User login
Daptomycin/fosfomycin: A new standard for MRSA bacteremia?
SAN FRANCISCO – Daptomycin plus fosfomycin is more effective than daptomycin alone for methicillin-resistant Staphylococcus aureus bacteremia, according to a multicenter, randomized trial from Spain.
“I think this is really an important study; I think it will change clinical practice for this infection” once it’s published, said lead investigator Miquel Pujol, MD, PhD, clinical head of infectious diseases at Bellvitge University Hospital in Barcelona.
The current standard for MRSA bacteremia is daptomycin (Cubicin) or vancomycin (Vancocin) monotherapy on both sides of the Atlantic, but mortality rates are way too high, more than 30% in some reviews. Dr. Pujol and his colleagues wanted to find something better.
Their lab work showed that daptomycin and fosfomycin (Monurol) were synergistic and rapidly bactericidal against MRSA, and anecdotal experience in Spain suggested the drugs improved bacteremia outcomes, so they decided to put the combination to the test.
They randomized 74 MRSA bacteremia patients to the combination, daptomycin 10mg/kg IV daily plus fosfomycin 2g IV q 6h. They randomized 81 other subjects to standard of care with daptomycin monotherapy, also at 10mg/kg IV daily. Treatment was 10-14 days for uncomplicated and 28-42 days for complicated bacteremia.
The open-label trial was conducted at 18 medical centers in Spain, where fosfomycin was discovered in dirt samples in the late 1960s and remains a matter of pride.
At day 7, 69 of the 74 combination patients (93.2%) were alive with clinical improvement, clearance of bacteremia, and no subsequent relapse, versus 62 of 81 patients (76.5%) on monotherapy (absolute difference 16.7%; 95% confidence interval, 5.4%-27.7%). Three people in the combination arm (4.1%) had died by day 7, versus six on monotherapy (7.4%).
Six weeks after the end of treatment at the test-of-cure visit, 40 of 74 combination patients (54.1%) were alive with resolution of all clinical signs and symptoms, negative blood cultures, and no previous or subsequent relapses; just 34 of 81 patients (42%) in the monotherapy arm hit that mark. The 12.1% difference was not statistically significant, nor was the difference in 12-week survival.
However, patients in the combination arm were 70% less likely to have complicated bacteremia at the test-of-cure visit (9.5% vs. 28.4%; relative risk 0.3; 95% CI, 0.2-0.7). There were no cases of persistent or recurrent infection in the combination arm, but nine persistent (11.1%) and five recurrent (6.2%) cases with daptomycin monotherapy. The differences were statistically significant.
The subjects all had at least one positive MRSA blood culture within 72 hours of randomization. Exclusion criteria included MRSA pneumonia, prosthetic valve endocarditis, end-stage liver disease, and moderate to severe heart failure.
There were no significant baseline differences between the groups. About half the subjects were men, and the mean age was about 73 years. The mean Charlson Comorbidity Index score was a bit under 4, and the mean Pitt bacteremia score a bit over 1. The leading source of infection was vascular catheter; acquisition was thought to be nosocomial in more than 40% of patients.
There were no discontinuations from drug side effects in the daptomycin arm, but there were five in the combination arm, including two for heart failure, two for respiratory insufficiency, and one for GI bleeding. Even so, the benefit outweighed the risk, Dr. Pujol said.
Intravenous fosfomycin is available in Europe, but the drug is approved in the United States only as an oral formulation. That could change soon; Nabriva Therapeutics plans to file its IV formulation (Contepo) for Food and Drug Administration approval in late 2018.
Though it is not standard of practice yet, the combination is increasingly being used in Spain for MRSA bacteremia, according to Dr. Pujol. “Patients probably need the combination [at least] initially, especially if they have complicated bacteremia” or fail monotherapy, he said at ID week, an annual scientific meeting on infectious diseases.
The work was funded by the Spanish government. Dr. Pujol said he had no relevant disclosures.
SOURCE: Pujol M et al. 2018 ID Week abstract LB3
SAN FRANCISCO – Daptomycin plus fosfomycin is more effective than daptomycin alone for methicillin-resistant Staphylococcus aureus bacteremia, according to a multicenter, randomized trial from Spain.
“I think this is really an important study; I think it will change clinical practice for this infection” once it’s published, said lead investigator Miquel Pujol, MD, PhD, clinical head of infectious diseases at Bellvitge University Hospital in Barcelona.
The current standard for MRSA bacteremia is daptomycin (Cubicin) or vancomycin (Vancocin) monotherapy on both sides of the Atlantic, but mortality rates are way too high, more than 30% in some reviews. Dr. Pujol and his colleagues wanted to find something better.
Their lab work showed that daptomycin and fosfomycin (Monurol) were synergistic and rapidly bactericidal against MRSA, and anecdotal experience in Spain suggested the drugs improved bacteremia outcomes, so they decided to put the combination to the test.
They randomized 74 MRSA bacteremia patients to the combination, daptomycin 10mg/kg IV daily plus fosfomycin 2g IV q 6h. They randomized 81 other subjects to standard of care with daptomycin monotherapy, also at 10mg/kg IV daily. Treatment was 10-14 days for uncomplicated and 28-42 days for complicated bacteremia.
The open-label trial was conducted at 18 medical centers in Spain, where fosfomycin was discovered in dirt samples in the late 1960s and remains a matter of pride.
At day 7, 69 of the 74 combination patients (93.2%) were alive with clinical improvement, clearance of bacteremia, and no subsequent relapse, versus 62 of 81 patients (76.5%) on monotherapy (absolute difference 16.7%; 95% confidence interval, 5.4%-27.7%). Three people in the combination arm (4.1%) had died by day 7, versus six on monotherapy (7.4%).
Six weeks after the end of treatment at the test-of-cure visit, 40 of 74 combination patients (54.1%) were alive with resolution of all clinical signs and symptoms, negative blood cultures, and no previous or subsequent relapses; just 34 of 81 patients (42%) in the monotherapy arm hit that mark. The 12.1% difference was not statistically significant, nor was the difference in 12-week survival.
However, patients in the combination arm were 70% less likely to have complicated bacteremia at the test-of-cure visit (9.5% vs. 28.4%; relative risk 0.3; 95% CI, 0.2-0.7). There were no cases of persistent or recurrent infection in the combination arm, but nine persistent (11.1%) and five recurrent (6.2%) cases with daptomycin monotherapy. The differences were statistically significant.
The subjects all had at least one positive MRSA blood culture within 72 hours of randomization. Exclusion criteria included MRSA pneumonia, prosthetic valve endocarditis, end-stage liver disease, and moderate to severe heart failure.
There were no significant baseline differences between the groups. About half the subjects were men, and the mean age was about 73 years. The mean Charlson Comorbidity Index score was a bit under 4, and the mean Pitt bacteremia score a bit over 1. The leading source of infection was vascular catheter; acquisition was thought to be nosocomial in more than 40% of patients.
There were no discontinuations from drug side effects in the daptomycin arm, but there were five in the combination arm, including two for heart failure, two for respiratory insufficiency, and one for GI bleeding. Even so, the benefit outweighed the risk, Dr. Pujol said.
Intravenous fosfomycin is available in Europe, but the drug is approved in the United States only as an oral formulation. That could change soon; Nabriva Therapeutics plans to file its IV formulation (Contepo) for Food and Drug Administration approval in late 2018.
Though it is not standard of practice yet, the combination is increasingly being used in Spain for MRSA bacteremia, according to Dr. Pujol. “Patients probably need the combination [at least] initially, especially if they have complicated bacteremia” or fail monotherapy, he said at ID week, an annual scientific meeting on infectious diseases.
The work was funded by the Spanish government. Dr. Pujol said he had no relevant disclosures.
SOURCE: Pujol M et al. 2018 ID Week abstract LB3
SAN FRANCISCO – Daptomycin plus fosfomycin is more effective than daptomycin alone for methicillin-resistant Staphylococcus aureus bacteremia, according to a multicenter, randomized trial from Spain.
“I think this is really an important study; I think it will change clinical practice for this infection” once it’s published, said lead investigator Miquel Pujol, MD, PhD, clinical head of infectious diseases at Bellvitge University Hospital in Barcelona.
The current standard for MRSA bacteremia is daptomycin (Cubicin) or vancomycin (Vancocin) monotherapy on both sides of the Atlantic, but mortality rates are way too high, more than 30% in some reviews. Dr. Pujol and his colleagues wanted to find something better.
Their lab work showed that daptomycin and fosfomycin (Monurol) were synergistic and rapidly bactericidal against MRSA, and anecdotal experience in Spain suggested the drugs improved bacteremia outcomes, so they decided to put the combination to the test.
They randomized 74 MRSA bacteremia patients to the combination, daptomycin 10mg/kg IV daily plus fosfomycin 2g IV q 6h. They randomized 81 other subjects to standard of care with daptomycin monotherapy, also at 10mg/kg IV daily. Treatment was 10-14 days for uncomplicated and 28-42 days for complicated bacteremia.
The open-label trial was conducted at 18 medical centers in Spain, where fosfomycin was discovered in dirt samples in the late 1960s and remains a matter of pride.
At day 7, 69 of the 74 combination patients (93.2%) were alive with clinical improvement, clearance of bacteremia, and no subsequent relapse, versus 62 of 81 patients (76.5%) on monotherapy (absolute difference 16.7%; 95% confidence interval, 5.4%-27.7%). Three people in the combination arm (4.1%) had died by day 7, versus six on monotherapy (7.4%).
Six weeks after the end of treatment at the test-of-cure visit, 40 of 74 combination patients (54.1%) were alive with resolution of all clinical signs and symptoms, negative blood cultures, and no previous or subsequent relapses; just 34 of 81 patients (42%) in the monotherapy arm hit that mark. The 12.1% difference was not statistically significant, nor was the difference in 12-week survival.
However, patients in the combination arm were 70% less likely to have complicated bacteremia at the test-of-cure visit (9.5% vs. 28.4%; relative risk 0.3; 95% CI, 0.2-0.7). There were no cases of persistent or recurrent infection in the combination arm, but nine persistent (11.1%) and five recurrent (6.2%) cases with daptomycin monotherapy. The differences were statistically significant.
The subjects all had at least one positive MRSA blood culture within 72 hours of randomization. Exclusion criteria included MRSA pneumonia, prosthetic valve endocarditis, end-stage liver disease, and moderate to severe heart failure.
There were no significant baseline differences between the groups. About half the subjects were men, and the mean age was about 73 years. The mean Charlson Comorbidity Index score was a bit under 4, and the mean Pitt bacteremia score a bit over 1. The leading source of infection was vascular catheter; acquisition was thought to be nosocomial in more than 40% of patients.
There were no discontinuations from drug side effects in the daptomycin arm, but there were five in the combination arm, including two for heart failure, two for respiratory insufficiency, and one for GI bleeding. Even so, the benefit outweighed the risk, Dr. Pujol said.
Intravenous fosfomycin is available in Europe, but the drug is approved in the United States only as an oral formulation. That could change soon; Nabriva Therapeutics plans to file its IV formulation (Contepo) for Food and Drug Administration approval in late 2018.
Though it is not standard of practice yet, the combination is increasingly being used in Spain for MRSA bacteremia, according to Dr. Pujol. “Patients probably need the combination [at least] initially, especially if they have complicated bacteremia” or fail monotherapy, he said at ID week, an annual scientific meeting on infectious diseases.
The work was funded by the Spanish government. Dr. Pujol said he had no relevant disclosures.
SOURCE: Pujol M et al. 2018 ID Week abstract LB3
REPORTING FROM ID WEEK 2018
Key clinical point:
Major finding: At day 93% of the combination patients were alive with clinical improvement, clearance of bacteremia, and no subsequent relapse, vs. 77% on monotherapy.
Study details: Randomized, open label trial in 155 patients with MRSA bacteremia.
Disclosures: The work was funded by the Spanish government. The lead investigator said he had no relevant disclosures.
Source: Pujol M et al. 2018 ID Week, Abstract LB3
Perioperative gabapentin’s effect on postoperative opioid use
Background: Previous studies have shown that perioperative gabapentin has no effect on remote pain cessation but have not linked it with effects on remote opioid cessation. Also, most trials were limited to immediate postoperative use during hospital admission; limited data were available with extensive postoperative longitudinal follow-up.
Study design: Randomized, double-blind, placebo-controlled study.
Setting: Tertiary referral teaching hospital.
Synopsis: A randomized, double-blind trial including a total of 1,805 patients aged 18-75 years who were scheduled for eligible surgery was conducted at a single-center, tertiary referral teaching hospital. The treatment group received 1,200 mg of gabapentin preoperatively followed by 600 mg 3 times a day postoperatively. Meanwhile, the placebo group received lorazepam 0.5 mg preoperatively followed by inactive placebo postoperatively for 72 hours. With use of intention to treat analysis, this study showed that perioperative gabapentin did not affect time to postoperative pain resolution. However, a modest increase in the rate of opioid cessation was uncovered. Specifically, there was a 24% increase in the rate (hazard ratio, 1.24; 95% confidence interval, 1.00-1.54; P = .05) of opioid cessation after hospital discharge, with a median time of 25 days in the gabapentin group versus 32 days in the placebo group.
One caveat to the outcomes is that use of a gabapentin regimen may have increased after discharge date, which could have biased the outcome.
Bottom line: Perioperative gabapentin may promote opioid cessation and prevent the development of chronic opioid use after surgery.
Citation: Hah J et al. Effect of perioperative gabapentin on postoperative pain resolution and opioid cessation in a mixed surgical cohort. JAMA Surg. 2018;153(4):303-11.
Dr. Katsouli is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Background: Previous studies have shown that perioperative gabapentin has no effect on remote pain cessation but have not linked it with effects on remote opioid cessation. Also, most trials were limited to immediate postoperative use during hospital admission; limited data were available with extensive postoperative longitudinal follow-up.
Study design: Randomized, double-blind, placebo-controlled study.
Setting: Tertiary referral teaching hospital.
Synopsis: A randomized, double-blind trial including a total of 1,805 patients aged 18-75 years who were scheduled for eligible surgery was conducted at a single-center, tertiary referral teaching hospital. The treatment group received 1,200 mg of gabapentin preoperatively followed by 600 mg 3 times a day postoperatively. Meanwhile, the placebo group received lorazepam 0.5 mg preoperatively followed by inactive placebo postoperatively for 72 hours. With use of intention to treat analysis, this study showed that perioperative gabapentin did not affect time to postoperative pain resolution. However, a modest increase in the rate of opioid cessation was uncovered. Specifically, there was a 24% increase in the rate (hazard ratio, 1.24; 95% confidence interval, 1.00-1.54; P = .05) of opioid cessation after hospital discharge, with a median time of 25 days in the gabapentin group versus 32 days in the placebo group.
One caveat to the outcomes is that use of a gabapentin regimen may have increased after discharge date, which could have biased the outcome.
