User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
The other epidemic: Violence against health care workers
After working two busy evening hospital shifts, I was eating breakfast with my children when I started reading about physicians confronted and verbally abused during school board meetings for advocating for face masks in school. The pandemic changed course with the Delta variant increasing hospitalizations, and it seems to me the public response to physicians and health care workers also changed.
During the first wave of the pandemic, public support accompanied health care workers’ sacrifices. Nightly applause rang through New York City, there were donations of food, and murals reflected public backing.
We as a nation rallied. We masked up and locked down. We produced vaccines. COVID cases decreased, and by spring, a hint of normalcy bloomed.
Then the virus changed, and the Delta variant spread. Pandemic fatigue set in. Health care workers asked for help with continued masking and increased vaccinations and instead were met with threats. The summer, already made difficult, makes the prospect of winter even more daunting.
This kind of abuse is persistent
Violence against health care workers is not a new dilemma. Stories abound of patients or family members physically attacking, verbally abusing, or harassing health care workers. A 2014 survey reported almost 80% of nurses attacked during their career. Data from the Bureau of Labor Statistics also reveals health care workers experience more nonfatal workplace violence, as compared with other professions.
Nurses, who often spend the most face-to-face time with patients, receive a litany of abuse. A 2019 nursing survey reported 59% of respondents experiencing verbal abuse from patients and more than 43% experiencing verbal abuse from patients’ families. Even more concerning is 23% of survey respondents reporting physical abuse, an increase from 20% in 2018.
Physicians, likewise, are not immune from the same maltreatment. A 2014 physician survey reported more than 71% of physicians in the United States have experienced at least one incident of workplace violence in their careers. Of the physician specialties, the highest rates of violence are in the emergency department and against less experienced physicians. This is likely caused by the higher rates of patient frustration in EDs as a result of long wait times, overcrowding, and boarding while awaiting an inpatient room.
These statistics are disheartening. However, what I find most discouraging is the almost submissive acceptance of this abuse in the health care field as almost 73% of health care workers feel that the abuse is part of the job.
COVID and the increase in violence against health care workers
As the Delta variant spreads, hospitals’ capacity to handle both COVID and non-COVID issues is further strained. Compounding this stress is the public’s pandemic fatigue and the ongoing battles with masking and vaccinations.
In San Antonio, health care workers faced verbal and physical abuse as they enforced masking and visitation restrictions for COVID patients. Online, health care workers, who advocate for masking or vaccination, are often subject to death threats, threats to family members, and verbal abuse on social media. Veiled threats of “we know who you are” and “we will find you” follow physicians who advocate for masking in schools.
This problem is not isolated to the United States. In Italy, a COVID patient spat at health care workers who asked them to wait, resulting in closure of an entire hospital ward. In the United Kingdom, health care workers were subject to the same abuse as those in San Antonio when trying to enforce masking in the hospital. In India, Pakistan, and Spain, a stigma exists against health care workers for being sources of contagion.
The presence of a growing divide between health care workers and those we serve threatens to undermine not only delivery of care but also our response to the pandemic. This is in addition to the mental health burden and compassion fatigue suffered by many health care workers who find their efforts in doubt. An already strained medical system will find it difficult to withstand the loss of its essential workforce.
Standing united against health care worker abuse
Despite the level of discord surrounding COVID-19, it is important that health care workers remain united. An effective response to the increase in violence toward health care workers will greatly depend on how we address the following.
First, we must actively work to combat the spread of misinformation that erodes the public trust in science and medicine. Transparency is paramount. Policy changes and plans for implementation should be open and free of political influence. This remains a challenge due to the CDC’s standing as both a federal and scientific institution. A steadfast and explicit presentation of scientific evidence by the CDC is a vital first step in repairing this trust.
In addition, we must become our own advocates. The passage of HR 1195, the Workplace Violence Prevention for Health Care and Social Service Workers Act, in the House of Representatives with bipartisan support is an indication that the time is ripe for sweeping change. Its supporters include the American Nurses Association, American Psychiatric Nurses Association, National Nurses United, and the American College of Emergency Physicians. Active opposition includes the American Hospital Association, which cites prohibitive cost as a source of objection.
HR 1195 now waits in the U.S. Senate for approval. We should alert local, state, and health system leadership to the violence against health care workers. We should demand increased protection for our most vulnerable colleagues in EDs and hospitals. Our advocacy will produce a paradigm shift away from the acceptance of this abuse.
Lastly, we must be mindful of compassion fatigue and health care worker burnout. Cynicism threatens to take away our greatest strengths of empathy and humanity. In our work environment, we must lift each other up and increase our awareness of when our colleagues need help. Self-care and creative outlets are encouraged. Admittedly, I am blogging as a personal safeguard against compassion fatigue and burnout.
The pandemic will have enduring implications both positive and negative. It is my hope that support for health care workers not only endures but is also enhanced long after the pandemic ends.
Giancarlo Toledanes, DO, is an assistant professor of pediatrics and a pediatric hospitalist at Texas Children’s Hospital and Baylor College of Medicine, both in Houston. He has no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
After working two busy evening hospital shifts, I was eating breakfast with my children when I started reading about physicians confronted and verbally abused during school board meetings for advocating for face masks in school. The pandemic changed course with the Delta variant increasing hospitalizations, and it seems to me the public response to physicians and health care workers also changed.
During the first wave of the pandemic, public support accompanied health care workers’ sacrifices. Nightly applause rang through New York City, there were donations of food, and murals reflected public backing.
We as a nation rallied. We masked up and locked down. We produced vaccines. COVID cases decreased, and by spring, a hint of normalcy bloomed.
Then the virus changed, and the Delta variant spread. Pandemic fatigue set in. Health care workers asked for help with continued masking and increased vaccinations and instead were met with threats. The summer, already made difficult, makes the prospect of winter even more daunting.
This kind of abuse is persistent
Violence against health care workers is not a new dilemma. Stories abound of patients or family members physically attacking, verbally abusing, or harassing health care workers. A 2014 survey reported almost 80% of nurses attacked during their career. Data from the Bureau of Labor Statistics also reveals health care workers experience more nonfatal workplace violence, as compared with other professions.
Nurses, who often spend the most face-to-face time with patients, receive a litany of abuse. A 2019 nursing survey reported 59% of respondents experiencing verbal abuse from patients and more than 43% experiencing verbal abuse from patients’ families. Even more concerning is 23% of survey respondents reporting physical abuse, an increase from 20% in 2018.
Physicians, likewise, are not immune from the same maltreatment. A 2014 physician survey reported more than 71% of physicians in the United States have experienced at least one incident of workplace violence in their careers. Of the physician specialties, the highest rates of violence are in the emergency department and against less experienced physicians. This is likely caused by the higher rates of patient frustration in EDs as a result of long wait times, overcrowding, and boarding while awaiting an inpatient room.
These statistics are disheartening. However, what I find most discouraging is the almost submissive acceptance of this abuse in the health care field as almost 73% of health care workers feel that the abuse is part of the job.
COVID and the increase in violence against health care workers
As the Delta variant spreads, hospitals’ capacity to handle both COVID and non-COVID issues is further strained. Compounding this stress is the public’s pandemic fatigue and the ongoing battles with masking and vaccinations.
In San Antonio, health care workers faced verbal and physical abuse as they enforced masking and visitation restrictions for COVID patients. Online, health care workers, who advocate for masking or vaccination, are often subject to death threats, threats to family members, and verbal abuse on social media. Veiled threats of “we know who you are” and “we will find you” follow physicians who advocate for masking in schools.
This problem is not isolated to the United States. In Italy, a COVID patient spat at health care workers who asked them to wait, resulting in closure of an entire hospital ward. In the United Kingdom, health care workers were subject to the same abuse as those in San Antonio when trying to enforce masking in the hospital. In India, Pakistan, and Spain, a stigma exists against health care workers for being sources of contagion.
The presence of a growing divide between health care workers and those we serve threatens to undermine not only delivery of care but also our response to the pandemic. This is in addition to the mental health burden and compassion fatigue suffered by many health care workers who find their efforts in doubt. An already strained medical system will find it difficult to withstand the loss of its essential workforce.
Standing united against health care worker abuse
Despite the level of discord surrounding COVID-19, it is important that health care workers remain united. An effective response to the increase in violence toward health care workers will greatly depend on how we address the following.
First, we must actively work to combat the spread of misinformation that erodes the public trust in science and medicine. Transparency is paramount. Policy changes and plans for implementation should be open and free of political influence. This remains a challenge due to the CDC’s standing as both a federal and scientific institution. A steadfast and explicit presentation of scientific evidence by the CDC is a vital first step in repairing this trust.
In addition, we must become our own advocates. The passage of HR 1195, the Workplace Violence Prevention for Health Care and Social Service Workers Act, in the House of Representatives with bipartisan support is an indication that the time is ripe for sweeping change. Its supporters include the American Nurses Association, American Psychiatric Nurses Association, National Nurses United, and the American College of Emergency Physicians. Active opposition includes the American Hospital Association, which cites prohibitive cost as a source of objection.
HR 1195 now waits in the U.S. Senate for approval. We should alert local, state, and health system leadership to the violence against health care workers. We should demand increased protection for our most vulnerable colleagues in EDs and hospitals. Our advocacy will produce a paradigm shift away from the acceptance of this abuse.
Lastly, we must be mindful of compassion fatigue and health care worker burnout. Cynicism threatens to take away our greatest strengths of empathy and humanity. In our work environment, we must lift each other up and increase our awareness of when our colleagues need help. Self-care and creative outlets are encouraged. Admittedly, I am blogging as a personal safeguard against compassion fatigue and burnout.
The pandemic will have enduring implications both positive and negative. It is my hope that support for health care workers not only endures but is also enhanced long after the pandemic ends.
Giancarlo Toledanes, DO, is an assistant professor of pediatrics and a pediatric hospitalist at Texas Children’s Hospital and Baylor College of Medicine, both in Houston. He has no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
After working two busy evening hospital shifts, I was eating breakfast with my children when I started reading about physicians confronted and verbally abused during school board meetings for advocating for face masks in school. The pandemic changed course with the Delta variant increasing hospitalizations, and it seems to me the public response to physicians and health care workers also changed.
During the first wave of the pandemic, public support accompanied health care workers’ sacrifices. Nightly applause rang through New York City, there were donations of food, and murals reflected public backing.
We as a nation rallied. We masked up and locked down. We produced vaccines. COVID cases decreased, and by spring, a hint of normalcy bloomed.
Then the virus changed, and the Delta variant spread. Pandemic fatigue set in. Health care workers asked for help with continued masking and increased vaccinations and instead were met with threats. The summer, already made difficult, makes the prospect of winter even more daunting.
This kind of abuse is persistent
Violence against health care workers is not a new dilemma. Stories abound of patients or family members physically attacking, verbally abusing, or harassing health care workers. A 2014 survey reported almost 80% of nurses attacked during their career. Data from the Bureau of Labor Statistics also reveals health care workers experience more nonfatal workplace violence, as compared with other professions.
Nurses, who often spend the most face-to-face time with patients, receive a litany of abuse. A 2019 nursing survey reported 59% of respondents experiencing verbal abuse from patients and more than 43% experiencing verbal abuse from patients’ families. Even more concerning is 23% of survey respondents reporting physical abuse, an increase from 20% in 2018.
Physicians, likewise, are not immune from the same maltreatment. A 2014 physician survey reported more than 71% of physicians in the United States have experienced at least one incident of workplace violence in their careers. Of the physician specialties, the highest rates of violence are in the emergency department and against less experienced physicians. This is likely caused by the higher rates of patient frustration in EDs as a result of long wait times, overcrowding, and boarding while awaiting an inpatient room.
These statistics are disheartening. However, what I find most discouraging is the almost submissive acceptance of this abuse in the health care field as almost 73% of health care workers feel that the abuse is part of the job.
COVID and the increase in violence against health care workers
As the Delta variant spreads, hospitals’ capacity to handle both COVID and non-COVID issues is further strained. Compounding this stress is the public’s pandemic fatigue and the ongoing battles with masking and vaccinations.
In San Antonio, health care workers faced verbal and physical abuse as they enforced masking and visitation restrictions for COVID patients. Online, health care workers, who advocate for masking or vaccination, are often subject to death threats, threats to family members, and verbal abuse on social media. Veiled threats of “we know who you are” and “we will find you” follow physicians who advocate for masking in schools.
This problem is not isolated to the United States. In Italy, a COVID patient spat at health care workers who asked them to wait, resulting in closure of an entire hospital ward. In the United Kingdom, health care workers were subject to the same abuse as those in San Antonio when trying to enforce masking in the hospital. In India, Pakistan, and Spain, a stigma exists against health care workers for being sources of contagion.
The presence of a growing divide between health care workers and those we serve threatens to undermine not only delivery of care but also our response to the pandemic. This is in addition to the mental health burden and compassion fatigue suffered by many health care workers who find their efforts in doubt. An already strained medical system will find it difficult to withstand the loss of its essential workforce.
Standing united against health care worker abuse
Despite the level of discord surrounding COVID-19, it is important that health care workers remain united. An effective response to the increase in violence toward health care workers will greatly depend on how we address the following.
First, we must actively work to combat the spread of misinformation that erodes the public trust in science and medicine. Transparency is paramount. Policy changes and plans for implementation should be open and free of political influence. This remains a challenge due to the CDC’s standing as both a federal and scientific institution. A steadfast and explicit presentation of scientific evidence by the CDC is a vital first step in repairing this trust.
In addition, we must become our own advocates. The passage of HR 1195, the Workplace Violence Prevention for Health Care and Social Service Workers Act, in the House of Representatives with bipartisan support is an indication that the time is ripe for sweeping change. Its supporters include the American Nurses Association, American Psychiatric Nurses Association, National Nurses United, and the American College of Emergency Physicians. Active opposition includes the American Hospital Association, which cites prohibitive cost as a source of objection.
HR 1195 now waits in the U.S. Senate for approval. We should alert local, state, and health system leadership to the violence against health care workers. We should demand increased protection for our most vulnerable colleagues in EDs and hospitals. Our advocacy will produce a paradigm shift away from the acceptance of this abuse.
Lastly, we must be mindful of compassion fatigue and health care worker burnout. Cynicism threatens to take away our greatest strengths of empathy and humanity. In our work environment, we must lift each other up and increase our awareness of when our colleagues need help. Self-care and creative outlets are encouraged. Admittedly, I am blogging as a personal safeguard against compassion fatigue and burnout.
The pandemic will have enduring implications both positive and negative. It is my hope that support for health care workers not only endures but is also enhanced long after the pandemic ends.
Giancarlo Toledanes, DO, is an assistant professor of pediatrics and a pediatric hospitalist at Texas Children’s Hospital and Baylor College of Medicine, both in Houston. He has no relevant financial conflicts of interest.
A version of this article first appeared on Medscape.com.
PA gets prison time for knowingly prescribing unneeded addictive drugs
A U.S. District Judge sentenced William Soyke, 68, of Hanover, Penn., for acting outside the scope of professional practice and not for a legitimate medical purpose, according to the U.S. Attorney’s Office in Maryland. The 37-month prison term will be followed by 3 years of supervised release.
According to the plea agreement, Mr. Soyke worked as a physician assistant with Rosen-Hoffberg Rehabilitation and Pain Management from 2011 to 2018, where he treated patients during follow-up doctor appointments. As a physician assistant, Mr. Soyke had privileges to prescribe controlled substance medications, but was required to operate under a delegation agreement with the Rosen-Hoffberg owners.
In his plea, Mr. Soyke said that he believed the owners, Norman Rosen, MD, and Howard Hoffberg, MD, prescribed excessive levels of opioids. Despite Mr. Soyke’s attempts to lower patient’s prescription doses, both doctors overruled the PA’s opinion, according to the plea agreement. Also, if another health care provider within the practice declined to treat a patient because of the patient’s aberrant behavior – such as failing a drug screening test for illicit drugs or selling their prescriptions – Dr. Rosen and Dr. Hoffberg would assume that patient’s care, the report continued.
As stated in the plea agreement, Mr. Sokye was aware that many of the patients presenting to Rosen-Hoffberg Rehabilitation and Pain Management did not have a legitimate medical need for the oxycodone, fentanyl, alprazolam, and methadone they were being prescribed. Nevertheless, Mr. Soyke issued prescriptions for these drugs to patients without a legitimate medical need and outside the bounds of acceptable medical practice, according to the release.
Mr. Soyke also admitted that in several instances he engaged in sexual, physical contact with female patients who were attempting to get prescriptions, the plea agreement stated. Specifically, Mr. Soyke asked some female customers to engage in a range of motion test, and while they were bending over, he would position himself behind them such that his genitalia would rub against the customers’ buttocks through their clothes. These patients often submitted to this sexual abuse for fear of not getting the medications to which they were addicted, according to the press release.
Although the female patients complained to Dr. Rosen and Dr. Hoffberg about Mr. Soyke’s behavior, the doctors did not fire Mr. Soyke because the PA saw the largest number of patients at the practice and generated significant revenue, according to federal officials.
Dr. Hoffberg, the associate medical director and part-owner of the practice, pleaded guilty in June to accepting kickbacks from pharmaceutical company Insys Therapeutics in exchange for prescribing an opioid drug called Subsys (a fentanyl sublingual spray) marketed by Insys for breakthrough pain in cancer patients for off-label purposes. He will be sentenced in September and faces a maximum of 5 years in federal prison.
