User login
More years of ice hockey play tied to higher CTE risk
new research suggests. Early results from a study that examined donor brains showed that each additional year of ice hockey play increased the risk for CTE by 23%.
This information should be on the “radar” of all clinicians, said coinvestigator Jesse Mez, MD, associate professor of neurology at Boston University. “When they’re talking to kids and families and parents about playing contact sports, they should discuss the benefits as well as the risks so all that information can be taken into consideration.”
Dr. Mez noted that clinicians should also consider the amount of hockey played when assessing patients for thinking and memory trouble later in life. “CTE could be in the differential diagnosis,” he said.
The study findings were presented at the 2022 annual meeting of the American Academy of Neurology.
Football data
CTE is a neurodegenerative disease associated with repetitive hits to the head. In previous research, the investigators showed that the more that athletes play American football, the more likely they are to develop CTE.
“Hockey, like football, involves repetitive head impacts as part of the game,” said Dr. Mez. “So we hypothesized that we would see a similar type of dose-response relationship in hockey.”
From two brain banks – the Veterans Affairs–Boston University–Concussion Legacy Foundation and the Framingham Heart Study – the researchers accessed 74 consecutive brains from donors who had played ice hockey. They collected information about hockey play during “pretty comprehensive” interviews with next of kin, Dr. Mez reported.
The study participants ranged in age from 13 to 91 years. The cause of death varied; most died with end-stage dementia and neurodegenerative disease, but some died of cardiovascular disease, and others from accidents.
For 9% of the individuals, the highest level of play was a youth league; 34% had reached the high school level, 30% reached the juniors/college level, and 26% played professionally. In addition, 46% played another contact sport – including 43% who played American football.
Primary outcomes included evidence of CTE from stage 0 (no CTE) to stage IV and severity of CTE, which was defined by the amount of neurofibrillary tangle (NFT) burden in 11 brain regions. For this burden, the score ranged from 0 (absent) to 3 (severe) in each region for a total range of 0-33.
Dr. Mez noted that, in CTE, tau protein accumulates abnormally. “It typically begins in the cortex in the frontal lobe and then spreads to other parts of the brain, including to the medial temporal structures, and is widespread by stage IV.”
The researchers estimated the association of duration of ice hockey play in years with each neuropathologic outcome and adjusted for age at death and duration of football play.
Consistent findings
Results showed that, of the 74 donors, 40 (54%) had CTE. Each additional year of hockey play corresponded to increased chances for having CTE (odds ratio, 1.23; 95% confidence interval, 11%-36%; P < .01). This increase in risk is similar to that which was found with football players, Dr. Mez noted. This was somewhat surprising, as hockey involves fewer “hits” than football.
“Hits are not as quintessential to the game of hockey as they are in football, where contacts occur with nearly every play,” he said. “In football, you have several hundred impacts over the course of a season.”
Researchers also found a 15% increase in odds for increasing one CTE stage (95% CI, 8%-22%; P < .01), and a .03 standard deviation increase in cumulative NFT burden (95% CI, 0.01-0.05; P < .01).
Dr. Mez noted that the fact that the results were consistent across different outcomes “improves the validity” of the findings.
In a sensitivity analysis that excluded participants who also played football, estimates “were pretty similar” to those in the full analysis, said Dr. Mez.
The investigators have not yet examined the effect of level of hockey play, such as professionally or at the college level, on CTE risk. However, in football players, they found that level of play is another “valuable predictor of CTE pathology,” Dr. Mez said, adding that level of play, position played, and years of play “are all probably contributing” to CTE risk.
Asking about years of play is useful in a clinical setting. “It’s very easy for a clinician to ask patients how many years of hockey they played,” said Dr. Mez.
Overall, the new results are important, as “millions of individuals” play contact sports, whether that is hockey, football, or European soccer, he added. “And for all sports, there seems to be this relationship between more play and risk of this disease.”
‘Skewed’ population?
Commenting on the findings, Frank Conidi, MD, director, Florida Center for Health and Sports Neurology, Port St. Lucie, said he was surprised the investigators found a 23% per year increase in risk for CTE among hockey players.
Dr. Conidi has played hockey himself and works with the Florida Panthers of the National Hockey League. In his practice, he treats retired professional football players who have neurodegenerative disorders. From his experience, the number of repetitive direct head impacts in football is significantly higher than in hockey. “Most of the forces seen in hockey are from hits to the body, where the force is transferred to the head,” said Dr. Conidi, who was not involved with the research.
He noted differences in the way hockey is played around the world. In European countries, for example, the ice surface is relatively large and the emphasis tends to be more on skill than hitting.
“It would have been interesting to have the study group analyze the data based on where the athlete grew up,” he said. Dr. Conidi would also like to know when the participants played hockey. “The game is vastly different now than it was in the 1970s, ‘80s, and early ‘90s, when there was more fighting, less protective gear, and more hitting in general.”
As is the case for most studies of CTE in athletes, the study population is “skewed” because the participants likely had neurocognitive and other problems that led to their decision to donate their brain, said Dr. Conidi.
He also doesn’t believe the study should be the sole factor in a decision to continue or stop playing hockey. “We are still in the infancy stages of understanding the effects of high-impact sports on athletes’ brains.”
The study received funding from the National Institute of Neurological Diseases and Stroke and the National Institute on Aging. Dr. Mez and Dr. Conidi have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests. Early results from a study that examined donor brains showed that each additional year of ice hockey play increased the risk for CTE by 23%.
This information should be on the “radar” of all clinicians, said coinvestigator Jesse Mez, MD, associate professor of neurology at Boston University. “When they’re talking to kids and families and parents about playing contact sports, they should discuss the benefits as well as the risks so all that information can be taken into consideration.”
Dr. Mez noted that clinicians should also consider the amount of hockey played when assessing patients for thinking and memory trouble later in life. “CTE could be in the differential diagnosis,” he said.
The study findings were presented at the 2022 annual meeting of the American Academy of Neurology.
Football data
CTE is a neurodegenerative disease associated with repetitive hits to the head. In previous research, the investigators showed that the more that athletes play American football, the more likely they are to develop CTE.
“Hockey, like football, involves repetitive head impacts as part of the game,” said Dr. Mez. “So we hypothesized that we would see a similar type of dose-response relationship in hockey.”
From two brain banks – the Veterans Affairs–Boston University–Concussion Legacy Foundation and the Framingham Heart Study – the researchers accessed 74 consecutive brains from donors who had played ice hockey. They collected information about hockey play during “pretty comprehensive” interviews with next of kin, Dr. Mez reported.
The study participants ranged in age from 13 to 91 years. The cause of death varied; most died with end-stage dementia and neurodegenerative disease, but some died of cardiovascular disease, and others from accidents.
For 9% of the individuals, the highest level of play was a youth league; 34% had reached the high school level, 30% reached the juniors/college level, and 26% played professionally. In addition, 46% played another contact sport – including 43% who played American football.
Primary outcomes included evidence of CTE from stage 0 (no CTE) to stage IV and severity of CTE, which was defined by the amount of neurofibrillary tangle (NFT) burden in 11 brain regions. For this burden, the score ranged from 0 (absent) to 3 (severe) in each region for a total range of 0-33.
Dr. Mez noted that, in CTE, tau protein accumulates abnormally. “It typically begins in the cortex in the frontal lobe and then spreads to other parts of the brain, including to the medial temporal structures, and is widespread by stage IV.”
The researchers estimated the association of duration of ice hockey play in years with each neuropathologic outcome and adjusted for age at death and duration of football play.
Consistent findings
Results showed that, of the 74 donors, 40 (54%) had CTE. Each additional year of hockey play corresponded to increased chances for having CTE (odds ratio, 1.23; 95% confidence interval, 11%-36%; P < .01). This increase in risk is similar to that which was found with football players, Dr. Mez noted. This was somewhat surprising, as hockey involves fewer “hits” than football.
“Hits are not as quintessential to the game of hockey as they are in football, where contacts occur with nearly every play,” he said. “In football, you have several hundred impacts over the course of a season.”
Researchers also found a 15% increase in odds for increasing one CTE stage (95% CI, 8%-22%; P < .01), and a .03 standard deviation increase in cumulative NFT burden (95% CI, 0.01-0.05; P < .01).
Dr. Mez noted that the fact that the results were consistent across different outcomes “improves the validity” of the findings.
In a sensitivity analysis that excluded participants who also played football, estimates “were pretty similar” to those in the full analysis, said Dr. Mez.
The investigators have not yet examined the effect of level of hockey play, such as professionally or at the college level, on CTE risk. However, in football players, they found that level of play is another “valuable predictor of CTE pathology,” Dr. Mez said, adding that level of play, position played, and years of play “are all probably contributing” to CTE risk.
Asking about years of play is useful in a clinical setting. “It’s very easy for a clinician to ask patients how many years of hockey they played,” said Dr. Mez.
Overall, the new results are important, as “millions of individuals” play contact sports, whether that is hockey, football, or European soccer, he added. “And for all sports, there seems to be this relationship between more play and risk of this disease.”
‘Skewed’ population?
Commenting on the findings, Frank Conidi, MD, director, Florida Center for Health and Sports Neurology, Port St. Lucie, said he was surprised the investigators found a 23% per year increase in risk for CTE among hockey players.
Dr. Conidi has played hockey himself and works with the Florida Panthers of the National Hockey League. In his practice, he treats retired professional football players who have neurodegenerative disorders. From his experience, the number of repetitive direct head impacts in football is significantly higher than in hockey. “Most of the forces seen in hockey are from hits to the body, where the force is transferred to the head,” said Dr. Conidi, who was not involved with the research.
He noted differences in the way hockey is played around the world. In European countries, for example, the ice surface is relatively large and the emphasis tends to be more on skill than hitting.
“It would have been interesting to have the study group analyze the data based on where the athlete grew up,” he said. Dr. Conidi would also like to know when the participants played hockey. “The game is vastly different now than it was in the 1970s, ‘80s, and early ‘90s, when there was more fighting, less protective gear, and more hitting in general.”
As is the case for most studies of CTE in athletes, the study population is “skewed” because the participants likely had neurocognitive and other problems that led to their decision to donate their brain, said Dr. Conidi.
He also doesn’t believe the study should be the sole factor in a decision to continue or stop playing hockey. “We are still in the infancy stages of understanding the effects of high-impact sports on athletes’ brains.”
The study received funding from the National Institute of Neurological Diseases and Stroke and the National Institute on Aging. Dr. Mez and Dr. Conidi have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests. Early results from a study that examined donor brains showed that each additional year of ice hockey play increased the risk for CTE by 23%.
This information should be on the “radar” of all clinicians, said coinvestigator Jesse Mez, MD, associate professor of neurology at Boston University. “When they’re talking to kids and families and parents about playing contact sports, they should discuss the benefits as well as the risks so all that information can be taken into consideration.”
Dr. Mez noted that clinicians should also consider the amount of hockey played when assessing patients for thinking and memory trouble later in life. “CTE could be in the differential diagnosis,” he said.
The study findings were presented at the 2022 annual meeting of the American Academy of Neurology.
Football data
CTE is a neurodegenerative disease associated with repetitive hits to the head. In previous research, the investigators showed that the more that athletes play American football, the more likely they are to develop CTE.
“Hockey, like football, involves repetitive head impacts as part of the game,” said Dr. Mez. “So we hypothesized that we would see a similar type of dose-response relationship in hockey.”
From two brain banks – the Veterans Affairs–Boston University–Concussion Legacy Foundation and the Framingham Heart Study – the researchers accessed 74 consecutive brains from donors who had played ice hockey. They collected information about hockey play during “pretty comprehensive” interviews with next of kin, Dr. Mez reported.
The study participants ranged in age from 13 to 91 years. The cause of death varied; most died with end-stage dementia and neurodegenerative disease, but some died of cardiovascular disease, and others from accidents.
For 9% of the individuals, the highest level of play was a youth league; 34% had reached the high school level, 30% reached the juniors/college level, and 26% played professionally. In addition, 46% played another contact sport – including 43% who played American football.
Primary outcomes included evidence of CTE from stage 0 (no CTE) to stage IV and severity of CTE, which was defined by the amount of neurofibrillary tangle (NFT) burden in 11 brain regions. For this burden, the score ranged from 0 (absent) to 3 (severe) in each region for a total range of 0-33.
Dr. Mez noted that, in CTE, tau protein accumulates abnormally. “It typically begins in the cortex in the frontal lobe and then spreads to other parts of the brain, including to the medial temporal structures, and is widespread by stage IV.”
The researchers estimated the association of duration of ice hockey play in years with each neuropathologic outcome and adjusted for age at death and duration of football play.
Consistent findings
Results showed that, of the 74 donors, 40 (54%) had CTE. Each additional year of hockey play corresponded to increased chances for having CTE (odds ratio, 1.23; 95% confidence interval, 11%-36%; P < .01). This increase in risk is similar to that which was found with football players, Dr. Mez noted. This was somewhat surprising, as hockey involves fewer “hits” than football.
“Hits are not as quintessential to the game of hockey as they are in football, where contacts occur with nearly every play,” he said. “In football, you have several hundred impacts over the course of a season.”
Researchers also found a 15% increase in odds for increasing one CTE stage (95% CI, 8%-22%; P < .01), and a .03 standard deviation increase in cumulative NFT burden (95% CI, 0.01-0.05; P < .01).
Dr. Mez noted that the fact that the results were consistent across different outcomes “improves the validity” of the findings.
In a sensitivity analysis that excluded participants who also played football, estimates “were pretty similar” to those in the full analysis, said Dr. Mez.
The investigators have not yet examined the effect of level of hockey play, such as professionally or at the college level, on CTE risk. However, in football players, they found that level of play is another “valuable predictor of CTE pathology,” Dr. Mez said, adding that level of play, position played, and years of play “are all probably contributing” to CTE risk.
Asking about years of play is useful in a clinical setting. “It’s very easy for a clinician to ask patients how many years of hockey they played,” said Dr. Mez.
Overall, the new results are important, as “millions of individuals” play contact sports, whether that is hockey, football, or European soccer, he added. “And for all sports, there seems to be this relationship between more play and risk of this disease.”
‘Skewed’ population?
