User login
ACEI/ARBs linked with survival in hypertensive, Chinese COVID-19 patients
Hospitalized COVID-19 patients with hypertension and on treatment with an renin-angiotensin system inhibiting drug had significantly better survival, compared with similar hypertensive patients not on these drugs, in observational, propensity score–matched analyses that drew from a pool of more than 3,430 patients hospitalized at any of nine Chinese hospitals during December 2019–February 2020.
“Among patients with hypertension hospitalized with COVID-19, inpatient treatment with ACEI [ACE inhibitor]/ARB [angiotensin receptor blocker] was associated with lower risk of all-cause mortality, compared with ACEI/ARB nonusers, during 28 days of follow-up. While study interpretation needs to consider the potential for residual confounders, it is unlikely that inpatient ACEI/ARB would be associated with an increased risk of mortality,” wrote Peng Zhang, MD, a cardiology researcher at Renmin Hospital of Wuhan University, China, and coauthors in Circulations Research, buttressing recent recommendations from several medical societies to maintain COVID-19 patients on these drugs.
“Our findings in this paper provide evidence supporting continuous use of ACEI/ARB for patients with hypertension infected with SARS-COV-2,” wrote the authors, backing up recent recommendations from cardiology societies that called for not stopping ACEI/ARB prescriptions in patients at risk for contracting or already have COVID-19 infection, including a statement from the American College of Cardiology, American Heart Association, and Heart Failure Society of America, and also guidance from the European Society of Cardiology.
The study included 1,128 patients with a history of hypertension, including 188 (17%) who received an ACEI/ARB drug during hospitalization. During 28-day follow-up, 99 died (9%), including 7 deaths among the 188 patients (4%) on an ACEI/ARB drug and 92 deaths among the 940 other hypertensive patients (10%).
The authors ran several analyses to try to adjust for the influence of possible confounders. A mixed-effect Cox model with four adjusted variables showed that treatment with an ACEI/ARB drug was tied to a statistically significant 58% lower death rate, compared with patients not receiving these drugs.
The researchers also ran several propensity score–adjusted analyses. One matched 174 of the patients who received an ACEI/ARB drug with 522 who did not, and comparing these two matched arms showed that ACEI/ARB use was linked with a statistically significant 63% cut in mortality, compared with patients not getting these drugs. A second propensity score–matched analysis first excluded the 383 patients who were hypertensive but received no antihypertensive medication during hospitalization. From the remaining 745 patients who received at least one antihypertensive medication, the authors identified 181 patients who received an ACEI/ARB and propensity-score matched them with 181 hypertensive patients on a different medication class, finding that ACEI/ARB use linked with a statistically significant 71% lower rate of all-cause mortality.
Additional analyses also showed that patients with hypertension had a statistically significant, 41% increased rate of all-cause death, compared with patients without hypertension, and another propensity score–matched analysis showed that among hypertensives treatment with an ACEI/ARB drug was linked with a statistically significant 68% reduced rate of septic shock.
Although this report was received with caution and some skepticism, it was also acknowledged as a step forward in the creation of an evidence base addressing ACEI/ARB treatment during COVID-19 infection.
“These drugs are lifesaving and should not be discontinued” for patients with hypertension, heart failure, and other cardiovascular disease, commented Gian Paolo Rossi, MD, professor and chair of medicine and director of the high blood pressure unit at the University of Padua (Italy). The analysis by Zhang and associates included the largest number of hospitalized COVID-19 patients with hypertension yet reported to assess the impact of treatment with ACEI/ARB drugs, and adds important evidence in favor of continuing these drugs in patients who develop COVID-19 infection, Dr. Rossi said in an interview. He recently coauthored a review that argued against ACEI/ARB discontinuation in COVID-19 patients based on previously reported evidence (Elife. 2020 Apr 6. doi: 10.7554/eLife.57278).
But other researchers take a wary view of the potential impact of ACEI/ARB agents. “If ACEI/ARB therapy increases ACE2 and the virus down-regulates it, and because ACE2 is the viral entry port into cells, why would ACE2-mediated down-regulation of the renin-angiotensin-aldosterone system lead to amelioration of [COVID-19] disease?” asked Laurence W. Busse, MD, a critical care physician at Emory University, Atlanta. “A number of issues could potentially confound the results, including the definition of COVID-19 and imbalance of antiviral therapy,” added Dr. Busse, who recently coauthored an editorial that posited using angiotensin II (Giapreza), an approved vasopressor drug, as an alternative renin-angiotensin system intervention for COVID-19 patients including both those in shock as well as potentially those not in shock (Crit Care. 2020 Apr 7. doi: 10.1186/s13054-020-02862-1). Despite these caveats, the new Chinese findings reported by Dr. Zhang and associates “are hypothesis generating and worth further exploration.”
The authors of an editorial that accompanied the Zhang study in Circulation Research made similar points. “While the investigators used standard techniques to attempt to reduce bias in this observational study via propensity matching, it is not a randomized study and the residual confounding inherent to this approach renders the conclusions hypothesis generating at best,” wrote Ravi V. Shah, MD, and two coauthors in the editorial (Circ Res. 2020 Apr 17. doi: 10.1161/CIRCRESAHA.120.317174). They also agreed with the several society statements that have supported continued use of ACEI/ARB drugs in COVID-19 patients. “Withdrawal of these medications in the context of those conditions in which they have proven benefit (e.g., heart failure with reduced left ventricular ejection fraction) may actually inflict more harm than good,” they warned. “In the end we must rely on randomized clinical science,” and while this level of evidence is currently lacking, “the study by Zhang and colleagues is a direct step toward that goal.”
Dr. Zhang and coauthors had no commercial disclosures. Dr. Rossi and Dr. Busse had no disclosures. The authors of the Circulation Research editorial reported several disclosures.
SOURCE: Zhang P et al. Circ Res. 2020 Apr 17. doi: 10.1161/CIRCRESAHA.120.317134.
Hospitalized COVID-19 patients with hypertension and on treatment with an renin-angiotensin system inhibiting drug had significantly better survival, compared with similar hypertensive patients not on these drugs, in observational, propensity score–matched analyses that drew from a pool of more than 3,430 patients hospitalized at any of nine Chinese hospitals during December 2019–February 2020.
“Among patients with hypertension hospitalized with COVID-19, inpatient treatment with ACEI [ACE inhibitor]/ARB [angiotensin receptor blocker] was associated with lower risk of all-cause mortality, compared with ACEI/ARB nonusers, during 28 days of follow-up. While study interpretation needs to consider the potential for residual confounders, it is unlikely that inpatient ACEI/ARB would be associated with an increased risk of mortality,” wrote Peng Zhang, MD, a cardiology researcher at Renmin Hospital of Wuhan University, China, and coauthors in Circulations Research, buttressing recent recommendations from several medical societies to maintain COVID-19 patients on these drugs.
“Our findings in this paper provide evidence supporting continuous use of ACEI/ARB for patients with hypertension infected with SARS-COV-2,” wrote the authors, backing up recent recommendations from cardiology societies that called for not stopping ACEI/ARB prescriptions in patients at risk for contracting or already have COVID-19 infection, including a statement from the American College of Cardiology, American Heart Association, and Heart Failure Society of America, and also guidance from the European Society of Cardiology.
The study included 1,128 patients with a history of hypertension, including 188 (17%) who received an ACEI/ARB drug during hospitalization. During 28-day follow-up, 99 died (9%), including 7 deaths among the 188 patients (4%) on an ACEI/ARB drug and 92 deaths among the 940 other hypertensive patients (10%).
The authors ran several analyses to try to adjust for the influence of possible confounders. A mixed-effect Cox model with four adjusted variables showed that treatment with an ACEI/ARB drug was tied to a statistically significant 58% lower death rate, compared with patients not receiving these drugs.
The researchers also ran several propensity score–adjusted analyses. One matched 174 of the patients who received an ACEI/ARB drug with 522 who did not, and comparing these two matched arms showed that ACEI/ARB use was linked with a statistically significant 63% cut in mortality, compared with patients not getting these drugs. A second propensity score–matched analysis first excluded the 383 patients who were hypertensive but received no antihypertensive medication during hospitalization. From the remaining 745 patients who received at least one antihypertensive medication, the authors identified 181 patients who received an ACEI/ARB and propensity-score matched them with 181 hypertensive patients on a different medication class, finding that ACEI/ARB use linked with a statistically significant 71% lower rate of all-cause mortality.
Additional analyses also showed that patients with hypertension had a statistically significant, 41% increased rate of all-cause death, compared with patients without hypertension, and another propensity score–matched analysis showed that among hypertensives treatment with an ACEI/ARB drug was linked with a statistically significant 68% reduced rate of septic shock.
Although this report was received with caution and some skepticism, it was also acknowledged as a step forward in the creation of an evidence base addressing ACEI/ARB treatment during COVID-19 infection.
“These drugs are lifesaving and should not be discontinued” for patients with hypertension, heart failure, and other cardiovascular disease, commented Gian Paolo Rossi, MD, professor and chair of medicine and director of the high blood pressure unit at the University of Padua (Italy). The analysis by Zhang and associates included the largest number of hospitalized COVID-19 patients with hypertension yet reported to assess the impact of treatment with ACEI/ARB drugs, and adds important evidence in favor of continuing these drugs in patients who develop COVID-19 infection, Dr. Rossi said in an interview. He recently coauthored a review that argued against ACEI/ARB discontinuation in COVID-19 patients based on previously reported evidence (Elife. 2020 Apr 6. doi: 10.7554/eLife.57278).
But other researchers take a wary view of the potential impact of ACEI/ARB agents. “If ACEI/ARB therapy increases ACE2 and the virus down-regulates it, and because ACE2 is the viral entry port into cells, why would ACE2-mediated down-regulation of the renin-angiotensin-aldosterone system lead to amelioration of [COVID-19] disease?” asked Laurence W. Busse, MD, a critical care physician at Emory University, Atlanta. “A number of issues could potentially confound the results, including the definition of COVID-19 and imbalance of antiviral therapy,” added Dr. Busse, who recently coauthored an editorial that posited using angiotensin II (Giapreza), an approved vasopressor drug, as an alternative renin-angiotensin system intervention for COVID-19 patients including both those in shock as well as potentially those not in shock (Crit Care. 2020 Apr 7. doi: 10.1186/s13054-020-02862-1). Despite these caveats, the new Chinese findings reported by Dr. Zhang and associates “are hypothesis generating and worth further exploration.”
The authors of an editorial that accompanied the Zhang study in Circulation Research made similar points. “While the investigators used standard techniques to attempt to reduce bias in this observational study via propensity matching, it is not a randomized study and the residual confounding inherent to this approach renders the conclusions hypothesis generating at best,” wrote Ravi V. Shah, MD, and two coauthors in the editorial (Circ Res. 2020 Apr 17. doi: 10.1161/CIRCRESAHA.120.317174). They also agreed with the several society statements that have supported continued use of ACEI/ARB drugs in COVID-19 patients. “Withdrawal of these medications in the context of those conditions in which they have proven benefit (e.g., heart failure with reduced left ventricular ejection fraction) may actually inflict more harm than good,” they warned. “In the end we must rely on randomized clinical science,” and while this level of evidence is currently lacking, “the study by Zhang and colleagues is a direct step toward that goal.”
Dr. Zhang and coauthors had no commercial disclosures. Dr. Rossi and Dr. Busse had no disclosures. The authors of the Circulation Research editorial reported several disclosures.
SOURCE: Zhang P et al. Circ Res. 2020 Apr 17. doi: 10.1161/CIRCRESAHA.120.317134.
Hospitalized COVID-19 patients with hypertension and on treatment with an renin-angiotensin system inhibiting drug had significantly better survival, compared with similar hypertensive patients not on these drugs, in observational, propensity score–matched analyses that drew from a pool of more than 3,430 patients hospitalized at any of nine Chinese hospitals during December 2019–February 2020.
“Among patients with hypertension hospitalized with COVID-19, inpatient treatment with ACEI [ACE inhibitor]/ARB [angiotensin receptor blocker] was associated with lower risk of all-cause mortality, compared with ACEI/ARB nonusers, during 28 days of follow-up. While study interpretation needs to consider the potential for residual confounders, it is unlikely that inpatient ACEI/ARB would be associated with an increased risk of mortality,” wrote Peng Zhang, MD, a cardiology researcher at Renmin Hospital of Wuhan University, China, and coauthors in Circulations Research, buttressing recent recommendations from several medical societies to maintain COVID-19 patients on these drugs.
“Our findings in this paper provide evidence supporting continuous use of ACEI/ARB for patients with hypertension infected with SARS-COV-2,” wrote the authors, backing up recent recommendations from cardiology societies that called for not stopping ACEI/ARB prescriptions in patients at risk for contracting or already have COVID-19 infection, including a statement from the American College of Cardiology, American Heart Association, and Heart Failure Society of America, and also guidance from the European Society of Cardiology.
The study included 1,128 patients with a history of hypertension, including 188 (17%) who received an ACEI/ARB drug during hospitalization. During 28-day follow-up, 99 died (9%), including 7 deaths among the 188 patients (4%) on an ACEI/ARB drug and 92 deaths among the 940 other hypertensive patients (10%).
The authors ran several analyses to try to adjust for the influence of possible confounders. A mixed-effect Cox model with four adjusted variables showed that treatment with an ACEI/ARB drug was tied to a statistically significant 58% lower death rate, compared with patients not receiving these drugs.
The researchers also ran several propensity score–adjusted analyses. One matched 174 of the patients who received an ACEI/ARB drug with 522 who did not, and comparing these two matched arms showed that ACEI/ARB use was linked with a statistically significant 63% cut in mortality, compared with patients not getting these drugs. A second propensity score–matched analysis first excluded the 383 patients who were hypertensive but received no antihypertensive medication during hospitalization. From the remaining 745 patients who received at least one antihypertensive medication, the authors identified 181 patients who received an ACEI/ARB and propensity-score matched them with 181 hypertensive patients on a different medication class, finding that ACEI/ARB use linked with a statistically significant 71% lower rate of all-cause mortality.
Additional analyses also showed that patients with hypertension had a statistically significant, 41% increased rate of all-cause death, compared with patients without hypertension, and another propensity score–matched analysis showed that among hypertensives treatment with an ACEI/ARB drug was linked with a statistically significant 68% reduced rate of septic shock.
Although this report was received with caution and some skepticism, it was also acknowledged as a step forward in the creation of an evidence base addressing ACEI/ARB treatment during COVID-19 infection.
“These drugs are lifesaving and should not be discontinued” for patients with hypertension, heart failure, and other cardiovascular disease, commented Gian Paolo Rossi, MD, professor and chair of medicine and director of the high blood pressure unit at the University of Padua (Italy). The analysis by Zhang and associates included the largest number of hospitalized COVID-19 patients with hypertension yet reported to assess the impact of treatment with ACEI/ARB drugs, and adds important evidence in favor of continuing these drugs in patients who develop COVID-19 infection, Dr. Rossi said in an interview. He recently coauthored a review that argued against ACEI/ARB discontinuation in COVID-19 patients based on previously reported evidence (Elife. 2020 Apr 6. doi: 10.7554/eLife.57278).
