User login
Omicron BA.2: What do we know so far?
Omicron has 30 mutations of the spike protein, compared with the original Wuhan-Hu-1 variant, with 15 mutations of the receptor-binding domain (which are linked to a decrease in antibody binding), mutations at the furin S1/S2 site (which improves furin binding and increases infectiousness), and mutations of the amino terminal domain (which is the main binding site for some of the therapeutic antibodies used to treat COVID-19 infections).
Omicron’s functional characteristics
Non–peer-reviewed studies have shown a replication of Omicron in pulmonary epithelial cells, which was shown to be less efficient, when compared with Delta and Wuhan-Hu-1. The number of viral copies from an Omicron infection in pulmonary epithelial cells was significantly lower, compared with infection with the Delta or Wuhan-Hu-1 variants. The association of these characteristics found an increase in the number of viral copies in human epithelial cells (taken from the nasal airways) infected with Omicron. This supports the understanding that Omicron is more transmissible but results in a less severe manifestation of the disease.
As for the phenotypic expression of the infection, attention has been focused on Omicron’s reduced capacity to cause syncytia in pulmonary tissue cultures, information which is relevant to its clinical significance, if we consider that the formation of syncytia has been associated with a more severe manifestation of the disease. Furthermore, it has emerged that Omicron can use different cellular entry routes, with a preference for endosomal fusion over superficial cellular fusion. This characteristic allows Omicron to significantly increase the number of types of cells it can infect.
Omicron BA.2 evolves
Between November and December 2021, Omicron progressed, evolving into a variant with characteristics similar to those of its predecessors (that is, it underwent a gradual and progressive increase in transmissibility). Early studies on the Omicron variant were mainly based on the BA.1 subvariant. Since the start of January 2022, there has been an unexpected increase in BA.2 in Europe and Asia. Since then, continued surveillance on the evolution of Omicron has shown an increased prevalence of two subvariants: BA.1 with a R346K mutation (BA.1 + R346K) and B.1.1.529.2 (BA.2), with the latter containing eight unique spike mutations and 13 missing spike mutations, compared with those found in BA.1.
From these differences, we cannot presume that their antigenic properties are similar or different, but they seem to be antigenically equidistant from wild-type SARS-CoV-2, likely jeopardizing in equal measures the efficacy of current COVID-19 vaccines. Furthermore, BA.2 shows significant resistance to 17 out of 19 neutralizing monoclonal antibodies tested in this study, demonstrating that current monoclonal antibody therapy may have significant limitations in terms of adequate coverage for all subvariants of the Omicron variant.
Omicron BA.2 and reinfection
BA.2 initially represented only 13% of Omicron sequences at a global level, quickly becoming the dominant form in some countries, such as Denmark. At the end of 2021, BA.2 represented around 20% of all Danish cases of SARS-CoV-2. Halfway through January 2022, this had increased to around 45%, data that indicate that BA.2 carries an advantage over BA.1 within the highly vaccinated population of Denmark.
BA.2 is associated with an increased susceptibility of infection for unvaccinated individuals (odds ratio, 2.19; 95% confidence interval, 1.58-3.04), fully vaccinated individuals (OR, 2.45; 95% CI, 1.77-3.40), and booster-vaccinated individuals (OR, 2.99; 95% CI, 2.11-4.24), compared with BA.1. The pattern of increased transmissibility in BA.2 households was not observed for fully vaccinated and booster-vaccinated primary cases, where the OR of transmission was below 1 for BA.2, compared with BA.1. These data confirm the immune-evasive properties of BA.2 that further reduce the protective effect of vaccination against infection, but do not increase its transmissibility from vaccinated individuals with breakthrough infections.
Omicron, BA.2, and vaccination
The understanding of serum neutralizing activity, in correlation to the efficacy of a vaccine, is a priority of research because of the growing epidemiological significance of BA.2. There is evidence to support the claim that the immune-evasive nature of BA.2 doesn›t seem to be as severe as that of BA.1, and it is possible that there are other viral or host factors that are enabling the rapid diffusion of BA.2. A study published in Science Immunology investigated humoral and cellular immune responses to Omicron and other variants of concern (VOCs), looking to understand how, and to what degree, vaccinated individuals are protected against Omicron. From the results, a very low level of antibody cross-neutralization of Omicron, or a lack thereof, was seen when compared with wild type, Beta, and Delta variants, which could be partially restored by a third booster vaccination. Furthermore, T lymphocytes were shown to recognize Omicron with the same efficacy as seen for the other VOCs, suggesting that vaccinated individuals maintain T lymphocyte immunity, an element that is capable of providing protection in the absence of neutralizing antibodies, limiting the chance of serious disease.
These results are consistent with those available from a study performed in a population from Qatar made up of 2,239,193 people who had received at least two doses of a BNT162b2 or mRNA-1273 vaccine. The efficacy of the booster against a symptomatic Omicron infection, compared with that from the primary series, was 49.4% (95% CI, 47.1-51.6). The efficacy of the booster against hospitalization for COVID-19 and the death rate from Omicron infection, compared with the primary series, was 76.5% (95% CI, 55.9-87.5). The efficacy of the BNT162b2 booster against a symptomatic Delta variant infection (or B.1.617.2), compared with the primary series, was 86.1% (95% CI, 67.3-94.1).
To summarize, the constant increase in the prevalence of BA.2 in more countries over the world has confirmed the growth advantage that this variant has compared with others. BA.2 reduces the protective effect of vaccination against infection. Omicron antibody cross-neutralization can be partially restored by a third booster vaccination, an aspect that becomes problematic in the context of a low vaccination rate, where peaks of Omicron may increase the likelihood of infection in the elderly and in other groups at a higher risk of severe disease. Omicron BA.2 opens up new evolution channels, but what do the experts think will happen?
A version of this article was originally published in Italian on Univadis.
Omicron has 30 mutations of the spike protein, compared with the original Wuhan-Hu-1 variant, with 15 mutations of the receptor-binding domain (which are linked to a decrease in antibody binding), mutations at the furin S1/S2 site (which improves furin binding and increases infectiousness), and mutations of the amino terminal domain (which is the main binding site for some of the therapeutic antibodies used to treat COVID-19 infections).
Omicron’s functional characteristics
Non–peer-reviewed studies have shown a replication of Omicron in pulmonary epithelial cells, which was shown to be less efficient, when compared with Delta and Wuhan-Hu-1. The number of viral copies from an Omicron infection in pulmonary epithelial cells was significantly lower, compared with infection with the Delta or Wuhan-Hu-1 variants. The association of these characteristics found an increase in the number of viral copies in human epithelial cells (taken from the nasal airways) infected with Omicron. This supports the understanding that Omicron is more transmissible but results in a less severe manifestation of the disease.
As for the phenotypic expression of the infection, attention has been focused on Omicron’s reduced capacity to cause syncytia in pulmonary tissue cultures, information which is relevant to its clinical significance, if we consider that the formation of syncytia has been associated with a more severe manifestation of the disease. Furthermore, it has emerged that Omicron can use different cellular entry routes, with a preference for endosomal fusion over superficial cellular fusion. This characteristic allows Omicron to significantly increase the number of types of cells it can infect.
Omicron BA.2 evolves
Between November and December 2021, Omicron progressed, evolving into a variant with characteristics similar to those of its predecessors (that is, it underwent a gradual and progressive increase in transmissibility). Early studies on the Omicron variant were mainly based on the BA.1 subvariant. Since the start of January 2022, there has been an unexpected increase in BA.2 in Europe and Asia. Since then, continued surveillance on the evolution of Omicron has shown an increased prevalence of two subvariants: BA.1 with a R346K mutation (BA.1 + R346K) and B.1.1.529.2 (BA.2), with the latter containing eight unique spike mutations and 13 missing spike mutations, compared with those found in BA.1.
From these differences, we cannot presume that their antigenic properties are similar or different, but they seem to be antigenically equidistant from wild-type SARS-CoV-2, likely jeopardizing in equal measures the efficacy of current COVID-19 vaccines. Furthermore, BA.2 shows significant resistance to 17 out of 19 neutralizing monoclonal antibodies tested in this study, demonstrating that current monoclonal antibody therapy may have significant limitations in terms of adequate coverage for all subvariants of the Omicron variant.
Omicron BA.2 and reinfection
BA.2 initially represented only 13% of Omicron sequences at a global level, quickly becoming the dominant form in some countries, such as Denmark. At the end of 2021, BA.2 represented around 20% of all Danish cases of SARS-CoV-2. Halfway through January 2022, this had increased to around 45%, data that indicate that BA.2 carries an advantage over BA.1 within the highly vaccinated population of Denmark.
BA.2 is associated with an increased susceptibility of infection for unvaccinated individuals (odds ratio, 2.19; 95% confidence interval, 1.58-3.04), fully vaccinated individuals (OR, 2.45; 95% CI, 1.77-3.40), and booster-vaccinated individuals (OR, 2.99; 95% CI, 2.11-4.24), compared with BA.1. The pattern of increased transmissibility in BA.2 households was not observed for fully vaccinated and booster-vaccinated primary cases, where the OR of transmission was below 1 for BA.2, compared with BA.1. These data confirm the immune-evasive properties of BA.2 that further reduce the protective effect of vaccination against infection, but do not increase its transmissibility from vaccinated individuals with breakthrough infections.
Omicron, BA.2, and vaccination
The understanding of serum neutralizing activity, in correlation to the efficacy of a vaccine, is a priority of research because of the growing epidemiological significance of BA.2. There is evidence to support the claim that the immune-evasive nature of BA.2 doesn›t seem to be as severe as that of BA.1, and it is possible that there are other viral or host factors that are enabling the rapid diffusion of BA.2. A study published in Science Immunology investigated humoral and cellular immune responses to Omicron and other variants of concern (VOCs), looking to understand how, and to what degree, vaccinated individuals are protected against Omicron. From the results, a very low level of antibody cross-neutralization of Omicron, or a lack thereof, was seen when compared with wild type, Beta, and Delta variants, which could be partially restored by a third booster vaccination. Furthermore, T lymphocytes were shown to recognize Omicron with the same efficacy as seen for the other VOCs, suggesting that vaccinated individuals maintain T lymphocyte immunity, an element that is capable of providing protection in the absence of neutralizing antibodies, limiting the chance of serious disease.
These results are consistent with those available from a study performed in a population from Qatar made up of 2,239,193 people who had received at least two doses of a BNT162b2 or mRNA-1273 vaccine. The efficacy of the booster against a symptomatic Omicron infection, compared with that from the primary series, was 49.4% (95% CI, 47.1-51.6). The efficacy of the booster against hospitalization for COVID-19 and the death rate from Omicron infection, compared with the primary series, was 76.5% (95% CI, 55.9-87.5). The efficacy of the BNT162b2 booster against a symptomatic Delta variant infection (or B.1.617.2), compared with the primary series, was 86.1% (95% CI, 67.3-94.1).
To summarize, the constant increase in the prevalence of BA.2 in more countries over the world has confirmed the growth advantage that this variant has compared with others. BA.2 reduces the protective effect of vaccination against infection. Omicron antibody cross-neutralization can be partially restored by a third booster vaccination, an aspect that becomes problematic in the context of a low vaccination rate, where peaks of Omicron may increase the likelihood of infection in the elderly and in other groups at a higher risk of severe disease. Omicron BA.2 opens up new evolution channels, but what do the experts think will happen?
A version of this article was originally published in Italian on Univadis.
Omicron has 30 mutations of the spike protein, compared with the original Wuhan-Hu-1 variant, with 15 mutations of the receptor-binding domain (which are linked to a decrease in antibody binding), mutations at the furin S1/S2 site (which improves furin binding and increases infectiousness), and mutations of the amino terminal domain (which is the main binding site for some of the therapeutic antibodies used to treat COVID-19 infections).
Omicron’s functional characteristics
Non–peer-reviewed studies have shown a replication of Omicron in pulmonary epithelial cells, which was shown to be less efficient, when compared with Delta and Wuhan-Hu-1. The number of viral copies from an Omicron infection in pulmonary epithelial cells was significantly lower, compared with infection with the Delta or Wuhan-Hu-1 variants. The association of these characteristics found an increase in the number of viral copies in human epithelial cells (taken from the nasal airways) infected with Omicron. This supports the understanding that Omicron is more transmissible but results in a less severe manifestation of the disease.
As for the phenotypic expression of the infection, attention has been focused on Omicron’s reduced capacity to cause syncytia in pulmonary tissue cultures, information which is relevant to its clinical significance, if we consider that the formation of syncytia has been associated with a more severe manifestation of the disease. Furthermore, it has emerged that Omicron can use different cellular entry routes, with a preference for endosomal fusion over superficial cellular fusion. This characteristic allows Omicron to significantly increase the number of types of cells it can infect.
Omicron BA.2 evolves
Between November and December 2021, Omicron progressed, evolving into a variant with characteristics similar to those of its predecessors (that is, it underwent a gradual and progressive increase in transmissibility). Early studies on the Omicron variant were mainly based on the BA.1 subvariant. Since the start of January 2022, there has been an unexpected increase in BA.2 in Europe and Asia. Since then, continued surveillance on the evolution of Omicron has shown an increased prevalence of two subvariants: BA.1 with a R346K mutation (BA.1 + R346K) and B.1.1.529.2 (BA.2), with the latter containing eight unique spike mutations and 13 missing spike mutations, compared with those found in BA.1.
From these differences, we cannot presume that their antigenic properties are similar or different, but they seem to be antigenically equidistant from wild-type SARS-CoV-2, likely jeopardizing in equal measures the efficacy of current COVID-19 vaccines. Furthermore, BA.2 shows significant resistance to 17 out of 19 neutralizing monoclonal antibodies tested in this study, demonstrating that current monoclonal antibody therapy may have significant limitations in terms of adequate coverage for all subvariants of the Omicron variant.
Omicron BA.2 and reinfection
BA.2 initially represented only 13% of Omicron sequences at a global level, quickly becoming the dominant form in some countries, such as Denmark. At the end of 2021, BA.2 represented around 20% of all Danish cases of SARS-CoV-2. Halfway through January 2022, this had increased to around 45%, data that indicate that BA.2 carries an advantage over BA.1 within the highly vaccinated population of Denmark.
BA.2 is associated with an increased susceptibility of infection for unvaccinated individuals (odds ratio, 2.19; 95% confidence interval, 1.58-3.04), fully vaccinated individuals (OR, 2.45; 95% CI, 1.77-3.40), and booster-vaccinated individuals (OR, 2.99; 95% CI, 2.11-4.24), compared with BA.1. The pattern of increased transmissibility in BA.2 households was not observed for fully vaccinated and booster-vaccinated primary cases, where the OR of transmission was below 1 for BA.2, compared with BA.1. These data confirm the immune-evasive properties of BA.2 that further reduce the protective effect of vaccination against infection, but do not increase its transmissibility from vaccinated individuals with breakthrough infections.
Omicron, BA.2, and vaccination
The understanding of serum neutralizing activity, in correlation to the efficacy of a vaccine, is a priority of research because of the growing epidemiological significance of BA.2. There is evidence to support the claim that the immune-evasive nature of BA.2 doesn›t seem to be as severe as that of BA.1, and it is possible that there are other viral or host factors that are enabling the rapid diffusion of BA.2. A study published in Science Immunology investigated humoral and cellular immune responses to Omicron and other variants of concern (VOCs), looking to understand how, and to what degree, vaccinated individuals are protected against Omicron. From the results, a very low level of antibody cross-neutralization of Omicron, or a lack thereof, was seen when compared with wild type, Beta, and Delta variants, which could be partially restored by a third booster vaccination. Furthermore, T lymphocytes were shown to recognize Omicron with the same efficacy as seen for the other VOCs, suggesting that vaccinated individuals maintain T lymphocyte immunity, an element that is capable of providing protection in the absence of neutralizing antibodies, limiting the chance of serious disease.
These results are consistent with those available from a study performed in a population from Qatar made up of 2,239,193 people who had received at least two doses of a BNT162b2 or mRNA-1273 vaccine. The efficacy of the booster against a symptomatic Omicron infection, compared with that from the primary series, was 49.4% (95% CI, 47.1-51.6). The efficacy of the booster against hospitalization for COVID-19 and the death rate from Omicron infection, compared with the primary series, was 76.5% (95% CI, 55.9-87.5). The efficacy of the BNT162b2 booster against a symptomatic Delta variant infection (or B.1.617.2), compared with the primary series, was 86.1% (95% CI, 67.3-94.1).
To summarize, the constant increase in the prevalence of BA.2 in more countries over the world has confirmed the growth advantage that this variant has compared with others. BA.2 reduces the protective effect of vaccination against infection. Omicron antibody cross-neutralization can be partially restored by a third booster vaccination, an aspect that becomes problematic in the context of a low vaccination rate, where peaks of Omicron may increase the likelihood of infection in the elderly and in other groups at a higher risk of severe disease. Omicron BA.2 opens up new evolution channels, but what do the experts think will happen?
A version of this article was originally published in Italian on Univadis.
Treat or refer? New primary care flow diagrams for allergy patients
Most patients with allergy problems first see PCPs, not allergists, the authors write in Allergy. The new flow diagrams help PCPs treat anaphylaxis, asthma, drug allergy, food allergy, and urticaria.
“The European Academy of Allergy and Clinical Immunology established the Logogram Task Force to create a set of simple flow diagrams to assist allergy nonspecialist, generalist, and primary care teams in the diagnosis of five common allergic diseases encountered in primary care,” lead author Dermot Ryan, MB BCh, BAO, FRGCP, of the University of Edinburgh told this news organization.
“The source documents were mainstream guidelines coupled with ancillary literature,” he added in an email. “A multi-disciplinary taskforce ... distilled these guidelines into accessible, comprehensible, usable, and context-specific flow diagrams.”
The flow diagrams developed in Europe can be used by providers in the United States and elsewhere
“These diagrams are consistent with practices in the U.S.,” Christina E. Ciaccio, MD, an associate professor of pediatrics and the section chief of pediatric allergy and immunology at the University of Chicago Medicine, said in an email. “They will prove helpful to PCPs in the U.S. and elsewhere, particularly to young physicians new to practice.
“Treating allergies is part of the ‘bread-and-butter’ practice of primary care physicians in the U.S.,” Dr. Ciaccio, who was not involved in developing the flow diagrams, explained. “Up to 30% of Americans are atopic, and the vast majority seek treatment advice from their PCP first.”
The flow diagrams can help providers in developing countries, where allergic diseases are common, provide the best patient care possible, she said.
At some point, a PCP may need to think beyond flow diagrams and refer the patient to an allergist
“If the treatment plan for a patient falls outside first- or second-line medications, or if a diagnosis is unclear with preliminary testing, a PCP may reach out to an allergy/immunology specialist to assist in providing care,” Dr. Ciaccio advised. “Allergists may provide treatment options, such as immunotherapy, that the PCP does not offer. PCPs also often reach out to allergy team members for help with patients whose allergies are not ‘run-of-the-mill.’
“The flow diagrams are complex and may not be practical in the middle of a busy clinic,” she cautioned. “However, when a patient comes into a primary care clinic with an atypical presentation of an allergic disease, the diagrams are likely to help a physician feel confident that an allergist is the right physician for consultation.”
Patricia Lynne Lugar, MD, an associate professor of medicine in pulmonary, allergy, and critical care medicine at Duke University in Durham, N.C., noted that providers in the U.S. can use the flow diagrams because the definitions, differential diagnosis, and treatments for the conditions they cover are similar.
“The flow diagrams are comprehensive, and they attempt to condense a great deal of information into summary points. They are very useful in the U.S., and not just for generalists,” Dr. Lugar, who also was not involved in the project, said. “Even emergency rooms would benefit from these flow diagrams, especially regarding the recognition of symptoms and differential diagnosis.”
Asthma and seasonal and environmental allergies are often managed by PCPs, and the flow diagrams would help them decide when to refer their patients to an allergist, she added in an email.
Dr. Lugar advises PCPs to “recognize the symptoms of an allergic condition, offer treatment based on confidence the diagnosis is correct, and offer a referral for testing to confirm the allergy.
“Because 50% or more of asthmatics are allergic, all asthmatics should be offered an allergy evaluation to determine their allergies and avoid exacerbating the asthma,” she added. “I do not see the flow diagrams as comprehensive enough to manage chronic urticaria, asthma, venom allergy, and drug allergy.”
With food allergy, environmental allergy, venom allergy, or anaphylaxis, “allergists are experts at considering the differential diagnosis and providing the next steps in the diagnostic workup,” Dr. Lugar said. “Allergists can also provide special treatments, such as allergen-specific immunotherapy or desensitization.”
