User login
News and Views that Matter to Physicians
Postop delirium linked to greater long-term cognitive decline
Patients with postoperative delirium have significantly worse preoperative short-term cognitive performance and significantly greater long-term cognitive decline, compared with patients without delirium, according to Sharon K. Inouye, MD, and her associates.
In a prospective cohort study of 560 patients aged 70 years and older, 134 patients were selected for the delirium group and 426 for the nondelirium group. The delirium group had a significantly greater decline (–1.03 points) at 1 month, compared with those without delirium (P = .003). After cognitive function had recovered at 2 months, there were no significant differences between groups (P = 0.99). After 2 months, both groups decline on average; however, the delirium group declined significantly more (–1.07) in adjusted mean scores at 36 months (P =.02).
From baseline to 36 months, there was a significant change for the delirium group (–1.30, P less than .01) and no significant change for the group without delirium (–0.23, P = .30). Researchers noted that the effect of delirium remains undiminished after consecutive rehospitalizations, intercurrent illnesses, and major postoperative complications were controlled for.
The patients underwent major noncardiac surgery, such as total hip or knee replacement, open abdominal aortic aneurysm repair, colectomy, and lower-extremity arterial bypass.
“This study provides a novel presentation of the biphasic relationship of delirium and cognitive trajectory, both its well-recognized acute effects but also long-term effects,” the researchers wrote. “Our results suggest that after a period of initial recovery, patients with delirium experience a substantially accelerated trajectory of cognitive aging.”
Read the full study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association (doi:10.1016/j.jalz.2016.03.005).
Patients with postoperative delirium have significantly worse preoperative short-term cognitive performance and significantly greater long-term cognitive decline, compared with patients without delirium, according to Sharon K. Inouye, MD, and her associates.
In a prospective cohort study of 560 patients aged 70 years and older, 134 patients were selected for the delirium group and 426 for the nondelirium group. The delirium group had a significantly greater decline (–1.03 points) at 1 month, compared with those without delirium (P = .003). After cognitive function had recovered at 2 months, there were no significant differences between groups (P = 0.99). After 2 months, both groups decline on average; however, the delirium group declined significantly more (–1.07) in adjusted mean scores at 36 months (P =.02).
From baseline to 36 months, there was a significant change for the delirium group (–1.30, P less than .01) and no significant change for the group without delirium (–0.23, P = .30). Researchers noted that the effect of delirium remains undiminished after consecutive rehospitalizations, intercurrent illnesses, and major postoperative complications were controlled for.
The patients underwent major noncardiac surgery, such as total hip or knee replacement, open abdominal aortic aneurysm repair, colectomy, and lower-extremity arterial bypass.
“This study provides a novel presentation of the biphasic relationship of delirium and cognitive trajectory, both its well-recognized acute effects but also long-term effects,” the researchers wrote. “Our results suggest that after a period of initial recovery, patients with delirium experience a substantially accelerated trajectory of cognitive aging.”
Read the full study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association (doi:10.1016/j.jalz.2016.03.005).
Patients with postoperative delirium have significantly worse preoperative short-term cognitive performance and significantly greater long-term cognitive decline, compared with patients without delirium, according to Sharon K. Inouye, MD, and her associates.
In a prospective cohort study of 560 patients aged 70 years and older, 134 patients were selected for the delirium group and 426 for the nondelirium group. The delirium group had a significantly greater decline (–1.03 points) at 1 month, compared with those without delirium (P = .003). After cognitive function had recovered at 2 months, there were no significant differences between groups (P = 0.99). After 2 months, both groups decline on average; however, the delirium group declined significantly more (–1.07) in adjusted mean scores at 36 months (P =.02).
From baseline to 36 months, there was a significant change for the delirium group (–1.30, P less than .01) and no significant change for the group without delirium (–0.23, P = .30). Researchers noted that the effect of delirium remains undiminished after consecutive rehospitalizations, intercurrent illnesses, and major postoperative complications were controlled for.
The patients underwent major noncardiac surgery, such as total hip or knee replacement, open abdominal aortic aneurysm repair, colectomy, and lower-extremity arterial bypass.
“This study provides a novel presentation of the biphasic relationship of delirium and cognitive trajectory, both its well-recognized acute effects but also long-term effects,” the researchers wrote. “Our results suggest that after a period of initial recovery, patients with delirium experience a substantially accelerated trajectory of cognitive aging.”
Read the full study in Alzheimer’s & Dementia: The Journal of the Alzheimer’s Association (doi:10.1016/j.jalz.2016.03.005).
FROM ALZHEIMER’S & DEMENTIA
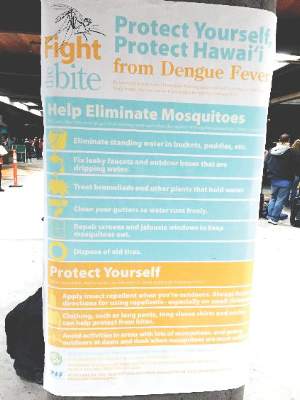
Skin rash in recent traveler? Think dengue fever
BOSTON – Maintain clinical suspicion for dengue fever among individuals with recent travel to endemic areas who present with a rash and other signs and symptoms of infection, an expert advised at the American Academy of Dermatology summer meeting.
Dengue fever accounts for nearly 10% of skin rashes among individuals returning from endemic areas, and related illness can range from mild to fatal, said Jose Dario Martinez, MD, chief of the Internal Medicine Clinic at University Hospital “J.E. Gonzalez,” UANL Monterrey, Mexico.
“This is the most prevalent arthropod-borne virus in the world at this time, and it is a resurgent disease in some countries, like Mexico, Brazil, and Colombia,” he noted.
Worldwide, more than 2.5 billion people are at risk of dengue infection, and between 50 million and 100 million cases occur each year, while about 250,000 to 500,000 cases of dengue hemorrhagic fever occur each year, and about 25,000 related deaths occur.
In 2005, there was a dengue outbreak in Texas, where 25 cases occurred; and in southern Florida, an outbreak of 90 cases was reported in 2009 and 2010. More recently, in 2015, there was an outbreak of 107 cases of locally-acquired dengue on the Big Island, Hawaii (MMWR). But in Mexico, 18,000 new cases occurred in 2015, Dr. Martinez said.
Of the RNA virus serotypes 1-4, type 1 (DENV1) is the most common, and DENV2 and 3 are the most severe, but up to 40% of cases are asymptomatic, he noted, adding that the virus has an incubation period of 2-8 days. When symptoms occur, they are representative of acute febrile illness, and may include headache, high fever, myalgia, arthralgia, retro-orbital pain, and fatigue. A faint, itchy, macular rash commonly occurs at 2-6 days into the illness. According to the World Health Organization, a probable dengue fever case includes acute febrile illness and at least two of either headache, retro-orbital pain, myalgia, arthralgia, rash, hemorrhagic manifestations, leukopenia, or supportive serology.
“Sometimes the nose bleeds, the gums bleed, and there is bruising in the patient,” Dr. Martinez said. “Most important are retro-orbital pain and hemorrhagic manifestations, but also supportive serology.”
About 1% of patients progress to dengue hemorrhagic fever or dengue shock syndrome during the critical phase (days 4-7) of illness. This is most likely in those with serotypes 2 and 3, but can occur with all serotypes. Warning signs of such severe disease include abdominal pain or tenderness, persistent vomiting, pleural effusion or ascites, and of particular importance – mucosal bleeding, Dr. Martinez said.
By the WHO definition, a diagnosis of dengue hemorrhagic fever requires the presence of fever for at least 2-7 days, hemorrhagic tendencies, thrombocytopenia, and evidence and signs of plasma leakage; dengue shock syndrome requires these, as well as evidence of circulatory failure, such as rapid and weak pulse, narrow pulse pressure, hypotension, and shock.
