User login
Enhanced recovery protocol for colectomy patients reduced hospital stay
SAN DIEGO – Multihospital collaboration and implementation of enhanced recovery have the potential to improve outcomes, in particular, length of hospital stay, results from a pilot study showed.
“Given the importance of patient engagement, enhanced recovery has the potential to improve patient experience and provide high-value health care,” Julia R. Berian, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Berian, the James C. Thompson Geriatric Surgery Research Fellow at the University of Chicago Medical Center, presented findings from the Enhanced Recovery in NSQIP (ERIN) Pilot, a collaborative effort by 16 ACS-NSQIP hospitals to improve length of stay in patients who undergo colectomy, a procedure that has been shown to have an adverse event rate of 28.9% and an average length of stay of 9.8 days for those who experience an adverse event (J Am Coll Surg. 2008; 207[5]:698-704).
Implementation of the ERIN Pilot showed reductions in length of hospital stay and morbidity among colectomy patients. The average length of stay decreased by 1.2 days (from a mean of 6.6 among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01), but the rate of readmission was 11% for both pre- and postimplementation cases. In the adjusted model, the enhanced recovery protocol decreased the risk of prolonged length of stay by 40% (odds ratio, 0.6; 95% confidence interval, 0.5-0.8).
For the ERIN Pilot, she and her associates participated in monthly conference calls for collaborative experience and expert guidance from project leaders Julie Thacker, MD, and Liane Feldman, MD. Enhanced recovery protocols were tailored to each individual hospital. Data were collected before and after implementation using 14 novel ERIN variables, including preoperative elements such as defining expectations and minimizing starvation, intraoperative variables such as optimizing fluid management and minimizing surgical trauma, and postoperative elements such as aggressive adherence to best practices including feeding, early ambulation, and minimizing the use of tethers such as urinary catheters.
The researchers evaluated procedure-targeted colectomy cases performed between July 2013 and June 2015, and excluded emergency cases or those with preoperative sepsis. They used bivariate analysis and multivariate logistic regression with forward selection, and the outcome of interest, prolonged hospital length of stay, was specified by the standard ACS NSQIP definition: greater than the 75th percentile of uncomplicated cases.
Dr. Berian reported results from 2,523 colectomies performed prior to implementation of the ERIN Pilot process and 823 colectomies performed after implementation of the process. The researchers observed no differences between the preimplementation and postimplementation cases in terms of sex, preoperative functional status, hypertension, renal failure, ascites, diabetes, disseminated cancer, or use of steroids for inflammatory bowel disease. However, compared with preimplementation colectomies, a significantly higher proportion of postimplementation cases were white (77% vs. 68%, respectively), had heart failure (2.8% vs. 1.2%), had chronic obstructive pulmonary disease (7.8% vs. 5.3%), were American Society of Anesthesiologists (ASA) class 1 and 2 ( 50.2% vs. 44.7%), were smokers (21.6% vs. 16.7%), had unintentional weight loss (7.7% vs. 5.7%), had used mechanical bowel prep (77% vs. 53%), and used more oral antibiotics (68% vs. 33%).
On the other hand, compared with preimplementation cases, there were significantly fewer bleeding disorders in the postimplementation colectomies (3.9% vs. 6.4%), as well as fewer cases with preoperative systemic inflammatory response syndrome (2.9% vs. 5.4%) and open surgery approaches (31.7% vs. 42.3%).
Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
SAN DIEGO – Multihospital collaboration and implementation of enhanced recovery have the potential to improve outcomes, in particular, length of hospital stay, results from a pilot study showed.
“Given the importance of patient engagement, enhanced recovery has the potential to improve patient experience and provide high-value health care,” Julia R. Berian, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Berian, the James C. Thompson Geriatric Surgery Research Fellow at the University of Chicago Medical Center, presented findings from the Enhanced Recovery in NSQIP (ERIN) Pilot, a collaborative effort by 16 ACS-NSQIP hospitals to improve length of stay in patients who undergo colectomy, a procedure that has been shown to have an adverse event rate of 28.9% and an average length of stay of 9.8 days for those who experience an adverse event (J Am Coll Surg. 2008; 207[5]:698-704).
Implementation of the ERIN Pilot showed reductions in length of hospital stay and morbidity among colectomy patients. The average length of stay decreased by 1.2 days (from a mean of 6.6 among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01), but the rate of readmission was 11% for both pre- and postimplementation cases. In the adjusted model, the enhanced recovery protocol decreased the risk of prolonged length of stay by 40% (odds ratio, 0.6; 95% confidence interval, 0.5-0.8).
For the ERIN Pilot, she and her associates participated in monthly conference calls for collaborative experience and expert guidance from project leaders Julie Thacker, MD, and Liane Feldman, MD. Enhanced recovery protocols were tailored to each individual hospital. Data were collected before and after implementation using 14 novel ERIN variables, including preoperative elements such as defining expectations and minimizing starvation, intraoperative variables such as optimizing fluid management and minimizing surgical trauma, and postoperative elements such as aggressive adherence to best practices including feeding, early ambulation, and minimizing the use of tethers such as urinary catheters.
The researchers evaluated procedure-targeted colectomy cases performed between July 2013 and June 2015, and excluded emergency cases or those with preoperative sepsis. They used bivariate analysis and multivariate logistic regression with forward selection, and the outcome of interest, prolonged hospital length of stay, was specified by the standard ACS NSQIP definition: greater than the 75th percentile of uncomplicated cases.
Dr. Berian reported results from 2,523 colectomies performed prior to implementation of the ERIN Pilot process and 823 colectomies performed after implementation of the process. The researchers observed no differences between the preimplementation and postimplementation cases in terms of sex, preoperative functional status, hypertension, renal failure, ascites, diabetes, disseminated cancer, or use of steroids for inflammatory bowel disease. However, compared with preimplementation colectomies, a significantly higher proportion of postimplementation cases were white (77% vs. 68%, respectively), had heart failure (2.8% vs. 1.2%), had chronic obstructive pulmonary disease (7.8% vs. 5.3%), were American Society of Anesthesiologists (ASA) class 1 and 2 ( 50.2% vs. 44.7%), were smokers (21.6% vs. 16.7%), had unintentional weight loss (7.7% vs. 5.7%), had used mechanical bowel prep (77% vs. 53%), and used more oral antibiotics (68% vs. 33%).
On the other hand, compared with preimplementation cases, there were significantly fewer bleeding disorders in the postimplementation colectomies (3.9% vs. 6.4%), as well as fewer cases with preoperative systemic inflammatory response syndrome (2.9% vs. 5.4%) and open surgery approaches (31.7% vs. 42.3%).
Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
SAN DIEGO – Multihospital collaboration and implementation of enhanced recovery have the potential to improve outcomes, in particular, length of hospital stay, results from a pilot study showed.
“Given the importance of patient engagement, enhanced recovery has the potential to improve patient experience and provide high-value health care,” Julia R. Berian, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Berian, the James C. Thompson Geriatric Surgery Research Fellow at the University of Chicago Medical Center, presented findings from the Enhanced Recovery in NSQIP (ERIN) Pilot, a collaborative effort by 16 ACS-NSQIP hospitals to improve length of stay in patients who undergo colectomy, a procedure that has been shown to have an adverse event rate of 28.9% and an average length of stay of 9.8 days for those who experience an adverse event (J Am Coll Surg. 2008; 207[5]:698-704).
Implementation of the ERIN Pilot showed reductions in length of hospital stay and morbidity among colectomy patients. The average length of stay decreased by 1.2 days (from a mean of 6.6 among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01), but the rate of readmission was 11% for both pre- and postimplementation cases. In the adjusted model, the enhanced recovery protocol decreased the risk of prolonged length of stay by 40% (odds ratio, 0.6; 95% confidence interval, 0.5-0.8).
For the ERIN Pilot, she and her associates participated in monthly conference calls for collaborative experience and expert guidance from project leaders Julie Thacker, MD, and Liane Feldman, MD. Enhanced recovery protocols were tailored to each individual hospital. Data were collected before and after implementation using 14 novel ERIN variables, including preoperative elements such as defining expectations and minimizing starvation, intraoperative variables such as optimizing fluid management and minimizing surgical trauma, and postoperative elements such as aggressive adherence to best practices including feeding, early ambulation, and minimizing the use of tethers such as urinary catheters.
The researchers evaluated procedure-targeted colectomy cases performed between July 2013 and June 2015, and excluded emergency cases or those with preoperative sepsis. They used bivariate analysis and multivariate logistic regression with forward selection, and the outcome of interest, prolonged hospital length of stay, was specified by the standard ACS NSQIP definition: greater than the 75th percentile of uncomplicated cases.
Dr. Berian reported results from 2,523 colectomies performed prior to implementation of the ERIN Pilot process and 823 colectomies performed after implementation of the process. The researchers observed no differences between the preimplementation and postimplementation cases in terms of sex, preoperative functional status, hypertension, renal failure, ascites, diabetes, disseminated cancer, or use of steroids for inflammatory bowel disease. However, compared with preimplementation colectomies, a significantly higher proportion of postimplementation cases were white (77% vs. 68%, respectively), had heart failure (2.8% vs. 1.2%), had chronic obstructive pulmonary disease (7.8% vs. 5.3%), were American Society of Anesthesiologists (ASA) class 1 and 2 ( 50.2% vs. 44.7%), were smokers (21.6% vs. 16.7%), had unintentional weight loss (7.7% vs. 5.7%), had used mechanical bowel prep (77% vs. 53%), and used more oral antibiotics (68% vs. 33%).
On the other hand, compared with preimplementation cases, there were significantly fewer bleeding disorders in the postimplementation colectomies (3.9% vs. 6.4%), as well as fewer cases with preoperative systemic inflammatory response syndrome (2.9% vs. 5.4%) and open surgery approaches (31.7% vs. 42.3%).
Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: A multihospital enhanced recovery process for colectomy patients decreased length of stay and morbidity.
Major finding: After implementation of an enhanced recovery protocol in colectomy patients, the average hospital length of stay decreased by 1.2 days (from a mean of 6.6 days among preimplementation cases to 5.4 days among post implementation cases; P less than .0001). Morbidity also decreased from 14% to 11% (P = .01).
Data source: An analysis of 2,523 colectomies performed prior to implementation of the Enhanced Recovery in NSQIP (ERIN) Pilot process and 823 colectomies performed after implementation of the process.
Disclosures: Dr. Berian disclosed that her fellowship position is funded by the John A. Hartford Foundation.
Simple colon surgery bundle accelerated outcomes improvement
SAN DIEGO – Implementation of a simple colon bundle decreased the rate of colonic and enteric resections faster, compared with improvements seen for other procedures, according to a study that involved 23 hospitals in Tennessee.
At the American College of Surgeons/National Surgical Quality Improvement Program National Conference, Brian J. Daley, MD, discussed findings from an analysis conducted by members of the Tennessee Surgical Quality Collaborative (TSQC), which he described as “a collection of surgeons who put aside their hospital and regional affiliations to work together to help each other and to help our fellow Tennesseans.” Established in 2008 with member hospitals, the TSQC has grown to 23 member hospitals, including 18 community hospitals and 5 academic medical centers. It provides data on nearly 600 surgeons across the state. “While this only represents about half of the surgical procedures in the state, there is sufficient statistical power to make comments about our surgical performance,” said Dr. Daley of the department of surgery at the University of Tennessee Medical Center, Knoxville.
To quantify TSQC’s impact on surgical outcomes, surgeons at the member hospitals evaluated the TSQC colon bundle, which was developed in 2012 and implemented in 2013. It bundles four processes of care: maintaining intraoperative oxygen delivery, maintaining a temperature of 36° C, making sure the patient’s blood glucose is normal, and choosing the appropriate antibiotics. “We kept it simple: easy, not expensive, and hopefully helpful,” Dr. Daley said.
With other procedures as a baseline, they used statistical analyses to determine if implementation of the bundle led to an incremental acceleration of reduced complications, compared with other improvements observed in other procedures. “To understand our outcomes, we needed to prove three points: that the trend improved [a negative trend in the resection rate], that this negative trend was more negative than trends for other comparator procedures, and that the trend for intercept was not equal to the comparator in any way,” Dr. Daley explained.
Following adoption of the bundle, he and his associates observed that the rate of decrease in postoperative recurrences was greater in colectomy, compared with that for all other surgical procedures (P less than .001 for both the trend and the intercept statistical models). Adoption of the bundle also positively impacted decreases in postoperative recurrences among enterectomy cases (P less than .001 for both the trend and the intercept statistical models).
“We were able to demonstrate that our TSQC bundle paid dividends in improving colectomy outcomes,” Dr. Daley concluded. “We have seen these efforts spill over into enterectomy. From this we can also infer that participation in the collaborative improves outcomes and is imperative to maintain the acceleration in surgical improvement.”