But other researchers take a wary view of the potential impact of ACEI/ARB agents. “If ACEI/ARB therapy increases ACE2 and the virus down-regulates it, and because ACE2 is the viral entry port into cells, why would ACE2-mediated down-regulation of the renin-angiotensin-aldosterone system lead to amelioration of [COVID-19] disease?” asked Laurence W. Busse, MD, a critical care physician at Emory University, Atlanta. “A number of issues could potentially confound the results, including the definition of COVID-19 and imbalance of antiviral therapy,” added Dr. Busse, who recently coauthored an editorial that posited using angiotensin II (Giapreza), an approved vasopressor drug, as an alternative renin-angiotensin system intervention for COVID-19 patients including both those in shock as well as potentially those not in shock (Crit Care. 2020 Apr 7. doi: 10.1186/s13054-020-02862-1). Despite these caveats, the new Chinese findings reported by Dr. Zhang and associates “are hypothesis generating and worth further exploration.”
The authors of an editorial that accompanied the Zhang study in Circulation Research made similar points. “While the investigators used standard techniques to attempt to reduce bias in this observational study via propensity matching, it is not a randomized study and the residual confounding inherent to this approach renders the conclusions hypothesis generating at best,” wrote Ravi V. Shah, MD, and two coauthors in the editorial (Circ Res. 2020 Apr 17. doi: 10.1161/CIRCRESAHA.120.317174). They also agreed with the several society statements that have supported continued use of ACEI/ARB drugs in COVID-19 patients. “Withdrawal of these medications in the context of those conditions in which they have proven benefit (e.g., heart failure with reduced left ventricular ejection fraction) may actually inflict more harm than good,” they warned. “In the end we must rely on randomized clinical science,” and while this level of evidence is currently lacking, “the study by Zhang and colleagues is a direct step toward that goal.”
Dr. Zhang and coauthors had no commercial disclosures. Dr. Rossi and Dr. Busse had no disclosures. The authors of the Circulation Research editorial reported several disclosures.
SOURCE: Zhang P et al. Circ Res. 2020 Apr 17. doi: 10.1161/CIRCRESAHA.120.317134.
FROM CIRCULATION RESEARCH
Doctors push back on treating COVID-19 as HAPE
For Luanne Freer, MD, an expert in high-altitude pulmonary edema (HAPE) and founder and director of Everest ER, a nonprofit seasonal clinic at the Mt. Everest base camp in Nepal (elevation, 17,600 ft), a sudden flurry of messages and questions she received about a possible COVID-19/HAPE link was startling.
“That’s why it kind of poked me in the eye,” she said, referencing her extensive experience treating HAPE, which she described as a pressure-related phenomenon. “My goodness, they are so completely different.”
Dr. Freer, an emergency physician, reached out to several pulmonary intensivists with experience treating both HAPE and COVID-19 to gauge their reactions, and within 36 hours, they had drafted their response. In the commentary, published in High Altitude Medicine & Biology, the clinicians note that the comparison between HAPE and COVID-19 is potentially risky.
“As a group of physicians who have in some cases cared for patients with COVID-19 and in all cases cared for patients with HAPE and studied its pathophysiology and management, we feel it important to correct this misconception, as continued amplification of this message could have adverse effects on management of these patients,” they wrote.
The suggestion that COVID-19 lung injury sometimes looks more like HAPE than like acute respiratory distress syndrome (ARDS) appeared in a journal review article in late March and was put forth by medical professionals on social media where it gained traction in recent weeks and was amplified in multiple media outlets, including this one.
“With COVID, we don’t understand everything that’s going on, but we know for sure it’s an inflammatory process – not a pressure-related problem,” Dr. Freer said. “I thought ... this could be so dangerous to load the medicines that we use when we’re treating HAPE onto patients with COVID-19.”
The pathophysiological mechanisms in HAPE are different than those in other respiratory syndromes, including those associated with COVID-19, said Andrew M. Luks, MD, of the UW Medicine, Seattle, and the first author on the commentary.
“HAPE is a noncardiogenic form of pulmonary edema, as are ARDS due to bacteria or viral pneumonia, re-expansion pulmonary edema, immersion pulmonary edema, negative pressure pulmonary edema, and neurogenic pulmonary edema,” Dr. Luks, Dr. Freer, and colleagues wrote in the commentary, explaining that all of these entities cause varying degrees of hypoxemia and diffuse bilateral opacities on chest imaging. “Importantly, in all of these cases, edema accumulates in the interstitial and alveolar spaces of the lung as a result of imbalance in Starling forces.”
A difference between these entities, however, is “the mechanism by which that imbalance develops,” they noted.
The excessive and uneven hypoxic pulmonary vasoconstriction that leads to a marked increase in pulmonary artery pressure, subsequent lung overperfusion, increased pulmonary capillary hydrostatic pressure, and leakage of fluid from the vascular space into the alveolar space as seen in HAPE, is a “fundamentally different phenomenon than what is seen in COVID-19-related ARDS, which involves viral-mediated inflammatory responses as the primary pathophysiological mechanism,” they added.
The authors described several other differences between the conditions, ultimately noting that “understanding the distinction between the pathophysiological mechanisms of these entities is critical for patient management.”
In HAPE, supplemental oxygen alone may be sufficient; in COVID-19, it may improve hypoxemia but won’t resolve the underlying inflammation or injury, they explained, adding that “only good supportive care including mechanical ventilation, quite often for long periods of time, allows some patients to survive until their disease resolves.”
Further, HAPE can be prevented or treated with pulmonary vasodilators such a nifedipine or sildenafil, which decrease pulmonary artery pressure and, as a result lower pulmonary capillary hydrostatic pressure, they said.
Use of such medications for COVID-19 might decrease pulmonary artery pressure and improve right ventricular function in COVID-19, but “by releasing hypoxic pulmonary vasoconstriction and increasing perfusion to nonventilated regions of the lung, they could also worsen ventilation-perfusion mismatch” and thereby worsen hypoxemia, they explained, adding that the treatments can also cause or worsen hypotension.
Efforts to share observations and experience are important in medicine, but sometimes, as in this circumstance, “they get out there, spread around – like a brushfire almost – and get [unwarranted] face validity,” Dr. Luks said, noting that in response to information circulating about COVID-19 and HAPE, he has already heard medical professionals floating the idea of treating COVID-19 with treatments used for HAPE.
It’s true that some COVID-19 lung injury cases are behaving differently than typical ARDS, he said, adding that presentation can vary.
“But trying to equate HAPE and COVID-19 is just wrong,” he said. “HAPE and COVID-19 may share several features ...but those are features that are shared by a lot of different forms of respiratory failure.”
In a recent video interview, WebMD’s chief medical officer John Whyte, MD, spoke with a New York City physician trained in critical care and emergency medicine, Cameron Kyle-Sidell, MD, who raised the need to consider different respiratory protocols for COVID-19, noting that standard protocols were falling short in many cases.
“What we’re seeing ... is something unusual, it’s something that we are not used to,” Dr. Kyle-Sidell of Maimonides Medical Center said in that interview, stressing that the presentation differed from that seen in typical ARDS. “The patterns I was seeing did not make sense.”
Like others, he noted that COVID-19 patients were presenting with illness that clinically looked more like HAPE, but that the pathophysiology is not necessary similar to HAPE.
At around the same time, Luciano Gattinoni, MD, of the Medical University of Göttingen in Germany and colleagues, published a letter to the editor in the American Journal of Respiratory and Critical Care Medicine stressing that the ARDS presentation in COVID-19 patients is atypical and requires a patient physiology–driven treatment approach, rather than a standard protocol–driven approach. Dr. Gattinoni and colleagues suggested that instead of high positive end-expiratory pressure (PEEP), physicians should consider the lowest possible PEEP and gentle ventilation.
Dr. Luks agreed that “some patients with COVID-19 do not have the same physiologic derangements that we see in a lot of other people with ARDS.”
“[Dr. Gattinoni] is making the point that we need to treat these people differently ... and I think that’s a valid point, and honestly, that’s a point that applied even before COVID-19,” he said. “Most of the things that we see in clinical practice – there’s a lot of heterogeneity between patients, and you have to be prepared to tailor your therapy in light of the differences that you’re picking up from your observations at the bedside and other data that you’re getting on the patient.”
The main concern Dr. Luks and his coauthors wanted to convey, they said, is making sure that the anecdotal experiences and observations of clinicians struggling to find answers don’t spiral out of control without proper vetting, thereby leading to patient harm.
“In this challenging time, we must identify the best means to care for these critically ill patients. That approach should be grounded in sound pulmonary physiology, clinical experience and, when available, evidence from clinical studies,” they concluded.
Dr. Luks and Dr. Freer reported having no financial disclosures.
For Luanne Freer, MD, an expert in high-altitude pulmonary edema (HAPE) and founder and director of Everest ER, a nonprofit seasonal clinic at the Mt. Everest base camp in Nepal (elevation, 17,600 ft), a sudden flurry of messages and questions she received about a possible COVID-19/HAPE link was startling.
“That’s why it kind of poked me in the eye,” she said, referencing her extensive experience treating HAPE, which she described as a pressure-related phenomenon. “My goodness, they are so completely different.”
Dr. Freer, an emergency physician, reached out to several pulmonary intensivists with experience treating both HAPE and COVID-19 to gauge their reactions, and within 36 hours, they had drafted their response. In the commentary, published in High Altitude Medicine & Biology, the clinicians note that the comparison between HAPE and COVID-19 is potentially risky.
“As a group of physicians who have in some cases cared for patients with COVID-19 and in all cases cared for patients with HAPE and studied its pathophysiology and management, we feel it important to correct this misconception, as continued amplification of this message could have adverse effects on management of these patients,” they wrote.
The suggestion that COVID-19 lung injury sometimes looks more like HAPE than like acute respiratory distress syndrome (ARDS) appeared in a journal review article in late March and was put forth by medical professionals on social media where it gained traction in recent weeks and was amplified in multiple media outlets, including this one.
“With COVID, we don’t understand everything that’s going on, but we know for sure it’s an inflammatory process – not a pressure-related problem,” Dr. Freer said. “I thought ... this could be so dangerous to load the medicines that we use when we’re treating HAPE onto patients with COVID-19.”
The pathophysiological mechanisms in HAPE are different than those in other respiratory syndromes, including those associated with COVID-19, said Andrew M. Luks, MD, of the UW Medicine, Seattle, and the first author on the commentary.
“HAPE is a noncardiogenic form of pulmonary edema, as are ARDS due to bacteria or viral pneumonia, re-expansion pulmonary edema, immersion pulmonary edema, negative pressure pulmonary edema, and neurogenic pulmonary edema,” Dr. Luks, Dr. Freer, and colleagues wrote in the commentary, explaining that all of these entities cause varying degrees of hypoxemia and diffuse bilateral opacities on chest imaging. “Importantly, in all of these cases, edema accumulates in the interstitial and alveolar spaces of the lung as a result of imbalance in Starling forces.”
A difference between these entities, however, is “the mechanism by which that imbalance develops,” they noted.
The excessive and uneven hypoxic pulmonary vasoconstriction that leads to a marked increase in pulmonary artery pressure, subsequent lung overperfusion, increased pulmonary capillary hydrostatic pressure, and leakage of fluid from the vascular space into the alveolar space as seen in HAPE, is a “fundamentally different phenomenon than what is seen in COVID-19-related ARDS, which involves viral-mediated inflammatory responses as the primary pathophysiological mechanism,” they added.
The authors described several other differences between the conditions, ultimately noting that “understanding the distinction between the pathophysiological mechanisms of these entities is critical for patient management.”
In HAPE, supplemental oxygen alone may be sufficient; in COVID-19, it may improve hypoxemia but won’t resolve the underlying inflammation or injury, they explained, adding that “only good supportive care including mechanical ventilation, quite often for long periods of time, allows some patients to survive until their disease resolves.”
Further, HAPE can be prevented or treated with pulmonary vasodilators such a nifedipine or sildenafil, which decrease pulmonary artery pressure and, as a result lower pulmonary capillary hydrostatic pressure, they said.
Use of such medications for COVID-19 might decrease pulmonary artery pressure and improve right ventricular function in COVID-19, but “by releasing hypoxic pulmonary vasoconstriction and increasing perfusion to nonventilated regions of the lung, they could also worsen ventilation-perfusion mismatch” and thereby worsen hypoxemia, they explained, adding that the treatments can also cause or worsen hypotension.
Efforts to share observations and experience are important in medicine, but sometimes, as in this circumstance, “they get out there, spread around – like a brushfire almost – and get [unwarranted] face validity,” Dr. Luks said, noting that in response to information circulating about COVID-19 and HAPE, he has already heard medical professionals floating the idea of treating COVID-19 with treatments used for HAPE.
It’s true that some COVID-19 lung injury cases are behaving differently than typical ARDS, he said, adding that presentation can vary.
“But trying to equate HAPE and COVID-19 is just wrong,” he said. “HAPE and COVID-19 may share several features ...but those are features that are shared by a lot of different forms of respiratory failure.”
In a recent video interview, WebMD’s chief medical officer John Whyte, MD, spoke with a New York City physician trained in critical care and emergency medicine, Cameron Kyle-Sidell, MD, who raised the need to consider different respiratory protocols for COVID-19, noting that standard protocols were falling short in many cases.
“What we’re seeing ... is something unusual, it’s something that we are not used to,” Dr. Kyle-Sidell of Maimonides Medical Center said in that interview, stressing that the presentation differed from that seen in typical ARDS. “The patterns I was seeing did not make sense.”
Like others, he noted that COVID-19 patients were presenting with illness that clinically looked more like HAPE, but that the pathophysiology is not necessary similar to HAPE.
At around the same time, Luciano Gattinoni, MD, of the Medical University of Göttingen in Germany and colleagues, published a letter to the editor in the American Journal of Respiratory and Critical Care Medicine stressing that the ARDS presentation in COVID-19 patients is atypical and requires a patient physiology–driven treatment approach, rather than a standard protocol–driven approach. Dr. Gattinoni and colleagues suggested that instead of high positive end-expiratory pressure (PEEP), physicians should consider the lowest possible PEEP and gentle ventilation.
Dr. Luks agreed that “some patients with COVID-19 do not have the same physiologic derangements that we see in a lot of other people with ARDS.”
“[Dr. Gattinoni] is making the point that we need to treat these people differently ... and I think that’s a valid point, and honestly, that’s a point that applied even before COVID-19,” he said. “Most of the things that we see in clinical practice – there’s a lot of heterogeneity between patients, and you have to be prepared to tailor your therapy in light of the differences that you’re picking up from your observations at the bedside and other data that you’re getting on the patient.”
The main concern Dr. Luks and his coauthors wanted to convey, they said, is making sure that the anecdotal experiences and observations of clinicians struggling to find answers don’t spiral out of control without proper vetting, thereby leading to patient harm.
“In this challenging time, we must identify the best means to care for these critically ill patients. That approach should be grounded in sound pulmonary physiology, clinical experience and, when available, evidence from clinical studies,” they concluded.
Dr. Luks and Dr. Freer reported having no financial disclosures.
For Luanne Freer, MD, an expert in high-altitude pulmonary edema (HAPE) and founder and director of Everest ER, a nonprofit seasonal clinic at the Mt. Everest base camp in Nepal (elevation, 17,600 ft), a sudden flurry of messages and questions she received about a possible COVID-19/HAPE link was startling.
“That’s why it kind of poked me in the eye,” she said, referencing her extensive experience treating HAPE, which she described as a pressure-related phenomenon. “My goodness, they are so completely different.”
