User login
Occlusion of Brachial Pseudoaneurysm After Periprosthetic Humerus Fracture
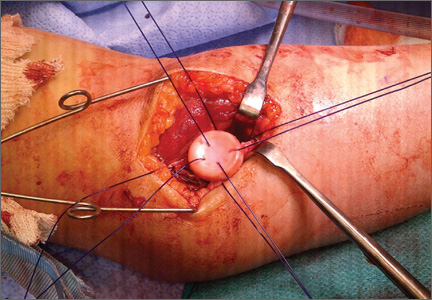
The Métaizeau Technique for Pediatric Radial Neck Fracture With Elbow Dislocation: Intraoperative Pitfalls and Associated Forearm Compartment Syndrome
Allograft Anterior Cruciate Ligament Reconstruction in Patients Younger Than 30 Years: A Matched-Pair Comparison of Bone– Patellar Tendon–Bone and Tibialis Anterior
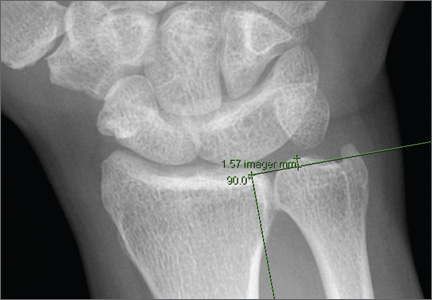
Compared With Magnetic Resonance Imaging, Radiographs Underestimate the Magnitude of Negative Ulnar Variance
Endoprosthetic Reconstruction After Resection of Musculoskeletal Tumors
Is It Safe to Place a Tibial Intramedullary Nail Through a Traumatic Knee Arthrotomy?
Use Online Coding Discussion Tools With Caution
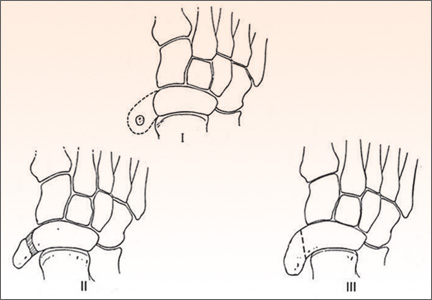
Surgical Treatment of Symptomatic Accessory Navicular in Children and Adolescents
The Orthopedic Stepchild
Throughout antiquity, physicians and surgeons have concerned themselves with maladies of the foot and ankle. The literature is rife with articles describing management of clubfoot deformities and traumatic amputations of feet and legs. Authors have described tenotomies and manipulation for clubfeet as well as optimal techniques and levels for amputations to promote healing and functional outcomes. In progressive and aggressive surgical centers in Austria and Germany, techniques for correction of the deformities created by disease and trauma formed the basis for today’s reconstructive methodologies.
During my orthopedic residency in the 1960s, we managed pediatric versions of clubfoot, vertical talus, and neuromuscular conditions of the lower extremity (myelomeningocele, muscular dystrophy, cerebral palsy); adolescent bunions and pathologic flat feet; and, in adults, residual polio, arthritis, bunions, lesser toe deformities, ankle disorders, and trauma. Then along came the excitement of total joint arthroplasty, with its spectacular results, and the thrill in devoting careers to athletes and their myriad problems. Other interesting subspecialties emerged, and the orthopedic focus on a significant part of our heritage, the issues of foot and ankle, was lost for decades. Care for these problems was left to a small cadre of pediatric doctors, and soon-to-retire orthopedists who tended to view the field as
less demanding. Dynamic young practitioners showed little or no interest in caring for foot and ankle patients, and no progress was made in clinical care, research, and development of orthopedic technology and devices.
