User login
Antiretroviral pill better at suppressing HIV in children
Dolutegravir suppresses HIV by inhibiting integrase, an enzyme that the virus needs to replicate.
The pill-based regimen, which researchers described as easier to take than standard treatment, reduced the chances of treatment failure among children aged 3-18 years by about 40%, compared with other treatments. Dolutegravir is already used for the suppression of HIV in adults.
“About 1.8 million children live with HIV but they have had limited treatment options, with medicines that taste unpalatable, that need to be taken twice a day, or that come in large pills that are difficult to swallow” said lead author Anna Turkova, MD, from the MRC clinical trials unit at UCL. “Dolutegravir is given in small tablets usually once a day and the baby pills can be dispersed in water, meaning it’s a lot easier for young children to take. This is important in encouraging uptake of the treatment and adherence to it over many years.
“Sadly, only about half of children living with HIV are currently receiving treatment, and those who are not treated face high risks of impaired immunity and worsening health.”
Study details
The randomized controlled trial, called ODYSSEY, involved more than 700 children from 29 clinical centers located in Africa, Europe, and Asia. The children were given either dolutegravir or standard anti-HIV drugs, and were followed up for at least 2 years.
The study showed that 14% of children receiving dolutegravir experienced treatment failure over 2 years, compared with 22% of those receiving standard treatment. Treatment failure was deemed to occur if measurable virus appeared in the blood or if the child had symptoms of HIV-related illness.
“Our findings provide strong evidence for the global rollout of dolutegravir for children with HIV,” said Diana Gibb, MD, also from the MRC clinical trials unit at UCL, principal investigator of the trial and one of the senior authors of the paper.
“Medical treatments for children often lag woefully behind those of adults because of the separate formulations and studies that are needed,” she added. “With the evidence from ODYSSEY which used simplified dosing of both adult and baby pills, this treatment gap has been reduced and we hope that countries can quickly scale up access to children globally.”
Simplified dosing
“Simplifying the dosing is crucial,” concurred Cissy Kityo Mutuluuza, MD, from the Joint Clinical Research Centre in Uganda, the country enrolling most children in the trial. “Older children being able to take the same tablets as adults immediately opens access to dolutegravir for the majority of children living with HIV. It greatly simplifies procurement for national health systems in low- and middle-income countries, and lowers costs.”
Evidence from adults shows dolutegravir has a high genetic barrier to resistance, meaning viruses are less likely to become resistant to it over time. This was confirmed in the ODYSSEY trial, with much less resistance occurring among children and adolescents on dolutegravir-based treatment. In addition, past studies of the drug have shown that it may be associated with weight gain in adults, but the findings were reassuring for children. Those given dolutegravir gained on average 1 kg more and grew 1 cm higher over the study period, indicating better growth rather than abnormal weight gain.
Early findings from the trial have informed new guidance by the World Health Organization, recommending the use of dolutegravir for children.
The study was sponsored by the Penta Foundation, an international independent research network, and funded by specialist pharmaceutical company ViiV Healthcare.
A version of this article first appeared on Medscape.com.
Dolutegravir suppresses HIV by inhibiting integrase, an enzyme that the virus needs to replicate.
The pill-based regimen, which researchers described as easier to take than standard treatment, reduced the chances of treatment failure among children aged 3-18 years by about 40%, compared with other treatments. Dolutegravir is already used for the suppression of HIV in adults.
“About 1.8 million children live with HIV but they have had limited treatment options, with medicines that taste unpalatable, that need to be taken twice a day, or that come in large pills that are difficult to swallow” said lead author Anna Turkova, MD, from the MRC clinical trials unit at UCL. “Dolutegravir is given in small tablets usually once a day and the baby pills can be dispersed in water, meaning it’s a lot easier for young children to take. This is important in encouraging uptake of the treatment and adherence to it over many years.
“Sadly, only about half of children living with HIV are currently receiving treatment, and those who are not treated face high risks of impaired immunity and worsening health.”
Study details
The randomized controlled trial, called ODYSSEY, involved more than 700 children from 29 clinical centers located in Africa, Europe, and Asia. The children were given either dolutegravir or standard anti-HIV drugs, and were followed up for at least 2 years.
The study showed that 14% of children receiving dolutegravir experienced treatment failure over 2 years, compared with 22% of those receiving standard treatment. Treatment failure was deemed to occur if measurable virus appeared in the blood or if the child had symptoms of HIV-related illness.
“Our findings provide strong evidence for the global rollout of dolutegravir for children with HIV,” said Diana Gibb, MD, also from the MRC clinical trials unit at UCL, principal investigator of the trial and one of the senior authors of the paper.
“Medical treatments for children often lag woefully behind those of adults because of the separate formulations and studies that are needed,” she added. “With the evidence from ODYSSEY which used simplified dosing of both adult and baby pills, this treatment gap has been reduced and we hope that countries can quickly scale up access to children globally.”
Simplified dosing
“Simplifying the dosing is crucial,” concurred Cissy Kityo Mutuluuza, MD, from the Joint Clinical Research Centre in Uganda, the country enrolling most children in the trial. “Older children being able to take the same tablets as adults immediately opens access to dolutegravir for the majority of children living with HIV. It greatly simplifies procurement for national health systems in low- and middle-income countries, and lowers costs.”
Evidence from adults shows dolutegravir has a high genetic barrier to resistance, meaning viruses are less likely to become resistant to it over time. This was confirmed in the ODYSSEY trial, with much less resistance occurring among children and adolescents on dolutegravir-based treatment. In addition, past studies of the drug have shown that it may be associated with weight gain in adults, but the findings were reassuring for children. Those given dolutegravir gained on average 1 kg more and grew 1 cm higher over the study period, indicating better growth rather than abnormal weight gain.
Early findings from the trial have informed new guidance by the World Health Organization, recommending the use of dolutegravir for children.
The study was sponsored by the Penta Foundation, an international independent research network, and funded by specialist pharmaceutical company ViiV Healthcare.
A version of this article first appeared on Medscape.com.
Dolutegravir suppresses HIV by inhibiting integrase, an enzyme that the virus needs to replicate.
The pill-based regimen, which researchers described as easier to take than standard treatment, reduced the chances of treatment failure among children aged 3-18 years by about 40%, compared with other treatments. Dolutegravir is already used for the suppression of HIV in adults.
“About 1.8 million children live with HIV but they have had limited treatment options, with medicines that taste unpalatable, that need to be taken twice a day, or that come in large pills that are difficult to swallow” said lead author Anna Turkova, MD, from the MRC clinical trials unit at UCL. “Dolutegravir is given in small tablets usually once a day and the baby pills can be dispersed in water, meaning it’s a lot easier for young children to take. This is important in encouraging uptake of the treatment and adherence to it over many years.
“Sadly, only about half of children living with HIV are currently receiving treatment, and those who are not treated face high risks of impaired immunity and worsening health.”
Study details
The randomized controlled trial, called ODYSSEY, involved more than 700 children from 29 clinical centers located in Africa, Europe, and Asia. The children were given either dolutegravir or standard anti-HIV drugs, and were followed up for at least 2 years.
The study showed that 14% of children receiving dolutegravir experienced treatment failure over 2 years, compared with 22% of those receiving standard treatment. Treatment failure was deemed to occur if measurable virus appeared in the blood or if the child had symptoms of HIV-related illness.
“Our findings provide strong evidence for the global rollout of dolutegravir for children with HIV,” said Diana Gibb, MD, also from the MRC clinical trials unit at UCL, principal investigator of the trial and one of the senior authors of the paper.
“Medical treatments for children often lag woefully behind those of adults because of the separate formulations and studies that are needed,” she added. “With the evidence from ODYSSEY which used simplified dosing of both adult and baby pills, this treatment gap has been reduced and we hope that countries can quickly scale up access to children globally.”
Simplified dosing
“Simplifying the dosing is crucial,” concurred Cissy Kityo Mutuluuza, MD, from the Joint Clinical Research Centre in Uganda, the country enrolling most children in the trial. “Older children being able to take the same tablets as adults immediately opens access to dolutegravir for the majority of children living with HIV. It greatly simplifies procurement for national health systems in low- and middle-income countries, and lowers costs.”
Evidence from adults shows dolutegravir has a high genetic barrier to resistance, meaning viruses are less likely to become resistant to it over time. This was confirmed in the ODYSSEY trial, with much less resistance occurring among children and adolescents on dolutegravir-based treatment. In addition, past studies of the drug have shown that it may be associated with weight gain in adults, but the findings were reassuring for children. Those given dolutegravir gained on average 1 kg more and grew 1 cm higher over the study period, indicating better growth rather than abnormal weight gain.
Early findings from the trial have informed new guidance by the World Health Organization, recommending the use of dolutegravir for children.
The study was sponsored by the Penta Foundation, an international independent research network, and funded by specialist pharmaceutical company ViiV Healthcare.
A version of this article first appeared on Medscape.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Pandemic screen time linked to anxiety, depression in older kids
However, the study doesn’t definitively prove that screen time is harmful, and an expert challenged the conclusions.
Still, the findings highlight the potential harms of excessive screen time, especially in the context of pandemic-era virtual learning. Clinicians “really need to advocate for policies that would be protective for children to reduce their screen time and social isolation and increase their involvement with school, sports, and academic activities,” Catherine S. Birken, MD, a pediatrician at the University of Toronto and study coauthor said in an interview.
The study appeared Dec. 28, 2021, in the journal JAMA Network Open (doi: 10.1001/jamanetworkopen.2021.40875).
Dr. Birken and colleagues launched the study to examine whether heightened levels of screen time during the pandemic disrupted mental health in kids. In particular, they wanted to break down different types of screen time, such as virtual learning, watching television, and playing video games.
“The bulk of the literature is supportive of a strong relationship between screen time and mental health symptoms like anxiety,” Dr. Birken said.
For the study, the researchers surveyed parents to track the screen time of 2,026 children between May 2020 and April 2021.
In a cohort of 532 younger children (average age, 5.9 years; 52% male; 58% of European ancestry), the researchers linked each extra daily hour of TV or use of digital media to worse behavior, as measured by the Strengths and Difficulties Questionnaire: 0.22 in an adjusted model for children aged 2-4;(95% confidence interval, 0.10-0.35; P < .001) and 0.07 in an adjusted model in those aged 4 and older (95% CI, 0.02-0.11; P = .007).
However, the researchers observed no statistically significant links to more anxiety/depression or hyperactivity/inattention in this group of children.
Among 1,494 older kids (mean age, 11.3; 57% male; 58% of European ancestry), researchers linked greater daily use of TV or digital media to higher levels of depression symptoms in a dose-dependent relationship, Dr. Birken said (1 hour: beta, 0.21; 95% CI, –1.28 to 0.78; 2-3 hours: beta, 1.81; 95% CI, 0.29-3.33; 4-5 hours: beta, 2.80; 95% CI, 1.15-4.44; 6-8 hours: beta, 5.16; 95% CI, 3.32-7.01; 9 hours: beta, 5.42; 95% CI, 3.30-7.54; overall P < .001).
“Similarly, higher TV or digital media time per day was associated with higher levels of anxiety symptoms,” the researchers reported. “TV or digital media time per day was also significantly associated with differences in symptoms of irritability, inattention, and hyperactivity/inattention.”
More time spent learning virtually was associated with higher levels of depression and anxiety in both groups of children, according to the researchers. Whether this finding reflects an effect of screens themselves or because the children most exposed to virtual learning may also have been the most exposed to the stressful disruptiveness of the pandemic is unclear.
The researchers also found “insufficient evidence” to link more virtual learning to irritability, inattention and hyperactivity, inattention, and hyperactivity/impulsivity in adjusted models.
Video chatting did not appear to have a protective effect, Dr. Birken said. The researchers also specifically analyzed children with autism and found no link between more screen time and various mental health/conduct problems.
Is it possible that kids with more anxiety, depression, and isolation simply turn to screens because they’re anxious, depressed, and isolated? Dr. Birken said the researchers adjusted the findings to account for previous mental health problems. And she noted that the study linked more pandemic-era virtual learning to more depression/anxiety. It’s “hard to imagine” how more mental health problems would cause more virtual learning.
Bad news or bad stats?
Chris Ferguson, PhD, a professor of psychology at Stetson University. DeLand, Fla., who studies screen time, criticized the study in an interview. “The observed effects are so tiny, it’s impossible to know if they are real or a false-positive artifact common to social science research,” he said. “Ultimately, this study is better evidence about how many scholars are bad at statistics than anything having to do with kids and screens.”
Dr. Ferguson said that the results may be confounded because kids turn to screens to reduce their anxiety. “For the most part, screens were a godsend during COVID-19,” he said. “They helped kids stay inside and gave them something to do while social distancing and allowed them to keep in touch with friends and families. Honestly, what else were we expecting kids to do, stare at the wallpaper?”
Children with depression and anxiety often retreat into screens or books to escape the unpleasantries of real life. “That doesn’t mean the screens or books are the culprits,” he said.
Instead of focusing on screen time, Dr. Ferguson suggested parents consider these factors: “Keeping in mind not every kid is a genius, is your kid doing about as well in school as you’d expect, given their natural ability? Are they getting at least some exercise every day? Are they getting adequate sleep? Are they able to socialize with friends in some context, either in real life or online? Are they happy?”
The study was funded by the Canadian Institutes of Health Research, the Center for Brain & Mental Health at The Hospital for Sick Children, the Ontario Ministry of Health, and the Miner’s Lamp Innovation Fund in Prevention and Early Detection of Severe Mental Illness at the University of Toronto. The study authors reported various financial relationships. Dr. Ferguson reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
However, the study doesn’t definitively prove that screen time is harmful, and an expert challenged the conclusions.
Still, the findings highlight the potential harms of excessive screen time, especially in the context of pandemic-era virtual learning. Clinicians “really need to advocate for policies that would be protective for children to reduce their screen time and social isolation and increase their involvement with school, sports, and academic activities,” Catherine S. Birken, MD, a pediatrician at the University of Toronto and study coauthor said in an interview.
The study appeared Dec. 28, 2021, in the journal JAMA Network Open (doi: 10.1001/jamanetworkopen.2021.40875).
Dr. Birken and colleagues launched the study to examine whether heightened levels of screen time during the pandemic disrupted mental health in kids. In particular, they wanted to break down different types of screen time, such as virtual learning, watching television, and playing video games.
“The bulk of the literature is supportive of a strong relationship between screen time and mental health symptoms like anxiety,” Dr. Birken said.
For the study, the researchers surveyed parents to track the screen time of 2,026 children between May 2020 and April 2021.
In a cohort of 532 younger children (average age, 5.9 years; 52% male; 58% of European ancestry), the researchers linked each extra daily hour of TV or use of digital media to worse behavior, as measured by the Strengths and Difficulties Questionnaire: 0.22 in an adjusted model for children aged 2-4;(95% confidence interval, 0.10-0.35; P < .001) and 0.07 in an adjusted model in those aged 4 and older (95% CI, 0.02-0.11; P = .007).
