User login
Burnout in medical profession higher among women, younger clinicians
The poster child for a burned-out physician is a young woman practicing in primary care, according to a new study of more than 1,300 clinicians.
The study, published in JAMA Network Open. investigated patterns in physician burnout among 1,373 physicians at Massachusetts General Physicians Organization, a hospital-owned group practice. It assessed burnout in 3 years: 2017, 2019, and 2021.
Respondents were queried about their satisfaction with their career and compensation, as well as their well-being, administrative workload, and leadership and diversity.
Female physicians exhibited a higher burnout rate than male physicians (odds ratio, 1.47; 95% confidence interval, 1.02-2.12), while among primary care physicians (PCPs), the burnout rate was almost three times higher than among those in internal medicine (OR, 2.82; 95% CI, 1.76-4.50). Among physicians with 30 or more years of experience, the burnout rate was lower than among those with 10 years of experience or less (OR, 0.21; 95% CI, 0.13-0.35).
The fact that burnout disproportionately affects female physicians could reflect the additional household and family obligations women are often expected to handle, as well as their desire to form relationships with their patients, according to Timothy Hoff, PhD, a professor of management, healthcare systems, and health policy at Northeastern University, Boston.
“Female physicians tend to practice differently than their male counterparts,” said Dr. Hoff, who studies primary care. “They may focus more on the relational aspects of care, and that could lead to a higher rate of burnout.”
The study used the Maslach Burnout Inventory and three burnout subscales: exhaustion, cynicism, and reduced personal efficacy. The cohort was composed of 50% men, 67% White respondents, and 87% non-Hispanic respondents. A little over two-thirds of physicians had from 11 to 20 years of experience.
About 93% of those surveyed responded; by comparison, response rates were between 27% and 32% in previous analyses of physician burnout, the study authors say. They attribute this high participation rate to the fact that they compensated each participant with $850, more than is usually offered.
Hilton Gomes, MD, a partner at a concierge primary care practice in Miami – who has been practicing medicine for more than 15 years – said the increased rates of burnout among his younger colleagues are partly the result of a recent shift in what is considered the ideal work-life balance.
“Younger generations of doctors enter the profession with a strong desire for a better work-life balance. Unfortunately, medicine does not typically lend itself to achieving this balance,” he said.
Dr. Gomes recalled a time in medical school when he tried to visit his former pediatrician, who couldn’t be found at home.
“His wife informed me that he was tending to an urgent sick visit at the hospital, while his wife had to deal with their own grandson’s fracture being treated at urgent care,” Dr. Gomes said. “This illustrates, in my experience, how older generations of physicians accepted the demands of the profession as part of their commitment, and this often involved putting our own families second.”
Dr. Gomes, like many other PCPs who have converted to concierge medicine, previously worked at a practice where he saw nearly two dozen patients a day for a maximum of 15 minutes each.
“The structure of managed care often results in primary care physicians spending less time with patients and more time on paperwork, which is not the reason why physicians enter the field of medicine,” Dr. Gomes said.
Physicians are not alone in their feelings of physical and mental exhaustion. In the Medscape Physician Assistant Burnout Report 2023, 16% of respondents said the burnout they experienced was so severe that they were thinking of leaving medicine.
In 2022, PCP burnout cost the United States $260 million in excess health care expenditures. Burnout has also increased rates of physician suicide over the past 50 years and has led to a rise in medical errors.
Physicians say that programs that teach them to perform yoga and take deep breaths – which are offered by their employers – are not the solution.
“We sort of know what the realities of physician burnout are now; the imperative is to address it,” Dr. Hoff said. “We need studies that focus on the concepts of sustainability.”
The study was funded by the Massachusetts General Physicians Organization. A coauthor reports receiving a grant from the American Heart Association. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
The poster child for a burned-out physician is a young woman practicing in primary care, according to a new study of more than 1,300 clinicians.
The study, published in JAMA Network Open. investigated patterns in physician burnout among 1,373 physicians at Massachusetts General Physicians Organization, a hospital-owned group practice. It assessed burnout in 3 years: 2017, 2019, and 2021.
Respondents were queried about their satisfaction with their career and compensation, as well as their well-being, administrative workload, and leadership and diversity.
Female physicians exhibited a higher burnout rate than male physicians (odds ratio, 1.47; 95% confidence interval, 1.02-2.12), while among primary care physicians (PCPs), the burnout rate was almost three times higher than among those in internal medicine (OR, 2.82; 95% CI, 1.76-4.50). Among physicians with 30 or more years of experience, the burnout rate was lower than among those with 10 years of experience or less (OR, 0.21; 95% CI, 0.13-0.35).
The fact that burnout disproportionately affects female physicians could reflect the additional household and family obligations women are often expected to handle, as well as their desire to form relationships with their patients, according to Timothy Hoff, PhD, a professor of management, healthcare systems, and health policy at Northeastern University, Boston.
“Female physicians tend to practice differently than their male counterparts,” said Dr. Hoff, who studies primary care. “They may focus more on the relational aspects of care, and that could lead to a higher rate of burnout.”
The study used the Maslach Burnout Inventory and three burnout subscales: exhaustion, cynicism, and reduced personal efficacy. The cohort was composed of 50% men, 67% White respondents, and 87% non-Hispanic respondents. A little over two-thirds of physicians had from 11 to 20 years of experience.
About 93% of those surveyed responded; by comparison, response rates were between 27% and 32% in previous analyses of physician burnout, the study authors say. They attribute this high participation rate to the fact that they compensated each participant with $850, more than is usually offered.
Hilton Gomes, MD, a partner at a concierge primary care practice in Miami – who has been practicing medicine for more than 15 years – said the increased rates of burnout among his younger colleagues are partly the result of a recent shift in what is considered the ideal work-life balance.
“Younger generations of doctors enter the profession with a strong desire for a better work-life balance. Unfortunately, medicine does not typically lend itself to achieving this balance,” he said.
Dr. Gomes recalled a time in medical school when he tried to visit his former pediatrician, who couldn’t be found at home.
“His wife informed me that he was tending to an urgent sick visit at the hospital, while his wife had to deal with their own grandson’s fracture being treated at urgent care,” Dr. Gomes said. “This illustrates, in my experience, how older generations of physicians accepted the demands of the profession as part of their commitment, and this often involved putting our own families second.”
Dr. Gomes, like many other PCPs who have converted to concierge medicine, previously worked at a practice where he saw nearly two dozen patients a day for a maximum of 15 minutes each.
“The structure of managed care often results in primary care physicians spending less time with patients and more time on paperwork, which is not the reason why physicians enter the field of medicine,” Dr. Gomes said.
Physicians are not alone in their feelings of physical and mental exhaustion. In the Medscape Physician Assistant Burnout Report 2023, 16% of respondents said the burnout they experienced was so severe that they were thinking of leaving medicine.
In 2022, PCP burnout cost the United States $260 million in excess health care expenditures. Burnout has also increased rates of physician suicide over the past 50 years and has led to a rise in medical errors.
Physicians say that programs that teach them to perform yoga and take deep breaths – which are offered by their employers – are not the solution.
“We sort of know what the realities of physician burnout are now; the imperative is to address it,” Dr. Hoff said. “We need studies that focus on the concepts of sustainability.”
The study was funded by the Massachusetts General Physicians Organization. A coauthor reports receiving a grant from the American Heart Association. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
The poster child for a burned-out physician is a young woman practicing in primary care, according to a new study of more than 1,300 clinicians.
The study, published in JAMA Network Open. investigated patterns in physician burnout among 1,373 physicians at Massachusetts General Physicians Organization, a hospital-owned group practice. It assessed burnout in 3 years: 2017, 2019, and 2021.
Respondents were queried about their satisfaction with their career and compensation, as well as their well-being, administrative workload, and leadership and diversity.
Female physicians exhibited a higher burnout rate than male physicians (odds ratio, 1.47; 95% confidence interval, 1.02-2.12), while among primary care physicians (PCPs), the burnout rate was almost three times higher than among those in internal medicine (OR, 2.82; 95% CI, 1.76-4.50). Among physicians with 30 or more years of experience, the burnout rate was lower than among those with 10 years of experience or less (OR, 0.21; 95% CI, 0.13-0.35).
The fact that burnout disproportionately affects female physicians could reflect the additional household and family obligations women are often expected to handle, as well as their desire to form relationships with their patients, according to Timothy Hoff, PhD, a professor of management, healthcare systems, and health policy at Northeastern University, Boston.
“Female physicians tend to practice differently than their male counterparts,” said Dr. Hoff, who studies primary care. “They may focus more on the relational aspects of care, and that could lead to a higher rate of burnout.”
The study used the Maslach Burnout Inventory and three burnout subscales: exhaustion, cynicism, and reduced personal efficacy. The cohort was composed of 50% men, 67% White respondents, and 87% non-Hispanic respondents. A little over two-thirds of physicians had from 11 to 20 years of experience.
About 93% of those surveyed responded; by comparison, response rates were between 27% and 32% in previous analyses of physician burnout, the study authors say. They attribute this high participation rate to the fact that they compensated each participant with $850, more than is usually offered.
Hilton Gomes, MD, a partner at a concierge primary care practice in Miami – who has been practicing medicine for more than 15 years – said the increased rates of burnout among his younger colleagues are partly the result of a recent shift in what is considered the ideal work-life balance.
“Younger generations of doctors enter the profession with a strong desire for a better work-life balance. Unfortunately, medicine does not typically lend itself to achieving this balance,” he said.
Dr. Gomes recalled a time in medical school when he tried to visit his former pediatrician, who couldn’t be found at home.
“His wife informed me that he was tending to an urgent sick visit at the hospital, while his wife had to deal with their own grandson’s fracture being treated at urgent care,” Dr. Gomes said. “This illustrates, in my experience, how older generations of physicians accepted the demands of the profession as part of their commitment, and this often involved putting our own families second.”
Dr. Gomes, like many other PCPs who have converted to concierge medicine, previously worked at a practice where he saw nearly two dozen patients a day for a maximum of 15 minutes each.
“The structure of managed care often results in primary care physicians spending less time with patients and more time on paperwork, which is not the reason why physicians enter the field of medicine,” Dr. Gomes said.
Physicians are not alone in their feelings of physical and mental exhaustion. In the Medscape Physician Assistant Burnout Report 2023, 16% of respondents said the burnout they experienced was so severe that they were thinking of leaving medicine.
In 2022, PCP burnout cost the United States $260 million in excess health care expenditures. Burnout has also increased rates of physician suicide over the past 50 years and has led to a rise in medical errors.
Physicians say that programs that teach them to perform yoga and take deep breaths – which are offered by their employers – are not the solution.
“We sort of know what the realities of physician burnout are now; the imperative is to address it,” Dr. Hoff said. “We need studies that focus on the concepts of sustainability.”
The study was funded by the Massachusetts General Physicians Organization. A coauthor reports receiving a grant from the American Heart Association. No other disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
History of depression, stress tied to Alzheimer’s, MCI risk
TOPLINE:
compared with those without either condition, a new study found.
METHODOLOGY:
- Longitudinal cohort study of 1,362,548 people with records in the Region Stockholm administrative health care database with a diagnosis of stress-induced exhaustion disorder (SED), depression, or both between 2012 and 2013.
- Cohort followed for diagnosis of MCI or AD between 2014 and 2022.
TAKEAWAY:
- SED diagnosed in 0.3%, depression in 2.9% and both SED and depression in 0.1%
- Compared with people without SED or depression, AD risk was more than double in patients with SED (adjusted odds ratio [aOR], 2.45; 99% confidence interval [CI], 1.22-4.91) or depression (aOR, 2.32; 99% CI, 1.85-2.90) and four times higher in patients with both SED and depression (aOR, 4.00; 99% CI, 1.67-9.58)
- Risk for MCI was also higher in people with SED (aOR, 1.87; 99% CI,1.20-2.91), depression (aOR, 2.85; 99% CI, 2.53-3.22) or both SED and depression (aOR, 3.87; 99% CI, 2.39-6.27) vs patients with no history of SED or depression.
- Only patients with depression had a higher risk for another dementia type (aOR, 2.39; 99% CI, 1.92-2.96).
IN PRACTICE:
“Future studies should examine the possibility that symptoms of depression and/or chronic stress could be prodromal symptoms of dementia rather than risk factors,” study authors wrote.
SOURCE:
The study was conducted by Johanna Wallensten, doctoral student, department of clinical sciences, Danderyd Hospital, Stockholm, and colleagues and funded by the Karolinska Institute. It was published online in Alzheimer’s Research and Therapy.
LIMITATIONS:
Use of a health care registry could have led to over- or underestimation of depression, MCI and AD. The study probably captures most people with depression but not most people with depressive symptoms.
DISCLOSURES:
The authors reported no relevant conflicts.
A version of this article appeared on Medscape.com.
TOPLINE:
compared with those without either condition, a new study found.
METHODOLOGY:
- Longitudinal cohort study of 1,362,548 people with records in the Region Stockholm administrative health care database with a diagnosis of stress-induced exhaustion disorder (SED), depression, or both between 2012 and 2013.
- Cohort followed for diagnosis of MCI or AD between 2014 and 2022.
