User login
Collagen filler succeeds against acne scars
SAN DIEGO – An injectable collagen-based filler significantly outperformed saline placebo for treating acne scars, with durable effects at 12 months, according to a randomized, double-blind crossover trial of 147 adults.
The study “successfully demonstrates the effectiveness and safety of polymethylmethacrylate in atrophic acne scars,” said Dr. James Spencer, who conducted the research while at Mount Sinai School of Medicine in New York. Dr. Spencer is now in private practice in St. Petersburg, Fla.
Six months after treatment, 64% of patients who received the polymethylmethacrylate-collagen filler (or PMMA) had at least half their scars improve by at least 2 points on an acne rating scale, Dr. Spencer and his associates said at the annual meeting of the American Society for Dermatologic Surgery. Only 32% of the control group achieved that result (P = .0005). Response rates for the filler were 61% at 9 months and 70% at 12 months, and “crossover subjects subsequently treated with PMMA collagen showed similar response levels,” they said.
The PMMA-collagen filler is easy to administer; “works well on deep, severe scars; and should also work very well on shallow scars,” the researchers noted. The treatment “may enable practitioners to effectively treat acne scarring with no need for capital equipment expenditure or the risks associated with resurfacing procedures,” they said.
About 61% of patients in the study were female, participants averaged 44 years of age, and 20% were Fitzpatrick skin type V or VI. To enter the study, participants had to have at least four facial acne scars that were soft contoured, rolling, distensible, and rated moderate to severe (3-4) on a 4-point acne rating scale.
The patients were treated every 2 weeks for a month, and again at months 3 and 6. At 6 months, patients in the placebo group crossed over and received the filler, and all patients were followed for another 6 months.
Adverse effects were uncommon and included mild transient pain at the injection site, swelling, bruising, and acne, the researchers said. “There was no evidence of granulomas, changes in pigmentation, or hypertrophic scarring,” they added.
No funding source was reported for the study. Dr. Spencer and his coauthors reported financial relationships with Photomedex, Genentech, and Leo Pharma.
SAN DIEGO – An injectable collagen-based filler significantly outperformed saline placebo for treating acne scars, with durable effects at 12 months, according to a randomized, double-blind crossover trial of 147 adults.
The study “successfully demonstrates the effectiveness and safety of polymethylmethacrylate in atrophic acne scars,” said Dr. James Spencer, who conducted the research while at Mount Sinai School of Medicine in New York. Dr. Spencer is now in private practice in St. Petersburg, Fla.
Six months after treatment, 64% of patients who received the polymethylmethacrylate-collagen filler (or PMMA) had at least half their scars improve by at least 2 points on an acne rating scale, Dr. Spencer and his associates said at the annual meeting of the American Society for Dermatologic Surgery. Only 32% of the control group achieved that result (P = .0005). Response rates for the filler were 61% at 9 months and 70% at 12 months, and “crossover subjects subsequently treated with PMMA collagen showed similar response levels,” they said.
The PMMA-collagen filler is easy to administer; “works well on deep, severe scars; and should also work very well on shallow scars,” the researchers noted. The treatment “may enable practitioners to effectively treat acne scarring with no need for capital equipment expenditure or the risks associated with resurfacing procedures,” they said.
About 61% of patients in the study were female, participants averaged 44 years of age, and 20% were Fitzpatrick skin type V or VI. To enter the study, participants had to have at least four facial acne scars that were soft contoured, rolling, distensible, and rated moderate to severe (3-4) on a 4-point acne rating scale.
The patients were treated every 2 weeks for a month, and again at months 3 and 6. At 6 months, patients in the placebo group crossed over and received the filler, and all patients were followed for another 6 months.
Adverse effects were uncommon and included mild transient pain at the injection site, swelling, bruising, and acne, the researchers said. “There was no evidence of granulomas, changes in pigmentation, or hypertrophic scarring,” they added.
No funding source was reported for the study. Dr. Spencer and his coauthors reported financial relationships with Photomedex, Genentech, and Leo Pharma.
SAN DIEGO – An injectable collagen-based filler significantly outperformed saline placebo for treating acne scars, with durable effects at 12 months, according to a randomized, double-blind crossover trial of 147 adults.
The study “successfully demonstrates the effectiveness and safety of polymethylmethacrylate in atrophic acne scars,” said Dr. James Spencer, who conducted the research while at Mount Sinai School of Medicine in New York. Dr. Spencer is now in private practice in St. Petersburg, Fla.
Six months after treatment, 64% of patients who received the polymethylmethacrylate-collagen filler (or PMMA) had at least half their scars improve by at least 2 points on an acne rating scale, Dr. Spencer and his associates said at the annual meeting of the American Society for Dermatologic Surgery. Only 32% of the control group achieved that result (P = .0005). Response rates for the filler were 61% at 9 months and 70% at 12 months, and “crossover subjects subsequently treated with PMMA collagen showed similar response levels,” they said.
The PMMA-collagen filler is easy to administer; “works well on deep, severe scars; and should also work very well on shallow scars,” the researchers noted. The treatment “may enable practitioners to effectively treat acne scarring with no need for capital equipment expenditure or the risks associated with resurfacing procedures,” they said.
About 61% of patients in the study were female, participants averaged 44 years of age, and 20% were Fitzpatrick skin type V or VI. To enter the study, participants had to have at least four facial acne scars that were soft contoured, rolling, distensible, and rated moderate to severe (3-4) on a 4-point acne rating scale.
The patients were treated every 2 weeks for a month, and again at months 3 and 6. At 6 months, patients in the placebo group crossed over and received the filler, and all patients were followed for another 6 months.
Adverse effects were uncommon and included mild transient pain at the injection site, swelling, bruising, and acne, the researchers said. “There was no evidence of granulomas, changes in pigmentation, or hypertrophic scarring,” they added.
No funding source was reported for the study. Dr. Spencer and his coauthors reported financial relationships with Photomedex, Genentech, and Leo Pharma.
Key clinical point: A collagen-based filler significantly improved the appearance of acne scars in adults, with persistent improvement at 12 months.
Major finding: At 6-month evaluation, 64% of the intervention group were considered responders, compared with 32% of the control group (P = .0005).
Data source: A prospective, randomized, double-blind, controlled, multicenter crossover study of 147 adults with acne scars.
Disclosures: The researchers did not report funding sources. Dr. Spencer and his coauthors reported financial relationships with Photomedex, Genentech, and Leo Pharma.
Fractional laser technology reduces facial acne scarring
Fractional laser technology, often used in the removal of unwanted tattoos, can improve the appearance and texture of facial acne scars, based on data published online Nov.19 in JAMA Dermatology.
“The evolution from traditional nanosecond to picosecond lasers has been observed to produce a photomechanical effect that causes fragmentation of tattoo ink or pigment,” wrote Dr. Jeremy A. Brauer, a dermatologist in group practice in New York, and his coinvestigators. “An innovative optical attachment for the picosecond laser, a diffractive lens array, has been developed that gauges distribution of energy to the treatment area. This specialized optic affects more surface area, has a greater pattern density per pulse, and may improve the appearance of acne scars,” they reported.
In a single-center, prospective study, Dr. Brauer and his associates enrolled 20 patients – 15 women and 5 men – based on screenings to ensure no history of skin cancer, keloidal scarring, localized or active infection, immunodeficiency disorders, and light hypersensitivity or use of medications with known phototoxic effects. Of that initial group, 17 completed all six treatments and presented for follow-up visits at 1 and 3 months. Patients were aged 27-66 (mean age, 44 years), and included Fitzpatrick skin types I (one patient), II (seven patients), III (six patients), and IV (three patients).
Subjects mostly had rolling-type scars, boxcar scars, and icepick lesions related to acne. Each subject underwent six treatments with a 755-nanometer alexandrite picosecond laser with a diffractive lens array; each treatment occurred every 4-8 weeks.
Subjects also provided a subjective score for pain experienced during each treatment on a scale of 0 (no pain) to 10 (extreme pain). The patients also used a scale of 0-4 to indicate their satisfaction with improvement of overall skin appearance and texture prior to their final treatment, at the 1-month follow-up, and at the 3-month follow-up (with 0 being total dissatisfaction and 4 total satisfaction).
At the 1-month and 3-month follow-ups, three independent dermatologists gave masked evaluations of each patient’s improvement on a 4-point scale, with 0 = 0%-25%, 1 = 26%-50%, 3 = 51%-75%, and 4 = 76%-100%.
All patients were either “satisfied” or “extremely satisfied” with the appearance and texture of their facial skin after receiving the full treatment regimen, and recorded an average pain score of 2.83 out of 10. The masked assessment scores also were favorable, averaging 1.5 of 3 and 1.4 of 3 at the 1-month and 3-month follow-ups, with a score of 0 indicating 0-25% improvement and a score of 3, greater than 75% improvement, the researchers reported.
Dr. Brauer and his associates also evaluated three-dimensional volumetric data for each subject, which showed an average of 24.0% improvement in scar volume at the 1-month follow-up and 27.2% at the 3-month follow-up. Furthermore, histologic analysis revealed elongation and increased density of elastic fibers, as well as an increase in dermal collagen and mucin.
“This is the first study, to our knowledge, that demonstrates favorable clinical outcomes in acne scar management with the 755[-nm] picosecond laser and diffractive lens array,” the researchers noted. “Observed improvement in pigmentation and texture of the surrounding skin suggests that there may be benefits for indications beyond scarring,” they wrote.
The authors disclosed that funding for this study was provided in part by Cynosure, manufacturer of the Food and Drug Administration–approved 755-nm picosecond alexandrite laser used in the study, and noted that “Cynosure had a role in the design of the study but not the conduct, collection, management, analysis, or interpretation of data. They approved the manuscript but did not prepare or decide to submit.” Dr. Brauer disclosed receiving honoraria from Cynosure/Palomar Medical Technologies and consulting for Miramar. Several other coauthors disclosed financial relationships with multiple companies, including Cynosure/Palomar Medical Technologies.
Fractional laser technology, often used in the removal of unwanted tattoos, can improve the appearance and texture of facial acne scars, based on data published online Nov.19 in JAMA Dermatology.
“The evolution from traditional nanosecond to picosecond lasers has been observed to produce a photomechanical effect that causes fragmentation of tattoo ink or pigment,” wrote Dr. Jeremy A. Brauer, a dermatologist in group practice in New York, and his coinvestigators. “An innovative optical attachment for the picosecond laser, a diffractive lens array, has been developed that gauges distribution of energy to the treatment area. This specialized optic affects more surface area, has a greater pattern density per pulse, and may improve the appearance of acne scars,” they reported.
In a single-center, prospective study, Dr. Brauer and his associates enrolled 20 patients – 15 women and 5 men – based on screenings to ensure no history of skin cancer, keloidal scarring, localized or active infection, immunodeficiency disorders, and light hypersensitivity or use of medications with known phototoxic effects. Of that initial group, 17 completed all six treatments and presented for follow-up visits at 1 and 3 months. Patients were aged 27-66 (mean age, 44 years), and included Fitzpatrick skin types I (one patient), II (seven patients), III (six patients), and IV (three patients).
Subjects mostly had rolling-type scars, boxcar scars, and icepick lesions related to acne. Each subject underwent six treatments with a 755-nanometer alexandrite picosecond laser with a diffractive lens array; each treatment occurred every 4-8 weeks.
Subjects also provided a subjective score for pain experienced during each treatment on a scale of 0 (no pain) to 10 (extreme pain). The patients also used a scale of 0-4 to indicate their satisfaction with improvement of overall skin appearance and texture prior to their final treatment, at the 1-month follow-up, and at the 3-month follow-up (with 0 being total dissatisfaction and 4 total satisfaction).
At the 1-month and 3-month follow-ups, three independent dermatologists gave masked evaluations of each patient’s improvement on a 4-point scale, with 0 = 0%-25%, 1 = 26%-50%, 3 = 51%-75%, and 4 = 76%-100%.
All patients were either “satisfied” or “extremely satisfied” with the appearance and texture of their facial skin after receiving the full treatment regimen, and recorded an average pain score of 2.83 out of 10. The masked assessment scores also were favorable, averaging 1.5 of 3 and 1.4 of 3 at the 1-month and 3-month follow-ups, with a score of 0 indicating 0-25% improvement and a score of 3, greater than 75% improvement, the researchers reported.
Dr. Brauer and his associates also evaluated three-dimensional volumetric data for each subject, which showed an average of 24.0% improvement in scar volume at the 1-month follow-up and 27.2% at the 3-month follow-up. Furthermore, histologic analysis revealed elongation and increased density of elastic fibers, as well as an increase in dermal collagen and mucin.
“This is the first study, to our knowledge, that demonstrates favorable clinical outcomes in acne scar management with the 755[-nm] picosecond laser and diffractive lens array,” the researchers noted. “Observed improvement in pigmentation and texture of the surrounding skin suggests that there may be benefits for indications beyond scarring,” they wrote.
The authors disclosed that funding for this study was provided in part by Cynosure, manufacturer of the Food and Drug Administration–approved 755-nm picosecond alexandrite laser used in the study, and noted that “Cynosure had a role in the design of the study but not the conduct, collection, management, analysis, or interpretation of data. They approved the manuscript but did not prepare or decide to submit.” Dr. Brauer disclosed receiving honoraria from Cynosure/Palomar Medical Technologies and consulting for Miramar. Several other coauthors disclosed financial relationships with multiple companies, including Cynosure/Palomar Medical Technologies.
Fractional laser technology, often used in the removal of unwanted tattoos, can improve the appearance and texture of facial acne scars, based on data published online Nov.19 in JAMA Dermatology.
“The evolution from traditional nanosecond to picosecond lasers has been observed to produce a photomechanical effect that causes fragmentation of tattoo ink or pigment,” wrote Dr. Jeremy A. Brauer, a dermatologist in group practice in New York, and his coinvestigators. “An innovative optical attachment for the picosecond laser, a diffractive lens array, has been developed that gauges distribution of energy to the treatment area. This specialized optic affects more surface area, has a greater pattern density per pulse, and may improve the appearance of acne scars,” they reported.
In a single-center, prospective study, Dr. Brauer and his associates enrolled 20 patients – 15 women and 5 men – based on screenings to ensure no history of skin cancer, keloidal scarring, localized or active infection, immunodeficiency disorders, and light hypersensitivity or use of medications with known phototoxic effects. Of that initial group, 17 completed all six treatments and presented for follow-up visits at 1 and 3 months. Patients were aged 27-66 (mean age, 44 years), and included Fitzpatrick skin types I (one patient), II (seven patients), III (six patients), and IV (three patients).
Subjects mostly had rolling-type scars, boxcar scars, and icepick lesions related to acne. Each subject underwent six treatments with a 755-nanometer alexandrite picosecond laser with a diffractive lens array; each treatment occurred every 4-8 weeks.
Subjects also provided a subjective score for pain experienced during each treatment on a scale of 0 (no pain) to 10 (extreme pain). The patients also used a scale of 0-4 to indicate their satisfaction with improvement of overall skin appearance and texture prior to their final treatment, at the 1-month follow-up, and at the 3-month follow-up (with 0 being total dissatisfaction and 4 total satisfaction).
At the 1-month and 3-month follow-ups, three independent dermatologists gave masked evaluations of each patient’s improvement on a 4-point scale, with 0 = 0%-25%, 1 = 26%-50%, 3 = 51%-75%, and 4 = 76%-100%.
All patients were either “satisfied” or “extremely satisfied” with the appearance and texture of their facial skin after receiving the full treatment regimen, and recorded an average pain score of 2.83 out of 10. The masked assessment scores also were favorable, averaging 1.5 of 3 and 1.4 of 3 at the 1-month and 3-month follow-ups, with a score of 0 indicating 0-25% improvement and a score of 3, greater than 75% improvement, the researchers reported.
Dr. Brauer and his associates also evaluated three-dimensional volumetric data for each subject, which showed an average of 24.0% improvement in scar volume at the 1-month follow-up and 27.2% at the 3-month follow-up. Furthermore, histologic analysis revealed elongation and increased density of elastic fibers, as well as an increase in dermal collagen and mucin.
“This is the first study, to our knowledge, that demonstrates favorable clinical outcomes in acne scar management with the 755[-nm] picosecond laser and diffractive lens array,” the researchers noted. “Observed improvement in pigmentation and texture of the surrounding skin suggests that there may be benefits for indications beyond scarring,” they wrote.
The authors disclosed that funding for this study was provided in part by Cynosure, manufacturer of the Food and Drug Administration–approved 755-nm picosecond alexandrite laser used in the study, and noted that “Cynosure had a role in the design of the study but not the conduct, collection, management, analysis, or interpretation of data. They approved the manuscript but did not prepare or decide to submit.” Dr. Brauer disclosed receiving honoraria from Cynosure/Palomar Medical Technologies and consulting for Miramar. Several other coauthors disclosed financial relationships with multiple companies, including Cynosure/Palomar Medical Technologies.
FROM JAMA DERMATOLOGY
Key clinical point: Treatment of facial acne scars with a diffractive lens array and a picosecond 755-nm alexandrite laser improves the appearance and texture of skin within 3 months.
Major finding: Masked assessments by a dermatologist found a 25%-50% global improvement at the 1-month postoperation follow-up visit, which was maintained at the 3-month follow-up.
Data source: A single-center, prospective study of 20 patients.
Disclosures: This study was supported in part by Cynosure. The authors disclosed several potential conflicts of interest.
VIDEO: Dr. Sheila F. Friedlander discusses when and why to worry about acne in young children
NEWPORT BEACH, CALIF.– “The group we worry about are the 1- to 7-year-olds,” when it comes to new-onset acne, Dr. Sheila Fallon Friedlander said at Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
In an interview at the meeting, Dr. Friedlander, a professor at the University of California, San Diego, explained the additional clinical signs that can indicate a serious problem, and what questions to ask parents.
Tune in for her tips on how to evaluate children aged 1-7 years with acne.
SDEF and this news organization are owned by Frontline Medical Communications.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEWPORT BEACH, CALIF.– “The group we worry about are the 1- to 7-year-olds,” when it comes to new-onset acne, Dr. Sheila Fallon Friedlander said at Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
In an interview at the meeting, Dr. Friedlander, a professor at the University of California, San Diego, explained the additional clinical signs that can indicate a serious problem, and what questions to ask parents.
Tune in for her tips on how to evaluate children aged 1-7 years with acne.
SDEF and this news organization are owned by Frontline Medical Communications.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEWPORT BEACH, CALIF.– “The group we worry about are the 1- to 7-year-olds,” when it comes to new-onset acne, Dr. Sheila Fallon Friedlander said at Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
In an interview at the meeting, Dr. Friedlander, a professor at the University of California, San Diego, explained the additional clinical signs that can indicate a serious problem, and what questions to ask parents.
Tune in for her tips on how to evaluate children aged 1-7 years with acne.
SDEF and this news organization are owned by Frontline Medical Communications.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT SDEF WOMEN’S & PEDIATRIC DERMATOLOGY SEMINAR
Rosacea’s comorbidities are more than skin deep
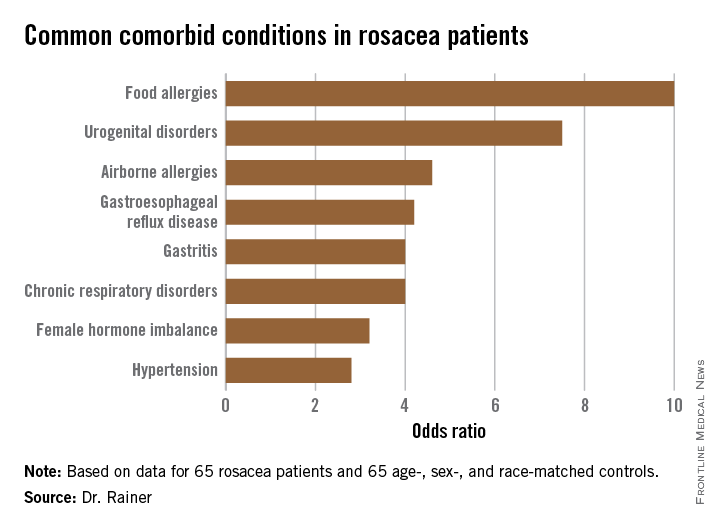
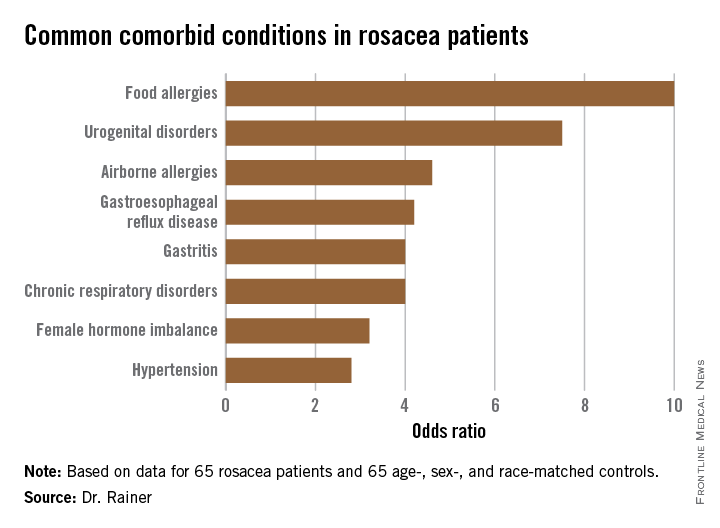
AMSTERDAM – Rosacea is associated with increased risk of a range of chronic systemic diseases, including allergies and urogential disorders, a case-control study showed.
