User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Reduced-lactose infant formula related to higher risk of obesity later
Doctors may want to advise parents against giving their infants lactose-reduced infant formula unless absolutely necessary, because doing so may be setting babies up for an increased risk of obesity in toddlerhood, new research shows.
Infants who drink infant formula instead of breast milk already carry an increased risk of obesity. But the new study, published in The American Journal of Clinical Nutrition, found a difference in types of formula and obesity outcomes for children.
Babies under 1 year who received lactose-reduced formula made partially of corn syrup solids were at a 10% greater risk (risk ratio, 1.10; 95% confidence interval, 1.02, 1.20; P = .02) of being obese by age 2 than infants who received regular cow’s milk formula.
“This is even another reason to not use a low-lactose formula,” said Mark R. Corkins, MD, division chief of pediatric gastroenterology, hepatology, and nutrition at the University of Tennessee Health Science Center, Memphis, who was not involved in the study. “Parents think if babies are fussy, or they spit up, they have lactose intolerance, but if you look at the actual numbers, lactose intolerance in infants is rare.”
Actual lactose intolerance in infancy is the result of a newborn receiving the same mutated gene from both parents, called congenital lactase deficiency, said Dr. Corkins.
“The reason the low-lactose formulas are even on the market is because parents want them, and they think their kid is lactose intolerant, but they are not,” Dr. Corkins said.
Researchers from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in southern California and the University of Southern California, Los Angeles, analyzed data from over 15,000 infants in southern California enrolled in WIC.
Records from infants born between Sept. 2012 and March 2016 were separated into two groups: infants that had stopped breastfeeding by month 3 and had started reduced-lactose formula and infants who received all other forms of formula. Over 80% of infants in both groups were Hispanic.
Infants who received the reduced-lactose formula with corn syrup solids were at an 8% increased risk of obesity by age 3 (RR = 1.08; 95% CI, 1.02, 1.15; P = .01), compared with children who received regular cow’s milk formula, and a 7% increased risk by age 4 (RR = 1.07; 95% CI; 1.01, 1.14; P = .01).
Tara Williams, MD, pediatrician and breastfeeding specialist associated with the Florida Chapter of American Academy of Pediatrics, said the findings should make pediatricians, parents, and others pause and consider what infant formulas contain.
She explained that babies who receive formula have higher obesity risk than babies who are breastfed overall. But research into the effects of different types of formula is relatively new. She said there may be a few reasons for the association between reduced-lactose, corn syrup solid formula and a higher risk of obesity.
“The addition of the corn syrup really starts to potentially teach that child to like sweet things,” Dr. Williams said, which in turn can lead to less healthy eating habits in childhood and adulthood.
Or, it may be that parents who tend to give their children lactose-reduced formula are less likely to be tolerant of fussy babies and end up feeding their babies more, Dr. Williams hypothesized.
In addition, emerging research shows corn syrup may act differently from other sugars in the gut microbiome and as it is metabolized in the liver, leading to weight gain.
Although parents make individual choices for what kind of formula to feed their infants, states play a large role in these choices. In 2018, 45% of babies in the United States were eligible for WIC, which is funded through the federal government but administered by states. State WIC programs request bids from formula manufacturers, and products chosen are then redeemed at retailers by parents.
“Now that we’re starting to see a signal that perhaps some formulas will have a potentially added risk of obesity for participants, states may say that when we’re helping mothers select among the formulas, we need to be very explicit about this additional risk,” said Christopher Anderson, PhD, MSPH, associate research scientist at the southern California Public Health Foundation Enterprises WIC and lead author of the study.
Dr. Williams said more research to do similar analyses in other populations is needed to draw cause and effect conclusions, while Dr. Corkins said he’d like to see more research into the amount of formula eaten and health connections to types of formula.
“We know as soon as you sign up for a baby registry at Target, you’re getting formula samples in the mail. You’re very aggressively marketed to; it’s a $55 billion industry,” Dr. Williams said. “And their goal is to sell their product – not to promote the health of infants. “This research certainly will cause us to pause and consider what we are feeding our infants in the United States and how we allow companies to market their products.”
Dr. Goran receives book royalties from Penguin Random House and is a scientific consultant for Yumi Foods and Else Nutrition. All other authors disclosed no conflicts of interest. Dr. Corkins reports working at a clinic that’s the site of a Takeda pharmaceutical research study. Dr. Williams reports no relevant financial relationships.
Doctors may want to advise parents against giving their infants lactose-reduced infant formula unless absolutely necessary, because doing so may be setting babies up for an increased risk of obesity in toddlerhood, new research shows.
Infants who drink infant formula instead of breast milk already carry an increased risk of obesity. But the new study, published in The American Journal of Clinical Nutrition, found a difference in types of formula and obesity outcomes for children.
Babies under 1 year who received lactose-reduced formula made partially of corn syrup solids were at a 10% greater risk (risk ratio, 1.10; 95% confidence interval, 1.02, 1.20; P = .02) of being obese by age 2 than infants who received regular cow’s milk formula.
“This is even another reason to not use a low-lactose formula,” said Mark R. Corkins, MD, division chief of pediatric gastroenterology, hepatology, and nutrition at the University of Tennessee Health Science Center, Memphis, who was not involved in the study. “Parents think if babies are fussy, or they spit up, they have lactose intolerance, but if you look at the actual numbers, lactose intolerance in infants is rare.”
Actual lactose intolerance in infancy is the result of a newborn receiving the same mutated gene from both parents, called congenital lactase deficiency, said Dr. Corkins.
“The reason the low-lactose formulas are even on the market is because parents want them, and they think their kid is lactose intolerant, but they are not,” Dr. Corkins said.
Researchers from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in southern California and the University of Southern California, Los Angeles, analyzed data from over 15,000 infants in southern California enrolled in WIC.
Records from infants born between Sept. 2012 and March 2016 were separated into two groups: infants that had stopped breastfeeding by month 3 and had started reduced-lactose formula and infants who received all other forms of formula. Over 80% of infants in both groups were Hispanic.
Infants who received the reduced-lactose formula with corn syrup solids were at an 8% increased risk of obesity by age 3 (RR = 1.08; 95% CI, 1.02, 1.15; P = .01), compared with children who received regular cow’s milk formula, and a 7% increased risk by age 4 (RR = 1.07; 95% CI; 1.01, 1.14; P = .01).
Tara Williams, MD, pediatrician and breastfeeding specialist associated with the Florida Chapter of American Academy of Pediatrics, said the findings should make pediatricians, parents, and others pause and consider what infant formulas contain.
She explained that babies who receive formula have higher obesity risk than babies who are breastfed overall. But research into the effects of different types of formula is relatively new. She said there may be a few reasons for the association between reduced-lactose, corn syrup solid formula and a higher risk of obesity.
“The addition of the corn syrup really starts to potentially teach that child to like sweet things,” Dr. Williams said, which in turn can lead to less healthy eating habits in childhood and adulthood.
Or, it may be that parents who tend to give their children lactose-reduced formula are less likely to be tolerant of fussy babies and end up feeding their babies more, Dr. Williams hypothesized.
In addition, emerging research shows corn syrup may act differently from other sugars in the gut microbiome and as it is metabolized in the liver, leading to weight gain.
Although parents make individual choices for what kind of formula to feed their infants, states play a large role in these choices. In 2018, 45% of babies in the United States were eligible for WIC, which is funded through the federal government but administered by states. State WIC programs request bids from formula manufacturers, and products chosen are then redeemed at retailers by parents.
“Now that we’re starting to see a signal that perhaps some formulas will have a potentially added risk of obesity for participants, states may say that when we’re helping mothers select among the formulas, we need to be very explicit about this additional risk,” said Christopher Anderson, PhD, MSPH, associate research scientist at the southern California Public Health Foundation Enterprises WIC and lead author of the study.
Dr. Williams said more research to do similar analyses in other populations is needed to draw cause and effect conclusions, while Dr. Corkins said he’d like to see more research into the amount of formula eaten and health connections to types of formula.
“We know as soon as you sign up for a baby registry at Target, you’re getting formula samples in the mail. You’re very aggressively marketed to; it’s a $55 billion industry,” Dr. Williams said. “And their goal is to sell their product – not to promote the health of infants. “This research certainly will cause us to pause and consider what we are feeding our infants in the United States and how we allow companies to market their products.”
Dr. Goran receives book royalties from Penguin Random House and is a scientific consultant for Yumi Foods and Else Nutrition. All other authors disclosed no conflicts of interest. Dr. Corkins reports working at a clinic that’s the site of a Takeda pharmaceutical research study. Dr. Williams reports no relevant financial relationships.
Doctors may want to advise parents against giving their infants lactose-reduced infant formula unless absolutely necessary, because doing so may be setting babies up for an increased risk of obesity in toddlerhood, new research shows.
Infants who drink infant formula instead of breast milk already carry an increased risk of obesity. But the new study, published in The American Journal of Clinical Nutrition, found a difference in types of formula and obesity outcomes for children.
Babies under 1 year who received lactose-reduced formula made partially of corn syrup solids were at a 10% greater risk (risk ratio, 1.10; 95% confidence interval, 1.02, 1.20; P = .02) of being obese by age 2 than infants who received regular cow’s milk formula.
“This is even another reason to not use a low-lactose formula,” said Mark R. Corkins, MD, division chief of pediatric gastroenterology, hepatology, and nutrition at the University of Tennessee Health Science Center, Memphis, who was not involved in the study. “Parents think if babies are fussy, or they spit up, they have lactose intolerance, but if you look at the actual numbers, lactose intolerance in infants is rare.”
Actual lactose intolerance in infancy is the result of a newborn receiving the same mutated gene from both parents, called congenital lactase deficiency, said Dr. Corkins.
“The reason the low-lactose formulas are even on the market is because parents want them, and they think their kid is lactose intolerant, but they are not,” Dr. Corkins said.
Researchers from the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) in southern California and the University of Southern California, Los Angeles, analyzed data from over 15,000 infants in southern California enrolled in WIC.
Records from infants born between Sept. 2012 and March 2016 were separated into two groups: infants that had stopped breastfeeding by month 3 and had started reduced-lactose formula and infants who received all other forms of formula. Over 80% of infants in both groups were Hispanic.
Infants who received the reduced-lactose formula with corn syrup solids were at an 8% increased risk of obesity by age 3 (RR = 1.08; 95% CI, 1.02, 1.15; P = .01), compared with children who received regular cow’s milk formula, and a 7% increased risk by age 4 (RR = 1.07; 95% CI; 1.01, 1.14; P = .01).
Tara Williams, MD, pediatrician and breastfeeding specialist associated with the Florida Chapter of American Academy of Pediatrics, said the findings should make pediatricians, parents, and others pause and consider what infant formulas contain.
She explained that babies who receive formula have higher obesity risk than babies who are breastfed overall. But research into the effects of different types of formula is relatively new. She said there may be a few reasons for the association between reduced-lactose, corn syrup solid formula and a higher risk of obesity.
“The addition of the corn syrup really starts to potentially teach that child to like sweet things,” Dr. Williams said, which in turn can lead to less healthy eating habits in childhood and adulthood.
Or, it may be that parents who tend to give their children lactose-reduced formula are less likely to be tolerant of fussy babies and end up feeding their babies more, Dr. Williams hypothesized.
In addition, emerging research shows corn syrup may act differently from other sugars in the gut microbiome and as it is metabolized in the liver, leading to weight gain.
Although parents make individual choices for what kind of formula to feed their infants, states play a large role in these choices. In 2018, 45% of babies in the United States were eligible for WIC, which is funded through the federal government but administered by states. State WIC programs request bids from formula manufacturers, and products chosen are then redeemed at retailers by parents.
“Now that we’re starting to see a signal that perhaps some formulas will have a potentially added risk of obesity for participants, states may say that when we’re helping mothers select among the formulas, we need to be very explicit about this additional risk,” said Christopher Anderson, PhD, MSPH, associate research scientist at the southern California Public Health Foundation Enterprises WIC and lead author of the study.
Dr. Williams said more research to do similar analyses in other populations is needed to draw cause and effect conclusions, while Dr. Corkins said he’d like to see more research into the amount of formula eaten and health connections to types of formula.
“We know as soon as you sign up for a baby registry at Target, you’re getting formula samples in the mail. You’re very aggressively marketed to; it’s a $55 billion industry,” Dr. Williams said. “And their goal is to sell their product – not to promote the health of infants. “This research certainly will cause us to pause and consider what we are feeding our infants in the United States and how we allow companies to market their products.”
Dr. Goran receives book royalties from Penguin Random House and is a scientific consultant for Yumi Foods and Else Nutrition. All other authors disclosed no conflicts of interest. Dr. Corkins reports working at a clinic that’s the site of a Takeda pharmaceutical research study. Dr. Williams reports no relevant financial relationships.
FROM AMERICAN JOURNAL OF CLINICAL NUTRITION
DOJ: Indiana nurses allowed controlled substances during opioid recovery
, according to a statement released Sept. 1.
In March, the U.S. Department of Justice (DOJ) announced the findings of its investigation, stating that the board “violated the ADA by prohibiting nurses who take medication to treat OUD from participating in the Indiana State Nursing Assistance Program [ISNAP].”
ISNAP rehabilitates and monitors nurses with substance use disorders, and the nursing board contracts with vendors to administer the program. Nurses seeking recovery must typically enroll in ISNAP and complete the 1-year program to maintain an active nursing license or have a license reinstated.
Following the investigation, the nursing board was instructed to implement corrective measures, such as revising policies and handbooks and training nursing board staff and vendors on ADA guidelines and nondiscriminatory practices.
The state’s professional organization for nurses said the remediation efforts will help nurses who are struggling with opioid addiction.
Katherine Feley, DNP, RN, chief executive officer of the Indiana State Nurses Association, told this news organization, “Allowing nurses who take medication to treat OUD to remain on their medication when participating in [ISNAP] will avoid making nurses choose between their health and their profession. This improvement will increase access to treatment resources, enabling more nurses to complete treatment and progress toward a safe return to work.”
The DOJ opened an investigation after receiving a complaint from a nurse in which she alleged that she was denied participation in ISNAP because of her use of prescription medication for OUD. In 2013, while participating in a methadone maintenance program, the nurse was told she had to taper off the medication because ISNAP utilizes an “abstinence-based” model. Because of these restrictions, she could not complete the program, and her nursing license was suspended in late 2014.
In 2016, her physician prescribed a new medication, buprenorphine, and the nurse attempted to enroll in ISNAP again. The program vendor instructed her to taper off the drug within 3 months of enrollment, something her physician believed “would come with a significant risk of relapse [and possibly] death.” The nurse was unable to qualify for reinstatement of her license.
As part of the settlement, the nursing board has agreed to pay a total of $70,000 in damages to the complainant and report compliance with new guidelines to the DOJ every 6 months.
The DOJ says ISNAP’s OUD abstinence policy does not conform with the state’s statute, which mandates that substance abuse rehabilitation services be provided for nurses.
“Indiana may not deny individuals lifesaving medications, including medications that treat [OUD], based on stereotypes and misinformation,” Assistant Attorney General Kristen Clarke of the Justice Department’s Civil Rights Division said of the settlement. “Requiring nurses to stop taking prescribed medication as a condition of maintaining a nursing license violates the ADA and not only creates barriers to recovery but inappropriately limits employment opportunities based on disability.”
In April, the DOJ issued guidance for protecting the civil rights of people with OUD under the ADA to ensure that individuals seeking treatment or recovery can continue participating in society and the workplace.
“The opioid epidemic has greatly impacted professionals and families of all walks of life, and Indiana nurses have the right to seek medically approved treatment for [OUD] under federal law,” U.S. Attorney Zachary A. Myers, of the Southern District of Indiana, said of the settlement. “Following the Justice Department’s findings and the parties’ settlement agreement, Indiana must now enact policies to ensure that Hoosier nurses will not be forced to choose between their recovery and their livelihoods.”
Under the terms of the agreement, the nursing board must allow nurses who are taking OUD medication to participate in ISNAP when the medication is prescribed by a licensed practitioner as part of a medically necessary treatment plan and is incorporated into a recovery monitoring agreement.
A version of this article first appeared on Medscape.com.
, according to a statement released Sept. 1.
In March, the U.S. Department of Justice (DOJ) announced the findings of its investigation, stating that the board “violated the ADA by prohibiting nurses who take medication to treat OUD from participating in the Indiana State Nursing Assistance Program [ISNAP].”
ISNAP rehabilitates and monitors nurses with substance use disorders, and the nursing board contracts with vendors to administer the program. Nurses seeking recovery must typically enroll in ISNAP and complete the 1-year program to maintain an active nursing license or have a license reinstated.
Following the investigation, the nursing board was instructed to implement corrective measures, such as revising policies and handbooks and training nursing board staff and vendors on ADA guidelines and nondiscriminatory practices.
The state’s professional organization for nurses said the remediation efforts will help nurses who are struggling with opioid addiction.
Katherine Feley, DNP, RN, chief executive officer of the Indiana State Nurses Association, told this news organization, “Allowing nurses who take medication to treat OUD to remain on their medication when participating in [ISNAP] will avoid making nurses choose between their health and their profession. This improvement will increase access to treatment resources, enabling more nurses to complete treatment and progress toward a safe return to work.”