Dr. Freer, an emergency physician, reached out to several pulmonary intensivists with experience treating both HAPE and COVID-19 to gauge their reactions, and within 36 hours, they had drafted their response. In the commentary, published in High Altitude Medicine & Biology, the clinicians note that the comparison between HAPE and COVID-19 is potentially risky.
“As a group of physicians who have in some cases cared for patients with COVID-19 and in all cases cared for patients with HAPE and studied its pathophysiology and management, we feel it important to correct this misconception, as continued amplification of this message could have adverse effects on management of these patients,” they wrote.
The suggestion that COVID-19 lung injury sometimes looks more like HAPE than like acute respiratory distress syndrome (ARDS) appeared in a journal review article in late March and was put forth by medical professionals on social media where it gained traction in recent weeks and was amplified in multiple media outlets, including this one.
“With COVID, we don’t understand everything that’s going on, but we know for sure it’s an inflammatory process – not a pressure-related problem,” Dr. Freer said. “I thought ... this could be so dangerous to load the medicines that we use when we’re treating HAPE onto patients with COVID-19.”
The pathophysiological mechanisms in HAPE are different than those in other respiratory syndromes, including those associated with COVID-19, said Andrew M. Luks, MD, of the UW Medicine, Seattle, and the first author on the commentary.
“HAPE is a noncardiogenic form of pulmonary edema, as are ARDS due to bacteria or viral pneumonia, re-expansion pulmonary edema, immersion pulmonary edema, negative pressure pulmonary edema, and neurogenic pulmonary edema,” Dr. Luks, Dr. Freer, and colleagues wrote in the commentary, explaining that all of these entities cause varying degrees of hypoxemia and diffuse bilateral opacities on chest imaging. “Importantly, in all of these cases, edema accumulates in the interstitial and alveolar spaces of the lung as a result of imbalance in Starling forces.”
A difference between these entities, however, is “the mechanism by which that imbalance develops,” they noted.
The excessive and uneven hypoxic pulmonary vasoconstriction that leads to a marked increase in pulmonary artery pressure, subsequent lung overperfusion, increased pulmonary capillary hydrostatic pressure, and leakage of fluid from the vascular space into the alveolar space as seen in HAPE, is a “fundamentally different phenomenon than what is seen in COVID-19-related ARDS, which involves viral-mediated inflammatory responses as the primary pathophysiological mechanism,” they added.
The authors described several other differences between the conditions, ultimately noting that “understanding the distinction between the pathophysiological mechanisms of these entities is critical for patient management.”
In HAPE, supplemental oxygen alone may be sufficient; in COVID-19, it may improve hypoxemia but won’t resolve the underlying inflammation or injury, they explained, adding that “only good supportive care including mechanical ventilation, quite often for long periods of time, allows some patients to survive until their disease resolves.”
Further, HAPE can be prevented or treated with pulmonary vasodilators such a nifedipine or sildenafil, which decrease pulmonary artery pressure and, as a result lower pulmonary capillary hydrostatic pressure, they said.
Use of such medications for COVID-19 might decrease pulmonary artery pressure and improve right ventricular function in COVID-19, but “by releasing hypoxic pulmonary vasoconstriction and increasing perfusion to nonventilated regions of the lung, they could also worsen ventilation-perfusion mismatch” and thereby worsen hypoxemia, they explained, adding that the treatments can also cause or worsen hypotension.
Efforts to share observations and experience are important in medicine, but sometimes, as in this circumstance, “they get out there, spread around – like a brushfire almost – and get [unwarranted] face validity,” Dr. Luks said, noting that in response to information circulating about COVID-19 and HAPE, he has already heard medical professionals floating the idea of treating COVID-19 with treatments used for HAPE.
It’s true that some COVID-19 lung injury cases are behaving differently than typical ARDS, he said, adding that presentation can vary.
“But trying to equate HAPE and COVID-19 is just wrong,” he said. “HAPE and COVID-19 may share several features ...but those are features that are shared by a lot of different forms of respiratory failure.”
In a recent video interview, WebMD’s chief medical officer John Whyte, MD, spoke with a New York City physician trained in critical care and emergency medicine, Cameron Kyle-Sidell, MD, who raised the need to consider different respiratory protocols for COVID-19, noting that standard protocols were falling short in many cases.
“What we’re seeing ... is something unusual, it’s something that we are not used to,” Dr. Kyle-Sidell of Maimonides Medical Center said in that interview, stressing that the presentation differed from that seen in typical ARDS. “The patterns I was seeing did not make sense.”
Like others, he noted that COVID-19 patients were presenting with illness that clinically looked more like HAPE, but that the pathophysiology is not necessary similar to HAPE.
At around the same time, Luciano Gattinoni, MD, of the Medical University of Göttingen in Germany and colleagues, published a letter to the editor in the American Journal of Respiratory and Critical Care Medicine stressing that the ARDS presentation in COVID-19 patients is atypical and requires a patient physiology–driven treatment approach, rather than a standard protocol–driven approach. Dr. Gattinoni and colleagues suggested that instead of high positive end-expiratory pressure (PEEP), physicians should consider the lowest possible PEEP and gentle ventilation.
Dr. Luks agreed that “some patients with COVID-19 do not have the same physiologic derangements that we see in a lot of other people with ARDS.”
“[Dr. Gattinoni] is making the point that we need to treat these people differently ... and I think that’s a valid point, and honestly, that’s a point that applied even before COVID-19,” he said. “Most of the things that we see in clinical practice – there’s a lot of heterogeneity between patients, and you have to be prepared to tailor your therapy in light of the differences that you’re picking up from your observations at the bedside and other data that you’re getting on the patient.”
The main concern Dr. Luks and his coauthors wanted to convey, they said, is making sure that the anecdotal experiences and observations of clinicians struggling to find answers don’t spiral out of control without proper vetting, thereby leading to patient harm.
“In this challenging time, we must identify the best means to care for these critically ill patients. That approach should be grounded in sound pulmonary physiology, clinical experience and, when available, evidence from clinical studies,” they concluded.
Dr. Luks and Dr. Freer reported having no financial disclosures.
Omalizumab shown to improve chronic rhinosinusitis with nasal polyps
The monoclonal antibody omalizumab, already approved to treat allergic asthma and urticaria, has been shown to improve symptoms of patients who have chronic rhinosinusitis and nasal polyps (CRSwNP), according to recent research released as an abstract from the American Academy of Allergy, Asthma, and Immunology annual meeting. The AAAAI canceled the meeting and provided abstracts and access to presenters for press coverage.
“When you give this drug to patients who have nasal polyposis and concomitant asthma, you are effectively treating both the upper and lower airway disease components,” Jonathan Corren, MD, of the University of California, Los Angeles, said in an interview. “Typically, people with nasal polyp disease have worse nasal disease than people without asthma. In addition, asthma is also generally worse in patients with nasal polyposis,” he added.
Dr. Corren reported results of a subset of patients with corticosteroid-refractory CRSwNP and comorbid asthma enrolled in phase III, placebo-controlled, 24-week, trials of omalizumab, POLYP1 (n = 74) and POLYP2 (n = 77). The analysis excluded patients who were on oral steroids or high-dose steroid inhaler therapy so the effectiveness of omalizumab could be evaluated without interfering factors, Dr. Corren explained. As a result, the study population consisted of patients with mild to moderate asthma. Dr. Corren is also principal investigator of the POLYP1 trial.
The analysis compared changes in Asthma Quality of Life Questionnaire (AQLQ) and sino-nasal outcome test (SNOT-22) measures after 24 weeks of treatment with those seen with placebo.
“With regard to asthma outcomes, we found there was a significant increase in the odds ratio that patients who received omalizumab would achieve a minimal, clinically important improvement in their asthma quality of life,” Dr. Corren said .
The study estimated the odds ratio for minimal clinically important difference in AQLQ at 24 weeks was 3.9 (95% confidence interval, 1.5-9.7; P = .0043), which Dr. Corren called “quite significant.” SNOT-22 scores showed a mean improvement of 23.3 from baseline to week 24, compared with a worsening of 8.4 in placebo (P = .0001).
Omalizumab is approved for treatment of perennial allergies and urticaria. Chronic rhinosinusitis with nasal polyps would be a third indication if the Food and Drug Administration approves it, Dr. Corren noted.
Genentech sponsored the subset analysis. Hoffmann-La Roche, Genentech’s parent company, is sponsor of the POLYP1 and POLYP2 trials. Dr. Corren disclosed financial relationships with Genentech.
SOURCE: Corren J et al. AAAAI, Session 4608, Abstract 813.
The monoclonal antibody omalizumab, already approved to treat allergic asthma and urticaria, has been shown to improve symptoms of patients who have chronic rhinosinusitis and nasal polyps (CRSwNP), according to recent research released as an abstract from the American Academy of Allergy, Asthma, and Immunology annual meeting. The AAAAI canceled the meeting and provided abstracts and access to presenters for press coverage.
“When you give this drug to patients who have nasal polyposis and concomitant asthma, you are effectively treating both the upper and lower airway disease components,” Jonathan Corren, MD, of the University of California, Los Angeles, said in an interview. “Typically, people with nasal polyp disease have worse nasal disease than people without asthma. In addition, asthma is also generally worse in patients with nasal polyposis,” he added.
Dr. Corren reported results of a subset of patients with corticosteroid-refractory CRSwNP and comorbid asthma enrolled in phase III, placebo-controlled, 24-week, trials of omalizumab, POLYP1 (n = 74) and POLYP2 (n = 77). The analysis excluded patients who were on oral steroids or high-dose steroid inhaler therapy so the effectiveness of omalizumab could be evaluated without interfering factors, Dr. Corren explained. As a result, the study population consisted of patients with mild to moderate asthma. Dr. Corren is also principal investigator of the POLYP1 trial.
The analysis compared changes in Asthma Quality of Life Questionnaire (AQLQ) and sino-nasal outcome test (SNOT-22) measures after 24 weeks of treatment with those seen with placebo.
“With regard to asthma outcomes, we found there was a significant increase in the odds ratio that patients who received omalizumab would achieve a minimal, clinically important improvement in their asthma quality of life,” Dr. Corren said .
The study estimated the odds ratio for minimal clinically important difference in AQLQ at 24 weeks was 3.9 (95% confidence interval, 1.5-9.7; P = .0043), which Dr. Corren called “quite significant.” SNOT-22 scores showed a mean improvement of 23.3 from baseline to week 24, compared with a worsening of 8.4 in placebo (P = .0001).
Omalizumab is approved for treatment of perennial allergies and urticaria. Chronic rhinosinusitis with nasal polyps would be a third indication if the Food and Drug Administration approves it, Dr. Corren noted.
Genentech sponsored the subset analysis. Hoffmann-La Roche, Genentech’s parent company, is sponsor of the POLYP1 and POLYP2 trials. Dr. Corren disclosed financial relationships with Genentech.
SOURCE: Corren J et al. AAAAI, Session 4608, Abstract 813.
The monoclonal antibody omalizumab, already approved to treat allergic asthma and urticaria, has been shown to improve symptoms of patients who have chronic rhinosinusitis and nasal polyps (CRSwNP), according to recent research released as an abstract from the American Academy of Allergy, Asthma, and Immunology annual meeting. The AAAAI canceled the meeting and provided abstracts and access to presenters for press coverage.
“When you give this drug to patients who have nasal polyposis and concomitant asthma, you are effectively treating both the upper and lower airway disease components,” Jonathan Corren, MD, of the University of California, Los Angeles, said in an interview. “Typically, people with nasal polyp disease have worse nasal disease than people without asthma. In addition, asthma is also generally worse in patients with nasal polyposis,” he added.
Dr. Corren reported results of a subset of patients with corticosteroid-refractory CRSwNP and comorbid asthma enrolled in phase III, placebo-controlled, 24-week, trials of omalizumab, POLYP1 (n = 74) and POLYP2 (n = 77). The analysis excluded patients who were on oral steroids or high-dose steroid inhaler therapy so the effectiveness of omalizumab could be evaluated without interfering factors, Dr. Corren explained. As a result, the study population consisted of patients with mild to moderate asthma. Dr. Corren is also principal investigator of the POLYP1 trial.
The analysis compared changes in Asthma Quality of Life Questionnaire (AQLQ) and sino-nasal outcome test (SNOT-22) measures after 24 weeks of treatment with those seen with placebo.
“With regard to asthma outcomes, we found there was a significant increase in the odds ratio that patients who received omalizumab would achieve a minimal, clinically important improvement in their asthma quality of life,” Dr. Corren said .
The study estimated the odds ratio for minimal clinically important difference in AQLQ at 24 weeks was 3.9 (95% confidence interval, 1.5-9.7; P = .0043), which Dr. Corren called “quite significant.” SNOT-22 scores showed a mean improvement of 23.3 from baseline to week 24, compared with a worsening of 8.4 in placebo (P = .0001).
Omalizumab is approved for treatment of perennial allergies and urticaria. Chronic rhinosinusitis with nasal polyps would be a third indication if the Food and Drug Administration approves it, Dr. Corren noted.
Genentech sponsored the subset analysis. Hoffmann-La Roche, Genentech’s parent company, is sponsor of the POLYP1 and POLYP2 trials. Dr. Corren disclosed financial relationships with Genentech.
SOURCE: Corren J et al. AAAAI, Session 4608, Abstract 813.
FROM AAAAI
Key clinical point: Omalizumab improved symptoms in people with chronic rhinosinusitis with nasal polyps.
Major finding: Sino-nasal outcome test scores improved 23.3 points in treated patients (P = .0001).
Study details: Subset analysis of 151 patients in the POLYP1 and POLYP2 Phase 2 trials of omalizumab.
Disclosures: Genentech sponsored the subset analysis. Hoffman-La Roche, Genentech’s parent company, is the sponsor of the POLYP1 and POLYP2 clinical trials. Dr. Corren is principal investigator of POLYP1 and disclosed financial relationships with Genentech.
Source: Corren J et al. AAAAI Session 4608, Abstract 813.
Interim guidance for CPR in patients with COVID-19
The American Heart Association (AHA) and seven other medical societies have issued interim guidance to inform treatment of victims of cardiac arrest with suspected or confirmed COVID-19, focusing on reducing provider exposure, and prioritizing oxygenation and ventilation strategies, goals of care, and appropriateness of resuscitation.
“We were very specific in calling this ‘interim guidance’ based on expert opinion because things are evolving so quickly and we are learning more and more every day as more and more patients with COVID-19 are taken care of,” corresponding author Comilla Sasson, MD, PhD, vice president, Emergency Cardiovascular Care (ECC) Science and Innovation, American Heart Association, told theheart.org | Medscape Cardiology.
“We wanted this to be a starting point for providing the clinical guidance that everyone is looking for and, as we collect more data, the guidance will change, as it has for CDC [Centers for Disease Control and Prevention] and WHO [World Health Organization],” she said.
“The guidance sought to balance the provision of timely, high-quality resuscitation to patients while simultaneously protecting rescuers,” she added.
The guidance was published online April 9 in Circulation. The AHA produced the guidelines in collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, the Society of Critical Care Anesthesiologists, and the American Society of Anesthesiologists, with support from the American Association of Critical Care Nurses and National EMS Physicians.
Respiratory Etiologies
“We think of cardiac arrest in adults, especially as related to cardiac etiologies, but we are now thinking of it in COVID-19 more as hypoxemia or respiratory failure, which can predispose patients to cardiac arrest,” Sasson explained.
Healthcare workers are the “highest-risk profession” for contracting the COVID-19, with resuscitations carrying “added risk” for several reasons, the authors note.