Mr. Soyke pled guilty to a federal drug charge in July 2019. In announcing the guilty plea then, U.S. Attorney Robert Hur said, “Opioid overdoses are killing thousands of Marylanders each year, and opioid addiction is fueled by health care providers who prescribe drugs for people without a legitimate medical need. Doctors and other medical professionals who irresponsibly write opioid prescriptions are acting like street-corner drug pushers.”
A version of this article first appeared on Medscape.com.
A U.S. District Judge sentenced William Soyke, 68, of Hanover, Penn., for acting outside the scope of professional practice and not for a legitimate medical purpose, according to the U.S. Attorney’s Office in Maryland. The 37-month prison term will be followed by 3 years of supervised release.
According to the plea agreement, Mr. Soyke worked as a physician assistant with Rosen-Hoffberg Rehabilitation and Pain Management from 2011 to 2018, where he treated patients during follow-up doctor appointments. As a physician assistant, Mr. Soyke had privileges to prescribe controlled substance medications, but was required to operate under a delegation agreement with the Rosen-Hoffberg owners.
In his plea, Mr. Soyke said that he believed the owners, Norman Rosen, MD, and Howard Hoffberg, MD, prescribed excessive levels of opioids. Despite Mr. Soyke’s attempts to lower patient’s prescription doses, both doctors overruled the PA’s opinion, according to the plea agreement. Also, if another health care provider within the practice declined to treat a patient because of the patient’s aberrant behavior – such as failing a drug screening test for illicit drugs or selling their prescriptions – Dr. Rosen and Dr. Hoffberg would assume that patient’s care, the report continued.
As stated in the plea agreement, Mr. Sokye was aware that many of the patients presenting to Rosen-Hoffberg Rehabilitation and Pain Management did not have a legitimate medical need for the oxycodone, fentanyl, alprazolam, and methadone they were being prescribed. Nevertheless, Mr. Soyke issued prescriptions for these drugs to patients without a legitimate medical need and outside the bounds of acceptable medical practice, according to the release.
Mr. Soyke also admitted that in several instances he engaged in sexual, physical contact with female patients who were attempting to get prescriptions, the plea agreement stated. Specifically, Mr. Soyke asked some female customers to engage in a range of motion test, and while they were bending over, he would position himself behind them such that his genitalia would rub against the customers’ buttocks through their clothes. These patients often submitted to this sexual abuse for fear of not getting the medications to which they were addicted, according to the press release.
Although the female patients complained to Dr. Rosen and Dr. Hoffberg about Mr. Soyke’s behavior, the doctors did not fire Mr. Soyke because the PA saw the largest number of patients at the practice and generated significant revenue, according to federal officials.
Dr. Hoffberg, the associate medical director and part-owner of the practice, pleaded guilty in June to accepting kickbacks from pharmaceutical company Insys Therapeutics in exchange for prescribing an opioid drug called Subsys (a fentanyl sublingual spray) marketed by Insys for breakthrough pain in cancer patients for off-label purposes. He will be sentenced in September and faces a maximum of 5 years in federal prison.
Mr. Soyke pled guilty to a federal drug charge in July 2019. In announcing the guilty plea then, U.S. Attorney Robert Hur said, “Opioid overdoses are killing thousands of Marylanders each year, and opioid addiction is fueled by health care providers who prescribe drugs for people without a legitimate medical need. Doctors and other medical professionals who irresponsibly write opioid prescriptions are acting like street-corner drug pushers.”
A version of this article first appeared on Medscape.com.
A U.S. District Judge sentenced William Soyke, 68, of Hanover, Penn., for acting outside the scope of professional practice and not for a legitimate medical purpose, according to the U.S. Attorney’s Office in Maryland. The 37-month prison term will be followed by 3 years of supervised release.
According to the plea agreement, Mr. Soyke worked as a physician assistant with Rosen-Hoffberg Rehabilitation and Pain Management from 2011 to 2018, where he treated patients during follow-up doctor appointments. As a physician assistant, Mr. Soyke had privileges to prescribe controlled substance medications, but was required to operate under a delegation agreement with the Rosen-Hoffberg owners.
In his plea, Mr. Soyke said that he believed the owners, Norman Rosen, MD, and Howard Hoffberg, MD, prescribed excessive levels of opioids. Despite Mr. Soyke’s attempts to lower patient’s prescription doses, both doctors overruled the PA’s opinion, according to the plea agreement. Also, if another health care provider within the practice declined to treat a patient because of the patient’s aberrant behavior – such as failing a drug screening test for illicit drugs or selling their prescriptions – Dr. Rosen and Dr. Hoffberg would assume that patient’s care, the report continued.
As stated in the plea agreement, Mr. Sokye was aware that many of the patients presenting to Rosen-Hoffberg Rehabilitation and Pain Management did not have a legitimate medical need for the oxycodone, fentanyl, alprazolam, and methadone they were being prescribed. Nevertheless, Mr. Soyke issued prescriptions for these drugs to patients without a legitimate medical need and outside the bounds of acceptable medical practice, according to the release.
Mr. Soyke also admitted that in several instances he engaged in sexual, physical contact with female patients who were attempting to get prescriptions, the plea agreement stated. Specifically, Mr. Soyke asked some female customers to engage in a range of motion test, and while they were bending over, he would position himself behind them such that his genitalia would rub against the customers’ buttocks through their clothes. These patients often submitted to this sexual abuse for fear of not getting the medications to which they were addicted, according to the press release.
Although the female patients complained to Dr. Rosen and Dr. Hoffberg about Mr. Soyke’s behavior, the doctors did not fire Mr. Soyke because the PA saw the largest number of patients at the practice and generated significant revenue, according to federal officials.
Dr. Hoffberg, the associate medical director and part-owner of the practice, pleaded guilty in June to accepting kickbacks from pharmaceutical company Insys Therapeutics in exchange for prescribing an opioid drug called Subsys (a fentanyl sublingual spray) marketed by Insys for breakthrough pain in cancer patients for off-label purposes. He will be sentenced in September and faces a maximum of 5 years in federal prison.
Mr. Soyke pled guilty to a federal drug charge in July 2019. In announcing the guilty plea then, U.S. Attorney Robert Hur said, “Opioid overdoses are killing thousands of Marylanders each year, and opioid addiction is fueled by health care providers who prescribe drugs for people without a legitimate medical need. Doctors and other medical professionals who irresponsibly write opioid prescriptions are acting like street-corner drug pushers.”
A version of this article first appeared on Medscape.com.
SSaSS: Salt substitute shows clear reduction in stroke, CV events, death
Switching from regular salt to a low-sodium salt substitute has major public health benefits, including a reduction in stroke, cardiovascular events, and death, a new landmark study shows.
The Salt Substitute and Stroke Study (SSaSS) was conducted in 21,000 people with a history of stroke or high blood pressure in rural China, with half of them using a lower-sodium salt substitute instead of regular salt.
Results showed that after 5 years, those using the salt substitute had a 14% reduction in stroke, a 13% reduction in major cardiovascular events, and a 12% reduction in death. These benefits were achieved without any apparent adverse effects.
The trial was presented by Bruce Neal, MB, George Institute for Global Health, Sydney, Australia, on Aug. 29 at the virtual European Society of Cardiology (ESC) Congress 2021. They were simultaneously published online in the New England Journal of Medicine.
“This is one of the largest dietary intervention trials ever conducted and has shown very clear evidence of protection against stroke, cardiovascular events, and premature death, with no adverse effects with a very simple and low-cost intervention,” Dr. Neal concluded. “This is a very easy thing to work into the diet. You just replace regular salt with a substitute that looks and tastes almost identical,” he added.
Addressing the issue of whether these results are generalizable to other populations, Dr. Neal said, “We believe the results are relevant to everyone who eats salt.
“The way the body manages sodium and potassium and their association with blood pressure is highly consistent across different populations,” he said. “Almost everyone, with the exception of a few people with serious kidney disease, should be avoiding salt or switching to a salt substitute and expect to see some benefit of this.”
Commentators at the ESC presentation lauded the study as “magnificent,” with “extraordinary” results and “very powerful implications.”
Designated discussant, hypertension expert Bryan Williams, MD, University College London, said the SSaSS was “probably the most important study with regards to public health that we will see.” He described the reductions in stroke, cardiovascular events, and death as “extraordinary for such a simple intervention.”
Dr. Williams added: “Those who have doubted the benefits of salt restriction must now admit they were wrong. The debate stops here. The data are in. Global health interventions to implement these findings must now begin.”
He also highlighted the large number of events in the trial. “This was a large, pragmatic, long-duration study in a high-risk population, and with 5,000 cardiovascular events it gives enormous power to show benefits.”
Chair of the ESC session, Barbara Casadei, MD, DPhil, John Radcliffe Hospital, Oxford (England), said the SSaSS “will change the way we think about salt and be remembered for years to come.”
Noting that the benefits were seen in all subgroups across the study, Bertram Pitt, MD, University of Michigan, Ann Arbor, was particularly excited about the stroke reduction seen in patients with diabetes, noting that several recent trials of new diabetes drugs have not managed to show a reduction in stroke.
“For patients with diabetes, this is a really important intervention,” he stated.
However, an editorial accompanying the NEJM publication gave a somewhat less enthusiastic response to the study than the ESC commentators.
Julie R. Ingelfinger, MD, deputy editor of the journal, points out that serial monitoring of potassium levels was not performed in the trial, so it is possible that hyperkalemic episodes were not detected, and persons with a history of medical conditions that may be associated with hyperkalemia were not studied.
She also noted that because the salt substitute was distributed to families, it would have been instructive to have data on the household members without risk factors, but no such data were obtained.
“Overall, the SSaSS provides some intriguing hints, but wider effectiveness is hard to predict, given limited generalizability,” she concluded.
Cluster-randomized trial
The SSaSS was an open-label, cluster-randomized trial involving 20,995 people from 600 villages in rural China who had a history of stroke or were 60 years of age or older and had uncontrolled hypertension. Patients with a history of severe kidney disease and those taking potassium supplements or potassium-sparing diuretics were excluded.
They were randomly assigned in a 1:1 ratio to the intervention group, in which the participants used a salt substitute (roughly 75% sodium chloride and 25% potassium chloride), or to the control group, in which the participants continued to use regular salt (100% sodium chloride).
Results showed that after a mean follow-up of 4.74 years, systolic blood pressure was reduced by 3.3 mm Hg in the salt substitute group.
The rate of stroke, the primary endpoint, was 29.14 events per 1,000 person-years in the salt substitute group vs. 33.65 events per 1,000 person-years with regular salt (rate ratio, 0.86; 95% confidence interval, 0.77-0.96; P = .006).
The rates of major cardiovascular events were 49.09 events per 1,000 person-years in the salt substitute group vs. 56.29 events per 1,000 person-years in those using regular salt (rate ratio, 0.87; 95% CI, 0.80-0.94; P < .001).
And the rate of death was 39.28 events per 1,000 person-years with the salt substitute vs. 44.61 events per 1,000 person-years with regular salt (rate ratio, 0.88; 95% CI, 0.82-0.95; P < .001).
The rate of serious adverse events attributed to hyperkalemia was not significantly higher with the salt substitute than with regular salt (3.35 events vs. 3.30 events per 1,000 person-years; rate ratio, 1.04; 95% CI, 0.80-1.37; P = .76).
Dr. Neal reported that 7%-8% of the control group started using salt substitute over the study period, so these results have likely underestimated the true effect of switching to a salt substitute product.
Noting that about 10 million cardiovascular events occur each year in China, he said the study results suggested that using salt substitute instead of regular salt could prevent about 10% of these events.
Food manufacturers must make changes
Dr. Neal acknowledged that a limitation of the study was the fact it was conducted in a single country, which would raise issues of generalizability. But he said he believes the results are generalizable to other populations.
Those who would get the most benefit from switching to a salt substitute are those who consume large amounts of discretionary salt – salt added at home at the time of cooking for preservation of food or seasoning. “This is salt that is easy to replace with salt substitute,” Dr. Neal noted.
“There are more than 5 billion people in the world that consume more than 50% of their salt intake as discretionary salt – mainly in the developing world. These people would expect to get significant health benefits from a switch to salt substitute.”
He pointed out that salt substitute is low cost and is easy to manufacture. “Salt substitutes cost around 50% more than regular salt, but this translates into just a dollar or two per person per year to make the switch.”
Dr. Neal said the results also apply to higher-income countries but must be implemented by governments and food manufactures, as most salt in these countries comes from processed foods.
“This study provides strong evidence to take to the food industry,” he concluded. “We would like to see food manufacturers switch to using salt substitute and for salt substitute products to be widely available on supermarket shelves. We also urge governments to take action to promote use of salt substitutes over regular salt. This could take the form of taxing regular salt or subsidies for use of salt substitutes.”
The SSaSS was supported by grants from the National Health and Medical Research Council of Australia. Dr. Neal reports no disclosures. Dr. Ingelfinger is employed by the New England Journal of Medicine as deputy editor.
A version of this article first appeared on Medscape.com.
Switching from regular salt to a low-sodium salt substitute has major public health benefits, including a reduction in stroke, cardiovascular events, and death, a new landmark study shows.
The Salt Substitute and Stroke Study (SSaSS) was conducted in 21,000 people with a history of stroke or high blood pressure in rural China, with half of them using a lower-sodium salt substitute instead of regular salt.
Results showed that after 5 years, those using the salt substitute had a 14% reduction in stroke, a 13% reduction in major cardiovascular events, and a 12% reduction in death. These benefits were achieved without any apparent adverse effects.
The trial was presented by Bruce Neal, MB, George Institute for Global Health, Sydney, Australia, on Aug. 29 at the virtual European Society of Cardiology (ESC) Congress 2021. They were simultaneously published online in the New England Journal of Medicine.
“This is one of the largest dietary intervention trials ever conducted and has shown very clear evidence of protection against stroke, cardiovascular events, and premature death, with no adverse effects with a very simple and low-cost intervention,” Dr. Neal concluded. “This is a very easy thing to work into the diet. You just replace regular salt with a substitute that looks and tastes almost identical,” he added.
Addressing the issue of whether these results are generalizable to other populations, Dr. Neal said, “We believe the results are relevant to everyone who eats salt.
“The way the body manages sodium and potassium and their association with blood pressure is highly consistent across different populations,” he said. “Almost everyone, with the exception of a few people with serious kidney disease, should be avoiding salt or switching to a salt substitute and expect to see some benefit of this.”
Commentators at the ESC presentation lauded the study as “magnificent,” with “extraordinary” results and “very powerful implications.”
Designated discussant, hypertension expert Bryan Williams, MD, University College London, said the SSaSS was “probably the most important study with regards to public health that we will see.” He described the reductions in stroke, cardiovascular events, and death as “extraordinary for such a simple intervention.”
Dr. Williams added: “Those who have doubted the benefits of salt restriction must now admit they were wrong. The debate stops here. The data are in. Global health interventions to implement these findings must now begin.”
He also highlighted the large number of events in the trial. “This was a large, pragmatic, long-duration study in a high-risk population, and with 5,000 cardiovascular events it gives enormous power to show benefits.”
Chair of the ESC session, Barbara Casadei, MD, DPhil, John Radcliffe Hospital, Oxford (England), said the SSaSS “will change the way we think about salt and be remembered for years to come.”
Noting that the benefits were seen in all subgroups across the study, Bertram Pitt, MD, University of Michigan, Ann Arbor, was particularly excited about the stroke reduction seen in patients with diabetes, noting that several recent trials of new diabetes drugs have not managed to show a reduction in stroke.
“For patients with diabetes, this is a really important intervention,” he stated.
However, an editorial accompanying the NEJM publication gave a somewhat less enthusiastic response to the study than the ESC commentators.
Julie R. Ingelfinger, MD, deputy editor of the journal, points out that serial monitoring of potassium levels was not performed in the trial, so it is possible that hyperkalemic episodes were not detected, and persons with a history of medical conditions that may be associated with hyperkalemia were not studied.
She also noted that because the salt substitute was distributed to families, it would have been instructive to have data on the household members without risk factors, but no such data were obtained.
“Overall, the SSaSS provides some intriguing hints, but wider effectiveness is hard to predict, given limited generalizability,” she concluded.
Cluster-randomized trial
The SSaSS was an open-label, cluster-randomized trial involving 20,995 people from 600 villages in rural China who had a history of stroke or were 60 years of age or older and had uncontrolled hypertension. Patients with a history of severe kidney disease and those taking potassium supplements or potassium-sparing diuretics were excluded.
They were randomly assigned in a 1:1 ratio to the intervention group, in which the participants used a salt substitute (roughly 75% sodium chloride and 25% potassium chloride), or to the control group, in which the participants continued to use regular salt (100% sodium chloride).
Results showed that after a mean follow-up of 4.74 years, systolic blood pressure was reduced by 3.3 mm Hg in the salt substitute group.
The rate of stroke, the primary endpoint, was 29.14 events per 1,000 person-years in the salt substitute group vs. 33.65 events per 1,000 person-years with regular salt (rate ratio, 0.86; 95% confidence interval, 0.77-0.96; P = .006).
The rates of major cardiovascular events were 49.09 events per 1,000 person-years in the salt substitute group vs. 56.29 events per 1,000 person-years in those using regular salt (rate ratio, 0.87; 95% CI, 0.80-0.94; P < .001).
And the rate of death was 39.28 events per 1,000 person-years with the salt substitute vs. 44.61 events per 1,000 person-years with regular salt (rate ratio, 0.88; 95% CI, 0.82-0.95; P < .001).