TAKEAWAY:
- SED diagnosed in 0.3%, depression in 2.9% and both SED and depression in 0.1%
- Compared with people without SED or depression, AD risk was more than double in patients with SED (adjusted odds ratio [aOR], 2.45; 99% confidence interval [CI], 1.22-4.91) or depression (aOR, 2.32; 99% CI, 1.85-2.90) and four times higher in patients with both SED and depression (aOR, 4.00; 99% CI, 1.67-9.58)
- Risk for MCI was also higher in people with SED (aOR, 1.87; 99% CI,1.20-2.91), depression (aOR, 2.85; 99% CI, 2.53-3.22) or both SED and depression (aOR, 3.87; 99% CI, 2.39-6.27) vs patients with no history of SED or depression.
- Only patients with depression had a higher risk for another dementia type (aOR, 2.39; 99% CI, 1.92-2.96).
IN PRACTICE:
“Future studies should examine the possibility that symptoms of depression and/or chronic stress could be prodromal symptoms of dementia rather than risk factors,” study authors wrote.
SOURCE:
The study was conducted by Johanna Wallensten, doctoral student, department of clinical sciences, Danderyd Hospital, Stockholm, and colleagues and funded by the Karolinska Institute. It was published online in Alzheimer’s Research and Therapy.
LIMITATIONS:
Use of a health care registry could have led to over- or underestimation of depression, MCI and AD. The study probably captures most people with depression but not most people with depressive symptoms.
DISCLOSURES:
The authors reported no relevant conflicts.
A version of this article appeared on Medscape.com.
TOPLINE:
compared with those without either condition, a new study found.
METHODOLOGY:
- Longitudinal cohort study of 1,362,548 people with records in the Region Stockholm administrative health care database with a diagnosis of stress-induced exhaustion disorder (SED), depression, or both between 2012 and 2013.
- Cohort followed for diagnosis of MCI or AD between 2014 and 2022.
TAKEAWAY:
- SED diagnosed in 0.3%, depression in 2.9% and both SED and depression in 0.1%
- Compared with people without SED or depression, AD risk was more than double in patients with SED (adjusted odds ratio [aOR], 2.45; 99% confidence interval [CI], 1.22-4.91) or depression (aOR, 2.32; 99% CI, 1.85-2.90) and four times higher in patients with both SED and depression (aOR, 4.00; 99% CI, 1.67-9.58)
- Risk for MCI was also higher in people with SED (aOR, 1.87; 99% CI,1.20-2.91), depression (aOR, 2.85; 99% CI, 2.53-3.22) or both SED and depression (aOR, 3.87; 99% CI, 2.39-6.27) vs patients with no history of SED or depression.
- Only patients with depression had a higher risk for another dementia type (aOR, 2.39; 99% CI, 1.92-2.96).
IN PRACTICE:
“Future studies should examine the possibility that symptoms of depression and/or chronic stress could be prodromal symptoms of dementia rather than risk factors,” study authors wrote.
SOURCE:
The study was conducted by Johanna Wallensten, doctoral student, department of clinical sciences, Danderyd Hospital, Stockholm, and colleagues and funded by the Karolinska Institute. It was published online in Alzheimer’s Research and Therapy.
LIMITATIONS:
Use of a health care registry could have led to over- or underestimation of depression, MCI and AD. The study probably captures most people with depression but not most people with depressive symptoms.
DISCLOSURES:
The authors reported no relevant conflicts.
A version of this article appeared on Medscape.com.
Depression tied to higher all-cause and cardiovascular mortality
In a large prospective study, a graded higher risk of all-cause mortality and mortality from cardiovascular disease (CVD) and ischemic heart disease (IHD) emerged in adults with moderate to severe depressive symptoms, compared with those with no such symptoms.
Participants with mild depressive symptoms had a 35%-49% higher risk of all-cause and CVD mortality, respectively, while for those with moderate to severe depressive symptoms, the risk of all-cause, CVD, and IHD mortality was 62%, 79%, and 121% higher, respectively.
“This information highlights the importance for clinicians to identify patients with depressive symptoms and help them engage in treatment,” lead author Zefeng Zhang, MD, PhD, of the division for heart disease and stroke prevention at the U.S. Centers for Disease Control and Prevention, Atlanta, said in an interview.
The study appears in JAMA Network Open.
A nonclassic risk factor for CVD death
This graded positive association between depressive symptoms and CVD death was observed in data from the National Health and Nutrition Examination Survey 2005-2018, which were linked with the National Death Index through 2019 for adults aged 20 and older. Data analysis occurred from March 1 to May 26, 2023. According to the authors, their analyses extend findings from previous research by assessing these associations in a large, diverse, and nationally representative sample. Using more nuanced CVD-related causes of death, depressive symptoms emerged as a nontraditional risk factor for CVD mortality.
The study
In a total cohort of 23,694, about half male, mean overall age 44.7 years, prevalences of mild and moderate to severe depression were 14.9% and 7.2%, respectively, with depressive symptoms assessed by the nine-item Patient Health Questionnaire asking about symptoms over the past 2 weeks.
Adults with depression had significantly lower CV health scores in six of the American Heart Association Life’s Essential 8 metrics for heart health. For all-cause mortality, hazard ratios were 1.35 (95% confidence interval, 1.07-1.72) for mild depressive symptoms vs. none and 1.62 (95% CI, 1.24-2.12) for moderate to severe depressive symptoms vs. none.
The corresponding hazard ratios were 1.49 (95% CI, 1.11-2.0) and 1.79 (95% CI,1.22-2.62) for CVD mortality and 0.96 (95% CI, 0.58-1.60) and 2.21 (95% CI, 1.24-3.91) for IHD death, with associations largely consistent across subgroups.
At the highest severity of depressive symptoms (almost daily for past 2 weeks), feeling tired or having little energy, poor appetite or overeating, and having little interest in doing things were significantly associated with all-cause and CVD mortality after adjusting for potential confounders.
Approximately 11%-16% of the positive associations could be explained by lifestyle factors such as excess alcohol consumption, overeating, and inactivity as per the AHA’s Life’s Essential 8 metrics.
“Taken together with the body of literature on associations between depression and CVD mortality, these findings can support public health efforts to develop a comprehensive, nationwide strategy to improve well-being, including both mental and cardiovascular health,” Dr. Zhang and associates wrote.
This research was funded by the U.S. Centers for Disease Control and Prevention. The authors had no conflicts of interest to disclose.
In a large prospective study, a graded higher risk of all-cause mortality and mortality from cardiovascular disease (CVD) and ischemic heart disease (IHD) emerged in adults with moderate to severe depressive symptoms, compared with those with no such symptoms.
Participants with mild depressive symptoms had a 35%-49% higher risk of all-cause and CVD mortality, respectively, while for those with moderate to severe depressive symptoms, the risk of all-cause, CVD, and IHD mortality was 62%, 79%, and 121% higher, respectively.
“This information highlights the importance for clinicians to identify patients with depressive symptoms and help them engage in treatment,” lead author Zefeng Zhang, MD, PhD, of the division for heart disease and stroke prevention at the U.S. Centers for Disease Control and Prevention, Atlanta, said in an interview.
The study appears in JAMA Network Open.
A nonclassic risk factor for CVD death
This graded positive association between depressive symptoms and CVD death was observed in data from the National Health and Nutrition Examination Survey 2005-2018, which were linked with the National Death Index through 2019 for adults aged 20 and older. Data analysis occurred from March 1 to May 26, 2023. According to the authors, their analyses extend findings from previous research by assessing these associations in a large, diverse, and nationally representative sample. Using more nuanced CVD-related causes of death, depressive symptoms emerged as a nontraditional risk factor for CVD mortality.
The study
In a total cohort of 23,694, about half male, mean overall age 44.7 years, prevalences of mild and moderate to severe depression were 14.9% and 7.2%, respectively, with depressive symptoms assessed by the nine-item Patient Health Questionnaire asking about symptoms over the past 2 weeks.
Adults with depression had significantly lower CV health scores in six of the American Heart Association Life’s Essential 8 metrics for heart health. For all-cause mortality, hazard ratios were 1.35 (95% confidence interval, 1.07-1.72) for mild depressive symptoms vs. none and 1.62 (95% CI, 1.24-2.12) for moderate to severe depressive symptoms vs. none.
The corresponding hazard ratios were 1.49 (95% CI, 1.11-2.0) and 1.79 (95% CI,1.22-2.62) for CVD mortality and 0.96 (95% CI, 0.58-1.60) and 2.21 (95% CI, 1.24-3.91) for IHD death, with associations largely consistent across subgroups.
At the highest severity of depressive symptoms (almost daily for past 2 weeks), feeling tired or having little energy, poor appetite or overeating, and having little interest in doing things were significantly associated with all-cause and CVD mortality after adjusting for potential confounders.
Approximately 11%-16% of the positive associations could be explained by lifestyle factors such as excess alcohol consumption, overeating, and inactivity as per the AHA’s Life’s Essential 8 metrics.
“Taken together with the body of literature on associations between depression and CVD mortality, these findings can support public health efforts to develop a comprehensive, nationwide strategy to improve well-being, including both mental and cardiovascular health,” Dr. Zhang and associates wrote.
This research was funded by the U.S. Centers for Disease Control and Prevention. The authors had no conflicts of interest to disclose.
In a large prospective study, a graded higher risk of all-cause mortality and mortality from cardiovascular disease (CVD) and ischemic heart disease (IHD) emerged in adults with moderate to severe depressive symptoms, compared with those with no such symptoms.
Participants with mild depressive symptoms had a 35%-49% higher risk of all-cause and CVD mortality, respectively, while for those with moderate to severe depressive symptoms, the risk of all-cause, CVD, and IHD mortality was 62%, 79%, and 121% higher, respectively.
“This information highlights the importance for clinicians to identify patients with depressive symptoms and help them engage in treatment,” lead author Zefeng Zhang, MD, PhD, of the division for heart disease and stroke prevention at the U.S. Centers for Disease Control and Prevention, Atlanta, said in an interview.
The study appears in JAMA Network Open.
A nonclassic risk factor for CVD death
This graded positive association between depressive symptoms and CVD death was observed in data from the National Health and Nutrition Examination Survey 2005-2018, which were linked with the National Death Index through 2019 for adults aged 20 and older. Data analysis occurred from March 1 to May 26, 2023. According to the authors, their analyses extend findings from previous research by assessing these associations in a large, diverse, and nationally representative sample. Using more nuanced CVD-related causes of death, depressive symptoms emerged as a nontraditional risk factor for CVD mortality.
The study
In a total cohort of 23,694, about half male, mean overall age 44.7 years, prevalences of mild and moderate to severe depression were 14.9% and 7.2%, respectively, with depressive symptoms assessed by the nine-item Patient Health Questionnaire asking about symptoms over the past 2 weeks.
Adults with depression had significantly lower CV health scores in six of the American Heart Association Life’s Essential 8 metrics for heart health. For all-cause mortality, hazard ratios were 1.35 (95% confidence interval, 1.07-1.72) for mild depressive symptoms vs. none and 1.62 (95% CI, 1.24-2.12) for moderate to severe depressive symptoms vs. none.
The corresponding hazard ratios were 1.49 (95% CI, 1.11-2.0) and 1.79 (95% CI,1.22-2.62) for CVD mortality and 0.96 (95% CI, 0.58-1.60) and 2.21 (95% CI, 1.24-3.91) for IHD death, with associations largely consistent across subgroups.
At the highest severity of depressive symptoms (almost daily for past 2 weeks), feeling tired or having little energy, poor appetite or overeating, and having little interest in doing things were significantly associated with all-cause and CVD mortality after adjusting for potential confounders.
Approximately 11%-16% of the positive associations could be explained by lifestyle factors such as excess alcohol consumption, overeating, and inactivity as per the AHA’s Life’s Essential 8 metrics.
“Taken together with the body of literature on associations between depression and CVD mortality, these findings can support public health efforts to develop a comprehensive, nationwide strategy to improve well-being, including both mental and cardiovascular health,” Dr. Zhang and associates wrote.
This research was funded by the U.S. Centers for Disease Control and Prevention. The authors had no conflicts of interest to disclose.
FROM JAMA NETWORK OPEN
Irritable temperament predicts bipolar disorder risk
When German psychiatrist Emil Kraepelin (1856-1926) studied emotions in patients with affective disorders, he identified four temperaments: the depressive (DT), the hyperthymic (HT), the irritable (IT), and the cyclothymic (CT). Subsequent researchers later identified an anxious temperament (AT).
“The notion that temperaments can be useful in predicting bipolar disorders sparked a plethora of research,” wrote Elie G. Karam, MD, of Saint George Hospital, Beirut, and colleagues. In particular, the cyclothymic (CT) and irritable (IT) temperament types have been targeted in studies of patients with bipolar disorders, but previous studies of temperament and bipolar have been limited by methodological issues, they said.
In a study published in European Psychiatry, the researchers reviewed data from 1,723 consecutive adult outpatients who presented to a university-based mental health clinic with various symptoms between January 2014 and September 2019.
Patients were assessed using the Hypomania Checklist-32 (HCL-32) and the Temperament Evaluation of Memphis, Pisa, Paris, and San Diego-Auto-questionnaire (TEMPS-A), then were diagnosed by psychiatrists using DSM-5 criteria. Patients with any bipolar types as defined by the DSM-5 underwent simple and multiple binary logistic regression analyses. The analysis included continuous scores and categorical normalized z-scores.
