User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
FDA okays extended-release exenatide for children with T2D
the agency announced July 22.
Previously approved in adults, the injectable is now the second glucagonlike peptide-1 receptor agonist approved for use in pediatric type 2 diabetes, after liraglutide (Victoza, Novo Nordisk) in 2019, and the first with once-weekly administration.
The two extended-release Bydureon products – which differ in delivery device and mixing procedure – are now indicated for use in addition to diet and exercise to improve glycemic control in pediatric patients 10 years of age or older with type 2 diabetes.
Exenatide extended release is not recommended as first-line treatment following diet and exercise.
The approval was based on a 24-week, double-blind, placebo-controlled study in 82 children with type 2 diabetes aged 10 and older. They were randomized to 2 mg once-weekly exenatide extended release or placebo. At week 24, hemoglobin A1c in those randomized to the drug had dropped by 0.25 percentage points, compared with a 0.45 percentage point increase in the placebo group.
Side effects were similar to those seen in adults, including injection site reactions, headaches, and gastrointestinal discomfort.
Currently, metformin is the only oral medication approved for treating pediatric type 2 diabetes, while the injectables also include insulin in addition to the two GLP-1 receptor agonists. During a symposium held in June 2021 at the annual scientific sessions of the American Diabetes Association, speakers expressed alarm about the rise in youth developing type 2 diabetes, noting that the condition typically progresses more rapidly and is less likely to respond well to metformin, compared with adults.
But, the panelists were also optimistic about extended-release exenatide as well as several other therapies for pediatric patients with type 2 diabetes in ongoing phase 3 trials, including the sodium-glucose cotransporter 2 inhibitors dapagliflozin and empagliflozin, and the dipeptidyl peptidase–4 inhibitors alogliptin and linagliptin. Results are expected in the next 1-2 years.
the agency announced July 22.
Previously approved in adults, the injectable is now the second glucagonlike peptide-1 receptor agonist approved for use in pediatric type 2 diabetes, after liraglutide (Victoza, Novo Nordisk) in 2019, and the first with once-weekly administration.
The two extended-release Bydureon products – which differ in delivery device and mixing procedure – are now indicated for use in addition to diet and exercise to improve glycemic control in pediatric patients 10 years of age or older with type 2 diabetes.
Exenatide extended release is not recommended as first-line treatment following diet and exercise.
The approval was based on a 24-week, double-blind, placebo-controlled study in 82 children with type 2 diabetes aged 10 and older. They were randomized to 2 mg once-weekly exenatide extended release or placebo. At week 24, hemoglobin A1c in those randomized to the drug had dropped by 0.25 percentage points, compared with a 0.45 percentage point increase in the placebo group.
Side effects were similar to those seen in adults, including injection site reactions, headaches, and gastrointestinal discomfort.
Currently, metformin is the only oral medication approved for treating pediatric type 2 diabetes, while the injectables also include insulin in addition to the two GLP-1 receptor agonists. During a symposium held in June 2021 at the annual scientific sessions of the American Diabetes Association, speakers expressed alarm about the rise in youth developing type 2 diabetes, noting that the condition typically progresses more rapidly and is less likely to respond well to metformin, compared with adults.
But, the panelists were also optimistic about extended-release exenatide as well as several other therapies for pediatric patients with type 2 diabetes in ongoing phase 3 trials, including the sodium-glucose cotransporter 2 inhibitors dapagliflozin and empagliflozin, and the dipeptidyl peptidase–4 inhibitors alogliptin and linagliptin. Results are expected in the next 1-2 years.
the agency announced July 22.
Previously approved in adults, the injectable is now the second glucagonlike peptide-1 receptor agonist approved for use in pediatric type 2 diabetes, after liraglutide (Victoza, Novo Nordisk) in 2019, and the first with once-weekly administration.
The two extended-release Bydureon products – which differ in delivery device and mixing procedure – are now indicated for use in addition to diet and exercise to improve glycemic control in pediatric patients 10 years of age or older with type 2 diabetes.
Exenatide extended release is not recommended as first-line treatment following diet and exercise.
The approval was based on a 24-week, double-blind, placebo-controlled study in 82 children with type 2 diabetes aged 10 and older. They were randomized to 2 mg once-weekly exenatide extended release or placebo. At week 24, hemoglobin A1c in those randomized to the drug had dropped by 0.25 percentage points, compared with a 0.45 percentage point increase in the placebo group.
Side effects were similar to those seen in adults, including injection site reactions, headaches, and gastrointestinal discomfort.
Currently, metformin is the only oral medication approved for treating pediatric type 2 diabetes, while the injectables also include insulin in addition to the two GLP-1 receptor agonists. During a symposium held in June 2021 at the annual scientific sessions of the American Diabetes Association, speakers expressed alarm about the rise in youth developing type 2 diabetes, noting that the condition typically progresses more rapidly and is less likely to respond well to metformin, compared with adults.
But, the panelists were also optimistic about extended-release exenatide as well as several other therapies for pediatric patients with type 2 diabetes in ongoing phase 3 trials, including the sodium-glucose cotransporter 2 inhibitors dapagliflozin and empagliflozin, and the dipeptidyl peptidase–4 inhibitors alogliptin and linagliptin. Results are expected in the next 1-2 years.
Two-drug dolutegravir treatment noninferior to 3/4 drug regimen
A two-drug fixed-dose tablet therapy of dolutegravir/lamivudine (Dovato, ViiV Healthcare; DTG/3TC) shows noninferiority in viral suppression among people with HIV-1 who switch from any type of three- or four-drug antiretroviral (ART) regimens. But, presented at the virtual meeting of the International AIDS Society.
The results on the switch to DTG/3TC are from the phase 3 SALSA trial, which compared patients with HIV-1 who either remained on any current three- or four-drug ART regimen or who switched to the two-drug dolutegravir option.
For the primary endpoint, rates of virologic failure at 48 weeks were noninferior in the DTG/3TC group versus the three- or four-drug regimen (.4% vs. 1.2; adjusted difference: –.8% [95% confidence interval, –2.4%, .8%]).
In addition, rates of virologic suppression at week 48 were noninferior, with 94.3% of patients achieving HIV-1 RNA < 50 c/mL in the DTG/3TC group versus 92.7% in the three- or four-drug regimen (adjusted difference: 1.6% [95% CI, –2.8%, 5.9%).
“These data build upon the previous TANGO study and support DTG/3TC as a robust switch option with high levels of efficacy, good safety and tolerability, and a high barrier of resistance,” first author Josep M. Llibre, MD, PhD, consultant, infectious diseases department, Germans Trias i Pujol University Hospital, Barcelona, said in presenting the findings.
The two-drug dolutegravir-based regimen had previously been shown in the phase 3 GEMINI-1 and GEMINI-2 trials to have virologic noninferiority and safety compared with three- or four-drug DTG plus tenofovir/emtricitabine (TDF/FTC) ART regimens in treatment-naive individuals, and, in the subsequent TANGO trial, the regimen was also noninferior versus tenofovir alafenamide–based regimens among treatment-experienced patients, at 144 weeks in both studies.
Trial details
The new SALSA trial, designed to broaden the comparison to treatment with any current three- or four-drug ART regimen, involved 493 patients at 120 study sites in 17 countries.
All patients were initially on a three- or four-drug regimen, with HIV-1 RNA of less than 50 c/mL for more than 6 months, and without prior virologic failure or nucleoside reverse transcriptase inhibitors or dolutegravir resistance-associated mutations.
The participants were randomized 1:1 to remain on their current regimen (n = 247) or to switch to the once-daily, fixed-dose tablet two-drug combination of dolutegravir 50 mg/lamivudine 300 mg (n = 246) for 52 weeks.
In addition to the noninferior virologic outcomes, there were no serious drug-related adverse events, no confirmed virologic withdrawals, and no resistance mutations in either group.
Of note, weight increase was higher in the DTG/3TC group (8%; n = 20) versus the current ART arm (2%; n = 5), as has been observed in previous studies. The adjusted mean change in weight from baseline to week 48 in the DTG arm was 2.1 kg versus 0.6 kg in the current ART arm.
Dr. Llibre pointed out that many of the participants who switched were discontinuing regimens such as TDF and efavirenz that are associated with weight loss, “so discontinuation could be more related to weight gain than the introduction of dolutegravir, but this deserves further study,” he noted.
There were no significant differences in changes in eGFR and fasting lipids, or in changes in inflammatory biomarkers between the groups.
Bone and renal biomarkers were more favorable in the dolutegravir two-drug arm, suggesting that bone and renal function was either maintained or even improved with the drug switch, Dr. Llibre noted.
Commenting on the research, Alexandra Calmy, PhD, of the HIV/AIDS Unit and LIPO & metabolism group, infectious disease division, Geneva University Hospitals, said that data on quality of life and patient satisfaction measures would be of particular interest.
“Indeed, it is not absolutely clear how a two-in-one versus a three-in-one pill may really influence treatment satisfaction and/or quality of life,” she said in an interview. “Validated scales and patient-reported outcomes with regards to treatment satisfaction would have been an added value to the study.”
Dr. Calmy coauthored a previous study looking at weight change and pharmacokinetic parameters in patients with HIV who switched to DTG-based regimens, and also found weight changes were increased with the DTG regimens. However, the weight gain was not associated with DTG plasma levels, thus supporting Dr. Llibre’s suggestion of possible withdrawal effects from other drugs.
STAT trial: Feasibility of two-drug DTG/3TC as first-line treatment
In further findings presented at the meeting on the STAT trial, researchers evaluated the feasibility not of switching to, but of initiating patients on, the two-drug DTG treatment as a first-line therapy, within 14 days of HIV-1 diagnosis.
The “test-and-treat” approach counters common belief that the regimen should be started only after the traditional three-drug regimens, because of the potential of transmitted resistance and baseline hepatitis B virus coinfection.
In the study of 131 patients, at week 48, 82% (107/131) of all participants and 97% (107/110) of those with available data achieved HIV-1 RNA levels of < 50 c/mL.
While two participants had confirmed virologic failure in the study, there were no treatment-emergent resistance-associated mutations, and neither patient discontinued the two-drug DTG treatment. There were low rates of drug-related adverse events (8%) and they were not serious.
“The STAT data is important as it shows us, for the first time, that in patients where potentially very little is known prior to treatment initiation, DTG/3TC can be very effectively used as a first-line regimen in a ‘test-and-treat’ approach without compromising on patient safety,” first author Charlotte-Paige Rolle, MD, director of research operations, Orlando (Fla.) Immunology Center, said in an interview.
Dr. Rolle added that “with careful monitoring of test results in the first weeks of therapy, we can appropriately and safely adjust therapy from DTG/3TC to a three-drug regimen if needed for patients that have transmitted drug resistance to DTG or 3TC, or hepatitis B coinfection, with both of these occurring at very low rates regardless.”
The SALSA and STAT studies received funding from ViiV Healthcare. Dr. Llibre has received honoraria or consultation fees from ViiV Healthcare, Gilead Sciences and Janssen-Cilag. Dr. Rolle has received grants from and served on advisory boards/speakers bureaus for ViiV Healthcare, Gilead, and Janssen. Dr. Calmy had no disclosures to report.
A two-drug fixed-dose tablet therapy of dolutegravir/lamivudine (Dovato, ViiV Healthcare; DTG/3TC) shows noninferiority in viral suppression among people with HIV-1 who switch from any type of three- or four-drug antiretroviral (ART) regimens. But, presented at the virtual meeting of the International AIDS Society.
The results on the switch to DTG/3TC are from the phase 3 SALSA trial, which compared patients with HIV-1 who either remained on any current three- or four-drug ART regimen or who switched to the two-drug dolutegravir option.
For the primary endpoint, rates of virologic failure at 48 weeks were noninferior in the DTG/3TC group versus the three- or four-drug regimen (.4% vs. 1.2; adjusted difference: –.8% [95% confidence interval, –2.4%, .8%]).
In addition, rates of virologic suppression at week 48 were noninferior, with 94.3% of patients achieving HIV-1 RNA < 50 c/mL in the DTG/3TC group versus 92.7% in the three- or four-drug regimen (adjusted difference: 1.6% [95% CI, –2.8%, 5.9%).
“These data build upon the previous TANGO study and support DTG/3TC as a robust switch option with high levels of efficacy, good safety and tolerability, and a high barrier of resistance,” first author Josep M. Llibre, MD, PhD, consultant, infectious diseases department, Germans Trias i Pujol University Hospital, Barcelona, said in presenting the findings.
The two-drug dolutegravir-based regimen had previously been shown in the phase 3 GEMINI-1 and GEMINI-2 trials to have virologic noninferiority and safety compared with three- or four-drug DTG plus tenofovir/emtricitabine (TDF/FTC) ART regimens in treatment-naive individuals, and, in the subsequent TANGO trial, the regimen was also noninferior versus tenofovir alafenamide–based regimens among treatment-experienced patients, at 144 weeks in both studies.
Trial details
The new SALSA trial, designed to broaden the comparison to treatment with any current three- or four-drug ART regimen, involved 493 patients at 120 study sites in 17 countries.
All patients were initially on a three- or four-drug regimen, with HIV-1 RNA of less than 50 c/mL for more than 6 months, and without prior virologic failure or nucleoside reverse transcriptase inhibitors or dolutegravir resistance-associated mutations.
The participants were randomized 1:1 to remain on their current regimen (n = 247) or to switch to the once-daily, fixed-dose tablet two-drug combination of dolutegravir 50 mg/lamivudine 300 mg (n = 246) for 52 weeks.
In addition to the noninferior virologic outcomes, there were no serious drug-related adverse events, no confirmed virologic withdrawals, and no resistance mutations in either group.
Of note, weight increase was higher in the DTG/3TC group (8%; n = 20) versus the current ART arm (2%; n = 5), as has been observed in previous studies. The adjusted mean change in weight from baseline to week 48 in the DTG arm was 2.1 kg versus 0.6 kg in the current ART arm.
Dr. Llibre pointed out that many of the participants who switched were discontinuing regimens such as TDF and efavirenz that are associated with weight loss, “so discontinuation could be more related to weight gain than the introduction of dolutegravir, but this deserves further study,” he noted.
There were no significant differences in changes in eGFR and fasting lipids, or in changes in inflammatory biomarkers between the groups.
Bone and renal biomarkers were more favorable in the dolutegravir two-drug arm, suggesting that bone and renal function was either maintained or even improved with the drug switch, Dr. Llibre noted.
Commenting on the research, Alexandra Calmy, PhD, of the HIV/AIDS Unit and LIPO & metabolism group, infectious disease division, Geneva University Hospitals, said that data on quality of life and patient satisfaction measures would be of particular interest.
“Indeed, it is not absolutely clear how a two-in-one versus a three-in-one pill may really influence treatment satisfaction and/or quality of life,” she said in an interview. “Validated scales and patient-reported outcomes with regards to treatment satisfaction would have been an added value to the study.”
Dr. Calmy coauthored a previous study looking at weight change and pharmacokinetic parameters in patients with HIV who switched to DTG-based regimens, and also found weight changes were increased with the DTG regimens. However, the weight gain was not associated with DTG plasma levels, thus supporting Dr. Llibre’s suggestion of possible withdrawal effects from other drugs.
STAT trial: Feasibility of two-drug DTG/3TC as first-line treatment
In further findings presented at the meeting on the STAT trial, researchers evaluated the feasibility not of switching to, but of initiating patients on, the two-drug DTG treatment as a first-line therapy, within 14 days of HIV-1 diagnosis.
The “test-and-treat” approach counters common belief that the regimen should be started only after the traditional three-drug regimens, because of the potential of transmitted resistance and baseline hepatitis B virus coinfection.
In the study of 131 patients, at week 48, 82% (107/131) of all participants and 97% (107/110) of those with available data achieved HIV-1 RNA levels of < 50 c/mL.
While two participants had confirmed virologic failure in the study, there were no treatment-emergent resistance-associated mutations, and neither patient discontinued the two-drug DTG treatment. There were low rates of drug-related adverse events (8%) and they were not serious.
“The STAT data is important as it shows us, for the first time, that in patients where potentially very little is known prior to treatment initiation, DTG/3TC can be very effectively used as a first-line regimen in a ‘test-and-treat’ approach without compromising on patient safety,” first author Charlotte-Paige Rolle, MD, director of research operations, Orlando (Fla.) Immunology Center, said in an interview.
Dr. Rolle added that “with careful monitoring of test results in the first weeks of therapy, we can appropriately and safely adjust therapy from DTG/3TC to a three-drug regimen if needed for patients that have transmitted drug resistance to DTG or 3TC, or hepatitis B coinfection, with both of these occurring at very low rates regardless.”
The SALSA and STAT studies received funding from ViiV Healthcare. Dr. Llibre has received honoraria or consultation fees from ViiV Healthcare, Gilead Sciences and Janssen-Cilag. Dr. Rolle has received grants from and served on advisory boards/speakers bureaus for ViiV Healthcare, Gilead, and Janssen. Dr. Calmy had no disclosures to report.
A two-drug fixed-dose tablet therapy of dolutegravir/lamivudine (Dovato, ViiV Healthcare; DTG/3TC) shows noninferiority in viral suppression among people with HIV-1 who switch from any type of three- or four-drug antiretroviral (ART) regimens. But, presented at the virtual meeting of the International AIDS Society.
The results on the switch to DTG/3TC are from the phase 3 SALSA trial, which compared patients with HIV-1 who either remained on any current three- or four-drug ART regimen or who switched to the two-drug dolutegravir option.
For the primary endpoint, rates of virologic failure at 48 weeks were noninferior in the DTG/3TC group versus the three- or four-drug regimen (.4% vs. 1.2; adjusted difference: –.8% [95% confidence interval, –2.4%, .8%]).
In addition, rates of virologic suppression at week 48 were noninferior, with 94.3% of patients achieving HIV-1 RNA < 50 c/mL in the DTG/3TC group versus 92.7% in the three- or four-drug regimen (adjusted difference: 1.6% [95% CI, –2.8%, 5.9%).
“These data build upon the previous TANGO study and support DTG/3TC as a robust switch option with high levels of efficacy, good safety and tolerability, and a high barrier of resistance,” first author Josep M. Llibre, MD, PhD, consultant, infectious diseases department, Germans Trias i Pujol University Hospital, Barcelona, said in presenting the findings.
The two-drug dolutegravir-based regimen had previously been shown in the phase 3 GEMINI-1 and GEMINI-2 trials to have virologic noninferiority and safety compared with three- or four-drug DTG plus tenofovir/emtricitabine (TDF/FTC) ART regimens in treatment-naive individuals, and, in the subsequent TANGO trial, the regimen was also noninferior versus tenofovir alafenamide–based regimens among treatment-experienced patients, at 144 weeks in both studies.
Trial details
The new SALSA trial, designed to broaden the comparison to treatment with any current three- or four-drug ART regimen, involved 493 patients at 120 study sites in 17 countries.
All patients were initially on a three- or four-drug regimen, with HIV-1 RNA of less than 50 c/mL for more than 6 months, and without prior virologic failure or nucleoside reverse transcriptase inhibitors or dolutegravir resistance-associated mutations.
The participants were randomized 1:1 to remain on their current regimen (n = 247) or to switch to the once-daily, fixed-dose tablet two-drug combination of dolutegravir 50 mg/lamivudine 300 mg (n = 246) for 52 weeks.
In addition to the noninferior virologic outcomes, there were no serious drug-related adverse events, no confirmed virologic withdrawals, and no resistance mutations in either group.
Of note, weight increase was higher in the DTG/3TC group (8%; n = 20) versus the current ART arm (2%; n = 5), as has been observed in previous studies. The adjusted mean change in weight from baseline to week 48 in the DTG arm was 2.1 kg versus 0.6 kg in the current ART arm.
Dr. Llibre pointed out that many of the participants who switched were discontinuing regimens such as TDF and efavirenz that are associated with weight loss, “so discontinuation could be more related to weight gain than the introduction of dolutegravir, but this deserves further study,” he noted.
There were no significant differences in changes in eGFR and fasting lipids, or in changes in inflammatory biomarkers between the groups.
Bone and renal biomarkers were more favorable in the dolutegravir two-drug arm, suggesting that bone and renal function was either maintained or even improved with the drug switch, Dr. Llibre noted.
Commenting on the research, Alexandra Calmy, PhD, of the HIV/AIDS Unit and LIPO & metabolism group, infectious disease division, Geneva University Hospitals, said that data on quality of life and patient satisfaction measures would be of particular interest.
“Indeed, it is not absolutely clear how a two-in-one versus a three-in-one pill may really influence treatment satisfaction and/or quality of life,” she said in an interview. “Validated scales and patient-reported outcomes with regards to treatment satisfaction would have been an added value to the study.”
Dr. Calmy coauthored a previous study looking at weight change and pharmacokinetic parameters in patients with HIV who switched to DTG-based regimens, and also found weight changes were increased with the DTG regimens. However, the weight gain was not associated with DTG plasma levels, thus supporting Dr. Llibre’s suggestion of possible withdrawal effects from other drugs.
STAT trial: Feasibility of two-drug DTG/3TC as first-line treatment
In further findings presented at the meeting on the STAT trial, researchers evaluated the feasibility not of switching to, but of initiating patients on, the two-drug DTG treatment as a first-line therapy, within 14 days of HIV-1 diagnosis.
The “test-and-treat” approach counters common belief that the regimen should be started only after the traditional three-drug regimens, because of the potential of transmitted resistance and baseline hepatitis B virus coinfection.
In the study of 131 patients, at week 48, 82% (107/131) of all participants and 97% (107/110) of those with available data achieved HIV-1 RNA levels of < 50 c/mL.