The rate of serious adverse events attributed to hyperkalemia was not significantly higher with the salt substitute than with regular salt (3.35 events vs. 3.30 events per 1,000 person-years; rate ratio, 1.04; 95% CI, 0.80-1.37; P = .76).
Dr. Neal reported that 7%-8% of the control group started using salt substitute over the study period, so these results have likely underestimated the true effect of switching to a salt substitute product.
Noting that about 10 million cardiovascular events occur each year in China, he said the study results suggested that using salt substitute instead of regular salt could prevent about 10% of these events.
Food manufacturers must make changes
Dr. Neal acknowledged that a limitation of the study was the fact it was conducted in a single country, which would raise issues of generalizability. But he said he believes the results are generalizable to other populations.
Those who would get the most benefit from switching to a salt substitute are those who consume large amounts of discretionary salt – salt added at home at the time of cooking for preservation of food or seasoning. “This is salt that is easy to replace with salt substitute,” Dr. Neal noted.
“There are more than 5 billion people in the world that consume more than 50% of their salt intake as discretionary salt – mainly in the developing world. These people would expect to get significant health benefits from a switch to salt substitute.”
He pointed out that salt substitute is low cost and is easy to manufacture. “Salt substitutes cost around 50% more than regular salt, but this translates into just a dollar or two per person per year to make the switch.”
Dr. Neal said the results also apply to higher-income countries but must be implemented by governments and food manufactures, as most salt in these countries comes from processed foods.
“This study provides strong evidence to take to the food industry,” he concluded. “We would like to see food manufacturers switch to using salt substitute and for salt substitute products to be widely available on supermarket shelves. We also urge governments to take action to promote use of salt substitutes over regular salt. This could take the form of taxing regular salt or subsidies for use of salt substitutes.”
The SSaSS was supported by grants from the National Health and Medical Research Council of Australia. Dr. Neal reports no disclosures. Dr. Ingelfinger is employed by the New England Journal of Medicine as deputy editor.
A version of this article first appeared on Medscape.com.
Switching from regular salt to a low-sodium salt substitute has major public health benefits, including a reduction in stroke, cardiovascular events, and death, a new landmark study shows.
The Salt Substitute and Stroke Study (SSaSS) was conducted in 21,000 people with a history of stroke or high blood pressure in rural China, with half of them using a lower-sodium salt substitute instead of regular salt.
Results showed that after 5 years, those using the salt substitute had a 14% reduction in stroke, a 13% reduction in major cardiovascular events, and a 12% reduction in death. These benefits were achieved without any apparent adverse effects.
The trial was presented by Bruce Neal, MB, George Institute for Global Health, Sydney, Australia, on Aug. 29 at the virtual European Society of Cardiology (ESC) Congress 2021. They were simultaneously published online in the New England Journal of Medicine.
“This is one of the largest dietary intervention trials ever conducted and has shown very clear evidence of protection against stroke, cardiovascular events, and premature death, with no adverse effects with a very simple and low-cost intervention,” Dr. Neal concluded. “This is a very easy thing to work into the diet. You just replace regular salt with a substitute that looks and tastes almost identical,” he added.
Addressing the issue of whether these results are generalizable to other populations, Dr. Neal said, “We believe the results are relevant to everyone who eats salt.
“The way the body manages sodium and potassium and their association with blood pressure is highly consistent across different populations,” he said. “Almost everyone, with the exception of a few people with serious kidney disease, should be avoiding salt or switching to a salt substitute and expect to see some benefit of this.”
Commentators at the ESC presentation lauded the study as “magnificent,” with “extraordinary” results and “very powerful implications.”
Designated discussant, hypertension expert Bryan Williams, MD, University College London, said the SSaSS was “probably the most important study with regards to public health that we will see.” He described the reductions in stroke, cardiovascular events, and death as “extraordinary for such a simple intervention.”
Dr. Williams added: “Those who have doubted the benefits of salt restriction must now admit they were wrong. The debate stops here. The data are in. Global health interventions to implement these findings must now begin.”
He also highlighted the large number of events in the trial. “This was a large, pragmatic, long-duration study in a high-risk population, and with 5,000 cardiovascular events it gives enormous power to show benefits.”
Chair of the ESC session, Barbara Casadei, MD, DPhil, John Radcliffe Hospital, Oxford (England), said the SSaSS “will change the way we think about salt and be remembered for years to come.”
Noting that the benefits were seen in all subgroups across the study, Bertram Pitt, MD, University of Michigan, Ann Arbor, was particularly excited about the stroke reduction seen in patients with diabetes, noting that several recent trials of new diabetes drugs have not managed to show a reduction in stroke.
“For patients with diabetes, this is a really important intervention,” he stated.
However, an editorial accompanying the NEJM publication gave a somewhat less enthusiastic response to the study than the ESC commentators.
Julie R. Ingelfinger, MD, deputy editor of the journal, points out that serial monitoring of potassium levels was not performed in the trial, so it is possible that hyperkalemic episodes were not detected, and persons with a history of medical conditions that may be associated with hyperkalemia were not studied.
She also noted that because the salt substitute was distributed to families, it would have been instructive to have data on the household members without risk factors, but no such data were obtained.
“Overall, the SSaSS provides some intriguing hints, but wider effectiveness is hard to predict, given limited generalizability,” she concluded.
Cluster-randomized trial
The SSaSS was an open-label, cluster-randomized trial involving 20,995 people from 600 villages in rural China who had a history of stroke or were 60 years of age or older and had uncontrolled hypertension. Patients with a history of severe kidney disease and those taking potassium supplements or potassium-sparing diuretics were excluded.
They were randomly assigned in a 1:1 ratio to the intervention group, in which the participants used a salt substitute (roughly 75% sodium chloride and 25% potassium chloride), or to the control group, in which the participants continued to use regular salt (100% sodium chloride).
Results showed that after a mean follow-up of 4.74 years, systolic blood pressure was reduced by 3.3 mm Hg in the salt substitute group.
The rate of stroke, the primary endpoint, was 29.14 events per 1,000 person-years in the salt substitute group vs. 33.65 events per 1,000 person-years with regular salt (rate ratio, 0.86; 95% confidence interval, 0.77-0.96; P = .006).
The rates of major cardiovascular events were 49.09 events per 1,000 person-years in the salt substitute group vs. 56.29 events per 1,000 person-years in those using regular salt (rate ratio, 0.87; 95% CI, 0.80-0.94; P < .001).
And the rate of death was 39.28 events per 1,000 person-years with the salt substitute vs. 44.61 events per 1,000 person-years with regular salt (rate ratio, 0.88; 95% CI, 0.82-0.95; P < .001).
The rate of serious adverse events attributed to hyperkalemia was not significantly higher with the salt substitute than with regular salt (3.35 events vs. 3.30 events per 1,000 person-years; rate ratio, 1.04; 95% CI, 0.80-1.37; P = .76).
Dr. Neal reported that 7%-8% of the control group started using salt substitute over the study period, so these results have likely underestimated the true effect of switching to a salt substitute product.
Noting that about 10 million cardiovascular events occur each year in China, he said the study results suggested that using salt substitute instead of regular salt could prevent about 10% of these events.
Food manufacturers must make changes
Dr. Neal acknowledged that a limitation of the study was the fact it was conducted in a single country, which would raise issues of generalizability. But he said he believes the results are generalizable to other populations.
Those who would get the most benefit from switching to a salt substitute are those who consume large amounts of discretionary salt – salt added at home at the time of cooking for preservation of food or seasoning. “This is salt that is easy to replace with salt substitute,” Dr. Neal noted.
“There are more than 5 billion people in the world that consume more than 50% of their salt intake as discretionary salt – mainly in the developing world. These people would expect to get significant health benefits from a switch to salt substitute.”
He pointed out that salt substitute is low cost and is easy to manufacture. “Salt substitutes cost around 50% more than regular salt, but this translates into just a dollar or two per person per year to make the switch.”
Dr. Neal said the results also apply to higher-income countries but must be implemented by governments and food manufactures, as most salt in these countries comes from processed foods.
“This study provides strong evidence to take to the food industry,” he concluded. “We would like to see food manufacturers switch to using salt substitute and for salt substitute products to be widely available on supermarket shelves. We also urge governments to take action to promote use of salt substitutes over regular salt. This could take the form of taxing regular salt or subsidies for use of salt substitutes.”
The SSaSS was supported by grants from the National Health and Medical Research Council of Australia. Dr. Neal reports no disclosures. Dr. Ingelfinger is employed by the New England Journal of Medicine as deputy editor.
A version of this article first appeared on Medscape.com.
‘High normal’ sodium, poor hydration linked to heart failure
– a heart failure (HF) precursor – and for HF itself, in older age, a new study suggests.
Compared with middle-aged adults in the Atherosclerosis Risk in Communities (ARIC) study with normal serum sodium, those with levels of 142-146 mmol/L were more likely to have left ventricular hypertrophy or HF when they were in their 70s and 80s, independent of other risk factors.
Natalia Dmitrieva, PhD, a research scientist at the National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, Md., presented the study findings in an e-poster on Aug. 27 at the European Society of Cardiology (ESC) Congress 2021.
“Our study suggests that maintaining good hydration can prevent or at least slow down the changes within the heart that lead to heart failure,” she said in a statement from the ESC.
It “suggests that all adults should aim for eight to ten glasses of liquid [daily] and keep salt intake low,” Dr. Dmitrieva said in an interview.
However, people should not rely completely on thirst, she cautioned, especially in middle age, when thirst sensation starts to deteriorate. And too much fluid intake can be harmful and even dangerous.
Normal serum sodium is usually defined as 135-146 mmol/L, Dr. Dmitrieva explained, and this study involved only patients in ARIC with sodium levels in this range, to try to exclude patients with genetic or water-salt balance diseases.
The findings suggest that a serum sodium level of 142-146 mmol/L, which would not be flagged as abnormal by a test lab, “can be used by clinicians as a warning sign” for a patient’s increased risk for HF, she noted.
Clinicians should explain this risk to patients and advise them to drink at least 2 L per day. However, people should not try to reduce their sodium levels by drinking more than 2 to 3 L per day, she cautioned, which can be harmful and even deadly, and they should consult their doctors.
Watch hydration
“An important finding of this study is that sodium values considered ‘normal’ may also be deleterious,” Jacob Joseph, MD, director, heart failure program, VA Boston Healthcare System, who was not involved with this study, said in an interview.
“These results are similar to studies we have conducted in heart failure with preserved ejection fraction,” noted Dr. Joseph, associate professor of medicine at Harvard Medical School, Boston.
Their studies showed a U-shaped relationship between serum sodium values and adverse outcomes, “indicating an ‘optimal’ range of serum sodium value that was narrower than the accepted normal laboratory value range,” he noted.
The study by Dmitrieva et al. was observational and the findings would need to be verified in a randomized controlled trial, Dr. Joseph pointed out; however, the research “supports the idea that even a high normal sodium level may indicate risk of future heart failure.
“Hence, patients should pay attention to hydration,” he continued, and “clinicians should not assume that a sodium level of 142 mmol/L is appropriate and should ensure that patients are paying attention to hydration.
“In today’s busy and stress-filled lifestyle, it is easy to forget about adequate fluid intake,” Dr. Joseph added.
More than 15,000 adults followed for 25 Years
To investigate the relationship between serum sodium, hydration, and future heart failure, Dr. Dmitrieva and colleagues analyzed data from 15,792 adults in ARIC who were 44-66 years of age at study entry, with serum sodium levels from 135 to 146 mmol/L.
The participants were evaluated over five visits until they reached 70-90 years.
They were divided into four groups based on their average serum sodium concentrations at study visits one and two (conducted in the first 3 years): 135 -139.5 mmol/L, 140-141.5 mmol/L, 142-143.5 mmol/L, and 144-146 mmol/L.
The researchers determined the percentage of people in each group who developed HF and left ventricular hypertrophy at visit five (25 years after study enrollment).
Patients with higher serum sodium levels had a significantly higher risk for HF and left ventricular hypertrophy, after adjustment for other risk factors, including age, blood pressure, kidney function, blood cholesterol, blood glucose, body mass index, sex, and smoking status.
Every 1 mmol/L increase in serum sodium concentration in midlife was associated with 1.20 and 1.11 increased odds of developing left ventricular hypertrophy and HF, respectively, 25 years later.
“More studies are needed to find out what proportion of people with serum sodium 142 mmol/L and higher have this [serum sodium] level because they do not drink enough and will be able to reduce it by making sure they consistently drink 2 to 2.5 L per day,” said Dr. Dmitrieva.
“It is likely that for some people, other factors that are related to genetics or diseases affecting water-salt balance could be causing their increased serum sodium levels,” she speculated.
The study was funded by the Intramural Program of the National Heart, Lung, and Blood Institute. The authors and Dr. Joseph have no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
– a heart failure (HF) precursor – and for HF itself, in older age, a new study suggests.
Compared with middle-aged adults in the Atherosclerosis Risk in Communities (ARIC) study with normal serum sodium, those with levels of 142-146 mmol/L were more likely to have left ventricular hypertrophy or HF when they were in their 70s and 80s, independent of other risk factors.
Natalia Dmitrieva, PhD, a research scientist at the National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, Md., presented the study findings in an e-poster on Aug. 27 at the European Society of Cardiology (ESC) Congress 2021.
“Our study suggests that maintaining good hydration can prevent or at least slow down the changes within the heart that lead to heart failure,” she said in a statement from the ESC.
It “suggests that all adults should aim for eight to ten glasses of liquid [daily] and keep salt intake low,” Dr. Dmitrieva said in an interview.
However, people should not rely completely on thirst, she cautioned, especially in middle age, when thirst sensation starts to deteriorate. And too much fluid intake can be harmful and even dangerous.
Normal serum sodium is usually defined as 135-146 mmol/L, Dr. Dmitrieva explained, and this study involved only patients in ARIC with sodium levels in this range, to try to exclude patients with genetic or water-salt balance diseases.
The findings suggest that a serum sodium level of 142-146 mmol/L, which would not be flagged as abnormal by a test lab, “can be used by clinicians as a warning sign” for a patient’s increased risk for HF, she noted.
Clinicians should explain this risk to patients and advise them to drink at least 2 L per day. However, people should not try to reduce their sodium levels by drinking more than 2 to 3 L per day, she cautioned, which can be harmful and even deadly, and they should consult their doctors.
Watch hydration
“An important finding of this study is that sodium values considered ‘normal’ may also be deleterious,” Jacob Joseph, MD, director, heart failure program, VA Boston Healthcare System, who was not involved with this study, said in an interview.
“These results are similar to studies we have conducted in heart failure with preserved ejection fraction,” noted Dr. Joseph, associate professor of medicine at Harvard Medical School, Boston.
Their studies showed a U-shaped relationship between serum sodium values and adverse outcomes, “indicating an ‘optimal’ range of serum sodium value that was narrower than the accepted normal laboratory value range,” he noted.
The study by Dmitrieva et al. was observational and the findings would need to be verified in a randomized controlled trial, Dr. Joseph pointed out; however, the research “supports the idea that even a high normal sodium level may indicate risk of future heart failure.
“Hence, patients should pay attention to hydration,” he continued, and “clinicians should not assume that a sodium level of 142 mmol/L is appropriate and should ensure that patients are paying attention to hydration.
“In today’s busy and stress-filled lifestyle, it is easy to forget about adequate fluid intake,” Dr. Joseph added.
More than 15,000 adults followed for 25 Years
To investigate the relationship between serum sodium, hydration, and future heart failure, Dr. Dmitrieva and colleagues analyzed data from 15,792 adults in ARIC who were 44-66 years of age at study entry, with serum sodium levels from 135 to 146 mmol/L.
The participants were evaluated over five visits until they reached 70-90 years.
They were divided into four groups based on their average serum sodium concentrations at study visits one and two (conducted in the first 3 years): 135 -139.5 mmol/L, 140-141.5 mmol/L, 142-143.5 mmol/L, and 144-146 mmol/L.
The researchers determined the percentage of people in each group who developed HF and left ventricular hypertrophy at visit five (25 years after study enrollment).
Patients with higher serum sodium levels had a significantly higher risk for HF and left ventricular hypertrophy, after adjustment for other risk factors, including age, blood pressure, kidney function, blood cholesterol, blood glucose, body mass index, sex, and smoking status.
Every 1 mmol/L increase in serum sodium concentration in midlife was associated with 1.20 and 1.11 increased odds of developing left ventricular hypertrophy and HF, respectively, 25 years later.
“More studies are needed to find out what proportion of people with serum sodium 142 mmol/L and higher have this [serum sodium] level because they do not drink enough and will be able to reduce it by making sure they consistently drink 2 to 2.5 L per day,” said Dr. Dmitrieva.
“It is likely that for some people, other factors that are related to genetics or diseases affecting water-salt balance could be causing their increased serum sodium levels,” she speculated.
The study was funded by the Intramural Program of the National Heart, Lung, and Blood Institute. The authors and Dr. Joseph have no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
– a heart failure (HF) precursor – and for HF itself, in older age, a new study suggests.
Compared with middle-aged adults in the Atherosclerosis Risk in Communities (ARIC) study with normal serum sodium, those with levels of 142-146 mmol/L were more likely to have left ventricular hypertrophy or HF when they were in their 70s and 80s, independent of other risk factors.
Natalia Dmitrieva, PhD, a research scientist at the National Heart, Lung, and Blood Institute, National Institutes of Health, Bethesda, Md., presented the study findings in an e-poster on Aug. 27 at the European Society of Cardiology (ESC) Congress 2021.
