User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
International expert group agrees on redefining psoriasis severity
It’s high time to say farewell to the traditional categorization of psoriasis severity into mild, moderate, or severe disease, according to the International Psoriasis Council.
The mild/moderate/severe categorization is vague and defined differently by different organizations and in different countries. It often underestimates disease severity because it ignores psoriasis involvement in particularly tough-to-treat special areas, including the scalp, palms, soles, face, nails, and genitalia, Bruce E. Strober, MD, PhD, asserted at MedscapeLive’s annual Las Vegas Dermatology Seminar, held virtually this year. He chaired an IPC project in which prominent psoriasis experts in 32 countries employed a Delphi consensus approach aimed at achieving agreement on a more practical recategorization of psoriasis severity for use in both daily clinical practice and enrolling appropriate participants in clinical trials. What emerged was a simplified dichotomous categorization system.
“What we came up with is a very sensible approach to defining whether patients should get either topical or systemic therapy. In fact, there are only two groups of patients in psoriasis: those who should get topicals alone, and those who should get systemic therapy. It’s topicals or systemics,” explained Dr. Strober, a dermatologist at Yale University, New Haven, Conn., who also works in private practice in Cromwell, Conn.
Under the IPC classification, psoriasis patients are candidates for systemic therapy if they meet at least one of three criteria: body surface area of involvement greater than 10%, disease involving the previously mentioned special areas, or failure of topical therapy.
“This approach is about practically treating patients who are in need,” Dr. Strober said. “If patients meet just one of these three criteria they can move on to our current toolbox of systemic therapies, be they older systemic treatments, apremilast, phototherapy, or 1 of the 11 biologics currently approved for the treatment of psoriasis. The key point is that for patients with moderate to severe psoriasis – or should I say, systemic therapy–appropriate psoriasis – treatment should be based on individual patient characteristics. We don’t work on a stepwise approach. If a patient walks in with more than 10% body surface area involved, don’t make them fail topicals; you can go right to systemics.”
European dermatologists often use the Psoriasis Area and Severity Index (PASI) score to characterize disease severity and monitor response to therapy. In contrast, American dermatologists generally find PASI too complex and time-consuming for use in clinical practice, relying instead on the amount of body surface area involved with psoriasis. Neither of these measures incorporates disease involvement in special areas, which when present ought to automatically place a patient in the systemic therapy–appropriate category, according to Dr. Strober.
“I find this [IPC recategorization] a very practical approach. I hope you write this down and use this in your own practice,” Dr. Strober said.
The full IPC report was published in the Journal of the American Academy of Dermatology.
The IPC psoriasis severity reclassification project was unfunded. Dr. Strober reported receiving institutional research funding from and serving as a paid consultant to more than two dozen pharmaceutical companies.
MedscapeLive and this news organization are owned by the same parent company.
It’s high time to say farewell to the traditional categorization of psoriasis severity into mild, moderate, or severe disease, according to the International Psoriasis Council.
The mild/moderate/severe categorization is vague and defined differently by different organizations and in different countries. It often underestimates disease severity because it ignores psoriasis involvement in particularly tough-to-treat special areas, including the scalp, palms, soles, face, nails, and genitalia, Bruce E. Strober, MD, PhD, asserted at MedscapeLive’s annual Las Vegas Dermatology Seminar, held virtually this year. He chaired an IPC project in which prominent psoriasis experts in 32 countries employed a Delphi consensus approach aimed at achieving agreement on a more practical recategorization of psoriasis severity for use in both daily clinical practice and enrolling appropriate participants in clinical trials. What emerged was a simplified dichotomous categorization system.
“What we came up with is a very sensible approach to defining whether patients should get either topical or systemic therapy. In fact, there are only two groups of patients in psoriasis: those who should get topicals alone, and those who should get systemic therapy. It’s topicals or systemics,” explained Dr. Strober, a dermatologist at Yale University, New Haven, Conn., who also works in private practice in Cromwell, Conn.
Under the IPC classification, psoriasis patients are candidates for systemic therapy if they meet at least one of three criteria: body surface area of involvement greater than 10%, disease involving the previously mentioned special areas, or failure of topical therapy.
“This approach is about practically treating patients who are in need,” Dr. Strober said. “If patients meet just one of these three criteria they can move on to our current toolbox of systemic therapies, be they older systemic treatments, apremilast, phototherapy, or 1 of the 11 biologics currently approved for the treatment of psoriasis. The key point is that for patients with moderate to severe psoriasis – or should I say, systemic therapy–appropriate psoriasis – treatment should be based on individual patient characteristics. We don’t work on a stepwise approach. If a patient walks in with more than 10% body surface area involved, don’t make them fail topicals; you can go right to systemics.”
European dermatologists often use the Psoriasis Area and Severity Index (PASI) score to characterize disease severity and monitor response to therapy. In contrast, American dermatologists generally find PASI too complex and time-consuming for use in clinical practice, relying instead on the amount of body surface area involved with psoriasis. Neither of these measures incorporates disease involvement in special areas, which when present ought to automatically place a patient in the systemic therapy–appropriate category, according to Dr. Strober.
“I find this [IPC recategorization] a very practical approach. I hope you write this down and use this in your own practice,” Dr. Strober said.
The full IPC report was published in the Journal of the American Academy of Dermatology.
The IPC psoriasis severity reclassification project was unfunded. Dr. Strober reported receiving institutional research funding from and serving as a paid consultant to more than two dozen pharmaceutical companies.
MedscapeLive and this news organization are owned by the same parent company.
It’s high time to say farewell to the traditional categorization of psoriasis severity into mild, moderate, or severe disease, according to the International Psoriasis Council.
The mild/moderate/severe categorization is vague and defined differently by different organizations and in different countries. It often underestimates disease severity because it ignores psoriasis involvement in particularly tough-to-treat special areas, including the scalp, palms, soles, face, nails, and genitalia, Bruce E. Strober, MD, PhD, asserted at MedscapeLive’s annual Las Vegas Dermatology Seminar, held virtually this year. He chaired an IPC project in which prominent psoriasis experts in 32 countries employed a Delphi consensus approach aimed at achieving agreement on a more practical recategorization of psoriasis severity for use in both daily clinical practice and enrolling appropriate participants in clinical trials. What emerged was a simplified dichotomous categorization system.
“What we came up with is a very sensible approach to defining whether patients should get either topical or systemic therapy. In fact, there are only two groups of patients in psoriasis: those who should get topicals alone, and those who should get systemic therapy. It’s topicals or systemics,” explained Dr. Strober, a dermatologist at Yale University, New Haven, Conn., who also works in private practice in Cromwell, Conn.
Under the IPC classification, psoriasis patients are candidates for systemic therapy if they meet at least one of three criteria: body surface area of involvement greater than 10%, disease involving the previously mentioned special areas, or failure of topical therapy.
“This approach is about practically treating patients who are in need,” Dr. Strober said. “If patients meet just one of these three criteria they can move on to our current toolbox of systemic therapies, be they older systemic treatments, apremilast, phototherapy, or 1 of the 11 biologics currently approved for the treatment of psoriasis. The key point is that for patients with moderate to severe psoriasis – or should I say, systemic therapy–appropriate psoriasis – treatment should be based on individual patient characteristics. We don’t work on a stepwise approach. If a patient walks in with more than 10% body surface area involved, don’t make them fail topicals; you can go right to systemics.”
European dermatologists often use the Psoriasis Area and Severity Index (PASI) score to characterize disease severity and monitor response to therapy. In contrast, American dermatologists generally find PASI too complex and time-consuming for use in clinical practice, relying instead on the amount of body surface area involved with psoriasis. Neither of these measures incorporates disease involvement in special areas, which when present ought to automatically place a patient in the systemic therapy–appropriate category, according to Dr. Strober.
“I find this [IPC recategorization] a very practical approach. I hope you write this down and use this in your own practice,” Dr. Strober said.
The full IPC report was published in the Journal of the American Academy of Dermatology.
The IPC psoriasis severity reclassification project was unfunded. Dr. Strober reported receiving institutional research funding from and serving as a paid consultant to more than two dozen pharmaceutical companies.
MedscapeLive and this news organization are owned by the same parent company.
FROM MEDSCAPELIVE LAS VEGAS DERMATOLOGY SEMINAR
Histologic remission fails to be related to UC relapse
Relapse in ulcerative colitis patients with endoscopic remission was unaffected by histologic remission status, based on data from a retrospective study of 269 adults.
Data from previous studies suggest that histologic remission may be the strongest predictor of prognosis of disease course, wrote Neeraj Narula, MD, of McMaster University, Hamilton, Ont., and colleagues.
“However, it is unclear if UC patients who have achieved endoscopic healing have additional benefit in clinical outcomes if they have achieved histologic remission as well compared to those with ongoing histology activity,” they said.
In a study published in Alimentary Pharmacology and Therapeutics, the researchers identified 269 adults with ulcerative colitis who had endoscopic remission. Of these, 53 had normal histology, 138 had histologically inactive colitis, and 78 had histologically active colitis.
Overall, clinical relapse occurred in 64 patients, including 12 with normal histology (22.6%), 32 with inactive colitis (23.2%), and 29 with active colitis (25.6%).
No significant difference occurred in the time to relapse in patients with inactive vs. active colitis (adjusted hazard ratio 1.17, P = .67) or in patients with normal histology vs. inactive histology (AHR 0.67, P = .39). The median time to relapse was 2.92 years, 3.0 years, and 4.0 years in the normal, inactive, and active groups, respectively. Factors associated with a shorter time to relapse included older age at colonoscopy, use of 5-aminosalicylic acid, and disease extent in cases of pancolitis and left-sided colitis.
The study findings were limited by several factors including the possibility of bias in histologic scoring, lack of objective measures of disease activity, and the lack of uniformity is histologic assessment, the researchers noted. However, the results were strengthened by the large size compared with previous studies and by the adjustments for known confounding factors, they said.
“While clinical and endoscopic remission [is the target] of therapy for patients with UC, our study does not support targeting histologic remission in patients who have already achieved endoscopic remission,” they concluded.
More research may support clinical applications
“I was rather surprised by the findings, as a majority of studies have shown that histologic healing more accurately predicts clinical relapse than endoscopic remission in UC,” Atsushi Sakuraba, MD, of the University of Chicago, said in an interview.
“Although of a good sample size, this was a retrospective study, so no firm conclusion can be made,” said Dr. Sakuraba. “Using histologic healing as a therapeutic goal is still an evolving field, and it is too early to draw a conclusion as to whether (or not) to introduce histologic healing in clinical decision making,” he emphasized.
Going forward, prospective studies are needed that match for confounders such as postendoscopy medication use, age, and disease extent, Dr. Sakuraba said.
The study received no outside funding. Lead author Dr. Narula disclosed honoraria from Janssen, AbbVie, Takeda, Pfizer, Merck, and Ferring. Dr. Sakuraba had no financial conflicts to disclose.
SOURCE: Narula N et al. Aliment Pharmacol Ther. 2020 Nov 1. doi: 10.1111/apt.16147.
Relapse in ulcerative colitis patients with endoscopic remission was unaffected by histologic remission status, based on data from a retrospective study of 269 adults.
Data from previous studies suggest that histologic remission may be the strongest predictor of prognosis of disease course, wrote Neeraj Narula, MD, of McMaster University, Hamilton, Ont., and colleagues.
“However, it is unclear if UC patients who have achieved endoscopic healing have additional benefit in clinical outcomes if they have achieved histologic remission as well compared to those with ongoing histology activity,” they said.
In a study published in Alimentary Pharmacology and Therapeutics, the researchers identified 269 adults with ulcerative colitis who had endoscopic remission. Of these, 53 had normal histology, 138 had histologically inactive colitis, and 78 had histologically active colitis.
Overall, clinical relapse occurred in 64 patients, including 12 with normal histology (22.6%), 32 with inactive colitis (23.2%), and 29 with active colitis (25.6%).
No significant difference occurred in the time to relapse in patients with inactive vs. active colitis (adjusted hazard ratio 1.17, P = .67) or in patients with normal histology vs. inactive histology (AHR 0.67, P = .39). The median time to relapse was 2.92 years, 3.0 years, and 4.0 years in the normal, inactive, and active groups, respectively. Factors associated with a shorter time to relapse included older age at colonoscopy, use of 5-aminosalicylic acid, and disease extent in cases of pancolitis and left-sided colitis.
The study findings were limited by several factors including the possibility of bias in histologic scoring, lack of objective measures of disease activity, and the lack of uniformity is histologic assessment, the researchers noted. However, the results were strengthened by the large size compared with previous studies and by the adjustments for known confounding factors, they said.
“While clinical and endoscopic remission [is the target] of therapy for patients with UC, our study does not support targeting histologic remission in patients who have already achieved endoscopic remission,” they concluded.
More research may support clinical applications
“I was rather surprised by the findings, as a majority of studies have shown that histologic healing more accurately predicts clinical relapse than endoscopic remission in UC,” Atsushi Sakuraba, MD, of the University of Chicago, said in an interview.
“Although of a good sample size, this was a retrospective study, so no firm conclusion can be made,” said Dr. Sakuraba. “Using histologic healing as a therapeutic goal is still an evolving field, and it is too early to draw a conclusion as to whether (or not) to introduce histologic healing in clinical decision making,” he emphasized.
Going forward, prospective studies are needed that match for confounders such as postendoscopy medication use, age, and disease extent, Dr. Sakuraba said.
The study received no outside funding. Lead author Dr. Narula disclosed honoraria from Janssen, AbbVie, Takeda, Pfizer, Merck, and Ferring. Dr. Sakuraba had no financial conflicts to disclose.
SOURCE: Narula N et al. Aliment Pharmacol Ther. 2020 Nov 1. doi: 10.1111/apt.16147.
Relapse in ulcerative colitis patients with endoscopic remission was unaffected by histologic remission status, based on data from a retrospective study of 269 adults.
Data from previous studies suggest that histologic remission may be the strongest predictor of prognosis of disease course, wrote Neeraj Narula, MD, of McMaster University, Hamilton, Ont., and colleagues.
“However, it is unclear if UC patients who have achieved endoscopic healing have additional benefit in clinical outcomes if they have achieved histologic remission as well compared to those with ongoing histology activity,” they said.
In a study published in Alimentary Pharmacology and Therapeutics, the researchers identified 269 adults with ulcerative colitis who had endoscopic remission. Of these, 53 had normal histology, 138 had histologically inactive colitis, and 78 had histologically active colitis.
Overall, clinical relapse occurred in 64 patients, including 12 with normal histology (22.6%), 32 with inactive colitis (23.2%), and 29 with active colitis (25.6%).
No significant difference occurred in the time to relapse in patients with inactive vs. active colitis (adjusted hazard ratio 1.17, P = .67) or in patients with normal histology vs. inactive histology (AHR 0.67, P = .39). The median time to relapse was 2.92 years, 3.0 years, and 4.0 years in the normal, inactive, and active groups, respectively. Factors associated with a shorter time to relapse included older age at colonoscopy, use of 5-aminosalicylic acid, and disease extent in cases of pancolitis and left-sided colitis.
The study findings were limited by several factors including the possibility of bias in histologic scoring, lack of objective measures of disease activity, and the lack of uniformity is histologic assessment, the researchers noted. However, the results were strengthened by the large size compared with previous studies and by the adjustments for known confounding factors, they said.
“While clinical and endoscopic remission [is the target] of therapy for patients with UC, our study does not support targeting histologic remission in patients who have already achieved endoscopic remission,” they concluded.
More research may support clinical applications
“I was rather surprised by the findings, as a majority of studies have shown that histologic healing more accurately predicts clinical relapse than endoscopic remission in UC,” Atsushi Sakuraba, MD, of the University of Chicago, said in an interview.
“Although of a good sample size, this was a retrospective study, so no firm conclusion can be made,” said Dr. Sakuraba. “Using histologic healing as a therapeutic goal is still an evolving field, and it is too early to draw a conclusion as to whether (or not) to introduce histologic healing in clinical decision making,” he emphasized.
Going forward, prospective studies are needed that match for confounders such as postendoscopy medication use, age, and disease extent, Dr. Sakuraba said.
The study received no outside funding. Lead author Dr. Narula disclosed honoraria from Janssen, AbbVie, Takeda, Pfizer, Merck, and Ferring. Dr. Sakuraba had no financial conflicts to disclose.
SOURCE: Narula N et al. Aliment Pharmacol Ther. 2020 Nov 1. doi: 10.1111/apt.16147.
FROM ALIMENTARY PHARMACOLOGY AND THERAPEUTICS
Inverse Distribution of Pink Macules and Patches
Punch biopsies from the right axilla (Figure) and right abdomen as well as a tangential biopsy from the left volar wrist papule showed an interstitial histiocytic infiltrate with focal palisading of histiocytes around central regions with collagen alteration and increased mucin. Grocott-Gomori methenamine-silver stain and acid-fast bacilli smear both were negative for organisms; these findings were consistent with a diagnosis of granuloma annulare (GA).