However, the researchers observed no statistically significant links to more anxiety/depression or hyperactivity/inattention in this group of children.
Among 1,494 older kids (mean age, 11.3; 57% male; 58% of European ancestry), researchers linked greater daily use of TV or digital media to higher levels of depression symptoms in a dose-dependent relationship, Dr. Birken said (1 hour: beta, 0.21; 95% CI, –1.28 to 0.78; 2-3 hours: beta, 1.81; 95% CI, 0.29-3.33; 4-5 hours: beta, 2.80; 95% CI, 1.15-4.44; 6-8 hours: beta, 5.16; 95% CI, 3.32-7.01; 9 hours: beta, 5.42; 95% CI, 3.30-7.54; overall P < .001).
“Similarly, higher TV or digital media time per day was associated with higher levels of anxiety symptoms,” the researchers reported. “TV or digital media time per day was also significantly associated with differences in symptoms of irritability, inattention, and hyperactivity/inattention.”
More time spent learning virtually was associated with higher levels of depression and anxiety in both groups of children, according to the researchers. Whether this finding reflects an effect of screens themselves or because the children most exposed to virtual learning may also have been the most exposed to the stressful disruptiveness of the pandemic is unclear.
The researchers also found “insufficient evidence” to link more virtual learning to irritability, inattention and hyperactivity, inattention, and hyperactivity/impulsivity in adjusted models.
Video chatting did not appear to have a protective effect, Dr. Birken said. The researchers also specifically analyzed children with autism and found no link between more screen time and various mental health/conduct problems.
Is it possible that kids with more anxiety, depression, and isolation simply turn to screens because they’re anxious, depressed, and isolated? Dr. Birken said the researchers adjusted the findings to account for previous mental health problems. And she noted that the study linked more pandemic-era virtual learning to more depression/anxiety. It’s “hard to imagine” how more mental health problems would cause more virtual learning.
Bad news or bad stats?
Chris Ferguson, PhD, a professor of psychology at Stetson University. DeLand, Fla., who studies screen time, criticized the study in an interview. “The observed effects are so tiny, it’s impossible to know if they are real or a false-positive artifact common to social science research,” he said. “Ultimately, this study is better evidence about how many scholars are bad at statistics than anything having to do with kids and screens.”
Dr. Ferguson said that the results may be confounded because kids turn to screens to reduce their anxiety. “For the most part, screens were a godsend during COVID-19,” he said. “They helped kids stay inside and gave them something to do while social distancing and allowed them to keep in touch with friends and families. Honestly, what else were we expecting kids to do, stare at the wallpaper?”
Children with depression and anxiety often retreat into screens or books to escape the unpleasantries of real life. “That doesn’t mean the screens or books are the culprits,” he said.
Instead of focusing on screen time, Dr. Ferguson suggested parents consider these factors: “Keeping in mind not every kid is a genius, is your kid doing about as well in school as you’d expect, given their natural ability? Are they getting at least some exercise every day? Are they getting adequate sleep? Are they able to socialize with friends in some context, either in real life or online? Are they happy?”
The study was funded by the Canadian Institutes of Health Research, the Center for Brain & Mental Health at The Hospital for Sick Children, the Ontario Ministry of Health, and the Miner’s Lamp Innovation Fund in Prevention and Early Detection of Severe Mental Illness at the University of Toronto. The study authors reported various financial relationships. Dr. Ferguson reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
However, the study doesn’t definitively prove that screen time is harmful, and an expert challenged the conclusions.
Still, the findings highlight the potential harms of excessive screen time, especially in the context of pandemic-era virtual learning. Clinicians “really need to advocate for policies that would be protective for children to reduce their screen time and social isolation and increase their involvement with school, sports, and academic activities,” Catherine S. Birken, MD, a pediatrician at the University of Toronto and study coauthor said in an interview.
The study appeared Dec. 28, 2021, in the journal JAMA Network Open (doi: 10.1001/jamanetworkopen.2021.40875).
Dr. Birken and colleagues launched the study to examine whether heightened levels of screen time during the pandemic disrupted mental health in kids. In particular, they wanted to break down different types of screen time, such as virtual learning, watching television, and playing video games.
“The bulk of the literature is supportive of a strong relationship between screen time and mental health symptoms like anxiety,” Dr. Birken said.
For the study, the researchers surveyed parents to track the screen time of 2,026 children between May 2020 and April 2021.
In a cohort of 532 younger children (average age, 5.9 years; 52% male; 58% of European ancestry), the researchers linked each extra daily hour of TV or use of digital media to worse behavior, as measured by the Strengths and Difficulties Questionnaire: 0.22 in an adjusted model for children aged 2-4;(95% confidence interval, 0.10-0.35; P < .001) and 0.07 in an adjusted model in those aged 4 and older (95% CI, 0.02-0.11; P = .007).
However, the researchers observed no statistically significant links to more anxiety/depression or hyperactivity/inattention in this group of children.
Among 1,494 older kids (mean age, 11.3; 57% male; 58% of European ancestry), researchers linked greater daily use of TV or digital media to higher levels of depression symptoms in a dose-dependent relationship, Dr. Birken said (1 hour: beta, 0.21; 95% CI, –1.28 to 0.78; 2-3 hours: beta, 1.81; 95% CI, 0.29-3.33; 4-5 hours: beta, 2.80; 95% CI, 1.15-4.44; 6-8 hours: beta, 5.16; 95% CI, 3.32-7.01; 9 hours: beta, 5.42; 95% CI, 3.30-7.54; overall P < .001).
“Similarly, higher TV or digital media time per day was associated with higher levels of anxiety symptoms,” the researchers reported. “TV or digital media time per day was also significantly associated with differences in symptoms of irritability, inattention, and hyperactivity/inattention.”
More time spent learning virtually was associated with higher levels of depression and anxiety in both groups of children, according to the researchers. Whether this finding reflects an effect of screens themselves or because the children most exposed to virtual learning may also have been the most exposed to the stressful disruptiveness of the pandemic is unclear.
The researchers also found “insufficient evidence” to link more virtual learning to irritability, inattention and hyperactivity, inattention, and hyperactivity/impulsivity in adjusted models.
Video chatting did not appear to have a protective effect, Dr. Birken said. The researchers also specifically analyzed children with autism and found no link between more screen time and various mental health/conduct problems.
Is it possible that kids with more anxiety, depression, and isolation simply turn to screens because they’re anxious, depressed, and isolated? Dr. Birken said the researchers adjusted the findings to account for previous mental health problems. And she noted that the study linked more pandemic-era virtual learning to more depression/anxiety. It’s “hard to imagine” how more mental health problems would cause more virtual learning.
Bad news or bad stats?
Chris Ferguson, PhD, a professor of psychology at Stetson University. DeLand, Fla., who studies screen time, criticized the study in an interview. “The observed effects are so tiny, it’s impossible to know if they are real or a false-positive artifact common to social science research,” he said. “Ultimately, this study is better evidence about how many scholars are bad at statistics than anything having to do with kids and screens.”
Dr. Ferguson said that the results may be confounded because kids turn to screens to reduce their anxiety. “For the most part, screens were a godsend during COVID-19,” he said. “They helped kids stay inside and gave them something to do while social distancing and allowed them to keep in touch with friends and families. Honestly, what else were we expecting kids to do, stare at the wallpaper?”
Children with depression and anxiety often retreat into screens or books to escape the unpleasantries of real life. “That doesn’t mean the screens or books are the culprits,” he said.
Instead of focusing on screen time, Dr. Ferguson suggested parents consider these factors: “Keeping in mind not every kid is a genius, is your kid doing about as well in school as you’d expect, given their natural ability? Are they getting at least some exercise every day? Are they getting adequate sleep? Are they able to socialize with friends in some context, either in real life or online? Are they happy?”
The study was funded by the Canadian Institutes of Health Research, the Center for Brain & Mental Health at The Hospital for Sick Children, the Ontario Ministry of Health, and the Miner’s Lamp Innovation Fund in Prevention and Early Detection of Severe Mental Illness at the University of Toronto. The study authors reported various financial relationships. Dr. Ferguson reported no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
FDA to review PDE4-inhibitor roflumilast for psoriasis
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
The , according to a statement from the manufacturer.
Roflumilast cream (also known as ARQ-151) is a small molecule inhibitor of PDE4, an enzyme that increases proinflammatory mediators and decreases anti-inflammatory mediators. PDE4 is an established treatment target in dermatology: The FDA approved PDE-4 inhibitor crisaborole (Eucrisa) as a topical treatment for mild to moderate atopic dermatitis in 2016, and an oral PDE-4 inhibitor, orismilast, is being studied for the treatment of plaque psoriasis.
Topical roflumilast, if approved, would be the first topical PDE4 inhibitor for psoriasis in particular, according to the Arcutis Biotherapeutics statement. The cream is designed for use on the entire body, including the face and sensitive intertriginous areas.
The NDA is based on data from a pair of phase 3 randomized, double-blind 8-week studies known as DERMIS 1 and DERMIS 2 (Trials of PDE4 Inhibition with Roflumilast for the Management of Plaque Psoriasis” One and Two) and a long-term phase 2b open-label study.
DERMIS 1 and DERMIS 2 were identical multinational, multicenter studies designed to assess the safety and efficacy of 0.3% roflumilast cream. In the studies, roflumilast met its primary endpoint and patients treated with it demonstrated an Investigator Global Assessment (IGA) success rate of 42.4% compared with 6.1% for the vehicle control (P < .0001), and 37.5% compared with 6.9% for the vehicle control (P < .0001), in the DERMIS 1 and 2 trials, respectively, according to Arcutis.
In the phase 2b study, the treatment effect lasted for 52-64 weeks. Roflumilast was well tolerated across the three studies.
Overall, the most common adverse events reported in the studies were diarrhea (3%), headache (2%), insomnia (1%), nausea (1%), upper respiratory tract infections (1%), and urinary tract infections (1%).
Roflumilast also showed statistically significant improvement compared to a vehicle on secondary endpoints including Intertriginous IGA (I-IGA) Success, Psoriasis Area Severity Index-75 (PASI-75), reductions in itch as measured by the Worst Itch-Numerical Rating Scale (WI-NRS), and patient perceptions of symptoms based on the Psoriasis Symptoms Diary (PSD).
The FDA has set a Prescription Drug User Fee Act (PDUFA) target action date of July 29, 2022, according to the manufacturer’s statement. An oral formulation of roflumilast was approved by the FDA in 2011, for reducing the risk of exacerbations of chronic obstructive pulmonary disease (COPD) in patients with severe COPD.
Children and COVID: Nearly 200,000 new cases reported in 1 week
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
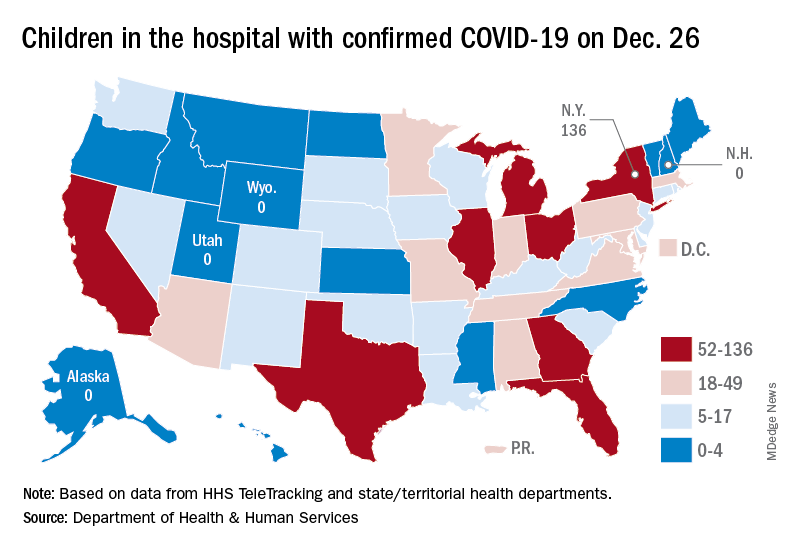
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
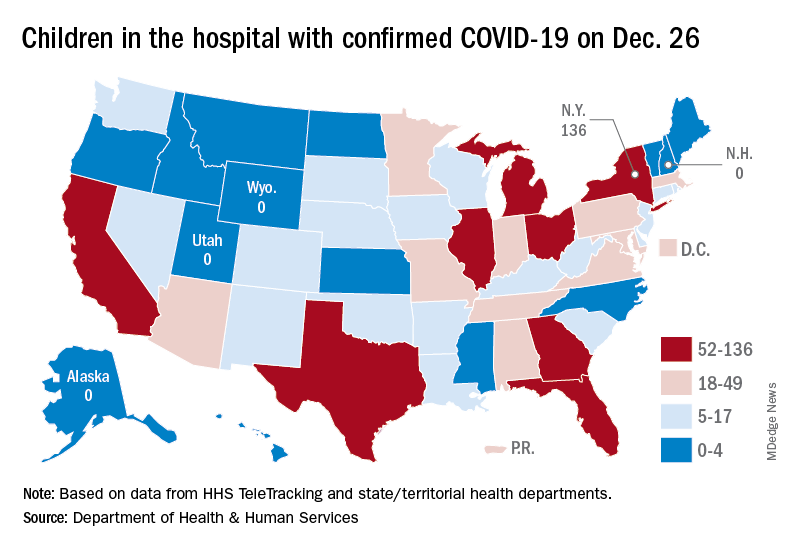
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
, according to the American Academy of Pediatrics and the Children’s Hospital Association.
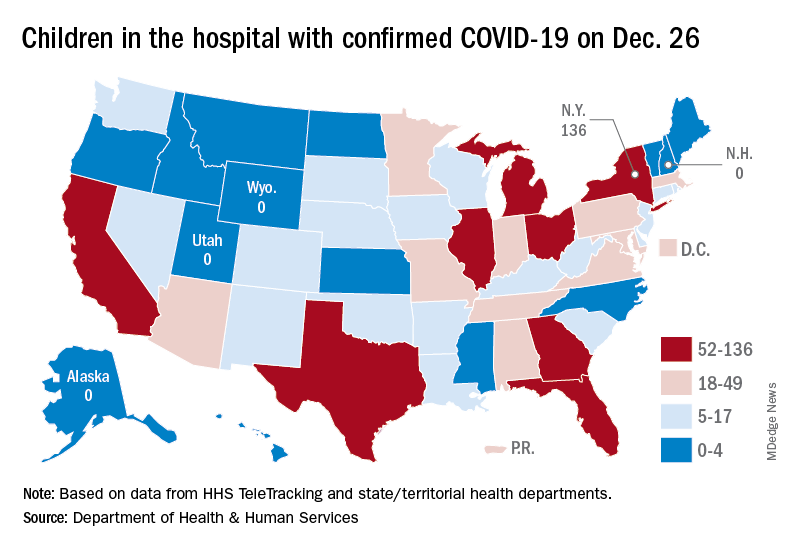
Available state data show that 198,551 child COVID cases were added during the week of Dec. 17-23 – up by 16.8% from the nearly 170,000 new cases reported the previous week and the highest 7-day figure since Sept. 17-23, when 207,000 cases were reported, the AAP and the CHA said in their weekly COVID report. Since Oct. 22-28, when the weekly count dropped to a seasonal low, the weekly count has nearly doubled.