Bottom line: Perioperative gabapentin may promote opioid cessation and prevent the development of chronic opioid use after surgery.
Citation: Hah J et al. Effect of perioperative gabapentin on postoperative pain resolution and opioid cessation in a mixed surgical cohort. JAMA Surg. 2018;153(4):303-11.
Dr. Katsouli is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Background: Previous studies have shown that perioperative gabapentin has no effect on remote pain cessation but have not linked it with effects on remote opioid cessation. Also, most trials were limited to immediate postoperative use during hospital admission; limited data were available with extensive postoperative longitudinal follow-up.
Study design: Randomized, double-blind, placebo-controlled study.
Setting: Tertiary referral teaching hospital.
Synopsis: A randomized, double-blind trial including a total of 1,805 patients aged 18-75 years who were scheduled for eligible surgery was conducted at a single-center, tertiary referral teaching hospital. The treatment group received 1,200 mg of gabapentin preoperatively followed by 600 mg 3 times a day postoperatively. Meanwhile, the placebo group received lorazepam 0.5 mg preoperatively followed by inactive placebo postoperatively for 72 hours. With use of intention to treat analysis, this study showed that perioperative gabapentin did not affect time to postoperative pain resolution. However, a modest increase in the rate of opioid cessation was uncovered. Specifically, there was a 24% increase in the rate (hazard ratio, 1.24; 95% confidence interval, 1.00-1.54; P = .05) of opioid cessation after hospital discharge, with a median time of 25 days in the gabapentin group versus 32 days in the placebo group.
One caveat to the outcomes is that use of a gabapentin regimen may have increased after discharge date, which could have biased the outcome.
Bottom line: Perioperative gabapentin may promote opioid cessation and prevent the development of chronic opioid use after surgery.
Citation: Hah J et al. Effect of perioperative gabapentin on postoperative pain resolution and opioid cessation in a mixed surgical cohort. JAMA Surg. 2018;153(4):303-11.
Dr. Katsouli is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Perioperative diabetes and HbA1c in mortality
Clinical question: Do preoperative hemoglobin A1c (HbA1c) and perioperative glucose predict outcomes in patients undergoing noncardiac and cardiac surgeries?
Background: Hyperglycemia in the perioperative period has been associated with infection, delayed wound healing, and postoperative mortality. Studies have investigated the effects of HbA1c or hyperglycemia on postoperative outcomes, but none have been performed to assess the effect of one while controlling for the other.
Study design: Retrospective analysis.
Setting: Single-center, Duke University Health System.
Synopsis: Using a database of electronic health records at Duke University Health System, Durham, N.C., investigators reviewed 13,077 surgeries (6,684 noncardiac and 6,393 cardiac) to determine the association of preoperative HbA1c with perioperative glucose and 30-day mortality. For noncardiac surgery, increased average perioperative glucose was associated with increased mortality (P = .04). In cardiac surgery both low and high average glucose was associated with increased mortality (P = .001). By contrast, HbA1c was not a significant predictor of postoperative mortality in cardiac surgery (P = .08), and in noncardiac surgery, HbA1C was negatively associated with 30-day mortality (P = .01). Overall, perioperative glucose was predictive of 30-day mortality, but HbA1c was not associated with 30-day mortality after researchers controlled for glucose.
Because the study is retrospective, no causal relationship can be established. Hospitalists involved in perioperative care should aim for optimization of glucose control regardless of preoperative HbA1c.
Bottom line: Perioperative glucose is related to surgical outcomes, but HbA1c is a less useful indicator of 30-day postoperative mortality.
Citation: Van den Boom W et al. Effect of A1C and glucose on postoperative mortality in noncardiac and cardiac surgeries. Diabetes Care. 2018 Feb;41:782-8.
Clinical question: Do preoperative hemoglobin A1c (HbA1c) and perioperative glucose predict outcomes in patients undergoing noncardiac and cardiac surgeries?
Background: Hyperglycemia in the perioperative period has been associated with infection, delayed wound healing, and postoperative mortality. Studies have investigated the effects of HbA1c or hyperglycemia on postoperative outcomes, but none have been performed to assess the effect of one while controlling for the other.
Study design: Retrospective analysis.
Setting: Single-center, Duke University Health System.
Synopsis: Using a database of electronic health records at Duke University Health System, Durham, N.C., investigators reviewed 13,077 surgeries (6,684 noncardiac and 6,393 cardiac) to determine the association of preoperative HbA1c with perioperative glucose and 30-day mortality. For noncardiac surgery, increased average perioperative glucose was associated with increased mortality (P = .04). In cardiac surgery both low and high average glucose was associated with increased mortality (P = .001). By contrast, HbA1c was not a significant predictor of postoperative mortality in cardiac surgery (P = .08), and in noncardiac surgery, HbA1C was negatively associated with 30-day mortality (P = .01). Overall, perioperative glucose was predictive of 30-day mortality, but HbA1c was not associated with 30-day mortality after researchers controlled for glucose.
Because the study is retrospective, no causal relationship can be established. Hospitalists involved in perioperative care should aim for optimization of glucose control regardless of preoperative HbA1c.
Bottom line: Perioperative glucose is related to surgical outcomes, but HbA1c is a less useful indicator of 30-day postoperative mortality.
Citation: Van den Boom W et al. Effect of A1C and glucose on postoperative mortality in noncardiac and cardiac surgeries. Diabetes Care. 2018 Feb;41:782-8.
Clinical question: Do preoperative hemoglobin A1c (HbA1c) and perioperative glucose predict outcomes in patients undergoing noncardiac and cardiac surgeries?
Background: Hyperglycemia in the perioperative period has been associated with infection, delayed wound healing, and postoperative mortality. Studies have investigated the effects of HbA1c or hyperglycemia on postoperative outcomes, but none have been performed to assess the effect of one while controlling for the other.
Study design: Retrospective analysis.
Setting: Single-center, Duke University Health System.
Synopsis: Using a database of electronic health records at Duke University Health System, Durham, N.C., investigators reviewed 13,077 surgeries (6,684 noncardiac and 6,393 cardiac) to determine the association of preoperative HbA1c with perioperative glucose and 30-day mortality. For noncardiac surgery, increased average perioperative glucose was associated with increased mortality (P = .04). In cardiac surgery both low and high average glucose was associated with increased mortality (P = .001). By contrast, HbA1c was not a significant predictor of postoperative mortality in cardiac surgery (P = .08), and in noncardiac surgery, HbA1C was negatively associated with 30-day mortality (P = .01). Overall, perioperative glucose was predictive of 30-day mortality, but HbA1c was not associated with 30-day mortality after researchers controlled for glucose.
Because the study is retrospective, no causal relationship can be established. Hospitalists involved in perioperative care should aim for optimization of glucose control regardless of preoperative HbA1c.
Bottom line: Perioperative glucose is related to surgical outcomes, but HbA1c is a less useful indicator of 30-day postoperative mortality.
Citation: Van den Boom W et al. Effect of A1C and glucose on postoperative mortality in noncardiac and cardiac surgeries. Diabetes Care. 2018 Feb;41:782-8.
Low-dose ketamine controls pain from severe chest injury, while sparing opioid consumption
SAN DIEGO – while reducing opioid consumption.
The anesthetic didn’t make much difference in pain control or opioid use overall in a randomized study of 93 patients with thoracic injury Nathan Kugler, MD, said at the annual meeting of the American Association for the Surgery of Trauma. But among severely injured patients, it cut the opioid mean equivalency dose by about 164 mg over the 48-hour infusion and by 328 mg over a mean hospital stay while maintaining pain control, said Dr. Kugler, a surgical resident at the Medical College of Wisconsin, Milwaukee.
“With increasing focus on multimodal pain strategies, opioid-based regimens continue to be the backbone of pain control,” he said. “We have used ketamine effectively for failure of maximum therapy and demonstrated an opioid-sparing effect.” This new research shows that the drug can be an effective adjunct for acute pain control for severely injured patients in the emergency setting.
The study recruited 93 patients with thoracic injury; they had a mean of six broken ribs, mostly caused by motor vehicle accidents. Most of the patients were male (75%), and their mean age was 46 years. The mean Injury Severity Score was about 15; about 30% had flail chest.
All patients received a standardized acute pain medication regime comprising acetaminophen, nonsteroidal anti-inflammatories, methocarbamol (Robaxin), and intravenous opioids. Regional therapies included rib block with an epidural catheter. In addition, they were randomized to placebo infusions or to 48 hours of IV ketamine at 2.5 mcg/kg per minute. “To put this in perspective, for a 70-kg patient, that is a mean of 10.5 mg/hour,” Dr. Kugler said.
The primary endpoint was a reduction of at least 2 points on an 11-point pain scale. Secondary endpoints included opioid use in oral morphine equivalents (OME); respiratory complications; and psychoactive events. The primary outcome was assessed with an area under the curve model.
In the overall group, there was no significant between-group difference in pain score. Nor were there differences in the total OME at 12-24 hours (184 mg ketamine vs. 230 mg placebo), or at 48 hours (86 vs. 113 mg).
Dr. Kugler also looked at these outcomes in patients who had only rib fractures independent of other chest injury. He saw no significant differences in pain scores or OME at 24 or 48 hours.
However, significant differences did emerge in the group of severely injured patients with an Injury Severity Score of more than 15. There were no differences in pain scores at either time point. However, ketamine allowed patients to achieve the same level of pain control with significantly less opioid medication. The OME at 12-24 hours was 50.5 mg vs 94 mg. At 24-48 hours, it was 87 mg vs. 64 mg.
This worked out to a mean OME savings of 148 mg over a patient’s entire hospitalization.
“We saw a very nice separation of opioid consumption that began early and continued to separate over the 48-hour infusion and even after it was discontinued,” Dr. Kugler said.
This benefit was achieved without any additional adverse events, he added. There were no significant differences in confusion; epidural placement; length of stay; respiratory event, sedation, hallucinations, delusions or disturbing dreams; or unplanned transfers to the ICU.
Dr. Kugler disclosed that he and primary investigator Thomas Carver, MD, also of the Medical College of Wisconsin, Milwaukee, are both paid consultants for InnoVital Systems.
SAN DIEGO – while reducing opioid consumption.
The anesthetic didn’t make much difference in pain control or opioid use overall in a randomized study of 93 patients with thoracic injury Nathan Kugler, MD, said at the annual meeting of the American Association for the Surgery of Trauma. But among severely injured patients, it cut the opioid mean equivalency dose by about 164 mg over the 48-hour infusion and by 328 mg over a mean hospital stay while maintaining pain control, said Dr. Kugler, a surgical resident at the Medical College of Wisconsin, Milwaukee.
“With increasing focus on multimodal pain strategies, opioid-based regimens continue to be the backbone of pain control,” he said. “We have used ketamine effectively for failure of maximum therapy and demonstrated an opioid-sparing effect.” This new research shows that the drug can be an effective adjunct for acute pain control for severely injured patients in the emergency setting.
The study recruited 93 patients with thoracic injury; they had a mean of six broken ribs, mostly caused by motor vehicle accidents. Most of the patients were male (75%), and their mean age was 46 years. The mean Injury Severity Score was about 15; about 30% had flail chest.
All patients received a standardized acute pain medication regime comprising acetaminophen, nonsteroidal anti-inflammatories, methocarbamol (Robaxin), and intravenous opioids. Regional therapies included rib block with an epidural catheter. In addition, they were randomized to placebo infusions or to 48 hours of IV ketamine at 2.5 mcg/kg per minute. “To put this in perspective, for a 70-kg patient, that is a mean of 10.5 mg/hour,” Dr. Kugler said.
The primary endpoint was a reduction of at least 2 points on an 11-point pain scale. Secondary endpoints included opioid use in oral morphine equivalents (OME); respiratory complications; and psychoactive events. The primary outcome was assessed with an area under the curve model.
In the overall group, there was no significant between-group difference in pain score. Nor were there differences in the total OME at 12-24 hours (184 mg ketamine vs. 230 mg placebo), or at 48 hours (86 vs. 113 mg).
Dr. Kugler also looked at these outcomes in patients who had only rib fractures independent of other chest injury. He saw no significant differences in pain scores or OME at 24 or 48 hours.
However, significant differences did emerge in the group of severely injured patients with an Injury Severity Score of more than 15. There were no differences in pain scores at either time point. However, ketamine allowed patients to achieve the same level of pain control with significantly less opioid medication. The OME at 12-24 hours was 50.5 mg vs 94 mg. At 24-48 hours, it was 87 mg vs. 64 mg.
This worked out to a mean OME savings of 148 mg over a patient’s entire hospitalization.
“We saw a very nice separation of opioid consumption that began early and continued to separate over the 48-hour infusion and even after it was discontinued,” Dr. Kugler said.
This benefit was achieved without any additional adverse events, he added. There were no significant differences in confusion; epidural placement; length of stay; respiratory event, sedation, hallucinations, delusions or disturbing dreams; or unplanned transfers to the ICU.
Dr. Kugler disclosed that he and primary investigator Thomas Carver, MD, also of the Medical College of Wisconsin, Milwaukee, are both paid consultants for InnoVital Systems.
SAN DIEGO – while reducing opioid consumption.
The anesthetic didn’t make much difference in pain control or opioid use overall in a randomized study of 93 patients with thoracic injury Nathan Kugler, MD, said at the annual meeting of the American Association for the Surgery of Trauma. But among severely injured patients, it cut the opioid mean equivalency dose by about 164 mg over the 48-hour infusion and by 328 mg over a mean hospital stay while maintaining pain control, said Dr. Kugler, a surgical resident at the Medical College of Wisconsin, Milwaukee.
“With increasing focus on multimodal pain strategies, opioid-based regimens continue to be the backbone of pain control,” he said. “We have used ketamine effectively for failure of maximum therapy and demonstrated an opioid-sparing effect.” This new research shows that the drug can be an effective adjunct for acute pain control for severely injured patients in the emergency setting.
The study recruited 93 patients with thoracic injury; they had a mean of six broken ribs, mostly caused by motor vehicle accidents. Most of the patients were male (75%), and their mean age was 46 years. The mean Injury Severity Score was about 15; about 30% had flail chest.
All patients received a standardized acute pain medication regime comprising acetaminophen, nonsteroidal anti-inflammatories, methocarbamol (Robaxin), and intravenous opioids. Regional therapies included rib block with an epidural catheter. In addition, they were randomized to placebo infusions or to 48 hours of IV ketamine at 2.5 mcg/kg per minute. “To put this in perspective, for a 70-kg patient, that is a mean of 10.5 mg/hour,” Dr. Kugler said.
The primary endpoint was a reduction of at least 2 points on an 11-point pain scale. Secondary endpoints included opioid use in oral morphine equivalents (OME); respiratory complications; and psychoactive events. The primary outcome was assessed with an area under the curve model.
In the overall group, there was no significant between-group difference in pain score. Nor were there differences in the total OME at 12-24 hours (184 mg ketamine vs. 230 mg placebo), or at 48 hours (86 vs. 113 mg).