While two participants had confirmed virologic failure in the study, there were no treatment-emergent resistance-associated mutations, and neither patient discontinued the two-drug DTG treatment. There were low rates of drug-related adverse events (8%) and they were not serious.
“The STAT data is important as it shows us, for the first time, that in patients where potentially very little is known prior to treatment initiation, DTG/3TC can be very effectively used as a first-line regimen in a ‘test-and-treat’ approach without compromising on patient safety,” first author Charlotte-Paige Rolle, MD, director of research operations, Orlando (Fla.) Immunology Center, said in an interview.
Dr. Rolle added that “with careful monitoring of test results in the first weeks of therapy, we can appropriately and safely adjust therapy from DTG/3TC to a three-drug regimen if needed for patients that have transmitted drug resistance to DTG or 3TC, or hepatitis B coinfection, with both of these occurring at very low rates regardless.”
The SALSA and STAT studies received funding from ViiV Healthcare. Dr. Llibre has received honoraria or consultation fees from ViiV Healthcare, Gilead Sciences and Janssen-Cilag. Dr. Rolle has received grants from and served on advisory boards/speakers bureaus for ViiV Healthcare, Gilead, and Janssen. Dr. Calmy had no disclosures to report.
FROM IAS 2021
Necessary or not, COVID booster shots are probably on the horizon
The drug maker Pfizer recently announced that vaccinated people are likely to need a booster shot to be effectively protected against new variants of COVID-19 and that the company would apply for Food and Drug Administration emergency use authorization for the shot. Top government health officials immediately and emphatically announced that the booster isn’t needed right now – and held firm to that position even after Pfizer’s top scientist made his case and shared preliminary data with them on July 12.
This has led to confusion. Is the protection that has allowed them to see loved ones and go out to dinner fading?
Ultimately, the question of whether a booster is needed is unlikely to determine the FDA’s decision. If recent history is predictive, booster shots will be here before long. That’s because of the outdated, 60-year-old basic standard the FDA uses to authorize medicines for sale: Is a new drug “safe and effective?”
The FDA, using that standard, will very likely have to authorize Pfizer’s booster for emergency use, as it did the company’s prior COVID shot. The booster is likely to be safe – hundreds of millions have taken the earlier shots – and Pfizer reported that it dramatically increases a vaccinated person’s antibodies against SARS-CoV-2. From that perspective, it may also be considered very effective.
But does that kind of efficacy matter? Is a higher level of antibodies needed to protect vaccinated Americans? Though antibody levels may wane some over time, the current vaccines deliver perfectly good immunity so far.
What if a booster is safe and effective in one sense but simply not needed – at least for now?
Reliance on the simple “safe and effective” standard – which certainly sounds reasonable – is a relic of a time when there were far fewer and simpler medicines available to treat diseases and before pharmaceutical manufacturing became one of the world’s biggest businesses.
The FDA’s 1938 landmark legislation focused primarily on safety after more than 100 Americans died from a raspberry-flavored liquid form of an early antibiotic because one of its ingredients was used as antifreeze. The 1962 Kefauver-Harris Amendments to the Federal Food, Drug, and Cosmetic Act set out more specific requirements for drug approval: Companies must scientifically prove a drug’s effectiveness through “adequate and well-controlled studies.”
In today’s pharmaceutical universe, a simple “safe and effective” determination is not always an adequate bar, and it can be manipulated to sell drugs of questionable value. There’s also big money involved: Pfizer is already projecting $26 billion in COVID revenue in 2021.
The United States’ continued use of this standard to let drugs into the market has led to the approval of expensive, not necessarily very effective drugs. In 2014, for example, the FDA approved a toenail fungus drug that can cost up to $1,500 a month and that studies showed cured fewer than 10% of patients after a year of treatment. That’s more effective than doing nothing but less effective and more costly than a number of other treatments for this bothersome malady.
It has also led to a plethora of high-priced drugs to treat diseases like cancers, multiple sclerosis and type 2 diabetes that are all more effective than a placebo but have often not been tested very much against one another to determine which are most effective.
In today’s complex world, clarification is needed to determine just what kind of effectiveness the FDA should demand. And should that be the job of the FDA alone?
For example, should drugmakers prove a drug is significantly more effective than products already on the market? Or demonstrate cost-effectiveness – the health value of a product relative to its price – a metric used by Britain’s health system? And in which cases is effectiveness against a surrogate marker – like an antibody level – a good enough stand-in for whether a drug will have a significant impact on a patient’s health?
In most industrialized countries, broad access to the national market is a two-step process, said Aaron Kesselheim, a professor of medicine at Harvard Medical School, Boston, who studies drug development, marketing and law and recently served on an FDA advisory committee. The first part certifies that a drug is sufficiently safe and effective. That is immediately followed by an independent health technology assessment to see where it fits in the treatment armamentarium, including, in some countries, whether it is useful enough to be sold at all at the stated price. But there’s no such automatic process in the United States.
When Pfizer applies for authorization, the FDA may well clear a booster for the U.S. market. The Centers for Disease Control and Prevention, likely with advice from National Institutes of Health experts, will then have to decide whether to recommend it and for whom. This judgment call usually determines whether insurers will cover it. Pfizer is likely to profit handsomely from a government authorization, and the company will gain some revenue even if only the worried well, who can pay out of pocket, decide to get the shot.
To make any recommendation on a booster, government experts say they need more data. They could, for example, as Anthony S. Fauci, MD, has suggested, eventually green-light the additional vaccine shot only for a small group of patients at high risk for a deadly infection, such as the very old or transplant recipients who take immunosuppressant drugs, as some other countries have done.
But until the United States refines the FDA’s “safe and effective” standard or adds a second layer of vetting, when new products hit the market and manufacturers promote them, Americans will be left to decipher whose version of effective and necessary matters to them.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The drug maker Pfizer recently announced that vaccinated people are likely to need a booster shot to be effectively protected against new variants of COVID-19 and that the company would apply for Food and Drug Administration emergency use authorization for the shot. Top government health officials immediately and emphatically announced that the booster isn’t needed right now – and held firm to that position even after Pfizer’s top scientist made his case and shared preliminary data with them on July 12.
This has led to confusion. Is the protection that has allowed them to see loved ones and go out to dinner fading?
Ultimately, the question of whether a booster is needed is unlikely to determine the FDA’s decision. If recent history is predictive, booster shots will be here before long. That’s because of the outdated, 60-year-old basic standard the FDA uses to authorize medicines for sale: Is a new drug “safe and effective?”
The FDA, using that standard, will very likely have to authorize Pfizer’s booster for emergency use, as it did the company’s prior COVID shot. The booster is likely to be safe – hundreds of millions have taken the earlier shots – and Pfizer reported that it dramatically increases a vaccinated person’s antibodies against SARS-CoV-2. From that perspective, it may also be considered very effective.
But does that kind of efficacy matter? Is a higher level of antibodies needed to protect vaccinated Americans? Though antibody levels may wane some over time, the current vaccines deliver perfectly good immunity so far.
What if a booster is safe and effective in one sense but simply not needed – at least for now?
Reliance on the simple “safe and effective” standard – which certainly sounds reasonable – is a relic of a time when there were far fewer and simpler medicines available to treat diseases and before pharmaceutical manufacturing became one of the world’s biggest businesses.
The FDA’s 1938 landmark legislation focused primarily on safety after more than 100 Americans died from a raspberry-flavored liquid form of an early antibiotic because one of its ingredients was used as antifreeze. The 1962 Kefauver-Harris Amendments to the Federal Food, Drug, and Cosmetic Act set out more specific requirements for drug approval: Companies must scientifically prove a drug’s effectiveness through “adequate and well-controlled studies.”
In today’s pharmaceutical universe, a simple “safe and effective” determination is not always an adequate bar, and it can be manipulated to sell drugs of questionable value. There’s also big money involved: Pfizer is already projecting $26 billion in COVID revenue in 2021.
The United States’ continued use of this standard to let drugs into the market has led to the approval of expensive, not necessarily very effective drugs. In 2014, for example, the FDA approved a toenail fungus drug that can cost up to $1,500 a month and that studies showed cured fewer than 10% of patients after a year of treatment. That’s more effective than doing nothing but less effective and more costly than a number of other treatments for this bothersome malady.
It has also led to a plethora of high-priced drugs to treat diseases like cancers, multiple sclerosis and type 2 diabetes that are all more effective than a placebo but have often not been tested very much against one another to determine which are most effective.
In today’s complex world, clarification is needed to determine just what kind of effectiveness the FDA should demand. And should that be the job of the FDA alone?
For example, should drugmakers prove a drug is significantly more effective than products already on the market? Or demonstrate cost-effectiveness – the health value of a product relative to its price – a metric used by Britain’s health system? And in which cases is effectiveness against a surrogate marker – like an antibody level – a good enough stand-in for whether a drug will have a significant impact on a patient’s health?
In most industrialized countries, broad access to the national market is a two-step process, said Aaron Kesselheim, a professor of medicine at Harvard Medical School, Boston, who studies drug development, marketing and law and recently served on an FDA advisory committee. The first part certifies that a drug is sufficiently safe and effective. That is immediately followed by an independent health technology assessment to see where it fits in the treatment armamentarium, including, in some countries, whether it is useful enough to be sold at all at the stated price. But there’s no such automatic process in the United States.
When Pfizer applies for authorization, the FDA may well clear a booster for the U.S. market. The Centers for Disease Control and Prevention, likely with advice from National Institutes of Health experts, will then have to decide whether to recommend it and for whom. This judgment call usually determines whether insurers will cover it. Pfizer is likely to profit handsomely from a government authorization, and the company will gain some revenue even if only the worried well, who can pay out of pocket, decide to get the shot.
To make any recommendation on a booster, government experts say they need more data. They could, for example, as Anthony S. Fauci, MD, has suggested, eventually green-light the additional vaccine shot only for a small group of patients at high risk for a deadly infection, such as the very old or transplant recipients who take immunosuppressant drugs, as some other countries have done.
But until the United States refines the FDA’s “safe and effective” standard or adds a second layer of vetting, when new products hit the market and manufacturers promote them, Americans will be left to decipher whose version of effective and necessary matters to them.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
The drug maker Pfizer recently announced that vaccinated people are likely to need a booster shot to be effectively protected against new variants of COVID-19 and that the company would apply for Food and Drug Administration emergency use authorization for the shot. Top government health officials immediately and emphatically announced that the booster isn’t needed right now – and held firm to that position even after Pfizer’s top scientist made his case and shared preliminary data with them on July 12.
This has led to confusion. Is the protection that has allowed them to see loved ones and go out to dinner fading?
Ultimately, the question of whether a booster is needed is unlikely to determine the FDA’s decision. If recent history is predictive, booster shots will be here before long. That’s because of the outdated, 60-year-old basic standard the FDA uses to authorize medicines for sale: Is a new drug “safe and effective?”
The FDA, using that standard, will very likely have to authorize Pfizer’s booster for emergency use, as it did the company’s prior COVID shot. The booster is likely to be safe – hundreds of millions have taken the earlier shots – and Pfizer reported that it dramatically increases a vaccinated person’s antibodies against SARS-CoV-2. From that perspective, it may also be considered very effective.
But does that kind of efficacy matter? Is a higher level of antibodies needed to protect vaccinated Americans? Though antibody levels may wane some over time, the current vaccines deliver perfectly good immunity so far.
What if a booster is safe and effective in one sense but simply not needed – at least for now?
Reliance on the simple “safe and effective” standard – which certainly sounds reasonable – is a relic of a time when there were far fewer and simpler medicines available to treat diseases and before pharmaceutical manufacturing became one of the world’s biggest businesses.
The FDA’s 1938 landmark legislation focused primarily on safety after more than 100 Americans died from a raspberry-flavored liquid form of an early antibiotic because one of its ingredients was used as antifreeze. The 1962 Kefauver-Harris Amendments to the Federal Food, Drug, and Cosmetic Act set out more specific requirements for drug approval: Companies must scientifically prove a drug’s effectiveness through “adequate and well-controlled studies.”
In today’s pharmaceutical universe, a simple “safe and effective” determination is not always an adequate bar, and it can be manipulated to sell drugs of questionable value. There’s also big money involved: Pfizer is already projecting $26 billion in COVID revenue in 2021.
The United States’ continued use of this standard to let drugs into the market has led to the approval of expensive, not necessarily very effective drugs. In 2014, for example, the FDA approved a toenail fungus drug that can cost up to $1,500 a month and that studies showed cured fewer than 10% of patients after a year of treatment. That’s more effective than doing nothing but less effective and more costly than a number of other treatments for this bothersome malady.
It has also led to a plethora of high-priced drugs to treat diseases like cancers, multiple sclerosis and type 2 diabetes that are all more effective than a placebo but have often not been tested very much against one another to determine which are most effective.
In today’s complex world, clarification is needed to determine just what kind of effectiveness the FDA should demand. And should that be the job of the FDA alone?
For example, should drugmakers prove a drug is significantly more effective than products already on the market? Or demonstrate cost-effectiveness – the health value of a product relative to its price – a metric used by Britain’s health system? And in which cases is effectiveness against a surrogate marker – like an antibody level – a good enough stand-in for whether a drug will have a significant impact on a patient’s health?
In most industrialized countries, broad access to the national market is a two-step process, said Aaron Kesselheim, a professor of medicine at Harvard Medical School, Boston, who studies drug development, marketing and law and recently served on an FDA advisory committee. The first part certifies that a drug is sufficiently safe and effective. That is immediately followed by an independent health technology assessment to see where it fits in the treatment armamentarium, including, in some countries, whether it is useful enough to be sold at all at the stated price. But there’s no such automatic process in the United States.
When Pfizer applies for authorization, the FDA may well clear a booster for the U.S. market. The Centers for Disease Control and Prevention, likely with advice from National Institutes of Health experts, will then have to decide whether to recommend it and for whom. This judgment call usually determines whether insurers will cover it. Pfizer is likely to profit handsomely from a government authorization, and the company will gain some revenue even if only the worried well, who can pay out of pocket, decide to get the shot.
To make any recommendation on a booster, government experts say they need more data. They could, for example, as Anthony S. Fauci, MD, has suggested, eventually green-light the additional vaccine shot only for a small group of patients at high risk for a deadly infection, such as the very old or transplant recipients who take immunosuppressant drugs, as some other countries have done.
But until the United States refines the FDA’s “safe and effective” standard or adds a second layer of vetting, when new products hit the market and manufacturers promote them, Americans will be left to decipher whose version of effective and necessary matters to them.
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
HIV-associated cryptococcal meningitis: Single-dose regimen found non-inferior
A single high dose of the antifungal agent liposomal amphotericin B (L-AmB; AmBisome, Gilead Sciences), with a background regimen of flucytosine and fluconazole, is non-inferior and significantly safer in preventing mortality in HIV-associated cryptococcal meningitis than a conventional seven-day regimen that is the current standard of care, according to a new study.
“The results of this phase 3 [AMBITION-cm] trial make it clear that this approach is just as good as the current World Health Organization-recommended first-line treatment in preventing death,” first author David S. Lawrence, MD, AMBITION study lead clinician, of the London School of Hygiene and Tropical Medicine, United Kingdom, said in an interview.
“The fact that this was the largest ever trial [on HIV-associated cryptococcal meningitis] conducted to date… gives us a high level of confidence in these results,” he said of the study, which was presented at the virtual annual meeting of the International AIDS Society.
“We believe that this should become the WHO-recommended first-line regimen,” he emphasized.
In commenting on the study, Meg Doherty, MD, PhD, director of global HIV, hepatitis, and STI programs at WHO, agreed that a shorter regimen could be vital, particularly in settings with limited resources.
“The results from the AMBITION trial are important for low- and middle-income countries, where the cost and complexity of implementing the current standard seven-day course of L-ambisome or cryptococcal meningitis treatment can put this out of reach for many,” she told this news organization.
“Simplification that maintains the highest quality of care is an important component of the public health approach for HIV treatment and care,” she added.
Dr. Doherty could not comment on any possible changes to WHO recommendations, which are formulated by an independent guideline development group, but a spokesperson said that “WHO is preparing an updated review of the evidence for treating cryptococcal disease as a first step towards updating guidance.”
Conventional treatment toxicities
Cryptococcal meningitis is a leading cause of death in HIV, and the conventional treatment of amphotericin B deoxycholate, though less expensive than L-AmB, is more toxic, causing anemia, renal impairment, and electrolyte abnormalities, Dr. Lawrence explained
Having previously shown a single 10 mg/kg dose of L-AmB to be as effective as the longer regimen of 14 daily doses in terms of clearing cryptococcus from the cerebrospinal fluid, Dr. Lawrence and his colleagues conducted the phase 3 AMBITION-Cm trial to evaluate the effect on mortality, enrolling 844 patients in Botswana, Malawi, South Africa, Uganda, and Zimbabwe who were HIV-positive and had a first episode of cryptococcal meningitis.
Participants in the study were randomized to treatment either with single, high-dose L-AmB (10 mg/kg), combined with 14 days of flucytosine 100 mg/kg/day and fluconazole 1,200 mg/day or to a control group receiving 7 daily doses of AmB deoxycholate (1 mg/kg) plus 7 days of flucytosine 100 mg/kg/day, followed by 7 days of fluconazole 1,200 mg/day.
All patients were also provided with consolidation therapy of fluconazole 800 mg/day for eight weeks. Of the patients, 60.2% were male, their median age was 37, and their median CD4 count was 27 cells/mm3.
For the primary endpoint in the intention-to-treat analysis of 814 patients, the 10-week mortality rate in the single-dose L-AmB group was 24.82% (101 of 407) and 28.75% (117 of 407) in the control arm, for a difference (-3.93%) that was well within the pre-specified non-inferiority margin of 10%.
As expected, the safety measures were significantly improved with the single-dose of L-AmB: Rates of grade 3 or 4 adverse events within the initial 21 days of treatment in the single-dose L-AmB group were 50% versus 62.3% in the control group, and severe anemia occurred in just 13% of single-dose L-AmB participants, compared with 41% in the AmB deoxycholate control arm (both P < .001), Dr. Lawrence reported.
Furthermore, the average decline in hemoglobin over the first week was 0.3 g/dL in the single-dose L-AmB arm and 1.9 g/dL in the control arm, resulting in the need for more blood transfusions in the control arm (P < .001).
The impact on kidney function was also worse in the higher dose arm, with an average increase in creatinine over the first week of 20.2% in the L-AmB group versus 49.7% in the control group, while hypokalemia and thrombophlebitis were also more common with the higher dose group, Dr. Lawrence noted.
In the adjusted analysis, the single-dose L-AmB measures were in fact superior after adjusting for factors including research site, age, sex, baseline Glasgow Coma Scale, CD4 count, CSF cryptococcal colony-forming units/mL, antiretroviral therapy status, hemoglobin, and CSF opening pressure.
Mortality rate still high – but significantly reduced
The mortality rate of about 25% in the study after the treatment is still significantly higher than typically seen in high-income countries such as the United States, where HIV-associated cryptococcal meningitis is less common and associated with a mortality of roughly 10-15%, Dr. Lawrence noted.
The rate is nevertheless among the lowest mortality rates ever reported within a clinical trial conducted in resource-limited settings, he explained.
“These results are a step in the right direction and a significant improvement on the rates of 40% to 45% reported with two-week L-AmB-based regimens in African settings,” Dr. Lawrence underscored.
Higher cost — but potentially more cost-effective
With a higher cost than AmB deoxycholate, L-AmB’s utilization in resource-limited settings has been a challenge: A single vial of L-AmB ranges from $80 to $200, according to some reports, and while 14-day dosing requires as many as 42 vials of L-AmB, even a 7-day regimen still requires 21 vials.
In comparison, the single-dose L-AmB regimen only requires an average of 10 to 11 vials per patient, but the regimen’s higher safety could translate to far greater cost savings, Dr. Lawrence explained.
“While the AmBisome regimen is technically more expensive in terms of drugs, we expect it to be cost-effective or possibly cost-saving when taking into account that there is less toxicity, fewer blood tests, less transfusions, etc., and possibly shorter duration of hospital admission,” he said.
Cost, supply controversy: ‘Black fungus’-related demand
The drug’s cost — as well as supply issues — have meanwhile become even more of a problem as L-AmB has unexpectedly also become urgently needed in the treatment of mucormycosis in India and Nepal, where the otherwise rare fungal disease, commonly known as “black fungus,” has been increasingly affecting COVID-19 patients and survivors.
Gilead had previously announced in 2018 its intention to make L-AmB more widely available at a price of $16.25 per vial, but “implementation of this has been slow,” Dr. Lawrence said.
As a result, Gilead is facing heightened pressure to implement the lower prices – and also improve substantial supply issues, with Médecins Sans Frontières (Doctors Without Borders) and dozens of other global organizations issuing an open letter to Gilead and partner Viatris in June calling for immediate action to implement the lower price and improve supply of L-AmB.
In a company statement, Gilead responded, detailing its “commit[ment] to the non-profit pricing for the treatment of cryptococcal meningitis” and to efforts to improve the public health crisis in India.
For their part, Dr. Lawrence and his colleagues are working on producing more research on the issue.
“We hope that the conclusive results of the AMBITION trial will give a much needed push to implement this program,” he said.
“We are also currently completing the cost-effectiveness analysis of the study, which we hope will provide additional evidence to support widespread implementation of this regimen and highlight further the urgent need to broaden access to AmBisome and flucytosine,” he said.
The trial was supported by a grant through the European Developing Countries Clinical Trials Partnership (EDCTP), the Swedish International Development Cooperation Agency (SIDA) (TRIA2015-1092), and the Wellcome Trust / Medical Research Council (UK)/UKAID Joint Global Health Trials (MR/P006922/1. The AmBisome was donated by Gilead Sciences. Dr. Lawrence had no disclosures to report.