Administering CPR involves performing numerous aerosol-generating procedures that can cause viral particles to remain suspended in the air and be inhaled by those nearby, with a half-life of approximately 1 hour, they point out.
Moreover, resuscitation efforts “require numerous providers to work in close proximity to one another and the patient,” and the high-stress emergent nature of these events may result in lapses in infection-control procedures.
The guidance is designed “to protect not only the patient but also the provider and involves strategies regarding oxygenation and ventilation that differ from what we’ve done in the past since we have a strong feeling that this is a different disease process that may require different approaches than what we’ve dealt with in the past,” Sasson commented.
Reducing Provider Exposure
Providers should don PPE to protect both themselves and their colleagues from unnecessary exposure, the authors advise, noting that recommendations for PPE standards may “vary considerably,” so health or emergency medical services (EMS) standards should be taken into account.
Moreover, it is important to allow only the most essential providers into the room or on the scene. In keeping with reducing the number of rescuers, the authors recommend replacing manual chest compressions with mechanical CPR devices for patients who meet height and weight criteria in settings with “protocols and expertise in place for their use.”
COVID-19 status should be communicated to any new providers prior to their arrival on the scene, the authors stress.
Oxygenation and Ventilation Strategies
“Reducing risk of aerosolization during the process of intubation is key,” Sasson emphasized.
For this reason, a high-efficiency particulate air HEPA filter (if available) should be attached to any manual or mechanical ventilation device, specifically in the path of exhaled gas, before any breaths are administered.
Moreover, it is important to intubate early with a cuffed tube and connect to a mechanical ventilator, if possible. The intubator should be engaged with the “highest chance of first-pass success,” and chest compression should be paused to intubate.
To further increase the chance of a successful first intubation, use of video laryngoscopy (if available) is helpful.
Additional guidance includes:
- Using a bag-mask device (or T-piece in neonates) with a HEPA filter and a tight seal prior to intubation
- Considering passive oxygenation with non-rebreathing face mask as an alternative to bag-mask device for short duration (in adults)
- Considering supraglottic airway if intubation is delayed
- Minimizing closed circuit disconnections.
Resuscitation Considerations
“One big take-home point of the guidance is to consider resuscitation appropriateness, starting with goals of care when the patient comes to us, and continuing or stopping resuscitation when needed, based on the discussion with the family as well as local protocol,” Sasson said.
A variety of factors need to be taken into account, including age, comorbidities, and illness severity to determine the appropriateness of resuscitation, and “the likelihood of success” must be balanced “against the risk to rescuers and patients from whom resources are being diverted,” the authors state.
An Array of Scenarios
“We divided bystander CPR into adults vs pediatrics and into those who are living with a person who is in cardiac arrest – because they have already been exposed [to COVID-19] – vs those who are not living with the patient,” Sasson reported. “We also addressed the role of lay bystanders.”
For lay rescuers:
- Household members should perform at least hands-only CPR, if willing and able to do so
- Use of a face mark or cloth covering of the mouth and nose of the rescuer and/or patient may reduce the risk of transmission to a nonhousehold member
- In children, lay rescuers should perform chest compressions and “consider mouth-to-mouth resuscitation,” especially if they are household members.
- If available, an automated external defibrillator should be used to assess and treat victims of out-of-hospital cardiac arrest (OHCA).
The authors offer additional guidance for in-hospital cardiac arrest (IHCA), including addressing advanced care directives, closing the door when possible to prevent airborne contamination of adjacent space, and considering leaving the patient on a mechanical ventilator with HEPA filter.
They additionally address the special needs of neonates, recommending the presence of a “skilled attendant prepared to resuscitate, irrespective of COVID-19 status,” and stressing the importance of PPE since the mother may be a “potential source of aerosolization for the neonatal team.” Additional measures include avoidance of routine airway suctioning and the use of endotracheal medications.
Critically ill pregnant women with COVID-19 are more vulnerable to acute decompensation because of the cardiopulmonary physiological changes associated with pregnancy, the authors note. Preparation for a potential perimortem delivery should take place after 4 minutes of resuscitation and be initiated early in the resuscitation algorithm so as to allow specialized obstetrical and neonatal teams with PPE to convene.
“We will be continually updating this guidance and we are encouraging people to ask questions,” Sasson summarized.
She noted that a hospital-based COVID-19 registry is being formed to collect “clinically relevant data” that will inform and update the current guidance.
Sasson reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper.
This article first appeared on Medscape.com.
The American Heart Association (AHA) and seven other medical societies have issued interim guidance to inform treatment of victims of cardiac arrest with suspected or confirmed COVID-19, focusing on reducing provider exposure, and prioritizing oxygenation and ventilation strategies, goals of care, and appropriateness of resuscitation.
“We were very specific in calling this ‘interim guidance’ based on expert opinion because things are evolving so quickly and we are learning more and more every day as more and more patients with COVID-19 are taken care of,” corresponding author Comilla Sasson, MD, PhD, vice president, Emergency Cardiovascular Care (ECC) Science and Innovation, American Heart Association, told theheart.org | Medscape Cardiology.
“We wanted this to be a starting point for providing the clinical guidance that everyone is looking for and, as we collect more data, the guidance will change, as it has for CDC [Centers for Disease Control and Prevention] and WHO [World Health Organization],” she said.
“The guidance sought to balance the provision of timely, high-quality resuscitation to patients while simultaneously protecting rescuers,” she added.
The guidance was published online April 9 in Circulation. The AHA produced the guidelines in collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, the Society of Critical Care Anesthesiologists, and the American Society of Anesthesiologists, with support from the American Association of Critical Care Nurses and National EMS Physicians.
Respiratory Etiologies
“We think of cardiac arrest in adults, especially as related to cardiac etiologies, but we are now thinking of it in COVID-19 more as hypoxemia or respiratory failure, which can predispose patients to cardiac arrest,” Sasson explained.
Healthcare workers are the “highest-risk profession” for contracting the COVID-19, with resuscitations carrying “added risk” for several reasons, the authors note.
Administering CPR involves performing numerous aerosol-generating procedures that can cause viral particles to remain suspended in the air and be inhaled by those nearby, with a half-life of approximately 1 hour, they point out.
Moreover, resuscitation efforts “require numerous providers to work in close proximity to one another and the patient,” and the high-stress emergent nature of these events may result in lapses in infection-control procedures.
The guidance is designed “to protect not only the patient but also the provider and involves strategies regarding oxygenation and ventilation that differ from what we’ve done in the past since we have a strong feeling that this is a different disease process that may require different approaches than what we’ve dealt with in the past,” Sasson commented.
Reducing Provider Exposure
Providers should don PPE to protect both themselves and their colleagues from unnecessary exposure, the authors advise, noting that recommendations for PPE standards may “vary considerably,” so health or emergency medical services (EMS) standards should be taken into account.
Moreover, it is important to allow only the most essential providers into the room or on the scene. In keeping with reducing the number of rescuers, the authors recommend replacing manual chest compressions with mechanical CPR devices for patients who meet height and weight criteria in settings with “protocols and expertise in place for their use.”
COVID-19 status should be communicated to any new providers prior to their arrival on the scene, the authors stress.
Oxygenation and Ventilation Strategies
“Reducing risk of aerosolization during the process of intubation is key,” Sasson emphasized.
For this reason, a high-efficiency particulate air HEPA filter (if available) should be attached to any manual or mechanical ventilation device, specifically in the path of exhaled gas, before any breaths are administered.
Moreover, it is important to intubate early with a cuffed tube and connect to a mechanical ventilator, if possible. The intubator should be engaged with the “highest chance of first-pass success,” and chest compression should be paused to intubate.
To further increase the chance of a successful first intubation, use of video laryngoscopy (if available) is helpful.
Additional guidance includes:
- Using a bag-mask device (or T-piece in neonates) with a HEPA filter and a tight seal prior to intubation
- Considering passive oxygenation with non-rebreathing face mask as an alternative to bag-mask device for short duration (in adults)
- Considering supraglottic airway if intubation is delayed
- Minimizing closed circuit disconnections.
Resuscitation Considerations
“One big take-home point of the guidance is to consider resuscitation appropriateness, starting with goals of care when the patient comes to us, and continuing or stopping resuscitation when needed, based on the discussion with the family as well as local protocol,” Sasson said.
A variety of factors need to be taken into account, including age, comorbidities, and illness severity to determine the appropriateness of resuscitation, and “the likelihood of success” must be balanced “against the risk to rescuers and patients from whom resources are being diverted,” the authors state.
An Array of Scenarios
“We divided bystander CPR into adults vs pediatrics and into those who are living with a person who is in cardiac arrest – because they have already been exposed [to COVID-19] – vs those who are not living with the patient,” Sasson reported. “We also addressed the role of lay bystanders.”
For lay rescuers:
- Household members should perform at least hands-only CPR, if willing and able to do so
- Use of a face mark or cloth covering of the mouth and nose of the rescuer and/or patient may reduce the risk of transmission to a nonhousehold member
- In children, lay rescuers should perform chest compressions and “consider mouth-to-mouth resuscitation,” especially if they are household members.
- If available, an automated external defibrillator should be used to assess and treat victims of out-of-hospital cardiac arrest (OHCA).
The authors offer additional guidance for in-hospital cardiac arrest (IHCA), including addressing advanced care directives, closing the door when possible to prevent airborne contamination of adjacent space, and considering leaving the patient on a mechanical ventilator with HEPA filter.
They additionally address the special needs of neonates, recommending the presence of a “skilled attendant prepared to resuscitate, irrespective of COVID-19 status,” and stressing the importance of PPE since the mother may be a “potential source of aerosolization for the neonatal team.” Additional measures include avoidance of routine airway suctioning and the use of endotracheal medications.
Critically ill pregnant women with COVID-19 are more vulnerable to acute decompensation because of the cardiopulmonary physiological changes associated with pregnancy, the authors note. Preparation for a potential perimortem delivery should take place after 4 minutes of resuscitation and be initiated early in the resuscitation algorithm so as to allow specialized obstetrical and neonatal teams with PPE to convene.
“We will be continually updating this guidance and we are encouraging people to ask questions,” Sasson summarized.
She noted that a hospital-based COVID-19 registry is being formed to collect “clinically relevant data” that will inform and update the current guidance.
Sasson reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper.
This article first appeared on Medscape.com.
The American Heart Association (AHA) and seven other medical societies have issued interim guidance to inform treatment of victims of cardiac arrest with suspected or confirmed COVID-19, focusing on reducing provider exposure, and prioritizing oxygenation and ventilation strategies, goals of care, and appropriateness of resuscitation.
“We were very specific in calling this ‘interim guidance’ based on expert opinion because things are evolving so quickly and we are learning more and more every day as more and more patients with COVID-19 are taken care of,” corresponding author Comilla Sasson, MD, PhD, vice president, Emergency Cardiovascular Care (ECC) Science and Innovation, American Heart Association, told theheart.org | Medscape Cardiology.
“We wanted this to be a starting point for providing the clinical guidance that everyone is looking for and, as we collect more data, the guidance will change, as it has for CDC [Centers for Disease Control and Prevention] and WHO [World Health Organization],” she said.
“The guidance sought to balance the provision of timely, high-quality resuscitation to patients while simultaneously protecting rescuers,” she added.
The guidance was published online April 9 in Circulation. The AHA produced the guidelines in collaboration with the American Academy of Pediatrics, American Association for Respiratory Care, American College of Emergency Physicians, the Society of Critical Care Anesthesiologists, and the American Society of Anesthesiologists, with support from the American Association of Critical Care Nurses and National EMS Physicians.
Respiratory Etiologies
“We think of cardiac arrest in adults, especially as related to cardiac etiologies, but we are now thinking of it in COVID-19 more as hypoxemia or respiratory failure, which can predispose patients to cardiac arrest,” Sasson explained.
Healthcare workers are the “highest-risk profession” for contracting the COVID-19, with resuscitations carrying “added risk” for several reasons, the authors note.
Administering CPR involves performing numerous aerosol-generating procedures that can cause viral particles to remain suspended in the air and be inhaled by those nearby, with a half-life of approximately 1 hour, they point out.
Moreover, resuscitation efforts “require numerous providers to work in close proximity to one another and the patient,” and the high-stress emergent nature of these events may result in lapses in infection-control procedures.
The guidance is designed “to protect not only the patient but also the provider and involves strategies regarding oxygenation and ventilation that differ from what we’ve done in the past since we have a strong feeling that this is a different disease process that may require different approaches than what we’ve dealt with in the past,” Sasson commented.
Reducing Provider Exposure
Providers should don PPE to protect both themselves and their colleagues from unnecessary exposure, the authors advise, noting that recommendations for PPE standards may “vary considerably,” so health or emergency medical services (EMS) standards should be taken into account.
Moreover, it is important to allow only the most essential providers into the room or on the scene. In keeping with reducing the number of rescuers, the authors recommend replacing manual chest compressions with mechanical CPR devices for patients who meet height and weight criteria in settings with “protocols and expertise in place for their use.”
COVID-19 status should be communicated to any new providers prior to their arrival on the scene, the authors stress.
Oxygenation and Ventilation Strategies
“Reducing risk of aerosolization during the process of intubation is key,” Sasson emphasized.
For this reason, a high-efficiency particulate air HEPA filter (if available) should be attached to any manual or mechanical ventilation device, specifically in the path of exhaled gas, before any breaths are administered.
Moreover, it is important to intubate early with a cuffed tube and connect to a mechanical ventilator, if possible. The intubator should be engaged with the “highest chance of first-pass success,” and chest compression should be paused to intubate.
To further increase the chance of a successful first intubation, use of video laryngoscopy (if available) is helpful.
Additional guidance includes:
- Using a bag-mask device (or T-piece in neonates) with a HEPA filter and a tight seal prior to intubation
- Considering passive oxygenation with non-rebreathing face mask as an alternative to bag-mask device for short duration (in adults)
- Considering supraglottic airway if intubation is delayed
- Minimizing closed circuit disconnections.
Resuscitation Considerations
“One big take-home point of the guidance is to consider resuscitation appropriateness, starting with goals of care when the patient comes to us, and continuing or stopping resuscitation when needed, based on the discussion with the family as well as local protocol,” Sasson said.
A variety of factors need to be taken into account, including age, comorbidities, and illness severity to determine the appropriateness of resuscitation, and “the likelihood of success” must be balanced “against the risk to rescuers and patients from whom resources are being diverted,” the authors state.
An Array of Scenarios
“We divided bystander CPR into adults vs pediatrics and into those who are living with a person who is in cardiac arrest – because they have already been exposed [to COVID-19] – vs those who are not living with the patient,” Sasson reported. “We also addressed the role of lay bystanders.”
For lay rescuers:
- Household members should perform at least hands-only CPR, if willing and able to do so
- Use of a face mark or cloth covering of the mouth and nose of the rescuer and/or patient may reduce the risk of transmission to a nonhousehold member
- In children, lay rescuers should perform chest compressions and “consider mouth-to-mouth resuscitation,” especially if they are household members.
- If available, an automated external defibrillator should be used to assess and treat victims of out-of-hospital cardiac arrest (OHCA).
The authors offer additional guidance for in-hospital cardiac arrest (IHCA), including addressing advanced care directives, closing the door when possible to prevent airborne contamination of adjacent space, and considering leaving the patient on a mechanical ventilator with HEPA filter.