The common denominator among this linked diverse collection of diseases is probably underlying systemic inflammation, Dr. Barbara M. Rainer explained at the annual congress of the European Academy of Dermatology and Venereology. But regardless of the pathophysiologic mechanisms at work, the important thing is that physicians be on the lookout for these comorbid conditions in their patients with rosacea.
Dr. Rainer of Johns Hopkins University in Baltimore presented a case-control study involving 130 subjects: 65 rosacea patients and an equal number of controls matched for age, sex, and race.
The most common comorbidity was food allergies (odds ratio, 10), followed by urogenital disorders (OR, 7.5).
The rosacea patients averaged 50 years of age and had a mean 11.8-year history of their skin disease. Body mass index, smoking status, alcohol intake, and coffee consumption were similar in cases and controls. Two-thirds of subjects were women. Relative risks for comorbid conditions were calculated using logistic regression analysis.
Dr. Rainer reported no relevant financial conflicts.
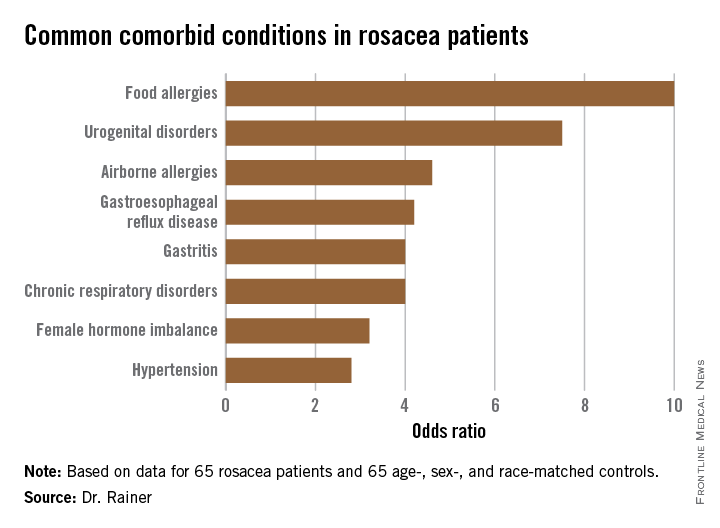
AMSTERDAM – Rosacea is associated with increased risk of a range of chronic systemic diseases, including allergies and urogential disorders, a case-control study showed.
The common denominator among this linked diverse collection of diseases is probably underlying systemic inflammation, Dr. Barbara M. Rainer explained at the annual congress of the European Academy of Dermatology and Venereology. But regardless of the pathophysiologic mechanisms at work, the important thing is that physicians be on the lookout for these comorbid conditions in their patients with rosacea.
Dr. Rainer of Johns Hopkins University in Baltimore presented a case-control study involving 130 subjects: 65 rosacea patients and an equal number of controls matched for age, sex, and race.
The most common comorbidity was food allergies (odds ratio, 10), followed by urogenital disorders (OR, 7.5).
The rosacea patients averaged 50 years of age and had a mean 11.8-year history of their skin disease. Body mass index, smoking status, alcohol intake, and coffee consumption were similar in cases and controls. Two-thirds of subjects were women. Relative risks for comorbid conditions were calculated using logistic regression analysis.
Dr. Rainer reported no relevant financial conflicts.
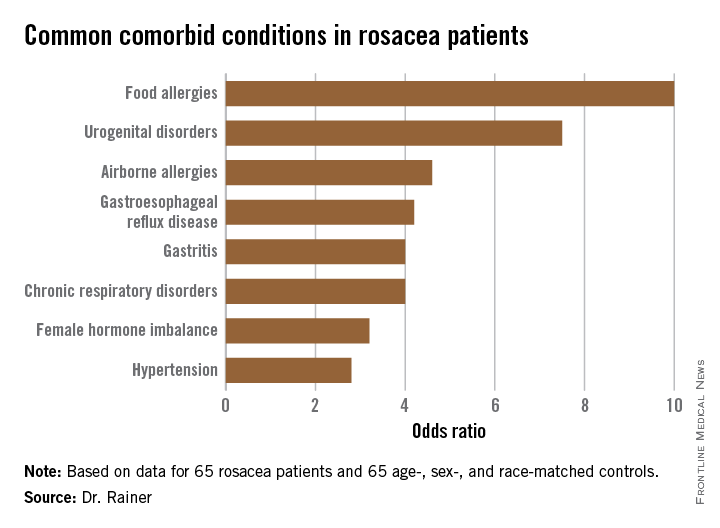
AMSTERDAM – Rosacea is associated with increased risk of a range of chronic systemic diseases, including allergies and urogential disorders, a case-control study showed.
The common denominator among this linked diverse collection of diseases is probably underlying systemic inflammation, Dr. Barbara M. Rainer explained at the annual congress of the European Academy of Dermatology and Venereology. But regardless of the pathophysiologic mechanisms at work, the important thing is that physicians be on the lookout for these comorbid conditions in their patients with rosacea.
Dr. Rainer of Johns Hopkins University in Baltimore presented a case-control study involving 130 subjects: 65 rosacea patients and an equal number of controls matched for age, sex, and race.
The most common comorbidity was food allergies (odds ratio, 10), followed by urogenital disorders (OR, 7.5).
The rosacea patients averaged 50 years of age and had a mean 11.8-year history of their skin disease. Body mass index, smoking status, alcohol intake, and coffee consumption were similar in cases and controls. Two-thirds of subjects were women. Relative risks for comorbid conditions were calculated using logistic regression analysis.
Dr. Rainer reported no relevant financial conflicts.
AT THE EADV CONGRESS
Key clinical point: Rosacea patients are at increased risk for an eclectic variety of chronic systemic comorbid conditions.
Major finding: The strongest associations seen with rosacea were for food allergies, with a 10-fold increased risk, and urogenital disorders, with a 7.5-fold relative risk.
Data source: A case-control study including 65 rosacea patients and an equal number of matched controls.
Disclosures: Dr. Rainer reported no relevant financial conflicts.
VIDEO: What’s unique about treating acne in adult women
NEWPORT BEACH, CALIF. – Do more women today really have acne? Or are they simply more likely to seek help because they learn of new and better medications?
Acne often causes more psychosocial and psychological stress in adult women than in men or adolescents, Dr. Hilary Baldwin of SUNY Downstate Medical Center, Brooklyn, N.Y., said at Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
In an interview at the meeting, Dr. Baldwin explained what makes the treatment of acne in adult women distinct from acne treatment for men and adolescents, and what underused medications can yield success.
SDEF and this news organization are owned by Frontline Medical Communications.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEWPORT BEACH, CALIF. – Do more women today really have acne? Or are they simply more likely to seek help because they learn of new and better medications?
Acne often causes more psychosocial and psychological stress in adult women than in men or adolescents, Dr. Hilary Baldwin of SUNY Downstate Medical Center, Brooklyn, N.Y., said at Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
In an interview at the meeting, Dr. Baldwin explained what makes the treatment of acne in adult women distinct from acne treatment for men and adolescents, and what underused medications can yield success.
SDEF and this news organization are owned by Frontline Medical Communications.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
NEWPORT BEACH, CALIF. – Do more women today really have acne? Or are they simply more likely to seek help because they learn of new and better medications?
Acne often causes more psychosocial and psychological stress in adult women than in men or adolescents, Dr. Hilary Baldwin of SUNY Downstate Medical Center, Brooklyn, N.Y., said at Skin Disease Education Foundation’s Women’s & Pediatric Dermatology Seminar.
In an interview at the meeting, Dr. Baldwin explained what makes the treatment of acne in adult women distinct from acne treatment for men and adolescents, and what underused medications can yield success.
SDEF and this news organization are owned by Frontline Medical Communications.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE SDEF WOMEN’S & PEDIATRIC DERMATOLOGY SEMINAR
Acne and rosacea management for men
In a report released March 2014 by the American Society of Aesthetic Plastic Surgery, the top five surgical procedures for men were liposuction, eyelid surgery, rhinoplasty, male breast reduction, and ear surgery. However, the rate of noninvasive cosmetic procedures and sales of men’s grooming products is one of the leading segments of the beauty industry.
Although most scientific research and media are focused on the female aesthetic, understanding the specific needs of your male patients is key to patient satisfaction. Most men are generally less aware than are women of the treatment options and risks and benefits of procedures. Men also prefer treatments with less downtime and natural-looking results. This column continues our miniseries on aesthetic dermatology for the male patient.
In a general dermatology practice, there are several skin concerns often identified by male patients, and acne and rosacea are among them.
Acne: Men generally have thicker, more sebaceous skin than that of women. Although acne is a very common problem in teens and young men, there is a growing trend of cases of cystic acne in adult men who consume popular protein meal replacement or muscle enhancing shakes that contain whey protein. Whey is a protein derived from cow’s milk. Milk and dairy products act by increasing insulin-like growth factor 1, which has been linked to acne. Although few case reports have shown a link between dietary whey supplementation and acne, in my practice, men with cystic acne who report using whey supplementation products have had almost complete resolution of their acne without medical intervention after discontinuing these products.
Rosacea: Men have a higher density of facial blood vessels than women do, and often seek treatment for telangiectasias and overall facial erythema. For papulopustular rosacea, common treatments include oral antibiotics, topical antibiotics, topical azaleic acid, and topical anti-inflammatory medications. For erythematotelangiectatic rosacea, Mirvaso (brimonidine), a topical vasoconstrictor, can be applied to the skin for 8-12 hours of marked reduction in facial erythema. Although theoretically a great option for patients suffering from erythema, the effects of topical brimonidine are transient, and the gel requires daily application with no long-term benefit. Vascular laser treatments are effective for telangiectasias for both men and women. However, men with more granulomatous or phymatous rosacea often need a combination of treatments including antibiotics, oral isotretinoin and fractional ablative lasers.
Resources:
American Society for Plastic Surgery 2012 statistics.
“Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes,” Cutis 2012;90:70-2.
Dr. Talakoub and Dr. Wesley are cocontributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
In a report released March 2014 by the American Society of Aesthetic Plastic Surgery, the top five surgical procedures for men were liposuction, eyelid surgery, rhinoplasty, male breast reduction, and ear surgery. However, the rate of noninvasive cosmetic procedures and sales of men’s grooming products is one of the leading segments of the beauty industry.
Although most scientific research and media are focused on the female aesthetic, understanding the specific needs of your male patients is key to patient satisfaction. Most men are generally less aware than are women of the treatment options and risks and benefits of procedures. Men also prefer treatments with less downtime and natural-looking results. This column continues our miniseries on aesthetic dermatology for the male patient.
In a general dermatology practice, there are several skin concerns often identified by male patients, and acne and rosacea are among them.
Acne: Men generally have thicker, more sebaceous skin than that of women. Although acne is a very common problem in teens and young men, there is a growing trend of cases of cystic acne in adult men who consume popular protein meal replacement or muscle enhancing shakes that contain whey protein. Whey is a protein derived from cow’s milk. Milk and dairy products act by increasing insulin-like growth factor 1, which has been linked to acne. Although few case reports have shown a link between dietary whey supplementation and acne, in my practice, men with cystic acne who report using whey supplementation products have had almost complete resolution of their acne without medical intervention after discontinuing these products.
Rosacea: Men have a higher density of facial blood vessels than women do, and often seek treatment for telangiectasias and overall facial erythema. For papulopustular rosacea, common treatments include oral antibiotics, topical antibiotics, topical azaleic acid, and topical anti-inflammatory medications. For erythematotelangiectatic rosacea, Mirvaso (brimonidine), a topical vasoconstrictor, can be applied to the skin for 8-12 hours of marked reduction in facial erythema. Although theoretically a great option for patients suffering from erythema, the effects of topical brimonidine are transient, and the gel requires daily application with no long-term benefit. Vascular laser treatments are effective for telangiectasias for both men and women. However, men with more granulomatous or phymatous rosacea often need a combination of treatments including antibiotics, oral isotretinoin and fractional ablative lasers.
Resources:
American Society for Plastic Surgery 2012 statistics.
“Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes,” Cutis 2012;90:70-2.
Dr. Talakoub and Dr. Wesley are cocontributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
In a report released March 2014 by the American Society of Aesthetic Plastic Surgery, the top five surgical procedures for men were liposuction, eyelid surgery, rhinoplasty, male breast reduction, and ear surgery. However, the rate of noninvasive cosmetic procedures and sales of men’s grooming products is one of the leading segments of the beauty industry.
Although most scientific research and media are focused on the female aesthetic, understanding the specific needs of your male patients is key to patient satisfaction. Most men are generally less aware than are women of the treatment options and risks and benefits of procedures. Men also prefer treatments with less downtime and natural-looking results. This column continues our miniseries on aesthetic dermatology for the male patient.
In a general dermatology practice, there are several skin concerns often identified by male patients, and acne and rosacea are among them.
Acne: Men generally have thicker, more sebaceous skin than that of women. Although acne is a very common problem in teens and young men, there is a growing trend of cases of cystic acne in adult men who consume popular protein meal replacement or muscle enhancing shakes that contain whey protein. Whey is a protein derived from cow’s milk. Milk and dairy products act by increasing insulin-like growth factor 1, which has been linked to acne. Although few case reports have shown a link between dietary whey supplementation and acne, in my practice, men with cystic acne who report using whey supplementation products have had almost complete resolution of their acne without medical intervention after discontinuing these products.
Rosacea: Men have a higher density of facial blood vessels than women do, and often seek treatment for telangiectasias and overall facial erythema. For papulopustular rosacea, common treatments include oral antibiotics, topical antibiotics, topical azaleic acid, and topical anti-inflammatory medications. For erythematotelangiectatic rosacea, Mirvaso (brimonidine), a topical vasoconstrictor, can be applied to the skin for 8-12 hours of marked reduction in facial erythema. Although theoretically a great option for patients suffering from erythema, the effects of topical brimonidine are transient, and the gel requires daily application with no long-term benefit. Vascular laser treatments are effective for telangiectasias for both men and women. However, men with more granulomatous or phymatous rosacea often need a combination of treatments including antibiotics, oral isotretinoin and fractional ablative lasers.
Resources:
American Society for Plastic Surgery 2012 statistics.
“Whey protein precipitating moderate to severe acne flares in 5 teenaged athletes,” Cutis 2012;90:70-2.
Dr. Talakoub and Dr. Wesley are cocontributors to a monthly Aesthetic Dermatology column in Skin & Allergy News. Dr. Talakoub is in private practice in McLean, Va. Dr. Wesley practices dermatology in Beverly Hills, Calif. This month’s column is by Dr. Talakoub.
Best Practices in Pulsed Dye Laser Treatment
For more information, access Dr. Ezra's article from the August 2014 issue, "Linear Scarring Following Treatment With a 595-nm Pulsed Dye Laser."
For more information, access Dr. Ezra's article from the August 2014 issue, "Linear Scarring Following Treatment With a 595-nm Pulsed Dye Laser."
For more information, access Dr. Ezra's article from the August 2014 issue, "Linear Scarring Following Treatment With a 595-nm Pulsed Dye Laser."
Pros and Cons of Devices for Rosacea
For more information, access Dr. Goldenberg's article from the July 2014 issue, "Devices and Topical Agents for Rosacea Management."
For more information, access Dr. Goldenberg's article from the July 2014 issue, "Devices and Topical Agents for Rosacea Management."
For more information, access Dr. Goldenberg's article from the July 2014 issue, "Devices and Topical Agents for Rosacea Management."
Devices and Topical Agents for Rosacea Management
Rosacea is a common chronic inflammatory disease that typically affects centrofacial skin, particularly the convexities of the forehead, nose, cheeks, and chin. Occasionally, involvement of the scalp, neck, or upper trunk can occur.1 Rosacea is more common in light-skinned individuals and has been called the “curse of the Celts,”2 but it also can affect Asian individuals and patients of African descent. Although rosacea affects women more frequently, men are more likely to develop severe disease with complications such as rhinophyma. Diagnosis is made on clinical grounds, and histologic confirmation rarely is necessary.
Despite its high incidence and recent advances, the pathogenesis of rosacea is still poorly understood. A combination of factors, such as aberrations in innate immunity,3 neurovascular dysregulation, dilated blood and lymphatic vessels, and a possible genetic predisposition seem to be involved.4 Presence of commensal Demodex folliculorum mites may be a contributing factor for papulopustular disease.
Patients can present with a range of clinical features, such as transient or persistent facial erythema, telangiectasia, papules, pustules, edema, thickening, plaque formation, and ocular manifestations. Associated burning and stinging also may occur. Rosacea-related erythema (eg, lesional and perilesional erythema) can be caused by inflammatory lesions or can present independent of lesions in the case of diffuse facial erythema. Due to the diversity of clinical signs and limited knowledge regarding its etiology, rosacea is best regarded as a syndrome and has been classified into 4 subtypes—erythematotelangiectatic, papulopustular, phymatous, and ocular—and 1 variant (granulomatous rosacea).5 The most common phymatous changes affect the nose, with hypertrophy and lymphedema of subcutaneous tissues. Other sites that can be affected are the ears, forehead, and chin. Ocular manifestations affect approximately 50% of rosacea patients,6 ranging from conjunctivitis and blepharitis to keratitis and corneal ulceration, thereby requiring ophthalmologic assessment.
Because rosacea affects facial appearance, it can have a devastating impact on the patient’s quality of life, leading to social isolation. Although there is no cure available for rosacea, lifestyle modification and treatment can reduce or control its features, which tend to exacerbate and remit. There are a number of possible triggers for rosacea that ideally should be avoided such as sun exposure, hot or cold weather, heavy exercise, emotional stress, and consumption of alcohol and spicy foods. It is essential to consider disease subtype as well as the signs and symptoms presenting in each individual patient when approaching therapy selection. Most well-established US Food and Drug Administration (FDA)–approved treatments of rosacea target the papulopustular aspect of disease, including the erythema associated with the lesions. These treatments include topical and systemic antibiotics and azelaic acid. Non–FDA-approved agents such as topical and systemic retinoids, topical calcineurin inhibitors, and topical benzoyl peroxide also are used, though there is limited evidence of their efficacy.7
Management options for diffuse facial erythema and telangiectasia, however, are limited. Standard rosacea treatments often are not efficacious in treating these aspects of the disease, thereby requiring an alternative approach. This article reviews devices and topical agents currently available for the management of rosacea.
Skin Care
The skin of rosacea patients often is sensitive and prone to irritation; therefore, a good skin care regimen is an integral part of disease management and should include a gentle cleanser, moisturizer, and sunscreen.8 Lipid-free liquid cleansers or synthetic detergent (syndet) cleansers with a neutral to slightly acidic pH (ie, similar to the pH of normal skin) are ideal.9 Following cleansing, the skin should be gently dried. It may be beneficial to wait up to 30 minutes before application of a moisturizer to avoid irritation. Hydrating moisturizers should be free of irritants or abrasives, allowing maintenance of stratum corneum pH in an acid range of 4 to 6. Green-tinted makeup can be a useful tool in covering areas of erythema.
Devices
A variety of devices targeting hemoglobin are reported to be effective for the management of erythema and telangiectasia in rosacea patients, including the 595-nm pulsed dye laser (PDL), the potassium titanyl phosphate (KTP) laser, the 1064-nm Nd:YAG laser, and noncoherent intense pulsed light (IPL) sources.
The major chromophore in blood vessels is oxyhemoglobin, with 2 major absorption bands in the visible light spectrum at 542 and 577 nm. There also is notable albeit lesser absorption in the near-infrared range from 700 to 1100 nm.10 Following absorption by oxyhemoglobin, light energy is converted to thermal energy, which diffuses in the blood vessel causing photocoagulation, mechanical injury, and finally thrombosis.
Pulsed Dye Laser (585–595 nm)
Among the vascular lasers, the PDL has a long safety record. It was the first laser that used the concept of selective photothermolysis for treatment of vascular lesions.11,12 The first PDLs had a wavelength of 577 nm, while current PDLs have wavelengths of 585 or 595 nm with longer pulse durations and circular or oval spot sizes that are ideal for treatment of dermal vessels. The main disadvantage of PDLs is the development of posttreatment purpura. The longer pulse durations of KTP lasers avoid damage to cutaneous vasculature and eliminate the risk for bruising. Nonetheless, the wavelength of the PDL provides a greater depth of penetration due to its substantial absorption by cutaneous vasculature compared to the shorter wavelength of the KTP laser.
