User login
Adolescent immunizations and protecting our children from COVID-19
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
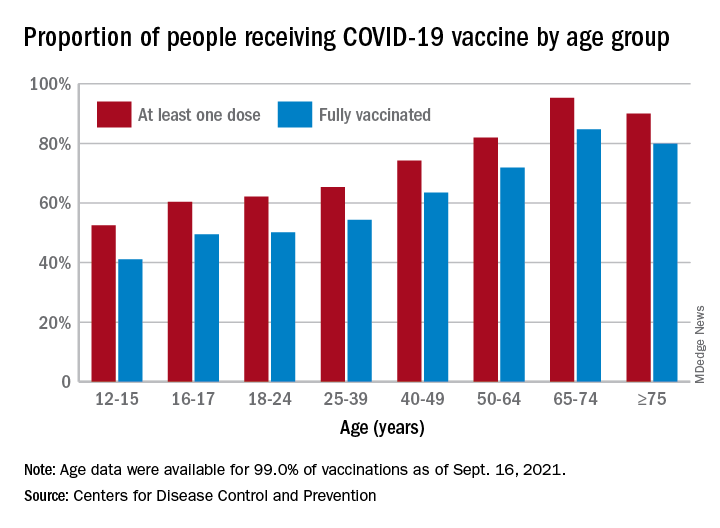
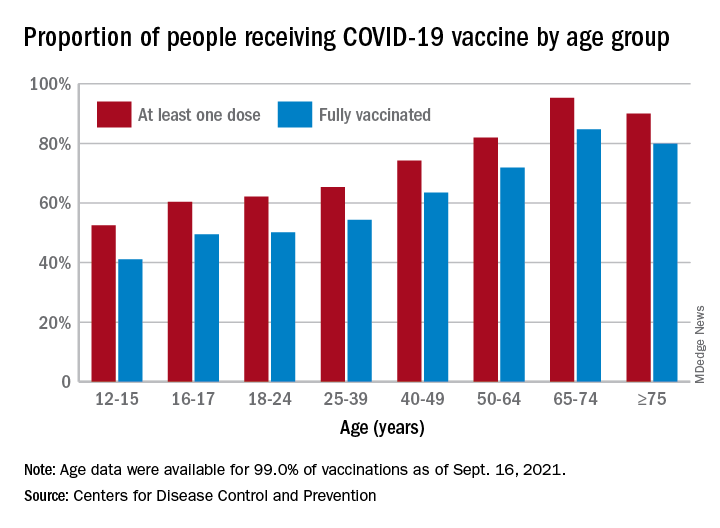
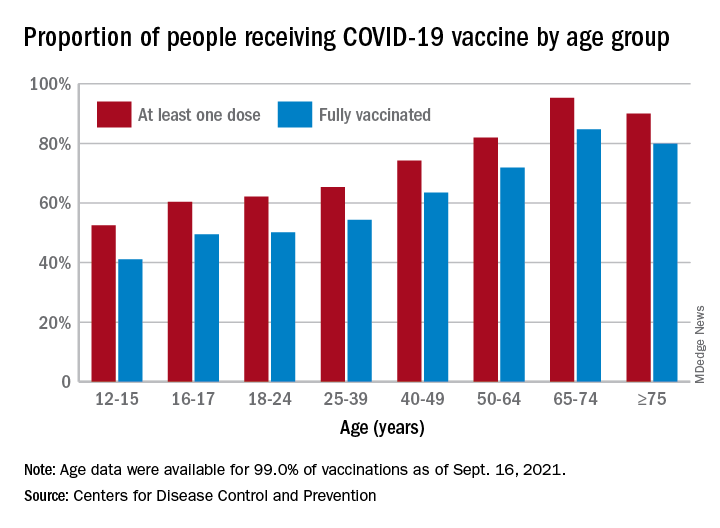
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)
It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)
It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
I began thinking of a topic for this column weeks ago determined to discuss anything except COVID-19. Yet, news reports from all sources blasted daily reminders of rising COVID-19 cases overall and specifically in children.
In August, school resumed for many of our patients and the battle over mandating masks for school attendance was in full swing. The fact that it is a Centers for Disease Control and Prevention recommendation supported by both the American Academy of Pediatrics and the Pediatric Infectious Disease Society fell on deaf ears. One day, I heard a report that over 25,000 students attending Texas public schools were diagnosed with COVID-19 between Aug. 23 and Aug. 29. This peak in activity occurred just 2 weeks after the start of school and led to the closure of 45 school districts. Texas does not have a monopoly on these rising cases. Delta, a more contagious variant, began circulating in June 2021 and by July it was the most predominant. Emergency department visits and hospitalizations have increased nationwide. During the latter 2 weeks of August 2021, COVID-19–related ED visits and hospitalizations for persons aged 0-17 years were 3.4 and 3.7 times higher in states with the lowest vaccination coverage, compared with states with high vaccination coverage (MMWR Morb Mortal Wkly Rep. 2021;70:1249-54). Specifically, the rates of hospitalization the week ending Aug. 14, 2021, were nearly 5 times the rates for the week ending June 26, 2021, for 0- to 17-year-olds and nearly 10 times the rates for children 0-4 years of age. Hospitalization rates were 10.1 times higher for unimmunized adolescents than for fully vaccinated ones (MMWR Morb Mortal Wkly Rep. 2021;70:1255-60).
Multiple elected state leaders have opposed interventions such as mandating masks in school, and our children are paying for it. These leaders have relinquished their responsibility to local school boards. Several have reinforced the no-mask mandate while others have had the courage and insight to ignore state government leaders and have established mask mandates.
How is this lack of enforcement of national recommendations affecting our patients? Let’s look at two neighboring school districts in Texas. School districts have COVID-19 dashboards that are updated daily and accessible to the general public. School District A requires masks for school entry. It serves 196,171 students and has 27,195 teachers and staff. Since school opened in August, 1,606 cumulative cases of COVID-19 in students (0.8%) and 282 in staff (1%) have been reported. Fifty-five percent of the student cases occurred in elementary schools. In contrast, School District B located in the adjacent county serves 64,517 students and has 3,906 teachers and staff with no mask mandate. Since August, there have been 4,506 cumulative COVID-19 cases in students (6.9%) and 578 (14.7%) in staff. Information regarding the specific school type was not provided; however, the dashboard indicates that 2,924 cases (64.8%) occurred in children younger than 11 years of age. County data indicate 62% of those older than 12 years of age were fully vaccinated in District A, compared with 54% of persons older than 12 years in District B. The county COVID-19 positivity rate in District A is 17.6% and in District B it is 20%. Both counties are experiencing increased COVID-19 activity yet have had strikingly different outcomes in the student/staff population. While supporting the case for wearing masks to prevent disease transmission, one can’t ignore the adolescents who were infected and vaccine eligible (District A: 706; District B: 1,582). Their vaccination status could not be determined.
As pediatricians we have played an integral part in the elimination of diseases through educating and administering vaccinations. Adolescents are relatively healthy, thus limiting the number of encounters with them. The majority complete the 11-year visit; however, many fail to return for the 16- to 18-year visit.
So how are we doing? CDC data from 10 U.S. jurisdictions demonstrated a substantial decrease in vaccine administration between March and May of 2020, compared with the same period in 2018 and 2019. A decline was anticipated because of the nationwide lockdown. Doses of HPV administered declined almost 64% and 71% for 9- to 12-year-olds and 13- to 17-year-olds, respectively. Tdap administration declined 66% and 61% for the same respective age groups. Although administered doses increased between June and September of 2020, it was not sufficient to achieve catch-up coverage. Compared to the same period in 2018-2019, administration of the HPV vaccine declined 12.8% and 28% (ages 9-12 and ages 13-17) and for Tdap it was 21% and 30% lower (ages 9-12 and ages 13-17) (MMWR Morb Mortal Wkly Rep. 2021;70:840-5).
Now, we have another adolescent vaccine to discuss and encourage our patients to receive. We also need to address their concerns and/or to at least direct them to a reliable source to obtain accurate information. For the first time, a recommended vaccine may not be available at their medical home. Many don’t know where to go to receive it (http://www.vaccines.gov). Results of a Kaiser Family Foundation COVID-19 survey (August 2021) indicated that parents trusted their pediatricians most often (78%) for vaccine advice. The respondents voiced concern about trusting the location where the child would be immunized and long-term effects especially related to fertility. Parents who received communications regarding the benefits of vaccination were twice as likely to have their adolescents immunized. Finally, remember: Like parent, like child. An immunized parent is more likely to immunize the adolescent. (See Fig. 1.)
It is beyond the scope of this column to discuss the psychosocial aspects of this disease: children experiencing the death of teachers, classmates, family members, and those viewing the vitriol between pro- and antimask proponents often exhibited on school premises. And let’s not forget the child who wants to wear a mask but may be ostracized or bullied for doing so.
Our job is to do our very best to advocate for and to protect our patients by promoting mandatory masks at schools and encouraging vaccination of adolescents as we patiently wait for vaccines to become available for all of our children.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Moderna vaccine more effective than Pfizer and J&J
the Centers for Disease Control and Protection has said.
“Among U.S. adults without immunocompromising conditions, vaccine effectiveness against COVID-19 hospitalization during March 11–Aug. 15, 2021, was higher for the Moderna vaccine (93%) than the Pfizer-BioNTech vaccine (88%) and the Janssen vaccine (71%),” the agency’s Morbidity and Mortality Weekly Report said. Janssen refers to the Johnson & Johnson vaccine.
The CDC said the data could help people make informed decisions.
“Understanding differences in VE [vaccine effectiveness] by vaccine product can guide individual choices and policy recommendations regarding vaccine boosters. All Food and Drug Administration–approved or authorized COVID-19 vaccines provide substantial protection against COVID-19 hospitalization,” the report said.
The study also broke down effectiveness for longer periods. Moderna came out on top again.
After 120 days, the Moderna vaccine provided 92% effectiveness against hospitalization, whereas the Pfizer vaccine’s effectiveness dropped to 77%, the CDC said. There was no similar calculation for the Johnson & Johnson vaccine.
The CDC studied 3,689 adults at 21 hospitals in 18 states who got the two-shot Pfizer or Moderna vaccine or the one-shot Johnson & Johnson vaccine between March and August.
The agency noted some factors that could have come into play.
“Differences in vaccine effectiveness between the Moderna and Pfizer-BioNTech vaccine might be due to higher mRNA content in the Moderna vaccine, differences in timing between doses (3 weeks for Pfizer-BioNTech vs. 4 weeks for Moderna), or possible differences between groups that received each vaccine that were not accounted for in the analysis,” the report said.
The CDC noted limitations in the findings. Children, immunocompromised adults, and vaccine effectiveness against COVID-19 that did not result in hospitalization were not studied.
Other studies have shown all three U.S. vaccines provide a high rate of protection against coronavirus.
A version of this article first appeared on WebMD.com.
the Centers for Disease Control and Protection has said.
“Among U.S. adults without immunocompromising conditions, vaccine effectiveness against COVID-19 hospitalization during March 11–Aug. 15, 2021, was higher for the Moderna vaccine (93%) than the Pfizer-BioNTech vaccine (88%) and the Janssen vaccine (71%),” the agency’s Morbidity and Mortality Weekly Report said. Janssen refers to the Johnson & Johnson vaccine.
The CDC said the data could help people make informed decisions.
“Understanding differences in VE [vaccine effectiveness] by vaccine product can guide individual choices and policy recommendations regarding vaccine boosters. All Food and Drug Administration–approved or authorized COVID-19 vaccines provide substantial protection against COVID-19 hospitalization,” the report said.
The study also broke down effectiveness for longer periods. Moderna came out on top again.
After 120 days, the Moderna vaccine provided 92% effectiveness against hospitalization, whereas the Pfizer vaccine’s effectiveness dropped to 77%, the CDC said. There was no similar calculation for the Johnson & Johnson vaccine.
The CDC studied 3,689 adults at 21 hospitals in 18 states who got the two-shot Pfizer or Moderna vaccine or the one-shot Johnson & Johnson vaccine between March and August.
The agency noted some factors that could have come into play.
“Differences in vaccine effectiveness between the Moderna and Pfizer-BioNTech vaccine might be due to higher mRNA content in the Moderna vaccine, differences in timing between doses (3 weeks for Pfizer-BioNTech vs. 4 weeks for Moderna), or possible differences between groups that received each vaccine that were not accounted for in the analysis,” the report said.
The CDC noted limitations in the findings. Children, immunocompromised adults, and vaccine effectiveness against COVID-19 that did not result in hospitalization were not studied.
Other studies have shown all three U.S. vaccines provide a high rate of protection against coronavirus.
A version of this article first appeared on WebMD.com.
the Centers for Disease Control and Protection has said.
“Among U.S. adults without immunocompromising conditions, vaccine effectiveness against COVID-19 hospitalization during March 11–Aug. 15, 2021, was higher for the Moderna vaccine (93%) than the Pfizer-BioNTech vaccine (88%) and the Janssen vaccine (71%),” the agency’s Morbidity and Mortality Weekly Report said. Janssen refers to the Johnson & Johnson vaccine.
The CDC said the data could help people make informed decisions.
“Understanding differences in VE [vaccine effectiveness] by vaccine product can guide individual choices and policy recommendations regarding vaccine boosters. All Food and Drug Administration–approved or authorized COVID-19 vaccines provide substantial protection against COVID-19 hospitalization,” the report said.
The study also broke down effectiveness for longer periods. Moderna came out on top again.
After 120 days, the Moderna vaccine provided 92% effectiveness against hospitalization, whereas the Pfizer vaccine’s effectiveness dropped to 77%, the CDC said. There was no similar calculation for the Johnson & Johnson vaccine.
The CDC studied 3,689 adults at 21 hospitals in 18 states who got the two-shot Pfizer or Moderna vaccine or the one-shot Johnson & Johnson vaccine between March and August.
The agency noted some factors that could have come into play.
“Differences in vaccine effectiveness between the Moderna and Pfizer-BioNTech vaccine might be due to higher mRNA content in the Moderna vaccine, differences in timing between doses (3 weeks for Pfizer-BioNTech vs. 4 weeks for Moderna), or possible differences between groups that received each vaccine that were not accounted for in the analysis,” the report said.
The CDC noted limitations in the findings. Children, immunocompromised adults, and vaccine effectiveness against COVID-19 that did not result in hospitalization were not studied.
Other studies have shown all three U.S. vaccines provide a high rate of protection against coronavirus.
A version of this article first appeared on WebMD.com.
COVID vaccine is safe, effective for children aged 5-11, Pfizer says
With record numbers of COVID-19 cases being reported in kids, Pfizer and its partner BioNTech have announced that their mRNA vaccine for COVID-19 is safe and appears to generate a protective immune response in children as young as 5.
The companies have been testing a lower dose of the vaccine -- just 10 milligrams -- in children between the ages of 5 and 11. That’s one-third the dose given to adults.
In a clinical trial that included more than 2,200 children, Pfizer says two doses of the vaccines given 3 weeks apart generated a high level of neutralizing antibodies, comparable to the level seen in older children who get a higher dose of the vaccine.
On the advice of its vaccine advisory committee, the Food and Drug Administration asked vaccine makers to include more children in these studies earlier this year.
Rather than testing whether the vaccines are preventing COVID-19 illness in children, as they did in adults, the pharmaceutical companies that make the COVID-19 vaccines are looking at the antibody levels generated by the vaccines instead. The FDA has approved the approach in hopes of speeding vaccines to children, who are now back in school full time in most parts of the United States.
With that in mind, Evan Anderson, MD, a doctor with Children’s Healthcare of Atlanta who is an investigator for the trial — and is therefore kept in the dark about its results — said it’s important to keep in mind that the company didn’t share any efficacy data today.
“We don’t know whether there were cases of COVID-19 among children that were enrolled in the study and how those compared in those who received placebo versus those that received vaccine,” he said.