The largest shares of the nearly 199,000 new cases were divided pretty equally between the Northeast and the South, while the West had just a small bump in cases and the Midwest was in the middle. The largest statewide percent increases came in the New England states, along with New Jersey, the District of Columbia, and Puerto Rico. New York State does not report age ranges for COVID cases, the AAP/CHA report noted.
Emergency department visits and hospital admissions are following a similar trend, as both have risen considerably over the last 2 months, data from the Centers for Disease Control and Prevention show.
COVID-related ED visits for children aged 0-11 years – measured as a proportion of all ED visits – are nearing the pandemic high of 4.1% set in late August, while visits in 12- to 15-year-olds have risen from 1.4% in early November to 5.6% on Dec. 24 and 16- to 17-year-olds have gone from 1.5% to 6% over the same period of time, the CDC reported on its COVID Data Tracker.
As for hospital admissions in children aged 0-17 years, the rate was down to 0.19 per 100,000 population on Nov. 11 but had risen to 0.38 per 100,000 as of Dec. 24. The highest point reached in children during the pandemic was 0.46 per 100,000 in early September, the CDC said.
On Dec. 23, 367 children were admitted to hospitals in the United States, the highest number since Sept. 7, when 374 were hospitalized. The highest 1-day total over the course of the pandemic, 394, came just a week before that, Aug. 31, according to the Department of Health & Human Services.
A look at the most recent HHS data shows that 1,161 children were being hospitalized in pediatric inpatient beds with confirmed COVID-19 on Dec. 26. The highest number by state was in New York (136), followed by Texas (90) and Illinois and Ohio, both with 83. There were four states – Alaska, New Hampshire, Utah, and Wyoming – with no hospitalized children, the HHS said. Puerto Rico, meanwhile, had 28 children in the hospital with COVID, more than 38 states.
How do digital technologies affect young people’s mental health?
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
For almost all of us, “screen time”—time spent using a device with a screen such as a smartphone, computer, television, or video game console—has become a large part of our daily lives. This is very much the case for children and adolescents. In the United States, children ages 8 to 12 years spend an average of 4 to 6 hours each day watching or using screens, and teens spend up to 9 hours.1 Because young people are continually adopting newer forms of entertainment and technologies, new digital technologies are an ongoing source of concern for parents and clinicians alike.2 Studies have suggested that excessive screen time is associated with numerous psychiatric symptoms and disorders, including poor sleep, weight gain, anxiety, depression, and attention-deficit/hyperactive disorder.3,4 However, a recent systematic review and meta-analysis found that individuals’ self-reports of media use were rarely an accurate reflection of their actual, logged media use, and that measures of problematic media use had an even weaker association with usage logs.5 Therefore, it is crucial to have an accurate understanding of how children and adolescents are affected by new technologies. In this article, we discuss a recent study that investigated variations in adolescents’ mental health over time, and the association of their mental health and their use of digital technologies.
Results were mixed
Vuorre et al6 conducted a study to examine a possible shift in the associations between adolescents’ technology use and mental health outcomes. To investigate whether technology engagement and mental health outcomes changed over time, these researchers evaluated the impact not only of smartphones and social media, but also of television, which in the mid- to late-20th century elicited comparable levels of academic, public, and policy concern about its potential impact on child development. They analyzed data from 3 large-scale studies of adolescents living in the United States (Monitoring the Future and Youth Risk Behavior Surveillance System) and the United Kingdom (Understanding Society) that included a total of 430,561 participants.
The results were mixed across types of technology and mental health outcomes. Television and social media were found to have a direct correlation with conduct problems and emotional problems. Suicidal ideation and behavior were associated with digital device use; however, no correlation was found between depression and technology use. Regarding social media use, researchers found that its association with conduct problems remained stable, decreased with depression, and increased with emotional problems. The magnitudes of the observed changes over time were small. These researchers concluded there is “little evidence for increases in the associations between adolescents’ technology engagement and mental health [problems]” and “drawing firm conclusions about changes in ... associations with mental health may be premature.”6
Future directions
The study by Vuorre et al6 has opened the door to better analysis of the association between screen use and mental health outcomes. More robust, detailed studies are required to fully understand the varying impact of technologies on the lives of children and adolescents. Collaborative efforts by technology companies and researchers can help to determine the impact of technology on young people’s mental health.
1. American Academy of Child & Adolescent Psychiatry. Screen time and children. Updated February 2020. Accessed October 7, 2021. http://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Children-And-Watching-TV-054.aspx
2. Orben A. The Sisyphean cycle of technology panics. Perspect Psychol Sci. 2020;15(5):1143-1157.
3. Paulich KN, Ross JM, Lessem JM, et al. Screen time and early adolescent mental health, academic, and social outcomes in 9- and 10-year old children: utilizing the Adolescent Brain Cognitive Development (ABCD) Study. PLoS One. 2021;16(9):e0256591. doi: 10.1371/journal.pone.0256591
4. Twenge JM, Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents: evidence from a population-based study. Prev Med Rep. 2018;12:271-283. doi: 10.1016/j.pmedr.2018.10.003
5. Parry DA, Davidson BI, Sewall CJR, et al. A systematic review and meta-analysis of discrepancies between logged and self-reported digital media use. Nat Hum Behav. 2021;5(11):1535-1547.
6. Vuorre M, Orben A, Przybylski AK. There is no evidence that associations between adolescents’ digital technology engagement and mental health problems have increased. Clin Psychol Sci. 2021;9(5):823-835.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
For almost all of us, “screen time”—time spent using a device with a screen such as a smartphone, computer, television, or video game console—has become a large part of our daily lives. This is very much the case for children and adolescents. In the United States, children ages 8 to 12 years spend an average of 4 to 6 hours each day watching or using screens, and teens spend up to 9 hours.1 Because young people are continually adopting newer forms of entertainment and technologies, new digital technologies are an ongoing source of concern for parents and clinicians alike.2 Studies have suggested that excessive screen time is associated with numerous psychiatric symptoms and disorders, including poor sleep, weight gain, anxiety, depression, and attention-deficit/hyperactive disorder.3,4 However, a recent systematic review and meta-analysis found that individuals’ self-reports of media use were rarely an accurate reflection of their actual, logged media use, and that measures of problematic media use had an even weaker association with usage logs.5 Therefore, it is crucial to have an accurate understanding of how children and adolescents are affected by new technologies. In this article, we discuss a recent study that investigated variations in adolescents’ mental health over time, and the association of their mental health and their use of digital technologies.
Results were mixed
Vuorre et al6 conducted a study to examine a possible shift in the associations between adolescents’ technology use and mental health outcomes. To investigate whether technology engagement and mental health outcomes changed over time, these researchers evaluated the impact not only of smartphones and social media, but also of television, which in the mid- to late-20th century elicited comparable levels of academic, public, and policy concern about its potential impact on child development. They analyzed data from 3 large-scale studies of adolescents living in the United States (Monitoring the Future and Youth Risk Behavior Surveillance System) and the United Kingdom (Understanding Society) that included a total of 430,561 participants.
The results were mixed across types of technology and mental health outcomes. Television and social media were found to have a direct correlation with conduct problems and emotional problems. Suicidal ideation and behavior were associated with digital device use; however, no correlation was found between depression and technology use. Regarding social media use, researchers found that its association with conduct problems remained stable, decreased with depression, and increased with emotional problems. The magnitudes of the observed changes over time were small. These researchers concluded there is “little evidence for increases in the associations between adolescents’ technology engagement and mental health [problems]” and “drawing firm conclusions about changes in ... associations with mental health may be premature.”6
Future directions
The study by Vuorre et al6 has opened the door to better analysis of the association between screen use and mental health outcomes. More robust, detailed studies are required to fully understand the varying impact of technologies on the lives of children and adolescents. Collaborative efforts by technology companies and researchers can help to determine the impact of technology on young people’s mental health.
Editor’s note: Readers’ Forum is a department for correspondence from readers that is not in response to articles published in
For almost all of us, “screen time”—time spent using a device with a screen such as a smartphone, computer, television, or video game console—has become a large part of our daily lives. This is very much the case for children and adolescents. In the United States, children ages 8 to 12 years spend an average of 4 to 6 hours each day watching or using screens, and teens spend up to 9 hours.1 Because young people are continually adopting newer forms of entertainment and technologies, new digital technologies are an ongoing source of concern for parents and clinicians alike.2 Studies have suggested that excessive screen time is associated with numerous psychiatric symptoms and disorders, including poor sleep, weight gain, anxiety, depression, and attention-deficit/hyperactive disorder.3,4 However, a recent systematic review and meta-analysis found that individuals’ self-reports of media use were rarely an accurate reflection of their actual, logged media use, and that measures of problematic media use had an even weaker association with usage logs.5 Therefore, it is crucial to have an accurate understanding of how children and adolescents are affected by new technologies. In this article, we discuss a recent study that investigated variations in adolescents’ mental health over time, and the association of their mental health and their use of digital technologies.
Results were mixed
Vuorre et al6 conducted a study to examine a possible shift in the associations between adolescents’ technology use and mental health outcomes. To investigate whether technology engagement and mental health outcomes changed over time, these researchers evaluated the impact not only of smartphones and social media, but also of television, which in the mid- to late-20th century elicited comparable levels of academic, public, and policy concern about its potential impact on child development. They analyzed data from 3 large-scale studies of adolescents living in the United States (Monitoring the Future and Youth Risk Behavior Surveillance System) and the United Kingdom (Understanding Society) that included a total of 430,561 participants.
The results were mixed across types of technology and mental health outcomes. Television and social media were found to have a direct correlation with conduct problems and emotional problems. Suicidal ideation and behavior were associated with digital device use; however, no correlation was found between depression and technology use. Regarding social media use, researchers found that its association with conduct problems remained stable, decreased with depression, and increased with emotional problems. The magnitudes of the observed changes over time were small. These researchers concluded there is “little evidence for increases in the associations between adolescents’ technology engagement and mental health [problems]” and “drawing firm conclusions about changes in ... associations with mental health may be premature.”6
Future directions
The study by Vuorre et al6 has opened the door to better analysis of the association between screen use and mental health outcomes. More robust, detailed studies are required to fully understand the varying impact of technologies on the lives of children and adolescents. Collaborative efforts by technology companies and researchers can help to determine the impact of technology on young people’s mental health.
1. American Academy of Child & Adolescent Psychiatry. Screen time and children. Updated February 2020. Accessed October 7, 2021. http://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Children-And-Watching-TV-054.aspx
2. Orben A. The Sisyphean cycle of technology panics. Perspect Psychol Sci. 2020;15(5):1143-1157.
3. Paulich KN, Ross JM, Lessem JM, et al. Screen time and early adolescent mental health, academic, and social outcomes in 9- and 10-year old children: utilizing the Adolescent Brain Cognitive Development (ABCD) Study. PLoS One. 2021;16(9):e0256591. doi: 10.1371/journal.pone.0256591
4. Twenge JM, Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents: evidence from a population-based study. Prev Med Rep. 2018;12:271-283. doi: 10.1016/j.pmedr.2018.10.003
5. Parry DA, Davidson BI, Sewall CJR, et al. A systematic review and meta-analysis of discrepancies between logged and self-reported digital media use. Nat Hum Behav. 2021;5(11):1535-1547.
6. Vuorre M, Orben A, Przybylski AK. There is no evidence that associations between adolescents’ digital technology engagement and mental health problems have increased. Clin Psychol Sci. 2021;9(5):823-835.
1. American Academy of Child & Adolescent Psychiatry. Screen time and children. Updated February 2020. Accessed October 7, 2021. http://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/Children-And-Watching-TV-054.aspx
2. Orben A. The Sisyphean cycle of technology panics. Perspect Psychol Sci. 2020;15(5):1143-1157.
3. Paulich KN, Ross JM, Lessem JM, et al. Screen time and early adolescent mental health, academic, and social outcomes in 9- and 10-year old children: utilizing the Adolescent Brain Cognitive Development (ABCD) Study. PLoS One. 2021;16(9):e0256591. doi: 10.1371/journal.pone.0256591
4. Twenge JM, Campbell WK. Associations between screen time and lower psychological well-being among children and adolescents: evidence from a population-based study. Prev Med Rep. 2018;12:271-283. doi: 10.1016/j.pmedr.2018.10.003
5. Parry DA, Davidson BI, Sewall CJR, et al. A systematic review and meta-analysis of discrepancies between logged and self-reported digital media use. Nat Hum Behav. 2021;5(11):1535-1547.
6. Vuorre M, Orben A, Przybylski AK. There is no evidence that associations between adolescents’ digital technology engagement and mental health problems have increased. Clin Psychol Sci. 2021;9(5):823-835.
AD burden may be greater for those with head, neck, face, and hand involvement
of patients with AD.
“While we know that head, neck, face, and hands seem to be significantly affected by patients with AD, there is a limited evidence basis regarding the prevalence and health-related quality of life impact of AD in these areas,” presenting author Lawrence F. Eichenfield, MD, said during a late-breaking abstract session at the Revolutionizing Atopic Dermatitis symposium.
For the study, Dr. Eichenfield, professor of dermatology and pediatrics at the University of California, San Diego, and colleagues evaluated 533 patients from the TARGET-DERM AD cohort, an ongoing, longitudinal, observational study launched in 2019 that captures patients with AD in 44 community or academic sites in the United States.
Adult, adolescent, and pediatric patients with moderate or severe Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD) scores at enrollment were included in the analysis. The researchers used the Patient-Oriented Scoring AD (PO-SCORAD) index to gather information on involvement of the head, neck, face, hands, or other areas, and the Patient-Oriented Eczema Measure (POEM) and Dermatology Life Quality Index/Children’s DLQI (CDLQI) to measure health-related quality of life outcomes.
Of the 533 study participants, 453 (85%) had AD affecting the head, neck, face, hands, and other areas, while 80 (15%) had AD located in other body regions not including the head, neck, face, or hands. About 38% of all patients were using systemic treatments; most were using topical treatments.
Comorbid immune system disorders (including allergic and hypersensitivity disorders) were noted in 44.8% of patients, infections in 32.5%, asthma in 26.5%, hypertension in 18.6%, depression in 15.8%, and anxiety in 12.4%, with similar proportions observed in those with or without head, neck, face, and hand involvement.