The flow diagrams guide nonspecialists in diagnosis and treatment of their patients with allergy, with supplementary information as needed. The diagrams recommend referral to a specialist when appropriate, as in cases of anaphylaxis, or chronic urticaria.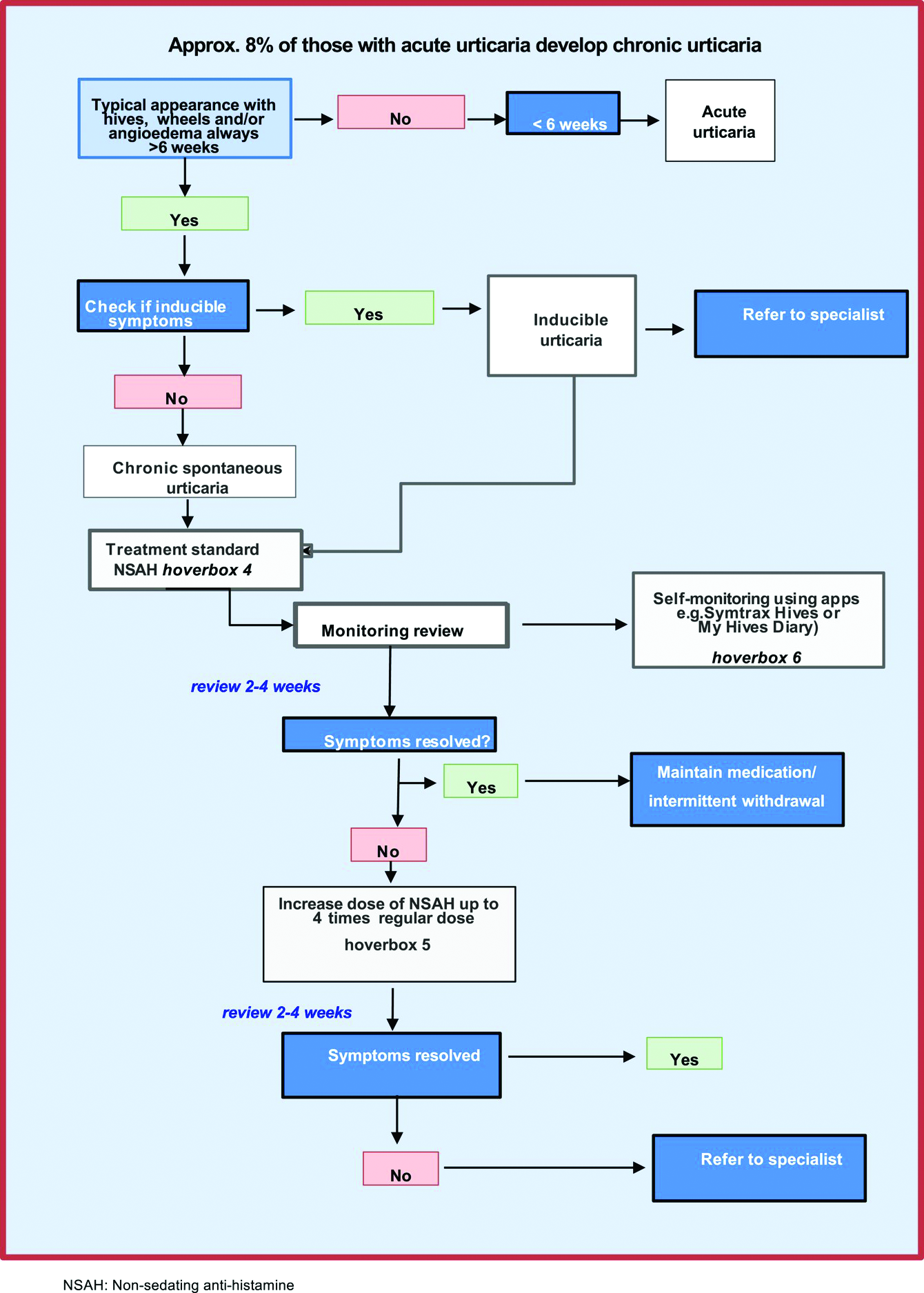
The task force was funded by EAACI. Dr. Ryan and several other authors report financial relationships with pharmaceutical companies. Dr. Ciaccio and Dr. Lugar report no such relationships.
A version of this article first appeared on Medscape.com.
Most patients with allergy problems first see PCPs, not allergists, the authors write in Allergy. The new flow diagrams help PCPs treat anaphylaxis, asthma, drug allergy, food allergy, and urticaria.
“The European Academy of Allergy and Clinical Immunology established the Logogram Task Force to create a set of simple flow diagrams to assist allergy nonspecialist, generalist, and primary care teams in the diagnosis of five common allergic diseases encountered in primary care,” lead author Dermot Ryan, MB BCh, BAO, FRGCP, of the University of Edinburgh told this news organization.
“The source documents were mainstream guidelines coupled with ancillary literature,” he added in an email. “A multi-disciplinary taskforce ... distilled these guidelines into accessible, comprehensible, usable, and context-specific flow diagrams.”
The flow diagrams developed in Europe can be used by providers in the United States and elsewhere
“These diagrams are consistent with practices in the U.S.,” Christina E. Ciaccio, MD, an associate professor of pediatrics and the section chief of pediatric allergy and immunology at the University of Chicago Medicine, said in an email. “They will prove helpful to PCPs in the U.S. and elsewhere, particularly to young physicians new to practice.
“Treating allergies is part of the ‘bread-and-butter’ practice of primary care physicians in the U.S.,” Dr. Ciaccio, who was not involved in developing the flow diagrams, explained. “Up to 30% of Americans are atopic, and the vast majority seek treatment advice from their PCP first.”
The flow diagrams can help providers in developing countries, where allergic diseases are common, provide the best patient care possible, she said.
At some point, a PCP may need to think beyond flow diagrams and refer the patient to an allergist
“If the treatment plan for a patient falls outside first- or second-line medications, or if a diagnosis is unclear with preliminary testing, a PCP may reach out to an allergy/immunology specialist to assist in providing care,” Dr. Ciaccio advised. “Allergists may provide treatment options, such as immunotherapy, that the PCP does not offer. PCPs also often reach out to allergy team members for help with patients whose allergies are not ‘run-of-the-mill.’
“The flow diagrams are complex and may not be practical in the middle of a busy clinic,” she cautioned. “However, when a patient comes into a primary care clinic with an atypical presentation of an allergic disease, the diagrams are likely to help a physician feel confident that an allergist is the right physician for consultation.”
Patricia Lynne Lugar, MD, an associate professor of medicine in pulmonary, allergy, and critical care medicine at Duke University in Durham, N.C., noted that providers in the U.S. can use the flow diagrams because the definitions, differential diagnosis, and treatments for the conditions they cover are similar.
“The flow diagrams are comprehensive, and they attempt to condense a great deal of information into summary points. They are very useful in the U.S., and not just for generalists,” Dr. Lugar, who also was not involved in the project, said. “Even emergency rooms would benefit from these flow diagrams, especially regarding the recognition of symptoms and differential diagnosis.”
Asthma and seasonal and environmental allergies are often managed by PCPs, and the flow diagrams would help them decide when to refer their patients to an allergist, she added in an email.
Dr. Lugar advises PCPs to “recognize the symptoms of an allergic condition, offer treatment based on confidence the diagnosis is correct, and offer a referral for testing to confirm the allergy.
“Because 50% or more of asthmatics are allergic, all asthmatics should be offered an allergy evaluation to determine their allergies and avoid exacerbating the asthma,” she added. “I do not see the flow diagrams as comprehensive enough to manage chronic urticaria, asthma, venom allergy, and drug allergy.”
With food allergy, environmental allergy, venom allergy, or anaphylaxis, “allergists are experts at considering the differential diagnosis and providing the next steps in the diagnostic workup,” Dr. Lugar said. “Allergists can also provide special treatments, such as allergen-specific immunotherapy or desensitization.”
The flow diagrams guide nonspecialists in diagnosis and treatment of their patients with allergy, with supplementary information as needed. The diagrams recommend referral to a specialist when appropriate, as in cases of anaphylaxis, or chronic urticaria.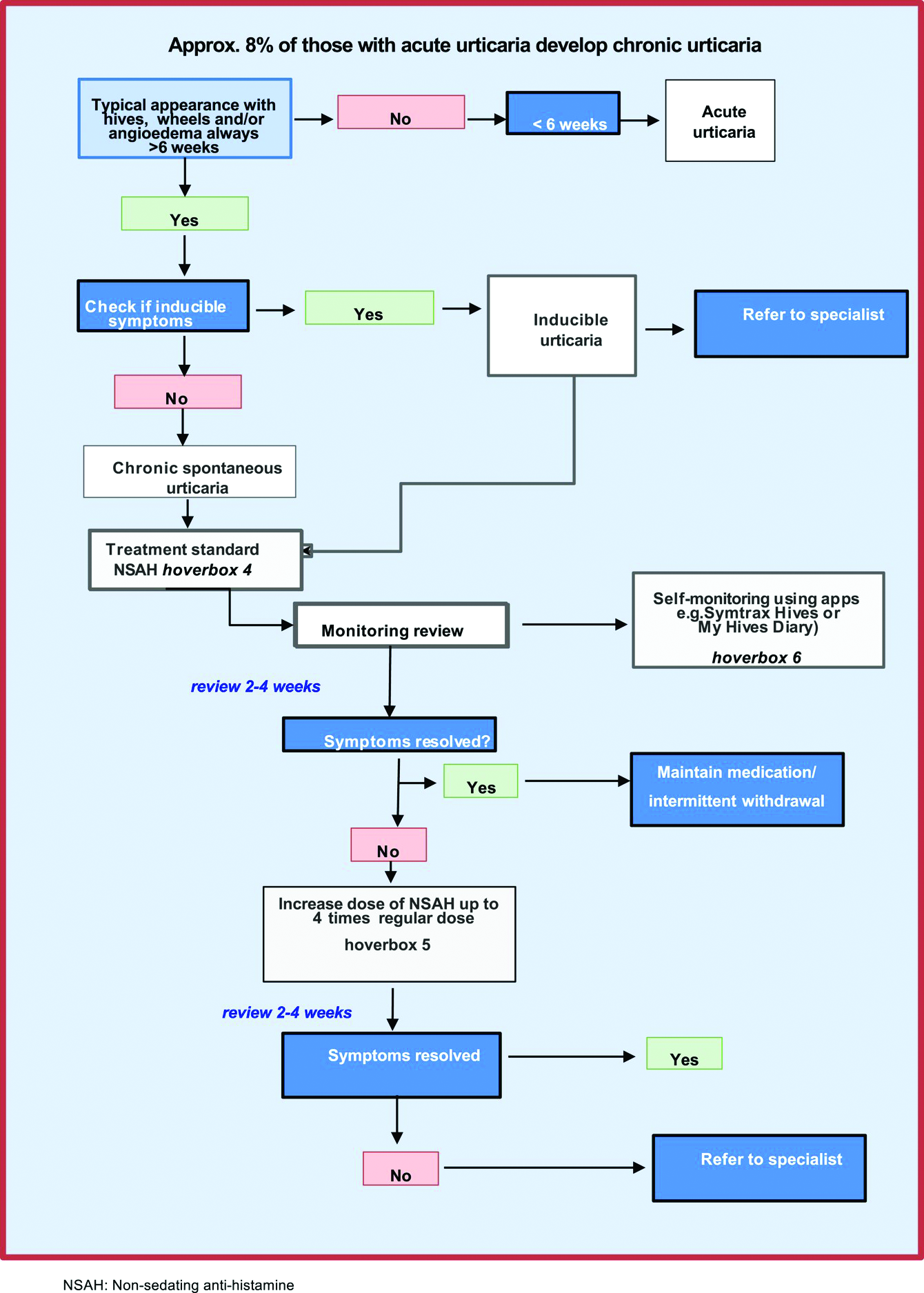
The task force was funded by EAACI. Dr. Ryan and several other authors report financial relationships with pharmaceutical companies. Dr. Ciaccio and Dr. Lugar report no such relationships.
A version of this article first appeared on Medscape.com.
Most patients with allergy problems first see PCPs, not allergists, the authors write in Allergy. The new flow diagrams help PCPs treat anaphylaxis, asthma, drug allergy, food allergy, and urticaria.
“The European Academy of Allergy and Clinical Immunology established the Logogram Task Force to create a set of simple flow diagrams to assist allergy nonspecialist, generalist, and primary care teams in the diagnosis of five common allergic diseases encountered in primary care,” lead author Dermot Ryan, MB BCh, BAO, FRGCP, of the University of Edinburgh told this news organization.
“The source documents were mainstream guidelines coupled with ancillary literature,” he added in an email. “A multi-disciplinary taskforce ... distilled these guidelines into accessible, comprehensible, usable, and context-specific flow diagrams.”
The flow diagrams developed in Europe can be used by providers in the United States and elsewhere
“These diagrams are consistent with practices in the U.S.,” Christina E. Ciaccio, MD, an associate professor of pediatrics and the section chief of pediatric allergy and immunology at the University of Chicago Medicine, said in an email. “They will prove helpful to PCPs in the U.S. and elsewhere, particularly to young physicians new to practice.
“Treating allergies is part of the ‘bread-and-butter’ practice of primary care physicians in the U.S.,” Dr. Ciaccio, who was not involved in developing the flow diagrams, explained. “Up to 30% of Americans are atopic, and the vast majority seek treatment advice from their PCP first.”
The flow diagrams can help providers in developing countries, where allergic diseases are common, provide the best patient care possible, she said.
At some point, a PCP may need to think beyond flow diagrams and refer the patient to an allergist
“If the treatment plan for a patient falls outside first- or second-line medications, or if a diagnosis is unclear with preliminary testing, a PCP may reach out to an allergy/immunology specialist to assist in providing care,” Dr. Ciaccio advised. “Allergists may provide treatment options, such as immunotherapy, that the PCP does not offer. PCPs also often reach out to allergy team members for help with patients whose allergies are not ‘run-of-the-mill.’
“The flow diagrams are complex and may not be practical in the middle of a busy clinic,” she cautioned. “However, when a patient comes into a primary care clinic with an atypical presentation of an allergic disease, the diagrams are likely to help a physician feel confident that an allergist is the right physician for consultation.”
Patricia Lynne Lugar, MD, an associate professor of medicine in pulmonary, allergy, and critical care medicine at Duke University in Durham, N.C., noted that providers in the U.S. can use the flow diagrams because the definitions, differential diagnosis, and treatments for the conditions they cover are similar.
“The flow diagrams are comprehensive, and they attempt to condense a great deal of information into summary points. They are very useful in the U.S., and not just for generalists,” Dr. Lugar, who also was not involved in the project, said. “Even emergency rooms would benefit from these flow diagrams, especially regarding the recognition of symptoms and differential diagnosis.”
Asthma and seasonal and environmental allergies are often managed by PCPs, and the flow diagrams would help them decide when to refer their patients to an allergist, she added in an email.
Dr. Lugar advises PCPs to “recognize the symptoms of an allergic condition, offer treatment based on confidence the diagnosis is correct, and offer a referral for testing to confirm the allergy.
“Because 50% or more of asthmatics are allergic, all asthmatics should be offered an allergy evaluation to determine their allergies and avoid exacerbating the asthma,” she added. “I do not see the flow diagrams as comprehensive enough to manage chronic urticaria, asthma, venom allergy, and drug allergy.”
With food allergy, environmental allergy, venom allergy, or anaphylaxis, “allergists are experts at considering the differential diagnosis and providing the next steps in the diagnostic workup,” Dr. Lugar said. “Allergists can also provide special treatments, such as allergen-specific immunotherapy or desensitization.”
The flow diagrams guide nonspecialists in diagnosis and treatment of their patients with allergy, with supplementary information as needed. The diagrams recommend referral to a specialist when appropriate, as in cases of anaphylaxis, or chronic urticaria.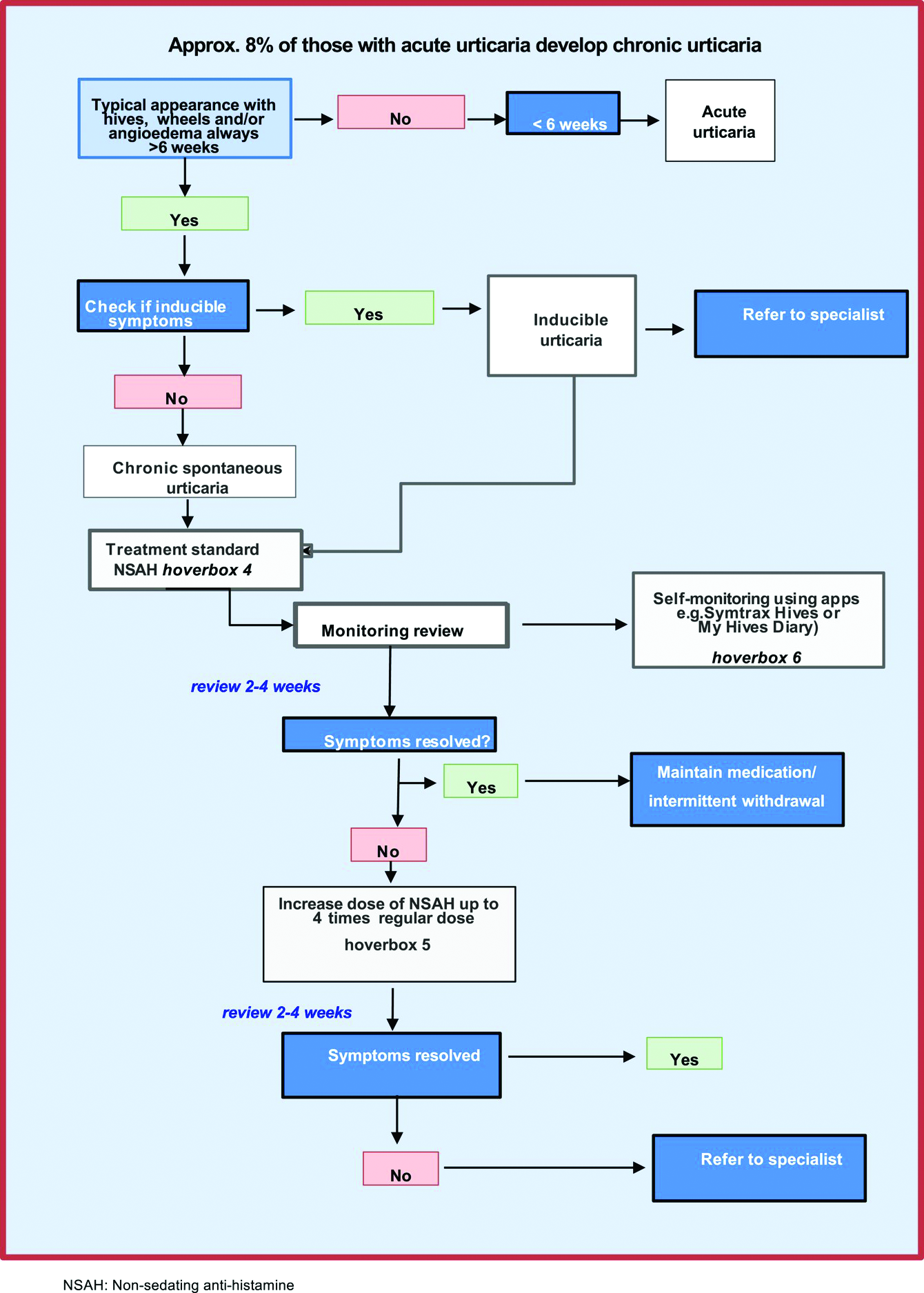
The task force was funded by EAACI. Dr. Ryan and several other authors report financial relationships with pharmaceutical companies. Dr. Ciaccio and Dr. Lugar report no such relationships.
A version of this article first appeared on Medscape.com.
FROM ALLERGY
Gaps in follow-up care put kids with asthma at risk of severe recurrence
Jo Ward’s twin boys have been to the emergency department for respiratory problems about as many times as the dozen years they’ve been alive. Both have asthma and bronchopulmonary dysplasia, a form of chronic airway damage that can occur in children born premature, as the twins were. But each time Ms. Ward took them in for treatment during an acute bout of breathing distress, the staff told her to schedule a follow-up visit for the children with their physician only if they didn’t get better, not regardless of the outcome – as medical guidelines recommend.
“They asked questions, they did the exams, but they really didn’t give you a lot of information to help you at home,” Ms. Ward told this news organization. If they had, she doesn’t think she’d have needed to take them in for emergency care so often.
A new study, published in Academic Pediatrics, suggests she’s right.
Current clinical guidelines for asthma recommend that patients who visit the ED for an asthma-related problem should have a follow-up appointment within a month after the visit, independent of how well they have recovered once home, according to Naomi S. Bardach, MD, a professor of pediatrics and health policy at the University of California, San Francisco, who led the new study.
Her research found that children who have a follow-up appointment within 2 weeks of such a visit are less likely to come back again the next year. Yet the study also found that only about one in five youth had a follow-up visit within that 2-week window.
“The emergency department visit is probably a sign that they need some additional attention for their asthma,” Dr. Bardach said. “We know we can prevent emergency department visits if they get the right kind of medication or if they figure out how to avoid the things that are going to cause an asthma exacerbation or flare.”
