User login
Get triage plans in place before COVID-19 surge hits, critical care experts say
, according to authors of recent reports that offer advice on how to prepare for surges in demand.
Even modest numbers of critically ill COVID-19 patients have already rapidly overwhelmed existing hospital capacity in hard-hit areas including Italy, Spain, and New York City, said authors of an expert panel report released in CHEST.
“The ethical burden this places on hospitals, health systems, and society is enormous,” said Ryan C. Maves, MD, FCCP, of the Naval Medical Center in San Diego, lead author of the expert panel report from the Task Force for Mass Critical Care and the American College of Chest Physicians (CHEST).
Triage decisions could be especially daunting for resource-intensive therapies such as extracorporeal membrane oxygenation (ECMO), as physicians may be forced to decide when and if to offer such support after demand outstrips a hospital’s ability to provide it.
“ECMO requires a lot of specialized capability to initiate on a patient, and then, it requires a lot of specialized capability to maintain and do safely,” said Steven P. Keller, MD, of the division of emergency critical care medicine in the department of emergency medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston.
Those resource requirements can present a challenge to health care systems already overtaxed by COVID-19, according to Dr. Keller, coauthor of a guidance document in Annals of the American Thoracic Society. The guidance suggests a pandemic approach to ECMO response that’s tiered depending on the intensity of the surge over usual hospital volumes.
Mild surges call for a focus on increasing ECMO capacity, while a moderate surge may indicate a need to focus on allocating scarce resources, and a major surge may signal the need to limit or defer use of scarce resources, according to the guidance.
“If your health care system is stretched from a resource standpoint, at what point do you say, ‘we don’t even have the capability to even safely do ECMO, and so, perhaps we should not even be offering the support’?” Dr. Keller said in an interview. “That’s what we tried to get at in the paper – helping institutions think about how to prepare for that pandemic, and then when to make decisions on when it should and should not be offered.”
Critical care guidance for COVID-19
The guidance from the Task Force for Mass Critical Care and CHEST offers nine specific actions that authors suggest as part of a framework for communities to establish the infrastructure needed to triage critical care resources and “equitably” meet the needs of the largest number of COVID-19 patients.
“It is the goal of the task force to minimize the need for allocation of scarce resources as much as possible,” the authors stated.
The framework starts with surge planning that includes an inventory of intensive care unit resources such as ventilators, beds, supplies, and staff that could be marshaled to meet a surge in demand, followed by establishing “identification triggers” for triage initiation by a regional authority, should clinical demand reach a crisis stage.
The next step is preparing the triage system, which includes creating a committee at the regional level, identifying members of tertiary triage teams and the support structures they will need, and preparing and distributing training materials.
Agreeing on a triage protocol is important to ensure equitable targeting of resources, and how to allocate limited life-sustaining measures needs to be considered, according to the panel of experts. They also recommend adaptations to the standards of care such as modification of end-of-life care policies, support for health care workers, family, and the public, and consideration of pediatric issues including transport, concentration of care at specific centers, and potential increases in age thresholds to accommodate surges.
Barriers to triage?
When asked about potential barriers to rolling out a triage plan, Dr. Maves said the first is acknowledging the possible need for such a plan: “It is a difficult concept for most in critical care to accept – the idea that we may not be able to provide an individual patient with interventions that we consider routine,” he said.
Beyond acknowledging need, other potential barriers to successful implementation include the limited evidence base to support development of these protocols, as well as the need to address public trust.
“If a triage system is perceived as unjust or biased, or if people think that triage favors or excludes certain groups unfairly, it will undermine any system,” Dr. Maves said. “Making sure the public both understands and has input into system development is critical if we are going to be able to make this work.”
Dr. Maves and coauthors reported that some of the authors of their guidance are United States government employees or military service members, and that their opinions and assertions do not reflect the official views or position of those institutions. Dr. Keller reported no disclosures related to the ECMO guidance.
SOURCES: Maves RC et al. Chest. 2020 Apr 11. pii: S0012-3692(20)30691-7. doi: 10.1016/j.chest.2020.03.063; Seethara R and Keller SP. Ann Am Thorac Soc. 2020 Apr 15. doi: 10.1513/AnnalsATS.202003-233PS.
, according to authors of recent reports that offer advice on how to prepare for surges in demand.
Even modest numbers of critically ill COVID-19 patients have already rapidly overwhelmed existing hospital capacity in hard-hit areas including Italy, Spain, and New York City, said authors of an expert panel report released in CHEST.
“The ethical burden this places on hospitals, health systems, and society is enormous,” said Ryan C. Maves, MD, FCCP, of the Naval Medical Center in San Diego, lead author of the expert panel report from the Task Force for Mass Critical Care and the American College of Chest Physicians (CHEST).
Triage decisions could be especially daunting for resource-intensive therapies such as extracorporeal membrane oxygenation (ECMO), as physicians may be forced to decide when and if to offer such support after demand outstrips a hospital’s ability to provide it.
“ECMO requires a lot of specialized capability to initiate on a patient, and then, it requires a lot of specialized capability to maintain and do safely,” said Steven P. Keller, MD, of the division of emergency critical care medicine in the department of emergency medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston.
Those resource requirements can present a challenge to health care systems already overtaxed by COVID-19, according to Dr. Keller, coauthor of a guidance document in Annals of the American Thoracic Society. The guidance suggests a pandemic approach to ECMO response that’s tiered depending on the intensity of the surge over usual hospital volumes.
Mild surges call for a focus on increasing ECMO capacity, while a moderate surge may indicate a need to focus on allocating scarce resources, and a major surge may signal the need to limit or defer use of scarce resources, according to the guidance.
“If your health care system is stretched from a resource standpoint, at what point do you say, ‘we don’t even have the capability to even safely do ECMO, and so, perhaps we should not even be offering the support’?” Dr. Keller said in an interview. “That’s what we tried to get at in the paper – helping institutions think about how to prepare for that pandemic, and then when to make decisions on when it should and should not be offered.”
Critical care guidance for COVID-19
The guidance from the Task Force for Mass Critical Care and CHEST offers nine specific actions that authors suggest as part of a framework for communities to establish the infrastructure needed to triage critical care resources and “equitably” meet the needs of the largest number of COVID-19 patients.
“It is the goal of the task force to minimize the need for allocation of scarce resources as much as possible,” the authors stated.
The framework starts with surge planning that includes an inventory of intensive care unit resources such as ventilators, beds, supplies, and staff that could be marshaled to meet a surge in demand, followed by establishing “identification triggers” for triage initiation by a regional authority, should clinical demand reach a crisis stage.
The next step is preparing the triage system, which includes creating a committee at the regional level, identifying members of tertiary triage teams and the support structures they will need, and preparing and distributing training materials.
Agreeing on a triage protocol is important to ensure equitable targeting of resources, and how to allocate limited life-sustaining measures needs to be considered, according to the panel of experts. They also recommend adaptations to the standards of care such as modification of end-of-life care policies, support for health care workers, family, and the public, and consideration of pediatric issues including transport, concentration of care at specific centers, and potential increases in age thresholds to accommodate surges.
Barriers to triage?
When asked about potential barriers to rolling out a triage plan, Dr. Maves said the first is acknowledging the possible need for such a plan: “It is a difficult concept for most in critical care to accept – the idea that we may not be able to provide an individual patient with interventions that we consider routine,” he said.
Beyond acknowledging need, other potential barriers to successful implementation include the limited evidence base to support development of these protocols, as well as the need to address public trust.
“If a triage system is perceived as unjust or biased, or if people think that triage favors or excludes certain groups unfairly, it will undermine any system,” Dr. Maves said. “Making sure the public both understands and has input into system development is critical if we are going to be able to make this work.”
Dr. Maves and coauthors reported that some of the authors of their guidance are United States government employees or military service members, and that their opinions and assertions do not reflect the official views or position of those institutions. Dr. Keller reported no disclosures related to the ECMO guidance.
SOURCES: Maves RC et al. Chest. 2020 Apr 11. pii: S0012-3692(20)30691-7. doi: 10.1016/j.chest.2020.03.063; Seethara R and Keller SP. Ann Am Thorac Soc. 2020 Apr 15. doi: 10.1513/AnnalsATS.202003-233PS.
, according to authors of recent reports that offer advice on how to prepare for surges in demand.
Even modest numbers of critically ill COVID-19 patients have already rapidly overwhelmed existing hospital capacity in hard-hit areas including Italy, Spain, and New York City, said authors of an expert panel report released in CHEST.
“The ethical burden this places on hospitals, health systems, and society is enormous,” said Ryan C. Maves, MD, FCCP, of the Naval Medical Center in San Diego, lead author of the expert panel report from the Task Force for Mass Critical Care and the American College of Chest Physicians (CHEST).
Triage decisions could be especially daunting for resource-intensive therapies such as extracorporeal membrane oxygenation (ECMO), as physicians may be forced to decide when and if to offer such support after demand outstrips a hospital’s ability to provide it.
“ECMO requires a lot of specialized capability to initiate on a patient, and then, it requires a lot of specialized capability to maintain and do safely,” said Steven P. Keller, MD, of the division of emergency critical care medicine in the department of emergency medicine at Brigham and Women’s Hospital and Harvard Medical School in Boston.
Those resource requirements can present a challenge to health care systems already overtaxed by COVID-19, according to Dr. Keller, coauthor of a guidance document in Annals of the American Thoracic Society. The guidance suggests a pandemic approach to ECMO response that’s tiered depending on the intensity of the surge over usual hospital volumes.
Mild surges call for a focus on increasing ECMO capacity, while a moderate surge may indicate a need to focus on allocating scarce resources, and a major surge may signal the need to limit or defer use of scarce resources, according to the guidance.
“If your health care system is stretched from a resource standpoint, at what point do you say, ‘we don’t even have the capability to even safely do ECMO, and so, perhaps we should not even be offering the support’?” Dr. Keller said in an interview. “That’s what we tried to get at in the paper – helping institutions think about how to prepare for that pandemic, and then when to make decisions on when it should and should not be offered.”
Critical care guidance for COVID-19
The guidance from the Task Force for Mass Critical Care and CHEST offers nine specific actions that authors suggest as part of a framework for communities to establish the infrastructure needed to triage critical care resources and “equitably” meet the needs of the largest number of COVID-19 patients.
“It is the goal of the task force to minimize the need for allocation of scarce resources as much as possible,” the authors stated.
The framework starts with surge planning that includes an inventory of intensive care unit resources such as ventilators, beds, supplies, and staff that could be marshaled to meet a surge in demand, followed by establishing “identification triggers” for triage initiation by a regional authority, should clinical demand reach a crisis stage.
The next step is preparing the triage system, which includes creating a committee at the regional level, identifying members of tertiary triage teams and the support structures they will need, and preparing and distributing training materials.
Agreeing on a triage protocol is important to ensure equitable targeting of resources, and how to allocate limited life-sustaining measures needs to be considered, according to the panel of experts. They also recommend adaptations to the standards of care such as modification of end-of-life care policies, support for health care workers, family, and the public, and consideration of pediatric issues including transport, concentration of care at specific centers, and potential increases in age thresholds to accommodate surges.
Barriers to triage?
When asked about potential barriers to rolling out a triage plan, Dr. Maves said the first is acknowledging the possible need for such a plan: “It is a difficult concept for most in critical care to accept – the idea that we may not be able to provide an individual patient with interventions that we consider routine,” he said.
Beyond acknowledging need, other potential barriers to successful implementation include the limited evidence base to support development of these protocols, as well as the need to address public trust.
“If a triage system is perceived as unjust or biased, or if people think that triage favors or excludes certain groups unfairly, it will undermine any system,” Dr. Maves said. “Making sure the public both understands and has input into system development is critical if we are going to be able to make this work.”
Dr. Maves and coauthors reported that some of the authors of their guidance are United States government employees or military service members, and that their opinions and assertions do not reflect the official views or position of those institutions. Dr. Keller reported no disclosures related to the ECMO guidance.