Granuloma annulare is a noninfectious granulomatous disease of unknown etiology. It most commonly appears as asymptomatic, flesh-colored, pink or violaceous annular patches or thin plaques favoring the trunk and extremities. Granuloma annulare has many documented presentations including generalized, patch, subcutaneous, and perforating forms. It can present as macules, papules, nodules, patches, or plaques. Reported associations include diabetes mellitus, hyperlipidemia, solid organ tumors, systemic infection, and thyroid disease.1 Granuloma annulare can occur in any age group but is most common between the ages of 20 and 40 years.2
Diagnosis most often is made clinically and can be confirmed by histopathology. Histologic examination most commonly shows histiocytes within the dermis that palisade around a central area of mucin deposition between degenerating collagen fibers. The histiocytes of GA stain positive with vimentin, lysozyme, and CD68. The increased mucin stains with colloidal iron and Alcian blue. Multinucleated giant cells and perivascular lymphocytic infiltrate also are commonly seen.3
Cutaneous B-cell lymphoma has a wide range of presentations but usually occurs as hyperpigmented plaques and patches with dermal atrophy. Psoriasis can present in an inverse distribution but will show epidermal changes including scale. Sarcoidosis presents as multiple erythematous plaques and papules and also can be accompanied by erythema nodosum. Tinea corporis likely would have resolved with antifungal treatment.
Many different treatments have been described as effective, including cryosurgery, topical and intralesional corticosteroids, antibiotics, immune modulators, phototherapy, and oral corticosteroids.1 We started our patient on triple-antibiotic therapy with rifampin 600 mg, minocycline 100 mg, and ofloxacin 400 mg all once monthly for 6 months, which has been shown to be efficacious in treating GA.4 The patient returned for follow-up 1 year after the initial presentation. At that time, she had faint pink patches on the waist and medial upper thighs, and the axillary lesions had cleared. In the interim, she developed more classic GA lesions—pink to violaceous smooth papules with no overlying epidermal changes—on the volar wrists and dorsal feet. These lesions were asymptomatic, and she currently is not undergoing any further treatment.
- Piette EW, Rosenbach M. Granuloma annulare: pathogenesis, disease associations and triggers, and therapeutic options. J Am Acad Dermatol. 2016;75:467-479.
- Piette EW, Rosenbach M. Granuloma annulare: clinical and histologic variants, epidemiology, and genetics. J Am Acad Dermatol. 2016;75:457-465.
- Patterson JW, Hosler GA. The granulomatous reaction pattern. Weedon’s Skin Pathology. 4th ed. China: Churchill Livingstone Elsevier; 2016:198-203.
- Marcus DV, Mahmoud BH, Hamzavi IH. Granuloma annulare treated with rifampin, ofloxacin, and minocycline combination therapy. Arch Dermatol. 2009;145:787-789.
Punch biopsies from the right axilla (Figure) and right abdomen as well as a tangential biopsy from the left volar wrist papule showed an interstitial histiocytic infiltrate with focal palisading of histiocytes around central regions with collagen alteration and increased mucin. Grocott-Gomori methenamine-silver stain and acid-fast bacilli smear both were negative for organisms; these findings were consistent with a diagnosis of granuloma annulare (GA).

Granuloma annulare is a noninfectious granulomatous disease of unknown etiology. It most commonly appears as asymptomatic, flesh-colored, pink or violaceous annular patches or thin plaques favoring the trunk and extremities. Granuloma annulare has many documented presentations including generalized, patch, subcutaneous, and perforating forms. It can present as macules, papules, nodules, patches, or plaques. Reported associations include diabetes mellitus, hyperlipidemia, solid organ tumors, systemic infection, and thyroid disease.1 Granuloma annulare can occur in any age group but is most common between the ages of 20 and 40 years.2
Diagnosis most often is made clinically and can be confirmed by histopathology. Histologic examination most commonly shows histiocytes within the dermis that palisade around a central area of mucin deposition between degenerating collagen fibers. The histiocytes of GA stain positive with vimentin, lysozyme, and CD68. The increased mucin stains with colloidal iron and Alcian blue. Multinucleated giant cells and perivascular lymphocytic infiltrate also are commonly seen.3
Cutaneous B-cell lymphoma has a wide range of presentations but usually occurs as hyperpigmented plaques and patches with dermal atrophy. Psoriasis can present in an inverse distribution but will show epidermal changes including scale. Sarcoidosis presents as multiple erythematous plaques and papules and also can be accompanied by erythema nodosum. Tinea corporis likely would have resolved with antifungal treatment.
Many different treatments have been described as effective, including cryosurgery, topical and intralesional corticosteroids, antibiotics, immune modulators, phototherapy, and oral corticosteroids.1 We started our patient on triple-antibiotic therapy with rifampin 600 mg, minocycline 100 mg, and ofloxacin 400 mg all once monthly for 6 months, which has been shown to be efficacious in treating GA.4 The patient returned for follow-up 1 year after the initial presentation. At that time, she had faint pink patches on the waist and medial upper thighs, and the axillary lesions had cleared. In the interim, she developed more classic GA lesions—pink to violaceous smooth papules with no overlying epidermal changes—on the volar wrists and dorsal feet. These lesions were asymptomatic, and she currently is not undergoing any further treatment.
Punch biopsies from the right axilla (Figure) and right abdomen as well as a tangential biopsy from the left volar wrist papule showed an interstitial histiocytic infiltrate with focal palisading of histiocytes around central regions with collagen alteration and increased mucin. Grocott-Gomori methenamine-silver stain and acid-fast bacilli smear both were negative for organisms; these findings were consistent with a diagnosis of granuloma annulare (GA).

Granuloma annulare is a noninfectious granulomatous disease of unknown etiology. It most commonly appears as asymptomatic, flesh-colored, pink or violaceous annular patches or thin plaques favoring the trunk and extremities. Granuloma annulare has many documented presentations including generalized, patch, subcutaneous, and perforating forms. It can present as macules, papules, nodules, patches, or plaques. Reported associations include diabetes mellitus, hyperlipidemia, solid organ tumors, systemic infection, and thyroid disease.1 Granuloma annulare can occur in any age group but is most common between the ages of 20 and 40 years.2
Diagnosis most often is made clinically and can be confirmed by histopathology. Histologic examination most commonly shows histiocytes within the dermis that palisade around a central area of mucin deposition between degenerating collagen fibers. The histiocytes of GA stain positive with vimentin, lysozyme, and CD68. The increased mucin stains with colloidal iron and Alcian blue. Multinucleated giant cells and perivascular lymphocytic infiltrate also are commonly seen.3
Cutaneous B-cell lymphoma has a wide range of presentations but usually occurs as hyperpigmented plaques and patches with dermal atrophy. Psoriasis can present in an inverse distribution but will show epidermal changes including scale. Sarcoidosis presents as multiple erythematous plaques and papules and also can be accompanied by erythema nodosum. Tinea corporis likely would have resolved with antifungal treatment.
Many different treatments have been described as effective, including cryosurgery, topical and intralesional corticosteroids, antibiotics, immune modulators, phototherapy, and oral corticosteroids.1 We started our patient on triple-antibiotic therapy with rifampin 600 mg, minocycline 100 mg, and ofloxacin 400 mg all once monthly for 6 months, which has been shown to be efficacious in treating GA.4 The patient returned for follow-up 1 year after the initial presentation. At that time, she had faint pink patches on the waist and medial upper thighs, and the axillary lesions had cleared. In the interim, she developed more classic GA lesions—pink to violaceous smooth papules with no overlying epidermal changes—on the volar wrists and dorsal feet. These lesions were asymptomatic, and she currently is not undergoing any further treatment.
- Piette EW, Rosenbach M. Granuloma annulare: pathogenesis, disease associations and triggers, and therapeutic options. J Am Acad Dermatol. 2016;75:467-479.
- Piette EW, Rosenbach M. Granuloma annulare: clinical and histologic variants, epidemiology, and genetics. J Am Acad Dermatol. 2016;75:457-465.
- Patterson JW, Hosler GA. The granulomatous reaction pattern. Weedon’s Skin Pathology. 4th ed. China: Churchill Livingstone Elsevier; 2016:198-203.
- Marcus DV, Mahmoud BH, Hamzavi IH. Granuloma annulare treated with rifampin, ofloxacin, and minocycline combination therapy. Arch Dermatol. 2009;145:787-789.
- Piette EW, Rosenbach M. Granuloma annulare: pathogenesis, disease associations and triggers, and therapeutic options. J Am Acad Dermatol. 2016;75:467-479.
- Piette EW, Rosenbach M. Granuloma annulare: clinical and histologic variants, epidemiology, and genetics. J Am Acad Dermatol. 2016;75:457-465.
- Patterson JW, Hosler GA. The granulomatous reaction pattern. Weedon’s Skin Pathology. 4th ed. China: Churchill Livingstone Elsevier; 2016:198-203.
- Marcus DV, Mahmoud BH, Hamzavi IH. Granuloma annulare treated with rifampin, ofloxacin, and minocycline combination therapy. Arch Dermatol. 2009;145:787-789.

A 73-year-old woman presented for evaluation of an asymptomatic progressive rash on the left wrist, waist, groin, and inner thighs of 2 months’ duration. Her primary care provider prescribed clotrimazole and fluconazole with no improvement. Review of systems was negative. Medications included omeprazole, candesartan hydrochlorothiazide, potassium chloride, and levothyroxine. Physical examination revealed many scattered, pink to violaceous macules and patches in the axillae (sparing the vaults) and inguinal folds as well as on the waist and medial upper thighs. The lesions were without scale or other epidermal change. She also had a pink papule on the left volar wrist. A Wood lamp examination was unremarkable, and punch biopsies were performed.
Rapid relief of opioid-induced constipation with MNTX
Subcutaneously administered methylnaltrexone (MNTX) (Relistor), a peripherally acting mu-opioid receptor antagonist, relieves opioid-induced constipation (OID) in both chronic, noncancer-related illness and cancer-related illness, a new analysis concludes.
“While these are two very different patient groups, the ability to have something to treat OIC in noncancer patients who stay on opioids for whatever reason helps, because [otherwise] these patients are not doing well,” said lead author Eric Shah, MD, motility director for the Dartmouth program at Dartmouth Hitchcock Health, Lebanon, N.H.
Importantly, peripherally acting mu-opioid receptor antagonists such as MNTX do not affect overall pain control to any significant extent, which is “reassuring,” he said in an interview.
These drugs decrease the constipating effects of opioids without reversing CNS-mediated opioid effects, he explained.
“Methylnaltrexone has already been approved for the treatment of OIC in adults with chronic noncancer pain as well as for OIC in adults with advanced illness who are receiving palliative care, which is often the case in patients with cancer-related pain,” he noted.
Dr. Shah discussed the new analysis during PAINWeek 2020, the American Society of Regional Anesthesia and Pain Medicine 19th Annual Pain Medicine Meeting.
The analysis was based on a review of data collected in two previously reported randomized, placebo-controlled studies (study 302 and 4000), which were used to gain approval.
The new analysis shows that “the drug works up front, and the effect is able to be maintained. I think the studies are clinically relevant in that patients are able to have a bowel movement quickly after you give them an injectable formulation when they are vomiting or otherwise can’t tolerate a pill and they are feeling miserable,” Dr. Shah commented. Many patients with OIC are constipated for reasons other than from opioid use. They often have other side effects from opioids, including bloating, nausea, and vomiting.
“When patients go to the emergency room, it’s not just that they are not able to have a bowel movement; they are often also vomiting, so it’s important to have agents that can be given in a manner that avoids the need for oral medication,” Dr. Shah said. MNTX is the only peripherally acting opioid antagonist available in a subcutaneous formulation.
Moreover, if patients are able to control these symptoms at home with an injectable formulation, they may not need to go to the ED for treatment of their gastrointestinal distress, he added.
Viable product
In a comment, Darren Brenner, MD, associate professor of medicine and surgery, Northwestern University, Chicago, who has worked with this subcutaneous formulation, said it is “definitely a viable product.
“The data presented here were in patients with advanced illness receiving palliative care when other laxatives have failed, and the difference and the potential benefit for MNTX is that it is the only peripherally acting mu-opioid receptor antagonist that is approved for advanced cancer,” he added. The other products that are currently approved, naloxegol (Movantik) and naldemedine (Symproic), are both indicated for chronic, noncancer pain.
The other potential benefit of subcutaneous MNTX is that it can work very rapidly for the patients who respond to it. “One of the things investigators did not mention in these two trials but which has been shown in previous studies is that almost half of patients who respond to this drug respond within the first 30 minutes of receiving the injection,” Dr. Brenner said in an interview.
This can be very beneficial in an emergency setting, because it may avoid having patients admitted to hospital. They can be discharged and sent home with enough drug to use on demand, Dr. Brenner suggested.
New analysis of data from studies 302 and 4000
Both studies were carried out in adults with advanced illness and OIC whose conditions were refractory to laxative use. Both of the studies were placebo controlled.
Study 302 involved 78 patients with cancer and 56 patients with noncancer-related OIC. MNTX was given at a dose of 0.15 mg/kg subcutaneously every other day for 2 weeks.
Study 4000 included 152 patients with cancer and OIC and 78 patients with noncancer-related OIC. In this study, the dose of MNTX was based on body weight. Seven or fewer doses of either 8 mg or 12 mg were given subcutaneously for 2 weeks.
The main endpoints of both studies was the proportion of patients who achieved a rescue-free laxation (RFL) response within 4 hours after the first dose and the proportion of patients with an RFL response within 4 hours for two or more of the first four doses within 24 hours.
Dr. Shah explained that RFL is a meaningful clinical endpoint. Patients could achieve a bowel movement with the two prespecified time endpoints in both studies.
Not all patients were hospitalized for OIC, Dr. Shah noted. Entry criteria were strict and included having fewer than three bowel movements during the previous week and no clinically significant laxation (defecation) within 48 hours of receiving the first dose of study drug.
“In both studies, a significantly greater proportion of patients treated with MNTX versus placebo achieved an RFL within 4 hours after the first dose among both cancer and noncancer patients,” the investigators reported.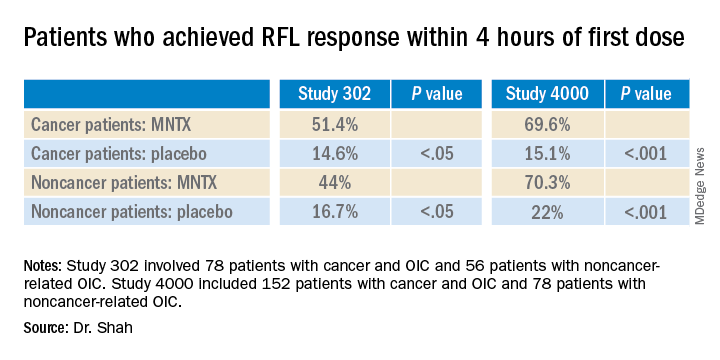
Results were relatively comparable between cancer and noncancer patients who were treated for OIC in study 4000, the investigators noted.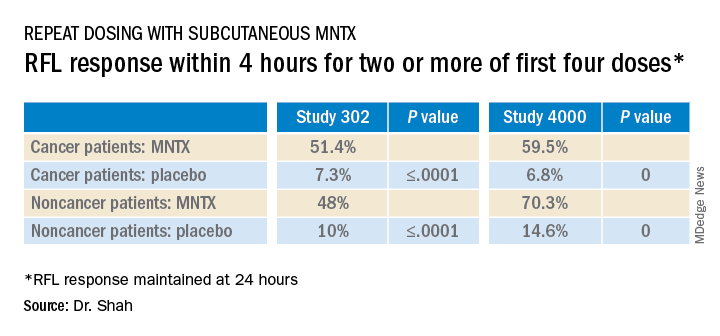
Both studies were sponsored by Salix Pharmaceuticals. Dr. Shah has received travel fees from Salix Pharmaceuticals. Dr. Brenner has served as a consultant for Salix Pharmaceuticals, AstraZeneca, and Purdue Pharma. AstraZeneca developed naloxegol.
This article first appeared on Medscape.com.
Subcutaneously administered methylnaltrexone (MNTX) (Relistor), a peripherally acting mu-opioid receptor antagonist, relieves opioid-induced constipation (OID) in both chronic, noncancer-related illness and cancer-related illness, a new analysis concludes.
“While these are two very different patient groups, the ability to have something to treat OIC in noncancer patients who stay on opioids for whatever reason helps, because [otherwise] these patients are not doing well,” said lead author Eric Shah, MD, motility director for the Dartmouth program at Dartmouth Hitchcock Health, Lebanon, N.H.
Importantly, peripherally acting mu-opioid receptor antagonists such as MNTX do not affect overall pain control to any significant extent, which is “reassuring,” he said in an interview.
These drugs decrease the constipating effects of opioids without reversing CNS-mediated opioid effects, he explained.
“Methylnaltrexone has already been approved for the treatment of OIC in adults with chronic noncancer pain as well as for OIC in adults with advanced illness who are receiving palliative care, which is often the case in patients with cancer-related pain,” he noted.