Although newer-generation PDLs still have the potential to cause purpura, various attempts have been made to minimize this risk, such as the use of longer pulse durations, multiple minipulses or “pulselets,”13 and multiple passes. Separate parameters may need to be used when treating linear vessels and diffuse erythema, with longer pulse durations required for larger vessels. The Figure shows a rosacea patient with facial telangiectasia before and after 1 treatment with a PDL.

According to Alam et al,14 purpuric settings were more efficacious in a comparison of variable-pulsed PDLs for facial telangiectasia. In 82% (9/11) of cases, greater reduction in telangiectasia density was noted on the side of the face that had been treated with purpuric settings versus the other side of the face.14 Purpuric settings are particularly effective in treating larger vessels, while finer telangiectatic vessels may respond to purpura-free settings.
In a study of 12 participants treated with a 595-nm PDL at a pulse duration of 6 ms and fluences from 7 to 9 J/cm2, no lasting purpura was seen; however, while 9 participants achieved more than 25% improvement after a single treatment, only 2 participants achieved more than 75% improvement.15 Nonetheless, some patients may prefer this potentially less effective treatment method to avoid the socially embarrassing side effect of purpura.
In a study of 12 rosacea patients, a 75% reduction in telangiectasia scores was noted after a mean of 3 treatments with the 585-nm PDL using 450-ms pulse durations. Purpura occurred in all patients.16 In another study by Madan and Ferguson,17 18 participants with nasal telangiectasia that had been resistant to the traditional round spot, 595-nm PDL and/or 532-nm KTP laser were treated with a 3x10-mm elliptical spot, ultra-long pulse, 595-nm PDL with a 40-ms pulse duration and double passes. Complete clearance was seen in 10 (55.6%) participants and 8 (44.4%) showed more than 80% improvement. No purpura was associated with the treatment.17
Further studies comparing the efficacy of nonpurpuric and purpuric settings in the same patient would allow us to determine the most effective option for future treatment.
KTP Laser (532 nm)
Potassium titanyl phosphate lasers have the disadvantage of higher melanin absorption, which can lead to epidermal damage with postinflammatory hyperpigmentation. Their use is limited to lighter skin types. Because of its shorter wavelength, the KTP laser is best used to treat superficial telangiectasia. The absence of posttreatment purpura can make KTP lasers a popular alternative to PDLs.17 Uebelhoer et al18 performed a split-face study in 15 participants to compare the 595-nm PDL and 532-nm KTP laser. Although both treatments were effective, the KTP laser achieved 62% clearance after the first treatment and 85% clearance 3 weeks after the third treatment compared to 49% and 75%, respectively, for the PDL. Interestingly, the degree of swelling and erythema posttreatment were greater on the KTP laser–treated side.18
Nd:YAG (1064 nm)
The wavelength of the Nd:YAG laser targets the lower absorption peak of oxyhemoglobin. In a study of 15 participants with facial telangiectasia who were treated with a 1064-nm Nd:YAG laser at day 0 and day 30 using a 3-mm spot size, a fluence of 120 to 170 J/cm,2 and 5- to 40-ms pulse durations, 73% (11/15) showed moderate to significant improvement at day 0 and day 30 and 80% improvement at 3 months’ follow-up.19 In a split-face study of 14 patients, treatment with the 595-nm PDL with a fluence of 7.5 J/cm2, pulse duration of 6 ms, and spot size of 10 mm was compared with the 1064-nm Nd:YAG laser with a fluence of 6 J/cm2, pulse duration of 0.3 ms, and spot size of 8 mm.20 Erythema improved by 6.4% from baseline on the side treated with the PDL. Although participants rated the Nd:YAG laser treatment as less painful, they were more satisfied with the results of the PDL treatment.20 In another split-face study comparing the 595-nm PDL and 1064-nm Nd:YAG laser, greater improvement was reported with the Nd:YAG laser, though the results were not statistically significant.21
Intense Pulsed Light
While lasers use selective photothermolysis, IPL devices emit noncoherent light at a wavelength of 500 to 1200 nm. Cutoff filters allow for selective tissue damage depending on the absorption spectra of the tissue. Longer wavelengths are effective for the treatment of deeper vessels, while shorter wavelengths target more superficial vessels; however, the shorter wavelengths can interact with melanin and should be avoided in darker skin types. In a phase 3 open trial, 34 participants were treated with IPL with a 560-nm cutoff filter and fluences of 24 to 32 J/cm2. The mean reduction of erythema following 4 treatments was 39% on the cheeks and 22% on the chin; side effects were minimal.22
Photodynamic Therapy
Photodynamic therapy is an effective and widely used treatment method for a number of skin conditions. Following its success in the treatment of acne, it also has been used in the management of rosacea, though the exact mechanism of action remains unclear.
Photodynamic therapy involves topical application of a photosensitizing agent (eg, 5-aminolevulinic acid, methyl aminolevulinate [MAL]) followed by exposure to red or blue light. The photosensitizing agent accumulates semiselectively in abnormal skin tissue and is converted to protoporphyrin IX, which induces a toxic skin reaction through reactive oxygen radicals in the presence of visible light.23 Photodynamic therapy generally is well tolerated. The primary side effects are pain, burning, and stinging.
In 3 of 4 (75%) patients treated with MAL and red light, rosacea clearance was noted after 2 to 3 sessions. Remission lasted for 3 months in 2 (66.7%) participants and for 9 months in 1 (33.3%) participant.24 In another study, 17 patients were treated with MAL and red light. Results were good in 10 participants (58.8%), fair in 4 (23.5%), and poor in 3 (17.6%).23
ALPHA-Adrenergic Receptor Agonists
Recently, the α-adrenergic receptor agonists brimonidine tartrate and oxymetazoline have been found to be effective in controlling diffuse facial erythema of rosacea, which is thought to arise from vasomotor instability and abnormal vasodilation of the superficial cutaneous vasculature. Brimonidine tartrate is a potent α2-agonist that is mainly used for treatment of open-angle glaucoma. In 2 phase 3 controlled studies, once-daily application of brimonidine tartrate gel 0.5% was found to be effective and safe in reducing the erythema of rosacea.25 Brimonidine tartrate gel is the first FDA-approved treatment of facial erythema associated with rosacea. Possible side effects are erythema worse than baseline (4%), flushing (3%), and burning (2%).26 Oxymetazoline is a potent α1- and partial α2-agonist that is available as a nasal decongestant. Oxymetazoline solution 0.05% used once daily has been shown in case reports to reduce rosacea-associated erythema for several hours.27
Nicotinamide
Nicotinamide is the amide form of niacin, which has both anti-inflammatory properties and a stabilizing effect on epidermal barrier function.28 Although topical application of nicotinamide has been used in the treatment of inflammatory dermatoses such as rosacea,28,29 niacin can lead to cutaneous vasodilation and thus flushing. It has been hypothesized to potentially enhance the effect of PDL if used as pretreatment for rosacea-associated erythema.30
Conclusion
Rosacea can have a substantial impact on patient quality of life. Recent advances in treatment options and rapidly advancing knowledge of laser therapy are providing dermatologists with powerful tools for rosacea clearance. Lasers and IPL are effective treatments of the erythematotelangiectatic aspect of the disease, and careful selection of devices and treatment parameters can reduce unwanted side effects.
- Ayres S Jr. Extrafacial rosacea is rare but does exist. J Am Acad Dermatol. 1987;16:391-392.
- Jansen T, Plewig G. Rosacea: classification and treatment. J R Soc Med. 1997;90:144-150.
- Yamasaki K, Gallo RL. Rosacea as a disease of cathelicidins and skin innate immunity. J Investig Dermatol Symp Proc. 2011;15:12-15.
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69(6, suppl 1):S15-S26.
- Wilkin J, Dahl M, Detmar M, et al; National Rosacea Society Expert Committee. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol. 2002;46:584-587.
- Webster G, Schaller M. Ocular rosacea: a dermatologic perspective. J Am Acad Dermatol. 2013;69(6, suppl 1):S42-S43.
- Del Rosso JQ, Thiboutot D, Gallo R, et al. Consensus recommendations from the American Acne & Rosacea Society on the management of rosacea, part 2: a status report on topical agents. Cutis. 2013;92:277-284.
- Levin J, Miller R. A guide to the ingredients and potential benefits of over-the-counter cleansers and moisturizers for rosacea patients. J Clin Aesthet Dermatol. 2011;4:31-49.
- Draelos ZD. The effect of Cetaphil gentle skin cleanser on the skin barrier of patients with rosacea. Cutis. 2006;77:27-33.
- Hare McCoppin HH, Goldberg DJ. Laser treatment of facial telangiectases: an update. Dermatol Surg. 2010;36:1221-1230.
- Garden JM, Polla LL, Tan OT. The treatment of port-wine stains by the pulsed dye laser. analysis of pulse duration and long-term therapy. Arch Dermatol. 1988;124:889-896.
- Anderson RR, Parrish JA. Microvasculature can be selectively damaged using dye lasers: a basic theory and experimental evidence in human skin. Lasers Surg Med. 1981;1:263-276.
- Bernstein EF, Kligman A. Rosacea treatment using the new-generation, high-energy, 595 nm, long pulse-duration pulsed-dye laser. Lasers Surg Med. 2008;40:233-239.
- Alam M, Dover JS, Arndt KA. Treatment of facial telangiectasia with variable-pulse high-fluence pulsed-dye laser: comparison of efficacy with fluences immediately above and below the purpura threshold. Dermatol Surg. 2003;29:681-684.
- Jasim ZF, Woo WK, Handley JM. Long-pulsed (6-ms) pulsed dye laser treatment of rosacea-associated telangiectasia using subpurpuric clinical threshold. Dermatol Surg. 2004;30:37-40.
- Clark SM, Lanigan SW, Marks R. Laser treatment of erythema and telangiectasia associated with rosacea. Lasers Med Sci. 2002;17:26-33.
- Madan V, Ferguson J. Using the ultra-long pulse width pulsed dye laser and elliptical spot to treat resistant nasal telangiectasia. Lasers Med Sci. 2010;25:151-154.
- Uebelhoer NS, Bogle MA, Stewart B, et al. A split-face comparison study of pulsed 532-nm KTP laser and 595-nm pulsed dye laser in the treatment of facial telangiectases and diffuse telangiectatic facial erythema. Dermatol Surg. 2007;33:441-448.
- Sarradet DM, Hussain M, Goldberg DJ. Millisecond 1064-nm neodymium:YAG laser treatment of facial telangiectases. Dermatol Surg. 2003;29:56-58.
- Alam M, Voravutinon N, Warycha M, et al. Comparative effectiveness of nonpurpuragenic 595-nm pulsed dye laser and microsecond 1064-nm neodymium:yttrium-aluminum-garnet laser for treatment of diffuse facial erythema: a double-blind randomized controlled trial. J Am Acad Dermatol. 2013;69:438-443.
- Salem SA, Abdel Fattah NS, Tantawy SM, et al. Neodymium-yttrium aluminum garnet laser versus pulsed dye laser in erythemato-telangiectatic rosacea:comparison of clinical efficacy and effect on cutaneoussubstance (P) expression. J Cosmet Dermatol. 2013;12:187-194.
- Papageorgiou P, Clayton W, Norwood S, et al. Treatment of rosacea with intense pulsed light: significant improvement and long-lasting results. Br J Dermatol. 2008;159:628-632.
- Bryld LE, Jemec GB. Photodynamic therapy in a series of rosacea patients. J Eur Acad Dermatol Venereol. 2007;21:1199-1202.
- Nybaek H, Jemec GB. Photodynamic therapy in the treatment of rosacea. Dermatology. 2005;211:135-138.
- Fowler J, Jackson M, Moore A, et al. Efficacy and safety of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of two randomized, double-blind, and vehicle-controlled pivotal studies. J Drugs Dermatol. 2013;12:650-656.
- Routt ET, Levitt JO. Rebound erythema and burning sensation from a new topical brimonidine tartrate gel 0.33%. J Am Acad Dermatol. 2014;70:E37-E38.
- Shanler SD, Ondo AL. Successful treatment of the erythema and flushing of rosacea using a topically applied selective alpha1-adrenergic receptor agonist, oxymetazoline. Arch Dermatol. 2007;143:1369-1371.
- Draelos ZD, Ertel K, Berge C. Niacinamide-containing facial moisturizer improves skin barrier and benefits subjects with rosacea. Cutis. 2005;76:135-141.
- Draelos ZD, Ertel KD, Berge CA. Facilitating facial retinization through barrier improvement. Cutis. 2006;78:275-281.
- Kim TG, Roh HJ, Cho SB, et al. Enhancing effect of pretreatment with topical niacin in the treatment of rosacea-associated erythema by 585-nm pulsed dye laser in Koreans: a randomized, prospective, split-face trial. Br J Dermatol. 2011;164:573-579.
Rosacea is a common chronic inflammatory disease that typically affects centrofacial skin, particularly the convexities of the forehead, nose, cheeks, and chin. Occasionally, involvement of the scalp, neck, or upper trunk can occur.1 Rosacea is more common in light-skinned individuals and has been called the “curse of the Celts,”2 but it also can affect Asian individuals and patients of African descent. Although rosacea affects women more frequently, men are more likely to develop severe disease with complications such as rhinophyma. Diagnosis is made on clinical grounds, and histologic confirmation rarely is necessary.
Despite its high incidence and recent advances, the pathogenesis of rosacea is still poorly understood. A combination of factors, such as aberrations in innate immunity,3 neurovascular dysregulation, dilated blood and lymphatic vessels, and a possible genetic predisposition seem to be involved.4 Presence of commensal Demodex folliculorum mites may be a contributing factor for papulopustular disease.
Patients can present with a range of clinical features, such as transient or persistent facial erythema, telangiectasia, papules, pustules, edema, thickening, plaque formation, and ocular manifestations. Associated burning and stinging also may occur. Rosacea-related erythema (eg, lesional and perilesional erythema) can be caused by inflammatory lesions or can present independent of lesions in the case of diffuse facial erythema. Due to the diversity of clinical signs and limited knowledge regarding its etiology, rosacea is best regarded as a syndrome and has been classified into 4 subtypes—erythematotelangiectatic, papulopustular, phymatous, and ocular—and 1 variant (granulomatous rosacea).5 The most common phymatous changes affect the nose, with hypertrophy and lymphedema of subcutaneous tissues. Other sites that can be affected are the ears, forehead, and chin. Ocular manifestations affect approximately 50% of rosacea patients,6 ranging from conjunctivitis and blepharitis to keratitis and corneal ulceration, thereby requiring ophthalmologic assessment.
Because rosacea affects facial appearance, it can have a devastating impact on the patient’s quality of life, leading to social isolation. Although there is no cure available for rosacea, lifestyle modification and treatment can reduce or control its features, which tend to exacerbate and remit. There are a number of possible triggers for rosacea that ideally should be avoided such as sun exposure, hot or cold weather, heavy exercise, emotional stress, and consumption of alcohol and spicy foods. It is essential to consider disease subtype as well as the signs and symptoms presenting in each individual patient when approaching therapy selection. Most well-established US Food and Drug Administration (FDA)–approved treatments of rosacea target the papulopustular aspect of disease, including the erythema associated with the lesions. These treatments include topical and systemic antibiotics and azelaic acid. Non–FDA-approved agents such as topical and systemic retinoids, topical calcineurin inhibitors, and topical benzoyl peroxide also are used, though there is limited evidence of their efficacy.7
Management options for diffuse facial erythema and telangiectasia, however, are limited. Standard rosacea treatments often are not efficacious in treating these aspects of the disease, thereby requiring an alternative approach. This article reviews devices and topical agents currently available for the management of rosacea.
Skin Care
The skin of rosacea patients often is sensitive and prone to irritation; therefore, a good skin care regimen is an integral part of disease management and should include a gentle cleanser, moisturizer, and sunscreen.8 Lipid-free liquid cleansers or synthetic detergent (syndet) cleansers with a neutral to slightly acidic pH (ie, similar to the pH of normal skin) are ideal.9 Following cleansing, the skin should be gently dried. It may be beneficial to wait up to 30 minutes before application of a moisturizer to avoid irritation. Hydrating moisturizers should be free of irritants or abrasives, allowing maintenance of stratum corneum pH in an acid range of 4 to 6. Green-tinted makeup can be a useful tool in covering areas of erythema.
Devices
A variety of devices targeting hemoglobin are reported to be effective for the management of erythema and telangiectasia in rosacea patients, including the 595-nm pulsed dye laser (PDL), the potassium titanyl phosphate (KTP) laser, the 1064-nm Nd:YAG laser, and noncoherent intense pulsed light (IPL) sources.
The major chromophore in blood vessels is oxyhemoglobin, with 2 major absorption bands in the visible light spectrum at 542 and 577 nm. There also is notable albeit lesser absorption in the near-infrared range from 700 to 1100 nm.10 Following absorption by oxyhemoglobin, light energy is converted to thermal energy, which diffuses in the blood vessel causing photocoagulation, mechanical injury, and finally thrombosis.
Pulsed Dye Laser (585–595 nm)
Among the vascular lasers, the PDL has a long safety record. It was the first laser that used the concept of selective photothermolysis for treatment of vascular lesions.11,12 The first PDLs had a wavelength of 577 nm, while current PDLs have wavelengths of 585 or 595 nm with longer pulse durations and circular or oval spot sizes that are ideal for treatment of dermal vessels. The main disadvantage of PDLs is the development of posttreatment purpura. The longer pulse durations of KTP lasers avoid damage to cutaneous vasculature and eliminate the risk for bruising. Nonetheless, the wavelength of the PDL provides a greater depth of penetration due to its substantial absorption by cutaneous vasculature compared to the shorter wavelength of the KTP laser.
Although newer-generation PDLs still have the potential to cause purpura, various attempts have been made to minimize this risk, such as the use of longer pulse durations, multiple minipulses or “pulselets,”13 and multiple passes. Separate parameters may need to be used when treating linear vessels and diffuse erythema, with longer pulse durations required for larger vessels. The Figure shows a rosacea patient with facial telangiectasia before and after 1 treatment with a PDL.

According to Alam et al,14 purpuric settings were more efficacious in a comparison of variable-pulsed PDLs for facial telangiectasia. In 82% (9/11) of cases, greater reduction in telangiectasia density was noted on the side of the face that had been treated with purpuric settings versus the other side of the face.14 Purpuric settings are particularly effective in treating larger vessels, while finer telangiectatic vessels may respond to purpura-free settings.
In a study of 12 participants treated with a 595-nm PDL at a pulse duration of 6 ms and fluences from 7 to 9 J/cm2, no lasting purpura was seen; however, while 9 participants achieved more than 25% improvement after a single treatment, only 2 participants achieved more than 75% improvement.15 Nonetheless, some patients may prefer this potentially less effective treatment method to avoid the socially embarrassing side effect of purpura.
In a study of 12 rosacea patients, a 75% reduction in telangiectasia scores was noted after a mean of 3 treatments with the 585-nm PDL using 450-ms pulse durations. Purpura occurred in all patients.16 In another study by Madan and Ferguson,17 18 participants with nasal telangiectasia that had been resistant to the traditional round spot, 595-nm PDL and/or 532-nm KTP laser were treated with a 3x10-mm elliptical spot, ultra-long pulse, 595-nm PDL with a 40-ms pulse duration and double passes. Complete clearance was seen in 10 (55.6%) participants and 8 (44.4%) showed more than 80% improvement. No purpura was associated with the treatment.17
Further studies comparing the efficacy of nonpurpuric and purpuric settings in the same patient would allow us to determine the most effective option for future treatment.