A single high dose of the antifungal agent liposomal amphotericin B (L-AmB; AmBisome, Gilead Sciences), with a background regimen of flucytosine and fluconazole, is non-inferior and significantly safer in preventing mortality in HIV-associated cryptococcal meningitis than a conventional seven-day regimen that is the current standard of care, according to a new study.
“The results of this phase 3 [AMBITION-cm] trial make it clear that this approach is just as good as the current World Health Organization-recommended first-line treatment in preventing death,” first author David S. Lawrence, MD, AMBITION study lead clinician, of the London School of Hygiene and Tropical Medicine, United Kingdom, said in an interview.
“The fact that this was the largest ever trial [on HIV-associated cryptococcal meningitis] conducted to date… gives us a high level of confidence in these results,” he said of the study, which was presented at the virtual annual meeting of the International AIDS Society.
“We believe that this should become the WHO-recommended first-line regimen,” he emphasized.
In commenting on the study, Meg Doherty, MD, PhD, director of global HIV, hepatitis, and STI programs at WHO, agreed that a shorter regimen could be vital, particularly in settings with limited resources.
“The results from the AMBITION trial are important for low- and middle-income countries, where the cost and complexity of implementing the current standard seven-day course of L-ambisome or cryptococcal meningitis treatment can put this out of reach for many,” she told this news organization.
“Simplification that maintains the highest quality of care is an important component of the public health approach for HIV treatment and care,” she added.
Dr. Doherty could not comment on any possible changes to WHO recommendations, which are formulated by an independent guideline development group, but a spokesperson said that “WHO is preparing an updated review of the evidence for treating cryptococcal disease as a first step towards updating guidance.”
Conventional treatment toxicities
Cryptococcal meningitis is a leading cause of death in HIV, and the conventional treatment of amphotericin B deoxycholate, though less expensive than L-AmB, is more toxic, causing anemia, renal impairment, and electrolyte abnormalities, Dr. Lawrence explained
Having previously shown a single 10 mg/kg dose of L-AmB to be as effective as the longer regimen of 14 daily doses in terms of clearing cryptococcus from the cerebrospinal fluid, Dr. Lawrence and his colleagues conducted the phase 3 AMBITION-Cm trial to evaluate the effect on mortality, enrolling 844 patients in Botswana, Malawi, South Africa, Uganda, and Zimbabwe who were HIV-positive and had a first episode of cryptococcal meningitis.
Participants in the study were randomized to treatment either with single, high-dose L-AmB (10 mg/kg), combined with 14 days of flucytosine 100 mg/kg/day and fluconazole 1,200 mg/day or to a control group receiving 7 daily doses of AmB deoxycholate (1 mg/kg) plus 7 days of flucytosine 100 mg/kg/day, followed by 7 days of fluconazole 1,200 mg/day.
All patients were also provided with consolidation therapy of fluconazole 800 mg/day for eight weeks. Of the patients, 60.2% were male, their median age was 37, and their median CD4 count was 27 cells/mm3.
For the primary endpoint in the intention-to-treat analysis of 814 patients, the 10-week mortality rate in the single-dose L-AmB group was 24.82% (101 of 407) and 28.75% (117 of 407) in the control arm, for a difference (-3.93%) that was well within the pre-specified non-inferiority margin of 10%.
As expected, the safety measures were significantly improved with the single-dose of L-AmB: Rates of grade 3 or 4 adverse events within the initial 21 days of treatment in the single-dose L-AmB group were 50% versus 62.3% in the control group, and severe anemia occurred in just 13% of single-dose L-AmB participants, compared with 41% in the AmB deoxycholate control arm (both P < .001), Dr. Lawrence reported.
Furthermore, the average decline in hemoglobin over the first week was 0.3 g/dL in the single-dose L-AmB arm and 1.9 g/dL in the control arm, resulting in the need for more blood transfusions in the control arm (P < .001).
The impact on kidney function was also worse in the higher dose arm, with an average increase in creatinine over the first week of 20.2% in the L-AmB group versus 49.7% in the control group, while hypokalemia and thrombophlebitis were also more common with the higher dose group, Dr. Lawrence noted.
In the adjusted analysis, the single-dose L-AmB measures were in fact superior after adjusting for factors including research site, age, sex, baseline Glasgow Coma Scale, CD4 count, CSF cryptococcal colony-forming units/mL, antiretroviral therapy status, hemoglobin, and CSF opening pressure.
Mortality rate still high – but significantly reduced
The mortality rate of about 25% in the study after the treatment is still significantly higher than typically seen in high-income countries such as the United States, where HIV-associated cryptococcal meningitis is less common and associated with a mortality of roughly 10-15%, Dr. Lawrence noted.
The rate is nevertheless among the lowest mortality rates ever reported within a clinical trial conducted in resource-limited settings, he explained.
“These results are a step in the right direction and a significant improvement on the rates of 40% to 45% reported with two-week L-AmB-based regimens in African settings,” Dr. Lawrence underscored.
Higher cost — but potentially more cost-effective
With a higher cost than AmB deoxycholate, L-AmB’s utilization in resource-limited settings has been a challenge: A single vial of L-AmB ranges from $80 to $200, according to some reports, and while 14-day dosing requires as many as 42 vials of L-AmB, even a 7-day regimen still requires 21 vials.
In comparison, the single-dose L-AmB regimen only requires an average of 10 to 11 vials per patient, but the regimen’s higher safety could translate to far greater cost savings, Dr. Lawrence explained.
“While the AmBisome regimen is technically more expensive in terms of drugs, we expect it to be cost-effective or possibly cost-saving when taking into account that there is less toxicity, fewer blood tests, less transfusions, etc., and possibly shorter duration of hospital admission,” he said.
Cost, supply controversy: ‘Black fungus’-related demand
The drug’s cost — as well as supply issues — have meanwhile become even more of a problem as L-AmB has unexpectedly also become urgently needed in the treatment of mucormycosis in India and Nepal, where the otherwise rare fungal disease, commonly known as “black fungus,” has been increasingly affecting COVID-19 patients and survivors.
Gilead had previously announced in 2018 its intention to make L-AmB more widely available at a price of $16.25 per vial, but “implementation of this has been slow,” Dr. Lawrence said.
As a result, Gilead is facing heightened pressure to implement the lower prices – and also improve substantial supply issues, with Médecins Sans Frontières (Doctors Without Borders) and dozens of other global organizations issuing an open letter to Gilead and partner Viatris in June calling for immediate action to implement the lower price and improve supply of L-AmB.
In a company statement, Gilead responded, detailing its “commit[ment] to the non-profit pricing for the treatment of cryptococcal meningitis” and to efforts to improve the public health crisis in India.
For their part, Dr. Lawrence and his colleagues are working on producing more research on the issue.
“We hope that the conclusive results of the AMBITION trial will give a much needed push to implement this program,” he said.
“We are also currently completing the cost-effectiveness analysis of the study, which we hope will provide additional evidence to support widespread implementation of this regimen and highlight further the urgent need to broaden access to AmBisome and flucytosine,” he said.
The trial was supported by a grant through the European Developing Countries Clinical Trials Partnership (EDCTP), the Swedish International Development Cooperation Agency (SIDA) (TRIA2015-1092), and the Wellcome Trust / Medical Research Council (UK)/UKAID Joint Global Health Trials (MR/P006922/1. The AmBisome was donated by Gilead Sciences. Dr. Lawrence had no disclosures to report.
A single high dose of the antifungal agent liposomal amphotericin B (L-AmB; AmBisome, Gilead Sciences), with a background regimen of flucytosine and fluconazole, is non-inferior and significantly safer in preventing mortality in HIV-associated cryptococcal meningitis than a conventional seven-day regimen that is the current standard of care, according to a new study.
“The results of this phase 3 [AMBITION-cm] trial make it clear that this approach is just as good as the current World Health Organization-recommended first-line treatment in preventing death,” first author David S. Lawrence, MD, AMBITION study lead clinician, of the London School of Hygiene and Tropical Medicine, United Kingdom, said in an interview.
“The fact that this was the largest ever trial [on HIV-associated cryptococcal meningitis] conducted to date… gives us a high level of confidence in these results,” he said of the study, which was presented at the virtual annual meeting of the International AIDS Society.
“We believe that this should become the WHO-recommended first-line regimen,” he emphasized.
In commenting on the study, Meg Doherty, MD, PhD, director of global HIV, hepatitis, and STI programs at WHO, agreed that a shorter regimen could be vital, particularly in settings with limited resources.
“The results from the AMBITION trial are important for low- and middle-income countries, where the cost and complexity of implementing the current standard seven-day course of L-ambisome or cryptococcal meningitis treatment can put this out of reach for many,” she told this news organization.
“Simplification that maintains the highest quality of care is an important component of the public health approach for HIV treatment and care,” she added.
Dr. Doherty could not comment on any possible changes to WHO recommendations, which are formulated by an independent guideline development group, but a spokesperson said that “WHO is preparing an updated review of the evidence for treating cryptococcal disease as a first step towards updating guidance.”
Conventional treatment toxicities
Cryptococcal meningitis is a leading cause of death in HIV, and the conventional treatment of amphotericin B deoxycholate, though less expensive than L-AmB, is more toxic, causing anemia, renal impairment, and electrolyte abnormalities, Dr. Lawrence explained
Having previously shown a single 10 mg/kg dose of L-AmB to be as effective as the longer regimen of 14 daily doses in terms of clearing cryptococcus from the cerebrospinal fluid, Dr. Lawrence and his colleagues conducted the phase 3 AMBITION-Cm trial to evaluate the effect on mortality, enrolling 844 patients in Botswana, Malawi, South Africa, Uganda, and Zimbabwe who were HIV-positive and had a first episode of cryptococcal meningitis.
Participants in the study were randomized to treatment either with single, high-dose L-AmB (10 mg/kg), combined with 14 days of flucytosine 100 mg/kg/day and fluconazole 1,200 mg/day or to a control group receiving 7 daily doses of AmB deoxycholate (1 mg/kg) plus 7 days of flucytosine 100 mg/kg/day, followed by 7 days of fluconazole 1,200 mg/day.
All patients were also provided with consolidation therapy of fluconazole 800 mg/day for eight weeks. Of the patients, 60.2% were male, their median age was 37, and their median CD4 count was 27 cells/mm3.
For the primary endpoint in the intention-to-treat analysis of 814 patients, the 10-week mortality rate in the single-dose L-AmB group was 24.82% (101 of 407) and 28.75% (117 of 407) in the control arm, for a difference (-3.93%) that was well within the pre-specified non-inferiority margin of 10%.
As expected, the safety measures were significantly improved with the single-dose of L-AmB: Rates of grade 3 or 4 adverse events within the initial 21 days of treatment in the single-dose L-AmB group were 50% versus 62.3% in the control group, and severe anemia occurred in just 13% of single-dose L-AmB participants, compared with 41% in the AmB deoxycholate control arm (both P < .001), Dr. Lawrence reported.
Furthermore, the average decline in hemoglobin over the first week was 0.3 g/dL in the single-dose L-AmB arm and 1.9 g/dL in the control arm, resulting in the need for more blood transfusions in the control arm (P < .001).
The impact on kidney function was also worse in the higher dose arm, with an average increase in creatinine over the first week of 20.2% in the L-AmB group versus 49.7% in the control group, while hypokalemia and thrombophlebitis were also more common with the higher dose group, Dr. Lawrence noted.
In the adjusted analysis, the single-dose L-AmB measures were in fact superior after adjusting for factors including research site, age, sex, baseline Glasgow Coma Scale, CD4 count, CSF cryptococcal colony-forming units/mL, antiretroviral therapy status, hemoglobin, and CSF opening pressure.
Mortality rate still high – but significantly reduced
The mortality rate of about 25% in the study after the treatment is still significantly higher than typically seen in high-income countries such as the United States, where HIV-associated cryptococcal meningitis is less common and associated with a mortality of roughly 10-15%, Dr. Lawrence noted.
The rate is nevertheless among the lowest mortality rates ever reported within a clinical trial conducted in resource-limited settings, he explained.
“These results are a step in the right direction and a significant improvement on the rates of 40% to 45% reported with two-week L-AmB-based regimens in African settings,” Dr. Lawrence underscored.
Higher cost — but potentially more cost-effective
With a higher cost than AmB deoxycholate, L-AmB’s utilization in resource-limited settings has been a challenge: A single vial of L-AmB ranges from $80 to $200, according to some reports, and while 14-day dosing requires as many as 42 vials of L-AmB, even a 7-day regimen still requires 21 vials.
In comparison, the single-dose L-AmB regimen only requires an average of 10 to 11 vials per patient, but the regimen’s higher safety could translate to far greater cost savings, Dr. Lawrence explained.
“While the AmBisome regimen is technically more expensive in terms of drugs, we expect it to be cost-effective or possibly cost-saving when taking into account that there is less toxicity, fewer blood tests, less transfusions, etc., and possibly shorter duration of hospital admission,” he said.
Cost, supply controversy: ‘Black fungus’-related demand
The drug’s cost — as well as supply issues — have meanwhile become even more of a problem as L-AmB has unexpectedly also become urgently needed in the treatment of mucormycosis in India and Nepal, where the otherwise rare fungal disease, commonly known as “black fungus,” has been increasingly affecting COVID-19 patients and survivors.
Gilead had previously announced in 2018 its intention to make L-AmB more widely available at a price of $16.25 per vial, but “implementation of this has been slow,” Dr. Lawrence said.
As a result, Gilead is facing heightened pressure to implement the lower prices – and also improve substantial supply issues, with Médecins Sans Frontières (Doctors Without Borders) and dozens of other global organizations issuing an open letter to Gilead and partner Viatris in June calling for immediate action to implement the lower price and improve supply of L-AmB.
In a company statement, Gilead responded, detailing its “commit[ment] to the non-profit pricing for the treatment of cryptococcal meningitis” and to efforts to improve the public health crisis in India.
For their part, Dr. Lawrence and his colleagues are working on producing more research on the issue.
“We hope that the conclusive results of the AMBITION trial will give a much needed push to implement this program,” he said.
“We are also currently completing the cost-effectiveness analysis of the study, which we hope will provide additional evidence to support widespread implementation of this regimen and highlight further the urgent need to broaden access to AmBisome and flucytosine,” he said.
The trial was supported by a grant through the European Developing Countries Clinical Trials Partnership (EDCTP), the Swedish International Development Cooperation Agency (SIDA) (TRIA2015-1092), and the Wellcome Trust / Medical Research Council (UK)/UKAID Joint Global Health Trials (MR/P006922/1. The AmBisome was donated by Gilead Sciences. Dr. Lawrence had no disclosures to report.
REPORTING FROM IAS 2021
‘Wild West’ and weak evidence for weight-loss supplements
“Purported” weight-loss products –12 dietary supplements and 2 alternative therapies – lack high-quality evidence to back up claims of efficacy, a systematic review by the Obesity Society reports.
Most of the more than 300 published randomized controlled trials in the review were small and short, and only 0.5% found a statistically significant weight loss of up to 5 kg, John A. Batsis, MD, from the University of North Carolina at Chapel Hill, and colleagues reported in the journal Obesity.
“Despite the poor quality of these studies with high degrees of bias, most still failed to show efficacy of the product they were testing,” Srividya Kidambi, MD, from the Medical College of Wisconsin, Milwaukee, and colleagues from the Obesity Society’s Clinical Committee pointed out in an accompanying commentary.
“Yet these are the studies that are often used to support manufacturers’ claims of ‘clinically proven’ in their marketing,” they noted.
Most consumers, they continued, are unaware that these nondrug weight-loss products are not regulated by the Food and Drug Administration, but rather, if their ingredients are “generally regarded as safe,” they are treated as dietary supplements and require little or no testing to show either efficacy or safety.
“Our patients need to become aware that dietary supplements for weight loss are nothing more than a pipe dream, and as clinicians we would do well to talk with our patients and help steer them toward science-based treatments rather than the ‘Wild West’ of dietary supplements that are marketed for weight loss,” Scott Kahan, MD, MPH, coauthor of the review and commentary, told this news organization.
The dietary supplement industry has a strong lobby against legislation for more rigorous requirements for claims, noted Dr. Kahan, of the National Center for Weight and Wellness as well as George Washington University, Washington.
However, “there has to be some level of protection for consumers” who are faced with ads by “healthy skinny people saying this [product] can change your life.”
Clinical providers need to guide patients to “evidence-based interventions to support weight loss such as behavioral weight-loss interventions, [FDA-approved] medications, or bariatric surgery,” said Dr. Batsis, who also coauthored the commentary.
There is a “critical need” for more rigorous trials, and a partnership between researchers, funders, and industry, he added.
According to Dr. Kidambi and colleagues, “the use of these products will continue as long as they are allowed to be marketed with the aforementioned limited federal oversight and there is a lack of access to evidence-based obesity treatments.”
The commentary authors “call on regulatory authorities to critically examine the dietary supplement industry, including their role in promoting misleading claims and marketing products that have the potential to harm patients.”
They also urged public and private health insurance plans to “provide adequate resources for obesity management.”
And clinicians should “consider the lack of evidence for non–FDA-approved dietary supplements and therapies and guide their patients toward tested weight-management approaches.”
Subpar evidence, booming industry
“Annual sales of dietary supplements for weight loss are booming with an industry valued at $30 billion worldwide, despite subpar evidence” of efficacy, the commentary authors wrote by way of background.
After the Dietary Supplement Health and Education Act of 1994, the National Institutes of Health’s Office of Dietary Supplements was established “to strengthen the knowledge and understanding of dietary supplements by evaluating scientific information, stimulating and supporting research, and educating the public,” they explained.
However, dietary supplements and alternative therapies are endorsed by influencers and celebrities and marketed as a panacea for obesity and weight gain.
Literature review finds scant evidence
Consumers may believe that the “clinically proven” claims of efficacy of these “natural” weight-loss treatments have been thoroughly evaluated for safety and efficacy by the FDA, and clinicians lack information to counsel patients about this.
Therefore, although the Office of Dietary Supplements’ work has importantly advanced the science, the review authors wrote, members of the Obesity Society believed it was important to evaluate and perform a qualitative synthesis of the evidence for efficacy of non–FDA-regulated weight-loss supplements and alternative therapies to better inform clinicians and consumers.
From more than 20,000 citations of 53 dietary supplements and alternative therapies promoted for weight loss, the researchers identified 314 randomized controlled trials of 14 products that each had at least 5 randomized controlled trials.
The two types of alternative therapies in the review were mind-body interventions – which included behavioral therapies (for example, mindfulness and stress management), hypnosis, meditation, or massage – and acupuncture.
Several popular and widely used products (for example, human chorionic gonadotropin, raspberry ketones, nicotinamide adenine dinucleotide, vitamin infusions) did not meet the predefined number of published randomized controlled trials to be eligible for inclusion in the review.
The greatest number of trials were for acupuncture (45 trials), green tea (38), conjugated linoleic acid (31), ephedra with or without caffeine (31), mind-body therapies (22), and calcium and vitamin D (22). There were fewer trials of garcinia and/or hydroxycitrate (15), chitosan (9), phaseolus (7), pyruvate (7), chocolate/cocoa (6), chromium (6), guar gum (5), and phenylpropylamine (5).
Of the 314 studies, only 52 studies (16.5%) demonstrated that the products were efficacious and low risk, and only 16 studies (0.5%) reported a statistically significant between-group weight loss (0.3-4.93 kg).
For more information, in addition to their review and commentary, the authors refer clinicians to a dietary supplement label database.
The study was supported in part by grants from the National Institute on Aging. Dr. Batsis reported equity in SynchroHealth. Dr. Kidambi reported being the medical director for TOPS Center for Metabolic Health at the Medical College of Wisconsin, which is supported by TOPS. Dr. Kahan reported serving as a consultant for Novo Nordisk, Vivus, Gelesis, and Pfizer.
“Purported” weight-loss products –12 dietary supplements and 2 alternative therapies – lack high-quality evidence to back up claims of efficacy, a systematic review by the Obesity Society reports.
Most of the more than 300 published randomized controlled trials in the review were small and short, and only 0.5% found a statistically significant weight loss of up to 5 kg, John A. Batsis, MD, from the University of North Carolina at Chapel Hill, and colleagues reported in the journal Obesity.
“Despite the poor quality of these studies with high degrees of bias, most still failed to show efficacy of the product they were testing,” Srividya Kidambi, MD, from the Medical College of Wisconsin, Milwaukee, and colleagues from the Obesity Society’s Clinical Committee pointed out in an accompanying commentary.
“Yet these are the studies that are often used to support manufacturers’ claims of ‘clinically proven’ in their marketing,” they noted.
Most consumers, they continued, are unaware that these nondrug weight-loss products are not regulated by the Food and Drug Administration, but rather, if their ingredients are “generally regarded as safe,” they are treated as dietary supplements and require little or no testing to show either efficacy or safety.
“Our patients need to become aware that dietary supplements for weight loss are nothing more than a pipe dream, and as clinicians we would do well to talk with our patients and help steer them toward science-based treatments rather than the ‘Wild West’ of dietary supplements that are marketed for weight loss,” Scott Kahan, MD, MPH, coauthor of the review and commentary, told this news organization.
The dietary supplement industry has a strong lobby against legislation for more rigorous requirements for claims, noted Dr. Kahan, of the National Center for Weight and Wellness as well as George Washington University, Washington.
However, “there has to be some level of protection for consumers” who are faced with ads by “healthy skinny people saying this [product] can change your life.”
Clinical providers need to guide patients to “evidence-based interventions to support weight loss such as behavioral weight-loss interventions, [FDA-approved] medications, or bariatric surgery,” said Dr. Batsis, who also coauthored the commentary.
There is a “critical need” for more rigorous trials, and a partnership between researchers, funders, and industry, he added.
