User login
Posttraumatic epilepsy is common, even after ‘mild’ TBI
, new research suggests.
Results from a multicenter, prospective cohort study showed 2.7% of nearly 1,500 participants with TBI reported also having posttraumatic epilepsy, and these patients had significantly worse outcomes than those without posttraumatic epilepsy.
“Posttraumatic epilepsy is common even in so-called mild TBI, and we should be on the lookout for patients reporting these kinds of spells,” said coinvestigator Ramon Diaz-Arrastia, MD, PhD, professor of neurology and director of the TBI Clinical Research Center, University of Pennsylvania, Philadelphia.
Dr. Diaz-Arrastia said he dislikes the term “mild TBI” because many of these injuries have “pretty substantial consequences.”
The findings were published online Dec. 29 in JAMA Network Open.
Novel study
Seizures can occur after TBI, most commonly after a severe brain injury, such as those leading to coma or bleeding in the brain or requiring surgical intervention. However, there have been “hints” that some patients with milder brain injuries are also at increased risk for epilepsy, said Dr. Diaz-Arrastia.
To investigate, the researchers assessed data from the large, multicenter Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI) database. Participants with TBI, defined as a Glasgow Coma Scale (GCS) score of 3-15, had presented to a level I trauma center within 24 hours of a head trauma needing evaluation with a CT scan.
The study included patients with relatively mild TBI (GCS score, 13-15), which is a “novel feature” of the study, the authors noted. Most prior studies of posttraumatic epilepsy focused on moderate to severe TBI.
The researchers included two sex- and age-matched control groups. The orthopedic trauma control (OTC) group consisted of patients with isolated trauma to the limbs, pelvis, and/or ribs. The “friend” or peer control group had backgrounds and lifestyles similar to those with TBI but had no history of TBI, concussion, or traumatic injury in the previous year.
The analysis included 1,885 participants (mean age, 41.3 years; 65.8% men). Of these, 1,493 had TBI, 182 were in the OTC group, and 210 were in the friends group. At 6- and 12-month follow-ups, investigators administered the Epilepsy Screening Questionnaire (ESQ), developed by the National Institute of Neurological Disorders and Stroke (NINDS).
Confirmatory data
Participants were asked about experiencing uncontrolled movements, unexplained changes in mental state, and repeated unusual attacks or convulsions, and whether they had been told they had epilepsy or seizures. If they answered yes to any of these questions, they received second-level screening, which asked about seizures.
Patients were deemed to have posttraumatic epilepsy if they answered affirmatively to any first-level screening item, experienced seizures 7 days after injury, and were diagnosed with epilepsy.
The primary outcome was rate of positive posttraumatic epilepsy diagnoses. At 12 months, 2.7% of those with TBI reported a posttraumatic epilepsy diagnosis compared with none of either of the control groups (P < .001).
This rate is consistent with prior literature and is “pretty close to what we expected,” said Dr. Diaz-Arrastia.
Among those with TBI and posttraumatic epilepsy, 12.2% had GCS scores of 3-8 (severe), 5.3% had scores of 9-12 (moderate), and 0.9% had scores of 13-15 (mild). That figure for mild TBI is not insignificant, said Dr. Diaz-Arrastia.
“Probably 90% of all those coming to the emergency room with a brain injury are diagnosed with mild TBI not requiring admission,” he noted.
The risk for posttraumatic epilepsy was higher the more severe the head injury, and among those with hemorrhage on head CT imaging. In patients with mild TBI, hemorrhage was associated with a two- to threefold risk of developing posttraumatic epilepsy.
“This prospective observational study confirms the epidemiologic data that even after mild brain injury, there is an increased risk for epilepsy,” said Dr. Diaz-Arrastia.
Universal screening?
The researchers also looked at whether seizures worsen other outcomes. Compared with those who had TBI but not posttraumatic epilepsy, those with posttraumatic epilepsy had significantly lower Glasgow Outcome Scale Extended (GOSE) scores (mean, 4.7 vs. 6.1; P < .001), higher Brief Symptom Inventory (BSI) scores (58.6 vs. 50.2; P = .02), and higher Rivermead Cognitive Metric (RCM) scores (5.3 vs. 3.1; P = .002) at 12 months after adjustment for age, initial GCS score, and imaging findings.
Higher GOSE and RCM scores reflect better outcomes, but a higher score on the BSI, which assesses overall mood, reflects a worse outcome, the investigators noted.
Previous evidence suggests prophylactic use of antiepileptic drugs in patients with TBI does not reduce risks. These drugs “are neither 100% safe nor 100% effective,” said Dr. Diaz-Arrastia. Some studies showed that certain agents actually worsen outcomes, he added.
What the field needs instead are antiepileptogenic drugs – those that interfere with the maladaptive synaptic plasticity that ends up in an epileptic circuit, he noted.
The new results suggest screening for posttraumatic epilepsy using the NINDS-ESQ “should be done pretty much routinely as a follow-up for all brain injuries,” Dr. Diaz-Arrastia said.
The investigators plan to have study participants assessed by an epileptologist later. A significant number of people with TBI, he noted, won’t develop posttraumatic epilepsy until 1-5 years after their injury – and even later in some cases.
A limitation of the study was that some patients reporting posttraumatic epilepsy may have had psychogenic nonepileptiform seizures, which are common in TBI patients, the investigators noted.
The study was supported by grants from One Mind, National Institutes of Health (NIH), National Institute of Neurological Disorders and Stroke (NINDS, and Department of Defence. Dr. Diaz-Arrastia reported receiving grants from the NIH, NINDS, and DOD during the conduct of the study.
A version of this article first appeared on Medscape.com.
, new research suggests.
Results from a multicenter, prospective cohort study showed 2.7% of nearly 1,500 participants with TBI reported also having posttraumatic epilepsy, and these patients had significantly worse outcomes than those without posttraumatic epilepsy.
“Posttraumatic epilepsy is common even in so-called mild TBI, and we should be on the lookout for patients reporting these kinds of spells,” said coinvestigator Ramon Diaz-Arrastia, MD, PhD, professor of neurology and director of the TBI Clinical Research Center, University of Pennsylvania, Philadelphia.
Dr. Diaz-Arrastia said he dislikes the term “mild TBI” because many of these injuries have “pretty substantial consequences.”
The findings were published online Dec. 29 in JAMA Network Open.
Novel study
Seizures can occur after TBI, most commonly after a severe brain injury, such as those leading to coma or bleeding in the brain or requiring surgical intervention. However, there have been “hints” that some patients with milder brain injuries are also at increased risk for epilepsy, said Dr. Diaz-Arrastia.
To investigate, the researchers assessed data from the large, multicenter Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI) database. Participants with TBI, defined as a Glasgow Coma Scale (GCS) score of 3-15, had presented to a level I trauma center within 24 hours of a head trauma needing evaluation with a CT scan.
The study included patients with relatively mild TBI (GCS score, 13-15), which is a “novel feature” of the study, the authors noted. Most prior studies of posttraumatic epilepsy focused on moderate to severe TBI.
The researchers included two sex- and age-matched control groups. The orthopedic trauma control (OTC) group consisted of patients with isolated trauma to the limbs, pelvis, and/or ribs. The “friend” or peer control group had backgrounds and lifestyles similar to those with TBI but had no history of TBI, concussion, or traumatic injury in the previous year.
The analysis included 1,885 participants (mean age, 41.3 years; 65.8% men). Of these, 1,493 had TBI, 182 were in the OTC group, and 210 were in the friends group. At 6- and 12-month follow-ups, investigators administered the Epilepsy Screening Questionnaire (ESQ), developed by the National Institute of Neurological Disorders and Stroke (NINDS).
Confirmatory data
Participants were asked about experiencing uncontrolled movements, unexplained changes in mental state, and repeated unusual attacks or convulsions, and whether they had been told they had epilepsy or seizures. If they answered yes to any of these questions, they received second-level screening, which asked about seizures.
Patients were deemed to have posttraumatic epilepsy if they answered affirmatively to any first-level screening item, experienced seizures 7 days after injury, and were diagnosed with epilepsy.
The primary outcome was rate of positive posttraumatic epilepsy diagnoses. At 12 months, 2.7% of those with TBI reported a posttraumatic epilepsy diagnosis compared with none of either of the control groups (P < .001).
This rate is consistent with prior literature and is “pretty close to what we expected,” said Dr. Diaz-Arrastia.
Among those with TBI and posttraumatic epilepsy, 12.2% had GCS scores of 3-8 (severe), 5.3% had scores of 9-12 (moderate), and 0.9% had scores of 13-15 (mild). That figure for mild TBI is not insignificant, said Dr. Diaz-Arrastia.
“Probably 90% of all those coming to the emergency room with a brain injury are diagnosed with mild TBI not requiring admission,” he noted.
The risk for posttraumatic epilepsy was higher the more severe the head injury, and among those with hemorrhage on head CT imaging. In patients with mild TBI, hemorrhage was associated with a two- to threefold risk of developing posttraumatic epilepsy.
“This prospective observational study confirms the epidemiologic data that even after mild brain injury, there is an increased risk for epilepsy,” said Dr. Diaz-Arrastia.
Universal screening?
The researchers also looked at whether seizures worsen other outcomes. Compared with those who had TBI but not posttraumatic epilepsy, those with posttraumatic epilepsy had significantly lower Glasgow Outcome Scale Extended (GOSE) scores (mean, 4.7 vs. 6.1; P < .001), higher Brief Symptom Inventory (BSI) scores (58.6 vs. 50.2; P = .02), and higher Rivermead Cognitive Metric (RCM) scores (5.3 vs. 3.1; P = .002) at 12 months after adjustment for age, initial GCS score, and imaging findings.
Higher GOSE and RCM scores reflect better outcomes, but a higher score on the BSI, which assesses overall mood, reflects a worse outcome, the investigators noted.
Previous evidence suggests prophylactic use of antiepileptic drugs in patients with TBI does not reduce risks. These drugs “are neither 100% safe nor 100% effective,” said Dr. Diaz-Arrastia. Some studies showed that certain agents actually worsen outcomes, he added.
What the field needs instead are antiepileptogenic drugs – those that interfere with the maladaptive synaptic plasticity that ends up in an epileptic circuit, he noted.
The new results suggest screening for posttraumatic epilepsy using the NINDS-ESQ “should be done pretty much routinely as a follow-up for all brain injuries,” Dr. Diaz-Arrastia said.
The investigators plan to have study participants assessed by an epileptologist later. A significant number of people with TBI, he noted, won’t develop posttraumatic epilepsy until 1-5 years after their injury – and even later in some cases.
A limitation of the study was that some patients reporting posttraumatic epilepsy may have had psychogenic nonepileptiform seizures, which are common in TBI patients, the investigators noted.
The study was supported by grants from One Mind, National Institutes of Health (NIH), National Institute of Neurological Disorders and Stroke (NINDS, and Department of Defence. Dr. Diaz-Arrastia reported receiving grants from the NIH, NINDS, and DOD during the conduct of the study.
A version of this article first appeared on Medscape.com.
, new research suggests.
Results from a multicenter, prospective cohort study showed 2.7% of nearly 1,500 participants with TBI reported also having posttraumatic epilepsy, and these patients had significantly worse outcomes than those without posttraumatic epilepsy.
“Posttraumatic epilepsy is common even in so-called mild TBI, and we should be on the lookout for patients reporting these kinds of spells,” said coinvestigator Ramon Diaz-Arrastia, MD, PhD, professor of neurology and director of the TBI Clinical Research Center, University of Pennsylvania, Philadelphia.
Dr. Diaz-Arrastia said he dislikes the term “mild TBI” because many of these injuries have “pretty substantial consequences.”
The findings were published online Dec. 29 in JAMA Network Open.
Novel study
Seizures can occur after TBI, most commonly after a severe brain injury, such as those leading to coma or bleeding in the brain or requiring surgical intervention. However, there have been “hints” that some patients with milder brain injuries are also at increased risk for epilepsy, said Dr. Diaz-Arrastia.
To investigate, the researchers assessed data from the large, multicenter Transforming Research and Clinical Knowledge in Traumatic Brain Injury (TRACK-TBI) database. Participants with TBI, defined as a Glasgow Coma Scale (GCS) score of 3-15, had presented to a level I trauma center within 24 hours of a head trauma needing evaluation with a CT scan.
The study included patients with relatively mild TBI (GCS score, 13-15), which is a “novel feature” of the study, the authors noted. Most prior studies of posttraumatic epilepsy focused on moderate to severe TBI.
The researchers included two sex- and age-matched control groups. The orthopedic trauma control (OTC) group consisted of patients with isolated trauma to the limbs, pelvis, and/or ribs. The “friend” or peer control group had backgrounds and lifestyles similar to those with TBI but had no history of TBI, concussion, or traumatic injury in the previous year.
The analysis included 1,885 participants (mean age, 41.3 years; 65.8% men). Of these, 1,493 had TBI, 182 were in the OTC group, and 210 were in the friends group. At 6- and 12-month follow-ups, investigators administered the Epilepsy Screening Questionnaire (ESQ), developed by the National Institute of Neurological Disorders and Stroke (NINDS).
Confirmatory data
Participants were asked about experiencing uncontrolled movements, unexplained changes in mental state, and repeated unusual attacks or convulsions, and whether they had been told they had epilepsy or seizures. If they answered yes to any of these questions, they received second-level screening, which asked about seizures.
Patients were deemed to have posttraumatic epilepsy if they answered affirmatively to any first-level screening item, experienced seizures 7 days after injury, and were diagnosed with epilepsy.
The primary outcome was rate of positive posttraumatic epilepsy diagnoses. At 12 months, 2.7% of those with TBI reported a posttraumatic epilepsy diagnosis compared with none of either of the control groups (P < .001).
This rate is consistent with prior literature and is “pretty close to what we expected,” said Dr. Diaz-Arrastia.
Among those with TBI and posttraumatic epilepsy, 12.2% had GCS scores of 3-8 (severe), 5.3% had scores of 9-12 (moderate), and 0.9% had scores of 13-15 (mild). That figure for mild TBI is not insignificant, said Dr. Diaz-Arrastia.
“Probably 90% of all those coming to the emergency room with a brain injury are diagnosed with mild TBI not requiring admission,” he noted.
The risk for posttraumatic epilepsy was higher the more severe the head injury, and among those with hemorrhage on head CT imaging. In patients with mild TBI, hemorrhage was associated with a two- to threefold risk of developing posttraumatic epilepsy.
“This prospective observational study confirms the epidemiologic data that even after mild brain injury, there is an increased risk for epilepsy,” said Dr. Diaz-Arrastia.
Universal screening?
The researchers also looked at whether seizures worsen other outcomes. Compared with those who had TBI but not posttraumatic epilepsy, those with posttraumatic epilepsy had significantly lower Glasgow Outcome Scale Extended (GOSE) scores (mean, 4.7 vs. 6.1; P < .001), higher Brief Symptom Inventory (BSI) scores (58.6 vs. 50.2; P = .02), and higher Rivermead Cognitive Metric (RCM) scores (5.3 vs. 3.1; P = .002) at 12 months after adjustment for age, initial GCS score, and imaging findings.
Higher GOSE and RCM scores reflect better outcomes, but a higher score on the BSI, which assesses overall mood, reflects a worse outcome, the investigators noted.
Previous evidence suggests prophylactic use of antiepileptic drugs in patients with TBI does not reduce risks. These drugs “are neither 100% safe nor 100% effective,” said Dr. Diaz-Arrastia. Some studies showed that certain agents actually worsen outcomes, he added.
What the field needs instead are antiepileptogenic drugs – those that interfere with the maladaptive synaptic plasticity that ends up in an epileptic circuit, he noted.
The new results suggest screening for posttraumatic epilepsy using the NINDS-ESQ “should be done pretty much routinely as a follow-up for all brain injuries,” Dr. Diaz-Arrastia said.
The investigators plan to have study participants assessed by an epileptologist later. A significant number of people with TBI, he noted, won’t develop posttraumatic epilepsy until 1-5 years after their injury – and even later in some cases.