For the study, Dr. Bardach and colleagues analyzed data from California, Vermont, and Massachusetts for all asthma-related emergency visits for patients aged 3-21 years between 2013 and 2016.
Out of the 90,267 such visits they identified, 22.6% of patients had a follow-up within 2 weeks, more often by patients who were younger, had commercial insurance, had evidence of prior asthma, or had complex chronic conditions.
Whereas 5.7% of patients who had follow-up visits returned to the ED within 60 days, 6.4% of those who didn’t came back – a 12% difference (P < .001). The gap was larger a year out, with 25% of those with follow-ups returning to the ED, compared with 28.3% of those without follow-ups returning (P < .001), according to the researchers.
Overall, Dr. Bardach’s group estimates that for every 30 children who have follow-up visits with a physician, one would avoid a return trip to the emergency department for asthma within a year.
But given the sheer number of asthma-related trips to the ED each year – 164,145 for kids age 1-17 years in the United States in 2016 alone – that translates into big numbers of kids not going back to the hospital: approximately 72,000 such trips avoided at a savings to the health care system of at least $8.6 million annually.
Missed opportunities
Had Ms. Ward’s boys been among the one in five to receive follow-up care earlier in their lives, she might have saved a significant amount of time, money, anxiety, and heartache. When the twins were 9 years old, she took them to a new pediatric pulmonologist. That changed everything. In that first visit, “they gave me way more information than I ever had in the first 9 years,” she said.
The doctor told Ms. Ward to keep steroids on hand, gave her a prescription for extra doses of the powerful medication, and explained that they needed to be used within 24 hours of the first sign of a breathing problem.
“She said if you give them the steroids right away, it keeps them out of the emergency room, and that’s actually worked,” Ms. Ward said. “She made sure we had care plans every visit and asked me each time if I still had it or we needed to rewrite it. They gave me signs to look for, for when to go to hospital visits. I think that when you go to the doctor, they should be telling you stuff like that.”
Dr. Bardach said visits with a primary care doctor or asthma specialist offer families a chance to receive information to keep the condition from becoming critical.
“Going to that follow-up visit, they can get access to education from the provider about how to avoid things that trigger asthma, and there’s medication that kids can take that keeps the lungs calm and less likely to have a big asthma reaction, so getting access to that medication can be really helpful,” she said.
That was the case for Amy Davenport, of Chapel Hill, N.C., whose 6-year-old son has been to the ED twice for his asthma.
The first time, when he was 3, he was having trouble breathing with a respiratory tract infection and received nebulizer treatment – although he received it in the ED since no beds were available in the ICU. The staff did tell Ms. Davenport to follow up with her primary care provider, but her son’s pediatrician was reluctant to diagnose him with asthma at such a young age and didn’t prescribe any maintenance medications.
A few months later, Ms. Davenport and her son found themselves back in the hospital, and an ICU bed was open this time. The critical care staff referred Davenport to a pediatric pulmonary specialist, and they haven’t been back to the hospital since. Ms. Davenport said she believes if they’d received a maintenance medication after the first visit, it likely would have prevented the second one.
“I’ve definitely seen now that, after the second admission, we got an asthma action plan and it said exactly what to do,” she said. “I felt like we had really good follow-up. We had that action plan on our refrigerator for a long time, and it helped us as parents with three small children to manage.”
Of course, follow-up care takes time – time away from work and school that not all families can spare, the researchers acknowledged. Telehealth may be an option, especially after its use expanded during the COVID-19 pandemic.
“We know that health systems have a hard time being flexible enough to actually have a kid be able to make an appointment within a short period of time, and we also know it’s hard for families sometimes to go back into a clinical setting within a certain period of time,” Dr. Bardach said. The urgency for the appointment may wane for those whose children seem to be doing better.
When the researchers adjusted their calculations for socioeconomic status, the results didn’t change much. But the study did find that patients with private insurance were about twice as likely to have follow-up visits as those on Medicaid (43.7% vs. 21.7%). And “the content and conduct” of the follow-up visit makes a difference as well.
Ms. Ward, whose boys are insured through Medicaid, recalled several visits to the ED where she had to push the staff to get the care her children needed. In one case, when one of her boys was a year old and struggling to breathe, the emergency doctor handed her a prescription and recommended she fill it at a neighborhood drugstore that would be cheaper than the hospital’s pharmacy. Then a nurse came in to begin the discharge process.
“I said no, ‘we’re not ready yet. Look at him,’” Ms. Ward said. The nurse took a pulse oximeter reading that showed the boy’s oxygen levels were at 84%, dangerously low. “If I wasn’t so knowledgeable and paid attention when they were born, since they were preemies, if it would have been somebody else, they probably would’ve went home and he’d have died.”
With the pediatric pulmonologist the boys have now, Ms. Ward said she feels more capable of managing their asthma and knowing how to reduce the likelihood that they’ll need to visit the ED.
“Part of what we’re seeing here is that having an existing and trusting relationship with a clinician can be helpful to kids with asthma,” Dr. Bardach said. “If we help establish and maintain those connections, and explain how important that connection can be, that can also help somebody with asthma overall.”
The research was funded by the Agency for Healthcare Research and Quality. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Jo Ward’s twin boys have been to the emergency department for respiratory problems about as many times as the dozen years they’ve been alive. Both have asthma and bronchopulmonary dysplasia, a form of chronic airway damage that can occur in children born premature, as the twins were. But each time Ms. Ward took them in for treatment during an acute bout of breathing distress, the staff told her to schedule a follow-up visit for the children with their physician only if they didn’t get better, not regardless of the outcome – as medical guidelines recommend.
“They asked questions, they did the exams, but they really didn’t give you a lot of information to help you at home,” Ms. Ward told this news organization. If they had, she doesn’t think she’d have needed to take them in for emergency care so often.
A new study, published in Academic Pediatrics, suggests she’s right.
Current clinical guidelines for asthma recommend that patients who visit the ED for an asthma-related problem should have a follow-up appointment within a month after the visit, independent of how well they have recovered once home, according to Naomi S. Bardach, MD, a professor of pediatrics and health policy at the University of California, San Francisco, who led the new study.
Her research found that children who have a follow-up appointment within 2 weeks of such a visit are less likely to come back again the next year. Yet the study also found that only about one in five youth had a follow-up visit within that 2-week window.
“The emergency department visit is probably a sign that they need some additional attention for their asthma,” Dr. Bardach said. “We know we can prevent emergency department visits if they get the right kind of medication or if they figure out how to avoid the things that are going to cause an asthma exacerbation or flare.”
For the study, Dr. Bardach and colleagues analyzed data from California, Vermont, and Massachusetts for all asthma-related emergency visits for patients aged 3-21 years between 2013 and 2016.
Out of the 90,267 such visits they identified, 22.6% of patients had a follow-up within 2 weeks, more often by patients who were younger, had commercial insurance, had evidence of prior asthma, or had complex chronic conditions.
Whereas 5.7% of patients who had follow-up visits returned to the ED within 60 days, 6.4% of those who didn’t came back – a 12% difference (P < .001). The gap was larger a year out, with 25% of those with follow-ups returning to the ED, compared with 28.3% of those without follow-ups returning (P < .001), according to the researchers.
Overall, Dr. Bardach’s group estimates that for every 30 children who have follow-up visits with a physician, one would avoid a return trip to the emergency department for asthma within a year.
But given the sheer number of asthma-related trips to the ED each year – 164,145 for kids age 1-17 years in the United States in 2016 alone – that translates into big numbers of kids not going back to the hospital: approximately 72,000 such trips avoided at a savings to the health care system of at least $8.6 million annually.
Missed opportunities
Had Ms. Ward’s boys been among the one in five to receive follow-up care earlier in their lives, she might have saved a significant amount of time, money, anxiety, and heartache. When the twins were 9 years old, she took them to a new pediatric pulmonologist. That changed everything. In that first visit, “they gave me way more information than I ever had in the first 9 years,” she said.
The doctor told Ms. Ward to keep steroids on hand, gave her a prescription for extra doses of the powerful medication, and explained that they needed to be used within 24 hours of the first sign of a breathing problem.
“She said if you give them the steroids right away, it keeps them out of the emergency room, and that’s actually worked,” Ms. Ward said. “She made sure we had care plans every visit and asked me each time if I still had it or we needed to rewrite it. They gave me signs to look for, for when to go to hospital visits. I think that when you go to the doctor, they should be telling you stuff like that.”
Dr. Bardach said visits with a primary care doctor or asthma specialist offer families a chance to receive information to keep the condition from becoming critical.
“Going to that follow-up visit, they can get access to education from the provider about how to avoid things that trigger asthma, and there’s medication that kids can take that keeps the lungs calm and less likely to have a big asthma reaction, so getting access to that medication can be really helpful,” she said.
That was the case for Amy Davenport, of Chapel Hill, N.C., whose 6-year-old son has been to the ED twice for his asthma.
The first time, when he was 3, he was having trouble breathing with a respiratory tract infection and received nebulizer treatment – although he received it in the ED since no beds were available in the ICU. The staff did tell Ms. Davenport to follow up with her primary care provider, but her son’s pediatrician was reluctant to diagnose him with asthma at such a young age and didn’t prescribe any maintenance medications.
A few months later, Ms. Davenport and her son found themselves back in the hospital, and an ICU bed was open this time. The critical care staff referred Davenport to a pediatric pulmonary specialist, and they haven’t been back to the hospital since. Ms. Davenport said she believes if they’d received a maintenance medication after the first visit, it likely would have prevented the second one.
“I’ve definitely seen now that, after the second admission, we got an asthma action plan and it said exactly what to do,” she said. “I felt like we had really good follow-up. We had that action plan on our refrigerator for a long time, and it helped us as parents with three small children to manage.”
Of course, follow-up care takes time – time away from work and school that not all families can spare, the researchers acknowledged. Telehealth may be an option, especially after its use expanded during the COVID-19 pandemic.
“We know that health systems have a hard time being flexible enough to actually have a kid be able to make an appointment within a short period of time, and we also know it’s hard for families sometimes to go back into a clinical setting within a certain period of time,” Dr. Bardach said. The urgency for the appointment may wane for those whose children seem to be doing better.
When the researchers adjusted their calculations for socioeconomic status, the results didn’t change much. But the study did find that patients with private insurance were about twice as likely to have follow-up visits as those on Medicaid (43.7% vs. 21.7%). And “the content and conduct” of the follow-up visit makes a difference as well.
Ms. Ward, whose boys are insured through Medicaid, recalled several visits to the ED where she had to push the staff to get the care her children needed. In one case, when one of her boys was a year old and struggling to breathe, the emergency doctor handed her a prescription and recommended she fill it at a neighborhood drugstore that would be cheaper than the hospital’s pharmacy. Then a nurse came in to begin the discharge process.
“I said no, ‘we’re not ready yet. Look at him,’” Ms. Ward said. The nurse took a pulse oximeter reading that showed the boy’s oxygen levels were at 84%, dangerously low. “If I wasn’t so knowledgeable and paid attention when they were born, since they were preemies, if it would have been somebody else, they probably would’ve went home and he’d have died.”
With the pediatric pulmonologist the boys have now, Ms. Ward said she feels more capable of managing their asthma and knowing how to reduce the likelihood that they’ll need to visit the ED.
“Part of what we’re seeing here is that having an existing and trusting relationship with a clinician can be helpful to kids with asthma,” Dr. Bardach said. “If we help establish and maintain those connections, and explain how important that connection can be, that can also help somebody with asthma overall.”
The research was funded by the Agency for Healthcare Research and Quality. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Jo Ward’s twin boys have been to the emergency department for respiratory problems about as many times as the dozen years they’ve been alive. Both have asthma and bronchopulmonary dysplasia, a form of chronic airway damage that can occur in children born premature, as the twins were. But each time Ms. Ward took them in for treatment during an acute bout of breathing distress, the staff told her to schedule a follow-up visit for the children with their physician only if they didn’t get better, not regardless of the outcome – as medical guidelines recommend.
“They asked questions, they did the exams, but they really didn’t give you a lot of information to help you at home,” Ms. Ward told this news organization. If they had, she doesn’t think she’d have needed to take them in for emergency care so often.
A new study, published in Academic Pediatrics, suggests she’s right.
Current clinical guidelines for asthma recommend that patients who visit the ED for an asthma-related problem should have a follow-up appointment within a month after the visit, independent of how well they have recovered once home, according to Naomi S. Bardach, MD, a professor of pediatrics and health policy at the University of California, San Francisco, who led the new study.
Her research found that children who have a follow-up appointment within 2 weeks of such a visit are less likely to come back again the next year. Yet the study also found that only about one in five youth had a follow-up visit within that 2-week window.
“The emergency department visit is probably a sign that they need some additional attention for their asthma,” Dr. Bardach said. “We know we can prevent emergency department visits if they get the right kind of medication or if they figure out how to avoid the things that are going to cause an asthma exacerbation or flare.”
For the study, Dr. Bardach and colleagues analyzed data from California, Vermont, and Massachusetts for all asthma-related emergency visits for patients aged 3-21 years between 2013 and 2016.
Out of the 90,267 such visits they identified, 22.6% of patients had a follow-up within 2 weeks, more often by patients who were younger, had commercial insurance, had evidence of prior asthma, or had complex chronic conditions.
Whereas 5.7% of patients who had follow-up visits returned to the ED within 60 days, 6.4% of those who didn’t came back – a 12% difference (P < .001). The gap was larger a year out, with 25% of those with follow-ups returning to the ED, compared with 28.3% of those without follow-ups returning (P < .001), according to the researchers.
Overall, Dr. Bardach’s group estimates that for every 30 children who have follow-up visits with a physician, one would avoid a return trip to the emergency department for asthma within a year.
But given the sheer number of asthma-related trips to the ED each year – 164,145 for kids age 1-17 years in the United States in 2016 alone – that translates into big numbers of kids not going back to the hospital: approximately 72,000 such trips avoided at a savings to the health care system of at least $8.6 million annually.
Missed opportunities
Had Ms. Ward’s boys been among the one in five to receive follow-up care earlier in their lives, she might have saved a significant amount of time, money, anxiety, and heartache. When the twins were 9 years old, she took them to a new pediatric pulmonologist. That changed everything. In that first visit, “they gave me way more information than I ever had in the first 9 years,” she said.
The doctor told Ms. Ward to keep steroids on hand, gave her a prescription for extra doses of the powerful medication, and explained that they needed to be used within 24 hours of the first sign of a breathing problem.
“She said if you give them the steroids right away, it keeps them out of the emergency room, and that’s actually worked,” Ms. Ward said. “She made sure we had care plans every visit and asked me each time if I still had it or we needed to rewrite it. They gave me signs to look for, for when to go to hospital visits. I think that when you go to the doctor, they should be telling you stuff like that.”
Dr. Bardach said visits with a primary care doctor or asthma specialist offer families a chance to receive information to keep the condition from becoming critical.
“Going to that follow-up visit, they can get access to education from the provider about how to avoid things that trigger asthma, and there’s medication that kids can take that keeps the lungs calm and less likely to have a big asthma reaction, so getting access to that medication can be really helpful,” she said.
That was the case for Amy Davenport, of Chapel Hill, N.C., whose 6-year-old son has been to the ED twice for his asthma.
The first time, when he was 3, he was having trouble breathing with a respiratory tract infection and received nebulizer treatment – although he received it in the ED since no beds were available in the ICU. The staff did tell Ms. Davenport to follow up with her primary care provider, but her son’s pediatrician was reluctant to diagnose him with asthma at such a young age and didn’t prescribe any maintenance medications.
A few months later, Ms. Davenport and her son found themselves back in the hospital, and an ICU bed was open this time. The critical care staff referred Davenport to a pediatric pulmonary specialist, and they haven’t been back to the hospital since. Ms. Davenport said she believes if they’d received a maintenance medication after the first visit, it likely would have prevented the second one.
“I’ve definitely seen now that, after the second admission, we got an asthma action plan and it said exactly what to do,” she said. “I felt like we had really good follow-up. We had that action plan on our refrigerator for a long time, and it helped us as parents with three small children to manage.”
Of course, follow-up care takes time – time away from work and school that not all families can spare, the researchers acknowledged. Telehealth may be an option, especially after its use expanded during the COVID-19 pandemic.
“We know that health systems have a hard time being flexible enough to actually have a kid be able to make an appointment within a short period of time, and we also know it’s hard for families sometimes to go back into a clinical setting within a certain period of time,” Dr. Bardach said. The urgency for the appointment may wane for those whose children seem to be doing better.
When the researchers adjusted their calculations for socioeconomic status, the results didn’t change much. But the study did find that patients with private insurance were about twice as likely to have follow-up visits as those on Medicaid (43.7% vs. 21.7%). And “the content and conduct” of the follow-up visit makes a difference as well.
Ms. Ward, whose boys are insured through Medicaid, recalled several visits to the ED where she had to push the staff to get the care her children needed. In one case, when one of her boys was a year old and struggling to breathe, the emergency doctor handed her a prescription and recommended she fill it at a neighborhood drugstore that would be cheaper than the hospital’s pharmacy. Then a nurse came in to begin the discharge process.
“I said no, ‘we’re not ready yet. Look at him,’” Ms. Ward said. The nurse took a pulse oximeter reading that showed the boy’s oxygen levels were at 84%, dangerously low. “If I wasn’t so knowledgeable and paid attention when they were born, since they were preemies, if it would have been somebody else, they probably would’ve went home and he’d have died.”
With the pediatric pulmonologist the boys have now, Ms. Ward said she feels more capable of managing their asthma and knowing how to reduce the likelihood that they’ll need to visit the ED.
“Part of what we’re seeing here is that having an existing and trusting relationship with a clinician can be helpful to kids with asthma,” Dr. Bardach said. “If we help establish and maintain those connections, and explain how important that connection can be, that can also help somebody with asthma overall.”
The research was funded by the Agency for Healthcare Research and Quality. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ACADEMIC PEDIATRICS
Nontuberculous mycobacterial lung disease can be challenging to treat
Living in coastal areas of Florida and California has great appeal for many, with the warm, sunny climate and nearby fresh water and salt water.
But, unknown to many, those balmy coasts also carry the risk of infection from nontuberculous (atypical) mycobacteria (NTM). Unlike its relative, tuberculosis, NTM is not transmitted from person to person, with one exception: patients with cystic fibrosis.
It is estimated that there were 181,000 people with NTM lung disease in the U.S. in 2015, and according to one study, the incidence is increasing by 8.2% annually among those aged 65 years and older. But NTM doesn’t only affect the elderly; it’s estimated that 31% of all NTM patients are younger than 65 years.
With the warm, moist soil and water, NTM is most commonly found in Florida, California, Hawaii, and the Gulf Coast states. The incidence is somewhat lower in states along the Great Lakes. Other states are not without risk – but NTM is perhaps even more likely to be overlooked in these states by physicians because of a lack of awareness of the disease.
Rebecca Prevots, PhD, MPH, chief of the epidemiology and population studies unit of the Division of Intramural Research at the National Institute of Allergy and Infectious Diseases, told this news organization that “why NTM is increasing is one of the most common questions” she gets, followed by whether it is due to climate change. “The short answer is, we don’t know.”
She suggests that the increase in diagnoses is due to a combination of increased awareness, host susceptibility, and perhaps environmental changes. One problem is that NTM is not a reportable disease. Also, public health resources have been decimated, both through funding cuts and loss of personnel. Dr. Prevots said, “It’s not just NTM surveillance that is important, but you can’t just make a certain condition reportable and expect to have good data without putting resources to it. ... Diseases are made reportable at the state level. There’s no mandated reporting up to CDC. So CDC is piloting reporting events through their emerging infectious program.”
Anthony Cannella, MD, assistant professor of infectious diseases at the University of South Florida (USF), is in the midst of NTM. He told this news organization that “there’s a huge circle with big old dots right over the center of the state.” He is adamant that “a soil-water survey has to occur. We need to know what the devil is happening.”
Florida legislators agreed to allocate $519,000 for NTM testing and surveillance in 2019. But Florida Governor Ron DeSantis vetoed that line item in the budget. WUSF (a National Public Radio affiliate on the USF campus) was unable to get a response to their query about this from the governor’s office.
Who gets NTM?
Mycobacterium avium complex primarily causes lung disease, which presents as two clinical syndromes.
“These infections don’t affect everyone,” Kenneth Olivier, MD, MPH, chief of pulmonary clinical medicine, Cardiovascular Pulmonary Branch of the National Heart, Lung, and Blood Institute, said in an interview. They affect “patients that have underlying genetic conditions that cause abnormalities in the airway clearance mechanisms, particularly cystic fibrosis and primary ciliary dyskinesia [and], to some extent, patients with COPD.”
