User login
Hematologic manifestations of COVID-19
While SARS-CoV-2 causes frequent and potentially severe pulmonary disease, extrapulmonary manifestations may be a prominent part of the clinical spectrum, according to a review published in Nature Medicine.
In this comprehensive literature review, Aakriti Gupta, MD, of New York-Presbyterian/Columbia University Irving Medical Center and colleagues detailed the epidemiologic and clinical multisystem effects of COVID-19. The authors explained what is known and/or suspected about the pathophysiology of those effects and outlined the resultant management considerations.
Key mechanisms for multiorgan injury include direct viral toxicity, endothelial cell damage with inflammatory mediation of thrombosis, aberrant immune response, and dysregulation of the renin-angiotensin-aldosterone system.
The relative importance of each pathway in the clinical presentation of COVID-19 and the mechanism for extrapulmonary spread of SARS-CoV-2 infection are imperfectly understood, Dr. Gupta and colleagues noted.
As for the hematologic effects of COVID-19, patients may present with several laboratory abnormalities, but the most clinically relevant complications are thromboembolic.
COVID-19-associated coagulopathy
Dr. Gupta and colleagues noted that COVID-19–associated coagulopathy (CAC) is accompanied by elevated levels of D-dimer and fibrinogen, with minor abnormalities in prothrombin time, activated partial thromboplastin time, and platelet counts in the initial stage of infection.
Elevated D-dimer levels have been reported in up to 46% of hospitalized patients, and a longitudinal increase while hospitalized is associated with higher mortality.
In initial reports from China and the Netherlands, thrombotic complications were seen in up to 30% of COVID-19 patients in ICUs. Thromboembolic events have been reported in 17%-22% of critically ill COVID-19 patients in studies from Italy and France.
Globally, in severely affected COVID-19 patients, there have been reports of thromboses in intravenous catheters and extracorporeal circuits as well as arterial vascular occlusive events, including myocardial infarction, acute limb ischemia, and stroke.
There have been multiple small studies in which critically ill COVID-19 patients were routinely screened for thrombotic disease. In these studies, rates of thrombotic complications ranged from 69% to 85%, despite thromboprophylaxis. Variability in prophylactic and screening protocols explain discrepancies in event rates.
Pathophysiology
The abnormally high blood levels of D-dimer and fibrinogen during the early stages of SARS-CoV-2 infection are reflective of excessive inflammation rather than overt disseminated intravascular coagulation (DIC), which may develop in later stages of illness, according to Dr. Gupta and colleagues. The authors theorized that uninhibited inflammation, along with hypoxia and direct viral-mediated cellular injury, contribute to thrombotic complications in COVID-19 patients.
“The increased expression of ACE2 in endothelial cells after infection with SARS-CoV-2 may perpetuate a vicious cycle of endothelialitis that promotes thromboinflammation,” the authors wrote. “Collectively, hemostatic and inflammatory changes, which reflect endothelial damage and activation as well as critical illness, constitute a prothrombotic milieu.”
The authors noted that small autopsy series have shown high rates of microvascular and macrovascular thromboses, particularly in the pulmonary circulation, in COVID-19 patients.
Management considerations
Dr. Gupta and colleagues referenced interim guidelines from the International Society of Thrombosis and Haemostasis that recommend serial complete blood counts, with white blood cell differential and assessment of D-dimer, prothrombin time, and fibrinogen for hospitalized patients with COVID-19. The authors also cited guidelines published in the Journal of the American College of Cardiology that recommend routine risk assessment for venous thromboembolism in all hospitalized patients with COVID-19 and the consideration of standard-dose pharmaco-prophylaxis in patients who lack absolute contraindications.
Empiric use of higher-than-routine prophylactic-dose or therapeutic-dose anticoagulation in ICU patients in the absence of proven thromboses has been implemented in some institutions, Dr. Gupta and colleagues noted. Parenteral anticoagulants (such as low-molecular-weight or unfractionated heparin) are preferred to oral anticoagulants because of short half-life, available reversal agents, and the potential for drug interactions between oral agents and antiviral and/or antibacterial treatment, according to the authors.
They wrote that randomized clinical trials “will be crucial to establishing effective and safe strategies” for anticoagulation in COVID-19 patients. To this point, few randomized trials have been published to guide management of COVID-19–associated extrapulmonary manifestations, including CAC.
Research priorities
A more complete understanding of the organ-specific pathophysiology of this multisystem disease is vital, according to Dr. Gupta and colleagues.
“Regional, national, and international collaborations of clinicians and scientists focused on high-quality, transparent, ethical, and evidence-based research practices would help propel the global community toward achieving success against this pandemic,” the authors wrote.
They noted that common definitions and data standards for research are key for cross-institutional and international collaborations.
Initial attention to high-quality prospective scientific documentation standards would have been valuable and will be required for dedicated trials to address the multisystem effects of COVID-19.
Community of learners
As much as at any prior time in their careers, during the COVID-19 pandemic, health care providers have been enveloped in a community of learners – a group of people who share values and beliefs and who actively engage in learning from one another.
Through a patchwork of sources – news media, social media, traditional medical journals, general and COVID-focused meetings, and, most importantly, patients – we have been living in a learning-centered environment. Academicians, clinicians, practicing physicians, researchers, patients, family members, and caregivers have been actively and intentionally building a knowledge base together.
Through their published review, Dr. Gupta and colleagues have contributed meaningfully to the understanding our learning community has of the various extrapulmonary manifestations of COVID-19. The authors have provided a nice template for further research and clinical advances.
Dr. Gupta and colleagues disclosed financial relationships with a range of pharmaceutical companies and other organizations.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Source: Gupta A et al. Nat Med. 2020 Jul;26(7):1017-32.
While SARS-CoV-2 causes frequent and potentially severe pulmonary disease, extrapulmonary manifestations may be a prominent part of the clinical spectrum, according to a review published in Nature Medicine.
In this comprehensive literature review, Aakriti Gupta, MD, of New York-Presbyterian/Columbia University Irving Medical Center and colleagues detailed the epidemiologic and clinical multisystem effects of COVID-19. The authors explained what is known and/or suspected about the pathophysiology of those effects and outlined the resultant management considerations.
Key mechanisms for multiorgan injury include direct viral toxicity, endothelial cell damage with inflammatory mediation of thrombosis, aberrant immune response, and dysregulation of the renin-angiotensin-aldosterone system.
The relative importance of each pathway in the clinical presentation of COVID-19 and the mechanism for extrapulmonary spread of SARS-CoV-2 infection are imperfectly understood, Dr. Gupta and colleagues noted.
As for the hematologic effects of COVID-19, patients may present with several laboratory abnormalities, but the most clinically relevant complications are thromboembolic.
COVID-19-associated coagulopathy
Dr. Gupta and colleagues noted that COVID-19–associated coagulopathy (CAC) is accompanied by elevated levels of D-dimer and fibrinogen, with minor abnormalities in prothrombin time, activated partial thromboplastin time, and platelet counts in the initial stage of infection.
Elevated D-dimer levels have been reported in up to 46% of hospitalized patients, and a longitudinal increase while hospitalized is associated with higher mortality.
In initial reports from China and the Netherlands, thrombotic complications were seen in up to 30% of COVID-19 patients in ICUs. Thromboembolic events have been reported in 17%-22% of critically ill COVID-19 patients in studies from Italy and France.
Globally, in severely affected COVID-19 patients, there have been reports of thromboses in intravenous catheters and extracorporeal circuits as well as arterial vascular occlusive events, including myocardial infarction, acute limb ischemia, and stroke.
There have been multiple small studies in which critically ill COVID-19 patients were routinely screened for thrombotic disease. In these studies, rates of thrombotic complications ranged from 69% to 85%, despite thromboprophylaxis. Variability in prophylactic and screening protocols explain discrepancies in event rates.
Pathophysiology
The abnormally high blood levels of D-dimer and fibrinogen during the early stages of SARS-CoV-2 infection are reflective of excessive inflammation rather than overt disseminated intravascular coagulation (DIC), which may develop in later stages of illness, according to Dr. Gupta and colleagues. The authors theorized that uninhibited inflammation, along with hypoxia and direct viral-mediated cellular injury, contribute to thrombotic complications in COVID-19 patients.
“The increased expression of ACE2 in endothelial cells after infection with SARS-CoV-2 may perpetuate a vicious cycle of endothelialitis that promotes thromboinflammation,” the authors wrote. “Collectively, hemostatic and inflammatory changes, which reflect endothelial damage and activation as well as critical illness, constitute a prothrombotic milieu.”
The authors noted that small autopsy series have shown high rates of microvascular and macrovascular thromboses, particularly in the pulmonary circulation, in COVID-19 patients.
Management considerations
Dr. Gupta and colleagues referenced interim guidelines from the International Society of Thrombosis and Haemostasis that recommend serial complete blood counts, with white blood cell differential and assessment of D-dimer, prothrombin time, and fibrinogen for hospitalized patients with COVID-19. The authors also cited guidelines published in the Journal of the American College of Cardiology that recommend routine risk assessment for venous thromboembolism in all hospitalized patients with COVID-19 and the consideration of standard-dose pharmaco-prophylaxis in patients who lack absolute contraindications.
Empiric use of higher-than-routine prophylactic-dose or therapeutic-dose anticoagulation in ICU patients in the absence of proven thromboses has been implemented in some institutions, Dr. Gupta and colleagues noted. Parenteral anticoagulants (such as low-molecular-weight or unfractionated heparin) are preferred to oral anticoagulants because of short half-life, available reversal agents, and the potential for drug interactions between oral agents and antiviral and/or antibacterial treatment, according to the authors.
They wrote that randomized clinical trials “will be crucial to establishing effective and safe strategies” for anticoagulation in COVID-19 patients. To this point, few randomized trials have been published to guide management of COVID-19–associated extrapulmonary manifestations, including CAC.
Research priorities
A more complete understanding of the organ-specific pathophysiology of this multisystem disease is vital, according to Dr. Gupta and colleagues.
“Regional, national, and international collaborations of clinicians and scientists focused on high-quality, transparent, ethical, and evidence-based research practices would help propel the global community toward achieving success against this pandemic,” the authors wrote.
They noted that common definitions and data standards for research are key for cross-institutional and international collaborations.
Initial attention to high-quality prospective scientific documentation standards would have been valuable and will be required for dedicated trials to address the multisystem effects of COVID-19.
Community of learners
As much as at any prior time in their careers, during the COVID-19 pandemic, health care providers have been enveloped in a community of learners – a group of people who share values and beliefs and who actively engage in learning from one another.
Through a patchwork of sources – news media, social media, traditional medical journals, general and COVID-focused meetings, and, most importantly, patients – we have been living in a learning-centered environment. Academicians, clinicians, practicing physicians, researchers, patients, family members, and caregivers have been actively and intentionally building a knowledge base together.
Through their published review, Dr. Gupta and colleagues have contributed meaningfully to the understanding our learning community has of the various extrapulmonary manifestations of COVID-19. The authors have provided a nice template for further research and clinical advances.
Dr. Gupta and colleagues disclosed financial relationships with a range of pharmaceutical companies and other organizations.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Source: Gupta A et al. Nat Med. 2020 Jul;26(7):1017-32.
While SARS-CoV-2 causes frequent and potentially severe pulmonary disease, extrapulmonary manifestations may be a prominent part of the clinical spectrum, according to a review published in Nature Medicine.
In this comprehensive literature review, Aakriti Gupta, MD, of New York-Presbyterian/Columbia University Irving Medical Center and colleagues detailed the epidemiologic and clinical multisystem effects of COVID-19. The authors explained what is known and/or suspected about the pathophysiology of those effects and outlined the resultant management considerations.
Key mechanisms for multiorgan injury include direct viral toxicity, endothelial cell damage with inflammatory mediation of thrombosis, aberrant immune response, and dysregulation of the renin-angiotensin-aldosterone system.
The relative importance of each pathway in the clinical presentation of COVID-19 and the mechanism for extrapulmonary spread of SARS-CoV-2 infection are imperfectly understood, Dr. Gupta and colleagues noted.
As for the hematologic effects of COVID-19, patients may present with several laboratory abnormalities, but the most clinically relevant complications are thromboembolic.
COVID-19-associated coagulopathy
Dr. Gupta and colleagues noted that COVID-19–associated coagulopathy (CAC) is accompanied by elevated levels of D-dimer and fibrinogen, with minor abnormalities in prothrombin time, activated partial thromboplastin time, and platelet counts in the initial stage of infection.
Elevated D-dimer levels have been reported in up to 46% of hospitalized patients, and a longitudinal increase while hospitalized is associated with higher mortality.
In initial reports from China and the Netherlands, thrombotic complications were seen in up to 30% of COVID-19 patients in ICUs. Thromboembolic events have been reported in 17%-22% of critically ill COVID-19 patients in studies from Italy and France.
Globally, in severely affected COVID-19 patients, there have been reports of thromboses in intravenous catheters and extracorporeal circuits as well as arterial vascular occlusive events, including myocardial infarction, acute limb ischemia, and stroke.
There have been multiple small studies in which critically ill COVID-19 patients were routinely screened for thrombotic disease. In these studies, rates of thrombotic complications ranged from 69% to 85%, despite thromboprophylaxis. Variability in prophylactic and screening protocols explain discrepancies in event rates.
Pathophysiology
The abnormally high blood levels of D-dimer and fibrinogen during the early stages of SARS-CoV-2 infection are reflective of excessive inflammation rather than overt disseminated intravascular coagulation (DIC), which may develop in later stages of illness, according to Dr. Gupta and colleagues. The authors theorized that uninhibited inflammation, along with hypoxia and direct viral-mediated cellular injury, contribute to thrombotic complications in COVID-19 patients.
“The increased expression of ACE2 in endothelial cells after infection with SARS-CoV-2 may perpetuate a vicious cycle of endothelialitis that promotes thromboinflammation,” the authors wrote. “Collectively, hemostatic and inflammatory changes, which reflect endothelial damage and activation as well as critical illness, constitute a prothrombotic milieu.”
The authors noted that small autopsy series have shown high rates of microvascular and macrovascular thromboses, particularly in the pulmonary circulation, in COVID-19 patients.
Management considerations
Dr. Gupta and colleagues referenced interim guidelines from the International Society of Thrombosis and Haemostasis that recommend serial complete blood counts, with white blood cell differential and assessment of D-dimer, prothrombin time, and fibrinogen for hospitalized patients with COVID-19. The authors also cited guidelines published in the Journal of the American College of Cardiology that recommend routine risk assessment for venous thromboembolism in all hospitalized patients with COVID-19 and the consideration of standard-dose pharmaco-prophylaxis in patients who lack absolute contraindications.
Empiric use of higher-than-routine prophylactic-dose or therapeutic-dose anticoagulation in ICU patients in the absence of proven thromboses has been implemented in some institutions, Dr. Gupta and colleagues noted. Parenteral anticoagulants (such as low-molecular-weight or unfractionated heparin) are preferred to oral anticoagulants because of short half-life, available reversal agents, and the potential for drug interactions between oral agents and antiviral and/or antibacterial treatment, according to the authors.
They wrote that randomized clinical trials “will be crucial to establishing effective and safe strategies” for anticoagulation in COVID-19 patients. To this point, few randomized trials have been published to guide management of COVID-19–associated extrapulmonary manifestations, including CAC.
Research priorities
A more complete understanding of the organ-specific pathophysiology of this multisystem disease is vital, according to Dr. Gupta and colleagues.
