User login
Quadrivalent flu vaccine okayed for 6 months and up
The expanded approval now includes persons aged 6-59 months; the quadrivalent vaccine had previously been approved for ages 5 years and up. A trivalent version of the Afluria influenza vaccine also now is indicated for people aged 6 months and up, according to an Oct. 4 communication from the FDA.
A total of 172 pediatric influenza-related deaths occurred in the United States during the 2017-2018 season, representing a new high in nonpandemic influenza seasons. About half of the pediatric influenza deaths occurred in otherwise healthy children, and about 22% of children who died were fully vaccinated, according to the Centers for Disease Control and Prevention, reporting U.S. data from 2010 to 2016.
“As we enter a new flu season, we are reminded of the enormous impact that influenza can have on public health,” Seqirus’ vice president of medical affairs Gregg Sylvester, MD, said in a press release announcing the extended indication. “Having another option to fight this disease can translate to saved lives and fewer flu-related hospitalizations this season and going forward.”
According to the CDC, the 2018-2019 influenza vaccine has been updated to provide a better match – and more protection against – viruses circulating in this influenza season. Specifically, says the CDC, the influenza B Victoria lineage and the influenza A(H3N2) components were updated.
In addition to providing protection against these two strains of influenza, trivalent vaccines for the 2018-2019 season are recommended to include protection against H1N1 influenza as well. Quadrivalent vaccines protect against a second influenza B lineage.
Most people will receive a quadrivalent vaccine this year, according to the CDC.
The expanded approval now includes persons aged 6-59 months; the quadrivalent vaccine had previously been approved for ages 5 years and up. A trivalent version of the Afluria influenza vaccine also now is indicated for people aged 6 months and up, according to an Oct. 4 communication from the FDA.
A total of 172 pediatric influenza-related deaths occurred in the United States during the 2017-2018 season, representing a new high in nonpandemic influenza seasons. About half of the pediatric influenza deaths occurred in otherwise healthy children, and about 22% of children who died were fully vaccinated, according to the Centers for Disease Control and Prevention, reporting U.S. data from 2010 to 2016.
“As we enter a new flu season, we are reminded of the enormous impact that influenza can have on public health,” Seqirus’ vice president of medical affairs Gregg Sylvester, MD, said in a press release announcing the extended indication. “Having another option to fight this disease can translate to saved lives and fewer flu-related hospitalizations this season and going forward.”
According to the CDC, the 2018-2019 influenza vaccine has been updated to provide a better match – and more protection against – viruses circulating in this influenza season. Specifically, says the CDC, the influenza B Victoria lineage and the influenza A(H3N2) components were updated.
In addition to providing protection against these two strains of influenza, trivalent vaccines for the 2018-2019 season are recommended to include protection against H1N1 influenza as well. Quadrivalent vaccines protect against a second influenza B lineage.
Most people will receive a quadrivalent vaccine this year, according to the CDC.
The expanded approval now includes persons aged 6-59 months; the quadrivalent vaccine had previously been approved for ages 5 years and up. A trivalent version of the Afluria influenza vaccine also now is indicated for people aged 6 months and up, according to an Oct. 4 communication from the FDA.
A total of 172 pediatric influenza-related deaths occurred in the United States during the 2017-2018 season, representing a new high in nonpandemic influenza seasons. About half of the pediatric influenza deaths occurred in otherwise healthy children, and about 22% of children who died were fully vaccinated, according to the Centers for Disease Control and Prevention, reporting U.S. data from 2010 to 2016.
“As we enter a new flu season, we are reminded of the enormous impact that influenza can have on public health,” Seqirus’ vice president of medical affairs Gregg Sylvester, MD, said in a press release announcing the extended indication. “Having another option to fight this disease can translate to saved lives and fewer flu-related hospitalizations this season and going forward.”
According to the CDC, the 2018-2019 influenza vaccine has been updated to provide a better match – and more protection against – viruses circulating in this influenza season. Specifically, says the CDC, the influenza B Victoria lineage and the influenza A(H3N2) components were updated.
In addition to providing protection against these two strains of influenza, trivalent vaccines for the 2018-2019 season are recommended to include protection against H1N1 influenza as well. Quadrivalent vaccines protect against a second influenza B lineage.
Most people will receive a quadrivalent vaccine this year, according to the CDC.
High-dose flu vaccine in RA patients beats standard dose
CHICAGO – The administration of high-dose vs. standard-dose influenza vaccine provided substantially better immune responses in seropositive rheumatoid arthritis patients in a randomized, active-controlled trial.
High-dose trivalent influenza vaccine is known to improve immune responses in the elderly, but the current findings, which were presented at the annual meeting of the American College of Rheumatology, are the first to document a successful intervention to enhance vaccine responses in immunocompromised patients, according to Inés Colmegna, MD, of McGill University, Montreal.
Dr. Colmegna and her colleagues assessed antibody responses to either standard-dose (15 mcg of hemagglutinin per strain) quadrivalent inactivated influenza vaccine (SD-QIV) or high-dose (60 mcg of hemagglutinin per strain) trivalent inactivated influenza vaccine (HD-TIV) in 140 and 139 patients, respectively.
Seroprotection rates prior to vaccination were comparable in the two groups, but the high-dose recipients had consistently higher overall responses to vaccination.
Seroconversion rates were 22.3% vs. 8.6% (odds ratio, 2.93) for the H3N2 strain (A/HongKong/4801/2014), and 44.6% vs. 28.6% (OR, 1.93) for the B Victoria Lin strain (B/Brisbane/60/2008). For the H1N1 strain A/California/7/2009 in 2016-2017 and closely related A/Michigan/45/2015 in 2017-2018, the seroconversion rates were 51.1% vs. 30.0% (OR, 2.91) and 46.4% vs. 24.6% (OR, 2.79), respectively. Seroprotection rates for the H3N2 strain were 48.5% vs. 30.9%, and for the B Victoria Lin strain, 60.0% vs. 50.7%. The seroprotection rates for the H1N1 strains together were and 80.4% vs. 73.5%, Dr. Colmegna said.
Seroconversion was defined as at least a fourfold serum hemagglutination inhibition (HI) antibody increase from prevaccination level (day 0), and seroprotection was defined as percent with HI titers of 1:40 or greater at postvaccination day 28.
After the researchers controlled for age, vaccine type, treatment type in the 3 months prior to vaccination and during the study period, Charlson comorbidity index, and RA duration, the only significant predictors of vaccine seroresponse were vaccine dose and age.
The findings are notable because RA patients have a nearly threefold increase in the risk of contracting influenza infection or related illness, compared with age-matched healthy controls, because of “inherent immune dysfunction associated with RA, comorbidities, the age of our patients, and immunosuppressive therapy,” Dr. Colmegna said.
For this reason, RA patients are a priority group for annual vaccination. However, while vaccination remains the most effective method for preventing influenza and its associated complications, vaccine-induced antibody responses and protection in RA are suboptimal, she explained, noting that this puts them at increased risk for severe influenza.
“There is a high priority to develop new approaches to try to decrease this risk,” she said.
It was unknown whether HD-TIV – the only currently available high-dose influenza vaccine – would safely enhance antibody production in RA as it does in the elderly, so she and her colleagues recruited patients from a tertiary care center during the 2016-2017 and 2017-2018 Northern Hemisphere influenza seasons for this study.
The mean age of the patients was 61 years, and 80% were women. All were on stable treatment with either disease-modifying antirheumatic drugs (DMARDs) or biologics for at least 3 months prior to vaccination; treatment types included DMARDs in 138 patients (49.5%), anticytokine therapy in 92 patients (33%), and anti-B-cell therapy and small molecules in 49 patients (17.6%). An analysis by treatment type showed a possible reduction in the rate of seroconversion in patients who received anti-B-cell therapy and small molecules, but the number of patients in the group was too small to make definitive conclusions, Dr. Colmegna said.
Treatment in all groups was safe, with no differences in adverse events between those receiving high- or standard-dose vaccine, and none of the adverse events were related to treatment.
Further, the high-dose vaccine was not associated with an increase in disease activity.
“We believe that these results will likely change clinical practice,” she concluded.
Dr. Colmegna reported having no disclosures.
SOURCE: Colmegna I et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 837.
CHICAGO – The administration of high-dose vs. standard-dose influenza vaccine provided substantially better immune responses in seropositive rheumatoid arthritis patients in a randomized, active-controlled trial.
High-dose trivalent influenza vaccine is known to improve immune responses in the elderly, but the current findings, which were presented at the annual meeting of the American College of Rheumatology, are the first to document a successful intervention to enhance vaccine responses in immunocompromised patients, according to Inés Colmegna, MD, of McGill University, Montreal.
Dr. Colmegna and her colleagues assessed antibody responses to either standard-dose (15 mcg of hemagglutinin per strain) quadrivalent inactivated influenza vaccine (SD-QIV) or high-dose (60 mcg of hemagglutinin per strain) trivalent inactivated influenza vaccine (HD-TIV) in 140 and 139 patients, respectively.
Seroprotection rates prior to vaccination were comparable in the two groups, but the high-dose recipients had consistently higher overall responses to vaccination.
Seroconversion rates were 22.3% vs. 8.6% (odds ratio, 2.93) for the H3N2 strain (A/HongKong/4801/2014), and 44.6% vs. 28.6% (OR, 1.93) for the B Victoria Lin strain (B/Brisbane/60/2008). For the H1N1 strain A/California/7/2009 in 2016-2017 and closely related A/Michigan/45/2015 in 2017-2018, the seroconversion rates were 51.1% vs. 30.0% (OR, 2.91) and 46.4% vs. 24.6% (OR, 2.79), respectively. Seroprotection rates for the H3N2 strain were 48.5% vs. 30.9%, and for the B Victoria Lin strain, 60.0% vs. 50.7%. The seroprotection rates for the H1N1 strains together were and 80.4% vs. 73.5%, Dr. Colmegna said.
Seroconversion was defined as at least a fourfold serum hemagglutination inhibition (HI) antibody increase from prevaccination level (day 0), and seroprotection was defined as percent with HI titers of 1:40 or greater at postvaccination day 28.