The company says side effects seen in the trial are comparable to those seen in older children. The company said there were no cases of heart inflammation called myocarditis observed. Pfizer says they plan to send their data to the FDA as soon as possible.
The company says side effects seen in the trial are comparable to those seen in older children. Pfizer says they plan to send their data to the FDA as soon as possible.
“We are pleased to be able to submit data to regulatory authorities for this group of school-aged children before the start of the winter season,” Ugur Sahin, MD, CEO and co-founder of BioNTech, said in a news release. “The safety profile and immunogenicity data in children aged 5 to 11 years vaccinated at a lower dose are consistent with those we have observed with our vaccine in other older populations at a higher dose.”
When asked how soon the FDA might act on Pfizer’s application, Anderson said others had speculated about timelines of 4 to 6 weeks, but he also noted that the FDA could still exercise its authority to ask the company for more information, which could slow the process down.
“As a parent myself, I would love to see that timeline occurring quickly. However, I do want the FDA to fully review the data and ask the necessary questions,” he said. “It’s a little speculative to get too definitive with timelines.”
A version of this article first appeared on WebMD.com.
With record numbers of COVID-19 cases being reported in kids, Pfizer and its partner BioNTech have announced that their mRNA vaccine for COVID-19 is safe and appears to generate a protective immune response in children as young as 5.
The companies have been testing a lower dose of the vaccine -- just 10 milligrams -- in children between the ages of 5 and 11. That’s one-third the dose given to adults.
In a clinical trial that included more than 2,200 children, Pfizer says two doses of the vaccines given 3 weeks apart generated a high level of neutralizing antibodies, comparable to the level seen in older children who get a higher dose of the vaccine.
On the advice of its vaccine advisory committee, the Food and Drug Administration asked vaccine makers to include more children in these studies earlier this year.
Rather than testing whether the vaccines are preventing COVID-19 illness in children, as they did in adults, the pharmaceutical companies that make the COVID-19 vaccines are looking at the antibody levels generated by the vaccines instead. The FDA has approved the approach in hopes of speeding vaccines to children, who are now back in school full time in most parts of the United States.
With that in mind, Evan Anderson, MD, a doctor with Children’s Healthcare of Atlanta who is an investigator for the trial — and is therefore kept in the dark about its results — said it’s important to keep in mind that the company didn’t share any efficacy data today.
“We don’t know whether there were cases of COVID-19 among children that were enrolled in the study and how those compared in those who received placebo versus those that received vaccine,” he said.
The company says side effects seen in the trial are comparable to those seen in older children. The company said there were no cases of heart inflammation called myocarditis observed. Pfizer says they plan to send their data to the FDA as soon as possible.
The company says side effects seen in the trial are comparable to those seen in older children. Pfizer says they plan to send their data to the FDA as soon as possible.
“We are pleased to be able to submit data to regulatory authorities for this group of school-aged children before the start of the winter season,” Ugur Sahin, MD, CEO and co-founder of BioNTech, said in a news release. “The safety profile and immunogenicity data in children aged 5 to 11 years vaccinated at a lower dose are consistent with those we have observed with our vaccine in other older populations at a higher dose.”
When asked how soon the FDA might act on Pfizer’s application, Anderson said others had speculated about timelines of 4 to 6 weeks, but he also noted that the FDA could still exercise its authority to ask the company for more information, which could slow the process down.
“As a parent myself, I would love to see that timeline occurring quickly. However, I do want the FDA to fully review the data and ask the necessary questions,” he said. “It’s a little speculative to get too definitive with timelines.”
A version of this article first appeared on WebMD.com.
With record numbers of COVID-19 cases being reported in kids, Pfizer and its partner BioNTech have announced that their mRNA vaccine for COVID-19 is safe and appears to generate a protective immune response in children as young as 5.
The companies have been testing a lower dose of the vaccine -- just 10 milligrams -- in children between the ages of 5 and 11. That’s one-third the dose given to adults.
In a clinical trial that included more than 2,200 children, Pfizer says two doses of the vaccines given 3 weeks apart generated a high level of neutralizing antibodies, comparable to the level seen in older children who get a higher dose of the vaccine.
On the advice of its vaccine advisory committee, the Food and Drug Administration asked vaccine makers to include more children in these studies earlier this year.
Rather than testing whether the vaccines are preventing COVID-19 illness in children, as they did in adults, the pharmaceutical companies that make the COVID-19 vaccines are looking at the antibody levels generated by the vaccines instead. The FDA has approved the approach in hopes of speeding vaccines to children, who are now back in school full time in most parts of the United States.
With that in mind, Evan Anderson, MD, a doctor with Children’s Healthcare of Atlanta who is an investigator for the trial — and is therefore kept in the dark about its results — said it’s important to keep in mind that the company didn’t share any efficacy data today.
“We don’t know whether there were cases of COVID-19 among children that were enrolled in the study and how those compared in those who received placebo versus those that received vaccine,” he said.
The company says side effects seen in the trial are comparable to those seen in older children. The company said there were no cases of heart inflammation called myocarditis observed. Pfizer says they plan to send their data to the FDA as soon as possible.
The company says side effects seen in the trial are comparable to those seen in older children. Pfizer says they plan to send their data to the FDA as soon as possible.
“We are pleased to be able to submit data to regulatory authorities for this group of school-aged children before the start of the winter season,” Ugur Sahin, MD, CEO and co-founder of BioNTech, said in a news release. “The safety profile and immunogenicity data in children aged 5 to 11 years vaccinated at a lower dose are consistent with those we have observed with our vaccine in other older populations at a higher dose.”
When asked how soon the FDA might act on Pfizer’s application, Anderson said others had speculated about timelines of 4 to 6 weeks, but he also noted that the FDA could still exercise its authority to ask the company for more information, which could slow the process down.
“As a parent myself, I would love to see that timeline occurring quickly. However, I do want the FDA to fully review the data and ask the necessary questions,” he said. “It’s a little speculative to get too definitive with timelines.”
A version of this article first appeared on WebMD.com.
FDA panel backs Pfizer's COVID booster for 65 and older, those at high risk
An expert panel that advises the Food and Drug Administration on its regulatory decisions voted Sept. 17 against recommending third doses of Pfizer’s COVID-19 vaccine for younger Americans.
But they didn’t kill the idea of booster shots completely.
In a dramatic, last-minute pivot, the 18 members of the FDA’s Vaccines and Related Biological Products Advisory Committee unanimously voted to recommend the FDA make boosters available for seniors and others at high risk of severe outcomes from COVID-19, including health care workers.
The 16-2 vote was a rebuttal to Pfizer’s initial request. The company had asked the FDA to allow it to offer third doses to all Americans over the age of 16 at least six months after their second shot.
The company requested an amendment to the full approval the FDA granted in August. That is the typical way boosters are authorized in the U.S., but it requires a higher bar of evidence and more regulatory scrutiny than the agency had been able to give since Pfizer filed for the change just days after its vaccine was granted full approval.
The committee’s actions were also a rebuff to the Biden administration, which announced before the FDA approved them that boosters would be rolled out to the general public Sept. 20. The announcement triggered the resignations of two of the agency’s top vaccine reviewers, who both participated in the Sept. 17 meeting.
After initially voting against Pfizer’s request to amend its license, the committee then worked on the fly with FDA officials to craft a strategy that would allow third doses to be offered under an emergency use authorization (EUA).
An EUA requires a lower standard of evidence and is more specific. It will restrict third doses to a more defined population than a change to the license would. It will also require Pfizer to continue to monitor the safety of third doses as they begin to be administered.
“This should demonstrate to the public that the members of this committee are independent of the FDA and that we do, in fact, bring our voices to the table when we are asked to serve on this committee,” said Archana Chattergee, MD, a pediatric infectious disease specialist who is dean of the Chicago Medical School at Rosalind Franklin University in Illinois.
The FDA doesn’t have to follow the committee’s recommendation, but almost certainly will, though regulators said they may still make some changes.
“We are not bound at FDA by your vote, we can tweak this,” said Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the FDA. Dr. Marks participated in the meeting and helped to draft the revised proposal.
If the FDA issues the recommended EUA, a council of independent advisors to the CDC will make specific recommendations about how the third doses should be given. After the CDC director weighs in, boosters will begin rolling out to the public.
Moderna submitted data to the FDA on Sept. 1 in support of adding a booster dose to its regimen. The agency has not yet scheduled a public review of that data.
The Biden administration is prepared to administer shots as soon as they get the green light, Surgeon General Vivek Murthy, MD, said at a White House briefing earlier Sept. 17.
"This process is consistent with what we outlined in August where our goals were to stay ahead of the virus," Dr. Murthy said. "Our goal then and now is to protect the health and well-being of the public. As soon as the FDA and CDC complete their evaluations, we will be ready to move forward accordingly."
He added, "We've used this time since our August announcement to communicate and coordinate with pharmacy partners, nursing homes, states, and localities."
White House COVID-19 Response Coordinator Jeff Zients said vaccine supply is "in good shape for all Americans to get boosters as recommended."
Taking cues from Israel
In considering Pfizer’s original request, the committee overwhelmingly felt that they didn’t have enough information to say that the benefits of an additional dose of vaccine in 16- and 17-year-olds would outweigh its risk. Teens have the highest risk of rare heart inflammation after vaccination, a side effect known as myocarditis. It is not known how the vaccines are causing these cases of heart swelling. Most who have been diagnosed with the condition have recovered, though some have needed hospital care.
Pfizer didn’t include 16- and 17-year-olds in its studies of boosters, which included about 300 people between the ages of 18 and 55. The company acknowledged that gap in its data but pointed to FDA guidance that said evidence from adults could be extrapolated to teens.
“We don’t know that much about risks,” said committee member Eric Rubin, MD, who is editor-in-chief of the New England Journal of Medicine.
Much of the data on the potential benefits and harms of third Pfizer doses comes from Israel, which first began rolling out boosters to older adults in July.
In a highly anticipated presentation, Sharon Alroy-Preis, Israel’s director of public health services, joined the meeting to describe Israel’s experience with boosters.
Israel began to see a third surge of COVID-19 cases in December.
“This was after having two waves and two lockdowns,” Ms. Alroy-Preis said. By the third surge, she said, Israelis were tired.
“We decided on a lockdown, but the compliance of the public wasn’t as it was in the previous two waves,” she said.
Then the vaccine arrived. Israel started vaccinations as soon as the FDA approved it, and they quickly vaccinated a high percentage of their population, about 3 months faster than the rest of the world.
All vaccinations are reported and tracked by the Ministry of Health, so the country is able to keep close tabs on how well the shots are working.
As vaccines rolled out, cases fell dramatically. The pandemic seemed to be behind them. Delta arrived in March. By June, their cases were doubling every 10 days, despite about 80% of their most vulnerable adults being fully vaccinated, she said.
Most concerning was that about 60% of severe cases were breakthrough cases in fully vaccinated individuals.
“We had to stop and figure out, was this a Delta issue,” she said. “Or was this a waning immunity issue.”
“We had some clue that it might not be the Delta variant, at least not alone,” she said.
People who had originally been first in line for the vaccines, seniors and health care workers, were having the highest rates of breakthrough infections. People further away from their second dose were more likely to get a breakthrough infection.
Ms. Alroy-Preis said that if they had not started booster doses in July, their hospitals would have been overwhelmed. They had projected that they would have 2,000 cases in the hospital each day.
Boosters have helped to flatten the curve, though they are still seeing a significant number of infections.
Data from Israel presented at the meeting show boosters are largely safe and effective at reducing severe outcomes in seniors. Israeli experience also showed that third doses, which generate very high levels of neutralizing antibodies—the first and fastest line of the body’s immune defense - -may also slow transmission of the virus.
Key differences in the U.S.
The benefit of slowing down the explosive spread of a highly contagious virus was tantalizing, but many members noted that circumstances in Israel are very different than in the United States. Israel went into its current Delta surge already having high levels of vaccination in its population. They also relied on the Pfizer vaccine almost exclusively for their campaign.
The United States used a different mix of vaccines – Pfizer, Moderna, and Johnson & Johnson -- and doesn’t have the same high level of vaccination coverage of its population.
In the United States, transmission is mainly being driven by unvaccinated people, Dr. Rubin noted.
“That really means the primary benefit is going to be in reducing disease,” he said, “And we know the people who are going to benefit from that … and those are the kinds of people the FDA has already approved a third dose for,” he said, referring to those with underlying health conditions.
But Israel only began vaccinating younger people a few weeks ago. Most are still within a window where rare risks like myocarditis could appear, Rubin noted.
He and other members of the committee said they wished they had more information about the safety of third doses in younger adults.
“We don’t have that right now, and I don’t think I would be comfortable giving it to a 16-year-old,” he said.
At the same time, the primary benefit for third doses would be in preventing severe disease, and overall, data from the United States and other countries show that two doses of the vaccines remain highly effective at preventing hospitalization and death.
Asked why Israel began to see more severe cases in fully vaccinated people, the CDC’s Sara Oliver, MD, a disease detective with the CDC, said it was probably due to a mix of factors including the fact that Israel defines severe cases a little differently.
In the United States, a severe case is generally a person who has to be hospitalized or who has died from the infection. In Israel, a person with a severe case is someone who has an elevated respiratory rate and someone who has a blood oxygen level less than 94%. In the United States, that kind of patient wouldn’t necessarily be hospitalized.
In the end, one of the two committee members who wanted full approval for Pfizer’s third doses said he was satisfied with the outcome.
Mark Sawyer, MD, a professor of pediatrics and infectious disease at the University of California at San Diego, said he voted yes on the first question because he thought full approval was the best way to give doctors the flexibility to prescribe the shots to vulnerable individuals.
“I’m really glad we authorized a vaccine for a third dose, and I plan to go out and get my vaccine this afternoon,” Dr. Sawyer said, noting that he was at high risk as a health care provider.
This article was updated 9/19/21.
A version of this article first appeared on Medscape.com.
An expert panel that advises the Food and Drug Administration on its regulatory decisions voted Sept. 17 against recommending third doses of Pfizer’s COVID-19 vaccine for younger Americans.
But they didn’t kill the idea of booster shots completely.
In a dramatic, last-minute pivot, the 18 members of the FDA’s Vaccines and Related Biological Products Advisory Committee unanimously voted to recommend the FDA make boosters available for seniors and others at high risk of severe outcomes from COVID-19, including health care workers.
The 16-2 vote was a rebuttal to Pfizer’s initial request. The company had asked the FDA to allow it to offer third doses to all Americans over the age of 16 at least six months after their second shot.
The company requested an amendment to the full approval the FDA granted in August. That is the typical way boosters are authorized in the U.S., but it requires a higher bar of evidence and more regulatory scrutiny than the agency had been able to give since Pfizer filed for the change just days after its vaccine was granted full approval.
The committee’s actions were also a rebuff to the Biden administration, which announced before the FDA approved them that boosters would be rolled out to the general public Sept. 20. The announcement triggered the resignations of two of the agency’s top vaccine reviewers, who both participated in the Sept. 17 meeting.
After initially voting against Pfizer’s request to amend its license, the committee then worked on the fly with FDA officials to craft a strategy that would allow third doses to be offered under an emergency use authorization (EUA).
An EUA requires a lower standard of evidence and is more specific. It will restrict third doses to a more defined population than a change to the license would. It will also require Pfizer to continue to monitor the safety of third doses as they begin to be administered.
“This should demonstrate to the public that the members of this committee are independent of the FDA and that we do, in fact, bring our voices to the table when we are asked to serve on this committee,” said Archana Chattergee, MD, a pediatric infectious disease specialist who is dean of the Chicago Medical School at Rosalind Franklin University in Illinois.
The FDA doesn’t have to follow the committee’s recommendation, but almost certainly will, though regulators said they may still make some changes.
“We are not bound at FDA by your vote, we can tweak this,” said Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the FDA. Dr. Marks participated in the meeting and helped to draft the revised proposal.
If the FDA issues the recommended EUA, a council of independent advisors to the CDC will make specific recommendations about how the third doses should be given. After the CDC director weighs in, boosters will begin rolling out to the public.