Dr. Shah discussed the new analysis during PAINWeek 2020, the American Society of Regional Anesthesia and Pain Medicine 19th Annual Pain Medicine Meeting.
The analysis was based on a review of data collected in two previously reported randomized, placebo-controlled studies (study 302 and 4000), which were used to gain approval.
The new analysis shows that “the drug works up front, and the effect is able to be maintained. I think the studies are clinically relevant in that patients are able to have a bowel movement quickly after you give them an injectable formulation when they are vomiting or otherwise can’t tolerate a pill and they are feeling miserable,” Dr. Shah commented. Many patients with OIC are constipated for reasons other than from opioid use. They often have other side effects from opioids, including bloating, nausea, and vomiting.
“When patients go to the emergency room, it’s not just that they are not able to have a bowel movement; they are often also vomiting, so it’s important to have agents that can be given in a manner that avoids the need for oral medication,” Dr. Shah said. MNTX is the only peripherally acting opioid antagonist available in a subcutaneous formulation.
Moreover, if patients are able to control these symptoms at home with an injectable formulation, they may not need to go to the ED for treatment of their gastrointestinal distress, he added.
Viable product
In a comment, Darren Brenner, MD, associate professor of medicine and surgery, Northwestern University, Chicago, who has worked with this subcutaneous formulation, said it is “definitely a viable product.
“The data presented here were in patients with advanced illness receiving palliative care when other laxatives have failed, and the difference and the potential benefit for MNTX is that it is the only peripherally acting mu-opioid receptor antagonist that is approved for advanced cancer,” he added. The other products that are currently approved, naloxegol (Movantik) and naldemedine (Symproic), are both indicated for chronic, noncancer pain.
The other potential benefit of subcutaneous MNTX is that it can work very rapidly for the patients who respond to it. “One of the things investigators did not mention in these two trials but which has been shown in previous studies is that almost half of patients who respond to this drug respond within the first 30 minutes of receiving the injection,” Dr. Brenner said in an interview.
This can be very beneficial in an emergency setting, because it may avoid having patients admitted to hospital. They can be discharged and sent home with enough drug to use on demand, Dr. Brenner suggested.
New analysis of data from studies 302 and 4000
Both studies were carried out in adults with advanced illness and OIC whose conditions were refractory to laxative use. Both of the studies were placebo controlled.
Study 302 involved 78 patients with cancer and 56 patients with noncancer-related OIC. MNTX was given at a dose of 0.15 mg/kg subcutaneously every other day for 2 weeks.
Study 4000 included 152 patients with cancer and OIC and 78 patients with noncancer-related OIC. In this study, the dose of MNTX was based on body weight. Seven or fewer doses of either 8 mg or 12 mg were given subcutaneously for 2 weeks.
The main endpoints of both studies was the proportion of patients who achieved a rescue-free laxation (RFL) response within 4 hours after the first dose and the proportion of patients with an RFL response within 4 hours for two or more of the first four doses within 24 hours.
Dr. Shah explained that RFL is a meaningful clinical endpoint. Patients could achieve a bowel movement with the two prespecified time endpoints in both studies.
Not all patients were hospitalized for OIC, Dr. Shah noted. Entry criteria were strict and included having fewer than three bowel movements during the previous week and no clinically significant laxation (defecation) within 48 hours of receiving the first dose of study drug.
“In both studies, a significantly greater proportion of patients treated with MNTX versus placebo achieved an RFL within 4 hours after the first dose among both cancer and noncancer patients,” the investigators reported.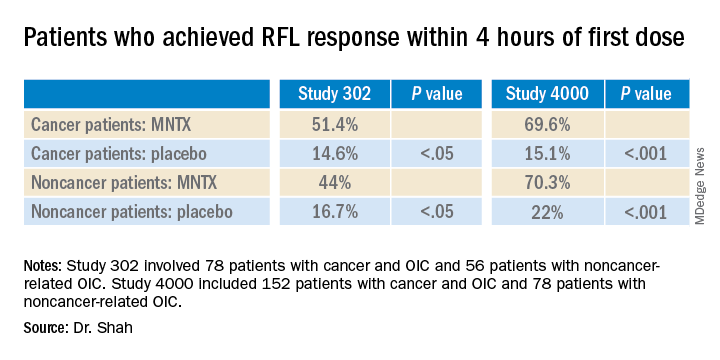
Results were relatively comparable between cancer and noncancer patients who were treated for OIC in study 4000, the investigators noted.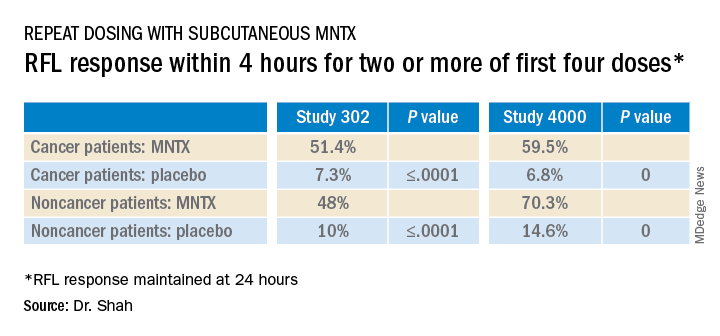
Both studies were sponsored by Salix Pharmaceuticals. Dr. Shah has received travel fees from Salix Pharmaceuticals. Dr. Brenner has served as a consultant for Salix Pharmaceuticals, AstraZeneca, and Purdue Pharma. AstraZeneca developed naloxegol.
This article first appeared on Medscape.com.
Subcutaneously administered methylnaltrexone (MNTX) (Relistor), a peripherally acting mu-opioid receptor antagonist, relieves opioid-induced constipation (OID) in both chronic, noncancer-related illness and cancer-related illness, a new analysis concludes.
“While these are two very different patient groups, the ability to have something to treat OIC in noncancer patients who stay on opioids for whatever reason helps, because [otherwise] these patients are not doing well,” said lead author Eric Shah, MD, motility director for the Dartmouth program at Dartmouth Hitchcock Health, Lebanon, N.H.
Importantly, peripherally acting mu-opioid receptor antagonists such as MNTX do not affect overall pain control to any significant extent, which is “reassuring,” he said in an interview.
These drugs decrease the constipating effects of opioids without reversing CNS-mediated opioid effects, he explained.
“Methylnaltrexone has already been approved for the treatment of OIC in adults with chronic noncancer pain as well as for OIC in adults with advanced illness who are receiving palliative care, which is often the case in patients with cancer-related pain,” he noted.
Dr. Shah discussed the new analysis during PAINWeek 2020, the American Society of Regional Anesthesia and Pain Medicine 19th Annual Pain Medicine Meeting.
The analysis was based on a review of data collected in two previously reported randomized, placebo-controlled studies (study 302 and 4000), which were used to gain approval.
The new analysis shows that “the drug works up front, and the effect is able to be maintained. I think the studies are clinically relevant in that patients are able to have a bowel movement quickly after you give them an injectable formulation when they are vomiting or otherwise can’t tolerate a pill and they are feeling miserable,” Dr. Shah commented. Many patients with OIC are constipated for reasons other than from opioid use. They often have other side effects from opioids, including bloating, nausea, and vomiting.
“When patients go to the emergency room, it’s not just that they are not able to have a bowel movement; they are often also vomiting, so it’s important to have agents that can be given in a manner that avoids the need for oral medication,” Dr. Shah said. MNTX is the only peripherally acting opioid antagonist available in a subcutaneous formulation.
Moreover, if patients are able to control these symptoms at home with an injectable formulation, they may not need to go to the ED for treatment of their gastrointestinal distress, he added.
Viable product
In a comment, Darren Brenner, MD, associate professor of medicine and surgery, Northwestern University, Chicago, who has worked with this subcutaneous formulation, said it is “definitely a viable product.
“The data presented here were in patients with advanced illness receiving palliative care when other laxatives have failed, and the difference and the potential benefit for MNTX is that it is the only peripherally acting mu-opioid receptor antagonist that is approved for advanced cancer,” he added. The other products that are currently approved, naloxegol (Movantik) and naldemedine (Symproic), are both indicated for chronic, noncancer pain.
The other potential benefit of subcutaneous MNTX is that it can work very rapidly for the patients who respond to it. “One of the things investigators did not mention in these two trials but which has been shown in previous studies is that almost half of patients who respond to this drug respond within the first 30 minutes of receiving the injection,” Dr. Brenner said in an interview.
This can be very beneficial in an emergency setting, because it may avoid having patients admitted to hospital. They can be discharged and sent home with enough drug to use on demand, Dr. Brenner suggested.
New analysis of data from studies 302 and 4000
Both studies were carried out in adults with advanced illness and OIC whose conditions were refractory to laxative use. Both of the studies were placebo controlled.
Study 302 involved 78 patients with cancer and 56 patients with noncancer-related OIC. MNTX was given at a dose of 0.15 mg/kg subcutaneously every other day for 2 weeks.
Study 4000 included 152 patients with cancer and OIC and 78 patients with noncancer-related OIC. In this study, the dose of MNTX was based on body weight. Seven or fewer doses of either 8 mg or 12 mg were given subcutaneously for 2 weeks.
The main endpoints of both studies was the proportion of patients who achieved a rescue-free laxation (RFL) response within 4 hours after the first dose and the proportion of patients with an RFL response within 4 hours for two or more of the first four doses within 24 hours.
Dr. Shah explained that RFL is a meaningful clinical endpoint. Patients could achieve a bowel movement with the two prespecified time endpoints in both studies.
Not all patients were hospitalized for OIC, Dr. Shah noted. Entry criteria were strict and included having fewer than three bowel movements during the previous week and no clinically significant laxation (defecation) within 48 hours of receiving the first dose of study drug.
“In both studies, a significantly greater proportion of patients treated with MNTX versus placebo achieved an RFL within 4 hours after the first dose among both cancer and noncancer patients,” the investigators reported.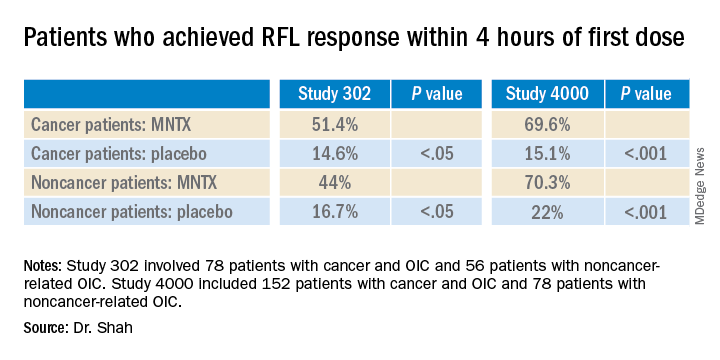
Results were relatively comparable between cancer and noncancer patients who were treated for OIC in study 4000, the investigators noted.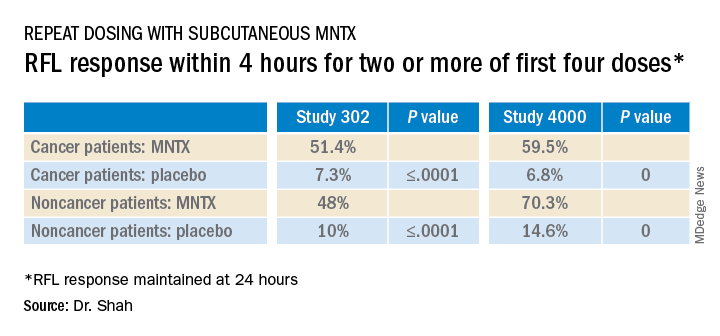
Both studies were sponsored by Salix Pharmaceuticals. Dr. Shah has received travel fees from Salix Pharmaceuticals. Dr. Brenner has served as a consultant for Salix Pharmaceuticals, AstraZeneca, and Purdue Pharma. AstraZeneca developed naloxegol.
This article first appeared on Medscape.com.
Prophylactic HIV treatment in female STI patients is rare
reported Kirk D. Henny, PhD, and colleagues of the Centers for Disease Control and Prevention.
In an effort to quantify HIV testing rates as well as the rate of pre-exposure prophylaxis (PrEP) among women with gonorrhea or syphilis, Dr. Henny and his colleagues performed a multivariate logistic regression analysis of 13,074 female patients aged 15-64 diagnosed with a STI in the absence of HIV. Data was pulled in 2017 from the IBM MarketScan commercial and Medicaid insurance databases, and the research was published in Obstetrics & Gynecology.
Medicaid patients were more likely to be tested for HIV
A total of 3,709 patients with commercial insurance were diagnosed with gonorrhea and 1,696 with syphilis. Among those with Medicaid, 6,172 were diagnosed with gonorrhea and 1,497 with syphilis. Medicaid patients diagnosed with either STI were more likely to be tested for HIV than the commercially insured patients. With an adjusted prevalence ratio, patients commercially insured with had either STI were more likely to be tested for HIV than patients who had no STI. Prophylactic treatment rates were similar in both insurance groups: 0.15% in the commercial insurance group and 0.26% in the Medicaid group. No patient from either group who was diagnosed with gonorrhea or syphilis and subsequently tested for HIV received pre-exposure prophylactic (PrEP) treatment.
STI diagnosis is a significant indicator of future HIV
Female patients diagnosed with either STI are more likely to contract HIV, the researchers noted. They cautioned that their findings of low HIV testing rates and the absence of prophylactic treatment means that “these missed opportunities for health care professionals to intervene with female patients diagnosed with gonorrhea or syphilis might have contributed to HIV infections that could have been averted.”
The researchers also pointed out that, in a recent analysis of pharmacy data, prophylactic prescribing for female patients with clinical indications for PrEP was 6.6%, less than one-third the coverage provided to male patients.
Future research should target understanding “individual and contextual factors associated with low HIV testing” and PrEP treatment in female patients, especially those with STIs, Dr. Henny and his colleagues advised.
In a separate interview, Constance Bohon, MD FACOG, observed: “The authors present data to document the low incidence of pre-exposure prophylaxis in women who are at substantial risk of acquiring HIV and possible causes for the low utilization of this treatment.” It is important to identify barriers to diagnosis, counseling, and treatment, she advised.
“Multicenter studies to determine the best methodologies to improve the identification, management, and treatment of these at-risk women need to be done, and the conclusions disseminated to health care providers caring for women,” Dr. Bohon said.
PrEP is an important, simple strategy for reducing HIV transmission
“Pre-exposure prophylaxis has been demonstrated to decrease HIV acquisition in those at risk by up to 90% when taken appropriately,” and yet prescribing rates are extremely low (2%-6%) in at-risk women and especially women of color. These disparities have only grown over time, with prophylactic prescriptions for women at 5% between 2012 and 2017, compared with 68% for men, Catherine S. Eppes, MD, MPH, and Jennifer McKinney, MD, MPH, said in a related editorial commenting on the Research Letter by Dr. Henny and colleagues in Obstetrics & Gynecology (2020 Dec;136[6]:1080-2).
Given the abundant research demonstrating the importance and ease of prescribing PrEP, the question remains: “why does preexposure prophylaxis uptake remain so low, especially for women and women of color? There are three important issues about preexposure prophylaxis raised by this study: the research gap, the implementation gap, and the effect of systemic racism and bias,” noted Dr. Eppes and Dr. McKinney.
Women constitute a significant portion of the population that would benefit from HIV-prevention strategies, yet they continue to be excluded from research, they noted. “Much focus on research into barriers and implementation interventions for preexposure prophylaxis have focused on men who have sex with men and transgender women,” the authors of the editorial wrote.
Most women eligible for treatment would be willing to consider it if they were aware of the option, but numerous studies have cited a lack of awareness, especially among high-risk women of color in the United States, Dr. Eppes and Dr. McKinney noted.
Clinicians also need to add it to their growing checklist of mandatory appointment discussion topics, the editorialists said. “We propose standardized inclusion of preexposure prophylaxis counseling during reproductive healthcare visits. This could be aided through an electronic medical record-based best practice advisory alert. … Standardized order sets with the medication and laboratory studies necessary for safe monitoring could facilitate ease of incorporating into routine visits,” they suggested.
“Preexposure prophylaxis is extremely effective in preventing HIV, is safe, and is the only prevention method that leaves control entirely in the hands of the female partner. As a specialty, we have a responsibility to make sure our patients know about this option,” the editorialists concluded.
The authors had no financial disclosures to report. Dr. Bohon had no conflicts of interest to report.
SOURCE: Henny KD et al. Obstet Gynecol. 2020 Dec;136(6):1083-5.
reported Kirk D. Henny, PhD, and colleagues of the Centers for Disease Control and Prevention.
In an effort to quantify HIV testing rates as well as the rate of pre-exposure prophylaxis (PrEP) among women with gonorrhea or syphilis, Dr. Henny and his colleagues performed a multivariate logistic regression analysis of 13,074 female patients aged 15-64 diagnosed with a STI in the absence of HIV. Data was pulled in 2017 from the IBM MarketScan commercial and Medicaid insurance databases, and the research was published in Obstetrics & Gynecology.
