User login
Modifier -25 and the New 2021 E/M Codes: Documentation of Separate and Distinct Just Got Easier
Insurers Target Modifier -25
Modifier -25 allows reporting of both a minor procedure (ie, one with a 0- or 10-day global period) and a separate and distinct evaluation and management (E/M) service on the same date of service.1 Because of the multicomplaint nature of dermatology, the ability to report a same-day procedure and an E/M service is critical for efficient, cost-effective, and patient-centered dermatologic care. However, it is well known that the use of modifier -25 has been under notable insurer scrutiny and is a common reason for medical record audits.2,3 Some insurers have responded to increased utilization of modifier -25 by cutting reimbursement for claims that include both a procedure and an E/M service or by denying one of the services altogether.4-6 The Centers for Medicare and Medicaid Services also have expressed concern about this coding combination with proposed cuts to reimbursement.7 Moreover, the Office of Inspector General has announced a work plan to investigate the frequent utilization of E/M codes and minor procedures by dermatologists.8 Clearly, modifier -25 is a continued target by insurers and regulators; therefore, dermatologists will want to make sure their coding and documentation meet all requirements and are updated for the new E/M codes for 2021.
The American Medical Association’s Current Procedural Terminology indicates that modifier -25 allows reporting of a “significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of a procedure or other service.”1 Given that dermatology patients typically present with multiple concerns, dermatologists commonly evaluate and treat numerous conditions during one visit. Understanding what constitutes a separately identifiable E/M service is critical to bill accurately and to pass insurer audits.
Global Surgical Package
To appropriately bill both a procedure and an E/M service, the physician must indicate that the patient’s condition required an E/M service above and beyond the usual work of the procedure. The compilation of evaluation and work included in the payment for a procedure is called the global surgical package.9 In general, the global surgical package includes local or topical anesthesia; the surgical service/procedure itself; immediate postoperative care, including dictating the operative note; meeting/discussing the patient’s procedure with family and other physicians; and writing orders for the patient. For minor procedures (ie, those with either 0- or 10-day global periods), the surgical package also includes same-day E/M services associated with the decision to perform surgery. An appropriate history and physical examination as well as a discussion of the differential diagnosis, treatment options, and risk and benefits of treatment are all included in the payment of a minor procedure itself. Therefore, an evaluation to discuss a patient’s condition or change in condition, alternatives to treatment, or next steps after a diagnosis related to a treatment or diagnostic procedure should not be separately reported. Moreover, the fact that the patient is new to the physician is not in itself sufficient to allow reporting of an E/M service with these minor procedures. For major procedures (ie, those with 90-day postoperative periods), the decision for surgery is excluded from the global surgical package.
2021 E/M Codes Simplify Documentation
The biggest coding change of 2021 was the new E/M codes.10 Prior to this year, the descriptors of E/M services recognized 7 components to define the levels of E/M services11: history and nature of the presenting problem; physical examination; medical decision-making (MDM); counseling; coordination of care; and time. Furthermore, history, physical examination, and MDM were all broken down into more granular elements that were summed to determine the level for each component; for example, the history of the presenting problem was defined as a chronological description of the development of the patient’s present illness, including the following elements: location, quality, severity, duration, timing, context, modifying factors, and associated signs and symptoms. Each of these categories would constitute bullet points to be summed to determine the level of history. Physical examination and MDM bullet points also would be summed to determine a proper coding level.11 Understandably, this coding scheme was complicated and burdensome to medical providers.
The redefinition of the E/M codes for 2021 substantially simplified the determination of coding level and documentation.10 The revisions to the E/M office visit code descriptors and documentation standards are now centered around how physicians think and take care of patients and not on mandatory standards and checking boxes. The main changes involve MDM as the prime determinant of the coding level. Elements of MDM affecting coding for an outpatient or office visit now include only 3 components: the number and complexity of problems addressed in the encounter, the amount or complexity of data to be reviewed and analyzed, and the risk of complications or morbidity of patient management. Gone are the requirements from the earlier criteria requiring so many bullet points for the history, physical examination, and MDM.
Dermatologists may ask, “How does the new E/M coding structure affect reporting and documenting an E/M and a procedure on the same day?” The answer is that the determination of separate and distinct is basically unchanged with the new E/M codes; however, the documentation requirements for modifier -25 using the new E/M codes are simplified.
As always, the key to determining whether a separate and distinct E/M service was provided and subsequently documented is to deconstruct the medical note. All evaluation services associated with the procedure—making a clinical diagnosis or differential diagnosis, decision to perform surgery, and discussion of alternative treatments—should be removed from one’s documentation as shown in the example below. If a complete E/M service still exists, then an E/M may be billed in addition to the procedure. Physical examination of the treatment area is included in the surgical package. With the prior E/M criteria, physical examination of the procedural area could not be used again as a bullet point to count for the E/M level. However, with the new 2021 coding requirements, the documentation of a separate MDM will be sufficient to meet criteria because documentation of physical examination is not a requirement.
Modifier -25 Examples
Let’s examine a typical dermatologist medical note. An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. The patient also complains of a growing tender lesion on the left elbow of 2 months’ duration. Physical examination reveals a linear vesicular eruption on the left wrist and a tender hyperkeratotic papule on the left elbow. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed. The decision is made to perform a tangential biopsy of the lesion on the left elbow because of the suspicion for malignancy. The biopsy is performed the same day.
This case clearly illustrates performance of an E/M service in the treatment of rhus dermatitis, which is separate and distinct from the biopsy procedure; however, in evaluating whether the case meets the documentation requirements for modifier -25, the information in the medical note inclusive to the procedure’s global surgical package, including history associated with establishing the diagnosis, physical examination of the procedure area(s), and discussion of treatment options, is eliminated, leaving the following notes: An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed.
Because the physical examination of the body part (left arm) is included in the procedure’s global surgical package, the examination of the left wrist cannot be used as coding support for the E/M service. This makes a difference for coding level in the prior E/M coding requirements, which required examination bullet points. However, with the 2021 E/M codes, documentation of physical examination bullet points is irrelevant to the coding level. Therefore, qualifying for a modifier -25 claim is more straightforward in this case with the new code set. Because bullet points are not integral to the 2021 E/M codes, qualifying and properly documenting for a higher level of service will likely be more common in dermatology.
Final Thoughts
Frequent use of modifier -25 is a critical part of a high-quality and cost-effective dermatology practice. Same-day performance of minor procedures and E/M services allows for more rapid and efficient diagnosis and treatment of various conditions as well as minimizing unnecessary office visits. The new E/M codes for 2021 actually make the documentation of a separate and distinct E/M service less complicated because the bullet point requirements associated with the old E/M codes have been eliminated. Understanding how the new E/M code descriptors affect modifier -25 reporting and clear documentation of separate, distinct, and medically necessary E/M services will be needed due to increased insurer scrutiny and audits.
- Current Procedural Terminology 2021, Professional Edition. American Medical Association; 2020.
- Rogers HW. Modifier −25 victory, but the battle is not over. Cutis. 2018;101:409-410.
- Rogers HW. One diagnosis and modifier −25: appropriate or audit target? Cutis. 2017;99:165-166.
- Update regarding E/M with modifier −25—professional. Anthem Blue Cross Blue Shield website. Published February 1, 2019. Accessed August 17, 2021. https://providernews.anthem.com/ohio/article/update-regarding-em-with-modifier-25-professional
- Payment policies—surgery. Harvard Pilgrim Health Care website. Updated May 2021. Accessed August 17, 2021. https://www.harvardpilgrim.org/provider/wp-content/uploads/sites/7/2020/07/H-6-Surgery-PM.pdf
- Modifier 25: frequently asked questions. Independence Blue Cross website. Updated September 25, 2017. Accessed August 17, 2021. https://provcomm.ibx.com/ibc/archive/pages/A86603B03881756B8525817E00768006.aspx
- Huang G. CMS 2019 fee schedule takes modifier 25 cuts, runs with them. Doctors Management website. Accessed August 17, 2021. https://www.doctors-management.com/cms-2019-feeschedule-modifier25/
- Dermatologist claims for evaluation and management services on the same day as minor surgical procedures. US Department of Health and Humans Services Office of Inspector General website. Accessed August 17, 2021. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000577.asp
- Global surgery booklet. Centers for Medicare and Medicaid Services website. Updated September 2018. Accessed August 17, 2021. https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/globallsurgery-icn907166.pdf
- American Medical Association. CPT® Evaluation and management (E/M)—office or other outpatient (99202-99215) and prolonged services (99354, 99355, 99356, 99417) code and guideline changes. Updated March 9, 2021. Accessed August 17, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
- 1997 documentation guidelines for evaluation and management services. Centers for Medicare and Medicaid Services website. Accessed August 17, 2021. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
Insurers Target Modifier -25
Modifier -25 allows reporting of both a minor procedure (ie, one with a 0- or 10-day global period) and a separate and distinct evaluation and management (E/M) service on the same date of service.1 Because of the multicomplaint nature of dermatology, the ability to report a same-day procedure and an E/M service is critical for efficient, cost-effective, and patient-centered dermatologic care. However, it is well known that the use of modifier -25 has been under notable insurer scrutiny and is a common reason for medical record audits.2,3 Some insurers have responded to increased utilization of modifier -25 by cutting reimbursement for claims that include both a procedure and an E/M service or by denying one of the services altogether.4-6 The Centers for Medicare and Medicaid Services also have expressed concern about this coding combination with proposed cuts to reimbursement.7 Moreover, the Office of Inspector General has announced a work plan to investigate the frequent utilization of E/M codes and minor procedures by dermatologists.8 Clearly, modifier -25 is a continued target by insurers and regulators; therefore, dermatologists will want to make sure their coding and documentation meet all requirements and are updated for the new E/M codes for 2021.
The American Medical Association’s Current Procedural Terminology indicates that modifier -25 allows reporting of a “significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of a procedure or other service.”1 Given that dermatology patients typically present with multiple concerns, dermatologists commonly evaluate and treat numerous conditions during one visit. Understanding what constitutes a separately identifiable E/M service is critical to bill accurately and to pass insurer audits.
Global Surgical Package
To appropriately bill both a procedure and an E/M service, the physician must indicate that the patient’s condition required an E/M service above and beyond the usual work of the procedure. The compilation of evaluation and work included in the payment for a procedure is called the global surgical package.9 In general, the global surgical package includes local or topical anesthesia; the surgical service/procedure itself; immediate postoperative care, including dictating the operative note; meeting/discussing the patient’s procedure with family and other physicians; and writing orders for the patient. For minor procedures (ie, those with either 0- or 10-day global periods), the surgical package also includes same-day E/M services associated with the decision to perform surgery. An appropriate history and physical examination as well as a discussion of the differential diagnosis, treatment options, and risk and benefits of treatment are all included in the payment of a minor procedure itself. Therefore, an evaluation to discuss a patient’s condition or change in condition, alternatives to treatment, or next steps after a diagnosis related to a treatment or diagnostic procedure should not be separately reported. Moreover, the fact that the patient is new to the physician is not in itself sufficient to allow reporting of an E/M service with these minor procedures. For major procedures (ie, those with 90-day postoperative periods), the decision for surgery is excluded from the global surgical package.
2021 E/M Codes Simplify Documentation
The biggest coding change of 2021 was the new E/M codes.10 Prior to this year, the descriptors of E/M services recognized 7 components to define the levels of E/M services11: history and nature of the presenting problem; physical examination; medical decision-making (MDM); counseling; coordination of care; and time. Furthermore, history, physical examination, and MDM were all broken down into more granular elements that were summed to determine the level for each component; for example, the history of the presenting problem was defined as a chronological description of the development of the patient’s present illness, including the following elements: location, quality, severity, duration, timing, context, modifying factors, and associated signs and symptoms. Each of these categories would constitute bullet points to be summed to determine the level of history. Physical examination and MDM bullet points also would be summed to determine a proper coding level.11 Understandably, this coding scheme was complicated and burdensome to medical providers.
The redefinition of the E/M codes for 2021 substantially simplified the determination of coding level and documentation.10 The revisions to the E/M office visit code descriptors and documentation standards are now centered around how physicians think and take care of patients and not on mandatory standards and checking boxes. The main changes involve MDM as the prime determinant of the coding level. Elements of MDM affecting coding for an outpatient or office visit now include only 3 components: the number and complexity of problems addressed in the encounter, the amount or complexity of data to be reviewed and analyzed, and the risk of complications or morbidity of patient management. Gone are the requirements from the earlier criteria requiring so many bullet points for the history, physical examination, and MDM.
Dermatologists may ask, “How does the new E/M coding structure affect reporting and documenting an E/M and a procedure on the same day?” The answer is that the determination of separate and distinct is basically unchanged with the new E/M codes; however, the documentation requirements for modifier -25 using the new E/M codes are simplified.
As always, the key to determining whether a separate and distinct E/M service was provided and subsequently documented is to deconstruct the medical note. All evaluation services associated with the procedure—making a clinical diagnosis or differential diagnosis, decision to perform surgery, and discussion of alternative treatments—should be removed from one’s documentation as shown in the example below. If a complete E/M service still exists, then an E/M may be billed in addition to the procedure. Physical examination of the treatment area is included in the surgical package. With the prior E/M criteria, physical examination of the procedural area could not be used again as a bullet point to count for the E/M level. However, with the new 2021 coding requirements, the documentation of a separate MDM will be sufficient to meet criteria because documentation of physical examination is not a requirement.
Modifier -25 Examples
Let’s examine a typical dermatologist medical note. An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. The patient also complains of a growing tender lesion on the left elbow of 2 months’ duration. Physical examination reveals a linear vesicular eruption on the left wrist and a tender hyperkeratotic papule on the left elbow. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed. The decision is made to perform a tangential biopsy of the lesion on the left elbow because of the suspicion for malignancy. The biopsy is performed the same day.
This case clearly illustrates performance of an E/M service in the treatment of rhus dermatitis, which is separate and distinct from the biopsy procedure; however, in evaluating whether the case meets the documentation requirements for modifier -25, the information in the medical note inclusive to the procedure’s global surgical package, including history associated with establishing the diagnosis, physical examination of the procedure area(s), and discussion of treatment options, is eliminated, leaving the following notes: An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed.
Because the physical examination of the body part (left arm) is included in the procedure’s global surgical package, the examination of the left wrist cannot be used as coding support for the E/M service. This makes a difference for coding level in the prior E/M coding requirements, which required examination bullet points. However, with the 2021 E/M codes, documentation of physical examination bullet points is irrelevant to the coding level. Therefore, qualifying for a modifier -25 claim is more straightforward in this case with the new code set. Because bullet points are not integral to the 2021 E/M codes, qualifying and properly documenting for a higher level of service will likely be more common in dermatology.
Final Thoughts
Frequent use of modifier -25 is a critical part of a high-quality and cost-effective dermatology practice. Same-day performance of minor procedures and E/M services allows for more rapid and efficient diagnosis and treatment of various conditions as well as minimizing unnecessary office visits. The new E/M codes for 2021 actually make the documentation of a separate and distinct E/M service less complicated because the bullet point requirements associated with the old E/M codes have been eliminated. Understanding how the new E/M code descriptors affect modifier -25 reporting and clear documentation of separate, distinct, and medically necessary E/M services will be needed due to increased insurer scrutiny and audits.
Insurers Target Modifier -25
Modifier -25 allows reporting of both a minor procedure (ie, one with a 0- or 10-day global period) and a separate and distinct evaluation and management (E/M) service on the same date of service.1 Because of the multicomplaint nature of dermatology, the ability to report a same-day procedure and an E/M service is critical for efficient, cost-effective, and patient-centered dermatologic care. However, it is well known that the use of modifier -25 has been under notable insurer scrutiny and is a common reason for medical record audits.2,3 Some insurers have responded to increased utilization of modifier -25 by cutting reimbursement for claims that include both a procedure and an E/M service or by denying one of the services altogether.4-6 The Centers for Medicare and Medicaid Services also have expressed concern about this coding combination with proposed cuts to reimbursement.7 Moreover, the Office of Inspector General has announced a work plan to investigate the frequent utilization of E/M codes and minor procedures by dermatologists.8 Clearly, modifier -25 is a continued target by insurers and regulators; therefore, dermatologists will want to make sure their coding and documentation meet all requirements and are updated for the new E/M codes for 2021.
The American Medical Association’s Current Procedural Terminology indicates that modifier -25 allows reporting of a “significant, separately identifiable evaluation and management service by the same physician or other qualified health care professional on the same day of a procedure or other service.”1 Given that dermatology patients typically present with multiple concerns, dermatologists commonly evaluate and treat numerous conditions during one visit. Understanding what constitutes a separately identifiable E/M service is critical to bill accurately and to pass insurer audits.
Global Surgical Package
To appropriately bill both a procedure and an E/M service, the physician must indicate that the patient’s condition required an E/M service above and beyond the usual work of the procedure. The compilation of evaluation and work included in the payment for a procedure is called the global surgical package.9 In general, the global surgical package includes local or topical anesthesia; the surgical service/procedure itself; immediate postoperative care, including dictating the operative note; meeting/discussing the patient’s procedure with family and other physicians; and writing orders for the patient. For minor procedures (ie, those with either 0- or 10-day global periods), the surgical package also includes same-day E/M services associated with the decision to perform surgery. An appropriate history and physical examination as well as a discussion of the differential diagnosis, treatment options, and risk and benefits of treatment are all included in the payment of a minor procedure itself. Therefore, an evaluation to discuss a patient’s condition or change in condition, alternatives to treatment, or next steps after a diagnosis related to a treatment or diagnostic procedure should not be separately reported. Moreover, the fact that the patient is new to the physician is not in itself sufficient to allow reporting of an E/M service with these minor procedures. For major procedures (ie, those with 90-day postoperative periods), the decision for surgery is excluded from the global surgical package.
2021 E/M Codes Simplify Documentation
The biggest coding change of 2021 was the new E/M codes.10 Prior to this year, the descriptors of E/M services recognized 7 components to define the levels of E/M services11: history and nature of the presenting problem; physical examination; medical decision-making (MDM); counseling; coordination of care; and time. Furthermore, history, physical examination, and MDM were all broken down into more granular elements that were summed to determine the level for each component; for example, the history of the presenting problem was defined as a chronological description of the development of the patient’s present illness, including the following elements: location, quality, severity, duration, timing, context, modifying factors, and associated signs and symptoms. Each of these categories would constitute bullet points to be summed to determine the level of history. Physical examination and MDM bullet points also would be summed to determine a proper coding level.11 Understandably, this coding scheme was complicated and burdensome to medical providers.
The redefinition of the E/M codes for 2021 substantially simplified the determination of coding level and documentation.10 The revisions to the E/M office visit code descriptors and documentation standards are now centered around how physicians think and take care of patients and not on mandatory standards and checking boxes. The main changes involve MDM as the prime determinant of the coding level. Elements of MDM affecting coding for an outpatient or office visit now include only 3 components: the number and complexity of problems addressed in the encounter, the amount or complexity of data to be reviewed and analyzed, and the risk of complications or morbidity of patient management. Gone are the requirements from the earlier criteria requiring so many bullet points for the history, physical examination, and MDM.
Dermatologists may ask, “How does the new E/M coding structure affect reporting and documenting an E/M and a procedure on the same day?” The answer is that the determination of separate and distinct is basically unchanged with the new E/M codes; however, the documentation requirements for modifier -25 using the new E/M codes are simplified.
As always, the key to determining whether a separate and distinct E/M service was provided and subsequently documented is to deconstruct the medical note. All evaluation services associated with the procedure—making a clinical diagnosis or differential diagnosis, decision to perform surgery, and discussion of alternative treatments—should be removed from one’s documentation as shown in the example below. If a complete E/M service still exists, then an E/M may be billed in addition to the procedure. Physical examination of the treatment area is included in the surgical package. With the prior E/M criteria, physical examination of the procedural area could not be used again as a bullet point to count for the E/M level. However, with the new 2021 coding requirements, the documentation of a separate MDM will be sufficient to meet criteria because documentation of physical examination is not a requirement.
Modifier -25 Examples
Let’s examine a typical dermatologist medical note. An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. The patient also complains of a growing tender lesion on the left elbow of 2 months’ duration. Physical examination reveals a linear vesicular eruption on the left wrist and a tender hyperkeratotic papule on the left elbow. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed. The decision is made to perform a tangential biopsy of the lesion on the left elbow because of the suspicion for malignancy. The biopsy is performed the same day.
This case clearly illustrates performance of an E/M service in the treatment of rhus dermatitis, which is separate and distinct from the biopsy procedure; however, in evaluating whether the case meets the documentation requirements for modifier -25, the information in the medical note inclusive to the procedure’s global surgical package, including history associated with establishing the diagnosis, physical examination of the procedure area(s), and discussion of treatment options, is eliminated, leaving the following notes: An established patient presents to the dermatologist complaining of an itchy rash on the left wrist after a hiking trip. Treatment with topical hydrocortisone 1% did not help. No data is evaluated. A diagnosis of acute rhus dermatitis of the left wrist is made, and betamethasone cream is prescribed.
Because the physical examination of the body part (left arm) is included in the procedure’s global surgical package, the examination of the left wrist cannot be used as coding support for the E/M service. This makes a difference for coding level in the prior E/M coding requirements, which required examination bullet points. However, with the 2021 E/M codes, documentation of physical examination bullet points is irrelevant to the coding level. Therefore, qualifying for a modifier -25 claim is more straightforward in this case with the new code set. Because bullet points are not integral to the 2021 E/M codes, qualifying and properly documenting for a higher level of service will likely be more common in dermatology.
Final Thoughts
Frequent use of modifier -25 is a critical part of a high-quality and cost-effective dermatology practice. Same-day performance of minor procedures and E/M services allows for more rapid and efficient diagnosis and treatment of various conditions as well as minimizing unnecessary office visits. The new E/M codes for 2021 actually make the documentation of a separate and distinct E/M service less complicated because the bullet point requirements associated with the old E/M codes have been eliminated. Understanding how the new E/M code descriptors affect modifier -25 reporting and clear documentation of separate, distinct, and medically necessary E/M services will be needed due to increased insurer scrutiny and audits.
- Current Procedural Terminology 2021, Professional Edition. American Medical Association; 2020.
- Rogers HW. Modifier −25 victory, but the battle is not over. Cutis. 2018;101:409-410.
- Rogers HW. One diagnosis and modifier −25: appropriate or audit target? Cutis. 2017;99:165-166.
- Update regarding E/M with modifier −25—professional. Anthem Blue Cross Blue Shield website. Published February 1, 2019. Accessed August 17, 2021. https://providernews.anthem.com/ohio/article/update-regarding-em-with-modifier-25-professional
- Payment policies—surgery. Harvard Pilgrim Health Care website. Updated May 2021. Accessed August 17, 2021. https://www.harvardpilgrim.org/provider/wp-content/uploads/sites/7/2020/07/H-6-Surgery-PM.pdf
- Modifier 25: frequently asked questions. Independence Blue Cross website. Updated September 25, 2017. Accessed August 17, 2021. https://provcomm.ibx.com/ibc/archive/pages/A86603B03881756B8525817E00768006.aspx
- Huang G. CMS 2019 fee schedule takes modifier 25 cuts, runs with them. Doctors Management website. Accessed August 17, 2021. https://www.doctors-management.com/cms-2019-feeschedule-modifier25/
- Dermatologist claims for evaluation and management services on the same day as minor surgical procedures. US Department of Health and Humans Services Office of Inspector General website. Accessed August 17, 2021. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000577.asp
- Global surgery booklet. Centers for Medicare and Medicaid Services website. Updated September 2018. Accessed August 17, 2021. https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/globallsurgery-icn907166.pdf
- American Medical Association. CPT® Evaluation and management (E/M)—office or other outpatient (99202-99215) and prolonged services (99354, 99355, 99356, 99417) code and guideline changes. Updated March 9, 2021. Accessed August 17, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
- 1997 documentation guidelines for evaluation and management services. Centers for Medicare and Medicaid Services website. Accessed August 17, 2021. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
- Current Procedural Terminology 2021, Professional Edition. American Medical Association; 2020.
- Rogers HW. Modifier −25 victory, but the battle is not over. Cutis. 2018;101:409-410.
- Rogers HW. One diagnosis and modifier −25: appropriate or audit target? Cutis. 2017;99:165-166.
- Update regarding E/M with modifier −25—professional. Anthem Blue Cross Blue Shield website. Published February 1, 2019. Accessed August 17, 2021. https://providernews.anthem.com/ohio/article/update-regarding-em-with-modifier-25-professional
- Payment policies—surgery. Harvard Pilgrim Health Care website. Updated May 2021. Accessed August 17, 2021. https://www.harvardpilgrim.org/provider/wp-content/uploads/sites/7/2020/07/H-6-Surgery-PM.pdf
- Modifier 25: frequently asked questions. Independence Blue Cross website. Updated September 25, 2017. Accessed August 17, 2021. https://provcomm.ibx.com/ibc/archive/pages/A86603B03881756B8525817E00768006.aspx
- Huang G. CMS 2019 fee schedule takes modifier 25 cuts, runs with them. Doctors Management website. Accessed August 17, 2021. https://www.doctors-management.com/cms-2019-feeschedule-modifier25/
- Dermatologist claims for evaluation and management services on the same day as minor surgical procedures. US Department of Health and Humans Services Office of Inspector General website. Accessed August 17, 2021. https://oig.hhs.gov/reports-and-publications/workplan/summary/wp-summary-0000577.asp
- Global surgery booklet. Centers for Medicare and Medicaid Services website. Updated September 2018. Accessed August 17, 2021. https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/globallsurgery-icn907166.pdf
- American Medical Association. CPT® Evaluation and management (E/M)—office or other outpatient (99202-99215) and prolonged services (99354, 99355, 99356, 99417) code and guideline changes. Updated March 9, 2021. Accessed August 17, 2021. https://www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf
- 1997 documentation guidelines for evaluation and management services. Centers for Medicare and Medicaid Services website. Accessed August 17, 2021. https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNEdWebGuide/Downloads/97Docguidelines.pdf
Practice Points
- Insurer scrutiny of same-day evaluation and management (E/M) and procedure services has increased, and dermatologists should be prepared for more frequent medical record reviews and audits.
- The new 2021 E/M codes actually reduce the hurdles for reporting a separate and distinct E/M service by eliminating the history and physical examination bullet points of the previous code set.
Supreme Court Case: Dobbs v Jackson Women’s Health Organization: What you need to know
This fall, the Supreme Court of the United States (SCOTUS) will announce when they will hear oral arguments for Dobbs v Jackson Women’s Health Organization. The court will examine a Mississippi law, known as the “Gestational Age Act,” originally passed in 2018, that sought to “limit abortions to fifteen weeks’ gestation except in a medical emergency or in cases of severe fetal abnormality.”1 This sets the stage for SCOTUS to make a major ruling on abortion, one which could affirm or upend landmark decisions and nearly 50 years of abortion legislative precedent. Additionally, SCOTUS’ recent decision to not intervene on Texas’ Senate Bill 8 (SB8), which essentially bans all abortions after 6 weeks’ gestational age, may foreshadow how this case will be decided. The current abortion restrictions in Texas and the implications of SB8 will be discussed in a forthcoming column.
SCOTUS and abortion rights
The decision to hear this case comes on the heels of another recent decision regarding a Louisiana law in June Medical Services v Russo. This case examined Louisiana Act 620, which would have required physicians to have hospital admitting privileges within 30 miles of where they provide abortion services.2 The law was deemed constitutionally invalid, with the majority noting the law would have drastically burdened a woman’s right to access abortion services. The Court ruled similarly in 2016 in Whole Women’s Health (WWH) v Hellerstedt, in which WWH challenged Texas House Bill 2, a nearly identical law requiring admitting privileges for abortion care providers. In both of these cases, SCOTUS pointed to precedent set by Southeastern Pennsylvania v Casey, which established that it is unconstitutional for a state to create an “undue burden” on a woman’s right to abortion prior to fetal viability.3 The precedent to this, Roe v Wade, and 5 decades of abortion legislation set may be upended by a SCOTUS decision this next term.