A limitation of the study was that some patients reporting posttraumatic epilepsy may have had psychogenic nonepileptiform seizures, which are common in TBI patients, the investigators noted.
The study was supported by grants from One Mind, National Institutes of Health (NIH), National Institute of Neurological Disorders and Stroke (NINDS, and Department of Defence. Dr. Diaz-Arrastia reported receiving grants from the NIH, NINDS, and DOD during the conduct of the study.
A version of this article first appeared on Medscape.com.
COVID affects executive functioning in young to middle-age adults: Study
than people in the general population with no such infection, according to new data published on the preprint server medRxiv.
Researchers, led by Peter A. Hall, PhD, with the University of Waterloo (Ont.), found that COVID infection is associated with executive dysfunction among young and middle-aged adults, including for those not exposed to intubation or hospitalization.
The findings have not been peer reviewed.
The study included a representative cohort of 1,958 community-dwelling young and middle-aged adults. It used a balanced proportion of infected and uninfected people to estimate the link between SARS-CoV-2 infection and cognitive/executive dysfunction.
The authors noted that the survey was conducted from Sept. 28 to Oct. 21, 2021, when the primary variant in Canada was Delta.
The research was a cross-sectional observational study with data from the ongoing Canadian COVID-19 Experiences Survey. It included equal representation of vaccinated and vaccine-hesitant adults aged 18-54 years. COVID-19 symptoms ranged from negligible to life-threatening cases requiring hospitalization.
Half in the cohort (50.2%) received two vaccine shots; 43.3% had received no shots; and 5.5% received one shot, but were not intending to receive a second shot.
Dose-response relationship
According to the paper, those with prior COVID-19 infection, regardless of symptom severity, reported a significantly higher number of symptoms of executive dysfunction than their noninfected counterparts (mechanical adjustment, 1.63, standard error, 0.08; 95% confidence interval, 1.47-1.80; P = .001).
The researchers also found a dose-response relationship between COVID-19 symptom severity and cognitive dysfunction. Those with moderate and very/extremely severe COVID-19 symptoms were linked with significantly greater dysfunction.
“This reinforces what we’re hearing about – that COVID is not ‘one and done.’ It can have lasting and quite subtle and damaging effects on the human body,” William Schaffner, MD, infectious disease specialist with Vanderbilt University, Nashville, Tenn., said in an interview.
Measuring executive functioning – including the ability to make sound decisions – is something other studies haven’t typically addressed, he said.
Men were likely to report more cognitive dysfunction symptoms than women (beta, 0.15; P < .001). Younger adults (25-39 years) were more likely to experience cognitive dysfunction than those age 40-54 (beta, 0.30; P < .001).
Dr. Schaffner said it was troubling that young people are more likely to experience the dysfunction.
“When we think of ‘brain fog’ we think of older persons who are already predisposed to have more memory lapses as they get older,” he said.
The link between cognitive dysfunction and COVID-19 infection has been shown in other studies, but many have not used representative samples and have not compared results with noninfected controls in the general population, the authors wrote.
Executive dysfunction was measured using four questions from the Deficits in Executive Functioning Scale. Respondents were asked how often they have experienced these scenarios in the past 6 months:
- “I am unable to inhibit my reactions or responses to events or to other people.”
- “I make impulsive comments to others.”
- “I am likely to do things without considering the consequences for doing them.”
- “I act without thinking.”
“This makes it even more important that we talk about vaccination,” Dr. Schaffner said, “because clearly the more seriously ill you are, the more likely this sort of thing is likely to happen and vaccines have been shown time and again to avert hospitalizations and more serious illness. It also makes more important the monoclonal antibody treatments we have and the antivirals, which will prevent the evolution of mild disease into something more serious.”
This research was supported by a grant from the Canadian Institutes for Health Research, Institute for Population and Public Health. The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
than people in the general population with no such infection, according to new data published on the preprint server medRxiv.
Researchers, led by Peter A. Hall, PhD, with the University of Waterloo (Ont.), found that COVID infection is associated with executive dysfunction among young and middle-aged adults, including for those not exposed to intubation or hospitalization.
The findings have not been peer reviewed.
The study included a representative cohort of 1,958 community-dwelling young and middle-aged adults. It used a balanced proportion of infected and uninfected people to estimate the link between SARS-CoV-2 infection and cognitive/executive dysfunction.
The authors noted that the survey was conducted from Sept. 28 to Oct. 21, 2021, when the primary variant in Canada was Delta.
The research was a cross-sectional observational study with data from the ongoing Canadian COVID-19 Experiences Survey. It included equal representation of vaccinated and vaccine-hesitant adults aged 18-54 years. COVID-19 symptoms ranged from negligible to life-threatening cases requiring hospitalization.
Half in the cohort (50.2%) received two vaccine shots; 43.3% had received no shots; and 5.5% received one shot, but were not intending to receive a second shot.
Dose-response relationship
According to the paper, those with prior COVID-19 infection, regardless of symptom severity, reported a significantly higher number of symptoms of executive dysfunction than their noninfected counterparts (mechanical adjustment, 1.63, standard error, 0.08; 95% confidence interval, 1.47-1.80; P = .001).
The researchers also found a dose-response relationship between COVID-19 symptom severity and cognitive dysfunction. Those with moderate and very/extremely severe COVID-19 symptoms were linked with significantly greater dysfunction.
“This reinforces what we’re hearing about – that COVID is not ‘one and done.’ It can have lasting and quite subtle and damaging effects on the human body,” William Schaffner, MD, infectious disease specialist with Vanderbilt University, Nashville, Tenn., said in an interview.
Measuring executive functioning – including the ability to make sound decisions – is something other studies haven’t typically addressed, he said.
Men were likely to report more cognitive dysfunction symptoms than women (beta, 0.15; P < .001). Younger adults (25-39 years) were more likely to experience cognitive dysfunction than those age 40-54 (beta, 0.30; P < .001).
Dr. Schaffner said it was troubling that young people are more likely to experience the dysfunction.
“When we think of ‘brain fog’ we think of older persons who are already predisposed to have more memory lapses as they get older,” he said.
The link between cognitive dysfunction and COVID-19 infection has been shown in other studies, but many have not used representative samples and have not compared results with noninfected controls in the general population, the authors wrote.
Executive dysfunction was measured using four questions from the Deficits in Executive Functioning Scale. Respondents were asked how often they have experienced these scenarios in the past 6 months:
- “I am unable to inhibit my reactions or responses to events or to other people.”
- “I make impulsive comments to others.”
- “I am likely to do things without considering the consequences for doing them.”
- “I act without thinking.”
“This makes it even more important that we talk about vaccination,” Dr. Schaffner said, “because clearly the more seriously ill you are, the more likely this sort of thing is likely to happen and vaccines have been shown time and again to avert hospitalizations and more serious illness. It also makes more important the monoclonal antibody treatments we have and the antivirals, which will prevent the evolution of mild disease into something more serious.”
This research was supported by a grant from the Canadian Institutes for Health Research, Institute for Population and Public Health. The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
than people in the general population with no such infection, according to new data published on the preprint server medRxiv.
Researchers, led by Peter A. Hall, PhD, with the University of Waterloo (Ont.), found that COVID infection is associated with executive dysfunction among young and middle-aged adults, including for those not exposed to intubation or hospitalization.
The findings have not been peer reviewed.
The study included a representative cohort of 1,958 community-dwelling young and middle-aged adults. It used a balanced proportion of infected and uninfected people to estimate the link between SARS-CoV-2 infection and cognitive/executive dysfunction.
The authors noted that the survey was conducted from Sept. 28 to Oct. 21, 2021, when the primary variant in Canada was Delta.
The research was a cross-sectional observational study with data from the ongoing Canadian COVID-19 Experiences Survey. It included equal representation of vaccinated and vaccine-hesitant adults aged 18-54 years. COVID-19 symptoms ranged from negligible to life-threatening cases requiring hospitalization.
Half in the cohort (50.2%) received two vaccine shots; 43.3% had received no shots; and 5.5% received one shot, but were not intending to receive a second shot.
Dose-response relationship
According to the paper, those with prior COVID-19 infection, regardless of symptom severity, reported a significantly higher number of symptoms of executive dysfunction than their noninfected counterparts (mechanical adjustment, 1.63, standard error, 0.08; 95% confidence interval, 1.47-1.80; P = .001).
The researchers also found a dose-response relationship between COVID-19 symptom severity and cognitive dysfunction. Those with moderate and very/extremely severe COVID-19 symptoms were linked with significantly greater dysfunction.
“This reinforces what we’re hearing about – that COVID is not ‘one and done.’ It can have lasting and quite subtle and damaging effects on the human body,” William Schaffner, MD, infectious disease specialist with Vanderbilt University, Nashville, Tenn., said in an interview.
Measuring executive functioning – including the ability to make sound decisions – is something other studies haven’t typically addressed, he said.
Men were likely to report more cognitive dysfunction symptoms than women (beta, 0.15; P < .001). Younger adults (25-39 years) were more likely to experience cognitive dysfunction than those age 40-54 (beta, 0.30; P < .001).
Dr. Schaffner said it was troubling that young people are more likely to experience the dysfunction.
“When we think of ‘brain fog’ we think of older persons who are already predisposed to have more memory lapses as they get older,” he said.
The link between cognitive dysfunction and COVID-19 infection has been shown in other studies, but many have not used representative samples and have not compared results with noninfected controls in the general population, the authors wrote.
Executive dysfunction was measured using four questions from the Deficits in Executive Functioning Scale. Respondents were asked how often they have experienced these scenarios in the past 6 months:
- “I am unable to inhibit my reactions or responses to events or to other people.”
- “I make impulsive comments to others.”
- “I am likely to do things without considering the consequences for doing them.”
- “I act without thinking.”
“This makes it even more important that we talk about vaccination,” Dr. Schaffner said, “because clearly the more seriously ill you are, the more likely this sort of thing is likely to happen and vaccines have been shown time and again to avert hospitalizations and more serious illness. It also makes more important the monoclonal antibody treatments we have and the antivirals, which will prevent the evolution of mild disease into something more serious.”
This research was supported by a grant from the Canadian Institutes for Health Research, Institute for Population and Public Health. The study authors and Dr. Schaffner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM MEDRXIV
Asthma treatment does not appear to raise risk of neuropsychiatric disease
Use of a leukotriene receptor antagonist (LTRA) for asthma management did not increase the risk of neuropsychiatric disease, based on data from more than 60,000 asthma patients.
Although LTRAs are established as an effective drug for asthma, the U.S. Food and Drug Administration warnings of the risk for neuropsychiatric (NP) drug reactions – including a boxed warning for montelukast (Singulair) – has raised concerns, writes Ji-Su Shim, MD, of Ewha Womans University, Seoul, South Korea, and colleagues.
However, evidence for such an association is limited, and previous studies have focused only on children and adolescents, and on a single LTRA (montelukast), the researchers say.
In a study published Dec. 1 in the Journal of Allergy and Clinical Immunology: In Practice, the researchers used a Korean national health insurance database to identify 61,571 adult patients with asthma aged 40 years and older between Jan. 2002 and Dec. 2015 with no history of LTRA use.
The patients underwent screening examinations between Jan. 2009 and Dec. 2010, which marked the start of a follow-up period ending on Dec. 31, 2015. The median age of the study population was 61 years, and the mean follow-up period for NPs or other outcomes was approximately 47.6 months for LTRA users and 46.5 months for nonusers. Overall, 11.1% of the study population used pranlukast (Onon), 11% used montelukast, and 0.24% used zafirlukast (Accolate).
A total of 12,168 patients took an LTRA during the follow-up period. The hazard ratio for newly diagnosed neuropsychiatric diseases was not significantly different between LTRA users and nonusers (hazard ratio, 1.01; P = .952) in an adjusted model that included age, sex, pack-years of smoking, alcohol use, physical activity, body mass index, comorbid conditions, other respiratory diseases, and use of other asthma medications.
(75.4% vs. 76.1% for dementia, 12.7% vs. 12.8% for mood disorders, and 5.6% vs. 3.5% for panic disorders).
A subgroup analysis for associations between the duration of LTRA use and NP disease risk also showed no significant difference between LTRA users and nonusers.
“The mechanism of the development of NP symptoms by LTRAs has not been identified,” the researchers write in their discussion of the study findings. “Because most of NP side effects due to montelukast occur in few patients within 2 weeks of drug administration, it also may have relation with the presence of some genetic polymorphisms involving modification of the normal action or metabolism of LTRAs,” they explained.
The FDA’s boxed warning for montelukast noting the risk of serious mental health side effects has renewed interest in the relationship between NPs and LTRAs, the researchers noted. However, the current study findings support previous randomized controlled trials and larger studies, and the current warnings are based mainly on pharmacovigilance studies, case series, and case reports, they said.
The study findings were limited by several factors, including the retrospective design, the potential for misclassification of asthma diagnosis, the exclusion of temporary NP symptoms that might prompt LTRA discontinuation, and the inability to detect possible differences in ethnicities other than Korean, the researchers note.
However, the results suggest that adverse NP symptoms should not prevent physicians from prescribing LTRAs to selected patients with asthma. Instead, the physician should accompany the prescription with “a word of caution in case any mood changes might occur,” the investigators wrote.
“Further studies, such as randomized controlled trials, are needed to reveal the association between the use of LTRAs and the risk of NP events and/or diseases,” they concluded.
Potential genetic predisposition may drive cases
The relatively rare occurrence of NP symptoms in asthma patients using LTRAs has prompted questions from the medical community on whether the relationship really exists, writes Désirée Larenas-Linnemann, MD, of Médica Sur Clinical Foundation and Hospital, Mexico City, in an accompanying editorial ).
The current study provides information about medications and possible adverse drug reactions, but “great care should be taken in the interpretation of the results from such a study,” she notes. Limitations include not only the possible misclassification of asthma and the homogeneous study population, but also the fact that some NPs, such as dementia, are already common in older adults..
Dr. Larenas-Linnemann shared a story of one of her patients, a 2½-year-old boy who began exhibiting hyperactivity and other strange behaviors while on an LRTA. The toddler’s father had previously reported “horrible nightmares, strange thoughts, and to feel upset, unsecure until he suspended the medication.” Cases such as this support a potential genetic predisposition, with drug metabolism playing a role, and clinicians should take genetic backgrounds into account, she said.
“Even though the current study did not show an association between LTRA use or duration of exposure and the occurrence of NP diseases in Korean adults with asthma, this does not imply such a relationship might be present in other age groups (children-adolescents-adults up to 50 years) or in patients with a different genetic background,” she emphasized.
However, “In the meantime, although LTRA should continue to be prescribed if indicated, an index of suspicion for possible NP effects should be maintained,” Dr. Larenas-Linnemann concluded.
“This study is timely, since the boxed warning for montelukast was issued approximately 1 year ago by the FDA,” Thomas B. Casale, MD, of the University of South Florida, Tampa, said in an interview.
Dr. Casale said he was not surprised by the findings, “since most of the data implicating a potential link between the use of montelukast and neuropsychiatric disorders have not been particularly compelling,” and much of the current information comes from case reports and retrospective studies.
“Furthermore, the data appeared to be somewhat stronger in the pediatric population,” Dr. Casale noted. “This study focused on elderly patients (mean age 61) and included two other leukotriene modifiers. The number of patients receiving montelukast was small (56), which may have also confounded the results,” he noted.
As for clinical implications, “I don’t think this study will change practice,” Dr. Casale said. “As indicated, it is in an elderly population, included only a limited number of patients receiving montelukast, and was in a Korean cohort. All of these factors could have influenced the results,” and the data may not be generalizable to patients elsewhere, including the United States, he said. “Also, the study only included patients with asthma and in the United States; the approval for rhinitis is another important indication to study,” he noted.
Additional research is needed in the form of better prospective studies examining the potential link between montelukast and neuropsychiatric disorders in both the pediatric and adult populations having either asthma or rhinitis, Dr. Casale concluded.