After the researchers controlled for age, vaccine type, treatment type in the 3 months prior to vaccination and during the study period, Charlson comorbidity index, and RA duration, the only significant predictors of vaccine seroresponse were vaccine dose and age.
The findings are notable because RA patients have a nearly threefold increase in the risk of contracting influenza infection or related illness, compared with age-matched healthy controls, because of “inherent immune dysfunction associated with RA, comorbidities, the age of our patients, and immunosuppressive therapy,” Dr. Colmegna said.
For this reason, RA patients are a priority group for annual vaccination. However, while vaccination remains the most effective method for preventing influenza and its associated complications, vaccine-induced antibody responses and protection in RA are suboptimal, she explained, noting that this puts them at increased risk for severe influenza.
“There is a high priority to develop new approaches to try to decrease this risk,” she said.
It was unknown whether HD-TIV – the only currently available high-dose influenza vaccine – would safely enhance antibody production in RA as it does in the elderly, so she and her colleagues recruited patients from a tertiary care center during the 2016-2017 and 2017-2018 Northern Hemisphere influenza seasons for this study.
The mean age of the patients was 61 years, and 80% were women. All were on stable treatment with either disease-modifying antirheumatic drugs (DMARDs) or biologics for at least 3 months prior to vaccination; treatment types included DMARDs in 138 patients (49.5%), anticytokine therapy in 92 patients (33%), and anti-B-cell therapy and small molecules in 49 patients (17.6%). An analysis by treatment type showed a possible reduction in the rate of seroconversion in patients who received anti-B-cell therapy and small molecules, but the number of patients in the group was too small to make definitive conclusions, Dr. Colmegna said.
Treatment in all groups was safe, with no differences in adverse events between those receiving high- or standard-dose vaccine, and none of the adverse events were related to treatment.
Further, the high-dose vaccine was not associated with an increase in disease activity.
“We believe that these results will likely change clinical practice,” she concluded.
Dr. Colmegna reported having no disclosures.
SOURCE: Colmegna I et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 837.
CHICAGO – The administration of high-dose vs. standard-dose influenza vaccine provided substantially better immune responses in seropositive rheumatoid arthritis patients in a randomized, active-controlled trial.
High-dose trivalent influenza vaccine is known to improve immune responses in the elderly, but the current findings, which were presented at the annual meeting of the American College of Rheumatology, are the first to document a successful intervention to enhance vaccine responses in immunocompromised patients, according to Inés Colmegna, MD, of McGill University, Montreal.
Dr. Colmegna and her colleagues assessed antibody responses to either standard-dose (15 mcg of hemagglutinin per strain) quadrivalent inactivated influenza vaccine (SD-QIV) or high-dose (60 mcg of hemagglutinin per strain) trivalent inactivated influenza vaccine (HD-TIV) in 140 and 139 patients, respectively.
Seroprotection rates prior to vaccination were comparable in the two groups, but the high-dose recipients had consistently higher overall responses to vaccination.
Seroconversion rates were 22.3% vs. 8.6% (odds ratio, 2.93) for the H3N2 strain (A/HongKong/4801/2014), and 44.6% vs. 28.6% (OR, 1.93) for the B Victoria Lin strain (B/Brisbane/60/2008). For the H1N1 strain A/California/7/2009 in 2016-2017 and closely related A/Michigan/45/2015 in 2017-2018, the seroconversion rates were 51.1% vs. 30.0% (OR, 2.91) and 46.4% vs. 24.6% (OR, 2.79), respectively. Seroprotection rates for the H3N2 strain were 48.5% vs. 30.9%, and for the B Victoria Lin strain, 60.0% vs. 50.7%. The seroprotection rates for the H1N1 strains together were and 80.4% vs. 73.5%, Dr. Colmegna said.
Seroconversion was defined as at least a fourfold serum hemagglutination inhibition (HI) antibody increase from prevaccination level (day 0), and seroprotection was defined as percent with HI titers of 1:40 or greater at postvaccination day 28.
After the researchers controlled for age, vaccine type, treatment type in the 3 months prior to vaccination and during the study period, Charlson comorbidity index, and RA duration, the only significant predictors of vaccine seroresponse were vaccine dose and age.
The findings are notable because RA patients have a nearly threefold increase in the risk of contracting influenza infection or related illness, compared with age-matched healthy controls, because of “inherent immune dysfunction associated with RA, comorbidities, the age of our patients, and immunosuppressive therapy,” Dr. Colmegna said.
For this reason, RA patients are a priority group for annual vaccination. However, while vaccination remains the most effective method for preventing influenza and its associated complications, vaccine-induced antibody responses and protection in RA are suboptimal, she explained, noting that this puts them at increased risk for severe influenza.
“There is a high priority to develop new approaches to try to decrease this risk,” she said.
It was unknown whether HD-TIV – the only currently available high-dose influenza vaccine – would safely enhance antibody production in RA as it does in the elderly, so she and her colleagues recruited patients from a tertiary care center during the 2016-2017 and 2017-2018 Northern Hemisphere influenza seasons for this study.
The mean age of the patients was 61 years, and 80% were women. All were on stable treatment with either disease-modifying antirheumatic drugs (DMARDs) or biologics for at least 3 months prior to vaccination; treatment types included DMARDs in 138 patients (49.5%), anticytokine therapy in 92 patients (33%), and anti-B-cell therapy and small molecules in 49 patients (17.6%). An analysis by treatment type showed a possible reduction in the rate of seroconversion in patients who received anti-B-cell therapy and small molecules, but the number of patients in the group was too small to make definitive conclusions, Dr. Colmegna said.
Treatment in all groups was safe, with no differences in adverse events between those receiving high- or standard-dose vaccine, and none of the adverse events were related to treatment.
Further, the high-dose vaccine was not associated with an increase in disease activity.
“We believe that these results will likely change clinical practice,” she concluded.
Dr. Colmegna reported having no disclosures.
SOURCE: Colmegna I et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 837.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: High- vs. standard-dose flu vaccine improves immune responses in RA patients.
Major finding: High-dose trivalent inactivated influenza vaccine was associated with greater odds of H3N2, B Victoria Lin, and H1N1 seroconversion.
Study details: A randomized, active-controlled trial of 279 RA patients
Disclosures: Dr. Colmegna reported having no disclosures.
Source: Colmegna I et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 837.
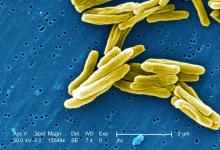
TB vaccine shows promise in previously infected
san francisco – A new The vaccine showed efficacy in young adults – an important finding because models suggest that inducing immunity in adolescents and young adults would be the fastest and most cost-effective approach to dealing with the global TB epidemic.
The study recruited adults who had previously been exposed to Mycobacterium tuberculosis, a population that receives no benefit from the long-standing bacillus Calmette-Guérin (BCG) vaccine. The overall efficacy of protection was 54%. “There isn’t any vaccine that’s been demonstrated to work in people who are already infected. It’s also the first vaccine to show this level of statistically significant protection in adults, and it’s adults who are the major transmitters of tuberculosis. The modeling has shown that even a vaccine that could protect infected adults at 20% vaccine efficacy would have a substantial impact on the epidemic and be cost effective,” said Ann Ginsberg, MD, PhD, chief medical officer at Aeras, which developed the vaccine and is now testing it in partnership with GlaxoSmithKline.
The results of the study were presented at ID Week 2018 and published in the New England Journal of Medicine (2018 Sep 25. doi: 10.1056/NEJMoa1803484).
The results address a major weakness of the BCG vaccine, which is that some studies have shown it offers little benefit to subjects who are already infected with the disease, which is the case for about a quarter of the world’s population, according to Dr. Ginsberg. The probable explanation is that previous infection with M. tuberculosis or a related bacteria is common in some populations and that this exposure grants some protection against progression to active disease.
The researchers tested the M72/AS01E vaccine, which includes two M. tuberculosis antigens that were identified from patients who had controlled their infection and also the AS01 adjuvant, which contains two immunostimulating agents and is a component of a developmental malaria vaccine and the recombinant zoster vaccine Shingrix.
In Kenya, South Africa, and Zambia, the researchers randomized 3,330 participants (mean age, 28.9 years; 43% female) to receive two doses 1 month apart of either vaccine or placebo. After a mean follow-up of 2.3 years, the protocol efficacy analysis showed that the vaccine had an efficacy rate of 54.0% (P = .04) for pulmonary tuberculosis.
The vaccine had greater efficacy in men (75.2%; P = .03) than it did in women (27.4%; P = .52) and among individuals aged 25 years or younger (84.4%; P = .01) than it did among older subjects (10.2%, P = .82).
The frequency of serious adverse events was similar between the vaccine (1.6%) and the placebo group (1.8%). Unsolicited reports of adverse events were more common in the vaccine group than the placebo group (67.4% vs. 45.4%, respectively), driven largely by more reports of injection site reactions and flu-like symptoms. Solicited reports of adverse events were highlighted by a greater frequency of injection site pain in the vaccine group (81.8% vs. 34.4%). A total of 24.3% of the vaccine recipients reported grade 3 pain, compared with 3.3% in the placebo arm. Rates of fatigue, headache, malaise, or myalgia were also higher in the vaccine group, as was fever.
All of the subjects in the vaccine group had seroconversion at month 2, and 99% remained seroconverted at 12 months.
Next, the researchers plan to conduct studies in HIV-infected individuals and to proceed with phase III trials.
The trial was funded by GlaxoSmithKline Biologicals and Aeras. Dr. Ginsberg is an employee of Aeras.
SOURCE: Ginsberg A et al. IDWeek 2018, Abstract 120
san francisco – A new The vaccine showed efficacy in young adults – an important finding because models suggest that inducing immunity in adolescents and young adults would be the fastest and most cost-effective approach to dealing with the global TB epidemic.