“Regional, national, and international collaborations of clinicians and scientists focused on high-quality, transparent, ethical, and evidence-based research practices would help propel the global community toward achieving success against this pandemic,” the authors wrote.
They noted that common definitions and data standards for research are key for cross-institutional and international collaborations.
Initial attention to high-quality prospective scientific documentation standards would have been valuable and will be required for dedicated trials to address the multisystem effects of COVID-19.
Community of learners
As much as at any prior time in their careers, during the COVID-19 pandemic, health care providers have been enveloped in a community of learners – a group of people who share values and beliefs and who actively engage in learning from one another.
Through a patchwork of sources – news media, social media, traditional medical journals, general and COVID-focused meetings, and, most importantly, patients – we have been living in a learning-centered environment. Academicians, clinicians, practicing physicians, researchers, patients, family members, and caregivers have been actively and intentionally building a knowledge base together.
Through their published review, Dr. Gupta and colleagues have contributed meaningfully to the understanding our learning community has of the various extrapulmonary manifestations of COVID-19. The authors have provided a nice template for further research and clinical advances.
Dr. Gupta and colleagues disclosed financial relationships with a range of pharmaceutical companies and other organizations.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Source: Gupta A et al. Nat Med. 2020 Jul;26(7):1017-32.
FROM NATURE MEDICINE
Low-dose prasugrel preserves efficacy but lowers bleeding in elderly
In elderly or low-weight patients with acute coronary syndrome (ACS), a reduced dose of prasugrel relative to a full-dose of ticagrelor is associated with lower numerical rates of ischemic events and bleeding events, according to a prespecified substudy of the ISAR-REACT 5 trial.
“The present study provides the strongest support for reduced-dose prasugrel as the standard for elderly and low-weight patients with ACS undergoing an invasive treatment strategy,” according to the senior author, Adnan Kastrati, MD, professor of cardiology and head of the Catheterization Laboratory at Deutsches Herzzentrum, Technical University of Munich.
The main results of ISAR-REACT 5, an open-label, head-to-head comparison of prasugrel and ticagrelor in patients with ACS, showed that the risk of the composite primary endpoint of death, myocardial infarction, or stroke 1 year after randomization was significantly higher for those on ticagrelor than prasugrel (hazard ratio, 1.39; P = .006). The bleeding risk on ticagrelor was also higher but not significantly different (5.4% vs. 4.8%; P = .46) (Schüpke S et al. N Engl J Med. 2019 Oct;381:1524-34).
In this substudy newly published in Annals of Internal Medicine, outcomes were compared in the 1,099 patients who were 75 years or older or weighed less than 60 kg. In this group, unlike those younger or weighing more, patients were randomized to receive a reduced maintenance dose of 5 mg of once-daily prasugrel (rather than 10 mg) or full dose ticagrelor (90 mg twice daily).
At 1 year, the low-dose prasugrel strategy relative to ticagrelor was associated with a lower rate of events (12.7% vs. 14.6%) and a lower rate of bleeding (8.1% vs. 10.6%), defined as Bleeding Academic Research Consortium (BARC) type 3-5 events.
Neither the 18% reduction for the efficacy endpoint (HR, 0.82; 95% CI 0.60-1.14) nor the 28% reduction in the bleeding endpoint (HR, 0.72; 95% CI 0.46-1.12) reached significance, but Dr. Kastrati reported that there was a significant “treatment effect-by-study-group interaction” for BARC 1-5 bleeding (P = .004) favoring prasugrel. This supports low-dose prasugrel as a strategy to prevent the excess bleeding risk previously observed with the standard 10-mg dose of prasugrel.
In other words, a reduced dose of prasugrel, compared with the standard dose of ticagrelor, in low-weight and elderly patients “is associated with maintained anti-ischemic efficacy while protecting these patients against the excess risk of bleeding,” he and his coinvestigators concluded.
Low-weight and older patients represented 27% of those enrolled in ISAR-REACT 5. When compared to the study population as a whole, the risk for both ischemic and bleeding events was at least twice as high, the authors of an accompanying editorial observed. They praised this effort to refine the optimal antiplatelet regimen in a very-high-risk ACS population.
“The current analysis suggests that the prasugrel dose reduction regimen for elderly or underweight patients with ACS is effective and safe,” according to the editorial coauthors, David Conen, MD, and P.J. Devereaux, MD, PhD, who are affiliated with the Population Health Research Institute, Hamilton, Ontario.
This substudy was underpowered to show superiority for the efficacy and safety outcomes in elderly and low-weight ACS patients, which makes these results “hypothesis generating,” but the authors believe that they provide the best available evidence for selecting antiplatelet therapy in this challenging subgroup. Although the exclusion of patients at very high risk of bleeding from ISAR-REACT 5 suggest findings might not be relevant to all elderly and low-weight individuals, the investigators believe the data do inform clinical practice.
“Our study is the first head-to-head randomized comparison of the reduced dose of prasugrel against standard dose of ticagrelor in elderly and low-weight patients,” said Dr. Kastrati in an interview. “Specifically designed studies for this subset of patients are very unlikely to be conducted in the future.”
Dr. Kastrati reported no potential conflicts of interest relevant to this study.
SOURCE: Menichelli M et al. Ann Intern Med. 2020 Jul 21. doi: 10.7326/M20-1806.
In elderly or low-weight patients with acute coronary syndrome (ACS), a reduced dose of prasugrel relative to a full-dose of ticagrelor is associated with lower numerical rates of ischemic events and bleeding events, according to a prespecified substudy of the ISAR-REACT 5 trial.
“The present study provides the strongest support for reduced-dose prasugrel as the standard for elderly and low-weight patients with ACS undergoing an invasive treatment strategy,” according to the senior author, Adnan Kastrati, MD, professor of cardiology and head of the Catheterization Laboratory at Deutsches Herzzentrum, Technical University of Munich.
The main results of ISAR-REACT 5, an open-label, head-to-head comparison of prasugrel and ticagrelor in patients with ACS, showed that the risk of the composite primary endpoint of death, myocardial infarction, or stroke 1 year after randomization was significantly higher for those on ticagrelor than prasugrel (hazard ratio, 1.39; P = .006). The bleeding risk on ticagrelor was also higher but not significantly different (5.4% vs. 4.8%; P = .46) (Schüpke S et al. N Engl J Med. 2019 Oct;381:1524-34).
In this substudy newly published in Annals of Internal Medicine, outcomes were compared in the 1,099 patients who were 75 years or older or weighed less than 60 kg. In this group, unlike those younger or weighing more, patients were randomized to receive a reduced maintenance dose of 5 mg of once-daily prasugrel (rather than 10 mg) or full dose ticagrelor (90 mg twice daily).
At 1 year, the low-dose prasugrel strategy relative to ticagrelor was associated with a lower rate of events (12.7% vs. 14.6%) and a lower rate of bleeding (8.1% vs. 10.6%), defined as Bleeding Academic Research Consortium (BARC) type 3-5 events.
Neither the 18% reduction for the efficacy endpoint (HR, 0.82; 95% CI 0.60-1.14) nor the 28% reduction in the bleeding endpoint (HR, 0.72; 95% CI 0.46-1.12) reached significance, but Dr. Kastrati reported that there was a significant “treatment effect-by-study-group interaction” for BARC 1-5 bleeding (P = .004) favoring prasugrel. This supports low-dose prasugrel as a strategy to prevent the excess bleeding risk previously observed with the standard 10-mg dose of prasugrel.
In other words, a reduced dose of prasugrel, compared with the standard dose of ticagrelor, in low-weight and elderly patients “is associated with maintained anti-ischemic efficacy while protecting these patients against the excess risk of bleeding,” he and his coinvestigators concluded.
Low-weight and older patients represented 27% of those enrolled in ISAR-REACT 5. When compared to the study population as a whole, the risk for both ischemic and bleeding events was at least twice as high, the authors of an accompanying editorial observed. They praised this effort to refine the optimal antiplatelet regimen in a very-high-risk ACS population.
“The current analysis suggests that the prasugrel dose reduction regimen for elderly or underweight patients with ACS is effective and safe,” according to the editorial coauthors, David Conen, MD, and P.J. Devereaux, MD, PhD, who are affiliated with the Population Health Research Institute, Hamilton, Ontario.
This substudy was underpowered to show superiority for the efficacy and safety outcomes in elderly and low-weight ACS patients, which makes these results “hypothesis generating,” but the authors believe that they provide the best available evidence for selecting antiplatelet therapy in this challenging subgroup. Although the exclusion of patients at very high risk of bleeding from ISAR-REACT 5 suggest findings might not be relevant to all elderly and low-weight individuals, the investigators believe the data do inform clinical practice.
“Our study is the first head-to-head randomized comparison of the reduced dose of prasugrel against standard dose of ticagrelor in elderly and low-weight patients,” said Dr. Kastrati in an interview. “Specifically designed studies for this subset of patients are very unlikely to be conducted in the future.”
Dr. Kastrati reported no potential conflicts of interest relevant to this study.
SOURCE: Menichelli M et al. Ann Intern Med. 2020 Jul 21. doi: 10.7326/M20-1806.
In elderly or low-weight patients with acute coronary syndrome (ACS), a reduced dose of prasugrel relative to a full-dose of ticagrelor is associated with lower numerical rates of ischemic events and bleeding events, according to a prespecified substudy of the ISAR-REACT 5 trial.
“The present study provides the strongest support for reduced-dose prasugrel as the standard for elderly and low-weight patients with ACS undergoing an invasive treatment strategy,” according to the senior author, Adnan Kastrati, MD, professor of cardiology and head of the Catheterization Laboratory at Deutsches Herzzentrum, Technical University of Munich.
The main results of ISAR-REACT 5, an open-label, head-to-head comparison of prasugrel and ticagrelor in patients with ACS, showed that the risk of the composite primary endpoint of death, myocardial infarction, or stroke 1 year after randomization was significantly higher for those on ticagrelor than prasugrel (hazard ratio, 1.39; P = .006). The bleeding risk on ticagrelor was also higher but not significantly different (5.4% vs. 4.8%; P = .46) (Schüpke S et al. N Engl J Med. 2019 Oct;381:1524-34).
In this substudy newly published in Annals of Internal Medicine, outcomes were compared in the 1,099 patients who were 75 years or older or weighed less than 60 kg. In this group, unlike those younger or weighing more, patients were randomized to receive a reduced maintenance dose of 5 mg of once-daily prasugrel (rather than 10 mg) or full dose ticagrelor (90 mg twice daily).
At 1 year, the low-dose prasugrel strategy relative to ticagrelor was associated with a lower rate of events (12.7% vs. 14.6%) and a lower rate of bleeding (8.1% vs. 10.6%), defined as Bleeding Academic Research Consortium (BARC) type 3-5 events.
Neither the 18% reduction for the efficacy endpoint (HR, 0.82; 95% CI 0.60-1.14) nor the 28% reduction in the bleeding endpoint (HR, 0.72; 95% CI 0.46-1.12) reached significance, but Dr. Kastrati reported that there was a significant “treatment effect-by-study-group interaction” for BARC 1-5 bleeding (P = .004) favoring prasugrel. This supports low-dose prasugrel as a strategy to prevent the excess bleeding risk previously observed with the standard 10-mg dose of prasugrel.
In other words, a reduced dose of prasugrel, compared with the standard dose of ticagrelor, in low-weight and elderly patients “is associated with maintained anti-ischemic efficacy while protecting these patients against the excess risk of bleeding,” he and his coinvestigators concluded.
Low-weight and older patients represented 27% of those enrolled in ISAR-REACT 5. When compared to the study population as a whole, the risk for both ischemic and bleeding events was at least twice as high, the authors of an accompanying editorial observed. They praised this effort to refine the optimal antiplatelet regimen in a very-high-risk ACS population.
“The current analysis suggests that the prasugrel dose reduction regimen for elderly or underweight patients with ACS is effective and safe,” according to the editorial coauthors, David Conen, MD, and P.J. Devereaux, MD, PhD, who are affiliated with the Population Health Research Institute, Hamilton, Ontario.
This substudy was underpowered to show superiority for the efficacy and safety outcomes in elderly and low-weight ACS patients, which makes these results “hypothesis generating,” but the authors believe that they provide the best available evidence for selecting antiplatelet therapy in this challenging subgroup. Although the exclusion of patients at very high risk of bleeding from ISAR-REACT 5 suggest findings might not be relevant to all elderly and low-weight individuals, the investigators believe the data do inform clinical practice.
“Our study is the first head-to-head randomized comparison of the reduced dose of prasugrel against standard dose of ticagrelor in elderly and low-weight patients,” said Dr. Kastrati in an interview. “Specifically designed studies for this subset of patients are very unlikely to be conducted in the future.”
Dr. Kastrati reported no potential conflicts of interest relevant to this study.
SOURCE: Menichelli M et al. Ann Intern Med. 2020 Jul 21. doi: 10.7326/M20-1806.
FROM ANNALS OF INTERNAL MEDICINE
New oral anticoagulants drive ACC consensus on bleeding
Patients on oral anticoagulants who experience a bleeding event may be able to discontinue therapy if certain circumstances apply, according to updated guidance from the American College of Cardiology.
The emergence of direct-acting oral anticoagulants (DOACs) to prevent venous thromboembolism and the introduction of new reversal strategies for factor Xa inhibitors prompted the creation of an Expert Consensus Decision Pathway to update the version from 2017, according to the ACC. Expert consensus decision pathways (ECDPs) are a component of the solution sets issued by the ACC to “address key questions facing care teams and attempt to provide practical guidance to be applied at the point of care.”
In an ECDP published in the Journal of the American College of Cardiology, the writing committee members developed treatment algorithms for managing bleeding in patients on DOACs and vitamin K antagonists (VKAs).
Bleeding was classified as major or nonmajor, with major defined as “bleeding that is associated with hemodynamic compromise, occurs in an anatomically critical site, requires transfusion of at least 2 units of packed red blood cells [RBCs]), or results in a hemoglobin drop greater than 2 g/dL. All other types of bleeding were classified as nonmajor.
The document includes a graphic algorithm for assessing bleed severity and managing major versus nonmajor bleeding, and a separate graphic describes considerations for reversal and use of hemostatic agents according to whether the patient is taking a VKA (warfarin and other coumarins), a direct thrombin inhibitor (dabigatran), the factor Xa inhibitors apixaban and rivaroxaban, or the factor Xa inhibitors betrixaban and edoxaban.
Another algorithm outlines whether to discontinue, delay, or restart anticoagulation. Considerations for restarting anticoagulation include whether the patient is pregnant, awaiting an invasive procedure, not able to receive medication by mouth, has a high risk of rebleeding, or is being bridged back to a vitamin K antagonist with high thrombotic risk.
In most cases of GI bleeding, for example, current data support restarting oral anticoagulants once hemostasis is achieved, but patients who experience intracranial hemorrhage should delay restarting any anticoagulation for at least 4 weeks if they are without high thrombotic risk, according to the document.
The report also recommends clinician-patient discussion before resuming anticoagulation, ideally with time allowed for patients to develop questions. Discussions should include the signs of bleeding, assessment of risk for a thromboembolic event, and the benefits of anticoagulation.
“The proliferation of oral anticoagulants (warfarin and DOACs) and growing indications for their use prompted the need for guidance on the management of these drugs,” said Gordon F. Tomaselli, MD, chair of the writing committee, in an interview. “This document provides guidance on management at the time of a bleeding complication. This includes acute management, starting and stopping drugs, and use of reversal agents,” he said. “This of course will be a dynamic document as the list of these drugs and their antidotes expand,” he noted.