According to Dr. Kidambi and colleagues, “the use of these products will continue as long as they are allowed to be marketed with the aforementioned limited federal oversight and there is a lack of access to evidence-based obesity treatments.”
The commentary authors “call on regulatory authorities to critically examine the dietary supplement industry, including their role in promoting misleading claims and marketing products that have the potential to harm patients.”
They also urged public and private health insurance plans to “provide adequate resources for obesity management.”
And clinicians should “consider the lack of evidence for non–FDA-approved dietary supplements and therapies and guide their patients toward tested weight-management approaches.”
Subpar evidence, booming industry
“Annual sales of dietary supplements for weight loss are booming with an industry valued at $30 billion worldwide, despite subpar evidence” of efficacy, the commentary authors wrote by way of background.
After the Dietary Supplement Health and Education Act of 1994, the National Institutes of Health’s Office of Dietary Supplements was established “to strengthen the knowledge and understanding of dietary supplements by evaluating scientific information, stimulating and supporting research, and educating the public,” they explained.
However, dietary supplements and alternative therapies are endorsed by influencers and celebrities and marketed as a panacea for obesity and weight gain.
Literature review finds scant evidence
Consumers may believe that the “clinically proven” claims of efficacy of these “natural” weight-loss treatments have been thoroughly evaluated for safety and efficacy by the FDA, and clinicians lack information to counsel patients about this.
Therefore, although the Office of Dietary Supplements’ work has importantly advanced the science, the review authors wrote, members of the Obesity Society believed it was important to evaluate and perform a qualitative synthesis of the evidence for efficacy of non–FDA-regulated weight-loss supplements and alternative therapies to better inform clinicians and consumers.
From more than 20,000 citations of 53 dietary supplements and alternative therapies promoted for weight loss, the researchers identified 314 randomized controlled trials of 14 products that each had at least 5 randomized controlled trials.
The two types of alternative therapies in the review were mind-body interventions – which included behavioral therapies (for example, mindfulness and stress management), hypnosis, meditation, or massage – and acupuncture.
Several popular and widely used products (for example, human chorionic gonadotropin, raspberry ketones, nicotinamide adenine dinucleotide, vitamin infusions) did not meet the predefined number of published randomized controlled trials to be eligible for inclusion in the review.
The greatest number of trials were for acupuncture (45 trials), green tea (38), conjugated linoleic acid (31), ephedra with or without caffeine (31), mind-body therapies (22), and calcium and vitamin D (22). There were fewer trials of garcinia and/or hydroxycitrate (15), chitosan (9), phaseolus (7), pyruvate (7), chocolate/cocoa (6), chromium (6), guar gum (5), and phenylpropylamine (5).
Of the 314 studies, only 52 studies (16.5%) demonstrated that the products were efficacious and low risk, and only 16 studies (0.5%) reported a statistically significant between-group weight loss (0.3-4.93 kg).
For more information, in addition to their review and commentary, the authors refer clinicians to a dietary supplement label database.
The study was supported in part by grants from the National Institute on Aging. Dr. Batsis reported equity in SynchroHealth. Dr. Kidambi reported being the medical director for TOPS Center for Metabolic Health at the Medical College of Wisconsin, which is supported by TOPS. Dr. Kahan reported serving as a consultant for Novo Nordisk, Vivus, Gelesis, and Pfizer.
“Purported” weight-loss products –12 dietary supplements and 2 alternative therapies – lack high-quality evidence to back up claims of efficacy, a systematic review by the Obesity Society reports.
Most of the more than 300 published randomized controlled trials in the review were small and short, and only 0.5% found a statistically significant weight loss of up to 5 kg, John A. Batsis, MD, from the University of North Carolina at Chapel Hill, and colleagues reported in the journal Obesity.
“Despite the poor quality of these studies with high degrees of bias, most still failed to show efficacy of the product they were testing,” Srividya Kidambi, MD, from the Medical College of Wisconsin, Milwaukee, and colleagues from the Obesity Society’s Clinical Committee pointed out in an accompanying commentary.
“Yet these are the studies that are often used to support manufacturers’ claims of ‘clinically proven’ in their marketing,” they noted.
Most consumers, they continued, are unaware that these nondrug weight-loss products are not regulated by the Food and Drug Administration, but rather, if their ingredients are “generally regarded as safe,” they are treated as dietary supplements and require little or no testing to show either efficacy or safety.
“Our patients need to become aware that dietary supplements for weight loss are nothing more than a pipe dream, and as clinicians we would do well to talk with our patients and help steer them toward science-based treatments rather than the ‘Wild West’ of dietary supplements that are marketed for weight loss,” Scott Kahan, MD, MPH, coauthor of the review and commentary, told this news organization.
The dietary supplement industry has a strong lobby against legislation for more rigorous requirements for claims, noted Dr. Kahan, of the National Center for Weight and Wellness as well as George Washington University, Washington.
However, “there has to be some level of protection for consumers” who are faced with ads by “healthy skinny people saying this [product] can change your life.”
Clinical providers need to guide patients to “evidence-based interventions to support weight loss such as behavioral weight-loss interventions, [FDA-approved] medications, or bariatric surgery,” said Dr. Batsis, who also coauthored the commentary.
There is a “critical need” for more rigorous trials, and a partnership between researchers, funders, and industry, he added.
According to Dr. Kidambi and colleagues, “the use of these products will continue as long as they are allowed to be marketed with the aforementioned limited federal oversight and there is a lack of access to evidence-based obesity treatments.”
The commentary authors “call on regulatory authorities to critically examine the dietary supplement industry, including their role in promoting misleading claims and marketing products that have the potential to harm patients.”
They also urged public and private health insurance plans to “provide adequate resources for obesity management.”
And clinicians should “consider the lack of evidence for non–FDA-approved dietary supplements and therapies and guide their patients toward tested weight-management approaches.”
Subpar evidence, booming industry
“Annual sales of dietary supplements for weight loss are booming with an industry valued at $30 billion worldwide, despite subpar evidence” of efficacy, the commentary authors wrote by way of background.
After the Dietary Supplement Health and Education Act of 1994, the National Institutes of Health’s Office of Dietary Supplements was established “to strengthen the knowledge and understanding of dietary supplements by evaluating scientific information, stimulating and supporting research, and educating the public,” they explained.
However, dietary supplements and alternative therapies are endorsed by influencers and celebrities and marketed as a panacea for obesity and weight gain.
Literature review finds scant evidence
Consumers may believe that the “clinically proven” claims of efficacy of these “natural” weight-loss treatments have been thoroughly evaluated for safety and efficacy by the FDA, and clinicians lack information to counsel patients about this.
Therefore, although the Office of Dietary Supplements’ work has importantly advanced the science, the review authors wrote, members of the Obesity Society believed it was important to evaluate and perform a qualitative synthesis of the evidence for efficacy of non–FDA-regulated weight-loss supplements and alternative therapies to better inform clinicians and consumers.
From more than 20,000 citations of 53 dietary supplements and alternative therapies promoted for weight loss, the researchers identified 314 randomized controlled trials of 14 products that each had at least 5 randomized controlled trials.
The two types of alternative therapies in the review were mind-body interventions – which included behavioral therapies (for example, mindfulness and stress management), hypnosis, meditation, or massage – and acupuncture.
Several popular and widely used products (for example, human chorionic gonadotropin, raspberry ketones, nicotinamide adenine dinucleotide, vitamin infusions) did not meet the predefined number of published randomized controlled trials to be eligible for inclusion in the review.
The greatest number of trials were for acupuncture (45 trials), green tea (38), conjugated linoleic acid (31), ephedra with or without caffeine (31), mind-body therapies (22), and calcium and vitamin D (22). There were fewer trials of garcinia and/or hydroxycitrate (15), chitosan (9), phaseolus (7), pyruvate (7), chocolate/cocoa (6), chromium (6), guar gum (5), and phenylpropylamine (5).
Of the 314 studies, only 52 studies (16.5%) demonstrated that the products were efficacious and low risk, and only 16 studies (0.5%) reported a statistically significant between-group weight loss (0.3-4.93 kg).
For more information, in addition to their review and commentary, the authors refer clinicians to a dietary supplement label database.
The study was supported in part by grants from the National Institute on Aging. Dr. Batsis reported equity in SynchroHealth. Dr. Kidambi reported being the medical director for TOPS Center for Metabolic Health at the Medical College of Wisconsin, which is supported by TOPS. Dr. Kahan reported serving as a consultant for Novo Nordisk, Vivus, Gelesis, and Pfizer.
FROM OBESITY
FDA OKs spinal cord stimulation for diabetic neuropathy pain
The Food and Drug Administration has approved the first high-frequency spinal cord stimulation (SCS) therapy for treating painful diabetic neuropathy (PDN).
The approval is specific for the treatment of chronic pain associated with PDN using the Nevro’s Senza System with 10 kHz stimulation. It is intended for patients whose pain is refractory to, or who can’t tolerate, conventional medical treatment. According to the company, there are currently about 2.3 million individuals with refractory PDN in the United States.
The 10 kHz device, called HFX, involves minimally invasive epidural implantation of the stimulator device, which delivers mild electrical impulses to the nerves to interrupt pain signal to the brain. Such spinal cord stimulation “is a straightforward, well-established treatment for chronic pain that’s been used for over 30 years,” according to the company, although this is the first approval of the modality specifically for PDN.
Asked to comment, Rodica Pop-Busui MD, PhD, the Larry D. Soderquist Professor in Diabetes at the University of Michigan, Ann Arbor, said that “the approval of the Nevro 10kHz high-frequency spinal cord stimulation to treat pain associated with diabetic neuropathy has the potential for benefit for many patients with diabetes and painful diabetic peripheral neuropathy.”
She noted that, “although there are several other pharmacological agents that currently carry the FDA approval for PDN, this is a condition that is notoriously difficult to treat, particularly when taking into account the actual number needed to treat with a specific agent to achieve a clinically meaningful pain reduction, as well as the spectrum of side effects and drug-drug interactions in a patient population that require many other additional agents to manage diabetes and comorbidities on a daily basis. Thus, this new therapeutic approach besides effective pain reduction has the additional benefit of bypassing drug interactions.” Dr. Pop-Busui was the lead author on the American Diabetes Association’s 2017 position statement on diabetic neuropathy.
She also cautioned, on the other hand, that “it is not very clear yet how easy it will be for all eligible patients to have access to this technology, what will be the actual costs, the insurance coverage, or the acceptance by patients across various sociodemographic backgrounds from the at-large clinical care. However, given the challenges we encounter to treat diabetic neuropathy and particularly the pain associated with it, it is quite encouraging to see that the tools available to help our patients are now broader.”
Both 6-and 12-month results show benefit
The FDA approval was based on 6-month data from a prospective, multicenter, open-label randomized clinical trial published in JAMA Neurology.
Use of the 10-kHz SCS device was compared with conventional treatment alone in 216 patients with PDN refractory to gabapentinoids and at least one other analgesic class and lower limb pain intensity of 5 cm or more on a 10-cm visual analog scale.
The primary endpoint, percentage of participants reporting 50% pain relief or more without worsening of baseline neurologic deficits at 3 months, was met by 5 of 94 (5%) patients in the conventional group, compared with 75 of 95 (79%) with the 10-kHz SCS plus conventional treatment (P < .001).
Infections requiring device explant occurred in two patients in the 10-kHz SCS group (2%).
At 12 months, those in the original SCS group plus 86% of subjects given the option to cross over from the conventional treatment group showed “clear and sustained” benefits of the 10-kHz SCS with regard to lower-limb pain, pain interference with daily living, sleep quality, and activity, Erika Petersen, MD, director of the section of functional and restorative neurosurgery at the University of Arkansas for Medical Sciences, Little Rock , reported at the 2021 annual scientific sessions of the ADA.
Infection was the most common study-related adverse event, affecting 8 of 154 patients with the SCS implants (5.2%). Three resolved with conservative treatment and five (3.2%) required removal of the device.
The patients will be followed for a total of 24 months.
Commercial launch of HFX in the United States will begin immediately, the company said.
Dr. Pop-Busui has received consultant fees in the last 12 months from Averitas Pharma, Boehringer Ingelheim, Nevro, and Novo Nordisk. Dr. Petersen has financial relationships with Nevro, Medtronic, and several other neuromodulator makers.
The Food and Drug Administration has approved the first high-frequency spinal cord stimulation (SCS) therapy for treating painful diabetic neuropathy (PDN).
The approval is specific for the treatment of chronic pain associated with PDN using the Nevro’s Senza System with 10 kHz stimulation. It is intended for patients whose pain is refractory to, or who can’t tolerate, conventional medical treatment. According to the company, there are currently about 2.3 million individuals with refractory PDN in the United States.
The 10 kHz device, called HFX, involves minimally invasive epidural implantation of the stimulator device, which delivers mild electrical impulses to the nerves to interrupt pain signal to the brain. Such spinal cord stimulation “is a straightforward, well-established treatment for chronic pain that’s been used for over 30 years,” according to the company, although this is the first approval of the modality specifically for PDN.
Asked to comment, Rodica Pop-Busui MD, PhD, the Larry D. Soderquist Professor in Diabetes at the University of Michigan, Ann Arbor, said that “the approval of the Nevro 10kHz high-frequency spinal cord stimulation to treat pain associated with diabetic neuropathy has the potential for benefit for many patients with diabetes and painful diabetic peripheral neuropathy.”
She noted that, “although there are several other pharmacological agents that currently carry the FDA approval for PDN, this is a condition that is notoriously difficult to treat, particularly when taking into account the actual number needed to treat with a specific agent to achieve a clinically meaningful pain reduction, as well as the spectrum of side effects and drug-drug interactions in a patient population that require many other additional agents to manage diabetes and comorbidities on a daily basis. Thus, this new therapeutic approach besides effective pain reduction has the additional benefit of bypassing drug interactions.” Dr. Pop-Busui was the lead author on the American Diabetes Association’s 2017 position statement on diabetic neuropathy.
She also cautioned, on the other hand, that “it is not very clear yet how easy it will be for all eligible patients to have access to this technology, what will be the actual costs, the insurance coverage, or the acceptance by patients across various sociodemographic backgrounds from the at-large clinical care. However, given the challenges we encounter to treat diabetic neuropathy and particularly the pain associated with it, it is quite encouraging to see that the tools available to help our patients are now broader.”
Both 6-and 12-month results show benefit
The FDA approval was based on 6-month data from a prospective, multicenter, open-label randomized clinical trial published in JAMA Neurology.
Use of the 10-kHz SCS device was compared with conventional treatment alone in 216 patients with PDN refractory to gabapentinoids and at least one other analgesic class and lower limb pain intensity of 5 cm or more on a 10-cm visual analog scale.
The primary endpoint, percentage of participants reporting 50% pain relief or more without worsening of baseline neurologic deficits at 3 months, was met by 5 of 94 (5%) patients in the conventional group, compared with 75 of 95 (79%) with the 10-kHz SCS plus conventional treatment (P < .001).
Infections requiring device explant occurred in two patients in the 10-kHz SCS group (2%).
At 12 months, those in the original SCS group plus 86% of subjects given the option to cross over from the conventional treatment group showed “clear and sustained” benefits of the 10-kHz SCS with regard to lower-limb pain, pain interference with daily living, sleep quality, and activity, Erika Petersen, MD, director of the section of functional and restorative neurosurgery at the University of Arkansas for Medical Sciences, Little Rock , reported at the 2021 annual scientific sessions of the ADA.
Infection was the most common study-related adverse event, affecting 8 of 154 patients with the SCS implants (5.2%). Three resolved with conservative treatment and five (3.2%) required removal of the device.
The patients will be followed for a total of 24 months.
Commercial launch of HFX in the United States will begin immediately, the company said.
Dr. Pop-Busui has received consultant fees in the last 12 months from Averitas Pharma, Boehringer Ingelheim, Nevro, and Novo Nordisk. Dr. Petersen has financial relationships with Nevro, Medtronic, and several other neuromodulator makers.
The Food and Drug Administration has approved the first high-frequency spinal cord stimulation (SCS) therapy for treating painful diabetic neuropathy (PDN).
The approval is specific for the treatment of chronic pain associated with PDN using the Nevro’s Senza System with 10 kHz stimulation. It is intended for patients whose pain is refractory to, or who can’t tolerate, conventional medical treatment. According to the company, there are currently about 2.3 million individuals with refractory PDN in the United States.
The 10 kHz device, called HFX, involves minimally invasive epidural implantation of the stimulator device, which delivers mild electrical impulses to the nerves to interrupt pain signal to the brain. Such spinal cord stimulation “is a straightforward, well-established treatment for chronic pain that’s been used for over 30 years,” according to the company, although this is the first approval of the modality specifically for PDN.
Asked to comment, Rodica Pop-Busui MD, PhD, the Larry D. Soderquist Professor in Diabetes at the University of Michigan, Ann Arbor, said that “the approval of the Nevro 10kHz high-frequency spinal cord stimulation to treat pain associated with diabetic neuropathy has the potential for benefit for many patients with diabetes and painful diabetic peripheral neuropathy.”
She noted that, “although there are several other pharmacological agents that currently carry the FDA approval for PDN, this is a condition that is notoriously difficult to treat, particularly when taking into account the actual number needed to treat with a specific agent to achieve a clinically meaningful pain reduction, as well as the spectrum of side effects and drug-drug interactions in a patient population that require many other additional agents to manage diabetes and comorbidities on a daily basis. Thus, this new therapeutic approach besides effective pain reduction has the additional benefit of bypassing drug interactions.” Dr. Pop-Busui was the lead author on the American Diabetes Association’s 2017 position statement on diabetic neuropathy.
She also cautioned, on the other hand, that “it is not very clear yet how easy it will be for all eligible patients to have access to this technology, what will be the actual costs, the insurance coverage, or the acceptance by patients across various sociodemographic backgrounds from the at-large clinical care. However, given the challenges we encounter to treat diabetic neuropathy and particularly the pain associated with it, it is quite encouraging to see that the tools available to help our patients are now broader.”
Both 6-and 12-month results show benefit
The FDA approval was based on 6-month data from a prospective, multicenter, open-label randomized clinical trial published in JAMA Neurology.
Use of the 10-kHz SCS device was compared with conventional treatment alone in 216 patients with PDN refractory to gabapentinoids and at least one other analgesic class and lower limb pain intensity of 5 cm or more on a 10-cm visual analog scale.
The primary endpoint, percentage of participants reporting 50% pain relief or more without worsening of baseline neurologic deficits at 3 months, was met by 5 of 94 (5%) patients in the conventional group, compared with 75 of 95 (79%) with the 10-kHz SCS plus conventional treatment (P < .001).
Infections requiring device explant occurred in two patients in the 10-kHz SCS group (2%).
At 12 months, those in the original SCS group plus 86% of subjects given the option to cross over from the conventional treatment group showed “clear and sustained” benefits of the 10-kHz SCS with regard to lower-limb pain, pain interference with daily living, sleep quality, and activity, Erika Petersen, MD, director of the section of functional and restorative neurosurgery at the University of Arkansas for Medical Sciences, Little Rock , reported at the 2021 annual scientific sessions of the ADA.
Infection was the most common study-related adverse event, affecting 8 of 154 patients with the SCS implants (5.2%). Three resolved with conservative treatment and five (3.2%) required removal of the device.
The patients will be followed for a total of 24 months.
Commercial launch of HFX in the United States will begin immediately, the company said.
Dr. Pop-Busui has received consultant fees in the last 12 months from Averitas Pharma, Boehringer Ingelheim, Nevro, and Novo Nordisk. Dr. Petersen has financial relationships with Nevro, Medtronic, and several other neuromodulator makers.
Twice-a-year lenacapavir shows viral suppression in drug-resistant HIV at 26 weeks
With regulatory approval, lenacapavir could become the only HIV-1 treatment option given every 6 months.
“These data support the use of lenacapavir in patients with multidrug-resistant viruses, and according to its long half-life of two subcutaneous injections per year, [it] could help reduce pill burden,” first author Jean-Michel Molina, MD, PhD, professor of infectious diseases and head of the infectious diseases department at the Saint-Louis and Lariboisière Hospitals, Paris, said in an interview.
Presenting the updated findings from the phase 2/3 CAPELLA trial at the virtual annual meeting of the International AIDS Society conference, Dr. Molina underscored the need for longer-term treatments.
“These patients with multidrug resistances are usually those who have not been fully adherent to their regimen,” he said. “Being able to provide the drug, given every 6 months subcutaneously, provides an ideal treatment for overcoming resistance and lack of adherence.”
The study showed that, after 26 weeks, 81% of heavily treatment-experienced people with HIV in a randomized cohort who were treated with a subcutaneous injection of lenacapavir (927 mg) combined with an optimized background antiretroviral regimen achieved sustained virologic suppression, with an undetectable viral load (<50 copies/mL).
In addition, the lenacapavir-treated patients had a clinically meaningful mean increase in CD4 counts of 81 cells/mcL over the 26 weeks.
The drug was well tolerated, with no drug-related serious adverse events or adverse events leading to discontinuation. The most common adverse events were injection-site reactions, which occurred in 56% of participants, with most being mild or moderate.
Importantly, four participants developed emergent resistances to lenacapavir. One was suppressed with a change in the background regimen and two others were suppressed without a change in regimen.
“We know that these mutations affect viral fitness,” Dr. Molina said in an interview. “We need more studies to assess the real impact of these mutations.”
Dr. Molina noted that a phase 2 study is already underway to evaluate how a pairing of lenacapavir with fellow investigational long-acting drug islatravir (Merck) could offset the risk of developing resistances.