They additionally address the special needs of neonates, recommending the presence of a “skilled attendant prepared to resuscitate, irrespective of COVID-19 status,” and stressing the importance of PPE since the mother may be a “potential source of aerosolization for the neonatal team.” Additional measures include avoidance of routine airway suctioning and the use of endotracheal medications.
Critically ill pregnant women with COVID-19 are more vulnerable to acute decompensation because of the cardiopulmonary physiological changes associated with pregnancy, the authors note. Preparation for a potential perimortem delivery should take place after 4 minutes of resuscitation and be initiated early in the resuscitation algorithm so as to allow specialized obstetrical and neonatal teams with PPE to convene.
“We will be continually updating this guidance and we are encouraging people to ask questions,” Sasson summarized.
She noted that a hospital-based COVID-19 registry is being formed to collect “clinically relevant data” that will inform and update the current guidance.
Sasson reports no relevant financial relationships. The other authors’ disclosures are listed on the original paper.
This article first appeared on Medscape.com.
Researchers investigate impact of smoking on COVID-19 risk
but quitting smoking is likely to lower the risk of developing more severe or fatal cases of the infection, according to research from several recent papers.
Interest in how tobacco use affects COVID-19 infection rates stems from research showing that men at the epicenter of the outbreak in China having a higher early mortality rate. Early reports from China showed a case fatality rate of 4.7% for men, compared with 2.8% for women, according to the World Health Organization. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2, is suspected to enter a cell using the ACE2 receptor. Since smoking up-regulates this receptor, one popular theory is that smoking can increase the risk of COVID-19 or exacerbate symptoms of an existing infection (Eur Respir J. 2020 Apr 8. doi: 10.1183/13993003.00688-2020). In China, about half of men are active smokers, compared with 2.7% of women (Transl Lung Cancer Res. 2019;8[Suppl 1]:S21-30), so this association would explain the severe cases and increased mortality in this group. In response to potential risk for public health, the World Health Organization, Centers for Disease Control and Prevention, the Attorney General of Massachusetts, and other organizations have warned that smoking may increase one’s risk of transmitting and developing COVID-19 or may worsen the infection.
“While it is easy to jump to the conclusion that more ACE2 means more susceptibility to severe infection, there is no evidence to support this,” Brandon Michael Henry, MD, of the cardiac intensive care unit and the Heart Institute at Cincinnati Children’s Hospital Medical Center, said in an interview. “Moreover, some would argue (including myself) that increased ACE2 may in fact be protective, as ACE2 decreases the levels of angiotensin-2 which likely plays a significant role in the pathophysiology of ARDS.”
Some researchers have examined the limited evidence of smoking on COVID-19 risk and come to preliminary conclusions. In a letter to the editor recently published in the European Journal of Internal Medicine, Dr. Henry and Giuseppe Lippi, MD, of the section of clinical biochemistry in the department of neuroscience, biomedicine, and movement at the University of Verona (Italy), performed a meta-analysis of papers examining smoking and COVID-19 up to March 9, 2020 and identified five articles with 1,399 COVID-19 cases (Eur J Intern Med. 2020 Mar 16. doi: 10.1016/j.ejim.2020.03.014).
“Given the fact that COVID-19 is a primarily respiratory illness, smoking was one of first risk factors we examined,” Dr. Henry said.
They noted that a study by Liu et al. in the Chinese Medical Journal was the only paper that showed a significant association between smoking status and COVID-19 case severity (Chin Med J [Engl]. 2020 Feb 28. doi: 10.1097/CM9.0000000000000775), while the four other studies showed no significant association. The pooled data of all five studies showed an association that was not statistically significant (odds ratio, 1.69; 95% confidence interval, 0.41-6.92; P = .254). When Dr. Lippi and Dr. Henry performed the analysis again after removing a paper by Guan et al. (N Engl J Med. 2020 Feb 28. doi: 10.1056/NEJMoa2002032) comprising 89.5% of patients in the pooled analysis, there was no significant association (OR, 4.35; 95% CI, 0.86-21.86; P = .129).
Constantine I. Vardavas, MD, FCCP, of the department of oral health policy and epidemiology at Harvard School of Dental Medicine, Boston, and Katerina Nikitara, of the University of Crete in Heraklion, Greece, also published a systematic review in Tobacco Induced Diseases of five studies evaluating smoking and COVID-19 (Tob Induc Dis. 2020. doi: 10.18332/tid/119324). Of the studies chosen for the review, four were shared with the paper by Dr. Lippi and Dr. Henry. They found “a higher percentage of smokers” made up severe COVID-19 cases, but acknowledged the majority of these were from the largest study by Guan et al. Overall, they calculated smokers carried a risk ratio of 1.4 (95% CI, 0.98-2.00) for developing severe COVID-19 symptoms, and were over twice as likely to be admitted to an ICU, require a mechanical ventilator, or die from COVID-19, compared with patients who did not smoke (RR, 2.4; 95% CI, 1.43-4.04).
“Although further research is warranted as the weight of the evidence increases, with the limited available data, and although the above results are unadjusted for other factors that may impact disease progression, smoking is most likely associated with the negative progression and adverse outcomes of COVID-19,” Dr. Vardavas and Ms. Nikitara concluded.
However, the association between smoking and severe disease was not significant, and it is not immediately clear how the analysis was performed based on the details in the editorial. “Both of our reports were limited by a lack of data adjusted for age, sex, and comorbidities which may influence any analysis on smoking,” Dr. Henry said.
Some researchers have proposed collecting information on smoking status and conducting further research on whether vaping devices like e-cigarettes also impact COVID-19 cases. An editorial by Samuel Brake and colleagues published in the Journal of Clinical Medicine proposed the ACE2-receptor binding site as an area of interest for COVID-19 and as a potential therapeutic target (J Clin Med. 2020 Mar 20. doi: 10.3390/jcm9030841).
Ultimately, whether smoking itself is associated with COVID-19 is still an open question. Nonetheless, encouraging patients to quit smoking should be a priority because long-term sequelae of smoking have been linked to worsened or fatal COVID-19 cases, said Dr. Henry.
“There is a lack of definitive data on smoking to date. Nonetheless, we do know that many illnesses associated with smoking, such as [chronic obstructive pulmonary disease, hypertension, and heart disease are all strong risk factors for severe and fatal COVID-19,” he said. “Thus, absolutely we should encourage the public to quit smoking, especially for older individuals and those with comorbidities.”
The papers by Lippi et al., Vardavas et al., and Brake et al. had no funding source, and the authors reported no relevant conflicts of interest.
but quitting smoking is likely to lower the risk of developing more severe or fatal cases of the infection, according to research from several recent papers.
Interest in how tobacco use affects COVID-19 infection rates stems from research showing that men at the epicenter of the outbreak in China having a higher early mortality rate. Early reports from China showed a case fatality rate of 4.7% for men, compared with 2.8% for women, according to the World Health Organization. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2, is suspected to enter a cell using the ACE2 receptor. Since smoking up-regulates this receptor, one popular theory is that smoking can increase the risk of COVID-19 or exacerbate symptoms of an existing infection (Eur Respir J. 2020 Apr 8. doi: 10.1183/13993003.00688-2020). In China, about half of men are active smokers, compared with 2.7% of women (Transl Lung Cancer Res. 2019;8[Suppl 1]:S21-30), so this association would explain the severe cases and increased mortality in this group. In response to potential risk for public health, the World Health Organization, Centers for Disease Control and Prevention, the Attorney General of Massachusetts, and other organizations have warned that smoking may increase one’s risk of transmitting and developing COVID-19 or may worsen the infection.
“While it is easy to jump to the conclusion that more ACE2 means more susceptibility to severe infection, there is no evidence to support this,” Brandon Michael Henry, MD, of the cardiac intensive care unit and the Heart Institute at Cincinnati Children’s Hospital Medical Center, said in an interview. “Moreover, some would argue (including myself) that increased ACE2 may in fact be protective, as ACE2 decreases the levels of angiotensin-2 which likely plays a significant role in the pathophysiology of ARDS.”
Some researchers have examined the limited evidence of smoking on COVID-19 risk and come to preliminary conclusions. In a letter to the editor recently published in the European Journal of Internal Medicine, Dr. Henry and Giuseppe Lippi, MD, of the section of clinical biochemistry in the department of neuroscience, biomedicine, and movement at the University of Verona (Italy), performed a meta-analysis of papers examining smoking and COVID-19 up to March 9, 2020 and identified five articles with 1,399 COVID-19 cases (Eur J Intern Med. 2020 Mar 16. doi: 10.1016/j.ejim.2020.03.014).
“Given the fact that COVID-19 is a primarily respiratory illness, smoking was one of first risk factors we examined,” Dr. Henry said.
They noted that a study by Liu et al. in the Chinese Medical Journal was the only paper that showed a significant association between smoking status and COVID-19 case severity (Chin Med J [Engl]. 2020 Feb 28. doi: 10.1097/CM9.0000000000000775), while the four other studies showed no significant association. The pooled data of all five studies showed an association that was not statistically significant (odds ratio, 1.69; 95% confidence interval, 0.41-6.92; P = .254). When Dr. Lippi and Dr. Henry performed the analysis again after removing a paper by Guan et al. (N Engl J Med. 2020 Feb 28. doi: 10.1056/NEJMoa2002032) comprising 89.5% of patients in the pooled analysis, there was no significant association (OR, 4.35; 95% CI, 0.86-21.86; P = .129).
Constantine I. Vardavas, MD, FCCP, of the department of oral health policy and epidemiology at Harvard School of Dental Medicine, Boston, and Katerina Nikitara, of the University of Crete in Heraklion, Greece, also published a systematic review in Tobacco Induced Diseases of five studies evaluating smoking and COVID-19 (Tob Induc Dis. 2020. doi: 10.18332/tid/119324). Of the studies chosen for the review, four were shared with the paper by Dr. Lippi and Dr. Henry. They found “a higher percentage of smokers” made up severe COVID-19 cases, but acknowledged the majority of these were from the largest study by Guan et al. Overall, they calculated smokers carried a risk ratio of 1.4 (95% CI, 0.98-2.00) for developing severe COVID-19 symptoms, and were over twice as likely to be admitted to an ICU, require a mechanical ventilator, or die from COVID-19, compared with patients who did not smoke (RR, 2.4; 95% CI, 1.43-4.04).
“Although further research is warranted as the weight of the evidence increases, with the limited available data, and although the above results are unadjusted for other factors that may impact disease progression, smoking is most likely associated with the negative progression and adverse outcomes of COVID-19,” Dr. Vardavas and Ms. Nikitara concluded.
However, the association between smoking and severe disease was not significant, and it is not immediately clear how the analysis was performed based on the details in the editorial. “Both of our reports were limited by a lack of data adjusted for age, sex, and comorbidities which may influence any analysis on smoking,” Dr. Henry said.
Some researchers have proposed collecting information on smoking status and conducting further research on whether vaping devices like e-cigarettes also impact COVID-19 cases. An editorial by Samuel Brake and colleagues published in the Journal of Clinical Medicine proposed the ACE2-receptor binding site as an area of interest for COVID-19 and as a potential therapeutic target (J Clin Med. 2020 Mar 20. doi: 10.3390/jcm9030841).
Ultimately, whether smoking itself is associated with COVID-19 is still an open question. Nonetheless, encouraging patients to quit smoking should be a priority because long-term sequelae of smoking have been linked to worsened or fatal COVID-19 cases, said Dr. Henry.
“There is a lack of definitive data on smoking to date. Nonetheless, we do know that many illnesses associated with smoking, such as [chronic obstructive pulmonary disease, hypertension, and heart disease are all strong risk factors for severe and fatal COVID-19,” he said. “Thus, absolutely we should encourage the public to quit smoking, especially for older individuals and those with comorbidities.”
The papers by Lippi et al., Vardavas et al., and Brake et al. had no funding source, and the authors reported no relevant conflicts of interest.
but quitting smoking is likely to lower the risk of developing more severe or fatal cases of the infection, according to research from several recent papers.
Interest in how tobacco use affects COVID-19 infection rates stems from research showing that men at the epicenter of the outbreak in China having a higher early mortality rate. Early reports from China showed a case fatality rate of 4.7% for men, compared with 2.8% for women, according to the World Health Organization. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus 2, is suspected to enter a cell using the ACE2 receptor. Since smoking up-regulates this receptor, one popular theory is that smoking can increase the risk of COVID-19 or exacerbate symptoms of an existing infection (Eur Respir J. 2020 Apr 8. doi: 10.1183/13993003.00688-2020). In China, about half of men are active smokers, compared with 2.7% of women (Transl Lung Cancer Res. 2019;8[Suppl 1]:S21-30), so this association would explain the severe cases and increased mortality in this group. In response to potential risk for public health, the World Health Organization, Centers for Disease Control and Prevention, the Attorney General of Massachusetts, and other organizations have warned that smoking may increase one’s risk of transmitting and developing COVID-19 or may worsen the infection.
“While it is easy to jump to the conclusion that more ACE2 means more susceptibility to severe infection, there is no evidence to support this,” Brandon Michael Henry, MD, of the cardiac intensive care unit and the Heart Institute at Cincinnati Children’s Hospital Medical Center, said in an interview. “Moreover, some would argue (including myself) that increased ACE2 may in fact be protective, as ACE2 decreases the levels of angiotensin-2 which likely plays a significant role in the pathophysiology of ARDS.”
Some researchers have examined the limited evidence of smoking on COVID-19 risk and come to preliminary conclusions. In a letter to the editor recently published in the European Journal of Internal Medicine, Dr. Henry and Giuseppe Lippi, MD, of the section of clinical biochemistry in the department of neuroscience, biomedicine, and movement at the University of Verona (Italy), performed a meta-analysis of papers examining smoking and COVID-19 up to March 9, 2020 and identified five articles with 1,399 COVID-19 cases (Eur J Intern Med. 2020 Mar 16. doi: 10.1016/j.ejim.2020.03.014).
“Given the fact that COVID-19 is a primarily respiratory illness, smoking was one of first risk factors we examined,” Dr. Henry said.
They noted that a study by Liu et al. in the Chinese Medical Journal was the only paper that showed a significant association between smoking status and COVID-19 case severity (Chin Med J [Engl]. 2020 Feb 28. doi: 10.1097/CM9.0000000000000775), while the four other studies showed no significant association. The pooled data of all five studies showed an association that was not statistically significant (odds ratio, 1.69; 95% confidence interval, 0.41-6.92; P = .254). When Dr. Lippi and Dr. Henry performed the analysis again after removing a paper by Guan et al. (N Engl J Med. 2020 Feb 28. doi: 10.1056/NEJMoa2002032) comprising 89.5% of patients in the pooled analysis, there was no significant association (OR, 4.35; 95% CI, 0.86-21.86; P = .129).
Constantine I. Vardavas, MD, FCCP, of the department of oral health policy and epidemiology at Harvard School of Dental Medicine, Boston, and Katerina Nikitara, of the University of Crete in Heraklion, Greece, also published a systematic review in Tobacco Induced Diseases of five studies evaluating smoking and COVID-19 (Tob Induc Dis. 2020. doi: 10.18332/tid/119324). Of the studies chosen for the review, four were shared with the paper by Dr. Lippi and Dr. Henry. They found “a higher percentage of smokers” made up severe COVID-19 cases, but acknowledged the majority of these were from the largest study by Guan et al. Overall, they calculated smokers carried a risk ratio of 1.4 (95% CI, 0.98-2.00) for developing severe COVID-19 symptoms, and were over twice as likely to be admitted to an ICU, require a mechanical ventilator, or die from COVID-19, compared with patients who did not smoke (RR, 2.4; 95% CI, 1.43-4.04).