The study received no outside funding. The researchers and Dr. Casale have disclosed no relevant financial relationships. Dr. Larenas-Linnemann disclosed personal fees from Allakos, Armstrong, AstraZeneca, Chiesi, DBV Technologies, Grünenthal, GSK, Mylan/Viatris, Menarini, MSD, Novartis, Pfizer, Sanofi, Siegfried, UCB, Alakos, Gossamer, and Carnot, and grants from Sanofi, AstraZeneca, Novartis, Circassia, UCB, GSK, and the Purina Institute.
A version of this article first appeared on Medscape.com.
Use of a leukotriene receptor antagonist (LTRA) for asthma management did not increase the risk of neuropsychiatric disease, based on data from more than 60,000 asthma patients.
Although LTRAs are established as an effective drug for asthma, the U.S. Food and Drug Administration warnings of the risk for neuropsychiatric (NP) drug reactions – including a boxed warning for montelukast (Singulair) – has raised concerns, writes Ji-Su Shim, MD, of Ewha Womans University, Seoul, South Korea, and colleagues.
However, evidence for such an association is limited, and previous studies have focused only on children and adolescents, and on a single LTRA (montelukast), the researchers say.
In a study published Dec. 1 in the Journal of Allergy and Clinical Immunology: In Practice, the researchers used a Korean national health insurance database to identify 61,571 adult patients with asthma aged 40 years and older between Jan. 2002 and Dec. 2015 with no history of LTRA use.
The patients underwent screening examinations between Jan. 2009 and Dec. 2010, which marked the start of a follow-up period ending on Dec. 31, 2015. The median age of the study population was 61 years, and the mean follow-up period for NPs or other outcomes was approximately 47.6 months for LTRA users and 46.5 months for nonusers. Overall, 11.1% of the study population used pranlukast (Onon), 11% used montelukast, and 0.24% used zafirlukast (Accolate).
A total of 12,168 patients took an LTRA during the follow-up period. The hazard ratio for newly diagnosed neuropsychiatric diseases was not significantly different between LTRA users and nonusers (hazard ratio, 1.01; P = .952) in an adjusted model that included age, sex, pack-years of smoking, alcohol use, physical activity, body mass index, comorbid conditions, other respiratory diseases, and use of other asthma medications.
(75.4% vs. 76.1% for dementia, 12.7% vs. 12.8% for mood disorders, and 5.6% vs. 3.5% for panic disorders).
A subgroup analysis for associations between the duration of LTRA use and NP disease risk also showed no significant difference between LTRA users and nonusers.
“The mechanism of the development of NP symptoms by LTRAs has not been identified,” the researchers write in their discussion of the study findings. “Because most of NP side effects due to montelukast occur in few patients within 2 weeks of drug administration, it also may have relation with the presence of some genetic polymorphisms involving modification of the normal action or metabolism of LTRAs,” they explained.
The FDA’s boxed warning for montelukast noting the risk of serious mental health side effects has renewed interest in the relationship between NPs and LTRAs, the researchers noted. However, the current study findings support previous randomized controlled trials and larger studies, and the current warnings are based mainly on pharmacovigilance studies, case series, and case reports, they said.
The study findings were limited by several factors, including the retrospective design, the potential for misclassification of asthma diagnosis, the exclusion of temporary NP symptoms that might prompt LTRA discontinuation, and the inability to detect possible differences in ethnicities other than Korean, the researchers note.
However, the results suggest that adverse NP symptoms should not prevent physicians from prescribing LTRAs to selected patients with asthma. Instead, the physician should accompany the prescription with “a word of caution in case any mood changes might occur,” the investigators wrote.
“Further studies, such as randomized controlled trials, are needed to reveal the association between the use of LTRAs and the risk of NP events and/or diseases,” they concluded.
Potential genetic predisposition may drive cases
The relatively rare occurrence of NP symptoms in asthma patients using LTRAs has prompted questions from the medical community on whether the relationship really exists, writes Désirée Larenas-Linnemann, MD, of Médica Sur Clinical Foundation and Hospital, Mexico City, in an accompanying editorial ).
The current study provides information about medications and possible adverse drug reactions, but “great care should be taken in the interpretation of the results from such a study,” she notes. Limitations include not only the possible misclassification of asthma and the homogeneous study population, but also the fact that some NPs, such as dementia, are already common in older adults..
Dr. Larenas-Linnemann shared a story of one of her patients, a 2½-year-old boy who began exhibiting hyperactivity and other strange behaviors while on an LRTA. The toddler’s father had previously reported “horrible nightmares, strange thoughts, and to feel upset, unsecure until he suspended the medication.” Cases such as this support a potential genetic predisposition, with drug metabolism playing a role, and clinicians should take genetic backgrounds into account, she said.
“Even though the current study did not show an association between LTRA use or duration of exposure and the occurrence of NP diseases in Korean adults with asthma, this does not imply such a relationship might be present in other age groups (children-adolescents-adults up to 50 years) or in patients with a different genetic background,” she emphasized.
However, “In the meantime, although LTRA should continue to be prescribed if indicated, an index of suspicion for possible NP effects should be maintained,” Dr. Larenas-Linnemann concluded.
“This study is timely, since the boxed warning for montelukast was issued approximately 1 year ago by the FDA,” Thomas B. Casale, MD, of the University of South Florida, Tampa, said in an interview.
Dr. Casale said he was not surprised by the findings, “since most of the data implicating a potential link between the use of montelukast and neuropsychiatric disorders have not been particularly compelling,” and much of the current information comes from case reports and retrospective studies.
“Furthermore, the data appeared to be somewhat stronger in the pediatric population,” Dr. Casale noted. “This study focused on elderly patients (mean age 61) and included two other leukotriene modifiers. The number of patients receiving montelukast was small (56), which may have also confounded the results,” he noted.
As for clinical implications, “I don’t think this study will change practice,” Dr. Casale said. “As indicated, it is in an elderly population, included only a limited number of patients receiving montelukast, and was in a Korean cohort. All of these factors could have influenced the results,” and the data may not be generalizable to patients elsewhere, including the United States, he said. “Also, the study only included patients with asthma and in the United States; the approval for rhinitis is another important indication to study,” he noted.
Additional research is needed in the form of better prospective studies examining the potential link between montelukast and neuropsychiatric disorders in both the pediatric and adult populations having either asthma or rhinitis, Dr. Casale concluded.
The study received no outside funding. The researchers and Dr. Casale have disclosed no relevant financial relationships. Dr. Larenas-Linnemann disclosed personal fees from Allakos, Armstrong, AstraZeneca, Chiesi, DBV Technologies, Grünenthal, GSK, Mylan/Viatris, Menarini, MSD, Novartis, Pfizer, Sanofi, Siegfried, UCB, Alakos, Gossamer, and Carnot, and grants from Sanofi, AstraZeneca, Novartis, Circassia, UCB, GSK, and the Purina Institute.
A version of this article first appeared on Medscape.com.
Use of a leukotriene receptor antagonist (LTRA) for asthma management did not increase the risk of neuropsychiatric disease, based on data from more than 60,000 asthma patients.
Although LTRAs are established as an effective drug for asthma, the U.S. Food and Drug Administration warnings of the risk for neuropsychiatric (NP) drug reactions – including a boxed warning for montelukast (Singulair) – has raised concerns, writes Ji-Su Shim, MD, of Ewha Womans University, Seoul, South Korea, and colleagues.
However, evidence for such an association is limited, and previous studies have focused only on children and adolescents, and on a single LTRA (montelukast), the researchers say.
In a study published Dec. 1 in the Journal of Allergy and Clinical Immunology: In Practice, the researchers used a Korean national health insurance database to identify 61,571 adult patients with asthma aged 40 years and older between Jan. 2002 and Dec. 2015 with no history of LTRA use.
The patients underwent screening examinations between Jan. 2009 and Dec. 2010, which marked the start of a follow-up period ending on Dec. 31, 2015. The median age of the study population was 61 years, and the mean follow-up period for NPs or other outcomes was approximately 47.6 months for LTRA users and 46.5 months for nonusers. Overall, 11.1% of the study population used pranlukast (Onon), 11% used montelukast, and 0.24% used zafirlukast (Accolate).
A total of 12,168 patients took an LTRA during the follow-up period. The hazard ratio for newly diagnosed neuropsychiatric diseases was not significantly different between LTRA users and nonusers (hazard ratio, 1.01; P = .952) in an adjusted model that included age, sex, pack-years of smoking, alcohol use, physical activity, body mass index, comorbid conditions, other respiratory diseases, and use of other asthma medications.
(75.4% vs. 76.1% for dementia, 12.7% vs. 12.8% for mood disorders, and 5.6% vs. 3.5% for panic disorders).
A subgroup analysis for associations between the duration of LTRA use and NP disease risk also showed no significant difference between LTRA users and nonusers.
“The mechanism of the development of NP symptoms by LTRAs has not been identified,” the researchers write in their discussion of the study findings. “Because most of NP side effects due to montelukast occur in few patients within 2 weeks of drug administration, it also may have relation with the presence of some genetic polymorphisms involving modification of the normal action or metabolism of LTRAs,” they explained.
The FDA’s boxed warning for montelukast noting the risk of serious mental health side effects has renewed interest in the relationship between NPs and LTRAs, the researchers noted. However, the current study findings support previous randomized controlled trials and larger studies, and the current warnings are based mainly on pharmacovigilance studies, case series, and case reports, they said.
The study findings were limited by several factors, including the retrospective design, the potential for misclassification of asthma diagnosis, the exclusion of temporary NP symptoms that might prompt LTRA discontinuation, and the inability to detect possible differences in ethnicities other than Korean, the researchers note.
However, the results suggest that adverse NP symptoms should not prevent physicians from prescribing LTRAs to selected patients with asthma. Instead, the physician should accompany the prescription with “a word of caution in case any mood changes might occur,” the investigators wrote.
“Further studies, such as randomized controlled trials, are needed to reveal the association between the use of LTRAs and the risk of NP events and/or diseases,” they concluded.
Potential genetic predisposition may drive cases
The relatively rare occurrence of NP symptoms in asthma patients using LTRAs has prompted questions from the medical community on whether the relationship really exists, writes Désirée Larenas-Linnemann, MD, of Médica Sur Clinical Foundation and Hospital, Mexico City, in an accompanying editorial ).
The current study provides information about medications and possible adverse drug reactions, but “great care should be taken in the interpretation of the results from such a study,” she notes. Limitations include not only the possible misclassification of asthma and the homogeneous study population, but also the fact that some NPs, such as dementia, are already common in older adults..
Dr. Larenas-Linnemann shared a story of one of her patients, a 2½-year-old boy who began exhibiting hyperactivity and other strange behaviors while on an LRTA. The toddler’s father had previously reported “horrible nightmares, strange thoughts, and to feel upset, unsecure until he suspended the medication.” Cases such as this support a potential genetic predisposition, with drug metabolism playing a role, and clinicians should take genetic backgrounds into account, she said.
“Even though the current study did not show an association between LTRA use or duration of exposure and the occurrence of NP diseases in Korean adults with asthma, this does not imply such a relationship might be present in other age groups (children-adolescents-adults up to 50 years) or in patients with a different genetic background,” she emphasized.
However, “In the meantime, although LTRA should continue to be prescribed if indicated, an index of suspicion for possible NP effects should be maintained,” Dr. Larenas-Linnemann concluded.
“This study is timely, since the boxed warning for montelukast was issued approximately 1 year ago by the FDA,” Thomas B. Casale, MD, of the University of South Florida, Tampa, said in an interview.
Dr. Casale said he was not surprised by the findings, “since most of the data implicating a potential link between the use of montelukast and neuropsychiatric disorders have not been particularly compelling,” and much of the current information comes from case reports and retrospective studies.
“Furthermore, the data appeared to be somewhat stronger in the pediatric population,” Dr. Casale noted. “This study focused on elderly patients (mean age 61) and included two other leukotriene modifiers. The number of patients receiving montelukast was small (56), which may have also confounded the results,” he noted.
As for clinical implications, “I don’t think this study will change practice,” Dr. Casale said. “As indicated, it is in an elderly population, included only a limited number of patients receiving montelukast, and was in a Korean cohort. All of these factors could have influenced the results,” and the data may not be generalizable to patients elsewhere, including the United States, he said. “Also, the study only included patients with asthma and in the United States; the approval for rhinitis is another important indication to study,” he noted.
Additional research is needed in the form of better prospective studies examining the potential link between montelukast and neuropsychiatric disorders in both the pediatric and adult populations having either asthma or rhinitis, Dr. Casale concluded.
The study received no outside funding. The researchers and Dr. Casale have disclosed no relevant financial relationships. Dr. Larenas-Linnemann disclosed personal fees from Allakos, Armstrong, AstraZeneca, Chiesi, DBV Technologies, Grünenthal, GSK, Mylan/Viatris, Menarini, MSD, Novartis, Pfizer, Sanofi, Siegfried, UCB, Alakos, Gossamer, and Carnot, and grants from Sanofi, AstraZeneca, Novartis, Circassia, UCB, GSK, and the Purina Institute.
A version of this article first appeared on Medscape.com.
New data support a causal role for depression in Alzheimer’s
Researchers have known for some time that depression is associated with Alzheimer’s disease (AD), but a causal link has been elusive. Now, using newly available data, they have uncovered genetic evidence of a causal role for depression in AD.
As depression typically affects those in early or midlife and dementia often occurs in later life, “it’s fascinating to see a connection between the two brain illnesses that manifest in different time windows,” coinvestigator Aliza P. Wingo, MD, associate professor of psychiatry and behavioral science, Emory University, Atlanta, said in an interview.
“If we can treat the depression early on, we may help reduce risk for dementia for our patients later in life,” Dr. Wingo said.
The findings were published online Dec. 16, 2021, in Biological Psychiatry.
Postmortem data
The investigators, who are all from the Emory University Center for Neurodegenerative Disease, wanted to clarify the genetic basis underlying the association between the established link between depression and dementia risk.
They used data from the largest and most recent genomewide association studies (GWAS). These included a 2019 analysis of depression among 807,553 individuals and a 2019 study of AD among 455,258 individuals, all of European ancestry. For sensitivity analyses, they used results from two additional AD GWAS.
The researchers also accessed postmortem brain samples from participants in the Religious Orders Study (ROS) and the Rush Memory and Aging Project (MAP). These participants were cognitively normal at enrollment, underwent annual clinical evaluations, and agreed to donate their brains.
They also assessed brain samples donated by participants in the Banner Sun Health Research Institute longitudinal study of healthy aging, Alzheimer’s, and Parkinson’s disease.
The brain samples allowed researchers to use deep brain proteomic data to help determine molecular links between depression and AD.
After quality control, the analysis included 8,356 proteins in 391 ROS/MAP participants and 7,854 proteins in 196 Banner participants.
suggesting the two conditions have a shared genetic basis.
The investigators also applied a framework called “Mendelian randomization” to determine causality between depression and AD.
After assessing the effect of 115 independent single-nucleotide polymorphisms (SNPs) from the GWAS of depression, they uncovered significant evidence “that the SNPs cause depression, which in turn cause AD,” said Dr. Wingo.
One-way relationship
The researchers conducted the same analysis on 61 significant SNPs from the GWAS of AD but did not find evidence to conclude AD causes depression.
“We found genetic evidence supporting a causal role of depression in AD but not vice versa,” Dr. Wingo said.
In addition, the investigators identified 75 brain transcripts (messenger RNA) and 28 brain proteins regulated by the depression-predisposing genetic variants. Of these, 46 brain transcripts and seven proteins were significantly associated with at least one AD feature – for example, beta-amyloid, tau tangles, and cognitive trajectory.
“These findings support the notion that the depression risk variants contribute to AD via regulating expression of their corresponding transcripts in the brain,” the investigators wrote.
It is only recently that large enough studies have allowed researchers sufficient power to reach these conclusions, coinvestigator Thomas Wingo, MD, said in an interview.