Commenting on the findings, Frank Conidi, MD, director, Florida Center for Health and Sports Neurology, Port St. Lucie, said he was surprised the investigators found a 23% per year increase in risk for CTE among hockey players.
Dr. Conidi has played hockey himself and works with the Florida Panthers of the National Hockey League. In his practice, he treats retired professional football players who have neurodegenerative disorders. From his experience, the number of repetitive direct head impacts in football is significantly higher than in hockey. “Most of the forces seen in hockey are from hits to the body, where the force is transferred to the head,” said Dr. Conidi, who was not involved with the research.
He noted differences in the way hockey is played around the world. In European countries, for example, the ice surface is relatively large and the emphasis tends to be more on skill than hitting.
“It would have been interesting to have the study group analyze the data based on where the athlete grew up,” he said. Dr. Conidi would also like to know when the participants played hockey. “The game is vastly different now than it was in the 1970s, ‘80s, and early ‘90s, when there was more fighting, less protective gear, and more hitting in general.”
As is the case for most studies of CTE in athletes, the study population is “skewed” because the participants likely had neurocognitive and other problems that led to their decision to donate their brain, said Dr. Conidi.
He also doesn’t believe the study should be the sole factor in a decision to continue or stop playing hockey. “We are still in the infancy stages of understanding the effects of high-impact sports on athletes’ brains.”
The study received funding from the National Institute of Neurological Diseases and Stroke and the National Institute on Aging. Dr. Mez and Dr. Conidi have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAN 2022
Give patients can’ts but also can do’s
On his last shift in the last hockey game of the regular season, our 14-year-old grandson broke his arm. Although this was his first fracture, the rest of the nuclear family has had ample experience with orthopedic trauma over the last year, both planned and unplanned.
As I drove Peter and my daughter-in-law to his first postsetting and casting appointment I told him how sorry I was that he had been told “no contact sports for the next 3 months.” This was a tough pill for a kid eager to begin his first high school lacrosse season. Then I asked him what the doctor had told him he could do in the way of activity.
Based on personal and professional experience I was not surprised when he told me that no one had suggested things he could be doing. In fact, being a cautious and thoughtful kid, he was concerned about what he should be doing around the house let alone any athletic activities. It turns out he wasn’t even lifting his laptop computer with two hands because some nurse had told him not to lift anything over 2 pounds.
I told him “Peter, even some of the most experienced doctors focus on the ‘can’ts’ and forget to tell you the ‘cans’ and ‘shoulds.’ While you’re in the waiting room make up a mental list of what you would like to be doing that you aren’t.”
As he climbed back in the car for the ride home I asked how the visit went. The x-ray showed good alignment and the doctor was pleased. But, as I predicted, they were already on the launch pad to the receptionist to make a follow-up appointment without the physician uttering a single word about what activities he could resume. Always a very coachable kid, Peter piped up with the list he had created in the waiting room and was relieved to hear that he could do anything as long as it didn’t hurt. In fact, the doctor encouraged him to use his fingers because it might speed the healing.
Not every patient, regardless of age, is as cautious as my grandson and in some circumstances the physician must err on the side of emphasizing the “don’ts.” However, in my experience, too many physicians forget to include a generous list of “can do’s” in their visit closing discussions. This oversight is a mistake for several reasons.
First, and maybe most importantly, even a brief discussion of “can do’s” can soften the depressing message that the patient will not be able to do things he or she enjoys. I can’t quote the references but I am sure there is plenty of evidence that depression slows the healing process.
Second, and this is particularly true in older patients with orthopedic problems – failure to include a plan for return to activity can hinder recovery. I can recall more than a few patients who were seen in the emergency department and diagnosed with sprains but not given even the simplest instructions on how to begin moving the injured joint. When they finally returned to see me we had to begin the painful and unnecessary project of thawing a frozen joint.
Fortunately, we have evolved past the era when best rest was near the top of the list of our recommended remedies. However, there still remains a bias against activity in some situations. The most recent example is the evolving strategies for the management of concussion. There is some evidence that involving the patient in a return to activity plan may shorten the time to recovery. The myth about brain rest has been slow to die.
Finally, providing the patient with a personalized list of “can do’s” makes good business sense because it can head off those time-gobbling call backs that tie up you and your office staff. As an experienced physician, you have probably learned the most frequently asked “Can Jason do ... ?” questions. Make your own list and give the patient your answers. An ounce of anticipatory guidance is worth hours on the telephone or sorting through the email inbox.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
On his last shift in the last hockey game of the regular season, our 14-year-old grandson broke his arm. Although this was his first fracture, the rest of the nuclear family has had ample experience with orthopedic trauma over the last year, both planned and unplanned.
As I drove Peter and my daughter-in-law to his first postsetting and casting appointment I told him how sorry I was that he had been told “no contact sports for the next 3 months.” This was a tough pill for a kid eager to begin his first high school lacrosse season. Then I asked him what the doctor had told him he could do in the way of activity.
Based on personal and professional experience I was not surprised when he told me that no one had suggested things he could be doing. In fact, being a cautious and thoughtful kid, he was concerned about what he should be doing around the house let alone any athletic activities. It turns out he wasn’t even lifting his laptop computer with two hands because some nurse had told him not to lift anything over 2 pounds.
I told him “Peter, even some of the most experienced doctors focus on the ‘can’ts’ and forget to tell you the ‘cans’ and ‘shoulds.’ While you’re in the waiting room make up a mental list of what you would like to be doing that you aren’t.”
As he climbed back in the car for the ride home I asked how the visit went. The x-ray showed good alignment and the doctor was pleased. But, as I predicted, they were already on the launch pad to the receptionist to make a follow-up appointment without the physician uttering a single word about what activities he could resume. Always a very coachable kid, Peter piped up with the list he had created in the waiting room and was relieved to hear that he could do anything as long as it didn’t hurt. In fact, the doctor encouraged him to use his fingers because it might speed the healing.
Not every patient, regardless of age, is as cautious as my grandson and in some circumstances the physician must err on the side of emphasizing the “don’ts.” However, in my experience, too many physicians forget to include a generous list of “can do’s” in their visit closing discussions. This oversight is a mistake for several reasons.
First, and maybe most importantly, even a brief discussion of “can do’s” can soften the depressing message that the patient will not be able to do things he or she enjoys. I can’t quote the references but I am sure there is plenty of evidence that depression slows the healing process.
Second, and this is particularly true in older patients with orthopedic problems – failure to include a plan for return to activity can hinder recovery. I can recall more than a few patients who were seen in the emergency department and diagnosed with sprains but not given even the simplest instructions on how to begin moving the injured joint. When they finally returned to see me we had to begin the painful and unnecessary project of thawing a frozen joint.
Fortunately, we have evolved past the era when best rest was near the top of the list of our recommended remedies. However, there still remains a bias against activity in some situations. The most recent example is the evolving strategies for the management of concussion. There is some evidence that involving the patient in a return to activity plan may shorten the time to recovery. The myth about brain rest has been slow to die.
Finally, providing the patient with a personalized list of “can do’s” makes good business sense because it can head off those time-gobbling call backs that tie up you and your office staff. As an experienced physician, you have probably learned the most frequently asked “Can Jason do ... ?” questions. Make your own list and give the patient your answers. An ounce of anticipatory guidance is worth hours on the telephone or sorting through the email inbox.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
On his last shift in the last hockey game of the regular season, our 14-year-old grandson broke his arm. Although this was his first fracture, the rest of the nuclear family has had ample experience with orthopedic trauma over the last year, both planned and unplanned.
As I drove Peter and my daughter-in-law to his first postsetting and casting appointment I told him how sorry I was that he had been told “no contact sports for the next 3 months.” This was a tough pill for a kid eager to begin his first high school lacrosse season. Then I asked him what the doctor had told him he could do in the way of activity.
Based on personal and professional experience I was not surprised when he told me that no one had suggested things he could be doing. In fact, being a cautious and thoughtful kid, he was concerned about what he should be doing around the house let alone any athletic activities. It turns out he wasn’t even lifting his laptop computer with two hands because some nurse had told him not to lift anything over 2 pounds.
I told him “Peter, even some of the most experienced doctors focus on the ‘can’ts’ and forget to tell you the ‘cans’ and ‘shoulds.’ While you’re in the waiting room make up a mental list of what you would like to be doing that you aren’t.”
As he climbed back in the car for the ride home I asked how the visit went. The x-ray showed good alignment and the doctor was pleased. But, as I predicted, they were already on the launch pad to the receptionist to make a follow-up appointment without the physician uttering a single word about what activities he could resume. Always a very coachable kid, Peter piped up with the list he had created in the waiting room and was relieved to hear that he could do anything as long as it didn’t hurt. In fact, the doctor encouraged him to use his fingers because it might speed the healing.
Not every patient, regardless of age, is as cautious as my grandson and in some circumstances the physician must err on the side of emphasizing the “don’ts.” However, in my experience, too many physicians forget to include a generous list of “can do’s” in their visit closing discussions. This oversight is a mistake for several reasons.
First, and maybe most importantly, even a brief discussion of “can do’s” can soften the depressing message that the patient will not be able to do things he or she enjoys. I can’t quote the references but I am sure there is plenty of evidence that depression slows the healing process.
Second, and this is particularly true in older patients with orthopedic problems – failure to include a plan for return to activity can hinder recovery. I can recall more than a few patients who were seen in the emergency department and diagnosed with sprains but not given even the simplest instructions on how to begin moving the injured joint. When they finally returned to see me we had to begin the painful and unnecessary project of thawing a frozen joint.
Fortunately, we have evolved past the era when best rest was near the top of the list of our recommended remedies. However, there still remains a bias against activity in some situations. The most recent example is the evolving strategies for the management of concussion. There is some evidence that involving the patient in a return to activity plan may shorten the time to recovery. The myth about brain rest has been slow to die.
Finally, providing the patient with a personalized list of “can do’s” makes good business sense because it can head off those time-gobbling call backs that tie up you and your office staff. As an experienced physician, you have probably learned the most frequently asked “Can Jason do ... ?” questions. Make your own list and give the patient your answers. An ounce of anticipatory guidance is worth hours on the telephone or sorting through the email inbox.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Is family reunification our goal?
This has been an unfortunate, but not an atypical year, for the children in Maine whose lives have intersected with the state’s Department of Health and Human Services. In 2021, 25 children died of abuse and neglect or in homes with prior involvement with the child protective system. Four cases not included in that number are currently listed as homicides. At a recent legislative hearing the grandmother of one of those victims told her story to the lawmaker.
Her grandson was removed from his mother’s custody at 3 months of age after a 2-year-old sibling overdosed on methadone. Father and grandmother became his caregivers but when the father was arrested the child was returned to the mother’s custody by a judge despite the pleas of the child’s court-appointed guardian. The child eventually returned to the care of his paternal aunt and father, but when the father was arrested again the then 3-year-old was returned to his mother. Within months he was dead with multiple fractures, including to his spine and with internal and intracranial bleeding (Overton P. Maine’s child welfare system failed a 3-year old who died, grandmother tells lawmakers. 2022 Feb 11. Portland Press Herald).
The grandmother questioned the legislators why a vulnerable child would be returned to the care of a woman with such an extensive history of involvement with the Department of Health and Human Services. While there may have been errors of judgment on the part of department staff, in large part the answer lies in the system’s emphasis on reunification. Like apple pie, motherhood, and more recently fatherhood, have been viewed as something deserving of our unquestioning efforts to preserve.
This is not a recent trend. Some of the most frustrating cases over my 40 years of practice involved the failure of the courts and in some cases social workers to place a child’s welfare in the proper perspective as court schedules and custody decisions were made. Too often the reunification of “the family” seemed to trump the needs of the child. Fortunately, I’m unaware of any of my patients who died as the result of these untimely and poorly made decisions. However, many of my patients lived in unsettled conditions never sure what the next week would bring while the system focused on giving an adult whose life was a mess one more chance to demonstrate his or her ability to parent.
Of course, there are occasions in which child protective workers have been too hasty in pulling a child from his or her parents. But, in my experience those cases pale next to the number of times in which children were exposed to home environments that threatened their psychological health and development. Yes, there are bad foster homes. Many foster homes might do a better job if they were working in a system that put a higher value on the emotional needs and safety of the children in making its custody decisions.
We have a governor here in Maine who has worked hard to do the right thing during the pandemic and has made child health a focus. However, her recent proposed appropriations bill appears to continue the focus on reunification by funneling money into programs such as family reunion training and coaching as well as a parent mentorship program. Certainly, one can’t argue that these kind of programs might be helpful to some families. On the other hand, we can’t let these programs create the impression that an intact family is our primary goal. Not every family is repairable, at least on a time schedule compatible with the emotional and health needs of the children.
I wouldn’t be surprised to learn that many of you have experienced a similar frustration when decisions based on an unrealistic goal of family reunification have put your patients at risk.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
This has been an unfortunate, but not an atypical year, for the children in Maine whose lives have intersected with the state’s Department of Health and Human Services. In 2021, 25 children died of abuse and neglect or in homes with prior involvement with the child protective system. Four cases not included in that number are currently listed as homicides. At a recent legislative hearing the grandmother of one of those victims told her story to the lawmaker.
Her grandson was removed from his mother’s custody at 3 months of age after a 2-year-old sibling overdosed on methadone. Father and grandmother became his caregivers but when the father was arrested the child was returned to the mother’s custody by a judge despite the pleas of the child’s court-appointed guardian. The child eventually returned to the care of his paternal aunt and father, but when the father was arrested again the then 3-year-old was returned to his mother. Within months he was dead with multiple fractures, including to his spine and with internal and intracranial bleeding (Overton P. Maine’s child welfare system failed a 3-year old who died, grandmother tells lawmakers. 2022 Feb 11. Portland Press Herald).
The grandmother questioned the legislators why a vulnerable child would be returned to the care of a woman with such an extensive history of involvement with the Department of Health and Human Services. While there may have been errors of judgment on the part of department staff, in large part the answer lies in the system’s emphasis on reunification. Like apple pie, motherhood, and more recently fatherhood, have been viewed as something deserving of our unquestioning efforts to preserve.