Dobbs v Jackson
On March 19, 2018, Mississippi enacted the “Gestational Age Act” into law. The newly enacted law would limit abortions to 15 weeks’ gestation except in a medical emergency or in cases of severe fetal anomalies. Jackson Women’s Health Organization, the only licensed abortion provider in the state, challenged the constitutionality of the law with legal support from Center for Reproductive Rights (CRR). The US District Court for the Southern District of Mississippi granted summary judgement in favor of the clinic and placed an injunction on the law’s enforcement. The state appealed to the Fifth Circuit Court of Appeals, which upheld the district court decision in a 3-0 decision in November 2019. Mississippi appealed to the Supreme Court, with their petition focusing on multiple questions from the appeals process. After repeatedly rescheduling the case, and multiple reviews in conference, SCOTUS agreed to hear the case. Most recently, the state has narrowed its argument, changing course, and attacking Roe v Wade directly. In a brief submitted in July 2021, the state argues the court should hold that all pre-viability prohibitions on elective abortions are constitutional.
Interestingly, during this time the Mississippi legislature also passed a law, House Bill 2116, also known as the “fetal heartbeat bill,” banning abortion with gestational ages after detection of a fetal heartbeat. This was also challenged, deemed unconstitutional, and affirmed on appeal by the Fifth US Circuit Court.
While recent challenges have focused on the “undue burden” state laws placed on those trying to access abortion care, this case will bring the issue of “viability” and gestational age limits to the forefront.4,5 In addition to Roe v Wade, the Court will have the opportunity to reexamine other relevant precedent, such as Southeastern Pennsylvania v Casey, in considering the most recent arguments of the state. In this most recent brief, the state argues that the Court should, “reject viability as a barrier to prohibiting elective abortions” and that a “viability rule has no constitutional basis.” The state goes on to argue the “Constitution does not protect a right to abortion or limit States’ authority to restrict it.”6 The language and tone in this brief are more direct and aggressive than the states’ petition submitted last June.
However, the composition of the Court is different than in the past. This case will be argued with Justice Amy Coney Barrett seated in place of Justice Ruth Bader Ginsburg, who was a strong advocate for women’s rights.7 She joins Justices Neil Gorsuch and Brett Kavanaugh, also appointed by President Donald Trump and widely viewed as conservative judges, tipping the scales to a more conservative Supreme Court. This case will also be argued in a polarized political environment.8,9 Given the conservative Supreme Court in the setting of an increasingly politically charged environment, reproductive right advocates are understandably worried that members of the anti-abortion movement view this as an opportunity to weaken or remove federal constitutional protections for abortion.
Continue to: Potential outcome of Dobbs v Jackson...
Potential outcome of Dobbs v Jackson
Should SCOTUS choose to rule in favor of Mississippi, it could severely weaken, or even overturn Roe v Wade. This would leave a legal path for states with pre-Roe abortion bans and currently unenforced post-Roe bans to take effect. These “trigger” laws are bans or severe restrictions on abortion providers and patients intended to take effect if Roe were to be overturned. Alternatively, the Court may overturn Southeastern Pennsylvania v Casey, but maintain Roe v Wade, essentially leaving the regulation of pre-viability abortion care to individual states. Currently 21 states have laws that would restrict the legal status of abortion.10 In addition, state legislatures are aggressively introducing abortion restrictions. As of June 2021, there have been 561 abortion restrictions, including 165 abortion bans, introduced across 47 states, putting 2021 on course to be the most devastating anti-abortion state legislative session in decades.11
The damage caused by such restriction on abortion care would be significant. It would block or push access out of reach for many. The negative effects of such legislative action would most heavily burden those already marginalized by systemic, structural inequalities including those of low socioeconomic status, people of color, young people, those in rural communities, and members of the LGBTQ community. The medical community has long recognized the harm caused by restricting access to abortion care. Restriction of access to safe abortion care paradoxically has been shown not to decrease the incidence of abortion, but rather increases the number of unsafe abortions.12 The American College of Obstetricians and Gynecologists (ACOG) acknowledge “individuals require access to safe, legal abortion” and that this represents “a necessary component for comprehensive health care.”13,14 They joined the American Medical Association and other professional groups in a 2019 amicus brief to SCOTUS opposing restrictions on abortion access.15 In addition, government laws restricting access to abortion care undermine the fundamental relationship between a person and their physician, limiting a physician’s obligation to honor patient autonomy and provide appropriate medical care.
By taking up the question whether all pre-viability bans on elective abortions violate the Constitution, SCOTUS is indicating a possible willingness to revisit the central holding of abortion jurisprudence. Their decision regarding this case will likely be the most significant ruling regarding the legal status of abortion care in decades, and will significantly affect the delivery of abortion care in the future.
Action items
- Reach out to your representatives to support the Women’s Health Protection Act, an initiative introduced to Congress to protect access to abortion care. If you reside in a state where your federal representatives support the Women’s Health Protection Act, reach out to friends and colleagues in states without supportive elected officials and ask them to call their representatives and ask them to support the bill.
- Get involved with local grassroots groups fighting to protect abortion access.
- Continue to speak out against laws and policies designed to limit access to safe abortion care.
- Connect with your local ACOG chapter for more ways to become involved.
- As always, make sure you are registered to vote, and exercise your right whenever you can.
- HB1510 (As Introduced) - 2018 Regular Session. http://billstatus.ls.state.ms.us/documents/2018/html/HB/1500-1599/HB1510IN.htm Accessed August 13, 2021.
- HB338. Louisiana State Legislature. 2014. http://www.legis.la.gov/legis/BillInfo.aspx?s=14RS&b=ACT620&sbi=y. Accessed August 13, 2021.
- Planned Parenthood of Southeastern Pennsylvania v. Casey. Cornell Law School Legal Information Institute. https://www.law.cornell.edu/supremecourt/text/505/833. Accessed August 13, 2021.
- 15-274 Whole Woman’s Health v. Hellerstedt (06/27/2016). Published online 2016:107.
- 18-1323 June Medical Services L. L. C. v. Russo (06/29/2020). Published online 2020:138.
- 19-1392 Dobbs v. Jackson Women’s Health Organization (07/22/2021). Published online 2021.
- What Ruth Bader Ginsburg said about abortion and Roe v. Wade. Time. August 2, 2018. https://time.com/5354490/ruth-bader-ginsburg-roe-v-wade/. Accessed August 13, 2021.
- Montanaro D. Poll: majority want to keep abortion legal, but they also want restrictions. NPR. June 7, 2019. https://www.npr.org/2019/06/07/730183531/poll-majority-want-to-keep-abortion-legal-but-they-also-want-restrictions. Accessed August 13, 2021.
- Abortion support remains steady despite growing partisan divide, survey finds. Washington Post. August 13, 2019. https://www.washingtonpost.com/health/2019/08/13/one-largest-ever-abortion-surveys-shows-growing-partisan-divide/. Accessed August 13, 2021.
- Abortion policy in the absence of Roe. Guttmacher Institute. September 1, 2021. https://www.guttmacher.org/state-policy/explore/abortion-policy-absence-roe#. Accessed September 8, 2021.
- 2021 is on track to become the most devastating antiabortion state legislative session in decades. Guttmacher Institute. Published April 30, 2021. Updated June 14, 2021. https://www.guttmacher.org/article/2021/04/2021-track-become-most-devastating-antiabortion-state-legislative-session-decades. Accessed August 13, 2021.
- Facts and consequences: legality, incidence and safety of abortion worldwide. Guttmacher Institute. November 20, 2009. https://www.guttmacher.org/gpr/2009/11/facts-and-consequences-legality-incidence-and-safety-abortion-worldwide. Accessed August 13, 2021.
- Increasing access to abortion. https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2020/12/increasing-access-to-abortion. Accessed August 13, 2021.
- ACOG statement on Dobbs vs. Jackson Women’s Health. May 17, 2021. https://www.acog.org/en/news/news-releases/2021/05/acog-statement-dobbs-vs-jackson-womens-health. Accessed August 13, 2021.
- Perryman SL, Parker KA, Hickman SA. Brief of amici curiae American College of Obstetricians and Gynecologists, American Medical Associations, American Academy of Family Physicians, American Academy of Nursing, American Academy of Pediatrics, et al. In support of June Medical Services, LLC, et al. https://www.supremecourt.gov/
DocketPDF/18/18-1323/124091/ . Accessed August 13, 2021.20191202145531124_18-1323% 2018-1460%20tsac%20American% 20College%20of% 20Obstetricians%20and% 20Gynecologists%20et%20al.pdf
This fall, the Supreme Court of the United States (SCOTUS) will announce when they will hear oral arguments for Dobbs v Jackson Women’s Health Organization. The court will examine a Mississippi law, known as the “Gestational Age Act,” originally passed in 2018, that sought to “limit abortions to fifteen weeks’ gestation except in a medical emergency or in cases of severe fetal abnormality.”1 This sets the stage for SCOTUS to make a major ruling on abortion, one which could affirm or upend landmark decisions and nearly 50 years of abortion legislative precedent. Additionally, SCOTUS’ recent decision to not intervene on Texas’ Senate Bill 8 (SB8), which essentially bans all abortions after 6 weeks’ gestational age, may foreshadow how this case will be decided. The current abortion restrictions in Texas and the implications of SB8 will be discussed in a forthcoming column.
SCOTUS and abortion rights
The decision to hear this case comes on the heels of another recent decision regarding a Louisiana law in June Medical Services v Russo. This case examined Louisiana Act 620, which would have required physicians to have hospital admitting privileges within 30 miles of where they provide abortion services.2 The law was deemed constitutionally invalid, with the majority noting the law would have drastically burdened a woman’s right to access abortion services. The Court ruled similarly in 2016 in Whole Women’s Health (WWH) v Hellerstedt, in which WWH challenged Texas House Bill 2, a nearly identical law requiring admitting privileges for abortion care providers. In both of these cases, SCOTUS pointed to precedent set by Southeastern Pennsylvania v Casey, which established that it is unconstitutional for a state to create an “undue burden” on a woman’s right to abortion prior to fetal viability.3 The precedent to this, Roe v Wade, and 5 decades of abortion legislation set may be upended by a SCOTUS decision this next term.
Dobbs v Jackson
On March 19, 2018, Mississippi enacted the “Gestational Age Act” into law. The newly enacted law would limit abortions to 15 weeks’ gestation except in a medical emergency or in cases of severe fetal anomalies. Jackson Women’s Health Organization, the only licensed abortion provider in the state, challenged the constitutionality of the law with legal support from Center for Reproductive Rights (CRR). The US District Court for the Southern District of Mississippi granted summary judgement in favor of the clinic and placed an injunction on the law’s enforcement. The state appealed to the Fifth Circuit Court of Appeals, which upheld the district court decision in a 3-0 decision in November 2019. Mississippi appealed to the Supreme Court, with their petition focusing on multiple questions from the appeals process. After repeatedly rescheduling the case, and multiple reviews in conference, SCOTUS agreed to hear the case. Most recently, the state has narrowed its argument, changing course, and attacking Roe v Wade directly. In a brief submitted in July 2021, the state argues the court should hold that all pre-viability prohibitions on elective abortions are constitutional.
Interestingly, during this time the Mississippi legislature also passed a law, House Bill 2116, also known as the “fetal heartbeat bill,” banning abortion with gestational ages after detection of a fetal heartbeat. This was also challenged, deemed unconstitutional, and affirmed on appeal by the Fifth US Circuit Court.
While recent challenges have focused on the “undue burden” state laws placed on those trying to access abortion care, this case will bring the issue of “viability” and gestational age limits to the forefront.4,5 In addition to Roe v Wade, the Court will have the opportunity to reexamine other relevant precedent, such as Southeastern Pennsylvania v Casey, in considering the most recent arguments of the state. In this most recent brief, the state argues that the Court should, “reject viability as a barrier to prohibiting elective abortions” and that a “viability rule has no constitutional basis.” The state goes on to argue the “Constitution does not protect a right to abortion or limit States’ authority to restrict it.”6 The language and tone in this brief are more direct and aggressive than the states’ petition submitted last June.
However, the composition of the Court is different than in the past. This case will be argued with Justice Amy Coney Barrett seated in place of Justice Ruth Bader Ginsburg, who was a strong advocate for women’s rights.7 She joins Justices Neil Gorsuch and Brett Kavanaugh, also appointed by President Donald Trump and widely viewed as conservative judges, tipping the scales to a more conservative Supreme Court. This case will also be argued in a polarized political environment.8,9 Given the conservative Supreme Court in the setting of an increasingly politically charged environment, reproductive right advocates are understandably worried that members of the anti-abortion movement view this as an opportunity to weaken or remove federal constitutional protections for abortion.
Continue to: Potential outcome of Dobbs v Jackson...
Potential outcome of Dobbs v Jackson
Should SCOTUS choose to rule in favor of Mississippi, it could severely weaken, or even overturn Roe v Wade. This would leave a legal path for states with pre-Roe abortion bans and currently unenforced post-Roe bans to take effect. These “trigger” laws are bans or severe restrictions on abortion providers and patients intended to take effect if Roe were to be overturned. Alternatively, the Court may overturn Southeastern Pennsylvania v Casey, but maintain Roe v Wade, essentially leaving the regulation of pre-viability abortion care to individual states. Currently 21 states have laws that would restrict the legal status of abortion.10 In addition, state legislatures are aggressively introducing abortion restrictions. As of June 2021, there have been 561 abortion restrictions, including 165 abortion bans, introduced across 47 states, putting 2021 on course to be the most devastating anti-abortion state legislative session in decades.11
The damage caused by such restriction on abortion care would be significant. It would block or push access out of reach for many. The negative effects of such legislative action would most heavily burden those already marginalized by systemic, structural inequalities including those of low socioeconomic status, people of color, young people, those in rural communities, and members of the LGBTQ community. The medical community has long recognized the harm caused by restricting access to abortion care. Restriction of access to safe abortion care paradoxically has been shown not to decrease the incidence of abortion, but rather increases the number of unsafe abortions.12 The American College of Obstetricians and Gynecologists (ACOG) acknowledge “individuals require access to safe, legal abortion” and that this represents “a necessary component for comprehensive health care.”13,14 They joined the American Medical Association and other professional groups in a 2019 amicus brief to SCOTUS opposing restrictions on abortion access.15 In addition, government laws restricting access to abortion care undermine the fundamental relationship between a person and their physician, limiting a physician’s obligation to honor patient autonomy and provide appropriate medical care.
By taking up the question whether all pre-viability bans on elective abortions violate the Constitution, SCOTUS is indicating a possible willingness to revisit the central holding of abortion jurisprudence. Their decision regarding this case will likely be the most significant ruling regarding the legal status of abortion care in decades, and will significantly affect the delivery of abortion care in the future.
Action items
- Reach out to your representatives to support the Women’s Health Protection Act, an initiative introduced to Congress to protect access to abortion care. If you reside in a state where your federal representatives support the Women’s Health Protection Act, reach out to friends and colleagues in states without supportive elected officials and ask them to call their representatives and ask them to support the bill.
- Get involved with local grassroots groups fighting to protect abortion access.
- Continue to speak out against laws and policies designed to limit access to safe abortion care.
- Connect with your local ACOG chapter for more ways to become involved.
- As always, make sure you are registered to vote, and exercise your right whenever you can.
This fall, the Supreme Court of the United States (SCOTUS) will announce when they will hear oral arguments for Dobbs v Jackson Women’s Health Organization. The court will examine a Mississippi law, known as the “Gestational Age Act,” originally passed in 2018, that sought to “limit abortions to fifteen weeks’ gestation except in a medical emergency or in cases of severe fetal abnormality.”1 This sets the stage for SCOTUS to make a major ruling on abortion, one which could affirm or upend landmark decisions and nearly 50 years of abortion legislative precedent. Additionally, SCOTUS’ recent decision to not intervene on Texas’ Senate Bill 8 (SB8), which essentially bans all abortions after 6 weeks’ gestational age, may foreshadow how this case will be decided. The current abortion restrictions in Texas and the implications of SB8 will be discussed in a forthcoming column.
SCOTUS and abortion rights
The decision to hear this case comes on the heels of another recent decision regarding a Louisiana law in June Medical Services v Russo. This case examined Louisiana Act 620, which would have required physicians to have hospital admitting privileges within 30 miles of where they provide abortion services.2 The law was deemed constitutionally invalid, with the majority noting the law would have drastically burdened a woman’s right to access abortion services. The Court ruled similarly in 2016 in Whole Women’s Health (WWH) v Hellerstedt, in which WWH challenged Texas House Bill 2, a nearly identical law requiring admitting privileges for abortion care providers. In both of these cases, SCOTUS pointed to precedent set by Southeastern Pennsylvania v Casey, which established that it is unconstitutional for a state to create an “undue burden” on a woman’s right to abortion prior to fetal viability.3 The precedent to this, Roe v Wade, and 5 decades of abortion legislation set may be upended by a SCOTUS decision this next term.
Dobbs v Jackson
On March 19, 2018, Mississippi enacted the “Gestational Age Act” into law. The newly enacted law would limit abortions to 15 weeks’ gestation except in a medical emergency or in cases of severe fetal anomalies. Jackson Women’s Health Organization, the only licensed abortion provider in the state, challenged the constitutionality of the law with legal support from Center for Reproductive Rights (CRR). The US District Court for the Southern District of Mississippi granted summary judgement in favor of the clinic and placed an injunction on the law’s enforcement. The state appealed to the Fifth Circuit Court of Appeals, which upheld the district court decision in a 3-0 decision in November 2019. Mississippi appealed to the Supreme Court, with their petition focusing on multiple questions from the appeals process. After repeatedly rescheduling the case, and multiple reviews in conference, SCOTUS agreed to hear the case. Most recently, the state has narrowed its argument, changing course, and attacking Roe v Wade directly. In a brief submitted in July 2021, the state argues the court should hold that all pre-viability prohibitions on elective abortions are constitutional.
Interestingly, during this time the Mississippi legislature also passed a law, House Bill 2116, also known as the “fetal heartbeat bill,” banning abortion with gestational ages after detection of a fetal heartbeat. This was also challenged, deemed unconstitutional, and affirmed on appeal by the Fifth US Circuit Court.
While recent challenges have focused on the “undue burden” state laws placed on those trying to access abortion care, this case will bring the issue of “viability” and gestational age limits to the forefront.4,5 In addition to Roe v Wade, the Court will have the opportunity to reexamine other relevant precedent, such as Southeastern Pennsylvania v Casey, in considering the most recent arguments of the state. In this most recent brief, the state argues that the Court should, “reject viability as a barrier to prohibiting elective abortions” and that a “viability rule has no constitutional basis.” The state goes on to argue the “Constitution does not protect a right to abortion or limit States’ authority to restrict it.”6 The language and tone in this brief are more direct and aggressive than the states’ petition submitted last June.
However, the composition of the Court is different than in the past. This case will be argued with Justice Amy Coney Barrett seated in place of Justice Ruth Bader Ginsburg, who was a strong advocate for women’s rights.7 She joins Justices Neil Gorsuch and Brett Kavanaugh, also appointed by President Donald Trump and widely viewed as conservative judges, tipping the scales to a more conservative Supreme Court. This case will also be argued in a polarized political environment.8,9 Given the conservative Supreme Court in the setting of an increasingly politically charged environment, reproductive right advocates are understandably worried that members of the anti-abortion movement view this as an opportunity to weaken or remove federal constitutional protections for abortion.
Continue to: Potential outcome of Dobbs v Jackson...
Potential outcome of Dobbs v Jackson
Should SCOTUS choose to rule in favor of Mississippi, it could severely weaken, or even overturn Roe v Wade. This would leave a legal path for states with pre-Roe abortion bans and currently unenforced post-Roe bans to take effect. These “trigger” laws are bans or severe restrictions on abortion providers and patients intended to take effect if Roe were to be overturned. Alternatively, the Court may overturn Southeastern Pennsylvania v Casey, but maintain Roe v Wade, essentially leaving the regulation of pre-viability abortion care to individual states. Currently 21 states have laws that would restrict the legal status of abortion.10 In addition, state legislatures are aggressively introducing abortion restrictions. As of June 2021, there have been 561 abortion restrictions, including 165 abortion bans, introduced across 47 states, putting 2021 on course to be the most devastating anti-abortion state legislative session in decades.11
The damage caused by such restriction on abortion care would be significant. It would block or push access out of reach for many. The negative effects of such legislative action would most heavily burden those already marginalized by systemic, structural inequalities including those of low socioeconomic status, people of color, young people, those in rural communities, and members of the LGBTQ community. The medical community has long recognized the harm caused by restricting access to abortion care. Restriction of access to safe abortion care paradoxically has been shown not to decrease the incidence of abortion, but rather increases the number of unsafe abortions.12 The American College of Obstetricians and Gynecologists (ACOG) acknowledge “individuals require access to safe, legal abortion” and that this represents “a necessary component for comprehensive health care.”13,14 They joined the American Medical Association and other professional groups in a 2019 amicus brief to SCOTUS opposing restrictions on abortion access.15 In addition, government laws restricting access to abortion care undermine the fundamental relationship between a person and their physician, limiting a physician’s obligation to honor patient autonomy and provide appropriate medical care.
By taking up the question whether all pre-viability bans on elective abortions violate the Constitution, SCOTUS is indicating a possible willingness to revisit the central holding of abortion jurisprudence. Their decision regarding this case will likely be the most significant ruling regarding the legal status of abortion care in decades, and will significantly affect the delivery of abortion care in the future.
Action items
- Reach out to your representatives to support the Women’s Health Protection Act, an initiative introduced to Congress to protect access to abortion care. If you reside in a state where your federal representatives support the Women’s Health Protection Act, reach out to friends and colleagues in states without supportive elected officials and ask them to call their representatives and ask them to support the bill.
- Get involved with local grassroots groups fighting to protect abortion access.
- Continue to speak out against laws and policies designed to limit access to safe abortion care.
- Connect with your local ACOG chapter for more ways to become involved.
- As always, make sure you are registered to vote, and exercise your right whenever you can.
- HB1510 (As Introduced) - 2018 Regular Session. http://billstatus.ls.state.ms.us/documents/2018/html/HB/1500-1599/HB1510IN.htm Accessed August 13, 2021.
- HB338. Louisiana State Legislature. 2014. http://www.legis.la.gov/legis/BillInfo.aspx?s=14RS&b=ACT620&sbi=y. Accessed August 13, 2021.
- Planned Parenthood of Southeastern Pennsylvania v. Casey. Cornell Law School Legal Information Institute. https://www.law.cornell.edu/supremecourt/text/505/833. Accessed August 13, 2021.
- 15-274 Whole Woman’s Health v. Hellerstedt (06/27/2016). Published online 2016:107.
- 18-1323 June Medical Services L. L. C. v. Russo (06/29/2020). Published online 2020:138.
- 19-1392 Dobbs v. Jackson Women’s Health Organization (07/22/2021). Published online 2021.
- What Ruth Bader Ginsburg said about abortion and Roe v. Wade. Time. August 2, 2018. https://time.com/5354490/ruth-bader-ginsburg-roe-v-wade/. Accessed August 13, 2021.
- Montanaro D. Poll: majority want to keep abortion legal, but they also want restrictions. NPR. June 7, 2019. https://www.npr.org/2019/06/07/730183531/poll-majority-want-to-keep-abortion-legal-but-they-also-want-restrictions. Accessed August 13, 2021.
- Abortion support remains steady despite growing partisan divide, survey finds. Washington Post. August 13, 2019. https://www.washingtonpost.com/health/2019/08/13/one-largest-ever-abortion-surveys-shows-growing-partisan-divide/. Accessed August 13, 2021.
- Abortion policy in the absence of Roe. Guttmacher Institute. September 1, 2021. https://www.guttmacher.org/state-policy/explore/abortion-policy-absence-roe#. Accessed September 8, 2021.
- 2021 is on track to become the most devastating antiabortion state legislative session in decades. Guttmacher Institute. Published April 30, 2021. Updated June 14, 2021. https://www.guttmacher.org/article/2021/04/2021-track-become-most-devastating-antiabortion-state-legislative-session-decades. Accessed August 13, 2021.
- Facts and consequences: legality, incidence and safety of abortion worldwide. Guttmacher Institute. November 20, 2009. https://www.guttmacher.org/gpr/2009/11/facts-and-consequences-legality-incidence-and-safety-abortion-worldwide. Accessed August 13, 2021.
- Increasing access to abortion. https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2020/12/increasing-access-to-abortion. Accessed August 13, 2021.
- ACOG statement on Dobbs vs. Jackson Women’s Health. May 17, 2021. https://www.acog.org/en/news/news-releases/2021/05/acog-statement-dobbs-vs-jackson-womens-health. Accessed August 13, 2021.
- Perryman SL, Parker KA, Hickman SA. Brief of amici curiae American College of Obstetricians and Gynecologists, American Medical Associations, American Academy of Family Physicians, American Academy of Nursing, American Academy of Pediatrics, et al. In support of June Medical Services, LLC, et al. https://www.supremecourt.gov/
DocketPDF/18/18-1323/124091/ . Accessed August 13, 2021.20191202145531124_18-1323% 2018-1460%20tsac%20American% 20College%20of% 20Obstetricians%20and% 20Gynecologists%20et%20al.pdf
- HB1510 (As Introduced) - 2018 Regular Session. http://billstatus.ls.state.ms.us/documents/2018/html/HB/1500-1599/HB1510IN.htm Accessed August 13, 2021.
- HB338. Louisiana State Legislature. 2014. http://www.legis.la.gov/legis/BillInfo.aspx?s=14RS&b=ACT620&sbi=y. Accessed August 13, 2021.
- Planned Parenthood of Southeastern Pennsylvania v. Casey. Cornell Law School Legal Information Institute. https://www.law.cornell.edu/supremecourt/text/505/833. Accessed August 13, 2021.
- 15-274 Whole Woman’s Health v. Hellerstedt (06/27/2016). Published online 2016:107.
- 18-1323 June Medical Services L. L. C. v. Russo (06/29/2020). Published online 2020:138.
- 19-1392 Dobbs v. Jackson Women’s Health Organization (07/22/2021). Published online 2021.
- What Ruth Bader Ginsburg said about abortion and Roe v. Wade. Time. August 2, 2018. https://time.com/5354490/ruth-bader-ginsburg-roe-v-wade/. Accessed August 13, 2021.
- Montanaro D. Poll: majority want to keep abortion legal, but they also want restrictions. NPR. June 7, 2019. https://www.npr.org/2019/06/07/730183531/poll-majority-want-to-keep-abortion-legal-but-they-also-want-restrictions. Accessed August 13, 2021.
- Abortion support remains steady despite growing partisan divide, survey finds. Washington Post. August 13, 2019. https://www.washingtonpost.com/health/2019/08/13/one-largest-ever-abortion-surveys-shows-growing-partisan-divide/. Accessed August 13, 2021.
- Abortion policy in the absence of Roe. Guttmacher Institute. September 1, 2021. https://www.guttmacher.org/state-policy/explore/abortion-policy-absence-roe#. Accessed September 8, 2021.
- 2021 is on track to become the most devastating antiabortion state legislative session in decades. Guttmacher Institute. Published April 30, 2021. Updated June 14, 2021. https://www.guttmacher.org/article/2021/04/2021-track-become-most-devastating-antiabortion-state-legislative-session-decades. Accessed August 13, 2021.
- Facts and consequences: legality, incidence and safety of abortion worldwide. Guttmacher Institute. November 20, 2009. https://www.guttmacher.org/gpr/2009/11/facts-and-consequences-legality-incidence-and-safety-abortion-worldwide. Accessed August 13, 2021.
- Increasing access to abortion. https://www.acog.org/en/clinical/clinical-guidance/committee-opinion/articles/2020/12/increasing-access-to-abortion. Accessed August 13, 2021.