The study recruited adults who had previously been exposed to Mycobacterium tuberculosis, a population that receives no benefit from the long-standing bacillus Calmette-Guérin (BCG) vaccine. The overall efficacy of protection was 54%. “There isn’t any vaccine that’s been demonstrated to work in people who are already infected. It’s also the first vaccine to show this level of statistically significant protection in adults, and it’s adults who are the major transmitters of tuberculosis. The modeling has shown that even a vaccine that could protect infected adults at 20% vaccine efficacy would have a substantial impact on the epidemic and be cost effective,” said Ann Ginsberg, MD, PhD, chief medical officer at Aeras, which developed the vaccine and is now testing it in partnership with GlaxoSmithKline.
The results of the study were presented at ID Week 2018 and published in the New England Journal of Medicine (2018 Sep 25. doi: 10.1056/NEJMoa1803484).
The results address a major weakness of the BCG vaccine, which is that some studies have shown it offers little benefit to subjects who are already infected with the disease, which is the case for about a quarter of the world’s population, according to Dr. Ginsberg. The probable explanation is that previous infection with M. tuberculosis or a related bacteria is common in some populations and that this exposure grants some protection against progression to active disease.
The researchers tested the M72/AS01E vaccine, which includes two M. tuberculosis antigens that were identified from patients who had controlled their infection and also the AS01 adjuvant, which contains two immunostimulating agents and is a component of a developmental malaria vaccine and the recombinant zoster vaccine Shingrix.
In Kenya, South Africa, and Zambia, the researchers randomized 3,330 participants (mean age, 28.9 years; 43% female) to receive two doses 1 month apart of either vaccine or placebo. After a mean follow-up of 2.3 years, the protocol efficacy analysis showed that the vaccine had an efficacy rate of 54.0% (P = .04) for pulmonary tuberculosis.
The vaccine had greater efficacy in men (75.2%; P = .03) than it did in women (27.4%; P = .52) and among individuals aged 25 years or younger (84.4%; P = .01) than it did among older subjects (10.2%, P = .82).
The frequency of serious adverse events was similar between the vaccine (1.6%) and the placebo group (1.8%). Unsolicited reports of adverse events were more common in the vaccine group than the placebo group (67.4% vs. 45.4%, respectively), driven largely by more reports of injection site reactions and flu-like symptoms. Solicited reports of adverse events were highlighted by a greater frequency of injection site pain in the vaccine group (81.8% vs. 34.4%). A total of 24.3% of the vaccine recipients reported grade 3 pain, compared with 3.3% in the placebo arm. Rates of fatigue, headache, malaise, or myalgia were also higher in the vaccine group, as was fever.
All of the subjects in the vaccine group had seroconversion at month 2, and 99% remained seroconverted at 12 months.
Next, the researchers plan to conduct studies in HIV-infected individuals and to proceed with phase III trials.
The trial was funded by GlaxoSmithKline Biologicals and Aeras. Dr. Ginsberg is an employee of Aeras.
SOURCE: Ginsberg A et al. IDWeek 2018, Abstract 120
san francisco – A new The vaccine showed efficacy in young adults – an important finding because models suggest that inducing immunity in adolescents and young adults would be the fastest and most cost-effective approach to dealing with the global TB epidemic.
The study recruited adults who had previously been exposed to Mycobacterium tuberculosis, a population that receives no benefit from the long-standing bacillus Calmette-Guérin (BCG) vaccine. The overall efficacy of protection was 54%. “There isn’t any vaccine that’s been demonstrated to work in people who are already infected. It’s also the first vaccine to show this level of statistically significant protection in adults, and it’s adults who are the major transmitters of tuberculosis. The modeling has shown that even a vaccine that could protect infected adults at 20% vaccine efficacy would have a substantial impact on the epidemic and be cost effective,” said Ann Ginsberg, MD, PhD, chief medical officer at Aeras, which developed the vaccine and is now testing it in partnership with GlaxoSmithKline.
The results of the study were presented at ID Week 2018 and published in the New England Journal of Medicine (2018 Sep 25. doi: 10.1056/NEJMoa1803484).
The results address a major weakness of the BCG vaccine, which is that some studies have shown it offers little benefit to subjects who are already infected with the disease, which is the case for about a quarter of the world’s population, according to Dr. Ginsberg. The probable explanation is that previous infection with M. tuberculosis or a related bacteria is common in some populations and that this exposure grants some protection against progression to active disease.
The researchers tested the M72/AS01E vaccine, which includes two M. tuberculosis antigens that were identified from patients who had controlled their infection and also the AS01 adjuvant, which contains two immunostimulating agents and is a component of a developmental malaria vaccine and the recombinant zoster vaccine Shingrix.
In Kenya, South Africa, and Zambia, the researchers randomized 3,330 participants (mean age, 28.9 years; 43% female) to receive two doses 1 month apart of either vaccine or placebo. After a mean follow-up of 2.3 years, the protocol efficacy analysis showed that the vaccine had an efficacy rate of 54.0% (P = .04) for pulmonary tuberculosis.
The vaccine had greater efficacy in men (75.2%; P = .03) than it did in women (27.4%; P = .52) and among individuals aged 25 years or younger (84.4%; P = .01) than it did among older subjects (10.2%, P = .82).
The frequency of serious adverse events was similar between the vaccine (1.6%) and the placebo group (1.8%). Unsolicited reports of adverse events were more common in the vaccine group than the placebo group (67.4% vs. 45.4%, respectively), driven largely by more reports of injection site reactions and flu-like symptoms. Solicited reports of adverse events were highlighted by a greater frequency of injection site pain in the vaccine group (81.8% vs. 34.4%). A total of 24.3% of the vaccine recipients reported grade 3 pain, compared with 3.3% in the placebo arm. Rates of fatigue, headache, malaise, or myalgia were also higher in the vaccine group, as was fever.
All of the subjects in the vaccine group had seroconversion at month 2, and 99% remained seroconverted at 12 months.
Next, the researchers plan to conduct studies in HIV-infected individuals and to proceed with phase III trials.
The trial was funded by GlaxoSmithKline Biologicals and Aeras. Dr. Ginsberg is an employee of Aeras.
SOURCE: Ginsberg A et al. IDWeek 2018, Abstract 120
REPORTING FROM IDWEEK 2018
Key clinical point: The vaccine is the first to show efficacy in patients previously exposed to the TB bacterium.
Major finding: The vaccine had a protective efficacy of 54%.
Study details: Randomized, controlled trial with 3,330 participants.
Disclosures: The trial was funded by GlaxoSmithKline Biologicals and Aeras. Dr. Ginsberg is an employee of Aeras.
Source: Ginsberg A et al. IDWeek 2018, Abstract 120.
Flu vaccination lags among patients with psoriasis
Psoriasis patients are more vulnerable to systemic infections, including influenza-related pneumonia, but a new study shows that they are less likely to receive the influenza vaccine than patients with RA.
Vaccination rates were higher in psoriasis patients aged over 50 years, those who were female, and those with other chronic medical conditions, however.
Megan H. Noe, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, and her coauthors referred to recent evidence suggesting that psoriasis involves systemic inflammation that increase the risk of comorbidities and that hospitalization rates for serious infections, including lower respiratory tract infections and pneumonia, are higher among adults with psoriasis than those who do not have psoriasis.
drawing from administrative and commercial claims data from OptumInsight Clinformatics Data Mart. They examined all adult patients with psoriasis, RA, or chronic hypertension who required oral antihypertensive medication. The study population included individuals tracked during the 2010-2011 flu season and 24 months prior (September 2008 to March 2011). This year was chosen because it was labeled as a “typical” season by the Centers for Disease Control and Prevention.
The primary outcome was a claim for an influenza vaccine, and covariates included age, length of residency, gender, and a clinical history of a range of conditions known to be associated with greater risk of influenza complications.
The population included 17,078 patients with psoriasis, 21,832 with RA, and 496,972 with chronic hypertension. After controlling for sex and age, the probability of getting a flu vaccine was similar between psoriasis and hypertension patients, but RA patients were more likely to be vaccinated than patients with psoriasis (odds ratio, 1.08; 95% confidence interval, 1.03-1.13). But the likelihood varied with age: 30-year-old patients with RA were more likely than a 30-year-old psoriasis patient to get a flu shot (OR, 1.30; 95% CI, 1.18-1.45), while a 70-year-old patient with RA was about as likely to get the flu vaccine as a 70-year-old patient with psoriasis.
Female psoriasis patients were more likely to get a flu shot than males (OR, 1.29; 95% CI, 1.20-1.38). Among the psoriasis patients, having some medical comorbidities were linked to a greater likelihood of being vaccinated, including asthma (OR, 1.58; 95% CI, 1.40-1.77), chronic liver disease (OR, 1.23; 95%, 1.03-1.47), diabetes (OR, 1.48; 95% CI, 1.36-1.63), HIV (OR, 3.68; 95% CI, 2.06-6.57), history of malignancy (OR, 1.21; 95% CI, 1.09-1.34), and psoriatic arthritis (OR, 1.40; 95% CI, 1.25-1.58).
There was no association between the use of an oral systemic therapy or biologic treatment and vaccination rates.
The authors suggested that psoriasis patients, especially younger ones, may not get adequate counseling on the value of the flu vaccine from their physicians. Studies have shown that, among the American public, health care providers are the most influential source of information about the flu vaccine. Among younger patients, the dermatologist may be a psoriasis patient’s primary health care provider, so it is important for dermatologists to counsel patients about the recommended vaccines, the authors wrote.
“Further research understanding why adults with psoriasis do not receive recommended vaccinations will help to create targeted interventions to improve vaccination rates and decrease hospitalizations in adults with psoriasis,” they concluded.
The study relied on administrative claims, so the results may not be generalizable to patients with insurance types other than those in the database or who are uninsured, the authors noted.
This study was funded by the National Psoriasis Foundation, the Dermatology Foundation, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Noe and three other authors did not report any disclosures, the fifth author reported multiple disclosures related to various pharmaceutical companies.
SOURCE: Noe MH et al. J Invest Dermatol. 2018 Oct 10. doi: 10.1016/j.jid.2018.09.012.