Dr. Daley reported that he and his coauthors had no relevant financial disclosures.
SAN DIEGO – Implementation of a simple colon bundle decreased the rate of colonic and enteric resections faster, compared with improvements seen for other procedures, according to a study that involved 23 hospitals in Tennessee.
At the American College of Surgeons/National Surgical Quality Improvement Program National Conference, Brian J. Daley, MD, discussed findings from an analysis conducted by members of the Tennessee Surgical Quality Collaborative (TSQC), which he described as “a collection of surgeons who put aside their hospital and regional affiliations to work together to help each other and to help our fellow Tennesseans.” Established in 2008 with member hospitals, the TSQC has grown to 23 member hospitals, including 18 community hospitals and 5 academic medical centers. It provides data on nearly 600 surgeons across the state. “While this only represents about half of the surgical procedures in the state, there is sufficient statistical power to make comments about our surgical performance,” said Dr. Daley of the department of surgery at the University of Tennessee Medical Center, Knoxville.
To quantify TSQC’s impact on surgical outcomes, surgeons at the member hospitals evaluated the TSQC colon bundle, which was developed in 2012 and implemented in 2013. It bundles four processes of care: maintaining intraoperative oxygen delivery, maintaining a temperature of 36° C, making sure the patient’s blood glucose is normal, and choosing the appropriate antibiotics. “We kept it simple: easy, not expensive, and hopefully helpful,” Dr. Daley said.
With other procedures as a baseline, they used statistical analyses to determine if implementation of the bundle led to an incremental acceleration of reduced complications, compared with other improvements observed in other procedures. “To understand our outcomes, we needed to prove three points: that the trend improved [a negative trend in the resection rate], that this negative trend was more negative than trends for other comparator procedures, and that the trend for intercept was not equal to the comparator in any way,” Dr. Daley explained.
Following adoption of the bundle, he and his associates observed that the rate of decrease in postoperative recurrences was greater in colectomy, compared with that for all other surgical procedures (P less than .001 for both the trend and the intercept statistical models). Adoption of the bundle also positively impacted decreases in postoperative recurrences among enterectomy cases (P less than .001 for both the trend and the intercept statistical models).
“We were able to demonstrate that our TSQC bundle paid dividends in improving colectomy outcomes,” Dr. Daley concluded. “We have seen these efforts spill over into enterectomy. From this we can also infer that participation in the collaborative improves outcomes and is imperative to maintain the acceleration in surgical improvement.”
Dr. Daley reported that he and his coauthors had no relevant financial disclosures.
SAN DIEGO – Implementation of a simple colon bundle decreased the rate of colonic and enteric resections faster, compared with improvements seen for other procedures, according to a study that involved 23 hospitals in Tennessee.
At the American College of Surgeons/National Surgical Quality Improvement Program National Conference, Brian J. Daley, MD, discussed findings from an analysis conducted by members of the Tennessee Surgical Quality Collaborative (TSQC), which he described as “a collection of surgeons who put aside their hospital and regional affiliations to work together to help each other and to help our fellow Tennesseans.” Established in 2008 with member hospitals, the TSQC has grown to 23 member hospitals, including 18 community hospitals and 5 academic medical centers. It provides data on nearly 600 surgeons across the state. “While this only represents about half of the surgical procedures in the state, there is sufficient statistical power to make comments about our surgical performance,” said Dr. Daley of the department of surgery at the University of Tennessee Medical Center, Knoxville.
To quantify TSQC’s impact on surgical outcomes, surgeons at the member hospitals evaluated the TSQC colon bundle, which was developed in 2012 and implemented in 2013. It bundles four processes of care: maintaining intraoperative oxygen delivery, maintaining a temperature of 36° C, making sure the patient’s blood glucose is normal, and choosing the appropriate antibiotics. “We kept it simple: easy, not expensive, and hopefully helpful,” Dr. Daley said.
With other procedures as a baseline, they used statistical analyses to determine if implementation of the bundle led to an incremental acceleration of reduced complications, compared with other improvements observed in other procedures. “To understand our outcomes, we needed to prove three points: that the trend improved [a negative trend in the resection rate], that this negative trend was more negative than trends for other comparator procedures, and that the trend for intercept was not equal to the comparator in any way,” Dr. Daley explained.
Following adoption of the bundle, he and his associates observed that the rate of decrease in postoperative recurrences was greater in colectomy, compared with that for all other surgical procedures (P less than .001 for both the trend and the intercept statistical models). Adoption of the bundle also positively impacted decreases in postoperative recurrences among enterectomy cases (P less than .001 for both the trend and the intercept statistical models).
“We were able to demonstrate that our TSQC bundle paid dividends in improving colectomy outcomes,” Dr. Daley concluded. “We have seen these efforts spill over into enterectomy. From this we can also infer that participation in the collaborative improves outcomes and is imperative to maintain the acceleration in surgical improvement.”
Dr. Daley reported that he and his coauthors had no relevant financial disclosures.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Adoption of a colon bundle by a collaborative of Tennessee hospitals improved certain colectomy outcomes.
Major finding: Following adoption of a colon bundle, the rate of decrease in postoperative recurrences was greater in colectomy than for all other surgical procedures (P less than .001 for both the trend and the intercept statistical models).
Data source: An analysis conducted by members of the Tennessee Surgical Quality Collaborative, which included 23 hospitals in the state.
Disclosures: The researchers reported having no relevant financial disclosures.
Postop delirium linked to greater long-term cognitive decline
Patients with postoperative delirium have significantly worse preoperative short-term cognitive performance and significantly greater long-term cognitive decline, compared with patients without delirium, according to Sharon K. Inouye, MD, and her associates.
In a prospective cohort study of 560 patients aged 70 years and older, 134 patients were selected for the delirium group and 426 for the nondelirium group. The delirium group had a significantly greater decline (–1.03 points) at 1 month, compared with those without delirium (P = .003). After cognitive function had recovered at 2 months, there were no significant differences between groups (P = 0.99). After 2 months, both groups decline on average; however, the delirium group declined significantly more (–1.07) in adjusted mean scores at 36 months (P =.02).
From baseline to 36 months, there was a significant change for the delirium group (–1.30, P less than .01) and no significant change for the group without delirium (–0.23, P = .30). Researchers noted that the effect of delirium remains undiminished after consecutive rehospitalizations, intercurrent illnesses, and major postoperative complications were controlled for.
The patients underwent major noncardiac surgery, such as total hip or knee replacement, open abdominal aortic aneurysm repair, colectomy, and lower-extremity arterial bypass.
“This study provides a novel presentation of the biphasic relationship of delirium and cognitive trajectory, both its well-recognized acute effects but also long-term effects,” the researchers wrote. “Our results suggest that after a period of initial recovery, patients with delirium experience a substantially accelerated trajectory of cognitive aging.”
Read the full study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association (doi:10.1016/j.jalz.2016.03.005).
Patients with postoperative delirium have significantly worse preoperative short-term cognitive performance and significantly greater long-term cognitive decline, compared with patients without delirium, according to Sharon K. Inouye, MD, and her associates.
In a prospective cohort study of 560 patients aged 70 years and older, 134 patients were selected for the delirium group and 426 for the nondelirium group. The delirium group had a significantly greater decline (–1.03 points) at 1 month, compared with those without delirium (P = .003). After cognitive function had recovered at 2 months, there were no significant differences between groups (P = 0.99). After 2 months, both groups decline on average; however, the delirium group declined significantly more (–1.07) in adjusted mean scores at 36 months (P =.02).
From baseline to 36 months, there was a significant change for the delirium group (–1.30, P less than .01) and no significant change for the group without delirium (–0.23, P = .30). Researchers noted that the effect of delirium remains undiminished after consecutive rehospitalizations, intercurrent illnesses, and major postoperative complications were controlled for.
The patients underwent major noncardiac surgery, such as total hip or knee replacement, open abdominal aortic aneurysm repair, colectomy, and lower-extremity arterial bypass.
“This study provides a novel presentation of the biphasic relationship of delirium and cognitive trajectory, both its well-recognized acute effects but also long-term effects,” the researchers wrote. “Our results suggest that after a period of initial recovery, patients with delirium experience a substantially accelerated trajectory of cognitive aging.”
Read the full study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association (doi:10.1016/j.jalz.2016.03.005).
Patients with postoperative delirium have significantly worse preoperative short-term cognitive performance and significantly greater long-term cognitive decline, compared with patients without delirium, according to Sharon K. Inouye, MD, and her associates.
In a prospective cohort study of 560 patients aged 70 years and older, 134 patients were selected for the delirium group and 426 for the nondelirium group. The delirium group had a significantly greater decline (–1.03 points) at 1 month, compared with those without delirium (P = .003). After cognitive function had recovered at 2 months, there were no significant differences between groups (P = 0.99). After 2 months, both groups decline on average; however, the delirium group declined significantly more (–1.07) in adjusted mean scores at 36 months (P =.02).
From baseline to 36 months, there was a significant change for the delirium group (–1.30, P less than .01) and no significant change for the group without delirium (–0.23, P = .30). Researchers noted that the effect of delirium remains undiminished after consecutive rehospitalizations, intercurrent illnesses, and major postoperative complications were controlled for.
The patients underwent major noncardiac surgery, such as total hip or knee replacement, open abdominal aortic aneurysm repair, colectomy, and lower-extremity arterial bypass.
“This study provides a novel presentation of the biphasic relationship of delirium and cognitive trajectory, both its well-recognized acute effects but also long-term effects,” the researchers wrote. “Our results suggest that after a period of initial recovery, patients with delirium experience a substantially accelerated trajectory of cognitive aging.”
Read the full study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association (doi:10.1016/j.jalz.2016.03.005).
FROM ALZHEIMER’S & DEMENTIA
No one-size-fits-all approach for reducing hospital readmissions
SAN DIEGO – Despite advances in the way surgeons practice their craft and measure outcomes in a meaningful way, the rate of hospital readmissions remains unacceptably high, according to an Emory University surgeon who has studied the readmission patterns.
“Readmission is a problem, not only from a cost and penalties standpoint but also from the rates of readmission affecting patients’ lives and expectations,” Jyotirmay Sharma, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Sharma, director of thyroid and endocrine surgery at Emory University Hospital, Atlanta, cited recent federal data estimating that among Medicare patients discharged from a hospital, 20% are rehospitalized within 30 days, and 34% are rehospitalized within 90 days. In 2013 alone, the Centers for Medicare & Medicaid Services levied readmission penalties against 2,213 hospitals to the tune of $280 million. “So clearly it’s a major issue,” he said.
In a study conducted by one of Dr. Sharma’s associates, researchers evaluated the risk factors for 30-day hospital readmission among general surgery patients treated at Emory University Hospital (J Am Coll Surg. 2012 Sep;215[3]:322-30). Pancreatectomy accounted for 18% of readmissions, followed by colectomy/colostomy (13%), small bowel resection (12%), and gastrectomy and ventral hernia repair (both 11%).
An unrelated analysis of a 498,875 operations found that lower extremity vascular bypass procedures accounted for 16% of readmissions, followed by colectomy or proctectomy (11%), bariatric surgery (5%), and ventral hernia repair (4%). In addition, the readmission rates were 6% among patients with no complications, 16% among those with one complications such as surgical site infections (SSIs), bleeding, and ileus, 37% among those with two or more complications, and 29% among those with three or more complications (JAMA 2015;313[3]:483-95). The most common complication overall was SSI (20%), followed by ileus (10%).
When the Emory study researchers drilled down on their data, they found that the following preexisting conditions were associated with readmissions among colectomy patients: steroid use, hypertension, readmission, cancer, COPD, smoking, poor functional status, and diabetes. At the same time, preexisting conditions associated with readmissions among vascular patients were diabetes and renal failure. The only preexisting condition associated with readmissions among thyroidectomy was renal failure. When the researchers evaluated the association between readmission risk and system-wide complications, they found that vascular surgery and urinary surgery conferred the highest risks (sixfold and fivefold, respectively).
“Just looking at your semiannual report quickly can give you a sense of which complications are associated with that readmission,” Dr. Sharma said. “There are many areas of potential intervention.” Preoperatively, he recommends screening surgery patients for obstructive sleep apnea, hypertension, and diabetes. “Looking at preexisting comorbid dyspnea, cancer, and renal failure can give you those target populations very quickly,” he said.
Intraoperatively, “it’s all about reduction of complications,” he said. These include using the WHO checklist, employing SSI prevention practices and considering certain anesthesia techniques such as low tidal volume ventilation and fluid limitation, control of hyperglycemia, and enhanced recovery after surgery protocols (ERAS).