KTP Laser (532 nm)
Potassium titanyl phosphate lasers have the disadvantage of higher melanin absorption, which can lead to epidermal damage with postinflammatory hyperpigmentation. Their use is limited to lighter skin types. Because of its shorter wavelength, the KTP laser is best used to treat superficial telangiectasia. The absence of posttreatment purpura can make KTP lasers a popular alternative to PDLs.17 Uebelhoer et al18 performed a split-face study in 15 participants to compare the 595-nm PDL and 532-nm KTP laser. Although both treatments were effective, the KTP laser achieved 62% clearance after the first treatment and 85% clearance 3 weeks after the third treatment compared to 49% and 75%, respectively, for the PDL. Interestingly, the degree of swelling and erythema posttreatment were greater on the KTP laser–treated side.18
Nd:YAG (1064 nm)
The wavelength of the Nd:YAG laser targets the lower absorption peak of oxyhemoglobin. In a study of 15 participants with facial telangiectasia who were treated with a 1064-nm Nd:YAG laser at day 0 and day 30 using a 3-mm spot size, a fluence of 120 to 170 J/cm,2 and 5- to 40-ms pulse durations, 73% (11/15) showed moderate to significant improvement at day 0 and day 30 and 80% improvement at 3 months’ follow-up.19 In a split-face study of 14 patients, treatment with the 595-nm PDL with a fluence of 7.5 J/cm2, pulse duration of 6 ms, and spot size of 10 mm was compared with the 1064-nm Nd:YAG laser with a fluence of 6 J/cm2, pulse duration of 0.3 ms, and spot size of 8 mm.20 Erythema improved by 6.4% from baseline on the side treated with the PDL. Although participants rated the Nd:YAG laser treatment as less painful, they were more satisfied with the results of the PDL treatment.20 In another split-face study comparing the 595-nm PDL and 1064-nm Nd:YAG laser, greater improvement was reported with the Nd:YAG laser, though the results were not statistically significant.21
Intense Pulsed Light
While lasers use selective photothermolysis, IPL devices emit noncoherent light at a wavelength of 500 to 1200 nm. Cutoff filters allow for selective tissue damage depending on the absorption spectra of the tissue. Longer wavelengths are effective for the treatment of deeper vessels, while shorter wavelengths target more superficial vessels; however, the shorter wavelengths can interact with melanin and should be avoided in darker skin types. In a phase 3 open trial, 34 participants were treated with IPL with a 560-nm cutoff filter and fluences of 24 to 32 J/cm2. The mean reduction of erythema following 4 treatments was 39% on the cheeks and 22% on the chin; side effects were minimal.22
Photodynamic Therapy
Photodynamic therapy is an effective and widely used treatment method for a number of skin conditions. Following its success in the treatment of acne, it also has been used in the management of rosacea, though the exact mechanism of action remains unclear.
Photodynamic therapy involves topical application of a photosensitizing agent (eg, 5-aminolevulinic acid, methyl aminolevulinate [MAL]) followed by exposure to red or blue light. The photosensitizing agent accumulates semiselectively in abnormal skin tissue and is converted to protoporphyrin IX, which induces a toxic skin reaction through reactive oxygen radicals in the presence of visible light.23 Photodynamic therapy generally is well tolerated. The primary side effects are pain, burning, and stinging.
In 3 of 4 (75%) patients treated with MAL and red light, rosacea clearance was noted after 2 to 3 sessions. Remission lasted for 3 months in 2 (66.7%) participants and for 9 months in 1 (33.3%) participant.24 In another study, 17 patients were treated with MAL and red light. Results were good in 10 participants (58.8%), fair in 4 (23.5%), and poor in 3 (17.6%).23
ALPHA-Adrenergic Receptor Agonists
Recently, the α-adrenergic receptor agonists brimonidine tartrate and oxymetazoline have been found to be effective in controlling diffuse facial erythema of rosacea, which is thought to arise from vasomotor instability and abnormal vasodilation of the superficial cutaneous vasculature. Brimonidine tartrate is a potent α2-agonist that is mainly used for treatment of open-angle glaucoma. In 2 phase 3 controlled studies, once-daily application of brimonidine tartrate gel 0.5% was found to be effective and safe in reducing the erythema of rosacea.25 Brimonidine tartrate gel is the first FDA-approved treatment of facial erythema associated with rosacea. Possible side effects are erythema worse than baseline (4%), flushing (3%), and burning (2%).26 Oxymetazoline is a potent α1- and partial α2-agonist that is available as a nasal decongestant. Oxymetazoline solution 0.05% used once daily has been shown in case reports to reduce rosacea-associated erythema for several hours.27
Nicotinamide
Nicotinamide is the amide form of niacin, which has both anti-inflammatory properties and a stabilizing effect on epidermal barrier function.28 Although topical application of nicotinamide has been used in the treatment of inflammatory dermatoses such as rosacea,28,29 niacin can lead to cutaneous vasodilation and thus flushing. It has been hypothesized to potentially enhance the effect of PDL if used as pretreatment for rosacea-associated erythema.30
Conclusion
Rosacea can have a substantial impact on patient quality of life. Recent advances in treatment options and rapidly advancing knowledge of laser therapy are providing dermatologists with powerful tools for rosacea clearance. Lasers and IPL are effective treatments of the erythematotelangiectatic aspect of the disease, and careful selection of devices and treatment parameters can reduce unwanted side effects.
Rosacea is a common chronic inflammatory disease that typically affects centrofacial skin, particularly the convexities of the forehead, nose, cheeks, and chin. Occasionally, involvement of the scalp, neck, or upper trunk can occur.1 Rosacea is more common in light-skinned individuals and has been called the “curse of the Celts,”2 but it also can affect Asian individuals and patients of African descent. Although rosacea affects women more frequently, men are more likely to develop severe disease with complications such as rhinophyma. Diagnosis is made on clinical grounds, and histologic confirmation rarely is necessary.
Despite its high incidence and recent advances, the pathogenesis of rosacea is still poorly understood. A combination of factors, such as aberrations in innate immunity,3 neurovascular dysregulation, dilated blood and lymphatic vessels, and a possible genetic predisposition seem to be involved.4 Presence of commensal Demodex folliculorum mites may be a contributing factor for papulopustular disease.
Patients can present with a range of clinical features, such as transient or persistent facial erythema, telangiectasia, papules, pustules, edema, thickening, plaque formation, and ocular manifestations. Associated burning and stinging also may occur. Rosacea-related erythema (eg, lesional and perilesional erythema) can be caused by inflammatory lesions or can present independent of lesions in the case of diffuse facial erythema. Due to the diversity of clinical signs and limited knowledge regarding its etiology, rosacea is best regarded as a syndrome and has been classified into 4 subtypes—erythematotelangiectatic, papulopustular, phymatous, and ocular—and 1 variant (granulomatous rosacea).5 The most common phymatous changes affect the nose, with hypertrophy and lymphedema of subcutaneous tissues. Other sites that can be affected are the ears, forehead, and chin. Ocular manifestations affect approximately 50% of rosacea patients,6 ranging from conjunctivitis and blepharitis to keratitis and corneal ulceration, thereby requiring ophthalmologic assessment.
Because rosacea affects facial appearance, it can have a devastating impact on the patient’s quality of life, leading to social isolation. Although there is no cure available for rosacea, lifestyle modification and treatment can reduce or control its features, which tend to exacerbate and remit. There are a number of possible triggers for rosacea that ideally should be avoided such as sun exposure, hot or cold weather, heavy exercise, emotional stress, and consumption of alcohol and spicy foods. It is essential to consider disease subtype as well as the signs and symptoms presenting in each individual patient when approaching therapy selection. Most well-established US Food and Drug Administration (FDA)–approved treatments of rosacea target the papulopustular aspect of disease, including the erythema associated with the lesions. These treatments include topical and systemic antibiotics and azelaic acid. Non–FDA-approved agents such as topical and systemic retinoids, topical calcineurin inhibitors, and topical benzoyl peroxide also are used, though there is limited evidence of their efficacy.7
Management options for diffuse facial erythema and telangiectasia, however, are limited. Standard rosacea treatments often are not efficacious in treating these aspects of the disease, thereby requiring an alternative approach. This article reviews devices and topical agents currently available for the management of rosacea.
Skin Care
The skin of rosacea patients often is sensitive and prone to irritation; therefore, a good skin care regimen is an integral part of disease management and should include a gentle cleanser, moisturizer, and sunscreen.8 Lipid-free liquid cleansers or synthetic detergent (syndet) cleansers with a neutral to slightly acidic pH (ie, similar to the pH of normal skin) are ideal.9 Following cleansing, the skin should be gently dried. It may be beneficial to wait up to 30 minutes before application of a moisturizer to avoid irritation. Hydrating moisturizers should be free of irritants or abrasives, allowing maintenance of stratum corneum pH in an acid range of 4 to 6. Green-tinted makeup can be a useful tool in covering areas of erythema.
Devices
A variety of devices targeting hemoglobin are reported to be effective for the management of erythema and telangiectasia in rosacea patients, including the 595-nm pulsed dye laser (PDL), the potassium titanyl phosphate (KTP) laser, the 1064-nm Nd:YAG laser, and noncoherent intense pulsed light (IPL) sources.
The major chromophore in blood vessels is oxyhemoglobin, with 2 major absorption bands in the visible light spectrum at 542 and 577 nm. There also is notable albeit lesser absorption in the near-infrared range from 700 to 1100 nm.10 Following absorption by oxyhemoglobin, light energy is converted to thermal energy, which diffuses in the blood vessel causing photocoagulation, mechanical injury, and finally thrombosis.
Pulsed Dye Laser (585–595 nm)
Among the vascular lasers, the PDL has a long safety record. It was the first laser that used the concept of selective photothermolysis for treatment of vascular lesions.11,12 The first PDLs had a wavelength of 577 nm, while current PDLs have wavelengths of 585 or 595 nm with longer pulse durations and circular or oval spot sizes that are ideal for treatment of dermal vessels. The main disadvantage of PDLs is the development of posttreatment purpura. The longer pulse durations of KTP lasers avoid damage to cutaneous vasculature and eliminate the risk for bruising. Nonetheless, the wavelength of the PDL provides a greater depth of penetration due to its substantial absorption by cutaneous vasculature compared to the shorter wavelength of the KTP laser.
Although newer-generation PDLs still have the potential to cause purpura, various attempts have been made to minimize this risk, such as the use of longer pulse durations, multiple minipulses or “pulselets,”13 and multiple passes. Separate parameters may need to be used when treating linear vessels and diffuse erythema, with longer pulse durations required for larger vessels. The Figure shows a rosacea patient with facial telangiectasia before and after 1 treatment with a PDL.

According to Alam et al,14 purpuric settings were more efficacious in a comparison of variable-pulsed PDLs for facial telangiectasia. In 82% (9/11) of cases, greater reduction in telangiectasia density was noted on the side of the face that had been treated with purpuric settings versus the other side of the face.14 Purpuric settings are particularly effective in treating larger vessels, while finer telangiectatic vessels may respond to purpura-free settings.
In a study of 12 participants treated with a 595-nm PDL at a pulse duration of 6 ms and fluences from 7 to 9 J/cm2, no lasting purpura was seen; however, while 9 participants achieved more than 25% improvement after a single treatment, only 2 participants achieved more than 75% improvement.15 Nonetheless, some patients may prefer this potentially less effective treatment method to avoid the socially embarrassing side effect of purpura.
In a study of 12 rosacea patients, a 75% reduction in telangiectasia scores was noted after a mean of 3 treatments with the 585-nm PDL using 450-ms pulse durations. Purpura occurred in all patients.16 In another study by Madan and Ferguson,17 18 participants with nasal telangiectasia that had been resistant to the traditional round spot, 595-nm PDL and/or 532-nm KTP laser were treated with a 3x10-mm elliptical spot, ultra-long pulse, 595-nm PDL with a 40-ms pulse duration and double passes. Complete clearance was seen in 10 (55.6%) participants and 8 (44.4%) showed more than 80% improvement. No purpura was associated with the treatment.17
Further studies comparing the efficacy of nonpurpuric and purpuric settings in the same patient would allow us to determine the most effective option for future treatment.
KTP Laser (532 nm)
Potassium titanyl phosphate lasers have the disadvantage of higher melanin absorption, which can lead to epidermal damage with postinflammatory hyperpigmentation. Their use is limited to lighter skin types. Because of its shorter wavelength, the KTP laser is best used to treat superficial telangiectasia. The absence of posttreatment purpura can make KTP lasers a popular alternative to PDLs.17 Uebelhoer et al18 performed a split-face study in 15 participants to compare the 595-nm PDL and 532-nm KTP laser. Although both treatments were effective, the KTP laser achieved 62% clearance after the first treatment and 85% clearance 3 weeks after the third treatment compared to 49% and 75%, respectively, for the PDL. Interestingly, the degree of swelling and erythema posttreatment were greater on the KTP laser–treated side.18
Nd:YAG (1064 nm)
The wavelength of the Nd:YAG laser targets the lower absorption peak of oxyhemoglobin. In a study of 15 participants with facial telangiectasia who were treated with a 1064-nm Nd:YAG laser at day 0 and day 30 using a 3-mm spot size, a fluence of 120 to 170 J/cm,2 and 5- to 40-ms pulse durations, 73% (11/15) showed moderate to significant improvement at day 0 and day 30 and 80% improvement at 3 months’ follow-up.19 In a split-face study of 14 patients, treatment with the 595-nm PDL with a fluence of 7.5 J/cm2, pulse duration of 6 ms, and spot size of 10 mm was compared with the 1064-nm Nd:YAG laser with a fluence of 6 J/cm2, pulse duration of 0.3 ms, and spot size of 8 mm.20 Erythema improved by 6.4% from baseline on the side treated with the PDL. Although participants rated the Nd:YAG laser treatment as less painful, they were more satisfied with the results of the PDL treatment.20 In another split-face study comparing the 595-nm PDL and 1064-nm Nd:YAG laser, greater improvement was reported with the Nd:YAG laser, though the results were not statistically significant.21
Intense Pulsed Light
While lasers use selective photothermolysis, IPL devices emit noncoherent light at a wavelength of 500 to 1200 nm. Cutoff filters allow for selective tissue damage depending on the absorption spectra of the tissue. Longer wavelengths are effective for the treatment of deeper vessels, while shorter wavelengths target more superficial vessels; however, the shorter wavelengths can interact with melanin and should be avoided in darker skin types. In a phase 3 open trial, 34 participants were treated with IPL with a 560-nm cutoff filter and fluences of 24 to 32 J/cm2. The mean reduction of erythema following 4 treatments was 39% on the cheeks and 22% on the chin; side effects were minimal.22
Photodynamic Therapy
Photodynamic therapy is an effective and widely used treatment method for a number of skin conditions. Following its success in the treatment of acne, it also has been used in the management of rosacea, though the exact mechanism of action remains unclear.
Photodynamic therapy involves topical application of a photosensitizing agent (eg, 5-aminolevulinic acid, methyl aminolevulinate [MAL]) followed by exposure to red or blue light. The photosensitizing agent accumulates semiselectively in abnormal skin tissue and is converted to protoporphyrin IX, which induces a toxic skin reaction through reactive oxygen radicals in the presence of visible light.23 Photodynamic therapy generally is well tolerated. The primary side effects are pain, burning, and stinging.
In 3 of 4 (75%) patients treated with MAL and red light, rosacea clearance was noted after 2 to 3 sessions. Remission lasted for 3 months in 2 (66.7%) participants and for 9 months in 1 (33.3%) participant.24 In another study, 17 patients were treated with MAL and red light. Results were good in 10 participants (58.8%), fair in 4 (23.5%), and poor in 3 (17.6%).23
ALPHA-Adrenergic Receptor Agonists
Recently, the α-adrenergic receptor agonists brimonidine tartrate and oxymetazoline have been found to be effective in controlling diffuse facial erythema of rosacea, which is thought to arise from vasomotor instability and abnormal vasodilation of the superficial cutaneous vasculature. Brimonidine tartrate is a potent α2-agonist that is mainly used for treatment of open-angle glaucoma. In 2 phase 3 controlled studies, once-daily application of brimonidine tartrate gel 0.5% was found to be effective and safe in reducing the erythema of rosacea.25 Brimonidine tartrate gel is the first FDA-approved treatment of facial erythema associated with rosacea. Possible side effects are erythema worse than baseline (4%), flushing (3%), and burning (2%).26 Oxymetazoline is a potent α1- and partial α2-agonist that is available as a nasal decongestant. Oxymetazoline solution 0.05% used once daily has been shown in case reports to reduce rosacea-associated erythema for several hours.27
Nicotinamide
Nicotinamide is the amide form of niacin, which has both anti-inflammatory properties and a stabilizing effect on epidermal barrier function.28 Although topical application of nicotinamide has been used in the treatment of inflammatory dermatoses such as rosacea,28,29 niacin can lead to cutaneous vasodilation and thus flushing. It has been hypothesized to potentially enhance the effect of PDL if used as pretreatment for rosacea-associated erythema.30
Conclusion
Rosacea can have a substantial impact on patient quality of life. Recent advances in treatment options and rapidly advancing knowledge of laser therapy are providing dermatologists with powerful tools for rosacea clearance. Lasers and IPL are effective treatments of the erythematotelangiectatic aspect of the disease, and careful selection of devices and treatment parameters can reduce unwanted side effects.
- Ayres S Jr. Extrafacial rosacea is rare but does exist. J Am Acad Dermatol. 1987;16:391-392.
- Jansen T, Plewig G. Rosacea: classification and treatment. J R Soc Med. 1997;90:144-150.
- Yamasaki K, Gallo RL. Rosacea as a disease of cathelicidins and skin innate immunity. J Investig Dermatol Symp Proc. 2011;15:12-15.
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69(6, suppl 1):S15-S26.
- Wilkin J, Dahl M, Detmar M, et al; National Rosacea Society Expert Committee. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol. 2002;46:584-587.
- Webster G, Schaller M. Ocular rosacea: a dermatologic perspective. J Am Acad Dermatol. 2013;69(6, suppl 1):S42-S43.
- Del Rosso JQ, Thiboutot D, Gallo R, et al. Consensus recommendations from the American Acne & Rosacea Society on the management of rosacea, part 2: a status report on topical agents. Cutis. 2013;92:277-284.
- Levin J, Miller R. A guide to the ingredients and potential benefits of over-the-counter cleansers and moisturizers for rosacea patients. J Clin Aesthet Dermatol. 2011;4:31-49.
- Draelos ZD. The effect of Cetaphil gentle skin cleanser on the skin barrier of patients with rosacea. Cutis. 2006;77:27-33.
- Hare McCoppin HH, Goldberg DJ. Laser treatment of facial telangiectases: an update. Dermatol Surg. 2010;36:1221-1230.
- Garden JM, Polla LL, Tan OT. The treatment of port-wine stains by the pulsed dye laser. analysis of pulse duration and long-term therapy. Arch Dermatol. 1988;124:889-896.
- Anderson RR, Parrish JA. Microvasculature can be selectively damaged using dye lasers: a basic theory and experimental evidence in human skin. Lasers Surg Med. 1981;1:263-276.
- Bernstein EF, Kligman A. Rosacea treatment using the new-generation, high-energy, 595 nm, long pulse-duration pulsed-dye laser. Lasers Surg Med. 2008;40:233-239.
- Alam M, Dover JS, Arndt KA. Treatment of facial telangiectasia with variable-pulse high-fluence pulsed-dye laser: comparison of efficacy with fluences immediately above and below the purpura threshold. Dermatol Surg. 2003;29:681-684.
- Jasim ZF, Woo WK, Handley JM. Long-pulsed (6-ms) pulsed dye laser treatment of rosacea-associated telangiectasia using subpurpuric clinical threshold. Dermatol Surg. 2004;30:37-40.
- Clark SM, Lanigan SW, Marks R. Laser treatment of erythema and telangiectasia associated with rosacea. Lasers Med Sci. 2002;17:26-33.
- Madan V, Ferguson J. Using the ultra-long pulse width pulsed dye laser and elliptical spot to treat resistant nasal telangiectasia. Lasers Med Sci. 2010;25:151-154.
- Uebelhoer NS, Bogle MA, Stewart B, et al. A split-face comparison study of pulsed 532-nm KTP laser and 595-nm pulsed dye laser in the treatment of facial telangiectases and diffuse telangiectatic facial erythema. Dermatol Surg. 2007;33:441-448.
- Sarradet DM, Hussain M, Goldberg DJ. Millisecond 1064-nm neodymium:YAG laser treatment of facial telangiectases. Dermatol Surg. 2003;29:56-58.
- Alam M, Voravutinon N, Warycha M, et al. Comparative effectiveness of nonpurpuragenic 595-nm pulsed dye laser and microsecond 1064-nm neodymium:yttrium-aluminum-garnet laser for treatment of diffuse facial erythema: a double-blind randomized controlled trial. J Am Acad Dermatol. 2013;69:438-443.
- Salem SA, Abdel Fattah NS, Tantawy SM, et al. Neodymium-yttrium aluminum garnet laser versus pulsed dye laser in erythemato-telangiectatic rosacea:comparison of clinical efficacy and effect on cutaneoussubstance (P) expression. J Cosmet Dermatol. 2013;12:187-194.
- Papageorgiou P, Clayton W, Norwood S, et al. Treatment of rosacea with intense pulsed light: significant improvement and long-lasting results. Br J Dermatol. 2008;159:628-632.
- Bryld LE, Jemec GB. Photodynamic therapy in a series of rosacea patients. J Eur Acad Dermatol Venereol. 2007;21:1199-1202.
- Nybaek H, Jemec GB. Photodynamic therapy in the treatment of rosacea. Dermatology. 2005;211:135-138.
- Fowler J, Jackson M, Moore A, et al. Efficacy and safety of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of two randomized, double-blind, and vehicle-controlled pivotal studies. J Drugs Dermatol. 2013;12:650-656.
- Routt ET, Levitt JO. Rebound erythema and burning sensation from a new topical brimonidine tartrate gel 0.33%. J Am Acad Dermatol. 2014;70:E37-E38.