Psoriasis patients are more vulnerable to systemic infections, including influenza-related pneumonia, but a new study shows that they are less likely to receive the influenza vaccine than patients with RA.
Vaccination rates were higher in psoriasis patients aged over 50 years, those who were female, and those with other chronic medical conditions, however.
Megan H. Noe, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, and her coauthors referred to recent evidence suggesting that psoriasis involves systemic inflammation that increase the risk of comorbidities and that hospitalization rates for serious infections, including lower respiratory tract infections and pneumonia, are higher among adults with psoriasis than those who do not have psoriasis.
drawing from administrative and commercial claims data from OptumInsight Clinformatics Data Mart. They examined all adult patients with psoriasis, RA, or chronic hypertension who required oral antihypertensive medication. The study population included individuals tracked during the 2010-2011 flu season and 24 months prior (September 2008 to March 2011). This year was chosen because it was labeled as a “typical” season by the Centers for Disease Control and Prevention.
The primary outcome was a claim for an influenza vaccine, and covariates included age, length of residency, gender, and a clinical history of a range of conditions known to be associated with greater risk of influenza complications.
The population included 17,078 patients with psoriasis, 21,832 with RA, and 496,972 with chronic hypertension. After controlling for sex and age, the probability of getting a flu vaccine was similar between psoriasis and hypertension patients, but RA patients were more likely to be vaccinated than patients with psoriasis (odds ratio, 1.08; 95% confidence interval, 1.03-1.13). But the likelihood varied with age: 30-year-old patients with RA were more likely than a 30-year-old psoriasis patient to get a flu shot (OR, 1.30; 95% CI, 1.18-1.45), while a 70-year-old patient with RA was about as likely to get the flu vaccine as a 70-year-old patient with psoriasis.
Female psoriasis patients were more likely to get a flu shot than males (OR, 1.29; 95% CI, 1.20-1.38). Among the psoriasis patients, having some medical comorbidities were linked to a greater likelihood of being vaccinated, including asthma (OR, 1.58; 95% CI, 1.40-1.77), chronic liver disease (OR, 1.23; 95%, 1.03-1.47), diabetes (OR, 1.48; 95% CI, 1.36-1.63), HIV (OR, 3.68; 95% CI, 2.06-6.57), history of malignancy (OR, 1.21; 95% CI, 1.09-1.34), and psoriatic arthritis (OR, 1.40; 95% CI, 1.25-1.58).
There was no association between the use of an oral systemic therapy or biologic treatment and vaccination rates.
The authors suggested that psoriasis patients, especially younger ones, may not get adequate counseling on the value of the flu vaccine from their physicians. Studies have shown that, among the American public, health care providers are the most influential source of information about the flu vaccine. Among younger patients, the dermatologist may be a psoriasis patient’s primary health care provider, so it is important for dermatologists to counsel patients about the recommended vaccines, the authors wrote.
“Further research understanding why adults with psoriasis do not receive recommended vaccinations will help to create targeted interventions to improve vaccination rates and decrease hospitalizations in adults with psoriasis,” they concluded.
The study relied on administrative claims, so the results may not be generalizable to patients with insurance types other than those in the database or who are uninsured, the authors noted.
This study was funded by the National Psoriasis Foundation, the Dermatology Foundation, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Noe and three other authors did not report any disclosures, the fifth author reported multiple disclosures related to various pharmaceutical companies.
SOURCE: Noe MH et al. J Invest Dermatol. 2018 Oct 10. doi: 10.1016/j.jid.2018.09.012.
Psoriasis patients are more vulnerable to systemic infections, including influenza-related pneumonia, but a new study shows that they are less likely to receive the influenza vaccine than patients with RA.
Vaccination rates were higher in psoriasis patients aged over 50 years, those who were female, and those with other chronic medical conditions, however.
Megan H. Noe, MD, of the department of dermatology at the University of Pennsylvania, Philadelphia, and her coauthors referred to recent evidence suggesting that psoriasis involves systemic inflammation that increase the risk of comorbidities and that hospitalization rates for serious infections, including lower respiratory tract infections and pneumonia, are higher among adults with psoriasis than those who do not have psoriasis.
drawing from administrative and commercial claims data from OptumInsight Clinformatics Data Mart. They examined all adult patients with psoriasis, RA, or chronic hypertension who required oral antihypertensive medication. The study population included individuals tracked during the 2010-2011 flu season and 24 months prior (September 2008 to March 2011). This year was chosen because it was labeled as a “typical” season by the Centers for Disease Control and Prevention.
The primary outcome was a claim for an influenza vaccine, and covariates included age, length of residency, gender, and a clinical history of a range of conditions known to be associated with greater risk of influenza complications.
The population included 17,078 patients with psoriasis, 21,832 with RA, and 496,972 with chronic hypertension. After controlling for sex and age, the probability of getting a flu vaccine was similar between psoriasis and hypertension patients, but RA patients were more likely to be vaccinated than patients with psoriasis (odds ratio, 1.08; 95% confidence interval, 1.03-1.13). But the likelihood varied with age: 30-year-old patients with RA were more likely than a 30-year-old psoriasis patient to get a flu shot (OR, 1.30; 95% CI, 1.18-1.45), while a 70-year-old patient with RA was about as likely to get the flu vaccine as a 70-year-old patient with psoriasis.
Female psoriasis patients were more likely to get a flu shot than males (OR, 1.29; 95% CI, 1.20-1.38). Among the psoriasis patients, having some medical comorbidities were linked to a greater likelihood of being vaccinated, including asthma (OR, 1.58; 95% CI, 1.40-1.77), chronic liver disease (OR, 1.23; 95%, 1.03-1.47), diabetes (OR, 1.48; 95% CI, 1.36-1.63), HIV (OR, 3.68; 95% CI, 2.06-6.57), history of malignancy (OR, 1.21; 95% CI, 1.09-1.34), and psoriatic arthritis (OR, 1.40; 95% CI, 1.25-1.58).
There was no association between the use of an oral systemic therapy or biologic treatment and vaccination rates.
The authors suggested that psoriasis patients, especially younger ones, may not get adequate counseling on the value of the flu vaccine from their physicians. Studies have shown that, among the American public, health care providers are the most influential source of information about the flu vaccine. Among younger patients, the dermatologist may be a psoriasis patient’s primary health care provider, so it is important for dermatologists to counsel patients about the recommended vaccines, the authors wrote.
“Further research understanding why adults with psoriasis do not receive recommended vaccinations will help to create targeted interventions to improve vaccination rates and decrease hospitalizations in adults with psoriasis,” they concluded.
The study relied on administrative claims, so the results may not be generalizable to patients with insurance types other than those in the database or who are uninsured, the authors noted.
This study was funded by the National Psoriasis Foundation, the Dermatology Foundation, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Dr. Noe and three other authors did not report any disclosures, the fifth author reported multiple disclosures related to various pharmaceutical companies.
SOURCE: Noe MH et al. J Invest Dermatol. 2018 Oct 10. doi: 10.1016/j.jid.2018.09.012.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
Key clinical point: Despite vulnerability to complications, fewer psoriasis patients received the vaccine, compared with RA patients.
Major finding: Patients with RA were 8% more likely to receive a flu vaccine than patients with psoriasis.
Study details: A retrospective cohort study of 535,882 subjects with psoriasis, RA, or hypertension.
Disclosures: This study was funded by the National Psoriasis Foundation, the Dermatology Foundation, and the National Institute of Arthritis and Musculoskeletal and Skin Diseases. Four authors did not report any disclosures; the fifth author reported multiple disclosures related to various pharmaceutical companies.
Source: Noe MH et al. J Invest Dermatol. 2018 Oct 10. doi: 10.1016/j.jid.2018.09.012.
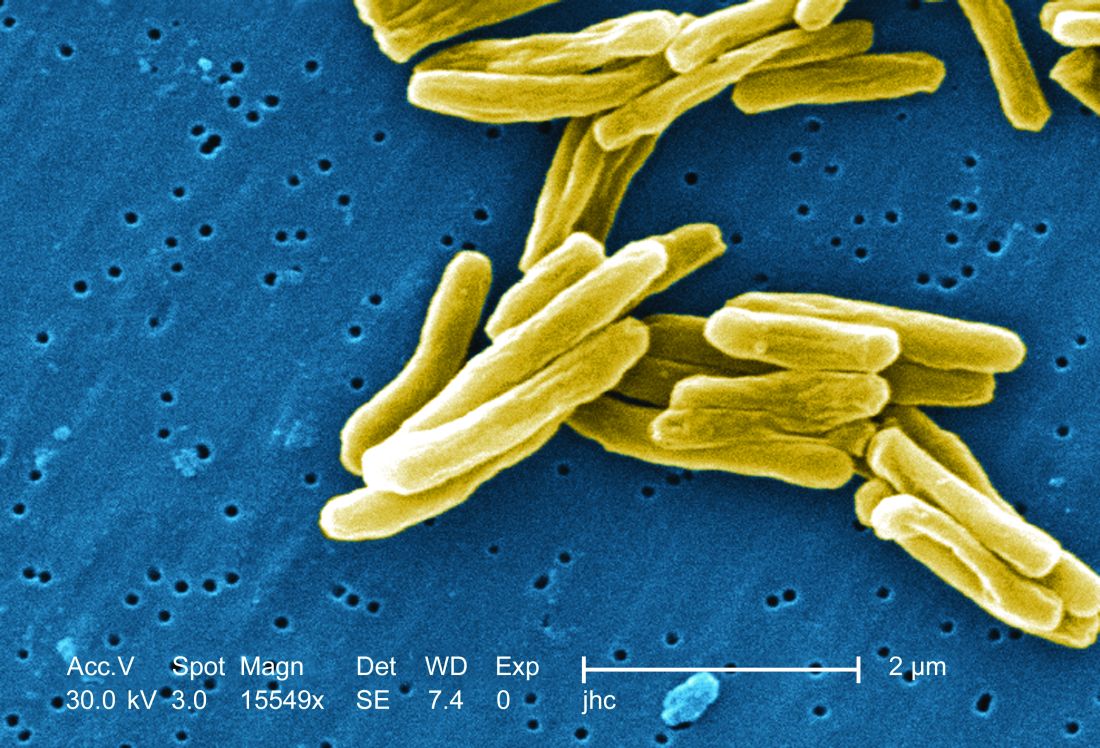
Novel recombinant vaccine protects animals from Lassa fever
An inactivated recombinant Lassa virus (LASV) and rabies vaccine candidate was developed that protects both mice and guinea pigs from Lassa fever. The vaccine also elicits a lasting humoral response against both LASV and rabies virus in both animal models. The novel vaccine, which uses a rabies virus–derived vector, expresses a codon-optimized LASV glycoprotein, according to Tiago Abreu Mota, a doctoral student at Jefferson University, Philadelphia, and his colleagues.