Dr. Kugler also looked at these outcomes in patients who had only rib fractures independent of other chest injury. He saw no significant differences in pain scores or OME at 24 or 48 hours.
However, significant differences did emerge in the group of severely injured patients with an Injury Severity Score of more than 15. There were no differences in pain scores at either time point. However, ketamine allowed patients to achieve the same level of pain control with significantly less opioid medication. The OME at 12-24 hours was 50.5 mg vs 94 mg. At 24-48 hours, it was 87 mg vs. 64 mg.
This worked out to a mean OME savings of 148 mg over a patient’s entire hospitalization.
“We saw a very nice separation of opioid consumption that began early and continued to separate over the 48-hour infusion and even after it was discontinued,” Dr. Kugler said.
This benefit was achieved without any additional adverse events, he added. There were no significant differences in confusion; epidural placement; length of stay; respiratory event, sedation, hallucinations, delusions or disturbing dreams; or unplanned transfers to the ICU.
Dr. Kugler disclosed that he and primary investigator Thomas Carver, MD, also of the Medical College of Wisconsin, Milwaukee, are both paid consultants for InnoVital Systems.
REPORTING FROM THE AAST ANNUAL MEETING
Key clinical point: Low-dose ketamine controlled pain while reducing opioid use among patients with severe thoracic injury.
Major finding: Compared with placebo, ketamine reduced opioids conferred OME savings of 148 mg over a patient’s entire hospitalization.
Study details: The randomized study comprised 93 patients with thoracic injury.
Disclosures: Dr. Kugler disclosed that he and primary investigator Thomas Carver, MD, are both paid consultants for InnoVital Systems.
Source: Carver T et al. AAST 2018, Oral abstract 2
Risk factors for postop cardiac events differ between vascular and general surgery
Predictive risk factors for cardiac events (CEs) after general and vascular surgery differed significantly, according to a large retrospective study. However, there was no significant difference seen in the overall incidence of CEs between the two types of surgery, reported Derrick Acheampong, MD, and his colleagues at the Icahn School of Medicine at Mount Sinai, New York.
They performed a retrospective data analysis of 8,441 adult patients at their large urban teaching hospital; these patients had undergone general or vascular surgery during 2013-2016 and, in the analysis, were grouped by whether they experienced postoperative CEs.
Univariate and multivariate analyses identified predictors of postoperative CE and the association of CEs with adverse postoperative outcomes. CEs were defined as myocardial infarction or cardiac arrest within the 30-day postoperative period.
A total of 157 patients (1.9%) experienced CEs after major general and vascular surgery, with no significant difference in incidence between the two types of surgery (P = .44), according to their report, published online in the Annals of Medicine and Surgery. CE-associated mortality among this group was high, at 55.4%.
The occurrence of a CE following surgery in both groups was significantly associated with increased mortality, as well as pulmonary, renal, and neurological complications, in addition to systemic sepsis, postoperative red blood cell transfusion, unplanned return to the operating room, and prolonged hospitalization, according to the researchers.
However, predictors of CEs risk between vascular and general surgery were significantly different.
For general surgery, American Society of Anesthesiologists (ASA) status greater than 3, dependent functional status, acute renal failure or dialysis, weight loss, creatinine greater than 1.2 mg/dL, international normalized ratio (INR) greater than 1.5, and partial thromboplastin time (PTT) less than 35 seconds were all unique independent predictors of postoperative CEs.
For vascular surgery, the unique significant predictors of postoperative CEs were age greater than 65 years, emergency surgery, diabetes, congestive heart failure, systemic sepsis, and operative time greater than 240 minutes.
The only common predictive risk factors for postoperative CEs for the two forms of surgery were hematocrit less than 34% and ventilator dependence.
“The present study corroborates reported studies that recommend separate predictive CE risk indices and risk stratification among different surgical specialties. Predictors for CE greatly differed between general and vascular surgery patients in our patient population,” the authors stated.
They concluded with the hope that their study “provides useful information to surgeons and allows for the necessary resources to be focused on identified at-risk patients to improve surgical outcomes.”
Dr. Acheampong and his colleagues reported having no disclosures.
SOURCE: Acheampong D et al. Ann Med Surg. 2018. doi: 10.1016/j.amsu.2018.08.001.
Predictive risk factors for cardiac events (CEs) after general and vascular surgery differed significantly, according to a large retrospective study. However, there was no significant difference seen in the overall incidence of CEs between the two types of surgery, reported Derrick Acheampong, MD, and his colleagues at the Icahn School of Medicine at Mount Sinai, New York.
They performed a retrospective data analysis of 8,441 adult patients at their large urban teaching hospital; these patients had undergone general or vascular surgery during 2013-2016 and, in the analysis, were grouped by whether they experienced postoperative CEs.
Univariate and multivariate analyses identified predictors of postoperative CE and the association of CEs with adverse postoperative outcomes. CEs were defined as myocardial infarction or cardiac arrest within the 30-day postoperative period.
A total of 157 patients (1.9%) experienced CEs after major general and vascular surgery, with no significant difference in incidence between the two types of surgery (P = .44), according to their report, published online in the Annals of Medicine and Surgery. CE-associated mortality among this group was high, at 55.4%.
The occurrence of a CE following surgery in both groups was significantly associated with increased mortality, as well as pulmonary, renal, and neurological complications, in addition to systemic sepsis, postoperative red blood cell transfusion, unplanned return to the operating room, and prolonged hospitalization, according to the researchers.
However, predictors of CEs risk between vascular and general surgery were significantly different.
For general surgery, American Society of Anesthesiologists (ASA) status greater than 3, dependent functional status, acute renal failure or dialysis, weight loss, creatinine greater than 1.2 mg/dL, international normalized ratio (INR) greater than 1.5, and partial thromboplastin time (PTT) less than 35 seconds were all unique independent predictors of postoperative CEs.
For vascular surgery, the unique significant predictors of postoperative CEs were age greater than 65 years, emergency surgery, diabetes, congestive heart failure, systemic sepsis, and operative time greater than 240 minutes.
The only common predictive risk factors for postoperative CEs for the two forms of surgery were hematocrit less than 34% and ventilator dependence.
“The present study corroborates reported studies that recommend separate predictive CE risk indices and risk stratification among different surgical specialties. Predictors for CE greatly differed between general and vascular surgery patients in our patient population,” the authors stated.
They concluded with the hope that their study “provides useful information to surgeons and allows for the necessary resources to be focused on identified at-risk patients to improve surgical outcomes.”
Dr. Acheampong and his colleagues reported having no disclosures.
SOURCE: Acheampong D et al. Ann Med Surg. 2018. doi: 10.1016/j.amsu.2018.08.001.
Predictive risk factors for cardiac events (CEs) after general and vascular surgery differed significantly, according to a large retrospective study. However, there was no significant difference seen in the overall incidence of CEs between the two types of surgery, reported Derrick Acheampong, MD, and his colleagues at the Icahn School of Medicine at Mount Sinai, New York.
They performed a retrospective data analysis of 8,441 adult patients at their large urban teaching hospital; these patients had undergone general or vascular surgery during 2013-2016 and, in the analysis, were grouped by whether they experienced postoperative CEs.
Univariate and multivariate analyses identified predictors of postoperative CE and the association of CEs with adverse postoperative outcomes. CEs were defined as myocardial infarction or cardiac arrest within the 30-day postoperative period.
A total of 157 patients (1.9%) experienced CEs after major general and vascular surgery, with no significant difference in incidence between the two types of surgery (P = .44), according to their report, published online in the Annals of Medicine and Surgery. CE-associated mortality among this group was high, at 55.4%.
The occurrence of a CE following surgery in both groups was significantly associated with increased mortality, as well as pulmonary, renal, and neurological complications, in addition to systemic sepsis, postoperative red blood cell transfusion, unplanned return to the operating room, and prolonged hospitalization, according to the researchers.
However, predictors of CEs risk between vascular and general surgery were significantly different.
For general surgery, American Society of Anesthesiologists (ASA) status greater than 3, dependent functional status, acute renal failure or dialysis, weight loss, creatinine greater than 1.2 mg/dL, international normalized ratio (INR) greater than 1.5, and partial thromboplastin time (PTT) less than 35 seconds were all unique independent predictors of postoperative CEs.
For vascular surgery, the unique significant predictors of postoperative CEs were age greater than 65 years, emergency surgery, diabetes, congestive heart failure, systemic sepsis, and operative time greater than 240 minutes.
The only common predictive risk factors for postoperative CEs for the two forms of surgery were hematocrit less than 34% and ventilator dependence.
“The present study corroborates reported studies that recommend separate predictive CE risk indices and risk stratification among different surgical specialties. Predictors for CE greatly differed between general and vascular surgery patients in our patient population,” the authors stated.
They concluded with the hope that their study “provides useful information to surgeons and allows for the necessary resources to be focused on identified at-risk patients to improve surgical outcomes.”
Dr. Acheampong and his colleagues reported having no disclosures.
SOURCE: Acheampong D et al. Ann Med Surg. 2018. doi: 10.1016/j.amsu.2018.08.001.
FROM ANNALS OF MEDICINE AND SURGERY
Key clinical point: There was a significant difference in predictive risk factors for postoperative cardiac events between vascular and general surgery.
Major finding: The 1.9% incidence of cardiac events following general or vascular surgery was associated with a mortality rate of 55%.
Study details: Retrospective study of 8,441 patients who underwent vascular or general surgery during 2013-2015.
Disclosures: The authors reported having no disclosures.
Source: Acheampong D et al. Ann Med Surg. 2018. doi: 10.1016/j.amsu.2018.08.001.
Frailty and risk of postoperative complications
Background: FTR is a quality measure defined as death after a serious, potentially preventable complication. Frailty incorporates different domains including physical performance, gait, mobility, nutritional status, mental health, and cognition. Although there are some studies linking frailty and FTR and postoperative morbidity, the degree and association with low-risk procedures is unclear.
Study design: Retrospective cohort study.
Setting: More than 600 hospitals participating in the American College of Surgeons’ National Surgical Quality Improvement Program database during 2005-2012.
Synopsis: The cohort included 984,550 adult patients who underwent inpatient procedure for general, vascular, thoracic, cardiac, and orthopedic operations. The Risk Analysis Index (RAI) score was used to calculate frailty. The rate of major complications increased as the RAI score was higher for both low-risk and high-risk surgery. For RAI scores less than 10, the rate was 7.4%; for RAI scores 11-20, the rate was 19.8%; for RAI scores 21-30, the rate was 41.1%; and for RAI scores above 40, the rate was 53.6%. Stratifying by the number of complications, significant increases in FTR were observed across the RAI categories for both low-risk and high-risk procedures.
Frailty assessment should be considered a part of the routine perioperative evaluation and should stimulate preoperative interventions aimed at reducing risk for postoperative complications.
Bottom line: This large retrospective study found an association between increasing frailty and both the number of complications and FTR for both low-risk and high-risk surgical procedures.
Citation: Shah R et al. Association of frailty with failure to rescue after low-risk and high-risk inpatient surgery. JAMA Surg. 2018 Mar 21;153(5):e180214.
Dr. Canepa is a hospitalist in the division of hospital medicine at the University of Kentucky, Lexington.
Background: FTR is a quality measure defined as death after a serious, potentially preventable complication. Frailty incorporates different domains including physical performance, gait, mobility, nutritional status, mental health, and cognition. Although there are some studies linking frailty and FTR and postoperative morbidity, the degree and association with low-risk procedures is unclear.
Study design: Retrospective cohort study.
Setting: More than 600 hospitals participating in the American College of Surgeons’ National Surgical Quality Improvement Program database during 2005-2012.
Synopsis: The cohort included 984,550 adult patients who underwent inpatient procedure for general, vascular, thoracic, cardiac, and orthopedic operations. The Risk Analysis Index (RAI) score was used to calculate frailty. The rate of major complications increased as the RAI score was higher for both low-risk and high-risk surgery. For RAI scores less than 10, the rate was 7.4%; for RAI scores 11-20, the rate was 19.8%; for RAI scores 21-30, the rate was 41.1%; and for RAI scores above 40, the rate was 53.6%. Stratifying by the number of complications, significant increases in FTR were observed across the RAI categories for both low-risk and high-risk procedures.
Frailty assessment should be considered a part of the routine perioperative evaluation and should stimulate preoperative interventions aimed at reducing risk for postoperative complications.
Bottom line: This large retrospective study found an association between increasing frailty and both the number of complications and FTR for both low-risk and high-risk surgical procedures.
Citation: Shah R et al. Association of frailty with failure to rescue after low-risk and high-risk inpatient surgery. JAMA Surg. 2018 Mar 21;153(5):e180214.
Dr. Canepa is a hospitalist in the division of hospital medicine at the University of Kentucky, Lexington.
Background: FTR is a quality measure defined as death after a serious, potentially preventable complication. Frailty incorporates different domains including physical performance, gait, mobility, nutritional status, mental health, and cognition. Although there are some studies linking frailty and FTR and postoperative morbidity, the degree and association with low-risk procedures is unclear.
Study design: Retrospective cohort study.
Setting: More than 600 hospitals participating in the American College of Surgeons’ National Surgical Quality Improvement Program database during 2005-2012.
Synopsis: The cohort included 984,550 adult patients who underwent inpatient procedure for general, vascular, thoracic, cardiac, and orthopedic operations. The Risk Analysis Index (RAI) score was used to calculate frailty. The rate of major complications increased as the RAI score was higher for both low-risk and high-risk surgery. For RAI scores less than 10, the rate was 7.4%; for RAI scores 11-20, the rate was 19.8%; for RAI scores 21-30, the rate was 41.1%; and for RAI scores above 40, the rate was 53.6%. Stratifying by the number of complications, significant increases in FTR were observed across the RAI categories for both low-risk and high-risk procedures.
Frailty assessment should be considered a part of the routine perioperative evaluation and should stimulate preoperative interventions aimed at reducing risk for postoperative complications.
Bottom line: This large retrospective study found an association between increasing frailty and both the number of complications and FTR for both low-risk and high-risk surgical procedures.
Citation: Shah R et al. Association of frailty with failure to rescue after low-risk and high-risk inpatient surgery. JAMA Surg. 2018 Mar 21;153(5):e180214.
Dr. Canepa is a hospitalist in the division of hospital medicine at the University of Kentucky, Lexington.
Enhanced recovery initiative improved bariatric length of stay
ORLANDO – Adopting a 28-point significantly reduced length of stay without significant effects on complications or readmissions, according to interim results of a large, nationwide surgical quality initiative.
Thirty-six centers participated in this pilot initiative, making it one of the largest national projects focused on enhanced recovery to date, according to Stacy A. Brethauer, MD, FACS, cochair of the Quality and Data Committee of the Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP).
The initiative, known as Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY), was developed in light of “huge gaps in literature and knowledge” about what best practices of enhanced recovery should look like for bariatric surgery, Dr. Brethauer said in a podium presentation at the American College of Surgeons Quality and Safety Conference.