This is not a recent trend. Some of the most frustrating cases over my 40 years of practice involved the failure of the courts and in some cases social workers to place a child’s welfare in the proper perspective as court schedules and custody decisions were made. Too often the reunification of “the family” seemed to trump the needs of the child. Fortunately, I’m unaware of any of my patients who died as the result of these untimely and poorly made decisions. However, many of my patients lived in unsettled conditions never sure what the next week would bring while the system focused on giving an adult whose life was a mess one more chance to demonstrate his or her ability to parent.
Of course, there are occasions in which child protective workers have been too hasty in pulling a child from his or her parents. But, in my experience those cases pale next to the number of times in which children were exposed to home environments that threatened their psychological health and development. Yes, there are bad foster homes. Many foster homes might do a better job if they were working in a system that put a higher value on the emotional needs and safety of the children in making its custody decisions.
We have a governor here in Maine who has worked hard to do the right thing during the pandemic and has made child health a focus. However, her recent proposed appropriations bill appears to continue the focus on reunification by funneling money into programs such as family reunion training and coaching as well as a parent mentorship program. Certainly, one can’t argue that these kind of programs might be helpful to some families. On the other hand, we can’t let these programs create the impression that an intact family is our primary goal. Not every family is repairable, at least on a time schedule compatible with the emotional and health needs of the children.
I wouldn’t be surprised to learn that many of you have experienced a similar frustration when decisions based on an unrealistic goal of family reunification have put your patients at risk.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
This has been an unfortunate, but not an atypical year, for the children in Maine whose lives have intersected with the state’s Department of Health and Human Services. In 2021, 25 children died of abuse and neglect or in homes with prior involvement with the child protective system. Four cases not included in that number are currently listed as homicides. At a recent legislative hearing the grandmother of one of those victims told her story to the lawmaker.
Her grandson was removed from his mother’s custody at 3 months of age after a 2-year-old sibling overdosed on methadone. Father and grandmother became his caregivers but when the father was arrested the child was returned to the mother’s custody by a judge despite the pleas of the child’s court-appointed guardian. The child eventually returned to the care of his paternal aunt and father, but when the father was arrested again the then 3-year-old was returned to his mother. Within months he was dead with multiple fractures, including to his spine and with internal and intracranial bleeding (Overton P. Maine’s child welfare system failed a 3-year old who died, grandmother tells lawmakers. 2022 Feb 11. Portland Press Herald).
The grandmother questioned the legislators why a vulnerable child would be returned to the care of a woman with such an extensive history of involvement with the Department of Health and Human Services. While there may have been errors of judgment on the part of department staff, in large part the answer lies in the system’s emphasis on reunification. Like apple pie, motherhood, and more recently fatherhood, have been viewed as something deserving of our unquestioning efforts to preserve.
This is not a recent trend. Some of the most frustrating cases over my 40 years of practice involved the failure of the courts and in some cases social workers to place a child’s welfare in the proper perspective as court schedules and custody decisions were made. Too often the reunification of “the family” seemed to trump the needs of the child. Fortunately, I’m unaware of any of my patients who died as the result of these untimely and poorly made decisions. However, many of my patients lived in unsettled conditions never sure what the next week would bring while the system focused on giving an adult whose life was a mess one more chance to demonstrate his or her ability to parent.
Of course, there are occasions in which child protective workers have been too hasty in pulling a child from his or her parents. But, in my experience those cases pale next to the number of times in which children were exposed to home environments that threatened their psychological health and development. Yes, there are bad foster homes. Many foster homes might do a better job if they were working in a system that put a higher value on the emotional needs and safety of the children in making its custody decisions.
We have a governor here in Maine who has worked hard to do the right thing during the pandemic and has made child health a focus. However, her recent proposed appropriations bill appears to continue the focus on reunification by funneling money into programs such as family reunion training and coaching as well as a parent mentorship program. Certainly, one can’t argue that these kind of programs might be helpful to some families. On the other hand, we can’t let these programs create the impression that an intact family is our primary goal. Not every family is repairable, at least on a time schedule compatible with the emotional and health needs of the children.
I wouldn’t be surprised to learn that many of you have experienced a similar frustration when decisions based on an unrealistic goal of family reunification have put your patients at risk.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Strangulation deaths spur FDA alert on pediatric enteral feeding kits
Enteral feeding kits pose a risk for strangulation in children, according to a safety alert from the U.S. Food and Drug Administration. The safety alert was prompted by two deaths linked to the medical devices.
The alert cites the deaths in 2021 of two toddlers who were strangled by tubes in the feeding sets that had become wrapped around their necks.
Clinicians should discuss the risk of strangulation with colleagues and caregivers and encourage them to take steps to keep tubing away from children as much as possible, the agency advised in a Feb. 8, 2022, safety communication.
“When caring for pediatric patients who receive enteral feeding and as part of an individual risk assessment, be aware of the risk of strangulation from the feeding set tubing and follow protocols to monitor medical line safety,” the FDA warned.
Parents should be aware of the risk and avoid leaving tubing where infants or children can become entangled, to the extent that is possible. They also should tell their child’s health care provider if their child has ever been tangled in the tubing and discuss precautions to ensure that tubing does not get wrapped around the neck, as well as any related concerns.
Enteral feeding sets provide nutrition to people who are unable meet their nutritional needs by eating or swallowing. Tubing delivers nutrition formulas, using gravity or a pump, directly to the stomach or small intestine through the nose, mouth, or an opening in the abdomen.
The two reported deaths involved children under the age of 2 years who were found with tubing wrapped around their necks after brief periods when their caregivers were not directly monitoring them. One report described the unsupervised period as about 10 minutes.
“While the FDA believes that death or serious injury from strangulation with enteral feeding set tubing in children is rare, health care providers and caregivers should be aware that these events can and do occur,” according to the alert. “It is also possible that some cases have not been reported to the FDA.”
Parents and health care providers can report injuries caused by these devices to the FDA.
A version of this article first appeared on Medscape.com.
Enteral feeding kits pose a risk for strangulation in children, according to a safety alert from the U.S. Food and Drug Administration. The safety alert was prompted by two deaths linked to the medical devices.
The alert cites the deaths in 2021 of two toddlers who were strangled by tubes in the feeding sets that had become wrapped around their necks.
Clinicians should discuss the risk of strangulation with colleagues and caregivers and encourage them to take steps to keep tubing away from children as much as possible, the agency advised in a Feb. 8, 2022, safety communication.
“When caring for pediatric patients who receive enteral feeding and as part of an individual risk assessment, be aware of the risk of strangulation from the feeding set tubing and follow protocols to monitor medical line safety,” the FDA warned.
Parents should be aware of the risk and avoid leaving tubing where infants or children can become entangled, to the extent that is possible. They also should tell their child’s health care provider if their child has ever been tangled in the tubing and discuss precautions to ensure that tubing does not get wrapped around the neck, as well as any related concerns.
Enteral feeding sets provide nutrition to people who are unable meet their nutritional needs by eating or swallowing. Tubing delivers nutrition formulas, using gravity or a pump, directly to the stomach or small intestine through the nose, mouth, or an opening in the abdomen.
The two reported deaths involved children under the age of 2 years who were found with tubing wrapped around their necks after brief periods when their caregivers were not directly monitoring them. One report described the unsupervised period as about 10 minutes.
“While the FDA believes that death or serious injury from strangulation with enteral feeding set tubing in children is rare, health care providers and caregivers should be aware that these events can and do occur,” according to the alert. “It is also possible that some cases have not been reported to the FDA.”
Parents and health care providers can report injuries caused by these devices to the FDA.
A version of this article first appeared on Medscape.com.
Enteral feeding kits pose a risk for strangulation in children, according to a safety alert from the U.S. Food and Drug Administration. The safety alert was prompted by two deaths linked to the medical devices.
The alert cites the deaths in 2021 of two toddlers who were strangled by tubes in the feeding sets that had become wrapped around their necks.
Clinicians should discuss the risk of strangulation with colleagues and caregivers and encourage them to take steps to keep tubing away from children as much as possible, the agency advised in a Feb. 8, 2022, safety communication.
“When caring for pediatric patients who receive enteral feeding and as part of an individual risk assessment, be aware of the risk of strangulation from the feeding set tubing and follow protocols to monitor medical line safety,” the FDA warned.
Parents should be aware of the risk and avoid leaving tubing where infants or children can become entangled, to the extent that is possible. They also should tell their child’s health care provider if their child has ever been tangled in the tubing and discuss precautions to ensure that tubing does not get wrapped around the neck, as well as any related concerns.
Enteral feeding sets provide nutrition to people who are unable meet their nutritional needs by eating or swallowing. Tubing delivers nutrition formulas, using gravity or a pump, directly to the stomach or small intestine through the nose, mouth, or an opening in the abdomen.
The two reported deaths involved children under the age of 2 years who were found with tubing wrapped around their necks after brief periods when their caregivers were not directly monitoring them. One report described the unsupervised period as about 10 minutes.
“While the FDA believes that death or serious injury from strangulation with enteral feeding set tubing in children is rare, health care providers and caregivers should be aware that these events can and do occur,” according to the alert. “It is also possible that some cases have not been reported to the FDA.”
Parents and health care providers can report injuries caused by these devices to the FDA.
A version of this article first appeared on Medscape.com.
‘Baby-wearing’ poses serious injury risks for infants, ED data show
Baby-wearing – carrying a child against your body in a sling, soft carrier, or other device – is associated with benefits like reduced crying and increased breastfeeding, studies have shown.
But this practice also entails risks. Babies can fall out of carriers, or be injured when an adult carrying them falls, for example.
researchers estimated in a study presented at the annual meeting of the American Academy of Pediatrics.
To characterize the epidemiology of these injuries, Samantha J. Rowe, MD, chief resident physician at Walter Reed National Military Medical Center in Bethesda, Md., and colleagues analyzed data from the National Electronic Injury Surveillance System between 2011 and 2020.
They included in their analysis data from patients aged 5 years and younger who sustained an injury associated with a baby-wearing product. Baby harnesses, carriers, slings, framed baby carriers, and soft baby carriers were among the devices included in the study. The researchers used 601 cases to generate national estimates.
An estimated 14,024 patients presented to EDs because of baby-wearing injuries, and 52% of the injuries occurred when a patient fell from the product.
Most injuries (61%) occurred in children aged 5 months and younger; 19.3% of these infants required hospitalization, most often for head injuries.
The investigators found that about 22% of the injuries were associated with a caregiver falling, noted Rachel Y. Moon, MD, who was not involved in the study.
“Carrying a baby changes your center of gravity – and can also obscure your vision of where you’re walking, so adults who use these devices should be cognizant of this,” said Dr. Moon, with the University of Virginia, Charlottesville.
Dr. Rowe often practiced baby-wearing with her daughter, and found that it was beneficial. And studies have demonstrated various benefits of baby-wearing, including improved thermoregulation and glycemic control.
Still, the new analysis illustrates the potential for baby-wearing products “to cause serious injury, especially in infants 5 months and younger,” Dr. Rowe said. “We need to provide more education to caregivers on safe baby-wearing and continue to improve our safety standards for baby-wearing products.”
Study coauthor Patrick T. Reeves, MD, with the Naval Medical Center at San Diego, offered additional guidance in a news release: “Like when buying a new pair of shoes, parents must be educated on the proper sizing, selection, and wear of baby carriers to prevent injury to themselves and their child.”
Parents also need to ensure that the child’s nose and mouth are not obstructed, Dr. Moon
In a recent article discussing the possible benefits of baby-wearing in terms of helping with breastfeeding, Dr. Moon also pointed out further safety considerations: “No matter which carrier is used, for safety reasons, we need to remind parents that the baby should be positioned so that the head is upright and the nose and mouth are not obstructed.”
The researchers and Dr. Moon had no relevant financial disclosures.
Baby-wearing – carrying a child against your body in a sling, soft carrier, or other device – is associated with benefits like reduced crying and increased breastfeeding, studies have shown.
But this practice also entails risks. Babies can fall out of carriers, or be injured when an adult carrying them falls, for example.
researchers estimated in a study presented at the annual meeting of the American Academy of Pediatrics.
To characterize the epidemiology of these injuries, Samantha J. Rowe, MD, chief resident physician at Walter Reed National Military Medical Center in Bethesda, Md., and colleagues analyzed data from the National Electronic Injury Surveillance System between 2011 and 2020.
They included in their analysis data from patients aged 5 years and younger who sustained an injury associated with a baby-wearing product. Baby harnesses, carriers, slings, framed baby carriers, and soft baby carriers were among the devices included in the study. The researchers used 601 cases to generate national estimates.
An estimated 14,024 patients presented to EDs because of baby-wearing injuries, and 52% of the injuries occurred when a patient fell from the product.
Most injuries (61%) occurred in children aged 5 months and younger; 19.3% of these infants required hospitalization, most often for head injuries.
The investigators found that about 22% of the injuries were associated with a caregiver falling, noted Rachel Y. Moon, MD, who was not involved in the study.
“Carrying a baby changes your center of gravity – and can also obscure your vision of where you’re walking, so adults who use these devices should be cognizant of this,” said Dr. Moon, with the University of Virginia, Charlottesville.
Dr. Rowe often practiced baby-wearing with her daughter, and found that it was beneficial. And studies have demonstrated various benefits of baby-wearing, including improved thermoregulation and glycemic control.
Still, the new analysis illustrates the potential for baby-wearing products “to cause serious injury, especially in infants 5 months and younger,” Dr. Rowe said. “We need to provide more education to caregivers on safe baby-wearing and continue to improve our safety standards for baby-wearing products.”
Study coauthor Patrick T. Reeves, MD, with the Naval Medical Center at San Diego, offered additional guidance in a news release: “Like when buying a new pair of shoes, parents must be educated on the proper sizing, selection, and wear of baby carriers to prevent injury to themselves and their child.”
Parents also need to ensure that the child’s nose and mouth are not obstructed, Dr. Moon
In a recent article discussing the possible benefits of baby-wearing in terms of helping with breastfeeding, Dr. Moon also pointed out further safety considerations: “No matter which carrier is used, for safety reasons, we need to remind parents that the baby should be positioned so that the head is upright and the nose and mouth are not obstructed.”
The researchers and Dr. Moon had no relevant financial disclosures.
Baby-wearing – carrying a child against your body in a sling, soft carrier, or other device – is associated with benefits like reduced crying and increased breastfeeding, studies have shown.