Moderna submitted data to the FDA on Sept. 1 in support of adding a booster dose to its regimen. The agency has not yet scheduled a public review of that data.
The Biden administration is prepared to administer shots as soon as they get the green light, Surgeon General Vivek Murthy, MD, said at a White House briefing earlier Sept. 17.
"This process is consistent with what we outlined in August where our goals were to stay ahead of the virus," Dr. Murthy said. "Our goal then and now is to protect the health and well-being of the public. As soon as the FDA and CDC complete their evaluations, we will be ready to move forward accordingly."
He added, "We've used this time since our August announcement to communicate and coordinate with pharmacy partners, nursing homes, states, and localities."
White House COVID-19 Response Coordinator Jeff Zients said vaccine supply is "in good shape for all Americans to get boosters as recommended."
Taking cues from Israel
In considering Pfizer’s original request, the committee overwhelmingly felt that they didn’t have enough information to say that the benefits of an additional dose of vaccine in 16- and 17-year-olds would outweigh its risk. Teens have the highest risk of rare heart inflammation after vaccination, a side effect known as myocarditis. It is not known how the vaccines are causing these cases of heart swelling. Most who have been diagnosed with the condition have recovered, though some have needed hospital care.
Pfizer didn’t include 16- and 17-year-olds in its studies of boosters, which included about 300 people between the ages of 18 and 55. The company acknowledged that gap in its data but pointed to FDA guidance that said evidence from adults could be extrapolated to teens.
“We don’t know that much about risks,” said committee member Eric Rubin, MD, who is editor-in-chief of the New England Journal of Medicine.
Much of the data on the potential benefits and harms of third Pfizer doses comes from Israel, which first began rolling out boosters to older adults in July.
In a highly anticipated presentation, Sharon Alroy-Preis, Israel’s director of public health services, joined the meeting to describe Israel’s experience with boosters.
Israel began to see a third surge of COVID-19 cases in December.
“This was after having two waves and two lockdowns,” Ms. Alroy-Preis said. By the third surge, she said, Israelis were tired.
“We decided on a lockdown, but the compliance of the public wasn’t as it was in the previous two waves,” she said.
Then the vaccine arrived. Israel started vaccinations as soon as the FDA approved it, and they quickly vaccinated a high percentage of their population, about 3 months faster than the rest of the world.
All vaccinations are reported and tracked by the Ministry of Health, so the country is able to keep close tabs on how well the shots are working.
As vaccines rolled out, cases fell dramatically. The pandemic seemed to be behind them. Delta arrived in March. By June, their cases were doubling every 10 days, despite about 80% of their most vulnerable adults being fully vaccinated, she said.
Most concerning was that about 60% of severe cases were breakthrough cases in fully vaccinated individuals.
“We had to stop and figure out, was this a Delta issue,” she said. “Or was this a waning immunity issue.”
“We had some clue that it might not be the Delta variant, at least not alone,” she said.
People who had originally been first in line for the vaccines, seniors and health care workers, were having the highest rates of breakthrough infections. People further away from their second dose were more likely to get a breakthrough infection.
Ms. Alroy-Preis said that if they had not started booster doses in July, their hospitals would have been overwhelmed. They had projected that they would have 2,000 cases in the hospital each day.
Boosters have helped to flatten the curve, though they are still seeing a significant number of infections.
Data from Israel presented at the meeting show boosters are largely safe and effective at reducing severe outcomes in seniors. Israeli experience also showed that third doses, which generate very high levels of neutralizing antibodies—the first and fastest line of the body’s immune defense - -may also slow transmission of the virus.
Key differences in the U.S.
The benefit of slowing down the explosive spread of a highly contagious virus was tantalizing, but many members noted that circumstances in Israel are very different than in the United States. Israel went into its current Delta surge already having high levels of vaccination in its population. They also relied on the Pfizer vaccine almost exclusively for their campaign.
The United States used a different mix of vaccines – Pfizer, Moderna, and Johnson & Johnson -- and doesn’t have the same high level of vaccination coverage of its population.
In the United States, transmission is mainly being driven by unvaccinated people, Dr. Rubin noted.
“That really means the primary benefit is going to be in reducing disease,” he said, “And we know the people who are going to benefit from that … and those are the kinds of people the FDA has already approved a third dose for,” he said, referring to those with underlying health conditions.
But Israel only began vaccinating younger people a few weeks ago. Most are still within a window where rare risks like myocarditis could appear, Rubin noted.
He and other members of the committee said they wished they had more information about the safety of third doses in younger adults.
“We don’t have that right now, and I don’t think I would be comfortable giving it to a 16-year-old,” he said.
At the same time, the primary benefit for third doses would be in preventing severe disease, and overall, data from the United States and other countries show that two doses of the vaccines remain highly effective at preventing hospitalization and death.
Asked why Israel began to see more severe cases in fully vaccinated people, the CDC’s Sara Oliver, MD, a disease detective with the CDC, said it was probably due to a mix of factors including the fact that Israel defines severe cases a little differently.
In the United States, a severe case is generally a person who has to be hospitalized or who has died from the infection. In Israel, a person with a severe case is someone who has an elevated respiratory rate and someone who has a blood oxygen level less than 94%. In the United States, that kind of patient wouldn’t necessarily be hospitalized.
In the end, one of the two committee members who wanted full approval for Pfizer’s third doses said he was satisfied with the outcome.
Mark Sawyer, MD, a professor of pediatrics and infectious disease at the University of California at San Diego, said he voted yes on the first question because he thought full approval was the best way to give doctors the flexibility to prescribe the shots to vulnerable individuals.
“I’m really glad we authorized a vaccine for a third dose, and I plan to go out and get my vaccine this afternoon,” Dr. Sawyer said, noting that he was at high risk as a health care provider.
This article was updated 9/19/21.
A version of this article first appeared on Medscape.com.
An expert panel that advises the Food and Drug Administration on its regulatory decisions voted Sept. 17 against recommending third doses of Pfizer’s COVID-19 vaccine for younger Americans.
But they didn’t kill the idea of booster shots completely.
In a dramatic, last-minute pivot, the 18 members of the FDA’s Vaccines and Related Biological Products Advisory Committee unanimously voted to recommend the FDA make boosters available for seniors and others at high risk of severe outcomes from COVID-19, including health care workers.
The 16-2 vote was a rebuttal to Pfizer’s initial request. The company had asked the FDA to allow it to offer third doses to all Americans over the age of 16 at least six months after their second shot.
The company requested an amendment to the full approval the FDA granted in August. That is the typical way boosters are authorized in the U.S., but it requires a higher bar of evidence and more regulatory scrutiny than the agency had been able to give since Pfizer filed for the change just days after its vaccine was granted full approval.
The committee’s actions were also a rebuff to the Biden administration, which announced before the FDA approved them that boosters would be rolled out to the general public Sept. 20. The announcement triggered the resignations of two of the agency’s top vaccine reviewers, who both participated in the Sept. 17 meeting.
After initially voting against Pfizer’s request to amend its license, the committee then worked on the fly with FDA officials to craft a strategy that would allow third doses to be offered under an emergency use authorization (EUA).
An EUA requires a lower standard of evidence and is more specific. It will restrict third doses to a more defined population than a change to the license would. It will also require Pfizer to continue to monitor the safety of third doses as they begin to be administered.
“This should demonstrate to the public that the members of this committee are independent of the FDA and that we do, in fact, bring our voices to the table when we are asked to serve on this committee,” said Archana Chattergee, MD, a pediatric infectious disease specialist who is dean of the Chicago Medical School at Rosalind Franklin University in Illinois.
The FDA doesn’t have to follow the committee’s recommendation, but almost certainly will, though regulators said they may still make some changes.
“We are not bound at FDA by your vote, we can tweak this,” said Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the FDA. Dr. Marks participated in the meeting and helped to draft the revised proposal.
If the FDA issues the recommended EUA, a council of independent advisors to the CDC will make specific recommendations about how the third doses should be given. After the CDC director weighs in, boosters will begin rolling out to the public.
Moderna submitted data to the FDA on Sept. 1 in support of adding a booster dose to its regimen. The agency has not yet scheduled a public review of that data.
The Biden administration is prepared to administer shots as soon as they get the green light, Surgeon General Vivek Murthy, MD, said at a White House briefing earlier Sept. 17.
"This process is consistent with what we outlined in August where our goals were to stay ahead of the virus," Dr. Murthy said. "Our goal then and now is to protect the health and well-being of the public. As soon as the FDA and CDC complete their evaluations, we will be ready to move forward accordingly."
He added, "We've used this time since our August announcement to communicate and coordinate with pharmacy partners, nursing homes, states, and localities."
White House COVID-19 Response Coordinator Jeff Zients said vaccine supply is "in good shape for all Americans to get boosters as recommended."
Taking cues from Israel
In considering Pfizer’s original request, the committee overwhelmingly felt that they didn’t have enough information to say that the benefits of an additional dose of vaccine in 16- and 17-year-olds would outweigh its risk. Teens have the highest risk of rare heart inflammation after vaccination, a side effect known as myocarditis. It is not known how the vaccines are causing these cases of heart swelling. Most who have been diagnosed with the condition have recovered, though some have needed hospital care.
Pfizer didn’t include 16- and 17-year-olds in its studies of boosters, which included about 300 people between the ages of 18 and 55. The company acknowledged that gap in its data but pointed to FDA guidance that said evidence from adults could be extrapolated to teens.
“We don’t know that much about risks,” said committee member Eric Rubin, MD, who is editor-in-chief of the New England Journal of Medicine.
Much of the data on the potential benefits and harms of third Pfizer doses comes from Israel, which first began rolling out boosters to older adults in July.
In a highly anticipated presentation, Sharon Alroy-Preis, Israel’s director of public health services, joined the meeting to describe Israel’s experience with boosters.
Israel began to see a third surge of COVID-19 cases in December.
“This was after having two waves and two lockdowns,” Ms. Alroy-Preis said. By the third surge, she said, Israelis were tired.
“We decided on a lockdown, but the compliance of the public wasn’t as it was in the previous two waves,” she said.
Then the vaccine arrived. Israel started vaccinations as soon as the FDA approved it, and they quickly vaccinated a high percentage of their population, about 3 months faster than the rest of the world.
All vaccinations are reported and tracked by the Ministry of Health, so the country is able to keep close tabs on how well the shots are working.
As vaccines rolled out, cases fell dramatically. The pandemic seemed to be behind them. Delta arrived in March. By June, their cases were doubling every 10 days, despite about 80% of their most vulnerable adults being fully vaccinated, she said.
Most concerning was that about 60% of severe cases were breakthrough cases in fully vaccinated individuals.
“We had to stop and figure out, was this a Delta issue,” she said. “Or was this a waning immunity issue.”
“We had some clue that it might not be the Delta variant, at least not alone,” she said.
People who had originally been first in line for the vaccines, seniors and health care workers, were having the highest rates of breakthrough infections. People further away from their second dose were more likely to get a breakthrough infection.
Ms. Alroy-Preis said that if they had not started booster doses in July, their hospitals would have been overwhelmed. They had projected that they would have 2,000 cases in the hospital each day.
Boosters have helped to flatten the curve, though they are still seeing a significant number of infections.
Data from Israel presented at the meeting show boosters are largely safe and effective at reducing severe outcomes in seniors. Israeli experience also showed that third doses, which generate very high levels of neutralizing antibodies—the first and fastest line of the body’s immune defense - -may also slow transmission of the virus.
Key differences in the U.S.
The benefit of slowing down the explosive spread of a highly contagious virus was tantalizing, but many members noted that circumstances in Israel are very different than in the United States. Israel went into its current Delta surge already having high levels of vaccination in its population. They also relied on the Pfizer vaccine almost exclusively for their campaign.
The United States used a different mix of vaccines – Pfizer, Moderna, and Johnson & Johnson -- and doesn’t have the same high level of vaccination coverage of its population.
In the United States, transmission is mainly being driven by unvaccinated people, Dr. Rubin noted.
“That really means the primary benefit is going to be in reducing disease,” he said, “And we know the people who are going to benefit from that … and those are the kinds of people the FDA has already approved a third dose for,” he said, referring to those with underlying health conditions.
But Israel only began vaccinating younger people a few weeks ago. Most are still within a window where rare risks like myocarditis could appear, Rubin noted.
He and other members of the committee said they wished they had more information about the safety of third doses in younger adults.
“We don’t have that right now, and I don’t think I would be comfortable giving it to a 16-year-old,” he said.
At the same time, the primary benefit for third doses would be in preventing severe disease, and overall, data from the United States and other countries show that two doses of the vaccines remain highly effective at preventing hospitalization and death.
Asked why Israel began to see more severe cases in fully vaccinated people, the CDC’s Sara Oliver, MD, a disease detective with the CDC, said it was probably due to a mix of factors including the fact that Israel defines severe cases a little differently.
In the United States, a severe case is generally a person who has to be hospitalized or who has died from the infection. In Israel, a person with a severe case is someone who has an elevated respiratory rate and someone who has a blood oxygen level less than 94%. In the United States, that kind of patient wouldn’t necessarily be hospitalized.
In the end, one of the two committee members who wanted full approval for Pfizer’s third doses said he was satisfied with the outcome.
Mark Sawyer, MD, a professor of pediatrics and infectious disease at the University of California at San Diego, said he voted yes on the first question because he thought full approval was the best way to give doctors the flexibility to prescribe the shots to vulnerable individuals.
“I’m really glad we authorized a vaccine for a third dose, and I plan to go out and get my vaccine this afternoon,” Dr. Sawyer said, noting that he was at high risk as a health care provider.
This article was updated 9/19/21.
A version of this article first appeared on Medscape.com.
Pandemic goal deficiency disorder
In August I shared with you my observations on two opposing op-ed pieces from two major newspapers, one was in favor of masking mandates for public schools, the other against. (Masking in school: A battle of the op-eds. MDedge Pediatrics. Letters from Maine, 2021 Aug 12). Neither group of authors could offer us evidence from controlled studies to support their views. However, both agreed that returning children to school deserves a high priority. But neither the authors nor I treaded into the uncharted waters of exactly how masking fits into our national goals for managing the pandemic because ... no one in this country has articulated what these goals should be. A third op-ed appearing 3 weeks later suggests why we are floundering in this goal-deficient limbo.
Writing in the New York Times, two epidemiologists in Boston ask the simple question: “What are we actually trying to achieve in the United States?” when it comes to the pandemic. (Allen AG and Jenkins H. The Hard Covid-19 Questions We’re Not Asking. 2021 Aug 30). Is our goal zero infections? Is it hammering on the virus until we can treat it like the seasonal flu? We do seem to agree that not having kids in school has been a disaster economically, educationally, and psychologically. But, where does the goal of getting them back in school fit into a larger and as yet undefined national goal? Without that target we have little idea of what compromises and risks we should be willing to accept.
How much serious pediatric disease is acceptable? It appears that the number of fatal complications in the pediatric population is very small in comparison with other demographic groups. Although few in number, there have been and there will continue to be pediatric deaths because of COVID. Is our goal zero pediatric deaths? If it is then this dictates a level of response that ripples back upstream to every child in every classroom and could threaten our overarching goal of returning children to school. Because none of us likes the thought of a child dying, some of us may be hesitant to even consider a strategy that doesn’t include zero pediatric deaths as a goal.
Are we looking to have zero serious pediatric infections? Achieving this goal is unlikely. Even if we develop a pediatric vaccine in the near future it probably won’t be in the arms of enough children by the end of this school year to make a significant dent in the number of serious pediatric infections. Waiting until an optimal number of children are immunized doesn’t feel like it will achieve a primary goal of getting kids back in school if we continue to focus on driving the level of serious pediatric infections to zero. We have already endured a year in which many communities made decisions that seemed to have prioritized an unstated goal of no school exposure–related educator deaths. Again, a goal based on little if any evidence.