“The biggest change from the previous guidelines are twofold: an update on laboratory assessment to monitor drug levels and use of reversal agents,” while the acute management strategies have otherwise remained similar to previous documents, said Dr. Tomaselli.
Dr. Tomaselli said that he was not surprised by the biological aspects of recent research while developing the statement. However, “the extent of the use of multiple anticoagulants and antiplatelet agents was a bit surprising and complicates therapy with each of the agents,” he noted.
The way the pathways are presented may make them challenging to follow in clinical practice, said Dr. Tomaselli. “The pathways are described linearly and in practice often many things have to happen at once,” he said. “The other main issue may be limitations in the availability of some of the newer reversal agents,” he added.
“The complication of bleeding is difficult to avoid,” said Dr. Tomaselli, and for future research, “the focus needs to continue to refine the indications for anticoagulation and appropriate use with other drugs that predispose to bleeding. We also need better methods and testing to monitor drugs levels and the effect on coagulation,” he said.
In accordance with the ACC Solution Set Oversight Committee, the writing committee members, including Dr. Tomaselli, had no relevant relationships with industry to disclose.
SOURCE: Tomaselli GF et al. J Am Coll Cardiol. 2020. doi: 10.1016/j.jacc.2020.04.053.
Patients on oral anticoagulants who experience a bleeding event may be able to discontinue therapy if certain circumstances apply, according to updated guidance from the American College of Cardiology.
The emergence of direct-acting oral anticoagulants (DOACs) to prevent venous thromboembolism and the introduction of new reversal strategies for factor Xa inhibitors prompted the creation of an Expert Consensus Decision Pathway to update the version from 2017, according to the ACC. Expert consensus decision pathways (ECDPs) are a component of the solution sets issued by the ACC to “address key questions facing care teams and attempt to provide practical guidance to be applied at the point of care.”
In an ECDP published in the Journal of the American College of Cardiology, the writing committee members developed treatment algorithms for managing bleeding in patients on DOACs and vitamin K antagonists (VKAs).
Bleeding was classified as major or nonmajor, with major defined as “bleeding that is associated with hemodynamic compromise, occurs in an anatomically critical site, requires transfusion of at least 2 units of packed red blood cells [RBCs]), or results in a hemoglobin drop greater than 2 g/dL. All other types of bleeding were classified as nonmajor.
The document includes a graphic algorithm for assessing bleed severity and managing major versus nonmajor bleeding, and a separate graphic describes considerations for reversal and use of hemostatic agents according to whether the patient is taking a VKA (warfarin and other coumarins), a direct thrombin inhibitor (dabigatran), the factor Xa inhibitors apixaban and rivaroxaban, or the factor Xa inhibitors betrixaban and edoxaban.
Another algorithm outlines whether to discontinue, delay, or restart anticoagulation. Considerations for restarting anticoagulation include whether the patient is pregnant, awaiting an invasive procedure, not able to receive medication by mouth, has a high risk of rebleeding, or is being bridged back to a vitamin K antagonist with high thrombotic risk.
In most cases of GI bleeding, for example, current data support restarting oral anticoagulants once hemostasis is achieved, but patients who experience intracranial hemorrhage should delay restarting any anticoagulation for at least 4 weeks if they are without high thrombotic risk, according to the document.
The report also recommends clinician-patient discussion before resuming anticoagulation, ideally with time allowed for patients to develop questions. Discussions should include the signs of bleeding, assessment of risk for a thromboembolic event, and the benefits of anticoagulation.
“The proliferation of oral anticoagulants (warfarin and DOACs) and growing indications for their use prompted the need for guidance on the management of these drugs,” said Gordon F. Tomaselli, MD, chair of the writing committee, in an interview. “This document provides guidance on management at the time of a bleeding complication. This includes acute management, starting and stopping drugs, and use of reversal agents,” he said. “This of course will be a dynamic document as the list of these drugs and their antidotes expand,” he noted.
“The biggest change from the previous guidelines are twofold: an update on laboratory assessment to monitor drug levels and use of reversal agents,” while the acute management strategies have otherwise remained similar to previous documents, said Dr. Tomaselli.
Dr. Tomaselli said that he was not surprised by the biological aspects of recent research while developing the statement. However, “the extent of the use of multiple anticoagulants and antiplatelet agents was a bit surprising and complicates therapy with each of the agents,” he noted.
The way the pathways are presented may make them challenging to follow in clinical practice, said Dr. Tomaselli. “The pathways are described linearly and in practice often many things have to happen at once,” he said. “The other main issue may be limitations in the availability of some of the newer reversal agents,” he added.
“The complication of bleeding is difficult to avoid,” said Dr. Tomaselli, and for future research, “the focus needs to continue to refine the indications for anticoagulation and appropriate use with other drugs that predispose to bleeding. We also need better methods and testing to monitor drugs levels and the effect on coagulation,” he said.
In accordance with the ACC Solution Set Oversight Committee, the writing committee members, including Dr. Tomaselli, had no relevant relationships with industry to disclose.
SOURCE: Tomaselli GF et al. J Am Coll Cardiol. 2020. doi: 10.1016/j.jacc.2020.04.053.
Patients on oral anticoagulants who experience a bleeding event may be able to discontinue therapy if certain circumstances apply, according to updated guidance from the American College of Cardiology.
The emergence of direct-acting oral anticoagulants (DOACs) to prevent venous thromboembolism and the introduction of new reversal strategies for factor Xa inhibitors prompted the creation of an Expert Consensus Decision Pathway to update the version from 2017, according to the ACC. Expert consensus decision pathways (ECDPs) are a component of the solution sets issued by the ACC to “address key questions facing care teams and attempt to provide practical guidance to be applied at the point of care.”
In an ECDP published in the Journal of the American College of Cardiology, the writing committee members developed treatment algorithms for managing bleeding in patients on DOACs and vitamin K antagonists (VKAs).
Bleeding was classified as major or nonmajor, with major defined as “bleeding that is associated with hemodynamic compromise, occurs in an anatomically critical site, requires transfusion of at least 2 units of packed red blood cells [RBCs]), or results in a hemoglobin drop greater than 2 g/dL. All other types of bleeding were classified as nonmajor.
The document includes a graphic algorithm for assessing bleed severity and managing major versus nonmajor bleeding, and a separate graphic describes considerations for reversal and use of hemostatic agents according to whether the patient is taking a VKA (warfarin and other coumarins), a direct thrombin inhibitor (dabigatran), the factor Xa inhibitors apixaban and rivaroxaban, or the factor Xa inhibitors betrixaban and edoxaban.
Another algorithm outlines whether to discontinue, delay, or restart anticoagulation. Considerations for restarting anticoagulation include whether the patient is pregnant, awaiting an invasive procedure, not able to receive medication by mouth, has a high risk of rebleeding, or is being bridged back to a vitamin K antagonist with high thrombotic risk.
In most cases of GI bleeding, for example, current data support restarting oral anticoagulants once hemostasis is achieved, but patients who experience intracranial hemorrhage should delay restarting any anticoagulation for at least 4 weeks if they are without high thrombotic risk, according to the document.
The report also recommends clinician-patient discussion before resuming anticoagulation, ideally with time allowed for patients to develop questions. Discussions should include the signs of bleeding, assessment of risk for a thromboembolic event, and the benefits of anticoagulation.
“The proliferation of oral anticoagulants (warfarin and DOACs) and growing indications for their use prompted the need for guidance on the management of these drugs,” said Gordon F. Tomaselli, MD, chair of the writing committee, in an interview. “This document provides guidance on management at the time of a bleeding complication. This includes acute management, starting and stopping drugs, and use of reversal agents,” he said. “This of course will be a dynamic document as the list of these drugs and their antidotes expand,” he noted.
“The biggest change from the previous guidelines are twofold: an update on laboratory assessment to monitor drug levels and use of reversal agents,” while the acute management strategies have otherwise remained similar to previous documents, said Dr. Tomaselli.
Dr. Tomaselli said that he was not surprised by the biological aspects of recent research while developing the statement. However, “the extent of the use of multiple anticoagulants and antiplatelet agents was a bit surprising and complicates therapy with each of the agents,” he noted.
The way the pathways are presented may make them challenging to follow in clinical practice, said Dr. Tomaselli. “The pathways are described linearly and in practice often many things have to happen at once,” he said. “The other main issue may be limitations in the availability of some of the newer reversal agents,” he added.
“The complication of bleeding is difficult to avoid,” said Dr. Tomaselli, and for future research, “the focus needs to continue to refine the indications for anticoagulation and appropriate use with other drugs that predispose to bleeding. We also need better methods and testing to monitor drugs levels and the effect on coagulation,” he said.
In accordance with the ACC Solution Set Oversight Committee, the writing committee members, including Dr. Tomaselli, had no relevant relationships with industry to disclose.
SOURCE: Tomaselli GF et al. J Am Coll Cardiol. 2020. doi: 10.1016/j.jacc.2020.04.053.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
PCI or not, mortality climbs with post-ACS bleeding complications
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
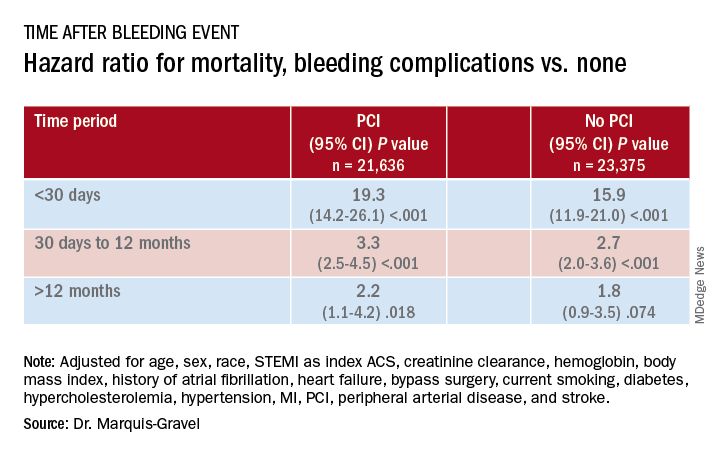
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
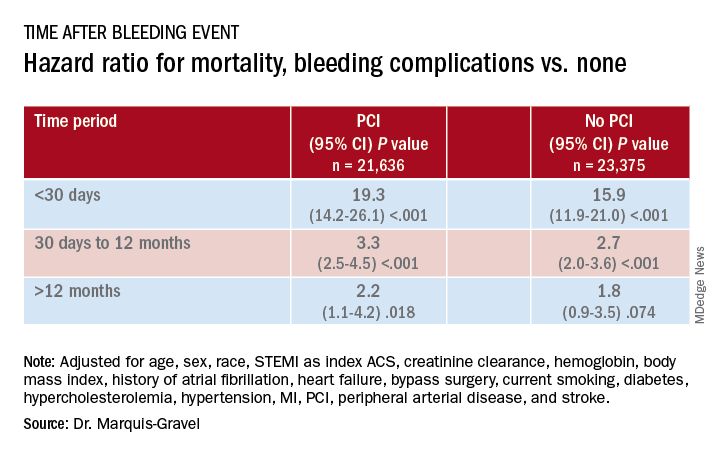
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
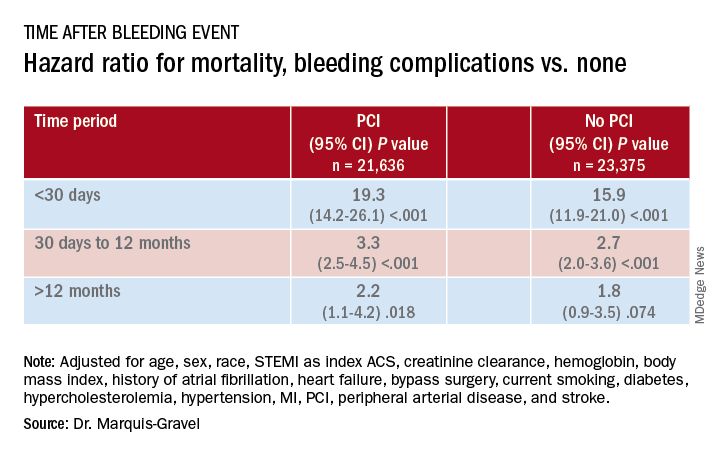
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Acetaminophen beats fentanyl in STEMI
Swapping out intravenous fentanyl in favor of IV acetaminophen in patients with ST-elevation MI (STEMI) provides comparable pain relief but with desirably higher blood levels of ticagrelor both immediately after primary percutaneous intervention and 1 hour post procedure.
That’s according to results of the Dutch ON-TIME 3 trial, presented by Anne H. Tavenier, MD, at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
“Our trial results have implications for the prehospital treatment of STEMI patients,” said Dr. Tavenier, a cardiologist at the Isala Clinic in Zwolle, the Netherlands.
The explanation for the success of this novel STEMI pain management strategy? The synthetic opioid fentanyl impairs gastrointestinal absorption of oral P2Y12 receptor antagonists such as ticagrelor. Opiates do so as well, whereas acetaminophen does not, she explained.
The potent platelet inhibition provided by oral P2Y12 inhibitors is crucial to successful primary PCI for STEMI. But these platelet inhibitory effects are inherently slowed in STEMI patients owing to hemodynamic changes and delayed GI absorption. And even though both American College of Cardiology/American Heart Association and European Society of Cardiology guidelines recommend the use of opioids for pain control in STEMI patients, the fact is that these medications further delay the absorption of oral P2Y12 inhibitors. And this delay is further exacerbated by the nausea and vomiting which are common side effects of IV fentanyl, she continued.
The impetus for the ON-TIME 3 trial was straightforward, the cardiologist said: “For years, STEMI patients have been treated with morphine or morphinelike drugs like fentanyl because of pain or sympathetic stress. To date, trials investigating alternative analgesics to opioids have been scarce.”
ON-TIME 3 was a multicenter, open-label, phase 4 clinical trial in which 195 STEMI patients with a self-reported pain score of at least 4 on a 0-10 scale received crushed ticagrelor in the ambulance along with either 1,000 mg of IV acetaminophen or fentanyl at 1-2 mcg/kg.
Ticagrelor blood levels were significantly higher in the IV acetaminophen group when measured just prior to primary PCI (151 ng/mL versus 60 ng/mL in the IV fentanyl group; immediately after PCI (326 versus 115 ng/mL), and 1 hour post PCI (488 versus 372 ng/mL).
However, there was no significant between-group difference in levels of platelet reactivity units measured immediately after primary PCI, Dr. Tavenier added.
Discussant Christoph K. Naber, MD, PhD, confessed that prior to ON-TIME 3 he was unaware that administering opioids to STEMI patients results in delayed absorption of oral P2Y12 inhibitors. Upon delving into the literature, however, he found that this is indeed a well-documented problem.
“The open question I have about this very elegant trial is whether the increased P2Y12 levels will translate into a measurable difference in clinical outcomes,” said Dr. Naber, an interventional cardiologist at the Wilhemshaven (Germany) Clinic.
The answer to that question would require a larger, longer-term trial. And he’s disinclined to wait around for that to happen.
“I think when we look at the risk balance, the risk of switching from an opioid to acetaminophen, if it works for the patient, is rather low. So this might be something to introduce in my practice,” the cardiologist said.