“Our study suggests that maintaining good hydration can prevent or at least slow down the changes within the heart that lead to heart failure,” she said in a statement from the ESC.
It “suggests that all adults should aim for eight to ten glasses of liquid [daily] and keep salt intake low,” Dr. Dmitrieva said in an interview.
However, people should not rely completely on thirst, she cautioned, especially in middle age, when thirst sensation starts to deteriorate. And too much fluid intake can be harmful and even dangerous.
Normal serum sodium is usually defined as 135-146 mmol/L, Dr. Dmitrieva explained, and this study involved only patients in ARIC with sodium levels in this range, to try to exclude patients with genetic or water-salt balance diseases.
The findings suggest that a serum sodium level of 142-146 mmol/L, which would not be flagged as abnormal by a test lab, “can be used by clinicians as a warning sign” for a patient’s increased risk for HF, she noted.
Clinicians should explain this risk to patients and advise them to drink at least 2 L per day. However, people should not try to reduce their sodium levels by drinking more than 2 to 3 L per day, she cautioned, which can be harmful and even deadly, and they should consult their doctors.
Watch hydration
“An important finding of this study is that sodium values considered ‘normal’ may also be deleterious,” Jacob Joseph, MD, director, heart failure program, VA Boston Healthcare System, who was not involved with this study, said in an interview.
“These results are similar to studies we have conducted in heart failure with preserved ejection fraction,” noted Dr. Joseph, associate professor of medicine at Harvard Medical School, Boston.
Their studies showed a U-shaped relationship between serum sodium values and adverse outcomes, “indicating an ‘optimal’ range of serum sodium value that was narrower than the accepted normal laboratory value range,” he noted.
The study by Dmitrieva et al. was observational and the findings would need to be verified in a randomized controlled trial, Dr. Joseph pointed out; however, the research “supports the idea that even a high normal sodium level may indicate risk of future heart failure.
“Hence, patients should pay attention to hydration,” he continued, and “clinicians should not assume that a sodium level of 142 mmol/L is appropriate and should ensure that patients are paying attention to hydration.
“In today’s busy and stress-filled lifestyle, it is easy to forget about adequate fluid intake,” Dr. Joseph added.
More than 15,000 adults followed for 25 Years
To investigate the relationship between serum sodium, hydration, and future heart failure, Dr. Dmitrieva and colleagues analyzed data from 15,792 adults in ARIC who were 44-66 years of age at study entry, with serum sodium levels from 135 to 146 mmol/L.
The participants were evaluated over five visits until they reached 70-90 years.
They were divided into four groups based on their average serum sodium concentrations at study visits one and two (conducted in the first 3 years): 135 -139.5 mmol/L, 140-141.5 mmol/L, 142-143.5 mmol/L, and 144-146 mmol/L.
The researchers determined the percentage of people in each group who developed HF and left ventricular hypertrophy at visit five (25 years after study enrollment).
Patients with higher serum sodium levels had a significantly higher risk for HF and left ventricular hypertrophy, after adjustment for other risk factors, including age, blood pressure, kidney function, blood cholesterol, blood glucose, body mass index, sex, and smoking status.
Every 1 mmol/L increase in serum sodium concentration in midlife was associated with 1.20 and 1.11 increased odds of developing left ventricular hypertrophy and HF, respectively, 25 years later.
“More studies are needed to find out what proportion of people with serum sodium 142 mmol/L and higher have this [serum sodium] level because they do not drink enough and will be able to reduce it by making sure they consistently drink 2 to 2.5 L per day,” said Dr. Dmitrieva.
“It is likely that for some people, other factors that are related to genetics or diseases affecting water-salt balance could be causing their increased serum sodium levels,” she speculated.
The study was funded by the Intramural Program of the National Heart, Lung, and Blood Institute. The authors and Dr. Joseph have no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Coffee drinking in midlife tied to heart benefits
Among middle-aged people without heart disease, drinking up to three cups of coffee per day was linked with a lower risk for stroke or death over the next decade, along with better heart structure and function, in a large, observational study.
Specifically, light-to-moderate coffee drinking, defined as 0.5 to 3 cups per day, was associated with a 21% lower risk for stroke, a 17% lower risk for death from cardiovascular disease (CVD), and a 12% lower risk for death from all causes, as well as more favorable cardiac MRI findings, compared with nondrinkers (< 0.5 cup per day) during a median 11-year follow-up.
Heavy coffee drinkers, defined as those consuming more than three cups per day, on the other hand, likewise had more favorable cardiac MRI findings, but with similar (not lower) rates of stroke and CVD or all-cause mortality compared with nondrinkers.
Judit Simon, MD, presented these findings, from close to 500,000 participants in the UK Biobank study, at a press conference before an e-poster session at the virtual annual congress of the European Society of Cardiology.
“To our knowledge, this is the largest study to systematically assess the cardiovascular effects of regular coffee consumption in a population without diagnosed heart disease,” Dr. Simon, a PhD student at the Heart and Vascular Centre, Semmelweis University, Budapest, Hungary, said in an ESC press release.
The results “suggest that regular coffee consumption is safe, as even high daily intake was not associated with adverse cardiovascular outcomes and all-cause mortality after a follow-up of 10 to 15 years,” she said.
The imaging analysis showed that “compared with participants who did not drink coffee regularly, daily consumers had healthier sized and better functioning hearts,” Dr. Simon continued, “consistent with reversing the detrimental effects of aging on the heart.”
“The observed benefits might be partly explained by positive alterations in cardiac structure and function,” she speculated, adding that further studies are needed to explain the underlying mechanisms.
Instant coffee most popular
In this population, the coffee drinkers mostly drank instant coffee (55%), followed by filtered/ground (23%), decaffeinated (20%), or other types of coffee (2%), Dr. Simon said in an interview.
Risk for myocardial infarction (MI) or heart failure did not significantly differ for different categories of coffee intake, she added. The researchers did not study the effect of coffee consumption on atrial fibrillation (AF), she noted.
Study limitations, Dr. Simon acknowledged, include that it was observational, so it cannot show causation, and that coffee consumption was self-reported in a questionnaire.
Invited to comment, Alice H. Lichtenstein, DSc, who was not involved with the research, said, “Consistent with prior data, this new study indicates there is no adverse effect of coffee consumption on cardiovascular health and there may be a benefit.”
However, “because of the nature of the data, it would not be recommended that an individual starting drinking coffee to improve cardiovascular health,” added Dr. Lichtenstein, director and senior scientist at the Cardiovascular Nutrition Laboratory at Tufts University, Boston.
But if people already drink coffee, “it is fine to continue, assuming that the coffee drinks are not high in added sugar and cream,” she said in an interview.
Coffee intake, CVD outcomes, and heart structure
To study the relationship between coffee intake and incident MI, stroke, and death, as well as heart structure, the researchers examined data from the UK Biobank, which recruited 500,000 people aged 40-69 years in 2006-2010 from across the United Kingdom.
They identified 468,629 participants with no signs of heart disease at recruitment and an average age of 56 years, of whom 56% were women.
The participants were divided into three groups based on usual coffee intake: none (22% of participants), light-to-moderate (58%), and high (20%).
Median tea intake was three cups per day overall, four cups per day in noncoffee drinkers, three cups per day in light-to-moderate coffee drinkers, and one cup per day in high coffee drinkers.
Compared to not drinking coffee, light-to-moderate coffee consumption was associated with lower risks for all-cause death (hazard ratio [HR], 0.88; P < .001), CVD death (HR, 0.83; P = .006), and stroke (HR, 0.79; P = .037), over a median follow-up of 11 years, after adjustment for sex; weight; height; smoking status; physical activity; high blood pressure; diabetes; cholesterol level; socioeconomic status; and usual intake of alcohol, meat, tea, fruit, and vegetables.
In the 30,650 participants who had cardiac MRI data, the study found that compared with not drinking coffee, both light-to-moderate and high coffee consumption were associated with significantly increased left and right ventricular end-systolic and end-diastolic volumes, and with greater left ventricular mass (all P < .001).
These differences were small but significant, Dr. Simon stressed, because this was a cohort of healthy patients who did not have CVD (heart failure, MI, stroke, AF) at baseline, although some had hypertension or diabetes.
Press conference chairperson, Steen Dalby Kristensen, MD, professor and cardiologist, Aarhus University Hospital, Denmark, a coffee lover himself, wanted to know if an amount such as two, three, or four cups of coffee was optimal to see these heart benefits, and whether there were differences in benefits seen with drinking different types of coffee.
The analysis did not identify an optimal coffee intake, Dr. Simon said. Compared with not drinking coffee, she continued, drinking instant coffee was associated with a lower risk for all-cause mortality, but not CVD mortality or stroke.
Drinking filtered coffee was associated with lower risks for all three outcomes, but there was no significant difference in risk for MI. Drinking decaffeinated coffee was associated with a lower risk for all-cause and CVD mortality.
“Decaffeinated coffee contains a small amount of caffeine,” Dr. Simon pointed out. “Something other than caffeine might have this protective impact,” she suggested.
The researchers and Dr. Lichtenstein declared having no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Among middle-aged people without heart disease, drinking up to three cups of coffee per day was linked with a lower risk for stroke or death over the next decade, along with better heart structure and function, in a large, observational study.
Specifically, light-to-moderate coffee drinking, defined as 0.5 to 3 cups per day, was associated with a 21% lower risk for stroke, a 17% lower risk for death from cardiovascular disease (CVD), and a 12% lower risk for death from all causes, as well as more favorable cardiac MRI findings, compared with nondrinkers (< 0.5 cup per day) during a median 11-year follow-up.
Heavy coffee drinkers, defined as those consuming more than three cups per day, on the other hand, likewise had more favorable cardiac MRI findings, but with similar (not lower) rates of stroke and CVD or all-cause mortality compared with nondrinkers.
Judit Simon, MD, presented these findings, from close to 500,000 participants in the UK Biobank study, at a press conference before an e-poster session at the virtual annual congress of the European Society of Cardiology.
“To our knowledge, this is the largest study to systematically assess the cardiovascular effects of regular coffee consumption in a population without diagnosed heart disease,” Dr. Simon, a PhD student at the Heart and Vascular Centre, Semmelweis University, Budapest, Hungary, said in an ESC press release.
The results “suggest that regular coffee consumption is safe, as even high daily intake was not associated with adverse cardiovascular outcomes and all-cause mortality after a follow-up of 10 to 15 years,” she said.
The imaging analysis showed that “compared with participants who did not drink coffee regularly, daily consumers had healthier sized and better functioning hearts,” Dr. Simon continued, “consistent with reversing the detrimental effects of aging on the heart.”
“The observed benefits might be partly explained by positive alterations in cardiac structure and function,” she speculated, adding that further studies are needed to explain the underlying mechanisms.
Instant coffee most popular
In this population, the coffee drinkers mostly drank instant coffee (55%), followed by filtered/ground (23%), decaffeinated (20%), or other types of coffee (2%), Dr. Simon said in an interview.
Risk for myocardial infarction (MI) or heart failure did not significantly differ for different categories of coffee intake, she added. The researchers did not study the effect of coffee consumption on atrial fibrillation (AF), she noted.
Study limitations, Dr. Simon acknowledged, include that it was observational, so it cannot show causation, and that coffee consumption was self-reported in a questionnaire.
Invited to comment, Alice H. Lichtenstein, DSc, who was not involved with the research, said, “Consistent with prior data, this new study indicates there is no adverse effect of coffee consumption on cardiovascular health and there may be a benefit.”
However, “because of the nature of the data, it would not be recommended that an individual starting drinking coffee to improve cardiovascular health,” added Dr. Lichtenstein, director and senior scientist at the Cardiovascular Nutrition Laboratory at Tufts University, Boston.
But if people already drink coffee, “it is fine to continue, assuming that the coffee drinks are not high in added sugar and cream,” she said in an interview.
Coffee intake, CVD outcomes, and heart structure
To study the relationship between coffee intake and incident MI, stroke, and death, as well as heart structure, the researchers examined data from the UK Biobank, which recruited 500,000 people aged 40-69 years in 2006-2010 from across the United Kingdom.
They identified 468,629 participants with no signs of heart disease at recruitment and an average age of 56 years, of whom 56% were women.
The participants were divided into three groups based on usual coffee intake: none (22% of participants), light-to-moderate (58%), and high (20%).
Median tea intake was three cups per day overall, four cups per day in noncoffee drinkers, three cups per day in light-to-moderate coffee drinkers, and one cup per day in high coffee drinkers.
Compared to not drinking coffee, light-to-moderate coffee consumption was associated with lower risks for all-cause death (hazard ratio [HR], 0.88; P < .001), CVD death (HR, 0.83; P = .006), and stroke (HR, 0.79; P = .037), over a median follow-up of 11 years, after adjustment for sex; weight; height; smoking status; physical activity; high blood pressure; diabetes; cholesterol level; socioeconomic status; and usual intake of alcohol, meat, tea, fruit, and vegetables.
In the 30,650 participants who had cardiac MRI data, the study found that compared with not drinking coffee, both light-to-moderate and high coffee consumption were associated with significantly increased left and right ventricular end-systolic and end-diastolic volumes, and with greater left ventricular mass (all P < .001).
These differences were small but significant, Dr. Simon stressed, because this was a cohort of healthy patients who did not have CVD (heart failure, MI, stroke, AF) at baseline, although some had hypertension or diabetes.
Press conference chairperson, Steen Dalby Kristensen, MD, professor and cardiologist, Aarhus University Hospital, Denmark, a coffee lover himself, wanted to know if an amount such as two, three, or four cups of coffee was optimal to see these heart benefits, and whether there were differences in benefits seen with drinking different types of coffee.
The analysis did not identify an optimal coffee intake, Dr. Simon said. Compared with not drinking coffee, she continued, drinking instant coffee was associated with a lower risk for all-cause mortality, but not CVD mortality or stroke.
Drinking filtered coffee was associated with lower risks for all three outcomes, but there was no significant difference in risk for MI. Drinking decaffeinated coffee was associated with a lower risk for all-cause and CVD mortality.
“Decaffeinated coffee contains a small amount of caffeine,” Dr. Simon pointed out. “Something other than caffeine might have this protective impact,” she suggested.
The researchers and Dr. Lichtenstein declared having no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
Among middle-aged people without heart disease, drinking up to three cups of coffee per day was linked with a lower risk for stroke or death over the next decade, along with better heart structure and function, in a large, observational study.
Specifically, light-to-moderate coffee drinking, defined as 0.5 to 3 cups per day, was associated with a 21% lower risk for stroke, a 17% lower risk for death from cardiovascular disease (CVD), and a 12% lower risk for death from all causes, as well as more favorable cardiac MRI findings, compared with nondrinkers (< 0.5 cup per day) during a median 11-year follow-up.
Heavy coffee drinkers, defined as those consuming more than three cups per day, on the other hand, likewise had more favorable cardiac MRI findings, but with similar (not lower) rates of stroke and CVD or all-cause mortality compared with nondrinkers.
Judit Simon, MD, presented these findings, from close to 500,000 participants in the UK Biobank study, at a press conference before an e-poster session at the virtual annual congress of the European Society of Cardiology.
“To our knowledge, this is the largest study to systematically assess the cardiovascular effects of regular coffee consumption in a population without diagnosed heart disease,” Dr. Simon, a PhD student at the Heart and Vascular Centre, Semmelweis University, Budapest, Hungary, said in an ESC press release.
The results “suggest that regular coffee consumption is safe, as even high daily intake was not associated with adverse cardiovascular outcomes and all-cause mortality after a follow-up of 10 to 15 years,” she said.
The imaging analysis showed that “compared with participants who did not drink coffee regularly, daily consumers had healthier sized and better functioning hearts,” Dr. Simon continued, “consistent with reversing the detrimental effects of aging on the heart.”
“The observed benefits might be partly explained by positive alterations in cardiac structure and function,” she speculated, adding that further studies are needed to explain the underlying mechanisms.
Instant coffee most popular
In this population, the coffee drinkers mostly drank instant coffee (55%), followed by filtered/ground (23%), decaffeinated (20%), or other types of coffee (2%), Dr. Simon said in an interview.
Risk for myocardial infarction (MI) or heart failure did not significantly differ for different categories of coffee intake, she added. The researchers did not study the effect of coffee consumption on atrial fibrillation (AF), she noted.
Study limitations, Dr. Simon acknowledged, include that it was observational, so it cannot show causation, and that coffee consumption was self-reported in a questionnaire.
Invited to comment, Alice H. Lichtenstein, DSc, who was not involved with the research, said, “Consistent with prior data, this new study indicates there is no adverse effect of coffee consumption on cardiovascular health and there may be a benefit.”
However, “because of the nature of the data, it would not be recommended that an individual starting drinking coffee to improve cardiovascular health,” added Dr. Lichtenstein, director and senior scientist at the Cardiovascular Nutrition Laboratory at Tufts University, Boston.
But if people already drink coffee, “it is fine to continue, assuming that the coffee drinks are not high in added sugar and cream,” she said in an interview.
Coffee intake, CVD outcomes, and heart structure
To study the relationship between coffee intake and incident MI, stroke, and death, as well as heart structure, the researchers examined data from the UK Biobank, which recruited 500,000 people aged 40-69 years in 2006-2010 from across the United Kingdom.
They identified 468,629 participants with no signs of heart disease at recruitment and an average age of 56 years, of whom 56% were women.