Postoperative strategies to reduce readmission risk include ERAS for multimodal analgesia, fluid restriction, oral intake, and ambulation, and being aggressive about follow-up with high-risk populations and discharge planning. “The strategies for readmission reduction should be based on the preoperative assessment and the ability to identify high-risk populations,” Dr. Sharma said. “At Emory, we found that ileostomy patients had the highest risk of readmission. This made sense from a dehydration standpoint. So a colorectal surgeon led the creation of an Emory-wide protocol for teaching patients and their families, giving them signs of dehydration, what to look for, direct access to a dedicated nurse for follow-up, and an arrangement with the infusion center for rehydration as needed.”
He concluded by noting that there is no one-size-fits-all approach to reducing hospital readmissions. “I think an overarching readmission improvement process is not the way to go, unless you’re talking about a preoperative assessment area,” he said. “Identifying high-risk patients and giving them a lifeline where they can call so you can intervene and avoid that readmission, is better.”
Dr. Sharma reported having no relevant disclosures.
SAN DIEGO – Despite advances in the way surgeons practice their craft and measure outcomes in a meaningful way, the rate of hospital readmissions remains unacceptably high, according to an Emory University surgeon who has studied the readmission patterns.
“Readmission is a problem, not only from a cost and penalties standpoint but also from the rates of readmission affecting patients’ lives and expectations,” Jyotirmay Sharma, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Sharma, director of thyroid and endocrine surgery at Emory University Hospital, Atlanta, cited recent federal data estimating that among Medicare patients discharged from a hospital, 20% are rehospitalized within 30 days, and 34% are rehospitalized within 90 days. In 2013 alone, the Centers for Medicare & Medicaid Services levied readmission penalties against 2,213 hospitals to the tune of $280 million. “So clearly it’s a major issue,” he said.
In a study conducted by one of Dr. Sharma’s associates, researchers evaluated the risk factors for 30-day hospital readmission among general surgery patients treated at Emory University Hospital (J Am Coll Surg. 2012 Sep;215[3]:322-30). Pancreatectomy accounted for 18% of readmissions, followed by colectomy/colostomy (13%), small bowel resection (12%), and gastrectomy and ventral hernia repair (both 11%).
An unrelated analysis of a 498,875 operations found that lower extremity vascular bypass procedures accounted for 16% of readmissions, followed by colectomy or proctectomy (11%), bariatric surgery (5%), and ventral hernia repair (4%). In addition, the readmission rates were 6% among patients with no complications, 16% among those with one complications such as surgical site infections (SSIs), bleeding, and ileus, 37% among those with two or more complications, and 29% among those with three or more complications (JAMA 2015;313[3]:483-95). The most common complication overall was SSI (20%), followed by ileus (10%).
When the Emory study researchers drilled down on their data, they found that the following preexisting conditions were associated with readmissions among colectomy patients: steroid use, hypertension, readmission, cancer, COPD, smoking, poor functional status, and diabetes. At the same time, preexisting conditions associated with readmissions among vascular patients were diabetes and renal failure. The only preexisting condition associated with readmissions among thyroidectomy was renal failure. When the researchers evaluated the association between readmission risk and system-wide complications, they found that vascular surgery and urinary surgery conferred the highest risks (sixfold and fivefold, respectively).
“Just looking at your semiannual report quickly can give you a sense of which complications are associated with that readmission,” Dr. Sharma said. “There are many areas of potential intervention.” Preoperatively, he recommends screening surgery patients for obstructive sleep apnea, hypertension, and diabetes. “Looking at preexisting comorbid dyspnea, cancer, and renal failure can give you those target populations very quickly,” he said.
Intraoperatively, “it’s all about reduction of complications,” he said. These include using the WHO checklist, employing SSI prevention practices and considering certain anesthesia techniques such as low tidal volume ventilation and fluid limitation, control of hyperglycemia, and enhanced recovery after surgery protocols (ERAS).
Postoperative strategies to reduce readmission risk include ERAS for multimodal analgesia, fluid restriction, oral intake, and ambulation, and being aggressive about follow-up with high-risk populations and discharge planning. “The strategies for readmission reduction should be based on the preoperative assessment and the ability to identify high-risk populations,” Dr. Sharma said. “At Emory, we found that ileostomy patients had the highest risk of readmission. This made sense from a dehydration standpoint. So a colorectal surgeon led the creation of an Emory-wide protocol for teaching patients and their families, giving them signs of dehydration, what to look for, direct access to a dedicated nurse for follow-up, and an arrangement with the infusion center for rehydration as needed.”
He concluded by noting that there is no one-size-fits-all approach to reducing hospital readmissions. “I think an overarching readmission improvement process is not the way to go, unless you’re talking about a preoperative assessment area,” he said. “Identifying high-risk patients and giving them a lifeline where they can call so you can intervene and avoid that readmission, is better.”
Dr. Sharma reported having no relevant disclosures.
SAN DIEGO – Despite advances in the way surgeons practice their craft and measure outcomes in a meaningful way, the rate of hospital readmissions remains unacceptably high, according to an Emory University surgeon who has studied the readmission patterns.
“Readmission is a problem, not only from a cost and penalties standpoint but also from the rates of readmission affecting patients’ lives and expectations,” Jyotirmay Sharma, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Sharma, director of thyroid and endocrine surgery at Emory University Hospital, Atlanta, cited recent federal data estimating that among Medicare patients discharged from a hospital, 20% are rehospitalized within 30 days, and 34% are rehospitalized within 90 days. In 2013 alone, the Centers for Medicare & Medicaid Services levied readmission penalties against 2,213 hospitals to the tune of $280 million. “So clearly it’s a major issue,” he said.
In a study conducted by one of Dr. Sharma’s associates, researchers evaluated the risk factors for 30-day hospital readmission among general surgery patients treated at Emory University Hospital (J Am Coll Surg. 2012 Sep;215[3]:322-30). Pancreatectomy accounted for 18% of readmissions, followed by colectomy/colostomy (13%), small bowel resection (12%), and gastrectomy and ventral hernia repair (both 11%).
An unrelated analysis of a 498,875 operations found that lower extremity vascular bypass procedures accounted for 16% of readmissions, followed by colectomy or proctectomy (11%), bariatric surgery (5%), and ventral hernia repair (4%). In addition, the readmission rates were 6% among patients with no complications, 16% among those with one complications such as surgical site infections (SSIs), bleeding, and ileus, 37% among those with two or more complications, and 29% among those with three or more complications (JAMA 2015;313[3]:483-95). The most common complication overall was SSI (20%), followed by ileus (10%).
When the Emory study researchers drilled down on their data, they found that the following preexisting conditions were associated with readmissions among colectomy patients: steroid use, hypertension, readmission, cancer, COPD, smoking, poor functional status, and diabetes. At the same time, preexisting conditions associated with readmissions among vascular patients were diabetes and renal failure. The only preexisting condition associated with readmissions among thyroidectomy was renal failure. When the researchers evaluated the association between readmission risk and system-wide complications, they found that vascular surgery and urinary surgery conferred the highest risks (sixfold and fivefold, respectively).
“Just looking at your semiannual report quickly can give you a sense of which complications are associated with that readmission,” Dr. Sharma said. “There are many areas of potential intervention.” Preoperatively, he recommends screening surgery patients for obstructive sleep apnea, hypertension, and diabetes. “Looking at preexisting comorbid dyspnea, cancer, and renal failure can give you those target populations very quickly,” he said.
Intraoperatively, “it’s all about reduction of complications,” he said. These include using the WHO checklist, employing SSI prevention practices and considering certain anesthesia techniques such as low tidal volume ventilation and fluid limitation, control of hyperglycemia, and enhanced recovery after surgery protocols (ERAS).
Postoperative strategies to reduce readmission risk include ERAS for multimodal analgesia, fluid restriction, oral intake, and ambulation, and being aggressive about follow-up with high-risk populations and discharge planning. “The strategies for readmission reduction should be based on the preoperative assessment and the ability to identify high-risk populations,” Dr. Sharma said. “At Emory, we found that ileostomy patients had the highest risk of readmission. This made sense from a dehydration standpoint. So a colorectal surgeon led the creation of an Emory-wide protocol for teaching patients and their families, giving them signs of dehydration, what to look for, direct access to a dedicated nurse for follow-up, and an arrangement with the infusion center for rehydration as needed.”
He concluded by noting that there is no one-size-fits-all approach to reducing hospital readmissions. “I think an overarching readmission improvement process is not the way to go, unless you’re talking about a preoperative assessment area,” he said. “Identifying high-risk patients and giving them a lifeline where they can call so you can intervene and avoid that readmission, is better.”
Dr. Sharma reported having no relevant disclosures.
EXPERT ANALYSIS AT THE ACS NSQIP NATIONAL CONFERENCE
The drive to cut readmissions after bariatric surgery continues with DROP project
SAN DIEGO – John Morton, MD, started his bariatric surgery career about the same time that demand for gastric bypass and other bariatric procedures began to skyrocket. But a troubling trend emerged.
“About 10-15 years ago, bariatric surgery had a problem when it came to mortality,” Dr. Morton said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “You can’t move forward without looking back.”
A 2005 study of early mortality among Medicare beneficiaries undergoing bariatric procedures found a 30-day mortality of 9% and a 1-year mortality of 21% (JAMA 2005 Oct. 19;294[15]:1903-8). Such data prompted Dr. Morton and other leaders in the field to push for accreditation in the field. In 2012, the ACS Bariatric Surgery Center Network program and the American Society for Metabolic and Bariatric Surgery (ASMBS) Bariatric Centers of Excellence program were extended accreditation in the joint Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). As a result, the mortality rate among patients undergoing bariatric procedures has dropped nearly 10-fold and now stands at 1 out of 1,000, said Dr. Morton, chief of bariatric and minimally invasive surgery at Stanford (Calif.) University. “That’s been a real success story for us,” he said. “Part of it has been the accreditation program, having the resources in place to accomplish those goals.”
Of the 802 participating centers in MBSAQIP, 647 are accredited. “One of the reasons we see such good results at accredited centers is the fact that they work as a multidisciplinary team, where you have the nutritionist, the psychologist, the internist, and the anesthesiologist working together,” said Dr. Morton, immediate past president of the American Society for Metabolic and Bariatric Surgery. “When you have that team, it allows you to marshal your resources, do appropriate risk assessment, and get those processes in place to have the very best outcomes.”
In an effort to reduce hospital readmissions among bariatric surgery patients, MBSAQIP launched a national project called Decreasing Readmissions through Opportunities Provided (DROP), which currently has 129 participating hospitals. “If you drill down on the reasons for bariatric surgery readmissions, many are preventable: dehydration, nausea, medication side effects, and patient expectations,” Dr. Morton said. “I have a formula called the Morton Formula: happiness equals reality divided by expectations. If you set expectations accordingly, you’ll get a happier patient. If my patients know they’re going to be discharged in 1 day, they can plan accordingly.”
These concepts were adopted from a study that Dr. Morton and his associates carried out at Stanford Health Care in an effort to reduce readmissions for complications within 30 days to below the national average. It involved “straightforward” strategy including improving patient education, discharge planning, and giving patients a direct phone number to call. “Anybody who has called a health center and has had to go through that phone tree knows how difficult that can be, so we provide a direct number,” he said. “The postop phone call is critical, because that’s a way to nip readmissions in the bud. We do same-day appointments so they come and see us in the clinic rather than going to the ER and getting the enormous workup. Infusion centers are our best friend, because many of these patients come in dehydrated.”
After implementing these strategies, the rate of readmission for complications at Stanford fell from 8% to 2.5%. This led to the creation of a readmission bundle for the DROP project with steps for preoperative, intraoperative, and postoperative aspects of care. For example, preoperatively, “we make sure that they have a postop appointment made [and] rather than waiting to give them a prescription when they get discharged, we make sure that they have those prescriptions earlier at the preoperative visit,” he said. “They are provided the clinic phone number and patients watch video vignettes from all members of the team: surgeon, nurse, nutritionist, pharmacist, and psychologist. Rather than the education being dependent on [the surgeon’s schedule], they can get the same dose of education and even watch these over and over again if they want to.”
Surgeons who participate in the DROP project also stratify high-risk patients by consulting with their primary care physicians and case managers to achieve optimal outcomes. They address modifiable risk factors. “Weight gain prior to bariatric surgery is not ideal, so we want to address that, and have a hemoglobin A1c of less than 10%,” Dr. Morton said. Patients receive a “HELP” card, which instructs them to contact the treating clinic if they have abdominal pain, dehydration, nausea and vomiting, diarrhea, and fatigue.
The inpatient part of the bundle includes a “clinical roadmap” with a fixed length of stay. “There are expectations every single day about what’s going to happen to their care,” Dr. Morton said. “We give them a water bottle with the logo of the hospital. It’s a reminder for them to stay hydrated. They have a nutritional consult and they go through a checklist before they get discharged.”