SOURCES: Maves RC et al. Chest. 2020 Apr 11. pii: S0012-3692(20)30691-7. doi: 10.1016/j.chest.2020.03.063; Seethara R and Keller SP. Ann Am Thorac Soc. 2020 Apr 15. doi: 10.1513/AnnalsATS.202003-233PS.
FROM CHEST AND ANNALS OF THE AMERICAN THORACIC SOCIETY
COVID-19 strikes hard at state-run veterans nursing homes
In early March, 35 residents in the Life Care Center in Kirkland, Washington, died due to complications associated with COVID-19. And that facility thus became the first example of how extremely vulnerable nursing home residents are to COVID-19. Since then, around the US, thousands of nursing home residents have died from complications of the virus. US Department of Veterans Affairs (VA) nursing homes, while rated high in VA health inspection reports, have not been exempt.
As of April 21, the VA had confirmed > 5,500 coronavirus cases in 50 states, the District of Columbia, and Puerto Rico. More than 350 veterans have died of COVID-19, according to VA data. The VA calculates its rates by health care system or VA medical center and does not provide separate data for the community living centers (CLCs).
The VA initiated an isolation strategy on March 10 that suspended most new admissions and barred outsiders from all of its 134 nursing homes. The only exception to the rule was when a patient was expected to die soon. The VA has taken other precautions as well, including extra screening and directing patients to use telehealth where possible.
State-run long-term care facilities for veterans have been hard hit across the country. At the Soldiers’ Home in Holyoke, Massachusetts, which is run by the state of Massachusetts, 5 of 11 veterans who died recently tested positive for COVID-19. At the 4 state-run nursing homes in Alabama, as of April 14, 45 people were confirmed positive and 2 residents had died. The largest outbreak was in the Bill Nichols State Veterans Home in Alexander City. Alabama State Rep. Ed Oliver and Commissioner Kent Davis, of the Alabama Department of Veterans Affairs (ADVA), are looking into how the outbreak started and whether it could have been prevented. “We have reports of lack of hand sanitizers, and those are the things we’re looking at right now,” Rep. Oliver said. The ADVA says residents who test positive are isolated for treatment, and infected employees are prohibited from entering the homes.
States have deployed National Guard troops to facilities following large scale outbreaks and multiple deaths. Pennsylvania deployed 30 National Guard troops to its Southeastern Veterans Center facility in Spring City after at least 10 veterans had died and at least 19 health care workers had tested positive for the virus. The facility is 1 of 6 extended-care facilities run by the Pennsylvania Department of Military and Veterans Affairs. In New Jersey, 40 National Guard troops, 25 New Jersey Department of Health nurses, and 90 VA nurses were deployed to 2 of its veterans facilities amid worsening outbreaks. At the Paramus facility, 155 residents had tested positive and 39 had died, and at the home in Edison, 86 veterans had tested positive and 25 died; 6 more died at a third state facility.
However, reporting remains inconsistent across many states and facilities. Only on April 19 did the Centers for Medicare and Medicaid Services (CMS) order nursing home facilities to inform residents and families about COVID-19 cases inside. This followed similar orders in New Jersey, New York, California, Washington, and other states.
“Nursing homes have been ground zero for COVID-19,” said CMS Administrator Seema Verma in a written statement. “Nursing home reporting to the [Centers for Disease Control and Prevention] is a critical component of the go-forward national COVID-19 surveillance system and to efforts to reopen America.”
In early March, 35 residents in the Life Care Center in Kirkland, Washington, died due to complications associated with COVID-19. And that facility thus became the first example of how extremely vulnerable nursing home residents are to COVID-19. Since then, around the US, thousands of nursing home residents have died from complications of the virus. US Department of Veterans Affairs (VA) nursing homes, while rated high in VA health inspection reports, have not been exempt.
As of April 21, the VA had confirmed > 5,500 coronavirus cases in 50 states, the District of Columbia, and Puerto Rico. More than 350 veterans have died of COVID-19, according to VA data. The VA calculates its rates by health care system or VA medical center and does not provide separate data for the community living centers (CLCs).
The VA initiated an isolation strategy on March 10 that suspended most new admissions and barred outsiders from all of its 134 nursing homes. The only exception to the rule was when a patient was expected to die soon. The VA has taken other precautions as well, including extra screening and directing patients to use telehealth where possible.
State-run long-term care facilities for veterans have been hard hit across the country. At the Soldiers’ Home in Holyoke, Massachusetts, which is run by the state of Massachusetts, 5 of 11 veterans who died recently tested positive for COVID-19. At the 4 state-run nursing homes in Alabama, as of April 14, 45 people were confirmed positive and 2 residents had died. The largest outbreak was in the Bill Nichols State Veterans Home in Alexander City. Alabama State Rep. Ed Oliver and Commissioner Kent Davis, of the Alabama Department of Veterans Affairs (ADVA), are looking into how the outbreak started and whether it could have been prevented. “We have reports of lack of hand sanitizers, and those are the things we’re looking at right now,” Rep. Oliver said. The ADVA says residents who test positive are isolated for treatment, and infected employees are prohibited from entering the homes.
States have deployed National Guard troops to facilities following large scale outbreaks and multiple deaths. Pennsylvania deployed 30 National Guard troops to its Southeastern Veterans Center facility in Spring City after at least 10 veterans had died and at least 19 health care workers had tested positive for the virus. The facility is 1 of 6 extended-care facilities run by the Pennsylvania Department of Military and Veterans Affairs. In New Jersey, 40 National Guard troops, 25 New Jersey Department of Health nurses, and 90 VA nurses were deployed to 2 of its veterans facilities amid worsening outbreaks. At the Paramus facility, 155 residents had tested positive and 39 had died, and at the home in Edison, 86 veterans had tested positive and 25 died; 6 more died at a third state facility.
However, reporting remains inconsistent across many states and facilities. Only on April 19 did the Centers for Medicare and Medicaid Services (CMS) order nursing home facilities to inform residents and families about COVID-19 cases inside. This followed similar orders in New Jersey, New York, California, Washington, and other states.
“Nursing homes have been ground zero for COVID-19,” said CMS Administrator Seema Verma in a written statement. “Nursing home reporting to the [Centers for Disease Control and Prevention] is a critical component of the go-forward national COVID-19 surveillance system and to efforts to reopen America.”
In early March, 35 residents in the Life Care Center in Kirkland, Washington, died due to complications associated with COVID-19. And that facility thus became the first example of how extremely vulnerable nursing home residents are to COVID-19. Since then, around the US, thousands of nursing home residents have died from complications of the virus. US Department of Veterans Affairs (VA) nursing homes, while rated high in VA health inspection reports, have not been exempt.
As of April 21, the VA had confirmed > 5,500 coronavirus cases in 50 states, the District of Columbia, and Puerto Rico. More than 350 veterans have died of COVID-19, according to VA data. The VA calculates its rates by health care system or VA medical center and does not provide separate data for the community living centers (CLCs).
The VA initiated an isolation strategy on March 10 that suspended most new admissions and barred outsiders from all of its 134 nursing homes. The only exception to the rule was when a patient was expected to die soon. The VA has taken other precautions as well, including extra screening and directing patients to use telehealth where possible.
State-run long-term care facilities for veterans have been hard hit across the country. At the Soldiers’ Home in Holyoke, Massachusetts, which is run by the state of Massachusetts, 5 of 11 veterans who died recently tested positive for COVID-19. At the 4 state-run nursing homes in Alabama, as of April 14, 45 people were confirmed positive and 2 residents had died. The largest outbreak was in the Bill Nichols State Veterans Home in Alexander City. Alabama State Rep. Ed Oliver and Commissioner Kent Davis, of the Alabama Department of Veterans Affairs (ADVA), are looking into how the outbreak started and whether it could have been prevented. “We have reports of lack of hand sanitizers, and those are the things we’re looking at right now,” Rep. Oliver said. The ADVA says residents who test positive are isolated for treatment, and infected employees are prohibited from entering the homes.
States have deployed National Guard troops to facilities following large scale outbreaks and multiple deaths. Pennsylvania deployed 30 National Guard troops to its Southeastern Veterans Center facility in Spring City after at least 10 veterans had died and at least 19 health care workers had tested positive for the virus. The facility is 1 of 6 extended-care facilities run by the Pennsylvania Department of Military and Veterans Affairs. In New Jersey, 40 National Guard troops, 25 New Jersey Department of Health nurses, and 90 VA nurses were deployed to 2 of its veterans facilities amid worsening outbreaks. At the Paramus facility, 155 residents had tested positive and 39 had died, and at the home in Edison, 86 veterans had tested positive and 25 died; 6 more died at a third state facility.
However, reporting remains inconsistent across many states and facilities. Only on April 19 did the Centers for Medicare and Medicaid Services (CMS) order nursing home facilities to inform residents and families about COVID-19 cases inside. This followed similar orders in New Jersey, New York, California, Washington, and other states.
“Nursing homes have been ground zero for COVID-19,” said CMS Administrator Seema Verma in a written statement. “Nursing home reporting to the [Centers for Disease Control and Prevention] is a critical component of the go-forward national COVID-19 surveillance system and to efforts to reopen America.”
Doctors push back on treating COVID-19 as HAPE
For Luanne Freer, MD, an expert in high-altitude pulmonary edema (HAPE) and founder and director of Everest ER, a nonprofit seasonal clinic at the Mt. Everest base camp in Nepal (elevation, 17,600 ft), a sudden flurry of messages and questions she received about a possible COVID-19/HAPE link was startling.
“That’s why it kind of poked me in the eye,” she said, referencing her extensive experience treating HAPE, which she described as a pressure-related phenomenon. “My goodness, they are so completely different.”
Dr. Freer, an emergency physician, reached out to several pulmonary intensivists with experience treating both HAPE and COVID-19 to gauge their reactions, and within 36 hours, they had drafted their response. In the commentary, published in High Altitude Medicine & Biology, the clinicians note that the comparison between HAPE and COVID-19 is potentially risky.
“As a group of physicians who have in some cases cared for patients with COVID-19 and in all cases cared for patients with HAPE and studied its pathophysiology and management, we feel it important to correct this misconception, as continued amplification of this message could have adverse effects on management of these patients,” they wrote.
The suggestion that COVID-19 lung injury sometimes looks more like HAPE than like acute respiratory distress syndrome (ARDS) appeared in a journal review article in late March and was put forth by medical professionals on social media where it gained traction in recent weeks and was amplified in multiple media outlets, including this one.
“With COVID, we don’t understand everything that’s going on, but we know for sure it’s an inflammatory process – not a pressure-related problem,” Dr. Freer said. “I thought ... this could be so dangerous to load the medicines that we use when we’re treating HAPE onto patients with COVID-19.”
The pathophysiological mechanisms in HAPE are different than those in other respiratory syndromes, including those associated with COVID-19, said Andrew M. Luks, MD, of the UW Medicine, Seattle, and the first author on the commentary.
“HAPE is a noncardiogenic form of pulmonary edema, as are ARDS due to bacteria or viral pneumonia, re-expansion pulmonary edema, immersion pulmonary edema, negative pressure pulmonary edema, and neurogenic pulmonary edema,” Dr. Luks, Dr. Freer, and colleagues wrote in the commentary, explaining that all of these entities cause varying degrees of hypoxemia and diffuse bilateral opacities on chest imaging. “Importantly, in all of these cases, edema accumulates in the interstitial and alveolar spaces of the lung as a result of imbalance in Starling forces.”
A difference between these entities, however, is “the mechanism by which that imbalance develops,” they noted.
The excessive and uneven hypoxic pulmonary vasoconstriction that leads to a marked increase in pulmonary artery pressure, subsequent lung overperfusion, increased pulmonary capillary hydrostatic pressure, and leakage of fluid from the vascular space into the alveolar space as seen in HAPE, is a “fundamentally different phenomenon than what is seen in COVID-19-related ARDS, which involves viral-mediated inflammatory responses as the primary pathophysiological mechanism,” they added.
The authors described several other differences between the conditions, ultimately noting that “understanding the distinction between the pathophysiological mechanisms of these entities is critical for patient management.”