The DOJ opened an investigation after receiving a complaint from a nurse in which she alleged that she was denied participation in ISNAP because of her use of prescription medication for OUD. In 2013, while participating in a methadone maintenance program, the nurse was told she had to taper off the medication because ISNAP utilizes an “abstinence-based” model. Because of these restrictions, she could not complete the program, and her nursing license was suspended in late 2014.
In 2016, her physician prescribed a new medication, buprenorphine, and the nurse attempted to enroll in ISNAP again. The program vendor instructed her to taper off the drug within 3 months of enrollment, something her physician believed “would come with a significant risk of relapse [and possibly] death.” The nurse was unable to qualify for reinstatement of her license.
As part of the settlement, the nursing board has agreed to pay a total of $70,000 in damages to the complainant and report compliance with new guidelines to the DOJ every 6 months.
The DOJ says ISNAP’s OUD abstinence policy does not conform with the state’s statute, which mandates that substance abuse rehabilitation services be provided for nurses.
“Indiana may not deny individuals lifesaving medications, including medications that treat [OUD], based on stereotypes and misinformation,” Assistant Attorney General Kristen Clarke of the Justice Department’s Civil Rights Division said of the settlement. “Requiring nurses to stop taking prescribed medication as a condition of maintaining a nursing license violates the ADA and not only creates barriers to recovery but inappropriately limits employment opportunities based on disability.”
In April, the DOJ issued guidance for protecting the civil rights of people with OUD under the ADA to ensure that individuals seeking treatment or recovery can continue participating in society and the workplace.
“The opioid epidemic has greatly impacted professionals and families of all walks of life, and Indiana nurses have the right to seek medically approved treatment for [OUD] under federal law,” U.S. Attorney Zachary A. Myers, of the Southern District of Indiana, said of the settlement. “Following the Justice Department’s findings and the parties’ settlement agreement, Indiana must now enact policies to ensure that Hoosier nurses will not be forced to choose between their recovery and their livelihoods.”
Under the terms of the agreement, the nursing board must allow nurses who are taking OUD medication to participate in ISNAP when the medication is prescribed by a licensed practitioner as part of a medically necessary treatment plan and is incorporated into a recovery monitoring agreement.
A version of this article first appeared on Medscape.com.
, according to a statement released Sept. 1.
In March, the U.S. Department of Justice (DOJ) announced the findings of its investigation, stating that the board “violated the ADA by prohibiting nurses who take medication to treat OUD from participating in the Indiana State Nursing Assistance Program [ISNAP].”
ISNAP rehabilitates and monitors nurses with substance use disorders, and the nursing board contracts with vendors to administer the program. Nurses seeking recovery must typically enroll in ISNAP and complete the 1-year program to maintain an active nursing license or have a license reinstated.
Following the investigation, the nursing board was instructed to implement corrective measures, such as revising policies and handbooks and training nursing board staff and vendors on ADA guidelines and nondiscriminatory practices.
The state’s professional organization for nurses said the remediation efforts will help nurses who are struggling with opioid addiction.
Katherine Feley, DNP, RN, chief executive officer of the Indiana State Nurses Association, told this news organization, “Allowing nurses who take medication to treat OUD to remain on their medication when participating in [ISNAP] will avoid making nurses choose between their health and their profession. This improvement will increase access to treatment resources, enabling more nurses to complete treatment and progress toward a safe return to work.”
The DOJ opened an investigation after receiving a complaint from a nurse in which she alleged that she was denied participation in ISNAP because of her use of prescription medication for OUD. In 2013, while participating in a methadone maintenance program, the nurse was told she had to taper off the medication because ISNAP utilizes an “abstinence-based” model. Because of these restrictions, she could not complete the program, and her nursing license was suspended in late 2014.
In 2016, her physician prescribed a new medication, buprenorphine, and the nurse attempted to enroll in ISNAP again. The program vendor instructed her to taper off the drug within 3 months of enrollment, something her physician believed “would come with a significant risk of relapse [and possibly] death.” The nurse was unable to qualify for reinstatement of her license.
As part of the settlement, the nursing board has agreed to pay a total of $70,000 in damages to the complainant and report compliance with new guidelines to the DOJ every 6 months.
The DOJ says ISNAP’s OUD abstinence policy does not conform with the state’s statute, which mandates that substance abuse rehabilitation services be provided for nurses.
“Indiana may not deny individuals lifesaving medications, including medications that treat [OUD], based on stereotypes and misinformation,” Assistant Attorney General Kristen Clarke of the Justice Department’s Civil Rights Division said of the settlement. “Requiring nurses to stop taking prescribed medication as a condition of maintaining a nursing license violates the ADA and not only creates barriers to recovery but inappropriately limits employment opportunities based on disability.”
In April, the DOJ issued guidance for protecting the civil rights of people with OUD under the ADA to ensure that individuals seeking treatment or recovery can continue participating in society and the workplace.
“The opioid epidemic has greatly impacted professionals and families of all walks of life, and Indiana nurses have the right to seek medically approved treatment for [OUD] under federal law,” U.S. Attorney Zachary A. Myers, of the Southern District of Indiana, said of the settlement. “Following the Justice Department’s findings and the parties’ settlement agreement, Indiana must now enact policies to ensure that Hoosier nurses will not be forced to choose between their recovery and their livelihoods.”
Under the terms of the agreement, the nursing board must allow nurses who are taking OUD medication to participate in ISNAP when the medication is prescribed by a licensed practitioner as part of a medically necessary treatment plan and is incorporated into a recovery monitoring agreement.
A version of this article first appeared on Medscape.com.
Taking the heat out of coffee’s esophageal cancer risk
Whether coffee is good or bad for health is a frequent debate in the media, fueled by apparently conflicting studies suggesting the plethora of bioactive chemicals in the popular brew could either raise or lower cancer risk.
Now, an analysis by Cambridge scientists has suggested that while coffee is not associated with enhanced overall risk of non–digestive system cancers among people genetically predicted to drink more of it,
, although this might be explained by a tendency for drinking it warm or hot, the study in the journal Clinical Nutrition suggested.
Regular coffee drinking has been linked to a slightly lower risk of all-cause mortality. However, it remains unclear whether coffee consumption is associated with a lower risk of dying from cancer.
Hotly debated
In 2016, a working group of international scientists convened by the International Agency for Research on Cancer (IARC) found no conclusive evidence for a carcinogenic effect of drinking coffee. However, the experts did find that drinking very hot beverages was a probable cause of esophageal cancer, making “the temperature, rather than the drinks themselves” the most likely cause, according to the organization’s director.
This latest study concurred. “We provide strong evidence for a causal relationship which is large in magnitude (threefold) and consistent across sensitivity analyses and in a replication study,” it stated.
The Cambridge researchers, assisted by colleagues at the Karolinska Institutet in Stockholm and Bristol Medical School, conducted a Mendelian randomization study to investigate causal associations between coffee consumption and 22 site-specific cancers using data of individuals of European descent in the UK Biobank.
They reported “no strong evidence supporting a causal relationship between genetically-predicted coffee consumption and the majority of cancers studied” (odds ratio [OR], in the main analysis 1.05, 95% confidence interval [CI], 0.98-1.14, P = .183), and remained without association after adjustments for predicted BMI, smoking, or alcohol consumption.
However, genetically predicted coffee consumption was linked to an increased risk of digestive system cancer (OR, 1.28, 95% CI, 1.09-1.51, P = .003), and the risk was largely attributed to “a strong association with esophageal cancer” (OR, 2.79, 95% CI, 1.73-4.50, P = 2.5x10-5). This risk association remained persistent after adjustment for confounders, the researchers said.
Coffee or tea?
Further analysis of the data found that increased risk of esophageal cancer was consistently associated with genetically predicted coffee consumption by individuals with a preference for warm and hot drinks. Among this group, a similar esophageal cancer risk profile among those who reported drinking one to three cups of coffee a day and those who said they did not drink coffee was most likely due to a high prevalence of tea drinking, the study authors said.
“It is, therefore, plausible that a carcinogenic effect of coffee relates to thermal injury broadly, rather than being specific to coffee or its constituents,” said the scientists, who highlighted that this was also pointed out by the IARC in its statement 6 years ago.
Genetically predicted coffee consumption was also found to be associated with increased risk of multiple myeloma (OR, 2.25, 95% CI, 1.30-3.89, P = .004) and reduced ovarian cancer risk (OR, 0.63, 95% CI, 0.43-0.93, P = .020).
The authors concluded there was “evidence for coffee consumption being causally associated with risk of esophageal cancer, with some evidence this is related to a temperature effect.” Otherwise, “our results do not support a linear causal association with the majority of cancer types studied, other than limited evidence for harmful and protective associations with multiple myeloma and ovarian cancers respectively.”
Further studies were needed to investigate “the possible mechanisms of coffee consumption in esophageal carcinogenesis,” they said.
A version of this article first appeared on Medscape UK.
Whether coffee is good or bad for health is a frequent debate in the media, fueled by apparently conflicting studies suggesting the plethora of bioactive chemicals in the popular brew could either raise or lower cancer risk.
Now, an analysis by Cambridge scientists has suggested that while coffee is not associated with enhanced overall risk of non–digestive system cancers among people genetically predicted to drink more of it,
, although this might be explained by a tendency for drinking it warm or hot, the study in the journal Clinical Nutrition suggested.
Regular coffee drinking has been linked to a slightly lower risk of all-cause mortality. However, it remains unclear whether coffee consumption is associated with a lower risk of dying from cancer.
Hotly debated
In 2016, a working group of international scientists convened by the International Agency for Research on Cancer (IARC) found no conclusive evidence for a carcinogenic effect of drinking coffee. However, the experts did find that drinking very hot beverages was a probable cause of esophageal cancer, making “the temperature, rather than the drinks themselves” the most likely cause, according to the organization’s director.
This latest study concurred. “We provide strong evidence for a causal relationship which is large in magnitude (threefold) and consistent across sensitivity analyses and in a replication study,” it stated.
The Cambridge researchers, assisted by colleagues at the Karolinska Institutet in Stockholm and Bristol Medical School, conducted a Mendelian randomization study to investigate causal associations between coffee consumption and 22 site-specific cancers using data of individuals of European descent in the UK Biobank.
They reported “no strong evidence supporting a causal relationship between genetically-predicted coffee consumption and the majority of cancers studied” (odds ratio [OR], in the main analysis 1.05, 95% confidence interval [CI], 0.98-1.14, P = .183), and remained without association after adjustments for predicted BMI, smoking, or alcohol consumption.
However, genetically predicted coffee consumption was linked to an increased risk of digestive system cancer (OR, 1.28, 95% CI, 1.09-1.51, P = .003), and the risk was largely attributed to “a strong association with esophageal cancer” (OR, 2.79, 95% CI, 1.73-4.50, P = 2.5x10-5). This risk association remained persistent after adjustment for confounders, the researchers said.
Coffee or tea?
Further analysis of the data found that increased risk of esophageal cancer was consistently associated with genetically predicted coffee consumption by individuals with a preference for warm and hot drinks. Among this group, a similar esophageal cancer risk profile among those who reported drinking one to three cups of coffee a day and those who said they did not drink coffee was most likely due to a high prevalence of tea drinking, the study authors said.
“It is, therefore, plausible that a carcinogenic effect of coffee relates to thermal injury broadly, rather than being specific to coffee or its constituents,” said the scientists, who highlighted that this was also pointed out by the IARC in its statement 6 years ago.
Genetically predicted coffee consumption was also found to be associated with increased risk of multiple myeloma (OR, 2.25, 95% CI, 1.30-3.89, P = .004) and reduced ovarian cancer risk (OR, 0.63, 95% CI, 0.43-0.93, P = .020).
The authors concluded there was “evidence for coffee consumption being causally associated with risk of esophageal cancer, with some evidence this is related to a temperature effect.” Otherwise, “our results do not support a linear causal association with the majority of cancer types studied, other than limited evidence for harmful and protective associations with multiple myeloma and ovarian cancers respectively.”
Further studies were needed to investigate “the possible mechanisms of coffee consumption in esophageal carcinogenesis,” they said.
A version of this article first appeared on Medscape UK.
Whether coffee is good or bad for health is a frequent debate in the media, fueled by apparently conflicting studies suggesting the plethora of bioactive chemicals in the popular brew could either raise or lower cancer risk.
Now, an analysis by Cambridge scientists has suggested that while coffee is not associated with enhanced overall risk of non–digestive system cancers among people genetically predicted to drink more of it,
, although this might be explained by a tendency for drinking it warm or hot, the study in the journal Clinical Nutrition suggested.
Regular coffee drinking has been linked to a slightly lower risk of all-cause mortality. However, it remains unclear whether coffee consumption is associated with a lower risk of dying from cancer.
Hotly debated
In 2016, a working group of international scientists convened by the International Agency for Research on Cancer (IARC) found no conclusive evidence for a carcinogenic effect of drinking coffee. However, the experts did find that drinking very hot beverages was a probable cause of esophageal cancer, making “the temperature, rather than the drinks themselves” the most likely cause, according to the organization’s director.
This latest study concurred. “We provide strong evidence for a causal relationship which is large in magnitude (threefold) and consistent across sensitivity analyses and in a replication study,” it stated.
The Cambridge researchers, assisted by colleagues at the Karolinska Institutet in Stockholm and Bristol Medical School, conducted a Mendelian randomization study to investigate causal associations between coffee consumption and 22 site-specific cancers using data of individuals of European descent in the UK Biobank.
They reported “no strong evidence supporting a causal relationship between genetically-predicted coffee consumption and the majority of cancers studied” (odds ratio [OR], in the main analysis 1.05, 95% confidence interval [CI], 0.98-1.14, P = .183), and remained without association after adjustments for predicted BMI, smoking, or alcohol consumption.
However, genetically predicted coffee consumption was linked to an increased risk of digestive system cancer (OR, 1.28, 95% CI, 1.09-1.51, P = .003), and the risk was largely attributed to “a strong association with esophageal cancer” (OR, 2.79, 95% CI, 1.73-4.50, P = 2.5x10-5). This risk association remained persistent after adjustment for confounders, the researchers said.
Coffee or tea?
Further analysis of the data found that increased risk of esophageal cancer was consistently associated with genetically predicted coffee consumption by individuals with a preference for warm and hot drinks. Among this group, a similar esophageal cancer risk profile among those who reported drinking one to three cups of coffee a day and those who said they did not drink coffee was most likely due to a high prevalence of tea drinking, the study authors said.
“It is, therefore, plausible that a carcinogenic effect of coffee relates to thermal injury broadly, rather than being specific to coffee or its constituents,” said the scientists, who highlighted that this was also pointed out by the IARC in its statement 6 years ago.
Genetically predicted coffee consumption was also found to be associated with increased risk of multiple myeloma (OR, 2.25, 95% CI, 1.30-3.89, P = .004) and reduced ovarian cancer risk (OR, 0.63, 95% CI, 0.43-0.93, P = .020).
The authors concluded there was “evidence for coffee consumption being causally associated with risk of esophageal cancer, with some evidence this is related to a temperature effect.” Otherwise, “our results do not support a linear causal association with the majority of cancer types studied, other than limited evidence for harmful and protective associations with multiple myeloma and ovarian cancers respectively.”
Further studies were needed to investigate “the possible mechanisms of coffee consumption in esophageal carcinogenesis,” they said.
A version of this article first appeared on Medscape UK.
FROM CLINICAL NUTRITION
How strength training can help you live longer
People who lift weights understand they’re playing a long game.
Once they get past the “newbie gains” – the quick and exciting increases in muscle strength and size – it takes time, effort, and patience to keep making progress.
Whether they know it or not, they’re also playing the longevity game.
A growing body of research shows that resistance training adds years to both lifespan and “healthspan” – the period of life when we’re in good health.
A 2022 study review from Japanese researchers linked “muscle-strengthening activities” to a 15% lower risk of all-cause mortality.
Resistance exercise was also linked to a lower risk of cardiovascular disease (17%), cancer (12%), and diabetes (17%).
We’ve known for a long time that strength is an excellent predictor of future health. Lots of research has shown that, if all else is equal, stronger men and women have a much lower risk of dying during a given period than people with less strength.
This new research shows that strength training offers similar protection, regardless of the results of that training. So even if you don’t think you’re getting as strong or as lean as you’d like to be, you should keep it up – because chances are, you’re still helping your health in a big way.
How strength training helps as you age
For longevity, strength training seems to be especially effective for older adults, says Roger Fielding, PhD, of Tufts University Medford, Mass., who’s been studying the role of exercise in the aging process since the early 1990s.
“With aging, we see clear deficits in muscle function and bone health,” he says. “That all can be slowed, attenuated, or reversed with appropriate exercise.”
His concept of “appropriate” has changed a lot in the past 3 decades. “When I first started studying this stuff, we would try to give people a very formalized prescription” for strength training, he says.
That strength-training prescription typically included a lot of sets (three per exercise), moderate reps (8-12 per set), and relatively heavy weights. It also required professional supervision in a well-equipped gym, which was both unappealing and impractical for most of the target population.
“What I’ve learned is that even lower-intensity strength training, at home, without a lot of specialized equipment, has some benefits,” he says.
Which benefits? That’s harder to say.
The research linking resistance exercise to lower mortality comes from large, population-wide surveys, looking at tens or even hundreds of thousands of people. The broad category of “muscle-strengthening exercises” can include anything from calisthenics in the living room to a serious bodybuilding or power-lifting program.