The participants were divided into three groups based on usual coffee intake: none (22% of participants), light-to-moderate (58%), and high (20%).
Median tea intake was three cups per day overall, four cups per day in noncoffee drinkers, three cups per day in light-to-moderate coffee drinkers, and one cup per day in high coffee drinkers.
Compared to not drinking coffee, light-to-moderate coffee consumption was associated with lower risks for all-cause death (hazard ratio [HR], 0.88; P < .001), CVD death (HR, 0.83; P = .006), and stroke (HR, 0.79; P = .037), over a median follow-up of 11 years, after adjustment for sex; weight; height; smoking status; physical activity; high blood pressure; diabetes; cholesterol level; socioeconomic status; and usual intake of alcohol, meat, tea, fruit, and vegetables.
In the 30,650 participants who had cardiac MRI data, the study found that compared with not drinking coffee, both light-to-moderate and high coffee consumption were associated with significantly increased left and right ventricular end-systolic and end-diastolic volumes, and with greater left ventricular mass (all P < .001).
These differences were small but significant, Dr. Simon stressed, because this was a cohort of healthy patients who did not have CVD (heart failure, MI, stroke, AF) at baseline, although some had hypertension or diabetes.
Press conference chairperson, Steen Dalby Kristensen, MD, professor and cardiologist, Aarhus University Hospital, Denmark, a coffee lover himself, wanted to know if an amount such as two, three, or four cups of coffee was optimal to see these heart benefits, and whether there were differences in benefits seen with drinking different types of coffee.
The analysis did not identify an optimal coffee intake, Dr. Simon said. Compared with not drinking coffee, she continued, drinking instant coffee was associated with a lower risk for all-cause mortality, but not CVD mortality or stroke.
Drinking filtered coffee was associated with lower risks for all three outcomes, but there was no significant difference in risk for MI. Drinking decaffeinated coffee was associated with a lower risk for all-cause and CVD mortality.
“Decaffeinated coffee contains a small amount of caffeine,” Dr. Simon pointed out. “Something other than caffeine might have this protective impact,” she suggested.
The researchers and Dr. Lichtenstein declared having no relevant financial disclosures.
A version of this article first appeared on Medscape.com.
FIDELITY: Finerenone benefits patients with T2D across CKD spectrum
New data on using the nonsteroidal mineralocorticoid receptor antagonist (MRA) finerenone to treat patients with type 2 diabetes and chronic kidney disease did more than further confirm this new drug’s efficacy in these patients for slowing progression to end-stage renal disease and reducing hospitalizations for heart failure.
It also strengthened the case for clinicians to be much more proactive in collecting urine specimens from patients with type 2 diabetes (T2D) to find those with albuminuria whose kidney function has not yet dropped below 60 mL/min per 1.73 m2, a population that the data show finerenone can help.
The FIDELITY prespecified meta-analysis combined data from two related pivotal trials of finerenone (Kerendia) in a total of more than 13,000 patients with T2D and chronic kidney disease (CKD). Each of these two trials, FIDELIO-DKD and FIGARO-DKD, identified patients with CKD by either of two methods, or a total of four different criteria.
In sum, the two trials enrolled patients with an estimated glomerular filtration rate (eGFR) of 25-90 mL/min per 1.73 m2 and a urinary albumin-to-creatinine ratio (UACR) of 30-299, or an eGFR of 25-75 mL/min per 1.73 m2 and a UACR of 300-5,000. The result was that 40% of enrolled patients had an eGFR of at least 60, levels that are considered normal, but they also had some level of albuminuria that defined them as having CKD.
The results showed that during a median follow-up of 36 months, patients with a normal eGFR and albuminuria had their combined incidence of cardiovascular disease events (cardiovascular death, MI, stroke, or hospitalization for heart failure) reduced by roughly the same amount as seen in patients with lower levels of eGFR and renal function, a finding that reimagines how clinicians need to routinely screen patients with T2D for CKD, Gerasimos Filippatos, MD, reported at the virtual annual congress of the European Society of Cardiology.
“Measuring UACR in patients with type 2 diabetes is important to identify patients who will benefit from finerenone treatment independent of their eGFR,” said Dr. Filippatos, professor of medicine at the University of Athens and director of the heart failure unit at Attikon University Hospital in Athens.
The combined FIDELITY analysis showed a significant overall cut in the combined cardiovascular disease endpoint of 14% relative to placebo, which reflected a 1.7% absolute reduction in events between the two arms during 3 years of treatment. The primary driver of this benefit was the significant drop in hospitalizations for heart failure on finerenone compared with placebo, which fell by a relative 22% and by an absolute 1.1%, Dr. Filippatos reported.
Routinely screening for albuminuria is ‘practice changing’
“This is really practice changing information for cardiologists,” said Rajiv L. Agarwal, MD, a copresenter of the FIDELITY analysis and a lead investigator of the two finerenone trials.
When cardiologists and possibly other specialists see patients with T2D, they traditionally have focused on measuring left ventricular ejection fraction and checking for other indications of heart failure. The new results from FIDELIO-DKD and FIGARO-DKD showed that finerenone treatment can prevent heart failure onset or worsening in patients with T2D with finerenone, which clinicians can accomplish by “simply measuring UACR,” as well as eGFR, and then treating patients with abnormal levels of either, explained Dr. Agarwal, a nephrologist and professor of medicine at Indiana University in Indianapolis.
“Diabetologists know that when they see patients with diabetes they need to collect a urine sample to check for albuminuria. But when some other clinicians see a patient with type 2 diabetes and a normal eGFR, they often think that the patient is okay and don’t get a urine specimen,” noted Bertram Pitt, MD, another collaborator of the finerenone trials and a heart failure specialist affiliated with the University of Michigan in Ann Arbor.
“We need to pay more attention to UACR and albuminuria; traditionally clinicians have mostly looked at eGFR,” agreed Dipti Itchhaporia, MD, a cardiologist at the Carlton Heart and Vascular Institute of Hoag Hospital in Newport Beach, Calif. UACR “is a marker that should be shared” between endocrinologists, nephrologists, and cardiologists as they together care for patients with T2D, suggested Dr. Itchhaporia, president of the American College of Cardiology.
Two pivotal trials with consistent findings
The FIDELITY analysis combined data from the FIDELIO-DKD trial, reported in 2020, and from the FIGARO-DKD trial that was first reported during the current congress as well as in a simultaneous report published online.
Results from the two trials were very consistent, although the primary endpoint in FIDELIO-DKD was a composite measure of renal disease with the combined cardiovascular disease metric a secondary endpoint, while this got flipped in FIGARO-DKD which had the cardiovascular disease composite as its primary endpoint as the combined renal outcomes as a secondary endpoint.
In addition to showing a consistent, significant reduction in both combined cardiovascular disease events and in the specific endpoint of hospitalization for heart failure, the two trials also showed a consistent benefit for slowing renal disease progression, including significantly fewer patients developing end-stage kidney disease. In the combined FIDELITY analysis, treatment with finerenone cut the incidence of end-stage kidney disease by a significant 20% compared with placebo, and by an absolute reduction of 0.6%.
Another common finding was a relatively low incidence of hyperkalemia compared with what’s usually seen using a steroidal MRA, spironolactone or eplerenone. In the combined analysis treatment with finerenone produced a 14% incidence of any hyperkalemia compared with 7% among placebo-treated patients, and the rate of patients stopping their treatment because of hyperkalemia was 1.7% on finerenone and 0.6% on placebo.
“Finerenone is much better tolerated” than the steroidal MRAs in causing clinically significant hyperkalemia, noted Dr. Pitt. “There are a lot of misconceptions” about the potassium-raising potential of MRAs, and “people get frightened” by the potential. Spreading the message of finerenone’s relative safety “will take a lot of education,” he acknowledged. Routine monitoring of potassium levels is a key step to minimizing the risk for hyperkalemia when using finerenone, he added.
Suggested benefit from combination treatment
Another intriguing observation from FIDELITY derived from the fact that roughly 7% of enrolled patients were also on treatment with a sodium-glucose cotransporter 2 (SGLT2) inhibitor at entry, and about 7% were on treatment with a glucagon-like peptide-1 (GLP-1) receptor agonist, and in both subgroups the incidence of the composite cardiovascular disease endpoint appeared to suggest additive effects of agents from either of these classes when combined with finerenone. Although the numbers of patients on combined treatment were too low to show a definitive result, “our expectation is that we will see an additive effect,” said Dr. Pitt. Ideally, patients with T2D and CKD “should be on both” an SGLT2 inhibitor and finerenone, he predicted.
SGLT2 inhibitors have now been embraced as a key treatment for patients with T2D or with heart failure with reduced ejection fraction, and the preliminary data suggest that combining these agents with finerenone can provide additional benefit, agreed Dr. Itchhaporia. Aside from the need for more evidence to prove this, there are also practical considerations of “How do we pay for all these fantastic therapies?” She expressed optimism that cost-benefit analyses will eventually show that the additive benefits justify the added cost.
Based largely on results from FIDELIO-DKD, finerenone received marketing approval from the Food and Drug Administration in July 2021 for the indication of treating patients with T2D and chronic kidney disease.
FIGARO-DKD, FIDELIO-DKD, and FIDELITY were sponsored by Bayer, the company that markets finerenone. Dr. Filippatos has received lecture fees from Bayer, and has had financial relationships with Amgen, Boehringer Ingelheim, Medtronic, Novartis, Servier, and Vifor. Dr. Agarwal received travel support from and has been a consultant to Bayer and to numerous other companies. Dr. Pitt has been a consultant to Bayer and to numerous other companies. Dr. Itchhaporia had no disclosures.
New data on using the nonsteroidal mineralocorticoid receptor antagonist (MRA) finerenone to treat patients with type 2 diabetes and chronic kidney disease did more than further confirm this new drug’s efficacy in these patients for slowing progression to end-stage renal disease and reducing hospitalizations for heart failure.
It also strengthened the case for clinicians to be much more proactive in collecting urine specimens from patients with type 2 diabetes (T2D) to find those with albuminuria whose kidney function has not yet dropped below 60 mL/min per 1.73 m2, a population that the data show finerenone can help.
The FIDELITY prespecified meta-analysis combined data from two related pivotal trials of finerenone (Kerendia) in a total of more than 13,000 patients with T2D and chronic kidney disease (CKD). Each of these two trials, FIDELIO-DKD and FIGARO-DKD, identified patients with CKD by either of two methods, or a total of four different criteria.
In sum, the two trials enrolled patients with an estimated glomerular filtration rate (eGFR) of 25-90 mL/min per 1.73 m2 and a urinary albumin-to-creatinine ratio (UACR) of 30-299, or an eGFR of 25-75 mL/min per 1.73 m2 and a UACR of 300-5,000. The result was that 40% of enrolled patients had an eGFR of at least 60, levels that are considered normal, but they also had some level of albuminuria that defined them as having CKD.
The results showed that during a median follow-up of 36 months, patients with a normal eGFR and albuminuria had their combined incidence of cardiovascular disease events (cardiovascular death, MI, stroke, or hospitalization for heart failure) reduced by roughly the same amount as seen in patients with lower levels of eGFR and renal function, a finding that reimagines how clinicians need to routinely screen patients with T2D for CKD, Gerasimos Filippatos, MD, reported at the virtual annual congress of the European Society of Cardiology.
“Measuring UACR in patients with type 2 diabetes is important to identify patients who will benefit from finerenone treatment independent of their eGFR,” said Dr. Filippatos, professor of medicine at the University of Athens and director of the heart failure unit at Attikon University Hospital in Athens.
The combined FIDELITY analysis showed a significant overall cut in the combined cardiovascular disease endpoint of 14% relative to placebo, which reflected a 1.7% absolute reduction in events between the two arms during 3 years of treatment. The primary driver of this benefit was the significant drop in hospitalizations for heart failure on finerenone compared with placebo, which fell by a relative 22% and by an absolute 1.1%, Dr. Filippatos reported.
Routinely screening for albuminuria is ‘practice changing’
“This is really practice changing information for cardiologists,” said Rajiv L. Agarwal, MD, a copresenter of the FIDELITY analysis and a lead investigator of the two finerenone trials.
When cardiologists and possibly other specialists see patients with T2D, they traditionally have focused on measuring left ventricular ejection fraction and checking for other indications of heart failure. The new results from FIDELIO-DKD and FIGARO-DKD showed that finerenone treatment can prevent heart failure onset or worsening in patients with T2D with finerenone, which clinicians can accomplish by “simply measuring UACR,” as well as eGFR, and then treating patients with abnormal levels of either, explained Dr. Agarwal, a nephrologist and professor of medicine at Indiana University in Indianapolis.
“Diabetologists know that when they see patients with diabetes they need to collect a urine sample to check for albuminuria. But when some other clinicians see a patient with type 2 diabetes and a normal eGFR, they often think that the patient is okay and don’t get a urine specimen,” noted Bertram Pitt, MD, another collaborator of the finerenone trials and a heart failure specialist affiliated with the University of Michigan in Ann Arbor.
“We need to pay more attention to UACR and albuminuria; traditionally clinicians have mostly looked at eGFR,” agreed Dipti Itchhaporia, MD, a cardiologist at the Carlton Heart and Vascular Institute of Hoag Hospital in Newport Beach, Calif. UACR “is a marker that should be shared” between endocrinologists, nephrologists, and cardiologists as they together care for patients with T2D, suggested Dr. Itchhaporia, president of the American College of Cardiology.
Two pivotal trials with consistent findings
The FIDELITY analysis combined data from the FIDELIO-DKD trial, reported in 2020, and from the FIGARO-DKD trial that was first reported during the current congress as well as in a simultaneous report published online.
Results from the two trials were very consistent, although the primary endpoint in FIDELIO-DKD was a composite measure of renal disease with the combined cardiovascular disease metric a secondary endpoint, while this got flipped in FIGARO-DKD which had the cardiovascular disease composite as its primary endpoint as the combined renal outcomes as a secondary endpoint.
In addition to showing a consistent, significant reduction in both combined cardiovascular disease events and in the specific endpoint of hospitalization for heart failure, the two trials also showed a consistent benefit for slowing renal disease progression, including significantly fewer patients developing end-stage kidney disease. In the combined FIDELITY analysis, treatment with finerenone cut the incidence of end-stage kidney disease by a significant 20% compared with placebo, and by an absolute reduction of 0.6%.
Another common finding was a relatively low incidence of hyperkalemia compared with what’s usually seen using a steroidal MRA, spironolactone or eplerenone. In the combined analysis treatment with finerenone produced a 14% incidence of any hyperkalemia compared with 7% among placebo-treated patients, and the rate of patients stopping their treatment because of hyperkalemia was 1.7% on finerenone and 0.6% on placebo.
“Finerenone is much better tolerated” than the steroidal MRAs in causing clinically significant hyperkalemia, noted Dr. Pitt. “There are a lot of misconceptions” about the potassium-raising potential of MRAs, and “people get frightened” by the potential. Spreading the message of finerenone’s relative safety “will take a lot of education,” he acknowledged. Routine monitoring of potassium levels is a key step to minimizing the risk for hyperkalemia when using finerenone, he added.
Suggested benefit from combination treatment
Another intriguing observation from FIDELITY derived from the fact that roughly 7% of enrolled patients were also on treatment with a sodium-glucose cotransporter 2 (SGLT2) inhibitor at entry, and about 7% were on treatment with a glucagon-like peptide-1 (GLP-1) receptor agonist, and in both subgroups the incidence of the composite cardiovascular disease endpoint appeared to suggest additive effects of agents from either of these classes when combined with finerenone. Although the numbers of patients on combined treatment were too low to show a definitive result, “our expectation is that we will see an additive effect,” said Dr. Pitt. Ideally, patients with T2D and CKD “should be on both” an SGLT2 inhibitor and finerenone, he predicted.
SGLT2 inhibitors have now been embraced as a key treatment for patients with T2D or with heart failure with reduced ejection fraction, and the preliminary data suggest that combining these agents with finerenone can provide additional benefit, agreed Dr. Itchhaporia. Aside from the need for more evidence to prove this, there are also practical considerations of “How do we pay for all these fantastic therapies?” She expressed optimism that cost-benefit analyses will eventually show that the additive benefits justify the added cost.
Based largely on results from FIDELIO-DKD, finerenone received marketing approval from the Food and Drug Administration in July 2021 for the indication of treating patients with T2D and chronic kidney disease.
FIGARO-DKD, FIDELIO-DKD, and FIDELITY were sponsored by Bayer, the company that markets finerenone. Dr. Filippatos has received lecture fees from Bayer, and has had financial relationships with Amgen, Boehringer Ingelheim, Medtronic, Novartis, Servier, and Vifor. Dr. Agarwal received travel support from and has been a consultant to Bayer and to numerous other companies. Dr. Pitt has been a consultant to Bayer and to numerous other companies. Dr. Itchhaporia had no disclosures.
New data on using the nonsteroidal mineralocorticoid receptor antagonist (MRA) finerenone to treat patients with type 2 diabetes and chronic kidney disease did more than further confirm this new drug’s efficacy in these patients for slowing progression to end-stage renal disease and reducing hospitalizations for heart failure.
It also strengthened the case for clinicians to be much more proactive in collecting urine specimens from patients with type 2 diabetes (T2D) to find those with albuminuria whose kidney function has not yet dropped below 60 mL/min per 1.73 m2, a population that the data show finerenone can help.