- ACOG statement on Dobbs vs. Jackson Women’s Health. May 17, 2021. https://www.acog.org/en/news/news-releases/2021/05/acog-statement-dobbs-vs-jackson-womens-health. Accessed August 13, 2021.
- Perryman SL, Parker KA, Hickman SA. Brief of amici curiae American College of Obstetricians and Gynecologists, American Medical Associations, American Academy of Family Physicians, American Academy of Nursing, American Academy of Pediatrics, et al. In support of June Medical Services, LLC, et al. https://www.supremecourt.gov/
DocketPDF/18/18-1323/124091/ . Accessed August 13, 2021.20191202145531124_18-1323% 2018-1460%20tsac%20American% 20College%20of% 20Obstetricians%20and% 20Gynecologists%20et%20al.pdf
I did peer review: I saw turf wars, ego, and unfairness
After making an insulting comment to a surgery scheduler, a surgeon become the subject of a peer review investigation.
The surgeon had been called in on a Saturday morning for surgery, but when he arrived at the hospital, staff informed him that the operating room had been incorrectly booked and asked him to come back that afternoon. When the surgeon returned, the room still wasn’t ready, recounted David Beran, DO, a peer reviewer and medical director for the emergency department at University Medical Center New Orleans, in Louisiana. After more waiting and staff uncertainty about which operating room was going to open, the surgeon became frustrated and said to the scheduler: “Any idiot could figure this out!”
During his peer review, the surgeon acknowledged that he shouldn’t have made the rude remark to the scheduler, Dr. Beran said. His exasperation stemmed from an ongoing problem – operating rooms at the hospital were being inefficiently managed.
“The surgeon acknowledged that even though there was a systems issue at the root, that’s not justification to speak to people unprofessionally,” Dr. Beran said. “So, there was education for the surgeon, but the surgeon was also able to explain the frustration that led to that point.”
System problems are commonly encountered by peer reviewers, said Dr. Beran.
“There’s a huge gap between administration and clinical professionals when it comes to peer review,” he said. “So many times, bad situations, whether they’re clinical or behavioral, often boil down to systems issues or some inadequacy, whether it’s an EMR [electronic medical record] problem, an inefficacy, or how complicated a process is for an end user. But having a peer review situation that then leads to a system-level change that prevents that problem from happening again is really unlikely. There’s a huge disconnect between those two.”
Peer review is generally a process that goes on behind closed doors. Although structures may differ, peer review is generally described as the process by which physicians assess the quality of their peers’ work to ensure that standards of care are being met. The process is often used to evaluate issues regarding clinical care as well as behavioral complaints against physicians.
Doctors who undergo peer review frequently share their experiences, but reviewers themselves rarely speak out. For this story,
“Peer review processes are in place to build stronger institutions and stronger practices, and they’re supposed to be helpful,” Dr. Beran said. “But because of how opaque they are, it immediately puts physicians on the defensive, and it doesn’t always succeed in what it’s trying to do. I think that’s one of the biggest challenges.”
Biased reviewers taint evaluations
A peer reviewer on and off throughout her career, Indiana family physician Lana Patch, MD, said she always strived to be fair when evaluating fellow physicians. But not every reviewer she encountered operated the same way, she said. Some were biased.
In one case, Dr. Patch peer reviewed a general surgeon who had performed a hysterectomy on a 16-year-old girl. The surgeon believed the teenager likely had an acute appendicitis, but it turned out she had a uterine pathology, Dr. Patch said. The surgeon saved the girl’s life, but the case came under review because of the patient’s age and the fact that her uterus was removed. A local obstetrician-gynecologist weighed in on the case.
“The local ob.gyn. saw it as a turf battle,” recalled Dr. Patch, who is now retired after 30 years of practice in eastern Indiana. “The doctor had nothing but bad to say about the surgeon. He was a competitor.”
Because it was a small hospital, the committee sometimes had trouble finding a specialist who was qualified to give an opinion and who wasn’t in competition with the physician in question, said Dr. Patch. Eventually they found an outside pediatric gynecologist who reviewed the case and concluded that the surgeon had followed the standard of care.
Personal agendas in can come from different directions, said Robert Marder, MD, the author of several books on peer review. Dr. Marder is a consultant who assists with peer review redesign. He has worked with hundreds of medical staff leaders and is a former vice president at the Greeley Company, a consulting firm in Danvers, Mass., that performs peer review redesign. Dr. Marder is president of Robert J. Marder Consulting.
“It goes both ways,” Dr. Marder said. “I’ve seen where somebody with a personal view decides to bring things to the peer review committee specifically because they want the peer review committee to have an adverse view of this person and get them off the medical staff. And I’ve seen hospitals that are uncomfortable with a certain person for whatever reason and want the peer review committee to address it, as opposed to addressing it from a human resource standpoint.”
Dr. Patch recalled a case in which reviewers and hospital leaders were at odds over the credentialing of a physician. Fifteen years earlier, while driving in California, the psychiatrist had been pulled over and was found with an ounce of marijuana, she said.
“We wanted to privilege him,” Dr. Patch said. “As staff physicians, we felt that was 15 years ago, people change over time. Doctors are human beings, too. He seemed to have good credentials and good training. The hospital said, ‘Oh no, we can’t have somebody like this.’ “
The psychiatrist was placed on probation and had to undergo a review every 90 days for about 3 years. Eventually, he was privileged, Dr. Patch said.
Bias among reviewers, including unintentional bias, is also a challenge, Dr. Marder noted. Some initial reviewers score a physician too harshly, he said, whereas others underscore.
“Underscoring is more insidious and more difficult to deal with,” Dr. Marder said. “Underscoring is where the reviewer is too nice. They tend to dismiss things from their colleagues rather than recognize them as an opportunity to help them improve. With underscoring, a lot of committees, if the initial reviewer says the care was appropriate, they don’t even look at the case. They just take that one person’s word for it.”
Reviewers: Looks can be deceiving
When first examining the documented details of a case, it can be easy for peer reviewers to make a quick judgment about what happened, Dr. Beran said.
“You get these complaints, and you read through it, and you think, ‘Oh man, this person really messed up,’ “ he said. “Then you hear the doctor’s side of it, and you realize, ‘No, there’s a much bigger picture at play.’ You realize both sides have valid perspectives on it.”
In one case, for example, Dr. Beran recalled a complaint against a physician who made a snarky remark to a nurse. The doctor had asked the nurse for a piece of equipment, and the nurse said she was busy preparing the room for a patient. The doctor made a comment along the lines of, “Well, would you like me to do that for you and also intubate the patient while you do some charting?!”
At first glance, it appeared that the physician lashed out inappropriately at the nurse. But when reviewers heard from the doctor, they learned that the nurses knew that a trauma patient was coming by ambulance and that he would likely require a ventilator, Dr. Beran said. As the minutes ticked by, however, the nurses were seen in the break room chatting. Nothing had been prepared in the room, including any airway supply.
“The patient had a prolonged course and a very difficult intubation and could have very easily wound up with a much worse outcome for something the nurses had been warned about prior to the patient’s arrival,” he said. “I can see anybody getting upset in that situation if I warned them 5 or 10 minutes beforehand, ‘Get this stuff ready,’ and then nothing was done.”
There was no direct penalty for the physician.
Just as some complaints can be misleading, the clinical record in some peer review cases can also lead reviewers astray.
Physicians frequently include too much irrelevant information in the record, which can cloud a peer review, said Hans Duvefelt, MD, a family physician at Pines Health Services, in Van Buren, Maine. Dr. Duvefelt is a former medical director at Bucksport Regional Health Center, in Ellsworth, Maine. Both facilities are federally qualified health centers where continuous, random peer reviews are required.
In one case, Dr. Duvefelt was peer reviewing a physician’s office note regarding an elderly patient with a low-grade fever. The final diagnosis was urinary tract infection. Dr. Duvefelt said he had trouble following the doctor’s line of thinking because of a plethora of unnecessary data in the 10-page document. The office note included past medical history, prior lab and imaging test results, and an extensive narrative section that included a mixture of active medical problems and ongoing relationships with specialists, he said.
After reading through the printout three times, Dr. Duvefelt said he finally found mention of increased urinary dribbling and details about an enlarged prostate. He also spotted a same-day urinalysis among nearly a dozen other previous lab tests that had no connection to body temperature. Dr. Duvefelt gave the physician a passing grade but also left a scathing note about all the irrelevant information.
“It’s very common,” Dr. Duvefelt said. “It’s a disaster. Other doctors can’t follow your thinking. A reviewer has a hard time determining whether the doctor acted reasonably.”
Slackers make bad reviewers
Although dedicated reviewers work hard to get to the bottom of cases, it’s not uncommon for some committee members to hardly work at all, according to experts.
Dr. Marder said he’s seen many instances in which reviewers were assigned a review but did not complete it for months. Most committees have set time frames in which reviewers must complete their review.
“That delays that review, and by that time, the review is older and it’s harder to remember things,” he said. “It’s not fair to the physician. If there was a problem the physician could fix and you don’t tell him for 3 or 4 months what it is, he may do the same thing again. The case might come before the committee again and it looks like he’s repeated something, but you never gave him the opportunity to improve.”
Other reviewers fail to attend meetings regularly. Peer review committee members are generally volunteers, and meetings are usually held in the early mornings or late evenings.
“There are reasons for not attending occasionally, but some people put on a committee just don’t take it seriously,” Dr. Marder said. “They don’t fulfill their responsibilities as well as they should. If you accept the job, do the job.”
For physicians considering becoming a peer reviewer, Dr. Beran offers these tips: Be transparent, help physicians understand next steps, and make yourself as available as allowed to answer questions.
Know your committee’s policies and procedures, and follow them, added Dr. Marder. It’s also a good idea to work with your hospital’s quality staff, he said.
Reviewers should keep in mind that they may not always be the one assessing someone else, Dr. Beran said.
“Realize very easily you could be on the other side of that table for things that are outside your control,” he said. “How would you want to be treated?”
A version of this article first appeared on Medscape.com.
After making an insulting comment to a surgery scheduler, a surgeon become the subject of a peer review investigation.
The surgeon had been called in on a Saturday morning for surgery, but when he arrived at the hospital, staff informed him that the operating room had been incorrectly booked and asked him to come back that afternoon. When the surgeon returned, the room still wasn’t ready, recounted David Beran, DO, a peer reviewer and medical director for the emergency department at University Medical Center New Orleans, in Louisiana. After more waiting and staff uncertainty about which operating room was going to open, the surgeon became frustrated and said to the scheduler: “Any idiot could figure this out!”
During his peer review, the surgeon acknowledged that he shouldn’t have made the rude remark to the scheduler, Dr. Beran said. His exasperation stemmed from an ongoing problem – operating rooms at the hospital were being inefficiently managed.
“The surgeon acknowledged that even though there was a systems issue at the root, that’s not justification to speak to people unprofessionally,” Dr. Beran said. “So, there was education for the surgeon, but the surgeon was also able to explain the frustration that led to that point.”
System problems are commonly encountered by peer reviewers, said Dr. Beran.
“There’s a huge gap between administration and clinical professionals when it comes to peer review,” he said. “So many times, bad situations, whether they’re clinical or behavioral, often boil down to systems issues or some inadequacy, whether it’s an EMR [electronic medical record] problem, an inefficacy, or how complicated a process is for an end user. But having a peer review situation that then leads to a system-level change that prevents that problem from happening again is really unlikely. There’s a huge disconnect between those two.”
Peer review is generally a process that goes on behind closed doors. Although structures may differ, peer review is generally described as the process by which physicians assess the quality of their peers’ work to ensure that standards of care are being met. The process is often used to evaluate issues regarding clinical care as well as behavioral complaints against physicians.
Doctors who undergo peer review frequently share their experiences, but reviewers themselves rarely speak out. For this story,
“Peer review processes are in place to build stronger institutions and stronger practices, and they’re supposed to be helpful,” Dr. Beran said. “But because of how opaque they are, it immediately puts physicians on the defensive, and it doesn’t always succeed in what it’s trying to do. I think that’s one of the biggest challenges.”
Biased reviewers taint evaluations
A peer reviewer on and off throughout her career, Indiana family physician Lana Patch, MD, said she always strived to be fair when evaluating fellow physicians. But not every reviewer she encountered operated the same way, she said. Some were biased.
In one case, Dr. Patch peer reviewed a general surgeon who had performed a hysterectomy on a 16-year-old girl. The surgeon believed the teenager likely had an acute appendicitis, but it turned out she had a uterine pathology, Dr. Patch said. The surgeon saved the girl’s life, but the case came under review because of the patient’s age and the fact that her uterus was removed. A local obstetrician-gynecologist weighed in on the case.
“The local ob.gyn. saw it as a turf battle,” recalled Dr. Patch, who is now retired after 30 years of practice in eastern Indiana. “The doctor had nothing but bad to say about the surgeon. He was a competitor.”
Because it was a small hospital, the committee sometimes had trouble finding a specialist who was qualified to give an opinion and who wasn’t in competition with the physician in question, said Dr. Patch. Eventually they found an outside pediatric gynecologist who reviewed the case and concluded that the surgeon had followed the standard of care.
Personal agendas in can come from different directions, said Robert Marder, MD, the author of several books on peer review. Dr. Marder is a consultant who assists with peer review redesign. He has worked with hundreds of medical staff leaders and is a former vice president at the Greeley Company, a consulting firm in Danvers, Mass., that performs peer review redesign. Dr. Marder is president of Robert J. Marder Consulting.
“It goes both ways,” Dr. Marder said. “I’ve seen where somebody with a personal view decides to bring things to the peer review committee specifically because they want the peer review committee to have an adverse view of this person and get them off the medical staff. And I’ve seen hospitals that are uncomfortable with a certain person for whatever reason and want the peer review committee to address it, as opposed to addressing it from a human resource standpoint.”
Dr. Patch recalled a case in which reviewers and hospital leaders were at odds over the credentialing of a physician. Fifteen years earlier, while driving in California, the psychiatrist had been pulled over and was found with an ounce of marijuana, she said.
“We wanted to privilege him,” Dr. Patch said. “As staff physicians, we felt that was 15 years ago, people change over time. Doctors are human beings, too. He seemed to have good credentials and good training. The hospital said, ‘Oh no, we can’t have somebody like this.’ “
The psychiatrist was placed on probation and had to undergo a review every 90 days for about 3 years. Eventually, he was privileged, Dr. Patch said.
Bias among reviewers, including unintentional bias, is also a challenge, Dr. Marder noted. Some initial reviewers score a physician too harshly, he said, whereas others underscore.
“Underscoring is more insidious and more difficult to deal with,” Dr. Marder said. “Underscoring is where the reviewer is too nice. They tend to dismiss things from their colleagues rather than recognize them as an opportunity to help them improve. With underscoring, a lot of committees, if the initial reviewer says the care was appropriate, they don’t even look at the case. They just take that one person’s word for it.”
Reviewers: Looks can be deceiving
When first examining the documented details of a case, it can be easy for peer reviewers to make a quick judgment about what happened, Dr. Beran said.
“You get these complaints, and you read through it, and you think, ‘Oh man, this person really messed up,’ “ he said. “Then you hear the doctor’s side of it, and you realize, ‘No, there’s a much bigger picture at play.’ You realize both sides have valid perspectives on it.”
In one case, for example, Dr. Beran recalled a complaint against a physician who made a snarky remark to a nurse. The doctor had asked the nurse for a piece of equipment, and the nurse said she was busy preparing the room for a patient. The doctor made a comment along the lines of, “Well, would you like me to do that for you and also intubate the patient while you do some charting?!”
At first glance, it appeared that the physician lashed out inappropriately at the nurse. But when reviewers heard from the doctor, they learned that the nurses knew that a trauma patient was coming by ambulance and that he would likely require a ventilator, Dr. Beran said. As the minutes ticked by, however, the nurses were seen in the break room chatting. Nothing had been prepared in the room, including any airway supply.
“The patient had a prolonged course and a very difficult intubation and could have very easily wound up with a much worse outcome for something the nurses had been warned about prior to the patient’s arrival,” he said. “I can see anybody getting upset in that situation if I warned them 5 or 10 minutes beforehand, ‘Get this stuff ready,’ and then nothing was done.”
There was no direct penalty for the physician.
Just as some complaints can be misleading, the clinical record in some peer review cases can also lead reviewers astray.
Physicians frequently include too much irrelevant information in the record, which can cloud a peer review, said Hans Duvefelt, MD, a family physician at Pines Health Services, in Van Buren, Maine. Dr. Duvefelt is a former medical director at Bucksport Regional Health Center, in Ellsworth, Maine. Both facilities are federally qualified health centers where continuous, random peer reviews are required.
In one case, Dr. Duvefelt was peer reviewing a physician’s office note regarding an elderly patient with a low-grade fever. The final diagnosis was urinary tract infection. Dr. Duvefelt said he had trouble following the doctor’s line of thinking because of a plethora of unnecessary data in the 10-page document. The office note included past medical history, prior lab and imaging test results, and an extensive narrative section that included a mixture of active medical problems and ongoing relationships with specialists, he said.
After reading through the printout three times, Dr. Duvefelt said he finally found mention of increased urinary dribbling and details about an enlarged prostate. He also spotted a same-day urinalysis among nearly a dozen other previous lab tests that had no connection to body temperature. Dr. Duvefelt gave the physician a passing grade but also left a scathing note about all the irrelevant information.
“It’s very common,” Dr. Duvefelt said. “It’s a disaster. Other doctors can’t follow your thinking. A reviewer has a hard time determining whether the doctor acted reasonably.”
Slackers make bad reviewers
Although dedicated reviewers work hard to get to the bottom of cases, it’s not uncommon for some committee members to hardly work at all, according to experts.
Dr. Marder said he’s seen many instances in which reviewers were assigned a review but did not complete it for months. Most committees have set time frames in which reviewers must complete their review.
“That delays that review, and by that time, the review is older and it’s harder to remember things,” he said. “It’s not fair to the physician. If there was a problem the physician could fix and you don’t tell him for 3 or 4 months what it is, he may do the same thing again. The case might come before the committee again and it looks like he’s repeated something, but you never gave him the opportunity to improve.”
Other reviewers fail to attend meetings regularly. Peer review committee members are generally volunteers, and meetings are usually held in the early mornings or late evenings.
“There are reasons for not attending occasionally, but some people put on a committee just don’t take it seriously,” Dr. Marder said. “They don’t fulfill their responsibilities as well as they should. If you accept the job, do the job.”
For physicians considering becoming a peer reviewer, Dr. Beran offers these tips: Be transparent, help physicians understand next steps, and make yourself as available as allowed to answer questions.
Know your committee’s policies and procedures, and follow them, added Dr. Marder. It’s also a good idea to work with your hospital’s quality staff, he said.
Reviewers should keep in mind that they may not always be the one assessing someone else, Dr. Beran said.
“Realize very easily you could be on the other side of that table for things that are outside your control,” he said. “How would you want to be treated?”
A version of this article first appeared on Medscape.com.
After making an insulting comment to a surgery scheduler, a surgeon become the subject of a peer review investigation.
The surgeon had been called in on a Saturday morning for surgery, but when he arrived at the hospital, staff informed him that the operating room had been incorrectly booked and asked him to come back that afternoon. When the surgeon returned, the room still wasn’t ready, recounted David Beran, DO, a peer reviewer and medical director for the emergency department at University Medical Center New Orleans, in Louisiana. After more waiting and staff uncertainty about which operating room was going to open, the surgeon became frustrated and said to the scheduler: “Any idiot could figure this out!”
During his peer review, the surgeon acknowledged that he shouldn’t have made the rude remark to the scheduler, Dr. Beran said. His exasperation stemmed from an ongoing problem – operating rooms at the hospital were being inefficiently managed.
“The surgeon acknowledged that even though there was a systems issue at the root, that’s not justification to speak to people unprofessionally,” Dr. Beran said. “So, there was education for the surgeon, but the surgeon was also able to explain the frustration that led to that point.”
System problems are commonly encountered by peer reviewers, said Dr. Beran.
“There’s a huge gap between administration and clinical professionals when it comes to peer review,” he said. “So many times, bad situations, whether they’re clinical or behavioral, often boil down to systems issues or some inadequacy, whether it’s an EMR [electronic medical record] problem, an inefficacy, or how complicated a process is for an end user. But having a peer review situation that then leads to a system-level change that prevents that problem from happening again is really unlikely. There’s a huge disconnect between those two.”
Peer review is generally a process that goes on behind closed doors. Although structures may differ, peer review is generally described as the process by which physicians assess the quality of their peers’ work to ensure that standards of care are being met. The process is often used to evaluate issues regarding clinical care as well as behavioral complaints against physicians.
Doctors who undergo peer review frequently share their experiences, but reviewers themselves rarely speak out. For this story,
“Peer review processes are in place to build stronger institutions and stronger practices, and they’re supposed to be helpful,” Dr. Beran said. “But because of how opaque they are, it immediately puts physicians on the defensive, and it doesn’t always succeed in what it’s trying to do. I think that’s one of the biggest challenges.”
Biased reviewers taint evaluations
A peer reviewer on and off throughout her career, Indiana family physician Lana Patch, MD, said she always strived to be fair when evaluating fellow physicians. But not every reviewer she encountered operated the same way, she said. Some were biased.
In one case, Dr. Patch peer reviewed a general surgeon who had performed a hysterectomy on a 16-year-old girl. The surgeon believed the teenager likely had an acute appendicitis, but it turned out she had a uterine pathology, Dr. Patch said. The surgeon saved the girl’s life, but the case came under review because of the patient’s age and the fact that her uterus was removed. A local obstetrician-gynecologist weighed in on the case.
“The local ob.gyn. saw it as a turf battle,” recalled Dr. Patch, who is now retired after 30 years of practice in eastern Indiana. “The doctor had nothing but bad to say about the surgeon. He was a competitor.”
Because it was a small hospital, the committee sometimes had trouble finding a specialist who was qualified to give an opinion and who wasn’t in competition with the physician in question, said Dr. Patch. Eventually they found an outside pediatric gynecologist who reviewed the case and concluded that the surgeon had followed the standard of care.
Personal agendas in can come from different directions, said Robert Marder, MD, the author of several books on peer review. Dr. Marder is a consultant who assists with peer review redesign. He has worked with hundreds of medical staff leaders and is a former vice president at the Greeley Company, a consulting firm in Danvers, Mass., that performs peer review redesign. Dr. Marder is president of Robert J. Marder Consulting.
“It goes both ways,” Dr. Marder said. “I’ve seen where somebody with a personal view decides to bring things to the peer review committee specifically because they want the peer review committee to have an adverse view of this person and get them off the medical staff. And I’ve seen hospitals that are uncomfortable with a certain person for whatever reason and want the peer review committee to address it, as opposed to addressing it from a human resource standpoint.”
Dr. Patch recalled a case in which reviewers and hospital leaders were at odds over the credentialing of a physician. Fifteen years earlier, while driving in California, the psychiatrist had been pulled over and was found with an ounce of marijuana, she said.
“We wanted to privilege him,” Dr. Patch said. “As staff physicians, we felt that was 15 years ago, people change over time. Doctors are human beings, too. He seemed to have good credentials and good training. The hospital said, ‘Oh no, we can’t have somebody like this.’ “
The psychiatrist was placed on probation and had to undergo a review every 90 days for about 3 years. Eventually, he was privileged, Dr. Patch said.
Bias among reviewers, including unintentional bias, is also a challenge, Dr. Marder noted. Some initial reviewers score a physician too harshly, he said, whereas others underscore.
“Underscoring is more insidious and more difficult to deal with,” Dr. Marder said. “Underscoring is where the reviewer is too nice. They tend to dismiss things from their colleagues rather than recognize them as an opportunity to help them improve. With underscoring, a lot of committees, if the initial reviewer says the care was appropriate, they don’t even look at the case. They just take that one person’s word for it.”
Reviewers: Looks can be deceiving
When first examining the documented details of a case, it can be easy for peer reviewers to make a quick judgment about what happened, Dr. Beran said.
“You get these complaints, and you read through it, and you think, ‘Oh man, this person really messed up,’ “ he said. “Then you hear the doctor’s side of it, and you realize, ‘No, there’s a much bigger picture at play.’ You realize both sides have valid perspectives on it.”
In one case, for example, Dr. Beran recalled a complaint against a physician who made a snarky remark to a nurse. The doctor had asked the nurse for a piece of equipment, and the nurse said she was busy preparing the room for a patient. The doctor made a comment along the lines of, “Well, would you like me to do that for you and also intubate the patient while you do some charting?!”
At first glance, it appeared that the physician lashed out inappropriately at the nurse. But when reviewers heard from the doctor, they learned that the nurses knew that a trauma patient was coming by ambulance and that he would likely require a ventilator, Dr. Beran said. As the minutes ticked by, however, the nurses were seen in the break room chatting. Nothing had been prepared in the room, including any airway supply.
“The patient had a prolonged course and a very difficult intubation and could have very easily wound up with a much worse outcome for something the nurses had been warned about prior to the patient’s arrival,” he said. “I can see anybody getting upset in that situation if I warned them 5 or 10 minutes beforehand, ‘Get this stuff ready,’ and then nothing was done.”
There was no direct penalty for the physician.
Just as some complaints can be misleading, the clinical record in some peer review cases can also lead reviewers astray.
Physicians frequently include too much irrelevant information in the record, which can cloud a peer review, said Hans Duvefelt, MD, a family physician at Pines Health Services, in Van Buren, Maine. Dr. Duvefelt is a former medical director at Bucksport Regional Health Center, in Ellsworth, Maine. Both facilities are federally qualified health centers where continuous, random peer reviews are required.
In one case, Dr. Duvefelt was peer reviewing a physician’s office note regarding an elderly patient with a low-grade fever. The final diagnosis was urinary tract infection. Dr. Duvefelt said he had trouble following the doctor’s line of thinking because of a plethora of unnecessary data in the 10-page document. The office note included past medical history, prior lab and imaging test results, and an extensive narrative section that included a mixture of active medical problems and ongoing relationships with specialists, he said.
After reading through the printout three times, Dr. Duvefelt said he finally found mention of increased urinary dribbling and details about an enlarged prostate. He also spotted a same-day urinalysis among nearly a dozen other previous lab tests that had no connection to body temperature. Dr. Duvefelt gave the physician a passing grade but also left a scathing note about all the irrelevant information.
“It’s very common,” Dr. Duvefelt said. “It’s a disaster. Other doctors can’t follow your thinking. A reviewer has a hard time determining whether the doctor acted reasonably.”
Slackers make bad reviewers
Although dedicated reviewers work hard to get to the bottom of cases, it’s not uncommon for some committee members to hardly work at all, according to experts.
Dr. Marder said he’s seen many instances in which reviewers were assigned a review but did not complete it for months. Most committees have set time frames in which reviewers must complete their review.
“That delays that review, and by that time, the review is older and it’s harder to remember things,” he said. “It’s not fair to the physician. If there was a problem the physician could fix and you don’t tell him for 3 or 4 months what it is, he may do the same thing again. The case might come before the committee again and it looks like he’s repeated something, but you never gave him the opportunity to improve.”
Other reviewers fail to attend meetings regularly. Peer review committee members are generally volunteers, and meetings are usually held in the early mornings or late evenings.
“There are reasons for not attending occasionally, but some people put on a committee just don’t take it seriously,” Dr. Marder said. “They don’t fulfill their responsibilities as well as they should. If you accept the job, do the job.”
For physicians considering becoming a peer reviewer, Dr. Beran offers these tips: Be transparent, help physicians understand next steps, and make yourself as available as allowed to answer questions.
Know your committee’s policies and procedures, and follow them, added Dr. Marder. It’s also a good idea to work with your hospital’s quality staff, he said.
Reviewers should keep in mind that they may not always be the one assessing someone else, Dr. Beran said.
“Realize very easily you could be on the other side of that table for things that are outside your control,” he said. “How would you want to be treated?”
A version of this article first appeared on Medscape.com.
