User login
Bundled payment for OA surgery linked to more emergency department visits
And therein lies a key lesson for health policy makers who have embraced bundled payments to reduce rising health care costs, Mayilee Canizares, PhD, observed at the OARSI 2019 World Congress.
In Ontario, with patients discharged sooner and directly to home, there was the negative impact of increased emergency department visits after surgery, Dr. Canizares, of the University Health Network in Toronto, said at OARSI 2019 World Congress, sponsored by the Osteoarthritis Research Society International. “Our findings highlight the importance of coordinating the appropriate support services as well as the need to continue assessing the optimal discharge care plan for osteoarthritis patients undergoing surgery.”
Dr. Canizares’ study of the Ontario-wide experience with orthopedic surgery for osteoarthritis during 2004-2016 received the OARSI 2019 award for the meeting’s top-rated study in clinical epidemiology/health services research.
Using administrative data from Canada’s national health care system, Dr. Canizares and her coinvestigators found that the number of individuals undergoing elective orthopedic surgery for osteoarthritis ballooned from 22,700 in 2004 to 41,900 in 2016, representing an increase from 246 to 381 procedures per 100,000 people. During this time, the mean length of stay declined from about 5 days to just under 3 days, the 30-day readmission rate dropped from 4.2% to 3.4%, and the rate of emergency department visits within 30 days post discharge rose steadily from 8.7% in 2004 to 14.1% in 2016.
Roughly half of the operations were total knee replacements and one-third were hip replacements. The profile of patients undergoing surgery changed little over the course of the 12-year study with the exception that in more recent years patients presented with more comorbidities: Indeed, three or more comorbid conditions were present in 2.9% of the surgical patients in 2004 compared to 4.2% in 2016.
In multivariate logistic regression analyses, patient characteristics didn’t explain the change over time in early readmission or unplanned emergency department visit rates. However, discharge disposition did: By 2014, more patients were being discharged home, and in nearly half of cases that was being done without support.
Dr. Canizares reported having no financial conflicts regarding her study, funded by the Toronto General and Western Hospital Foundation.
SOURCE: Canizares M. OARSI, Abstract 16.
And therein lies a key lesson for health policy makers who have embraced bundled payments to reduce rising health care costs, Mayilee Canizares, PhD, observed at the OARSI 2019 World Congress.
In Ontario, with patients discharged sooner and directly to home, there was the negative impact of increased emergency department visits after surgery, Dr. Canizares, of the University Health Network in Toronto, said at OARSI 2019 World Congress, sponsored by the Osteoarthritis Research Society International. “Our findings highlight the importance of coordinating the appropriate support services as well as the need to continue assessing the optimal discharge care plan for osteoarthritis patients undergoing surgery.”
Dr. Canizares’ study of the Ontario-wide experience with orthopedic surgery for osteoarthritis during 2004-2016 received the OARSI 2019 award for the meeting’s top-rated study in clinical epidemiology/health services research.
Using administrative data from Canada’s national health care system, Dr. Canizares and her coinvestigators found that the number of individuals undergoing elective orthopedic surgery for osteoarthritis ballooned from 22,700 in 2004 to 41,900 in 2016, representing an increase from 246 to 381 procedures per 100,000 people. During this time, the mean length of stay declined from about 5 days to just under 3 days, the 30-day readmission rate dropped from 4.2% to 3.4%, and the rate of emergency department visits within 30 days post discharge rose steadily from 8.7% in 2004 to 14.1% in 2016.
Roughly half of the operations were total knee replacements and one-third were hip replacements. The profile of patients undergoing surgery changed little over the course of the 12-year study with the exception that in more recent years patients presented with more comorbidities: Indeed, three or more comorbid conditions were present in 2.9% of the surgical patients in 2004 compared to 4.2% in 2016.
In multivariate logistic regression analyses, patient characteristics didn’t explain the change over time in early readmission or unplanned emergency department visit rates. However, discharge disposition did: By 2014, more patients were being discharged home, and in nearly half of cases that was being done without support.
Dr. Canizares reported having no financial conflicts regarding her study, funded by the Toronto General and Western Hospital Foundation.
SOURCE: Canizares M. OARSI, Abstract 16.
And therein lies a key lesson for health policy makers who have embraced bundled payments to reduce rising health care costs, Mayilee Canizares, PhD, observed at the OARSI 2019 World Congress.
In Ontario, with patients discharged sooner and directly to home, there was the negative impact of increased emergency department visits after surgery, Dr. Canizares, of the University Health Network in Toronto, said at OARSI 2019 World Congress, sponsored by the Osteoarthritis Research Society International. “Our findings highlight the importance of coordinating the appropriate support services as well as the need to continue assessing the optimal discharge care plan for osteoarthritis patients undergoing surgery.”
Dr. Canizares’ study of the Ontario-wide experience with orthopedic surgery for osteoarthritis during 2004-2016 received the OARSI 2019 award for the meeting’s top-rated study in clinical epidemiology/health services research.
Using administrative data from Canada’s national health care system, Dr. Canizares and her coinvestigators found that the number of individuals undergoing elective orthopedic surgery for osteoarthritis ballooned from 22,700 in 2004 to 41,900 in 2016, representing an increase from 246 to 381 procedures per 100,000 people. During this time, the mean length of stay declined from about 5 days to just under 3 days, the 30-day readmission rate dropped from 4.2% to 3.4%, and the rate of emergency department visits within 30 days post discharge rose steadily from 8.7% in 2004 to 14.1% in 2016.
Roughly half of the operations were total knee replacements and one-third were hip replacements. The profile of patients undergoing surgery changed little over the course of the 12-year study with the exception that in more recent years patients presented with more comorbidities: Indeed, three or more comorbid conditions were present in 2.9% of the surgical patients in 2004 compared to 4.2% in 2016.
In multivariate logistic regression analyses, patient characteristics didn’t explain the change over time in early readmission or unplanned emergency department visit rates. However, discharge disposition did: By 2014, more patients were being discharged home, and in nearly half of cases that was being done without support.
Dr. Canizares reported having no financial conflicts regarding her study, funded by the Toronto General and Western Hospital Foundation.
SOURCE: Canizares M. OARSI, Abstract 16.
REPORTING FROM OARSI 2019
PT beats steroid injections for knee OA
TORONTO – Eight physical therapy sessions spread over 4-6 weeks in patients with knee osteoarthritis provided significantly greater and longer-lasting improvements in both pain and function than an intra-articular corticosteroid injection in a randomized, multicenter trial with 12 months of prospective, blinded follow-up, Daniel I. Rhon, DPT, DSc, reported at the OARSI 2019 World Congress.
“Considering the very low utilization rate of physical therapy prior to arthroplasty, perhaps we should more often give it a try before declaring that conservative care has failed and moving on to surgical management,” concluded Dr. Rhon, director of the primary care musculoskeletal research center at Brooke Army Medical Center in San Antonio.
Various studies have shown that close to 50% of patients with knee OA receive one or more intra-articular corticosteroid injections within 5 years prior to undergoing total knee arthroplasty, compared with physical therapy in only about 10% of patients, even though most guidelines rate both as first-line therapies, he noted at the meeting sponsored by the Osteoarthritis Research Society International.
He presented a randomized trial of 156 patients who sought treatment for pain caused by knee OA at army medical center primary care clinics. To his knowledge, this was the first-ever randomized, head-to-head comparison of the effectiveness of a physical therapy regimen versus corticosteroid injections for knee OA. Because he and his coinvestigators wanted a pragmatic study giving each treatment strategy its due, booster therapy was available to patients who requested it. Patients in the corticosteroid arm were able to receive up to two additional spaced intra-articular injections as needed, while those assigned to the individualized manual physical therapy intervention, which utilized exercises targeting the typical strength and movement deficits found in patients with knee OA, could have up to three additional sessions. At the outset, all participants received education about the benefits of regular low-impact physical activity, weight reduction, and strength and flexibility exercises.
The two treatment groups were comparable except that the physical therapy group had a longer disease duration – a mean of 123 months as compared with 89 in the corticosteroid group – and more radiographically severe disease. Indeed, 60% of patients randomized to physical therapy were Kellgren-Lawrence scale grade III-IV, versus 45% of those assigned to intra-articular corticosteroid injection.
The primary outcome in the study was change in Western Ontario & McMaster Universities Arthritis Index (WOMAC) score at 12 months. As early as 4 weeks into the study, the physical therapy group showed significantly greater improvement than in the comparison arm: from a mean baseline WOMAC score of 115 to 42.9 at 4 weeks, 42.5 at 6 months, and 38.4 at 1 year. The comparable figures in the intra-articular corticosteroid group were 113.3 at baseline, 53.3 at 4 weeks, 57.9 at 6 months, and 53.8 at 1 year.
“Physical therapy provided clinically important benefit that was superior to corticosteroid injection out to 1 year, while also providing the short-term benefit typically sought from corticosteroid injection,” Dr. Rhon observed.
The median improvement in WOMAC score at 1 year was 52% in the corticosteroid group and 71% in the physical therapy arm. About 59% of the physical therapy group experienced at least a 50% reduction in WOMAC score at 12 months, as did 38% of intra-articular injection recipients. The number needed to treat with physical therapy instead of intra-articular corticosteroids in order for one additional patient to achieve at least a 50% improvement in WOMAC score through 1 year of follow-up was four.
“We were a little bit surprised that there was such a large effect size in the study. The effect size in the injection group was bigger than reported in some other trials,” according to Dr. Rhon.
In terms of downstream utilization of health care, there were two knee arthroplasties and one arthroscopy in the study population, all in the intra-articular corticosteroid group. Seven patients in the intra-articular steroid group received more than three injections, including one patient with nine. And 13 patients in the physical therapy arm went outside the study in order to receive at least one corticosteroid injection.
One audience member pointed out that the physical therapy approach offers an important side benefit: In addition to improving pain and function, the exercise regimen has a favorable effect on comorbid metabolic diseases commonly associated with knee OA.
“An injection doesn’t achieve that,” he noted.
Dr. Rhon reported having no financial conflicts of interest regarding the randomized trial, sponsored by Madigan Army Medical Center. He receives research funding from the National Institutes of Health and the Congressionally Directed Medical Research Programs.
SOURCE: Rhon DI et al. Osteoarthritis Cartilage. 2019 Apr;27[suppl 1]:S32, Abstract 13
TORONTO – Eight physical therapy sessions spread over 4-6 weeks in patients with knee osteoarthritis provided significantly greater and longer-lasting improvements in both pain and function than an intra-articular corticosteroid injection in a randomized, multicenter trial with 12 months of prospective, blinded follow-up, Daniel I. Rhon, DPT, DSc, reported at the OARSI 2019 World Congress.
“Considering the very low utilization rate of physical therapy prior to arthroplasty, perhaps we should more often give it a try before declaring that conservative care has failed and moving on to surgical management,” concluded Dr. Rhon, director of the primary care musculoskeletal research center at Brooke Army Medical Center in San Antonio.
Various studies have shown that close to 50% of patients with knee OA receive one or more intra-articular corticosteroid injections within 5 years prior to undergoing total knee arthroplasty, compared with physical therapy in only about 10% of patients, even though most guidelines rate both as first-line therapies, he noted at the meeting sponsored by the Osteoarthritis Research Society International.
He presented a randomized trial of 156 patients who sought treatment for pain caused by knee OA at army medical center primary care clinics. To his knowledge, this was the first-ever randomized, head-to-head comparison of the effectiveness of a physical therapy regimen versus corticosteroid injections for knee OA. Because he and his coinvestigators wanted a pragmatic study giving each treatment strategy its due, booster therapy was available to patients who requested it. Patients in the corticosteroid arm were able to receive up to two additional spaced intra-articular injections as needed, while those assigned to the individualized manual physical therapy intervention, which utilized exercises targeting the typical strength and movement deficits found in patients with knee OA, could have up to three additional sessions. At the outset, all participants received education about the benefits of regular low-impact physical activity, weight reduction, and strength and flexibility exercises.
The two treatment groups were comparable except that the physical therapy group had a longer disease duration – a mean of 123 months as compared with 89 in the corticosteroid group – and more radiographically severe disease. Indeed, 60% of patients randomized to physical therapy were Kellgren-Lawrence scale grade III-IV, versus 45% of those assigned to intra-articular corticosteroid injection.
The primary outcome in the study was change in Western Ontario & McMaster Universities Arthritis Index (WOMAC) score at 12 months. As early as 4 weeks into the study, the physical therapy group showed significantly greater improvement than in the comparison arm: from a mean baseline WOMAC score of 115 to 42.9 at 4 weeks, 42.5 at 6 months, and 38.4 at 1 year. The comparable figures in the intra-articular corticosteroid group were 113.3 at baseline, 53.3 at 4 weeks, 57.9 at 6 months, and 53.8 at 1 year.
“Physical therapy provided clinically important benefit that was superior to corticosteroid injection out to 1 year, while also providing the short-term benefit typically sought from corticosteroid injection,” Dr. Rhon observed.
The median improvement in WOMAC score at 1 year was 52% in the corticosteroid group and 71% in the physical therapy arm. About 59% of the physical therapy group experienced at least a 50% reduction in WOMAC score at 12 months, as did 38% of intra-articular injection recipients. The number needed to treat with physical therapy instead of intra-articular corticosteroids in order for one additional patient to achieve at least a 50% improvement in WOMAC score through 1 year of follow-up was four.
“We were a little bit surprised that there was such a large effect size in the study. The effect size in the injection group was bigger than reported in some other trials,” according to Dr. Rhon.
In terms of downstream utilization of health care, there were two knee arthroplasties and one arthroscopy in the study population, all in the intra-articular corticosteroid group. Seven patients in the intra-articular steroid group received more than three injections, including one patient with nine. And 13 patients in the physical therapy arm went outside the study in order to receive at least one corticosteroid injection.
One audience member pointed out that the physical therapy approach offers an important side benefit: In addition to improving pain and function, the exercise regimen has a favorable effect on comorbid metabolic diseases commonly associated with knee OA.
“An injection doesn’t achieve that,” he noted.
Dr. Rhon reported having no financial conflicts of interest regarding the randomized trial, sponsored by Madigan Army Medical Center. He receives research funding from the National Institutes of Health and the Congressionally Directed Medical Research Programs.
SOURCE: Rhon DI et al. Osteoarthritis Cartilage. 2019 Apr;27[suppl 1]:S32, Abstract 13
TORONTO – Eight physical therapy sessions spread over 4-6 weeks in patients with knee osteoarthritis provided significantly greater and longer-lasting improvements in both pain and function than an intra-articular corticosteroid injection in a randomized, multicenter trial with 12 months of prospective, blinded follow-up, Daniel I. Rhon, DPT, DSc, reported at the OARSI 2019 World Congress.
“Considering the very low utilization rate of physical therapy prior to arthroplasty, perhaps we should more often give it a try before declaring that conservative care has failed and moving on to surgical management,” concluded Dr. Rhon, director of the primary care musculoskeletal research center at Brooke Army Medical Center in San Antonio.
Various studies have shown that close to 50% of patients with knee OA receive one or more intra-articular corticosteroid injections within 5 years prior to undergoing total knee arthroplasty, compared with physical therapy in only about 10% of patients, even though most guidelines rate both as first-line therapies, he noted at the meeting sponsored by the Osteoarthritis Research Society International.
He presented a randomized trial of 156 patients who sought treatment for pain caused by knee OA at army medical center primary care clinics. To his knowledge, this was the first-ever randomized, head-to-head comparison of the effectiveness of a physical therapy regimen versus corticosteroid injections for knee OA. Because he and his coinvestigators wanted a pragmatic study giving each treatment strategy its due, booster therapy was available to patients who requested it. Patients in the corticosteroid arm were able to receive up to two additional spaced intra-articular injections as needed, while those assigned to the individualized manual physical therapy intervention, which utilized exercises targeting the typical strength and movement deficits found in patients with knee OA, could have up to three additional sessions. At the outset, all participants received education about the benefits of regular low-impact physical activity, weight reduction, and strength and flexibility exercises.
The two treatment groups were comparable except that the physical therapy group had a longer disease duration – a mean of 123 months as compared with 89 in the corticosteroid group – and more radiographically severe disease. Indeed, 60% of patients randomized to physical therapy were Kellgren-Lawrence scale grade III-IV, versus 45% of those assigned to intra-articular corticosteroid injection.
The primary outcome in the study was change in Western Ontario & McMaster Universities Arthritis Index (WOMAC) score at 12 months. As early as 4 weeks into the study, the physical therapy group showed significantly greater improvement than in the comparison arm: from a mean baseline WOMAC score of 115 to 42.9 at 4 weeks, 42.5 at 6 months, and 38.4 at 1 year. The comparable figures in the intra-articular corticosteroid group were 113.3 at baseline, 53.3 at 4 weeks, 57.9 at 6 months, and 53.8 at 1 year.
