User login
HCC surveillance after anti-HCV therapy cost effective only for patients with cirrhosis
For patients with hepatitis C virus (HCV)–related cirrhosis (F4), but not those with advanced fibrosis (F3), hepatocellular carcinoma (HCC) surveillance after a sustained virologic response (SVR) is cost effective, according to investigators.
Current international guidelines call for HCC surveillance among all patients with advanced fibrosis (F3) or cirrhosis (F4) who have achieved SVR, but this is “very unlikely to be cost effective,” reported lead author Hooman Farhang Zangneh, MD, of Toronto General Hospital and colleagues. “HCV-related HCC rarely occurs in patients without cirrhosis,” the investigators explained in Clinical Gastroenterology and Hepatology. “With cirrhosis present, HCC incidence is 1.4% to 4.9% per year. If found early, options for curative therapy include radiofrequency ablation (RFA), surgical resection, and liver transplantation.”
The investigators developed a Markov model to determine which at-risk patients could undergo surveillance while remaining below willingness-to-pay thresholds. Specifically, cost-effectiveness was assessed for ultrasound screenings annually (every year) or biannually (twice a year) among patients with advanced fibrosis (F3) or compensated cirrhosis (F4) who were aged 50 years and had an SVR. Relevant data were drawn from expert opinions, medical literature, and Canada Life Tables. Various HCC incidence rates were tested, including a constant annual rate, rates based on type of antiviral treatment (direct-acting and interferon-based therapies), others based on stage of fibrosis, and another that increased with age. The model was validated by applying it to patients with F3 or F4 fibrosis who had not yet achieved an SVR. All monetary values were reported in 2015 Canadian dollars.
Representative of current guidelines, the investigators first tested costs when conducting surveillance among all patients with F3 or F4 fibrosis with an assumed constant HCC annual incidence rate of 0.5%. Biannual ultrasound surveillance after SVR caught more cases of HCC still in a curable stage (78%) than no surveillance (29%); however, false-positives were relatively common at 21.8% and 15.7% for biannual and annual surveillance, respectively. The investigators noted that in the real world, some of these false-positives are not detected by more advanced imaging, so patients go on to receive unnecessary RFA, which incurs additional costs. Partly for this reason, while biannual surveillance was more effective, it was also more expensive, with an incremental cost-effectiveness ratio (ICER) of $106,792 per quality-adjusted life-years (QALY), compared with $72,105 per QALY for annual surveillance.
Including only patients with F3 fibrosis after interferon-based therapy, using an HCC incidence of 0.23%, biannual and annual ICERs rose to $484,160 and $204,708 per QALY, respectively, both of which exceed standard willingness-to-pay thresholds. In comparison, annual and biannual ICERs were at most $55,850 and $42,305 per QALY, respectively, among patients with cirrhosis before interferon-induced SVR, using an HCC incidence rate of up to 1.39% per year.
“These results suggest that biannual (or annual) HCC surveillance is likely to be cost effective for patients with cirrhosis, but not for patients with F3 fibrosis before SVR,” the investigators wrote.
Costs for HCC surveillance among cirrhosis patients after direct-acting antiviral-induced SVR were still lower, at $43,229 and $34,307 per QALY, which were far lower than costs for patients with F3 fibrosis, which were $188,157 and $111,667 per QALY.
Focusing on the evident savings associated with surveillance of patients with cirrhosis, the investigators tested two diagnostic thresholds within this population with the aim of reducing costs further. They found that surveillance of patients with a pretreatment aspartate aminotransferase to platelet ratio index (APRI) greater than 2.0 (HCC incidence, 0.89%) was associated with biannual and annual ICERs of $48,729 and $37,806 per QALY, respectively, but when APRI was less than 2.0 (HCC incidence, 0.093%), surveillance was less effective and more expensive than no surveillance at all. A similar trend was found for an FIB-4 threshold of 3.25.
Employment of age-stratified risk of HCC also reduced costs of screening for patients with cirrhosis. With this strategy, ICER was $48,432 per QALY for biannual surveillance and $37,201 per QALY for annual surveillance.
“These data suggest that, if we assume HCC incidence increases with age, biannual or annual surveillance will be cost effective for the vast majority, if not all, patients with cirrhosis before SVR,” the investigators wrote.
“Our analysis suggests that HCC surveillance is very unlikely to be cost effective in patients with F3 fibrosis, whereas both annual and biannual modalities are likely to be cost effective at standard willingness-to-pay thresholds for patients with cirrhosis compared with no surveillance,” the investigators wrote.
“Additional long-term follow-up data are required to help identify patients at highest risk of HCC after SVR to tailor surveillance guidelines,” the investigators concluded.
The study was funded by the Toronto Centre for Liver Disease. The investigators declared no conflicts of interest.
This story was updated on 7/12/2019.
SOURCE: Zangneh et al. Clin Gastroenterol Hepatol. 2018 Dec 20. doi: 10.1016/j.cgh.2018.12.018.
For patients with hepatitis C virus (HCV)–related cirrhosis (F4), but not those with advanced fibrosis (F3), hepatocellular carcinoma (HCC) surveillance after a sustained virologic response (SVR) is cost effective, according to investigators.
Current international guidelines call for HCC surveillance among all patients with advanced fibrosis (F3) or cirrhosis (F4) who have achieved SVR, but this is “very unlikely to be cost effective,” reported lead author Hooman Farhang Zangneh, MD, of Toronto General Hospital and colleagues. “HCV-related HCC rarely occurs in patients without cirrhosis,” the investigators explained in Clinical Gastroenterology and Hepatology. “With cirrhosis present, HCC incidence is 1.4% to 4.9% per year. If found early, options for curative therapy include radiofrequency ablation (RFA), surgical resection, and liver transplantation.”
The investigators developed a Markov model to determine which at-risk patients could undergo surveillance while remaining below willingness-to-pay thresholds. Specifically, cost-effectiveness was assessed for ultrasound screenings annually (every year) or biannually (twice a year) among patients with advanced fibrosis (F3) or compensated cirrhosis (F4) who were aged 50 years and had an SVR. Relevant data were drawn from expert opinions, medical literature, and Canada Life Tables. Various HCC incidence rates were tested, including a constant annual rate, rates based on type of antiviral treatment (direct-acting and interferon-based therapies), others based on stage of fibrosis, and another that increased with age. The model was validated by applying it to patients with F3 or F4 fibrosis who had not yet achieved an SVR. All monetary values were reported in 2015 Canadian dollars.
Representative of current guidelines, the investigators first tested costs when conducting surveillance among all patients with F3 or F4 fibrosis with an assumed constant HCC annual incidence rate of 0.5%. Biannual ultrasound surveillance after SVR caught more cases of HCC still in a curable stage (78%) than no surveillance (29%); however, false-positives were relatively common at 21.8% and 15.7% for biannual and annual surveillance, respectively. The investigators noted that in the real world, some of these false-positives are not detected by more advanced imaging, so patients go on to receive unnecessary RFA, which incurs additional costs. Partly for this reason, while biannual surveillance was more effective, it was also more expensive, with an incremental cost-effectiveness ratio (ICER) of $106,792 per quality-adjusted life-years (QALY), compared with $72,105 per QALY for annual surveillance.
Including only patients with F3 fibrosis after interferon-based therapy, using an HCC incidence of 0.23%, biannual and annual ICERs rose to $484,160 and $204,708 per QALY, respectively, both of which exceed standard willingness-to-pay thresholds. In comparison, annual and biannual ICERs were at most $55,850 and $42,305 per QALY, respectively, among patients with cirrhosis before interferon-induced SVR, using an HCC incidence rate of up to 1.39% per year.
“These results suggest that biannual (or annual) HCC surveillance is likely to be cost effective for patients with cirrhosis, but not for patients with F3 fibrosis before SVR,” the investigators wrote.
Costs for HCC surveillance among cirrhosis patients after direct-acting antiviral-induced SVR were still lower, at $43,229 and $34,307 per QALY, which were far lower than costs for patients with F3 fibrosis, which were $188,157 and $111,667 per QALY.
Focusing on the evident savings associated with surveillance of patients with cirrhosis, the investigators tested two diagnostic thresholds within this population with the aim of reducing costs further. They found that surveillance of patients with a pretreatment aspartate aminotransferase to platelet ratio index (APRI) greater than 2.0 (HCC incidence, 0.89%) was associated with biannual and annual ICERs of $48,729 and $37,806 per QALY, respectively, but when APRI was less than 2.0 (HCC incidence, 0.093%), surveillance was less effective and more expensive than no surveillance at all. A similar trend was found for an FIB-4 threshold of 3.25.
Employment of age-stratified risk of HCC also reduced costs of screening for patients with cirrhosis. With this strategy, ICER was $48,432 per QALY for biannual surveillance and $37,201 per QALY for annual surveillance.
“These data suggest that, if we assume HCC incidence increases with age, biannual or annual surveillance will be cost effective for the vast majority, if not all, patients with cirrhosis before SVR,” the investigators wrote.
“Our analysis suggests that HCC surveillance is very unlikely to be cost effective in patients with F3 fibrosis, whereas both annual and biannual modalities are likely to be cost effective at standard willingness-to-pay thresholds for patients with cirrhosis compared with no surveillance,” the investigators wrote.
“Additional long-term follow-up data are required to help identify patients at highest risk of HCC after SVR to tailor surveillance guidelines,” the investigators concluded.
The study was funded by the Toronto Centre for Liver Disease. The investigators declared no conflicts of interest.
This story was updated on 7/12/2019.
SOURCE: Zangneh et al. Clin Gastroenterol Hepatol. 2018 Dec 20. doi: 10.1016/j.cgh.2018.12.018.
For patients with hepatitis C virus (HCV)–related cirrhosis (F4), but not those with advanced fibrosis (F3), hepatocellular carcinoma (HCC) surveillance after a sustained virologic response (SVR) is cost effective, according to investigators.
Current international guidelines call for HCC surveillance among all patients with advanced fibrosis (F3) or cirrhosis (F4) who have achieved SVR, but this is “very unlikely to be cost effective,” reported lead author Hooman Farhang Zangneh, MD, of Toronto General Hospital and colleagues. “HCV-related HCC rarely occurs in patients without cirrhosis,” the investigators explained in Clinical Gastroenterology and Hepatology. “With cirrhosis present, HCC incidence is 1.4% to 4.9% per year. If found early, options for curative therapy include radiofrequency ablation (RFA), surgical resection, and liver transplantation.”
The investigators developed a Markov model to determine which at-risk patients could undergo surveillance while remaining below willingness-to-pay thresholds. Specifically, cost-effectiveness was assessed for ultrasound screenings annually (every year) or biannually (twice a year) among patients with advanced fibrosis (F3) or compensated cirrhosis (F4) who were aged 50 years and had an SVR. Relevant data were drawn from expert opinions, medical literature, and Canada Life Tables. Various HCC incidence rates were tested, including a constant annual rate, rates based on type of antiviral treatment (direct-acting and interferon-based therapies), others based on stage of fibrosis, and another that increased with age. The model was validated by applying it to patients with F3 or F4 fibrosis who had not yet achieved an SVR. All monetary values were reported in 2015 Canadian dollars.
Representative of current guidelines, the investigators first tested costs when conducting surveillance among all patients with F3 or F4 fibrosis with an assumed constant HCC annual incidence rate of 0.5%. Biannual ultrasound surveillance after SVR caught more cases of HCC still in a curable stage (78%) than no surveillance (29%); however, false-positives were relatively common at 21.8% and 15.7% for biannual and annual surveillance, respectively. The investigators noted that in the real world, some of these false-positives are not detected by more advanced imaging, so patients go on to receive unnecessary RFA, which incurs additional costs. Partly for this reason, while biannual surveillance was more effective, it was also more expensive, with an incremental cost-effectiveness ratio (ICER) of $106,792 per quality-adjusted life-years (QALY), compared with $72,105 per QALY for annual surveillance.
Including only patients with F3 fibrosis after interferon-based therapy, using an HCC incidence of 0.23%, biannual and annual ICERs rose to $484,160 and $204,708 per QALY, respectively, both of which exceed standard willingness-to-pay thresholds. In comparison, annual and biannual ICERs were at most $55,850 and $42,305 per QALY, respectively, among patients with cirrhosis before interferon-induced SVR, using an HCC incidence rate of up to 1.39% per year.
“These results suggest that biannual (or annual) HCC surveillance is likely to be cost effective for patients with cirrhosis, but not for patients with F3 fibrosis before SVR,” the investigators wrote.
Costs for HCC surveillance among cirrhosis patients after direct-acting antiviral-induced SVR were still lower, at $43,229 and $34,307 per QALY, which were far lower than costs for patients with F3 fibrosis, which were $188,157 and $111,667 per QALY.
Focusing on the evident savings associated with surveillance of patients with cirrhosis, the investigators tested two diagnostic thresholds within this population with the aim of reducing costs further. They found that surveillance of patients with a pretreatment aspartate aminotransferase to platelet ratio index (APRI) greater than 2.0 (HCC incidence, 0.89%) was associated with biannual and annual ICERs of $48,729 and $37,806 per QALY, respectively, but when APRI was less than 2.0 (HCC incidence, 0.093%), surveillance was less effective and more expensive than no surveillance at all. A similar trend was found for an FIB-4 threshold of 3.25.
Employment of age-stratified risk of HCC also reduced costs of screening for patients with cirrhosis. With this strategy, ICER was $48,432 per QALY for biannual surveillance and $37,201 per QALY for annual surveillance.
“These data suggest that, if we assume HCC incidence increases with age, biannual or annual surveillance will be cost effective for the vast majority, if not all, patients with cirrhosis before SVR,” the investigators wrote.
“Our analysis suggests that HCC surveillance is very unlikely to be cost effective in patients with F3 fibrosis, whereas both annual and biannual modalities are likely to be cost effective at standard willingness-to-pay thresholds for patients with cirrhosis compared with no surveillance,” the investigators wrote.
“Additional long-term follow-up data are required to help identify patients at highest risk of HCC after SVR to tailor surveillance guidelines,” the investigators concluded.
The study was funded by the Toronto Centre for Liver Disease. The investigators declared no conflicts of interest.
This story was updated on 7/12/2019.
SOURCE: Zangneh et al. Clin Gastroenterol Hepatol. 2018 Dec 20. doi: 10.1016/j.cgh.2018.12.018.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
FDA approves first treatment for neuromyelitis optica spectrum disorder
Soliris, a complement inhibitor, is the first FDA-approved treatment for NMOSD, a rare autoimmune disease of the central nervous system that mainly affects the optic nerves and spinal cord, according to a news release.
About 73% of patients with NMOSD test positive for anti-AQP4 antibodies, and complement activation resulting from anti-AQP4 antibodies is an underlying cause of the disease, according to the news release from Alexion, the company that markets the drug. The average age of NMOSD onset is 39 years, and the disease can lead to permanent visual impairment and paralysis. The condition, previously known as Devic’s disease, may affect between 4,000 and 8,000 people in the United States. NMOSD may be confused with other neurologic conditions such as multiple sclerosis.
Investigators studied the drug’s effectiveness in a placebo-controlled clinical trial of 143 patients with NMOSD who had anti-AQP4 antibodies. Compared with placebo, Soliris reduced the number of NMOSD relapses by 94% during the 48-week study. Nearly 98% of patients in the PREVENT trial who received Soliris were relapse-free after 48 weeks, compared with 63% of patients who received placebo.
Soliris also reduced hospitalizations and the need for corticosteroids and plasma exchange to treat acute attacks.
Soliris includes a boxed warning about life-threatening and fatal meningococcal infections that have occurred in patients treated with Soliris. Patients should be monitored and evaluated immediately if infection is suspected, according to the FDA announcement. In addition, health care professionals should use caution when administering Soliris to patients with any other infection. No cases of meningococcal infection were observed in the PREVENT trial.
Soliris is available through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS). Prescribers must counsel patients about the risk of meningococcal infection and ensure that patients have been vaccinated with meningococcal vaccines.
Adverse reactions in the NMOSD clinical trial included upper respiratory infection, nasopharyngitis, diarrhea, back pain, dizziness, influenza, joint pain, sore throat, and confusion.
The drug’s use for NMOSD received Orphan Drug designation, which provides incentives for the development of drugs for rare diseases.
Eculizumab first was approved by the FDA in 2007 and also may be used to treat paroxysmal nocturnal hemoglobinuria, atypical hemolytic uremic syndrome, and myasthenia gravis.
Soliris, a complement inhibitor, is the first FDA-approved treatment for NMOSD, a rare autoimmune disease of the central nervous system that mainly affects the optic nerves and spinal cord, according to a news release.
About 73% of patients with NMOSD test positive for anti-AQP4 antibodies, and complement activation resulting from anti-AQP4 antibodies is an underlying cause of the disease, according to the news release from Alexion, the company that markets the drug. The average age of NMOSD onset is 39 years, and the disease can lead to permanent visual impairment and paralysis. The condition, previously known as Devic’s disease, may affect between 4,000 and 8,000 people in the United States. NMOSD may be confused with other neurologic conditions such as multiple sclerosis.
Investigators studied the drug’s effectiveness in a placebo-controlled clinical trial of 143 patients with NMOSD who had anti-AQP4 antibodies. Compared with placebo, Soliris reduced the number of NMOSD relapses by 94% during the 48-week study. Nearly 98% of patients in the PREVENT trial who received Soliris were relapse-free after 48 weeks, compared with 63% of patients who received placebo.
Soliris also reduced hospitalizations and the need for corticosteroids and plasma exchange to treat acute attacks.
Soliris includes a boxed warning about life-threatening and fatal meningococcal infections that have occurred in patients treated with Soliris. Patients should be monitored and evaluated immediately if infection is suspected, according to the FDA announcement. In addition, health care professionals should use caution when administering Soliris to patients with any other infection. No cases of meningococcal infection were observed in the PREVENT trial.
Soliris is available through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS). Prescribers must counsel patients about the risk of meningococcal infection and ensure that patients have been vaccinated with meningococcal vaccines.
Adverse reactions in the NMOSD clinical trial included upper respiratory infection, nasopharyngitis, diarrhea, back pain, dizziness, influenza, joint pain, sore throat, and confusion.
The drug’s use for NMOSD received Orphan Drug designation, which provides incentives for the development of drugs for rare diseases.
Eculizumab first was approved by the FDA in 2007 and also may be used to treat paroxysmal nocturnal hemoglobinuria, atypical hemolytic uremic syndrome, and myasthenia gravis.