How the 2022 proposed Medicare payment rules impact GI
In July 2021, the Centers for Medicare & Medicaid Services released the Medicare Physician Fee Schedule (PFS) and Hospital Outpatient Prospective Payment System (OPPS)/Ambulatory Surgery Center (ASC) proposed rules for calendar year (CY) 2022. While the OPPS/ASC proposed rule was largely positive for gastroenterology, the PFS proposed rule was more of a mixed bag for practices.
No more colonoscopy coinsurance “loophole”: After nearly a decade of advocacy, the Removing Barriers to Colorectal Cancer Screening Act was finally signed into law this year and will take effect Jan. 1, 2023. The legislation phases out Medicare beneficiary cost-sharing obligations when a polyp or lesion is found and biopsied or removed as part of a screening colonoscopy or flexible sigmoidoscopy. The American Gastroenterological Association is pleased this will finally eliminate a surprise bill for patients and remove a barrier to colorectal cancer screening.
The phase out timeline is as follows:
- 80% payment for services furnished during CY 2022 (coinsurance, 20%).
- 85% payment for services furnished during CY 2023 through CY 2026 (coinsurance, 15%).
- 90% payment for services furnished during CY 2027 through CY 2029 (coinsurance, 10%).
- 100% payment for services furnished from CY 2030 onward (coinsurance, 0%).
Providers must continue to report HCPCS modifier “PT” in the hospital outpatient and ASC during the transition period to indicate that a planned colorectal cancer screening service converted to a diagnostic service.
Proposed 2022 PFS conversion factor could fall 3.75% unless Congress acts: The proposed 2022 PFS conversion factor is $33.58. The decrease reflects the expiration of the 3.75% payment increase provided by the Consolidated Appropriations Act. This congressional intervention averted a significant cut in Medicare physician payment that would have resulted in an almost 10% cut to GI services. The GI societies are working with Congress to avert cuts to physician payments next year as practices continue to recover from the pandemic.
GI procedure payments to increase 3% for hospital outpatient and ASCs: A 2.3% increase has been proposed for the conversion factors, resulting in $84.46 for hospitals and $50.04 for ASCs meeting quality reporting requirements. However, GI endoscopy procedure payments are expected to increase on average 3% in CY 2022.
Colon capsule endoscopy and POEM get new codes and payments: CMS accepted new CPT codes for colon capsule endoscopy (CCE) and peroral endoscopic myotomy (POEM) beginning Jan. 1, 2022.
CMS’s proposed CCE value of 2.41 physician work relative value units (wRVUs) reflects the recommendation of the American Medical Association RVS Update Committee (RUC), which is based on data from physicians who perform the procedure. The proposed national-level physician payments are $116.52 for the professional component and $664.21 for the technical component.
However, CMS did not accept the RUC’s recommendation of 15.50 wRVUs for POEM and, instead, proposed that POEM is similar in work to hemodialysis access CPT code 36819, which has a wRVU of 13.29 and a payment of $792.82. The RUC’s valuation of 15.50 wRVUs was based on data from nearly 120 physicians who perform POEM, and we are disappointed CMS chose to reject the robust survey data. The GI societies will defend the 15.50 wRVU in our comments.
The proposed facility fee for POEM is $3,160.76 in the hospital outpatient setting and $1,848.32 in the ASC. CMS’s proposed facility fee for colon capsule endoscopy is $814.44 in the hospital outpatient setting.
CMS moves physicians to MVPs and plans to phase out MIPS: CMS proposes to revise and phase out the Merit-Based Incentive Payment System (MIPS) and move physicians towards the MIPS Value Pathways (MVPs) system beginning in the 2023 performance year (PY). No GI MVPs were proposed for PY 2023. The GI societies are working with CMS as they develop MVPs to ensure any gastroenterology-related MVPs do not harm gastroenterologists.
CMS is statutorily required to weigh the MIPS Cost and Quality performance categories equally beginning with PY 2022. The proposed PY 2022 MIPS performance categories are:
- Quality: 30%.
- Cost: 30%.
- Promoting Interoperability: 25% (no change from 2021).
- Improvement Activities: 15% (no change from 2021).
CMS is also required by law beginning in 2022 to set the MIPS performance threshold to either the mean or median of the final scores for all MIPS eligible clinicians for a prior period. CMS proposes to use the mean final score from MIPS 2017 performance year/MIPS 2019 payment year, which would result in a performance threshold of 75 points and an additional performance threshold set at 89 points for exceptional performance.
CMS keeps all AGA-stewarded measures in MIPS 2022 program year: CMS has proposed to keep all AGA-stewarded measures in the MIPS program for the 2022 program year and accepted the substantive changes for the one-time screening for hepatitis C virus measure we received last year from the Physician Consortium for Performance Improvement. CMS proposed removal of the claims reporting option of American Society for Gastrointestinal Endoscopy–stewarded measure for photodocumentation of cecal intubation because it is topped-out; however, the registry version is still available in MIPS.
OQR Program includes colonoscopy measure for disparities reporting: CMS has identified six priority measures included in the Hospital Outpatient Quality Reporting (OQR) Program as candidate measures for disparities reporting stratified by dual eligibility, one of which is the Facility 7-Day Risk-Standardized Hospital Visit Rate After Outpatient Colonoscopy (OP-32).
The GI societies will jointly comment on issues in the 2022 PFS and OPPS/ASC proposed rules impacting gastroenterologists. We may also organize members to take action by submitting letters during the comment period, so watch your inbox for invitations to participate. We need your help to influence change.
Shivan Mehta, MD, MBA, is with the division of gastroenterology and hepatology at the University of Pennsylvania, Philadelphia, and is an AGA adviser to the American Medical Association RVS Update Committee. David A. Leiman, MD, MSHP, is with the division of gastroenterology at Duke University, Durham, N.C., and is the chair of the AGA Quality Committee. Neither have conflicts to declare.
In July 2021, the Centers for Medicare & Medicaid Services released the Medicare Physician Fee Schedule (PFS) and Hospital Outpatient Prospective Payment System (OPPS)/Ambulatory Surgery Center (ASC) proposed rules for calendar year (CY) 2022. While the OPPS/ASC proposed rule was largely positive for gastroenterology, the PFS proposed rule was more of a mixed bag for practices.
No more colonoscopy coinsurance “loophole”: After nearly a decade of advocacy, the Removing Barriers to Colorectal Cancer Screening Act was finally signed into law this year and will take effect Jan. 1, 2023. The legislation phases out Medicare beneficiary cost-sharing obligations when a polyp or lesion is found and biopsied or removed as part of a screening colonoscopy or flexible sigmoidoscopy. The American Gastroenterological Association is pleased this will finally eliminate a surprise bill for patients and remove a barrier to colorectal cancer screening.
The phase out timeline is as follows:
- 80% payment for services furnished during CY 2022 (coinsurance, 20%).
- 85% payment for services furnished during CY 2023 through CY 2026 (coinsurance, 15%).
- 90% payment for services furnished during CY 2027 through CY 2029 (coinsurance, 10%).
- 100% payment for services furnished from CY 2030 onward (coinsurance, 0%).
Providers must continue to report HCPCS modifier “PT” in the hospital outpatient and ASC during the transition period to indicate that a planned colorectal cancer screening service converted to a diagnostic service.
Proposed 2022 PFS conversion factor could fall 3.75% unless Congress acts: The proposed 2022 PFS conversion factor is $33.58. The decrease reflects the expiration of the 3.75% payment increase provided by the Consolidated Appropriations Act. This congressional intervention averted a significant cut in Medicare physician payment that would have resulted in an almost 10% cut to GI services. The GI societies are working with Congress to avert cuts to physician payments next year as practices continue to recover from the pandemic.
GI procedure payments to increase 3% for hospital outpatient and ASCs: A 2.3% increase has been proposed for the conversion factors, resulting in $84.46 for hospitals and $50.04 for ASCs meeting quality reporting requirements. However, GI endoscopy procedure payments are expected to increase on average 3% in CY 2022.
Colon capsule endoscopy and POEM get new codes and payments: CMS accepted new CPT codes for colon capsule endoscopy (CCE) and peroral endoscopic myotomy (POEM) beginning Jan. 1, 2022.
CMS’s proposed CCE value of 2.41 physician work relative value units (wRVUs) reflects the recommendation of the American Medical Association RVS Update Committee (RUC), which is based on data from physicians who perform the procedure. The proposed national-level physician payments are $116.52 for the professional component and $664.21 for the technical component.
However, CMS did not accept the RUC’s recommendation of 15.50 wRVUs for POEM and, instead, proposed that POEM is similar in work to hemodialysis access CPT code 36819, which has a wRVU of 13.29 and a payment of $792.82. The RUC’s valuation of 15.50 wRVUs was based on data from nearly 120 physicians who perform POEM, and we are disappointed CMS chose to reject the robust survey data. The GI societies will defend the 15.50 wRVU in our comments.
The proposed facility fee for POEM is $3,160.76 in the hospital outpatient setting and $1,848.32 in the ASC. CMS’s proposed facility fee for colon capsule endoscopy is $814.44 in the hospital outpatient setting.
CMS moves physicians to MVPs and plans to phase out MIPS: CMS proposes to revise and phase out the Merit-Based Incentive Payment System (MIPS) and move physicians towards the MIPS Value Pathways (MVPs) system beginning in the 2023 performance year (PY). No GI MVPs were proposed for PY 2023. The GI societies are working with CMS as they develop MVPs to ensure any gastroenterology-related MVPs do not harm gastroenterologists.
CMS is statutorily required to weigh the MIPS Cost and Quality performance categories equally beginning with PY 2022. The proposed PY 2022 MIPS performance categories are:
- Quality: 30%.
- Cost: 30%.
- Promoting Interoperability: 25% (no change from 2021).
- Improvement Activities: 15% (no change from 2021).
CMS is also required by law beginning in 2022 to set the MIPS performance threshold to either the mean or median of the final scores for all MIPS eligible clinicians for a prior period. CMS proposes to use the mean final score from MIPS 2017 performance year/MIPS 2019 payment year, which would result in a performance threshold of 75 points and an additional performance threshold set at 89 points for exceptional performance.
CMS keeps all AGA-stewarded measures in MIPS 2022 program year: CMS has proposed to keep all AGA-stewarded measures in the MIPS program for the 2022 program year and accepted the substantive changes for the one-time screening for hepatitis C virus measure we received last year from the Physician Consortium for Performance Improvement. CMS proposed removal of the claims reporting option of American Society for Gastrointestinal Endoscopy–stewarded measure for photodocumentation of cecal intubation because it is topped-out; however, the registry version is still available in MIPS.
OQR Program includes colonoscopy measure for disparities reporting: CMS has identified six priority measures included in the Hospital Outpatient Quality Reporting (OQR) Program as candidate measures for disparities reporting stratified by dual eligibility, one of which is the Facility 7-Day Risk-Standardized Hospital Visit Rate After Outpatient Colonoscopy (OP-32).
The GI societies will jointly comment on issues in the 2022 PFS and OPPS/ASC proposed rules impacting gastroenterologists. We may also organize members to take action by submitting letters during the comment period, so watch your inbox for invitations to participate. We need your help to influence change.
Shivan Mehta, MD, MBA, is with the division of gastroenterology and hepatology at the University of Pennsylvania, Philadelphia, and is an AGA adviser to the American Medical Association RVS Update Committee. David A. Leiman, MD, MSHP, is with the division of gastroenterology at Duke University, Durham, N.C., and is the chair of the AGA Quality Committee. Neither have conflicts to declare.
In July 2021, the Centers for Medicare & Medicaid Services released the Medicare Physician Fee Schedule (PFS) and Hospital Outpatient Prospective Payment System (OPPS)/Ambulatory Surgery Center (ASC) proposed rules for calendar year (CY) 2022. While the OPPS/ASC proposed rule was largely positive for gastroenterology, the PFS proposed rule was more of a mixed bag for practices.
No more colonoscopy coinsurance “loophole”: After nearly a decade of advocacy, the Removing Barriers to Colorectal Cancer Screening Act was finally signed into law this year and will take effect Jan. 1, 2023. The legislation phases out Medicare beneficiary cost-sharing obligations when a polyp or lesion is found and biopsied or removed as part of a screening colonoscopy or flexible sigmoidoscopy. The American Gastroenterological Association is pleased this will finally eliminate a surprise bill for patients and remove a barrier to colorectal cancer screening.
The phase out timeline is as follows:
- 80% payment for services furnished during CY 2022 (coinsurance, 20%).
- 85% payment for services furnished during CY 2023 through CY 2026 (coinsurance, 15%).
- 90% payment for services furnished during CY 2027 through CY 2029 (coinsurance, 10%).
- 100% payment for services furnished from CY 2030 onward (coinsurance, 0%).
Providers must continue to report HCPCS modifier “PT” in the hospital outpatient and ASC during the transition period to indicate that a planned colorectal cancer screening service converted to a diagnostic service.
Proposed 2022 PFS conversion factor could fall 3.75% unless Congress acts: The proposed 2022 PFS conversion factor is $33.58. The decrease reflects the expiration of the 3.75% payment increase provided by the Consolidated Appropriations Act. This congressional intervention averted a significant cut in Medicare physician payment that would have resulted in an almost 10% cut to GI services. The GI societies are working with Congress to avert cuts to physician payments next year as practices continue to recover from the pandemic.
GI procedure payments to increase 3% for hospital outpatient and ASCs: A 2.3% increase has been proposed for the conversion factors, resulting in $84.46 for hospitals and $50.04 for ASCs meeting quality reporting requirements. However, GI endoscopy procedure payments are expected to increase on average 3% in CY 2022.
Colon capsule endoscopy and POEM get new codes and payments: CMS accepted new CPT codes for colon capsule endoscopy (CCE) and peroral endoscopic myotomy (POEM) beginning Jan. 1, 2022.
CMS’s proposed CCE value of 2.41 physician work relative value units (wRVUs) reflects the recommendation of the American Medical Association RVS Update Committee (RUC), which is based on data from physicians who perform the procedure. The proposed national-level physician payments are $116.52 for the professional component and $664.21 for the technical component.
However, CMS did not accept the RUC’s recommendation of 15.50 wRVUs for POEM and, instead, proposed that POEM is similar in work to hemodialysis access CPT code 36819, which has a wRVU of 13.29 and a payment of $792.82. The RUC’s valuation of 15.50 wRVUs was based on data from nearly 120 physicians who perform POEM, and we are disappointed CMS chose to reject the robust survey data. The GI societies will defend the 15.50 wRVU in our comments.
The proposed facility fee for POEM is $3,160.76 in the hospital outpatient setting and $1,848.32 in the ASC. CMS’s proposed facility fee for colon capsule endoscopy is $814.44 in the hospital outpatient setting.
CMS moves physicians to MVPs and plans to phase out MIPS: CMS proposes to revise and phase out the Merit-Based Incentive Payment System (MIPS) and move physicians towards the MIPS Value Pathways (MVPs) system beginning in the 2023 performance year (PY). No GI MVPs were proposed for PY 2023. The GI societies are working with CMS as they develop MVPs to ensure any gastroenterology-related MVPs do not harm gastroenterologists.
CMS is statutorily required to weigh the MIPS Cost and Quality performance categories equally beginning with PY 2022. The proposed PY 2022 MIPS performance categories are:
- Quality: 30%.
- Cost: 30%.
- Promoting Interoperability: 25% (no change from 2021).
- Improvement Activities: 15% (no change from 2021).
CMS is also required by law beginning in 2022 to set the MIPS performance threshold to either the mean or median of the final scores for all MIPS eligible clinicians for a prior period. CMS proposes to use the mean final score from MIPS 2017 performance year/MIPS 2019 payment year, which would result in a performance threshold of 75 points and an additional performance threshold set at 89 points for exceptional performance.
CMS keeps all AGA-stewarded measures in MIPS 2022 program year: CMS has proposed to keep all AGA-stewarded measures in the MIPS program for the 2022 program year and accepted the substantive changes for the one-time screening for hepatitis C virus measure we received last year from the Physician Consortium for Performance Improvement. CMS proposed removal of the claims reporting option of American Society for Gastrointestinal Endoscopy–stewarded measure for photodocumentation of cecal intubation because it is topped-out; however, the registry version is still available in MIPS.
OQR Program includes colonoscopy measure for disparities reporting: CMS has identified six priority measures included in the Hospital Outpatient Quality Reporting (OQR) Program as candidate measures for disparities reporting stratified by dual eligibility, one of which is the Facility 7-Day Risk-Standardized Hospital Visit Rate After Outpatient Colonoscopy (OP-32).
The GI societies will jointly comment on issues in the 2022 PFS and OPPS/ASC proposed rules impacting gastroenterologists. We may also organize members to take action by submitting letters during the comment period, so watch your inbox for invitations to participate. We need your help to influence change.
Shivan Mehta, MD, MBA, is with the division of gastroenterology and hepatology at the University of Pennsylvania, Philadelphia, and is an AGA adviser to the American Medical Association RVS Update Committee. David A. Leiman, MD, MSHP, is with the division of gastroenterology at Duke University, Durham, N.C., and is the chair of the AGA Quality Committee. Neither have conflicts to declare.
Pregnancy and parental leave during gastroenterology fellowship training: A program perspective
Due to broad social changes and efforts from leaders in GI, there is renewed interest in family planning and parental leave policies for GI trainees. The American Board of Medical Specialties now permits trainees a minimum of 6 weeks away during training, without automatically requiring an extension of training time or completely depleting vacation time, for boards eligibility.1,2 However, national and institutional guidance for family planning and pregnancy during GI fellowship is lacking. How can gastroenterology fellowship programs support fellows taking parental leave and enact fair policies? We review the scope of the problem, describe our experience in developing resources within our GI fellowship program, and highlight areas that require further development.
The scope of the issue
There is no national data yet on the number of GI fellows that are parents prior to starting fellowship or who become parents during fellowship. We estimate that approximately 25% of fellows enter training as parents or become parents during fellowship, although 40%-50% may have an intention to have children.3,4 Fellows may be worried that they will “fall behind” or be perceived as less committed if they devote time to childrearing or take parental leave.5-7 Indeed, worries about discrimination based on pregnancy and parental leave are borne out by the experiences of older physicians (in particular, female physicians).8,9
State- and institution-specific benefits vary from program to program. Nationally, the Family and Medical Leave Act provides only unpaid leave and applies only to trainees who have been employed for greater than 12 months.10 Benefits may not always be well advertised, and even when they are, trainees (and attendings) may feel uncomfortable taking full advantage. One survey of GIs revealed that, although two-thirds believed that 6-8 weeks of maternity leave was inadequate, half took less than that amount due to fears about financial and professional consequences.8
Pregnancy during GI fellowship is a special concern. GI fellowship consists of long work hours, includes night call, and can be physically demanding. All three of these factors have been associated with preterm delivery, infertility, and miscarriage.11,12 In addition, there are no guidelines for ergonomic adjustments or infection precautions for pregnant endoscopists. We have compiled information about infection prevention guidance in pregnancy (available from the authors on request) derived from guidance from the National Institute for Occupational Safety and Health, which recommends the same precautions for pregnant health care workers as for nonpregnant health care workers.13 In regards to SARS-CoV-2, we believe that the decision to perform procedures on patients with COVID-19 infection should be individualized, although vaccinated endoscopists should be reassured by the exceedingly low rates of infection after vaccination and with appropriate personal protective equipment. Radiation is yet another concern. There are limited data on radiation dosages incurred by workers in the endoscopy suite and no pregnancy-specific data, which may lead trainees to avoid fluoroscopic procedures and unnecessarily double up on lead gowns.8,11,14-17
Breastfeeding accommodations, and access to lactation rooms for trainees, are required by federal law for a minimum of 12 months.18 Should a trainee choose to breastfeed, education of staff and attendings is critical because many may be unaware of the specific needs pertaining to lactation. Staff should be aware that 30-45 minutes are needed to prepare, pump, and store milk. Trainees should not be solely responsible for educating their attendings and staff.
Our Experience in Creating a Policy
We developed a formal fellowship program policy on parental leave and pregnancy in the setting of a broader discussion about fellow workload and wellness. We agreed that trainees should be allowed to make changes to their schedule with co-fellows as needed for medical appointments or procedures and that our backup policy should be flexible enough to provide spot coverage for unexpected complications and family emergencies. We also incorporated a GI psychologist to provide wellness resources and suggestions for reducing burnout for our fellows.
We strove to follow certain principles in creating this policy. Trainees who are parents should have a comparable clinical experience to their nonparenting colleagues and should take the lead in rearranging their own schedule. Nonbirthing parents, adopting parents, and parents using surrogacy should be included in any parental leave policy. Fellowship leaders have an important responsibility in helping fellows proactively plan to meet requirements for graduation and maximize learning and exposure (Figure). We also recognized the importance of equitable coverage. For example, there is sometimes a perception that fellows with children “burden” fellows who are not parents.3,19 On the other hand, fellows without children may feel that they are called on more than their colleagues with children to cover those with childcare issues. In addition, as a recent study of general surgery residency program directors indicates, there are complex interpersonal issues that play into a colleague’s willingness to provide coverage.20 It behooves program leadership to be cognizant of group dynamics that might cause conflict over what should be a straightforward coverage situation.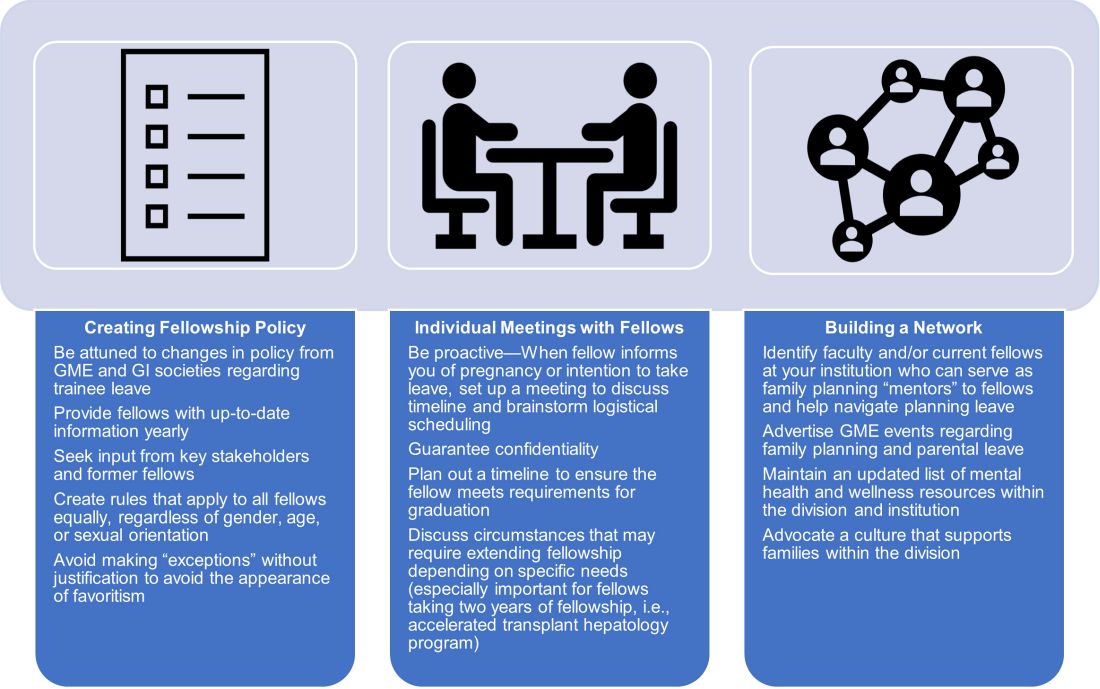
We first researched national and societal guidelines if available, as well as our institution’s graduate medical education (GME) website. We categorized benefits by whether they were federal, state-mandated, or institutional. It is important to note that any concerns about trainee salaries should be discussed with one’s GME office to ensure the leave policy is in accordance with federal funding policies.21 We solicited experiences and advice from former and current fellows who had gone through, or were planning, pregnancy and parental leave. A few faculty members volunteered to serve as a resource for fellows; these “ambassadors” discussed their experiences during a lunchtime panel, as well as offered to provide one-on-one advice and participate in future panels. We also reached out to our infection control experts to review the literature and federal policies on infections of special consideration during pregnancy and endoscopy. As for radiation safety, given the importance of education and active monitoring, we offer the option of reaching out to our radiation safety officer for individualized counseling.22
Based on these efforts, we drafted a written policy designed for pregnant fellows and fellows planning parental leave on expectations for the program and fellows, benefits, and advice, including childcare options, lactation room locations, and financial planning tips. We shared this document with fellows and incorporated feedback. As a “living document” it is subject to change and will be updated as needed (at least annually).
Additional planning considerations for fellows
Research childcare options (ideally 6 months or more before leave).
- Start to explore your institution’s resources for leave and childcare options (daycare waitlists may be greater than 1 year in some cities).
Inform your program director (4-5 months before leave).
- Consider informing your program director about pregnancy at the beginning of the second trimester.
- Discuss Accreditation Council for Graduate Medical Education requirements and scheduling responsibilities.
- Explicitly discuss whether you plan to graduate on time or extend fellowship.
Inform your colleagues and patients (at least 3-4 months before leave).
- If comfortable, consider getting advice from a co-fellow and/or faculty mentor parent to facilitate transition to parenthood.
- When you feel ready, begin trading rotations and calls with co-fellows. If you have a results inbox or pager, discuss who can help cover those during your leave.
- Inform research collaborators about your leave and make preparations to keep projects progressing during your leave.
- If you have “active” clinic patients, when appropriate, begin to inform them that you will be away and provide reassurance that a colleague will be covering you. Leave clear plans with contingencies for these patients in your last progress notes.
Complete institutional paperwork and map out facilities (at least 2-3 months before leave).
- Review your options for using time toward leave, including vacation, research, or Family and Medical Leave Act–provided leave (unpaid), and what paperwork you need to fill out.
- Contact your payroll and/or human resources office to inform them of birth/adoption.
- Research potential program parental benefits, such as dependent daycare and/or health care flexible spending accounts.
- If choosing to breastfeed, explore the lactation rooms that are closest to your workroom and endoscopy suite and determine how much time you will need to set aside for pumping.
Be prepared to make adjustments as needed.
- Endoscopy-heavy rotations may be more difficult in the third trimester of pregnancy.
- Make contingency plans for early or late delivery dates, as well as if you undergo a cesarean that requires additional recovery time.
- Consider scheduling elective rotations (research, clinic) toward the end of leave and for the first month of “return to work.”
- If you plan to join limited clinic or outpatient endoscopy blocks later in your leave, make early arrangements to work regularly with these attendings.
Conclusion
Trainee needs assessments in gastroenterology fellowship similar to those in other specialties should be performed, and are in fact underway.19,23,24 There is a lack of data regarding the availability of fellowship program guidance and, specifically, adherence to required policies, and more data from program directors at a national level need to be collected.20 We recommend that programs engage in identifying specific needs at their institutions with the goal of eventually sharing this knowledge with other programs. Gastroenterology society recommendations for performing endoscopy while pregnant, with regard to ergonomics, infection control, and radiation exposure, would be instrumental. GI fellowships should consolidate institutional knowledge and engage key stakeholders – including trainees, prior trainees, occupational safety experts, radiation safety offices, wellness experts, and GME – to create program-specific policies that are flexible but rigorous and generous but equitable.
Dr. Liu and Dr. Summa are gastroenterology fellows at Northwestern University, Chicago. Dr. Patel is an assistant professor of medicine and a gastroenterology fellowship assistant program director at Northwestern University, Chicago. Dr. Donnan and Dr. Guentner are assistant professors of medicine at Northwestern University. Dr. Kia is an assistant professor of medicine and the gastroenterology fellowship program director at Northwestern University. They have no conflicts of interest to disclose. The authors would like to thank Michelle Clermont, MD, and Maureen K. Bolon, MD, for their discussion and assistance during the drafting of this article.
References
1. Section on Medical Students, Residents, and Fellowship Trainees; Committee on Early Childhood. Pediatrics. 2013;131(2):387-90.