The second group is “comprised mainly of postmenopausal women, many of whom have had no predisposing medical problems prior to onset of generally frequent throat clearing or chronic cough, which is what brings them to medical attention.” Dr. Olivier added that “many of these patients have a fairly unique appearance. They tend to have a high prevalence of curvature of the spine, scoliosis, indentation of the chest wall (pectus excavatum), and physical characteristics that overlap heritable connective tissue disorders like Marfan syndrome or Ehlers-Danlos syndrome.”
Dr. Olivier pointed out a major problem in NTM diagnosis and treatment: “The guidelines-based approach to chronic cough generally calls for treating postnasal drip, airway reactivity, asthma type symptoms first empirically, before doing different diagnostic studies. That generally causes a delay in obtaining things like CT scan, where you can see the characteristic changes.”
Dr. Cannella added, “People are starting to become more aware of it. It’s kind of like pneumocystis back in the 80s. ... We’ve had patients who have had long periods of febrile neutropenia, and NTM wasn’t on the radar. Now we’ve picked up at least seven or eight.”
In addition to pulmonary infections, nosocomial outbreaks have occurred, owing to contaminated heater-cooler units, catheter infections, nail salons, or to medical tourism. These more commonly involve rapidly growing species, such as M abscessus, M chelonae, and M fortuitum. Clinicians should also be aware of skin infections from M marinum, which come from wounds from aquariums, fish, or shellfish. Incubation can occur over months, highlighting the importance of a detailed history and special cultures.
Diagnostics
The diagnosis of NTM is delayed for several reasons. One is the lack of awareness among clinicians about NTM and its risk factors, including hobbies such as gardening or working in places where dirt is aerosolized, such as on road crews, or even from hot tubs. A thorough history is critical.
Another is not recognizing the need for an acid-fast bacilli (AFB) culture, which requires specialized media. Fortunately, NTM can be picked up on fungal cultures, Dr. Cannella noted. Clinicians are sometimes discouraged from culturing AFB because doing so may not be cost-effective. And many hospital laboratories are increasingly sending cultures to outside labs, and it can take days – sometimes even more than a week – to receive a report of results.
Charles Daley, MD, chief of the Division of Mycobacterial and Respiratory Infections at National Jewish Health, expressed his frustration about labs in an interview, saying diagnostics is “an important hole in the U.S., as our laboratories do not provide clinicians with the results that they need to make good decisions. Most laboratories in the U.S. just don’t speciate the organisms or subspeciate in the setting of abscesses. They don’t tell the clinician enough about the susceptibility, particularly whether there’s inducible resistance. As a clinician, you just don’t have the information to make the right decisions. ... We need to improve diagnostics in NTM. Everything is there and available. They just don’t want to do it because it increases the costs.”
Men tend to have fibrocavitary disease, which shows on ordinary chest x-rays, but CT scans are essential for women because women tend to have either nodular disease or bronchiectasis, which does not show on a plain film.
Treatment
A standard treatment for NTM lung disease includes three or four medications – clarithromycin or azithromycin, rifampin or rifabutin, ethambutol, and streptomycin or amikacin. In vitro resistance is important in predicting the clinical response to a macrolide or amikacin.
For bronchiectatic disease, National Jewish Hospital recommends treatment three times per week rather than daily therapy, as it is better tolerated. Azithromycin is preferred over clarithromycin. Amikacin should be added if there is cavitary or severe disease, and the macrolide is then given daily.
Dr. Olivier suggested that physicians stagger the initiation of those drugs to improve the tolerability of the difficult regimen. Generally, treatment is for 18 months – a year after sputum cultures become negative.
If therapy fails – that is, sputum is persistently positive at 6 months – amikacin liposomal inhalation solution (Arikayce) is likely to be added. Patients should be monitored with monthly safety labs, sputum cultures, and an audiogram (if receiving amikacin). Every 3 months, vestibular tests, eye exams, and spirometry should be conducted, and every 6 months, physicians should order a CT, an audiogram, and an electrocardiogram.
Despite completing such a rigorous regimen, about half of patients experience reinfection because of their underlying host susceptibility. Genomic sequencing shows that these are new infections, not relapses, Dr. Prevots said. She also noted that gastroesophageal reflux disease is a significant risk factor because of chronic aspiration.
Dr. Daley outlined the newer treatments being studied. They include Arikayce, omadocycline, and bedaquiline. He added, “There’s a neutrophil elastase inhibitor trial that’s ongoing, a huge trial. There’s another one looking at basically eosinophilic inflammation.”
Other trials are in the offing, he said, all focusing on the inflammatory response – a development he described as exciting, because for the longest time, there were few if any NTM trials.
Dr. Cannella is also buoyed by the potential synergy of dual beta-lactam therapy with ceftaroline and a carbapenem for M abscessus infections, which are notoriously difficult to treat.
There are unique problems facing drug development for NTM because, for approval, the U.S. Food and Drug Administration requires the drug to “improve how a patient feels, functions, or survives.” NTM is associated with low mortality, so that “is off the table,” Dr. Daley explained. It’s hard to quantify improvement in function. The top two symptoms to measure are coughing and fatigue, he said. But both are difficult to measure, and some of the medicines worsen cough. Some research groups are now trying to validate patient-reported outcome instruments to satisfy the FDA’s requirements.
Tips for patients and physicians
The experts this news organization spoke to had very consistent recommendations for patients:
- NTM is resistant to chlorine and bromine, so tap water is a major source of infection. Patients should consider to greater than 130° F and using metal showerheads or bathing rather than showering.
- Good bathroom ventilation helps.
- Patients should consider using a water filter that filters entities less than 5 mcm in size – but not carbon filters, which concentrate the organisms.
- Humidifiers and hot tubs should be avoided.
- A good face mask, such as an N95, should be worn when gardening or repotting plants.
Dr. Olivier stressed that clinicians should familiarize themselves with the guidelines for diagnosing and treating NTM. In particular, clinicians should be aware that using azithromycin for bronchitis might cause resistance in NTM. “Macrolide resistance turns what may be a slowly progressive or bothersome infection into a lethal infection with a 1-year mortality of 35%.”
He concluded, “I would just urge that if the patient’s on their second or third Z-Pak within a year, it’s probably time to look for other causes of what might be happening.”
Dr. Cannella, Dr. Prevots, and Dr. Olivier reported no relevant financial relationships. Dr. Cannella adds, “My views are not those of my employers, the U.S. Dept of VA, or the University of South Florida Morsani College of Medicine.” Dr. Daley reports research grants/contracts with AN2, Beyond Air, Bugworks, Insmed, and Paratek and service on advisory boards or as a consultant for AN2, AstraZeneca, Genentech, Insmed, Matinas, Paratek, Pfizer, and Spero.
A version of this article first appeared on Medscape.com.
Living in coastal areas of Florida and California has great appeal for many, with the warm, sunny climate and nearby fresh water and salt water.
But, unknown to many, those balmy coasts also carry the risk of infection from nontuberculous (atypical) mycobacteria (NTM). Unlike its relative, tuberculosis, NTM is not transmitted from person to person, with one exception: patients with cystic fibrosis.
It is estimated that there were 181,000 people with NTM lung disease in the U.S. in 2015, and according to one study, the incidence is increasing by 8.2% annually among those aged 65 years and older. But NTM doesn’t only affect the elderly; it’s estimated that 31% of all NTM patients are younger than 65 years.
With the warm, moist soil and water, NTM is most commonly found in Florida, California, Hawaii, and the Gulf Coast states. The incidence is somewhat lower in states along the Great Lakes. Other states are not without risk – but NTM is perhaps even more likely to be overlooked in these states by physicians because of a lack of awareness of the disease.
Rebecca Prevots, PhD, MPH, chief of the epidemiology and population studies unit of the Division of Intramural Research at the National Institute of Allergy and Infectious Diseases, told this news organization that “why NTM is increasing is one of the most common questions” she gets, followed by whether it is due to climate change. “The short answer is, we don’t know.”
She suggests that the increase in diagnoses is due to a combination of increased awareness, host susceptibility, and perhaps environmental changes. One problem is that NTM is not a reportable disease. Also, public health resources have been decimated, both through funding cuts and loss of personnel. Dr. Prevots said, “It’s not just NTM surveillance that is important, but you can’t just make a certain condition reportable and expect to have good data without putting resources to it. ... Diseases are made reportable at the state level. There’s no mandated reporting up to CDC. So CDC is piloting reporting events through their emerging infectious program.”
Anthony Cannella, MD, assistant professor of infectious diseases at the University of South Florida (USF), is in the midst of NTM. He told this news organization that “there’s a huge circle with big old dots right over the center of the state.” He is adamant that “a soil-water survey has to occur. We need to know what the devil is happening.”
Florida legislators agreed to allocate $519,000 for NTM testing and surveillance in 2019. But Florida Governor Ron DeSantis vetoed that line item in the budget. WUSF (a National Public Radio affiliate on the USF campus) was unable to get a response to their query about this from the governor’s office.
Who gets NTM?
Mycobacterium avium complex primarily causes lung disease, which presents as two clinical syndromes.
“These infections don’t affect everyone,” Kenneth Olivier, MD, MPH, chief of pulmonary clinical medicine, Cardiovascular Pulmonary Branch of the National Heart, Lung, and Blood Institute, said in an interview. They affect “patients that have underlying genetic conditions that cause abnormalities in the airway clearance mechanisms, particularly cystic fibrosis and primary ciliary dyskinesia [and], to some extent, patients with COPD.”
The second group is “comprised mainly of postmenopausal women, many of whom have had no predisposing medical problems prior to onset of generally frequent throat clearing or chronic cough, which is what brings them to medical attention.” Dr. Olivier added that “many of these patients have a fairly unique appearance. They tend to have a high prevalence of curvature of the spine, scoliosis, indentation of the chest wall (pectus excavatum), and physical characteristics that overlap heritable connective tissue disorders like Marfan syndrome or Ehlers-Danlos syndrome.”
Dr. Olivier pointed out a major problem in NTM diagnosis and treatment: “The guidelines-based approach to chronic cough generally calls for treating postnasal drip, airway reactivity, asthma type symptoms first empirically, before doing different diagnostic studies. That generally causes a delay in obtaining things like CT scan, where you can see the characteristic changes.”
Dr. Cannella added, “People are starting to become more aware of it. It’s kind of like pneumocystis back in the 80s. ... We’ve had patients who have had long periods of febrile neutropenia, and NTM wasn’t on the radar. Now we’ve picked up at least seven or eight.”
In addition to pulmonary infections, nosocomial outbreaks have occurred, owing to contaminated heater-cooler units, catheter infections, nail salons, or to medical tourism. These more commonly involve rapidly growing species, such as M abscessus, M chelonae, and M fortuitum. Clinicians should also be aware of skin infections from M marinum, which come from wounds from aquariums, fish, or shellfish. Incubation can occur over months, highlighting the importance of a detailed history and special cultures.
Diagnostics
The diagnosis of NTM is delayed for several reasons. One is the lack of awareness among clinicians about NTM and its risk factors, including hobbies such as gardening or working in places where dirt is aerosolized, such as on road crews, or even from hot tubs. A thorough history is critical.
Another is not recognizing the need for an acid-fast bacilli (AFB) culture, which requires specialized media. Fortunately, NTM can be picked up on fungal cultures, Dr. Cannella noted. Clinicians are sometimes discouraged from culturing AFB because doing so may not be cost-effective. And many hospital laboratories are increasingly sending cultures to outside labs, and it can take days – sometimes even more than a week – to receive a report of results.
Charles Daley, MD, chief of the Division of Mycobacterial and Respiratory Infections at National Jewish Health, expressed his frustration about labs in an interview, saying diagnostics is “an important hole in the U.S., as our laboratories do not provide clinicians with the results that they need to make good decisions. Most laboratories in the U.S. just don’t speciate the organisms or subspeciate in the setting of abscesses. They don’t tell the clinician enough about the susceptibility, particularly whether there’s inducible resistance. As a clinician, you just don’t have the information to make the right decisions. ... We need to improve diagnostics in NTM. Everything is there and available. They just don’t want to do it because it increases the costs.”
Men tend to have fibrocavitary disease, which shows on ordinary chest x-rays, but CT scans are essential for women because women tend to have either nodular disease or bronchiectasis, which does not show on a plain film.
Treatment
A standard treatment for NTM lung disease includes three or four medications – clarithromycin or azithromycin, rifampin or rifabutin, ethambutol, and streptomycin or amikacin. In vitro resistance is important in predicting the clinical response to a macrolide or amikacin.
For bronchiectatic disease, National Jewish Hospital recommends treatment three times per week rather than daily therapy, as it is better tolerated. Azithromycin is preferred over clarithromycin. Amikacin should be added if there is cavitary or severe disease, and the macrolide is then given daily.
Dr. Olivier suggested that physicians stagger the initiation of those drugs to improve the tolerability of the difficult regimen. Generally, treatment is for 18 months – a year after sputum cultures become negative.
If therapy fails – that is, sputum is persistently positive at 6 months – amikacin liposomal inhalation solution (Arikayce) is likely to be added. Patients should be monitored with monthly safety labs, sputum cultures, and an audiogram (if receiving amikacin). Every 3 months, vestibular tests, eye exams, and spirometry should be conducted, and every 6 months, physicians should order a CT, an audiogram, and an electrocardiogram.
Despite completing such a rigorous regimen, about half of patients experience reinfection because of their underlying host susceptibility. Genomic sequencing shows that these are new infections, not relapses, Dr. Prevots said. She also noted that gastroesophageal reflux disease is a significant risk factor because of chronic aspiration.
Dr. Daley outlined the newer treatments being studied. They include Arikayce, omadocycline, and bedaquiline. He added, “There’s a neutrophil elastase inhibitor trial that’s ongoing, a huge trial. There’s another one looking at basically eosinophilic inflammation.”
Other trials are in the offing, he said, all focusing on the inflammatory response – a development he described as exciting, because for the longest time, there were few if any NTM trials.
Dr. Cannella is also buoyed by the potential synergy of dual beta-lactam therapy with ceftaroline and a carbapenem for M abscessus infections, which are notoriously difficult to treat.
There are unique problems facing drug development for NTM because, for approval, the U.S. Food and Drug Administration requires the drug to “improve how a patient feels, functions, or survives.” NTM is associated with low mortality, so that “is off the table,” Dr. Daley explained. It’s hard to quantify improvement in function. The top two symptoms to measure are coughing and fatigue, he said. But both are difficult to measure, and some of the medicines worsen cough. Some research groups are now trying to validate patient-reported outcome instruments to satisfy the FDA’s requirements.
Tips for patients and physicians
The experts this news organization spoke to had very consistent recommendations for patients:
- NTM is resistant to chlorine and bromine, so tap water is a major source of infection. Patients should consider to greater than 130° F and using metal showerheads or bathing rather than showering.
- Good bathroom ventilation helps.
- Patients should consider using a water filter that filters entities less than 5 mcm in size – but not carbon filters, which concentrate the organisms.
- Humidifiers and hot tubs should be avoided.
- A good face mask, such as an N95, should be worn when gardening or repotting plants.
Dr. Olivier stressed that clinicians should familiarize themselves with the guidelines for diagnosing and treating NTM. In particular, clinicians should be aware that using azithromycin for bronchitis might cause resistance in NTM. “Macrolide resistance turns what may be a slowly progressive or bothersome infection into a lethal infection with a 1-year mortality of 35%.”
He concluded, “I would just urge that if the patient’s on their second or third Z-Pak within a year, it’s probably time to look for other causes of what might be happening.”
Dr. Cannella, Dr. Prevots, and Dr. Olivier reported no relevant financial relationships. Dr. Cannella adds, “My views are not those of my employers, the U.S. Dept of VA, or the University of South Florida Morsani College of Medicine.” Dr. Daley reports research grants/contracts with AN2, Beyond Air, Bugworks, Insmed, and Paratek and service on advisory boards or as a consultant for AN2, AstraZeneca, Genentech, Insmed, Matinas, Paratek, Pfizer, and Spero.
A version of this article first appeared on Medscape.com.
Living in coastal areas of Florida and California has great appeal for many, with the warm, sunny climate and nearby fresh water and salt water.
But, unknown to many, those balmy coasts also carry the risk of infection from nontuberculous (atypical) mycobacteria (NTM). Unlike its relative, tuberculosis, NTM is not transmitted from person to person, with one exception: patients with cystic fibrosis.
It is estimated that there were 181,000 people with NTM lung disease in the U.S. in 2015, and according to one study, the incidence is increasing by 8.2% annually among those aged 65 years and older. But NTM doesn’t only affect the elderly; it’s estimated that 31% of all NTM patients are younger than 65 years.
With the warm, moist soil and water, NTM is most commonly found in Florida, California, Hawaii, and the Gulf Coast states. The incidence is somewhat lower in states along the Great Lakes. Other states are not without risk – but NTM is perhaps even more likely to be overlooked in these states by physicians because of a lack of awareness of the disease.
Rebecca Prevots, PhD, MPH, chief of the epidemiology and population studies unit of the Division of Intramural Research at the National Institute of Allergy and Infectious Diseases, told this news organization that “why NTM is increasing is one of the most common questions” she gets, followed by whether it is due to climate change. “The short answer is, we don’t know.”
She suggests that the increase in diagnoses is due to a combination of increased awareness, host susceptibility, and perhaps environmental changes. One problem is that NTM is not a reportable disease. Also, public health resources have been decimated, both through funding cuts and loss of personnel. Dr. Prevots said, “It’s not just NTM surveillance that is important, but you can’t just make a certain condition reportable and expect to have good data without putting resources to it. ... Diseases are made reportable at the state level. There’s no mandated reporting up to CDC. So CDC is piloting reporting events through their emerging infectious program.”
Anthony Cannella, MD, assistant professor of infectious diseases at the University of South Florida (USF), is in the midst of NTM. He told this news organization that “there’s a huge circle with big old dots right over the center of the state.” He is adamant that “a soil-water survey has to occur. We need to know what the devil is happening.”
Florida legislators agreed to allocate $519,000 for NTM testing and surveillance in 2019. But Florida Governor Ron DeSantis vetoed that line item in the budget. WUSF (a National Public Radio affiliate on the USF campus) was unable to get a response to their query about this from the governor’s office.
Who gets NTM?
Mycobacterium avium complex primarily causes lung disease, which presents as two clinical syndromes.
“These infections don’t affect everyone,” Kenneth Olivier, MD, MPH, chief of pulmonary clinical medicine, Cardiovascular Pulmonary Branch of the National Heart, Lung, and Blood Institute, said in an interview. They affect “patients that have underlying genetic conditions that cause abnormalities in the airway clearance mechanisms, particularly cystic fibrosis and primary ciliary dyskinesia [and], to some extent, patients with COPD.”
The second group is “comprised mainly of postmenopausal women, many of whom have had no predisposing medical problems prior to onset of generally frequent throat clearing or chronic cough, which is what brings them to medical attention.” Dr. Olivier added that “many of these patients have a fairly unique appearance. They tend to have a high prevalence of curvature of the spine, scoliosis, indentation of the chest wall (pectus excavatum), and physical characteristics that overlap heritable connective tissue disorders like Marfan syndrome or Ehlers-Danlos syndrome.”
Dr. Olivier pointed out a major problem in NTM diagnosis and treatment: “The guidelines-based approach to chronic cough generally calls for treating postnasal drip, airway reactivity, asthma type symptoms first empirically, before doing different diagnostic studies. That generally causes a delay in obtaining things like CT scan, where you can see the characteristic changes.”
Dr. Cannella added, “People are starting to become more aware of it. It’s kind of like pneumocystis back in the 80s. ... We’ve had patients who have had long periods of febrile neutropenia, and NTM wasn’t on the radar. Now we’ve picked up at least seven or eight.”
In addition to pulmonary infections, nosocomial outbreaks have occurred, owing to contaminated heater-cooler units, catheter infections, nail salons, or to medical tourism. These more commonly involve rapidly growing species, such as M abscessus, M chelonae, and M fortuitum. Clinicians should also be aware of skin infections from M marinum, which come from wounds from aquariums, fish, or shellfish. Incubation can occur over months, highlighting the importance of a detailed history and special cultures.
Diagnostics
The diagnosis of NTM is delayed for several reasons. One is the lack of awareness among clinicians about NTM and its risk factors, including hobbies such as gardening or working in places where dirt is aerosolized, such as on road crews, or even from hot tubs. A thorough history is critical.
Another is not recognizing the need for an acid-fast bacilli (AFB) culture, which requires specialized media. Fortunately, NTM can be picked up on fungal cultures, Dr. Cannella noted. Clinicians are sometimes discouraged from culturing AFB because doing so may not be cost-effective. And many hospital laboratories are increasingly sending cultures to outside labs, and it can take days – sometimes even more than a week – to receive a report of results.