It is important to maintain clinical suspicion for dengue fever, particularly in anyone who has traveled to an endemic area in the 2 weeks before presentation. Serologic tests are important to detect anti-dengue antibodies. IgG is important, because its presence could suggest recurrent infection and thus the potential for severe disease, Dr. Martinez said. Polymerase chain reaction can be used for detection in the first 4-5 days of infection, and the NS1 rapid test can be positive on the first day, he noted.
The differential diagnosis for dengue fever is broad, and can include chikungunya fever, malaria, leptospirosis, meningococcemia, drug eruption, and Zika fever.
Management of dengue fever includes bed rest, liquids, and mosquito net isolation to prevent re-infection, as more severe disease can occur after re-infection. Acetaminophen can be used for pain relief; aspirin should be avoided due to risk of bleeding, Dr. Martinez said.
Hospitalization and supportive care are required for those with dengue hemorrhagic fever or dengue shock syndrome. Intensive care unit admission may be required.
Of note, a vaccine against dengue fever has shown promise in phase III trials. The vaccine has been approved in Mexico and Brazil, but not yet in the U.S.
Dr Martinez reported having no disclosures.
BOSTON – Maintain clinical suspicion for dengue fever among individuals with recent travel to endemic areas who present with a rash and other signs and symptoms of infection, an expert advised at the American Academy of Dermatology summer meeting.
Dengue fever accounts for nearly 10% of skin rashes among individuals returning from endemic areas, and related illness can range from mild to fatal, said Jose Dario Martinez, MD, chief of the Internal Medicine Clinic at University Hospital “J.E. Gonzalez,” UANL Monterrey, Mexico.
“This is the most prevalent arthropod-borne virus in the world at this time, and it is a resurgent disease in some countries, like Mexico, Brazil, and Colombia,” he noted.
Worldwide, more than 2.5 billion people are at risk of dengue infection, and between 50 million and 100 million cases occur each year, while about 250,000 to 500,000 cases of dengue hemorrhagic fever occur each year, and about 25,000 related deaths occur.
In 2005, there was a dengue outbreak in Texas, where 25 cases occurred; and in southern Florida, an outbreak of 90 cases was reported in 2009 and 2010. More recently, in 2015, there was an outbreak of 107 cases of locally-acquired dengue on the Big Island, Hawaii (MMWR). But in Mexico, 18,000 new cases occurred in 2015, Dr. Martinez said.
Of the RNA virus serotypes 1-4, type 1 (DENV1) is the most common, and DENV2 and 3 are the most severe, but up to 40% of cases are asymptomatic, he noted, adding that the virus has an incubation period of 2-8 days. When symptoms occur, they are representative of acute febrile illness, and may include headache, high fever, myalgia, arthralgia, retro-orbital pain, and fatigue. A faint, itchy, macular rash commonly occurs at 2-6 days into the illness. According to the World Health Organization, a probable dengue fever case includes acute febrile illness and at least two of either headache, retro-orbital pain, myalgia, arthralgia, rash, hemorrhagic manifestations, leukopenia, or supportive serology.
“Sometimes the nose bleeds, the gums bleed, and there is bruising in the patient,” Dr. Martinez said. “Most important are retro-orbital pain and hemorrhagic manifestations, but also supportive serology.”
About 1% of patients progress to dengue hemorrhagic fever or dengue shock syndrome during the critical phase (days 4-7) of illness. This is most likely in those with serotypes 2 and 3, but can occur with all serotypes. Warning signs of such severe disease include abdominal pain or tenderness, persistent vomiting, pleural effusion or ascites, and of particular importance – mucosal bleeding, Dr. Martinez said.
By the WHO definition, a diagnosis of dengue hemorrhagic fever requires the presence of fever for at least 2-7 days, hemorrhagic tendencies, thrombocytopenia, and evidence and signs of plasma leakage; dengue shock syndrome requires these, as well as evidence of circulatory failure, such as rapid and weak pulse, narrow pulse pressure, hypotension, and shock.
It is important to maintain clinical suspicion for dengue fever, particularly in anyone who has traveled to an endemic area in the 2 weeks before presentation. Serologic tests are important to detect anti-dengue antibodies. IgG is important, because its presence could suggest recurrent infection and thus the potential for severe disease, Dr. Martinez said. Polymerase chain reaction can be used for detection in the first 4-5 days of infection, and the NS1 rapid test can be positive on the first day, he noted.
The differential diagnosis for dengue fever is broad, and can include chikungunya fever, malaria, leptospirosis, meningococcemia, drug eruption, and Zika fever.
Management of dengue fever includes bed rest, liquids, and mosquito net isolation to prevent re-infection, as more severe disease can occur after re-infection. Acetaminophen can be used for pain relief; aspirin should be avoided due to risk of bleeding, Dr. Martinez said.
Hospitalization and supportive care are required for those with dengue hemorrhagic fever or dengue shock syndrome. Intensive care unit admission may be required.
Of note, a vaccine against dengue fever has shown promise in phase III trials. The vaccine has been approved in Mexico and Brazil, but not yet in the U.S.
Dr Martinez reported having no disclosures.
BOSTON – Maintain clinical suspicion for dengue fever among individuals with recent travel to endemic areas who present with a rash and other signs and symptoms of infection, an expert advised at the American Academy of Dermatology summer meeting.
Dengue fever accounts for nearly 10% of skin rashes among individuals returning from endemic areas, and related illness can range from mild to fatal, said Jose Dario Martinez, MD, chief of the Internal Medicine Clinic at University Hospital “J.E. Gonzalez,” UANL Monterrey, Mexico.
“This is the most prevalent arthropod-borne virus in the world at this time, and it is a resurgent disease in some countries, like Mexico, Brazil, and Colombia,” he noted.
Worldwide, more than 2.5 billion people are at risk of dengue infection, and between 50 million and 100 million cases occur each year, while about 250,000 to 500,000 cases of dengue hemorrhagic fever occur each year, and about 25,000 related deaths occur.
In 2005, there was a dengue outbreak in Texas, where 25 cases occurred; and in southern Florida, an outbreak of 90 cases was reported in 2009 and 2010. More recently, in 2015, there was an outbreak of 107 cases of locally-acquired dengue on the Big Island, Hawaii (MMWR). But in Mexico, 18,000 new cases occurred in 2015, Dr. Martinez said.
Of the RNA virus serotypes 1-4, type 1 (DENV1) is the most common, and DENV2 and 3 are the most severe, but up to 40% of cases are asymptomatic, he noted, adding that the virus has an incubation period of 2-8 days. When symptoms occur, they are representative of acute febrile illness, and may include headache, high fever, myalgia, arthralgia, retro-orbital pain, and fatigue. A faint, itchy, macular rash commonly occurs at 2-6 days into the illness. According to the World Health Organization, a probable dengue fever case includes acute febrile illness and at least two of either headache, retro-orbital pain, myalgia, arthralgia, rash, hemorrhagic manifestations, leukopenia, or supportive serology.
“Sometimes the nose bleeds, the gums bleed, and there is bruising in the patient,” Dr. Martinez said. “Most important are retro-orbital pain and hemorrhagic manifestations, but also supportive serology.”
About 1% of patients progress to dengue hemorrhagic fever or dengue shock syndrome during the critical phase (days 4-7) of illness. This is most likely in those with serotypes 2 and 3, but can occur with all serotypes. Warning signs of such severe disease include abdominal pain or tenderness, persistent vomiting, pleural effusion or ascites, and of particular importance – mucosal bleeding, Dr. Martinez said.