Lassa fever, a World Health Organization priority disease with a biosafety level of 4, is a hemorrhagic fever caused by the Lassa virus, which has no approved vaccine or potent antiviral treatment, according to the report published online in Nature Communications. So the development of a vaccine would be an important step in protecting the West African population from this deadly disease, which infects an estimated 100,000-300,000 people annually. As many as 80% of Lassa fever exposures are mildly symptomatic and thus go unreported; however, the case fatality rate of full-blown Lassa fever has been reported to reach as high as 50%, according to Mr. Mota and his colleagues.
An advantage to the new vaccine is that it is inactivated and thus could potentially be used in pregnant women and immunosuppressed patients, both of which are major risk groups for Lassa fever, according to the researchers. The vaccine could also protect against rabies, which is another major health concern in the regions affected by the Lassa virus.
In terms of mechanism of action, the vaccine did not induce virus-neutralizing antibodies, but rather appeared to trigger cell-mediated protection through activating natural killer cells to promote significantly more killing of virus-infected cells than nontriggered NK cells (P less than .01), as seen through in vitro testing.
The ability to assay for this form of vaccine effectiveness was a key development, according to the researchers. “The neutralizing antibody has been something of a gold standard in vaccine development. High levels are usually a good indication that the immune reaction is strong enough to deflect viral disease. In the case of Lassa virus, however, neutralizing antibodies have not been very good surrogates, since they are produced in much lower quantities. ... The new surrogate of protection will aid in the development of a more potent vaccine against Lassa virus,” according to a press release by Jefferson University.
This work was supported by various grants from the National Institutes of Health. Mr. Mota and two of his colleagues are inventors on a U.S. provisional patent application for a recombinant Lassa-rabies vaccine.
SOURCE: Mota TA et al. Nat Commun. 2018;9:4223. doi: 10.1038/s41467-018-06741-w.
An inactivated recombinant Lassa virus (LASV) and rabies vaccine candidate was developed that protects both mice and guinea pigs from Lassa fever. The vaccine also elicits a lasting humoral response against both LASV and rabies virus in both animal models. The novel vaccine, which uses a rabies virus–derived vector, expresses a codon-optimized LASV glycoprotein, according to Tiago Abreu Mota, a doctoral student at Jefferson University, Philadelphia, and his colleagues.
Lassa fever, a World Health Organization priority disease with a biosafety level of 4, is a hemorrhagic fever caused by the Lassa virus, which has no approved vaccine or potent antiviral treatment, according to the report published online in Nature Communications. So the development of a vaccine would be an important step in protecting the West African population from this deadly disease, which infects an estimated 100,000-300,000 people annually. As many as 80% of Lassa fever exposures are mildly symptomatic and thus go unreported; however, the case fatality rate of full-blown Lassa fever has been reported to reach as high as 50%, according to Mr. Mota and his colleagues.
An advantage to the new vaccine is that it is inactivated and thus could potentially be used in pregnant women and immunosuppressed patients, both of which are major risk groups for Lassa fever, according to the researchers. The vaccine could also protect against rabies, which is another major health concern in the regions affected by the Lassa virus.
In terms of mechanism of action, the vaccine did not induce virus-neutralizing antibodies, but rather appeared to trigger cell-mediated protection through activating natural killer cells to promote significantly more killing of virus-infected cells than nontriggered NK cells (P less than .01), as seen through in vitro testing.
The ability to assay for this form of vaccine effectiveness was a key development, according to the researchers. “The neutralizing antibody has been something of a gold standard in vaccine development. High levels are usually a good indication that the immune reaction is strong enough to deflect viral disease. In the case of Lassa virus, however, neutralizing antibodies have not been very good surrogates, since they are produced in much lower quantities. ... The new surrogate of protection will aid in the development of a more potent vaccine against Lassa virus,” according to a press release by Jefferson University.
This work was supported by various grants from the National Institutes of Health. Mr. Mota and two of his colleagues are inventors on a U.S. provisional patent application for a recombinant Lassa-rabies vaccine.
SOURCE: Mota TA et al. Nat Commun. 2018;9:4223. doi: 10.1038/s41467-018-06741-w.
An inactivated recombinant Lassa virus (LASV) and rabies vaccine candidate was developed that protects both mice and guinea pigs from Lassa fever. The vaccine also elicits a lasting humoral response against both LASV and rabies virus in both animal models. The novel vaccine, which uses a rabies virus–derived vector, expresses a codon-optimized LASV glycoprotein, according to Tiago Abreu Mota, a doctoral student at Jefferson University, Philadelphia, and his colleagues.
Lassa fever, a World Health Organization priority disease with a biosafety level of 4, is a hemorrhagic fever caused by the Lassa virus, which has no approved vaccine or potent antiviral treatment, according to the report published online in Nature Communications. So the development of a vaccine would be an important step in protecting the West African population from this deadly disease, which infects an estimated 100,000-300,000 people annually. As many as 80% of Lassa fever exposures are mildly symptomatic and thus go unreported; however, the case fatality rate of full-blown Lassa fever has been reported to reach as high as 50%, according to Mr. Mota and his colleagues.
An advantage to the new vaccine is that it is inactivated and thus could potentially be used in pregnant women and immunosuppressed patients, both of which are major risk groups for Lassa fever, according to the researchers. The vaccine could also protect against rabies, which is another major health concern in the regions affected by the Lassa virus.
In terms of mechanism of action, the vaccine did not induce virus-neutralizing antibodies, but rather appeared to trigger cell-mediated protection through activating natural killer cells to promote significantly more killing of virus-infected cells than nontriggered NK cells (P less than .01), as seen through in vitro testing.
The ability to assay for this form of vaccine effectiveness was a key development, according to the researchers. “The neutralizing antibody has been something of a gold standard in vaccine development. High levels are usually a good indication that the immune reaction is strong enough to deflect viral disease. In the case of Lassa virus, however, neutralizing antibodies have not been very good surrogates, since they are produced in much lower quantities. ... The new surrogate of protection will aid in the development of a more potent vaccine against Lassa virus,” according to a press release by Jefferson University.
This work was supported by various grants from the National Institutes of Health. Mr. Mota and two of his colleagues are inventors on a U.S. provisional patent application for a recombinant Lassa-rabies vaccine.
SOURCE: Mota TA et al. Nat Commun. 2018;9:4223. doi: 10.1038/s41467-018-06741-w.
FROM NATURE COMMUNICATIONS
Key clinical point: A novel recombinant Lassa virus vaccine protected guinea pigs and mice against Lassa fever.
Major finding: A novel recombinant Lassa virus vaccine elicited strong humeral antibody response in guinea pigs and mice against Lassa and rabies viruses.
Study details: Animal models and an in vitro cellular system were used to assay for the effectiveness of a novel Lassa fever vaccine.
Disclosures: This work was supported by grants from the National Institutes of Health. Mr. Mota and two of his colleagues are inventors on a U.S. provisional patent application for a recombinant Lassa-rabies vaccine.
Source: Mota TA et al. Nat Commun. 2018;9:4223. doi: 10.1038/s41467-018-06741-w.
Third trimester Tdap vaccination raises antibodies in newborns
Immunization of pregnant women with the Tdap vaccine during weeks 27-30 of pregnancy yielded the higher concentration of protective pertussis toxin antibodies in neonates, compared with neonates not exposed to the vaccine, based on data from more than 600 pregnancies.
The Centers for Disease Control and Prevention recommends Tdap vaccination for pregnant women between 27 and 35 weeks’ gestation, but “data on pertussis antibody concentrations following maternal Tdap immunization are limited because of small cohort size or differing immunization schedules,” wrote C. Mary Healy, MD, of Baylor College of Medicine, Houston and her colleagues.
In an observational study published in JAMA, the researchers reviewed data from 626 pregnancies and births at a single tertiary care center in Texas. The average age of the mothers was 30 years; 41% were white, 27% Hispanic, 26% black, 5% Asian, and 1% another ethnicity. Of these, 312 received the Tdap vaccine at an average gestation of 31 weeks, while 314 women were not immunized.
Overall, the geometric mean concentration (GMC) of neonatal umbilical cord pertussis toxin antibodies among infants exposed to Tdap was 47.3 IU/mL, compared with 12.9 IU/mL for unexposed infants, yielding a GMC ratio of 3.6 (P less than .001).
In addition, pertussis toxin antibody concentrations of 15 IU/mL or higher, 30 IU/mL or higher, and 40 IU/mL or higher were significantly more common in Tdap-exposed vs. Tdap-unexposed neonates (86% vs. 37%, 72% vs. 17%, 59% vs. 12%, respectively).
The GMC of pertussis toxin antibodies was highest when the vaccine was given during weeks 27-30, after which the GMC declined, the researchers noted.
The study was limited by several factors including the observational design, which does not support causes and effect analysis, the use of data from a single center, and the lack of pre- and postimmunization serum samples for comparison, and the absence of data on women immunized during the second trimester, the researchers wrote.
However, the results support data from previous studies, and were strengthened by the large study population. The findings suggest that “following U.S. immunization recommendations and in accordance with current understanding of the kinetics of placental transfer, optimal time to administer Tdap vaccine to maximize pertussis toxin antibodies at birth may be early in the third trimester, with the window of 27 through 30 weeks of gestation yielding the highest cord blood levels,” the researchers said.