They’re also based on self-reporting by the people studied. Because of that, “we should be careful how we interpret some of these studies,” Dr. Fielding says.
How much strength training should you do?
That warning seems especially appropriate for the study’s most surprising conclusion: The maximum longevity benefit comes from one or two resistance exercise sessions a week totaling 30-60 minutes.
The study adds that it’s unclear why more strength training would have diminishing or even negative returns.
Robert Linkul, owner of Training the Older Adult in Shingle Springs, Calif., thinks the answer is perfectly clear.
“Less might be more for the beginning lifter,” he says. That’s why his new clients typically begin with two 50-minute workouts a week. But after 3 months, they need to train three times a week to continue seeing gains.
He currently has 14 clients who have been with him at least 16 years. Most of them started in their 50s and are now in their 60s or 70s. If there were any downside to working out more than two times a week, he’s pretty sure he would’ve seen it by now.
Live longer and move longer, too
Mr. Linkul says that his training program includes a lot more than lifting. Clients start each workout with 10-15 minutes of mobility and warm-up exercises. That’s followed by 15 minutes of strength training and 15 minutes of high-intensity resistance training (HIRT).
HIRT uses functional exercises – lifting and carrying dumbbells or kettlebells; pushing or pulling a weighted sled – to improve strength and endurance at the same time.
“Most of the clients I get are training for real-life function,” Mr. Linkul says.
Falling is one of their biggest concerns, and for good reason: According to the World Health Organization, it’s the second-leading cause of unintentional injury–related deaths worldwide, behind only traffic accidents.
Their other major concern is losing their independence, which often follows a fall. “They want to feel they’re not near using a cane or a walker or being stuck in a wheelchair,” he says. “The more we train, the further we get from that.”
That’s where strength training offers its most unique advantages, according to a 2019 study from researchers at McMaster University, Hamilton, Ont. Resistance exercise is “particularly potent for maintaining mobility in older adults,” the study says.
Training for life
Traditional aerobic exercise also offers many of the same benefits, including longer life and a lower risk of cardiovascular disease, cancer, and diabetes.
But there’s no need to choose one or the other. As a recent study) noted, combining aerobic and strength exercises leads to a lower risk of early death than either of them separately.
Which makes perfect sense to Dr. Fielding.
“Usually, people who’re physically active aren’t just doing strength training alone,” he says. “Some exercise is better than no exercise,” and more is usually better than less. “People have to find things they like to do and want to do and are able to do consistently.”
A version of this article first appeared on WebMD.com.
People who lift weights understand they’re playing a long game.
Once they get past the “newbie gains” – the quick and exciting increases in muscle strength and size – it takes time, effort, and patience to keep making progress.
Whether they know it or not, they’re also playing the longevity game.
A growing body of research shows that resistance training adds years to both lifespan and “healthspan” – the period of life when we’re in good health.
A 2022 study review from Japanese researchers linked “muscle-strengthening activities” to a 15% lower risk of all-cause mortality.
Resistance exercise was also linked to a lower risk of cardiovascular disease (17%), cancer (12%), and diabetes (17%).
We’ve known for a long time that strength is an excellent predictor of future health. Lots of research has shown that, if all else is equal, stronger men and women have a much lower risk of dying during a given period than people with less strength.
This new research shows that strength training offers similar protection, regardless of the results of that training. So even if you don’t think you’re getting as strong or as lean as you’d like to be, you should keep it up – because chances are, you’re still helping your health in a big way.
How strength training helps as you age
For longevity, strength training seems to be especially effective for older adults, says Roger Fielding, PhD, of Tufts University Medford, Mass., who’s been studying the role of exercise in the aging process since the early 1990s.
“With aging, we see clear deficits in muscle function and bone health,” he says. “That all can be slowed, attenuated, or reversed with appropriate exercise.”
His concept of “appropriate” has changed a lot in the past 3 decades. “When I first started studying this stuff, we would try to give people a very formalized prescription” for strength training, he says.
That strength-training prescription typically included a lot of sets (three per exercise), moderate reps (8-12 per set), and relatively heavy weights. It also required professional supervision in a well-equipped gym, which was both unappealing and impractical for most of the target population.
“What I’ve learned is that even lower-intensity strength training, at home, without a lot of specialized equipment, has some benefits,” he says.
Which benefits? That’s harder to say.
The research linking resistance exercise to lower mortality comes from large, population-wide surveys, looking at tens or even hundreds of thousands of people. The broad category of “muscle-strengthening exercises” can include anything from calisthenics in the living room to a serious bodybuilding or power-lifting program.
They’re also based on self-reporting by the people studied. Because of that, “we should be careful how we interpret some of these studies,” Dr. Fielding says.
How much strength training should you do?
That warning seems especially appropriate for the study’s most surprising conclusion: The maximum longevity benefit comes from one or two resistance exercise sessions a week totaling 30-60 minutes.
The study adds that it’s unclear why more strength training would have diminishing or even negative returns.
Robert Linkul, owner of Training the Older Adult in Shingle Springs, Calif., thinks the answer is perfectly clear.
“Less might be more for the beginning lifter,” he says. That’s why his new clients typically begin with two 50-minute workouts a week. But after 3 months, they need to train three times a week to continue seeing gains.
He currently has 14 clients who have been with him at least 16 years. Most of them started in their 50s and are now in their 60s or 70s. If there were any downside to working out more than two times a week, he’s pretty sure he would’ve seen it by now.
Live longer and move longer, too
Mr. Linkul says that his training program includes a lot more than lifting. Clients start each workout with 10-15 minutes of mobility and warm-up exercises. That’s followed by 15 minutes of strength training and 15 minutes of high-intensity resistance training (HIRT).
HIRT uses functional exercises – lifting and carrying dumbbells or kettlebells; pushing or pulling a weighted sled – to improve strength and endurance at the same time.
“Most of the clients I get are training for real-life function,” Mr. Linkul says.
Falling is one of their biggest concerns, and for good reason: According to the World Health Organization, it’s the second-leading cause of unintentional injury–related deaths worldwide, behind only traffic accidents.
Their other major concern is losing their independence, which often follows a fall. “They want to feel they’re not near using a cane or a walker or being stuck in a wheelchair,” he says. “The more we train, the further we get from that.”
That’s where strength training offers its most unique advantages, according to a 2019 study from researchers at McMaster University, Hamilton, Ont. Resistance exercise is “particularly potent for maintaining mobility in older adults,” the study says.
Training for life
Traditional aerobic exercise also offers many of the same benefits, including longer life and a lower risk of cardiovascular disease, cancer, and diabetes.
But there’s no need to choose one or the other. As a recent study) noted, combining aerobic and strength exercises leads to a lower risk of early death than either of them separately.
Which makes perfect sense to Dr. Fielding.
“Usually, people who’re physically active aren’t just doing strength training alone,” he says. “Some exercise is better than no exercise,” and more is usually better than less. “People have to find things they like to do and want to do and are able to do consistently.”
A version of this article first appeared on WebMD.com.
People who lift weights understand they’re playing a long game.
Once they get past the “newbie gains” – the quick and exciting increases in muscle strength and size – it takes time, effort, and patience to keep making progress.
Whether they know it or not, they’re also playing the longevity game.
A growing body of research shows that resistance training adds years to both lifespan and “healthspan” – the period of life when we’re in good health.
A 2022 study review from Japanese researchers linked “muscle-strengthening activities” to a 15% lower risk of all-cause mortality.
Resistance exercise was also linked to a lower risk of cardiovascular disease (17%), cancer (12%), and diabetes (17%).
We’ve known for a long time that strength is an excellent predictor of future health. Lots of research has shown that, if all else is equal, stronger men and women have a much lower risk of dying during a given period than people with less strength.
This new research shows that strength training offers similar protection, regardless of the results of that training. So even if you don’t think you’re getting as strong or as lean as you’d like to be, you should keep it up – because chances are, you’re still helping your health in a big way.
How strength training helps as you age
For longevity, strength training seems to be especially effective for older adults, says Roger Fielding, PhD, of Tufts University Medford, Mass., who’s been studying the role of exercise in the aging process since the early 1990s.
“With aging, we see clear deficits in muscle function and bone health,” he says. “That all can be slowed, attenuated, or reversed with appropriate exercise.”
His concept of “appropriate” has changed a lot in the past 3 decades. “When I first started studying this stuff, we would try to give people a very formalized prescription” for strength training, he says.
That strength-training prescription typically included a lot of sets (three per exercise), moderate reps (8-12 per set), and relatively heavy weights. It also required professional supervision in a well-equipped gym, which was both unappealing and impractical for most of the target population.
“What I’ve learned is that even lower-intensity strength training, at home, without a lot of specialized equipment, has some benefits,” he says.
Which benefits? That’s harder to say.
The research linking resistance exercise to lower mortality comes from large, population-wide surveys, looking at tens or even hundreds of thousands of people. The broad category of “muscle-strengthening exercises” can include anything from calisthenics in the living room to a serious bodybuilding or power-lifting program.
They’re also based on self-reporting by the people studied. Because of that, “we should be careful how we interpret some of these studies,” Dr. Fielding says.
How much strength training should you do?
That warning seems especially appropriate for the study’s most surprising conclusion: The maximum longevity benefit comes from one or two resistance exercise sessions a week totaling 30-60 minutes.
The study adds that it’s unclear why more strength training would have diminishing or even negative returns.
Robert Linkul, owner of Training the Older Adult in Shingle Springs, Calif., thinks the answer is perfectly clear.
“Less might be more for the beginning lifter,” he says. That’s why his new clients typically begin with two 50-minute workouts a week. But after 3 months, they need to train three times a week to continue seeing gains.
He currently has 14 clients who have been with him at least 16 years. Most of them started in their 50s and are now in their 60s or 70s. If there were any downside to working out more than two times a week, he’s pretty sure he would’ve seen it by now.
Live longer and move longer, too
Mr. Linkul says that his training program includes a lot more than lifting. Clients start each workout with 10-15 minutes of mobility and warm-up exercises. That’s followed by 15 minutes of strength training and 15 minutes of high-intensity resistance training (HIRT).
HIRT uses functional exercises – lifting and carrying dumbbells or kettlebells; pushing or pulling a weighted sled – to improve strength and endurance at the same time.
“Most of the clients I get are training for real-life function,” Mr. Linkul says.
Falling is one of their biggest concerns, and for good reason: According to the World Health Organization, it’s the second-leading cause of unintentional injury–related deaths worldwide, behind only traffic accidents.
Their other major concern is losing their independence, which often follows a fall. “They want to feel they’re not near using a cane or a walker or being stuck in a wheelchair,” he says. “The more we train, the further we get from that.”
That’s where strength training offers its most unique advantages, according to a 2019 study from researchers at McMaster University, Hamilton, Ont. Resistance exercise is “particularly potent for maintaining mobility in older adults,” the study says.
Training for life
Traditional aerobic exercise also offers many of the same benefits, including longer life and a lower risk of cardiovascular disease, cancer, and diabetes.
But there’s no need to choose one or the other. As a recent study) noted, combining aerobic and strength exercises leads to a lower risk of early death than either of them separately.
Which makes perfect sense to Dr. Fielding.
“Usually, people who’re physically active aren’t just doing strength training alone,” he says. “Some exercise is better than no exercise,” and more is usually better than less. “People have to find things they like to do and want to do and are able to do consistently.”
A version of this article first appeared on WebMD.com.
Early rhythm control improves cardiovascular outcomes in AFib patients regardless of stroke risk
These findings broaden support for early rhythm control, suggesting that physicians should be presenting the option to all patients diagnosed with AFib in routine clinical practice, lead author Daehoon Kim, MD, of Yonsei University, Seoul, South Korea, and colleagues reported.
In 2020, the EAST-AFNET 4 trial showed that early rhythm control was better than rate control for reducing adverse cardiovascular outcomes, but the trial only included patients at risk of stroke with a CHA2DS2-VASc score of at least 2, leaving it unclear whether healthier patients might benefit from the same approach.
“Although the primary indication for rhythm control is to alleviate AF[ib]-related symptoms and improve quality of life, the current guidelines suggest younger age and no or few comorbid conditions as factors favoring rhythm control,” the investigators wrote in Annals of Internal Medicine. “Thus, the effect of rhythm control on cardiovascular outcomes in this population requires elucidation.”
Methods and results
The present study aimed to address this knowledge gap by reviewing data from 54,216 patients with AFib who had rhythm control (ablation or medication) or rate control within one year of diagnosis. Among these patients, 69.3% would have qualified for the EAST-AFNET 4 trial based on higher stroke risk, while the remaining 30.7% of patients would not have been eligible because of lower stroke risk. Median age, consequently, was higher in the former group, at 70 years, versus 54 years in the latter group.
Evaluating the same primary composite outcome as the EAST-AFNET 4 trial (cardiovascular death, ischemic stroke, hospitalization for heart failure, or MI) showed that patients benefited from rhythm control over rate control regardless of risk group.
Those in the higher risk group had a 14% reduced risk of negative cardiovascular outcomes (weighted hazard ratio, 0.86; 95% confidence interval, 0.81-0.92), while those in the lower risk group had a 19% reduced risk of adverse cardiovascular outcomes (weighted HR, 0.81; 95% CI, 0.66-0.98). Safety profiles were similar across groups and management strategies.
Rhythm control well supported from statistical perspective
“We think that physicians should pursue early rhythm control in all patients diagnosed with AF[ib],” principal author Boyoung Joung, MD, PhD, of Yonsei University said in an interview. “Like catheter ablation, we support the idea that early rhythm control can be more effective and safely performed in younger and less frail populations.”
Xiaoxi Yao, PhD, MPH, associate professor of health services research at Mayo Clinic, Rochester, Minn., agreed that rhythm control is now well supported from a statistical perspective, but patients and physicians need to look beyond relative risk improvements, and remain pragmatic.
“There is a benefit, but the benefit is consistent in terms of hazard ratio, or relative risk,” Dr. Yao said in an interview. “You still find a smaller absolute risk difference.”
Patients in the United States – versus Korea where the investigators are based – also need to consider the out-of-pocket costs involved in rhythm control, Dr. Yao said, noting that unclear cost effectiveness may also prevent changes to American guidelines. Medication side effects and procedural risks should also be considered, she added, as well as time off from work needed for ablation.
Dr. Yao, who published a similar paper in June and previously evaluated the role of catheter ablation in routine practice, suggested that the youngest patients may have the most to gain from rhythm control. This is because even a small absolute benefit is magnified with time, she said.
“Since [younger patients] have another several decades to live ... then yes, there might be very significant long-term effects in terms of both symptom control and cardiovascular death and stroke,” Dr. Yao said.
For optimal patient selection, however, more advanced tools are needed, which is why Dr. Yao and her colleagues are exploring new technologies to improve risk-benefit analysis.
“We are not only interested in [a patient’s] baseline high or low risk, but also the extent of risk reduction [that rhythm control provides],” Dr. Yao said. “We are trying to see if there is an [artificial intelligence] or machine-learning approach that can help us provide each patient with a more accurate, individualized estimate to help them make their decision.”
Until then, Dr. Yao encouraged physicians to engage in shared decision-making with patients, making sure to discuss both statistical and practical considerations.
The study was funded by the Ministry of Health and Welfare and the Ministry of Food and Drug Safety of the Republic of Korea. The investigators and Dr. Yao reported no conflicts.
These findings broaden support for early rhythm control, suggesting that physicians should be presenting the option to all patients diagnosed with AFib in routine clinical practice, lead author Daehoon Kim, MD, of Yonsei University, Seoul, South Korea, and colleagues reported.
In 2020, the EAST-AFNET 4 trial showed that early rhythm control was better than rate control for reducing adverse cardiovascular outcomes, but the trial only included patients at risk of stroke with a CHA2DS2-VASc score of at least 2, leaving it unclear whether healthier patients might benefit from the same approach.
“Although the primary indication for rhythm control is to alleviate AF[ib]-related symptoms and improve quality of life, the current guidelines suggest younger age and no or few comorbid conditions as factors favoring rhythm control,” the investigators wrote in Annals of Internal Medicine. “Thus, the effect of rhythm control on cardiovascular outcomes in this population requires elucidation.”
Methods and results
The present study aimed to address this knowledge gap by reviewing data from 54,216 patients with AFib who had rhythm control (ablation or medication) or rate control within one year of diagnosis. Among these patients, 69.3% would have qualified for the EAST-AFNET 4 trial based on higher stroke risk, while the remaining 30.7% of patients would not have been eligible because of lower stroke risk. Median age, consequently, was higher in the former group, at 70 years, versus 54 years in the latter group.
Evaluating the same primary composite outcome as the EAST-AFNET 4 trial (cardiovascular death, ischemic stroke, hospitalization for heart failure, or MI) showed that patients benefited from rhythm control over rate control regardless of risk group.
Those in the higher risk group had a 14% reduced risk of negative cardiovascular outcomes (weighted hazard ratio, 0.86; 95% confidence interval, 0.81-0.92), while those in the lower risk group had a 19% reduced risk of adverse cardiovascular outcomes (weighted HR, 0.81; 95% CI, 0.66-0.98). Safety profiles were similar across groups and management strategies.