“Physical therapy provided clinically important benefit that was superior to corticosteroid injection out to 1 year, while also providing the short-term benefit typically sought from corticosteroid injection,” Dr. Rhon observed.
The median improvement in WOMAC score at 1 year was 52% in the corticosteroid group and 71% in the physical therapy arm. About 59% of the physical therapy group experienced at least a 50% reduction in WOMAC score at 12 months, as did 38% of intra-articular injection recipients. The number needed to treat with physical therapy instead of intra-articular corticosteroids in order for one additional patient to achieve at least a 50% improvement in WOMAC score through 1 year of follow-up was four.
“We were a little bit surprised that there was such a large effect size in the study. The effect size in the injection group was bigger than reported in some other trials,” according to Dr. Rhon.
In terms of downstream utilization of health care, there were two knee arthroplasties and one arthroscopy in the study population, all in the intra-articular corticosteroid group. Seven patients in the intra-articular steroid group received more than three injections, including one patient with nine. And 13 patients in the physical therapy arm went outside the study in order to receive at least one corticosteroid injection.
One audience member pointed out that the physical therapy approach offers an important side benefit: In addition to improving pain and function, the exercise regimen has a favorable effect on comorbid metabolic diseases commonly associated with knee OA.
“An injection doesn’t achieve that,” he noted.
Dr. Rhon reported having no financial conflicts of interest regarding the randomized trial, sponsored by Madigan Army Medical Center. He receives research funding from the National Institutes of Health and the Congressionally Directed Medical Research Programs.
SOURCE: Rhon DI et al. Osteoarthritis Cartilage. 2019 Apr;27[suppl 1]:S32, Abstract 13
REPORTING FROM OARSI 2019
High-intensity statins may cut risk of joint replacement
TORONTO – comparing nearly 180,000 statin users with an equal number of propensity-matched nonusers, Jie Wei, PhD, reported at the OARSI 2019 World Congress.
Less intensive statin therapy was associated with significantly less need for joint replacement surgery in rheumatoid arthritis patients, but not in those with osteoarthritis, she said at the meeting, sponsored by the Osteoarthritis Research Society International.
“In summary, statins may reduce the risk of joint replacement, especially when given at high strength and in people with rheumatoid arthritis,” said Dr. Wei, an epidemiologist at Massachusetts General Hospital, Boston, and Central South University in Changsha, Hunan, China.
She was quick to note that this study can’t be considered the final, definitive word on the topic, since other investigators’ studies of the relationship between statin usage and joint replacement surgery for arthritis have yielded conflicting results. However, given the thoroughly established super-favorable risk/benefit ratio of statins for the prevention of cardiovascular morbidity and mortality, the possibility of a prospective, randomized, controlled trial addressing the joint surgery issue is for ethical reasons a train that’s left the station.
Dr. Wei presented an analysis drawn from the U.K. Clinical Practice Research Datalink for the years 1989 through mid-2017. The initial sample included the medical records of 17.1 million patients, or 26% of the total U.K. population. From that massive pool, she and her coinvestigators zeroed in on 178,467 statin users and an equal number of non–statin-user controls under the care of 718 primary care physicians, with the pairs propensity score-matched on the basis of age, gender, locality, comorbid conditions, nonstatin medications, lifestyle factors, and duration of rheumatoid arthritis or osteoarthritis. The mean age of the matched pairs was 62 years, 52% were women, and the mean prospective follow-up was 6.5 years.
The use of high-intensity statin therapy – for example, atorvastatin at 40-80 mg/day or rosuvastatin (Crestor) at 20-40 mg/day – was independently associated with a 21% reduction in the risk of knee or hip replacement surgery for osteoarthritis and a 90% reduction for rheumatoid arthritis, compared with statin nonusers. Notably, joint replacement surgery for osteoarthritis was roughly 25-fold more common than for rheumatoid arthritis.
Statin therapy overall, including the more widely prescribed low- and intermediate-intensity regimens, was associated with a 23% reduction in joint replacement surgery for rheumatoid arthritis, compared with statin nonusers, but had no significant impact on surgery for the osteoarthritis population.
A couple of distinguished American rheumatologists in the audience rose to voice reluctance about drawing broad conclusions from this study.
“Bias, as you’ve said yourself, is a bit of a concern,” said David T. Felson, MD, professor of medicine and public health and director of clinical epidemiology at Boston University.
He was troubled that the study design was such that anyone who filled as few as two statin prescriptions during the more than 6-year study period was categorized as a statin user. That, he said, muddies the waters. Does the database contain information on duration of statin therapy, and whether joint replacement surgery was more likely to occur when patients were on or off statin therapy? he asked.
It does, Dr. Wei replied, adding that she will take that suggestion for additional analysis back to her international team of coinvestigators.
“It seems to me,” said Jeffrey N. Katz, MD, “that the major risk of potential bias is that people who were provided high-intensity statins were prescribed that because they were at risk for or had cardiac disease.”
That high cardiovascular risk might have curbed orthopedic surgeons’ enthusiasm to operate. Thus, it would be helpful to learn whether patients who underwent joint replacement were less likely to have undergone coronary revascularization or other cardiac interventions than were those without joint replacement, according to Dr. Katz, professor of medicine and orthopedic surgery at Harvard Medical School, Boston.
Dr. Wei agreed that confounding by indication is always a possibility in an observational study such as this. Identification of a plausible mechanism by which statins might reduce the risk of joint replacement surgery in rheumatoid arthritis – something that hasn’t happened yet – would help counter such concerns.
She noted that a separate recent analysis of the U.K. Clinical Practice Research Datalink by other investigators concluded that statin therapy started up to 5 years following total hip or knee replacement was associated with a significantly reduced risk of revision arthroplasty. Moreover, the benefit was treatment duration-dependent: Patients on statin therapy for more than 5 years were 26% less likely to undergo revision arthroplasty than were those on a statin for less than 1 year (J Rheumatol. 2019 Mar 15. doi: 10.3899/jrheum.180574).
On the other hand, Swedish investigators found that statin use wasn’t associated with a reduced risk of consultation or surgery for osteoarthritis in a pooled analysis of four cohort studies totaling more than 132,000 Swedes followed for 7.5 years (Osteoarthritis Cartilage. 2017 Nov;25[11]:1804-13).
Dr. Wei reported having no financial conflicts regarding the study, which was supported by the National Clinical Research Center of Geriatric Disorders in Hunan, China, and several British universities.
SOURCE: Sarmanova A et al. Osteoarthritis cartilage. 2019 Apr;27[suppl 1]:S78-S79. Abstract 77.
TORONTO – comparing nearly 180,000 statin users with an equal number of propensity-matched nonusers, Jie Wei, PhD, reported at the OARSI 2019 World Congress.
Less intensive statin therapy was associated with significantly less need for joint replacement surgery in rheumatoid arthritis patients, but not in those with osteoarthritis, she said at the meeting, sponsored by the Osteoarthritis Research Society International.
“In summary, statins may reduce the risk of joint replacement, especially when given at high strength and in people with rheumatoid arthritis,” said Dr. Wei, an epidemiologist at Massachusetts General Hospital, Boston, and Central South University in Changsha, Hunan, China.
She was quick to note that this study can’t be considered the final, definitive word on the topic, since other investigators’ studies of the relationship between statin usage and joint replacement surgery for arthritis have yielded conflicting results. However, given the thoroughly established super-favorable risk/benefit ratio of statins for the prevention of cardiovascular morbidity and mortality, the possibility of a prospective, randomized, controlled trial addressing the joint surgery issue is for ethical reasons a train that’s left the station.
Dr. Wei presented an analysis drawn from the U.K. Clinical Practice Research Datalink for the years 1989 through mid-2017. The initial sample included the medical records of 17.1 million patients, or 26% of the total U.K. population. From that massive pool, she and her coinvestigators zeroed in on 178,467 statin users and an equal number of non–statin-user controls under the care of 718 primary care physicians, with the pairs propensity score-matched on the basis of age, gender, locality, comorbid conditions, nonstatin medications, lifestyle factors, and duration of rheumatoid arthritis or osteoarthritis. The mean age of the matched pairs was 62 years, 52% were women, and the mean prospective follow-up was 6.5 years.
The use of high-intensity statin therapy – for example, atorvastatin at 40-80 mg/day or rosuvastatin (Crestor) at 20-40 mg/day – was independently associated with a 21% reduction in the risk of knee or hip replacement surgery for osteoarthritis and a 90% reduction for rheumatoid arthritis, compared with statin nonusers. Notably, joint replacement surgery for osteoarthritis was roughly 25-fold more common than for rheumatoid arthritis.
Statin therapy overall, including the more widely prescribed low- and intermediate-intensity regimens, was associated with a 23% reduction in joint replacement surgery for rheumatoid arthritis, compared with statin nonusers, but had no significant impact on surgery for the osteoarthritis population.
A couple of distinguished American rheumatologists in the audience rose to voice reluctance about drawing broad conclusions from this study.
“Bias, as you’ve said yourself, is a bit of a concern,” said David T. Felson, MD, professor of medicine and public health and director of clinical epidemiology at Boston University.
He was troubled that the study design was such that anyone who filled as few as two statin prescriptions during the more than 6-year study period was categorized as a statin user. That, he said, muddies the waters. Does the database contain information on duration of statin therapy, and whether joint replacement surgery was more likely to occur when patients were on or off statin therapy? he asked.
It does, Dr. Wei replied, adding that she will take that suggestion for additional analysis back to her international team of coinvestigators.
“It seems to me,” said Jeffrey N. Katz, MD, “that the major risk of potential bias is that people who were provided high-intensity statins were prescribed that because they were at risk for or had cardiac disease.”
That high cardiovascular risk might have curbed orthopedic surgeons’ enthusiasm to operate. Thus, it would be helpful to learn whether patients who underwent joint replacement were less likely to have undergone coronary revascularization or other cardiac interventions than were those without joint replacement, according to Dr. Katz, professor of medicine and orthopedic surgery at Harvard Medical School, Boston.
Dr. Wei agreed that confounding by indication is always a possibility in an observational study such as this. Identification of a plausible mechanism by which statins might reduce the risk of joint replacement surgery in rheumatoid arthritis – something that hasn’t happened yet – would help counter such concerns.
She noted that a separate recent analysis of the U.K. Clinical Practice Research Datalink by other investigators concluded that statin therapy started up to 5 years following total hip or knee replacement was associated with a significantly reduced risk of revision arthroplasty. Moreover, the benefit was treatment duration-dependent: Patients on statin therapy for more than 5 years were 26% less likely to undergo revision arthroplasty than were those on a statin for less than 1 year (J Rheumatol. 2019 Mar 15. doi: 10.3899/jrheum.180574).
On the other hand, Swedish investigators found that statin use wasn’t associated with a reduced risk of consultation or surgery for osteoarthritis in a pooled analysis of four cohort studies totaling more than 132,000 Swedes followed for 7.5 years (Osteoarthritis Cartilage. 2017 Nov;25[11]:1804-13).
Dr. Wei reported having no financial conflicts regarding the study, which was supported by the National Clinical Research Center of Geriatric Disorders in Hunan, China, and several British universities.
SOURCE: Sarmanova A et al. Osteoarthritis cartilage. 2019 Apr;27[suppl 1]:S78-S79. Abstract 77.
TORONTO – comparing nearly 180,000 statin users with an equal number of propensity-matched nonusers, Jie Wei, PhD, reported at the OARSI 2019 World Congress.
Less intensive statin therapy was associated with significantly less need for joint replacement surgery in rheumatoid arthritis patients, but not in those with osteoarthritis, she said at the meeting, sponsored by the Osteoarthritis Research Society International.
“In summary, statins may reduce the risk of joint replacement, especially when given at high strength and in people with rheumatoid arthritis,” said Dr. Wei, an epidemiologist at Massachusetts General Hospital, Boston, and Central South University in Changsha, Hunan, China.
She was quick to note that this study can’t be considered the final, definitive word on the topic, since other investigators’ studies of the relationship between statin usage and joint replacement surgery for arthritis have yielded conflicting results. However, given the thoroughly established super-favorable risk/benefit ratio of statins for the prevention of cardiovascular morbidity and mortality, the possibility of a prospective, randomized, controlled trial addressing the joint surgery issue is for ethical reasons a train that’s left the station.
Dr. Wei presented an analysis drawn from the U.K. Clinical Practice Research Datalink for the years 1989 through mid-2017. The initial sample included the medical records of 17.1 million patients, or 26% of the total U.K. population. From that massive pool, she and her coinvestigators zeroed in on 178,467 statin users and an equal number of non–statin-user controls under the care of 718 primary care physicians, with the pairs propensity score-matched on the basis of age, gender, locality, comorbid conditions, nonstatin medications, lifestyle factors, and duration of rheumatoid arthritis or osteoarthritis. The mean age of the matched pairs was 62 years, 52% were women, and the mean prospective follow-up was 6.5 years.
The use of high-intensity statin therapy – for example, atorvastatin at 40-80 mg/day or rosuvastatin (Crestor) at 20-40 mg/day – was independently associated with a 21% reduction in the risk of knee or hip replacement surgery for osteoarthritis and a 90% reduction for rheumatoid arthritis, compared with statin nonusers. Notably, joint replacement surgery for osteoarthritis was roughly 25-fold more common than for rheumatoid arthritis.
Statin therapy overall, including the more widely prescribed low- and intermediate-intensity regimens, was associated with a 23% reduction in joint replacement surgery for rheumatoid arthritis, compared with statin nonusers, but had no significant impact on surgery for the osteoarthritis population.
A couple of distinguished American rheumatologists in the audience rose to voice reluctance about drawing broad conclusions from this study.
“Bias, as you’ve said yourself, is a bit of a concern,” said David T. Felson, MD, professor of medicine and public health and director of clinical epidemiology at Boston University.
He was troubled that the study design was such that anyone who filled as few as two statin prescriptions during the more than 6-year study period was categorized as a statin user. That, he said, muddies the waters. Does the database contain information on duration of statin therapy, and whether joint replacement surgery was more likely to occur when patients were on or off statin therapy? he asked.
It does, Dr. Wei replied, adding that she will take that suggestion for additional analysis back to her international team of coinvestigators.
“It seems to me,” said Jeffrey N. Katz, MD, “that the major risk of potential bias is that people who were provided high-intensity statins were prescribed that because they were at risk for or had cardiac disease.”
That high cardiovascular risk might have curbed orthopedic surgeons’ enthusiasm to operate. Thus, it would be helpful to learn whether patients who underwent joint replacement were less likely to have undergone coronary revascularization or other cardiac interventions than were those without joint replacement, according to Dr. Katz, professor of medicine and orthopedic surgery at Harvard Medical School, Boston.
Dr. Wei agreed that confounding by indication is always a possibility in an observational study such as this. Identification of a plausible mechanism by which statins might reduce the risk of joint replacement surgery in rheumatoid arthritis – something that hasn’t happened yet – would help counter such concerns.
She noted that a separate recent analysis of the U.K. Clinical Practice Research Datalink by other investigators concluded that statin therapy started up to 5 years following total hip or knee replacement was associated with a significantly reduced risk of revision arthroplasty. Moreover, the benefit was treatment duration-dependent: Patients on statin therapy for more than 5 years were 26% less likely to undergo revision arthroplasty than were those on a statin for less than 1 year (J Rheumatol. 2019 Mar 15. doi: 10.3899/jrheum.180574).
On the other hand, Swedish investigators found that statin use wasn’t associated with a reduced risk of consultation or surgery for osteoarthritis in a pooled analysis of four cohort studies totaling more than 132,000 Swedes followed for 7.5 years (Osteoarthritis Cartilage. 2017 Nov;25[11]:1804-13).
Dr. Wei reported having no financial conflicts regarding the study, which was supported by the National Clinical Research Center of Geriatric Disorders in Hunan, China, and several British universities.
SOURCE: Sarmanova A et al. Osteoarthritis cartilage. 2019 Apr;27[suppl 1]:S78-S79. Abstract 77.
REPORTING FROM OARSI 2019
Key clinical point: High-intensity statin therapy may reduce need for joint replacement in arthritis.
Major finding: The risk of knee or hip replacement surgery for rheumatoid arthritis was slashed by 90%, and by 21% for osteoarthritis.
Study details: This study included nearly 180,000 statin users propensity score-matched to an equal number of nonusers and prospectively followed for a mean of 6.5 years.
Disclosures: The study was supported by the National Clinical Research Center of Geriatric Disorders at Central South University in Hunan, China, and by several British universities. The presenter reported having no financial conflicts of interest.
Source: Sarmanova A et al. Osteoarthritis Cartilage. 2019 Apr;27[suppl 1]:S78-S79. Abstract 77.
Restricting opioids after knee surgery did not increase refills
according to a study in the Journal of Arthroplasty.
Contrary to concerns that restrictive opioid prescribing might increase the number of patient call-ins and refill requests, one academic institution had significantly fewer call-ins and refills after it implemented a strict postoperative opioid prescribing protocol on Jan. 1, 2018.