Soliris, a complement inhibitor, is the first FDA-approved treatment for NMOSD, a rare autoimmune disease of the central nervous system that mainly affects the optic nerves and spinal cord, according to a news release.
About 73% of patients with NMOSD test positive for anti-AQP4 antibodies, and complement activation resulting from anti-AQP4 antibodies is an underlying cause of the disease, according to the news release from Alexion, the company that markets the drug. The average age of NMOSD onset is 39 years, and the disease can lead to permanent visual impairment and paralysis. The condition, previously known as Devic’s disease, may affect between 4,000 and 8,000 people in the United States. NMOSD may be confused with other neurologic conditions such as multiple sclerosis.
Investigators studied the drug’s effectiveness in a placebo-controlled clinical trial of 143 patients with NMOSD who had anti-AQP4 antibodies. Compared with placebo, Soliris reduced the number of NMOSD relapses by 94% during the 48-week study. Nearly 98% of patients in the PREVENT trial who received Soliris were relapse-free after 48 weeks, compared with 63% of patients who received placebo.
Soliris also reduced hospitalizations and the need for corticosteroids and plasma exchange to treat acute attacks.
Soliris includes a boxed warning about life-threatening and fatal meningococcal infections that have occurred in patients treated with Soliris. Patients should be monitored and evaluated immediately if infection is suspected, according to the FDA announcement. In addition, health care professionals should use caution when administering Soliris to patients with any other infection. No cases of meningococcal infection were observed in the PREVENT trial.
Soliris is available through a restricted program under a Risk Evaluation and Mitigation Strategy (REMS). Prescribers must counsel patients about the risk of meningococcal infection and ensure that patients have been vaccinated with meningococcal vaccines.
Adverse reactions in the NMOSD clinical trial included upper respiratory infection, nasopharyngitis, diarrhea, back pain, dizziness, influenza, joint pain, sore throat, and confusion.
The drug’s use for NMOSD received Orphan Drug designation, which provides incentives for the development of drugs for rare diseases.
Eculizumab first was approved by the FDA in 2007 and also may be used to treat paroxysmal nocturnal hemoglobinuria, atypical hemolytic uremic syndrome, and myasthenia gravis.
Tocilizumab preserves lung function in systemic sclerosis
MADRID – , according to a secondary endpoint analysis of the phase 3, double-blind, randomized, controlled focuSSced trial.

After 48 weeks, a significantly lower proportion of patients treated with tocilizumab than placebo experienced any decline in lung function from baseline (50.5% versus 70.3% (P = .015), as defined by the percentage increase in predicted forced vital capacity (%pFVC). When only patients with interstitial lung disease (ILD) were considered, the respective percentages were 51.7% and 75.5% (P = .003).
In SSc-ILD patients, a clinically meaningful decline of 10% or more of the %pFVC in lung function was seen in 24.5% given placebo but in just 8.6% of those treated with tocilizumab.
“ILD is a major complication of scleroderma; it has high morbidity and mortality ... and it’s largely irreversible,” Dinesh Khanna, MD, said at the European Congress of Rheumatology.
“In this day and age, when we treat ILD, we wait for a patient to develop clinical ILD,” added Dr. Khanna, director of the scleroderma program at the University of Michigan, Ann Arbor. Clinical ILD can be defined by symptoms, abnormal pulmonary function tests, and marked abnormalities on high resolution computed tomography (HRCT) scans. He indicated that if improving ILD was not possible, then the next best thing would be to stabilize the disease and ensure there was no worsening in lung function.
As yet, there are no disease-modifying treatments available to treat SSc but there are “ample data that interleukin-6 plays a very important role in the pathogenesis of scleroderma,” Dr. Khanna observed. Tocilizumab is a humanized monoclonal antibody against the interleukin-6 receptor.
Data from the phase 2 faSScinate trial showed initial promise for the drug in SSc where a numerical, but not statistically significant, improvement in skin thickening was seen, and the results had hinted at a possible benefit on lung function (Lancet. 2016 Jun 25;387:2630-40).
However, in the phase 3 focuSSced trial, there was no statistically significant difference in the change from baseline to week 48 modified Rodnan skin score (mRSS) between tocilizumab and placebo, which was the primary endpoint. The least square mean change in mRSS was –6.14 for tocilizumab and –4.41 for placebo (P = .0983).
A total of 205 patients with SSc were studied and randomized, 1:1 in a double-blind fashion, to receive either a once-weekly, subcutaneous dose of 162 mg tocilizumab or a weekly subcutaneous placebo injection for 48 weeks.
For inclusion in the study, patients had to have SSc that met American College of Rheumatology and European League Against Rheumatism (EULAR) criteria and be diagnosed less than 60 months previously. Patients had to have an mRSS of 10-35 units and active disease with one or more of the following: C-reactive protein of 6 mg/L or higher; erythrocyte sedimentation rate of 28 mm/h or higher; and platelet count of330 x 109 L.
“What was astonishing in the trial was that every patient had HRCT at baseline and at the end of the study,” Dr. Khanna reported. These scans showed that 64% of patients had evidence of ILD at baseline and that those treated with tocilizumab had less evidence of fibrosis at week 48 versus placebo, indicating a stabilization rather than worsening of disease.
A time to treatment failure analysis also favored tocilizumab over placebo, but there were no significant changes in patient-reported outcomes.
Dr. Khanna’s slides stated that “given that the primary endpoint for mRSS was not met, all other P values are presented for information purposes only and cannot be considered statistically significant despite the strength of the evidence.” During the Q&A after his presentation, he noted that it was unlikely that the study’s sponsors (Roche/Genentech) will now pursue a license for tocilizumab in SSc.
Nevertheless, Dr. Khanna concluded, “we have the opportunity, based on these data, to treat these patients early on, where you can preserve the lung function, which is a paradigm shift versus waiting for the lung function to decline, become clinically meaningful, significant, and then treat this patient population.”
Roche/Genentech sponsored the study. Dr. Khanna acts as a consultant to Roche/Genentech and eight other pharmaceutical companies. He owns stock in Eicos Sciences.
SOURCE: Khanna D et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):202-3. Abstract OP0245, doi: 10.1136/annrheumdis-2019-eular.2120
MADRID – , according to a secondary endpoint analysis of the phase 3, double-blind, randomized, controlled focuSSced trial.

After 48 weeks, a significantly lower proportion of patients treated with tocilizumab than placebo experienced any decline in lung function from baseline (50.5% versus 70.3% (P = .015), as defined by the percentage increase in predicted forced vital capacity (%pFVC). When only patients with interstitial lung disease (ILD) were considered, the respective percentages were 51.7% and 75.5% (P = .003).
In SSc-ILD patients, a clinically meaningful decline of 10% or more of the %pFVC in lung function was seen in 24.5% given placebo but in just 8.6% of those treated with tocilizumab.
“ILD is a major complication of scleroderma; it has high morbidity and mortality ... and it’s largely irreversible,” Dinesh Khanna, MD, said at the European Congress of Rheumatology.
“In this day and age, when we treat ILD, we wait for a patient to develop clinical ILD,” added Dr. Khanna, director of the scleroderma program at the University of Michigan, Ann Arbor. Clinical ILD can be defined by symptoms, abnormal pulmonary function tests, and marked abnormalities on high resolution computed tomography (HRCT) scans. He indicated that if improving ILD was not possible, then the next best thing would be to stabilize the disease and ensure there was no worsening in lung function.
As yet, there are no disease-modifying treatments available to treat SSc but there are “ample data that interleukin-6 plays a very important role in the pathogenesis of scleroderma,” Dr. Khanna observed. Tocilizumab is a humanized monoclonal antibody against the interleukin-6 receptor.
Data from the phase 2 faSScinate trial showed initial promise for the drug in SSc where a numerical, but not statistically significant, improvement in skin thickening was seen, and the results had hinted at a possible benefit on lung function (Lancet. 2016 Jun 25;387:2630-40).
However, in the phase 3 focuSSced trial, there was no statistically significant difference in the change from baseline to week 48 modified Rodnan skin score (mRSS) between tocilizumab and placebo, which was the primary endpoint. The least square mean change in mRSS was –6.14 for tocilizumab and –4.41 for placebo (P = .0983).
A total of 205 patients with SSc were studied and randomized, 1:1 in a double-blind fashion, to receive either a once-weekly, subcutaneous dose of 162 mg tocilizumab or a weekly subcutaneous placebo injection for 48 weeks.
For inclusion in the study, patients had to have SSc that met American College of Rheumatology and European League Against Rheumatism (EULAR) criteria and be diagnosed less than 60 months previously. Patients had to have an mRSS of 10-35 units and active disease with one or more of the following: C-reactive protein of 6 mg/L or higher; erythrocyte sedimentation rate of 28 mm/h or higher; and platelet count of330 x 109 L.
“What was astonishing in the trial was that every patient had HRCT at baseline and at the end of the study,” Dr. Khanna reported. These scans showed that 64% of patients had evidence of ILD at baseline and that those treated with tocilizumab had less evidence of fibrosis at week 48 versus placebo, indicating a stabilization rather than worsening of disease.
A time to treatment failure analysis also favored tocilizumab over placebo, but there were no significant changes in patient-reported outcomes.
Dr. Khanna’s slides stated that “given that the primary endpoint for mRSS was not met, all other P values are presented for information purposes only and cannot be considered statistically significant despite the strength of the evidence.” During the Q&A after his presentation, he noted that it was unlikely that the study’s sponsors (Roche/Genentech) will now pursue a license for tocilizumab in SSc.
Nevertheless, Dr. Khanna concluded, “we have the opportunity, based on these data, to treat these patients early on, where you can preserve the lung function, which is a paradigm shift versus waiting for the lung function to decline, become clinically meaningful, significant, and then treat this patient population.”
Roche/Genentech sponsored the study. Dr. Khanna acts as a consultant to Roche/Genentech and eight other pharmaceutical companies. He owns stock in Eicos Sciences.
SOURCE: Khanna D et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):202-3. Abstract OP0245, doi: 10.1136/annrheumdis-2019-eular.2120
MADRID – , according to a secondary endpoint analysis of the phase 3, double-blind, randomized, controlled focuSSced trial.

After 48 weeks, a significantly lower proportion of patients treated with tocilizumab than placebo experienced any decline in lung function from baseline (50.5% versus 70.3% (P = .015), as defined by the percentage increase in predicted forced vital capacity (%pFVC). When only patients with interstitial lung disease (ILD) were considered, the respective percentages were 51.7% and 75.5% (P = .003).
In SSc-ILD patients, a clinically meaningful decline of 10% or more of the %pFVC in lung function was seen in 24.5% given placebo but in just 8.6% of those treated with tocilizumab.
“ILD is a major complication of scleroderma; it has high morbidity and mortality ... and it’s largely irreversible,” Dinesh Khanna, MD, said at the European Congress of Rheumatology.
“In this day and age, when we treat ILD, we wait for a patient to develop clinical ILD,” added Dr. Khanna, director of the scleroderma program at the University of Michigan, Ann Arbor. Clinical ILD can be defined by symptoms, abnormal pulmonary function tests, and marked abnormalities on high resolution computed tomography (HRCT) scans. He indicated that if improving ILD was not possible, then the next best thing would be to stabilize the disease and ensure there was no worsening in lung function.
As yet, there are no disease-modifying treatments available to treat SSc but there are “ample data that interleukin-6 plays a very important role in the pathogenesis of scleroderma,” Dr. Khanna observed. Tocilizumab is a humanized monoclonal antibody against the interleukin-6 receptor.
Data from the phase 2 faSScinate trial showed initial promise for the drug in SSc where a numerical, but not statistically significant, improvement in skin thickening was seen, and the results had hinted at a possible benefit on lung function (Lancet. 2016 Jun 25;387:2630-40).
However, in the phase 3 focuSSced trial, there was no statistically significant difference in the change from baseline to week 48 modified Rodnan skin score (mRSS) between tocilizumab and placebo, which was the primary endpoint. The least square mean change in mRSS was –6.14 for tocilizumab and –4.41 for placebo (P = .0983).
A total of 205 patients with SSc were studied and randomized, 1:1 in a double-blind fashion, to receive either a once-weekly, subcutaneous dose of 162 mg tocilizumab or a weekly subcutaneous placebo injection for 48 weeks.
For inclusion in the study, patients had to have SSc that met American College of Rheumatology and European League Against Rheumatism (EULAR) criteria and be diagnosed less than 60 months previously. Patients had to have an mRSS of 10-35 units and active disease with one or more of the following: C-reactive protein of 6 mg/L or higher; erythrocyte sedimentation rate of 28 mm/h or higher; and platelet count of330 x 109 L.
“What was astonishing in the trial was that every patient had HRCT at baseline and at the end of the study,” Dr. Khanna reported. These scans showed that 64% of patients had evidence of ILD at baseline and that those treated with tocilizumab had less evidence of fibrosis at week 48 versus placebo, indicating a stabilization rather than worsening of disease.
A time to treatment failure analysis also favored tocilizumab over placebo, but there were no significant changes in patient-reported outcomes.
Dr. Khanna’s slides stated that “given that the primary endpoint for mRSS was not met, all other P values are presented for information purposes only and cannot be considered statistically significant despite the strength of the evidence.” During the Q&A after his presentation, he noted that it was unlikely that the study’s sponsors (Roche/Genentech) will now pursue a license for tocilizumab in SSc.
Nevertheless, Dr. Khanna concluded, “we have the opportunity, based on these data, to treat these patients early on, where you can preserve the lung function, which is a paradigm shift versus waiting for the lung function to decline, become clinically meaningful, significant, and then treat this patient population.”
Roche/Genentech sponsored the study. Dr. Khanna acts as a consultant to Roche/Genentech and eight other pharmaceutical companies. He owns stock in Eicos Sciences.
SOURCE: Khanna D et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):202-3. Abstract OP0245, doi: 10.1136/annrheumdis-2019-eular.2120
REPORTING FROM THE EULAR 2019 CONGRESS
Rozanolixizumab may offer new treatment paradigm for ITP
AMSTERDAM – Rozanolixizumab, a subcutaneous antibody for the human neonatal Fc receptor, provides clinically meaningful improvements in platelet count for patients with primary immune thrombocytopenia, according to results from a recent phase 2 trial.
Rozanolixizumab was well tolerated across all dose groups, with higher doses delivering faster responses, reported lead author Tadeusz Robak, MD, PhD, of the Medical University of Lodz (Poland).
Targeting the Fc receptor interrupts recirculation of IgG, a key autoantibody in immune thrombocytopenia (ITP) pathogenesis, Dr. Robak explained during a presentation at the annual congress of the European Hematology Association. This approach represents an emerging treatment paradigm, he said, noting that rozanolixizumab is also being studied for the treatment of other IgG-driven autoimmune diseases, such as myasthenia gravis and chronic inflammatory demyelinating polyneuropathy.
The present open-label, dose-escalation study involved 54 adult patients with primary ITP of at least 3 months duration and platelet counts of less than 30 x 109/L at screening and 35 x 109/L at baseline. Eligibility required a previous response to ITP therapy. Enrolled patients were randomized into four dose groups: 4 mg/kg (five doses), 7 mg/kg (three doses), 10 mg/kg (two doses), or 15 mg/kg (one dose). After dosing, patients were followed for 8 weeks. Clinically relevant efficacy was defined as a platelet count of at least 50 x 109/L. Decreases in IgG were also reported.
A safety analysis showed that the regimen was well tolerated across all dose groups. In total, 20.4% of patients experienced at least one treatment-related adverse event. The most common adverse events were headache (31.5%), diarrhea (11.1%), and vomiting (3.7%); all of which were mild or moderate. Headache appeared to be dose related, as 42% of patients in the 15-mg/kg group reported headache, compared with 8% in the 10-mg/kg group, 7% in the 7-mg/kg group, and none in the 4-mg/kg group. Out of four reported serious adverse events, none were considered treatment related.
Concerning efficacy, higher doses were associated with higher response rates and faster response times. In the 4-mg/kg group, 33% of patients achieved a platelet count of at least 50 x 109/L, compared with 33% of the 7-mg/kg group, 50% of the 10-mg/kg group, and 67% of the 15-mg/kg group. Of the patients that achieved clinically meaningful responses, 20% of the 4-mg/kg group did so within 8 days, compared with 40% of 7-mg/kg responders, 50% of 10-mg/kg responders, and 87.5% of 15-mg/kg responders. Additional observations included dose-dependent decreases in IgG titer and longer response durations after multiple lower doses.
“Data from this study indicate that we can achieve effective increases in platelet levels, we can observe decreasing IgG levels, and the treatment was safe for the patients,” Dr. Robak said.
When asked about the intended clinical application of rozanolixizumab, Dr. Robak suggested that the agent may have a role in the postacute care setting. “We should develop a method of prolonged administration of [rozanolixizumab], as we saw that lower, multiple doses gave longer response durations.”
Still, he noted that more research is needed, since responses in diverse patient populations remain unknown. “We do not know how the drug will be active in truly refractory patients and we need this response before we establish the indication for the drug.”
The investigators reported financial relationships with Celgene, Roche, GlaxoSmithKline, Amgen, AbbVie, and other companies.
SOURCE: Robak T et al. EHA Congress, Abstract S850.
AMSTERDAM – Rozanolixizumab, a subcutaneous antibody for the human neonatal Fc receptor, provides clinically meaningful improvements in platelet count for patients with primary immune thrombocytopenia, according to results from a recent phase 2 trial.
Rozanolixizumab was well tolerated across all dose groups, with higher doses delivering faster responses, reported lead author Tadeusz Robak, MD, PhD, of the Medical University of Lodz (Poland).
Targeting the Fc receptor interrupts recirculation of IgG, a key autoantibody in immune thrombocytopenia (ITP) pathogenesis, Dr. Robak explained during a presentation at the annual congress of the European Hematology Association. This approach represents an emerging treatment paradigm, he said, noting that rozanolixizumab is also being studied for the treatment of other IgG-driven autoimmune diseases, such as myasthenia gravis and chronic inflammatory demyelinating polyneuropathy.
The present open-label, dose-escalation study involved 54 adult patients with primary ITP of at least 3 months duration and platelet counts of less than 30 x 109/L at screening and 35 x 109/L at baseline. Eligibility required a previous response to ITP therapy. Enrolled patients were randomized into four dose groups: 4 mg/kg (five doses), 7 mg/kg (three doses), 10 mg/kg (two doses), or 15 mg/kg (one dose). After dosing, patients were followed for 8 weeks. Clinically relevant efficacy was defined as a platelet count of at least 50 x 109/L. Decreases in IgG were also reported.