2. American Board of Medical Specialties. ABMS Announces Progressive Leave Policy for Residents and Fellows. July 13, 2020. Accessed May 1, 2021. https://www.abms.org/news-events/abms-announces-progressive-leave-policy-for-residents-and-fellows/.
3. Magudia K et al. J Grad Med Educ. 2020;12(2):162-7.
4. Blair JE et al. Acad Med. 2016;91(7):972-8.
5. Feld LD. Am J Gastroenterol. 2021;116(3):505-8.
6. Roubaud MS. Plast Reconstr Surg Glob Open. 2019. doi: 10.1097/GOX.0000000000002104.
7. Price J, Dunbar K. Gastrointest Endosc. 2009;69(1):121-3.
8. David YN et al. Gastrointest Endosc. 2020;91(6):AB75-AB76.
9. Webb AMB et al. Acad Med J Assoc Am Med Coll. 2019;94(11):1631-4.
10. Weinstein DF et al. N Engl J Med. 2019 Sep 12;381(11):995-7.
11. Anderson M, Goldman RH. JAMA Surg. 2020;155(3):243-9.
12. Palmer KT et al. Occup Environ Med. 2013;70(4):213-22.
13. Siegel JD et al; Healthcare Infection, Control Practices Advisory Committee. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007). 2007. Last reviewed July 22, 2019. Accessed April 28, 2021. https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html
14. David YN et al. Am J Gastroenterol. 2021;116(3):539-50.
15. Sethi S et al. Dig Dis Sci. 2019;64(9):2455-66.
16. Alzimami K et al. Gastroenterol Res Pract. 2013;2013:587574.
17. Hayashi S et al. World J Clin Cases. 2018;6(16):1087-93.
18. U.S. Department of Labor, Wage and Hour Division. “Frequently Asked Questions – Break Time for Nursing Mothers.” Accessed May 1, 2021. https://www.dol.gov/agencies/whd/nursing-mothers/faq.
19. Mwakyanjala EJ et al. J Am Heart Assoc. 2019. doi: 10.1161/JAHA.119.012137.
20. Castillo-Angeles M et al. JAMA Surg. 2021 Jul 1;156(7):647-53.
21. Prasad S et al. J Grad Med Educ. 2021 Jun;13(3):349-54.
22. Ho IKH et al. Am J Gastroenterol. 2014;109(8):1180-94.
23. Sherbaf FG et al. AJNR Am J Neuroradiol. 2020;41(8):1348-54.
24. Altieri MS et al. JAMA Surg. 2019;154(10):952-58.
Due to broad social changes and efforts from leaders in GI, there is renewed interest in family planning and parental leave policies for GI trainees. The American Board of Medical Specialties now permits trainees a minimum of 6 weeks away during training, without automatically requiring an extension of training time or completely depleting vacation time, for boards eligibility.1,2 However, national and institutional guidance for family planning and pregnancy during GI fellowship is lacking. How can gastroenterology fellowship programs support fellows taking parental leave and enact fair policies? We review the scope of the problem, describe our experience in developing resources within our GI fellowship program, and highlight areas that require further development.
The scope of the issue
There is no national data yet on the number of GI fellows that are parents prior to starting fellowship or who become parents during fellowship. We estimate that approximately 25% of fellows enter training as parents or become parents during fellowship, although 40%-50% may have an intention to have children.3,4 Fellows may be worried that they will “fall behind” or be perceived as less committed if they devote time to childrearing or take parental leave.5-7 Indeed, worries about discrimination based on pregnancy and parental leave are borne out by the experiences of older physicians (in particular, female physicians).8,9
State- and institution-specific benefits vary from program to program. Nationally, the Family and Medical Leave Act provides only unpaid leave and applies only to trainees who have been employed for greater than 12 months.10 Benefits may not always be well advertised, and even when they are, trainees (and attendings) may feel uncomfortable taking full advantage. One survey of GIs revealed that, although two-thirds believed that 6-8 weeks of maternity leave was inadequate, half took less than that amount due to fears about financial and professional consequences.8
Pregnancy during GI fellowship is a special concern. GI fellowship consists of long work hours, includes night call, and can be physically demanding. All three of these factors have been associated with preterm delivery, infertility, and miscarriage.11,12 In addition, there are no guidelines for ergonomic adjustments or infection precautions for pregnant endoscopists. We have compiled information about infection prevention guidance in pregnancy (available from the authors on request) derived from guidance from the National Institute for Occupational Safety and Health, which recommends the same precautions for pregnant health care workers as for nonpregnant health care workers.13 In regards to SARS-CoV-2, we believe that the decision to perform procedures on patients with COVID-19 infection should be individualized, although vaccinated endoscopists should be reassured by the exceedingly low rates of infection after vaccination and with appropriate personal protective equipment. Radiation is yet another concern. There are limited data on radiation dosages incurred by workers in the endoscopy suite and no pregnancy-specific data, which may lead trainees to avoid fluoroscopic procedures and unnecessarily double up on lead gowns.8,11,14-17
Breastfeeding accommodations, and access to lactation rooms for trainees, are required by federal law for a minimum of 12 months.18 Should a trainee choose to breastfeed, education of staff and attendings is critical because many may be unaware of the specific needs pertaining to lactation. Staff should be aware that 30-45 minutes are needed to prepare, pump, and store milk. Trainees should not be solely responsible for educating their attendings and staff.
Our Experience in Creating a Policy
We developed a formal fellowship program policy on parental leave and pregnancy in the setting of a broader discussion about fellow workload and wellness. We agreed that trainees should be allowed to make changes to their schedule with co-fellows as needed for medical appointments or procedures and that our backup policy should be flexible enough to provide spot coverage for unexpected complications and family emergencies. We also incorporated a GI psychologist to provide wellness resources and suggestions for reducing burnout for our fellows.
We strove to follow certain principles in creating this policy. Trainees who are parents should have a comparable clinical experience to their nonparenting colleagues and should take the lead in rearranging their own schedule. Nonbirthing parents, adopting parents, and parents using surrogacy should be included in any parental leave policy. Fellowship leaders have an important responsibility in helping fellows proactively plan to meet requirements for graduation and maximize learning and exposure (Figure). We also recognized the importance of equitable coverage. For example, there is sometimes a perception that fellows with children “burden” fellows who are not parents.3,19 On the other hand, fellows without children may feel that they are called on more than their colleagues with children to cover those with childcare issues. In addition, as a recent study of general surgery residency program directors indicates, there are complex interpersonal issues that play into a colleague’s willingness to provide coverage.20 It behooves program leadership to be cognizant of group dynamics that might cause conflict over what should be a straightforward coverage situation.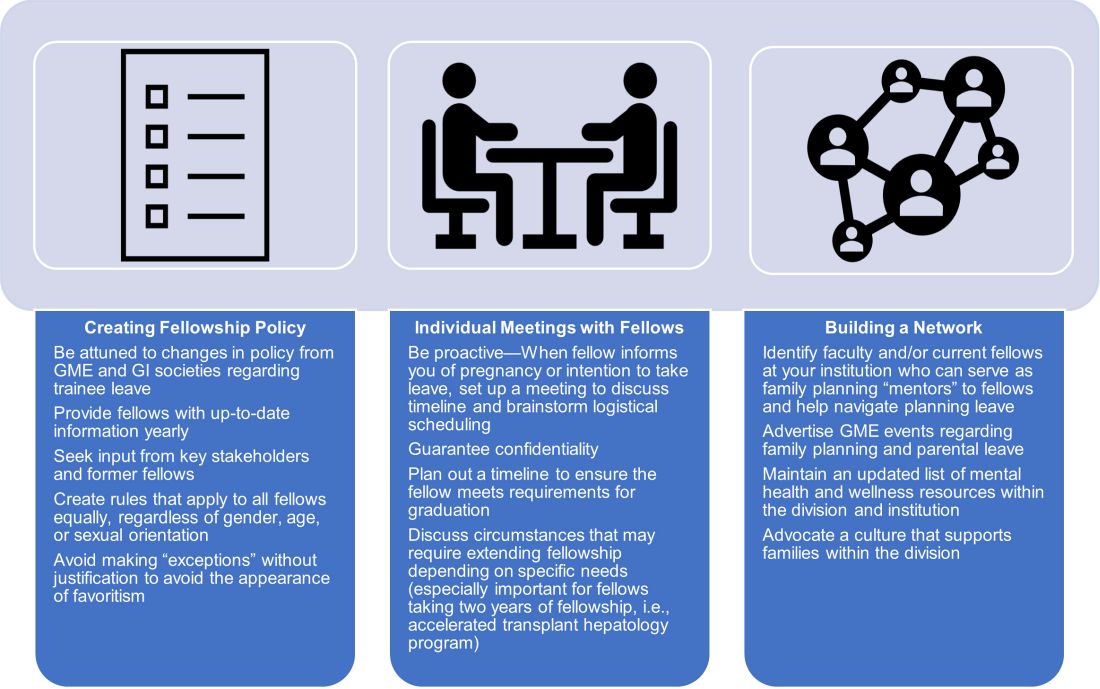
We first researched national and societal guidelines if available, as well as our institution’s graduate medical education (GME) website. We categorized benefits by whether they were federal, state-mandated, or institutional. It is important to note that any concerns about trainee salaries should be discussed with one’s GME office to ensure the leave policy is in accordance with federal funding policies.21 We solicited experiences and advice from former and current fellows who had gone through, or were planning, pregnancy and parental leave. A few faculty members volunteered to serve as a resource for fellows; these “ambassadors” discussed their experiences during a lunchtime panel, as well as offered to provide one-on-one advice and participate in future panels. We also reached out to our infection control experts to review the literature and federal policies on infections of special consideration during pregnancy and endoscopy. As for radiation safety, given the importance of education and active monitoring, we offer the option of reaching out to our radiation safety officer for individualized counseling.22
Based on these efforts, we drafted a written policy designed for pregnant fellows and fellows planning parental leave on expectations for the program and fellows, benefits, and advice, including childcare options, lactation room locations, and financial planning tips. We shared this document with fellows and incorporated feedback. As a “living document” it is subject to change and will be updated as needed (at least annually).
Additional planning considerations for fellows
Research childcare options (ideally 6 months or more before leave).
- Start to explore your institution’s resources for leave and childcare options (daycare waitlists may be greater than 1 year in some cities).
Inform your program director (4-5 months before leave).
- Consider informing your program director about pregnancy at the beginning of the second trimester.
- Discuss Accreditation Council for Graduate Medical Education requirements and scheduling responsibilities.
- Explicitly discuss whether you plan to graduate on time or extend fellowship.
Inform your colleagues and patients (at least 3-4 months before leave).
- If comfortable, consider getting advice from a co-fellow and/or faculty mentor parent to facilitate transition to parenthood.
- When you feel ready, begin trading rotations and calls with co-fellows. If you have a results inbox or pager, discuss who can help cover those during your leave.
- Inform research collaborators about your leave and make preparations to keep projects progressing during your leave.
- If you have “active” clinic patients, when appropriate, begin to inform them that you will be away and provide reassurance that a colleague will be covering you. Leave clear plans with contingencies for these patients in your last progress notes.
Complete institutional paperwork and map out facilities (at least 2-3 months before leave).
- Review your options for using time toward leave, including vacation, research, or Family and Medical Leave Act–provided leave (unpaid), and what paperwork you need to fill out.
- Contact your payroll and/or human resources office to inform them of birth/adoption.
- Research potential program parental benefits, such as dependent daycare and/or health care flexible spending accounts.
- If choosing to breastfeed, explore the lactation rooms that are closest to your workroom and endoscopy suite and determine how much time you will need to set aside for pumping.
Be prepared to make adjustments as needed.
- Endoscopy-heavy rotations may be more difficult in the third trimester of pregnancy.
- Make contingency plans for early or late delivery dates, as well as if you undergo a cesarean that requires additional recovery time.
- Consider scheduling elective rotations (research, clinic) toward the end of leave and for the first month of “return to work.”
- If you plan to join limited clinic or outpatient endoscopy blocks later in your leave, make early arrangements to work regularly with these attendings.
Conclusion
Trainee needs assessments in gastroenterology fellowship similar to those in other specialties should be performed, and are in fact underway.19,23,24 There is a lack of data regarding the availability of fellowship program guidance and, specifically, adherence to required policies, and more data from program directors at a national level need to be collected.20 We recommend that programs engage in identifying specific needs at their institutions with the goal of eventually sharing this knowledge with other programs. Gastroenterology society recommendations for performing endoscopy while pregnant, with regard to ergonomics, infection control, and radiation exposure, would be instrumental. GI fellowships should consolidate institutional knowledge and engage key stakeholders – including trainees, prior trainees, occupational safety experts, radiation safety offices, wellness experts, and GME – to create program-specific policies that are flexible but rigorous and generous but equitable.
Dr. Liu and Dr. Summa are gastroenterology fellows at Northwestern University, Chicago. Dr. Patel is an assistant professor of medicine and a gastroenterology fellowship assistant program director at Northwestern University, Chicago. Dr. Donnan and Dr. Guentner are assistant professors of medicine at Northwestern University. Dr. Kia is an assistant professor of medicine and the gastroenterology fellowship program director at Northwestern University. They have no conflicts of interest to disclose. The authors would like to thank Michelle Clermont, MD, and Maureen K. Bolon, MD, for their discussion and assistance during the drafting of this article.
References
1. Section on Medical Students, Residents, and Fellowship Trainees; Committee on Early Childhood. Pediatrics. 2013;131(2):387-90.
2. American Board of Medical Specialties. ABMS Announces Progressive Leave Policy for Residents and Fellows. July 13, 2020. Accessed May 1, 2021. https://www.abms.org/news-events/abms-announces-progressive-leave-policy-for-residents-and-fellows/.
3. Magudia K et al. J Grad Med Educ. 2020;12(2):162-7.
4. Blair JE et al. Acad Med. 2016;91(7):972-8.
5. Feld LD. Am J Gastroenterol. 2021;116(3):505-8.
6. Roubaud MS. Plast Reconstr Surg Glob Open. 2019. doi: 10.1097/GOX.0000000000002104.
7. Price J, Dunbar K. Gastrointest Endosc. 2009;69(1):121-3.
8. David YN et al. Gastrointest Endosc. 2020;91(6):AB75-AB76.
9. Webb AMB et al. Acad Med J Assoc Am Med Coll. 2019;94(11):1631-4.
10. Weinstein DF et al. N Engl J Med. 2019 Sep 12;381(11):995-7.
11. Anderson M, Goldman RH. JAMA Surg. 2020;155(3):243-9.
12. Palmer KT et al. Occup Environ Med. 2013;70(4):213-22.
13. Siegel JD et al; Healthcare Infection, Control Practices Advisory Committee. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007). 2007. Last reviewed July 22, 2019. Accessed April 28, 2021. https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html
14. David YN et al. Am J Gastroenterol. 2021;116(3):539-50.
15. Sethi S et al. Dig Dis Sci. 2019;64(9):2455-66.
16. Alzimami K et al. Gastroenterol Res Pract. 2013;2013:587574.
17. Hayashi S et al. World J Clin Cases. 2018;6(16):1087-93.
18. U.S. Department of Labor, Wage and Hour Division. “Frequently Asked Questions – Break Time for Nursing Mothers.” Accessed May 1, 2021. https://www.dol.gov/agencies/whd/nursing-mothers/faq.
19. Mwakyanjala EJ et al. J Am Heart Assoc. 2019. doi: 10.1161/JAHA.119.012137.
20. Castillo-Angeles M et al. JAMA Surg. 2021 Jul 1;156(7):647-53.
21. Prasad S et al. J Grad Med Educ. 2021 Jun;13(3):349-54.
22. Ho IKH et al. Am J Gastroenterol. 2014;109(8):1180-94.
23. Sherbaf FG et al. AJNR Am J Neuroradiol. 2020;41(8):1348-54.
24. Altieri MS et al. JAMA Surg. 2019;154(10):952-58.
Due to broad social changes and efforts from leaders in GI, there is renewed interest in family planning and parental leave policies for GI trainees. The American Board of Medical Specialties now permits trainees a minimum of 6 weeks away during training, without automatically requiring an extension of training time or completely depleting vacation time, for boards eligibility.1,2 However, national and institutional guidance for family planning and pregnancy during GI fellowship is lacking. How can gastroenterology fellowship programs support fellows taking parental leave and enact fair policies? We review the scope of the problem, describe our experience in developing resources within our GI fellowship program, and highlight areas that require further development.
The scope of the issue
There is no national data yet on the number of GI fellows that are parents prior to starting fellowship or who become parents during fellowship. We estimate that approximately 25% of fellows enter training as parents or become parents during fellowship, although 40%-50% may have an intention to have children.3,4 Fellows may be worried that they will “fall behind” or be perceived as less committed if they devote time to childrearing or take parental leave.5-7 Indeed, worries about discrimination based on pregnancy and parental leave are borne out by the experiences of older physicians (in particular, female physicians).8,9
State- and institution-specific benefits vary from program to program. Nationally, the Family and Medical Leave Act provides only unpaid leave and applies only to trainees who have been employed for greater than 12 months.10 Benefits may not always be well advertised, and even when they are, trainees (and attendings) may feel uncomfortable taking full advantage. One survey of GIs revealed that, although two-thirds believed that 6-8 weeks of maternity leave was inadequate, half took less than that amount due to fears about financial and professional consequences.8
Pregnancy during GI fellowship is a special concern. GI fellowship consists of long work hours, includes night call, and can be physically demanding. All three of these factors have been associated with preterm delivery, infertility, and miscarriage.11,12 In addition, there are no guidelines for ergonomic adjustments or infection precautions for pregnant endoscopists. We have compiled information about infection prevention guidance in pregnancy (available from the authors on request) derived from guidance from the National Institute for Occupational Safety and Health, which recommends the same precautions for pregnant health care workers as for nonpregnant health care workers.13 In regards to SARS-CoV-2, we believe that the decision to perform procedures on patients with COVID-19 infection should be individualized, although vaccinated endoscopists should be reassured by the exceedingly low rates of infection after vaccination and with appropriate personal protective equipment. Radiation is yet another concern. There are limited data on radiation dosages incurred by workers in the endoscopy suite and no pregnancy-specific data, which may lead trainees to avoid fluoroscopic procedures and unnecessarily double up on lead gowns.8,11,14-17
Breastfeeding accommodations, and access to lactation rooms for trainees, are required by federal law for a minimum of 12 months.18 Should a trainee choose to breastfeed, education of staff and attendings is critical because many may be unaware of the specific needs pertaining to lactation. Staff should be aware that 30-45 minutes are needed to prepare, pump, and store milk. Trainees should not be solely responsible for educating their attendings and staff.
Our Experience in Creating a Policy
We developed a formal fellowship program policy on parental leave and pregnancy in the setting of a broader discussion about fellow workload and wellness. We agreed that trainees should be allowed to make changes to their schedule with co-fellows as needed for medical appointments or procedures and that our backup policy should be flexible enough to provide spot coverage for unexpected complications and family emergencies. We also incorporated a GI psychologist to provide wellness resources and suggestions for reducing burnout for our fellows.
We strove to follow certain principles in creating this policy. Trainees who are parents should have a comparable clinical experience to their nonparenting colleagues and should take the lead in rearranging their own schedule. Nonbirthing parents, adopting parents, and parents using surrogacy should be included in any parental leave policy. Fellowship leaders have an important responsibility in helping fellows proactively plan to meet requirements for graduation and maximize learning and exposure (Figure). We also recognized the importance of equitable coverage. For example, there is sometimes a perception that fellows with children “burden” fellows who are not parents.3,19 On the other hand, fellows without children may feel that they are called on more than their colleagues with children to cover those with childcare issues. In addition, as a recent study of general surgery residency program directors indicates, there are complex interpersonal issues that play into a colleague’s willingness to provide coverage.20 It behooves program leadership to be cognizant of group dynamics that might cause conflict over what should be a straightforward coverage situation.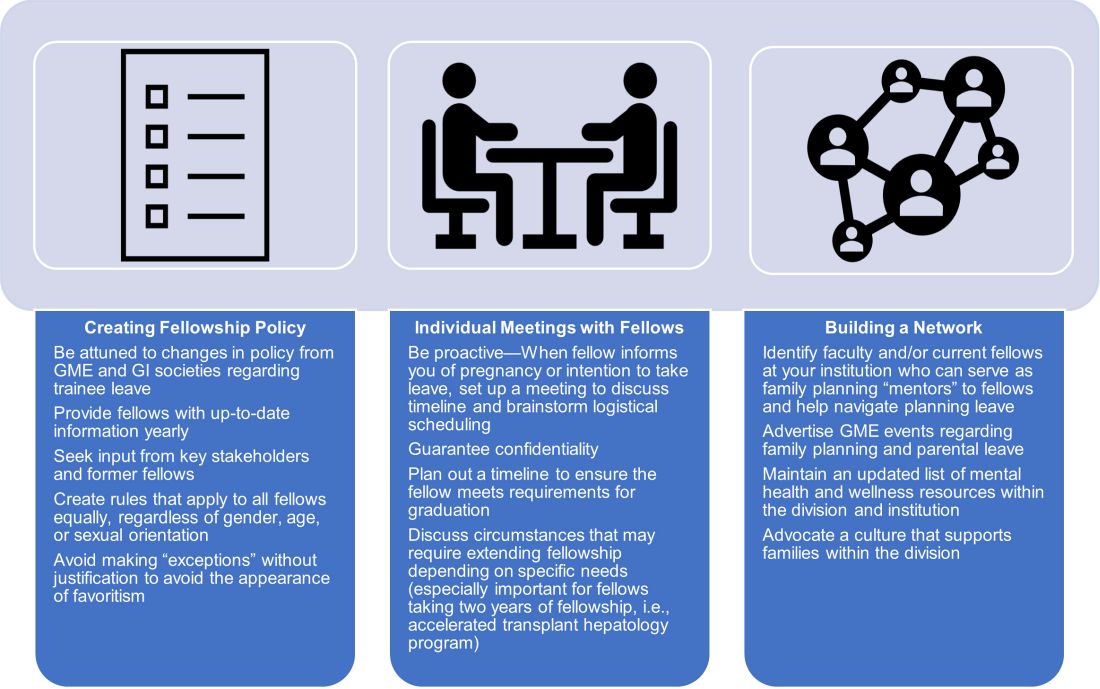
We first researched national and societal guidelines if available, as well as our institution’s graduate medical education (GME) website. We categorized benefits by whether they were federal, state-mandated, or institutional. It is important to note that any concerns about trainee salaries should be discussed with one’s GME office to ensure the leave policy is in accordance with federal funding policies.21 We solicited experiences and advice from former and current fellows who had gone through, or were planning, pregnancy and parental leave. A few faculty members volunteered to serve as a resource for fellows; these “ambassadors” discussed their experiences during a lunchtime panel, as well as offered to provide one-on-one advice and participate in future panels. We also reached out to our infection control experts to review the literature and federal policies on infections of special consideration during pregnancy and endoscopy. As for radiation safety, given the importance of education and active monitoring, we offer the option of reaching out to our radiation safety officer for individualized counseling.22
Based on these efforts, we drafted a written policy designed for pregnant fellows and fellows planning parental leave on expectations for the program and fellows, benefits, and advice, including childcare options, lactation room locations, and financial planning tips. We shared this document with fellows and incorporated feedback. As a “living document” it is subject to change and will be updated as needed (at least annually).
Additional planning considerations for fellows
Research childcare options (ideally 6 months or more before leave).
- Start to explore your institution’s resources for leave and childcare options (daycare waitlists may be greater than 1 year in some cities).
Inform your program director (4-5 months before leave).
- Consider informing your program director about pregnancy at the beginning of the second trimester.
- Discuss Accreditation Council for Graduate Medical Education requirements and scheduling responsibilities.
- Explicitly discuss whether you plan to graduate on time or extend fellowship.
Inform your colleagues and patients (at least 3-4 months before leave).
- If comfortable, consider getting advice from a co-fellow and/or faculty mentor parent to facilitate transition to parenthood.
- When you feel ready, begin trading rotations and calls with co-fellows. If you have a results inbox or pager, discuss who can help cover those during your leave.
- Inform research collaborators about your leave and make preparations to keep projects progressing during your leave.
- If you have “active” clinic patients, when appropriate, begin to inform them that you will be away and provide reassurance that a colleague will be covering you. Leave clear plans with contingencies for these patients in your last progress notes.
Complete institutional paperwork and map out facilities (at least 2-3 months before leave).
- Review your options for using time toward leave, including vacation, research, or Family and Medical Leave Act–provided leave (unpaid), and what paperwork you need to fill out.
- Contact your payroll and/or human resources office to inform them of birth/adoption.
- Research potential program parental benefits, such as dependent daycare and/or health care flexible spending accounts.
- If choosing to breastfeed, explore the lactation rooms that are closest to your workroom and endoscopy suite and determine how much time you will need to set aside for pumping.
Be prepared to make adjustments as needed.
- Endoscopy-heavy rotations may be more difficult in the third trimester of pregnancy.
- Make contingency plans for early or late delivery dates, as well as if you undergo a cesarean that requires additional recovery time.
- Consider scheduling elective rotations (research, clinic) toward the end of leave and for the first month of “return to work.”
- If you plan to join limited clinic or outpatient endoscopy blocks later in your leave, make early arrangements to work regularly with these attendings.
Conclusion
Trainee needs assessments in gastroenterology fellowship similar to those in other specialties should be performed, and are in fact underway.19,23,24 There is a lack of data regarding the availability of fellowship program guidance and, specifically, adherence to required policies, and more data from program directors at a national level need to be collected.20 We recommend that programs engage in identifying specific needs at their institutions with the goal of eventually sharing this knowledge with other programs. Gastroenterology society recommendations for performing endoscopy while pregnant, with regard to ergonomics, infection control, and radiation exposure, would be instrumental. GI fellowships should consolidate institutional knowledge and engage key stakeholders – including trainees, prior trainees, occupational safety experts, radiation safety offices, wellness experts, and GME – to create program-specific policies that are flexible but rigorous and generous but equitable.
Dr. Liu and Dr. Summa are gastroenterology fellows at Northwestern University, Chicago. Dr. Patel is an assistant professor of medicine and a gastroenterology fellowship assistant program director at Northwestern University, Chicago. Dr. Donnan and Dr. Guentner are assistant professors of medicine at Northwestern University. Dr. Kia is an assistant professor of medicine and the gastroenterology fellowship program director at Northwestern University. They have no conflicts of interest to disclose. The authors would like to thank Michelle Clermont, MD, and Maureen K. Bolon, MD, for their discussion and assistance during the drafting of this article.
References
1. Section on Medical Students, Residents, and Fellowship Trainees; Committee on Early Childhood. Pediatrics. 2013;131(2):387-90.
2. American Board of Medical Specialties. ABMS Announces Progressive Leave Policy for Residents and Fellows. July 13, 2020. Accessed May 1, 2021. https://www.abms.org/news-events/abms-announces-progressive-leave-policy-for-residents-and-fellows/.
3. Magudia K et al. J Grad Med Educ. 2020;12(2):162-7.
4. Blair JE et al. Acad Med. 2016;91(7):972-8.
5. Feld LD. Am J Gastroenterol. 2021;116(3):505-8.
6. Roubaud MS. Plast Reconstr Surg Glob Open. 2019. doi: 10.1097/GOX.0000000000002104.
7. Price J, Dunbar K. Gastrointest Endosc. 2009;69(1):121-3.
8. David YN et al. Gastrointest Endosc. 2020;91(6):AB75-AB76.
9. Webb AMB et al. Acad Med J Assoc Am Med Coll. 2019;94(11):1631-4.
10. Weinstein DF et al. N Engl J Med. 2019 Sep 12;381(11):995-7.
11. Anderson M, Goldman RH. JAMA Surg. 2020;155(3):243-9.
12. Palmer KT et al. Occup Environ Med. 2013;70(4):213-22.
13. Siegel JD et al; Healthcare Infection, Control Practices Advisory Committee. Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings (2007). 2007. Last reviewed July 22, 2019. Accessed April 28, 2021. https://www.cdc.gov/infectioncontrol/guidelines/isolation/index.html
14. David YN et al. Am J Gastroenterol. 2021;116(3):539-50.
15. Sethi S et al. Dig Dis Sci. 2019;64(9):2455-66.
16. Alzimami K et al. Gastroenterol Res Pract. 2013;2013:587574.
17. Hayashi S et al. World J Clin Cases. 2018;6(16):1087-93.
18. U.S. Department of Labor, Wage and Hour Division. “Frequently Asked Questions – Break Time for Nursing Mothers.” Accessed May 1, 2021. https://www.dol.gov/agencies/whd/nursing-mothers/faq.