“Orthopedic surgeons might be reluctant to change practice without evidence that new, more-restrictive practice will not impede patient care,” the researchers wrote. “As the current study demonstrates, there is room to significantly decrease postoperative opioid prescriptions in total joint arthroplasty. This places patients at lower risk of opioid abuse and diversion without significantly altering the risk of postoperative complications or compromising postoperative pain control.”
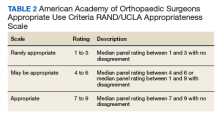
Opioid overuse is a major public health concern, and orthopedic surgeons may overprescribe opioids after surgery. The University of Iowa Hospitals and Clinics in Iowa City implemented strict postoperative opioid prescription guidelines that are based on the American Academy of Orthopedic Surgeons Clinical Practice Guidelines. As part of the protocol, patients receive a preoperative education session that emphasizes risks associated with opioid use. Before initiating this protocol, postoperative drug choice and quantity had not been standardized.
To examine changes in opioid prescriptions and the number of call-ins, postoperative complications, and prescription refill requests after the implementation of the restrictive opioid prescribing protocol, investigators at the institution conducted a retrospective study.
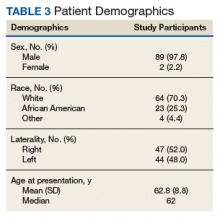
Andrew J. Holte, a researcher in the department of orthopedics and rehabilitation, and his colleagues reviewed cases from June 2017 to February 2018. Their analysis included 399 patients who underwent total hip arthroplasty or total knee arthroplasty.
In all, 282 patients underwent surgery before the restrictive protocol (the historical cohort) and 117 after (the restrictive cohort). In the historical cohort, about 48% of the patients underwent total knee arthroplasty. In the restrictive cohort, about 44% underwent total knee arthroplasty. Patients had an average age of about 61 years, and approximately 52% were women.
According to comparisons of morphine mg equivalents (MME), the historical cohort received significantly larger mean initial opioid prescriptions (752 MME vs. 387 MME), significantly more refills per patient (0.5 vs. 0.3), and significantly more medication through refills (253 MME vs. 84 MME).
“For reference, 50 pills of 5 mg oxycodone is equivalent to 300 MMEs,” the authors noted.
A multivariable model found that younger age and total knee arthroplasty, compared with total hip arthroplasty, were associated with increased likelihood of requests for refills and patient call-ins.
“Surprisingly, there were significantly more patient call-ins and requests for refills of opioids in the historical cohort,” Mr. Holte and his colleagues said. “Although this study did not collect direct data on patient pain scores, we believe that call-ins and requests for refills are sufficient surrogate markers for inadequate pain control.”
The study does not account for prescriptions from other providers or whether patients took none, some, or all of their filled prescriptions. Future studies are needed to assess how reduced opioid prescriptions affect pain and functional outcomes in the long term, the researchers said.
One or more study authors disclosed potential conflicts of interest. The disclosures can be found in Appendix A, Supplementary Data, at the end of the journal article.
SOURCE: Holte AJ et al. J Arthroplasty. 2019 Feb 20. doi: 10.1016/j.arth.2019.02.022.
according to a study in the Journal of Arthroplasty.
Contrary to concerns that restrictive opioid prescribing might increase the number of patient call-ins and refill requests, one academic institution had significantly fewer call-ins and refills after it implemented a strict postoperative opioid prescribing protocol on Jan. 1, 2018.
“Orthopedic surgeons might be reluctant to change practice without evidence that new, more-restrictive practice will not impede patient care,” the researchers wrote. “As the current study demonstrates, there is room to significantly decrease postoperative opioid prescriptions in total joint arthroplasty. This places patients at lower risk of opioid abuse and diversion without significantly altering the risk of postoperative complications or compromising postoperative pain control.”
Opioid overuse is a major public health concern, and orthopedic surgeons may overprescribe opioids after surgery. The University of Iowa Hospitals and Clinics in Iowa City implemented strict postoperative opioid prescription guidelines that are based on the American Academy of Orthopedic Surgeons Clinical Practice Guidelines. As part of the protocol, patients receive a preoperative education session that emphasizes risks associated with opioid use. Before initiating this protocol, postoperative drug choice and quantity had not been standardized.
To examine changes in opioid prescriptions and the number of call-ins, postoperative complications, and prescription refill requests after the implementation of the restrictive opioid prescribing protocol, investigators at the institution conducted a retrospective study.
Andrew J. Holte, a researcher in the department of orthopedics and rehabilitation, and his colleagues reviewed cases from June 2017 to February 2018. Their analysis included 399 patients who underwent total hip arthroplasty or total knee arthroplasty.
In all, 282 patients underwent surgery before the restrictive protocol (the historical cohort) and 117 after (the restrictive cohort). In the historical cohort, about 48% of the patients underwent total knee arthroplasty. In the restrictive cohort, about 44% underwent total knee arthroplasty. Patients had an average age of about 61 years, and approximately 52% were women.
According to comparisons of morphine mg equivalents (MME), the historical cohort received significantly larger mean initial opioid prescriptions (752 MME vs. 387 MME), significantly more refills per patient (0.5 vs. 0.3), and significantly more medication through refills (253 MME vs. 84 MME).
“For reference, 50 pills of 5 mg oxycodone is equivalent to 300 MMEs,” the authors noted.
A multivariable model found that younger age and total knee arthroplasty, compared with total hip arthroplasty, were associated with increased likelihood of requests for refills and patient call-ins.
“Surprisingly, there were significantly more patient call-ins and requests for refills of opioids in the historical cohort,” Mr. Holte and his colleagues said. “Although this study did not collect direct data on patient pain scores, we believe that call-ins and requests for refills are sufficient surrogate markers for inadequate pain control.”
The study does not account for prescriptions from other providers or whether patients took none, some, or all of their filled prescriptions. Future studies are needed to assess how reduced opioid prescriptions affect pain and functional outcomes in the long term, the researchers said.
One or more study authors disclosed potential conflicts of interest. The disclosures can be found in Appendix A, Supplementary Data, at the end of the journal article.
SOURCE: Holte AJ et al. J Arthroplasty. 2019 Feb 20. doi: 10.1016/j.arth.2019.02.022.
according to a study in the Journal of Arthroplasty.
Contrary to concerns that restrictive opioid prescribing might increase the number of patient call-ins and refill requests, one academic institution had significantly fewer call-ins and refills after it implemented a strict postoperative opioid prescribing protocol on Jan. 1, 2018.
“Orthopedic surgeons might be reluctant to change practice without evidence that new, more-restrictive practice will not impede patient care,” the researchers wrote. “As the current study demonstrates, there is room to significantly decrease postoperative opioid prescriptions in total joint arthroplasty. This places patients at lower risk of opioid abuse and diversion without significantly altering the risk of postoperative complications or compromising postoperative pain control.”
Opioid overuse is a major public health concern, and orthopedic surgeons may overprescribe opioids after surgery. The University of Iowa Hospitals and Clinics in Iowa City implemented strict postoperative opioid prescription guidelines that are based on the American Academy of Orthopedic Surgeons Clinical Practice Guidelines. As part of the protocol, patients receive a preoperative education session that emphasizes risks associated with opioid use. Before initiating this protocol, postoperative drug choice and quantity had not been standardized.
To examine changes in opioid prescriptions and the number of call-ins, postoperative complications, and prescription refill requests after the implementation of the restrictive opioid prescribing protocol, investigators at the institution conducted a retrospective study.
Andrew J. Holte, a researcher in the department of orthopedics and rehabilitation, and his colleagues reviewed cases from June 2017 to February 2018. Their analysis included 399 patients who underwent total hip arthroplasty or total knee arthroplasty.
In all, 282 patients underwent surgery before the restrictive protocol (the historical cohort) and 117 after (the restrictive cohort). In the historical cohort, about 48% of the patients underwent total knee arthroplasty. In the restrictive cohort, about 44% underwent total knee arthroplasty. Patients had an average age of about 61 years, and approximately 52% were women.
According to comparisons of morphine mg equivalents (MME), the historical cohort received significantly larger mean initial opioid prescriptions (752 MME vs. 387 MME), significantly more refills per patient (0.5 vs. 0.3), and significantly more medication through refills (253 MME vs. 84 MME).
“For reference, 50 pills of 5 mg oxycodone is equivalent to 300 MMEs,” the authors noted.
A multivariable model found that younger age and total knee arthroplasty, compared with total hip arthroplasty, were associated with increased likelihood of requests for refills and patient call-ins.
“Surprisingly, there were significantly more patient call-ins and requests for refills of opioids in the historical cohort,” Mr. Holte and his colleagues said. “Although this study did not collect direct data on patient pain scores, we believe that call-ins and requests for refills are sufficient surrogate markers for inadequate pain control.”
The study does not account for prescriptions from other providers or whether patients took none, some, or all of their filled prescriptions. Future studies are needed to assess how reduced opioid prescriptions affect pain and functional outcomes in the long term, the researchers said.
One or more study authors disclosed potential conflicts of interest. The disclosures can be found in Appendix A, Supplementary Data, at the end of the journal article.
SOURCE: Holte AJ et al. J Arthroplasty. 2019 Feb 20. doi: 10.1016/j.arth.2019.02.022.
FROM THE JOURNAL OF ARTHROPLASTY
Platelet-rich plasma shows promise in hemophilic arthropathy of the knee
A single intra-articular injection of platelet-rich plasma showed better pain and function scores at 6 months than did weekly injections of hyaluronic acid in patients with hemophilic arthropathy of the knee.
“In patients with chronic knee joint pain, our study shows that treatment with intra-articular [platelet-rich plasma] injection could reduce pain, improve hyperaemia and enhance knee joint function,” wrote Tsung-Ying Li, MD, of Tri-Service General Hospital in Taipei, Taiwan, and his colleagues. The results of the comparison study were published in Haemophilia.
Researchers conducted a nonrandomized, single-center, open-label comparison study of 22 patients with hemophilia A who had chronic hemophilic arthropathy of the knee. Patients were stratified into two treatment groups using a matched sampling method.
“Patients who could commit to hyaluronic acid treatment were allocated to the hyaluronic acid group, otherwise patients were allocated to the platelet‐rich plasma group,” the researchers wrote.
Participants in the hyaluronic acid arm were given five sequential weekly injections and those in the platelet-rich plasma arm received only a single injection. Outcomes were measured via the visual analogue scale (VAS), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Chinese Version, and ultrasonography to determine synovial change.
Pain and function scores were significantly lower in patients administered intra-articular platelet-rich plasma versus hyaluronic acid at 6 months (P less than .05), the researchers reported. However, comparative analysis found no significant differences at earlier follow-up time points.
“Both treatments were found to be effective in reducing pain and improving functional status of the knee,” the researchers wrote.
They acknowledged a key limitation of the study was the short duration of follow-up, which was due to budget restrictions at the treatment facility.
“Further investigation using rigorous research methodology is warranted to establish the benefit of [platelet-rich plasma] on hemophilic arthropathy and standardized [platelet-rich plasma] preparation and dosing regimens,” they wrote.
The study was supported by grant funding from Tri-Service General Hospital in Taiwan. Three of the authors reported receiving research grants from Shire.
SOURCE: Li TY et al. Haemophilia. 2019 Mar 13. doi: 10.1111/hae.13711.
A single intra-articular injection of platelet-rich plasma showed better pain and function scores at 6 months than did weekly injections of hyaluronic acid in patients with hemophilic arthropathy of the knee.
“In patients with chronic knee joint pain, our study shows that treatment with intra-articular [platelet-rich plasma] injection could reduce pain, improve hyperaemia and enhance knee joint function,” wrote Tsung-Ying Li, MD, of Tri-Service General Hospital in Taipei, Taiwan, and his colleagues. The results of the comparison study were published in Haemophilia.
Researchers conducted a nonrandomized, single-center, open-label comparison study of 22 patients with hemophilia A who had chronic hemophilic arthropathy of the knee. Patients were stratified into two treatment groups using a matched sampling method.
“Patients who could commit to hyaluronic acid treatment were allocated to the hyaluronic acid group, otherwise patients were allocated to the platelet‐rich plasma group,” the researchers wrote.
Participants in the hyaluronic acid arm were given five sequential weekly injections and those in the platelet-rich plasma arm received only a single injection. Outcomes were measured via the visual analogue scale (VAS), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Chinese Version, and ultrasonography to determine synovial change.
Pain and function scores were significantly lower in patients administered intra-articular platelet-rich plasma versus hyaluronic acid at 6 months (P less than .05), the researchers reported. However, comparative analysis found no significant differences at earlier follow-up time points.
“Both treatments were found to be effective in reducing pain and improving functional status of the knee,” the researchers wrote.
They acknowledged a key limitation of the study was the short duration of follow-up, which was due to budget restrictions at the treatment facility.
“Further investigation using rigorous research methodology is warranted to establish the benefit of [platelet-rich plasma] on hemophilic arthropathy and standardized [platelet-rich plasma] preparation and dosing regimens,” they wrote.
The study was supported by grant funding from Tri-Service General Hospital in Taiwan. Three of the authors reported receiving research grants from Shire.
SOURCE: Li TY et al. Haemophilia. 2019 Mar 13. doi: 10.1111/hae.13711.
A single intra-articular injection of platelet-rich plasma showed better pain and function scores at 6 months than did weekly injections of hyaluronic acid in patients with hemophilic arthropathy of the knee.
“In patients with chronic knee joint pain, our study shows that treatment with intra-articular [platelet-rich plasma] injection could reduce pain, improve hyperaemia and enhance knee joint function,” wrote Tsung-Ying Li, MD, of Tri-Service General Hospital in Taipei, Taiwan, and his colleagues. The results of the comparison study were published in Haemophilia.
Researchers conducted a nonrandomized, single-center, open-label comparison study of 22 patients with hemophilia A who had chronic hemophilic arthropathy of the knee. Patients were stratified into two treatment groups using a matched sampling method.
“Patients who could commit to hyaluronic acid treatment were allocated to the hyaluronic acid group, otherwise patients were allocated to the platelet‐rich plasma group,” the researchers wrote.
Participants in the hyaluronic acid arm were given five sequential weekly injections and those in the platelet-rich plasma arm received only a single injection. Outcomes were measured via the visual analogue scale (VAS), the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) Chinese Version, and ultrasonography to determine synovial change.
Pain and function scores were significantly lower in patients administered intra-articular platelet-rich plasma versus hyaluronic acid at 6 months (P less than .05), the researchers reported. However, comparative analysis found no significant differences at earlier follow-up time points.
“Both treatments were found to be effective in reducing pain and improving functional status of the knee,” the researchers wrote.
They acknowledged a key limitation of the study was the short duration of follow-up, which was due to budget restrictions at the treatment facility.
“Further investigation using rigorous research methodology is warranted to establish the benefit of [platelet-rich plasma] on hemophilic arthropathy and standardized [platelet-rich plasma] preparation and dosing regimens,” they wrote.
The study was supported by grant funding from Tri-Service General Hospital in Taiwan. Three of the authors reported receiving research grants from Shire.
SOURCE: Li TY et al. Haemophilia. 2019 Mar 13. doi: 10.1111/hae.13711.
FROM HAEMOPHILIA
Four biomarkers could distinguish psoriatic arthritis from osteoarthritis
A panel of four biomarkers of cartilage metabolism, metabolic syndrome, and inflammation could help physicians to distinguish between osteoarthritis and psoriatic arthritis, new research suggests.
Such a test for distinguishing between the two conditions, which have “similarities in the distribution of joints involved,” could offer a way to make earlier diagnoses and avoid inappropriate treatment, according to Vinod Chandran, MD, PhD, of the department of medicine at the University of Toronto and Toronto Western Hospital and his colleagues. Dr. Chandran was first author on a study published online in Annals of the Rheumatic Diseases that analyzed serum samples from the University of Toronto Psoriatic Arthritis Program and University Health Network Arthritis Program for differences in certain biomarkers from 201 individuals with osteoarthritis, 77 with psoriatic arthritis, and 76 healthy controls.
The samples were tested for 15 biomarkers, including those related to cartilage metabolism (cartilage oligomeric matrix protein and hyaluronan), to metabolic syndrome (adiponectin, adipsin, resistin, hepatocyte growth factor, insulin, and leptin), and to inflammation (C-reactive protein, interleukin-1-beta, interleukin-6, interleukin-8, tumor necrosis factor alpha, monocyte chemoattractant protein–1, and nerve growth factor).
Researchers found that levels of 12 of these markers were different in patients with psoriatic arthritis, osteoarthritis, or controls, and 9 markers showed altered expression in psoriatic arthritis, compared with osteoarthritis.