The postoperative component of the DROP bundle includes a phone call to the patient following discharge. “They also get an appointment with a nutritionist within a month of surgery,” he said. “We treat readmissions seriously, like a complication.”
Data from a study of 18,296 primary bariatric surgery patients gleaned from 2012 ACS-NSQIP Participant Use Data Files found a 30-day readmission rate of 5.2% (Am J Surg 2016 Jul;212[1]:76-80). Compared with the patients’ counterparts who did not require readmission within 30 days, risk factors for those who did included body mass index greater than 50 kg/m2 (30.2% vs. 24.6%, respectively; P = .001); longer operative time (132 vs. 115 minutes; P = .001); length of stay greater than 4 days (9.57% vs. 3.36%; P = .001); surgical site infection (15.5% vs. 1.15%; P less than .001); urinary tract infection (3.15% vs. .65%; P less than .001), and deep vein thrombosis (3.58% vs. .13%; P less than .001). Common reasons for readmissions were GI-related (45%), dietary (33.5%), and bleeding (6.57%). Dr. Morton went on to report preliminary findings from 19,648 cases included in the DROP project, which began collecting data in March 2015 and has a yearlong goal of reducing national admission rates by 20%. The preintervention readmission rate was 4.79%. By the end of October 2015 the readmission rate had dropped to 4.30%. “One of the things we realized is that the hospitals with the higher readmission rates were the ones who had the greatest improvement,” Dr. Morton said. “They went from about 8% down to about 5.51%. We anticipate that for each quarter that we do this, we’ll continue to see improvement.”
Individual center results were made available in late January 2016 and reviewed with mentors. “They also received aggregated reports to see how they stacked up others as a benchmark,” Dr. Morton said.
Final results from DROP are expected to be released later in 2016.
Dr. Morton reported having no financial disclosures.
SAN DIEGO – John Morton, MD, started his bariatric surgery career about the same time that demand for gastric bypass and other bariatric procedures began to skyrocket. But a troubling trend emerged.
“About 10-15 years ago, bariatric surgery had a problem when it came to mortality,” Dr. Morton said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “You can’t move forward without looking back.”
A 2005 study of early mortality among Medicare beneficiaries undergoing bariatric procedures found a 30-day mortality of 9% and a 1-year mortality of 21% (JAMA 2005 Oct. 19;294[15]:1903-8). Such data prompted Dr. Morton and other leaders in the field to push for accreditation in the field. In 2012, the ACS Bariatric Surgery Center Network program and the American Society for Metabolic and Bariatric Surgery (ASMBS) Bariatric Centers of Excellence program were extended accreditation in the joint Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). As a result, the mortality rate among patients undergoing bariatric procedures has dropped nearly 10-fold and now stands at 1 out of 1,000, said Dr. Morton, chief of bariatric and minimally invasive surgery at Stanford (Calif.) University. “That’s been a real success story for us,” he said. “Part of it has been the accreditation program, having the resources in place to accomplish those goals.”
Of the 802 participating centers in MBSAQIP, 647 are accredited. “One of the reasons we see such good results at accredited centers is the fact that they work as a multidisciplinary team, where you have the nutritionist, the psychologist, the internist, and the anesthesiologist working together,” said Dr. Morton, immediate past president of the American Society for Metabolic and Bariatric Surgery. “When you have that team, it allows you to marshal your resources, do appropriate risk assessment, and get those processes in place to have the very best outcomes.”
In an effort to reduce hospital readmissions among bariatric surgery patients, MBSAQIP launched a national project called Decreasing Readmissions through Opportunities Provided (DROP), which currently has 129 participating hospitals. “If you drill down on the reasons for bariatric surgery readmissions, many are preventable: dehydration, nausea, medication side effects, and patient expectations,” Dr. Morton said. “I have a formula called the Morton Formula: happiness equals reality divided by expectations. If you set expectations accordingly, you’ll get a happier patient. If my patients know they’re going to be discharged in 1 day, they can plan accordingly.”
These concepts were adopted from a study that Dr. Morton and his associates carried out at Stanford Health Care in an effort to reduce readmissions for complications within 30 days to below the national average. It involved “straightforward” strategy including improving patient education, discharge planning, and giving patients a direct phone number to call. “Anybody who has called a health center and has had to go through that phone tree knows how difficult that can be, so we provide a direct number,” he said. “The postop phone call is critical, because that’s a way to nip readmissions in the bud. We do same-day appointments so they come and see us in the clinic rather than going to the ER and getting the enormous workup. Infusion centers are our best friend, because many of these patients come in dehydrated.”
After implementing these strategies, the rate of readmission for complications at Stanford fell from 8% to 2.5%. This led to the creation of a readmission bundle for the DROP project with steps for preoperative, intraoperative, and postoperative aspects of care. For example, preoperatively, “we make sure that they have a postop appointment made [and] rather than waiting to give them a prescription when they get discharged, we make sure that they have those prescriptions earlier at the preoperative visit,” he said. “They are provided the clinic phone number and patients watch video vignettes from all members of the team: surgeon, nurse, nutritionist, pharmacist, and psychologist. Rather than the education being dependent on [the surgeon’s schedule], they can get the same dose of education and even watch these over and over again if they want to.”
Surgeons who participate in the DROP project also stratify high-risk patients by consulting with their primary care physicians and case managers to achieve optimal outcomes. They address modifiable risk factors. “Weight gain prior to bariatric surgery is not ideal, so we want to address that, and have a hemoglobin A1c of less than 10%,” Dr. Morton said. Patients receive a “HELP” card, which instructs them to contact the treating clinic if they have abdominal pain, dehydration, nausea and vomiting, diarrhea, and fatigue.
The inpatient part of the bundle includes a “clinical roadmap” with a fixed length of stay. “There are expectations every single day about what’s going to happen to their care,” Dr. Morton said. “We give them a water bottle with the logo of the hospital. It’s a reminder for them to stay hydrated. They have a nutritional consult and they go through a checklist before they get discharged.”
The postoperative component of the DROP bundle includes a phone call to the patient following discharge. “They also get an appointment with a nutritionist within a month of surgery,” he said. “We treat readmissions seriously, like a complication.”
Data from a study of 18,296 primary bariatric surgery patients gleaned from 2012 ACS-NSQIP Participant Use Data Files found a 30-day readmission rate of 5.2% (Am J Surg 2016 Jul;212[1]:76-80). Compared with the patients’ counterparts who did not require readmission within 30 days, risk factors for those who did included body mass index greater than 50 kg/m2 (30.2% vs. 24.6%, respectively; P = .001); longer operative time (132 vs. 115 minutes; P = .001); length of stay greater than 4 days (9.57% vs. 3.36%; P = .001); surgical site infection (15.5% vs. 1.15%; P less than .001); urinary tract infection (3.15% vs. .65%; P less than .001), and deep vein thrombosis (3.58% vs. .13%; P less than .001). Common reasons for readmissions were GI-related (45%), dietary (33.5%), and bleeding (6.57%). Dr. Morton went on to report preliminary findings from 19,648 cases included in the DROP project, which began collecting data in March 2015 and has a yearlong goal of reducing national admission rates by 20%. The preintervention readmission rate was 4.79%. By the end of October 2015 the readmission rate had dropped to 4.30%. “One of the things we realized is that the hospitals with the higher readmission rates were the ones who had the greatest improvement,” Dr. Morton said. “They went from about 8% down to about 5.51%. We anticipate that for each quarter that we do this, we’ll continue to see improvement.”
Individual center results were made available in late January 2016 and reviewed with mentors. “They also received aggregated reports to see how they stacked up others as a benchmark,” Dr. Morton said.
Final results from DROP are expected to be released later in 2016.
Dr. Morton reported having no financial disclosures.
SAN DIEGO – John Morton, MD, started his bariatric surgery career about the same time that demand for gastric bypass and other bariatric procedures began to skyrocket. But a troubling trend emerged.
“About 10-15 years ago, bariatric surgery had a problem when it came to mortality,” Dr. Morton said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “You can’t move forward without looking back.”
A 2005 study of early mortality among Medicare beneficiaries undergoing bariatric procedures found a 30-day mortality of 9% and a 1-year mortality of 21% (JAMA 2005 Oct. 19;294[15]:1903-8). Such data prompted Dr. Morton and other leaders in the field to push for accreditation in the field. In 2012, the ACS Bariatric Surgery Center Network program and the American Society for Metabolic and Bariatric Surgery (ASMBS) Bariatric Centers of Excellence program were extended accreditation in the joint Metabolic and Bariatric Surgery Accreditation and Quality Improvement Program (MBSAQIP). As a result, the mortality rate among patients undergoing bariatric procedures has dropped nearly 10-fold and now stands at 1 out of 1,000, said Dr. Morton, chief of bariatric and minimally invasive surgery at Stanford (Calif.) University. “That’s been a real success story for us,” he said. “Part of it has been the accreditation program, having the resources in place to accomplish those goals.”
Of the 802 participating centers in MBSAQIP, 647 are accredited. “One of the reasons we see such good results at accredited centers is the fact that they work as a multidisciplinary team, where you have the nutritionist, the psychologist, the internist, and the anesthesiologist working together,” said Dr. Morton, immediate past president of the American Society for Metabolic and Bariatric Surgery. “When you have that team, it allows you to marshal your resources, do appropriate risk assessment, and get those processes in place to have the very best outcomes.”
In an effort to reduce hospital readmissions among bariatric surgery patients, MBSAQIP launched a national project called Decreasing Readmissions through Opportunities Provided (DROP), which currently has 129 participating hospitals. “If you drill down on the reasons for bariatric surgery readmissions, many are preventable: dehydration, nausea, medication side effects, and patient expectations,” Dr. Morton said. “I have a formula called the Morton Formula: happiness equals reality divided by expectations. If you set expectations accordingly, you’ll get a happier patient. If my patients know they’re going to be discharged in 1 day, they can plan accordingly.”
These concepts were adopted from a study that Dr. Morton and his associates carried out at Stanford Health Care in an effort to reduce readmissions for complications within 30 days to below the national average. It involved “straightforward” strategy including improving patient education, discharge planning, and giving patients a direct phone number to call. “Anybody who has called a health center and has had to go through that phone tree knows how difficult that can be, so we provide a direct number,” he said. “The postop phone call is critical, because that’s a way to nip readmissions in the bud. We do same-day appointments so they come and see us in the clinic rather than going to the ER and getting the enormous workup. Infusion centers are our best friend, because many of these patients come in dehydrated.”
After implementing these strategies, the rate of readmission for complications at Stanford fell from 8% to 2.5%. This led to the creation of a readmission bundle for the DROP project with steps for preoperative, intraoperative, and postoperative aspects of care. For example, preoperatively, “we make sure that they have a postop appointment made [and] rather than waiting to give them a prescription when they get discharged, we make sure that they have those prescriptions earlier at the preoperative visit,” he said. “They are provided the clinic phone number and patients watch video vignettes from all members of the team: surgeon, nurse, nutritionist, pharmacist, and psychologist. Rather than the education being dependent on [the surgeon’s schedule], they can get the same dose of education and even watch these over and over again if they want to.”
Surgeons who participate in the DROP project also stratify high-risk patients by consulting with their primary care physicians and case managers to achieve optimal outcomes. They address modifiable risk factors. “Weight gain prior to bariatric surgery is not ideal, so we want to address that, and have a hemoglobin A1c of less than 10%,” Dr. Morton said. Patients receive a “HELP” card, which instructs them to contact the treating clinic if they have abdominal pain, dehydration, nausea and vomiting, diarrhea, and fatigue.
The inpatient part of the bundle includes a “clinical roadmap” with a fixed length of stay. “There are expectations every single day about what’s going to happen to their care,” Dr. Morton said. “We give them a water bottle with the logo of the hospital. It’s a reminder for them to stay hydrated. They have a nutritional consult and they go through a checklist before they get discharged.”
The postoperative component of the DROP bundle includes a phone call to the patient following discharge. “They also get an appointment with a nutritionist within a month of surgery,” he said. “We treat readmissions seriously, like a complication.”
Data from a study of 18,296 primary bariatric surgery patients gleaned from 2012 ACS-NSQIP Participant Use Data Files found a 30-day readmission rate of 5.2% (Am J Surg 2016 Jul;212[1]:76-80). Compared with the patients’ counterparts who did not require readmission within 30 days, risk factors for those who did included body mass index greater than 50 kg/m2 (30.2% vs. 24.6%, respectively; P = .001); longer operative time (132 vs. 115 minutes; P = .001); length of stay greater than 4 days (9.57% vs. 3.36%; P = .001); surgical site infection (15.5% vs. 1.15%; P less than .001); urinary tract infection (3.15% vs. .65%; P less than .001), and deep vein thrombosis (3.58% vs. .13%; P less than .001). Common reasons for readmissions were GI-related (45%), dietary (33.5%), and bleeding (6.57%). Dr. Morton went on to report preliminary findings from 19,648 cases included in the DROP project, which began collecting data in March 2015 and has a yearlong goal of reducing national admission rates by 20%. The preintervention readmission rate was 4.79%. By the end of October 2015 the readmission rate had dropped to 4.30%. “One of the things we realized is that the hospitals with the higher readmission rates were the ones who had the greatest improvement,” Dr. Morton said. “They went from about 8% down to about 5.51%. We anticipate that for each quarter that we do this, we’ll continue to see improvement.”