Charles Daley, MD, chief of the Division of Mycobacterial and Respiratory Infections at National Jewish Health, expressed his frustration about labs in an interview, saying diagnostics is “an important hole in the U.S., as our laboratories do not provide clinicians with the results that they need to make good decisions. Most laboratories in the U.S. just don’t speciate the organisms or subspeciate in the setting of abscesses. They don’t tell the clinician enough about the susceptibility, particularly whether there’s inducible resistance. As a clinician, you just don’t have the information to make the right decisions. ... We need to improve diagnostics in NTM. Everything is there and available. They just don’t want to do it because it increases the costs.”
Men tend to have fibrocavitary disease, which shows on ordinary chest x-rays, but CT scans are essential for women because women tend to have either nodular disease or bronchiectasis, which does not show on a plain film.
Treatment
A standard treatment for NTM lung disease includes three or four medications – clarithromycin or azithromycin, rifampin or rifabutin, ethambutol, and streptomycin or amikacin. In vitro resistance is important in predicting the clinical response to a macrolide or amikacin.
For bronchiectatic disease, National Jewish Hospital recommends treatment three times per week rather than daily therapy, as it is better tolerated. Azithromycin is preferred over clarithromycin. Amikacin should be added if there is cavitary or severe disease, and the macrolide is then given daily.
Dr. Olivier suggested that physicians stagger the initiation of those drugs to improve the tolerability of the difficult regimen. Generally, treatment is for 18 months – a year after sputum cultures become negative.
If therapy fails – that is, sputum is persistently positive at 6 months – amikacin liposomal inhalation solution (Arikayce) is likely to be added. Patients should be monitored with monthly safety labs, sputum cultures, and an audiogram (if receiving amikacin). Every 3 months, vestibular tests, eye exams, and spirometry should be conducted, and every 6 months, physicians should order a CT, an audiogram, and an electrocardiogram.
Despite completing such a rigorous regimen, about half of patients experience reinfection because of their underlying host susceptibility. Genomic sequencing shows that these are new infections, not relapses, Dr. Prevots said. She also noted that gastroesophageal reflux disease is a significant risk factor because of chronic aspiration.
Dr. Daley outlined the newer treatments being studied. They include Arikayce, omadocycline, and bedaquiline. He added, “There’s a neutrophil elastase inhibitor trial that’s ongoing, a huge trial. There’s another one looking at basically eosinophilic inflammation.”
Other trials are in the offing, he said, all focusing on the inflammatory response – a development he described as exciting, because for the longest time, there were few if any NTM trials.
Dr. Cannella is also buoyed by the potential synergy of dual beta-lactam therapy with ceftaroline and a carbapenem for M abscessus infections, which are notoriously difficult to treat.
There are unique problems facing drug development for NTM because, for approval, the U.S. Food and Drug Administration requires the drug to “improve how a patient feels, functions, or survives.” NTM is associated with low mortality, so that “is off the table,” Dr. Daley explained. It’s hard to quantify improvement in function. The top two symptoms to measure are coughing and fatigue, he said. But both are difficult to measure, and some of the medicines worsen cough. Some research groups are now trying to validate patient-reported outcome instruments to satisfy the FDA’s requirements.
Tips for patients and physicians
The experts this news organization spoke to had very consistent recommendations for patients:
- NTM is resistant to chlorine and bromine, so tap water is a major source of infection. Patients should consider to greater than 130° F and using metal showerheads or bathing rather than showering.
- Good bathroom ventilation helps.
- Patients should consider using a water filter that filters entities less than 5 mcm in size – but not carbon filters, which concentrate the organisms.
- Humidifiers and hot tubs should be avoided.
- A good face mask, such as an N95, should be worn when gardening or repotting plants.
Dr. Olivier stressed that clinicians should familiarize themselves with the guidelines for diagnosing and treating NTM. In particular, clinicians should be aware that using azithromycin for bronchitis might cause resistance in NTM. “Macrolide resistance turns what may be a slowly progressive or bothersome infection into a lethal infection with a 1-year mortality of 35%.”
He concluded, “I would just urge that if the patient’s on their second or third Z-Pak within a year, it’s probably time to look for other causes of what might be happening.”
Dr. Cannella, Dr. Prevots, and Dr. Olivier reported no relevant financial relationships. Dr. Cannella adds, “My views are not those of my employers, the U.S. Dept of VA, or the University of South Florida Morsani College of Medicine.” Dr. Daley reports research grants/contracts with AN2, Beyond Air, Bugworks, Insmed, and Paratek and service on advisory boards or as a consultant for AN2, AstraZeneca, Genentech, Insmed, Matinas, Paratek, Pfizer, and Spero.
A version of this article first appeared on Medscape.com.
Scientists find microplastics in human lung tissue
U.K. scientists said microplastics may pose even more of a threat than previously thought after confirming their presence in lung tissue taken from living people.
Microplastics were identified in all lung regions, but significantly higher levels were found in the lower lung.
The results supported inhalation as an exposure risk, according to the team from the University of Hull and Hull York Medical School (England), who said their findings could support further investigations into the effects of airborne microplastics on respiratory health.
The study, published in Science of the Total Environment, used lung tissue collected from surgical procedures on patients during routine medical care at Castle Hill Hospital in East Yorkshire.
Polypropylene and polyethylene
It found 39 microplastics in 11 of the 13 lung tissue samples tested using micro-Fourier-transform infrared (μFTIR) analysis, which the scientists said was considerably higher than results from previous laboratory tests.
Of microplastics detected, 12 polymer types were identified, of which the most common were polypropylene, (23%) polyethylene terephthalate (18%), and resin (15%). The fibers are commonly found in packaging, bottles, clothing, rope and twine manufacture, and other industries, the scientists said.
Microplastics with dimensions as small as 4 μm were found, but the scientists said they were surprised to discover samples as large as greater than 2 mm within all lung region samples, with the majority being fibrous and fragmented.
The study identified 11 microplastics in the upper part of the lung, seven in the mid part, and 21 in the lower part of the lung.
Laura Sadofsky, the study’s lead author, said: “Microplastics have previously been found in human cadaver autopsy samples. This is the first robust study to show microplastics in lungs from live people. It also shows that they are in the lower parts of the lung. Lung airways are very narrow, so no one thought they could possibly get there, but they clearly have.”
There were also considerably higher levels of microplastics found in male patients, compared with female patients.
Future investigations into health implications
“The characterization of types and levels of microplastics we have found can now inform realistic conditions for laboratory exposure experiments with the aim of determining health impacts,” said Laura Sadofsky, who is a senior lecturer in respiratory medicine in the Centre for Atherothrombotic and Metabolic Research at Hull York Medical School.
The latest investigation followed previous research by the medical school and the University of Hull, which found high levels of atmospheric microplastics within the Humber region.
That study, published in Atmosphere, identified resins, which could have originated from degraded roads, paint marking, or tire rubber, as well as polyethylene fibers.
A version of this article first appeared on Medscape UK.
U.K. scientists said microplastics may pose even more of a threat than previously thought after confirming their presence in lung tissue taken from living people.
Microplastics were identified in all lung regions, but significantly higher levels were found in the lower lung.
The results supported inhalation as an exposure risk, according to the team from the University of Hull and Hull York Medical School (England), who said their findings could support further investigations into the effects of airborne microplastics on respiratory health.
The study, published in Science of the Total Environment, used lung tissue collected from surgical procedures on patients during routine medical care at Castle Hill Hospital in East Yorkshire.
Polypropylene and polyethylene
It found 39 microplastics in 11 of the 13 lung tissue samples tested using micro-Fourier-transform infrared (μFTIR) analysis, which the scientists said was considerably higher than results from previous laboratory tests.
Of microplastics detected, 12 polymer types were identified, of which the most common were polypropylene, (23%) polyethylene terephthalate (18%), and resin (15%). The fibers are commonly found in packaging, bottles, clothing, rope and twine manufacture, and other industries, the scientists said.
Microplastics with dimensions as small as 4 μm were found, but the scientists said they were surprised to discover samples as large as greater than 2 mm within all lung region samples, with the majority being fibrous and fragmented.
The study identified 11 microplastics in the upper part of the lung, seven in the mid part, and 21 in the lower part of the lung.
Laura Sadofsky, the study’s lead author, said: “Microplastics have previously been found in human cadaver autopsy samples. This is the first robust study to show microplastics in lungs from live people. It also shows that they are in the lower parts of the lung. Lung airways are very narrow, so no one thought they could possibly get there, but they clearly have.”
There were also considerably higher levels of microplastics found in male patients, compared with female patients.
Future investigations into health implications
“The characterization of types and levels of microplastics we have found can now inform realistic conditions for laboratory exposure experiments with the aim of determining health impacts,” said Laura Sadofsky, who is a senior lecturer in respiratory medicine in the Centre for Atherothrombotic and Metabolic Research at Hull York Medical School.
The latest investigation followed previous research by the medical school and the University of Hull, which found high levels of atmospheric microplastics within the Humber region.
That study, published in Atmosphere, identified resins, which could have originated from degraded roads, paint marking, or tire rubber, as well as polyethylene fibers.
A version of this article first appeared on Medscape UK.
U.K. scientists said microplastics may pose even more of a threat than previously thought after confirming their presence in lung tissue taken from living people.
Microplastics were identified in all lung regions, but significantly higher levels were found in the lower lung.
The results supported inhalation as an exposure risk, according to the team from the University of Hull and Hull York Medical School (England), who said their findings could support further investigations into the effects of airborne microplastics on respiratory health.
The study, published in Science of the Total Environment, used lung tissue collected from surgical procedures on patients during routine medical care at Castle Hill Hospital in East Yorkshire.
Polypropylene and polyethylene
It found 39 microplastics in 11 of the 13 lung tissue samples tested using micro-Fourier-transform infrared (μFTIR) analysis, which the scientists said was considerably higher than results from previous laboratory tests.
Of microplastics detected, 12 polymer types were identified, of which the most common were polypropylene, (23%) polyethylene terephthalate (18%), and resin (15%). The fibers are commonly found in packaging, bottles, clothing, rope and twine manufacture, and other industries, the scientists said.
Microplastics with dimensions as small as 4 μm were found, but the scientists said they were surprised to discover samples as large as greater than 2 mm within all lung region samples, with the majority being fibrous and fragmented.
The study identified 11 microplastics in the upper part of the lung, seven in the mid part, and 21 in the lower part of the lung.
Laura Sadofsky, the study’s lead author, said: “Microplastics have previously been found in human cadaver autopsy samples. This is the first robust study to show microplastics in lungs from live people. It also shows that they are in the lower parts of the lung. Lung airways are very narrow, so no one thought they could possibly get there, but they clearly have.”
There were also considerably higher levels of microplastics found in male patients, compared with female patients.
Future investigations into health implications
“The characterization of types and levels of microplastics we have found can now inform realistic conditions for laboratory exposure experiments with the aim of determining health impacts,” said Laura Sadofsky, who is a senior lecturer in respiratory medicine in the Centre for Atherothrombotic and Metabolic Research at Hull York Medical School.
The latest investigation followed previous research by the medical school and the University of Hull, which found high levels of atmospheric microplastics within the Humber region.
That study, published in Atmosphere, identified resins, which could have originated from degraded roads, paint marking, or tire rubber, as well as polyethylene fibers.
A version of this article first appeared on Medscape UK.
Sex differences in COPD slow to be recognized, treated
When Sigmund Freud claimed that “anatomy is destiny” he was referring to anatomical sex as a determinant of personality traits. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,”
That notion has been widely discredited, but Freud appears to be inadvertently right in one respect: When it comes to chronic obstructive pulmonary disease (COPD), anatomy really is destiny, and sex may be as well, pulmonary researchers say.
There is a growing body of evidence to indicate that COPD affects men and women differently, and that men and women patients with COPD require different clinical management. Yet women are often underdiagnosed or misdiagnosed, partly because of poorly understood sex differences, but also because of cultural biases.
But plunging any farther into the weeds, it’s important to define terms. Although various investigators have used the terms “sex” and “gender” interchangeably, sex is the preferred term when referring to biological attributes of individual patients, while gender refers to personal identity.
These distinctions are important, contended Amik Sodhi, MBBS, MPH, from the division of allergy, pulmonology, and critical care medicine at the University of Wisconsin–Madison.
“Sex is essentially a biologic construct, so it’s got to do with the sex chromosomes, the genetics of that person, and it refers to the anatomic variations that can change susceptibility to different diseases,” she said in an interview.
An example of sex differences or “sexual dimorphism” can be found in a recent meta-analysis of sex-based genetic associations by Megan Hardin, MD, MPH from Brigham & Women’s Hospital in Boston and colleagues.
They reported that CELSR1, a gene involved in fetal lung development, was expressed more among women than among men and that a single nucleotide polymorphism in the gene was associated with COPD among women smokers, but not among men smokers.
The finding points to a potential risk locus for COPD in women, and could help shed light on sexual dimorphism in COPD, Dr. Hardin and colleagues said.
In contrast to sex, “gender is more of a psychosocial construct which can impact how diseases manifest themselves, how they are potentially managed, and what outcomes might occur for that particular disease,” Dr. Sodhi said.
She and her colleagues recently published a review of sex and gender in common lung disorders and sleep in the journal CHEST, where they wrote that the “influence of sex and gender is portrayed in epidemiological data, disease pathogenesis and pathophysiology, clinical manifestations, response to treatment, access to care, and health outcomes. Hence, sex and gender should be considered in all types of research, clinical practice and educational curricula.”
For example, as previously reported at the 2021 annual meeting of the American Thoracic Society, sex-specific differences in the severity of symptoms and prevalence of comorbidities in patients with COPD may point to different criteria for diagnosing cardiac comorbidities in women and men.
Those conclusions came from a retrospective analysis of data on 795 women and 1,251 men with GOLD (Global Initiative for Chronic Obstructive Lung Disease) class 1-3 disease.
The investigators looked at the patients’ clinical history, comorbidities, lung function, COPD Assessment Test scores, and modified Medical Research Council (mMRC) dyspnea score, and found significant differences between men and women for most functional parameters and comorbidities, and for CAT items of cough, phlegm, and energy.
In logistic regression analysis, predictors for cardiac disease in men were energy, mMRC score, smoking status, body mass index, age, and spirometric lung function, but in women only age was significantly predictive for cardiac disease.
An example of gender effects on COPD differences in men and women is the increase in cigarette advertising aimed at women in the 1960s and the advent of women-targeted brands such as Virginia Slims, which in turn lead to increased smoking rates among women. In addition, in the developing world, where the sex/gender gap in COPD is narrowing, women tend to have greater exposure to wood smoke and cooking fuels in unventilated or poorly ventilated spaces, compared with men.
Increasing incidence among women
According to the Centers for Disease Control and Prevention, chronic lower respiratory diseases, primarily COPD, were the fourth-leading cause of death in women in the United States in 2018, following only heart disease, cancer, and accidents/injuries.
And as a CDC analysis of data from the 2013 Behavioral Risk Factor Surveillance System showed, women were more likely to report being told by a physician that they had COPD than did men (6.6%, compared with 5.4%).
Dr. Sodhi and colleagues noted that, at all time points examined from 2005 to 2014, women had a higher proportion than men of COPD hospitalizations and in-hospital deaths. They also noted that female sex is associated with a threefold risk for severe early-onset COPD, and that women with COPD have lower diffusion capacity of lungs for carbon monoxide, despite having higher predicted forced expiratory volume in 1 second, compared with men.
“Historically, COPD wasn’t a disease that was so prevalent in women. It’s been in the past 20 years that the trends have changed,” said Patricia Silveyra, MSc, PhD, ATSF, associate professor of environmental and occupational health at Indiana University, Bloomington.
The increasing prevalence of COPD among women cannot be explained by smoking alone, she said in an interview.
“It used to be thought that it was because more women smoked, but actually a lot of women who don’t smoke can develop COPD, so it appears to be probably something environmental, but because it used to be a disease of older men, in the clinic there was also a bias to diagnose men with COPD, and women with asthma, so a lot of women went underdiagnosed,” Dr. Silveyra said.
In their review, Dr. Sodhi and colleagues noted that women with COPD “may be underdiagnosed as a result of having different symptoms from those classically recognized. Reasons for underdiagnosis or a delay in diagnosis may also be due to lack of a formal evaluation with spirometry, women seeking care later in the course of disease, physician bias, or associated fatigue or depression misdirecting diagnostic strategies. Underdiagnosis may be associated with psychological distress and worse health-related quality of life.”
Although the evidence is mixed, women tend to present more frequently with the chronic bronchitis phenotype of COPD, compared with the emphysema phenotype, and women tend to have greater degrees of pulmonary function impairment when exposed to tobacco smoke, even after controlling for differences in height and weight.
“For the same amount of exposure to tobacco smoke, females are likely to develop more severe airflow limitation at an earlier age than males, and have more exacerbation,” Dr. Sodhi and colleagues wrote.
Both Dr. Silveyra and Dr. Sodhi said that reason why men and women differ in their physiological reactions to smoke are still unknown.
Sex differences in drug responses
There is only limited evidence to indicate that women and men respond differently to various therapeutic agents, but what is clear is that more research into this area is needed, Dr. Sodhi and Dr. Silveyra said.
For example, among the few studies that have documented sex differences, one showed no sex differences in the efficacy of salmeterol/fluticasone combination therapy for reducing exacerbations or improving quality of life, whereas another showed that women were more likely than men to experience COPD symptoms or exacerbations after stopping inhaled corticosteroids, Dr. Sodhi and colleagues noted.
Both Dr. Sodhi and Dr. Silveyra emphasized the need for clinical trials that study the effects of sex on treatment outcomes in COPD, which could lead to better, more personalized therapeutic regimens that take sex and gender into account.
Dr. Sodhi and colleagues offered the following advice to clinicians: “Interaction with female patients should take into account that their symptoms may not conform to traditionally accepted presentations. Challenges exist for female patients at all levels of health care interaction and as clinicians we need to acknowledge the bias and willfully work toward recognition and elimination of unconscious and conscious bias. Empowering our patients to have frank discussions with their health care team when they perceive bias is another step to help promote equity.”
The review by Dr. Sodhi and colleagues was supported by grants from the National Institutes of Health. Dr. Sodhi and Dr. Silveyra reported having no conflicts of interest to disclose.
When Sigmund Freud claimed that “anatomy is destiny” he was referring to anatomical sex as a determinant of personality traits. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,”
That notion has been widely discredited, but Freud appears to be inadvertently right in one respect: When it comes to chronic obstructive pulmonary disease (COPD), anatomy really is destiny, and sex may be as well, pulmonary researchers say.
There is a growing body of evidence to indicate that COPD affects men and women differently, and that men and women patients with COPD require different clinical management. Yet women are often underdiagnosed or misdiagnosed, partly because of poorly understood sex differences, but also because of cultural biases.
But plunging any farther into the weeds, it’s important to define terms. Although various investigators have used the terms “sex” and “gender” interchangeably, sex is the preferred term when referring to biological attributes of individual patients, while gender refers to personal identity.
These distinctions are important, contended Amik Sodhi, MBBS, MPH, from the division of allergy, pulmonology, and critical care medicine at the University of Wisconsin–Madison.
“Sex is essentially a biologic construct, so it’s got to do with the sex chromosomes, the genetics of that person, and it refers to the anatomic variations that can change susceptibility to different diseases,” she said in an interview.
An example of sex differences or “sexual dimorphism” can be found in a recent meta-analysis of sex-based genetic associations by Megan Hardin, MD, MPH from Brigham & Women’s Hospital in Boston and colleagues.
They reported that CELSR1, a gene involved in fetal lung development, was expressed more among women than among men and that a single nucleotide polymorphism in the gene was associated with COPD among women smokers, but not among men smokers.
The finding points to a potential risk locus for COPD in women, and could help shed light on sexual dimorphism in COPD, Dr. Hardin and colleagues said.
In contrast to sex, “gender is more of a psychosocial construct which can impact how diseases manifest themselves, how they are potentially managed, and what outcomes might occur for that particular disease,” Dr. Sodhi said.
She and her colleagues recently published a review of sex and gender in common lung disorders and sleep in the journal CHEST, where they wrote that the “influence of sex and gender is portrayed in epidemiological data, disease pathogenesis and pathophysiology, clinical manifestations, response to treatment, access to care, and health outcomes. Hence, sex and gender should be considered in all types of research, clinical practice and educational curricula.”
For example, as previously reported at the 2021 annual meeting of the American Thoracic Society, sex-specific differences in the severity of symptoms and prevalence of comorbidities in patients with COPD may point to different criteria for diagnosing cardiac comorbidities in women and men.
Those conclusions came from a retrospective analysis of data on 795 women and 1,251 men with GOLD (Global Initiative for Chronic Obstructive Lung Disease) class 1-3 disease.
The investigators looked at the patients’ clinical history, comorbidities, lung function, COPD Assessment Test scores, and modified Medical Research Council (mMRC) dyspnea score, and found significant differences between men and women for most functional parameters and comorbidities, and for CAT items of cough, phlegm, and energy.
In logistic regression analysis, predictors for cardiac disease in men were energy, mMRC score, smoking status, body mass index, age, and spirometric lung function, but in women only age was significantly predictive for cardiac disease.