Further analysis showed that levels of cartilage oligomeric matrix protein, resistin, monocyte chemoattractant protein–1, and nerve growth factor were significantly different between patients with psoriatic arthritis and those with osteoarthritis. The ROC curve for a model based on these four biomarkers that also incorporated age and sex had an area under the curve of 0.9984.
Researchers then validated the four biomarkers in an independent set of 75 patients with osteoarthritis and 73 with psoriatic arthritis and found these biomarkers were able to discriminate between the two conditions beyond what would be achieved based on age and sex alone.
The authors noted that previous research has observed high expression of monocyte chemoattractant protein–1 and resistin in patients with psoriatic arthritis when compared with those with osteoarthritis.
Nerve growth factor has been seen at elevated levels in the synovial fluid of individuals with osteoarthritis and is known to play a role in the chronic pain associated with that disease.
Similarly, higher cartilage oligomeric matrix protein levels are associated with a higher risk of knee osteoarthritis.
However, the authors noted that individuals with osteoarthritis in the study were all undergoing joint replacement surgery and therefore may not be typical of patients presenting to family practices or rheumatology clinics.
The University of Toronto Psoriatic Arthritis Program is supported by the Krembil Foundation. No conflicts of interest were declared.
SOURCE: Chandran V et al. Ann Rheum Dis. 2019 Mar 25. doi: 10.1136/annrheumdis-2018-214737.
A panel of four biomarkers of cartilage metabolism, metabolic syndrome, and inflammation could help physicians to distinguish between osteoarthritis and psoriatic arthritis, new research suggests.
Such a test for distinguishing between the two conditions, which have “similarities in the distribution of joints involved,” could offer a way to make earlier diagnoses and avoid inappropriate treatment, according to Vinod Chandran, MD, PhD, of the department of medicine at the University of Toronto and Toronto Western Hospital and his colleagues. Dr. Chandran was first author on a study published online in Annals of the Rheumatic Diseases that analyzed serum samples from the University of Toronto Psoriatic Arthritis Program and University Health Network Arthritis Program for differences in certain biomarkers from 201 individuals with osteoarthritis, 77 with psoriatic arthritis, and 76 healthy controls.
The samples were tested for 15 biomarkers, including those related to cartilage metabolism (cartilage oligomeric matrix protein and hyaluronan), to metabolic syndrome (adiponectin, adipsin, resistin, hepatocyte growth factor, insulin, and leptin), and to inflammation (C-reactive protein, interleukin-1-beta, interleukin-6, interleukin-8, tumor necrosis factor alpha, monocyte chemoattractant protein–1, and nerve growth factor).
Researchers found that levels of 12 of these markers were different in patients with psoriatic arthritis, osteoarthritis, or controls, and 9 markers showed altered expression in psoriatic arthritis, compared with osteoarthritis.
Further analysis showed that levels of cartilage oligomeric matrix protein, resistin, monocyte chemoattractant protein–1, and nerve growth factor were significantly different between patients with psoriatic arthritis and those with osteoarthritis. The ROC curve for a model based on these four biomarkers that also incorporated age and sex had an area under the curve of 0.9984.
Researchers then validated the four biomarkers in an independent set of 75 patients with osteoarthritis and 73 with psoriatic arthritis and found these biomarkers were able to discriminate between the two conditions beyond what would be achieved based on age and sex alone.
The authors noted that previous research has observed high expression of monocyte chemoattractant protein–1 and resistin in patients with psoriatic arthritis when compared with those with osteoarthritis.
Nerve growth factor has been seen at elevated levels in the synovial fluid of individuals with osteoarthritis and is known to play a role in the chronic pain associated with that disease.
Similarly, higher cartilage oligomeric matrix protein levels are associated with a higher risk of knee osteoarthritis.
However, the authors noted that individuals with osteoarthritis in the study were all undergoing joint replacement surgery and therefore may not be typical of patients presenting to family practices or rheumatology clinics.
The University of Toronto Psoriatic Arthritis Program is supported by the Krembil Foundation. No conflicts of interest were declared.
SOURCE: Chandran V et al. Ann Rheum Dis. 2019 Mar 25. doi: 10.1136/annrheumdis-2018-214737.
A panel of four biomarkers of cartilage metabolism, metabolic syndrome, and inflammation could help physicians to distinguish between osteoarthritis and psoriatic arthritis, new research suggests.
Such a test for distinguishing between the two conditions, which have “similarities in the distribution of joints involved,” could offer a way to make earlier diagnoses and avoid inappropriate treatment, according to Vinod Chandran, MD, PhD, of the department of medicine at the University of Toronto and Toronto Western Hospital and his colleagues. Dr. Chandran was first author on a study published online in Annals of the Rheumatic Diseases that analyzed serum samples from the University of Toronto Psoriatic Arthritis Program and University Health Network Arthritis Program for differences in certain biomarkers from 201 individuals with osteoarthritis, 77 with psoriatic arthritis, and 76 healthy controls.
The samples were tested for 15 biomarkers, including those related to cartilage metabolism (cartilage oligomeric matrix protein and hyaluronan), to metabolic syndrome (adiponectin, adipsin, resistin, hepatocyte growth factor, insulin, and leptin), and to inflammation (C-reactive protein, interleukin-1-beta, interleukin-6, interleukin-8, tumor necrosis factor alpha, monocyte chemoattractant protein–1, and nerve growth factor).
Researchers found that levels of 12 of these markers were different in patients with psoriatic arthritis, osteoarthritis, or controls, and 9 markers showed altered expression in psoriatic arthritis, compared with osteoarthritis.
Further analysis showed that levels of cartilage oligomeric matrix protein, resistin, monocyte chemoattractant protein–1, and nerve growth factor were significantly different between patients with psoriatic arthritis and those with osteoarthritis. The ROC curve for a model based on these four biomarkers that also incorporated age and sex had an area under the curve of 0.9984.
Researchers then validated the four biomarkers in an independent set of 75 patients with osteoarthritis and 73 with psoriatic arthritis and found these biomarkers were able to discriminate between the two conditions beyond what would be achieved based on age and sex alone.
The authors noted that previous research has observed high expression of monocyte chemoattractant protein–1 and resistin in patients with psoriatic arthritis when compared with those with osteoarthritis.
Nerve growth factor has been seen at elevated levels in the synovial fluid of individuals with osteoarthritis and is known to play a role in the chronic pain associated with that disease.
Similarly, higher cartilage oligomeric matrix protein levels are associated with a higher risk of knee osteoarthritis.
However, the authors noted that individuals with osteoarthritis in the study were all undergoing joint replacement surgery and therefore may not be typical of patients presenting to family practices or rheumatology clinics.
The University of Toronto Psoriatic Arthritis Program is supported by the Krembil Foundation. No conflicts of interest were declared.
SOURCE: Chandran V et al. Ann Rheum Dis. 2019 Mar 25. doi: 10.1136/annrheumdis-2018-214737.
FROM ANNALS OF THE RHEUMATIC DISEASES
Bariatric surgery may be appropriate for class 1 obesity
LAS VEGAS – Once reserved for the most obese patients, bariatric surgery is on the road to becoming an option for millions of Americans who are just a step beyond overweight, even those with a body mass index as low as 30 kg/m2.
In regard to patients with lower levels of obesity, “we should be intervening in this chronic disease earlier rather than later,” said Stacy A. Brethauer, MD, professor of surgery at the Ohio State University, Columbus, in a presentation about new standards for bariatric surgery at the 2019 Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education.
Bariatric treatment “should be offered after nonsurgical [weight-loss] therapy has failed,” he said. “That’s not where you stop. You continue to escalate as you would for heart disease or cancer.”
As Dr. Brethauer noted, research suggests that all categories of obesity – including so-called class 1 obesity (defined as a BMI from 30.0 to 34.9 kg/m2) – boost the risk of multiple diseases, including hypertension, coronary artery disease, congestive heart failure, stroke, asthma, pulmonary embolism, gallbladder disease, several types of cancer, osteoarthritis, knee pain and chronic back pain.
“There is no question that class 1 obesity is clearly putting people at risk,” he said. “Ultimately, you can conclude from all this evidence that class 1 is a chronic disease, and it deserves to be treated effectively.”
There are, of course, various nonsurgical treatments for obesity, including diet and exercise and pharmacotherapy. However, systematic reviews have found that people find it extremely difficult to keep the weight off after 1 year regardless of the strategy they adopt.
Beyond a year, Dr. Brethauer said, “you get poor maintenance of weight control, and you get poor control of metabolic burden. You don’t have a durable efficacy.”
In the past, bariatric surgery wasn’t considered an option for patients with class 1 obesity. It’s traditionally been reserved for patients with BMIs at or above 35 kg/m2. But this standard has evolved in recent years.
In 2018, Dr. Brethauer coauthored an updated position statement by the American Society for Metabolic and Bariatric Surgery that encouraged bariatric surgery in certain mildly obese patients.
“For most people with class I obesity,” the statement on bariatric surgery states, “it is clear that the nonsurgical group of therapies will not provide a durable solution to their disease of obesity.”
The statement went on to say that “surgical intervention should be considered after failure of nonsurgical treatments” in the class 1 population.
Bariatric surgery in the class 1 population does more than reduce obesity, Dr. Brethauer said. “Over the last 5 years or so, a large body of literature has emerged,” he said, and both systematic reviews and randomized trails have shown significant postsurgery improvements in comorbidities such as diabetes.
“It’s important to emphasize that these patients don’t become underweight,” he said. “The body finds a healthy set point. They don’t become underweight or malnourished because you’re operating on a lower-weight group.”
Are weight-loss operations safe in class 1 patients? The American Society for Metabolic and Bariatric Surgery statement says that research has found “bariatric surgery is associated with modest morbidity and very low mortality in patients with class I obesity.”
In fact, Dr. Brethauer said, the mortality rate in this population is “less than gallbladder surgery, less than hip surgery, less than hysterectomy, less than knee surgery – operations people are being referred for and undergoing all the time.”
He added: “The case can be made very clearly based on this data that these operations are safe in this patient population. Not only are they safe, they have durable and significant impact on comorbidities.”
Global Academy for Medical Education and this news organization are owned by the same parent company. Dr. Brethauer discloses relationships with Medtronic (speaker) and GI Windows (consultant).
LAS VEGAS – Once reserved for the most obese patients, bariatric surgery is on the road to becoming an option for millions of Americans who are just a step beyond overweight, even those with a body mass index as low as 30 kg/m2.
In regard to patients with lower levels of obesity, “we should be intervening in this chronic disease earlier rather than later,” said Stacy A. Brethauer, MD, professor of surgery at the Ohio State University, Columbus, in a presentation about new standards for bariatric surgery at the 2019 Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education.
Bariatric treatment “should be offered after nonsurgical [weight-loss] therapy has failed,” he said. “That’s not where you stop. You continue to escalate as you would for heart disease or cancer.”
As Dr. Brethauer noted, research suggests that all categories of obesity – including so-called class 1 obesity (defined as a BMI from 30.0 to 34.9 kg/m2) – boost the risk of multiple diseases, including hypertension, coronary artery disease, congestive heart failure, stroke, asthma, pulmonary embolism, gallbladder disease, several types of cancer, osteoarthritis, knee pain and chronic back pain.
“There is no question that class 1 obesity is clearly putting people at risk,” he said. “Ultimately, you can conclude from all this evidence that class 1 is a chronic disease, and it deserves to be treated effectively.”
There are, of course, various nonsurgical treatments for obesity, including diet and exercise and pharmacotherapy. However, systematic reviews have found that people find it extremely difficult to keep the weight off after 1 year regardless of the strategy they adopt.
Beyond a year, Dr. Brethauer said, “you get poor maintenance of weight control, and you get poor control of metabolic burden. You don’t have a durable efficacy.”
In the past, bariatric surgery wasn’t considered an option for patients with class 1 obesity. It’s traditionally been reserved for patients with BMIs at or above 35 kg/m2. But this standard has evolved in recent years.
In 2018, Dr. Brethauer coauthored an updated position statement by the American Society for Metabolic and Bariatric Surgery that encouraged bariatric surgery in certain mildly obese patients.
“For most people with class I obesity,” the statement on bariatric surgery states, “it is clear that the nonsurgical group of therapies will not provide a durable solution to their disease of obesity.”
The statement went on to say that “surgical intervention should be considered after failure of nonsurgical treatments” in the class 1 population.
Bariatric surgery in the class 1 population does more than reduce obesity, Dr. Brethauer said. “Over the last 5 years or so, a large body of literature has emerged,” he said, and both systematic reviews and randomized trails have shown significant postsurgery improvements in comorbidities such as diabetes.
“It’s important to emphasize that these patients don’t become underweight,” he said. “The body finds a healthy set point. They don’t become underweight or malnourished because you’re operating on a lower-weight group.”
Are weight-loss operations safe in class 1 patients? The American Society for Metabolic and Bariatric Surgery statement says that research has found “bariatric surgery is associated with modest morbidity and very low mortality in patients with class I obesity.”
In fact, Dr. Brethauer said, the mortality rate in this population is “less than gallbladder surgery, less than hip surgery, less than hysterectomy, less than knee surgery – operations people are being referred for and undergoing all the time.”
He added: “The case can be made very clearly based on this data that these operations are safe in this patient population. Not only are they safe, they have durable and significant impact on comorbidities.”
Global Academy for Medical Education and this news organization are owned by the same parent company. Dr. Brethauer discloses relationships with Medtronic (speaker) and GI Windows (consultant).
LAS VEGAS – Once reserved for the most obese patients, bariatric surgery is on the road to becoming an option for millions of Americans who are just a step beyond overweight, even those with a body mass index as low as 30 kg/m2.
In regard to patients with lower levels of obesity, “we should be intervening in this chronic disease earlier rather than later,” said Stacy A. Brethauer, MD, professor of surgery at the Ohio State University, Columbus, in a presentation about new standards for bariatric surgery at the 2019 Annual Minimally Invasive Surgery Symposium by Global Academy for Medical Education.
Bariatric treatment “should be offered after nonsurgical [weight-loss] therapy has failed,” he said. “That’s not where you stop. You continue to escalate as you would for heart disease or cancer.”
As Dr. Brethauer noted, research suggests that all categories of obesity – including so-called class 1 obesity (defined as a BMI from 30.0 to 34.9 kg/m2) – boost the risk of multiple diseases, including hypertension, coronary artery disease, congestive heart failure, stroke, asthma, pulmonary embolism, gallbladder disease, several types of cancer, osteoarthritis, knee pain and chronic back pain.
“There is no question that class 1 obesity is clearly putting people at risk,” he said. “Ultimately, you can conclude from all this evidence that class 1 is a chronic disease, and it deserves to be treated effectively.”
There are, of course, various nonsurgical treatments for obesity, including diet and exercise and pharmacotherapy. However, systematic reviews have found that people find it extremely difficult to keep the weight off after 1 year regardless of the strategy they adopt.
Beyond a year, Dr. Brethauer said, “you get poor maintenance of weight control, and you get poor control of metabolic burden. You don’t have a durable efficacy.”
In the past, bariatric surgery wasn’t considered an option for patients with class 1 obesity. It’s traditionally been reserved for patients with BMIs at or above 35 kg/m2. But this standard has evolved in recent years.
In 2018, Dr. Brethauer coauthored an updated position statement by the American Society for Metabolic and Bariatric Surgery that encouraged bariatric surgery in certain mildly obese patients.
“For most people with class I obesity,” the statement on bariatric surgery states, “it is clear that the nonsurgical group of therapies will not provide a durable solution to their disease of obesity.”
The statement went on to say that “surgical intervention should be considered after failure of nonsurgical treatments” in the class 1 population.
Bariatric surgery in the class 1 population does more than reduce obesity, Dr. Brethauer said. “Over the last 5 years or so, a large body of literature has emerged,” he said, and both systematic reviews and randomized trails have shown significant postsurgery improvements in comorbidities such as diabetes.
“It’s important to emphasize that these patients don’t become underweight,” he said. “The body finds a healthy set point. They don’t become underweight or malnourished because you’re operating on a lower-weight group.”
Are weight-loss operations safe in class 1 patients? The American Society for Metabolic and Bariatric Surgery statement says that research has found “bariatric surgery is associated with modest morbidity and very low mortality in patients with class I obesity.”
In fact, Dr. Brethauer said, the mortality rate in this population is “less than gallbladder surgery, less than hip surgery, less than hysterectomy, less than knee surgery – operations people are being referred for and undergoing all the time.”
He added: “The case can be made very clearly based on this data that these operations are safe in this patient population. Not only are they safe, they have durable and significant impact on comorbidities.”
Global Academy for Medical Education and this news organization are owned by the same parent company. Dr. Brethauer discloses relationships with Medtronic (speaker) and GI Windows (consultant).
REPORTING FROM MISS
Possible mortality risk seen with tramadol in osteoarthritis
Tramadol appears to be associated with higher mortality risk among older patients with osteoarthritis when compared against common NSAIDs, according to findings from a study published online March 12 in JAMA.