Individual center results were made available in late January 2016 and reviewed with mentors. “They also received aggregated reports to see how they stacked up others as a benchmark,” Dr. Morton said.
Final results from DROP are expected to be released later in 2016.
Dr. Morton reported having no financial disclosures.
EXPERT ANALYSIS AT THE ACS NSQIP NATIONAL CONFERENCE
Blood management strategy leads to cost savings, less waste
SAN DIEGO – A process intended to optimize blood management led to a 30% reduction in blood use and a savings of $2 million, results from a single-center study showed.
“Blood is a limited resource and we have a responsibility as a health care provider to optimize the use of a resource that is difficult to get and only available through altruistic donations,” lead study author Barbara J. Martin, RN, said in a press release. The study was presented in a poster session at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
In an effort to evaluate how they could implement evidence-based guidelines around restrictive transfusion, Ms. Martin and her colleagues at Vanderbilt University Medical Center, Nashville, Tenn., first changed provider orders to support a single unit order and then follow-up order for more blood if necessary. The previous process was to order two units of blood, which was at times more blood than was needed. “The data on restrictive transfusion has been out for years documenting that patients have better outcomes with a more restrictive transfusion strategy,” Ms. Martin, of the Vanderbilt Center for Clinical Improvement, said in the press release. “We were looking at whether we could guide providers to treat symptomatic anemia with a single unit of blood rather than the usual two units.”
The researchers enhanced the Computerized Provider Order Entry (CPOE) system to allow blood ordering practices to be based on a specific assessment of each case rather than on a standard order of two units. As a result, red blood cell transfusions at Vanderbilt declined from 675 units per 1,000 discharges in 2011 to 432 units per 1,000 discharges in 2015, a decrease of more than 30%.
In an effort to reduce inefficiencies in the way blood is ordered, transported, and stored, Ms. Martin and her multidisciplinary team developed the following guidelines for perioperative handling:
• When more than one unit of blood is ordered, it is sent in a cooler rather than the pneumatic tube.
• Coolers are reconfigured to optimize temperature management.
• A specific staff member is tasked with “ownership” of the blood products, including returning unused product to the blood bank.
• Individual unit wastage is reported to clinical leaders for review; aggregate data are reported monthly.
After implementation of these practices, fewer than 80 units of blood were wasted at Vanderbilt in 2015, a drop from 300 in 2011. Collectively, the blood management strategies resulted in a savings of $2 million. Ms. Martin said that such guidelines can be implemented at other medical centers, but “you have to prioritize what your initiatives are. At Vanderbilt we had a lot of opportunities with blood transfusion and blood wastage and we made huge gains. Any incremental improvement would take additional resources.”
The researchers reported having no relevant disclosures.
SAN DIEGO – A process intended to optimize blood management led to a 30% reduction in blood use and a savings of $2 million, results from a single-center study showed.
“Blood is a limited resource and we have a responsibility as a health care provider to optimize the use of a resource that is difficult to get and only available through altruistic donations,” lead study author Barbara J. Martin, RN, said in a press release. The study was presented in a poster session at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
In an effort to evaluate how they could implement evidence-based guidelines around restrictive transfusion, Ms. Martin and her colleagues at Vanderbilt University Medical Center, Nashville, Tenn., first changed provider orders to support a single unit order and then follow-up order for more blood if necessary. The previous process was to order two units of blood, which was at times more blood than was needed. “The data on restrictive transfusion has been out for years documenting that patients have better outcomes with a more restrictive transfusion strategy,” Ms. Martin, of the Vanderbilt Center for Clinical Improvement, said in the press release. “We were looking at whether we could guide providers to treat symptomatic anemia with a single unit of blood rather than the usual two units.”
The researchers enhanced the Computerized Provider Order Entry (CPOE) system to allow blood ordering practices to be based on a specific assessment of each case rather than on a standard order of two units. As a result, red blood cell transfusions at Vanderbilt declined from 675 units per 1,000 discharges in 2011 to 432 units per 1,000 discharges in 2015, a decrease of more than 30%.
In an effort to reduce inefficiencies in the way blood is ordered, transported, and stored, Ms. Martin and her multidisciplinary team developed the following guidelines for perioperative handling:
• When more than one unit of blood is ordered, it is sent in a cooler rather than the pneumatic tube.
• Coolers are reconfigured to optimize temperature management.
• A specific staff member is tasked with “ownership” of the blood products, including returning unused product to the blood bank.
• Individual unit wastage is reported to clinical leaders for review; aggregate data are reported monthly.
After implementation of these practices, fewer than 80 units of blood were wasted at Vanderbilt in 2015, a drop from 300 in 2011. Collectively, the blood management strategies resulted in a savings of $2 million. Ms. Martin said that such guidelines can be implemented at other medical centers, but “you have to prioritize what your initiatives are. At Vanderbilt we had a lot of opportunities with blood transfusion and blood wastage and we made huge gains. Any incremental improvement would take additional resources.”
The researchers reported having no relevant disclosures.
SAN DIEGO – A process intended to optimize blood management led to a 30% reduction in blood use and a savings of $2 million, results from a single-center study showed.
“Blood is a limited resource and we have a responsibility as a health care provider to optimize the use of a resource that is difficult to get and only available through altruistic donations,” lead study author Barbara J. Martin, RN, said in a press release. The study was presented in a poster session at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
In an effort to evaluate how they could implement evidence-based guidelines around restrictive transfusion, Ms. Martin and her colleagues at Vanderbilt University Medical Center, Nashville, Tenn., first changed provider orders to support a single unit order and then follow-up order for more blood if necessary. The previous process was to order two units of blood, which was at times more blood than was needed. “The data on restrictive transfusion has been out for years documenting that patients have better outcomes with a more restrictive transfusion strategy,” Ms. Martin, of the Vanderbilt Center for Clinical Improvement, said in the press release. “We were looking at whether we could guide providers to treat symptomatic anemia with a single unit of blood rather than the usual two units.”
The researchers enhanced the Computerized Provider Order Entry (CPOE) system to allow blood ordering practices to be based on a specific assessment of each case rather than on a standard order of two units. As a result, red blood cell transfusions at Vanderbilt declined from 675 units per 1,000 discharges in 2011 to 432 units per 1,000 discharges in 2015, a decrease of more than 30%.
In an effort to reduce inefficiencies in the way blood is ordered, transported, and stored, Ms. Martin and her multidisciplinary team developed the following guidelines for perioperative handling:
• When more than one unit of blood is ordered, it is sent in a cooler rather than the pneumatic tube.
• Coolers are reconfigured to optimize temperature management.
• A specific staff member is tasked with “ownership” of the blood products, including returning unused product to the blood bank.
• Individual unit wastage is reported to clinical leaders for review; aggregate data are reported monthly.
After implementation of these practices, fewer than 80 units of blood were wasted at Vanderbilt in 2015, a drop from 300 in 2011. Collectively, the blood management strategies resulted in a savings of $2 million. Ms. Martin said that such guidelines can be implemented at other medical centers, but “you have to prioritize what your initiatives are. At Vanderbilt we had a lot of opportunities with blood transfusion and blood wastage and we made huge gains. Any incremental improvement would take additional resources.”
The researchers reported having no relevant disclosures.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: A multidisciplinary effort to improve the process of blood product management led to a significantly reduced use of blood products.
Major finding: Red blood cell transfusions declined from 675 units per 1,000 discharges in 2011 to 432 units per 1,000 discharges in 2015, a decrease of more than 30%.
Data source: An alteration of the Computerized Provider Order Entry (CPOE) system at Vanderbilt University Medical Center to allow blood ordering practices to be based on a specific assessment of each case rather than on a standard order of two units.
Disclosures: The researchers reported having no financial disclosures.
Common surgeries linked to chronic opioid use among opioid-naive patients
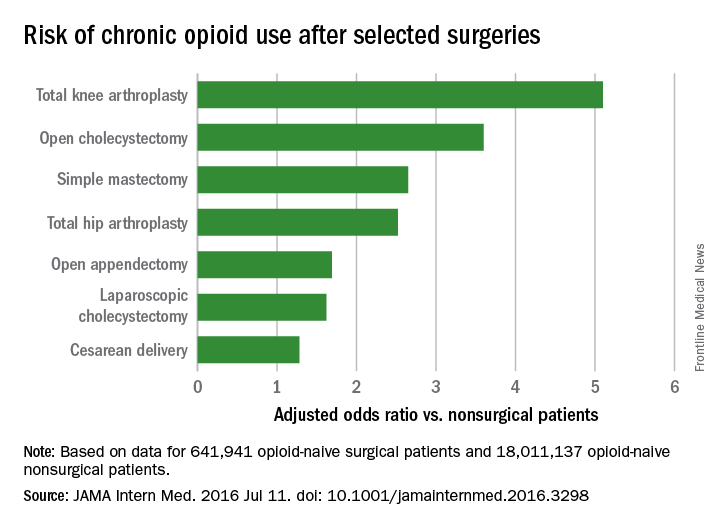
Common surgeries increase the risk of chronic opioid use in opioid-naive adults, especially those using antidepressants or benzodiazepines before their operations, and those with substance abuse histories, according to an insurance claims analysis from Stanford (Calif.) University.
The researchers reviewed opioid prescribing in the first postop year – excluding the first 90 days – for 641,941 patients and compared that information with opioid prescribing for 18,011,137 adult patients who did not have surgery. None of the subjects had filled an opioid prescription in the previous year (JAMA Intern Med. 2016 Jul 11. doi: 10.1001/jamainternmed.2016.3298).
Chronic opioid use, defined as filling at least 120 days of opioid prescriptions within the first year of surgery, ranged up to 1.41% for total knee replacement, versus 0.136% in the nonsurgical controls. After adjustment for potential confounders, knee replacement increased the risk fivefold; open cholecystectomy almost fourfold; total hip replacement and simple mastectomy almost threefold; and laparoscopic cholecystectomy and open appendectomy almost twofold. Cesarean delivery increased the risk of chronic use by 28%.
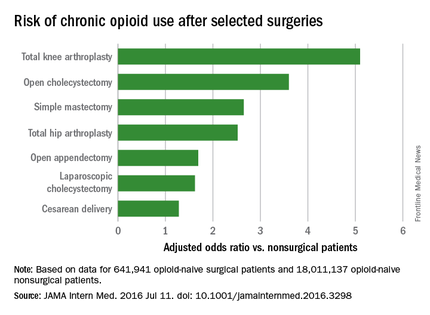
With the exception of knee and hip replacements, “these procedures are not indicated to relieve pain and are not thought to place patients at risk for long-term pain ... Our results suggest that primary care clinicians and surgeons should monitor opioid use closely in the postsurgical period,” wrote Eric C. Sun, MD, PhD, of the department of anesthesiology, perioperative and pain medicine at Stanford (Calif.) University, and his colleagues.
Preoperative antidepressants and benzodiazepines carried about the same risk of chronic use as alcohol abuse (odds ratio 1.83; P less than .001), while drug abuse history increased the risk even more (OR 3.15; P less than .001). Male sex, age over 50 years, and history of depression were also associated with chronic use on multivariate analysis. Meanwhile, transurethral prostatectomy, laparoscopic appendectomy, functional endoscopic sinus surgery, and cataract surgery did not increase chronic use risk.
“Surgical patients, particularly those at higher risk for chronic opioid use, may benefit from techniques to reduce the risk such as multimodal analgesia and regional anesthesia, particularly in light of literature suggesting that these interventions may improve other perioperative outcomes ... Patients may also benefit from other preoperative and postoperative interventions, such as evidence-based psychobehavioral pain management skills,” the investigators said.
It wasn’t clear until now that even opioid-naive patients are at risk for opioid problems after surgery. Stanford’s investigation is not the first to link surgery and opioid abuse, but previous studies tended to focus on patients with preexisting use and more painful operations.
The study included prescriptions for oral and patch fentanyl, hydrocodone, oral hydromorphone, methadone, morphine, oxymorphone, and oxycodone. Hydrocodone cough remedies and acetaminophen/codeine analgesics were excluded.
Nonsurgical patients tended to be younger than their surgical peers (mean 42 vs. 44 years) and more likely to be male (49% vs. 26%).