A safety analysis showed that the regimen was well tolerated across all dose groups. In total, 20.4% of patients experienced at least one treatment-related adverse event. The most common adverse events were headache (31.5%), diarrhea (11.1%), and vomiting (3.7%); all of which were mild or moderate. Headache appeared to be dose related, as 42% of patients in the 15-mg/kg group reported headache, compared with 8% in the 10-mg/kg group, 7% in the 7-mg/kg group, and none in the 4-mg/kg group. Out of four reported serious adverse events, none were considered treatment related.
Concerning efficacy, higher doses were associated with higher response rates and faster response times. In the 4-mg/kg group, 33% of patients achieved a platelet count of at least 50 x 109/L, compared with 33% of the 7-mg/kg group, 50% of the 10-mg/kg group, and 67% of the 15-mg/kg group. Of the patients that achieved clinically meaningful responses, 20% of the 4-mg/kg group did so within 8 days, compared with 40% of 7-mg/kg responders, 50% of 10-mg/kg responders, and 87.5% of 15-mg/kg responders. Additional observations included dose-dependent decreases in IgG titer and longer response durations after multiple lower doses.
“Data from this study indicate that we can achieve effective increases in platelet levels, we can observe decreasing IgG levels, and the treatment was safe for the patients,” Dr. Robak said.
When asked about the intended clinical application of rozanolixizumab, Dr. Robak suggested that the agent may have a role in the postacute care setting. “We should develop a method of prolonged administration of [rozanolixizumab], as we saw that lower, multiple doses gave longer response durations.”
Still, he noted that more research is needed, since responses in diverse patient populations remain unknown. “We do not know how the drug will be active in truly refractory patients and we need this response before we establish the indication for the drug.”
The investigators reported financial relationships with Celgene, Roche, GlaxoSmithKline, Amgen, AbbVie, and other companies.
SOURCE: Robak T et al. EHA Congress, Abstract S850.
AMSTERDAM – Rozanolixizumab, a subcutaneous antibody for the human neonatal Fc receptor, provides clinically meaningful improvements in platelet count for patients with primary immune thrombocytopenia, according to results from a recent phase 2 trial.
Rozanolixizumab was well tolerated across all dose groups, with higher doses delivering faster responses, reported lead author Tadeusz Robak, MD, PhD, of the Medical University of Lodz (Poland).
Targeting the Fc receptor interrupts recirculation of IgG, a key autoantibody in immune thrombocytopenia (ITP) pathogenesis, Dr. Robak explained during a presentation at the annual congress of the European Hematology Association. This approach represents an emerging treatment paradigm, he said, noting that rozanolixizumab is also being studied for the treatment of other IgG-driven autoimmune diseases, such as myasthenia gravis and chronic inflammatory demyelinating polyneuropathy.
The present open-label, dose-escalation study involved 54 adult patients with primary ITP of at least 3 months duration and platelet counts of less than 30 x 109/L at screening and 35 x 109/L at baseline. Eligibility required a previous response to ITP therapy. Enrolled patients were randomized into four dose groups: 4 mg/kg (five doses), 7 mg/kg (three doses), 10 mg/kg (two doses), or 15 mg/kg (one dose). After dosing, patients were followed for 8 weeks. Clinically relevant efficacy was defined as a platelet count of at least 50 x 109/L. Decreases in IgG were also reported.
A safety analysis showed that the regimen was well tolerated across all dose groups. In total, 20.4% of patients experienced at least one treatment-related adverse event. The most common adverse events were headache (31.5%), diarrhea (11.1%), and vomiting (3.7%); all of which were mild or moderate. Headache appeared to be dose related, as 42% of patients in the 15-mg/kg group reported headache, compared with 8% in the 10-mg/kg group, 7% in the 7-mg/kg group, and none in the 4-mg/kg group. Out of four reported serious adverse events, none were considered treatment related.
Concerning efficacy, higher doses were associated with higher response rates and faster response times. In the 4-mg/kg group, 33% of patients achieved a platelet count of at least 50 x 109/L, compared with 33% of the 7-mg/kg group, 50% of the 10-mg/kg group, and 67% of the 15-mg/kg group. Of the patients that achieved clinically meaningful responses, 20% of the 4-mg/kg group did so within 8 days, compared with 40% of 7-mg/kg responders, 50% of 10-mg/kg responders, and 87.5% of 15-mg/kg responders. Additional observations included dose-dependent decreases in IgG titer and longer response durations after multiple lower doses.
“Data from this study indicate that we can achieve effective increases in platelet levels, we can observe decreasing IgG levels, and the treatment was safe for the patients,” Dr. Robak said.
When asked about the intended clinical application of rozanolixizumab, Dr. Robak suggested that the agent may have a role in the postacute care setting. “We should develop a method of prolonged administration of [rozanolixizumab], as we saw that lower, multiple doses gave longer response durations.”
Still, he noted that more research is needed, since responses in diverse patient populations remain unknown. “We do not know how the drug will be active in truly refractory patients and we need this response before we establish the indication for the drug.”
The investigators reported financial relationships with Celgene, Roche, GlaxoSmithKline, Amgen, AbbVie, and other companies.
SOURCE: Robak T et al. EHA Congress, Abstract S850.
REPORTING FROM EHA CONGRESS
Budesonide tablets considerably outperformed placebo for active EoE
Budesonide orodispersible tablets (BOTs) are highly effective in inducing disease remission in adults with active eosinophilic esophagitis (EOE), according to a study of the tablets versus placebo in European patients.
“A 6-week treatment with 1 mg budesonide twice daily was highly superior over placebo with regard to all predefined primary and secondary outcomes,” wrote Alfredo J. Lucendo, MD, of Hospital General de Tomelloso in Real, Spain, and his coauthors. The study was published in Gastroenterology.
To assess the effectiveness and tolerability of BOT in adults with EOE, Dr. Lucendo and his fellow researchers launched a randomized, placebo-controlled trial made up of 88 European adults with active EoE. Patients were assigned to either a group that received BOT twice daily (n = 59) or a group that received placebo (n = 29). The primary endpoint was complete remission.
After 6 weeks, 34 of 59 patients (58%) receiving BOT had achieved complete remission, compared with 0 patients receiving placebo (P less than .0001). After 12 weeks, 50 of 59 patients (85%) in the BOT group had achieved complete remission. BOT was also well tolerated; no serious adverse event was reported, and no differences were observed between groups with regard to commonly reported adverse events.
The coauthors acknowledged their study’s limitations, including the fact that it was designed to demonstrate budesonide’s superiority to placebo at 6 weeks, not to identify the time of its maximal effect. In addition, the researchers did not identify a minimally effective dose; they did, however, note their belief that a lower dose could still achieve similar rates of remission and “a higher dose would not achieve a higher clinico-remission rate.”
The study was funded by Dr. Falk Pharma. The authors reported numerous conflicts of interest, including receiving research funding and speaker fees from various pharmaceutical companies and foundations.
SOURCE: Lucendo AJ et al. Gastroenterology. 2019 Mar 25. doi: 10.1053/j.gastro.2019.03.025.
Budesonide orodispersible tablets (BOTs) are highly effective in inducing disease remission in adults with active eosinophilic esophagitis (EOE), according to a study of the tablets versus placebo in European patients.
“A 6-week treatment with 1 mg budesonide twice daily was highly superior over placebo with regard to all predefined primary and secondary outcomes,” wrote Alfredo J. Lucendo, MD, of Hospital General de Tomelloso in Real, Spain, and his coauthors. The study was published in Gastroenterology.
To assess the effectiveness and tolerability of BOT in adults with EOE, Dr. Lucendo and his fellow researchers launched a randomized, placebo-controlled trial made up of 88 European adults with active EoE. Patients were assigned to either a group that received BOT twice daily (n = 59) or a group that received placebo (n = 29). The primary endpoint was complete remission.
After 6 weeks, 34 of 59 patients (58%) receiving BOT had achieved complete remission, compared with 0 patients receiving placebo (P less than .0001). After 12 weeks, 50 of 59 patients (85%) in the BOT group had achieved complete remission. BOT was also well tolerated; no serious adverse event was reported, and no differences were observed between groups with regard to commonly reported adverse events.
The coauthors acknowledged their study’s limitations, including the fact that it was designed to demonstrate budesonide’s superiority to placebo at 6 weeks, not to identify the time of its maximal effect. In addition, the researchers did not identify a minimally effective dose; they did, however, note their belief that a lower dose could still achieve similar rates of remission and “a higher dose would not achieve a higher clinico-remission rate.”
The study was funded by Dr. Falk Pharma. The authors reported numerous conflicts of interest, including receiving research funding and speaker fees from various pharmaceutical companies and foundations.
SOURCE: Lucendo AJ et al. Gastroenterology. 2019 Mar 25. doi: 10.1053/j.gastro.2019.03.025.
Budesonide orodispersible tablets (BOTs) are highly effective in inducing disease remission in adults with active eosinophilic esophagitis (EOE), according to a study of the tablets versus placebo in European patients.
“A 6-week treatment with 1 mg budesonide twice daily was highly superior over placebo with regard to all predefined primary and secondary outcomes,” wrote Alfredo J. Lucendo, MD, of Hospital General de Tomelloso in Real, Spain, and his coauthors. The study was published in Gastroenterology.
To assess the effectiveness and tolerability of BOT in adults with EOE, Dr. Lucendo and his fellow researchers launched a randomized, placebo-controlled trial made up of 88 European adults with active EoE. Patients were assigned to either a group that received BOT twice daily (n = 59) or a group that received placebo (n = 29). The primary endpoint was complete remission.
After 6 weeks, 34 of 59 patients (58%) receiving BOT had achieved complete remission, compared with 0 patients receiving placebo (P less than .0001). After 12 weeks, 50 of 59 patients (85%) in the BOT group had achieved complete remission. BOT was also well tolerated; no serious adverse event was reported, and no differences were observed between groups with regard to commonly reported adverse events.
The coauthors acknowledged their study’s limitations, including the fact that it was designed to demonstrate budesonide’s superiority to placebo at 6 weeks, not to identify the time of its maximal effect. In addition, the researchers did not identify a minimally effective dose; they did, however, note their belief that a lower dose could still achieve similar rates of remission and “a higher dose would not achieve a higher clinico-remission rate.”
The study was funded by Dr. Falk Pharma. The authors reported numerous conflicts of interest, including receiving research funding and speaker fees from various pharmaceutical companies and foundations.
SOURCE: Lucendo AJ et al. Gastroenterology. 2019 Mar 25. doi: 10.1053/j.gastro.2019.03.025.
FROM GASTROENTEROLOGY
Efforts toward producing CNO/CRMO classification criteria show first results
MADRID – according to recent findings from international surveys of pediatric rheumatologists that were presented at the European Congress of Rheumatology.
Melissa Oliver, MD, a pediatric rheumatologist at Riley Hospital for Children, Indianapolis, and colleagues recently undertook the multiphase study as part of an international collaborative effort led by the Childhood Arthritis and Rheumatology Research Alliance to establish consensus-based diagnostic and classification criteria for CNO, an autoinflammatory bone disease of unknown cause that primarily affects children and adolescents. CNO is also known as chronic recurrent multifocal osteomyelitis (CRMO). If this disease is not diagnosed and treated appropriately in a timely fashion, damage and long-term disability is possible. In the absence of widely accepted, consensus-driven criteria, treatment is based largely on expert opinion, Dr. Oliver explained in an interview.
“There is an urgent need for a new and more robust set of classification criteria for CRMO, based on large expert consensus and the analysis of a large sample of patients and controls,” she said.
There are two proposed diagnostic criteria, the 2007 classification of nonbacterial osteitis and the 2016 Bristol diagnostic criteria for CRMO, but both are derived from single-center cohort studies and have not been validated, Dr. Oliver explained.
The list of candidate items that have come out of the study is moving clinicians a step closer toward the design of a practical patient data collection form that appropriately weighs each item included in the classification criteria.
The study employed anonymous survey and nominal group techniques with the goal of developing a set of classification criteria sensitive and specific enough to identify CRMO/CNO patients. In phase 1, a Delphi survey was administered among international rheumatologists to generate candidate criteria items. Phase 2 sought to reduce candidate criteria items through consensus processes via input from physicians managing CNO and patients or caregivers of children with CNO.
Altogether, 259 of 865 pediatric rheumatologists (30%) completed an online questionnaire addressing features key to the classification of CNO, including 77 who practice in Europe (30%), 132 in North America (51%), and 50 on other continents (19%). Of these, 138 (53%) had greater than 10 years of clinical practice experience, and 108 (42%) had managed more than 10 CNO patients.
Initially, Dr. Oliver and colleagues identified 33 candidate criteria items that fell into six domains: clinical presentation, physical exam, laboratory findings, imaging findings, bone biopsy, and treatment response. The top eight weighted items that increased the likelihood of CNO/CRMO were exclusion of malignancy by bone biopsy; multifocal bone lesions; presence of bone pain, swelling, and/or warmth; signs of fibrosis and/or inflammation on bone biopsy; typical location of CNO/CRMO lesion, such as the clavicle, metaphysis of long bones, the mandible, and vertebrae; presence of CNO/CRMO–related comorbidities; normal C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR); and typical MRI findings of CNO/CRMO.
By phase 2, candidate items, which were presented to 39 rheumatologists and 7 parents, were refined or eliminated using item-reduction techniques. A second survey was issued to 77 of 82 members of a work group so that the remaining items could be ranked by their power of distinguishing CNO from conditions that merely mimicked the disease. The greatest mean discriminatory scores were identified with multifocal lesions (ruling out malignancy and infection) and typical location on imaging. Normal C-reactive protein and/or an erythrocyte sedimentation rate more than three times the upper limit of normal had the greatest negative mean discriminatory scores.
The next steps will be to form an expert panel who will use 1000minds software to determine the final criteria and identify a threshold for disease. The investigators hope to build a large multinational case repository of at least 500 patients with CNO/CRMO and 500 patients with mimicking conditions from which to derive a development cohort and an external validation cohort. So far, 10 sites, including 4 in Europe, have obtained approval from an institutional review board. The group has also submitted a proposal for classification criteria to the American College of Rheumatology and the European League Against Rheumatism, Dr. Oliver said.
Dr. Oliver had no disclosures to report, but several coauthors reported financial ties to industry.
SOURCE: Oliver M et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):254-5, Abstract OP0342. doi: 10.1136/annrheumdis-2019-eular.1539.
MADRID – according to recent findings from international surveys of pediatric rheumatologists that were presented at the European Congress of Rheumatology.
Melissa Oliver, MD, a pediatric rheumatologist at Riley Hospital for Children, Indianapolis, and colleagues recently undertook the multiphase study as part of an international collaborative effort led by the Childhood Arthritis and Rheumatology Research Alliance to establish consensus-based diagnostic and classification criteria for CNO, an autoinflammatory bone disease of unknown cause that primarily affects children and adolescents. CNO is also known as chronic recurrent multifocal osteomyelitis (CRMO). If this disease is not diagnosed and treated appropriately in a timely fashion, damage and long-term disability is possible. In the absence of widely accepted, consensus-driven criteria, treatment is based largely on expert opinion, Dr. Oliver explained in an interview.
“There is an urgent need for a new and more robust set of classification criteria for CRMO, based on large expert consensus and the analysis of a large sample of patients and controls,” she said.
There are two proposed diagnostic criteria, the 2007 classification of nonbacterial osteitis and the 2016 Bristol diagnostic criteria for CRMO, but both are derived from single-center cohort studies and have not been validated, Dr. Oliver explained.
The list of candidate items that have come out of the study is moving clinicians a step closer toward the design of a practical patient data collection form that appropriately weighs each item included in the classification criteria.
The study employed anonymous survey and nominal group techniques with the goal of developing a set of classification criteria sensitive and specific enough to identify CRMO/CNO patients. In phase 1, a Delphi survey was administered among international rheumatologists to generate candidate criteria items. Phase 2 sought to reduce candidate criteria items through consensus processes via input from physicians managing CNO and patients or caregivers of children with CNO.
Altogether, 259 of 865 pediatric rheumatologists (30%) completed an online questionnaire addressing features key to the classification of CNO, including 77 who practice in Europe (30%), 132 in North America (51%), and 50 on other continents (19%). Of these, 138 (53%) had greater than 10 years of clinical practice experience, and 108 (42%) had managed more than 10 CNO patients.
Initially, Dr. Oliver and colleagues identified 33 candidate criteria items that fell into six domains: clinical presentation, physical exam, laboratory findings, imaging findings, bone biopsy, and treatment response. The top eight weighted items that increased the likelihood of CNO/CRMO were exclusion of malignancy by bone biopsy; multifocal bone lesions; presence of bone pain, swelling, and/or warmth; signs of fibrosis and/or inflammation on bone biopsy; typical location of CNO/CRMO lesion, such as the clavicle, metaphysis of long bones, the mandible, and vertebrae; presence of CNO/CRMO–related comorbidities; normal C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR); and typical MRI findings of CNO/CRMO.
By phase 2, candidate items, which were presented to 39 rheumatologists and 7 parents, were refined or eliminated using item-reduction techniques. A second survey was issued to 77 of 82 members of a work group so that the remaining items could be ranked by their power of distinguishing CNO from conditions that merely mimicked the disease. The greatest mean discriminatory scores were identified with multifocal lesions (ruling out malignancy and infection) and typical location on imaging. Normal C-reactive protein and/or an erythrocyte sedimentation rate more than three times the upper limit of normal had the greatest negative mean discriminatory scores.
The next steps will be to form an expert panel who will use 1000minds software to determine the final criteria and identify a threshold for disease. The investigators hope to build a large multinational case repository of at least 500 patients with CNO/CRMO and 500 patients with mimicking conditions from which to derive a development cohort and an external validation cohort. So far, 10 sites, including 4 in Europe, have obtained approval from an institutional review board. The group has also submitted a proposal for classification criteria to the American College of Rheumatology and the European League Against Rheumatism, Dr. Oliver said.
Dr. Oliver had no disclosures to report, but several coauthors reported financial ties to industry.
SOURCE: Oliver M et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):254-5, Abstract OP0342. doi: 10.1136/annrheumdis-2019-eular.1539.