By the WHO definition, a diagnosis of dengue hemorrhagic fever requires the presence of fever for at least 2-7 days, hemorrhagic tendencies, thrombocytopenia, and evidence and signs of plasma leakage; dengue shock syndrome requires these, as well as evidence of circulatory failure, such as rapid and weak pulse, narrow pulse pressure, hypotension, and shock.
It is important to maintain clinical suspicion for dengue fever, particularly in anyone who has traveled to an endemic area in the 2 weeks before presentation. Serologic tests are important to detect anti-dengue antibodies. IgG is important, because its presence could suggest recurrent infection and thus the potential for severe disease, Dr. Martinez said. Polymerase chain reaction can be used for detection in the first 4-5 days of infection, and the NS1 rapid test can be positive on the first day, he noted.
The differential diagnosis for dengue fever is broad, and can include chikungunya fever, malaria, leptospirosis, meningococcemia, drug eruption, and Zika fever.
Management of dengue fever includes bed rest, liquids, and mosquito net isolation to prevent re-infection, as more severe disease can occur after re-infection. Acetaminophen can be used for pain relief; aspirin should be avoided due to risk of bleeding, Dr. Martinez said.
Hospitalization and supportive care are required for those with dengue hemorrhagic fever or dengue shock syndrome. Intensive care unit admission may be required.
Of note, a vaccine against dengue fever has shown promise in phase III trials. The vaccine has been approved in Mexico and Brazil, but not yet in the U.S.
Dr Martinez reported having no disclosures.
EXPERT ANALYSIS FROM THE AAD SUMMER ACADEMY 2016
GLP-1 receptor agonist lixisenatide approved for type 2 diabetes
The Food and Drug Administration has approved the once-daily injectable lixisenatide, a glucagonlike peptide-1 (GLP-1) receptor agonist, as an adjunct to diet and exercise for improved glycemic control in adults with type 2 diabetes.
The safety and effectiveness of lixisenatide (Adlyxin, Sanofi) were evaluated either as a standalone therapy or in combination with other FDA-approved treatments in a series of clinical trials that enrolled 5,400 adults with poorly controlled type 2 diabetes. The combinations tested in the GetGoal Duo2 studies included lixisenatide with metformin, sulfonylureas, pioglitazone, or basal insulin. Lixisenatide successfully met the primary endpoint of improved hemoglobin A1c levels.
Sanofi, the drug’s manufacturer, withdrew its original 2013 application for lixisenatide’s approval pending evaluation of its cardiovascular safety profile using data from the randomized, controlled Evaluation of Lixisenatide in Acute Coronary Syndrome ELIXA trial. In that study of more than 6,000 adults with type 2 diabetes at risk for atherosclerotic cardiovascular disease, lixisenatide did not increase the risk of cardiovascular adverse events, which occurred in 13.2% of placebo patients and 13.4% of treatment group patients (N Engl J Med. 2015;373:2247-57).
The drug’s most common side effects are nausea, vomiting, headache, diarrhea, dizziness, and hypoglycemia. Severe hypersensitivity reactions, including anaphylaxis, also were reported in the clinical trials.
Lixisenatide should not be used to treat people with type 1 diabetes or patients with diabetic ketoacidosis.
The drug will be marketed in disposable, 20-mcg single-dose pens to be injected postprandially, once daily, following initial treatment with a once-daily dose of 10 mcg for 14 days.
Lixisenatide is approved in more than 60 countries and marketed as Lyxumia in over 40, according to information on the manufacturer’s website.
Postmarketing studies for lixisenatide will be required to evaluate dosing, efficacy, and safety in pediatric patients, and to evaluate the drug’s immunogenicity, according to an FDA statement.
“The FDA continues to support the development of new drug therapies for diabetes management,” said Mary Thanh Hai Parks, MD, deputy director, Office of Drug Evaluation II in the FDA’s Center for Drug Evaluation and Research. “Adlyxin will add to the available treatment options to control blood sugar levels for those with type 2.”
On Twitter @whitneymcknight
The Food and Drug Administration has approved the once-daily injectable lixisenatide, a glucagonlike peptide-1 (GLP-1) receptor agonist, as an adjunct to diet and exercise for improved glycemic control in adults with type 2 diabetes.
The safety and effectiveness of lixisenatide (Adlyxin, Sanofi) were evaluated either as a standalone therapy or in combination with other FDA-approved treatments in a series of clinical trials that enrolled 5,400 adults with poorly controlled type 2 diabetes. The combinations tested in the GetGoal Duo2 studies included lixisenatide with metformin, sulfonylureas, pioglitazone, or basal insulin. Lixisenatide successfully met the primary endpoint of improved hemoglobin A1c levels.
Sanofi, the drug’s manufacturer, withdrew its original 2013 application for lixisenatide’s approval pending evaluation of its cardiovascular safety profile using data from the randomized, controlled Evaluation of Lixisenatide in Acute Coronary Syndrome ELIXA trial. In that study of more than 6,000 adults with type 2 diabetes at risk for atherosclerotic cardiovascular disease, lixisenatide did not increase the risk of cardiovascular adverse events, which occurred in 13.2% of placebo patients and 13.4% of treatment group patients (N Engl J Med. 2015;373:2247-57).
The drug’s most common side effects are nausea, vomiting, headache, diarrhea, dizziness, and hypoglycemia. Severe hypersensitivity reactions, including anaphylaxis, also were reported in the clinical trials.
Lixisenatide should not be used to treat people with type 1 diabetes or patients with diabetic ketoacidosis.
The drug will be marketed in disposable, 20-mcg single-dose pens to be injected postprandially, once daily, following initial treatment with a once-daily dose of 10 mcg for 14 days.
Lixisenatide is approved in more than 60 countries and marketed as Lyxumia in over 40, according to information on the manufacturer’s website.
Postmarketing studies for lixisenatide will be required to evaluate dosing, efficacy, and safety in pediatric patients, and to evaluate the drug’s immunogenicity, according to an FDA statement.
“The FDA continues to support the development of new drug therapies for diabetes management,” said Mary Thanh Hai Parks, MD, deputy director, Office of Drug Evaluation II in the FDA’s Center for Drug Evaluation and Research. “Adlyxin will add to the available treatment options to control blood sugar levels for those with type 2.”
On Twitter @whitneymcknight
The Food and Drug Administration has approved the once-daily injectable lixisenatide, a glucagonlike peptide-1 (GLP-1) receptor agonist, as an adjunct to diet and exercise for improved glycemic control in adults with type 2 diabetes.
The safety and effectiveness of lixisenatide (Adlyxin, Sanofi) were evaluated either as a standalone therapy or in combination with other FDA-approved treatments in a series of clinical trials that enrolled 5,400 adults with poorly controlled type 2 diabetes. The combinations tested in the GetGoal Duo2 studies included lixisenatide with metformin, sulfonylureas, pioglitazone, or basal insulin. Lixisenatide successfully met the primary endpoint of improved hemoglobin A1c levels.
Sanofi, the drug’s manufacturer, withdrew its original 2013 application for lixisenatide’s approval pending evaluation of its cardiovascular safety profile using data from the randomized, controlled Evaluation of Lixisenatide in Acute Coronary Syndrome ELIXA trial. In that study of more than 6,000 adults with type 2 diabetes at risk for atherosclerotic cardiovascular disease, lixisenatide did not increase the risk of cardiovascular adverse events, which occurred in 13.2% of placebo patients and 13.4% of treatment group patients (N Engl J Med. 2015;373:2247-57).
The drug’s most common side effects are nausea, vomiting, headache, diarrhea, dizziness, and hypoglycemia. Severe hypersensitivity reactions, including anaphylaxis, also were reported in the clinical trials.