A total of 369 patients had confirmed DSM-5 diagnosis of bipolar disorder (52 with type I, 176 with type II, 102 with other specified bipolar and related disorder, and 39 with substance- or medication-induced bipolar disorder. The mean age of the participants was 38 years, and 54% were female.
In a bivariate analysis, all continuous temperament scores were significant predictors of bipolar disorder; all except AT remained significant in multivariate analysis. Increasing scores of IT, CT, and HT were associated with bipolar disorder, but increasing scores of DT were reflective of lower chance of bipolar disorder, the researchers noted.
In multivariate analysis of categorical normalized z-scores, IT and CT were significant predictors of bipolar disorder. At the highest point, CT was the stronger predictor, compared with IT (odds ratio, 3.84 vs. 2.55); having a higher DT score significantly reduced the odds of bipolar disorder (OR, 0.50).
However, “after adjusting for the presence of all temperaments as well as age and gender, only IT remained a significant predictor of patients with bipolar I disorder with adjusted OR of 1.19,” the researchers wrote.
“Correlations among temperaments were solid whether looking at patients with bipolarity or not, further emphasizing the necessity of controlling for them,” the researchers wrote in their discussion.
The findings were limited by several factors including the lack of structured interviews, the use of an outpatient-only sample, and the small number of bipolar I patients, the researchers noted.
However, the result suggest that IT can serve as a predictor of bipolar I and bipolar II disorders they said. Given the underdiagnosis of bipolar disorder in many studies, the incorporation of temperaments into the assessment of patients and research participants alike is likely to help us detect the presence of bipolarity more readily and quite importantly help us in our quest to understand their genesis,” they concluded.
The study was supported in part by anonymous private unrestricted donations to IDRAAC, Lebanon, and by Eli Lilly. The researchers had no financial conflicts to disclose.
When German psychiatrist Emil Kraepelin (1856-1926) studied emotions in patients with affective disorders, he identified four temperaments: the depressive (DT), the hyperthymic (HT), the irritable (IT), and the cyclothymic (CT). Subsequent researchers later identified an anxious temperament (AT).
“The notion that temperaments can be useful in predicting bipolar disorders sparked a plethora of research,” wrote Elie G. Karam, MD, of Saint George Hospital, Beirut, and colleagues. In particular, the cyclothymic (CT) and irritable (IT) temperament types have been targeted in studies of patients with bipolar disorders, but previous studies of temperament and bipolar have been limited by methodological issues, they said.
In a study published in European Psychiatry, the researchers reviewed data from 1,723 consecutive adult outpatients who presented to a university-based mental health clinic with various symptoms between January 2014 and September 2019.
Patients were assessed using the Hypomania Checklist-32 (HCL-32) and the Temperament Evaluation of Memphis, Pisa, Paris, and San Diego-Auto-questionnaire (TEMPS-A), then were diagnosed by psychiatrists using DSM-5 criteria. Patients with any bipolar types as defined by the DSM-5 underwent simple and multiple binary logistic regression analyses. The analysis included continuous scores and categorical normalized z-scores.
A total of 369 patients had confirmed DSM-5 diagnosis of bipolar disorder (52 with type I, 176 with type II, 102 with other specified bipolar and related disorder, and 39 with substance- or medication-induced bipolar disorder. The mean age of the participants was 38 years, and 54% were female.
In a bivariate analysis, all continuous temperament scores were significant predictors of bipolar disorder; all except AT remained significant in multivariate analysis. Increasing scores of IT, CT, and HT were associated with bipolar disorder, but increasing scores of DT were reflective of lower chance of bipolar disorder, the researchers noted.
In multivariate analysis of categorical normalized z-scores, IT and CT were significant predictors of bipolar disorder. At the highest point, CT was the stronger predictor, compared with IT (odds ratio, 3.84 vs. 2.55); having a higher DT score significantly reduced the odds of bipolar disorder (OR, 0.50).
However, “after adjusting for the presence of all temperaments as well as age and gender, only IT remained a significant predictor of patients with bipolar I disorder with adjusted OR of 1.19,” the researchers wrote.
“Correlations among temperaments were solid whether looking at patients with bipolarity or not, further emphasizing the necessity of controlling for them,” the researchers wrote in their discussion.
The findings were limited by several factors including the lack of structured interviews, the use of an outpatient-only sample, and the small number of bipolar I patients, the researchers noted.
However, the result suggest that IT can serve as a predictor of bipolar I and bipolar II disorders they said. Given the underdiagnosis of bipolar disorder in many studies, the incorporation of temperaments into the assessment of patients and research participants alike is likely to help us detect the presence of bipolarity more readily and quite importantly help us in our quest to understand their genesis,” they concluded.
The study was supported in part by anonymous private unrestricted donations to IDRAAC, Lebanon, and by Eli Lilly. The researchers had no financial conflicts to disclose.
When German psychiatrist Emil Kraepelin (1856-1926) studied emotions in patients with affective disorders, he identified four temperaments: the depressive (DT), the hyperthymic (HT), the irritable (IT), and the cyclothymic (CT). Subsequent researchers later identified an anxious temperament (AT).
“The notion that temperaments can be useful in predicting bipolar disorders sparked a plethora of research,” wrote Elie G. Karam, MD, of Saint George Hospital, Beirut, and colleagues. In particular, the cyclothymic (CT) and irritable (IT) temperament types have been targeted in studies of patients with bipolar disorders, but previous studies of temperament and bipolar have been limited by methodological issues, they said.
In a study published in European Psychiatry, the researchers reviewed data from 1,723 consecutive adult outpatients who presented to a university-based mental health clinic with various symptoms between January 2014 and September 2019.
Patients were assessed using the Hypomania Checklist-32 (HCL-32) and the Temperament Evaluation of Memphis, Pisa, Paris, and San Diego-Auto-questionnaire (TEMPS-A), then were diagnosed by psychiatrists using DSM-5 criteria. Patients with any bipolar types as defined by the DSM-5 underwent simple and multiple binary logistic regression analyses. The analysis included continuous scores and categorical normalized z-scores.
A total of 369 patients had confirmed DSM-5 diagnosis of bipolar disorder (52 with type I, 176 with type II, 102 with other specified bipolar and related disorder, and 39 with substance- or medication-induced bipolar disorder. The mean age of the participants was 38 years, and 54% were female.
In a bivariate analysis, all continuous temperament scores were significant predictors of bipolar disorder; all except AT remained significant in multivariate analysis. Increasing scores of IT, CT, and HT were associated with bipolar disorder, but increasing scores of DT were reflective of lower chance of bipolar disorder, the researchers noted.
In multivariate analysis of categorical normalized z-scores, IT and CT were significant predictors of bipolar disorder. At the highest point, CT was the stronger predictor, compared with IT (odds ratio, 3.84 vs. 2.55); having a higher DT score significantly reduced the odds of bipolar disorder (OR, 0.50).
However, “after adjusting for the presence of all temperaments as well as age and gender, only IT remained a significant predictor of patients with bipolar I disorder with adjusted OR of 1.19,” the researchers wrote.
“Correlations among temperaments were solid whether looking at patients with bipolarity or not, further emphasizing the necessity of controlling for them,” the researchers wrote in their discussion.
The findings were limited by several factors including the lack of structured interviews, the use of an outpatient-only sample, and the small number of bipolar I patients, the researchers noted.
However, the result suggest that IT can serve as a predictor of bipolar I and bipolar II disorders they said. Given the underdiagnosis of bipolar disorder in many studies, the incorporation of temperaments into the assessment of patients and research participants alike is likely to help us detect the presence of bipolarity more readily and quite importantly help us in our quest to understand their genesis,” they concluded.
The study was supported in part by anonymous private unrestricted donations to IDRAAC, Lebanon, and by Eli Lilly. The researchers had no financial conflicts to disclose.
FROM EUROPEAN PSYCHIATRY
Substance-induced psychosis tied to schizophrenia risk
TOPLINE:
Three years after an initial ER visit, 18.5% of those with substance-induced psychosis were diagnosed with an SSD. Cannabis-induced psychosis was associated with the greatest risk.
METHODOLOGY:
- In this retrospective, population-based cohort study, investigators evaluated the risk of transition to a diagnosis of SSD for individuals with an ER visit for substance use versus the general population.
- Investigators at The Ottawa Hospital and the Institute for Clinical Evaluative Sciences, both in Ontario, analyzed data from six linked databases containing health information on nearly 10 million Ontario residents aged 14-65 years eligible for medical coverage.
- Investigators collected the health data between January 2008 and March 2022 on residents with substance use–related ER visits with, and without, psychosis.
TAKEAWAY:
- There were nearly 408,000 individuals with an ER visit for substance use, of which 13,800 (3.4%) of the visits were for substance-induced psychosis.
- Individuals with substance-induced psychosis were at a 163-fold (age- and sex-adjusted hazard ratio, 163.2; 95% confidence interval, 156.1-170.5) increased risk of transitioning to an SSD, relative to the general population (3-year risk, 18.5% vs. 0.1%).
- Individuals with an ER visit for substance use without psychosis had a lower relative risk of transitioning (aHR, 9.8; 95% CI, 9.5-10.2; 3-year risk, 1.4%) but incurred more than three times the absolute number of transitions (9,969 vs. 3,029).
- ER visits related to cannabis use had the highest transition risk among visits with psychosis (aHR, 241.6; 95% CI, 225.5-258.9) and the third-highest risk among visits without psychosis (aHR, 14.3; 95% CI, 13.5-15.2).
- Younger age and male sex were associated with a higher risk of transition, and the risk of male sex was greater in younger, compared with older, individuals particularly for cannabis use.
IN PRACTICE:
“Primary prevention efforts aimed at reducing substance use and substance use disorders could substantially reduce the population-level burden of chronic psychoses,” the investigators write. “Our findings also highlight the need for targeted secondary prevention providing early intervention and reducing substance use in the highest-risk groups, which may delay or prevent transition to schizophrenia spectrum disorders.”
SOURCE:
Daniel T. Myran, MD, MPH, of the Ottawa Hospital Research Institute, led the study, which was funded by the Canadian Institutes of Health Research and the University of Ottawa department of family medicine. The study was published online in JAMA Psychiatry.
LIMITATIONS:
Investigators did not have access to detailed data on substance-related outpatient visits or patterns of substance use, which could provide additional prognostic information.
DISCLOSURES:
Dr. Myran reported receiving grants from the Canadian Institutes of Health Research during the conduct of the study. Dr. Solmi reported receiving honoraria for participation on advisory boards or presentations from AbbVie, Angelini, Lundbeck, and Otsuka outside the submitted work. The remaining authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
Three years after an initial ER visit, 18.5% of those with substance-induced psychosis were diagnosed with an SSD. Cannabis-induced psychosis was associated with the greatest risk.
METHODOLOGY:
- In this retrospective, population-based cohort study, investigators evaluated the risk of transition to a diagnosis of SSD for individuals with an ER visit for substance use versus the general population.
- Investigators at The Ottawa Hospital and the Institute for Clinical Evaluative Sciences, both in Ontario, analyzed data from six linked databases containing health information on nearly 10 million Ontario residents aged 14-65 years eligible for medical coverage.
- Investigators collected the health data between January 2008 and March 2022 on residents with substance use–related ER visits with, and without, psychosis.
TAKEAWAY:
- There were nearly 408,000 individuals with an ER visit for substance use, of which 13,800 (3.4%) of the visits were for substance-induced psychosis.
- Individuals with substance-induced psychosis were at a 163-fold (age- and sex-adjusted hazard ratio, 163.2; 95% confidence interval, 156.1-170.5) increased risk of transitioning to an SSD, relative to the general population (3-year risk, 18.5% vs. 0.1%).
- Individuals with an ER visit for substance use without psychosis had a lower relative risk of transitioning (aHR, 9.8; 95% CI, 9.5-10.2; 3-year risk, 1.4%) but incurred more than three times the absolute number of transitions (9,969 vs. 3,029).
- ER visits related to cannabis use had the highest transition risk among visits with psychosis (aHR, 241.6; 95% CI, 225.5-258.9) and the third-highest risk among visits without psychosis (aHR, 14.3; 95% CI, 13.5-15.2).
- Younger age and male sex were associated with a higher risk of transition, and the risk of male sex was greater in younger, compared with older, individuals particularly for cannabis use.
IN PRACTICE:
“Primary prevention efforts aimed at reducing substance use and substance use disorders could substantially reduce the population-level burden of chronic psychoses,” the investigators write. “Our findings also highlight the need for targeted secondary prevention providing early intervention and reducing substance use in the highest-risk groups, which may delay or prevent transition to schizophrenia spectrum disorders.”
SOURCE:
Daniel T. Myran, MD, MPH, of the Ottawa Hospital Research Institute, led the study, which was funded by the Canadian Institutes of Health Research and the University of Ottawa department of family medicine. The study was published online in JAMA Psychiatry.
LIMITATIONS:
Investigators did not have access to detailed data on substance-related outpatient visits or patterns of substance use, which could provide additional prognostic information.