MADRID – according to recent findings from international surveys of pediatric rheumatologists that were presented at the European Congress of Rheumatology.
Melissa Oliver, MD, a pediatric rheumatologist at Riley Hospital for Children, Indianapolis, and colleagues recently undertook the multiphase study as part of an international collaborative effort led by the Childhood Arthritis and Rheumatology Research Alliance to establish consensus-based diagnostic and classification criteria for CNO, an autoinflammatory bone disease of unknown cause that primarily affects children and adolescents. CNO is also known as chronic recurrent multifocal osteomyelitis (CRMO). If this disease is not diagnosed and treated appropriately in a timely fashion, damage and long-term disability is possible. In the absence of widely accepted, consensus-driven criteria, treatment is based largely on expert opinion, Dr. Oliver explained in an interview.
“There is an urgent need for a new and more robust set of classification criteria for CRMO, based on large expert consensus and the analysis of a large sample of patients and controls,” she said.
There are two proposed diagnostic criteria, the 2007 classification of nonbacterial osteitis and the 2016 Bristol diagnostic criteria for CRMO, but both are derived from single-center cohort studies and have not been validated, Dr. Oliver explained.
The list of candidate items that have come out of the study is moving clinicians a step closer toward the design of a practical patient data collection form that appropriately weighs each item included in the classification criteria.
The study employed anonymous survey and nominal group techniques with the goal of developing a set of classification criteria sensitive and specific enough to identify CRMO/CNO patients. In phase 1, a Delphi survey was administered among international rheumatologists to generate candidate criteria items. Phase 2 sought to reduce candidate criteria items through consensus processes via input from physicians managing CNO and patients or caregivers of children with CNO.
Altogether, 259 of 865 pediatric rheumatologists (30%) completed an online questionnaire addressing features key to the classification of CNO, including 77 who practice in Europe (30%), 132 in North America (51%), and 50 on other continents (19%). Of these, 138 (53%) had greater than 10 years of clinical practice experience, and 108 (42%) had managed more than 10 CNO patients.
Initially, Dr. Oliver and colleagues identified 33 candidate criteria items that fell into six domains: clinical presentation, physical exam, laboratory findings, imaging findings, bone biopsy, and treatment response. The top eight weighted items that increased the likelihood of CNO/CRMO were exclusion of malignancy by bone biopsy; multifocal bone lesions; presence of bone pain, swelling, and/or warmth; signs of fibrosis and/or inflammation on bone biopsy; typical location of CNO/CRMO lesion, such as the clavicle, metaphysis of long bones, the mandible, and vertebrae; presence of CNO/CRMO–related comorbidities; normal C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR); and typical MRI findings of CNO/CRMO.
By phase 2, candidate items, which were presented to 39 rheumatologists and 7 parents, were refined or eliminated using item-reduction techniques. A second survey was issued to 77 of 82 members of a work group so that the remaining items could be ranked by their power of distinguishing CNO from conditions that merely mimicked the disease. The greatest mean discriminatory scores were identified with multifocal lesions (ruling out malignancy and infection) and typical location on imaging. Normal C-reactive protein and/or an erythrocyte sedimentation rate more than three times the upper limit of normal had the greatest negative mean discriminatory scores.
The next steps will be to form an expert panel who will use 1000minds software to determine the final criteria and identify a threshold for disease. The investigators hope to build a large multinational case repository of at least 500 patients with CNO/CRMO and 500 patients with mimicking conditions from which to derive a development cohort and an external validation cohort. So far, 10 sites, including 4 in Europe, have obtained approval from an institutional review board. The group has also submitted a proposal for classification criteria to the American College of Rheumatology and the European League Against Rheumatism, Dr. Oliver said.
Dr. Oliver had no disclosures to report, but several coauthors reported financial ties to industry.
SOURCE: Oliver M et al. Ann Rheum Dis. Jun 2019;78(Suppl 2):254-5, Abstract OP0342. doi: 10.1136/annrheumdis-2019-eular.1539.
REPORTING FROM EULAR 2019 CONGRESS
R2 appears active in high-risk FL and MZL
CHICAGO – Lenalidomide plus rituximab (R2) demonstrated activity against relapsed or refractory follicular lymphoma (FL) and marginal zone lymphoma (MZL) in the phase 3b MAGNIFY trial.
R2 produced responses in FL and MZL patients, including those who had previously experienced early relapse and patients who were refractory to rituximab or both lenalidomide and rituximab at baseline.
David Jacob Andorsky, MD, of Rocky Mountain Cancer Centers in Boulder, Colo., and colleagues presented these results in a poster at the annual meeting of the American Society of Clinical Oncology.
The ongoing MAGNIFY trial has enrolled 370 patients with relapsed/refractory FL (grade 1-3a) or MZL.
For induction, patients receive lenalidomide (20 mg per day on days 1-21 for 12 cycles) and rituximab (375 mg/m2 per week in cycle 1 and then on day 1 of cycles 3, 5, 7, 9, and 11). Patients who achieve stable disease or better on R2 induction are randomized to maintenance with R2 or rituximab alone.
Dr. Andorsky and colleagues presented results of R2 induction in 310 evaluable patients – 247 with FL and 63 with MZL.
The patients had a median age of 66 years (range, 35-91 years) at baseline, and they had received a median of two prior therapies (range, one to eight). Some patients had experienced early relapse (37%, n = 115), were refractory to rituximab (36%, n = 113), or were refractory to both rituximab and lenalidomide (20%, n = 63) at baseline.
Results
At a median follow-up of 16.7 months, the overall response rate was 73%, and the complete response rate was 45%. The overall response rate was 74% in FL patients, 65% in MZL patients, 63% in rituximab-refractory patients, 51% in double-refractory patients, and 68% in patients with an early relapse.
The median duration of response was 36.8 months in all patients, 35.8 months in MZL patients, and not reached in FL patients. The median duration of response was 35.8 months in patients who were rituximab refractory and was not reached in patients who were not refractory to rituximab.
The median progression-free survival was 36 months overall, 30 months in FL patients, 38 months in MZL patients, 23 months in patients with early relapse, and 15.5 months in double-refractory patients.
“While these [subgroup analyses of efficacy] were exploratory endpoints, I think this suggests that [R2] is a promising regimen for patients that are in the high-risk subgroup,” said Carla Casulo, MD, of the University of Rochester (N.Y.), who reviewed this study in a poster discussion session.
The most common adverse events in this trial were fatigue (48%), neutropenia (40%), diarrhea (35%), nausea (30%), and constipation (29%). The most common grade 3/4 adverse event was neutropenia (34%).
The MAGNIFY trial is sponsored by Celgene. Dr. Andorsky reported financial relationships with Celgene, CTI BioPharma, and Gilead Sciences. Dr. Casulo reported financial relationships with Gilead Sciences, Celgene, and Roche.
SOURCE: Andorsky DJ et al. ASCO 2019, Abstract 7513.
CHICAGO – Lenalidomide plus rituximab (R2) demonstrated activity against relapsed or refractory follicular lymphoma (FL) and marginal zone lymphoma (MZL) in the phase 3b MAGNIFY trial.
R2 produced responses in FL and MZL patients, including those who had previously experienced early relapse and patients who were refractory to rituximab or both lenalidomide and rituximab at baseline.
David Jacob Andorsky, MD, of Rocky Mountain Cancer Centers in Boulder, Colo., and colleagues presented these results in a poster at the annual meeting of the American Society of Clinical Oncology.
The ongoing MAGNIFY trial has enrolled 370 patients with relapsed/refractory FL (grade 1-3a) or MZL.
For induction, patients receive lenalidomide (20 mg per day on days 1-21 for 12 cycles) and rituximab (375 mg/m2 per week in cycle 1 and then on day 1 of cycles 3, 5, 7, 9, and 11). Patients who achieve stable disease or better on R2 induction are randomized to maintenance with R2 or rituximab alone.
Dr. Andorsky and colleagues presented results of R2 induction in 310 evaluable patients – 247 with FL and 63 with MZL.
The patients had a median age of 66 years (range, 35-91 years) at baseline, and they had received a median of two prior therapies (range, one to eight). Some patients had experienced early relapse (37%, n = 115), were refractory to rituximab (36%, n = 113), or were refractory to both rituximab and lenalidomide (20%, n = 63) at baseline.
Results
At a median follow-up of 16.7 months, the overall response rate was 73%, and the complete response rate was 45%. The overall response rate was 74% in FL patients, 65% in MZL patients, 63% in rituximab-refractory patients, 51% in double-refractory patients, and 68% in patients with an early relapse.
The median duration of response was 36.8 months in all patients, 35.8 months in MZL patients, and not reached in FL patients. The median duration of response was 35.8 months in patients who were rituximab refractory and was not reached in patients who were not refractory to rituximab.
The median progression-free survival was 36 months overall, 30 months in FL patients, 38 months in MZL patients, 23 months in patients with early relapse, and 15.5 months in double-refractory patients.
“While these [subgroup analyses of efficacy] were exploratory endpoints, I think this suggests that [R2] is a promising regimen for patients that are in the high-risk subgroup,” said Carla Casulo, MD, of the University of Rochester (N.Y.), who reviewed this study in a poster discussion session.
The most common adverse events in this trial were fatigue (48%), neutropenia (40%), diarrhea (35%), nausea (30%), and constipation (29%). The most common grade 3/4 adverse event was neutropenia (34%).
The MAGNIFY trial is sponsored by Celgene. Dr. Andorsky reported financial relationships with Celgene, CTI BioPharma, and Gilead Sciences. Dr. Casulo reported financial relationships with Gilead Sciences, Celgene, and Roche.
SOURCE: Andorsky DJ et al. ASCO 2019, Abstract 7513.
CHICAGO – Lenalidomide plus rituximab (R2) demonstrated activity against relapsed or refractory follicular lymphoma (FL) and marginal zone lymphoma (MZL) in the phase 3b MAGNIFY trial.
R2 produced responses in FL and MZL patients, including those who had previously experienced early relapse and patients who were refractory to rituximab or both lenalidomide and rituximab at baseline.
David Jacob Andorsky, MD, of Rocky Mountain Cancer Centers in Boulder, Colo., and colleagues presented these results in a poster at the annual meeting of the American Society of Clinical Oncology.
The ongoing MAGNIFY trial has enrolled 370 patients with relapsed/refractory FL (grade 1-3a) or MZL.
For induction, patients receive lenalidomide (20 mg per day on days 1-21 for 12 cycles) and rituximab (375 mg/m2 per week in cycle 1 and then on day 1 of cycles 3, 5, 7, 9, and 11). Patients who achieve stable disease or better on R2 induction are randomized to maintenance with R2 or rituximab alone.
Dr. Andorsky and colleagues presented results of R2 induction in 310 evaluable patients – 247 with FL and 63 with MZL.
The patients had a median age of 66 years (range, 35-91 years) at baseline, and they had received a median of two prior therapies (range, one to eight). Some patients had experienced early relapse (37%, n = 115), were refractory to rituximab (36%, n = 113), or were refractory to both rituximab and lenalidomide (20%, n = 63) at baseline.
Results
At a median follow-up of 16.7 months, the overall response rate was 73%, and the complete response rate was 45%. The overall response rate was 74% in FL patients, 65% in MZL patients, 63% in rituximab-refractory patients, 51% in double-refractory patients, and 68% in patients with an early relapse.
The median duration of response was 36.8 months in all patients, 35.8 months in MZL patients, and not reached in FL patients. The median duration of response was 35.8 months in patients who were rituximab refractory and was not reached in patients who were not refractory to rituximab.
The median progression-free survival was 36 months overall, 30 months in FL patients, 38 months in MZL patients, 23 months in patients with early relapse, and 15.5 months in double-refractory patients.
“While these [subgroup analyses of efficacy] were exploratory endpoints, I think this suggests that [R2] is a promising regimen for patients that are in the high-risk subgroup,” said Carla Casulo, MD, of the University of Rochester (N.Y.), who reviewed this study in a poster discussion session.
The most common adverse events in this trial were fatigue (48%), neutropenia (40%), diarrhea (35%), nausea (30%), and constipation (29%). The most common grade 3/4 adverse event was neutropenia (34%).
The MAGNIFY trial is sponsored by Celgene. Dr. Andorsky reported financial relationships with Celgene, CTI BioPharma, and Gilead Sciences. Dr. Casulo reported financial relationships with Gilead Sciences, Celgene, and Roche.
SOURCE: Andorsky DJ et al. ASCO 2019, Abstract 7513.
REPORTING FROM ASCO 2019
Novel genetic therapy reduces key protein in Huntington’s disease
according to a study published in the New England Journal of Medicine.
Huntington’s disease is an autosomal-dominant neurodegenerative disease caused by CAG trinucleotide repeat expansion in HTT, resulting in a mutant huntingtin protein. No disease-modifying treatment currently exists. The experimental therapy tested in this trial, developed by Ionis Pharmaceuticals and licensed to Roche as HTTRx, is an antisense oligonucleotide that inhibits HTT messenger RNA signaling specific to the production of the mutant huntingtin protein implicated in Huntington’s disease. Whether HTTRx, which is delivered intrathecally, can produce functional or cognitive improvement is yet unclear, as this randomized, double-blinded, multiple-ascending-dose, placebo-controlled trial, which enrolled 46 patients in Canada, Germany, and the United Kingdom, was primarily a safety study.
For the phase 1-2a trial, lead author Sarah J. Tabrizi, MB, ChB, PhD, of University College London and colleagues assigned patients with early Huntington’s disease to monthly intrathecal injections of one of five different doses of HTTRx (10, 30, 60, 90 or 120 mg), or placebo. Most patients (n = 34) received active drug. After the 85-day treatment period, in which four doses were delivered, patients were followed for 4 months.
The treatment groups saw a mean dose-dependent reduction from baseline in the concentration of CSF mutant huntingtin of between –20% and –42% at 28 days post dosing, while the placebo arm saw an increase of a mean 10%. The most common adverse events seen in the trial were procedure-related pain and headache following spinal puncture.
Other endpoints in the study included concentrations of mutant huntingtin in plasma, the effect of treatment on other neurodegenerative biomarkers, and cognitive scores.
The median peak plasma concentrations of HTTRx were reached within 4 hours after the bolus intrathecal administration and declined to less than 30% of the peak concentration by 24 hours after administration. There was no evidence of accumulation of concentration in plasma 24 hours after dose administration.
Functional, cognitive, psychiatric, and neurologic clinical outcomes were generally unchanged at the dose-group level during the trial, and no meaningful differences were observed between patients who received placebo and patients who received active treatment, regardless of the dose level.
An open-label, follow-up study in the same group of patients, all of whom have been assigned to the 120-mg dose monthly or every other month, is expected to end in October 2019. While the extension study is also mainly a safety study, it will also look at biomarkers and cognitive scores over a longer treatment period.
The study was funded by Ionis Pharmaceuticals and F. Hoffmann–La Roche, and most of the authors, including Dr. Tabrizi, reported financial relationships with one or both entities.
SOURCE: Tabrizi SJ et al. N Eng J Med. 2019:380;2307-16.
according to a study published in the New England Journal of Medicine.
Huntington’s disease is an autosomal-dominant neurodegenerative disease caused by CAG trinucleotide repeat expansion in HTT, resulting in a mutant huntingtin protein. No disease-modifying treatment currently exists. The experimental therapy tested in this trial, developed by Ionis Pharmaceuticals and licensed to Roche as HTTRx, is an antisense oligonucleotide that inhibits HTT messenger RNA signaling specific to the production of the mutant huntingtin protein implicated in Huntington’s disease. Whether HTTRx, which is delivered intrathecally, can produce functional or cognitive improvement is yet unclear, as this randomized, double-blinded, multiple-ascending-dose, placebo-controlled trial, which enrolled 46 patients in Canada, Germany, and the United Kingdom, was primarily a safety study.
For the phase 1-2a trial, lead author Sarah J. Tabrizi, MB, ChB, PhD, of University College London and colleagues assigned patients with early Huntington’s disease to monthly intrathecal injections of one of five different doses of HTTRx (10, 30, 60, 90 or 120 mg), or placebo. Most patients (n = 34) received active drug. After the 85-day treatment period, in which four doses were delivered, patients were followed for 4 months.
The treatment groups saw a mean dose-dependent reduction from baseline in the concentration of CSF mutant huntingtin of between –20% and –42% at 28 days post dosing, while the placebo arm saw an increase of a mean 10%. The most common adverse events seen in the trial were procedure-related pain and headache following spinal puncture.
Other endpoints in the study included concentrations of mutant huntingtin in plasma, the effect of treatment on other neurodegenerative biomarkers, and cognitive scores.
The median peak plasma concentrations of HTTRx were reached within 4 hours after the bolus intrathecal administration and declined to less than 30% of the peak concentration by 24 hours after administration. There was no evidence of accumulation of concentration in plasma 24 hours after dose administration.
Functional, cognitive, psychiatric, and neurologic clinical outcomes were generally unchanged at the dose-group level during the trial, and no meaningful differences were observed between patients who received placebo and patients who received active treatment, regardless of the dose level.
An open-label, follow-up study in the same group of patients, all of whom have been assigned to the 120-mg dose monthly or every other month, is expected to end in October 2019. While the extension study is also mainly a safety study, it will also look at biomarkers and cognitive scores over a longer treatment period.
The study was funded by Ionis Pharmaceuticals and F. Hoffmann–La Roche, and most of the authors, including Dr. Tabrizi, reported financial relationships with one or both entities.
SOURCE: Tabrizi SJ et al. N Eng J Med. 2019:380;2307-16.
according to a study published in the New England Journal of Medicine.
Huntington’s disease is an autosomal-dominant neurodegenerative disease caused by CAG trinucleotide repeat expansion in HTT, resulting in a mutant huntingtin protein. No disease-modifying treatment currently exists. The experimental therapy tested in this trial, developed by Ionis Pharmaceuticals and licensed to Roche as HTTRx, is an antisense oligonucleotide that inhibits HTT messenger RNA signaling specific to the production of the mutant huntingtin protein implicated in Huntington’s disease. Whether HTTRx, which is delivered intrathecally, can produce functional or cognitive improvement is yet unclear, as this randomized, double-blinded, multiple-ascending-dose, placebo-controlled trial, which enrolled 46 patients in Canada, Germany, and the United Kingdom, was primarily a safety study.