But this practice also entails risks. Babies can fall out of carriers, or be injured when an adult carrying them falls, for example.
researchers estimated in a study presented at the annual meeting of the American Academy of Pediatrics.
To characterize the epidemiology of these injuries, Samantha J. Rowe, MD, chief resident physician at Walter Reed National Military Medical Center in Bethesda, Md., and colleagues analyzed data from the National Electronic Injury Surveillance System between 2011 and 2020.
They included in their analysis data from patients aged 5 years and younger who sustained an injury associated with a baby-wearing product. Baby harnesses, carriers, slings, framed baby carriers, and soft baby carriers were among the devices included in the study. The researchers used 601 cases to generate national estimates.
An estimated 14,024 patients presented to EDs because of baby-wearing injuries, and 52% of the injuries occurred when a patient fell from the product.
Most injuries (61%) occurred in children aged 5 months and younger; 19.3% of these infants required hospitalization, most often for head injuries.
The investigators found that about 22% of the injuries were associated with a caregiver falling, noted Rachel Y. Moon, MD, who was not involved in the study.
“Carrying a baby changes your center of gravity – and can also obscure your vision of where you’re walking, so adults who use these devices should be cognizant of this,” said Dr. Moon, with the University of Virginia, Charlottesville.
Dr. Rowe often practiced baby-wearing with her daughter, and found that it was beneficial. And studies have demonstrated various benefits of baby-wearing, including improved thermoregulation and glycemic control.
Still, the new analysis illustrates the potential for baby-wearing products “to cause serious injury, especially in infants 5 months and younger,” Dr. Rowe said. “We need to provide more education to caregivers on safe baby-wearing and continue to improve our safety standards for baby-wearing products.”
Study coauthor Patrick T. Reeves, MD, with the Naval Medical Center at San Diego, offered additional guidance in a news release: “Like when buying a new pair of shoes, parents must be educated on the proper sizing, selection, and wear of baby carriers to prevent injury to themselves and their child.”
Parents also need to ensure that the child’s nose and mouth are not obstructed, Dr. Moon
In a recent article discussing the possible benefits of baby-wearing in terms of helping with breastfeeding, Dr. Moon also pointed out further safety considerations: “No matter which carrier is used, for safety reasons, we need to remind parents that the baby should be positioned so that the head is upright and the nose and mouth are not obstructed.”
The researchers and Dr. Moon had no relevant financial disclosures.
FROM AAP 2021
Pediatricians can effectively promote gun safety
When pediatricians and other pediatric providers are given training and resource materials, levels of firearm screenings and anticipatory guidance about firearm safety increase significantly, according to two new studies presented at the annual meeting of the American Academy of Pediatrics.
“With the rise in firearm sales and injuries during the COVID-19 pandemic, it is more important than ever that pediatricians address the firearm epidemic,” said Alexandra Byrne, MD, a pediatric resident at the University of Florida in Gainesville, who presented one of the studies.
There were 4.3 million more firearms purchased from March through July 2020 than expected, a recent study estimates, and 4,075 more firearm injuries than expected from April through July 2020.
In states with more excess purchases, firearm injuries related to domestic violence increased in April (rate ratio, 2.60; 95% CI, 1.32-5.93) and May (RR, 1.79; 95% CI, 1.19-2.91) 2020. However, excess gun purchases had no effect on rates of firearm violence outside the home.
In addition to the link between firearms in the home and domestic violence, they are also linked to a three- to fourfold greater risk for teen suicide, and both depression and suicidal thoughts have risen in teens during the pandemic.
“The data are pretty clear that if you have an unlocked, loaded weapon in your home, and you have a kid who’s depressed or anxious or dysregulated or doing maladaptive things for the pandemic, they’re much more likely to inadvertently take their own or someone else’s life by grabbing [a gun],” said Cora Breuner, MD, MPH, professor of pediatrics at Seattle Children’s Hospital.
However, there is no difference in gun ownership or gun-safety measures between homes with and without at-risk children, previous research shows.
Training, guidance, and locks
Previous research has also shown that there has been a reluctance by pediatricians to conduct firearm screenings and counsel parents about gun safety in the home.
For their two-step program, Dr. Byrne’s team used a plan-do-study-act approach. They started by providing training on firearm safety, evidence-based recommendations for firearm screening, and anticipatory guidance regarding safe firearm storage to members of the general pediatrics division at the University of Florida. And they supplied clinics with free firearm locks.
Next they supplied clinics with posters and educational cards from the Be SMART campaign, an initiative of the Everytown for Gun Safety Support Fund, which provides materials for anyone, including physicians, to use.
During their study, the researchers sent three anonymous six-question online surveys – at baseline and 3 to 4 months after each of the two steps – to pediatric residents, physician assistants, advanced practice registered nurses, and attendings to assess the project. There were 52 responses to the first survey, for a response rate of 58.4%, 42 responses to the second survey, for a response rate of 47.2%, and 23 responses to the third survey, for a rate of response 25.8%.
The program nearly doubled screenings during well-child visits and dramatically increased the proportion of families who received a firearm lock when they told providers they had a firearm at home.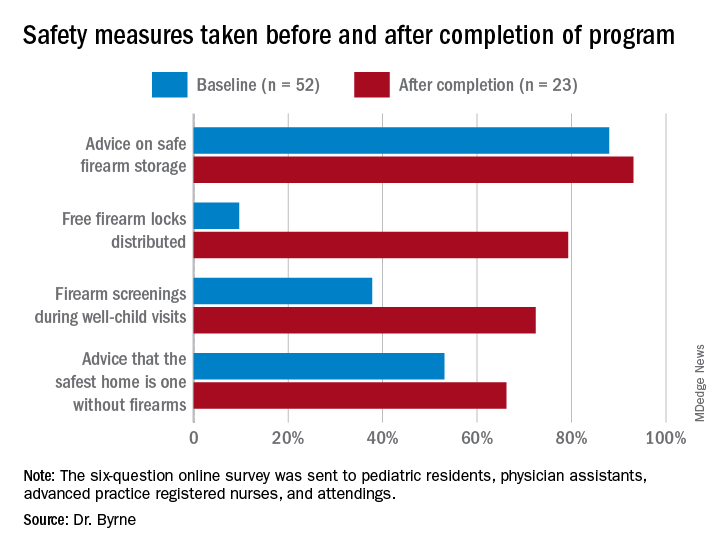
Previous research has shown “a significant increase in safe firearm storage when firearm locks were provided to families in clinic compared to verbal counseling alone,” Dr. Byrne said. “We know that safe firearm storage reduces injuries. Roughly one in three children in the United States lives in a home with a firearm. Individuals with a firearm are at two times the risk of homicide and three to four times the risk of suicide, so it is essential we further study how pediatricians can be most effective when it comes to firearm counseling.”
The difference in lock distribution as a result of the program is a “tremendous increase,” said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine in Houston, who was not involved in the research.
“Locks could go a long way to minimizing the risk,” he said in an interview, adding that nearly half of all teen suicide deaths that occurred over a decade in Houston involved a firearm.
Adding a social-history component
A program to increase firearm screening was also presented at the AAP conference.
After random review of medical records from 30 patients admitted to the hospital documented zero firearm screenings, Marjorie Farrington, MD, and Samantha Gunkelman, MD, from Akron Children’s Hospital in Ohio, implemented a program that they hope will increase firearm screenings during inpatient admissions to at least 50%.
They started their ongoing program in April 2020 by adding a social-history component to the history and physical (H&P) exam template and educating residents on how to screen and included guidance on safe firearm storage.
They also had physicians with firearm expertise give gun-safety lectures, and they plan to involve the Family Resource Center at their hospital in the creation of resources that can be incorporated into discharge instructions.
From April 2020 to June 2021, after the addition to the H&P template, 63% of the 5196 patients admitted to the hospital underwent a firearm screening. Of the 25% of patients who reported guns at home, 3% were not storing their firearms safely.
The pair used the “Store It Safe” Physician Handout provided by the Ohio chapter of the AAP.
Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic.
The BulletPoints Project — developed by the Violence Prevention Research Program at the University of California, Davis — can also help physicians talk to patients about guns.
“Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic,” Dr. Byrne said in an interview. “Additionally, it is a challenging topic that can often be met with resistance from patients and families. Lack of time during visits is also a huge barrier.”
Lack of training is an obstacle to greater firearm screenings, Dr. Greeley agreed, as are the feeling that guidance simply won’t make a difference and concerns about political pressure and divineness. The lack of research on firearm injuries and the impact of firearm screenings and anticipatory guidance is a challenge, he added, although that is starting to change.
Pediatricians need education on how to make a difference when it comes to firearm safety, and should follow AAP guidelines, Dr. Greeley said.
Counseling on firearm safety is in the same category as immunizations, seatbelts, substance use, helmets, and other public-health issues that are important to address at visits, regardless of how difficult it might be, Dr. Breuner told this news organization.
“It is our mission, as pediatricians, to provide every ounce of prevention in our well-child and anticipatory guidance visits,” she said. “It’s our job, so we shouldn’t shy away from it even though it’s hard.”
Doctors are more comfortable discussing firearm safety if they are firearm owners, previous research has shown, so she advises pediatricians who feel unqualified to discuss firearms to seek guidance from their peers on how to approach screenings and anticipatory guidance, she noted.
The firearm study being done in an academic center gives me great pause. The populations are often very different than private practice.
Both of these studies were conducted at single institutions and might not reflect what would work in private clinics.
“The firearm study being done in an academic center gives me great pause,” Dr. Greeley said. “The populations are often very different than private practice. I think that there is still a lot that remains unknown about decreasing household firearm injury and death.”
And the degree to which findings from these two gun-safety programs can be generalized to other academic centers or children’s hospitals is unclear.
“There are states where, I suspect, firearm screening is much more common. Some states have very pro-firearm cultures and others are anti-firearm,” Dr. Greeley said. “There are also likely differences within states,” particularly between urban and rural regions.
“Firearms are often a very personal issue for families, and pediatricians in ‘pro-firearm’ communities may have greater resistance to working on this,” he pointed out.
Nevertheless, Dr. Greeley said, “this is a promising strategy that could be part of a broad injury prevention initiative.”
Neither study noted any external funding. Dr. Byrne is a member of the Moms Demand Action Gainesville Chapter, which donated the firearm locks for the project. Dr. Breuner, Dr. Greeley, and Dr. Farrington have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When pediatricians and other pediatric providers are given training and resource materials, levels of firearm screenings and anticipatory guidance about firearm safety increase significantly, according to two new studies presented at the annual meeting of the American Academy of Pediatrics.
“With the rise in firearm sales and injuries during the COVID-19 pandemic, it is more important than ever that pediatricians address the firearm epidemic,” said Alexandra Byrne, MD, a pediatric resident at the University of Florida in Gainesville, who presented one of the studies.
There were 4.3 million more firearms purchased from March through July 2020 than expected, a recent study estimates, and 4,075 more firearm injuries than expected from April through July 2020.
In states with more excess purchases, firearm injuries related to domestic violence increased in April (rate ratio, 2.60; 95% CI, 1.32-5.93) and May (RR, 1.79; 95% CI, 1.19-2.91) 2020. However, excess gun purchases had no effect on rates of firearm violence outside the home.
In addition to the link between firearms in the home and domestic violence, they are also linked to a three- to fourfold greater risk for teen suicide, and both depression and suicidal thoughts have risen in teens during the pandemic.
“The data are pretty clear that if you have an unlocked, loaded weapon in your home, and you have a kid who’s depressed or anxious or dysregulated or doing maladaptive things for the pandemic, they’re much more likely to inadvertently take their own or someone else’s life by grabbing [a gun],” said Cora Breuner, MD, MPH, professor of pediatrics at Seattle Children’s Hospital.
However, there is no difference in gun ownership or gun-safety measures between homes with and without at-risk children, previous research shows.
Training, guidance, and locks
Previous research has also shown that there has been a reluctance by pediatricians to conduct firearm screenings and counsel parents about gun safety in the home.
For their two-step program, Dr. Byrne’s team used a plan-do-study-act approach. They started by providing training on firearm safety, evidence-based recommendations for firearm screening, and anticipatory guidance regarding safe firearm storage to members of the general pediatrics division at the University of Florida. And they supplied clinics with free firearm locks.
Next they supplied clinics with posters and educational cards from the Be SMART campaign, an initiative of the Everytown for Gun Safety Support Fund, which provides materials for anyone, including physicians, to use.
During their study, the researchers sent three anonymous six-question online surveys – at baseline and 3 to 4 months after each of the two steps – to pediatric residents, physician assistants, advanced practice registered nurses, and attendings to assess the project. There were 52 responses to the first survey, for a response rate of 58.4%, 42 responses to the second survey, for a response rate of 47.2%, and 23 responses to the third survey, for a rate of response 25.8%.
The program nearly doubled screenings during well-child visits and dramatically increased the proportion of families who received a firearm lock when they told providers they had a firearm at home.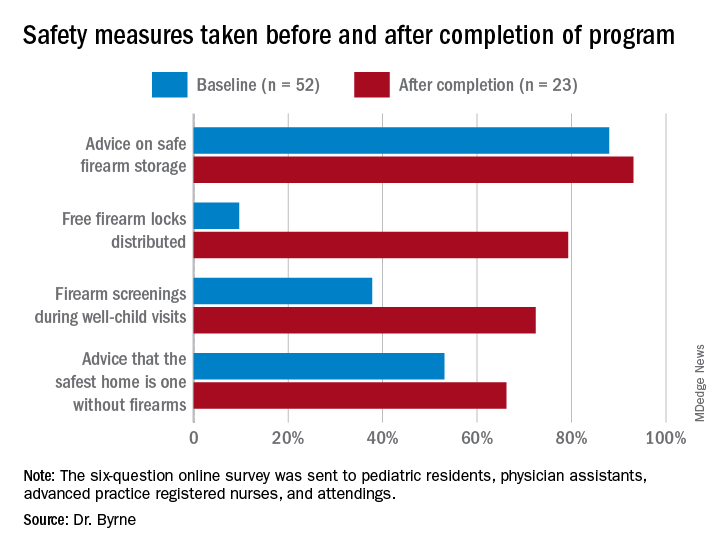
Previous research has shown “a significant increase in safe firearm storage when firearm locks were provided to families in clinic compared to verbal counseling alone,” Dr. Byrne said. “We know that safe firearm storage reduces injuries. Roughly one in three children in the United States lives in a home with a firearm. Individuals with a firearm are at two times the risk of homicide and three to four times the risk of suicide, so it is essential we further study how pediatricians can be most effective when it comes to firearm counseling.”
