reported symptoms of the coronavirus. In many cases, health care providers recommend that people with mild versions of these symptoms stay at home.
Helpful tips
The Epilepsy Foundation offers tips on signs to look for when trying to figure out when a seizure requires an ER visit. These are:
- Seizures in which awareness is lost for more than 5 minutes and no reversal medications are available.
- Seizures with an unusual pattern or duration.
- Seizures that cannot be treated safely at home or are not responding to rescue medication even after the medication has had enough time to work.
- Seizures that occur after a severe blow to the head.
Additionally, while COVID-19 can cause death and sudden death in patients, the virus does not cause sudden unexpected death in epilepsy (SUDEP). Because SUDEP is extremely rare, Dr. Benbadis said that there is no information to suggest that contracting the coronavirus will increase the risk,
Finally, no shortages of seizures medications have been reported as a result of COVID-19. However, there were shortages of generic levetiracetam immediate-release and levetiracetam extended-release medications prior to and during COVID-19. Experts expect the shortage to continue.
Overall, people who have epilepsy should be able to stay healthy – provided they exercise healthy and preventative habits.
“The majority of epilepsy patients should be reassured that if they continue their usual care, take their meds as directed, get adequate sleep, nutritious diet, they’re not at any increased risk compared to the general population,” said Dr. Wilner.
Dr. Benbadis reported the following disclosures: consultant for Bioserenity (DigiTrace), Brain Sentinel, Cavion, Ceribell, Eisai, Greenwich, LivaNova, Neuropace, SK biopharmaceuticals, Sunovion; speakers bureau for Eisai, Greenwich, LivaNova, Sunovion; Florida Medical Director of Stratus/Alliance; Member: Epilepsy Study Consortium; grant support from Cavion, LivaNova, Greenwich, SK biopharmaceuticals, Sunovion, Takeda, UCB, Xenon; royalties as an author or editor for Emedicine-Medscape-WebMD, UpToDate; editorial board for the Epilepsy.com (Epilepsy Foundation) controversy section, Emedicine-Medscape-WebMD, Epileptic Disorders, Epilepsy and Behavior, and Expert Review of Neurotherapeutics. Dr. Wilner reports Medical Advisory Board of Accordant Health Services, Greensboro, S.C., and book royalties: “The Locum Life: A Physician’s Guide to Locum Tenens,” Lulu Press.
COVID-19 antibody tests proliferate, but what do they show?
Noopur Raje, MD, has been sitting at home for 5 weeks waiting for her COVID-19 test to turn negative so she can get back to work. She’s a cancer specialist – head of the Massachusetts General Hospital’s Center for Multiple Myeloma – but Raje says as soon as she’s allowed back to the hospital, she’ll head straight to the front line of COVID-19 caregivers.
“It’s people like us who have to get back in the trenches and do the work now,” she told Medscape Medical News.
“I still will be at risk,” she said. But, having nursed her physician husband through COVID-19 at home until he was admitted to an intensive care unit, she is determined to help in the COVID-19 wards.
“I will be the first one to volunteer to take care of these patients,” she said. “I can’t wait, as I want to give these folks hope. They are so scared.”
Around the world, it’s assumed that she and others like her who’ve recovered from COVID-19 will be immune to the infection.
Some have suggested that with antibodies to the virus coursing through their veins, these survivors might be given immunity passports. They could be the ones to jump-start people’s lives again ― the first to be let out from lockdown, and in healthcare, the ones to head the ongoing battle against this pandemic.
So, there has been a race to develop COVID-19 antibody tests to identify these people.
Circumventing the Usual Clearance Process
To speed up the process, the US Food and Drug Administration (FDA) made a much-criticized move to allow a free-for-all for developers to begin marketing antibody tests that had not gone through the agency’s usual evaluation process. The result was a flood of more than 90 unapproved tests “that have, frankly, dubious quality,” said Scott Becker, CEO of the Association of Public Health Laboratories (APHL), which represents local and state public laboratories.
The APHL spoke out in dismay – its chief program officer, Eric Blank, decried the “Wild West” of tests unleashed on the public.
“These tests create more uncertainty than before,” said Kelly Wroblewski, APHL’s director of infectious diseases, in a news conference on April 14. “Having many inaccurate tests is worse than having no tests at all.”
The APHL and the FDA, working with the Centers for Disease Control and Prevention and the National Institutes of Health (NIH), have moved quickly into damage control, conducting evaluations of the tests in an effort to distinguish the potentially useful from the useless.
So far, they have succeeded in issuing emergency use authorizations (EUAs) to only four tests, those marketed by Cellex, Ortho Clinical Diagnostics, Chembio Diagnostic Systems, and the Mount Sinai Laboratory.
For all the other antibody tests on the market that do not have an EUA, “They’re trusting that the test developer has done a good job in validation,” Becker said. But there are worrying anecdotes. “Our members have reported that they’ve seen fraudulent marketing.... We’ve seen the FDA clamp down on some companies... [and] a number of cities and health departments have issued warnings because of what they’ve seen,” he added.
In particular, Wroblewski said, some companies are marketing tests for use in physicians’ offices or pharmacies. “Today, there are no serology tests approved for point-of-care settings,” she warned. “We don’t know how to interpret the test results, if the presence of antibodies indicates immunity, how long it will last, or what titer might be sufficient.”
Uncertainty Emphasized
The FDA emphasized the uncertainty about antibody tests in a statement released on April 18.
Although the tests can identify people who have been exposed and who developed an immune response to the virus, the agency noted, “we don’t yet know that just because someone has developed antibodies, that they are fully protected from reinfection, or how long any immunity lasts.”
The FDA says that the role of these antibody tests, at present, lies in providing information to “help us track the spread of the virus nationwide and assess the impact of our public health efforts now, while also informing our COVID-19 response as we continue to move forward.”
The World Health Organization (WHO) also emphasized the current uncertainty over antibody tests at a press briefing on April 17. “Nobody is sure about the length of protection that antibodies may give and whether they fully protect against ... the disease,” said Mike Ryan, MD, executive director of the WHO’s emergencies program. There is also a concern that such tests may give false assurance or be misused. “There is still a lot of work that needs to be done to validate these antibody tests,” he added.
“The WHO are right to highlight that any antibody test, if we get one, won’t be able to definitely say whether someone is immune to the infection, because we just don’t know enough yet about how immunity works with COVID-19,” commented Prof. Chris Dye, Oxford Martin School, University of Oxford, in reaction on the UK Science Media Center.
Expanding on this point on the same site, Andrew Easton PhD, professor of virology at the University of Warwick, noted that “a serology test does not discriminate between neutralising and non-neutralising antibodies; a discriminatory test is much more complex and slow.”
Only the neutralizing antibodies have the ability to inactivate the invading virus, he noted.
“When people are infected, the proportions of neutralising and non-neutralising antibodies can differ. It is not always understood what makes an antibody neutralising and another non-neutralising, or why an infection leads to production of more of one of these types of antibodies,” he explained. “The initial immune response immediately following infection sets the memory of the immune system, so if the person had generated mostly non-neutralising antibodies, the next time that person encounters the same virus, they may not be able to prevent an infection.”
So at present, the information from antibody testing is largely unhelpful to individuals, but it could be valuable to epidemiologists and policy makers.
“States are looking at ways they can integrate reliable serologic tests for surveillance,” explained APHL’s Blank.
Knowing how widespread the infection has been within a community could guide research and possibly public health decisions, Wroblewski said at the APHL press conference. But she’s hesitant here, too. “I know there has been a lot of talk about using this testing to ease restrictions, but I do think we need to be cautious on how quickly we move in that direction.” If people don’t have antibodies, it means they haven’t been exposed and that they’re still vulnerable, she noted. “If nothing else, that still informs policy decisions, even if they’re not the policy decisions we want.”
Trials Recruiting, Medical Centers Develop Own Tests
Despite the uncertainties over antibody testing, many efforts are still being guided by this strategy.
The NIH is recruiting volunteers to its antibody testing study and suggests that immunity is “likely” for those who test positive.
In addition, several large medical centers have developed their own antibody tests, including Stanford, the Yale New Haven Hospital, and the Mayo Clinic.
The Stanford test detects two types of antibodies: IgM, which is made early in an immune response and usually wanes quickly, and IgG, which rises more slowly after infection but usually persists longer.
“There’s limited data out of China and Europe showing that this appears to be the response pattern followed with this virus,” commented Thomas Montine, MD, PhD, professor and chair of pathology at Stanford University. “But no one has had this long enough to know how long after infection the antibodies persist,” he added.
“There is enormous demand for serologic testing,” said William Morice, MD, PhD, president of Mayo Clinic Laboratories. “At this time, serology testing needs to be prioritized for efforts to identify individuals in areas where potential immunity is key ― supporting healthcare workers, screening for potential plasma donors, and helping advance the most promising vaccine candidates.”
During a recent webinar with the Association for Value-Based Cancer Care, the largest physician-owned oncology-hematology practice in the country, the president, Lucio Gordan, MD, said his organization was looking into antibody testing for staff. “They wanted to see how many have been exposed,” he said, although “what it means is uncertain.”
When Medscape Medical News checked back with him a few weeks later, Gordan, president of Florida Cancer Specialists and Research Institute, reported that no progress had been made.
“We unfortunately have not been able to test yet, due to concerns with reliability of kits. We are waiting for a better solution so we can reassess our strategy,” he said.
This article first appeared on Medscape.com.
Noopur Raje, MD, has been sitting at home for 5 weeks waiting for her COVID-19 test to turn negative so she can get back to work. She’s a cancer specialist – head of the Massachusetts General Hospital’s Center for Multiple Myeloma – but Raje says as soon as she’s allowed back to the hospital, she’ll head straight to the front line of COVID-19 caregivers.
“It’s people like us who have to get back in the trenches and do the work now,” she told Medscape Medical News.
“I still will be at risk,” she said. But, having nursed her physician husband through COVID-19 at home until he was admitted to an intensive care unit, she is determined to help in the COVID-19 wards.
“I will be the first one to volunteer to take care of these patients,” she said. “I can’t wait, as I want to give these folks hope. They are so scared.”
Around the world, it’s assumed that she and others like her who’ve recovered from COVID-19 will be immune to the infection.
Some have suggested that with antibodies to the virus coursing through their veins, these survivors might be given immunity passports. They could be the ones to jump-start people’s lives again ― the first to be let out from lockdown, and in healthcare, the ones to head the ongoing battle against this pandemic.
So, there has been a race to develop COVID-19 antibody tests to identify these people.
Circumventing the Usual Clearance Process
To speed up the process, the US Food and Drug Administration (FDA) made a much-criticized move to allow a free-for-all for developers to begin marketing antibody tests that had not gone through the agency’s usual evaluation process. The result was a flood of more than 90 unapproved tests “that have, frankly, dubious quality,” said Scott Becker, CEO of the Association of Public Health Laboratories (APHL), which represents local and state public laboratories.
The APHL spoke out in dismay – its chief program officer, Eric Blank, decried the “Wild West” of tests unleashed on the public.
“These tests create more uncertainty than before,” said Kelly Wroblewski, APHL’s director of infectious diseases, in a news conference on April 14. “Having many inaccurate tests is worse than having no tests at all.”
The APHL and the FDA, working with the Centers for Disease Control and Prevention and the National Institutes of Health (NIH), have moved quickly into damage control, conducting evaluations of the tests in an effort to distinguish the potentially useful from the useless.
So far, they have succeeded in issuing emergency use authorizations (EUAs) to only four tests, those marketed by Cellex, Ortho Clinical Diagnostics, Chembio Diagnostic Systems, and the Mount Sinai Laboratory.
For all the other antibody tests on the market that do not have an EUA, “They’re trusting that the test developer has done a good job in validation,” Becker said. But there are worrying anecdotes. “Our members have reported that they’ve seen fraudulent marketing.... We’ve seen the FDA clamp down on some companies... [and] a number of cities and health departments have issued warnings because of what they’ve seen,” he added.
In particular, Wroblewski said, some companies are marketing tests for use in physicians’ offices or pharmacies. “Today, there are no serology tests approved for point-of-care settings,” she warned. “We don’t know how to interpret the test results, if the presence of antibodies indicates immunity, how long it will last, or what titer might be sufficient.”
Uncertainty Emphasized
The FDA emphasized the uncertainty about antibody tests in a statement released on April 18.
Although the tests can identify people who have been exposed and who developed an immune response to the virus, the agency noted, “we don’t yet know that just because someone has developed antibodies, that they are fully protected from reinfection, or how long any immunity lasts.”
The FDA says that the role of these antibody tests, at present, lies in providing information to “help us track the spread of the virus nationwide and assess the impact of our public health efforts now, while also informing our COVID-19 response as we continue to move forward.”
The World Health Organization (WHO) also emphasized the current uncertainty over antibody tests at a press briefing on April 17. “Nobody is sure about the length of protection that antibodies may give and whether they fully protect against ... the disease,” said Mike Ryan, MD, executive director of the WHO’s emergencies program. There is also a concern that such tests may give false assurance or be misused. “There is still a lot of work that needs to be done to validate these antibody tests,” he added.
“The WHO are right to highlight that any antibody test, if we get one, won’t be able to definitely say whether someone is immune to the infection, because we just don’t know enough yet about how immunity works with COVID-19,” commented Prof. Chris Dye, Oxford Martin School, University of Oxford, in reaction on the UK Science Media Center.
Expanding on this point on the same site, Andrew Easton PhD, professor of virology at the University of Warwick, noted that “a serology test does not discriminate between neutralising and non-neutralising antibodies; a discriminatory test is much more complex and slow.”
Only the neutralizing antibodies have the ability to inactivate the invading virus, he noted.
“When people are infected, the proportions of neutralising and non-neutralising antibodies can differ. It is not always understood what makes an antibody neutralising and another non-neutralising, or why an infection leads to production of more of one of these types of antibodies,” he explained. “The initial immune response immediately following infection sets the memory of the immune system, so if the person had generated mostly non-neutralising antibodies, the next time that person encounters the same virus, they may not be able to prevent an infection.”
So at present, the information from antibody testing is largely unhelpful to individuals, but it could be valuable to epidemiologists and policy makers.
“States are looking at ways they can integrate reliable serologic tests for surveillance,” explained APHL’s Blank.
Knowing how widespread the infection has been within a community could guide research and possibly public health decisions, Wroblewski said at the APHL press conference. But she’s hesitant here, too. “I know there has been a lot of talk about using this testing to ease restrictions, but I do think we need to be cautious on how quickly we move in that direction.” If people don’t have antibodies, it means they haven’t been exposed and that they’re still vulnerable, she noted. “If nothing else, that still informs policy decisions, even if they’re not the policy decisions we want.”
Trials Recruiting, Medical Centers Develop Own Tests
Despite the uncertainties over antibody testing, many efforts are still being guided by this strategy.
The NIH is recruiting volunteers to its antibody testing study and suggests that immunity is “likely” for those who test positive.
In addition, several large medical centers have developed their own antibody tests, including Stanford, the Yale New Haven Hospital, and the Mayo Clinic.
The Stanford test detects two types of antibodies: IgM, which is made early in an immune response and usually wanes quickly, and IgG, which rises more slowly after infection but usually persists longer.
“There’s limited data out of China and Europe showing that this appears to be the response pattern followed with this virus,” commented Thomas Montine, MD, PhD, professor and chair of pathology at Stanford University. “But no one has had this long enough to know how long after infection the antibodies persist,” he added.
“There is enormous demand for serologic testing,” said William Morice, MD, PhD, president of Mayo Clinic Laboratories. “At this time, serology testing needs to be prioritized for efforts to identify individuals in areas where potential immunity is key ― supporting healthcare workers, screening for potential plasma donors, and helping advance the most promising vaccine candidates.”
During a recent webinar with the Association for Value-Based Cancer Care, the largest physician-owned oncology-hematology practice in the country, the president, Lucio Gordan, MD, said his organization was looking into antibody testing for staff. “They wanted to see how many have been exposed,” he said, although “what it means is uncertain.”
When Medscape Medical News checked back with him a few weeks later, Gordan, president of Florida Cancer Specialists and Research Institute, reported that no progress had been made.
“We unfortunately have not been able to test yet, due to concerns with reliability of kits. We are waiting for a better solution so we can reassess our strategy,” he said.
This article first appeared on Medscape.com.
Noopur Raje, MD, has been sitting at home for 5 weeks waiting for her COVID-19 test to turn negative so she can get back to work. She’s a cancer specialist – head of the Massachusetts General Hospital’s Center for Multiple Myeloma – but Raje says as soon as she’s allowed back to the hospital, she’ll head straight to the front line of COVID-19 caregivers.
“It’s people like us who have to get back in the trenches and do the work now,” she told Medscape Medical News.
“I still will be at risk,” she said. But, having nursed her physician husband through COVID-19 at home until he was admitted to an intensive care unit, she is determined to help in the COVID-19 wards.
“I will be the first one to volunteer to take care of these patients,” she said. “I can’t wait, as I want to give these folks hope. They are so scared.”
Around the world, it’s assumed that she and others like her who’ve recovered from COVID-19 will be immune to the infection.