The study was supported in part by the Centers for Disease Control and Prevention. Dr. Healy disclosed relationships with Sanofi Pasteur, Novartis Vaccines, Pfizer, and Novavax.
SOURCE: Healy C et al. JAMA. 2018 Oct 9;320(14):1464-70.
Immunization of pregnant women with the Tdap vaccine during weeks 27-30 of pregnancy yielded the higher concentration of protective pertussis toxin antibodies in neonates, compared with neonates not exposed to the vaccine, based on data from more than 600 pregnancies.
The Centers for Disease Control and Prevention recommends Tdap vaccination for pregnant women between 27 and 35 weeks’ gestation, but “data on pertussis antibody concentrations following maternal Tdap immunization are limited because of small cohort size or differing immunization schedules,” wrote C. Mary Healy, MD, of Baylor College of Medicine, Houston and her colleagues.
In an observational study published in JAMA, the researchers reviewed data from 626 pregnancies and births at a single tertiary care center in Texas. The average age of the mothers was 30 years; 41% were white, 27% Hispanic, 26% black, 5% Asian, and 1% another ethnicity. Of these, 312 received the Tdap vaccine at an average gestation of 31 weeks, while 314 women were not immunized.
Overall, the geometric mean concentration (GMC) of neonatal umbilical cord pertussis toxin antibodies among infants exposed to Tdap was 47.3 IU/mL, compared with 12.9 IU/mL for unexposed infants, yielding a GMC ratio of 3.6 (P less than .001).
In addition, pertussis toxin antibody concentrations of 15 IU/mL or higher, 30 IU/mL or higher, and 40 IU/mL or higher were significantly more common in Tdap-exposed vs. Tdap-unexposed neonates (86% vs. 37%, 72% vs. 17%, 59% vs. 12%, respectively).
The GMC of pertussis toxin antibodies was highest when the vaccine was given during weeks 27-30, after which the GMC declined, the researchers noted.
The study was limited by several factors including the observational design, which does not support causes and effect analysis, the use of data from a single center, and the lack of pre- and postimmunization serum samples for comparison, and the absence of data on women immunized during the second trimester, the researchers wrote.
However, the results support data from previous studies, and were strengthened by the large study population. The findings suggest that “following U.S. immunization recommendations and in accordance with current understanding of the kinetics of placental transfer, optimal time to administer Tdap vaccine to maximize pertussis toxin antibodies at birth may be early in the third trimester, with the window of 27 through 30 weeks of gestation yielding the highest cord blood levels,” the researchers said.
The study was supported in part by the Centers for Disease Control and Prevention. Dr. Healy disclosed relationships with Sanofi Pasteur, Novartis Vaccines, Pfizer, and Novavax.
SOURCE: Healy C et al. JAMA. 2018 Oct 9;320(14):1464-70.
Immunization of pregnant women with the Tdap vaccine during weeks 27-30 of pregnancy yielded the higher concentration of protective pertussis toxin antibodies in neonates, compared with neonates not exposed to the vaccine, based on data from more than 600 pregnancies.
The Centers for Disease Control and Prevention recommends Tdap vaccination for pregnant women between 27 and 35 weeks’ gestation, but “data on pertussis antibody concentrations following maternal Tdap immunization are limited because of small cohort size or differing immunization schedules,” wrote C. Mary Healy, MD, of Baylor College of Medicine, Houston and her colleagues.
In an observational study published in JAMA, the researchers reviewed data from 626 pregnancies and births at a single tertiary care center in Texas. The average age of the mothers was 30 years; 41% were white, 27% Hispanic, 26% black, 5% Asian, and 1% another ethnicity. Of these, 312 received the Tdap vaccine at an average gestation of 31 weeks, while 314 women were not immunized.
Overall, the geometric mean concentration (GMC) of neonatal umbilical cord pertussis toxin antibodies among infants exposed to Tdap was 47.3 IU/mL, compared with 12.9 IU/mL for unexposed infants, yielding a GMC ratio of 3.6 (P less than .001).
In addition, pertussis toxin antibody concentrations of 15 IU/mL or higher, 30 IU/mL or higher, and 40 IU/mL or higher were significantly more common in Tdap-exposed vs. Tdap-unexposed neonates (86% vs. 37%, 72% vs. 17%, 59% vs. 12%, respectively).
The GMC of pertussis toxin antibodies was highest when the vaccine was given during weeks 27-30, after which the GMC declined, the researchers noted.
The study was limited by several factors including the observational design, which does not support causes and effect analysis, the use of data from a single center, and the lack of pre- and postimmunization serum samples for comparison, and the absence of data on women immunized during the second trimester, the researchers wrote.
However, the results support data from previous studies, and were strengthened by the large study population. The findings suggest that “following U.S. immunization recommendations and in accordance with current understanding of the kinetics of placental transfer, optimal time to administer Tdap vaccine to maximize pertussis toxin antibodies at birth may be early in the third trimester, with the window of 27 through 30 weeks of gestation yielding the highest cord blood levels,” the researchers said.
The study was supported in part by the Centers for Disease Control and Prevention. Dr. Healy disclosed relationships with Sanofi Pasteur, Novartis Vaccines, Pfizer, and Novavax.
SOURCE: Healy C et al. JAMA. 2018 Oct 9;320(14):1464-70.
FROM JAMA
Key clinical point:
Major finding: The geometric mean concentration of neonatal cord pertussis toxin antibodies was 47.3 IU/mL among newborns exposed to Tdap, compared with 12.9 IU/mL among unexposed (P less than .001).
Study details: The data come from an observational study of 626 pregnancies.
Disclosures: The study was supported in part by the Centers for Disease Control and Prevention. Dr. Healy disclosed relationships with Sanofi Pasteur, Novartis Vaccines, Pfizer, and Novavax.
Source: Healy C et al. JAMA. 2018 Oct 9;320(14):1464-70.
How to vaccinate patients on biologics
SAN FRANCISCO – The new herpes zoster subunit vaccine (Shingrix) is on the short list of essential vaccines for immunocompromised adults, including those on biologics.
Ongoing research is demonstrating efficacy and safety in renal transplants patients, as well as those with hematologic cancer and stem cell transplants, according to Lorry Rubin, MD, director of pediatric infectious diseases at Cohen Children’s Medical Center, Queens, and professor of pediatrics at Hofstra University, Hempstead, N.Y.
Immunocompromised people, including those on biologics, should be immunized against a variety of diseases just like everyone else, but it’s tricky. There’s considerable variability in how biologics affect the immune system and subsequent vaccine potency. Timing is important, and although live vaccines are generally a no-go, there’s one class of biologics with which they’re safe, he said.
In a wide-ranging interview at IDWeek 2018, an annual scientific meeting on infectious diseases, Dr. Rubin shared his advice on immunizing the immunocompromised, including the other vaccines on the short list. He also tackled the common concern that vaccinations might trigger rejection in transplant patients.
He’s well qualified to address the issues: Dr. Rubin was lead author on the 2013 Infectious Diseases Society of America guidelines on vaccinating immunocompromised patients.
SAN FRANCISCO – The new herpes zoster subunit vaccine (Shingrix) is on the short list of essential vaccines for immunocompromised adults, including those on biologics.
Ongoing research is demonstrating efficacy and safety in renal transplants patients, as well as those with hematologic cancer and stem cell transplants, according to Lorry Rubin, MD, director of pediatric infectious diseases at Cohen Children’s Medical Center, Queens, and professor of pediatrics at Hofstra University, Hempstead, N.Y.
Immunocompromised people, including those on biologics, should be immunized against a variety of diseases just like everyone else, but it’s tricky. There’s considerable variability in how biologics affect the immune system and subsequent vaccine potency. Timing is important, and although live vaccines are generally a no-go, there’s one class of biologics with which they’re safe, he said.
In a wide-ranging interview at IDWeek 2018, an annual scientific meeting on infectious diseases, Dr. Rubin shared his advice on immunizing the immunocompromised, including the other vaccines on the short list. He also tackled the common concern that vaccinations might trigger rejection in transplant patients.
He’s well qualified to address the issues: Dr. Rubin was lead author on the 2013 Infectious Diseases Society of America guidelines on vaccinating immunocompromised patients.
SAN FRANCISCO – The new herpes zoster subunit vaccine (Shingrix) is on the short list of essential vaccines for immunocompromised adults, including those on biologics.
Ongoing research is demonstrating efficacy and safety in renal transplants patients, as well as those with hematologic cancer and stem cell transplants, according to Lorry Rubin, MD, director of pediatric infectious diseases at Cohen Children’s Medical Center, Queens, and professor of pediatrics at Hofstra University, Hempstead, N.Y.
Immunocompromised people, including those on biologics, should be immunized against a variety of diseases just like everyone else, but it’s tricky. There’s considerable variability in how biologics affect the immune system and subsequent vaccine potency. Timing is important, and although live vaccines are generally a no-go, there’s one class of biologics with which they’re safe, he said.
In a wide-ranging interview at IDWeek 2018, an annual scientific meeting on infectious diseases, Dr. Rubin shared his advice on immunizing the immunocompromised, including the other vaccines on the short list. He also tackled the common concern that vaccinations might trigger rejection in transplant patients.
He’s well qualified to address the issues: Dr. Rubin was lead author on the 2013 Infectious Diseases Society of America guidelines on vaccinating immunocompromised patients.
REPORTING FROM IDWEEK 2018
FDA expands approval of 9-valent HPV vaccine
The , men and women aged 27-45 years, the Food and Drug Administration announced on Oct. 5.
The vaccine (Gardasil 9) was previously approved for those aged 9-26 years.
The approval “represents an important opportunity to help prevent HPV-related diseases and cancers in a broader age range,” Peter Marks, M.D., Ph.D., director of the FDA’s Center for Biologics Evaluation and Research, said in the FDA statement announcing the approval.
“The Centers for Disease Control and Prevention has stated that HPV vaccination prior to becoming infected with the HPV types covered by the vaccine has the potential to prevent more than 90 percent of these cancers, or 31,200 cases every year, from ever developing,” he added.