In the late 1960s, a small group of middle-aged and senior devotees of the specialty met in New York to form the American Orthopaedic Foot Society (AOFS), later to become the American Orthopaedic Foot and Ankle Society (AOFAS). The group’s goal was to renew interest in the foot and ankle specialty among orthopedic surgeons. As everyone knows, AOFAS has flourished and become one of the most progressive, innovative, and dynamic of all the orthopedic subspecialty
groups. In 1985, John Gartland, president of the American Academy of Orthopaedic Surgeons, called together the leaders in the foot and ankle field to formulate a long-range plan to reclaim foot and ankle from the morass of substandard care
and to advance the subspecialty in every quarter. As AOFS (and later AOFAS) president, I was part of Gartland’s team. I recall we aimed to convince orthopedic chairs, the Residency Review Committee for Orthopaedic Surgery, and the Board
of Orthopaedic Surgery to increase training requirements, to develop foot and ankle educators, and to promote the area in training programs. Orthopedic educators developed fellowships (essentially nonexistent up until then) and organized and taught beginner and advanced continuing education courses at annual meetings and throughout the year.
There were other needs to be addressed. One was to educate nonorthopedic doctors to appreciate that foot and ankle problems had good nonoperative and surgical solutions, that there was an orthopedic subspecialty for these conditions, and that foot and ankle patients should be referred to its practitioners. Second, these patients’ public advocacy groups needed to know what knowledgeable orthopedists could provide and needed to be encouraged to seek care from these physicians rather than from less qualified providers and nonspecialists.
To an extraordinary degree, the goal of educating orthopedists has been achieved, and the field is now populated with young, energetic leaders, teachers, and practitioners. We have been less successful in educating potential referring physicians, the public, public advocacy groups, and third-party payers, including the US government. Progress has been made with private insurers and, as advisors, with the Centers for Medicare and Medicaid Services and state government health committees.
Driven by emerging market opportunities, the orthopedic device industry has made unanticipated and enormous advances in the distal lower extremity realm. Small
companies have been founded, and larger companies have dedicated entire divisions to making fixation devices and prosthetic implants for every procedure involving the foot or the ankle. Biomedical engineers, metallurgists, orthopedic
consultant researchers, and well-funded projects have led the surge to develop the best foot and ankle technology. In addition, industry courses and scholarships for residents, fellows, teaching programs, and young physicians have been generating interest in these advances. Although it may be argued that entrepreneurship brings enormous bias, it must be conceded that interest in the foot and ankle field has increased tremendously. Outreach programs for foot and ankle care in the Third World have emerged as an additional humanitarian benefit of the expansion of the field.
From its strong start as a medical specialty to its fall into ignorance and neglect, the foot and ankle field, the unwanted stepchild of medicine and orthopedics, has made a dramatic recovery and has become a premier example of what medicine can achieve through focused effort. As leaders in orthopedic medicine in North America, we must also acknowledge the huge contributions made by a sterling array of international researchers, educators, and practitioners.
Some journals in the United States and other countries now concentrate solely on foot and ankle. Nevertheless, it is appropriate that The American Journal of Orthopedics and other general orthopedic surgery publications focus on foot and
ankle (and other specialties) in an annual issue. As each orthopedist tends mainly to his or her own area of interest, it is essential that we all stay current on the field as a whole. The basic science, innovations, and concepts of one specialty are often applicable to the entire field, and a casual notation of an idea from such a focused issue may have unimagined benefits for the readership and their patients. ◾
Throughout antiquity, physicians and surgeons have concerned themselves with maladies of the foot and ankle. The literature is rife with articles describing management of clubfoot deformities and traumatic amputations of feet and legs. Authors have described tenotomies and manipulation for clubfeet as well as optimal techniques and levels for amputations to promote healing and functional outcomes. In progressive and aggressive surgical centers in Austria and Germany, techniques for correction of the deformities created by disease and trauma formed the basis for today’s reconstructive methodologies.
During my orthopedic residency in the 1960s, we managed pediatric versions of clubfoot, vertical talus, and neuromuscular conditions of the lower extremity (myelomeningocele, muscular dystrophy, cerebral palsy); adolescent bunions and pathologic flat feet; and, in adults, residual polio, arthritis, bunions, lesser toe deformities, ankle disorders, and trauma. Then along came the excitement of total joint arthroplasty, with its spectacular results, and the thrill in devoting careers to athletes and their myriad problems. Other interesting subspecialties emerged, and the orthopedic focus on a significant part of our heritage, the issues of foot and ankle, was lost for decades. Care for these problems was left to a small cadre of pediatric doctors, and soon-to-retire orthopedists who tended to view the field as
less demanding. Dynamic young practitioners showed little or no interest in caring for foot and ankle patients, and no progress was made in clinical care, research, and development of orthopedic technology and devices.