The problem we face in this country is that our response to the pandemic has been nonuniform. Here in Brunswick, Maine, 99% of the eligible adults have been vaccinated. Even with the recent surge, we may be ready for a strategy that avoids wholesale quarantining. A targeted and robust antibody testing system might work for us and make an unproven and unpopular masking mandate unnecessary. Britain seems to be moving in a similar direction to meet its goal of keeping children in school.
However, there are large population groups in regions of this country that have stumbled at taking the initial steps to get the pandemic under control. Articulating a national goal that covers both communities where the response to the pandemic has been less thoughtful and robust along with states that have been more successful is going to be difficult. But it must be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
In August I shared with you my observations on two opposing op-ed pieces from two major newspapers, one was in favor of masking mandates for public schools, the other against. (Masking in school: A battle of the op-eds. MDedge Pediatrics. Letters from Maine, 2021 Aug 12). Neither group of authors could offer us evidence from controlled studies to support their views. However, both agreed that returning children to school deserves a high priority. But neither the authors nor I treaded into the uncharted waters of exactly how masking fits into our national goals for managing the pandemic because ... no one in this country has articulated what these goals should be. A third op-ed appearing 3 weeks later suggests why we are floundering in this goal-deficient limbo.
Writing in the New York Times, two epidemiologists in Boston ask the simple question: “What are we actually trying to achieve in the United States?” when it comes to the pandemic. (Allen AG and Jenkins H. The Hard Covid-19 Questions We’re Not Asking. 2021 Aug 30). Is our goal zero infections? Is it hammering on the virus until we can treat it like the seasonal flu? We do seem to agree that not having kids in school has been a disaster economically, educationally, and psychologically. But, where does the goal of getting them back in school fit into a larger and as yet undefined national goal? Without that target we have little idea of what compromises and risks we should be willing to accept.
How much serious pediatric disease is acceptable? It appears that the number of fatal complications in the pediatric population is very small in comparison with other demographic groups. Although few in number, there have been and there will continue to be pediatric deaths because of COVID. Is our goal zero pediatric deaths? If it is then this dictates a level of response that ripples back upstream to every child in every classroom and could threaten our overarching goal of returning children to school. Because none of us likes the thought of a child dying, some of us may be hesitant to even consider a strategy that doesn’t include zero pediatric deaths as a goal.
Are we looking to have zero serious pediatric infections? Achieving this goal is unlikely. Even if we develop a pediatric vaccine in the near future it probably won’t be in the arms of enough children by the end of this school year to make a significant dent in the number of serious pediatric infections. Waiting until an optimal number of children are immunized doesn’t feel like it will achieve a primary goal of getting kids back in school if we continue to focus on driving the level of serious pediatric infections to zero. We have already endured a year in which many communities made decisions that seemed to have prioritized an unstated goal of no school exposure–related educator deaths. Again, a goal based on little if any evidence.
The problem we face in this country is that our response to the pandemic has been nonuniform. Here in Brunswick, Maine, 99% of the eligible adults have been vaccinated. Even with the recent surge, we may be ready for a strategy that avoids wholesale quarantining. A targeted and robust antibody testing system might work for us and make an unproven and unpopular masking mandate unnecessary. Britain seems to be moving in a similar direction to meet its goal of keeping children in school.
However, there are large population groups in regions of this country that have stumbled at taking the initial steps to get the pandemic under control. Articulating a national goal that covers both communities where the response to the pandemic has been less thoughtful and robust along with states that have been more successful is going to be difficult. But it must be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
In August I shared with you my observations on two opposing op-ed pieces from two major newspapers, one was in favor of masking mandates for public schools, the other against. (Masking in school: A battle of the op-eds. MDedge Pediatrics. Letters from Maine, 2021 Aug 12). Neither group of authors could offer us evidence from controlled studies to support their views. However, both agreed that returning children to school deserves a high priority. But neither the authors nor I treaded into the uncharted waters of exactly how masking fits into our national goals for managing the pandemic because ... no one in this country has articulated what these goals should be. A third op-ed appearing 3 weeks later suggests why we are floundering in this goal-deficient limbo.
Writing in the New York Times, two epidemiologists in Boston ask the simple question: “What are we actually trying to achieve in the United States?” when it comes to the pandemic. (Allen AG and Jenkins H. The Hard Covid-19 Questions We’re Not Asking. 2021 Aug 30). Is our goal zero infections? Is it hammering on the virus until we can treat it like the seasonal flu? We do seem to agree that not having kids in school has been a disaster economically, educationally, and psychologically. But, where does the goal of getting them back in school fit into a larger and as yet undefined national goal? Without that target we have little idea of what compromises and risks we should be willing to accept.
How much serious pediatric disease is acceptable? It appears that the number of fatal complications in the pediatric population is very small in comparison with other demographic groups. Although few in number, there have been and there will continue to be pediatric deaths because of COVID. Is our goal zero pediatric deaths? If it is then this dictates a level of response that ripples back upstream to every child in every classroom and could threaten our overarching goal of returning children to school. Because none of us likes the thought of a child dying, some of us may be hesitant to even consider a strategy that doesn’t include zero pediatric deaths as a goal.
Are we looking to have zero serious pediatric infections? Achieving this goal is unlikely. Even if we develop a pediatric vaccine in the near future it probably won’t be in the arms of enough children by the end of this school year to make a significant dent in the number of serious pediatric infections. Waiting until an optimal number of children are immunized doesn’t feel like it will achieve a primary goal of getting kids back in school if we continue to focus on driving the level of serious pediatric infections to zero. We have already endured a year in which many communities made decisions that seemed to have prioritized an unstated goal of no school exposure–related educator deaths. Again, a goal based on little if any evidence.
The problem we face in this country is that our response to the pandemic has been nonuniform. Here in Brunswick, Maine, 99% of the eligible adults have been vaccinated. Even with the recent surge, we may be ready for a strategy that avoids wholesale quarantining. A targeted and robust antibody testing system might work for us and make an unproven and unpopular masking mandate unnecessary. Britain seems to be moving in a similar direction to meet its goal of keeping children in school.
However, there are large population groups in regions of this country that have stumbled at taking the initial steps to get the pandemic under control. Articulating a national goal that covers both communities where the response to the pandemic has been less thoughtful and robust along with states that have been more successful is going to be difficult. But it must be done.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Other than a Littman stethoscope he accepted as a first-year medical student in 1966, Dr. Wilkoff reports having nothing to disclose. Email him at [email protected].
HPV infection during pregnancy ups risk of premature birth
Persistent human papillomavirus (HPV) 16 and HPV 18 during a pregnancy may be associated with an increased risk of premature birth.
Findings published online in JAMA Network Open found that 15.9% of individuals who had a persistent HPV 16 or 18 infection during the first and third trimesters of their pregnancy gave birth prematurely, compared with 5.6% of those who did not have an HPV infection at all.
The findings prompted the question of “the pathophysiology of HPV in pregnancy and how the virus is affecting the placenta,” said Lisette Davidson Tanner, MD, MPH, FACOG, who was not involved in the study.
Researchers said the findings are the first to show the association between preterm birth and HPV, which is an incurable virus that most sexually active individuals will get at some point in their lives, according to the Centers for Disease Control and Prevention.
“The results of this study are very important in helping us understand the burden caused by HPV in pregnancy,” study author Helen Trottier, MSc, PhD, researcher at the Centre Hospitalier Universitaire Sainte-Justine, said in an interview. “We may have just pinpointed an important cause of preterm birth that has so far been unexplained.”
Dr. Trottier and colleagues examined data from 1,052 pregnant women from three university-affiliated health care centers in Montreal between Nov. 8, 2010, and Oct. 16, 2016.
Only 5.6% of those who did not have an HPV infection had a premature birth, compared with 6.9% of those who tested positive for any HPV infection in the first trimester.
When looking at the first trimester, researchers found 12% of those diagnosed with HPV 16 and 18 had a preterm birth, compared to 4.9% of those who had a high-risk HPV infection other than HPV 16/18. When looking at the third trimester, researchers found that 15.9% of those with HPV 16/18 had an increased risk of giving birth prematurely, compared to those who had other high-risk HPV infections.
When researchers looked at the persistence of these HPV infections, they found that most HPV infections detected in the first trimester persist to the third trimester. The findings also revealed that persistent vaginal HPV 16/18 detection was significantly associated with all preterm births and spontaneous preterm births. This association was also found among those who had HPV infections detected in their placentas.
Meanwhile, 5.8% of those who had an HPV infection only during the first trimester experienced a preterm birth.
The researchers also found that HPV infections were frequent in pregnancy even among populations “considered to be at low risk based on sociodemographic and sexual history characteristics,” they wrote. Dr. Trottier said she hopes the findings will strengthen support for HPV vaccination.
Dr. Trottier’s study adds to a growing body of research regarding the adverse effects of HPV, according to Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta. “It is already well known that HPV is associated with a number of anogenital and oropharyngeal cancers,” Dr. Tanner said in an interview. “The potential association with preterm birth only adds weight to the recommendations to screen for and prevent HPV infection.”
HPV 16 and 18 are high-risk types that cause about 70% of cervical cancers and precancerous cervical lesions, according to the World Health Organization. However, there are three HPV vaccines – 9-valent HPV vaccine (Gardasil), quadrivalent HPV vaccine (Gardasil®, 4vHPV), and bivalent HPV vaccine (Cervarix) – that help protect against HPV 16/18.
The findings strengthen the benefits of HPV vaccination, Dr. Trottier explained. “There is no cure when the HPV infection is present,” Dr. Trottier said. “If the link [between preterm birth and HPV infections] is indeed causal, we can expect a greater risk of preterm delivery in these women. The effective tool we have is the HPV vaccination, but it should ideally be received before the start of sexual activity in order to prevent future infections that could occur in women.”
The American College of Obstetricians and Gynecologists recommends HPV vaccination for girls and women between the ages of 11 and 26 years old. However, Dr. Tanner said, women aged 27-45 who were previously unvaccinated may still receive benefit from the vaccine.
“Despite the known efficacy of the vaccine, only 50% of patients are up to date with their HPV vaccination,” Dr. Tanner explained. “This study further highlights the need to educate and encourage patients to be vaccinated.”
The researchers said future studies should investigate the association of HPV vaccination and vaccination programs with the risk of preterm birth.
The experts disclosed no conflicts of interest.
Persistent human papillomavirus (HPV) 16 and HPV 18 during a pregnancy may be associated with an increased risk of premature birth.
Findings published online in JAMA Network Open found that 15.9% of individuals who had a persistent HPV 16 or 18 infection during the first and third trimesters of their pregnancy gave birth prematurely, compared with 5.6% of those who did not have an HPV infection at all.
The findings prompted the question of “the pathophysiology of HPV in pregnancy and how the virus is affecting the placenta,” said Lisette Davidson Tanner, MD, MPH, FACOG, who was not involved in the study.
Researchers said the findings are the first to show the association between preterm birth and HPV, which is an incurable virus that most sexually active individuals will get at some point in their lives, according to the Centers for Disease Control and Prevention.
“The results of this study are very important in helping us understand the burden caused by HPV in pregnancy,” study author Helen Trottier, MSc, PhD, researcher at the Centre Hospitalier Universitaire Sainte-Justine, said in an interview. “We may have just pinpointed an important cause of preterm birth that has so far been unexplained.”
Dr. Trottier and colleagues examined data from 1,052 pregnant women from three university-affiliated health care centers in Montreal between Nov. 8, 2010, and Oct. 16, 2016.
Only 5.6% of those who did not have an HPV infection had a premature birth, compared with 6.9% of those who tested positive for any HPV infection in the first trimester.
When looking at the first trimester, researchers found 12% of those diagnosed with HPV 16 and 18 had a preterm birth, compared to 4.9% of those who had a high-risk HPV infection other than HPV 16/18. When looking at the third trimester, researchers found that 15.9% of those with HPV 16/18 had an increased risk of giving birth prematurely, compared to those who had other high-risk HPV infections.
When researchers looked at the persistence of these HPV infections, they found that most HPV infections detected in the first trimester persist to the third trimester. The findings also revealed that persistent vaginal HPV 16/18 detection was significantly associated with all preterm births and spontaneous preterm births. This association was also found among those who had HPV infections detected in their placentas.
Meanwhile, 5.8% of those who had an HPV infection only during the first trimester experienced a preterm birth.
The researchers also found that HPV infections were frequent in pregnancy even among populations “considered to be at low risk based on sociodemographic and sexual history characteristics,” they wrote. Dr. Trottier said she hopes the findings will strengthen support for HPV vaccination.
Dr. Trottier’s study adds to a growing body of research regarding the adverse effects of HPV, according to Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta. “It is already well known that HPV is associated with a number of anogenital and oropharyngeal cancers,” Dr. Tanner said in an interview. “The potential association with preterm birth only adds weight to the recommendations to screen for and prevent HPV infection.”
HPV 16 and 18 are high-risk types that cause about 70% of cervical cancers and precancerous cervical lesions, according to the World Health Organization. However, there are three HPV vaccines – 9-valent HPV vaccine (Gardasil), quadrivalent HPV vaccine (Gardasil®, 4vHPV), and bivalent HPV vaccine (Cervarix) – that help protect against HPV 16/18.
The findings strengthen the benefits of HPV vaccination, Dr. Trottier explained. “There is no cure when the HPV infection is present,” Dr. Trottier said. “If the link [between preterm birth and HPV infections] is indeed causal, we can expect a greater risk of preterm delivery in these women. The effective tool we have is the HPV vaccination, but it should ideally be received before the start of sexual activity in order to prevent future infections that could occur in women.”
The American College of Obstetricians and Gynecologists recommends HPV vaccination for girls and women between the ages of 11 and 26 years old. However, Dr. Tanner said, women aged 27-45 who were previously unvaccinated may still receive benefit from the vaccine.
“Despite the known efficacy of the vaccine, only 50% of patients are up to date with their HPV vaccination,” Dr. Tanner explained. “This study further highlights the need to educate and encourage patients to be vaccinated.”
The researchers said future studies should investigate the association of HPV vaccination and vaccination programs with the risk of preterm birth.
The experts disclosed no conflicts of interest.
Persistent human papillomavirus (HPV) 16 and HPV 18 during a pregnancy may be associated with an increased risk of premature birth.
Findings published online in JAMA Network Open found that 15.9% of individuals who had a persistent HPV 16 or 18 infection during the first and third trimesters of their pregnancy gave birth prematurely, compared with 5.6% of those who did not have an HPV infection at all.
The findings prompted the question of “the pathophysiology of HPV in pregnancy and how the virus is affecting the placenta,” said Lisette Davidson Tanner, MD, MPH, FACOG, who was not involved in the study.
Researchers said the findings are the first to show the association between preterm birth and HPV, which is an incurable virus that most sexually active individuals will get at some point in their lives, according to the Centers for Disease Control and Prevention.
“The results of this study are very important in helping us understand the burden caused by HPV in pregnancy,” study author Helen Trottier, MSc, PhD, researcher at the Centre Hospitalier Universitaire Sainte-Justine, said in an interview. “We may have just pinpointed an important cause of preterm birth that has so far been unexplained.”
Dr. Trottier and colleagues examined data from 1,052 pregnant women from three university-affiliated health care centers in Montreal between Nov. 8, 2010, and Oct. 16, 2016.
Only 5.6% of those who did not have an HPV infection had a premature birth, compared with 6.9% of those who tested positive for any HPV infection in the first trimester.
When looking at the first trimester, researchers found 12% of those diagnosed with HPV 16 and 18 had a preterm birth, compared to 4.9% of those who had a high-risk HPV infection other than HPV 16/18. When looking at the third trimester, researchers found that 15.9% of those with HPV 16/18 had an increased risk of giving birth prematurely, compared to those who had other high-risk HPV infections.
When researchers looked at the persistence of these HPV infections, they found that most HPV infections detected in the first trimester persist to the third trimester. The findings also revealed that persistent vaginal HPV 16/18 detection was significantly associated with all preterm births and spontaneous preterm births. This association was also found among those who had HPV infections detected in their placentas.