The difference in lock distribution as a result of the program is a “tremendous increase,” said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine in Houston, who was not involved in the research.
“Locks could go a long way to minimizing the risk,” he said in an interview, adding that nearly half of all teen suicide deaths that occurred over a decade in Houston involved a firearm.
Adding a social-history component
A program to increase firearm screening was also presented at the AAP conference.
After random review of medical records from 30 patients admitted to the hospital documented zero firearm screenings, Marjorie Farrington, MD, and Samantha Gunkelman, MD, from Akron Children’s Hospital in Ohio, implemented a program that they hope will increase firearm screenings during inpatient admissions to at least 50%.
They started their ongoing program in April 2020 by adding a social-history component to the history and physical (H&P) exam template and educating residents on how to screen and included guidance on safe firearm storage.
They also had physicians with firearm expertise give gun-safety lectures, and they plan to involve the Family Resource Center at their hospital in the creation of resources that can be incorporated into discharge instructions.
From April 2020 to June 2021, after the addition to the H&P template, 63% of the 5196 patients admitted to the hospital underwent a firearm screening. Of the 25% of patients who reported guns at home, 3% were not storing their firearms safely.
The pair used the “Store It Safe” Physician Handout provided by the Ohio chapter of the AAP.
Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic.
The BulletPoints Project — developed by the Violence Prevention Research Program at the University of California, Davis — can also help physicians talk to patients about guns.
“Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic,” Dr. Byrne said in an interview. “Additionally, it is a challenging topic that can often be met with resistance from patients and families. Lack of time during visits is also a huge barrier.”
Lack of training is an obstacle to greater firearm screenings, Dr. Greeley agreed, as are the feeling that guidance simply won’t make a difference and concerns about political pressure and divineness. The lack of research on firearm injuries and the impact of firearm screenings and anticipatory guidance is a challenge, he added, although that is starting to change.
Pediatricians need education on how to make a difference when it comes to firearm safety, and should follow AAP guidelines, Dr. Greeley said.
Counseling on firearm safety is in the same category as immunizations, seatbelts, substance use, helmets, and other public-health issues that are important to address at visits, regardless of how difficult it might be, Dr. Breuner told this news organization.
“It is our mission, as pediatricians, to provide every ounce of prevention in our well-child and anticipatory guidance visits,” she said. “It’s our job, so we shouldn’t shy away from it even though it’s hard.”
Doctors are more comfortable discussing firearm safety if they are firearm owners, previous research has shown, so she advises pediatricians who feel unqualified to discuss firearms to seek guidance from their peers on how to approach screenings and anticipatory guidance, she noted.
The firearm study being done in an academic center gives me great pause. The populations are often very different than private practice.
Both of these studies were conducted at single institutions and might not reflect what would work in private clinics.
“The firearm study being done in an academic center gives me great pause,” Dr. Greeley said. “The populations are often very different than private practice. I think that there is still a lot that remains unknown about decreasing household firearm injury and death.”
And the degree to which findings from these two gun-safety programs can be generalized to other academic centers or children’s hospitals is unclear.
“There are states where, I suspect, firearm screening is much more common. Some states have very pro-firearm cultures and others are anti-firearm,” Dr. Greeley said. “There are also likely differences within states,” particularly between urban and rural regions.
“Firearms are often a very personal issue for families, and pediatricians in ‘pro-firearm’ communities may have greater resistance to working on this,” he pointed out.
Nevertheless, Dr. Greeley said, “this is a promising strategy that could be part of a broad injury prevention initiative.”
Neither study noted any external funding. Dr. Byrne is a member of the Moms Demand Action Gainesville Chapter, which donated the firearm locks for the project. Dr. Breuner, Dr. Greeley, and Dr. Farrington have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
When pediatricians and other pediatric providers are given training and resource materials, levels of firearm screenings and anticipatory guidance about firearm safety increase significantly, according to two new studies presented at the annual meeting of the American Academy of Pediatrics.
“With the rise in firearm sales and injuries during the COVID-19 pandemic, it is more important than ever that pediatricians address the firearm epidemic,” said Alexandra Byrne, MD, a pediatric resident at the University of Florida in Gainesville, who presented one of the studies.
There were 4.3 million more firearms purchased from March through July 2020 than expected, a recent study estimates, and 4,075 more firearm injuries than expected from April through July 2020.
In states with more excess purchases, firearm injuries related to domestic violence increased in April (rate ratio, 2.60; 95% CI, 1.32-5.93) and May (RR, 1.79; 95% CI, 1.19-2.91) 2020. However, excess gun purchases had no effect on rates of firearm violence outside the home.
In addition to the link between firearms in the home and domestic violence, they are also linked to a three- to fourfold greater risk for teen suicide, and both depression and suicidal thoughts have risen in teens during the pandemic.
“The data are pretty clear that if you have an unlocked, loaded weapon in your home, and you have a kid who’s depressed or anxious or dysregulated or doing maladaptive things for the pandemic, they’re much more likely to inadvertently take their own or someone else’s life by grabbing [a gun],” said Cora Breuner, MD, MPH, professor of pediatrics at Seattle Children’s Hospital.
However, there is no difference in gun ownership or gun-safety measures between homes with and without at-risk children, previous research shows.
Training, guidance, and locks
Previous research has also shown that there has been a reluctance by pediatricians to conduct firearm screenings and counsel parents about gun safety in the home.
For their two-step program, Dr. Byrne’s team used a plan-do-study-act approach. They started by providing training on firearm safety, evidence-based recommendations for firearm screening, and anticipatory guidance regarding safe firearm storage to members of the general pediatrics division at the University of Florida. And they supplied clinics with free firearm locks.
Next they supplied clinics with posters and educational cards from the Be SMART campaign, an initiative of the Everytown for Gun Safety Support Fund, which provides materials for anyone, including physicians, to use.
During their study, the researchers sent three anonymous six-question online surveys – at baseline and 3 to 4 months after each of the two steps – to pediatric residents, physician assistants, advanced practice registered nurses, and attendings to assess the project. There were 52 responses to the first survey, for a response rate of 58.4%, 42 responses to the second survey, for a response rate of 47.2%, and 23 responses to the third survey, for a rate of response 25.8%.
The program nearly doubled screenings during well-child visits and dramatically increased the proportion of families who received a firearm lock when they told providers they had a firearm at home.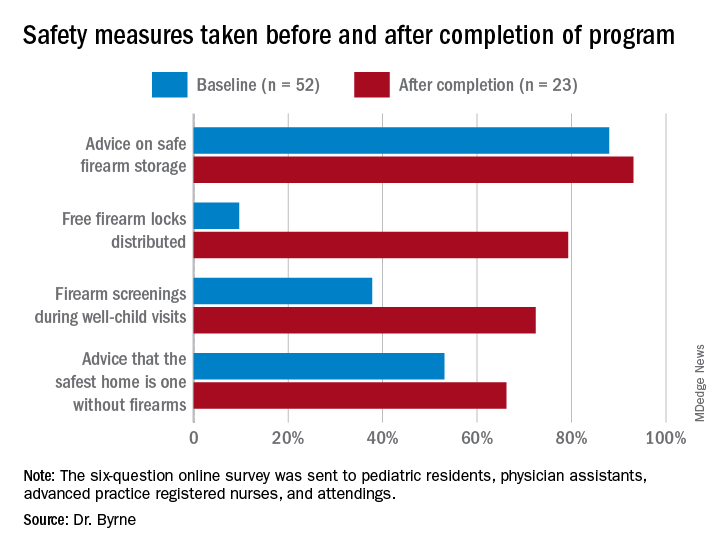
Previous research has shown “a significant increase in safe firearm storage when firearm locks were provided to families in clinic compared to verbal counseling alone,” Dr. Byrne said. “We know that safe firearm storage reduces injuries. Roughly one in three children in the United States lives in a home with a firearm. Individuals with a firearm are at two times the risk of homicide and three to four times the risk of suicide, so it is essential we further study how pediatricians can be most effective when it comes to firearm counseling.”
The difference in lock distribution as a result of the program is a “tremendous increase,” said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine in Houston, who was not involved in the research.
“Locks could go a long way to minimizing the risk,” he said in an interview, adding that nearly half of all teen suicide deaths that occurred over a decade in Houston involved a firearm.
Adding a social-history component
A program to increase firearm screening was also presented at the AAP conference.
After random review of medical records from 30 patients admitted to the hospital documented zero firearm screenings, Marjorie Farrington, MD, and Samantha Gunkelman, MD, from Akron Children’s Hospital in Ohio, implemented a program that they hope will increase firearm screenings during inpatient admissions to at least 50%.
They started their ongoing program in April 2020 by adding a social-history component to the history and physical (H&P) exam template and educating residents on how to screen and included guidance on safe firearm storage.
They also had physicians with firearm expertise give gun-safety lectures, and they plan to involve the Family Resource Center at their hospital in the creation of resources that can be incorporated into discharge instructions.
From April 2020 to June 2021, after the addition to the H&P template, 63% of the 5196 patients admitted to the hospital underwent a firearm screening. Of the 25% of patients who reported guns at home, 3% were not storing their firearms safely.
The pair used the “Store It Safe” Physician Handout provided by the Ohio chapter of the AAP.
Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic.
The BulletPoints Project — developed by the Violence Prevention Research Program at the University of California, Davis — can also help physicians talk to patients about guns.
“Many pediatricians and pediatric trainees are not comfortable counseling on firearm safety, often a result of inadequate training on the topic,” Dr. Byrne said in an interview. “Additionally, it is a challenging topic that can often be met with resistance from patients and families. Lack of time during visits is also a huge barrier.”
Lack of training is an obstacle to greater firearm screenings, Dr. Greeley agreed, as are the feeling that guidance simply won’t make a difference and concerns about political pressure and divineness. The lack of research on firearm injuries and the impact of firearm screenings and anticipatory guidance is a challenge, he added, although that is starting to change.
Pediatricians need education on how to make a difference when it comes to firearm safety, and should follow AAP guidelines, Dr. Greeley said.
Counseling on firearm safety is in the same category as immunizations, seatbelts, substance use, helmets, and other public-health issues that are important to address at visits, regardless of how difficult it might be, Dr. Breuner told this news organization.
“It is our mission, as pediatricians, to provide every ounce of prevention in our well-child and anticipatory guidance visits,” she said. “It’s our job, so we shouldn’t shy away from it even though it’s hard.”
Doctors are more comfortable discussing firearm safety if they are firearm owners, previous research has shown, so she advises pediatricians who feel unqualified to discuss firearms to seek guidance from their peers on how to approach screenings and anticipatory guidance, she noted.
The firearm study being done in an academic center gives me great pause. The populations are often very different than private practice.
Both of these studies were conducted at single institutions and might not reflect what would work in private clinics.
“The firearm study being done in an academic center gives me great pause,” Dr. Greeley said. “The populations are often very different than private practice. I think that there is still a lot that remains unknown about decreasing household firearm injury and death.”
And the degree to which findings from these two gun-safety programs can be generalized to other academic centers or children’s hospitals is unclear.
“There are states where, I suspect, firearm screening is much more common. Some states have very pro-firearm cultures and others are anti-firearm,” Dr. Greeley said. “There are also likely differences within states,” particularly between urban and rural regions.
“Firearms are often a very personal issue for families, and pediatricians in ‘pro-firearm’ communities may have greater resistance to working on this,” he pointed out.
Nevertheless, Dr. Greeley said, “this is a promising strategy that could be part of a broad injury prevention initiative.”
Neither study noted any external funding. Dr. Byrne is a member of the Moms Demand Action Gainesville Chapter, which donated the firearm locks for the project. Dr. Breuner, Dr. Greeley, and Dr. Farrington have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AAP 2021
You’ve been uneasy about the mother’s boyfriend: This may be why
The first patient of the afternoon is a 4-month-old in for his health maintenance visit. You’ve known his 20-year-old mother since she was a toddler. This infant has a 2-year-old sister. Also in the exam room is a young man you don’t recognize whom the mother introduces as Jason, her new boyfriend. He never makes eye contact and despite your best efforts you can’t get him to engage.
At the child’s next visit you are relieved to see the 6-month-old is alive and well and learn that your former patient and her two children have moved back in with her parents and Jason is no longer in the picture.
You don’t have to have been doing pediatrics very long to have learned that a “family” that includes an infant and a young adult male who is probably not the father is an environment in which the infant’s health and well-being is at significant risk. It is a situation in which child abuse even to the point of infanticide should be waving a red flag in your face.
Infanticide occurs in many animal species including our own. As abhorrent we may find the act, it occurs often enough to be, if not normal, at least not unexpected in certain circumstances. Theories abound as to what advantage the act of infanticide might convey to the success of a species. However, little if anything is known about any possible mechanisms that would allow it to occur.
Recently, a professor of molecular and cellular biology at Harvard University discovered a specific set of neurons in the mouse brain that controls aggressive behavior toward infants (Biological triggers for infant abuse, by Juan Siliezar, The Harvard Gazette, Sept 27, 2021). This same set of neurons also appears to trigger avoidance and neglect behaviors as well.
Research in other animal species has found that these antiparental behaviors occur in both virgins and sexually mature males who are strangers to the group. Interestingly, the behaviors switch off once individuals have their own offspring or have had the opportunity to familiarize themselves with infants. Not surprisingly, other studies have found that in some species environmental stress such as food shortage or threats of predation have triggered females to attack or ignore their offspring.
I think it is safe to assume a similar collection of neurons controlling aggressive behavior also exists in humans. One can imagine some well-read defense attorney dredging up this study and claiming that because his client had not yet fathered a child of his own that it was his nervous system’s normal response that made him toss his girlfriend’s baby against the wall.
The lead author of the study intends to study this collection of neurons in more depth to discover more about the process. It is conceivable that with more information her initial findings may help in the development of treatment and specific prevention strategies. Until that happens, we must rely on our intuition and keep our antennae tuned and alert for high-risk scenarios like the one I described at the opening of this letter.