However, patients with head, face, neck, and hand involvement, when compared with patients without those affected areas, were more likely to have severe vIGA scores (28.5% vs. 16.3%, P = .02) and a higher median total body surface area affected (15% vs. 10%, P ≤ .01). Also, while bivariable analyses did not detect statistical differences in POEM and DLQI/CDLQI by body region involvement, multivariable-adjusted models showed that patients with head, neck, face, and hand involvement were more than twice as likely to report higher DLQI/CDLQI (odds ratio, 2.09) and POEM (OR, 2.51) scores than those without head, face, neck, and hand involvement.
“These findings highlight the importance of detailed assessment of specific areas affected by AD to personalize treatment approaches to the needs of patients,” Dr. Eichenfield concluded.
Raj Chovatiya MD, PhD, assistant professor of dermatology at Northwestern University, Chicago, who was asked to comment on the study, said that the findings confirm clinical suspicions about the unique and heightened impact of facial, head/neck, and hand dermatitis. “These data show that a detailed skin examination is necessary for a complete assessment of AD,” he said. “Future studies should focus on characterizing the optimal treatment approaches for each of these special sites.”
“This is important data,” added primary study author Jonathan I. Silverberg, MD, PhD, MPH, director of clinical research in the division of dermatology at George Washington University, Washington. “We need more high-quality studies like this; we need to create long-term longitudinal data to better understand [the impact of AD on] this and other cohorts.”
TARGET-DERM is sponsored by Target RWE. Dr. Eichenfield disclosed that he has served as a consultant to or investigator for numerous pharmaceutical companies. Dr. Chovatiya disclosed that he is a consultant to, a speaker for, and/or a member of the advisory board for AbbVie, Arena, Arcutis, Incyte, Pfizer, Regeneron, and Sanofi-Genzyme. Dr. Silverberg disclosed that he is a consultant to numerous pharmaceutical companies, receives fees for non-CME/CE services from Eli Lilly, Leo Pharma, Pfizer, Regeneron, and Sanofi Genzyme, as well as contracted research fees from Galderma.
Commentary by Robert Sidbury, MD, MPH
Patients with atopic dermatitis (AD) in “visible” areas such as the head, neck, and hands experience a higher impact on their quality of life than those who do not have these areas of involvement. This is a self-evident and unsurprising result but also a particularly important one to document for several reasons. First, evidence-based demonstration of quality-of-life impact is critical as we petition carriers to support the use of newer, more expensive medications. Second, from a topical therapy standpoint, we often use different medications on the head, neck, face, and hands relative to other areas. On the head and neck area we often use either weaker topical steroids to avoid side effects or nonsteroids like topical calcineurin or phosphodiesterase inhibitors; conversely, on the hands we use stronger steroids and are less likely to use nonsteroidal agents that are perceived to be less potent. These data emphasize the need to tailor therapy but ascertain whether standard approaches are satisfactory. If patients are not responding, particularly in these sensitive areas, providers should consider the outsized impact AD may be having on quality of life.
Dr. Sidbury is chief of dermatology at Seattle Children's Hospital and professor, department of pediatrics, University of Washington, Seattle. He is a site principal investigator for dupilumab trials, for which the hospital has a contract with Regeneron.
A version of this article first appeared on Medscape.com.
This article was updated 6/10/22.
of patients with AD.
“While we know that head, neck, face, and hands seem to be significantly affected by patients with AD, there is a limited evidence basis regarding the prevalence and health-related quality of life impact of AD in these areas,” presenting author Lawrence F. Eichenfield, MD, said during a late-breaking abstract session at the Revolutionizing Atopic Dermatitis symposium.
For the study, Dr. Eichenfield, professor of dermatology and pediatrics at the University of California, San Diego, and colleagues evaluated 533 patients from the TARGET-DERM AD cohort, an ongoing, longitudinal, observational study launched in 2019 that captures patients with AD in 44 community or academic sites in the United States.
Adult, adolescent, and pediatric patients with moderate or severe Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD) scores at enrollment were included in the analysis. The researchers used the Patient-Oriented Scoring AD (PO-SCORAD) index to gather information on involvement of the head, neck, face, hands, or other areas, and the Patient-Oriented Eczema Measure (POEM) and Dermatology Life Quality Index/Children’s DLQI (CDLQI) to measure health-related quality of life outcomes.
Of the 533 study participants, 453 (85%) had AD affecting the head, neck, face, hands, and other areas, while 80 (15%) had AD located in other body regions not including the head, neck, face, or hands. About 38% of all patients were using systemic treatments; most were using topical treatments.
Comorbid immune system disorders (including allergic and hypersensitivity disorders) were noted in 44.8% of patients, infections in 32.5%, asthma in 26.5%, hypertension in 18.6%, depression in 15.8%, and anxiety in 12.4%, with similar proportions observed in those with or without head, neck, face, and hand involvement.
However, patients with head, face, neck, and hand involvement, when compared with patients without those affected areas, were more likely to have severe vIGA scores (28.5% vs. 16.3%, P = .02) and a higher median total body surface area affected (15% vs. 10%, P ≤ .01). Also, while bivariable analyses did not detect statistical differences in POEM and DLQI/CDLQI by body region involvement, multivariable-adjusted models showed that patients with head, neck, face, and hand involvement were more than twice as likely to report higher DLQI/CDLQI (odds ratio, 2.09) and POEM (OR, 2.51) scores than those without head, face, neck, and hand involvement.
“These findings highlight the importance of detailed assessment of specific areas affected by AD to personalize treatment approaches to the needs of patients,” Dr. Eichenfield concluded.
Raj Chovatiya MD, PhD, assistant professor of dermatology at Northwestern University, Chicago, who was asked to comment on the study, said that the findings confirm clinical suspicions about the unique and heightened impact of facial, head/neck, and hand dermatitis. “These data show that a detailed skin examination is necessary for a complete assessment of AD,” he said. “Future studies should focus on characterizing the optimal treatment approaches for each of these special sites.”
“This is important data,” added primary study author Jonathan I. Silverberg, MD, PhD, MPH, director of clinical research in the division of dermatology at George Washington University, Washington. “We need more high-quality studies like this; we need to create long-term longitudinal data to better understand [the impact of AD on] this and other cohorts.”
TARGET-DERM is sponsored by Target RWE. Dr. Eichenfield disclosed that he has served as a consultant to or investigator for numerous pharmaceutical companies. Dr. Chovatiya disclosed that he is a consultant to, a speaker for, and/or a member of the advisory board for AbbVie, Arena, Arcutis, Incyte, Pfizer, Regeneron, and Sanofi-Genzyme. Dr. Silverberg disclosed that he is a consultant to numerous pharmaceutical companies, receives fees for non-CME/CE services from Eli Lilly, Leo Pharma, Pfizer, Regeneron, and Sanofi Genzyme, as well as contracted research fees from Galderma.
Commentary by Robert Sidbury, MD, MPH
Patients with atopic dermatitis (AD) in “visible” areas such as the head, neck, and hands experience a higher impact on their quality of life than those who do not have these areas of involvement. This is a self-evident and unsurprising result but also a particularly important one to document for several reasons. First, evidence-based demonstration of quality-of-life impact is critical as we petition carriers to support the use of newer, more expensive medications. Second, from a topical therapy standpoint, we often use different medications on the head, neck, face, and hands relative to other areas. On the head and neck area we often use either weaker topical steroids to avoid side effects or nonsteroids like topical calcineurin or phosphodiesterase inhibitors; conversely, on the hands we use stronger steroids and are less likely to use nonsteroidal agents that are perceived to be less potent. These data emphasize the need to tailor therapy but ascertain whether standard approaches are satisfactory. If patients are not responding, particularly in these sensitive areas, providers should consider the outsized impact AD may be having on quality of life.
Dr. Sidbury is chief of dermatology at Seattle Children's Hospital and professor, department of pediatrics, University of Washington, Seattle. He is a site principal investigator for dupilumab trials, for which the hospital has a contract with Regeneron.
A version of this article first appeared on Medscape.com.
This article was updated 6/10/22.
of patients with AD.
“While we know that head, neck, face, and hands seem to be significantly affected by patients with AD, there is a limited evidence basis regarding the prevalence and health-related quality of life impact of AD in these areas,” presenting author Lawrence F. Eichenfield, MD, said during a late-breaking abstract session at the Revolutionizing Atopic Dermatitis symposium.
For the study, Dr. Eichenfield, professor of dermatology and pediatrics at the University of California, San Diego, and colleagues evaluated 533 patients from the TARGET-DERM AD cohort, an ongoing, longitudinal, observational study launched in 2019 that captures patients with AD in 44 community or academic sites in the United States.
Adult, adolescent, and pediatric patients with moderate or severe Validated Investigator Global Assessment for Atopic Dermatitis (vIGA-AD) scores at enrollment were included in the analysis. The researchers used the Patient-Oriented Scoring AD (PO-SCORAD) index to gather information on involvement of the head, neck, face, hands, or other areas, and the Patient-Oriented Eczema Measure (POEM) and Dermatology Life Quality Index/Children’s DLQI (CDLQI) to measure health-related quality of life outcomes.
Of the 533 study participants, 453 (85%) had AD affecting the head, neck, face, hands, and other areas, while 80 (15%) had AD located in other body regions not including the head, neck, face, or hands. About 38% of all patients were using systemic treatments; most were using topical treatments.
Comorbid immune system disorders (including allergic and hypersensitivity disorders) were noted in 44.8% of patients, infections in 32.5%, asthma in 26.5%, hypertension in 18.6%, depression in 15.8%, and anxiety in 12.4%, with similar proportions observed in those with or without head, neck, face, and hand involvement.
However, patients with head, face, neck, and hand involvement, when compared with patients without those affected areas, were more likely to have severe vIGA scores (28.5% vs. 16.3%, P = .02) and a higher median total body surface area affected (15% vs. 10%, P ≤ .01). Also, while bivariable analyses did not detect statistical differences in POEM and DLQI/CDLQI by body region involvement, multivariable-adjusted models showed that patients with head, neck, face, and hand involvement were more than twice as likely to report higher DLQI/CDLQI (odds ratio, 2.09) and POEM (OR, 2.51) scores than those without head, face, neck, and hand involvement.
“These findings highlight the importance of detailed assessment of specific areas affected by AD to personalize treatment approaches to the needs of patients,” Dr. Eichenfield concluded.
Raj Chovatiya MD, PhD, assistant professor of dermatology at Northwestern University, Chicago, who was asked to comment on the study, said that the findings confirm clinical suspicions about the unique and heightened impact of facial, head/neck, and hand dermatitis. “These data show that a detailed skin examination is necessary for a complete assessment of AD,” he said. “Future studies should focus on characterizing the optimal treatment approaches for each of these special sites.”
“This is important data,” added primary study author Jonathan I. Silverberg, MD, PhD, MPH, director of clinical research in the division of dermatology at George Washington University, Washington. “We need more high-quality studies like this; we need to create long-term longitudinal data to better understand [the impact of AD on] this and other cohorts.”
TARGET-DERM is sponsored by Target RWE. Dr. Eichenfield disclosed that he has served as a consultant to or investigator for numerous pharmaceutical companies. Dr. Chovatiya disclosed that he is a consultant to, a speaker for, and/or a member of the advisory board for AbbVie, Arena, Arcutis, Incyte, Pfizer, Regeneron, and Sanofi-Genzyme. Dr. Silverberg disclosed that he is a consultant to numerous pharmaceutical companies, receives fees for non-CME/CE services from Eli Lilly, Leo Pharma, Pfizer, Regeneron, and Sanofi Genzyme, as well as contracted research fees from Galderma.
Commentary by Robert Sidbury, MD, MPH
Patients with atopic dermatitis (AD) in “visible” areas such as the head, neck, and hands experience a higher impact on their quality of life than those who do not have these areas of involvement. This is a self-evident and unsurprising result but also a particularly important one to document for several reasons. First, evidence-based demonstration of quality-of-life impact is critical as we petition carriers to support the use of newer, more expensive medications. Second, from a topical therapy standpoint, we often use different medications on the head, neck, face, and hands relative to other areas. On the head and neck area we often use either weaker topical steroids to avoid side effects or nonsteroids like topical calcineurin or phosphodiesterase inhibitors; conversely, on the hands we use stronger steroids and are less likely to use nonsteroidal agents that are perceived to be less potent. These data emphasize the need to tailor therapy but ascertain whether standard approaches are satisfactory. If patients are not responding, particularly in these sensitive areas, providers should consider the outsized impact AD may be having on quality of life.
Dr. Sidbury is chief of dermatology at Seattle Children's Hospital and professor, department of pediatrics, University of Washington, Seattle. He is a site principal investigator for dupilumab trials, for which the hospital has a contract with Regeneron.
A version of this article first appeared on Medscape.com.
This article was updated 6/10/22.
FROM REVOLUTIONIZING AD 2021
iPLEDGE rollout: As frustration mounts, FDA agrees to help solve issues
, according to dermatologists, pharmacists, and patients.
When the new website and call center launched Dec. 13, hours-long hold times and repeated crashing of the website were reported as the norm, not the exception, triggering the American Academy of Dermatology Association (AADA) to request – and get – an emergency meeting on Dec. 16 with the U.S. Food and Drug Administration, which mandates the risk evaluation and mitigation strategy (REMS) for isotretinoin due to the teratogenicity of the acne medication.
At that meeting, ‘’the FDA and HHS [U.S. Department of Health and Human Services] acknowledged the concerns of dermatologists and the need for stakeholders to work collaboratively to find a solution,” Ilona Frieden, MD, chair of the AADA’s iPLEDGE workgroup and professor of dermatology at the University of California, San Francisco, said in an email interview. At the meeting, the AADA representatives described the severe impact on patient access to treatment that is resulting from the issues. The AADA also ‘’reiterated our call for a temporary pause to the program while stakeholders work to resolve the urgent issues with the platform,” she said.
The new approach, which is intended to make the experience more inclusive for transgender patients, reduces the previous three risk categories (females of reproductive potential, females not of reproductive potential, and males) to just two (those capable of getting pregnant and those not capable). The program requires physicians, patients, and pharmacists who prescribe, use, or dispense the drug to be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy tests by patients capable of becoming pregnant.
With reduced or no access during the technology glitches, access to the medicine was delayed for some patients. And dermatologists, pharmacists, and their staffs reported grueling hold times trying to reach the call center when the website had issues.
While the FDA agreed to help find a solution, it noted that the solution ‘’was to be found with dermatologists and pharmacists who are on the ground living the program every day,” Dr. Frieden said. No timeline for solving the issues was provided, so on Dec. 21, the AADA asked the FDA for a constructive dialogue among stakeholders within the next 24 hours, Dr. Frieden told this news organization.