“Bariatric surgery is very pathway driven, but the pathway can be very cumbersome and very antiquated if you don’t keep it up to date and evidence based,” said Dr. Brethauer, associate professor of surgery at the Cleveland Clinic.
Invitations to join in the ENERGY pilot were targeted to the 80 or so MBSAQIP-accredited centers in the top decile of programs for length of stay. “That’s the needle that we want to move,” Dr. Brethauer said.
ENERGY includes interventions in the preoperative, perioperative, and postoperative setting for each patient who undergoes a primary band, lap sleeve, or lap bypass procedure.
The 36 participating centers were asked to document 28 discrete process measures, starting with “did the patient stop smoking before surgery?” and ending with “did the patient have a follow-up clinic appointment scheduled?” Each one was entered by a trained clinical reviewer. The program included monthly audits for each participating center.
Data collection started on July 1, 2017, and continued to June 30, 2018, following a 6-month run-up period to allow centers to incorporate the measures.
The interim analysis presented included 4,700 patients who underwent procedures in the first 6 months of the data collection period. Nearly 60% (2,790 patients) had a laparoscopic sleeve gastrectomy, while about 40% (1,896 patients) underwent laparoscopic gastric bypass, and 0.1% (6 patients) had a band procedure.
Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers (P less than .001), Dr. Brethauer reported.
Similarly, the rate of extended length of stay was 4.4% in the first 6 months of the pilot, down from 8.2% in 2016. Extended length of stay decreased with increasing adherence to the protocol, Dr. Brethauer and his colleagues found in their analysis.
Those length-of-stay reductions were accomplished with no increase in bleeding rates, all-cause reoperation rates, or readmissions. “We’re not doing this at the expense of other complications,” Dr. Brethauer said in a comment on the results.
Adherence to the 28 ENERGY measures increased from 26% in the first month of the pilot to 80.2% in March 2017, the latest month included in the interim analysis.
Opioid-sparing pain management strategies are incorporated into ENERGY. Over the first six months of the pilot, the average proportion of patients receiving no opioids postoperatively was 26.8%.
The ultimate goal of ENERGY is a large-scale rollout of enhanced recovery strategies, according to Dr. Brethauer.
ENERGY is the second national quality improvement project of the MBSAQIP. In the first, known as Decreasing Readmissions through Opportunities Provided (DROP), 128 U.S. hospitals implemented a set of standard processes organized into preoperative, inpatient, and postoperative care bundles. Results of a yearlong study of the DROP intervention demonstrated a significant reduction in 30-day all-cause hospital readmissions following sleeve gastrectomy.
“If you look at what’s happened in our specialty, and all the changes and all the work that’s been done, it’s really quite impressive,” Dr. Brethauer told attendees at the meeting. “It’s something that we’re very proud of. “
Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
ORLANDO – Adopting a 28-point significantly reduced length of stay without significant effects on complications or readmissions, according to interim results of a large, nationwide surgical quality initiative.
Thirty-six centers participated in this pilot initiative, making it one of the largest national projects focused on enhanced recovery to date, according to Stacy A. Brethauer, MD, FACS, cochair of the Quality and Data Committee of the Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP).
The initiative, known as Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY), was developed in light of “huge gaps in literature and knowledge” about what best practices of enhanced recovery should look like for bariatric surgery, Dr. Brethauer said in a podium presentation at the American College of Surgeons Quality and Safety Conference.
“Bariatric surgery is very pathway driven, but the pathway can be very cumbersome and very antiquated if you don’t keep it up to date and evidence based,” said Dr. Brethauer, associate professor of surgery at the Cleveland Clinic.
Invitations to join in the ENERGY pilot were targeted to the 80 or so MBSAQIP-accredited centers in the top decile of programs for length of stay. “That’s the needle that we want to move,” Dr. Brethauer said.
ENERGY includes interventions in the preoperative, perioperative, and postoperative setting for each patient who undergoes a primary band, lap sleeve, or lap bypass procedure.
The 36 participating centers were asked to document 28 discrete process measures, starting with “did the patient stop smoking before surgery?” and ending with “did the patient have a follow-up clinic appointment scheduled?” Each one was entered by a trained clinical reviewer. The program included monthly audits for each participating center.
Data collection started on July 1, 2017, and continued to June 30, 2018, following a 6-month run-up period to allow centers to incorporate the measures.
The interim analysis presented included 4,700 patients who underwent procedures in the first 6 months of the data collection period. Nearly 60% (2,790 patients) had a laparoscopic sleeve gastrectomy, while about 40% (1,896 patients) underwent laparoscopic gastric bypass, and 0.1% (6 patients) had a band procedure.
Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers (P less than .001), Dr. Brethauer reported.
Similarly, the rate of extended length of stay was 4.4% in the first 6 months of the pilot, down from 8.2% in 2016. Extended length of stay decreased with increasing adherence to the protocol, Dr. Brethauer and his colleagues found in their analysis.
Those length-of-stay reductions were accomplished with no increase in bleeding rates, all-cause reoperation rates, or readmissions. “We’re not doing this at the expense of other complications,” Dr. Brethauer said in a comment on the results.
Adherence to the 28 ENERGY measures increased from 26% in the first month of the pilot to 80.2% in March 2017, the latest month included in the interim analysis.
Opioid-sparing pain management strategies are incorporated into ENERGY. Over the first six months of the pilot, the average proportion of patients receiving no opioids postoperatively was 26.8%.
The ultimate goal of ENERGY is a large-scale rollout of enhanced recovery strategies, according to Dr. Brethauer.
ENERGY is the second national quality improvement project of the MBSAQIP. In the first, known as Decreasing Readmissions through Opportunities Provided (DROP), 128 U.S. hospitals implemented a set of standard processes organized into preoperative, inpatient, and postoperative care bundles. Results of a yearlong study of the DROP intervention demonstrated a significant reduction in 30-day all-cause hospital readmissions following sleeve gastrectomy.
“If you look at what’s happened in our specialty, and all the changes and all the work that’s been done, it’s really quite impressive,” Dr. Brethauer told attendees at the meeting. “It’s something that we’re very proud of. “
Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
ORLANDO – Adopting a 28-point significantly reduced length of stay without significant effects on complications or readmissions, according to interim results of a large, nationwide surgical quality initiative.
Thirty-six centers participated in this pilot initiative, making it one of the largest national projects focused on enhanced recovery to date, according to Stacy A. Brethauer, MD, FACS, cochair of the Quality and Data Committee of the Metabolic and Bariatric Surgery Accreditation Quality Improvement Program (MBSAQIP).
The initiative, known as Employing New Enhanced Recovery Goals for Bariatric Surgery (ENERGY), was developed in light of “huge gaps in literature and knowledge” about what best practices of enhanced recovery should look like for bariatric surgery, Dr. Brethauer said in a podium presentation at the American College of Surgeons Quality and Safety Conference.
“Bariatric surgery is very pathway driven, but the pathway can be very cumbersome and very antiquated if you don’t keep it up to date and evidence based,” said Dr. Brethauer, associate professor of surgery at the Cleveland Clinic.
Invitations to join in the ENERGY pilot were targeted to the 80 or so MBSAQIP-accredited centers in the top decile of programs for length of stay. “That’s the needle that we want to move,” Dr. Brethauer said.
ENERGY includes interventions in the preoperative, perioperative, and postoperative setting for each patient who undergoes a primary band, lap sleeve, or lap bypass procedure.
The 36 participating centers were asked to document 28 discrete process measures, starting with “did the patient stop smoking before surgery?” and ending with “did the patient have a follow-up clinic appointment scheduled?” Each one was entered by a trained clinical reviewer. The program included monthly audits for each participating center.
Data collection started on July 1, 2017, and continued to June 30, 2018, following a 6-month run-up period to allow centers to incorporate the measures.
The interim analysis presented included 4,700 patients who underwent procedures in the first 6 months of the data collection period. Nearly 60% (2,790 patients) had a laparoscopic sleeve gastrectomy, while about 40% (1,896 patients) underwent laparoscopic gastric bypass, and 0.1% (6 patients) had a band procedure.
Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers (P less than .001), Dr. Brethauer reported.
Similarly, the rate of extended length of stay was 4.4% in the first 6 months of the pilot, down from 8.2% in 2016. Extended length of stay decreased with increasing adherence to the protocol, Dr. Brethauer and his colleagues found in their analysis.
Those length-of-stay reductions were accomplished with no increase in bleeding rates, all-cause reoperation rates, or readmissions. “We’re not doing this at the expense of other complications,” Dr. Brethauer said in a comment on the results.
Adherence to the 28 ENERGY measures increased from 26% in the first month of the pilot to 80.2% in March 2017, the latest month included in the interim analysis.
Opioid-sparing pain management strategies are incorporated into ENERGY. Over the first six months of the pilot, the average proportion of patients receiving no opioids postoperatively was 26.8%.
The ultimate goal of ENERGY is a large-scale rollout of enhanced recovery strategies, according to Dr. Brethauer.
ENERGY is the second national quality improvement project of the MBSAQIP. In the first, known as Decreasing Readmissions through Opportunities Provided (DROP), 128 U.S. hospitals implemented a set of standard processes organized into preoperative, inpatient, and postoperative care bundles. Results of a yearlong study of the DROP intervention demonstrated a significant reduction in 30-day all-cause hospital readmissions following sleeve gastrectomy.
“If you look at what’s happened in our specialty, and all the changes and all the work that’s been done, it’s really quite impressive,” Dr. Brethauer told attendees at the meeting. “It’s something that we’re very proud of. “
Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
REPORTING FROM ACSQSC 2018
Key clinical point: An evidence-based enhanced recovery protocol reduced length of stay for bariatric surgery patients.
Major finding: Average length of stay was 1.76 days in the first 6 months of the pilot, down from 2.24 days in 2016 for those same participating centers.
Study details: Data on 36 bariatric surgery centers and 4,700 patients who underwent procedures in the first 6 months of the data collection period.
Disclosures: Dr. Brethauer reported disclosures related to Medtronic and Ethicon outside of the scope of this presentation.
Internist comanagement of orthopedic inpatients boosts outcomes
NEW ORLEANS – Comanagement of orthopedic inpatients by an internist or hospitalist can improve outcomes in myriad ways, Mary Anderson Wallace, MD, said at the annual meeting of the American College of Physicians.
She focused on patients undergoing total hip or knee arthroplasty (THA/TKA). In 2014, there were 400,000 of them under Medicare alone, accounting for $7 billion in hospitalization costs and nearly as much again in the cost of related postdischarge care.
So, changes in management that improve key outcomes in this population by even a small increment reap huge benefits when spread across this enormous patient population, noted Dr. Wallace, an internist and hospitalist at the University of Colorado, Denver.
Among the examples she highlighted where comanagement can have a favorable impact were optimization of perioperative pain management pathways; how to handle the use of disease-modifying antirheumatic drugs (DMARDs) in patients undergoing THA/TKA; the latest thinking on the appropriateness of low-dose aspirin for deep vein thrombosis (DVT) prophylaxis; a simple way to predict postop delirium in older individuals without known dementia; how to decide which postoperative fevers warrant a costly infectious disease workup; and the optimal wait time from arrival at the hospital with a fractured hip and THA.
These are all issues where a well-informed internist/hospitalist can be of enormous assistance to a busy orthopedic surgeon in providing high-value care, she explained.
Optimizing perioperative pain management pathways
As of 2015, orthopedists ranked as the third highest prescribers of opioids. Impressively, a retrospective cohort study of 641,941 opioid-naive, privately insured patients undergoing 1 of 11 types of surgery demonstrated that TKA was associated with a 5.1-fold increased risk for subsequent chronic opioid use in the first year after surgery, compared with 18 million opioid-naive nonsurgical controls. Indeed, TKA was the highest-risk of the 11 surgical procedures examined (JAMA Intern Med. 2016 Sep 1;176[9]:1286-93).
Another study that points to a need to develop best practices for opioid prescribing in orthopedic surgery – and other types of surgery as well – was a systematic review of six studies of patients who received prescription opioid analgesics in conjunction with seven types of surgery.
Opioid oversupply was identified as a clear problem: 67%-92% of patients in the six studies reported unused opioids. Up to 71% of opioid tablets went unused, mainly because patients felt they’d achieved adequate pain control and didn’t need them. Rates of safe disposal of unused opioids were in the single digits, suggesting that overprescribing provides a large potential reservoir of opioids that can be diverted to nonmedical use (JAMA Surg. 2017 Nov 1;152[11]:1066-71).
Moreover, a recent retrospective study of more than 1 million opioid-naive patients undergoing surgery showed that 56% of them received postoperative opioids. And each additional week of use was associated with a 44% increase in the relative risk of the composite endpoint of opioid dependence, abuse, or overdose. Duration of opioid use was a stronger predictor of this adverse outcome than was dosage (BMJ. 2018 Jan 17;360:j5790).
Other studies have shown that multimodal analgesia is utilized in only 25%-50% of surgical patients, even though it is considered the standard of care. Only 20% of patients undergoing THA/TKA receive peripheral nerve and neuraxial blocks. So, there is an opportunity for optimization of perioperative pain management pathways in orthopedic surgery patients, including avoidance of unnecessary p.r.n. prescribing, to favorably impact the national opioid epidemic, Dr. Wallace observed.
A surprise benefit of multimodal pain management that includes acetaminophen and a nonsteroidal anti-inflammatory agent is that it markedly reduces the incidence of postoperative fevers after total joint arthroplasty, compared with opioid-based pain management.
That was demonstrated in a retrospective study of 2,417 THA/TKAs in which multimodal pain management was used, and 1,484 procedures that relied on opioid-based pain relief. All of the operations were performed by the same three orthopedic surgeons. Only 5% of patients in the multimodal pain management group developed a fever greater than 38.5 degrees Celsius during the first 5 postoperative days, compared with 25% of those in the opioid-based analgesia group.
Moreover, an infectious disease workup was ordered in 2% of the multimodal analgesia group, versus 10% in the opioid-based pain management cohort, with no difference in the positive workup rates between the two groups (Clin Orthop Relat Res. 2014 May;472[5]:1489-95).
“It’s interesting that multimodal pain management has the side effect of putting you in a better position to practice high-value care, with less fever and fewer infectious disease workups,” Dr. Wallace said.
Perioperative management of DMARDs
Recent joint guidelines from the American College of Rheumatology and American Association of Hip and Knee Surgeons specifically address this issue in patients undergoing elective joint replacement (Arthritis Rheumatol. 2017 Aug;69[8]:1538-51).
“The quality of evidence isn’t high, but at least it’s a starting point,” Dr. Wallace said.
Patients with rheumatoid arthritis, systemic lupus erythematosus, spondyloarthropathies, and other rheumatic diseases who are on methotrexate or other nonbiologic DMARDs should be maintained on their current dose, according to the guidelines.