These additional “insights” into the relationship between depression and AD might “motivate” clinicians more to screen for and treat depressive symptoms, Dr. Aliza Wingo noted.
The new results also have implications for developing therapeutics to treat depression, she said. “If we target the genes, the brain proteins, that are shared risk between depression and AD, the medications that target that gene might mitigate risk for AD later on.”
However, the investigators advised caution. “A lot of this is still unknown,” said Dr. Thomas Wingo.
For example, it is not clear whether successfully treating depression mitigates the eventual risk of dementia, which is “a very important topic of inquiry and one we continue to work on,” he said, adding that a significant number of patients do not respond well to existing antidepressants such as SSRIs.
Need for further research
Commenting on the findings, Claire Sexton, DPhil, director of scientific programs and outreach, Alzheimer’s Association, said the study contributes to the debate about whether depression increases risk for AD, whether AD increases risk for depression, or both.
“These newly published findings strengthen our understanding of the role of depression as a risk factor for Alzheimer’s dementia,” said Dr. Sexton, who was not involved with the research.
While experts do not yet fully understand the impact of treating depression on dementia risk, “the findings emphasize the importance of assessing mental health status, particularly depression, and getting it properly diagnosed and treated in a timely manner,” she said.
However, she agreed more research in this area is needed. “Importantly, these findings need replication in broader, more diverse study populations,” Dr. Sexton said.
A study funded by the Alzheimer’s Association may provide more information on the link between depression and AD. It will investigate whether machine learning, an advanced computer science technique, can better predict cognitive decline, compared with traditional methods.
Over a period of 6 months, researchers will collect smartphone conversations from 225 older adults with dementia, mild cognitive impairment, or no cognitive impairment. They will also have data from cognitive tests, brain scans, and biomarkers such as cerebrospinal fluid samples to study brain changes associated with AD.
The novel method of analysis should be able to identify subtle differences in speech quality to indicate which depressive symptoms an individual might be experiencing.
“The study could help us further understand the potential impact of depression in the risk of developing dementia,” said Dr. Sexton.
Dr. Aliza Wingo and Dr. Thomas Wingo reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers have known for some time that depression is associated with Alzheimer’s disease (AD), but a causal link has been elusive. Now, using newly available data, they have uncovered genetic evidence of a causal role for depression in AD.
As depression typically affects those in early or midlife and dementia often occurs in later life, “it’s fascinating to see a connection between the two brain illnesses that manifest in different time windows,” coinvestigator Aliza P. Wingo, MD, associate professor of psychiatry and behavioral science, Emory University, Atlanta, said in an interview.
“If we can treat the depression early on, we may help reduce risk for dementia for our patients later in life,” Dr. Wingo said.
The findings were published online Dec. 16, 2021, in Biological Psychiatry.
Postmortem data
The investigators, who are all from the Emory University Center for Neurodegenerative Disease, wanted to clarify the genetic basis underlying the association between the established link between depression and dementia risk.
They used data from the largest and most recent genomewide association studies (GWAS). These included a 2019 analysis of depression among 807,553 individuals and a 2019 study of AD among 455,258 individuals, all of European ancestry. For sensitivity analyses, they used results from two additional AD GWAS.
The researchers also accessed postmortem brain samples from participants in the Religious Orders Study (ROS) and the Rush Memory and Aging Project (MAP). These participants were cognitively normal at enrollment, underwent annual clinical evaluations, and agreed to donate their brains.
They also assessed brain samples donated by participants in the Banner Sun Health Research Institute longitudinal study of healthy aging, Alzheimer’s, and Parkinson’s disease.
The brain samples allowed researchers to use deep brain proteomic data to help determine molecular links between depression and AD.
After quality control, the analysis included 8,356 proteins in 391 ROS/MAP participants and 7,854 proteins in 196 Banner participants.
suggesting the two conditions have a shared genetic basis.
The investigators also applied a framework called “Mendelian randomization” to determine causality between depression and AD.
After assessing the effect of 115 independent single-nucleotide polymorphisms (SNPs) from the GWAS of depression, they uncovered significant evidence “that the SNPs cause depression, which in turn cause AD,” said Dr. Wingo.
One-way relationship
The researchers conducted the same analysis on 61 significant SNPs from the GWAS of AD but did not find evidence to conclude AD causes depression.
“We found genetic evidence supporting a causal role of depression in AD but not vice versa,” Dr. Wingo said.
In addition, the investigators identified 75 brain transcripts (messenger RNA) and 28 brain proteins regulated by the depression-predisposing genetic variants. Of these, 46 brain transcripts and seven proteins were significantly associated with at least one AD feature – for example, beta-amyloid, tau tangles, and cognitive trajectory.
“These findings support the notion that the depression risk variants contribute to AD via regulating expression of their corresponding transcripts in the brain,” the investigators wrote.
It is only recently that large enough studies have allowed researchers sufficient power to reach these conclusions, coinvestigator Thomas Wingo, MD, said in an interview.
These additional “insights” into the relationship between depression and AD might “motivate” clinicians more to screen for and treat depressive symptoms, Dr. Aliza Wingo noted.
The new results also have implications for developing therapeutics to treat depression, she said. “If we target the genes, the brain proteins, that are shared risk between depression and AD, the medications that target that gene might mitigate risk for AD later on.”
However, the investigators advised caution. “A lot of this is still unknown,” said Dr. Thomas Wingo.
For example, it is not clear whether successfully treating depression mitigates the eventual risk of dementia, which is “a very important topic of inquiry and one we continue to work on,” he said, adding that a significant number of patients do not respond well to existing antidepressants such as SSRIs.
Need for further research
Commenting on the findings, Claire Sexton, DPhil, director of scientific programs and outreach, Alzheimer’s Association, said the study contributes to the debate about whether depression increases risk for AD, whether AD increases risk for depression, or both.
“These newly published findings strengthen our understanding of the role of depression as a risk factor for Alzheimer’s dementia,” said Dr. Sexton, who was not involved with the research.
While experts do not yet fully understand the impact of treating depression on dementia risk, “the findings emphasize the importance of assessing mental health status, particularly depression, and getting it properly diagnosed and treated in a timely manner,” she said.
However, she agreed more research in this area is needed. “Importantly, these findings need replication in broader, more diverse study populations,” Dr. Sexton said.
A study funded by the Alzheimer’s Association may provide more information on the link between depression and AD. It will investigate whether machine learning, an advanced computer science technique, can better predict cognitive decline, compared with traditional methods.
Over a period of 6 months, researchers will collect smartphone conversations from 225 older adults with dementia, mild cognitive impairment, or no cognitive impairment. They will also have data from cognitive tests, brain scans, and biomarkers such as cerebrospinal fluid samples to study brain changes associated with AD.
The novel method of analysis should be able to identify subtle differences in speech quality to indicate which depressive symptoms an individual might be experiencing.
“The study could help us further understand the potential impact of depression in the risk of developing dementia,” said Dr. Sexton.
Dr. Aliza Wingo and Dr. Thomas Wingo reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Researchers have known for some time that depression is associated with Alzheimer’s disease (AD), but a causal link has been elusive. Now, using newly available data, they have uncovered genetic evidence of a causal role for depression in AD.
As depression typically affects those in early or midlife and dementia often occurs in later life, “it’s fascinating to see a connection between the two brain illnesses that manifest in different time windows,” coinvestigator Aliza P. Wingo, MD, associate professor of psychiatry and behavioral science, Emory University, Atlanta, said in an interview.
“If we can treat the depression early on, we may help reduce risk for dementia for our patients later in life,” Dr. Wingo said.
The findings were published online Dec. 16, 2021, in Biological Psychiatry.
Postmortem data
The investigators, who are all from the Emory University Center for Neurodegenerative Disease, wanted to clarify the genetic basis underlying the association between the established link between depression and dementia risk.
They used data from the largest and most recent genomewide association studies (GWAS). These included a 2019 analysis of depression among 807,553 individuals and a 2019 study of AD among 455,258 individuals, all of European ancestry. For sensitivity analyses, they used results from two additional AD GWAS.
The researchers also accessed postmortem brain samples from participants in the Religious Orders Study (ROS) and the Rush Memory and Aging Project (MAP). These participants were cognitively normal at enrollment, underwent annual clinical evaluations, and agreed to donate their brains.
They also assessed brain samples donated by participants in the Banner Sun Health Research Institute longitudinal study of healthy aging, Alzheimer’s, and Parkinson’s disease.
The brain samples allowed researchers to use deep brain proteomic data to help determine molecular links between depression and AD.
After quality control, the analysis included 8,356 proteins in 391 ROS/MAP participants and 7,854 proteins in 196 Banner participants.
suggesting the two conditions have a shared genetic basis.
The investigators also applied a framework called “Mendelian randomization” to determine causality between depression and AD.
After assessing the effect of 115 independent single-nucleotide polymorphisms (SNPs) from the GWAS of depression, they uncovered significant evidence “that the SNPs cause depression, which in turn cause AD,” said Dr. Wingo.
One-way relationship
The researchers conducted the same analysis on 61 significant SNPs from the GWAS of AD but did not find evidence to conclude AD causes depression.
“We found genetic evidence supporting a causal role of depression in AD but not vice versa,” Dr. Wingo said.
In addition, the investigators identified 75 brain transcripts (messenger RNA) and 28 brain proteins regulated by the depression-predisposing genetic variants. Of these, 46 brain transcripts and seven proteins were significantly associated with at least one AD feature – for example, beta-amyloid, tau tangles, and cognitive trajectory.
“These findings support the notion that the depression risk variants contribute to AD via regulating expression of their corresponding transcripts in the brain,” the investigators wrote.
It is only recently that large enough studies have allowed researchers sufficient power to reach these conclusions, coinvestigator Thomas Wingo, MD, said in an interview.
These additional “insights” into the relationship between depression and AD might “motivate” clinicians more to screen for and treat depressive symptoms, Dr. Aliza Wingo noted.
The new results also have implications for developing therapeutics to treat depression, she said. “If we target the genes, the brain proteins, that are shared risk between depression and AD, the medications that target that gene might mitigate risk for AD later on.”
However, the investigators advised caution. “A lot of this is still unknown,” said Dr. Thomas Wingo.
For example, it is not clear whether successfully treating depression mitigates the eventual risk of dementia, which is “a very important topic of inquiry and one we continue to work on,” he said, adding that a significant number of patients do not respond well to existing antidepressants such as SSRIs.
Need for further research
Commenting on the findings, Claire Sexton, DPhil, director of scientific programs and outreach, Alzheimer’s Association, said the study contributes to the debate about whether depression increases risk for AD, whether AD increases risk for depression, or both.
“These newly published findings strengthen our understanding of the role of depression as a risk factor for Alzheimer’s dementia,” said Dr. Sexton, who was not involved with the research.
While experts do not yet fully understand the impact of treating depression on dementia risk, “the findings emphasize the importance of assessing mental health status, particularly depression, and getting it properly diagnosed and treated in a timely manner,” she said.
However, she agreed more research in this area is needed. “Importantly, these findings need replication in broader, more diverse study populations,” Dr. Sexton said.
A study funded by the Alzheimer’s Association may provide more information on the link between depression and AD. It will investigate whether machine learning, an advanced computer science technique, can better predict cognitive decline, compared with traditional methods.
Over a period of 6 months, researchers will collect smartphone conversations from 225 older adults with dementia, mild cognitive impairment, or no cognitive impairment. They will also have data from cognitive tests, brain scans, and biomarkers such as cerebrospinal fluid samples to study brain changes associated with AD.
The novel method of analysis should be able to identify subtle differences in speech quality to indicate which depressive symptoms an individual might be experiencing.
“The study could help us further understand the potential impact of depression in the risk of developing dementia,” said Dr. Sexton.
Dr. Aliza Wingo and Dr. Thomas Wingo reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM BIOLOGICAL PSYCHIATRY
Positive phase 3 topline results for early Parkinson’s drug
Topline results from a phase 3 trial of P2B001, a fixed-dose combination of extended release (ER) formulations of pramipexole and rasagiline, showed it was superior to its individual components as a first-line treatment for early Parkinson’s disease.
Study participants also reported less daytime sleepiness with P2B001, according to a statement from the drug’s manufacturer.
while mitigating the side effects typically associated with this class of medicine such as somnolence, orthostatic hypotension, and hallucinations,” Sheila Oren, MD, chief executive officer of Pharma Two B, said in a statement.
“This is important for PD patients of all ages and is critical for the elderly, who typically do not tolerate side effects of dopamine agonists,” Dr. Oren added.
Promising results
The 12-week, international, randomized, double-blind trial was designed to study the efficacy, safety, and tolerability of P2B001 compared to its individual components and to a calibration arm of pramipexole ER in 544 patients with early PD.
Participants received P2B001, a once-daily ER combination product composed of pramipexole 0.6 mg and rasagiline 0.75 mg; pramipexole ER capsule 0.6 mg once daily; rasagiline ER capsule 0.75 mg once daily; or the currently marketed product pramipexole ER capsules titrated to an optimal dose for each individual patient (1.5-4.5 mg).
The adjusted mean change from baseline in total Unified Parkinson’s Disease Rating Scale (UPDRS) score was –2.66 points for P2B001 versus pramipexole (P = .0018) and –3.30 points for P2B001 versus rasagiline (P = .0001). There was no significant difference in UPDRS scores between P2B001 and pramipexole ER.
The adjusted mean change from baseline in the Epworth Sleepiness Scale score for P2B001 versus pramipexole ER was –2.66 points (P < .0001).
Treatment-related adverse events were mostly mild or moderate and were similar among groups.
“The initiation of treatment of patients with Parkinson’s disease represents an area of unmet need due to the side effects associated with current treatments,” Warren Olanow, MD, professor emeritus of neurology and neuroscience at the Icahn School of Medicine at Mount Sinai in New York, said in a statement from the manufacturer.
“Based on the data from this well-designed, rigorous, active-controlled study, P2B001 has the potential to become a leading treatment option for PD, particularly as first line therapy for early-stage patients of all ages,” Dr. Olanow added.
The company plans to file a new drug application in 2022.
A version of this article first appeared on Medscape.com.
Topline results from a phase 3 trial of P2B001, a fixed-dose combination of extended release (ER) formulations of pramipexole and rasagiline, showed it was superior to its individual components as a first-line treatment for early Parkinson’s disease.
Study participants also reported less daytime sleepiness with P2B001, according to a statement from the drug’s manufacturer.
while mitigating the side effects typically associated with this class of medicine such as somnolence, orthostatic hypotension, and hallucinations,” Sheila Oren, MD, chief executive officer of Pharma Two B, said in a statement.
“This is important for PD patients of all ages and is critical for the elderly, who typically do not tolerate side effects of dopamine agonists,” Dr. Oren added.
Promising results
The 12-week, international, randomized, double-blind trial was designed to study the efficacy, safety, and tolerability of P2B001 compared to its individual components and to a calibration arm of pramipexole ER in 544 patients with early PD.
Participants received P2B001, a once-daily ER combination product composed of pramipexole 0.6 mg and rasagiline 0.75 mg; pramipexole ER capsule 0.6 mg once daily; rasagiline ER capsule 0.75 mg once daily; or the currently marketed product pramipexole ER capsules titrated to an optimal dose for each individual patient (1.5-4.5 mg).
The adjusted mean change from baseline in total Unified Parkinson’s Disease Rating Scale (UPDRS) score was –2.66 points for P2B001 versus pramipexole (P = .0018) and –3.30 points for P2B001 versus rasagiline (P = .0001). There was no significant difference in UPDRS scores between P2B001 and pramipexole ER.
The adjusted mean change from baseline in the Epworth Sleepiness Scale score for P2B001 versus pramipexole ER was –2.66 points (P < .0001).
Treatment-related adverse events were mostly mild or moderate and were similar among groups.
“The initiation of treatment of patients with Parkinson’s disease represents an area of unmet need due to the side effects associated with current treatments,” Warren Olanow, MD, professor emeritus of neurology and neuroscience at the Icahn School of Medicine at Mount Sinai in New York, said in a statement from the manufacturer.