While Dr. Frieden sees progress, ‘’we are disappointed that this situation continues to drag on for more than a week later, with more patients losing access to their needed medication each day.” While some prescribers have been able to log onto the portal and enter the information required, confirming some patients, large gaps remain, she said. Patients and pharmacists still report difficulties logging on. When that happens and they try to reach the call center, there are often hours-long hold times, dropped calls, or a message saying to call back.
The iPLEDGE administrator is Syneos Health, but a spokesperson for Syneos, Gary Gatyas, said the company does not maintain the system or the contact center.
So who does manage the call center and website? “The AADA has asked stakeholders, including Syneos Health, for clarification on who manages the call center and website but has not received a response,” Dr. Frieden said. “In the meeting [Dec. 16], representatives from the FDA made clear that the iPLEDGE sponsors are ultimately responsible for this REMS program,” Dr. Frieden said.
According to the FDA, isotretinoin manufacturers are part of the iPLEDGE program. On the iPLEDGE website, 12 isotretinoin products are listed, made by eight different companies.
One dermatologist maneuvering the new website who registered successfully as a provider told this news organization that he received a follow-up survey from United BioSource about the new website. This news organization contacted that company to confirm it runs the website but has not yet received a response.
Meanwhile, dermatologists continue to help frustrated patients cope with the new website and registration details. Neil S. Goldberg, MD, a dermatologist in Westchester County, New York, heard from two mothers who helped their teen daughters complete the forms by attesting they would use abstinence as contraception but then couldn’t figure out how to answer another question. As a result, their answers were interpreted as the patients saying they were using abstinence but didn’t commit to not having sexual contact with a partner capable of impregnating them. So Dr. Goldberg got an automated message back from the iPLEDGE program that the answers were a mismatch.
And in the comments section following a previous story on the problematic rollout, one reader offered a suggestion for reducing hold times to the call center: choose the Spanish option.
Dr. Frieden and Dr. Goldberg have no relevant disclosures.
A version of this article first appeared on Medscape.com.
, according to dermatologists, pharmacists, and patients.
When the new website and call center launched Dec. 13, hours-long hold times and repeated crashing of the website were reported as the norm, not the exception, triggering the American Academy of Dermatology Association (AADA) to request – and get – an emergency meeting on Dec. 16 with the U.S. Food and Drug Administration, which mandates the risk evaluation and mitigation strategy (REMS) for isotretinoin due to the teratogenicity of the acne medication.
At that meeting, ‘’the FDA and HHS [U.S. Department of Health and Human Services] acknowledged the concerns of dermatologists and the need for stakeholders to work collaboratively to find a solution,” Ilona Frieden, MD, chair of the AADA’s iPLEDGE workgroup and professor of dermatology at the University of California, San Francisco, said in an email interview. At the meeting, the AADA representatives described the severe impact on patient access to treatment that is resulting from the issues. The AADA also ‘’reiterated our call for a temporary pause to the program while stakeholders work to resolve the urgent issues with the platform,” she said.
The new approach, which is intended to make the experience more inclusive for transgender patients, reduces the previous three risk categories (females of reproductive potential, females not of reproductive potential, and males) to just two (those capable of getting pregnant and those not capable). The program requires physicians, patients, and pharmacists who prescribe, use, or dispense the drug to be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy tests by patients capable of becoming pregnant.
With reduced or no access during the technology glitches, access to the medicine was delayed for some patients. And dermatologists, pharmacists, and their staffs reported grueling hold times trying to reach the call center when the website had issues.
While the FDA agreed to help find a solution, it noted that the solution ‘’was to be found with dermatologists and pharmacists who are on the ground living the program every day,” Dr. Frieden said. No timeline for solving the issues was provided, so on Dec. 21, the AADA asked the FDA for a constructive dialogue among stakeholders within the next 24 hours, Dr. Frieden told this news organization.
While Dr. Frieden sees progress, ‘’we are disappointed that this situation continues to drag on for more than a week later, with more patients losing access to their needed medication each day.” While some prescribers have been able to log onto the portal and enter the information required, confirming some patients, large gaps remain, she said. Patients and pharmacists still report difficulties logging on. When that happens and they try to reach the call center, there are often hours-long hold times, dropped calls, or a message saying to call back.
The iPLEDGE administrator is Syneos Health, but a spokesperson for Syneos, Gary Gatyas, said the company does not maintain the system or the contact center.
So who does manage the call center and website? “The AADA has asked stakeholders, including Syneos Health, for clarification on who manages the call center and website but has not received a response,” Dr. Frieden said. “In the meeting [Dec. 16], representatives from the FDA made clear that the iPLEDGE sponsors are ultimately responsible for this REMS program,” Dr. Frieden said.
According to the FDA, isotretinoin manufacturers are part of the iPLEDGE program. On the iPLEDGE website, 12 isotretinoin products are listed, made by eight different companies.
One dermatologist maneuvering the new website who registered successfully as a provider told this news organization that he received a follow-up survey from United BioSource about the new website. This news organization contacted that company to confirm it runs the website but has not yet received a response.
Meanwhile, dermatologists continue to help frustrated patients cope with the new website and registration details. Neil S. Goldberg, MD, a dermatologist in Westchester County, New York, heard from two mothers who helped their teen daughters complete the forms by attesting they would use abstinence as contraception but then couldn’t figure out how to answer another question. As a result, their answers were interpreted as the patients saying they were using abstinence but didn’t commit to not having sexual contact with a partner capable of impregnating them. So Dr. Goldberg got an automated message back from the iPLEDGE program that the answers were a mismatch.
And in the comments section following a previous story on the problematic rollout, one reader offered a suggestion for reducing hold times to the call center: choose the Spanish option.
Dr. Frieden and Dr. Goldberg have no relevant disclosures.
A version of this article first appeared on Medscape.com.
, according to dermatologists, pharmacists, and patients.
When the new website and call center launched Dec. 13, hours-long hold times and repeated crashing of the website were reported as the norm, not the exception, triggering the American Academy of Dermatology Association (AADA) to request – and get – an emergency meeting on Dec. 16 with the U.S. Food and Drug Administration, which mandates the risk evaluation and mitigation strategy (REMS) for isotretinoin due to the teratogenicity of the acne medication.
At that meeting, ‘’the FDA and HHS [U.S. Department of Health and Human Services] acknowledged the concerns of dermatologists and the need for stakeholders to work collaboratively to find a solution,” Ilona Frieden, MD, chair of the AADA’s iPLEDGE workgroup and professor of dermatology at the University of California, San Francisco, said in an email interview. At the meeting, the AADA representatives described the severe impact on patient access to treatment that is resulting from the issues. The AADA also ‘’reiterated our call for a temporary pause to the program while stakeholders work to resolve the urgent issues with the platform,” she said.
The new approach, which is intended to make the experience more inclusive for transgender patients, reduces the previous three risk categories (females of reproductive potential, females not of reproductive potential, and males) to just two (those capable of getting pregnant and those not capable). The program requires physicians, patients, and pharmacists who prescribe, use, or dispense the drug to be registered, with requirements that include the use of two forms of an effective contraceptive and regular pregnancy tests by patients capable of becoming pregnant.
With reduced or no access during the technology glitches, access to the medicine was delayed for some patients. And dermatologists, pharmacists, and their staffs reported grueling hold times trying to reach the call center when the website had issues.
While the FDA agreed to help find a solution, it noted that the solution ‘’was to be found with dermatologists and pharmacists who are on the ground living the program every day,” Dr. Frieden said. No timeline for solving the issues was provided, so on Dec. 21, the AADA asked the FDA for a constructive dialogue among stakeholders within the next 24 hours, Dr. Frieden told this news organization.
While Dr. Frieden sees progress, ‘’we are disappointed that this situation continues to drag on for more than a week later, with more patients losing access to their needed medication each day.” While some prescribers have been able to log onto the portal and enter the information required, confirming some patients, large gaps remain, she said. Patients and pharmacists still report difficulties logging on. When that happens and they try to reach the call center, there are often hours-long hold times, dropped calls, or a message saying to call back.
The iPLEDGE administrator is Syneos Health, but a spokesperson for Syneos, Gary Gatyas, said the company does not maintain the system or the contact center.
So who does manage the call center and website? “The AADA has asked stakeholders, including Syneos Health, for clarification on who manages the call center and website but has not received a response,” Dr. Frieden said. “In the meeting [Dec. 16], representatives from the FDA made clear that the iPLEDGE sponsors are ultimately responsible for this REMS program,” Dr. Frieden said.
According to the FDA, isotretinoin manufacturers are part of the iPLEDGE program. On the iPLEDGE website, 12 isotretinoin products are listed, made by eight different companies.
One dermatologist maneuvering the new website who registered successfully as a provider told this news organization that he received a follow-up survey from United BioSource about the new website. This news organization contacted that company to confirm it runs the website but has not yet received a response.
Meanwhile, dermatologists continue to help frustrated patients cope with the new website and registration details. Neil S. Goldberg, MD, a dermatologist in Westchester County, New York, heard from two mothers who helped their teen daughters complete the forms by attesting they would use abstinence as contraception but then couldn’t figure out how to answer another question. As a result, their answers were interpreted as the patients saying they were using abstinence but didn’t commit to not having sexual contact with a partner capable of impregnating them. So Dr. Goldberg got an automated message back from the iPLEDGE program that the answers were a mismatch.
And in the comments section following a previous story on the problematic rollout, one reader offered a suggestion for reducing hold times to the call center: choose the Spanish option.
Dr. Frieden and Dr. Goldberg have no relevant disclosures.
A version of this article first appeared on Medscape.com.
Increased AD severity linked to more frequent baths and showers, but not with duration
of showers or baths, results from a prospective observational study found.
“Patients may benefit most from counseling on showering or bathing once daily and regularly applying moisturizer after showering or bathing,” one of the study authors, Uros Rakita, MSc, told this news organization. “Recommending less than daily shower frequencies or counseling on specific shower durations may not be necessary.”
During a late-breaking abstract session at the Revolutionizing Atopic Dermatitis symposium, Mr. Rakita, a fourth-year student at Chicago Medical School, North Chicago, presented findings from a prospective, practice-based dermatology study that investigated the longitudinal relationship between different bathing practices and AD severity to help inform patient counseling about optimal bathing practices.
“AD is a chronic, inflammatory skin condition with a diverse set of environmental triggers and exacerbating factors,” Mr. Rakita said during the meeting. “Maintaining adequate skin hydration, skin hygiene, and avoiding triggers are key aspects of AD management across all disease severities. Therefore, understanding optimal shower or bath and moisturizing practices is essential.” In fact, he added, “bathing has been shown to not only hydrate the skin, but also to improve symptoms, remove allergens, and decrease [Staphylococcus] aureus colonization. However, at the same time, concern exists for the potential of inappropriate shower or bathing frequency or durations, as well as inconsistent moisturizer application to worsen disease severity and potentially compromise disease management.”
He noted that current guidelines on bathing frequency and duration among AD patients lack consensus, are limited, and are largely based on studies of pediatric populations.
Mr. Rakita, along with primary study author Jonathan I. Silverberg, MD, PhD, MPH, director of clinical research in the division of dermatology at George Washington University, Washington, and Trisha Kaundinya, a medical student at Northwestern University, Chicago, prospectively evaluated 509 adults with AD who made an average of 2.3 visits at a single dermatology clinic between 2013 and 2020. At each visit, severity of AD signs and symptoms, as well as bathing and moisturizing practices, were assessed.
AD severity was assessed using the objective component of Scoring Atopic Dermatitis (o-SCORAD), intensity of pruritus in the past 3 days (SCORAD-itch), Eczema Area and Severity Index (EASI), Patient-Oriented Eczema Measure (POEM), and Dermatology Life Quality Index (DLQI). The researchers constructed repeated measures regression models to examine associations of bathing and moisturizing practices with change in AD severity outcome measure scores over time. Multivariable models controlled for age, sex, and race.
In adjusted linear regression models, showering or bathing more than once a day versus once daily was associated with significantly higher scores for SCORAD-itch (0.74; P = .0456), o-SCORAD (4.27; P = .0171), EASI (4.20; P = .0028), POEM (2.61; P = .0021), and DLQI (2.77; P = .0004).
The researchers also found that consistent application of moisturizer after the shower or bath was associated with significantly lower scores for o-SCORAD (–7.22; P < .0001), EASI (–3.91; P = .001) and POEM (–2.68; P = .0002), compared against not applying moisturizer after a shower or bath. However, shower or bath duration of more than, compared against fewer than, 15 minutes was not associated with significantly lower scores for o-SCORAD (1.26; P = .2868), SCORAD-itch (0.17; P = .4987), EASI (0.85; P = .3454), POEM (0.24; P = .6627) or DLQI (–0.40; P = .4318).
“Interestingly, this pattern was present when the reference shower or bath durations were under 10 minutes as well as under 5 minutes,” Mr. Rakita said. “Also, shower or bath frequencies of less than daily, relative to daily frequencies, were not significantly related to longitudinal AD severity.”
Mr. Rakita acknowledged certain limitations of the study, including the fact that the researchers did not examine the potential influence of specific soap and moisturizing products, water hardness, or other bathing features such as water temperature and bath additives.
Lawrence J. Green, MD, who was asked to comment on the study, said that he was not surprised by the finding that moisturizing after bathing improved AD signs and symptoms. “On the other hand, a long-held belief that longer duration of shower/bath time worsens AD was not found to be true,” said Dr. Green, a dermatologist who practices in Rockville, Md., and is also clinical professor of dermatology at George Washington University.
“This provides useful information for practicing dermatologists who wish to provide evidenced-based education about moisturizing and bathing to their AD patients,” he said.
The study was supported by the Agency for Healthcare Research and Quality and the Dermatology Foundation. Dr. Silverberg disclosed that he is a consultant to numerous pharmaceutical companies, receives fees for non-CME/CE services from Eli Lilly, Leo Pharma, Pfizer, Regeneron, and Sanofi Genzyme, as well as contracted research fees from Galderma. Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies. There were no other disclosures.
A version of this article first appeared on Medscape.com.
of showers or baths, results from a prospective observational study found.
“Patients may benefit most from counseling on showering or bathing once daily and regularly applying moisturizer after showering or bathing,” one of the study authors, Uros Rakita, MSc, told this news organization. “Recommending less than daily shower frequencies or counseling on specific shower durations may not be necessary.”
During a late-breaking abstract session at the Revolutionizing Atopic Dermatitis symposium, Mr. Rakita, a fourth-year student at Chicago Medical School, North Chicago, presented findings from a prospective, practice-based dermatology study that investigated the longitudinal relationship between different bathing practices and AD severity to help inform patient counseling about optimal bathing practices.