In HAPE, supplemental oxygen alone may be sufficient; in COVID-19, it may improve hypoxemia but won’t resolve the underlying inflammation or injury, they explained, adding that “only good supportive care including mechanical ventilation, quite often for long periods of time, allows some patients to survive until their disease resolves.”
Further, HAPE can be prevented or treated with pulmonary vasodilators such a nifedipine or sildenafil, which decrease pulmonary artery pressure and, as a result lower pulmonary capillary hydrostatic pressure, they said.
Use of such medications for COVID-19 might decrease pulmonary artery pressure and improve right ventricular function in COVID-19, but “by releasing hypoxic pulmonary vasoconstriction and increasing perfusion to nonventilated regions of the lung, they could also worsen ventilation-perfusion mismatch” and thereby worsen hypoxemia, they explained, adding that the treatments can also cause or worsen hypotension.
Efforts to share observations and experience are important in medicine, but sometimes, as in this circumstance, “they get out there, spread around – like a brushfire almost – and get [unwarranted] face validity,” Dr. Luks said, noting that in response to information circulating about COVID-19 and HAPE, he has already heard medical professionals floating the idea of treating COVID-19 with treatments used for HAPE.
It’s true that some COVID-19 lung injury cases are behaving differently than typical ARDS, he said, adding that presentation can vary.
“But trying to equate HAPE and COVID-19 is just wrong,” he said. “HAPE and COVID-19 may share several features ...but those are features that are shared by a lot of different forms of respiratory failure.”
In a recent video interview, WebMD’s chief medical officer John Whyte, MD, spoke with a New York City physician trained in critical care and emergency medicine, Cameron Kyle-Sidell, MD, who raised the need to consider different respiratory protocols for COVID-19, noting that standard protocols were falling short in many cases.
“What we’re seeing ... is something unusual, it’s something that we are not used to,” Dr. Kyle-Sidell of Maimonides Medical Center said in that interview, stressing that the presentation differed from that seen in typical ARDS. “The patterns I was seeing did not make sense.”
Like others, he noted that COVID-19 patients were presenting with illness that clinically looked more like HAPE, but that the pathophysiology is not necessary similar to HAPE.
At around the same time, Luciano Gattinoni, MD, of the Medical University of Göttingen in Germany and colleagues, published a letter to the editor in the American Journal of Respiratory and Critical Care Medicine stressing that the ARDS presentation in COVID-19 patients is atypical and requires a patient physiology–driven treatment approach, rather than a standard protocol–driven approach. Dr. Gattinoni and colleagues suggested that instead of high positive end-expiratory pressure (PEEP), physicians should consider the lowest possible PEEP and gentle ventilation.
Dr. Luks agreed that “some patients with COVID-19 do not have the same physiologic derangements that we see in a lot of other people with ARDS.”
“[Dr. Gattinoni] is making the point that we need to treat these people differently ... and I think that’s a valid point, and honestly, that’s a point that applied even before COVID-19,” he said. “Most of the things that we see in clinical practice – there’s a lot of heterogeneity between patients, and you have to be prepared to tailor your therapy in light of the differences that you’re picking up from your observations at the bedside and other data that you’re getting on the patient.”
The main concern Dr. Luks and his coauthors wanted to convey, they said, is making sure that the anecdotal experiences and observations of clinicians struggling to find answers don’t spiral out of control without proper vetting, thereby leading to patient harm.
“In this challenging time, we must identify the best means to care for these critically ill patients. That approach should be grounded in sound pulmonary physiology, clinical experience and, when available, evidence from clinical studies,” they concluded.
Dr. Luks and Dr. Freer reported having no financial disclosures.
For Luanne Freer, MD, an expert in high-altitude pulmonary edema (HAPE) and founder and director of Everest ER, a nonprofit seasonal clinic at the Mt. Everest base camp in Nepal (elevation, 17,600 ft), a sudden flurry of messages and questions she received about a possible COVID-19/HAPE link was startling.
“That’s why it kind of poked me in the eye,” she said, referencing her extensive experience treating HAPE, which she described as a pressure-related phenomenon. “My goodness, they are so completely different.”
Dr. Freer, an emergency physician, reached out to several pulmonary intensivists with experience treating both HAPE and COVID-19 to gauge their reactions, and within 36 hours, they had drafted their response. In the commentary, published in High Altitude Medicine & Biology, the clinicians note that the comparison between HAPE and COVID-19 is potentially risky.
“As a group of physicians who have in some cases cared for patients with COVID-19 and in all cases cared for patients with HAPE and studied its pathophysiology and management, we feel it important to correct this misconception, as continued amplification of this message could have adverse effects on management of these patients,” they wrote.
The suggestion that COVID-19 lung injury sometimes looks more like HAPE than like acute respiratory distress syndrome (ARDS) appeared in a journal review article in late March and was put forth by medical professionals on social media where it gained traction in recent weeks and was amplified in multiple media outlets, including this one.
“With COVID, we don’t understand everything that’s going on, but we know for sure it’s an inflammatory process – not a pressure-related problem,” Dr. Freer said. “I thought ... this could be so dangerous to load the medicines that we use when we’re treating HAPE onto patients with COVID-19.”
The pathophysiological mechanisms in HAPE are different than those in other respiratory syndromes, including those associated with COVID-19, said Andrew M. Luks, MD, of the UW Medicine, Seattle, and the first author on the commentary.
“HAPE is a noncardiogenic form of pulmonary edema, as are ARDS due to bacteria or viral pneumonia, re-expansion pulmonary edema, immersion pulmonary edema, negative pressure pulmonary edema, and neurogenic pulmonary edema,” Dr. Luks, Dr. Freer, and colleagues wrote in the commentary, explaining that all of these entities cause varying degrees of hypoxemia and diffuse bilateral opacities on chest imaging. “Importantly, in all of these cases, edema accumulates in the interstitial and alveolar spaces of the lung as a result of imbalance in Starling forces.”
A difference between these entities, however, is “the mechanism by which that imbalance develops,” they noted.
The excessive and uneven hypoxic pulmonary vasoconstriction that leads to a marked increase in pulmonary artery pressure, subsequent lung overperfusion, increased pulmonary capillary hydrostatic pressure, and leakage of fluid from the vascular space into the alveolar space as seen in HAPE, is a “fundamentally different phenomenon than what is seen in COVID-19-related ARDS, which involves viral-mediated inflammatory responses as the primary pathophysiological mechanism,” they added.
The authors described several other differences between the conditions, ultimately noting that “understanding the distinction between the pathophysiological mechanisms of these entities is critical for patient management.”
In HAPE, supplemental oxygen alone may be sufficient; in COVID-19, it may improve hypoxemia but won’t resolve the underlying inflammation or injury, they explained, adding that “only good supportive care including mechanical ventilation, quite often for long periods of time, allows some patients to survive until their disease resolves.”
Further, HAPE can be prevented or treated with pulmonary vasodilators such a nifedipine or sildenafil, which decrease pulmonary artery pressure and, as a result lower pulmonary capillary hydrostatic pressure, they said.
Use of such medications for COVID-19 might decrease pulmonary artery pressure and improve right ventricular function in COVID-19, but “by releasing hypoxic pulmonary vasoconstriction and increasing perfusion to nonventilated regions of the lung, they could also worsen ventilation-perfusion mismatch” and thereby worsen hypoxemia, they explained, adding that the treatments can also cause or worsen hypotension.
Efforts to share observations and experience are important in medicine, but sometimes, as in this circumstance, “they get out there, spread around – like a brushfire almost – and get [unwarranted] face validity,” Dr. Luks said, noting that in response to information circulating about COVID-19 and HAPE, he has already heard medical professionals floating the idea of treating COVID-19 with treatments used for HAPE.
It’s true that some COVID-19 lung injury cases are behaving differently than typical ARDS, he said, adding that presentation can vary.
“But trying to equate HAPE and COVID-19 is just wrong,” he said. “HAPE and COVID-19 may share several features ...but those are features that are shared by a lot of different forms of respiratory failure.”
In a recent video interview, WebMD’s chief medical officer John Whyte, MD, spoke with a New York City physician trained in critical care and emergency medicine, Cameron Kyle-Sidell, MD, who raised the need to consider different respiratory protocols for COVID-19, noting that standard protocols were falling short in many cases.
“What we’re seeing ... is something unusual, it’s something that we are not used to,” Dr. Kyle-Sidell of Maimonides Medical Center said in that interview, stressing that the presentation differed from that seen in typical ARDS. “The patterns I was seeing did not make sense.”
Like others, he noted that COVID-19 patients were presenting with illness that clinically looked more like HAPE, but that the pathophysiology is not necessary similar to HAPE.
At around the same time, Luciano Gattinoni, MD, of the Medical University of Göttingen in Germany and colleagues, published a letter to the editor in the American Journal of Respiratory and Critical Care Medicine stressing that the ARDS presentation in COVID-19 patients is atypical and requires a patient physiology–driven treatment approach, rather than a standard protocol–driven approach. Dr. Gattinoni and colleagues suggested that instead of high positive end-expiratory pressure (PEEP), physicians should consider the lowest possible PEEP and gentle ventilation.
Dr. Luks agreed that “some patients with COVID-19 do not have the same physiologic derangements that we see in a lot of other people with ARDS.”
“[Dr. Gattinoni] is making the point that we need to treat these people differently ... and I think that’s a valid point, and honestly, that’s a point that applied even before COVID-19,” he said. “Most of the things that we see in clinical practice – there’s a lot of heterogeneity between patients, and you have to be prepared to tailor your therapy in light of the differences that you’re picking up from your observations at the bedside and other data that you’re getting on the patient.”
The main concern Dr. Luks and his coauthors wanted to convey, they said, is making sure that the anecdotal experiences and observations of clinicians struggling to find answers don’t spiral out of control without proper vetting, thereby leading to patient harm.
“In this challenging time, we must identify the best means to care for these critically ill patients. That approach should be grounded in sound pulmonary physiology, clinical experience and, when available, evidence from clinical studies,” they concluded.
Dr. Luks and Dr. Freer reported having no financial disclosures.
For Luanne Freer, MD, an expert in high-altitude pulmonary edema (HAPE) and founder and director of Everest ER, a nonprofit seasonal clinic at the Mt. Everest base camp in Nepal (elevation, 17,600 ft), a sudden flurry of messages and questions she received about a possible COVID-19/HAPE link was startling.
“That’s why it kind of poked me in the eye,” she said, referencing her extensive experience treating HAPE, which she described as a pressure-related phenomenon. “My goodness, they are so completely different.”
Dr. Freer, an emergency physician, reached out to several pulmonary intensivists with experience treating both HAPE and COVID-19 to gauge their reactions, and within 36 hours, they had drafted their response. In the commentary, published in High Altitude Medicine & Biology, the clinicians note that the comparison between HAPE and COVID-19 is potentially risky.
“As a group of physicians who have in some cases cared for patients with COVID-19 and in all cases cared for patients with HAPE and studied its pathophysiology and management, we feel it important to correct this misconception, as continued amplification of this message could have adverse effects on management of these patients,” they wrote.
The suggestion that COVID-19 lung injury sometimes looks more like HAPE than like acute respiratory distress syndrome (ARDS) appeared in a journal review article in late March and was put forth by medical professionals on social media where it gained traction in recent weeks and was amplified in multiple media outlets, including this one.
“With COVID, we don’t understand everything that’s going on, but we know for sure it’s an inflammatory process – not a pressure-related problem,” Dr. Freer said. “I thought ... this could be so dangerous to load the medicines that we use when we’re treating HAPE onto patients with COVID-19.”
The pathophysiological mechanisms in HAPE are different than those in other respiratory syndromes, including those associated with COVID-19, said Andrew M. Luks, MD, of the UW Medicine, Seattle, and the first author on the commentary.