Medicaid patients were more likely to be tested for HIV
A total of 3,709 patients with commercial insurance were diagnosed with gonorrhea and 1,696 with syphilis. Among those with Medicaid, 6,172 were diagnosed with gonorrhea and 1,497 with syphilis. Medicaid patients diagnosed with either STI were more likely to be tested for HIV than the commercially insured patients. With an adjusted prevalence ratio, patients commercially insured with had either STI were more likely to be tested for HIV than patients who had no STI. Prophylactic treatment rates were similar in both insurance groups: 0.15% in the commercial insurance group and 0.26% in the Medicaid group. No patient from either group who was diagnosed with gonorrhea or syphilis and subsequently tested for HIV received pre-exposure prophylactic (PrEP) treatment.
STI diagnosis is a significant indicator of future HIV
Female patients diagnosed with either STI are more likely to contract HIV, the researchers noted. They cautioned that their findings of low HIV testing rates and the absence of prophylactic treatment means that “these missed opportunities for health care professionals to intervene with female patients diagnosed with gonorrhea or syphilis might have contributed to HIV infections that could have been averted.”
The researchers also pointed out that, in a recent analysis of pharmacy data, prophylactic prescribing for female patients with clinical indications for PrEP was 6.6%, less than one-third the coverage provided to male patients.
Future research should target understanding “individual and contextual factors associated with low HIV testing” and PrEP treatment in female patients, especially those with STIs, Dr. Henny and his colleagues advised.
In a separate interview, Constance Bohon, MD FACOG, observed: “The authors present data to document the low incidence of pre-exposure prophylaxis in women who are at substantial risk of acquiring HIV and possible causes for the low utilization of this treatment.” It is important to identify barriers to diagnosis, counseling, and treatment, she advised.
“Multicenter studies to determine the best methodologies to improve the identification, management, and treatment of these at-risk women need to be done, and the conclusions disseminated to health care providers caring for women,” Dr. Bohon said.
PrEP is an important, simple strategy for reducing HIV transmission
“Pre-exposure prophylaxis has been demonstrated to decrease HIV acquisition in those at risk by up to 90% when taken appropriately,” and yet prescribing rates are extremely low (2%-6%) in at-risk women and especially women of color. These disparities have only grown over time, with prophylactic prescriptions for women at 5% between 2012 and 2017, compared with 68% for men, Catherine S. Eppes, MD, MPH, and Jennifer McKinney, MD, MPH, said in a related editorial commenting on the Research Letter by Dr. Henny and colleagues in Obstetrics & Gynecology (2020 Dec;136[6]:1080-2).
Given the abundant research demonstrating the importance and ease of prescribing PrEP, the question remains: “why does preexposure prophylaxis uptake remain so low, especially for women and women of color? There are three important issues about preexposure prophylaxis raised by this study: the research gap, the implementation gap, and the effect of systemic racism and bias,” noted Dr. Eppes and Dr. McKinney.
Women constitute a significant portion of the population that would benefit from HIV-prevention strategies, yet they continue to be excluded from research, they noted. “Much focus on research into barriers and implementation interventions for preexposure prophylaxis have focused on men who have sex with men and transgender women,” the authors of the editorial wrote.
Most women eligible for treatment would be willing to consider it if they were aware of the option, but numerous studies have cited a lack of awareness, especially among high-risk women of color in the United States, Dr. Eppes and Dr. McKinney noted.
Clinicians also need to add it to their growing checklist of mandatory appointment discussion topics, the editorialists said. “We propose standardized inclusion of preexposure prophylaxis counseling during reproductive healthcare visits. This could be aided through an electronic medical record-based best practice advisory alert. … Standardized order sets with the medication and laboratory studies necessary for safe monitoring could facilitate ease of incorporating into routine visits,” they suggested.
“Preexposure prophylaxis is extremely effective in preventing HIV, is safe, and is the only prevention method that leaves control entirely in the hands of the female partner. As a specialty, we have a responsibility to make sure our patients know about this option,” the editorialists concluded.
The authors had no financial disclosures to report. Dr. Bohon had no conflicts of interest to report.
SOURCE: Henny KD et al. Obstet Gynecol. 2020 Dec;136(6):1083-5.
reported Kirk D. Henny, PhD, and colleagues of the Centers for Disease Control and Prevention.
In an effort to quantify HIV testing rates as well as the rate of pre-exposure prophylaxis (PrEP) among women with gonorrhea or syphilis, Dr. Henny and his colleagues performed a multivariate logistic regression analysis of 13,074 female patients aged 15-64 diagnosed with a STI in the absence of HIV. Data was pulled in 2017 from the IBM MarketScan commercial and Medicaid insurance databases, and the research was published in Obstetrics & Gynecology.
Medicaid patients were more likely to be tested for HIV
A total of 3,709 patients with commercial insurance were diagnosed with gonorrhea and 1,696 with syphilis. Among those with Medicaid, 6,172 were diagnosed with gonorrhea and 1,497 with syphilis. Medicaid patients diagnosed with either STI were more likely to be tested for HIV than the commercially insured patients. With an adjusted prevalence ratio, patients commercially insured with had either STI were more likely to be tested for HIV than patients who had no STI. Prophylactic treatment rates were similar in both insurance groups: 0.15% in the commercial insurance group and 0.26% in the Medicaid group. No patient from either group who was diagnosed with gonorrhea or syphilis and subsequently tested for HIV received pre-exposure prophylactic (PrEP) treatment.
STI diagnosis is a significant indicator of future HIV
Female patients diagnosed with either STI are more likely to contract HIV, the researchers noted. They cautioned that their findings of low HIV testing rates and the absence of prophylactic treatment means that “these missed opportunities for health care professionals to intervene with female patients diagnosed with gonorrhea or syphilis might have contributed to HIV infections that could have been averted.”
The researchers also pointed out that, in a recent analysis of pharmacy data, prophylactic prescribing for female patients with clinical indications for PrEP was 6.6%, less than one-third the coverage provided to male patients.
Future research should target understanding “individual and contextual factors associated with low HIV testing” and PrEP treatment in female patients, especially those with STIs, Dr. Henny and his colleagues advised.
In a separate interview, Constance Bohon, MD FACOG, observed: “The authors present data to document the low incidence of pre-exposure prophylaxis in women who are at substantial risk of acquiring HIV and possible causes for the low utilization of this treatment.” It is important to identify barriers to diagnosis, counseling, and treatment, she advised.
“Multicenter studies to determine the best methodologies to improve the identification, management, and treatment of these at-risk women need to be done, and the conclusions disseminated to health care providers caring for women,” Dr. Bohon said.
PrEP is an important, simple strategy for reducing HIV transmission
“Pre-exposure prophylaxis has been demonstrated to decrease HIV acquisition in those at risk by up to 90% when taken appropriately,” and yet prescribing rates are extremely low (2%-6%) in at-risk women and especially women of color. These disparities have only grown over time, with prophylactic prescriptions for women at 5% between 2012 and 2017, compared with 68% for men, Catherine S. Eppes, MD, MPH, and Jennifer McKinney, MD, MPH, said in a related editorial commenting on the Research Letter by Dr. Henny and colleagues in Obstetrics & Gynecology (2020 Dec;136[6]:1080-2).
Given the abundant research demonstrating the importance and ease of prescribing PrEP, the question remains: “why does preexposure prophylaxis uptake remain so low, especially for women and women of color? There are three important issues about preexposure prophylaxis raised by this study: the research gap, the implementation gap, and the effect of systemic racism and bias,” noted Dr. Eppes and Dr. McKinney.
Women constitute a significant portion of the population that would benefit from HIV-prevention strategies, yet they continue to be excluded from research, they noted. “Much focus on research into barriers and implementation interventions for preexposure prophylaxis have focused on men who have sex with men and transgender women,” the authors of the editorial wrote.
Most women eligible for treatment would be willing to consider it if they were aware of the option, but numerous studies have cited a lack of awareness, especially among high-risk women of color in the United States, Dr. Eppes and Dr. McKinney noted.
Clinicians also need to add it to their growing checklist of mandatory appointment discussion topics, the editorialists said. “We propose standardized inclusion of preexposure prophylaxis counseling during reproductive healthcare visits. This could be aided through an electronic medical record-based best practice advisory alert. … Standardized order sets with the medication and laboratory studies necessary for safe monitoring could facilitate ease of incorporating into routine visits,” they suggested.
“Preexposure prophylaxis is extremely effective in preventing HIV, is safe, and is the only prevention method that leaves control entirely in the hands of the female partner. As a specialty, we have a responsibility to make sure our patients know about this option,” the editorialists concluded.
The authors had no financial disclosures to report. Dr. Bohon had no conflicts of interest to report.
SOURCE: Henny KD et al. Obstet Gynecol. 2020 Dec;136(6):1083-5.
FROM OBSTETRICS & GYNECOLOGY
Liquid oxygen recommended for mobile patients with lung disease
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
People with chronic lung disease who need significant amounts of oxygen should be able to take it in liquid form when they are able to leave home, according to a new guideline from the American Thoracic Society.
“For those patients, often the other types of devices either can’t supply enough oxygen or are not portable enough,” said Anne Holland, PT, PhD, a professor of physiotherapy at Monash University and Alfred Hospital in Melbourne. “They’re heavy and cumbersome to use.”
Dr. Holland and colleagues also gave a more general recommendation to prescribe ambulatory oxygen – though not necessarily in liquid form – for adults with chronic obstructive pulmonary disease (COPD) or interstitial lung disease (ILD) who have severe exertional room air hypoxemia.
They published the recommendations as part of the ATS’ first-ever guideline on home oxygen therapy for adults with chronic lung disease in the American Journal of Respiratory and Critical Care Medicine.
The ATS identified the need for an updated guideline because of new research, and because an online survey of almost 2,000 U.S. oxygen users showed they were having problems accessing and using oxygen.
For long-term oxygen therapy, the guideline reinforces what most practitioners are already doing, Dr. Holland said. It recommends that adults with COPD or ILD who have severe chronic resting room air hypoxemia receive oxygen therapy at least 15 hours per day.
On the other hand, in adults with COPD who have moderate chronic resting room-air hypoxemia, the guideline recommends against long-term oxygen therapy.
The recommendation to prescribe ambulatory oxygen for people with severe exertional room-air hypoxemia may have more effect on practice, Dr. Holland said. Laboratory-based tests have suggested oxygen can improve exercise capacity, but clinical trials used during daily life have had inconsistent results.
The evidence is particularly lacking for patients with ILD, Dr. Holland said in an interview. “It’s such an important part of practice to maintain oxygen therapy that it’s ethically very difficult to conduct such a trial. So, we did have to make use of indirect evidence from patients with COPD” for the guidelines.
The portable equipment comes with burdens, including managing its weight and bulk, social stigma, fear of cylinders running out, and equipment noise.
“We tried to clearly set out both the benefits and burdens of that therapy and made a conditional recommendation, and also a really strong call for shared decision-making with patients and health professionals,” Dr. Holland said.
In addition to looking at the evidence, the panel took into consideration the concerns identified by patients. This included the challenge of figuring out how to use the equipment. “All the oxygen equipment was ‘dumped’ on me,” wrote one oxygen user quoted in the guideline. “I knew nothing and was in a daze. I am sure that the delivery guy gave me some instructions when it was delivered but I retained nothing.”
For this reason, the guideline describes instruction and training on the use and maintenance of the equipment, including smoking cessation, fire prevention, and tripping hazards, as a “best practice.”
Nothing about the guideline is surprising, said MeiLan K. Han, MD, a spokesperson for the American Lung Association and professor of pulmonary and critical care medicine at the University of Michigan Health System in Ann Arbor. “I don’t think they’ve actually come to any new conclusion,” she said in an interview. “This is pretty much how I practice already.”
But the guideline could have an effect on policy, she said. The panel noted research showing that lower Medicare reimbursement to durable medical equipment companies since 2011 has forced many patients to switch from small, easily portable liquid oxygen to home-fill oxygen systems that include heavy cylinders.
“The impact of this decline in the availability and adequacy of portable oxygen devices in the United States has been profound,” Dr. Holland and colleagues wrote. “Supplemental oxygen users reported numerous problems, with the overarching theme being restricted mobility and isolation due to inadequate portable options.”
For this reason, the guideline recommends liquid oxygen for patients with chronic lung disease who are mobile outside of the home and require continuous oxygen flow rates of >3 L/min during exertion.
Many of Dr. Han’s patients have struggled with this problem, she said. “The clunkiest, most painful form of ‘ambulatory oxygen’ are these really large metal cylinders. They’re huge. And you have to carry them on a cart. It’s portable in theory only.”
Some of her patients have resorted to buying their own equipment on eBay, she said.
The authors report multiple disclosures including serving as advisory board members to foundations and pharmaceutical companies, and some are company employees or stockholders.
A version of this article originally appeared on Medscape.com.
TNF inhibitor–induced psoriasis treatment algorithm maintains TNF inhibitor if possible
In a single-center retrospective analysis of 102 patients with psoriasis induced by tumor necrosis factor (TNF) inhibitors, most cases improved or resolved with use of topical medications or with discontinuation of the inciting TNF inhibitor, with or without other interventions. All patients were treated and diagnosed by dermatologists.
While TNF inhibitors have revolutionized management of numerous debilitating chronic inflammatory diseases, they are associated with mild and potentially serious adverse reactions, including de novo psoriasiform eruptions, noted Sean E. Mazloom, MD, and colleagues, at the Cleveland Clinic, Cleveland, Ohio, in the Journal of the American Academy of Dermatology. Despite the fact that it has been more than 15 years since the first reports of TNF inhibitor-induced psoriasis, optimal treatment strategies still remain poorly understood.
IBD and RA most common
Dr. Mazloom and colleagues identified 102 patients (median onset, 41 years; 72.5% female) with TNF inhibitor-induced psoriasis seen at a single tertiary care institution (the Cleveland Clinic) over a 10-year period. The authors proposed a treatment algorithm based on their findings.
Inciting TNF inhibitors were prescribed most commonly for inflammatory bowel disease (IBD) (52%) and rheumatoid arthritis (RA) (24.5%). The most common inciting TNF inhibitor was infliximab (52%). TNF inhibitor-induced psoriasis improved or resolved with topical medications alone in 63.5% of patients, and cyclosporine and methotrexate (10 mg weekly) were often effective (cyclosporine in five of five patients; methotrexate in 7 of 13) if topicals failed.
Noting that the success with topicals in this cohort exceeded that of earlier reports, the authors suggested that more accurate diagnoses and optimal strategies attributable to the involvement of dermatologists may be explanatory.
In 67% of refractory cases, discontinuation of the inciting TNF inhibitor with or without other interventions improved or resolved TNF inhibitor-induced psoriasis. With switching of TNF inhibitors, persistence or worsening of TNF inhibitor-induced psoriasis was reported in 16 of 25 patients (64%).
Algorithm aims at balancing control
The treatment algorithm proposed by Dr. Mazloom and colleagues aims at balancing control of the primary disease with minimization of skin symptom discomfort and continuation of the inciting TNF inhibitor if possible. Only with cyclosporine or methotrexate failure amid severe symptoms and less-than-optimal primary disease control should TNF inhibitors be discontinued and biologics and/or small-molecule inhibitors with alternative mechanisms of action be introduced. Transitioning to other TNF inhibitors may be tried before alternative strategies when the underlying disease is well-controlled but TNF inhibitor-induced psoriasis remains severe.
“Most dermatologists who see TNF-induced psoriasis often are likely already using strategies like the one proposed in the algorithm,” commented senior author Anthony Fernandez, MD, PhD, of the Cleveland (Ohio) Clinic, in an interview. “The concern is over those who may not see TNF inhibitor-induced psoriasis very often, and who may, as a knee-jerk response to TNF-induced psoriasis, stop the inciting medication. When strong side effects occur in IBD and RA, it’s critical to know how well the TNF inhibitor is controlling the underlying disease because lack of control can lead to permanent damage.”
Risk to benefit ratio favors retaining TNF inhibitors
The dermatologist’s goal, if the TNF inhibitor is working well, should be to exhaust all reasonable options to control the psoriasiform eruption and keep the patient on the TNF inhibitor rather than turn to potentially less effective alternatives, Dr. Fernandez added. “The risk:benefit ratio still usually favors adding more immune therapies to treat these reactions in order to enable patients to stay” on their TNF inhibitors.
Study authors disclosed no direct funding for the study. Dr Fernandez, the senior author, receives research funding from Pfizer, Mallinckrodt, and Novartis, consults for AbbVie and Celgene, and is a speaker for AbbVie and Mallinckrodt.
SOURCE: Mazloom SE et al. J Am Acad Dermatol. 2020 Dec;83(6):1590-8.
In a single-center retrospective analysis of 102 patients with psoriasis induced by tumor necrosis factor (TNF) inhibitors, most cases improved or resolved with use of topical medications or with discontinuation of the inciting TNF inhibitor, with or without other interventions. All patients were treated and diagnosed by dermatologists.