Rhythm control well supported from statistical perspective
“We think that physicians should pursue early rhythm control in all patients diagnosed with AF[ib],” principal author Boyoung Joung, MD, PhD, of Yonsei University said in an interview. “Like catheter ablation, we support the idea that early rhythm control can be more effective and safely performed in younger and less frail populations.”
Xiaoxi Yao, PhD, MPH, associate professor of health services research at Mayo Clinic, Rochester, Minn., agreed that rhythm control is now well supported from a statistical perspective, but patients and physicians need to look beyond relative risk improvements, and remain pragmatic.
“There is a benefit, but the benefit is consistent in terms of hazard ratio, or relative risk,” Dr. Yao said in an interview. “You still find a smaller absolute risk difference.”
Patients in the United States – versus Korea where the investigators are based – also need to consider the out-of-pocket costs involved in rhythm control, Dr. Yao said, noting that unclear cost effectiveness may also prevent changes to American guidelines. Medication side effects and procedural risks should also be considered, she added, as well as time off from work needed for ablation.
Dr. Yao, who published a similar paper in June and previously evaluated the role of catheter ablation in routine practice, suggested that the youngest patients may have the most to gain from rhythm control. This is because even a small absolute benefit is magnified with time, she said.
“Since [younger patients] have another several decades to live ... then yes, there might be very significant long-term effects in terms of both symptom control and cardiovascular death and stroke,” Dr. Yao said.
For optimal patient selection, however, more advanced tools are needed, which is why Dr. Yao and her colleagues are exploring new technologies to improve risk-benefit analysis.
“We are not only interested in [a patient’s] baseline high or low risk, but also the extent of risk reduction [that rhythm control provides],” Dr. Yao said. “We are trying to see if there is an [artificial intelligence] or machine-learning approach that can help us provide each patient with a more accurate, individualized estimate to help them make their decision.”
Until then, Dr. Yao encouraged physicians to engage in shared decision-making with patients, making sure to discuss both statistical and practical considerations.
The study was funded by the Ministry of Health and Welfare and the Ministry of Food and Drug Safety of the Republic of Korea. The investigators and Dr. Yao reported no conflicts.
These findings broaden support for early rhythm control, suggesting that physicians should be presenting the option to all patients diagnosed with AFib in routine clinical practice, lead author Daehoon Kim, MD, of Yonsei University, Seoul, South Korea, and colleagues reported.
In 2020, the EAST-AFNET 4 trial showed that early rhythm control was better than rate control for reducing adverse cardiovascular outcomes, but the trial only included patients at risk of stroke with a CHA2DS2-VASc score of at least 2, leaving it unclear whether healthier patients might benefit from the same approach.
“Although the primary indication for rhythm control is to alleviate AF[ib]-related symptoms and improve quality of life, the current guidelines suggest younger age and no or few comorbid conditions as factors favoring rhythm control,” the investigators wrote in Annals of Internal Medicine. “Thus, the effect of rhythm control on cardiovascular outcomes in this population requires elucidation.”
Methods and results
The present study aimed to address this knowledge gap by reviewing data from 54,216 patients with AFib who had rhythm control (ablation or medication) or rate control within one year of diagnosis. Among these patients, 69.3% would have qualified for the EAST-AFNET 4 trial based on higher stroke risk, while the remaining 30.7% of patients would not have been eligible because of lower stroke risk. Median age, consequently, was higher in the former group, at 70 years, versus 54 years in the latter group.
Evaluating the same primary composite outcome as the EAST-AFNET 4 trial (cardiovascular death, ischemic stroke, hospitalization for heart failure, or MI) showed that patients benefited from rhythm control over rate control regardless of risk group.
Those in the higher risk group had a 14% reduced risk of negative cardiovascular outcomes (weighted hazard ratio, 0.86; 95% confidence interval, 0.81-0.92), while those in the lower risk group had a 19% reduced risk of adverse cardiovascular outcomes (weighted HR, 0.81; 95% CI, 0.66-0.98). Safety profiles were similar across groups and management strategies.
Rhythm control well supported from statistical perspective
“We think that physicians should pursue early rhythm control in all patients diagnosed with AF[ib],” principal author Boyoung Joung, MD, PhD, of Yonsei University said in an interview. “Like catheter ablation, we support the idea that early rhythm control can be more effective and safely performed in younger and less frail populations.”
Xiaoxi Yao, PhD, MPH, associate professor of health services research at Mayo Clinic, Rochester, Minn., agreed that rhythm control is now well supported from a statistical perspective, but patients and physicians need to look beyond relative risk improvements, and remain pragmatic.
“There is a benefit, but the benefit is consistent in terms of hazard ratio, or relative risk,” Dr. Yao said in an interview. “You still find a smaller absolute risk difference.”
Patients in the United States – versus Korea where the investigators are based – also need to consider the out-of-pocket costs involved in rhythm control, Dr. Yao said, noting that unclear cost effectiveness may also prevent changes to American guidelines. Medication side effects and procedural risks should also be considered, she added, as well as time off from work needed for ablation.
Dr. Yao, who published a similar paper in June and previously evaluated the role of catheter ablation in routine practice, suggested that the youngest patients may have the most to gain from rhythm control. This is because even a small absolute benefit is magnified with time, she said.
“Since [younger patients] have another several decades to live ... then yes, there might be very significant long-term effects in terms of both symptom control and cardiovascular death and stroke,” Dr. Yao said.
For optimal patient selection, however, more advanced tools are needed, which is why Dr. Yao and her colleagues are exploring new technologies to improve risk-benefit analysis.
“We are not only interested in [a patient’s] baseline high or low risk, but also the extent of risk reduction [that rhythm control provides],” Dr. Yao said. “We are trying to see if there is an [artificial intelligence] or machine-learning approach that can help us provide each patient with a more accurate, individualized estimate to help them make their decision.”
Until then, Dr. Yao encouraged physicians to engage in shared decision-making with patients, making sure to discuss both statistical and practical considerations.
The study was funded by the Ministry of Health and Welfare and the Ministry of Food and Drug Safety of the Republic of Korea. The investigators and Dr. Yao reported no conflicts.
FROM ANNALS OF INTERNAL MEDICINE
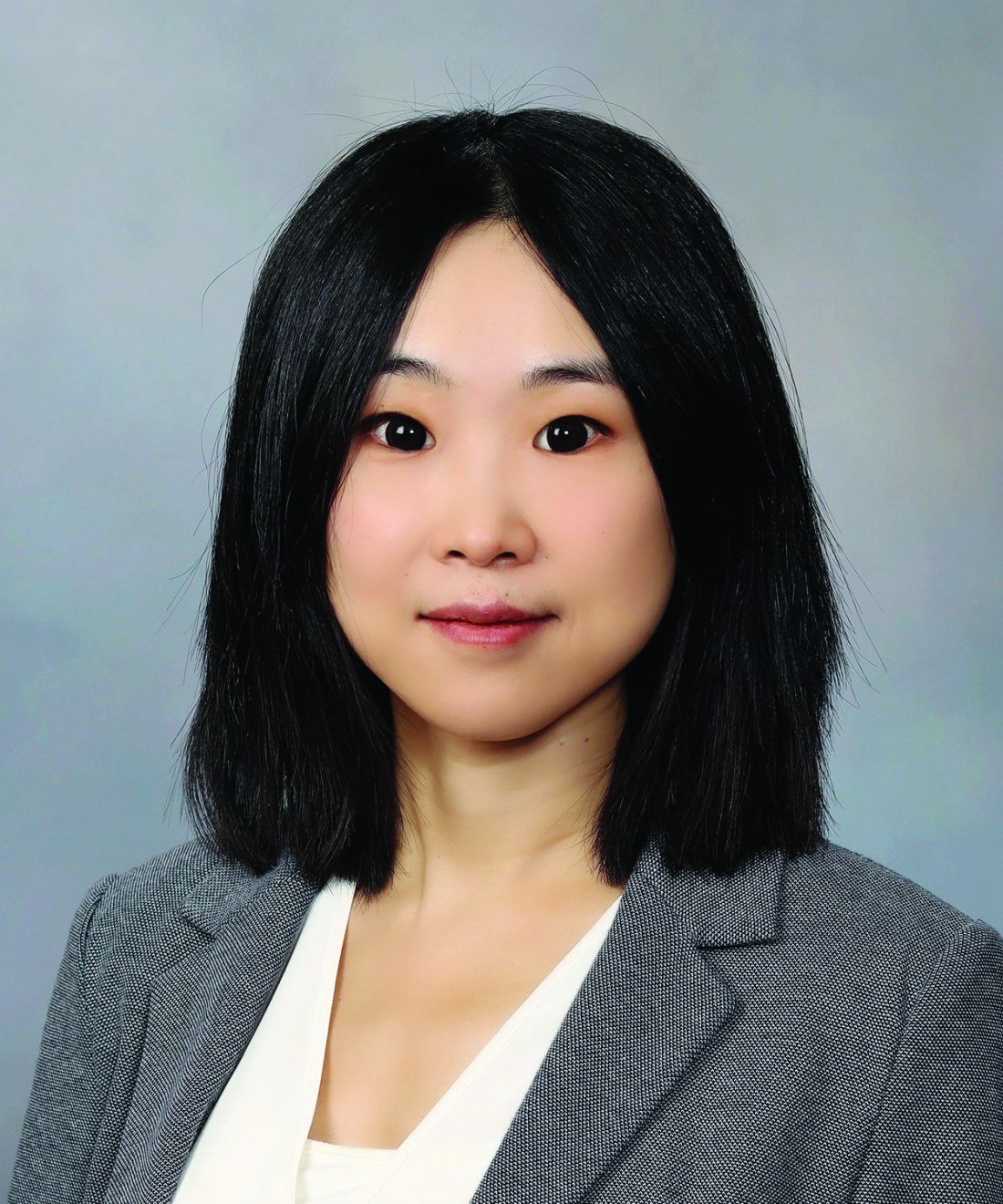
Linear Hypopigmentation on the Right Arm
The Diagnosis: Chemical Leukoderma
A clinical diagnosis of chemical leukoderma was made. In our patient, the observed linear hypopigmentation likely resulted from the prior treatment for De Quervain tenosynovitis in which an intralesional corticosteroid entered the lymphatic channel causing a linear distribution of chemical leukoderma. The hypopigmentation self-resolved at 6-month follow-up, and the patient was counseled to continue steroid injections if indicated.
Chemical leukoderma is an acquired depigmenting dermatosis that displays vitiligolike patterning. Detailed personal and family history in addition to complete physical examination are crucial given the inability to distinguish chemical leukoderma from vitiligo on histopathology. A set of clinical criteria proposed by Ghosh and Mukhopadhyay1 includes the presence of acquired depigmented macules and patches resembling vitiligo, history of repeat exposure to certain chemical substances, hypopigmentation at the site of exposure, and/ or confettilike white macules. Three of these 4 clinical findings must be present to establish a diagnosis of chemical leukoderma. The extent of disease involvement may be graded as follows: Stage I is defined as leukoderma only at the site of contact to the offending agent. Stage II involvement is characterized by local spread beyond the exposure site via the lymphatic system. Stages IIIA and IIIB leukoderma entail hematogenous spread distant to the site of chemical exposure. Although stage IIIA leukoderma is limited to cutaneous involvement, stage IIIB findings are marked by systemic organ involvement. Stage IV disease is defined by the distant spread of hypopigmented macules and patches that continues following 1 year of strict avoidance of the causative agent.1
The pathogenesis behind chemical leukoderma is not completely understood. Studies have suggested that individuals with certain genetic susceptibilities are predisposed to developing the condition after being exposed to chemicals with melanocytotoxic properties.2,3 It has been proposed that the chemicals accelerate pre-existing cellular stress cascades within melanocytes to levels higher than what healthy cells can tolerate. Genetic factors can increase an individual’s total melanocytic stress or establish a lower cellular threshold for stress than what the immune system can manage.4 These influences culminate in an inflammatory response that results in melanocytic destruction and subsequent cutaneous hypopigmentation.
The most well-known offending chemical agents are phenol and catechol derivatives, such as hydroquinone, which is used in topical bleaching agents to treat diseases of hyperpigmentation, including melasma.2 Potent topical or intralesional corticosteroids also may precipitate chemical leukoderma, most notably in individuals with darker skin tones. Hypomelanosis induced by intralesional steroids frequently occurs weeks to months after administration and commonly is observed in a stellate or linear pattern with an irregular outline.5 Other offending chemical agents include sulfhydryls, mercurials, arsenic, benzoyl peroxide, azelaic acid, imiquimod, chloroquine, and tyrosine kinase inhibitors.2,5
Segmental vitiligo is characterized by unilateral hypopigmentation in a linear or blocklike distribution that does not cross the midline. However, onset of segmental vitiligo classically occurs prior to 30 years of age and frequently is related with early leukotrichia.6 Additionally, the hypomelanosis associated with segmental vitiligo more often presents as broad bands or patches that occasionally have a blaschkoid distribution and most commonly appear on the face.5 Lichen striatus is a lichenoid dermatosis that presents as asymptomatic pink or hypopigmented papules that follow the Blaschko lines, often favoring the extremities. Postinflammatory hypopigmentation also may occur as an associated sequela of resolved lichen striatus. Although the disease onset of lichen striatus may occur in adulthood, it typically appears in childhood and is triggered by factors such as trauma, hypersensitivity reactions, viral infections, and medications. Physical injuries such as trauma following surgical procedures also can lead to hypomelanosis; however, our patient denied any relevant surgical history. Progressive macular hypomelanosis is a skin condition presenting as ill-defined, nummular, hypopigmented macules or patches that commonly affects women with darker skin tones with an ethnic background from a tropical location or residing in a tropical environment.5 Lesions frequently appear on the trunk and rarely progress to the proximal extremities, making it an unlikely diagnosis for our patient.
In most cases of chemical leukoderma, spontaneous repigmentation often occurs within 12 months after the elimination of the offending substance; however, hypopigmented lesions may persist or continue to develop at sites distant from the initial site despite discontinuing the causative agent.1 Therapies for vitiligo, such as topical corticosteroids, topical immunosuppressants, narrowband UVB phototherapy, and psoralen plus UVA photochemotherapy, may be utilized for chemical leukoderma that does not self-resolve.
- Ghosh S, Mukhopadhyay S. Chemical leucoderma: a clinicoaetiological study of 864 cases in the perspective of a developing country [published online September 6, 2008]. Br J Dermatol. 2009;160:40-47.
- Ghosh S. Chemical leukoderma: what’s new on etiopathological and clinical aspects? Indian J Dermatol. 2010;55:255.
- Boissy RE, Manga P. On the etiology of contact/occupational vitiligo. Pigment Cell Res. 2004;17:208-214.
- Harris J. Chemical-induced vitiligo. Dermatol Clin. 2017; 35:151-161.
- Bolognia JL, Schaffer JV, Cerroni L, et al. Vitiligo and other disorders of hypopigmentation. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Mosby/Elsevier; 2018:1087-1114.
- Rodrigues M, Ezzedine K, Hamzavi I, et al. New discoveries in the pathogenesis and classification of vitiligo. J Am Acad Dermatol. 2017;77:1-13.
The Diagnosis: Chemical Leukoderma
A clinical diagnosis of chemical leukoderma was made. In our patient, the observed linear hypopigmentation likely resulted from the prior treatment for De Quervain tenosynovitis in which an intralesional corticosteroid entered the lymphatic channel causing a linear distribution of chemical leukoderma. The hypopigmentation self-resolved at 6-month follow-up, and the patient was counseled to continue steroid injections if indicated.
Chemical leukoderma is an acquired depigmenting dermatosis that displays vitiligolike patterning. Detailed personal and family history in addition to complete physical examination are crucial given the inability to distinguish chemical leukoderma from vitiligo on histopathology. A set of clinical criteria proposed by Ghosh and Mukhopadhyay1 includes the presence of acquired depigmented macules and patches resembling vitiligo, history of repeat exposure to certain chemical substances, hypopigmentation at the site of exposure, and/ or confettilike white macules. Three of these 4 clinical findings must be present to establish a diagnosis of chemical leukoderma. The extent of disease involvement may be graded as follows: Stage I is defined as leukoderma only at the site of contact to the offending agent. Stage II involvement is characterized by local spread beyond the exposure site via the lymphatic system. Stages IIIA and IIIB leukoderma entail hematogenous spread distant to the site of chemical exposure. Although stage IIIA leukoderma is limited to cutaneous involvement, stage IIIB findings are marked by systemic organ involvement. Stage IV disease is defined by the distant spread of hypopigmented macules and patches that continues following 1 year of strict avoidance of the causative agent.1
The pathogenesis behind chemical leukoderma is not completely understood. Studies have suggested that individuals with certain genetic susceptibilities are predisposed to developing the condition after being exposed to chemicals with melanocytotoxic properties.2,3 It has been proposed that the chemicals accelerate pre-existing cellular stress cascades within melanocytes to levels higher than what healthy cells can tolerate. Genetic factors can increase an individual’s total melanocytic stress or establish a lower cellular threshold for stress than what the immune system can manage.4 These influences culminate in an inflammatory response that results in melanocytic destruction and subsequent cutaneous hypopigmentation.