The findings from the retrospective cohort study are worth noting despite their susceptibility to confounding by indication because “tramadol is a weak opioid agonist and has been considered a potential alternative to NSAIDs and traditional opioids because of its assumed relatively lower risk of serious cardiovascular and gastrointestinal adverse effects than NSAIDs, as well as a lower risk of addiction and respiratory depression compared with other opioids,” wrote Chao Zeng, MD, PhD, of Xiangya Hospital of Central South University, Changsha, China, and his coauthors.
The investigators analyzed data from a combined total of 88,902 individuals aged 50 years and older with knee, hip, or hand osteoarthritis who were seen during 2000-2015 and had visits recorded in the United Kingdom’s The Health Improvement Network (THIN) electronic medical records database. Participants were matched on sociodemographic and lifestyle factors, as well as osteoarthritis duration, comorbidities, other prescriptions, and health care utilization prior to the index date of the study.
Over 1 year of follow-up, researchers saw a 71% higher risk of all-cause mortality in patients taking tramadol than that in seen in those taking naproxen, 88% higher than in those taking diclofenac, 70% higher than in those taking celecoxib, and about twice as high as in patients taking etoricoxib.
However, there was no significant difference in risk of all-cause mortality between tramadol and codeine, the researchers found.
The authors suggested that tramadol may have adverse effects on the neurologic system by inhibiting central serotonin and norepinephrine uptake, which could potentially lead to serotonin syndrome. They also speculated that it could increase the risk of postoperative delirium, cause fatal poisoning or respiratory depression if taken in conjunction with alcohol or other drugs, or increase the risk of hypoglycemia, hyponatremia, fractures, or falls.
The numbers of deaths from cardiovascular, gastrointestinal, infection, cancer, and respiratory diseases were all higher in the tramadol group, compared with patients taking NSAIDs, but the differences were not statistically significant because of the relatively small number of deaths, the authors said.
Overall, 44,451 patients were taking tramadol, 12,397 were taking naproxen, 6,512 were taking diclofenac, 5,674 were taking celecoxib, 2,946 were taking etoricoxib, and 16,922 were taking codeine.
Patients in the tramadol cohort were generally older, with higher body mass index, a longer duration of osteoarthritis, and had a higher prevalence of comorbidities, higher health care utilization, and more prescriptions of other medications.
The authors noted that, while the patients from each medication cohort were matched on propensity score, the results were still susceptible to confounding by indication and should be interpreted with caution.
The study was supported by grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Natural Science Foundation of China. One author declared funding from the National Institute on Drug Abuse during the conduct of the study and grants from Optum Labs outside the study. No other conflicts of interest were declared.
SOURCE: Zeng C et al. JAMA. 2019;321:969-82.
Tramadol appears to be associated with higher mortality risk among older patients with osteoarthritis when compared against common NSAIDs, according to findings from a study published online March 12 in JAMA.
The findings from the retrospective cohort study are worth noting despite their susceptibility to confounding by indication because “tramadol is a weak opioid agonist and has been considered a potential alternative to NSAIDs and traditional opioids because of its assumed relatively lower risk of serious cardiovascular and gastrointestinal adverse effects than NSAIDs, as well as a lower risk of addiction and respiratory depression compared with other opioids,” wrote Chao Zeng, MD, PhD, of Xiangya Hospital of Central South University, Changsha, China, and his coauthors.
The investigators analyzed data from a combined total of 88,902 individuals aged 50 years and older with knee, hip, or hand osteoarthritis who were seen during 2000-2015 and had visits recorded in the United Kingdom’s The Health Improvement Network (THIN) electronic medical records database. Participants were matched on sociodemographic and lifestyle factors, as well as osteoarthritis duration, comorbidities, other prescriptions, and health care utilization prior to the index date of the study.
Over 1 year of follow-up, researchers saw a 71% higher risk of all-cause mortality in patients taking tramadol than that in seen in those taking naproxen, 88% higher than in those taking diclofenac, 70% higher than in those taking celecoxib, and about twice as high as in patients taking etoricoxib.
However, there was no significant difference in risk of all-cause mortality between tramadol and codeine, the researchers found.
The authors suggested that tramadol may have adverse effects on the neurologic system by inhibiting central serotonin and norepinephrine uptake, which could potentially lead to serotonin syndrome. They also speculated that it could increase the risk of postoperative delirium, cause fatal poisoning or respiratory depression if taken in conjunction with alcohol or other drugs, or increase the risk of hypoglycemia, hyponatremia, fractures, or falls.
The numbers of deaths from cardiovascular, gastrointestinal, infection, cancer, and respiratory diseases were all higher in the tramadol group, compared with patients taking NSAIDs, but the differences were not statistically significant because of the relatively small number of deaths, the authors said.
Overall, 44,451 patients were taking tramadol, 12,397 were taking naproxen, 6,512 were taking diclofenac, 5,674 were taking celecoxib, 2,946 were taking etoricoxib, and 16,922 were taking codeine.
Patients in the tramadol cohort were generally older, with higher body mass index, a longer duration of osteoarthritis, and had a higher prevalence of comorbidities, higher health care utilization, and more prescriptions of other medications.
The authors noted that, while the patients from each medication cohort were matched on propensity score, the results were still susceptible to confounding by indication and should be interpreted with caution.
The study was supported by grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Natural Science Foundation of China. One author declared funding from the National Institute on Drug Abuse during the conduct of the study and grants from Optum Labs outside the study. No other conflicts of interest were declared.
SOURCE: Zeng C et al. JAMA. 2019;321:969-82.
Tramadol appears to be associated with higher mortality risk among older patients with osteoarthritis when compared against common NSAIDs, according to findings from a study published online March 12 in JAMA.
The findings from the retrospective cohort study are worth noting despite their susceptibility to confounding by indication because “tramadol is a weak opioid agonist and has been considered a potential alternative to NSAIDs and traditional opioids because of its assumed relatively lower risk of serious cardiovascular and gastrointestinal adverse effects than NSAIDs, as well as a lower risk of addiction and respiratory depression compared with other opioids,” wrote Chao Zeng, MD, PhD, of Xiangya Hospital of Central South University, Changsha, China, and his coauthors.
The investigators analyzed data from a combined total of 88,902 individuals aged 50 years and older with knee, hip, or hand osteoarthritis who were seen during 2000-2015 and had visits recorded in the United Kingdom’s The Health Improvement Network (THIN) electronic medical records database. Participants were matched on sociodemographic and lifestyle factors, as well as osteoarthritis duration, comorbidities, other prescriptions, and health care utilization prior to the index date of the study.
Over 1 year of follow-up, researchers saw a 71% higher risk of all-cause mortality in patients taking tramadol than that in seen in those taking naproxen, 88% higher than in those taking diclofenac, 70% higher than in those taking celecoxib, and about twice as high as in patients taking etoricoxib.
However, there was no significant difference in risk of all-cause mortality between tramadol and codeine, the researchers found.
The authors suggested that tramadol may have adverse effects on the neurologic system by inhibiting central serotonin and norepinephrine uptake, which could potentially lead to serotonin syndrome. They also speculated that it could increase the risk of postoperative delirium, cause fatal poisoning or respiratory depression if taken in conjunction with alcohol or other drugs, or increase the risk of hypoglycemia, hyponatremia, fractures, or falls.
The numbers of deaths from cardiovascular, gastrointestinal, infection, cancer, and respiratory diseases were all higher in the tramadol group, compared with patients taking NSAIDs, but the differences were not statistically significant because of the relatively small number of deaths, the authors said.
Overall, 44,451 patients were taking tramadol, 12,397 were taking naproxen, 6,512 were taking diclofenac, 5,674 were taking celecoxib, 2,946 were taking etoricoxib, and 16,922 were taking codeine.
Patients in the tramadol cohort were generally older, with higher body mass index, a longer duration of osteoarthritis, and had a higher prevalence of comorbidities, higher health care utilization, and more prescriptions of other medications.
The authors noted that, while the patients from each medication cohort were matched on propensity score, the results were still susceptible to confounding by indication and should be interpreted with caution.
The study was supported by grants from the National Institute of Arthritis and Musculoskeletal and Skin Diseases and the National Natural Science Foundation of China. One author declared funding from the National Institute on Drug Abuse during the conduct of the study and grants from Optum Labs outside the study. No other conflicts of interest were declared.
SOURCE: Zeng C et al. JAMA. 2019;321:969-82.
FROM JAMA
Evaluation of the American Academy of Orthopaedic Surgeons Appropriate Use Criteria for the Nonarthroplasty Treatment of Knee Osteoarthritis in Veterans
Knee osteoarthritis (OA) affects almost 9.3 million adults in the US and accounts for $27 billion in annual health care expenses.1,2 Due to the increasing cost of health care and an aging population, there has been renewed interest in establishing criteria for nonarthroplasty treatment of knee OA.
In 2013, using the RAND/UCLA Appropriateness method, the American Academy of Orthopaedic Surgeons (AAOS) developed an appropriate use criteria (AUC) for nonarthroplasty management of primary OA of the knee, based on orthopaedic literature and expert opinion.3 Interventions such as activity modification, weight loss, prescribed physical therapy, nonsteroidal anti-inflammatory drugs, tramadol, prescribed oral or transcutaneous opioids, acetaminophen, intra-articular corticosteroids, hinged or unloading knee braces, arthroscopic partial menisectomy or loose body removal, and realignment osteotomy were assessed. An algorithm was developed for 576 patients scenarios that incorporated patient-specific, prognostic/predictor variables to assign designations of “appropriate,” “may be appropriate,” or “rarely appropriate,” to treatment interventions.4,5 An online version of the algorithm (orthoguidelines.org) is available for physicians and surgeons to judge appropriateness of nonarthroplasty treatments; however, it is not intended to mandate candidacy for treatment or intervention.
Clinical evaluation of the AAOS AUC is necessary to determine how treatment recommendations correlate with current practice. A recent examination of the AAOS Appropriateness System for Surgical Management of Knee OA found that prognostic/predictor variables, such as patient age, OA severity, and pattern of knee OA involvement were more heavily weighted when determining arthroplasty appropriateness than was pain severity or functional loss.6 Furthermore, non-AAOS AUC prognostic/predictor variables, such as race and gender, have been linked to disparities in utilization of knee OA interventions.7-9 Such disparities can be costly not just from a patient perceptive, but also employer and societal perspectives.10
The Department of Veterans Affairs (VA) health care system represents a model of equal-access-to care system in the US that is ideal for examination of issues about health care utilization and any disparities within the AAOS AUC model and has previously been used to assess utilization of total knee arthroplasty.9 The aim of this study was to characterize utilization of the AAOS AUC for nonarthroplasty treatment of knee OA in a VA patient population. We asked the following questions: (1) What variables are predictive of receiving a greater number of AAOS AUC evaluated nonarthroplasty treatments? (2) What variables are predictive of receiving “rarely appropriate” AAOS AUC evaluated nonarthroplasty treatment? (3) What factors are predictive of duration of nonarthroplasty care until total knee arthroplasty (TKA)?
Methods
The institutional review board at the Louis Stokes Cleveland VA Medical Center in Ohio approved a retrospective chart review of nonarthroplasty treatments utilized by patients presenting to its orthopaedic section who subsequently underwent knee arthroplasty between 2013 and 2016. Eligibility criteria included patients aged ≥ 30 years with a diagnosis of unilateral or bilateral primary knee OA. Patients with posttraumatic OA, inflammatory arthritis, and a history of infectious arthritis or Charcot arthropathy of the knee were excluded. Patients with a body mass index (BMI) > 40 or a hemoglobin A1c > 8.0 at presentation were excluded as nonarthroplasty care was the recommended course of treatment above these thresholds.
Data collected included race, gender, duration of nonarthroplasty treatment, BMI, and Kellgren-Lawrence classification of knee OA at time of presentation for symptomatic knee OA.11 All AAOS AUC-evaluated nonarthroplasty treatments utilized prior to arthroplasty intervention also were recorded (Table 1).
Statistical Analysis
Statistical analysis was completed with GraphPad Software Prism 7.0a (La Jolla, CA) and Mathworks MatLab R2016b software (Natick, MA). Univariate analysis with Student t tests with Welch corrections in the setting of unequal variance, Mann-Whitney nonparametric tests, and Fisher exact test were generated in the appropriate setting. Multivariable analyses also were conducted. For continuous outcomes, stepwise multiple linear regression was used to generate predictive models; for binary outcomes, binomial logistic regression was used.
Factors analyzed in regression modeling for the total number of AAOS AUC evaluated nonarthroplasty treatments utilized and the likelihood of receiving a rarely appropriate treatment included gender, race, function-limiting pain, range of motion (ROM), ligamentous instability, arthritis pattern, limb alignment, mechanical symptoms, BMI, age, and Kellgren-Lawrence grade. Factors analyzed in timing of TKA included the above variables plus the total number of AUC interventions, whether the patient received an inappropriate intervention, and average appropriateness of the interventions received. Residual analysis with Cook’s distance was used to identify outliers in regression. Observations with Cook’s distance > 3 times the mean Cook’s distance were identified as potential outliers, and models were adjusted accordingly. All statistical analyses were 2-tailed. Statistical significance was set to P ≤ .05 for all outputs.
Results
In the study, 97.8% of participants identified as male, and the mean age was 62.8 years (Table 3).
Appropriate Use Criteria Interventions
Patients received a mean of 5.2 AAOS AUC evaluated interventions before undergoing arthroplasty management at a mean of 32.3 months (range 2-181 months) from initial presentation. The majority of these interventions were classified as either appropriate or may be appropriate, according to the AUC definitions (95.1%). Self-management and physical therapy programs were widely utilized (100% and 90.1%, respectively), with all use of these interventions classified as appropriate.
Hinged or unloader knee braces were utilized in about half the study patients; this intervention was classified as rarely appropriate in 4.4% of these patients. Medical therapy was also widely used, with all use of NSAIDs, acetaminophen, and tramadol classified as appropriate or may be appropriate. Oral or transcutaneous opioid medications were prescribed in 14.3% of patients, with 92.3% of this use classified as rarely appropriate. Although the opioid medication prescribing provider was not specifically evaluated, there were no instances in which the orthopaedic service provided an oral or transcutaneous opioid prescriptions. Procedural interventions, with the exception of corticosteroid injections, were uncommon; no patient received realignment osteotomy, and only 12.1% of patients underwent arthroscopy. The use of arthroscopy was deemed rarely appropriate in 72.7% of these cases.
Factors Associated With AAOS AUC Intervention Use
There was no difference in the number of AAOS AUC evaluated interventions received based on BMI (mean [SD] BMI < 35, 5.2 [1.0] vs BMI ≥ 35, 5.3 [1.1], P = .49), age (mean [SD] aged < 60 years, 5.4 [1.0] vs aged ≥ 60 years, 5.1 [1.2], P = .23), or Kellgren-Lawrence arthritic grade (mean [SD] grade ≤ 2, 5.5 [1.0] vs grade > 2, 5.1 [1.1], P = .06). These variables also were not associated with receiving a rarely appropriate intervention (mean [SD] BMI < 35, 0.27 [0.5] vs BMI > 35, 0.2 [0.4], P = .81; aged > 60 years, 0.3 [0.5] vs aged < 60 years, 0.2 [0.4], P = .26; Kellgren-Lawrence grade < 2, 0.4 [0.6] vs grade > 2, 0.2 [0.4], P = .1).
Regression modeling to predict total number of AAOS AUC evaluated interventions received produced a significant model (R2 = 0.111, P = .006). The presence of ligamentous instability (β coefficient, -1.61) and the absence of mechanical symptoms (β coefficient, -0.67) were negative predictors of number of AUC interventions received. Variance inflation factors were 1.014 and 1.012, respectively. Likewise, regression modeling to identify factors predictive of receiving a rarely appropriate intervention also produced a significant model (pseudo R2= 0.06, P = .025), with lower Kellgren-Lawrence grade the only significant predictor of receiving a rarely appropriate intervention (odds ratio [OR] 0.54; 95% CI, 0.42 -0.72, per unit increase).
Timing from presentation to arthroplasty intervention was also evaluated. Age was a negative predictor (β coefficient -1.61), while positive predictors were reduced ROM (β coefficient 15.72) and having more AUC interventions (β coefficient 7.31) (model R2= 0.29, P = < .001). Age was the most significant predictor. Variance inflations factors were 1.02, 1.01, and 1.03, respectively. Receiving a rarely appropriate intervention was not associated with TKA timing.
Discussion
This single-center retrospective study examined the utilization of AAOS AUC-evaluated nonarthroplasty interventions for symptomatic knee OA prior to TKA. The aims of this study were to validate the AAOS AUC in a clinical setting and identify predictors of AAOS AUC utilization. In particular, this study focused on the number of interventions utilized prior to knee arthroplasty, whether interventions receiving a designation of rarely appropriate were used, and the duration of nonarthroplasty treatment.