“HAPE is a noncardiogenic form of pulmonary edema, as are ARDS due to bacteria or viral pneumonia, re-expansion pulmonary edema, immersion pulmonary edema, negative pressure pulmonary edema, and neurogenic pulmonary edema,” Dr. Luks, Dr. Freer, and colleagues wrote in the commentary, explaining that all of these entities cause varying degrees of hypoxemia and diffuse bilateral opacities on chest imaging. “Importantly, in all of these cases, edema accumulates in the interstitial and alveolar spaces of the lung as a result of imbalance in Starling forces.”
A difference between these entities, however, is “the mechanism by which that imbalance develops,” they noted.
The excessive and uneven hypoxic pulmonary vasoconstriction that leads to a marked increase in pulmonary artery pressure, subsequent lung overperfusion, increased pulmonary capillary hydrostatic pressure, and leakage of fluid from the vascular space into the alveolar space as seen in HAPE, is a “fundamentally different phenomenon than what is seen in COVID-19-related ARDS, which involves viral-mediated inflammatory responses as the primary pathophysiological mechanism,” they added.
The authors described several other differences between the conditions, ultimately noting that “understanding the distinction between the pathophysiological mechanisms of these entities is critical for patient management.”
In HAPE, supplemental oxygen alone may be sufficient; in COVID-19, it may improve hypoxemia but won’t resolve the underlying inflammation or injury, they explained, adding that “only good supportive care including mechanical ventilation, quite often for long periods of time, allows some patients to survive until their disease resolves.”
Further, HAPE can be prevented or treated with pulmonary vasodilators such a nifedipine or sildenafil, which decrease pulmonary artery pressure and, as a result lower pulmonary capillary hydrostatic pressure, they said.
Use of such medications for COVID-19 might decrease pulmonary artery pressure and improve right ventricular function in COVID-19, but “by releasing hypoxic pulmonary vasoconstriction and increasing perfusion to nonventilated regions of the lung, they could also worsen ventilation-perfusion mismatch” and thereby worsen hypoxemia, they explained, adding that the treatments can also cause or worsen hypotension.
Efforts to share observations and experience are important in medicine, but sometimes, as in this circumstance, “they get out there, spread around – like a brushfire almost – and get [unwarranted] face validity,” Dr. Luks said, noting that in response to information circulating about COVID-19 and HAPE, he has already heard medical professionals floating the idea of treating COVID-19 with treatments used for HAPE.
It’s true that some COVID-19 lung injury cases are behaving differently than typical ARDS, he said, adding that presentation can vary.
“But trying to equate HAPE and COVID-19 is just wrong,” he said. “HAPE and COVID-19 may share several features ...but those are features that are shared by a lot of different forms of respiratory failure.”
In a recent video interview, WebMD’s chief medical officer John Whyte, MD, spoke with a New York City physician trained in critical care and emergency medicine, Cameron Kyle-Sidell, MD, who raised the need to consider different respiratory protocols for COVID-19, noting that standard protocols were falling short in many cases.
“What we’re seeing ... is something unusual, it’s something that we are not used to,” Dr. Kyle-Sidell of Maimonides Medical Center said in that interview, stressing that the presentation differed from that seen in typical ARDS. “The patterns I was seeing did not make sense.”
Like others, he noted that COVID-19 patients were presenting with illness that clinically looked more like HAPE, but that the pathophysiology is not necessary similar to HAPE.
At around the same time, Luciano Gattinoni, MD, of the Medical University of Göttingen in Germany and colleagues, published a letter to the editor in the American Journal of Respiratory and Critical Care Medicine stressing that the ARDS presentation in COVID-19 patients is atypical and requires a patient physiology–driven treatment approach, rather than a standard protocol–driven approach. Dr. Gattinoni and colleagues suggested that instead of high positive end-expiratory pressure (PEEP), physicians should consider the lowest possible PEEP and gentle ventilation.
Dr. Luks agreed that “some patients with COVID-19 do not have the same physiologic derangements that we see in a lot of other people with ARDS.”
“[Dr. Gattinoni] is making the point that we need to treat these people differently ... and I think that’s a valid point, and honestly, that’s a point that applied even before COVID-19,” he said. “Most of the things that we see in clinical practice – there’s a lot of heterogeneity between patients, and you have to be prepared to tailor your therapy in light of the differences that you’re picking up from your observations at the bedside and other data that you’re getting on the patient.”
The main concern Dr. Luks and his coauthors wanted to convey, they said, is making sure that the anecdotal experiences and observations of clinicians struggling to find answers don’t spiral out of control without proper vetting, thereby leading to patient harm.
“In this challenging time, we must identify the best means to care for these critically ill patients. That approach should be grounded in sound pulmonary physiology, clinical experience and, when available, evidence from clinical studies,” they concluded.
Dr. Luks and Dr. Freer reported having no financial disclosures.
Overcoming COVID-related stress
As a department chief managing during this crisis, everyone greets me sympathetically: “This must be so stressful for you! Are you doing OK?” “Um, I’m great,” I answer contritely. Yes, this is hard, yet I feel fine. But why? Shouldn’t I be fretting the damage done by the COVID cyclone? Our operations are smashed and our staff scrambled, my family and friends are out of work; these are difficult times. But a harmful effect on my health or yours is not inevitable. There are things we can do to inoculate ourselves.
No doubt, exercise (if you can find weights!), eating well, sleeping, and meditating help, but they are secondary. None of these protect much if you still believe stress is killing you. You must first reframe what is happening. Health psychologist Kelly McGonigal, PhD, from Stanford (Calif.) University, is a world expert on this topic. If you’ve not seen her TED talk about stress, then watch it now. She teaches how stress is indeed harmful to your health – but only if you believe it to be so. Many studies have borne this out. One showed that people who reported high stress in the previous year were 43% more likely to die than those who did not. But that risk held only when they believed stress was harmful to them. Those who did not think that stress was harmful not only fared better but also had the lowest likelihood of death, lower even than those who reported little stress! So it wasn’t the stress that mattered, it was the physiologic response to it. And that you can control.
Changing your beliefs is no easy feat. There is work to be done, Dr. McGonigal would argue. You must not only reframe our stress as healthful, but also act in ways to make this true. This is easier for us as physicians. First, we understand better than most that difficulty is a normal part of life. We have countless stories of hardship, tragedy, pain and suffering from the work we do. The pandemic may be extraordinary in breadth, but not in depth. We’ve seen worse happen to patients. Second, we have firsthand experience that suffering ends and often leads to strength and resilience. Even in our own lives, it was by traveling through the extraordinary stress of medical school and residency that we arrived here.
Cortisol increases when we are under duress. So does oxytocin. The former gets most of the press, the latter is more interesting. That oxytocin release during stress conferred survival benefits to us as a species: When a threat arrived, we not only ran, but also grabbed the kids, too! Oxytocin is the “tend and befriend” compliment to cortisol’s “fight or flight.” Focusing on this priming to strengthen social ties, listen, spend (Zoom) time together, and provide emotional support is key to our recovery. Even small acts of giving for our staff, friends, family, and strangers can significantly shift consequences of this stress from harmful to beneficial.
Last year, my uncle died in a tragic accident. My aunt, who is alone, is now also isolated. She’s lost her partner, her guardian, and she is afraid. Rather than succumb to the stress, she imagined something she could do to wrest some control. Last week, she filled her minivan with pink and yellow tulips bunched in bouquets and tied with handwritten notes of encouragement. She then drove up and down the streets in her North Attleboro, Mass., neighborhood and left the flowers on doorsteps until her van was empty. She did so to share with them the bit of joy that spring brings, she says, and to encourage people to stay inside!
This is a difficult time for us, and yet even more difficult for others. Perhaps the best we can do is to find ways to bring a bit of joy or comfort to others.
“In some ways suffering ceases to be suffering at the moment it finds a meaning, such as the meaning of a sacrifice.” – Viktor Frankl
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He had no relevant disclosures. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
As a department chief managing during this crisis, everyone greets me sympathetically: “This must be so stressful for you! Are you doing OK?” “Um, I’m great,” I answer contritely. Yes, this is hard, yet I feel fine. But why? Shouldn’t I be fretting the damage done by the COVID cyclone? Our operations are smashed and our staff scrambled, my family and friends are out of work; these are difficult times. But a harmful effect on my health or yours is not inevitable. There are things we can do to inoculate ourselves.
No doubt, exercise (if you can find weights!), eating well, sleeping, and meditating help, but they are secondary. None of these protect much if you still believe stress is killing you. You must first reframe what is happening. Health psychologist Kelly McGonigal, PhD, from Stanford (Calif.) University, is a world expert on this topic. If you’ve not seen her TED talk about stress, then watch it now. She teaches how stress is indeed harmful to your health – but only if you believe it to be so. Many studies have borne this out. One showed that people who reported high stress in the previous year were 43% more likely to die than those who did not. But that risk held only when they believed stress was harmful to them. Those who did not think that stress was harmful not only fared better but also had the lowest likelihood of death, lower even than those who reported little stress! So it wasn’t the stress that mattered, it was the physiologic response to it. And that you can control.
Changing your beliefs is no easy feat. There is work to be done, Dr. McGonigal would argue. You must not only reframe our stress as healthful, but also act in ways to make this true. This is easier for us as physicians. First, we understand better than most that difficulty is a normal part of life. We have countless stories of hardship, tragedy, pain and suffering from the work we do. The pandemic may be extraordinary in breadth, but not in depth. We’ve seen worse happen to patients. Second, we have firsthand experience that suffering ends and often leads to strength and resilience. Even in our own lives, it was by traveling through the extraordinary stress of medical school and residency that we arrived here.
Cortisol increases when we are under duress. So does oxytocin. The former gets most of the press, the latter is more interesting. That oxytocin release during stress conferred survival benefits to us as a species: When a threat arrived, we not only ran, but also grabbed the kids, too! Oxytocin is the “tend and befriend” compliment to cortisol’s “fight or flight.” Focusing on this priming to strengthen social ties, listen, spend (Zoom) time together, and provide emotional support is key to our recovery. Even small acts of giving for our staff, friends, family, and strangers can significantly shift consequences of this stress from harmful to beneficial.
Last year, my uncle died in a tragic accident. My aunt, who is alone, is now also isolated. She’s lost her partner, her guardian, and she is afraid. Rather than succumb to the stress, she imagined something she could do to wrest some control. Last week, she filled her minivan with pink and yellow tulips bunched in bouquets and tied with handwritten notes of encouragement. She then drove up and down the streets in her North Attleboro, Mass., neighborhood and left the flowers on doorsteps until her van was empty. She did so to share with them the bit of joy that spring brings, she says, and to encourage people to stay inside!
This is a difficult time for us, and yet even more difficult for others. Perhaps the best we can do is to find ways to bring a bit of joy or comfort to others.
“In some ways suffering ceases to be suffering at the moment it finds a meaning, such as the meaning of a sacrifice.” – Viktor Frankl
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He had no relevant disclosures. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
As a department chief managing during this crisis, everyone greets me sympathetically: “This must be so stressful for you! Are you doing OK?” “Um, I’m great,” I answer contritely. Yes, this is hard, yet I feel fine. But why? Shouldn’t I be fretting the damage done by the COVID cyclone? Our operations are smashed and our staff scrambled, my family and friends are out of work; these are difficult times. But a harmful effect on my health or yours is not inevitable. There are things we can do to inoculate ourselves.
No doubt, exercise (if you can find weights!), eating well, sleeping, and meditating help, but they are secondary. None of these protect much if you still believe stress is killing you. You must first reframe what is happening. Health psychologist Kelly McGonigal, PhD, from Stanford (Calif.) University, is a world expert on this topic. If you’ve not seen her TED talk about stress, then watch it now. She teaches how stress is indeed harmful to your health – but only if you believe it to be so. Many studies have borne this out. One showed that people who reported high stress in the previous year were 43% more likely to die than those who did not. But that risk held only when they believed stress was harmful to them. Those who did not think that stress was harmful not only fared better but also had the lowest likelihood of death, lower even than those who reported little stress! So it wasn’t the stress that mattered, it was the physiologic response to it. And that you can control.