The most well-known offending chemical agents are phenol and catechol derivatives, such as hydroquinone, which is used in topical bleaching agents to treat diseases of hyperpigmentation, including melasma.2 Potent topical or intralesional corticosteroids also may precipitate chemical leukoderma, most notably in individuals with darker skin tones. Hypomelanosis induced by intralesional steroids frequently occurs weeks to months after administration and commonly is observed in a stellate or linear pattern with an irregular outline.5 Other offending chemical agents include sulfhydryls, mercurials, arsenic, benzoyl peroxide, azelaic acid, imiquimod, chloroquine, and tyrosine kinase inhibitors.2,5
Segmental vitiligo is characterized by unilateral hypopigmentation in a linear or blocklike distribution that does not cross the midline. However, onset of segmental vitiligo classically occurs prior to 30 years of age and frequently is related with early leukotrichia.6 Additionally, the hypomelanosis associated with segmental vitiligo more often presents as broad bands or patches that occasionally have a blaschkoid distribution and most commonly appear on the face.5 Lichen striatus is a lichenoid dermatosis that presents as asymptomatic pink or hypopigmented papules that follow the Blaschko lines, often favoring the extremities. Postinflammatory hypopigmentation also may occur as an associated sequela of resolved lichen striatus. Although the disease onset of lichen striatus may occur in adulthood, it typically appears in childhood and is triggered by factors such as trauma, hypersensitivity reactions, viral infections, and medications. Physical injuries such as trauma following surgical procedures also can lead to hypomelanosis; however, our patient denied any relevant surgical history. Progressive macular hypomelanosis is a skin condition presenting as ill-defined, nummular, hypopigmented macules or patches that commonly affects women with darker skin tones with an ethnic background from a tropical location or residing in a tropical environment.5 Lesions frequently appear on the trunk and rarely progress to the proximal extremities, making it an unlikely diagnosis for our patient.
In most cases of chemical leukoderma, spontaneous repigmentation often occurs within 12 months after the elimination of the offending substance; however, hypopigmented lesions may persist or continue to develop at sites distant from the initial site despite discontinuing the causative agent.1 Therapies for vitiligo, such as topical corticosteroids, topical immunosuppressants, narrowband UVB phototherapy, and psoralen plus UVA photochemotherapy, may be utilized for chemical leukoderma that does not self-resolve.
The Diagnosis: Chemical Leukoderma
A clinical diagnosis of chemical leukoderma was made. In our patient, the observed linear hypopigmentation likely resulted from the prior treatment for De Quervain tenosynovitis in which an intralesional corticosteroid entered the lymphatic channel causing a linear distribution of chemical leukoderma. The hypopigmentation self-resolved at 6-month follow-up, and the patient was counseled to continue steroid injections if indicated.
Chemical leukoderma is an acquired depigmenting dermatosis that displays vitiligolike patterning. Detailed personal and family history in addition to complete physical examination are crucial given the inability to distinguish chemical leukoderma from vitiligo on histopathology. A set of clinical criteria proposed by Ghosh and Mukhopadhyay1 includes the presence of acquired depigmented macules and patches resembling vitiligo, history of repeat exposure to certain chemical substances, hypopigmentation at the site of exposure, and/ or confettilike white macules. Three of these 4 clinical findings must be present to establish a diagnosis of chemical leukoderma. The extent of disease involvement may be graded as follows: Stage I is defined as leukoderma only at the site of contact to the offending agent. Stage II involvement is characterized by local spread beyond the exposure site via the lymphatic system. Stages IIIA and IIIB leukoderma entail hematogenous spread distant to the site of chemical exposure. Although stage IIIA leukoderma is limited to cutaneous involvement, stage IIIB findings are marked by systemic organ involvement. Stage IV disease is defined by the distant spread of hypopigmented macules and patches that continues following 1 year of strict avoidance of the causative agent.1
The pathogenesis behind chemical leukoderma is not completely understood. Studies have suggested that individuals with certain genetic susceptibilities are predisposed to developing the condition after being exposed to chemicals with melanocytotoxic properties.2,3 It has been proposed that the chemicals accelerate pre-existing cellular stress cascades within melanocytes to levels higher than what healthy cells can tolerate. Genetic factors can increase an individual’s total melanocytic stress or establish a lower cellular threshold for stress than what the immune system can manage.4 These influences culminate in an inflammatory response that results in melanocytic destruction and subsequent cutaneous hypopigmentation.
The most well-known offending chemical agents are phenol and catechol derivatives, such as hydroquinone, which is used in topical bleaching agents to treat diseases of hyperpigmentation, including melasma.2 Potent topical or intralesional corticosteroids also may precipitate chemical leukoderma, most notably in individuals with darker skin tones. Hypomelanosis induced by intralesional steroids frequently occurs weeks to months after administration and commonly is observed in a stellate or linear pattern with an irregular outline.5 Other offending chemical agents include sulfhydryls, mercurials, arsenic, benzoyl peroxide, azelaic acid, imiquimod, chloroquine, and tyrosine kinase inhibitors.2,5
Segmental vitiligo is characterized by unilateral hypopigmentation in a linear or blocklike distribution that does not cross the midline. However, onset of segmental vitiligo classically occurs prior to 30 years of age and frequently is related with early leukotrichia.6 Additionally, the hypomelanosis associated with segmental vitiligo more often presents as broad bands or patches that occasionally have a blaschkoid distribution and most commonly appear on the face.5 Lichen striatus is a lichenoid dermatosis that presents as asymptomatic pink or hypopigmented papules that follow the Blaschko lines, often favoring the extremities. Postinflammatory hypopigmentation also may occur as an associated sequela of resolved lichen striatus. Although the disease onset of lichen striatus may occur in adulthood, it typically appears in childhood and is triggered by factors such as trauma, hypersensitivity reactions, viral infections, and medications. Physical injuries such as trauma following surgical procedures also can lead to hypomelanosis; however, our patient denied any relevant surgical history. Progressive macular hypomelanosis is a skin condition presenting as ill-defined, nummular, hypopigmented macules or patches that commonly affects women with darker skin tones with an ethnic background from a tropical location or residing in a tropical environment.5 Lesions frequently appear on the trunk and rarely progress to the proximal extremities, making it an unlikely diagnosis for our patient.
In most cases of chemical leukoderma, spontaneous repigmentation often occurs within 12 months after the elimination of the offending substance; however, hypopigmented lesions may persist or continue to develop at sites distant from the initial site despite discontinuing the causative agent.1 Therapies for vitiligo, such as topical corticosteroids, topical immunosuppressants, narrowband UVB phototherapy, and psoralen plus UVA photochemotherapy, may be utilized for chemical leukoderma that does not self-resolve.
- Ghosh S, Mukhopadhyay S. Chemical leucoderma: a clinicoaetiological study of 864 cases in the perspective of a developing country [published online September 6, 2008]. Br J Dermatol. 2009;160:40-47.
- Ghosh S. Chemical leukoderma: what’s new on etiopathological and clinical aspects? Indian J Dermatol. 2010;55:255.
- Boissy RE, Manga P. On the etiology of contact/occupational vitiligo. Pigment Cell Res. 2004;17:208-214.
- Harris J. Chemical-induced vitiligo. Dermatol Clin. 2017; 35:151-161.
- Bolognia JL, Schaffer JV, Cerroni L, et al. Vitiligo and other disorders of hypopigmentation. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Mosby/Elsevier; 2018:1087-1114.
- Rodrigues M, Ezzedine K, Hamzavi I, et al. New discoveries in the pathogenesis and classification of vitiligo. J Am Acad Dermatol. 2017;77:1-13.
- Ghosh S, Mukhopadhyay S. Chemical leucoderma: a clinicoaetiological study of 864 cases in the perspective of a developing country [published online September 6, 2008]. Br J Dermatol. 2009;160:40-47.
- Ghosh S. Chemical leukoderma: what’s new on etiopathological and clinical aspects? Indian J Dermatol. 2010;55:255.
- Boissy RE, Manga P. On the etiology of contact/occupational vitiligo. Pigment Cell Res. 2004;17:208-214.
- Harris J. Chemical-induced vitiligo. Dermatol Clin. 2017; 35:151-161.
- Bolognia JL, Schaffer JV, Cerroni L, et al. Vitiligo and other disorders of hypopigmentation. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology. 4th ed. Mosby/Elsevier; 2018:1087-1114.
- Rodrigues M, Ezzedine K, Hamzavi I, et al. New discoveries in the pathogenesis and classification of vitiligo. J Am Acad Dermatol. 2017;77:1-13.
A 73-year-old woman presented to the dermatology clinic with hypopigmentation along the right arm. Her medical history was notable for prior treatment with intralesional triamcinolone injections for De Quervain tenosynovitis. Two months after receiving the steroid injections she noted progressive spreading of an asymptomatic white discoloration originating on the right wrist. Physical examination revealed a hypopigmented atrophic patch on the medial aspect of the right wrist (left) with linear hypopigmented patches extending proximally up the forearm (right).
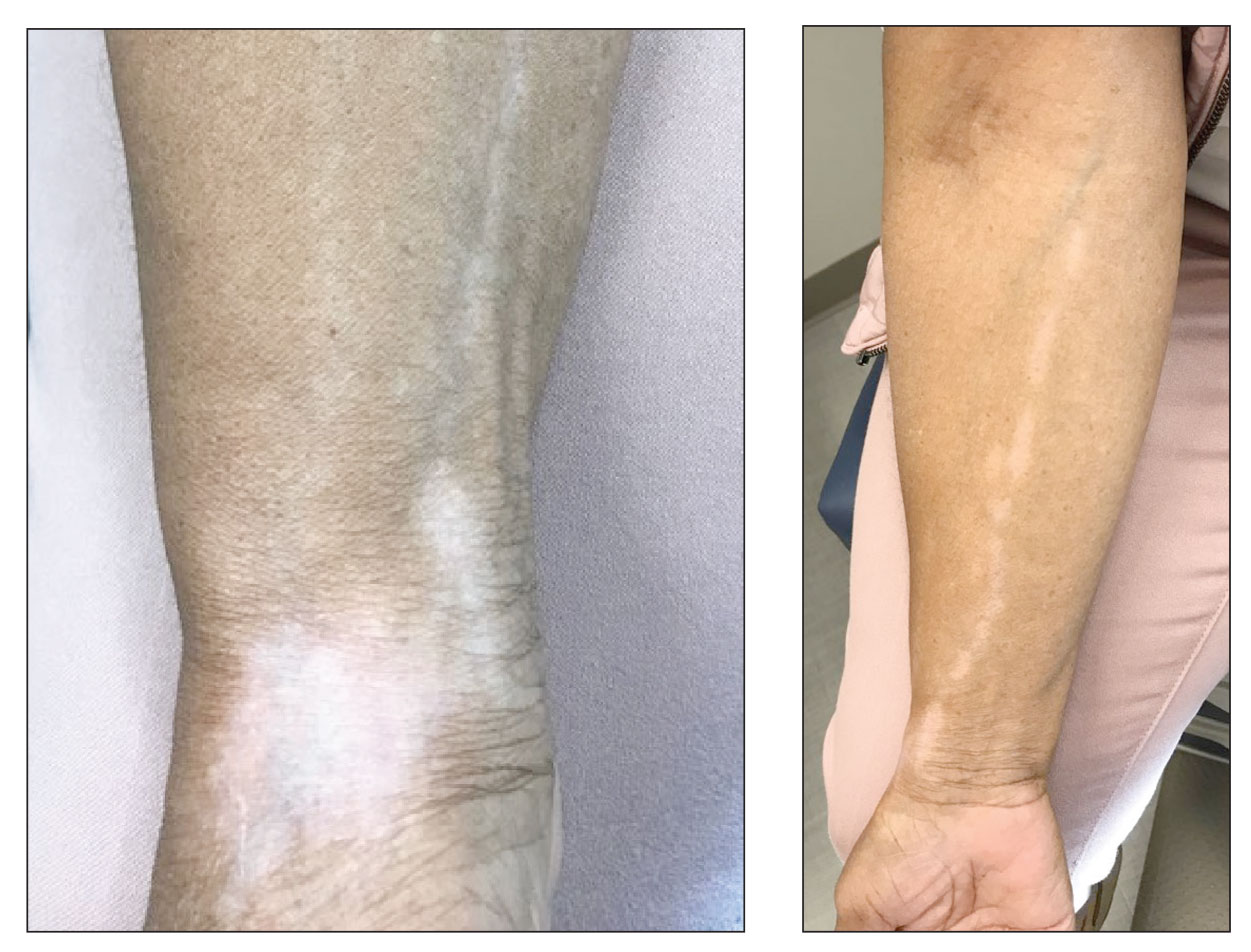
Blue light from cell phones and other devices could be causing wrinkles
Blue light from screens on smartphones, computers, and other gadgets “may have detrimental effects on a wide range of cells in our body, from skin and fat cells to sensory neurons,” Oregon State University scientist Jadwiga Giebultowicz, PhD, said of the study, which was published in the journal Frontiers in Aging.
“Our study suggests that avoidance of excessive blue light exposure may be a good anti-aging strategy,” Dr. Giebultowicz added.
Ultraviolet rays from the sun harm skin appearance and health. Doctors are continuing to study the damage caused by the screens of devices that most people are exposed to throughout the day. These devices emit blue light.
“Aging occurs in various ways, but on a cellular level, we age when cells stop repairing and producing new healthy cells. And cells that aren’t functioning properly are more likely to self destruct – which has ramifications not only in terms of appearance but for the whole body,” the New York Post wrote. “It’s the reason why the elderly take longer to heal, and their bones and organs begin to deteriorate.”
Dr. Giebultowicz said the study shows that certain substances in the body, called metabolites, are essential indicators of how a cell functions. These metabolites are naturally occurring as the body converts food and drinks into energy. Research indicates that these substances are altered by blue light exposure.
More specifically, researchers found that levels of succinate, or succinic acid, in fruit flies increased under excessive blue light, while glutamate decreased, the newspaper wrote.
Researchers said the insects “make an appropriate analog for humans” because the same signaling devices are shared.
The flies were exposed with more blue light than people usually get. Dr. Giebultowicz said future research is needed on human cells.
A version of this article first appeared on WebMD.com.
Blue light from screens on smartphones, computers, and other gadgets “may have detrimental effects on a wide range of cells in our body, from skin and fat cells to sensory neurons,” Oregon State University scientist Jadwiga Giebultowicz, PhD, said of the study, which was published in the journal Frontiers in Aging.
“Our study suggests that avoidance of excessive blue light exposure may be a good anti-aging strategy,” Dr. Giebultowicz added.
Ultraviolet rays from the sun harm skin appearance and health. Doctors are continuing to study the damage caused by the screens of devices that most people are exposed to throughout the day. These devices emit blue light.
“Aging occurs in various ways, but on a cellular level, we age when cells stop repairing and producing new healthy cells. And cells that aren’t functioning properly are more likely to self destruct – which has ramifications not only in terms of appearance but for the whole body,” the New York Post wrote. “It’s the reason why the elderly take longer to heal, and their bones and organs begin to deteriorate.”
Dr. Giebultowicz said the study shows that certain substances in the body, called metabolites, are essential indicators of how a cell functions. These metabolites are naturally occurring as the body converts food and drinks into energy. Research indicates that these substances are altered by blue light exposure.
More specifically, researchers found that levels of succinate, or succinic acid, in fruit flies increased under excessive blue light, while glutamate decreased, the newspaper wrote.
Researchers said the insects “make an appropriate analog for humans” because the same signaling devices are shared.
The flies were exposed with more blue light than people usually get. Dr. Giebultowicz said future research is needed on human cells.
A version of this article first appeared on WebMD.com.
Blue light from screens on smartphones, computers, and other gadgets “may have detrimental effects on a wide range of cells in our body, from skin and fat cells to sensory neurons,” Oregon State University scientist Jadwiga Giebultowicz, PhD, said of the study, which was published in the journal Frontiers in Aging.
“Our study suggests that avoidance of excessive blue light exposure may be a good anti-aging strategy,” Dr. Giebultowicz added.
Ultraviolet rays from the sun harm skin appearance and health. Doctors are continuing to study the damage caused by the screens of devices that most people are exposed to throughout the day. These devices emit blue light.
“Aging occurs in various ways, but on a cellular level, we age when cells stop repairing and producing new healthy cells. And cells that aren’t functioning properly are more likely to self destruct – which has ramifications not only in terms of appearance but for the whole body,” the New York Post wrote. “It’s the reason why the elderly take longer to heal, and their bones and organs begin to deteriorate.”
Dr. Giebultowicz said the study shows that certain substances in the body, called metabolites, are essential indicators of how a cell functions. These metabolites are naturally occurring as the body converts food and drinks into energy. Research indicates that these substances are altered by blue light exposure.
More specifically, researchers found that levels of succinate, or succinic acid, in fruit flies increased under excessive blue light, while glutamate decreased, the newspaper wrote.
Researchers said the insects “make an appropriate analog for humans” because the same signaling devices are shared.
The flies were exposed with more blue light than people usually get. Dr. Giebultowicz said future research is needed on human cells.
A version of this article first appeared on WebMD.com.
FROM FRONTIERS IN AGING
Low physical function tied to cardiac events in older adults
including coronary heart disease (CHD), stroke, and heart failure (HF) in older adults, according to new observational data from the Atherosclerosis Risk in Communities (ARIC) study.