The FIDELITY prespecified meta-analysis combined data from two related pivotal trials of finerenone (Kerendia) in a total of more than 13,000 patients with T2D and chronic kidney disease (CKD). Each of these two trials, FIDELIO-DKD and FIGARO-DKD, identified patients with CKD by either of two methods, or a total of four different criteria.
In sum, the two trials enrolled patients with an estimated glomerular filtration rate (eGFR) of 25-90 mL/min per 1.73 m2 and a urinary albumin-to-creatinine ratio (UACR) of 30-299, or an eGFR of 25-75 mL/min per 1.73 m2 and a UACR of 300-5,000. The result was that 40% of enrolled patients had an eGFR of at least 60, levels that are considered normal, but they also had some level of albuminuria that defined them as having CKD.
The results showed that during a median follow-up of 36 months, patients with a normal eGFR and albuminuria had their combined incidence of cardiovascular disease events (cardiovascular death, MI, stroke, or hospitalization for heart failure) reduced by roughly the same amount as seen in patients with lower levels of eGFR and renal function, a finding that reimagines how clinicians need to routinely screen patients with T2D for CKD, Gerasimos Filippatos, MD, reported at the virtual annual congress of the European Society of Cardiology.
“Measuring UACR in patients with type 2 diabetes is important to identify patients who will benefit from finerenone treatment independent of their eGFR,” said Dr. Filippatos, professor of medicine at the University of Athens and director of the heart failure unit at Attikon University Hospital in Athens.
The combined FIDELITY analysis showed a significant overall cut in the combined cardiovascular disease endpoint of 14% relative to placebo, which reflected a 1.7% absolute reduction in events between the two arms during 3 years of treatment. The primary driver of this benefit was the significant drop in hospitalizations for heart failure on finerenone compared with placebo, which fell by a relative 22% and by an absolute 1.1%, Dr. Filippatos reported.
Routinely screening for albuminuria is ‘practice changing’
“This is really practice changing information for cardiologists,” said Rajiv L. Agarwal, MD, a copresenter of the FIDELITY analysis and a lead investigator of the two finerenone trials.
When cardiologists and possibly other specialists see patients with T2D, they traditionally have focused on measuring left ventricular ejection fraction and checking for other indications of heart failure. The new results from FIDELIO-DKD and FIGARO-DKD showed that finerenone treatment can prevent heart failure onset or worsening in patients with T2D with finerenone, which clinicians can accomplish by “simply measuring UACR,” as well as eGFR, and then treating patients with abnormal levels of either, explained Dr. Agarwal, a nephrologist and professor of medicine at Indiana University in Indianapolis.
“Diabetologists know that when they see patients with diabetes they need to collect a urine sample to check for albuminuria. But when some other clinicians see a patient with type 2 diabetes and a normal eGFR, they often think that the patient is okay and don’t get a urine specimen,” noted Bertram Pitt, MD, another collaborator of the finerenone trials and a heart failure specialist affiliated with the University of Michigan in Ann Arbor.
“We need to pay more attention to UACR and albuminuria; traditionally clinicians have mostly looked at eGFR,” agreed Dipti Itchhaporia, MD, a cardiologist at the Carlton Heart and Vascular Institute of Hoag Hospital in Newport Beach, Calif. UACR “is a marker that should be shared” between endocrinologists, nephrologists, and cardiologists as they together care for patients with T2D, suggested Dr. Itchhaporia, president of the American College of Cardiology.
Two pivotal trials with consistent findings
The FIDELITY analysis combined data from the FIDELIO-DKD trial, reported in 2020, and from the FIGARO-DKD trial that was first reported during the current congress as well as in a simultaneous report published online.
Results from the two trials were very consistent, although the primary endpoint in FIDELIO-DKD was a composite measure of renal disease with the combined cardiovascular disease metric a secondary endpoint, while this got flipped in FIGARO-DKD which had the cardiovascular disease composite as its primary endpoint as the combined renal outcomes as a secondary endpoint.
In addition to showing a consistent, significant reduction in both combined cardiovascular disease events and in the specific endpoint of hospitalization for heart failure, the two trials also showed a consistent benefit for slowing renal disease progression, including significantly fewer patients developing end-stage kidney disease. In the combined FIDELITY analysis, treatment with finerenone cut the incidence of end-stage kidney disease by a significant 20% compared with placebo, and by an absolute reduction of 0.6%.
Another common finding was a relatively low incidence of hyperkalemia compared with what’s usually seen using a steroidal MRA, spironolactone or eplerenone. In the combined analysis treatment with finerenone produced a 14% incidence of any hyperkalemia compared with 7% among placebo-treated patients, and the rate of patients stopping their treatment because of hyperkalemia was 1.7% on finerenone and 0.6% on placebo.
“Finerenone is much better tolerated” than the steroidal MRAs in causing clinically significant hyperkalemia, noted Dr. Pitt. “There are a lot of misconceptions” about the potassium-raising potential of MRAs, and “people get frightened” by the potential. Spreading the message of finerenone’s relative safety “will take a lot of education,” he acknowledged. Routine monitoring of potassium levels is a key step to minimizing the risk for hyperkalemia when using finerenone, he added.
Suggested benefit from combination treatment
Another intriguing observation from FIDELITY derived from the fact that roughly 7% of enrolled patients were also on treatment with a sodium-glucose cotransporter 2 (SGLT2) inhibitor at entry, and about 7% were on treatment with a glucagon-like peptide-1 (GLP-1) receptor agonist, and in both subgroups the incidence of the composite cardiovascular disease endpoint appeared to suggest additive effects of agents from either of these classes when combined with finerenone. Although the numbers of patients on combined treatment were too low to show a definitive result, “our expectation is that we will see an additive effect,” said Dr. Pitt. Ideally, patients with T2D and CKD “should be on both” an SGLT2 inhibitor and finerenone, he predicted.
SGLT2 inhibitors have now been embraced as a key treatment for patients with T2D or with heart failure with reduced ejection fraction, and the preliminary data suggest that combining these agents with finerenone can provide additional benefit, agreed Dr. Itchhaporia. Aside from the need for more evidence to prove this, there are also practical considerations of “How do we pay for all these fantastic therapies?” She expressed optimism that cost-benefit analyses will eventually show that the additive benefits justify the added cost.
Based largely on results from FIDELIO-DKD, finerenone received marketing approval from the Food and Drug Administration in July 2021 for the indication of treating patients with T2D and chronic kidney disease.
FIGARO-DKD, FIDELIO-DKD, and FIDELITY were sponsored by Bayer, the company that markets finerenone. Dr. Filippatos has received lecture fees from Bayer, and has had financial relationships with Amgen, Boehringer Ingelheim, Medtronic, Novartis, Servier, and Vifor. Dr. Agarwal received travel support from and has been a consultant to Bayer and to numerous other companies. Dr. Pitt has been a consultant to Bayer and to numerous other companies. Dr. Itchhaporia had no disclosures.
FROM ESC CONGRESS 2021
Dapagliflozin in HFrEF may cut arrhythmias, sudden death: DAPA-HF
Dapagliflozin might reduce the risk for ventricular arrhythmias and sudden death in patients with heart failure and reduced ejection fraction (HFrEF), a post hoc analysis of the DAPA-HF trial suggests.
The addition of dapagliflozin to standard therapy reduced the relative risk for the primary composite endpoint of any serious ventricular arrhythmia, resuscitated cardiac arrest, or sudden death by 21%, compared with placebo (hazard ratio, 0.79; 95% confidence interval, 0.63-0.99). The absolute risk reduction was 1.5% (5.9% vs. 7.4%).
The benefit was consistent in a competing-risks analysis that included all-cause mortality (HR, 0.80; P = .043) and across the individual components of the composite outcome, James Curtain, MD, Cardiovascular Research Centre of Glasgow, said at the annual congress of the European Society of Cardiology.
As previously reported from the main trial, treatment with the sodium-glucose cotransporter 2 (SGLT2) inhibitor cut the primary endpoint of cardiovascular death or worsening heart failure by 26% among 4,744 patients with HFrEF and in New York Heart Association functional class 2-4.
Cochair of the late-breaking science session, Lars Lund, MD, Karolinska Institute, Stockholm, pointed out that dapagliflozin reduced sudden cardiac deaths and related events to an extent similar to that observed for cardiovascular deaths, total mortality, and the main trial’s primary endpoint.
“So does that mean it has any particular effect on arrhythmic events or does it mean, such as a beta-blocker, for example, [it] reduces calcium transience and improves handling of calcium, or does it have an effect simply by improving heart failure?” he asked.
Dr. Curtain replied they are still trying to understand the effects of this new class of drug but that studies have shown dapagliflozin and other SGLT2 inhibitors have favorable effects on adverse cardiac remodeling, which contributes to sudden death and ventricular arrhythmia. They’ve also been shown to reduce cardiac chamber size, left ventricular hypertrophy, and N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels over time, consistent with a reduction in myocardial wall stress. “So it could indeed be one of several mechanisms by which they may exert a beneficial cardiac effect.”
Speaking with this news organization, Dr. Curtain pointed out that the Kaplan-Meier curves for the composite outcome began to separate early on, but that the clearest separation was after 9 months, suggestive of a positive action on adverse cardiac remodeling over time.
“This would improve the patients’ heart failure situation, but also thick ventricles are a key risk factor for the occurrence of sudden death and ventricular arrhythmias,” he said. “The effects on adverse cardiac remodeling, given its plausibility in terms of our Kaplan-Meier curves, are one [mechanism] that I’d look to in the first instance, but I’m sure there are more than one actions at play.”
According to the new analysis, the primary outcome occurred in 315 (6.6%) patients; there were 203 adjudicated sudden deaths (64%), 104 investigator-reported ventricular arrhythmias (33%), and 8 resuscitated cardiac arrests (3%). Independent predictors of the primary outcome were higher NT-proBNP levels (odds ratio, 1.54), previous ventricular arrhythmia (OR, 1.93), previous myocardial infarction (OR, 1.42), male sex (OR, 1.53), and higher body mass index (OR, 1.03).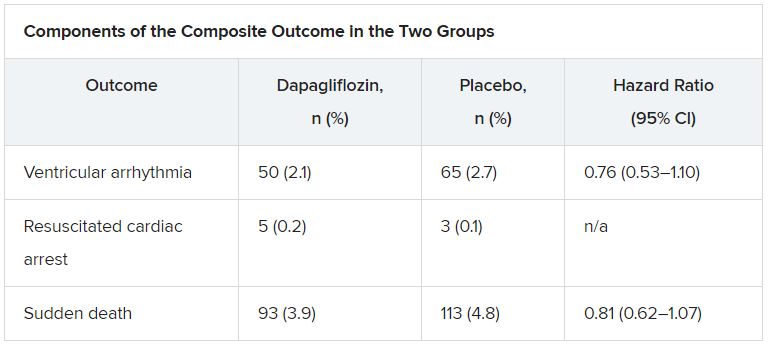
The effect of dapagliflozin on the primary outcome was consistent in several sensitivity analyses and “generally consistent” across key subgroups, Dr. Curtain said.
During a discussion of the results, session cochair Mitja Lainscak, MD, General Hospital Murska Sobota, Slovenia, called out two exceptions. “With regard to patients with implanted ICDs, the effect was neutral, and in the patients without diabetes, the benefit was less than in diabetic patients. Any explanations for that?”
Dr. Curtain responded that “it’s important to note that in the subgroup analyses the point estimates were all on the side favoring dapagliflozin and the interaction test was not significant in that subgroup. The numbers of patients who were in the defibrillator group were modest, and there was a relatively smaller number of events, so it may be harder to show benefit in that group.”
In the dapagliflozin and placebo groups, the event rates per 100 person-years were 3.9 and 5.8, respectively, in patients with diabetes, and 4.1 and 4.7, respectively, in those without diabetes (P for interaction = .273).
Event rates per 100 person-years were 5.8 and 5.9, respectively, in patients with a defibrillator at baseline, and 3.5 and 4.9, respectively, in those without a defibrillator (P for interaction = .174).
Asked to comment on the study, which was simultaneously published in the European Heart Journal, Milton Packer, MD, Baylor University Medical Center, Dallas, said he had “very little confidence” in the findings.
“This was entirely post hoc and the investigators combined events – with markedly different levels of clinical importance – in order to achieve a P value less than 0.05,” he told this news organization. “If one takes asymptomatic ventricular arrhythmias out of the analysis, the effect is no longer statistically significant. Furthermore, half of sudden deaths in patients with heart failure are not related to a ventricular arrhythmia.”
The authors note in their report that the analysis was not prespecified and the findings should be regarded as “hypothesis generating and require confirmation,” but also point out that a recent meta-analysis showed that SGLT2 inhibitor use was associated with a lower risk for ventricular tachycardia. Other limitations to the post hoc analysis are that adverse-event reporting likely underestimated the true prevalence of ventricular arrhythmias, and that these events were not adjudicated.
DAPA-HF was funded by AstraZeneca. Dr. Curtain reports no relevant financial relationships. Disclosures for the coauthors are listed in the paper.
A version of this article first appeared on Medscape.com.
Dapagliflozin might reduce the risk for ventricular arrhythmias and sudden death in patients with heart failure and reduced ejection fraction (HFrEF), a post hoc analysis of the DAPA-HF trial suggests.
The addition of dapagliflozin to standard therapy reduced the relative risk for the primary composite endpoint of any serious ventricular arrhythmia, resuscitated cardiac arrest, or sudden death by 21%, compared with placebo (hazard ratio, 0.79; 95% confidence interval, 0.63-0.99). The absolute risk reduction was 1.5% (5.9% vs. 7.4%).
The benefit was consistent in a competing-risks analysis that included all-cause mortality (HR, 0.80; P = .043) and across the individual components of the composite outcome, James Curtain, MD, Cardiovascular Research Centre of Glasgow, said at the annual congress of the European Society of Cardiology.
As previously reported from the main trial, treatment with the sodium-glucose cotransporter 2 (SGLT2) inhibitor cut the primary endpoint of cardiovascular death or worsening heart failure by 26% among 4,744 patients with HFrEF and in New York Heart Association functional class 2-4.
Cochair of the late-breaking science session, Lars Lund, MD, Karolinska Institute, Stockholm, pointed out that dapagliflozin reduced sudden cardiac deaths and related events to an extent similar to that observed for cardiovascular deaths, total mortality, and the main trial’s primary endpoint.
“So does that mean it has any particular effect on arrhythmic events or does it mean, such as a beta-blocker, for example, [it] reduces calcium transience and improves handling of calcium, or does it have an effect simply by improving heart failure?” he asked.
Dr. Curtain replied they are still trying to understand the effects of this new class of drug but that studies have shown dapagliflozin and other SGLT2 inhibitors have favorable effects on adverse cardiac remodeling, which contributes to sudden death and ventricular arrhythmia. They’ve also been shown to reduce cardiac chamber size, left ventricular hypertrophy, and N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels over time, consistent with a reduction in myocardial wall stress. “So it could indeed be one of several mechanisms by which they may exert a beneficial cardiac effect.”
Speaking with this news organization, Dr. Curtain pointed out that the Kaplan-Meier curves for the composite outcome began to separate early on, but that the clearest separation was after 9 months, suggestive of a positive action on adverse cardiac remodeling over time.
“This would improve the patients’ heart failure situation, but also thick ventricles are a key risk factor for the occurrence of sudden death and ventricular arrhythmias,” he said. “The effects on adverse cardiac remodeling, given its plausibility in terms of our Kaplan-Meier curves, are one [mechanism] that I’d look to in the first instance, but I’m sure there are more than one actions at play.”
According to the new analysis, the primary outcome occurred in 315 (6.6%) patients; there were 203 adjudicated sudden deaths (64%), 104 investigator-reported ventricular arrhythmias (33%), and 8 resuscitated cardiac arrests (3%). Independent predictors of the primary outcome were higher NT-proBNP levels (odds ratio, 1.54), previous ventricular arrhythmia (OR, 1.93), previous myocardial infarction (OR, 1.42), male sex (OR, 1.53), and higher body mass index (OR, 1.03).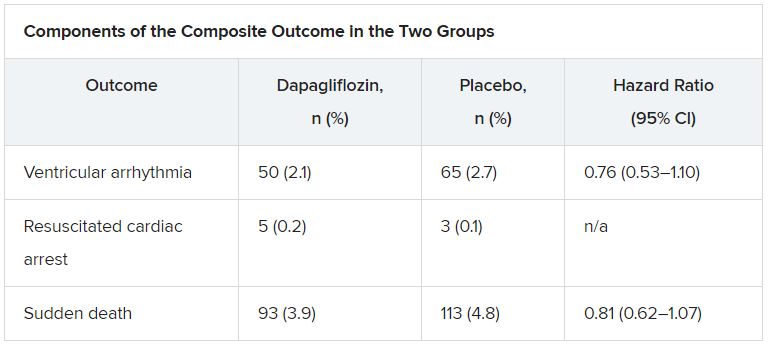
The effect of dapagliflozin on the primary outcome was consistent in several sensitivity analyses and “generally consistent” across key subgroups, Dr. Curtain said.
During a discussion of the results, session cochair Mitja Lainscak, MD, General Hospital Murska Sobota, Slovenia, called out two exceptions. “With regard to patients with implanted ICDs, the effect was neutral, and in the patients without diabetes, the benefit was less than in diabetic patients. Any explanations for that?”
Dr. Curtain responded that “it’s important to note that in the subgroup analyses the point estimates were all on the side favoring dapagliflozin and the interaction test was not significant in that subgroup. The numbers of patients who were in the defibrillator group were modest, and there was a relatively smaller number of events, so it may be harder to show benefit in that group.”