While TNF inhibitors have revolutionized management of numerous debilitating chronic inflammatory diseases, they are associated with mild and potentially serious adverse reactions, including de novo psoriasiform eruptions, noted Sean E. Mazloom, MD, and colleagues, at the Cleveland Clinic, Cleveland, Ohio, in the Journal of the American Academy of Dermatology. Despite the fact that it has been more than 15 years since the first reports of TNF inhibitor-induced psoriasis, optimal treatment strategies still remain poorly understood.
IBD and RA most common
Dr. Mazloom and colleagues identified 102 patients (median onset, 41 years; 72.5% female) with TNF inhibitor-induced psoriasis seen at a single tertiary care institution (the Cleveland Clinic) over a 10-year period. The authors proposed a treatment algorithm based on their findings.
Inciting TNF inhibitors were prescribed most commonly for inflammatory bowel disease (IBD) (52%) and rheumatoid arthritis (RA) (24.5%). The most common inciting TNF inhibitor was infliximab (52%). TNF inhibitor-induced psoriasis improved or resolved with topical medications alone in 63.5% of patients, and cyclosporine and methotrexate (10 mg weekly) were often effective (cyclosporine in five of five patients; methotrexate in 7 of 13) if topicals failed.
Noting that the success with topicals in this cohort exceeded that of earlier reports, the authors suggested that more accurate diagnoses and optimal strategies attributable to the involvement of dermatologists may be explanatory.
In 67% of refractory cases, discontinuation of the inciting TNF inhibitor with or without other interventions improved or resolved TNF inhibitor-induced psoriasis. With switching of TNF inhibitors, persistence or worsening of TNF inhibitor-induced psoriasis was reported in 16 of 25 patients (64%).
Algorithm aims at balancing control
The treatment algorithm proposed by Dr. Mazloom and colleagues aims at balancing control of the primary disease with minimization of skin symptom discomfort and continuation of the inciting TNF inhibitor if possible. Only with cyclosporine or methotrexate failure amid severe symptoms and less-than-optimal primary disease control should TNF inhibitors be discontinued and biologics and/or small-molecule inhibitors with alternative mechanisms of action be introduced. Transitioning to other TNF inhibitors may be tried before alternative strategies when the underlying disease is well-controlled but TNF inhibitor-induced psoriasis remains severe.
“Most dermatologists who see TNF-induced psoriasis often are likely already using strategies like the one proposed in the algorithm,” commented senior author Anthony Fernandez, MD, PhD, of the Cleveland (Ohio) Clinic, in an interview. “The concern is over those who may not see TNF inhibitor-induced psoriasis very often, and who may, as a knee-jerk response to TNF-induced psoriasis, stop the inciting medication. When strong side effects occur in IBD and RA, it’s critical to know how well the TNF inhibitor is controlling the underlying disease because lack of control can lead to permanent damage.”
Risk to benefit ratio favors retaining TNF inhibitors
The dermatologist’s goal, if the TNF inhibitor is working well, should be to exhaust all reasonable options to control the psoriasiform eruption and keep the patient on the TNF inhibitor rather than turn to potentially less effective alternatives, Dr. Fernandez added. “The risk:benefit ratio still usually favors adding more immune therapies to treat these reactions in order to enable patients to stay” on their TNF inhibitors.
Study authors disclosed no direct funding for the study. Dr Fernandez, the senior author, receives research funding from Pfizer, Mallinckrodt, and Novartis, consults for AbbVie and Celgene, and is a speaker for AbbVie and Mallinckrodt.
SOURCE: Mazloom SE et al. J Am Acad Dermatol. 2020 Dec;83(6):1590-8.
In a single-center retrospective analysis of 102 patients with psoriasis induced by tumor necrosis factor (TNF) inhibitors, most cases improved or resolved with use of topical medications or with discontinuation of the inciting TNF inhibitor, with or without other interventions. All patients were treated and diagnosed by dermatologists.
While TNF inhibitors have revolutionized management of numerous debilitating chronic inflammatory diseases, they are associated with mild and potentially serious adverse reactions, including de novo psoriasiform eruptions, noted Sean E. Mazloom, MD, and colleagues, at the Cleveland Clinic, Cleveland, Ohio, in the Journal of the American Academy of Dermatology. Despite the fact that it has been more than 15 years since the first reports of TNF inhibitor-induced psoriasis, optimal treatment strategies still remain poorly understood.
IBD and RA most common
Dr. Mazloom and colleagues identified 102 patients (median onset, 41 years; 72.5% female) with TNF inhibitor-induced psoriasis seen at a single tertiary care institution (the Cleveland Clinic) over a 10-year period. The authors proposed a treatment algorithm based on their findings.
Inciting TNF inhibitors were prescribed most commonly for inflammatory bowel disease (IBD) (52%) and rheumatoid arthritis (RA) (24.5%). The most common inciting TNF inhibitor was infliximab (52%). TNF inhibitor-induced psoriasis improved or resolved with topical medications alone in 63.5% of patients, and cyclosporine and methotrexate (10 mg weekly) were often effective (cyclosporine in five of five patients; methotrexate in 7 of 13) if topicals failed.
Noting that the success with topicals in this cohort exceeded that of earlier reports, the authors suggested that more accurate diagnoses and optimal strategies attributable to the involvement of dermatologists may be explanatory.
In 67% of refractory cases, discontinuation of the inciting TNF inhibitor with or without other interventions improved or resolved TNF inhibitor-induced psoriasis. With switching of TNF inhibitors, persistence or worsening of TNF inhibitor-induced psoriasis was reported in 16 of 25 patients (64%).
Algorithm aims at balancing control
The treatment algorithm proposed by Dr. Mazloom and colleagues aims at balancing control of the primary disease with minimization of skin symptom discomfort and continuation of the inciting TNF inhibitor if possible. Only with cyclosporine or methotrexate failure amid severe symptoms and less-than-optimal primary disease control should TNF inhibitors be discontinued and biologics and/or small-molecule inhibitors with alternative mechanisms of action be introduced. Transitioning to other TNF inhibitors may be tried before alternative strategies when the underlying disease is well-controlled but TNF inhibitor-induced psoriasis remains severe.
“Most dermatologists who see TNF-induced psoriasis often are likely already using strategies like the one proposed in the algorithm,” commented senior author Anthony Fernandez, MD, PhD, of the Cleveland (Ohio) Clinic, in an interview. “The concern is over those who may not see TNF inhibitor-induced psoriasis very often, and who may, as a knee-jerk response to TNF-induced psoriasis, stop the inciting medication. When strong side effects occur in IBD and RA, it’s critical to know how well the TNF inhibitor is controlling the underlying disease because lack of control can lead to permanent damage.”
Risk to benefit ratio favors retaining TNF inhibitors
The dermatologist’s goal, if the TNF inhibitor is working well, should be to exhaust all reasonable options to control the psoriasiform eruption and keep the patient on the TNF inhibitor rather than turn to potentially less effective alternatives, Dr. Fernandez added. “The risk:benefit ratio still usually favors adding more immune therapies to treat these reactions in order to enable patients to stay” on their TNF inhibitors.
Study authors disclosed no direct funding for the study. Dr Fernandez, the senior author, receives research funding from Pfizer, Mallinckrodt, and Novartis, consults for AbbVie and Celgene, and is a speaker for AbbVie and Mallinckrodt.
SOURCE: Mazloom SE et al. J Am Acad Dermatol. 2020 Dec;83(6):1590-8.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Golimumab preserves insulin production in type 1 diabetes
The human monoclonal antibody golimumab (Simponi) preserved endogenous insulin secretion in patients with new-onset type 1 diabetes and reduced their exogenous insulin requirements at 1 year, newly published phase 2 data indicate.
Results from the multicenter, double-blind, placebo-controlled trial were first reported as a poster at the virtual American Diabetes Association 80th Scientific Sessions in June. They were published online Nov. 18 in the New England Journal of Medicine.
In the 52-week study of 84 children and adults with new-onset type 1 diabetes, those given golimumab injections every 2 weeks had significantly higher levels of C-peptide, a marker of insulin secretion, and required less injected or infused insulin than did those who received placebo injections. There were no treatment-associated serious adverse events.
Golimumab is a human monoclonal antibody specific for tumor necrosis factor–alpha. It is approved for the treatment of several autoimmune diseases, including rheumatoid arthritis and ulcerative colitis, in the United States, Europe, and elsewhere.
An intermediate step toward a cure
Although none of the patients were able to stop taking insulin entirely, the results have important clinical implications, lead author Teresa Quattrin, MD, said in an interview.
“People want a cure, but the fact is, a cure is not available yet. So, this is an intermediate step towards a cure.... There are advantages to being on a small insulin dose,” including lower rates of hypoglycemia and maintenance of intraportal insulin, said Dr. Quattrin, of the State University of New York at Buffalo.
But in an accompanying editorial, Domenico Accili, MD, points to potential risks from immunotherapy and from attempting additional interventions at an “emotionally fraught” time when patients and families are coping with the new diabetes diagnosis.
He said of golimumab, “the effect is actually very small. ... There’s nothing wrong in and of itself with improving those outcomes. I just wouldn’t assign them as game changers.”
If this or a similar immunotherapeutic intervention were approved for this indication, “I would tell patients it exists and let them make the decision whether they want to try it. I wouldn’t say you must try it,” said Dr. Accili, of the Columbia University Diabetes and Endocrinology Research Center, New York.
With golimumab, higher C-peptide, lower insulin requirement
Of the 84 patients, who ranged in age from 6 to 21 years, 56 were randomly assigned within 100 days of being diagnosed with type 1 diabetes to receive golimumab, and 28 were assigned to receive placebo injections, given every 2 weeks.
The drug resulted in lower insulin use (0.51U/Kg per day vs. 0.69 U/kg per day), and the increase in insulin use over 52 weeks was less with golimumab than with placebo (0.07 vs. 0.24 U/kg per day; P = .001).
The mean percent decrease of C-peptide production from baseline was 12% with golimumab versus 56% with placebo.
Although the mean number of overall hypoglycemic events was similar, the mean number of level 2 hypoglycemic events (<54 mg/dL) was 36% lower with golimumab (11.5 vs. 17.6). There were no severe cases of hypoglycemia in either group.
No severe or serious infections occurred in either group, although mild to moderate infections were reported in 71% with golimumab versus 61% with placebo. More patients in the golimumab group experienced a decrease in neutrophils (29% vs. 19%).
Immunotherapy: Which one, and when should it start?
These findings come on the heels of the 2019 landmark results with another monoclonal antibody, the investigational anti-CD3 teplizumab (PRV-031). Among patients at risk, a diagnosis of type 1 diabetes was delayed by 2 years, and continued benefit was seen at 3 years.
However, Dr. Quattrin said teplizumab is limited by the fact that it must be administered via a 14-day infusion, whereas golimumab can be injected by patients themselves at home.
Moreover, the phase 2 teplizumab study was conducted in people who had antibodies that placed them at high risk for type 1 diabetes, but those patients did not yet have the condition. They were identified because they had close relatives with type 1 diabetes and were enrolled in the federally funded TrialNet screening program.
Dr. Quattrin is now participating in an ongoing phase 3 study of teplizumab that involves patients newly diagnosed with type 1 diabetes.
A Janssen spokesperson said in an interview that the company isn’t planning to further develop golimumab for use in type 1 diabetes.
“Our focus is to apply insights from the phase 2 ... proof-of-concept study to progress what we believe are novel, immunologically targeted pipeline candidates in stage 2 disease or presymptomatic stages of type 1 diabetes, which is consistent with our mission to intercept and prevent type 1 diabetes,” the spokesperson said.
To identify more individuals at risk for type 1 diabetes beyond the close relatives of those who already have it, so as to be able to intervene at a presymptomatic stage, Janssen is organizing a public-private effort to advocate for routine population screening for type 1 diabetes–related autoantibodies.
Dr. Quattrin said: “Preserving some insulin is key. Having somebody with beta cell functioning still is an intermediate step to a cure and will make their life easier, and that’s what people should care about.”
Dr. Accili, who cofounded and leads a company working on a novel approach to type 1 diabetes treatment, writes in his editorial: “We should also be mindful that this treatment debate is first world–centric.
“Current treatments for type 1 diabetes require resources not readily available in most parts of the world, where something as simple as refrigeration of insulin can become a logistic nightmare. While combinations of [approaches] tailored to individual risk and potential benefits are likely to make inroads in clinical practice, the need for a simpler, safer, and equally effective alternative to insulin remains,” he wrote.
Dr. Quattrin is a researcher and consultant for Janssen and conducts clinical trials for Provention Bio, Opko, and Ascendis. Dr. Accili is founder and director of Forkhead Therapeutics.
A version of this article originally appeared on Medscape.com.
The human monoclonal antibody golimumab (Simponi) preserved endogenous insulin secretion in patients with new-onset type 1 diabetes and reduced their exogenous insulin requirements at 1 year, newly published phase 2 data indicate.
Results from the multicenter, double-blind, placebo-controlled trial were first reported as a poster at the virtual American Diabetes Association 80th Scientific Sessions in June. They were published online Nov. 18 in the New England Journal of Medicine.
In the 52-week study of 84 children and adults with new-onset type 1 diabetes, those given golimumab injections every 2 weeks had significantly higher levels of C-peptide, a marker of insulin secretion, and required less injected or infused insulin than did those who received placebo injections. There were no treatment-associated serious adverse events.
Golimumab is a human monoclonal antibody specific for tumor necrosis factor–alpha. It is approved for the treatment of several autoimmune diseases, including rheumatoid arthritis and ulcerative colitis, in the United States, Europe, and elsewhere.
An intermediate step toward a cure
Although none of the patients were able to stop taking insulin entirely, the results have important clinical implications, lead author Teresa Quattrin, MD, said in an interview.
“People want a cure, but the fact is, a cure is not available yet. So, this is an intermediate step towards a cure.... There are advantages to being on a small insulin dose,” including lower rates of hypoglycemia and maintenance of intraportal insulin, said Dr. Quattrin, of the State University of New York at Buffalo.
But in an accompanying editorial, Domenico Accili, MD, points to potential risks from immunotherapy and from attempting additional interventions at an “emotionally fraught” time when patients and families are coping with the new diabetes diagnosis.
He said of golimumab, “the effect is actually very small. ... There’s nothing wrong in and of itself with improving those outcomes. I just wouldn’t assign them as game changers.”
If this or a similar immunotherapeutic intervention were approved for this indication, “I would tell patients it exists and let them make the decision whether they want to try it. I wouldn’t say you must try it,” said Dr. Accili, of the Columbia University Diabetes and Endocrinology Research Center, New York.
With golimumab, higher C-peptide, lower insulin requirement
Of the 84 patients, who ranged in age from 6 to 21 years, 56 were randomly assigned within 100 days of being diagnosed with type 1 diabetes to receive golimumab, and 28 were assigned to receive placebo injections, given every 2 weeks.
The drug resulted in lower insulin use (0.51U/Kg per day vs. 0.69 U/kg per day), and the increase in insulin use over 52 weeks was less with golimumab than with placebo (0.07 vs. 0.24 U/kg per day; P = .001).
The mean percent decrease of C-peptide production from baseline was 12% with golimumab versus 56% with placebo.
Although the mean number of overall hypoglycemic events was similar, the mean number of level 2 hypoglycemic events (<54 mg/dL) was 36% lower with golimumab (11.5 vs. 17.6). There were no severe cases of hypoglycemia in either group.
No severe or serious infections occurred in either group, although mild to moderate infections were reported in 71% with golimumab versus 61% with placebo. More patients in the golimumab group experienced a decrease in neutrophils (29% vs. 19%).
Immunotherapy: Which one, and when should it start?
These findings come on the heels of the 2019 landmark results with another monoclonal antibody, the investigational anti-CD3 teplizumab (PRV-031). Among patients at risk, a diagnosis of type 1 diabetes was delayed by 2 years, and continued benefit was seen at 3 years.
However, Dr. Quattrin said teplizumab is limited by the fact that it must be administered via a 14-day infusion, whereas golimumab can be injected by patients themselves at home.
Moreover, the phase 2 teplizumab study was conducted in people who had antibodies that placed them at high risk for type 1 diabetes, but those patients did not yet have the condition. They were identified because they had close relatives with type 1 diabetes and were enrolled in the federally funded TrialNet screening program.
Dr. Quattrin is now participating in an ongoing phase 3 study of teplizumab that involves patients newly diagnosed with type 1 diabetes.
A Janssen spokesperson said in an interview that the company isn’t planning to further develop golimumab for use in type 1 diabetes.
“Our focus is to apply insights from the phase 2 ... proof-of-concept study to progress what we believe are novel, immunologically targeted pipeline candidates in stage 2 disease or presymptomatic stages of type 1 diabetes, which is consistent with our mission to intercept and prevent type 1 diabetes,” the spokesperson said.