Lixisenatide should not be used to treat people with type 1 diabetes or patients with diabetic ketoacidosis.
The drug will be marketed in disposable, 20-mcg single-dose pens to be injected postprandially, once daily, following initial treatment with a once-daily dose of 10 mcg for 14 days.
Lixisenatide is approved in more than 60 countries and marketed as Lyxumia in over 40, according to information on the manufacturer’s website.
Postmarketing studies for lixisenatide will be required to evaluate dosing, efficacy, and safety in pediatric patients, and to evaluate the drug’s immunogenicity, according to an FDA statement.
“The FDA continues to support the development of new drug therapies for diabetes management,” said Mary Thanh Hai Parks, MD, deputy director, Office of Drug Evaluation II in the FDA’s Center for Drug Evaluation and Research. “Adlyxin will add to the available treatment options to control blood sugar levels for those with type 2.”
On Twitter @whitneymcknight
Law & Medicine: Discovery rule and statute of limitations
Question: In July 2002, a patient in California underwent surgery for a herniated T8-9 disk, but the surgeon instead removed the T6-7 and T7-8 disks. On Sept. 11, 2002, the surgeon discussed with the patient the MRI findings showing his mistake. On Sept. 17, 2003, the patient filed a malpractice lawsuit, just 6 days beyond California’s 1-year limitations period. California subscribes to the discovery rule, that is, a cause of action accrues only when a claimant discovers or should have discovered injury was the result of negligence.
Which of the following choices is best?
A. The lawsuit filed Sept. 17, 2003, is time barred, as the negligent surgery took place in July 2002.
B. On its face, the lawsuit was filed too late, being 1 year and 6 days after the Sept. 11, 2002, discussion date.
C. The lawsuit was timely filed, so long as the claimant can prove he was out of town for more than 6 days of that year.
D. The patient should sue as an action in battery, which has a longer statute of limitations.
E. All choices except A are correct.
Answer: E. At common law, there was no time limit that barred a plaintiff from bringing a claim, although an equitable doctrine of laches existed to foreclose an action that had long lapsed. Statutory changes in the law now require that lawsuits be brought in a timely manner so that the evidence remains fresh, accurate, and reliable.
Another reason is to provide repose to the wrongdoer, that is, relief from worrying for an indefinite period of time whether a lawsuit will be brought. This time period, during which a lawsuit must be filed or it will be barred, is termed the statute of limitations. It is 2 years for the tort of negligence in most jurisdictions, with states such as California and Tennessee placing a 1-year limit on medical malpractice claims. In California, the running of the statute is tolled (temporarily halted) for the days a claimant is out of state.
The above case scenario is taken from Kaplan v. Mamelak,1 where the plaintiff’s lawsuit was not barred to allow him to identify the number of days he was out of town. The court also permitted a cause of action in battery, which is covered under a longer statute of limitations, as well as one sounding in malpractice.
Patients who are injured from malpractice may not always be aware that a negligent act had taken place, and some injuries may remain latent for a long period. Recognizing this, statutes of limitation emphasize the date when the plaintiff first discovered that the injury resulted from negligence. This is termed the discovery rule.
Stated more formally, the limitations period commences at the time the cause of action (negligence or other wrongs) accrues, and this usually means when the claimant knew (actual knowledge) or should have known (constructive knowledge).
The rule, in the words of one court, is meant to balance the need for “prompt assertion of claims” against a policy “favoring adjudication of claims on the merits and ensuring that a party with a valid claim will be given an opportunity to present it.”
As is typical of other jurisdictions, Hawaii sought to clarify the discovery rule in a series of court cases, beginning with Yoshizaki v. Hilo Hospital,2 where the court deemed a cause of action “does not begin to run until the plaintiff knew or should have known of the defendant’s negligence.”
Subsequently, Hawaii’s Intermediate Court of Appeals explained that the state’s 2-year limitations statute commences when the plaintiff discovers, or through the use of reasonable diligence should have discovered, 1) the damage; 2) the violation of the duty; and 3) the causal connection between the violation of the duty and the damage.3
The court subsequently held that the rule prevents the running of the limitations period until “the plaintiff [has] knowledge of those facts which are necessary for an actionable claim.”4 In 1999, the Hawaii Supreme Court clarified that it was “factual knowledge,” rather than “legal knowledge,” that starts the clock running, and that legal knowledge of a defendant’s negligence was not required.5
More recently, litigation over the time barring of claims was evident in Moon v. Rhode,6 where Dr. Clarissa Rhode and Central Illinois Radiological Associates were sued for negligently misreading a patient’s CT scans.
The 90-year-old patient, Kathryn Moon, was admitted to Proctor Hospital May 18, 2009, and died 11 days later following surgery and complications of fluid overload and a pneumoperitoneum. Dr. Rhode, a radiologist, interpreted two CT scans, which an independent expert in 2013 determined were negligently misread. A lawsuit was then brought against Dr. Rhode, who was not a named defendant when the plaintiff had timely filed a medical negligence action back in 2011 against the surgeon and the attending doctor.
The court of appeals held that the discovery rule can be applied to wrongful death and survival actions, and that the statute of limitations begins to run when the plaintiff knows or should have known that the death was “wrongfully caused.” However, this did not necessarily mean knowledge of a specific defendant’s negligent conduct or knowledge of the existence of a cause of action.
The court stated: “Plaintiff filed his complaint long after he became possessed with sufficient information, which put him on inquiry to determine whether actionable conduct was involved.” The court ruled that the relevant inquiry was not when the plaintiff became aware that Dr. Rhode may have committed medical negligence, but when any defendant may have committed medical negligence against the patient Kathryn. The case is currently on appeal to the Supreme Court of Illinois.
In addition to the discovery rule, other situations may toll the limitations period. One example is fraudulent concealment of a right of action, where the statute may be tolled during the period of concealment. And in all jurisdictions, the running of the time period is halted in malpractice complaints involving treatment of a minor until that minor reaches a certain age, such as age of majority, or after a stipulated number of years, for example, 6 years.
Occasionally, a health care provider may overlook an important tolling provision. California, for example, has a rule that any “payment” made to an injured party must be accompanied by a written statement regarding the applicable statute of limitations.
In the recent Coastal Surgical Institute v. Blevins case,7 the defendant surgeon made a payment of $4,118.23 for medical expenses incurred by an unrepresented plaintiff, but had neglected to attach a release or a written notice regarding the statute of limitations. The plaintiff subsequently decided to file a lawsuit, even though more than a year – the statutory period – had lapsed.
Under the facts, the limitation period was tolled, and the trial court allowed the case to go forward, ultimately finding liability and awarding damages of $500,000, later reduced to $285,114. The court of appeals affirmed the decision.
This case has prompted MIEC, a malpractice insurance carrier, to emphasize putting in writing the restrictions imposed by the limitations statute to any unrepresented patient. MIEC also warned that the term “payment” might be construed liberally, citing case examples that include a free counseling session and the provision of specialized care for a student injured by a school’s gym equipment.
References
1. Kaplan v. Mamelak, 162 Cal. App. 4th 637 (2008).
2. Yoshizaki v. Hilo Hospital, 433 P.2d 220 (1967).
3. Jacoby v. Kaiser Foundation Hospital, 622 P.2d 613 (1981).
4. Yamaguchi v. Queen’s Medical Center, 648 P.2d 689 (1982).
5. Buck v. Miles, 971 P.2d 717 (1999).
6. Moon v. Rhode, IL. 2015 App. 3d 130613.
7. Coastal Surgical Institute v. Blevins, 232 Cal. App. 4th 1321 (2015).
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. It is adapted from the author’s book, “Medical Malpractice: Understanding the Law, Managing the Risk” (2006). For additional information, readers may contact the author at [email protected].