“Although further research is warranted as the weight of the evidence increases, with the limited available data, and although the above results are unadjusted for other factors that may impact disease progression, smoking is most likely associated with the negative progression and adverse outcomes of COVID-19,” Dr. Vardavas and Ms. Nikitara concluded.
However, the association between smoking and severe disease was not significant, and it is not immediately clear how the analysis was performed based on the details in the editorial. “Both of our reports were limited by a lack of data adjusted for age, sex, and comorbidities which may influence any analysis on smoking,” Dr. Henry said.
Some researchers have proposed collecting information on smoking status and conducting further research on whether vaping devices like e-cigarettes also impact COVID-19 cases. An editorial by Samuel Brake and colleagues published in the Journal of Clinical Medicine proposed the ACE2-receptor binding site as an area of interest for COVID-19 and as a potential therapeutic target (J Clin Med. 2020 Mar 20. doi: 10.3390/jcm9030841).
Ultimately, whether smoking itself is associated with COVID-19 is still an open question. Nonetheless, encouraging patients to quit smoking should be a priority because long-term sequelae of smoking have been linked to worsened or fatal COVID-19 cases, said Dr. Henry.
“There is a lack of definitive data on smoking to date. Nonetheless, we do know that many illnesses associated with smoking, such as [chronic obstructive pulmonary disease, hypertension, and heart disease are all strong risk factors for severe and fatal COVID-19,” he said. “Thus, absolutely we should encourage the public to quit smoking, especially for older individuals and those with comorbidities.”
The papers by Lippi et al., Vardavas et al., and Brake et al. had no funding source, and the authors reported no relevant conflicts of interest.
Switching gears at high speed
Michigan hospitalists prepare for COVID-19 care
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
Michigan hospitalists prepare for COVID-19 care
Michigan hospitalists prepare for COVID-19 care
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
When March began, Valerie Vaughn, MD, split her time between caring for general inpatients at the University of Michigan’s hospitals in Ann Arbor and doing research on how to reduce overuse of antibiotics in hospitals nationwide.
By the time the month was over, she had helped create a new kind of hospital team focused on caring for patients with COVID-19, learned how to provide an intensive level of care for the sickest among them, trained hundreds of physicians in how to do the same, and created free online learning tools for physicians nationwide.
Call it switching gears while driving a race car. Changing horses in the middle of a raging river. Or going to medical boot camp. Whatever the metaphor, Dr. Vaughn and her colleagues did it.
And now they’re hoping that sharing what they learned will help others if their hospitals go through the same thing.
Near the epicenter
Michigan Medicine, the University of Michigan’s academic medical center, is a few dozen miles west of the Detroit hospitals that have become a national epicenter for COVID-19 cases. It’s gotten plenty of direct and transferred COVID-19 patients since mid-March.
When Dr. Vaughn’s boss, division of hospital medicine chief Vineet Chopra, MD, was tapped to lead the creation of an all-COVID unit, he asked Dr. Vaughn to work with him and the team of hospitalists, nurse practitioners, physician assistants, nurses, respiratory therapists, and other staff that had volunteered for the team.
They had 3 days to prepare.
The “SWAT team”, as Dr. Vaughn calls it, opened the RICU, or Regional Infectious Containment Unit, on March 16. They doubled the number of beds 2 weeks later.
By the end of March, the team had handed over the reins to a team of experienced intensive care professionals so the unit could focus on the sickest patients. And the RICU team had moved on to transforming other areas of the hospital, and training their staff, in the same way.
By early April, more than 200 beds across the University of Michigan’s hospitals were devoted to COVID-19 care. General medicine physicians who hadn’t practiced inside a hospital since their residency days – thanks to the ability to hand off to hospitalists – were being pulled into inpatient duty. Hospitalists were being pulled into caring for patients who would normally have been in the care of an intensive care team.
“What’s amazed me most is how much people have stepped up to the challenge,” says Dr. Vaughn. “As hard and uncomfortable as it is to do something you’re not typically doing, it can also be therapeutic to say how can I help, let me do something. Yes, they’re anxious, but they want to know how they can be as prepared as they can be, to be as helpful as possible to these patients.”
Dr. Chopra agrees. “The silver lining in all of this is that I have personally seen the best in us come to the surface. Nurses, physicians, pharmacists, and therapists have come together and have shown selflessness, kindness, empathy and resilience in profound ways.”
Making the leap
Even though they didn’t choose hospital medicine, or ICU medicine, as their specialty, physicians may greatly underestimate how useful they can be with a little just-in-time training and the help of residents, fellows, advanced practice providers, and experienced nurses and respiratory therapists.
That training is now available for free through Michigan Medicine’s new online COVID-19 CME portal. The session in “Inpatient Management of COVID-19 patients” provides an important overview for those who have never cared for a case, especially if they haven’t been on inpatient duty in a while. The ICU Bootcamp is for those who will be caring for sicker COVID-19 patients but haven’t practiced in an ICU for a while.
One of the most important roles of a COVID-19 inpatient physician, Dr. Vaughn notes, doesn’t involve new skills. Rather, it draws on the doctoring skills that general medicine and hospital medicine physicians have already honed: the ability to assess and treat the entire patient, to talk with families who can’t be with their loved ones, to humanize the experience for patients and their loved ones as much as possible, and to bring messages of love from the family back to the bedside.
By pairing a general medicine physician newly placed on inpatient duty with a resident, nurse practitioner, or physician assistant who can handle inpatient charting duties, the team can make the most of each kind of provider’s time. Administrators, too, can reduce the burden on the entire team by simplifying processes for what must be charted and recorded in the EMR.
“Hospitals facing a COVID-19 crunch need to make it easier for teams to focus on the medicine and the human connection” and to shorten the learning curve for those shifting into unfamiliar duties, she advises.
Other lessons learned
Placing COVID-19 patients on the same unit, and keeping non–COVID-19 patients in another area of the hospital, isn’t just a good idea for protecting uninfected patients, Dr. Vaughn notes. It’s also good for providers who are getting used to treating COVID-19 because they don’t have to shift between the needs of different types of patients as they go from room to room.
“The learning curve is steep, but after a couple of days taking care of these patients, you have a good feeling about how to care for them and a great sense of camaraderie with the rest of the team involved in caring for them,” she says. “Everyone jumps in to help because they know we’re in this as a team and that it’s OK for respiratory therapists to step up to help a physician who doesn’t know as much about ventilator care or for nurses to suggest medications based on what other physicians have used.”
The flattening of professional hierarchies long ingrained in hospitals may be a side effect of the tremendous and urgent sense of mission that has developed around responding to COVID-19, Dr. Vaughn notes.
Those stepping into new roles should invite their colleagues to alert them when they see them about to slip up on protective practices that might be new to them. Similarly, they should help each other resist the urge to rush into a COVID-19 patient’s room unprotected in order to help with an urgent situation. The safety of providers – to preserve their ability to care for the many more patients who will need them – must be paramount.
“To handle this pandemic, we need to all be all-in and working toward a common goal, without competing priorities,” she says. “We need to use everyone’s skill sets to the fullest, without creating burnout. We’re going to be different when all this is done.”
Avoiding provider burnout is harder than ever because team members caring for COVID-19 must stay apart from family at home and avoid in-person visits with loved ones and friends. Those who are switching to inpatient or ICU-level care should make a point of focusing on exercise, sleep, virtual connections with loved ones, and healthy eating in between shifts.
“You’re no good to anyone else if you’re not healthy,” Dr. Vaughn says. “Your mental and physical health have to come first because they enable you to help others.”
Paying attention to the appreciation that the community is showing health care workers can also brighten the day of a stressed COVID-19 inpatient clinician, she notes.
“All the little signs of love from the community – the thank you signs, sidewalk chalk drawings, hearts in people’s windows – really do help.”
This article is published courtesy of the University of Michigan Health Lab, where it appeared originally.
2019-2020 flu season ends with ‘very high’ activity in New Jersey
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
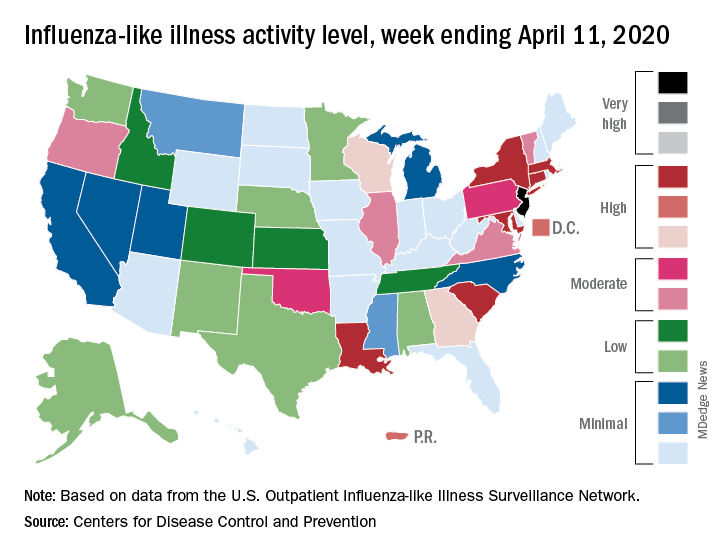
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
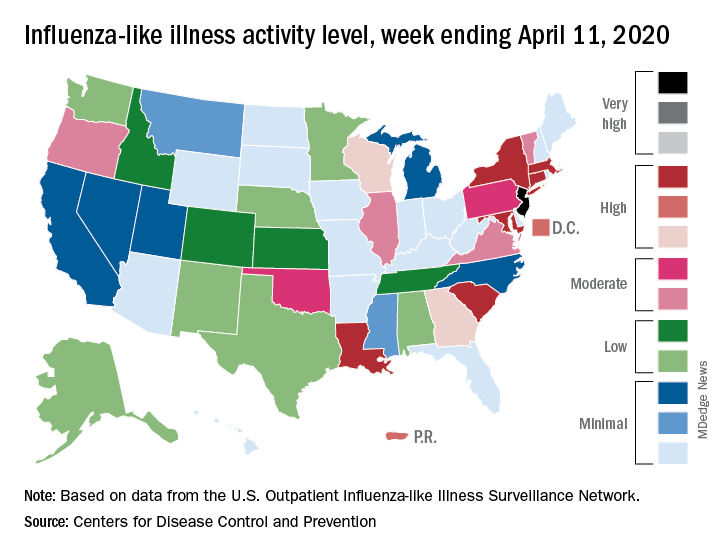
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
The 2019-2020 flu season is ending, but not without a revised map to reflect the COVID-induced new world order.
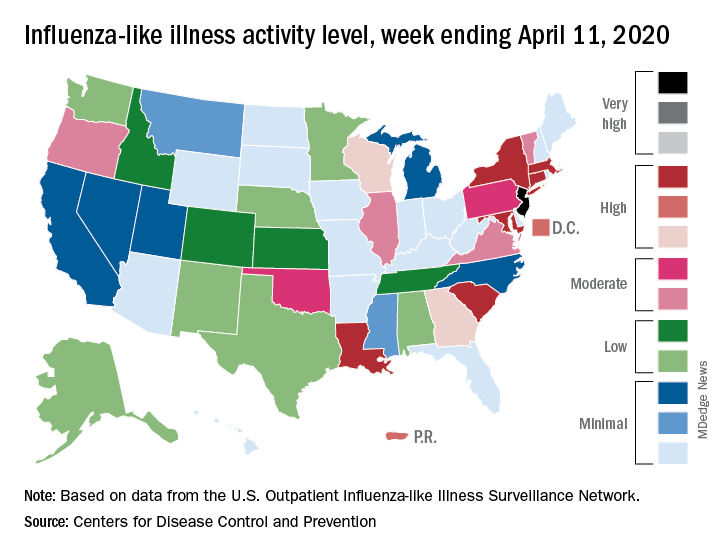
For the week ending April 11, those additions encompass only New Jersey at level 13 and New York City at level 12, the CDC reported April 17.
Eight states, plus the District of Columbia and Puerto Rico, were in the “high” range of flu activity, which runs from level 8 to level 10, for the same week. Those eight states included Connecticut, Georgia, Louisiana, Maryland, Massachusetts, New York, South Carolina, and Wisconsin.
The CDC’s influenza division included this note with its latest FluView report: “The COVID-19 pandemic is affecting healthcare seeking behavior. The number of persons and their reasons for seeking care in the outpatient and ED settings is changing. These changes impact data from ILINet [Outpatient Influenza-like Illness Surveillance Network] in ways that are difficult to differentiate from changes in illness levels, therefore ILINet data should be interpreted with caution.”
Outpatient visits for influenza-like illness made up 2.9% of all visits to health care providers for the week ending April 11, which is the 23rd consecutive week that it’s been at or above the national baseline level of 2.4%. Twenty-three weeks is longer than this has occurred during any flu season since the CDC started setting a baseline in 2007, according to ILINet data.
Mortality from pneumonia and influenza, at 11.7%, was well above the epidemic threshold of 7.0%, although, again, pneumonia mortality “is being driven primarily by an increase in non-influenza pneumonia deaths due to COVID-19,” the CDC wrote.
The total number of influenza-related deaths in children, with reports of two more added this week, is 168 for the season – higher than two of the last three seasons: 144 in 2018-2019, 188 in 2017-2018, and 110 in 2016-2017, according to the CDC.
COVID-19 mythconceptions
Let’s start with a case:
A 37-year-old woman is seen in clinic for a 5-day history of cough, fever, chest tightness, and onset of dyspnea on the day of her office visit.
An exam reveals her blood pressure is 100/60 mm Hg, her pulse is 100 beats per minute, her temperature is 38.7° C, her oxygen saturation is 93%, and her respiratory rate is 20 breaths per minute.
Auscultation of the chest revealed bilateral wheezing and rhonchi. A nasopharyngeal swab is sent for COVID-19 and is negative; she also tests negative for influenza.
Her hemoglobin level is 13 g/dL, hematocrit was 39%, platelet count was 155,000 per mcL of blood, and D-dimer level was 8.4 mcg/mL (normal is less than 0.4 mcg/mL.) Her white blood cell count was 6,000 per mcL of blood (neutrophils, 4,900; lymphocytes, 800; basophils, 200). Her chest x-ray showed bilateral lower lobe infiltrates.
What do you recommend?
A. Begin azithromycin plus ceftriaxone
B. Begin azithromycin
C. Begin oseltamivir
D. Obtain chest CT
E. Repeat COVID-19 test
With the massive amount of information coming out every day on COVID-19, it is hard to keep up with all of it, and sort out accurate, reviewed studies. We are in a position where we need to take in what we can and assess the best data available.
In the case above, I think choices D or E would make sense. This patient very likely has COVID-19 based on clinical symptoms and lab parameters. The negative COVID-19 test gives us pause, but several studies show that false negative tests are not uncommon.
Long et al. reported on 36 patients who had received both chest CT and real-time reverse transcription polymerase chain reaction (rRT-PCR) for COVID-19.1 All were eventually diagnosed with COVID-19 pneumonia. The CT scan had a very high sensitivity (35/36) of 97.2%, whereas the rRT-PCR had a lower sensitivity (30/36) of 83%. All six of the patients with a negative COVID-19 test initially were positive on repeat testing (three on the second test, three on the third test).