“Based on the data from this well-designed, rigorous, active-controlled study, P2B001 has the potential to become a leading treatment option for PD, particularly as first line therapy for early-stage patients of all ages,” Dr. Olanow added.
The company plans to file a new drug application in 2022.
A version of this article first appeared on Medscape.com.
Topline results from a phase 3 trial of P2B001, a fixed-dose combination of extended release (ER) formulations of pramipexole and rasagiline, showed it was superior to its individual components as a first-line treatment for early Parkinson’s disease.
Study participants also reported less daytime sleepiness with P2B001, according to a statement from the drug’s manufacturer.
while mitigating the side effects typically associated with this class of medicine such as somnolence, orthostatic hypotension, and hallucinations,” Sheila Oren, MD, chief executive officer of Pharma Two B, said in a statement.
“This is important for PD patients of all ages and is critical for the elderly, who typically do not tolerate side effects of dopamine agonists,” Dr. Oren added.
Promising results
The 12-week, international, randomized, double-blind trial was designed to study the efficacy, safety, and tolerability of P2B001 compared to its individual components and to a calibration arm of pramipexole ER in 544 patients with early PD.
Participants received P2B001, a once-daily ER combination product composed of pramipexole 0.6 mg and rasagiline 0.75 mg; pramipexole ER capsule 0.6 mg once daily; rasagiline ER capsule 0.75 mg once daily; or the currently marketed product pramipexole ER capsules titrated to an optimal dose for each individual patient (1.5-4.5 mg).
The adjusted mean change from baseline in total Unified Parkinson’s Disease Rating Scale (UPDRS) score was –2.66 points for P2B001 versus pramipexole (P = .0018) and –3.30 points for P2B001 versus rasagiline (P = .0001). There was no significant difference in UPDRS scores between P2B001 and pramipexole ER.
The adjusted mean change from baseline in the Epworth Sleepiness Scale score for P2B001 versus pramipexole ER was –2.66 points (P < .0001).
Treatment-related adverse events were mostly mild or moderate and were similar among groups.
“The initiation of treatment of patients with Parkinson’s disease represents an area of unmet need due to the side effects associated with current treatments,” Warren Olanow, MD, professor emeritus of neurology and neuroscience at the Icahn School of Medicine at Mount Sinai in New York, said in a statement from the manufacturer.
“Based on the data from this well-designed, rigorous, active-controlled study, P2B001 has the potential to become a leading treatment option for PD, particularly as first line therapy for early-stage patients of all ages,” Dr. Olanow added.
The company plans to file a new drug application in 2022.
A version of this article first appeared on Medscape.com.
Formaldehyde exposure tied to cognitive impairment
Long-term exposure to formaldehyde on the job is linked to cognitive impairment down the road, new research suggests.
In a large observational study of adults aged 45-70 years, researchers found a 17% higher risk for cognitive problems in those with occupational formaldehyde exposure – and higher risks for those with longer duration of exposure.
“The effect of formaldehyde on the brain has been previously shown mainly in animal experiments, but very few studies have been done on humans,” lead author Noemie Letellier, PhD, Institute for Neurosciences of Montpellier, University of Montpellier (France), said in an interview.
“Our results show that being or having been occupationally exposed to formaldehyde is associated with cognitive impairment in a relatively young population,” Dr. Letellier said.
The findings were published online Dec. 22, 2021, in the journal Neurology.
Dose-effect relationship
The investigators assessed a representative sample of 75,322 adults in France (median age, 57.5 years; 53% women). All were part of the CONSTANCES cohort, an observational cohort with a focus on occupational and environmental factors.
A total of 6,026 participants (8%) were exposed to formaldehyde during their careers. Their occupations included nurses, caregivers, medical technicians, workers in the textile, chemistry and metal industries, carpenters, and cleaners.
The researchers calculated lifetime formaldehyde exposure using a French job-exposure matrix created to estimate a person’s exposure to potential health hazards in different occupations.
Individuals were divided into three equal groups according to their years of exposure to formaldehyde. “Low” was considered to be 6 or fewer years of exposure, “medium” was 7-21 years, and “high” was 22 or more years.
Participants were also split into three groups according to their cumulative exposure (total lifetime formaldehyde exposure based on the probability, intensity, and frequency of exposure).
Prevention efforts needed
After adjusting for age, sex, education and other confounders, participants exposed to formaldehyde were at higher risk for global cognitive impairment (adjusted relative risk, 1.17; 95% confidence interval, 1.1-1.2).
Longer duration of exposure and high cumulative lifetime exposure were associated with worse cognitive impairment, “with a dose-effect relationship for exposure duration,” the researchers reported.
Those exposed to formaldehyde for 22 years or more had a 21% higher risk of global cognitive impairment and workers with the highest cumulative exposure had a 19% higher risk of cognitive impairment, compared with workers with no exposure.
Although workers with recent exposure showed higher cognitive impairment, “time may not fully attenuate formaldehyde-associated cognitive deficits, especially in highly exposed but also in moderately exposed workers,” the researchers wrote.
They caution that their findings only show an association and does not prove that exposure to formaldehyde causes cognitive impairment.
Nonetheless, Dr. Letellier encourages health care providers to “be aware of lifetime occupational exposure to target prevention efforts to the identified occupational groups.” This especially includes the care sector where the most people are exposed to formaldehyde, such as nurses, caregivers, and medical technicians.
“Despite the restrictions on the use of formaldehyde due to the better knowledge of its toxicity, especially its carcinogenic effect, formaldehyde is still widely used in many sectors. These results encourage prevention efforts to further limit worker exposure to formaldehyde,” Dr. Letellier said.
Relevant to health care workers
Commenting on the study, Shaheen E. Lakhan, MD, PhD, a neurologist in Newton, Mass., said in an interview that exposure to some degree of formaldehyde is found in every home and workplace, “from the floors to furniture.”
“If you have cigarette smoke in the environment, your exposure rises sharply. When limiting your exposure, it’s not only cancer that you are preventing, but also your brain health,” added Dr. Lakhan, who was not involved with the research.
He said the disturbances in cognitive function noted in the current study were “particularly relevant to health care workers, given the use of formaldehyde in sterilization, tissue pathology processing, and embalming.”
“Interestingly, with only past exposure, there seems to be some degree of cognitive recovery,” but it does not return to a level before any exposure when corrected for age and other factors, Dr. Lakhan said.
Some caveats should also be noted, he pointed out. The study included a French population, but regulators such as the U.S. Occupational Safety and Health Administration and the California Office of Environmental Health Hazard Assessment have strict standards on formaldehyde use in a variety of work settings.
On the flip side, given the COVID-19 pandemic, there has been greater use of chemical disinfectants in and out the workplace, some of which contain formaldehyde, Dr. Lakhan said.
In addition, he noted the study assessed data from 1950 to 2018, so prepandemic.
“A word of advice from a brain doc: Check with your employer on the level of occupational exposure to formaldehyde, heavy metals, and other toxic substances – and cross-reference with your local environmental standards,” Dr. Lakhan concluded.
The research was supported by a grant from the French Agency for Food, Environmental, and Occupational Health & Safety. The investigators and Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term exposure to formaldehyde on the job is linked to cognitive impairment down the road, new research suggests.
In a large observational study of adults aged 45-70 years, researchers found a 17% higher risk for cognitive problems in those with occupational formaldehyde exposure – and higher risks for those with longer duration of exposure.
“The effect of formaldehyde on the brain has been previously shown mainly in animal experiments, but very few studies have been done on humans,” lead author Noemie Letellier, PhD, Institute for Neurosciences of Montpellier, University of Montpellier (France), said in an interview.
“Our results show that being or having been occupationally exposed to formaldehyde is associated with cognitive impairment in a relatively young population,” Dr. Letellier said.
The findings were published online Dec. 22, 2021, in the journal Neurology.
Dose-effect relationship
The investigators assessed a representative sample of 75,322 adults in France (median age, 57.5 years; 53% women). All were part of the CONSTANCES cohort, an observational cohort with a focus on occupational and environmental factors.
A total of 6,026 participants (8%) were exposed to formaldehyde during their careers. Their occupations included nurses, caregivers, medical technicians, workers in the textile, chemistry and metal industries, carpenters, and cleaners.
The researchers calculated lifetime formaldehyde exposure using a French job-exposure matrix created to estimate a person’s exposure to potential health hazards in different occupations.
Individuals were divided into three equal groups according to their years of exposure to formaldehyde. “Low” was considered to be 6 or fewer years of exposure, “medium” was 7-21 years, and “high” was 22 or more years.
Participants were also split into three groups according to their cumulative exposure (total lifetime formaldehyde exposure based on the probability, intensity, and frequency of exposure).
Prevention efforts needed
After adjusting for age, sex, education and other confounders, participants exposed to formaldehyde were at higher risk for global cognitive impairment (adjusted relative risk, 1.17; 95% confidence interval, 1.1-1.2).
Longer duration of exposure and high cumulative lifetime exposure were associated with worse cognitive impairment, “with a dose-effect relationship for exposure duration,” the researchers reported.
Those exposed to formaldehyde for 22 years or more had a 21% higher risk of global cognitive impairment and workers with the highest cumulative exposure had a 19% higher risk of cognitive impairment, compared with workers with no exposure.
Although workers with recent exposure showed higher cognitive impairment, “time may not fully attenuate formaldehyde-associated cognitive deficits, especially in highly exposed but also in moderately exposed workers,” the researchers wrote.
They caution that their findings only show an association and does not prove that exposure to formaldehyde causes cognitive impairment.
Nonetheless, Dr. Letellier encourages health care providers to “be aware of lifetime occupational exposure to target prevention efforts to the identified occupational groups.” This especially includes the care sector where the most people are exposed to formaldehyde, such as nurses, caregivers, and medical technicians.
“Despite the restrictions on the use of formaldehyde due to the better knowledge of its toxicity, especially its carcinogenic effect, formaldehyde is still widely used in many sectors. These results encourage prevention efforts to further limit worker exposure to formaldehyde,” Dr. Letellier said.
Relevant to health care workers
Commenting on the study, Shaheen E. Lakhan, MD, PhD, a neurologist in Newton, Mass., said in an interview that exposure to some degree of formaldehyde is found in every home and workplace, “from the floors to furniture.”
“If you have cigarette smoke in the environment, your exposure rises sharply. When limiting your exposure, it’s not only cancer that you are preventing, but also your brain health,” added Dr. Lakhan, who was not involved with the research.
He said the disturbances in cognitive function noted in the current study were “particularly relevant to health care workers, given the use of formaldehyde in sterilization, tissue pathology processing, and embalming.”
“Interestingly, with only past exposure, there seems to be some degree of cognitive recovery,” but it does not return to a level before any exposure when corrected for age and other factors, Dr. Lakhan said.
Some caveats should also be noted, he pointed out. The study included a French population, but regulators such as the U.S. Occupational Safety and Health Administration and the California Office of Environmental Health Hazard Assessment have strict standards on formaldehyde use in a variety of work settings.
On the flip side, given the COVID-19 pandemic, there has been greater use of chemical disinfectants in and out the workplace, some of which contain formaldehyde, Dr. Lakhan said.
In addition, he noted the study assessed data from 1950 to 2018, so prepandemic.
“A word of advice from a brain doc: Check with your employer on the level of occupational exposure to formaldehyde, heavy metals, and other toxic substances – and cross-reference with your local environmental standards,” Dr. Lakhan concluded.
The research was supported by a grant from the French Agency for Food, Environmental, and Occupational Health & Safety. The investigators and Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Long-term exposure to formaldehyde on the job is linked to cognitive impairment down the road, new research suggests.
In a large observational study of adults aged 45-70 years, researchers found a 17% higher risk for cognitive problems in those with occupational formaldehyde exposure – and higher risks for those with longer duration of exposure.
“The effect of formaldehyde on the brain has been previously shown mainly in animal experiments, but very few studies have been done on humans,” lead author Noemie Letellier, PhD, Institute for Neurosciences of Montpellier, University of Montpellier (France), said in an interview.
“Our results show that being or having been occupationally exposed to formaldehyde is associated with cognitive impairment in a relatively young population,” Dr. Letellier said.
The findings were published online Dec. 22, 2021, in the journal Neurology.
Dose-effect relationship
The investigators assessed a representative sample of 75,322 adults in France (median age, 57.5 years; 53% women). All were part of the CONSTANCES cohort, an observational cohort with a focus on occupational and environmental factors.
A total of 6,026 participants (8%) were exposed to formaldehyde during their careers. Their occupations included nurses, caregivers, medical technicians, workers in the textile, chemistry and metal industries, carpenters, and cleaners.
The researchers calculated lifetime formaldehyde exposure using a French job-exposure matrix created to estimate a person’s exposure to potential health hazards in different occupations.
Individuals were divided into three equal groups according to their years of exposure to formaldehyde. “Low” was considered to be 6 or fewer years of exposure, “medium” was 7-21 years, and “high” was 22 or more years.
Participants were also split into three groups according to their cumulative exposure (total lifetime formaldehyde exposure based on the probability, intensity, and frequency of exposure).
Prevention efforts needed
After adjusting for age, sex, education and other confounders, participants exposed to formaldehyde were at higher risk for global cognitive impairment (adjusted relative risk, 1.17; 95% confidence interval, 1.1-1.2).
Longer duration of exposure and high cumulative lifetime exposure were associated with worse cognitive impairment, “with a dose-effect relationship for exposure duration,” the researchers reported.
Those exposed to formaldehyde for 22 years or more had a 21% higher risk of global cognitive impairment and workers with the highest cumulative exposure had a 19% higher risk of cognitive impairment, compared with workers with no exposure.
Although workers with recent exposure showed higher cognitive impairment, “time may not fully attenuate formaldehyde-associated cognitive deficits, especially in highly exposed but also in moderately exposed workers,” the researchers wrote.
They caution that their findings only show an association and does not prove that exposure to formaldehyde causes cognitive impairment.
Nonetheless, Dr. Letellier encourages health care providers to “be aware of lifetime occupational exposure to target prevention efforts to the identified occupational groups.” This especially includes the care sector where the most people are exposed to formaldehyde, such as nurses, caregivers, and medical technicians.
“Despite the restrictions on the use of formaldehyde due to the better knowledge of its toxicity, especially its carcinogenic effect, formaldehyde is still widely used in many sectors. These results encourage prevention efforts to further limit worker exposure to formaldehyde,” Dr. Letellier said.
Relevant to health care workers
Commenting on the study, Shaheen E. Lakhan, MD, PhD, a neurologist in Newton, Mass., said in an interview that exposure to some degree of formaldehyde is found in every home and workplace, “from the floors to furniture.”
“If you have cigarette smoke in the environment, your exposure rises sharply. When limiting your exposure, it’s not only cancer that you are preventing, but also your brain health,” added Dr. Lakhan, who was not involved with the research.
He said the disturbances in cognitive function noted in the current study were “particularly relevant to health care workers, given the use of formaldehyde in sterilization, tissue pathology processing, and embalming.”
“Interestingly, with only past exposure, there seems to be some degree of cognitive recovery,” but it does not return to a level before any exposure when corrected for age and other factors, Dr. Lakhan said.
Some caveats should also be noted, he pointed out. The study included a French population, but regulators such as the U.S. Occupational Safety and Health Administration and the California Office of Environmental Health Hazard Assessment have strict standards on formaldehyde use in a variety of work settings.
On the flip side, given the COVID-19 pandemic, there has been greater use of chemical disinfectants in and out the workplace, some of which contain formaldehyde, Dr. Lakhan said.
In addition, he noted the study assessed data from 1950 to 2018, so prepandemic.
“A word of advice from a brain doc: Check with your employer on the level of occupational exposure to formaldehyde, heavy metals, and other toxic substances – and cross-reference with your local environmental standards,” Dr. Lakhan concluded.