Question: In July 2002, a patient in California underwent surgery for a herniated T8-9 disk, but the surgeon instead removed the T6-7 and T7-8 disks. On Sept. 11, 2002, the surgeon discussed with the patient the MRI findings showing his mistake. On Sept. 17, 2003, the patient filed a malpractice lawsuit, just 6 days beyond California’s 1-year limitations period. California subscribes to the discovery rule, that is, a cause of action accrues only when a claimant discovers or should have discovered injury was the result of negligence.
Which of the following choices is best?
A. The lawsuit filed Sept. 17, 2003, is time barred, as the negligent surgery took place in July 2002.
B. On its face, the lawsuit was filed too late, being 1 year and 6 days after the Sept. 11, 2002, discussion date.
C. The lawsuit was timely filed, so long as the claimant can prove he was out of town for more than 6 days of that year.
D. The patient should sue as an action in battery, which has a longer statute of limitations.
E. All choices except A are correct.
Answer: E. At common law, there was no time limit that barred a plaintiff from bringing a claim, although an equitable doctrine of laches existed to foreclose an action that had long lapsed. Statutory changes in the law now require that lawsuits be brought in a timely manner so that the evidence remains fresh, accurate, and reliable.
Another reason is to provide repose to the wrongdoer, that is, relief from worrying for an indefinite period of time whether a lawsuit will be brought. This time period, during which a lawsuit must be filed or it will be barred, is termed the statute of limitations. It is 2 years for the tort of negligence in most jurisdictions, with states such as California and Tennessee placing a 1-year limit on medical malpractice claims. In California, the running of the statute is tolled (temporarily halted) for the days a claimant is out of state.
The above case scenario is taken from Kaplan v. Mamelak,1 where the plaintiff’s lawsuit was not barred to allow him to identify the number of days he was out of town. The court also permitted a cause of action in battery, which is covered under a longer statute of limitations, as well as one sounding in malpractice.
Patients who are injured from malpractice may not always be aware that a negligent act had taken place, and some injuries may remain latent for a long period. Recognizing this, statutes of limitation emphasize the date when the plaintiff first discovered that the injury resulted from negligence. This is termed the discovery rule.
Stated more formally, the limitations period commences at the time the cause of action (negligence or other wrongs) accrues, and this usually means when the claimant knew (actual knowledge) or should have known (constructive knowledge).
The rule, in the words of one court, is meant to balance the need for “prompt assertion of claims” against a policy “favoring adjudication of claims on the merits and ensuring that a party with a valid claim will be given an opportunity to present it.”
As is typical of other jurisdictions, Hawaii sought to clarify the discovery rule in a series of court cases, beginning with Yoshizaki v. Hilo Hospital,2 where the court deemed a cause of action “does not begin to run until the plaintiff knew or should have known of the defendant’s negligence.”
Subsequently, Hawaii’s Intermediate Court of Appeals explained that the state’s 2-year limitations statute commences when the plaintiff discovers, or through the use of reasonable diligence should have discovered, 1) the damage; 2) the violation of the duty; and 3) the causal connection between the violation of the duty and the damage.3
The court subsequently held that the rule prevents the running of the limitations period until “the plaintiff [has] knowledge of those facts which are necessary for an actionable claim.”4 In 1999, the Hawaii Supreme Court clarified that it was “factual knowledge,” rather than “legal knowledge,” that starts the clock running, and that legal knowledge of a defendant’s negligence was not required.5
More recently, litigation over the time barring of claims was evident in Moon v. Rhode,6 where Dr. Clarissa Rhode and Central Illinois Radiological Associates were sued for negligently misreading a patient’s CT scans.
The 90-year-old patient, Kathryn Moon, was admitted to Proctor Hospital May 18, 2009, and died 11 days later following surgery and complications of fluid overload and a pneumoperitoneum. Dr. Rhode, a radiologist, interpreted two CT scans, which an independent expert in 2013 determined were negligently misread. A lawsuit was then brought against Dr. Rhode, who was not a named defendant when the plaintiff had timely filed a medical negligence action back in 2011 against the surgeon and the attending doctor.
The court of appeals held that the discovery rule can be applied to wrongful death and survival actions, and that the statute of limitations begins to run when the plaintiff knows or should have known that the death was “wrongfully caused.” However, this did not necessarily mean knowledge of a specific defendant’s negligent conduct or knowledge of the existence of a cause of action.
The court stated: “Plaintiff filed his complaint long after he became possessed with sufficient information, which put him on inquiry to determine whether actionable conduct was involved.” The court ruled that the relevant inquiry was not when the plaintiff became aware that Dr. Rhode may have committed medical negligence, but when any defendant may have committed medical negligence against the patient Kathryn. The case is currently on appeal to the Supreme Court of Illinois.
In addition to the discovery rule, other situations may toll the limitations period. One example is fraudulent concealment of a right of action, where the statute may be tolled during the period of concealment. And in all jurisdictions, the running of the time period is halted in malpractice complaints involving treatment of a minor until that minor reaches a certain age, such as age of majority, or after a stipulated number of years, for example, 6 years.
Occasionally, a health care provider may overlook an important tolling provision. California, for example, has a rule that any “payment” made to an injured party must be accompanied by a written statement regarding the applicable statute of limitations.
In the recent Coastal Surgical Institute v. Blevins case,7 the defendant surgeon made a payment of $4,118.23 for medical expenses incurred by an unrepresented plaintiff, but had neglected to attach a release or a written notice regarding the statute of limitations. The plaintiff subsequently decided to file a lawsuit, even though more than a year – the statutory period – had lapsed.
Under the facts, the limitation period was tolled, and the trial court allowed the case to go forward, ultimately finding liability and awarding damages of $500,000, later reduced to $285,114. The court of appeals affirmed the decision.
This case has prompted MIEC, a malpractice insurance carrier, to emphasize putting in writing the restrictions imposed by the limitations statute to any unrepresented patient. MIEC also warned that the term “payment” might be construed liberally, citing case examples that include a free counseling session and the provision of specialized care for a student injured by a school’s gym equipment.
References
1. Kaplan v. Mamelak, 162 Cal. App. 4th 637 (2008).
2. Yoshizaki v. Hilo Hospital, 433 P.2d 220 (1967).
3. Jacoby v. Kaiser Foundation Hospital, 622 P.2d 613 (1981).
4. Yamaguchi v. Queen’s Medical Center, 648 P.2d 689 (1982).
5. Buck v. Miles, 971 P.2d 717 (1999).
6. Moon v. Rhode, IL. 2015 App. 3d 130613.
7. Coastal Surgical Institute v. Blevins, 232 Cal. App. 4th 1321 (2015).
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. It is adapted from the author’s book, “Medical Malpractice: Understanding the Law, Managing the Risk” (2006). For additional information, readers may contact the author at [email protected].
Question: In July 2002, a patient in California underwent surgery for a herniated T8-9 disk, but the surgeon instead removed the T6-7 and T7-8 disks. On Sept. 11, 2002, the surgeon discussed with the patient the MRI findings showing his mistake. On Sept. 17, 2003, the patient filed a malpractice lawsuit, just 6 days beyond California’s 1-year limitations period. California subscribes to the discovery rule, that is, a cause of action accrues only when a claimant discovers or should have discovered injury was the result of negligence.
Which of the following choices is best?