The authors had no disclosures. The work was funded in part by the Foundation for Anesthesia Education and Research and the Anesthesia Quality Institute. Claims data came from MarketScan (Truven Health Analytics).
Common surgeries increase the risk of chronic opioid use in opioid-naive adults, especially those using antidepressants or benzodiazepines before their operations, and those with substance abuse histories, according to an insurance claims analysis from Stanford (Calif.) University.
The researchers reviewed opioid prescribing in the first postop year – excluding the first 90 days – for 641,941 patients and compared that information with opioid prescribing for 18,011,137 adult patients who did not have surgery. None of the subjects had filled an opioid prescription in the previous year (JAMA Intern Med. 2016 Jul 11. doi: 10.1001/jamainternmed.2016.3298).
Chronic opioid use, defined as filling at least 120 days of opioid prescriptions within the first year of surgery, ranged up to 1.41% for total knee replacement, versus 0.136% in the nonsurgical controls. After adjustment for potential confounders, knee replacement increased the risk fivefold; open cholecystectomy almost fourfold; total hip replacement and simple mastectomy almost threefold; and laparoscopic cholecystectomy and open appendectomy almost twofold. Cesarean delivery increased the risk of chronic use by 28%.
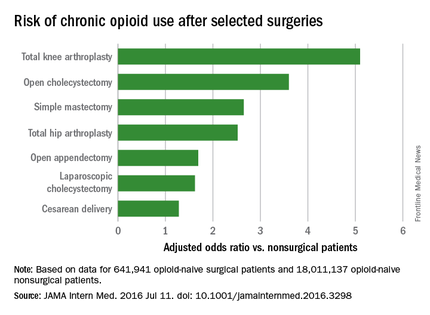
With the exception of knee and hip replacements, “these procedures are not indicated to relieve pain and are not thought to place patients at risk for long-term pain ... Our results suggest that primary care clinicians and surgeons should monitor opioid use closely in the postsurgical period,” wrote Eric C. Sun, MD, PhD, of the department of anesthesiology, perioperative and pain medicine at Stanford (Calif.) University, and his colleagues.
Preoperative antidepressants and benzodiazepines carried about the same risk of chronic use as alcohol abuse (odds ratio 1.83; P less than .001), while drug abuse history increased the risk even more (OR 3.15; P less than .001). Male sex, age over 50 years, and history of depression were also associated with chronic use on multivariate analysis. Meanwhile, transurethral prostatectomy, laparoscopic appendectomy, functional endoscopic sinus surgery, and cataract surgery did not increase chronic use risk.
“Surgical patients, particularly those at higher risk for chronic opioid use, may benefit from techniques to reduce the risk such as multimodal analgesia and regional anesthesia, particularly in light of literature suggesting that these interventions may improve other perioperative outcomes ... Patients may also benefit from other preoperative and postoperative interventions, such as evidence-based psychobehavioral pain management skills,” the investigators said.
It wasn’t clear until now that even opioid-naive patients are at risk for opioid problems after surgery. Stanford’s investigation is not the first to link surgery and opioid abuse, but previous studies tended to focus on patients with preexisting use and more painful operations.
The study included prescriptions for oral and patch fentanyl, hydrocodone, oral hydromorphone, methadone, morphine, oxymorphone, and oxycodone. Hydrocodone cough remedies and acetaminophen/codeine analgesics were excluded.
Nonsurgical patients tended to be younger than their surgical peers (mean 42 vs. 44 years) and more likely to be male (49% vs. 26%).
The authors had no disclosures. The work was funded in part by the Foundation for Anesthesia Education and Research and the Anesthesia Quality Institute. Claims data came from MarketScan (Truven Health Analytics).
Common surgeries increase the risk of chronic opioid use in opioid-naive adults, especially those using antidepressants or benzodiazepines before their operations, and those with substance abuse histories, according to an insurance claims analysis from Stanford (Calif.) University.
The researchers reviewed opioid prescribing in the first postop year – excluding the first 90 days – for 641,941 patients and compared that information with opioid prescribing for 18,011,137 adult patients who did not have surgery. None of the subjects had filled an opioid prescription in the previous year (JAMA Intern Med. 2016 Jul 11. doi: 10.1001/jamainternmed.2016.3298).
Chronic opioid use, defined as filling at least 120 days of opioid prescriptions within the first year of surgery, ranged up to 1.41% for total knee replacement, versus 0.136% in the nonsurgical controls. After adjustment for potential confounders, knee replacement increased the risk fivefold; open cholecystectomy almost fourfold; total hip replacement and simple mastectomy almost threefold; and laparoscopic cholecystectomy and open appendectomy almost twofold. Cesarean delivery increased the risk of chronic use by 28%.
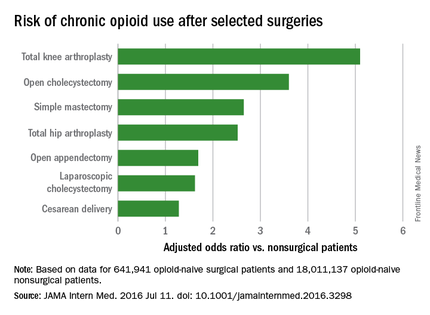
With the exception of knee and hip replacements, “these procedures are not indicated to relieve pain and are not thought to place patients at risk for long-term pain ... Our results suggest that primary care clinicians and surgeons should monitor opioid use closely in the postsurgical period,” wrote Eric C. Sun, MD, PhD, of the department of anesthesiology, perioperative and pain medicine at Stanford (Calif.) University, and his colleagues.
Preoperative antidepressants and benzodiazepines carried about the same risk of chronic use as alcohol abuse (odds ratio 1.83; P less than .001), while drug abuse history increased the risk even more (OR 3.15; P less than .001). Male sex, age over 50 years, and history of depression were also associated with chronic use on multivariate analysis. Meanwhile, transurethral prostatectomy, laparoscopic appendectomy, functional endoscopic sinus surgery, and cataract surgery did not increase chronic use risk.
“Surgical patients, particularly those at higher risk for chronic opioid use, may benefit from techniques to reduce the risk such as multimodal analgesia and regional anesthesia, particularly in light of literature suggesting that these interventions may improve other perioperative outcomes ... Patients may also benefit from other preoperative and postoperative interventions, such as evidence-based psychobehavioral pain management skills,” the investigators said.
It wasn’t clear until now that even opioid-naive patients are at risk for opioid problems after surgery. Stanford’s investigation is not the first to link surgery and opioid abuse, but previous studies tended to focus on patients with preexisting use and more painful operations.
The study included prescriptions for oral and patch fentanyl, hydrocodone, oral hydromorphone, methadone, morphine, oxymorphone, and oxycodone. Hydrocodone cough remedies and acetaminophen/codeine analgesics were excluded.
Nonsurgical patients tended to be younger than their surgical peers (mean 42 vs. 44 years) and more likely to be male (49% vs. 26%).
The authors had no disclosures. The work was funded in part by the Foundation for Anesthesia Education and Research and the Anesthesia Quality Institute. Claims data came from MarketScan (Truven Health Analytics).
FROM JAMA INTERNAL MEDICINE
Key clinical point: Common surgeries increase the risk of chronic opioid use in opioid-naive adults, especially among those using antidepressants or benzodiazepines before their operations, and those with substance abuse histories.
Major finding: After adjustment for potential confounders, knee replacement increased the risk fivefold; open cholecystectomy almost fourfold; and total hip replacement and simple mastectomy almost threefold.
Data source: Insurance claims of more than 18 million people.
Disclosures: The authors had no disclosures. The work was funded in part by the Foundation for Anesthesia Education and Research and the Anesthesia Quality Institute. Claims data came from MarketScan (Truven Health Analytics).
Syndecan-1 may predict kidney injury after ped heart surgery
Acute kidney injury is a common complication after pediatric cardiac surgery, but measuring for a specific genetic protein immediately after cardiac surgery may improve cardiac surgeons’ ability to predict patients at higher risk of AKI, according to researchers from Brazil. The study results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152-178-86).
“Plasma syndecan-1 levels measured early in the postoperative period were independently associated with severe acute kidney injury,” wrote Candice Torres de Melo Bezerra Cavalcante, MD, of Heart Hospital of Messejana and Federal University of Ceará.
Their prospective cohort study involved 289 pediatric patients who had cardiac surgery at their institution between September 2013 and December 2014.
Dr. Cavalcante and colleagues acknowledged that the traditional biomarker for renal function, serum creatinine, only increases appreciably after the glomerular filtration rate declines 50%, impairing physicians’ ability to detect AKI early enough to treat it. “This delay can explain, in part the, negative results in AKI therapeutic clinical trials,” they wrote.
They evaluated two different endothelial biomarkers in addition to syndecan-1 with regard to their capacity for predicting severe AKI: plasma ICAM-1, a marker of endothelial cell activation; and E-selectin, an endothelial cell adhesion molecule. Syndecan-1 works as a biomarker of injury to the glycocalyx protein that surrounds endothelial cell membranes that acts as a permeability barrier and prevents the cells from adhering to blood. They found that median syndecan-1 levels soon after surgery were higher in patients with severe AKI, 103.6 vs. 42.3 ng/mL.
“Although syndecan-1 is not a renal-specific biomarker, there has been recent increasing evidence that endothelial injury has an important role in AKI pathophysiology,” the researchers noted.
Study results showed the higher the level of syndecan-1, the greater the adjusted odds ratio (OR) for severe AKI. Levels of less than 17 ng/mL were considered normal; 17.1-46.7 ng/mL carried an adjusted OR of 1.42; 47.4-93.1 ng/mL had an adjusted OR of 2.05; and levels 96.3 or greater had an OR of 8.87.
“Maintenance of endothelial glycocalyx integrity can be a therapeutic target to reduce AKI in this setting,” the researchers wrote.
The authors acknowledged that the study was done at a single center that had dialysis and death rates three and five times higher, respectively, than those of developed countries; and it measured syndecan-1 at only one time point almost immediately after the operation.
“Adding postoperative syndecan-1, even when using a clinical model that already incorporates variables from renal angina index, results in significant improvement in the capacity to predict severe AKI,” Dr. Cavalcante and colleagues concluded.
They had no financial relationships to disclose.
Results of AKI in heart surgery patients have been “sobering,” with up to 56% of these patients being diagnosed with AKI, but research such as that by Dr. Cavalcante and colleagues represents a new approach to improving outcomes by combining clinical risk factors with specific biomarkers to identify patients at risk, Petros V. Anagnostopoulos, MD, of American Family Children’s Hospital, University of Wisconsin, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152[1]:187-8).
Dr. Anagnostopoulos acknowledged problems with traditional markers for renal function. “An ideal biomarker should be sensitive, easy to measure, reproducible, and inexpensive,” he said. “Finally, when combined with clinical prediction models, it should potentiate the discrimination of these models.”
Syndecan-1 answers that call, he said. “It peaks early and is cheap, fast, and easy to measure with readily available methods, which makes it an ideal early biomarker of AKI,” Dr. Anagnostopoulos said. Even so, he pointed out potential shortcomings of syndecan-1: It is not renal specific and it does not increase before the operation.
But he applauded Dr. Cavalcante and colleagues for pursuing research to combine clinical risk factors with specific biomarkers. “It is very likely that this type of clinical research will become prevalent in the near future and will hopefully produce results that will allow better individual patient-specific risk stratification,” Dr. Anagnostopoulos said.
He had no financial relationships to disclose.
Results of AKI in heart surgery patients have been “sobering,” with up to 56% of these patients being diagnosed with AKI, but research such as that by Dr. Cavalcante and colleagues represents a new approach to improving outcomes by combining clinical risk factors with specific biomarkers to identify patients at risk, Petros V. Anagnostopoulos, MD, of American Family Children’s Hospital, University of Wisconsin, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152[1]:187-8).
Dr. Anagnostopoulos acknowledged problems with traditional markers for renal function. “An ideal biomarker should be sensitive, easy to measure, reproducible, and inexpensive,” he said. “Finally, when combined with clinical prediction models, it should potentiate the discrimination of these models.”
Syndecan-1 answers that call, he said. “It peaks early and is cheap, fast, and easy to measure with readily available methods, which makes it an ideal early biomarker of AKI,” Dr. Anagnostopoulos said. Even so, he pointed out potential shortcomings of syndecan-1: It is not renal specific and it does not increase before the operation.
But he applauded Dr. Cavalcante and colleagues for pursuing research to combine clinical risk factors with specific biomarkers. “It is very likely that this type of clinical research will become prevalent in the near future and will hopefully produce results that will allow better individual patient-specific risk stratification,” Dr. Anagnostopoulos said.
He had no financial relationships to disclose.