- Shanler SD, Ondo AL. Successful treatment of the erythema and flushing of rosacea using a topically applied selective alpha1-adrenergic receptor agonist, oxymetazoline. Arch Dermatol. 2007;143:1369-1371.
- Draelos ZD, Ertel K, Berge C. Niacinamide-containing facial moisturizer improves skin barrier and benefits subjects with rosacea. Cutis. 2005;76:135-141.
- Draelos ZD, Ertel KD, Berge CA. Facilitating facial retinization through barrier improvement. Cutis. 2006;78:275-281.
- Kim TG, Roh HJ, Cho SB, et al. Enhancing effect of pretreatment with topical niacin in the treatment of rosacea-associated erythema by 585-nm pulsed dye laser in Koreans: a randomized, prospective, split-face trial. Br J Dermatol. 2011;164:573-579.
- Ayres S Jr. Extrafacial rosacea is rare but does exist. J Am Acad Dermatol. 1987;16:391-392.
- Jansen T, Plewig G. Rosacea: classification and treatment. J R Soc Med. 1997;90:144-150.
- Yamasaki K, Gallo RL. Rosacea as a disease of cathelicidins and skin innate immunity. J Investig Dermatol Symp Proc. 2011;15:12-15.
- Steinhoff M, Schauber J, Leyden JJ. New insights into rosacea pathophysiology: a review of recent findings. J Am Acad Dermatol. 2013;69(6, suppl 1):S15-S26.
- Wilkin J, Dahl M, Detmar M, et al; National Rosacea Society Expert Committee. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol. 2002;46:584-587.
- Webster G, Schaller M. Ocular rosacea: a dermatologic perspective. J Am Acad Dermatol. 2013;69(6, suppl 1):S42-S43.
- Del Rosso JQ, Thiboutot D, Gallo R, et al. Consensus recommendations from the American Acne & Rosacea Society on the management of rosacea, part 2: a status report on topical agents. Cutis. 2013;92:277-284.
- Levin J, Miller R. A guide to the ingredients and potential benefits of over-the-counter cleansers and moisturizers for rosacea patients. J Clin Aesthet Dermatol. 2011;4:31-49.
- Draelos ZD. The effect of Cetaphil gentle skin cleanser on the skin barrier of patients with rosacea. Cutis. 2006;77:27-33.
- Hare McCoppin HH, Goldberg DJ. Laser treatment of facial telangiectases: an update. Dermatol Surg. 2010;36:1221-1230.
- Garden JM, Polla LL, Tan OT. The treatment of port-wine stains by the pulsed dye laser. analysis of pulse duration and long-term therapy. Arch Dermatol. 1988;124:889-896.
- Anderson RR, Parrish JA. Microvasculature can be selectively damaged using dye lasers: a basic theory and experimental evidence in human skin. Lasers Surg Med. 1981;1:263-276.
- Bernstein EF, Kligman A. Rosacea treatment using the new-generation, high-energy, 595 nm, long pulse-duration pulsed-dye laser. Lasers Surg Med. 2008;40:233-239.
- Alam M, Dover JS, Arndt KA. Treatment of facial telangiectasia with variable-pulse high-fluence pulsed-dye laser: comparison of efficacy with fluences immediately above and below the purpura threshold. Dermatol Surg. 2003;29:681-684.
- Jasim ZF, Woo WK, Handley JM. Long-pulsed (6-ms) pulsed dye laser treatment of rosacea-associated telangiectasia using subpurpuric clinical threshold. Dermatol Surg. 2004;30:37-40.
- Clark SM, Lanigan SW, Marks R. Laser treatment of erythema and telangiectasia associated with rosacea. Lasers Med Sci. 2002;17:26-33.
- Madan V, Ferguson J. Using the ultra-long pulse width pulsed dye laser and elliptical spot to treat resistant nasal telangiectasia. Lasers Med Sci. 2010;25:151-154.
- Uebelhoer NS, Bogle MA, Stewart B, et al. A split-face comparison study of pulsed 532-nm KTP laser and 595-nm pulsed dye laser in the treatment of facial telangiectases and diffuse telangiectatic facial erythema. Dermatol Surg. 2007;33:441-448.
- Sarradet DM, Hussain M, Goldberg DJ. Millisecond 1064-nm neodymium:YAG laser treatment of facial telangiectases. Dermatol Surg. 2003;29:56-58.
- Alam M, Voravutinon N, Warycha M, et al. Comparative effectiveness of nonpurpuragenic 595-nm pulsed dye laser and microsecond 1064-nm neodymium:yttrium-aluminum-garnet laser for treatment of diffuse facial erythema: a double-blind randomized controlled trial. J Am Acad Dermatol. 2013;69:438-443.
- Salem SA, Abdel Fattah NS, Tantawy SM, et al. Neodymium-yttrium aluminum garnet laser versus pulsed dye laser in erythemato-telangiectatic rosacea:comparison of clinical efficacy and effect on cutaneoussubstance (P) expression. J Cosmet Dermatol. 2013;12:187-194.
- Papageorgiou P, Clayton W, Norwood S, et al. Treatment of rosacea with intense pulsed light: significant improvement and long-lasting results. Br J Dermatol. 2008;159:628-632.
- Bryld LE, Jemec GB. Photodynamic therapy in a series of rosacea patients. J Eur Acad Dermatol Venereol. 2007;21:1199-1202.
- Nybaek H, Jemec GB. Photodynamic therapy in the treatment of rosacea. Dermatology. 2005;211:135-138.
- Fowler J, Jackson M, Moore A, et al. Efficacy and safety of once-daily topical brimonidine tartrate gel 0.5% for the treatment of moderate to severe facial erythema of rosacea: results of two randomized, double-blind, and vehicle-controlled pivotal studies. J Drugs Dermatol. 2013;12:650-656.
- Routt ET, Levitt JO. Rebound erythema and burning sensation from a new topical brimonidine tartrate gel 0.33%. J Am Acad Dermatol. 2014;70:E37-E38.
- Shanler SD, Ondo AL. Successful treatment of the erythema and flushing of rosacea using a topically applied selective alpha1-adrenergic receptor agonist, oxymetazoline. Arch Dermatol. 2007;143:1369-1371.
- Draelos ZD, Ertel K, Berge C. Niacinamide-containing facial moisturizer improves skin barrier and benefits subjects with rosacea. Cutis. 2005;76:135-141.
- Draelos ZD, Ertel KD, Berge CA. Facilitating facial retinization through barrier improvement. Cutis. 2006;78:275-281.
- Kim TG, Roh HJ, Cho SB, et al. Enhancing effect of pretreatment with topical niacin in the treatment of rosacea-associated erythema by 585-nm pulsed dye laser in Koreans: a randomized, prospective, split-face trial. Br J Dermatol. 2011;164:573-579.
Practice Points
- Rosacea patients should be advised on appropriate skin care.
- Purpuric settings of the pulsed dye laser may be more effective in treating rosacea-associated erythema.
- Topical brimodine tartrate can control facial erythema, but patients should be warned of the potential risk for rebound erythema.
The Great Mimickers of Rosacea
Although rosacea is one of the most common conditions treated by dermatologists, it also is one of the most misunderstood. Historically, large noses due to rhinomegaly were associated with indulgence in wine and wealth.1 The term rosacea is derived from the Latin adjective meaning “like roses.” Rosacea was first medically described in French as goutterose (pink droplet) and pustule de vin (pimples of wine).1 This article reviews the characteristics of rosacea compared to several mimickers of rosacea that physicians should consider.
Rosacea Characteristics
Rosacea is a chronic disorder affecting the central parts of the face that is characterized by frequent flushing; persistent erythema (ie, lasting for at least 3 months); telangiectasia; and interspersed episodes of inflammation with swelling, papules, and pustules.2 It is most commonly seen in adults older than 30 years and is considered to have a strong hereditary component, as it is more commonly seen in individuals of Celtic and Northern European descent as well as those with fair skin. Furthermore, approximately 30% to 40% of patients report a family member with the condition.2
Rosacea Subtypes
In a 2002 meeting held to standardize the diagnostic criteria for rosacea, the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea described 4 broad clinical subtypes of rosacea: erythematotelangiectatic, papulopustular, phymatous, and ocular.3 More than 1 subtype may present in the same patient. A progression from one subtype to another can occur in cases of severe papulopustular or glandular rosacea that eventuate into the phymatous form.2 Moreover, not all of the disease features are present in every patient. Secondary features of rosacea include burning or stinging, edema, plaques, dry appearance of the skin, ocular manifestations, peripheral site involvement, and phymatous changes.
In erythematotelangiectatic rosacea, episodic flushing occurs, which can last longer than 10 minutes with the central face exhibiting the most intense color. The redness also may involve the peripheral portion of the face as well as extrafacial areas (eg, ears, scalp, neck, chest). Periocular skin is spared. The stimuli that may bring on flushing include short-term emotional stress, hot drinks, alcohol, spicy foods, exercise, cold or hot weather, and hot water.3
Patients with papulopustular rosacea generally present with redness of the central portion of the face along with persistent or intermittent flares characterized by small papules and pinpoint pustules. There also is an almost universal sparing of the periocular skin, and a history of flushing often is present; however, flushing usually is milder than in the erythematotelangiectatic subtype. The constant inflammation may lead to chronic edema and phymatous changes, which occur more commonly in men than in women.3
Phymatous rosacea is characterized by marked skin thickening and irregular surface nodularities, most commonly involving the nose (rhinophyma), though the chin (gnathophyma), forehead (metophyma), ears (otophyma), and eyelids (blepharophyma) also are occasionally affected. There are 4 variants of rhinophyma with distinct histopathologic features: glandular, fibrous, fibroangiomatous, and actinic.3 The glandular variant is most often seen in men who have thick sebaceous skin. Edematous papules and pustules often are large and may be accompanied by nodulocystic lesions. Frequently, affected patients will have a history of adolescent acne with scarring.
Ocular rosacea may precede cutaneous findings by many years; however, in most cases the ocular findings occur concurrently or develop later on in the disease course. The most consistent findings in ocular rosacea are blepharitis and conjunctivitis. Symptoms of burning or stinging, itching, light sensitivity, and a foreign body sensation are common in these patients.3
Pathogenesis
Several investigators have proposed that Demodex folliculorum may play a pathogenic role in rosacea. Demodex is a common inhabitant of normal human skin, and its role in human disease is a matter of controversy.3Demodex has a predilection for the regions of the skin that are most often affected by rosacea, such as the nose and cheeks. The clinical manifestations of rosacea tend to appear later in life, which parallels the increase in the density of Demodex mites that occurs with age.4 It has been hypothesized that beneficial effects of metronidazole in the treatment of rosacea may be related to an antiparasitic effect on Demodex; however, these mites can survive high concentrations of the drug.3 Moreover, modern techniques that employ cyanoacrylate surface biopsies, which are extremely sensitive, estimate that the prevalence of Demodex in healthy skin approaches 100%.4 Consequently, the simple identification of Demodex is by no means proof of pathogenesis. Whether Demodex is truly pathogenic or simply an inhabitant of follicles in rosacea-prone skin remains a subject for future investigation.
Demodicosis occurs mainly in immunosuppressed patients because immunosuppression influences the number of Demodex mites and the treatment response. Multiple patients with AIDS and/or those with a CD4 lymphocyte count below 200/mm3 have been reported to have demodicosis.5-11 In immunocompetent patients, pruritic papular, papulopustular, and nodular lesions occur on the face, but in immunocompromised patients, the eruption may be more diffuse, affecting the back, presternal area, and upper limbs.6 A correct diagnosis relies on suggestive clinical signs, the presence of numerous parasites on direct examination, and a good clinical response to acaricide treatment.
Helicobacter pylori seropositivity has been associated with various dermatologic disorders, including rosacea.12 However, robust support for a causal association between H pylori and rosacea does not exist. Several studies have demonstrated high prevalence rates of H pylori in rosacea patients, some even in comparison with age- and sex-matched controls.13,14 Moreover, treatments aimed at eradicating H pylori also beneficially influence the clinical outcome of rosacea; for instance, metronidazole, a common treatment of roscea, is an effective agent against H pylori.
Understanding the clinical variants and disease course of rosacea is important to differentiate this entity from other conditions that can mimic rosacea. Laboratory studies and histopathologic examination via skin biopsy may be needed to differentiate between rosacea and rosacealike conditions.
Common Rosacealike Conditions
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is a chronic inflammatory disease that has protean clinical manifestations and follows a relapsing and remitting course. Characteristic malar erythema appears in approximately 50% of patients and may accompany or precede other symptoms of lupus. The affected skin generally feels warm and appears slightly edematous. The erythema may last for hours to days and often recurs, particularly with sun exposure. The malar erythema of SLE can be confused with the redness of erythematotelangiectatic rosacea. Nevertheless, the color of the skin in SLE has a violaceous quality and may show a more abrupt cutoff, especially at its most lateral margins. Marzano et al15 reported 4 cases in which lupus erythematosus was misdiagnosed as rosacea. All 4 patients presented with erythema that was localized to the central face along with a few raised, smooth, round, erythematous to violaceous papules over the malar areas and the forehead. This presentation evolved rapidly and was aggravated by sun exposure. The patients were all treated with medication for rosacea but showed no improvement. These patients originally presented with limited skin involvement in the absence of any systemic sign or symptoms of SLE.15
Dermatomyositis
Dermatomyositis (DM) is an inflammatory myopathy characterized by varying degrees of muscle weakness and distinctive skin erythema (Figure 1); however, some patients lack muscular involvement and initially present with skin manifestations only. Sontheimer16 described criteria for defining skin involvement in DM. Major criteria include the heliotrope rash, Gottron papules, and Gottron sign, while minor criteria include macular violaceous erythema (MVE), periungual telangiectasia of the nail fold, poikiloderma, mechanic’s hands, cutaneous calcinosis, cutaneous ulcers, and pruritus. With the exception of the heliotrope rash, facial erythema has drawn little attention in prior studies of DM-associated skin manifestations. Therefore, Okiyama et al17 performed a retrospective study on the skin manifestations of DM in 33 patients. The investigators observed that MVE in the seborrheic area of the face was most frequent.17 Therefore, it is critical to consider DM in the differential diagnosis of rosacea because the MVE seen in DM might be confused with the erythema seen in rosacea.

|
| Figure 1. Macular violaceous erythema of the face in a patient with dermatomyositis. Photograph courtesy of Marc Silverstein, MD, Sacramento, California. |

|
Figure 2. Polymorphous light eruption manifesting as erythematous papules over the cheek and dorsal aspect of the nose. Photograph courtesy of Marc Silverstein, MD, Sacramento, California. |
Polymorphous Light Eruption
Polymorphous light eruption (PMLE), the most common of the idiopathic photodermatoses, is characterized by erythematous papules, papulovesicles, and plaques on sun-exposed surfaces (Figure 2). The areas of the skin that are most commonly affected are the face, neck, outer aspects of the arms, and dorsal surfaces of the hands.18 Lesions may appear immediately but often develop several hours after sun exposure. Symptoms of itching and/or burning usually are mild and transient. The etiology of PMLE is unknown, though it is likely to be multifactorial.
Similarities between PMLE and rosacea include exacerbation by sun exposure and a higher prevalence in fair-skinned individuals.19 Also, in both conditions erythematous papules appear on the face and may be pruritic and in some instances painful; however, unlike rosacea, which is chronic, PMLE tends to be intermittent and recurrent, typically occurring in the spring and early summer months. In contrast to rosacea, the onset of the erythema in PMLE is abrupt, appearing quickly after sun exposure and subsiding within 1 to 7 days. Furthermore, patients with PMLE may experience systemic flulike symptoms after sun exposure.19
Seborrheic Dermatitis
Seborrheic dermatitis is a chronic relapsing papulosquamous skin disease most commonly involving sebum-rich areas such as the scalp and face. The prevalence of seborrheic dermatitis is higher in human immunodeficiency virus–positive individuals and in patients with neurologic conditions such as Parkinson disease. The pathogenesis of seborrheic dermatitis has been linked to the yeast of Malassezia species, immunologic abnormalities, and activation of complements. A clinical diagnosis usually is made based on a history of waxing and waning in severity and by the sites of involvement.20
Similar to rosacea, seborrheic dermatitis is a chronic and relapsing erythematous rash with well-demarcated erythematous patches, papules, or plaques; however, unlike rosacea, the distribution varies from minimal asymptomatic scaliness of the scalp to more widespread involvement (eg, scalp, ears, upper aspect of the trunk, intertriginous areas). Also, although macular erythema and scaling involving the perinasal area (Figure 3) may be seen in either rosacea or seborrheic dermatitis, a greasy quality to the scales and involvement of other sites such as the scalp, retroauricular skin, and eyebrows suggest a diagnosis of seborrheic dermatitis.
Acne Vulgaris
Acne vulgaris is the most common skin disease in the United States.21 It is characterized by noninflammatory; open or closed comedones; and inflammatory papules, pustules, and nodules. Acne vulgaris typically affects the areas of skin with the highest density of sebaceous follicles including the face, upper aspect of the chest, and back.22 It is the most common skin disease in the differential diagnosis of the papulopustular form of rosacea. Inflammatory lesions in both acne vulgaris and rosacea may be clinically identical; however, unlike acne vulgaris, rosacea is characterized by a complete absence of comedones. A prominent centrofacial distribution also favors rosacea. As a general rule, acne peaks in adolescence, years before papulopustular rosacea usually becomes prominent. However, some acne patients who are prone to flushing and blushing may develop rosacea later in life.
Topical Steroid–Induced Acne
Chronic use of topical corticosteroids on the face for several months can result in the appearance of monomorphic inflammatory papules (Figure 4). Corticosteroids can cause a dry scaly eruption with scattered follicular pustules around the mouth (perioral dermatitis).23 This acneform eruption is indistinguishable from rosacea. However, the monomorphic inflammatory papules generally resolve within 1 to 2 months following discontinuation of the corticosteroid therapy.
Multiple pathways have been proposed as the mechanism for such reactions, including rebound vasodilation and proinflammatory cytokine release by chronic intermittent steroid exposure.24 At first, the vasoconstrictive and anti-inflammatory effects of the steroids result in what seems to be clearance of the primary dermatitis for which the steroids were being used. Unfortunately, persistent use of steroids, particularly high-potency products, leads to epidermal atrophy, degeneration of dermal structures, and destruction of collagen, rendering the skin vulnerable to bacterial, viral, and fungal infections. In the end, the skin has the appearance of bright red rosacea with red scaly papules.
Rare Rosacealike Conditions
Carcinoid Syndrome
Carcinoid syndrome typically develops after hepatic metastasis from a carcinoid tumor when the circulating neuroendocrine mediators produced by the tumor can no longer be adequately cleared. Flushing is characteristic of carcinoid syndrome and usually presents on the face, neck, and upper trunk. Although rare, other types of cutaneous involvement also have been reported.25 Bell et al25 concluded that skin involvement is not uncommon in carcinoid syndrome, as all 25 patients with carcinoid syndrome showed cutaneous involvement in their case series. The investigators observed that chronic flushing eventually may become permanent and evolve into a rosacealike picture.25
Cases of carcinoid syndrome that were misdiagnosed as rosacea have been reported in the literature.26-28 Creamer et al26 reported a case of a 67-year-old woman who initially was diagnosed with rosacea; it took 1 year to finally arrive at the correct diagnosis of multiple endocrine neoplasia type 1 after developing a malignant carcinoid tumor and a parathyroid tumor.