We are left with leaning heavily on our community social work networks to keep close tabs on these high-risk families, offering both financial and emotional support. Parenting classes may be helpful, but some of this research leads me to suspect that immersing these young parents-to-be in hands-on child care situations might provide the best protection we can offer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
The first patient of the afternoon is a 4-month-old in for his health maintenance visit. You’ve known his 20-year-old mother since she was a toddler. This infant has a 2-year-old sister. Also in the exam room is a young man you don’t recognize whom the mother introduces as Jason, her new boyfriend. He never makes eye contact and despite your best efforts you can’t get him to engage.
At the child’s next visit you are relieved to see the 6-month-old is alive and well and learn that your former patient and her two children have moved back in with her parents and Jason is no longer in the picture.
You don’t have to have been doing pediatrics very long to have learned that a “family” that includes an infant and a young adult male who is probably not the father is an environment in which the infant’s health and well-being is at significant risk. It is a situation in which child abuse even to the point of infanticide should be waving a red flag in your face.
Infanticide occurs in many animal species including our own. As abhorrent we may find the act, it occurs often enough to be, if not normal, at least not unexpected in certain circumstances. Theories abound as to what advantage the act of infanticide might convey to the success of a species. However, little if anything is known about any possible mechanisms that would allow it to occur.
Recently, a professor of molecular and cellular biology at Harvard University discovered a specific set of neurons in the mouse brain that controls aggressive behavior toward infants (Biological triggers for infant abuse, by Juan Siliezar, The Harvard Gazette, Sept 27, 2021). This same set of neurons also appears to trigger avoidance and neglect behaviors as well.
Research in other animal species has found that these antiparental behaviors occur in both virgins and sexually mature males who are strangers to the group. Interestingly, the behaviors switch off once individuals have their own offspring or have had the opportunity to familiarize themselves with infants. Not surprisingly, other studies have found that in some species environmental stress such as food shortage or threats of predation have triggered females to attack or ignore their offspring.
I think it is safe to assume a similar collection of neurons controlling aggressive behavior also exists in humans. One can imagine some well-read defense attorney dredging up this study and claiming that because his client had not yet fathered a child of his own that it was his nervous system’s normal response that made him toss his girlfriend’s baby against the wall.
The lead author of the study intends to study this collection of neurons in more depth to discover more about the process. It is conceivable that with more information her initial findings may help in the development of treatment and specific prevention strategies. Until that happens, we must rely on our intuition and keep our antennae tuned and alert for high-risk scenarios like the one I described at the opening of this letter.
We are left with leaning heavily on our community social work networks to keep close tabs on these high-risk families, offering both financial and emotional support. Parenting classes may be helpful, but some of this research leads me to suspect that immersing these young parents-to-be in hands-on child care situations might provide the best protection we can offer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
The first patient of the afternoon is a 4-month-old in for his health maintenance visit. You’ve known his 20-year-old mother since she was a toddler. This infant has a 2-year-old sister. Also in the exam room is a young man you don’t recognize whom the mother introduces as Jason, her new boyfriend. He never makes eye contact and despite your best efforts you can’t get him to engage.
At the child’s next visit you are relieved to see the 6-month-old is alive and well and learn that your former patient and her two children have moved back in with her parents and Jason is no longer in the picture.
You don’t have to have been doing pediatrics very long to have learned that a “family” that includes an infant and a young adult male who is probably not the father is an environment in which the infant’s health and well-being is at significant risk. It is a situation in which child abuse even to the point of infanticide should be waving a red flag in your face.
Infanticide occurs in many animal species including our own. As abhorrent we may find the act, it occurs often enough to be, if not normal, at least not unexpected in certain circumstances. Theories abound as to what advantage the act of infanticide might convey to the success of a species. However, little if anything is known about any possible mechanisms that would allow it to occur.
Recently, a professor of molecular and cellular biology at Harvard University discovered a specific set of neurons in the mouse brain that controls aggressive behavior toward infants (Biological triggers for infant abuse, by Juan Siliezar, The Harvard Gazette, Sept 27, 2021). This same set of neurons also appears to trigger avoidance and neglect behaviors as well.
Research in other animal species has found that these antiparental behaviors occur in both virgins and sexually mature males who are strangers to the group. Interestingly, the behaviors switch off once individuals have their own offspring or have had the opportunity to familiarize themselves with infants. Not surprisingly, other studies have found that in some species environmental stress such as food shortage or threats of predation have triggered females to attack or ignore their offspring.
I think it is safe to assume a similar collection of neurons controlling aggressive behavior also exists in humans. One can imagine some well-read defense attorney dredging up this study and claiming that because his client had not yet fathered a child of his own that it was his nervous system’s normal response that made him toss his girlfriend’s baby against the wall.
The lead author of the study intends to study this collection of neurons in more depth to discover more about the process. It is conceivable that with more information her initial findings may help in the development of treatment and specific prevention strategies. Until that happens, we must rely on our intuition and keep our antennae tuned and alert for high-risk scenarios like the one I described at the opening of this letter.
We are left with leaning heavily on our community social work networks to keep close tabs on these high-risk families, offering both financial and emotional support. Parenting classes may be helpful, but some of this research leads me to suspect that immersing these young parents-to-be in hands-on child care situations might provide the best protection we can offer.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
Bystander actions can reduce children’s risk of drowning
The likelihood that a child will survive a near-drowning without long-term damage is substantially greater if a bystander attempts a rescue, even if that person doesn’t perform cardiopulmonary resuscitation (CPR), according to new research presented October 10 at the American Academy of Pediatrics (AAP) 2021 National Conference.
“The extent to which bystander rescue is associated with reduced odds of unfavorable drowning outcomes was surprising,” said lead investigator Rohit P. Shenoi, MD, professor of pediatrics at Baylor College of Medicine and attending physician at Texas Children’s Hospital, Houston.
“While we do know that early rescue and resuscitation is helpful in preventing severe drowning injury, the degree of benefit from bystander rescue in all cases of pediatric drowning has not been described so far,” he told this news organization.
The fact that a bystander’s rescue attempt improves a child’s odds of a good outcome is not surprising on its own, but the magnitude of the finding really affirms the importance of bystander intervention, said Benjamin Hoffman, MD, professor of pediatrics at the Oregon Health & Science University School of Medicine and medical director of the Tom Sargent Safety Center at the Doernbecher Children’s Hospital, Portland.
“If an adult finds a child in the water, even if they don’t administer formal CPR, they’re going to be doing things” to try to help, Dr. Hoffman, who was not involved in this research but who specializes in child injury prevention, said in an interview. The act of intervening – whether it’s formal CPR or a CPR attempt or even just calling appropriate first responders – “likely impacts the duration of the submersion” and “clearly makes a difference.”
Drowning is the leading cause of death for children younger than 4 years, Dr. Hoffman noted, adding that the AAP recommends swimming lessons for children older than 1 year to reduce that risk.
In their cross-sectional study, Dr. Shenoi and his colleagues analyzed data on drownings and near-drownings in children and adolescents younger than 18 years using hospital, emergency medical services, and child fatality records from Harris County, Texas.
They analyzed 237 incidents from 2010 to 2013 in which the young person was submerged. Median age of the victims was 3.2 years, 60% were male, 64% were Black, Hispanic, or Native American, and 78% occurred in a swimming pool.
Unfavorable outcomes – defined as death or severe impairment after hospital discharge – were experienced by 38 victims (16%) and were significantly associated with being submerged for longer than 5 minutes (P < .001).
The odds of an unfavorable outcome dropped by 80% if a bystander attempted a rescue, whether or not they performed CPR (adjusted odds ratio, 0.2; P = .004). If the bystander performed CPR, the odds of an unfavorable outcome dropped by a similar amount, but the difference was not statistically significant (aOR, 0.22; P = .07).
However, previous research has shown a significant reduction in poor outcomes when CPR is administered to children who have been submerged, Dr. Hoffman explained.
The most important thing a bystander can do is simply get a submerged child out of the water. “Early rescue in drowning terminates what is initially a respiratory arrest from progressing to a full cardiopulmonary arrest with severe hypoxic brain injury and death,” Dr. Shenoi said.
“CPR is also very important, and rescue and resuscitation go hand in hand. We encourage all laypersons to be trained in CPR so that they can administer correct CPR techniques,” he added.
Both Dr. Shenoi and Dr. Hoffman emphasized the value of CPR training for adults, as the AAP recommends, and the importance of other precautions that reduce the risk of drowning.
“Drowning prevention should consist of multiple layers of prevention,” Dr. Shenoi said. These consist of “close, constant, and attentive supervision; isolation fencing for swimming pools; and water competency, including water-safety knowledge, basic swim skills, and the ability to recognize and respond to a swimmer in trouble, use of life jackets, and early bystander CPR.”
The relative importance of each of those layers depends on geography and circumstances, Dr. Hoffman said. Pools are the most common drowning sites in the United States overall, but they’re much more common in warmer states, such as California, Florida, and Texas, which have more pools. In contrast, drownings in Oregon are more likely to occur in rivers, so prevention is more about access to life jackets and increasing access to swim lessons.
The findings from this study drive home how important it is for physicians to provide anticipatory guidance to families on reducing the risk of drowning. Pediatricians should convey to families the need for different layers of protection, he added.
“If your family spends a lot of time around water, whether open water or swimming pools, the more layers you can provide, the better off you’re going to be,” Dr. Hoffman said.
Dr. Shenoi echoed this sentiment.
“The take-home message is to be observant if you are entrusted with the care of a child around water,” Dr. Shenoi said. “If you notice the child to be drowning, either attempt rescue yourself if it is safe to do so or enlist the help of others to save the victim as soon as possible. However, the rescuer should not place himself or herself in danger when attempting rescue.”
The five steps in the “drowning chain of survival” – preventing drowning, recognizing distress, providing flotation, removing the victim from the water, and providing care and CPR as needed – are key to reducing drowning deaths and injury, Dr. Shenoi emphasized.
Dr. Shenoi has disclosed no relevant financial relationships. Dr. Hoffman is a paid consultant on child drowning prevention for the nonprofit Anonymous Philanthropy.
A version of this article first appeared on Medscape.com.
The likelihood that a child will survive a near-drowning without long-term damage is substantially greater if a bystander attempts a rescue, even if that person doesn’t perform cardiopulmonary resuscitation (CPR), according to new research presented October 10 at the American Academy of Pediatrics (AAP) 2021 National Conference.
“The extent to which bystander rescue is associated with reduced odds of unfavorable drowning outcomes was surprising,” said lead investigator Rohit P. Shenoi, MD, professor of pediatrics at Baylor College of Medicine and attending physician at Texas Children’s Hospital, Houston.
“While we do know that early rescue and resuscitation is helpful in preventing severe drowning injury, the degree of benefit from bystander rescue in all cases of pediatric drowning has not been described so far,” he told this news organization.
The fact that a bystander’s rescue attempt improves a child’s odds of a good outcome is not surprising on its own, but the magnitude of the finding really affirms the importance of bystander intervention, said Benjamin Hoffman, MD, professor of pediatrics at the Oregon Health & Science University School of Medicine and medical director of the Tom Sargent Safety Center at the Doernbecher Children’s Hospital, Portland.
“If an adult finds a child in the water, even if they don’t administer formal CPR, they’re going to be doing things” to try to help, Dr. Hoffman, who was not involved in this research but who specializes in child injury prevention, said in an interview. The act of intervening – whether it’s formal CPR or a CPR attempt or even just calling appropriate first responders – “likely impacts the duration of the submersion” and “clearly makes a difference.”
Drowning is the leading cause of death for children younger than 4 years, Dr. Hoffman noted, adding that the AAP recommends swimming lessons for children older than 1 year to reduce that risk.
In their cross-sectional study, Dr. Shenoi and his colleagues analyzed data on drownings and near-drownings in children and adolescents younger than 18 years using hospital, emergency medical services, and child fatality records from Harris County, Texas.
They analyzed 237 incidents from 2010 to 2013 in which the young person was submerged. Median age of the victims was 3.2 years, 60% were male, 64% were Black, Hispanic, or Native American, and 78% occurred in a swimming pool.
Unfavorable outcomes – defined as death or severe impairment after hospital discharge – were experienced by 38 victims (16%) and were significantly associated with being submerged for longer than 5 minutes (P < .001).
The odds of an unfavorable outcome dropped by 80% if a bystander attempted a rescue, whether or not they performed CPR (adjusted odds ratio, 0.2; P = .004). If the bystander performed CPR, the odds of an unfavorable outcome dropped by a similar amount, but the difference was not statistically significant (aOR, 0.22; P = .07).
However, previous research has shown a significant reduction in poor outcomes when CPR is administered to children who have been submerged, Dr. Hoffman explained.
The most important thing a bystander can do is simply get a submerged child out of the water. “Early rescue in drowning terminates what is initially a respiratory arrest from progressing to a full cardiopulmonary arrest with severe hypoxic brain injury and death,” Dr. Shenoi said.
“CPR is also very important, and rescue and resuscitation go hand in hand. We encourage all laypersons to be trained in CPR so that they can administer correct CPR techniques,” he added.
Both Dr. Shenoi and Dr. Hoffman emphasized the value of CPR training for adults, as the AAP recommends, and the importance of other precautions that reduce the risk of drowning.
“Drowning prevention should consist of multiple layers of prevention,” Dr. Shenoi said. These consist of “close, constant, and attentive supervision; isolation fencing for swimming pools; and water competency, including water-safety knowledge, basic swim skills, and the ability to recognize and respond to a swimmer in trouble, use of life jackets, and early bystander CPR.”
The relative importance of each of those layers depends on geography and circumstances, Dr. Hoffman said. Pools are the most common drowning sites in the United States overall, but they’re much more common in warmer states, such as California, Florida, and Texas, which have more pools. In contrast, drownings in Oregon are more likely to occur in rivers, so prevention is more about access to life jackets and increasing access to swim lessons.
The findings from this study drive home how important it is for physicians to provide anticipatory guidance to families on reducing the risk of drowning. Pediatricians should convey to families the need for different layers of protection, he added.
“If your family spends a lot of time around water, whether open water or swimming pools, the more layers you can provide, the better off you’re going to be,” Dr. Hoffman said.
Dr. Shenoi echoed this sentiment.