19. Mwakyanjala EJ et al. J Am Heart Assoc. 2019. doi: 10.1161/JAHA.119.012137.
20. Castillo-Angeles M et al. JAMA Surg. 2021 Jul 1;156(7):647-53.
21. Prasad S et al. J Grad Med Educ. 2021 Jun;13(3):349-54.
22. Ho IKH et al. Am J Gastroenterol. 2014;109(8):1180-94.
23. Sherbaf FG et al. AJNR Am J Neuroradiol. 2020;41(8):1348-54.
24. Altieri MS et al. JAMA Surg. 2019;154(10):952-58.
CMS’s proposed 22% cut to radiation oncology is ‘tone deaf’
The changes, proposed by the Centers for Medicare & Medicaid Services to their Radiation Oncology (RO) Model, have been challenged primarily by the American Society for Radiation Oncology (ASTRO), but by other groups as well.
These excessive reductions will jeopardize access to lifesaving radiation therapy services for Medicare beneficiaries at a time when the U.S. health care system needs “all doors open” to treat patients with cancer, says ASTRO.
The proposed cuts are scheduled to take effect Jan. 1 and will be mandatory for the 30% of providers that will be randomly selected to participate.
The timing could not be worse, says the Community Oncology Alliance. “How can payment be ratcheted down on a vital aspect of cancer in the middle of a pandemic?” said Ted Okon, MBA, executive director of COA. “What was CMS thinking? These are extreme circumstances, and this is so ill-timed and so tone deaf that it just takes my breath away.”
He pointed out that with hospitals being overrun with COVID-19 patients, community practices have to keep their doors open to treat patients. “This is an extended public health emergency, and a variant can reignite the surge,” said Mr. Okon. “CMS should be asking practices what they can do to help them – and not trying to make drastic cuts.”
Mr. Okon is also concerned that as a result of the pandemic, “we are going to be seeing more advanced cancers, which are more difficult and expensive to treat, and radiation therapy is going to come into play,” he said. “These are serious and unintended consequences, and CMS needs to come out of their [Washington] D.C. bubble and see what’s really going on.”
The timing of the rollout is particularly precarious, given the financial upheaval caused by the COVID-19 pandemic, agrees Constantine Mantz, MD, ASTRO’s Health Policy Council vice-chair.
“Medicare’s proposed cuts, unfortunately, compound the enormous financial challenges imposed by the COVID-19 pandemic on physicians and their practices,” said Dr. Mantz. “Radiation oncology is particularly at risk given its dependence on expensive treatment equipment to deliver cancer care.”
The high costs of maintaining this equipment remain the same whether the equipment is used or not. “This means that fewer patients being seen during the pandemic combined with these steep reimbursement cuts in the near future risk the continued viability of many centers and their ability to provide lifesaving cancer treatment,” he said.
ASTRO calls on Congress to intervene
ASTRO has asked President Biden and Congress to intervene immediately on not only the Radiation Oncology model but the severe cuts that were proposed for the 2022 Medicare Physician Fee Schedule.
“The RO Model, which was last updated in the 2022 Medicare Hospital Outpatient Prospective Payment System Proposed Rule, would cut payments for radiation therapy services by 3.75% for physicians and 4.75% for facilities,” said Dr. Mantz. “This cut would be in addition to an 8.75% cut to radiation oncology in the 2022 Medicare Physician Fee Schedule Proposed Rule.”
As a result, the physicians and facilities that are required to participate in the RO Model are facing steep declines in Medicare reimbursement. “This amounts to well over 10% for their patients covered by Medicare next year,” Dr. Mantz told this news organization.
The radiation oncology model
The goal of the RO Model is to test a change in the way radiation therapy services are paid – from the current “fee-for-service” payments” to prospective, site-neutral, modality-agnostic, episode-based payments that incentivize physicians to deliver higher-value care. It requires mandatory participation of practices.
The Center for Medicare and Medicaid Innovation published a final rule in September 2020 that established the RO Model, which was to begin on Jan. 1, 2021. However, because of the ongoing COVID-19 pandemic, the start of the RO Model was delayed until July 1, 2021, and subsequently, the Consolidated Appropriations Act, 2021, included a provision that prohibits implementation of the RO Model before Jan. 1, 2022.
Further changes to the RO model were proposed last month, which included some slight revisions to the discount factor. But ASTRO points out that these revisions did not address numerous concerns raised by both the radiation oncology community and a broad coalition of medical provider groups, patients, hospitals, health systems, and bipartisan members of Congress.
The new model would provide an alternative to the traditional fee-for-service payments. Instead, the payments are prospective and episode-based, and based on the cancer diagnosis. It would cover radiation therapy that is administered during a 90-day episode, and would meet the included cancer type criteria described in the final rule.
The RO model would use “site-neutral payment” by establishing a common, adjusted national base payment amount for the episode, regardless of the setting where it is administered.
The episode payments would be divided into professional and technical components to allow the current claims systems for the Physician Fee Schedule (PFS) and the Outpatient Prospective Payment System (OPPS) to be used to adjudicate claims as well as to maintain consistency with existing business relationships.
Another aspect is that the model links “payment” to “quality” using reporting and performance on quality measures, clinical data reporting, and patient experience as factors when determining payment to RO participants. Finally, providers will be randomly selected and participation is mandatory.
Mr. Okon feels that the idea of a mandatory model is wrong. “They are going to be taking 30% of practices to participate in an experiment,” he said. “Mandatory means that you can’t get enough people to participate so it is mandated to force them into it.”
Dr. Mantz also noted that the model is going to have a widespread impact on a wide range of issues. “Sharply reduced reimbursement for radiation therapy services under the RO Model is expected to delay, if not prevent, the equipment upgrades and other improvements that are necessary for practices to continue to provide high-quality, high-value cancer care.
“These problematic barriers to access advanced treatment technology also come at a critical time for radiation oncology, in that we already are seeing more difficult-to-treat cancers and caring for patients with more advanced-stage diseases due to delayed diagnoses during the peak of the pandemic last year.”
In addition, the RO model, in its current inception, is expected to further widen existing gaps in access to cancer care, disproportionately harming patients from marginalized groups, such as poor patients and medically underserved patients.
“For example, ASTRO analyses have demonstrated that patients in rural areas currently face significantly reduced access to stereotactic radiotherapy and lifesaving brachytherapy treatments, compared to patients in urban areas,” said Dr. Mantz. “It’s difficult to imagine that these serious health inequities could even begin to be addressed with the aggregate payment cuts imposed by the RO model.”
A version of this article first appeared on Medscape.com.
The changes, proposed by the Centers for Medicare & Medicaid Services to their Radiation Oncology (RO) Model, have been challenged primarily by the American Society for Radiation Oncology (ASTRO), but by other groups as well.
These excessive reductions will jeopardize access to lifesaving radiation therapy services for Medicare beneficiaries at a time when the U.S. health care system needs “all doors open” to treat patients with cancer, says ASTRO.
The proposed cuts are scheduled to take effect Jan. 1 and will be mandatory for the 30% of providers that will be randomly selected to participate.
The timing could not be worse, says the Community Oncology Alliance. “How can payment be ratcheted down on a vital aspect of cancer in the middle of a pandemic?” said Ted Okon, MBA, executive director of COA. “What was CMS thinking? These are extreme circumstances, and this is so ill-timed and so tone deaf that it just takes my breath away.”
He pointed out that with hospitals being overrun with COVID-19 patients, community practices have to keep their doors open to treat patients. “This is an extended public health emergency, and a variant can reignite the surge,” said Mr. Okon. “CMS should be asking practices what they can do to help them – and not trying to make drastic cuts.”
Mr. Okon is also concerned that as a result of the pandemic, “we are going to be seeing more advanced cancers, which are more difficult and expensive to treat, and radiation therapy is going to come into play,” he said. “These are serious and unintended consequences, and CMS needs to come out of their [Washington] D.C. bubble and see what’s really going on.”
The timing of the rollout is particularly precarious, given the financial upheaval caused by the COVID-19 pandemic, agrees Constantine Mantz, MD, ASTRO’s Health Policy Council vice-chair.
“Medicare’s proposed cuts, unfortunately, compound the enormous financial challenges imposed by the COVID-19 pandemic on physicians and their practices,” said Dr. Mantz. “Radiation oncology is particularly at risk given its dependence on expensive treatment equipment to deliver cancer care.”
The high costs of maintaining this equipment remain the same whether the equipment is used or not. “This means that fewer patients being seen during the pandemic combined with these steep reimbursement cuts in the near future risk the continued viability of many centers and their ability to provide lifesaving cancer treatment,” he said.
ASTRO calls on Congress to intervene
ASTRO has asked President Biden and Congress to intervene immediately on not only the Radiation Oncology model but the severe cuts that were proposed for the 2022 Medicare Physician Fee Schedule.
“The RO Model, which was last updated in the 2022 Medicare Hospital Outpatient Prospective Payment System Proposed Rule, would cut payments for radiation therapy services by 3.75% for physicians and 4.75% for facilities,” said Dr. Mantz. “This cut would be in addition to an 8.75% cut to radiation oncology in the 2022 Medicare Physician Fee Schedule Proposed Rule.”
As a result, the physicians and facilities that are required to participate in the RO Model are facing steep declines in Medicare reimbursement. “This amounts to well over 10% for their patients covered by Medicare next year,” Dr. Mantz told this news organization.
The radiation oncology model
The goal of the RO Model is to test a change in the way radiation therapy services are paid – from the current “fee-for-service” payments” to prospective, site-neutral, modality-agnostic, episode-based payments that incentivize physicians to deliver higher-value care. It requires mandatory participation of practices.
The Center for Medicare and Medicaid Innovation published a final rule in September 2020 that established the RO Model, which was to begin on Jan. 1, 2021. However, because of the ongoing COVID-19 pandemic, the start of the RO Model was delayed until July 1, 2021, and subsequently, the Consolidated Appropriations Act, 2021, included a provision that prohibits implementation of the RO Model before Jan. 1, 2022.
Further changes to the RO model were proposed last month, which included some slight revisions to the discount factor. But ASTRO points out that these revisions did not address numerous concerns raised by both the radiation oncology community and a broad coalition of medical provider groups, patients, hospitals, health systems, and bipartisan members of Congress.
The new model would provide an alternative to the traditional fee-for-service payments. Instead, the payments are prospective and episode-based, and based on the cancer diagnosis. It would cover radiation therapy that is administered during a 90-day episode, and would meet the included cancer type criteria described in the final rule.
The RO model would use “site-neutral payment” by establishing a common, adjusted national base payment amount for the episode, regardless of the setting where it is administered.
The episode payments would be divided into professional and technical components to allow the current claims systems for the Physician Fee Schedule (PFS) and the Outpatient Prospective Payment System (OPPS) to be used to adjudicate claims as well as to maintain consistency with existing business relationships.
Another aspect is that the model links “payment” to “quality” using reporting and performance on quality measures, clinical data reporting, and patient experience as factors when determining payment to RO participants. Finally, providers will be randomly selected and participation is mandatory.
Mr. Okon feels that the idea of a mandatory model is wrong. “They are going to be taking 30% of practices to participate in an experiment,” he said. “Mandatory means that you can’t get enough people to participate so it is mandated to force them into it.”
Dr. Mantz also noted that the model is going to have a widespread impact on a wide range of issues. “Sharply reduced reimbursement for radiation therapy services under the RO Model is expected to delay, if not prevent, the equipment upgrades and other improvements that are necessary for practices to continue to provide high-quality, high-value cancer care.
“These problematic barriers to access advanced treatment technology also come at a critical time for radiation oncology, in that we already are seeing more difficult-to-treat cancers and caring for patients with more advanced-stage diseases due to delayed diagnoses during the peak of the pandemic last year.”
In addition, the RO model, in its current inception, is expected to further widen existing gaps in access to cancer care, disproportionately harming patients from marginalized groups, such as poor patients and medically underserved patients.
“For example, ASTRO analyses have demonstrated that patients in rural areas currently face significantly reduced access to stereotactic radiotherapy and lifesaving brachytherapy treatments, compared to patients in urban areas,” said Dr. Mantz. “It’s difficult to imagine that these serious health inequities could even begin to be addressed with the aggregate payment cuts imposed by the RO model.”
A version of this article first appeared on Medscape.com.
The changes, proposed by the Centers for Medicare & Medicaid Services to their Radiation Oncology (RO) Model, have been challenged primarily by the American Society for Radiation Oncology (ASTRO), but by other groups as well.
These excessive reductions will jeopardize access to lifesaving radiation therapy services for Medicare beneficiaries at a time when the U.S. health care system needs “all doors open” to treat patients with cancer, says ASTRO.
The proposed cuts are scheduled to take effect Jan. 1 and will be mandatory for the 30% of providers that will be randomly selected to participate.
The timing could not be worse, says the Community Oncology Alliance. “How can payment be ratcheted down on a vital aspect of cancer in the middle of a pandemic?” said Ted Okon, MBA, executive director of COA. “What was CMS thinking? These are extreme circumstances, and this is so ill-timed and so tone deaf that it just takes my breath away.”
He pointed out that with hospitals being overrun with COVID-19 patients, community practices have to keep their doors open to treat patients. “This is an extended public health emergency, and a variant can reignite the surge,” said Mr. Okon. “CMS should be asking practices what they can do to help them – and not trying to make drastic cuts.”
Mr. Okon is also concerned that as a result of the pandemic, “we are going to be seeing more advanced cancers, which are more difficult and expensive to treat, and radiation therapy is going to come into play,” he said. “These are serious and unintended consequences, and CMS needs to come out of their [Washington] D.C. bubble and see what’s really going on.”
The timing of the rollout is particularly precarious, given the financial upheaval caused by the COVID-19 pandemic, agrees Constantine Mantz, MD, ASTRO’s Health Policy Council vice-chair.
“Medicare’s proposed cuts, unfortunately, compound the enormous financial challenges imposed by the COVID-19 pandemic on physicians and their practices,” said Dr. Mantz. “Radiation oncology is particularly at risk given its dependence on expensive treatment equipment to deliver cancer care.”
The high costs of maintaining this equipment remain the same whether the equipment is used or not. “This means that fewer patients being seen during the pandemic combined with these steep reimbursement cuts in the near future risk the continued viability of many centers and their ability to provide lifesaving cancer treatment,” he said.
ASTRO calls on Congress to intervene
ASTRO has asked President Biden and Congress to intervene immediately on not only the Radiation Oncology model but the severe cuts that were proposed for the 2022 Medicare Physician Fee Schedule.
“The RO Model, which was last updated in the 2022 Medicare Hospital Outpatient Prospective Payment System Proposed Rule, would cut payments for radiation therapy services by 3.75% for physicians and 4.75% for facilities,” said Dr. Mantz. “This cut would be in addition to an 8.75% cut to radiation oncology in the 2022 Medicare Physician Fee Schedule Proposed Rule.”
As a result, the physicians and facilities that are required to participate in the RO Model are facing steep declines in Medicare reimbursement. “This amounts to well over 10% for their patients covered by Medicare next year,” Dr. Mantz told this news organization.
The radiation oncology model
The goal of the RO Model is to test a change in the way radiation therapy services are paid – from the current “fee-for-service” payments” to prospective, site-neutral, modality-agnostic, episode-based payments that incentivize physicians to deliver higher-value care. It requires mandatory participation of practices.
The Center for Medicare and Medicaid Innovation published a final rule in September 2020 that established the RO Model, which was to begin on Jan. 1, 2021. However, because of the ongoing COVID-19 pandemic, the start of the RO Model was delayed until July 1, 2021, and subsequently, the Consolidated Appropriations Act, 2021, included a provision that prohibits implementation of the RO Model before Jan. 1, 2022.
Further changes to the RO model were proposed last month, which included some slight revisions to the discount factor. But ASTRO points out that these revisions did not address numerous concerns raised by both the radiation oncology community and a broad coalition of medical provider groups, patients, hospitals, health systems, and bipartisan members of Congress.
The new model would provide an alternative to the traditional fee-for-service payments. Instead, the payments are prospective and episode-based, and based on the cancer diagnosis. It would cover radiation therapy that is administered during a 90-day episode, and would meet the included cancer type criteria described in the final rule.
The RO model would use “site-neutral payment” by establishing a common, adjusted national base payment amount for the episode, regardless of the setting where it is administered.
The episode payments would be divided into professional and technical components to allow the current claims systems for the Physician Fee Schedule (PFS) and the Outpatient Prospective Payment System (OPPS) to be used to adjudicate claims as well as to maintain consistency with existing business relationships.
Another aspect is that the model links “payment” to “quality” using reporting and performance on quality measures, clinical data reporting, and patient experience as factors when determining payment to RO participants. Finally, providers will be randomly selected and participation is mandatory.
Mr. Okon feels that the idea of a mandatory model is wrong. “They are going to be taking 30% of practices to participate in an experiment,” he said. “Mandatory means that you can’t get enough people to participate so it is mandated to force them into it.”
Dr. Mantz also noted that the model is going to have a widespread impact on a wide range of issues. “Sharply reduced reimbursement for radiation therapy services under the RO Model is expected to delay, if not prevent, the equipment upgrades and other improvements that are necessary for practices to continue to provide high-quality, high-value cancer care.
“These problematic barriers to access advanced treatment technology also come at a critical time for radiation oncology, in that we already are seeing more difficult-to-treat cancers and caring for patients with more advanced-stage diseases due to delayed diagnoses during the peak of the pandemic last year.”
In addition, the RO model, in its current inception, is expected to further widen existing gaps in access to cancer care, disproportionately harming patients from marginalized groups, such as poor patients and medically underserved patients.
“For example, ASTRO analyses have demonstrated that patients in rural areas currently face significantly reduced access to stereotactic radiotherapy and lifesaving brachytherapy treatments, compared to patients in urban areas,” said Dr. Mantz. “It’s difficult to imagine that these serious health inequities could even begin to be addressed with the aggregate payment cuts imposed by the RO model.”
A version of this article first appeared on Medscape.com.
Study calls higher surgery costs at NCI centers into question
according to a recent report in JAMA Network Open.
“While acceptable to pay higher prices for care that is expected to be of higher quality, we found no differences in short-term postsurgical outcomes,” said authors led by Samuel Takvorian, MD, a medical oncologist at the University of Pennsylvania, Philadelphia.
The team looked at what insurance companies paid for incident breast, colon, and lung cancer surgeries, which together account for most cancer surgeries, among 66,878 patients treated from 2011 to 2014 at almost 3,000 U.S. hospitals.
Three-quarters had surgery at a community hospital, and 8.3% were treated at one of the nation’s 71 NCI centers, which are recognized by the NCI as meeting rigorous standards in cancer care. The remaining patients were treated at non-NCI academic hospitals.
The mean surgery-specific insurer prices paid at NCI centers was $18,526 versus $14,772 at community hospitals, a difference of $3,755 (P < .001) that was driven primarily by higher facility payments at NCI centers, a mean of $17,704 versus $14,120 at community hospitals.
Mean 90-day postdischarge payments were also $5,744 higher at NCI centers, $47,035 versus $41,291 at community hospitals (P = .006).
The team used postsurgical acute care utilization as a marker of quality but found no differences between the two settings. Mean length of stay was 5.1 days and the probability of ED utilization just over 13% in both, and both had a 90-day readmission rate of just over 10%.
Who should be treated at an NCI center?
The data didn’t allow for direct comparison of surgical quality, such as margin status, number of lymph nodes assessed, or postoperative complications, but the postsurgery utilization outcomes “suggest that quality may have been similar,” said Nancy Keating, MD, a health care policy and medicine professor at Harvard Medical School, Boston, in an invited commentary.
The price differences are probably because NCI centers, with their comprehensive offerings, market share, and prestige, can negotiate higher reimbursement rates from insurers, the researchers said.
There is also evidence of better outcomes at NCI centers, particularly for more advanced and complex cases. However, “this study focused on common cancer surgical procedures ... revealing that there is a premium associated with receipt of surgical cancer care at NCI centers.” Further research “is necessary to judge whether and under what circumstances the premium price of NCI centers is justified,” the investigators said.
Dr. Keating noted that “it is likely that some patients benefit from the highly specialized care available at NCI-designated cancer centers ... but it is also likely that many other patients will do equally well regardless of where they receive their care.”
Amid ever-increasing cancer care costs and the need to strategically allocate financial resources, more research is needed to “identify subgroups of patients for whom highly specialized care is particularly necessary to achieve better outcomes. Such data could also be used by payers considering tiered networks and by physician organizations participating in risk contracts for decisions about where to refer patients with cancer for treatment,” she said.
Rectifying a ‘misalignment’
The researchers also said the findings reveal competing incentives, with commercial payers wanting to steer patients away from high-cost hospitals but health systems hoping to maximize surgical volume at lucrative referral centers.
“Value-based or bundled payment reimbursement for surgical episodes, particularly when paired with mandatory reporting on surgical outcomes, could help to rectify this misalignment,” they said.
Out-of-pocket spending wasn’t analyzed in the study, so it’s unknown how the higher prices at NCI centers hit patients in the pocketbook.
Meanwhile, non-NCI academic hospitals also had higher insurer prices paid than community hospitals, but the differences were not statistically significant, nor were differences in the study’s utilization outcomes.
Over half the patients had breast cancer, about one-third had colon cancer, and the rest had lung tumors. Patients treated at NCI centers tended to be younger than those treated at community hospitals and more likely to be women, but comorbidity scores were similar between the groups.
NCI centers, compared with community hospitals, were larger with higher surgical volumes and in more populated areas. They also had higher rates of laparoscopic partial colectomies and pneumonectomies.
Data came from the Health Care Cost Institute’s national commercial claims data set, which includes claims from three of the country’s five largest commercial insurers: Aetna, Humana, and UnitedHealthcare.
The work was funded by the Commonwealth of Pennsylvania and the National Cancer Institute. Dr. Takvorian and Dr. Keating didn’t have any disclosures. One of Dr. Takvorian’s coauthors reported grants and/or personal fees from several sources, including Pfizer, UnitedHealthcare, and Blue Cross Blue Shield of North Carolina.
according to a recent report in JAMA Network Open.
“While acceptable to pay higher prices for care that is expected to be of higher quality, we found no differences in short-term postsurgical outcomes,” said authors led by Samuel Takvorian, MD, a medical oncologist at the University of Pennsylvania, Philadelphia.
The team looked at what insurance companies paid for incident breast, colon, and lung cancer surgeries, which together account for most cancer surgeries, among 66,878 patients treated from 2011 to 2014 at almost 3,000 U.S. hospitals.
Three-quarters had surgery at a community hospital, and 8.3% were treated at one of the nation’s 71 NCI centers, which are recognized by the NCI as meeting rigorous standards in cancer care. The remaining patients were treated at non-NCI academic hospitals.
The mean surgery-specific insurer prices paid at NCI centers was $18,526 versus $14,772 at community hospitals, a difference of $3,755 (P < .001) that was driven primarily by higher facility payments at NCI centers, a mean of $17,704 versus $14,120 at community hospitals.
Mean 90-day postdischarge payments were also $5,744 higher at NCI centers, $47,035 versus $41,291 at community hospitals (P = .006).
The team used postsurgical acute care utilization as a marker of quality but found no differences between the two settings. Mean length of stay was 5.1 days and the probability of ED utilization just over 13% in both, and both had a 90-day readmission rate of just over 10%.
Who should be treated at an NCI center?
The data didn’t allow for direct comparison of surgical quality, such as margin status, number of lymph nodes assessed, or postoperative complications, but the postsurgery utilization outcomes “suggest that quality may have been similar,” said Nancy Keating, MD, a health care policy and medicine professor at Harvard Medical School, Boston, in an invited commentary.
The price differences are probably because NCI centers, with their comprehensive offerings, market share, and prestige, can negotiate higher reimbursement rates from insurers, the researchers said.
There is also evidence of better outcomes at NCI centers, particularly for more advanced and complex cases. However, “this study focused on common cancer surgical procedures ... revealing that there is a premium associated with receipt of surgical cancer care at NCI centers.” Further research “is necessary to judge whether and under what circumstances the premium price of NCI centers is justified,” the investigators said.
Dr. Keating noted that “it is likely that some patients benefit from the highly specialized care available at NCI-designated cancer centers ... but it is also likely that many other patients will do equally well regardless of where they receive their care.”
Amid ever-increasing cancer care costs and the need to strategically allocate financial resources, more research is needed to “identify subgroups of patients for whom highly specialized care is particularly necessary to achieve better outcomes. Such data could also be used by payers considering tiered networks and by physician organizations participating in risk contracts for decisions about where to refer patients with cancer for treatment,” she said.
Rectifying a ‘misalignment’
The researchers also said the findings reveal competing incentives, with commercial payers wanting to steer patients away from high-cost hospitals but health systems hoping to maximize surgical volume at lucrative referral centers.
“Value-based or bundled payment reimbursement for surgical episodes, particularly when paired with mandatory reporting on surgical outcomes, could help to rectify this misalignment,” they said.
Out-of-pocket spending wasn’t analyzed in the study, so it’s unknown how the higher prices at NCI centers hit patients in the pocketbook.
Meanwhile, non-NCI academic hospitals also had higher insurer prices paid than community hospitals, but the differences were not statistically significant, nor were differences in the study’s utilization outcomes.
Over half the patients had breast cancer, about one-third had colon cancer, and the rest had lung tumors. Patients treated at NCI centers tended to be younger than those treated at community hospitals and more likely to be women, but comorbidity scores were similar between the groups.
NCI centers, compared with community hospitals, were larger with higher surgical volumes and in more populated areas. They also had higher rates of laparoscopic partial colectomies and pneumonectomies.
Data came from the Health Care Cost Institute’s national commercial claims data set, which includes claims from three of the country’s five largest commercial insurers: Aetna, Humana, and UnitedHealthcare.
The work was funded by the Commonwealth of Pennsylvania and the National Cancer Institute. Dr. Takvorian and Dr. Keating didn’t have any disclosures. One of Dr. Takvorian’s coauthors reported grants and/or personal fees from several sources, including Pfizer, UnitedHealthcare, and Blue Cross Blue Shield of North Carolina.
according to a recent report in JAMA Network Open.
“While acceptable to pay higher prices for care that is expected to be of higher quality, we found no differences in short-term postsurgical outcomes,” said authors led by Samuel Takvorian, MD, a medical oncologist at the University of Pennsylvania, Philadelphia.
The team looked at what insurance companies paid for incident breast, colon, and lung cancer surgeries, which together account for most cancer surgeries, among 66,878 patients treated from 2011 to 2014 at almost 3,000 U.S. hospitals.
Three-quarters had surgery at a community hospital, and 8.3% were treated at one of the nation’s 71 NCI centers, which are recognized by the NCI as meeting rigorous standards in cancer care. The remaining patients were treated at non-NCI academic hospitals.
The mean surgery-specific insurer prices paid at NCI centers was $18,526 versus $14,772 at community hospitals, a difference of $3,755 (P < .001) that was driven primarily by higher facility payments at NCI centers, a mean of $17,704 versus $14,120 at community hospitals.
Mean 90-day postdischarge payments were also $5,744 higher at NCI centers, $47,035 versus $41,291 at community hospitals (P = .006).