For the phase 1-2a trial, lead author Sarah J. Tabrizi, MB, ChB, PhD, of University College London and colleagues assigned patients with early Huntington’s disease to monthly intrathecal injections of one of five different doses of HTTRx (10, 30, 60, 90 or 120 mg), or placebo. Most patients (n = 34) received active drug. After the 85-day treatment period, in which four doses were delivered, patients were followed for 4 months.
The treatment groups saw a mean dose-dependent reduction from baseline in the concentration of CSF mutant huntingtin of between –20% and –42% at 28 days post dosing, while the placebo arm saw an increase of a mean 10%. The most common adverse events seen in the trial were procedure-related pain and headache following spinal puncture.
Other endpoints in the study included concentrations of mutant huntingtin in plasma, the effect of treatment on other neurodegenerative biomarkers, and cognitive scores.
The median peak plasma concentrations of HTTRx were reached within 4 hours after the bolus intrathecal administration and declined to less than 30% of the peak concentration by 24 hours after administration. There was no evidence of accumulation of concentration in plasma 24 hours after dose administration.
Functional, cognitive, psychiatric, and neurologic clinical outcomes were generally unchanged at the dose-group level during the trial, and no meaningful differences were observed between patients who received placebo and patients who received active treatment, regardless of the dose level.
An open-label, follow-up study in the same group of patients, all of whom have been assigned to the 120-mg dose monthly or every other month, is expected to end in October 2019. While the extension study is also mainly a safety study, it will also look at biomarkers and cognitive scores over a longer treatment period.
The study was funded by Ionis Pharmaceuticals and F. Hoffmann–La Roche, and most of the authors, including Dr. Tabrizi, reported financial relationships with one or both entities.
SOURCE: Tabrizi SJ et al. N Eng J Med. 2019:380;2307-16.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Mutant huntingtin and neurofilament light are potential biomarkers in Huntington’s disease
PHILADELPHIA – according to an investigation presented at the annual meeting of the American Academy of Neurology. These biomarkers appear to reflect the earliest detectable changes in the natural history of Huntington’s disease, but the longitudinal prognostic value of changes in these biomarkers requires further investigation, the researchers said.
Huntington’s disease has a long prodromal phase and is associated with long survival. Investigators still need well-validated biomarkers of disease progression, prognosis, and pharmacodynamics to aid drug development, said Filipe B. Rodrigues, MD, clinical research fellow at University College London. After several years of study, Dr. Rodrigues and colleagues found mutant huntingtin and neurofilament light (NfL) to be the most promising potential biomarkers in Huntington’s disease. They sought to understand how these two biomarkers compare with each other, what their predictive ability is, and how they change longitudinally.
To this end, Dr. Rodrigues and colleagues designed the HD-CSF study, a prospective, observational, longitudinal cohort study with a 2-year follow-up. They recruited 20 healthy controls, 20 patients with premanifest Huntington’s disease, and 40 patients with manifest Huntington’s disease. All participants underwent regular clinical assessments and standardized collections of cerebrospinal fluid (CSF) and blood. They also had the option of undergoing brain MRI scans.
The investigators analyzed their data using multiple linear regression models, Pearson’s correlations, receiver operating characteristic curves, and sample size calculations. They used an event-based model to evaluate the temporal sequence of changes in Huntington’s disease-related biomarkers.
Dr. Rodrigues and colleagues first observed that all three biomarkers successfully distinguished between healthy controls, patients with premanifest Huntington’s disease, and patients with Huntington’s disease. Mutant huntingtin, the pathogenic agent in Huntington’s disease, discriminated perfectly between healthy controls and mutation carriers, as the researchers had expected. CSF and plasma levels of NfL also discriminated well between healthy controls and mutation carriers. These biomarkers had areas under the ROC curve greater than 0.9. NfL in plasma and CSF also distinguished well between patients with premanifest Huntington’s disease and those with manifest Huntington’s disease, with areas under the curve greater than 0.9. Their discriminative ability in this regard was significantly better than that of mutant huntingtin.
When the researchers examined the relationship between the three biomarkers, they found that CSF levels of NfL were strongly correlated in a linear fashion with plasma levels of NfL. CSF levels of mutant huntingtin were moderately associated with CSF levels of NfL.
Levels of all three biomarkers increased significantly as the disease progressed and were associated with all clinical scales and imaging measures. CSF and plasma levels of NfL had superior predictive ability for clinical and imaging measures, compared with mutant huntingtin. CSF and plasma NfL were associated with brain volume, but mutant huntingtin was not.
All three biomarkers were stable during a 6-week period. Dr. Rodrigues and colleagues calculated sample sizes for a two-arm interventional trial involving various hypothetical therapeutic effects. They found that the required sample sizes were small enough to be incorporated easily into ongoing and future clinical trials.
In silico modeling suggested among the markers measured in the HD-CSF study, the three biofluid biomarkers were the first factors to be altered in the course of Huntington’s disease. Alterations in the biomarkers were followed by changes in imaging markers, and then by changes in clinical markers (for example, motor and cognitive function).
Finally, Dr. Rodrigues and colleagues found preliminary evidence that levels of NfL in CSF and plasma increase over time at different rates in patients with Huntington’s disease, compared with healthy controls. NfL appears to be more useful than mutant huntingtin for evaluating the rate of disease progression than for gauging response to treatment, said Dr. Rodrigues. “If [we] can prove that we can assess response to treatment by measuring NfL, I think that would be great.”
The investigators are currently analyzing the longitudinal predictive value of changes in these biomarkers. They also have begun analyzing other markers such as tau and brain-derived neurotrophic factor.
This study was funded by the Medical Research Council UK, the CHDI Foundation, and F. Hoffmann-La Roche.
This article was updated 6/18/19.
SOURCE: Rodrigues FB et al. AAN 2019, Abstract S16.003.
PHILADELPHIA – according to an investigation presented at the annual meeting of the American Academy of Neurology. These biomarkers appear to reflect the earliest detectable changes in the natural history of Huntington’s disease, but the longitudinal prognostic value of changes in these biomarkers requires further investigation, the researchers said.
Huntington’s disease has a long prodromal phase and is associated with long survival. Investigators still need well-validated biomarkers of disease progression, prognosis, and pharmacodynamics to aid drug development, said Filipe B. Rodrigues, MD, clinical research fellow at University College London. After several years of study, Dr. Rodrigues and colleagues found mutant huntingtin and neurofilament light (NfL) to be the most promising potential biomarkers in Huntington’s disease. They sought to understand how these two biomarkers compare with each other, what their predictive ability is, and how they change longitudinally.
To this end, Dr. Rodrigues and colleagues designed the HD-CSF study, a prospective, observational, longitudinal cohort study with a 2-year follow-up. They recruited 20 healthy controls, 20 patients with premanifest Huntington’s disease, and 40 patients with manifest Huntington’s disease. All participants underwent regular clinical assessments and standardized collections of cerebrospinal fluid (CSF) and blood. They also had the option of undergoing brain MRI scans.
The investigators analyzed their data using multiple linear regression models, Pearson’s correlations, receiver operating characteristic curves, and sample size calculations. They used an event-based model to evaluate the temporal sequence of changes in Huntington’s disease-related biomarkers.
Dr. Rodrigues and colleagues first observed that all three biomarkers successfully distinguished between healthy controls, patients with premanifest Huntington’s disease, and patients with Huntington’s disease. Mutant huntingtin, the pathogenic agent in Huntington’s disease, discriminated perfectly between healthy controls and mutation carriers, as the researchers had expected. CSF and plasma levels of NfL also discriminated well between healthy controls and mutation carriers. These biomarkers had areas under the ROC curve greater than 0.9. NfL in plasma and CSF also distinguished well between patients with premanifest Huntington’s disease and those with manifest Huntington’s disease, with areas under the curve greater than 0.9. Their discriminative ability in this regard was significantly better than that of mutant huntingtin.
When the researchers examined the relationship between the three biomarkers, they found that CSF levels of NfL were strongly correlated in a linear fashion with plasma levels of NfL. CSF levels of mutant huntingtin were moderately associated with CSF levels of NfL.
Levels of all three biomarkers increased significantly as the disease progressed and were associated with all clinical scales and imaging measures. CSF and plasma levels of NfL had superior predictive ability for clinical and imaging measures, compared with mutant huntingtin. CSF and plasma NfL were associated with brain volume, but mutant huntingtin was not.
All three biomarkers were stable during a 6-week period. Dr. Rodrigues and colleagues calculated sample sizes for a two-arm interventional trial involving various hypothetical therapeutic effects. They found that the required sample sizes were small enough to be incorporated easily into ongoing and future clinical trials.
In silico modeling suggested among the markers measured in the HD-CSF study, the three biofluid biomarkers were the first factors to be altered in the course of Huntington’s disease. Alterations in the biomarkers were followed by changes in imaging markers, and then by changes in clinical markers (for example, motor and cognitive function).
Finally, Dr. Rodrigues and colleagues found preliminary evidence that levels of NfL in CSF and plasma increase over time at different rates in patients with Huntington’s disease, compared with healthy controls. NfL appears to be more useful than mutant huntingtin for evaluating the rate of disease progression than for gauging response to treatment, said Dr. Rodrigues. “If [we] can prove that we can assess response to treatment by measuring NfL, I think that would be great.”
The investigators are currently analyzing the longitudinal predictive value of changes in these biomarkers. They also have begun analyzing other markers such as tau and brain-derived neurotrophic factor.
This study was funded by the Medical Research Council UK, the CHDI Foundation, and F. Hoffmann-La Roche.
This article was updated 6/18/19.
SOURCE: Rodrigues FB et al. AAN 2019, Abstract S16.003.
PHILADELPHIA – according to an investigation presented at the annual meeting of the American Academy of Neurology. These biomarkers appear to reflect the earliest detectable changes in the natural history of Huntington’s disease, but the longitudinal prognostic value of changes in these biomarkers requires further investigation, the researchers said.
Huntington’s disease has a long prodromal phase and is associated with long survival. Investigators still need well-validated biomarkers of disease progression, prognosis, and pharmacodynamics to aid drug development, said Filipe B. Rodrigues, MD, clinical research fellow at University College London. After several years of study, Dr. Rodrigues and colleagues found mutant huntingtin and neurofilament light (NfL) to be the most promising potential biomarkers in Huntington’s disease. They sought to understand how these two biomarkers compare with each other, what their predictive ability is, and how they change longitudinally.
To this end, Dr. Rodrigues and colleagues designed the HD-CSF study, a prospective, observational, longitudinal cohort study with a 2-year follow-up. They recruited 20 healthy controls, 20 patients with premanifest Huntington’s disease, and 40 patients with manifest Huntington’s disease. All participants underwent regular clinical assessments and standardized collections of cerebrospinal fluid (CSF) and blood. They also had the option of undergoing brain MRI scans.
The investigators analyzed their data using multiple linear regression models, Pearson’s correlations, receiver operating characteristic curves, and sample size calculations. They used an event-based model to evaluate the temporal sequence of changes in Huntington’s disease-related biomarkers.
Dr. Rodrigues and colleagues first observed that all three biomarkers successfully distinguished between healthy controls, patients with premanifest Huntington’s disease, and patients with Huntington’s disease. Mutant huntingtin, the pathogenic agent in Huntington’s disease, discriminated perfectly between healthy controls and mutation carriers, as the researchers had expected. CSF and plasma levels of NfL also discriminated well between healthy controls and mutation carriers. These biomarkers had areas under the ROC curve greater than 0.9. NfL in plasma and CSF also distinguished well between patients with premanifest Huntington’s disease and those with manifest Huntington’s disease, with areas under the curve greater than 0.9. Their discriminative ability in this regard was significantly better than that of mutant huntingtin.
When the researchers examined the relationship between the three biomarkers, they found that CSF levels of NfL were strongly correlated in a linear fashion with plasma levels of NfL. CSF levels of mutant huntingtin were moderately associated with CSF levels of NfL.
Levels of all three biomarkers increased significantly as the disease progressed and were associated with all clinical scales and imaging measures. CSF and plasma levels of NfL had superior predictive ability for clinical and imaging measures, compared with mutant huntingtin. CSF and plasma NfL were associated with brain volume, but mutant huntingtin was not.
All three biomarkers were stable during a 6-week period. Dr. Rodrigues and colleagues calculated sample sizes for a two-arm interventional trial involving various hypothetical therapeutic effects. They found that the required sample sizes were small enough to be incorporated easily into ongoing and future clinical trials.
In silico modeling suggested among the markers measured in the HD-CSF study, the three biofluid biomarkers were the first factors to be altered in the course of Huntington’s disease. Alterations in the biomarkers were followed by changes in imaging markers, and then by changes in clinical markers (for example, motor and cognitive function).
Finally, Dr. Rodrigues and colleagues found preliminary evidence that levels of NfL in CSF and plasma increase over time at different rates in patients with Huntington’s disease, compared with healthy controls. NfL appears to be more useful than mutant huntingtin for evaluating the rate of disease progression than for gauging response to treatment, said Dr. Rodrigues. “If [we] can prove that we can assess response to treatment by measuring NfL, I think that would be great.”
The investigators are currently analyzing the longitudinal predictive value of changes in these biomarkers. They also have begun analyzing other markers such as tau and brain-derived neurotrophic factor.
This study was funded by the Medical Research Council UK, the CHDI Foundation, and F. Hoffmann-La Roche.
This article was updated 6/18/19.
SOURCE: Rodrigues FB et al. AAN 2019, Abstract S16.003.
REPORTING FROM AAN 2019
Key clinical point: Mutant huntingtin and plasma and cerebrospinal fluid levels of neurofilament light are useful potential biomarkers in Huntington’s disease.
Major finding: Levels of neurofilament light in plasma are correlated with those in cerebrospinal fluid.
Study details: A prospective, observational, longitudinal cohort study including 80 participants with and without Huntington’s disease.
Disclosures: This study was funded by the Medical Research Council UK, the CHDI Foundation, and F. Hoffmann-La Roche.
Source: Rodrigues FB et al. AAN 2019, Abstract S16.003.
Acroangiodermatitis of Mali and Stewart-Bluefarb Syndrome
Case Reports
Patient 1
A 56-year-old white man with a history of hypertension, hyperlipidemia, sleep apnea, bilateral knee replacement, and cataract removal presented to the emergency department with a worsening rash on the left posterior medial leg of 6 months’ duration. He reported associated redness and tenderness with the plaques as well as increased swelling and firmness of the leg. He was admitted to the hospital where the infectious disease team treated him with cefazolin for presumed cellulitis. His condition did not improve, and another course of cefazolin was started in addition to oral fluconazole and clotrimazole–betamethasone dipropionate lotion for a possible fungal cause. Again, treatment provided no improvement.
He was then evaluated by dermatology. On physical examination, the patient had edema, warmth, and induration of the left lower leg. There also was an annular and serpiginous indurated plaque with minimal scale on the left lower leg (Figure 1). A firm, dark red to purple plaque on the left medial thigh with mild scale was present. There also was scaling of the right plantar foot.

Skin biopsy revealed a dermal capillary proliferation with a scattering of inflammatory cells including eosinophils as well as dermal fibrosis (Figure 2). Periodic acid–Schiff and human herpesvirus 8 (HHV-8) immunostains were negative. Considering the degree and depth of vascular proliferation, Mali-type acroangiodermatitis (AAD) was the favored diagnosis.
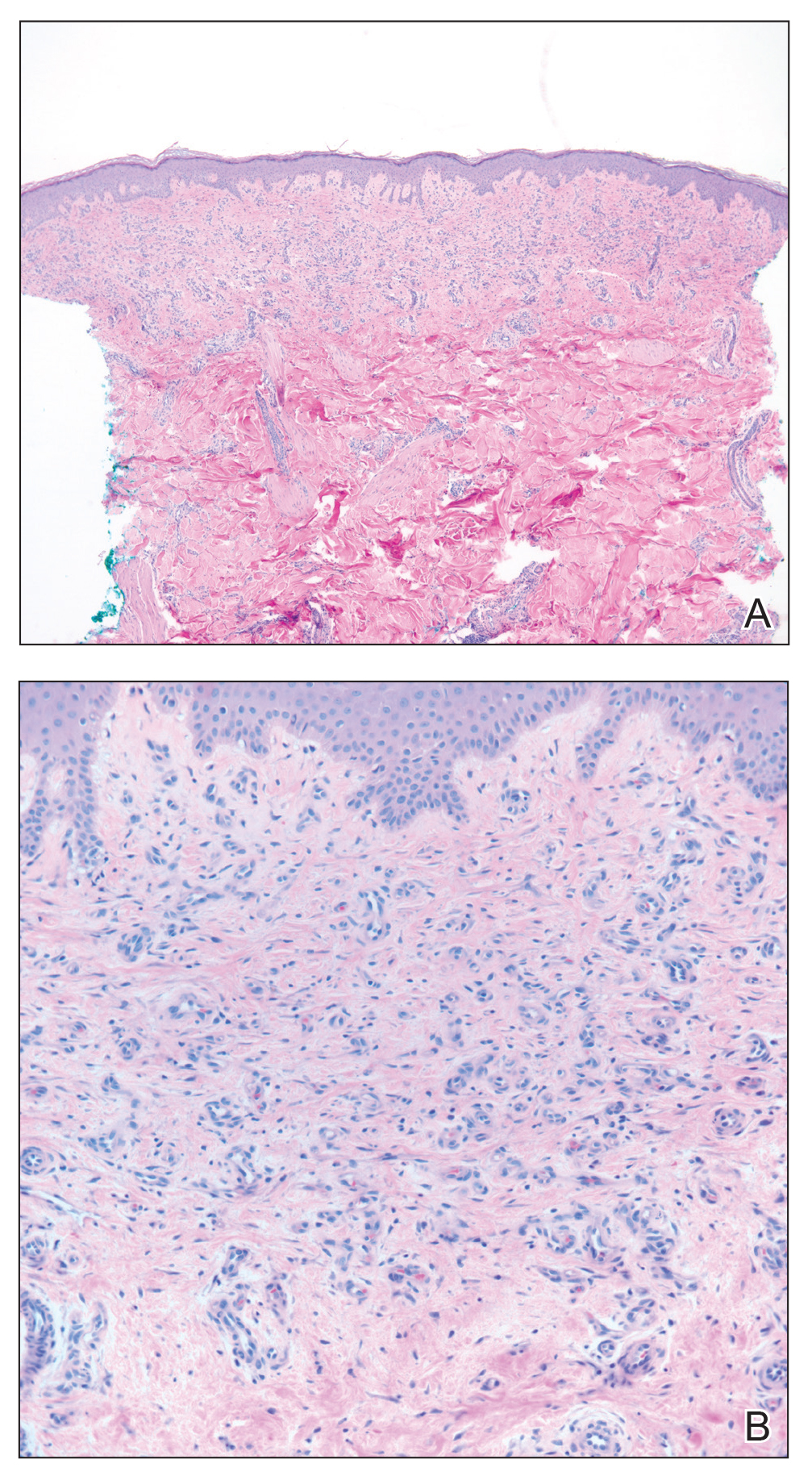
Patient 2
A 72-year-old white man presented with a firm asymptomatic growth on the left dorsal forearm of 3 months’ duration. It was located near the site of a prior squamous cell carcinoma that was excised 1 year prior to presentation. The patient had no treatment or biopsy of the presenting lesion. His medical and surgical history included polycystic kidney disease and renal transplantation 4 years prior to presentation. He also had an arteriovenous fistula of the left arm. His other chronic diseases included chronic obstructive lung disease, congestive heart failure, hypertension, type 2 diabetes mellitus, and obstructive sleep apnea.