DISCLOSURES:
Dr. Myran reported receiving grants from the Canadian Institutes of Health Research during the conduct of the study. Dr. Solmi reported receiving honoraria for participation on advisory boards or presentations from AbbVie, Angelini, Lundbeck, and Otsuka outside the submitted work. The remaining authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
Three years after an initial ER visit, 18.5% of those with substance-induced psychosis were diagnosed with an SSD. Cannabis-induced psychosis was associated with the greatest risk.
METHODOLOGY:
- In this retrospective, population-based cohort study, investigators evaluated the risk of transition to a diagnosis of SSD for individuals with an ER visit for substance use versus the general population.
- Investigators at The Ottawa Hospital and the Institute for Clinical Evaluative Sciences, both in Ontario, analyzed data from six linked databases containing health information on nearly 10 million Ontario residents aged 14-65 years eligible for medical coverage.
- Investigators collected the health data between January 2008 and March 2022 on residents with substance use–related ER visits with, and without, psychosis.
TAKEAWAY:
- There were nearly 408,000 individuals with an ER visit for substance use, of which 13,800 (3.4%) of the visits were for substance-induced psychosis.
- Individuals with substance-induced psychosis were at a 163-fold (age- and sex-adjusted hazard ratio, 163.2; 95% confidence interval, 156.1-170.5) increased risk of transitioning to an SSD, relative to the general population (3-year risk, 18.5% vs. 0.1%).
- Individuals with an ER visit for substance use without psychosis had a lower relative risk of transitioning (aHR, 9.8; 95% CI, 9.5-10.2; 3-year risk, 1.4%) but incurred more than three times the absolute number of transitions (9,969 vs. 3,029).
- ER visits related to cannabis use had the highest transition risk among visits with psychosis (aHR, 241.6; 95% CI, 225.5-258.9) and the third-highest risk among visits without psychosis (aHR, 14.3; 95% CI, 13.5-15.2).
- Younger age and male sex were associated with a higher risk of transition, and the risk of male sex was greater in younger, compared with older, individuals particularly for cannabis use.
IN PRACTICE:
“Primary prevention efforts aimed at reducing substance use and substance use disorders could substantially reduce the population-level burden of chronic psychoses,” the investigators write. “Our findings also highlight the need for targeted secondary prevention providing early intervention and reducing substance use in the highest-risk groups, which may delay or prevent transition to schizophrenia spectrum disorders.”
SOURCE:
Daniel T. Myran, MD, MPH, of the Ottawa Hospital Research Institute, led the study, which was funded by the Canadian Institutes of Health Research and the University of Ottawa department of family medicine. The study was published online in JAMA Psychiatry.
LIMITATIONS:
Investigators did not have access to detailed data on substance-related outpatient visits or patterns of substance use, which could provide additional prognostic information.
DISCLOSURES:
Dr. Myran reported receiving grants from the Canadian Institutes of Health Research during the conduct of the study. Dr. Solmi reported receiving honoraria for participation on advisory boards or presentations from AbbVie, Angelini, Lundbeck, and Otsuka outside the submitted work. The remaining authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA PSYCHIATRY
Adolescents’ acute care use for eating disorders has risen
In a repeated cross-sectional study that examined population-based data from January 2017 through August 2022, ED visits increased by 121% above expected levels, and hospital admissions increased by 54% above expected among patients aged 10-17 years during the pandemic.
“We are hoping this study continues to heighten awareness of the importance of eating disorders, and also to bolster support for eating disorder programs so that we can adequately care for patients and address the increasing demand for treatment and services,” lead author Alene Toulany, MD, adolescent medicine specialist and researcher at the Hospital for Sick Children in Toronto, told this news organization.
The study was published in the Canadian Medical Association Journal.
‘A pressing concern’
The researchers used linked health administrative databases that included all patients in Ontario who were eligible for the Ontario Health Insurance Plan, which is publicly funded. They compared observed and expected rates of ED visits and hospitalizations for eating disorders between a prepandemic period (Jan. 1, 2017, to Feb. 29, 2020) and a pandemic period (Mar. 1, 2020, to Aug. 31, 2022). The researchers examined the following four age categories: adolescents (aged 10-17 years), young adults (aged 18-26 years), adults (aged 27-40 years), and older adults (aged 41-105 years).
Among adolescents, the observed rate of ED visits during the 30 pandemic months studied was 7.38 per 100,000 population, compared with 3.33 per 100,000 before the pandemic (incidence rate ratio [IRR], 2.21).
The rate of ED visits among young adults increased by 13% above the expected rate. It reached 2.79 per 100,000, compared with 2.46 per 100,000 in the prepandemic period (IRR, 1.13).
Among older adults, ED visits increased from 0.11 per 100,000 in the prepandemic period to 0.14 per 100,000 in the pandemic period (IRR, 1.15). The rate of ED visits among adults remained approximately the same.
The rate of hospital admissions among adolescents increased by 54% above the expected rate during the pandemic. The observed rate of hospital admissions before the pandemic was 5.74 per 100,000, vs. 8.82 per 100,000 during the pandemic (IRR, 1.54). Hospital admissions remained stable or decreased for the other age groups.
“Eating disorders have increased globally in children and adolescents during COVID,” said Dr. Toulany. “There are a number of risk factors contributing to this pandemic rise, including isolation, more time on social media, decreased access to care (as many in-person services were not available due to the pandemic), as well as fear of getting infected. All of these could contribute to an increased risk of developing an eating disorder or of making an existing one worse.”
Regardless of the cause, more investment in eating disorders research and eating disorder programs for adolescents and adults is needed, she said.
“The pandemic served as a catalyst, because it started to shed light on the prevalence of eating disorders, especially in young people. But it’s very important that we recognize that this has been a long-standing issue and a pressing concern that has been consistently overlooked and underfunded,” said Dr. Toulany.
Surging eating disorders
Commenting on the findings, Victor Fornari, MD, director of child and adolescent psychiatry at Zucker Hillside Hospital/Northwell Health in Glen Oaks, N.Y., said, “Our experience in the United States parallels what is described in this Canadian paper. This was a surge of eating disorders the likes of which I had not experienced in my career.” Dr. Fornari did not participate in the current study.
“I’ve been here for over 40 years, and the average number of our inpatients in our eating disorder program has been three to five and about a dozen patients in our day clinic at any one time. But in the spring of 2020, we surged to 20 inpatients and over 20 day patients,” Dr. Fornari said.
“We can speculate as to the reasons for this,” he continued. “Kids were isolated. School was closed. They spent more time on social media and the Internet. Their sports activities were curtailed. There was anxiety because the guidance that we were all offered to prevent contagion was increasing people’s anxiety about safety and danger. So, I think we saw dramatic rises in eating disorders in the same way we saw dramatic rises in anxiety and depression in adolescents, as well.”
Dr. Fornari cited social media as an important contributing factor to eating disorders, especially among vulnerable teenagers. “Many of these vulnerable kids are looking at pictures of people who are very thin and comparing themselves, feeling inadequate, feeling sad. Social media is one of the reasons why the rates of psychopathology amongst teens has skyrocketed in the last decade. The surgeon general recently said we should delay access to social media until age 16 because the younger kids are impressionable and vulnerable. I think there is wisdom there, but it is very hard to actually put into practice.”
Worsening mental health
“I thought this was very relevant research and an important contribution to our understanding of eating disorders during pandemic times,” said Simon Sherry, PhD, professor of psychology and neuroscience at Dalhousie University in Halifax, Nova Scotia. “It also dovetails with my own experience as a practitioner.” Dr. Sherry was not involved in the research.
The pandemic has been difficult for people with disordered eating for many reasons, Dr. Sherry said. “There was a massive disruption or ‘loss of normal’ around food. Restaurants closed, grocery shopping was disrupted, scarcity of food occurred, hoarding of food occurred. That meant that eating was difficult for all of us, but especially for individuals who were rigid and controlling around the consumption of food. In this COVID era, you would need flexibility and acceptance around eating, but if you had a narrow range of preferred foods and preferred shopping locations, no doubt the pandemic made this a lot worse.”
Certain forms of disordered eating would be much more likely during the pandemic, Dr. Sherry noted. “For example, binge eating is often triggered by psychological, social, and environmental events,” and those triggers were abundant at the beginning of the pandemic. Boredom, anxiety, depression, stress, loneliness, confinement, and isolation are among the triggers. “COVID-19-related stress was and is very fertile ground for the growth of emotional eating, binge eating, or turning to food to cope. Eating disorders tend to fester amid silence and isolation and inactivity, and that was very much our experience during the lockdown phase of the pandemic,” he said.
Dr. Sherry agrees with the need for more funding for eating disorders research. “We know in Canada that eating disorders are a very important and deadly issue that is chronically underfunded. We are not funding disordered eating in proportion to its prevalence or in proportion to the amount of harm and destruction it creates for individuals, their family members, and our society at large. The authors are absolutely correct to advocate for care in proportion to the prevalence and the damage associated with eating disorders,” he said.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health, the Ministry of Long-Term Care, and the Canadian Institutes of Health Research (CIHR). Dr. Toulany, Dr. Fornari, and Dr. Sherry reported no relevant financial relationships. One study author reported receiving personal fees from the BMJ Group’s Archives of Diseases in Childhood and grants from CIHR, the Ontario Ministry of Health, the Centre for Addiction and Mental Health, and the Hospital for Sick Children. A second author reported funding from CIHR.
A version of this article first appeared on Medscape.com.
In a repeated cross-sectional study that examined population-based data from January 2017 through August 2022, ED visits increased by 121% above expected levels, and hospital admissions increased by 54% above expected among patients aged 10-17 years during the pandemic.
“We are hoping this study continues to heighten awareness of the importance of eating disorders, and also to bolster support for eating disorder programs so that we can adequately care for patients and address the increasing demand for treatment and services,” lead author Alene Toulany, MD, adolescent medicine specialist and researcher at the Hospital for Sick Children in Toronto, told this news organization.
The study was published in the Canadian Medical Association Journal.
‘A pressing concern’
The researchers used linked health administrative databases that included all patients in Ontario who were eligible for the Ontario Health Insurance Plan, which is publicly funded. They compared observed and expected rates of ED visits and hospitalizations for eating disorders between a prepandemic period (Jan. 1, 2017, to Feb. 29, 2020) and a pandemic period (Mar. 1, 2020, to Aug. 31, 2022). The researchers examined the following four age categories: adolescents (aged 10-17 years), young adults (aged 18-26 years), adults (aged 27-40 years), and older adults (aged 41-105 years).
Among adolescents, the observed rate of ED visits during the 30 pandemic months studied was 7.38 per 100,000 population, compared with 3.33 per 100,000 before the pandemic (incidence rate ratio [IRR], 2.21).
The rate of ED visits among young adults increased by 13% above the expected rate. It reached 2.79 per 100,000, compared with 2.46 per 100,000 in the prepandemic period (IRR, 1.13).
Among older adults, ED visits increased from 0.11 per 100,000 in the prepandemic period to 0.14 per 100,000 in the pandemic period (IRR, 1.15). The rate of ED visits among adults remained approximately the same.
The rate of hospital admissions among adolescents increased by 54% above the expected rate during the pandemic. The observed rate of hospital admissions before the pandemic was 5.74 per 100,000, vs. 8.82 per 100,000 during the pandemic (IRR, 1.54). Hospital admissions remained stable or decreased for the other age groups.
“Eating disorders have increased globally in children and adolescents during COVID,” said Dr. Toulany. “There are a number of risk factors contributing to this pandemic rise, including isolation, more time on social media, decreased access to care (as many in-person services were not available due to the pandemic), as well as fear of getting infected. All of these could contribute to an increased risk of developing an eating disorder or of making an existing one worse.”
Regardless of the cause, more investment in eating disorders research and eating disorder programs for adolescents and adults is needed, she said.
“The pandemic served as a catalyst, because it started to shed light on the prevalence of eating disorders, especially in young people. But it’s very important that we recognize that this has been a long-standing issue and a pressing concern that has been consistently overlooked and underfunded,” said Dr. Toulany.
Surging eating disorders
Commenting on the findings, Victor Fornari, MD, director of child and adolescent psychiatry at Zucker Hillside Hospital/Northwell Health in Glen Oaks, N.Y., said, “Our experience in the United States parallels what is described in this Canadian paper. This was a surge of eating disorders the likes of which I had not experienced in my career.” Dr. Fornari did not participate in the current study.
“I’ve been here for over 40 years, and the average number of our inpatients in our eating disorder program has been three to five and about a dozen patients in our day clinic at any one time. But in the spring of 2020, we surged to 20 inpatients and over 20 day patients,” Dr. Fornari said.
“We can speculate as to the reasons for this,” he continued. “Kids were isolated. School was closed. They spent more time on social media and the Internet. Their sports activities were curtailed. There was anxiety because the guidance that we were all offered to prevent contagion was increasing people’s anxiety about safety and danger. So, I think we saw dramatic rises in eating disorders in the same way we saw dramatic rises in anxiety and depression in adolescents, as well.”
Dr. Fornari cited social media as an important contributing factor to eating disorders, especially among vulnerable teenagers. “Many of these vulnerable kids are looking at pictures of people who are very thin and comparing themselves, feeling inadequate, feeling sad. Social media is one of the reasons why the rates of psychopathology amongst teens has skyrocketed in the last decade. The surgeon general recently said we should delay access to social media until age 16 because the younger kids are impressionable and vulnerable. I think there is wisdom there, but it is very hard to actually put into practice.”