An example of gender effects on COPD differences in men and women is the increase in cigarette advertising aimed at women in the 1960s and the advent of women-targeted brands such as Virginia Slims, which in turn lead to increased smoking rates among women. In addition, in the developing world, where the sex/gender gap in COPD is narrowing, women tend to have greater exposure to wood smoke and cooking fuels in unventilated or poorly ventilated spaces, compared with men.
Increasing incidence among women
According to the Centers for Disease Control and Prevention, chronic lower respiratory diseases, primarily COPD, were the fourth-leading cause of death in women in the United States in 2018, following only heart disease, cancer, and accidents/injuries.
And as a CDC analysis of data from the 2013 Behavioral Risk Factor Surveillance System showed, women were more likely to report being told by a physician that they had COPD than did men (6.6%, compared with 5.4%).
Dr. Sodhi and colleagues noted that, at all time points examined from 2005 to 2014, women had a higher proportion than men of COPD hospitalizations and in-hospital deaths. They also noted that female sex is associated with a threefold risk for severe early-onset COPD, and that women with COPD have lower diffusion capacity of lungs for carbon monoxide, despite having higher predicted forced expiratory volume in 1 second, compared with men.
“Historically, COPD wasn’t a disease that was so prevalent in women. It’s been in the past 20 years that the trends have changed,” said Patricia Silveyra, MSc, PhD, ATSF, associate professor of environmental and occupational health at Indiana University, Bloomington.
The increasing prevalence of COPD among women cannot be explained by smoking alone, she said in an interview.
“It used to be thought that it was because more women smoked, but actually a lot of women who don’t smoke can develop COPD, so it appears to be probably something environmental, but because it used to be a disease of older men, in the clinic there was also a bias to diagnose men with COPD, and women with asthma, so a lot of women went underdiagnosed,” Dr. Silveyra said.
In their review, Dr. Sodhi and colleagues noted that women with COPD “may be underdiagnosed as a result of having different symptoms from those classically recognized. Reasons for underdiagnosis or a delay in diagnosis may also be due to lack of a formal evaluation with spirometry, women seeking care later in the course of disease, physician bias, or associated fatigue or depression misdirecting diagnostic strategies. Underdiagnosis may be associated with psychological distress and worse health-related quality of life.”
Although the evidence is mixed, women tend to present more frequently with the chronic bronchitis phenotype of COPD, compared with the emphysema phenotype, and women tend to have greater degrees of pulmonary function impairment when exposed to tobacco smoke, even after controlling for differences in height and weight.
“For the same amount of exposure to tobacco smoke, females are likely to develop more severe airflow limitation at an earlier age than males, and have more exacerbation,” Dr. Sodhi and colleagues wrote.
Both Dr. Silveyra and Dr. Sodhi said that reason why men and women differ in their physiological reactions to smoke are still unknown.
Sex differences in drug responses
There is only limited evidence to indicate that women and men respond differently to various therapeutic agents, but what is clear is that more research into this area is needed, Dr. Sodhi and Dr. Silveyra said.
For example, among the few studies that have documented sex differences, one showed no sex differences in the efficacy of salmeterol/fluticasone combination therapy for reducing exacerbations or improving quality of life, whereas another showed that women were more likely than men to experience COPD symptoms or exacerbations after stopping inhaled corticosteroids, Dr. Sodhi and colleagues noted.
Both Dr. Sodhi and Dr. Silveyra emphasized the need for clinical trials that study the effects of sex on treatment outcomes in COPD, which could lead to better, more personalized therapeutic regimens that take sex and gender into account.
Dr. Sodhi and colleagues offered the following advice to clinicians: “Interaction with female patients should take into account that their symptoms may not conform to traditionally accepted presentations. Challenges exist for female patients at all levels of health care interaction and as clinicians we need to acknowledge the bias and willfully work toward recognition and elimination of unconscious and conscious bias. Empowering our patients to have frank discussions with their health care team when they perceive bias is another step to help promote equity.”
The review by Dr. Sodhi and colleagues was supported by grants from the National Institutes of Health. Dr. Sodhi and Dr. Silveyra reported having no conflicts of interest to disclose.
When Sigmund Freud claimed that “anatomy is destiny” he was referring to anatomical sex as a determinant of personality traits. Expert consensus statements have previously offered some recommendations for managing these syndromes, but clinical data are scarce, so the present review “is intended to establish a starting point for future research,”
That notion has been widely discredited, but Freud appears to be inadvertently right in one respect: When it comes to chronic obstructive pulmonary disease (COPD), anatomy really is destiny, and sex may be as well, pulmonary researchers say.
There is a growing body of evidence to indicate that COPD affects men and women differently, and that men and women patients with COPD require different clinical management. Yet women are often underdiagnosed or misdiagnosed, partly because of poorly understood sex differences, but also because of cultural biases.
But plunging any farther into the weeds, it’s important to define terms. Although various investigators have used the terms “sex” and “gender” interchangeably, sex is the preferred term when referring to biological attributes of individual patients, while gender refers to personal identity.
These distinctions are important, contended Amik Sodhi, MBBS, MPH, from the division of allergy, pulmonology, and critical care medicine at the University of Wisconsin–Madison.
“Sex is essentially a biologic construct, so it’s got to do with the sex chromosomes, the genetics of that person, and it refers to the anatomic variations that can change susceptibility to different diseases,” she said in an interview.
An example of sex differences or “sexual dimorphism” can be found in a recent meta-analysis of sex-based genetic associations by Megan Hardin, MD, MPH from Brigham & Women’s Hospital in Boston and colleagues.
They reported that CELSR1, a gene involved in fetal lung development, was expressed more among women than among men and that a single nucleotide polymorphism in the gene was associated with COPD among women smokers, but not among men smokers.
The finding points to a potential risk locus for COPD in women, and could help shed light on sexual dimorphism in COPD, Dr. Hardin and colleagues said.
In contrast to sex, “gender is more of a psychosocial construct which can impact how diseases manifest themselves, how they are potentially managed, and what outcomes might occur for that particular disease,” Dr. Sodhi said.
She and her colleagues recently published a review of sex and gender in common lung disorders and sleep in the journal CHEST, where they wrote that the “influence of sex and gender is portrayed in epidemiological data, disease pathogenesis and pathophysiology, clinical manifestations, response to treatment, access to care, and health outcomes. Hence, sex and gender should be considered in all types of research, clinical practice and educational curricula.”
For example, as previously reported at the 2021 annual meeting of the American Thoracic Society, sex-specific differences in the severity of symptoms and prevalence of comorbidities in patients with COPD may point to different criteria for diagnosing cardiac comorbidities in women and men.
Those conclusions came from a retrospective analysis of data on 795 women and 1,251 men with GOLD (Global Initiative for Chronic Obstructive Lung Disease) class 1-3 disease.
The investigators looked at the patients’ clinical history, comorbidities, lung function, COPD Assessment Test scores, and modified Medical Research Council (mMRC) dyspnea score, and found significant differences between men and women for most functional parameters and comorbidities, and for CAT items of cough, phlegm, and energy.
In logistic regression analysis, predictors for cardiac disease in men were energy, mMRC score, smoking status, body mass index, age, and spirometric lung function, but in women only age was significantly predictive for cardiac disease.
An example of gender effects on COPD differences in men and women is the increase in cigarette advertising aimed at women in the 1960s and the advent of women-targeted brands such as Virginia Slims, which in turn lead to increased smoking rates among women. In addition, in the developing world, where the sex/gender gap in COPD is narrowing, women tend to have greater exposure to wood smoke and cooking fuels in unventilated or poorly ventilated spaces, compared with men.
Increasing incidence among women
According to the Centers for Disease Control and Prevention, chronic lower respiratory diseases, primarily COPD, were the fourth-leading cause of death in women in the United States in 2018, following only heart disease, cancer, and accidents/injuries.
And as a CDC analysis of data from the 2013 Behavioral Risk Factor Surveillance System showed, women were more likely to report being told by a physician that they had COPD than did men (6.6%, compared with 5.4%).
Dr. Sodhi and colleagues noted that, at all time points examined from 2005 to 2014, women had a higher proportion than men of COPD hospitalizations and in-hospital deaths. They also noted that female sex is associated with a threefold risk for severe early-onset COPD, and that women with COPD have lower diffusion capacity of lungs for carbon monoxide, despite having higher predicted forced expiratory volume in 1 second, compared with men.
“Historically, COPD wasn’t a disease that was so prevalent in women. It’s been in the past 20 years that the trends have changed,” said Patricia Silveyra, MSc, PhD, ATSF, associate professor of environmental and occupational health at Indiana University, Bloomington.
The increasing prevalence of COPD among women cannot be explained by smoking alone, she said in an interview.
“It used to be thought that it was because more women smoked, but actually a lot of women who don’t smoke can develop COPD, so it appears to be probably something environmental, but because it used to be a disease of older men, in the clinic there was also a bias to diagnose men with COPD, and women with asthma, so a lot of women went underdiagnosed,” Dr. Silveyra said.
In their review, Dr. Sodhi and colleagues noted that women with COPD “may be underdiagnosed as a result of having different symptoms from those classically recognized. Reasons for underdiagnosis or a delay in diagnosis may also be due to lack of a formal evaluation with spirometry, women seeking care later in the course of disease, physician bias, or associated fatigue or depression misdirecting diagnostic strategies. Underdiagnosis may be associated with psychological distress and worse health-related quality of life.”
Although the evidence is mixed, women tend to present more frequently with the chronic bronchitis phenotype of COPD, compared with the emphysema phenotype, and women tend to have greater degrees of pulmonary function impairment when exposed to tobacco smoke, even after controlling for differences in height and weight.
“For the same amount of exposure to tobacco smoke, females are likely to develop more severe airflow limitation at an earlier age than males, and have more exacerbation,” Dr. Sodhi and colleagues wrote.
Both Dr. Silveyra and Dr. Sodhi said that reason why men and women differ in their physiological reactions to smoke are still unknown.
Sex differences in drug responses
There is only limited evidence to indicate that women and men respond differently to various therapeutic agents, but what is clear is that more research into this area is needed, Dr. Sodhi and Dr. Silveyra said.
For example, among the few studies that have documented sex differences, one showed no sex differences in the efficacy of salmeterol/fluticasone combination therapy for reducing exacerbations or improving quality of life, whereas another showed that women were more likely than men to experience COPD symptoms or exacerbations after stopping inhaled corticosteroids, Dr. Sodhi and colleagues noted.
Both Dr. Sodhi and Dr. Silveyra emphasized the need for clinical trials that study the effects of sex on treatment outcomes in COPD, which could lead to better, more personalized therapeutic regimens that take sex and gender into account.
Dr. Sodhi and colleagues offered the following advice to clinicians: “Interaction with female patients should take into account that their symptoms may not conform to traditionally accepted presentations. Challenges exist for female patients at all levels of health care interaction and as clinicians we need to acknowledge the bias and willfully work toward recognition and elimination of unconscious and conscious bias. Empowering our patients to have frank discussions with their health care team when they perceive bias is another step to help promote equity.”
The review by Dr. Sodhi and colleagues was supported by grants from the National Institutes of Health. Dr. Sodhi and Dr. Silveyra reported having no conflicts of interest to disclose.
Continuous remote patient monitoring
The SARS-CoV-2 pandemic required health care systems around the world to rapidly innovate and adapt to unprecedented operational and clinical strain. Many health care systems leveraged virtual care capabilities as an innovative approach to safely and efficiently manage patients while reducing staff exposure and medical resource constraints (Healthcare [Basel]. 2020 Nov;8[4]:517; JMIR Form Res. 2021 Jan; 5[1]:e23190). With Medicare insurance claims data demonstrating a 30% reduction of in-person health visits, telemedicine has become an essential means to fill the gaps in providing essential medical services (JAMA Intern Med. 2021 Mar;181[3]:388-91). A vast majority of virtual health care visits come via telephonic encounters, which have inherent limitations in the ability to monitor patients with complex or critical medical conditions (Front Public Health. 2020;8:410; N Engl J Med. 2020 Apr;382[18]:1679-81). Remote patient monitoring (RPM) has been established in multiple clinical models as an effective adjunct in telemedicine encounters in order to ensure treatment regimen adherence, make real-time treatment adjustments, and identify patients at risk for early decompensation.
Long-term RPM data has demonstrated cost reduction, reduced burden of in-office visits, expedited management of significant clinical events, and decreased all-cause mortality rates. Previously RPM was limited to the care of patients with chronic conditions, particularly cardiac patients with congestive heart failure and invasive devices, such as pacemakers or implantable cardioverter–defibrillators (JMIR Form Res. 2021 Jan;5[1]:e23190; Front Public Health. 2020; 8:410). In response to the pandemic, the Centers for Medicare and Medicaid Services (CMS) added RPM billing codes in 2019 and then included coverage of acute conditions in 2020 that permitted a more extensive role of RPM in telemedicine. This change in financial reimbursement led to a more aggressive expansion of RPM devices to assess physiologic parameters, such as weight, blood pressure, oxygen saturation, and blood glucose levels for clinicians to review.
Currently, RPM devices fall within a low-risk FDA category that do not require clinical trials for validation prior to being cleared for CMS billing in a fee-for-service reimbursement model (N Engl J Med. 2021 Apr;384[15]:1384-6). A shortage of evidence-based publications to guide clinicians in this new landscape creates challenges from underuse, misuse, or abuse of RPM tools. In order to maximize the clinical benefits of RPM, standardized processes and device specifications derived from up-to-date research need to be established in professional society guidelines.
Formalized RPM protocols should play a key role in overcoming the hesitancy of health institutions becoming early adopters of RPM technologies. Some significant challenges leading to reluctance of executing an RPM program were recently highlighted at the REPROGRAM international consortium of telemedicine. These concerns involved building a technological infrastructure, training clinical staff, ensuring remote connectivity with broadband Internet, and working with patients of various technologic literacy (Front Public Health. 2020;8:410). We attempted to address these challenges by using a COVID-19 remote patient monitoring (CRPM) strategy within our Military Health System (MHS). By using the well-established responsible, accountable, consulted, and informed (RACI) matrix process mapping tool, we created a standardized enrollment process of high-risk patients across eight military treatment facilities (MTFs). High risk patients included those with COVID-19 pneumonia and persistent hypoxemia, those recovering from acute exacerbations of congestive heart failure, those with cardiopulmonary instability associated with malignancy, and other conditions that required continuous monitoring outside of the hospital setting.
In our CRPM process, the hospital inpatient unit or ED refer high-risk patients to a primary designated provider at each MTF for enrollment prior to discharge. Enrolled patients are equipped with an FDA-approved home monitoring kit that contains an electronic tablet, a network hub that operates independently of and/or in conjunction with Wi-Fi, and an armband containing a coin-sized monitor. The system has the capability to pair with additional smart-enabled accessories, such as a blood pressure cuff, temperature patch, and digital spirometer. With continuous bio-physiologic and symptom-based monitoring, a team of teleworking critical-care nurses monitor patients continuously. In case of a decompensation necessitating a higher level of care, an emergency action plan (EAP) is activated to ensure patients urgently receive emergency medical services. Once released from the CRPM program, discharged patients use prepaid shipping boxes to facilitate contactless repackaging, sanitization, and pickup for redistribution of devices to the MTF.
Given the increased number of hospital admissions noted during the COVID-19 global pandemic, the CRPM program has allowed us to address overutilization of hospital beds. Furthermore, it has allowed us to address issues of screening and resource utilization as we consider patients for safe implementation of home monitoring. While data concerning the outcome of the CRPM program are pending, we are encouraged about the ability to provide high quality care in a remote setting. To that end, we have addressed technologic difficulties, communication between remote providers and patients in the home environment, and communication between health care providers in various settings, such as the ED, inpatient wards, and the outpatient clinic.
To be sure, there are many challenges in making sure that CRPM adequately addresses the needs of patients, who may have persistent perturbations in cardiopulmonary status, tremendous anxiety about the progress or deterioration in their health status, and lack of understanding about their medical condition. Furthermore, providers face the challenge of making clinical decisions sometimes without the advantage of in-person examinations. Sometimes decisions must be made with incomplete information or when the status of the patient does not follow presupposed algorithms. Nevertheless, like many issues during the COVID-19 pandemic, patients and providers have evolved, pivoted, and made necessary adjustments to address an unprecedented time in recent history.
Ultimately, we believe that a continuous remote patient monitoring program can be designed, implemented, and maintained across a multifacility health care system for safe, effective, and efficient health care delivery. Limitations in implementing such a program might include lack of adequate Internet services, lack of telephonic communication, inadequate home facilities, lack of adequate home support, and, perhaps, lack of available emergency services. However, if the conditions for home monitoring are optimized, CRPM holds the promise of reducing the burden on emergency and inpatient hospital services, particularly when those services are strained in circumstances such as the ongoing global pandemic due to COVID-19. With further study, standardization, and evolution, remote monitoring will likely become a more acceptable and necessary form of health care delivery in the future.
Dr. Salomon is an Internal Medicine Resident (PGY-2); Dr. Muller is an Internal Medicine Resident (PGY-2); Dr. Boster is a Pulmonary and Critical Care Fellow; Dr. Loudermilk is a Pulmonary and Critical Care Fellow; and Dr. Kemp is Pulmonary and Critical Care staff, San Antonio Military Medical Center, Fort Sam Houston, Texas.
The SARS-CoV-2 pandemic required health care systems around the world to rapidly innovate and adapt to unprecedented operational and clinical strain. Many health care systems leveraged virtual care capabilities as an innovative approach to safely and efficiently manage patients while reducing staff exposure and medical resource constraints (Healthcare [Basel]. 2020 Nov;8[4]:517; JMIR Form Res. 2021 Jan; 5[1]:e23190). With Medicare insurance claims data demonstrating a 30% reduction of in-person health visits, telemedicine has become an essential means to fill the gaps in providing essential medical services (JAMA Intern Med. 2021 Mar;181[3]:388-91). A vast majority of virtual health care visits come via telephonic encounters, which have inherent limitations in the ability to monitor patients with complex or critical medical conditions (Front Public Health. 2020;8:410; N Engl J Med. 2020 Apr;382[18]:1679-81). Remote patient monitoring (RPM) has been established in multiple clinical models as an effective adjunct in telemedicine encounters in order to ensure treatment regimen adherence, make real-time treatment adjustments, and identify patients at risk for early decompensation.
Long-term RPM data has demonstrated cost reduction, reduced burden of in-office visits, expedited management of significant clinical events, and decreased all-cause mortality rates. Previously RPM was limited to the care of patients with chronic conditions, particularly cardiac patients with congestive heart failure and invasive devices, such as pacemakers or implantable cardioverter–defibrillators (JMIR Form Res. 2021 Jan;5[1]:e23190; Front Public Health. 2020; 8:410). In response to the pandemic, the Centers for Medicare and Medicaid Services (CMS) added RPM billing codes in 2019 and then included coverage of acute conditions in 2020 that permitted a more extensive role of RPM in telemedicine. This change in financial reimbursement led to a more aggressive expansion of RPM devices to assess physiologic parameters, such as weight, blood pressure, oxygen saturation, and blood glucose levels for clinicians to review.
Currently, RPM devices fall within a low-risk FDA category that do not require clinical trials for validation prior to being cleared for CMS billing in a fee-for-service reimbursement model (N Engl J Med. 2021 Apr;384[15]:1384-6). A shortage of evidence-based publications to guide clinicians in this new landscape creates challenges from underuse, misuse, or abuse of RPM tools. In order to maximize the clinical benefits of RPM, standardized processes and device specifications derived from up-to-date research need to be established in professional society guidelines.
Formalized RPM protocols should play a key role in overcoming the hesitancy of health institutions becoming early adopters of RPM technologies. Some significant challenges leading to reluctance of executing an RPM program were recently highlighted at the REPROGRAM international consortium of telemedicine. These concerns involved building a technological infrastructure, training clinical staff, ensuring remote connectivity with broadband Internet, and working with patients of various technologic literacy (Front Public Health. 2020;8:410). We attempted to address these challenges by using a COVID-19 remote patient monitoring (CRPM) strategy within our Military Health System (MHS). By using the well-established responsible, accountable, consulted, and informed (RACI) matrix process mapping tool, we created a standardized enrollment process of high-risk patients across eight military treatment facilities (MTFs). High risk patients included those with COVID-19 pneumonia and persistent hypoxemia, those recovering from acute exacerbations of congestive heart failure, those with cardiopulmonary instability associated with malignancy, and other conditions that required continuous monitoring outside of the hospital setting.