Some have suggested that with antibodies to the virus coursing through their veins, these survivors might be given immunity passports. They could be the ones to jump-start people’s lives again ― the first to be let out from lockdown, and in healthcare, the ones to head the ongoing battle against this pandemic.
So, there has been a race to develop COVID-19 antibody tests to identify these people.
Circumventing the Usual Clearance Process
To speed up the process, the US Food and Drug Administration (FDA) made a much-criticized move to allow a free-for-all for developers to begin marketing antibody tests that had not gone through the agency’s usual evaluation process. The result was a flood of more than 90 unapproved tests “that have, frankly, dubious quality,” said Scott Becker, CEO of the Association of Public Health Laboratories (APHL), which represents local and state public laboratories.
The APHL spoke out in dismay – its chief program officer, Eric Blank, decried the “Wild West” of tests unleashed on the public.
“These tests create more uncertainty than before,” said Kelly Wroblewski, APHL’s director of infectious diseases, in a news conference on April 14. “Having many inaccurate tests is worse than having no tests at all.”
The APHL and the FDA, working with the Centers for Disease Control and Prevention and the National Institutes of Health (NIH), have moved quickly into damage control, conducting evaluations of the tests in an effort to distinguish the potentially useful from the useless.
So far, they have succeeded in issuing emergency use authorizations (EUAs) to only four tests, those marketed by Cellex, Ortho Clinical Diagnostics, Chembio Diagnostic Systems, and the Mount Sinai Laboratory.
For all the other antibody tests on the market that do not have an EUA, “They’re trusting that the test developer has done a good job in validation,” Becker said. But there are worrying anecdotes. “Our members have reported that they’ve seen fraudulent marketing.... We’ve seen the FDA clamp down on some companies... [and] a number of cities and health departments have issued warnings because of what they’ve seen,” he added.
In particular, Wroblewski said, some companies are marketing tests for use in physicians’ offices or pharmacies. “Today, there are no serology tests approved for point-of-care settings,” she warned. “We don’t know how to interpret the test results, if the presence of antibodies indicates immunity, how long it will last, or what titer might be sufficient.”
Uncertainty Emphasized
The FDA emphasized the uncertainty about antibody tests in a statement released on April 18.
Although the tests can identify people who have been exposed and who developed an immune response to the virus, the agency noted, “we don’t yet know that just because someone has developed antibodies, that they are fully protected from reinfection, or how long any immunity lasts.”
The FDA says that the role of these antibody tests, at present, lies in providing information to “help us track the spread of the virus nationwide and assess the impact of our public health efforts now, while also informing our COVID-19 response as we continue to move forward.”
The World Health Organization (WHO) also emphasized the current uncertainty over antibody tests at a press briefing on April 17. “Nobody is sure about the length of protection that antibodies may give and whether they fully protect against ... the disease,” said Mike Ryan, MD, executive director of the WHO’s emergencies program. There is also a concern that such tests may give false assurance or be misused. “There is still a lot of work that needs to be done to validate these antibody tests,” he added.
“The WHO are right to highlight that any antibody test, if we get one, won’t be able to definitely say whether someone is immune to the infection, because we just don’t know enough yet about how immunity works with COVID-19,” commented Prof. Chris Dye, Oxford Martin School, University of Oxford, in reaction on the UK Science Media Center.
Expanding on this point on the same site, Andrew Easton PhD, professor of virology at the University of Warwick, noted that “a serology test does not discriminate between neutralising and non-neutralising antibodies; a discriminatory test is much more complex and slow.”
Only the neutralizing antibodies have the ability to inactivate the invading virus, he noted.
“When people are infected, the proportions of neutralising and non-neutralising antibodies can differ. It is not always understood what makes an antibody neutralising and another non-neutralising, or why an infection leads to production of more of one of these types of antibodies,” he explained. “The initial immune response immediately following infection sets the memory of the immune system, so if the person had generated mostly non-neutralising antibodies, the next time that person encounters the same virus, they may not be able to prevent an infection.”
So at present, the information from antibody testing is largely unhelpful to individuals, but it could be valuable to epidemiologists and policy makers.
“States are looking at ways they can integrate reliable serologic tests for surveillance,” explained APHL’s Blank.
Knowing how widespread the infection has been within a community could guide research and possibly public health decisions, Wroblewski said at the APHL press conference. But she’s hesitant here, too. “I know there has been a lot of talk about using this testing to ease restrictions, but I do think we need to be cautious on how quickly we move in that direction.” If people don’t have antibodies, it means they haven’t been exposed and that they’re still vulnerable, she noted. “If nothing else, that still informs policy decisions, even if they’re not the policy decisions we want.”
Trials Recruiting, Medical Centers Develop Own Tests
Despite the uncertainties over antibody testing, many efforts are still being guided by this strategy.
The NIH is recruiting volunteers to its antibody testing study and suggests that immunity is “likely” for those who test positive.
In addition, several large medical centers have developed their own antibody tests, including Stanford, the Yale New Haven Hospital, and the Mayo Clinic.
The Stanford test detects two types of antibodies: IgM, which is made early in an immune response and usually wanes quickly, and IgG, which rises more slowly after infection but usually persists longer.
“There’s limited data out of China and Europe showing that this appears to be the response pattern followed with this virus,” commented Thomas Montine, MD, PhD, professor and chair of pathology at Stanford University. “But no one has had this long enough to know how long after infection the antibodies persist,” he added.
“There is enormous demand for serologic testing,” said William Morice, MD, PhD, president of Mayo Clinic Laboratories. “At this time, serology testing needs to be prioritized for efforts to identify individuals in areas where potential immunity is key ― supporting healthcare workers, screening for potential plasma donors, and helping advance the most promising vaccine candidates.”
During a recent webinar with the Association for Value-Based Cancer Care, the largest physician-owned oncology-hematology practice in the country, the president, Lucio Gordan, MD, said his organization was looking into antibody testing for staff. “They wanted to see how many have been exposed,” he said, although “what it means is uncertain.”
When Medscape Medical News checked back with him a few weeks later, Gordan, president of Florida Cancer Specialists and Research Institute, reported that no progress had been made.
“We unfortunately have not been able to test yet, due to concerns with reliability of kits. We are waiting for a better solution so we can reassess our strategy,” he said.
This article first appeared on Medscape.com.
Sudden loss of taste and smell should be part of COVID-19 screen
A number of new publications show that a high proportion of people infected with COVID-19 report loss of smell and/or taste, with their authors adding to the clamor to recognize these symptoms as potentially indicative of the infection.
In particular, there is a belief that these signs may be present in many with asymptomatic COVID-19, and therefore asking about them could be a way to prioritize people for initial testing for the SARS-CoV-2 virus in the absence of other symptoms.
Anyone testing positive could then quarantine, and their contacts could be traced.
Despite this, the World Health Organization (WHO) has not listed loss of smell or taste as potential symptoms of SARS-CoV-2 infection.
But the US Centers for Disease Control and Prevention (CDC) has now added “new loss of taste or smell” as a symptom on its COVID-19 information page.
American Academy of Otolaryngology—Head and Neck Surgery (AAO-HNS) executive vice president and CEO James C. Denneny III, MD, believes the symptoms may be an early warning signal.
And there’s no downside to checking for these, Denneny told Medscape Medical News.
“Given the fact that this doesn’t require any surgical procedure, biopsy, or specific treatment, I think the upside of getting it early is great,” he said. “The downside of using it as a symptom, and if someone doesn’t turn out to have it, is virtually zero.”
Claire Hopkins, MD, president of the British Rhinological Society, and colleagues, writing in Lancet Infectious Diseases, agree.
“Physicians evaluating patients with acute-onset loss of smell or taste, particularly in the context of a patent nasal airway, should have a high index of suspicion for concomitant SARS-CoV-2 infection.”
They also observe that this appears to occur, in contrast to other respiratory infections, “in the absence of nasal congestion or rhinorrhea.”
Newest Publications Find Smell and Taste Loss Is Common
Author of one of the newly published studies, Carol H. Yan, MD, an otolaryngologist and head and neck surgeon at the University of California, San Diego, also thinks that sudden smell and taste loss seem to be fairly specific markers of COVID-19.
In her survey of patients who presented to UC San Diego Health for SARS-CoV-2 testing, Yan and colleagues reported that 68% (40 of 59) of COVID-19–positive patients reported olfactory impairment and 71% (42 of 59) reported taste impairment.
Among the 203 people in the “control” group who were polymerase chain reaction–negative (PCR–) for SARS-CoV-2, just 16% had smell loss and 17% had taste loss, according to their results published in the International Forum of Allergy & Rhinology.
“Based on our study, if you have smell and taste loss, you are more than 10 times more likely to have COVID-19 infection than other causes of infection. The most common first sign of a COVID-19 infection remains fever, but fatigue and loss of smell and taste follow as other very common initial symptoms,” said Yan.
“We know COVID-19 is an extremely contagious virus. This study supports the need to be aware of smell and taste loss as early signs of COVID-19.”
Yan told Medscape Medical News that another not-yet-published analysis indicates that sudden loss of smell or taste “may be more representative of a mild form of disease.”
Getting these people tested and isolated could therefore help prevent spread of COVID-19, she urged.
Based on Yan’s report and other case reports, the UC San Diego Health system is now asking all callers to its COVID-19 hotlines, and all visitors and staff, if they’ve had a sudden loss of taste or smell in the last few weeks, she explained.
And Ahmad R. Sedaghat, MD, PhD, at the University of Cincinnati, Ohio, takes a similar view.
In a new systematic review of the topic published April 14 in Laryngoscope Investigative Otolaryngology, Sedaghat and colleagues write: “Anosmia (total loss of smell) without nasal obstruction, in particular, appears to be a highly specific indicator of COVID-19.”
Sedaghat said a sudden loss of sense of smell wouldn’t necessarily lead people to think they have COVID-19, particularly if they remain asymptomatic, so “these individuals could continue business as usual and spread the disease as a carrier.”
“If someone experiences anosmia without nasal obstruction, aside from quarantining, it would not be unreasonable to reach out to one’s primary care physician about getting tested,” he said in a statement from his institution.
Symptom Checkers Add Weight
Several organizations around the world have begun collecting symptom reports from patients and clinicians, which has shone more light on the sudden loss of taste and smell as potential flags for COVID-19.
In an April 14 Morbidity and Mortality Weekly report from the CDC on COVID-19 infections in healthcare workers, of the 5000 who reported symptoms, 750 (16%) wrote “loss of smell or taste” as an “other” symptom.
Meanwhile, the COVID Symptom Tracker smartphone app, a joint effort by Massachusetts General Hospital, Boston, Stanford (Calif.) University, and King’s College, London, which as of press time, was monitoring some 2.5 million people, has had similar findings.
In a preprint publication on 400,000 people reporting one or more symptoms between March 24 and 29 on the tracker, 18% had lost their sense of smell or taste — more than the 10% who reported fever, but far less than the 53% who reported fatigue.
Only 1702 of the 400,000 had received a COVID-19 test.
Of those, 579 had tested positive and 1123 were negative.
The organizers estimated that of those who were positive, 59% reported losing smell or taste, compared with just 18% who tested negative.
“When combined with other symptoms, people with loss of smell and taste appear to be three times more likely to have contracted COVID-19 according to our data,” said Tim Spector, MD, a genetic epidemiologist at King’s College and the app’s lead researcher, on the symptom tracker’s website.
These people “should therefore self-isolate for 7 days to reduce the spread of the disease,” he urged.
Anosmia Is the Initial Symptom in Many Patients With COVID-19
The AAO-HNS also began collecting data from physicians and patients on March 25 through its Web-based 16-question symptom tracking tool.
It has received more than 500 reports of sudden taste or smell loss, said Denneny.
In a report on the first 237 responses, published in Otolaryngology-Head and Neck Surgery, anosmia (profound loss of smell) was found in 73% of subjects before a COVID-19 diagnosis and was the initial symptom in 27% of those subjects.
That latter determination “was the single most important finding,” said Denneny, noting it shows that smell and taste loss are “a sentinel symptom.”
Anosmia led to testing in only 40% of the cases.
Half of the reports came from otolaryngologists, but a large number came from other medical specialties, especially from family medicine.
Just 2% of reports came from patients in that first group, which was based on responses through April 3.
Denneny said that more reports are now coming in from patients, which he attributes to widespread media coverage about the loss of taste and smell.
It’s still not entirely clear why SARS-CoV-2 might inhibit taste or smell. More common viruses like influenza and other coronaviruses can also cause smell and taste loss.
So far, it seems like the sensory recovery is faster for SARS-CoV-2 than the other viruses, which suggests a potentially different mechanism of action, said Yan. Patients she surveyed at UC San Diego recovered the senses within a few weeks to a month, compared to months or a year with the more common viruses.
Yan’s study was partially supported by the National Institutes of Health. Sedaghat has reported no relevant financial relationships. The COVID Symptom Tracker is supported by Zoe Global Limited and has received grants from the Wellcome Trust, Medical Research Council/British Heart Foundation, and Biological Informative Markers for Stratification of Hypertension.
This article first appeared on Medscape.com.
A number of new publications show that a high proportion of people infected with COVID-19 report loss of smell and/or taste, with their authors adding to the clamor to recognize these symptoms as potentially indicative of the infection.
In particular, there is a belief that these signs may be present in many with asymptomatic COVID-19, and therefore asking about them could be a way to prioritize people for initial testing for the SARS-CoV-2 virus in the absence of other symptoms.
Anyone testing positive could then quarantine, and their contacts could be traced.
Despite this, the World Health Organization (WHO) has not listed loss of smell or taste as potential symptoms of SARS-CoV-2 infection.
But the US Centers for Disease Control and Prevention (CDC) has now added “new loss of taste or smell” as a symptom on its COVID-19 information page.
American Academy of Otolaryngology—Head and Neck Surgery (AAO-HNS) executive vice president and CEO James C. Denneny III, MD, believes the symptoms may be an early warning signal.
And there’s no downside to checking for these, Denneny told Medscape Medical News.
“Given the fact that this doesn’t require any surgical procedure, biopsy, or specific treatment, I think the upside of getting it early is great,” he said. “The downside of using it as a symptom, and if someone doesn’t turn out to have it, is virtually zero.”
Claire Hopkins, MD, president of the British Rhinological Society, and colleagues, writing in Lancet Infectious Diseases, agree.
“Physicians evaluating patients with acute-onset loss of smell or taste, particularly in the context of a patent nasal airway, should have a high index of suspicion for concomitant SARS-CoV-2 infection.”
They also observe that this appears to occur, in contrast to other respiratory infections, “in the absence of nasal congestion or rhinorrhea.”
Newest Publications Find Smell and Taste Loss Is Common
Author of one of the newly published studies, Carol H. Yan, MD, an otolaryngologist and head and neck surgeon at the University of California, San Diego, also thinks that sudden smell and taste loss seem to be fairly specific markers of COVID-19.
In her survey of patients who presented to UC San Diego Health for SARS-CoV-2 testing, Yan and colleagues reported that 68% (40 of 59) of COVID-19–positive patients reported olfactory impairment and 71% (42 of 59) reported taste impairment.
Among the 203 people in the “control” group who were polymerase chain reaction–negative (PCR–) for SARS-CoV-2, just 16% had smell loss and 17% had taste loss, according to their results published in the International Forum of Allergy & Rhinology.
“Based on our study, if you have smell and taste loss, you are more than 10 times more likely to have COVID-19 infection than other causes of infection. The most common first sign of a COVID-19 infection remains fever, but fatigue and loss of smell and taste follow as other very common initial symptoms,” said Yan.
“We know COVID-19 is an extremely contagious virus. This study supports the need to be aware of smell and taste loss as early signs of COVID-19.”
Yan told Medscape Medical News that another not-yet-published analysis indicates that sudden loss of smell or taste “may be more representative of a mild form of disease.”
Getting these people tested and isolated could therefore help prevent spread of COVID-19, she urged.
Based on Yan’s report and other case reports, the UC San Diego Health system is now asking all callers to its COVID-19 hotlines, and all visitors and staff, if they’ve had a sudden loss of taste or smell in the last few weeks, she explained.
And Ahmad R. Sedaghat, MD, PhD, at the University of Cincinnati, Ohio, takes a similar view.
In a new systematic review of the topic published April 14 in Laryngoscope Investigative Otolaryngology, Sedaghat and colleagues write: “Anosmia (total loss of smell) without nasal obstruction, in particular, appears to be a highly specific indicator of COVID-19.”
Sedaghat said a sudden loss of sense of smell wouldn’t necessarily lead people to think they have COVID-19, particularly if they remain asymptomatic, so “these individuals could continue business as usual and spread the disease as a carrier.”
“If someone experiences anosmia without nasal obstruction, aside from quarantining, it would not be unreasonable to reach out to one’s primary care physician about getting tested,” he said in a statement from his institution.
Symptom Checkers Add Weight
Several organizations around the world have begun collecting symptom reports from patients and clinicians, which has shone more light on the sudden loss of taste and smell as potential flags for COVID-19.