In contrast, all biologic agents should be withheld prior to surgery, which should be scheduled to coincide with the end of the dosing cycle for that specific biologic. The biologic agent should be resumed only once adequate wound healing has occurred, typically about 14 days post-THA/TKA.
Patients on daily glucocorticoids should continue on their current dose; supraphysiologic stress dosing is to be avoided.
Low-dose aspirin for VTE prophylaxis
“It seems like nothing has been such an enduring controversy in the comanagement literature as the question of whether aspirin is an effective prophylactic agent for prevention of DVT post THA/TKA,” according to Dr. Wallace.
She noted that in the space of just 4 years between the eighth and ninth editions of the American College of Chest Physician guidelines, that organization underwent a 180-degree reversal on the issue – whipsawing from a grade 1A recommendation against aspirin in 2008 to a 1B recommendation for it in 2012.
The literature is increasingly supportive of the use of aspirin for venous thromboembolism (VTE) prophylaxis in low-risk THA/TKA patients. Separate guidelines from the American Academy of Orthopaedic Surgeons (AAOS) and the Surgical Care Improvement Project, as well as the chest physicians, support the practice.
The hitch is that there is as yet no single validated risk-stratification protocol. AAOS recommends 325 mg of aspirin twice daily for 6 weeks. But a prospective crossover study of more than 4,600 total joint arthroplasty patients conducted by investigators at Thomas Jefferson University in Philadelphia showed that 81 mg BID for 4 weeks was just as effective as was 325 mg b.i.d., albeit with an incidence of GI bleeding that to their surprise wasn’t significantly lower (J Bone Joint Surg Am. 2017 Jan 18;99[2]:91-8).
Dr. Wallace anticipates definitive answers on VTE prophylaxis to come from the ongoing Patient-Centered Outcomes Research Institute-supported PEPPER (Comparative Effectiveness of Pulmonary Embolism Prevention After Hip and Knee Replacement) trial. In that study, roughly 25,000 patients undergoing THA/TKA are being randomized to prophylactic aspirin at 81 mg b.i.d., warfarin at an International Normalized Ratio of 2.0, or rivaroxaban (Xarelto). Endpoints include mortality, VTE, and bleeding. Results are expected in 2021.
Preoperative prediction of postop delirium
Unrecognized preoperative cognitive impairment in older patients without dementia who are undergoing THA/TKA is a common and powerful risk factor for postop delirium and other complications, as demonstrated recently by investigators at Harvard University and affiliated hospitals.
They had 211 patients aged 65 or older, none with known dementia, take the Mini-Cog screening test prior to their surgery. Fully 24% had probable cognitive impairment as reflected in a score of 2 or less out of a possible 5 points on this simple test, which consists of a three-word recall and clock drawing.
“I was very surprised at this high rate. These are patients who are at risk for delirium in the hospital when you’re taking care of them,” Dr. Wallace observed.
In the Harvard study, the incidence of postop delirium was 21% in patients with a Mini-Cog score of 2 or less, compared with 7% who scored 3-5, for an odds ratio of 4.5 in an age-adjusted multivariate analysis. Moreover, 67% of the low scorers were discharged somewhere other than home, in contrast to 34% of patients with a preop Mini-Cog score of 3-5, for an adjusted 3.9-fold increased risk. The group with a Mini-Cog score of 2 or less also had a significantly longer hospital length of stay (Anesthesiology. 2017 Nov;127[5]:765-74).
Perioperative gabapentin is often added to the medication regimen of older surgical patients to reduce postop delirium. The latest evidence indicates that doesn’t work, as demonstrated in a recent 697-patient randomized trial. The incidence of delirium during the first 3 days post surgery as measured by the Confusion Assessment Method was 22.4% in patients randomized to 900 mg of gabapentin per day, and 20.8% with placebo. Nearly 200 participants had THA or TKA, and in that subgroup, there was an even stronger – albeit still not statistically significant – trend for a higher delirium rate with gabapentin than with placebo (Anesthesiology. 2017 Oct.127[4]:633-44).
“Think twice about adding gabapentin to the pain regimen for THA/TKA/spine patients for the purpose of preventing postop delirium,” she advised.
When is postop fever a concern?
Up to half of patients develop fever early after THA/TKA. In most cases, this is a self-limited ancillary effect of cytokine release, with the temperature peaking on postop day 1-2.
Three strong predictors of a positive infectious disease workup are fever after postop day 3, with an associated 23.3-fold increased risk; multiple days of fever, with an odds ratio of 8.6; and a maximum temperature greater than 39.0 degrees Celsius, with a 2.4-fold increased risk. In this 7-year-old study, the cost of infectious disease workup per change in patient management was a hefty $8,209 (J Arthroplasty. 2010 Sep;25[6 Suppl]:43-8).
A retrospective study of nearly 125,000 THA/TKA patients in the American College of Surgeons National Surgical Quality Improvement Program database has important implications for clinical surveillance for postop adverse events. Stroke occurred early, on median postop day 1. The median time of acute MI and pulmonary embolism was postop day 3, and pneumonia day 4.
The key take-home message was that the median time to DVT was postop day 6, by which point most patients had been discharged. Thus, 60% of postoperative DVTs occurred after discharge. And the time to diagnosis of DVT differed markedly by surgical procedure: The median day of diagnosis was day 5 in TKA patients, compared with day 13 for THA patients. Sixty-eight percent of urinary tract infections occurred post discharge. Sepsis occurred on median day 10 post surgery, surgical site infections on day 17 (Clin Orthop Relat Res. 2017 Dec;475[12]:2952-9).
In light of ever-shortening hospital lengths of stay, Dr. Wallace noted, the findings underscore the importance of comprehensive predischarge patient counseling.
Optimal time window for hip fracture surgery
AAOS guidelines recommend that hip fracture surgery should take place within 48 hours, assuming medical comorbidities are stabilized, because complication rates go up with longer wait times.
But that is controversial. A University of Toronto retrospective cohort study of 42,430 adults with hip fracture treated at 72 Canadian hospitals during 2009-2014 found that the inflection point was 24 hours. Among 13,731 patients whose elapsed time from hospital arrival to surgery was 24 hours or less, 30-day mortality was 5.8%, significantly less than the 6.5% rate in an equal number of propensity score–matched patients with a longer wait time.
The 90- and 365-day mortality rates in the patients who received surgery within 24 hours were 10.7% and 19.3%, both significantly lower than the 12.0% and 21.6% figures in patients with longer wait times.
For the 30-day composite outcome of death, myocardial infarction, pulmonary embolism, DVT, or pneumonia, the rates were 10.1% and 12.2% – again, statistically significant and clinically meaningful. The 90- and 365-day composite outcomes followed suit (JAMA. 2017 Nov 28;318[20]:1994-2003).
But the Canadian study won’t be the final word. The ongoing international multicenter HIP ATTACK (Hip Fracture Accelerated Surgical Treatment and Care Track) trial is comparing outcomes in 3,000 patients randomized to hip fracture surgery within 6 hours versus 24 hours. Endpoints include mortality, myocardial infarction, pulmonary embolism, pneumonia, stroke, sepsis, and life-threatening and major bleeding.
Dr. Wallace reported having no financial conflicts regarding her presentation.
NEW ORLEANS – Comanagement of orthopedic inpatients by an internist or hospitalist can improve outcomes in myriad ways, Mary Anderson Wallace, MD, said at the annual meeting of the American College of Physicians.
She focused on patients undergoing total hip or knee arthroplasty (THA/TKA). In 2014, there were 400,000 of them under Medicare alone, accounting for $7 billion in hospitalization costs and nearly as much again in the cost of related postdischarge care.
So, changes in management that improve key outcomes in this population by even a small increment reap huge benefits when spread across this enormous patient population, noted Dr. Wallace, an internist and hospitalist at the University of Colorado, Denver.
Among the examples she highlighted where comanagement can have a favorable impact were optimization of perioperative pain management pathways; how to handle the use of disease-modifying antirheumatic drugs (DMARDs) in patients undergoing THA/TKA; the latest thinking on the appropriateness of low-dose aspirin for deep vein thrombosis (DVT) prophylaxis; a simple way to predict postop delirium in older individuals without known dementia; how to decide which postoperative fevers warrant a costly infectious disease workup; and the optimal wait time from arrival at the hospital with a fractured hip and THA.
These are all issues where a well-informed internist/hospitalist can be of enormous assistance to a busy orthopedic surgeon in providing high-value care, she explained.
Optimizing perioperative pain management pathways
As of 2015, orthopedists ranked as the third highest prescribers of opioids. Impressively, a retrospective cohort study of 641,941 opioid-naive, privately insured patients undergoing 1 of 11 types of surgery demonstrated that TKA was associated with a 5.1-fold increased risk for subsequent chronic opioid use in the first year after surgery, compared with 18 million opioid-naive nonsurgical controls. Indeed, TKA was the highest-risk of the 11 surgical procedures examined (JAMA Intern Med. 2016 Sep 1;176[9]:1286-93).
Another study that points to a need to develop best practices for opioid prescribing in orthopedic surgery – and other types of surgery as well – was a systematic review of six studies of patients who received prescription opioid analgesics in conjunction with seven types of surgery.
Opioid oversupply was identified as a clear problem: 67%-92% of patients in the six studies reported unused opioids. Up to 71% of opioid tablets went unused, mainly because patients felt they’d achieved adequate pain control and didn’t need them. Rates of safe disposal of unused opioids were in the single digits, suggesting that overprescribing provides a large potential reservoir of opioids that can be diverted to nonmedical use (JAMA Surg. 2017 Nov 1;152[11]:1066-71).
Moreover, a recent retrospective study of more than 1 million opioid-naive patients undergoing surgery showed that 56% of them received postoperative opioids. And each additional week of use was associated with a 44% increase in the relative risk of the composite endpoint of opioid dependence, abuse, or overdose. Duration of opioid use was a stronger predictor of this adverse outcome than was dosage (BMJ. 2018 Jan 17;360:j5790).
Other studies have shown that multimodal analgesia is utilized in only 25%-50% of surgical patients, even though it is considered the standard of care. Only 20% of patients undergoing THA/TKA receive peripheral nerve and neuraxial blocks. So, there is an opportunity for optimization of perioperative pain management pathways in orthopedic surgery patients, including avoidance of unnecessary p.r.n. prescribing, to favorably impact the national opioid epidemic, Dr. Wallace observed.
A surprise benefit of multimodal pain management that includes acetaminophen and a nonsteroidal anti-inflammatory agent is that it markedly reduces the incidence of postoperative fevers after total joint arthroplasty, compared with opioid-based pain management.
That was demonstrated in a retrospective study of 2,417 THA/TKAs in which multimodal pain management was used, and 1,484 procedures that relied on opioid-based pain relief. All of the operations were performed by the same three orthopedic surgeons. Only 5% of patients in the multimodal pain management group developed a fever greater than 38.5 degrees Celsius during the first 5 postoperative days, compared with 25% of those in the opioid-based analgesia group.
Moreover, an infectious disease workup was ordered in 2% of the multimodal analgesia group, versus 10% in the opioid-based pain management cohort, with no difference in the positive workup rates between the two groups (Clin Orthop Relat Res. 2014 May;472[5]:1489-95).
“It’s interesting that multimodal pain management has the side effect of putting you in a better position to practice high-value care, with less fever and fewer infectious disease workups,” Dr. Wallace said.
Perioperative management of DMARDs
Recent joint guidelines from the American College of Rheumatology and American Association of Hip and Knee Surgeons specifically address this issue in patients undergoing elective joint replacement (Arthritis Rheumatol. 2017 Aug;69[8]:1538-51).
“The quality of evidence isn’t high, but at least it’s a starting point,” Dr. Wallace said.
Patients with rheumatoid arthritis, systemic lupus erythematosus, spondyloarthropathies, and other rheumatic diseases who are on methotrexate or other nonbiologic DMARDs should be maintained on their current dose, according to the guidelines.
In contrast, all biologic agents should be withheld prior to surgery, which should be scheduled to coincide with the end of the dosing cycle for that specific biologic. The biologic agent should be resumed only once adequate wound healing has occurred, typically about 14 days post-THA/TKA.
Patients on daily glucocorticoids should continue on their current dose; supraphysiologic stress dosing is to be avoided.
Low-dose aspirin for VTE prophylaxis
“It seems like nothing has been such an enduring controversy in the comanagement literature as the question of whether aspirin is an effective prophylactic agent for prevention of DVT post THA/TKA,” according to Dr. Wallace.
She noted that in the space of just 4 years between the eighth and ninth editions of the American College of Chest Physician guidelines, that organization underwent a 180-degree reversal on the issue – whipsawing from a grade 1A recommendation against aspirin in 2008 to a 1B recommendation for it in 2012.
The literature is increasingly supportive of the use of aspirin for venous thromboembolism (VTE) prophylaxis in low-risk THA/TKA patients. Separate guidelines from the American Academy of Orthopaedic Surgeons (AAOS) and the Surgical Care Improvement Project, as well as the chest physicians, support the practice.
The hitch is that there is as yet no single validated risk-stratification protocol. AAOS recommends 325 mg of aspirin twice daily for 6 weeks. But a prospective crossover study of more than 4,600 total joint arthroplasty patients conducted by investigators at Thomas Jefferson University in Philadelphia showed that 81 mg BID for 4 weeks was just as effective as was 325 mg b.i.d., albeit with an incidence of GI bleeding that to their surprise wasn’t significantly lower (J Bone Joint Surg Am. 2017 Jan 18;99[2]:91-8).
Dr. Wallace anticipates definitive answers on VTE prophylaxis to come from the ongoing Patient-Centered Outcomes Research Institute-supported PEPPER (Comparative Effectiveness of Pulmonary Embolism Prevention After Hip and Knee Replacement) trial. In that study, roughly 25,000 patients undergoing THA/TKA are being randomized to prophylactic aspirin at 81 mg b.i.d., warfarin at an International Normalized Ratio of 2.0, or rivaroxaban (Xarelto). Endpoints include mortality, VTE, and bleeding. Results are expected in 2021.
Preoperative prediction of postop delirium
Unrecognized preoperative cognitive impairment in older patients without dementia who are undergoing THA/TKA is a common and powerful risk factor for postop delirium and other complications, as demonstrated recently by investigators at Harvard University and affiliated hospitals.
They had 211 patients aged 65 or older, none with known dementia, take the Mini-Cog screening test prior to their surgery. Fully 24% had probable cognitive impairment as reflected in a score of 2 or less out of a possible 5 points on this simple test, which consists of a three-word recall and clock drawing.
“I was very surprised at this high rate. These are patients who are at risk for delirium in the hospital when you’re taking care of them,” Dr. Wallace observed.
In the Harvard study, the incidence of postop delirium was 21% in patients with a Mini-Cog score of 2 or less, compared with 7% who scored 3-5, for an odds ratio of 4.5 in an age-adjusted multivariate analysis. Moreover, 67% of the low scorers were discharged somewhere other than home, in contrast to 34% of patients with a preop Mini-Cog score of 3-5, for an adjusted 3.9-fold increased risk. The group with a Mini-Cog score of 2 or less also had a significantly longer hospital length of stay (Anesthesiology. 2017 Nov;127[5]:765-74).
