User login
Welcome to Current Psychiatry, a leading source of information, online and in print, for practitioners of psychiatry and its related subspecialties, including addiction psychiatry, child and adolescent psychiatry, and geriatric psychiatry. This Web site contains evidence-based reviews of the prevention, diagnosis, and treatment of mental illness and psychological disorders; case reports; updates on psychopharmacology; news about the specialty of psychiatry; pearls for practice; and other topics of interest and use to this audience.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-current-psychiatry')]
div[contains(@class, 'pane-pub-home-current-psychiatry')]
div[contains(@class, 'pane-pub-topic-current-psychiatry')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Are the people we serve ‘patients’ or ‘customers’?
Dear Dr. Mossman,
At the multispecialty hospital where I work, administrators refer to patients as “customers” and tell us that, by improving “the customer experience,” we can reduce complaints and avoid malpractice suits. This business lingo offends me. Doesn’t providing good care do more to prevent malpractice claims than calling sick patients “customers”?
Submitted by “Dr. H”
“All words are pegs to hang ideas on.” As was true when Reverend Henry Ward Beecher uttered this phrase in the 19th century,1 names affect how we relate to and feel about people. Many doctors don’t think of themselves as “selling” services, and they find calling patients “customers” distasteful.
But for at least 4 decades, mental health professionals themselves have used a “customer approach” to think about certain aspects of psychiatrist–patient encounters.2 More pertinent to Dr. H’s questions, many attorneys who advise physicians are convinced that giving patients a satisfying “customer experience” is a sound strategy for reducing the risk of malpractice litigation.3
If the attorneys are right, taking a customer service perspective can lower the likelihood that psychiatrists will be sued. To understand why, this article looks at:
• terms for referring to health care recipients
• the feelings those terms generate
• how the “customer service” perspective has become a malpractice prevention
strategy.
Off-putting connotations
All the currently used ways of referring to persons served by doctors have off-putting features.
The word “patient” dates back to the 14th century and comes from Latin present
participles of pati, “to suffer.” Although Alpha Omega Alpha’s motto—“be worthy
to serve the suffering”4—expresses doctors’ commitment to help others, “patient”
carries emotional baggage. A “patient” is “a sick individual” who seeks treatment
from a physician,5 a circumstance that most people (including doctors) find unpleasant and hope is only temporary. The adjective “patient” means “bearing pains or trials calmly or without complaint” and “manifesting forbearance under provocation or strain,”5 phrases associated with passivity, deference, and a long wait to see the doctor.
Because “patient” evokes notions of helplessness and need for direction, non-medical psychotherapists often use “client” to designate care recipients. “Client” has the same Latin root as “to lean” and refers to someone “under the protection of another.” More pertinent to discussions of mental health care, a “client” also is “a person who pays a professional person or organization for services” or “a customer.”5 The latter definition explains what makes “client” feel wrong to medical practitioners, who regard those they treat as deserving more compassion and sacrifice than someone who simply purchases professional services.
“Consumer,” a word of French origin derived from the Latin consumere (“to take
up”), refers to “a person who buys goods and services.”5 If “consumers” are buyers, then those from whom they make purchases are merchants or sellers. Western marketplace concepts often regard consumers as sovereign judges of their needs, and the role of commodity producers is to try to satisfy those needs.6
The problem with viewing health care recipients this way is that sellers don’t caution customers about buying things when only principles of supply-and-demand govern exchange relationships.7 Quite the contrary: producers sometimes promote their products through “advertising [that] distorts reality and creates artificial needs to make profit for a firm.”8 If physicians behave this way, however, they get criticism and deserve it.
A “customer” in 15th-century Middle English was a tax collector, but in modern
usage, a customer is someone who, like a consumer, “purchases some commodity or service.”5 By the early 20th century, “customer” became associated with notions of empowerment embodied in the merchants’ credo, “The customer is always right.”9 Chronic illnesses often require self-management and collaboration with those labeled the “givers” and “recipients” of medical care. Research shows that “patients are more trusting of, and committed to, physicians who adopt an empowering communication style with them,” which suggests “that empowering
patients presents a means to improve the patient–physician relationship.”10
Feelings about names
People have strong feelings about what they are called. In opposing calling patients “consumers,” Nobel Prize-winning economist Paul Krugman explains: “Medical care is an area in which crucial decisions—life and death decisions—must be made; yet making those decisions intelligently requires a vast amount of specialized knowledge; and often those decisions must also be made under conditions in which the patient …needs action immediately, with no time for discussion, let alone comparison shopping. …That’s why doctors have traditionally…been expected to behave according to higher standards than the average professional…The idea that all this can be reduced to money—that doctors are just people selling services to consumers of health care—is, well, sickening.”11
Less famous recipients of nonpsychiatric medical services also prefer being called
“patients” over “clients” or “consumers.”12-14 Recipients of mental health services have a different view, however. In some surveys, “patient” gets a plurality or majority of service recipients’ votes,15,16 but in others, recipients prefer to be called “clients” or other terms.17,18 Of note, people who prefer being called “patients” tend to strongly dislike being called “clients.”19 On the professional
side, psychiatrists—along with other physicians—prefer to speak of treating “patients” and to criticize letting economic phrases infect medical discourse.20-22
Names: A practical difference?
Does what psychiatrists call those they serve make any practical difference? Perhaps not, but evidence suggests that the attitudes that doctors take toward patients affects economic success and malpractice risk.
When they have choices about where they can seek health care, medical patients value physicians’ competence, but they also consider nonclinical factors such as family members’ opinions and convenience.23 Knowing this, the federal government’s Centers for Medicare & Medicaid Services publishes results from its Hospital Consumer Assessment of Healthcare Providers and Systems to “create incentives for hospitals to improve their quality of care.”24
Nonclinical factors play a big part in patients’ decisions about suing their doctors, too. Many malpractice claims turn out to be groundless in the sense that they do not involve medical errors,25 and most errors that result in injury do not lead to malpractice suits.26
What explains this disparity? Often when a lawsuit is filed, whatever injury may have occurred is coupled with an aggravating factor, such as a communication gaffe,27 a physician’s domineering tone of voice,28 or failure to acknowledge error.29 The lower a physician’s patient satisfaction ratings, the higher the physician’s likelihood of receiving complaints and getting sued for malpractice.30,31
These kinds of considerations probably lie behind the recommendation of one hospital manager to doctors: “Continue to call them patients but treat them like
customers.”32 More insights into this view come from responses solicited from Yale
students, staff members, and alumni about whether it seems preferable to be a “patient” or a “customer” (Box).33
Bottom Line
When patients get injured during medical care, evidence suggests that how they feel about their doctors makes a big difference in whether they decide to file suit. If you’re like most psychiatrists, you prefer to call persons whom you treat “patients.” But watching and improving the things that affect your patients’ “customer experience” may help you avoid malpractice litigation.
Related Resource
• Goldhill D. To fix healthcare, turn patients into customers. Bloomberg Personal Finance. www.bloomberg.com/news/2013-01-03/to-fix-health-care-turn-patients-intocustomers.html.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Beecher HW, Drysdale W. Proverbs from Plymouth pulpit. New York, NY: D. Appleton & Co.;1887.
2. Lazare A, Eisenthal S, Wasserman L. The customer approach to patienthood: attending to patient requests in a walk-in clinic. Arch Gen Psychiatry. 1975;32:553-558.
3. Schleiter KE. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
4. Alpha Omega Alpha Honor Medical Society. Alpha Omega Alpha constitution. http://www.alphaomegaalpha.org/constitution.html. Accessed December 13, 2013. Accessed December 13, 2013.
5. Merriam-Webster. Dictionary. http://www.merriamwebster.com. Accessed December 9, 2013.
6. Kotler P, Burton S, Deans K, et al. Marketing, 9th ed. Frenchs Forest, Australia: Pearson Education Australia; 2013.
7. Deber RB. Getting what we pay for: myths and realities about financing Canada’s health care system. Health Law Can. 2000;21(2):9-56.
8. Takala T, Uusitalo O. An alternative view of relationship marketing: a framework for ethical analysis. Eur J Mark. 1996;30:45-60.
9. Van Vuren FS. The Yankee who taught Britishers that ‘the customer is always right.’ Milwaukee Journal. http://www.wisconsinhistory.org/wlhba/articleView.
asp?pg=1&id=11176. Published September 9, 1932. Accessed December 20, 2013.
10. Ouschan T, Sweeney J, Johnson L. Customer empowerment and relationship outcomes in healthcare consultations. Eur J Mark. 2006;40:1068-1086.
11. Krugman P. Patients are not consumers. The New York Times. http://krugman.blogs.nytimes.com/2011/04/20/patients-are-not-consumers. Published April 20, 2011. Accessed December 13, 2013.
12. Nair BR. Patient, client or customer? Med J Aust. 1998;169:593.
13. Wing PC. Patient or client? If in doubt, ask. CMAJ. 1997;157:287-289.
14. Deber RB, Kraetschmer N, Urowitz S, et al. Patient, consumer, client, or customer: what do people want to be called? Health Expect. 2005;8(4):345-351.
15. Sharma V, Whitney D, Kazarian SS, et al. Preferred terms for users of mental health services among service providers and recipients. Psychiatr Serv. 2000;51(2): 203-209.
16. Simmons P, Hawley CJ, Gale TM, et al. Service user, patient, client, user or survivor: describing recipients of mental health services. Psychiatrist. 2010;34:20-23.
17. Lloyd C, King R, Bassett H, et al. Patient, client or consumer? A survey of preferred terms. Australas Psychiatry. 2001; 9(4):321-324.
18. Covell NH, McCorkle BH, Weissman EM, et al. What’s in a name? Terms preferred by service recipients. Adm Policy Ment Health. 2007;34(5):443-447.
19. Ritchie CW, Hayes D, Ames DJ. Patient or client? The opinions of people attending a psychiatric clinic. Psychiatrist. 2000;24(12):447-450.
20. Andreasen NC. Clients, consumers, providers, and products: where will it all end? Am J Psychiatry. 1995;152:1107-1109.
21. Editorial. What’s in a name? Lancet. 2000;356(9248):2111.
22. Torrey EF. Patients, clients, consumers, survivors et al: what’s in a name? Schizophr Bull. 2011;37(3):466-468.
23. Wilson CT, Woloshin S, Schwartz L. Choosing where to have major surgery: who makes the decision? Arch Surg. 2007;142(3):242-246.
24. Centers for Medicare & Medicaid Services. Hospital consumer assessment of healthcare providers and systems. http://www.hcahpsonline.org. Accessed
January 26, 2014.
25. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354:2024-2033.
26. Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence—results of the Harvard Medical Practice Study III. N Engl J Med. 1991;325:245-251.
27. Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Bayl Univ Med Cent. 2003;16(2):157-161.
28. Ambady N, Laplante D, Nguyen T, et al. Surgeons’ tone of voice: a clue to malpractice history. Surgery. 2002;132(1):5-9.
29. Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. Arch Intern Med. 1996;156(22):2565-2569.
30. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):
1126-1133.
31. Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk. JAMA. 2002;287(22):2951-2957.
32. Bain W. Do we need a new word for patients? Continue to call them patients but treat them like customers. BMJ. 1999;319(7222):1436.
33. Johnson R, Moskowitz E, Thomas J, et al. Would you rather be treated as a patient or a customer? Yale Insights. http://insights.som.yale.edu/insights/would-you-rather-betreated-patient-or-customer. Accessed December 13, 2013.
Dear Dr. Mossman,
At the multispecialty hospital where I work, administrators refer to patients as “customers” and tell us that, by improving “the customer experience,” we can reduce complaints and avoid malpractice suits. This business lingo offends me. Doesn’t providing good care do more to prevent malpractice claims than calling sick patients “customers”?
Submitted by “Dr. H”
“All words are pegs to hang ideas on.” As was true when Reverend Henry Ward Beecher uttered this phrase in the 19th century,1 names affect how we relate to and feel about people. Many doctors don’t think of themselves as “selling” services, and they find calling patients “customers” distasteful.
But for at least 4 decades, mental health professionals themselves have used a “customer approach” to think about certain aspects of psychiatrist–patient encounters.2 More pertinent to Dr. H’s questions, many attorneys who advise physicians are convinced that giving patients a satisfying “customer experience” is a sound strategy for reducing the risk of malpractice litigation.3
If the attorneys are right, taking a customer service perspective can lower the likelihood that psychiatrists will be sued. To understand why, this article looks at:
• terms for referring to health care recipients
• the feelings those terms generate
• how the “customer service” perspective has become a malpractice prevention
strategy.
Off-putting connotations
All the currently used ways of referring to persons served by doctors have off-putting features.
The word “patient” dates back to the 14th century and comes from Latin present
participles of pati, “to suffer.” Although Alpha Omega Alpha’s motto—“be worthy
to serve the suffering”4—expresses doctors’ commitment to help others, “patient”
carries emotional baggage. A “patient” is “a sick individual” who seeks treatment
from a physician,5 a circumstance that most people (including doctors) find unpleasant and hope is only temporary. The adjective “patient” means “bearing pains or trials calmly or without complaint” and “manifesting forbearance under provocation or strain,”5 phrases associated with passivity, deference, and a long wait to see the doctor.
Because “patient” evokes notions of helplessness and need for direction, non-medical psychotherapists often use “client” to designate care recipients. “Client” has the same Latin root as “to lean” and refers to someone “under the protection of another.” More pertinent to discussions of mental health care, a “client” also is “a person who pays a professional person or organization for services” or “a customer.”5 The latter definition explains what makes “client” feel wrong to medical practitioners, who regard those they treat as deserving more compassion and sacrifice than someone who simply purchases professional services.
“Consumer,” a word of French origin derived from the Latin consumere (“to take
up”), refers to “a person who buys goods and services.”5 If “consumers” are buyers, then those from whom they make purchases are merchants or sellers. Western marketplace concepts often regard consumers as sovereign judges of their needs, and the role of commodity producers is to try to satisfy those needs.6
The problem with viewing health care recipients this way is that sellers don’t caution customers about buying things when only principles of supply-and-demand govern exchange relationships.7 Quite the contrary: producers sometimes promote their products through “advertising [that] distorts reality and creates artificial needs to make profit for a firm.”8 If physicians behave this way, however, they get criticism and deserve it.
A “customer” in 15th-century Middle English was a tax collector, but in modern
usage, a customer is someone who, like a consumer, “purchases some commodity or service.”5 By the early 20th century, “customer” became associated with notions of empowerment embodied in the merchants’ credo, “The customer is always right.”9 Chronic illnesses often require self-management and collaboration with those labeled the “givers” and “recipients” of medical care. Research shows that “patients are more trusting of, and committed to, physicians who adopt an empowering communication style with them,” which suggests “that empowering
patients presents a means to improve the patient–physician relationship.”10
Feelings about names
People have strong feelings about what they are called. In opposing calling patients “consumers,” Nobel Prize-winning economist Paul Krugman explains: “Medical care is an area in which crucial decisions—life and death decisions—must be made; yet making those decisions intelligently requires a vast amount of specialized knowledge; and often those decisions must also be made under conditions in which the patient …needs action immediately, with no time for discussion, let alone comparison shopping. …That’s why doctors have traditionally…been expected to behave according to higher standards than the average professional…The idea that all this can be reduced to money—that doctors are just people selling services to consumers of health care—is, well, sickening.”11
Less famous recipients of nonpsychiatric medical services also prefer being called
“patients” over “clients” or “consumers.”12-14 Recipients of mental health services have a different view, however. In some surveys, “patient” gets a plurality or majority of service recipients’ votes,15,16 but in others, recipients prefer to be called “clients” or other terms.17,18 Of note, people who prefer being called “patients” tend to strongly dislike being called “clients.”19 On the professional
side, psychiatrists—along with other physicians—prefer to speak of treating “patients” and to criticize letting economic phrases infect medical discourse.20-22
Names: A practical difference?
Does what psychiatrists call those they serve make any practical difference? Perhaps not, but evidence suggests that the attitudes that doctors take toward patients affects economic success and malpractice risk.
When they have choices about where they can seek health care, medical patients value physicians’ competence, but they also consider nonclinical factors such as family members’ opinions and convenience.23 Knowing this, the federal government’s Centers for Medicare & Medicaid Services publishes results from its Hospital Consumer Assessment of Healthcare Providers and Systems to “create incentives for hospitals to improve their quality of care.”24
Nonclinical factors play a big part in patients’ decisions about suing their doctors, too. Many malpractice claims turn out to be groundless in the sense that they do not involve medical errors,25 and most errors that result in injury do not lead to malpractice suits.26
What explains this disparity? Often when a lawsuit is filed, whatever injury may have occurred is coupled with an aggravating factor, such as a communication gaffe,27 a physician’s domineering tone of voice,28 or failure to acknowledge error.29 The lower a physician’s patient satisfaction ratings, the higher the physician’s likelihood of receiving complaints and getting sued for malpractice.30,31
These kinds of considerations probably lie behind the recommendation of one hospital manager to doctors: “Continue to call them patients but treat them like
customers.”32 More insights into this view come from responses solicited from Yale
students, staff members, and alumni about whether it seems preferable to be a “patient” or a “customer” (Box).33
Bottom Line
When patients get injured during medical care, evidence suggests that how they feel about their doctors makes a big difference in whether they decide to file suit. If you’re like most psychiatrists, you prefer to call persons whom you treat “patients.” But watching and improving the things that affect your patients’ “customer experience” may help you avoid malpractice litigation.
Related Resource
• Goldhill D. To fix healthcare, turn patients into customers. Bloomberg Personal Finance. www.bloomberg.com/news/2013-01-03/to-fix-health-care-turn-patients-intocustomers.html.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
Dear Dr. Mossman,
At the multispecialty hospital where I work, administrators refer to patients as “customers” and tell us that, by improving “the customer experience,” we can reduce complaints and avoid malpractice suits. This business lingo offends me. Doesn’t providing good care do more to prevent malpractice claims than calling sick patients “customers”?
Submitted by “Dr. H”
“All words are pegs to hang ideas on.” As was true when Reverend Henry Ward Beecher uttered this phrase in the 19th century,1 names affect how we relate to and feel about people. Many doctors don’t think of themselves as “selling” services, and they find calling patients “customers” distasteful.
But for at least 4 decades, mental health professionals themselves have used a “customer approach” to think about certain aspects of psychiatrist–patient encounters.2 More pertinent to Dr. H’s questions, many attorneys who advise physicians are convinced that giving patients a satisfying “customer experience” is a sound strategy for reducing the risk of malpractice litigation.3
If the attorneys are right, taking a customer service perspective can lower the likelihood that psychiatrists will be sued. To understand why, this article looks at:
• terms for referring to health care recipients
• the feelings those terms generate
• how the “customer service” perspective has become a malpractice prevention
strategy.
Off-putting connotations
All the currently used ways of referring to persons served by doctors have off-putting features.
The word “patient” dates back to the 14th century and comes from Latin present
participles of pati, “to suffer.” Although Alpha Omega Alpha’s motto—“be worthy
to serve the suffering”4—expresses doctors’ commitment to help others, “patient”
carries emotional baggage. A “patient” is “a sick individual” who seeks treatment
from a physician,5 a circumstance that most people (including doctors) find unpleasant and hope is only temporary. The adjective “patient” means “bearing pains or trials calmly or without complaint” and “manifesting forbearance under provocation or strain,”5 phrases associated with passivity, deference, and a long wait to see the doctor.
Because “patient” evokes notions of helplessness and need for direction, non-medical psychotherapists often use “client” to designate care recipients. “Client” has the same Latin root as “to lean” and refers to someone “under the protection of another.” More pertinent to discussions of mental health care, a “client” also is “a person who pays a professional person or organization for services” or “a customer.”5 The latter definition explains what makes “client” feel wrong to medical practitioners, who regard those they treat as deserving more compassion and sacrifice than someone who simply purchases professional services.
“Consumer,” a word of French origin derived from the Latin consumere (“to take
up”), refers to “a person who buys goods and services.”5 If “consumers” are buyers, then those from whom they make purchases are merchants or sellers. Western marketplace concepts often regard consumers as sovereign judges of their needs, and the role of commodity producers is to try to satisfy those needs.6
The problem with viewing health care recipients this way is that sellers don’t caution customers about buying things when only principles of supply-and-demand govern exchange relationships.7 Quite the contrary: producers sometimes promote their products through “advertising [that] distorts reality and creates artificial needs to make profit for a firm.”8 If physicians behave this way, however, they get criticism and deserve it.
A “customer” in 15th-century Middle English was a tax collector, but in modern
usage, a customer is someone who, like a consumer, “purchases some commodity or service.”5 By the early 20th century, “customer” became associated with notions of empowerment embodied in the merchants’ credo, “The customer is always right.”9 Chronic illnesses often require self-management and collaboration with those labeled the “givers” and “recipients” of medical care. Research shows that “patients are more trusting of, and committed to, physicians who adopt an empowering communication style with them,” which suggests “that empowering
patients presents a means to improve the patient–physician relationship.”10
Feelings about names
People have strong feelings about what they are called. In opposing calling patients “consumers,” Nobel Prize-winning economist Paul Krugman explains: “Medical care is an area in which crucial decisions—life and death decisions—must be made; yet making those decisions intelligently requires a vast amount of specialized knowledge; and often those decisions must also be made under conditions in which the patient …needs action immediately, with no time for discussion, let alone comparison shopping. …That’s why doctors have traditionally…been expected to behave according to higher standards than the average professional…The idea that all this can be reduced to money—that doctors are just people selling services to consumers of health care—is, well, sickening.”11
Less famous recipients of nonpsychiatric medical services also prefer being called
“patients” over “clients” or “consumers.”12-14 Recipients of mental health services have a different view, however. In some surveys, “patient” gets a plurality or majority of service recipients’ votes,15,16 but in others, recipients prefer to be called “clients” or other terms.17,18 Of note, people who prefer being called “patients” tend to strongly dislike being called “clients.”19 On the professional
side, psychiatrists—along with other physicians—prefer to speak of treating “patients” and to criticize letting economic phrases infect medical discourse.20-22
Names: A practical difference?
Does what psychiatrists call those they serve make any practical difference? Perhaps not, but evidence suggests that the attitudes that doctors take toward patients affects economic success and malpractice risk.