In an April 14 Morbidity and Mortality Weekly report from the CDC on COVID-19 infections in healthcare workers, of the 5000 who reported symptoms, 750 (16%) wrote “loss of smell or taste” as an “other” symptom.
Meanwhile, the COVID Symptom Tracker smartphone app, a joint effort by Massachusetts General Hospital, Boston, Stanford (Calif.) University, and King’s College, London, which as of press time, was monitoring some 2.5 million people, has had similar findings.
In a preprint publication on 400,000 people reporting one or more symptoms between March 24 and 29 on the tracker, 18% had lost their sense of smell or taste — more than the 10% who reported fever, but far less than the 53% who reported fatigue.
Only 1702 of the 400,000 had received a COVID-19 test.
Of those, 579 had tested positive and 1123 were negative.
The organizers estimated that of those who were positive, 59% reported losing smell or taste, compared with just 18% who tested negative.
“When combined with other symptoms, people with loss of smell and taste appear to be three times more likely to have contracted COVID-19 according to our data,” said Tim Spector, MD, a genetic epidemiologist at King’s College and the app’s lead researcher, on the symptom tracker’s website.
These people “should therefore self-isolate for 7 days to reduce the spread of the disease,” he urged.
Anosmia Is the Initial Symptom in Many Patients With COVID-19
The AAO-HNS also began collecting data from physicians and patients on March 25 through its Web-based 16-question symptom tracking tool.
It has received more than 500 reports of sudden taste or smell loss, said Denneny.
In a report on the first 237 responses, published in Otolaryngology-Head and Neck Surgery, anosmia (profound loss of smell) was found in 73% of subjects before a COVID-19 diagnosis and was the initial symptom in 27% of those subjects.
That latter determination “was the single most important finding,” said Denneny, noting it shows that smell and taste loss are “a sentinel symptom.”
Anosmia led to testing in only 40% of the cases.
Half of the reports came from otolaryngologists, but a large number came from other medical specialties, especially from family medicine.
Just 2% of reports came from patients in that first group, which was based on responses through April 3.
Denneny said that more reports are now coming in from patients, which he attributes to widespread media coverage about the loss of taste and smell.
It’s still not entirely clear why SARS-CoV-2 might inhibit taste or smell. More common viruses like influenza and other coronaviruses can also cause smell and taste loss.
So far, it seems like the sensory recovery is faster for SARS-CoV-2 than the other viruses, which suggests a potentially different mechanism of action, said Yan. Patients she surveyed at UC San Diego recovered the senses within a few weeks to a month, compared to months or a year with the more common viruses.
Yan’s study was partially supported by the National Institutes of Health. Sedaghat has reported no relevant financial relationships. The COVID Symptom Tracker is supported by Zoe Global Limited and has received grants from the Wellcome Trust, Medical Research Council/British Heart Foundation, and Biological Informative Markers for Stratification of Hypertension.
This article first appeared on Medscape.com.
A number of new publications show that a high proportion of people infected with COVID-19 report loss of smell and/or taste, with their authors adding to the clamor to recognize these symptoms as potentially indicative of the infection.
In particular, there is a belief that these signs may be present in many with asymptomatic COVID-19, and therefore asking about them could be a way to prioritize people for initial testing for the SARS-CoV-2 virus in the absence of other symptoms.
Anyone testing positive could then quarantine, and their contacts could be traced.
Despite this, the World Health Organization (WHO) has not listed loss of smell or taste as potential symptoms of SARS-CoV-2 infection.
But the US Centers for Disease Control and Prevention (CDC) has now added “new loss of taste or smell” as a symptom on its COVID-19 information page.
American Academy of Otolaryngology—Head and Neck Surgery (AAO-HNS) executive vice president and CEO James C. Denneny III, MD, believes the symptoms may be an early warning signal.
And there’s no downside to checking for these, Denneny told Medscape Medical News.
“Given the fact that this doesn’t require any surgical procedure, biopsy, or specific treatment, I think the upside of getting it early is great,” he said. “The downside of using it as a symptom, and if someone doesn’t turn out to have it, is virtually zero.”
Claire Hopkins, MD, president of the British Rhinological Society, and colleagues, writing in Lancet Infectious Diseases, agree.
“Physicians evaluating patients with acute-onset loss of smell or taste, particularly in the context of a patent nasal airway, should have a high index of suspicion for concomitant SARS-CoV-2 infection.”
They also observe that this appears to occur, in contrast to other respiratory infections, “in the absence of nasal congestion or rhinorrhea.”
Newest Publications Find Smell and Taste Loss Is Common
Author of one of the newly published studies, Carol H. Yan, MD, an otolaryngologist and head and neck surgeon at the University of California, San Diego, also thinks that sudden smell and taste loss seem to be fairly specific markers of COVID-19.
In her survey of patients who presented to UC San Diego Health for SARS-CoV-2 testing, Yan and colleagues reported that 68% (40 of 59) of COVID-19–positive patients reported olfactory impairment and 71% (42 of 59) reported taste impairment.
Among the 203 people in the “control” group who were polymerase chain reaction–negative (PCR–) for SARS-CoV-2, just 16% had smell loss and 17% had taste loss, according to their results published in the International Forum of Allergy & Rhinology.
“Based on our study, if you have smell and taste loss, you are more than 10 times more likely to have COVID-19 infection than other causes of infection. The most common first sign of a COVID-19 infection remains fever, but fatigue and loss of smell and taste follow as other very common initial symptoms,” said Yan.
“We know COVID-19 is an extremely contagious virus. This study supports the need to be aware of smell and taste loss as early signs of COVID-19.”
Yan told Medscape Medical News that another not-yet-published analysis indicates that sudden loss of smell or taste “may be more representative of a mild form of disease.”
Getting these people tested and isolated could therefore help prevent spread of COVID-19, she urged.
Based on Yan’s report and other case reports, the UC San Diego Health system is now asking all callers to its COVID-19 hotlines, and all visitors and staff, if they’ve had a sudden loss of taste or smell in the last few weeks, she explained.
And Ahmad R. Sedaghat, MD, PhD, at the University of Cincinnati, Ohio, takes a similar view.
In a new systematic review of the topic published April 14 in Laryngoscope Investigative Otolaryngology, Sedaghat and colleagues write: “Anosmia (total loss of smell) without nasal obstruction, in particular, appears to be a highly specific indicator of COVID-19.”
Sedaghat said a sudden loss of sense of smell wouldn’t necessarily lead people to think they have COVID-19, particularly if they remain asymptomatic, so “these individuals could continue business as usual and spread the disease as a carrier.”
“If someone experiences anosmia without nasal obstruction, aside from quarantining, it would not be unreasonable to reach out to one’s primary care physician about getting tested,” he said in a statement from his institution.
Symptom Checkers Add Weight
Several organizations around the world have begun collecting symptom reports from patients and clinicians, which has shone more light on the sudden loss of taste and smell as potential flags for COVID-19.
In an April 14 Morbidity and Mortality Weekly report from the CDC on COVID-19 infections in healthcare workers, of the 5000 who reported symptoms, 750 (16%) wrote “loss of smell or taste” as an “other” symptom.
Meanwhile, the COVID Symptom Tracker smartphone app, a joint effort by Massachusetts General Hospital, Boston, Stanford (Calif.) University, and King’s College, London, which as of press time, was monitoring some 2.5 million people, has had similar findings.
In a preprint publication on 400,000 people reporting one or more symptoms between March 24 and 29 on the tracker, 18% had lost their sense of smell or taste — more than the 10% who reported fever, but far less than the 53% who reported fatigue.
Only 1702 of the 400,000 had received a COVID-19 test.
Of those, 579 had tested positive and 1123 were negative.
The organizers estimated that of those who were positive, 59% reported losing smell or taste, compared with just 18% who tested negative.
“When combined with other symptoms, people with loss of smell and taste appear to be three times more likely to have contracted COVID-19 according to our data,” said Tim Spector, MD, a genetic epidemiologist at King’s College and the app’s lead researcher, on the symptom tracker’s website.
These people “should therefore self-isolate for 7 days to reduce the spread of the disease,” he urged.
Anosmia Is the Initial Symptom in Many Patients With COVID-19
The AAO-HNS also began collecting data from physicians and patients on March 25 through its Web-based 16-question symptom tracking tool.
It has received more than 500 reports of sudden taste or smell loss, said Denneny.
In a report on the first 237 responses, published in Otolaryngology-Head and Neck Surgery, anosmia (profound loss of smell) was found in 73% of subjects before a COVID-19 diagnosis and was the initial symptom in 27% of those subjects.
That latter determination “was the single most important finding,” said Denneny, noting it shows that smell and taste loss are “a sentinel symptom.”
Anosmia led to testing in only 40% of the cases.
Half of the reports came from otolaryngologists, but a large number came from other medical specialties, especially from family medicine.
Just 2% of reports came from patients in that first group, which was based on responses through April 3.
Denneny said that more reports are now coming in from patients, which he attributes to widespread media coverage about the loss of taste and smell.
It’s still not entirely clear why SARS-CoV-2 might inhibit taste or smell. More common viruses like influenza and other coronaviruses can also cause smell and taste loss.
So far, it seems like the sensory recovery is faster for SARS-CoV-2 than the other viruses, which suggests a potentially different mechanism of action, said Yan. Patients she surveyed at UC San Diego recovered the senses within a few weeks to a month, compared to months or a year with the more common viruses.
Yan’s study was partially supported by the National Institutes of Health. Sedaghat has reported no relevant financial relationships. The COVID Symptom Tracker is supported by Zoe Global Limited and has received grants from the Wellcome Trust, Medical Research Council/British Heart Foundation, and Biological Informative Markers for Stratification of Hypertension.
This article first appeared on Medscape.com.
During a pandemic, infusion center nursing team pitches in to keep patients on track
How do you run a chemotherapy infusion center during a pandemic?
Quick action, innovative staffing solutions, and nimble leadership are allowing one cancer center to continue providing care for the most vulnerable patients, while keeping patients and staff safe.
When nursing leaders at Atrium Health’s Levine Cancer Institute in Charlotte, N.C., realized that business was not going to continue as usual for American health care during the COVID-19 pandemic, they knew they had to act quickly to keep the institute’s 82-chair infusion center up and running.
North Carolina had already imposed restrictions on mass gatherings and closed educational facilities and some businesses by mid-March. Stay-at-home orders were being issued in surrounding states (North Carolina came under a statewide order on March 30). Physical distancing and a healthy, resilient team were prerequisites to an effective COVID-19 solution for the infusion clinic, said Angela Hosking, MBA, MSN, RN, director of nursing for Levine Cancer Institute. In an interview, she said that, at meetings on Monday, March 23, “we divided the team exactly in half.”
Infusion center staff members were broken into an “A” and a “B” rotation, with each team either on site or remotely for a 14-day stretch, and then switching at the 2-week mark. The 14-day rotation, she said, was chosen so that each cohort would have a full 2 weeks away after having been in clinic to ensure they were symptom free before returning. The cohorting scheme also serves to minimize between-staff exposure and risk of transmission.
These changes were implemented immediately, said Ms. Hosking, and included all but the most senior leadership – Ms. Hosking alternates days on site with another senior colleague to help with continuity.
Infusion center patients were triaged to determine “who absolutely needed to be seen,” and clinic staff started making phone calls and reshuffling the schedule so the clinic could continue at half-strength staffing.
The clinic was rearranged to ensure each infusion chair had appropriate space but the nursing work flow was still safe with reduced staff, said Jessica Stewart, MSN, RN, Levine Cancer Institute’s hematology–sickle cell nurse manager.
Patients were receptive, said Ms. Stewart. The team that was working remotely made sure all patients were called the day before their appointments, so they could understand what to expect when they arrived. Any needed updates to the medical history and patient teaching can also be done over the phone the day before the visit, she said, noting that patients are also queried about any concerning symptoms such as fever or cough.
In the spirit of providing information and managing expectations, patients are also informed that they will not be able to bring a visitor along and are advised to expect additional screening when they arrive. In addition to a repeat of symptom screening, patients are checked for fever with a temporal thermometer.
Any patient who arrives reporting symptoms or who has a fever is then subject to additional screening. Physician phone consultation is available, if needed, and patients may be routed to a drive-through screening and testing setup, or to the ED if there are concerns the patient may be seriously ill.
Several weeks into the new operations, Ms. Stewart said, “we’ve fine-tuned the processes we currently have in place. There’s new practices with virtual visits to make reaching our patients easier. Our senior leadership is communicating in a weekly video sent to all [Levine Cancer Institute] teammates for updates; it’s very transparent and the team is appreciative of being kept in the loop.”
Thus far, said Ms. Hosking, “it’s gone well – we’ve successfully operationalized this plan. … I think it shows that people that care about each other and their mission can collaborate with each other” to make change happen in a hurry.
Though it’s too soon to know exactly what the future holds once the pandemic has passed, some aspects of the new way of doing things may carry forward, said Ms. Stewart. “Communication has been massively streamlined,” and staff has found the previsit phone calls an efficient and effective way to gather and impart information.
A staff nurse at the infusion center, Whitney Hollifield, RN, added that patients have seen – and appreciate – the added precautions taken by all. “I feel that we have done well with protecting our patients from unneeded exposure and patients have expressed this to me,” said Ms. Hollifield. “They have said: ‘Thank you for doing this because I am scared to come in right now so I appreciate that your office is thinking of protecting us.’ ”
Ms. Hollifield added that “patients have been very responsive to our strategy for their care because we are truly concerned for them and I think that this shows. I believe that we are doing everything we can to keep them safe during a tumultuous time, and they feel genuine care for them during a frightening time is reassuring.”
On the practical side of things, Ms. Stewart noted, patients and families have provided infusion center staff with a seemingly endless supply of food: “We have never been more well fed!”
Rhonda Davis, RN, is a nurse at the Levine Cancer Institute. Speaking of the changes that have been made in recent weeks, she said, “Some of the changes that I think have been meaningful these last 3 weeks are making sure that the patients are the No. 1 priority. We are doing this by allowing patients options such as phone and virtual visits. This helps patients have some control over their health during this scary time for all.”
Ms. Davis acknowledged her own feelings about the uncertain times ahead. “As an individual with good health, I am scared, so to imagine the fear that these patients are facing must be overwhelming to them. Along that line, one of the most meaningful things that has happened for me is calling patients and having them concerned about my health and telling me to be safe.”
Despite her trepidation, she said, it’s meaningful for her to hear from patients who are in the clinic that they appreciate her presence. She found it heartening “that they are also considering our safety as well as their own.”
The two-cohort scheme has been well received by nursing staff, both administrators and clinic staff agreed. “I think that allowing staff to work 2 weeks on and 2 weeks at home helps keep patients and teammates safe,” Ms. Davis said.
Another infusion nurse, Ursel Wallace, RN, said that she appreciated the speed and efficiency with which the pandemic adaptations were made, including the nuts and bolts of reshuffling a complicated infusion schedule. “I know there were many different moving parts and it took a village” to move with such alacrity without dropping balls, she said.
The infusion nursing team’s spirit was summed up by Patricia Ashworth, RN: “Together, we will prevail!”
How do you run a chemotherapy infusion center during a pandemic?
Quick action, innovative staffing solutions, and nimble leadership are allowing one cancer center to continue providing care for the most vulnerable patients, while keeping patients and staff safe.
When nursing leaders at Atrium Health’s Levine Cancer Institute in Charlotte, N.C., realized that business was not going to continue as usual for American health care during the COVID-19 pandemic, they knew they had to act quickly to keep the institute’s 82-chair infusion center up and running.
North Carolina had already imposed restrictions on mass gatherings and closed educational facilities and some businesses by mid-March. Stay-at-home orders were being issued in surrounding states (North Carolina came under a statewide order on March 30). Physical distancing and a healthy, resilient team were prerequisites to an effective COVID-19 solution for the infusion clinic, said Angela Hosking, MBA, MSN, RN, director of nursing for Levine Cancer Institute. In an interview, she said that, at meetings on Monday, March 23, “we divided the team exactly in half.”
Infusion center staff members were broken into an “A” and a “B” rotation, with each team either on site or remotely for a 14-day stretch, and then switching at the 2-week mark. The 14-day rotation, she said, was chosen so that each cohort would have a full 2 weeks away after having been in clinic to ensure they were symptom free before returning. The cohorting scheme also serves to minimize between-staff exposure and risk of transmission.
These changes were implemented immediately, said Ms. Hosking, and included all but the most senior leadership – Ms. Hosking alternates days on site with another senior colleague to help with continuity.
Infusion center patients were triaged to determine “who absolutely needed to be seen,” and clinic staff started making phone calls and reshuffling the schedule so the clinic could continue at half-strength staffing.
The clinic was rearranged to ensure each infusion chair had appropriate space but the nursing work flow was still safe with reduced staff, said Jessica Stewart, MSN, RN, Levine Cancer Institute’s hematology–sickle cell nurse manager.
Patients were receptive, said Ms. Stewart. The team that was working remotely made sure all patients were called the day before their appointments, so they could understand what to expect when they arrived. Any needed updates to the medical history and patient teaching can also be done over the phone the day before the visit, she said, noting that patients are also queried about any concerning symptoms such as fever or cough.