Changing your beliefs is no easy feat. There is work to be done, Dr. McGonigal would argue. You must not only reframe our stress as healthful, but also act in ways to make this true. This is easier for us as physicians. First, we understand better than most that difficulty is a normal part of life. We have countless stories of hardship, tragedy, pain and suffering from the work we do. The pandemic may be extraordinary in breadth, but not in depth. We’ve seen worse happen to patients. Second, we have firsthand experience that suffering ends and often leads to strength and resilience. Even in our own lives, it was by traveling through the extraordinary stress of medical school and residency that we arrived here.
Cortisol increases when we are under duress. So does oxytocin. The former gets most of the press, the latter is more interesting. That oxytocin release during stress conferred survival benefits to us as a species: When a threat arrived, we not only ran, but also grabbed the kids, too! Oxytocin is the “tend and befriend” compliment to cortisol’s “fight or flight.” Focusing on this priming to strengthen social ties, listen, spend (Zoom) time together, and provide emotional support is key to our recovery. Even small acts of giving for our staff, friends, family, and strangers can significantly shift consequences of this stress from harmful to beneficial.
Last year, my uncle died in a tragic accident. My aunt, who is alone, is now also isolated. She’s lost her partner, her guardian, and she is afraid. Rather than succumb to the stress, she imagined something she could do to wrest some control. Last week, she filled her minivan with pink and yellow tulips bunched in bouquets and tied with handwritten notes of encouragement. She then drove up and down the streets in her North Attleboro, Mass., neighborhood and left the flowers on doorsteps until her van was empty. She did so to share with them the bit of joy that spring brings, she says, and to encourage people to stay inside!
This is a difficult time for us, and yet even more difficult for others. Perhaps the best we can do is to find ways to bring a bit of joy or comfort to others.
“In some ways suffering ceases to be suffering at the moment it finds a meaning, such as the meaning of a sacrifice.” – Viktor Frankl
Dr. Benabio is director of Healthcare Transformation and chief of dermatology at Kaiser Permanente San Diego. The opinions expressed in this column are his own and do not represent those of Kaiser Permanente. He had no relevant disclosures. Dr. Benabio is @Dermdoc on Twitter. Write to him at [email protected].
FDA authorizes first COVID-19 test kit with home collection option
a reissue of the emergency use authorization allowing for testing of samples self-collected by patients at home with the Pixel by LabCorp COVID-19 RT-PCR Test.
The reissued authorization allows for testing of a sample taken from the nose by way of a self-collection kit that contains nasal swabs and saline, according to the FDA press release. After self-swabbing, users should send the samples in an insulated package to a LabCorp laboratory for testing. LabCorp intends to make the Pixel test available to consumers in most states, accessible through doctors’ orders.
The Pixel test includes a specific Q-tip–style cotton swab for patients to use to collect their samples, the FDA noted. Because of concerns with sterility and cross-reactivity caused by inherent genetic material in cotton swabs, generic cotton swabs should not be used as a substitute. The FDA will work with test developers to determine if generic cotton swabs can be used safely and effectively with other tests.
“Throughout this pandemic we have been facilitating test development to ensure patients’ access to accurate diagnostics, which includes supporting the development of reliable and accurate at-home sample collection options. ... [The FDA] worked with LabCorp to ensure the data demonstrated from at-home patient sample collection is as safe and accurate as sample collection at a doctor’s office, hospital, or other testing site. With this action, there is now a convenient and reliable option for patient sample collection from the comfort and safety of their home,” FDA Commissioner Stephen M. Hahn, MD, said in the press release.
a reissue of the emergency use authorization allowing for testing of samples self-collected by patients at home with the Pixel by LabCorp COVID-19 RT-PCR Test.
The reissued authorization allows for testing of a sample taken from the nose by way of a self-collection kit that contains nasal swabs and saline, according to the FDA press release. After self-swabbing, users should send the samples in an insulated package to a LabCorp laboratory for testing. LabCorp intends to make the Pixel test available to consumers in most states, accessible through doctors’ orders.
The Pixel test includes a specific Q-tip–style cotton swab for patients to use to collect their samples, the FDA noted. Because of concerns with sterility and cross-reactivity caused by inherent genetic material in cotton swabs, generic cotton swabs should not be used as a substitute. The FDA will work with test developers to determine if generic cotton swabs can be used safely and effectively with other tests.
“Throughout this pandemic we have been facilitating test development to ensure patients’ access to accurate diagnostics, which includes supporting the development of reliable and accurate at-home sample collection options. ... [The FDA] worked with LabCorp to ensure the data demonstrated from at-home patient sample collection is as safe and accurate as sample collection at a doctor’s office, hospital, or other testing site. With this action, there is now a convenient and reliable option for patient sample collection from the comfort and safety of their home,” FDA Commissioner Stephen M. Hahn, MD, said in the press release.
a reissue of the emergency use authorization allowing for testing of samples self-collected by patients at home with the Pixel by LabCorp COVID-19 RT-PCR Test.
The reissued authorization allows for testing of a sample taken from the nose by way of a self-collection kit that contains nasal swabs and saline, according to the FDA press release. After self-swabbing, users should send the samples in an insulated package to a LabCorp laboratory for testing. LabCorp intends to make the Pixel test available to consumers in most states, accessible through doctors’ orders.
The Pixel test includes a specific Q-tip–style cotton swab for patients to use to collect their samples, the FDA noted. Because of concerns with sterility and cross-reactivity caused by inherent genetic material in cotton swabs, generic cotton swabs should not be used as a substitute. The FDA will work with test developers to determine if generic cotton swabs can be used safely and effectively with other tests.
“Throughout this pandemic we have been facilitating test development to ensure patients’ access to accurate diagnostics, which includes supporting the development of reliable and accurate at-home sample collection options. ... [The FDA] worked with LabCorp to ensure the data demonstrated from at-home patient sample collection is as safe and accurate as sample collection at a doctor’s office, hospital, or other testing site. With this action, there is now a convenient and reliable option for patient sample collection from the comfort and safety of their home,” FDA Commissioner Stephen M. Hahn, MD, said in the press release.
EHA and TIF explore how COVID-19 is affecting thalassemia and SCD patients
In a webinar designed to guide physicians in the care of hematology patients during the COVID-19 pandemic, three world experts on thalassemia and sickle cell disease (SCD) provided on-the-ground information from physicians who were dealing with the height of the crisis in their countries.
The webinar was organized by the European Hematology Association (EHA) and the Thalassemia International Federation (TIF).
Moderator Francesco Cerisoli, MD, head of research and mentoring at EHA, led the discussion with three guest speakers: Maria-Domenica Cappellini, MD, PhD, professor of hematology at the University of Milan; Androulla Eleftheriou, MD, executive director of TIF in Cyprus; and Raffaella Colombatti , MD, of the University of Padova in Italy, coordinator of the Red Cell Reserve Working Group of the Italian Association of Pediatric Hematology and Oncology.
Italian experience with thalassemia and COVID-19
Dr. Cappellini discussed the Italian experience with 11 thalassemia patients followed by a network survey who developed COVID-19 in the northern part of Italy, where the pandemic has been most widespread.
There are no published data focusing specifically on SARS-CoV-2 infection in patients with thalassemic syndromes, but patients with preexisting comorbidities are likely to be more severely affected by SARS-CoV-2, according to Dr. Cappellini.
Of particular concern is the fact that patients with thalassemia, especially older ones, are frequently splenectomized, which renders them more vulnerable to bacterial infections and can trigger life-threatening sepsis. However, splenectomy is not known to increase the risk of viral infection or severe viral illness. Of additional concern is the fact that many thalassemia patients need routine and frequent transfusions.
Overall, the 11 thalassemia patients who developed COVID-19 experienced only mild to moderate symptoms. This is despite the fact that 72% of the patients were splenectomized, which did not appear to affect the clinical course, and all of the patients had thalassemia-related comorbidities.
Around half of the patients were hospitalized, but none of them required transfer to the ICU. One patient who was treated with chemotherapy for diffuse large B-cell lymphoma in 2019 but is now in remission required more intense ventilation support with the use of continuous positive airway pressure.
Only three patients received specific treatment for COVID-19: one with hydroxychloroquine (HCQ) alone, one with HCQ plus anakinra, and one with HCQ plus ritonavir/darunavir.
Overall, “the number of infected thalassemia patients was lower than expected, likely due to earlier and more vigilant self-isolation compared to the general population,” Dr. Cappellini said. She pointed out that the first early response in February by thalassemia physicians was to warn their patients via email and phone calls about the need for self-isolation and precautions against the pandemic.
Physicians “rapidly reorganized activities, postponing nonessential ones” and managed to provide patients “a safe track at the hospital to receive their life-saving treatment in COVID-19–free areas with health care personnel wearing protective equipment” and assessment of all entering patients for COVID-19 infection, Dr. Cappellini said.
Results in additional thalassemia patients and SCD patients
Dr. Eleftheriou described 51 cases of thalassemia patients with SARS-CoV-2 infection reported to TIF as of April 16. Patients were from Cyprus, Italy, the United Kingdom, France, Turkey, Iran, Pakistan, and Indonesia.
Of the 51 patients, 46 presented with mild to moderate symptoms. Five patients had severe respiratory symptoms and required hospitalization, two were hospitalized and discharged, and three died between day 5 and day 15 post hospitalization.
Dr. Colombatti followed with a brief presentation of the intersection of COVID-19 with SCD patients. She presented anecdotal data involving 32 SCD patients who exhibited COVID-19 symptoms. Dr. Colombatti obtained the data via personal communication with Pablo Bartolucci, of Hôpitaux Universitaires Henri Mondor in Créteil, France.
All 32 SCD patients were screened and treated for COVID-19, and 17 of them continued treatment for 10 days. In all, 22 patients were hospitalized, 11 were transferred to the ICU, and 1 died.
Ensuring adequate blood supply
Dr. Eleftheriou also discussed the TIF response to the COVID-19 pandemic, which focused on the adequacy of blood supplies for these patients who so often need transfusions.
Dr. Eleftheriou stated that a shortage of blood was reported in 75% of the 62 member countries of the TIF, with 58% reporting severe shortages and 35% reporting moderate to severe shortages.
The shortages resulted in many countries returning to older family/friends donation practices, rare use of whole blood transfusions, and the use of older blood transfusions (older than 28 days).
In addition, physicians have modified their transfusion strategy. They have reduced the amount of blood given to thalassemia patients from two units to one unit during any transfusion, while making arrangements for more frequent transfusions; for example, one transfusion per week but with precautions made to “limit the time spent in the clinic and to control blood supplies while safeguarding that all [thalassemia] patients will be able to get their transfusion,” Dr. Eleftheriou said.
The information in the webinar was provided with the caveat that “no general evidence-based guidance can be derived from this discussion.” There were no other disclosures given.
In a webinar designed to guide physicians in the care of hematology patients during the COVID-19 pandemic, three world experts on thalassemia and sickle cell disease (SCD) provided on-the-ground information from physicians who were dealing with the height of the crisis in their countries.
The webinar was organized by the European Hematology Association (EHA) and the Thalassemia International Federation (TIF).
Moderator Francesco Cerisoli, MD, head of research and mentoring at EHA, led the discussion with three guest speakers: Maria-Domenica Cappellini, MD, PhD, professor of hematology at the University of Milan; Androulla Eleftheriou, MD, executive director of TIF in Cyprus; and Raffaella Colombatti , MD, of the University of Padova in Italy, coordinator of the Red Cell Reserve Working Group of the Italian Association of Pediatric Hematology and Oncology.
Italian experience with thalassemia and COVID-19
Dr. Cappellini discussed the Italian experience with 11 thalassemia patients followed by a network survey who developed COVID-19 in the northern part of Italy, where the pandemic has been most widespread.
There are no published data focusing specifically on SARS-CoV-2 infection in patients with thalassemic syndromes, but patients with preexisting comorbidities are likely to be more severely affected by SARS-CoV-2, according to Dr. Cappellini.
Of particular concern is the fact that patients with thalassemia, especially older ones, are frequently splenectomized, which renders them more vulnerable to bacterial infections and can trigger life-threatening sepsis. However, splenectomy is not known to increase the risk of viral infection or severe viral illness. Of additional concern is the fact that many thalassemia patients need routine and frequent transfusions.