“The take-home message is to be observant if you are entrusted with the care of a child around water,” Dr. Shenoi said. “If you notice the child to be drowning, either attempt rescue yourself if it is safe to do so or enlist the help of others to save the victim as soon as possible. However, the rescuer should not place himself or herself in danger when attempting rescue.”
The five steps in the “drowning chain of survival” – preventing drowning, recognizing distress, providing flotation, removing the victim from the water, and providing care and CPR as needed – are key to reducing drowning deaths and injury, Dr. Shenoi emphasized.
Dr. Shenoi has disclosed no relevant financial relationships. Dr. Hoffman is a paid consultant on child drowning prevention for the nonprofit Anonymous Philanthropy.
A version of this article first appeared on Medscape.com.
The likelihood that a child will survive a near-drowning without long-term damage is substantially greater if a bystander attempts a rescue, even if that person doesn’t perform cardiopulmonary resuscitation (CPR), according to new research presented October 10 at the American Academy of Pediatrics (AAP) 2021 National Conference.
“The extent to which bystander rescue is associated with reduced odds of unfavorable drowning outcomes was surprising,” said lead investigator Rohit P. Shenoi, MD, professor of pediatrics at Baylor College of Medicine and attending physician at Texas Children’s Hospital, Houston.
“While we do know that early rescue and resuscitation is helpful in preventing severe drowning injury, the degree of benefit from bystander rescue in all cases of pediatric drowning has not been described so far,” he told this news organization.
The fact that a bystander’s rescue attempt improves a child’s odds of a good outcome is not surprising on its own, but the magnitude of the finding really affirms the importance of bystander intervention, said Benjamin Hoffman, MD, professor of pediatrics at the Oregon Health & Science University School of Medicine and medical director of the Tom Sargent Safety Center at the Doernbecher Children’s Hospital, Portland.
“If an adult finds a child in the water, even if they don’t administer formal CPR, they’re going to be doing things” to try to help, Dr. Hoffman, who was not involved in this research but who specializes in child injury prevention, said in an interview. The act of intervening – whether it’s formal CPR or a CPR attempt or even just calling appropriate first responders – “likely impacts the duration of the submersion” and “clearly makes a difference.”
Drowning is the leading cause of death for children younger than 4 years, Dr. Hoffman noted, adding that the AAP recommends swimming lessons for children older than 1 year to reduce that risk.
In their cross-sectional study, Dr. Shenoi and his colleagues analyzed data on drownings and near-drownings in children and adolescents younger than 18 years using hospital, emergency medical services, and child fatality records from Harris County, Texas.
They analyzed 237 incidents from 2010 to 2013 in which the young person was submerged. Median age of the victims was 3.2 years, 60% were male, 64% were Black, Hispanic, or Native American, and 78% occurred in a swimming pool.
Unfavorable outcomes – defined as death or severe impairment after hospital discharge – were experienced by 38 victims (16%) and were significantly associated with being submerged for longer than 5 minutes (P < .001).
The odds of an unfavorable outcome dropped by 80% if a bystander attempted a rescue, whether or not they performed CPR (adjusted odds ratio, 0.2; P = .004). If the bystander performed CPR, the odds of an unfavorable outcome dropped by a similar amount, but the difference was not statistically significant (aOR, 0.22; P = .07).
However, previous research has shown a significant reduction in poor outcomes when CPR is administered to children who have been submerged, Dr. Hoffman explained.
The most important thing a bystander can do is simply get a submerged child out of the water. “Early rescue in drowning terminates what is initially a respiratory arrest from progressing to a full cardiopulmonary arrest with severe hypoxic brain injury and death,” Dr. Shenoi said.
“CPR is also very important, and rescue and resuscitation go hand in hand. We encourage all laypersons to be trained in CPR so that they can administer correct CPR techniques,” he added.
Both Dr. Shenoi and Dr. Hoffman emphasized the value of CPR training for adults, as the AAP recommends, and the importance of other precautions that reduce the risk of drowning.
“Drowning prevention should consist of multiple layers of prevention,” Dr. Shenoi said. These consist of “close, constant, and attentive supervision; isolation fencing for swimming pools; and water competency, including water-safety knowledge, basic swim skills, and the ability to recognize and respond to a swimmer in trouble, use of life jackets, and early bystander CPR.”
The relative importance of each of those layers depends on geography and circumstances, Dr. Hoffman said. Pools are the most common drowning sites in the United States overall, but they’re much more common in warmer states, such as California, Florida, and Texas, which have more pools. In contrast, drownings in Oregon are more likely to occur in rivers, so prevention is more about access to life jackets and increasing access to swim lessons.
The findings from this study drive home how important it is for physicians to provide anticipatory guidance to families on reducing the risk of drowning. Pediatricians should convey to families the need for different layers of protection, he added.
“If your family spends a lot of time around water, whether open water or swimming pools, the more layers you can provide, the better off you’re going to be,” Dr. Hoffman said.
Dr. Shenoi echoed this sentiment.
“The take-home message is to be observant if you are entrusted with the care of a child around water,” Dr. Shenoi said. “If you notice the child to be drowning, either attempt rescue yourself if it is safe to do so or enlist the help of others to save the victim as soon as possible. However, the rescuer should not place himself or herself in danger when attempting rescue.”
The five steps in the “drowning chain of survival” – preventing drowning, recognizing distress, providing flotation, removing the victim from the water, and providing care and CPR as needed – are key to reducing drowning deaths and injury, Dr. Shenoi emphasized.
Dr. Shenoi has disclosed no relevant financial relationships. Dr. Hoffman is a paid consultant on child drowning prevention for the nonprofit Anonymous Philanthropy.
A version of this article first appeared on Medscape.com.
Family violence patterns change during pandemic
Among adolescents treated for injuries caused by family-member violence, the proportion of incidents that involved illegal drugs or weapons more than doubled during the pandemic, and incidents that involved alcohol nearly doubled, according to data presented October 10 at the American Academy of Pediatrics 2021 National Conference.
“The COVID-19 pandemic amplified risk factors known to increase family interpersonal violence, such as increased need for parental supervision, parental stress, financial hardship, poor mental health, and isolation,” said investigator Mattea Miller, an MD candidate at the Johns Hopkins University School of Medicine, Baltimore.
To examine the issue, she and her colleagues “sought to characterize the prevalence and circumstances of adolescent injuries resulting from family interpersonal violence,” Ms. Miller told this news organization.
Their retrospective analysis involved children 10 to 15 years of age seen before or during the pandemic in the emergency department at Johns Hopkins Children’s Center for injuries that resulted from a violent incident with a family member.
Of the 819 incidents of violence-related injuries seen during the study period – the prepandemic ran from Jan. 1, 2019 to March 29, 2020, and the pandemic period ran from March 30, 2020, the date a stay-at-home order was first issued in Maryland, to Dec. 31, 2020 – 448 (54.7%) involved a family member. The proportion of such injuries was similar before and during the pandemic (54.6% vs. 54.9%; P = .99).
Most (83.9%) of these incidents occurred at home, 76.6% involved a parent or guardian, and 66.7% involved the youth being transported to the hospital by police.
It is surprising that families accounted for such a high level of violence involving adolescents, said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine, Houston, who was not involved in the research.
“The most common source of child physical abuse in younger children – infants and toddlers – [is the] parents,” who account for about 75% of cases, “but to see that amount of violence in adolescents was unexpected,” he told this news organization.
Patients in the study cohort were more likely to be Black than the hospital’s overall emergency-department population (84.4% vs. 60.0%), and more likely to be covered by public insurance (71.2% vs. 60.0%).
In the study cohort, 54.0% of the patients were female.
“We were surprised to see that 8% of visits did not have a referral to a social worker” – 92% of patients in the study cohort received a social work consult during their visit to the emergency department – and that number “did not vary during the COVID-19 pandemic,” Ms. Miller said. The pandemic exacerbated the types of stresses that social workers can help address, so “this potentially represents a gap in care that is important to address,” she added.
Increase in use of alcohol, drugs, weapons
The most significant increases from the prepandemic period to the pandemic period were in incidents that involved alcohol (10.0% vs. 18.8%; P ≤ .001), illegal drugs (6.5% vs. 14.9%; P ≤ .001), and weapons, most often a knife (10.7% vs. 23.8%; P ≤ .001).
“An obvious potential explanation for the increase in alcohol, drug, and weapons [involvement] would be the mental health impact of the pandemic in conjunction with the economic stressors that some families may be feeling,” Dr. Greeley said. Teachers are the most common reporters of child abuse, so it’s possible that reports of violence decreased when schools switched to remote learning. But with most schools back to in-person learning, data have not yet shown a surge in reporting, he noted.
The “epidemiology of family violence may be impacted by increased time at home, disruptions in school and family routines, exacerbations in mental health conditions, and financial stresses common during the pandemic,” said senior study investigator Leticia Ryan, MD, MPH, director of research in pediatrics at Johns Hopkins Medicine.
And research has shown increases in the use of alcohol and illegal drugs during the pandemic, she noted.
“As we transition to postpandemic life, it will be important to identify at-risk adolescents and families and provide supports,” Dr. Ryan told this news organization. “The emergency department is an appropriate setting to intervene with youth who have experienced family violence and initiate preventive strategies to avoid future violence.”
Among the strategies to identify and intervene for at-risk patients is the CRAFFT substance use screening tool. Furthermore, “case management, involvement of child protection services, and linkage with relevant support services may all be appropriate, depending on circumstances,” Ms. Miller added.
“Exposure to family violence at a young age increases the likelihood that a child will be exposed to additional violence or become a perpetrator of violence in the future, continuing a cycle of violence,” Ms. Miller explained. “Given that studies of adolescent violence often focus on peer violence, a better understanding of the epidemiology of violence-related injuries resulting from family violence is needed to better inform the development of more comprehensive prevention strategies.”
This study did not note any external funding. Ms. Miller, Dr. Greeley, and Dr. Ryan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among adolescents treated for injuries caused by family-member violence, the proportion of incidents that involved illegal drugs or weapons more than doubled during the pandemic, and incidents that involved alcohol nearly doubled, according to data presented October 10 at the American Academy of Pediatrics 2021 National Conference.
“The COVID-19 pandemic amplified risk factors known to increase family interpersonal violence, such as increased need for parental supervision, parental stress, financial hardship, poor mental health, and isolation,” said investigator Mattea Miller, an MD candidate at the Johns Hopkins University School of Medicine, Baltimore.
To examine the issue, she and her colleagues “sought to characterize the prevalence and circumstances of adolescent injuries resulting from family interpersonal violence,” Ms. Miller told this news organization.
Their retrospective analysis involved children 10 to 15 years of age seen before or during the pandemic in the emergency department at Johns Hopkins Children’s Center for injuries that resulted from a violent incident with a family member.
Of the 819 incidents of violence-related injuries seen during the study period – the prepandemic ran from Jan. 1, 2019 to March 29, 2020, and the pandemic period ran from March 30, 2020, the date a stay-at-home order was first issued in Maryland, to Dec. 31, 2020 – 448 (54.7%) involved a family member. The proportion of such injuries was similar before and during the pandemic (54.6% vs. 54.9%; P = .99).
Most (83.9%) of these incidents occurred at home, 76.6% involved a parent or guardian, and 66.7% involved the youth being transported to the hospital by police.
It is surprising that families accounted for such a high level of violence involving adolescents, said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine, Houston, who was not involved in the research.
“The most common source of child physical abuse in younger children – infants and toddlers – [is the] parents,” who account for about 75% of cases, “but to see that amount of violence in adolescents was unexpected,” he told this news organization.
Patients in the study cohort were more likely to be Black than the hospital’s overall emergency-department population (84.4% vs. 60.0%), and more likely to be covered by public insurance (71.2% vs. 60.0%).
In the study cohort, 54.0% of the patients were female.
“We were surprised to see that 8% of visits did not have a referral to a social worker” – 92% of patients in the study cohort received a social work consult during their visit to the emergency department – and that number “did not vary during the COVID-19 pandemic,” Ms. Miller said. The pandemic exacerbated the types of stresses that social workers can help address, so “this potentially represents a gap in care that is important to address,” she added.
Increase in use of alcohol, drugs, weapons
The most significant increases from the prepandemic period to the pandemic period were in incidents that involved alcohol (10.0% vs. 18.8%; P ≤ .001), illegal drugs (6.5% vs. 14.9%; P ≤ .001), and weapons, most often a knife (10.7% vs. 23.8%; P ≤ .001).
“An obvious potential explanation for the increase in alcohol, drug, and weapons [involvement] would be the mental health impact of the pandemic in conjunction with the economic stressors that some families may be feeling,” Dr. Greeley said. Teachers are the most common reporters of child abuse, so it’s possible that reports of violence decreased when schools switched to remote learning. But with most schools back to in-person learning, data have not yet shown a surge in reporting, he noted.
The “epidemiology of family violence may be impacted by increased time at home, disruptions in school and family routines, exacerbations in mental health conditions, and financial stresses common during the pandemic,” said senior study investigator Leticia Ryan, MD, MPH, director of research in pediatrics at Johns Hopkins Medicine.
And research has shown increases in the use of alcohol and illegal drugs during the pandemic, she noted.
“As we transition to postpandemic life, it will be important to identify at-risk adolescents and families and provide supports,” Dr. Ryan told this news organization. “The emergency department is an appropriate setting to intervene with youth who have experienced family violence and initiate preventive strategies to avoid future violence.”
Among the strategies to identify and intervene for at-risk patients is the CRAFFT substance use screening tool. Furthermore, “case management, involvement of child protection services, and linkage with relevant support services may all be appropriate, depending on circumstances,” Ms. Miller added.
“Exposure to family violence at a young age increases the likelihood that a child will be exposed to additional violence or become a perpetrator of violence in the future, continuing a cycle of violence,” Ms. Miller explained. “Given that studies of adolescent violence often focus on peer violence, a better understanding of the epidemiology of violence-related injuries resulting from family violence is needed to better inform the development of more comprehensive prevention strategies.”
This study did not note any external funding. Ms. Miller, Dr. Greeley, and Dr. Ryan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Among adolescents treated for injuries caused by family-member violence, the proportion of incidents that involved illegal drugs or weapons more than doubled during the pandemic, and incidents that involved alcohol nearly doubled, according to data presented October 10 at the American Academy of Pediatrics 2021 National Conference.