Gardasil 9, approved in 2014, covers the four HPV types included in the original Gardasil vaccine approved in 2006, plus five additional HPV types.
The approval is based on the results of a study and follow-up of about 3,200 women aged 27-45 years, followed for an average of 3.5 years, which found that the vaccine was 88% percent effective “in the prevention of a combined endpoint of persistent infection, genital warts, vulvar and vaginal precancerous lesions, cervical precancerous lesions, and cervical cancer related to HPV types covered by the vaccine,” according to the FDA. The vaccine’s effectiveness in men in this age group is “inferred” from these results and from data on Gardasil in men aged 16-26 years, as well as “immunogenicity data from a clinical trial in which 150 men, 27 through 45 years of age, received a 3-dose regimen of Gardasil over 6 months,” the FDA statement noted.
Based on safety data in about 13,000 men and women, injection-site pain, swelling, redness, and headaches are the most common adverse reactions associated with Gardasil 9, the statement said. Gardasil 9 is manufactured by Merck.
The , men and women aged 27-45 years, the Food and Drug Administration announced on Oct. 5.
The vaccine (Gardasil 9) was previously approved for those aged 9-26 years.
The approval “represents an important opportunity to help prevent HPV-related diseases and cancers in a broader age range,” Peter Marks, M.D., Ph.D., director of the FDA’s Center for Biologics Evaluation and Research, said in the FDA statement announcing the approval.
“The Centers for Disease Control and Prevention has stated that HPV vaccination prior to becoming infected with the HPV types covered by the vaccine has the potential to prevent more than 90 percent of these cancers, or 31,200 cases every year, from ever developing,” he added.
Gardasil 9, approved in 2014, covers the four HPV types included in the original Gardasil vaccine approved in 2006, plus five additional HPV types.
The approval is based on the results of a study and follow-up of about 3,200 women aged 27-45 years, followed for an average of 3.5 years, which found that the vaccine was 88% percent effective “in the prevention of a combined endpoint of persistent infection, genital warts, vulvar and vaginal precancerous lesions, cervical precancerous lesions, and cervical cancer related to HPV types covered by the vaccine,” according to the FDA. The vaccine’s effectiveness in men in this age group is “inferred” from these results and from data on Gardasil in men aged 16-26 years, as well as “immunogenicity data from a clinical trial in which 150 men, 27 through 45 years of age, received a 3-dose regimen of Gardasil over 6 months,” the FDA statement noted.
Based on safety data in about 13,000 men and women, injection-site pain, swelling, redness, and headaches are the most common adverse reactions associated with Gardasil 9, the statement said. Gardasil 9 is manufactured by Merck.
The , men and women aged 27-45 years, the Food and Drug Administration announced on Oct. 5.
The vaccine (Gardasil 9) was previously approved for those aged 9-26 years.
The approval “represents an important opportunity to help prevent HPV-related diseases and cancers in a broader age range,” Peter Marks, M.D., Ph.D., director of the FDA’s Center for Biologics Evaluation and Research, said in the FDA statement announcing the approval.
“The Centers for Disease Control and Prevention has stated that HPV vaccination prior to becoming infected with the HPV types covered by the vaccine has the potential to prevent more than 90 percent of these cancers, or 31,200 cases every year, from ever developing,” he added.
Gardasil 9, approved in 2014, covers the four HPV types included in the original Gardasil vaccine approved in 2006, plus five additional HPV types.
The approval is based on the results of a study and follow-up of about 3,200 women aged 27-45 years, followed for an average of 3.5 years, which found that the vaccine was 88% percent effective “in the prevention of a combined endpoint of persistent infection, genital warts, vulvar and vaginal precancerous lesions, cervical precancerous lesions, and cervical cancer related to HPV types covered by the vaccine,” according to the FDA. The vaccine’s effectiveness in men in this age group is “inferred” from these results and from data on Gardasil in men aged 16-26 years, as well as “immunogenicity data from a clinical trial in which 150 men, 27 through 45 years of age, received a 3-dose regimen of Gardasil over 6 months,” the FDA statement noted.
Based on safety data in about 13,000 men and women, injection-site pain, swelling, redness, and headaches are the most common adverse reactions associated with Gardasil 9, the statement said. Gardasil 9 is manufactured by Merck.
Encourage influenza vaccination in pregnant women
They are at greater risk for more severe illness, and influenza can lead to adverse outcomes in infants. The good news is that recent studies have shown that flu vaccines are safe and effective in pregnant women.
The bad news is that many women are hesitant to be vaccinated out of concerns over safety, in a trend that reflects broader societal worries over vaccination, said Dr. Chu, of the University of Washington, Seattle. In a video interview at an annual scientific meeting on infectious diseases, Dr. Chu advised steps to ensure that pregnant women are aware of the safety and efficacy of flu vaccines, and the benefits to the infant who acquires immunity through the mother. It’s also a good idea to have vaccine on hand to be able to offer it immediately during an office visit.
They are at greater risk for more severe illness, and influenza can lead to adverse outcomes in infants. The good news is that recent studies have shown that flu vaccines are safe and effective in pregnant women.
The bad news is that many women are hesitant to be vaccinated out of concerns over safety, in a trend that reflects broader societal worries over vaccination, said Dr. Chu, of the University of Washington, Seattle. In a video interview at an annual scientific meeting on infectious diseases, Dr. Chu advised steps to ensure that pregnant women are aware of the safety and efficacy of flu vaccines, and the benefits to the infant who acquires immunity through the mother. It’s also a good idea to have vaccine on hand to be able to offer it immediately during an office visit.
They are at greater risk for more severe illness, and influenza can lead to adverse outcomes in infants. The good news is that recent studies have shown that flu vaccines are safe and effective in pregnant women.
The bad news is that many women are hesitant to be vaccinated out of concerns over safety, in a trend that reflects broader societal worries over vaccination, said Dr. Chu, of the University of Washington, Seattle. In a video interview at an annual scientific meeting on infectious diseases, Dr. Chu advised steps to ensure that pregnant women are aware of the safety and efficacy of flu vaccines, and the benefits to the infant who acquires immunity through the mother. It’s also a good idea to have vaccine on hand to be able to offer it immediately during an office visit.
REPORTING FROM ID WEEK 2018
Flu outbreaks may be more intense in small cities
Influenza outbreaks in the United States tend to be concentrated and intense in small cities and more evenly spread throughout the season in large cities, results of a recent study show.
Swings in humidity further intensified the influenza spikes in small cities, but didn’t seem to have as much of an effect in large cities, the results suggest.
These findings help explain differences in influenza transmission patterns between cities that have similar climates and virus epidemiology, according to researcher Benjamin D. Dalziel, PhD, of the departments of integrative biology and mathematics at Oregon State University in Corvallis.
“City size and structure can play a role in determining how other factors such as climate affect and influence transmission,” Dr. Dalziel said in a press conference.
“Our results show how metropolises play a disproportionately important role in this process, as epidemic foci, and as potential sentinel hubs, where epidemiological observatories could integrate local strain dynamics to predict larger-scale patterns. As the growth and form of cities affect their function as climate-driven incubators of infectious disease, it may be possible to design smarter cities that better control epidemics in the face of accelerating global change,” the researchers wrote in their study.
Dr. Dalziel and his coauthors analyzed the weekly incidence of influenza-like illness across 603 U.S. ZIP codes using data obtained from medical claims from 2002 to 2008. They used epidemic intensity as a summary statistic to compare cities. By this variable, low epidemic intensity indicated a diffuse spread evenly across weeks of the flu season, whereas high epidemic intensity indicated intensively focused outbreaks on particular weeks.
In small cities, epidemics were more intensely focused on shorter periods at the peak of flu season, they found. In large cities, incidence was more diffuse, according to results published in Science.
Patterns of where people live and work in a city may account for the more diffuse and prolonged outbreaks seen in large cities, the authors wrote. Large cities have organized population movement patterns and crowding. In more highly established work locations, for example, the population density is pronounced during the day.
“We found the structure makes a difference for how the flu spreads at different times of year,” Dr. Dalziel said of the study, which used U.S. Census data to evaluate spatial population distributions. “In large cities with more highly organized patterns, conditions play a relatively smaller role in flu transmission.”
Humidity’s lower impact on outbreaks in large cities might also be explained by population effects: “If an infected person is sitting beside you, it matters less what the specific humidity is,” Dr. Dalziel said, adding that the proximity helps the virus find hosts even when climatic conditions are not at their most favorable.
The study findings may have implications for health care resources in small cities, which could be strained by intense outbreaks, said coinvestigator Cecile Viboud, PhD, of the Division of International Epidemiology and Population Studies, Fogarty International Center, National Institutes of Health, Bethesda, Md.
Intense outbreaks could overload the health care system, making it challenging to respond, especially around the peak of the epidemic. Pressure on the health care system may be less intense in cities such as Miami or New York, where flu epidemics are more diffuse and spread out during the year, she said.
Variations in vaccination coverage were not associated with variations in epidemic intensity at the state level. However, the data period that was analyzed ended in 2008, a time when flu vaccination rates were much lower than they are today, according to Dr. Viboud.
“It would be important to revisit the effect of city structure and humidity on flu transmission in a high vaccination regime in more recent years, especially if there is a lot of interest in developing broadly cross-protective flu vaccines, which might become available in the market in the future,” she said.
The researchers declared no competing interests related to their research, which was supported by a grant from the Bill & Melinda Gates Foundation, the RAPIDD program of the Science and Technology Directorate Department of Homeland Security, and the Fogarty International Center, National Institutes of Health.
SOURCE: Dalziel BD et al. Science. 2018 Oct 5;362(6410):75-9.
Public health policy makers may need to switch up their thinking about infection control during influenza outbreaks. Instead of targeting the population at large, it may make sense to focus on specific small towns or metropolitan areas for control.
Summary statistics, such as epidemic intensity, help to identify which places require more surge capacity to deal with peak health care demand. They also help to guide locations for active influenza surveillance where long transmission chains of influenza occur, and where new genetic variants of the influenza virus can be detected.