A. The lawsuit filed Sept. 17, 2003, is time barred, as the negligent surgery took place in July 2002.
B. On its face, the lawsuit was filed too late, being 1 year and 6 days after the Sept. 11, 2002, discussion date.
C. The lawsuit was timely filed, so long as the claimant can prove he was out of town for more than 6 days of that year.
D. The patient should sue as an action in battery, which has a longer statute of limitations.
E. All choices except A are correct.
Answer: E. At common law, there was no time limit that barred a plaintiff from bringing a claim, although an equitable doctrine of laches existed to foreclose an action that had long lapsed. Statutory changes in the law now require that lawsuits be brought in a timely manner so that the evidence remains fresh, accurate, and reliable.
Another reason is to provide repose to the wrongdoer, that is, relief from worrying for an indefinite period of time whether a lawsuit will be brought. This time period, during which a lawsuit must be filed or it will be barred, is termed the statute of limitations. It is 2 years for the tort of negligence in most jurisdictions, with states such as California and Tennessee placing a 1-year limit on medical malpractice claims. In California, the running of the statute is tolled (temporarily halted) for the days a claimant is out of state.
The above case scenario is taken from Kaplan v. Mamelak,1 where the plaintiff’s lawsuit was not barred to allow him to identify the number of days he was out of town. The court also permitted a cause of action in battery, which is covered under a longer statute of limitations, as well as one sounding in malpractice.
Patients who are injured from malpractice may not always be aware that a negligent act had taken place, and some injuries may remain latent for a long period. Recognizing this, statutes of limitation emphasize the date when the plaintiff first discovered that the injury resulted from negligence. This is termed the discovery rule.
Stated more formally, the limitations period commences at the time the cause of action (negligence or other wrongs) accrues, and this usually means when the claimant knew (actual knowledge) or should have known (constructive knowledge).
The rule, in the words of one court, is meant to balance the need for “prompt assertion of claims” against a policy “favoring adjudication of claims on the merits and ensuring that a party with a valid claim will be given an opportunity to present it.”
As is typical of other jurisdictions, Hawaii sought to clarify the discovery rule in a series of court cases, beginning with Yoshizaki v. Hilo Hospital,2 where the court deemed a cause of action “does not begin to run until the plaintiff knew or should have known of the defendant’s negligence.”
Subsequently, Hawaii’s Intermediate Court of Appeals explained that the state’s 2-year limitations statute commences when the plaintiff discovers, or through the use of reasonable diligence should have discovered, 1) the damage; 2) the violation of the duty; and 3) the causal connection between the violation of the duty and the damage.3
The court subsequently held that the rule prevents the running of the limitations period until “the plaintiff [has] knowledge of those facts which are necessary for an actionable claim.”4 In 1999, the Hawaii Supreme Court clarified that it was “factual knowledge,” rather than “legal knowledge,” that starts the clock running, and that legal knowledge of a defendant’s negligence was not required.5
More recently, litigation over the time barring of claims was evident in Moon v. Rhode,6 where Dr. Clarissa Rhode and Central Illinois Radiological Associates were sued for negligently misreading a patient’s CT scans.
The 90-year-old patient, Kathryn Moon, was admitted to Proctor Hospital May 18, 2009, and died 11 days later following surgery and complications of fluid overload and a pneumoperitoneum. Dr. Rhode, a radiologist, interpreted two CT scans, which an independent expert in 2013 determined were negligently misread. A lawsuit was then brought against Dr. Rhode, who was not a named defendant when the plaintiff had timely filed a medical negligence action back in 2011 against the surgeon and the attending doctor.
The court of appeals held that the discovery rule can be applied to wrongful death and survival actions, and that the statute of limitations begins to run when the plaintiff knows or should have known that the death was “wrongfully caused.” However, this did not necessarily mean knowledge of a specific defendant’s negligent conduct or knowledge of the existence of a cause of action.
The court stated: “Plaintiff filed his complaint long after he became possessed with sufficient information, which put him on inquiry to determine whether actionable conduct was involved.” The court ruled that the relevant inquiry was not when the plaintiff became aware that Dr. Rhode may have committed medical negligence, but when any defendant may have committed medical negligence against the patient Kathryn. The case is currently on appeal to the Supreme Court of Illinois.
In addition to the discovery rule, other situations may toll the limitations period. One example is fraudulent concealment of a right of action, where the statute may be tolled during the period of concealment. And in all jurisdictions, the running of the time period is halted in malpractice complaints involving treatment of a minor until that minor reaches a certain age, such as age of majority, or after a stipulated number of years, for example, 6 years.
Occasionally, a health care provider may overlook an important tolling provision. California, for example, has a rule that any “payment” made to an injured party must be accompanied by a written statement regarding the applicable statute of limitations.
In the recent Coastal Surgical Institute v. Blevins case,7 the defendant surgeon made a payment of $4,118.23 for medical expenses incurred by an unrepresented plaintiff, but had neglected to attach a release or a written notice regarding the statute of limitations. The plaintiff subsequently decided to file a lawsuit, even though more than a year – the statutory period – had lapsed.
Under the facts, the limitation period was tolled, and the trial court allowed the case to go forward, ultimately finding liability and awarding damages of $500,000, later reduced to $285,114. The court of appeals affirmed the decision.
This case has prompted MIEC, a malpractice insurance carrier, to emphasize putting in writing the restrictions imposed by the limitations statute to any unrepresented patient. MIEC also warned that the term “payment” might be construed liberally, citing case examples that include a free counseling session and the provision of specialized care for a student injured by a school’s gym equipment.
References
1. Kaplan v. Mamelak, 162 Cal. App. 4th 637 (2008).
2. Yoshizaki v. Hilo Hospital, 433 P.2d 220 (1967).
3. Jacoby v. Kaiser Foundation Hospital, 622 P.2d 613 (1981).
4. Yamaguchi v. Queen’s Medical Center, 648 P.2d 689 (1982).
5. Buck v. Miles, 971 P.2d 717 (1999).
6. Moon v. Rhode, IL. 2015 App. 3d 130613.
7. Coastal Surgical Institute v. Blevins, 232 Cal. App. 4th 1321 (2015).
Dr. Tan is emeritus professor of medicine and a former adjunct professor of law at the University of Hawaii. This article is meant to be educational and does not constitute medical, ethical, or legal advice. It is adapted from the author’s book, “Medical Malpractice: Understanding the Law, Managing the Risk” (2006). For additional information, readers may contact the author at [email protected].
Outpatient parenteral antimicrobial therapy for homeless patients saves lives, cuts costs
Prolonged hospitalizations for complicated patients with severe infections who need long courses of intravenous antibiotics, are common in many institutions.
Outpatient parenteral antimicrobial therapy (OPAT) is a safe and cost-effective way to administer intravenous (IV) antimicrobial therapy to patients with the potential to decrease hospital length of stay (LOS). OPAT programs train motivated patients in self-administration of IV medications at home, in a stable environment. Ideally, infectious disease (ID) consultation should be involved to determine appropriate candidates for OPAT as well as a suitable drug regimen and duration of therapy.
A potential barrier to successful utilization of OPAT programs is the need for stable housing at discharge for home infusion services.
Challenge facing homeless patients
There is very little published data regarding the use of OPAT at a medical respite facility for homeless patients. This may be due to perceived concerns of difficulty in administering OPAT to these disadvantaged patients for multiple reasons such as unstable or no housing, inability to stay engaged in medical care, and underlying mental illness and substance abuse problems. In particular, active substance abuse, specifically injection drug use (IDU), is a significant problem.
Traditionally, homeless patients requiring ongoing parenteral therapy have remained inpatient for the duration of their course, which can cause significant inpatient discharge delays and increased LOS. Recommending long-term parenteral therapy as an inpatient for all patients who are homeless or have a history of IDU can lead to prolonged hospitalizations, increased health care costs and contribute to conflicts between patients and staff.