In the dapagliflozin and placebo groups, the event rates per 100 person-years were 3.9 and 5.8, respectively, in patients with diabetes, and 4.1 and 4.7, respectively, in those without diabetes (P for interaction = .273).
Event rates per 100 person-years were 5.8 and 5.9, respectively, in patients with a defibrillator at baseline, and 3.5 and 4.9, respectively, in those without a defibrillator (P for interaction = .174).
Asked to comment on the study, which was simultaneously published in the European Heart Journal, Milton Packer, MD, Baylor University Medical Center, Dallas, said he had “very little confidence” in the findings.
“This was entirely post hoc and the investigators combined events – with markedly different levels of clinical importance – in order to achieve a P value less than 0.05,” he told this news organization. “If one takes asymptomatic ventricular arrhythmias out of the analysis, the effect is no longer statistically significant. Furthermore, half of sudden deaths in patients with heart failure are not related to a ventricular arrhythmia.”
The authors note in their report that the analysis was not prespecified and the findings should be regarded as “hypothesis generating and require confirmation,” but also point out that a recent meta-analysis showed that SGLT2 inhibitor use was associated with a lower risk for ventricular tachycardia. Other limitations to the post hoc analysis are that adverse-event reporting likely underestimated the true prevalence of ventricular arrhythmias, and that these events were not adjudicated.
DAPA-HF was funded by AstraZeneca. Dr. Curtain reports no relevant financial relationships. Disclosures for the coauthors are listed in the paper.
A version of this article first appeared on Medscape.com.
Dapagliflozin might reduce the risk for ventricular arrhythmias and sudden death in patients with heart failure and reduced ejection fraction (HFrEF), a post hoc analysis of the DAPA-HF trial suggests.
The addition of dapagliflozin to standard therapy reduced the relative risk for the primary composite endpoint of any serious ventricular arrhythmia, resuscitated cardiac arrest, or sudden death by 21%, compared with placebo (hazard ratio, 0.79; 95% confidence interval, 0.63-0.99). The absolute risk reduction was 1.5% (5.9% vs. 7.4%).
The benefit was consistent in a competing-risks analysis that included all-cause mortality (HR, 0.80; P = .043) and across the individual components of the composite outcome, James Curtain, MD, Cardiovascular Research Centre of Glasgow, said at the annual congress of the European Society of Cardiology.
As previously reported from the main trial, treatment with the sodium-glucose cotransporter 2 (SGLT2) inhibitor cut the primary endpoint of cardiovascular death or worsening heart failure by 26% among 4,744 patients with HFrEF and in New York Heart Association functional class 2-4.
Cochair of the late-breaking science session, Lars Lund, MD, Karolinska Institute, Stockholm, pointed out that dapagliflozin reduced sudden cardiac deaths and related events to an extent similar to that observed for cardiovascular deaths, total mortality, and the main trial’s primary endpoint.
“So does that mean it has any particular effect on arrhythmic events or does it mean, such as a beta-blocker, for example, [it] reduces calcium transience and improves handling of calcium, or does it have an effect simply by improving heart failure?” he asked.
Dr. Curtain replied they are still trying to understand the effects of this new class of drug but that studies have shown dapagliflozin and other SGLT2 inhibitors have favorable effects on adverse cardiac remodeling, which contributes to sudden death and ventricular arrhythmia. They’ve also been shown to reduce cardiac chamber size, left ventricular hypertrophy, and N-terminal pro-B-type natriuretic peptide (NT-proBNP) levels over time, consistent with a reduction in myocardial wall stress. “So it could indeed be one of several mechanisms by which they may exert a beneficial cardiac effect.”
Speaking with this news organization, Dr. Curtain pointed out that the Kaplan-Meier curves for the composite outcome began to separate early on, but that the clearest separation was after 9 months, suggestive of a positive action on adverse cardiac remodeling over time.
“This would improve the patients’ heart failure situation, but also thick ventricles are a key risk factor for the occurrence of sudden death and ventricular arrhythmias,” he said. “The effects on adverse cardiac remodeling, given its plausibility in terms of our Kaplan-Meier curves, are one [mechanism] that I’d look to in the first instance, but I’m sure there are more than one actions at play.”
According to the new analysis, the primary outcome occurred in 315 (6.6%) patients; there were 203 adjudicated sudden deaths (64%), 104 investigator-reported ventricular arrhythmias (33%), and 8 resuscitated cardiac arrests (3%). Independent predictors of the primary outcome were higher NT-proBNP levels (odds ratio, 1.54), previous ventricular arrhythmia (OR, 1.93), previous myocardial infarction (OR, 1.42), male sex (OR, 1.53), and higher body mass index (OR, 1.03).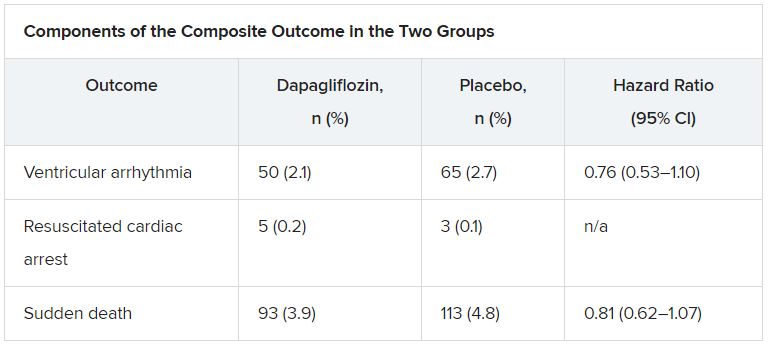
The effect of dapagliflozin on the primary outcome was consistent in several sensitivity analyses and “generally consistent” across key subgroups, Dr. Curtain said.
During a discussion of the results, session cochair Mitja Lainscak, MD, General Hospital Murska Sobota, Slovenia, called out two exceptions. “With regard to patients with implanted ICDs, the effect was neutral, and in the patients without diabetes, the benefit was less than in diabetic patients. Any explanations for that?”
Dr. Curtain responded that “it’s important to note that in the subgroup analyses the point estimates were all on the side favoring dapagliflozin and the interaction test was not significant in that subgroup. The numbers of patients who were in the defibrillator group were modest, and there was a relatively smaller number of events, so it may be harder to show benefit in that group.”
In the dapagliflozin and placebo groups, the event rates per 100 person-years were 3.9 and 5.8, respectively, in patients with diabetes, and 4.1 and 4.7, respectively, in those without diabetes (P for interaction = .273).
Event rates per 100 person-years were 5.8 and 5.9, respectively, in patients with a defibrillator at baseline, and 3.5 and 4.9, respectively, in those without a defibrillator (P for interaction = .174).
Asked to comment on the study, which was simultaneously published in the European Heart Journal, Milton Packer, MD, Baylor University Medical Center, Dallas, said he had “very little confidence” in the findings.
“This was entirely post hoc and the investigators combined events – with markedly different levels of clinical importance – in order to achieve a P value less than 0.05,” he told this news organization. “If one takes asymptomatic ventricular arrhythmias out of the analysis, the effect is no longer statistically significant. Furthermore, half of sudden deaths in patients with heart failure are not related to a ventricular arrhythmia.”
The authors note in their report that the analysis was not prespecified and the findings should be regarded as “hypothesis generating and require confirmation,” but also point out that a recent meta-analysis showed that SGLT2 inhibitor use was associated with a lower risk for ventricular tachycardia. Other limitations to the post hoc analysis are that adverse-event reporting likely underestimated the true prevalence of ventricular arrhythmias, and that these events were not adjudicated.
DAPA-HF was funded by AstraZeneca. Dr. Curtain reports no relevant financial relationships. Disclosures for the coauthors are listed in the paper.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2021
NIH to study COVID vaccine booster in people with autoimmune disease
In the wake of the Centers for Disease Control and Prevention’s recommendation for a third COVID-19 mRNA vaccine dose for immunocompromised people and the Food and Drug Administration’s authorization of the third dose, the according to an announcement.
The investigators of the trial, called COVID‐19 Booster Vaccine in Autoimmune Disease Non‐Responders, also want to determine if pausing immunosuppressive therapy for autoimmune disease improves the antibody response to an extra dose of a COVID-19 vaccine.
The trial will specifically look at the effects of mycophenolate mofetil (MMF) or mycophenolic acid (MPA), and methotrexate (MTX), or receipt of B cell–depletion therapy such as rituximab within the past 12 months on immune response to a booster dose in people with systemic lupus erythematosus, rheumatoid arthritis, multiple sclerosis, systemic sclerosis, or pemphigus. They have to have either no serologic response to their initial COVID-19 vaccine regimen or a suboptimal response, defined as a Roche Elecsys Anti-SARS-CoV-2 S (RBD) result greater than or equal to 50 U/mL.
The results of studies conducted in solid-organ transplant recipients who take immunosuppressants showed that an extra dose of vaccine could improve the immune response to the vaccine in many of the individuals, which suggests that the same approach might work in people with autoimmune disease who need treatment with immunosuppressive drugs. Improving the immune response of people with autoimmune disease to COVID-19 vaccines is important because higher rates of severe COVID-19 and death have been reported in this group of patients than in the general population, and it is unclear whether this is attributable to the autoimmune disease, the immunosuppressive medications taken to treat it, or both.
The open-label trial, conducted by the NIAID-funded Autoimmunity Centers of Excellence, aims to enroll 600 people aged 18 years and older with those conditions at 15-20 sites in the United States.
Because medications commonly taken by people with these conditions have been associated with poorer immune responses to vaccines, the trial will randomize the following two cohorts to stop or continue taking their immunosuppressive medication(s) or stop them before and after the booster according to protocol:
- Cohort 1 includes people who are taking MMF or MPA, without additional B cell–depleting medications or MTX.
- Cohort 2 includes people who are taking MTX without additional B cell–depleting medications or MMF/MPA.
A third, nonrandomized cohort consists of people who have received B cell–depletion therapy within the past 12 months regardless of whether they are also taking MMF/MPA or MTX.
Besides the cohort-specific exclusions, other rheumatic disease medications, including biologics, are allowed in the groups.
The primary outcome of the trial is the proportion of participants who have a protective antibody response at week 4. Secondary outcomes will examine various antibody responses at intervals, changes in disease activity across autoimmune diseases, adverse events, and SARS-CoV-2 infections out to 48 weeks.
Study participants will be followed for a total of 13 months. Preliminary results are expected in November 2021, according to the National Institutes of Health.
The trial is being led by Judith James, MD, PhD; Meggan Mackay, MD, MS; Dinesh Khanna, MBBS, MSc; and Amit Bar-Or, MD.
In the wake of the Centers for Disease Control and Prevention’s recommendation for a third COVID-19 mRNA vaccine dose for immunocompromised people and the Food and Drug Administration’s authorization of the third dose, the according to an announcement.
The investigators of the trial, called COVID‐19 Booster Vaccine in Autoimmune Disease Non‐Responders, also want to determine if pausing immunosuppressive therapy for autoimmune disease improves the antibody response to an extra dose of a COVID-19 vaccine.
The trial will specifically look at the effects of mycophenolate mofetil (MMF) or mycophenolic acid (MPA), and methotrexate (MTX), or receipt of B cell–depletion therapy such as rituximab within the past 12 months on immune response to a booster dose in people with systemic lupus erythematosus, rheumatoid arthritis, multiple sclerosis, systemic sclerosis, or pemphigus. They have to have either no serologic response to their initial COVID-19 vaccine regimen or a suboptimal response, defined as a Roche Elecsys Anti-SARS-CoV-2 S (RBD) result greater than or equal to 50 U/mL.
The results of studies conducted in solid-organ transplant recipients who take immunosuppressants showed that an extra dose of vaccine could improve the immune response to the vaccine in many of the individuals, which suggests that the same approach might work in people with autoimmune disease who need treatment with immunosuppressive drugs. Improving the immune response of people with autoimmune disease to COVID-19 vaccines is important because higher rates of severe COVID-19 and death have been reported in this group of patients than in the general population, and it is unclear whether this is attributable to the autoimmune disease, the immunosuppressive medications taken to treat it, or both.
The open-label trial, conducted by the NIAID-funded Autoimmunity Centers of Excellence, aims to enroll 600 people aged 18 years and older with those conditions at 15-20 sites in the United States.
Because medications commonly taken by people with these conditions have been associated with poorer immune responses to vaccines, the trial will randomize the following two cohorts to stop or continue taking their immunosuppressive medication(s) or stop them before and after the booster according to protocol:
- Cohort 1 includes people who are taking MMF or MPA, without additional B cell–depleting medications or MTX.
- Cohort 2 includes people who are taking MTX without additional B cell–depleting medications or MMF/MPA.
A third, nonrandomized cohort consists of people who have received B cell–depletion therapy within the past 12 months regardless of whether they are also taking MMF/MPA or MTX.
Besides the cohort-specific exclusions, other rheumatic disease medications, including biologics, are allowed in the groups.
The primary outcome of the trial is the proportion of participants who have a protective antibody response at week 4. Secondary outcomes will examine various antibody responses at intervals, changes in disease activity across autoimmune diseases, adverse events, and SARS-CoV-2 infections out to 48 weeks.
Study participants will be followed for a total of 13 months. Preliminary results are expected in November 2021, according to the National Institutes of Health.
The trial is being led by Judith James, MD, PhD; Meggan Mackay, MD, MS; Dinesh Khanna, MBBS, MSc; and Amit Bar-Or, MD.
In the wake of the Centers for Disease Control and Prevention’s recommendation for a third COVID-19 mRNA vaccine dose for immunocompromised people and the Food and Drug Administration’s authorization of the third dose, the according to an announcement.
The investigators of the trial, called COVID‐19 Booster Vaccine in Autoimmune Disease Non‐Responders, also want to determine if pausing immunosuppressive therapy for autoimmune disease improves the antibody response to an extra dose of a COVID-19 vaccine.
The trial will specifically look at the effects of mycophenolate mofetil (MMF) or mycophenolic acid (MPA), and methotrexate (MTX), or receipt of B cell–depletion therapy such as rituximab within the past 12 months on immune response to a booster dose in people with systemic lupus erythematosus, rheumatoid arthritis, multiple sclerosis, systemic sclerosis, or pemphigus. They have to have either no serologic response to their initial COVID-19 vaccine regimen or a suboptimal response, defined as a Roche Elecsys Anti-SARS-CoV-2 S (RBD) result greater than or equal to 50 U/mL.
The results of studies conducted in solid-organ transplant recipients who take immunosuppressants showed that an extra dose of vaccine could improve the immune response to the vaccine in many of the individuals, which suggests that the same approach might work in people with autoimmune disease who need treatment with immunosuppressive drugs. Improving the immune response of people with autoimmune disease to COVID-19 vaccines is important because higher rates of severe COVID-19 and death have been reported in this group of patients than in the general population, and it is unclear whether this is attributable to the autoimmune disease, the immunosuppressive medications taken to treat it, or both.
The open-label trial, conducted by the NIAID-funded Autoimmunity Centers of Excellence, aims to enroll 600 people aged 18 years and older with those conditions at 15-20 sites in the United States.
Because medications commonly taken by people with these conditions have been associated with poorer immune responses to vaccines, the trial will randomize the following two cohorts to stop or continue taking their immunosuppressive medication(s) or stop them before and after the booster according to protocol:
- Cohort 1 includes people who are taking MMF or MPA, without additional B cell–depleting medications or MTX.
- Cohort 2 includes people who are taking MTX without additional B cell–depleting medications or MMF/MPA.
A third, nonrandomized cohort consists of people who have received B cell–depletion therapy within the past 12 months regardless of whether they are also taking MMF/MPA or MTX.
Besides the cohort-specific exclusions, other rheumatic disease medications, including biologics, are allowed in the groups.
The primary outcome of the trial is the proportion of participants who have a protective antibody response at week 4. Secondary outcomes will examine various antibody responses at intervals, changes in disease activity across autoimmune diseases, adverse events, and SARS-CoV-2 infections out to 48 weeks.
Study participants will be followed for a total of 13 months. Preliminary results are expected in November 2021, according to the National Institutes of Health.
The trial is being led by Judith James, MD, PhD; Meggan Mackay, MD, MS; Dinesh Khanna, MBBS, MSc; and Amit Bar-Or, MD.
Study evaluates OTC treatments for molluscum contagiosum
“It’s important for clinicians who see children with molluscum to be aware of the many products marketed to patients and to be able to provide objective information about them,” senior author Elaine Siegfried, MD, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the abstract was presented during a poster session.
In the text of their abstract, Dr. Siegfried, professor of pediatrics and dermatology at Saint Louis University, and coauthors Isaac Hoft, of Open Mind Holistics in Ft. Collins, Colo., and Samantha K. Ong, BA, a student at SLU, noted that MC primarily infects children, with an annual incidence of 8%. “Although the disease is self-limited, associated symptoms, contagion and an average 1-year duration prompt concern and frequent medical visits,” they wrote.
The optimal treatment for MC has not been defined and there is currently no approved medication approved for the condition, although three products are in development: VP-102 (cantharidin) by Verrica Pharmaceuticals; SB206, a topical antiviral by Novan; and 10%-15% KOH formulation by the Gurina Foundation.