In our CRPM process, the hospital inpatient unit or ED refer high-risk patients to a primary designated provider at each MTF for enrollment prior to discharge. Enrolled patients are equipped with an FDA-approved home monitoring kit that contains an electronic tablet, a network hub that operates independently of and/or in conjunction with Wi-Fi, and an armband containing a coin-sized monitor. The system has the capability to pair with additional smart-enabled accessories, such as a blood pressure cuff, temperature patch, and digital spirometer. With continuous bio-physiologic and symptom-based monitoring, a team of teleworking critical-care nurses monitor patients continuously. In case of a decompensation necessitating a higher level of care, an emergency action plan (EAP) is activated to ensure patients urgently receive emergency medical services. Once released from the CRPM program, discharged patients use prepaid shipping boxes to facilitate contactless repackaging, sanitization, and pickup for redistribution of devices to the MTF.
Given the increased number of hospital admissions noted during the COVID-19 global pandemic, the CRPM program has allowed us to address overutilization of hospital beds. Furthermore, it has allowed us to address issues of screening and resource utilization as we consider patients for safe implementation of home monitoring. While data concerning the outcome of the CRPM program are pending, we are encouraged about the ability to provide high quality care in a remote setting. To that end, we have addressed technologic difficulties, communication between remote providers and patients in the home environment, and communication between health care providers in various settings, such as the ED, inpatient wards, and the outpatient clinic.
To be sure, there are many challenges in making sure that CRPM adequately addresses the needs of patients, who may have persistent perturbations in cardiopulmonary status, tremendous anxiety about the progress or deterioration in their health status, and lack of understanding about their medical condition. Furthermore, providers face the challenge of making clinical decisions sometimes without the advantage of in-person examinations. Sometimes decisions must be made with incomplete information or when the status of the patient does not follow presupposed algorithms. Nevertheless, like many issues during the COVID-19 pandemic, patients and providers have evolved, pivoted, and made necessary adjustments to address an unprecedented time in recent history.
Ultimately, we believe that a continuous remote patient monitoring program can be designed, implemented, and maintained across a multifacility health care system for safe, effective, and efficient health care delivery. Limitations in implementing such a program might include lack of adequate Internet services, lack of telephonic communication, inadequate home facilities, lack of adequate home support, and, perhaps, lack of available emergency services. However, if the conditions for home monitoring are optimized, CRPM holds the promise of reducing the burden on emergency and inpatient hospital services, particularly when those services are strained in circumstances such as the ongoing global pandemic due to COVID-19. With further study, standardization, and evolution, remote monitoring will likely become a more acceptable and necessary form of health care delivery in the future.
Dr. Salomon is an Internal Medicine Resident (PGY-2); Dr. Muller is an Internal Medicine Resident (PGY-2); Dr. Boster is a Pulmonary and Critical Care Fellow; Dr. Loudermilk is a Pulmonary and Critical Care Fellow; and Dr. Kemp is Pulmonary and Critical Care staff, San Antonio Military Medical Center, Fort Sam Houston, Texas.
The SARS-CoV-2 pandemic required health care systems around the world to rapidly innovate and adapt to unprecedented operational and clinical strain. Many health care systems leveraged virtual care capabilities as an innovative approach to safely and efficiently manage patients while reducing staff exposure and medical resource constraints (Healthcare [Basel]. 2020 Nov;8[4]:517; JMIR Form Res. 2021 Jan; 5[1]:e23190). With Medicare insurance claims data demonstrating a 30% reduction of in-person health visits, telemedicine has become an essential means to fill the gaps in providing essential medical services (JAMA Intern Med. 2021 Mar;181[3]:388-91). A vast majority of virtual health care visits come via telephonic encounters, which have inherent limitations in the ability to monitor patients with complex or critical medical conditions (Front Public Health. 2020;8:410; N Engl J Med. 2020 Apr;382[18]:1679-81). Remote patient monitoring (RPM) has been established in multiple clinical models as an effective adjunct in telemedicine encounters in order to ensure treatment regimen adherence, make real-time treatment adjustments, and identify patients at risk for early decompensation.
Long-term RPM data has demonstrated cost reduction, reduced burden of in-office visits, expedited management of significant clinical events, and decreased all-cause mortality rates. Previously RPM was limited to the care of patients with chronic conditions, particularly cardiac patients with congestive heart failure and invasive devices, such as pacemakers or implantable cardioverter–defibrillators (JMIR Form Res. 2021 Jan;5[1]:e23190; Front Public Health. 2020; 8:410). In response to the pandemic, the Centers for Medicare and Medicaid Services (CMS) added RPM billing codes in 2019 and then included coverage of acute conditions in 2020 that permitted a more extensive role of RPM in telemedicine. This change in financial reimbursement led to a more aggressive expansion of RPM devices to assess physiologic parameters, such as weight, blood pressure, oxygen saturation, and blood glucose levels for clinicians to review.
Currently, RPM devices fall within a low-risk FDA category that do not require clinical trials for validation prior to being cleared for CMS billing in a fee-for-service reimbursement model (N Engl J Med. 2021 Apr;384[15]:1384-6). A shortage of evidence-based publications to guide clinicians in this new landscape creates challenges from underuse, misuse, or abuse of RPM tools. In order to maximize the clinical benefits of RPM, standardized processes and device specifications derived from up-to-date research need to be established in professional society guidelines.
Formalized RPM protocols should play a key role in overcoming the hesitancy of health institutions becoming early adopters of RPM technologies. Some significant challenges leading to reluctance of executing an RPM program were recently highlighted at the REPROGRAM international consortium of telemedicine. These concerns involved building a technological infrastructure, training clinical staff, ensuring remote connectivity with broadband Internet, and working with patients of various technologic literacy (Front Public Health. 2020;8:410). We attempted to address these challenges by using a COVID-19 remote patient monitoring (CRPM) strategy within our Military Health System (MHS). By using the well-established responsible, accountable, consulted, and informed (RACI) matrix process mapping tool, we created a standardized enrollment process of high-risk patients across eight military treatment facilities (MTFs). High risk patients included those with COVID-19 pneumonia and persistent hypoxemia, those recovering from acute exacerbations of congestive heart failure, those with cardiopulmonary instability associated with malignancy, and other conditions that required continuous monitoring outside of the hospital setting.
In our CRPM process, the hospital inpatient unit or ED refer high-risk patients to a primary designated provider at each MTF for enrollment prior to discharge. Enrolled patients are equipped with an FDA-approved home monitoring kit that contains an electronic tablet, a network hub that operates independently of and/or in conjunction with Wi-Fi, and an armband containing a coin-sized monitor. The system has the capability to pair with additional smart-enabled accessories, such as a blood pressure cuff, temperature patch, and digital spirometer. With continuous bio-physiologic and symptom-based monitoring, a team of teleworking critical-care nurses monitor patients continuously. In case of a decompensation necessitating a higher level of care, an emergency action plan (EAP) is activated to ensure patients urgently receive emergency medical services. Once released from the CRPM program, discharged patients use prepaid shipping boxes to facilitate contactless repackaging, sanitization, and pickup for redistribution of devices to the MTF.
Given the increased number of hospital admissions noted during the COVID-19 global pandemic, the CRPM program has allowed us to address overutilization of hospital beds. Furthermore, it has allowed us to address issues of screening and resource utilization as we consider patients for safe implementation of home monitoring. While data concerning the outcome of the CRPM program are pending, we are encouraged about the ability to provide high quality care in a remote setting. To that end, we have addressed technologic difficulties, communication between remote providers and patients in the home environment, and communication between health care providers in various settings, such as the ED, inpatient wards, and the outpatient clinic.
To be sure, there are many challenges in making sure that CRPM adequately addresses the needs of patients, who may have persistent perturbations in cardiopulmonary status, tremendous anxiety about the progress or deterioration in their health status, and lack of understanding about their medical condition. Furthermore, providers face the challenge of making clinical decisions sometimes without the advantage of in-person examinations. Sometimes decisions must be made with incomplete information or when the status of the patient does not follow presupposed algorithms. Nevertheless, like many issues during the COVID-19 pandemic, patients and providers have evolved, pivoted, and made necessary adjustments to address an unprecedented time in recent history.
Ultimately, we believe that a continuous remote patient monitoring program can be designed, implemented, and maintained across a multifacility health care system for safe, effective, and efficient health care delivery. Limitations in implementing such a program might include lack of adequate Internet services, lack of telephonic communication, inadequate home facilities, lack of adequate home support, and, perhaps, lack of available emergency services. However, if the conditions for home monitoring are optimized, CRPM holds the promise of reducing the burden on emergency and inpatient hospital services, particularly when those services are strained in circumstances such as the ongoing global pandemic due to COVID-19. With further study, standardization, and evolution, remote monitoring will likely become a more acceptable and necessary form of health care delivery in the future.
Dr. Salomon is an Internal Medicine Resident (PGY-2); Dr. Muller is an Internal Medicine Resident (PGY-2); Dr. Boster is a Pulmonary and Critical Care Fellow; Dr. Loudermilk is a Pulmonary and Critical Care Fellow; and Dr. Kemp is Pulmonary and Critical Care staff, San Antonio Military Medical Center, Fort Sam Houston, Texas.
Denosumab boosts bone strength in glucocorticoid users
Bone strength and microarchitecture remained stronger at 24 months after treatment with denosumab compared to risedronate, in a study of 110 adults using glucocorticoids.
Patients using glucocorticoids are at increased risk for vertebral and nonvertebral fractures at both the start of treatment or as treatment continues, wrote Piet Geusens, MD, of Maastricht University, the Netherlands, and colleagues.
Imaging data collected via high-resolution peripheral quantitative computed tomography (HR-pQCT) allow for the assessment of bone microarchitecture and strength, but specific data comparing the impact of bone treatment in patients using glucocorticoids are lacking, they said.
In a study published in the Journal of Bone and Mineral Research, the researchers identified a subset of 56 patients randomized to denosumab and 54 to risedronate patients out of a total of 590 patients who were enrolled in a phase 3 randomized, controlled trial of denosumab vs. risedronate for bone mineral density. The main results of the larger trial – presented at EULAR 2018 – showed greater increases in bone strength with denosumab over risedronate in patients receiving glucocorticoids.
In the current study, the researchers reviewed HR-pQCT scans of the distal radius and tibia at baseline, 12 months, and 24 months. Bone strength and microarchitecture were defined in terms of failure load (FL) as a primary outcome. Patients also were divided into subpopulations of those initiating glucocorticoid treatment (GC-I) and continuing treatment (GC-C).
Baseline characteristics were mainly balanced among the treatment groups within the GC-I and GC-C categories.
Among the GC-I patients, in the denosumab group, FL increased significantly from baseline to 12 months at the radius at tibia (1.8% and 1.7%, respectively) but did not change significantly in the risedronate group, which translated to a significant treatment difference between the drugs of 3.3% for radius and 2.5% for tibia.
At 24 months, the radius measure of FL was unchanged from baseline in denosumab patients but significantly decreased in risedronate patients, with a difference of –4.1%, which translated to a significant between-treatment difference at the radius of 5.6% (P < .001). Changes at the tibia were not significantly different between the groups at 24 months.
Among the GC-C patients, FL was unchanged from baseline to 12 months for both the denosumab and risedronate groups. However, FL significantly increased with denosumab (4.3%) and remained unchanged in the risedronate group.
The researchers also found significant differences between denosumab and risedronate in percentage changes in cortical bone mineral density, and less prominent changes and differences in trabecular bone mineral density.
The study findings were limited by several factors including the use of the HR-pQCT scanner, which limits the measurement of trabecular microarchitecture, and the use of only standard HR-pQCT parameters, which do not allow insight into endosteal changes, and the inability to correct for multiplicity of data, the researchers noted.
However, the results support the superiority of denosumab over risedronate for preventing FL and total bone mineral density loss at the radius and tibia in new glucocorticoid users, and for increasing FL and total bone mineral density at the radius in long-term glucocorticoid users, they said.
Denosumab therefore could be a useful therapeutic option and could inform decision-making in patients initiating GC-therapy or on long-term GC-therapy, they concluded.
The study was supported by Amgen. Dr. Geusens disclosed grants from Amgen, Celgene, Lilly, Merck, Pfizer, Roche, UCB, Fresenius, Mylan, and Sandoz, and grants and other funding from AbbVie, outside the current study.
Bone strength and microarchitecture remained stronger at 24 months after treatment with denosumab compared to risedronate, in a study of 110 adults using glucocorticoids.
Patients using glucocorticoids are at increased risk for vertebral and nonvertebral fractures at both the start of treatment or as treatment continues, wrote Piet Geusens, MD, of Maastricht University, the Netherlands, and colleagues.
Imaging data collected via high-resolution peripheral quantitative computed tomography (HR-pQCT) allow for the assessment of bone microarchitecture and strength, but specific data comparing the impact of bone treatment in patients using glucocorticoids are lacking, they said.
In a study published in the Journal of Bone and Mineral Research, the researchers identified a subset of 56 patients randomized to denosumab and 54 to risedronate patients out of a total of 590 patients who were enrolled in a phase 3 randomized, controlled trial of denosumab vs. risedronate for bone mineral density. The main results of the larger trial – presented at EULAR 2018 – showed greater increases in bone strength with denosumab over risedronate in patients receiving glucocorticoids.
In the current study, the researchers reviewed HR-pQCT scans of the distal radius and tibia at baseline, 12 months, and 24 months. Bone strength and microarchitecture were defined in terms of failure load (FL) as a primary outcome. Patients also were divided into subpopulations of those initiating glucocorticoid treatment (GC-I) and continuing treatment (GC-C).
Baseline characteristics were mainly balanced among the treatment groups within the GC-I and GC-C categories.
Among the GC-I patients, in the denosumab group, FL increased significantly from baseline to 12 months at the radius at tibia (1.8% and 1.7%, respectively) but did not change significantly in the risedronate group, which translated to a significant treatment difference between the drugs of 3.3% for radius and 2.5% for tibia.
At 24 months, the radius measure of FL was unchanged from baseline in denosumab patients but significantly decreased in risedronate patients, with a difference of –4.1%, which translated to a significant between-treatment difference at the radius of 5.6% (P < .001). Changes at the tibia were not significantly different between the groups at 24 months.
Among the GC-C patients, FL was unchanged from baseline to 12 months for both the denosumab and risedronate groups. However, FL significantly increased with denosumab (4.3%) and remained unchanged in the risedronate group.
The researchers also found significant differences between denosumab and risedronate in percentage changes in cortical bone mineral density, and less prominent changes and differences in trabecular bone mineral density.
The study findings were limited by several factors including the use of the HR-pQCT scanner, which limits the measurement of trabecular microarchitecture, and the use of only standard HR-pQCT parameters, which do not allow insight into endosteal changes, and the inability to correct for multiplicity of data, the researchers noted.
However, the results support the superiority of denosumab over risedronate for preventing FL and total bone mineral density loss at the radius and tibia in new glucocorticoid users, and for increasing FL and total bone mineral density at the radius in long-term glucocorticoid users, they said.
Denosumab therefore could be a useful therapeutic option and could inform decision-making in patients initiating GC-therapy or on long-term GC-therapy, they concluded.
The study was supported by Amgen. Dr. Geusens disclosed grants from Amgen, Celgene, Lilly, Merck, Pfizer, Roche, UCB, Fresenius, Mylan, and Sandoz, and grants and other funding from AbbVie, outside the current study.
Bone strength and microarchitecture remained stronger at 24 months after treatment with denosumab compared to risedronate, in a study of 110 adults using glucocorticoids.
Patients using glucocorticoids are at increased risk for vertebral and nonvertebral fractures at both the start of treatment or as treatment continues, wrote Piet Geusens, MD, of Maastricht University, the Netherlands, and colleagues.
Imaging data collected via high-resolution peripheral quantitative computed tomography (HR-pQCT) allow for the assessment of bone microarchitecture and strength, but specific data comparing the impact of bone treatment in patients using glucocorticoids are lacking, they said.
In a study published in the Journal of Bone and Mineral Research, the researchers identified a subset of 56 patients randomized to denosumab and 54 to risedronate patients out of a total of 590 patients who were enrolled in a phase 3 randomized, controlled trial of denosumab vs. risedronate for bone mineral density. The main results of the larger trial – presented at EULAR 2018 – showed greater increases in bone strength with denosumab over risedronate in patients receiving glucocorticoids.
In the current study, the researchers reviewed HR-pQCT scans of the distal radius and tibia at baseline, 12 months, and 24 months. Bone strength and microarchitecture were defined in terms of failure load (FL) as a primary outcome. Patients also were divided into subpopulations of those initiating glucocorticoid treatment (GC-I) and continuing treatment (GC-C).
Baseline characteristics were mainly balanced among the treatment groups within the GC-I and GC-C categories.
Among the GC-I patients, in the denosumab group, FL increased significantly from baseline to 12 months at the radius at tibia (1.8% and 1.7%, respectively) but did not change significantly in the risedronate group, which translated to a significant treatment difference between the drugs of 3.3% for radius and 2.5% for tibia.
At 24 months, the radius measure of FL was unchanged from baseline in denosumab patients but significantly decreased in risedronate patients, with a difference of –4.1%, which translated to a significant between-treatment difference at the radius of 5.6% (P < .001). Changes at the tibia were not significantly different between the groups at 24 months.
Among the GC-C patients, FL was unchanged from baseline to 12 months for both the denosumab and risedronate groups. However, FL significantly increased with denosumab (4.3%) and remained unchanged in the risedronate group.
The researchers also found significant differences between denosumab and risedronate in percentage changes in cortical bone mineral density, and less prominent changes and differences in trabecular bone mineral density.
The study findings were limited by several factors including the use of the HR-pQCT scanner, which limits the measurement of trabecular microarchitecture, and the use of only standard HR-pQCT parameters, which do not allow insight into endosteal changes, and the inability to correct for multiplicity of data, the researchers noted.
However, the results support the superiority of denosumab over risedronate for preventing FL and total bone mineral density loss at the radius and tibia in new glucocorticoid users, and for increasing FL and total bone mineral density at the radius in long-term glucocorticoid users, they said.
Denosumab therefore could be a useful therapeutic option and could inform decision-making in patients initiating GC-therapy or on long-term GC-therapy, they concluded.
The study was supported by Amgen. Dr. Geusens disclosed grants from Amgen, Celgene, Lilly, Merck, Pfizer, Roche, UCB, Fresenius, Mylan, and Sandoz, and grants and other funding from AbbVie, outside the current study.
FROM THE JOURNAL OF BONE AND MINERAL RESEARCH
Surgeons in China ‘are the executioners,’ procuring organs before brain death
In a deep dive into obscure Chinese language transplant journals, a pair of researchers from Australia and Israel have added a new layer of horror to what’s already known about forced organ harvesting in China.
Searching for documentation that vital organs are being harvested from nonconsenting executed prisoners, a practice that the China Tribunal confirmed “beyond any reasonable doubt” in 2020, Jacob Lavee, MD, an Israeli heart transplant surgeon, and Matthew Roberston, a PhD student at Australian National University, uncovered something even more shocking: that vital organs are being explanted from patients who are still alive.
“We have shown for the first time that the transplant surgeons are the executioners – that the mode of execution is organ procurement. These are self-admissions of executing the patient,” Dr. Lavee told this news organization. “Up until now, there has been what we call circumstantial evidence of this, but our paper is what you’d call the smoking gun, because it’s in the words of the physicians themselves that they are doing it. In the words of these surgeons, intubation was done only after the beginning of surgery, which means the patients were breathing spontaneously up until the moment the operation started ... meaning they were not brain dead.”
The research, published in the American Journal of Transplantation, involved intricate analysis of thousands of Chinese language transplant articles and identified 71 articles in which transplant surgeons describe starting organ procurement surgery before declaring their patients brain dead.
“What we found were improper, illegitimate, nonexistent, or false declarations of brain death,” Mr. Robertson said in an interview. He explained that this violates what’s known as the dead donor rule, which is fundamental in transplant ethics. “The surgeons wrote that the donor was brain dead, but according to everything we know about medical science, they could not possibly have been brain dead because there was no apnea test performed. Brain death is not just something you say, there’s this whole battery of tests, and the key is the apnea test, [in which] the patient is already intubated and ventilated, they turn the machine off, and they’re looking for carbon dioxide in the blood above a certain level.”
Mr. Robertson and Dr. Lavee have painstakingly documented “incriminating sentences” in each of the 71 articles proving that brain death had not occurred before the organ explantation procedure began. “There were two criteria by which we claimed a problematic brain death declaration,” said Mr. Robertson, who translated the Chinese. “One was where the patient was not ventilated and was only intubated after they were declared brain dead; the other was that the intubation took place immediately prior to the surgery beginning.”
“It was mind-boggling,” said Dr. Lavee, from Tel Aviv University. “When I first started reading, my initial reaction is, ‘This can’t be.’ I read it once, and again, and I insisted that Matt get another independent translation of the Chinese just to be sure. I told him, ‘There’s no way a physician, a surgeon could write this – it doesn’t make sense.’ But the more of these papers we read, we saw it was a pattern – and they didn’t come out of a single medical center, they are spread all over China.”