On physical examination, the patient had a 1-cm violaceous nodule on the extensor surface of the left mid forearm. An arteriovenous fistula was present proximal to the lesion on the left arm (Figure 3).

Skin biopsy revealed a tightly packed proliferation of small vascular channels that tested negative for HHV-8, tumor protein p63, and cytokeratin 5/6. Erythrocytes were noted in the lumen of some of these vessels. Neutrophils were scattered and clustered throughout the specimen (Figure 4A). Blood vessels were highlighted with CD34 (Figure 4B). Grocott-Gomori methenamine-silver stain was negative for infectious agents. These findings favored AAD secondary to an arteriovenous malformation, consistent with Stewart-Bluefarb syndrome (SBS).
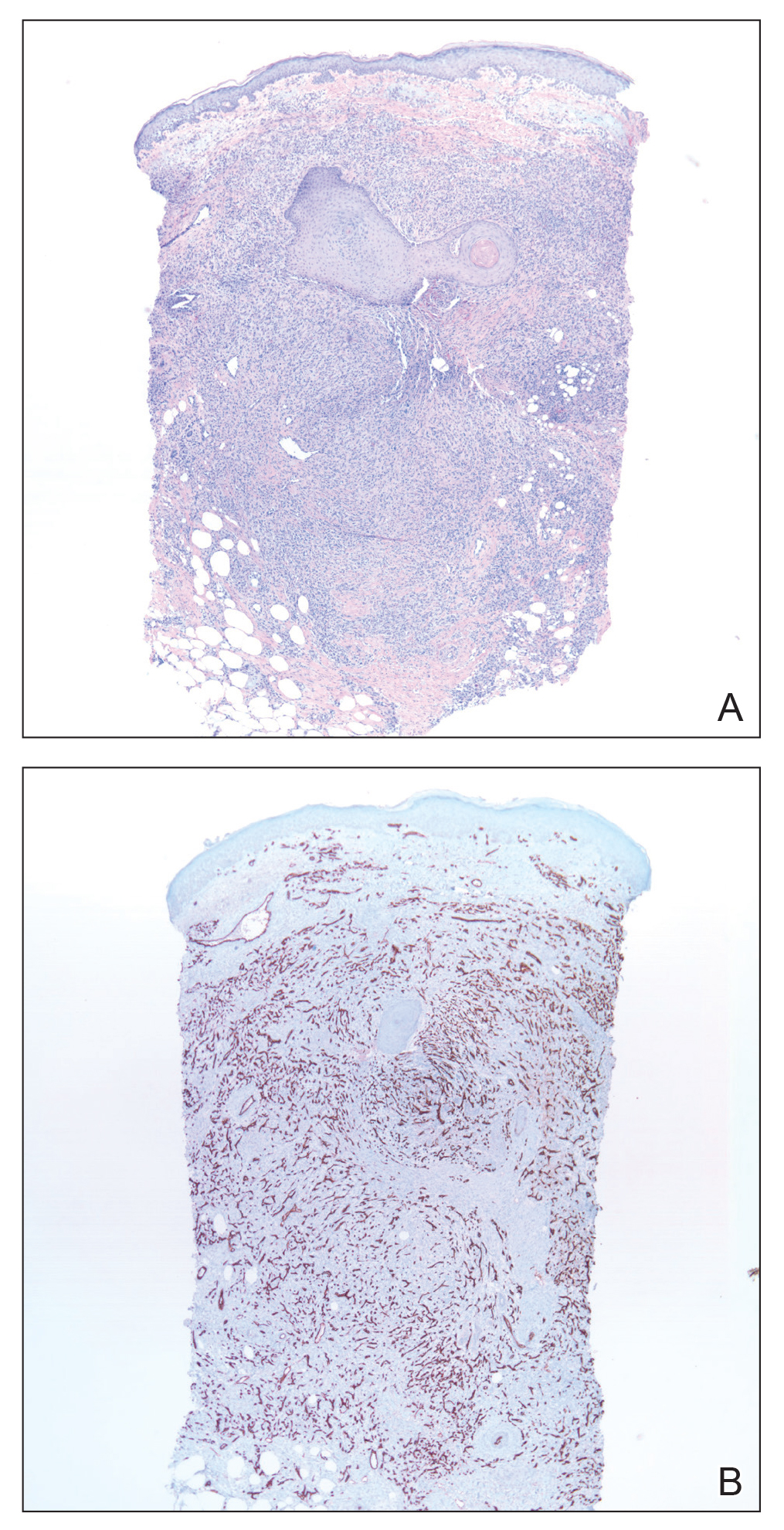
Comment
Presentation of AAD
Acroangiodermatitis is a rare chronic inflammatory skin process involving a reactive proliferation of capillaries and fibrosis of the skin that resembles Kaposi sarcoma both clinically and histopathologically. The condition has been reported in patients with chronic venous insufficiency,1 congenital arteriovenous malformation,2 acquired iatrogenic arteriovenous fistula,3 paralyzed extremity,4 suction socket lower limb prosthesis (amputees),5 and minor trauma.6-8 The lesions of AAD tend to be circumscribed, slowly evolving, red-violaceous (or brown or dusky) macules, papules, or plaques that may become verrucous or develop into painful ulcerations. They generally occur on the distal dorsal aspects of the lower legs and feet.110
Variants of AAD
Mali et al9 first reported cutaneous manifestations resembling Kaposi sarcoma in 18 patients with chronic venous insufficiency in 1965. Two years later, Bluefarb and Adams10 described kaposiform skin lesions in one patient with a congenital arteriovenous malformation without chronic venous insufficiency. It was not until 1974, however, that Earhart et al11 proposed the term pseudo-Kaposi sarcoma.10,11 Based on these findings, AAD is described as 2 variants: Mali type and SBS.
Mali-type AAD is more common and typically occurs in elderly men. It classically presents bilaterally on the lower extremities in association with severe chronic venous insufficiency.5 Skin lesions usually occur on the medial aspect of the lower legs (as in patient 1), dorsum of the heel, hallux, or second toe.12
The etiology of Mali-type AAD is poorly understood. The leading theory is that the condition involves reduced perfusion due to chronic edema, resulting in neovascularization, fibroblast proliferation, hypertrophy, and inflammatory skin changes. When AAD occurs in the setting of a suction socket prosthesis, the negative pressure of the stump-socket environment is thought to alter local circulation, leading to proliferation of small blood vessels.5,13
Stewart-Bluefarb syndrome usually involves a single extremity in young adults with congenital arteriovenous malformations, amputees, and individuals with hemiplegia or iatrogenic arteriovenous fistulae (as in patient 2).1 It was once thought to occur secondary to Klippel-Trenaunay-Weber syndrome; however, SBS rarely is accompanied by limb hypertrophy.9 Pathogenesis is thought to involve an angiogenic response to a high perfusion rate and high oxygen saturation, which leads to fibroblast proliferation and reactive endothelial hyperplasia.1,14
Diagnosis and Differential Diagnosis
Prompt identification of an underlying arteriovenous anomaly is critical, given the sequelae of high-flow shunts, which may result in skin ulceration, limb length discrepancy, cortical thinning of bone with regional osteoporosis, and congestive heart failure.1,5 Duplex ultrasonography is the first-line diagnostic modality because it is noninvasive and widely available. The key doppler feature of an arteriovenous malformation is low resistance and high diastolic pulsatile flow,1 which should be confirmed with magnetic resonance angiography or computed tomography angiography if present on ultrasonography.
The differential diagnosis of AAD includes Kaposi sarcoma, reactive angioendotheliomatosis, diffuse dermal angiomatosis, intravascular histiocytosis, glomeruloid angioendotheliomatosis, and angiopericytomatosis.15,16 These entities present as multiple erythematous, violaceous, purpuric patches and plaques generally on the extremities but can have a widely varied distribution. Some lesions evolve to necrosis or ulceration. Histopathologic analysis is useful to differentiate these entities.
Histopathology
The histopathologic features of AAD can be nonspecific; clinicopathologic correlation often is necessary to establish the diagnosis. Features include a proliferation of small thick-walled vessels, often in a lobular arrangement, in an edematous papillary dermis. Small thrombi may be observed. There may be increased fibroblasts; plump endothelial cells; a superficial mixed infiltrate comprised of lymphocytes, histiocytes, and eosinophils; and deposition of hemosiderin.2,5 These characteristics overlap with features of Kaposi sarcoma; AAD, however, lacks slitlike vascular spaces, perivascular CD34+ expression, and nuclear atypia. A negative HHV-8 stain will assist in ruling out Kaposi sarcoma.1,17
Management
Treatment reports are anecdotal. The goal is to correct underlying venous hypertension. Conservative measures with compression garments, intermittent pneumatic compression, and limb elevation are first line.18 Oral antibiotics and local wound care with topical emollients and corticosteroids have been shown to be effective treatments.19-21
Oral erythromycin 500 mg 4 times daily for 3 weeks and clobetasol propionate cream 0.05% healed a lower extremity ulcer in a patient with Mali-type AAD.21 In another patient, conservative treatment of Mali-type AAD failed, but rapid improvement of 2 lower extremity ulcers resulted after 3 weeks of oral dapsone 50 mg twice daily.22
Conclusion
Acroangiodermatitis is a rare entity that is characterized by erythematous violaceous papules and plaques of the extremities, commonly in the setting of chronic venous insufficiency or an arteriovenous shunt. Histopathologic analysis shows proliferation of capillaries with fibrosis, extravasation of erythrocytes, and deposition of hemosiderin without the spindle cells and slitlike vascular spaces characteristic of Kaposi sarcoma. Detection of an underlying arteriovenous malformation is essential, as the disease can have local and systemic consequences, such as skin ulceration and congestive heart failure.1 Treatment options are conservative, directed toward local wound care, compression, and management of complications, such as ulceration and infection, as well as obliterating any underlying arteriovenous malformation.
- Parsi K, O’Connor AA, Bester L. Stewart-Bluefarb syndrome: report of five cases and a review of literature. Phlebology. 2015;30:505-514.
- Larralde M, Gonzalez V, Marietti R, et al. Pseudo-Kaposi sarcoma with arteriovenous malformation. Pediatr Dermatol. 2001;18:325-327.
- Nakanishi G, Tachibana T, Soga H, et al. Pseudo-Kaposi’s sarcoma of the hand associated with acquired iatrogenic arteriovenous fistula. Indian J Dermatol. 2014;59:415-416.
- Landthaler M, Langehenke H, Holzmann H, et al. Mali’s acroangiodermatitis (pseudo-Kaposi) in paralyzed legs. Hautarzt. 1988;39:304-307.
- Trindade F, Requena L. Pseudo-Kaposi’s sarcoma because of suction socket lower limb prosthesis. J Cutan Pathol. 2009;36:482-485.
- Yu-Lu W, Tao Q, Hong-Zhong J, et al. Non-tender pedal plaques and nodules: pseudo-Kaposi’s sarcoma (Stewart-Bluefarb type) induced by trauma. J Dtsch Dermatol Ges. 2015;13:927-930.
- Del-Río E, Aguilar A, Ambrojo P, et al. Pseudo-Kaposi sarcoma induced by minor trauma in a patient with Klippel-Trenaunay-Weber syndrome. Clin Exp Dermatol. 1993;18:151-153.
- Archie M, Khademi S, Aungst D, et al. A rare case of acroangiodermatitis associated with a congenital arteriovenous malformation (Stewart-Bluefarb Syndrome) in a young veteran: case report and review of the literature. Ann Vasc Surg. 2015;29:1448.e5-1448.e10.
- Mali JW, Kuiper JP, Hamers AA. Acro-angiodermatitis of the foot. Arch Dermatol. 1965;92:515-518.
- Bluefarb SM, Adams LA. Arteriovenous malformation with angiodermatitis. stasis dermatitis simulating Kaposi’s disease. Arch Dermatol. 1967;96:176-181.
- Earhart RN, Aeling JA, Nuss DD, et al. Pseudo-Kaposi sarcoma. A patient with arteriovenous malformation and skin lesions simulating Kaposi sarcoma. Arch Dermatol. 1974;110:907-910.
- Lugovic´ L, Pusic´ J, Situm M, et al. Acroangiodermatitis (pseudo-Kaposi sarcoma): three case reports. Acta Dermatovenerol Croat. 2007;15:152-157.
- Horiguchi Y, Takahashi K, Tanizaki H, et al. Case of bilateral acroangiodermatitis due to symmetrical arteriovenous fistulas of the soles. J Dermatol. 2015;42:989-991.
- Dog˘an S, Boztepe G, Karaduman A. Pseudo-Kaposi sarcoma: a challenging vascular phenomenon. Dermatol Online J. 2007;13:22.
- Mazloom SE, Stallings A, Kyei A. Differentiating intralymphatic histiocytosis, intravascular histiocytosis, and subtypes of reactive angioendotheliomatosis: review of clinical and histologic features of all cases reported to date. Am J Dermatopathol. 2017;39:33-39.
- Rongioletti F, Rebora A. Cutaneous reactive angiomatoses: patterns and classification of reactive vascular proliferation. J Am Acad Dermatol. 2003;49:887-896.
- Kanitakis J, Narvaez D, Claudy A. Expression of the CD34 antigen distinguishes Kaposi’s sarcoma from pseudo-Kaposi’s sarcoma (acroangiodermatitis). Br J Dermatol. 1996;134:44-46.
- Pires A, Depairon M, Ricci C, et al. Effect of compression therapy on a pseudo-Kaposi sarcoma. Dermatology. 1999;198:439-441.
- Hayek S, Atiyeh B, Zgheib E. Stewart-Bluefarb syndrome: review of the literature and case report of chronic ulcer treatment with heparan sulphate (Cacipliq20®). Int Wound J. 2015;12:169-172.
- Varyani N, Thukral A, Kumar N, et al. Nonhealing ulcer: acroangiodermatitis of Mali. Case Rep Dermatol Med. 2011;2011:909383.
- Mehta AA, Pereira RR, Nayak C, et al. Acroangiodermatitis of Mali: a rare vascular phenomenon. Indian J Dermatol Venereol Leprol. 2010;76:553-556.
- Rashkovsky I, Gilead L, Schamroth J, et al. Acro-angiodermatitis: review of the literature and report of a case. Acta Derm Venereol. 1995;75:475-478.
Case Reports
Patient 1
A 56-year-old white man with a history of hypertension, hyperlipidemia, sleep apnea, bilateral knee replacement, and cataract removal presented to the emergency department with a worsening rash on the left posterior medial leg of 6 months’ duration. He reported associated redness and tenderness with the plaques as well as increased swelling and firmness of the leg. He was admitted to the hospital where the infectious disease team treated him with cefazolin for presumed cellulitis. His condition did not improve, and another course of cefazolin was started in addition to oral fluconazole and clotrimazole–betamethasone dipropionate lotion for a possible fungal cause. Again, treatment provided no improvement.
He was then evaluated by dermatology. On physical examination, the patient had edema, warmth, and induration of the left lower leg. There also was an annular and serpiginous indurated plaque with minimal scale on the left lower leg (Figure 1). A firm, dark red to purple plaque on the left medial thigh with mild scale was present. There also was scaling of the right plantar foot.

Skin biopsy revealed a dermal capillary proliferation with a scattering of inflammatory cells including eosinophils as well as dermal fibrosis (Figure 2). Periodic acid–Schiff and human herpesvirus 8 (HHV-8) immunostains were negative. Considering the degree and depth of vascular proliferation, Mali-type acroangiodermatitis (AAD) was the favored diagnosis.