The research was supported by a grant from the French Agency for Food, Environmental, and Occupational Health & Safety. The investigators and Dr. Lakhan disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
Epilepsy in older adults: Misdiagnosis and case complexity are common
, a neurologist told an audience at the annual meeting of the American Epilepsy Society. She urged colleagues to focus on possible interactions with other neurological conditions, consider various complicating factors, and embrace a team strategy.
“There are lots of nuances,” said Rebecca O’Dwyer, MD, an adult epilepsy specialist with Rush Epilepsy Center in Chicago. “It takes a lot of time and requires a multidisciplinary approach. Taking care of older individuals with epilepsy truly is a team sport.”
According to a 2014 report highlighted by Dr. O’Dwyer, “nearly 25% of new-onset seizures occur after age 65. The incidence of epilepsy in this age group is almost twice the rate in children, and in people over age 80, it is triple the rate in children.”
Research suggests it can take up to 2 years to correctly diagnose epilepsy in older people, Dr. O’Dwyer said, and nearly two-thirds of cases may be misdiagnosed. “Some of it is just limited awareness. There’s this perception in the public that epilepsy is something that occurs in younger adults or young children, and that when you come to a certain age, you cannot have epilepsy. Also, there are differences in the clinical manifestations of their seizures, and many comorbid possibilities could also present in similar fashion to epilepsy. Some of our usual tools that we use to come to the diagnosis such as EEG are also known to be less sensitive in this age group.”
According to the 2014 report, research finds that the elderly are much more likely than young adults to have postictal sleepiness or unresponsiveness and seizures manifesting as brief moments of subtle confusion. They’re much less likely to have epileptic aura and generalized tonic seizures.
“An epileptic seizure in an older adult tends to be less dramatic with fewer motor manifestations, and they often tend to be monophasic. They may be so subtle that they’re missed by family members and other medical providers,” Dr. O’Dwyer said. “I had a patient whose seizure consisted of her tapping her left shoulder. She had been doing this for at least 6 months, and she came to my clinic after her daughter realized that she was a little confused afterward. She’d already seen a behavioral neurologist and been given the diagnosis of dementia. We were fortunate enough to catch one of these episodes while we were doing an EEG, and we diagnosed her with focal epilepsy. With one antiseizure medication, we stopped the seizures, and her memory came back.”
Make sure to take detailed histories and keep an eye out for descriptions of behaviors that are episodic but perhaps not typical of seizures, she said.
Epilepsy can be misdiagnosed as a variety of conditions, she said, such as syncope, Alzheimer’s disease, stroke, Parkinson’s disease, and atrial fibrillation. “When you do diagnose somebody older with new-onset epilepsy, you should work them up for a stroke. Because we know that within the first 4 weeks after their first seizure the likelihood that they could have a stroke is three times higher.”
It’s also possible that neurological conditions can be followed by new-onset epilepsy, she said, making dementia even worse. Low-dose antiepileptic drugs can be helpful in these patients.
But seniors are especially vulnerable to side effects of antiepileptic drugs such as sedation, dizziness, and cardiac-conduction abnormalities. “You must adhere to the mantra of going low and going slow because they are exquisitely susceptible,” Dr. O’Dwyer said.
She recommends lamotrigine, which is well tolerated with helpful mood-stabilizing effects, and levetiracetam, which attenuates cognitive decline in dementia but may cause side effects such as irritable mood. Zonisamide is showing promise in patients with parkinsonian syndromes, she said, and it may be helpful to maximize drugs that patients are already taking such as gabapentin or pregabalin.
Finally, Dr. O’Dwyer urged colleagues to work in teams that include caregivers, primary care doctors, social workers, and pharmacists. “Sometimes in all this,” she said, “my job is the easiest.”
Dr. O’Dwyer discloses research support from the Shapiro Foundation.
, a neurologist told an audience at the annual meeting of the American Epilepsy Society. She urged colleagues to focus on possible interactions with other neurological conditions, consider various complicating factors, and embrace a team strategy.
“There are lots of nuances,” said Rebecca O’Dwyer, MD, an adult epilepsy specialist with Rush Epilepsy Center in Chicago. “It takes a lot of time and requires a multidisciplinary approach. Taking care of older individuals with epilepsy truly is a team sport.”
According to a 2014 report highlighted by Dr. O’Dwyer, “nearly 25% of new-onset seizures occur after age 65. The incidence of epilepsy in this age group is almost twice the rate in children, and in people over age 80, it is triple the rate in children.”
Research suggests it can take up to 2 years to correctly diagnose epilepsy in older people, Dr. O’Dwyer said, and nearly two-thirds of cases may be misdiagnosed. “Some of it is just limited awareness. There’s this perception in the public that epilepsy is something that occurs in younger adults or young children, and that when you come to a certain age, you cannot have epilepsy. Also, there are differences in the clinical manifestations of their seizures, and many comorbid possibilities could also present in similar fashion to epilepsy. Some of our usual tools that we use to come to the diagnosis such as EEG are also known to be less sensitive in this age group.”
According to the 2014 report, research finds that the elderly are much more likely than young adults to have postictal sleepiness or unresponsiveness and seizures manifesting as brief moments of subtle confusion. They’re much less likely to have epileptic aura and generalized tonic seizures.
“An epileptic seizure in an older adult tends to be less dramatic with fewer motor manifestations, and they often tend to be monophasic. They may be so subtle that they’re missed by family members and other medical providers,” Dr. O’Dwyer said. “I had a patient whose seizure consisted of her tapping her left shoulder. She had been doing this for at least 6 months, and she came to my clinic after her daughter realized that she was a little confused afterward. She’d already seen a behavioral neurologist and been given the diagnosis of dementia. We were fortunate enough to catch one of these episodes while we were doing an EEG, and we diagnosed her with focal epilepsy. With one antiseizure medication, we stopped the seizures, and her memory came back.”
Make sure to take detailed histories and keep an eye out for descriptions of behaviors that are episodic but perhaps not typical of seizures, she said.
Epilepsy can be misdiagnosed as a variety of conditions, she said, such as syncope, Alzheimer’s disease, stroke, Parkinson’s disease, and atrial fibrillation. “When you do diagnose somebody older with new-onset epilepsy, you should work them up for a stroke. Because we know that within the first 4 weeks after their first seizure the likelihood that they could have a stroke is three times higher.”
It’s also possible that neurological conditions can be followed by new-onset epilepsy, she said, making dementia even worse. Low-dose antiepileptic drugs can be helpful in these patients.
But seniors are especially vulnerable to side effects of antiepileptic drugs such as sedation, dizziness, and cardiac-conduction abnormalities. “You must adhere to the mantra of going low and going slow because they are exquisitely susceptible,” Dr. O’Dwyer said.
She recommends lamotrigine, which is well tolerated with helpful mood-stabilizing effects, and levetiracetam, which attenuates cognitive decline in dementia but may cause side effects such as irritable mood. Zonisamide is showing promise in patients with parkinsonian syndromes, she said, and it may be helpful to maximize drugs that patients are already taking such as gabapentin or pregabalin.
Finally, Dr. O’Dwyer urged colleagues to work in teams that include caregivers, primary care doctors, social workers, and pharmacists. “Sometimes in all this,” she said, “my job is the easiest.”
Dr. O’Dwyer discloses research support from the Shapiro Foundation.
, a neurologist told an audience at the annual meeting of the American Epilepsy Society. She urged colleagues to focus on possible interactions with other neurological conditions, consider various complicating factors, and embrace a team strategy.
“There are lots of nuances,” said Rebecca O’Dwyer, MD, an adult epilepsy specialist with Rush Epilepsy Center in Chicago. “It takes a lot of time and requires a multidisciplinary approach. Taking care of older individuals with epilepsy truly is a team sport.”
According to a 2014 report highlighted by Dr. O’Dwyer, “nearly 25% of new-onset seizures occur after age 65. The incidence of epilepsy in this age group is almost twice the rate in children, and in people over age 80, it is triple the rate in children.”
Research suggests it can take up to 2 years to correctly diagnose epilepsy in older people, Dr. O’Dwyer said, and nearly two-thirds of cases may be misdiagnosed. “Some of it is just limited awareness. There’s this perception in the public that epilepsy is something that occurs in younger adults or young children, and that when you come to a certain age, you cannot have epilepsy. Also, there are differences in the clinical manifestations of their seizures, and many comorbid possibilities could also present in similar fashion to epilepsy. Some of our usual tools that we use to come to the diagnosis such as EEG are also known to be less sensitive in this age group.”
According to the 2014 report, research finds that the elderly are much more likely than young adults to have postictal sleepiness or unresponsiveness and seizures manifesting as brief moments of subtle confusion. They’re much less likely to have epileptic aura and generalized tonic seizures.
“An epileptic seizure in an older adult tends to be less dramatic with fewer motor manifestations, and they often tend to be monophasic. They may be so subtle that they’re missed by family members and other medical providers,” Dr. O’Dwyer said. “I had a patient whose seizure consisted of her tapping her left shoulder. She had been doing this for at least 6 months, and she came to my clinic after her daughter realized that she was a little confused afterward. She’d already seen a behavioral neurologist and been given the diagnosis of dementia. We were fortunate enough to catch one of these episodes while we were doing an EEG, and we diagnosed her with focal epilepsy. With one antiseizure medication, we stopped the seizures, and her memory came back.”
Make sure to take detailed histories and keep an eye out for descriptions of behaviors that are episodic but perhaps not typical of seizures, she said.
Epilepsy can be misdiagnosed as a variety of conditions, she said, such as syncope, Alzheimer’s disease, stroke, Parkinson’s disease, and atrial fibrillation. “When you do diagnose somebody older with new-onset epilepsy, you should work them up for a stroke. Because we know that within the first 4 weeks after their first seizure the likelihood that they could have a stroke is three times higher.”
It’s also possible that neurological conditions can be followed by new-onset epilepsy, she said, making dementia even worse. Low-dose antiepileptic drugs can be helpful in these patients.
But seniors are especially vulnerable to side effects of antiepileptic drugs such as sedation, dizziness, and cardiac-conduction abnormalities. “You must adhere to the mantra of going low and going slow because they are exquisitely susceptible,” Dr. O’Dwyer said.
She recommends lamotrigine, which is well tolerated with helpful mood-stabilizing effects, and levetiracetam, which attenuates cognitive decline in dementia but may cause side effects such as irritable mood. Zonisamide is showing promise in patients with parkinsonian syndromes, she said, and it may be helpful to maximize drugs that patients are already taking such as gabapentin or pregabalin.
Finally, Dr. O’Dwyer urged colleagues to work in teams that include caregivers, primary care doctors, social workers, and pharmacists. “Sometimes in all this,” she said, “my job is the easiest.”
Dr. O’Dwyer discloses research support from the Shapiro Foundation.
FROM AES 2021
Even light physical activity linked to lower dementia risk
Older adults who participate in even light physical activity (LPA) may have a lower risk of developing dementia, new research suggests.
In a retrospective analysis of more than 62,000 individuals aged 65 or older without preexisting dementia, 6% developed dementia.
Compared with inactive individuals, “insufficiently active,” “active,” and “highly active” individuals all had a 10%, 20%, and 28% lower risk for dementia, respectively. And this association was consistent regardless of age, sex, other comorbidities, or after the researchers censored for stroke.
Even the lowest amount of LPA was associated with reduced dementia risk, investigators noted.
“In older adults, an increased physical activity level, including a low amount of LPA, was associated with a reduced risk of dementia,” Minjae Yoon, MD, division of cardiology, Severance Cardiovascular Hospital, Yonsei University, Seoul, South Korea, and colleagues wrote.
“Promotion of LPA might reduce the risk of dementia in older adults,” they added.
The findings were published online in JAMA Network Open.
Reverse causation?
Physical activity has been shown previously to be associated with reduced dementia risk. Current World Health Organization guidelines recommend that adults with normal cognition should engage in PA to reduce their risk for cognitive decline.
However, some studies have not yielded this result, “suggesting that previous findings showing a lower risk of dementia in physically active people could be attributed to reverse causation,” the investigators noted. Additionally, previous research regarding exercise intensity has been “inconsistent” concerning the role of LPA in reducing dementia risk.
Many older adults with frailty and comorbidity cannot perform intense or even moderate PA, therefore “these adults would have to gain the benefits of physical activity from LPA,” the researchers noted.
To clarify the potential association between PA and new-onset dementia, they focused specifically on the “dose-response association” between PA and dementia – especially LPA.
Between 2009 and 2012, the investigators enrolled 62,286 older individuals (60.4% women; mean age, 73.2 years) with available health checkup data from the National Health Insurance Service–Senior Database of Korea. All had no history of dementia.
Leisure-time PA was assessed with self-report questionnaires that used a 7-day recall method and included three questions regarding usual frequency (in days per week):
- Vigorous PA (VPA) for at least 20 minutes
- Moderate-intensity PA (MPA) for at least 30 minutes
- LPA for at least 30 minutes
VPA was defined as “intense exercise that caused severe shortness of breath, MPA was defined as activity causing mild shortness of breath, and LPA was defined as “walking at a slow or leisurely pace.”
PA-related energy expenditure was also calculated in metabolic equivalent (MET) minutes per week by “summing the product of frequency, intensity, and duration,” the investigators noted.
Participants were stratified on the basis of their weekly total PA levels into the following groups:
- Inactive (no LPA beyond basic movements)
- Insufficiently active (less than the recommended target range of 1-499 MET-min/wk)
- Active (meeting the recommended target range of 500-999 MET-min/wk)
- Highly active (exceeding the recommended target range of at least 1,000 MET-min/wk)
Of all participants, 35% were categorized as inactive, 25% were insufficiently active, 24.4% were active, and 15.2% were highly active.
Controversy remains
During the total median follow-up of 42 months, 6% of participants had all-cause dementia. After the researchers excluded the first 2 years, incidence of dementia was 21.6 per 1000 person-years during follow-up.
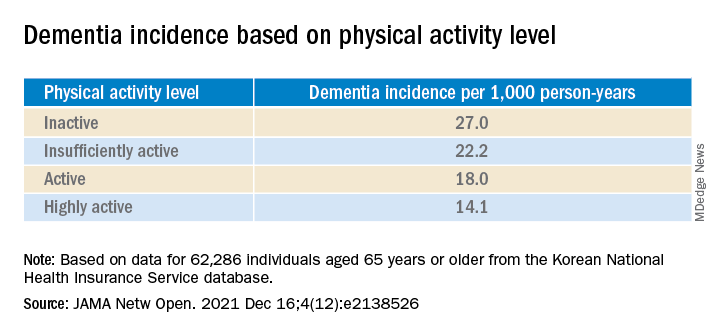
“The cumulative incidence of dementia was associated with a progressively decreasing trend with increasing physical activity” (P = .001 for trend), the investigators reported.
When using a competing-risk multivariable regression model, they found that higher levels of PA were associated with lower risk for dementia, compared with the inactive group.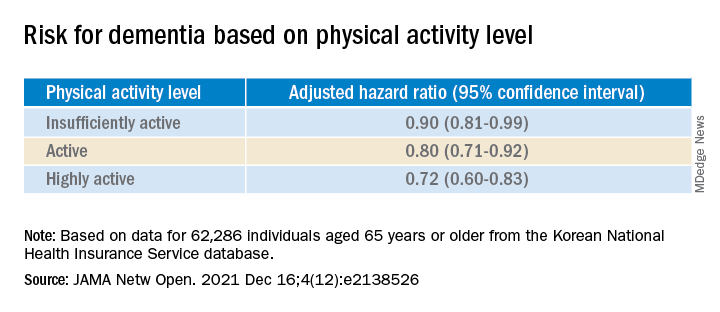
Similar findings were obtained after censoring for stroke, and were consistent for all follow-up periods. In subgroup analysis, the association between PA level and dementia risk remained consistent, regardless of age, sex, and comorbidities.
Even a low amount of LPA (1-299 MET-min/wk) was linked to reduced risk for dementia versus total sedentary behavior (adjusted HR, 0.86; 95% CI, 0.74-0.99).
The investigators noted that some “controversy” remains regarding the possibility of reverse causation and, because their study was observational in nature, “it cannot be used to establish causal relationship.”