Dr. Tavenier and Dr. Naber reported having no financial conflicts of interest.
SOURCE: Tavenier AH. EuroPCR 2020.
Swapping out intravenous fentanyl in favor of IV acetaminophen in patients with ST-elevation MI (STEMI) provides comparable pain relief but with desirably higher blood levels of ticagrelor both immediately after primary percutaneous intervention and 1 hour post procedure.
That’s according to results of the Dutch ON-TIME 3 trial, presented by Anne H. Tavenier, MD, at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
“Our trial results have implications for the prehospital treatment of STEMI patients,” said Dr. Tavenier, a cardiologist at the Isala Clinic in Zwolle, the Netherlands.
The explanation for the success of this novel STEMI pain management strategy? The synthetic opioid fentanyl impairs gastrointestinal absorption of oral P2Y12 receptor antagonists such as ticagrelor. Opiates do so as well, whereas acetaminophen does not, she explained.
The potent platelet inhibition provided by oral P2Y12 inhibitors is crucial to successful primary PCI for STEMI. But these platelet inhibitory effects are inherently slowed in STEMI patients owing to hemodynamic changes and delayed GI absorption. And even though both American College of Cardiology/American Heart Association and European Society of Cardiology guidelines recommend the use of opioids for pain control in STEMI patients, the fact is that these medications further delay the absorption of oral P2Y12 inhibitors. And this delay is further exacerbated by the nausea and vomiting which are common side effects of IV fentanyl, she continued.
The impetus for the ON-TIME 3 trial was straightforward, the cardiologist said: “For years, STEMI patients have been treated with morphine or morphinelike drugs like fentanyl because of pain or sympathetic stress. To date, trials investigating alternative analgesics to opioids have been scarce.”
ON-TIME 3 was a multicenter, open-label, phase 4 clinical trial in which 195 STEMI patients with a self-reported pain score of at least 4 on a 0-10 scale received crushed ticagrelor in the ambulance along with either 1,000 mg of IV acetaminophen or fentanyl at 1-2 mcg/kg.
Ticagrelor blood levels were significantly higher in the IV acetaminophen group when measured just prior to primary PCI (151 ng/mL versus 60 ng/mL in the IV fentanyl group; immediately after PCI (326 versus 115 ng/mL), and 1 hour post PCI (488 versus 372 ng/mL).
However, there was no significant between-group difference in levels of platelet reactivity units measured immediately after primary PCI, Dr. Tavenier added.
Discussant Christoph K. Naber, MD, PhD, confessed that prior to ON-TIME 3 he was unaware that administering opioids to STEMI patients results in delayed absorption of oral P2Y12 inhibitors. Upon delving into the literature, however, he found that this is indeed a well-documented problem.
“The open question I have about this very elegant trial is whether the increased P2Y12 levels will translate into a measurable difference in clinical outcomes,” said Dr. Naber, an interventional cardiologist at the Wilhemshaven (Germany) Clinic.
The answer to that question would require a larger, longer-term trial. And he’s disinclined to wait around for that to happen.
“I think when we look at the risk balance, the risk of switching from an opioid to acetaminophen, if it works for the patient, is rather low. So this might be something to introduce in my practice,” the cardiologist said.
Dr. Tavenier and Dr. Naber reported having no financial conflicts of interest.
SOURCE: Tavenier AH. EuroPCR 2020.
Swapping out intravenous fentanyl in favor of IV acetaminophen in patients with ST-elevation MI (STEMI) provides comparable pain relief but with desirably higher blood levels of ticagrelor both immediately after primary percutaneous intervention and 1 hour post procedure.
That’s according to results of the Dutch ON-TIME 3 trial, presented by Anne H. Tavenier, MD, at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
“Our trial results have implications for the prehospital treatment of STEMI patients,” said Dr. Tavenier, a cardiologist at the Isala Clinic in Zwolle, the Netherlands.
The explanation for the success of this novel STEMI pain management strategy? The synthetic opioid fentanyl impairs gastrointestinal absorption of oral P2Y12 receptor antagonists such as ticagrelor. Opiates do so as well, whereas acetaminophen does not, she explained.
The potent platelet inhibition provided by oral P2Y12 inhibitors is crucial to successful primary PCI for STEMI. But these platelet inhibitory effects are inherently slowed in STEMI patients owing to hemodynamic changes and delayed GI absorption. And even though both American College of Cardiology/American Heart Association and European Society of Cardiology guidelines recommend the use of opioids for pain control in STEMI patients, the fact is that these medications further delay the absorption of oral P2Y12 inhibitors. And this delay is further exacerbated by the nausea and vomiting which are common side effects of IV fentanyl, she continued.
The impetus for the ON-TIME 3 trial was straightforward, the cardiologist said: “For years, STEMI patients have been treated with morphine or morphinelike drugs like fentanyl because of pain or sympathetic stress. To date, trials investigating alternative analgesics to opioids have been scarce.”
ON-TIME 3 was a multicenter, open-label, phase 4 clinical trial in which 195 STEMI patients with a self-reported pain score of at least 4 on a 0-10 scale received crushed ticagrelor in the ambulance along with either 1,000 mg of IV acetaminophen or fentanyl at 1-2 mcg/kg.
Ticagrelor blood levels were significantly higher in the IV acetaminophen group when measured just prior to primary PCI (151 ng/mL versus 60 ng/mL in the IV fentanyl group; immediately after PCI (326 versus 115 ng/mL), and 1 hour post PCI (488 versus 372 ng/mL).
However, there was no significant between-group difference in levels of platelet reactivity units measured immediately after primary PCI, Dr. Tavenier added.
Discussant Christoph K. Naber, MD, PhD, confessed that prior to ON-TIME 3 he was unaware that administering opioids to STEMI patients results in delayed absorption of oral P2Y12 inhibitors. Upon delving into the literature, however, he found that this is indeed a well-documented problem.
“The open question I have about this very elegant trial is whether the increased P2Y12 levels will translate into a measurable difference in clinical outcomes,” said Dr. Naber, an interventional cardiologist at the Wilhemshaven (Germany) Clinic.
The answer to that question would require a larger, longer-term trial. And he’s disinclined to wait around for that to happen.
“I think when we look at the risk balance, the risk of switching from an opioid to acetaminophen, if it works for the patient, is rather low. So this might be something to introduce in my practice,” the cardiologist said.
Dr. Tavenier and Dr. Naber reported having no financial conflicts of interest.
SOURCE: Tavenier AH. EuroPCR 2020.
REPORTING FROM EUROPCR 2020
Post-PCI mortality higher in Blacks vs. Whites, regardless of comorbidities
A combined analysis of 10 prospective trials, intended to shed light on racial disparities in percutaneous coronary intervention (PCI) outcomes, saw sharply higher risks of death and myocardial infarction (MI) for Blacks compared with Whites.
The burden of comorbidities, including diabetes, was greater for Hispanics and Blacks, compared with Whites, but only in Blacks were PCI outcomes significantly worse even after controlling for such conditions and other baseline risk factors.
The analysis based on more than 22,000 patients was published July 6 in JACC: Cardiovascular Interventions,with lead author Mordechai Golomb, MD, Cardiovascular Research Foundation, New York.
In the study based on patient-level data from the different trials, the adjusted risk of MI after PCI was increased 45% at 1 year and 55% after 5 years for Blacks, compared with Whites. Their risk of death at 1 year was doubled, and their risk of major adverse cardiac events (MACE) was up by 28% at 5 years.
“Improving health care and outcomes for minorities is essential, and we are hopeful that our work may help direct these efforts, senior author Gregg W. Stone, MD, Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“But this won’t happen without active, concerted efforts to promote change and opportunity, a task for government, regulators, payers, hospital administrators, physicians, and all health care providers,” he said. “Understanding patient outcomes according to race and ethnicity is essential to optimize health for all patients,” but “most prior studies in this regard have looked at population-based data.”
In contrast, the current study used hospital source records – which are considered more accurate than administrative databases – and event coding reports, Dr. Stone said, plus angiographic core laboratory analyses for all patients, which allows “an independent assessment of the extent and type of coronary artery disease and procedural outcomes.”
The analysis “demonstrated that even when upfront treatments are presumably similar [across racial groups] in a clinical trial setting, longitudinal outcomes still differ by race,” Michael Nanna, MD, said in an interview.
The “troubling” results “highlight the persistence of racial disparities in health care and the need to renew our focus on closing these gaps [and] is yet another call to action for clinicians, researchers, and the health care system at large,” said Dr. Nanna, of Duke University Medical Center, Durham, N.C., and lead author on an editorial accompanying the published analysis.
Of the 10 randomized controlled trials included in the study, which encompassed 22,638 patients, 9 were stent comparisons and 1 compared antithrombotic regimens in patients with acute coronary syndromes (ACS), the authors noted. The median follow-up was about 1,100 days.
White patients made up 90.9% of the combined cohort, Black patients comprised 4.1%, Hispanics 2.1%, and Asians 1.8% – figures that “confirm the well-known fact that minority groups are underrepresented in clinical trials,” Dr. Stone said.
There were notable demographic and clinical differences at baseline between the four groups.
For example, Black patients tended to be younger than White, Hispanic, and Asian patients. Black and Hispanic patients were also less likely to be male, compared with White patients.
Both Black and Hispanic patients had more comorbidities than Whites did at baseline, the authors observe. For example, Black and Hispanic patients had a greater body mass index, compared with Whites, whereas it was lower for Asians; and they had more diabetes and more hypertension than Whites (P < .0001 for all differences). Hispanics were more likely to have ACS at baseline, compared with Whites, and less likely to have stable coronary artery disease (CAD) (P < .0001 for all differences). Similar proportions of Blacks and of Whites had stable CAD (about 32% of each) and ACS (about 68% in both cases). Rates of hyperlipidemia and stable CAD were greater and rates of ACS was lower in Asians than the other three race groups (P < .0001 for each difference). In adjusted analysis, the risk of MACE at 5 years was significantly increased for Blacks, compared with Whites (hazard ratio, 1.28; 95% CI, 1.05-1.57; P = .01). The same applied to MI (HR, 1.55; 95% CI, 1.15-2.09; P = .004). At 1 year, Blacks showed higher risks for death (HR, 2.06; 95% CI, 1.26-3.36; P = .004) and for MI (HR, 1.45; 95% CI, 1.01-2.10; P = .045), compared with Whites.
No significant increases in risk for outcomes at 1 and 5 years were seen for Hispanics or Asians, compared with Whites.
Covariates in the analyses included age, sex, body mass index, diabetes, current smoking, hypertension, hyperlipidemia, history of MI or coronary revascularization, clinical CAD presentation, category of stent, and race stratified by study.
Even with underlying genotypic differences between Blacks and Whites, much of the difference in risk for outcomes “should have been accounted for when the researchers adjusted for these clinical phenotypes,” the editorial notes.
Some of the difference in risk must have derived from uncontrolled-for variables, and “[b]eyond genetics, it is clear that race is also a surrogate for other socioeconomic factors that influence both medical care and patient outcomes,” the editorialists wrote.
The adjusted analysis, noted Golomb et al, suggests “that for Hispanic patients, the excess risk for adverse clinical outcomes may have been attributable to a higher prevalence of risk factors. In contrast, the excess risk for adverse clinical outcomes for Black patients persisted even after adjustment for baseline risk factors.”
As such, they agreed: “The observed increased risk may be explained by differences that are not fully captured in traditional cardiovascular risk factor assessment, including socioeconomic differences and education, treatment compliance rates, and yet-to-be-elucidated genetic differences and/or other factors.”
Dr. Stone said that such socioeconomic considerations may include reduced access to care and insurance coverage; lack of preventive care, disease awareness, and education; delayed presentation; and varying levels of provided care.
“Possible genetic or environmental-related differences in the development and progression of atherosclerosis and other disease processes” may also be involved.
“Achieving representative proportions of minorities in clinical trials is essential but has proved challenging,” Dr. Stone said. “We must ensure that adequate numbers of hospitals and providers that are serving these patients participate in multicenter trials, and trust has to be developed so that minority populations have confidence to enroll in studies.”
Dr. Stone reported holding equity options in Ancora, Qool Therapeutics, Cagent, Applied Therapeutics, the Biostar family of funds, SpectraWave, Orchestro Biomed, Aria, Cardiac Success, the MedFocus family of funds, and Valfix and receiving consulting fees from Valfix, TherOx, Vascular Dynamics, Robocath, HeartFlow, Gore Ablative Solutions, Miracor, Neovasc, W-Wave, Abiomed, and others. Disclosures for the other authors are in the report. Nanna reports no relevant financial relationships; other coauthor disclosures are provided with the editorial.
A version of this article originally appeared on Medscape.com.
A combined analysis of 10 prospective trials, intended to shed light on racial disparities in percutaneous coronary intervention (PCI) outcomes, saw sharply higher risks of death and myocardial infarction (MI) for Blacks compared with Whites.
The burden of comorbidities, including diabetes, was greater for Hispanics and Blacks, compared with Whites, but only in Blacks were PCI outcomes significantly worse even after controlling for such conditions and other baseline risk factors.
The analysis based on more than 22,000 patients was published July 6 in JACC: Cardiovascular Interventions,with lead author Mordechai Golomb, MD, Cardiovascular Research Foundation, New York.
In the study based on patient-level data from the different trials, the adjusted risk of MI after PCI was increased 45% at 1 year and 55% after 5 years for Blacks, compared with Whites. Their risk of death at 1 year was doubled, and their risk of major adverse cardiac events (MACE) was up by 28% at 5 years.
“Improving health care and outcomes for minorities is essential, and we are hopeful that our work may help direct these efforts, senior author Gregg W. Stone, MD, Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“But this won’t happen without active, concerted efforts to promote change and opportunity, a task for government, regulators, payers, hospital administrators, physicians, and all health care providers,” he said. “Understanding patient outcomes according to race and ethnicity is essential to optimize health for all patients,” but “most prior studies in this regard have looked at population-based data.”
In contrast, the current study used hospital source records – which are considered more accurate than administrative databases – and event coding reports, Dr. Stone said, plus angiographic core laboratory analyses for all patients, which allows “an independent assessment of the extent and type of coronary artery disease and procedural outcomes.”
The analysis “demonstrated that even when upfront treatments are presumably similar [across racial groups] in a clinical trial setting, longitudinal outcomes still differ by race,” Michael Nanna, MD, said in an interview.
The “troubling” results “highlight the persistence of racial disparities in health care and the need to renew our focus on closing these gaps [and] is yet another call to action for clinicians, researchers, and the health care system at large,” said Dr. Nanna, of Duke University Medical Center, Durham, N.C., and lead author on an editorial accompanying the published analysis.
Of the 10 randomized controlled trials included in the study, which encompassed 22,638 patients, 9 were stent comparisons and 1 compared antithrombotic regimens in patients with acute coronary syndromes (ACS), the authors noted. The median follow-up was about 1,100 days.
White patients made up 90.9% of the combined cohort, Black patients comprised 4.1%, Hispanics 2.1%, and Asians 1.8% – figures that “confirm the well-known fact that minority groups are underrepresented in clinical trials,” Dr. Stone said.
There were notable demographic and clinical differences at baseline between the four groups.
For example, Black patients tended to be younger than White, Hispanic, and Asian patients. Black and Hispanic patients were also less likely to be male, compared with White patients.