“We found that physical function in older adults predicts future cardiovascular disease (CVD) beyond traditional heart disease risk factors, regardless of whether an individual has a history of cardiovascular disease,” senior author Kunihiro Matsushita, MD, PhD, division of cardiology, Johns Hopkins University, Baltimore, said in a news release.
The study was published online in the Journal of the American Heart Association.
Keeping fit with age
The researchers analyzed health data collected between 2011 and 2013 for 5,570 ARIC participants (mean age, 75 years; 58% women, 22% Black persons). They assessed physical function using the Short Physical Performance Battery (SPPB), which measures walking speed, leg strength, and balance.
On the basis of the results, participants were categorized into three physical function groups: low (score, 0-6; 13% of the cohort), intermediate (score, 7-9; 30%) and high (score, 10-12; 57%).
During a median follow up of 7 years, there were 930 composite CVD events (386 CHD, 251 stroke, and 529 HF).
Adults with lower SPPB scores had a higher cumulative incidence of composite CVD outcomes.
The 5-year cumulative incidence of the composite CVD outcome in the low- and intermediate-SPPB categories was about three times (23.4%) and two times (15.3%) higher than in the high-SPPB category (8.6%), the researchers reported.
In addition, continuous SPPB scores showed significant associations with composite and individual CVD outcomes in all models. A 1-point lower SPPB score was associated with 6%-10% higher risk for CVD events after adjusting for potential confounders.
In the fully adjusted model, the risk for composite CVD outcomes was 47% higher (hazard ratio, 1.47; 95% confidence interval, 1.20-1.79) in those with low physical function and 25% higher in those with intermediate physical function (HR, 1.25; 95% CI, 1.07-1.46) compared with peers with high physical function.
For the individual outcomes, low physical function was associated with higher risk for stroke (HR, 1.81; 95% CI, 1.24-2.64) and HF (HR, 1.33; 95% CI, 1.02-1.73), whereas the association for CHD was not significant.
The associations were largely consistent across subgroups, including those with CVD at baseline.
The addition of SPPB scores significantly improved risk prediction of CVD events beyond traditional CVD risk factors in adults regardless of prior CVD history, suggesting that this tool may be useful for classifying CVD risk in older adults, the researchers said.
Meaningful impact on care?
“Our findings highlight the value of assessing the physical function level of older adults in clinical practice,” lead author Xiao Hu, MHS, with the department of epidemiology at Johns Hopkins, said in the news release. “In addition to heart health, older adults are at higher risk for falls and disability. The assessment of physical function may also inform the risk of these concerning conditions in older adults.”
Weighing in on the study, Jonathan Halperin, MD, cardiologist at Mount Sinai Heart and professor of medicine (cardiology) at the Icahn School of Medicine at Mount Sinai, both in New York, said that “It’s known that cardiorespiratory fitness is an important predictor of cardiovascular risk, but it is one of the few physiological risk factors that are subjectively queried but not objectively assessed in routine clinical practice.”
In this study, Dr. Halperin noted, the investigators found that a battery of physical performance assessments, including a walk test, chair standing, and balance testing, improved cardiovascular risk prediction.
Dr. Halperin cautioned, however, that “since even the short sequence of tests takes time to perform and interpret, and is not currently reimbursed under most health insurance policies, it is not clear whether the report will have a meaningful impact on patient care.”
This research was funded by the National Institutes of Health. Dr. Matsushita and Dr. Halperin have no relevant disclosures.
A version of this article first appeared on Medscape.com.
including coronary heart disease (CHD), stroke, and heart failure (HF) in older adults, according to new observational data from the Atherosclerosis Risk in Communities (ARIC) study.
“We found that physical function in older adults predicts future cardiovascular disease (CVD) beyond traditional heart disease risk factors, regardless of whether an individual has a history of cardiovascular disease,” senior author Kunihiro Matsushita, MD, PhD, division of cardiology, Johns Hopkins University, Baltimore, said in a news release.
The study was published online in the Journal of the American Heart Association.
Keeping fit with age
The researchers analyzed health data collected between 2011 and 2013 for 5,570 ARIC participants (mean age, 75 years; 58% women, 22% Black persons). They assessed physical function using the Short Physical Performance Battery (SPPB), which measures walking speed, leg strength, and balance.
On the basis of the results, participants were categorized into three physical function groups: low (score, 0-6; 13% of the cohort), intermediate (score, 7-9; 30%) and high (score, 10-12; 57%).
During a median follow up of 7 years, there were 930 composite CVD events (386 CHD, 251 stroke, and 529 HF).
Adults with lower SPPB scores had a higher cumulative incidence of composite CVD outcomes.
The 5-year cumulative incidence of the composite CVD outcome in the low- and intermediate-SPPB categories was about three times (23.4%) and two times (15.3%) higher than in the high-SPPB category (8.6%), the researchers reported.
In addition, continuous SPPB scores showed significant associations with composite and individual CVD outcomes in all models. A 1-point lower SPPB score was associated with 6%-10% higher risk for CVD events after adjusting for potential confounders.
In the fully adjusted model, the risk for composite CVD outcomes was 47% higher (hazard ratio, 1.47; 95% confidence interval, 1.20-1.79) in those with low physical function and 25% higher in those with intermediate physical function (HR, 1.25; 95% CI, 1.07-1.46) compared with peers with high physical function.
For the individual outcomes, low physical function was associated with higher risk for stroke (HR, 1.81; 95% CI, 1.24-2.64) and HF (HR, 1.33; 95% CI, 1.02-1.73), whereas the association for CHD was not significant.
The associations were largely consistent across subgroups, including those with CVD at baseline.
The addition of SPPB scores significantly improved risk prediction of CVD events beyond traditional CVD risk factors in adults regardless of prior CVD history, suggesting that this tool may be useful for classifying CVD risk in older adults, the researchers said.
Meaningful impact on care?
“Our findings highlight the value of assessing the physical function level of older adults in clinical practice,” lead author Xiao Hu, MHS, with the department of epidemiology at Johns Hopkins, said in the news release. “In addition to heart health, older adults are at higher risk for falls and disability. The assessment of physical function may also inform the risk of these concerning conditions in older adults.”
Weighing in on the study, Jonathan Halperin, MD, cardiologist at Mount Sinai Heart and professor of medicine (cardiology) at the Icahn School of Medicine at Mount Sinai, both in New York, said that “It’s known that cardiorespiratory fitness is an important predictor of cardiovascular risk, but it is one of the few physiological risk factors that are subjectively queried but not objectively assessed in routine clinical practice.”
In this study, Dr. Halperin noted, the investigators found that a battery of physical performance assessments, including a walk test, chair standing, and balance testing, improved cardiovascular risk prediction.
Dr. Halperin cautioned, however, that “since even the short sequence of tests takes time to perform and interpret, and is not currently reimbursed under most health insurance policies, it is not clear whether the report will have a meaningful impact on patient care.”
This research was funded by the National Institutes of Health. Dr. Matsushita and Dr. Halperin have no relevant disclosures.
A version of this article first appeared on Medscape.com.
including coronary heart disease (CHD), stroke, and heart failure (HF) in older adults, according to new observational data from the Atherosclerosis Risk in Communities (ARIC) study.
“We found that physical function in older adults predicts future cardiovascular disease (CVD) beyond traditional heart disease risk factors, regardless of whether an individual has a history of cardiovascular disease,” senior author Kunihiro Matsushita, MD, PhD, division of cardiology, Johns Hopkins University, Baltimore, said in a news release.
The study was published online in the Journal of the American Heart Association.
Keeping fit with age
The researchers analyzed health data collected between 2011 and 2013 for 5,570 ARIC participants (mean age, 75 years; 58% women, 22% Black persons). They assessed physical function using the Short Physical Performance Battery (SPPB), which measures walking speed, leg strength, and balance.
On the basis of the results, participants were categorized into three physical function groups: low (score, 0-6; 13% of the cohort), intermediate (score, 7-9; 30%) and high (score, 10-12; 57%).
During a median follow up of 7 years, there were 930 composite CVD events (386 CHD, 251 stroke, and 529 HF).
Adults with lower SPPB scores had a higher cumulative incidence of composite CVD outcomes.
The 5-year cumulative incidence of the composite CVD outcome in the low- and intermediate-SPPB categories was about three times (23.4%) and two times (15.3%) higher than in the high-SPPB category (8.6%), the researchers reported.
In addition, continuous SPPB scores showed significant associations with composite and individual CVD outcomes in all models. A 1-point lower SPPB score was associated with 6%-10% higher risk for CVD events after adjusting for potential confounders.
In the fully adjusted model, the risk for composite CVD outcomes was 47% higher (hazard ratio, 1.47; 95% confidence interval, 1.20-1.79) in those with low physical function and 25% higher in those with intermediate physical function (HR, 1.25; 95% CI, 1.07-1.46) compared with peers with high physical function.
For the individual outcomes, low physical function was associated with higher risk for stroke (HR, 1.81; 95% CI, 1.24-2.64) and HF (HR, 1.33; 95% CI, 1.02-1.73), whereas the association for CHD was not significant.
The associations were largely consistent across subgroups, including those with CVD at baseline.
The addition of SPPB scores significantly improved risk prediction of CVD events beyond traditional CVD risk factors in adults regardless of prior CVD history, suggesting that this tool may be useful for classifying CVD risk in older adults, the researchers said.
Meaningful impact on care?
“Our findings highlight the value of assessing the physical function level of older adults in clinical practice,” lead author Xiao Hu, MHS, with the department of epidemiology at Johns Hopkins, said in the news release. “In addition to heart health, older adults are at higher risk for falls and disability. The assessment of physical function may also inform the risk of these concerning conditions in older adults.”
Weighing in on the study, Jonathan Halperin, MD, cardiologist at Mount Sinai Heart and professor of medicine (cardiology) at the Icahn School of Medicine at Mount Sinai, both in New York, said that “It’s known that cardiorespiratory fitness is an important predictor of cardiovascular risk, but it is one of the few physiological risk factors that are subjectively queried but not objectively assessed in routine clinical practice.”
In this study, Dr. Halperin noted, the investigators found that a battery of physical performance assessments, including a walk test, chair standing, and balance testing, improved cardiovascular risk prediction.
Dr. Halperin cautioned, however, that “since even the short sequence of tests takes time to perform and interpret, and is not currently reimbursed under most health insurance policies, it is not clear whether the report will have a meaningful impact on patient care.”
This research was funded by the National Institutes of Health. Dr. Matsushita and Dr. Halperin have no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN HEART ASSOCIATION
Asymptomatic infections drive many epidemics, including monkeypox, polio, and COVID
Monkeypox, COVID, and polio: These three very different diseases have been dominating news cycles recently, but they share at least one common characteristic: some people can become infected – and in turn infect others – while showing no symptoms.
In 1883, the famous bacteriologist Friedrich Loeffler (1852-1915) recognized that an individual’s asymptomatic carriage of bacteria could lead to diphtheria in others.
“Typhoid Mary” is perhaps the quintessential example of asymptomatic transmission of infections leading to illness and death. At the turn of the 20th century, young Mary Mallon emigrated from Ireland to New York, where she soon became a cook for wealthy Manhattan families.
George Soper, a sanitary engineer, was hired by a stricken family to investigate. After epidemiologic study, he suspected that Mary was a carrier of Salmonella typhi, the bacterial cause of typhoid fever. He persuaded the New York Department of Health to test her – against her will – for infection. After her stool was found to test positive for Salmonella, Mary was forcibly moved to North Brother Island, where she remained largely isolated from others for the next 2 years. In 1910, she was released by a new commissioner after promising not to work as a cook.
However, working under an assumed name, Mary resumed cooking at the Sloane Hospital for Women in Manhattan. Over the next 3 months, at least 25 staff members became ill. Having been found out, Mary was again exiled to the island, where she spent the rest of her life. She died in 1938 after having infected at least 122 people, five of whom died.
COVID
Asymptomatic infections are primary drivers of COVID. Earlier in the pandemic, a meta-analysis suggested a 40% rate of asymptomatic infections, although some early reports arrived at lower estimates. A 2021 JAMA Network Open modeling study indicated a 60% rate.
Those rates are changing with the Omicron variants, of which even more cases are asymptomatic. Is this from a mutation in the virus? Some suggest that it is most likely attributable to prior vaccination resulting in boosted immunity and infections being milder. Of concern is that, although people may be asymptomatic, they still have the same viral load in their nose and can readily transmit infection.
Vincent Racaniello, PhD, a professor of virology at Columbia University in New York, told this news organization that “SARS-CoV-2 COVID is so effective at transmitting because it does this asymptomatic transmission. And so you’re out and about; you have no idea that you’re infected. You’re effectively doing what we call community transmission.”
This distinguishes SARS-CoV-2 from SARS-CoV-1. SARS-CoV-1 – which caused the SARS epidemic in 2002–2004 – had very little asymptomatic shedding. With COVID, on the other hand, “A lot of people are infected but never transmit,” Dr. Racaniello added. “I think 80% of transmissions are done by 20% of infected people because those are the ones who are shedding the most virus.”
Polio
The August case of paralytic polio in Rockland County, N.Y., is “the first case of polio reported in the United States in nearly 10 years, and only the second instance of community transmission identified in the U.S. since 1979,” a spokesperson for the Centers for Disease Control and Prevention said in an email. “Although no additional cases of polio have been reported at this time, recent wastewater findings elevate concerns that poliovirus is present in these communities, posing a risk to those who are unvaccinated.”
Poliovirus has now been found in the wastewater of New York City and three surrounding counties: Rockland, Orange, and Sullivan.
Unlike COVID, which is spread through air and respiratory secretions, polio has primarily fecal-oral transmission, meaning it is spread by people ingesting food or water contaminated with stool.
According to the World Health Organization, up to 90% of infections are unrecognized because the person has no to minimal symptoms. Symptoms are nonspecific in the remainder. Only a small proportion of those infected go on to develop paralysis.
Paul Offit, MD, a virologist and director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, told this news organization that before widespread immunization, polio “caused 25,000 – 30,000 children every year to be paralyzed and 1,500 to die. Roughly 1 of every 200 children who was infected was paralyzed. We had the inactivated vaccine followed by the oral polio vaccine (OPV). The price that we paid for the OPV was that rarely it could revert to the so-called neurovirulent type, a paralytic type.”
Use of the OPV was discontinued in 2000 in the United States but is still widely used worldwide because it is inexpensive and easier to administer than injections. It appeared that we were close to completely eradicating polio, as we had smallpox, but then vaccine-derived polio virus (VDPV) started cropping up in Africa, the Middle East, and Asia. They are mainly from the type 2 virus, as is the New York case. There have been three other cases of VDPV in the United States since 2000.
Now, Dr. Offit estimates that only 1 in 2,000 of those infected become paralyzed. This is why the CDC and epidemiologists are so concerned about the Rockland patient – that one case of paralysis could represent a large pool of people who are infected with polio and are asymptomatic, continuing to shed infectious virus into the sewage.
The CDC confirmed that it began conducting wastewater testing for polio in August 2022. In their interviews for this article, Dr. Offit and Dr. Racaniello were both critical of this, stressing that it is essential to do wastewater testing nationally, since asymptomatic polio can be expected to crop up from international travelers who have received OPV.
Many countries conduct that kind of wastewater surveillance. Dr. Racaniello was particularly critical of the CDC. “We’ve been telling CDC for years, at least a decade, Why don’t you check the wastewater?,” Dr. Racaniello said, “It’s been known for many years that we should be looking to monitor the circulation of these viruses. So we are using paralysis as a sentinel to say that this virus is in the wastewater, which is just not acceptable!”
Apparently there was some concern that the public would not understand. Dr. Offit viewed it as one more piece of necessary education: “You shouldn’t be alarmed about this as long as you’re vaccinated. If you’re not vaccinated, realize that this is a risk you’re taking.”
Monkeypox
Monkeypox cases have been skyrocketing in the United States in recent weeks. More than 18,000 cases have been reported since the first case in Boston on May 19, 2022.
“Monkeypox was such a rare zoonotic disease, and the disease always historically was introduced through animal contact,” Stuart Isaacs, MD, a pox virologist at the University of Pennsylvania, said in an interview. “And then the infected person would have potential spread within the household as the most common human-to-human spread, The sexual transmission is driving a lot of this infection and potentially allowing this to efficiently spread from person to person.”
A recent study from Belgium, available only as a preprint, created concerns about potential asymptomatic transmission of monkeypox Three men had undergone testing for anogenital chlamydia and gonorrhea but showed no clinical signs of monkeypox. The same samples were later tested by polymerase chain reaction (PCR), and their viral load in anorectal swabs was similar to or slightly lower than that of symptomatic patients. While no cultures were done, the patients seroconverted by later antibody testing, confirming infection.
Via email, a CDC spokesperson noted, “At this time, CDC does not have enough data to support transmission from aerosolized virus for the ongoing monkeypox outbreak, or to assess the risks for transmission from asymptomatic people. The data supports the main source of transmission currently as close contact with someone who is infected with monkeypox.”
Dr. Isaacs agreed, saying studies of smallpox, a related orthopox virus, also suggested this.
In the United Kingdom, the Institute of Tropical Medicine is offering PCR testing for monkeypox to all patients who come for gonorrhea/chlamydia screening. Dr. Racaniello said, “I think that would be great to get a sense of who is infected. Then you could look at the results and say what fraction of people go on to develop lesions, and they give you a sense of the asymptomatic rate, which we don’t know at this point.”