“AD is a chronic, inflammatory skin condition with a diverse set of environmental triggers and exacerbating factors,” Mr. Rakita said during the meeting. “Maintaining adequate skin hydration, skin hygiene, and avoiding triggers are key aspects of AD management across all disease severities. Therefore, understanding optimal shower or bath and moisturizing practices is essential.” In fact, he added, “bathing has been shown to not only hydrate the skin, but also to improve symptoms, remove allergens, and decrease [Staphylococcus] aureus colonization. However, at the same time, concern exists for the potential of inappropriate shower or bathing frequency or durations, as well as inconsistent moisturizer application to worsen disease severity and potentially compromise disease management.”
He noted that current guidelines on bathing frequency and duration among AD patients lack consensus, are limited, and are largely based on studies of pediatric populations.
Mr. Rakita, along with primary study author Jonathan I. Silverberg, MD, PhD, MPH, director of clinical research in the division of dermatology at George Washington University, Washington, and Trisha Kaundinya, a medical student at Northwestern University, Chicago, prospectively evaluated 509 adults with AD who made an average of 2.3 visits at a single dermatology clinic between 2013 and 2020. At each visit, severity of AD signs and symptoms, as well as bathing and moisturizing practices, were assessed.
AD severity was assessed using the objective component of Scoring Atopic Dermatitis (o-SCORAD), intensity of pruritus in the past 3 days (SCORAD-itch), Eczema Area and Severity Index (EASI), Patient-Oriented Eczema Measure (POEM), and Dermatology Life Quality Index (DLQI). The researchers constructed repeated measures regression models to examine associations of bathing and moisturizing practices with change in AD severity outcome measure scores over time. Multivariable models controlled for age, sex, and race.
In adjusted linear regression models, showering or bathing more than once a day versus once daily was associated with significantly higher scores for SCORAD-itch (0.74; P = .0456), o-SCORAD (4.27; P = .0171), EASI (4.20; P = .0028), POEM (2.61; P = .0021), and DLQI (2.77; P = .0004).
The researchers also found that consistent application of moisturizer after the shower or bath was associated with significantly lower scores for o-SCORAD (–7.22; P < .0001), EASI (–3.91; P = .001) and POEM (–2.68; P = .0002), compared against not applying moisturizer after a shower or bath. However, shower or bath duration of more than, compared against fewer than, 15 minutes was not associated with significantly lower scores for o-SCORAD (1.26; P = .2868), SCORAD-itch (0.17; P = .4987), EASI (0.85; P = .3454), POEM (0.24; P = .6627) or DLQI (–0.40; P = .4318).
“Interestingly, this pattern was present when the reference shower or bath durations were under 10 minutes as well as under 5 minutes,” Mr. Rakita said. “Also, shower or bath frequencies of less than daily, relative to daily frequencies, were not significantly related to longitudinal AD severity.”
Mr. Rakita acknowledged certain limitations of the study, including the fact that the researchers did not examine the potential influence of specific soap and moisturizing products, water hardness, or other bathing features such as water temperature and bath additives.
Lawrence J. Green, MD, who was asked to comment on the study, said that he was not surprised by the finding that moisturizing after bathing improved AD signs and symptoms. “On the other hand, a long-held belief that longer duration of shower/bath time worsens AD was not found to be true,” said Dr. Green, a dermatologist who practices in Rockville, Md., and is also clinical professor of dermatology at George Washington University.
“This provides useful information for practicing dermatologists who wish to provide evidenced-based education about moisturizing and bathing to their AD patients,” he said.
The study was supported by the Agency for Healthcare Research and Quality and the Dermatology Foundation. Dr. Silverberg disclosed that he is a consultant to numerous pharmaceutical companies, receives fees for non-CME/CE services from Eli Lilly, Leo Pharma, Pfizer, Regeneron, and Sanofi Genzyme, as well as contracted research fees from Galderma. Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies. There were no other disclosures.
A version of this article first appeared on Medscape.com.
of showers or baths, results from a prospective observational study found.
“Patients may benefit most from counseling on showering or bathing once daily and regularly applying moisturizer after showering or bathing,” one of the study authors, Uros Rakita, MSc, told this news organization. “Recommending less than daily shower frequencies or counseling on specific shower durations may not be necessary.”
During a late-breaking abstract session at the Revolutionizing Atopic Dermatitis symposium, Mr. Rakita, a fourth-year student at Chicago Medical School, North Chicago, presented findings from a prospective, practice-based dermatology study that investigated the longitudinal relationship between different bathing practices and AD severity to help inform patient counseling about optimal bathing practices.
“AD is a chronic, inflammatory skin condition with a diverse set of environmental triggers and exacerbating factors,” Mr. Rakita said during the meeting. “Maintaining adequate skin hydration, skin hygiene, and avoiding triggers are key aspects of AD management across all disease severities. Therefore, understanding optimal shower or bath and moisturizing practices is essential.” In fact, he added, “bathing has been shown to not only hydrate the skin, but also to improve symptoms, remove allergens, and decrease [Staphylococcus] aureus colonization. However, at the same time, concern exists for the potential of inappropriate shower or bathing frequency or durations, as well as inconsistent moisturizer application to worsen disease severity and potentially compromise disease management.”
He noted that current guidelines on bathing frequency and duration among AD patients lack consensus, are limited, and are largely based on studies of pediatric populations.
Mr. Rakita, along with primary study author Jonathan I. Silverberg, MD, PhD, MPH, director of clinical research in the division of dermatology at George Washington University, Washington, and Trisha Kaundinya, a medical student at Northwestern University, Chicago, prospectively evaluated 509 adults with AD who made an average of 2.3 visits at a single dermatology clinic between 2013 and 2020. At each visit, severity of AD signs and symptoms, as well as bathing and moisturizing practices, were assessed.
AD severity was assessed using the objective component of Scoring Atopic Dermatitis (o-SCORAD), intensity of pruritus in the past 3 days (SCORAD-itch), Eczema Area and Severity Index (EASI), Patient-Oriented Eczema Measure (POEM), and Dermatology Life Quality Index (DLQI). The researchers constructed repeated measures regression models to examine associations of bathing and moisturizing practices with change in AD severity outcome measure scores over time. Multivariable models controlled for age, sex, and race.
In adjusted linear regression models, showering or bathing more than once a day versus once daily was associated with significantly higher scores for SCORAD-itch (0.74; P = .0456), o-SCORAD (4.27; P = .0171), EASI (4.20; P = .0028), POEM (2.61; P = .0021), and DLQI (2.77; P = .0004).
The researchers also found that consistent application of moisturizer after the shower or bath was associated with significantly lower scores for o-SCORAD (–7.22; P < .0001), EASI (–3.91; P = .001) and POEM (–2.68; P = .0002), compared against not applying moisturizer after a shower or bath. However, shower or bath duration of more than, compared against fewer than, 15 minutes was not associated with significantly lower scores for o-SCORAD (1.26; P = .2868), SCORAD-itch (0.17; P = .4987), EASI (0.85; P = .3454), POEM (0.24; P = .6627) or DLQI (–0.40; P = .4318).
“Interestingly, this pattern was present when the reference shower or bath durations were under 10 minutes as well as under 5 minutes,” Mr. Rakita said. “Also, shower or bath frequencies of less than daily, relative to daily frequencies, were not significantly related to longitudinal AD severity.”
Mr. Rakita acknowledged certain limitations of the study, including the fact that the researchers did not examine the potential influence of specific soap and moisturizing products, water hardness, or other bathing features such as water temperature and bath additives.
Lawrence J. Green, MD, who was asked to comment on the study, said that he was not surprised by the finding that moisturizing after bathing improved AD signs and symptoms. “On the other hand, a long-held belief that longer duration of shower/bath time worsens AD was not found to be true,” said Dr. Green, a dermatologist who practices in Rockville, Md., and is also clinical professor of dermatology at George Washington University.
“This provides useful information for practicing dermatologists who wish to provide evidenced-based education about moisturizing and bathing to their AD patients,” he said.
The study was supported by the Agency for Healthcare Research and Quality and the Dermatology Foundation. Dr. Silverberg disclosed that he is a consultant to numerous pharmaceutical companies, receives fees for non-CME/CE services from Eli Lilly, Leo Pharma, Pfizer, Regeneron, and Sanofi Genzyme, as well as contracted research fees from Galderma. Dr. Green disclosed that he is a speaker, consultant, or investigator for numerous pharmaceutical companies. There were no other disclosures.
A version of this article first appeared on Medscape.com.
FROM REVOLUTIONIZING AD 2021
Pandemic poses short- and long-term risks to babies, especially boys
The pandemic has created a hostile environment for pregnant people and their babies.
Stress levels among expectant mothers have soared. Pregnant women with COVID are 5 times as likely as uninfected pregnant people to require intensive care and 22 times as likely to die. Infected moms are four times as likely to have a stillborn child.
Yet some of the pandemic’s greatest threats to infants’ health may not be apparent for years or even decades.
That’s because babies of COVID-infected moms are 60% more likely to be born very prematurely, which increases the danger of infant mortality and long-term disabilities such as cerebral palsy, asthma, and hearing loss, as well as a child’s risk of adult disease, including depression, anxiety, heart disease, and kidney disease.
Studies have linked fever and infection during pregnancy to developmental and psychiatric conditions such as autism, depression, and schizophrenia.
“Some of these conditions do not show up until middle childhood or early adult life, but they have their origins in fetal life,” said Evdokia Anagnostou, MD, a child neurologist at Holland Bloorview Kids Rehabilitation Hospital and a pediatrics professor at the University of Toronto.
For fetuses exposed to COVID, the greatest danger is usually not the coronavirus itself, but the mother’s immune system.
Both severe COVID infections and the strain of the pandemic can expose fetuses to harmful inflammation, which can occur when a mother’s immune system is fighting a virus or when stress hormones send nonstop alarm signals.
Prenatal inflammation “changes the way the brain develops and, depending on the timing of the infection, it can change the way the heart or kidneys develop,” Dr. Anagnostou said.
Although health officials have strongly recommended COVID vaccines for pregnant people, only 35% are fully vaccinated.
At least 150,000 pregnant women have been diagnosed with COVID; more than 25,000 of them have been hospitalized, and 249 have died, according to the Centers for Disease Control and Prevention.
Although most babies will be fine, even a small increase in the percentage of children with special medical or educational needs could have a large effect on the population, given the huge number of COVID infections, Dr. Anagnostou said.
“If someone has a baby who is doing well, that is what they should focus on,” Dr. Anagnostou said. “But from a public health point of view, we need to follow women who experienced severe COVID and their babies to understand the impact.”
Learning from history
Researchers in the United States and other countries are already studying “the COVID generation” to see whether these children have more health issues than those conceived or born before 2020.
Previous crises have shown that the challenges fetuses face in the womb – such as maternal infections, hunger, stress, and hormone-disrupting chemicals – can leave a lasting imprint on their health, as well as that of their children and grandchildren, said Frederick Kaskel, MD, director of pediatric nephrology at the Children’s Hospital at Montefiore, New York.
People whose mothers were pregnant during surges in the 1918 influenza pandemic, for example, had poorer health throughout their lives, compared with Americans born at other times, said John McCarthy, who is a medical student at Albert Einstein College of Medicine, New York, and cowrote a recent review in JAMA Pediatrics with Dr. Kaskel.
Researchers don’t know exactly which moms were infected with pandemic flu, Mr. McCarthy said. But women who were pregnant during major surges – when infection was widespread – had children with higher rates of heart disease or diabetes. These children were also less successful in school, less economically productive, and more likely to live with a disability.
Because organ systems develop during different periods of pregnancy, fetuses exposed during the first trimester may face different risks than those exposed toward the end of pregnancy, Mr. McCarthy said. For example, people born in the fall of 1918 were 50% more likely than others to develop kidney disease; that may reflect an exposure to the pandemic in the third trimester, while the kidneys were still developing.
Nearly 2 years into the COVID pandemic, researchers have begun to publish preliminary observations of infants exposed to COVID infections and stress before birth.
Although Dr. Anagnostou noted that it’s too early to reach definitive conclusions, “there is evidence that babies born to moms with severe COVID infections have changes to their immune system,” she said. “It’s enough to make us worry a little bit.”
Damaging a fetal security system
The good news about the coronavirus is that it seldom crosses the placenta, the organ tasked with protecting a developing fetus from infections and providing it with oxygen. So moms with COVID rarely give the virus to their children before birth.
That’s important, because some viruses that directly infect the fetus – such as Zika – can cause devastating birth defects, said Karin Nielsen-Saines, MD, a specialist in pediatric infectious diseases at University of California, Los Angeles.
But studies also suggest that inflammation from a mother’s COVID infection can injure the placenta, said Jeffery Goldstein, MD, an assistant professor of pathology at Northwestern University, Chicago. In a study published in American Journal of Clinical Pathology , Dr. Goldstein and his coauthors found that placentas from COVID-infected moms had more abnormal blood vessels than placentas from patients without COVID, making it harder for them to deliver sufficient oxygen to the fetus.
Placental damage can also lead to preeclampsia, a serious complication of pregnancy that can cause a mother’s blood pressure to spike.
Preeclampsia occurs when blood vessels in the placenta don’t develop or function properly, forcing the mother’s heart to work harder to get blood to the fetus, which may not receive enough oxygen and nutrients. Preeclampsia also predisposes women to heart attacks and strokes later in life.
Rewiring the immune system
In some cases, COVID also appears to rewire a baby’s immune response, Dr. Nielsen-Saines said.
In an October study in the journal Cell Reports Medicine, Dr. Nielsen-Saines and her coauthors found that infants born to people with severe COVID infections had a different mix of immune cells and proteins than other babies. None of the newborns tested positive for the coronavirus.
The immune changes are concerning, Dr. Nielsen-Saines said, because this pattern of immune cells and proteins has previously been found in infants with respiratory problems and in some cases poor neurodevelopment.
Notably, all the babies in her study appear healthy, said Dr. Nielsen-Saines, who plans to follow them for 3 years to see whether these early signals translate into developmental delays, such as problems talking, walking, or interacting with others.
“How big of a difference does any of this make in the baby?” asked Dr. Anagnostou. “We won’t know for a few years. All we can do is try to be as prepared as possible.”
Increasing the risk for boys
Boys could face higher risks from COVID, even before birth.
Males are generally more vulnerable than females as fetuses and newborns; they’re more likely to be born prematurely and to die as infants. Preterm boys also have a higher risk of disability and death.
But coronavirus infection poses special dangers, said Sabra Klein, PhD, a professor of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health, Baltimore.
That’s because boys are disproportionately affected by conditions linked to maternal infections. Boys are four times as likely as girls to be diagnosed with autism or attention-deficit/hyperactivity disorder, for example, while men are 75% more likely than women to develop schizophrenia.