In the late 1960s, a small group of middle-aged and senior devotees of the specialty met in New York to form the American Orthopaedic Foot Society (AOFS), later to become the American Orthopaedic Foot and Ankle Society (AOFAS). The group’s goal was to renew interest in the foot and ankle specialty among orthopedic surgeons. As everyone knows, AOFAS has flourished and become one of the most progressive, innovative, and dynamic of all the orthopedic subspecialty
groups. In 1985, John Gartland, president of the American Academy of Orthopaedic Surgeons, called together the leaders in the foot and ankle field to formulate a long-range plan to reclaim foot and ankle from the morass of substandard care
and to advance the subspecialty in every quarter. As AOFS (and later AOFAS) president, I was part of Gartland’s team. I recall we aimed to convince orthopedic chairs, the Residency Review Committee for Orthopaedic Surgery, and the Board
of Orthopaedic Surgery to increase training requirements, to develop foot and ankle educators, and to promote the area in training programs. Orthopedic educators developed fellowships (essentially nonexistent up until then) and organized and taught beginner and advanced continuing education courses at annual meetings and throughout the year.
There were other needs to be addressed. One was to educate nonorthopedic doctors to appreciate that foot and ankle problems had good nonoperative and surgical solutions, that there was an orthopedic subspecialty for these conditions, and that foot and ankle patients should be referred to its practitioners. Second, these patients’ public advocacy groups needed to know what knowledgeable orthopedists could provide and needed to be encouraged to seek care from these physicians rather than from less qualified providers and nonspecialists.
To an extraordinary degree, the goal of educating orthopedists has been achieved, and the field is now populated with young, energetic leaders, teachers, and practitioners. We have been less successful in educating potential referring physicians, the public, public advocacy groups, and third-party payers, including the US government. Progress has been made with private insurers and, as advisors, with the Centers for Medicare and Medicaid Services and state government health committees.
Driven by emerging market opportunities, the orthopedic device industry has made unanticipated and enormous advances in the distal lower extremity realm. Small
companies have been founded, and larger companies have dedicated entire divisions to making fixation devices and prosthetic implants for every procedure involving the foot or the ankle. Biomedical engineers, metallurgists, orthopedic
consultant researchers, and well-funded projects have led the surge to develop the best foot and ankle technology. In addition, industry courses and scholarships for residents, fellows, teaching programs, and young physicians have been generating interest in these advances. Although it may be argued that entrepreneurship brings enormous bias, it must be conceded that interest in the foot and ankle field has increased tremendously. Outreach programs for foot and ankle care in the Third World have emerged as an additional humanitarian benefit of the expansion of the field.
From its strong start as a medical specialty to its fall into ignorance and neglect, the foot and ankle field, the unwanted stepchild of medicine and orthopedics, has made a dramatic recovery and has become a premier example of what medicine can achieve through focused effort. As leaders in orthopedic medicine in North America, we must also acknowledge the huge contributions made by a sterling array of international researchers, educators, and practitioners.
Some journals in the United States and other countries now concentrate solely on foot and ankle. Nevertheless, it is appropriate that The American Journal of Orthopedics and other general orthopedic surgery publications focus on foot and
ankle (and other specialties) in an annual issue. As each orthopedist tends mainly to his or her own area of interest, it is essential that we all stay current on the field as a whole. The basic science, innovations, and concepts of one specialty are often applicable to the entire field, and a casual notation of an idea from such a focused issue may have unimagined benefits for the readership and their patients. ◾
Throughout antiquity, physicians and surgeons have concerned themselves with maladies of the foot and ankle. The literature is rife with articles describing management of clubfoot deformities and traumatic amputations of feet and legs. Authors have described tenotomies and manipulation for clubfeet as well as optimal techniques and levels for amputations to promote healing and functional outcomes. In progressive and aggressive surgical centers in Austria and Germany, techniques for correction of the deformities created by disease and trauma formed the basis for today’s reconstructive methodologies.