Meanwhile, 5.8% of those who had an HPV infection only during the first trimester experienced a preterm birth.
The researchers also found that HPV infections were frequent in pregnancy even among populations “considered to be at low risk based on sociodemographic and sexual history characteristics,” they wrote. Dr. Trottier said she hopes the findings will strengthen support for HPV vaccination.
Dr. Trottier’s study adds to a growing body of research regarding the adverse effects of HPV, according to Dr. Tanner, assistant professor of gynecology and obstetrics at Emory University, Atlanta. “It is already well known that HPV is associated with a number of anogenital and oropharyngeal cancers,” Dr. Tanner said in an interview. “The potential association with preterm birth only adds weight to the recommendations to screen for and prevent HPV infection.”
HPV 16 and 18 are high-risk types that cause about 70% of cervical cancers and precancerous cervical lesions, according to the World Health Organization. However, there are three HPV vaccines – 9-valent HPV vaccine (Gardasil), quadrivalent HPV vaccine (Gardasil®, 4vHPV), and bivalent HPV vaccine (Cervarix) – that help protect against HPV 16/18.
The findings strengthen the benefits of HPV vaccination, Dr. Trottier explained. “There is no cure when the HPV infection is present,” Dr. Trottier said. “If the link [between preterm birth and HPV infections] is indeed causal, we can expect a greater risk of preterm delivery in these women. The effective tool we have is the HPV vaccination, but it should ideally be received before the start of sexual activity in order to prevent future infections that could occur in women.”
The American College of Obstetricians and Gynecologists recommends HPV vaccination for girls and women between the ages of 11 and 26 years old. However, Dr. Tanner said, women aged 27-45 who were previously unvaccinated may still receive benefit from the vaccine.
“Despite the known efficacy of the vaccine, only 50% of patients are up to date with their HPV vaccination,” Dr. Tanner explained. “This study further highlights the need to educate and encourage patients to be vaccinated.”
The researchers said future studies should investigate the association of HPV vaccination and vaccination programs with the risk of preterm birth.
The experts disclosed no conflicts of interest.
FROM JAMA NETWORK OPEN
New Moderna vaccine data ‘support’ booster shot after 8 months
Moderna has released new data that it said support the argument for COVID-19 booster shots – specifically showing that people who received a first shot of their mRNA vaccine a median of 13 months ago are more likely to experience a breakthrough infection compared to individuals who received a first shot a median of 8 months ago.
The findings come from the ongoing phase 3 COVE clinical trial, the results of which the Food and Drug Administration considered in granting emergency use authorization for the vaccine. In the initial stage of the trial, people were randomly assigned to receive the company’s mRNA vaccine or placebo.
according to the analysis of the open-label extension of the study during which placebo participants could cross over and get immunized as well.
The updated COVE trial data show that 88 breakthrough cases of COVID-19 occurred among 11,431 participants vaccinated between December 2020 and March 2021 (49.0 cases per 1,000 person-years).
In contrast, there were 162 breakthrough cases among 14,746 people vaccinated between July and October 2020 (77.1 cases per 1,000 person-years).
The breakthrough infections include 19 severe cases. Although not statically different, there was a trend toward fewer severe cases among the more recently vaccinated, at a rate of 3.3 per 1,000 person-years, compared with 6.2 per 1,000 person-years in the group vaccinated in 2020
The findings were posted as a preprint to the medRxiv server and have not yet been peer reviewed.
“The increased risk of breakthrough infections in COVE study participants who were vaccinated last year compared to more recently illustrates the impact of waning immunity and supports the need for a booster to maintain high levels of protection,” Moderna CEO Stéphane Bancel said in a company statement.
An FDA advisory committee is meeting Sept. 17 to look at the available evidence on boosters to help the agency decide whether the additional shots are warranted.
There is still a lot of debate in the medical community about the need for boosters. U.S. physicians and nurses are divided about the need for them and about how the country should prioritize its vaccine supplies, according to a Medscape poll of more than 1,700 clinicians that collected responses from Aug. 25 to Sept. 6, 2020.
The research was funded by Moderna, and also supported by the Office of the Assistant Secretary for Preparedness and Response, Biomedical Advanced Research and Development Authority, and by the National Institute of Allergy and Infectious Diseases.
A version of this article first appeared on Medscape.com.
Moderna has released new data that it said support the argument for COVID-19 booster shots – specifically showing that people who received a first shot of their mRNA vaccine a median of 13 months ago are more likely to experience a breakthrough infection compared to individuals who received a first shot a median of 8 months ago.
The findings come from the ongoing phase 3 COVE clinical trial, the results of which the Food and Drug Administration considered in granting emergency use authorization for the vaccine. In the initial stage of the trial, people were randomly assigned to receive the company’s mRNA vaccine or placebo.
according to the analysis of the open-label extension of the study during which placebo participants could cross over and get immunized as well.
The updated COVE trial data show that 88 breakthrough cases of COVID-19 occurred among 11,431 participants vaccinated between December 2020 and March 2021 (49.0 cases per 1,000 person-years).
In contrast, there were 162 breakthrough cases among 14,746 people vaccinated between July and October 2020 (77.1 cases per 1,000 person-years).
The breakthrough infections include 19 severe cases. Although not statically different, there was a trend toward fewer severe cases among the more recently vaccinated, at a rate of 3.3 per 1,000 person-years, compared with 6.2 per 1,000 person-years in the group vaccinated in 2020
The findings were posted as a preprint to the medRxiv server and have not yet been peer reviewed.
“The increased risk of breakthrough infections in COVE study participants who were vaccinated last year compared to more recently illustrates the impact of waning immunity and supports the need for a booster to maintain high levels of protection,” Moderna CEO Stéphane Bancel said in a company statement.
An FDA advisory committee is meeting Sept. 17 to look at the available evidence on boosters to help the agency decide whether the additional shots are warranted.
There is still a lot of debate in the medical community about the need for boosters. U.S. physicians and nurses are divided about the need for them and about how the country should prioritize its vaccine supplies, according to a Medscape poll of more than 1,700 clinicians that collected responses from Aug. 25 to Sept. 6, 2020.
The research was funded by Moderna, and also supported by the Office of the Assistant Secretary for Preparedness and Response, Biomedical Advanced Research and Development Authority, and by the National Institute of Allergy and Infectious Diseases.
A version of this article first appeared on Medscape.com.
Moderna has released new data that it said support the argument for COVID-19 booster shots – specifically showing that people who received a first shot of their mRNA vaccine a median of 13 months ago are more likely to experience a breakthrough infection compared to individuals who received a first shot a median of 8 months ago.
The findings come from the ongoing phase 3 COVE clinical trial, the results of which the Food and Drug Administration considered in granting emergency use authorization for the vaccine. In the initial stage of the trial, people were randomly assigned to receive the company’s mRNA vaccine or placebo.
according to the analysis of the open-label extension of the study during which placebo participants could cross over and get immunized as well.
The updated COVE trial data show that 88 breakthrough cases of COVID-19 occurred among 11,431 participants vaccinated between December 2020 and March 2021 (49.0 cases per 1,000 person-years).
In contrast, there were 162 breakthrough cases among 14,746 people vaccinated between July and October 2020 (77.1 cases per 1,000 person-years).
The breakthrough infections include 19 severe cases. Although not statically different, there was a trend toward fewer severe cases among the more recently vaccinated, at a rate of 3.3 per 1,000 person-years, compared with 6.2 per 1,000 person-years in the group vaccinated in 2020
The findings were posted as a preprint to the medRxiv server and have not yet been peer reviewed.
“The increased risk of breakthrough infections in COVE study participants who were vaccinated last year compared to more recently illustrates the impact of waning immunity and supports the need for a booster to maintain high levels of protection,” Moderna CEO Stéphane Bancel said in a company statement.
An FDA advisory committee is meeting Sept. 17 to look at the available evidence on boosters to help the agency decide whether the additional shots are warranted.
There is still a lot of debate in the medical community about the need for boosters. U.S. physicians and nurses are divided about the need for them and about how the country should prioritize its vaccine supplies, according to a Medscape poll of more than 1,700 clinicians that collected responses from Aug. 25 to Sept. 6, 2020.
The research was funded by Moderna, and also supported by the Office of the Assistant Secretary for Preparedness and Response, Biomedical Advanced Research and Development Authority, and by the National Institute of Allergy and Infectious Diseases.
A version of this article first appeared on Medscape.com.
COVID vaccine preprint study prompts Twitter outrage
A preprint study finding that the Pfizer-BioNTech mRNA COVID vaccine is associated with an increased risk for cardiac adverse events in teenage boys has elicited a firestorm on Twitter. Although some people issued thoughtful critiques, others lobbed insults against the authors, and still others accused them of either being antivaccine or stoking the fires of the vaccine skeptic movement.
The controversy began soon after the study was posted online September 8 on medRxiv. The authors conclude that for boys, the risk for a cardiac adverse event or hospitalization after the second dose of the Pfizer mRNA vaccine was “considerably higher” than the 120-day risk for hospitalization for COVID-19, “even at times of peak disease prevalence.” This was especially true for those aged 12 to 15 years and even those with no underlying health conditions.
The conclusion – as well as the paper’s source, the Vaccine Adverse Event Reporting System (VAERS), and its methodology, modeled after the Centers for Disease Control and Prevention assessment of the database – did not sit well with many.
“Your methodology hugely overestimates risk, which many commentators who are specialists in the field have highlighted,” tweeted Deepti Gurdasani, senior lecturer in epidemiology at Queen Mary University of London. “Why make this claim when you must know it’s wrong?”
“The authors don’t know what they are doing and they are following their own ideology,” tweeted Boback Ziaeian, MD, PhD, assistant professor of medicine at the University of California, Los Angeles, in the cardiology division. Dr. Ziaeian also tweeted, “I believe the CDC is doing honest work and not dredging slop like you are.”
“Holy shit. Truly terrible methods in that paper,” tweeted Michael Mina, MD, PhD, an epidemiologist and immunologist at the Harvard School of Public Health, Boston, more bluntly.
Some pointed out that VAERS is often used by vaccine skeptics to spread misinformation. “‘Dumpster diving’ describes studies using #VAERS by authors (almost always antivaxxers) who don’t understand its limitations,” tweeted David Gorski, MD, PhD, the editor of Science-Based Medicine, who says in his Twitter bio that he “exposes quackery.”
Added Dr. Gorski: “Doctors fell into this trap with their study suggesting #CovidVaccine is more dangerous to children than #COVID19.”
Dr. Gorski said he did not think that the authors were antivaccine. But, he tweeted, “I’d argue that at least one of the authors (Stevenson) is grossly unqualified to analyze the data. Mandrola? Marginal. The other two *might* be qualified in public health/epi, but they clearly either had no clue about #VAERS limitations or didn’t take them seriously enough.”
Two of the authors, John Mandrola, MD, a cardiac electrophysiologist who is also a columnist for Medscape, and Tracy Beth Hoeg, MD, PhD, an epidemiologist and sports medicine specialist, told this news organization that their estimates are not definitive, owing to the nature of the VAERS database.
“I want to emphasize that our signal is hypothesis-generating,” said Dr. Mandrola. “There’s obviously more research that needs to be done.”
“I don’t think it should be used to establish a for-certain rate,” said Dr. Hoeg, about the study. “It’s not a perfect way of establishing what the rate of cardiac adverse events was, but it gives you an estimate, and generally with VAERS, it’s a significant underestimate.”
Both Dr. Hoeg and Dr. Mandrola said their analysis showed enough of a signal that it warranted a rush to publish. “We felt that it was super time-sensitive,” Dr. Mandrola said.
Vaccine risks versus COVID harm
The authors searched the VAERS system for children aged 12 to 17 years who had received one or two doses of an mRNA vaccine and had symptoms of myocarditis, pericarditis, myopericarditis, or chest pain, and also troponin levels available in the lab data.
Of the 257 patients they examined, 211 had peak troponin values available for analysis. All but one received the Pfizer vaccine. Results were stratified by age and sex.
The authors found that the rates of cardiac adverse events (CAEs) after dose 1 were 12.0 per million for 12- to 15-year-old boys and 8.2 per million for 16- and 17-year-old boys, compared with 0.0 per million and 2.0 per million for girls the same ages.
The estimates for the 12- to 15-year-old boys were 22% to 150% higher than what the CDC had previously reported.
After the second dose, the rate of CAEs for boys 12 to 15 years was 162.2 per million (143% to 280% higher than the CDC estimate) and for boys 16 and 17 years, it was 94.0 per million, or 30% to 40% higher than CDC estimate.
Dr. Mandrola said he and his colleagues found potentially more cases by using slightly broader search terms than those employed by the CDC but agreed with some critics that a limitation was that they did not call the reporting physicians, as is typical with CDC follow-up on VAERS reports.
The authors point to troponin levels as valid indicators of myocardial damage. Peak troponin levels exceeded 2 ng/mL in 71% of the 12- to 15-year-olds and 82% of 16- and 17-year-olds.
The study shows that for boys 12 to 15 years with no comorbidities, the risk for a CAE after the second dose would be 22.8 times higher than the risk for hospitalization for COVID-19 during periods of low disease burden, 6.0 times higher during periods of moderate transmission, and 4.3 times higher during periods of high transmission.
The authors acknowledge in the paper that their analysis “does not take into account any benefits the vaccine provides against transmission to others, long-term COVID-19 disease risk, or protection from nonsevere COVID-19 symptoms.”
Both Dr. Mandrola and Dr. Hoeg told this news organization that they are currently recalculating their estimates because of the rising numbers of pediatric hospitalizations from the Delta variant surge.
Paper rejected by journals
Dr. Hoeg said in an interview that the paper went through peer-review at three journals but was rejected by all three, for reasons that were not made clear.
She and the other authors incorporated the reviewers’ feedback at each turn and included all of their suggestions in the paper that was ultimately uploaded to medRxiv, said Dr. Hoeg.
They decided to put it out as a preprint after the U.S. Food and Drug Administration issued its data and then a warning on June 25 about myocarditis with use of the Pfizer vaccine in children 12 to 15 years of age.
The preprint study was picked up by some media outlets, including The Telegraph and The Guardian newspapers, and tweeted out by vaccine skeptics like Robert W. Malone, MD.
Rep. Marjorie Taylor Greene (R-Georgia), an outspoken vaccine skeptic, tweeted out the Guardian story saying that the findings mean “there is every reason to stop the covid vaccine mandates.”
Dr. Gorski noted in tweets and in a blog post that one of the paper’s coauthors, Josh Stevenson, is part of Rational Ground, a group that supports the Great Barrington Declaration and is against lockdowns and mask mandates.
Mr. Stevenson did not disclose his affiliation in the paper, and Dr. Hoeg said in an interview that she was unaware of the group and Mr. Stevenson’s association with it and that she did not have the impression that he was altering the data to show any bias.
Both Dr. Mandrola and Dr. Hoeg said they are provaccine and that they were dismayed to find their work being used to support any agenda. “It’s very frustrating,” said Dr. Hoeg, adding that she understands that “when you publish research on a controversial topic, people are going to take it and use it for their agendas.”
Some on Twitter blamed the open and free-wheeling nature of preprints.
Harlan Krumholz, MD, SM, the Harold H. Hines, junior professor of medicine and public health at Yale University, New Haven, Conn., which oversees medRxiv, tweeted, “Do you get that the discussion about the preprint is exactly the purpose of #preprints. So that way when someone claims something, you can look at the source and experts can comment.”
But Dr. Ziaeian tweeted back, “Preprints like this one can be weaponized to stir anti-vaccine lies and damage public health.”
In turn, the Yale physician replied, “Unfortunately these days, almost anything can be weaponized, distorted, misunderstood.” Dr. Krumholz added: “There is no question that this preprint is worthy of deep vetting and discussion. But there is a #preprint artifact to examine.”
Measured support
Some clinicians signaled their support for open debate and the preprint’s findings.