“The COVID-19 pandemic amplified risk factors known to increase family interpersonal violence, such as increased need for parental supervision, parental stress, financial hardship, poor mental health, and isolation,” said investigator Mattea Miller, an MD candidate at the Johns Hopkins University School of Medicine, Baltimore.
To examine the issue, she and her colleagues “sought to characterize the prevalence and circumstances of adolescent injuries resulting from family interpersonal violence,” Ms. Miller told this news organization.
Their retrospective analysis involved children 10 to 15 years of age seen before or during the pandemic in the emergency department at Johns Hopkins Children’s Center for injuries that resulted from a violent incident with a family member.
Of the 819 incidents of violence-related injuries seen during the study period – the prepandemic ran from Jan. 1, 2019 to March 29, 2020, and the pandemic period ran from March 30, 2020, the date a stay-at-home order was first issued in Maryland, to Dec. 31, 2020 – 448 (54.7%) involved a family member. The proportion of such injuries was similar before and during the pandemic (54.6% vs. 54.9%; P = .99).
Most (83.9%) of these incidents occurred at home, 76.6% involved a parent or guardian, and 66.7% involved the youth being transported to the hospital by police.
It is surprising that families accounted for such a high level of violence involving adolescents, said Christopher S. Greeley, MD, MS, chief of the division of public health pediatrics at Texas Children’s Hospital and professor of pediatrics at Baylor College of Medicine, Houston, who was not involved in the research.
“The most common source of child physical abuse in younger children – infants and toddlers – [is the] parents,” who account for about 75% of cases, “but to see that amount of violence in adolescents was unexpected,” he told this news organization.
Patients in the study cohort were more likely to be Black than the hospital’s overall emergency-department population (84.4% vs. 60.0%), and more likely to be covered by public insurance (71.2% vs. 60.0%).
In the study cohort, 54.0% of the patients were female.
“We were surprised to see that 8% of visits did not have a referral to a social worker” – 92% of patients in the study cohort received a social work consult during their visit to the emergency department – and that number “did not vary during the COVID-19 pandemic,” Ms. Miller said. The pandemic exacerbated the types of stresses that social workers can help address, so “this potentially represents a gap in care that is important to address,” she added.
Increase in use of alcohol, drugs, weapons
The most significant increases from the prepandemic period to the pandemic period were in incidents that involved alcohol (10.0% vs. 18.8%; P ≤ .001), illegal drugs (6.5% vs. 14.9%; P ≤ .001), and weapons, most often a knife (10.7% vs. 23.8%; P ≤ .001).
“An obvious potential explanation for the increase in alcohol, drug, and weapons [involvement] would be the mental health impact of the pandemic in conjunction with the economic stressors that some families may be feeling,” Dr. Greeley said. Teachers are the most common reporters of child abuse, so it’s possible that reports of violence decreased when schools switched to remote learning. But with most schools back to in-person learning, data have not yet shown a surge in reporting, he noted.
The “epidemiology of family violence may be impacted by increased time at home, disruptions in school and family routines, exacerbations in mental health conditions, and financial stresses common during the pandemic,” said senior study investigator Leticia Ryan, MD, MPH, director of research in pediatrics at Johns Hopkins Medicine.
And research has shown increases in the use of alcohol and illegal drugs during the pandemic, she noted.
“As we transition to postpandemic life, it will be important to identify at-risk adolescents and families and provide supports,” Dr. Ryan told this news organization. “The emergency department is an appropriate setting to intervene with youth who have experienced family violence and initiate preventive strategies to avoid future violence.”
Among the strategies to identify and intervene for at-risk patients is the CRAFFT substance use screening tool. Furthermore, “case management, involvement of child protection services, and linkage with relevant support services may all be appropriate, depending on circumstances,” Ms. Miller added.
“Exposure to family violence at a young age increases the likelihood that a child will be exposed to additional violence or become a perpetrator of violence in the future, continuing a cycle of violence,” Ms. Miller explained. “Given that studies of adolescent violence often focus on peer violence, a better understanding of the epidemiology of violence-related injuries resulting from family violence is needed to better inform the development of more comprehensive prevention strategies.”
This study did not note any external funding. Ms. Miller, Dr. Greeley, and Dr. Ryan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Adolescents who exercised after a concussion recovered faster in RCT
After a concussion, resuming aerobic exercise relatively early on – at an intensity that does not worsen symptoms – may help young athletes recover sooner, compared with stretching, a randomized controlled trial (RCT) shows.
The study adds to emerging evidence that clinicians should prescribe exercise, rather than strict rest, to facilitate concussion recovery, researchers said.
Tamara McLeod, PhD, ATC, professor and director of athletic training programs at A.T. Still University in Mesa, Ariz., hopes the findings help clinicians see that “this is an approach that should be taken.”
“Too often with concussion, patients are given a laundry list of things they are NOT allowed to do,” including sports, school, and social activities, said Dr. McLeod, who was not involved in the study.
The research, published in The Lancet Child & Adolescent Health, largely replicates the findings of a prior trial while addressing limitations of the previous study’s design, researchers said.
For the trial, John J. Leddy, MD, with the State University of New York at Buffalo and colleagues recruited 118 male and female adolescent athletes aged 13-18 years who had had a sport-related concussion in the past 10 days. Investigators at three community and hospital-affiliated sports medicine concussion centers in the United States randomly assigned the athletes to individualized subsymptom-threshold aerobic exercise (61 participants) or stretching exercise (57 participants) at least 20 minutes per day for up to 4 weeks. Aerobic exercise included walking, jogging, or stationary cycling at home.
“It is important that the general clinician community appreciates that prolonged rest and avoidance of physical activity until spontaneous symptom resolution is no longer an acceptable approach to caring for adolescents with concussion,” Dr. Leddy and coauthors said.
The investigators improved on the “the scientific rigor of their previous RCT by including intention-to-treat and per-protocol analyses, daily symptom reporting, objective exercise adherence measurements, and greater heterogeneity of concussion severity,” said Carolyn A. Emery, PhD, and Jonathan Smirl, PhD, both with the University of Calgary (Alta.), in a related commentary. The new study is the first to show that early targeted heart rate subsymptom-threshold aerobic exercise, relative to stretching, shortened recovery time within 4 weeks after sport-related concussion (hazard ratio, 0.52) when controlling for sex, study site, and average daily exercise time, Dr. Emery and Dr. Smirl said.
A larger proportion of athletes assigned to stretching did not recover by 4 weeks, compared with those assigned to aerobic exercise (32% vs. 21%). The median time to full recovery was longer for the stretching group than for the aerobic exercise group (19 days vs. 14 days).
Among athletes who adhered to their assigned regimens, the differences were more pronounced: The median recovery time was 21 days for the stretching group, compared with 12 days for the aerobic exercise group. The rate of postconcussion symptoms beyond 28 days was 9% in the aerobic exercise group versus 31% in the stretching group, among adherent participants.
More research is needed to establish the efficacy of postconcussion aerobic exercise in adults and for nonsport injury, the researchers noted. Possible mechanisms underlying aerobic exercise’s benefits could include increased parasympathetic autonomic tone, improved cerebral blood flow regulation, or enhanced neuron repair, they suggested.
The right amount and timing of exercise, and doing so at an intensity that does not exacerbate symptoms, may be key. Other research has suggested that too much exercise, too soon may delay recovery, Dr. Emery said in an interview. “But there is now a lot of evidence to support low and moderate levels of physical activity to expedite recovery,” she said.
The study was funded by the American Medical Society for Sports Medicine. The study and commentary authors and Dr. McLeod had no disclosures.
After a concussion, resuming aerobic exercise relatively early on – at an intensity that does not worsen symptoms – may help young athletes recover sooner, compared with stretching, a randomized controlled trial (RCT) shows.
The study adds to emerging evidence that clinicians should prescribe exercise, rather than strict rest, to facilitate concussion recovery, researchers said.
Tamara McLeod, PhD, ATC, professor and director of athletic training programs at A.T. Still University in Mesa, Ariz., hopes the findings help clinicians see that “this is an approach that should be taken.”
“Too often with concussion, patients are given a laundry list of things they are NOT allowed to do,” including sports, school, and social activities, said Dr. McLeod, who was not involved in the study.
The research, published in The Lancet Child & Adolescent Health, largely replicates the findings of a prior trial while addressing limitations of the previous study’s design, researchers said.
For the trial, John J. Leddy, MD, with the State University of New York at Buffalo and colleagues recruited 118 male and female adolescent athletes aged 13-18 years who had had a sport-related concussion in the past 10 days. Investigators at three community and hospital-affiliated sports medicine concussion centers in the United States randomly assigned the athletes to individualized subsymptom-threshold aerobic exercise (61 participants) or stretching exercise (57 participants) at least 20 minutes per day for up to 4 weeks. Aerobic exercise included walking, jogging, or stationary cycling at home.
“It is important that the general clinician community appreciates that prolonged rest and avoidance of physical activity until spontaneous symptom resolution is no longer an acceptable approach to caring for adolescents with concussion,” Dr. Leddy and coauthors said.
The investigators improved on the “the scientific rigor of their previous RCT by including intention-to-treat and per-protocol analyses, daily symptom reporting, objective exercise adherence measurements, and greater heterogeneity of concussion severity,” said Carolyn A. Emery, PhD, and Jonathan Smirl, PhD, both with the University of Calgary (Alta.), in a related commentary. The new study is the first to show that early targeted heart rate subsymptom-threshold aerobic exercise, relative to stretching, shortened recovery time within 4 weeks after sport-related concussion (hazard ratio, 0.52) when controlling for sex, study site, and average daily exercise time, Dr. Emery and Dr. Smirl said.
A larger proportion of athletes assigned to stretching did not recover by 4 weeks, compared with those assigned to aerobic exercise (32% vs. 21%). The median time to full recovery was longer for the stretching group than for the aerobic exercise group (19 days vs. 14 days).
Among athletes who adhered to their assigned regimens, the differences were more pronounced: The median recovery time was 21 days for the stretching group, compared with 12 days for the aerobic exercise group. The rate of postconcussion symptoms beyond 28 days was 9% in the aerobic exercise group versus 31% in the stretching group, among adherent participants.
More research is needed to establish the efficacy of postconcussion aerobic exercise in adults and for nonsport injury, the researchers noted. Possible mechanisms underlying aerobic exercise’s benefits could include increased parasympathetic autonomic tone, improved cerebral blood flow regulation, or enhanced neuron repair, they suggested.
The right amount and timing of exercise, and doing so at an intensity that does not exacerbate symptoms, may be key. Other research has suggested that too much exercise, too soon may delay recovery, Dr. Emery said in an interview. “But there is now a lot of evidence to support low and moderate levels of physical activity to expedite recovery,” she said.
The study was funded by the American Medical Society for Sports Medicine. The study and commentary authors and Dr. McLeod had no disclosures.
After a concussion, resuming aerobic exercise relatively early on – at an intensity that does not worsen symptoms – may help young athletes recover sooner, compared with stretching, a randomized controlled trial (RCT) shows.
The study adds to emerging evidence that clinicians should prescribe exercise, rather than strict rest, to facilitate concussion recovery, researchers said.
Tamara McLeod, PhD, ATC, professor and director of athletic training programs at A.T. Still University in Mesa, Ariz., hopes the findings help clinicians see that “this is an approach that should be taken.”
“Too often with concussion, patients are given a laundry list of things they are NOT allowed to do,” including sports, school, and social activities, said Dr. McLeod, who was not involved in the study.
The research, published in The Lancet Child & Adolescent Health, largely replicates the findings of a prior trial while addressing limitations of the previous study’s design, researchers said.
For the trial, John J. Leddy, MD, with the State University of New York at Buffalo and colleagues recruited 118 male and female adolescent athletes aged 13-18 years who had had a sport-related concussion in the past 10 days. Investigators at three community and hospital-affiliated sports medicine concussion centers in the United States randomly assigned the athletes to individualized subsymptom-threshold aerobic exercise (61 participants) or stretching exercise (57 participants) at least 20 minutes per day for up to 4 weeks. Aerobic exercise included walking, jogging, or stationary cycling at home.
“It is important that the general clinician community appreciates that prolonged rest and avoidance of physical activity until spontaneous symptom resolution is no longer an acceptable approach to caring for adolescents with concussion,” Dr. Leddy and coauthors said.
The investigators improved on the “the scientific rigor of their previous RCT by including intention-to-treat and per-protocol analyses, daily symptom reporting, objective exercise adherence measurements, and greater heterogeneity of concussion severity,” said Carolyn A. Emery, PhD, and Jonathan Smirl, PhD, both with the University of Calgary (Alta.), in a related commentary. The new study is the first to show that early targeted heart rate subsymptom-threshold aerobic exercise, relative to stretching, shortened recovery time within 4 weeks after sport-related concussion (hazard ratio, 0.52) when controlling for sex, study site, and average daily exercise time, Dr. Emery and Dr. Smirl said.
A larger proportion of athletes assigned to stretching did not recover by 4 weeks, compared with those assigned to aerobic exercise (32% vs. 21%). The median time to full recovery was longer for the stretching group than for the aerobic exercise group (19 days vs. 14 days).
Among athletes who adhered to their assigned regimens, the differences were more pronounced: The median recovery time was 21 days for the stretching group, compared with 12 days for the aerobic exercise group. The rate of postconcussion symptoms beyond 28 days was 9% in the aerobic exercise group versus 31% in the stretching group, among adherent participants.
More research is needed to establish the efficacy of postconcussion aerobic exercise in adults and for nonsport injury, the researchers noted. Possible mechanisms underlying aerobic exercise’s benefits could include increased parasympathetic autonomic tone, improved cerebral blood flow regulation, or enhanced neuron repair, they suggested.
The right amount and timing of exercise, and doing so at an intensity that does not exacerbate symptoms, may be key. Other research has suggested that too much exercise, too soon may delay recovery, Dr. Emery said in an interview. “But there is now a lot of evidence to support low and moderate levels of physical activity to expedite recovery,” she said.
The study was funded by the American Medical Society for Sports Medicine. The study and commentary authors and Dr. McLeod had no disclosures.
FROM THE LANCET CHILD & ADOLESCENT HEALTH