When they have choices about where they can seek health care, medical patients value physicians’ competence, but they also consider nonclinical factors such as family members’ opinions and convenience.23 Knowing this, the federal government’s Centers for Medicare & Medicaid Services publishes results from its Hospital Consumer Assessment of Healthcare Providers and Systems to “create incentives for hospitals to improve their quality of care.”24
Nonclinical factors play a big part in patients’ decisions about suing their doctors, too. Many malpractice claims turn out to be groundless in the sense that they do not involve medical errors,25 and most errors that result in injury do not lead to malpractice suits.26
What explains this disparity? Often when a lawsuit is filed, whatever injury may have occurred is coupled with an aggravating factor, such as a communication gaffe,27 a physician’s domineering tone of voice,28 or failure to acknowledge error.29 The lower a physician’s patient satisfaction ratings, the higher the physician’s likelihood of receiving complaints and getting sued for malpractice.30,31
These kinds of considerations probably lie behind the recommendation of one hospital manager to doctors: “Continue to call them patients but treat them like
customers.”32 More insights into this view come from responses solicited from Yale
students, staff members, and alumni about whether it seems preferable to be a “patient” or a “customer” (Box).33
Bottom Line
When patients get injured during medical care, evidence suggests that how they feel about their doctors makes a big difference in whether they decide to file suit. If you’re like most psychiatrists, you prefer to call persons whom you treat “patients.” But watching and improving the things that affect your patients’ “customer experience” may help you avoid malpractice litigation.
Related Resource
• Goldhill D. To fix healthcare, turn patients into customers. Bloomberg Personal Finance. www.bloomberg.com/news/2013-01-03/to-fix-health-care-turn-patients-intocustomers.html.
Disclosure
Dr. Mossman reports no financial relationship with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Beecher HW, Drysdale W. Proverbs from Plymouth pulpit. New York, NY: D. Appleton & Co.;1887.
2. Lazare A, Eisenthal S, Wasserman L. The customer approach to patienthood: attending to patient requests in a walk-in clinic. Arch Gen Psychiatry. 1975;32:553-558.
3. Schleiter KE. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
4. Alpha Omega Alpha Honor Medical Society. Alpha Omega Alpha constitution. http://www.alphaomegaalpha.org/constitution.html. Accessed December 13, 2013. Accessed December 13, 2013.
5. Merriam-Webster. Dictionary. http://www.merriamwebster.com. Accessed December 9, 2013.
6. Kotler P, Burton S, Deans K, et al. Marketing, 9th ed. Frenchs Forest, Australia: Pearson Education Australia; 2013.
7. Deber RB. Getting what we pay for: myths and realities about financing Canada’s health care system. Health Law Can. 2000;21(2):9-56.
8. Takala T, Uusitalo O. An alternative view of relationship marketing: a framework for ethical analysis. Eur J Mark. 1996;30:45-60.
9. Van Vuren FS. The Yankee who taught Britishers that ‘the customer is always right.’ Milwaukee Journal. http://www.wisconsinhistory.org/wlhba/articleView.
asp?pg=1&id=11176. Published September 9, 1932. Accessed December 20, 2013.
10. Ouschan T, Sweeney J, Johnson L. Customer empowerment and relationship outcomes in healthcare consultations. Eur J Mark. 2006;40:1068-1086.
11. Krugman P. Patients are not consumers. The New York Times. http://krugman.blogs.nytimes.com/2011/04/20/patients-are-not-consumers. Published April 20, 2011. Accessed December 13, 2013.
12. Nair BR. Patient, client or customer? Med J Aust. 1998;169:593.
13. Wing PC. Patient or client? If in doubt, ask. CMAJ. 1997;157:287-289.
14. Deber RB, Kraetschmer N, Urowitz S, et al. Patient, consumer, client, or customer: what do people want to be called? Health Expect. 2005;8(4):345-351.
15. Sharma V, Whitney D, Kazarian SS, et al. Preferred terms for users of mental health services among service providers and recipients. Psychiatr Serv. 2000;51(2): 203-209.
16. Simmons P, Hawley CJ, Gale TM, et al. Service user, patient, client, user or survivor: describing recipients of mental health services. Psychiatrist. 2010;34:20-23.
17. Lloyd C, King R, Bassett H, et al. Patient, client or consumer? A survey of preferred terms. Australas Psychiatry. 2001; 9(4):321-324.
18. Covell NH, McCorkle BH, Weissman EM, et al. What’s in a name? Terms preferred by service recipients. Adm Policy Ment Health. 2007;34(5):443-447.
19. Ritchie CW, Hayes D, Ames DJ. Patient or client? The opinions of people attending a psychiatric clinic. Psychiatrist. 2000;24(12):447-450.
20. Andreasen NC. Clients, consumers, providers, and products: where will it all end? Am J Psychiatry. 1995;152:1107-1109.
21. Editorial. What’s in a name? Lancet. 2000;356(9248):2111.
22. Torrey EF. Patients, clients, consumers, survivors et al: what’s in a name? Schizophr Bull. 2011;37(3):466-468.
23. Wilson CT, Woloshin S, Schwartz L. Choosing where to have major surgery: who makes the decision? Arch Surg. 2007;142(3):242-246.
24. Centers for Medicare & Medicaid Services. Hospital consumer assessment of healthcare providers and systems. http://www.hcahpsonline.org. Accessed
January 26, 2014.
25. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354:2024-2033.
26. Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence—results of the Harvard Medical Practice Study III. N Engl J Med. 1991;325:245-251.
27. Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Bayl Univ Med Cent. 2003;16(2):157-161.
28. Ambady N, Laplante D, Nguyen T, et al. Surgeons’ tone of voice: a clue to malpractice history. Surgery. 2002;132(1):5-9.
29. Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. Arch Intern Med. 1996;156(22):2565-2569.
30. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):
1126-1133.
31. Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk. JAMA. 2002;287(22):2951-2957.
32. Bain W. Do we need a new word for patients? Continue to call them patients but treat them like customers. BMJ. 1999;319(7222):1436.
33. Johnson R, Moskowitz E, Thomas J, et al. Would you rather be treated as a patient or a customer? Yale Insights. http://insights.som.yale.edu/insights/would-you-rather-betreated-patient-or-customer. Accessed December 13, 2013.
1. Beecher HW, Drysdale W. Proverbs from Plymouth pulpit. New York, NY: D. Appleton & Co.;1887.
2. Lazare A, Eisenthal S, Wasserman L. The customer approach to patienthood: attending to patient requests in a walk-in clinic. Arch Gen Psychiatry. 1975;32:553-558.
3. Schleiter KE. Difficult patient-physician relationships and the risk of medical malpractice litigation. Virtual Mentor. 2009;11:242-246.
4. Alpha Omega Alpha Honor Medical Society. Alpha Omega Alpha constitution. http://www.alphaomegaalpha.org/constitution.html. Accessed December 13, 2013. Accessed December 13, 2013.
5. Merriam-Webster. Dictionary. http://www.merriamwebster.com. Accessed December 9, 2013.
6. Kotler P, Burton S, Deans K, et al. Marketing, 9th ed. Frenchs Forest, Australia: Pearson Education Australia; 2013.
7. Deber RB. Getting what we pay for: myths and realities about financing Canada’s health care system. Health Law Can. 2000;21(2):9-56.
8. Takala T, Uusitalo O. An alternative view of relationship marketing: a framework for ethical analysis. Eur J Mark. 1996;30:45-60.
9. Van Vuren FS. The Yankee who taught Britishers that ‘the customer is always right.’ Milwaukee Journal. http://www.wisconsinhistory.org/wlhba/articleView.
asp?pg=1&id=11176. Published September 9, 1932. Accessed December 20, 2013.
10. Ouschan T, Sweeney J, Johnson L. Customer empowerment and relationship outcomes in healthcare consultations. Eur J Mark. 2006;40:1068-1086.
11. Krugman P. Patients are not consumers. The New York Times. http://krugman.blogs.nytimes.com/2011/04/20/patients-are-not-consumers. Published April 20, 2011. Accessed December 13, 2013.
12. Nair BR. Patient, client or customer? Med J Aust. 1998;169:593.
13. Wing PC. Patient or client? If in doubt, ask. CMAJ. 1997;157:287-289.
14. Deber RB, Kraetschmer N, Urowitz S, et al. Patient, consumer, client, or customer: what do people want to be called? Health Expect. 2005;8(4):345-351.
15. Sharma V, Whitney D, Kazarian SS, et al. Preferred terms for users of mental health services among service providers and recipients. Psychiatr Serv. 2000;51(2): 203-209.
16. Simmons P, Hawley CJ, Gale TM, et al. Service user, patient, client, user or survivor: describing recipients of mental health services. Psychiatrist. 2010;34:20-23.
17. Lloyd C, King R, Bassett H, et al. Patient, client or consumer? A survey of preferred terms. Australas Psychiatry. 2001; 9(4):321-324.
18. Covell NH, McCorkle BH, Weissman EM, et al. What’s in a name? Terms preferred by service recipients. Adm Policy Ment Health. 2007;34(5):443-447.
19. Ritchie CW, Hayes D, Ames DJ. Patient or client? The opinions of people attending a psychiatric clinic. Psychiatrist. 2000;24(12):447-450.
20. Andreasen NC. Clients, consumers, providers, and products: where will it all end? Am J Psychiatry. 1995;152:1107-1109.
21. Editorial. What’s in a name? Lancet. 2000;356(9248):2111.
22. Torrey EF. Patients, clients, consumers, survivors et al: what’s in a name? Schizophr Bull. 2011;37(3):466-468.
23. Wilson CT, Woloshin S, Schwartz L. Choosing where to have major surgery: who makes the decision? Arch Surg. 2007;142(3):242-246.
24. Centers for Medicare & Medicaid Services. Hospital consumer assessment of healthcare providers and systems. http://www.hcahpsonline.org. Accessed
January 26, 2014.
25. Studdert DM, Mello MM, Gawande AA, et al. Claims, errors, and compensation payments in medical malpractice litigation. N Engl J Med. 2006;354:2024-2033.
26. Localio AR, Lawthers AG, Brennan TA, et al. Relation between malpractice claims and adverse events due to negligence—results of the Harvard Medical Practice Study III. N Engl J Med. 1991;325:245-251.
27. Huntington B, Kuhn N. Communication gaffes: a root cause of malpractice claims. Bayl Univ Med Cent. 2003;16(2):157-161.
28. Ambady N, Laplante D, Nguyen T, et al. Surgeons’ tone of voice: a clue to malpractice history. Surgery. 2002;132(1):5-9.
29. Witman AB, Park DM, Hardin SB. How do patients want physicians to handle mistakes? A survey of internal medicine patients in an academic setting. Arch Intern Med. 1996;156(22):2565-2569.
30. Stelfox HT, Gandhi TK, Orav EJ, et al. The relation of patient satisfaction with complaints against physicians and malpractice lawsuits. Am J Med. 2005;118(10):
1126-1133.
31. Hickson GB, Federspiel CF, Pichert JW, et al. Patient complaints and malpractice risk. JAMA. 2002;287(22):2951-2957.
32. Bain W. Do we need a new word for patients? Continue to call them patients but treat them like customers. BMJ. 1999;319(7222):1436.
33. Johnson R, Moskowitz E, Thomas J, et al. Would you rather be treated as a patient or a customer? Yale Insights. http://insights.som.yale.edu/insights/would-you-rather-betreated-patient-or-customer. Accessed December 13, 2013.
Answers to 7 questions about using neuropsychological testing in your practice
Neuropsychological evaluation, consisting of a thorough examination of cognitive and behavioral functioning, can make an invaluable contribution to the care of psychiatric patients. Through the vehicle of standardized measures of abilities, patients’ cognitive strengths and weaknesses can be elucidated—revealing potential areas for further interventions or to explain impediments to treatment. A licensed clinical psychologist provides this service.
You, as a consumer of reported findings, can use the results to inform your diagnosis and treatment plan. Recommendations from the neuropsychologist often address dispositional planning, cognitive intervention, psychiatric intervention, and work and school accommodations.
Probing the brain−behavior relationship
Neuropsychology is a subspecialty of clinical psychology that is focused on understanding the brain–behavior relationship. Drawing information from multiple disciplines, including psychiatry and neurology, neuropsychology seeks to uncover the cognitive, behavioral, and emotional difficulties that can result from known or suspected brain dysfunction. Increasingly, to protect the public and referral sources, clinical psychologists who perform neuropsychological testing demonstrate their competence through board certification (eg, the American Board of Clinical Neuropsychology).
How is testing conducted? Evaluations comprise measures that are standardized, scored objectively, and have established psychometric properties. Testing can performed on an outpatient or inpatient basis; the duration of testing depends on the question for which the referring practitioner seeks an answer.
Measures typically are administered by paper and pencil, although computer-based
assessments are increasingly being employed. Because of the influence of demographic variables (age, sex, years of education, race), scores are compared with normative samples that resemble those of the patient’s background as closely as possible.
A thorough clinical interview with the patient, a collateral interview with caregivers
and family, and review of relevant medical records are crucial parts of the assessment. Multiple areas of cognition are assessed:
• intelligence
• academic functioning
• attention
• working memory
• speed of processing
• learning and memory
• visual spatial skills
• fine motor skills
• executive functioning.
Essentially, the evaluation speaks to a patient’s neurocognitive functioning and cerebral integrity.
How are results scored? Interpretation of test scores is contingent on expectations of how a patient should perform in the absence of neurologic or psychiatric illness (ie, based on normative data and performancebased estimates of premorbid functioning).1 The overall pattern of intact scores and deficit scores can be used to form specific impressions about a diagnosis, cognitive strengths and weaknesses, and strategies for intervention.
Personality testing. In addition to the cognitive aspect of the evaluation, personality measures are incorporated when relevant to the referral question or presenting concern.
Personality tests can be broadly divided into objective and projective measures.
Objective personality measures, such as the Minnesota Multiphasic Personality
Inventory-Second Edition, require the examinee to respond to a set of items as
true or false or on a Likert-type scale from strongly agree to disagree. Responses are then scored in standardized fashion, making comparisons to normative data, which are then analyzed to determine the extent to which the examinee experiences psychiatric symptoms.
As part of testing, patients’ responses to ambiguous or unstructured standard
stimuli—such as a series of drawings, abstract patterns, or incomplete sentences—
are analyzed to determine underlying personality traits, feelings, and attitudes.
Classic examples of these measures include the Rorschach Test and the Thematic
Apperception Test.
Personality measures and psychiatric testing are designed to answer questions
related to patients’ emotional status. These measures assess psychiatric symptoms and diagnoses, whereas neuropsychological measures provide an understanding of patients’ cognitive assets and limitations.
7 Common questions about neuropsychological testing
1 Will my patient’s insurance cover these assessments? The question is common from practitioners who are considering requesting an assessment for a patient. The short answer is “Yes.”
Most payers follow Medicare guidelines for reimbursement of neuropsychological
testing; if testing is determined to be medically necessary, insurance companies often cover the assessment. Medicaid also pays for psychometric testing services. Neuropsychologists who have a hospital-based practice typically include patients
with all types of insurance coverage. For example, 40% of patients seen in a hospital are covered by Medicare or Medicaid.2
A caveat: Local intermediaries interpret policies and procedures in different ways,
so there is variability in coverage by geographic region. That is why it is crucial
for neuropsychologists to obtain preauthorization, as would be the case with other medical procedures and services sought by referral.
Last, insurance companies do not pay for assessment of a learning disability. The
rationale typically offered for this lack of coverage? The assessment is for academic, not medical, purposes. In such a situation, patients and their families are offered a private-pay option.
2 What are the indications for neuropsychological assessment? Psychiatric practitioners are one of the top medical specialties that refer their patients for neuropsychological testing.3 This is because many patients with a psychiatric or
neurologic disorder experience changes in cognition, mood, and personality. Such
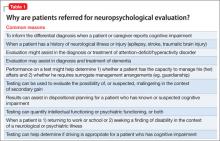
changes can range in severity from subtle to dramatic, and might reflect an underlying disease state or a side effect of medication or other treatment. Whatever the nature of a patient’s problem, careful assessment might help elucidate specific areas with which he (she) is struggling—so that you can better target your interventions. Table 1 lists common reasons for referring a patient for neuropsychological evaluation. Throughout this discussion, we describe examples of clinical situations in which neuropsychological testing is useful for establishing a differential diagnosis and dispositional planning.
3 How does neuropsychological testing help with the differential diagnosis? As an example, one area in which cognitive testing can be beneficial is in geriatric psychiatry.Dementia. Aging often is accompanied by a normal decline in memory and other cognitive functions. But because subtle changes in memory and cognition also canbe the sign of a progressive cognitive disorder, differentiating normal aging from early dementia is essential. Table 2 summarizes typical changes in cognition with aging.
Neuropsychologists, through knowledge of psychometric testing and the brain−behavior relationship, can help you detect dementia and plan treatment early. To determine if cognitive changes are progressive, patients might undergo re-evaluation—typically, every 6 to 12 months—to ascertain if changes have occurred. Mood disorders. Neuropsychological evaluation can be useful in building a differential diagnosis when determining whether cognitive symptoms are attributable to a mood disorder or a medical illness. Cognitive deficits associated with an affective disturbance generally include impairments in attention, memory, and executive functioning.4 The severity of deficits has been linked to severity of illness. When patients with a mood disorder demonstrate localizing impairments or those of greater severity than expected, suspicion arises that another cause likely better explains those deficits, and further medical testing then is often recommended. Medical procedures. Increasingly, neuropsychological assessment is used to assist in determining the appropriateness of medical procedures. For example, neurosurgical patients being considered for deep brain stimulation, brain tumor resectioning, and epilepsy surgery often are referred for preoperative and postoperative testing. Treating clinicians need an understanding of current cognitive status, localization of functioning, and psychological status to make appropriate decisions about a patient’s candidacy for one of these procedures,and to understand associated risk.
4 How is neuropsychological testing used for dispositional planning? The
results of cognitive and psychological testing have implications for dispositional
planning for patients who are receiving psychiatric care. The primary issue often is
to determine the patient’s level of independence and ability to make decisions about his affairs.5
Neuropsychological testing can help determine if cognitive deficits limit aspects of functional independence—for example, can the patient live alone, or must he live with family or in a residential care facility? Generally, the greater the cognitive impairment, the more supervision and assistance are required. This relationship between cognitive ability and independence in activities of daily living has been demonstrated in many groups of psychiatric patients, including older adults with dementia,6 patients with schizophrenia,7 and those with bipolar disorder.8
Specific recommendations can be made regarding management of finances, administering medications, and driving. To formulate an appropriate dispositional plan, the referring psychiatrist might integrate recommendations from the neuropsychological assessment with findings of other evaluations and with information that has been collected about the patient.
5 Can neuropsychological testing be used to refer a patient for neurological and cognitive rehabilitation? Yes. The neuropsychologist is singularly qualified to make recommendations about a range of interventions for cognitive deficits that have been identified on formal testing.
Typically, recommendations for addressing cognitive deficits involve rehabilitation
focused on development and use of compensatory strategies and modification to promote brain health.9,10 Rehabilitation therapy typically is aimed at increasing functioning independence and reducing physical and cognitive deficits associated
with illness (eg, traumatic brain injury [TBI], stroke, orthopedic injury, debility).
Patients who have a TBI or who have had a stroke often have comorbid psychiatric problems, including mood and anxiety disorders, that can exacerbate deficits and impede engagement in rehabilitation. The neuropsychological evaluation can determine if this is the case and if psychiatric consultation is warranted to assist with managing symptoms.
Premorbid psychiatric illness can affect rehabilitation. Formal neuropsychological testing can assist with parsing out deficits associated with new-onset illness compared with premorbid psychiatric problems. The evaluation of a patient before he begins rehabilitation also can be compared with evaluations made during treatment and after discharge to 1) assess for changes and 2) update recommendations about management.
Recommendations about cognitive interventions might include specific compensatory strategies to address areas of weakness and capitalize on strengths. Such strategies can include using internal mnemonics, such as visual imagery (ie, using a visual image to help encode verbal information) or semantic elaboration (using semantic cues to aid in encoding and recall of information). Methods can help train patients to capitalize on areas of stronger cognitive functioning in compensating for their weaknesses; an example is the spaced-retrieval technique, which relies on repetition of information that is to be learned over time.11
Perhaps the most practical strategies for addressing areas of weakness are nonmnemonic-based external memory aids, such as diaries, notebooks, calendars, alarms, and lists.12 For example, for a patient with a TBI who has impaired memory, recommendations might include using written notes or a calendar system; using a pillbox for medication management; and using labels to promote structure and consistency in the home. These strategies are meant to promote increased independence and to minimize the effect of cognitive deficits on daily functioning.
Recommended strategies can include lifestyle changes to promote improved cognitive functioning and overall health, such as:
• sleep hygiene, to reduce the effects of fatigue
• encouraging the patient to adhere to a diet, take prescribed medications, and follow up with his health care providers
• developing cognitive and physical exercise routines.
In addition, a patient who has had a stroke or who have a TBI might benefit from psychotherapy or referral to a group program or community resources to help cope with the effects of illness.13
6 How does neuropsychological testing help determine the appropriate psychiatric intervention for a patient? Results of neuropsychological testing can help determine appropriate interventions for a psychiatric condition that might be the principal factor affecting the patient’s functioning.
Concerning psychoactive medications, consider the following:
Mood and anxiety disorders. Neuropsychological measures can help substantiate the need for pharmacotherapy in a comorbid mood or anxiety disorder in a patient who has a neurologic illness, such as stroke or TBI.
ADHD. In a patient who has attentiondeficit/hyperactivity disorder (ADHD), results of cognitive testing might help determine if attention issues undermine daily functioning. Testing provides information beyond rating scale scores to justify diagnosis and psychopharmacotherapy.14
Dementia. Geriatric patients who have dementia often have coexisting behavioral and mood changes that, once evaluated, might improve with pharmacotherapy.
Other areas. Cognitive side effects of medications can be monitored by conducting testing before and after medication is started. The evaluation can address the patient’s ability to engage in psychotherapeutic interventions. Patients who have severe cognitive deficits might have greater difficulty engaging in psychotherapy, compared with patients who have less severe, or no, cognitive
impairment.15
7 Does neuropsychological testing help patients make return-to-work
and return-to-school decisions? Yes. Cognitive and psychiatric functioning have
implications for decisions about occupational and academic pursuits.
Patients who have severe cognitive or psychiatric symptoms might be or might not be able to maintain gainful employment or participate in school. Testing can help 1) document and justify disability and 2) establish recommendations about disability status. Those whose cognitive impairments or psychiatric symptoms are less severe might benefit from neuropsychological testing so that recommendations can be made regarding accommodations at work or in school, such as:
• reduced work or school schedule
• reduced level of occupational or academic demand
• change in supervision or evaluation procedures by employer or school.
Cognitive strengths and weaknesses can be used to help a patient devise and implement compensatory strategies at work or school, such as:
• note-taking
• audio recording of meetings and lectures
• using a calendar.