“I’ve been very critical of preprints that are too quickly disseminated in the media, and this one is no exception,” tweeted Walid Gellad, MD, MPH, associate professor of medicine at the University of Pittsburgh. “On the other hand, I think the vitriol directed at these authors is wrong,” he added.
“Like it or not, the issue of myocarditis in kids is an issue. Other countries have made vaccination decisions because of this issue, not because they’re driven by some ideology,” he tweeted.
Dr. Gellad also notes that the FDA has estimated the risk could be as high as one in 5,000 and that the preprint numbers could actually be underestimates.
In a long thread, Frank Han, MD, an adult congenital and pediatric cardiologist at the University of Illinois, tweets that relying on the VAERS reports might be faulty and that advanced cardiac imaging – guided by strict criteria – is the best way to determine myocarditis. And, he tweeted, “Physician review of VAERS reports really matters.”
Dr. Han concluded that vaccination “trades in a significant risk with a much smaller risk. That’s what counts in the end.”
In a response, Dr. Mandrola called Han’s tweets “reasoned criticism of our analysis.” He adds that his and Dr. Hoeg’s study have limits, but “our point is not to avoid protecting kids, but how to do so most safely.”
Both Dr. Mandrola and Dr. Hoeg said they welcomed critiques, but they felt blindsided by the vehemence of some of the Twitter debate.
“Some of the vitriol was surprising,” Dr. Mandrola said. “I kind of have this naive notion that people would assume that we’re not bad people,” he added.
However, Dr. Mandrola is known on Twitter for sometimes being highly critical of other researchers’ work, referring to some studies as “howlers,” and has in the past called out others for citing those papers.
Dr. Hoeg said she found critiques about weaknesses in the methods to be helpful. But she said many tweets were “attacking us as people, or not really attacking anything about our study, but just attacking the finding,” which does not help anyone “figure out what we should do about the safety signal or how we can research it further.”
Said Dr. Mandrola: “Why would we just ignore that and go forward with two-shot vaccination as a mandate when other countries are looking at other strategies?”
He noted that the United Kingdom has announced that children 12 to 15 years of age should receive just one shot of the mRNA vaccines instead of two because of the risk for myocarditis. Sixteen- to 18-year-olds have already been advised to get only one dose.
A version of this article first appeared on Medscape.com.
A preprint study finding that the Pfizer-BioNTech mRNA COVID vaccine is associated with an increased risk for cardiac adverse events in teenage boys has elicited a firestorm on Twitter. Although some people issued thoughtful critiques, others lobbed insults against the authors, and still others accused them of either being antivaccine or stoking the fires of the vaccine skeptic movement.
The controversy began soon after the study was posted online September 8 on medRxiv. The authors conclude that for boys, the risk for a cardiac adverse event or hospitalization after the second dose of the Pfizer mRNA vaccine was “considerably higher” than the 120-day risk for hospitalization for COVID-19, “even at times of peak disease prevalence.” This was especially true for those aged 12 to 15 years and even those with no underlying health conditions.
The conclusion – as well as the paper’s source, the Vaccine Adverse Event Reporting System (VAERS), and its methodology, modeled after the Centers for Disease Control and Prevention assessment of the database – did not sit well with many.
“Your methodology hugely overestimates risk, which many commentators who are specialists in the field have highlighted,” tweeted Deepti Gurdasani, senior lecturer in epidemiology at Queen Mary University of London. “Why make this claim when you must know it’s wrong?”
“The authors don’t know what they are doing and they are following their own ideology,” tweeted Boback Ziaeian, MD, PhD, assistant professor of medicine at the University of California, Los Angeles, in the cardiology division. Dr. Ziaeian also tweeted, “I believe the CDC is doing honest work and not dredging slop like you are.”
“Holy shit. Truly terrible methods in that paper,” tweeted Michael Mina, MD, PhD, an epidemiologist and immunologist at the Harvard School of Public Health, Boston, more bluntly.
Some pointed out that VAERS is often used by vaccine skeptics to spread misinformation. “‘Dumpster diving’ describes studies using #VAERS by authors (almost always antivaxxers) who don’t understand its limitations,” tweeted David Gorski, MD, PhD, the editor of Science-Based Medicine, who says in his Twitter bio that he “exposes quackery.”
Added Dr. Gorski: “Doctors fell into this trap with their study suggesting #CovidVaccine is more dangerous to children than #COVID19.”
Dr. Gorski said he did not think that the authors were antivaccine. But, he tweeted, “I’d argue that at least one of the authors (Stevenson) is grossly unqualified to analyze the data. Mandrola? Marginal. The other two *might* be qualified in public health/epi, but they clearly either had no clue about #VAERS limitations or didn’t take them seriously enough.”
Two of the authors, John Mandrola, MD, a cardiac electrophysiologist who is also a columnist for Medscape, and Tracy Beth Hoeg, MD, PhD, an epidemiologist and sports medicine specialist, told this news organization that their estimates are not definitive, owing to the nature of the VAERS database.
“I want to emphasize that our signal is hypothesis-generating,” said Dr. Mandrola. “There’s obviously more research that needs to be done.”
“I don’t think it should be used to establish a for-certain rate,” said Dr. Hoeg, about the study. “It’s not a perfect way of establishing what the rate of cardiac adverse events was, but it gives you an estimate, and generally with VAERS, it’s a significant underestimate.”
Both Dr. Hoeg and Dr. Mandrola said their analysis showed enough of a signal that it warranted a rush to publish. “We felt that it was super time-sensitive,” Dr. Mandrola said.
Vaccine risks versus COVID harm
The authors searched the VAERS system for children aged 12 to 17 years who had received one or two doses of an mRNA vaccine and had symptoms of myocarditis, pericarditis, myopericarditis, or chest pain, and also troponin levels available in the lab data.
Of the 257 patients they examined, 211 had peak troponin values available for analysis. All but one received the Pfizer vaccine. Results were stratified by age and sex.
The authors found that the rates of cardiac adverse events (CAEs) after dose 1 were 12.0 per million for 12- to 15-year-old boys and 8.2 per million for 16- and 17-year-old boys, compared with 0.0 per million and 2.0 per million for girls the same ages.
The estimates for the 12- to 15-year-old boys were 22% to 150% higher than what the CDC had previously reported.
After the second dose, the rate of CAEs for boys 12 to 15 years was 162.2 per million (143% to 280% higher than the CDC estimate) and for boys 16 and 17 years, it was 94.0 per million, or 30% to 40% higher than CDC estimate.
Dr. Mandrola said he and his colleagues found potentially more cases by using slightly broader search terms than those employed by the CDC but agreed with some critics that a limitation was that they did not call the reporting physicians, as is typical with CDC follow-up on VAERS reports.
The authors point to troponin levels as valid indicators of myocardial damage. Peak troponin levels exceeded 2 ng/mL in 71% of the 12- to 15-year-olds and 82% of 16- and 17-year-olds.
The study shows that for boys 12 to 15 years with no comorbidities, the risk for a CAE after the second dose would be 22.8 times higher than the risk for hospitalization for COVID-19 during periods of low disease burden, 6.0 times higher during periods of moderate transmission, and 4.3 times higher during periods of high transmission.
The authors acknowledge in the paper that their analysis “does not take into account any benefits the vaccine provides against transmission to others, long-term COVID-19 disease risk, or protection from nonsevere COVID-19 symptoms.”
Both Dr. Mandrola and Dr. Hoeg told this news organization that they are currently recalculating their estimates because of the rising numbers of pediatric hospitalizations from the Delta variant surge.
Paper rejected by journals
Dr. Hoeg said in an interview that the paper went through peer-review at three journals but was rejected by all three, for reasons that were not made clear.
She and the other authors incorporated the reviewers’ feedback at each turn and included all of their suggestions in the paper that was ultimately uploaded to medRxiv, said Dr. Hoeg.
They decided to put it out as a preprint after the U.S. Food and Drug Administration issued its data and then a warning on June 25 about myocarditis with use of the Pfizer vaccine in children 12 to 15 years of age.
The preprint study was picked up by some media outlets, including The Telegraph and The Guardian newspapers, and tweeted out by vaccine skeptics like Robert W. Malone, MD.
Rep. Marjorie Taylor Greene (R-Georgia), an outspoken vaccine skeptic, tweeted out the Guardian story saying that the findings mean “there is every reason to stop the covid vaccine mandates.”
Dr. Gorski noted in tweets and in a blog post that one of the paper’s coauthors, Josh Stevenson, is part of Rational Ground, a group that supports the Great Barrington Declaration and is against lockdowns and mask mandates.
Mr. Stevenson did not disclose his affiliation in the paper, and Dr. Hoeg said in an interview that she was unaware of the group and Mr. Stevenson’s association with it and that she did not have the impression that he was altering the data to show any bias.
Both Dr. Mandrola and Dr. Hoeg said they are provaccine and that they were dismayed to find their work being used to support any agenda. “It’s very frustrating,” said Dr. Hoeg, adding that she understands that “when you publish research on a controversial topic, people are going to take it and use it for their agendas.”
Some on Twitter blamed the open and free-wheeling nature of preprints.
Harlan Krumholz, MD, SM, the Harold H. Hines, junior professor of medicine and public health at Yale University, New Haven, Conn., which oversees medRxiv, tweeted, “Do you get that the discussion about the preprint is exactly the purpose of #preprints. So that way when someone claims something, you can look at the source and experts can comment.”
But Dr. Ziaeian tweeted back, “Preprints like this one can be weaponized to stir anti-vaccine lies and damage public health.”
In turn, the Yale physician replied, “Unfortunately these days, almost anything can be weaponized, distorted, misunderstood.” Dr. Krumholz added: “There is no question that this preprint is worthy of deep vetting and discussion. But there is a #preprint artifact to examine.”
Measured support
Some clinicians signaled their support for open debate and the preprint’s findings.
“I’ve been very critical of preprints that are too quickly disseminated in the media, and this one is no exception,” tweeted Walid Gellad, MD, MPH, associate professor of medicine at the University of Pittsburgh. “On the other hand, I think the vitriol directed at these authors is wrong,” he added.
“Like it or not, the issue of myocarditis in kids is an issue. Other countries have made vaccination decisions because of this issue, not because they’re driven by some ideology,” he tweeted.
Dr. Gellad also notes that the FDA has estimated the risk could be as high as one in 5,000 and that the preprint numbers could actually be underestimates.
In a long thread, Frank Han, MD, an adult congenital and pediatric cardiologist at the University of Illinois, tweets that relying on the VAERS reports might be faulty and that advanced cardiac imaging – guided by strict criteria – is the best way to determine myocarditis. And, he tweeted, “Physician review of VAERS reports really matters.”
Dr. Han concluded that vaccination “trades in a significant risk with a much smaller risk. That’s what counts in the end.”
In a response, Dr. Mandrola called Han’s tweets “reasoned criticism of our analysis.” He adds that his and Dr. Hoeg’s study have limits, but “our point is not to avoid protecting kids, but how to do so most safely.”
Both Dr. Mandrola and Dr. Hoeg said they welcomed critiques, but they felt blindsided by the vehemence of some of the Twitter debate.
“Some of the vitriol was surprising,” Dr. Mandrola said. “I kind of have this naive notion that people would assume that we’re not bad people,” he added.
However, Dr. Mandrola is known on Twitter for sometimes being highly critical of other researchers’ work, referring to some studies as “howlers,” and has in the past called out others for citing those papers.
Dr. Hoeg said she found critiques about weaknesses in the methods to be helpful. But she said many tweets were “attacking us as people, or not really attacking anything about our study, but just attacking the finding,” which does not help anyone “figure out what we should do about the safety signal or how we can research it further.”
Said Dr. Mandrola: “Why would we just ignore that and go forward with two-shot vaccination as a mandate when other countries are looking at other strategies?”
He noted that the United Kingdom has announced that children 12 to 15 years of age should receive just one shot of the mRNA vaccines instead of two because of the risk for myocarditis. Sixteen- to 18-year-olds have already been advised to get only one dose.
A version of this article first appeared on Medscape.com.
A preprint study finding that the Pfizer-BioNTech mRNA COVID vaccine is associated with an increased risk for cardiac adverse events in teenage boys has elicited a firestorm on Twitter. Although some people issued thoughtful critiques, others lobbed insults against the authors, and still others accused them of either being antivaccine or stoking the fires of the vaccine skeptic movement.
The controversy began soon after the study was posted online September 8 on medRxiv. The authors conclude that for boys, the risk for a cardiac adverse event or hospitalization after the second dose of the Pfizer mRNA vaccine was “considerably higher” than the 120-day risk for hospitalization for COVID-19, “even at times of peak disease prevalence.” This was especially true for those aged 12 to 15 years and even those with no underlying health conditions.
The conclusion – as well as the paper’s source, the Vaccine Adverse Event Reporting System (VAERS), and its methodology, modeled after the Centers for Disease Control and Prevention assessment of the database – did not sit well with many.
“Your methodology hugely overestimates risk, which many commentators who are specialists in the field have highlighted,” tweeted Deepti Gurdasani, senior lecturer in epidemiology at Queen Mary University of London. “Why make this claim when you must know it’s wrong?”
“The authors don’t know what they are doing and they are following their own ideology,” tweeted Boback Ziaeian, MD, PhD, assistant professor of medicine at the University of California, Los Angeles, in the cardiology division. Dr. Ziaeian also tweeted, “I believe the CDC is doing honest work and not dredging slop like you are.”
“Holy shit. Truly terrible methods in that paper,” tweeted Michael Mina, MD, PhD, an epidemiologist and immunologist at the Harvard School of Public Health, Boston, more bluntly.
Some pointed out that VAERS is often used by vaccine skeptics to spread misinformation. “‘Dumpster diving’ describes studies using #VAERS by authors (almost always antivaxxers) who don’t understand its limitations,” tweeted David Gorski, MD, PhD, the editor of Science-Based Medicine, who says in his Twitter bio that he “exposes quackery.”
Added Dr. Gorski: “Doctors fell into this trap with their study suggesting #CovidVaccine is more dangerous to children than #COVID19.”
Dr. Gorski said he did not think that the authors were antivaccine. But, he tweeted, “I’d argue that at least one of the authors (Stevenson) is grossly unqualified to analyze the data. Mandrola? Marginal. The other two *might* be qualified in public health/epi, but they clearly either had no clue about #VAERS limitations or didn’t take them seriously enough.”
Two of the authors, John Mandrola, MD, a cardiac electrophysiologist who is also a columnist for Medscape, and Tracy Beth Hoeg, MD, PhD, an epidemiologist and sports medicine specialist, told this news organization that their estimates are not definitive, owing to the nature of the VAERS database.
“I want to emphasize that our signal is hypothesis-generating,” said Dr. Mandrola. “There’s obviously more research that needs to be done.”
“I don’t think it should be used to establish a for-certain rate,” said Dr. Hoeg, about the study. “It’s not a perfect way of establishing what the rate of cardiac adverse events was, but it gives you an estimate, and generally with VAERS, it’s a significant underestimate.”
Both Dr. Hoeg and Dr. Mandrola said their analysis showed enough of a signal that it warranted a rush to publish. “We felt that it was super time-sensitive,” Dr. Mandrola said.
Vaccine risks versus COVID harm
The authors searched the VAERS system for children aged 12 to 17 years who had received one or two doses of an mRNA vaccine and had symptoms of myocarditis, pericarditis, myopericarditis, or chest pain, and also troponin levels available in the lab data.
Of the 257 patients they examined, 211 had peak troponin values available for analysis. All but one received the Pfizer vaccine. Results were stratified by age and sex.
The authors found that the rates of cardiac adverse events (CAEs) after dose 1 were 12.0 per million for 12- to 15-year-old boys and 8.2 per million for 16- and 17-year-old boys, compared with 0.0 per million and 2.0 per million for girls the same ages.
The estimates for the 12- to 15-year-old boys were 22% to 150% higher than what the CDC had previously reported.