Worsening mental health
“I thought this was very relevant research and an important contribution to our understanding of eating disorders during pandemic times,” said Simon Sherry, PhD, professor of psychology and neuroscience at Dalhousie University in Halifax, Nova Scotia. “It also dovetails with my own experience as a practitioner.” Dr. Sherry was not involved in the research.
The pandemic has been difficult for people with disordered eating for many reasons, Dr. Sherry said. “There was a massive disruption or ‘loss of normal’ around food. Restaurants closed, grocery shopping was disrupted, scarcity of food occurred, hoarding of food occurred. That meant that eating was difficult for all of us, but especially for individuals who were rigid and controlling around the consumption of food. In this COVID era, you would need flexibility and acceptance around eating, but if you had a narrow range of preferred foods and preferred shopping locations, no doubt the pandemic made this a lot worse.”
Certain forms of disordered eating would be much more likely during the pandemic, Dr. Sherry noted. “For example, binge eating is often triggered by psychological, social, and environmental events,” and those triggers were abundant at the beginning of the pandemic. Boredom, anxiety, depression, stress, loneliness, confinement, and isolation are among the triggers. “COVID-19-related stress was and is very fertile ground for the growth of emotional eating, binge eating, or turning to food to cope. Eating disorders tend to fester amid silence and isolation and inactivity, and that was very much our experience during the lockdown phase of the pandemic,” he said.
Dr. Sherry agrees with the need for more funding for eating disorders research. “We know in Canada that eating disorders are a very important and deadly issue that is chronically underfunded. We are not funding disordered eating in proportion to its prevalence or in proportion to the amount of harm and destruction it creates for individuals, their family members, and our society at large. The authors are absolutely correct to advocate for care in proportion to the prevalence and the damage associated with eating disorders,” he said.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health, the Ministry of Long-Term Care, and the Canadian Institutes of Health Research (CIHR). Dr. Toulany, Dr. Fornari, and Dr. Sherry reported no relevant financial relationships. One study author reported receiving personal fees from the BMJ Group’s Archives of Diseases in Childhood and grants from CIHR, the Ontario Ministry of Health, the Centre for Addiction and Mental Health, and the Hospital for Sick Children. A second author reported funding from CIHR.
A version of this article first appeared on Medscape.com.
In a repeated cross-sectional study that examined population-based data from January 2017 through August 2022, ED visits increased by 121% above expected levels, and hospital admissions increased by 54% above expected among patients aged 10-17 years during the pandemic.
“We are hoping this study continues to heighten awareness of the importance of eating disorders, and also to bolster support for eating disorder programs so that we can adequately care for patients and address the increasing demand for treatment and services,” lead author Alene Toulany, MD, adolescent medicine specialist and researcher at the Hospital for Sick Children in Toronto, told this news organization.
The study was published in the Canadian Medical Association Journal.
‘A pressing concern’
The researchers used linked health administrative databases that included all patients in Ontario who were eligible for the Ontario Health Insurance Plan, which is publicly funded. They compared observed and expected rates of ED visits and hospitalizations for eating disorders between a prepandemic period (Jan. 1, 2017, to Feb. 29, 2020) and a pandemic period (Mar. 1, 2020, to Aug. 31, 2022). The researchers examined the following four age categories: adolescents (aged 10-17 years), young adults (aged 18-26 years), adults (aged 27-40 years), and older adults (aged 41-105 years).
Among adolescents, the observed rate of ED visits during the 30 pandemic months studied was 7.38 per 100,000 population, compared with 3.33 per 100,000 before the pandemic (incidence rate ratio [IRR], 2.21).
The rate of ED visits among young adults increased by 13% above the expected rate. It reached 2.79 per 100,000, compared with 2.46 per 100,000 in the prepandemic period (IRR, 1.13).
Among older adults, ED visits increased from 0.11 per 100,000 in the prepandemic period to 0.14 per 100,000 in the pandemic period (IRR, 1.15). The rate of ED visits among adults remained approximately the same.
The rate of hospital admissions among adolescents increased by 54% above the expected rate during the pandemic. The observed rate of hospital admissions before the pandemic was 5.74 per 100,000, vs. 8.82 per 100,000 during the pandemic (IRR, 1.54). Hospital admissions remained stable or decreased for the other age groups.
“Eating disorders have increased globally in children and adolescents during COVID,” said Dr. Toulany. “There are a number of risk factors contributing to this pandemic rise, including isolation, more time on social media, decreased access to care (as many in-person services were not available due to the pandemic), as well as fear of getting infected. All of these could contribute to an increased risk of developing an eating disorder or of making an existing one worse.”
Regardless of the cause, more investment in eating disorders research and eating disorder programs for adolescents and adults is needed, she said.
“The pandemic served as a catalyst, because it started to shed light on the prevalence of eating disorders, especially in young people. But it’s very important that we recognize that this has been a long-standing issue and a pressing concern that has been consistently overlooked and underfunded,” said Dr. Toulany.
Surging eating disorders
Commenting on the findings, Victor Fornari, MD, director of child and adolescent psychiatry at Zucker Hillside Hospital/Northwell Health in Glen Oaks, N.Y., said, “Our experience in the United States parallels what is described in this Canadian paper. This was a surge of eating disorders the likes of which I had not experienced in my career.” Dr. Fornari did not participate in the current study.
“I’ve been here for over 40 years, and the average number of our inpatients in our eating disorder program has been three to five and about a dozen patients in our day clinic at any one time. But in the spring of 2020, we surged to 20 inpatients and over 20 day patients,” Dr. Fornari said.
“We can speculate as to the reasons for this,” he continued. “Kids were isolated. School was closed. They spent more time on social media and the Internet. Their sports activities were curtailed. There was anxiety because the guidance that we were all offered to prevent contagion was increasing people’s anxiety about safety and danger. So, I think we saw dramatic rises in eating disorders in the same way we saw dramatic rises in anxiety and depression in adolescents, as well.”
Dr. Fornari cited social media as an important contributing factor to eating disorders, especially among vulnerable teenagers. “Many of these vulnerable kids are looking at pictures of people who are very thin and comparing themselves, feeling inadequate, feeling sad. Social media is one of the reasons why the rates of psychopathology amongst teens has skyrocketed in the last decade. The surgeon general recently said we should delay access to social media until age 16 because the younger kids are impressionable and vulnerable. I think there is wisdom there, but it is very hard to actually put into practice.”
Worsening mental health
“I thought this was very relevant research and an important contribution to our understanding of eating disorders during pandemic times,” said Simon Sherry, PhD, professor of psychology and neuroscience at Dalhousie University in Halifax, Nova Scotia. “It also dovetails with my own experience as a practitioner.” Dr. Sherry was not involved in the research.
The pandemic has been difficult for people with disordered eating for many reasons, Dr. Sherry said. “There was a massive disruption or ‘loss of normal’ around food. Restaurants closed, grocery shopping was disrupted, scarcity of food occurred, hoarding of food occurred. That meant that eating was difficult for all of us, but especially for individuals who were rigid and controlling around the consumption of food. In this COVID era, you would need flexibility and acceptance around eating, but if you had a narrow range of preferred foods and preferred shopping locations, no doubt the pandemic made this a lot worse.”
Certain forms of disordered eating would be much more likely during the pandemic, Dr. Sherry noted. “For example, binge eating is often triggered by psychological, social, and environmental events,” and those triggers were abundant at the beginning of the pandemic. Boredom, anxiety, depression, stress, loneliness, confinement, and isolation are among the triggers. “COVID-19-related stress was and is very fertile ground for the growth of emotional eating, binge eating, or turning to food to cope. Eating disorders tend to fester amid silence and isolation and inactivity, and that was very much our experience during the lockdown phase of the pandemic,” he said.
Dr. Sherry agrees with the need for more funding for eating disorders research. “We know in Canada that eating disorders are a very important and deadly issue that is chronically underfunded. We are not funding disordered eating in proportion to its prevalence or in proportion to the amount of harm and destruction it creates for individuals, their family members, and our society at large. The authors are absolutely correct to advocate for care in proportion to the prevalence and the damage associated with eating disorders,” he said.
The study was supported by ICES, which is funded by an annual grant from the Ontario Ministry of Health, the Ministry of Long-Term Care, and the Canadian Institutes of Health Research (CIHR). Dr. Toulany, Dr. Fornari, and Dr. Sherry reported no relevant financial relationships. One study author reported receiving personal fees from the BMJ Group’s Archives of Diseases in Childhood and grants from CIHR, the Ontario Ministry of Health, the Centre for Addiction and Mental Health, and the Hospital for Sick Children. A second author reported funding from CIHR.
A version of this article first appeared on Medscape.com.
FROM THE CANADIAN MEDICAL ASSOCIATION JOURNAL
New insight into genetic link between schizophrenia and CVD
TOPLINE:
There is an extensive genetic overlap between schizophrenia and smoking, but there are also schizophrenia genes that may protect against obesity, illustrating the bidirectional effects of shared loci across cardiovascular disease (CVD) risk factors, results of new research suggest.
METHODOLOGY:
- Researchers obtained what they call an “unprecedentedly large” set of GWAS samples, including schizophrenia (53,386 patients and 77,258 controls) and various CVD risk factors.
- They used analytic approaches to identify genetic links between schizophrenia and CVD risk factors, including bivariate causal mixture model (MiXeR), which estimates the number of shared genetic variants between pairs of phenotypes, and conditional and conjunctional false discovery rate (condFDR and conjFDR), to identify specific genetic loci; these approaches can identify genetic overlap regardless of the effect directions.
TAKEAWAY:
- Using MiXeR, the study showed that several genetic variants underlying schizophrenia also influence CVD phenotypes, particularly risk factors of smoking and BMI.
- A total of 825 distinct loci were jointly associated with schizophrenia and CVD phenotypes at conjFDR < .05.
- Most of the loci shared with smoking were in line with positive genetic correlations; the authors noted individuals with schizophrenia are more nicotine dependent than the general population, and they experience greater reinforcing effects of nicotine and worse withdrawal symptoms during abstinence than the general population.
- The overlapping loci with BMI had effect directions consistent with negative genetic correlations, suggesting people with schizophrenia are genetically predisposed to lower BMI; this is in line with evidence of low BMI being a risk factor for schizophrenia, although obesity is more common in people with schizophrenia.
- There was a pattern of mixed effect directions among loci jointly associated with schizophrenia and lipids, blood pressure, type 2 diabetes, waist-to-hip ratio, and coronary artery disease, which may reflect variation in genetic susceptibility to CVD across subgroups of schizophrenia.
IN PRACTICE:
The new results “shed light” on biological pathways associated with comorbidity between CVD and schizophrenia, said the authors, adding future work could provide insights into mechanisms underlying the comorbidity and could facilitate development of antipsychotics with lower metabolic side effects, which could help prevent comorbid CVD, “thereby helping to mitigate a major clinical and health care problem.”
SOURCE:
The study was led by Linn Rødevand, PhD, Norwegian Center for Mental Disorders Research, Division of Mental Health and Addiction, Institute of Clinical Medicine, Oslo University Hospital, University of Oslo, and colleagues. It was published online in the American Journal of Psychiatry.
LIMITATIONS:
Methods used in the study are limited by uncertainties in translating genetic loci to causal variants, which restricts the biological interpretation of the shared genetic variants. Among other methodological limitations are that discrepancies between the linkage disequilibrium structure of the samples used for the GWAS and that of the reference panel may have biased estimates underlying MiXeR.
DISCLOSURES:
The study received support from the Research Council of Norway, Norwegian Health Association, South-East Norway Regional Health Authority, and the European Union. Dr. Rødevand reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
There is an extensive genetic overlap between schizophrenia and smoking, but there are also schizophrenia genes that may protect against obesity, illustrating the bidirectional effects of shared loci across cardiovascular disease (CVD) risk factors, results of new research suggest.
METHODOLOGY:
- Researchers obtained what they call an “unprecedentedly large” set of GWAS samples, including schizophrenia (53,386 patients and 77,258 controls) and various CVD risk factors.
- They used analytic approaches to identify genetic links between schizophrenia and CVD risk factors, including bivariate causal mixture model (MiXeR), which estimates the number of shared genetic variants between pairs of phenotypes, and conditional and conjunctional false discovery rate (condFDR and conjFDR), to identify specific genetic loci; these approaches can identify genetic overlap regardless of the effect directions.
TAKEAWAY:
- Using MiXeR, the study showed that several genetic variants underlying schizophrenia also influence CVD phenotypes, particularly risk factors of smoking and BMI.
- A total of 825 distinct loci were jointly associated with schizophrenia and CVD phenotypes at conjFDR < .05.
- Most of the loci shared with smoking were in line with positive genetic correlations; the authors noted individuals with schizophrenia are more nicotine dependent than the general population, and they experience greater reinforcing effects of nicotine and worse withdrawal symptoms during abstinence than the general population.
- The overlapping loci with BMI had effect directions consistent with negative genetic correlations, suggesting people with schizophrenia are genetically predisposed to lower BMI; this is in line with evidence of low BMI being a risk factor for schizophrenia, although obesity is more common in people with schizophrenia.