Results of AKI in heart surgery patients have been “sobering,” with up to 56% of these patients being diagnosed with AKI, but research such as that by Dr. Cavalcante and colleagues represents a new approach to improving outcomes by combining clinical risk factors with specific biomarkers to identify patients at risk, Petros V. Anagnostopoulos, MD, of American Family Children’s Hospital, University of Wisconsin, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152[1]:187-8).
Dr. Anagnostopoulos acknowledged problems with traditional markers for renal function. “An ideal biomarker should be sensitive, easy to measure, reproducible, and inexpensive,” he said. “Finally, when combined with clinical prediction models, it should potentiate the discrimination of these models.”
Syndecan-1 answers that call, he said. “It peaks early and is cheap, fast, and easy to measure with readily available methods, which makes it an ideal early biomarker of AKI,” Dr. Anagnostopoulos said. Even so, he pointed out potential shortcomings of syndecan-1: It is not renal specific and it does not increase before the operation.
But he applauded Dr. Cavalcante and colleagues for pursuing research to combine clinical risk factors with specific biomarkers. “It is very likely that this type of clinical research will become prevalent in the near future and will hopefully produce results that will allow better individual patient-specific risk stratification,” Dr. Anagnostopoulos said.
He had no financial relationships to disclose.
Acute kidney injury is a common complication after pediatric cardiac surgery, but measuring for a specific genetic protein immediately after cardiac surgery may improve cardiac surgeons’ ability to predict patients at higher risk of AKI, according to researchers from Brazil. The study results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152-178-86).
“Plasma syndecan-1 levels measured early in the postoperative period were independently associated with severe acute kidney injury,” wrote Candice Torres de Melo Bezerra Cavalcante, MD, of Heart Hospital of Messejana and Federal University of Ceará.
Their prospective cohort study involved 289 pediatric patients who had cardiac surgery at their institution between September 2013 and December 2014.
Dr. Cavalcante and colleagues acknowledged that the traditional biomarker for renal function, serum creatinine, only increases appreciably after the glomerular filtration rate declines 50%, impairing physicians’ ability to detect AKI early enough to treat it. “This delay can explain, in part the, negative results in AKI therapeutic clinical trials,” they wrote.
They evaluated two different endothelial biomarkers in addition to syndecan-1 with regard to their capacity for predicting severe AKI: plasma ICAM-1, a marker of endothelial cell activation; and E-selectin, an endothelial cell adhesion molecule. Syndecan-1 works as a biomarker of injury to the glycocalyx protein that surrounds endothelial cell membranes that acts as a permeability barrier and prevents the cells from adhering to blood. They found that median syndecan-1 levels soon after surgery were higher in patients with severe AKI, 103.6 vs. 42.3 ng/mL.
“Although syndecan-1 is not a renal-specific biomarker, there has been recent increasing evidence that endothelial injury has an important role in AKI pathophysiology,” the researchers noted.
Study results showed the higher the level of syndecan-1, the greater the adjusted odds ratio (OR) for severe AKI. Levels of less than 17 ng/mL were considered normal; 17.1-46.7 ng/mL carried an adjusted OR of 1.42; 47.4-93.1 ng/mL had an adjusted OR of 2.05; and levels 96.3 or greater had an OR of 8.87.
“Maintenance of endothelial glycocalyx integrity can be a therapeutic target to reduce AKI in this setting,” the researchers wrote.
The authors acknowledged that the study was done at a single center that had dialysis and death rates three and five times higher, respectively, than those of developed countries; and it measured syndecan-1 at only one time point almost immediately after the operation.
“Adding postoperative syndecan-1, even when using a clinical model that already incorporates variables from renal angina index, results in significant improvement in the capacity to predict severe AKI,” Dr. Cavalcante and colleagues concluded.
They had no financial relationships to disclose.
Acute kidney injury is a common complication after pediatric cardiac surgery, but measuring for a specific genetic protein immediately after cardiac surgery may improve cardiac surgeons’ ability to predict patients at higher risk of AKI, according to researchers from Brazil. The study results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152-178-86).
“Plasma syndecan-1 levels measured early in the postoperative period were independently associated with severe acute kidney injury,” wrote Candice Torres de Melo Bezerra Cavalcante, MD, of Heart Hospital of Messejana and Federal University of Ceará.
Their prospective cohort study involved 289 pediatric patients who had cardiac surgery at their institution between September 2013 and December 2014.
Dr. Cavalcante and colleagues acknowledged that the traditional biomarker for renal function, serum creatinine, only increases appreciably after the glomerular filtration rate declines 50%, impairing physicians’ ability to detect AKI early enough to treat it. “This delay can explain, in part the, negative results in AKI therapeutic clinical trials,” they wrote.
They evaluated two different endothelial biomarkers in addition to syndecan-1 with regard to their capacity for predicting severe AKI: plasma ICAM-1, a marker of endothelial cell activation; and E-selectin, an endothelial cell adhesion molecule. Syndecan-1 works as a biomarker of injury to the glycocalyx protein that surrounds endothelial cell membranes that acts as a permeability barrier and prevents the cells from adhering to blood. They found that median syndecan-1 levels soon after surgery were higher in patients with severe AKI, 103.6 vs. 42.3 ng/mL.
“Although syndecan-1 is not a renal-specific biomarker, there has been recent increasing evidence that endothelial injury has an important role in AKI pathophysiology,” the researchers noted.
Study results showed the higher the level of syndecan-1, the greater the adjusted odds ratio (OR) for severe AKI. Levels of less than 17 ng/mL were considered normal; 17.1-46.7 ng/mL carried an adjusted OR of 1.42; 47.4-93.1 ng/mL had an adjusted OR of 2.05; and levels 96.3 or greater had an OR of 8.87.
“Maintenance of endothelial glycocalyx integrity can be a therapeutic target to reduce AKI in this setting,” the researchers wrote.
The authors acknowledged that the study was done at a single center that had dialysis and death rates three and five times higher, respectively, than those of developed countries; and it measured syndecan-1 at only one time point almost immediately after the operation.
“Adding postoperative syndecan-1, even when using a clinical model that already incorporates variables from renal angina index, results in significant improvement in the capacity to predict severe AKI,” Dr. Cavalcante and colleagues concluded.
They had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The biomarker syndecan-1 may aid in determining acute kidney injury risk for children having cardiac surgery.
Major finding: Children with elevated levels of syndecan-1 had a two- to ninefold greater risk of acute kidney injury.
Data source: Single-institution, prospective cohort study of 289 pediatric patients who had cardiac surgery from September 2013 to December 2014.
Disclosures: Dr. Cavalcante and coauthors had no financial relationships to disclose.
Prevention of postop GI disorders may reduce ‘failed discharges’ for laparoscopic hernia surgery
Postoperative hospital readmissions after ventral hernia repair may be both predictable and preventable if type of operation and patient characteristics are taken into account, a large retrospective study has found.
Early readmissions, or ‘failed discharges,’ are potentially more preventable than are later readmissions, according to Adam C. Celio, MD, of East Carolina University, Greenville, N.C., and his colleagues. Medical literature “demonstrates that patients readmitted within a few days of discharge return for different reasons than patients who are readmitted later; very early readmissions are likely due to poor coordination of care or inadequate recognition of postdischarge needs, while later readmissions (still within the 30-day window) are more likely due to patient disease or procedural complications.”
Dr. Celio and his coinvestigators examined data from the American College of Surgeons’ National Surgical Quality Improvement Program, looking for patients who underwent either open (n = 9,009) or laparoscopic (n = 3,360) ventral hernia repair (VHR) in 2012. The primary endpoint was defined as readmission within 30 days of discharge following a VHR procedure; early readmission was defined as occurring within 5 days of discharge for laparoscopic VHR and within 9 days of discharge for open VHR, while late readmission was defined as any readmission that occurred after the aforementioned time frames (Surgery. 2016;160[2]:413-17).
The researchers analyzed each readmission to determine its cause among nine classifications: bleeding, cardiovascular events, dehydration, gastrointestinal causes (nausea, emesis, ileus, and bowel obstruction), pain, venous thromboembolic event, wound occurrences (superficial site infection, deep operative site infection, wound disruptions), other infection, and other causes.
Of the 12,369 individuals included in the study, 1,057 (8.5%) were readmitted within 30 days of undergoing VHR. Generally, the patients who had open procedures had higher ASA scores than did those who had laparoscopic surgery, reflecting a greater likelihood of preoperative physical impairment and chronic disease. The researchers then analyzed which patients were mostly likely to be readmitted and the correlation between type of operation, cause of readmission, and timing of readmission (early or late).
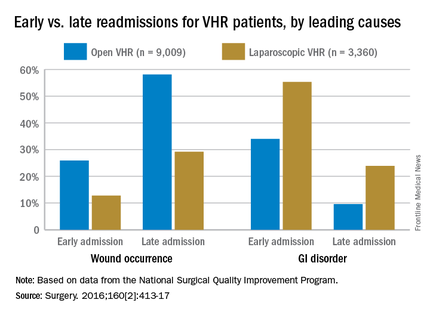
Open-VHR patients were more likely to be readmitted within 30 days than were those who underwent laparoscopic VHR: 9.2% vs. 6.9% readmission rates, respectively (OR 0.73, 95% CI 0.63-0.85). Among all the patients readmitted, wound complications were the most common cause (32.2%), followed by gastrointestinal disorders (14.3%), most which were attributed to emesis or nausea.
Wound complications were more highly associated with late readmission than with early ones, at 52% vs. 23%, respectively (OR 3.68, 95% CI 2.56-5.29). As might be expected, wound complications were more likely to occur in open-VHR patients than in laparoscopic-VHR patients: 49.6% vs. 24.4% (OR 3.05, 95% CI 2.06-4.52).
Of the entire cohort, 279 patients (2.3%) were classified as early readmissions, and gastrointestinal causes were more highly associated with early readmission than with late ones: 39% vs.13% (OR 4.45, 95% CI 3.06-6.47). Gastrointestinal issues occurred more often after laparoscopic VHR than after open VHR: 33% vs. 16% (OR 2.59, 95% CI 1.75-3.84). These early readmissions, occurring within days of discharge, are potentially preventable with a stepped up focus on control of nausea and emesis experienced by these patients, the researchers noted.
A funding source for this study was not disclosed. Dr. Celio and his coauthors did not report any relevant disclosures.
Postoperative hospital readmissions after ventral hernia repair may be both predictable and preventable if type of operation and patient characteristics are taken into account, a large retrospective study has found.
Early readmissions, or ‘failed discharges,’ are potentially more preventable than are later readmissions, according to Adam C. Celio, MD, of East Carolina University, Greenville, N.C., and his colleagues. Medical literature “demonstrates that patients readmitted within a few days of discharge return for different reasons than patients who are readmitted later; very early readmissions are likely due to poor coordination of care or inadequate recognition of postdischarge needs, while later readmissions (still within the 30-day window) are more likely due to patient disease or procedural complications.”
Dr. Celio and his coinvestigators examined data from the American College of Surgeons’ National Surgical Quality Improvement Program, looking for patients who underwent either open (n = 9,009) or laparoscopic (n = 3,360) ventral hernia repair (VHR) in 2012. The primary endpoint was defined as readmission within 30 days of discharge following a VHR procedure; early readmission was defined as occurring within 5 days of discharge for laparoscopic VHR and within 9 days of discharge for open VHR, while late readmission was defined as any readmission that occurred after the aforementioned time frames (Surgery. 2016;160[2]:413-17).
The researchers analyzed each readmission to determine its cause among nine classifications: bleeding, cardiovascular events, dehydration, gastrointestinal causes (nausea, emesis, ileus, and bowel obstruction), pain, venous thromboembolic event, wound occurrences (superficial site infection, deep operative site infection, wound disruptions), other infection, and other causes.
Of the 12,369 individuals included in the study, 1,057 (8.5%) were readmitted within 30 days of undergoing VHR. Generally, the patients who had open procedures had higher ASA scores than did those who had laparoscopic surgery, reflecting a greater likelihood of preoperative physical impairment and chronic disease. The researchers then analyzed which patients were mostly likely to be readmitted and the correlation between type of operation, cause of readmission, and timing of readmission (early or late).
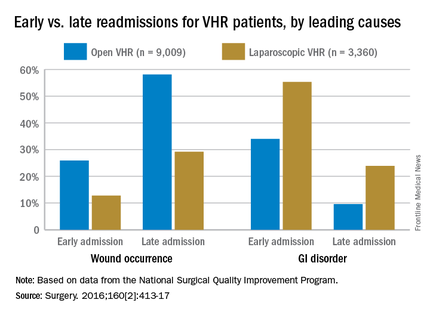
Open-VHR patients were more likely to be readmitted within 30 days than were those who underwent laparoscopic VHR: 9.2% vs. 6.9% readmission rates, respectively (OR 0.73, 95% CI 0.63-0.85). Among all the patients readmitted, wound complications were the most common cause (32.2%), followed by gastrointestinal disorders (14.3%), most which were attributed to emesis or nausea.