Perioperative gabapentin is often added to the medication regimen of older surgical patients to reduce postop delirium. The latest evidence indicates that doesn’t work, as demonstrated in a recent 697-patient randomized trial. The incidence of delirium during the first 3 days post surgery as measured by the Confusion Assessment Method was 22.4% in patients randomized to 900 mg of gabapentin per day, and 20.8% with placebo. Nearly 200 participants had THA or TKA, and in that subgroup, there was an even stronger – albeit still not statistically significant – trend for a higher delirium rate with gabapentin than with placebo (Anesthesiology. 2017 Oct.127[4]:633-44).
“Think twice about adding gabapentin to the pain regimen for THA/TKA/spine patients for the purpose of preventing postop delirium,” she advised.
When is postop fever a concern?
Up to half of patients develop fever early after THA/TKA. In most cases, this is a self-limited ancillary effect of cytokine release, with the temperature peaking on postop day 1-2.
Three strong predictors of a positive infectious disease workup are fever after postop day 3, with an associated 23.3-fold increased risk; multiple days of fever, with an odds ratio of 8.6; and a maximum temperature greater than 39.0 degrees Celsius, with a 2.4-fold increased risk. In this 7-year-old study, the cost of infectious disease workup per change in patient management was a hefty $8,209 (J Arthroplasty. 2010 Sep;25[6 Suppl]:43-8).
A retrospective study of nearly 125,000 THA/TKA patients in the American College of Surgeons National Surgical Quality Improvement Program database has important implications for clinical surveillance for postop adverse events. Stroke occurred early, on median postop day 1. The median time of acute MI and pulmonary embolism was postop day 3, and pneumonia day 4.
The key take-home message was that the median time to DVT was postop day 6, by which point most patients had been discharged. Thus, 60% of postoperative DVTs occurred after discharge. And the time to diagnosis of DVT differed markedly by surgical procedure: The median day of diagnosis was day 5 in TKA patients, compared with day 13 for THA patients. Sixty-eight percent of urinary tract infections occurred post discharge. Sepsis occurred on median day 10 post surgery, surgical site infections on day 17 (Clin Orthop Relat Res. 2017 Dec;475[12]:2952-9).
In light of ever-shortening hospital lengths of stay, Dr. Wallace noted, the findings underscore the importance of comprehensive predischarge patient counseling.
Optimal time window for hip fracture surgery
AAOS guidelines recommend that hip fracture surgery should take place within 48 hours, assuming medical comorbidities are stabilized, because complication rates go up with longer wait times.
But that is controversial. A University of Toronto retrospective cohort study of 42,430 adults with hip fracture treated at 72 Canadian hospitals during 2009-2014 found that the inflection point was 24 hours. Among 13,731 patients whose elapsed time from hospital arrival to surgery was 24 hours or less, 30-day mortality was 5.8%, significantly less than the 6.5% rate in an equal number of propensity score–matched patients with a longer wait time.
The 90- and 365-day mortality rates in the patients who received surgery within 24 hours were 10.7% and 19.3%, both significantly lower than the 12.0% and 21.6% figures in patients with longer wait times.
For the 30-day composite outcome of death, myocardial infarction, pulmonary embolism, DVT, or pneumonia, the rates were 10.1% and 12.2% – again, statistically significant and clinically meaningful. The 90- and 365-day composite outcomes followed suit (JAMA. 2017 Nov 28;318[20]:1994-2003).
But the Canadian study won’t be the final word. The ongoing international multicenter HIP ATTACK (Hip Fracture Accelerated Surgical Treatment and Care Track) trial is comparing outcomes in 3,000 patients randomized to hip fracture surgery within 6 hours versus 24 hours. Endpoints include mortality, myocardial infarction, pulmonary embolism, pneumonia, stroke, sepsis, and life-threatening and major bleeding.
Dr. Wallace reported having no financial conflicts regarding her presentation.
NEW ORLEANS – Comanagement of orthopedic inpatients by an internist or hospitalist can improve outcomes in myriad ways, Mary Anderson Wallace, MD, said at the annual meeting of the American College of Physicians.
She focused on patients undergoing total hip or knee arthroplasty (THA/TKA). In 2014, there were 400,000 of them under Medicare alone, accounting for $7 billion in hospitalization costs and nearly as much again in the cost of related postdischarge care.
So, changes in management that improve key outcomes in this population by even a small increment reap huge benefits when spread across this enormous patient population, noted Dr. Wallace, an internist and hospitalist at the University of Colorado, Denver.
Among the examples she highlighted where comanagement can have a favorable impact were optimization of perioperative pain management pathways; how to handle the use of disease-modifying antirheumatic drugs (DMARDs) in patients undergoing THA/TKA; the latest thinking on the appropriateness of low-dose aspirin for deep vein thrombosis (DVT) prophylaxis; a simple way to predict postop delirium in older individuals without known dementia; how to decide which postoperative fevers warrant a costly infectious disease workup; and the optimal wait time from arrival at the hospital with a fractured hip and THA.
These are all issues where a well-informed internist/hospitalist can be of enormous assistance to a busy orthopedic surgeon in providing high-value care, she explained.
Optimizing perioperative pain management pathways
As of 2015, orthopedists ranked as the third highest prescribers of opioids. Impressively, a retrospective cohort study of 641,941 opioid-naive, privately insured patients undergoing 1 of 11 types of surgery demonstrated that TKA was associated with a 5.1-fold increased risk for subsequent chronic opioid use in the first year after surgery, compared with 18 million opioid-naive nonsurgical controls. Indeed, TKA was the highest-risk of the 11 surgical procedures examined (JAMA Intern Med. 2016 Sep 1;176[9]:1286-93).
Another study that points to a need to develop best practices for opioid prescribing in orthopedic surgery – and other types of surgery as well – was a systematic review of six studies of patients who received prescription opioid analgesics in conjunction with seven types of surgery.
Opioid oversupply was identified as a clear problem: 67%-92% of patients in the six studies reported unused opioids. Up to 71% of opioid tablets went unused, mainly because patients felt they’d achieved adequate pain control and didn’t need them. Rates of safe disposal of unused opioids were in the single digits, suggesting that overprescribing provides a large potential reservoir of opioids that can be diverted to nonmedical use (JAMA Surg. 2017 Nov 1;152[11]:1066-71).
Moreover, a recent retrospective study of more than 1 million opioid-naive patients undergoing surgery showed that 56% of them received postoperative opioids. And each additional week of use was associated with a 44% increase in the relative risk of the composite endpoint of opioid dependence, abuse, or overdose. Duration of opioid use was a stronger predictor of this adverse outcome than was dosage (BMJ. 2018 Jan 17;360:j5790).
Other studies have shown that multimodal analgesia is utilized in only 25%-50% of surgical patients, even though it is considered the standard of care. Only 20% of patients undergoing THA/TKA receive peripheral nerve and neuraxial blocks. So, there is an opportunity for optimization of perioperative pain management pathways in orthopedic surgery patients, including avoidance of unnecessary p.r.n. prescribing, to favorably impact the national opioid epidemic, Dr. Wallace observed.
A surprise benefit of multimodal pain management that includes acetaminophen and a nonsteroidal anti-inflammatory agent is that it markedly reduces the incidence of postoperative fevers after total joint arthroplasty, compared with opioid-based pain management.
That was demonstrated in a retrospective study of 2,417 THA/TKAs in which multimodal pain management was used, and 1,484 procedures that relied on opioid-based pain relief. All of the operations were performed by the same three orthopedic surgeons. Only 5% of patients in the multimodal pain management group developed a fever greater than 38.5 degrees Celsius during the first 5 postoperative days, compared with 25% of those in the opioid-based analgesia group.
Moreover, an infectious disease workup was ordered in 2% of the multimodal analgesia group, versus 10% in the opioid-based pain management cohort, with no difference in the positive workup rates between the two groups (Clin Orthop Relat Res. 2014 May;472[5]:1489-95).
“It’s interesting that multimodal pain management has the side effect of putting you in a better position to practice high-value care, with less fever and fewer infectious disease workups,” Dr. Wallace said.
Perioperative management of DMARDs
Recent joint guidelines from the American College of Rheumatology and American Association of Hip and Knee Surgeons specifically address this issue in patients undergoing elective joint replacement (Arthritis Rheumatol. 2017 Aug;69[8]:1538-51).
“The quality of evidence isn’t high, but at least it’s a starting point,” Dr. Wallace said.
Patients with rheumatoid arthritis, systemic lupus erythematosus, spondyloarthropathies, and other rheumatic diseases who are on methotrexate or other nonbiologic DMARDs should be maintained on their current dose, according to the guidelines.
In contrast, all biologic agents should be withheld prior to surgery, which should be scheduled to coincide with the end of the dosing cycle for that specific biologic. The biologic agent should be resumed only once adequate wound healing has occurred, typically about 14 days post-THA/TKA.
Patients on daily glucocorticoids should continue on their current dose; supraphysiologic stress dosing is to be avoided.
Low-dose aspirin for VTE prophylaxis
“It seems like nothing has been such an enduring controversy in the comanagement literature as the question of whether aspirin is an effective prophylactic agent for prevention of DVT post THA/TKA,” according to Dr. Wallace.
She noted that in the space of just 4 years between the eighth and ninth editions of the American College of Chest Physician guidelines, that organization underwent a 180-degree reversal on the issue – whipsawing from a grade 1A recommendation against aspirin in 2008 to a 1B recommendation for it in 2012.
The literature is increasingly supportive of the use of aspirin for venous thromboembolism (VTE) prophylaxis in low-risk THA/TKA patients. Separate guidelines from the American Academy of Orthopaedic Surgeons (AAOS) and the Surgical Care Improvement Project, as well as the chest physicians, support the practice.
The hitch is that there is as yet no single validated risk-stratification protocol. AAOS recommends 325 mg of aspirin twice daily for 6 weeks. But a prospective crossover study of more than 4,600 total joint arthroplasty patients conducted by investigators at Thomas Jefferson University in Philadelphia showed that 81 mg BID for 4 weeks was just as effective as was 325 mg b.i.d., albeit with an incidence of GI bleeding that to their surprise wasn’t significantly lower (J Bone Joint Surg Am. 2017 Jan 18;99[2]:91-8).
Dr. Wallace anticipates definitive answers on VTE prophylaxis to come from the ongoing Patient-Centered Outcomes Research Institute-supported PEPPER (Comparative Effectiveness of Pulmonary Embolism Prevention After Hip and Knee Replacement) trial. In that study, roughly 25,000 patients undergoing THA/TKA are being randomized to prophylactic aspirin at 81 mg b.i.d., warfarin at an International Normalized Ratio of 2.0, or rivaroxaban (Xarelto). Endpoints include mortality, VTE, and bleeding. Results are expected in 2021.
Preoperative prediction of postop delirium
Unrecognized preoperative cognitive impairment in older patients without dementia who are undergoing THA/TKA is a common and powerful risk factor for postop delirium and other complications, as demonstrated recently by investigators at Harvard University and affiliated hospitals.
They had 211 patients aged 65 or older, none with known dementia, take the Mini-Cog screening test prior to their surgery. Fully 24% had probable cognitive impairment as reflected in a score of 2 or less out of a possible 5 points on this simple test, which consists of a three-word recall and clock drawing.
“I was very surprised at this high rate. These are patients who are at risk for delirium in the hospital when you’re taking care of them,” Dr. Wallace observed.
In the Harvard study, the incidence of postop delirium was 21% in patients with a Mini-Cog score of 2 or less, compared with 7% who scored 3-5, for an odds ratio of 4.5 in an age-adjusted multivariate analysis. Moreover, 67% of the low scorers were discharged somewhere other than home, in contrast to 34% of patients with a preop Mini-Cog score of 3-5, for an adjusted 3.9-fold increased risk. The group with a Mini-Cog score of 2 or less also had a significantly longer hospital length of stay (Anesthesiology. 2017 Nov;127[5]:765-74).
Perioperative gabapentin is often added to the medication regimen of older surgical patients to reduce postop delirium. The latest evidence indicates that doesn’t work, as demonstrated in a recent 697-patient randomized trial. The incidence of delirium during the first 3 days post surgery as measured by the Confusion Assessment Method was 22.4% in patients randomized to 900 mg of gabapentin per day, and 20.8% with placebo. Nearly 200 participants had THA or TKA, and in that subgroup, there was an even stronger – albeit still not statistically significant – trend for a higher delirium rate with gabapentin than with placebo (Anesthesiology. 2017 Oct.127[4]:633-44).
“Think twice about adding gabapentin to the pain regimen for THA/TKA/spine patients for the purpose of preventing postop delirium,” she advised.
When is postop fever a concern?
Up to half of patients develop fever early after THA/TKA. In most cases, this is a self-limited ancillary effect of cytokine release, with the temperature peaking on postop day 1-2.
Three strong predictors of a positive infectious disease workup are fever after postop day 3, with an associated 23.3-fold increased risk; multiple days of fever, with an odds ratio of 8.6; and a maximum temperature greater than 39.0 degrees Celsius, with a 2.4-fold increased risk. In this 7-year-old study, the cost of infectious disease workup per change in patient management was a hefty $8,209 (J Arthroplasty. 2010 Sep;25[6 Suppl]:43-8).
A retrospective study of nearly 125,000 THA/TKA patients in the American College of Surgeons National Surgical Quality Improvement Program database has important implications for clinical surveillance for postop adverse events. Stroke occurred early, on median postop day 1. The median time of acute MI and pulmonary embolism was postop day 3, and pneumonia day 4.
The key take-home message was that the median time to DVT was postop day 6, by which point most patients had been discharged. Thus, 60% of postoperative DVTs occurred after discharge. And the time to diagnosis of DVT differed markedly by surgical procedure: The median day of diagnosis was day 5 in TKA patients, compared with day 13 for THA patients. Sixty-eight percent of urinary tract infections occurred post discharge. Sepsis occurred on median day 10 post surgery, surgical site infections on day 17 (Clin Orthop Relat Res. 2017 Dec;475[12]:2952-9).
In light of ever-shortening hospital lengths of stay, Dr. Wallace noted, the findings underscore the importance of comprehensive predischarge patient counseling.
Optimal time window for hip fracture surgery
AAOS guidelines recommend that hip fracture surgery should take place within 48 hours, assuming medical comorbidities are stabilized, because complication rates go up with longer wait times.
But that is controversial. A University of Toronto retrospective cohort study of 42,430 adults with hip fracture treated at 72 Canadian hospitals during 2009-2014 found that the inflection point was 24 hours. Among 13,731 patients whose elapsed time from hospital arrival to surgery was 24 hours or less, 30-day mortality was 5.8%, significantly less than the 6.5% rate in an equal number of propensity score–matched patients with a longer wait time.