- There was a pattern of mixed effect directions among loci jointly associated with schizophrenia and lipids, blood pressure, type 2 diabetes, waist-to-hip ratio, and coronary artery disease, which may reflect variation in genetic susceptibility to CVD across subgroups of schizophrenia.
IN PRACTICE:
The new results “shed light” on biological pathways associated with comorbidity between CVD and schizophrenia, said the authors, adding future work could provide insights into mechanisms underlying the comorbidity and could facilitate development of antipsychotics with lower metabolic side effects, which could help prevent comorbid CVD, “thereby helping to mitigate a major clinical and health care problem.”
SOURCE:
The study was led by Linn Rødevand, PhD, Norwegian Center for Mental Disorders Research, Division of Mental Health and Addiction, Institute of Clinical Medicine, Oslo University Hospital, University of Oslo, and colleagues. It was published online in the American Journal of Psychiatry.
LIMITATIONS:
Methods used in the study are limited by uncertainties in translating genetic loci to causal variants, which restricts the biological interpretation of the shared genetic variants. Among other methodological limitations are that discrepancies between the linkage disequilibrium structure of the samples used for the GWAS and that of the reference panel may have biased estimates underlying MiXeR.
DISCLOSURES:
The study received support from the Research Council of Norway, Norwegian Health Association, South-East Norway Regional Health Authority, and the European Union. Dr. Rødevand reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
TOPLINE:
There is an extensive genetic overlap between schizophrenia and smoking, but there are also schizophrenia genes that may protect against obesity, illustrating the bidirectional effects of shared loci across cardiovascular disease (CVD) risk factors, results of new research suggest.
METHODOLOGY:
- Researchers obtained what they call an “unprecedentedly large” set of GWAS samples, including schizophrenia (53,386 patients and 77,258 controls) and various CVD risk factors.
- They used analytic approaches to identify genetic links between schizophrenia and CVD risk factors, including bivariate causal mixture model (MiXeR), which estimates the number of shared genetic variants between pairs of phenotypes, and conditional and conjunctional false discovery rate (condFDR and conjFDR), to identify specific genetic loci; these approaches can identify genetic overlap regardless of the effect directions.
TAKEAWAY:
- Using MiXeR, the study showed that several genetic variants underlying schizophrenia also influence CVD phenotypes, particularly risk factors of smoking and BMI.
- A total of 825 distinct loci were jointly associated with schizophrenia and CVD phenotypes at conjFDR < .05.
- Most of the loci shared with smoking were in line with positive genetic correlations; the authors noted individuals with schizophrenia are more nicotine dependent than the general population, and they experience greater reinforcing effects of nicotine and worse withdrawal symptoms during abstinence than the general population.
- The overlapping loci with BMI had effect directions consistent with negative genetic correlations, suggesting people with schizophrenia are genetically predisposed to lower BMI; this is in line with evidence of low BMI being a risk factor for schizophrenia, although obesity is more common in people with schizophrenia.
- There was a pattern of mixed effect directions among loci jointly associated with schizophrenia and lipids, blood pressure, type 2 diabetes, waist-to-hip ratio, and coronary artery disease, which may reflect variation in genetic susceptibility to CVD across subgroups of schizophrenia.
IN PRACTICE:
The new results “shed light” on biological pathways associated with comorbidity between CVD and schizophrenia, said the authors, adding future work could provide insights into mechanisms underlying the comorbidity and could facilitate development of antipsychotics with lower metabolic side effects, which could help prevent comorbid CVD, “thereby helping to mitigate a major clinical and health care problem.”
SOURCE:
The study was led by Linn Rødevand, PhD, Norwegian Center for Mental Disorders Research, Division of Mental Health and Addiction, Institute of Clinical Medicine, Oslo University Hospital, University of Oslo, and colleagues. It was published online in the American Journal of Psychiatry.
LIMITATIONS:
Methods used in the study are limited by uncertainties in translating genetic loci to causal variants, which restricts the biological interpretation of the shared genetic variants. Among other methodological limitations are that discrepancies between the linkage disequilibrium structure of the samples used for the GWAS and that of the reference panel may have biased estimates underlying MiXeR.
DISCLOSURES:
The study received support from the Research Council of Norway, Norwegian Health Association, South-East Norway Regional Health Authority, and the European Union. Dr. Rødevand reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF PSYCHIATRY
The surprising link between loneliness and Parkinson’s disease
This transcript has been edited for clarity.
On May 3, 2023, Surgeon General Vivek Murthy issued an advisory raising an alarm about what he called an “epidemic of loneliness” in the United States.
Now, I am not saying that Vivek Murthy read my book, “How Medicine Works and When It Doesn’t” – released in January and available in bookstores now – where, in chapter 11, I call attention to the problem of loneliness and its relationship to the exponential rise in deaths of despair. But Vivek, if you did, let me know. I could use the publicity.
No, of course the idea that loneliness is a public health issue is not new, but I’m glad to see it finally getting attention. At this point, studies have linked loneliness to heart disease, stroke, dementia, and premature death.
The UK Biobank is really a treasure trove of data for epidemiologists. I must see three to four studies a week coming out of this mega-dataset. This one, appearing in JAMA Neurology, caught my eye for its focus specifically on loneliness as a risk factor – something I’m hoping to see more of in the future.
The study examines data from just under 500,000 individuals in the United Kingdom who answered a survey including the question “Do you often feel lonely?” between 2006 and 2010; 18.4% of people answered yes. Individuals’ electronic health record data were then monitored over time to see who would get a new diagnosis code consistent with Parkinson’s disease. Through 2021, 2822 people did – that’s just over half a percent.
So, now we do the statistics thing. Of the nonlonely folks, 2,273 went on to develop Parkinson’s disease. Of those who said they often feel lonely, 549 people did. The raw numbers here, to be honest, aren’t that compelling. Lonely people had an absolute risk for Parkinson’s disease about 0.03% higher than that of nonlonely people. Put another way, you’d need to take over 3,000 lonely souls and make them not lonely to prevent 1 case of Parkinson’s disease.
Still, the costs of loneliness are not measured exclusively in Parkinson’s disease, and I would argue that the real risks here come from other sources: alcohol abuse, drug abuse, and suicide. Nevertheless, the weak but significant association with Parkinson’s disease reminds us that loneliness is a neurologic phenomenon. There is something about social connection that affects our brain in a way that is not just spiritual; it is actually biological.
Of course, people who say they are often lonely are different in other ways from people who report not being lonely. Lonely people, in this dataset, were younger, more likely to be female, less likely to have a college degree, in worse physical health, and engaged in more high-risk health behaviors like smoking.
The authors adjusted for all of these factors and found that, on the relative scale, lonely people were still about 20%-30% more likely to develop Parkinson’s disease.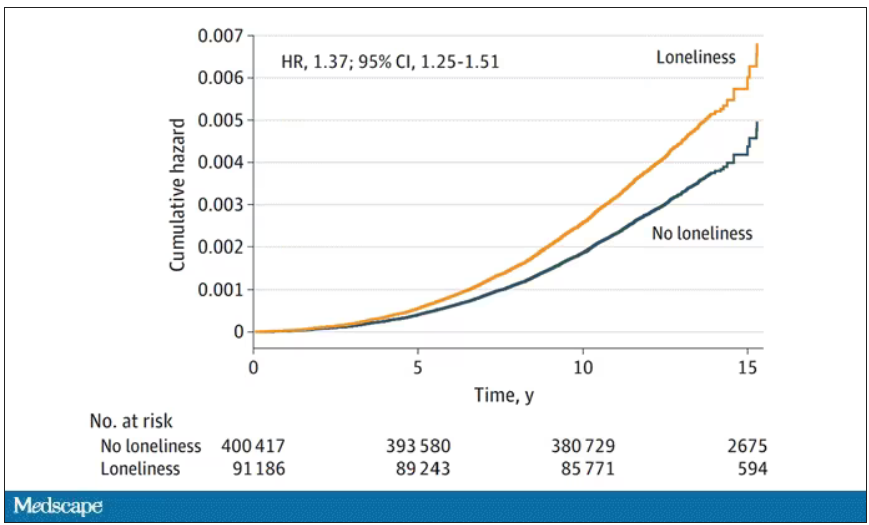
So, what do we do about this? There is no pill for loneliness, and God help us if there ever is. Recognizing the problem is a good start. But there are some policy things we can do to reduce loneliness. We can invest in public spaces that bring people together – parks, museums, libraries – and public transportation. We can deal with tech companies that are so optimized at capturing our attention that we cease to engage with other humans. And, individually, we can just reach out a bit more. We’ve spent the past few pandemic years with our attention focused sharply inward. It’s time to look out again.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
On May 3, 2023, Surgeon General Vivek Murthy issued an advisory raising an alarm about what he called an “epidemic of loneliness” in the United States.
Now, I am not saying that Vivek Murthy read my book, “How Medicine Works and When It Doesn’t” – released in January and available in bookstores now – where, in chapter 11, I call attention to the problem of loneliness and its relationship to the exponential rise in deaths of despair. But Vivek, if you did, let me know. I could use the publicity.
No, of course the idea that loneliness is a public health issue is not new, but I’m glad to see it finally getting attention. At this point, studies have linked loneliness to heart disease, stroke, dementia, and premature death.
The UK Biobank is really a treasure trove of data for epidemiologists. I must see three to four studies a week coming out of this mega-dataset. This one, appearing in JAMA Neurology, caught my eye for its focus specifically on loneliness as a risk factor – something I’m hoping to see more of in the future.
The study examines data from just under 500,000 individuals in the United Kingdom who answered a survey including the question “Do you often feel lonely?” between 2006 and 2010; 18.4% of people answered yes. Individuals’ electronic health record data were then monitored over time to see who would get a new diagnosis code consistent with Parkinson’s disease. Through 2021, 2822 people did – that’s just over half a percent.
So, now we do the statistics thing. Of the nonlonely folks, 2,273 went on to develop Parkinson’s disease. Of those who said they often feel lonely, 549 people did. The raw numbers here, to be honest, aren’t that compelling. Lonely people had an absolute risk for Parkinson’s disease about 0.03% higher than that of nonlonely people. Put another way, you’d need to take over 3,000 lonely souls and make them not lonely to prevent 1 case of Parkinson’s disease.
Still, the costs of loneliness are not measured exclusively in Parkinson’s disease, and I would argue that the real risks here come from other sources: alcohol abuse, drug abuse, and suicide. Nevertheless, the weak but significant association with Parkinson’s disease reminds us that loneliness is a neurologic phenomenon. There is something about social connection that affects our brain in a way that is not just spiritual; it is actually biological.
Of course, people who say they are often lonely are different in other ways from people who report not being lonely. Lonely people, in this dataset, were younger, more likely to be female, less likely to have a college degree, in worse physical health, and engaged in more high-risk health behaviors like smoking.
The authors adjusted for all of these factors and found that, on the relative scale, lonely people were still about 20%-30% more likely to develop Parkinson’s disease.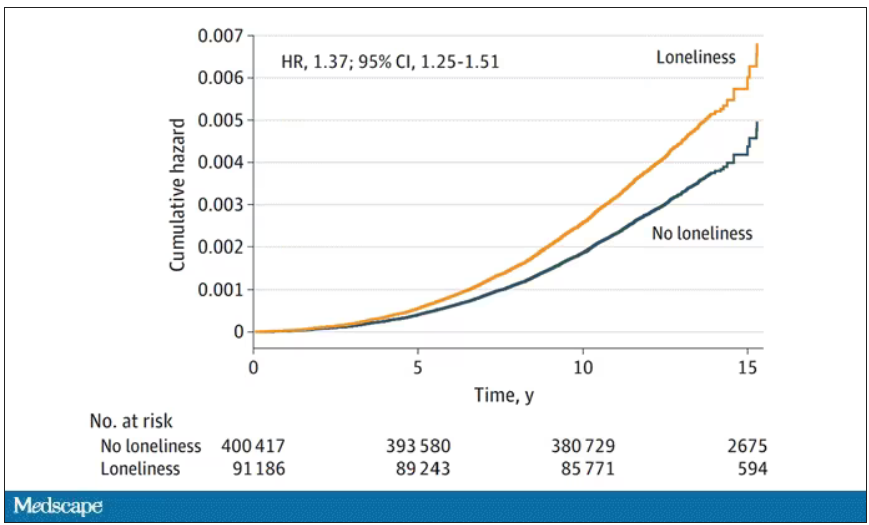
So, what do we do about this? There is no pill for loneliness, and God help us if there ever is. Recognizing the problem is a good start. But there are some policy things we can do to reduce loneliness. We can invest in public spaces that bring people together – parks, museums, libraries – and public transportation. We can deal with tech companies that are so optimized at capturing our attention that we cease to engage with other humans. And, individually, we can just reach out a bit more. We’ve spent the past few pandemic years with our attention focused sharply inward. It’s time to look out again.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
On May 3, 2023, Surgeon General Vivek Murthy issued an advisory raising an alarm about what he called an “epidemic of loneliness” in the United States.
Now, I am not saying that Vivek Murthy read my book, “How Medicine Works and When It Doesn’t” – released in January and available in bookstores now – where, in chapter 11, I call attention to the problem of loneliness and its relationship to the exponential rise in deaths of despair. But Vivek, if you did, let me know. I could use the publicity.