Asked by an audience member whether a two-drug regimen with something like islatravir is likely to successfully prevent resistances, Dr. Molina responded that “it’s too early to know what’s going to happen with [combinations], but these first results are really encouraging when you see the very high rate of being fully suppressed after 26 weeks. The efficacy that we’ve seen after [a previous 2-week analysis] is long lasting.”
Lenacapavir targets multiple viral stages
Unlike other antiviral drugs that target just a single stage of viral replication, lenacapavir takes aim at multiple steps in the viral life cycle, including capsid-mediated uptake of HIV-1 proviral DNA, virus assembly and release, and capsid core formation, Dr. Molina explained.
The CAPELLA trial included participants at research centers in North America, Europe, and Asia, with a median age of 52 years; 25% were female, 38% were Black, and their mean HIV-1 RNA (viral load) was 4.17 log copies/mL.
Overall, 72 patients were divided into two cohorts of 36 patients each, including a randomized and nonrandomized cohort. Dr. Molina primarily reported results from the randomized group.
In that group, patients received either a lead-in of oral lenacapavir (600 mg on day 1 and 2 and 300 mg on day 8) or placebo, in combination with patients’ current failing drug regimens in both groups.
At day 15, all participants were switched to the investigator-selected, optimized background treatment regimen, tailored according to patients’ drug-resistance profiles, and those in the lenacapavir group received the subcutaneous injection of lenacapavir; those in the placebo group were switched to the oral lead-in, followed by subcutaneous lenacapavir every 6 months.
Combined data that included six patients from the nonrandomized cohort showed that 79% of patients had a viral load of less than 50 copies/mL at week 26. The 81% viral suppression rate represented the randomized group (29 of 36).
International AIDS Society cochair Hendrik Streeck, MD, director of the Institute of Virology and Institute for HIV Research at the University Bonn (Germany), said a twice-a-year drug could possibly have profound benefits with a reduction in daily pill burden.
“What makes this an interesting drug is that it is long acting, so one can imagine it has the potential to treat individuals such as those who are not very adherent to the antiretroviral therapy, or who can’t easily access treatment, for example in resource-limited settings,” he said in an interview. “The option to treat patients for the next months in advance could be a very important next step.”
Further data from CALIBRATE
Additional data on lenacapavir from the phase 2 CALIBRATE study, presented in a separate session, further showed the drug, given orally or subcutaneously in combination with oral daily emtricitabine/tenofovir alafenamide, resulted in high rates of viral suppression among 94% of 157 treatment-naive patients after 28 weeks.
Commenting on the research, session moderator Alexandra Calmy, MD, PhD, of the HIV/AIDS unit and LIPO & Metabolism group, infectious diseases division, Geneva University Hospitals, noted the study offered “interesting data indeed” – with some caveats: “Why position a new drug class in naive patients [when] we already have good options, available for a large range of various populations?”
Dr. Calmy noted that, in general, lenacapavir “would certainly be an added value with an adapted 6-monthly companion drug.”
But she raised another key issue: “When will we have data on pregnancy that would allow lenacapavir to really be a game changer worldwide?”
The study was funded by Gilead Sciences. Dr. Molina reported receiving research funding from Gilead and being on advisory boards for Gilead, Merck, ViiV, and Janssen. Dr. Calmy and Dr. Streeck reported no relevant financial relationships.
With regulatory approval, lenacapavir could become the only HIV-1 treatment option given every 6 months.
“These data support the use of lenacapavir in patients with multidrug-resistant viruses, and according to its long half-life of two subcutaneous injections per year, [it] could help reduce pill burden,” first author Jean-Michel Molina, MD, PhD, professor of infectious diseases and head of the infectious diseases department at the Saint-Louis and Lariboisière Hospitals, Paris, said in an interview.
Presenting the updated findings from the phase 2/3 CAPELLA trial at the virtual annual meeting of the International AIDS Society conference, Dr. Molina underscored the need for longer-term treatments.
“These patients with multidrug resistances are usually those who have not been fully adherent to their regimen,” he said. “Being able to provide the drug, given every 6 months subcutaneously, provides an ideal treatment for overcoming resistance and lack of adherence.”
The study showed that, after 26 weeks, 81% of heavily treatment-experienced people with HIV in a randomized cohort who were treated with a subcutaneous injection of lenacapavir (927 mg) combined with an optimized background antiretroviral regimen achieved sustained virologic suppression, with an undetectable viral load (<50 copies/mL).
In addition, the lenacapavir-treated patients had a clinically meaningful mean increase in CD4 counts of 81 cells/mcL over the 26 weeks.
The drug was well tolerated, with no drug-related serious adverse events or adverse events leading to discontinuation. The most common adverse events were injection-site reactions, which occurred in 56% of participants, with most being mild or moderate.
Importantly, four participants developed emergent resistances to lenacapavir. One was suppressed with a change in the background regimen and two others were suppressed without a change in regimen.
“We know that these mutations affect viral fitness,” Dr. Molina said in an interview. “We need more studies to assess the real impact of these mutations.”
Dr. Molina noted that a phase 2 study is already underway to evaluate how a pairing of lenacapavir with fellow investigational long-acting drug islatravir (Merck) could offset the risk of developing resistances.
Asked by an audience member whether a two-drug regimen with something like islatravir is likely to successfully prevent resistances, Dr. Molina responded that “it’s too early to know what’s going to happen with [combinations], but these first results are really encouraging when you see the very high rate of being fully suppressed after 26 weeks. The efficacy that we’ve seen after [a previous 2-week analysis] is long lasting.”
Lenacapavir targets multiple viral stages
Unlike other antiviral drugs that target just a single stage of viral replication, lenacapavir takes aim at multiple steps in the viral life cycle, including capsid-mediated uptake of HIV-1 proviral DNA, virus assembly and release, and capsid core formation, Dr. Molina explained.
The CAPELLA trial included participants at research centers in North America, Europe, and Asia, with a median age of 52 years; 25% were female, 38% were Black, and their mean HIV-1 RNA (viral load) was 4.17 log copies/mL.
Overall, 72 patients were divided into two cohorts of 36 patients each, including a randomized and nonrandomized cohort. Dr. Molina primarily reported results from the randomized group.
In that group, patients received either a lead-in of oral lenacapavir (600 mg on day 1 and 2 and 300 mg on day 8) or placebo, in combination with patients’ current failing drug regimens in both groups.
At day 15, all participants were switched to the investigator-selected, optimized background treatment regimen, tailored according to patients’ drug-resistance profiles, and those in the lenacapavir group received the subcutaneous injection of lenacapavir; those in the placebo group were switched to the oral lead-in, followed by subcutaneous lenacapavir every 6 months.
Combined data that included six patients from the nonrandomized cohort showed that 79% of patients had a viral load of less than 50 copies/mL at week 26. The 81% viral suppression rate represented the randomized group (29 of 36).
International AIDS Society cochair Hendrik Streeck, MD, director of the Institute of Virology and Institute for HIV Research at the University Bonn (Germany), said a twice-a-year drug could possibly have profound benefits with a reduction in daily pill burden.
“What makes this an interesting drug is that it is long acting, so one can imagine it has the potential to treat individuals such as those who are not very adherent to the antiretroviral therapy, or who can’t easily access treatment, for example in resource-limited settings,” he said in an interview. “The option to treat patients for the next months in advance could be a very important next step.”
Further data from CALIBRATE
Additional data on lenacapavir from the phase 2 CALIBRATE study, presented in a separate session, further showed the drug, given orally or subcutaneously in combination with oral daily emtricitabine/tenofovir alafenamide, resulted in high rates of viral suppression among 94% of 157 treatment-naive patients after 28 weeks.
Commenting on the research, session moderator Alexandra Calmy, MD, PhD, of the HIV/AIDS unit and LIPO & Metabolism group, infectious diseases division, Geneva University Hospitals, noted the study offered “interesting data indeed” – with some caveats: “Why position a new drug class in naive patients [when] we already have good options, available for a large range of various populations?”
Dr. Calmy noted that, in general, lenacapavir “would certainly be an added value with an adapted 6-monthly companion drug.”
But she raised another key issue: “When will we have data on pregnancy that would allow lenacapavir to really be a game changer worldwide?”
The study was funded by Gilead Sciences. Dr. Molina reported receiving research funding from Gilead and being on advisory boards for Gilead, Merck, ViiV, and Janssen. Dr. Calmy and Dr. Streeck reported no relevant financial relationships.
With regulatory approval, lenacapavir could become the only HIV-1 treatment option given every 6 months.
“These data support the use of lenacapavir in patients with multidrug-resistant viruses, and according to its long half-life of two subcutaneous injections per year, [it] could help reduce pill burden,” first author Jean-Michel Molina, MD, PhD, professor of infectious diseases and head of the infectious diseases department at the Saint-Louis and Lariboisière Hospitals, Paris, said in an interview.
Presenting the updated findings from the phase 2/3 CAPELLA trial at the virtual annual meeting of the International AIDS Society conference, Dr. Molina underscored the need for longer-term treatments.
“These patients with multidrug resistances are usually those who have not been fully adherent to their regimen,” he said. “Being able to provide the drug, given every 6 months subcutaneously, provides an ideal treatment for overcoming resistance and lack of adherence.”
The study showed that, after 26 weeks, 81% of heavily treatment-experienced people with HIV in a randomized cohort who were treated with a subcutaneous injection of lenacapavir (927 mg) combined with an optimized background antiretroviral regimen achieved sustained virologic suppression, with an undetectable viral load (<50 copies/mL).
In addition, the lenacapavir-treated patients had a clinically meaningful mean increase in CD4 counts of 81 cells/mcL over the 26 weeks.
The drug was well tolerated, with no drug-related serious adverse events or adverse events leading to discontinuation. The most common adverse events were injection-site reactions, which occurred in 56% of participants, with most being mild or moderate.
Importantly, four participants developed emergent resistances to lenacapavir. One was suppressed with a change in the background regimen and two others were suppressed without a change in regimen.
“We know that these mutations affect viral fitness,” Dr. Molina said in an interview. “We need more studies to assess the real impact of these mutations.”
Dr. Molina noted that a phase 2 study is already underway to evaluate how a pairing of lenacapavir with fellow investigational long-acting drug islatravir (Merck) could offset the risk of developing resistances.
Asked by an audience member whether a two-drug regimen with something like islatravir is likely to successfully prevent resistances, Dr. Molina responded that “it’s too early to know what’s going to happen with [combinations], but these first results are really encouraging when you see the very high rate of being fully suppressed after 26 weeks. The efficacy that we’ve seen after [a previous 2-week analysis] is long lasting.”
Lenacapavir targets multiple viral stages
Unlike other antiviral drugs that target just a single stage of viral replication, lenacapavir takes aim at multiple steps in the viral life cycle, including capsid-mediated uptake of HIV-1 proviral DNA, virus assembly and release, and capsid core formation, Dr. Molina explained.
The CAPELLA trial included participants at research centers in North America, Europe, and Asia, with a median age of 52 years; 25% were female, 38% were Black, and their mean HIV-1 RNA (viral load) was 4.17 log copies/mL.
Overall, 72 patients were divided into two cohorts of 36 patients each, including a randomized and nonrandomized cohort. Dr. Molina primarily reported results from the randomized group.
In that group, patients received either a lead-in of oral lenacapavir (600 mg on day 1 and 2 and 300 mg on day 8) or placebo, in combination with patients’ current failing drug regimens in both groups.
At day 15, all participants were switched to the investigator-selected, optimized background treatment regimen, tailored according to patients’ drug-resistance profiles, and those in the lenacapavir group received the subcutaneous injection of lenacapavir; those in the placebo group were switched to the oral lead-in, followed by subcutaneous lenacapavir every 6 months.
Combined data that included six patients from the nonrandomized cohort showed that 79% of patients had a viral load of less than 50 copies/mL at week 26. The 81% viral suppression rate represented the randomized group (29 of 36).
International AIDS Society cochair Hendrik Streeck, MD, director of the Institute of Virology and Institute for HIV Research at the University Bonn (Germany), said a twice-a-year drug could possibly have profound benefits with a reduction in daily pill burden.
“What makes this an interesting drug is that it is long acting, so one can imagine it has the potential to treat individuals such as those who are not very adherent to the antiretroviral therapy, or who can’t easily access treatment, for example in resource-limited settings,” he said in an interview. “The option to treat patients for the next months in advance could be a very important next step.”
Further data from CALIBRATE
Additional data on lenacapavir from the phase 2 CALIBRATE study, presented in a separate session, further showed the drug, given orally or subcutaneously in combination with oral daily emtricitabine/tenofovir alafenamide, resulted in high rates of viral suppression among 94% of 157 treatment-naive patients after 28 weeks.
Commenting on the research, session moderator Alexandra Calmy, MD, PhD, of the HIV/AIDS unit and LIPO & Metabolism group, infectious diseases division, Geneva University Hospitals, noted the study offered “interesting data indeed” – with some caveats: “Why position a new drug class in naive patients [when] we already have good options, available for a large range of various populations?”
Dr. Calmy noted that, in general, lenacapavir “would certainly be an added value with an adapted 6-monthly companion drug.”
But she raised another key issue: “When will we have data on pregnancy that would allow lenacapavir to really be a game changer worldwide?”
The study was funded by Gilead Sciences. Dr. Molina reported receiving research funding from Gilead and being on advisory boards for Gilead, Merck, ViiV, and Janssen. Dr. Calmy and Dr. Streeck reported no relevant financial relationships.
FROM IAS 2021
Analysis supports CAC for personalizing statin use
In patients with intermediate risk of atherosclerotic cardiovascular disease along with risk-enhancing factors, coronary artery calcium scoring may help more precisely calculate their need for statin therapy.
Furthermore, when the need for statin treatment isn’t so clear and patients need additional risk assessment, the scoring can provide further information to personalize clinical decision making, according to a cross-sectional study of 1,688 participants in the Multi-Ethnic Study of Atherosclerosis (MESA) published in JAMA Cardiology.
And regardless of coronary artery calcium (CAC), a low ankle brachial index (ABI) score is a marker for statin therapy, the study found.
The study looked at CAC scoring in the context of ABI and other risk-enhancing factors identified in the 2018 American Heart Association/American College of Cardiology cholesterol management guidelines: a family history of premature atherosclerotic cardiovascular disease (ASCVD), lipid and inflammatory biomarkers, chronic kidney disease, chronic inflammatory conditions, premature menopause or preeclampsia, and South Asian ancestry.
Any number of these factors can indicate the need for statins in people with borderline or intermediate risk. The guidelines also call for selective use of CAC to aid the decision-making process for statin therapy when the risk for developing atherosclerosis isn’t so clear.
“The novel risk-enhancing factors are not perfect,” said lead author Jaideep Patel, MD, director of preventive cardiology at Johns Hopkins Heart Center at Greater Baltimore Medical Center. He noted that the 2018 dyslipidemia guidelines suggested the risk for cardiovascular events rises when new risk-enhancing factors emerge, and that it was difficult to predict the extent to which each enhancer could change the 10-year risk.
Utility of CAC
“In this setting, the most significant finding that supports the utility of CAC scoring is when CAC is absent – a CAC of 0 – even in the setting of any of these enhancers, whether it be single or multiple, the 10-year risk remains extremely low – at the very least below the accepted threshold to initiate statin therapy,” Dr. Patel said.
That threshold is below the 7.5% 10-year ASCVD incidence rate. Over the 12-year mean study follow-up, the ASCVD incidence rate among patients with a CAC score of 0 for all risk-enhancing factors was 7.5 events per 1,000 person years, with one exception: ABI had an incidence rate of 10.4 events per 1,000 person years. “A low ABI score should trigger statin initiation irrespective of CAC score,” Dr. Patel said.
The study found a CAC score of 0 in 45.7% of those with one or two risk-enhancing factors versus 40.3% in those with three or more. “Across all the risk enhancers (except low ABI), the prevalence of CAC of 0 was greater than 50% in women; that is, enhancers overestimate risk,” Dr. Patel said. “The prevalence of CAC of 0 was approximately 40% across all risk enhancers; that is, enhancers overestimate risk.”
Dr. Patel said previous studies have suggested the risk of a major cardiovascular event was almost identical for statin and nonstatin users with a CAC score of 0. “If there is uncertainty about statin use after the physician-patient risk discussion,” he said, “CAC scoring may be helpful to guide the use of statin therapy.”
Senior author Mahmoud Al Rifai, MD, MPH, added: “For example, if CAC was absent, a statin could be deprescribed if there’s disutility on the part of the patient, with ongoing lifestyle and risk factor modification efforts.” Dr. Al Rifai is a cardiology fellow at Baylor College of Medicine, Houston.
Dr. Patel said: “Alternatively, if CAC was present, then it would be prudent to continue statin therapy.”
While South Asian ethnicity is a risk enhancing factor, the investigators acknowledged that MESA didn’t recruit this population group.
Study confirms guidelines
The study “supports the contention of the [AHA/ACC] guidelines that, in people who are in this intermediate risk range, there may be factors that either favor statin treatment or suggest that statin treatment could be deferred,” said Neil J. Stone, MD, of Northwestern University, Chicago, and author of the 2013 ASCVD risk calculator. “The guidelines pointed out that risk-enhancing factors may be associated with an increase in lifetime risk, not necessarily short term, and so could inform a more personalized risk discussion.”
The study findings validate the utility of CAC for guiding statin therapy, Dr. Stone said. “For those who have felt that a calcium score is not useful,” he said, “this is additional evidence to show that, in the context of making a decision in those at intermediate risk as proposed by the guidelines, a calcium score is indeed very useful.”
Dr. Stone added: “An important clinical point not mentioned by the authors is that, when the patient has a CAC score of 0 and risk factors, this may be exactly the time to be aggressive with lifestyle to prevent them from developing a positive CAC score and atherosclerosis, because once atherosclerosis is present, treatment may not restore the risk back to the original lower state.”
Dr. Patel, Dr. Al Rifai, and Dr. Stone have no relevant relationships to disclose. A number of study coauthors disclosed multiple financial relationships.
In patients with intermediate risk of atherosclerotic cardiovascular disease along with risk-enhancing factors, coronary artery calcium scoring may help more precisely calculate their need for statin therapy.
Furthermore, when the need for statin treatment isn’t so clear and patients need additional risk assessment, the scoring can provide further information to personalize clinical decision making, according to a cross-sectional study of 1,688 participants in the Multi-Ethnic Study of Atherosclerosis (MESA) published in JAMA Cardiology.
And regardless of coronary artery calcium (CAC), a low ankle brachial index (ABI) score is a marker for statin therapy, the study found.
The study looked at CAC scoring in the context of ABI and other risk-enhancing factors identified in the 2018 American Heart Association/American College of Cardiology cholesterol management guidelines: a family history of premature atherosclerotic cardiovascular disease (ASCVD), lipid and inflammatory biomarkers, chronic kidney disease, chronic inflammatory conditions, premature menopause or preeclampsia, and South Asian ancestry.
Any number of these factors can indicate the need for statins in people with borderline or intermediate risk. The guidelines also call for selective use of CAC to aid the decision-making process for statin therapy when the risk for developing atherosclerosis isn’t so clear.
“The novel risk-enhancing factors are not perfect,” said lead author Jaideep Patel, MD, director of preventive cardiology at Johns Hopkins Heart Center at Greater Baltimore Medical Center. He noted that the 2018 dyslipidemia guidelines suggested the risk for cardiovascular events rises when new risk-enhancing factors emerge, and that it was difficult to predict the extent to which each enhancer could change the 10-year risk.
Utility of CAC
“In this setting, the most significant finding that supports the utility of CAC scoring is when CAC is absent – a CAC of 0 – even in the setting of any of these enhancers, whether it be single or multiple, the 10-year risk remains extremely low – at the very least below the accepted threshold to initiate statin therapy,” Dr. Patel said.
That threshold is below the 7.5% 10-year ASCVD incidence rate. Over the 12-year mean study follow-up, the ASCVD incidence rate among patients with a CAC score of 0 for all risk-enhancing factors was 7.5 events per 1,000 person years, with one exception: ABI had an incidence rate of 10.4 events per 1,000 person years. “A low ABI score should trigger statin initiation irrespective of CAC score,” Dr. Patel said.
The study found a CAC score of 0 in 45.7% of those with one or two risk-enhancing factors versus 40.3% in those with three or more. “Across all the risk enhancers (except low ABI), the prevalence of CAC of 0 was greater than 50% in women; that is, enhancers overestimate risk,” Dr. Patel said. “The prevalence of CAC of 0 was approximately 40% across all risk enhancers; that is, enhancers overestimate risk.”
Dr. Patel said previous studies have suggested the risk of a major cardiovascular event was almost identical for statin and nonstatin users with a CAC score of 0. “If there is uncertainty about statin use after the physician-patient risk discussion,” he said, “CAC scoring may be helpful to guide the use of statin therapy.”
Senior author Mahmoud Al Rifai, MD, MPH, added: “For example, if CAC was absent, a statin could be deprescribed if there’s disutility on the part of the patient, with ongoing lifestyle and risk factor modification efforts.” Dr. Al Rifai is a cardiology fellow at Baylor College of Medicine, Houston.
Dr. Patel said: “Alternatively, if CAC was present, then it would be prudent to continue statin therapy.”
While South Asian ethnicity is a risk enhancing factor, the investigators acknowledged that MESA didn’t recruit this population group.
Study confirms guidelines
The study “supports the contention of the [AHA/ACC] guidelines that, in people who are in this intermediate risk range, there may be factors that either favor statin treatment or suggest that statin treatment could be deferred,” said Neil J. Stone, MD, of Northwestern University, Chicago, and author of the 2013 ASCVD risk calculator. “The guidelines pointed out that risk-enhancing factors may be associated with an increase in lifetime risk, not necessarily short term, and so could inform a more personalized risk discussion.”