Both Black and Hispanic patients had more comorbidities than Whites did at baseline, the authors observe. For example, Black and Hispanic patients had a greater body mass index, compared with Whites, whereas it was lower for Asians; and they had more diabetes and more hypertension than Whites (P < .0001 for all differences). Hispanics were more likely to have ACS at baseline, compared with Whites, and less likely to have stable coronary artery disease (CAD) (P < .0001 for all differences). Similar proportions of Blacks and of Whites had stable CAD (about 32% of each) and ACS (about 68% in both cases). Rates of hyperlipidemia and stable CAD were greater and rates of ACS was lower in Asians than the other three race groups (P < .0001 for each difference). In adjusted analysis, the risk of MACE at 5 years was significantly increased for Blacks, compared with Whites (hazard ratio, 1.28; 95% CI, 1.05-1.57; P = .01). The same applied to MI (HR, 1.55; 95% CI, 1.15-2.09; P = .004). At 1 year, Blacks showed higher risks for death (HR, 2.06; 95% CI, 1.26-3.36; P = .004) and for MI (HR, 1.45; 95% CI, 1.01-2.10; P = .045), compared with Whites.
No significant increases in risk for outcomes at 1 and 5 years were seen for Hispanics or Asians, compared with Whites.
Covariates in the analyses included age, sex, body mass index, diabetes, current smoking, hypertension, hyperlipidemia, history of MI or coronary revascularization, clinical CAD presentation, category of stent, and race stratified by study.
Even with underlying genotypic differences between Blacks and Whites, much of the difference in risk for outcomes “should have been accounted for when the researchers adjusted for these clinical phenotypes,” the editorial notes.
Some of the difference in risk must have derived from uncontrolled-for variables, and “[b]eyond genetics, it is clear that race is also a surrogate for other socioeconomic factors that influence both medical care and patient outcomes,” the editorialists wrote.
The adjusted analysis, noted Golomb et al, suggests “that for Hispanic patients, the excess risk for adverse clinical outcomes may have been attributable to a higher prevalence of risk factors. In contrast, the excess risk for adverse clinical outcomes for Black patients persisted even after adjustment for baseline risk factors.”
As such, they agreed: “The observed increased risk may be explained by differences that are not fully captured in traditional cardiovascular risk factor assessment, including socioeconomic differences and education, treatment compliance rates, and yet-to-be-elucidated genetic differences and/or other factors.”
Dr. Stone said that such socioeconomic considerations may include reduced access to care and insurance coverage; lack of preventive care, disease awareness, and education; delayed presentation; and varying levels of provided care.
“Possible genetic or environmental-related differences in the development and progression of atherosclerosis and other disease processes” may also be involved.
“Achieving representative proportions of minorities in clinical trials is essential but has proved challenging,” Dr. Stone said. “We must ensure that adequate numbers of hospitals and providers that are serving these patients participate in multicenter trials, and trust has to be developed so that minority populations have confidence to enroll in studies.”
Dr. Stone reported holding equity options in Ancora, Qool Therapeutics, Cagent, Applied Therapeutics, the Biostar family of funds, SpectraWave, Orchestro Biomed, Aria, Cardiac Success, the MedFocus family of funds, and Valfix and receiving consulting fees from Valfix, TherOx, Vascular Dynamics, Robocath, HeartFlow, Gore Ablative Solutions, Miracor, Neovasc, W-Wave, Abiomed, and others. Disclosures for the other authors are in the report. Nanna reports no relevant financial relationships; other coauthor disclosures are provided with the editorial.
A version of this article originally appeared on Medscape.com.
A combined analysis of 10 prospective trials, intended to shed light on racial disparities in percutaneous coronary intervention (PCI) outcomes, saw sharply higher risks of death and myocardial infarction (MI) for Blacks compared with Whites.
The burden of comorbidities, including diabetes, was greater for Hispanics and Blacks, compared with Whites, but only in Blacks were PCI outcomes significantly worse even after controlling for such conditions and other baseline risk factors.
The analysis based on more than 22,000 patients was published July 6 in JACC: Cardiovascular Interventions,with lead author Mordechai Golomb, MD, Cardiovascular Research Foundation, New York.
In the study based on patient-level data from the different trials, the adjusted risk of MI after PCI was increased 45% at 1 year and 55% after 5 years for Blacks, compared with Whites. Their risk of death at 1 year was doubled, and their risk of major adverse cardiac events (MACE) was up by 28% at 5 years.
“Improving health care and outcomes for minorities is essential, and we are hopeful that our work may help direct these efforts, senior author Gregg W. Stone, MD, Icahn School of Medicine at Mount Sinai, New York, said in an interview.
“But this won’t happen without active, concerted efforts to promote change and opportunity, a task for government, regulators, payers, hospital administrators, physicians, and all health care providers,” he said. “Understanding patient outcomes according to race and ethnicity is essential to optimize health for all patients,” but “most prior studies in this regard have looked at population-based data.”
In contrast, the current study used hospital source records – which are considered more accurate than administrative databases – and event coding reports, Dr. Stone said, plus angiographic core laboratory analyses for all patients, which allows “an independent assessment of the extent and type of coronary artery disease and procedural outcomes.”
The analysis “demonstrated that even when upfront treatments are presumably similar [across racial groups] in a clinical trial setting, longitudinal outcomes still differ by race,” Michael Nanna, MD, said in an interview.
The “troubling” results “highlight the persistence of racial disparities in health care and the need to renew our focus on closing these gaps [and] is yet another call to action for clinicians, researchers, and the health care system at large,” said Dr. Nanna, of Duke University Medical Center, Durham, N.C., and lead author on an editorial accompanying the published analysis.
Of the 10 randomized controlled trials included in the study, which encompassed 22,638 patients, 9 were stent comparisons and 1 compared antithrombotic regimens in patients with acute coronary syndromes (ACS), the authors noted. The median follow-up was about 1,100 days.
White patients made up 90.9% of the combined cohort, Black patients comprised 4.1%, Hispanics 2.1%, and Asians 1.8% – figures that “confirm the well-known fact that minority groups are underrepresented in clinical trials,” Dr. Stone said.
There were notable demographic and clinical differences at baseline between the four groups.
For example, Black patients tended to be younger than White, Hispanic, and Asian patients. Black and Hispanic patients were also less likely to be male, compared with White patients.
Both Black and Hispanic patients had more comorbidities than Whites did at baseline, the authors observe. For example, Black and Hispanic patients had a greater body mass index, compared with Whites, whereas it was lower for Asians; and they had more diabetes and more hypertension than Whites (P < .0001 for all differences). Hispanics were more likely to have ACS at baseline, compared with Whites, and less likely to have stable coronary artery disease (CAD) (P < .0001 for all differences). Similar proportions of Blacks and of Whites had stable CAD (about 32% of each) and ACS (about 68% in both cases). Rates of hyperlipidemia and stable CAD were greater and rates of ACS was lower in Asians than the other three race groups (P < .0001 for each difference). In adjusted analysis, the risk of MACE at 5 years was significantly increased for Blacks, compared with Whites (hazard ratio, 1.28; 95% CI, 1.05-1.57; P = .01). The same applied to MI (HR, 1.55; 95% CI, 1.15-2.09; P = .004). At 1 year, Blacks showed higher risks for death (HR, 2.06; 95% CI, 1.26-3.36; P = .004) and for MI (HR, 1.45; 95% CI, 1.01-2.10; P = .045), compared with Whites.
No significant increases in risk for outcomes at 1 and 5 years were seen for Hispanics or Asians, compared with Whites.
Covariates in the analyses included age, sex, body mass index, diabetes, current smoking, hypertension, hyperlipidemia, history of MI or coronary revascularization, clinical CAD presentation, category of stent, and race stratified by study.
Even with underlying genotypic differences between Blacks and Whites, much of the difference in risk for outcomes “should have been accounted for when the researchers adjusted for these clinical phenotypes,” the editorial notes.
Some of the difference in risk must have derived from uncontrolled-for variables, and “[b]eyond genetics, it is clear that race is also a surrogate for other socioeconomic factors that influence both medical care and patient outcomes,” the editorialists wrote.
The adjusted analysis, noted Golomb et al, suggests “that for Hispanic patients, the excess risk for adverse clinical outcomes may have been attributable to a higher prevalence of risk factors. In contrast, the excess risk for adverse clinical outcomes for Black patients persisted even after adjustment for baseline risk factors.”
As such, they agreed: “The observed increased risk may be explained by differences that are not fully captured in traditional cardiovascular risk factor assessment, including socioeconomic differences and education, treatment compliance rates, and yet-to-be-elucidated genetic differences and/or other factors.”
Dr. Stone said that such socioeconomic considerations may include reduced access to care and insurance coverage; lack of preventive care, disease awareness, and education; delayed presentation; and varying levels of provided care.
“Possible genetic or environmental-related differences in the development and progression of atherosclerosis and other disease processes” may also be involved.
“Achieving representative proportions of minorities in clinical trials is essential but has proved challenging,” Dr. Stone said. “We must ensure that adequate numbers of hospitals and providers that are serving these patients participate in multicenter trials, and trust has to be developed so that minority populations have confidence to enroll in studies.”
Dr. Stone reported holding equity options in Ancora, Qool Therapeutics, Cagent, Applied Therapeutics, the Biostar family of funds, SpectraWave, Orchestro Biomed, Aria, Cardiac Success, the MedFocus family of funds, and Valfix and receiving consulting fees from Valfix, TherOx, Vascular Dynamics, Robocath, HeartFlow, Gore Ablative Solutions, Miracor, Neovasc, W-Wave, Abiomed, and others. Disclosures for the other authors are in the report. Nanna reports no relevant financial relationships; other coauthor disclosures are provided with the editorial.
A version of this article originally appeared on Medscape.com.
Anticoagulation in cirrhosis: Best practices
Background: Alterations to the coagulation cascade put cirrhotic patients at higher risk for bleeding and thrombotic complications.
Study design: Expert review.
Setting: Literature review.
Synopsis: The authors provide 12 best practice recommendations, including use blood products sparingly in the absence of active bleeding out of concern for raising portal pressures; low-risk paracentesis, thoracentesis, and upper endoscopy do not require routine correction of thrombocytopenia or coagulopathy; for active bleeding or high-risk procedures, correct hematocrit to above 25%, platelets to more than 50,000, and fibrinogen to above 120 mg/dL; the risk of thrombosis, including venous thromboembolism and portal vein thrombosis, is high in these patients despite elevated INR values.
As such, pharmacologic VTE prophylaxis is often underutilized in patients admitted with cirrhosis; for patients requiring therapeutic anticoagulation, direct oral anticoagulants are safe in stable patients with mild cirrhosis, but should be avoided in Child-Pugh B and C patients.
Bottom line: Cirrhotic patients do not require routine correction of coagulopathy prior to low-risk procedures.
Citation: O’Leary JG et al. AGA Clinical Practice Update: Coagulation in cirrhosis. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.03.070.
Dr. Lublin is a hospitalist at the University of Colorado at Denver, Aurora.
Background: Alterations to the coagulation cascade put cirrhotic patients at higher risk for bleeding and thrombotic complications.
Study design: Expert review.
Setting: Literature review.
Synopsis: The authors provide 12 best practice recommendations, including use blood products sparingly in the absence of active bleeding out of concern for raising portal pressures; low-risk paracentesis, thoracentesis, and upper endoscopy do not require routine correction of thrombocytopenia or coagulopathy; for active bleeding or high-risk procedures, correct hematocrit to above 25%, platelets to more than 50,000, and fibrinogen to above 120 mg/dL; the risk of thrombosis, including venous thromboembolism and portal vein thrombosis, is high in these patients despite elevated INR values.
As such, pharmacologic VTE prophylaxis is often underutilized in patients admitted with cirrhosis; for patients requiring therapeutic anticoagulation, direct oral anticoagulants are safe in stable patients with mild cirrhosis, but should be avoided in Child-Pugh B and C patients.
Bottom line: Cirrhotic patients do not require routine correction of coagulopathy prior to low-risk procedures.
Citation: O’Leary JG et al. AGA Clinical Practice Update: Coagulation in cirrhosis. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.03.070.
Dr. Lublin is a hospitalist at the University of Colorado at Denver, Aurora.
Background: Alterations to the coagulation cascade put cirrhotic patients at higher risk for bleeding and thrombotic complications.
Study design: Expert review.
Setting: Literature review.
Synopsis: The authors provide 12 best practice recommendations, including use blood products sparingly in the absence of active bleeding out of concern for raising portal pressures; low-risk paracentesis, thoracentesis, and upper endoscopy do not require routine correction of thrombocytopenia or coagulopathy; for active bleeding or high-risk procedures, correct hematocrit to above 25%, platelets to more than 50,000, and fibrinogen to above 120 mg/dL; the risk of thrombosis, including venous thromboembolism and portal vein thrombosis, is high in these patients despite elevated INR values.
As such, pharmacologic VTE prophylaxis is often underutilized in patients admitted with cirrhosis; for patients requiring therapeutic anticoagulation, direct oral anticoagulants are safe in stable patients with mild cirrhosis, but should be avoided in Child-Pugh B and C patients.
Bottom line: Cirrhotic patients do not require routine correction of coagulopathy prior to low-risk procedures.
Citation: O’Leary JG et al. AGA Clinical Practice Update: Coagulation in cirrhosis. Gastroenterology. 2019. doi: 10.1053/j.gastro.2019.03.070.
Dr. Lublin is a hospitalist at the University of Colorado at Denver, Aurora.
Chewed prasugrel for primary PCI? Forget it!
And cangrelor, in turn, is superior to oral prasugrel, according to the randomized FABOLUS FASTER trial, Marco Valgimigli, MD, PhD, reported at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Moreover, contrary to conventional wisdom, chewed prasugrel (Effient) proved no better than swallowing the tablets whole for platelet inhibition, said Dr. Valgimigli, an interventional cardiologist at the University of Bern (Switzerland).
He explained that standard administration of the newer oral P2Y12 inhibitors prasugrel and ticagrelor (Brilinta) in patients undergoing percutaneous coronary intervention (PCI) for ST-elevation MI (STEMI) does not provide optimal early inhibition of platelet aggregation. The parenteral antiplatelet drugs tirofiban and cangrelor have been shown to provide faster and more prolonged inhibition of platelet aggregation than the oral P2Y12 inhibitors.
But there has been no head-to-head comparative data for the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat) and the P2Y12 inhibitor cangrelor (Kengreal) in the setting of primary PCI for STEMI. This was the impetus for FABOLUS FASTER, the first study to compare the pharmacodynamic effects of the two parenteral antiplatelet agents. The trial also looked at how these potent parenteral drugs, compared with chewed prasugrel, another previously unexamined yet highly practical issue.
The three-center, multinational, open-label FABOLUS FASTER trial randomized 122 patients undergoing primary PCI for STEMI to one of three arms: a standard intravenous bolus and 2-hour infusion of either the P2Y12 inhibitor cangrelor (Kengreal) or the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat), followed in either case by 60 mg of oral prasugrel, or a third arm in which patients didn’t receive either drug but were instead randomized to a 60-mg loading dose of chewed or whole prasugrel tablets.
The primary study endpoint was inhibition of platelet aggregation at 30 minutes as measured by light transmittance aggregometry in response to 20 mcmol/L of adenosine diphosphate (ADP).
Tirofiban was the unequivocal winner with 95% inhibition, as compared with 34.1% with cangrelor, 10.5% with chewed prasugrel, and 6.3% with prasugrel swallowed whole, even though the concentration of prasugrel’s active metabolite was far greater at 62.3 ng/mL after prasugrel was chewed, compared with 17.1 ng/mL when swallowed in integral tablet form.