In the spirit of providing information and managing expectations, patients are also informed that they will not be able to bring a visitor along and are advised to expect additional screening when they arrive. In addition to a repeat of symptom screening, patients are checked for fever with a temporal thermometer.
Any patient who arrives reporting symptoms or who has a fever is then subject to additional screening. Physician phone consultation is available, if needed, and patients may be routed to a drive-through screening and testing setup, or to the ED if there are concerns the patient may be seriously ill.
Several weeks into the new operations, Ms. Stewart said, “we’ve fine-tuned the processes we currently have in place. There’s new practices with virtual visits to make reaching our patients easier. Our senior leadership is communicating in a weekly video sent to all [Levine Cancer Institute] teammates for updates; it’s very transparent and the team is appreciative of being kept in the loop.”
Thus far, said Ms. Hosking, “it’s gone well – we’ve successfully operationalized this plan. … I think it shows that people that care about each other and their mission can collaborate with each other” to make change happen in a hurry.
Though it’s too soon to know exactly what the future holds once the pandemic has passed, some aspects of the new way of doing things may carry forward, said Ms. Stewart. “Communication has been massively streamlined,” and staff has found the previsit phone calls an efficient and effective way to gather and impart information.
A staff nurse at the infusion center, Whitney Hollifield, RN, added that patients have seen – and appreciate – the added precautions taken by all. “I feel that we have done well with protecting our patients from unneeded exposure and patients have expressed this to me,” said Ms. Hollifield. “They have said: ‘Thank you for doing this because I am scared to come in right now so I appreciate that your office is thinking of protecting us.’ ”
Ms. Hollifield added that “patients have been very responsive to our strategy for their care because we are truly concerned for them and I think that this shows. I believe that we are doing everything we can to keep them safe during a tumultuous time, and they feel genuine care for them during a frightening time is reassuring.”
On the practical side of things, Ms. Stewart noted, patients and families have provided infusion center staff with a seemingly endless supply of food: “We have never been more well fed!”
Rhonda Davis, RN, is a nurse at the Levine Cancer Institute. Speaking of the changes that have been made in recent weeks, she said, “Some of the changes that I think have been meaningful these last 3 weeks are making sure that the patients are the No. 1 priority. We are doing this by allowing patients options such as phone and virtual visits. This helps patients have some control over their health during this scary time for all.”
Ms. Davis acknowledged her own feelings about the uncertain times ahead. “As an individual with good health, I am scared, so to imagine the fear that these patients are facing must be overwhelming to them. Along that line, one of the most meaningful things that has happened for me is calling patients and having them concerned about my health and telling me to be safe.”
Despite her trepidation, she said, it’s meaningful for her to hear from patients who are in the clinic that they appreciate her presence. She found it heartening “that they are also considering our safety as well as their own.”
The two-cohort scheme has been well received by nursing staff, both administrators and clinic staff agreed. “I think that allowing staff to work 2 weeks on and 2 weeks at home helps keep patients and teammates safe,” Ms. Davis said.
Another infusion nurse, Ursel Wallace, RN, said that she appreciated the speed and efficiency with which the pandemic adaptations were made, including the nuts and bolts of reshuffling a complicated infusion schedule. “I know there were many different moving parts and it took a village” to move with such alacrity without dropping balls, she said.
The infusion nursing team’s spirit was summed up by Patricia Ashworth, RN: “Together, we will prevail!”
How do you run a chemotherapy infusion center during a pandemic?
Quick action, innovative staffing solutions, and nimble leadership are allowing one cancer center to continue providing care for the most vulnerable patients, while keeping patients and staff safe.
When nursing leaders at Atrium Health’s Levine Cancer Institute in Charlotte, N.C., realized that business was not going to continue as usual for American health care during the COVID-19 pandemic, they knew they had to act quickly to keep the institute’s 82-chair infusion center up and running.
North Carolina had already imposed restrictions on mass gatherings and closed educational facilities and some businesses by mid-March. Stay-at-home orders were being issued in surrounding states (North Carolina came under a statewide order on March 30). Physical distancing and a healthy, resilient team were prerequisites to an effective COVID-19 solution for the infusion clinic, said Angela Hosking, MBA, MSN, RN, director of nursing for Levine Cancer Institute. In an interview, she said that, at meetings on Monday, March 23, “we divided the team exactly in half.”
Infusion center staff members were broken into an “A” and a “B” rotation, with each team either on site or remotely for a 14-day stretch, and then switching at the 2-week mark. The 14-day rotation, she said, was chosen so that each cohort would have a full 2 weeks away after having been in clinic to ensure they were symptom free before returning. The cohorting scheme also serves to minimize between-staff exposure and risk of transmission.
These changes were implemented immediately, said Ms. Hosking, and included all but the most senior leadership – Ms. Hosking alternates days on site with another senior colleague to help with continuity.
Infusion center patients were triaged to determine “who absolutely needed to be seen,” and clinic staff started making phone calls and reshuffling the schedule so the clinic could continue at half-strength staffing.
The clinic was rearranged to ensure each infusion chair had appropriate space but the nursing work flow was still safe with reduced staff, said Jessica Stewart, MSN, RN, Levine Cancer Institute’s hematology–sickle cell nurse manager.
Patients were receptive, said Ms. Stewart. The team that was working remotely made sure all patients were called the day before their appointments, so they could understand what to expect when they arrived. Any needed updates to the medical history and patient teaching can also be done over the phone the day before the visit, she said, noting that patients are also queried about any concerning symptoms such as fever or cough.
In the spirit of providing information and managing expectations, patients are also informed that they will not be able to bring a visitor along and are advised to expect additional screening when they arrive. In addition to a repeat of symptom screening, patients are checked for fever with a temporal thermometer.
Any patient who arrives reporting symptoms or who has a fever is then subject to additional screening. Physician phone consultation is available, if needed, and patients may be routed to a drive-through screening and testing setup, or to the ED if there are concerns the patient may be seriously ill.
Several weeks into the new operations, Ms. Stewart said, “we’ve fine-tuned the processes we currently have in place. There’s new practices with virtual visits to make reaching our patients easier. Our senior leadership is communicating in a weekly video sent to all [Levine Cancer Institute] teammates for updates; it’s very transparent and the team is appreciative of being kept in the loop.”
Thus far, said Ms. Hosking, “it’s gone well – we’ve successfully operationalized this plan. … I think it shows that people that care about each other and their mission can collaborate with each other” to make change happen in a hurry.
Though it’s too soon to know exactly what the future holds once the pandemic has passed, some aspects of the new way of doing things may carry forward, said Ms. Stewart. “Communication has been massively streamlined,” and staff has found the previsit phone calls an efficient and effective way to gather and impart information.
A staff nurse at the infusion center, Whitney Hollifield, RN, added that patients have seen – and appreciate – the added precautions taken by all. “I feel that we have done well with protecting our patients from unneeded exposure and patients have expressed this to me,” said Ms. Hollifield. “They have said: ‘Thank you for doing this because I am scared to come in right now so I appreciate that your office is thinking of protecting us.’ ”
Ms. Hollifield added that “patients have been very responsive to our strategy for their care because we are truly concerned for them and I think that this shows. I believe that we are doing everything we can to keep them safe during a tumultuous time, and they feel genuine care for them during a frightening time is reassuring.”
On the practical side of things, Ms. Stewart noted, patients and families have provided infusion center staff with a seemingly endless supply of food: “We have never been more well fed!”
Rhonda Davis, RN, is a nurse at the Levine Cancer Institute. Speaking of the changes that have been made in recent weeks, she said, “Some of the changes that I think have been meaningful these last 3 weeks are making sure that the patients are the No. 1 priority. We are doing this by allowing patients options such as phone and virtual visits. This helps patients have some control over their health during this scary time for all.”
Ms. Davis acknowledged her own feelings about the uncertain times ahead. “As an individual with good health, I am scared, so to imagine the fear that these patients are facing must be overwhelming to them. Along that line, one of the most meaningful things that has happened for me is calling patients and having them concerned about my health and telling me to be safe.”
Despite her trepidation, she said, it’s meaningful for her to hear from patients who are in the clinic that they appreciate her presence. She found it heartening “that they are also considering our safety as well as their own.”
The two-cohort scheme has been well received by nursing staff, both administrators and clinic staff agreed. “I think that allowing staff to work 2 weeks on and 2 weeks at home helps keep patients and teammates safe,” Ms. Davis said.
Another infusion nurse, Ursel Wallace, RN, said that she appreciated the speed and efficiency with which the pandemic adaptations were made, including the nuts and bolts of reshuffling a complicated infusion schedule. “I know there were many different moving parts and it took a village” to move with such alacrity without dropping balls, she said.
The infusion nursing team’s spirit was summed up by Patricia Ashworth, RN: “Together, we will prevail!”
COVID-19: Helping health care workers on front lines
Psychiatrists are intervening with less conventional strategies
Across the country, psychiatrists are stepping up to provide urgent care to fellow health care workers in need amid the coronavirus pandemic. They’re offering stress management strategies, spearheading unusual partnerships, and discovering that psychotherapy and medication might not be their most helpful tools to help their colleagues at this time.
“This is completely the opposite of the way we practice psychiatry,” said Allison Cotton, MD, of the University of Nevada, Reno. “Our interventions are quite different from a psychotherapeutic standpoint.”
In March, she worked with four colleagues, Suzan Song, MD, MPH, PhD; Ben Cheng, MD; Smita Gautam, MD; and Mona S. Masood, DO, to create the Physician Support Line, a confidential and free hotline that links physicians to volunteer psychiatrists who are available to listen and offer advice on coping. The hotline (888-409-0141) is available every day from 8 a.m. to midnight Eastern time. Calls typically take 15-45 minutes; no appointment is needed, and conversations are not reportable to state medical boards.

“The calls can be very intense,” Dr. Cotton said, and they’re unusual for several reasons. The hotline is not like a suicide or crisis hotline, when “a person calls because they need help, and then they can go get that help – they go to the hospital and get admitted to a psychiatric unit. Our callers don’t have that luxury.”
It’s also impossible to take an extensive history and create a sophisticated, long-term treatment plan as psychiatrists would during normal office visits. At the hotline, Dr. Cotton said, “we’re really focusing on the caller’s strengths and helping them come up with a plan for today to get through whatever they’re facing,” she said.
Stress management is critical
Psychiatrists at the University of Colorado Anschutz Medical Campus are embracing a similar approach to help health care workers cope, said Steven Berkowitz, MD. “We focus on stress management, and the notion that they are generally healthy and understandably struggling with extraordinary circumstances,” he said. “We are conservative in our use of medications and really only prescribe medications, such as trazodone, to help with sleep. We do not use benzodiazepines unless there is a history of more severe psychiatric problems.”
The pressure on health care workers during the pandemic is intense. A survey of 1,257 workers in 34 Chinese hospitals found high levels of symptoms of depression (50%), anxiety (45%), insomnia (35%), and distress (72%). Several groups appeared to be more vulnerable: women, nurses, front-line health care workers, and those in the coronavirus-stricken city of Wuhan (JAMA Netw Open. 2020;3[3]:e203976).
In Colorado, “providers are depleted,” Dr. Berkowitz said. “We are hearing about sleep disturbances and even some traumatic nightmares from ICU staff. During our support sessions, tears come most frequently when they talk about the struggle to care for their families and how they’re putting them at risk.”
Also, he said, “one of the most upsetting issues has been around language and cultural issues. Because of the language barriers, providers cannot explain why families can’t be with their sick members, which has led to acrimony.”
Guilt is a prevailing theme
Guilt also is a common emotion among health care workers, said psychiatrist Tia Konzer, DO, of Charlotte, N.C. “The ones on the front line question whether they were able to do enough to save someone or if they could have done more. Those of us not on the front lines feel guilty that we’re not there with our colleagues, that we don’t face the same fears and are in the safety of our outpatient clinics.”
The focus on social distancing is creating its own strains, she said. “A lot of people are recognizing the power of human touch and how comforting that is,” she said. “The healers aren’t able to comfort the loved ones of the deceased, and we’re not able to comfort each other. And people are having a hard time not being able to hug their kids and their spouses, having to ward off their kids when they come home or avoid them until they’ve showered.”
How can mental health professionals be most helpful to health care workers in need? The simple act of listening is crucial, several such professionals said in interviews.
“Your main job is to bear witness to their experiences and to hear their story, then secondarily to make sure they have a basic self-care plan to recover from what they’re doing each day,” said psychologist Leah Welch, PhD, of the Scripps Health network in San Diego. “Don’t talk too much or try to give advice too quickly before you’ve listened to what the caregiver has shared. They’re accumulating small traumas and need time and space to sort them out, and that takes patience and a listening ear on the part of the provider. Rushing in too quickly with advice deprives them of making sense of their own experience.”
She added that “they should also be thanked for what they’re doing, because it requires skill, empathy, and courage. They are being heroic, and they need to know they’re appreciated by those of us not on the front lines for what they’re putting themselves through.”
Partnerships are forming
At Zuckerberg San Francisco General Hospital and Trauma Center, psychiatry chief Lisa Fortuna, MD, MPH, MDiv, said her team has had success by working closely with the hospital’s chaplains. “A lot of the staff are not saying: ‘We’re stressing out; help us.’ The chaplains had starting rounding, asking how they’re doing, and they’d open up because there was already a relationship. The chaplains are very well trained in dealing with being support for people under situations of death, loss, and immediate stress.”
The chaplains themselves became overwhelmed, and the hospital responded by reaching out to bring in more chaplains. The psychiatry team, meanwhile, worked to partner with the chaplains to provide a continuum of support for staff. “We have an opportunity to build on the trust that they have,” said Dr. Fortuna, who is an ordained Episcopal minister. “They’re the perfect partners.”
What happens now? Dr. Fortuna has seen the long-term aftermath of a crisis. She previously worked in Massachusetts and helped to support health care workers in that state after the Boston Marathon bombing.
She cautioned that health care workers may first run on adrenaline in a crisis, spurred by “heroic high energy.” But then, the full extent of the tragedy begins to set in, and they start to process their feelings. “You have to keep people going through those phases,” she said.
Going forward, she said, “there will be a prolonged tail of stress,” especially if virus outbreaks recur. “We’ll have a long time enduring this.”
Don’t forget the self-care
There was a time during the pandemic when Dr. Cotton had become so overwhelmed by anxiety that she called the Physician Support Line to get some support from fellow psychiatrists.
“I thought, ‘Why not?’” she recalled. “I helped create the hotline. Why wouldn’t I call it?”
The calls took only a few minutes but they made a difference to Dr. Cotton, who had been severely ill with what she believed was an unconfirmed case of the novel coronavirus. “I immediately felt more like I improved my outlook by focusing on what I could control,” she said, “and accepting the things I could not control.”
Many psychiatrists are finding themselves in similar situations. Fortunately, colleagues are highlighting ways for psychiatrists to care for themselves just as they care for patients.
“One of the challenges clinicians are facing is that they are living through a shared experience in this global pandemic with their patients right now,” said psychologist Randi Pochtar, PhD, who is managing support groups for front-line workers at NYU Langone Health in New York City. “Some might find the work to be overwhelming and anxiety-inducing, and others might find their work to be helpful in managing their own anxiety and stress about the pandemic and its impact.”
Dr. Cotton said her breaking points came when she felt panic amid the pandemic. “I had watched too much news, and I’d seen protesters not taking it seriously, and I was scared for my family and myself. I just needed to feel like someone heard me feeling that way.”
The calls to the hotline were helpful, she said, and so was sharing news about her illness with friends. “So many people reached out to me and checked in on me, people I haven’t seen in years, and that was immensely helpful,” she said.
This sort of personal exposure may not come naturally to physicians and nurses, she said. “We don’t seek that kind of attention when we’re ill. Instead, we say: ‘I’m fine; how are you doing?’ That’s what we do every day of our lives at work.”
How can clinicians help themselves and one another? “Clinicians in our practice have been coping and supporting each other through peer supervision, connecting with colleagues in team meetings, and simply checking in on one another,” said Dr. Pochtar. “In addition, we can adopt many of the strategies that we are likely recommending to our patients, such as maintaining routines as much as possible, engaging in regular exercise, eating well and consistently, and connecting with friends and family.”
Managers can play important roles, said Dr. Fortuna. “I’ve been checking in with my faculty, being as supportive as I can be and highlighting the extraordinary things that people are doing, like going from zero to 100 percent in setting up telehealth.”
Dr. Konzer offered another perspective on recognizing the value of the work that psychiatrists are doing. “We’re on the front line of helping heal the front line, and in that responsibility comes an additional stress,” she said. “But there’s an additional gift of being able to contribute where we are most beneficial. We can try to be present now, versus worrying about what may happen or what lies ahead, and appreciate the beauty in the helpers and the small joys of life.”
Dr. Cotton, Dr. Berkowitz, Dr. Konzer, Dr. Welch, Dr. Fortuna, and Dr. Pochtar reported no relevant disclosures.