During my orthopedic residency in the 1960s, we managed pediatric versions of clubfoot, vertical talus, and neuromuscular conditions of the lower extremity (myelomeningocele, muscular dystrophy, cerebral palsy); adolescent bunions and pathologic flat feet; and, in adults, residual polio, arthritis, bunions, lesser toe deformities, ankle disorders, and trauma. Then along came the excitement of total joint arthroplasty, with its spectacular results, and the thrill in devoting careers to athletes and their myriad problems. Other interesting subspecialties emerged, and the orthopedic focus on a significant part of our heritage, the issues of foot and ankle, was lost for decades. Care for these problems was left to a small cadre of pediatric doctors, and soon-to-retire orthopedists who tended to view the field as
less demanding. Dynamic young practitioners showed little or no interest in caring for foot and ankle patients, and no progress was made in clinical care, research, and development of orthopedic technology and devices.
In the late 1960s, a small group of middle-aged and senior devotees of the specialty met in New York to form the American Orthopaedic Foot Society (AOFS), later to become the American Orthopaedic Foot and Ankle Society (AOFAS). The group’s goal was to renew interest in the foot and ankle specialty among orthopedic surgeons. As everyone knows, AOFAS has flourished and become one of the most progressive, innovative, and dynamic of all the orthopedic subspecialty
groups. In 1985, John Gartland, president of the American Academy of Orthopaedic Surgeons, called together the leaders in the foot and ankle field to formulate a long-range plan to reclaim foot and ankle from the morass of substandard care
and to advance the subspecialty in every quarter. As AOFS (and later AOFAS) president, I was part of Gartland’s team. I recall we aimed to convince orthopedic chairs, the Residency Review Committee for Orthopaedic Surgery, and the Board
of Orthopaedic Surgery to increase training requirements, to develop foot and ankle educators, and to promote the area in training programs. Orthopedic educators developed fellowships (essentially nonexistent up until then) and organized and taught beginner and advanced continuing education courses at annual meetings and throughout the year.
There were other needs to be addressed. One was to educate nonorthopedic doctors to appreciate that foot and ankle problems had good nonoperative and surgical solutions, that there was an orthopedic subspecialty for these conditions, and that foot and ankle patients should be referred to its practitioners. Second, these patients’ public advocacy groups needed to know what knowledgeable orthopedists could provide and needed to be encouraged to seek care from these physicians rather than from less qualified providers and nonspecialists.
To an extraordinary degree, the goal of educating orthopedists has been achieved, and the field is now populated with young, energetic leaders, teachers, and practitioners. We have been less successful in educating potential referring physicians, the public, public advocacy groups, and third-party payers, including the US government. Progress has been made with private insurers and, as advisors, with the Centers for Medicare and Medicaid Services and state government health committees.
Driven by emerging market opportunities, the orthopedic device industry has made unanticipated and enormous advances in the distal lower extremity realm. Small
companies have been founded, and larger companies have dedicated entire divisions to making fixation devices and prosthetic implants for every procedure involving the foot or the ankle. Biomedical engineers, metallurgists, orthopedic
consultant researchers, and well-funded projects have led the surge to develop the best foot and ankle technology. In addition, industry courses and scholarships for residents, fellows, teaching programs, and young physicians have been generating interest in these advances. Although it may be argued that entrepreneurship brings enormous bias, it must be conceded that interest in the foot and ankle field has increased tremendously. Outreach programs for foot and ankle care in the Third World have emerged as an additional humanitarian benefit of the expansion of the field.
From its strong start as a medical specialty to its fall into ignorance and neglect, the foot and ankle field, the unwanted stepchild of medicine and orthopedics, has made a dramatic recovery and has become a premier example of what medicine can achieve through focused effort. As leaders in orthopedic medicine in North America, we must also acknowledge the huge contributions made by a sterling array of international researchers, educators, and practitioners.