Patients sometimes benefit from formal vocational rehabilitation services to facilitate finding appropriate employment, returning to employment, and implementing workplace accommodations.
In conclusion
Neuropsychological evaluation, typically covered by health insurance, provides the
referring clinician with objective information about patients’ cognitive assets and limitations. In turn, this information can help you make a diagnosis and plan
treatment.
Unlike psychological testing, in which the patient is assessed for psychiatric
symptoms and conditions, neuropsychological measures offer insight into such
abilities as attention, memory, and reasoning. Neuropsychological evaluations also
can add insight to your determination of the cause of symptoms, thereby influencing decisions about medical therapy.
Last, these evaluations can aid with decision-making about dispositional planning
and whether adjunctive services, such as rehabilitation, would be of benefit.
Bottom Line
Neuropsychological assessments are a useful consultation to consider for patients
in a psychiatric setting. These evaluations can aid you in building and narrowing the differential diagnosis; identifying patients’ strengths and weakness; and making informed recommendations about functional independence.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Donders J. A survey of report writing by neuropsychologists, I: general characteristics and content. Clin Neuropsychol. 2001;15(2):137-149.
2. Lamberty GT, Courtney JC, Heilbronner RC. The practice of clinical neuropsychology: a survey of practices and settings. New York, NY: Taylor & Francis; 2005.
3. Sweet JJ, Meyer DG, Nelson NW, et al. The TCN/AACN 2010 “salary survey”: professional practices, beliefs, and incomes of U.S. neuropsychologists. Clin Neuropsychol. 2011;25(1):12-61.
4. Marvel CL, Paradiso S. Cognitive and neurologic impairment in mood disorders. Psychiatr Clin North Am. 2004;27(1):19-36,vii-viii.
5. Moberg PJ, Rick JH. Decision-making capacity and competency in the elderly: a clinical and neuropsychological perspective. NeuroRehabilitation. 2008;23(5):
403-413.
6. Bradshaw LE, Goldberg SE, Lewis SA, et al. Six-month outcomes following an emergency hospital admission for older adults with co-morbid mental health problems indicate complexity of care needs. Age Ageing. 2013; 42(5):582-588.
7. Medalia A, Lim RW. Self-awareness of cognitive functioning in schizophrenia. Schizophr Res. 2004;71(2-3):331-338.
8. Andreou C, Bozikas VP. The predictive significance of neurocognitive factors for functional outcome in bipolar disorder. Curr Opin Psychiatry. 2013;26(1):54-59.
9. Stuss DT, Winocur G, Robertson IH, eds. Cognitive neurorehabilitation: evidence and application. 2nd ed. New York, NY: Cambridge University Press; 2008.
10. Raskin SA, ed. Neuroplasticity and rehabilitation. New York, NY: The Guilford Press; 2011.
11. Glisky EL, Glisky ML. Memory rehabilitation in older adults. In: Stuss DT, Winocur G, Robertson IH. Cognitive neurorehabilitation. 1st ed. New York, NY: Cambridge University Press; 2008.
12. Kapur N, Glisky EL, Wilson BA. External memory aids and computers in memory rehabilitation. In: Baddeley AD, Kopelman MD, Wilson BA. Handbook of memory disorders. Chichester, United Kingdom: Wiley; 2002:757-784.
13. Stalder-Luthy F, Messerli-Burgy N, Hofer H, et al. Effect of psychological interventions on depressive symptoms in long-term rehabilitation after an acquired brain injury: a systematic review and meta-analysis. Arch Phys Med Rehabil.
2013;94(7):1386-1397.
14. Hale JB, Reddy LA, Semrud-Clikeman M, et al. Executive impairment determines ADHD medication response: implications for academic achievement. J Learn Disabil. 2011;44(2):196-212.
15. Medalia A, Lim R. Treatment of cognitive dysfunction in psychiatric disorders. J Psychiatr Pract. 2004;10(1):17-25.
Neuropsychological evaluation, consisting of a thorough examination of cognitive and behavioral functioning, can make an invaluable contribution to the care of psychiatric patients. Through the vehicle of standardized measures of abilities, patients’ cognitive strengths and weaknesses can be elucidated—revealing potential areas for further interventions or to explain impediments to treatment. A licensed clinical psychologist provides this service.
You, as a consumer of reported findings, can use the results to inform your diagnosis and treatment plan. Recommendations from the neuropsychologist often address dispositional planning, cognitive intervention, psychiatric intervention, and work and school accommodations.
Probing the brain−behavior relationship
Neuropsychology is a subspecialty of clinical psychology that is focused on understanding the brain–behavior relationship. Drawing information from multiple disciplines, including psychiatry and neurology, neuropsychology seeks to uncover the cognitive, behavioral, and emotional difficulties that can result from known or suspected brain dysfunction. Increasingly, to protect the public and referral sources, clinical psychologists who perform neuropsychological testing demonstrate their competence through board certification (eg, the American Board of Clinical Neuropsychology).
How is testing conducted? Evaluations comprise measures that are standardized, scored objectively, and have established psychometric properties. Testing can performed on an outpatient or inpatient basis; the duration of testing depends on the question for which the referring practitioner seeks an answer.
Measures typically are administered by paper and pencil, although computer-based
assessments are increasingly being employed. Because of the influence of demographic variables (age, sex, years of education, race), scores are compared with normative samples that resemble those of the patient’s background as closely as possible.
A thorough clinical interview with the patient, a collateral interview with caregivers
and family, and review of relevant medical records are crucial parts of the assessment. Multiple areas of cognition are assessed:
• intelligence
• academic functioning
• attention
• working memory
• speed of processing
• learning and memory
• visual spatial skills
• fine motor skills
• executive functioning.
Essentially, the evaluation speaks to a patient’s neurocognitive functioning and cerebral integrity.
How are results scored? Interpretation of test scores is contingent on expectations of how a patient should perform in the absence of neurologic or psychiatric illness (ie, based on normative data and performancebased estimates of premorbid functioning).1 The overall pattern of intact scores and deficit scores can be used to form specific impressions about a diagnosis, cognitive strengths and weaknesses, and strategies for intervention.
Personality testing. In addition to the cognitive aspect of the evaluation, personality measures are incorporated when relevant to the referral question or presenting concern.
Personality tests can be broadly divided into objective and projective measures.
Objective personality measures, such as the Minnesota Multiphasic Personality
Inventory-Second Edition, require the examinee to respond to a set of items as
true or false or on a Likert-type scale from strongly agree to disagree. Responses are then scored in standardized fashion, making comparisons to normative data, which are then analyzed to determine the extent to which the examinee experiences psychiatric symptoms.
As part of testing, patients’ responses to ambiguous or unstructured standard
stimuli—such as a series of drawings, abstract patterns, or incomplete sentences—
are analyzed to determine underlying personality traits, feelings, and attitudes.
Classic examples of these measures include the Rorschach Test and the Thematic
Apperception Test.
Personality measures and psychiatric testing are designed to answer questions
related to patients’ emotional status. These measures assess psychiatric symptoms and diagnoses, whereas neuropsychological measures provide an understanding of patients’ cognitive assets and limitations.
7 Common questions about neuropsychological testing
1 Will my patient’s insurance cover these assessments? The question is common from practitioners who are considering requesting an assessment for a patient. The short answer is “Yes.”
Most payers follow Medicare guidelines for reimbursement of neuropsychological
testing; if testing is determined to be medically necessary, insurance companies often cover the assessment. Medicaid also pays for psychometric testing services. Neuropsychologists who have a hospital-based practice typically include patients
with all types of insurance coverage. For example, 40% of patients seen in a hospital are covered by Medicare or Medicaid.2
A caveat: Local intermediaries interpret policies and procedures in different ways,
so there is variability in coverage by geographic region. That is why it is crucial
for neuropsychologists to obtain preauthorization, as would be the case with other medical procedures and services sought by referral.
Last, insurance companies do not pay for assessment of a learning disability. The
rationale typically offered for this lack of coverage? The assessment is for academic, not medical, purposes. In such a situation, patients and their families are offered a private-pay option.
2 What are the indications for neuropsychological assessment? Psychiatric practitioners are one of the top medical specialties that refer their patients for neuropsychological testing.3 This is because many patients with a psychiatric or
neurologic disorder experience changes in cognition, mood, and personality. Such
changes can range in severity from subtle to dramatic, and might reflect an underlying disease state or a side effect of medication or other treatment. Whatever the nature of a patient’s problem, careful assessment might help elucidate specific areas with which he (she) is struggling—so that you can better target your interventions. Table 1 lists common reasons for referring a patient for neuropsychological evaluation. Throughout this discussion, we describe examples of clinical situations in which neuropsychological testing is useful for establishing a differential diagnosis and dispositional planning.
3 How does neuropsychological testing help with the differential diagnosis? As an example, one area in which cognitive testing can be beneficial is in geriatric psychiatry.Dementia. Aging often is accompanied by a normal decline in memory and other cognitive functions. But because subtle changes in memory and cognition also canbe the sign of a progressive cognitive disorder, differentiating normal aging from early dementia is essential. Table 2 summarizes typical changes in cognition with aging.
Neuropsychologists, through knowledge of psychometric testing and the brain−behavior relationship, can help you detect dementia and plan treatment early. To determine if cognitive changes are progressive, patients might undergo re-evaluation—typically, every 6 to 12 months—to ascertain if changes have occurred. Mood disorders. Neuropsychological evaluation can be useful in building a differential diagnosis when determining whether cognitive symptoms are attributable to a mood disorder or a medical illness. Cognitive deficits associated with an affective disturbance generally include impairments in attention, memory, and executive functioning.4 The severity of deficits has been linked to severity of illness. When patients with a mood disorder demonstrate localizing impairments or those of greater severity than expected, suspicion arises that another cause likely better explains those deficits, and further medical testing then is often recommended. Medical procedures. Increasingly, neuropsychological assessment is used to assist in determining the appropriateness of medical procedures. For example, neurosurgical patients being considered for deep brain stimulation, brain tumor resectioning, and epilepsy surgery often are referred for preoperative and postoperative testing. Treating clinicians need an understanding of current cognitive status, localization of functioning, and psychological status to make appropriate decisions about a patient’s candidacy for one of these procedures,and to understand associated risk.
4 How is neuropsychological testing used for dispositional planning? The
results of cognitive and psychological testing have implications for dispositional
planning for patients who are receiving psychiatric care. The primary issue often is
to determine the patient’s level of independence and ability to make decisions about his affairs.5
Neuropsychological testing can help determine if cognitive deficits limit aspects of functional independence—for example, can the patient live alone, or must he live with family or in a residential care facility? Generally, the greater the cognitive impairment, the more supervision and assistance are required. This relationship between cognitive ability and independence in activities of daily living has been demonstrated in many groups of psychiatric patients, including older adults with dementia,6 patients with schizophrenia,7 and those with bipolar disorder.8
Specific recommendations can be made regarding management of finances, administering medications, and driving. To formulate an appropriate dispositional plan, the referring psychiatrist might integrate recommendations from the neuropsychological assessment with findings of other evaluations and with information that has been collected about the patient.
5 Can neuropsychological testing be used to refer a patient for neurological and cognitive rehabilitation? Yes. The neuropsychologist is singularly qualified to make recommendations about a range of interventions for cognitive deficits that have been identified on formal testing.
Typically, recommendations for addressing cognitive deficits involve rehabilitation
focused on development and use of compensatory strategies and modification to promote brain health.9,10 Rehabilitation therapy typically is aimed at increasing functioning independence and reducing physical and cognitive deficits associated
with illness (eg, traumatic brain injury [TBI], stroke, orthopedic injury, debility).
Patients who have a TBI or who have had a stroke often have comorbid psychiatric problems, including mood and anxiety disorders, that can exacerbate deficits and impede engagement in rehabilitation. The neuropsychological evaluation can determine if this is the case and if psychiatric consultation is warranted to assist with managing symptoms.
Premorbid psychiatric illness can affect rehabilitation. Formal neuropsychological testing can assist with parsing out deficits associated with new-onset illness compared with premorbid psychiatric problems. The evaluation of a patient before he begins rehabilitation also can be compared with evaluations made during treatment and after discharge to 1) assess for changes and 2) update recommendations about management.
Recommendations about cognitive interventions might include specific compensatory strategies to address areas of weakness and capitalize on strengths. Such strategies can include using internal mnemonics, such as visual imagery (ie, using a visual image to help encode verbal information) or semantic elaboration (using semantic cues to aid in encoding and recall of information). Methods can help train patients to capitalize on areas of stronger cognitive functioning in compensating for their weaknesses; an example is the spaced-retrieval technique, which relies on repetition of information that is to be learned over time.11
Perhaps the most practical strategies for addressing areas of weakness are nonmnemonic-based external memory aids, such as diaries, notebooks, calendars, alarms, and lists.12 For example, for a patient with a TBI who has impaired memory, recommendations might include using written notes or a calendar system; using a pillbox for medication management; and using labels to promote structure and consistency in the home. These strategies are meant to promote increased independence and to minimize the effect of cognitive deficits on daily functioning.
Recommended strategies can include lifestyle changes to promote improved cognitive functioning and overall health, such as:
• sleep hygiene, to reduce the effects of fatigue
• encouraging the patient to adhere to a diet, take prescribed medications, and follow up with his health care providers
• developing cognitive and physical exercise routines.
In addition, a patient who has had a stroke or who have a TBI might benefit from psychotherapy or referral to a group program or community resources to help cope with the effects of illness.13
6 How does neuropsychological testing help determine the appropriate psychiatric intervention for a patient? Results of neuropsychological testing can help determine appropriate interventions for a psychiatric condition that might be the principal factor affecting the patient’s functioning.
Concerning psychoactive medications, consider the following:
Mood and anxiety disorders. Neuropsychological measures can help substantiate the need for pharmacotherapy in a comorbid mood or anxiety disorder in a patient who has a neurologic illness, such as stroke or TBI.
ADHD. In a patient who has attentiondeficit/hyperactivity disorder (ADHD), results of cognitive testing might help determine if attention issues undermine daily functioning. Testing provides information beyond rating scale scores to justify diagnosis and psychopharmacotherapy.14
Dementia. Geriatric patients who have dementia often have coexisting behavioral and mood changes that, once evaluated, might improve with pharmacotherapy.
Other areas. Cognitive side effects of medications can be monitored by conducting testing before and after medication is started. The evaluation can address the patient’s ability to engage in psychotherapeutic interventions. Patients who have severe cognitive deficits might have greater difficulty engaging in psychotherapy, compared with patients who have less severe, or no, cognitive
impairment.15
7 Does neuropsychological testing help patients make return-to-work
and return-to-school decisions? Yes. Cognitive and psychiatric functioning have
implications for decisions about occupational and academic pursuits.
Patients who have severe cognitive or psychiatric symptoms might be or might not be able to maintain gainful employment or participate in school. Testing can help 1) document and justify disability and 2) establish recommendations about disability status. Those whose cognitive impairments or psychiatric symptoms are less severe might benefit from neuropsychological testing so that recommendations can be made regarding accommodations at work or in school, such as:
• reduced work or school schedule
• reduced level of occupational or academic demand
• change in supervision or evaluation procedures by employer or school.
Cognitive strengths and weaknesses can be used to help a patient devise and implement compensatory strategies at work or school, such as:
• note-taking
• audio recording of meetings and lectures
• using a calendar.
Patients sometimes benefit from formal vocational rehabilitation services to facilitate finding appropriate employment, returning to employment, and implementing workplace accommodations.
In conclusion
Neuropsychological evaluation, typically covered by health insurance, provides the
referring clinician with objective information about patients’ cognitive assets and limitations. In turn, this information can help you make a diagnosis and plan
treatment.
Unlike psychological testing, in which the patient is assessed for psychiatric
symptoms and conditions, neuropsychological measures offer insight into such
abilities as attention, memory, and reasoning. Neuropsychological evaluations also
can add insight to your determination of the cause of symptoms, thereby influencing decisions about medical therapy.
Last, these evaluations can aid with decision-making about dispositional planning
and whether adjunctive services, such as rehabilitation, would be of benefit.
Bottom Line
Neuropsychological assessments are a useful consultation to consider for patients
in a psychiatric setting. These evaluations can aid you in building and narrowing the differential diagnosis; identifying patients’ strengths and weakness; and making informed recommendations about functional independence.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Neuropsychological evaluation, consisting of a thorough examination of cognitive and behavioral functioning, can make an invaluable contribution to the care of psychiatric patients. Through the vehicle of standardized measures of abilities, patients’ cognitive strengths and weaknesses can be elucidated—revealing potential areas for further interventions or to explain impediments to treatment. A licensed clinical psychologist provides this service.
You, as a consumer of reported findings, can use the results to inform your diagnosis and treatment plan. Recommendations from the neuropsychologist often address dispositional planning, cognitive intervention, psychiatric intervention, and work and school accommodations.
Probing the brain−behavior relationship
Neuropsychology is a subspecialty of clinical psychology that is focused on understanding the brain–behavior relationship. Drawing information from multiple disciplines, including psychiatry and neurology, neuropsychology seeks to uncover the cognitive, behavioral, and emotional difficulties that can result from known or suspected brain dysfunction. Increasingly, to protect the public and referral sources, clinical psychologists who perform neuropsychological testing demonstrate their competence through board certification (eg, the American Board of Clinical Neuropsychology).
How is testing conducted? Evaluations comprise measures that are standardized, scored objectively, and have established psychometric properties. Testing can performed on an outpatient or inpatient basis; the duration of testing depends on the question for which the referring practitioner seeks an answer.
Measures typically are administered by paper and pencil, although computer-based
assessments are increasingly being employed. Because of the influence of demographic variables (age, sex, years of education, race), scores are compared with normative samples that resemble those of the patient’s background as closely as possible.
A thorough clinical interview with the patient, a collateral interview with caregivers
and family, and review of relevant medical records are crucial parts of the assessment. Multiple areas of cognition are assessed:
• intelligence
• academic functioning
• attention
• working memory
• speed of processing
• learning and memory
• visual spatial skills
• fine motor skills
• executive functioning.
Essentially, the evaluation speaks to a patient’s neurocognitive functioning and cerebral integrity.
How are results scored? Interpretation of test scores is contingent on expectations of how a patient should perform in the absence of neurologic or psychiatric illness (ie, based on normative data and performancebased estimates of premorbid functioning).1 The overall pattern of intact scores and deficit scores can be used to form specific impressions about a diagnosis, cognitive strengths and weaknesses, and strategies for intervention.
Personality testing. In addition to the cognitive aspect of the evaluation, personality measures are incorporated when relevant to the referral question or presenting concern.
Personality tests can be broadly divided into objective and projective measures.
Objective personality measures, such as the Minnesota Multiphasic Personality
Inventory-Second Edition, require the examinee to respond to a set of items as
true or false or on a Likert-type scale from strongly agree to disagree. Responses are then scored in standardized fashion, making comparisons to normative data, which are then analyzed to determine the extent to which the examinee experiences psychiatric symptoms.
As part of testing, patients’ responses to ambiguous or unstructured standard
stimuli—such as a series of drawings, abstract patterns, or incomplete sentences—
are analyzed to determine underlying personality traits, feelings, and attitudes.
Classic examples of these measures include the Rorschach Test and the Thematic
Apperception Test.
Personality measures and psychiatric testing are designed to answer questions
related to patients’ emotional status. These measures assess psychiatric symptoms and diagnoses, whereas neuropsychological measures provide an understanding of patients’ cognitive assets and limitations.
7 Common questions about neuropsychological testing
1 Will my patient’s insurance cover these assessments? The question is common from practitioners who are considering requesting an assessment for a patient. The short answer is “Yes.”
Most payers follow Medicare guidelines for reimbursement of neuropsychological
testing; if testing is determined to be medically necessary, insurance companies often cover the assessment. Medicaid also pays for psychometric testing services. Neuropsychologists who have a hospital-based practice typically include patients
with all types of insurance coverage. For example, 40% of patients seen in a hospital are covered by Medicare or Medicaid.2
A caveat: Local intermediaries interpret policies and procedures in different ways,
so there is variability in coverage by geographic region. That is why it is crucial
for neuropsychologists to obtain preauthorization, as would be the case with other medical procedures and services sought by referral.
Last, insurance companies do not pay for assessment of a learning disability. The
rationale typically offered for this lack of coverage? The assessment is for academic, not medical, purposes. In such a situation, patients and their families are offered a private-pay option.
2 What are the indications for neuropsychological assessment? Psychiatric practitioners are one of the top medical specialties that refer their patients for neuropsychological testing.3 This is because many patients with a psychiatric or
neurologic disorder experience changes in cognition, mood, and personality. Such
changes can range in severity from subtle to dramatic, and might reflect an underlying disease state or a side effect of medication or other treatment. Whatever the nature of a patient’s problem, careful assessment might help elucidate specific areas with which he (she) is struggling—so that you can better target your interventions. Table 1 lists common reasons for referring a patient for neuropsychological evaluation. Throughout this discussion, we describe examples of clinical situations in which neuropsychological testing is useful for establishing a differential diagnosis and dispositional planning.
3 How does neuropsychological testing help with the differential diagnosis? As an example, one area in which cognitive testing can be beneficial is in geriatric psychiatry.Dementia. Aging often is accompanied by a normal decline in memory and other cognitive functions. But because subtle changes in memory and cognition also canbe the sign of a progressive cognitive disorder, differentiating normal aging from early dementia is essential. Table 2 summarizes typical changes in cognition with aging.
Neuropsychologists, through knowledge of psychometric testing and the brain−behavior relationship, can help you detect dementia and plan treatment early. To determine if cognitive changes are progressive, patients might undergo re-evaluation—typically, every 6 to 12 months—to ascertain if changes have occurred. Mood disorders. Neuropsychological evaluation can be useful in building a differential diagnosis when determining whether cognitive symptoms are attributable to a mood disorder or a medical illness. Cognitive deficits associated with an affective disturbance generally include impairments in attention, memory, and executive functioning.4 The severity of deficits has been linked to severity of illness. When patients with a mood disorder demonstrate localizing impairments or those of greater severity than expected, suspicion arises that another cause likely better explains those deficits, and further medical testing then is often recommended. Medical procedures. Increasingly, neuropsychological assessment is used to assist in determining the appropriateness of medical procedures. For example, neurosurgical patients being considered for deep brain stimulation, brain tumor resectioning, and epilepsy surgery often are referred for preoperative and postoperative testing. Treating clinicians need an understanding of current cognitive status, localization of functioning, and psychological status to make appropriate decisions about a patient’s candidacy for one of these procedures,and to understand associated risk.