Overall, the 11 thalassemia patients who developed COVID-19 experienced only mild to moderate symptoms. This is despite the fact that 72% of the patients were splenectomized, which did not appear to affect the clinical course, and all of the patients had thalassemia-related comorbidities.
Around half of the patients were hospitalized, but none of them required transfer to the ICU. One patient who was treated with chemotherapy for diffuse large B-cell lymphoma in 2019 but is now in remission required more intense ventilation support with the use of continuous positive airway pressure.
Only three patients received specific treatment for COVID-19: one with hydroxychloroquine (HCQ) alone, one with HCQ plus anakinra, and one with HCQ plus ritonavir/darunavir.
Overall, “the number of infected thalassemia patients was lower than expected, likely due to earlier and more vigilant self-isolation compared to the general population,” Dr. Cappellini said. She pointed out that the first early response in February by thalassemia physicians was to warn their patients via email and phone calls about the need for self-isolation and precautions against the pandemic.
Physicians “rapidly reorganized activities, postponing nonessential ones” and managed to provide patients “a safe track at the hospital to receive their life-saving treatment in COVID-19–free areas with health care personnel wearing protective equipment” and assessment of all entering patients for COVID-19 infection, Dr. Cappellini said.
Results in additional thalassemia patients and SCD patients
Dr. Eleftheriou described 51 cases of thalassemia patients with SARS-CoV-2 infection reported to TIF as of April 16. Patients were from Cyprus, Italy, the United Kingdom, France, Turkey, Iran, Pakistan, and Indonesia.
Of the 51 patients, 46 presented with mild to moderate symptoms. Five patients had severe respiratory symptoms and required hospitalization, two were hospitalized and discharged, and three died between day 5 and day 15 post hospitalization.
Dr. Colombatti followed with a brief presentation of the intersection of COVID-19 with SCD patients. She presented anecdotal data involving 32 SCD patients who exhibited COVID-19 symptoms. Dr. Colombatti obtained the data via personal communication with Pablo Bartolucci, of Hôpitaux Universitaires Henri Mondor in Créteil, France.
All 32 SCD patients were screened and treated for COVID-19, and 17 of them continued treatment for 10 days. In all, 22 patients were hospitalized, 11 were transferred to the ICU, and 1 died.
Ensuring adequate blood supply
Dr. Eleftheriou also discussed the TIF response to the COVID-19 pandemic, which focused on the adequacy of blood supplies for these patients who so often need transfusions.
Dr. Eleftheriou stated that a shortage of blood was reported in 75% of the 62 member countries of the TIF, with 58% reporting severe shortages and 35% reporting moderate to severe shortages.
The shortages resulted in many countries returning to older family/friends donation practices, rare use of whole blood transfusions, and the use of older blood transfusions (older than 28 days).
In addition, physicians have modified their transfusion strategy. They have reduced the amount of blood given to thalassemia patients from two units to one unit during any transfusion, while making arrangements for more frequent transfusions; for example, one transfusion per week but with precautions made to “limit the time spent in the clinic and to control blood supplies while safeguarding that all [thalassemia] patients will be able to get their transfusion,” Dr. Eleftheriou said.
The information in the webinar was provided with the caveat that “no general evidence-based guidance can be derived from this discussion.” There were no other disclosures given.
In a webinar designed to guide physicians in the care of hematology patients during the COVID-19 pandemic, three world experts on thalassemia and sickle cell disease (SCD) provided on-the-ground information from physicians who were dealing with the height of the crisis in their countries.
The webinar was organized by the European Hematology Association (EHA) and the Thalassemia International Federation (TIF).
Moderator Francesco Cerisoli, MD, head of research and mentoring at EHA, led the discussion with three guest speakers: Maria-Domenica Cappellini, MD, PhD, professor of hematology at the University of Milan; Androulla Eleftheriou, MD, executive director of TIF in Cyprus; and Raffaella Colombatti , MD, of the University of Padova in Italy, coordinator of the Red Cell Reserve Working Group of the Italian Association of Pediatric Hematology and Oncology.
Italian experience with thalassemia and COVID-19
Dr. Cappellini discussed the Italian experience with 11 thalassemia patients followed by a network survey who developed COVID-19 in the northern part of Italy, where the pandemic has been most widespread.
There are no published data focusing specifically on SARS-CoV-2 infection in patients with thalassemic syndromes, but patients with preexisting comorbidities are likely to be more severely affected by SARS-CoV-2, according to Dr. Cappellini.
Of particular concern is the fact that patients with thalassemia, especially older ones, are frequently splenectomized, which renders them more vulnerable to bacterial infections and can trigger life-threatening sepsis. However, splenectomy is not known to increase the risk of viral infection or severe viral illness. Of additional concern is the fact that many thalassemia patients need routine and frequent transfusions.
Overall, the 11 thalassemia patients who developed COVID-19 experienced only mild to moderate symptoms. This is despite the fact that 72% of the patients were splenectomized, which did not appear to affect the clinical course, and all of the patients had thalassemia-related comorbidities.
Around half of the patients were hospitalized, but none of them required transfer to the ICU. One patient who was treated with chemotherapy for diffuse large B-cell lymphoma in 2019 but is now in remission required more intense ventilation support with the use of continuous positive airway pressure.
Only three patients received specific treatment for COVID-19: one with hydroxychloroquine (HCQ) alone, one with HCQ plus anakinra, and one with HCQ plus ritonavir/darunavir.
Overall, “the number of infected thalassemia patients was lower than expected, likely due to earlier and more vigilant self-isolation compared to the general population,” Dr. Cappellini said. She pointed out that the first early response in February by thalassemia physicians was to warn their patients via email and phone calls about the need for self-isolation and precautions against the pandemic.
Physicians “rapidly reorganized activities, postponing nonessential ones” and managed to provide patients “a safe track at the hospital to receive their life-saving treatment in COVID-19–free areas with health care personnel wearing protective equipment” and assessment of all entering patients for COVID-19 infection, Dr. Cappellini said.
Results in additional thalassemia patients and SCD patients
Dr. Eleftheriou described 51 cases of thalassemia patients with SARS-CoV-2 infection reported to TIF as of April 16. Patients were from Cyprus, Italy, the United Kingdom, France, Turkey, Iran, Pakistan, and Indonesia.
Of the 51 patients, 46 presented with mild to moderate symptoms. Five patients had severe respiratory symptoms and required hospitalization, two were hospitalized and discharged, and three died between day 5 and day 15 post hospitalization.
Dr. Colombatti followed with a brief presentation of the intersection of COVID-19 with SCD patients. She presented anecdotal data involving 32 SCD patients who exhibited COVID-19 symptoms. Dr. Colombatti obtained the data via personal communication with Pablo Bartolucci, of Hôpitaux Universitaires Henri Mondor in Créteil, France.
All 32 SCD patients were screened and treated for COVID-19, and 17 of them continued treatment for 10 days. In all, 22 patients were hospitalized, 11 were transferred to the ICU, and 1 died.
Ensuring adequate blood supply
Dr. Eleftheriou also discussed the TIF response to the COVID-19 pandemic, which focused on the adequacy of blood supplies for these patients who so often need transfusions.
Dr. Eleftheriou stated that a shortage of blood was reported in 75% of the 62 member countries of the TIF, with 58% reporting severe shortages and 35% reporting moderate to severe shortages.
The shortages resulted in many countries returning to older family/friends donation practices, rare use of whole blood transfusions, and the use of older blood transfusions (older than 28 days).
In addition, physicians have modified their transfusion strategy. They have reduced the amount of blood given to thalassemia patients from two units to one unit during any transfusion, while making arrangements for more frequent transfusions; for example, one transfusion per week but with precautions made to “limit the time spent in the clinic and to control blood supplies while safeguarding that all [thalassemia] patients will be able to get their transfusion,” Dr. Eleftheriou said.
The information in the webinar was provided with the caveat that “no general evidence-based guidance can be derived from this discussion.” There were no other disclosures given.
Researchers investigate impact of smoking on COVID-19 risk
but quitting smoking is likely to lower the risk of developing more severe or fatal cases of the infection, according to research from several recent papers.
Interest in how tobacco use affects COVID-19 infection rates stems from research showing that men at the epicenter of the outbreak in China having a higher early mortality rate. Early reports from China showed a case fatality rate of 4.7% for men, compared with 2.8% for women, according to the World Health Organization. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2, is suspected to enter a cell using the ACE2 receptor. Since smoking up-regulates this receptor, one popular theory is that smoking can increase the risk of COVID-19 or exacerbate symptoms of an existing infection (Eur Respir J. 2020 Apr 8. doi: 10.1183/13993003.00688-2020). In China, about half of men are active smokers, compared with 2.7% of women (Transl Lung Cancer Res. 2019;8[Suppl 1]:S21-30), so this association would explain the severe cases and increased mortality in this group. In response to potential risk for public health, the World Health Organization, Centers for Disease Control and Prevention, the Attorney General of Massachusetts, and other organizations have warned that smoking may increase one’s risk of transmitting and developing COVID-19 or may worsen the infection.
“While it is easy to jump to the conclusion that more ACE2 means more susceptibility to severe infection, there is no evidence to support this,” Brandon Michael Henry, MD, of the cardiac intensive care unit and the Heart Institute at Cincinnati Children’s Hospital Medical Center, said in an interview. “Moreover, some would argue (including myself) that increased ACE2 may in fact be protective, as ACE2 decreases the levels of angiotensin-2 which likely plays a significant role in the pathophysiology of ARDS.”
Some researchers have examined the limited evidence of smoking on COVID-19 risk and come to preliminary conclusions. In a letter to the editor recently published in the European Journal of Internal Medicine, Dr. Henry and Giuseppe Lippi, MD, of the section of clinical biochemistry in the department of neuroscience, biomedicine, and movement at the University of Verona (Italy), performed a meta-analysis of papers examining smoking and COVID-19 up to March 9, 2020 and identified five articles with 1,399 COVID-19 cases (Eur J Intern Med. 2020 Mar 16. doi: 10.1016/j.ejim.2020.03.014).
“Given the fact that COVID-19 is a primarily respiratory illness, smoking was one of first risk factors we examined,” Dr. Henry said.
They noted that a study by Liu et al. in the Chinese Medical Journal was the only paper that showed a significant association between smoking status and COVID-19 case severity (Chin Med J [Engl]. 2020 Feb 28. doi: 10.1097/CM9.0000000000000775), while the four other studies showed no significant association. The pooled data of all five studies showed an association that was not statistically significant (odds ratio, 1.69; 95% confidence interval, 0.41-6.92; P = .254). When Dr. Lippi and Dr. Henry performed the analysis again after removing a paper by Guan et al. (N Engl J Med. 2020 Feb 28. doi: 10.1056/NEJMoa2002032) comprising 89.5% of patients in the pooled analysis, there was no significant association (OR, 4.35; 95% CI, 0.86-21.86; P = .129).
Constantine I. Vardavas, MD, FCCP, of the department of oral health policy and epidemiology at Harvard School of Dental Medicine, Boston, and Katerina Nikitara, of the University of Crete in Heraklion, Greece, also published a systematic review in Tobacco Induced Diseases of five studies evaluating smoking and COVID-19 (Tob Induc Dis. 2020. doi: 10.18332/tid/119324). Of the studies chosen for the review, four were shared with the paper by Dr. Lippi and Dr. Henry. They found “a higher percentage of smokers” made up severe COVID-19 cases, but acknowledged the majority of these were from the largest study by Guan et al. Overall, they calculated smokers carried a risk ratio of 1.4 (95% CI, 0.98-2.00) for developing severe COVID-19 symptoms, and were over twice as likely to be admitted to an ICU, require a mechanical ventilator, or die from COVID-19, compared with patients who did not smoke (RR, 2.4; 95% CI, 1.43-4.04).
“Although further research is warranted as the weight of the evidence increases, with the limited available data, and although the above results are unadjusted for other factors that may impact disease progression, smoking is most likely associated with the negative progression and adverse outcomes of COVID-19,” Dr. Vardavas and Ms. Nikitara concluded.