Some journals in the United States and other countries now concentrate solely on foot and ankle. Nevertheless, it is appropriate that The American Journal of Orthopedics and other general orthopedic surgery publications focus on foot and
ankle (and other specialties) in an annual issue. As each orthopedist tends mainly to his or her own area of interest, it is essential that we all stay current on the field as a whole. The basic science, innovations, and concepts of one specialty are often applicable to the entire field, and a casual notation of an idea from such a focused issue may have unimagined benefits for the readership and their patients. ◾
Arthroplasty for rheumatoid arthritis doesn’t boost cardiovascular risk
SNOWMASS, COLO. – During a recent 15-year period in which the annual arthroplasty rate for osteoarthritis and other noninflammatory arthritides doubled, the arthroplasty rate for rheumatoid arthritis actually declined. Moreover, the mean age at the time of arthroplasty for RA rose.
"In a time frame when utilization of total knee and total hip replacement for osteoarthritis is really skyrocketing, with younger and younger patients, I think this speaks to something pretty good going on with our RA patients," Dr. Susan M. Goodman observed at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
She presented data from a soon to be published study of nearly 2.8 million arthroplasties included in 10 state databases. The arthroplasty rate for noninflammatory arthritis – the great majority of which is osteoarthritis (OA) – zoomed from 124.5/100,000 population in 1991 to 247.5/100,000 in 2005.
Meanwhile the rate of arthroplasty for RA fell slightly, albeit statistically significantly, from 4.6 to 4.5 per 100,000. The mean age at the time of arthroplasty for RA rose from 63.4 years in 1991 to 64.9 years in 2005, reported Dr. Goodman, a rheumatologist at the Hospital for Special Surgery in New York.
She turned to data from other sources to address issues related to the morbidity of arthroplasty for RA.
For example, it’s well documented that rheumatoid arthritis is associated with elevated cardiovascular risk, such that the typical RA patient has a cardiovascular morbidity burden comparable to that of someone without RA who’s 5 years older. So what does this mean for the many RA patients who come into the hospital for total hip or knee replacement?
Surprisingly, nothing. That is, data from multiple sources indicate RA patients are at no greater perioperative risk of cardiovascular events than are patients with OA undergoing the same procedures.
The take-away message? "Clearly we’re doing something right in managing our patients with RA," Dr. Goodman commented.
Similarly, an analysis of 7.75 million patients in the Nationwide Inpatient Sample database found that among RA patients undergoing intermediate-risk noncardiac surgery, such as total joint arthroplasty, the perioperative cardiovascular event rate was 0.34%, significantly less than the 1.07% rate in diabetic patients undergoing intermediate-risk surgeries. Moreover, perioperative mortality was 0.30% in the RA patients, less than half the 0.65% figure in diabetics (Arthritis Rheum. 2012;64:2429-37). These findings disproved the study hypothesis, which was that the two groups would have similar cardiovascular event rates, since both diseases are – unlike osteoarthritis – systemic inflammatory conditions associated with increased cardiovascular mortality.
"I think this means that we as rheumatologists are taking better care of our patients than the endocrinologists next door whose patients have a similar atherosclerotic burden," she continued.
Dr. Goodman was a coinvestigator in a population-based study of 351,103 total knee replacements and 157,775 total hip replacements done at 400 hospitals during 2006-2010. This retrospective analysis of an administrative database included 11,755 total knee and 5,400 total hip replacements for RA.
The prevalence of a prior history of MI, peripheral vascular disease, or cerebrovascular disease was closely similar in the RA and OA patients undergoing surgery. However, the prevalence of baseline COPD was significantly greater in the RA patients, at roughly 17.5%, or an absolute 3%-4% more than in the osteoarthritis patients.
The 30-day rates of cardiac events, venous thromboembolism, and cerebrovascular events were closely similar in the RA and OA arthroplasty patients. The RA patients undergoing total hip replacement had significantly higher rates of pulmonary compromise, infections, blood product transfusions, mechanical ventilation, and length of stay than did OA patients (Clin. Exp. Rheumatol. 2013;31:889-95). The RA patients with total knee replacement differed from their OA counterparts only in terms of greater need for transfusions and lengthier hospital stays (J. Arthroplasty 2014;29:308-13).