4 How is neuropsychological testing used for dispositional planning? The
results of cognitive and psychological testing have implications for dispositional
planning for patients who are receiving psychiatric care. The primary issue often is
to determine the patient’s level of independence and ability to make decisions about his affairs.5
Neuropsychological testing can help determine if cognitive deficits limit aspects of functional independence—for example, can the patient live alone, or must he live with family or in a residential care facility? Generally, the greater the cognitive impairment, the more supervision and assistance are required. This relationship between cognitive ability and independence in activities of daily living has been demonstrated in many groups of psychiatric patients, including older adults with dementia,6 patients with schizophrenia,7 and those with bipolar disorder.8
Specific recommendations can be made regarding management of finances, administering medications, and driving. To formulate an appropriate dispositional plan, the referring psychiatrist might integrate recommendations from the neuropsychological assessment with findings of other evaluations and with information that has been collected about the patient.
5 Can neuropsychological testing be used to refer a patient for neurological and cognitive rehabilitation? Yes. The neuropsychologist is singularly qualified to make recommendations about a range of interventions for cognitive deficits that have been identified on formal testing.
Typically, recommendations for addressing cognitive deficits involve rehabilitation
focused on development and use of compensatory strategies and modification to promote brain health.9,10 Rehabilitation therapy typically is aimed at increasing functioning independence and reducing physical and cognitive deficits associated
with illness (eg, traumatic brain injury [TBI], stroke, orthopedic injury, debility).
Patients who have a TBI or who have had a stroke often have comorbid psychiatric problems, including mood and anxiety disorders, that can exacerbate deficits and impede engagement in rehabilitation. The neuropsychological evaluation can determine if this is the case and if psychiatric consultation is warranted to assist with managing symptoms.
Premorbid psychiatric illness can affect rehabilitation. Formal neuropsychological testing can assist with parsing out deficits associated with new-onset illness compared with premorbid psychiatric problems. The evaluation of a patient before he begins rehabilitation also can be compared with evaluations made during treatment and after discharge to 1) assess for changes and 2) update recommendations about management.
Recommendations about cognitive interventions might include specific compensatory strategies to address areas of weakness and capitalize on strengths. Such strategies can include using internal mnemonics, such as visual imagery (ie, using a visual image to help encode verbal information) or semantic elaboration (using semantic cues to aid in encoding and recall of information). Methods can help train patients to capitalize on areas of stronger cognitive functioning in compensating for their weaknesses; an example is the spaced-retrieval technique, which relies on repetition of information that is to be learned over time.11
Perhaps the most practical strategies for addressing areas of weakness are nonmnemonic-based external memory aids, such as diaries, notebooks, calendars, alarms, and lists.12 For example, for a patient with a TBI who has impaired memory, recommendations might include using written notes or a calendar system; using a pillbox for medication management; and using labels to promote structure and consistency in the home. These strategies are meant to promote increased independence and to minimize the effect of cognitive deficits on daily functioning.
Recommended strategies can include lifestyle changes to promote improved cognitive functioning and overall health, such as:
• sleep hygiene, to reduce the effects of fatigue
• encouraging the patient to adhere to a diet, take prescribed medications, and follow up with his health care providers
• developing cognitive and physical exercise routines.
In addition, a patient who has had a stroke or who have a TBI might benefit from psychotherapy or referral to a group program or community resources to help cope with the effects of illness.13
6 How does neuropsychological testing help determine the appropriate psychiatric intervention for a patient? Results of neuropsychological testing can help determine appropriate interventions for a psychiatric condition that might be the principal factor affecting the patient’s functioning.
Concerning psychoactive medications, consider the following:
Mood and anxiety disorders. Neuropsychological measures can help substantiate the need for pharmacotherapy in a comorbid mood or anxiety disorder in a patient who has a neurologic illness, such as stroke or TBI.
ADHD. In a patient who has attentiondeficit/hyperactivity disorder (ADHD), results of cognitive testing might help determine if attention issues undermine daily functioning. Testing provides information beyond rating scale scores to justify diagnosis and psychopharmacotherapy.14
Dementia. Geriatric patients who have dementia often have coexisting behavioral and mood changes that, once evaluated, might improve with pharmacotherapy.
Other areas. Cognitive side effects of medications can be monitored by conducting testing before and after medication is started. The evaluation can address the patient’s ability to engage in psychotherapeutic interventions. Patients who have severe cognitive deficits might have greater difficulty engaging in psychotherapy, compared with patients who have less severe, or no, cognitive
impairment.15
7 Does neuropsychological testing help patients make return-to-work
and return-to-school decisions? Yes. Cognitive and psychiatric functioning have
implications for decisions about occupational and academic pursuits.
Patients who have severe cognitive or psychiatric symptoms might be or might not be able to maintain gainful employment or participate in school. Testing can help 1) document and justify disability and 2) establish recommendations about disability status. Those whose cognitive impairments or psychiatric symptoms are less severe might benefit from neuropsychological testing so that recommendations can be made regarding accommodations at work or in school, such as:
• reduced work or school schedule
• reduced level of occupational or academic demand
• change in supervision or evaluation procedures by employer or school.
Cognitive strengths and weaknesses can be used to help a patient devise and implement compensatory strategies at work or school, such as:
• note-taking
• audio recording of meetings and lectures
• using a calendar.
Patients sometimes benefit from formal vocational rehabilitation services to facilitate finding appropriate employment, returning to employment, and implementing workplace accommodations.
In conclusion
Neuropsychological evaluation, typically covered by health insurance, provides the
referring clinician with objective information about patients’ cognitive assets and limitations. In turn, this information can help you make a diagnosis and plan
treatment.
Unlike psychological testing, in which the patient is assessed for psychiatric
symptoms and conditions, neuropsychological measures offer insight into such
abilities as attention, memory, and reasoning. Neuropsychological evaluations also
can add insight to your determination of the cause of symptoms, thereby influencing decisions about medical therapy.
Last, these evaluations can aid with decision-making about dispositional planning
and whether adjunctive services, such as rehabilitation, would be of benefit.
Bottom Line
Neuropsychological assessments are a useful consultation to consider for patients
in a psychiatric setting. These evaluations can aid you in building and narrowing the differential diagnosis; identifying patients’ strengths and weakness; and making informed recommendations about functional independence.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Donders J. A survey of report writing by neuropsychologists, I: general characteristics and content. Clin Neuropsychol. 2001;15(2):137-149.
2. Lamberty GT, Courtney JC, Heilbronner RC. The practice of clinical neuropsychology: a survey of practices and settings. New York, NY: Taylor & Francis; 2005.
3. Sweet JJ, Meyer DG, Nelson NW, et al. The TCN/AACN 2010 “salary survey”: professional practices, beliefs, and incomes of U.S. neuropsychologists. Clin Neuropsychol. 2011;25(1):12-61.
4. Marvel CL, Paradiso S. Cognitive and neurologic impairment in mood disorders. Psychiatr Clin North Am. 2004;27(1):19-36,vii-viii.
5. Moberg PJ, Rick JH. Decision-making capacity and competency in the elderly: a clinical and neuropsychological perspective. NeuroRehabilitation. 2008;23(5):
403-413.
6. Bradshaw LE, Goldberg SE, Lewis SA, et al. Six-month outcomes following an emergency hospital admission for older adults with co-morbid mental health problems indicate complexity of care needs. Age Ageing. 2013; 42(5):582-588.
7. Medalia A, Lim RW. Self-awareness of cognitive functioning in schizophrenia. Schizophr Res. 2004;71(2-3):331-338.
8. Andreou C, Bozikas VP. The predictive significance of neurocognitive factors for functional outcome in bipolar disorder. Curr Opin Psychiatry. 2013;26(1):54-59.
9. Stuss DT, Winocur G, Robertson IH, eds. Cognitive neurorehabilitation: evidence and application. 2nd ed. New York, NY: Cambridge University Press; 2008.
10. Raskin SA, ed. Neuroplasticity and rehabilitation. New York, NY: The Guilford Press; 2011.
11. Glisky EL, Glisky ML. Memory rehabilitation in older adults. In: Stuss DT, Winocur G, Robertson IH. Cognitive neurorehabilitation. 1st ed. New York, NY: Cambridge University Press; 2008.
12. Kapur N, Glisky EL, Wilson BA. External memory aids and computers in memory rehabilitation. In: Baddeley AD, Kopelman MD, Wilson BA. Handbook of memory disorders. Chichester, United Kingdom: Wiley; 2002:757-784.
13. Stalder-Luthy F, Messerli-Burgy N, Hofer H, et al. Effect of psychological interventions on depressive symptoms in long-term rehabilitation after an acquired brain injury: a systematic review and meta-analysis. Arch Phys Med Rehabil.
2013;94(7):1386-1397.
14. Hale JB, Reddy LA, Semrud-Clikeman M, et al. Executive impairment determines ADHD medication response: implications for academic achievement. J Learn Disabil. 2011;44(2):196-212.
15. Medalia A, Lim R. Treatment of cognitive dysfunction in psychiatric disorders. J Psychiatr Pract. 2004;10(1):17-25.
1. Donders J. A survey of report writing by neuropsychologists, I: general characteristics and content. Clin Neuropsychol. 2001;15(2):137-149.
2. Lamberty GT, Courtney JC, Heilbronner RC. The practice of clinical neuropsychology: a survey of practices and settings. New York, NY: Taylor & Francis; 2005.
3. Sweet JJ, Meyer DG, Nelson NW, et al. The TCN/AACN 2010 “salary survey”: professional practices, beliefs, and incomes of U.S. neuropsychologists. Clin Neuropsychol. 2011;25(1):12-61.
4. Marvel CL, Paradiso S. Cognitive and neurologic impairment in mood disorders. Psychiatr Clin North Am. 2004;27(1):19-36,vii-viii.
5. Moberg PJ, Rick JH. Decision-making capacity and competency in the elderly: a clinical and neuropsychological perspective. NeuroRehabilitation. 2008;23(5):
403-413.
6. Bradshaw LE, Goldberg SE, Lewis SA, et al. Six-month outcomes following an emergency hospital admission for older adults with co-morbid mental health problems indicate complexity of care needs. Age Ageing. 2013; 42(5):582-588.
7. Medalia A, Lim RW. Self-awareness of cognitive functioning in schizophrenia. Schizophr Res. 2004;71(2-3):331-338.
8. Andreou C, Bozikas VP. The predictive significance of neurocognitive factors for functional outcome in bipolar disorder. Curr Opin Psychiatry. 2013;26(1):54-59.
9. Stuss DT, Winocur G, Robertson IH, eds. Cognitive neurorehabilitation: evidence and application. 2nd ed. New York, NY: Cambridge University Press; 2008.
10. Raskin SA, ed. Neuroplasticity and rehabilitation. New York, NY: The Guilford Press; 2011.
11. Glisky EL, Glisky ML. Memory rehabilitation in older adults. In: Stuss DT, Winocur G, Robertson IH. Cognitive neurorehabilitation. 1st ed. New York, NY: Cambridge University Press; 2008.
12. Kapur N, Glisky EL, Wilson BA. External memory aids and computers in memory rehabilitation. In: Baddeley AD, Kopelman MD, Wilson BA. Handbook of memory disorders. Chichester, United Kingdom: Wiley; 2002:757-784.
13. Stalder-Luthy F, Messerli-Burgy N, Hofer H, et al. Effect of psychological interventions on depressive symptoms in long-term rehabilitation after an acquired brain injury: a systematic review and meta-analysis. Arch Phys Med Rehabil.
2013;94(7):1386-1397.
14. Hale JB, Reddy LA, Semrud-Clikeman M, et al. Executive impairment determines ADHD medication response: implications for academic achievement. J Learn Disabil. 2011;44(2):196-212.
15. Medalia A, Lim R. Treatment of cognitive dysfunction in psychiatric disorders. J Psychiatr Pract. 2004;10(1):17-25.
Zolpidem may cause visual distortions and other psychotic symptoms
Zolpidem, an imidazopyridine hypnotic, has been used as an alternative to benzodiazepines for treating short-term insomnia because it has a relatively favorable side effect profile and less potential for abuse.1
However, several cases of zolpidemrelated psychotic symptoms have been reported,2 including a report of an association between zolpidem and hallucinations.1 The case illustrated here describes distortion of visual perception that can occur after ingestion of more than the recommended dosage of zolpidem.
CASE: Terrified and paranoid with distorted vision
Ms. K, age 33, an English-speaking woman from Portugal with a history of schizoaffective disorder, is brought to the emergency department in a terrified state. She describes visual distortion and paranoia because she fears losing her vision. She complains of suicidal ideation, depressed mood, insomnia, auditory
hallucinations, and distortion of visual perception. She reports seeing shadows, recurring movements of the ceiling bearing down on her, and molding or melting walls.
Ms. K reports that the visual distortions began when she started zolpidem, 10 mg/d, 2 months earlier, after her mother in Portugal gave it to her.
Ms. K describes feeling disoriented and disconnected from reality. She reports taking extra doses of zolpidem (40 mg)—recommended maximum dosage is 10 mg3—and clonazepam (1 mg) to address her insomnia.
On examination, Ms. K appears shaky and tremulous, and we note that her eyeballs roll upward. Vital signs are within normal limits, and she is awake, alert, and oriented to person, place, and time.
We diagnose exacerbation of schizoaffective disorder.
Ms. K is admitted to the inpatient psychiatric unit for observation and treatment. Quetiapine, 100 mg at bedtime, and sertraline, 100 mg/d, are started and zolpidem is discontinued.
The morning after admission, Ms. K reports that her vision has improved and that she no longer sees shadows or colored spots. All visual distortions resolve within 1 day after discontinuing zolpidem.
Discussion
Ms. K had no history of ophthalmologic or neurologic disease or alcohol or substance use. Physical and neurologic examination and laboratory testing failed to reveal any abnormality that accounts for her clinical presentation. Also, she reported visual distortions in the absence of drowsiness,4 thereby ruling out hypnagogic hallucination.5
Visual hallucinations are uncommon in schizoaffective disorder, but have been shown to occur with zolpidem use.1,4 The clinical manifestations in Ms. K’s case are
consistent with those of 3 reports, in which patients reported visual symptoms shortly after an initial dose of zolpidem, 10 mg.1,6 In those cases, symptoms resolved soon after zolpidem was discontinued.
Ms. K’s case is similar to other reports in regard to time of onset and manifestations of visual distortions. Iruela and colleagues documented that hallucinations could be reproduced with a lower challenge dose of zolpidem (5 or 2.5 mg), and that, with such a challenge, symptoms should be less severe.7 How zolpidem induces visual hallucinations remains unknown. Several studies have looked at variables that might predispose a patient taking zolpidem to visual
perceptual distortions.1
Sex might play an important role.1,7 After administering the same dosage of zolpidem, women age 20 to 40 had a blood concentration of the drug that was, on average, 45% higher than those measured in men.6 This difference in serum concentration is more remarkable in older women; the blood concentration of the drug in women age >60 was 63% higher than that of men.
Influence of hormones. Pharmacokinetics of zolpidem seem to be related to endocrine factors associated with cytochrome P450 (CYP) 3A4 metabolism. A low plasma concentration of free testosterone may contribute to lower CYP3A activity, with women achieving as much as a 50% higher plasma level of zolpidem, whereas exposure to testosterone activates biotransformation via CYP3A.8
Body weight is important when dosing zolpidem. Zolpidem-induced macropsia
has been reported in women with anorexia.7 The protein-binding capacity of zolpidem is approximately 92%, mainly to albumin (66%) and α1-acid glycoprotein (56.6%).4 In malnourished patients with anorexia nervosa, hypoalbuminemia is common and, therefore, unbound drug concentration is higher. This effect could account for, or contribute to, zolpidem toxicity.7
Ms. K did not have anorexia nervosa and was not underweight, and her liver function and kidney function were within normal limits. However, prescribing guidelines call for an initial dosage of 5 mg/d for women (10 mg/d for men)3; Ms. K ingested 8 times the recommended daily dosage.
The lesson for practitioners? When you encounter a patient who has a psychiatric disorder with psychotic features, explore causes unrelated to their primary disorder—such as taking a hypnotic or multiple psychoactive medications—as a possible source of the presenting symptoms (Box). In Ms. K’s case, her unusual symptoms resolved after a change in pharmacotherapy, leading us to conclude that her visual distortions likely were secondary to zolpidem and not to her schizoaffective disorder—a confounding factor.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Huang CL, Chang CJ, Hung CF, et al. Zolpidem-induced distortion in visual perception. Ann Pharmacother. 2003;37(5):683-686.
2. Ansseau M, Pitchot W, Hansenne M, et al. Psychotic reaction to zolpidem (letter). Lancet. 1992;339(8796):809.
3. Ambien [package insert]. Bridgewater, NJ: sanofi-aventis U.S. LLC; 2013.
4. van Puijenbroek EP, Egberts AC, Krom HJ. Visual hallucinations and amnesia associated with the use of zolpidem (letter). Int J Clin Pharmacol Ther. 1996;34(7):318.
5. Morselli PL. Zolpidem side-effects (letter). Lancet. 1993; 342(8875):868-869.
6. Salvà P, Costa J. Clinical pharmacokinetics and pharmacodynamics of zolpidem. Therapeutic implications. Clin Pharmacokinet. 1995;29(3):142-153.
7. Iruela LM, Ibañez-Rojo V, Baca E. Zolpidem-induced macropsia in anorexic woman (letter). Lancet. 1993; 342(8868):443-444.
8. Cubała WJ, Wiglusz M, Burkiewicz A, et al. Zolpidem pharmacokinetics and pharmacodynamics in metabolic interactions involving CYP3A: sex as a differentiating factor. Eur J Clin Pharmacol. 2010;66(9):955.
Zolpidem, an imidazopyridine hypnotic, has been used as an alternative to benzodiazepines for treating short-term insomnia because it has a relatively favorable side effect profile and less potential for abuse.1
However, several cases of zolpidemrelated psychotic symptoms have been reported,2 including a report of an association between zolpidem and hallucinations.1 The case illustrated here describes distortion of visual perception that can occur after ingestion of more than the recommended dosage of zolpidem.
CASE: Terrified and paranoid with distorted vision
Ms. K, age 33, an English-speaking woman from Portugal with a history of schizoaffective disorder, is brought to the emergency department in a terrified state. She describes visual distortion and paranoia because she fears losing her vision. She complains of suicidal ideation, depressed mood, insomnia, auditory
hallucinations, and distortion of visual perception. She reports seeing shadows, recurring movements of the ceiling bearing down on her, and molding or melting walls.
Ms. K reports that the visual distortions began when she started zolpidem, 10 mg/d, 2 months earlier, after her mother in Portugal gave it to her.
Ms. K describes feeling disoriented and disconnected from reality. She reports taking extra doses of zolpidem (40 mg)—recommended maximum dosage is 10 mg3—and clonazepam (1 mg) to address her insomnia.
On examination, Ms. K appears shaky and tremulous, and we note that her eyeballs roll upward. Vital signs are within normal limits, and she is awake, alert, and oriented to person, place, and time.
We diagnose exacerbation of schizoaffective disorder.
Ms. K is admitted to the inpatient psychiatric unit for observation and treatment. Quetiapine, 100 mg at bedtime, and sertraline, 100 mg/d, are started and zolpidem is discontinued.
The morning after admission, Ms. K reports that her vision has improved and that she no longer sees shadows or colored spots. All visual distortions resolve within 1 day after discontinuing zolpidem.
Discussion
Ms. K had no history of ophthalmologic or neurologic disease or alcohol or substance use. Physical and neurologic examination and laboratory testing failed to reveal any abnormality that accounts for her clinical presentation. Also, she reported visual distortions in the absence of drowsiness,4 thereby ruling out hypnagogic hallucination.5
Visual hallucinations are uncommon in schizoaffective disorder, but have been shown to occur with zolpidem use.1,4 The clinical manifestations in Ms. K’s case are
consistent with those of 3 reports, in which patients reported visual symptoms shortly after an initial dose of zolpidem, 10 mg.1,6 In those cases, symptoms resolved soon after zolpidem was discontinued.
Ms. K’s case is similar to other reports in regard to time of onset and manifestations of visual distortions. Iruela and colleagues documented that hallucinations could be reproduced with a lower challenge dose of zolpidem (5 or 2.5 mg), and that, with such a challenge, symptoms should be less severe.7 How zolpidem induces visual hallucinations remains unknown. Several studies have looked at variables that might predispose a patient taking zolpidem to visual
perceptual distortions.1
Sex might play an important role.1,7 After administering the same dosage of zolpidem, women age 20 to 40 had a blood concentration of the drug that was, on average, 45% higher than those measured in men.6 This difference in serum concentration is more remarkable in older women; the blood concentration of the drug in women age >60 was 63% higher than that of men.
Influence of hormones. Pharmacokinetics of zolpidem seem to be related to endocrine factors associated with cytochrome P450 (CYP) 3A4 metabolism. A low plasma concentration of free testosterone may contribute to lower CYP3A activity, with women achieving as much as a 50% higher plasma level of zolpidem, whereas exposure to testosterone activates biotransformation via CYP3A.8
Body weight is important when dosing zolpidem. Zolpidem-induced macropsia
has been reported in women with anorexia.7 The protein-binding capacity of zolpidem is approximately 92%, mainly to albumin (66%) and α1-acid glycoprotein (56.6%).4 In malnourished patients with anorexia nervosa, hypoalbuminemia is common and, therefore, unbound drug concentration is higher. This effect could account for, or contribute to, zolpidem toxicity.7
Ms. K did not have anorexia nervosa and was not underweight, and her liver function and kidney function were within normal limits. However, prescribing guidelines call for an initial dosage of 5 mg/d for women (10 mg/d for men)3; Ms. K ingested 8 times the recommended daily dosage.
The lesson for practitioners? When you encounter a patient who has a psychiatric disorder with psychotic features, explore causes unrelated to their primary disorder—such as taking a hypnotic or multiple psychoactive medications—as a possible source of the presenting symptoms (Box). In Ms. K’s case, her unusual symptoms resolved after a change in pharmacotherapy, leading us to conclude that her visual distortions likely were secondary to zolpidem and not to her schizoaffective disorder—a confounding factor.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
Zolpidem, an imidazopyridine hypnotic, has been used as an alternative to benzodiazepines for treating short-term insomnia because it has a relatively favorable side effect profile and less potential for abuse.1
However, several cases of zolpidemrelated psychotic symptoms have been reported,2 including a report of an association between zolpidem and hallucinations.1 The case illustrated here describes distortion of visual perception that can occur after ingestion of more than the recommended dosage of zolpidem.