Patients with knee instability used fewer total AAOS AUC evaluated interventions prior to TKA. Subjective instability has been reported as high as 27% in patients with OA and has been associated with fear of falling, poor balance confidence, activity limitations, and lower Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) physical function scores.12 However, it has not been found to correlate with knee laxity.13 Nevertheless, significant functional impairment with the risk of falling may reduce the number of nonarthroplasty interventions attempted. On the other hand, the presence of mechanical symptoms resulted in greater utilization of nonarthroplasty interventions. This is likely due to the greater utilization of arthroscopic partial menisectomy or loose body removal in this group of patients. Despite its inclusion as an AAOS AUC evaluated intervention, arthroscopy remains a contentious treatment for symptomatic knee pain in the setting of OA.14,15
For every unit decrease in Kellgren-Lawrence OA grade, patients were 54% more likely to receive a rarely appropriate intervention prior to knee arthroplasty. This is supported by the recent literature examining the AAOS AUC for surgical management of knee OA. Riddle and colleagues developed a classification tree to determine the contributions of various prognostic variables in final classifications of the 864 clinical vignettes used to develop the appropriateness algorithm and found that OA severity was strongly favored, with only 4 of the 432 vignettes with severe knee OA judged as rarely appropriate for surgical intervention.6
Our findings, too, may be explained by an AAOS AUC system that too heavily weighs radiographic severity of knee OA, resulting in more frequent rarely appropriate interventions in patients with less severe arthritis, including nonarthroplasty treatments. It is likely that rarely appropriate interventions were attempted in this subset of our study cohort based on patient’s subjective symptoms and functional status, both of which have been shown to be discordant with radiographic severity of knee OA.16
Oral or transcutaneous prescribed opioid medications were the most frequent intervention that received a rarely appropriate designation. Patients with preoperative opioid use undergoing TKA have been shown to have a greater risk for postoperative complications and longer hospital stay, particularly those patients aged < 75 years. Younger age, use of more interventions, and decreased knee ROM at presentation were predictive of longer duration of nonarthroplasty treatment. The use of more AAOS AUC evaluated interventions in these patients suggests that the AAOS AUC model may effectively be used to manage symptomatic OA, increasing the time from presentation to knee arthroplasty.
Interestingly, the use of rarely appropriate interventions did not affect TKA timing, as would be expected in a clinically effective nonarthroplasty treatment model. The reasons for rarely appropriate nonsurgical interventions are complex and require further investigation. One possible explanation is that decreased ROM was a marker for mechanical symptoms that necessitated additional intervention in the form of knee arthroscopy, delaying time to TKA.
Limitations
There are several limitations of this study. First, the small sample size (N = 90) requires acknowledgment; however, this limitation reflects the difficulty in following patients for years prior to an operative intervention. Second, the study population consists of veterans using the VA system and may not be reflective of the general population, differing with respect to gender, racial, and socioeconomic factors. Nevertheless, studies examining TKA utilization found, aside from racial and ethnic variability, patient gender and age do not affect arthroplasty utilization rate in the VA system.17
Additional limitations stem from the retrospective nature of this study. While the Computerized Patient Record System and centralized care of the VA system allows for review of all physical therapy consultations, orthotic consultations, and medications within the VA system, any treatments and intervention delivered by non-VA providers were not captured. Furthermore, the ability to assess for confounding variables limiting the prescription of certain medications, such as chronic kidney disease with NSAIDs or liver disease with acetaminophen, was limited by our study design.
Although our study suffers from selection bias with respect to examination of nonarthroplasty treatment in patients who have ultimately undergone TKA, we feel that this subset of patients with symptomatic knee OA represents the majority of patients evaluated for knee OA by orthopaedic surgeons in the clinic setting. It should be noted that although realignment osteotomies were sometimes indicated as appropriate by AAOS AUC model in our study population, this intervention was never performed due to patient and surgeon preference. Additionally, although it is not an AAOS AUC evaluated intervention, viscosupplementation was sporadically used during the study period; however, it is now off formulary at the investigation institution.
Conclusion
Our study suggests that patients without knee instability use more nonarthroplasty treatments over a longer period before TKA, and those patients with less severe knee OA are at risk of receiving an intervention judged to be rarely appropriate by the AAOS AUC. Such interventions do not affect timing of TKA. Nonarthroplasty care should be individualized to patients’ needs, and the decision to proceed with arthroplasty should be considered only after exhausting appropriate conservative measures. We recommend that providers use the AAOS AUC, especially when treating younger patients with less severe knee OA, particularly if considering opiate therapy or knee arthroscopy.
Acknowledgments
The authors would like to acknowledge Patrick Getty, MD, for his surgical care of some of the study patients. This material is the result of work supported with resources and the use of facilities at the Louis Stokes Cleveland VA Medical Center in Ohio.
1. Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(7):1323-1330.
2. Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169(12):1113-1121; discussion 1121-1122.
3. Members of the Writing, Review, and Voting Panels of the AUC on the Non-Arthroplasty Treatment of Osteoarthritis of the Knee, Sanders JO, Heggeness MH, Murray J, Pezold R, Donnelly P. The American Academy of Orthopaedic Surgeons Appropriate Use Criteria on the Non-Arthroplasty Treatment of Osteoarthritis of the Knee. J Bone Joint Surg Am. 2014;96(14):1220-1221.
4. Sanders JO, Murray J, Gross L. Non-arthroplasty treatment of osteoarthritis of the knee. J Am Acad Orthop Surg. 2014;22(4):256-260.
5. Yates AJ Jr, McGrory BJ, Starz TW, Vincent KR, McCardel B, Golightly YM. AAOS appropriate use criteria: optimizing the non-arthroplasty management of osteoarthritis of the knee. J Am Acad Orthop Surg. 2014;22(4):261-267.
6. Riddle DL, Perera RA. Appropriateness and total knee arthroplasty: an examination of the American Academy of Orthopaedic Surgeons appropriateness rating system. Osteoarthritis Cartilage. 2017;25(12):1994-1998.
7. Morgan RC Jr, Slover J. Breakout session: ethnic and racial disparities in joint arthroplasty. Clin Orthop Relat Res. 2011;469(7):1886-1890.
8. O’Connor MI, Hooten EG. Breakout session: gender disparities in knee osteoarthritis and TKA. Clin Orthop Relat Res. 2011;469(7):1883-1885.
9. Ibrahim SA. Racial and ethnic disparities in hip and knee joint replacement: a review of research in the Veterans Affairs Health Care System. J Am Acad Orthop Surg. 2007;15(suppl 1):S87-S94.
10. Karmarkar TD, Maurer A, Parks ML, et al. A fresh perspective on a familiar problem: examining disparities in knee osteoarthritis using a Markov model. Med Care. 2017;55(12):993-1000.
11. Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016;474(8):1886-1893.
12. Nguyen U, Felson DT, Niu J, et al. The impact of knee instability with and without buckling on balance confidence, fear of falling and physical function: the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage. 2014;22(4):527-534.
13. Schmitt LC, Fitzgerald GK, Reisman AS, Rudolph KS. Instability, laxity, and physical function in patients with medial knee osteoarthritis. Phys Ther. 2008;88(12):1506-1516.
14. Laupattarakasem W, Laopaiboon M, Laupattarakasem P, Sumananont C. Arthroscopic debridement for knee osteoarthritis. Cochrane Database Syst Rev. 2008;(1):CD005118.
15. Lamplot JD, Brophy RH. The role for arthroscopic partial meniscectomy in knees with degenerative changes: a systematic review. Bone Joint J. 2016;98-B(7):934-938.
16. Whittle R, Jordan KP, Thomas E, Peat G. Average symptom trajectories following incident radiographic knee osteoarthritis: data from the Osteoarthritis Initiative. RMD Open. 2016;2(2):e000281.
17. Jones A, Kwoh CK, Kelley ME, Ibrahim SA. Racial disparity in knee arthroplasty utilization in the Veterans Health Administration. Arthritis Rheum. 2005;53(6):979-981.
Knee osteoarthritis (OA) affects almost 9.3 million adults in the US and accounts for $27 billion in annual health care expenses.1,2 Due to the increasing cost of health care and an aging population, there has been renewed interest in establishing criteria for nonarthroplasty treatment of knee OA.
In 2013, using the RAND/UCLA Appropriateness method, the American Academy of Orthopaedic Surgeons (AAOS) developed an appropriate use criteria (AUC) for nonarthroplasty management of primary OA of the knee, based on orthopaedic literature and expert opinion.3 Interventions such as activity modification, weight loss, prescribed physical therapy, nonsteroidal anti-inflammatory drugs, tramadol, prescribed oral or transcutaneous opioids, acetaminophen, intra-articular corticosteroids, hinged or unloading knee braces, arthroscopic partial menisectomy or loose body removal, and realignment osteotomy were assessed. An algorithm was developed for 576 patients scenarios that incorporated patient-specific, prognostic/predictor variables to assign designations of “appropriate,” “may be appropriate,” or “rarely appropriate,” to treatment interventions.4,5 An online version of the algorithm (orthoguidelines.org) is available for physicians and surgeons to judge appropriateness of nonarthroplasty treatments; however, it is not intended to mandate candidacy for treatment or intervention.
Clinical evaluation of the AAOS AUC is necessary to determine how treatment recommendations correlate with current practice. A recent examination of the AAOS Appropriateness System for Surgical Management of Knee OA found that prognostic/predictor variables, such as patient age, OA severity, and pattern of knee OA involvement were more heavily weighted when determining arthroplasty appropriateness than was pain severity or functional loss.6 Furthermore, non-AAOS AUC prognostic/predictor variables, such as race and gender, have been linked to disparities in utilization of knee OA interventions.7-9 Such disparities can be costly not just from a patient perceptive, but also employer and societal perspectives.10
The Department of Veterans Affairs (VA) health care system represents a model of equal-access-to care system in the US that is ideal for examination of issues about health care utilization and any disparities within the AAOS AUC model and has previously been used to assess utilization of total knee arthroplasty.9 The aim of this study was to characterize utilization of the AAOS AUC for nonarthroplasty treatment of knee OA in a VA patient population. We asked the following questions: (1) What variables are predictive of receiving a greater number of AAOS AUC evaluated nonarthroplasty treatments? (2) What variables are predictive of receiving “rarely appropriate” AAOS AUC evaluated nonarthroplasty treatment? (3) What factors are predictive of duration of nonarthroplasty care until total knee arthroplasty (TKA)?
Methods
The institutional review board at the Louis Stokes Cleveland VA Medical Center in Ohio approved a retrospective chart review of nonarthroplasty treatments utilized by patients presenting to its orthopaedic section who subsequently underwent knee arthroplasty between 2013 and 2016. Eligibility criteria included patients aged ≥ 30 years with a diagnosis of unilateral or bilateral primary knee OA. Patients with posttraumatic OA, inflammatory arthritis, and a history of infectious arthritis or Charcot arthropathy of the knee were excluded. Patients with a body mass index (BMI) > 40 or a hemoglobin A1c > 8.0 at presentation were excluded as nonarthroplasty care was the recommended course of treatment above these thresholds.
Data collected included race, gender, duration of nonarthroplasty treatment, BMI, and Kellgren-Lawrence classification of knee OA at time of presentation for symptomatic knee OA.11 All AAOS AUC-evaluated nonarthroplasty treatments utilized prior to arthroplasty intervention also were recorded (Table 1).
Statistical Analysis
Statistical analysis was completed with GraphPad Software Prism 7.0a (La Jolla, CA) and Mathworks MatLab R2016b software (Natick, MA). Univariate analysis with Student t tests with Welch corrections in the setting of unequal variance, Mann-Whitney nonparametric tests, and Fisher exact test were generated in the appropriate setting. Multivariable analyses also were conducted. For continuous outcomes, stepwise multiple linear regression was used to generate predictive models; for binary outcomes, binomial logistic regression was used.
Factors analyzed in regression modeling for the total number of AAOS AUC evaluated nonarthroplasty treatments utilized and the likelihood of receiving a rarely appropriate treatment included gender, race, function-limiting pain, range of motion (ROM), ligamentous instability, arthritis pattern, limb alignment, mechanical symptoms, BMI, age, and Kellgren-Lawrence grade. Factors analyzed in timing of TKA included the above variables plus the total number of AUC interventions, whether the patient received an inappropriate intervention, and average appropriateness of the interventions received. Residual analysis with Cook’s distance was used to identify outliers in regression. Observations with Cook’s distance > 3 times the mean Cook’s distance were identified as potential outliers, and models were adjusted accordingly. All statistical analyses were 2-tailed. Statistical significance was set to P ≤ .05 for all outputs.
Results
In the study, 97.8% of participants identified as male, and the mean age was 62.8 years (Table 3).
Appropriate Use Criteria Interventions
Patients received a mean of 5.2 AAOS AUC evaluated interventions before undergoing arthroplasty management at a mean of 32.3 months (range 2-181 months) from initial presentation. The majority of these interventions were classified as either appropriate or may be appropriate, according to the AUC definitions (95.1%). Self-management and physical therapy programs were widely utilized (100% and 90.1%, respectively), with all use of these interventions classified as appropriate.
Hinged or unloader knee braces were utilized in about half the study patients; this intervention was classified as rarely appropriate in 4.4% of these patients. Medical therapy was also widely used, with all use of NSAIDs, acetaminophen, and tramadol classified as appropriate or may be appropriate. Oral or transcutaneous opioid medications were prescribed in 14.3% of patients, with 92.3% of this use classified as rarely appropriate. Although the opioid medication prescribing provider was not specifically evaluated, there were no instances in which the orthopaedic service provided an oral or transcutaneous opioid prescriptions. Procedural interventions, with the exception of corticosteroid injections, were uncommon; no patient received realignment osteotomy, and only 12.1% of patients underwent arthroscopy. The use of arthroscopy was deemed rarely appropriate in 72.7% of these cases.
Factors Associated With AAOS AUC Intervention Use
There was no difference in the number of AAOS AUC evaluated interventions received based on BMI (mean [SD] BMI < 35, 5.2 [1.0] vs BMI ≥ 35, 5.3 [1.1], P = .49), age (mean [SD] aged < 60 years, 5.4 [1.0] vs aged ≥ 60 years, 5.1 [1.2], P = .23), or Kellgren-Lawrence arthritic grade (mean [SD] grade ≤ 2, 5.5 [1.0] vs grade > 2, 5.1 [1.1], P = .06). These variables also were not associated with receiving a rarely appropriate intervention (mean [SD] BMI < 35, 0.27 [0.5] vs BMI > 35, 0.2 [0.4], P = .81; aged > 60 years, 0.3 [0.5] vs aged < 60 years, 0.2 [0.4], P = .26; Kellgren-Lawrence grade < 2, 0.4 [0.6] vs grade > 2, 0.2 [0.4], P = .1).
Regression modeling to predict total number of AAOS AUC evaluated interventions received produced a significant model (R2 = 0.111, P = .006). The presence of ligamentous instability (β coefficient, -1.61) and the absence of mechanical symptoms (β coefficient, -0.67) were negative predictors of number of AUC interventions received. Variance inflation factors were 1.014 and 1.012, respectively. Likewise, regression modeling to identify factors predictive of receiving a rarely appropriate intervention also produced a significant model (pseudo R2= 0.06, P = .025), with lower Kellgren-Lawrence grade the only significant predictor of receiving a rarely appropriate intervention (odds ratio [OR] 0.54; 95% CI, 0.42 -0.72, per unit increase).
Timing from presentation to arthroplasty intervention was also evaluated. Age was a negative predictor (β coefficient -1.61), while positive predictors were reduced ROM (β coefficient 15.72) and having more AUC interventions (β coefficient 7.31) (model R2= 0.29, P = < .001). Age was the most significant predictor. Variance inflations factors were 1.02, 1.01, and 1.03, respectively. Receiving a rarely appropriate intervention was not associated with TKA timing.
Discussion
This single-center retrospective study examined the utilization of AAOS AUC-evaluated nonarthroplasty interventions for symptomatic knee OA prior to TKA. The aims of this study were to validate the AAOS AUC in a clinical setting and identify predictors of AAOS AUC utilization. In particular, this study focused on the number of interventions utilized prior to knee arthroplasty, whether interventions receiving a designation of rarely appropriate were used, and the duration of nonarthroplasty treatment.