However, an analysis of the Hospital for Special Surgery experience failed to confirm the increased complication risks found in this study of a large administrative database. This retrospective review of adverse events within 6 months of total knee replacement in 156 RA patients and 318 OA controls showed no differences between the two groups in pneumonia, other infections, or venous thromboembolism. Moreover, the reoperation rate was 2.5% in the RA patients, compared with 8.8% in the OA group.
"The advantage of a smaller study like this is you really know who has RA and you have a lot of very granular information about the drugs they’re taking. The disadvantage, of course, is that you’re really not powered to look at major adverse events. But boy, there wasn’t even a hint of an increase in the complication rate amongst these RA patients," according to Dr. Goodman.
In a study she presented at the 2013 European Congress of Rheumatology, she compared 2-year outcomes post arthroplasty in RA and OA patients in the contemporary era of high use of biologic agents and traditional DMARDs for RA. The 178 RA patients who had total knee replacement had significantly greater comorbidities preoperatively than the 5,206 OA patients. Yet by 2 years postoperatively, they had fully caught up in terms of improved Western Ontario and McMaster Osteoarthritis Index (WOMAC) function and pain scores.
Total hip replacement was a very different story. The 202 RA patients were four times more likely to have poor WOMAC functional outcome and three times more likely to have poor pain outcome scores at 2 years, compared with 5,810 OA patients. In a multivariate analysis, higher expectations for surgery, better preoperative mental health, and more advanced education were associated with better 2-year outcomes.
"I’m not sure why our hip replacement patients with RA aren’t doing as well as the knee replacement patients, but they’re clearly not," according to the rheumatologist.
She reported having no financial disclosures.
SNOWMASS, COLO. – During a recent 15-year period in which the annual arthroplasty rate for osteoarthritis and other noninflammatory arthritides doubled, the arthroplasty rate for rheumatoid arthritis actually declined. Moreover, the mean age at the time of arthroplasty for RA rose.
"In a time frame when utilization of total knee and total hip replacement for osteoarthritis is really skyrocketing, with younger and younger patients, I think this speaks to something pretty good going on with our RA patients," Dr. Susan M. Goodman observed at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
She presented data from a soon to be published study of nearly 2.8 million arthroplasties included in 10 state databases. The arthroplasty rate for noninflammatory arthritis – the great majority of which is osteoarthritis (OA) – zoomed from 124.5/100,000 population in 1991 to 247.5/100,000 in 2005.
Meanwhile the rate of arthroplasty for RA fell slightly, albeit statistically significantly, from 4.6 to 4.5 per 100,000. The mean age at the time of arthroplasty for RA rose from 63.4 years in 1991 to 64.9 years in 2005, reported Dr. Goodman, a rheumatologist at the Hospital for Special Surgery in New York.
She turned to data from other sources to address issues related to the morbidity of arthroplasty for RA.
For example, it’s well documented that rheumatoid arthritis is associated with elevated cardiovascular risk, such that the typical RA patient has a cardiovascular morbidity burden comparable to that of someone without RA who’s 5 years older. So what does this mean for the many RA patients who come into the hospital for total hip or knee replacement?
Surprisingly, nothing. That is, data from multiple sources indicate RA patients are at no greater perioperative risk of cardiovascular events than are patients with OA undergoing the same procedures.
The take-away message? "Clearly we’re doing something right in managing our patients with RA," Dr. Goodman commented.
Similarly, an analysis of 7.75 million patients in the Nationwide Inpatient Sample database found that among RA patients undergoing intermediate-risk noncardiac surgery, such as total joint arthroplasty, the perioperative cardiovascular event rate was 0.34%, significantly less than the 1.07% rate in diabetic patients undergoing intermediate-risk surgeries. Moreover, perioperative mortality was 0.30% in the RA patients, less than half the 0.65% figure in diabetics (Arthritis Rheum. 2012;64:2429-37). These findings disproved the study hypothesis, which was that the two groups would have similar cardiovascular event rates, since both diseases are – unlike osteoarthritis – systemic inflammatory conditions associated with increased cardiovascular mortality.
"I think this means that we as rheumatologists are taking better care of our patients than the endocrinologists next door whose patients have a similar atherosclerotic burden," she continued.