Our study, recently published in the Journal of Hospital Medicine (J Hosp Med. 2016 Apr 27. doi: 10.1002/jhm.2597), aimed to evaluate our experience with administering OPAT to homeless patients at a medical respite facility and to determine if patients could complete a successful treatment course of antibiotics for a variety of illnesses.
We demonstrated that 87% of homeless patients were able to complete a defined course of antibiotic therapy, and 64% were successfully treated with OPAT at medical respite. To our knowledge this is the first study evaluating this specific population (including those with homelessness, mental illness, substance abuse) in which OPAT was received at medical respite.
Our rate of adverse events was 7%, similar to other OPAT studies in the published literature. Our total readmission rate of 30% was similar to what current literature suggests. Our data suggest that providing OPAT to homeless patients is feasible at a medical respite facility with care coordination between members of a multidisciplinary team, including nursing, home infusion pharmacist, and ID clinic.
Partnering with medical respite programs is important, as home infusion services are not available otherwise to homeless patients. The recommendation for ID consultation is beneficial to determine candidacy for OPAT, including close scrutiny of social behaviors in the OPAT patient selection process, and can assist with transitions in care from inpatient to outpatient setting.
Homeless IDU patients remain a challenging population to treat with long term IV antibiotics. However, in certain circumstances, IDU alone may not be a reason to fully exclude someone from OPAT candidacy. Careful review of substance abuse history and evaluation of psychosocial factors are needed. Furthermore, an evaluation of the patient’s willingness to comply with care agreements while inpatient and at medical respite, and ensuring appropriate resources for chemical dependency treatment are needed. Early consideration of oral antimicrobial options if the patient is readmitted for complications/non-adherence should be encouraged.
Medical respite programs
Treating homeless IDU patients with OPAT is possible under close supervision at medical respite. Our patients sign an agreement to refrain from using their IV access for drug use. Security seals are used on all connections and tubing to prevent tampering. The IV access sites are inspected daily, and ID providers are contacted to discuss any patients suspicious of tampering with their IV to determine plan of care – either readmission or transition to oral antibiotics.
Medical respite programs are gaining in popularity in the United States. Medical respite can help engage patients in follow-up care and provide linkage to housing, mental health, and chemical dependency services. Many programs support harm reduction IDU practices and offer referrals for substance abuse treatment programs, which are not typically offered during inpatient admission in most hospitals.
Medical respite may continue to be a site of OPAT expansion, as there is continued pressure to discharge nonacute patients from the hospital. Moving forward, it may be beneficial for hospitals, public health departments, and communities to support these programs, which can assist with close monitoring of homeless patients receiving OPAT.
There are ongoing challenges for housed IDU patients who require OPAT, as medical respite placement and home infusion are generally not options, and skilled nursing facility placement can be difficult. Careful review of substance abuse history; evaluation of psychosocial factors, such as housing status; mental health history; and outpatient support systems are needed.
Again, ID consultation is highly recommended to determine appropriate IV therapy, and if possible, early transition to oral antimicrobial therapy, as well as duration of treatment for specific illnesses on a case-by-case basis. Close follow-up is needed to ensure patient compliance with prescribed antimicrobial regimen, sometimes requiring weekly visits.
OPAT is effective for many patients, and it is optimal to utilize ID consultation to determine appropriate candidates – particularly among homeless and IDU patients. OPAT can be successful in a closely monitored medical respite setting for homeless patients with multiple comorbidities, with the help of a multidisciplinary team. Medical respite OPAT can decrease LOS in patients who would otherwise require long hospitalizations, resulting in overall cost savings.
Shireesha Dhanireddy, MD, is medical director of the infectious disease clinic at Harborview Medical Center, Seattle. Alison Beieler, PA-C, MPAS, runs the OPAT program in the infectious disease clinic at Harborview Medical Center.
Prolonged hospitalizations for complicated patients with severe infections who need long courses of intravenous antibiotics, are common in many institutions.
Outpatient parenteral antimicrobial therapy (OPAT) is a safe and cost-effective way to administer intravenous (IV) antimicrobial therapy to patients with the potential to decrease hospital length of stay (LOS). OPAT programs train motivated patients in self-administration of IV medications at home, in a stable environment. Ideally, infectious disease (ID) consultation should be involved to determine appropriate candidates for OPAT as well as a suitable drug regimen and duration of therapy.
A potential barrier to successful utilization of OPAT programs is the need for stable housing at discharge for home infusion services.
Challenge facing homeless patients
There is very little published data regarding the use of OPAT at a medical respite facility for homeless patients. This may be due to perceived concerns of difficulty in administering OPAT to these disadvantaged patients for multiple reasons such as unstable or no housing, inability to stay engaged in medical care, and underlying mental illness and substance abuse problems. In particular, active substance abuse, specifically injection drug use (IDU), is a significant problem.
Traditionally, homeless patients requiring ongoing parenteral therapy have remained inpatient for the duration of their course, which can cause significant inpatient discharge delays and increased LOS. Recommending long-term parenteral therapy as an inpatient for all patients who are homeless or have a history of IDU can lead to prolonged hospitalizations, increased health care costs and contribute to conflicts between patients and staff.
Our study, recently published in the Journal of Hospital Medicine (J Hosp Med. 2016 Apr 27. doi: 10.1002/jhm.2597), aimed to evaluate our experience with administering OPAT to homeless patients at a medical respite facility and to determine if patients could complete a successful treatment course of antibiotics for a variety of illnesses.
We demonstrated that 87% of homeless patients were able to complete a defined course of antibiotic therapy, and 64% were successfully treated with OPAT at medical respite. To our knowledge this is the first study evaluating this specific population (including those with homelessness, mental illness, substance abuse) in which OPAT was received at medical respite.
Our rate of adverse events was 7%, similar to other OPAT studies in the published literature. Our total readmission rate of 30% was similar to what current literature suggests. Our data suggest that providing OPAT to homeless patients is feasible at a medical respite facility with care coordination between members of a multidisciplinary team, including nursing, home infusion pharmacist, and ID clinic.
Partnering with medical respite programs is important, as home infusion services are not available otherwise to homeless patients. The recommendation for ID consultation is beneficial to determine candidacy for OPAT, including close scrutiny of social behaviors in the OPAT patient selection process, and can assist with transitions in care from inpatient to outpatient setting.
Homeless IDU patients remain a challenging population to treat with long term IV antibiotics. However, in certain circumstances, IDU alone may not be a reason to fully exclude someone from OPAT candidacy. Careful review of substance abuse history and evaluation of psychosocial factors are needed. Furthermore, an evaluation of the patient’s willingness to comply with care agreements while inpatient and at medical respite, and ensuring appropriate resources for chemical dependency treatment are needed. Early consideration of oral antimicrobial options if the patient is readmitted for complications/non-adherence should be encouraged.
Medical respite programs
Treating homeless IDU patients with OPAT is possible under close supervision at medical respite. Our patients sign an agreement to refrain from using their IV access for drug use. Security seals are used on all connections and tubing to prevent tampering. The IV access sites are inspected daily, and ID providers are contacted to discuss any patients suspicious of tampering with their IV to determine plan of care – either readmission or transition to oral antibiotics.
Medical respite programs are gaining in popularity in the United States. Medical respite can help engage patients in follow-up care and provide linkage to housing, mental health, and chemical dependency services. Many programs support harm reduction IDU practices and offer referrals for substance abuse treatment programs, which are not typically offered during inpatient admission in most hospitals.