Psychiatrists are intervening with less conventional strategies
Psychiatrists are intervening with less conventional strategies
Across the country, psychiatrists are stepping up to provide urgent care to fellow health care workers in need amid the coronavirus pandemic. They’re offering stress management strategies, spearheading unusual partnerships, and discovering that psychotherapy and medication might not be their most helpful tools to help their colleagues at this time.
“This is completely the opposite of the way we practice psychiatry,” said Allison Cotton, MD, of the University of Nevada, Reno. “Our interventions are quite different from a psychotherapeutic standpoint.”
In March, she worked with four colleagues, Suzan Song, MD, MPH, PhD; Ben Cheng, MD; Smita Gautam, MD; and Mona S. Masood, DO, to create the Physician Support Line, a confidential and free hotline that links physicians to volunteer psychiatrists who are available to listen and offer advice on coping. The hotline (888-409-0141) is available every day from 8 a.m. to midnight Eastern time. Calls typically take 15-45 minutes; no appointment is needed, and conversations are not reportable to state medical boards.

“The calls can be very intense,” Dr. Cotton said, and they’re unusual for several reasons. The hotline is not like a suicide or crisis hotline, when “a person calls because they need help, and then they can go get that help – they go to the hospital and get admitted to a psychiatric unit. Our callers don’t have that luxury.”
It’s also impossible to take an extensive history and create a sophisticated, long-term treatment plan as psychiatrists would during normal office visits. At the hotline, Dr. Cotton said, “we’re really focusing on the caller’s strengths and helping them come up with a plan for today to get through whatever they’re facing,” she said.
Stress management is critical
Psychiatrists at the University of Colorado Anschutz Medical Campus are embracing a similar approach to help health care workers cope, said Steven Berkowitz, MD. “We focus on stress management, and the notion that they are generally healthy and understandably struggling with extraordinary circumstances,” he said. “We are conservative in our use of medications and really only prescribe medications, such as trazodone, to help with sleep. We do not use benzodiazepines unless there is a history of more severe psychiatric problems.”
The pressure on health care workers during the pandemic is intense. A survey of 1,257 workers in 34 Chinese hospitals found high levels of symptoms of depression (50%), anxiety (45%), insomnia (35%), and distress (72%). Several groups appeared to be more vulnerable: women, nurses, front-line health care workers, and those in the coronavirus-stricken city of Wuhan (JAMA Netw Open. 2020;3[3]:e203976).
In Colorado, “providers are depleted,” Dr. Berkowitz said. “We are hearing about sleep disturbances and even some traumatic nightmares from ICU staff. During our support sessions, tears come most frequently when they talk about the struggle to care for their families and how they’re putting them at risk.”
Also, he said, “one of the most upsetting issues has been around language and cultural issues. Because of the language barriers, providers cannot explain why families can’t be with their sick members, which has led to acrimony.”
Guilt is a prevailing theme
Guilt also is a common emotion among health care workers, said psychiatrist Tia Konzer, DO, of Charlotte, N.C. “The ones on the front line question whether they were able to do enough to save someone or if they could have done more. Those of us not on the front lines feel guilty that we’re not there with our colleagues, that we don’t face the same fears and are in the safety of our outpatient clinics.”
The focus on social distancing is creating its own strains, she said. “A lot of people are recognizing the power of human touch and how comforting that is,” she said. “The healers aren’t able to comfort the loved ones of the deceased, and we’re not able to comfort each other. And people are having a hard time not being able to hug their kids and their spouses, having to ward off their kids when they come home or avoid them until they’ve showered.”
How can mental health professionals be most helpful to health care workers in need? The simple act of listening is crucial, several such professionals said in interviews.
“Your main job is to bear witness to their experiences and to hear their story, then secondarily to make sure they have a basic self-care plan to recover from what they’re doing each day,” said psychologist Leah Welch, PhD, of the Scripps Health network in San Diego. “Don’t talk too much or try to give advice too quickly before you’ve listened to what the caregiver has shared. They’re accumulating small traumas and need time and space to sort them out, and that takes patience and a listening ear on the part of the provider. Rushing in too quickly with advice deprives them of making sense of their own experience.”
She added that “they should also be thanked for what they’re doing, because it requires skill, empathy, and courage. They are being heroic, and they need to know they’re appreciated by those of us not on the front lines for what they’re putting themselves through.”
Partnerships are forming
At Zuckerberg San Francisco General Hospital and Trauma Center, psychiatry chief Lisa Fortuna, MD, MPH, MDiv, said her team has had success by working closely with the hospital’s chaplains. “A lot of the staff are not saying: ‘We’re stressing out; help us.’ The chaplains had starting rounding, asking how they’re doing, and they’d open up because there was already a relationship. The chaplains are very well trained in dealing with being support for people under situations of death, loss, and immediate stress.”
The chaplains themselves became overwhelmed, and the hospital responded by reaching out to bring in more chaplains. The psychiatry team, meanwhile, worked to partner with the chaplains to provide a continuum of support for staff. “We have an opportunity to build on the trust that they have,” said Dr. Fortuna, who is an ordained Episcopal minister. “They’re the perfect partners.”
What happens now? Dr. Fortuna has seen the long-term aftermath of a crisis. She previously worked in Massachusetts and helped to support health care workers in that state after the Boston Marathon bombing.
She cautioned that health care workers may first run on adrenaline in a crisis, spurred by “heroic high energy.” But then, the full extent of the tragedy begins to set in, and they start to process their feelings. “You have to keep people going through those phases,” she said.
Going forward, she said, “there will be a prolonged tail of stress,” especially if virus outbreaks recur. “We’ll have a long time enduring this.”
Don’t forget the self-care
There was a time during the pandemic when Dr. Cotton had become so overwhelmed by anxiety that she called the Physician Support Line to get some support from fellow psychiatrists.
“I thought, ‘Why not?’” she recalled. “I helped create the hotline. Why wouldn’t I call it?”
The calls took only a few minutes but they made a difference to Dr. Cotton, who had been severely ill with what she believed was an unconfirmed case of the novel coronavirus. “I immediately felt more like I improved my outlook by focusing on what I could control,” she said, “and accepting the things I could not control.”
Many psychiatrists are finding themselves in similar situations. Fortunately, colleagues are highlighting ways for psychiatrists to care for themselves just as they care for patients.
“One of the challenges clinicians are facing is that they are living through a shared experience in this global pandemic with their patients right now,” said psychologist Randi Pochtar, PhD, who is managing support groups for front-line workers at NYU Langone Health in New York City. “Some might find the work to be overwhelming and anxiety-inducing, and others might find their work to be helpful in managing their own anxiety and stress about the pandemic and its impact.”
Dr. Cotton said her breaking points came when she felt panic amid the pandemic. “I had watched too much news, and I’d seen protesters not taking it seriously, and I was scared for my family and myself. I just needed to feel like someone heard me feeling that way.”
The calls to the hotline were helpful, she said, and so was sharing news about her illness with friends. “So many people reached out to me and checked in on me, people I haven’t seen in years, and that was immensely helpful,” she said.
This sort of personal exposure may not come naturally to physicians and nurses, she said. “We don’t seek that kind of attention when we’re ill. Instead, we say: ‘I’m fine; how are you doing?’ That’s what we do every day of our lives at work.”
How can clinicians help themselves and one another? “Clinicians in our practice have been coping and supporting each other through peer supervision, connecting with colleagues in team meetings, and simply checking in on one another,” said Dr. Pochtar. “In addition, we can adopt many of the strategies that we are likely recommending to our patients, such as maintaining routines as much as possible, engaging in regular exercise, eating well and consistently, and connecting with friends and family.”
Managers can play important roles, said Dr. Fortuna. “I’ve been checking in with my faculty, being as supportive as I can be and highlighting the extraordinary things that people are doing, like going from zero to 100 percent in setting up telehealth.”
Dr. Konzer offered another perspective on recognizing the value of the work that psychiatrists are doing. “We’re on the front line of helping heal the front line, and in that responsibility comes an additional stress,” she said. “But there’s an additional gift of being able to contribute where we are most beneficial. We can try to be present now, versus worrying about what may happen or what lies ahead, and appreciate the beauty in the helpers and the small joys of life.”
Dr. Cotton, Dr. Berkowitz, Dr. Konzer, Dr. Welch, Dr. Fortuna, and Dr. Pochtar reported no relevant disclosures.
Across the country, psychiatrists are stepping up to provide urgent care to fellow health care workers in need amid the coronavirus pandemic. They’re offering stress management strategies, spearheading unusual partnerships, and discovering that psychotherapy and medication might not be their most helpful tools to help their colleagues at this time.
“This is completely the opposite of the way we practice psychiatry,” said Allison Cotton, MD, of the University of Nevada, Reno. “Our interventions are quite different from a psychotherapeutic standpoint.”
In March, she worked with four colleagues, Suzan Song, MD, MPH, PhD; Ben Cheng, MD; Smita Gautam, MD; and Mona S. Masood, DO, to create the Physician Support Line, a confidential and free hotline that links physicians to volunteer psychiatrists who are available to listen and offer advice on coping. The hotline (888-409-0141) is available every day from 8 a.m. to midnight Eastern time. Calls typically take 15-45 minutes; no appointment is needed, and conversations are not reportable to state medical boards.

“The calls can be very intense,” Dr. Cotton said, and they’re unusual for several reasons. The hotline is not like a suicide or crisis hotline, when “a person calls because they need help, and then they can go get that help – they go to the hospital and get admitted to a psychiatric unit. Our callers don’t have that luxury.”
It’s also impossible to take an extensive history and create a sophisticated, long-term treatment plan as psychiatrists would during normal office visits. At the hotline, Dr. Cotton said, “we’re really focusing on the caller’s strengths and helping them come up with a plan for today to get through whatever they’re facing,” she said.
Stress management is critical
Psychiatrists at the University of Colorado Anschutz Medical Campus are embracing a similar approach to help health care workers cope, said Steven Berkowitz, MD. “We focus on stress management, and the notion that they are generally healthy and understandably struggling with extraordinary circumstances,” he said. “We are conservative in our use of medications and really only prescribe medications, such as trazodone, to help with sleep. We do not use benzodiazepines unless there is a history of more severe psychiatric problems.”
The pressure on health care workers during the pandemic is intense. A survey of 1,257 workers in 34 Chinese hospitals found high levels of symptoms of depression (50%), anxiety (45%), insomnia (35%), and distress (72%). Several groups appeared to be more vulnerable: women, nurses, front-line health care workers, and those in the coronavirus-stricken city of Wuhan (JAMA Netw Open. 2020;3[3]:e203976).
In Colorado, “providers are depleted,” Dr. Berkowitz said. “We are hearing about sleep disturbances and even some traumatic nightmares from ICU staff. During our support sessions, tears come most frequently when they talk about the struggle to care for their families and how they’re putting them at risk.”
Also, he said, “one of the most upsetting issues has been around language and cultural issues. Because of the language barriers, providers cannot explain why families can’t be with their sick members, which has led to acrimony.”
Guilt is a prevailing theme
Guilt also is a common emotion among health care workers, said psychiatrist Tia Konzer, DO, of Charlotte, N.C. “The ones on the front line question whether they were able to do enough to save someone or if they could have done more. Those of us not on the front lines feel guilty that we’re not there with our colleagues, that we don’t face the same fears and are in the safety of our outpatient clinics.”
The focus on social distancing is creating its own strains, she said. “A lot of people are recognizing the power of human touch and how comforting that is,” she said. “The healers aren’t able to comfort the loved ones of the deceased, and we’re not able to comfort each other. And people are having a hard time not being able to hug their kids and their spouses, having to ward off their kids when they come home or avoid them until they’ve showered.”
How can mental health professionals be most helpful to health care workers in need? The simple act of listening is crucial, several such professionals said in interviews.
“Your main job is to bear witness to their experiences and to hear their story, then secondarily to make sure they have a basic self-care plan to recover from what they’re doing each day,” said psychologist Leah Welch, PhD, of the Scripps Health network in San Diego. “Don’t talk too much or try to give advice too quickly before you’ve listened to what the caregiver has shared. They’re accumulating small traumas and need time and space to sort them out, and that takes patience and a listening ear on the part of the provider. Rushing in too quickly with advice deprives them of making sense of their own experience.”
She added that “they should also be thanked for what they’re doing, because it requires skill, empathy, and courage. They are being heroic, and they need to know they’re appreciated by those of us not on the front lines for what they’re putting themselves through.”
Partnerships are forming
At Zuckerberg San Francisco General Hospital and Trauma Center, psychiatry chief Lisa Fortuna, MD, MPH, MDiv, said her team has had success by working closely with the hospital’s chaplains. “A lot of the staff are not saying: ‘We’re stressing out; help us.’ The chaplains had starting rounding, asking how they’re doing, and they’d open up because there was already a relationship. The chaplains are very well trained in dealing with being support for people under situations of death, loss, and immediate stress.”
The chaplains themselves became overwhelmed, and the hospital responded by reaching out to bring in more chaplains. The psychiatry team, meanwhile, worked to partner with the chaplains to provide a continuum of support for staff. “We have an opportunity to build on the trust that they have,” said Dr. Fortuna, who is an ordained Episcopal minister. “They’re the perfect partners.”
What happens now? Dr. Fortuna has seen the long-term aftermath of a crisis. She previously worked in Massachusetts and helped to support health care workers in that state after the Boston Marathon bombing.
She cautioned that health care workers may first run on adrenaline in a crisis, spurred by “heroic high energy.” But then, the full extent of the tragedy begins to set in, and they start to process their feelings. “You have to keep people going through those phases,” she said.
Going forward, she said, “there will be a prolonged tail of stress,” especially if virus outbreaks recur. “We’ll have a long time enduring this.”
Don’t forget the self-care
There was a time during the pandemic when Dr. Cotton had become so overwhelmed by anxiety that she called the Physician Support Line to get some support from fellow psychiatrists.
“I thought, ‘Why not?’” she recalled. “I helped create the hotline. Why wouldn’t I call it?”
The calls took only a few minutes but they made a difference to Dr. Cotton, who had been severely ill with what she believed was an unconfirmed case of the novel coronavirus. “I immediately felt more like I improved my outlook by focusing on what I could control,” she said, “and accepting the things I could not control.”
Many psychiatrists are finding themselves in similar situations. Fortunately, colleagues are highlighting ways for psychiatrists to care for themselves just as they care for patients.
“One of the challenges clinicians are facing is that they are living through a shared experience in this global pandemic with their patients right now,” said psychologist Randi Pochtar, PhD, who is managing support groups for front-line workers at NYU Langone Health in New York City. “Some might find the work to be overwhelming and anxiety-inducing, and others might find their work to be helpful in managing their own anxiety and stress about the pandemic and its impact.”
Dr. Cotton said her breaking points came when she felt panic amid the pandemic. “I had watched too much news, and I’d seen protesters not taking it seriously, and I was scared for my family and myself. I just needed to feel like someone heard me feeling that way.”
The calls to the hotline were helpful, she said, and so was sharing news about her illness with friends. “So many people reached out to me and checked in on me, people I haven’t seen in years, and that was immensely helpful,” she said.
This sort of personal exposure may not come naturally to physicians and nurses, she said. “We don’t seek that kind of attention when we’re ill. Instead, we say: ‘I’m fine; how are you doing?’ That’s what we do every day of our lives at work.”
How can clinicians help themselves and one another? “Clinicians in our practice have been coping and supporting each other through peer supervision, connecting with colleagues in team meetings, and simply checking in on one another,” said Dr. Pochtar. “In addition, we can adopt many of the strategies that we are likely recommending to our patients, such as maintaining routines as much as possible, engaging in regular exercise, eating well and consistently, and connecting with friends and family.”
Managers can play important roles, said Dr. Fortuna. “I’ve been checking in with my faculty, being as supportive as I can be and highlighting the extraordinary things that people are doing, like going from zero to 100 percent in setting up telehealth.”
Dr. Konzer offered another perspective on recognizing the value of the work that psychiatrists are doing. “We’re on the front line of helping heal the front line, and in that responsibility comes an additional stress,” she said. “But there’s an additional gift of being able to contribute where we are most beneficial. We can try to be present now, versus worrying about what may happen or what lies ahead, and appreciate the beauty in the helpers and the small joys of life.”
Dr. Cotton, Dr. Berkowitz, Dr. Konzer, Dr. Welch, Dr. Fortuna, and Dr. Pochtar reported no relevant disclosures.
Double Masking and Decontamination: A Doctor's COVID-19 Routine

This transcript has been edited for clarity.
Gary S. Ferenchick, MD, MS: I'm Gary Ferenchick with Hannah Ferenchick, who has agreed to join us to talk about the PPE and decontamination processes she's using. Why don't you introduce yourself?
Hannah R.B. Ferenchick, MD: I am Hannah Ferenchick. I'm an ER physician and medical intensivist. I split my time between the medical ICU and the emergency department at Detroit Medical Center.
PPE Routine at the Hospital
Dr Gary Ferenchick: You've developed your own PPE and decontamination routines. It's about protecting yourself at work but also about protecting your loved ones by not carrying the virus home. Could you walk us through it? I'll show it on the screen.