CASE: Terrified and paranoid with distorted vision
Ms. K, age 33, an English-speaking woman from Portugal with a history of schizoaffective disorder, is brought to the emergency department in a terrified state. She describes visual distortion and paranoia because she fears losing her vision. She complains of suicidal ideation, depressed mood, insomnia, auditory
hallucinations, and distortion of visual perception. She reports seeing shadows, recurring movements of the ceiling bearing down on her, and molding or melting walls.
Ms. K reports that the visual distortions began when she started zolpidem, 10 mg/d, 2 months earlier, after her mother in Portugal gave it to her.
Ms. K describes feeling disoriented and disconnected from reality. She reports taking extra doses of zolpidem (40 mg)—recommended maximum dosage is 10 mg3—and clonazepam (1 mg) to address her insomnia.
On examination, Ms. K appears shaky and tremulous, and we note that her eyeballs roll upward. Vital signs are within normal limits, and she is awake, alert, and oriented to person, place, and time.
We diagnose exacerbation of schizoaffective disorder.
Ms. K is admitted to the inpatient psychiatric unit for observation and treatment. Quetiapine, 100 mg at bedtime, and sertraline, 100 mg/d, are started and zolpidem is discontinued.
The morning after admission, Ms. K reports that her vision has improved and that she no longer sees shadows or colored spots. All visual distortions resolve within 1 day after discontinuing zolpidem.
Discussion
Ms. K had no history of ophthalmologic or neurologic disease or alcohol or substance use. Physical and neurologic examination and laboratory testing failed to reveal any abnormality that accounts for her clinical presentation. Also, she reported visual distortions in the absence of drowsiness,4 thereby ruling out hypnagogic hallucination.5
Visual hallucinations are uncommon in schizoaffective disorder, but have been shown to occur with zolpidem use.1,4 The clinical manifestations in Ms. K’s case are
consistent with those of 3 reports, in which patients reported visual symptoms shortly after an initial dose of zolpidem, 10 mg.1,6 In those cases, symptoms resolved soon after zolpidem was discontinued.
Ms. K’s case is similar to other reports in regard to time of onset and manifestations of visual distortions. Iruela and colleagues documented that hallucinations could be reproduced with a lower challenge dose of zolpidem (5 or 2.5 mg), and that, with such a challenge, symptoms should be less severe.7 How zolpidem induces visual hallucinations remains unknown. Several studies have looked at variables that might predispose a patient taking zolpidem to visual
perceptual distortions.1
Sex might play an important role.1,7 After administering the same dosage of zolpidem, women age 20 to 40 had a blood concentration of the drug that was, on average, 45% higher than those measured in men.6 This difference in serum concentration is more remarkable in older women; the blood concentration of the drug in women age >60 was 63% higher than that of men.
Influence of hormones. Pharmacokinetics of zolpidem seem to be related to endocrine factors associated with cytochrome P450 (CYP) 3A4 metabolism. A low plasma concentration of free testosterone may contribute to lower CYP3A activity, with women achieving as much as a 50% higher plasma level of zolpidem, whereas exposure to testosterone activates biotransformation via CYP3A.8
Body weight is important when dosing zolpidem. Zolpidem-induced macropsia
has been reported in women with anorexia.7 The protein-binding capacity of zolpidem is approximately 92%, mainly to albumin (66%) and α1-acid glycoprotein (56.6%).4 In malnourished patients with anorexia nervosa, hypoalbuminemia is common and, therefore, unbound drug concentration is higher. This effect could account for, or contribute to, zolpidem toxicity.7
Ms. K did not have anorexia nervosa and was not underweight, and her liver function and kidney function were within normal limits. However, prescribing guidelines call for an initial dosage of 5 mg/d for women (10 mg/d for men)3; Ms. K ingested 8 times the recommended daily dosage.
The lesson for practitioners? When you encounter a patient who has a psychiatric disorder with psychotic features, explore causes unrelated to their primary disorder—such as taking a hypnotic or multiple psychoactive medications—as a possible source of the presenting symptoms (Box). In Ms. K’s case, her unusual symptoms resolved after a change in pharmacotherapy, leading us to conclude that her visual distortions likely were secondary to zolpidem and not to her schizoaffective disorder—a confounding factor.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Huang CL, Chang CJ, Hung CF, et al. Zolpidem-induced distortion in visual perception. Ann Pharmacother. 2003;37(5):683-686.
2. Ansseau M, Pitchot W, Hansenne M, et al. Psychotic reaction to zolpidem (letter). Lancet. 1992;339(8796):809.
3. Ambien [package insert]. Bridgewater, NJ: sanofi-aventis U.S. LLC; 2013.
4. van Puijenbroek EP, Egberts AC, Krom HJ. Visual hallucinations and amnesia associated with the use of zolpidem (letter). Int J Clin Pharmacol Ther. 1996;34(7):318.
5. Morselli PL. Zolpidem side-effects (letter). Lancet. 1993; 342(8875):868-869.
6. Salvà P, Costa J. Clinical pharmacokinetics and pharmacodynamics of zolpidem. Therapeutic implications. Clin Pharmacokinet. 1995;29(3):142-153.
7. Iruela LM, Ibañez-Rojo V, Baca E. Zolpidem-induced macropsia in anorexic woman (letter). Lancet. 1993; 342(8868):443-444.
8. Cubała WJ, Wiglusz M, Burkiewicz A, et al. Zolpidem pharmacokinetics and pharmacodynamics in metabolic interactions involving CYP3A: sex as a differentiating factor. Eur J Clin Pharmacol. 2010;66(9):955.
1. Huang CL, Chang CJ, Hung CF, et al. Zolpidem-induced distortion in visual perception. Ann Pharmacother. 2003;37(5):683-686.
2. Ansseau M, Pitchot W, Hansenne M, et al. Psychotic reaction to zolpidem (letter). Lancet. 1992;339(8796):809.
3. Ambien [package insert]. Bridgewater, NJ: sanofi-aventis U.S. LLC; 2013.
4. van Puijenbroek EP, Egberts AC, Krom HJ. Visual hallucinations and amnesia associated with the use of zolpidem (letter). Int J Clin Pharmacol Ther. 1996;34(7):318.
5. Morselli PL. Zolpidem side-effects (letter). Lancet. 1993; 342(8875):868-869.
6. Salvà P, Costa J. Clinical pharmacokinetics and pharmacodynamics of zolpidem. Therapeutic implications. Clin Pharmacokinet. 1995;29(3):142-153.
7. Iruela LM, Ibañez-Rojo V, Baca E. Zolpidem-induced macropsia in anorexic woman (letter). Lancet. 1993; 342(8868):443-444.
8. Cubała WJ, Wiglusz M, Burkiewicz A, et al. Zolpidem pharmacokinetics and pharmacodynamics in metabolic interactions involving CYP3A: sex as a differentiating factor. Eur J Clin Pharmacol. 2010;66(9):955.
Passive suicidal ideation: Still a high-risk clinical scenario
The commonly held belief that passive suicidal ideation poses less risk for suicide than active suicidal ideation is steeped in the lore of psychiatric practice. “Passive suicidal ideation” appears countless times in psychiatric records, articles, texts, guidelines, and clinical discourse. When a patient reports passive suicide ideation, the clinician may seize upon it as an indicator of low risk of suicide. The clinician may feel relieved and not perform a thorough suicide risk assessment.
Whether suicide ideation is active or passive, the goal is the same—terminating one’s life. Suicidal ideation, such as the wish to die during sleep, to be killed in an accident, or to develop terminal cancer, may seem relatively innocuous, but it can be just as ominous as thoughts of hanging oneself. Although passive suicidal ideation may allow time for interventions, passive ideation can suddenly turn active.
CASE "I love my family too much to hurt myself"
Mr. F, a 52-year-old business executive, is brought to the hospital emergency room by his wife. His business is heading to bankruptcy and he is unable to go to the office and face his employees. Mr. F cannot sleep or eat, spending most of the day on the couch crying. His wife has threatened her husband with separation if he does not seek psychiatric treatment.
Mr. F tells the emergency room psychiatrist, “I am stressed but have no intention of hurting myself. I love my wife and kids too much to put them through that.” He admits to having wishes to die during sleep, but reports, “I can’t sleep anyway.” His wife finds a loaded gun in the glove compartment of his car, but he says the “gun is for my protection.” He angrily denies any suicidal ideation and protests, “I do not need to be here.” His wife insists that he be treated, stating, “I will not take my husband home in his condition.”
Mr. F refuses psychiatric hospitalization but changes his mind when confronted with the alternative of involuntary hospitalization. He admits that, unknown to his wife, he recently purchased a $2 million life insurance policy and made funeral arrangements. He planned to kill himself with his revolver. A thorough suicide risk assessment reveals a number of evidence-based risk factors that place the patient at acute, high risk for suicide.
Passive ideation is active
When a patient reports passive suicidal ideation, active suicidal ideation invariably is present. No bright line separates them. Suicidal ideation, active or passive, contains a dynamic mix of ambivalent thoughts and feelings along a continuum of severity. It reflects ongoing change in the patient’s psychiatric disorder.1
Reynolds et al2 assessed the clinical correlates of active suicidal ideation vs passive death wishes in geriatric patients with recurrent major depression. Their data challenged the utility of distinguishing active and passive suicidal ideation. The authors also noted that the patient’s ideation can change from passive to active during an episode of illness. They recommended that clinicians be no less vigilant with patients expressing passive suicidal ideation.
Suicidal ideation that expresses active or passive methods of suicide usually reflects psychodynamic, cultural, religious, and moral issues as well as evasiveness, guardedness, denial, and other factors. Assessing passive suicidal ideation may reveal few protective factors, which may increase the patient’s suicide risk.
Patients often find it easier to talk about protective factors than suicidal thoughts. Patients whose culture or religion strongly condemns suicide may feel less conflicted reporting suicide ideation in the passive mode, if at all. For the patient who is determined to commit suicide, passive expression of suicide intent may indicate minimizing risk or deception, as seen in the case described here.3
“Fleeting” suicidal ideation, a frequent companion of “passive” suicidal ideation, also requires careful evaluation. In a study of 100 patients who made severe suicide attempts, Hall et al4 found that 69 reported only fleeting or no suicidal ideation before their attempt. “Fleeting” thoughts of suicide must not be accepted at face value but require thorough assessment.
Structured assessments instruments for evaluating suicide ideation are available. The Chronological Assessment of Suicidal Events (case approach) is designed to uncover detailed information related to the patient’s suicidal ideation.5 The Scale for Suicide Ideation, and the later version, Beck Scale for Suicide Ideation,6 rates passive suicidal ideation on a 3-point Likerttype scale as:
0 “would take precautions to save life”
1 “would leave life/death to chance (eg, carelessly crossing a busy street)”
2 “would avoid steps necessary to save or maintain life (eg, diabetic ceasing to take insulin).”
Although the Beck scales have psychometric properties (reliability and validity), no scale can substitute for thorough clinical assessment of suicidal ideation. If used, ratings scales or checklists of suicidal ideation can alert clinicians to thoroughly assess this crucial symptom of suicide risk.
When treating a suicidal patient, clinicians often experience complex, distressing feelings. Maltzberger and Buie7 describe anger, frustration, despair, and even hate toward the suicidal patient. In addition to the devastating loss of one’s patient, fears of a lawsuits and damage to one’s professional competence and reputation may arise if the patient attempts or completes suicide. These can all lead a clinician to prematurely accept a patient’s statement regarding passive suicidal ideation rather than conduct a thorough suicide risk assessment. Consultation should be considered.
The necessity of action
Suicidal ideation must be carefully assessed—not labeled. Passive suicidal ideation should not deter a clinician from performing a thorough suicide risk assessment. A patient’s report of passive suicidal ideation is not an end but a beginning of thorough suicide risk assessment.8
Bottom Line
Passive suicidal ideation, such as a wish to die during sleep or being killed in an accident, does not indicate that a patient is at a low risk of suicide. A thorough suicide risk assessment may reveal active suicidal ideation that informs treatment and management interventions.
Related Resources
• Simon RI. Suicide rehearsals: A high risk psychiatric emergency. Current Psychiatry. 2012;11(7):28-32.
• Baca-Garcia E, Perez-Rodriguez MM, Oquendo MA, et al. Estimating risk for suicide attempt: are we asking the right questions? Passive suicidal ideation as a marker for suicidal behavior. J Affect Disord. 2011;134(1-3):327-332.
1. Isometsä ET, Lönnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173:531-535.
2. Szanto K, Reynolds CF, Frank E, et al. Suicide in elderly depressed patients: is active vs. passive suicidal ideation a clinically valid distinction? Am J Geriatr Psychiatry. 1996;4(3):197-207.
3. Simon RI. Behavioral risk assessment of the guarded suicidal patient. Suicide Life Threat Behav. 2008;38(5):517-522.
4. Hall RC, Platt DE, Hall RC. Suicide risk assessment: a review of risk factors for suicide in 100 patients who made severe suicide attempts. Evaluations of suicide risk in a time of managed care. Psychosomatics. 1999;40(1):18-27.
5. Shea SC. The interpersonal art of suicide assessment interviewing techniques for uncovering suicidal intent, ideation and actions. In: Simon RI, Hale RE, eds. American Psychiatric Publishing textbook of suicide assessment and management. Arlington, VA: American Psychiatric Publishing; 2012:29-56.
6. Rush AJ Jr, First MB, Blacker D. Suicide risk measures. In: Rush AJ Jr, First MB, Blacker D, eds. Handbook of psychiatric measures, 2nd ed. Arlington, VA: American Psychiatric Publishing; 2008:242-244.
7. Maltzberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974; 30(5):625-633.
8. Simon RI. Suicide risk assessment: gateway to treatment and management. In: Simon RI, Hale RE, eds. American Psychiatric Publishing textbook of suicide assessment and management. Arlington, VA: American Psychiatric Publishing; 2012:3-28.
The commonly held belief that passive suicidal ideation poses less risk for suicide than active suicidal ideation is steeped in the lore of psychiatric practice. “Passive suicidal ideation” appears countless times in psychiatric records, articles, texts, guidelines, and clinical discourse. When a patient reports passive suicide ideation, the clinician may seize upon it as an indicator of low risk of suicide. The clinician may feel relieved and not perform a thorough suicide risk assessment.
Whether suicide ideation is active or passive, the goal is the same—terminating one’s life. Suicidal ideation, such as the wish to die during sleep, to be killed in an accident, or to develop terminal cancer, may seem relatively innocuous, but it can be just as ominous as thoughts of hanging oneself. Although passive suicidal ideation may allow time for interventions, passive ideation can suddenly turn active.
CASE "I love my family too much to hurt myself"
Mr. F, a 52-year-old business executive, is brought to the hospital emergency room by his wife. His business is heading to bankruptcy and he is unable to go to the office and face his employees. Mr. F cannot sleep or eat, spending most of the day on the couch crying. His wife has threatened her husband with separation if he does not seek psychiatric treatment.
Mr. F tells the emergency room psychiatrist, “I am stressed but have no intention of hurting myself. I love my wife and kids too much to put them through that.” He admits to having wishes to die during sleep, but reports, “I can’t sleep anyway.” His wife finds a loaded gun in the glove compartment of his car, but he says the “gun is for my protection.” He angrily denies any suicidal ideation and protests, “I do not need to be here.” His wife insists that he be treated, stating, “I will not take my husband home in his condition.”
Mr. F refuses psychiatric hospitalization but changes his mind when confronted with the alternative of involuntary hospitalization. He admits that, unknown to his wife, he recently purchased a $2 million life insurance policy and made funeral arrangements. He planned to kill himself with his revolver. A thorough suicide risk assessment reveals a number of evidence-based risk factors that place the patient at acute, high risk for suicide.
Passive ideation is active
When a patient reports passive suicidal ideation, active suicidal ideation invariably is present. No bright line separates them. Suicidal ideation, active or passive, contains a dynamic mix of ambivalent thoughts and feelings along a continuum of severity. It reflects ongoing change in the patient’s psychiatric disorder.1
Reynolds et al2 assessed the clinical correlates of active suicidal ideation vs passive death wishes in geriatric patients with recurrent major depression. Their data challenged the utility of distinguishing active and passive suicidal ideation. The authors also noted that the patient’s ideation can change from passive to active during an episode of illness. They recommended that clinicians be no less vigilant with patients expressing passive suicidal ideation.
Suicidal ideation that expresses active or passive methods of suicide usually reflects psychodynamic, cultural, religious, and moral issues as well as evasiveness, guardedness, denial, and other factors. Assessing passive suicidal ideation may reveal few protective factors, which may increase the patient’s suicide risk.
Patients often find it easier to talk about protective factors than suicidal thoughts. Patients whose culture or religion strongly condemns suicide may feel less conflicted reporting suicide ideation in the passive mode, if at all. For the patient who is determined to commit suicide, passive expression of suicide intent may indicate minimizing risk or deception, as seen in the case described here.3
“Fleeting” suicidal ideation, a frequent companion of “passive” suicidal ideation, also requires careful evaluation. In a study of 100 patients who made severe suicide attempts, Hall et al4 found that 69 reported only fleeting or no suicidal ideation before their attempt. “Fleeting” thoughts of suicide must not be accepted at face value but require thorough assessment.
Structured assessments instruments for evaluating suicide ideation are available. The Chronological Assessment of Suicidal Events (case approach) is designed to uncover detailed information related to the patient’s suicidal ideation.5 The Scale for Suicide Ideation, and the later version, Beck Scale for Suicide Ideation,6 rates passive suicidal ideation on a 3-point Likerttype scale as:
0 “would take precautions to save life”
1 “would leave life/death to chance (eg, carelessly crossing a busy street)”
2 “would avoid steps necessary to save or maintain life (eg, diabetic ceasing to take insulin).”
Although the Beck scales have psychometric properties (reliability and validity), no scale can substitute for thorough clinical assessment of suicidal ideation. If used, ratings scales or checklists of suicidal ideation can alert clinicians to thoroughly assess this crucial symptom of suicide risk.
When treating a suicidal patient, clinicians often experience complex, distressing feelings. Maltzberger and Buie7 describe anger, frustration, despair, and even hate toward the suicidal patient. In addition to the devastating loss of one’s patient, fears of a lawsuits and damage to one’s professional competence and reputation may arise if the patient attempts or completes suicide. These can all lead a clinician to prematurely accept a patient’s statement regarding passive suicidal ideation rather than conduct a thorough suicide risk assessment. Consultation should be considered.
The necessity of action
Suicidal ideation must be carefully assessed—not labeled. Passive suicidal ideation should not deter a clinician from performing a thorough suicide risk assessment. A patient’s report of passive suicidal ideation is not an end but a beginning of thorough suicide risk assessment.8
Bottom Line
Passive suicidal ideation, such as a wish to die during sleep or being killed in an accident, does not indicate that a patient is at a low risk of suicide. A thorough suicide risk assessment may reveal active suicidal ideation that informs treatment and management interventions.
Related Resources
• Simon RI. Suicide rehearsals: A high risk psychiatric emergency. Current Psychiatry. 2012;11(7):28-32.
• Baca-Garcia E, Perez-Rodriguez MM, Oquendo MA, et al. Estimating risk for suicide attempt: are we asking the right questions? Passive suicidal ideation as a marker for suicidal behavior. J Affect Disord. 2011;134(1-3):327-332.
The commonly held belief that passive suicidal ideation poses less risk for suicide than active suicidal ideation is steeped in the lore of psychiatric practice. “Passive suicidal ideation” appears countless times in psychiatric records, articles, texts, guidelines, and clinical discourse. When a patient reports passive suicide ideation, the clinician may seize upon it as an indicator of low risk of suicide. The clinician may feel relieved and not perform a thorough suicide risk assessment.
Whether suicide ideation is active or passive, the goal is the same—terminating one’s life. Suicidal ideation, such as the wish to die during sleep, to be killed in an accident, or to develop terminal cancer, may seem relatively innocuous, but it can be just as ominous as thoughts of hanging oneself. Although passive suicidal ideation may allow time for interventions, passive ideation can suddenly turn active.
CASE "I love my family too much to hurt myself"
Mr. F, a 52-year-old business executive, is brought to the hospital emergency room by his wife. His business is heading to bankruptcy and he is unable to go to the office and face his employees. Mr. F cannot sleep or eat, spending most of the day on the couch crying. His wife has threatened her husband with separation if he does not seek psychiatric treatment.
Mr. F tells the emergency room psychiatrist, “I am stressed but have no intention of hurting myself. I love my wife and kids too much to put them through that.” He admits to having wishes to die during sleep, but reports, “I can’t sleep anyway.” His wife finds a loaded gun in the glove compartment of his car, but he says the “gun is for my protection.” He angrily denies any suicidal ideation and protests, “I do not need to be here.” His wife insists that he be treated, stating, “I will not take my husband home in his condition.”
Mr. F refuses psychiatric hospitalization but changes his mind when confronted with the alternative of involuntary hospitalization. He admits that, unknown to his wife, he recently purchased a $2 million life insurance policy and made funeral arrangements. He planned to kill himself with his revolver. A thorough suicide risk assessment reveals a number of evidence-based risk factors that place the patient at acute, high risk for suicide.
Passive ideation is active
When a patient reports passive suicidal ideation, active suicidal ideation invariably is present. No bright line separates them. Suicidal ideation, active or passive, contains a dynamic mix of ambivalent thoughts and feelings along a continuum of severity. It reflects ongoing change in the patient’s psychiatric disorder.1
Reynolds et al2 assessed the clinical correlates of active suicidal ideation vs passive death wishes in geriatric patients with recurrent major depression. Their data challenged the utility of distinguishing active and passive suicidal ideation. The authors also noted that the patient’s ideation can change from passive to active during an episode of illness. They recommended that clinicians be no less vigilant with patients expressing passive suicidal ideation.
Suicidal ideation that expresses active or passive methods of suicide usually reflects psychodynamic, cultural, religious, and moral issues as well as evasiveness, guardedness, denial, and other factors. Assessing passive suicidal ideation may reveal few protective factors, which may increase the patient’s suicide risk.
Patients often find it easier to talk about protective factors than suicidal thoughts. Patients whose culture or religion strongly condemns suicide may feel less conflicted reporting suicide ideation in the passive mode, if at all. For the patient who is determined to commit suicide, passive expression of suicide intent may indicate minimizing risk or deception, as seen in the case described here.3
“Fleeting” suicidal ideation, a frequent companion of “passive” suicidal ideation, also requires careful evaluation. In a study of 100 patients who made severe suicide attempts, Hall et al4 found that 69 reported only fleeting or no suicidal ideation before their attempt. “Fleeting” thoughts of suicide must not be accepted at face value but require thorough assessment.