The 90- and 365-day mortality rates in the patients who received surgery within 24 hours were 10.7% and 19.3%, both significantly lower than the 12.0% and 21.6% figures in patients with longer wait times.
For the 30-day composite outcome of death, myocardial infarction, pulmonary embolism, DVT, or pneumonia, the rates were 10.1% and 12.2% – again, statistically significant and clinically meaningful. The 90- and 365-day composite outcomes followed suit (JAMA. 2017 Nov 28;318[20]:1994-2003).
But the Canadian study won’t be the final word. The ongoing international multicenter HIP ATTACK (Hip Fracture Accelerated Surgical Treatment and Care Track) trial is comparing outcomes in 3,000 patients randomized to hip fracture surgery within 6 hours versus 24 hours. Endpoints include mortality, myocardial infarction, pulmonary embolism, pneumonia, stroke, sepsis, and life-threatening and major bleeding.
Dr. Wallace reported having no financial conflicts regarding her presentation.
REPORTING FROM ACP INTERNAL MEDICINE
Nearly one-quarter of presurgery patients already using opioids
at a large academic medical center, a cross-sectional observational study has determined.
Prescription or illegal opioid use can have profound implications for surgical outcomes and continued postoperative medication abuse. “Preoperative opioid use was associated with a greater burden of comorbid disease and multiple risk factors for poor recovery. ... Opioid-tolerant patients are at risk for opioid-associated adverse events and are less likely to discontinue opioid-based therapy after their surgery,” wrote Paul E. Hilliard, MD, and a team of researchers at the University of Michigan Health System. Although the question of preoperative opioid use has been examined and the Michigan findings are consistent with earlier estimates of prevalence (Ann Surg. 2017;265[4]:695-701), this study sought a more detailed profile of both the characteristics of these patients and the types of procedures correlated with opioid use.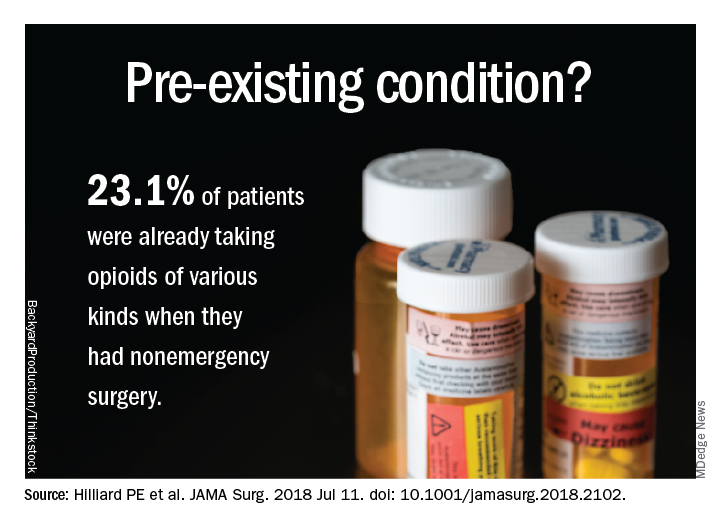
Patient data were derived primarily from two ongoing institutional registries, the Michigan Genomics Initiative and the Analgesic Outcomes Study. Each of these projects involved recruiting nonemergency surgery patients to participate and self-report on pain and affect issues. Opioid use data were extracted from the preop anesthesia history and from physical examination. A total of 34,186 patients were recruited for this study; 54.2% were women, 89.1% were white, and the mean age was 53.1 years. Overall, 23.1% of these patients were taking opioids of various kinds, mostly by prescription along with nonprescription opioids and illegal drugs of other kinds.
The most common opioids found in this patient sample were hydrocodone bitartrate (59.4%), tramadol hydrochloride (21.2%) and oxycodone hydrochloride (18.5%), although the duration or frequency of use was not determined.
“In our experience, in surveys like this patients are pretty honest. [The data do not] track to their medical record, but was done privately for research. That having been said, I am sure there is significant underreporting,” study coauthor Michael J. Englesbe, MD, FACS, said in an interview. In addition to some nondisclosure by study participants, the exclusion of patients admitted to surgery from the ED could mean that 23.1% is a conservative estimate, he noted.
Patient characteristics included in the study (tobacco use, alcohol use, sleep apnea, pain, life satisfaction, depression, anxiety) were self-reported and validated using tools such as the Brief Pain Inventory, the Fibromyalgia Survey, and the Hospital Anxiety and Depression Scale. Procedural data were derived from patient records and ICD-10 data and rated via the ASA score and Charlson Comorbidity Index.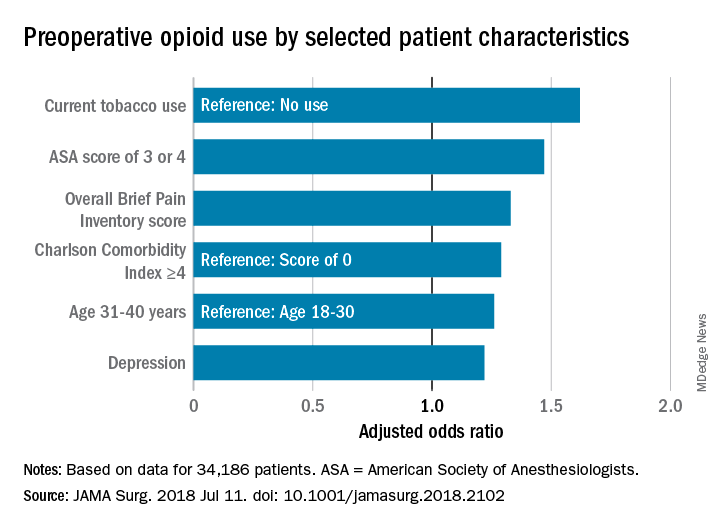
A multivariate analysis of patient characteristics found that age between 31 and 40, tobacco use, heavy alcohol use, pain score, depression, comorbidities reflected in a higher ASA score, and Charlson Comorbidity Score were all significant risk factors for presurgical opiate use.
Patients who were scheduled for surgical procedures involving lower extremities (adjusted odds ratio 3.61, 95% confidence interval, 2.81-4.64) were at the highest risk for opioid use, followed by pelvis surgery, excluding hip (aOR, 3.09, 95% CI, 1.88-5.08), upper arm or elbow (aOR, 3.07, 95% CI, 2.12-4.45), and spine surgery (aOR, 2.68, 95% CI, 2.15-3.32).
The study also broke out the data by presurgery opioid usage and surgery service. Of patients having spine neurosurgery, 55.1% were already taking opioids, and among those having orthopedic spine surgery, 65.1% were taking opioids. General surgery patients were not among those mostly likely to be using opioids (gastrointestinal surgery, 19.3% and endocrine surgery 14.3%). “Certain surgical services may be more likely to encounter patients with high comorbidities for opioid use, and more targeted opioid education strategies aimed at those services may help to mitigate risk in the postoperative period,” the authors wrote.
“All surgeons should take a preop pain history. They should ask about current pain and previous pain experiences. They should also ask about a history of substance use disorder. This should lead into a discussion of the pain expectations from the procedure. Patients should expect to be in pain, that is normal. Pain-free surgery is rare. If a patient has a complex pain history or takes chronic opioids, the surgeon should consider referring them to anesthesia for formal preop pain management planning and potentially weaning of opioid dose prior to elective surgery,” noted Dr. Englesbe, the Cyrenus G. Darling Sr., MD and Cyrenus G Darling Jr., MD Professor of Surgery, and faculty at the Center for Healthcare Outcomes & Policy, University of Michigan, Ann Arbor.
Surgeons are likely to see patients with a past history of opioid dependence or who are recovering from substance abuse. “Every effort should be made to avoid opioids in these patients. We have developed a Pain Optimization Pathway which facilitates no postoperative opioids for these and other patients. These patients are at high risk to relapse and surgeons must know who these patients are so they can provide optimal care,” Dr. Englesbe added.The limitations of this study as reported by the authors include the single-center design, the nondiverse racial makeup of the sample, and the difficulty of ascertaining the dosing and duration of opioid use, both prescription and illegal.
The investigators reported no disclosures relevant to this study. This study was supported by the National Institute on Drug Abuse, National Institutes of Health, the American College of Surgeons, and other noncommercial sources.
SOURCE: Hilliard PE et al. JAMA Surg. 2018 Jul 11. doi: 10.1001/jamasurg.2018.2102.
at a large academic medical center, a cross-sectional observational study has determined.
Prescription or illegal opioid use can have profound implications for surgical outcomes and continued postoperative medication abuse. “Preoperative opioid use was associated with a greater burden of comorbid disease and multiple risk factors for poor recovery. ... Opioid-tolerant patients are at risk for opioid-associated adverse events and are less likely to discontinue opioid-based therapy after their surgery,” wrote Paul E. Hilliard, MD, and a team of researchers at the University of Michigan Health System. Although the question of preoperative opioid use has been examined and the Michigan findings are consistent with earlier estimates of prevalence (Ann Surg. 2017;265[4]:695-701), this study sought a more detailed profile of both the characteristics of these patients and the types of procedures correlated with opioid use.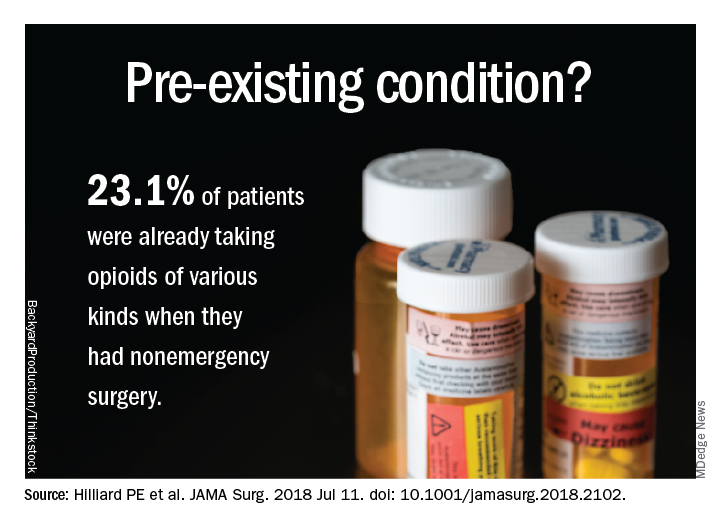
Patient data were derived primarily from two ongoing institutional registries, the Michigan Genomics Initiative and the Analgesic Outcomes Study. Each of these projects involved recruiting nonemergency surgery patients to participate and self-report on pain and affect issues. Opioid use data were extracted from the preop anesthesia history and from physical examination. A total of 34,186 patients were recruited for this study; 54.2% were women, 89.1% were white, and the mean age was 53.1 years. Overall, 23.1% of these patients were taking opioids of various kinds, mostly by prescription along with nonprescription opioids and illegal drugs of other kinds.
The most common opioids found in this patient sample were hydrocodone bitartrate (59.4%), tramadol hydrochloride (21.2%) and oxycodone hydrochloride (18.5%), although the duration or frequency of use was not determined.
“In our experience, in surveys like this patients are pretty honest. [The data do not] track to their medical record, but was done privately for research. That having been said, I am sure there is significant underreporting,” study coauthor Michael J. Englesbe, MD, FACS, said in an interview. In addition to some nondisclosure by study participants, the exclusion of patients admitted to surgery from the ED could mean that 23.1% is a conservative estimate, he noted.
Patient characteristics included in the study (tobacco use, alcohol use, sleep apnea, pain, life satisfaction, depression, anxiety) were self-reported and validated using tools such as the Brief Pain Inventory, the Fibromyalgia Survey, and the Hospital Anxiety and Depression Scale. Procedural data were derived from patient records and ICD-10 data and rated via the ASA score and Charlson Comorbidity Index.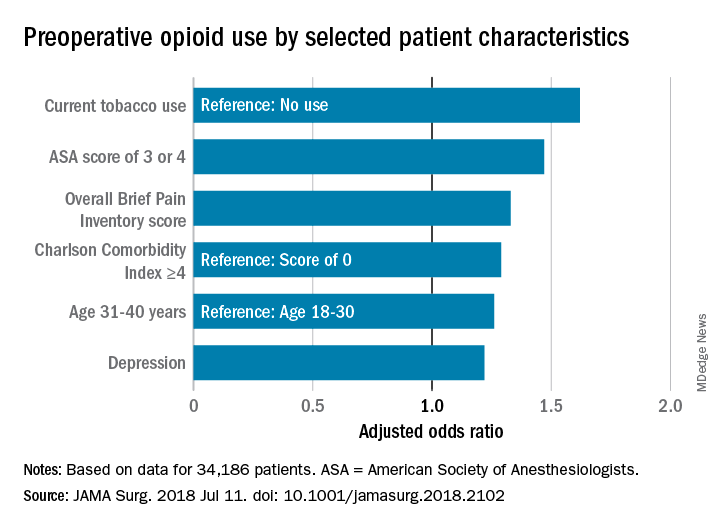
A multivariate analysis of patient characteristics found that age between 31 and 40, tobacco use, heavy alcohol use, pain score, depression, comorbidities reflected in a higher ASA score, and Charlson Comorbidity Score were all significant risk factors for presurgical opiate use.
Patients who were scheduled for surgical procedures involving lower extremities (adjusted odds ratio 3.61, 95% confidence interval, 2.81-4.64) were at the highest risk for opioid use, followed by pelvis surgery, excluding hip (aOR, 3.09, 95% CI, 1.88-5.08), upper arm or elbow (aOR, 3.07, 95% CI, 2.12-4.45), and spine surgery (aOR, 2.68, 95% CI, 2.15-3.32).
The study also broke out the data by presurgery opioid usage and surgery service. Of patients having spine neurosurgery, 55.1% were already taking opioids, and among those having orthopedic spine surgery, 65.1% were taking opioids. General surgery patients were not among those mostly likely to be using opioids (gastrointestinal surgery, 19.3% and endocrine surgery 14.3%). “Certain surgical services may be more likely to encounter patients with high comorbidities for opioid use, and more targeted opioid education strategies aimed at those services may help to mitigate risk in the postoperative period,” the authors wrote.
“All surgeons should take a preop pain history. They should ask about current pain and previous pain experiences. They should also ask about a history of substance use disorder. This should lead into a discussion of the pain expectations from the procedure. Patients should expect to be in pain, that is normal. Pain-free surgery is rare. If a patient has a complex pain history or takes chronic opioids, the surgeon should consider referring them to anesthesia for formal preop pain management planning and potentially weaning of opioid dose prior to elective surgery,” noted Dr. Englesbe, the Cyrenus G. Darling Sr., MD and Cyrenus G Darling Jr., MD Professor of Surgery, and faculty at the Center for Healthcare Outcomes & Policy, University of Michigan, Ann Arbor.