Cutaneous Lymphoma
B-cell neoplasms with skin involvement can present as primary cutaneous lymphomas or as secondary processes, including specific infiltrates of nodal or extranodal lymphoma or leukemia.29 B-cell lymphomas involving the skin have a distinct clinical appearance, presenting as isolated, grouped, or multiple erythematous to violaceous papules, plaques, or nodules, usually in an asymmetric distribution (Figure 5). B-cell lymphoproliferative diseases simulating rosacea are extremely rare.29 Nevertheless, B-cell lymphoma mimicking rhinophyma has been documented in the literature.29-35
Barzilai et al29 described 12 patients with B-cell lymphoproliferative neoplasms presenting with facial eruptions that clinically mimicked rosacea or rhinophyma. The clinical presentation included small papules on the nose, cheeks, and around the eyes mimicking granulomatous rosacea, and/or nodules on the nose, cheeks, chin, or forehead simulating phymatous rosacea. Three patients had preexisting erythematotelangiectatic rosacea and 1 had rhinophyma.29
Lupus Miliaris Disseminatus Faciei
Lupus miliaris disseminatus faciei (LMDF) is an uncommon chronic inflammatory skin disorder characterized by the appearance of asymptomatic small, red to yellowish brown papules on the face.36 This rare dermatologic disease usually is self-limited with spontaneous resolution of the lesions occurring within months or years; however, residual disfiguring scars may persist and usually are characteristic of LMDF.36,37 The pathogenesis of LMDF is unclear, and controversy remains as to whether it is a distinct cutaneous entity or a variant of granulomatous rosacea.38,39 It usually develops slowly as small, dome-shaped, red to yellowish brown papules in adults, most commonly appearing in men.39 Lupus miliaris disseminatus faciei shares several common features with both acne vulgaris and rosacea. For example, the inflammatory lesions of LMDF are located on the central face and usually respond to treatments that typically are used to treat acne vulgaris and rosacea. However, LMDF can be distinguished histologically by more intense granulomatous inflammation and central caseation, occurring in the absence of an apparent infectious origin.36
Tyrosinase Kinase Inhibitor Drug Eruptions
Sorafenib and sunitinib malate are multitargeted kinase inhibitors approved for the treatment of cancers such as renal cell carcinoma.40 A study by Lee et al40 reported that approximately 75% of patients treated with either sorafenib (n=109) or sunitinib (n=119) went on to develop at least one cutaneous reaction. Although hand-foot skin reaction was the most common and serious cutaneous side effect, other dermatologic manifestations, including alopecia, stomatitis, discoloration (hair or face), subungual splinter hemorrhages, facial swelling, facial erythema, and xerosis, were described. Facial changes such as swelling, yellowish discoloration, erythema, and acneform eruptions were described more frequently in patients treated with sunitinib than in those treated with sorafenib.40
Other reports have described facial erythematous papules with sorafenib.41 In these patients, facial erythema usually occurs within 1 to 2 weeks after initiation of treatment, unlike hand-foot skin reaction, which usually develops later.42
Epidermal Growth Factor Receptor Inhibitor Drug Eruptions
Monoclonal antibodies against the epidermal growth factor receptor (EGFR) (eg, cetuximab, panitumumab) and EGFR tyrosine kinase inhibitors (eg, gefitinib, erlotinib) are used in the treatment of several cancers. Use of these drugs has been associated with various dermatologic side effects, including rashes, paronychia and fissuring of the nail bed, hair changes, dry skin, hypersensitivity reactions, and mucositis.43 The most frequent dermatologic side effect is a sterile follicular and pustular rash, often affecting the face, that is seen in more than half of the patients treated with these drugs.43,44 These rosacealike facial lesions are accompanied by diffuse erythema and telangiectasia. In some cases, the pustules leave areas of erythema covered with greasy scaling, thus resembling seborrheic dermatitis.43 In general, the pustular rash manifests within 1 to 3 weeks after the onset of treatment with EGFR inhibitors. The reaction typically resolves within 4 weeks of stopping treatment.44 The etiology of the rash is unknown, but inhibition of EGFR may result in occlusion of hair follicles and their associated sebaceous glands, producing a rosacealike appearance.45
Conclusion
Since its first medical description, rosacea has undergone extensive study regarding its pathogenesis and management. The most current investigations indicate microorganisms such as D folliculorum and H pylori as etiologic factors, though several other possibilities (eg, vascular abnormalities) have been suggested. Understanding the clinical variants and disease course of rosacea is important in differentiating this entity from other conditions that can mimic rosacea.
Acknowledgments—The authors thank Jennifer Rullan, MD, San Diego, California, and Jose Gonzalez-Chavez, MD, San Juan, Puerto Rico, for their assistance.
1. Bateman T, Thomson AT, Willan R. A Practical Synopsis of Cutaneous Diseases According to the Arrangement of Dr. Willan, Exhibiting a Concise View of the Diagnostic Symptoms and the Method of Treatment. London, England: Longman, Hurst, Rees, Orme, and Browne; 1813.
2. Plewig G, Kligman AM. Acne and Rosacea. 3rd ed. Germany: Springer-Verlag; 2000.
3. Wilkin J, Dahl M, Detmar M, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol. 2002;46:584-587.
4. Crawford GH, Pelle MT, James WD. Rosacea: i. etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004;51:327-341.
5. Clyti E, Nacher M, Sainte-Marie D, et al. Ivermectin treatment of three cases of demodicosis during human immunodeficiency virus infection. Int J Dermatol. 2006;45:1066-1068.
6. Aquilina C, Viraben R, Sire S. Ivermectin-responsive Demodex infestation during human immunodeficiency virus infection. a case report and literature review. Dermatology. 2002;205:394-397.
7. Brutti CS, Artus G, Luzzatto L, et al. Crusted rosacea-like demodicidosis in an HIV-positive female. J Am Acad Dermatol. 2011;65:e131-e132.
8. Clyti E, Sayavong K, Chanthavisouk K. Demodicosis in a patient infected by HIV: successful treatment with ivermectin. Ann Dermatol Venereol. 2005;132:459-461.
9. Patrizi A, Neri I, Chieregato C, et al. Demodicosis in immunocompetent young children: report of eight cases. Dermatology. 1997;195:239-242.
10. Barrio J, Lecona M, Hernanz JM, et al. Rosacea-like demodicosis in an HIV-positive child. Dermatology. 1996;192:143-145.
11. Vin-Christian K, Maurer TA, Berger TG. Acne rosacea as a cutaneous manifestation of HIV infection. J Am Acad Dermatol. 1994;30:139-140.
12. Tüzün Y, Keskin S, Kote E. The role of Helicobacter pylori infection in skin diseases: facts and controversies. Clin Dermatol. 2010;28:478-482.
13. El-Khalawany M, Mahmoud A, Mosbeh AS, et al. Role of Helicobacter pylori in common rosacea subtypes: a genotypic comparative study of Egyptian patients. J Dermatol. 2012;39:989-995.
14. Boixeda de Miquel D, Vázquez Romero M, Vázquez Sequeiros E, et al. Effect of Helicobacter pylori eradication therapy in rosacea patients [in Spanish]. Rev Esp Enferm Dig. 2006;98:501-509.
15. Marzano AV, Lazzari R, Polloni I, et al. Rosacea-like cutaneous lupus erythematosus: an atypical presentation responding to antimalarials. Acta Derm Venereol. 2013;93:106-107.
16. Sontheimer RD. Cutaneous features of classic dermatomyositis and amyopathic dermatomyositis. Curr Opin Rheumatol. 1999;11:475-482.
17. Okiyama N, Kohsaka H, Ueda N, et al. Seborrheic area erythema as a common skin manifestation in Japanese patients with dermatomyositis. Dermatology. 2008;217:374-377.
18. Naleway AL, Greenlee RT, Melski JW. Characteristics of diagnosed polymorphous light eruption. Photodermatol Photoimmunol Photomed. 2006;22:205-207.
19. Tutrone WD. Polymorphic light eruption. Dermatol Ther. 2003;16:28-39.
20. Sampaio AL, Mameri AC, Vargas TJ, et al. Seborrheic dermatitis [in Portuguese]. An Bras Dermatol. 2011;86:1061-1071.
21. Cordain L, Lindberg S, Hurtado M, et al. Acne vulgaris: a disease of Western civilization. Arch Dermatol. 2002;138:1584-1590.
22. Titus S, Hodge J. Diagnosis and treatment of acne. Am Fam Physician. 2012;86:734-740.
23. Poulos GA, Brodell RT. Perioral dermatitis associated with an inhaled corticosteroid. Arch Dermatol. 2007;143:1460.
24. Bhat YJ, Manzoor S, Qayoom S. Steroid-induced rosacea: a clinical study of 200 patients. Indian J Dermatol. 2011;56:30-32.
25. Bell HK, Poston GJ, Vora J, et al. Cutaneous manifestations of the malignant carcinoid syndrome. Br J Dermatol. 2005;152:71-75.
26. Creamer JD, Whittaker SJ, Griffiths WA. Multiple endocrine neoplasia type 1 presenting as rosacea. Clin Exp Dermatol. 1996;21:170-171.
27. Reichert S, Truchetet F, Cuny JF, et al. Carcinoid tumor with revealed by skin manifestation [in French]. Ann Dermatol Venereol. 1994;121:485-488.
28. Findlay GH, Simson IW. Leonine hypertrophic rosacea associated with a benign bronchial carcinoid tumour. Clin Exp Dermatol. 1977;2:175-176.
29. Barzilai A, Feuerman H, Quaglino P, et al. Cutaneous B-cell neoplasms mimicking granulomatous rosacea or rhinophyma. Arch Dermatol. 2012;148:824-831.
30. Moulonguet I, Ghnassia M, Molina T, et al. Miliarial-type perifollicular B-cell pseudolymphoma (lymphocytoma cutis): a misleading eruption in two women. J Cutan Pathol. 2012;39:1016-1021.
31. Soon CW, Pincus LB, Ai WZ, et al. Acneiform presentation of primary cutaneous follicle center lymphoma. J Am Acad Dermatol. 2011;65:887-889.
32. Rosmaninho A, Alves R, Lima M, et al. Red nose: primary cutaneous marginal zone B-cell lymphoma. Leuk Res. 2010;34:682-684.
33. Ogden S, Coulson IH. B-cell lymphoma mimicking rhinophyma. Clin Exp Dermatol. 2008;33:213-214.
34. Seward JL, Malone JC, Callen JP. Rhinophymalike swelling in an 86-year-old woman. Primary cutaneous B-cell lymphoma of the nose. Arch Dermatol. 2004;140:751-756.
35. Colvin JH, Lamerson CL, Cualing H, et al. Cutaneous lymphoplasmacytoid lymphoma (immunocytoma) with Waldenström’s macroglobulinemia mimicking rosacea. J Am Acad Dermatol. 2003;49:1159-1162.
36. Jih MH, Friedman PM, Kimyai-Asadi A, et al. Lupus miliaris disseminatus faciei treatment with the 1450-nm diode laser. Arch Dermatol. 2005;141:143-145.
37. Abdullah L, Abbas O. Dermacase. can you identify this condition? lupus miliaris disseminatus faciei. Can Fam Physician. 2011;57:795-796.
38. van de Scheur MR, van der Waal RI, Starink TM. Lupus miliaris disseminatus faciei: a distinctive rosacea-like syndrome and not a granulomatous form of rosacea. Dermatology. 2003;206:120-123.
39. Skowron F, Causeret AS, Pabion C, et al. F.I.GU.R.E.: facial idiopathic granulomas with regressive evolution. is ‘lupus miliaris disseminatus faciei’ still an acceptable diagnosis in the third millennium? Dermatology. 2000;201:287-289.
40. Lee WJ, Lee JL, Chang SE, et al. Cutaneous adverse effects in patients treated with the multitargeted kinase inhibitors sorafenib and sunitinib. Br J Dermatol. 2009;161:1045-1051.
41. Kim DH, Son IP, Lee JW, et al. Sorafenib (Nexavar®, BAY 43-9006)–induced hand-foot skin reaction with facial erythema. Ann Dermatol. 2011;23:119-122.
42. Sahai S, Swick BL. Hyperkeratotic eruption, hand-foot skin reaction, facial erythema, and stomatitis secondary to multi-targeted kinase inhibitor sorafenib. Int J Dermatol. 2010;49:1203-1206.
43. Segaert S, Van Cutsem E. Clinical signs, pathophysiology and management of skin toxicity during therapy with epidermal growth factor receptor inhibitors. Ann Oncol. 2005;16:1425-1433.
44. Agero AL, Dusza SW, Benvenuto-Andrade C, et al. Dermatologic side effects associated with the epidermal growth factor receptor inhibitors. J Am Acad Dermatol. 2006;55:657-670.
45. Acharya J, Lyon C, Bottomley DM. Folliculitis-perifolliculitis related to erlotinib therapy spares previously irradiated skin. J Am Acad Dermatol. 2009;60:154-157.
Although rosacea is one of the most common conditions treated by dermatologists, it also is one of the most misunderstood. Historically, large noses due to rhinomegaly were associated with indulgence in wine and wealth.1 The term rosacea is derived from the Latin adjective meaning “like roses.” Rosacea was first medically described in French as goutterose (pink droplet) and pustule de vin (pimples of wine).1 This article reviews the characteristics of rosacea compared to several mimickers of rosacea that physicians should consider.
Rosacea Characteristics
Rosacea is a chronic disorder affecting the central parts of the face that is characterized by frequent flushing; persistent erythema (ie, lasting for at least 3 months); telangiectasia; and interspersed episodes of inflammation with swelling, papules, and pustules.2 It is most commonly seen in adults older than 30 years and is considered to have a strong hereditary component, as it is more commonly seen in individuals of Celtic and Northern European descent as well as those with fair skin. Furthermore, approximately 30% to 40% of patients report a family member with the condition.2
Rosacea Subtypes
In a 2002 meeting held to standardize the diagnostic criteria for rosacea, the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea described 4 broad clinical subtypes of rosacea: erythematotelangiectatic, papulopustular, phymatous, and ocular.3 More than 1 subtype may present in the same patient. A progression from one subtype to another can occur in cases of severe papulopustular or glandular rosacea that eventuate into the phymatous form.2 Moreover, not all of the disease features are present in every patient. Secondary features of rosacea include burning or stinging, edema, plaques, dry appearance of the skin, ocular manifestations, peripheral site involvement, and phymatous changes.
In erythematotelangiectatic rosacea, episodic flushing occurs, which can last longer than 10 minutes with the central face exhibiting the most intense color. The redness also may involve the peripheral portion of the face as well as extrafacial areas (eg, ears, scalp, neck, chest). Periocular skin is spared. The stimuli that may bring on flushing include short-term emotional stress, hot drinks, alcohol, spicy foods, exercise, cold or hot weather, and hot water.3
Patients with papulopustular rosacea generally present with redness of the central portion of the face along with persistent or intermittent flares characterized by small papules and pinpoint pustules. There also is an almost universal sparing of the periocular skin, and a history of flushing often is present; however, flushing usually is milder than in the erythematotelangiectatic subtype. The constant inflammation may lead to chronic edema and phymatous changes, which occur more commonly in men than in women.3
Phymatous rosacea is characterized by marked skin thickening and irregular surface nodularities, most commonly involving the nose (rhinophyma), though the chin (gnathophyma), forehead (metophyma), ears (otophyma), and eyelids (blepharophyma) also are occasionally affected. There are 4 variants of rhinophyma with distinct histopathologic features: glandular, fibrous, fibroangiomatous, and actinic.3 The glandular variant is most often seen in men who have thick sebaceous skin. Edematous papules and pustules often are large and may be accompanied by nodulocystic lesions. Frequently, affected patients will have a history of adolescent acne with scarring.
Ocular rosacea may precede cutaneous findings by many years; however, in most cases the ocular findings occur concurrently or develop later on in the disease course. The most consistent findings in ocular rosacea are blepharitis and conjunctivitis. Symptoms of burning or stinging, itching, light sensitivity, and a foreign body sensation are common in these patients.3
Pathogenesis
Several investigators have proposed that Demodex folliculorum may play a pathogenic role in rosacea. Demodex is a common inhabitant of normal human skin, and its role in human disease is a matter of controversy.3Demodex has a predilection for the regions of the skin that are most often affected by rosacea, such as the nose and cheeks. The clinical manifestations of rosacea tend to appear later in life, which parallels the increase in the density of Demodex mites that occurs with age.4 It has been hypothesized that beneficial effects of metronidazole in the treatment of rosacea may be related to an antiparasitic effect on Demodex; however, these mites can survive high concentrations of the drug.3 Moreover, modern techniques that employ cyanoacrylate surface biopsies, which are extremely sensitive, estimate that the prevalence of Demodex in healthy skin approaches 100%.4 Consequently, the simple identification of Demodex is by no means proof of pathogenesis. Whether Demodex is truly pathogenic or simply an inhabitant of follicles in rosacea-prone skin remains a subject for future investigation.
Demodicosis occurs mainly in immunosuppressed patients because immunosuppression influences the number of Demodex mites and the treatment response. Multiple patients with AIDS and/or those with a CD4 lymphocyte count below 200/mm3 have been reported to have demodicosis.5-11 In immunocompetent patients, pruritic papular, papulopustular, and nodular lesions occur on the face, but in immunocompromised patients, the eruption may be more diffuse, affecting the back, presternal area, and upper limbs.6 A correct diagnosis relies on suggestive clinical signs, the presence of numerous parasites on direct examination, and a good clinical response to acaricide treatment.
Helicobacter pylori seropositivity has been associated with various dermatologic disorders, including rosacea.12 However, robust support for a causal association between H pylori and rosacea does not exist. Several studies have demonstrated high prevalence rates of H pylori in rosacea patients, some even in comparison with age- and sex-matched controls.13,14 Moreover, treatments aimed at eradicating H pylori also beneficially influence the clinical outcome of rosacea; for instance, metronidazole, a common treatment of roscea, is an effective agent against H pylori.
Understanding the clinical variants and disease course of rosacea is important to differentiate this entity from other conditions that can mimic rosacea. Laboratory studies and histopathologic examination via skin biopsy may be needed to differentiate between rosacea and rosacealike conditions.
Common Rosacealike Conditions
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is a chronic inflammatory disease that has protean clinical manifestations and follows a relapsing and remitting course. Characteristic malar erythema appears in approximately 50% of patients and may accompany or precede other symptoms of lupus. The affected skin generally feels warm and appears slightly edematous. The erythema may last for hours to days and often recurs, particularly with sun exposure. The malar erythema of SLE can be confused with the redness of erythematotelangiectatic rosacea. Nevertheless, the color of the skin in SLE has a violaceous quality and may show a more abrupt cutoff, especially at its most lateral margins. Marzano et al15 reported 4 cases in which lupus erythematosus was misdiagnosed as rosacea. All 4 patients presented with erythema that was localized to the central face along with a few raised, smooth, round, erythematous to violaceous papules over the malar areas and the forehead. This presentation evolved rapidly and was aggravated by sun exposure. The patients were all treated with medication for rosacea but showed no improvement. These patients originally presented with limited skin involvement in the absence of any systemic sign or symptoms of SLE.15
Dermatomyositis
Dermatomyositis (DM) is an inflammatory myopathy characterized by varying degrees of muscle weakness and distinctive skin erythema (Figure 1); however, some patients lack muscular involvement and initially present with skin manifestations only. Sontheimer16 described criteria for defining skin involvement in DM. Major criteria include the heliotrope rash, Gottron papules, and Gottron sign, while minor criteria include macular violaceous erythema (MVE), periungual telangiectasia of the nail fold, poikiloderma, mechanic’s hands, cutaneous calcinosis, cutaneous ulcers, and pruritus. With the exception of the heliotrope rash, facial erythema has drawn little attention in prior studies of DM-associated skin manifestations. Therefore, Okiyama et al17 performed a retrospective study on the skin manifestations of DM in 33 patients. The investigators observed that MVE in the seborrheic area of the face was most frequent.17 Therefore, it is critical to consider DM in the differential diagnosis of rosacea because the MVE seen in DM might be confused with the erythema seen in rosacea.

|
| Figure 1. Macular violaceous erythema of the face in a patient with dermatomyositis. Photograph courtesy of Marc Silverstein, MD, Sacramento, California. |

|
Figure 2. Polymorphous light eruption manifesting as erythematous papules over the cheek and dorsal aspect of the nose. Photograph courtesy of Marc Silverstein, MD, Sacramento, California. |
Polymorphous Light Eruption
Polymorphous light eruption (PMLE), the most common of the idiopathic photodermatoses, is characterized by erythematous papules, papulovesicles, and plaques on sun-exposed surfaces (Figure 2). The areas of the skin that are most commonly affected are the face, neck, outer aspects of the arms, and dorsal surfaces of the hands.18 Lesions may appear immediately but often develop several hours after sun exposure. Symptoms of itching and/or burning usually are mild and transient. The etiology of PMLE is unknown, though it is likely to be multifactorial.
Similarities between PMLE and rosacea include exacerbation by sun exposure and a higher prevalence in fair-skinned individuals.19 Also, in both conditions erythematous papules appear on the face and may be pruritic and in some instances painful; however, unlike rosacea, which is chronic, PMLE tends to be intermittent and recurrent, typically occurring in the spring and early summer months. In contrast to rosacea, the onset of the erythema in PMLE is abrupt, appearing quickly after sun exposure and subsiding within 1 to 7 days. Furthermore, patients with PMLE may experience systemic flulike symptoms after sun exposure.19
Seborrheic Dermatitis
Seborrheic dermatitis is a chronic relapsing papulosquamous skin disease most commonly involving sebum-rich areas such as the scalp and face. The prevalence of seborrheic dermatitis is higher in human immunodeficiency virus–positive individuals and in patients with neurologic conditions such as Parkinson disease. The pathogenesis of seborrheic dermatitis has been linked to the yeast of Malassezia species, immunologic abnormalities, and activation of complements. A clinical diagnosis usually is made based on a history of waxing and waning in severity and by the sites of involvement.20
Similar to rosacea, seborrheic dermatitis is a chronic and relapsing erythematous rash with well-demarcated erythematous patches, papules, or plaques; however, unlike rosacea, the distribution varies from minimal asymptomatic scaliness of the scalp to more widespread involvement (eg, scalp, ears, upper aspect of the trunk, intertriginous areas). Also, although macular erythema and scaling involving the perinasal area (Figure 3) may be seen in either rosacea or seborrheic dermatitis, a greasy quality to the scales and involvement of other sites such as the scalp, retroauricular skin, and eyebrows suggest a diagnosis of seborrheic dermatitis.