Unfortunately, to be tested for monkeypox in the United States requires that the patient have a lesion. “This is part of the dropped ball of public health in the U.S.,” Dr. Racaniello said. “We’re not thinking about this. .... We need to be doing [infectivity] experiments. So then the question is, how much infectious virus do you need to transmit?”
Conclusion
We’ve seen that asymptomatic carriage of bacteria and viruses occurs readily with typhoid, COVID, diphtheria, and polio (among many other organisms, such as methicillin-resistant Staphylococcus aureus or group A strep) and is far less likely with monkeypox.
Two common denominators emerged from these interviews. The first and biggest hurdle is identifying asymptomatic carriers, which is hampered by the politicization of the CDC and funding cuts to public health. “It used to be the CDC was all about public health, and now it’s administrators, unfortunately,” said Dr. Racaniello, citing science writer Laurie Garrett, author of the influential 1994 book, “The Coming Plague”.
We don’t conduct proper surveillance, he pointed out. Wastewater surveillance has been neglected for more than a decade. It has been used for SARS-CoV-2 but is only now being initiated for polio and monkeypox. Norovirus testing would also be especially helpful in reducing foodborne outbreaks, Dr. Racaniello suggested.
The second common denominator is the need to increase the availability and uptake of vaccines. As Dr. Racaniello said about COVID, “The virus is here to stay. It’s never going to go away. It’s in humans. It’s in a lot of animals. So we’re stuck with it. We’re going to have outbreaks every year. So what do you do? Get vaccinated.” And he added, “Vaccination is the most important strategy to go on with our lives.”
Dr. Isaacs was a bit more tempered, not wanting to oversell the vaccine. He said, “The vaccine is just part of the toolkit,” which includes education, testing, isolation, and reducing risk, all of which decrease the transmission cycles.
Speaking of how antivaccine advocates had specifically targeted the Hasidic community in New York State’s Rockland County, Dr. Offit noted, “I don’t think it’s a knowledge deficit as much as a trust deficit.” He said officials should identify people in communities such as these who are trusted and have them become the influencers.
The final major hurdle to controlling these outbreaks remains global disparities in care. Monkeypox has been endemic in Nigeria for decades. It was only when it spread to Europe and America that it received attention. Polio has been actively circulating in Africa and the Middle East but is only getting attention because of the New York case.
Africa was unable to afford COVID vaccines until recently. While many in the United States are on their fourth booster, as of December 2021, more than 80% of people in Africa had not yet received a single dose, according to an article by Munyaradzi Makoni in The Lancet Respiratory Medicine.
Echoing Dr. Peter Hotez’s long-standing plea for “vaccine diplomacy,” Dr. Racaniello concluded, “My philosophy has always been we should give [vaccines] to them. I mean, we spend trillions on guns. Can’t we spend a few hundred million on vaccines? We should give away everything in terms of medicine to countries that need it, and people would like us a lot better than they do now. I think it would be such a great way of getting countries to like us. … So what if it costs a billion dollars a year? It’s a drop in the bucket for us.”
Given globalization, an infectious outbreak anywhere is a risk to all.
Dr. Racaniello and Dr. Offit report no relevant financial relationships. Dr. Isaacs receives royalties from UpToDate.
A version of this article first appeared on Medscape.com.
Monkeypox, COVID, and polio: These three very different diseases have been dominating news cycles recently, but they share at least one common characteristic: some people can become infected – and in turn infect others – while showing no symptoms.
In 1883, the famous bacteriologist Friedrich Loeffler (1852-1915) recognized that an individual’s asymptomatic carriage of bacteria could lead to diphtheria in others.
“Typhoid Mary” is perhaps the quintessential example of asymptomatic transmission of infections leading to illness and death. At the turn of the 20th century, young Mary Mallon emigrated from Ireland to New York, where she soon became a cook for wealthy Manhattan families.
George Soper, a sanitary engineer, was hired by a stricken family to investigate. After epidemiologic study, he suspected that Mary was a carrier of Salmonella typhi, the bacterial cause of typhoid fever. He persuaded the New York Department of Health to test her – against her will – for infection. After her stool was found to test positive for Salmonella, Mary was forcibly moved to North Brother Island, where she remained largely isolated from others for the next 2 years. In 1910, she was released by a new commissioner after promising not to work as a cook.
However, working under an assumed name, Mary resumed cooking at the Sloane Hospital for Women in Manhattan. Over the next 3 months, at least 25 staff members became ill. Having been found out, Mary was again exiled to the island, where she spent the rest of her life. She died in 1938 after having infected at least 122 people, five of whom died.
COVID
Asymptomatic infections are primary drivers of COVID. Earlier in the pandemic, a meta-analysis suggested a 40% rate of asymptomatic infections, although some early reports arrived at lower estimates. A 2021 JAMA Network Open modeling study indicated a 60% rate.
Those rates are changing with the Omicron variants, of which even more cases are asymptomatic. Is this from a mutation in the virus? Some suggest that it is most likely attributable to prior vaccination resulting in boosted immunity and infections being milder. Of concern is that, although people may be asymptomatic, they still have the same viral load in their nose and can readily transmit infection.
Vincent Racaniello, PhD, a professor of virology at Columbia University in New York, told this news organization that “SARS-CoV-2 COVID is so effective at transmitting because it does this asymptomatic transmission. And so you’re out and about; you have no idea that you’re infected. You’re effectively doing what we call community transmission.”
This distinguishes SARS-CoV-2 from SARS-CoV-1. SARS-CoV-1 – which caused the SARS epidemic in 2002–2004 – had very little asymptomatic shedding. With COVID, on the other hand, “A lot of people are infected but never transmit,” Dr. Racaniello added. “I think 80% of transmissions are done by 20% of infected people because those are the ones who are shedding the most virus.”
Polio
The August case of paralytic polio in Rockland County, N.Y., is “the first case of polio reported in the United States in nearly 10 years, and only the second instance of community transmission identified in the U.S. since 1979,” a spokesperson for the Centers for Disease Control and Prevention said in an email. “Although no additional cases of polio have been reported at this time, recent wastewater findings elevate concerns that poliovirus is present in these communities, posing a risk to those who are unvaccinated.”
Poliovirus has now been found in the wastewater of New York City and three surrounding counties: Rockland, Orange, and Sullivan.
Unlike COVID, which is spread through air and respiratory secretions, polio has primarily fecal-oral transmission, meaning it is spread by people ingesting food or water contaminated with stool.
According to the World Health Organization, up to 90% of infections are unrecognized because the person has no to minimal symptoms. Symptoms are nonspecific in the remainder. Only a small proportion of those infected go on to develop paralysis.
Paul Offit, MD, a virologist and director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, told this news organization that before widespread immunization, polio “caused 25,000 – 30,000 children every year to be paralyzed and 1,500 to die. Roughly 1 of every 200 children who was infected was paralyzed. We had the inactivated vaccine followed by the oral polio vaccine (OPV). The price that we paid for the OPV was that rarely it could revert to the so-called neurovirulent type, a paralytic type.”
Use of the OPV was discontinued in 2000 in the United States but is still widely used worldwide because it is inexpensive and easier to administer than injections. It appeared that we were close to completely eradicating polio, as we had smallpox, but then vaccine-derived polio virus (VDPV) started cropping up in Africa, the Middle East, and Asia. They are mainly from the type 2 virus, as is the New York case. There have been three other cases of VDPV in the United States since 2000.
Now, Dr. Offit estimates that only 1 in 2,000 of those infected become paralyzed. This is why the CDC and epidemiologists are so concerned about the Rockland patient – that one case of paralysis could represent a large pool of people who are infected with polio and are asymptomatic, continuing to shed infectious virus into the sewage.
The CDC confirmed that it began conducting wastewater testing for polio in August 2022. In their interviews for this article, Dr. Offit and Dr. Racaniello were both critical of this, stressing that it is essential to do wastewater testing nationally, since asymptomatic polio can be expected to crop up from international travelers who have received OPV.
Many countries conduct that kind of wastewater surveillance. Dr. Racaniello was particularly critical of the CDC. “We’ve been telling CDC for years, at least a decade, Why don’t you check the wastewater?,” Dr. Racaniello said, “It’s been known for many years that we should be looking to monitor the circulation of these viruses. So we are using paralysis as a sentinel to say that this virus is in the wastewater, which is just not acceptable!”
Apparently there was some concern that the public would not understand. Dr. Offit viewed it as one more piece of necessary education: “You shouldn’t be alarmed about this as long as you’re vaccinated. If you’re not vaccinated, realize that this is a risk you’re taking.”
Monkeypox
Monkeypox cases have been skyrocketing in the United States in recent weeks. More than 18,000 cases have been reported since the first case in Boston on May 19, 2022.
“Monkeypox was such a rare zoonotic disease, and the disease always historically was introduced through animal contact,” Stuart Isaacs, MD, a pox virologist at the University of Pennsylvania, said in an interview. “And then the infected person would have potential spread within the household as the most common human-to-human spread, The sexual transmission is driving a lot of this infection and potentially allowing this to efficiently spread from person to person.”
A recent study from Belgium, available only as a preprint, created concerns about potential asymptomatic transmission of monkeypox Three men had undergone testing for anogenital chlamydia and gonorrhea but showed no clinical signs of monkeypox. The same samples were later tested by polymerase chain reaction (PCR), and their viral load in anorectal swabs was similar to or slightly lower than that of symptomatic patients. While no cultures were done, the patients seroconverted by later antibody testing, confirming infection.
Via email, a CDC spokesperson noted, “At this time, CDC does not have enough data to support transmission from aerosolized virus for the ongoing monkeypox outbreak, or to assess the risks for transmission from asymptomatic people. The data supports the main source of transmission currently as close contact with someone who is infected with monkeypox.”
Dr. Isaacs agreed, saying studies of smallpox, a related orthopox virus, also suggested this.
In the United Kingdom, the Institute of Tropical Medicine is offering PCR testing for monkeypox to all patients who come for gonorrhea/chlamydia screening. Dr. Racaniello said, “I think that would be great to get a sense of who is infected. Then you could look at the results and say what fraction of people go on to develop lesions, and they give you a sense of the asymptomatic rate, which we don’t know at this point.”
Unfortunately, to be tested for monkeypox in the United States requires that the patient have a lesion. “This is part of the dropped ball of public health in the U.S.,” Dr. Racaniello said. “We’re not thinking about this. .... We need to be doing [infectivity] experiments. So then the question is, how much infectious virus do you need to transmit?”
Conclusion
We’ve seen that asymptomatic carriage of bacteria and viruses occurs readily with typhoid, COVID, diphtheria, and polio (among many other organisms, such as methicillin-resistant Staphylococcus aureus or group A strep) and is far less likely with monkeypox.
Two common denominators emerged from these interviews. The first and biggest hurdle is identifying asymptomatic carriers, which is hampered by the politicization of the CDC and funding cuts to public health. “It used to be the CDC was all about public health, and now it’s administrators, unfortunately,” said Dr. Racaniello, citing science writer Laurie Garrett, author of the influential 1994 book, “The Coming Plague”.
We don’t conduct proper surveillance, he pointed out. Wastewater surveillance has been neglected for more than a decade. It has been used for SARS-CoV-2 but is only now being initiated for polio and monkeypox. Norovirus testing would also be especially helpful in reducing foodborne outbreaks, Dr. Racaniello suggested.
The second common denominator is the need to increase the availability and uptake of vaccines. As Dr. Racaniello said about COVID, “The virus is here to stay. It’s never going to go away. It’s in humans. It’s in a lot of animals. So we’re stuck with it. We’re going to have outbreaks every year. So what do you do? Get vaccinated.” And he added, “Vaccination is the most important strategy to go on with our lives.”
Dr. Isaacs was a bit more tempered, not wanting to oversell the vaccine. He said, “The vaccine is just part of the toolkit,” which includes education, testing, isolation, and reducing risk, all of which decrease the transmission cycles.
Speaking of how antivaccine advocates had specifically targeted the Hasidic community in New York State’s Rockland County, Dr. Offit noted, “I don’t think it’s a knowledge deficit as much as a trust deficit.” He said officials should identify people in communities such as these who are trusted and have them become the influencers.
The final major hurdle to controlling these outbreaks remains global disparities in care. Monkeypox has been endemic in Nigeria for decades. It was only when it spread to Europe and America that it received attention. Polio has been actively circulating in Africa and the Middle East but is only getting attention because of the New York case.
Africa was unable to afford COVID vaccines until recently. While many in the United States are on their fourth booster, as of December 2021, more than 80% of people in Africa had not yet received a single dose, according to an article by Munyaradzi Makoni in The Lancet Respiratory Medicine.
Echoing Dr. Peter Hotez’s long-standing plea for “vaccine diplomacy,” Dr. Racaniello concluded, “My philosophy has always been we should give [vaccines] to them. I mean, we spend trillions on guns. Can’t we spend a few hundred million on vaccines? We should give away everything in terms of medicine to countries that need it, and people would like us a lot better than they do now. I think it would be such a great way of getting countries to like us. … So what if it costs a billion dollars a year? It’s a drop in the bucket for us.”
Given globalization, an infectious outbreak anywhere is a risk to all.
Dr. Racaniello and Dr. Offit report no relevant financial relationships. Dr. Isaacs receives royalties from UpToDate.
A version of this article first appeared on Medscape.com.
Monkeypox, COVID, and polio: These three very different diseases have been dominating news cycles recently, but they share at least one common characteristic: some people can become infected – and in turn infect others – while showing no symptoms.
In 1883, the famous bacteriologist Friedrich Loeffler (1852-1915) recognized that an individual’s asymptomatic carriage of bacteria could lead to diphtheria in others.
“Typhoid Mary” is perhaps the quintessential example of asymptomatic transmission of infections leading to illness and death. At the turn of the 20th century, young Mary Mallon emigrated from Ireland to New York, where she soon became a cook for wealthy Manhattan families.
George Soper, a sanitary engineer, was hired by a stricken family to investigate. After epidemiologic study, he suspected that Mary was a carrier of Salmonella typhi, the bacterial cause of typhoid fever. He persuaded the New York Department of Health to test her – against her will – for infection. After her stool was found to test positive for Salmonella, Mary was forcibly moved to North Brother Island, where she remained largely isolated from others for the next 2 years. In 1910, she was released by a new commissioner after promising not to work as a cook.
However, working under an assumed name, Mary resumed cooking at the Sloane Hospital for Women in Manhattan. Over the next 3 months, at least 25 staff members became ill. Having been found out, Mary was again exiled to the island, where she spent the rest of her life. She died in 1938 after having infected at least 122 people, five of whom died.
COVID
Asymptomatic infections are primary drivers of COVID. Earlier in the pandemic, a meta-analysis suggested a 40% rate of asymptomatic infections, although some early reports arrived at lower estimates. A 2021 JAMA Network Open modeling study indicated a 60% rate.
Those rates are changing with the Omicron variants, of which even more cases are asymptomatic. Is this from a mutation in the virus? Some suggest that it is most likely attributable to prior vaccination resulting in boosted immunity and infections being milder. Of concern is that, although people may be asymptomatic, they still have the same viral load in their nose and can readily transmit infection.
Vincent Racaniello, PhD, a professor of virology at Columbia University in New York, told this news organization that “SARS-CoV-2 COVID is so effective at transmitting because it does this asymptomatic transmission. And so you’re out and about; you have no idea that you’re infected. You’re effectively doing what we call community transmission.”
This distinguishes SARS-CoV-2 from SARS-CoV-1. SARS-CoV-1 – which caused the SARS epidemic in 2002–2004 – had very little asymptomatic shedding. With COVID, on the other hand, “A lot of people are infected but never transmit,” Dr. Racaniello added. “I think 80% of transmissions are done by 20% of infected people because those are the ones who are shedding the most virus.”
Polio
The August case of paralytic polio in Rockland County, N.Y., is “the first case of polio reported in the United States in nearly 10 years, and only the second instance of community transmission identified in the U.S. since 1979,” a spokesperson for the Centers for Disease Control and Prevention said in an email. “Although no additional cases of polio have been reported at this time, recent wastewater findings elevate concerns that poliovirus is present in these communities, posing a risk to those who are unvaccinated.”
Poliovirus has now been found in the wastewater of New York City and three surrounding counties: Rockland, Orange, and Sullivan.
Unlike COVID, which is spread through air and respiratory secretions, polio has primarily fecal-oral transmission, meaning it is spread by people ingesting food or water contaminated with stool.
According to the World Health Organization, up to 90% of infections are unrecognized because the person has no to minimal symptoms. Symptoms are nonspecific in the remainder. Only a small proportion of those infected go on to develop paralysis.
Paul Offit, MD, a virologist and director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, told this news organization that before widespread immunization, polio “caused 25,000 – 30,000 children every year to be paralyzed and 1,500 to die. Roughly 1 of every 200 children who was infected was paralyzed. We had the inactivated vaccine followed by the oral polio vaccine (OPV). The price that we paid for the OPV was that rarely it could revert to the so-called neurovirulent type, a paralytic type.”