To identify more individuals at risk for type 1 diabetes beyond the close relatives of those who already have it, so as to be able to intervene at a presymptomatic stage, Janssen is organizing a public-private effort to advocate for routine population screening for type 1 diabetes–related autoantibodies.
Dr. Quattrin said: “Preserving some insulin is key. Having somebody with beta cell functioning still is an intermediate step to a cure and will make their life easier, and that’s what people should care about.”
Dr. Accili, who cofounded and leads a company working on a novel approach to type 1 diabetes treatment, writes in his editorial: “We should also be mindful that this treatment debate is first world–centric.
“Current treatments for type 1 diabetes require resources not readily available in most parts of the world, where something as simple as refrigeration of insulin can become a logistic nightmare. While combinations of [approaches] tailored to individual risk and potential benefits are likely to make inroads in clinical practice, the need for a simpler, safer, and equally effective alternative to insulin remains,” he wrote.
Dr. Quattrin is a researcher and consultant for Janssen and conducts clinical trials for Provention Bio, Opko, and Ascendis. Dr. Accili is founder and director of Forkhead Therapeutics.
A version of this article originally appeared on Medscape.com.
The human monoclonal antibody golimumab (Simponi) preserved endogenous insulin secretion in patients with new-onset type 1 diabetes and reduced their exogenous insulin requirements at 1 year, newly published phase 2 data indicate.
Results from the multicenter, double-blind, placebo-controlled trial were first reported as a poster at the virtual American Diabetes Association 80th Scientific Sessions in June. They were published online Nov. 18 in the New England Journal of Medicine.
In the 52-week study of 84 children and adults with new-onset type 1 diabetes, those given golimumab injections every 2 weeks had significantly higher levels of C-peptide, a marker of insulin secretion, and required less injected or infused insulin than did those who received placebo injections. There were no treatment-associated serious adverse events.
Golimumab is a human monoclonal antibody specific for tumor necrosis factor–alpha. It is approved for the treatment of several autoimmune diseases, including rheumatoid arthritis and ulcerative colitis, in the United States, Europe, and elsewhere.
An intermediate step toward a cure
Although none of the patients were able to stop taking insulin entirely, the results have important clinical implications, lead author Teresa Quattrin, MD, said in an interview.
“People want a cure, but the fact is, a cure is not available yet. So, this is an intermediate step towards a cure.... There are advantages to being on a small insulin dose,” including lower rates of hypoglycemia and maintenance of intraportal insulin, said Dr. Quattrin, of the State University of New York at Buffalo.
But in an accompanying editorial, Domenico Accili, MD, points to potential risks from immunotherapy and from attempting additional interventions at an “emotionally fraught” time when patients and families are coping with the new diabetes diagnosis.
He said of golimumab, “the effect is actually very small. ... There’s nothing wrong in and of itself with improving those outcomes. I just wouldn’t assign them as game changers.”
If this or a similar immunotherapeutic intervention were approved for this indication, “I would tell patients it exists and let them make the decision whether they want to try it. I wouldn’t say you must try it,” said Dr. Accili, of the Columbia University Diabetes and Endocrinology Research Center, New York.
With golimumab, higher C-peptide, lower insulin requirement
Of the 84 patients, who ranged in age from 6 to 21 years, 56 were randomly assigned within 100 days of being diagnosed with type 1 diabetes to receive golimumab, and 28 were assigned to receive placebo injections, given every 2 weeks.
The drug resulted in lower insulin use (0.51U/Kg per day vs. 0.69 U/kg per day), and the increase in insulin use over 52 weeks was less with golimumab than with placebo (0.07 vs. 0.24 U/kg per day; P = .001).
The mean percent decrease of C-peptide production from baseline was 12% with golimumab versus 56% with placebo.
Although the mean number of overall hypoglycemic events was similar, the mean number of level 2 hypoglycemic events (<54 mg/dL) was 36% lower with golimumab (11.5 vs. 17.6). There were no severe cases of hypoglycemia in either group.
No severe or serious infections occurred in either group, although mild to moderate infections were reported in 71% with golimumab versus 61% with placebo. More patients in the golimumab group experienced a decrease in neutrophils (29% vs. 19%).
Immunotherapy: Which one, and when should it start?
These findings come on the heels of the 2019 landmark results with another monoclonal antibody, the investigational anti-CD3 teplizumab (PRV-031). Among patients at risk, a diagnosis of type 1 diabetes was delayed by 2 years, and continued benefit was seen at 3 years.
However, Dr. Quattrin said teplizumab is limited by the fact that it must be administered via a 14-day infusion, whereas golimumab can be injected by patients themselves at home.
Moreover, the phase 2 teplizumab study was conducted in people who had antibodies that placed them at high risk for type 1 diabetes, but those patients did not yet have the condition. They were identified because they had close relatives with type 1 diabetes and were enrolled in the federally funded TrialNet screening program.
Dr. Quattrin is now participating in an ongoing phase 3 study of teplizumab that involves patients newly diagnosed with type 1 diabetes.
A Janssen spokesperson said in an interview that the company isn’t planning to further develop golimumab for use in type 1 diabetes.
“Our focus is to apply insights from the phase 2 ... proof-of-concept study to progress what we believe are novel, immunologically targeted pipeline candidates in stage 2 disease or presymptomatic stages of type 1 diabetes, which is consistent with our mission to intercept and prevent type 1 diabetes,” the spokesperson said.
To identify more individuals at risk for type 1 diabetes beyond the close relatives of those who already have it, so as to be able to intervene at a presymptomatic stage, Janssen is organizing a public-private effort to advocate for routine population screening for type 1 diabetes–related autoantibodies.
Dr. Quattrin said: “Preserving some insulin is key. Having somebody with beta cell functioning still is an intermediate step to a cure and will make their life easier, and that’s what people should care about.”
Dr. Accili, who cofounded and leads a company working on a novel approach to type 1 diabetes treatment, writes in his editorial: “We should also be mindful that this treatment debate is first world–centric.
“Current treatments for type 1 diabetes require resources not readily available in most parts of the world, where something as simple as refrigeration of insulin can become a logistic nightmare. While combinations of [approaches] tailored to individual risk and potential benefits are likely to make inroads in clinical practice, the need for a simpler, safer, and equally effective alternative to insulin remains,” he wrote.
Dr. Quattrin is a researcher and consultant for Janssen and conducts clinical trials for Provention Bio, Opko, and Ascendis. Dr. Accili is founder and director of Forkhead Therapeutics.
A version of this article originally appeared on Medscape.com.
Statins beneficial in elderly, guidelines should be strengthened
Contrary to historical evidence, two new studies show.
“By contrast with previous historical studies, our data show that LDL cholesterol is an important risk factor for myocardial infarction and atherosclerotic cardiovascular disease in a contemporary primary prevention cohort of individuals aged 70 to 100 years,” Borge Nordestgaard, MD, of the University of Copenhagen, and colleagues noted in the first of the two studies, published this week in the Lancet.
“By lowering LDL cholesterol in healthy individuals aged 70-100 years, the potential for preventing myocardial infarctions and atherosclerotic cardiovascular disease is huge, and at a substantially lower number needed to treat when compared with those aged 20-69 years,” they added.
“These findings support the concept of the cumulative burden of LDL cholesterol over one’s lifetime and the progressive increase in risk for atherosclerotic cardiovascular disease, including myocardial infarction, with age,” added Frederick J. Raal, PhD, and Farzahna Mohamed, MB BCh, of the University of the Witwatersrand, Johannesburg, South Africa, in an editorial published with both new studies in the Lancet (2020 Nov 10. doi: 10.1016/S0140-6736[20]32333-3).
The studies underscore the need for clinicians to consider continued risks associated with elevated LDL cholesterol in older age, they stressed, adding that statins are also beneficial for younger persons at risk to prevent conditions from worsening.
“The average age of patients in all the trials analyzed was older than 60 years, an age when atherosclerotic cardiovascular disease is already well established,” the editorialists wrote.
“Lipid-lowering therapy should be initiated at a younger age, preferably before age 40 years, in those at risk to delay the onset of atherosclerosis, rather than try to manage the condition once fully established or advanced,” they stressed.
No RCTs have included patients older than 70
For persons aged 40-75 years, elevated LDL cholesterol levels are a known risk factor for MI and atherosclerotic cardiovascular disease, and there is consensus in guidelines regarding treatment with statins.
However, the risk for people older than 70 is controversial. Some studies show little or no association between elevated LDL cholesterol levels and an increased risk for MI.
Contributing to the uncertainty is that few of the randomized, controlled trials that have investigated the question have included patients aged older than 70 years.
As a consequence, many practice guidelines have noted that the level of evidence in older patients is low, and some organizations have lowered the strength of recommendations regarding the treatment for older patients in comparison with younger patients.
Primary prevention: CV events increase with elevated LDL cholesterol in older age
Dr. Nordestgaard and colleagues studied data on 91,131 people living in Copenhagen who did not have atherosclerotic cardiovascular disease or diabetes at baseline and were not taking statins.
Of the participants, 10,592 were aged 70-79 years, and 3,188 participants were aged 80-100 years.
Over an average follow-up period of 7.7 years, 1,515 participants had a first MI, and 3,389 developed atherosclerotic cardiovascular disease.
In the primary-prevention cohort, after multivariate adjustment, the risk of having a heart attack per 1.0 mmol/L increase in LDL cholesterol was increased in the group overall (hazard ratio, 1.34). The increased risk was observed for all age groups, including those aged 80-100 years (HR, 1.28), 70-79 (HR, 1.25), 60-69 (HR, 1.29), 50-59 (HR, 1.28), and 20-49 (HR, 1.68).
Risk for atherosclerotic cardiovascular disease was also raised per 1.0 mmol/L increase in LDL cholesterol overall (HR, 1.16) and in all age groups, particularly those aged 70-100 years.
Greater elevations in LDL cholesterol (5.0 mmol/L or higher, indicative of possible familial hypercholesterolemia) were associated with a notably higher risk for heart attack after multivariate adjustment in people aged 80-100 (HR, 2.99). Risk was also higher among those aged 70-79 (HR, 1.82).
The highest incidence was in those older than 70. The rate was 8.5 heart attacks per 1,000 people per year among those aged 80-100 and 5.2 heart attacks per 1,000 in those aged 70-79. The rates were 2.5 per 1,000 among those 60-69, 1.8 for those aged 50-59, and 0.8 for those aged 20-49.
“The absolute risk [of cardiovascular events] is of course much higher in the elderly than those under the age of 75, but what was a surprise was how clear our results were on a relative risk scale, that the risk associated with elevated LDL [cholesterol] was as high in people aged 80-100 as the younger patients,” Dr. Nordestgaard said in an interview.
With regard to the benefits of cholesterol-lowering drugs, the study showed that the number needed to prevent one heart attack over 5 years was 80 among those aged 80-100; the number was 439 for people aged 50-59.
With regard to stronger statins, when moderate-intensity statins were used, the number needed to treat to prevent one cardiovascular disease event of any type dropped to 42 for patients aged 80-100. It was 88 for those aged 70-79, 164 for those aged 60-69, 345 for those aged 50-59, and 769 for those aged 20-49.
“The clinical significance of this is that it appears those in older age groups indeed benefit from cholesterol-lowering therapy,” Dr. Nordestgaard said. “I think many people have this idea that LDL [cholesterol] is not important over the age of about 70-75, but that’s not the case.”
“These robust findings are novel,” he and his colleagues stressed.
Despite these observational findings, the South African editorialists noted that “whether lipid-lowering therapy should be initiated for primary prevention in people aged 75 years or older is unclear,” owing to the host of risks and benefits that need to be balanced.
The findings of an ongoing randomized, placebo-controlled trial (STAREE) may answer this question, they wrote. It is investigating primary prevention in 18,000 older patients (≥70 years) who are being randomly assigned to receive atorvastatin 40 mg/d or placebo. The study is seeking to determine whether statin treatment extends the length of a disability-free life, which will be assessed on the basis of survival outside permanent residential care. Results are expected in 2022-2023.
Unequivocal reductions in events in elderly, comparable with younger patients
In the second study (Lancet. 2020 Nov 10. doi: 10.1016/S0140-6736[20]32332-1), Baris Gencer, MD, of Brigham and Women’s Hospital, Boston, =and colleagues evaluated the effects of statins and other cholesterol-lowering drugs, including ezetimibe and proprotein convertase subtilisin/kexin type 9 inhibitors, in older versus younger patients.
The systematic review and meta-analysis of 29 randomized controlled trials, also published in the Lancet, were presented virtually as a poster as part of the 2020 American Heart Association scientific session. It included data on 244,090 patients, including 21,492 aged 75 years and older.
The meta-analysis included studies of cardiovascular outcomes of a guideline-recommended LDL cholesterol–lowering drug, with a median follow-up of at least 2 years and inclusion of data on patients aged 75 years and older.
The results showed that over a median follow-up of 2.2 to 6 years, statin use by older patients was associated with a relative risk reduction of major vascular events of 26% per 1 mmol/L reduction in LDL cholesterol (P = .0019), which was comparable with a risk reduction of 15% per 1 mmol/L reduction in LDL cholesterol for patients younger than 75 years (P = .37, compared with older patients).
Treatment of older patients with LDL cholesterol–lowering drugs was also associated with significantly improved outcomes in cardiovascular death (risk ratio, 0.85), MI (RR, 0.80), stroke (RR, 0.73), and coronary revascularization (RR, 0.80).
“We found an unequivocal reduction in the risk of major vascular events with both statin and nonstatin LDL cholesterol-lowering treatments, which was similar to that seen in younger patients,” the authors wrote.
“Cholesterol-lowering medications are affordable drugs that have reduced risk of heart disease for millions of people worldwide, but until now, their benefits for older people have remained less certain,” said lead author Marc Sabatine, MD, also of Brigham and Women’s Hospital, in a Lancet press release.
“Our analysis indicates that these therapies are as effective in reducing cardiovascular events and deaths in people aged 75 years and over as they are in younger people. We found no offsetting safety concerns, and together, these results should strengthen guideline recommendations for the use of cholesterol-lowering medications, including statin and nonstatin therapy, in elderly people.”
The editorialists agreed: “More than 80% of fatal cardiovascular events occur in individuals older than 65 years, and the incidence of cardiovascular events is increasing in those older than 80 years; therefore, the findings of Gencer and colleagues’ study should encourage the use of lipid-lowering therapy in older patients.”
The authors of the two studies have disclosed no relevant financial relationships. Dr. Raal has received research grants, honoraria, or consulting fees for advisory board membership, professional input, and lectures on lipid-lowering drug therapy from Amgen, Regeneron, Sanofi, Novartis, and the Medicines Company.
A version of this article originally appeared on Medscape.com.
Contrary to historical evidence, two new studies show.
“By contrast with previous historical studies, our data show that LDL cholesterol is an important risk factor for myocardial infarction and atherosclerotic cardiovascular disease in a contemporary primary prevention cohort of individuals aged 70 to 100 years,” Borge Nordestgaard, MD, of the University of Copenhagen, and colleagues noted in the first of the two studies, published this week in the Lancet.
“By lowering LDL cholesterol in healthy individuals aged 70-100 years, the potential for preventing myocardial infarctions and atherosclerotic cardiovascular disease is huge, and at a substantially lower number needed to treat when compared with those aged 20-69 years,” they added.
“These findings support the concept of the cumulative burden of LDL cholesterol over one’s lifetime and the progressive increase in risk for atherosclerotic cardiovascular disease, including myocardial infarction, with age,” added Frederick J. Raal, PhD, and Farzahna Mohamed, MB BCh, of the University of the Witwatersrand, Johannesburg, South Africa, in an editorial published with both new studies in the Lancet (2020 Nov 10. doi: 10.1016/S0140-6736[20]32333-3).
The studies underscore the need for clinicians to consider continued risks associated with elevated LDL cholesterol in older age, they stressed, adding that statins are also beneficial for younger persons at risk to prevent conditions from worsening.
“The average age of patients in all the trials analyzed was older than 60 years, an age when atherosclerotic cardiovascular disease is already well established,” the editorialists wrote.
“Lipid-lowering therapy should be initiated at a younger age, preferably before age 40 years, in those at risk to delay the onset of atherosclerosis, rather than try to manage the condition once fully established or advanced,” they stressed.
No RCTs have included patients older than 70
For persons aged 40-75 years, elevated LDL cholesterol levels are a known risk factor for MI and atherosclerotic cardiovascular disease, and there is consensus in guidelines regarding treatment with statins.
However, the risk for people older than 70 is controversial. Some studies show little or no association between elevated LDL cholesterol levels and an increased risk for MI.
Contributing to the uncertainty is that few of the randomized, controlled trials that have investigated the question have included patients aged older than 70 years.
As a consequence, many practice guidelines have noted that the level of evidence in older patients is low, and some organizations have lowered the strength of recommendations regarding the treatment for older patients in comparison with younger patients.
Primary prevention: CV events increase with elevated LDL cholesterol in older age
Dr. Nordestgaard and colleagues studied data on 91,131 people living in Copenhagen who did not have atherosclerotic cardiovascular disease or diabetes at baseline and were not taking statins.