Dr Hannah Ferenchick: At work I wear scrubs, and I try to minimize any additional clothing. I don't wear a jacket over my scrubs, and I don't wear any T-shirts under my scrubs. If I'm going to be in a situation that might involve exposure to patient secretions or bodily fluids, then I also wear shoe covers.
Because so many of our patients are infected and we may be called upon at any time to do an aerosol-generating procedure, in the ED we have all taken to wearing N95 masks for our entire shift. I wear a fitted N95 mask. I cover that with a surgical mask.
We are anticipating N95 shortages because our use of the masks has increased exponentially. Every hospital has to think about how to protect their healthcare workers while conserving PPE. We cover the N95 mask with a surgical mask, so that if there is any soiling or droplets reaching the mask, we are able to change the surgical mask and continue to use the same N95.
In addition, eye protection is important. Generally throughout the shift I wear my own goggles. If I'm going to be involved in any procedure with the potential for aerosolization (intubation, performing CPR, bronchoscopy) then I wear a creation of my own, which is a welder's shield.
Many of our providers have chosen to use their own equipment, although we are still able to use hospital-provided equipment. There is probably no difference in effectiveness between these devices.
Cell Phones and Stethoscopes
I carry a personal cell phone at work (which I often use to look things up, use the calculator, and for other purposes), and I'm cognizant that when I touch it, I am potentially transmitting pathogens to my phone or its cover. So I've taken to keeping my phone in a plastic sandwich bag, which I disinfect a couple of times throughout the shift. The phone still works normally.
After my shift, in my "decontamination phase," I remove the phone from the plastic bag and disinfect the phone again.
I try to avoid bringing objects into the vicinity of the patient. That's different from my normal routine—I usually like to write down what the patient has told me—but unfortunately, carrying pen and paper or a clipboard into a patient's room is not feasible at this point. During this time, I've also avoided using my personal stethoscope.
There's also transmission risk associated with shared equipment. We share hospital-provided phones and they must be disinfected. We are each disinfecting our own workspaces: computer, keyboard, mouse, and countertop.
Obviously you are trying to minimize any contact with your mouth or face. You don't want to rub your eyes, touch your nose, or eat anything with your hands while you are at work. The assumption is that you are doing very frequent hand hygiene.
Decontamination Routine
One of our concerns as healthcare providers is the possibility that we could, either asymptomatically or through the objects that we use at work, be bringing the disease home. We want to protect the people who may be at higher risk just because they live with a healthcare provider. These are the decontamination practices I've developed for my own situation, taken from best practices and suggestions from others.
I remove my dirty scrubs and leave them at work, and I change into a clean pair of scrubs or clean clothes. I disinfect any inanimate objects that my hands may have touched during the shift using alcohol, sanitizer wipes, bleach wipes, or hospital-grade chemical wipes.
To keep those objects clean after disinfecting, I place them in clean plastic bags away from other objects (eg, a wallet or purse) that may not be easy to disinfect. Then I store those bags in the trunk of my car for my next shift, so I'm not taking them into my home.
I also change my shoes, leaving my work shoes in the trunk of my car, and wear another pair of shoes into the house.
When I get home, I basically do everything again. I disinfect my phone, I wash my hands, and I shower immediately. At that point, I consider myself sufficiently "disinfected."
Gary S. Ferenchick, MD, MS, is a family physician and professor in the Department of Medicine at Michigan State University in East Lansing, Michigan. His daughter, Hannah R.B. Ferenchick, MD, is an assistant professor in the Department of Emergency Medicine, Division of Pulmonary & Critical Care and Sleep Medicine at Wayne State University, Detroit, Michigan, and a medical intensivist and emergency medicine physician at Detroit Medical Center.

This transcript has been edited for clarity.
Gary S. Ferenchick, MD, MS: I'm Gary Ferenchick with Hannah Ferenchick, who has agreed to join us to talk about the PPE and decontamination processes she's using. Why don't you introduce yourself?
Hannah R.B. Ferenchick, MD: I am Hannah Ferenchick. I'm an ER physician and medical intensivist. I split my time between the medical ICU and the emergency department at Detroit Medical Center.
PPE Routine at the Hospital
Dr Gary Ferenchick: You've developed your own PPE and decontamination routines. It's about protecting yourself at work but also about protecting your loved ones by not carrying the virus home. Could you walk us through it? I'll show it on the screen.
Dr Hannah Ferenchick: At work I wear scrubs, and I try to minimize any additional clothing. I don't wear a jacket over my scrubs, and I don't wear any T-shirts under my scrubs. If I'm going to be in a situation that might involve exposure to patient secretions or bodily fluids, then I also wear shoe covers.
Because so many of our patients are infected and we may be called upon at any time to do an aerosol-generating procedure, in the ED we have all taken to wearing N95 masks for our entire shift. I wear a fitted N95 mask. I cover that with a surgical mask.
We are anticipating N95 shortages because our use of the masks has increased exponentially. Every hospital has to think about how to protect their healthcare workers while conserving PPE. We cover the N95 mask with a surgical mask, so that if there is any soiling or droplets reaching the mask, we are able to change the surgical mask and continue to use the same N95.
In addition, eye protection is important. Generally throughout the shift I wear my own goggles. If I'm going to be involved in any procedure with the potential for aerosolization (intubation, performing CPR, bronchoscopy) then I wear a creation of my own, which is a welder's shield.
Many of our providers have chosen to use their own equipment, although we are still able to use hospital-provided equipment. There is probably no difference in effectiveness between these devices.
Cell Phones and Stethoscopes
I carry a personal cell phone at work (which I often use to look things up, use the calculator, and for other purposes), and I'm cognizant that when I touch it, I am potentially transmitting pathogens to my phone or its cover. So I've taken to keeping my phone in a plastic sandwich bag, which I disinfect a couple of times throughout the shift. The phone still works normally.
After my shift, in my "decontamination phase," I remove the phone from the plastic bag and disinfect the phone again.
I try to avoid bringing objects into the vicinity of the patient. That's different from my normal routine—I usually like to write down what the patient has told me—but unfortunately, carrying pen and paper or a clipboard into a patient's room is not feasible at this point. During this time, I've also avoided using my personal stethoscope.
There's also transmission risk associated with shared equipment. We share hospital-provided phones and they must be disinfected. We are each disinfecting our own workspaces: computer, keyboard, mouse, and countertop.
Obviously you are trying to minimize any contact with your mouth or face. You don't want to rub your eyes, touch your nose, or eat anything with your hands while you are at work. The assumption is that you are doing very frequent hand hygiene.
Decontamination Routine
One of our concerns as healthcare providers is the possibility that we could, either asymptomatically or through the objects that we use at work, be bringing the disease home. We want to protect the people who may be at higher risk just because they live with a healthcare provider. These are the decontamination practices I've developed for my own situation, taken from best practices and suggestions from others.
I remove my dirty scrubs and leave them at work, and I change into a clean pair of scrubs or clean clothes. I disinfect any inanimate objects that my hands may have touched during the shift using alcohol, sanitizer wipes, bleach wipes, or hospital-grade chemical wipes.
To keep those objects clean after disinfecting, I place them in clean plastic bags away from other objects (eg, a wallet or purse) that may not be easy to disinfect. Then I store those bags in the trunk of my car for my next shift, so I'm not taking them into my home.
I also change my shoes, leaving my work shoes in the trunk of my car, and wear another pair of shoes into the house.
When I get home, I basically do everything again. I disinfect my phone, I wash my hands, and I shower immediately. At that point, I consider myself sufficiently "disinfected."
Gary S. Ferenchick, MD, MS, is a family physician and professor in the Department of Medicine at Michigan State University in East Lansing, Michigan. His daughter, Hannah R.B. Ferenchick, MD, is an assistant professor in the Department of Emergency Medicine, Division of Pulmonary & Critical Care and Sleep Medicine at Wayne State University, Detroit, Michigan, and a medical intensivist and emergency medicine physician at Detroit Medical Center.

This transcript has been edited for clarity.
Gary S. Ferenchick, MD, MS: I'm Gary Ferenchick with Hannah Ferenchick, who has agreed to join us to talk about the PPE and decontamination processes she's using. Why don't you introduce yourself?
Hannah R.B. Ferenchick, MD: I am Hannah Ferenchick. I'm an ER physician and medical intensivist. I split my time between the medical ICU and the emergency department at Detroit Medical Center.
PPE Routine at the Hospital
Dr Gary Ferenchick: You've developed your own PPE and decontamination routines. It's about protecting yourself at work but also about protecting your loved ones by not carrying the virus home. Could you walk us through it? I'll show it on the screen.
Dr Hannah Ferenchick: At work I wear scrubs, and I try to minimize any additional clothing. I don't wear a jacket over my scrubs, and I don't wear any T-shirts under my scrubs. If I'm going to be in a situation that might involve exposure to patient secretions or bodily fluids, then I also wear shoe covers.
Because so many of our patients are infected and we may be called upon at any time to do an aerosol-generating procedure, in the ED we have all taken to wearing N95 masks for our entire shift. I wear a fitted N95 mask. I cover that with a surgical mask.
We are anticipating N95 shortages because our use of the masks has increased exponentially. Every hospital has to think about how to protect their healthcare workers while conserving PPE. We cover the N95 mask with a surgical mask, so that if there is any soiling or droplets reaching the mask, we are able to change the surgical mask and continue to use the same N95.
In addition, eye protection is important. Generally throughout the shift I wear my own goggles. If I'm going to be involved in any procedure with the potential for aerosolization (intubation, performing CPR, bronchoscopy) then I wear a creation of my own, which is a welder's shield.
Many of our providers have chosen to use their own equipment, although we are still able to use hospital-provided equipment. There is probably no difference in effectiveness between these devices.
Cell Phones and Stethoscopes
I carry a personal cell phone at work (which I often use to look things up, use the calculator, and for other purposes), and I'm cognizant that when I touch it, I am potentially transmitting pathogens to my phone or its cover. So I've taken to keeping my phone in a plastic sandwich bag, which I disinfect a couple of times throughout the shift. The phone still works normally.
After my shift, in my "decontamination phase," I remove the phone from the plastic bag and disinfect the phone again.
I try to avoid bringing objects into the vicinity of the patient. That's different from my normal routine—I usually like to write down what the patient has told me—but unfortunately, carrying pen and paper or a clipboard into a patient's room is not feasible at this point. During this time, I've also avoided using my personal stethoscope.
There's also transmission risk associated with shared equipment. We share hospital-provided phones and they must be disinfected. We are each disinfecting our own workspaces: computer, keyboard, mouse, and countertop.
Obviously you are trying to minimize any contact with your mouth or face. You don't want to rub your eyes, touch your nose, or eat anything with your hands while you are at work. The assumption is that you are doing very frequent hand hygiene.
Decontamination Routine
One of our concerns as healthcare providers is the possibility that we could, either asymptomatically or through the objects that we use at work, be bringing the disease home. We want to protect the people who may be at higher risk just because they live with a healthcare provider. These are the decontamination practices I've developed for my own situation, taken from best practices and suggestions from others.
I remove my dirty scrubs and leave them at work, and I change into a clean pair of scrubs or clean clothes. I disinfect any inanimate objects that my hands may have touched during the shift using alcohol, sanitizer wipes, bleach wipes, or hospital-grade chemical wipes.
To keep those objects clean after disinfecting, I place them in clean plastic bags away from other objects (eg, a wallet or purse) that may not be easy to disinfect. Then I store those bags in the trunk of my car for my next shift, so I'm not taking them into my home.
I also change my shoes, leaving my work shoes in the trunk of my car, and wear another pair of shoes into the house.
When I get home, I basically do everything again. I disinfect my phone, I wash my hands, and I shower immediately. At that point, I consider myself sufficiently "disinfected."
Gary S. Ferenchick, MD, MS, is a family physician and professor in the Department of Medicine at Michigan State University in East Lansing, Michigan. His daughter, Hannah R.B. Ferenchick, MD, is an assistant professor in the Department of Emergency Medicine, Division of Pulmonary & Critical Care and Sleep Medicine at Wayne State University, Detroit, Michigan, and a medical intensivist and emergency medicine physician at Detroit Medical Center.
Pruritic Papules on the Face and Chest
The Diagnosis: Eosinophilic Folliculitis
A shave biopsy specimen of an intact pustule on the left side of the chest was obtained. Histopathologic examination revealed follicular inflammation with copious eosinophils (Figure, A and B). Based on the histopathology and clinical presentation, a diagnosis of human immunodeficiency virus (HIV)-associated eosinophilic folliculitis (EF) was made.
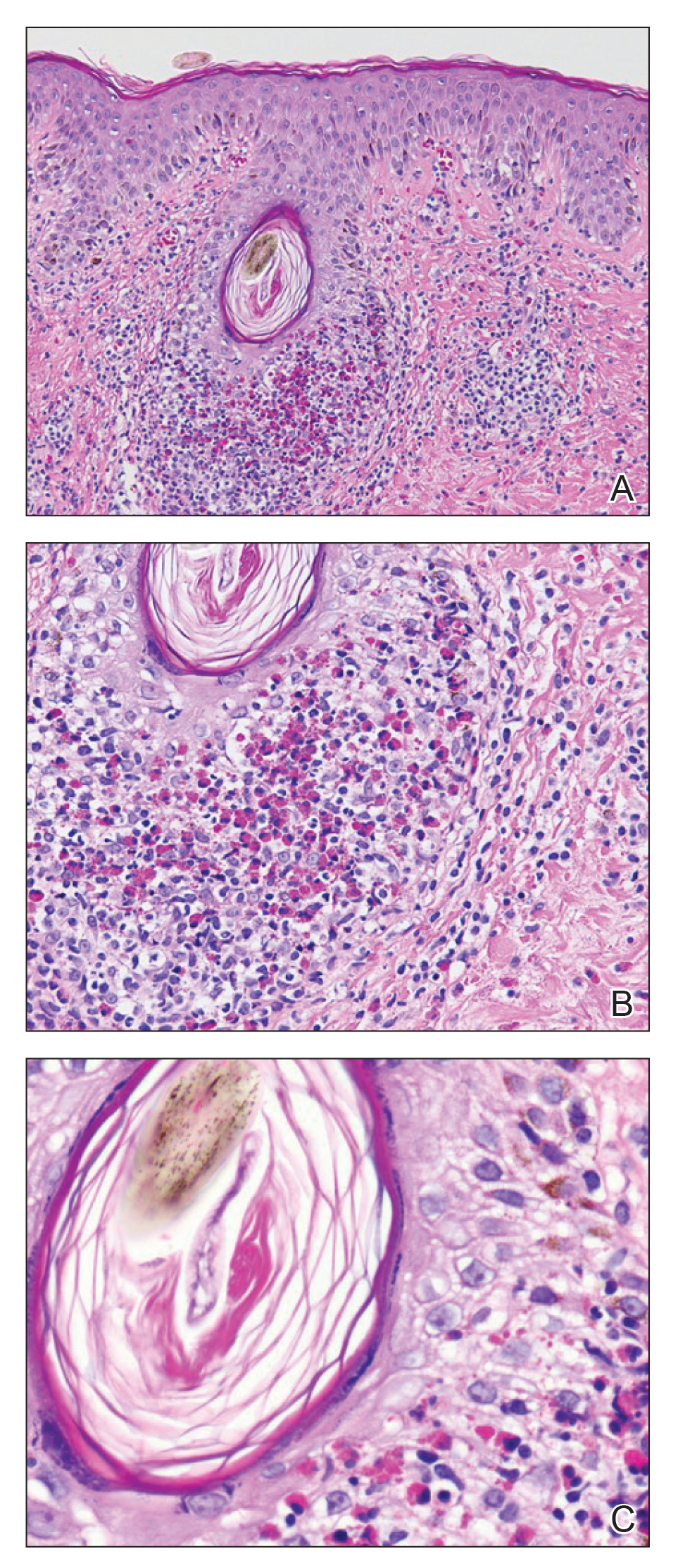
The patient was started on triamcinolone ointment 0.1% twice daily to active lesions, oral cetirizine 10 mg in the morning, and oral hydroxyzine 25 mg at bedtime. Laboratory evaluation at the time of diagnosis showed eosinophilia with a peripheral blood eosinophil count of 0.5 K/μL (reference range, 0.03–0.48 K/μL).
Human immunodeficiency virus-associated EF is a pruritic follicular eruption that occurs in HIV-positive individuals with advanced disease. Clinically, it is characterized by intermittent, urticarial, red or flesh-colored, 2- to 5-mm papules with sparse pustules involving the head, neck, arms, and upper trunk.1,2 The cardinal clinical feature of the disorder is intense pruritus, with overlying crusts and excoriations present on physical examination.3
Patients usually have a CD4 count of less than 250 cells/mm3.2,3 Patients with HIV can develop an exacerbation of EF in the first 3 to 6 months after initiating antiretroviral therapy. This clinical pattern is believed to be due to the reconstituted immune system and increased circulation of inflammatory cells.4 Peripheral eosinophilia and elevated serum IgE levels are found in 25% to 50% of patients with HIV-associated EF.2,3
Clinically, the differential diagnosis of intensely pruritic papules with excoriations should include scabies.3 Other diagnoses to consider include opportunistic infections and papular urticaria.5 Acne vulgaris and Demodex folliculitis also may present with lesions similar to HIV-associated EF; however, these lesions tend not to be as intensely pruritic.1,5
The etiology of HIV-associated EF is unknown.3 One proposed mechanism involves a hypersensitivity reaction to Pityrosporum or Demodex mite fragments, as evidenced by studies that found fragments of these microorganisms in biopsied lesions of HIV-associated EF.3,6 In our patient's histopathology, it was noted that the afflicted hair follicle held a single Demodex mite (Figure, C).