After the second dose, the rate of CAEs for boys 12 to 15 years was 162.2 per million (143% to 280% higher than the CDC estimate) and for boys 16 and 17 years, it was 94.0 per million, or 30% to 40% higher than CDC estimate.
Dr. Mandrola said he and his colleagues found potentially more cases by using slightly broader search terms than those employed by the CDC but agreed with some critics that a limitation was that they did not call the reporting physicians, as is typical with CDC follow-up on VAERS reports.
The authors point to troponin levels as valid indicators of myocardial damage. Peak troponin levels exceeded 2 ng/mL in 71% of the 12- to 15-year-olds and 82% of 16- and 17-year-olds.
The study shows that for boys 12 to 15 years with no comorbidities, the risk for a CAE after the second dose would be 22.8 times higher than the risk for hospitalization for COVID-19 during periods of low disease burden, 6.0 times higher during periods of moderate transmission, and 4.3 times higher during periods of high transmission.
The authors acknowledge in the paper that their analysis “does not take into account any benefits the vaccine provides against transmission to others, long-term COVID-19 disease risk, or protection from nonsevere COVID-19 symptoms.”
Both Dr. Mandrola and Dr. Hoeg told this news organization that they are currently recalculating their estimates because of the rising numbers of pediatric hospitalizations from the Delta variant surge.
Paper rejected by journals
Dr. Hoeg said in an interview that the paper went through peer-review at three journals but was rejected by all three, for reasons that were not made clear.
She and the other authors incorporated the reviewers’ feedback at each turn and included all of their suggestions in the paper that was ultimately uploaded to medRxiv, said Dr. Hoeg.
They decided to put it out as a preprint after the U.S. Food and Drug Administration issued its data and then a warning on June 25 about myocarditis with use of the Pfizer vaccine in children 12 to 15 years of age.
The preprint study was picked up by some media outlets, including The Telegraph and The Guardian newspapers, and tweeted out by vaccine skeptics like Robert W. Malone, MD.
Rep. Marjorie Taylor Greene (R-Georgia), an outspoken vaccine skeptic, tweeted out the Guardian story saying that the findings mean “there is every reason to stop the covid vaccine mandates.”
Dr. Gorski noted in tweets and in a blog post that one of the paper’s coauthors, Josh Stevenson, is part of Rational Ground, a group that supports the Great Barrington Declaration and is against lockdowns and mask mandates.
Mr. Stevenson did not disclose his affiliation in the paper, and Dr. Hoeg said in an interview that she was unaware of the group and Mr. Stevenson’s association with it and that she did not have the impression that he was altering the data to show any bias.
Both Dr. Mandrola and Dr. Hoeg said they are provaccine and that they were dismayed to find their work being used to support any agenda. “It’s very frustrating,” said Dr. Hoeg, adding that she understands that “when you publish research on a controversial topic, people are going to take it and use it for their agendas.”
Some on Twitter blamed the open and free-wheeling nature of preprints.
Harlan Krumholz, MD, SM, the Harold H. Hines, junior professor of medicine and public health at Yale University, New Haven, Conn., which oversees medRxiv, tweeted, “Do you get that the discussion about the preprint is exactly the purpose of #preprints. So that way when someone claims something, you can look at the source and experts can comment.”
But Dr. Ziaeian tweeted back, “Preprints like this one can be weaponized to stir anti-vaccine lies and damage public health.”
In turn, the Yale physician replied, “Unfortunately these days, almost anything can be weaponized, distorted, misunderstood.” Dr. Krumholz added: “There is no question that this preprint is worthy of deep vetting and discussion. But there is a #preprint artifact to examine.”
Measured support
Some clinicians signaled their support for open debate and the preprint’s findings.
“I’ve been very critical of preprints that are too quickly disseminated in the media, and this one is no exception,” tweeted Walid Gellad, MD, MPH, associate professor of medicine at the University of Pittsburgh. “On the other hand, I think the vitriol directed at these authors is wrong,” he added.
“Like it or not, the issue of myocarditis in kids is an issue. Other countries have made vaccination decisions because of this issue, not because they’re driven by some ideology,” he tweeted.
Dr. Gellad also notes that the FDA has estimated the risk could be as high as one in 5,000 and that the preprint numbers could actually be underestimates.
In a long thread, Frank Han, MD, an adult congenital and pediatric cardiologist at the University of Illinois, tweets that relying on the VAERS reports might be faulty and that advanced cardiac imaging – guided by strict criteria – is the best way to determine myocarditis. And, he tweeted, “Physician review of VAERS reports really matters.”
Dr. Han concluded that vaccination “trades in a significant risk with a much smaller risk. That’s what counts in the end.”
In a response, Dr. Mandrola called Han’s tweets “reasoned criticism of our analysis.” He adds that his and Dr. Hoeg’s study have limits, but “our point is not to avoid protecting kids, but how to do so most safely.”
Both Dr. Mandrola and Dr. Hoeg said they welcomed critiques, but they felt blindsided by the vehemence of some of the Twitter debate.
“Some of the vitriol was surprising,” Dr. Mandrola said. “I kind of have this naive notion that people would assume that we’re not bad people,” he added.
However, Dr. Mandrola is known on Twitter for sometimes being highly critical of other researchers’ work, referring to some studies as “howlers,” and has in the past called out others for citing those papers.
Dr. Hoeg said she found critiques about weaknesses in the methods to be helpful. But she said many tweets were “attacking us as people, or not really attacking anything about our study, but just attacking the finding,” which does not help anyone “figure out what we should do about the safety signal or how we can research it further.”
Said Dr. Mandrola: “Why would we just ignore that and go forward with two-shot vaccination as a mandate when other countries are looking at other strategies?”
He noted that the United Kingdom has announced that children 12 to 15 years of age should receive just one shot of the mRNA vaccines instead of two because of the risk for myocarditis. Sixteen- to 18-year-olds have already been advised to get only one dose.
A version of this article first appeared on Medscape.com.
FDA could authorize COVID-19 vaccine for ages 5-11 in October
The timeline is based on the expectation that Pfizer will have enough data from clinical trials to request Food and Drug Administration emergency use authorization for the age group near the end of September. Then the FDA would likely make a decision about the vaccine’s safety and effectiveness in children within about 3 weeks, two sources told Reuters.
Anthony Fauci, MD, chief medical adviser to President Joe Biden and director of the National Institute of Allergy and Infectious Diseases, spoke about the timeline during an online town hall meeting Friday, Reuters reported. The meeting was attended by thousands of staff members at the National Institutes of Health.
If Pfizer submits paperwork to the FDA by the end of September, the vaccine could be available for kids around mid-October, Dr. Fauci said, and approval for the Moderna vaccine could come in November. Moderna will take about 3 weeks longer to collect and analyze data for ages 5-11.
Pfizer has said it would have enough data for ages 5-11 in September and would submit its documentation for FDA authorization soon after. Moderna told investors on Sept. 9 that data for ages 6-11 would be available by the end of the year.
On Sept. 10, the FDA said it would work to approve COVID-19 vaccines for children quickly once companies submit their data, according to Reuters. The agency said it would consider applications for emergency use, which would allow for faster approval.
Pfizer’s vaccine is the only one to receive full FDA approval, but only for people ages 16 and older. Adolescents ages 12-15 can receive the Pfizer vaccine under the FDA’s emergency use authorization.
For emergency use authorization, companies must submit 2 months of safety data versus 6 months for full approval. The FDA said on Sept. 10 that children in clinical trials should be monitored for at least 2 months to observe side effects.
BioNTech, Pfizer’s vaccine manufacturing partner, told a news outlet in Germany that it plans to request authorization globally for ages 5-11 in coming weeks, according to Reuters.
“Already over the next few weeks, we will file the results of our trial in 5- to 11-year-olds with regulators across the world and will request approval of the vaccine in this age group, also here in Europe,” Oezlem Tuereci, MD, the chief medical officer for BioNTech, told Der Spiegel.
The company is completing the final production steps to make the vaccine at lower doses for the younger age group, she said. Pfizer and BioNTech will also seek vaccine approval for ages 6 months to 2 years later this year.
“Things are looking good, everything is going according to plan,” Ugur Sahin, MD, the CEO of BioNTech, told Der Spiegel.
A version of this article first appeared on WebMD.com.
The timeline is based on the expectation that Pfizer will have enough data from clinical trials to request Food and Drug Administration emergency use authorization for the age group near the end of September. Then the FDA would likely make a decision about the vaccine’s safety and effectiveness in children within about 3 weeks, two sources told Reuters.
Anthony Fauci, MD, chief medical adviser to President Joe Biden and director of the National Institute of Allergy and Infectious Diseases, spoke about the timeline during an online town hall meeting Friday, Reuters reported. The meeting was attended by thousands of staff members at the National Institutes of Health.
If Pfizer submits paperwork to the FDA by the end of September, the vaccine could be available for kids around mid-October, Dr. Fauci said, and approval for the Moderna vaccine could come in November. Moderna will take about 3 weeks longer to collect and analyze data for ages 5-11.
Pfizer has said it would have enough data for ages 5-11 in September and would submit its documentation for FDA authorization soon after. Moderna told investors on Sept. 9 that data for ages 6-11 would be available by the end of the year.
On Sept. 10, the FDA said it would work to approve COVID-19 vaccines for children quickly once companies submit their data, according to Reuters. The agency said it would consider applications for emergency use, which would allow for faster approval.
Pfizer’s vaccine is the only one to receive full FDA approval, but only for people ages 16 and older. Adolescents ages 12-15 can receive the Pfizer vaccine under the FDA’s emergency use authorization.
For emergency use authorization, companies must submit 2 months of safety data versus 6 months for full approval. The FDA said on Sept. 10 that children in clinical trials should be monitored for at least 2 months to observe side effects.
BioNTech, Pfizer’s vaccine manufacturing partner, told a news outlet in Germany that it plans to request authorization globally for ages 5-11 in coming weeks, according to Reuters.
“Already over the next few weeks, we will file the results of our trial in 5- to 11-year-olds with regulators across the world and will request approval of the vaccine in this age group, also here in Europe,” Oezlem Tuereci, MD, the chief medical officer for BioNTech, told Der Spiegel.
The company is completing the final production steps to make the vaccine at lower doses for the younger age group, she said. Pfizer and BioNTech will also seek vaccine approval for ages 6 months to 2 years later this year.
“Things are looking good, everything is going according to plan,” Ugur Sahin, MD, the CEO of BioNTech, told Der Spiegel.
A version of this article first appeared on WebMD.com.
The timeline is based on the expectation that Pfizer will have enough data from clinical trials to request Food and Drug Administration emergency use authorization for the age group near the end of September. Then the FDA would likely make a decision about the vaccine’s safety and effectiveness in children within about 3 weeks, two sources told Reuters.
Anthony Fauci, MD, chief medical adviser to President Joe Biden and director of the National Institute of Allergy and Infectious Diseases, spoke about the timeline during an online town hall meeting Friday, Reuters reported. The meeting was attended by thousands of staff members at the National Institutes of Health.
If Pfizer submits paperwork to the FDA by the end of September, the vaccine could be available for kids around mid-October, Dr. Fauci said, and approval for the Moderna vaccine could come in November. Moderna will take about 3 weeks longer to collect and analyze data for ages 5-11.
Pfizer has said it would have enough data for ages 5-11 in September and would submit its documentation for FDA authorization soon after. Moderna told investors on Sept. 9 that data for ages 6-11 would be available by the end of the year.
On Sept. 10, the FDA said it would work to approve COVID-19 vaccines for children quickly once companies submit their data, according to Reuters. The agency said it would consider applications for emergency use, which would allow for faster approval.
Pfizer’s vaccine is the only one to receive full FDA approval, but only for people ages 16 and older. Adolescents ages 12-15 can receive the Pfizer vaccine under the FDA’s emergency use authorization.
For emergency use authorization, companies must submit 2 months of safety data versus 6 months for full approval. The FDA said on Sept. 10 that children in clinical trials should be monitored for at least 2 months to observe side effects.
BioNTech, Pfizer’s vaccine manufacturing partner, told a news outlet in Germany that it plans to request authorization globally for ages 5-11 in coming weeks, according to Reuters.
“Already over the next few weeks, we will file the results of our trial in 5- to 11-year-olds with regulators across the world and will request approval of the vaccine in this age group, also here in Europe,” Oezlem Tuereci, MD, the chief medical officer for BioNTech, told Der Spiegel.
The company is completing the final production steps to make the vaccine at lower doses for the younger age group, she said. Pfizer and BioNTech will also seek vaccine approval for ages 6 months to 2 years later this year.
“Things are looking good, everything is going according to plan,” Ugur Sahin, MD, the CEO of BioNTech, told Der Spiegel.
A version of this article first appeared on WebMD.com.
Researchers describe first reports of breakthrough COVID infections, booster shots in rheumatology patients
Although breakthrough COVID-19 infections appear to be infrequent in people with inflammatory rheumatic and musculoskeletal diseases (iRMDs), these patients’ comparatively low antibodies after their initial vaccine series validate the recommendation that booster doses could reinforce their immune responses. These findings were highlighted in three letters recently published in Annals of the Rheumatic Diseases.
In the first letter, the researchers assessed breakthrough COVID-19 infections among vaccinated patients with iRMDs who were treated within the Mass General Brigham health care system in the Boston area. Of the 340 COVID-19 infections in patients with iRMDs after vaccinations were approved by the Food and Drug Administration for emergency use, 16 (4.7%) were breakthrough infections. All but one of the breakthrough infections were symptomatic, and six of the patients were hospitalized.
Patients who had breakthrough infections took disease-modifying antirheumatic drugs (DMARDs) that included rituximab and glucocorticoids (five patients each), mycophenolate mofetil or mycophenolic acid (four patients), and methotrexate (three patients). Two of the patients died, both of whom were on rituximab and had interstitial lung disease.
“Some DMARD users may require alternative risk-mitigation strategies, including passive immunity or booster vaccines, and may need to continue shielding practices,” the authors wrote.
“Honestly, it’s hard to know what to make of that rate of breakthrough infections,” Camille Kotton, MD, clinical director of transplant and immunocompromised host infectious diseases in the infectious diseases division at Massachusetts General Hospital in Boston, said in an interview. “People who are immunocompromised were strongly advised to change behavior so as to avoid infection, which probably greatly alters their risk of breakthrough infection. It’s thus hard to evaluate vaccine efficacy.
“Also, 93% were symptomatic, which is fairly high,” she added. “I’m not sure if these patients were more likely to be symptomatic or if there was some bias in testing based on symptoms.”
In the second letter, the researchers assessed postvaccination COVID-19 infections in European patients with iRMDs. Two COVID-19 registries with thousands of patients were reviewed, with less than 1% of patients in each deemed eligible for this study. Of the 34 patients who were ultimately analyzed with available COVID-19 outcomes – 10 were fully vaccinated and 24 were partially vaccinated – 28 fully recovered, 3 recovered with ongoing sequelae, and 3 patients died. The three patients who died were all over 70 years old and had been treated with glucocorticoids and mycophenolate mofetil, glucocorticoids, and rituximab, respectively.
The medications most frequently used by the iRMDs patients with breakthrough cases included glucocorticoids (32%), methotrexate (26%), and tumor necrosis factor inhibitors (26%).
“Overall, the low numbers of SARS-CoV-2 infection post vaccination in both registries are encouraging,” the authors wrote, adding that “all three deceased patients were treated with medications that are potential negative influences on postvaccination SARS-CoV-2 immunogenicity in the RMD population.”
Patients with RMDs: Consider COVID-19 booster shots
In the third letter, the researchers investigated booster doses of COVID-19 vaccine in patients with autoimmune diseases. Of the 18 participants who received a booster dose, 14 were on antimetabolite therapy and 8 of those were on mycophenolate. At a median of 29 days after completion of their initial vaccine series, antispike antibodies were negative in 10 of the participants and low positive in 6 others, with a median antispike antibody level of less than 0.4 U/mL (interquartile range, <0.4-222 U/mL).