The study findings validate the utility of CAC for guiding statin therapy, Dr. Stone said. “For those who have felt that a calcium score is not useful,” he said, “this is additional evidence to show that, in the context of making a decision in those at intermediate risk as proposed by the guidelines, a calcium score is indeed very useful.”
Dr. Stone added: “An important clinical point not mentioned by the authors is that, when the patient has a CAC score of 0 and risk factors, this may be exactly the time to be aggressive with lifestyle to prevent them from developing a positive CAC score and atherosclerosis, because once atherosclerosis is present, treatment may not restore the risk back to the original lower state.”
Dr. Patel, Dr. Al Rifai, and Dr. Stone have no relevant relationships to disclose. A number of study coauthors disclosed multiple financial relationships.
In patients with intermediate risk of atherosclerotic cardiovascular disease along with risk-enhancing factors, coronary artery calcium scoring may help more precisely calculate their need for statin therapy.
Furthermore, when the need for statin treatment isn’t so clear and patients need additional risk assessment, the scoring can provide further information to personalize clinical decision making, according to a cross-sectional study of 1,688 participants in the Multi-Ethnic Study of Atherosclerosis (MESA) published in JAMA Cardiology.
And regardless of coronary artery calcium (CAC), a low ankle brachial index (ABI) score is a marker for statin therapy, the study found.
The study looked at CAC scoring in the context of ABI and other risk-enhancing factors identified in the 2018 American Heart Association/American College of Cardiology cholesterol management guidelines: a family history of premature atherosclerotic cardiovascular disease (ASCVD), lipid and inflammatory biomarkers, chronic kidney disease, chronic inflammatory conditions, premature menopause or preeclampsia, and South Asian ancestry.
Any number of these factors can indicate the need for statins in people with borderline or intermediate risk. The guidelines also call for selective use of CAC to aid the decision-making process for statin therapy when the risk for developing atherosclerosis isn’t so clear.
“The novel risk-enhancing factors are not perfect,” said lead author Jaideep Patel, MD, director of preventive cardiology at Johns Hopkins Heart Center at Greater Baltimore Medical Center. He noted that the 2018 dyslipidemia guidelines suggested the risk for cardiovascular events rises when new risk-enhancing factors emerge, and that it was difficult to predict the extent to which each enhancer could change the 10-year risk.
Utility of CAC
“In this setting, the most significant finding that supports the utility of CAC scoring is when CAC is absent – a CAC of 0 – even in the setting of any of these enhancers, whether it be single or multiple, the 10-year risk remains extremely low – at the very least below the accepted threshold to initiate statin therapy,” Dr. Patel said.
That threshold is below the 7.5% 10-year ASCVD incidence rate. Over the 12-year mean study follow-up, the ASCVD incidence rate among patients with a CAC score of 0 for all risk-enhancing factors was 7.5 events per 1,000 person years, with one exception: ABI had an incidence rate of 10.4 events per 1,000 person years. “A low ABI score should trigger statin initiation irrespective of CAC score,” Dr. Patel said.
The study found a CAC score of 0 in 45.7% of those with one or two risk-enhancing factors versus 40.3% in those with three or more. “Across all the risk enhancers (except low ABI), the prevalence of CAC of 0 was greater than 50% in women; that is, enhancers overestimate risk,” Dr. Patel said. “The prevalence of CAC of 0 was approximately 40% across all risk enhancers; that is, enhancers overestimate risk.”
Dr. Patel said previous studies have suggested the risk of a major cardiovascular event was almost identical for statin and nonstatin users with a CAC score of 0. “If there is uncertainty about statin use after the physician-patient risk discussion,” he said, “CAC scoring may be helpful to guide the use of statin therapy.”
Senior author Mahmoud Al Rifai, MD, MPH, added: “For example, if CAC was absent, a statin could be deprescribed if there’s disutility on the part of the patient, with ongoing lifestyle and risk factor modification efforts.” Dr. Al Rifai is a cardiology fellow at Baylor College of Medicine, Houston.
Dr. Patel said: “Alternatively, if CAC was present, then it would be prudent to continue statin therapy.”
While South Asian ethnicity is a risk enhancing factor, the investigators acknowledged that MESA didn’t recruit this population group.
Study confirms guidelines
The study “supports the contention of the [AHA/ACC] guidelines that, in people who are in this intermediate risk range, there may be factors that either favor statin treatment or suggest that statin treatment could be deferred,” said Neil J. Stone, MD, of Northwestern University, Chicago, and author of the 2013 ASCVD risk calculator. “The guidelines pointed out that risk-enhancing factors may be associated with an increase in lifetime risk, not necessarily short term, and so could inform a more personalized risk discussion.”
The study findings validate the utility of CAC for guiding statin therapy, Dr. Stone said. “For those who have felt that a calcium score is not useful,” he said, “this is additional evidence to show that, in the context of making a decision in those at intermediate risk as proposed by the guidelines, a calcium score is indeed very useful.”
Dr. Stone added: “An important clinical point not mentioned by the authors is that, when the patient has a CAC score of 0 and risk factors, this may be exactly the time to be aggressive with lifestyle to prevent them from developing a positive CAC score and atherosclerosis, because once atherosclerosis is present, treatment may not restore the risk back to the original lower state.”
Dr. Patel, Dr. Al Rifai, and Dr. Stone have no relevant relationships to disclose. A number of study coauthors disclosed multiple financial relationships.
FROM JAMA CARDIOLOGY
Erythematous ear with drainage
A 6-year-old boy was seen in the hospital in consultation for a 3-week history of suspected cellulitis of the right ear. Drainage from the right ear was refractory to treatment with a 7-day course of cephalexin 15 mL po bid of 250 mg/5 mL solution and clindamycin 24.4 mL po tid of 75 mg/5 mL solution. Treatment was followed by admission to the hospital for treatment with intravenous (IV) cefazolin 1000 mg q6h and IV vancomycin 825 mg q6h for 1 week.
The patient had a significant past medical history for asthma, allergic rhinitis, and severe atopic dermatitis that had been treated with methotrexate 10 mg per week for 6 months beginning when the child was 5 years of age. When the methotrexate proved to be ineffective, the patient was started on Aquaphor and mometasone 0.1% ointment. A 6-month trial of these agents failed as well.
Physical examination revealed that the right ear and skin around it were edematous, erythematous, pruritic, and tender. There was also purulent drainage coming from the ear (FIGURE 1).
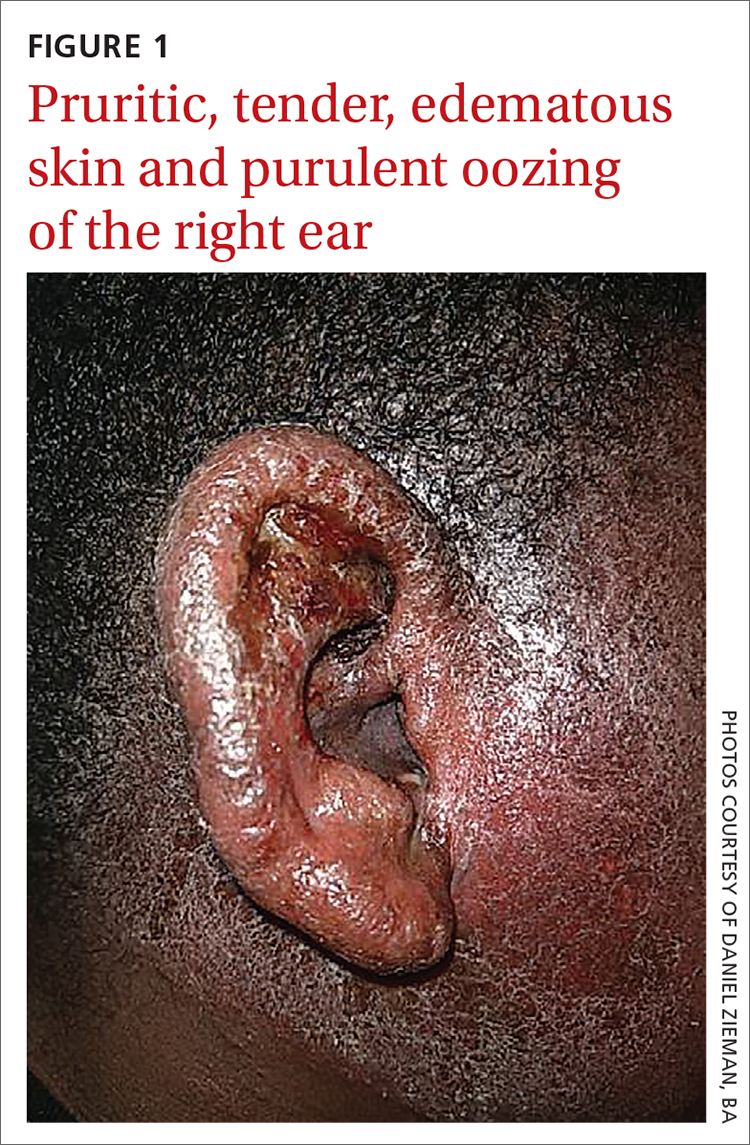
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Infectious eczematoid dermatitis
The patient was referred to a dermatologist after seeing an ear, nose, and throat (ENT) specialist who made the diagnosis of otitis externa when the rash failed to respond to topical and systemic antibiotics. The patient’s tender, pruritic, oozing, edematous eruption was recognized as an infectious eczematoid dermatitis (IED).
Although it is not an uncommon condition, IED may be underrecognized. It accounted for 2.9% of admissions to a dermatology-run inpatient service between 2000 and 2010.1 IED results from cutaneous sensitization to purulent drainage secondary to acute otitis externa or another primary infection.2 In fact, cultures from the purulent drainage in this patient grew methicillin-resistant Staphylococcus aureus. The patient’s right otitis externa drainage may have been associated with the previous history of atopic dermatitis. Atopic dermatitis is associated with an increased risk of skin infections due to decreased inflammatory mediators (defensins).
Cellulitis and herpes zoster oticus are part of the differential
The differential diagnosis in this case includes bacterial cellulitis, acute otitis media, and herpes zoster oticus.
Bacterial cellulitis manifests with erythema, edema, and tenderness with blistering when associated with bullous impetigo rather than pruritus. The clinical appearance of the patient’s diffuse, weeping, edematous external ear, the lack of response to guided antibiotic therapy, and the pruritus experienced by the patient argue against the diagnosis of bacterial cellulitis.
Acute otitis media, like otitis externa, produces ear discharge usually associated with significant pain. Thus, it is important when working through the differential to define the source of the ear discharge. In this case, a consultation with an ENT specialist confirmed that there was an intact tympanic membrane with no middle ear involvement, ruling out the diagnosis of acute otitis media.
Continue to: Herpes zoster oticus
Herpes zoster oticus. The absence of grouped vesicles at any point during the eruption, itching rather than pain, and negative viral culture and polymerase chain reaction studies for herpes simplex and varicella zoster virus excluded the diagnosis of herpes zoster oticus.
Diagnostic criteria were met
This case was compatible with the characterizations of IED as initially described by Engman3 in 1902 and further detailed by Sutton,4 who provided the following criteria for diagnosis:
- an initial eczematous or pustular lesion
- extension peripherally by autoinoculation
- an absence of central clearing
- Staphylococcus on culture of the initial lesion
- a history of infection.
Case reports have added to our understanding of the mechanism of autosensitization of surrounding skin.5 Yamany and Schwartz have proposed the diagnostic criteria summarized in the TABLE.2
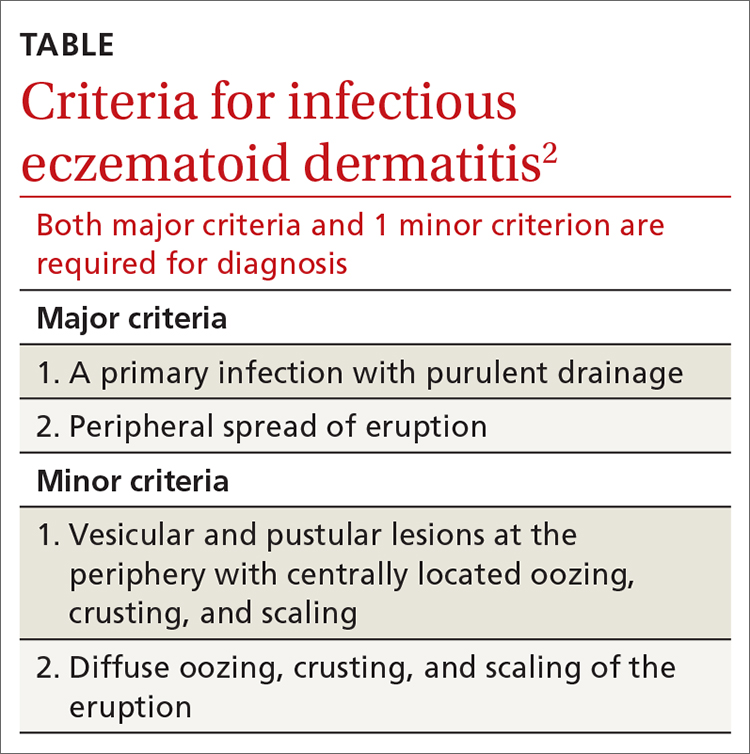
Age factors into location. The ears, nose, and face are predominantly involved in cases of IED in the pediatric population, while the lower extremities are predominantly involved in adults.6 Laboratory tests and imaging may aid in excluding other potential diagnoses or complications, but the diagnosis remains clinical and requires the clinician to avoid jumping to the conclusion that every moist, erythematous crusting eruption is purely infectious in nature.
Tx and prevention hinge on a combination of antibiotics, steroids
The management of IED should be aimed at fighting the infection, eliminating the allergic contact dermatitis associated with infectious products, and improving barrier protection. Topical and/or systemic antibiotics guided by culture focus on killing bacteria. The allergic immune response is dampened by systemic steroids. Topical steroids, however, are difficult to utilize on moist, draining skin. In the case of otitis externa, a combination topical antibiotic and steroid otic drop can be utilized. As healing begins, emollients are applied to aid in skin repair.2 Topical antibiotics containing neomycin or polymyxin should be avoided to eliminate the possibility of developing contact sensitivity to these agents.
For our patient, inpatient wound cultures demonstrated methicillin-resistant S aureus, and empiric treatment with IV cefepime and vancomycin was transitioned to IV clindamycin based on sensitivities and then transitioned to a 12-day course of oral clindamycin 150 mg bid. In addition, the patient received ciprofloxacin/dexamethasone otic drops 3 times/d to treat his otitis externa. After initiating prednisone 30 mg (1 mg/kg/d) for 10 days to cover the allergic component, the patient showed prompt clinical improvement. Gentle cleansing of the right ear with hypoallergenic soap and water followed by application of petrolatum ointment 4 times/d was used to promote healing and improve barrier function (FIGURE 2). The patient’s mother indicated during a follow-up call that the affected area had dramatically improved.
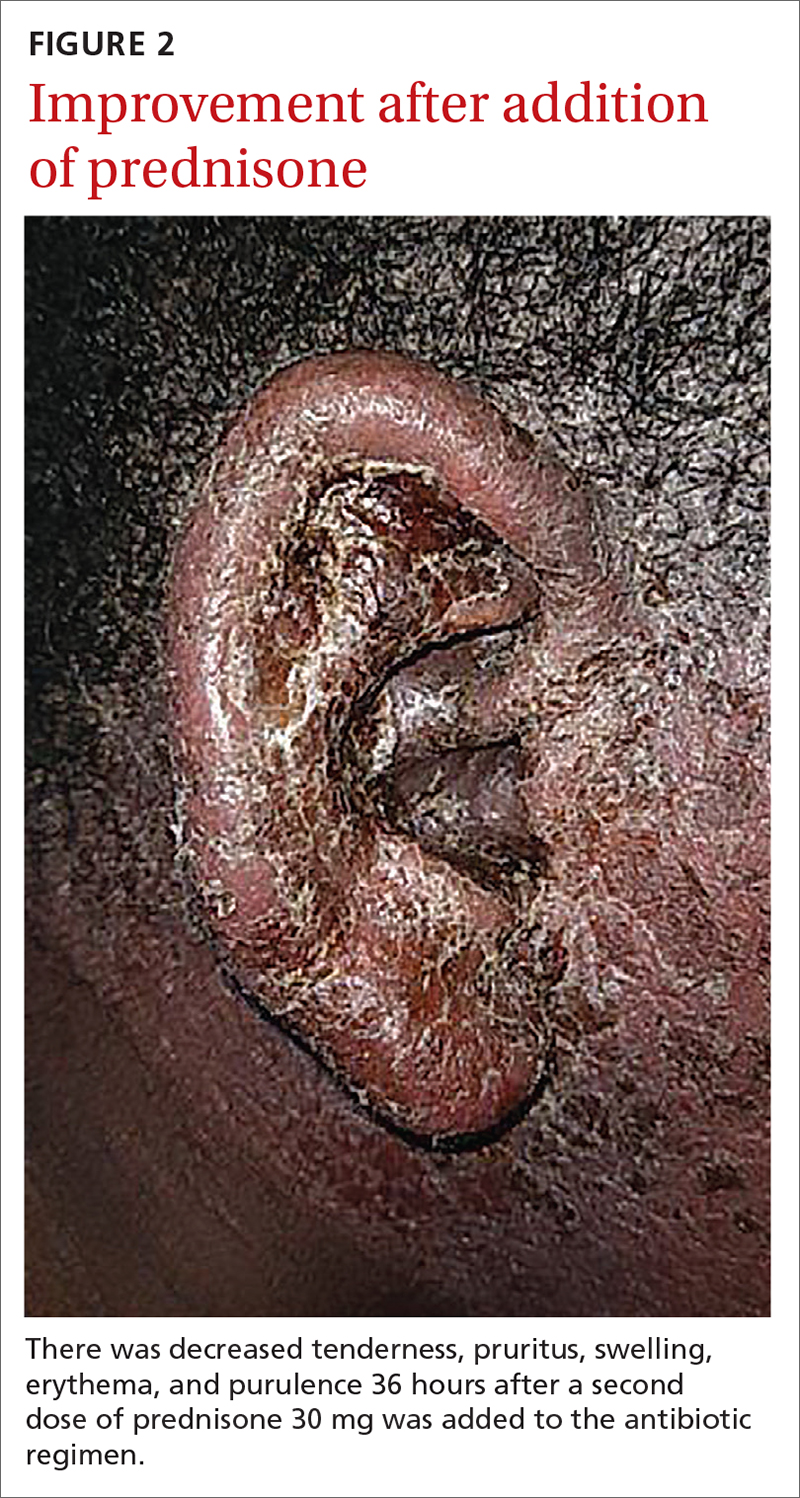
1. Storan ER, McEvoy MT, Wetter DA, et al. Experience with the dermatology inpatient hospital service for adults: Mayo Clinic, 2000–2010. J Eur Acad Dermatol Venereol. 2013;27:1360-1365. doi: 10.1111/jdv.12010
2. Yamany T, Schwartz RA. Infectious eczematoid dermatitis: a comprehensive review. J Eur Acad Dermatol Venereol. 2015;29:203-208. doi: 10.1111/jdv.12715
. An infectious form of an eczematoid dermatitis. St. Louis Courier of Med. 1902;27:401414.
4. Infectious eczematoid dermatitis. J Am Med Assoc. 1920;75:976-979.
, , . Autosensitization dermatitis: report of five cases and protocol of an experiment. Arch Derm Syphilol. 1949;59:68-77. doi: 10.1001/archderm.1949.01520260072010
, . Autosensitization in infectious eczematoid dermatitis. AMA Arch Derm Syphilol. 1950;62:703-704. doi: 10.1001/archderm.1950.01530180092021
A 6-year-old boy was seen in the hospital in consultation for a 3-week history of suspected cellulitis of the right ear. Drainage from the right ear was refractory to treatment with a 7-day course of cephalexin 15 mL po bid of 250 mg/5 mL solution and clindamycin 24.4 mL po tid of 75 mg/5 mL solution. Treatment was followed by admission to the hospital for treatment with intravenous (IV) cefazolin 1000 mg q6h and IV vancomycin 825 mg q6h for 1 week.
The patient had a significant past medical history for asthma, allergic rhinitis, and severe atopic dermatitis that had been treated with methotrexate 10 mg per week for 6 months beginning when the child was 5 years of age. When the methotrexate proved to be ineffective, the patient was started on Aquaphor and mometasone 0.1% ointment. A 6-month trial of these agents failed as well.
Physical examination revealed that the right ear and skin around it were edematous, erythematous, pruritic, and tender. There was also purulent drainage coming from the ear (FIGURE 1).