However, the association between smoking and severe disease was not significant, and it is not immediately clear how the analysis was performed based on the details in the editorial. “Both of our reports were limited by a lack of data adjusted for age, sex, and comorbidities which may influence any analysis on smoking,” Dr. Henry said.
Some researchers have proposed collecting information on smoking status and conducting further research on whether vaping devices like e-cigarettes also impact COVID-19 cases. An editorial by Samuel Brake and colleagues published in the Journal of Clinical Medicine proposed the ACE2-receptor binding site as an area of interest for COVID-19 and as a potential therapeutic target (J Clin Med. 2020 Mar 20. doi: 10.3390/jcm9030841).
Ultimately, whether smoking itself is associated with COVID-19 is still an open question. Nonetheless, encouraging patients to quit smoking should be a priority because long-term sequelae of smoking have been linked to worsened or fatal COVID-19 cases, said Dr. Henry.
“There is a lack of definitive data on smoking to date. Nonetheless, we do know that many illnesses associated with smoking, such as [chronic obstructive pulmonary disease, hypertension, and heart disease are all strong risk factors for severe and fatal COVID-19,” he said. “Thus, absolutely we should encourage the public to quit smoking, especially for older individuals and those with comorbidities.”
The papers by Lippi et al., Vardavas et al., and Brake et al. had no funding source, and the authors reported no relevant conflicts of interest.
but quitting smoking is likely to lower the risk of developing more severe or fatal cases of the infection, according to research from several recent papers.
Interest in how tobacco use affects COVID-19 infection rates stems from research showing that men at the epicenter of the outbreak in China having a higher early mortality rate. Early reports from China showed a case fatality rate of 4.7% for men, compared with 2.8% for women, according to the World Health Organization. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2, is suspected to enter a cell using the ACE2 receptor. Since smoking up-regulates this receptor, one popular theory is that smoking can increase the risk of COVID-19 or exacerbate symptoms of an existing infection (Eur Respir J. 2020 Apr 8. doi: 10.1183/13993003.00688-2020). In China, about half of men are active smokers, compared with 2.7% of women (Transl Lung Cancer Res. 2019;8[Suppl 1]:S21-30), so this association would explain the severe cases and increased mortality in this group. In response to potential risk for public health, the World Health Organization, Centers for Disease Control and Prevention, the Attorney General of Massachusetts, and other organizations have warned that smoking may increase one’s risk of transmitting and developing COVID-19 or may worsen the infection.
“While it is easy to jump to the conclusion that more ACE2 means more susceptibility to severe infection, there is no evidence to support this,” Brandon Michael Henry, MD, of the cardiac intensive care unit and the Heart Institute at Cincinnati Children’s Hospital Medical Center, said in an interview. “Moreover, some would argue (including myself) that increased ACE2 may in fact be protective, as ACE2 decreases the levels of angiotensin-2 which likely plays a significant role in the pathophysiology of ARDS.”
Some researchers have examined the limited evidence of smoking on COVID-19 risk and come to preliminary conclusions. In a letter to the editor recently published in the European Journal of Internal Medicine, Dr. Henry and Giuseppe Lippi, MD, of the section of clinical biochemistry in the department of neuroscience, biomedicine, and movement at the University of Verona (Italy), performed a meta-analysis of papers examining smoking and COVID-19 up to March 9, 2020 and identified five articles with 1,399 COVID-19 cases (Eur J Intern Med. 2020 Mar 16. doi: 10.1016/j.ejim.2020.03.014).
“Given the fact that COVID-19 is a primarily respiratory illness, smoking was one of first risk factors we examined,” Dr. Henry said.
They noted that a study by Liu et al. in the Chinese Medical Journal was the only paper that showed a significant association between smoking status and COVID-19 case severity (Chin Med J [Engl]. 2020 Feb 28. doi: 10.1097/CM9.0000000000000775), while the four other studies showed no significant association. The pooled data of all five studies showed an association that was not statistically significant (odds ratio, 1.69; 95% confidence interval, 0.41-6.92; P = .254). When Dr. Lippi and Dr. Henry performed the analysis again after removing a paper by Guan et al. (N Engl J Med. 2020 Feb 28. doi: 10.1056/NEJMoa2002032) comprising 89.5% of patients in the pooled analysis, there was no significant association (OR, 4.35; 95% CI, 0.86-21.86; P = .129).
Constantine I. Vardavas, MD, FCCP, of the department of oral health policy and epidemiology at Harvard School of Dental Medicine, Boston, and Katerina Nikitara, of the University of Crete in Heraklion, Greece, also published a systematic review in Tobacco Induced Diseases of five studies evaluating smoking and COVID-19 (Tob Induc Dis. 2020. doi: 10.18332/tid/119324). Of the studies chosen for the review, four were shared with the paper by Dr. Lippi and Dr. Henry. They found “a higher percentage of smokers” made up severe COVID-19 cases, but acknowledged the majority of these were from the largest study by Guan et al. Overall, they calculated smokers carried a risk ratio of 1.4 (95% CI, 0.98-2.00) for developing severe COVID-19 symptoms, and were over twice as likely to be admitted to an ICU, require a mechanical ventilator, or die from COVID-19, compared with patients who did not smoke (RR, 2.4; 95% CI, 1.43-4.04).
“Although further research is warranted as the weight of the evidence increases, with the limited available data, and although the above results are unadjusted for other factors that may impact disease progression, smoking is most likely associated with the negative progression and adverse outcomes of COVID-19,” Dr. Vardavas and Ms. Nikitara concluded.
However, the association between smoking and severe disease was not significant, and it is not immediately clear how the analysis was performed based on the details in the editorial. “Both of our reports were limited by a lack of data adjusted for age, sex, and comorbidities which may influence any analysis on smoking,” Dr. Henry said.
Some researchers have proposed collecting information on smoking status and conducting further research on whether vaping devices like e-cigarettes also impact COVID-19 cases. An editorial by Samuel Brake and colleagues published in the Journal of Clinical Medicine proposed the ACE2-receptor binding site as an area of interest for COVID-19 and as a potential therapeutic target (J Clin Med. 2020 Mar 20. doi: 10.3390/jcm9030841).
Ultimately, whether smoking itself is associated with COVID-19 is still an open question. Nonetheless, encouraging patients to quit smoking should be a priority because long-term sequelae of smoking have been linked to worsened or fatal COVID-19 cases, said Dr. Henry.
“There is a lack of definitive data on smoking to date. Nonetheless, we do know that many illnesses associated with smoking, such as [chronic obstructive pulmonary disease, hypertension, and heart disease are all strong risk factors for severe and fatal COVID-19,” he said. “Thus, absolutely we should encourage the public to quit smoking, especially for older individuals and those with comorbidities.”
The papers by Lippi et al., Vardavas et al., and Brake et al. had no funding source, and the authors reported no relevant conflicts of interest.
but quitting smoking is likely to lower the risk of developing more severe or fatal cases of the infection, according to research from several recent papers.
Interest in how tobacco use affects COVID-19 infection rates stems from research showing that men at the epicenter of the outbreak in China having a higher early mortality rate. Early reports from China showed a case fatality rate of 4.7% for men, compared with 2.8% for women, according to the World Health Organization. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2, is suspected to enter a cell using the ACE2 receptor. Since smoking up-regulates this receptor, one popular theory is that smoking can increase the risk of COVID-19 or exacerbate symptoms of an existing infection (Eur Respir J. 2020 Apr 8. doi: 10.1183/13993003.00688-2020). In China, about half of men are active smokers, compared with 2.7% of women (Transl Lung Cancer Res. 2019;8[Suppl 1]:S21-30), so this association would explain the severe cases and increased mortality in this group. In response to potential risk for public health, the World Health Organization, Centers for Disease Control and Prevention, the Attorney General of Massachusetts, and other organizations have warned that smoking may increase one’s risk of transmitting and developing COVID-19 or may worsen the infection.
“While it is easy to jump to the conclusion that more ACE2 means more susceptibility to severe infection, there is no evidence to support this,” Brandon Michael Henry, MD, of the cardiac intensive care unit and the Heart Institute at Cincinnati Children’s Hospital Medical Center, said in an interview. “Moreover, some would argue (including myself) that increased ACE2 may in fact be protective, as ACE2 decreases the levels of angiotensin-2 which likely plays a significant role in the pathophysiology of ARDS.”
Some researchers have examined the limited evidence of smoking on COVID-19 risk and come to preliminary conclusions. In a letter to the editor recently published in the European Journal of Internal Medicine, Dr. Henry and Giuseppe Lippi, MD, of the section of clinical biochemistry in the department of neuroscience, biomedicine, and movement at the University of Verona (Italy), performed a meta-analysis of papers examining smoking and COVID-19 up to March 9, 2020 and identified five articles with 1,399 COVID-19 cases (Eur J Intern Med. 2020 Mar 16. doi: 10.1016/j.ejim.2020.03.014).
“Given the fact that COVID-19 is a primarily respiratory illness, smoking was one of first risk factors we examined,” Dr. Henry said.
They noted that a study by Liu et al. in the Chinese Medical Journal was the only paper that showed a significant association between smoking status and COVID-19 case severity (Chin Med J [Engl]. 2020 Feb 28. doi: 10.1097/CM9.0000000000000775), while the four other studies showed no significant association. The pooled data of all five studies showed an association that was not statistically significant (odds ratio, 1.69; 95% confidence interval, 0.41-6.92; P = .254). When Dr. Lippi and Dr. Henry performed the analysis again after removing a paper by Guan et al. (N Engl J Med. 2020 Feb 28. doi: 10.1056/NEJMoa2002032) comprising 89.5% of patients in the pooled analysis, there was no significant association (OR, 4.35; 95% CI, 0.86-21.86; P = .129).
Constantine I. Vardavas, MD, FCCP, of the department of oral health policy and epidemiology at Harvard School of Dental Medicine, Boston, and Katerina Nikitara, of the University of Crete in Heraklion, Greece, also published a systematic review in Tobacco Induced Diseases of five studies evaluating smoking and COVID-19 (Tob Induc Dis. 2020. doi: 10.18332/tid/119324). Of the studies chosen for the review, four were shared with the paper by Dr. Lippi and Dr. Henry. They found “a higher percentage of smokers” made up severe COVID-19 cases, but acknowledged the majority of these were from the largest study by Guan et al. Overall, they calculated smokers carried a risk ratio of 1.4 (95% CI, 0.98-2.00) for developing severe COVID-19 symptoms, and were over twice as likely to be admitted to an ICU, require a mechanical ventilator, or die from COVID-19, compared with patients who did not smoke (RR, 2.4; 95% CI, 1.43-4.04).
“Although further research is warranted as the weight of the evidence increases, with the limited available data, and although the above results are unadjusted for other factors that may impact disease progression, smoking is most likely associated with the negative progression and adverse outcomes of COVID-19,” Dr. Vardavas and Ms. Nikitara concluded.
However, the association between smoking and severe disease was not significant, and it is not immediately clear how the analysis was performed based on the details in the editorial. “Both of our reports were limited by a lack of data adjusted for age, sex, and comorbidities which may influence any analysis on smoking,” Dr. Henry said.
Some researchers have proposed collecting information on smoking status and conducting further research on whether vaping devices like e-cigarettes also impact COVID-19 cases. An editorial by Samuel Brake and colleagues published in the Journal of Clinical Medicine proposed the ACE2-receptor binding site as an area of interest for COVID-19 and as a potential therapeutic target (J Clin Med. 2020 Mar 20. doi: 10.3390/jcm9030841).
Ultimately, whether smoking itself is associated with COVID-19 is still an open question. Nonetheless, encouraging patients to quit smoking should be a priority because long-term sequelae of smoking have been linked to worsened or fatal COVID-19 cases, said Dr. Henry.