Wound complications were more highly associated with late readmission than with early ones, at 52% vs. 23%, respectively (OR 3.68, 95% CI 2.56-5.29). As might be expected, wound complications were more likely to occur in open-VHR patients than in laparoscopic-VHR patients: 49.6% vs. 24.4% (OR 3.05, 95% CI 2.06-4.52).
Of the entire cohort, 279 patients (2.3%) were classified as early readmissions, and gastrointestinal causes were more highly associated with early readmission than with late ones: 39% vs.13% (OR 4.45, 95% CI 3.06-6.47). Gastrointestinal issues occurred more often after laparoscopic VHR than after open VHR: 33% vs. 16% (OR 2.59, 95% CI 1.75-3.84). These early readmissions, occurring within days of discharge, are potentially preventable with a stepped up focus on control of nausea and emesis experienced by these patients, the researchers noted.
A funding source for this study was not disclosed. Dr. Celio and his coauthors did not report any relevant disclosures.
Postoperative hospital readmissions after ventral hernia repair may be both predictable and preventable if type of operation and patient characteristics are taken into account, a large retrospective study has found.
Early readmissions, or ‘failed discharges,’ are potentially more preventable than are later readmissions, according to Adam C. Celio, MD, of East Carolina University, Greenville, N.C., and his colleagues. Medical literature “demonstrates that patients readmitted within a few days of discharge return for different reasons than patients who are readmitted later; very early readmissions are likely due to poor coordination of care or inadequate recognition of postdischarge needs, while later readmissions (still within the 30-day window) are more likely due to patient disease or procedural complications.”
Dr. Celio and his coinvestigators examined data from the American College of Surgeons’ National Surgical Quality Improvement Program, looking for patients who underwent either open (n = 9,009) or laparoscopic (n = 3,360) ventral hernia repair (VHR) in 2012. The primary endpoint was defined as readmission within 30 days of discharge following a VHR procedure; early readmission was defined as occurring within 5 days of discharge for laparoscopic VHR and within 9 days of discharge for open VHR, while late readmission was defined as any readmission that occurred after the aforementioned time frames (Surgery. 2016;160[2]:413-17).
The researchers analyzed each readmission to determine its cause among nine classifications: bleeding, cardiovascular events, dehydration, gastrointestinal causes (nausea, emesis, ileus, and bowel obstruction), pain, venous thromboembolic event, wound occurrences (superficial site infection, deep operative site infection, wound disruptions), other infection, and other causes.
Of the 12,369 individuals included in the study, 1,057 (8.5%) were readmitted within 30 days of undergoing VHR. Generally, the patients who had open procedures had higher ASA scores than did those who had laparoscopic surgery, reflecting a greater likelihood of preoperative physical impairment and chronic disease. The researchers then analyzed which patients were mostly likely to be readmitted and the correlation between type of operation, cause of readmission, and timing of readmission (early or late).
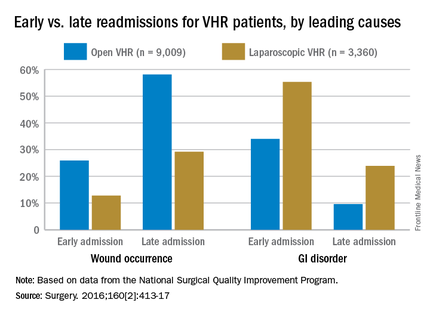
Open-VHR patients were more likely to be readmitted within 30 days than were those who underwent laparoscopic VHR: 9.2% vs. 6.9% readmission rates, respectively (OR 0.73, 95% CI 0.63-0.85). Among all the patients readmitted, wound complications were the most common cause (32.2%), followed by gastrointestinal disorders (14.3%), most which were attributed to emesis or nausea.
Wound complications were more highly associated with late readmission than with early ones, at 52% vs. 23%, respectively (OR 3.68, 95% CI 2.56-5.29). As might be expected, wound complications were more likely to occur in open-VHR patients than in laparoscopic-VHR patients: 49.6% vs. 24.4% (OR 3.05, 95% CI 2.06-4.52).
Of the entire cohort, 279 patients (2.3%) were classified as early readmissions, and gastrointestinal causes were more highly associated with early readmission than with late ones: 39% vs.13% (OR 4.45, 95% CI 3.06-6.47). Gastrointestinal issues occurred more often after laparoscopic VHR than after open VHR: 33% vs. 16% (OR 2.59, 95% CI 1.75-3.84). These early readmissions, occurring within days of discharge, are potentially preventable with a stepped up focus on control of nausea and emesis experienced by these patients, the researchers noted.
A funding source for this study was not disclosed. Dr. Celio and his coauthors did not report any relevant disclosures.
FROM SURGERY
Key clinical point: Postoperative complications and likelihood of readmission differ according to the type of ventral hernia repair procedure (open or laparoscopic).
Major finding: Thirty-day readmissions occurred among 6.9% of patients who had laparoscopic surgery, compared with 9.2% of open-procedure patients; gastrointestinal disorders were more common in early readmissions but wound occurrences were more common in late readmissions.
Data source: Retrospective cohort study of 12,369 ventral hernia repair patients (open and laparoscopic) in 2012.
Disclosures: Funding source not disclosed. Authors did not report any relevant financial disclosures.
Not enough evidence to support LAA closure by device or surgery for atrial fib
FROM CIRCULATION: CARDIOVASCULAR QUALITY OUTCOMES
Insufficient evidence exists to routinely recommend surgical closure of the left atrial appendage, either surgically or with a LAA exclusion device, for patients who have atrial fibrillation, a large data review has concluded.
None of the devices so far examined is more effective than oral anticoagulation therapy in reducing AF-related stroke risk, but they appear to be riskier, with up to 1 in 15 patients experiencing a serious adverse event during or after percutaneous placement, North Noelck, MD, and his colleagues wrote (Circ Cardiovasc Qual Outcomes. 2016 Jul 12. doi: 10.1161/CIRCOUTCOMES.115.002539).
Surgical studies, which also have found no benefit, are poor in quality and provide no strong data in favor of any technique, wrote Dr. Noelck of Oregon Health and Science University, Portland.
The meta-analysis comprised 13 studies of the benefits and risks of percutaneous LAA exclusion and 7 of the benefits and harms of surgical LAA closure.
The team found “limited evidence” that one device, the Watchman (Boston Scientific), may be an effective alternative to long-term oral anticoagulation treatment in some patients. But the Watchman was also associated with “significant, procedural-related harms,” in almost 11% of patients in one large study, PROTECT-AF. These included pericardial effusions with and without associated tamponade, bleeding, device thrombus, and device embolization. However, the benefit conferred by the device appeared marginal. Neither PROTECT-AF nor the subsequent PREVAIL studies of the Watchman found that it conferred significant clinical benefit above the comparator arm of warfarin therapy. Indeed, in PREVAIL, a composite outcome of death, ischemic/hemorrhagic stroke, or systemic embolism occurred in 5.2% of the device group and in 2.9% of the warfarin group.
Three randomized studies and two observational studies examined surgical LAA closure relative to usual medical care. The authors said the randomized studies were underpowered to show clinical benefit. Neither of the observational studies showed significant advantages in stroke-free survival, but the team noted, “data such as information about anticoagulation use among the groups [were] lacking.”
“Overall, there is insufficient evidence to support the routine use of surgical LAA exclusion to reduce stroke risk or the future need for anticoagulant therapy,” wrote Dr. Noelck and his coinvestigators. However, they said, several ongoing studies “should add substantively to this body of evidence during the next several years.”
The study was funded by the Department of Veterans Affairs. None of the authors had any relevant financial disclosure.
FROM CIRCULATION: CARDIOVASCULAR QUALITY OUTCOMES
Insufficient evidence exists to routinely recommend surgical closure of the left atrial appendage, either surgically or with a LAA exclusion device, for patients who have atrial fibrillation, a large data review has concluded.
None of the devices so far examined is more effective than oral anticoagulation therapy in reducing AF-related stroke risk, but they appear to be riskier, with up to 1 in 15 patients experiencing a serious adverse event during or after percutaneous placement, North Noelck, MD, and his colleagues wrote (Circ Cardiovasc Qual Outcomes. 2016 Jul 12. doi: 10.1161/CIRCOUTCOMES.115.002539).
Surgical studies, which also have found no benefit, are poor in quality and provide no strong data in favor of any technique, wrote Dr. Noelck of Oregon Health and Science University, Portland.
The meta-analysis comprised 13 studies of the benefits and risks of percutaneous LAA exclusion and 7 of the benefits and harms of surgical LAA closure.
The team found “limited evidence” that one device, the Watchman (Boston Scientific), may be an effective alternative to long-term oral anticoagulation treatment in some patients. But the Watchman was also associated with “significant, procedural-related harms,” in almost 11% of patients in one large study, PROTECT-AF. These included pericardial effusions with and without associated tamponade, bleeding, device thrombus, and device embolization. However, the benefit conferred by the device appeared marginal. Neither PROTECT-AF nor the subsequent PREVAIL studies of the Watchman found that it conferred significant clinical benefit above the comparator arm of warfarin therapy. Indeed, in PREVAIL, a composite outcome of death, ischemic/hemorrhagic stroke, or systemic embolism occurred in 5.2% of the device group and in 2.9% of the warfarin group.
Three randomized studies and two observational studies examined surgical LAA closure relative to usual medical care. The authors said the randomized studies were underpowered to show clinical benefit. Neither of the observational studies showed significant advantages in stroke-free survival, but the team noted, “data such as information about anticoagulation use among the groups [were] lacking.”
“Overall, there is insufficient evidence to support the routine use of surgical LAA exclusion to reduce stroke risk or the future need for anticoagulant therapy,” wrote Dr. Noelck and his coinvestigators. However, they said, several ongoing studies “should add substantively to this body of evidence during the next several years.”
The study was funded by the Department of Veterans Affairs. None of the authors had any relevant financial disclosure.
FROM CIRCULATION: CARDIOVASCULAR QUALITY OUTCOMES
Insufficient evidence exists to routinely recommend surgical closure of the left atrial appendage, either surgically or with a LAA exclusion device, for patients who have atrial fibrillation, a large data review has concluded.
None of the devices so far examined is more effective than oral anticoagulation therapy in reducing AF-related stroke risk, but they appear to be riskier, with up to 1 in 15 patients experiencing a serious adverse event during or after percutaneous placement, North Noelck, MD, and his colleagues wrote (Circ Cardiovasc Qual Outcomes. 2016 Jul 12. doi: 10.1161/CIRCOUTCOMES.115.002539).
Surgical studies, which also have found no benefit, are poor in quality and provide no strong data in favor of any technique, wrote Dr. Noelck of Oregon Health and Science University, Portland.
The meta-analysis comprised 13 studies of the benefits and risks of percutaneous LAA exclusion and 7 of the benefits and harms of surgical LAA closure.
The team found “limited evidence” that one device, the Watchman (Boston Scientific), may be an effective alternative to long-term oral anticoagulation treatment in some patients. But the Watchman was also associated with “significant, procedural-related harms,” in almost 11% of patients in one large study, PROTECT-AF. These included pericardial effusions with and without associated tamponade, bleeding, device thrombus, and device embolization. However, the benefit conferred by the device appeared marginal. Neither PROTECT-AF nor the subsequent PREVAIL studies of the Watchman found that it conferred significant clinical benefit above the comparator arm of warfarin therapy. Indeed, in PREVAIL, a composite outcome of death, ischemic/hemorrhagic stroke, or systemic embolism occurred in 5.2% of the device group and in 2.9% of the warfarin group.
Three randomized studies and two observational studies examined surgical LAA closure relative to usual medical care. The authors said the randomized studies were underpowered to show clinical benefit. Neither of the observational studies showed significant advantages in stroke-free survival, but the team noted, “data such as information about anticoagulation use among the groups [were] lacking.”
“Overall, there is insufficient evidence to support the routine use of surgical LAA exclusion to reduce stroke risk or the future need for anticoagulant therapy,” wrote Dr. Noelck and his coinvestigators. However, they said, several ongoing studies “should add substantively to this body of evidence during the next several years.”
The study was funded by the Department of Veterans Affairs. None of the authors had any relevant financial disclosure.
Key clinical point: There is insufficient evidence to recommend LAA closure over oral anticoagulation for stroke prevention in patients with atrial fibrillation.
Major finding: Device closure was not more effective than oral anticoagulation but was associated with a 1 in 15 patient incidence of procedural adverse events.
Data source: The meta-analysis comprised 13 studies of LAA device closure and 7 studies of surgical closure.
Disclosures: The study was funded by the Department of Veterans Affairs. None of the authors had any relevant financial disclosure.