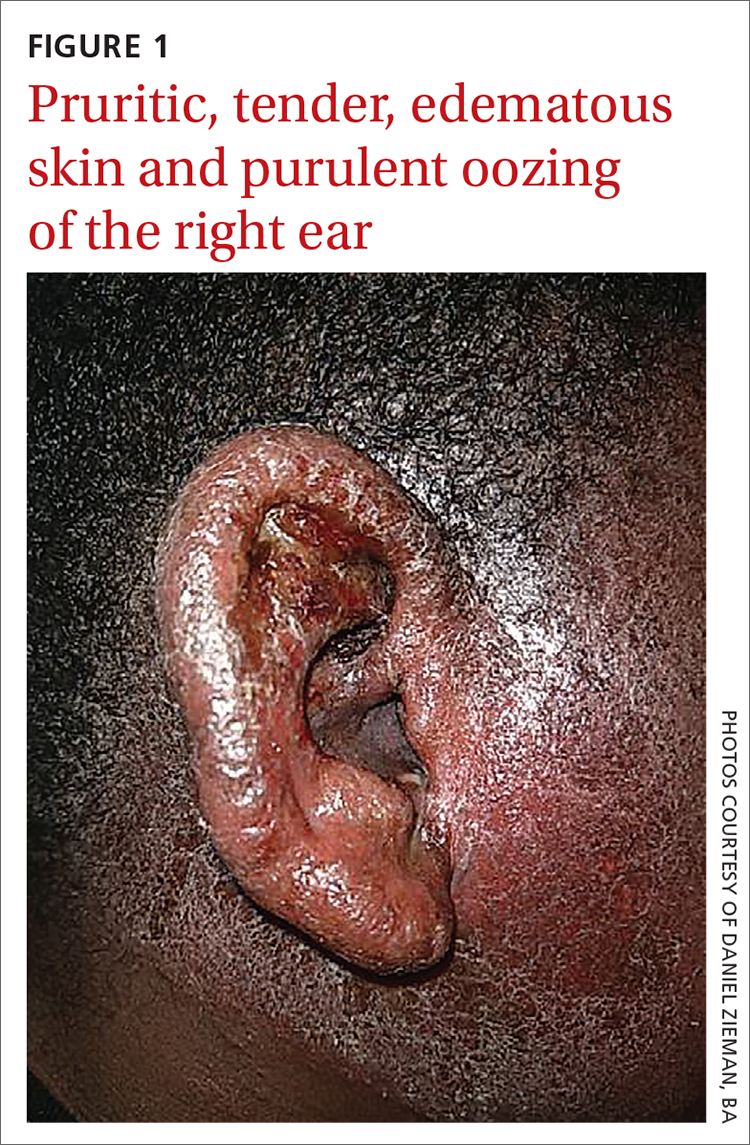
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Infectious eczematoid dermatitis
The patient was referred to a dermatologist after seeing an ear, nose, and throat (ENT) specialist who made the diagnosis of otitis externa when the rash failed to respond to topical and systemic antibiotics. The patient’s tender, pruritic, oozing, edematous eruption was recognized as an infectious eczematoid dermatitis (IED).
Although it is not an uncommon condition, IED may be underrecognized. It accounted for 2.9% of admissions to a dermatology-run inpatient service between 2000 and 2010.1 IED results from cutaneous sensitization to purulent drainage secondary to acute otitis externa or another primary infection.2 In fact, cultures from the purulent drainage in this patient grew methicillin-resistant Staphylococcus aureus. The patient’s right otitis externa drainage may have been associated with the previous history of atopic dermatitis. Atopic dermatitis is associated with an increased risk of skin infections due to decreased inflammatory mediators (defensins).
Cellulitis and herpes zoster oticus are part of the differential
The differential diagnosis in this case includes bacterial cellulitis, acute otitis media, and herpes zoster oticus.
Bacterial cellulitis manifests with erythema, edema, and tenderness with blistering when associated with bullous impetigo rather than pruritus. The clinical appearance of the patient’s diffuse, weeping, edematous external ear, the lack of response to guided antibiotic therapy, and the pruritus experienced by the patient argue against the diagnosis of bacterial cellulitis.
Acute otitis media, like otitis externa, produces ear discharge usually associated with significant pain. Thus, it is important when working through the differential to define the source of the ear discharge. In this case, a consultation with an ENT specialist confirmed that there was an intact tympanic membrane with no middle ear involvement, ruling out the diagnosis of acute otitis media.
Continue to: Herpes zoster oticus
Herpes zoster oticus. The absence of grouped vesicles at any point during the eruption, itching rather than pain, and negative viral culture and polymerase chain reaction studies for herpes simplex and varicella zoster virus excluded the diagnosis of herpes zoster oticus.
Diagnostic criteria were met
This case was compatible with the characterizations of IED as initially described by Engman3 in 1902 and further detailed by Sutton,4 who provided the following criteria for diagnosis:
- an initial eczematous or pustular lesion
- extension peripherally by autoinoculation
- an absence of central clearing
- Staphylococcus on culture of the initial lesion
- a history of infection.
Case reports have added to our understanding of the mechanism of autosensitization of surrounding skin.5 Yamany and Schwartz have proposed the diagnostic criteria summarized in the TABLE.2
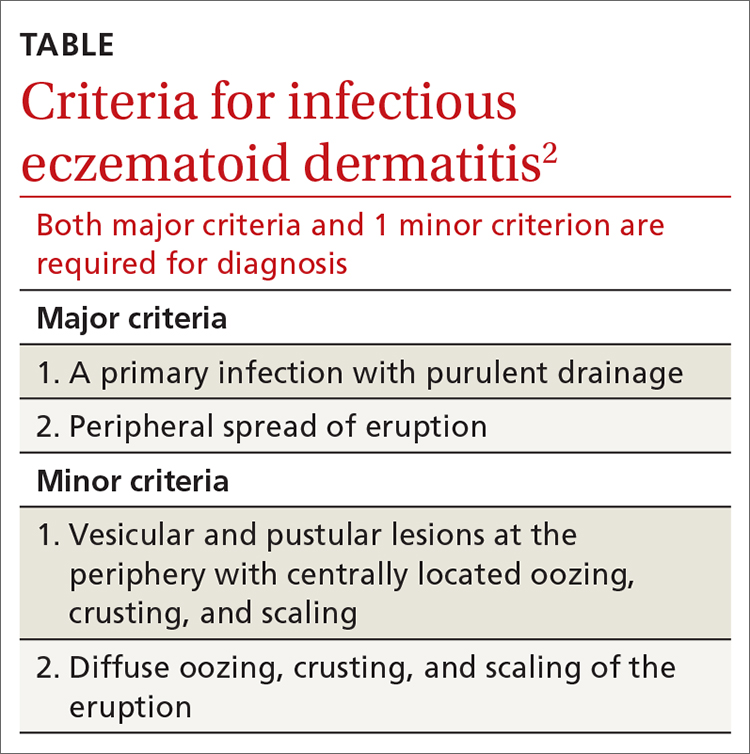
Age factors into location. The ears, nose, and face are predominantly involved in cases of IED in the pediatric population, while the lower extremities are predominantly involved in adults.6 Laboratory tests and imaging may aid in excluding other potential diagnoses or complications, but the diagnosis remains clinical and requires the clinician to avoid jumping to the conclusion that every moist, erythematous crusting eruption is purely infectious in nature.
Tx and prevention hinge on a combination of antibiotics, steroids
The management of IED should be aimed at fighting the infection, eliminating the allergic contact dermatitis associated with infectious products, and improving barrier protection. Topical and/or systemic antibiotics guided by culture focus on killing bacteria. The allergic immune response is dampened by systemic steroids. Topical steroids, however, are difficult to utilize on moist, draining skin. In the case of otitis externa, a combination topical antibiotic and steroid otic drop can be utilized. As healing begins, emollients are applied to aid in skin repair.2 Topical antibiotics containing neomycin or polymyxin should be avoided to eliminate the possibility of developing contact sensitivity to these agents.
For our patient, inpatient wound cultures demonstrated methicillin-resistant S aureus, and empiric treatment with IV cefepime and vancomycin was transitioned to IV clindamycin based on sensitivities and then transitioned to a 12-day course of oral clindamycin 150 mg bid. In addition, the patient received ciprofloxacin/dexamethasone otic drops 3 times/d to treat his otitis externa. After initiating prednisone 30 mg (1 mg/kg/d) for 10 days to cover the allergic component, the patient showed prompt clinical improvement. Gentle cleansing of the right ear with hypoallergenic soap and water followed by application of petrolatum ointment 4 times/d was used to promote healing and improve barrier function (FIGURE 2). The patient’s mother indicated during a follow-up call that the affected area had dramatically improved.
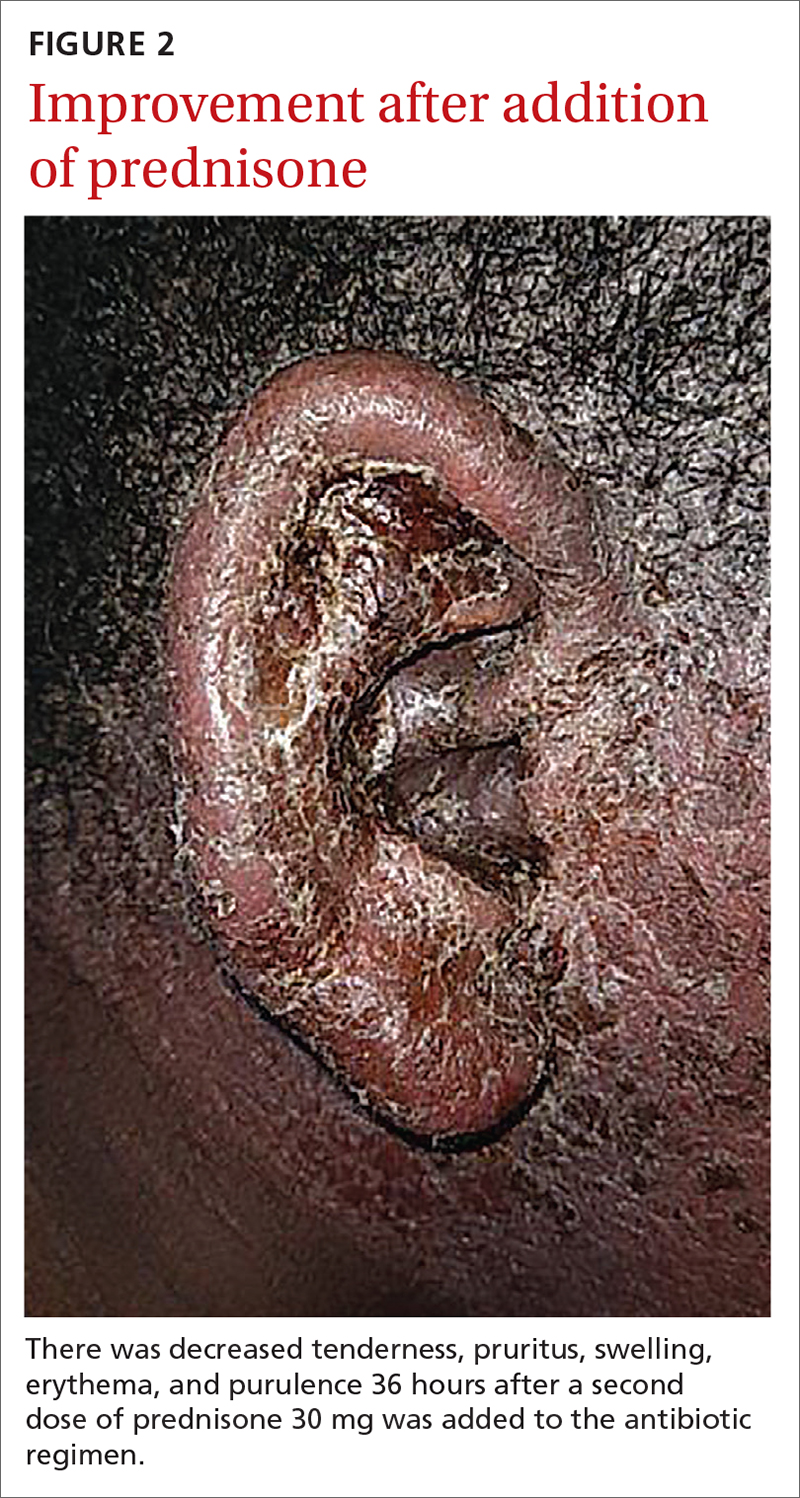
A 6-year-old boy was seen in the hospital in consultation for a 3-week history of suspected cellulitis of the right ear. Drainage from the right ear was refractory to treatment with a 7-day course of cephalexin 15 mL po bid of 250 mg/5 mL solution and clindamycin 24.4 mL po tid of 75 mg/5 mL solution. Treatment was followed by admission to the hospital for treatment with intravenous (IV) cefazolin 1000 mg q6h and IV vancomycin 825 mg q6h for 1 week.
The patient had a significant past medical history for asthma, allergic rhinitis, and severe atopic dermatitis that had been treated with methotrexate 10 mg per week for 6 months beginning when the child was 5 years of age. When the methotrexate proved to be ineffective, the patient was started on Aquaphor and mometasone 0.1% ointment. A 6-month trial of these agents failed as well.
Physical examination revealed that the right ear and skin around it were edematous, erythematous, pruritic, and tender. There was also purulent drainage coming from the ear (FIGURE 1).
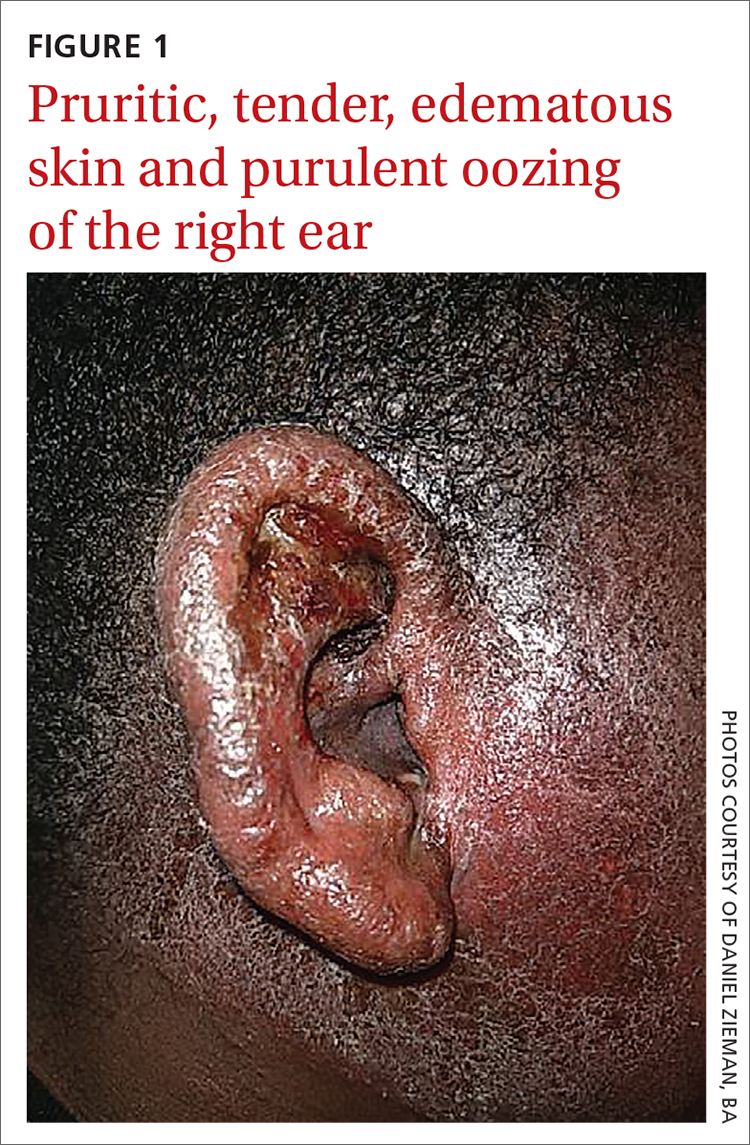
WHAT IS YOUR DIAGNOSIS?
HOW WOULD YOU TREAT THIS PATIENT?
Diagnosis: Infectious eczematoid dermatitis
The patient was referred to a dermatologist after seeing an ear, nose, and throat (ENT) specialist who made the diagnosis of otitis externa when the rash failed to respond to topical and systemic antibiotics. The patient’s tender, pruritic, oozing, edematous eruption was recognized as an infectious eczematoid dermatitis (IED).
Although it is not an uncommon condition, IED may be underrecognized. It accounted for 2.9% of admissions to a dermatology-run inpatient service between 2000 and 2010.1 IED results from cutaneous sensitization to purulent drainage secondary to acute otitis externa or another primary infection.2 In fact, cultures from the purulent drainage in this patient grew methicillin-resistant Staphylococcus aureus. The patient’s right otitis externa drainage may have been associated with the previous history of atopic dermatitis. Atopic dermatitis is associated with an increased risk of skin infections due to decreased inflammatory mediators (defensins).
Cellulitis and herpes zoster oticus are part of the differential
The differential diagnosis in this case includes bacterial cellulitis, acute otitis media, and herpes zoster oticus.
Bacterial cellulitis manifests with erythema, edema, and tenderness with blistering when associated with bullous impetigo rather than pruritus. The clinical appearance of the patient’s diffuse, weeping, edematous external ear, the lack of response to guided antibiotic therapy, and the pruritus experienced by the patient argue against the diagnosis of bacterial cellulitis.
Acute otitis media, like otitis externa, produces ear discharge usually associated with significant pain. Thus, it is important when working through the differential to define the source of the ear discharge. In this case, a consultation with an ENT specialist confirmed that there was an intact tympanic membrane with no middle ear involvement, ruling out the diagnosis of acute otitis media.
Continue to: Herpes zoster oticus
Herpes zoster oticus. The absence of grouped vesicles at any point during the eruption, itching rather than pain, and negative viral culture and polymerase chain reaction studies for herpes simplex and varicella zoster virus excluded the diagnosis of herpes zoster oticus.
Diagnostic criteria were met
This case was compatible with the characterizations of IED as initially described by Engman3 in 1902 and further detailed by Sutton,4 who provided the following criteria for diagnosis:
- an initial eczematous or pustular lesion
- extension peripherally by autoinoculation
- an absence of central clearing
- Staphylococcus on culture of the initial lesion
- a history of infection.
Case reports have added to our understanding of the mechanism of autosensitization of surrounding skin.5 Yamany and Schwartz have proposed the diagnostic criteria summarized in the TABLE.2
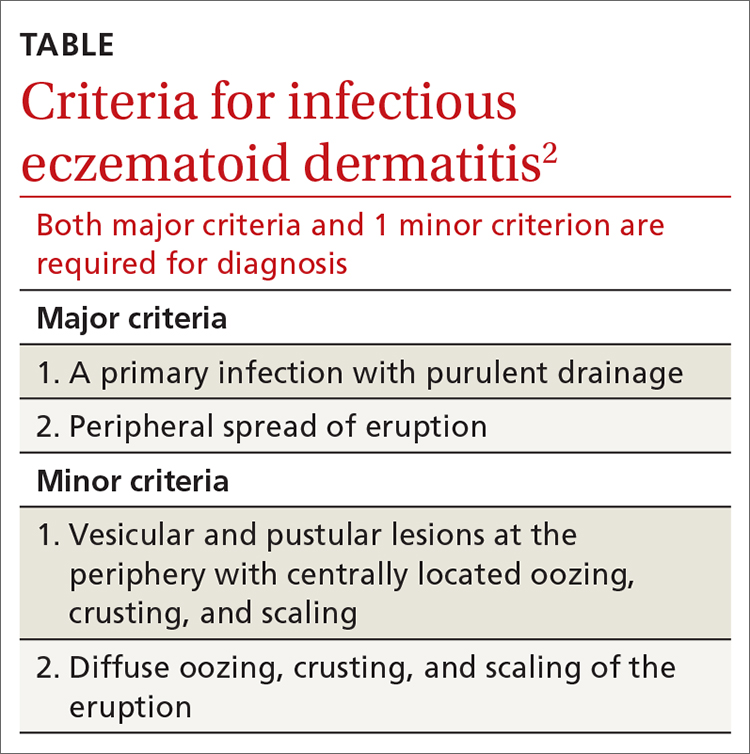
Age factors into location. The ears, nose, and face are predominantly involved in cases of IED in the pediatric population, while the lower extremities are predominantly involved in adults.6 Laboratory tests and imaging may aid in excluding other potential diagnoses or complications, but the diagnosis remains clinical and requires the clinician to avoid jumping to the conclusion that every moist, erythematous crusting eruption is purely infectious in nature.
Tx and prevention hinge on a combination of antibiotics, steroids
The management of IED should be aimed at fighting the infection, eliminating the allergic contact dermatitis associated with infectious products, and improving barrier protection. Topical and/or systemic antibiotics guided by culture focus on killing bacteria. The allergic immune response is dampened by systemic steroids. Topical steroids, however, are difficult to utilize on moist, draining skin. In the case of otitis externa, a combination topical antibiotic and steroid otic drop can be utilized. As healing begins, emollients are applied to aid in skin repair.2 Topical antibiotics containing neomycin or polymyxin should be avoided to eliminate the possibility of developing contact sensitivity to these agents.
For our patient, inpatient wound cultures demonstrated methicillin-resistant S aureus, and empiric treatment with IV cefepime and vancomycin was transitioned to IV clindamycin based on sensitivities and then transitioned to a 12-day course of oral clindamycin 150 mg bid. In addition, the patient received ciprofloxacin/dexamethasone otic drops 3 times/d to treat his otitis externa. After initiating prednisone 30 mg (1 mg/kg/d) for 10 days to cover the allergic component, the patient showed prompt clinical improvement. Gentle cleansing of the right ear with hypoallergenic soap and water followed by application of petrolatum ointment 4 times/d was used to promote healing and improve barrier function (FIGURE 2). The patient’s mother indicated during a follow-up call that the affected area had dramatically improved.