“There is a lack of definitive data on smoking to date. Nonetheless, we do know that many illnesses associated with smoking, such as [chronic obstructive pulmonary disease, hypertension, and heart disease are all strong risk factors for severe and fatal COVID-19,” he said. “Thus, absolutely we should encourage the public to quit smoking, especially for older individuals and those with comorbidities.”
The papers by Lippi et al., Vardavas et al., and Brake et al. had no funding source, and the authors reported no relevant conflicts of interest.
Switching gears at high speed
Michigan hospitalists prepare for COVID-19 care
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
Michigan hospitalists prepare for COVID-19 care
Michigan hospitalists prepare for COVID-19 care
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
2019-2020 flu season ends with ‘very high’ activity in New Jersey
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
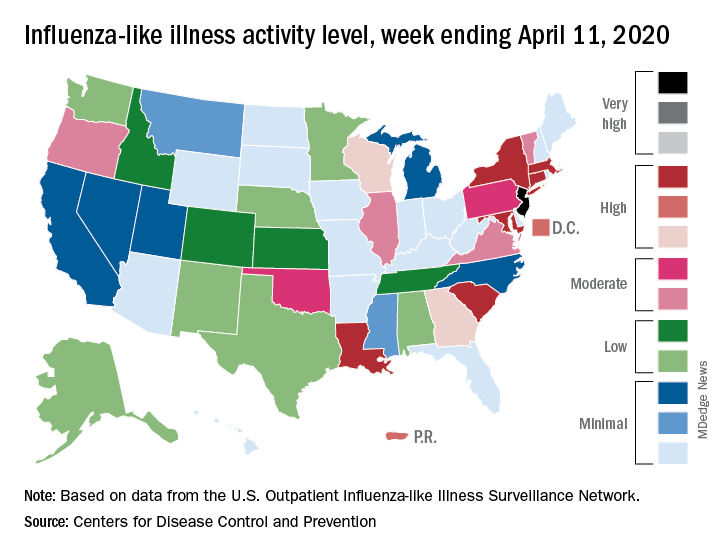
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
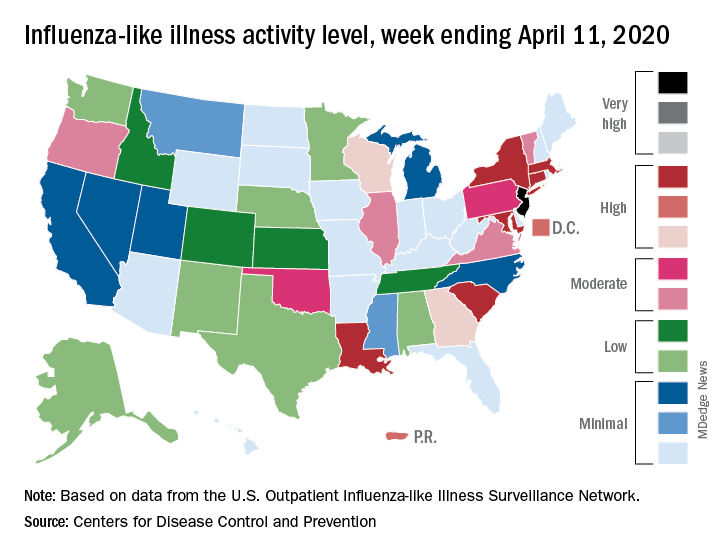
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
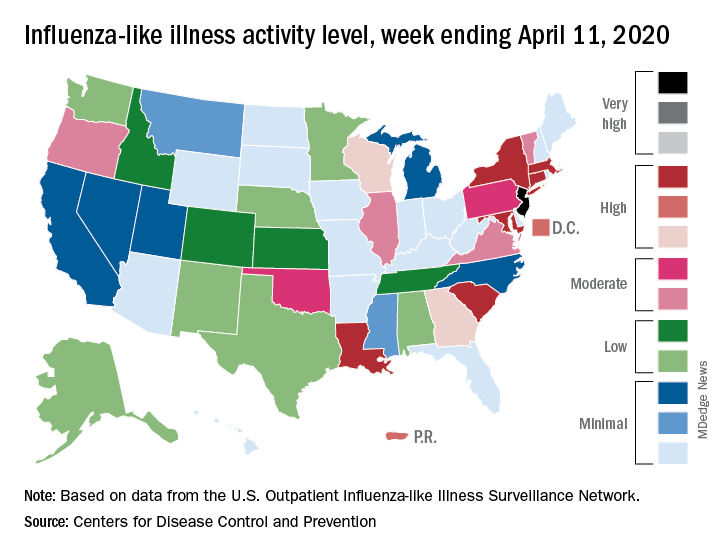
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
Infectious disease experts say testing is key to reopening
The key to opening up the American economy rests on the ability to conduct mass testing, according to the Infectious Diseases Society of America (IDSA).
As policymakers weigh how to safely reopen parts of the United States, the IDSA, along with its HIV Medicine Association, issued a set of recommendations outlining the steps that would be necessary in order to begin easing physical distancing measures.
“A stepwise approach to reopening should reflect early diagnosis and enhanced surveillance for COVID-19 cases, linkage of cases to appropriate levels of care, isolation and/or quarantine, contact tracing, and data processing capabilities for state and local public health departments,” according to the recommendation document.
Some of the recommended steps include the following:
- Widespread testing and surveillance, including use of validated nucleic acid amplification assays and anti–SARS-CoV-2 antibody detection.
- The ability to diagnose, treat, and isolate individuals with COVID-19.
- Scaling up of health care capacity and supplies to manage recurrent episodic outbreaks.
- Maintaining a degree of physical distancing to prevent recurrent outbreaks, including use of masks, limiting gatherings, and continued distancing for susceptible adults.
“The recommendations stress that physical distancing policy changes must be based on relevant data and adequate public health resources and capacities and calls for a rolling and incremental approach to lifting these restrictions, ” Thomas File Jr., MD, IDSA president and a professor at Northeastern Ohio Universities, Rootstown, said during an April 17 press briefing.
The rolling approach “must reflect state and regional capacities for diagnosing, isolating, and treating people with the virus, tracing their contacts, protecting health care workers, and addressing the needs of populations disproportionately affected by COVID-19,” he continued.
In order to fully lift physical distancing restrictions, there would need to be effective treatments for COVID-19 and a protective vaccine that can be deployed to key at-risk populations, according to the recommendations.
During the call, Tina Q. Tan, MD, professor of pediatrics at Northwestern University, Chicago, and a member of the IDSA board of directors, said that easing social distancing requirements requires comprehensive data and that “one of the major missing data points” is the number of people who are currently infected or have been infected. She warned that easing restrictions too soon could have “disastrous consequences,” including an increase in spread of infection, hospitalization, and death rates, as well as overwhelming health care facilities.
“In order to reopen, we have to have the ability to safely, successfully, and rapidly diagnose and treat, as well as isolate, individuals with COVID-19, as well as track their contacts,” she said.
The implementation of more widespread, comprehensive testing would better enable targeting of resources, such as personal protective equipment, ICU beds, and ventilators, Dr. Tan said. “This is needed in order to ensure that, if there is an outbreak and it does occur again, the health care system and the first responders are ready for this,” she said.
The key to opening up the American economy rests on the ability to conduct mass testing, according to the Infectious Diseases Society of America (IDSA).
As policymakers weigh how to safely reopen parts of the United States, the IDSA, along with its HIV Medicine Association, issued a set of recommendations outlining the steps that would be necessary in order to begin easing physical distancing measures.
“A stepwise approach to reopening should reflect early diagnosis and enhanced surveillance for COVID-19 cases, linkage of cases to appropriate levels of care, isolation and/or quarantine, contact tracing, and data processing capabilities for state and local public health departments,” according to the recommendation document.
Some of the recommended steps include the following:
- Widespread testing and surveillance, including use of validated nucleic acid amplification assays and anti–SARS-CoV-2 antibody detection.
- The ability to diagnose, treat, and isolate individuals with COVID-19.
- Scaling up of health care capacity and supplies to manage recurrent episodic outbreaks.
- Maintaining a degree of physical distancing to prevent recurrent outbreaks, including use of masks, limiting gatherings, and continued distancing for susceptible adults.
“The recommendations stress that physical distancing policy changes must be based on relevant data and adequate public health resources and capacities and calls for a rolling and incremental approach to lifting these restrictions, ” Thomas File Jr., MD, IDSA president and a professor at Northeastern Ohio Universities, Rootstown, said during an April 17 press briefing.
The rolling approach “must reflect state and regional capacities for diagnosing, isolating, and treating people with the virus, tracing their contacts, protecting health care workers, and addressing the needs of populations disproportionately affected by COVID-19,” he continued.
In order to fully lift physical distancing restrictions, there would need to be effective treatments for COVID-19 and a protective vaccine that can be deployed to key at-risk populations, according to the recommendations.
During the call, Tina Q. Tan, MD, professor of pediatrics at Northwestern University, Chicago, and a member of the IDSA board of directors, said that easing social distancing requirements requires comprehensive data and that “one of the major missing data points” is the number of people who are currently infected or have been infected. She warned that easing restrictions too soon could have “disastrous consequences,” including an increase in spread of infection, hospitalization, and death rates, as well as overwhelming health care facilities.
“In order to reopen, we have to have the ability to safely, successfully, and rapidly diagnose and treat, as well as isolate, individuals with COVID-19, as well as track their contacts,” she said.
The implementation of more widespread, comprehensive testing would better enable targeting of resources, such as personal protective equipment, ICU beds, and ventilators, Dr. Tan said. “This is needed in order to ensure that, if there is an outbreak and it does occur again, the health care system and the first responders are ready for this,” she said.
The key to opening up the American economy rests on the ability to conduct mass testing, according to the Infectious Diseases Society of America (IDSA).
As policymakers weigh how to safely reopen parts of the United States, the IDSA, along with its HIV Medicine Association, issued a set of recommendations outlining the steps that would be necessary in order to begin easing physical distancing measures.
“A stepwise approach to reopening should reflect early diagnosis and enhanced surveillance for COVID-19 cases, linkage of cases to appropriate levels of care, isolation and/or quarantine, contact tracing, and data processing capabilities for state and local public health departments,” according to the recommendation document.
Some of the recommended steps include the following:
- Widespread testing and surveillance, including use of validated nucleic acid amplification assays and anti–SARS-CoV-2 antibody detection.
- The ability to diagnose, treat, and isolate individuals with COVID-19.
- Scaling up of health care capacity and supplies to manage recurrent episodic outbreaks.
- Maintaining a degree of physical distancing to prevent recurrent outbreaks, including use of masks, limiting gatherings, and continued distancing for susceptible adults.
“The recommendations stress that physical distancing policy changes must be based on relevant data and adequate public health resources and capacities and calls for a rolling and incremental approach to lifting these restrictions, ” Thomas File Jr., MD, IDSA president and a professor at Northeastern Ohio Universities, Rootstown, said during an April 17 press briefing.
The rolling approach “must reflect state and regional capacities for diagnosing, isolating, and treating people with the virus, tracing their contacts, protecting health care workers, and addressing the needs of populations disproportionately affected by COVID-19,” he continued.
In order to fully lift physical distancing restrictions, there would need to be effective treatments for COVID-19 and a protective vaccine that can be deployed to key at-risk populations, according to the recommendations.
During the call, Tina Q. Tan, MD, professor of pediatrics at Northwestern University, Chicago, and a member of the IDSA board of directors, said that easing social distancing requirements requires comprehensive data and that “one of the major missing data points” is the number of people who are currently infected or have been infected. She warned that easing restrictions too soon could have “disastrous consequences,” including an increase in spread of infection, hospitalization, and death rates, as well as overwhelming health care facilities.
“In order to reopen, we have to have the ability to safely, successfully, and rapidly diagnose and treat, as well as isolate, individuals with COVID-19, as well as track their contacts,” she said.
The implementation of more widespread, comprehensive testing would better enable targeting of resources, such as personal protective equipment, ICU beds, and ventilators, Dr. Tan said. “This is needed in order to ensure that, if there is an outbreak and it does occur again, the health care system and the first responders are ready for this,” she said.