The team used postsurgical acute care utilization as a marker of quality but found no differences between the two settings. Mean length of stay was 5.1 days and the probability of ED utilization just over 13% in both, and both had a 90-day readmission rate of just over 10%.
Who should be treated at an NCI center?
The data didn’t allow for direct comparison of surgical quality, such as margin status, number of lymph nodes assessed, or postoperative complications, but the postsurgery utilization outcomes “suggest that quality may have been similar,” said Nancy Keating, MD, a health care policy and medicine professor at Harvard Medical School, Boston, in an invited commentary.
The price differences are probably because NCI centers, with their comprehensive offerings, market share, and prestige, can negotiate higher reimbursement rates from insurers, the researchers said.
There is also evidence of better outcomes at NCI centers, particularly for more advanced and complex cases. However, “this study focused on common cancer surgical procedures ... revealing that there is a premium associated with receipt of surgical cancer care at NCI centers.” Further research “is necessary to judge whether and under what circumstances the premium price of NCI centers is justified,” the investigators said.
Dr. Keating noted that “it is likely that some patients benefit from the highly specialized care available at NCI-designated cancer centers ... but it is also likely that many other patients will do equally well regardless of where they receive their care.”
Amid ever-increasing cancer care costs and the need to strategically allocate financial resources, more research is needed to “identify subgroups of patients for whom highly specialized care is particularly necessary to achieve better outcomes. Such data could also be used by payers considering tiered networks and by physician organizations participating in risk contracts for decisions about where to refer patients with cancer for treatment,” she said.
Rectifying a ‘misalignment’
The researchers also said the findings reveal competing incentives, with commercial payers wanting to steer patients away from high-cost hospitals but health systems hoping to maximize surgical volume at lucrative referral centers.
“Value-based or bundled payment reimbursement for surgical episodes, particularly when paired with mandatory reporting on surgical outcomes, could help to rectify this misalignment,” they said.
Out-of-pocket spending wasn’t analyzed in the study, so it’s unknown how the higher prices at NCI centers hit patients in the pocketbook.
Meanwhile, non-NCI academic hospitals also had higher insurer prices paid than community hospitals, but the differences were not statistically significant, nor were differences in the study’s utilization outcomes.
Over half the patients had breast cancer, about one-third had colon cancer, and the rest had lung tumors. Patients treated at NCI centers tended to be younger than those treated at community hospitals and more likely to be women, but comorbidity scores were similar between the groups.
NCI centers, compared with community hospitals, were larger with higher surgical volumes and in more populated areas. They also had higher rates of laparoscopic partial colectomies and pneumonectomies.
Data came from the Health Care Cost Institute’s national commercial claims data set, which includes claims from three of the country’s five largest commercial insurers: Aetna, Humana, and UnitedHealthcare.
The work was funded by the Commonwealth of Pennsylvania and the National Cancer Institute. Dr. Takvorian and Dr. Keating didn’t have any disclosures. One of Dr. Takvorian’s coauthors reported grants and/or personal fees from several sources, including Pfizer, UnitedHealthcare, and Blue Cross Blue Shield of North Carolina.
FROM JAMA NETWORK OPEN
Volunteer Opportunities Within Dermatology: More than Skin Deep
The adage “so much to do, so little time” aptly describes the daily challenges facing dermatologists and dermatology residents. The time and attention required by direct patient care, writing notes, navigating electronic health records, and engaging in education and research as well as family commitments can drain even the most tireless clinician. In addition, dermatologists are expected to play a critical role in clinic and practice management to successfully curate an online presence and adapt their skills to successfully manage a teledermatology practice. Coupled with the time spent socializing with friends or colleagues and time for personal hobbies or exercise, it’s easy to see how sleep deprivation is common in many of our colleagues.
What’s being left out of these jam-packed schedules? Increasingly, it is the time and expertise dedicated to volunteering in our local communities. Two recent research letters highlighted how a dramatic increase in the number of research projects and publications is not mirrored by a similar increase in volunteer experiences as dermatology residency selection becomes more competitive.1,2
Although the rate of volunteerism among practicing dermatologists has yet to be studied, a brief review suggests a component of unmet dermatology need within our communities. It’s estimated that approximately 5% to 10% of all emergency department visits are for dermatologic concerns.3-5 In many cases, the reason for the visit is nonurgent and instead reflects a lack of other options for care. However, the need for dermatologists extends beyond the emergency department setting. A review of the prevalence of patients presenting for care to a group of regional free clinics found that 8% (N=5553) of all visitors sought care for dermatologic concerns.6 The benefit is not just for those seated on the examination table; research has shown that while many of the underlying factors resulting in physician burnout stem from systemic issues, participating in volunteer opportunities helps combat burnout in ourselves and our colleagues.7-9 Herein, opportunities that exist for dermatologists to reconnect with their communities, advocate for causes distinctive to the specialty, and care for neighbors most in need are highlighted.
Camp Wonder
Every year, children from across the United States living with chronic and debilitating skin conditions get the opportunity to join fellow campers and spend a week just being kids without the constant focus on being a patient. Camp Wonder’s founder and director, Francesca Tenconi, describes the camp as a place where kids “can form a community and can feel free to be themselves, without judgment, without stares. They get the chance to forget about their skin disease and be themselves” (oral communication, June 18, 2021). Tenconi and the camp’s cofounders and medical directors, Drs. Jenny Kim and Stefani Takahashi, envisioned the camp as a place for all campers regardless of their skin condition to feel safe and welcome. This overall mission guides camp leadership and staff every year over the course of the camp week where campers participate in a mix of traditional and nontraditional summer activities that are safe and accessible for all, from spending time in the pool to arts and crafts and a ropes course.
Camp Wonder is in its 21st year of hosting children and adolescents from across North America at its camp in Livermore, California. This year, Tenconi expects about 100 campers during the last week in July. Camp Wonder relies on medical staff volunteers to make the camp setting safe, inclusive, and fun. “Our dermatology residents and dermatology volunteers are a huge part of why we’re able to have camp,” said Tenconi. “A lot of our kids require very specific medical care throughout the week. We are able to provide this camp experience for them because we have this medical support system available, this specialized dermatology knowledge.” She also noted the benefit to the volunteers themselves, saying,“The feedback we get a lot from residents and dermatologists is that camp gave them a chance to understand the true-life impact of some of the skin diseases these kids and families are living with. Kids will open up to them and tell them how their disease has impacted them personally” (oral communication, June 18, 2021).
Volunteer medical providers help manage the medical needs of the campers beginning at check-in and work shifts in the infirmary as well as help with dispensing and administering medications, changing dressings, and applying ointments or other topical medications. When not assisting with medical care, medical staff can get to know the campers; help out with arts and crafts, games, sports, and other camp activities; and put on skits and plays for campers at nightly camp hangouts (Figure 1).

How to Get Involved
Visit the website (https://www.csdf.org/camp-wonder) for information on becoming a medical volunteer for 2022. Donations to help keep the camp running also are greatly appreciated, as attendance, including travel costs, is free for families through the Children’s Skin Disease Foundation. Finally, dermatologists can help by keeping their young patients with skin disease in mind as future campers. The camp welcomes kids from across the United States and Canada and invites questions from dermatologists and families on how to become a camper and what the experience is like.
Native American Health Services Rotation
Located in the southwestern United States, the Navajo Nation is North America’s largest Native American tribe by enrollment and resides on the largest reservation in the United States.10 Comprised of 27,000 square miles within portions of Arizona, New Mexico, and Utah, the reservation’s total area is greater than that of Massachusetts, Vermont, and New Hampshire combined.11 The reservation is home to an estimated 180,000 Navajo people, a population roughly the size of Salt Lake City, Utah. Yet, many homes on the reservation are without electricity, running water, telephones, or broadband access, and many roads on the reservation remain unpaved. Prior to the COVID-19 pandemic, 4 dermatology residents were selected each year to travel to this unique and remote location to work with the staff of the Chinle Comprehensive Health Care Facility (Chinle, Arizona), an Indian Health Service facility, as part of the American Academy of Dermatology (AAD)–sponsored Native American Health Services Resident Rotation (NAHSRR).
Dr. Lucinda Kohn, Assistant Professor of Dermatology at the University of Colorado and the director of the NAHSRR program discovered the value of this rotation firsthand as a dermatology resident. In 2017, she traveled to the area to spend 2 weeks serving within the community. “I went because of a personal connection. My husband is Native American, although not Navajo. I wanted to experience what it was like to provide dermatologic care for Native Americans. I found the Navajo people to be so friendly and so grateful for our care. The clinicians we worked with at Chinle were excited to have us share our expertise and to pass on their knowledge to us,” said Dr. Kohn (personal communication, June 24, 2021).
Rotating residents provide dermatologic care for the Navajo people and share their unique medical skill set to local primary care clinicians serving as preceptors. They also may have an opportunity to learn from Native healers about traditional Navajo beliefs and ceremonies used as part of a holistic approach to healing.
The program, similar to volunteer programs across the country, was put on hold during the height of the COVID-19 pandemic. “The Navajo nation witnessed a really tragic surge of COVID cases that required that limited medical resources be diverted to help cope with the pandemic,” says Dr. Kohn. “It really wasn’t safe for residents to travel to the reservation either, so the rotation had to be put on hold.” However, in April 2021, the health care staff of the Chinle Comprehensive Care Facility reached out to revive the program, which is now pending the green light from the AAD. It is unclear if or when AAD leadership will allow this rotation to restart. Dr. Kohn hopes to be able to start accepting new applications soon. “This rotation provides a wealth of benefits to all those involved, from the residents who get the chance to work with a unique population in need to the clinicians who gain a diverse understanding of dermatology treatment techniques. And of course, for the patients, who are so appreciative of the care they receive from our volunteers” (personal communication, June 25, 2021).
How to Get Involved
Dr. Kohn is happy to field questions regarding the rotation and requests for more information via email ([email protected]). Residents interested in this program also may reach out to the AAD’s Education and Volunteers Abroad Committee to express interest in the NAHSRR program’s reinstatement.
Destination Healthy Skin
Since 2017, the Skin Cancer Foundation’s Destination Healthy Skin (DHS) RV has been the setting for more than 3800 free skin cancer screenings provided by volunteers within underserved populations across the United States (Figure 2). After a year hiatus due to the pandemic, DHS hit the road again, starting in New York City on August 1 to 3, 2021. From there, the DHS RV will traverse the country in one large loop, starting with visits to large and small cities in the Midwest and the West Coast. Following a visit to San Diego, California, in early October, the RV will turn east, with stops in Arizona, Texas, and several southern states before ending in Philadelphia, Pennsylvania. Dr. Elizabeth Hale, Senior Vice President of the Skin Cancer Foundation, feels that increasing awareness of the importance of regular skin cancer screening for those at risk is more important than ever. “We know that many people in the past year put routine cancer screening on the back burner, but we’re beginning to appreciate that this has led to significant delays in skin cancer diagnosis and potentially more significant disease when cases are diagnosed.” Dr. Hale noted that as the country continues to return to a degree of normalcy, the backlog of patients now seeking their routine screening has led to longer wait times. She expects DHS may offer some relief. “There are no appointments necessary. If the RV is close to their hometown, patients have an advantage in being able to be seen first come, first served, without having to wait for an appointment or make sure their insurance is accepted. It’s a free screening that can increase access to dermatologists” (personal communication, June 21, 2021).

The program’s organizers acknowledge that DHS is not a long-term solution for improving dermatology access in the United States and recognize that more needs to be done to raise awareness, both of the value that screenings can provide and the importance of sun-protective behavior. “This is an important first step,” says Dr. Hale. “It’s important that we disseminate that no one is immune to skin cancer. It’s about education, and this is a tool to educate patients that everyone should have a skin check once a year, regardless of where you live or what your skin type is” (personal communication, June 21, 2021).
Volunteer dermatologists are needed to assist with screenings when the DHS RV arrives in their community. Providers complete a screening form identifying any concerning lesions and can document specific lesions using the patient’s cell phone. Following the screenings, participating dermatologists are welcome to invite participants to make appointments at their practices or suggest local clinics for follow-up care.
How to Get Involved
The schedule for this year’s screening events can be found online (https://www.skincancer.org/early-detection/destination-healthy-skin/). Consider volunteering (https://www.skincancer.org/early-detection/destination-healthy-skin/physician-volunteers/) or helping to raise awareness by reaching out to local dermatology societies or free clinics in your area. Residents and physician’s assistants are welcome to volunteer as well, as long as they are under the on-site supervision of a board-certified dermatologist.
Final Thoughts
As medical professionals, we all recognize there are valuable contributions we can make to groups and organizations that need our help. The stresses and pressure of work and everyday life can make finding the time to offer that help seem impossible. Although it may seem counterintuitive, volunteering our time to help others can help us better navigate the professional burnout that many medical professionals experience today.
- Ezekor M, Pona A, Cline A, et al. An increasing trend in the number of publications and research projects among dermatology residency applicants. J Am Acad Dermatol. 2020;83:214-216.
- Atluri S, Seivright JR, Shi VY, et al. Volunteer and work experiences among dermatology residency applicants. J Am Acad Dermatol. 2021;84:E97-E98.
- Abokwidir M, Davis SA, Fleischer AB, et al. Use of the emergency department for dermatologic care in the United States by ethnic group. J Dermatolog Treat. 2015;26:392-394.
- Uscher-Pines L, Pines J, Kellermann A, et al. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19:47-59.
- Jack AR, Spence AA, Nichols BJ, et al. Cutaneous conditions leading to dermatology consultations in the emergency department. West J Emerg Med. 2011;12:551-555.
- Ayoubi N, Mirza A-S, Swanson J, et al. Dermatologic care of uninsured patients managed at free clinics. J Am Acad Dermatol. 2019;81:433-437.
- Wright AA, Katz IT. Beyond burnout—redesigning care to restore meaning and sanity for physicians. N Engl J Med. 2018;378:309-311.
- Bull C, Aucoin JB. Voluntary association participation and life satisfaction: a replication note. J Gerontol. 1975;30:73-76.
- Iserson KV. Burnout syndrome: global medicine volunteering as a possible treatment strategy. J Emerg Med. 2018;54:516-521.
- Romero S. Navajo Nation becomes largest tribe in U.S. after pandemic enrollment surge. New York Times. May 21, 2021. Accessed August 19, 2021. https://www.nytimes.com/2021/05/21/us/navajo-cherokee-population.html
- Moore GR, Benally J, Tuttle S. The Navajo Nation: quick facts. University of Arizona website. Accessed August 19, 2021. https://extension.arizona.edu/sites/extension.arizona.edu/files/pubs/az1471.pdf
The adage “so much to do, so little time” aptly describes the daily challenges facing dermatologists and dermatology residents. The time and attention required by direct patient care, writing notes, navigating electronic health records, and engaging in education and research as well as family commitments can drain even the most tireless clinician. In addition, dermatologists are expected to play a critical role in clinic and practice management to successfully curate an online presence and adapt their skills to successfully manage a teledermatology practice. Coupled with the time spent socializing with friends or colleagues and time for personal hobbies or exercise, it’s easy to see how sleep deprivation is common in many of our colleagues.
What’s being left out of these jam-packed schedules? Increasingly, it is the time and expertise dedicated to volunteering in our local communities. Two recent research letters highlighted how a dramatic increase in the number of research projects and publications is not mirrored by a similar increase in volunteer experiences as dermatology residency selection becomes more competitive.1,2
Although the rate of volunteerism among practicing dermatologists has yet to be studied, a brief review suggests a component of unmet dermatology need within our communities. It’s estimated that approximately 5% to 10% of all emergency department visits are for dermatologic concerns.3-5 In many cases, the reason for the visit is nonurgent and instead reflects a lack of other options for care. However, the need for dermatologists extends beyond the emergency department setting. A review of the prevalence of patients presenting for care to a group of regional free clinics found that 8% (N=5553) of all visitors sought care for dermatologic concerns.6 The benefit is not just for those seated on the examination table; research has shown that while many of the underlying factors resulting in physician burnout stem from systemic issues, participating in volunteer opportunities helps combat burnout in ourselves and our colleagues.7-9 Herein, opportunities that exist for dermatologists to reconnect with their communities, advocate for causes distinctive to the specialty, and care for neighbors most in need are highlighted.
Camp Wonder
Every year, children from across the United States living with chronic and debilitating skin conditions get the opportunity to join fellow campers and spend a week just being kids without the constant focus on being a patient. Camp Wonder’s founder and director, Francesca Tenconi, describes the camp as a place where kids “can form a community and can feel free to be themselves, without judgment, without stares. They get the chance to forget about their skin disease and be themselves” (oral communication, June 18, 2021). Tenconi and the camp’s cofounders and medical directors, Drs. Jenny Kim and Stefani Takahashi, envisioned the camp as a place for all campers regardless of their skin condition to feel safe and welcome. This overall mission guides camp leadership and staff every year over the course of the camp week where campers participate in a mix of traditional and nontraditional summer activities that are safe and accessible for all, from spending time in the pool to arts and crafts and a ropes course.
Camp Wonder is in its 21st year of hosting children and adolescents from across North America at its camp in Livermore, California. This year, Tenconi expects about 100 campers during the last week in July. Camp Wonder relies on medical staff volunteers to make the camp setting safe, inclusive, and fun. “Our dermatology residents and dermatology volunteers are a huge part of why we’re able to have camp,” said Tenconi. “A lot of our kids require very specific medical care throughout the week. We are able to provide this camp experience for them because we have this medical support system available, this specialized dermatology knowledge.” She also noted the benefit to the volunteers themselves, saying,“The feedback we get a lot from residents and dermatologists is that camp gave them a chance to understand the true-life impact of some of the skin diseases these kids and families are living with. Kids will open up to them and tell them how their disease has impacted them personally” (oral communication, June 18, 2021).
Volunteer medical providers help manage the medical needs of the campers beginning at check-in and work shifts in the infirmary as well as help with dispensing and administering medications, changing dressings, and applying ointments or other topical medications. When not assisting with medical care, medical staff can get to know the campers; help out with arts and crafts, games, sports, and other camp activities; and put on skits and plays for campers at nightly camp hangouts (Figure 1).

How to Get Involved
Visit the website (https://www.csdf.org/camp-wonder) for information on becoming a medical volunteer for 2022. Donations to help keep the camp running also are greatly appreciated, as attendance, including travel costs, is free for families through the Children’s Skin Disease Foundation. Finally, dermatologists can help by keeping their young patients with skin disease in mind as future campers. The camp welcomes kids from across the United States and Canada and invites questions from dermatologists and families on how to become a camper and what the experience is like.
Native American Health Services Rotation
Located in the southwestern United States, the Navajo Nation is North America’s largest Native American tribe by enrollment and resides on the largest reservation in the United States.10 Comprised of 27,000 square miles within portions of Arizona, New Mexico, and Utah, the reservation’s total area is greater than that of Massachusetts, Vermont, and New Hampshire combined.11 The reservation is home to an estimated 180,000 Navajo people, a population roughly the size of Salt Lake City, Utah. Yet, many homes on the reservation are without electricity, running water, telephones, or broadband access, and many roads on the reservation remain unpaved. Prior to the COVID-19 pandemic, 4 dermatology residents were selected each year to travel to this unique and remote location to work with the staff of the Chinle Comprehensive Health Care Facility (Chinle, Arizona), an Indian Health Service facility, as part of the American Academy of Dermatology (AAD)–sponsored Native American Health Services Resident Rotation (NAHSRR).
Dr. Lucinda Kohn, Assistant Professor of Dermatology at the University of Colorado and the director of the NAHSRR program discovered the value of this rotation firsthand as a dermatology resident. In 2017, she traveled to the area to spend 2 weeks serving within the community. “I went because of a personal connection. My husband is Native American, although not Navajo. I wanted to experience what it was like to provide dermatologic care for Native Americans. I found the Navajo people to be so friendly and so grateful for our care. The clinicians we worked with at Chinle were excited to have us share our expertise and to pass on their knowledge to us,” said Dr. Kohn (personal communication, June 24, 2021).
Rotating residents provide dermatologic care for the Navajo people and share their unique medical skill set to local primary care clinicians serving as preceptors. They also may have an opportunity to learn from Native healers about traditional Navajo beliefs and ceremonies used as part of a holistic approach to healing.
The program, similar to volunteer programs across the country, was put on hold during the height of the COVID-19 pandemic. “The Navajo nation witnessed a really tragic surge of COVID cases that required that limited medical resources be diverted to help cope with the pandemic,” says Dr. Kohn. “It really wasn’t safe for residents to travel to the reservation either, so the rotation had to be put on hold.” However, in April 2021, the health care staff of the Chinle Comprehensive Care Facility reached out to revive the program, which is now pending the green light from the AAD. It is unclear if or when AAD leadership will allow this rotation to restart. Dr. Kohn hopes to be able to start accepting new applications soon. “This rotation provides a wealth of benefits to all those involved, from the residents who get the chance to work with a unique population in need to the clinicians who gain a diverse understanding of dermatology treatment techniques. And of course, for the patients, who are so appreciative of the care they receive from our volunteers” (personal communication, June 25, 2021).
How to Get Involved
Dr. Kohn is happy to field questions regarding the rotation and requests for more information via email ([email protected]). Residents interested in this program also may reach out to the AAD’s Education and Volunteers Abroad Committee to express interest in the NAHSRR program’s reinstatement.
Destination Healthy Skin
Since 2017, the Skin Cancer Foundation’s Destination Healthy Skin (DHS) RV has been the setting for more than 3800 free skin cancer screenings provided by volunteers within underserved populations across the United States (Figure 2). After a year hiatus due to the pandemic, DHS hit the road again, starting in New York City on August 1 to 3, 2021. From there, the DHS RV will traverse the country in one large loop, starting with visits to large and small cities in the Midwest and the West Coast. Following a visit to San Diego, California, in early October, the RV will turn east, with stops in Arizona, Texas, and several southern states before ending in Philadelphia, Pennsylvania. Dr. Elizabeth Hale, Senior Vice President of the Skin Cancer Foundation, feels that increasing awareness of the importance of regular skin cancer screening for those at risk is more important than ever. “We know that many people in the past year put routine cancer screening on the back burner, but we’re beginning to appreciate that this has led to significant delays in skin cancer diagnosis and potentially more significant disease when cases are diagnosed.” Dr. Hale noted that as the country continues to return to a degree of normalcy, the backlog of patients now seeking their routine screening has led to longer wait times. She expects DHS may offer some relief. “There are no appointments necessary. If the RV is close to their hometown, patients have an advantage in being able to be seen first come, first served, without having to wait for an appointment or make sure their insurance is accepted. It’s a free screening that can increase access to dermatologists” (personal communication, June 21, 2021).

The program’s organizers acknowledge that DHS is not a long-term solution for improving dermatology access in the United States and recognize that more needs to be done to raise awareness, both of the value that screenings can provide and the importance of sun-protective behavior. “This is an important first step,” says Dr. Hale. “It’s important that we disseminate that no one is immune to skin cancer. It’s about education, and this is a tool to educate patients that everyone should have a skin check once a year, regardless of where you live or what your skin type is” (personal communication, June 21, 2021).
Volunteer dermatologists are needed to assist with screenings when the DHS RV arrives in their community. Providers complete a screening form identifying any concerning lesions and can document specific lesions using the patient’s cell phone. Following the screenings, participating dermatologists are welcome to invite participants to make appointments at their practices or suggest local clinics for follow-up care.
How to Get Involved
The schedule for this year’s screening events can be found online (https://www.skincancer.org/early-detection/destination-healthy-skin/). Consider volunteering (https://www.skincancer.org/early-detection/destination-healthy-skin/physician-volunteers/) or helping to raise awareness by reaching out to local dermatology societies or free clinics in your area. Residents and physician’s assistants are welcome to volunteer as well, as long as they are under the on-site supervision of a board-certified dermatologist.
Final Thoughts
As medical professionals, we all recognize there are valuable contributions we can make to groups and organizations that need our help. The stresses and pressure of work and everyday life can make finding the time to offer that help seem impossible. Although it may seem counterintuitive, volunteering our time to help others can help us better navigate the professional burnout that many medical professionals experience today.
The adage “so much to do, so little time” aptly describes the daily challenges facing dermatologists and dermatology residents. The time and attention required by direct patient care, writing notes, navigating electronic health records, and engaging in education and research as well as family commitments can drain even the most tireless clinician. In addition, dermatologists are expected to play a critical role in clinic and practice management to successfully curate an online presence and adapt their skills to successfully manage a teledermatology practice. Coupled with the time spent socializing with friends or colleagues and time for personal hobbies or exercise, it’s easy to see how sleep deprivation is common in many of our colleagues.
What’s being left out of these jam-packed schedules? Increasingly, it is the time and expertise dedicated to volunteering in our local communities. Two recent research letters highlighted how a dramatic increase in the number of research projects and publications is not mirrored by a similar increase in volunteer experiences as dermatology residency selection becomes more competitive.1,2
Although the rate of volunteerism among practicing dermatologists has yet to be studied, a brief review suggests a component of unmet dermatology need within our communities. It’s estimated that approximately 5% to 10% of all emergency department visits are for dermatologic concerns.3-5 In many cases, the reason for the visit is nonurgent and instead reflects a lack of other options for care. However, the need for dermatologists extends beyond the emergency department setting. A review of the prevalence of patients presenting for care to a group of regional free clinics found that 8% (N=5553) of all visitors sought care for dermatologic concerns.6 The benefit is not just for those seated on the examination table; research has shown that while many of the underlying factors resulting in physician burnout stem from systemic issues, participating in volunteer opportunities helps combat burnout in ourselves and our colleagues.7-9 Herein, opportunities that exist for dermatologists to reconnect with their communities, advocate for causes distinctive to the specialty, and care for neighbors most in need are highlighted.
Camp Wonder
Every year, children from across the United States living with chronic and debilitating skin conditions get the opportunity to join fellow campers and spend a week just being kids without the constant focus on being a patient. Camp Wonder’s founder and director, Francesca Tenconi, describes the camp as a place where kids “can form a community and can feel free to be themselves, without judgment, without stares. They get the chance to forget about their skin disease and be themselves” (oral communication, June 18, 2021). Tenconi and the camp’s cofounders and medical directors, Drs. Jenny Kim and Stefani Takahashi, envisioned the camp as a place for all campers regardless of their skin condition to feel safe and welcome. This overall mission guides camp leadership and staff every year over the course of the camp week where campers participate in a mix of traditional and nontraditional summer activities that are safe and accessible for all, from spending time in the pool to arts and crafts and a ropes course.
Camp Wonder is in its 21st year of hosting children and adolescents from across North America at its camp in Livermore, California. This year, Tenconi expects about 100 campers during the last week in July. Camp Wonder relies on medical staff volunteers to make the camp setting safe, inclusive, and fun. “Our dermatology residents and dermatology volunteers are a huge part of why we’re able to have camp,” said Tenconi. “A lot of our kids require very specific medical care throughout the week. We are able to provide this camp experience for them because we have this medical support system available, this specialized dermatology knowledge.” She also noted the benefit to the volunteers themselves, saying,“The feedback we get a lot from residents and dermatologists is that camp gave them a chance to understand the true-life impact of some of the skin diseases these kids and families are living with. Kids will open up to them and tell them how their disease has impacted them personally” (oral communication, June 18, 2021).
Volunteer medical providers help manage the medical needs of the campers beginning at check-in and work shifts in the infirmary as well as help with dispensing and administering medications, changing dressings, and applying ointments or other topical medications. When not assisting with medical care, medical staff can get to know the campers; help out with arts and crafts, games, sports, and other camp activities; and put on skits and plays for campers at nightly camp hangouts (Figure 1).

How to Get Involved
Visit the website (https://www.csdf.org/camp-wonder) for information on becoming a medical volunteer for 2022. Donations to help keep the camp running also are greatly appreciated, as attendance, including travel costs, is free for families through the Children’s Skin Disease Foundation. Finally, dermatologists can help by keeping their young patients with skin disease in mind as future campers. The camp welcomes kids from across the United States and Canada and invites questions from dermatologists and families on how to become a camper and what the experience is like.