Acne Vulgaris
Acne vulgaris is the most common skin disease in the United States.21 It is characterized by noninflammatory; open or closed comedones; and inflammatory papules, pustules, and nodules. Acne vulgaris typically affects the areas of skin with the highest density of sebaceous follicles including the face, upper aspect of the chest, and back.22 It is the most common skin disease in the differential diagnosis of the papulopustular form of rosacea. Inflammatory lesions in both acne vulgaris and rosacea may be clinically identical; however, unlike acne vulgaris, rosacea is characterized by a complete absence of comedones. A prominent centrofacial distribution also favors rosacea. As a general rule, acne peaks in adolescence, years before papulopustular rosacea usually becomes prominent. However, some acne patients who are prone to flushing and blushing may develop rosacea later in life.
Topical Steroid–Induced Acne
Chronic use of topical corticosteroids on the face for several months can result in the appearance of monomorphic inflammatory papules (Figure 4). Corticosteroids can cause a dry scaly eruption with scattered follicular pustules around the mouth (perioral dermatitis).23 This acneform eruption is indistinguishable from rosacea. However, the monomorphic inflammatory papules generally resolve within 1 to 2 months following discontinuation of the corticosteroid therapy.
Multiple pathways have been proposed as the mechanism for such reactions, including rebound vasodilation and proinflammatory cytokine release by chronic intermittent steroid exposure.24 At first, the vasoconstrictive and anti-inflammatory effects of the steroids result in what seems to be clearance of the primary dermatitis for which the steroids were being used. Unfortunately, persistent use of steroids, particularly high-potency products, leads to epidermal atrophy, degeneration of dermal structures, and destruction of collagen, rendering the skin vulnerable to bacterial, viral, and fungal infections. In the end, the skin has the appearance of bright red rosacea with red scaly papules.
Rare Rosacealike Conditions
Carcinoid Syndrome
Carcinoid syndrome typically develops after hepatic metastasis from a carcinoid tumor when the circulating neuroendocrine mediators produced by the tumor can no longer be adequately cleared. Flushing is characteristic of carcinoid syndrome and usually presents on the face, neck, and upper trunk. Although rare, other types of cutaneous involvement also have been reported.25 Bell et al25 concluded that skin involvement is not uncommon in carcinoid syndrome, as all 25 patients with carcinoid syndrome showed cutaneous involvement in their case series. The investigators observed that chronic flushing eventually may become permanent and evolve into a rosacealike picture.25
Cases of carcinoid syndrome that were misdiagnosed as rosacea have been reported in the literature.26-28 Creamer et al26 reported a case of a 67-year-old woman who initially was diagnosed with rosacea; it took 1 year to finally arrive at the correct diagnosis of multiple endocrine neoplasia type 1 after developing a malignant carcinoid tumor and a parathyroid tumor.
Cutaneous Lymphoma
B-cell neoplasms with skin involvement can present as primary cutaneous lymphomas or as secondary processes, including specific infiltrates of nodal or extranodal lymphoma or leukemia.29 B-cell lymphomas involving the skin have a distinct clinical appearance, presenting as isolated, grouped, or multiple erythematous to violaceous papules, plaques, or nodules, usually in an asymmetric distribution (Figure 5). B-cell lymphoproliferative diseases simulating rosacea are extremely rare.29 Nevertheless, B-cell lymphoma mimicking rhinophyma has been documented in the literature.29-35
Barzilai et al29 described 12 patients with B-cell lymphoproliferative neoplasms presenting with facial eruptions that clinically mimicked rosacea or rhinophyma. The clinical presentation included small papules on the nose, cheeks, and around the eyes mimicking granulomatous rosacea, and/or nodules on the nose, cheeks, chin, or forehead simulating phymatous rosacea. Three patients had preexisting erythematotelangiectatic rosacea and 1 had rhinophyma.29
Lupus Miliaris Disseminatus Faciei
Lupus miliaris disseminatus faciei (LMDF) is an uncommon chronic inflammatory skin disorder characterized by the appearance of asymptomatic small, red to yellowish brown papules on the face.36 This rare dermatologic disease usually is self-limited with spontaneous resolution of the lesions occurring within months or years; however, residual disfiguring scars may persist and usually are characteristic of LMDF.36,37 The pathogenesis of LMDF is unclear, and controversy remains as to whether it is a distinct cutaneous entity or a variant of granulomatous rosacea.38,39 It usually develops slowly as small, dome-shaped, red to yellowish brown papules in adults, most commonly appearing in men.39 Lupus miliaris disseminatus faciei shares several common features with both acne vulgaris and rosacea. For example, the inflammatory lesions of LMDF are located on the central face and usually respond to treatments that typically are used to treat acne vulgaris and rosacea. However, LMDF can be distinguished histologically by more intense granulomatous inflammation and central caseation, occurring in the absence of an apparent infectious origin.36
Tyrosinase Kinase Inhibitor Drug Eruptions
Sorafenib and sunitinib malate are multitargeted kinase inhibitors approved for the treatment of cancers such as renal cell carcinoma.40 A study by Lee et al40 reported that approximately 75% of patients treated with either sorafenib (n=109) or sunitinib (n=119) went on to develop at least one cutaneous reaction. Although hand-foot skin reaction was the most common and serious cutaneous side effect, other dermatologic manifestations, including alopecia, stomatitis, discoloration (hair or face), subungual splinter hemorrhages, facial swelling, facial erythema, and xerosis, were described. Facial changes such as swelling, yellowish discoloration, erythema, and acneform eruptions were described more frequently in patients treated with sunitinib than in those treated with sorafenib.40
Other reports have described facial erythematous papules with sorafenib.41 In these patients, facial erythema usually occurs within 1 to 2 weeks after initiation of treatment, unlike hand-foot skin reaction, which usually develops later.42
Epidermal Growth Factor Receptor Inhibitor Drug Eruptions
Monoclonal antibodies against the epidermal growth factor receptor (EGFR) (eg, cetuximab, panitumumab) and EGFR tyrosine kinase inhibitors (eg, gefitinib, erlotinib) are used in the treatment of several cancers. Use of these drugs has been associated with various dermatologic side effects, including rashes, paronychia and fissuring of the nail bed, hair changes, dry skin, hypersensitivity reactions, and mucositis.43 The most frequent dermatologic side effect is a sterile follicular and pustular rash, often affecting the face, that is seen in more than half of the patients treated with these drugs.43,44 These rosacealike facial lesions are accompanied by diffuse erythema and telangiectasia. In some cases, the pustules leave areas of erythema covered with greasy scaling, thus resembling seborrheic dermatitis.43 In general, the pustular rash manifests within 1 to 3 weeks after the onset of treatment with EGFR inhibitors. The reaction typically resolves within 4 weeks of stopping treatment.44 The etiology of the rash is unknown, but inhibition of EGFR may result in occlusion of hair follicles and their associated sebaceous glands, producing a rosacealike appearance.45
Conclusion
Since its first medical description, rosacea has undergone extensive study regarding its pathogenesis and management. The most current investigations indicate microorganisms such as D folliculorum and H pylori as etiologic factors, though several other possibilities (eg, vascular abnormalities) have been suggested. Understanding the clinical variants and disease course of rosacea is important in differentiating this entity from other conditions that can mimic rosacea.
Acknowledgments—The authors thank Jennifer Rullan, MD, San Diego, California, and Jose Gonzalez-Chavez, MD, San Juan, Puerto Rico, for their assistance.
Although rosacea is one of the most common conditions treated by dermatologists, it also is one of the most misunderstood. Historically, large noses due to rhinomegaly were associated with indulgence in wine and wealth.1 The term rosacea is derived from the Latin adjective meaning “like roses.” Rosacea was first medically described in French as goutterose (pink droplet) and pustule de vin (pimples of wine).1 This article reviews the characteristics of rosacea compared to several mimickers of rosacea that physicians should consider.
Rosacea Characteristics
Rosacea is a chronic disorder affecting the central parts of the face that is characterized by frequent flushing; persistent erythema (ie, lasting for at least 3 months); telangiectasia; and interspersed episodes of inflammation with swelling, papules, and pustules.2 It is most commonly seen in adults older than 30 years and is considered to have a strong hereditary component, as it is more commonly seen in individuals of Celtic and Northern European descent as well as those with fair skin. Furthermore, approximately 30% to 40% of patients report a family member with the condition.2
Rosacea Subtypes
In a 2002 meeting held to standardize the diagnostic criteria for rosacea, the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea described 4 broad clinical subtypes of rosacea: erythematotelangiectatic, papulopustular, phymatous, and ocular.3 More than 1 subtype may present in the same patient. A progression from one subtype to another can occur in cases of severe papulopustular or glandular rosacea that eventuate into the phymatous form.2 Moreover, not all of the disease features are present in every patient. Secondary features of rosacea include burning or stinging, edema, plaques, dry appearance of the skin, ocular manifestations, peripheral site involvement, and phymatous changes.
In erythematotelangiectatic rosacea, episodic flushing occurs, which can last longer than 10 minutes with the central face exhibiting the most intense color. The redness also may involve the peripheral portion of the face as well as extrafacial areas (eg, ears, scalp, neck, chest). Periocular skin is spared. The stimuli that may bring on flushing include short-term emotional stress, hot drinks, alcohol, spicy foods, exercise, cold or hot weather, and hot water.3
Patients with papulopustular rosacea generally present with redness of the central portion of the face along with persistent or intermittent flares characterized by small papules and pinpoint pustules. There also is an almost universal sparing of the periocular skin, and a history of flushing often is present; however, flushing usually is milder than in the erythematotelangiectatic subtype. The constant inflammation may lead to chronic edema and phymatous changes, which occur more commonly in men than in women.3
Phymatous rosacea is characterized by marked skin thickening and irregular surface nodularities, most commonly involving the nose (rhinophyma), though the chin (gnathophyma), forehead (metophyma), ears (otophyma), and eyelids (blepharophyma) also are occasionally affected. There are 4 variants of rhinophyma with distinct histopathologic features: glandular, fibrous, fibroangiomatous, and actinic.3 The glandular variant is most often seen in men who have thick sebaceous skin. Edematous papules and pustules often are large and may be accompanied by nodulocystic lesions. Frequently, affected patients will have a history of adolescent acne with scarring.
Ocular rosacea may precede cutaneous findings by many years; however, in most cases the ocular findings occur concurrently or develop later on in the disease course. The most consistent findings in ocular rosacea are blepharitis and conjunctivitis. Symptoms of burning or stinging, itching, light sensitivity, and a foreign body sensation are common in these patients.3
Pathogenesis
Several investigators have proposed that Demodex folliculorum may play a pathogenic role in rosacea. Demodex is a common inhabitant of normal human skin, and its role in human disease is a matter of controversy.3Demodex has a predilection for the regions of the skin that are most often affected by rosacea, such as the nose and cheeks. The clinical manifestations of rosacea tend to appear later in life, which parallels the increase in the density of Demodex mites that occurs with age.4 It has been hypothesized that beneficial effects of metronidazole in the treatment of rosacea may be related to an antiparasitic effect on Demodex; however, these mites can survive high concentrations of the drug.3 Moreover, modern techniques that employ cyanoacrylate surface biopsies, which are extremely sensitive, estimate that the prevalence of Demodex in healthy skin approaches 100%.4 Consequently, the simple identification of Demodex is by no means proof of pathogenesis. Whether Demodex is truly pathogenic or simply an inhabitant of follicles in rosacea-prone skin remains a subject for future investigation.
Demodicosis occurs mainly in immunosuppressed patients because immunosuppression influences the number of Demodex mites and the treatment response. Multiple patients with AIDS and/or those with a CD4 lymphocyte count below 200/mm3 have been reported to have demodicosis.5-11 In immunocompetent patients, pruritic papular, papulopustular, and nodular lesions occur on the face, but in immunocompromised patients, the eruption may be more diffuse, affecting the back, presternal area, and upper limbs.6 A correct diagnosis relies on suggestive clinical signs, the presence of numerous parasites on direct examination, and a good clinical response to acaricide treatment.
Helicobacter pylori seropositivity has been associated with various dermatologic disorders, including rosacea.12 However, robust support for a causal association between H pylori and rosacea does not exist. Several studies have demonstrated high prevalence rates of H pylori in rosacea patients, some even in comparison with age- and sex-matched controls.13,14 Moreover, treatments aimed at eradicating H pylori also beneficially influence the clinical outcome of rosacea; for instance, metronidazole, a common treatment of roscea, is an effective agent against H pylori.
Understanding the clinical variants and disease course of rosacea is important to differentiate this entity from other conditions that can mimic rosacea. Laboratory studies and histopathologic examination via skin biopsy may be needed to differentiate between rosacea and rosacealike conditions.
Common Rosacealike Conditions
Systemic Lupus Erythematosus
Systemic lupus erythematosus (SLE) is a chronic inflammatory disease that has protean clinical manifestations and follows a relapsing and remitting course. Characteristic malar erythema appears in approximately 50% of patients and may accompany or precede other symptoms of lupus. The affected skin generally feels warm and appears slightly edematous. The erythema may last for hours to days and often recurs, particularly with sun exposure. The malar erythema of SLE can be confused with the redness of erythematotelangiectatic rosacea. Nevertheless, the color of the skin in SLE has a violaceous quality and may show a more abrupt cutoff, especially at its most lateral margins. Marzano et al15 reported 4 cases in which lupus erythematosus was misdiagnosed as rosacea. All 4 patients presented with erythema that was localized to the central face along with a few raised, smooth, round, erythematous to violaceous papules over the malar areas and the forehead. This presentation evolved rapidly and was aggravated by sun exposure. The patients were all treated with medication for rosacea but showed no improvement. These patients originally presented with limited skin involvement in the absence of any systemic sign or symptoms of SLE.15
Dermatomyositis
Dermatomyositis (DM) is an inflammatory myopathy characterized by varying degrees of muscle weakness and distinctive skin erythema (Figure 1); however, some patients lack muscular involvement and initially present with skin manifestations only. Sontheimer16 described criteria for defining skin involvement in DM. Major criteria include the heliotrope rash, Gottron papules, and Gottron sign, while minor criteria include macular violaceous erythema (MVE), periungual telangiectasia of the nail fold, poikiloderma, mechanic’s hands, cutaneous calcinosis, cutaneous ulcers, and pruritus. With the exception of the heliotrope rash, facial erythema has drawn little attention in prior studies of DM-associated skin manifestations. Therefore, Okiyama et al17 performed a retrospective study on the skin manifestations of DM in 33 patients. The investigators observed that MVE in the seborrheic area of the face was most frequent.17 Therefore, it is critical to consider DM in the differential diagnosis of rosacea because the MVE seen in DM might be confused with the erythema seen in rosacea.

|
| Figure 1. Macular violaceous erythema of the face in a patient with dermatomyositis. Photograph courtesy of Marc Silverstein, MD, Sacramento, California. |

|
Figure 2. Polymorphous light eruption manifesting as erythematous papules over the cheek and dorsal aspect of the nose. Photograph courtesy of Marc Silverstein, MD, Sacramento, California. |
Polymorphous Light Eruption
Polymorphous light eruption (PMLE), the most common of the idiopathic photodermatoses, is characterized by erythematous papules, papulovesicles, and plaques on sun-exposed surfaces (Figure 2). The areas of the skin that are most commonly affected are the face, neck, outer aspects of the arms, and dorsal surfaces of the hands.18 Lesions may appear immediately but often develop several hours after sun exposure. Symptoms of itching and/or burning usually are mild and transient. The etiology of PMLE is unknown, though it is likely to be multifactorial.
Similarities between PMLE and rosacea include exacerbation by sun exposure and a higher prevalence in fair-skinned individuals.19 Also, in both conditions erythematous papules appear on the face and may be pruritic and in some instances painful; however, unlike rosacea, which is chronic, PMLE tends to be intermittent and recurrent, typically occurring in the spring and early summer months. In contrast to rosacea, the onset of the erythema in PMLE is abrupt, appearing quickly after sun exposure and subsiding within 1 to 7 days. Furthermore, patients with PMLE may experience systemic flulike symptoms after sun exposure.19
Seborrheic Dermatitis
Seborrheic dermatitis is a chronic relapsing papulosquamous skin disease most commonly involving sebum-rich areas such as the scalp and face. The prevalence of seborrheic dermatitis is higher in human immunodeficiency virus–positive individuals and in patients with neurologic conditions such as Parkinson disease. The pathogenesis of seborrheic dermatitis has been linked to the yeast of Malassezia species, immunologic abnormalities, and activation of complements. A clinical diagnosis usually is made based on a history of waxing and waning in severity and by the sites of involvement.20
Similar to rosacea, seborrheic dermatitis is a chronic and relapsing erythematous rash with well-demarcated erythematous patches, papules, or plaques; however, unlike rosacea, the distribution varies from minimal asymptomatic scaliness of the scalp to more widespread involvement (eg, scalp, ears, upper aspect of the trunk, intertriginous areas). Also, although macular erythema and scaling involving the perinasal area (Figure 3) may be seen in either rosacea or seborrheic dermatitis, a greasy quality to the scales and involvement of other sites such as the scalp, retroauricular skin, and eyebrows suggest a diagnosis of seborrheic dermatitis.
Acne Vulgaris
Acne vulgaris is the most common skin disease in the United States.21 It is characterized by noninflammatory; open or closed comedones; and inflammatory papules, pustules, and nodules. Acne vulgaris typically affects the areas of skin with the highest density of sebaceous follicles including the face, upper aspect of the chest, and back.22 It is the most common skin disease in the differential diagnosis of the papulopustular form of rosacea. Inflammatory lesions in both acne vulgaris and rosacea may be clinically identical; however, unlike acne vulgaris, rosacea is characterized by a complete absence of comedones. A prominent centrofacial distribution also favors rosacea. As a general rule, acne peaks in adolescence, years before papulopustular rosacea usually becomes prominent. However, some acne patients who are prone to flushing and blushing may develop rosacea later in life.
Topical Steroid–Induced Acne
Chronic use of topical corticosteroids on the face for several months can result in the appearance of monomorphic inflammatory papules (Figure 4). Corticosteroids can cause a dry scaly eruption with scattered follicular pustules around the mouth (perioral dermatitis).23 This acneform eruption is indistinguishable from rosacea. However, the monomorphic inflammatory papules generally resolve within 1 to 2 months following discontinuation of the corticosteroid therapy.
Multiple pathways have been proposed as the mechanism for such reactions, including rebound vasodilation and proinflammatory cytokine release by chronic intermittent steroid exposure.24 At first, the vasoconstrictive and anti-inflammatory effects of the steroids result in what seems to be clearance of the primary dermatitis for which the steroids were being used. Unfortunately, persistent use of steroids, particularly high-potency products, leads to epidermal atrophy, degeneration of dermal structures, and destruction of collagen, rendering the skin vulnerable to bacterial, viral, and fungal infections. In the end, the skin has the appearance of bright red rosacea with red scaly papules.
Rare Rosacealike Conditions
Carcinoid Syndrome
Carcinoid syndrome typically develops after hepatic metastasis from a carcinoid tumor when the circulating neuroendocrine mediators produced by the tumor can no longer be adequately cleared. Flushing is characteristic of carcinoid syndrome and usually presents on the face, neck, and upper trunk. Although rare, other types of cutaneous involvement also have been reported.25 Bell et al25 concluded that skin involvement is not uncommon in carcinoid syndrome, as all 25 patients with carcinoid syndrome showed cutaneous involvement in their case series. The investigators observed that chronic flushing eventually may become permanent and evolve into a rosacealike picture.25
Cases of carcinoid syndrome that were misdiagnosed as rosacea have been reported in the literature.26-28 Creamer et al26 reported a case of a 67-year-old woman who initially was diagnosed with rosacea; it took 1 year to finally arrive at the correct diagnosis of multiple endocrine neoplasia type 1 after developing a malignant carcinoid tumor and a parathyroid tumor.