The rate of nonresponsiveness to tirofiban as defined by greater than 59% platelet aggregation was zero for tirofiban during its 2-hour infusion, then a scant 8% thereafter during repeated testing at 3 and 4-6 hours. In contrast, the cangrelor nonresponsiveness rate was 50%-58% during the 2-hour infusion, rising to 82% at 3 hours.
FABOLUS FASTER, while not powered for clinical endpoints, might nevertheless have important clinical implications, according to Dr. Valgimigli. First, the superiority of the intravenous drugs tirofiban and cangrelor over prasugrel for early, strong platelet inhibition underscores the importance of giving parenteral antiplatelet drugs over oral therapy during the acute phase of STEMI therapy. Moreover, tirofiban’s outstanding performance – and the high residual platelet reactivity associated with cangrelor – makes a strong case for large comparative, randomized trials of the two drugs, with hard clinical endpoints.
Discussant Christoph K. Naber, MD, PhD, opined that he personally doesn’t consider the FABOLUS FASTER results practice changing, for a couple of reasons.
“Platelet inhibition measured by ADP in vitro is not necessarily related to true effects in vivo. We know that platelets are activated by multiple mechanisms, and the ADP pathway is just one of them,” said Dr. Naber, an interventional cardiologist at the Wilhemshaven (Germany) Clinic.
Also, there’s a good reason why no glycoprotein IIb/IIIA inhibitors are approved for treatment of STEMI, and why tirofiban, despite its impressive antiplatelet effects, is currently largely reserved for bailout situations, such as complex lesions with large thrombus burden. It’s because tirofiban’s potent antiplatelet activity is accompanied by a high risk of bleeding, he added.
However, Dr. Valgimigli noted that this conviction about excessive bleeding risk is mainly based on older studies in which glycoprotein IIb/IIIA inhibitors were administered for prolonged duration through femoral access sites. He argued that it’s time for large clinical trials examining the risk/benefit ratio of short infusion of these agents in the contemporary practice of primary PCI for STEMI.
Simultaneously with Dr. Valgimigli’s presentation, the FABOLUS FASTER results were published online (Circulation. 2020 Jun 27; doi: 10.1161/CIRCULATIONAHA.120.046928).
Dr. Valgimigli reported that Medicure, the sponsor of the FABOLUS FASTER trial, provided an institutional research grant to conduct the study. He also disclosed receiving research grants and personal fees outside the scope of this study from a dozen pharmaceutical and medical device companies. Dr. Naber reported having no financial conflicts.
And cangrelor, in turn, is superior to oral prasugrel, according to the randomized FABOLUS FASTER trial, Marco Valgimigli, MD, PhD, reported at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Moreover, contrary to conventional wisdom, chewed prasugrel (Effient) proved no better than swallowing the tablets whole for platelet inhibition, said Dr. Valgimigli, an interventional cardiologist at the University of Bern (Switzerland).
He explained that standard administration of the newer oral P2Y12 inhibitors prasugrel and ticagrelor (Brilinta) in patients undergoing percutaneous coronary intervention (PCI) for ST-elevation MI (STEMI) does not provide optimal early inhibition of platelet aggregation. The parenteral antiplatelet drugs tirofiban and cangrelor have been shown to provide faster and more prolonged inhibition of platelet aggregation than the oral P2Y12 inhibitors.
But there has been no head-to-head comparative data for the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat) and the P2Y12 inhibitor cangrelor (Kengreal) in the setting of primary PCI for STEMI. This was the impetus for FABOLUS FASTER, the first study to compare the pharmacodynamic effects of the two parenteral antiplatelet agents. The trial also looked at how these potent parenteral drugs, compared with chewed prasugrel, another previously unexamined yet highly practical issue.
The three-center, multinational, open-label FABOLUS FASTER trial randomized 122 patients undergoing primary PCI for STEMI to one of three arms: a standard intravenous bolus and 2-hour infusion of either the P2Y12 inhibitor cangrelor (Kengreal) or the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat), followed in either case by 60 mg of oral prasugrel, or a third arm in which patients didn’t receive either drug but were instead randomized to a 60-mg loading dose of chewed or whole prasugrel tablets.
The primary study endpoint was inhibition of platelet aggregation at 30 minutes as measured by light transmittance aggregometry in response to 20 mcmol/L of adenosine diphosphate (ADP).
Tirofiban was the unequivocal winner with 95% inhibition, as compared with 34.1% with cangrelor, 10.5% with chewed prasugrel, and 6.3% with prasugrel swallowed whole, even though the concentration of prasugrel’s active metabolite was far greater at 62.3 ng/mL after prasugrel was chewed, compared with 17.1 ng/mL when swallowed in integral tablet form.
The rate of nonresponsiveness to tirofiban as defined by greater than 59% platelet aggregation was zero for tirofiban during its 2-hour infusion, then a scant 8% thereafter during repeated testing at 3 and 4-6 hours. In contrast, the cangrelor nonresponsiveness rate was 50%-58% during the 2-hour infusion, rising to 82% at 3 hours.
FABOLUS FASTER, while not powered for clinical endpoints, might nevertheless have important clinical implications, according to Dr. Valgimigli. First, the superiority of the intravenous drugs tirofiban and cangrelor over prasugrel for early, strong platelet inhibition underscores the importance of giving parenteral antiplatelet drugs over oral therapy during the acute phase of STEMI therapy. Moreover, tirofiban’s outstanding performance – and the high residual platelet reactivity associated with cangrelor – makes a strong case for large comparative, randomized trials of the two drugs, with hard clinical endpoints.
Discussant Christoph K. Naber, MD, PhD, opined that he personally doesn’t consider the FABOLUS FASTER results practice changing, for a couple of reasons.
“Platelet inhibition measured by ADP in vitro is not necessarily related to true effects in vivo. We know that platelets are activated by multiple mechanisms, and the ADP pathway is just one of them,” said Dr. Naber, an interventional cardiologist at the Wilhemshaven (Germany) Clinic.
Also, there’s a good reason why no glycoprotein IIb/IIIA inhibitors are approved for treatment of STEMI, and why tirofiban, despite its impressive antiplatelet effects, is currently largely reserved for bailout situations, such as complex lesions with large thrombus burden. It’s because tirofiban’s potent antiplatelet activity is accompanied by a high risk of bleeding, he added.
However, Dr. Valgimigli noted that this conviction about excessive bleeding risk is mainly based on older studies in which glycoprotein IIb/IIIA inhibitors were administered for prolonged duration through femoral access sites. He argued that it’s time for large clinical trials examining the risk/benefit ratio of short infusion of these agents in the contemporary practice of primary PCI for STEMI.
Simultaneously with Dr. Valgimigli’s presentation, the FABOLUS FASTER results were published online (Circulation. 2020 Jun 27; doi: 10.1161/CIRCULATIONAHA.120.046928).
Dr. Valgimigli reported that Medicure, the sponsor of the FABOLUS FASTER trial, provided an institutional research grant to conduct the study. He also disclosed receiving research grants and personal fees outside the scope of this study from a dozen pharmaceutical and medical device companies. Dr. Naber reported having no financial conflicts.
And cangrelor, in turn, is superior to oral prasugrel, according to the randomized FABOLUS FASTER trial, Marco Valgimigli, MD, PhD, reported at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Moreover, contrary to conventional wisdom, chewed prasugrel (Effient) proved no better than swallowing the tablets whole for platelet inhibition, said Dr. Valgimigli, an interventional cardiologist at the University of Bern (Switzerland).
He explained that standard administration of the newer oral P2Y12 inhibitors prasugrel and ticagrelor (Brilinta) in patients undergoing percutaneous coronary intervention (PCI) for ST-elevation MI (STEMI) does not provide optimal early inhibition of platelet aggregation. The parenteral antiplatelet drugs tirofiban and cangrelor have been shown to provide faster and more prolonged inhibition of platelet aggregation than the oral P2Y12 inhibitors.
But there has been no head-to-head comparative data for the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat) and the P2Y12 inhibitor cangrelor (Kengreal) in the setting of primary PCI for STEMI. This was the impetus for FABOLUS FASTER, the first study to compare the pharmacodynamic effects of the two parenteral antiplatelet agents. The trial also looked at how these potent parenteral drugs, compared with chewed prasugrel, another previously unexamined yet highly practical issue.
The three-center, multinational, open-label FABOLUS FASTER trial randomized 122 patients undergoing primary PCI for STEMI to one of three arms: a standard intravenous bolus and 2-hour infusion of either the P2Y12 inhibitor cangrelor (Kengreal) or the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat), followed in either case by 60 mg of oral prasugrel, or a third arm in which patients didn’t receive either drug but were instead randomized to a 60-mg loading dose of chewed or whole prasugrel tablets.
The primary study endpoint was inhibition of platelet aggregation at 30 minutes as measured by light transmittance aggregometry in response to 20 mcmol/L of adenosine diphosphate (ADP).
Tirofiban was the unequivocal winner with 95% inhibition, as compared with 34.1% with cangrelor, 10.5% with chewed prasugrel, and 6.3% with prasugrel swallowed whole, even though the concentration of prasugrel’s active metabolite was far greater at 62.3 ng/mL after prasugrel was chewed, compared with 17.1 ng/mL when swallowed in integral tablet form.
The rate of nonresponsiveness to tirofiban as defined by greater than 59% platelet aggregation was zero for tirofiban during its 2-hour infusion, then a scant 8% thereafter during repeated testing at 3 and 4-6 hours. In contrast, the cangrelor nonresponsiveness rate was 50%-58% during the 2-hour infusion, rising to 82% at 3 hours.
FABOLUS FASTER, while not powered for clinical endpoints, might nevertheless have important clinical implications, according to Dr. Valgimigli. First, the superiority of the intravenous drugs tirofiban and cangrelor over prasugrel for early, strong platelet inhibition underscores the importance of giving parenteral antiplatelet drugs over oral therapy during the acute phase of STEMI therapy. Moreover, tirofiban’s outstanding performance – and the high residual platelet reactivity associated with cangrelor – makes a strong case for large comparative, randomized trials of the two drugs, with hard clinical endpoints.
Discussant Christoph K. Naber, MD, PhD, opined that he personally doesn’t consider the FABOLUS FASTER results practice changing, for a couple of reasons.
“Platelet inhibition measured by ADP in vitro is not necessarily related to true effects in vivo. We know that platelets are activated by multiple mechanisms, and the ADP pathway is just one of them,” said Dr. Naber, an interventional cardiologist at the Wilhemshaven (Germany) Clinic.
Also, there’s a good reason why no glycoprotein IIb/IIIA inhibitors are approved for treatment of STEMI, and why tirofiban, despite its impressive antiplatelet effects, is currently largely reserved for bailout situations, such as complex lesions with large thrombus burden. It’s because tirofiban’s potent antiplatelet activity is accompanied by a high risk of bleeding, he added.
However, Dr. Valgimigli noted that this conviction about excessive bleeding risk is mainly based on older studies in which glycoprotein IIb/IIIA inhibitors were administered for prolonged duration through femoral access sites. He argued that it’s time for large clinical trials examining the risk/benefit ratio of short infusion of these agents in the contemporary practice of primary PCI for STEMI.
Simultaneously with Dr. Valgimigli’s presentation, the FABOLUS FASTER results were published online (Circulation. 2020 Jun 27; doi: 10.1161/CIRCULATIONAHA.120.046928).
Dr. Valgimigli reported that Medicure, the sponsor of the FABOLUS FASTER trial, provided an institutional research grant to conduct the study. He also disclosed receiving research grants and personal fees outside the scope of this study from a dozen pharmaceutical and medical device companies. Dr. Naber reported having no financial conflicts.
REPORTING FROM EUROPCR 2020
Endothelial injury may play a major role in COVID-19–associated coagulopathy
A striking clinical feature of illness from SARS-CoV-2 is a marked increase in thrombotic and microvascular complications, or COVID-19–associated coagulopathy (CAC).
A new study suggests endothelial cell injury plays a major role in the pathogenesis of CAC, and blood levels of soluble thrombomodulin correlate with mortality.
George Goshua, MD, of Yale University, New Haven, Conn., presented this study as a late-breaking abstract at the virtual annual congress of the European Hematology Association.
Dr. Goshua cited past research showing CAC to be highly prevalent among hospitalized patients. Venous thromboembolism was found in 17% to 69% of patients, despite thromboprophylaxis.1-4 Arterial thrombosis has been seen in 3.6% to 4.0% of patients,1-3 and autopsy findings have shown microvascular thrombosis in as many as 87% of patients.5-7
For their study, Dr. Goshua and colleagues assessed endothelial cell damage, platelet activation, and hemostatic and fibrinolytic cascade effects of CAC.
The investigators measured markers of endothelial cell injury and platelet activation, plasminogen activation inhibitor 1 (PAI-1), and coagulation factors in stable and critically ill patients hospitalized with COVID-19. In addition, the team sought to identify biomarkers of mortality in hospitalized patients.
Dr. Goshua and colleagues studied 68 adults hospitalized for suspected COVID-19 – 48 in the ICU and 20 outside the ICU. Patients in the ICU received mechanical ventilation, while the non-ICU patients required supplemental oxygen (≤3 L/min per nasal cannula).
There were more men than women (69% vs. 31%) in the ICU population but not in the non-ICU population (40% vs. 60%). There were no statistically significant differences in age or comorbid conditions between the ICU and non-ICU patients.
Results and interpretation
Consistent with augmentation of the coagulation cascade – and as expected – D-dimer and thrombin-antithrombin levels were high in both the ICU and non-ICU populations, but levels were significantly higher (P < .001) among the ICU patients.
Endogenous anticoagulants (antithrombin and proteins C and S) and fibrinolytic enzymes (alpha 2-antiplasmin) were preserved, verifying that CAC is distinct from disseminated intravascular coagulation. Classic fibrinolysis did not occur, as PAI-1 was high in ICU and non-ICU patients, and lysis-30 was normal in nearly all ICU patients (96%).
Von Willebrand factor antigen and activity levels and factor VIII levels were markedly elevated in non-ICU and ICU patients, but they were significantly higher (P < .001) in the ICU cohort. This supports the hypothesis that endothelial cell damage and platelet activation play major roles in CAC.
Similarly, soluble P-selectin, which is shed from endothelial cells and platelets, was dramatically elevated in ICU patients in comparison with controls and non-ICU patients (P < .001 for both comparisons).
Levels of soluble thrombomodulin, which is released from endothelial cells, were not significantly different in ICU patients and controls. However, given thrombomodulin’s significant role in the coagulation cascade, Dr. Goshua and colleagues plotted receiver operating curves to see if soluble thrombomodulin levels were predictive of mortality.
The results showed that soluble thrombomodulin correlated with the probability of survival, both overall and in ICU patients. Soluble thrombomodulin levels greater than 3.26 ng/mL were associated with significantly worse survival in all patients (P = .0087) and ICU patients (P = .0309).
Influence on therapy
Laboratory perturbations were detected in both ICU and non-ICU patients, and otherwise healthy outpatients have exhibited potentially life-threatening CAC, according to Dr. Goshua.
These findings suggest the prothrombotic state occurs early in the pathogenesis of SARS-CoV-2 infection, is driven by platelet activation and endotheliopathy, and becomes more pronounced with worsening severity of infection.