Structured assessments instruments for evaluating suicide ideation are available. The Chronological Assessment of Suicidal Events (case approach) is designed to uncover detailed information related to the patient’s suicidal ideation.5 The Scale for Suicide Ideation, and the later version, Beck Scale for Suicide Ideation,6 rates passive suicidal ideation on a 3-point Likerttype scale as:
0 “would take precautions to save life”
1 “would leave life/death to chance (eg, carelessly crossing a busy street)”
2 “would avoid steps necessary to save or maintain life (eg, diabetic ceasing to take insulin).”
Although the Beck scales have psychometric properties (reliability and validity), no scale can substitute for thorough clinical assessment of suicidal ideation. If used, ratings scales or checklists of suicidal ideation can alert clinicians to thoroughly assess this crucial symptom of suicide risk.
When treating a suicidal patient, clinicians often experience complex, distressing feelings. Maltzberger and Buie7 describe anger, frustration, despair, and even hate toward the suicidal patient. In addition to the devastating loss of one’s patient, fears of a lawsuits and damage to one’s professional competence and reputation may arise if the patient attempts or completes suicide. These can all lead a clinician to prematurely accept a patient’s statement regarding passive suicidal ideation rather than conduct a thorough suicide risk assessment. Consultation should be considered.
The necessity of action
Suicidal ideation must be carefully assessed—not labeled. Passive suicidal ideation should not deter a clinician from performing a thorough suicide risk assessment. A patient’s report of passive suicidal ideation is not an end but a beginning of thorough suicide risk assessment.8
Bottom Line
Passive suicidal ideation, such as a wish to die during sleep or being killed in an accident, does not indicate that a patient is at a low risk of suicide. A thorough suicide risk assessment may reveal active suicidal ideation that informs treatment and management interventions.
Related Resources
• Simon RI. Suicide rehearsals: A high risk psychiatric emergency. Current Psychiatry. 2012;11(7):28-32.
• Baca-Garcia E, Perez-Rodriguez MM, Oquendo MA, et al. Estimating risk for suicide attempt: are we asking the right questions? Passive suicidal ideation as a marker for suicidal behavior. J Affect Disord. 2011;134(1-3):327-332.
1. Isometsä ET, Lönnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173:531-535.
2. Szanto K, Reynolds CF, Frank E, et al. Suicide in elderly depressed patients: is active vs. passive suicidal ideation a clinically valid distinction? Am J Geriatr Psychiatry. 1996;4(3):197-207.
3. Simon RI. Behavioral risk assessment of the guarded suicidal patient. Suicide Life Threat Behav. 2008;38(5):517-522.
4. Hall RC, Platt DE, Hall RC. Suicide risk assessment: a review of risk factors for suicide in 100 patients who made severe suicide attempts. Evaluations of suicide risk in a time of managed care. Psychosomatics. 1999;40(1):18-27.
5. Shea SC. The interpersonal art of suicide assessment interviewing techniques for uncovering suicidal intent, ideation and actions. In: Simon RI, Hale RE, eds. American Psychiatric Publishing textbook of suicide assessment and management. Arlington, VA: American Psychiatric Publishing; 2012:29-56.
6. Rush AJ Jr, First MB, Blacker D. Suicide risk measures. In: Rush AJ Jr, First MB, Blacker D, eds. Handbook of psychiatric measures, 2nd ed. Arlington, VA: American Psychiatric Publishing; 2008:242-244.
7. Maltzberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974; 30(5):625-633.
8. Simon RI. Suicide risk assessment: gateway to treatment and management. In: Simon RI, Hale RE, eds. American Psychiatric Publishing textbook of suicide assessment and management. Arlington, VA: American Psychiatric Publishing; 2012:3-28.
1. Isometsä ET, Lönnqvist JK. Suicide attempts preceding completed suicide. Br J Psychiatry. 1998;173:531-535.
2. Szanto K, Reynolds CF, Frank E, et al. Suicide in elderly depressed patients: is active vs. passive suicidal ideation a clinically valid distinction? Am J Geriatr Psychiatry. 1996;4(3):197-207.
3. Simon RI. Behavioral risk assessment of the guarded suicidal patient. Suicide Life Threat Behav. 2008;38(5):517-522.
4. Hall RC, Platt DE, Hall RC. Suicide risk assessment: a review of risk factors for suicide in 100 patients who made severe suicide attempts. Evaluations of suicide risk in a time of managed care. Psychosomatics. 1999;40(1):18-27.
5. Shea SC. The interpersonal art of suicide assessment interviewing techniques for uncovering suicidal intent, ideation and actions. In: Simon RI, Hale RE, eds. American Psychiatric Publishing textbook of suicide assessment and management. Arlington, VA: American Psychiatric Publishing; 2012:29-56.
6. Rush AJ Jr, First MB, Blacker D. Suicide risk measures. In: Rush AJ Jr, First MB, Blacker D, eds. Handbook of psychiatric measures, 2nd ed. Arlington, VA: American Psychiatric Publishing; 2008:242-244.
7. Maltzberger JT, Buie DH. Countertransference hate in the treatment of suicidal patients. Arch Gen Psychiatry. 1974; 30(5):625-633.
8. Simon RI. Suicide risk assessment: gateway to treatment and management. In: Simon RI, Hale RE, eds. American Psychiatric Publishing textbook of suicide assessment and management. Arlington, VA: American Psychiatric Publishing; 2012:3-28.
A brave new era of IV psychopharmacotherapy
Most psychiatrists generally avoid starting an IV line on their patients these days, but delivering psychotropic medications by infusion has been employed in psychiatry for decades—mainly in cases of acute psychiatric emergencies.
IV pharmacotherapy might be evolving, however, to address the treatment of severe, chronic, intractable, and disabling disorders that have failed to respond to multiple oral formulations. In addition, IV therapy might be exploited to hasten onset of a therapeutic response.
In short, IV delivery of psychotropics might soon become a routine psychiatric “procedure.”
In the past
Apart from the desperate measures of pentylenetetrazol-induced seizures for depression and insulin coma for schizophrenia—both eventually discarded—psychiatrists have used IV pharmacotherapeutic interventions since the dawn of psychopharmacology in the 1950s. These include:
• Droperidol (the highly sedating cousin of haloperidol) for severe agitation
or aggressive behavior in an emergency setting
• Haloperidol for delirium in the intensive care unit
• Benzodiazepines for severe anxiety and panic attacks (although the IM
route is preferable)
• Clomipramine to potentiate the effect of a selective serotonin reuptake inhibitor in treatment-resistant depression
• Valproate to accelerate mood stabilization in acute mania.
The present
Recently, a mini-avalanche of novel studies has signaled a paradigm shift to IV therapy for refractory unipolar and bipolar depression.
Ketamine. Administering the N-methyl-d-aspartate (NMDA) glutamate receptor antagonist ketamine (a cousin of phencyclidine and a well-known drug of abuse with psychotogenic properties) by IV infusion (0.5 mg/kg) produces rapid improvement, sometimes complete remission, of chronic, treatment-resistant depression. The effect seen in 1 or 2 hours matches what oral antidepressants accomplish in 6 to 8 weeks in a responsive patient.1,2 The response to IV ketamine lasts approximately 1 week and is initially associated with transient dissociation.
Another reported benefit of IV ketamine is rapid reversal of suicidal intent.3 This effect is envisioned as a future alternative to hospitalizing patients brought to the emergency room after a suicide attempt.
To be clear: The long-term (maintenance) safety and efficacy of repeated infusions of IV ketamine to maintain response in chronic, treatment-resistant depression has not been studied.
IV ketamine therapy for severe depression is a dual paradigm shift: 1) it uses the IV route and 2) it modulates the glutamate ion-channel receptor NMDA—a major departure from the 50-year-old monoamine hypothesis of depression, in which a deficit of serotonin and/or norepinephrine was proposed. The mechanism of action of IV ketamine appears to be instant triggering of neuroplasticity in the mammalian target of rapamycin (mTOR), as observed in animal studies. A significant surge in brain-derived neurotrophic factor appears to be involved as well.
Scopolamine. Another novel IV treatment for depression was reported recently,4 based on old studies in which tearfulness and dysphoria were induced by increasing cholinergic activity with IV physostigmine. The anticholinergic drug scopolamine was administered to depressed patients by pulsed IV infusion (4.0 μg/kg over 15 minutes), and rapid improvement in depression was observed within 72 hours in patients with unipolar and bipolar depression. Anticholinergic side effects were mild; women responded better than men.
Nitroprusside. A similar breakthrough with IV pharmacotherapy was recently reported in schizophrenia, in which traditional oral antipsychotic treatment is limited to suppressing positive symptoms, leaving negative symptoms and cognitive deficits unchanged. The old antihypertensive drug nitroprusside, which modulates nitrous oxide and, by extension, NMDA, was administered IV to a small sample of patients with schizophrenia.5 Significant improvement was observed not only in positive (psychotic) symptoms, but also in negative and cognitive symptoms. Improvement occurred within a few hours and lasted for as long as 4 weeks. Studies are underway to replicate the investigators’ findings about this potentially ground-breaking and novel approach to schizophrenia.
For the future
Given these recent successes, it is reasonable to speculate that IV drugs might someday become a major tool in the practice of psychiatry—transcending emergent uses (suicidal, homicidal, and delirious states) and becoming a mainstream treatment for acute episodes of psychosis, mania, depression, and anxiety. In addition, research might reveal that medications already approved for oral delivery exert a more robust response and a more rapid onset of action when delivered IV—assuming no serious safety issues arise.
Advances in our understanding of the neurobiologic basis and pathophysiology of psychiatric disorders might provide clues to agents that are not even on the current radar screen of psychiatry’s pharmacopoeia. Treatment-resistant conditions are obvious initial candidates for IV pharmacotherapy, but so might be acute episodes of psychosis, mania, and depression, and panic attacks. Just as status epilepticus requires IV, rather than oral, delivery of an anticonvulsant, we might conceptualize acute psychotic, mood, and anxiety episodes as emergent conditions of status psychiatricus that require rapid stabilization with IV medication instead of a pill.
The bottom line?
IV delivery of drugs might soon be a routine psychiatric “procedure.” Better brush up on your skills for starting an infusion!
Drug Brand Names
Benztropine • Cogentin Pentylenetetrazol • Metrazol
Clomipramine • Anafranil Physostigmine • Antilirium
Diphenhydramine• Benadryl Scopolamine • Scopace, Transderm-Scop
Droperidol • Inapsine Valproate • Depacon
Haloperidol • Haldol
Ketamine • Ketalar
Nitroprusside • Nitropress
1. DiazGranados N, Ibrahim LA, Brutsche NE, et al. Rapid resolution of suicidal ideation after a single infusion of an N-methyl-D-aspartate antagonist in patients with treatment-resistant major depressive disorder. J Clin Psychiatry. 2010;71(12):1605-1611.
2. Rasmussen KG, Lineberry TW, Galardy CW, et al. Serial infusions of low-dose ketamine for major depression. J Psychopharmacol. 2013;27(5):444-450.
3. Zarate CA Jr, Brutsche NE, Ibrahim L, et al. Replication of ketamine’s antidepressant efficacy in bipolar depression: a randomized controlled add-on trial. Biol Psychiatry. 2012;71(11):939-946.
4. Drevets WC, Furey ML. Replication of scopolamine’s antidepressant efficacy in major depressive disorder: a randomized, placebo-controlled clinical trial. Biol Psychiatry. 2010;67(5):432-438.
5. Hallak JE, Maia-de-Oliveira JP, Abrao J, et al. Rapid improvement of acute schizophrenia symptoms after intravenous sodium nitroprusside: a randomized, double-blind, placebo-controlled trial. JAMA Psychiatry. 2013;70(7):668-676.
Most psychiatrists generally avoid starting an IV line on their patients these days, but delivering psychotropic medications by infusion has been employed in psychiatry for decades—mainly in cases of acute psychiatric emergencies.
IV pharmacotherapy might be evolving, however, to address the treatment of severe, chronic, intractable, and disabling disorders that have failed to respond to multiple oral formulations. In addition, IV therapy might be exploited to hasten onset of a therapeutic response.
In short, IV delivery of psychotropics might soon become a routine psychiatric “procedure.”
In the past
Apart from the desperate measures of pentylenetetrazol-induced seizures for depression and insulin coma for schizophrenia—both eventually discarded—psychiatrists have used IV pharmacotherapeutic interventions since the dawn of psychopharmacology in the 1950s. These include:
• Droperidol (the highly sedating cousin of haloperidol) for severe agitation
or aggressive behavior in an emergency setting
• Haloperidol for delirium in the intensive care unit
• Benzodiazepines for severe anxiety and panic attacks (although the IM
route is preferable)
• Clomipramine to potentiate the effect of a selective serotonin reuptake inhibitor in treatment-resistant depression
• Valproate to accelerate mood stabilization in acute mania.
The present
Recently, a mini-avalanche of novel studies has signaled a paradigm shift to IV therapy for refractory unipolar and bipolar depression.
Ketamine. Administering the N-methyl-d-aspartate (NMDA) glutamate receptor antagonist ketamine (a cousin of phencyclidine and a well-known drug of abuse with psychotogenic properties) by IV infusion (0.5 mg/kg) produces rapid improvement, sometimes complete remission, of chronic, treatment-resistant depression. The effect seen in 1 or 2 hours matches what oral antidepressants accomplish in 6 to 8 weeks in a responsive patient.1,2 The response to IV ketamine lasts approximately 1 week and is initially associated with transient dissociation.
Another reported benefit of IV ketamine is rapid reversal of suicidal intent.3 This effect is envisioned as a future alternative to hospitalizing patients brought to the emergency room after a suicide attempt.
To be clear: The long-term (maintenance) safety and efficacy of repeated infusions of IV ketamine to maintain response in chronic, treatment-resistant depression has not been studied.
IV ketamine therapy for severe depression is a dual paradigm shift: 1) it uses the IV route and 2) it modulates the glutamate ion-channel receptor NMDA—a major departure from the 50-year-old monoamine hypothesis of depression, in which a deficit of serotonin and/or norepinephrine was proposed. The mechanism of action of IV ketamine appears to be instant triggering of neuroplasticity in the mammalian target of rapamycin (mTOR), as observed in animal studies. A significant surge in brain-derived neurotrophic factor appears to be involved as well.
Scopolamine. Another novel IV treatment for depression was reported recently,4 based on old studies in which tearfulness and dysphoria were induced by increasing cholinergic activity with IV physostigmine. The anticholinergic drug scopolamine was administered to depressed patients by pulsed IV infusion (4.0 μg/kg over 15 minutes), and rapid improvement in depression was observed within 72 hours in patients with unipolar and bipolar depression. Anticholinergic side effects were mild; women responded better than men.
Nitroprusside. A similar breakthrough with IV pharmacotherapy was recently reported in schizophrenia, in which traditional oral antipsychotic treatment is limited to suppressing positive symptoms, leaving negative symptoms and cognitive deficits unchanged. The old antihypertensive drug nitroprusside, which modulates nitrous oxide and, by extension, NMDA, was administered IV to a small sample of patients with schizophrenia.5 Significant improvement was observed not only in positive (psychotic) symptoms, but also in negative and cognitive symptoms. Improvement occurred within a few hours and lasted for as long as 4 weeks. Studies are underway to replicate the investigators’ findings about this potentially ground-breaking and novel approach to schizophrenia.
For the future
Given these recent successes, it is reasonable to speculate that IV drugs might someday become a major tool in the practice of psychiatry—transcending emergent uses (suicidal, homicidal, and delirious states) and becoming a mainstream treatment for acute episodes of psychosis, mania, depression, and anxiety. In addition, research might reveal that medications already approved for oral delivery exert a more robust response and a more rapid onset of action when delivered IV—assuming no serious safety issues arise.
Advances in our understanding of the neurobiologic basis and pathophysiology of psychiatric disorders might provide clues to agents that are not even on the current radar screen of psychiatry’s pharmacopoeia. Treatment-resistant conditions are obvious initial candidates for IV pharmacotherapy, but so might be acute episodes of psychosis, mania, and depression, and panic attacks. Just as status epilepticus requires IV, rather than oral, delivery of an anticonvulsant, we might conceptualize acute psychotic, mood, and anxiety episodes as emergent conditions of status psychiatricus that require rapid stabilization with IV medication instead of a pill.
The bottom line?
IV delivery of drugs might soon be a routine psychiatric “procedure.” Better brush up on your skills for starting an infusion!
Drug Brand Names
Benztropine • Cogentin Pentylenetetrazol • Metrazol
Clomipramine • Anafranil Physostigmine • Antilirium
Diphenhydramine• Benadryl Scopolamine • Scopace, Transderm-Scop
Droperidol • Inapsine Valproate • Depacon
Haloperidol • Haldol
Ketamine • Ketalar
Nitroprusside • Nitropress
Most psychiatrists generally avoid starting an IV line on their patients these days, but delivering psychotropic medications by infusion has been employed in psychiatry for decades—mainly in cases of acute psychiatric emergencies.
IV pharmacotherapy might be evolving, however, to address the treatment of severe, chronic, intractable, and disabling disorders that have failed to respond to multiple oral formulations. In addition, IV therapy might be exploited to hasten onset of a therapeutic response.
In short, IV delivery of psychotropics might soon become a routine psychiatric “procedure.”
In the past
Apart from the desperate measures of pentylenetetrazol-induced seizures for depression and insulin coma for schizophrenia—both eventually discarded—psychiatrists have used IV pharmacotherapeutic interventions since the dawn of psychopharmacology in the 1950s. These include:
• Droperidol (the highly sedating cousin of haloperidol) for severe agitation
or aggressive behavior in an emergency setting
• Haloperidol for delirium in the intensive care unit
• Benzodiazepines for severe anxiety and panic attacks (although the IM
route is preferable)
• Clomipramine to potentiate the effect of a selective serotonin reuptake inhibitor in treatment-resistant depression
• Valproate to accelerate mood stabilization in acute mania.
The present
Recently, a mini-avalanche of novel studies has signaled a paradigm shift to IV therapy for refractory unipolar and bipolar depression.
Ketamine. Administering the N-methyl-d-aspartate (NMDA) glutamate receptor antagonist ketamine (a cousin of phencyclidine and a well-known drug of abuse with psychotogenic properties) by IV infusion (0.5 mg/kg) produces rapid improvement, sometimes complete remission, of chronic, treatment-resistant depression. The effect seen in 1 or 2 hours matches what oral antidepressants accomplish in 6 to 8 weeks in a responsive patient.1,2 The response to IV ketamine lasts approximately 1 week and is initially associated with transient dissociation.
Another reported benefit of IV ketamine is rapid reversal of suicidal intent.3 This effect is envisioned as a future alternative to hospitalizing patients brought to the emergency room after a suicide attempt.
To be clear: The long-term (maintenance) safety and efficacy of repeated infusions of IV ketamine to maintain response in chronic, treatment-resistant depression has not been studied.
IV ketamine therapy for severe depression is a dual paradigm shift: 1) it uses the IV route and 2) it modulates the glutamate ion-channel receptor NMDA—a major departure from the 50-year-old monoamine hypothesis of depression, in which a deficit of serotonin and/or norepinephrine was proposed. The mechanism of action of IV ketamine appears to be instant triggering of neuroplasticity in the mammalian target of rapamycin (mTOR), as observed in animal studies. A significant surge in brain-derived neurotrophic factor appears to be involved as well.
Scopolamine. Another novel IV treatment for depression was reported recently,4 based on old studies in which tearfulness and dysphoria were induced by increasing cholinergic activity with IV physostigmine. The anticholinergic drug scopolamine was administered to depressed patients by pulsed IV infusion (4.0 μg/kg over 15 minutes), and rapid improvement in depression was observed within 72 hours in patients with unipolar and bipolar depression. Anticholinergic side effects were mild; women responded better than men.
Nitroprusside. A similar breakthrough with IV pharmacotherapy was recently reported in schizophrenia, in which traditional oral antipsychotic treatment is limited to suppressing positive symptoms, leaving negative symptoms and cognitive deficits unchanged. The old antihypertensive drug nitroprusside, which modulates nitrous oxide and, by extension, NMDA, was administered IV to a small sample of patients with schizophrenia.5 Significant improvement was observed not only in positive (psychotic) symptoms, but also in negative and cognitive symptoms. Improvement occurred within a few hours and lasted for as long as 4 weeks. Studies are underway to replicate the investigators’ findings about this potentially ground-breaking and novel approach to schizophrenia.
For the future
Given these recent successes, it is reasonable to speculate that IV drugs might someday become a major tool in the practice of psychiatry—transcending emergent uses (suicidal, homicidal, and delirious states) and becoming a mainstream treatment for acute episodes of psychosis, mania, depression, and anxiety. In addition, research might reveal that medications already approved for oral delivery exert a more robust response and a more rapid onset of action when delivered IV—assuming no serious safety issues arise.
Advances in our understanding of the neurobiologic basis and pathophysiology of psychiatric disorders might provide clues to agents that are not even on the current radar screen of psychiatry’s pharmacopoeia. Treatment-resistant conditions are obvious initial candidates for IV pharmacotherapy, but so might be acute episodes of psychosis, mania, and depression, and panic attacks. Just as status epilepticus requires IV, rather than oral, delivery of an anticonvulsant, we might conceptualize acute psychotic, mood, and anxiety episodes as emergent conditions of status psychiatricus that require rapid stabilization with IV medication instead of a pill.
The bottom line?
IV delivery of drugs might soon be a routine psychiatric “procedure.” Better brush up on your skills for starting an infusion!
Drug Brand Names
Benztropine • Cogentin Pentylenetetrazol • Metrazol
Clomipramine • Anafranil Physostigmine • Antilirium
Diphenhydramine• Benadryl Scopolamine • Scopace, Transderm-Scop
Droperidol • Inapsine Valproate • Depacon
Haloperidol • Haldol
Ketamine • Ketalar
Nitroprusside • Nitropress
1. DiazGranados N, Ibrahim LA, Brutsche NE, et al. Rapid resolution of suicidal ideation after a single infusion of an N-methyl-D-aspartate antagonist in patients with treatment-resistant major depressive disorder. J Clin Psychiatry. 2010;71(12):1605-1611.
2. Rasmussen KG, Lineberry TW, Galardy CW, et al. Serial infusions of low-dose ketamine for major depression. J Psychopharmacol. 2013;27(5):444-450.
3. Zarate CA Jr, Brutsche NE, Ibrahim L, et al. Replication of ketamine’s antidepressant efficacy in bipolar depression: a randomized controlled add-on trial. Biol Psychiatry. 2012;71(11):939-946.
4. Drevets WC, Furey ML. Replication of scopolamine’s antidepressant efficacy in major depressive disorder: a randomized, placebo-controlled clinical trial. Biol Psychiatry. 2010;67(5):432-438.