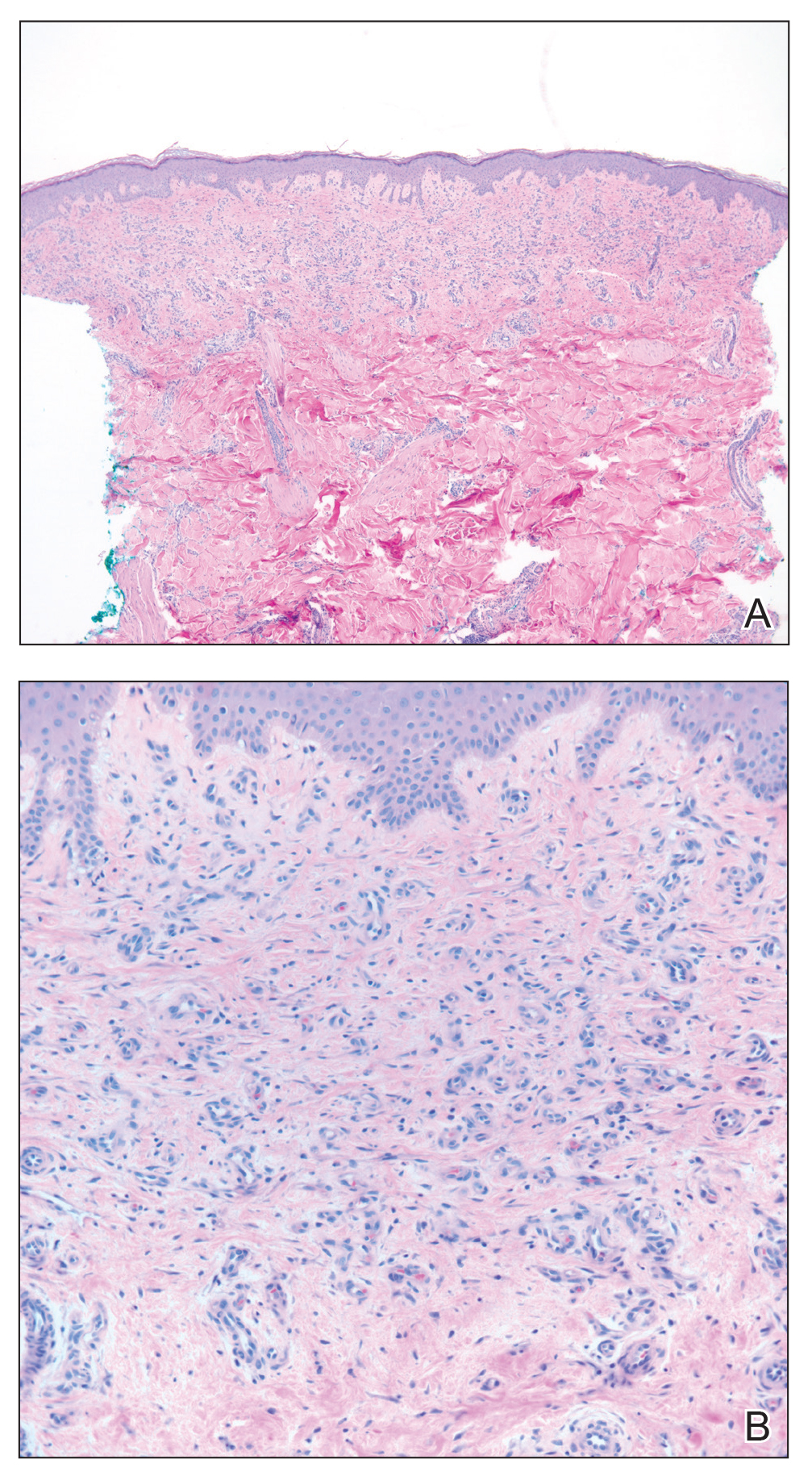
Patient 2
A 72-year-old white man presented with a firm asymptomatic growth on the left dorsal forearm of 3 months’ duration. It was located near the site of a prior squamous cell carcinoma that was excised 1 year prior to presentation. The patient had no treatment or biopsy of the presenting lesion. His medical and surgical history included polycystic kidney disease and renal transplantation 4 years prior to presentation. He also had an arteriovenous fistula of the left arm. His other chronic diseases included chronic obstructive lung disease, congestive heart failure, hypertension, type 2 diabetes mellitus, and obstructive sleep apnea.
On physical examination, the patient had a 1-cm violaceous nodule on the extensor surface of the left mid forearm. An arteriovenous fistula was present proximal to the lesion on the left arm (Figure 3).

Skin biopsy revealed a tightly packed proliferation of small vascular channels that tested negative for HHV-8, tumor protein p63, and cytokeratin 5/6. Erythrocytes were noted in the lumen of some of these vessels. Neutrophils were scattered and clustered throughout the specimen (Figure 4A). Blood vessels were highlighted with CD34 (Figure 4B). Grocott-Gomori methenamine-silver stain was negative for infectious agents. These findings favored AAD secondary to an arteriovenous malformation, consistent with Stewart-Bluefarb syndrome (SBS).
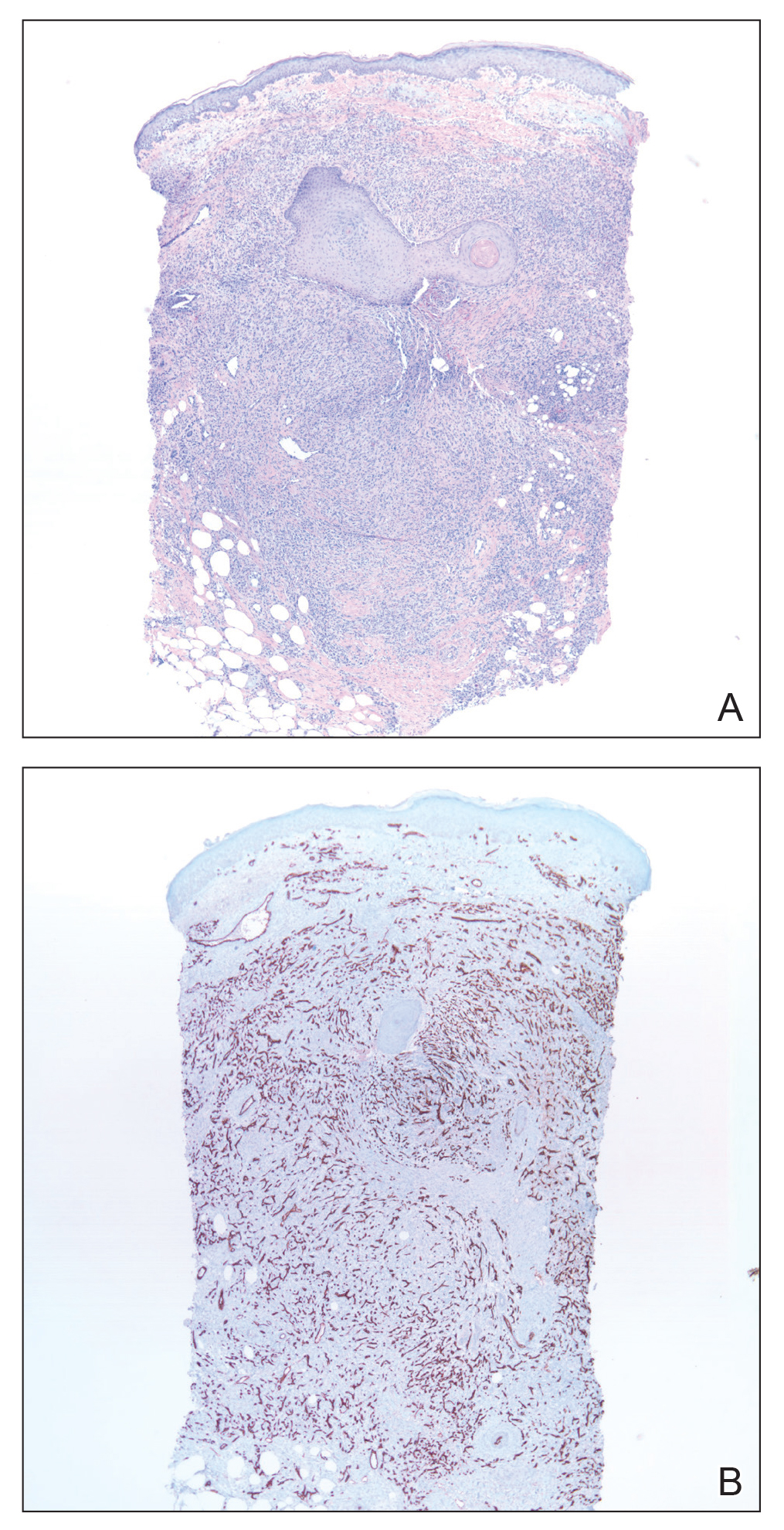
Comment
Presentation of AAD
Acroangiodermatitis is a rare chronic inflammatory skin process involving a reactive proliferation of capillaries and fibrosis of the skin that resembles Kaposi sarcoma both clinically and histopathologically. The condition has been reported in patients with chronic venous insufficiency,1 congenital arteriovenous malformation,2 acquired iatrogenic arteriovenous fistula,3 paralyzed extremity,4 suction socket lower limb prosthesis (amputees),5 and minor trauma.6-8 The lesions of AAD tend to be circumscribed, slowly evolving, red-violaceous (or brown or dusky) macules, papules, or plaques that may become verrucous or develop into painful ulcerations. They generally occur on the distal dorsal aspects of the lower legs and feet.110
Variants of AAD
Mali et al9 first reported cutaneous manifestations resembling Kaposi sarcoma in 18 patients with chronic venous insufficiency in 1965. Two years later, Bluefarb and Adams10 described kaposiform skin lesions in one patient with a congenital arteriovenous malformation without chronic venous insufficiency. It was not until 1974, however, that Earhart et al11 proposed the term pseudo-Kaposi sarcoma.10,11 Based on these findings, AAD is described as 2 variants: Mali type and SBS.
Mali-type AAD is more common and typically occurs in elderly men. It classically presents bilaterally on the lower extremities in association with severe chronic venous insufficiency.5 Skin lesions usually occur on the medial aspect of the lower legs (as in patient 1), dorsum of the heel, hallux, or second toe.12
The etiology of Mali-type AAD is poorly understood. The leading theory is that the condition involves reduced perfusion due to chronic edema, resulting in neovascularization, fibroblast proliferation, hypertrophy, and inflammatory skin changes. When AAD occurs in the setting of a suction socket prosthesis, the negative pressure of the stump-socket environment is thought to alter local circulation, leading to proliferation of small blood vessels.5,13
Stewart-Bluefarb syndrome usually involves a single extremity in young adults with congenital arteriovenous malformations, amputees, and individuals with hemiplegia or iatrogenic arteriovenous fistulae (as in patient 2).1 It was once thought to occur secondary to Klippel-Trenaunay-Weber syndrome; however, SBS rarely is accompanied by limb hypertrophy.9 Pathogenesis is thought to involve an angiogenic response to a high perfusion rate and high oxygen saturation, which leads to fibroblast proliferation and reactive endothelial hyperplasia.1,14
Diagnosis and Differential Diagnosis
Prompt identification of an underlying arteriovenous anomaly is critical, given the sequelae of high-flow shunts, which may result in skin ulceration, limb length discrepancy, cortical thinning of bone with regional osteoporosis, and congestive heart failure.1,5 Duplex ultrasonography is the first-line diagnostic modality because it is noninvasive and widely available. The key doppler feature of an arteriovenous malformation is low resistance and high diastolic pulsatile flow,1 which should be confirmed with magnetic resonance angiography or computed tomography angiography if present on ultrasonography.
The differential diagnosis of AAD includes Kaposi sarcoma, reactive angioendotheliomatosis, diffuse dermal angiomatosis, intravascular histiocytosis, glomeruloid angioendotheliomatosis, and angiopericytomatosis.15,16 These entities present as multiple erythematous, violaceous, purpuric patches and plaques generally on the extremities but can have a widely varied distribution. Some lesions evolve to necrosis or ulceration. Histopathologic analysis is useful to differentiate these entities.
Histopathology
The histopathologic features of AAD can be nonspecific; clinicopathologic correlation often is necessary to establish the diagnosis. Features include a proliferation of small thick-walled vessels, often in a lobular arrangement, in an edematous papillary dermis. Small thrombi may be observed. There may be increased fibroblasts; plump endothelial cells; a superficial mixed infiltrate comprised of lymphocytes, histiocytes, and eosinophils; and deposition of hemosiderin.2,5 These characteristics overlap with features of Kaposi sarcoma; AAD, however, lacks slitlike vascular spaces, perivascular CD34+ expression, and nuclear atypia. A negative HHV-8 stain will assist in ruling out Kaposi sarcoma.1,17
Management
Treatment reports are anecdotal. The goal is to correct underlying venous hypertension. Conservative measures with compression garments, intermittent pneumatic compression, and limb elevation are first line.18 Oral antibiotics and local wound care with topical emollients and corticosteroids have been shown to be effective treatments.19-21
Oral erythromycin 500 mg 4 times daily for 3 weeks and clobetasol propionate cream 0.05% healed a lower extremity ulcer in a patient with Mali-type AAD.21 In another patient, conservative treatment of Mali-type AAD failed, but rapid improvement of 2 lower extremity ulcers resulted after 3 weeks of oral dapsone 50 mg twice daily.22
Conclusion
Acroangiodermatitis is a rare entity that is characterized by erythematous violaceous papules and plaques of the extremities, commonly in the setting of chronic venous insufficiency or an arteriovenous shunt. Histopathologic analysis shows proliferation of capillaries with fibrosis, extravasation of erythrocytes, and deposition of hemosiderin without the spindle cells and slitlike vascular spaces characteristic of Kaposi sarcoma. Detection of an underlying arteriovenous malformation is essential, as the disease can have local and systemic consequences, such as skin ulceration and congestive heart failure.1 Treatment options are conservative, directed toward local wound care, compression, and management of complications, such as ulceration and infection, as well as obliterating any underlying arteriovenous malformation.
Case Reports
Patient 1
A 56-year-old white man with a history of hypertension, hyperlipidemia, sleep apnea, bilateral knee replacement, and cataract removal presented to the emergency department with a worsening rash on the left posterior medial leg of 6 months’ duration. He reported associated redness and tenderness with the plaques as well as increased swelling and firmness of the leg. He was admitted to the hospital where the infectious disease team treated him with cefazolin for presumed cellulitis. His condition did not improve, and another course of cefazolin was started in addition to oral fluconazole and clotrimazole–betamethasone dipropionate lotion for a possible fungal cause. Again, treatment provided no improvement.
He was then evaluated by dermatology. On physical examination, the patient had edema, warmth, and induration of the left lower leg. There also was an annular and serpiginous indurated plaque with minimal scale on the left lower leg (Figure 1). A firm, dark red to purple plaque on the left medial thigh with mild scale was present. There also was scaling of the right plantar foot.

Skin biopsy revealed a dermal capillary proliferation with a scattering of inflammatory cells including eosinophils as well as dermal fibrosis (Figure 2). Periodic acid–Schiff and human herpesvirus 8 (HHV-8) immunostains were negative. Considering the degree and depth of vascular proliferation, Mali-type acroangiodermatitis (AAD) was the favored diagnosis.
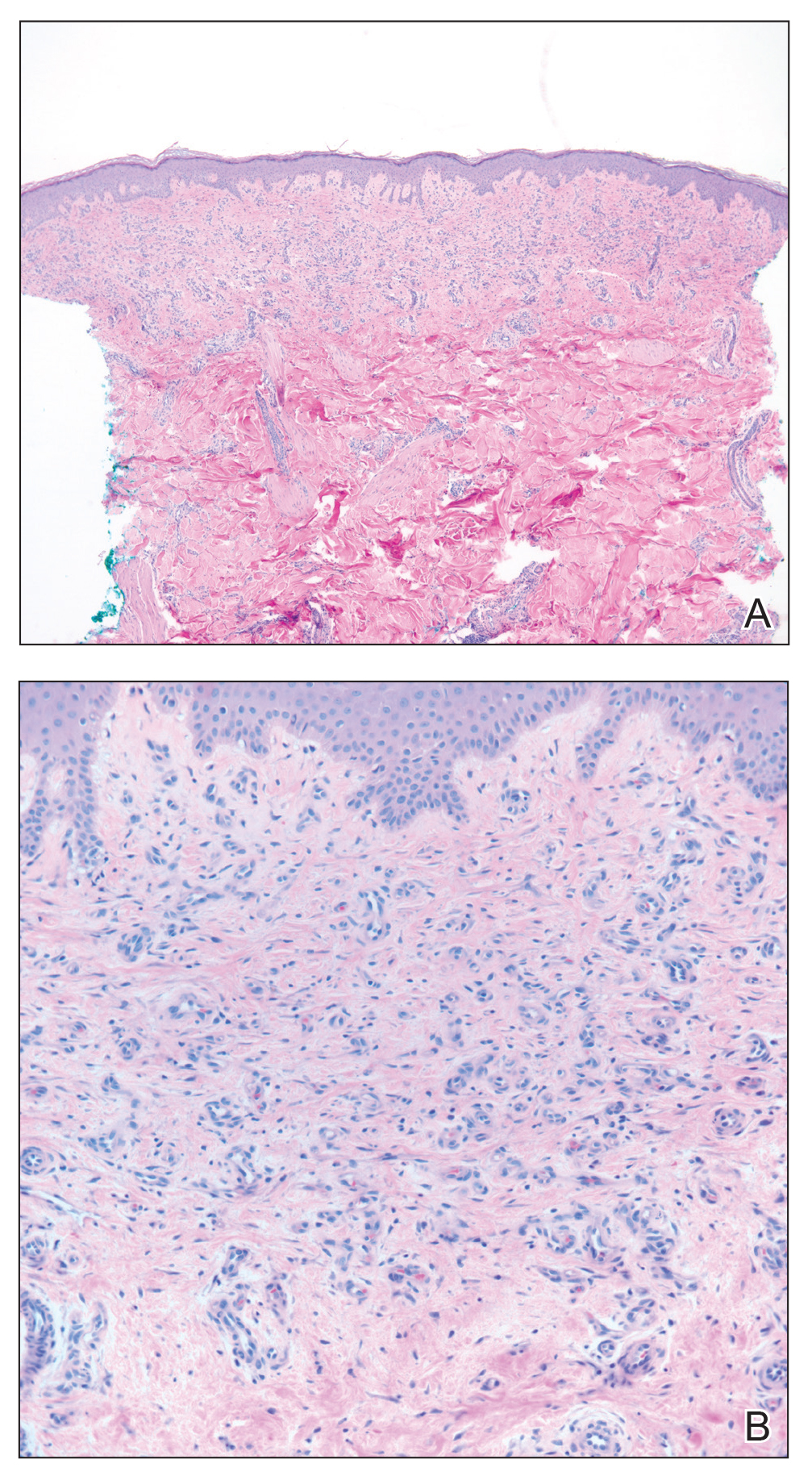
Patient 2
A 72-year-old white man presented with a firm asymptomatic growth on the left dorsal forearm of 3 months’ duration. It was located near the site of a prior squamous cell carcinoma that was excised 1 year prior to presentation. The patient had no treatment or biopsy of the presenting lesion. His medical and surgical history included polycystic kidney disease and renal transplantation 4 years prior to presentation. He also had an arteriovenous fistula of the left arm. His other chronic diseases included chronic obstructive lung disease, congestive heart failure, hypertension, type 2 diabetes mellitus, and obstructive sleep apnea.
On physical examination, the patient had a 1-cm violaceous nodule on the extensor surface of the left mid forearm. An arteriovenous fistula was present proximal to the lesion on the left arm (Figure 3).

Skin biopsy revealed a tightly packed proliferation of small vascular channels that tested negative for HHV-8, tumor protein p63, and cytokeratin 5/6. Erythrocytes were noted in the lumen of some of these vessels. Neutrophils were scattered and clustered throughout the specimen (Figure 4A). Blood vessels were highlighted with CD34 (Figure 4B). Grocott-Gomori methenamine-silver stain was negative for infectious agents. These findings favored AAD secondary to an arteriovenous malformation, consistent with Stewart-Bluefarb syndrome (SBS).