No, of course the idea that loneliness is a public health issue is not new, but I’m glad to see it finally getting attention. At this point, studies have linked loneliness to heart disease, stroke, dementia, and premature death.
The UK Biobank is really a treasure trove of data for epidemiologists. I must see three to four studies a week coming out of this mega-dataset. This one, appearing in JAMA Neurology, caught my eye for its focus specifically on loneliness as a risk factor – something I’m hoping to see more of in the future.
The study examines data from just under 500,000 individuals in the United Kingdom who answered a survey including the question “Do you often feel lonely?” between 2006 and 2010; 18.4% of people answered yes. Individuals’ electronic health record data were then monitored over time to see who would get a new diagnosis code consistent with Parkinson’s disease. Through 2021, 2822 people did – that’s just over half a percent.
So, now we do the statistics thing. Of the nonlonely folks, 2,273 went on to develop Parkinson’s disease. Of those who said they often feel lonely, 549 people did. The raw numbers here, to be honest, aren’t that compelling. Lonely people had an absolute risk for Parkinson’s disease about 0.03% higher than that of nonlonely people. Put another way, you’d need to take over 3,000 lonely souls and make them not lonely to prevent 1 case of Parkinson’s disease.
Still, the costs of loneliness are not measured exclusively in Parkinson’s disease, and I would argue that the real risks here come from other sources: alcohol abuse, drug abuse, and suicide. Nevertheless, the weak but significant association with Parkinson’s disease reminds us that loneliness is a neurologic phenomenon. There is something about social connection that affects our brain in a way that is not just spiritual; it is actually biological.
Of course, people who say they are often lonely are different in other ways from people who report not being lonely. Lonely people, in this dataset, were younger, more likely to be female, less likely to have a college degree, in worse physical health, and engaged in more high-risk health behaviors like smoking.
The authors adjusted for all of these factors and found that, on the relative scale, lonely people were still about 20%-30% more likely to develop Parkinson’s disease.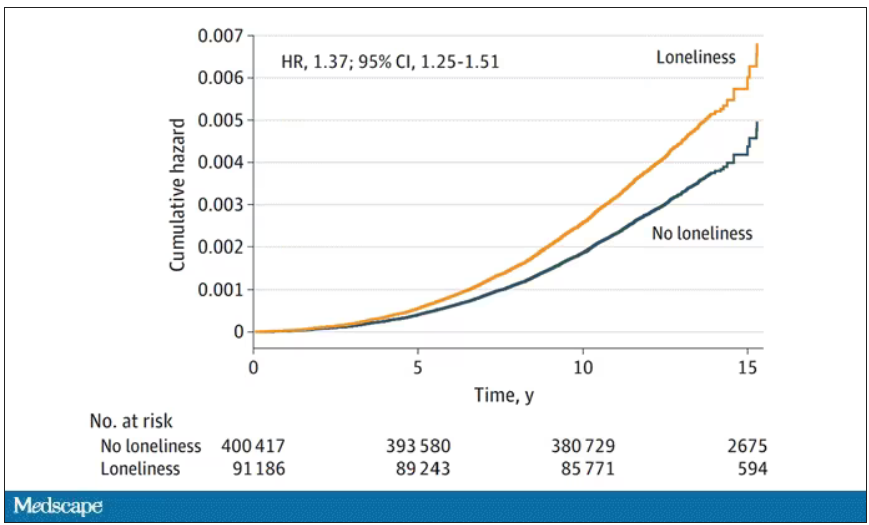
So, what do we do about this? There is no pill for loneliness, and God help us if there ever is. Recognizing the problem is a good start. But there are some policy things we can do to reduce loneliness. We can invest in public spaces that bring people together – parks, museums, libraries – and public transportation. We can deal with tech companies that are so optimized at capturing our attention that we cease to engage with other humans. And, individually, we can just reach out a bit more. We’ve spent the past few pandemic years with our attention focused sharply inward. It’s time to look out again.
F. Perry Wilson, MD, MSCE, is an associate professor of medicine and public health and director of Yale University’s Clinical and Translational Research Accelerator in New Haven, Conn. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
CBT effectively treats sexual concerns in menopausal women
PHILADELPHIA – . Four CBT sessions specifically focused on sexual concerns resulted in decreased sexual distress and concern, reduced depressive and menopausal symptoms, and increased sexual desire and functioning, as well as improved body image and relationship satisfaction.
An estimated 68%-87% of perimenopausal and postmenopausal women report sexual concerns, Sheryl Green, PhD, CPsych, an associate professor of psychiatry and behavioral neurosciences at McMaster University and a psychologist at St. Joseph’s Healthcare’s Women’s Health Concerns Clinic, both in Hamilton, Ont., told attendees at the meeting.
“Sexual concerns over the menopausal transition are not just physical, but they’re also psychological and emotional,” Dr. Green said. “Three common challenges include decreased sexual desire, a reduction in physical arousal and ability to achieve an orgasm, and sexual pain and discomfort during intercourse.”
The reasons for these concerns are multifactorial, she said. Decreased sexual desire can stem from stress, medical problems, their relationship with their partner, or other causes. A woman’s difficulty with reduced physical arousal or ability to have an orgasm can result from changes in hormone levels and vaginal changes, such as vaginal atrophy, which can also contribute to the sexual pain or discomfort reported by 17%-45% of postmenopausal women.
Two pharmacologic treatments exist for sexual concerns: oral flibanserin (Addyi) and injectable bremelanotide (Vyleesi). But many women may be unable or unwilling to take medication for their concerns. Previous research from Lori Brotto has found cognitive behavioral therapy and mindfulness interventions to effectively improve sexual functioning in women treated for gynecologic cancer and in women without a history of cancer.
“Sexual function needs to be understood from a bio-psychosocial model, looking at the biologic factors, the psychological factors, the sociocultural factors, and the interpersonal factors,” Sheryl Kingsberg, PhD, a professor of psychiatry and reproductive biology at Case Western Reserve University and a psychologist at University Hospitals in Cleveland, said in an interview.
“They can all overlap, and the clinician can ask a few pointed questions that help identify what the source of the problem is,” said Dr. Kingsberg, who was not involved in this study. She noted that the International Society for the Study of Women’s Sexual Health has an algorithm that can help in determining the source of the problems.
“Sometimes it’s going to be a biologic condition for which pharmacologic options are nice, but even if it is primarily pharmacologic, psychotherapy is always useful,” Dr. Kingsberg said. “Once the problem is there, even if it’s biologically based, then you have all the things in terms of the cognitive distortion, anxiety,” and other issues that a cognitive behavioral approach can help address. “And access is now much wider because of telehealth,” she added.
‘Psychology of menopause’
The study led by Dr. Green focused on peri- and postmenopausal women, with an average age of 50, who were experiencing primary sexual concerns based on a score of at least 26 on the Female Sexual Function Index (FSFI). Among the 20 women recruited for the study, 6 had already been prescribed hormone therapy for sexual concerns.
All reported decreased sexual desire, 17 reported decreased sexual arousal, 14 had body image dissatisfaction related to sexual concerns, and 6 reported urogenital problems. Nine of the women were in full remission from major depressive disorder, one had post-traumatic stress syndrome, and one had subclinical generalized anxiety disorder.
After spending 4 weeks on a wait list as self-control group for the study, the 15 women who completed the trial underwent four individual CBT sessions focusing on sexual concerns. The first session focused on psychoeducation and thought monitoring, and the second focused on cognitive distortions, cognitive strategies, and unhelpful beliefs or expectations related to sexual concerns. The third session looked at the role of problematic behaviors and behavioral experiments, and the fourth focused on continuation of strategies, long-term goals, and maintaining gains.
The participants completed eight measures at baseline, after the 4 weeks on the wait list, and after the four CBT sessions to assess the following:
- Sexual satisfaction, distress, and desire, using the FSFI, the Female Sexual Distress Scale-Revised (FSDS-R), and the Female Sexual Desire Questionnaire (FSDQ).
- Menopause symptoms, using the Greene Climacteric Scale (GCS).
- Body image, using the Dresden Body Image Questionnaire (DBIQ).
- Relationship satisfaction, using the Couples Satisfaction Index (CSI).
- Depression, using the Beck Depression Inventory-II (BDI-II).
- Anxiety, using the Hamilton Anxiety Rating Scale (HAM-A).
The women did not experience any significant changes while on the wait list except a slight decrease on the FSDQ concern subscale. Following the CBT sessions, however, the women experienced a significant decrease in sexual distress and concern as well as an increase in sexual dyadic desire and sexual functioning (P = .003 for FSFI, P = .002 for FSDS-R, and P = .003 for FSDQ).
Participants also experienced a decrease in depression (P < .0001) and menopausal symptoms (P = .001) and an increase in body-image satisfaction (P = .018) and relationship satisfaction (P = .0011) after the CBT sessions. The researchers assessed participants’ satisfaction with the Client Satisfaction Questionnaire after the CBT sessions and reported some of the qualitative findings.
“The treatment program was able to assist me with recognizing that some of my sexual concerns were normal, emotional as well as physical and hormonal, and provided me the ability to delve more deeply into the psychology of menopause and how to work through symptoms and concerns in more manageable pieces,” one participant wrote. Another found helpful the “homework exercises of recognizing a thought/feeling/emotion surrounding how I feel about myself/body and working through. More positive thought pattern/restructuring a response the most helpful.”
The main complaint about the program was that it was too short, with women wanting more sessions to help continue their progress.
Not an ‘either-or’ approach
Dr. Kingsberg said ISSWSH has a variety of sexual medicine practitioners, including providers who can provide CBT for sexual concerns, and the American Association of Sexuality Educators, Counselors and Therapists has a referral directory.
“Keeping in mind the bio-psychosocial model, sometimes psychotherapy is going to be a really effective treatment for sexual concerns,” Dr. Kingsberg said. “Sometimes the pharmacologic option is going to be a really effective treatment for some concerns, and sometimes the combination is going to have a really nice treatment effect. So it’s not a one-size-fits-all, and it doesn’t have to be an either-or.”
The sexual concerns of women still do not get adequately addressed in medical schools and residencies, Dr. Kingsberg said, which is distinctly different from how male sexual concerns are addressed in health care.
“Erectile dysfunction is kind of in the norm, and women are still a little hesitant to bring up their sexual concerns,” Dr. Kingsberg said. “They don’t know if it’s appropriate and they’re hoping that their clinician will ask.”
One way clinicians can do that is with a global question for all their patients: “Most of my patients have sexual questions or concerns; what concerns do you have?”
“They don’t have to go through a checklist of 10 things,” Dr. Kingsberg said. If the patient does not bring anything up, providers can then ask a single follow up question: “Do you have any concerns with desire, arousal, orgasm, or pain?” That question, Dr. Kingsberg said, covers the four main areas of concern.
The study was funded by the Canadian Institute of Health Research. Dr. Green reported no disclosures. Dr. Kingsberg has consulted for or served on the advisory board for Alloy, Astellas, Bayer, Dare Bioscience, Freya, Reunion Neuroscience, Materna Medical, Madorra, Palatin, Pfizer, ReJoy, Sprout, Strategic Science Technologies, and MsMedicine.
PHILADELPHIA – . Four CBT sessions specifically focused on sexual concerns resulted in decreased sexual distress and concern, reduced depressive and menopausal symptoms, and increased sexual desire and functioning, as well as improved body image and relationship satisfaction.
An estimated 68%-87% of perimenopausal and postmenopausal women report sexual concerns, Sheryl Green, PhD, CPsych, an associate professor of psychiatry and behavioral neurosciences at McMaster University and a psychologist at St. Joseph’s Healthcare’s Women’s Health Concerns Clinic, both in Hamilton, Ont., told attendees at the meeting.
“Sexual concerns over the menopausal transition are not just physical, but they’re also psychological and emotional,” Dr. Green said. “Three common challenges include decreased sexual desire, a reduction in physical arousal and ability to achieve an orgasm, and sexual pain and discomfort during intercourse.”
The reasons for these concerns are multifactorial, she said. Decreased sexual desire can stem from stress, medical problems, their relationship with their partner, or other causes. A woman’s difficulty with reduced physical arousal or ability to have an orgasm can result from changes in hormone levels and vaginal changes, such as vaginal atrophy, which can also contribute to the sexual pain or discomfort reported by 17%-45% of postmenopausal women.
Two pharmacologic treatments exist for sexual concerns: oral flibanserin (Addyi) and injectable bremelanotide (Vyleesi). But many women may be unable or unwilling to take medication for their concerns. Previous research from Lori Brotto has found cognitive behavioral therapy and mindfulness interventions to effectively improve sexual functioning in women treated for gynecologic cancer and in women without a history of cancer.
“Sexual function needs to be understood from a bio-psychosocial model, looking at the biologic factors, the psychological factors, the sociocultural factors, and the interpersonal factors,” Sheryl Kingsberg, PhD, a professor of psychiatry and reproductive biology at Case Western Reserve University and a psychologist at University Hospitals in Cleveland, said in an interview.
“They can all overlap, and the clinician can ask a few pointed questions that help identify what the source of the problem is,” said Dr. Kingsberg, who was not involved in this study. She noted that the International Society for the Study of Women’s Sexual Health has an algorithm that can help in determining the source of the problems.