The findings of this study could foster the development of more accurate short-term, small-scale forecasts of the expected health care demand in a season. Most important, they could guide long-term projections that reveal how the shifting demography, growth of cities, and the changing climate alter infection dynamics and required control efforts.
Prof. Jacco Wallinga is with the Center for Infectious Disease Control, National Institute for Public Health and the Environment, Bilthoven, the Netherlands, and the Department of Biomedical Data Sciences, Leiden (the Netherlands) University Medical Center. These comments appeared in his editorial in Science (2018 Oct 5;362[6410]:29-30).
Public health policy makers may need to switch up their thinking about infection control during influenza outbreaks. Instead of targeting the population at large, it may make sense to focus on specific small towns or metropolitan areas for control.
Summary statistics, such as epidemic intensity, help to identify which places require more surge capacity to deal with peak health care demand. They also help to guide locations for active influenza surveillance where long transmission chains of influenza occur, and where new genetic variants of the influenza virus can be detected.
The findings of this study could foster the development of more accurate short-term, small-scale forecasts of the expected health care demand in a season. Most important, they could guide long-term projections that reveal how the shifting demography, growth of cities, and the changing climate alter infection dynamics and required control efforts.
Prof. Jacco Wallinga is with the Center for Infectious Disease Control, National Institute for Public Health and the Environment, Bilthoven, the Netherlands, and the Department of Biomedical Data Sciences, Leiden (the Netherlands) University Medical Center. These comments appeared in his editorial in Science (2018 Oct 5;362[6410]:29-30).
Public health policy makers may need to switch up their thinking about infection control during influenza outbreaks. Instead of targeting the population at large, it may make sense to focus on specific small towns or metropolitan areas for control.
Summary statistics, such as epidemic intensity, help to identify which places require more surge capacity to deal with peak health care demand. They also help to guide locations for active influenza surveillance where long transmission chains of influenza occur, and where new genetic variants of the influenza virus can be detected.
The findings of this study could foster the development of more accurate short-term, small-scale forecasts of the expected health care demand in a season. Most important, they could guide long-term projections that reveal how the shifting demography, growth of cities, and the changing climate alter infection dynamics and required control efforts.
Prof. Jacco Wallinga is with the Center for Infectious Disease Control, National Institute for Public Health and the Environment, Bilthoven, the Netherlands, and the Department of Biomedical Data Sciences, Leiden (the Netherlands) University Medical Center. These comments appeared in his editorial in Science (2018 Oct 5;362[6410]:29-30).
Influenza outbreaks in the United States tend to be concentrated and intense in small cities and more evenly spread throughout the season in large cities, results of a recent study show.
Swings in humidity further intensified the influenza spikes in small cities, but didn’t seem to have as much of an effect in large cities, the results suggest.
These findings help explain differences in influenza transmission patterns between cities that have similar climates and virus epidemiology, according to researcher Benjamin D. Dalziel, PhD, of the departments of integrative biology and mathematics at Oregon State University in Corvallis.
“City size and structure can play a role in determining how other factors such as climate affect and influence transmission,” Dr. Dalziel said in a press conference.
“Our results show how metropolises play a disproportionately important role in this process, as epidemic foci, and as potential sentinel hubs, where epidemiological observatories could integrate local strain dynamics to predict larger-scale patterns. As the growth and form of cities affect their function as climate-driven incubators of infectious disease, it may be possible to design smarter cities that better control epidemics in the face of accelerating global change,” the researchers wrote in their study.
Dr. Dalziel and his coauthors analyzed the weekly incidence of influenza-like illness across 603 U.S. ZIP codes using data obtained from medical claims from 2002 to 2008. They used epidemic intensity as a summary statistic to compare cities. By this variable, low epidemic intensity indicated a diffuse spread evenly across weeks of the flu season, whereas high epidemic intensity indicated intensively focused outbreaks on particular weeks.
In small cities, epidemics were more intensely focused on shorter periods at the peak of flu season, they found. In large cities, incidence was more diffuse, according to results published in Science.
Patterns of where people live and work in a city may account for the more diffuse and prolonged outbreaks seen in large cities, the authors wrote. Large cities have organized population movement patterns and crowding. In more highly established work locations, for example, the population density is pronounced during the day.
“We found the structure makes a difference for how the flu spreads at different times of year,” Dr. Dalziel said of the study, which used U.S. Census data to evaluate spatial population distributions. “In large cities with more highly organized patterns, conditions play a relatively smaller role in flu transmission.”
Humidity’s lower impact on outbreaks in large cities might also be explained by population effects: “If an infected person is sitting beside you, it matters less what the specific humidity is,” Dr. Dalziel said, adding that the proximity helps the virus find hosts even when climatic conditions are not at their most favorable.
The study findings may have implications for health care resources in small cities, which could be strained by intense outbreaks, said coinvestigator Cecile Viboud, PhD, of the Division of International Epidemiology and Population Studies, Fogarty International Center, National Institutes of Health, Bethesda, Md.
Intense outbreaks could overload the health care system, making it challenging to respond, especially around the peak of the epidemic. Pressure on the health care system may be less intense in cities such as Miami or New York, where flu epidemics are more diffuse and spread out during the year, she said.
Variations in vaccination coverage were not associated with variations in epidemic intensity at the state level. However, the data period that was analyzed ended in 2008, a time when flu vaccination rates were much lower than they are today, according to Dr. Viboud.
“It would be important to revisit the effect of city structure and humidity on flu transmission in a high vaccination regime in more recent years, especially if there is a lot of interest in developing broadly cross-protective flu vaccines, which might become available in the market in the future,” she said.
The researchers declared no competing interests related to their research, which was supported by a grant from the Bill & Melinda Gates Foundation, the RAPIDD program of the Science and Technology Directorate Department of Homeland Security, and the Fogarty International Center, National Institutes of Health.
SOURCE: Dalziel BD et al. Science. 2018 Oct 5;362(6410):75-9.
Influenza outbreaks in the United States tend to be concentrated and intense in small cities and more evenly spread throughout the season in large cities, results of a recent study show.
Swings in humidity further intensified the influenza spikes in small cities, but didn’t seem to have as much of an effect in large cities, the results suggest.
These findings help explain differences in influenza transmission patterns between cities that have similar climates and virus epidemiology, according to researcher Benjamin D. Dalziel, PhD, of the departments of integrative biology and mathematics at Oregon State University in Corvallis.
“City size and structure can play a role in determining how other factors such as climate affect and influence transmission,” Dr. Dalziel said in a press conference.
“Our results show how metropolises play a disproportionately important role in this process, as epidemic foci, and as potential sentinel hubs, where epidemiological observatories could integrate local strain dynamics to predict larger-scale patterns. As the growth and form of cities affect their function as climate-driven incubators of infectious disease, it may be possible to design smarter cities that better control epidemics in the face of accelerating global change,” the researchers wrote in their study.
Dr. Dalziel and his coauthors analyzed the weekly incidence of influenza-like illness across 603 U.S. ZIP codes using data obtained from medical claims from 2002 to 2008. They used epidemic intensity as a summary statistic to compare cities. By this variable, low epidemic intensity indicated a diffuse spread evenly across weeks of the flu season, whereas high epidemic intensity indicated intensively focused outbreaks on particular weeks.
In small cities, epidemics were more intensely focused on shorter periods at the peak of flu season, they found. In large cities, incidence was more diffuse, according to results published in Science.
Patterns of where people live and work in a city may account for the more diffuse and prolonged outbreaks seen in large cities, the authors wrote. Large cities have organized population movement patterns and crowding. In more highly established work locations, for example, the population density is pronounced during the day.
“We found the structure makes a difference for how the flu spreads at different times of year,” Dr. Dalziel said of the study, which used U.S. Census data to evaluate spatial population distributions. “In large cities with more highly organized patterns, conditions play a relatively smaller role in flu transmission.”
Humidity’s lower impact on outbreaks in large cities might also be explained by population effects: “If an infected person is sitting beside you, it matters less what the specific humidity is,” Dr. Dalziel said, adding that the proximity helps the virus find hosts even when climatic conditions are not at their most favorable.
The study findings may have implications for health care resources in small cities, which could be strained by intense outbreaks, said coinvestigator Cecile Viboud, PhD, of the Division of International Epidemiology and Population Studies, Fogarty International Center, National Institutes of Health, Bethesda, Md.
Intense outbreaks could overload the health care system, making it challenging to respond, especially around the peak of the epidemic. Pressure on the health care system may be less intense in cities such as Miami or New York, where flu epidemics are more diffuse and spread out during the year, she said.
Variations in vaccination coverage were not associated with variations in epidemic intensity at the state level. However, the data period that was analyzed ended in 2008, a time when flu vaccination rates were much lower than they are today, according to Dr. Viboud.
“It would be important to revisit the effect of city structure and humidity on flu transmission in a high vaccination regime in more recent years, especially if there is a lot of interest in developing broadly cross-protective flu vaccines, which might become available in the market in the future,” she said.
The researchers declared no competing interests related to their research, which was supported by a grant from the Bill & Melinda Gates Foundation, the RAPIDD program of the Science and Technology Directorate Department of Homeland Security, and the Fogarty International Center, National Institutes of Health.
SOURCE: Dalziel BD et al. Science. 2018 Oct 5;362(6410):75-9.
FROM SCIENCE
Key clinical point: The intensity of influenza epidemics in U.S. cities varies according to population.
Major finding: Smaller cities had more intense outbreaks concentrated around the peak of flu season, while larger cities had cases spread throughout the season.
Study details: Analysis of weekly influenza-like illness incidence for 603 U.S. ZIP codes in medical claims data from 2002 to 2008.
Disclosures: The authors declared no competing interests. Funding came from the Bill & Melinda Gates Foundation, the Science and Technology Directorate Department of Homeland Security, and the Fogarty International Center, National Institutes of Health.
Source: Dalziel BD et al. Science. 2018 Oct 5;362(6410):75-9.