Nevertheless, the study had important strengths, including the large number of older adults with available data, the assessment of dose-response association between PA and dementia, and the sensitivity analyses they performed, the researchers added.
Piece of important evidence
Commenting on the findings, Takashi Tarumi, PhD, senior research investigator, National Institute of Advanced Industrial Science and Technology, Ibaraki, Japan, said previous studies have suggested “an inverse association between physical activity and dementia risk, such that older adults performing a higher dose of exercise may have a greater benefit for reducing the dementia risk.”
Dr. Tarumi, an associate editor at the Journal of Alzheimer’s Disease, added the current study “significantly extends our knowledge by showing that dementia risk can also be reduced by light physical activities when they are performed for longer hours.”
This provides “another piece of important evidence” to support clinicians recommending regular physical activity for the prevention of dementia in later life, said Dr. Tarumi, who was not involved with the research.
Also commenting, Martin Underwood, MD, Warwick Medical School, Coventry, England, described the association between reduced physical inactivity and dementia as well established – and noted the current study “appears to confirm earlier observational data showing this relationship.”
The current results have “still not been able to fully exclude the possibility of reverse causation,” said Dr. Underwood, who was also not associated with the study.
However, the finding that more physically active individuals are less likely to develop dementia “only becomes of real interest if we can show that increased physical activity prevents the onset, or slows the progression, of dementia,” he noted.
“To my knowledge this has not yet been established” in randomized clinical trials, Dr. Underwood added.
The study was supported by grants from the Patient-Centered Clinical Research Coordinating Center, funded by the Ministry of Health & Welfare, Republic of Korea; and by a research grant from Yonsei University. One coauthor reported serving as a speaker for Bayer, Bristol-Myers Squibb/Pfizer, Medtronic, and Daiichi-Sankyo, and receiving research funds from Medtronic and Abbott. No other author disclosures were reported. Dr. Tarumi and Dr. Underwood have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults who participate in even light physical activity (LPA) may have a lower risk of developing dementia, new research suggests.
In a retrospective analysis of more than 62,000 individuals aged 65 or older without preexisting dementia, 6% developed dementia.
Compared with inactive individuals, “insufficiently active,” “active,” and “highly active” individuals all had a 10%, 20%, and 28% lower risk for dementia, respectively. And this association was consistent regardless of age, sex, other comorbidities, or after the researchers censored for stroke.
Even the lowest amount of LPA was associated with reduced dementia risk, investigators noted.
“In older adults, an increased physical activity level, including a low amount of LPA, was associated with a reduced risk of dementia,” Minjae Yoon, MD, division of cardiology, Severance Cardiovascular Hospital, Yonsei University, Seoul, South Korea, and colleagues wrote.
“Promotion of LPA might reduce the risk of dementia in older adults,” they added.
The findings were published online in JAMA Network Open.
Reverse causation?
Physical activity has been shown previously to be associated with reduced dementia risk. Current World Health Organization guidelines recommend that adults with normal cognition should engage in PA to reduce their risk for cognitive decline.
However, some studies have not yielded this result, “suggesting that previous findings showing a lower risk of dementia in physically active people could be attributed to reverse causation,” the investigators noted. Additionally, previous research regarding exercise intensity has been “inconsistent” concerning the role of LPA in reducing dementia risk.
Many older adults with frailty and comorbidity cannot perform intense or even moderate PA, therefore “these adults would have to gain the benefits of physical activity from LPA,” the researchers noted.
To clarify the potential association between PA and new-onset dementia, they focused specifically on the “dose-response association” between PA and dementia – especially LPA.
Between 2009 and 2012, the investigators enrolled 62,286 older individuals (60.4% women; mean age, 73.2 years) with available health checkup data from the National Health Insurance Service–Senior Database of Korea. All had no history of dementia.
Leisure-time PA was assessed with self-report questionnaires that used a 7-day recall method and included three questions regarding usual frequency (in days per week):
- Vigorous PA (VPA) for at least 20 minutes
- Moderate-intensity PA (MPA) for at least 30 minutes
- LPA for at least 30 minutes
VPA was defined as “intense exercise that caused severe shortness of breath, MPA was defined as activity causing mild shortness of breath, and LPA was defined as “walking at a slow or leisurely pace.”
PA-related energy expenditure was also calculated in metabolic equivalent (MET) minutes per week by “summing the product of frequency, intensity, and duration,” the investigators noted.
Participants were stratified on the basis of their weekly total PA levels into the following groups:
- Inactive (no LPA beyond basic movements)
- Insufficiently active (less than the recommended target range of 1-499 MET-min/wk)
- Active (meeting the recommended target range of 500-999 MET-min/wk)
- Highly active (exceeding the recommended target range of at least 1,000 MET-min/wk)
Of all participants, 35% were categorized as inactive, 25% were insufficiently active, 24.4% were active, and 15.2% were highly active.
Controversy remains
During the total median follow-up of 42 months, 6% of participants had all-cause dementia. After the researchers excluded the first 2 years, incidence of dementia was 21.6 per 1000 person-years during follow-up.
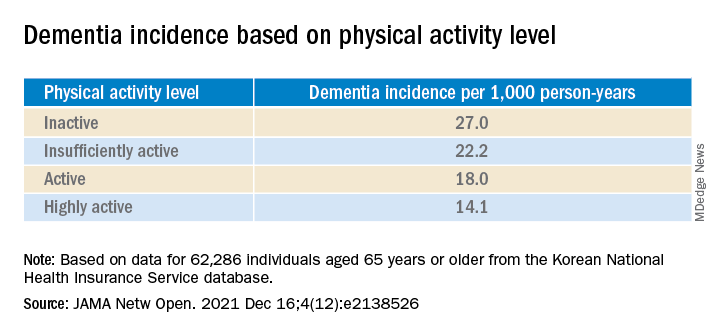
“The cumulative incidence of dementia was associated with a progressively decreasing trend with increasing physical activity” (P = .001 for trend), the investigators reported.
When using a competing-risk multivariable regression model, they found that higher levels of PA were associated with lower risk for dementia, compared with the inactive group.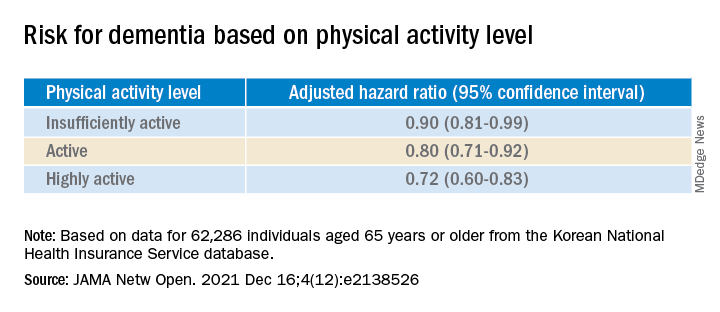
Similar findings were obtained after censoring for stroke, and were consistent for all follow-up periods. In subgroup analysis, the association between PA level and dementia risk remained consistent, regardless of age, sex, and comorbidities.
Even a low amount of LPA (1-299 MET-min/wk) was linked to reduced risk for dementia versus total sedentary behavior (adjusted HR, 0.86; 95% CI, 0.74-0.99).
The investigators noted that some “controversy” remains regarding the possibility of reverse causation and, because their study was observational in nature, “it cannot be used to establish causal relationship.”
Nevertheless, the study had important strengths, including the large number of older adults with available data, the assessment of dose-response association between PA and dementia, and the sensitivity analyses they performed, the researchers added.
Piece of important evidence
Commenting on the findings, Takashi Tarumi, PhD, senior research investigator, National Institute of Advanced Industrial Science and Technology, Ibaraki, Japan, said previous studies have suggested “an inverse association between physical activity and dementia risk, such that older adults performing a higher dose of exercise may have a greater benefit for reducing the dementia risk.”
Dr. Tarumi, an associate editor at the Journal of Alzheimer’s Disease, added the current study “significantly extends our knowledge by showing that dementia risk can also be reduced by light physical activities when they are performed for longer hours.”
This provides “another piece of important evidence” to support clinicians recommending regular physical activity for the prevention of dementia in later life, said Dr. Tarumi, who was not involved with the research.
Also commenting, Martin Underwood, MD, Warwick Medical School, Coventry, England, described the association between reduced physical inactivity and dementia as well established – and noted the current study “appears to confirm earlier observational data showing this relationship.”
The current results have “still not been able to fully exclude the possibility of reverse causation,” said Dr. Underwood, who was also not associated with the study.
However, the finding that more physically active individuals are less likely to develop dementia “only becomes of real interest if we can show that increased physical activity prevents the onset, or slows the progression, of dementia,” he noted.
“To my knowledge this has not yet been established” in randomized clinical trials, Dr. Underwood added.
The study was supported by grants from the Patient-Centered Clinical Research Coordinating Center, funded by the Ministry of Health & Welfare, Republic of Korea; and by a research grant from Yonsei University. One coauthor reported serving as a speaker for Bayer, Bristol-Myers Squibb/Pfizer, Medtronic, and Daiichi-Sankyo, and receiving research funds from Medtronic and Abbott. No other author disclosures were reported. Dr. Tarumi and Dr. Underwood have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults who participate in even light physical activity (LPA) may have a lower risk of developing dementia, new research suggests.
In a retrospective analysis of more than 62,000 individuals aged 65 or older without preexisting dementia, 6% developed dementia.
Compared with inactive individuals, “insufficiently active,” “active,” and “highly active” individuals all had a 10%, 20%, and 28% lower risk for dementia, respectively. And this association was consistent regardless of age, sex, other comorbidities, or after the researchers censored for stroke.
Even the lowest amount of LPA was associated with reduced dementia risk, investigators noted.
“In older adults, an increased physical activity level, including a low amount of LPA, was associated with a reduced risk of dementia,” Minjae Yoon, MD, division of cardiology, Severance Cardiovascular Hospital, Yonsei University, Seoul, South Korea, and colleagues wrote.
“Promotion of LPA might reduce the risk of dementia in older adults,” they added.
The findings were published online in JAMA Network Open.
Reverse causation?
Physical activity has been shown previously to be associated with reduced dementia risk. Current World Health Organization guidelines recommend that adults with normal cognition should engage in PA to reduce their risk for cognitive decline.
However, some studies have not yielded this result, “suggesting that previous findings showing a lower risk of dementia in physically active people could be attributed to reverse causation,” the investigators noted. Additionally, previous research regarding exercise intensity has been “inconsistent” concerning the role of LPA in reducing dementia risk.
Many older adults with frailty and comorbidity cannot perform intense or even moderate PA, therefore “these adults would have to gain the benefits of physical activity from LPA,” the researchers noted.
To clarify the potential association between PA and new-onset dementia, they focused specifically on the “dose-response association” between PA and dementia – especially LPA.
Between 2009 and 2012, the investigators enrolled 62,286 older individuals (60.4% women; mean age, 73.2 years) with available health checkup data from the National Health Insurance Service–Senior Database of Korea. All had no history of dementia.
Leisure-time PA was assessed with self-report questionnaires that used a 7-day recall method and included three questions regarding usual frequency (in days per week):
- Vigorous PA (VPA) for at least 20 minutes
- Moderate-intensity PA (MPA) for at least 30 minutes
- LPA for at least 30 minutes
VPA was defined as “intense exercise that caused severe shortness of breath, MPA was defined as activity causing mild shortness of breath, and LPA was defined as “walking at a slow or leisurely pace.”
PA-related energy expenditure was also calculated in metabolic equivalent (MET) minutes per week by “summing the product of frequency, intensity, and duration,” the investigators noted.
Participants were stratified on the basis of their weekly total PA levels into the following groups:
- Inactive (no LPA beyond basic movements)
- Insufficiently active (less than the recommended target range of 1-499 MET-min/wk)
- Active (meeting the recommended target range of 500-999 MET-min/wk)
- Highly active (exceeding the recommended target range of at least 1,000 MET-min/wk)
Of all participants, 35% were categorized as inactive, 25% were insufficiently active, 24.4% were active, and 15.2% were highly active.
Controversy remains
During the total median follow-up of 42 months, 6% of participants had all-cause dementia. After the researchers excluded the first 2 years, incidence of dementia was 21.6 per 1000 person-years during follow-up.
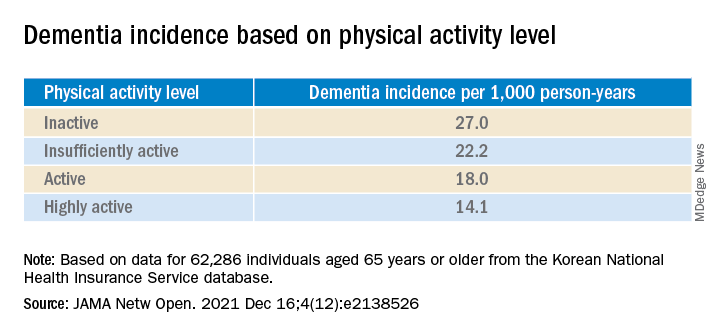
“The cumulative incidence of dementia was associated with a progressively decreasing trend with increasing physical activity” (P = .001 for trend), the investigators reported.
When using a competing-risk multivariable regression model, they found that higher levels of PA were associated with lower risk for dementia, compared with the inactive group.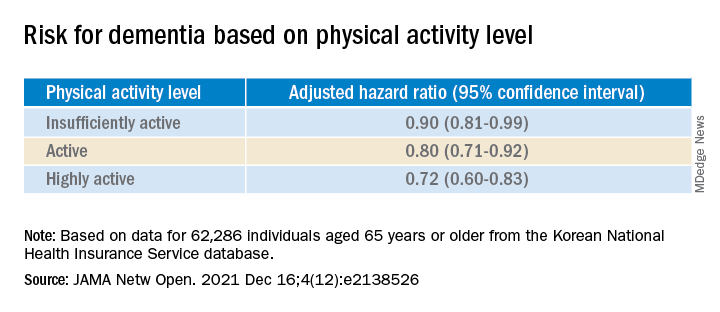
Similar findings were obtained after censoring for stroke, and were consistent for all follow-up periods. In subgroup analysis, the association between PA level and dementia risk remained consistent, regardless of age, sex, and comorbidities.
Even a low amount of LPA (1-299 MET-min/wk) was linked to reduced risk for dementia versus total sedentary behavior (adjusted HR, 0.86; 95% CI, 0.74-0.99).
The investigators noted that some “controversy” remains regarding the possibility of reverse causation and, because their study was observational in nature, “it cannot be used to establish causal relationship.”
Nevertheless, the study had important strengths, including the large number of older adults with available data, the assessment of dose-response association between PA and dementia, and the sensitivity analyses they performed, the researchers added.
Piece of important evidence
Commenting on the findings, Takashi Tarumi, PhD, senior research investigator, National Institute of Advanced Industrial Science and Technology, Ibaraki, Japan, said previous studies have suggested “an inverse association between physical activity and dementia risk, such that older adults performing a higher dose of exercise may have a greater benefit for reducing the dementia risk.”
Dr. Tarumi, an associate editor at the Journal of Alzheimer’s Disease, added the current study “significantly extends our knowledge by showing that dementia risk can also be reduced by light physical activities when they are performed for longer hours.”
This provides “another piece of important evidence” to support clinicians recommending regular physical activity for the prevention of dementia in later life, said Dr. Tarumi, who was not involved with the research.
Also commenting, Martin Underwood, MD, Warwick Medical School, Coventry, England, described the association between reduced physical inactivity and dementia as well established – and noted the current study “appears to confirm earlier observational data showing this relationship.”
The current results have “still not been able to fully exclude the possibility of reverse causation,” said Dr. Underwood, who was also not associated with the study.
However, the finding that more physically active individuals are less likely to develop dementia “only becomes of real interest if we can show that increased physical activity prevents the onset, or slows the progression, of dementia,” he noted.
“To my knowledge this has not yet been established” in randomized clinical trials, Dr. Underwood added.