Of the participants, 10,592 were aged 70-79 years, and 3,188 participants were aged 80-100 years.
Over an average follow-up period of 7.7 years, 1,515 participants had a first MI, and 3,389 developed atherosclerotic cardiovascular disease.
In the primary-prevention cohort, after multivariate adjustment, the risk of having a heart attack per 1.0 mmol/L increase in LDL cholesterol was increased in the group overall (hazard ratio, 1.34). The increased risk was observed for all age groups, including those aged 80-100 years (HR, 1.28), 70-79 (HR, 1.25), 60-69 (HR, 1.29), 50-59 (HR, 1.28), and 20-49 (HR, 1.68).
Risk for atherosclerotic cardiovascular disease was also raised per 1.0 mmol/L increase in LDL cholesterol overall (HR, 1.16) and in all age groups, particularly those aged 70-100 years.
Greater elevations in LDL cholesterol (5.0 mmol/L or higher, indicative of possible familial hypercholesterolemia) were associated with a notably higher risk for heart attack after multivariate adjustment in people aged 80-100 (HR, 2.99). Risk was also higher among those aged 70-79 (HR, 1.82).
The highest incidence was in those older than 70. The rate was 8.5 heart attacks per 1,000 people per year among those aged 80-100 and 5.2 heart attacks per 1,000 in those aged 70-79. The rates were 2.5 per 1,000 among those 60-69, 1.8 for those aged 50-59, and 0.8 for those aged 20-49.
“The absolute risk [of cardiovascular events] is of course much higher in the elderly than those under the age of 75, but what was a surprise was how clear our results were on a relative risk scale, that the risk associated with elevated LDL [cholesterol] was as high in people aged 80-100 as the younger patients,” Dr. Nordestgaard said in an interview.
With regard to the benefits of cholesterol-lowering drugs, the study showed that the number needed to prevent one heart attack over 5 years was 80 among those aged 80-100; the number was 439 for people aged 50-59.
With regard to stronger statins, when moderate-intensity statins were used, the number needed to treat to prevent one cardiovascular disease event of any type dropped to 42 for patients aged 80-100. It was 88 for those aged 70-79, 164 for those aged 60-69, 345 for those aged 50-59, and 769 for those aged 20-49.
“The clinical significance of this is that it appears those in older age groups indeed benefit from cholesterol-lowering therapy,” Dr. Nordestgaard said. “I think many people have this idea that LDL [cholesterol] is not important over the age of about 70-75, but that’s not the case.”
“These robust findings are novel,” he and his colleagues stressed.
Despite these observational findings, the South African editorialists noted that “whether lipid-lowering therapy should be initiated for primary prevention in people aged 75 years or older is unclear,” owing to the host of risks and benefits that need to be balanced.
The findings of an ongoing randomized, placebo-controlled trial (STAREE) may answer this question, they wrote. It is investigating primary prevention in 18,000 older patients (≥70 years) who are being randomly assigned to receive atorvastatin 40 mg/d or placebo. The study is seeking to determine whether statin treatment extends the length of a disability-free life, which will be assessed on the basis of survival outside permanent residential care. Results are expected in 2022-2023.
Unequivocal reductions in events in elderly, comparable with younger patients
In the second study (Lancet. 2020 Nov 10. doi: 10.1016/S0140-6736[20]32332-1), Baris Gencer, MD, of Brigham and Women’s Hospital, Boston, =and colleagues evaluated the effects of statins and other cholesterol-lowering drugs, including ezetimibe and proprotein convertase subtilisin/kexin type 9 inhibitors, in older versus younger patients.
The systematic review and meta-analysis of 29 randomized controlled trials, also published in the Lancet, were presented virtually as a poster as part of the 2020 American Heart Association scientific session. It included data on 244,090 patients, including 21,492 aged 75 years and older.
The meta-analysis included studies of cardiovascular outcomes of a guideline-recommended LDL cholesterol–lowering drug, with a median follow-up of at least 2 years and inclusion of data on patients aged 75 years and older.
The results showed that over a median follow-up of 2.2 to 6 years, statin use by older patients was associated with a relative risk reduction of major vascular events of 26% per 1 mmol/L reduction in LDL cholesterol (P = .0019), which was comparable with a risk reduction of 15% per 1 mmol/L reduction in LDL cholesterol for patients younger than 75 years (P = .37, compared with older patients).
Treatment of older patients with LDL cholesterol–lowering drugs was also associated with significantly improved outcomes in cardiovascular death (risk ratio, 0.85), MI (RR, 0.80), stroke (RR, 0.73), and coronary revascularization (RR, 0.80).
“We found an unequivocal reduction in the risk of major vascular events with both statin and nonstatin LDL cholesterol-lowering treatments, which was similar to that seen in younger patients,” the authors wrote.
“Cholesterol-lowering medications are affordable drugs that have reduced risk of heart disease for millions of people worldwide, but until now, their benefits for older people have remained less certain,” said lead author Marc Sabatine, MD, also of Brigham and Women’s Hospital, in a Lancet press release.
“Our analysis indicates that these therapies are as effective in reducing cardiovascular events and deaths in people aged 75 years and over as they are in younger people. We found no offsetting safety concerns, and together, these results should strengthen guideline recommendations for the use of cholesterol-lowering medications, including statin and nonstatin therapy, in elderly people.”
The editorialists agreed: “More than 80% of fatal cardiovascular events occur in individuals older than 65 years, and the incidence of cardiovascular events is increasing in those older than 80 years; therefore, the findings of Gencer and colleagues’ study should encourage the use of lipid-lowering therapy in older patients.”
The authors of the two studies have disclosed no relevant financial relationships. Dr. Raal has received research grants, honoraria, or consulting fees for advisory board membership, professional input, and lectures on lipid-lowering drug therapy from Amgen, Regeneron, Sanofi, Novartis, and the Medicines Company.
A version of this article originally appeared on Medscape.com.
Contrary to historical evidence, two new studies show.
“By contrast with previous historical studies, our data show that LDL cholesterol is an important risk factor for myocardial infarction and atherosclerotic cardiovascular disease in a contemporary primary prevention cohort of individuals aged 70 to 100 years,” Borge Nordestgaard, MD, of the University of Copenhagen, and colleagues noted in the first of the two studies, published this week in the Lancet.
“By lowering LDL cholesterol in healthy individuals aged 70-100 years, the potential for preventing myocardial infarctions and atherosclerotic cardiovascular disease is huge, and at a substantially lower number needed to treat when compared with those aged 20-69 years,” they added.
“These findings support the concept of the cumulative burden of LDL cholesterol over one’s lifetime and the progressive increase in risk for atherosclerotic cardiovascular disease, including myocardial infarction, with age,” added Frederick J. Raal, PhD, and Farzahna Mohamed, MB BCh, of the University of the Witwatersrand, Johannesburg, South Africa, in an editorial published with both new studies in the Lancet (2020 Nov 10. doi: 10.1016/S0140-6736[20]32333-3).
The studies underscore the need for clinicians to consider continued risks associated with elevated LDL cholesterol in older age, they stressed, adding that statins are also beneficial for younger persons at risk to prevent conditions from worsening.
“The average age of patients in all the trials analyzed was older than 60 years, an age when atherosclerotic cardiovascular disease is already well established,” the editorialists wrote.
“Lipid-lowering therapy should be initiated at a younger age, preferably before age 40 years, in those at risk to delay the onset of atherosclerosis, rather than try to manage the condition once fully established or advanced,” they stressed.
No RCTs have included patients older than 70
For persons aged 40-75 years, elevated LDL cholesterol levels are a known risk factor for MI and atherosclerotic cardiovascular disease, and there is consensus in guidelines regarding treatment with statins.
However, the risk for people older than 70 is controversial. Some studies show little or no association between elevated LDL cholesterol levels and an increased risk for MI.
Contributing to the uncertainty is that few of the randomized, controlled trials that have investigated the question have included patients aged older than 70 years.
As a consequence, many practice guidelines have noted that the level of evidence in older patients is low, and some organizations have lowered the strength of recommendations regarding the treatment for older patients in comparison with younger patients.
Primary prevention: CV events increase with elevated LDL cholesterol in older age
Dr. Nordestgaard and colleagues studied data on 91,131 people living in Copenhagen who did not have atherosclerotic cardiovascular disease or diabetes at baseline and were not taking statins.
Of the participants, 10,592 were aged 70-79 years, and 3,188 participants were aged 80-100 years.
Over an average follow-up period of 7.7 years, 1,515 participants had a first MI, and 3,389 developed atherosclerotic cardiovascular disease.
In the primary-prevention cohort, after multivariate adjustment, the risk of having a heart attack per 1.0 mmol/L increase in LDL cholesterol was increased in the group overall (hazard ratio, 1.34). The increased risk was observed for all age groups, including those aged 80-100 years (HR, 1.28), 70-79 (HR, 1.25), 60-69 (HR, 1.29), 50-59 (HR, 1.28), and 20-49 (HR, 1.68).
Risk for atherosclerotic cardiovascular disease was also raised per 1.0 mmol/L increase in LDL cholesterol overall (HR, 1.16) and in all age groups, particularly those aged 70-100 years.
Greater elevations in LDL cholesterol (5.0 mmol/L or higher, indicative of possible familial hypercholesterolemia) were associated with a notably higher risk for heart attack after multivariate adjustment in people aged 80-100 (HR, 2.99). Risk was also higher among those aged 70-79 (HR, 1.82).
The highest incidence was in those older than 70. The rate was 8.5 heart attacks per 1,000 people per year among those aged 80-100 and 5.2 heart attacks per 1,000 in those aged 70-79. The rates were 2.5 per 1,000 among those 60-69, 1.8 for those aged 50-59, and 0.8 for those aged 20-49.
“The absolute risk [of cardiovascular events] is of course much higher in the elderly than those under the age of 75, but what was a surprise was how clear our results were on a relative risk scale, that the risk associated with elevated LDL [cholesterol] was as high in people aged 80-100 as the younger patients,” Dr. Nordestgaard said in an interview.
With regard to the benefits of cholesterol-lowering drugs, the study showed that the number needed to prevent one heart attack over 5 years was 80 among those aged 80-100; the number was 439 for people aged 50-59.
With regard to stronger statins, when moderate-intensity statins were used, the number needed to treat to prevent one cardiovascular disease event of any type dropped to 42 for patients aged 80-100. It was 88 for those aged 70-79, 164 for those aged 60-69, 345 for those aged 50-59, and 769 for those aged 20-49.
“The clinical significance of this is that it appears those in older age groups indeed benefit from cholesterol-lowering therapy,” Dr. Nordestgaard said. “I think many people have this idea that LDL [cholesterol] is not important over the age of about 70-75, but that’s not the case.”
“These robust findings are novel,” he and his colleagues stressed.
Despite these observational findings, the South African editorialists noted that “whether lipid-lowering therapy should be initiated for primary prevention in people aged 75 years or older is unclear,” owing to the host of risks and benefits that need to be balanced.
The findings of an ongoing randomized, placebo-controlled trial (STAREE) may answer this question, they wrote. It is investigating primary prevention in 18,000 older patients (≥70 years) who are being randomly assigned to receive atorvastatin 40 mg/d or placebo. The study is seeking to determine whether statin treatment extends the length of a disability-free life, which will be assessed on the basis of survival outside permanent residential care. Results are expected in 2022-2023.
Unequivocal reductions in events in elderly, comparable with younger patients
In the second study (Lancet. 2020 Nov 10. doi: 10.1016/S0140-6736[20]32332-1), Baris Gencer, MD, of Brigham and Women’s Hospital, Boston, =and colleagues evaluated the effects of statins and other cholesterol-lowering drugs, including ezetimibe and proprotein convertase subtilisin/kexin type 9 inhibitors, in older versus younger patients.
The systematic review and meta-analysis of 29 randomized controlled trials, also published in the Lancet, were presented virtually as a poster as part of the 2020 American Heart Association scientific session. It included data on 244,090 patients, including 21,492 aged 75 years and older.
The meta-analysis included studies of cardiovascular outcomes of a guideline-recommended LDL cholesterol–lowering drug, with a median follow-up of at least 2 years and inclusion of data on patients aged 75 years and older.
The results showed that over a median follow-up of 2.2 to 6 years, statin use by older patients was associated with a relative risk reduction of major vascular events of 26% per 1 mmol/L reduction in LDL cholesterol (P = .0019), which was comparable with a risk reduction of 15% per 1 mmol/L reduction in LDL cholesterol for patients younger than 75 years (P = .37, compared with older patients).
Treatment of older patients with LDL cholesterol–lowering drugs was also associated with significantly improved outcomes in cardiovascular death (risk ratio, 0.85), MI (RR, 0.80), stroke (RR, 0.73), and coronary revascularization (RR, 0.80).
“We found an unequivocal reduction in the risk of major vascular events with both statin and nonstatin LDL cholesterol-lowering treatments, which was similar to that seen in younger patients,” the authors wrote.
“Cholesterol-lowering medications are affordable drugs that have reduced risk of heart disease for millions of people worldwide, but until now, their benefits for older people have remained less certain,” said lead author Marc Sabatine, MD, also of Brigham and Women’s Hospital, in a Lancet press release.
“Our analysis indicates that these therapies are as effective in reducing cardiovascular events and deaths in people aged 75 years and over as they are in younger people. We found no offsetting safety concerns, and together, these results should strengthen guideline recommendations for the use of cholesterol-lowering medications, including statin and nonstatin therapy, in elderly people.”
The editorialists agreed: “More than 80% of fatal cardiovascular events occur in individuals older than 65 years, and the incidence of cardiovascular events is increasing in those older than 80 years; therefore, the findings of Gencer and colleagues’ study should encourage the use of lipid-lowering therapy in older patients.”
The authors of the two studies have disclosed no relevant financial relationships. Dr. Raal has received research grants, honoraria, or consulting fees for advisory board membership, professional input, and lectures on lipid-lowering drug therapy from Amgen, Regeneron, Sanofi, Novartis, and the Medicines Company.
A version of this article originally appeared on Medscape.com.
Rationale for baricitinib’s use in COVID-19 patients demonstrated
It should not be surprising that the RA drug baricitinib (Olumiant), a Janus kinase (JAK) 1/2 inhibitor, might be beneficial in controlling the cytokine storm of hyperinflammation that can follow severe SARS-CoV-2 infections and lead to lung damage and acute respiratory distress syndrome – the leading cause of death from the virus.
But to demonstrate within a matter of months, at least preliminarily, that baricitinib reduces mortality and morbidity in hospitalized patients with COVID-19 pneumonia required a widely cross-disciplinary international team of researchers from 10 countries working at breakneck speed, said Justin Stebbing, PhD, the principal investigator of a new baricitinib study published Nov. 13 in Science Advances. “We went from modeling and mechanistic investigations to clinical tests in a number of settings and laboratory analysis in record time.”
The international team of 50 researchers included medical specialists in rheumatology, virology, geriatrics, oncology, and general medicine, along with experts in molecular and cellular biology, bioinformatics, statistics and trial design, computer modeling, pathology, genetics, and super-resolution microscopy, Dr. Stebbing, professor of cancer medicine and medical oncology at Imperial College, London, said in an interview.
Artificial intelligence, provided by the London-based firm BenevolentAI, was used to sift through a huge repository of structured medical information to identify drugs that might block the SARS-CoV-2 infection process. It predicted that baricitinib would be a promising candidate to inhibit inflammation and reduce viral load in COVID-19. Previous reports by Dr. Stebbing and colleagues (here and here) describe this AI-mediated testing, which was validated by the new study.
The researchers also used three-dimensional miniature human liver organoids in vitro and super-resolution microscopy to perform further lab investigations, which showed that baricitinib reversed expression of the SARS-CoV-2 receptor ACE2 triggered by type I interferons. Baricitinib inhibited the significant increase in ACE2 expression caused by interferon alpha-2, and thus cytokine-mediated inflammation, and also reduced infectivity, Dr. Stebbing said. “Our study of baricitinib shows that it has both antiviral and anticytokine effects and appears to be safe.”
71% mortality reduction
The team found a 71% reduction in mortality for a group of 83 hospitalized patients with COVID-19 pneumonia in Italy and Spain – early epicenters of the pandemic – who received baricitinib along with standard care, compared with propensity-matched groups that received only standard care. At that time, between mid-March and mid-April, standard COVID-19 care included antibiotics, glucocorticoids, hydroxychloroquine, low-molecular-weight heparin, and the antiretroviral combination lopinavir/ritonavir.
In the Spanish and Italian cohorts, baricitinib was generally well tolerated, although not without side effects, including bacterial infections and increases in liver enzyme levels, which may not have been related to baricitinib. Patients showed reductions in inflammation within days of starting treatment. “We did not observe thrombotic or vascular events in our cohorts, but most of the patients were receiving low molecular weight heparin,” he said.