There are concerns about what the sensitivity of the rRT-PCR tests being run in the United States are. At this point, I think that, when the pretest probability of COVID-19 infection is very high based on local epidemiology and clinical symptoms, a negative COVID rRT-PCR does not eliminate the diagnosis. In many cases, COVID-19 may still be the most likely diagnosis.
Early in the pandemic, the symptoms that were emphasized were fever, cough, and dyspnea. Those were all crucial symptoms for a disease that causes pneumonia. GI symptoms were initially deemphasized. In an early study released from Wuhan, China, only about 5% of COVID-19 patients had nausea or diarrhea.2 In a study of 305 patients focused on gastrointestinal symptoms, half of the patients had diarrhea, half had anorexia and 30% had nausea.3 In a small series of nine patients who presented with only GI symptoms, four of these patients never developed fever or pulmonary symptoms.3
On March 14, the French health minister, Olivier Véran, tweeted that “taking anti-inflammatory drugs (ibuprofen, cortisone ...) could be an aggravating factor for the infection. If you have a fever, take paracetamol.” This was picked up by many news services, and soon became standard recommendations, despite no data.
There is reason for concern for NSAIDs, as regular NSAID use has been tied to more complications in patients with respiratory tract infections.4 I have never been a proponent of regular NSAID use in patients who are infected, because the likelihood of toxicity is elevated in patients who are volume depleted or under physiologic stress. But at this time, there is no evidence on problems with episodic NSAID use in patients with COVID-19.
Another widely disseminated decree was that patients with COVID-19 should not use ACE inhibitors and angiotensin II receptor blockers (ARBs). COVID-19 binds to their target cells through ACE2, which is expressed by epithelial cells of the lung, intestine and kidney. Patients who are treated with ACE inhibitors and ARBs have been shown to have more ACE2 expression.
In a letter to the editor by Fang et al. published in Lancet Respiratory Medicine, the authors raised the question of whether patients might be better served to be switched from ACE inhibitors and ARBs to calcium-channel blockers for the treatment of hypertension.5 A small study by Meng et al. looked at outcomes of patients on these drugs who had COVID-19 infection.6 They looked at 417 patients admitted to a hospital in China with COVID-19 infection. A total of 42 patients were on medications for hypertension. Group 1 were patients on ACE inhibitors/ARBs (17 patients) and group 2 were patients on other antihypertensives (25 patients). During hospitalization 12 patients (48%) in group 2 were categorized as having severe disease and 1 patient died. In group 1 (the ACE inhibitor/ARB–treated patients) only four (23%) were categorized as having severe disease, and no patients in this group died.
Vaduganathan et al. published a special report in the New England Journal of Medicine strongly arguing the point that “[u]ntil further data are available, we think that [renin-angiotensin-aldosterone system] inhibitors should be continued in patients in otherwise stable condition who are at risk for, being evaluated for, or with COVID-19”.7 This position is supported by the American Heart Association, the American College of Cardiology, the American College of Physicians, and 11 other medical organizations.
Take-home messages
- Testing isn’t perfect – if you have strong suspicion for COVID-19 disease, retest.
- GI symptoms appear to be common, and rarely may be the only symptoms initially.
- NSAIDs are always risky in really sick patients, but data specific to COVID-19 is lacking.
- ACE inhibitors/ARBs should not be avoided in patients with COVID-19.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact Dr. Paauw at [email protected].
References
1. Long C et al. Diagnosis of the Coronavirus disease (COVID-19): rRT-PCR or CT? Eur J Radiol. 2020 Mar 25;126:108961.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Tian Y et al. Review article: Gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;00:1–9.
4. Voiriot G et al. Risks related to the use of nonsteroidal anti-inflammatory drugs in community-acquired pneumonia in adult and pediatric patients. J Clin Med. 2019;8:E786.
5. Fang L et al. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020 Mar 11. doi:10.1016/S2213-2600(20)30116-8.
6. Meng J et al. Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Emerg Microbes Infect. 2020 Dec;9(1):757-60.
7. Vaduganathan M et al. Renin-angiotensin-aldosterone system inhibitors in patients with COVID-19. N Engl J Med. 2020 Mar 30. doi: 10.1056/NEJMsr2005760.
Let’s start with a case:
A 37-year-old woman is seen in clinic for a 5-day history of cough, fever, chest tightness, and onset of dyspnea on the day of her office visit.
An exam reveals her blood pressure is 100/60 mm Hg, her pulse is 100 beats per minute, her temperature is 38.7° C, her oxygen saturation is 93%, and her respiratory rate is 20 breaths per minute.
Auscultation of the chest revealed bilateral wheezing and rhonchi. A nasopharyngeal swab is sent for COVID-19 and is negative; she also tests negative for influenza.
Her hemoglobin level is 13 g/dL, hematocrit was 39%, platelet count was 155,000 per mcL of blood, and D-dimer level was 8.4 mcg/mL (normal is less than 0.4 mcg/mL.) Her white blood cell count was 6,000 per mcL of blood (neutrophils, 4,900; lymphocytes, 800; basophils, 200). Her chest x-ray showed bilateral lower lobe infiltrates.
What do you recommend?
A. Begin azithromycin plus ceftriaxone
B. Begin azithromycin
C. Begin oseltamivir
D. Obtain chest CT
E. Repeat COVID-19 test
With the massive amount of information coming out every day on COVID-19, it is hard to keep up with all of it, and sort out accurate, reviewed studies. We are in a position where we need to take in what we can and assess the best data available.
In the case above, I think choices D or E would make sense. This patient very likely has COVID-19 based on clinical symptoms and lab parameters. The negative COVID-19 test gives us pause, but several studies show that false negative tests are not uncommon.
Long et al. reported on 36 patients who had received both chest CT and real-time reverse transcription polymerase chain reaction (rRT-PCR) for COVID-19.1 All were eventually diagnosed with COVID-19 pneumonia. The CT scan had a very high sensitivity (35/36) of 97.2%, whereas the rRT-PCR had a lower sensitivity (30/36) of 83%. All six of the patients with a negative COVID-19 test initially were positive on repeat testing (three on the second test, three on the third test).
There are concerns about what the sensitivity of the rRT-PCR tests being run in the United States are. At this point, I think that, when the pretest probability of COVID-19 infection is very high based on local epidemiology and clinical symptoms, a negative COVID rRT-PCR does not eliminate the diagnosis. In many cases, COVID-19 may still be the most likely diagnosis.
Early in the pandemic, the symptoms that were emphasized were fever, cough, and dyspnea. Those were all crucial symptoms for a disease that causes pneumonia. GI symptoms were initially deemphasized. In an early study released from Wuhan, China, only about 5% of COVID-19 patients had nausea or diarrhea.2 In a study of 305 patients focused on gastrointestinal symptoms, half of the patients had diarrhea, half had anorexia and 30% had nausea.3 In a small series of nine patients who presented with only GI symptoms, four of these patients never developed fever or pulmonary symptoms.3
On March 14, the French health minister, Olivier Véran, tweeted that “taking anti-inflammatory drugs (ibuprofen, cortisone ...) could be an aggravating factor for the infection. If you have a fever, take paracetamol.” This was picked up by many news services, and soon became standard recommendations, despite no data.
There is reason for concern for NSAIDs, as regular NSAID use has been tied to more complications in patients with respiratory tract infections.4 I have never been a proponent of regular NSAID use in patients who are infected, because the likelihood of toxicity is elevated in patients who are volume depleted or under physiologic stress. But at this time, there is no evidence on problems with episodic NSAID use in patients with COVID-19.
Another widely disseminated decree was that patients with COVID-19 should not use ACE inhibitors and angiotensin II receptor blockers (ARBs). COVID-19 binds to their target cells through ACE2, which is expressed by epithelial cells of the lung, intestine and kidney. Patients who are treated with ACE inhibitors and ARBs have been shown to have more ACE2 expression.
In a letter to the editor by Fang et al. published in Lancet Respiratory Medicine, the authors raised the question of whether patients might be better served to be switched from ACE inhibitors and ARBs to calcium-channel blockers for the treatment of hypertension.5 A small study by Meng et al. looked at outcomes of patients on these drugs who had COVID-19 infection.6 They looked at 417 patients admitted to a hospital in China with COVID-19 infection. A total of 42 patients were on medications for hypertension. Group 1 were patients on ACE inhibitors/ARBs (17 patients) and group 2 were patients on other antihypertensives (25 patients). During hospitalization 12 patients (48%) in group 2 were categorized as having severe disease and 1 patient died. In group 1 (the ACE inhibitor/ARB–treated patients) only four (23%) were categorized as having severe disease, and no patients in this group died.
Vaduganathan et al. published a special report in the New England Journal of Medicine strongly arguing the point that “[u]ntil further data are available, we think that [renin-angiotensin-aldosterone system] inhibitors should be continued in patients in otherwise stable condition who are at risk for, being evaluated for, or with COVID-19”.7 This position is supported by the American Heart Association, the American College of Cardiology, the American College of Physicians, and 11 other medical organizations.
Take-home messages
- Testing isn’t perfect – if you have strong suspicion for COVID-19 disease, retest.
- GI symptoms appear to be common, and rarely may be the only symptoms initially.
- NSAIDs are always risky in really sick patients, but data specific to COVID-19 is lacking.
- ACE inhibitors/ARBs should not be avoided in patients with COVID-19.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact Dr. Paauw at [email protected].
References
1. Long C et al. Diagnosis of the Coronavirus disease (COVID-19): rRT-PCR or CT? Eur J Radiol. 2020 Mar 25;126:108961.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Tian Y et al. Review article: Gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;00:1–9.
4. Voiriot G et al. Risks related to the use of nonsteroidal anti-inflammatory drugs in community-acquired pneumonia in adult and pediatric patients. J Clin Med. 2019;8:E786.
5. Fang L et al. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020 Mar 11. doi:10.1016/S2213-2600(20)30116-8.
6. Meng J et al. Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Emerg Microbes Infect. 2020 Dec;9(1):757-60.
7. Vaduganathan M et al. Renin-angiotensin-aldosterone system inhibitors in patients with COVID-19. N Engl J Med. 2020 Mar 30. doi: 10.1056/NEJMsr2005760.
Let’s start with a case:
A 37-year-old woman is seen in clinic for a 5-day history of cough, fever, chest tightness, and onset of dyspnea on the day of her office visit.
An exam reveals her blood pressure is 100/60 mm Hg, her pulse is 100 beats per minute, her temperature is 38.7° C, her oxygen saturation is 93%, and her respiratory rate is 20 breaths per minute.
Auscultation of the chest revealed bilateral wheezing and rhonchi. A nasopharyngeal swab is sent for COVID-19 and is negative; she also tests negative for influenza.
Her hemoglobin level is 13 g/dL, hematocrit was 39%, platelet count was 155,000 per mcL of blood, and D-dimer level was 8.4 mcg/mL (normal is less than 0.4 mcg/mL.) Her white blood cell count was 6,000 per mcL of blood (neutrophils, 4,900; lymphocytes, 800; basophils, 200). Her chest x-ray showed bilateral lower lobe infiltrates.
What do you recommend?
A. Begin azithromycin plus ceftriaxone
B. Begin azithromycin
C. Begin oseltamivir
D. Obtain chest CT
E. Repeat COVID-19 test
With the massive amount of information coming out every day on COVID-19, it is hard to keep up with all of it, and sort out accurate, reviewed studies. We are in a position where we need to take in what we can and assess the best data available.
In the case above, I think choices D or E would make sense. This patient very likely has COVID-19 based on clinical symptoms and lab parameters. The negative COVID-19 test gives us pause, but several studies show that false negative tests are not uncommon.
Long et al. reported on 36 patients who had received both chest CT and real-time reverse transcription polymerase chain reaction (rRT-PCR) for COVID-19.1 All were eventually diagnosed with COVID-19 pneumonia. The CT scan had a very high sensitivity (35/36) of 97.2%, whereas the rRT-PCR had a lower sensitivity (30/36) of 83%. All six of the patients with a negative COVID-19 test initially were positive on repeat testing (three on the second test, three on the third test).
There are concerns about what the sensitivity of the rRT-PCR tests being run in the United States are. At this point, I think that, when the pretest probability of COVID-19 infection is very high based on local epidemiology and clinical symptoms, a negative COVID rRT-PCR does not eliminate the diagnosis. In many cases, COVID-19 may still be the most likely diagnosis.
Early in the pandemic, the symptoms that were emphasized were fever, cough, and dyspnea. Those were all crucial symptoms for a disease that causes pneumonia. GI symptoms were initially deemphasized. In an early study released from Wuhan, China, only about 5% of COVID-19 patients had nausea or diarrhea.2 In a study of 305 patients focused on gastrointestinal symptoms, half of the patients had diarrhea, half had anorexia and 30% had nausea.3 In a small series of nine patients who presented with only GI symptoms, four of these patients never developed fever or pulmonary symptoms.3
On March 14, the French health minister, Olivier Véran, tweeted that “taking anti-inflammatory drugs (ibuprofen, cortisone ...) could be an aggravating factor for the infection. If you have a fever, take paracetamol.” This was picked up by many news services, and soon became standard recommendations, despite no data.
There is reason for concern for NSAIDs, as regular NSAID use has been tied to more complications in patients with respiratory tract infections.4 I have never been a proponent of regular NSAID use in patients who are infected, because the likelihood of toxicity is elevated in patients who are volume depleted or under physiologic stress. But at this time, there is no evidence on problems with episodic NSAID use in patients with COVID-19.
Another widely disseminated decree was that patients with COVID-19 should not use ACE inhibitors and angiotensin II receptor blockers (ARBs). COVID-19 binds to their target cells through ACE2, which is expressed by epithelial cells of the lung, intestine and kidney. Patients who are treated with ACE inhibitors and ARBs have been shown to have more ACE2 expression.
In a letter to the editor by Fang et al. published in Lancet Respiratory Medicine, the authors raised the question of whether patients might be better served to be switched from ACE inhibitors and ARBs to calcium-channel blockers for the treatment of hypertension.5 A small study by Meng et al. looked at outcomes of patients on these drugs who had COVID-19 infection.6 They looked at 417 patients admitted to a hospital in China with COVID-19 infection. A total of 42 patients were on medications for hypertension. Group 1 were patients on ACE inhibitors/ARBs (17 patients) and group 2 were patients on other antihypertensives (25 patients). During hospitalization 12 patients (48%) in group 2 were categorized as having severe disease and 1 patient died. In group 1 (the ACE inhibitor/ARB–treated patients) only four (23%) were categorized as having severe disease, and no patients in this group died.
Vaduganathan et al. published a special report in the New England Journal of Medicine strongly arguing the point that “[u]ntil further data are available, we think that [renin-angiotensin-aldosterone system] inhibitors should be continued in patients in otherwise stable condition who are at risk for, being evaluated for, or with COVID-19”.7 This position is supported by the American Heart Association, the American College of Cardiology, the American College of Physicians, and 11 other medical organizations.
Take-home messages
- Testing isn’t perfect – if you have strong suspicion for COVID-19 disease, retest.
- GI symptoms appear to be common, and rarely may be the only symptoms initially.
- NSAIDs are always risky in really sick patients, but data specific to COVID-19 is lacking.
- ACE inhibitors/ARBs should not be avoided in patients with COVID-19.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact Dr. Paauw at [email protected].