Surgeons are likely to see patients with a past history of opioid dependence or who are recovering from substance abuse. “Every effort should be made to avoid opioids in these patients. We have developed a Pain Optimization Pathway which facilitates no postoperative opioids for these and other patients. These patients are at high risk to relapse and surgeons must know who these patients are so they can provide optimal care,” Dr. Englesbe added.The limitations of this study as reported by the authors include the single-center design, the nondiverse racial makeup of the sample, and the difficulty of ascertaining the dosing and duration of opioid use, both prescription and illegal.
The investigators reported no disclosures relevant to this study. This study was supported by the National Institute on Drug Abuse, National Institutes of Health, the American College of Surgeons, and other noncommercial sources.
SOURCE: Hilliard PE et al. JAMA Surg. 2018 Jul 11. doi: 10.1001/jamasurg.2018.2102.
at a large academic medical center, a cross-sectional observational study has determined.
Prescription or illegal opioid use can have profound implications for surgical outcomes and continued postoperative medication abuse. “Preoperative opioid use was associated with a greater burden of comorbid disease and multiple risk factors for poor recovery. ... Opioid-tolerant patients are at risk for opioid-associated adverse events and are less likely to discontinue opioid-based therapy after their surgery,” wrote Paul E. Hilliard, MD, and a team of researchers at the University of Michigan Health System. Although the question of preoperative opioid use has been examined and the Michigan findings are consistent with earlier estimates of prevalence (Ann Surg. 2017;265[4]:695-701), this study sought a more detailed profile of both the characteristics of these patients and the types of procedures correlated with opioid use.
Patient data were derived primarily from two ongoing institutional registries, the Michigan Genomics Initiative and the Analgesic Outcomes Study. Each of these projects involved recruiting nonemergency surgery patients to participate and self-report on pain and affect issues. Opioid use data were extracted from the preop anesthesia history and from physical examination. A total of 34,186 patients were recruited for this study; 54.2% were women, 89.1% were white, and the mean age was 53.1 years. Overall, 23.1% of these patients were taking opioids of various kinds, mostly by prescription along with nonprescription opioids and illegal drugs of other kinds.
The most common opioids found in this patient sample were hydrocodone bitartrate (59.4%), tramadol hydrochloride (21.2%) and oxycodone hydrochloride (18.5%), although the duration or frequency of use was not determined.
“In our experience, in surveys like this patients are pretty honest. [The data do not] track to their medical record, but was done privately for research. That having been said, I am sure there is significant underreporting,” study coauthor Michael J. Englesbe, MD, FACS, said in an interview. In addition to some nondisclosure by study participants, the exclusion of patients admitted to surgery from the ED could mean that 23.1% is a conservative estimate, he noted.
Patient characteristics included in the study (tobacco use, alcohol use, sleep apnea, pain, life satisfaction, depression, anxiety) were self-reported and validated using tools such as the Brief Pain Inventory, the Fibromyalgia Survey, and the Hospital Anxiety and Depression Scale. Procedural data were derived from patient records and ICD-10 data and rated via the ASA score and Charlson Comorbidity Index.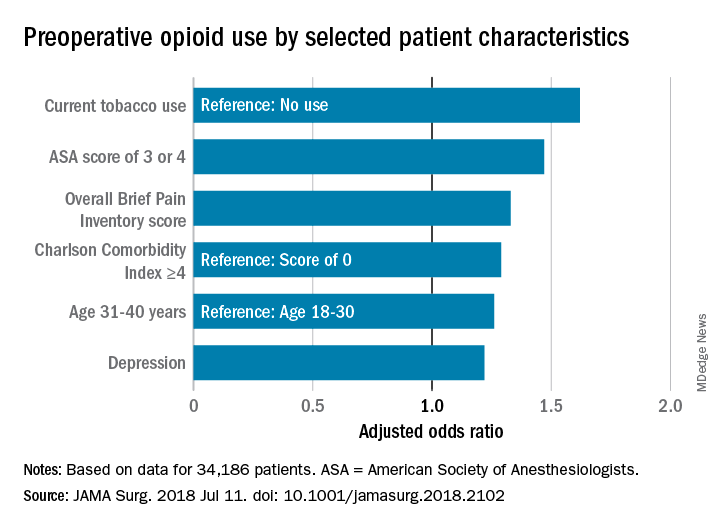
A multivariate analysis of patient characteristics found that age between 31 and 40, tobacco use, heavy alcohol use, pain score, depression, comorbidities reflected in a higher ASA score, and Charlson Comorbidity Score were all significant risk factors for presurgical opiate use.
Patients who were scheduled for surgical procedures involving lower extremities (adjusted odds ratio 3.61, 95% confidence interval, 2.81-4.64) were at the highest risk for opioid use, followed by pelvis surgery, excluding hip (aOR, 3.09, 95% CI, 1.88-5.08), upper arm or elbow (aOR, 3.07, 95% CI, 2.12-4.45), and spine surgery (aOR, 2.68, 95% CI, 2.15-3.32).
The study also broke out the data by presurgery opioid usage and surgery service. Of patients having spine neurosurgery, 55.1% were already taking opioids, and among those having orthopedic spine surgery, 65.1% were taking opioids. General surgery patients were not among those mostly likely to be using opioids (gastrointestinal surgery, 19.3% and endocrine surgery 14.3%). “Certain surgical services may be more likely to encounter patients with high comorbidities for opioid use, and more targeted opioid education strategies aimed at those services may help to mitigate risk in the postoperative period,” the authors wrote.
“All surgeons should take a preop pain history. They should ask about current pain and previous pain experiences. They should also ask about a history of substance use disorder. This should lead into a discussion of the pain expectations from the procedure. Patients should expect to be in pain, that is normal. Pain-free surgery is rare. If a patient has a complex pain history or takes chronic opioids, the surgeon should consider referring them to anesthesia for formal preop pain management planning and potentially weaning of opioid dose prior to elective surgery,” noted Dr. Englesbe, the Cyrenus G. Darling Sr., MD and Cyrenus G Darling Jr., MD Professor of Surgery, and faculty at the Center for Healthcare Outcomes & Policy, University of Michigan, Ann Arbor.
Surgeons are likely to see patients with a past history of opioid dependence or who are recovering from substance abuse. “Every effort should be made to avoid opioids in these patients. We have developed a Pain Optimization Pathway which facilitates no postoperative opioids for these and other patients. These patients are at high risk to relapse and surgeons must know who these patients are so they can provide optimal care,” Dr. Englesbe added.The limitations of this study as reported by the authors include the single-center design, the nondiverse racial makeup of the sample, and the difficulty of ascertaining the dosing and duration of opioid use, both prescription and illegal.
The investigators reported no disclosures relevant to this study. This study was supported by the National Institute on Drug Abuse, National Institutes of Health, the American College of Surgeons, and other noncommercial sources.
SOURCE: Hilliard PE et al. JAMA Surg. 2018 Jul 11. doi: 10.1001/jamasurg.2018.2102.
FROM JAMA SURGERY
Key clinical point: Preoperative opioid use is prevalent in patients who are having spinal surgery and have depression.
Major finding:
Study details: An observational study of 34,186 surgical patients in the University of Michigan Health system.
Disclosures: The investigators reported no disclosures relevant to this study. This study was supported by the National Institute on Drug Abuse, National Institutes of Health, the American College of Surgeons, and other noncommercial sources.
Source: Hilliard P E et al. JAMA Surg. 2018 Jul 11;. doi:10.1001/jamasurg.2018.2102.
MI risk prediction after noncardiac surgery simplified
ORLANDO – The risk of perioperative MI or death associated with noncardiac surgery is vanishingly low in patients free of diabetes, hypertension, and smoking, Tanya Wilcox, MD, reported at the annual meeting of the American College of Cardiology.
How small is the risk? A mere 1 in 1,000, according to her analysis of more than 3.8 million major noncardiac surgeries in the American College of Surgeons National Surgical Quality Improvement Program database for 2009-2015, according to Dr. Wilcox of New York University.
Physicians are frequently asked by surgeons to clear patients for noncardiac surgery in terms of cardiovascular risk. Because current risk scores are complex, aren’t amenable to rapid bedside calculations, and may entail cardiac stress testing, Dr. Wilcox decided it was worth assessing the impact of three straightforward cardiovascular risk factors – current smoking and treatment for hypertension or diabetes – on 30-day postoperative MI-free survival. For this purpose she turned to the National Surgical Quality Improvement Program database, a validated, risk-adjusted, outcomes-based program to measure and improve the quality of surgical care utilizing data from 250 U.S. surgical centers.
Of the 3,817,113 patients who underwent major noncardiac surgery, 1,586,020 (42%) of them had none of the three cardiovascular risk factors of interest, 1,541,846 (40%) had one, 643,424 (17%) had two, and 45,823, or 1.2%, had all three. The patients’ mean age was 57, 75% were white, and 57% were women. About half of all patients underwent various operations within the realm of general surgery; next most frequent were orthopedic procedures, accounting for 18% of total noncardiac surgery. Of note, only 23% of patients with zero risk factors were American Society of Anesthesiologists Class 3-5, compared with 51% of those with one cardiovascular risk factor, 76% with two, and 71% with all three.
The incidence of acute MI or death within 30 days of noncardiac surgery climbed in stepwise fashion according to a patient’s risk factor burden. In a multivariate analysis adjusted for age, race, and gender, patients with any one of the cardiovascular risk factors had a 30-day risk of acute MI or death that was 1.52 times greater than those with no risk factors, patients with two risk factors were at 2.4-fold increased risk, and those with all three were at 3.63-fold greater risk than those with none. The degree of increased risk associated with any single risk factor ranged from 1.47-fold for hypertension to 1.94-fold for smoking.
“Further study is needed to determine whether aggressive risk factor modifications in the form of blood pressure control, glycemic control, and smoking cessation could reduce the incidence of postoperative MI,” Dr. Wilcox observed.
She reported having no financial conflicts regarding her study.
ORLANDO – The risk of perioperative MI or death associated with noncardiac surgery is vanishingly low in patients free of diabetes, hypertension, and smoking, Tanya Wilcox, MD, reported at the annual meeting of the American College of Cardiology.
How small is the risk? A mere 1 in 1,000, according to her analysis of more than 3.8 million major noncardiac surgeries in the American College of Surgeons National Surgical Quality Improvement Program database for 2009-2015, according to Dr. Wilcox of New York University.
Physicians are frequently asked by surgeons to clear patients for noncardiac surgery in terms of cardiovascular risk. Because current risk scores are complex, aren’t amenable to rapid bedside calculations, and may entail cardiac stress testing, Dr. Wilcox decided it was worth assessing the impact of three straightforward cardiovascular risk factors – current smoking and treatment for hypertension or diabetes – on 30-day postoperative MI-free survival. For this purpose she turned to the National Surgical Quality Improvement Program database, a validated, risk-adjusted, outcomes-based program to measure and improve the quality of surgical care utilizing data from 250 U.S. surgical centers.
Of the 3,817,113 patients who underwent major noncardiac surgery, 1,586,020 (42%) of them had none of the three cardiovascular risk factors of interest, 1,541,846 (40%) had one, 643,424 (17%) had two, and 45,823, or 1.2%, had all three. The patients’ mean age was 57, 75% were white, and 57% were women. About half of all patients underwent various operations within the realm of general surgery; next most frequent were orthopedic procedures, accounting for 18% of total noncardiac surgery. Of note, only 23% of patients with zero risk factors were American Society of Anesthesiologists Class 3-5, compared with 51% of those with one cardiovascular risk factor, 76% with two, and 71% with all three.
The incidence of acute MI or death within 30 days of noncardiac surgery climbed in stepwise fashion according to a patient’s risk factor burden. In a multivariate analysis adjusted for age, race, and gender, patients with any one of the cardiovascular risk factors had a 30-day risk of acute MI or death that was 1.52 times greater than those with no risk factors, patients with two risk factors were at 2.4-fold increased risk, and those with all three were at 3.63-fold greater risk than those with none. The degree of increased risk associated with any single risk factor ranged from 1.47-fold for hypertension to 1.94-fold for smoking.
“Further study is needed to determine whether aggressive risk factor modifications in the form of blood pressure control, glycemic control, and smoking cessation could reduce the incidence of postoperative MI,” Dr. Wilcox observed.
She reported having no financial conflicts regarding her study.
ORLANDO – The risk of perioperative MI or death associated with noncardiac surgery is vanishingly low in patients free of diabetes, hypertension, and smoking, Tanya Wilcox, MD, reported at the annual meeting of the American College of Cardiology.
How small is the risk? A mere 1 in 1,000, according to her analysis of more than 3.8 million major noncardiac surgeries in the American College of Surgeons National Surgical Quality Improvement Program database for 2009-2015, according to Dr. Wilcox of New York University.
Physicians are frequently asked by surgeons to clear patients for noncardiac surgery in terms of cardiovascular risk. Because current risk scores are complex, aren’t amenable to rapid bedside calculations, and may entail cardiac stress testing, Dr. Wilcox decided it was worth assessing the impact of three straightforward cardiovascular risk factors – current smoking and treatment for hypertension or diabetes – on 30-day postoperative MI-free survival. For this purpose she turned to the National Surgical Quality Improvement Program database, a validated, risk-adjusted, outcomes-based program to measure and improve the quality of surgical care utilizing data from 250 U.S. surgical centers.
Of the 3,817,113 patients who underwent major noncardiac surgery, 1,586,020 (42%) of them had none of the three cardiovascular risk factors of interest, 1,541,846 (40%) had one, 643,424 (17%) had two, and 45,823, or 1.2%, had all three. The patients’ mean age was 57, 75% were white, and 57% were women. About half of all patients underwent various operations within the realm of general surgery; next most frequent were orthopedic procedures, accounting for 18% of total noncardiac surgery. Of note, only 23% of patients with zero risk factors were American Society of Anesthesiologists Class 3-5, compared with 51% of those with one cardiovascular risk factor, 76% with two, and 71% with all three.
The incidence of acute MI or death within 30 days of noncardiac surgery climbed in stepwise fashion according to a patient’s risk factor burden. In a multivariate analysis adjusted for age, race, and gender, patients with any one of the cardiovascular risk factors had a 30-day risk of acute MI or death that was 1.52 times greater than those with no risk factors, patients with two risk factors were at 2.4-fold increased risk, and those with all three were at 3.63-fold greater risk than those with none. The degree of increased risk associated with any single risk factor ranged from 1.47-fold for hypertension to 1.94-fold for smoking.
“Further study is needed to determine whether aggressive risk factor modifications in the form of blood pressure control, glycemic control, and smoking cessation could reduce the incidence of postoperative MI,” Dr. Wilcox observed.
She reported having no financial conflicts regarding her study.
REPORTING FROM ACC 2018
Key clinical point: Noncardiac surgery patients can breathe easier regarding perioperative cardiovascular risk provided they don’t smoke and aren’t hypertensive or diabetic.
Major finding: .
Study details: This was a retrospective analysis of more than 3.8 million noncardiac surgeries contained in the American College of Surgeons National Surgical Quality Improvement Program database for 2009-2015.
Disclosures: The study presenter reported having no financial conflicts.