Patients with knee instability used fewer total AAOS AUC evaluated interventions prior to TKA. Subjective instability has been reported as high as 27% in patients with OA and has been associated with fear of falling, poor balance confidence, activity limitations, and lower Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) physical function scores.12 However, it has not been found to correlate with knee laxity.13 Nevertheless, significant functional impairment with the risk of falling may reduce the number of nonarthroplasty interventions attempted. On the other hand, the presence of mechanical symptoms resulted in greater utilization of nonarthroplasty interventions. This is likely due to the greater utilization of arthroscopic partial menisectomy or loose body removal in this group of patients. Despite its inclusion as an AAOS AUC evaluated intervention, arthroscopy remains a contentious treatment for symptomatic knee pain in the setting of OA.14,15
For every unit decrease in Kellgren-Lawrence OA grade, patients were 54% more likely to receive a rarely appropriate intervention prior to knee arthroplasty. This is supported by the recent literature examining the AAOS AUC for surgical management of knee OA. Riddle and colleagues developed a classification tree to determine the contributions of various prognostic variables in final classifications of the 864 clinical vignettes used to develop the appropriateness algorithm and found that OA severity was strongly favored, with only 4 of the 432 vignettes with severe knee OA judged as rarely appropriate for surgical intervention.6
Our findings, too, may be explained by an AAOS AUC system that too heavily weighs radiographic severity of knee OA, resulting in more frequent rarely appropriate interventions in patients with less severe arthritis, including nonarthroplasty treatments. It is likely that rarely appropriate interventions were attempted in this subset of our study cohort based on patient’s subjective symptoms and functional status, both of which have been shown to be discordant with radiographic severity of knee OA.16
Oral or transcutaneous prescribed opioid medications were the most frequent intervention that received a rarely appropriate designation. Patients with preoperative opioid use undergoing TKA have been shown to have a greater risk for postoperative complications and longer hospital stay, particularly those patients aged < 75 years. Younger age, use of more interventions, and decreased knee ROM at presentation were predictive of longer duration of nonarthroplasty treatment. The use of more AAOS AUC evaluated interventions in these patients suggests that the AAOS AUC model may effectively be used to manage symptomatic OA, increasing the time from presentation to knee arthroplasty.
Interestingly, the use of rarely appropriate interventions did not affect TKA timing, as would be expected in a clinically effective nonarthroplasty treatment model. The reasons for rarely appropriate nonsurgical interventions are complex and require further investigation. One possible explanation is that decreased ROM was a marker for mechanical symptoms that necessitated additional intervention in the form of knee arthroscopy, delaying time to TKA.
Limitations
There are several limitations of this study. First, the small sample size (N = 90) requires acknowledgment; however, this limitation reflects the difficulty in following patients for years prior to an operative intervention. Second, the study population consists of veterans using the VA system and may not be reflective of the general population, differing with respect to gender, racial, and socioeconomic factors. Nevertheless, studies examining TKA utilization found, aside from racial and ethnic variability, patient gender and age do not affect arthroplasty utilization rate in the VA system.17
Additional limitations stem from the retrospective nature of this study. While the Computerized Patient Record System and centralized care of the VA system allows for review of all physical therapy consultations, orthotic consultations, and medications within the VA system, any treatments and intervention delivered by non-VA providers were not captured. Furthermore, the ability to assess for confounding variables limiting the prescription of certain medications, such as chronic kidney disease with NSAIDs or liver disease with acetaminophen, was limited by our study design.
Although our study suffers from selection bias with respect to examination of nonarthroplasty treatment in patients who have ultimately undergone TKA, we feel that this subset of patients with symptomatic knee OA represents the majority of patients evaluated for knee OA by orthopaedic surgeons in the clinic setting. It should be noted that although realignment osteotomies were sometimes indicated as appropriate by AAOS AUC model in our study population, this intervention was never performed due to patient and surgeon preference. Additionally, although it is not an AAOS AUC evaluated intervention, viscosupplementation was sporadically used during the study period; however, it is now off formulary at the investigation institution.
Conclusion
Our study suggests that patients without knee instability use more nonarthroplasty treatments over a longer period before TKA, and those patients with less severe knee OA are at risk of receiving an intervention judged to be rarely appropriate by the AAOS AUC. Such interventions do not affect timing of TKA. Nonarthroplasty care should be individualized to patients’ needs, and the decision to proceed with arthroplasty should be considered only after exhausting appropriate conservative measures. We recommend that providers use the AAOS AUC, especially when treating younger patients with less severe knee OA, particularly if considering opiate therapy or knee arthroscopy.
Acknowledgments
The authors would like to acknowledge Patrick Getty, MD, for his surgical care of some of the study patients. This material is the result of work supported with resources and the use of facilities at the Louis Stokes Cleveland VA Medical Center in Ohio.
Knee osteoarthritis (OA) affects almost 9.3 million adults in the US and accounts for $27 billion in annual health care expenses.1,2 Due to the increasing cost of health care and an aging population, there has been renewed interest in establishing criteria for nonarthroplasty treatment of knee OA.
In 2013, using the RAND/UCLA Appropriateness method, the American Academy of Orthopaedic Surgeons (AAOS) developed an appropriate use criteria (AUC) for nonarthroplasty management of primary OA of the knee, based on orthopaedic literature and expert opinion.3 Interventions such as activity modification, weight loss, prescribed physical therapy, nonsteroidal anti-inflammatory drugs, tramadol, prescribed oral or transcutaneous opioids, acetaminophen, intra-articular corticosteroids, hinged or unloading knee braces, arthroscopic partial menisectomy or loose body removal, and realignment osteotomy were assessed. An algorithm was developed for 576 patients scenarios that incorporated patient-specific, prognostic/predictor variables to assign designations of “appropriate,” “may be appropriate,” or “rarely appropriate,” to treatment interventions.4,5 An online version of the algorithm (orthoguidelines.org) is available for physicians and surgeons to judge appropriateness of nonarthroplasty treatments; however, it is not intended to mandate candidacy for treatment or intervention.
Clinical evaluation of the AAOS AUC is necessary to determine how treatment recommendations correlate with current practice. A recent examination of the AAOS Appropriateness System for Surgical Management of Knee OA found that prognostic/predictor variables, such as patient age, OA severity, and pattern of knee OA involvement were more heavily weighted when determining arthroplasty appropriateness than was pain severity or functional loss.6 Furthermore, non-AAOS AUC prognostic/predictor variables, such as race and gender, have been linked to disparities in utilization of knee OA interventions.7-9 Such disparities can be costly not just from a patient perceptive, but also employer and societal perspectives.10
The Department of Veterans Affairs (VA) health care system represents a model of equal-access-to care system in the US that is ideal for examination of issues about health care utilization and any disparities within the AAOS AUC model and has previously been used to assess utilization of total knee arthroplasty.9 The aim of this study was to characterize utilization of the AAOS AUC for nonarthroplasty treatment of knee OA in a VA patient population. We asked the following questions: (1) What variables are predictive of receiving a greater number of AAOS AUC evaluated nonarthroplasty treatments? (2) What variables are predictive of receiving “rarely appropriate” AAOS AUC evaluated nonarthroplasty treatment? (3) What factors are predictive of duration of nonarthroplasty care until total knee arthroplasty (TKA)?
Methods
The institutional review board at the Louis Stokes Cleveland VA Medical Center in Ohio approved a retrospective chart review of nonarthroplasty treatments utilized by patients presenting to its orthopaedic section who subsequently underwent knee arthroplasty between 2013 and 2016. Eligibility criteria included patients aged ≥ 30 years with a diagnosis of unilateral or bilateral primary knee OA. Patients with posttraumatic OA, inflammatory arthritis, and a history of infectious arthritis or Charcot arthropathy of the knee were excluded. Patients with a body mass index (BMI) > 40 or a hemoglobin A1c > 8.0 at presentation were excluded as nonarthroplasty care was the recommended course of treatment above these thresholds.
Data collected included race, gender, duration of nonarthroplasty treatment, BMI, and Kellgren-Lawrence classification of knee OA at time of presentation for symptomatic knee OA.11 All AAOS AUC-evaluated nonarthroplasty treatments utilized prior to arthroplasty intervention also were recorded (Table 1).
Statistical Analysis
Statistical analysis was completed with GraphPad Software Prism 7.0a (La Jolla, CA) and Mathworks MatLab R2016b software (Natick, MA). Univariate analysis with Student t tests with Welch corrections in the setting of unequal variance, Mann-Whitney nonparametric tests, and Fisher exact test were generated in the appropriate setting. Multivariable analyses also were conducted. For continuous outcomes, stepwise multiple linear regression was used to generate predictive models; for binary outcomes, binomial logistic regression was used.
Factors analyzed in regression modeling for the total number of AAOS AUC evaluated nonarthroplasty treatments utilized and the likelihood of receiving a rarely appropriate treatment included gender, race, function-limiting pain, range of motion (ROM), ligamentous instability, arthritis pattern, limb alignment, mechanical symptoms, BMI, age, and Kellgren-Lawrence grade. Factors analyzed in timing of TKA included the above variables plus the total number of AUC interventions, whether the patient received an inappropriate intervention, and average appropriateness of the interventions received. Residual analysis with Cook’s distance was used to identify outliers in regression. Observations with Cook’s distance > 3 times the mean Cook’s distance were identified as potential outliers, and models were adjusted accordingly. All statistical analyses were 2-tailed. Statistical significance was set to P ≤ .05 for all outputs.
Results
In the study, 97.8% of participants identified as male, and the mean age was 62.8 years (Table 3).
Appropriate Use Criteria Interventions
Patients received a mean of 5.2 AAOS AUC evaluated interventions before undergoing arthroplasty management at a mean of 32.3 months (range 2-181 months) from initial presentation. The majority of these interventions were classified as either appropriate or may be appropriate, according to the AUC definitions (95.1%). Self-management and physical therapy programs were widely utilized (100% and 90.1%, respectively), with all use of these interventions classified as appropriate.
Hinged or unloader knee braces were utilized in about half the study patients; this intervention was classified as rarely appropriate in 4.4% of these patients. Medical therapy was also widely used, with all use of NSAIDs, acetaminophen, and tramadol classified as appropriate or may be appropriate. Oral or transcutaneous opioid medications were prescribed in 14.3% of patients, with 92.3% of this use classified as rarely appropriate. Although the opioid medication prescribing provider was not specifically evaluated, there were no instances in which the orthopaedic service provided an oral or transcutaneous opioid prescriptions. Procedural interventions, with the exception of corticosteroid injections, were uncommon; no patient received realignment osteotomy, and only 12.1% of patients underwent arthroscopy. The use of arthroscopy was deemed rarely appropriate in 72.7% of these cases.
Factors Associated With AAOS AUC Intervention Use
There was no difference in the number of AAOS AUC evaluated interventions received based on BMI (mean [SD] BMI < 35, 5.2 [1.0] vs BMI ≥ 35, 5.3 [1.1], P = .49), age (mean [SD] aged < 60 years, 5.4 [1.0] vs aged ≥ 60 years, 5.1 [1.2], P = .23), or Kellgren-Lawrence arthritic grade (mean [SD] grade ≤ 2, 5.5 [1.0] vs grade > 2, 5.1 [1.1], P = .06). These variables also were not associated with receiving a rarely appropriate intervention (mean [SD] BMI < 35, 0.27 [0.5] vs BMI > 35, 0.2 [0.4], P = .81; aged > 60 years, 0.3 [0.5] vs aged < 60 years, 0.2 [0.4], P = .26; Kellgren-Lawrence grade < 2, 0.4 [0.6] vs grade > 2, 0.2 [0.4], P = .1).
Regression modeling to predict total number of AAOS AUC evaluated interventions received produced a significant model (R2 = 0.111, P = .006). The presence of ligamentous instability (β coefficient, -1.61) and the absence of mechanical symptoms (β coefficient, -0.67) were negative predictors of number of AUC interventions received. Variance inflation factors were 1.014 and 1.012, respectively. Likewise, regression modeling to identify factors predictive of receiving a rarely appropriate intervention also produced a significant model (pseudo R2= 0.06, P = .025), with lower Kellgren-Lawrence grade the only significant predictor of receiving a rarely appropriate intervention (odds ratio [OR] 0.54; 95% CI, 0.42 -0.72, per unit increase).
Timing from presentation to arthroplasty intervention was also evaluated. Age was a negative predictor (β coefficient -1.61), while positive predictors were reduced ROM (β coefficient 15.72) and having more AUC interventions (β coefficient 7.31) (model R2= 0.29, P = < .001). Age was the most significant predictor. Variance inflations factors were 1.02, 1.01, and 1.03, respectively. Receiving a rarely appropriate intervention was not associated with TKA timing.
Discussion
This single-center retrospective study examined the utilization of AAOS AUC-evaluated nonarthroplasty interventions for symptomatic knee OA prior to TKA. The aims of this study were to validate the AAOS AUC in a clinical setting and identify predictors of AAOS AUC utilization. In particular, this study focused on the number of interventions utilized prior to knee arthroplasty, whether interventions receiving a designation of rarely appropriate were used, and the duration of nonarthroplasty treatment.
Patients with knee instability used fewer total AAOS AUC evaluated interventions prior to TKA. Subjective instability has been reported as high as 27% in patients with OA and has been associated with fear of falling, poor balance confidence, activity limitations, and lower Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) physical function scores.12 However, it has not been found to correlate with knee laxity.13 Nevertheless, significant functional impairment with the risk of falling may reduce the number of nonarthroplasty interventions attempted. On the other hand, the presence of mechanical symptoms resulted in greater utilization of nonarthroplasty interventions. This is likely due to the greater utilization of arthroscopic partial menisectomy or loose body removal in this group of patients. Despite its inclusion as an AAOS AUC evaluated intervention, arthroscopy remains a contentious treatment for symptomatic knee pain in the setting of OA.14,15
For every unit decrease in Kellgren-Lawrence OA grade, patients were 54% more likely to receive a rarely appropriate intervention prior to knee arthroplasty. This is supported by the recent literature examining the AAOS AUC for surgical management of knee OA. Riddle and colleagues developed a classification tree to determine the contributions of various prognostic variables in final classifications of the 864 clinical vignettes used to develop the appropriateness algorithm and found that OA severity was strongly favored, with only 4 of the 432 vignettes with severe knee OA judged as rarely appropriate for surgical intervention.6
Our findings, too, may be explained by an AAOS AUC system that too heavily weighs radiographic severity of knee OA, resulting in more frequent rarely appropriate interventions in patients with less severe arthritis, including nonarthroplasty treatments. It is likely that rarely appropriate interventions were attempted in this subset of our study cohort based on patient’s subjective symptoms and functional status, both of which have been shown to be discordant with radiographic severity of knee OA.16
Oral or transcutaneous prescribed opioid medications were the most frequent intervention that received a rarely appropriate designation. Patients with preoperative opioid use undergoing TKA have been shown to have a greater risk for postoperative complications and longer hospital stay, particularly those patients aged < 75 years. Younger age, use of more interventions, and decreased knee ROM at presentation were predictive of longer duration of nonarthroplasty treatment. The use of more AAOS AUC evaluated interventions in these patients suggests that the AAOS AUC model may effectively be used to manage symptomatic OA, increasing the time from presentation to knee arthroplasty.
Interestingly, the use of rarely appropriate interventions did not affect TKA timing, as would be expected in a clinically effective nonarthroplasty treatment model. The reasons for rarely appropriate nonsurgical interventions are complex and require further investigation. One possible explanation is that decreased ROM was a marker for mechanical symptoms that necessitated additional intervention in the form of knee arthroscopy, delaying time to TKA.
Limitations
There are several limitations of this study. First, the small sample size (N = 90) requires acknowledgment; however, this limitation reflects the difficulty in following patients for years prior to an operative intervention. Second, the study population consists of veterans using the VA system and may not be reflective of the general population, differing with respect to gender, racial, and socioeconomic factors. Nevertheless, studies examining TKA utilization found, aside from racial and ethnic variability, patient gender and age do not affect arthroplasty utilization rate in the VA system.17
Additional limitations stem from the retrospective nature of this study. While the Computerized Patient Record System and centralized care of the VA system allows for review of all physical therapy consultations, orthotic consultations, and medications within the VA system, any treatments and intervention delivered by non-VA providers were not captured. Furthermore, the ability to assess for confounding variables limiting the prescription of certain medications, such as chronic kidney disease with NSAIDs or liver disease with acetaminophen, was limited by our study design.
Although our study suffers from selection bias with respect to examination of nonarthroplasty treatment in patients who have ultimately undergone TKA, we feel that this subset of patients with symptomatic knee OA represents the majority of patients evaluated for knee OA by orthopaedic surgeons in the clinic setting. It should be noted that although realignment osteotomies were sometimes indicated as appropriate by AAOS AUC model in our study population, this intervention was never performed due to patient and surgeon preference. Additionally, although it is not an AAOS AUC evaluated intervention, viscosupplementation was sporadically used during the study period; however, it is now off formulary at the investigation institution.
Conclusion
Our study suggests that patients without knee instability use more nonarthroplasty treatments over a longer period before TKA, and those patients with less severe knee OA are at risk of receiving an intervention judged to be rarely appropriate by the AAOS AUC. Such interventions do not affect timing of TKA. Nonarthroplasty care should be individualized to patients’ needs, and the decision to proceed with arthroplasty should be considered only after exhausting appropriate conservative measures. We recommend that providers use the AAOS AUC, especially when treating younger patients with less severe knee OA, particularly if considering opiate therapy or knee arthroscopy.