Scientists don’t fully understand why boys appear more fragile in the womb, although testosterone – which can dampen immune response – may play a role, said Kristina Adams Waldorf, MD, a professor of obstetrics and gynecology at the University of Washington.
Men generally mount weaker immune responses than women and more often develop severe COVID infections. Recent research suggests boys with COVID are more likely than girls to become seriously ill or develop a rare inflammatory condition called multisystem inflammatory syndrome.
New research on COVID could help illuminate this vulnerability.
In a study published in October, researchers found that the sex of a fetus influences the way its placenta responds to COVID, as well as how its mother’s immune system responds.
Pregnant people infected with COVID made fewer antibodies against the coronavirus if they were carrying male fetuses than if they were carrying females. Mothers also transferred fewer antibodies to boys than to girls, said Andrea Edlow, MD, senior author of the study and a maternal-fetal medicine specialist at Massachusetts General Hospital, Boston.
When examining the placentas of male fetuses after delivery, researchers found changes that could leave boys less protected against damaging inflammation.
The sex of a fetus can influence its mother’s response to other illnesses, as well.
For example, research shows that pregnant women with asthma have worse symptoms if they’re carrying a female. Women carrying males are slightly more likely to develop gestational diabetes.
Dr. Edlow said her findings raise questions about the “cross talk” between mother and baby. “The mom’s immune system is sensing there is a male fetus,” Dr. Edlow said. “And the fetus is actively communicating with the mom’s immune system.”
Boosting toxic stress
Rates of depression and stress among pregnant women have increased dramatically during the pandemic.
That’s concerning because chronic stress can lead to inflammation, affecting the babies of both infected and uninfected women, Dr. Anagnostou said.
Studies consistently show that infants born to mothers who experience significant stress during pregnancy have higher rates of short- and long-term health damage – including heart defects and obesity – than babies born to women with less stress.
“We know that inflammation directly influences the way a baby’s brain develops,” said Elinor Sullivan, PhD, an associate professor in psychiatry at Oregon Health & Science University, Portland.
Lockdowns, travel restrictions and physical distancing left many pregnant women without the support of family and friends. The stress of losing a loved one, a job, or a home further heightens the risks to moms and babies, said Dr. Sullivan, who is following children born during the pandemic for 5 years.
In research that has not yet been published, Dr. Sullivan found that babies of women who were pregnant during the pandemic showed more sadness and negative emotions in the first year of life, compared with infants of women who were pregnant before the pandemic.
The findings show the importance of helping and protecting pregnant people before and after delivery, said Dr. Sullivan, who conducted a separate study that found women who received more social support were less depressed.
Italian researchers are also studying the effect of maternal stress on infants’ behavior, as well as the way their genes are regulated.
Although stress-related inflammation doesn’t alter the structure of a baby’s genes, it can influence whether they’re turned on and off, said Livio Provenzi, PhD, a psychologist at the C. Mondino National Institute of Neurology Foundation in Pavia, Italy.
In Dr. Provenzi’s study of 163 mother-baby pairs he found differences in how genes that regulate the stress response were activated. Genes that help people respond to stress were more likely to be turned off in babies whose moms reported the most stress during pregnancy. The same moms also reported that their babies cried more and were fussier when they were 3 months old.
Researchers usually prefer to make in-person observations of babies as they interact with their mothers, Dr. Provenzi said. But because of the pandemic, Dr. Provenzi asked mothers to fill out questionnaires about infant behavior. He plans to observe mothers and babies in person when the children are 12 months old.
While vaccinating pregnant people is the best way to protect them and their fetuses from the virus, Dr. Anagnostou said, society needs to do more to preserve expectant mothers’ mental health.
“We can’t escape the fact that we’ve lived through 2 years of a pandemic,” Dr. Anagnostou said. “But we can think about opportunities for reducing the risk.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The pandemic has created a hostile environment for pregnant people and their babies.
Stress levels among expectant mothers have soared. Pregnant women with COVID are 5 times as likely as uninfected pregnant people to require intensive care and 22 times as likely to die. Infected moms are four times as likely to have a stillborn child.
Yet some of the pandemic’s greatest threats to infants’ health may not be apparent for years or even decades.
That’s because babies of COVID-infected moms are 60% more likely to be born very prematurely, which increases the danger of infant mortality and long-term disabilities such as cerebral palsy, asthma, and hearing loss, as well as a child’s risk of adult disease, including depression, anxiety, heart disease, and kidney disease.
Studies have linked fever and infection during pregnancy to developmental and psychiatric conditions such as autism, depression, and schizophrenia.
“Some of these conditions do not show up until middle childhood or early adult life, but they have their origins in fetal life,” said Evdokia Anagnostou, MD, a child neurologist at Holland Bloorview Kids Rehabilitation Hospital and a pediatrics professor at the University of Toronto.
For fetuses exposed to COVID, the greatest danger is usually not the coronavirus itself, but the mother’s immune system.
Both severe COVID infections and the strain of the pandemic can expose fetuses to harmful inflammation, which can occur when a mother’s immune system is fighting a virus or when stress hormones send nonstop alarm signals.
Prenatal inflammation “changes the way the brain develops and, depending on the timing of the infection, it can change the way the heart or kidneys develop,” Dr. Anagnostou said.
Although health officials have strongly recommended COVID vaccines for pregnant people, only 35% are fully vaccinated.
At least 150,000 pregnant women have been diagnosed with COVID; more than 25,000 of them have been hospitalized, and 249 have died, according to the Centers for Disease Control and Prevention.
Although most babies will be fine, even a small increase in the percentage of children with special medical or educational needs could have a large effect on the population, given the huge number of COVID infections, Dr. Anagnostou said.
“If someone has a baby who is doing well, that is what they should focus on,” Dr. Anagnostou said. “But from a public health point of view, we need to follow women who experienced severe COVID and their babies to understand the impact.”
Learning from history
Researchers in the United States and other countries are already studying “the COVID generation” to see whether these children have more health issues than those conceived or born before 2020.
Previous crises have shown that the challenges fetuses face in the womb – such as maternal infections, hunger, stress, and hormone-disrupting chemicals – can leave a lasting imprint on their health, as well as that of their children and grandchildren, said Frederick Kaskel, MD, director of pediatric nephrology at the Children’s Hospital at Montefiore, New York.
People whose mothers were pregnant during surges in the 1918 influenza pandemic, for example, had poorer health throughout their lives, compared with Americans born at other times, said John McCarthy, who is a medical student at Albert Einstein College of Medicine, New York, and cowrote a recent review in JAMA Pediatrics with Dr. Kaskel.
Researchers don’t know exactly which moms were infected with pandemic flu, Mr. McCarthy said. But women who were pregnant during major surges – when infection was widespread – had children with higher rates of heart disease or diabetes. These children were also less successful in school, less economically productive, and more likely to live with a disability.
Because organ systems develop during different periods of pregnancy, fetuses exposed during the first trimester may face different risks than those exposed toward the end of pregnancy, Mr. McCarthy said. For example, people born in the fall of 1918 were 50% more likely than others to develop kidney disease; that may reflect an exposure to the pandemic in the third trimester, while the kidneys were still developing.
Nearly 2 years into the COVID pandemic, researchers have begun to publish preliminary observations of infants exposed to COVID infections and stress before birth.
Although Dr. Anagnostou noted that it’s too early to reach definitive conclusions, “there is evidence that babies born to moms with severe COVID infections have changes to their immune system,” she said. “It’s enough to make us worry a little bit.”
Damaging a fetal security system
The good news about the coronavirus is that it seldom crosses the placenta, the organ tasked with protecting a developing fetus from infections and providing it with oxygen. So moms with COVID rarely give the virus to their children before birth.
That’s important, because some viruses that directly infect the fetus – such as Zika – can cause devastating birth defects, said Karin Nielsen-Saines, MD, a specialist in pediatric infectious diseases at University of California, Los Angeles.
But studies also suggest that inflammation from a mother’s COVID infection can injure the placenta, said Jeffery Goldstein, MD, an assistant professor of pathology at Northwestern University, Chicago. In a study published in American Journal of Clinical Pathology , Dr. Goldstein and his coauthors found that placentas from COVID-infected moms had more abnormal blood vessels than placentas from patients without COVID, making it harder for them to deliver sufficient oxygen to the fetus.
Placental damage can also lead to preeclampsia, a serious complication of pregnancy that can cause a mother’s blood pressure to spike.
Preeclampsia occurs when blood vessels in the placenta don’t develop or function properly, forcing the mother’s heart to work harder to get blood to the fetus, which may not receive enough oxygen and nutrients. Preeclampsia also predisposes women to heart attacks and strokes later in life.
Rewiring the immune system
In some cases, COVID also appears to rewire a baby’s immune response, Dr. Nielsen-Saines said.
In an October study in the journal Cell Reports Medicine, Dr. Nielsen-Saines and her coauthors found that infants born to people with severe COVID infections had a different mix of immune cells and proteins than other babies. None of the newborns tested positive for the coronavirus.
The immune changes are concerning, Dr. Nielsen-Saines said, because this pattern of immune cells and proteins has previously been found in infants with respiratory problems and in some cases poor neurodevelopment.
Notably, all the babies in her study appear healthy, said Dr. Nielsen-Saines, who plans to follow them for 3 years to see whether these early signals translate into developmental delays, such as problems talking, walking, or interacting with others.
“How big of a difference does any of this make in the baby?” asked Dr. Anagnostou. “We won’t know for a few years. All we can do is try to be as prepared as possible.”
Increasing the risk for boys
Boys could face higher risks from COVID, even before birth.
Males are generally more vulnerable than females as fetuses and newborns; they’re more likely to be born prematurely and to die as infants. Preterm boys also have a higher risk of disability and death.
But coronavirus infection poses special dangers, said Sabra Klein, PhD, a professor of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health, Baltimore.
That’s because boys are disproportionately affected by conditions linked to maternal infections. Boys are four times as likely as girls to be diagnosed with autism or attention-deficit/hyperactivity disorder, for example, while men are 75% more likely than women to develop schizophrenia.
Scientists don’t fully understand why boys appear more fragile in the womb, although testosterone – which can dampen immune response – may play a role, said Kristina Adams Waldorf, MD, a professor of obstetrics and gynecology at the University of Washington.
Men generally mount weaker immune responses than women and more often develop severe COVID infections. Recent research suggests boys with COVID are more likely than girls to become seriously ill or develop a rare inflammatory condition called multisystem inflammatory syndrome.
New research on COVID could help illuminate this vulnerability.
In a study published in October, researchers found that the sex of a fetus influences the way its placenta responds to COVID, as well as how its mother’s immune system responds.
Pregnant people infected with COVID made fewer antibodies against the coronavirus if they were carrying male fetuses than if they were carrying females. Mothers also transferred fewer antibodies to boys than to girls, said Andrea Edlow, MD, senior author of the study and a maternal-fetal medicine specialist at Massachusetts General Hospital, Boston.
When examining the placentas of male fetuses after delivery, researchers found changes that could leave boys less protected against damaging inflammation.
The sex of a fetus can influence its mother’s response to other illnesses, as well.
For example, research shows that pregnant women with asthma have worse symptoms if they’re carrying a female. Women carrying males are slightly more likely to develop gestational diabetes.
Dr. Edlow said her findings raise questions about the “cross talk” between mother and baby. “The mom’s immune system is sensing there is a male fetus,” Dr. Edlow said. “And the fetus is actively communicating with the mom’s immune system.”
Boosting toxic stress
Rates of depression and stress among pregnant women have increased dramatically during the pandemic.
That’s concerning because chronic stress can lead to inflammation, affecting the babies of both infected and uninfected women, Dr. Anagnostou said.
Studies consistently show that infants born to mothers who experience significant stress during pregnancy have higher rates of short- and long-term health damage – including heart defects and obesity – than babies born to women with less stress.
“We know that inflammation directly influences the way a baby’s brain develops,” said Elinor Sullivan, PhD, an associate professor in psychiatry at Oregon Health & Science University, Portland.
Lockdowns, travel restrictions and physical distancing left many pregnant women without the support of family and friends. The stress of losing a loved one, a job, or a home further heightens the risks to moms and babies, said Dr. Sullivan, who is following children born during the pandemic for 5 years.
In research that has not yet been published, Dr. Sullivan found that babies of women who were pregnant during the pandemic showed more sadness and negative emotions in the first year of life, compared with infants of women who were pregnant before the pandemic.
The findings show the importance of helping and protecting pregnant people before and after delivery, said Dr. Sullivan, who conducted a separate study that found women who received more social support were less depressed.
Italian researchers are also studying the effect of maternal stress on infants’ behavior, as well as the way their genes are regulated.
Although stress-related inflammation doesn’t alter the structure of a baby’s genes, it can influence whether they’re turned on and off, said Livio Provenzi, PhD, a psychologist at the C. Mondino National Institute of Neurology Foundation in Pavia, Italy.
In Dr. Provenzi’s study of 163 mother-baby pairs he found differences in how genes that regulate the stress response were activated. Genes that help people respond to stress were more likely to be turned off in babies whose moms reported the most stress during pregnancy. The same moms also reported that their babies cried more and were fussier when they were 3 months old.
Researchers usually prefer to make in-person observations of babies as they interact with their mothers, Dr. Provenzi said. But because of the pandemic, Dr. Provenzi asked mothers to fill out questionnaires about infant behavior. He plans to observe mothers and babies in person when the children are 12 months old.
While vaccinating pregnant people is the best way to protect them and their fetuses from the virus, Dr. Anagnostou said, society needs to do more to preserve expectant mothers’ mental health.
“We can’t escape the fact that we’ve lived through 2 years of a pandemic,” Dr. Anagnostou said. “But we can think about opportunities for reducing the risk.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The pandemic has created a hostile environment for pregnant people and their babies.
Stress levels among expectant mothers have soared. Pregnant women with COVID are 5 times as likely as uninfected pregnant people to require intensive care and 22 times as likely to die. Infected moms are four times as likely to have a stillborn child.
Yet some of the pandemic’s greatest threats to infants’ health may not be apparent for years or even decades.
That’s because babies of COVID-infected moms are 60% more likely to be born very prematurely, which increases the danger of infant mortality and long-term disabilities such as cerebral palsy, asthma, and hearing loss, as well as a child’s risk of adult disease, including depression, anxiety, heart disease, and kidney disease.
Studies have linked fever and infection during pregnancy to developmental and psychiatric conditions such as autism, depression, and schizophrenia.
“Some of these conditions do not show up until middle childhood or early adult life, but they have their origins in fetal life,” said Evdokia Anagnostou, MD, a child neurologist at Holland Bloorview Kids Rehabilitation Hospital and a pediatrics professor at the University of Toronto.
For fetuses exposed to COVID, the greatest danger is usually not the coronavirus itself, but the mother’s immune system.
Both severe COVID infections and the strain of the pandemic can expose fetuses to harmful inflammation, which can occur when a mother’s immune system is fighting a virus or when stress hormones send nonstop alarm signals.