Cutaneous Lymphoma
B-cell neoplasms with skin involvement can present as primary cutaneous lymphomas or as secondary processes, including specific infiltrates of nodal or extranodal lymphoma or leukemia.29 B-cell lymphomas involving the skin have a distinct clinical appearance, presenting as isolated, grouped, or multiple erythematous to violaceous papules, plaques, or nodules, usually in an asymmetric distribution (Figure 5). B-cell lymphoproliferative diseases simulating rosacea are extremely rare.29 Nevertheless, B-cell lymphoma mimicking rhinophyma has been documented in the literature.29-35
Barzilai et al29 described 12 patients with B-cell lymphoproliferative neoplasms presenting with facial eruptions that clinically mimicked rosacea or rhinophyma. The clinical presentation included small papules on the nose, cheeks, and around the eyes mimicking granulomatous rosacea, and/or nodules on the nose, cheeks, chin, or forehead simulating phymatous rosacea. Three patients had preexisting erythematotelangiectatic rosacea and 1 had rhinophyma.29
Lupus Miliaris Disseminatus Faciei
Lupus miliaris disseminatus faciei (LMDF) is an uncommon chronic inflammatory skin disorder characterized by the appearance of asymptomatic small, red to yellowish brown papules on the face.36 This rare dermatologic disease usually is self-limited with spontaneous resolution of the lesions occurring within months or years; however, residual disfiguring scars may persist and usually are characteristic of LMDF.36,37 The pathogenesis of LMDF is unclear, and controversy remains as to whether it is a distinct cutaneous entity or a variant of granulomatous rosacea.38,39 It usually develops slowly as small, dome-shaped, red to yellowish brown papules in adults, most commonly appearing in men.39 Lupus miliaris disseminatus faciei shares several common features with both acne vulgaris and rosacea. For example, the inflammatory lesions of LMDF are located on the central face and usually respond to treatments that typically are used to treat acne vulgaris and rosacea. However, LMDF can be distinguished histologically by more intense granulomatous inflammation and central caseation, occurring in the absence of an apparent infectious origin.36
Tyrosinase Kinase Inhibitor Drug Eruptions
Sorafenib and sunitinib malate are multitargeted kinase inhibitors approved for the treatment of cancers such as renal cell carcinoma.40 A study by Lee et al40 reported that approximately 75% of patients treated with either sorafenib (n=109) or sunitinib (n=119) went on to develop at least one cutaneous reaction. Although hand-foot skin reaction was the most common and serious cutaneous side effect, other dermatologic manifestations, including alopecia, stomatitis, discoloration (hair or face), subungual splinter hemorrhages, facial swelling, facial erythema, and xerosis, were described. Facial changes such as swelling, yellowish discoloration, erythema, and acneform eruptions were described more frequently in patients treated with sunitinib than in those treated with sorafenib.40
Other reports have described facial erythematous papules with sorafenib.41 In these patients, facial erythema usually occurs within 1 to 2 weeks after initiation of treatment, unlike hand-foot skin reaction, which usually develops later.42
Epidermal Growth Factor Receptor Inhibitor Drug Eruptions
Monoclonal antibodies against the epidermal growth factor receptor (EGFR) (eg, cetuximab, panitumumab) and EGFR tyrosine kinase inhibitors (eg, gefitinib, erlotinib) are used in the treatment of several cancers. Use of these drugs has been associated with various dermatologic side effects, including rashes, paronychia and fissuring of the nail bed, hair changes, dry skin, hypersensitivity reactions, and mucositis.43 The most frequent dermatologic side effect is a sterile follicular and pustular rash, often affecting the face, that is seen in more than half of the patients treated with these drugs.43,44 These rosacealike facial lesions are accompanied by diffuse erythema and telangiectasia. In some cases, the pustules leave areas of erythema covered with greasy scaling, thus resembling seborrheic dermatitis.43 In general, the pustular rash manifests within 1 to 3 weeks after the onset of treatment with EGFR inhibitors. The reaction typically resolves within 4 weeks of stopping treatment.44 The etiology of the rash is unknown, but inhibition of EGFR may result in occlusion of hair follicles and their associated sebaceous glands, producing a rosacealike appearance.45
Conclusion
Since its first medical description, rosacea has undergone extensive study regarding its pathogenesis and management. The most current investigations indicate microorganisms such as D folliculorum and H pylori as etiologic factors, though several other possibilities (eg, vascular abnormalities) have been suggested. Understanding the clinical variants and disease course of rosacea is important in differentiating this entity from other conditions that can mimic rosacea.
Acknowledgments—The authors thank Jennifer Rullan, MD, San Diego, California, and Jose Gonzalez-Chavez, MD, San Juan, Puerto Rico, for their assistance.
1. Bateman T, Thomson AT, Willan R. A Practical Synopsis of Cutaneous Diseases According to the Arrangement of Dr. Willan, Exhibiting a Concise View of the Diagnostic Symptoms and the Method of Treatment. London, England: Longman, Hurst, Rees, Orme, and Browne; 1813.
2. Plewig G, Kligman AM. Acne and Rosacea. 3rd ed. Germany: Springer-Verlag; 2000.
3. Wilkin J, Dahl M, Detmar M, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol. 2002;46:584-587.
4. Crawford GH, Pelle MT, James WD. Rosacea: i. etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004;51:327-341.
5. Clyti E, Nacher M, Sainte-Marie D, et al. Ivermectin treatment of three cases of demodicosis during human immunodeficiency virus infection. Int J Dermatol. 2006;45:1066-1068.
6. Aquilina C, Viraben R, Sire S. Ivermectin-responsive Demodex infestation during human immunodeficiency virus infection. a case report and literature review. Dermatology. 2002;205:394-397.
7. Brutti CS, Artus G, Luzzatto L, et al. Crusted rosacea-like demodicidosis in an HIV-positive female. J Am Acad Dermatol. 2011;65:e131-e132.
8. Clyti E, Sayavong K, Chanthavisouk K. Demodicosis in a patient infected by HIV: successful treatment with ivermectin. Ann Dermatol Venereol. 2005;132:459-461.
9. Patrizi A, Neri I, Chieregato C, et al. Demodicosis in immunocompetent young children: report of eight cases. Dermatology. 1997;195:239-242.
10. Barrio J, Lecona M, Hernanz JM, et al. Rosacea-like demodicosis in an HIV-positive child. Dermatology. 1996;192:143-145.
11. Vin-Christian K, Maurer TA, Berger TG. Acne rosacea as a cutaneous manifestation of HIV infection. J Am Acad Dermatol. 1994;30:139-140.
12. Tüzün Y, Keskin S, Kote E. The role of Helicobacter pylori infection in skin diseases: facts and controversies. Clin Dermatol. 2010;28:478-482.
13. El-Khalawany M, Mahmoud A, Mosbeh AS, et al. Role of Helicobacter pylori in common rosacea subtypes: a genotypic comparative study of Egyptian patients. J Dermatol. 2012;39:989-995.
14. Boixeda de Miquel D, Vázquez Romero M, Vázquez Sequeiros E, et al. Effect of Helicobacter pylori eradication therapy in rosacea patients [in Spanish]. Rev Esp Enferm Dig. 2006;98:501-509.
15. Marzano AV, Lazzari R, Polloni I, et al. Rosacea-like cutaneous lupus erythematosus: an atypical presentation responding to antimalarials. Acta Derm Venereol. 2013;93:106-107.
16. Sontheimer RD. Cutaneous features of classic dermatomyositis and amyopathic dermatomyositis. Curr Opin Rheumatol. 1999;11:475-482.
17. Okiyama N, Kohsaka H, Ueda N, et al. Seborrheic area erythema as a common skin manifestation in Japanese patients with dermatomyositis. Dermatology. 2008;217:374-377.
18. Naleway AL, Greenlee RT, Melski JW. Characteristics of diagnosed polymorphous light eruption. Photodermatol Photoimmunol Photomed. 2006;22:205-207.
19. Tutrone WD. Polymorphic light eruption. Dermatol Ther. 2003;16:28-39.
20. Sampaio AL, Mameri AC, Vargas TJ, et al. Seborrheic dermatitis [in Portuguese]. An Bras Dermatol. 2011;86:1061-1071.
21. Cordain L, Lindberg S, Hurtado M, et al. Acne vulgaris: a disease of Western civilization. Arch Dermatol. 2002;138:1584-1590.
22. Titus S, Hodge J. Diagnosis and treatment of acne. Am Fam Physician. 2012;86:734-740.
23. Poulos GA, Brodell RT. Perioral dermatitis associated with an inhaled corticosteroid. Arch Dermatol. 2007;143:1460.
24. Bhat YJ, Manzoor S, Qayoom S. Steroid-induced rosacea: a clinical study of 200 patients. Indian J Dermatol. 2011;56:30-32.
25. Bell HK, Poston GJ, Vora J, et al. Cutaneous manifestations of the malignant carcinoid syndrome. Br J Dermatol. 2005;152:71-75.
26. Creamer JD, Whittaker SJ, Griffiths WA. Multiple endocrine neoplasia type 1 presenting as rosacea. Clin Exp Dermatol. 1996;21:170-171.
27. Reichert S, Truchetet F, Cuny JF, et al. Carcinoid tumor with revealed by skin manifestation [in French]. Ann Dermatol Venereol. 1994;121:485-488.
28. Findlay GH, Simson IW. Leonine hypertrophic rosacea associated with a benign bronchial carcinoid tumour. Clin Exp Dermatol. 1977;2:175-176.
29. Barzilai A, Feuerman H, Quaglino P, et al. Cutaneous B-cell neoplasms mimicking granulomatous rosacea or rhinophyma. Arch Dermatol. 2012;148:824-831.
30. Moulonguet I, Ghnassia M, Molina T, et al. Miliarial-type perifollicular B-cell pseudolymphoma (lymphocytoma cutis): a misleading eruption in two women. J Cutan Pathol. 2012;39:1016-1021.
31. Soon CW, Pincus LB, Ai WZ, et al. Acneiform presentation of primary cutaneous follicle center lymphoma. J Am Acad Dermatol. 2011;65:887-889.
32. Rosmaninho A, Alves R, Lima M, et al. Red nose: primary cutaneous marginal zone B-cell lymphoma. Leuk Res. 2010;34:682-684.
33. Ogden S, Coulson IH. B-cell lymphoma mimicking rhinophyma. Clin Exp Dermatol. 2008;33:213-214.
34. Seward JL, Malone JC, Callen JP. Rhinophymalike swelling in an 86-year-old woman. Primary cutaneous B-cell lymphoma of the nose. Arch Dermatol. 2004;140:751-756.
35. Colvin JH, Lamerson CL, Cualing H, et al. Cutaneous lymphoplasmacytoid lymphoma (immunocytoma) with Waldenström’s macroglobulinemia mimicking rosacea. J Am Acad Dermatol. 2003;49:1159-1162.
36. Jih MH, Friedman PM, Kimyai-Asadi A, et al. Lupus miliaris disseminatus faciei treatment with the 1450-nm diode laser. Arch Dermatol. 2005;141:143-145.
37. Abdullah L, Abbas O. Dermacase. can you identify this condition? lupus miliaris disseminatus faciei. Can Fam Physician. 2011;57:795-796.
38. van de Scheur MR, van der Waal RI, Starink TM. Lupus miliaris disseminatus faciei: a distinctive rosacea-like syndrome and not a granulomatous form of rosacea. Dermatology. 2003;206:120-123.
39. Skowron F, Causeret AS, Pabion C, et al. F.I.GU.R.E.: facial idiopathic granulomas with regressive evolution. is ‘lupus miliaris disseminatus faciei’ still an acceptable diagnosis in the third millennium? Dermatology. 2000;201:287-289.
40. Lee WJ, Lee JL, Chang SE, et al. Cutaneous adverse effects in patients treated with the multitargeted kinase inhibitors sorafenib and sunitinib. Br J Dermatol. 2009;161:1045-1051.
41. Kim DH, Son IP, Lee JW, et al. Sorafenib (Nexavar®, BAY 43-9006)–induced hand-foot skin reaction with facial erythema. Ann Dermatol. 2011;23:119-122.
42. Sahai S, Swick BL. Hyperkeratotic eruption, hand-foot skin reaction, facial erythema, and stomatitis secondary to multi-targeted kinase inhibitor sorafenib. Int J Dermatol. 2010;49:1203-1206.
43. Segaert S, Van Cutsem E. Clinical signs, pathophysiology and management of skin toxicity during therapy with epidermal growth factor receptor inhibitors. Ann Oncol. 2005;16:1425-1433.
44. Agero AL, Dusza SW, Benvenuto-Andrade C, et al. Dermatologic side effects associated with the epidermal growth factor receptor inhibitors. J Am Acad Dermatol. 2006;55:657-670.
45. Acharya J, Lyon C, Bottomley DM. Folliculitis-perifolliculitis related to erlotinib therapy spares previously irradiated skin. J Am Acad Dermatol. 2009;60:154-157.
1. Bateman T, Thomson AT, Willan R. A Practical Synopsis of Cutaneous Diseases According to the Arrangement of Dr. Willan, Exhibiting a Concise View of the Diagnostic Symptoms and the Method of Treatment. London, England: Longman, Hurst, Rees, Orme, and Browne; 1813.
2. Plewig G, Kligman AM. Acne and Rosacea. 3rd ed. Germany: Springer-Verlag; 2000.
3. Wilkin J, Dahl M, Detmar M, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the Classification and Staging of Rosacea. J Am Acad Dermatol. 2002;46:584-587.
4. Crawford GH, Pelle MT, James WD. Rosacea: i. etiology, pathogenesis, and subtype classification. J Am Acad Dermatol. 2004;51:327-341.
5. Clyti E, Nacher M, Sainte-Marie D, et al. Ivermectin treatment of three cases of demodicosis during human immunodeficiency virus infection. Int J Dermatol. 2006;45:1066-1068.
6. Aquilina C, Viraben R, Sire S. Ivermectin-responsive Demodex infestation during human immunodeficiency virus infection. a case report and literature review. Dermatology. 2002;205:394-397.
7. Brutti CS, Artus G, Luzzatto L, et al. Crusted rosacea-like demodicidosis in an HIV-positive female. J Am Acad Dermatol. 2011;65:e131-e132.
8. Clyti E, Sayavong K, Chanthavisouk K. Demodicosis in a patient infected by HIV: successful treatment with ivermectin. Ann Dermatol Venereol. 2005;132:459-461.
9. Patrizi A, Neri I, Chieregato C, et al. Demodicosis in immunocompetent young children: report of eight cases. Dermatology. 1997;195:239-242.
10. Barrio J, Lecona M, Hernanz JM, et al. Rosacea-like demodicosis in an HIV-positive child. Dermatology. 1996;192:143-145.
11. Vin-Christian K, Maurer TA, Berger TG. Acne rosacea as a cutaneous manifestation of HIV infection. J Am Acad Dermatol. 1994;30:139-140.
12. Tüzün Y, Keskin S, Kote E. The role of Helicobacter pylori infection in skin diseases: facts and controversies. Clin Dermatol. 2010;28:478-482.
13. El-Khalawany M, Mahmoud A, Mosbeh AS, et al. Role of Helicobacter pylori in common rosacea subtypes: a genotypic comparative study of Egyptian patients. J Dermatol. 2012;39:989-995.
14. Boixeda de Miquel D, Vázquez Romero M, Vázquez Sequeiros E, et al. Effect of Helicobacter pylori eradication therapy in rosacea patients [in Spanish]. Rev Esp Enferm Dig. 2006;98:501-509.
15. Marzano AV, Lazzari R, Polloni I, et al. Rosacea-like cutaneous lupus erythematosus: an atypical presentation responding to antimalarials. Acta Derm Venereol. 2013;93:106-107.
16. Sontheimer RD. Cutaneous features of classic dermatomyositis and amyopathic dermatomyositis. Curr Opin Rheumatol. 1999;11:475-482.
17. Okiyama N, Kohsaka H, Ueda N, et al. Seborrheic area erythema as a common skin manifestation in Japanese patients with dermatomyositis. Dermatology. 2008;217:374-377.
18. Naleway AL, Greenlee RT, Melski JW. Characteristics of diagnosed polymorphous light eruption. Photodermatol Photoimmunol Photomed. 2006;22:205-207.
19. Tutrone WD. Polymorphic light eruption. Dermatol Ther. 2003;16:28-39.
20. Sampaio AL, Mameri AC, Vargas TJ, et al. Seborrheic dermatitis [in Portuguese]. An Bras Dermatol. 2011;86:1061-1071.
21. Cordain L, Lindberg S, Hurtado M, et al. Acne vulgaris: a disease of Western civilization. Arch Dermatol. 2002;138:1584-1590.
22. Titus S, Hodge J. Diagnosis and treatment of acne. Am Fam Physician. 2012;86:734-740.
23. Poulos GA, Brodell RT. Perioral dermatitis associated with an inhaled corticosteroid. Arch Dermatol. 2007;143:1460.
24. Bhat YJ, Manzoor S, Qayoom S. Steroid-induced rosacea: a clinical study of 200 patients. Indian J Dermatol. 2011;56:30-32.
25. Bell HK, Poston GJ, Vora J, et al. Cutaneous manifestations of the malignant carcinoid syndrome. Br J Dermatol. 2005;152:71-75.
26. Creamer JD, Whittaker SJ, Griffiths WA. Multiple endocrine neoplasia type 1 presenting as rosacea. Clin Exp Dermatol. 1996;21:170-171.
27. Reichert S, Truchetet F, Cuny JF, et al. Carcinoid tumor with revealed by skin manifestation [in French]. Ann Dermatol Venereol. 1994;121:485-488.
28. Findlay GH, Simson IW. Leonine hypertrophic rosacea associated with a benign bronchial carcinoid tumour. Clin Exp Dermatol. 1977;2:175-176.
29. Barzilai A, Feuerman H, Quaglino P, et al. Cutaneous B-cell neoplasms mimicking granulomatous rosacea or rhinophyma. Arch Dermatol. 2012;148:824-831.
30. Moulonguet I, Ghnassia M, Molina T, et al. Miliarial-type perifollicular B-cell pseudolymphoma (lymphocytoma cutis): a misleading eruption in two women. J Cutan Pathol. 2012;39:1016-1021.
31. Soon CW, Pincus LB, Ai WZ, et al. Acneiform presentation of primary cutaneous follicle center lymphoma. J Am Acad Dermatol. 2011;65:887-889.
32. Rosmaninho A, Alves R, Lima M, et al. Red nose: primary cutaneous marginal zone B-cell lymphoma. Leuk Res. 2010;34:682-684.
33. Ogden S, Coulson IH. B-cell lymphoma mimicking rhinophyma. Clin Exp Dermatol. 2008;33:213-214.
34. Seward JL, Malone JC, Callen JP. Rhinophymalike swelling in an 86-year-old woman. Primary cutaneous B-cell lymphoma of the nose. Arch Dermatol. 2004;140:751-756.
35. Colvin JH, Lamerson CL, Cualing H, et al. Cutaneous lymphoplasmacytoid lymphoma (immunocytoma) with Waldenström’s macroglobulinemia mimicking rosacea. J Am Acad Dermatol. 2003;49:1159-1162.
36. Jih MH, Friedman PM, Kimyai-Asadi A, et al. Lupus miliaris disseminatus faciei treatment with the 1450-nm diode laser. Arch Dermatol. 2005;141:143-145.
37. Abdullah L, Abbas O. Dermacase. can you identify this condition? lupus miliaris disseminatus faciei. Can Fam Physician. 2011;57:795-796.
38. van de Scheur MR, van der Waal RI, Starink TM. Lupus miliaris disseminatus faciei: a distinctive rosacea-like syndrome and not a granulomatous form of rosacea. Dermatology. 2003;206:120-123.
39. Skowron F, Causeret AS, Pabion C, et al. F.I.GU.R.E.: facial idiopathic granulomas with regressive evolution. is ‘lupus miliaris disseminatus faciei’ still an acceptable diagnosis in the third millennium? Dermatology. 2000;201:287-289.
40. Lee WJ, Lee JL, Chang SE, et al. Cutaneous adverse effects in patients treated with the multitargeted kinase inhibitors sorafenib and sunitinib. Br J Dermatol. 2009;161:1045-1051.
41. Kim DH, Son IP, Lee JW, et al. Sorafenib (Nexavar®, BAY 43-9006)–induced hand-foot skin reaction with facial erythema. Ann Dermatol. 2011;23:119-122.
42. Sahai S, Swick BL. Hyperkeratotic eruption, hand-foot skin reaction, facial erythema, and stomatitis secondary to multi-targeted kinase inhibitor sorafenib. Int J Dermatol. 2010;49:1203-1206.
43. Segaert S, Van Cutsem E. Clinical signs, pathophysiology and management of skin toxicity during therapy with epidermal growth factor receptor inhibitors. Ann Oncol. 2005;16:1425-1433.
44. Agero AL, Dusza SW, Benvenuto-Andrade C, et al. Dermatologic side effects associated with the epidermal growth factor receptor inhibitors. J Am Acad Dermatol. 2006;55:657-670.
45. Acharya J, Lyon C, Bottomley DM. Folliculitis-perifolliculitis related to erlotinib therapy spares previously irradiated skin. J Am Acad Dermatol. 2009;60:154-157.
Practice Points
- Rosacea is characterized by frequent flushing; persistent erythema (ie, lasting for at least 3 months); telangiectasia; and interspersed episodes of inflammation with swelling, papules, and pustules.
- Rosacea is most commonly seen in adults older than 30 years and is considered to have a strong hereditary component, as it is more commonly seen in individuals of Celtic and Northern European descent as well as those with fair skin.