Acknowledgments
The authors would like to acknowledge Patrick Getty, MD, for his surgical care of some of the study patients. This material is the result of work supported with resources and the use of facilities at the Louis Stokes Cleveland VA Medical Center in Ohio.
1. Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(7):1323-1330.
2. Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169(12):1113-1121; discussion 1121-1122.
3. Members of the Writing, Review, and Voting Panels of the AUC on the Non-Arthroplasty Treatment of Osteoarthritis of the Knee, Sanders JO, Heggeness MH, Murray J, Pezold R, Donnelly P. The American Academy of Orthopaedic Surgeons Appropriate Use Criteria on the Non-Arthroplasty Treatment of Osteoarthritis of the Knee. J Bone Joint Surg Am. 2014;96(14):1220-1221.
4. Sanders JO, Murray J, Gross L. Non-arthroplasty treatment of osteoarthritis of the knee. J Am Acad Orthop Surg. 2014;22(4):256-260.
5. Yates AJ Jr, McGrory BJ, Starz TW, Vincent KR, McCardel B, Golightly YM. AAOS appropriate use criteria: optimizing the non-arthroplasty management of osteoarthritis of the knee. J Am Acad Orthop Surg. 2014;22(4):261-267.
6. Riddle DL, Perera RA. Appropriateness and total knee arthroplasty: an examination of the American Academy of Orthopaedic Surgeons appropriateness rating system. Osteoarthritis Cartilage. 2017;25(12):1994-1998.
7. Morgan RC Jr, Slover J. Breakout session: ethnic and racial disparities in joint arthroplasty. Clin Orthop Relat Res. 2011;469(7):1886-1890.
8. O’Connor MI, Hooten EG. Breakout session: gender disparities in knee osteoarthritis and TKA. Clin Orthop Relat Res. 2011;469(7):1883-1885.
9. Ibrahim SA. Racial and ethnic disparities in hip and knee joint replacement: a review of research in the Veterans Affairs Health Care System. J Am Acad Orthop Surg. 2007;15(suppl 1):S87-S94.
10. Karmarkar TD, Maurer A, Parks ML, et al. A fresh perspective on a familiar problem: examining disparities in knee osteoarthritis using a Markov model. Med Care. 2017;55(12):993-1000.
11. Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016;474(8):1886-1893.
12. Nguyen U, Felson DT, Niu J, et al. The impact of knee instability with and without buckling on balance confidence, fear of falling and physical function: the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage. 2014;22(4):527-534.
13. Schmitt LC, Fitzgerald GK, Reisman AS, Rudolph KS. Instability, laxity, and physical function in patients with medial knee osteoarthritis. Phys Ther. 2008;88(12):1506-1516.
14. Laupattarakasem W, Laopaiboon M, Laupattarakasem P, Sumananont C. Arthroscopic debridement for knee osteoarthritis. Cochrane Database Syst Rev. 2008;(1):CD005118.
15. Lamplot JD, Brophy RH. The role for arthroscopic partial meniscectomy in knees with degenerative changes: a systematic review. Bone Joint J. 2016;98-B(7):934-938.
16. Whittle R, Jordan KP, Thomas E, Peat G. Average symptom trajectories following incident radiographic knee osteoarthritis: data from the Osteoarthritis Initiative. RMD Open. 2016;2(2):e000281.
17. Jones A, Kwoh CK, Kelley ME, Ibrahim SA. Racial disparity in knee arthroplasty utilization in the Veterans Health Administration. Arthritis Rheum. 2005;53(6):979-981.
1. Cross M, Smith E, Hoy D, et al. The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Ann Rheum Dis. 2014;73(7):1323-1330.
2. Losina E, Walensky RP, Kessler CL, et al. Cost-effectiveness of total knee arthroplasty in the United States: patient risk and hospital volume. Arch Intern Med. 2009;169(12):1113-1121; discussion 1121-1122.
3. Members of the Writing, Review, and Voting Panels of the AUC on the Non-Arthroplasty Treatment of Osteoarthritis of the Knee, Sanders JO, Heggeness MH, Murray J, Pezold R, Donnelly P. The American Academy of Orthopaedic Surgeons Appropriate Use Criteria on the Non-Arthroplasty Treatment of Osteoarthritis of the Knee. J Bone Joint Surg Am. 2014;96(14):1220-1221.
4. Sanders JO, Murray J, Gross L. Non-arthroplasty treatment of osteoarthritis of the knee. J Am Acad Orthop Surg. 2014;22(4):256-260.
5. Yates AJ Jr, McGrory BJ, Starz TW, Vincent KR, McCardel B, Golightly YM. AAOS appropriate use criteria: optimizing the non-arthroplasty management of osteoarthritis of the knee. J Am Acad Orthop Surg. 2014;22(4):261-267.
6. Riddle DL, Perera RA. Appropriateness and total knee arthroplasty: an examination of the American Academy of Orthopaedic Surgeons appropriateness rating system. Osteoarthritis Cartilage. 2017;25(12):1994-1998.
7. Morgan RC Jr, Slover J. Breakout session: ethnic and racial disparities in joint arthroplasty. Clin Orthop Relat Res. 2011;469(7):1886-1890.
8. O’Connor MI, Hooten EG. Breakout session: gender disparities in knee osteoarthritis and TKA. Clin Orthop Relat Res. 2011;469(7):1883-1885.
9. Ibrahim SA. Racial and ethnic disparities in hip and knee joint replacement: a review of research in the Veterans Affairs Health Care System. J Am Acad Orthop Surg. 2007;15(suppl 1):S87-S94.
10. Karmarkar TD, Maurer A, Parks ML, et al. A fresh perspective on a familiar problem: examining disparities in knee osteoarthritis using a Markov model. Med Care. 2017;55(12):993-1000.
11. Kohn MD, Sassoon AA, Fernando ND. Classifications in brief: Kellgren-Lawrence Classification of Osteoarthritis. Clin Orthop Relat Res. 2016;474(8):1886-1893.
12. Nguyen U, Felson DT, Niu J, et al. The impact of knee instability with and without buckling on balance confidence, fear of falling and physical function: the Multicenter Osteoarthritis Study. Osteoarthritis Cartilage. 2014;22(4):527-534.
13. Schmitt LC, Fitzgerald GK, Reisman AS, Rudolph KS. Instability, laxity, and physical function in patients with medial knee osteoarthritis. Phys Ther. 2008;88(12):1506-1516.
14. Laupattarakasem W, Laopaiboon M, Laupattarakasem P, Sumananont C. Arthroscopic debridement for knee osteoarthritis. Cochrane Database Syst Rev. 2008;(1):CD005118.
15. Lamplot JD, Brophy RH. The role for arthroscopic partial meniscectomy in knees with degenerative changes: a systematic review. Bone Joint J. 2016;98-B(7):934-938.
16. Whittle R, Jordan KP, Thomas E, Peat G. Average symptom trajectories following incident radiographic knee osteoarthritis: data from the Osteoarthritis Initiative. RMD Open. 2016;2(2):e000281.
17. Jones A, Kwoh CK, Kelley ME, Ibrahim SA. Racial disparity in knee arthroplasty utilization in the Veterans Health Administration. Arthritis Rheum. 2005;53(6):979-981.
Emicizumab performs well in surgical setting
PRAGUE – Emicizumab appears safe and effective for patients with hemophilia A undergoing surgical procedures, based on experience with a subpopulation of HAVEN 3 trial participants.
Out of 28 minor procedures performed without preventive factor VIII (FVIII), only 2 were associated with postoperative bleeds requiring treatment, reported lead author Elena Santagostino, MD, PhD, of Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico in Milan, and her colleagues.
All events requiring bleeding treatment were associated with dental procedures, highlighting an area where clinicians and dentists may need to exercise caution. Still, overall results supported emicizumab in a surgical setting.
“There were no thrombotic complications or other unexpected events, including inhibitor development,” Dr. Santagostino said at the annual congress of the European Association for Haemophilia and Allied Disorders.
The findings were drawn from 30 patients who underwent 50 surgeries (46 minor, 4 major) during HAVEN 3, a previously reported phase 3 trial investigating the use of emicizumab, a humanized bispecific monoclonal antibody for patients with hemophilia A without inhibitors.
The minor surgeries included dental or orthopedic procedures, esophagogastroduodenoscopy, or colonoscopy. The four major procedures were all orthopedic (knee arthroscopic synovectomy, biceps femoris tear repair, total ankle arthroplasty, and total hip replacement). The investigators analyzed surgery-related bleeds and the nature of FVIII usage.
Preventive FVIII was used in 18 procedures; infusion duration was 24 hours or less in 14 procedures, between 25 hours and 48 hours in 2 procedures, and more than 72 hours in 2 procedures. The median cumulative preventive FVIII dose per procedure was 30 IU/kg.
Of the 46 minor procedures, 28 (61%) were performed without preventive FVIII, and 2 (7.1%) were associated with bleeding requiring treatment, both after dental procedures. Two other participants who received preventive FVIII also needed postoperative bleeding treatment. Of note, these events were also after dental procedures, meaning all four instances of bleeding requiring treatment during the trial were associated with dentistry.
“[I]n this experience, dental procedures were somewhat tricky because the bleeding complications were mainly there,” Dr. Santagostino said.
When asked by an audience member if this trend was unique to mucosal bleeding, Dr. Santagostino said it was too early to draw such a conclusion but offered some insight. “To control and prevent bleeding during a dental procedure is not trivial, because … sometimes if you stop factor VIII treatment quite early, you may have late bleeding, mainly due to local reasons, because … dental procedures are very heterogenous.”
Among three other participants who had postoperative bleeding but did not require treatment, two underwent dental procedures, further supporting this association. Although the study numbers are relatively small, the findings may at least support caution, if not preventive FVIII in the dental setting, Dr. Santagostino said.
The four major procedures – all orthopedic – were knee arthroscopic synovectomy, biceps femoris tear repair, total ankle arthroplasty, and total hip replacement. Along with preoperative preventive FVIII, three of four patients undergoing major surgery received preventive FVIII for 14-18 days postoperatively. Doses ranged from 99-522 IU/kg. No postoperative bleeds occurred in this subgroup.
Study funding was provided by F. Hoffmann–La Roche and Chugai Pharmaceutical. The investigators reported financial relationships with Bayer, Shire, Pfizer, Novo Nordisk, and others.
SOURCE: Santagostino E et al. EAHAD 2019, Abstract OR15.
PRAGUE – Emicizumab appears safe and effective for patients with hemophilia A undergoing surgical procedures, based on experience with a subpopulation of HAVEN 3 trial participants.
Out of 28 minor procedures performed without preventive factor VIII (FVIII), only 2 were associated with postoperative bleeds requiring treatment, reported lead author Elena Santagostino, MD, PhD, of Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico in Milan, and her colleagues.
All events requiring bleeding treatment were associated with dental procedures, highlighting an area where clinicians and dentists may need to exercise caution. Still, overall results supported emicizumab in a surgical setting.
“There were no thrombotic complications or other unexpected events, including inhibitor development,” Dr. Santagostino said at the annual congress of the European Association for Haemophilia and Allied Disorders.
The findings were drawn from 30 patients who underwent 50 surgeries (46 minor, 4 major) during HAVEN 3, a previously reported phase 3 trial investigating the use of emicizumab, a humanized bispecific monoclonal antibody for patients with hemophilia A without inhibitors.
The minor surgeries included dental or orthopedic procedures, esophagogastroduodenoscopy, or colonoscopy. The four major procedures were all orthopedic (knee arthroscopic synovectomy, biceps femoris tear repair, total ankle arthroplasty, and total hip replacement). The investigators analyzed surgery-related bleeds and the nature of FVIII usage.
Preventive FVIII was used in 18 procedures; infusion duration was 24 hours or less in 14 procedures, between 25 hours and 48 hours in 2 procedures, and more than 72 hours in 2 procedures. The median cumulative preventive FVIII dose per procedure was 30 IU/kg.
Of the 46 minor procedures, 28 (61%) were performed without preventive FVIII, and 2 (7.1%) were associated with bleeding requiring treatment, both after dental procedures. Two other participants who received preventive FVIII also needed postoperative bleeding treatment. Of note, these events were also after dental procedures, meaning all four instances of bleeding requiring treatment during the trial were associated with dentistry.
“[I]n this experience, dental procedures were somewhat tricky because the bleeding complications were mainly there,” Dr. Santagostino said.
When asked by an audience member if this trend was unique to mucosal bleeding, Dr. Santagostino said it was too early to draw such a conclusion but offered some insight. “To control and prevent bleeding during a dental procedure is not trivial, because … sometimes if you stop factor VIII treatment quite early, you may have late bleeding, mainly due to local reasons, because … dental procedures are very heterogenous.”
Among three other participants who had postoperative bleeding but did not require treatment, two underwent dental procedures, further supporting this association. Although the study numbers are relatively small, the findings may at least support caution, if not preventive FVIII in the dental setting, Dr. Santagostino said.
The four major procedures – all orthopedic – were knee arthroscopic synovectomy, biceps femoris tear repair, total ankle arthroplasty, and total hip replacement. Along with preoperative preventive FVIII, three of four patients undergoing major surgery received preventive FVIII for 14-18 days postoperatively. Doses ranged from 99-522 IU/kg. No postoperative bleeds occurred in this subgroup.
Study funding was provided by F. Hoffmann–La Roche and Chugai Pharmaceutical. The investigators reported financial relationships with Bayer, Shire, Pfizer, Novo Nordisk, and others.
SOURCE: Santagostino E et al. EAHAD 2019, Abstract OR15.
PRAGUE – Emicizumab appears safe and effective for patients with hemophilia A undergoing surgical procedures, based on experience with a subpopulation of HAVEN 3 trial participants.
Out of 28 minor procedures performed without preventive factor VIII (FVIII), only 2 were associated with postoperative bleeds requiring treatment, reported lead author Elena Santagostino, MD, PhD, of Fondazione IRCCS Ca’ Granda Ospedale Maggiore Policlinico in Milan, and her colleagues.
All events requiring bleeding treatment were associated with dental procedures, highlighting an area where clinicians and dentists may need to exercise caution. Still, overall results supported emicizumab in a surgical setting.
“There were no thrombotic complications or other unexpected events, including inhibitor development,” Dr. Santagostino said at the annual congress of the European Association for Haemophilia and Allied Disorders.
The findings were drawn from 30 patients who underwent 50 surgeries (46 minor, 4 major) during HAVEN 3, a previously reported phase 3 trial investigating the use of emicizumab, a humanized bispecific monoclonal antibody for patients with hemophilia A without inhibitors.
The minor surgeries included dental or orthopedic procedures, esophagogastroduodenoscopy, or colonoscopy. The four major procedures were all orthopedic (knee arthroscopic synovectomy, biceps femoris tear repair, total ankle arthroplasty, and total hip replacement). The investigators analyzed surgery-related bleeds and the nature of FVIII usage.
Preventive FVIII was used in 18 procedures; infusion duration was 24 hours or less in 14 procedures, between 25 hours and 48 hours in 2 procedures, and more than 72 hours in 2 procedures. The median cumulative preventive FVIII dose per procedure was 30 IU/kg.
Of the 46 minor procedures, 28 (61%) were performed without preventive FVIII, and 2 (7.1%) were associated with bleeding requiring treatment, both after dental procedures. Two other participants who received preventive FVIII also needed postoperative bleeding treatment. Of note, these events were also after dental procedures, meaning all four instances of bleeding requiring treatment during the trial were associated with dentistry.
“[I]n this experience, dental procedures were somewhat tricky because the bleeding complications were mainly there,” Dr. Santagostino said.
When asked by an audience member if this trend was unique to mucosal bleeding, Dr. Santagostino said it was too early to draw such a conclusion but offered some insight. “To control and prevent bleeding during a dental procedure is not trivial, because … sometimes if you stop factor VIII treatment quite early, you may have late bleeding, mainly due to local reasons, because … dental procedures are very heterogenous.”
Among three other participants who had postoperative bleeding but did not require treatment, two underwent dental procedures, further supporting this association. Although the study numbers are relatively small, the findings may at least support caution, if not preventive FVIII in the dental setting, Dr. Santagostino said.
The four major procedures – all orthopedic – were knee arthroscopic synovectomy, biceps femoris tear repair, total ankle arthroplasty, and total hip replacement. Along with preoperative preventive FVIII, three of four patients undergoing major surgery received preventive FVIII for 14-18 days postoperatively. Doses ranged from 99-522 IU/kg. No postoperative bleeds occurred in this subgroup.
Study funding was provided by F. Hoffmann–La Roche and Chugai Pharmaceutical. The investigators reported financial relationships with Bayer, Shire, Pfizer, Novo Nordisk, and others.
SOURCE: Santagostino E et al. EAHAD 2019, Abstract OR15.
REPORTING FROM EAHAD 2019