Dr. Goodman was a coinvestigator in a population-based study of 351,103 total knee replacements and 157,775 total hip replacements done at 400 hospitals during 2006-2010. This retrospective analysis of an administrative database included 11,755 total knee and 5,400 total hip replacements for RA.
The prevalence of a prior history of MI, peripheral vascular disease, or cerebrovascular disease was closely similar in the RA and OA patients undergoing surgery. However, the prevalence of baseline COPD was significantly greater in the RA patients, at roughly 17.5%, or an absolute 3%-4% more than in the osteoarthritis patients.
The 30-day rates of cardiac events, venous thromboembolism, and cerebrovascular events were closely similar in the RA and OA arthroplasty patients. The RA patients undergoing total hip replacement had significantly higher rates of pulmonary compromise, infections, blood product transfusions, mechanical ventilation, and length of stay than did OA patients (Clin. Exp. Rheumatol. 2013;31:889-95). The RA patients with total knee replacement differed from their OA counterparts only in terms of greater need for transfusions and lengthier hospital stays (J. Arthroplasty 2014;29:308-13).
However, an analysis of the Hospital for Special Surgery experience failed to confirm the increased complication risks found in this study of a large administrative database. This retrospective review of adverse events within 6 months of total knee replacement in 156 RA patients and 318 OA controls showed no differences between the two groups in pneumonia, other infections, or venous thromboembolism. Moreover, the reoperation rate was 2.5% in the RA patients, compared with 8.8% in the OA group.
"The advantage of a smaller study like this is you really know who has RA and you have a lot of very granular information about the drugs they’re taking. The disadvantage, of course, is that you’re really not powered to look at major adverse events. But boy, there wasn’t even a hint of an increase in the complication rate amongst these RA patients," according to Dr. Goodman.
In a study she presented at the 2013 European Congress of Rheumatology, she compared 2-year outcomes post arthroplasty in RA and OA patients in the contemporary era of high use of biologic agents and traditional DMARDs for RA. The 178 RA patients who had total knee replacement had significantly greater comorbidities preoperatively than the 5,206 OA patients. Yet by 2 years postoperatively, they had fully caught up in terms of improved Western Ontario and McMaster Osteoarthritis Index (WOMAC) function and pain scores.
Total hip replacement was a very different story. The 202 RA patients were four times more likely to have poor WOMAC functional outcome and three times more likely to have poor pain outcome scores at 2 years, compared with 5,810 OA patients. In a multivariate analysis, higher expectations for surgery, better preoperative mental health, and more advanced education were associated with better 2-year outcomes.
"I’m not sure why our hip replacement patients with RA aren’t doing as well as the knee replacement patients, but they’re clearly not," according to the rheumatologist.
She reported having no financial disclosures.
SNOWMASS, COLO. – During a recent 15-year period in which the annual arthroplasty rate for osteoarthritis and other noninflammatory arthritides doubled, the arthroplasty rate for rheumatoid arthritis actually declined. Moreover, the mean age at the time of arthroplasty for RA rose.
"In a time frame when utilization of total knee and total hip replacement for osteoarthritis is really skyrocketing, with younger and younger patients, I think this speaks to something pretty good going on with our RA patients," Dr. Susan M. Goodman observed at the Winter Rheumatology Symposium sponsored by the American College of Rheumatology.
She presented data from a soon to be published study of nearly 2.8 million arthroplasties included in 10 state databases. The arthroplasty rate for noninflammatory arthritis – the great majority of which is osteoarthritis (OA) – zoomed from 124.5/100,000 population in 1991 to 247.5/100,000 in 2005.
Meanwhile the rate of arthroplasty for RA fell slightly, albeit statistically significantly, from 4.6 to 4.5 per 100,000. The mean age at the time of arthroplasty for RA rose from 63.4 years in 1991 to 64.9 years in 2005, reported Dr. Goodman, a rheumatologist at the Hospital for Special Surgery in New York.
She turned to data from other sources to address issues related to the morbidity of arthroplasty for RA.