“Sometimes it’s going to be a biologic condition for which pharmacologic options are nice, but even if it is primarily pharmacologic, psychotherapy is always useful,” Dr. Kingsberg said. “Once the problem is there, even if it’s biologically based, then you have all the things in terms of the cognitive distortion, anxiety,” and other issues that a cognitive behavioral approach can help address. “And access is now much wider because of telehealth,” she added.
‘Psychology of menopause’
The study led by Dr. Green focused on peri- and postmenopausal women, with an average age of 50, who were experiencing primary sexual concerns based on a score of at least 26 on the Female Sexual Function Index (FSFI). Among the 20 women recruited for the study, 6 had already been prescribed hormone therapy for sexual concerns.
All reported decreased sexual desire, 17 reported decreased sexual arousal, 14 had body image dissatisfaction related to sexual concerns, and 6 reported urogenital problems. Nine of the women were in full remission from major depressive disorder, one had post-traumatic stress syndrome, and one had subclinical generalized anxiety disorder.
After spending 4 weeks on a wait list as self-control group for the study, the 15 women who completed the trial underwent four individual CBT sessions focusing on sexual concerns. The first session focused on psychoeducation and thought monitoring, and the second focused on cognitive distortions, cognitive strategies, and unhelpful beliefs or expectations related to sexual concerns. The third session looked at the role of problematic behaviors and behavioral experiments, and the fourth focused on continuation of strategies, long-term goals, and maintaining gains.
The participants completed eight measures at baseline, after the 4 weeks on the wait list, and after the four CBT sessions to assess the following:
- Sexual satisfaction, distress, and desire, using the FSFI, the Female Sexual Distress Scale-Revised (FSDS-R), and the Female Sexual Desire Questionnaire (FSDQ).
- Menopause symptoms, using the Greene Climacteric Scale (GCS).
- Body image, using the Dresden Body Image Questionnaire (DBIQ).
- Relationship satisfaction, using the Couples Satisfaction Index (CSI).
- Depression, using the Beck Depression Inventory-II (BDI-II).
- Anxiety, using the Hamilton Anxiety Rating Scale (HAM-A).
The women did not experience any significant changes while on the wait list except a slight decrease on the FSDQ concern subscale. Following the CBT sessions, however, the women experienced a significant decrease in sexual distress and concern as well as an increase in sexual dyadic desire and sexual functioning (P = .003 for FSFI, P = .002 for FSDS-R, and P = .003 for FSDQ).
Participants also experienced a decrease in depression (P < .0001) and menopausal symptoms (P = .001) and an increase in body-image satisfaction (P = .018) and relationship satisfaction (P = .0011) after the CBT sessions. The researchers assessed participants’ satisfaction with the Client Satisfaction Questionnaire after the CBT sessions and reported some of the qualitative findings.
“The treatment program was able to assist me with recognizing that some of my sexual concerns were normal, emotional as well as physical and hormonal, and provided me the ability to delve more deeply into the psychology of menopause and how to work through symptoms and concerns in more manageable pieces,” one participant wrote. Another found helpful the “homework exercises of recognizing a thought/feeling/emotion surrounding how I feel about myself/body and working through. More positive thought pattern/restructuring a response the most helpful.”
The main complaint about the program was that it was too short, with women wanting more sessions to help continue their progress.
Not an ‘either-or’ approach
Dr. Kingsberg said ISSWSH has a variety of sexual medicine practitioners, including providers who can provide CBT for sexual concerns, and the American Association of Sexuality Educators, Counselors and Therapists has a referral directory.
“Keeping in mind the bio-psychosocial model, sometimes psychotherapy is going to be a really effective treatment for sexual concerns,” Dr. Kingsberg said. “Sometimes the pharmacologic option is going to be a really effective treatment for some concerns, and sometimes the combination is going to have a really nice treatment effect. So it’s not a one-size-fits-all, and it doesn’t have to be an either-or.”
The sexual concerns of women still do not get adequately addressed in medical schools and residencies, Dr. Kingsberg said, which is distinctly different from how male sexual concerns are addressed in health care.
“Erectile dysfunction is kind of in the norm, and women are still a little hesitant to bring up their sexual concerns,” Dr. Kingsberg said. “They don’t know if it’s appropriate and they’re hoping that their clinician will ask.”
One way clinicians can do that is with a global question for all their patients: “Most of my patients have sexual questions or concerns; what concerns do you have?”
“They don’t have to go through a checklist of 10 things,” Dr. Kingsberg said. If the patient does not bring anything up, providers can then ask a single follow up question: “Do you have any concerns with desire, arousal, orgasm, or pain?” That question, Dr. Kingsberg said, covers the four main areas of concern.
The study was funded by the Canadian Institute of Health Research. Dr. Green reported no disclosures. Dr. Kingsberg has consulted for or served on the advisory board for Alloy, Astellas, Bayer, Dare Bioscience, Freya, Reunion Neuroscience, Materna Medical, Madorra, Palatin, Pfizer, ReJoy, Sprout, Strategic Science Technologies, and MsMedicine.
PHILADELPHIA – . Four CBT sessions specifically focused on sexual concerns resulted in decreased sexual distress and concern, reduced depressive and menopausal symptoms, and increased sexual desire and functioning, as well as improved body image and relationship satisfaction.
An estimated 68%-87% of perimenopausal and postmenopausal women report sexual concerns, Sheryl Green, PhD, CPsych, an associate professor of psychiatry and behavioral neurosciences at McMaster University and a psychologist at St. Joseph’s Healthcare’s Women’s Health Concerns Clinic, both in Hamilton, Ont., told attendees at the meeting.
“Sexual concerns over the menopausal transition are not just physical, but they’re also psychological and emotional,” Dr. Green said. “Three common challenges include decreased sexual desire, a reduction in physical arousal and ability to achieve an orgasm, and sexual pain and discomfort during intercourse.”
The reasons for these concerns are multifactorial, she said. Decreased sexual desire can stem from stress, medical problems, their relationship with their partner, or other causes. A woman’s difficulty with reduced physical arousal or ability to have an orgasm can result from changes in hormone levels and vaginal changes, such as vaginal atrophy, which can also contribute to the sexual pain or discomfort reported by 17%-45% of postmenopausal women.
Two pharmacologic treatments exist for sexual concerns: oral flibanserin (Addyi) and injectable bremelanotide (Vyleesi). But many women may be unable or unwilling to take medication for their concerns. Previous research from Lori Brotto has found cognitive behavioral therapy and mindfulness interventions to effectively improve sexual functioning in women treated for gynecologic cancer and in women without a history of cancer.
“Sexual function needs to be understood from a bio-psychosocial model, looking at the biologic factors, the psychological factors, the sociocultural factors, and the interpersonal factors,” Sheryl Kingsberg, PhD, a professor of psychiatry and reproductive biology at Case Western Reserve University and a psychologist at University Hospitals in Cleveland, said in an interview.
“They can all overlap, and the clinician can ask a few pointed questions that help identify what the source of the problem is,” said Dr. Kingsberg, who was not involved in this study. She noted that the International Society for the Study of Women’s Sexual Health has an algorithm that can help in determining the source of the problems.
“Sometimes it’s going to be a biologic condition for which pharmacologic options are nice, but even if it is primarily pharmacologic, psychotherapy is always useful,” Dr. Kingsberg said. “Once the problem is there, even if it’s biologically based, then you have all the things in terms of the cognitive distortion, anxiety,” and other issues that a cognitive behavioral approach can help address. “And access is now much wider because of telehealth,” she added.
‘Psychology of menopause’
The study led by Dr. Green focused on peri- and postmenopausal women, with an average age of 50, who were experiencing primary sexual concerns based on a score of at least 26 on the Female Sexual Function Index (FSFI). Among the 20 women recruited for the study, 6 had already been prescribed hormone therapy for sexual concerns.
All reported decreased sexual desire, 17 reported decreased sexual arousal, 14 had body image dissatisfaction related to sexual concerns, and 6 reported urogenital problems. Nine of the women were in full remission from major depressive disorder, one had post-traumatic stress syndrome, and one had subclinical generalized anxiety disorder.
After spending 4 weeks on a wait list as self-control group for the study, the 15 women who completed the trial underwent four individual CBT sessions focusing on sexual concerns. The first session focused on psychoeducation and thought monitoring, and the second focused on cognitive distortions, cognitive strategies, and unhelpful beliefs or expectations related to sexual concerns. The third session looked at the role of problematic behaviors and behavioral experiments, and the fourth focused on continuation of strategies, long-term goals, and maintaining gains.
The participants completed eight measures at baseline, after the 4 weeks on the wait list, and after the four CBT sessions to assess the following:
- Sexual satisfaction, distress, and desire, using the FSFI, the Female Sexual Distress Scale-Revised (FSDS-R), and the Female Sexual Desire Questionnaire (FSDQ).
- Menopause symptoms, using the Greene Climacteric Scale (GCS).
- Body image, using the Dresden Body Image Questionnaire (DBIQ).
- Relationship satisfaction, using the Couples Satisfaction Index (CSI).
- Depression, using the Beck Depression Inventory-II (BDI-II).
- Anxiety, using the Hamilton Anxiety Rating Scale (HAM-A).
The women did not experience any significant changes while on the wait list except a slight decrease on the FSDQ concern subscale. Following the CBT sessions, however, the women experienced a significant decrease in sexual distress and concern as well as an increase in sexual dyadic desire and sexual functioning (P = .003 for FSFI, P = .002 for FSDS-R, and P = .003 for FSDQ).
Participants also experienced a decrease in depression (P < .0001) and menopausal symptoms (P = .001) and an increase in body-image satisfaction (P = .018) and relationship satisfaction (P = .0011) after the CBT sessions. The researchers assessed participants’ satisfaction with the Client Satisfaction Questionnaire after the CBT sessions and reported some of the qualitative findings.
“The treatment program was able to assist me with recognizing that some of my sexual concerns were normal, emotional as well as physical and hormonal, and provided me the ability to delve more deeply into the psychology of menopause and how to work through symptoms and concerns in more manageable pieces,” one participant wrote. Another found helpful the “homework exercises of recognizing a thought/feeling/emotion surrounding how I feel about myself/body and working through. More positive thought pattern/restructuring a response the most helpful.”
The main complaint about the program was that it was too short, with women wanting more sessions to help continue their progress.
Not an ‘either-or’ approach
Dr. Kingsberg said ISSWSH has a variety of sexual medicine practitioners, including providers who can provide CBT for sexual concerns, and the American Association of Sexuality Educators, Counselors and Therapists has a referral directory.
“Keeping in mind the bio-psychosocial model, sometimes psychotherapy is going to be a really effective treatment for sexual concerns,” Dr. Kingsberg said. “Sometimes the pharmacologic option is going to be a really effective treatment for some concerns, and sometimes the combination is going to have a really nice treatment effect. So it’s not a one-size-fits-all, and it doesn’t have to be an either-or.”
The sexual concerns of women still do not get adequately addressed in medical schools and residencies, Dr. Kingsberg said, which is distinctly different from how male sexual concerns are addressed in health care.
“Erectile dysfunction is kind of in the norm, and women are still a little hesitant to bring up their sexual concerns,” Dr. Kingsberg said. “They don’t know if it’s appropriate and they’re hoping that their clinician will ask.”
One way clinicians can do that is with a global question for all their patients: “Most of my patients have sexual questions or concerns; what concerns do you have?”
“They don’t have to go through a checklist of 10 things,” Dr. Kingsberg said. If the patient does not bring anything up, providers can then ask a single follow up question: “Do you have any concerns with desire, arousal, orgasm, or pain?” That question, Dr. Kingsberg said, covers the four main areas of concern.
The study was funded by the Canadian Institute of Health Research. Dr. Green reported no disclosures. Dr. Kingsberg has consulted for or served on the advisory board for Alloy, Astellas, Bayer, Dare Bioscience, Freya, Reunion Neuroscience, Materna Medical, Madorra, Palatin, Pfizer, ReJoy, Sprout, Strategic Science Technologies, and MsMedicine.
AT NAMS 2023
Federal Health Care Data Trends 2023
Federal Health Care Data Trends (click to view the digital edition) is a special supplement to Federal Practitioner, highlighting the latest research and study outcomes related to the health of veteran and active-duty populations.
In this issue:
- Limb Loss and Prostheses
- Neurology
- Cardiology
- Mental Health
- Diabetes
- Rheumatoid Arthritis
- Respiratory illnesses
- Women's Health
- HPV and Related Cancers
Federal Health Care Data Trends (click to view the digital edition) is a special supplement to Federal Practitioner, highlighting the latest research and study outcomes related to the health of veteran and active-duty populations.
In this issue:
- Limb Loss and Prostheses
- Neurology
- Cardiology
- Mental Health
- Diabetes
- Rheumatoid Arthritis
- Respiratory illnesses
- Women's Health
- HPV and Related Cancers
Federal Health Care Data Trends (click to view the digital edition) is a special supplement to Federal Practitioner, highlighting the latest research and study outcomes related to the health of veteran and active-duty populations.
In this issue:
- Limb Loss and Prostheses
- Neurology
- Cardiology
- Mental Health
- Diabetes
- Rheumatoid Arthritis
- Respiratory illnesses
- Women's Health
- HPV and Related Cancers