But many OTC products have been marketed to treat the condition. To identify the OTC products and to assess accompanying information related to safety, efficacy, and cost, the researchers performed an internet search using the terms “molluscum” plus “treatment,” “treatment at home,” “relief,” and “medication.” Eight products were identified for analysis: Conzerol (Elroselabs), Molleave (Innovative Med), Mollenol (Jeva Laboratories), MolluscumBLAST (Revitalize Life Organics), Molluscum Away Patches (Molluscum Away), Naturasil (Nature’s Innovation), Terrasil (Advanced Skincare % Topical Solutions), and Zymaderm (Naturopathix). Package sizes ranged from 0.78 to 1.5 ounces, and prices ranged from about $19 to almost $55.
Dr. Siegfried and colleagues found that all products provided instructions on application and use but most package labels did not include sufficient information about their plant-based ingredients or appropriate dosing. Six of the eight products contained Thuja occidentalis (Arbor vitae), a coniferous cedar whose essential oil has been used in homeopathic products for its anti-inflammatory and antiviral properties. Lemon extract, tea tree oil, and other botanicals were present in no more than three products each. Only two of the products provided information about the number of lesions that could be treated per package.
“The lack of national oversight as well as robust methods for high-level data analysis make safety and efficacy unclear for a Thuja extract marketed to treat MC,” the researchers wrote. “Numerous adverse drug events and positive intradermal skin tests related to Thuja have been reported.”
Dr. Siegfried added that many OTC products offer a money-back guarantee, “so when seeing a patient who failed to respond to one of these products, encourage them, at least, to request a refund, but to also submit a comment about lack of efficacy, in order to provide more balanced Internet information.”
Dr. Siegfried disclosed that she has served as an investigator and consultant for Verrica Pharmaceuticals, and as a consultant and Data Safety Monitoring board member for Novan, two of the companies currently developing drugs to treat molluscum. Her coauthors had no conflicts of interest to disclose.
“It’s important for clinicians who see children with molluscum to be aware of the many products marketed to patients and to be able to provide objective information about them,” senior author Elaine Siegfried, MD, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the abstract was presented during a poster session.
In the text of their abstract, Dr. Siegfried, professor of pediatrics and dermatology at Saint Louis University, and coauthors Isaac Hoft, of Open Mind Holistics in Ft. Collins, Colo., and Samantha K. Ong, BA, a student at SLU, noted that MC primarily infects children, with an annual incidence of 8%. “Although the disease is self-limited, associated symptoms, contagion and an average 1-year duration prompt concern and frequent medical visits,” they wrote.
The optimal treatment for MC has not been defined and there is currently no approved medication approved for the condition, although three products are in development: VP-102 (cantharidin) by Verrica Pharmaceuticals; SB206, a topical antiviral by Novan; and 10%-15% KOH formulation by the Gurina Foundation.
But many OTC products have been marketed to treat the condition. To identify the OTC products and to assess accompanying information related to safety, efficacy, and cost, the researchers performed an internet search using the terms “molluscum” plus “treatment,” “treatment at home,” “relief,” and “medication.” Eight products were identified for analysis: Conzerol (Elroselabs), Molleave (Innovative Med), Mollenol (Jeva Laboratories), MolluscumBLAST (Revitalize Life Organics), Molluscum Away Patches (Molluscum Away), Naturasil (Nature’s Innovation), Terrasil (Advanced Skincare % Topical Solutions), and Zymaderm (Naturopathix). Package sizes ranged from 0.78 to 1.5 ounces, and prices ranged from about $19 to almost $55.
Dr. Siegfried and colleagues found that all products provided instructions on application and use but most package labels did not include sufficient information about their plant-based ingredients or appropriate dosing. Six of the eight products contained Thuja occidentalis (Arbor vitae), a coniferous cedar whose essential oil has been used in homeopathic products for its anti-inflammatory and antiviral properties. Lemon extract, tea tree oil, and other botanicals were present in no more than three products each. Only two of the products provided information about the number of lesions that could be treated per package.
“The lack of national oversight as well as robust methods for high-level data analysis make safety and efficacy unclear for a Thuja extract marketed to treat MC,” the researchers wrote. “Numerous adverse drug events and positive intradermal skin tests related to Thuja have been reported.”
Dr. Siegfried added that many OTC products offer a money-back guarantee, “so when seeing a patient who failed to respond to one of these products, encourage them, at least, to request a refund, but to also submit a comment about lack of efficacy, in order to provide more balanced Internet information.”
Dr. Siegfried disclosed that she has served as an investigator and consultant for Verrica Pharmaceuticals, and as a consultant and Data Safety Monitoring board member for Novan, two of the companies currently developing drugs to treat molluscum. Her coauthors had no conflicts of interest to disclose.
“It’s important for clinicians who see children with molluscum to be aware of the many products marketed to patients and to be able to provide objective information about them,” senior author Elaine Siegfried, MD, said in an interview following the annual meeting of the Society for Pediatric Dermatology, where the abstract was presented during a poster session.
In the text of their abstract, Dr. Siegfried, professor of pediatrics and dermatology at Saint Louis University, and coauthors Isaac Hoft, of Open Mind Holistics in Ft. Collins, Colo., and Samantha K. Ong, BA, a student at SLU, noted that MC primarily infects children, with an annual incidence of 8%. “Although the disease is self-limited, associated symptoms, contagion and an average 1-year duration prompt concern and frequent medical visits,” they wrote.
The optimal treatment for MC has not been defined and there is currently no approved medication approved for the condition, although three products are in development: VP-102 (cantharidin) by Verrica Pharmaceuticals; SB206, a topical antiviral by Novan; and 10%-15% KOH formulation by the Gurina Foundation.
But many OTC products have been marketed to treat the condition. To identify the OTC products and to assess accompanying information related to safety, efficacy, and cost, the researchers performed an internet search using the terms “molluscum” plus “treatment,” “treatment at home,” “relief,” and “medication.” Eight products were identified for analysis: Conzerol (Elroselabs), Molleave (Innovative Med), Mollenol (Jeva Laboratories), MolluscumBLAST (Revitalize Life Organics), Molluscum Away Patches (Molluscum Away), Naturasil (Nature’s Innovation), Terrasil (Advanced Skincare % Topical Solutions), and Zymaderm (Naturopathix). Package sizes ranged from 0.78 to 1.5 ounces, and prices ranged from about $19 to almost $55.
Dr. Siegfried and colleagues found that all products provided instructions on application and use but most package labels did not include sufficient information about their plant-based ingredients or appropriate dosing. Six of the eight products contained Thuja occidentalis (Arbor vitae), a coniferous cedar whose essential oil has been used in homeopathic products for its anti-inflammatory and antiviral properties. Lemon extract, tea tree oil, and other botanicals were present in no more than three products each. Only two of the products provided information about the number of lesions that could be treated per package.
“The lack of national oversight as well as robust methods for high-level data analysis make safety and efficacy unclear for a Thuja extract marketed to treat MC,” the researchers wrote. “Numerous adverse drug events and positive intradermal skin tests related to Thuja have been reported.”
Dr. Siegfried added that many OTC products offer a money-back guarantee, “so when seeing a patient who failed to respond to one of these products, encourage them, at least, to request a refund, but to also submit a comment about lack of efficacy, in order to provide more balanced Internet information.”
Dr. Siegfried disclosed that she has served as an investigator and consultant for Verrica Pharmaceuticals, and as a consultant and Data Safety Monitoring board member for Novan, two of the companies currently developing drugs to treat molluscum. Her coauthors had no conflicts of interest to disclose.
FROM SPD 2021
Stop blaming the unvaccinated
As politicians battle over masks and mandates, heated rhetoric has been used to describe the fourth heartbreaking surge in COVID as a “pandemic of the unvaccinated.”
While it may serve to further divide red and blue states, I disagree with the assertion that the current surge in cases is driven simply by the unvaccinated. Why? First, the premise would assume complete efficacy with our vaccinated population, which is statistically incorrect (at least 15 million of the U.S. population never completed a second round of injections), which means they were not considered “fully vaccinated.”
Alternately, we need to examine what has occurred in nations with significantly higher vaccination rates than ours (the United Kingdom and Israel) to realize that variants have overrun the dramatic success achieved in those countries as well. Israel, once considered to be the most vaccinated country in the world, is facing a brutal fourth wave of COVID that has sent the country spiraling into another heartbreaking lockdown.
The unvaccinated could hardly be blamed for what is happening in either of these highly vaccinated countries.
The concept of blame
So why use blame? It defeats the purpose of encouraging those who are hesitant or possibly misinformed or disenfranchised to move forward. It lacks compassion. It does not encompass the art and science of nursing (for example, the University of Southern Indiana), such as those that hospitals have used to frame optimal nursing care. I abhor the idea of labeling because it denies the prospect of future comprehension.
Labeling reminds me of one of the saddest cases in my career.
An unfortunate case
I was the nurse caring for a man from a motor vehicular accident where an entire family was brutally killed. My patient was alleged to be the cause, with a blood alcohol level of 0.40%+ post hydration, intubated and ventilated, with a flailed chest and multiple orthopedic injuries as well as blunt head trauma. He was secured to the bed with handcuffs, although that was unnecessary. Multiple times I was asked how I could possibly care for such an individual, by the police and even a few colleagues. But it was not my place to judge the man.
He was in pain, and he was dying. I comforted him for the 2 weeks it took his battered body to pass into the next realm. No one visited him except the police, eagerly waiting for the man to wake up to explain the tragic events that occurred. It was my job to ease what pain I could and protect him from labels. Did he deserve the labels? Who knew? I did not care. I cared about his writhing and his physical anguish.
The comparison
Blame did not help the situation then, nor does it help us move forward now. As nurses, we seek to work within a framework of understanding. As we tire of caring for thousands of COVID patients, we do not stop to ask if they “deserve” care or if they have taken precautions and lived reasonably prior to seeking assistance for disease. We would not be nurses if we did this.
Think about Gov. Greg Abbott, who has asked that Texans not be allowed to mandate masks for children returning to school. He has recently been diagnosed with COVID, despite assuring the public he is fully vaccinated. Politically, his diagnosis could be visualized as a fiasco for a purple state where he has been adamant in denying the efficacy of masks for children.
Yet, his diagnosis should not be fodder for the press. The first concern should be his health and well-being, similar for any man of his age and potential comorbidity.
Conclusion
We should be people first, human beings that remain interconnected by our need for care and survival, not conservatives, independents, or liberals, not “vaccinated or unvaccinated,” not seen as “breakthrough” infections, or the immunosuppressed possibly unable to mount a robust response to COVID.
Labels do not define the ability to effectively defeat coronavirus or variants, as highly vaccinated countries have demonstrated in recent months. We are in the midst of a global pandemic, and the battle is raging onward.
In fact, the longer this pandemic continues, the more likely it is we will need to live with this as an endemic disease, so we should stop blaming those who become ill and need support.
It could be any of us.
A version of this article first appeared on Medscape.com.
As politicians battle over masks and mandates, heated rhetoric has been used to describe the fourth heartbreaking surge in COVID as a “pandemic of the unvaccinated.”
While it may serve to further divide red and blue states, I disagree with the assertion that the current surge in cases is driven simply by the unvaccinated. Why? First, the premise would assume complete efficacy with our vaccinated population, which is statistically incorrect (at least 15 million of the U.S. population never completed a second round of injections), which means they were not considered “fully vaccinated.”
Alternately, we need to examine what has occurred in nations with significantly higher vaccination rates than ours (the United Kingdom and Israel) to realize that variants have overrun the dramatic success achieved in those countries as well. Israel, once considered to be the most vaccinated country in the world, is facing a brutal fourth wave of COVID that has sent the country spiraling into another heartbreaking lockdown.
The unvaccinated could hardly be blamed for what is happening in either of these highly vaccinated countries.
The concept of blame
So why use blame? It defeats the purpose of encouraging those who are hesitant or possibly misinformed or disenfranchised to move forward. It lacks compassion. It does not encompass the art and science of nursing (for example, the University of Southern Indiana), such as those that hospitals have used to frame optimal nursing care. I abhor the idea of labeling because it denies the prospect of future comprehension.
Labeling reminds me of one of the saddest cases in my career.
An unfortunate case
I was the nurse caring for a man from a motor vehicular accident where an entire family was brutally killed. My patient was alleged to be the cause, with a blood alcohol level of 0.40%+ post hydration, intubated and ventilated, with a flailed chest and multiple orthopedic injuries as well as blunt head trauma. He was secured to the bed with handcuffs, although that was unnecessary. Multiple times I was asked how I could possibly care for such an individual, by the police and even a few colleagues. But it was not my place to judge the man.
He was in pain, and he was dying. I comforted him for the 2 weeks it took his battered body to pass into the next realm. No one visited him except the police, eagerly waiting for the man to wake up to explain the tragic events that occurred. It was my job to ease what pain I could and protect him from labels. Did he deserve the labels? Who knew? I did not care. I cared about his writhing and his physical anguish.
The comparison
Blame did not help the situation then, nor does it help us move forward now. As nurses, we seek to work within a framework of understanding. As we tire of caring for thousands of COVID patients, we do not stop to ask if they “deserve” care or if they have taken precautions and lived reasonably prior to seeking assistance for disease. We would not be nurses if we did this.
Think about Gov. Greg Abbott, who has asked that Texans not be allowed to mandate masks for children returning to school. He has recently been diagnosed with COVID, despite assuring the public he is fully vaccinated. Politically, his diagnosis could be visualized as a fiasco for a purple state where he has been adamant in denying the efficacy of masks for children.
Yet, his diagnosis should not be fodder for the press. The first concern should be his health and well-being, similar for any man of his age and potential comorbidity.
Conclusion
We should be people first, human beings that remain interconnected by our need for care and survival, not conservatives, independents, or liberals, not “vaccinated or unvaccinated,” not seen as “breakthrough” infections, or the immunosuppressed possibly unable to mount a robust response to COVID.
Labels do not define the ability to effectively defeat coronavirus or variants, as highly vaccinated countries have demonstrated in recent months. We are in the midst of a global pandemic, and the battle is raging onward.
In fact, the longer this pandemic continues, the more likely it is we will need to live with this as an endemic disease, so we should stop blaming those who become ill and need support.
It could be any of us.
A version of this article first appeared on Medscape.com.
As politicians battle over masks and mandates, heated rhetoric has been used to describe the fourth heartbreaking surge in COVID as a “pandemic of the unvaccinated.”
While it may serve to further divide red and blue states, I disagree with the assertion that the current surge in cases is driven simply by the unvaccinated. Why? First, the premise would assume complete efficacy with our vaccinated population, which is statistically incorrect (at least 15 million of the U.S. population never completed a second round of injections), which means they were not considered “fully vaccinated.”
Alternately, we need to examine what has occurred in nations with significantly higher vaccination rates than ours (the United Kingdom and Israel) to realize that variants have overrun the dramatic success achieved in those countries as well. Israel, once considered to be the most vaccinated country in the world, is facing a brutal fourth wave of COVID that has sent the country spiraling into another heartbreaking lockdown.
The unvaccinated could hardly be blamed for what is happening in either of these highly vaccinated countries.
The concept of blame
So why use blame? It defeats the purpose of encouraging those who are hesitant or possibly misinformed or disenfranchised to move forward. It lacks compassion. It does not encompass the art and science of nursing (for example, the University of Southern Indiana), such as those that hospitals have used to frame optimal nursing care. I abhor the idea of labeling because it denies the prospect of future comprehension.
Labeling reminds me of one of the saddest cases in my career.
An unfortunate case
I was the nurse caring for a man from a motor vehicular accident where an entire family was brutally killed. My patient was alleged to be the cause, with a blood alcohol level of 0.40%+ post hydration, intubated and ventilated, with a flailed chest and multiple orthopedic injuries as well as blunt head trauma. He was secured to the bed with handcuffs, although that was unnecessary. Multiple times I was asked how I could possibly care for such an individual, by the police and even a few colleagues. But it was not my place to judge the man.
He was in pain, and he was dying. I comforted him for the 2 weeks it took his battered body to pass into the next realm. No one visited him except the police, eagerly waiting for the man to wake up to explain the tragic events that occurred. It was my job to ease what pain I could and protect him from labels. Did he deserve the labels? Who knew? I did not care. I cared about his writhing and his physical anguish.
The comparison
Blame did not help the situation then, nor does it help us move forward now. As nurses, we seek to work within a framework of understanding. As we tire of caring for thousands of COVID patients, we do not stop to ask if they “deserve” care or if they have taken precautions and lived reasonably prior to seeking assistance for disease. We would not be nurses if we did this.
Think about Gov. Greg Abbott, who has asked that Texans not be allowed to mandate masks for children returning to school. He has recently been diagnosed with COVID, despite assuring the public he is fully vaccinated. Politically, his diagnosis could be visualized as a fiasco for a purple state where he has been adamant in denying the efficacy of masks for children.
Yet, his diagnosis should not be fodder for the press. The first concern should be his health and well-being, similar for any man of his age and potential comorbidity.
Conclusion
We should be people first, human beings that remain interconnected by our need for care and survival, not conservatives, independents, or liberals, not “vaccinated or unvaccinated,” not seen as “breakthrough” infections, or the immunosuppressed possibly unable to mount a robust response to COVID.
Labels do not define the ability to effectively defeat coronavirus or variants, as highly vaccinated countries have demonstrated in recent months. We are in the midst of a global pandemic, and the battle is raging onward.
In fact, the longer this pandemic continues, the more likely it is we will need to live with this as an endemic disease, so we should stop blaming those who become ill and need support.
It could be any of us.
A version of this article first appeared on Medscape.com.