The histopathology is characterized by a perifollicular inflammatory infiltrate of eosinophils and CD8+ lymphocytes with areas of sebaceous lysis.3,6 Spongiosis of the follicular epithelium is seen in early lesions of HIV-associated EF.6
The first-line treatment of HIV-associated EF includes antiretroviral therapy with topical steroids and antihistamines. Human immunodeficiency virus-associated EF improves as CD4 helper T-cell counts rise above 250 cells/mm3 with continued antiretroviral therapy, though it initially can cause a flare of the condition.4 High-potency steroids and antihistamines are added during this period to treat the severe pruritus.1,7 In particular, daily cetirizine has been shown to be effective, which may be due to its ability to block eosinophil migration in addition to H1-receptor antagonist properties.3,7
Various alternative therapies have been described in case reports and case series; however, there have been no controlled studies comparing therapies. Phototherapy with UVB light 3 times weekly for 3 to 6 weeks has been effective and curative in recalcitrant cases.7 Other frequently used treatments include oral metronidazole, oral itraconazole, and permethrin cream 5%. The effectiveness of the latter 2 treatments is believed to be related to the proposed role of Pityrosporum and Demodex in the pathogenesis.3
Acknowledgment
The authors thank Garth Fraga, MD (Kansas City, Kansas), for his help compiling the histopathological images and their diagnostic descriptions.
- Parker SR, Parker DC, McCall CO. Eosinophilic folliculitis in HIV-infected women: case series and review. Am J Clin Dermatol. 2006;7:193-200.
- Rosenthal D, LeBoit PE, Klumpp L, et al. Human immunodeficiency virus-associated eosinophilic folliculitis. a unique dermatosis associated with advanced human immunodeficiency virus infection. Arch Dermatol. 1991;127:206-209.
- Fearfield LA, Rowe A, Francis N, et al. Itchy folliculitis and human immunodeficiency virus infection: clinicopathological and immunological features, pathogenesis, and treatment. Br J Dermatol. 1999;141:3-11.
- Rajendran PM, Dolev JC, Heaphy MR, et al. Eosinophilic folliculitis: before and after the introduction of antiretroviral therapy. Arch Dermatol. 2005;141:1227-1231.
- Nervi SJ, Schwartz RA, Dmochowski M. Eosinophilic pustular folliculitis: a 40 year retrospect. J Am Acad Dermatol. 2006;55:285-289.
- McCalmont TH, Altemus D, Maurer T, et al. Eosinophilic folliculitis: the histological spectrum. Am J Dermatopathol. 1995;17:439-446.
- Ellis E, Scheinfeld N. Eosinophilic pustular folliculitis: a comprehensive review of treatment options. Am J Clin Dermatol. 2004;5:189-197.
The Diagnosis: Eosinophilic Folliculitis
A shave biopsy specimen of an intact pustule on the left side of the chest was obtained. Histopathologic examination revealed follicular inflammation with copious eosinophils (Figure, A and B). Based on the histopathology and clinical presentation, a diagnosis of human immunodeficiency virus (HIV)-associated eosinophilic folliculitis (EF) was made.
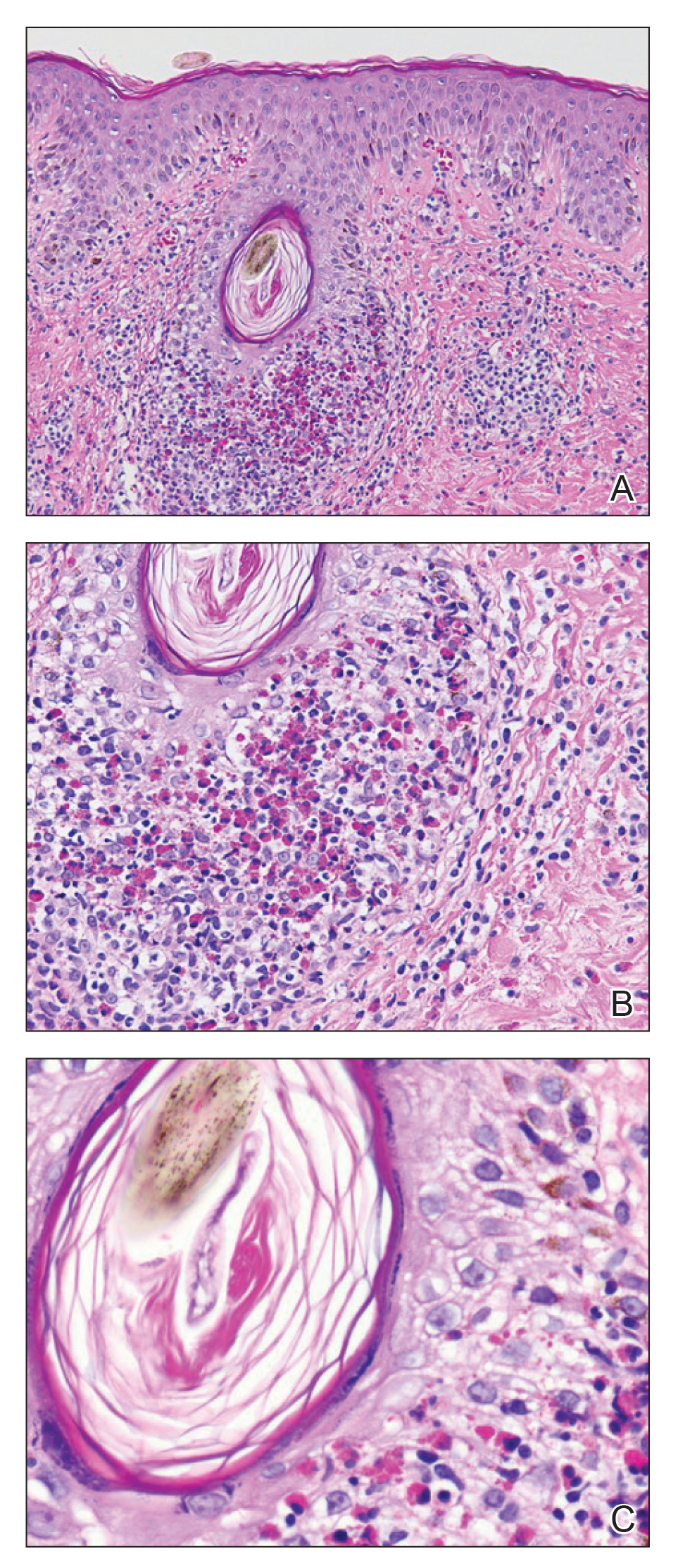
The patient was started on triamcinolone ointment 0.1% twice daily to active lesions, oral cetirizine 10 mg in the morning, and oral hydroxyzine 25 mg at bedtime. Laboratory evaluation at the time of diagnosis showed eosinophilia with a peripheral blood eosinophil count of 0.5 K/μL (reference range, 0.03–0.48 K/μL).
Human immunodeficiency virus-associated EF is a pruritic follicular eruption that occurs in HIV-positive individuals with advanced disease. Clinically, it is characterized by intermittent, urticarial, red or flesh-colored, 2- to 5-mm papules with sparse pustules involving the head, neck, arms, and upper trunk.1,2 The cardinal clinical feature of the disorder is intense pruritus, with overlying crusts and excoriations present on physical examination.3
Patients usually have a CD4 count of less than 250 cells/mm3.2,3 Patients with HIV can develop an exacerbation of EF in the first 3 to 6 months after initiating antiretroviral therapy. This clinical pattern is believed to be due to the reconstituted immune system and increased circulation of inflammatory cells.4 Peripheral eosinophilia and elevated serum IgE levels are found in 25% to 50% of patients with HIV-associated EF.2,3
Clinically, the differential diagnosis of intensely pruritic papules with excoriations should include scabies.3 Other diagnoses to consider include opportunistic infections and papular urticaria.5 Acne vulgaris and Demodex folliculitis also may present with lesions similar to HIV-associated EF; however, these lesions tend not to be as intensely pruritic.1,5
The etiology of HIV-associated EF is unknown.3 One proposed mechanism involves a hypersensitivity reaction to Pityrosporum or Demodex mite fragments, as evidenced by studies that found fragments of these microorganisms in biopsied lesions of HIV-associated EF.3,6 In our patient's histopathology, it was noted that the afflicted hair follicle held a single Demodex mite (Figure, C).
The histopathology is characterized by a perifollicular inflammatory infiltrate of eosinophils and CD8+ lymphocytes with areas of sebaceous lysis.3,6 Spongiosis of the follicular epithelium is seen in early lesions of HIV-associated EF.6
The first-line treatment of HIV-associated EF includes antiretroviral therapy with topical steroids and antihistamines. Human immunodeficiency virus-associated EF improves as CD4 helper T-cell counts rise above 250 cells/mm3 with continued antiretroviral therapy, though it initially can cause a flare of the condition.4 High-potency steroids and antihistamines are added during this period to treat the severe pruritus.1,7 In particular, daily cetirizine has been shown to be effective, which may be due to its ability to block eosinophil migration in addition to H1-receptor antagonist properties.3,7
Various alternative therapies have been described in case reports and case series; however, there have been no controlled studies comparing therapies. Phototherapy with UVB light 3 times weekly for 3 to 6 weeks has been effective and curative in recalcitrant cases.7 Other frequently used treatments include oral metronidazole, oral itraconazole, and permethrin cream 5%. The effectiveness of the latter 2 treatments is believed to be related to the proposed role of Pityrosporum and Demodex in the pathogenesis.3
Acknowledgment
The authors thank Garth Fraga, MD (Kansas City, Kansas), for his help compiling the histopathological images and their diagnostic descriptions.
The Diagnosis: Eosinophilic Folliculitis
A shave biopsy specimen of an intact pustule on the left side of the chest was obtained. Histopathologic examination revealed follicular inflammation with copious eosinophils (Figure, A and B). Based on the histopathology and clinical presentation, a diagnosis of human immunodeficiency virus (HIV)-associated eosinophilic folliculitis (EF) was made.
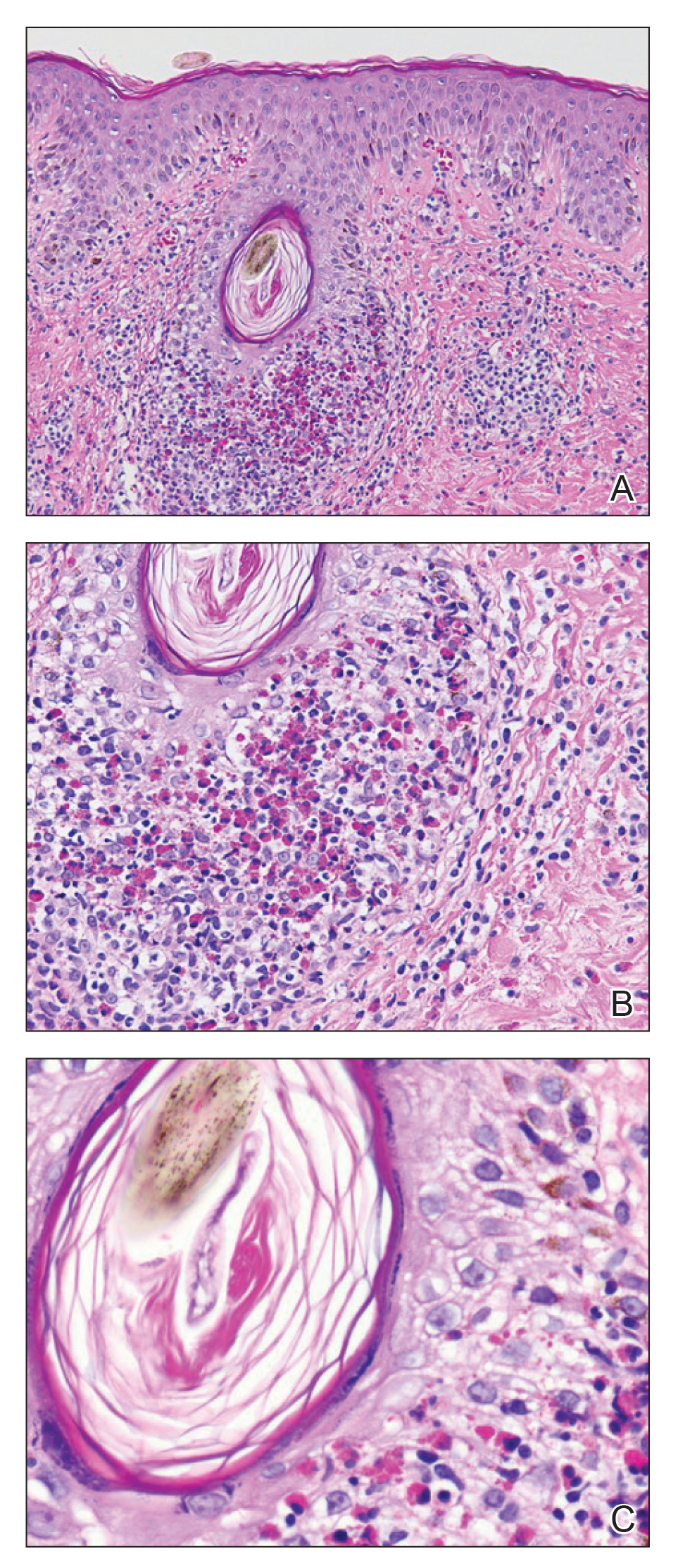
The patient was started on triamcinolone ointment 0.1% twice daily to active lesions, oral cetirizine 10 mg in the morning, and oral hydroxyzine 25 mg at bedtime. Laboratory evaluation at the time of diagnosis showed eosinophilia with a peripheral blood eosinophil count of 0.5 K/μL (reference range, 0.03–0.48 K/μL).
Human immunodeficiency virus-associated EF is a pruritic follicular eruption that occurs in HIV-positive individuals with advanced disease. Clinically, it is characterized by intermittent, urticarial, red or flesh-colored, 2- to 5-mm papules with sparse pustules involving the head, neck, arms, and upper trunk.1,2 The cardinal clinical feature of the disorder is intense pruritus, with overlying crusts and excoriations present on physical examination.3
Patients usually have a CD4 count of less than 250 cells/mm3.2,3 Patients with HIV can develop an exacerbation of EF in the first 3 to 6 months after initiating antiretroviral therapy. This clinical pattern is believed to be due to the reconstituted immune system and increased circulation of inflammatory cells.4 Peripheral eosinophilia and elevated serum IgE levels are found in 25% to 50% of patients with HIV-associated EF.2,3
Clinically, the differential diagnosis of intensely pruritic papules with excoriations should include scabies.3 Other diagnoses to consider include opportunistic infections and papular urticaria.5 Acne vulgaris and Demodex folliculitis also may present with lesions similar to HIV-associated EF; however, these lesions tend not to be as intensely pruritic.1,5
The etiology of HIV-associated EF is unknown.3 One proposed mechanism involves a hypersensitivity reaction to Pityrosporum or Demodex mite fragments, as evidenced by studies that found fragments of these microorganisms in biopsied lesions of HIV-associated EF.3,6 In our patient's histopathology, it was noted that the afflicted hair follicle held a single Demodex mite (Figure, C).
The histopathology is characterized by a perifollicular inflammatory infiltrate of eosinophils and CD8+ lymphocytes with areas of sebaceous lysis.3,6 Spongiosis of the follicular epithelium is seen in early lesions of HIV-associated EF.6
The first-line treatment of HIV-associated EF includes antiretroviral therapy with topical steroids and antihistamines. Human immunodeficiency virus-associated EF improves as CD4 helper T-cell counts rise above 250 cells/mm3 with continued antiretroviral therapy, though it initially can cause a flare of the condition.4 High-potency steroids and antihistamines are added during this period to treat the severe pruritus.1,7 In particular, daily cetirizine has been shown to be effective, which may be due to its ability to block eosinophil migration in addition to H1-receptor antagonist properties.3,7
Various alternative therapies have been described in case reports and case series; however, there have been no controlled studies comparing therapies. Phototherapy with UVB light 3 times weekly for 3 to 6 weeks has been effective and curative in recalcitrant cases.7 Other frequently used treatments include oral metronidazole, oral itraconazole, and permethrin cream 5%. The effectiveness of the latter 2 treatments is believed to be related to the proposed role of Pityrosporum and Demodex in the pathogenesis.3
Acknowledgment
The authors thank Garth Fraga, MD (Kansas City, Kansas), for his help compiling the histopathological images and their diagnostic descriptions.
- Parker SR, Parker DC, McCall CO. Eosinophilic folliculitis in HIV-infected women: case series and review. Am J Clin Dermatol. 2006;7:193-200.