Native American Health Services Rotation
Located in the southwestern United States, the Navajo Nation is North America’s largest Native American tribe by enrollment and resides on the largest reservation in the United States.10 Comprised of 27,000 square miles within portions of Arizona, New Mexico, and Utah, the reservation’s total area is greater than that of Massachusetts, Vermont, and New Hampshire combined.11 The reservation is home to an estimated 180,000 Navajo people, a population roughly the size of Salt Lake City, Utah. Yet, many homes on the reservation are without electricity, running water, telephones, or broadband access, and many roads on the reservation remain unpaved. Prior to the COVID-19 pandemic, 4 dermatology residents were selected each year to travel to this unique and remote location to work with the staff of the Chinle Comprehensive Health Care Facility (Chinle, Arizona), an Indian Health Service facility, as part of the American Academy of Dermatology (AAD)–sponsored Native American Health Services Resident Rotation (NAHSRR).
Dr. Lucinda Kohn, Assistant Professor of Dermatology at the University of Colorado and the director of the NAHSRR program discovered the value of this rotation firsthand as a dermatology resident. In 2017, she traveled to the area to spend 2 weeks serving within the community. “I went because of a personal connection. My husband is Native American, although not Navajo. I wanted to experience what it was like to provide dermatologic care for Native Americans. I found the Navajo people to be so friendly and so grateful for our care. The clinicians we worked with at Chinle were excited to have us share our expertise and to pass on their knowledge to us,” said Dr. Kohn (personal communication, June 24, 2021).
Rotating residents provide dermatologic care for the Navajo people and share their unique medical skill set to local primary care clinicians serving as preceptors. They also may have an opportunity to learn from Native healers about traditional Navajo beliefs and ceremonies used as part of a holistic approach to healing.
The program, similar to volunteer programs across the country, was put on hold during the height of the COVID-19 pandemic. “The Navajo nation witnessed a really tragic surge of COVID cases that required that limited medical resources be diverted to help cope with the pandemic,” says Dr. Kohn. “It really wasn’t safe for residents to travel to the reservation either, so the rotation had to be put on hold.” However, in April 2021, the health care staff of the Chinle Comprehensive Care Facility reached out to revive the program, which is now pending the green light from the AAD. It is unclear if or when AAD leadership will allow this rotation to restart. Dr. Kohn hopes to be able to start accepting new applications soon. “This rotation provides a wealth of benefits to all those involved, from the residents who get the chance to work with a unique population in need to the clinicians who gain a diverse understanding of dermatology treatment techniques. And of course, for the patients, who are so appreciative of the care they receive from our volunteers” (personal communication, June 25, 2021).
How to Get Involved
Dr. Kohn is happy to field questions regarding the rotation and requests for more information via email ([email protected]). Residents interested in this program also may reach out to the AAD’s Education and Volunteers Abroad Committee to express interest in the NAHSRR program’s reinstatement.
Destination Healthy Skin
Since 2017, the Skin Cancer Foundation’s Destination Healthy Skin (DHS) RV has been the setting for more than 3800 free skin cancer screenings provided by volunteers within underserved populations across the United States (Figure 2). After a year hiatus due to the pandemic, DHS hit the road again, starting in New York City on August 1 to 3, 2021. From there, the DHS RV will traverse the country in one large loop, starting with visits to large and small cities in the Midwest and the West Coast. Following a visit to San Diego, California, in early October, the RV will turn east, with stops in Arizona, Texas, and several southern states before ending in Philadelphia, Pennsylvania. Dr. Elizabeth Hale, Senior Vice President of the Skin Cancer Foundation, feels that increasing awareness of the importance of regular skin cancer screening for those at risk is more important than ever. “We know that many people in the past year put routine cancer screening on the back burner, but we’re beginning to appreciate that this has led to significant delays in skin cancer diagnosis and potentially more significant disease when cases are diagnosed.” Dr. Hale noted that as the country continues to return to a degree of normalcy, the backlog of patients now seeking their routine screening has led to longer wait times. She expects DHS may offer some relief. “There are no appointments necessary. If the RV is close to their hometown, patients have an advantage in being able to be seen first come, first served, without having to wait for an appointment or make sure their insurance is accepted. It’s a free screening that can increase access to dermatologists” (personal communication, June 21, 2021).

The program’s organizers acknowledge that DHS is not a long-term solution for improving dermatology access in the United States and recognize that more needs to be done to raise awareness, both of the value that screenings can provide and the importance of sun-protective behavior. “This is an important first step,” says Dr. Hale. “It’s important that we disseminate that no one is immune to skin cancer. It’s about education, and this is a tool to educate patients that everyone should have a skin check once a year, regardless of where you live or what your skin type is” (personal communication, June 21, 2021).
Volunteer dermatologists are needed to assist with screenings when the DHS RV arrives in their community. Providers complete a screening form identifying any concerning lesions and can document specific lesions using the patient’s cell phone. Following the screenings, participating dermatologists are welcome to invite participants to make appointments at their practices or suggest local clinics for follow-up care.
How to Get Involved
The schedule for this year’s screening events can be found online (https://www.skincancer.org/early-detection/destination-healthy-skin/). Consider volunteering (https://www.skincancer.org/early-detection/destination-healthy-skin/physician-volunteers/) or helping to raise awareness by reaching out to local dermatology societies or free clinics in your area. Residents and physician’s assistants are welcome to volunteer as well, as long as they are under the on-site supervision of a board-certified dermatologist.
Final Thoughts
As medical professionals, we all recognize there are valuable contributions we can make to groups and organizations that need our help. The stresses and pressure of work and everyday life can make finding the time to offer that help seem impossible. Although it may seem counterintuitive, volunteering our time to help others can help us better navigate the professional burnout that many medical professionals experience today.
- Ezekor M, Pona A, Cline A, et al. An increasing trend in the number of publications and research projects among dermatology residency applicants. J Am Acad Dermatol. 2020;83:214-216.
- Atluri S, Seivright JR, Shi VY, et al. Volunteer and work experiences among dermatology residency applicants. J Am Acad Dermatol. 2021;84:E97-E98.
- Abokwidir M, Davis SA, Fleischer AB, et al. Use of the emergency department for dermatologic care in the United States by ethnic group. J Dermatolog Treat. 2015;26:392-394.
- Uscher-Pines L, Pines J, Kellermann A, et al. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19:47-59.
- Jack AR, Spence AA, Nichols BJ, et al. Cutaneous conditions leading to dermatology consultations in the emergency department. West J Emerg Med. 2011;12:551-555.
- Ayoubi N, Mirza A-S, Swanson J, et al. Dermatologic care of uninsured patients managed at free clinics. J Am Acad Dermatol. 2019;81:433-437.
- Wright AA, Katz IT. Beyond burnout—redesigning care to restore meaning and sanity for physicians. N Engl J Med. 2018;378:309-311.
- Bull C, Aucoin JB. Voluntary association participation and life satisfaction: a replication note. J Gerontol. 1975;30:73-76.
- Iserson KV. Burnout syndrome: global medicine volunteering as a possible treatment strategy. J Emerg Med. 2018;54:516-521.
- Romero S. Navajo Nation becomes largest tribe in U.S. after pandemic enrollment surge. New York Times. May 21, 2021. Accessed August 19, 2021. https://www.nytimes.com/2021/05/21/us/navajo-cherokee-population.html
- Moore GR, Benally J, Tuttle S. The Navajo Nation: quick facts. University of Arizona website. Accessed August 19, 2021. https://extension.arizona.edu/sites/extension.arizona.edu/files/pubs/az1471.pdf
- Ezekor M, Pona A, Cline A, et al. An increasing trend in the number of publications and research projects among dermatology residency applicants. J Am Acad Dermatol. 2020;83:214-216.
- Atluri S, Seivright JR, Shi VY, et al. Volunteer and work experiences among dermatology residency applicants. J Am Acad Dermatol. 2021;84:E97-E98.
- Abokwidir M, Davis SA, Fleischer AB, et al. Use of the emergency department for dermatologic care in the United States by ethnic group. J Dermatolog Treat. 2015;26:392-394.
- Uscher-Pines L, Pines J, Kellermann A, et al. Emergency department visits for nonurgent conditions: systematic literature review. Am J Manag Care. 2013;19:47-59.
- Jack AR, Spence AA, Nichols BJ, et al. Cutaneous conditions leading to dermatology consultations in the emergency department. West J Emerg Med. 2011;12:551-555.
- Ayoubi N, Mirza A-S, Swanson J, et al. Dermatologic care of uninsured patients managed at free clinics. J Am Acad Dermatol. 2019;81:433-437.
- Wright AA, Katz IT. Beyond burnout—redesigning care to restore meaning and sanity for physicians. N Engl J Med. 2018;378:309-311.
- Bull C, Aucoin JB. Voluntary association participation and life satisfaction: a replication note. J Gerontol. 1975;30:73-76.
- Iserson KV. Burnout syndrome: global medicine volunteering as a possible treatment strategy. J Emerg Med. 2018;54:516-521.
- Romero S. Navajo Nation becomes largest tribe in U.S. after pandemic enrollment surge. New York Times. May 21, 2021. Accessed August 19, 2021. https://www.nytimes.com/2021/05/21/us/navajo-cherokee-population.html
- Moore GR, Benally J, Tuttle S. The Navajo Nation: quick facts. University of Arizona website. Accessed August 19, 2021. https://extension.arizona.edu/sites/extension.arizona.edu/files/pubs/az1471.pdf
Resident Pearl
- Volunteerism rates among dermatology residents seem to be decreasing. We should work to combat this trend by finding ways to give back to our communities and spur our colleagues to do the same.
Report urges complete residency overhaul
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
from the Graduate Medical Education Review Committee (UGRC) of the Coalition for Physician Accountability.
The 275-page report presents preliminary findings that were released in April 2021 and a long list of stakeholder comments. According to the report, the coalition will meet soon to discuss the final recommendations and consider next steps toward implementation.
The UGRC includes representatives of national medical organizations, medical schools, and residency programs. Among the organizations that participated in the report’s creation are the American Medical Association, the National Board of Medical Examiners, the American Osteopathic Association, the National Board of Osteopathic Medical Examiners, the Educational Commission for Foreign Medical Graduates, and the Association of American Medical Colleges.
The report identifies a list of challenges that affect the transition of medical students into residency programs and beyond. They include:
- Too much focus on finding and filling residency positions instead of “assuring learner competence and readiness for residency training”
- Inattention to assuring congruence between applicant goals and program missions
- Overreliance on licensure exam scores rather than “valid, trustworthy measures of students’ competence and clinical abilities”
- Increasing financial costs to students
- Individual and systemic biases in the UME-GME transition, as well as inequities related to international medical graduates
Seeking a common framework for competence
Overall, the report calls for increased standardization of how students are evaluated in medical school and how residency programs evaluate students. Less reliance should be placed on the numerical scores of the U.S. Medical Licensing Examination (USMLE), the report says, and more attention should be paid to the direct observation of student performance in clinical situations. In addition, the various organizations involved in the UME-GME transition process are asked to work better together.
To develop better methods of evaluating medical students and residents, UME and GME educators should jointly define and implement a common framework and set of competencies to apply to learners across the UME-GME transition, the report suggests.
While emphasizing the need for a broader student assessment framework, the report says, USMLE scores should also continue to be used in judging residency applicants. “Assessment information should be shared in residency applications and a postmatch learner handover. Licensing examinations should be used for their intended purpose to ensure requisite competence.”
Among the committee’s three dozen recommendations are the following:
- The Centers for Medicare & Medicaid Services should change the GME funding structure so that the initial residency period is calculated starting with the second year of postgraduate training. This change would allow residents to reconsider their career choices. Currently, if a resident decides to switch to another program or specialty after beginning training, the hospital may not receive full GME funding, so may be less likely to approve the change.
- Residency programs should improve recruitment practices to increase specialty-specific diversity of residents. Medical educators should also receive additional training regarding antiracism, avoiding bias, and ensuring equity.
- The self-reported demographic information of applicants to residency programs should be measured and shared with stakeholders, including the programs and medical schools, to promote equity. “A residency program that finds bias in its selection process could go back in real time to find qualified applicants who may have been missed, potentially improving outcomes,” the report notes.
- An interactive database of GME program and specialty track information should be created and made available to all applicants, medical schools, and residency programs at no cost to applicants. “Applicants and their advisors should be able to sort the information according to demographic and educational features that may significantly impact the likelihood of matching at a program.”
Less than half of applicants get in-depth reviews
The 2020 National Resident Matching Program Program Director Survey found that only 49% of applications received in-depth review. In light of this, the report suggests that the application system be updated to use modern information technology, including discrete fields for key data to expedite application reviews.
Many applications have been discarded because of various filters used to block consideration of certain applications. The report suggests that new filters be designed to ensure that each detects meaningful differences among applicants and promotes review based on mission alignment and likelihood of success in a program. Filters should be improved to decrease the likelihood of random exclusions of qualified applicants.
Specialty-specific, just-in-time training for all incoming first-year residents is also suggested to support the transition from the role of student to a physician ready to assume increased responsibility for patient care. In addition, the report urges adequate time be allowed between medical school graduation and residency to enable new residents to relocate and find homes.
The report also calls for a standardized process in the United States for initial licensing of doctors at entrance to residency in order to streamline the process of credentialing for both residency training and continuing practice.
Osteopathic students’ dilemma
To promote equitable treatment of applicants regardless of licensure examination requirements, comparable exams with different scales (COMLEX-USA and USMLE) should be reported within the electronic application system in a single field, the report said.
Osteopathic students, who make up 25% of U.S. medical students, must take the COMLEX-USA exam, but residency programs may filter them out if they don’t also take the USMLE exam. Thus, many osteopathic students take both exams, incurring extra time, cost, and stress.
The UGRC recommends creating a combined field in the electronic residency application service that normalizes the scores between the two exams. Residency programs could then filter applications based only on the single normalized score.
This approach makes sense from the viewpoint that it would reduce the pressure on osteopathic students to take the USMLE, Bryan Carmody, MD, an outspoken critic of various current training policies, said in an interview. But it could also have serious disadvantages.
For one thing, only osteopathic students can take the COMLEX-USA exam, he noted. If they don’t like their score, they can then take the USMLE test to get a higher score – an option that allopathic students don’t have. It’s not clear that they’d be prevented from doing this under the UGRC recommendation.
Second, he said, osteopathic students, on average, don’t do as well as allopathic students on the UMSLE exam. If they only take the COMLEX-USA test, they’re competing against other students who don’t do as well on tests as allopathic students do. If their scores were normalized with those of the USMLE test takers, they’d gain an unfair advantage against students who can only take the USMLE, including international medical graduates.
Although Dr. Carmody admitted that osteopathic students face a harder challenge than allopathic students in matching to residency programs, he said that the UGRC approach to the licensing exams might actually penalize them further. As a result of the scores of the two exams being averaged, residency program directors might discount the scores of all osteopathic students.
A version of this article first appeared on Medscape.com.
Self-described ‘assassin,’ now doctor, indicted for 1M illegal opioid doses
A according to the U.S. Department of Justice. The substances include oxycodone and morphine.
Adrian Dexter Talbot, MD, 55, of Slidell, La., is also charged with maintaining a medical clinic for the purpose of illegally distributing controlled substances, per the indictment.
Because the opioid prescriptions were filled using beneficiaries’ health insurance, Dr. Talbot is also charged with defrauding Medicare, Medicaid, and Blue Cross and Blue Shield of Louisiana of more than $5.1 million.
When contacted by this news organization for comment on the case via Twitter, Dr. Talbot or a representative responded with a link to his self-published book on Amazon. In his author bio, Dr. Talbot refers to himself as “a former assassin,” “retired military commander,” and “leader of the Medellin Cartel’s New York operations at the age of 16.” The Medellin Cartel is a notorious drug distribution empire.
Dr. Talbot is listed as the author of another book on Google Books detailing his time as a “former teenage assassin” and leader of the cartel, told as he struggles with early onset Alzheimer’s.
Dr. Talbot could spend decades in prison
According to the National Institute on Drug Abuse, 444 residents of the Bayou State lost their lives because of an opioid-related drug overdose in 2018. During that year, the state’s health care providers wrote more than 79.4 opioid prescriptions for every 100 persons, which puts the state in the top five in the United States in 2018, when the average U.S. rate was 51.4 prescriptions per 100 persons.
Charged with one count each of conspiracy to unlawfully distribute and dispense controlled substances and maintaining drug-involved premises and conspiracy to commit health care fraud, Dr. Talbot is also charged with four counts of unlawfully distributing and dispensing controlled substances. He is scheduled for a federal court appearance on September 10.
In addition to presigning prescriptions for individuals he didn’t meet or examine, federal officials allege Dr. Talbot hired another health care provider to similarly presign prescriptions for people who weren’t examined at a medical practice in Slidell, where Dr. Talbot was employed. The DOJ says Dr. Talbot took a full-time job in Pineville, La., and presigned prescriptions while no longer physically present at the Slidell clinic.
A speaker’s bio for Dr. Talbot indicates he worked as chief of medical services for the Alexandria Veterans Affairs Health Care System in Pineville.
According to the DOJ’s indictment, Dr. Talbot was aware that patients were filling the prescriptions that were provided outside the scope of professional practice and not for a legitimate medical purpose. This is what triggered the DOJ’s fraudulent billing claim.
Dr. Talbot faces a maximum penalty of 10 years for conspiracy to commit health care fraud and 20 years each for the other counts, if convicted.
Dr. Talbot was candidate for local coroner
In February 2015, Dr. Talbot announced his candidacy for coroner for St. Tammany Parish, about an hour’s drive south of New Orleans, reported the Times Picayune. The seat was open because the previous coroner had resigned and ultimately pleaded guilty to a federal corruption charge.
The Times Picayune reported at the time that Dr. Talbot was a U.S. Navy veteran, in addition to serving as medical director and a primary care physician at the Medical Care Center in Slidell. Among the services provided to his patients were evaluations and treatment for substance use and mental health disorders, according to a press release issued by Dr. Talbot’s campaign.
Dr. Talbot’s medical license was issued in 1999 and inactive as of 2017, per the Louisiana State Board of Medical Examiners.
Louisiana expects $325M in multistate settlement with opioid companies
Louisiana is a party to a multistate and multijurisdictional lawsuit where the state is expected to receive more than $325 million in a settlement reached with drug distributors Cardinal, McKesson, and AmerisourceBergen, and drug manufacturer Johnson & Johnson, reported the Louisiana Illuminator in July. The total settlement may reach $26 billion dollars.
The Associated Press reported in July that there have been at least $40 billion in completed or proposed settlements, penalties, and fines between governments as a result of the opioid epidemic since 2007.
That total doesn’t include a proposed settlement involving members of the Sackler family, who own Purdue Pharmaceuticals, which manufactured and marketed the opioid painkiller OxyContin. The Sackler family have agreed to pay approximately $4.3 billion and surrender ownership of their bankrupt company, reported NPR. The family’s proposed settlement is part of a deal involving Purdue Pharmaceuticals worth more than $10 billion, reported Reuters.
In 2020, there were more than 81,000 drug overdose deaths, the highest number recorded in a 12-month period, per the U.S. Centers for Disease Control and Prevention. Fentanyl, an illicitly manufactured synthetic opioid, was the lead driver of those deaths.
A version of this article first appeared on Medscape.com.
A according to the U.S. Department of Justice. The substances include oxycodone and morphine.
Adrian Dexter Talbot, MD, 55, of Slidell, La., is also charged with maintaining a medical clinic for the purpose of illegally distributing controlled substances, per the indictment.
Because the opioid prescriptions were filled using beneficiaries’ health insurance, Dr. Talbot is also charged with defrauding Medicare, Medicaid, and Blue Cross and Blue Shield of Louisiana of more than $5.1 million.
When contacted by this news organization for comment on the case via Twitter, Dr. Talbot or a representative responded with a link to his self-published book on Amazon. In his author bio, Dr. Talbot refers to himself as “a former assassin,” “retired military commander,” and “leader of the Medellin Cartel’s New York operations at the age of 16.” The Medellin Cartel is a notorious drug distribution empire.
Dr. Talbot is listed as the author of another book on Google Books detailing his time as a “former teenage assassin” and leader of the cartel, told as he struggles with early onset Alzheimer’s.
Dr. Talbot could spend decades in prison
According to the National Institute on Drug Abuse, 444 residents of the Bayou State lost their lives because of an opioid-related drug overdose in 2018. During that year, the state’s health care providers wrote more than 79.4 opioid prescriptions for every 100 persons, which puts the state in the top five in the United States in 2018, when the average U.S. rate was 51.4 prescriptions per 100 persons.
Charged with one count each of conspiracy to unlawfully distribute and dispense controlled substances and maintaining drug-involved premises and conspiracy to commit health care fraud, Dr. Talbot is also charged with four counts of unlawfully distributing and dispensing controlled substances. He is scheduled for a federal court appearance on September 10.
In addition to presigning prescriptions for individuals he didn’t meet or examine, federal officials allege Dr. Talbot hired another health care provider to similarly presign prescriptions for people who weren’t examined at a medical practice in Slidell, where Dr. Talbot was employed. The DOJ says Dr. Talbot took a full-time job in Pineville, La., and presigned prescriptions while no longer physically present at the Slidell clinic.
A speaker’s bio for Dr. Talbot indicates he worked as chief of medical services for the Alexandria Veterans Affairs Health Care System in Pineville.
According to the DOJ’s indictment, Dr. Talbot was aware that patients were filling the prescriptions that were provided outside the scope of professional practice and not for a legitimate medical purpose. This is what triggered the DOJ’s fraudulent billing claim.
Dr. Talbot faces a maximum penalty of 10 years for conspiracy to commit health care fraud and 20 years each for the other counts, if convicted.
Dr. Talbot was candidate for local coroner
In February 2015, Dr. Talbot announced his candidacy for coroner for St. Tammany Parish, about an hour’s drive south of New Orleans, reported the Times Picayune. The seat was open because the previous coroner had resigned and ultimately pleaded guilty to a federal corruption charge.
The Times Picayune reported at the time that Dr. Talbot was a U.S. Navy veteran, in addition to serving as medical director and a primary care physician at the Medical Care Center in Slidell. Among the services provided to his patients were evaluations and treatment for substance use and mental health disorders, according to a press release issued by Dr. Talbot’s campaign.
Dr. Talbot’s medical license was issued in 1999 and inactive as of 2017, per the Louisiana State Board of Medical Examiners.
Louisiana expects $325M in multistate settlement with opioid companies
Louisiana is a party to a multistate and multijurisdictional lawsuit where the state is expected to receive more than $325 million in a settlement reached with drug distributors Cardinal, McKesson, and AmerisourceBergen, and drug manufacturer Johnson & Johnson, reported the Louisiana Illuminator in July. The total settlement may reach $26 billion dollars.
The Associated Press reported in July that there have been at least $40 billion in completed or proposed settlements, penalties, and fines between governments as a result of the opioid epidemic since 2007.
That total doesn’t include a proposed settlement involving members of the Sackler family, who own Purdue Pharmaceuticals, which manufactured and marketed the opioid painkiller OxyContin. The Sackler family have agreed to pay approximately $4.3 billion and surrender ownership of their bankrupt company, reported NPR. The family’s proposed settlement is part of a deal involving Purdue Pharmaceuticals worth more than $10 billion, reported Reuters.
In 2020, there were more than 81,000 drug overdose deaths, the highest number recorded in a 12-month period, per the U.S. Centers for Disease Control and Prevention. Fentanyl, an illicitly manufactured synthetic opioid, was the lead driver of those deaths.
A version of this article first appeared on Medscape.com.
A according to the U.S. Department of Justice. The substances include oxycodone and morphine.
Adrian Dexter Talbot, MD, 55, of Slidell, La., is also charged with maintaining a medical clinic for the purpose of illegally distributing controlled substances, per the indictment.
Because the opioid prescriptions were filled using beneficiaries’ health insurance, Dr. Talbot is also charged with defrauding Medicare, Medicaid, and Blue Cross and Blue Shield of Louisiana of more than $5.1 million.
When contacted by this news organization for comment on the case via Twitter, Dr. Talbot or a representative responded with a link to his self-published book on Amazon. In his author bio, Dr. Talbot refers to himself as “a former assassin,” “retired military commander,” and “leader of the Medellin Cartel’s New York operations at the age of 16.” The Medellin Cartel is a notorious drug distribution empire.
Dr. Talbot is listed as the author of another book on Google Books detailing his time as a “former teenage assassin” and leader of the cartel, told as he struggles with early onset Alzheimer’s.
Dr. Talbot could spend decades in prison
According to the National Institute on Drug Abuse, 444 residents of the Bayou State lost their lives because of an opioid-related drug overdose in 2018. During that year, the state’s health care providers wrote more than 79.4 opioid prescriptions for every 100 persons, which puts the state in the top five in the United States in 2018, when the average U.S. rate was 51.4 prescriptions per 100 persons.
Charged with one count each of conspiracy to unlawfully distribute and dispense controlled substances and maintaining drug-involved premises and conspiracy to commit health care fraud, Dr. Talbot is also charged with four counts of unlawfully distributing and dispensing controlled substances. He is scheduled for a federal court appearance on September 10.
In addition to presigning prescriptions for individuals he didn’t meet or examine, federal officials allege Dr. Talbot hired another health care provider to similarly presign prescriptions for people who weren’t examined at a medical practice in Slidell, where Dr. Talbot was employed. The DOJ says Dr. Talbot took a full-time job in Pineville, La., and presigned prescriptions while no longer physically present at the Slidell clinic.
A speaker’s bio for Dr. Talbot indicates he worked as chief of medical services for the Alexandria Veterans Affairs Health Care System in Pineville.
According to the DOJ’s indictment, Dr. Talbot was aware that patients were filling the prescriptions that were provided outside the scope of professional practice and not for a legitimate medical purpose. This is what triggered the DOJ’s fraudulent billing claim.
Dr. Talbot faces a maximum penalty of 10 years for conspiracy to commit health care fraud and 20 years each for the other counts, if convicted.
Dr. Talbot was candidate for local coroner
In February 2015, Dr. Talbot announced his candidacy for coroner for St. Tammany Parish, about an hour’s drive south of New Orleans, reported the Times Picayune. The seat was open because the previous coroner had resigned and ultimately pleaded guilty to a federal corruption charge.
The Times Picayune reported at the time that Dr. Talbot was a U.S. Navy veteran, in addition to serving as medical director and a primary care physician at the Medical Care Center in Slidell. Among the services provided to his patients were evaluations and treatment for substance use and mental health disorders, according to a press release issued by Dr. Talbot’s campaign.
Dr. Talbot’s medical license was issued in 1999 and inactive as of 2017, per the Louisiana State Board of Medical Examiners.
Louisiana expects $325M in multistate settlement with opioid companies
Louisiana is a party to a multistate and multijurisdictional lawsuit where the state is expected to receive more than $325 million in a settlement reached with drug distributors Cardinal, McKesson, and AmerisourceBergen, and drug manufacturer Johnson & Johnson, reported the Louisiana Illuminator in July. The total settlement may reach $26 billion dollars.
The Associated Press reported in July that there have been at least $40 billion in completed or proposed settlements, penalties, and fines between governments as a result of the opioid epidemic since 2007.
That total doesn’t include a proposed settlement involving members of the Sackler family, who own Purdue Pharmaceuticals, which manufactured and marketed the opioid painkiller OxyContin. The Sackler family have agreed to pay approximately $4.3 billion and surrender ownership of their bankrupt company, reported NPR. The family’s proposed settlement is part of a deal involving Purdue Pharmaceuticals worth more than $10 billion, reported Reuters.
In 2020, there were more than 81,000 drug overdose deaths, the highest number recorded in a 12-month period, per the U.S. Centers for Disease Control and Prevention. Fentanyl, an illicitly manufactured synthetic opioid, was the lead driver of those deaths.
A version of this article first appeared on Medscape.com.