Prenatal inflammation “changes the way the brain develops and, depending on the timing of the infection, it can change the way the heart or kidneys develop,” Dr. Anagnostou said.
Although health officials have strongly recommended COVID vaccines for pregnant people, only 35% are fully vaccinated.
At least 150,000 pregnant women have been diagnosed with COVID; more than 25,000 of them have been hospitalized, and 249 have died, according to the Centers for Disease Control and Prevention.
Although most babies will be fine, even a small increase in the percentage of children with special medical or educational needs could have a large effect on the population, given the huge number of COVID infections, Dr. Anagnostou said.
“If someone has a baby who is doing well, that is what they should focus on,” Dr. Anagnostou said. “But from a public health point of view, we need to follow women who experienced severe COVID and their babies to understand the impact.”
Learning from history
Researchers in the United States and other countries are already studying “the COVID generation” to see whether these children have more health issues than those conceived or born before 2020.
Previous crises have shown that the challenges fetuses face in the womb – such as maternal infections, hunger, stress, and hormone-disrupting chemicals – can leave a lasting imprint on their health, as well as that of their children and grandchildren, said Frederick Kaskel, MD, director of pediatric nephrology at the Children’s Hospital at Montefiore, New York.
People whose mothers were pregnant during surges in the 1918 influenza pandemic, for example, had poorer health throughout their lives, compared with Americans born at other times, said John McCarthy, who is a medical student at Albert Einstein College of Medicine, New York, and cowrote a recent review in JAMA Pediatrics with Dr. Kaskel.
Researchers don’t know exactly which moms were infected with pandemic flu, Mr. McCarthy said. But women who were pregnant during major surges – when infection was widespread – had children with higher rates of heart disease or diabetes. These children were also less successful in school, less economically productive, and more likely to live with a disability.
Because organ systems develop during different periods of pregnancy, fetuses exposed during the first trimester may face different risks than those exposed toward the end of pregnancy, Mr. McCarthy said. For example, people born in the fall of 1918 were 50% more likely than others to develop kidney disease; that may reflect an exposure to the pandemic in the third trimester, while the kidneys were still developing.
Nearly 2 years into the COVID pandemic, researchers have begun to publish preliminary observations of infants exposed to COVID infections and stress before birth.
Although Dr. Anagnostou noted that it’s too early to reach definitive conclusions, “there is evidence that babies born to moms with severe COVID infections have changes to their immune system,” she said. “It’s enough to make us worry a little bit.”
Damaging a fetal security system
The good news about the coronavirus is that it seldom crosses the placenta, the organ tasked with protecting a developing fetus from infections and providing it with oxygen. So moms with COVID rarely give the virus to their children before birth.
That’s important, because some viruses that directly infect the fetus – such as Zika – can cause devastating birth defects, said Karin Nielsen-Saines, MD, a specialist in pediatric infectious diseases at University of California, Los Angeles.
But studies also suggest that inflammation from a mother’s COVID infection can injure the placenta, said Jeffery Goldstein, MD, an assistant professor of pathology at Northwestern University, Chicago. In a study published in American Journal of Clinical Pathology , Dr. Goldstein and his coauthors found that placentas from COVID-infected moms had more abnormal blood vessels than placentas from patients without COVID, making it harder for them to deliver sufficient oxygen to the fetus.
Placental damage can also lead to preeclampsia, a serious complication of pregnancy that can cause a mother’s blood pressure to spike.
Preeclampsia occurs when blood vessels in the placenta don’t develop or function properly, forcing the mother’s heart to work harder to get blood to the fetus, which may not receive enough oxygen and nutrients. Preeclampsia also predisposes women to heart attacks and strokes later in life.
Rewiring the immune system
In some cases, COVID also appears to rewire a baby’s immune response, Dr. Nielsen-Saines said.
In an October study in the journal Cell Reports Medicine, Dr. Nielsen-Saines and her coauthors found that infants born to people with severe COVID infections had a different mix of immune cells and proteins than other babies. None of the newborns tested positive for the coronavirus.
The immune changes are concerning, Dr. Nielsen-Saines said, because this pattern of immune cells and proteins has previously been found in infants with respiratory problems and in some cases poor neurodevelopment.
Notably, all the babies in her study appear healthy, said Dr. Nielsen-Saines, who plans to follow them for 3 years to see whether these early signals translate into developmental delays, such as problems talking, walking, or interacting with others.
“How big of a difference does any of this make in the baby?” asked Dr. Anagnostou. “We won’t know for a few years. All we can do is try to be as prepared as possible.”
Increasing the risk for boys
Boys could face higher risks from COVID, even before birth.
Males are generally more vulnerable than females as fetuses and newborns; they’re more likely to be born prematurely and to die as infants. Preterm boys also have a higher risk of disability and death.
But coronavirus infection poses special dangers, said Sabra Klein, PhD, a professor of molecular microbiology and immunology at the Johns Hopkins Bloomberg School of Public Health, Baltimore.
That’s because boys are disproportionately affected by conditions linked to maternal infections. Boys are four times as likely as girls to be diagnosed with autism or attention-deficit/hyperactivity disorder, for example, while men are 75% more likely than women to develop schizophrenia.
Scientists don’t fully understand why boys appear more fragile in the womb, although testosterone – which can dampen immune response – may play a role, said Kristina Adams Waldorf, MD, a professor of obstetrics and gynecology at the University of Washington.
Men generally mount weaker immune responses than women and more often develop severe COVID infections. Recent research suggests boys with COVID are more likely than girls to become seriously ill or develop a rare inflammatory condition called multisystem inflammatory syndrome.
New research on COVID could help illuminate this vulnerability.
In a study published in October, researchers found that the sex of a fetus influences the way its placenta responds to COVID, as well as how its mother’s immune system responds.
Pregnant people infected with COVID made fewer antibodies against the coronavirus if they were carrying male fetuses than if they were carrying females. Mothers also transferred fewer antibodies to boys than to girls, said Andrea Edlow, MD, senior author of the study and a maternal-fetal medicine specialist at Massachusetts General Hospital, Boston.
When examining the placentas of male fetuses after delivery, researchers found changes that could leave boys less protected against damaging inflammation.
The sex of a fetus can influence its mother’s response to other illnesses, as well.
For example, research shows that pregnant women with asthma have worse symptoms if they’re carrying a female. Women carrying males are slightly more likely to develop gestational diabetes.
Dr. Edlow said her findings raise questions about the “cross talk” between mother and baby. “The mom’s immune system is sensing there is a male fetus,” Dr. Edlow said. “And the fetus is actively communicating with the mom’s immune system.”
Boosting toxic stress
Rates of depression and stress among pregnant women have increased dramatically during the pandemic.
That’s concerning because chronic stress can lead to inflammation, affecting the babies of both infected and uninfected women, Dr. Anagnostou said.
Studies consistently show that infants born to mothers who experience significant stress during pregnancy have higher rates of short- and long-term health damage – including heart defects and obesity – than babies born to women with less stress.
“We know that inflammation directly influences the way a baby’s brain develops,” said Elinor Sullivan, PhD, an associate professor in psychiatry at Oregon Health & Science University, Portland.
Lockdowns, travel restrictions and physical distancing left many pregnant women without the support of family and friends. The stress of losing a loved one, a job, or a home further heightens the risks to moms and babies, said Dr. Sullivan, who is following children born during the pandemic for 5 years.
In research that has not yet been published, Dr. Sullivan found that babies of women who were pregnant during the pandemic showed more sadness and negative emotions in the first year of life, compared with infants of women who were pregnant before the pandemic.
The findings show the importance of helping and protecting pregnant people before and after delivery, said Dr. Sullivan, who conducted a separate study that found women who received more social support were less depressed.
Italian researchers are also studying the effect of maternal stress on infants’ behavior, as well as the way their genes are regulated.
Although stress-related inflammation doesn’t alter the structure of a baby’s genes, it can influence whether they’re turned on and off, said Livio Provenzi, PhD, a psychologist at the C. Mondino National Institute of Neurology Foundation in Pavia, Italy.
In Dr. Provenzi’s study of 163 mother-baby pairs he found differences in how genes that regulate the stress response were activated. Genes that help people respond to stress were more likely to be turned off in babies whose moms reported the most stress during pregnancy. The same moms also reported that their babies cried more and were fussier when they were 3 months old.
Researchers usually prefer to make in-person observations of babies as they interact with their mothers, Dr. Provenzi said. But because of the pandemic, Dr. Provenzi asked mothers to fill out questionnaires about infant behavior. He plans to observe mothers and babies in person when the children are 12 months old.
While vaccinating pregnant people is the best way to protect them and their fetuses from the virus, Dr. Anagnostou said, society needs to do more to preserve expectant mothers’ mental health.
“We can’t escape the fact that we’ve lived through 2 years of a pandemic,” Dr. Anagnostou said. “But we can think about opportunities for reducing the risk.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Children and COVID: New cases up slightly, vaccinations continue to slow
New COVID-19 vaccinations in children were down by almost 24% in the last week as new cases rose by just 3.5%, based on new data.
That fairly low number suggests the latest case count from the American Academy of Pediatrics and the Children’s Hospital Association has not caught up yet to the reality of the Omicron variant, which has sent new cases climbing among all ages and now represents the majority of COVID-19 infections nationwide, the Centers for Disease Control and Prevention said.
Meanwhile, in the midst of the latest surge, the United States just passed yet another sobering COVID milestone: 1,000 deaths in children aged 17 and under. The total as of Dec. 20 was 1,015, according to the CDC, with the largest share, almost 32%, occurring in children less than 5 years of age.
Regionally, the majority of that increase came in the Northeast, with a small rise in the South and decreases in the Midwest and West, the AAP and CHA said in their weekly COVID report.
At the state level, the largest percent increases in cases over the past 2 weeks were seen in Maine and New Hampshire, as well as Vermont, which has the nation’s highest vaccination rates for children aged 5-11 (51%) and 12-17 (84%), the AAP said in its vaccination trends report.
Nationally, new COVID vaccinations in children continue to trend downward. The number of children aged 5-17 years who had received at least one dose increased by about 498,000 for the week of Dec. 13-19, down from 654,000 (–23.9%) the previous week. Children aged 5-11 years still represented the largest share (22.7%) of all vaccine initiators in the last 2 weeks, but that proportion was 42.8% just before Thanksgiving, according to data from the CDC.
On a more positive note, children aged 5-11 made up 51% of all Americans who completed the vaccine regimen during the 2 weeks ending Dec. 20. The cumulative completion count is 3.6 million in that age group, along with almost 13.4 million children aged 12-17, and the CDC data show that 6.1 million children aged 5-11 and 15.9 million children aged 12-17 have received at least one dose.
On a less positive note, however, that means almost half (47%) of 12- to 17-year-olds still are not fully vaccinated and that over a third (37%) have received no vaccine at all, according to the COVID Data Tracker.
New COVID-19 vaccinations in children were down by almost 24% in the last week as new cases rose by just 3.5%, based on new data.
That fairly low number suggests the latest case count from the American Academy of Pediatrics and the Children’s Hospital Association has not caught up yet to the reality of the Omicron variant, which has sent new cases climbing among all ages and now represents the majority of COVID-19 infections nationwide, the Centers for Disease Control and Prevention said.
Meanwhile, in the midst of the latest surge, the United States just passed yet another sobering COVID milestone: 1,000 deaths in children aged 17 and under. The total as of Dec. 20 was 1,015, according to the CDC, with the largest share, almost 32%, occurring in children less than 5 years of age.
Regionally, the majority of that increase came in the Northeast, with a small rise in the South and decreases in the Midwest and West, the AAP and CHA said in their weekly COVID report.
At the state level, the largest percent increases in cases over the past 2 weeks were seen in Maine and New Hampshire, as well as Vermont, which has the nation’s highest vaccination rates for children aged 5-11 (51%) and 12-17 (84%), the AAP said in its vaccination trends report.
Nationally, new COVID vaccinations in children continue to trend downward. The number of children aged 5-17 years who had received at least one dose increased by about 498,000 for the week of Dec. 13-19, down from 654,000 (–23.9%) the previous week. Children aged 5-11 years still represented the largest share (22.7%) of all vaccine initiators in the last 2 weeks, but that proportion was 42.8% just before Thanksgiving, according to data from the CDC.
On a more positive note, children aged 5-11 made up 51% of all Americans who completed the vaccine regimen during the 2 weeks ending Dec. 20. The cumulative completion count is 3.6 million in that age group, along with almost 13.4 million children aged 12-17, and the CDC data show that 6.1 million children aged 5-11 and 15.9 million children aged 12-17 have received at least one dose.
On a less positive note, however, that means almost half (47%) of 12- to 17-year-olds still are not fully vaccinated and that over a third (37%) have received no vaccine at all, according to the COVID Data Tracker.
New COVID-19 vaccinations in children were down by almost 24% in the last week as new cases rose by just 3.5%, based on new data.
That fairly low number suggests the latest case count from the American Academy of Pediatrics and the Children’s Hospital Association has not caught up yet to the reality of the Omicron variant, which has sent new cases climbing among all ages and now represents the majority of COVID-19 infections nationwide, the Centers for Disease Control and Prevention said.
Meanwhile, in the midst of the latest surge, the United States just passed yet another sobering COVID milestone: 1,000 deaths in children aged 17 and under. The total as of Dec. 20 was 1,015, according to the CDC, with the largest share, almost 32%, occurring in children less than 5 years of age.
Regionally, the majority of that increase came in the Northeast, with a small rise in the South and decreases in the Midwest and West, the AAP and CHA said in their weekly COVID report.
At the state level, the largest percent increases in cases over the past 2 weeks were seen in Maine and New Hampshire, as well as Vermont, which has the nation’s highest vaccination rates for children aged 5-11 (51%) and 12-17 (84%), the AAP said in its vaccination trends report.
Nationally, new COVID vaccinations in children continue to trend downward. The number of children aged 5-17 years who had received at least one dose increased by about 498,000 for the week of Dec. 13-19, down from 654,000 (–23.9%) the previous week. Children aged 5-11 years still represented the largest share (22.7%) of all vaccine initiators in the last 2 weeks, but that proportion was 42.8% just before Thanksgiving, according to data from the CDC.
On a more positive note, children aged 5-11 made up 51% of all Americans who completed the vaccine regimen during the 2 weeks ending Dec. 20. The cumulative completion count is 3.6 million in that age group, along with almost 13.4 million children aged 12-17, and the CDC data show that 6.1 million children aged 5-11 and 15.9 million children aged 12-17 have received at least one dose.
On a less positive note, however, that means almost half (47%) of 12- to 17-year-olds still are not fully vaccinated and that over a third (37%) have received no vaccine at all, according to the COVID Data Tracker.