The results of this study prompted a change in how Yale–New Haven Hospital manages COVID-19 patients. Patients without a clinical contraindication now receive aspirin at 81 mg daily in addition to the anticoagulation regimen typically used for all hospitalized COVID-19 patients.
Investigations regarding other medications that can influence platelet-endothelial cell interactions and modulate endothelial cell damage in CAC – such as dipyridamole, defibrotide, and eculizumab – are planned.
Challenges and unanswered questions
Virchow’s triad was described by the eminent German physician, Rudolf Virchow, MD, in the 19th century. It refers to the three broad categories of factors that can predispose patients to thrombosis — circulatory stasis, hypercoagulability, and endothelial injury.
Although all of these elements could be operative in CAC, the current study suggests platelet activation and endothelial cell injury in CAC may be of primary importance.
Because of the limited ability to test critically ill patients and concerns regarding exposure of additional hospital personnel to COVID-19 patients, the current report lacked clarity about the relationship of the detected laboratory abnormalities to confirmed thrombotic events.
It is unknown whether endothelial cells in different organs are damaged uniformly. It is also unclear if the laboratory abnormalities identified in this analysis can be used to monitor response to therapy, to guide follow-up management of discharged patients with CAC, or to identify infected outpatients who should receive prophylactic anticoagulation.
The mechanism by which SARS-CoV-2 injures endothelial cells is not explained by these data. Neutrophil defensins and other prothrombotic peptides or markers of inflammation could play key roles in pathogenesis, assessment of disease severity, or monitoring for therapeutic efficacy.
Today, we have more sophisticated diagnostic tools than Dr. Virchow had. We also have the ability to record and rapidly disseminate information globally. Still, with regard to the COVID-19 pandemic, clinicians face many of the same challenges that confronted Dr. Virchow in his era.
The analysis conducted by Dr. Goshua and colleagues goes a long way toward elucidating some of the mechanisms and therapeutic targets to meet these challenges.
Dr. Goshua disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Goshua G et al. EHA Congress. Abstract LB2605.
References
1. Klok FA et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50. doi: 10.1016/j.thromres.2020.04.041.
2. Thomas W et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at a teaching hospital in the United Kingdom. Thromb Res. 2020;191:76-7. doi: 10.1016/j.thromres.2020.04.028
3. Lodigiani C et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9-14. doi: 10.1016/j.thromres.2020.04.024
4. Llitjos JF et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients [published online ahead of print, 2020 Apr 22]. J Thromb Haemost. 2020;10.1111/jth.14869. doi: 10.1111/jth.14869
5. Carsana L et al. Pulmonary post-mortem findings in a large series of COVID-19 cases from Northern Italy. medRxiv 2020.04.19.20054262; doi: 10.1101/2020.04.19.20054262v1.
6. Menter T et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction [published online ahead of print, 2020 May 4]. Histopathology. 2020;10.1111/his.14134. doi: 10.1111/his.14134
7. Lax SF, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: Results from a prospective, single-center, clinicopathologic case series [published online ahead of print, 2020 May 14]. Ann Intern Med. 2020;M20-2566. doi: 10.7326/M20-2566.
A striking clinical feature of illness from SARS-CoV-2 is a marked increase in thrombotic and microvascular complications, or COVID-19–associated coagulopathy (CAC).
A new study suggests endothelial cell injury plays a major role in the pathogenesis of CAC, and blood levels of soluble thrombomodulin correlate with mortality.
George Goshua, MD, of Yale University, New Haven, Conn., presented this study as a late-breaking abstract at the virtual annual congress of the European Hematology Association.
Dr. Goshua cited past research showing CAC to be highly prevalent among hospitalized patients. Venous thromboembolism was found in 17% to 69% of patients, despite thromboprophylaxis.1-4 Arterial thrombosis has been seen in 3.6% to 4.0% of patients,1-3 and autopsy findings have shown microvascular thrombosis in as many as 87% of patients.5-7
For their study, Dr. Goshua and colleagues assessed endothelial cell damage, platelet activation, and hemostatic and fibrinolytic cascade effects of CAC.
The investigators measured markers of endothelial cell injury and platelet activation, plasminogen activation inhibitor 1 (PAI-1), and coagulation factors in stable and critically ill patients hospitalized with COVID-19. In addition, the team sought to identify biomarkers of mortality in hospitalized patients.
Dr. Goshua and colleagues studied 68 adults hospitalized for suspected COVID-19 – 48 in the ICU and 20 outside the ICU. Patients in the ICU received mechanical ventilation, while the non-ICU patients required supplemental oxygen (≤3 L/min per nasal cannula).
There were more men than women (69% vs. 31%) in the ICU population but not in the non-ICU population (40% vs. 60%). There were no statistically significant differences in age or comorbid conditions between the ICU and non-ICU patients.
Results and interpretation
Consistent with augmentation of the coagulation cascade – and as expected – D-dimer and thrombin-antithrombin levels were high in both the ICU and non-ICU populations, but levels were significantly higher (P < .001) among the ICU patients.
Endogenous anticoagulants (antithrombin and proteins C and S) and fibrinolytic enzymes (alpha 2-antiplasmin) were preserved, verifying that CAC is distinct from disseminated intravascular coagulation. Classic fibrinolysis did not occur, as PAI-1 was high in ICU and non-ICU patients, and lysis-30 was normal in nearly all ICU patients (96%).
Von Willebrand factor antigen and activity levels and factor VIII levels were markedly elevated in non-ICU and ICU patients, but they were significantly higher (P < .001) in the ICU cohort. This supports the hypothesis that endothelial cell damage and platelet activation play major roles in CAC.
Similarly, soluble P-selectin, which is shed from endothelial cells and platelets, was dramatically elevated in ICU patients in comparison with controls and non-ICU patients (P < .001 for both comparisons).
Levels of soluble thrombomodulin, which is released from endothelial cells, were not significantly different in ICU patients and controls. However, given thrombomodulin’s significant role in the coagulation cascade, Dr. Goshua and colleagues plotted receiver operating curves to see if soluble thrombomodulin levels were predictive of mortality.
The results showed that soluble thrombomodulin correlated with the probability of survival, both overall and in ICU patients. Soluble thrombomodulin levels greater than 3.26 ng/mL were associated with significantly worse survival in all patients (P = .0087) and ICU patients (P = .0309).
Influence on therapy
Laboratory perturbations were detected in both ICU and non-ICU patients, and otherwise healthy outpatients have exhibited potentially life-threatening CAC, according to Dr. Goshua.
These findings suggest the prothrombotic state occurs early in the pathogenesis of SARS-CoV-2 infection, is driven by platelet activation and endotheliopathy, and becomes more pronounced with worsening severity of infection.
The results of this study prompted a change in how Yale–New Haven Hospital manages COVID-19 patients. Patients without a clinical contraindication now receive aspirin at 81 mg daily in addition to the anticoagulation regimen typically used for all hospitalized COVID-19 patients.
Investigations regarding other medications that can influence platelet-endothelial cell interactions and modulate endothelial cell damage in CAC – such as dipyridamole, defibrotide, and eculizumab – are planned.
Challenges and unanswered questions
Virchow’s triad was described by the eminent German physician, Rudolf Virchow, MD, in the 19th century. It refers to the three broad categories of factors that can predispose patients to thrombosis — circulatory stasis, hypercoagulability, and endothelial injury.
Although all of these elements could be operative in CAC, the current study suggests platelet activation and endothelial cell injury in CAC may be of primary importance.
Because of the limited ability to test critically ill patients and concerns regarding exposure of additional hospital personnel to COVID-19 patients, the current report lacked clarity about the relationship of the detected laboratory abnormalities to confirmed thrombotic events.
It is unknown whether endothelial cells in different organs are damaged uniformly. It is also unclear if the laboratory abnormalities identified in this analysis can be used to monitor response to therapy, to guide follow-up management of discharged patients with CAC, or to identify infected outpatients who should receive prophylactic anticoagulation.
The mechanism by which SARS-CoV-2 injures endothelial cells is not explained by these data. Neutrophil defensins and other prothrombotic peptides or markers of inflammation could play key roles in pathogenesis, assessment of disease severity, or monitoring for therapeutic efficacy.
Today, we have more sophisticated diagnostic tools than Dr. Virchow had. We also have the ability to record and rapidly disseminate information globally. Still, with regard to the COVID-19 pandemic, clinicians face many of the same challenges that confronted Dr. Virchow in his era.
The analysis conducted by Dr. Goshua and colleagues goes a long way toward elucidating some of the mechanisms and therapeutic targets to meet these challenges.
Dr. Goshua disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Goshua G et al. EHA Congress. Abstract LB2605.
References
1. Klok FA et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50. doi: 10.1016/j.thromres.2020.04.041.
2. Thomas W et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at a teaching hospital in the United Kingdom. Thromb Res. 2020;191:76-7. doi: 10.1016/j.thromres.2020.04.028
3. Lodigiani C et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9-14. doi: 10.1016/j.thromres.2020.04.024
4. Llitjos JF et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients [published online ahead of print, 2020 Apr 22]. J Thromb Haemost. 2020;10.1111/jth.14869. doi: 10.1111/jth.14869
5. Carsana L et al. Pulmonary post-mortem findings in a large series of COVID-19 cases from Northern Italy. medRxiv 2020.04.19.20054262; doi: 10.1101/2020.04.19.20054262v1.
6. Menter T et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction [published online ahead of print, 2020 May 4]. Histopathology. 2020;10.1111/his.14134. doi: 10.1111/his.14134
7. Lax SF, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: Results from a prospective, single-center, clinicopathologic case series [published online ahead of print, 2020 May 14]. Ann Intern Med. 2020;M20-2566. doi: 10.7326/M20-2566.
A striking clinical feature of illness from SARS-CoV-2 is a marked increase in thrombotic and microvascular complications, or COVID-19–associated coagulopathy (CAC).
A new study suggests endothelial cell injury plays a major role in the pathogenesis of CAC, and blood levels of soluble thrombomodulin correlate with mortality.
George Goshua, MD, of Yale University, New Haven, Conn., presented this study as a late-breaking abstract at the virtual annual congress of the European Hematology Association.
Dr. Goshua cited past research showing CAC to be highly prevalent among hospitalized patients. Venous thromboembolism was found in 17% to 69% of patients, despite thromboprophylaxis.1-4 Arterial thrombosis has been seen in 3.6% to 4.0% of patients,1-3 and autopsy findings have shown microvascular thrombosis in as many as 87% of patients.5-7
For their study, Dr. Goshua and colleagues assessed endothelial cell damage, platelet activation, and hemostatic and fibrinolytic cascade effects of CAC.
The investigators measured markers of endothelial cell injury and platelet activation, plasminogen activation inhibitor 1 (PAI-1), and coagulation factors in stable and critically ill patients hospitalized with COVID-19. In addition, the team sought to identify biomarkers of mortality in hospitalized patients.
Dr. Goshua and colleagues studied 68 adults hospitalized for suspected COVID-19 – 48 in the ICU and 20 outside the ICU. Patients in the ICU received mechanical ventilation, while the non-ICU patients required supplemental oxygen (≤3 L/min per nasal cannula).
There were more men than women (69% vs. 31%) in the ICU population but not in the non-ICU population (40% vs. 60%). There were no statistically significant differences in age or comorbid conditions between the ICU and non-ICU patients.
Results and interpretation
Consistent with augmentation of the coagulation cascade – and as expected – D-dimer and thrombin-antithrombin levels were high in both the ICU and non-ICU populations, but levels were significantly higher (P < .001) among the ICU patients.
Endogenous anticoagulants (antithrombin and proteins C and S) and fibrinolytic enzymes (alpha 2-antiplasmin) were preserved, verifying that CAC is distinct from disseminated intravascular coagulation. Classic fibrinolysis did not occur, as PAI-1 was high in ICU and non-ICU patients, and lysis-30 was normal in nearly all ICU patients (96%).
Von Willebrand factor antigen and activity levels and factor VIII levels were markedly elevated in non-ICU and ICU patients, but they were significantly higher (P < .001) in the ICU cohort. This supports the hypothesis that endothelial cell damage and platelet activation play major roles in CAC.
Similarly, soluble P-selectin, which is shed from endothelial cells and platelets, was dramatically elevated in ICU patients in comparison with controls and non-ICU patients (P < .001 for both comparisons).
Levels of soluble thrombomodulin, which is released from endothelial cells, were not significantly different in ICU patients and controls. However, given thrombomodulin’s significant role in the coagulation cascade, Dr. Goshua and colleagues plotted receiver operating curves to see if soluble thrombomodulin levels were predictive of mortality.
The results showed that soluble thrombomodulin correlated with the probability of survival, both overall and in ICU patients. Soluble thrombomodulin levels greater than 3.26 ng/mL were associated with significantly worse survival in all patients (P = .0087) and ICU patients (P = .0309).
Influence on therapy
Laboratory perturbations were detected in both ICU and non-ICU patients, and otherwise healthy outpatients have exhibited potentially life-threatening CAC, according to Dr. Goshua.
These findings suggest the prothrombotic state occurs early in the pathogenesis of SARS-CoV-2 infection, is driven by platelet activation and endotheliopathy, and becomes more pronounced with worsening severity of infection.
The results of this study prompted a change in how Yale–New Haven Hospital manages COVID-19 patients. Patients without a clinical contraindication now receive aspirin at 81 mg daily in addition to the anticoagulation regimen typically used for all hospitalized COVID-19 patients.
Investigations regarding other medications that can influence platelet-endothelial cell interactions and modulate endothelial cell damage in CAC – such as dipyridamole, defibrotide, and eculizumab – are planned.
Challenges and unanswered questions
Virchow’s triad was described by the eminent German physician, Rudolf Virchow, MD, in the 19th century. It refers to the three broad categories of factors that can predispose patients to thrombosis — circulatory stasis, hypercoagulability, and endothelial injury.
Although all of these elements could be operative in CAC, the current study suggests platelet activation and endothelial cell injury in CAC may be of primary importance.
Because of the limited ability to test critically ill patients and concerns regarding exposure of additional hospital personnel to COVID-19 patients, the current report lacked clarity about the relationship of the detected laboratory abnormalities to confirmed thrombotic events.
It is unknown whether endothelial cells in different organs are damaged uniformly. It is also unclear if the laboratory abnormalities identified in this analysis can be used to monitor response to therapy, to guide follow-up management of discharged patients with CAC, or to identify infected outpatients who should receive prophylactic anticoagulation.
The mechanism by which SARS-CoV-2 injures endothelial cells is not explained by these data. Neutrophil defensins and other prothrombotic peptides or markers of inflammation could play key roles in pathogenesis, assessment of disease severity, or monitoring for therapeutic efficacy.
Today, we have more sophisticated diagnostic tools than Dr. Virchow had. We also have the ability to record and rapidly disseminate information globally. Still, with regard to the COVID-19 pandemic, clinicians face many of the same challenges that confronted Dr. Virchow in his era.
The analysis conducted by Dr. Goshua and colleagues goes a long way toward elucidating some of the mechanisms and therapeutic targets to meet these challenges.
Dr. Goshua disclosed no conflicts of interest.
Dr. Lyss was a community-based medical oncologist and clinical researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
SOURCE: Goshua G et al. EHA Congress. Abstract LB2605.
References
1. Klok FA et al. Confirmation of the high cumulative incidence of thrombotic complications in critically ill ICU patients with COVID-19: An updated analysis. Thromb Res. 2020;191:148-50. doi: 10.1016/j.thromres.2020.04.041.