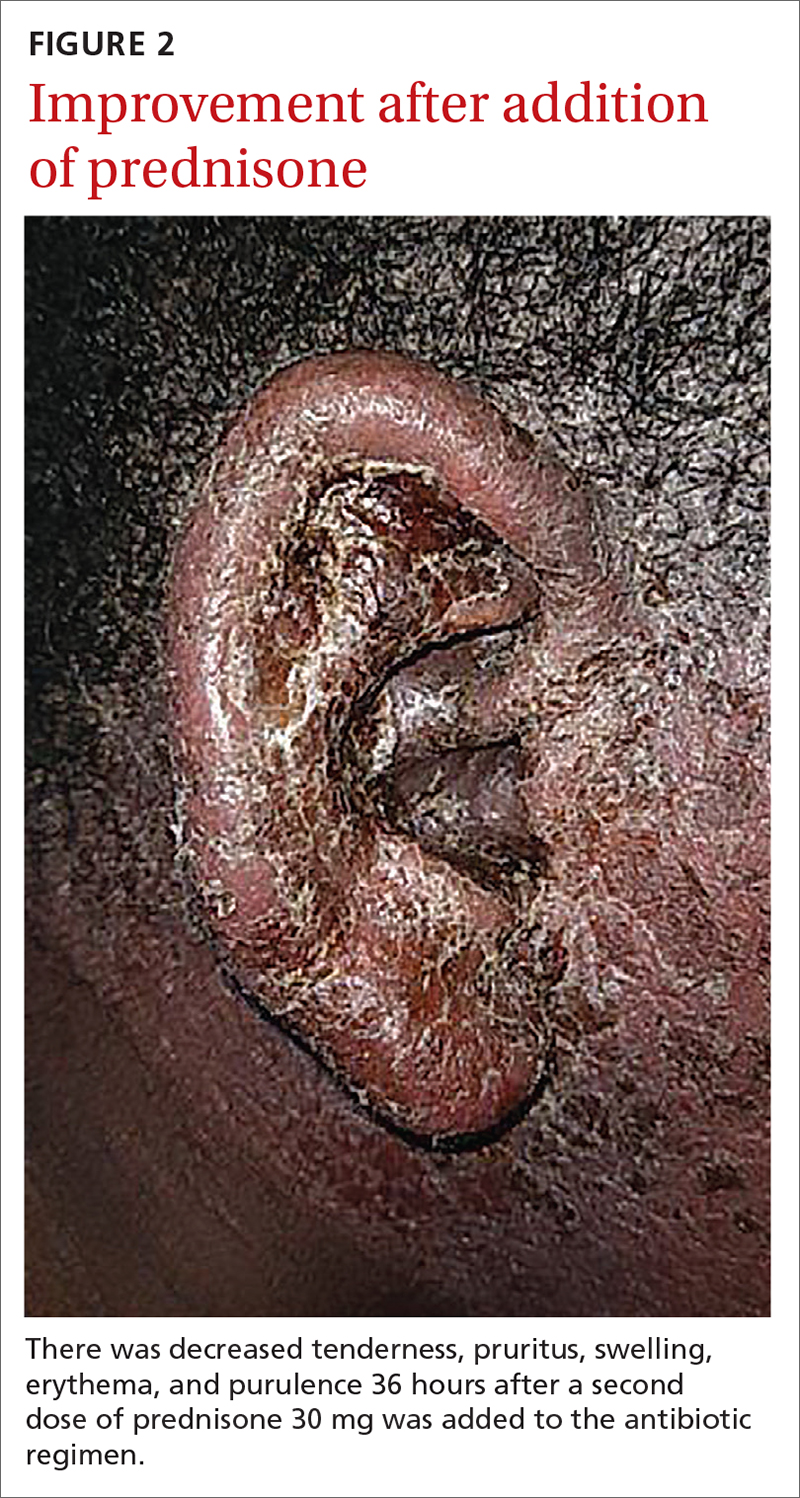
1. Storan ER, McEvoy MT, Wetter DA, et al. Experience with the dermatology inpatient hospital service for adults: Mayo Clinic, 2000–2010. J Eur Acad Dermatol Venereol. 2013;27:1360-1365. doi: 10.1111/jdv.12010
2. Yamany T, Schwartz RA. Infectious eczematoid dermatitis: a comprehensive review. J Eur Acad Dermatol Venereol. 2015;29:203-208. doi: 10.1111/jdv.12715
. An infectious form of an eczematoid dermatitis. St. Louis Courier of Med. 1902;27:401414.
4. Infectious eczematoid dermatitis. J Am Med Assoc. 1920;75:976-979.
, , . Autosensitization dermatitis: report of five cases and protocol of an experiment. Arch Derm Syphilol. 1949;59:68-77. doi: 10.1001/archderm.1949.01520260072010
, . Autosensitization in infectious eczematoid dermatitis. AMA Arch Derm Syphilol. 1950;62:703-704. doi: 10.1001/archderm.1950.01530180092021
1. Storan ER, McEvoy MT, Wetter DA, et al. Experience with the dermatology inpatient hospital service for adults: Mayo Clinic, 2000–2010. J Eur Acad Dermatol Venereol. 2013;27:1360-1365. doi: 10.1111/jdv.12010
2. Yamany T, Schwartz RA. Infectious eczematoid dermatitis: a comprehensive review. J Eur Acad Dermatol Venereol. 2015;29:203-208. doi: 10.1111/jdv.12715
. An infectious form of an eczematoid dermatitis. St. Louis Courier of Med. 1902;27:401414.
4. Infectious eczematoid dermatitis. J Am Med Assoc. 1920;75:976-979.
, , . Autosensitization dermatitis: report of five cases and protocol of an experiment. Arch Derm Syphilol. 1949;59:68-77. doi: 10.1001/archderm.1949.01520260072010
, . Autosensitization in infectious eczematoid dermatitis. AMA Arch Derm Syphilol. 1950;62:703-704. doi: 10.1001/archderm.1950.01530180092021
HIV: Could another two-drug regimen be on the horizon?
Headache was the most common adverse event (AE) people experienced in 72 weeks of taking the once-daily investigational two-drug HIV treatment islatravir (ISL; Merck) plus doravirine (DOR; Merck), and those AEs were short-lived and mild, according to a safety analysis presented at the International AIDS Society (IAS) Conference 2021.
That finding, combined with other data showing few changes in metabolic markers, is potentially good news for people living with HIV, inasmuch as two-drug regimens generally have fewer side effects than traditional three- or four-drug regimens, said Jean-Michel Molina, MD, PhD, of Sant-Louis and Lariboisière Hospitals, Paris, who previously presented efficacy data on the combination at the HIV Glasgow 2020 Virtual Conference.
“At this point, it’s encouraging,” Dr. Molina told this news organization. “Safety is good, efficacy seems good. But the data are limited, and it’s too early to tell.”
If it makes it to the clinic, IS/DOR would be the fourth two-drug regimen approved for HIV treatment, following the U.S. Food and Drug Administration approval of dolutegravir/lamivudine (Dovato), dolutegravir/rilpivirine (Juluca), and the monthly injectable cabotegravir long-acting/rilpivirine long-acting (Cabenuva).
DOR, a non-nucleoside reverse transcriptase inhibitor (NNRTI), is currently approved and is part of the three-drug single-pill regimen Delstrigo (doravirine/lamivudine/tenofovir disoproxil fumarate, DOR/3TC/TDF, Merck). ISL is still under development for treatment and prevention. Dr. Molina had previously presented data showing that 81.1% of people living with HIV maintained undetectable viral loads (defined as <50 copies/mL) compared to 80.6% of people who continued treatment with DOR/3TC/TDF. Data on ISL/DOR versus DOR/3TC/TDF for people new to HIV treatment were published May 14 in The Lancet HIV.
The ISL/DOR trial was designed to assess the safety of three doses of ISL with 100 mg of DOR – 0.25 mg, 0.75 mg, and 2.25 mg – as a daily treatment. The investigators randomly assigned 29, 30, and 31 participants, respectively, to each of the dual-therapy arms and 31 people to the DOR/3TC/TDF arm after a 24-week lead-in course of DOR/3TC/TDF. At week 60, everyone in the two-drug arms received 0.75 mg of ISL with DOR.
At HIV Glasgow, Dr. Molina didn’t present details about the safety profile of the two-drug combination. Douglas Cunningham, DO, a primary care provider at Pueblo Family Physicians, Phoenix, presented such data at IAS 2021. What he showed was that over the first 96 weeks of the trial, there were a total of 118 AEs among the 90 participants in the ISL plus DOR arms and 42 among the 31 participants in the three-drug regimen arm, but there were only seven drug-related AEs for people in the ISL plus DOR arm, and all of those occurred during the first 48 weeks. There were none from weeks 48 to 96.
In total, there were no drug-related serious AEs for ISL/DOR; there was one in the DOR/3TC/TDF arm. The most common AE was headache, which occurred in a total of 10 participants in the ISL/DOR arms. There were nine cases of vitamin D deficiency, eight cases of nausea, seven cases of arthralgia, diarrhea, sinus pain, and vomiting, and six cases each of anxiety and rash. Four people experienced pain in their extremities.
In the three-drug combination arm, side effects were far fewer – just 18 occurred in at least 10% of participants. The most common AE among people on the three-drug combination was diarrhea, which occurred in six participants. Nausea occurred in three; vomiting and headache in two; and there was one instance each of vitamin D deficiency, arthralgia, sinus pain, rash, and pain in extremities.
“The majority of these events were mild, transient, and not related to study drug,” Dr. Cunningham said.
Three ISL/DOR participants experienced an increase in fasting triglyceride level of >500-1,000 mg/dL, and six patients experienced grade 4 changes in creatine kinase level of ≥20 IU/L. Dr. Cunningham said that all but one of the cases of an increase in creatinine level were the result of physical exertion by the participants, and all of those changes were found to have resolved at future visits. The bottom line is that the two-drug combination was safe.
“In the islatravir and doravirine arm, there were no serious drug related serious AEs and no discontinuations due to drug-related AEs from week 48 to week 96,” said Dr. Cunningham. “Islatravir in combination with doravirine was generally well tolerated through week 96 with few drug-related AEs.”
Still, the value of this combination is unclear for Laura Waters, MD, consulting physician in HIV and sexual health at Central and Northwest London NHS Trust. She pointed out that the data are preliminary and that islatravir hasn’t yet been shown to lessen the chances of development of treatment-resistant mutations – a big deal for two-drug regimens, inasmuch as early attempts at using only two drugs resulted in incomplete suppression of the virus and resistance. Merck is planning a study of the combination in heavily pretreated individuals.
Merck presented data at IAS on another NNRTI, the investigational MK-8507, in combination with islatravir. MK-8507 has the potential to be used weekly instead of daily. Dr. Waters said she suspects that this trial is just a proof of concept of islatravir in combination with an NNRTI. Merck has signed an agreement with Gilead Sciences to co-develop islatravir with long-acting lenacapravir. Additionally, the two-drug combination of dolutegravir and lamivudine has been very successful.
“I’d be surprised if they developed islatravir/doravirine as a usable combo,” she said. “It’s just too soon to say. My personal view is that people are a bit too overoptimistic about it.”
The study was funded by Merck. Dr. Molina has received grants from Gilead Sciences, Merck, ViiV Healthcare, and Sanofi. Dr. Waters has received speaker or advisory fees during the past 2 years from Gilead Sciences, ViiV Healthcare, Merck, Janssen, Theratech, Sipla, and Mylan.
A version of this article first appeared on Medscape.com.
Headache was the most common adverse event (AE) people experienced in 72 weeks of taking the once-daily investigational two-drug HIV treatment islatravir (ISL; Merck) plus doravirine (DOR; Merck), and those AEs were short-lived and mild, according to a safety analysis presented at the International AIDS Society (IAS) Conference 2021.
That finding, combined with other data showing few changes in metabolic markers, is potentially good news for people living with HIV, inasmuch as two-drug regimens generally have fewer side effects than traditional three- or four-drug regimens, said Jean-Michel Molina, MD, PhD, of Sant-Louis and Lariboisière Hospitals, Paris, who previously presented efficacy data on the combination at the HIV Glasgow 2020 Virtual Conference.
“At this point, it’s encouraging,” Dr. Molina told this news organization. “Safety is good, efficacy seems good. But the data are limited, and it’s too early to tell.”
If it makes it to the clinic, IS/DOR would be the fourth two-drug regimen approved for HIV treatment, following the U.S. Food and Drug Administration approval of dolutegravir/lamivudine (Dovato), dolutegravir/rilpivirine (Juluca), and the monthly injectable cabotegravir long-acting/rilpivirine long-acting (Cabenuva).
DOR, a non-nucleoside reverse transcriptase inhibitor (NNRTI), is currently approved and is part of the three-drug single-pill regimen Delstrigo (doravirine/lamivudine/tenofovir disoproxil fumarate, DOR/3TC/TDF, Merck). ISL is still under development for treatment and prevention. Dr. Molina had previously presented data showing that 81.1% of people living with HIV maintained undetectable viral loads (defined as <50 copies/mL) compared to 80.6% of people who continued treatment with DOR/3TC/TDF. Data on ISL/DOR versus DOR/3TC/TDF for people new to HIV treatment were published May 14 in The Lancet HIV.
The ISL/DOR trial was designed to assess the safety of three doses of ISL with 100 mg of DOR – 0.25 mg, 0.75 mg, and 2.25 mg – as a daily treatment. The investigators randomly assigned 29, 30, and 31 participants, respectively, to each of the dual-therapy arms and 31 people to the DOR/3TC/TDF arm after a 24-week lead-in course of DOR/3TC/TDF. At week 60, everyone in the two-drug arms received 0.75 mg of ISL with DOR.
At HIV Glasgow, Dr. Molina didn’t present details about the safety profile of the two-drug combination. Douglas Cunningham, DO, a primary care provider at Pueblo Family Physicians, Phoenix, presented such data at IAS 2021. What he showed was that over the first 96 weeks of the trial, there were a total of 118 AEs among the 90 participants in the ISL plus DOR arms and 42 among the 31 participants in the three-drug regimen arm, but there were only seven drug-related AEs for people in the ISL plus DOR arm, and all of those occurred during the first 48 weeks. There were none from weeks 48 to 96.
In total, there were no drug-related serious AEs for ISL/DOR; there was one in the DOR/3TC/TDF arm. The most common AE was headache, which occurred in a total of 10 participants in the ISL/DOR arms. There were nine cases of vitamin D deficiency, eight cases of nausea, seven cases of arthralgia, diarrhea, sinus pain, and vomiting, and six cases each of anxiety and rash. Four people experienced pain in their extremities.
In the three-drug combination arm, side effects were far fewer – just 18 occurred in at least 10% of participants. The most common AE among people on the three-drug combination was diarrhea, which occurred in six participants. Nausea occurred in three; vomiting and headache in two; and there was one instance each of vitamin D deficiency, arthralgia, sinus pain, rash, and pain in extremities.
“The majority of these events were mild, transient, and not related to study drug,” Dr. Cunningham said.
Three ISL/DOR participants experienced an increase in fasting triglyceride level of >500-1,000 mg/dL, and six patients experienced grade 4 changes in creatine kinase level of ≥20 IU/L. Dr. Cunningham said that all but one of the cases of an increase in creatinine level were the result of physical exertion by the participants, and all of those changes were found to have resolved at future visits. The bottom line is that the two-drug combination was safe.
“In the islatravir and doravirine arm, there were no serious drug related serious AEs and no discontinuations due to drug-related AEs from week 48 to week 96,” said Dr. Cunningham. “Islatravir in combination with doravirine was generally well tolerated through week 96 with few drug-related AEs.”
Still, the value of this combination is unclear for Laura Waters, MD, consulting physician in HIV and sexual health at Central and Northwest London NHS Trust. She pointed out that the data are preliminary and that islatravir hasn’t yet been shown to lessen the chances of development of treatment-resistant mutations – a big deal for two-drug regimens, inasmuch as early attempts at using only two drugs resulted in incomplete suppression of the virus and resistance. Merck is planning a study of the combination in heavily pretreated individuals.
Merck presented data at IAS on another NNRTI, the investigational MK-8507, in combination with islatravir. MK-8507 has the potential to be used weekly instead of daily. Dr. Waters said she suspects that this trial is just a proof of concept of islatravir in combination with an NNRTI. Merck has signed an agreement with Gilead Sciences to co-develop islatravir with long-acting lenacapravir. Additionally, the two-drug combination of dolutegravir and lamivudine has been very successful.
“I’d be surprised if they developed islatravir/doravirine as a usable combo,” she said. “It’s just too soon to say. My personal view is that people are a bit too overoptimistic about it.”
The study was funded by Merck. Dr. Molina has received grants from Gilead Sciences, Merck, ViiV Healthcare, and Sanofi. Dr. Waters has received speaker or advisory fees during the past 2 years from Gilead Sciences, ViiV Healthcare, Merck, Janssen, Theratech, Sipla, and Mylan.
A version of this article first appeared on Medscape.com.
Headache was the most common adverse event (AE) people experienced in 72 weeks of taking the once-daily investigational two-drug HIV treatment islatravir (ISL; Merck) plus doravirine (DOR; Merck), and those AEs were short-lived and mild, according to a safety analysis presented at the International AIDS Society (IAS) Conference 2021.
That finding, combined with other data showing few changes in metabolic markers, is potentially good news for people living with HIV, inasmuch as two-drug regimens generally have fewer side effects than traditional three- or four-drug regimens, said Jean-Michel Molina, MD, PhD, of Sant-Louis and Lariboisière Hospitals, Paris, who previously presented efficacy data on the combination at the HIV Glasgow 2020 Virtual Conference.
“At this point, it’s encouraging,” Dr. Molina told this news organization. “Safety is good, efficacy seems good. But the data are limited, and it’s too early to tell.”
If it makes it to the clinic, IS/DOR would be the fourth two-drug regimen approved for HIV treatment, following the U.S. Food and Drug Administration approval of dolutegravir/lamivudine (Dovato), dolutegravir/rilpivirine (Juluca), and the monthly injectable cabotegravir long-acting/rilpivirine long-acting (Cabenuva).
DOR, a non-nucleoside reverse transcriptase inhibitor (NNRTI), is currently approved and is part of the three-drug single-pill regimen Delstrigo (doravirine/lamivudine/tenofovir disoproxil fumarate, DOR/3TC/TDF, Merck). ISL is still under development for treatment and prevention. Dr. Molina had previously presented data showing that 81.1% of people living with HIV maintained undetectable viral loads (defined as <50 copies/mL) compared to 80.6% of people who continued treatment with DOR/3TC/TDF. Data on ISL/DOR versus DOR/3TC/TDF for people new to HIV treatment were published May 14 in The Lancet HIV.
The ISL/DOR trial was designed to assess the safety of three doses of ISL with 100 mg of DOR – 0.25 mg, 0.75 mg, and 2.25 mg – as a daily treatment. The investigators randomly assigned 29, 30, and 31 participants, respectively, to each of the dual-therapy arms and 31 people to the DOR/3TC/TDF arm after a 24-week lead-in course of DOR/3TC/TDF. At week 60, everyone in the two-drug arms received 0.75 mg of ISL with DOR.
At HIV Glasgow, Dr. Molina didn’t present details about the safety profile of the two-drug combination. Douglas Cunningham, DO, a primary care provider at Pueblo Family Physicians, Phoenix, presented such data at IAS 2021. What he showed was that over the first 96 weeks of the trial, there were a total of 118 AEs among the 90 participants in the ISL plus DOR arms and 42 among the 31 participants in the three-drug regimen arm, but there were only seven drug-related AEs for people in the ISL plus DOR arm, and all of those occurred during the first 48 weeks. There were none from weeks 48 to 96.
In total, there were no drug-related serious AEs for ISL/DOR; there was one in the DOR/3TC/TDF arm. The most common AE was headache, which occurred in a total of 10 participants in the ISL/DOR arms. There were nine cases of vitamin D deficiency, eight cases of nausea, seven cases of arthralgia, diarrhea, sinus pain, and vomiting, and six cases each of anxiety and rash. Four people experienced pain in their extremities.
In the three-drug combination arm, side effects were far fewer – just 18 occurred in at least 10% of participants. The most common AE among people on the three-drug combination was diarrhea, which occurred in six participants. Nausea occurred in three; vomiting and headache in two; and there was one instance each of vitamin D deficiency, arthralgia, sinus pain, rash, and pain in extremities.
“The majority of these events were mild, transient, and not related to study drug,” Dr. Cunningham said.
Three ISL/DOR participants experienced an increase in fasting triglyceride level of >500-1,000 mg/dL, and six patients experienced grade 4 changes in creatine kinase level of ≥20 IU/L. Dr. Cunningham said that all but one of the cases of an increase in creatinine level were the result of physical exertion by the participants, and all of those changes were found to have resolved at future visits. The bottom line is that the two-drug combination was safe.
“In the islatravir and doravirine arm, there were no serious drug related serious AEs and no discontinuations due to drug-related AEs from week 48 to week 96,” said Dr. Cunningham. “Islatravir in combination with doravirine was generally well tolerated through week 96 with few drug-related AEs.”
Still, the value of this combination is unclear for Laura Waters, MD, consulting physician in HIV and sexual health at Central and Northwest London NHS Trust. She pointed out that the data are preliminary and that islatravir hasn’t yet been shown to lessen the chances of development of treatment-resistant mutations – a big deal for two-drug regimens, inasmuch as early attempts at using only two drugs resulted in incomplete suppression of the virus and resistance. Merck is planning a study of the combination in heavily pretreated individuals.
Merck presented data at IAS on another NNRTI, the investigational MK-8507, in combination with islatravir. MK-8507 has the potential to be used weekly instead of daily. Dr. Waters said she suspects that this trial is just a proof of concept of islatravir in combination with an NNRTI. Merck has signed an agreement with Gilead Sciences to co-develop islatravir with long-acting lenacapravir. Additionally, the two-drug combination of dolutegravir and lamivudine has been very successful.
“I’d be surprised if they developed islatravir/doravirine as a usable combo,” she said. “It’s just too soon to say. My personal view is that people are a bit too overoptimistic about it.”
The study was funded by Merck. Dr. Molina has received grants from Gilead Sciences, Merck, ViiV Healthcare, and Sanofi. Dr. Waters has received speaker or advisory fees during the past 2 years from Gilead Sciences, ViiV Healthcare, Merck, Janssen, Theratech, Sipla, and Mylan.
A version of this article first appeared on Medscape.com.