Use of the OPV was discontinued in 2000 in the United States but is still widely used worldwide because it is inexpensive and easier to administer than injections. It appeared that we were close to completely eradicating polio, as we had smallpox, but then vaccine-derived polio virus (VDPV) started cropping up in Africa, the Middle East, and Asia. They are mainly from the type 2 virus, as is the New York case. There have been three other cases of VDPV in the United States since 2000.
Now, Dr. Offit estimates that only 1 in 2,000 of those infected become paralyzed. This is why the CDC and epidemiologists are so concerned about the Rockland patient – that one case of paralysis could represent a large pool of people who are infected with polio and are asymptomatic, continuing to shed infectious virus into the sewage.
The CDC confirmed that it began conducting wastewater testing for polio in August 2022. In their interviews for this article, Dr. Offit and Dr. Racaniello were both critical of this, stressing that it is essential to do wastewater testing nationally, since asymptomatic polio can be expected to crop up from international travelers who have received OPV.
Many countries conduct that kind of wastewater surveillance. Dr. Racaniello was particularly critical of the CDC. “We’ve been telling CDC for years, at least a decade, Why don’t you check the wastewater?,” Dr. Racaniello said, “It’s been known for many years that we should be looking to monitor the circulation of these viruses. So we are using paralysis as a sentinel to say that this virus is in the wastewater, which is just not acceptable!”
Apparently there was some concern that the public would not understand. Dr. Offit viewed it as one more piece of necessary education: “You shouldn’t be alarmed about this as long as you’re vaccinated. If you’re not vaccinated, realize that this is a risk you’re taking.”
Monkeypox
Monkeypox cases have been skyrocketing in the United States in recent weeks. More than 18,000 cases have been reported since the first case in Boston on May 19, 2022.
“Monkeypox was such a rare zoonotic disease, and the disease always historically was introduced through animal contact,” Stuart Isaacs, MD, a pox virologist at the University of Pennsylvania, said in an interview. “And then the infected person would have potential spread within the household as the most common human-to-human spread, The sexual transmission is driving a lot of this infection and potentially allowing this to efficiently spread from person to person.”
A recent study from Belgium, available only as a preprint, created concerns about potential asymptomatic transmission of monkeypox Three men had undergone testing for anogenital chlamydia and gonorrhea but showed no clinical signs of monkeypox. The same samples were later tested by polymerase chain reaction (PCR), and their viral load in anorectal swabs was similar to or slightly lower than that of symptomatic patients. While no cultures were done, the patients seroconverted by later antibody testing, confirming infection.
Via email, a CDC spokesperson noted, “At this time, CDC does not have enough data to support transmission from aerosolized virus for the ongoing monkeypox outbreak, or to assess the risks for transmission from asymptomatic people. The data supports the main source of transmission currently as close contact with someone who is infected with monkeypox.”
Dr. Isaacs agreed, saying studies of smallpox, a related orthopox virus, also suggested this.
In the United Kingdom, the Institute of Tropical Medicine is offering PCR testing for monkeypox to all patients who come for gonorrhea/chlamydia screening. Dr. Racaniello said, “I think that would be great to get a sense of who is infected. Then you could look at the results and say what fraction of people go on to develop lesions, and they give you a sense of the asymptomatic rate, which we don’t know at this point.”
Unfortunately, to be tested for monkeypox in the United States requires that the patient have a lesion. “This is part of the dropped ball of public health in the U.S.,” Dr. Racaniello said. “We’re not thinking about this. .... We need to be doing [infectivity] experiments. So then the question is, how much infectious virus do you need to transmit?”
Conclusion
We’ve seen that asymptomatic carriage of bacteria and viruses occurs readily with typhoid, COVID, diphtheria, and polio (among many other organisms, such as methicillin-resistant Staphylococcus aureus or group A strep) and is far less likely with monkeypox.
Two common denominators emerged from these interviews. The first and biggest hurdle is identifying asymptomatic carriers, which is hampered by the politicization of the CDC and funding cuts to public health. “It used to be the CDC was all about public health, and now it’s administrators, unfortunately,” said Dr. Racaniello, citing science writer Laurie Garrett, author of the influential 1994 book, “The Coming Plague”.
We don’t conduct proper surveillance, he pointed out. Wastewater surveillance has been neglected for more than a decade. It has been used for SARS-CoV-2 but is only now being initiated for polio and monkeypox. Norovirus testing would also be especially helpful in reducing foodborne outbreaks, Dr. Racaniello suggested.
The second common denominator is the need to increase the availability and uptake of vaccines. As Dr. Racaniello said about COVID, “The virus is here to stay. It’s never going to go away. It’s in humans. It’s in a lot of animals. So we’re stuck with it. We’re going to have outbreaks every year. So what do you do? Get vaccinated.” And he added, “Vaccination is the most important strategy to go on with our lives.”
Dr. Isaacs was a bit more tempered, not wanting to oversell the vaccine. He said, “The vaccine is just part of the toolkit,” which includes education, testing, isolation, and reducing risk, all of which decrease the transmission cycles.
Speaking of how antivaccine advocates had specifically targeted the Hasidic community in New York State’s Rockland County, Dr. Offit noted, “I don’t think it’s a knowledge deficit as much as a trust deficit.” He said officials should identify people in communities such as these who are trusted and have them become the influencers.
The final major hurdle to controlling these outbreaks remains global disparities in care. Monkeypox has been endemic in Nigeria for decades. It was only when it spread to Europe and America that it received attention. Polio has been actively circulating in Africa and the Middle East but is only getting attention because of the New York case.
Africa was unable to afford COVID vaccines until recently. While many in the United States are on their fourth booster, as of December 2021, more than 80% of people in Africa had not yet received a single dose, according to an article by Munyaradzi Makoni in The Lancet Respiratory Medicine.
Echoing Dr. Peter Hotez’s long-standing plea for “vaccine diplomacy,” Dr. Racaniello concluded, “My philosophy has always been we should give [vaccines] to them. I mean, we spend trillions on guns. Can’t we spend a few hundred million on vaccines? We should give away everything in terms of medicine to countries that need it, and people would like us a lot better than they do now. I think it would be such a great way of getting countries to like us. … So what if it costs a billion dollars a year? It’s a drop in the bucket for us.”
Given globalization, an infectious outbreak anywhere is a risk to all.
Dr. Racaniello and Dr. Offit report no relevant financial relationships. Dr. Isaacs receives royalties from UpToDate.
A version of this article first appeared on Medscape.com.
Yoga, CBT provide long-term improvement in insomnia, worry
new research suggests.
The study is the first to compare the long-term effects from the two interventions; and the results offer clinicians and patients two effective choices for reducing worry and anxiety, researchers noted.
“Anxiety can be a really big problem for older adults,” lead investigator Suzanne Danhauer, PhD, professor of social sciences and health policy at Wake Forest University, Winston-Salem, N.C., said in an interview.
“So to find something they can do that lasts ... and has some enduring impact on their quality of life and their mental health, and they’re both nonpharmacologic treatments, I think for a lot of older people that’s really attractive,” Dr. Danhauer said.
The findings are published in the September issue of the American Journal of Geriatric Psychiatry.
Long-term benefits
The two-stage randomized preference trial included 500 community-dwelling individuals over age 60 who scored 26 or above on the Penn State Worry Questionnaire–Abbreviated (PSWQ-A), indicating heightened anxiety and worry.
Half the group took part in a randomized, controlled trial comparing CBT (n = 125) with yoga (n = 125). The other half participated in a preference trial where they were allowed to choose between CBT (n = 120) and yoga (n = 130).
Participants completed 20 yoga sessions over 10 weeks or 10 weekly CBT calls between May 2017 and November 2018.
Measures used included the PSWQ-A, the Insomnia Severity Index (ISI), the Patient Reported Outcomes Measurement Information System (PROMIS) Short Form v1.0 – Anxiety 8a, and the PROMIS-29 to assess depression, fatigue, physical function, social participation, and pain.
In 2020, the researchers published results at 11 weeks showing improvements from baseline in all areas. The scores for anxiety and worry were similar between the CBT and yoga groups, but CBT yielded significantly higher improvement in insomnia.
At 37 weeks, about 6 months after the interventions had ended, the investigators found even greater improvements from baseline in all areas measured – except physical function.
However, at that point, there were no significant differences between the two interventions in either the randomized controlled trial or the preference trial. There were also no differences in the results between the two trial designs.
“There were some little differences, but by and large we found both interventions to be efficacious,” Dr. Danhauer said. “This gives clinicians [the] choice to be able to say, ‘you can try either one of these and they’re probably going to help.’ ”
Beyond statistically significant
The researchers also found the improvements were not just statistically significant, but were also clinically meaningful for worry, anxiety, and insomnia.
Meaningful changes were defined as a decrease of at least 5.5 points on the PSWQ-A for worry, a decrease of at least 3 points on the PROMIS Anxiety scale for anxiety, and a decrease of at least 6 points in the ISI for insomnia.
At long-term follow-up, the majority of participants in both the CBT and yoga arms of the randomized, controlled trial demonstrated meaningful change in worry (85.7% and 77.6%, respectively), anxiety (82.1% and 80.8%), and insomnia (52.8% and 44.3%).
The majority of participants also reported meaningful improvements in generalized anxiety symptoms, depressive symptoms, and fatigue, but not for physical function, pain interference, or pain intensity.
“That’s the part to me that’s particularly notable. The improvements weren’t just statistically significant, they were clinically meaningful as well,” Dr. Danhauer said.
“When it comes right down to people’s lives, they want differences they can feel and see and not just what a P value looks like,” she added.
Real-world impact
In an accompanying editorial, Carmen Andreescu, MD, associate professor of psychiatry at the University of Pittsburgh, agreed that the results have “real-world impact.”
“Clinicians can direct their patients toward interventions that may be beneficial, consolidate the results over time and avoid fueling the well-trained worry cognitive loop with concerns related to potential side effects,” Dr. Andreescu wrote.
She adds that interventions such as these “may increase accessibility and provide relief for the immediate suffering of our patients.”
The study was funded by the Patient-Centered Outcomes Research Institute Program. Dr. Danhauer and Dr. Andreescu reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
The study is the first to compare the long-term effects from the two interventions; and the results offer clinicians and patients two effective choices for reducing worry and anxiety, researchers noted.
“Anxiety can be a really big problem for older adults,” lead investigator Suzanne Danhauer, PhD, professor of social sciences and health policy at Wake Forest University, Winston-Salem, N.C., said in an interview.
“So to find something they can do that lasts ... and has some enduring impact on their quality of life and their mental health, and they’re both nonpharmacologic treatments, I think for a lot of older people that’s really attractive,” Dr. Danhauer said.
The findings are published in the September issue of the American Journal of Geriatric Psychiatry.
Long-term benefits
The two-stage randomized preference trial included 500 community-dwelling individuals over age 60 who scored 26 or above on the Penn State Worry Questionnaire–Abbreviated (PSWQ-A), indicating heightened anxiety and worry.
Half the group took part in a randomized, controlled trial comparing CBT (n = 125) with yoga (n = 125). The other half participated in a preference trial where they were allowed to choose between CBT (n = 120) and yoga (n = 130).
Participants completed 20 yoga sessions over 10 weeks or 10 weekly CBT calls between May 2017 and November 2018.
Measures used included the PSWQ-A, the Insomnia Severity Index (ISI), the Patient Reported Outcomes Measurement Information System (PROMIS) Short Form v1.0 – Anxiety 8a, and the PROMIS-29 to assess depression, fatigue, physical function, social participation, and pain.
In 2020, the researchers published results at 11 weeks showing improvements from baseline in all areas. The scores for anxiety and worry were similar between the CBT and yoga groups, but CBT yielded significantly higher improvement in insomnia.
At 37 weeks, about 6 months after the interventions had ended, the investigators found even greater improvements from baseline in all areas measured – except physical function.
However, at that point, there were no significant differences between the two interventions in either the randomized controlled trial or the preference trial. There were also no differences in the results between the two trial designs.
“There were some little differences, but by and large we found both interventions to be efficacious,” Dr. Danhauer said. “This gives clinicians [the] choice to be able to say, ‘you can try either one of these and they’re probably going to help.’ ”
Beyond statistically significant
The researchers also found the improvements were not just statistically significant, but were also clinically meaningful for worry, anxiety, and insomnia.
Meaningful changes were defined as a decrease of at least 5.5 points on the PSWQ-A for worry, a decrease of at least 3 points on the PROMIS Anxiety scale for anxiety, and a decrease of at least 6 points in the ISI for insomnia.
At long-term follow-up, the majority of participants in both the CBT and yoga arms of the randomized, controlled trial demonstrated meaningful change in worry (85.7% and 77.6%, respectively), anxiety (82.1% and 80.8%), and insomnia (52.8% and 44.3%).
The majority of participants also reported meaningful improvements in generalized anxiety symptoms, depressive symptoms, and fatigue, but not for physical function, pain interference, or pain intensity.
“That’s the part to me that’s particularly notable. The improvements weren’t just statistically significant, they were clinically meaningful as well,” Dr. Danhauer said.
“When it comes right down to people’s lives, they want differences they can feel and see and not just what a P value looks like,” she added.
Real-world impact
In an accompanying editorial, Carmen Andreescu, MD, associate professor of psychiatry at the University of Pittsburgh, agreed that the results have “real-world impact.”
“Clinicians can direct their patients toward interventions that may be beneficial, consolidate the results over time and avoid fueling the well-trained worry cognitive loop with concerns related to potential side effects,” Dr. Andreescu wrote.
She adds that interventions such as these “may increase accessibility and provide relief for the immediate suffering of our patients.”
The study was funded by the Patient-Centered Outcomes Research Institute Program. Dr. Danhauer and Dr. Andreescu reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research suggests.
The study is the first to compare the long-term effects from the two interventions; and the results offer clinicians and patients two effective choices for reducing worry and anxiety, researchers noted.
“Anxiety can be a really big problem for older adults,” lead investigator Suzanne Danhauer, PhD, professor of social sciences and health policy at Wake Forest University, Winston-Salem, N.C., said in an interview.
“So to find something they can do that lasts ... and has some enduring impact on their quality of life and their mental health, and they’re both nonpharmacologic treatments, I think for a lot of older people that’s really attractive,” Dr. Danhauer said.
The findings are published in the September issue of the American Journal of Geriatric Psychiatry.
Long-term benefits
The two-stage randomized preference trial included 500 community-dwelling individuals over age 60 who scored 26 or above on the Penn State Worry Questionnaire–Abbreviated (PSWQ-A), indicating heightened anxiety and worry.
Half the group took part in a randomized, controlled trial comparing CBT (n = 125) with yoga (n = 125). The other half participated in a preference trial where they were allowed to choose between CBT (n = 120) and yoga (n = 130).
Participants completed 20 yoga sessions over 10 weeks or 10 weekly CBT calls between May 2017 and November 2018.
Measures used included the PSWQ-A, the Insomnia Severity Index (ISI), the Patient Reported Outcomes Measurement Information System (PROMIS) Short Form v1.0 – Anxiety 8a, and the PROMIS-29 to assess depression, fatigue, physical function, social participation, and pain.
In 2020, the researchers published results at 11 weeks showing improvements from baseline in all areas. The scores for anxiety and worry were similar between the CBT and yoga groups, but CBT yielded significantly higher improvement in insomnia.
At 37 weeks, about 6 months after the interventions had ended, the investigators found even greater improvements from baseline in all areas measured – except physical function.
However, at that point, there were no significant differences between the two interventions in either the randomized controlled trial or the preference trial. There were also no differences in the results between the two trial designs.
“There were some little differences, but by and large we found both interventions to be efficacious,” Dr. Danhauer said. “This gives clinicians [the] choice to be able to say, ‘you can try either one of these and they’re probably going to help.’ ”
Beyond statistically significant
The researchers also found the improvements were not just statistically significant, but were also clinically meaningful for worry, anxiety, and insomnia.
Meaningful changes were defined as a decrease of at least 5.5 points on the PSWQ-A for worry, a decrease of at least 3 points on the PROMIS Anxiety scale for anxiety, and a decrease of at least 6 points in the ISI for insomnia.
At long-term follow-up, the majority of participants in both the CBT and yoga arms of the randomized, controlled trial demonstrated meaningful change in worry (85.7% and 77.6%, respectively), anxiety (82.1% and 80.8%), and insomnia (52.8% and 44.3%).
The majority of participants also reported meaningful improvements in generalized anxiety symptoms, depressive symptoms, and fatigue, but not for physical function, pain interference, or pain intensity.
“That’s the part to me that’s particularly notable. The improvements weren’t just statistically significant, they were clinically meaningful as well,” Dr. Danhauer said.
“When it comes right down to people’s lives, they want differences they can feel and see and not just what a P value looks like,” she added.
Real-world impact
In an accompanying editorial, Carmen Andreescu, MD, associate professor of psychiatry at the University of Pittsburgh, agreed that the results have “real-world impact.”
“Clinicians can direct their patients toward interventions that may be beneficial, consolidate the results over time and avoid fueling the well-trained worry cognitive loop with concerns related to potential side effects,” Dr. Andreescu wrote.
She adds that interventions such as these “may increase accessibility and provide relief for the immediate suffering of our patients.”
The study was funded by the Patient-Centered Outcomes Research Institute Program. Dr. Danhauer and Dr. Andreescu reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM AMERICAN JOURNAL OF GERIATRIC PSYCHIATRY