The study was supported by grants from the Patient-Centered Clinical Research Coordinating Center, funded by the Ministry of Health & Welfare, Republic of Korea; and by a research grant from Yonsei University. One coauthor reported serving as a speaker for Bayer, Bristol-Myers Squibb/Pfizer, Medtronic, and Daiichi-Sankyo, and receiving research funds from Medtronic and Abbott. No other author disclosures were reported. Dr. Tarumi and Dr. Underwood have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Ophthalmologist who developed medical botox dies at 89
his family confirmed to National Public Radio.
Four decades ago, Alan Brown Scott, MD, a native of Berkeley, Calif., turned the drug, once a deadly poison, into a revolutionary treatment for obscure eye diseases. It later became a well-known blockbuster treatment for reducing the appearance of wrinkles and treating hyperhidrosis (excessive sweating). Other approved medical uses include treatment of overactive bladder and urinary incontinence.
According to the American Society of Plastic Surgeons, its popularity for cosmetic use was boosted further during the pandemic and it was the No. 1 minimally invasive cosmetic procedure performed in 2020. Among the 13.3 million procedures, 4.4 million involved Botox.
According to Bloomberg Businessweek, Ed Schantz, who was working in the military’s biological weapons program, was the one to first send the toxin to Dr. Scott, who wanted to explore its properties for medical use.
The same Bloomberg article also noted that the original botulinum toxin itself “is so powerful that a tiny amount can suffocate a person by paralyzing the muscles used for breathing.”
Dr. Scott was looking for a way to help his patients avoid extensive surgeries.
“Specifically, he was aiming to treat people with strabismus, or cross-eyes, and blepharospasm, which is an uncontrollable closure of eyes. Today, it’s also used as a treatment to help with migraines, hair loss, and drooling,” NPR reported.
The New York Times once described Botox as “medicine’s answer to duct tape.”
Dr. Scott was the executive director of the Smith-Kettlewell Eye Research Institute in San Francisco when he did his pioneering research with botulinum toxin in the 1970s and 1980s, according to a 2002 article in SFGate.
In 1991, Dr. Scott sold the drug to Allergan, when it was called Oculinum. The next year, the name was officially changed to Botox.
In 2002, Dr. Scott told SFGate, when asked about the more popular use for the drug, “I think that’s a charming, slightly frivolous use,” adding, “but it’s not along the lines of what I was into, applications for serious disorders.”
According to Scientific American in 2016, Dr. Scott, then age 83, kept working on the noncosmetic benefits of botulism-toxin injections for eye-related disorders at the Strabismus Research Foundation,
He told Scientific American he was proud that his efforts “are directly helpful to people.”
“There are interesting and difficult problems still to be solved, and I’m a practicing physician and I see them every day,” he said.
Dr. Scott’s daughter, Ann Scott, told NPR: “He definitely loved his work and he was also a really great father.” She said her dad involved his children in his research and work.
She added, “He was a really calm, more of a quiet reserved person,” and said he was committed to teaching his students, many of them international students.
“That was what he really loved,” she said.
Dr. Scott, who died Dec. 16, was in intensive care for the last 10 days from an unspecified illness, his daughter told NPR.
A version of this article first appeared on Medscape.com.
his family confirmed to National Public Radio.
Four decades ago, Alan Brown Scott, MD, a native of Berkeley, Calif., turned the drug, once a deadly poison, into a revolutionary treatment for obscure eye diseases. It later became a well-known blockbuster treatment for reducing the appearance of wrinkles and treating hyperhidrosis (excessive sweating). Other approved medical uses include treatment of overactive bladder and urinary incontinence.
According to the American Society of Plastic Surgeons, its popularity for cosmetic use was boosted further during the pandemic and it was the No. 1 minimally invasive cosmetic procedure performed in 2020. Among the 13.3 million procedures, 4.4 million involved Botox.
According to Bloomberg Businessweek, Ed Schantz, who was working in the military’s biological weapons program, was the one to first send the toxin to Dr. Scott, who wanted to explore its properties for medical use.
The same Bloomberg article also noted that the original botulinum toxin itself “is so powerful that a tiny amount can suffocate a person by paralyzing the muscles used for breathing.”
Dr. Scott was looking for a way to help his patients avoid extensive surgeries.
“Specifically, he was aiming to treat people with strabismus, or cross-eyes, and blepharospasm, which is an uncontrollable closure of eyes. Today, it’s also used as a treatment to help with migraines, hair loss, and drooling,” NPR reported.
The New York Times once described Botox as “medicine’s answer to duct tape.”
Dr. Scott was the executive director of the Smith-Kettlewell Eye Research Institute in San Francisco when he did his pioneering research with botulinum toxin in the 1970s and 1980s, according to a 2002 article in SFGate.
In 1991, Dr. Scott sold the drug to Allergan, when it was called Oculinum. The next year, the name was officially changed to Botox.
In 2002, Dr. Scott told SFGate, when asked about the more popular use for the drug, “I think that’s a charming, slightly frivolous use,” adding, “but it’s not along the lines of what I was into, applications for serious disorders.”
According to Scientific American in 2016, Dr. Scott, then age 83, kept working on the noncosmetic benefits of botulism-toxin injections for eye-related disorders at the Strabismus Research Foundation,
He told Scientific American he was proud that his efforts “are directly helpful to people.”
“There are interesting and difficult problems still to be solved, and I’m a practicing physician and I see them every day,” he said.
Dr. Scott’s daughter, Ann Scott, told NPR: “He definitely loved his work and he was also a really great father.” She said her dad involved his children in his research and work.
She added, “He was a really calm, more of a quiet reserved person,” and said he was committed to teaching his students, many of them international students.
“That was what he really loved,” she said.
Dr. Scott, who died Dec. 16, was in intensive care for the last 10 days from an unspecified illness, his daughter told NPR.
A version of this article first appeared on Medscape.com.
his family confirmed to National Public Radio.
Four decades ago, Alan Brown Scott, MD, a native of Berkeley, Calif., turned the drug, once a deadly poison, into a revolutionary treatment for obscure eye diseases. It later became a well-known blockbuster treatment for reducing the appearance of wrinkles and treating hyperhidrosis (excessive sweating). Other approved medical uses include treatment of overactive bladder and urinary incontinence.
According to the American Society of Plastic Surgeons, its popularity for cosmetic use was boosted further during the pandemic and it was the No. 1 minimally invasive cosmetic procedure performed in 2020. Among the 13.3 million procedures, 4.4 million involved Botox.
According to Bloomberg Businessweek, Ed Schantz, who was working in the military’s biological weapons program, was the one to first send the toxin to Dr. Scott, who wanted to explore its properties for medical use.
The same Bloomberg article also noted that the original botulinum toxin itself “is so powerful that a tiny amount can suffocate a person by paralyzing the muscles used for breathing.”
Dr. Scott was looking for a way to help his patients avoid extensive surgeries.
“Specifically, he was aiming to treat people with strabismus, or cross-eyes, and blepharospasm, which is an uncontrollable closure of eyes. Today, it’s also used as a treatment to help with migraines, hair loss, and drooling,” NPR reported.
The New York Times once described Botox as “medicine’s answer to duct tape.”
Dr. Scott was the executive director of the Smith-Kettlewell Eye Research Institute in San Francisco when he did his pioneering research with botulinum toxin in the 1970s and 1980s, according to a 2002 article in SFGate.
In 1991, Dr. Scott sold the drug to Allergan, when it was called Oculinum. The next year, the name was officially changed to Botox.
In 2002, Dr. Scott told SFGate, when asked about the more popular use for the drug, “I think that’s a charming, slightly frivolous use,” adding, “but it’s not along the lines of what I was into, applications for serious disorders.”
According to Scientific American in 2016, Dr. Scott, then age 83, kept working on the noncosmetic benefits of botulism-toxin injections for eye-related disorders at the Strabismus Research Foundation,
He told Scientific American he was proud that his efforts “are directly helpful to people.”
“There are interesting and difficult problems still to be solved, and I’m a practicing physician and I see them every day,” he said.
Dr. Scott’s daughter, Ann Scott, told NPR: “He definitely loved his work and he was also a really great father.” She said her dad involved his children in his research and work.
She added, “He was a really calm, more of a quiet reserved person,” and said he was committed to teaching his students, many of them international students.
“That was what he really loved,” she said.
Dr. Scott, who died Dec. 16, was in intensive care for the last 10 days from an unspecified illness, his daughter told NPR.
A version of this article first appeared on Medscape.com.
FDA approves new myasthenia gravis drug
“There are significant unmet medical needs for people living with myasthenia gravis, as with many other rare diseases,” Billy Dunn, MD, director, office of neuroscience, FDA Center for Drug Evaluation and Research, said in a news release.
This approval represents “an important step in providing a novel therapy option for patients and underscores the agency’s commitment to help make new treatment options available for people living with rare diseases,” Dr. Dunn added.
Effective, well tolerated
The rare and chronic autoimmune neuromuscular disorder of gMG causes debilitating and potentially life-threatening muscle weakness and significantly impaired independence and quality of life. Most patients with gMG have IgG antibodies, which are most often directed against skeletal muscle nicotinic acetylcholine receptors.
Efgartigimod is an antibody fragment designed to reduce pathogenic IgG antibodies and block the IgG recycling process in patients with gMG.
The novel agent binds to the neonatal Fc receptor (FcRn), which is widely expressed throughout the body and plays a central role in rescuing IgG antibodies from degradation. Blocking FcRn reduces IgG antibody levels.
As previously reported, efgartigimod was effective and well tolerated in the phase 3, randomized, placebo-controlled ADAPT trial, which enrolled 187 adults with gMG regardless of acetylcholine receptor antibody status. All had a Myasthenia Gravis–Activities of Daily Living score of at least 5 (>50% nonocular) on a background of a stable dose of at least one MG drug.
For 26 weeks, 84 patients were randomly assigned to receive efgartigimod 10 mg/kg and 83 to receive matching placebo. Both treatments were administered as four infusions per cycle at one infusion per week. The process was repeated as needed, depending on clinical response no sooner than 8 weeks after initiation of the previous cycle.
Treatment with efgartigimod reduced disease burden and improved strength and quality of life in patients with gMG across four MG-specific scales. In addition, these benefits were observed early and were reproducible and durable.
The results were published in Lancet Neurology.
‘Important new advance’
Efgartigimod is a “very rapidly acting drug relative to other treatments that may take 4, 6, sometimes 10 months before they start to work; and the side-effect profile is much like placebo,” said principal investigator James Howard Jr., MD, department of neurology, University of North Carolina at Chapel Hill.
The FDA granted efgartigimod fast track and orphan drug designation.
“People living with gMG have been in need of new treatment options that are targeted to the underlying pathogenesis of the disease and supported by clinical data,” Dr. Howard said in a company news release issued upon approval.
This approval “represents an important new advance for gMG patients and families affected by this debilitating disease. This therapy has the potential to reduce the disease burden of gMG and transform the way we treat this disease,” Dr. Howard added.
A version of this article first appeared on Medscape.com.
“There are significant unmet medical needs for people living with myasthenia gravis, as with many other rare diseases,” Billy Dunn, MD, director, office of neuroscience, FDA Center for Drug Evaluation and Research, said in a news release.
This approval represents “an important step in providing a novel therapy option for patients and underscores the agency’s commitment to help make new treatment options available for people living with rare diseases,” Dr. Dunn added.
Effective, well tolerated
The rare and chronic autoimmune neuromuscular disorder of gMG causes debilitating and potentially life-threatening muscle weakness and significantly impaired independence and quality of life. Most patients with gMG have IgG antibodies, which are most often directed against skeletal muscle nicotinic acetylcholine receptors.
Efgartigimod is an antibody fragment designed to reduce pathogenic IgG antibodies and block the IgG recycling process in patients with gMG.
The novel agent binds to the neonatal Fc receptor (FcRn), which is widely expressed throughout the body and plays a central role in rescuing IgG antibodies from degradation. Blocking FcRn reduces IgG antibody levels.
As previously reported, efgartigimod was effective and well tolerated in the phase 3, randomized, placebo-controlled ADAPT trial, which enrolled 187 adults with gMG regardless of acetylcholine receptor antibody status. All had a Myasthenia Gravis–Activities of Daily Living score of at least 5 (>50% nonocular) on a background of a stable dose of at least one MG drug.
For 26 weeks, 84 patients were randomly assigned to receive efgartigimod 10 mg/kg and 83 to receive matching placebo. Both treatments were administered as four infusions per cycle at one infusion per week. The process was repeated as needed, depending on clinical response no sooner than 8 weeks after initiation of the previous cycle.
Treatment with efgartigimod reduced disease burden and improved strength and quality of life in patients with gMG across four MG-specific scales. In addition, these benefits were observed early and were reproducible and durable.
The results were published in Lancet Neurology.
‘Important new advance’
Efgartigimod is a “very rapidly acting drug relative to other treatments that may take 4, 6, sometimes 10 months before they start to work; and the side-effect profile is much like placebo,” said principal investigator James Howard Jr., MD, department of neurology, University of North Carolina at Chapel Hill.
The FDA granted efgartigimod fast track and orphan drug designation.
“People living with gMG have been in need of new treatment options that are targeted to the underlying pathogenesis of the disease and supported by clinical data,” Dr. Howard said in a company news release issued upon approval.
This approval “represents an important new advance for gMG patients and families affected by this debilitating disease. This therapy has the potential to reduce the disease burden of gMG and transform the way we treat this disease,” Dr. Howard added.
A version of this article first appeared on Medscape.com.
“There are significant unmet medical needs for people living with myasthenia gravis, as with many other rare diseases,” Billy Dunn, MD, director, office of neuroscience, FDA Center for Drug Evaluation and Research, said in a news release.
This approval represents “an important step in providing a novel therapy option for patients and underscores the agency’s commitment to help make new treatment options available for people living with rare diseases,” Dr. Dunn added.
Effective, well tolerated
The rare and chronic autoimmune neuromuscular disorder of gMG causes debilitating and potentially life-threatening muscle weakness and significantly impaired independence and quality of life. Most patients with gMG have IgG antibodies, which are most often directed against skeletal muscle nicotinic acetylcholine receptors.
Efgartigimod is an antibody fragment designed to reduce pathogenic IgG antibodies and block the IgG recycling process in patients with gMG.
The novel agent binds to the neonatal Fc receptor (FcRn), which is widely expressed throughout the body and plays a central role in rescuing IgG antibodies from degradation. Blocking FcRn reduces IgG antibody levels.
As previously reported, efgartigimod was effective and well tolerated in the phase 3, randomized, placebo-controlled ADAPT trial, which enrolled 187 adults with gMG regardless of acetylcholine receptor antibody status. All had a Myasthenia Gravis–Activities of Daily Living score of at least 5 (>50% nonocular) on a background of a stable dose of at least one MG drug.
For 26 weeks, 84 patients were randomly assigned to receive efgartigimod 10 mg/kg and 83 to receive matching placebo. Both treatments were administered as four infusions per cycle at one infusion per week. The process was repeated as needed, depending on clinical response no sooner than 8 weeks after initiation of the previous cycle.
Treatment with efgartigimod reduced disease burden and improved strength and quality of life in patients with gMG across four MG-specific scales. In addition, these benefits were observed early and were reproducible and durable.
The results were published in Lancet Neurology.
‘Important new advance’
Efgartigimod is a “very rapidly acting drug relative to other treatments that may take 4, 6, sometimes 10 months before they start to work; and the side-effect profile is much like placebo,” said principal investigator James Howard Jr., MD, department of neurology, University of North Carolina at Chapel Hill.
The FDA granted efgartigimod fast track and orphan drug designation.
“People living with gMG have been in need of new treatment options that are targeted to the underlying pathogenesis of the disease and supported by clinical data,” Dr. Howard said in a company news release issued upon approval.
This approval “represents an important new advance for gMG patients and families affected by this debilitating disease. This therapy has the potential to reduce the disease burden of gMG and transform the way we treat this disease,” Dr. Howard added.
A version of this article first appeared on Medscape.com.