- Rosenthal D, LeBoit PE, Klumpp L, et al. Human immunodeficiency virus-associated eosinophilic folliculitis. a unique dermatosis associated with advanced human immunodeficiency virus infection. Arch Dermatol. 1991;127:206-209.
- Fearfield LA, Rowe A, Francis N, et al. Itchy folliculitis and human immunodeficiency virus infection: clinicopathological and immunological features, pathogenesis, and treatment. Br J Dermatol. 1999;141:3-11.
- Rajendran PM, Dolev JC, Heaphy MR, et al. Eosinophilic folliculitis: before and after the introduction of antiretroviral therapy. Arch Dermatol. 2005;141:1227-1231.
- Nervi SJ, Schwartz RA, Dmochowski M. Eosinophilic pustular folliculitis: a 40 year retrospect. J Am Acad Dermatol. 2006;55:285-289.
- McCalmont TH, Altemus D, Maurer T, et al. Eosinophilic folliculitis: the histological spectrum. Am J Dermatopathol. 1995;17:439-446.
- Ellis E, Scheinfeld N. Eosinophilic pustular folliculitis: a comprehensive review of treatment options. Am J Clin Dermatol. 2004;5:189-197.
- Parker SR, Parker DC, McCall CO. Eosinophilic folliculitis in HIV-infected women: case series and review. Am J Clin Dermatol. 2006;7:193-200.
- Rosenthal D, LeBoit PE, Klumpp L, et al. Human immunodeficiency virus-associated eosinophilic folliculitis. a unique dermatosis associated with advanced human immunodeficiency virus infection. Arch Dermatol. 1991;127:206-209.
- Fearfield LA, Rowe A, Francis N, et al. Itchy folliculitis and human immunodeficiency virus infection: clinicopathological and immunological features, pathogenesis, and treatment. Br J Dermatol. 1999;141:3-11.
- Rajendran PM, Dolev JC, Heaphy MR, et al. Eosinophilic folliculitis: before and after the introduction of antiretroviral therapy. Arch Dermatol. 2005;141:1227-1231.
- Nervi SJ, Schwartz RA, Dmochowski M. Eosinophilic pustular folliculitis: a 40 year retrospect. J Am Acad Dermatol. 2006;55:285-289.
- McCalmont TH, Altemus D, Maurer T, et al. Eosinophilic folliculitis: the histological spectrum. Am J Dermatopathol. 1995;17:439-446.
- Ellis E, Scheinfeld N. Eosinophilic pustular folliculitis: a comprehensive review of treatment options. Am J Clin Dermatol. 2004;5:189-197.

A 31-year-old man presented with a severely pruritic rash of 2 weeks' duration. Physical examination revealed numerous urticarial papules and rare erythematous pustules over the face (top), upper chest (bottom), and proximal arms; most lesions were excoriated. Additionally, there were numerous hyperpigmented papules with central hypopigmentation on the upper chest and arms. The lower half of the body was spared. His medical history was notable for human immunodeficiency virus/AIDS with a prior episode of Pneumocystis pneumonia. He had been noncompliant with antiretroviral therapy for the last 2 years but restarted therapy 3 weeks prior to presentation. Laboratory test results revealed a CD4 cell count of 13 cells/mm3 (reference range, 500-1500 cells/mm3) with a viral load of 179 copies/mL (reference range, undetectable).
Management of infants born to mothers with COVID-19
Initial guidance for pediatric hospitalists
Clinical question: How should we care for newborns born to mothers with COVID-19?
Background: Around the United States, the SARS-CoV-2 virus is infecting pregnant mothers and causing COVID-19. Current limited data demonstrates that children under the age of 1 year are at risk for severe disease. Clinicians are caring for infants born to mothers with COVID-19 during the pandemic with minimal guidance.
Study design: Clinical practice guidelines.
Synopsis: The American Academy of Pediatrics’ Committee on Fetus and Newborn, Section on Neonatal and Perinatal Medicine and Committee of Infectious Diseases developed guidelines of care for infants born to COVID-19 mothers to help clinicians care for newborns using limited data published before March 30, 2020.
- Neonates should be considered persons under investigation (PUIs) if they are born to mothers with diagnosed COVID-19 or with COVID-19 tests pending at the time of delivery.
- Neonatal clinicians should attend deliveries based on their center’s policies. If clinicians are required to perform stabilization they should use airborne, droplet, and contact personal protective equipment (PPE). This includes, gown, gloves, eye protection (goggles or face shield), and N95 respirator mask or an air-purifying respirator.
- Mother and newborn should be separated to minimize the infant’s risk of postnatal infection.
- Well newborns born at or near term may be admitted to areas physically separated from newborns unaffected by maternal COVID-19. Alternatively, a mother may room-in with her infant with 6 feet of separation between mother and infant. Newborn PUIs should be bathed as soon as possible.
- Newborns requiring intensive care should be admitted to a single negative-pressure room. Alternatively, COVID-19–exposed infants should be grouped with a minimum of 6 feet of separation, or placed in air temperature-controlled isolettes.
- Until the newborn PUI’s virologic status is known, clinical staff caring for the infant should use droplet and contact PPE. This includes gown, gloves, eye protection (goggles or face shield), and a standard surgical mask. Airborne, droplet, and contact precautions should be used for infants requiring CPAP or any form of mechanical ventilation.
- COVID-19–positive mothers who want to breastfeed may feed expressed breast milk using proper breast and hand hygiene or directly breastfeed their infants wearing a mask while practicing proper breast and hand hygiene.
- If testing is available, newborns should be tested for SARS-CoV-2 using molecular arrays. If testing is unavailable, clinicians may monitor newborns clinically. Infants should be tested if they require prolonged intensive care.
- Optimal timing and extent of testing is unknown. Tests should be performed around 24 hours of life and 48 hours of life. If discharge is planned for a well appearing infant before 48 hours of life, the clinician may choose not to do the 48-hour test. A single swab should be taken from the throat followed by the nasopharynx to perform the test.
- Newborns should receive all newborn care, including circumcision if requested.
- Infants who are asymptomatic with positive or pending SARS-CoV-2 tests may be discharged home with plans for frequent outpatient follow-up through 14 days after birth. Infants with negative SARS-CoV-2 testing should be discharged to the care of a noninfected caregiver. If the mother lives in the same household, she must keep a distance of 6 feet as often as possible. When not possible, the mother should wear a mask and practice hand hygiene. The mother may resume caring for her infant normally when she has been afebrile for more than 72 hours (without antipyretics) and has been asymptomatic for 7 days. Alternatively, the mother may resume care if she has two consecutive negative SARS-CoV-2 nasopharyngeal swabs taken more than 24 hours apart.
- Visitation to infants requiring intensive care should be limited for mothers with COVID-19 until her fever has resolved for more than 72 hours and has improvement of respiratory symptoms and has had two consecutive negative SARS-CoV-2 nasopharyngeal swabs taken more than 24 hours apart.
Bottom line: Clinicians should protect themselves with contact and droplet PPE at all times until the infant’s viral status is known. Clinicians should use airborne, contact, and droplet PPE when resuscitating the infant and/or when using CPAP/mechanical ventilation. Mothers should be encouraged to feed their infants expressed breast milk while practicing proper hygiene or directly breastfeed while wearing a mask and practicing proper hygiene. Viral testing of every infant born to a mother with COVID-19 should be performed after the infant is 24 hours old. Mothers should resume caring for their infants normally after they have met criteria suggesting they are no longer actively infected.
Article citation: Puopolo KM, Hudak ML, Kimberlin DW, Cummings J. Initial Guidance: Management of Infants born to Mothers with COVID-19. 2020 Apr 2. https://downloads.aap.org/AAP/PDF/COVID%2019%20Initial%20Newborn%20Guidance.pdf. Accessed Apr 2, 2020.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s. She is a clinical assistant professor of pediatrics at Case Western Reserve University, Cleveland, and serves as the Pediatrics Editor for The Hospitalist.
Initial guidance for pediatric hospitalists
Initial guidance for pediatric hospitalists
Clinical question: How should we care for newborns born to mothers with COVID-19?
Background: Around the United States, the SARS-CoV-2 virus is infecting pregnant mothers and causing COVID-19. Current limited data demonstrates that children under the age of 1 year are at risk for severe disease. Clinicians are caring for infants born to mothers with COVID-19 during the pandemic with minimal guidance.
Study design: Clinical practice guidelines.
Synopsis: The American Academy of Pediatrics’ Committee on Fetus and Newborn, Section on Neonatal and Perinatal Medicine and Committee of Infectious Diseases developed guidelines of care for infants born to COVID-19 mothers to help clinicians care for newborns using limited data published before March 30, 2020.
- Neonates should be considered persons under investigation (PUIs) if they are born to mothers with diagnosed COVID-19 or with COVID-19 tests pending at the time of delivery.
- Neonatal clinicians should attend deliveries based on their center’s policies. If clinicians are required to perform stabilization they should use airborne, droplet, and contact personal protective equipment (PPE). This includes, gown, gloves, eye protection (goggles or face shield), and N95 respirator mask or an air-purifying respirator.
- Mother and newborn should be separated to minimize the infant’s risk of postnatal infection.
- Well newborns born at or near term may be admitted to areas physically separated from newborns unaffected by maternal COVID-19. Alternatively, a mother may room-in with her infant with 6 feet of separation between mother and infant. Newborn PUIs should be bathed as soon as possible.
- Newborns requiring intensive care should be admitted to a single negative-pressure room. Alternatively, COVID-19–exposed infants should be grouped with a minimum of 6 feet of separation, or placed in air temperature-controlled isolettes.
- Until the newborn PUI’s virologic status is known, clinical staff caring for the infant should use droplet and contact PPE. This includes gown, gloves, eye protection (goggles or face shield), and a standard surgical mask. Airborne, droplet, and contact precautions should be used for infants requiring CPAP or any form of mechanical ventilation.
- COVID-19–positive mothers who want to breastfeed may feed expressed breast milk using proper breast and hand hygiene or directly breastfeed their infants wearing a mask while practicing proper breast and hand hygiene.
- If testing is available, newborns should be tested for SARS-CoV-2 using molecular arrays. If testing is unavailable, clinicians may monitor newborns clinically. Infants should be tested if they require prolonged intensive care.
- Optimal timing and extent of testing is unknown. Tests should be performed around 24 hours of life and 48 hours of life. If discharge is planned for a well appearing infant before 48 hours of life, the clinician may choose not to do the 48-hour test. A single swab should be taken from the throat followed by the nasopharynx to perform the test.
- Newborns should receive all newborn care, including circumcision if requested.
- Infants who are asymptomatic with positive or pending SARS-CoV-2 tests may be discharged home with plans for frequent outpatient follow-up through 14 days after birth. Infants with negative SARS-CoV-2 testing should be discharged to the care of a noninfected caregiver. If the mother lives in the same household, she must keep a distance of 6 feet as often as possible. When not possible, the mother should wear a mask and practice hand hygiene. The mother may resume caring for her infant normally when she has been afebrile for more than 72 hours (without antipyretics) and has been asymptomatic for 7 days. Alternatively, the mother may resume care if she has two consecutive negative SARS-CoV-2 nasopharyngeal swabs taken more than 24 hours apart.
- Visitation to infants requiring intensive care should be limited for mothers with COVID-19 until her fever has resolved for more than 72 hours and has improvement of respiratory symptoms and has had two consecutive negative SARS-CoV-2 nasopharyngeal swabs taken more than 24 hours apart.
Bottom line: Clinicians should protect themselves with contact and droplet PPE at all times until the infant’s viral status is known. Clinicians should use airborne, contact, and droplet PPE when resuscitating the infant and/or when using CPAP/mechanical ventilation. Mothers should be encouraged to feed their infants expressed breast milk while practicing proper hygiene or directly breastfeed while wearing a mask and practicing proper hygiene. Viral testing of every infant born to a mother with COVID-19 should be performed after the infant is 24 hours old. Mothers should resume caring for their infants normally after they have met criteria suggesting they are no longer actively infected.
Article citation: Puopolo KM, Hudak ML, Kimberlin DW, Cummings J. Initial Guidance: Management of Infants born to Mothers with COVID-19. 2020 Apr 2. https://downloads.aap.org/AAP/PDF/COVID%2019%20Initial%20Newborn%20Guidance.pdf. Accessed Apr 2, 2020.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s. She is a clinical assistant professor of pediatrics at Case Western Reserve University, Cleveland, and serves as the Pediatrics Editor for The Hospitalist.
Clinical question: How should we care for newborns born to mothers with COVID-19?
Background: Around the United States, the SARS-CoV-2 virus is infecting pregnant mothers and causing COVID-19. Current limited data demonstrates that children under the age of 1 year are at risk for severe disease. Clinicians are caring for infants born to mothers with COVID-19 during the pandemic with minimal guidance.
Study design: Clinical practice guidelines.
Synopsis: The American Academy of Pediatrics’ Committee on Fetus and Newborn, Section on Neonatal and Perinatal Medicine and Committee of Infectious Diseases developed guidelines of care for infants born to COVID-19 mothers to help clinicians care for newborns using limited data published before March 30, 2020.
- Neonates should be considered persons under investigation (PUIs) if they are born to mothers with diagnosed COVID-19 or with COVID-19 tests pending at the time of delivery.
- Neonatal clinicians should attend deliveries based on their center’s policies. If clinicians are required to perform stabilization they should use airborne, droplet, and contact personal protective equipment (PPE). This includes, gown, gloves, eye protection (goggles or face shield), and N95 respirator mask or an air-purifying respirator.
- Mother and newborn should be separated to minimize the infant’s risk of postnatal infection.
- Well newborns born at or near term may be admitted to areas physically separated from newborns unaffected by maternal COVID-19. Alternatively, a mother may room-in with her infant with 6 feet of separation between mother and infant. Newborn PUIs should be bathed as soon as possible.
- Newborns requiring intensive care should be admitted to a single negative-pressure room. Alternatively, COVID-19–exposed infants should be grouped with a minimum of 6 feet of separation, or placed in air temperature-controlled isolettes.
- Until the newborn PUI’s virologic status is known, clinical staff caring for the infant should use droplet and contact PPE. This includes gown, gloves, eye protection (goggles or face shield), and a standard surgical mask. Airborne, droplet, and contact precautions should be used for infants requiring CPAP or any form of mechanical ventilation.
- COVID-19–positive mothers who want to breastfeed may feed expressed breast milk using proper breast and hand hygiene or directly breastfeed their infants wearing a mask while practicing proper breast and hand hygiene.
- If testing is available, newborns should be tested for SARS-CoV-2 using molecular arrays. If testing is unavailable, clinicians may monitor newborns clinically. Infants should be tested if they require prolonged intensive care.
- Optimal timing and extent of testing is unknown. Tests should be performed around 24 hours of life and 48 hours of life. If discharge is planned for a well appearing infant before 48 hours of life, the clinician may choose not to do the 48-hour test. A single swab should be taken from the throat followed by the nasopharynx to perform the test.
- Newborns should receive all newborn care, including circumcision if requested.
- Infants who are asymptomatic with positive or pending SARS-CoV-2 tests may be discharged home with plans for frequent outpatient follow-up through 14 days after birth. Infants with negative SARS-CoV-2 testing should be discharged to the care of a noninfected caregiver. If the mother lives in the same household, she must keep a distance of 6 feet as often as possible. When not possible, the mother should wear a mask and practice hand hygiene. The mother may resume caring for her infant normally when she has been afebrile for more than 72 hours (without antipyretics) and has been asymptomatic for 7 days. Alternatively, the mother may resume care if she has two consecutive negative SARS-CoV-2 nasopharyngeal swabs taken more than 24 hours apart.
- Visitation to infants requiring intensive care should be limited for mothers with COVID-19 until her fever has resolved for more than 72 hours and has improvement of respiratory symptoms and has had two consecutive negative SARS-CoV-2 nasopharyngeal swabs taken more than 24 hours apart.
Bottom line: Clinicians should protect themselves with contact and droplet PPE at all times until the infant’s viral status is known. Clinicians should use airborne, contact, and droplet PPE when resuscitating the infant and/or when using CPAP/mechanical ventilation. Mothers should be encouraged to feed their infants expressed breast milk while practicing proper hygiene or directly breastfeed while wearing a mask and practicing proper hygiene. Viral testing of every infant born to a mother with COVID-19 should be performed after the infant is 24 hours old. Mothers should resume caring for their infants normally after they have met criteria suggesting they are no longer actively infected.
Article citation: Puopolo KM, Hudak ML, Kimberlin DW, Cummings J. Initial Guidance: Management of Infants born to Mothers with COVID-19. 2020 Apr 2. https://downloads.aap.org/AAP/PDF/COVID%2019%20Initial%20Newborn%20Guidance.pdf. Accessed Apr 2, 2020.
Dr. Kumar is a pediatric hospitalist at Cleveland Clinic Children’s. She is a clinical assistant professor of pediatrics at Case Western Reserve University, Cleveland, and serves as the Pediatrics Editor for The Hospitalist.