2. Thomas W et al. Thrombotic complications of patients admitted to intensive care with COVID-19 at a teaching hospital in the United Kingdom. Thromb Res. 2020;191:76-7. doi: 10.1016/j.thromres.2020.04.028
3. Lodigiani C et al. Venous and arterial thromboembolic complications in COVID-19 patients admitted to an academic hospital in Milan, Italy. Thromb Res. 2020;191:9-14. doi: 10.1016/j.thromres.2020.04.024
4. Llitjos JF et al. High incidence of venous thromboembolic events in anticoagulated severe COVID-19 patients [published online ahead of print, 2020 Apr 22]. J Thromb Haemost. 2020;10.1111/jth.14869. doi: 10.1111/jth.14869
5. Carsana L et al. Pulmonary post-mortem findings in a large series of COVID-19 cases from Northern Italy. medRxiv 2020.04.19.20054262; doi: 10.1101/2020.04.19.20054262v1.
6. Menter T et al. Post-mortem examination of COVID19 patients reveals diffuse alveolar damage with severe capillary congestion and variegated findings of lungs and other organs suggesting vascular dysfunction [published online ahead of print, 2020 May 4]. Histopathology. 2020;10.1111/his.14134. doi: 10.1111/his.14134
7. Lax SF, et al. Pulmonary arterial thrombosis in COVID-19 with fatal outcome: Results from a prospective, single-center, clinicopathologic case series [published online ahead of print, 2020 May 14]. Ann Intern Med. 2020;M20-2566. doi: 10.7326/M20-2566.
FROM EHA CONGRESS
LAA Closure noninferior to DOACs to prevent AF-related events
Left atrial appendage closure was noninferior to use of direct oral anticoagulants for the prevention of atrial fibrillation (AFib)–related events in high-risk patients, based on data from 402 adults.
Given the limitations of vitamin K antagonists for preventing stroke in AFib, “a novel site-specific therapeutic alternative, mechanical left atrial appendage occlusion [LAAO], entered clinical practice,” but has not been compared with current safe and effective oral anticoagulants, wrote Pavel Osmancik, MD, of University Hospital Kralovske Vinohrady, Prague, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers randomized 201 moderate- or high-risk adults with nonvalvular AFib to LAAO and another 201 to direct oral anticoagulants (DOAC).
Patients in the LAAO group underwent transesophageal echocardiography to exclude left atrial thrombi and underwent implantation with Boston Scientific’s Watchman, Watchman-FLX, or Abbott’s Amulet devices. Patients in the DOAC group received rivaroxaban, apixaban, or dabigatran at the manufacturer-recommended dose.
The primary outcome was a composite of complications related to procedures or devices, thromboembolic events (including stroke), and clinically significant bleeding. After an average of 20 months follow-up, 35 patients in the LAAO group and 41 in the DOAC group met the primary outcome (11% per 100 patient-years vs. 13% per 100 patient-years).
In addition, no differences appeared between the groups for the endpoint components of all-stroke/transient ischemic attack event (subdistribution hazard ratio, 1.00), clinically significantly bleeding (sHR, 0.81), or cardiovascular death (sHR, 0.75).
Nine patients experienced major complications related to LAAO, including clinically significant bleeding (sHR, 0.81; 95% CI, 0.44-1.52) and cardiovascular death (sHR, 0.75; 95% CI, 0.34-1.62). Major LAAO-related complications occurred in nine (4.5%) patients, with a short-term (up to 7 days or hospital discharge) complication rate of 2.1% and a 2.7% late complication rate. The late complications included three pericardial effusions, one of which resulted in death, the researchers wrote.
The study findings were limited by several factors, including the inability to assess the differences among the components of the composite primary endpoint. For example, “Regarding the primary endpoint, stroke reduction may be more important than bleeding reduction,” the investigators wrote.
The results were strengthened, however, by the enrollment of a high-risk AF population and is the first known randomized trial to compare percutaneous LAAO and DOACs for stroke prevention in this group. But the late complication rate of 2.7% is “suboptimal” and safety issues reinforce the need for refinement of operator technique and device technology with LAAO, they concluded.
‘Important step forward,’ with caveats
“How LAAO might stack up against DOAC therapy has remained an open question: Compared with warfarin, DOACs are easier to use and are associated with a reduction in mortality, driven by a substantially lower risk of intracranial hemorrhage and fatal bleeding,” wrote Matthew J. Price, MD, of the Scripps Clinic in La Jolla, Calif., and Jacqueline Saw, MD, of Vancouver General Hospital, in an accompanying editorial.
Previous studies of LAAO have shown a reduced risk of gastrointestinal bleeding, but procedure hazards interfered with long-term benefits, they said. The current study findings of similar rates of stroke and lower bleeding rates with LAAO, compared with DOAC, “are provocative given the clinical consensus that DOACs are safer, well tolerated, and generally better than warfarin, which was an easy target for transcatheter LAAO, given warfarin’s extensive limitations,” the editorialists wrote. Although the findings lend support to the use of LAAO, clinicians should consider several caveats such as the inclusion of patients who were “not optimal candidates for long-term OAC but were selected because they were at high risk for bleeding or because OAC treatment had already failed.”
However, “despite its imperfections, PRAGUE-17 is an important step forward and reinforces the role of transcatheter LAAO as a stroke-prevention strategy for patients with [AFib] at high risk of bleeding or medical treatment failure, even in the modern era of the DOACs,” they concluded. “Going forward, successful enrollment in ongoing and planned clinical trials while avoiding off-label procedures will be critical to define the appropriate use of transcatheter LAAO in expanded patient populations.”
The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot. Dr. Price’s financial disclosures included honoraria, speaker bureau fees, and/or research grants from Abbott Vascular, AstraZeneca, Boston Scientific, Chiesi USA, Daiichi Sankyo, and Medtronic. Dr. Saw disclosed receiving unrestricted research grant support several Canadian research institutes and fees and honoraria from AstraZeneca, Abbott Vascular, Boston Scientific, and Servier, among other drug companies.
SOURCES: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
Left atrial appendage closure was noninferior to use of direct oral anticoagulants for the prevention of atrial fibrillation (AFib)–related events in high-risk patients, based on data from 402 adults.
Given the limitations of vitamin K antagonists for preventing stroke in AFib, “a novel site-specific therapeutic alternative, mechanical left atrial appendage occlusion [LAAO], entered clinical practice,” but has not been compared with current safe and effective oral anticoagulants, wrote Pavel Osmancik, MD, of University Hospital Kralovske Vinohrady, Prague, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers randomized 201 moderate- or high-risk adults with nonvalvular AFib to LAAO and another 201 to direct oral anticoagulants (DOAC).
Patients in the LAAO group underwent transesophageal echocardiography to exclude left atrial thrombi and underwent implantation with Boston Scientific’s Watchman, Watchman-FLX, or Abbott’s Amulet devices. Patients in the DOAC group received rivaroxaban, apixaban, or dabigatran at the manufacturer-recommended dose.
The primary outcome was a composite of complications related to procedures or devices, thromboembolic events (including stroke), and clinically significant bleeding. After an average of 20 months follow-up, 35 patients in the LAAO group and 41 in the DOAC group met the primary outcome (11% per 100 patient-years vs. 13% per 100 patient-years).
In addition, no differences appeared between the groups for the endpoint components of all-stroke/transient ischemic attack event (subdistribution hazard ratio, 1.00), clinically significantly bleeding (sHR, 0.81), or cardiovascular death (sHR, 0.75).
Nine patients experienced major complications related to LAAO, including clinically significant bleeding (sHR, 0.81; 95% CI, 0.44-1.52) and cardiovascular death (sHR, 0.75; 95% CI, 0.34-1.62). Major LAAO-related complications occurred in nine (4.5%) patients, with a short-term (up to 7 days or hospital discharge) complication rate of 2.1% and a 2.7% late complication rate. The late complications included three pericardial effusions, one of which resulted in death, the researchers wrote.
The study findings were limited by several factors, including the inability to assess the differences among the components of the composite primary endpoint. For example, “Regarding the primary endpoint, stroke reduction may be more important than bleeding reduction,” the investigators wrote.
The results were strengthened, however, by the enrollment of a high-risk AF population and is the first known randomized trial to compare percutaneous LAAO and DOACs for stroke prevention in this group. But the late complication rate of 2.7% is “suboptimal” and safety issues reinforce the need for refinement of operator technique and device technology with LAAO, they concluded.
‘Important step forward,’ with caveats
“How LAAO might stack up against DOAC therapy has remained an open question: Compared with warfarin, DOACs are easier to use and are associated with a reduction in mortality, driven by a substantially lower risk of intracranial hemorrhage and fatal bleeding,” wrote Matthew J. Price, MD, of the Scripps Clinic in La Jolla, Calif., and Jacqueline Saw, MD, of Vancouver General Hospital, in an accompanying editorial.
Previous studies of LAAO have shown a reduced risk of gastrointestinal bleeding, but procedure hazards interfered with long-term benefits, they said. The current study findings of similar rates of stroke and lower bleeding rates with LAAO, compared with DOAC, “are provocative given the clinical consensus that DOACs are safer, well tolerated, and generally better than warfarin, which was an easy target for transcatheter LAAO, given warfarin’s extensive limitations,” the editorialists wrote. Although the findings lend support to the use of LAAO, clinicians should consider several caveats such as the inclusion of patients who were “not optimal candidates for long-term OAC but were selected because they were at high risk for bleeding or because OAC treatment had already failed.”
However, “despite its imperfections, PRAGUE-17 is an important step forward and reinforces the role of transcatheter LAAO as a stroke-prevention strategy for patients with [AFib] at high risk of bleeding or medical treatment failure, even in the modern era of the DOACs,” they concluded. “Going forward, successful enrollment in ongoing and planned clinical trials while avoiding off-label procedures will be critical to define the appropriate use of transcatheter LAAO in expanded patient populations.”
The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot. Dr. Price’s financial disclosures included honoraria, speaker bureau fees, and/or research grants from Abbott Vascular, AstraZeneca, Boston Scientific, Chiesi USA, Daiichi Sankyo, and Medtronic. Dr. Saw disclosed receiving unrestricted research grant support several Canadian research institutes and fees and honoraria from AstraZeneca, Abbott Vascular, Boston Scientific, and Servier, among other drug companies.
SOURCES: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
Left atrial appendage closure was noninferior to use of direct oral anticoagulants for the prevention of atrial fibrillation (AFib)–related events in high-risk patients, based on data from 402 adults.
Given the limitations of vitamin K antagonists for preventing stroke in AFib, “a novel site-specific therapeutic alternative, mechanical left atrial appendage occlusion [LAAO], entered clinical practice,” but has not been compared with current safe and effective oral anticoagulants, wrote Pavel Osmancik, MD, of University Hospital Kralovske Vinohrady, Prague, and colleagues.
In a study published in the Journal of the American College of Cardiology, the researchers randomized 201 moderate- or high-risk adults with nonvalvular AFib to LAAO and another 201 to direct oral anticoagulants (DOAC).
Patients in the LAAO group underwent transesophageal echocardiography to exclude left atrial thrombi and underwent implantation with Boston Scientific’s Watchman, Watchman-FLX, or Abbott’s Amulet devices. Patients in the DOAC group received rivaroxaban, apixaban, or dabigatran at the manufacturer-recommended dose.
The primary outcome was a composite of complications related to procedures or devices, thromboembolic events (including stroke), and clinically significant bleeding. After an average of 20 months follow-up, 35 patients in the LAAO group and 41 in the DOAC group met the primary outcome (11% per 100 patient-years vs. 13% per 100 patient-years).
In addition, no differences appeared between the groups for the endpoint components of all-stroke/transient ischemic attack event (subdistribution hazard ratio, 1.00), clinically significantly bleeding (sHR, 0.81), or cardiovascular death (sHR, 0.75).
Nine patients experienced major complications related to LAAO, including clinically significant bleeding (sHR, 0.81; 95% CI, 0.44-1.52) and cardiovascular death (sHR, 0.75; 95% CI, 0.34-1.62). Major LAAO-related complications occurred in nine (4.5%) patients, with a short-term (up to 7 days or hospital discharge) complication rate of 2.1% and a 2.7% late complication rate. The late complications included three pericardial effusions, one of which resulted in death, the researchers wrote.
The study findings were limited by several factors, including the inability to assess the differences among the components of the composite primary endpoint. For example, “Regarding the primary endpoint, stroke reduction may be more important than bleeding reduction,” the investigators wrote.
The results were strengthened, however, by the enrollment of a high-risk AF population and is the first known randomized trial to compare percutaneous LAAO and DOACs for stroke prevention in this group. But the late complication rate of 2.7% is “suboptimal” and safety issues reinforce the need for refinement of operator technique and device technology with LAAO, they concluded.
‘Important step forward,’ with caveats
“How LAAO might stack up against DOAC therapy has remained an open question: Compared with warfarin, DOACs are easier to use and are associated with a reduction in mortality, driven by a substantially lower risk of intracranial hemorrhage and fatal bleeding,” wrote Matthew J. Price, MD, of the Scripps Clinic in La Jolla, Calif., and Jacqueline Saw, MD, of Vancouver General Hospital, in an accompanying editorial.
Previous studies of LAAO have shown a reduced risk of gastrointestinal bleeding, but procedure hazards interfered with long-term benefits, they said. The current study findings of similar rates of stroke and lower bleeding rates with LAAO, compared with DOAC, “are provocative given the clinical consensus that DOACs are safer, well tolerated, and generally better than warfarin, which was an easy target for transcatheter LAAO, given warfarin’s extensive limitations,” the editorialists wrote. Although the findings lend support to the use of LAAO, clinicians should consider several caveats such as the inclusion of patients who were “not optimal candidates for long-term OAC but were selected because they were at high risk for bleeding or because OAC treatment had already failed.”
However, “despite its imperfections, PRAGUE-17 is an important step forward and reinforces the role of transcatheter LAAO as a stroke-prevention strategy for patients with [AFib] at high risk of bleeding or medical treatment failure, even in the modern era of the DOACs,” they concluded. “Going forward, successful enrollment in ongoing and planned clinical trials while avoiding off-label procedures will be critical to define the appropriate use of transcatheter LAAO in expanded patient populations.”
The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot. Dr. Price’s financial disclosures included honoraria, speaker bureau fees, and/or research grants from Abbott Vascular, AstraZeneca, Boston Scientific, Chiesi USA, Daiichi Sankyo, and Medtronic. Dr. Saw disclosed receiving unrestricted research grant support several Canadian research institutes and fees and honoraria from AstraZeneca, Abbott Vascular, Boston Scientific, and Servier, among other drug companies.
SOURCES: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point:
Major finding: A composite primary outcome including stroke and death was not significantly different in high-risk patients randomized to left atrial appendage occlusion or direct oral anticoagulants at roughly 20 months’ follow-up (11% vs. 13%, respectively).
Study details: The data come from the PRAGUE-17 study, a randomized trial of 402 adults at increased risk for atrial fibrillation.
Disclosures: The study was supported by the Ministry of Health of the Czech Republic. Dr. Osmancik disclosed speaking honoraria from Bayer and Abbot.
Sources: Osmancik P et al. J Am Coll Cardiol. 2020;75:3122-35; Price MJ, Saw J. J Am Coll Cardiol. 2020;75:3136-9.