The fact that baricitinib is approved by the Food and Drug Administration, is already well studied for safety, can be taken conveniently as a once-daily oral tablet, and is less expensive than many other antiviral treatments all make it an good target for further study, including randomized, controlled trials that are already underway, Dr. Stebbing noted. His study cohort also included elderly patients (median age, 81 years) who are the most likely to experience severe disease or death from COVID-19.
The National Library of Medicine’s clinicaltrials.gov registry of federally funded clinical studies lists 15 current research initiatives involving baricitinib and COVID-19. Dr. Stebbing suggested that data generated so far are helping to guide ongoing studies on dose and duration of treatment – in other words, who it works for, when to give it, and at what dose it should be taken and for how long.
Manufacturer Eli Lilly, which markets baricitinib in 2-mg or 4-mg tablets, announced in October that initial data are starting to emerge from 1,000-plus patients enrolled in ACTT-2 (the Adaptive COVID-19 Treatment Trial 2). ACTT-2 compared patients on the broad-spectrum intravenous antiviral drug remdesivir (Veklury) with those receiving remdesivir in combination with baricitinib. Based on ACTT-2 results that suggested a reduced time to recovery and improved clinical outcomes for the combination group, the FDA issued an emergency-use authorization on Nov. 19 for the combination of baricitinib and remdesivir for the treatment of suspected or laboratory confirmed COVID-19 in hospitalized adults and pediatric patients aged 2 years or older requiring supplemental oxygen, invasive mechanical ventilation, or extracorporeal membrane oxygenation.
Interrupting the cytokine outbreak
Baricitinib has the potential to reduce or interrupt the passage of SARS-CoV-2 into cells, and thus to inhibit the JAK1- and JAK2-mediated cytokine outbreak, researcher Heinz-Josef Lenz, MD, professor of medicine and preventive medicine at the University of Southern California’s Norris Comprehensive Cancer Center in Los Angeles, said in a comment. Baricitinib was also identified, using BenevolentAI’s proprietary, artificial intelligence-derived knowledge graph, as a numb-associated kinase inhibitor, with high affinity for AP2-associated protein kinase 1, an important endocytosis regulator.
Early clinical data suggest a potent biologic effect of baricitinib 2 mg or 4 mg daily on circulating interleukin-6 levels and other inflammatory markers, including C-reactive protein. Dr. Lenz said the evidence for advantageous action of baricitinib on viral endocytosis and excessive cytokine release constitutes the rationale for using it in combination with other antivirals such as remdesivir in patients with moderate to severe COVID-19 illness.
“Although baricitinib may display antiviral activity on its own, its anti-inflammatory effects could hypothetically delay viral clearance,” Dr. Lenz added. “The data from Stebbing et al. confirm the dual actions of baricitinib, demonstrating its ability to inhibit viral entry into primary human hepatocyte spheroids and the reduction in inflammatory markers in COVID-19 patients.”
Other JAK inhibitors were not advanced as promising candidates for the research team’s attention by its artificial intelligence search, Dr. Stebbing noted. “The history of the pandemic has taught us the importance of well-designed observational studies as well as randomized, controlled trials. When it comes to COVID, pyrite looks much like gold, as failed studies of four antivirals have shown.”
Although the current translational research study did not use a placebo group, it is an important next step toward future randomized, controlled trials. “What’s great about this study is its high degree of collaboration, done with real urgency,” he added. “It’s harder to produce a paper that crosses multiple boundaries, like this one does, than a single-focused piece of work. But we wanted to link all of these threads together.”
The study was supported by the Imperial Biomedical Research Centre and Experimental Cancer Medicine Centre, the National Institute for Health Research, and the U.K. National Health Service’s Accelerated Access Collaborative. Dr. Stebbing has served on scientific advisory boards for Eli Lilly and other companies. Dr. Lenz had no relevant disclosures to report.
SOURCE: Stebbing J et al. Sci Adv. 2020 Nov 13. doi: 10.1126/sciadv.abe4724.
It should not be surprising that the RA drug baricitinib (Olumiant), a Janus kinase (JAK) 1/2 inhibitor, might be beneficial in controlling the cytokine storm of hyperinflammation that can follow severe SARS-CoV-2 infections and lead to lung damage and acute respiratory distress syndrome – the leading cause of death from the virus.
But to demonstrate within a matter of months, at least preliminarily, that baricitinib reduces mortality and morbidity in hospitalized patients with COVID-19 pneumonia required a widely cross-disciplinary international team of researchers from 10 countries working at breakneck speed, said Justin Stebbing, PhD, the principal investigator of a new baricitinib study published Nov. 13 in Science Advances. “We went from modeling and mechanistic investigations to clinical tests in a number of settings and laboratory analysis in record time.”
The international team of 50 researchers included medical specialists in rheumatology, virology, geriatrics, oncology, and general medicine, along with experts in molecular and cellular biology, bioinformatics, statistics and trial design, computer modeling, pathology, genetics, and super-resolution microscopy, Dr. Stebbing, professor of cancer medicine and medical oncology at Imperial College, London, said in an interview.
Artificial intelligence, provided by the London-based firm BenevolentAI, was used to sift through a huge repository of structured medical information to identify drugs that might block the SARS-CoV-2 infection process. It predicted that baricitinib would be a promising candidate to inhibit inflammation and reduce viral load in COVID-19. Previous reports by Dr. Stebbing and colleagues (here and here) describe this AI-mediated testing, which was validated by the new study.
The researchers also used three-dimensional miniature human liver organoids in vitro and super-resolution microscopy to perform further lab investigations, which showed that baricitinib reversed expression of the SARS-CoV-2 receptor ACE2 triggered by type I interferons. Baricitinib inhibited the significant increase in ACE2 expression caused by interferon alpha-2, and thus cytokine-mediated inflammation, and also reduced infectivity, Dr. Stebbing said. “Our study of baricitinib shows that it has both antiviral and anticytokine effects and appears to be safe.”
71% mortality reduction
The team found a 71% reduction in mortality for a group of 83 hospitalized patients with COVID-19 pneumonia in Italy and Spain – early epicenters of the pandemic – who received baricitinib along with standard care, compared with propensity-matched groups that received only standard care. At that time, between mid-March and mid-April, standard COVID-19 care included antibiotics, glucocorticoids, hydroxychloroquine, low-molecular-weight heparin, and the antiretroviral combination lopinavir/ritonavir.
In the Spanish and Italian cohorts, baricitinib was generally well tolerated, although not without side effects, including bacterial infections and increases in liver enzyme levels, which may not have been related to baricitinib. Patients showed reductions in inflammation within days of starting treatment. “We did not observe thrombotic or vascular events in our cohorts, but most of the patients were receiving low molecular weight heparin,” he said.
The fact that baricitinib is approved by the Food and Drug Administration, is already well studied for safety, can be taken conveniently as a once-daily oral tablet, and is less expensive than many other antiviral treatments all make it an good target for further study, including randomized, controlled trials that are already underway, Dr. Stebbing noted. His study cohort also included elderly patients (median age, 81 years) who are the most likely to experience severe disease or death from COVID-19.
The National Library of Medicine’s clinicaltrials.gov registry of federally funded clinical studies lists 15 current research initiatives involving baricitinib and COVID-19. Dr. Stebbing suggested that data generated so far are helping to guide ongoing studies on dose and duration of treatment – in other words, who it works for, when to give it, and at what dose it should be taken and for how long.
Manufacturer Eli Lilly, which markets baricitinib in 2-mg or 4-mg tablets, announced in October that initial data are starting to emerge from 1,000-plus patients enrolled in ACTT-2 (the Adaptive COVID-19 Treatment Trial 2). ACTT-2 compared patients on the broad-spectrum intravenous antiviral drug remdesivir (Veklury) with those receiving remdesivir in combination with baricitinib. Based on ACTT-2 results that suggested a reduced time to recovery and improved clinical outcomes for the combination group, the FDA issued an emergency-use authorization on Nov. 19 for the combination of baricitinib and remdesivir for the treatment of suspected or laboratory confirmed COVID-19 in hospitalized adults and pediatric patients aged 2 years or older requiring supplemental oxygen, invasive mechanical ventilation, or extracorporeal membrane oxygenation.
Interrupting the cytokine outbreak
Baricitinib has the potential to reduce or interrupt the passage of SARS-CoV-2 into cells, and thus to inhibit the JAK1- and JAK2-mediated cytokine outbreak, researcher Heinz-Josef Lenz, MD, professor of medicine and preventive medicine at the University of Southern California’s Norris Comprehensive Cancer Center in Los Angeles, said in a comment. Baricitinib was also identified, using BenevolentAI’s proprietary, artificial intelligence-derived knowledge graph, as a numb-associated kinase inhibitor, with high affinity for AP2-associated protein kinase 1, an important endocytosis regulator.
Early clinical data suggest a potent biologic effect of baricitinib 2 mg or 4 mg daily on circulating interleukin-6 levels and other inflammatory markers, including C-reactive protein. Dr. Lenz said the evidence for advantageous action of baricitinib on viral endocytosis and excessive cytokine release constitutes the rationale for using it in combination with other antivirals such as remdesivir in patients with moderate to severe COVID-19 illness.
“Although baricitinib may display antiviral activity on its own, its anti-inflammatory effects could hypothetically delay viral clearance,” Dr. Lenz added. “The data from Stebbing et al. confirm the dual actions of baricitinib, demonstrating its ability to inhibit viral entry into primary human hepatocyte spheroids and the reduction in inflammatory markers in COVID-19 patients.”
Other JAK inhibitors were not advanced as promising candidates for the research team’s attention by its artificial intelligence search, Dr. Stebbing noted. “The history of the pandemic has taught us the importance of well-designed observational studies as well as randomized, controlled trials. When it comes to COVID, pyrite looks much like gold, as failed studies of four antivirals have shown.”
Although the current translational research study did not use a placebo group, it is an important next step toward future randomized, controlled trials. “What’s great about this study is its high degree of collaboration, done with real urgency,” he added. “It’s harder to produce a paper that crosses multiple boundaries, like this one does, than a single-focused piece of work. But we wanted to link all of these threads together.”
The study was supported by the Imperial Biomedical Research Centre and Experimental Cancer Medicine Centre, the National Institute for Health Research, and the U.K. National Health Service’s Accelerated Access Collaborative. Dr. Stebbing has served on scientific advisory boards for Eli Lilly and other companies. Dr. Lenz had no relevant disclosures to report.
SOURCE: Stebbing J et al. Sci Adv. 2020 Nov 13. doi: 10.1126/sciadv.abe4724.
It should not be surprising that the RA drug baricitinib (Olumiant), a Janus kinase (JAK) 1/2 inhibitor, might be beneficial in controlling the cytokine storm of hyperinflammation that can follow severe SARS-CoV-2 infections and lead to lung damage and acute respiratory distress syndrome – the leading cause of death from the virus.
But to demonstrate within a matter of months, at least preliminarily, that baricitinib reduces mortality and morbidity in hospitalized patients with COVID-19 pneumonia required a widely cross-disciplinary international team of researchers from 10 countries working at breakneck speed, said Justin Stebbing, PhD, the principal investigator of a new baricitinib study published Nov. 13 in Science Advances. “We went from modeling and mechanistic investigations to clinical tests in a number of settings and laboratory analysis in record time.”
The international team of 50 researchers included medical specialists in rheumatology, virology, geriatrics, oncology, and general medicine, along with experts in molecular and cellular biology, bioinformatics, statistics and trial design, computer modeling, pathology, genetics, and super-resolution microscopy, Dr. Stebbing, professor of cancer medicine and medical oncology at Imperial College, London, said in an interview.
Artificial intelligence, provided by the London-based firm BenevolentAI, was used to sift through a huge repository of structured medical information to identify drugs that might block the SARS-CoV-2 infection process. It predicted that baricitinib would be a promising candidate to inhibit inflammation and reduce viral load in COVID-19. Previous reports by Dr. Stebbing and colleagues (here and here) describe this AI-mediated testing, which was validated by the new study.
The researchers also used three-dimensional miniature human liver organoids in vitro and super-resolution microscopy to perform further lab investigations, which showed that baricitinib reversed expression of the SARS-CoV-2 receptor ACE2 triggered by type I interferons. Baricitinib inhibited the significant increase in ACE2 expression caused by interferon alpha-2, and thus cytokine-mediated inflammation, and also reduced infectivity, Dr. Stebbing said. “Our study of baricitinib shows that it has both antiviral and anticytokine effects and appears to be safe.”
71% mortality reduction
The team found a 71% reduction in mortality for a group of 83 hospitalized patients with COVID-19 pneumonia in Italy and Spain – early epicenters of the pandemic – who received baricitinib along with standard care, compared with propensity-matched groups that received only standard care. At that time, between mid-March and mid-April, standard COVID-19 care included antibiotics, glucocorticoids, hydroxychloroquine, low-molecular-weight heparin, and the antiretroviral combination lopinavir/ritonavir.
In the Spanish and Italian cohorts, baricitinib was generally well tolerated, although not without side effects, including bacterial infections and increases in liver enzyme levels, which may not have been related to baricitinib. Patients showed reductions in inflammation within days of starting treatment. “We did not observe thrombotic or vascular events in our cohorts, but most of the patients were receiving low molecular weight heparin,” he said.
The fact that baricitinib is approved by the Food and Drug Administration, is already well studied for safety, can be taken conveniently as a once-daily oral tablet, and is less expensive than many other antiviral treatments all make it an good target for further study, including randomized, controlled trials that are already underway, Dr. Stebbing noted. His study cohort also included elderly patients (median age, 81 years) who are the most likely to experience severe disease or death from COVID-19.
The National Library of Medicine’s clinicaltrials.gov registry of federally funded clinical studies lists 15 current research initiatives involving baricitinib and COVID-19. Dr. Stebbing suggested that data generated so far are helping to guide ongoing studies on dose and duration of treatment – in other words, who it works for, when to give it, and at what dose it should be taken and for how long.
Manufacturer Eli Lilly, which markets baricitinib in 2-mg or 4-mg tablets, announced in October that initial data are starting to emerge from 1,000-plus patients enrolled in ACTT-2 (the Adaptive COVID-19 Treatment Trial 2). ACTT-2 compared patients on the broad-spectrum intravenous antiviral drug remdesivir (Veklury) with those receiving remdesivir in combination with baricitinib. Based on ACTT-2 results that suggested a reduced time to recovery and improved clinical outcomes for the combination group, the FDA issued an emergency-use authorization on Nov. 19 for the combination of baricitinib and remdesivir for the treatment of suspected or laboratory confirmed COVID-19 in hospitalized adults and pediatric patients aged 2 years or older requiring supplemental oxygen, invasive mechanical ventilation, or extracorporeal membrane oxygenation.
Interrupting the cytokine outbreak
Baricitinib has the potential to reduce or interrupt the passage of SARS-CoV-2 into cells, and thus to inhibit the JAK1- and JAK2-mediated cytokine outbreak, researcher Heinz-Josef Lenz, MD, professor of medicine and preventive medicine at the University of Southern California’s Norris Comprehensive Cancer Center in Los Angeles, said in a comment. Baricitinib was also identified, using BenevolentAI’s proprietary, artificial intelligence-derived knowledge graph, as a numb-associated kinase inhibitor, with high affinity for AP2-associated protein kinase 1, an important endocytosis regulator.
Early clinical data suggest a potent biologic effect of baricitinib 2 mg or 4 mg daily on circulating interleukin-6 levels and other inflammatory markers, including C-reactive protein. Dr. Lenz said the evidence for advantageous action of baricitinib on viral endocytosis and excessive cytokine release constitutes the rationale for using it in combination with other antivirals such as remdesivir in patients with moderate to severe COVID-19 illness.
“Although baricitinib may display antiviral activity on its own, its anti-inflammatory effects could hypothetically delay viral clearance,” Dr. Lenz added. “The data from Stebbing et al. confirm the dual actions of baricitinib, demonstrating its ability to inhibit viral entry into primary human hepatocyte spheroids and the reduction in inflammatory markers in COVID-19 patients.”
Other JAK inhibitors were not advanced as promising candidates for the research team’s attention by its artificial intelligence search, Dr. Stebbing noted. “The history of the pandemic has taught us the importance of well-designed observational studies as well as randomized, controlled trials. When it comes to COVID, pyrite looks much like gold, as failed studies of four antivirals have shown.”
Although the current translational research study did not use a placebo group, it is an important next step toward future randomized, controlled trials. “What’s great about this study is its high degree of collaboration, done with real urgency,” he added. “It’s harder to produce a paper that crosses multiple boundaries, like this one does, than a single-focused piece of work. But we wanted to link all of these threads together.”
The study was supported by the Imperial Biomedical Research Centre and Experimental Cancer Medicine Centre, the National Institute for Health Research, and the U.K. National Health Service’s Accelerated Access Collaborative. Dr. Stebbing has served on scientific advisory boards for Eli Lilly and other companies. Dr. Lenz had no relevant disclosures to report.
SOURCE: Stebbing J et al. Sci Adv. 2020 Nov 13. doi: 10.1126/sciadv.abe4724.
FROM SCIENCE ADVANCES