5. Hallak JE, Maia-de-Oliveira JP, Abrao J, et al. Rapid improvement of acute schizophrenia symptoms after intravenous sodium nitroprusside: a randomized, double-blind, placebo-controlled trial. JAMA Psychiatry. 2013;70(7):668-676.
1. DiazGranados N, Ibrahim LA, Brutsche NE, et al. Rapid resolution of suicidal ideation after a single infusion of an N-methyl-D-aspartate antagonist in patients with treatment-resistant major depressive disorder. J Clin Psychiatry. 2010;71(12):1605-1611.
2. Rasmussen KG, Lineberry TW, Galardy CW, et al. Serial infusions of low-dose ketamine for major depression. J Psychopharmacol. 2013;27(5):444-450.
3. Zarate CA Jr, Brutsche NE, Ibrahim L, et al. Replication of ketamine’s antidepressant efficacy in bipolar depression: a randomized controlled add-on trial. Biol Psychiatry. 2012;71(11):939-946.
4. Drevets WC, Furey ML. Replication of scopolamine’s antidepressant efficacy in major depressive disorder: a randomized, placebo-controlled clinical trial. Biol Psychiatry. 2010;67(5):432-438.
5. Hallak JE, Maia-de-Oliveira JP, Abrao J, et al. Rapid improvement of acute schizophrenia symptoms after intravenous sodium nitroprusside: a randomized, double-blind, placebo-controlled trial. JAMA Psychiatry. 2013;70(7):668-676.
Clozapine for schizophrenia
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
First signs of a psychotic disorder
Schizophrenia prodrome: An optimal approach
In studies of schizophrenia, one of the more striking findings is the delay in the initiation of treatment. That delay ranges from 1 to 2 years for patients experiencing psychotic symptoms to several years if the prodromal phase is taken into account.1 Yet duration of untreated psychosis has been found to be a critical factor in prognosis, including psychosocial functioning, in patients with schizophrenia.2,3 Identification of individuals in the prodromal phase not only offers an opportunity to intervene at an earlier symptomatic stage, but might be associated with a better response to antipsychotics and a better overall treatment outcome as well.
What’s in a name?
Several terms, including ultra high risk, clinical high risk, at-risk mental state, psychosis risk syndrome, and schizophrenia/psychosis prodrome, have been used to describe the prodromal phase of schizophrenia. The proposal to include attenuated psychosis syndrome (APS) in the DSM-5—originally intended to capture those with subthreshold delusions, hallucinations, or disorganized behavior, occurring at least once a week for the past month and worsening over the past year—generated a debate about the validity of such a diagnostic category4,5 that culminated in the inclusion of APS as a condition for further study but not as a term for clinical use.6 Its presence in the DSM-5 brings to the forefront the importance of early clinical intervention in patients at risk of developing psychotic illness.
Schizophrenia is not inevitable
The prodromal phase can be viewed as a sequence of evolving symptoms7 (Box 18,9), starting with subtle differences evident only to the person experiencing them and often progressing to brief limited intermittent psychosis (BLIPS) or attenuated psychosis.8
In fact, prodrome is a retrospective diagnosis. The predictive power of conversion to psychosis has been found to fluctuate from as low as 9% to as high as 76%,10 prompting ethical concerns about a high false-positive rate, the assumption of inevitability associated with the term “schizophrenia prodrome,”9 and the potential for overdiagnosis and misdiagnosis. Concerns about psychosocial stigma and exposure to antipsychotic medications have been expressed as well.11
A case for early engagement
In retrospect, patients who eventually progress to psychotic illness are commonly found to have been in the prodromal phase for several years. Yet many patients’ first contact with psychiatric services occurs during a florid episode of acute psychosis. Identifying patients in the early prodromal period offers the opportunity to more effectively engage them and form a therapeutic alliance.12 Any young adult who presents with a decline in academic or occupational function, social withdrawal, perplexity, and apparent distress or agitation (Table 113-16) without a clear precipitating factor should therefore be closely monitored, particularly if he (she) has a family history of psychosis.
Screening tools. A variety of interviews and rating scales (Table 28) have been developed to assess and monitor at-risk persons, a number of which have been designed to detect basic symptoms in the early phase of prodrome. In addition to the structured scales, several self-report tools—including the Prodromal Questionnaire-Brief (PQ-B), Youth Psychosis At Risk Questionnaire-Brief (YPARQ-B), Prime Screen-Revised, and PROD-screen (Screen for prodromal symptoms of psychosis)—have been found to be useful in screening a large sample to identify those who might need further evaluation.17
Increased risk of conversion. Several clinical factors are associated with an increased risk of conversion to psychotic illness.9 In addition to family history, these include:
• greater severity and longer duration of attenuated positive symptoms
• presence of bizarre thoughts and behavior
• paranoia
• decline in global assessment of functioning score over the previous year
• use of either Cannabis or amphetamines.
A history of childhood trauma, increased sensitivity to psychosocial stressors, and dysregulation of the hypothalamicpituitary axis also have been associated with progression to psychosis.18
Recent evidence suggests that the prodromal phase is a predictor not only for psychosis but also for other disabling psychiatric illnesses, such as bipolar disorder and obsessive-compulsive disorder.19
From a phenomenological standpoint, disturbance of the sense of self—characterized by features such as depersonalization, derealization, decreased reactivity to other people and the environment, and intense reflectivity to oneself or others—has been proposed as a critical marker for progression to psychosis.20 Another predictor is the perception of negativity of others toward oneself. Examples include heightened sensitivity to rejection or shame, which seems to emerge from a pattern of insecure attachment, and the outsider status experienced by immigrants faced with multiple social, cultural, and language barriers.21 The presence of obsessivecompulsive symptoms during the prodromal phase has been linked to significant impairment in functioning, an acute switch to psychosis, and an increased risk of suicide.22
Monitor or treat? An optimal approach
A key dilemma in the management of patients who exhibit signs and symptoms of schizophrenia prodrome is whether to simply monitor closely or to initiate treatment.
International clinical practice guidelines recommend several practical steps in the monitoring of patients in a prepsychotic state (Table 3),23 but caution against the use of antipsychotic agents unless the patient meets diagnostic criteria for a psychotic disorder.
CBT. Some evidence supports the initiation of cognitive-behavioral therapy (CBT) during the initial prodromal phase and the addition of alow-dose atypical antipsychotic if the patient progresses to a later phase, characterized by BLIPS/APS.24,25 Evidence also suggests that a combination of CBT and antipsychotic medication might delay, but not prevent, the progression to a psychotic episode.9 Any risk of adverse metabolic complications precludes use ofan atypical antipsychotic.One potential alternative is the use of omega-3 polyunsaturated fatty acids (Box 2).26,27
A clinically useful approach would be to view schizophrenia/psychosis prodrome not as a distinct diagnostic category but as a cluster of signs and symptoms associated with an increased risk of psychosis, with persons in this phase in need of close follow-up and, possibly, early initiation of an antipsychotic agent. It is important to engage the patient and his family at an early stage to educate them about the diagnostic uncertainty; to help them deal with the stigma; to manage risk factors; and, collaboratively, to decide on an intervention strategy.23,28
Bottom Line
Despite several drawbacks, the concept of schizophrenia/psychosis prodrome may
be viewed as a cluster of signs and symptoms (rather than a distinct diagnostic category) associated with increased risk for psychosis that need close follow up. Follow up may involve psychoeducational and psychotherapeutic interventions and, need be, early initiation of antipsychotics. In addition, such symptoms may be associated with other psychiatric disorders such as bipolar disorder and obsessive- compulsive disorder. Timely attention and early intervention may alter the course
and improve overall prognosis.
Related Resources
• Early intervention in psychosis. WPA Education Committee’s recommended roles of the psychiatrist. www.wpanet.org/uploads/Education/Educational_Resources/earlyintervention-psychosis.pdf.
• Early Psychosis Prevention and Intervention Centre, Melbourne, Australia. http://eppic.org.au/psychosis.
• International Early Psychosis Association Writing Group. International clinical practice guidelines for early psychosis. Br J Psychiatry. 2005;187:s120-124. http://bjp.rcpsych.org/content/187/48/s120.full.
Disclosures
Dr. Madaan is an employee of University of Virginia Health System. As an employee with the University of Virginia, Dr. Madaan has received research support from Eli Lilly and Company, Forest, Merck, Otsuka, Pfizer, Shire, and Sunovion. He also has served as a consultant for the NOW Coalition for Bipolar Disorder, and on the American Psychiatric Association’s Focus Self-Assessment editorial board. Drs. Bestha and Kolli report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Salokangas RK, McGlashan TH. Early detection and intervention of psychosis. A review. Nord J Psychiatry. 2008;62:92-105.
2. Perkins DO, Gu H, Boteva K, et al. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry. 2005;162(10): 1785-1804.
3. Stefanopoulou E, Lafuente AR, Fonseca AS, et al. Global assessment of psychosocial functioning and predictors of outcome in schizophrenia. Int J Psychiatry Clin Pract. 2011;15(1):62-68.
4. Yung AR, Nelson B, Thompson AD, et al. Should a “Risk Syndrome for Psychosis” be included in the DSMV? Schizophr Res. 2010;120(1-3):7-15.
5. Corcoran CM, First MB, Cornblatt B. The psychosis risk syndrome and its proposed inclusion in the DSM-V: a risk-benefit analysis. Schizophr Res. 2010;120(1-3):16-22.
6. Diagnostic and statistical manual of mental disorders, 5th ed, text rev. Washington, DC: American Psychiatric Association; 2013.
7. Schultze-Lutter F, Ruhrmann S, Berning J, et al. Basic symptoms and ultrahigh risk criteria: symptom development in the initial prodromal state. Schizophr Bull. 2010;36(1):182-191.
8. Correll CU, Hauser M, Auther AM, et al. Research in people with psychosis risk syndrome: a review of the current evidence and future directions. J Child Psychol
Psychiatry. 2010;51(4):390-431.
9. Addington J, Heinssen R. Prediction and prevention of psychosis in youth at clinical high risk. Annu Rev Clin Psychol. 2012;8:269-289.
10. Cannon TD, Cadenhead K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65(1):28-37.
11. Singh F, Mirzakhanian H, Fusar-Poli P, et al. Ethical implications for clinical practice and future research in “at risk” individuals. Curr Pharm Des. 2012;18(4):606-612.
12. Bota RG, Munro JS, Ricci WF, et al. The dynamics of insight in the prodrome of schizophrenia. CNS Spectr. 2006;11(5):355-362.
13. Phillips LJ, Yung AR, McGorry PD. Identification of young people at risk of psychosis: validation of Personal Assessment and Crisis Evaluation Clinic intake criteria. Aust N Z J Psychiatry. 2000;34(suppl):S164-S169.
14. Miller TJ, McGlashan TH, Woods SW, et al. Symptom assessment in schizophrenic prodromal states. Psychiatr Q. 1999;70(4):273-287.
15. Schultze-Lutter F, Klosterkötter J, Picker H. Predicting first-episode psychosis by basic symptom criteria. Clinical Neuropsychiatry. 2007;4(1):11-22.
16. Schultze-Lutter F, Ruhrmann S, Picker H, et al. Basic symptoms in early psychotic and depressive disorders. Br J Psychiatry Suppl. 2007;51:s31-s37.
17. Kline E, Wilson C, Ereshefsky S, et al. Convergent and discriminant validity of attenuated psychosis screening tools. Schizophr Res. 2012;134(1):49-53.
18. Holtzman CW, Shapiro DI, Trotman HD, et al. Stress and the prodromal phase of psychosis. Curr Pharm Des. 2012;18(4):527-533.
19. Rössler W, Hengartner MP, Ajdacic-Gross V, et al. Subclinical psychosis symptoms in young adults are risk factors for subsequent common mental disorders. Schizophr Res. 2011;131(1-3):18-23.
20. Nelson B, Yung AR, Bechdolf A, et al. The phenomenological critique and self-disturbance: implications for ultra-high risk (“prodrome”) research. Schizophr Bull. 2008;34(2):381-392.
21. Salokangas RK, Heinimaa M, Svirskis T, et al. Perceived negative attitude of others as an early sign of psychosis. Eur Psychiatry. 2009;24(4):233-238.
22. Niendam TA, Berzak J, Cannon TD, et al. Obsessive compulsive symptoms in the psychosis prodrome:correlates of clinical and functional outcome. Schizophr
Res. 2009;108(1-3):170-175.
23. Addington J, Amminger GP, Barbato A. International clinical practice guidelines for early psychosis. Br J Psychiatry. 2005;187:s120-s124.
24. Klosterkötter J, Schultze-Lutter F, Bechdolf A, et al. Prediction and prevention of schizophrenia: what has been achieved and where to go next? World Psychiatry.
2011;10(3):165-174.
25. Stafford MR, Jackson H, Mayo-Wilson E, et al. Early interventions to prevent psychosis: systematic review and meta-analysis. BMJ. 2013;346:f185.
In studies of schizophrenia, one of the more striking findings is the delay in the initiation of treatment. That delay ranges from 1 to 2 years for patients experiencing psychotic symptoms to several years if the prodromal phase is taken into account.1 Yet duration of untreated psychosis has been found to be a critical factor in prognosis, including psychosocial functioning, in patients with schizophrenia.2,3 Identification of individuals in the prodromal phase not only offers an opportunity to intervene at an earlier symptomatic stage, but might be associated with a better response to antipsychotics and a better overall treatment outcome as well.
What’s in a name?
Several terms, including ultra high risk, clinical high risk, at-risk mental state, psychosis risk syndrome, and schizophrenia/psychosis prodrome, have been used to describe the prodromal phase of schizophrenia. The proposal to include attenuated psychosis syndrome (APS) in the DSM-5—originally intended to capture those with subthreshold delusions, hallucinations, or disorganized behavior, occurring at least once a week for the past month and worsening over the past year—generated a debate about the validity of such a diagnostic category4,5 that culminated in the inclusion of APS as a condition for further study but not as a term for clinical use.6 Its presence in the DSM-5 brings to the forefront the importance of early clinical intervention in patients at risk of developing psychotic illness.
Schizophrenia is not inevitable
The prodromal phase can be viewed as a sequence of evolving symptoms7 (Box 18,9), starting with subtle differences evident only to the person experiencing them and often progressing to brief limited intermittent psychosis (BLIPS) or attenuated psychosis.8
In fact, prodrome is a retrospective diagnosis. The predictive power of conversion to psychosis has been found to fluctuate from as low as 9% to as high as 76%,10 prompting ethical concerns about a high false-positive rate, the assumption of inevitability associated with the term “schizophrenia prodrome,”9 and the potential for overdiagnosis and misdiagnosis. Concerns about psychosocial stigma and exposure to antipsychotic medications have been expressed as well.11
A case for early engagement
In retrospect, patients who eventually progress to psychotic illness are commonly found to have been in the prodromal phase for several years. Yet many patients’ first contact with psychiatric services occurs during a florid episode of acute psychosis. Identifying patients in the early prodromal period offers the opportunity to more effectively engage them and form a therapeutic alliance.12 Any young adult who presents with a decline in academic or occupational function, social withdrawal, perplexity, and apparent distress or agitation (Table 113-16) without a clear precipitating factor should therefore be closely monitored, particularly if he (she) has a family history of psychosis.
Screening tools. A variety of interviews and rating scales (Table 28) have been developed to assess and monitor at-risk persons, a number of which have been designed to detect basic symptoms in the early phase of prodrome. In addition to the structured scales, several self-report tools—including the Prodromal Questionnaire-Brief (PQ-B), Youth Psychosis At Risk Questionnaire-Brief (YPARQ-B), Prime Screen-Revised, and PROD-screen (Screen for prodromal symptoms of psychosis)—have been found to be useful in screening a large sample to identify those who might need further evaluation.17
Increased risk of conversion. Several clinical factors are associated with an increased risk of conversion to psychotic illness.9 In addition to family history, these include:
• greater severity and longer duration of attenuated positive symptoms
• presence of bizarre thoughts and behavior
• paranoia
• decline in global assessment of functioning score over the previous year
• use of either Cannabis or amphetamines.
A history of childhood trauma, increased sensitivity to psychosocial stressors, and dysregulation of the hypothalamicpituitary axis also have been associated with progression to psychosis.18
Recent evidence suggests that the prodromal phase is a predictor not only for psychosis but also for other disabling psychiatric illnesses, such as bipolar disorder and obsessive-compulsive disorder.19
From a phenomenological standpoint, disturbance of the sense of self—characterized by features such as depersonalization, derealization, decreased reactivity to other people and the environment, and intense reflectivity to oneself or others—has been proposed as a critical marker for progression to psychosis.20 Another predictor is the perception of negativity of others toward oneself. Examples include heightened sensitivity to rejection or shame, which seems to emerge from a pattern of insecure attachment, and the outsider status experienced by immigrants faced with multiple social, cultural, and language barriers.21 The presence of obsessivecompulsive symptoms during the prodromal phase has been linked to significant impairment in functioning, an acute switch to psychosis, and an increased risk of suicide.22
Monitor or treat? An optimal approach
A key dilemma in the management of patients who exhibit signs and symptoms of schizophrenia prodrome is whether to simply monitor closely or to initiate treatment.
International clinical practice guidelines recommend several practical steps in the monitoring of patients in a prepsychotic state (Table 3),23 but caution against the use of antipsychotic agents unless the patient meets diagnostic criteria for a psychotic disorder.
CBT. Some evidence supports the initiation of cognitive-behavioral therapy (CBT) during the initial prodromal phase and the addition of alow-dose atypical antipsychotic if the patient progresses to a later phase, characterized by BLIPS/APS.24,25 Evidence also suggests that a combination of CBT and antipsychotic medication might delay, but not prevent, the progression to a psychotic episode.9 Any risk of adverse metabolic complications precludes use ofan atypical antipsychotic.One potential alternative is the use of omega-3 polyunsaturated fatty acids (Box 2).26,27
A clinically useful approach would be to view schizophrenia/psychosis prodrome not as a distinct diagnostic category but as a cluster of signs and symptoms associated with an increased risk of psychosis, with persons in this phase in need of close follow-up and, possibly, early initiation of an antipsychotic agent. It is important to engage the patient and his family at an early stage to educate them about the diagnostic uncertainty; to help them deal with the stigma; to manage risk factors; and, collaboratively, to decide on an intervention strategy.23,28
Bottom Line
Despite several drawbacks, the concept of schizophrenia/psychosis prodrome may
be viewed as a cluster of signs and symptoms (rather than a distinct diagnostic category) associated with increased risk for psychosis that need close follow up. Follow up may involve psychoeducational and psychotherapeutic interventions and, need be, early initiation of antipsychotics. In addition, such symptoms may be associated with other psychiatric disorders such as bipolar disorder and obsessive- compulsive disorder. Timely attention and early intervention may alter the course
and improve overall prognosis.
Related Resources
• Early intervention in psychosis. WPA Education Committee’s recommended roles of the psychiatrist. www.wpanet.org/uploads/Education/Educational_Resources/earlyintervention-psychosis.pdf.
• Early Psychosis Prevention and Intervention Centre, Melbourne, Australia. http://eppic.org.au/psychosis.
• International Early Psychosis Association Writing Group. International clinical practice guidelines for early psychosis. Br J Psychiatry. 2005;187:s120-124. http://bjp.rcpsych.org/content/187/48/s120.full.
Disclosures
Dr. Madaan is an employee of University of Virginia Health System. As an employee with the University of Virginia, Dr. Madaan has received research support from Eli Lilly and Company, Forest, Merck, Otsuka, Pfizer, Shire, and Sunovion. He also has served as a consultant for the NOW Coalition for Bipolar Disorder, and on the American Psychiatric Association’s Focus Self-Assessment editorial board. Drs. Bestha and Kolli report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
In studies of schizophrenia, one of the more striking findings is the delay in the initiation of treatment. That delay ranges from 1 to 2 years for patients experiencing psychotic symptoms to several years if the prodromal phase is taken into account.1 Yet duration of untreated psychosis has been found to be a critical factor in prognosis, including psychosocial functioning, in patients with schizophrenia.2,3 Identification of individuals in the prodromal phase not only offers an opportunity to intervene at an earlier symptomatic stage, but might be associated with a better response to antipsychotics and a better overall treatment outcome as well.
What’s in a name?
Several terms, including ultra high risk, clinical high risk, at-risk mental state, psychosis risk syndrome, and schizophrenia/psychosis prodrome, have been used to describe the prodromal phase of schizophrenia. The proposal to include attenuated psychosis syndrome (APS) in the DSM-5—originally intended to capture those with subthreshold delusions, hallucinations, or disorganized behavior, occurring at least once a week for the past month and worsening over the past year—generated a debate about the validity of such a diagnostic category4,5 that culminated in the inclusion of APS as a condition for further study but not as a term for clinical use.6 Its presence in the DSM-5 brings to the forefront the importance of early clinical intervention in patients at risk of developing psychotic illness.
Schizophrenia is not inevitable
The prodromal phase can be viewed as a sequence of evolving symptoms7 (Box 18,9), starting with subtle differences evident only to the person experiencing them and often progressing to brief limited intermittent psychosis (BLIPS) or attenuated psychosis.8
In fact, prodrome is a retrospective diagnosis. The predictive power of conversion to psychosis has been found to fluctuate from as low as 9% to as high as 76%,10 prompting ethical concerns about a high false-positive rate, the assumption of inevitability associated with the term “schizophrenia prodrome,”9 and the potential for overdiagnosis and misdiagnosis. Concerns about psychosocial stigma and exposure to antipsychotic medications have been expressed as well.11
A case for early engagement
In retrospect, patients who eventually progress to psychotic illness are commonly found to have been in the prodromal phase for several years. Yet many patients’ first contact with psychiatric services occurs during a florid episode of acute psychosis. Identifying patients in the early prodromal period offers the opportunity to more effectively engage them and form a therapeutic alliance.12 Any young adult who presents with a decline in academic or occupational function, social withdrawal, perplexity, and apparent distress or agitation (Table 113-16) without a clear precipitating factor should therefore be closely monitored, particularly if he (she) has a family history of psychosis.
Screening tools. A variety of interviews and rating scales (Table 28) have been developed to assess and monitor at-risk persons, a number of which have been designed to detect basic symptoms in the early phase of prodrome. In addition to the structured scales, several self-report tools—including the Prodromal Questionnaire-Brief (PQ-B), Youth Psychosis At Risk Questionnaire-Brief (YPARQ-B), Prime Screen-Revised, and PROD-screen (Screen for prodromal symptoms of psychosis)—have been found to be useful in screening a large sample to identify those who might need further evaluation.17
Increased risk of conversion. Several clinical factors are associated with an increased risk of conversion to psychotic illness.9 In addition to family history, these include:
• greater severity and longer duration of attenuated positive symptoms
• presence of bizarre thoughts and behavior
• paranoia
• decline in global assessment of functioning score over the previous year
• use of either Cannabis or amphetamines.