References
1. Long C et al. Diagnosis of the Coronavirus disease (COVID-19): rRT-PCR or CT? Eur J Radiol. 2020 Mar 25;126:108961.
2. Zhou F et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: A retrospective cohort study. Lancet. 2020 Mar 28;395(10229):1054-62.
3. Tian Y et al. Review article: Gastrointestinal features in COVID-19 and the possibility of faecal transmission. Aliment Pharmacol Ther. 2020;00:1–9.
4. Voiriot G et al. Risks related to the use of nonsteroidal anti-inflammatory drugs in community-acquired pneumonia in adult and pediatric patients. J Clin Med. 2019;8:E786.
5. Fang L et al. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med. 2020 Mar 11. doi:10.1016/S2213-2600(20)30116-8.
6. Meng J et al. Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Renin-angiotensin system inhibitors improve the clinical outcomes of COVID-19 patients with hypertension. Emerg Microbes Infect. 2020 Dec;9(1):757-60.
7. Vaduganathan M et al. Renin-angiotensin-aldosterone system inhibitors in patients with COVID-19. N Engl J Med. 2020 Mar 30. doi: 10.1056/NEJMsr2005760.
Should ART for HIV be initiated prior to tuberculosis testing results?
Tuberculosis symptoms as defined by the World Health Organization were effective in identifying patients with TB for the purposes of same-day antiretroviral therapy (ART) initiation in patients diagnosed with HIV, according to a pooled study of patients in two clinical trials. Guidelines suggest that patients with one or more TB symptoms be investigated for active TB before initiation of ART.
However, more than 80% of patients with TB symptoms did not have the disease and faced a delay of ART initiation, despite the many benefits of same-day ART initiation, according to the study presented online at the Conference on Retroviruses & Opportunistic Infections. This year CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
In her presentation, Alana T. Brennan, PhD, of the Boston University School of Public Health discussed the pooled results of 834 patients in the SLATE (Simple Algorithm for Treatment Eligibility) I and SLATE II trials. These two trials, conducted in South Africa and Kenya, respectively, assessed two variations of a simplified algorithm for eligibility for same-day ART initiation.
A total of 834 patients at baseline reported any self-described symptoms of TB using the WHO four-symptom TB screen (cough, fever, weight loss, night sweats). Those patients with any TB symptoms were assessed by sputum samples. The outcomes were prevalence of TB symptoms, TB diagnosis, and treatment.
Among the 834 patients, 493 (60%) reported no symptoms; 215 (26%) reported one to two symptoms, and 120 (14%) reported three to four symptoms. Only 66% of the patients with one to two symptoms were tested for TB; 78% of the patients with three to four symptoms were tested. Of these, only 1% of the patients with one to two symptoms tested positive for TB, and only 2% of the patients with three to four symptoms tested positive, according to Dr. Brennan.
“More than 80% of patients with TB symptoms did not have TB, but faced delay in ART initiation. No same-day [ART] initiators reported adverse events, so we hope that there would be some reconsideration of the requirement of TB testing prior to ART initiation due to any symptom of TB. … A potential consideration of the severity of the symptoms a patient has is necessary,” Dr. Brennan concluded.
Dr. Brennan reported that there were no disclosures.
SOURCE: Brennan AT et al. CROI 2020, Abstract 720.
Tuberculosis symptoms as defined by the World Health Organization were effective in identifying patients with TB for the purposes of same-day antiretroviral therapy (ART) initiation in patients diagnosed with HIV, according to a pooled study of patients in two clinical trials. Guidelines suggest that patients with one or more TB symptoms be investigated for active TB before initiation of ART.
However, more than 80% of patients with TB symptoms did not have the disease and faced a delay of ART initiation, despite the many benefits of same-day ART initiation, according to the study presented online at the Conference on Retroviruses & Opportunistic Infections. This year CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
In her presentation, Alana T. Brennan, PhD, of the Boston University School of Public Health discussed the pooled results of 834 patients in the SLATE (Simple Algorithm for Treatment Eligibility) I and SLATE II trials. These two trials, conducted in South Africa and Kenya, respectively, assessed two variations of a simplified algorithm for eligibility for same-day ART initiation.
A total of 834 patients at baseline reported any self-described symptoms of TB using the WHO four-symptom TB screen (cough, fever, weight loss, night sweats). Those patients with any TB symptoms were assessed by sputum samples. The outcomes were prevalence of TB symptoms, TB diagnosis, and treatment.
Among the 834 patients, 493 (60%) reported no symptoms; 215 (26%) reported one to two symptoms, and 120 (14%) reported three to four symptoms. Only 66% of the patients with one to two symptoms were tested for TB; 78% of the patients with three to four symptoms were tested. Of these, only 1% of the patients with one to two symptoms tested positive for TB, and only 2% of the patients with three to four symptoms tested positive, according to Dr. Brennan.
“More than 80% of patients with TB symptoms did not have TB, but faced delay in ART initiation. No same-day [ART] initiators reported adverse events, so we hope that there would be some reconsideration of the requirement of TB testing prior to ART initiation due to any symptom of TB. … A potential consideration of the severity of the symptoms a patient has is necessary,” Dr. Brennan concluded.
Dr. Brennan reported that there were no disclosures.
SOURCE: Brennan AT et al. CROI 2020, Abstract 720.
Tuberculosis symptoms as defined by the World Health Organization were effective in identifying patients with TB for the purposes of same-day antiretroviral therapy (ART) initiation in patients diagnosed with HIV, according to a pooled study of patients in two clinical trials. Guidelines suggest that patients with one or more TB symptoms be investigated for active TB before initiation of ART.
However, more than 80% of patients with TB symptoms did not have the disease and faced a delay of ART initiation, despite the many benefits of same-day ART initiation, according to the study presented online at the Conference on Retroviruses & Opportunistic Infections. This year CROI organizers chose to hold a virtual meeting because of concerns about the spread of COVID-19.
In her presentation, Alana T. Brennan, PhD, of the Boston University School of Public Health discussed the pooled results of 834 patients in the SLATE (Simple Algorithm for Treatment Eligibility) I and SLATE II trials. These two trials, conducted in South Africa and Kenya, respectively, assessed two variations of a simplified algorithm for eligibility for same-day ART initiation.
A total of 834 patients at baseline reported any self-described symptoms of TB using the WHO four-symptom TB screen (cough, fever, weight loss, night sweats). Those patients with any TB symptoms were assessed by sputum samples. The outcomes were prevalence of TB symptoms, TB diagnosis, and treatment.
Among the 834 patients, 493 (60%) reported no symptoms; 215 (26%) reported one to two symptoms, and 120 (14%) reported three to four symptoms. Only 66% of the patients with one to two symptoms were tested for TB; 78% of the patients with three to four symptoms were tested. Of these, only 1% of the patients with one to two symptoms tested positive for TB, and only 2% of the patients with three to four symptoms tested positive, according to Dr. Brennan.
“More than 80% of patients with TB symptoms did not have TB, but faced delay in ART initiation. No same-day [ART] initiators reported adverse events, so we hope that there would be some reconsideration of the requirement of TB testing prior to ART initiation due to any symptom of TB. … A potential consideration of the severity of the symptoms a patient has is necessary,” Dr. Brennan concluded.
Dr. Brennan reported that there were no disclosures.
SOURCE: Brennan AT et al. CROI 2020, Abstract 720.
FROM CROI 2020
OSA increases odds of hospital readmission after COPD exacerbation
more than threefold, according to results from a single-center study published in CHEST.
Mario Naranjo, MD, and colleagues retrospectively examined data from Albert Einstein Medical Center in Philadelphia to assess the impact of OSA on hospital readmission within 30 days of discharge after treatment for a COPD exacerbation. Dr. Naranjo is affiliated with Johns Hopkins Medicine, Baltimore.
The researchers analyzed data from 238 patients admitted for COPD exacerbation between May 2017 and July 2018 who were screened for previously unrecognized and untreated OSA and underwent a high-resolution pulse-oximetry or portable sleep monitoring study. In all, 111 (46.6%) had OSA; 28.6% had mild OSA, 9.7% had moderate OSA, and 8.4% had severe OSA.
Most baseline characteristics were similar among patients with and without OSA, but patients with OSA had a greater mean body mass index (33.9 vs. 30.3 kg/m2) and were more likely to have comorbid heart failure (19.8% vs. 7.1%), compared with patients without OSA. In addition, the proportion of male patients was greater in the cohort with OSA (60.4% vs. 49.6%).
For patients with mild OSA (oxygen desaturation index [ODI] ≥ 5 and < 15/hour), the odds of 30-day readmission were 2.05 times higher, compared with patients without OSA (32.4% vs. 18.9%). With moderate OSA (ODI ≥ 15 and < 30/hour), the odds of 30-day readmission were 6.68 times higher (60.9% vs. 18.9%). For severe OSA (ODI ≥ 30/hour), the odds were 10.01 times higher (70.0% vs. 18.9%). “For combined OSA severity categories, the odds of 30-day readmission were 3.5 times higher,” said Dr. Naranjo and colleagues. In addition, 90- and 180-day readmission rates and 6-month mortality rates were higher among patients with OSA.
“These findings have important implications for the evaluation and care of patients admitted to the hospital for COPD exacerbations,” Dr. Naranjo and colleagues said. “Although the combination of COPD and OSA (also known as the “overlap syndrome”) in ambulatory settings has been shown to have worse outcomes in terms of COPD exacerbations and mortality, these findings have not been reported previously for hospitalized COPD patients.”
Greater degrees of nocturnal hypoxemia and hypercapnia, worse functional status, and daytime sleepiness and fatigue may contribute to the relationship between OSA and the likelihood of hospital readmission, according to the authors. A multicenter study is warranted to confirm the results, they said.
Dr. Naranjo had no conflicts of interest. Coauthors have received grants from ResMed, Dayzz, and the National Institutes of Health and consulted for Jazz Pharmaceuticals, Best Doctors, and ResMed. One author is a committee chair for the American Academy of Sleep Medicine.
SOURCE: Naranjo M et al. Chest. 2020 Apr 2. doi: 10.1016/j.chest.2020.03.036.
more than threefold, according to results from a single-center study published in CHEST.
Mario Naranjo, MD, and colleagues retrospectively examined data from Albert Einstein Medical Center in Philadelphia to assess the impact of OSA on hospital readmission within 30 days of discharge after treatment for a COPD exacerbation. Dr. Naranjo is affiliated with Johns Hopkins Medicine, Baltimore.
The researchers analyzed data from 238 patients admitted for COPD exacerbation between May 2017 and July 2018 who were screened for previously unrecognized and untreated OSA and underwent a high-resolution pulse-oximetry or portable sleep monitoring study. In all, 111 (46.6%) had OSA; 28.6% had mild OSA, 9.7% had moderate OSA, and 8.4% had severe OSA.
Most baseline characteristics were similar among patients with and without OSA, but patients with OSA had a greater mean body mass index (33.9 vs. 30.3 kg/m2) and were more likely to have comorbid heart failure (19.8% vs. 7.1%), compared with patients without OSA. In addition, the proportion of male patients was greater in the cohort with OSA (60.4% vs. 49.6%).
For patients with mild OSA (oxygen desaturation index [ODI] ≥ 5 and < 15/hour), the odds of 30-day readmission were 2.05 times higher, compared with patients without OSA (32.4% vs. 18.9%). With moderate OSA (ODI ≥ 15 and < 30/hour), the odds of 30-day readmission were 6.68 times higher (60.9% vs. 18.9%). For severe OSA (ODI ≥ 30/hour), the odds were 10.01 times higher (70.0% vs. 18.9%). “For combined OSA severity categories, the odds of 30-day readmission were 3.5 times higher,” said Dr. Naranjo and colleagues. In addition, 90- and 180-day readmission rates and 6-month mortality rates were higher among patients with OSA.
“These findings have important implications for the evaluation and care of patients admitted to the hospital for COPD exacerbations,” Dr. Naranjo and colleagues said. “Although the combination of COPD and OSA (also known as the “overlap syndrome”) in ambulatory settings has been shown to have worse outcomes in terms of COPD exacerbations and mortality, these findings have not been reported previously for hospitalized COPD patients.”
Greater degrees of nocturnal hypoxemia and hypercapnia, worse functional status, and daytime sleepiness and fatigue may contribute to the relationship between OSA and the likelihood of hospital readmission, according to the authors. A multicenter study is warranted to confirm the results, they said.
Dr. Naranjo had no conflicts of interest. Coauthors have received grants from ResMed, Dayzz, and the National Institutes of Health and consulted for Jazz Pharmaceuticals, Best Doctors, and ResMed. One author is a committee chair for the American Academy of Sleep Medicine.
SOURCE: Naranjo M et al. Chest. 2020 Apr 2. doi: 10.1016/j.chest.2020.03.036.
more than threefold, according to results from a single-center study published in CHEST.
Mario Naranjo, MD, and colleagues retrospectively examined data from Albert Einstein Medical Center in Philadelphia to assess the impact of OSA on hospital readmission within 30 days of discharge after treatment for a COPD exacerbation. Dr. Naranjo is affiliated with Johns Hopkins Medicine, Baltimore.
The researchers analyzed data from 238 patients admitted for COPD exacerbation between May 2017 and July 2018 who were screened for previously unrecognized and untreated OSA and underwent a high-resolution pulse-oximetry or portable sleep monitoring study. In all, 111 (46.6%) had OSA; 28.6% had mild OSA, 9.7% had moderate OSA, and 8.4% had severe OSA.
Most baseline characteristics were similar among patients with and without OSA, but patients with OSA had a greater mean body mass index (33.9 vs. 30.3 kg/m2) and were more likely to have comorbid heart failure (19.8% vs. 7.1%), compared with patients without OSA. In addition, the proportion of male patients was greater in the cohort with OSA (60.4% vs. 49.6%).
For patients with mild OSA (oxygen desaturation index [ODI] ≥ 5 and < 15/hour), the odds of 30-day readmission were 2.05 times higher, compared with patients without OSA (32.4% vs. 18.9%). With moderate OSA (ODI ≥ 15 and < 30/hour), the odds of 30-day readmission were 6.68 times higher (60.9% vs. 18.9%). For severe OSA (ODI ≥ 30/hour), the odds were 10.01 times higher (70.0% vs. 18.9%). “For combined OSA severity categories, the odds of 30-day readmission were 3.5 times higher,” said Dr. Naranjo and colleagues. In addition, 90- and 180-day readmission rates and 6-month mortality rates were higher among patients with OSA.
“These findings have important implications for the evaluation and care of patients admitted to the hospital for COPD exacerbations,” Dr. Naranjo and colleagues said. “Although the combination of COPD and OSA (also known as the “overlap syndrome”) in ambulatory settings has been shown to have worse outcomes in terms of COPD exacerbations and mortality, these findings have not been reported previously for hospitalized COPD patients.”
Greater degrees of nocturnal hypoxemia and hypercapnia, worse functional status, and daytime sleepiness and fatigue may contribute to the relationship between OSA and the likelihood of hospital readmission, according to the authors. A multicenter study is warranted to confirm the results, they said.
Dr. Naranjo had no conflicts of interest. Coauthors have received grants from ResMed, Dayzz, and the National Institutes of Health and consulted for Jazz Pharmaceuticals, Best Doctors, and ResMed. One author is a committee chair for the American Academy of Sleep Medicine.
SOURCE: Naranjo M et al. Chest. 2020 Apr 2. doi: 10.1016/j.chest.2020.03.036.
FROM CHEST