For the analysis, Mr. Robertson wrote code and customized an algorithm to examine 124,770 medical articles from official Chinese databases between 1980 and 2020. The 71 articles revealing cases involving problematic brain death came from 56 hospitals (of which 12 were military) in 33 cities across 15 provinces, they report. In total, 348 surgeons, nurses, anesthesiologists, and other medical workers or researchers were listed as authors of these publications.
Why would these medical personnel write such self-incriminating evidence? The researchers say it’s unclear. “They don’t think anyone’s reading this stuff,” Mr. Robertson suggests. “Sometimes it’s revealed in just five or six characters in a paper of eight pages.” Dr. Lavee wonders if it’s also ignorance. “If this has been a practice for 20 or 30 years in China, I guess nobody at that time was aware they were doing something wrong, although how to declare brain death is something that is known in China. They’ve published a lot about it.”
The article is “evidence that this barbarity continues and is a very valuable contribution that continues to bring attention to an enormous human rights violation,” said Arthur Caplan, PhD, head of the Division of Medical Ethics at New York University’s Grossman School of Medicine. “What they’ve reported has been going on for many, many years, the data are very clear that China’s doing many more transplants than they have cadaver organ donors,” he said, adding that the country’s well-documented and lucrative involvement in transplant tourism “means you have to have a donor ready when the would-be recipient appears; you have to have a matched organ available, and that’s hard to do waiting on a cadaver donor.”
Although the researchers found no incriminating publications after 2015, they speculate that this is likely due to growing awareness among Chinese surgeons that publishing the information would attract international condemnation. “We think these practices are continuing to go on,” said Dr. Lavee. He acknowledged that a voluntary organ donation program is slowly developing in parallel to this. He said, given China’s place as the world’s second largest transplant country behind the U.S., as well as its low rate of voluntary donation, it’s reasonable to conclude that the main source of organs remains prisoners on death row.
Dr. Caplan and the researchers have called for academic institutions and medical journals to resume their previous boycotts of Chinese transplant publications and speakers, but as long as China denies the practices, economic and political leaders will turn a blind eye. “In the past, I don’t think the question of China’s medical professional involvement in the execution of donors has been taken as seriously as it should have,” said Mr. Robertson. “I certainly hope that with the publication of this paper in the leading journal in the field, this will change.”
The study was supported by the Google Cloud Research Credits program, the Australian Government Research Training Program Scholarship, and the Victims of Communism Memorial Foundation. Mr. Robertson, Dr. Lavee, and Dr. Caplan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a deep dive into obscure Chinese language transplant journals, a pair of researchers from Australia and Israel have added a new layer of horror to what’s already known about forced organ harvesting in China.
Searching for documentation that vital organs are being harvested from nonconsenting executed prisoners, a practice that the China Tribunal confirmed “beyond any reasonable doubt” in 2020, Jacob Lavee, MD, an Israeli heart transplant surgeon, and Matthew Roberston, a PhD student at Australian National University, uncovered something even more shocking: that vital organs are being explanted from patients who are still alive.
“We have shown for the first time that the transplant surgeons are the executioners – that the mode of execution is organ procurement. These are self-admissions of executing the patient,” Dr. Lavee told this news organization. “Up until now, there has been what we call circumstantial evidence of this, but our paper is what you’d call the smoking gun, because it’s in the words of the physicians themselves that they are doing it. In the words of these surgeons, intubation was done only after the beginning of surgery, which means the patients were breathing spontaneously up until the moment the operation started ... meaning they were not brain dead.”
The research, published in the American Journal of Transplantation, involved intricate analysis of thousands of Chinese language transplant articles and identified 71 articles in which transplant surgeons describe starting organ procurement surgery before declaring their patients brain dead.
“What we found were improper, illegitimate, nonexistent, or false declarations of brain death,” Mr. Robertson said in an interview. He explained that this violates what’s known as the dead donor rule, which is fundamental in transplant ethics. “The surgeons wrote that the donor was brain dead, but according to everything we know about medical science, they could not possibly have been brain dead because there was no apnea test performed. Brain death is not just something you say, there’s this whole battery of tests, and the key is the apnea test, [in which] the patient is already intubated and ventilated, they turn the machine off, and they’re looking for carbon dioxide in the blood above a certain level.”
Mr. Robertson and Dr. Lavee have painstakingly documented “incriminating sentences” in each of the 71 articles proving that brain death had not occurred before the organ explantation procedure began. “There were two criteria by which we claimed a problematic brain death declaration,” said Mr. Robertson, who translated the Chinese. “One was where the patient was not ventilated and was only intubated after they were declared brain dead; the other was that the intubation took place immediately prior to the surgery beginning.”
“It was mind-boggling,” said Dr. Lavee, from Tel Aviv University. “When I first started reading, my initial reaction is, ‘This can’t be.’ I read it once, and again, and I insisted that Matt get another independent translation of the Chinese just to be sure. I told him, ‘There’s no way a physician, a surgeon could write this – it doesn’t make sense.’ But the more of these papers we read, we saw it was a pattern – and they didn’t come out of a single medical center, they are spread all over China.”
For the analysis, Mr. Robertson wrote code and customized an algorithm to examine 124,770 medical articles from official Chinese databases between 1980 and 2020. The 71 articles revealing cases involving problematic brain death came from 56 hospitals (of which 12 were military) in 33 cities across 15 provinces, they report. In total, 348 surgeons, nurses, anesthesiologists, and other medical workers or researchers were listed as authors of these publications.
Why would these medical personnel write such self-incriminating evidence? The researchers say it’s unclear. “They don’t think anyone’s reading this stuff,” Mr. Robertson suggests. “Sometimes it’s revealed in just five or six characters in a paper of eight pages.” Dr. Lavee wonders if it’s also ignorance. “If this has been a practice for 20 or 30 years in China, I guess nobody at that time was aware they were doing something wrong, although how to declare brain death is something that is known in China. They’ve published a lot about it.”
The article is “evidence that this barbarity continues and is a very valuable contribution that continues to bring attention to an enormous human rights violation,” said Arthur Caplan, PhD, head of the Division of Medical Ethics at New York University’s Grossman School of Medicine. “What they’ve reported has been going on for many, many years, the data are very clear that China’s doing many more transplants than they have cadaver organ donors,” he said, adding that the country’s well-documented and lucrative involvement in transplant tourism “means you have to have a donor ready when the would-be recipient appears; you have to have a matched organ available, and that’s hard to do waiting on a cadaver donor.”
Although the researchers found no incriminating publications after 2015, they speculate that this is likely due to growing awareness among Chinese surgeons that publishing the information would attract international condemnation. “We think these practices are continuing to go on,” said Dr. Lavee. He acknowledged that a voluntary organ donation program is slowly developing in parallel to this. He said, given China’s place as the world’s second largest transplant country behind the U.S., as well as its low rate of voluntary donation, it’s reasonable to conclude that the main source of organs remains prisoners on death row.
Dr. Caplan and the researchers have called for academic institutions and medical journals to resume their previous boycotts of Chinese transplant publications and speakers, but as long as China denies the practices, economic and political leaders will turn a blind eye. “In the past, I don’t think the question of China’s medical professional involvement in the execution of donors has been taken as seriously as it should have,” said Mr. Robertson. “I certainly hope that with the publication of this paper in the leading journal in the field, this will change.”
The study was supported by the Google Cloud Research Credits program, the Australian Government Research Training Program Scholarship, and the Victims of Communism Memorial Foundation. Mr. Robertson, Dr. Lavee, and Dr. Caplan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
In a deep dive into obscure Chinese language transplant journals, a pair of researchers from Australia and Israel have added a new layer of horror to what’s already known about forced organ harvesting in China.
Searching for documentation that vital organs are being harvested from nonconsenting executed prisoners, a practice that the China Tribunal confirmed “beyond any reasonable doubt” in 2020, Jacob Lavee, MD, an Israeli heart transplant surgeon, and Matthew Roberston, a PhD student at Australian National University, uncovered something even more shocking: that vital organs are being explanted from patients who are still alive.
“We have shown for the first time that the transplant surgeons are the executioners – that the mode of execution is organ procurement. These are self-admissions of executing the patient,” Dr. Lavee told this news organization. “Up until now, there has been what we call circumstantial evidence of this, but our paper is what you’d call the smoking gun, because it’s in the words of the physicians themselves that they are doing it. In the words of these surgeons, intubation was done only after the beginning of surgery, which means the patients were breathing spontaneously up until the moment the operation started ... meaning they were not brain dead.”
The research, published in the American Journal of Transplantation, involved intricate analysis of thousands of Chinese language transplant articles and identified 71 articles in which transplant surgeons describe starting organ procurement surgery before declaring their patients brain dead.
“What we found were improper, illegitimate, nonexistent, or false declarations of brain death,” Mr. Robertson said in an interview. He explained that this violates what’s known as the dead donor rule, which is fundamental in transplant ethics. “The surgeons wrote that the donor was brain dead, but according to everything we know about medical science, they could not possibly have been brain dead because there was no apnea test performed. Brain death is not just something you say, there’s this whole battery of tests, and the key is the apnea test, [in which] the patient is already intubated and ventilated, they turn the machine off, and they’re looking for carbon dioxide in the blood above a certain level.”
Mr. Robertson and Dr. Lavee have painstakingly documented “incriminating sentences” in each of the 71 articles proving that brain death had not occurred before the organ explantation procedure began. “There were two criteria by which we claimed a problematic brain death declaration,” said Mr. Robertson, who translated the Chinese. “One was where the patient was not ventilated and was only intubated after they were declared brain dead; the other was that the intubation took place immediately prior to the surgery beginning.”
“It was mind-boggling,” said Dr. Lavee, from Tel Aviv University. “When I first started reading, my initial reaction is, ‘This can’t be.’ I read it once, and again, and I insisted that Matt get another independent translation of the Chinese just to be sure. I told him, ‘There’s no way a physician, a surgeon could write this – it doesn’t make sense.’ But the more of these papers we read, we saw it was a pattern – and they didn’t come out of a single medical center, they are spread all over China.”
For the analysis, Mr. Robertson wrote code and customized an algorithm to examine 124,770 medical articles from official Chinese databases between 1980 and 2020. The 71 articles revealing cases involving problematic brain death came from 56 hospitals (of which 12 were military) in 33 cities across 15 provinces, they report. In total, 348 surgeons, nurses, anesthesiologists, and other medical workers or researchers were listed as authors of these publications.
Why would these medical personnel write such self-incriminating evidence? The researchers say it’s unclear. “They don’t think anyone’s reading this stuff,” Mr. Robertson suggests. “Sometimes it’s revealed in just five or six characters in a paper of eight pages.” Dr. Lavee wonders if it’s also ignorance. “If this has been a practice for 20 or 30 years in China, I guess nobody at that time was aware they were doing something wrong, although how to declare brain death is something that is known in China. They’ve published a lot about it.”
The article is “evidence that this barbarity continues and is a very valuable contribution that continues to bring attention to an enormous human rights violation,” said Arthur Caplan, PhD, head of the Division of Medical Ethics at New York University’s Grossman School of Medicine. “What they’ve reported has been going on for many, many years, the data are very clear that China’s doing many more transplants than they have cadaver organ donors,” he said, adding that the country’s well-documented and lucrative involvement in transplant tourism “means you have to have a donor ready when the would-be recipient appears; you have to have a matched organ available, and that’s hard to do waiting on a cadaver donor.”
Although the researchers found no incriminating publications after 2015, they speculate that this is likely due to growing awareness among Chinese surgeons that publishing the information would attract international condemnation. “We think these practices are continuing to go on,” said Dr. Lavee. He acknowledged that a voluntary organ donation program is slowly developing in parallel to this. He said, given China’s place as the world’s second largest transplant country behind the U.S., as well as its low rate of voluntary donation, it’s reasonable to conclude that the main source of organs remains prisoners on death row.
Dr. Caplan and the researchers have called for academic institutions and medical journals to resume their previous boycotts of Chinese transplant publications and speakers, but as long as China denies the practices, economic and political leaders will turn a blind eye. “In the past, I don’t think the question of China’s medical professional involvement in the execution of donors has been taken as seriously as it should have,” said Mr. Robertson. “I certainly hope that with the publication of this paper in the leading journal in the field, this will change.”
The study was supported by the Google Cloud Research Credits program, the Australian Government Research Training Program Scholarship, and the Victims of Communism Memorial Foundation. Mr. Robertson, Dr. Lavee, and Dr. Caplan have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pneumonia shows strong connection to chronic otitis media
Individuals with a prior diagnosis of pneumonia were significantly more likely to develop chronic otitis media (COM) than were those without a history of pneumonia, based on data from a nationwide cohort study of more than 100,000 patients.
“Recently, middle ear diseases, including COM, have been recognized as respiratory tract diseases beyond the pathophysiological concepts of ventilation dysfunction, with recurrent infection that occurs from anatomically adjacent structures such as the middle ear, mastoid cavity, and eustachian tube,” but the potential link between pneumonia and chronic otitis media and adults in particular has not been examined, wrote Sung Kyun Kim, MD, of Hallym University, Dongtan, South Korea, and colleagues.
In a study recently published in the International Journal of Infectious Diseases, the researchers identified 23,436 adults with COM and 93,744 controls aged 40 years and older from a Korean health insurance database between 2002 and 2015.
The overall incidence of pneumonia in the study population was significantly higher in the COM group compared with controls (9.3% vs. 7.2%, P <.001). The odds ratios of pneumonia were significantly higher in the COM group compared with controls, and a history of pneumonia increased the odds of COM regardless of sex and across all ages.
Pneumonia was defined as when a patient had a diagnosis of pneumonia based on ICD-10 codes and underwent a chest x-ray or chest CT scan. Chronic otitis media was defined as when a patient had a diagnosis based on ICD-10 codes at least two times with one of the following conditions: chronic serous otitis media, chronic mucoid otitis media, other chronic nonsuppurative otitis media, unspecified nonsuppurative otitis media, chronic tubotympanic suppurative otitis media, chronic atticoantral suppurative otitis media, other chronic suppurative otitis media, or unspecified suppurative otitis media.
Age groups were divided into 5-year intervals, and patients were classified into income groups and rural vs. urban residence.
In a further sensitivity analysis, individuals who were diagnosed with pneumonia five or more times before the index date had a significantly higher odds ratio for COM compared with those with less than five diagnoses of pneumonia (adjusted odds ratio, 1.34; P < .001).
Microbiome dysbiosis may explain part of the connection between pneumonia and COM, the researchers wrote in their discussion. Pathogens in the lungs can prompt changes in the microbiome dynamics, as might the use of antibiotics, they said. In addition, “Mucus plugging in the airway caused by pneumonia induces hypoxic conditions and leads to the expression of inflammatory markers in the eustachian tube and middle ear mucosa,” they noted.
The study findings were limited by several factors, including the retrospective design and lack of data on microbiological cultures for antibiotic susceptibility, radiologic findings on the severity of pneumonia, results of pulmonary function tests, and hearing thresholds, the researchers noted. Other limitations were the exclusion of the frequency of upper respiratory infections and antibiotic use due to lack of data, they said.
However, the results show an association between pneumonia diagnoses and increased incidence of COM, which suggests a novel perspective that “infection of the lower respiratory tract may affect the function of the eustachian tube and the middle ear to later cause COM,” they concluded.
The study received no outside funding. The researchers have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with a prior diagnosis of pneumonia were significantly more likely to develop chronic otitis media (COM) than were those without a history of pneumonia, based on data from a nationwide cohort study of more than 100,000 patients.
“Recently, middle ear diseases, including COM, have been recognized as respiratory tract diseases beyond the pathophysiological concepts of ventilation dysfunction, with recurrent infection that occurs from anatomically adjacent structures such as the middle ear, mastoid cavity, and eustachian tube,” but the potential link between pneumonia and chronic otitis media and adults in particular has not been examined, wrote Sung Kyun Kim, MD, of Hallym University, Dongtan, South Korea, and colleagues.
In a study recently published in the International Journal of Infectious Diseases, the researchers identified 23,436 adults with COM and 93,744 controls aged 40 years and older from a Korean health insurance database between 2002 and 2015.
The overall incidence of pneumonia in the study population was significantly higher in the COM group compared with controls (9.3% vs. 7.2%, P <.001). The odds ratios of pneumonia were significantly higher in the COM group compared with controls, and a history of pneumonia increased the odds of COM regardless of sex and across all ages.
Pneumonia was defined as when a patient had a diagnosis of pneumonia based on ICD-10 codes and underwent a chest x-ray or chest CT scan. Chronic otitis media was defined as when a patient had a diagnosis based on ICD-10 codes at least two times with one of the following conditions: chronic serous otitis media, chronic mucoid otitis media, other chronic nonsuppurative otitis media, unspecified nonsuppurative otitis media, chronic tubotympanic suppurative otitis media, chronic atticoantral suppurative otitis media, other chronic suppurative otitis media, or unspecified suppurative otitis media.
Age groups were divided into 5-year intervals, and patients were classified into income groups and rural vs. urban residence.
In a further sensitivity analysis, individuals who were diagnosed with pneumonia five or more times before the index date had a significantly higher odds ratio for COM compared with those with less than five diagnoses of pneumonia (adjusted odds ratio, 1.34; P < .001).
Microbiome dysbiosis may explain part of the connection between pneumonia and COM, the researchers wrote in their discussion. Pathogens in the lungs can prompt changes in the microbiome dynamics, as might the use of antibiotics, they said. In addition, “Mucus plugging in the airway caused by pneumonia induces hypoxic conditions and leads to the expression of inflammatory markers in the eustachian tube and middle ear mucosa,” they noted.
The study findings were limited by several factors, including the retrospective design and lack of data on microbiological cultures for antibiotic susceptibility, radiologic findings on the severity of pneumonia, results of pulmonary function tests, and hearing thresholds, the researchers noted. Other limitations were the exclusion of the frequency of upper respiratory infections and antibiotic use due to lack of data, they said.
However, the results show an association between pneumonia diagnoses and increased incidence of COM, which suggests a novel perspective that “infection of the lower respiratory tract may affect the function of the eustachian tube and the middle ear to later cause COM,” they concluded.
The study received no outside funding. The researchers have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Individuals with a prior diagnosis of pneumonia were significantly more likely to develop chronic otitis media (COM) than were those without a history of pneumonia, based on data from a nationwide cohort study of more than 100,000 patients.
“Recently, middle ear diseases, including COM, have been recognized as respiratory tract diseases beyond the pathophysiological concepts of ventilation dysfunction, with recurrent infection that occurs from anatomically adjacent structures such as the middle ear, mastoid cavity, and eustachian tube,” but the potential link between pneumonia and chronic otitis media and adults in particular has not been examined, wrote Sung Kyun Kim, MD, of Hallym University, Dongtan, South Korea, and colleagues.
In a study recently published in the International Journal of Infectious Diseases, the researchers identified 23,436 adults with COM and 93,744 controls aged 40 years and older from a Korean health insurance database between 2002 and 2015.
The overall incidence of pneumonia in the study population was significantly higher in the COM group compared with controls (9.3% vs. 7.2%, P <.001). The odds ratios of pneumonia were significantly higher in the COM group compared with controls, and a history of pneumonia increased the odds of COM regardless of sex and across all ages.
Pneumonia was defined as when a patient had a diagnosis of pneumonia based on ICD-10 codes and underwent a chest x-ray or chest CT scan. Chronic otitis media was defined as when a patient had a diagnosis based on ICD-10 codes at least two times with one of the following conditions: chronic serous otitis media, chronic mucoid otitis media, other chronic nonsuppurative otitis media, unspecified nonsuppurative otitis media, chronic tubotympanic suppurative otitis media, chronic atticoantral suppurative otitis media, other chronic suppurative otitis media, or unspecified suppurative otitis media.
Age groups were divided into 5-year intervals, and patients were classified into income groups and rural vs. urban residence.
In a further sensitivity analysis, individuals who were diagnosed with pneumonia five or more times before the index date had a significantly higher odds ratio for COM compared with those with less than five diagnoses of pneumonia (adjusted odds ratio, 1.34; P < .001).
Microbiome dysbiosis may explain part of the connection between pneumonia and COM, the researchers wrote in their discussion. Pathogens in the lungs can prompt changes in the microbiome dynamics, as might the use of antibiotics, they said. In addition, “Mucus plugging in the airway caused by pneumonia induces hypoxic conditions and leads to the expression of inflammatory markers in the eustachian tube and middle ear mucosa,” they noted.
The study findings were limited by several factors, including the retrospective design and lack of data on microbiological cultures for antibiotic susceptibility, radiologic findings on the severity of pneumonia, results of pulmonary function tests, and hearing thresholds, the researchers noted. Other limitations were the exclusion of the frequency of upper respiratory infections and antibiotic use due to lack of data, they said.
However, the results show an association between pneumonia diagnoses and increased incidence of COM, which suggests a novel perspective that “infection of the lower respiratory tract may affect the function of the eustachian tube and the middle ear to later cause COM,” they concluded.
The study received no outside funding. The researchers have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE INTERNATIONAL JOURNAL OF INFECTIOUS DISEASES