A history of childhood trauma, increased sensitivity to psychosocial stressors, and dysregulation of the hypothalamicpituitary axis also have been associated with progression to psychosis.18
Recent evidence suggests that the prodromal phase is a predictor not only for psychosis but also for other disabling psychiatric illnesses, such as bipolar disorder and obsessive-compulsive disorder.19
From a phenomenological standpoint, disturbance of the sense of self—characterized by features such as depersonalization, derealization, decreased reactivity to other people and the environment, and intense reflectivity to oneself or others—has been proposed as a critical marker for progression to psychosis.20 Another predictor is the perception of negativity of others toward oneself. Examples include heightened sensitivity to rejection or shame, which seems to emerge from a pattern of insecure attachment, and the outsider status experienced by immigrants faced with multiple social, cultural, and language barriers.21 The presence of obsessivecompulsive symptoms during the prodromal phase has been linked to significant impairment in functioning, an acute switch to psychosis, and an increased risk of suicide.22
Monitor or treat? An optimal approach
A key dilemma in the management of patients who exhibit signs and symptoms of schizophrenia prodrome is whether to simply monitor closely or to initiate treatment.
International clinical practice guidelines recommend several practical steps in the monitoring of patients in a prepsychotic state (Table 3),23 but caution against the use of antipsychotic agents unless the patient meets diagnostic criteria for a psychotic disorder.
CBT. Some evidence supports the initiation of cognitive-behavioral therapy (CBT) during the initial prodromal phase and the addition of alow-dose atypical antipsychotic if the patient progresses to a later phase, characterized by BLIPS/APS.24,25 Evidence also suggests that a combination of CBT and antipsychotic medication might delay, but not prevent, the progression to a psychotic episode.9 Any risk of adverse metabolic complications precludes use ofan atypical antipsychotic.One potential alternative is the use of omega-3 polyunsaturated fatty acids (Box 2).26,27
A clinically useful approach would be to view schizophrenia/psychosis prodrome not as a distinct diagnostic category but as a cluster of signs and symptoms associated with an increased risk of psychosis, with persons in this phase in need of close follow-up and, possibly, early initiation of an antipsychotic agent. It is important to engage the patient and his family at an early stage to educate them about the diagnostic uncertainty; to help them deal with the stigma; to manage risk factors; and, collaboratively, to decide on an intervention strategy.23,28
Bottom Line
Despite several drawbacks, the concept of schizophrenia/psychosis prodrome may
be viewed as a cluster of signs and symptoms (rather than a distinct diagnostic category) associated with increased risk for psychosis that need close follow up. Follow up may involve psychoeducational and psychotherapeutic interventions and, need be, early initiation of antipsychotics. In addition, such symptoms may be associated with other psychiatric disorders such as bipolar disorder and obsessive- compulsive disorder. Timely attention and early intervention may alter the course
and improve overall prognosis.
Related Resources
• Early intervention in psychosis. WPA Education Committee’s recommended roles of the psychiatrist. www.wpanet.org/uploads/Education/Educational_Resources/earlyintervention-psychosis.pdf.
• Early Psychosis Prevention and Intervention Centre, Melbourne, Australia. http://eppic.org.au/psychosis.
• International Early Psychosis Association Writing Group. International clinical practice guidelines for early psychosis. Br J Psychiatry. 2005;187:s120-124. http://bjp.rcpsych.org/content/187/48/s120.full.
Disclosures
Dr. Madaan is an employee of University of Virginia Health System. As an employee with the University of Virginia, Dr. Madaan has received research support from Eli Lilly and Company, Forest, Merck, Otsuka, Pfizer, Shire, and Sunovion. He also has served as a consultant for the NOW Coalition for Bipolar Disorder, and on the American Psychiatric Association’s Focus Self-Assessment editorial board. Drs. Bestha and Kolli report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. Salokangas RK, McGlashan TH. Early detection and intervention of psychosis. A review. Nord J Psychiatry. 2008;62:92-105.
2. Perkins DO, Gu H, Boteva K, et al. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry. 2005;162(10): 1785-1804.
3. Stefanopoulou E, Lafuente AR, Fonseca AS, et al. Global assessment of psychosocial functioning and predictors of outcome in schizophrenia. Int J Psychiatry Clin Pract. 2011;15(1):62-68.
4. Yung AR, Nelson B, Thompson AD, et al. Should a “Risk Syndrome for Psychosis” be included in the DSMV? Schizophr Res. 2010;120(1-3):7-15.
5. Corcoran CM, First MB, Cornblatt B. The psychosis risk syndrome and its proposed inclusion in the DSM-V: a risk-benefit analysis. Schizophr Res. 2010;120(1-3):16-22.
6. Diagnostic and statistical manual of mental disorders, 5th ed, text rev. Washington, DC: American Psychiatric Association; 2013.
7. Schultze-Lutter F, Ruhrmann S, Berning J, et al. Basic symptoms and ultrahigh risk criteria: symptom development in the initial prodromal state. Schizophr Bull. 2010;36(1):182-191.
8. Correll CU, Hauser M, Auther AM, et al. Research in people with psychosis risk syndrome: a review of the current evidence and future directions. J Child Psychol
Psychiatry. 2010;51(4):390-431.
9. Addington J, Heinssen R. Prediction and prevention of psychosis in youth at clinical high risk. Annu Rev Clin Psychol. 2012;8:269-289.
10. Cannon TD, Cadenhead K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65(1):28-37.
11. Singh F, Mirzakhanian H, Fusar-Poli P, et al. Ethical implications for clinical practice and future research in “at risk” individuals. Curr Pharm Des. 2012;18(4):606-612.
12. Bota RG, Munro JS, Ricci WF, et al. The dynamics of insight in the prodrome of schizophrenia. CNS Spectr. 2006;11(5):355-362.
13. Phillips LJ, Yung AR, McGorry PD. Identification of young people at risk of psychosis: validation of Personal Assessment and Crisis Evaluation Clinic intake criteria. Aust N Z J Psychiatry. 2000;34(suppl):S164-S169.
14. Miller TJ, McGlashan TH, Woods SW, et al. Symptom assessment in schizophrenic prodromal states. Psychiatr Q. 1999;70(4):273-287.
15. Schultze-Lutter F, Klosterkötter J, Picker H. Predicting first-episode psychosis by basic symptom criteria. Clinical Neuropsychiatry. 2007;4(1):11-22.
16. Schultze-Lutter F, Ruhrmann S, Picker H, et al. Basic symptoms in early psychotic and depressive disorders. Br J Psychiatry Suppl. 2007;51:s31-s37.
17. Kline E, Wilson C, Ereshefsky S, et al. Convergent and discriminant validity of attenuated psychosis screening tools. Schizophr Res. 2012;134(1):49-53.
18. Holtzman CW, Shapiro DI, Trotman HD, et al. Stress and the prodromal phase of psychosis. Curr Pharm Des. 2012;18(4):527-533.
19. Rössler W, Hengartner MP, Ajdacic-Gross V, et al. Subclinical psychosis symptoms in young adults are risk factors for subsequent common mental disorders. Schizophr Res. 2011;131(1-3):18-23.
20. Nelson B, Yung AR, Bechdolf A, et al. The phenomenological critique and self-disturbance: implications for ultra-high risk (“prodrome”) research. Schizophr Bull. 2008;34(2):381-392.
21. Salokangas RK, Heinimaa M, Svirskis T, et al. Perceived negative attitude of others as an early sign of psychosis. Eur Psychiatry. 2009;24(4):233-238.
22. Niendam TA, Berzak J, Cannon TD, et al. Obsessive compulsive symptoms in the psychosis prodrome:correlates of clinical and functional outcome. Schizophr
Res. 2009;108(1-3):170-175.
23. Addington J, Amminger GP, Barbato A. International clinical practice guidelines for early psychosis. Br J Psychiatry. 2005;187:s120-s124.
24. Klosterkötter J, Schultze-Lutter F, Bechdolf A, et al. Prediction and prevention of schizophrenia: what has been achieved and where to go next? World Psychiatry.
2011;10(3):165-174.
25. Stafford MR, Jackson H, Mayo-Wilson E, et al. Early interventions to prevent psychosis: systematic review and meta-analysis. BMJ. 2013;346:f185.
1. Salokangas RK, McGlashan TH. Early detection and intervention of psychosis. A review. Nord J Psychiatry. 2008;62:92-105.
2. Perkins DO, Gu H, Boteva K, et al. Relationship between duration of untreated psychosis and outcome in first-episode schizophrenia: a critical review and meta-analysis. Am J Psychiatry. 2005;162(10): 1785-1804.
3. Stefanopoulou E, Lafuente AR, Fonseca AS, et al. Global assessment of psychosocial functioning and predictors of outcome in schizophrenia. Int J Psychiatry Clin Pract. 2011;15(1):62-68.
4. Yung AR, Nelson B, Thompson AD, et al. Should a “Risk Syndrome for Psychosis” be included in the DSMV? Schizophr Res. 2010;120(1-3):7-15.
5. Corcoran CM, First MB, Cornblatt B. The psychosis risk syndrome and its proposed inclusion in the DSM-V: a risk-benefit analysis. Schizophr Res. 2010;120(1-3):16-22.
6. Diagnostic and statistical manual of mental disorders, 5th ed, text rev. Washington, DC: American Psychiatric Association; 2013.
7. Schultze-Lutter F, Ruhrmann S, Berning J, et al. Basic symptoms and ultrahigh risk criteria: symptom development in the initial prodromal state. Schizophr Bull. 2010;36(1):182-191.
8. Correll CU, Hauser M, Auther AM, et al. Research in people with psychosis risk syndrome: a review of the current evidence and future directions. J Child Psychol
Psychiatry. 2010;51(4):390-431.
9. Addington J, Heinssen R. Prediction and prevention of psychosis in youth at clinical high risk. Annu Rev Clin Psychol. 2012;8:269-289.
10. Cannon TD, Cadenhead K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008;65(1):28-37.
11. Singh F, Mirzakhanian H, Fusar-Poli P, et al. Ethical implications for clinical practice and future research in “at risk” individuals. Curr Pharm Des. 2012;18(4):606-612.
12. Bota RG, Munro JS, Ricci WF, et al. The dynamics of insight in the prodrome of schizophrenia. CNS Spectr. 2006;11(5):355-362.
13. Phillips LJ, Yung AR, McGorry PD. Identification of young people at risk of psychosis: validation of Personal Assessment and Crisis Evaluation Clinic intake criteria. Aust N Z J Psychiatry. 2000;34(suppl):S164-S169.
14. Miller TJ, McGlashan TH, Woods SW, et al. Symptom assessment in schizophrenic prodromal states. Psychiatr Q. 1999;70(4):273-287.
15. Schultze-Lutter F, Klosterkötter J, Picker H. Predicting first-episode psychosis by basic symptom criteria. Clinical Neuropsychiatry. 2007;4(1):11-22.
16. Schultze-Lutter F, Ruhrmann S, Picker H, et al. Basic symptoms in early psychotic and depressive disorders. Br J Psychiatry Suppl. 2007;51:s31-s37.
17. Kline E, Wilson C, Ereshefsky S, et al. Convergent and discriminant validity of attenuated psychosis screening tools. Schizophr Res. 2012;134(1):49-53.
18. Holtzman CW, Shapiro DI, Trotman HD, et al. Stress and the prodromal phase of psychosis. Curr Pharm Des. 2012;18(4):527-533.
19. Rössler W, Hengartner MP, Ajdacic-Gross V, et al. Subclinical psychosis symptoms in young adults are risk factors for subsequent common mental disorders. Schizophr Res. 2011;131(1-3):18-23.
20. Nelson B, Yung AR, Bechdolf A, et al. The phenomenological critique and self-disturbance: implications for ultra-high risk (“prodrome”) research. Schizophr Bull. 2008;34(2):381-392.
21. Salokangas RK, Heinimaa M, Svirskis T, et al. Perceived negative attitude of others as an early sign of psychosis. Eur Psychiatry. 2009;24(4):233-238.
22. Niendam TA, Berzak J, Cannon TD, et al. Obsessive compulsive symptoms in the psychosis prodrome:correlates of clinical and functional outcome. Schizophr
Res. 2009;108(1-3):170-175.
23. Addington J, Amminger GP, Barbato A. International clinical practice guidelines for early psychosis. Br J Psychiatry. 2005;187:s120-s124.
24. Klosterkötter J, Schultze-Lutter F, Bechdolf A, et al. Prediction and prevention of schizophrenia: what has been achieved and where to go next? World Psychiatry.
2011;10(3):165-174.
25. Stafford MR, Jackson H, Mayo-Wilson E, et al. Early interventions to prevent psychosis: systematic review and meta-analysis. BMJ. 2013;346:f185.
Treating depression with combination therapy
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Once-weekly exenatide can be especially useful to treat diabetes in schizophrenia
The incidence of diabetes in people with schizophrenia is 2- to 3-fold that of the general population—which has been attributed to several variables, including adverse effects of antipsychotic drugs, susceptibility related to mental illness, lifestyle, and social health determinants.1 Controlling diabetes is important because cardiovascular consequences of the disease contribute to the shortened life expectancy seen in patients with schizophrenia.2
The dosing frequency of a newer formulation of exenatide, a glucose-lowering drug that has been available for almost a decade, can help manage type 2 diabetes mellitus in your patient with schizophrenia.
What is the new formulation and why is it appealing?
Exenatide is a glucagon-like peptide-1 (GLP-1) receptor agonist indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2
diabetes mellitus. GLP-1 agonists lower the blood glucose level by enhancing glucose-dependent insulin secretion, suppressing glucagon secretion, slowing gastric emptying, and enhancing satiety. Exenatide was approved by the FDA
in 2005 as a twice-daily subcutaneous injection (brand name, Byetta); the once-weekly formulation, also for subcutaneous injection (brand name, Bydureon), was approved in 2012.
Practical use for psychiatric patients
Because psychiatric patients face medication adherence challenges, the once-
weekly formulation of exenatide is appealing. The patient or a member of his (her) care team can administer the once-weekly injection.
Practitioners might be concerned that patients with comorbid psychiatric illness and diabetes will overreact to an elevated blood glucose reading by overusing medications such as oral hypoglycemics and insulin. The fixed-dosage of weekly exenatide minimizes the risk that a patient will react to a single elevated blood glucose reading.
Exenatide can produce weight loss, which might benefit patients who suffer from the metabolic adverse effects of an atypical antipsychotic, including an elevated blood glucose level and weight gain.
Real-world application
We have used once-weekly exenatide successfully in a female patient with schizophrenia who was taking quetiapine and haloperidol, and had uncontrolled diabetes resulting from medication nonadherence and lack of insight into diabetes.
The patient’s hemoglobin A1c level remained at 8.8% (target A1c, <7%, as set by the American Diabetes Association), despite taking 3 oral diabetes medications at maximum dosage.
The care team determined that daily insulin injections were too risky, given the patient’s compulsive behavior; she had a history of medication overuse in response to significantly elevated blood glucose.
Once-weekly exenatide, however, was a feasible alternative. Three months after she was started on once-weekly exenatide, and with additional lifestyle modifications, her hemoglobin A1c level had fallen to 6.4%, without any hypoglycemic episodes.
Select patients carefully
Exenatide is not a first-line therapy because of its potential side effects (Table), route of administration, and cost. Consider the once-weekly formulation of the drug on a patient-by-patient basis for patients with schizophrenia whose diabetes otherwise cannot be controlled.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. De Hert M, van Winkel R, Van Eyck D, et al. Prevalence of diabetes, metabolic syndrome and metabolic abnormalities in schizophrenia over the course of the illness: a cross-sectional study. Clin Pract Epidemiol Ment Health. 2006;2:14.
2. Laursen TM, Munk-Olsen T, Vestergaard M. Life expectancy and cardiovascular mortality in persons with schizophrenia. Curr Opin Psychiatry. 2012;25(2):83-88.
3. Bydureon [package insert]. San Diego, CA: Amylin Pharmaceuticals, Inc.; 2012.
The incidence of diabetes in people with schizophrenia is 2- to 3-fold that of the general population—which has been attributed to several variables, including adverse effects of antipsychotic drugs, susceptibility related to mental illness, lifestyle, and social health determinants.1 Controlling diabetes is important because cardiovascular consequences of the disease contribute to the shortened life expectancy seen in patients with schizophrenia.2
The dosing frequency of a newer formulation of exenatide, a glucose-lowering drug that has been available for almost a decade, can help manage type 2 diabetes mellitus in your patient with schizophrenia.
What is the new formulation and why is it appealing?
Exenatide is a glucagon-like peptide-1 (GLP-1) receptor agonist indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2
diabetes mellitus. GLP-1 agonists lower the blood glucose level by enhancing glucose-dependent insulin secretion, suppressing glucagon secretion, slowing gastric emptying, and enhancing satiety. Exenatide was approved by the FDA
in 2005 as a twice-daily subcutaneous injection (brand name, Byetta); the once-weekly formulation, also for subcutaneous injection (brand name, Bydureon), was approved in 2012.
Practical use for psychiatric patients
Because psychiatric patients face medication adherence challenges, the once-
weekly formulation of exenatide is appealing. The patient or a member of his (her) care team can administer the once-weekly injection.
Practitioners might be concerned that patients with comorbid psychiatric illness and diabetes will overreact to an elevated blood glucose reading by overusing medications such as oral hypoglycemics and insulin. The fixed-dosage of weekly exenatide minimizes the risk that a patient will react to a single elevated blood glucose reading.
Exenatide can produce weight loss, which might benefit patients who suffer from the metabolic adverse effects of an atypical antipsychotic, including an elevated blood glucose level and weight gain.
Real-world application
We have used once-weekly exenatide successfully in a female patient with schizophrenia who was taking quetiapine and haloperidol, and had uncontrolled diabetes resulting from medication nonadherence and lack of insight into diabetes.
The patient’s hemoglobin A1c level remained at 8.8% (target A1c, <7%, as set by the American Diabetes Association), despite taking 3 oral diabetes medications at maximum dosage.
The care team determined that daily insulin injections were too risky, given the patient’s compulsive behavior; she had a history of medication overuse in response to significantly elevated blood glucose.
Once-weekly exenatide, however, was a feasible alternative. Three months after she was started on once-weekly exenatide, and with additional lifestyle modifications, her hemoglobin A1c level had fallen to 6.4%, without any hypoglycemic episodes.
Select patients carefully
Exenatide is not a first-line therapy because of its potential side effects (Table), route of administration, and cost. Consider the once-weekly formulation of the drug on a patient-by-patient basis for patients with schizophrenia whose diabetes otherwise cannot be controlled.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
The incidence of diabetes in people with schizophrenia is 2- to 3-fold that of the general population—which has been attributed to several variables, including adverse effects of antipsychotic drugs, susceptibility related to mental illness, lifestyle, and social health determinants.1 Controlling diabetes is important because cardiovascular consequences of the disease contribute to the shortened life expectancy seen in patients with schizophrenia.2
The dosing frequency of a newer formulation of exenatide, a glucose-lowering drug that has been available for almost a decade, can help manage type 2 diabetes mellitus in your patient with schizophrenia.
What is the new formulation and why is it appealing?
Exenatide is a glucagon-like peptide-1 (GLP-1) receptor agonist indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2
diabetes mellitus. GLP-1 agonists lower the blood glucose level by enhancing glucose-dependent insulin secretion, suppressing glucagon secretion, slowing gastric emptying, and enhancing satiety. Exenatide was approved by the FDA
in 2005 as a twice-daily subcutaneous injection (brand name, Byetta); the once-weekly formulation, also for subcutaneous injection (brand name, Bydureon), was approved in 2012.
Practical use for psychiatric patients
Because psychiatric patients face medication adherence challenges, the once-
weekly formulation of exenatide is appealing. The patient or a member of his (her) care team can administer the once-weekly injection.
Practitioners might be concerned that patients with comorbid psychiatric illness and diabetes will overreact to an elevated blood glucose reading by overusing medications such as oral hypoglycemics and insulin. The fixed-dosage of weekly exenatide minimizes the risk that a patient will react to a single elevated blood glucose reading.
Exenatide can produce weight loss, which might benefit patients who suffer from the metabolic adverse effects of an atypical antipsychotic, including an elevated blood glucose level and weight gain.
Real-world application
We have used once-weekly exenatide successfully in a female patient with schizophrenia who was taking quetiapine and haloperidol, and had uncontrolled diabetes resulting from medication nonadherence and lack of insight into diabetes.
The patient’s hemoglobin A1c level remained at 8.8% (target A1c, <7%, as set by the American Diabetes Association), despite taking 3 oral diabetes medications at maximum dosage.
The care team determined that daily insulin injections were too risky, given the patient’s compulsive behavior; she had a history of medication overuse in response to significantly elevated blood glucose.
Once-weekly exenatide, however, was a feasible alternative. Three months after she was started on once-weekly exenatide, and with additional lifestyle modifications, her hemoglobin A1c level had fallen to 6.4%, without any hypoglycemic episodes.
Select patients carefully
Exenatide is not a first-line therapy because of its potential side effects (Table), route of administration, and cost. Consider the once-weekly formulation of the drug on a patient-by-patient basis for patients with schizophrenia whose diabetes otherwise cannot be controlled.
Disclosure
The authors report no financial relationships with any company whose products are mentioned in this article or with manufacturers of competing products.
1. De Hert M, van Winkel R, Van Eyck D, et al. Prevalence of diabetes, metabolic syndrome and metabolic abnormalities in schizophrenia over the course of the illness: a cross-sectional study. Clin Pract Epidemiol Ment Health. 2006;2:14.
2. Laursen TM, Munk-Olsen T, Vestergaard M. Life expectancy and cardiovascular mortality in persons with schizophrenia. Curr Opin Psychiatry. 2012;25(2):83-88.
3. Bydureon [package insert]. San Diego, CA: Amylin Pharmaceuticals, Inc.; 2012.
1. De Hert M, van Winkel R, Van Eyck D, et al. Prevalence of diabetes, metabolic syndrome and metabolic abnormalities in schizophrenia over the course of the illness: a cross-sectional study. Clin Pract Epidemiol Ment Health. 2006;2:14.
2. Laursen TM, Munk-Olsen T, Vestergaard M. Life expectancy and cardiovascular mortality in persons with schizophrenia. Curr Opin Psychiatry. 2012;25(2):83-88.
3. Bydureon [package insert]. San Diego, CA: Amylin Pharmaceuticals, Inc.; 2012.