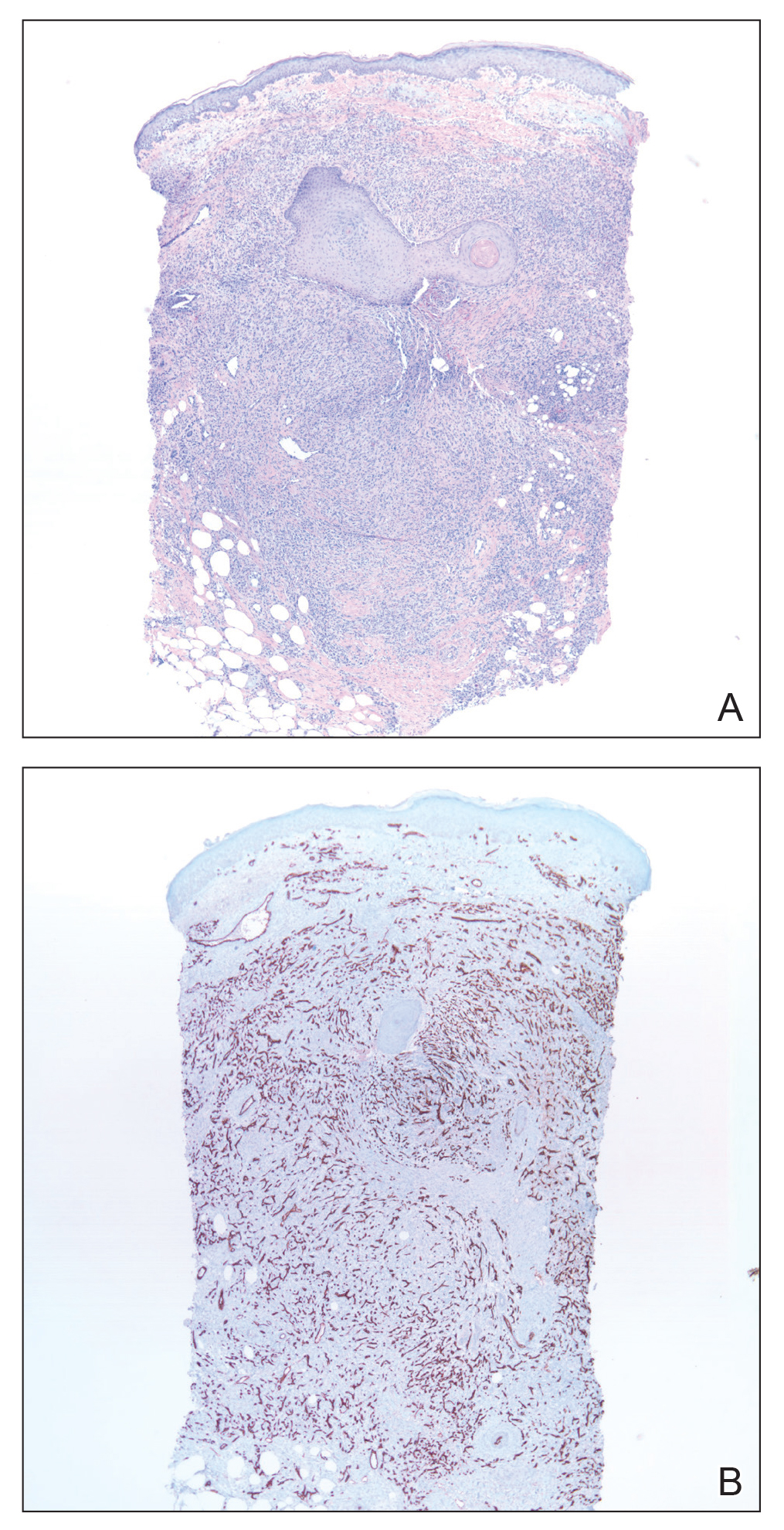
Comment
Presentation of AAD
Acroangiodermatitis is a rare chronic inflammatory skin process involving a reactive proliferation of capillaries and fibrosis of the skin that resembles Kaposi sarcoma both clinically and histopathologically. The condition has been reported in patients with chronic venous insufficiency,1 congenital arteriovenous malformation,2 acquired iatrogenic arteriovenous fistula,3 paralyzed extremity,4 suction socket lower limb prosthesis (amputees),5 and minor trauma.6-8 The lesions of AAD tend to be circumscribed, slowly evolving, red-violaceous (or brown or dusky) macules, papules, or plaques that may become verrucous or develop into painful ulcerations. They generally occur on the distal dorsal aspects of the lower legs and feet.110
Variants of AAD
Mali et al9 first reported cutaneous manifestations resembling Kaposi sarcoma in 18 patients with chronic venous insufficiency in 1965. Two years later, Bluefarb and Adams10 described kaposiform skin lesions in one patient with a congenital arteriovenous malformation without chronic venous insufficiency. It was not until 1974, however, that Earhart et al11 proposed the term pseudo-Kaposi sarcoma.10,11 Based on these findings, AAD is described as 2 variants: Mali type and SBS.
Mali-type AAD is more common and typically occurs in elderly men. It classically presents bilaterally on the lower extremities in association with severe chronic venous insufficiency.5 Skin lesions usually occur on the medial aspect of the lower legs (as in patient 1), dorsum of the heel, hallux, or second toe.12
The etiology of Mali-type AAD is poorly understood. The leading theory is that the condition involves reduced perfusion due to chronic edema, resulting in neovascularization, fibroblast proliferation, hypertrophy, and inflammatory skin changes. When AAD occurs in the setting of a suction socket prosthesis, the negative pressure of the stump-socket environment is thought to alter local circulation, leading to proliferation of small blood vessels.5,13
Stewart-Bluefarb syndrome usually involves a single extremity in young adults with congenital arteriovenous malformations, amputees, and individuals with hemiplegia or iatrogenic arteriovenous fistulae (as in patient 2).1 It was once thought to occur secondary to Klippel-Trenaunay-Weber syndrome; however, SBS rarely is accompanied by limb hypertrophy.9 Pathogenesis is thought to involve an angiogenic response to a high perfusion rate and high oxygen saturation, which leads to fibroblast proliferation and reactive endothelial hyperplasia.1,14
Diagnosis and Differential Diagnosis
Prompt identification of an underlying arteriovenous anomaly is critical, given the sequelae of high-flow shunts, which may result in skin ulceration, limb length discrepancy, cortical thinning of bone with regional osteoporosis, and congestive heart failure.1,5 Duplex ultrasonography is the first-line diagnostic modality because it is noninvasive and widely available. The key doppler feature of an arteriovenous malformation is low resistance and high diastolic pulsatile flow,1 which should be confirmed with magnetic resonance angiography or computed tomography angiography if present on ultrasonography.
The differential diagnosis of AAD includes Kaposi sarcoma, reactive angioendotheliomatosis, diffuse dermal angiomatosis, intravascular histiocytosis, glomeruloid angioendotheliomatosis, and angiopericytomatosis.15,16 These entities present as multiple erythematous, violaceous, purpuric patches and plaques generally on the extremities but can have a widely varied distribution. Some lesions evolve to necrosis or ulceration. Histopathologic analysis is useful to differentiate these entities.
Histopathology
The histopathologic features of AAD can be nonspecific; clinicopathologic correlation often is necessary to establish the diagnosis. Features include a proliferation of small thick-walled vessels, often in a lobular arrangement, in an edematous papillary dermis. Small thrombi may be observed. There may be increased fibroblasts; plump endothelial cells; a superficial mixed infiltrate comprised of lymphocytes, histiocytes, and eosinophils; and deposition of hemosiderin.2,5 These characteristics overlap with features of Kaposi sarcoma; AAD, however, lacks slitlike vascular spaces, perivascular CD34+ expression, and nuclear atypia. A negative HHV-8 stain will assist in ruling out Kaposi sarcoma.1,17
Management
Treatment reports are anecdotal. The goal is to correct underlying venous hypertension. Conservative measures with compression garments, intermittent pneumatic compression, and limb elevation are first line.18 Oral antibiotics and local wound care with topical emollients and corticosteroids have been shown to be effective treatments.19-21
Oral erythromycin 500 mg 4 times daily for 3 weeks and clobetasol propionate cream 0.05% healed a lower extremity ulcer in a patient with Mali-type AAD.21 In another patient, conservative treatment of Mali-type AAD failed, but rapid improvement of 2 lower extremity ulcers resulted after 3 weeks of oral dapsone 50 mg twice daily.22
Conclusion
Acroangiodermatitis is a rare entity that is characterized by erythematous violaceous papules and plaques of the extremities, commonly in the setting of chronic venous insufficiency or an arteriovenous shunt. Histopathologic analysis shows proliferation of capillaries with fibrosis, extravasation of erythrocytes, and deposition of hemosiderin without the spindle cells and slitlike vascular spaces characteristic of Kaposi sarcoma. Detection of an underlying arteriovenous malformation is essential, as the disease can have local and systemic consequences, such as skin ulceration and congestive heart failure.1 Treatment options are conservative, directed toward local wound care, compression, and management of complications, such as ulceration and infection, as well as obliterating any underlying arteriovenous malformation.
- Parsi K, O’Connor AA, Bester L. Stewart-Bluefarb syndrome: report of five cases and a review of literature. Phlebology. 2015;30:505-514.
- Larralde M, Gonzalez V, Marietti R, et al. Pseudo-Kaposi sarcoma with arteriovenous malformation. Pediatr Dermatol. 2001;18:325-327.
- Nakanishi G, Tachibana T, Soga H, et al. Pseudo-Kaposi’s sarcoma of the hand associated with acquired iatrogenic arteriovenous fistula. Indian J Dermatol. 2014;59:415-416.
- Landthaler M, Langehenke H, Holzmann H, et al. Mali’s acroangiodermatitis (pseudo-Kaposi) in paralyzed legs. Hautarzt. 1988;39:304-307.
- Trindade F, Requena L. Pseudo-Kaposi’s sarcoma because of suction socket lower limb prosthesis. J Cutan Pathol. 2009;36:482-485.
- Yu-Lu W, Tao Q, Hong-Zhong J, et al. Non-tender pedal plaques and nodules: pseudo-Kaposi’s sarcoma (Stewart-Bluefarb type) induced by trauma. J Dtsch Dermatol Ges. 2015;13:927-930.
- Del-Río E, Aguilar A, Ambrojo P, et al. Pseudo-Kaposi sarcoma induced by minor trauma in a patient with Klippel-Trenaunay-Weber syndrome. Clin Exp Dermatol. 1993;18:151-153.
- Archie M, Khademi S, Aungst D, et al. A rare case of acroangiodermatitis associated with a congenital arteriovenous malformation (Stewart-Bluefarb Syndrome) in a young veteran: case report and review of the literature. Ann Vasc Surg. 2015;29:1448.e5-1448.e10.
- Mali JW, Kuiper JP, Hamers AA. Acro-angiodermatitis of the foot. Arch Dermatol. 1965;92:515-518.
- Bluefarb SM, Adams LA. Arteriovenous malformation with angiodermatitis. stasis dermatitis simulating Kaposi’s disease. Arch Dermatol. 1967;96:176-181.
- Earhart RN, Aeling JA, Nuss DD, et al. Pseudo-Kaposi sarcoma. A patient with arteriovenous malformation and skin lesions simulating Kaposi sarcoma. Arch Dermatol. 1974;110:907-910.
- Lugovic´ L, Pusic´ J, Situm M, et al. Acroangiodermatitis (pseudo-Kaposi sarcoma): three case reports. Acta Dermatovenerol Croat. 2007;15:152-157.
- Horiguchi Y, Takahashi K, Tanizaki H, et al. Case of bilateral acroangiodermatitis due to symmetrical arteriovenous fistulas of the soles. J Dermatol. 2015;42:989-991.
- Dog˘an S, Boztepe G, Karaduman A. Pseudo-Kaposi sarcoma: a challenging vascular phenomenon. Dermatol Online J. 2007;13:22.
- Mazloom SE, Stallings A, Kyei A. Differentiating intralymphatic histiocytosis, intravascular histiocytosis, and subtypes of reactive angioendotheliomatosis: review of clinical and histologic features of all cases reported to date. Am J Dermatopathol. 2017;39:33-39.
- Rongioletti F, Rebora A. Cutaneous reactive angiomatoses: patterns and classification of reactive vascular proliferation. J Am Acad Dermatol. 2003;49:887-896.
- Kanitakis J, Narvaez D, Claudy A. Expression of the CD34 antigen distinguishes Kaposi’s sarcoma from pseudo-Kaposi’s sarcoma (acroangiodermatitis). Br J Dermatol. 1996;134:44-46.
- Pires A, Depairon M, Ricci C, et al. Effect of compression therapy on a pseudo-Kaposi sarcoma. Dermatology. 1999;198:439-441.
- Hayek S, Atiyeh B, Zgheib E. Stewart-Bluefarb syndrome: review of the literature and case report of chronic ulcer treatment with heparan sulphate (Cacipliq20®). Int Wound J. 2015;12:169-172.
- Varyani N, Thukral A, Kumar N, et al. Nonhealing ulcer: acroangiodermatitis of Mali. Case Rep Dermatol Med. 2011;2011:909383.
- Mehta AA, Pereira RR, Nayak C, et al. Acroangiodermatitis of Mali: a rare vascular phenomenon. Indian J Dermatol Venereol Leprol. 2010;76:553-556.
- Rashkovsky I, Gilead L, Schamroth J, et al. Acro-angiodermatitis: review of the literature and report of a case. Acta Derm Venereol. 1995;75:475-478.
- Parsi K, O’Connor AA, Bester L. Stewart-Bluefarb syndrome: report of five cases and a review of literature. Phlebology. 2015;30:505-514.
- Larralde M, Gonzalez V, Marietti R, et al. Pseudo-Kaposi sarcoma with arteriovenous malformation. Pediatr Dermatol. 2001;18:325-327.
- Nakanishi G, Tachibana T, Soga H, et al. Pseudo-Kaposi’s sarcoma of the hand associated with acquired iatrogenic arteriovenous fistula. Indian J Dermatol. 2014;59:415-416.
- Landthaler M, Langehenke H, Holzmann H, et al. Mali’s acroangiodermatitis (pseudo-Kaposi) in paralyzed legs. Hautarzt. 1988;39:304-307.
- Trindade F, Requena L. Pseudo-Kaposi’s sarcoma because of suction socket lower limb prosthesis. J Cutan Pathol. 2009;36:482-485.
- Yu-Lu W, Tao Q, Hong-Zhong J, et al. Non-tender pedal plaques and nodules: pseudo-Kaposi’s sarcoma (Stewart-Bluefarb type) induced by trauma. J Dtsch Dermatol Ges. 2015;13:927-930.
- Del-Río E, Aguilar A, Ambrojo P, et al. Pseudo-Kaposi sarcoma induced by minor trauma in a patient with Klippel-Trenaunay-Weber syndrome. Clin Exp Dermatol. 1993;18:151-153.
- Archie M, Khademi S, Aungst D, et al. A rare case of acroangiodermatitis associated with a congenital arteriovenous malformation (Stewart-Bluefarb Syndrome) in a young veteran: case report and review of the literature. Ann Vasc Surg. 2015;29:1448.e5-1448.e10.
- Mali JW, Kuiper JP, Hamers AA. Acro-angiodermatitis of the foot. Arch Dermatol. 1965;92:515-518.
- Bluefarb SM, Adams LA. Arteriovenous malformation with angiodermatitis. stasis dermatitis simulating Kaposi’s disease. Arch Dermatol. 1967;96:176-181.
- Earhart RN, Aeling JA, Nuss DD, et al. Pseudo-Kaposi sarcoma. A patient with arteriovenous malformation and skin lesions simulating Kaposi sarcoma. Arch Dermatol. 1974;110:907-910.
- Lugovic´ L, Pusic´ J, Situm M, et al. Acroangiodermatitis (pseudo-Kaposi sarcoma): three case reports. Acta Dermatovenerol Croat. 2007;15:152-157.
- Horiguchi Y, Takahashi K, Tanizaki H, et al. Case of bilateral acroangiodermatitis due to symmetrical arteriovenous fistulas of the soles. J Dermatol. 2015;42:989-991.
- Dog˘an S, Boztepe G, Karaduman A. Pseudo-Kaposi sarcoma: a challenging vascular phenomenon. Dermatol Online J. 2007;13:22.
- Mazloom SE, Stallings A, Kyei A. Differentiating intralymphatic histiocytosis, intravascular histiocytosis, and subtypes of reactive angioendotheliomatosis: review of clinical and histologic features of all cases reported to date. Am J Dermatopathol. 2017;39:33-39.
- Rongioletti F, Rebora A. Cutaneous reactive angiomatoses: patterns and classification of reactive vascular proliferation. J Am Acad Dermatol. 2003;49:887-896.
- Kanitakis J, Narvaez D, Claudy A. Expression of the CD34 antigen distinguishes Kaposi’s sarcoma from pseudo-Kaposi’s sarcoma (acroangiodermatitis). Br J Dermatol. 1996;134:44-46.
- Pires A, Depairon M, Ricci C, et al. Effect of compression therapy on a pseudo-Kaposi sarcoma. Dermatology. 1999;198:439-441.
- Hayek S, Atiyeh B, Zgheib E. Stewart-Bluefarb syndrome: review of the literature and case report of chronic ulcer treatment with heparan sulphate (Cacipliq20®). Int Wound J. 2015;12:169-172.
- Varyani N, Thukral A, Kumar N, et al. Nonhealing ulcer: acroangiodermatitis of Mali. Case Rep Dermatol Med. 2011;2011:909383.
- Mehta AA, Pereira RR, Nayak C, et al. Acroangiodermatitis of Mali: a rare vascular phenomenon. Indian J Dermatol Venereol Leprol. 2010;76:553-556.
- Rashkovsky I, Gilead L, Schamroth J, et al. Acro-angiodermatitis: review of the literature and report of a case. Acta Derm Venereol. 1995;75:475-478.
Practice Points
- Acroangiodermatitis (AAD) may mimic Kaposi sarcoma clinically and histopathologically. A human herpesvirus 8 stain is helpful to differentiate these two entities.
- Diagnosis of AAD should prompt investigation of an underlying arteriovenous malformation, as the disease may have systemic consequences such as congestive heart failure.