Booster doses were administered at a median of 77 days after completion of the initial series. At a median of 30 days after booster dose, 89% of the participants had an augmented humoral response, with a median antispike antibody level of 2,500 (IQR, 885-2,500 U/mL). Of the 10 participants who had negative anti-spike antibodies after the initial series, 80% were positive after the booster.
“I think this study supports the wealth of evidence that contributed to the [Centers for Disease Control and Prevention]’s and the FDA’s recommendation to get the third dose of the COVID vaccination,” coauthor Julie J. Paik, MD, of Johns Hopkins University, Baltimore, said in an interview. “Our patients are a very vulnerable group, including lupus patients or myositis patients, both of whom can get severe COVID if they were to contract it. They think they’re protected after a two-dose series, but in reality they’re not.
“We were just happy that they had a response,” she added. “Most of them had absolutely no response whatsoever after the first series.”
One other recently published case report in Arthritis & Rheumatology describes booster vaccination with the viral vector Johnson & Johnson vaccine in a man with seropositive RA who had previously received both doses of the Moderna mRNA-1273 vaccine. The 74-year-old man, who had low disease activity over the past 5 years on hydroxychloroquine, etanercept, and leflunomide, received the booster dose of his own accord after undergoing testing that showed a semiquantitative spike protein receptor binding domain (RBD) antibody level of 53.9 U/mL (reference range, 0-2,500 U/mL) and a negative SARS-CoV-2 antispike (S1/RBD) IgG test, as well as less than 10% blocking activity on an assay designed to detect blocking of the interaction between the SARS-CoV-2 spike protein RBD and the human ACE2 receptor and a negative interferon-gamma release assay detecting SARS-CoV-2–specific T cells. Several weeks after the booster dose, a repeat semiquantitative spike protein RBD antibody level was 2,455.0 U/mL and the S1/RBD IgG level was positive. An ACE2 blocking assay demonstrated 90%-100% blocking activity, but the interferon-gamma release assay remained negative.
“I would recommend abiding by the CDC guidelines regarding boosters for immunocompromised patients,” Dr. Kotton stated. “Patients with rheumatologic disease generally fit into the last category on that list. We don’t have an antibody titer that ensures protection, and as per CDC guidance, we don’t recommend checking antibody titers. Furthermore, boosters were given for this study before the CDC recommendation came out.”
Dr. Paik and coauthors acknowledged their study’s limitations, including a small, inhomogeneous sample and a lack of data on memory B-cell and T-cell response. They also echoed Dr. Kotton’s thoughts by noting that, although this subset of patients had notably limited antibody responses, “no antibody titer has been defined to correlate with protection.”
“Of course, the humoral response isn’t the whole story,” Dr. Paik said. “Some studies are showing that some vaccine recipients may not have the antibodies but their T-cell response may still be intact; it just takes time, and we’re not picking it up. Even if the antibody test is coming up negative, there may be some immunogenicity to the vaccine that we’re not detecting.
“Hopefully at some point, we’ll have more T-cell immunophenotyping to provide better insight into the full vaccine response.”
The Boston-area breakthrough study and the booster shot study were both funded primarily by grants from various institutes within the National Institutes of Health. The European study was financially supported by the European Alliance of Associations for Rheumatology.
Although breakthrough COVID-19 infections appear to be infrequent in people with inflammatory rheumatic and musculoskeletal diseases (iRMDs), these patients’ comparatively low antibodies after their initial vaccine series validate the recommendation that booster doses could reinforce their immune responses. These findings were highlighted in three letters recently published in Annals of the Rheumatic Diseases.
In the first letter, the researchers assessed breakthrough COVID-19 infections among vaccinated patients with iRMDs who were treated within the Mass General Brigham health care system in the Boston area. Of the 340 COVID-19 infections in patients with iRMDs after vaccinations were approved by the Food and Drug Administration for emergency use, 16 (4.7%) were breakthrough infections. All but one of the breakthrough infections were symptomatic, and six of the patients were hospitalized.
Patients who had breakthrough infections took disease-modifying antirheumatic drugs (DMARDs) that included rituximab and glucocorticoids (five patients each), mycophenolate mofetil or mycophenolic acid (four patients), and methotrexate (three patients). Two of the patients died, both of whom were on rituximab and had interstitial lung disease.
“Some DMARD users may require alternative risk-mitigation strategies, including passive immunity or booster vaccines, and may need to continue shielding practices,” the authors wrote.
“Honestly, it’s hard to know what to make of that rate of breakthrough infections,” Camille Kotton, MD, clinical director of transplant and immunocompromised host infectious diseases in the infectious diseases division at Massachusetts General Hospital in Boston, said in an interview. “People who are immunocompromised were strongly advised to change behavior so as to avoid infection, which probably greatly alters their risk of breakthrough infection. It’s thus hard to evaluate vaccine efficacy.
“Also, 93% were symptomatic, which is fairly high,” she added. “I’m not sure if these patients were more likely to be symptomatic or if there was some bias in testing based on symptoms.”
In the second letter, the researchers assessed postvaccination COVID-19 infections in European patients with iRMDs. Two COVID-19 registries with thousands of patients were reviewed, with less than 1% of patients in each deemed eligible for this study. Of the 34 patients who were ultimately analyzed with available COVID-19 outcomes – 10 were fully vaccinated and 24 were partially vaccinated – 28 fully recovered, 3 recovered with ongoing sequelae, and 3 patients died. The three patients who died were all over 70 years old and had been treated with glucocorticoids and mycophenolate mofetil, glucocorticoids, and rituximab, respectively.
The medications most frequently used by the iRMDs patients with breakthrough cases included glucocorticoids (32%), methotrexate (26%), and tumor necrosis factor inhibitors (26%).
“Overall, the low numbers of SARS-CoV-2 infection post vaccination in both registries are encouraging,” the authors wrote, adding that “all three deceased patients were treated with medications that are potential negative influences on postvaccination SARS-CoV-2 immunogenicity in the RMD population.”
Patients with RMDs: Consider COVID-19 booster shots
In the third letter, the researchers investigated booster doses of COVID-19 vaccine in patients with autoimmune diseases. Of the 18 participants who received a booster dose, 14 were on antimetabolite therapy and 8 of those were on mycophenolate. At a median of 29 days after completion of their initial vaccine series, antispike antibodies were negative in 10 of the participants and low positive in 6 others, with a median antispike antibody level of less than 0.4 U/mL (interquartile range, <0.4-222 U/mL).
Booster doses were administered at a median of 77 days after completion of the initial series. At a median of 30 days after booster dose, 89% of the participants had an augmented humoral response, with a median antispike antibody level of 2,500 (IQR, 885-2,500 U/mL). Of the 10 participants who had negative anti-spike antibodies after the initial series, 80% were positive after the booster.
“I think this study supports the wealth of evidence that contributed to the [Centers for Disease Control and Prevention]’s and the FDA’s recommendation to get the third dose of the COVID vaccination,” coauthor Julie J. Paik, MD, of Johns Hopkins University, Baltimore, said in an interview. “Our patients are a very vulnerable group, including lupus patients or myositis patients, both of whom can get severe COVID if they were to contract it. They think they’re protected after a two-dose series, but in reality they’re not.
“We were just happy that they had a response,” she added. “Most of them had absolutely no response whatsoever after the first series.”
One other recently published case report in Arthritis & Rheumatology describes booster vaccination with the viral vector Johnson & Johnson vaccine in a man with seropositive RA who had previously received both doses of the Moderna mRNA-1273 vaccine. The 74-year-old man, who had low disease activity over the past 5 years on hydroxychloroquine, etanercept, and leflunomide, received the booster dose of his own accord after undergoing testing that showed a semiquantitative spike protein receptor binding domain (RBD) antibody level of 53.9 U/mL (reference range, 0-2,500 U/mL) and a negative SARS-CoV-2 antispike (S1/RBD) IgG test, as well as less than 10% blocking activity on an assay designed to detect blocking of the interaction between the SARS-CoV-2 spike protein RBD and the human ACE2 receptor and a negative interferon-gamma release assay detecting SARS-CoV-2–specific T cells. Several weeks after the booster dose, a repeat semiquantitative spike protein RBD antibody level was 2,455.0 U/mL and the S1/RBD IgG level was positive. An ACE2 blocking assay demonstrated 90%-100% blocking activity, but the interferon-gamma release assay remained negative.
“I would recommend abiding by the CDC guidelines regarding boosters for immunocompromised patients,” Dr. Kotton stated. “Patients with rheumatologic disease generally fit into the last category on that list. We don’t have an antibody titer that ensures protection, and as per CDC guidance, we don’t recommend checking antibody titers. Furthermore, boosters were given for this study before the CDC recommendation came out.”
Dr. Paik and coauthors acknowledged their study’s limitations, including a small, inhomogeneous sample and a lack of data on memory B-cell and T-cell response. They also echoed Dr. Kotton’s thoughts by noting that, although this subset of patients had notably limited antibody responses, “no antibody titer has been defined to correlate with protection.”
“Of course, the humoral response isn’t the whole story,” Dr. Paik said. “Some studies are showing that some vaccine recipients may not have the antibodies but their T-cell response may still be intact; it just takes time, and we’re not picking it up. Even if the antibody test is coming up negative, there may be some immunogenicity to the vaccine that we’re not detecting.
“Hopefully at some point, we’ll have more T-cell immunophenotyping to provide better insight into the full vaccine response.”
The Boston-area breakthrough study and the booster shot study were both funded primarily by grants from various institutes within the National Institutes of Health. The European study was financially supported by the European Alliance of Associations for Rheumatology.
Although breakthrough COVID-19 infections appear to be infrequent in people with inflammatory rheumatic and musculoskeletal diseases (iRMDs), these patients’ comparatively low antibodies after their initial vaccine series validate the recommendation that booster doses could reinforce their immune responses. These findings were highlighted in three letters recently published in Annals of the Rheumatic Diseases.
In the first letter, the researchers assessed breakthrough COVID-19 infections among vaccinated patients with iRMDs who were treated within the Mass General Brigham health care system in the Boston area. Of the 340 COVID-19 infections in patients with iRMDs after vaccinations were approved by the Food and Drug Administration for emergency use, 16 (4.7%) were breakthrough infections. All but one of the breakthrough infections were symptomatic, and six of the patients were hospitalized.
Patients who had breakthrough infections took disease-modifying antirheumatic drugs (DMARDs) that included rituximab and glucocorticoids (five patients each), mycophenolate mofetil or mycophenolic acid (four patients), and methotrexate (three patients). Two of the patients died, both of whom were on rituximab and had interstitial lung disease.
“Some DMARD users may require alternative risk-mitigation strategies, including passive immunity or booster vaccines, and may need to continue shielding practices,” the authors wrote.
“Honestly, it’s hard to know what to make of that rate of breakthrough infections,” Camille Kotton, MD, clinical director of transplant and immunocompromised host infectious diseases in the infectious diseases division at Massachusetts General Hospital in Boston, said in an interview. “People who are immunocompromised were strongly advised to change behavior so as to avoid infection, which probably greatly alters their risk of breakthrough infection. It’s thus hard to evaluate vaccine efficacy.
“Also, 93% were symptomatic, which is fairly high,” she added. “I’m not sure if these patients were more likely to be symptomatic or if there was some bias in testing based on symptoms.”
In the second letter, the researchers assessed postvaccination COVID-19 infections in European patients with iRMDs. Two COVID-19 registries with thousands of patients were reviewed, with less than 1% of patients in each deemed eligible for this study. Of the 34 patients who were ultimately analyzed with available COVID-19 outcomes – 10 were fully vaccinated and 24 were partially vaccinated – 28 fully recovered, 3 recovered with ongoing sequelae, and 3 patients died. The three patients who died were all over 70 years old and had been treated with glucocorticoids and mycophenolate mofetil, glucocorticoids, and rituximab, respectively.
The medications most frequently used by the iRMDs patients with breakthrough cases included glucocorticoids (32%), methotrexate (26%), and tumor necrosis factor inhibitors (26%).
“Overall, the low numbers of SARS-CoV-2 infection post vaccination in both registries are encouraging,” the authors wrote, adding that “all three deceased patients were treated with medications that are potential negative influences on postvaccination SARS-CoV-2 immunogenicity in the RMD population.”
Patients with RMDs: Consider COVID-19 booster shots
In the third letter, the researchers investigated booster doses of COVID-19 vaccine in patients with autoimmune diseases. Of the 18 participants who received a booster dose, 14 were on antimetabolite therapy and 8 of those were on mycophenolate. At a median of 29 days after completion of their initial vaccine series, antispike antibodies were negative in 10 of the participants and low positive in 6 others, with a median antispike antibody level of less than 0.4 U/mL (interquartile range, <0.4-222 U/mL).
Booster doses were administered at a median of 77 days after completion of the initial series. At a median of 30 days after booster dose, 89% of the participants had an augmented humoral response, with a median antispike antibody level of 2,500 (IQR, 885-2,500 U/mL). Of the 10 participants who had negative anti-spike antibodies after the initial series, 80% were positive after the booster.
“I think this study supports the wealth of evidence that contributed to the [Centers for Disease Control and Prevention]’s and the FDA’s recommendation to get the third dose of the COVID vaccination,” coauthor Julie J. Paik, MD, of Johns Hopkins University, Baltimore, said in an interview. “Our patients are a very vulnerable group, including lupus patients or myositis patients, both of whom can get severe COVID if they were to contract it. They think they’re protected after a two-dose series, but in reality they’re not.
“We were just happy that they had a response,” she added. “Most of them had absolutely no response whatsoever after the first series.”
One other recently published case report in Arthritis & Rheumatology describes booster vaccination with the viral vector Johnson & Johnson vaccine in a man with seropositive RA who had previously received both doses of the Moderna mRNA-1273 vaccine. The 74-year-old man, who had low disease activity over the past 5 years on hydroxychloroquine, etanercept, and leflunomide, received the booster dose of his own accord after undergoing testing that showed a semiquantitative spike protein receptor binding domain (RBD) antibody level of 53.9 U/mL (reference range, 0-2,500 U/mL) and a negative SARS-CoV-2 antispike (S1/RBD) IgG test, as well as less than 10% blocking activity on an assay designed to detect blocking of the interaction between the SARS-CoV-2 spike protein RBD and the human ACE2 receptor and a negative interferon-gamma release assay detecting SARS-CoV-2–specific T cells. Several weeks after the booster dose, a repeat semiquantitative spike protein RBD antibody level was 2,455.0 U/mL and the S1/RBD IgG level was positive. An ACE2 blocking assay demonstrated 90%-100% blocking activity, but the interferon-gamma release assay remained negative.
“I would recommend abiding by the CDC guidelines regarding boosters for immunocompromised patients,” Dr. Kotton stated. “Patients with rheumatologic disease generally fit into the last category on that list. We don’t have an antibody titer that ensures protection, and as per CDC guidance, we don’t recommend checking antibody titers. Furthermore, boosters were given for this study before the CDC recommendation came out.”
Dr. Paik and coauthors acknowledged their study’s limitations, including a small, inhomogeneous sample and a lack of data on memory B-cell and T-cell response. They also echoed Dr. Kotton’s thoughts by noting that, although this subset of patients had notably limited antibody responses, “no antibody titer has been defined to correlate with protection.”
“Of course, the humoral response isn’t the whole story,” Dr. Paik said. “Some studies are showing that some vaccine recipients may not have the antibodies but their T-cell response may still be intact; it just takes time, and we’re not picking it up. Even if the antibody test is coming up negative, there may be some immunogenicity to the vaccine that we’re not detecting.
“Hopefully at some point, we’ll have more T-cell immunophenotyping to provide better insight into the full vaccine response.”
The Boston-area breakthrough study and the booster shot study were both funded primarily by grants from various institutes within the National Institutes of Health. The European study was financially supported by the European Alliance of Associations for Rheumatology.
FROM ANNALS OF THE RHEUMATIC DISEASES