For example, it’s well documented that rheumatoid arthritis is associated with elevated cardiovascular risk, such that the typical RA patient has a cardiovascular morbidity burden comparable to that of someone without RA who’s 5 years older. So what does this mean for the many RA patients who come into the hospital for total hip or knee replacement?
Surprisingly, nothing. That is, data from multiple sources indicate RA patients are at no greater perioperative risk of cardiovascular events than are patients with OA undergoing the same procedures.
The take-away message? "Clearly we’re doing something right in managing our patients with RA," Dr. Goodman commented.
Similarly, an analysis of 7.75 million patients in the Nationwide Inpatient Sample database found that among RA patients undergoing intermediate-risk noncardiac surgery, such as total joint arthroplasty, the perioperative cardiovascular event rate was 0.34%, significantly less than the 1.07% rate in diabetic patients undergoing intermediate-risk surgeries. Moreover, perioperative mortality was 0.30% in the RA patients, less than half the 0.65% figure in diabetics (Arthritis Rheum. 2012;64:2429-37). These findings disproved the study hypothesis, which was that the two groups would have similar cardiovascular event rates, since both diseases are – unlike osteoarthritis – systemic inflammatory conditions associated with increased cardiovascular mortality.
"I think this means that we as rheumatologists are taking better care of our patients than the endocrinologists next door whose patients have a similar atherosclerotic burden," she continued.
Dr. Goodman was a coinvestigator in a population-based study of 351,103 total knee replacements and 157,775 total hip replacements done at 400 hospitals during 2006-2010. This retrospective analysis of an administrative database included 11,755 total knee and 5,400 total hip replacements for RA.
The prevalence of a prior history of MI, peripheral vascular disease, or cerebrovascular disease was closely similar in the RA and OA patients undergoing surgery. However, the prevalence of baseline COPD was significantly greater in the RA patients, at roughly 17.5%, or an absolute 3%-4% more than in the osteoarthritis patients.
The 30-day rates of cardiac events, venous thromboembolism, and cerebrovascular events were closely similar in the RA and OA arthroplasty patients. The RA patients undergoing total hip replacement had significantly higher rates of pulmonary compromise, infections, blood product transfusions, mechanical ventilation, and length of stay than did OA patients (Clin. Exp. Rheumatol. 2013;31:889-95). The RA patients with total knee replacement differed from their OA counterparts only in terms of greater need for transfusions and lengthier hospital stays (J. Arthroplasty 2014;29:308-13).
However, an analysis of the Hospital for Special Surgery experience failed to confirm the increased complication risks found in this study of a large administrative database. This retrospective review of adverse events within 6 months of total knee replacement in 156 RA patients and 318 OA controls showed no differences between the two groups in pneumonia, other infections, or venous thromboembolism. Moreover, the reoperation rate was 2.5% in the RA patients, compared with 8.8% in the OA group.
"The advantage of a smaller study like this is you really know who has RA and you have a lot of very granular information about the drugs they’re taking. The disadvantage, of course, is that you’re really not powered to look at major adverse events. But boy, there wasn’t even a hint of an increase in the complication rate amongst these RA patients," according to Dr. Goodman.
In a study she presented at the 2013 European Congress of Rheumatology, she compared 2-year outcomes post arthroplasty in RA and OA patients in the contemporary era of high use of biologic agents and traditional DMARDs for RA. The 178 RA patients who had total knee replacement had significantly greater comorbidities preoperatively than the 5,206 OA patients. Yet by 2 years postoperatively, they had fully caught up in terms of improved Western Ontario and McMaster Osteoarthritis Index (WOMAC) function and pain scores.
Total hip replacement was a very different story. The 202 RA patients were four times more likely to have poor WOMAC functional outcome and three times more likely to have poor pain outcome scores at 2 years, compared with 5,810 OA patients. In a multivariate analysis, higher expectations for surgery, better preoperative mental health, and more advanced education were associated with better 2-year outcomes.
"I’m not sure why our hip replacement patients with RA aren’t doing as well as the knee replacement patients, but they’re clearly not," according to the rheumatologist.
She reported having no financial disclosures.
EXPERT ANALYSIS FROM THE WINTER RHEUMATOLOGY SYMPOSIUM