Medical respite may continue to be a site of OPAT expansion, as there is continued pressure to discharge nonacute patients from the hospital. Moving forward, it may be beneficial for hospitals, public health departments, and communities to support these programs, which can assist with close monitoring of homeless patients receiving OPAT.
There are ongoing challenges for housed IDU patients who require OPAT, as medical respite placement and home infusion are generally not options, and skilled nursing facility placement can be difficult. Careful review of substance abuse history; evaluation of psychosocial factors, such as housing status; mental health history; and outpatient support systems are needed.
Again, ID consultation is highly recommended to determine appropriate IV therapy, and if possible, early transition to oral antimicrobial therapy, as well as duration of treatment for specific illnesses on a case-by-case basis. Close follow-up is needed to ensure patient compliance with prescribed antimicrobial regimen, sometimes requiring weekly visits.
OPAT is effective for many patients, and it is optimal to utilize ID consultation to determine appropriate candidates – particularly among homeless and IDU patients. OPAT can be successful in a closely monitored medical respite setting for homeless patients with multiple comorbidities, with the help of a multidisciplinary team. Medical respite OPAT can decrease LOS in patients who would otherwise require long hospitalizations, resulting in overall cost savings.
Shireesha Dhanireddy, MD, is medical director of the infectious disease clinic at Harborview Medical Center, Seattle. Alison Beieler, PA-C, MPAS, runs the OPAT program in the infectious disease clinic at Harborview Medical Center.
Prolonged hospitalizations for complicated patients with severe infections who need long courses of intravenous antibiotics, are common in many institutions.
Outpatient parenteral antimicrobial therapy (OPAT) is a safe and cost-effective way to administer intravenous (IV) antimicrobial therapy to patients with the potential to decrease hospital length of stay (LOS). OPAT programs train motivated patients in self-administration of IV medications at home, in a stable environment. Ideally, infectious disease (ID) consultation should be involved to determine appropriate candidates for OPAT as well as a suitable drug regimen and duration of therapy.
A potential barrier to successful utilization of OPAT programs is the need for stable housing at discharge for home infusion services.
Challenge facing homeless patients
There is very little published data regarding the use of OPAT at a medical respite facility for homeless patients. This may be due to perceived concerns of difficulty in administering OPAT to these disadvantaged patients for multiple reasons such as unstable or no housing, inability to stay engaged in medical care, and underlying mental illness and substance abuse problems. In particular, active substance abuse, specifically injection drug use (IDU), is a significant problem.
Traditionally, homeless patients requiring ongoing parenteral therapy have remained inpatient for the duration of their course, which can cause significant inpatient discharge delays and increased LOS. Recommending long-term parenteral therapy as an inpatient for all patients who are homeless or have a history of IDU can lead to prolonged hospitalizations, increased health care costs and contribute to conflicts between patients and staff.
Our study, recently published in the Journal of Hospital Medicine (J Hosp Med. 2016 Apr 27. doi: 10.1002/jhm.2597), aimed to evaluate our experience with administering OPAT to homeless patients at a medical respite facility and to determine if patients could complete a successful treatment course of antibiotics for a variety of illnesses.
We demonstrated that 87% of homeless patients were able to complete a defined course of antibiotic therapy, and 64% were successfully treated with OPAT at medical respite. To our knowledge this is the first study evaluating this specific population (including those with homelessness, mental illness, substance abuse) in which OPAT was received at medical respite.
Our rate of adverse events was 7%, similar to other OPAT studies in the published literature. Our total readmission rate of 30% was similar to what current literature suggests. Our data suggest that providing OPAT to homeless patients is feasible at a medical respite facility with care coordination between members of a multidisciplinary team, including nursing, home infusion pharmacist, and ID clinic.
Partnering with medical respite programs is important, as home infusion services are not available otherwise to homeless patients. The recommendation for ID consultation is beneficial to determine candidacy for OPAT, including close scrutiny of social behaviors in the OPAT patient selection process, and can assist with transitions in care from inpatient to outpatient setting.
Homeless IDU patients remain a challenging population to treat with long term IV antibiotics. However, in certain circumstances, IDU alone may not be a reason to fully exclude someone from OPAT candidacy. Careful review of substance abuse history and evaluation of psychosocial factors are needed. Furthermore, an evaluation of the patient’s willingness to comply with care agreements while inpatient and at medical respite, and ensuring appropriate resources for chemical dependency treatment are needed. Early consideration of oral antimicrobial options if the patient is readmitted for complications/non-adherence should be encouraged.
Medical respite programs
Treating homeless IDU patients with OPAT is possible under close supervision at medical respite. Our patients sign an agreement to refrain from using their IV access for drug use. Security seals are used on all connections and tubing to prevent tampering. The IV access sites are inspected daily, and ID providers are contacted to discuss any patients suspicious of tampering with their IV to determine plan of care – either readmission or transition to oral antibiotics.
Medical respite programs are gaining in popularity in the United States. Medical respite can help engage patients in follow-up care and provide linkage to housing, mental health, and chemical dependency services. Many programs support harm reduction IDU practices and offer referrals for substance abuse treatment programs, which are not typically offered during inpatient admission in most hospitals.
Medical respite may continue to be a site of OPAT expansion, as there is continued pressure to discharge nonacute patients from the hospital. Moving forward, it may be beneficial for hospitals, public health departments, and communities to support these programs, which can assist with close monitoring of homeless patients receiving OPAT.
There are ongoing challenges for housed IDU patients who require OPAT, as medical respite placement and home infusion are generally not options, and skilled nursing facility placement can be difficult. Careful review of substance abuse history; evaluation of psychosocial factors, such as housing status; mental health history; and outpatient support systems are needed.
Again, ID consultation is highly recommended to determine appropriate IV therapy, and if possible, early transition to oral antimicrobial therapy, as well as duration of treatment for specific illnesses on a case-by-case basis. Close follow-up is needed to ensure patient compliance with prescribed antimicrobial regimen, sometimes requiring weekly visits.
OPAT is effective for many patients, and it is optimal to utilize ID consultation to determine appropriate candidates – particularly among homeless and IDU patients. OPAT can be successful in a closely monitored medical respite setting for homeless patients with multiple comorbidities, with the help of a multidisciplinary team. Medical respite OPAT can decrease LOS in patients who would otherwise require long hospitalizations, resulting in overall cost savings.
Shireesha Dhanireddy, MD, is medical director of the infectious disease clinic at Harborview Medical Center, Seattle. Alison Beieler, PA-C, MPAS, runs the OPAT program in the infectious disease clinic at Harborview Medical Center.
Hemophilia guideline recommends integrated care model
ORLANDO – An integrated care model that includes a hematologist, a specialized hematology nurse, a physical therapist, a social worker, and 24/7 access to a specialized coagulation laboratory is recommended in a new hemophilia care guideline jointly developed by the National Hemophilia Foundation and McMaster University in Hamilton, Ontario.
The guideline has been formally accepted for inclusion in the National Guideline Clearinghouse (NGC), the National Hemophilia Foundation announced at its annual meeting, held immediately before the World Hemophilia Foundation World Congress here.
“The integrated care model, as is utilized within the U.S. federally funded network of hemophilia treatment centers (HTCs), should be advocated for optimal care of persons with hemophilia,” wrote guideline coauthors Steven W. Pipe, MD, from the University of Michigan School of Medicine in Ann Arbor, and Craig M. Kessler, MD, from Georgetown University in Washington, in an introduction to the guideline, published in the journal Hemophilia.
Developed according to evidence-based principles, the guideline is hoped to “promote harmonization of care delivery and reduce practice variations within the U.S. HTC network. This guideline will inform the HTC network how best to prioritize additional ‘high-value’ research to fill data gaps or strengthen the evidence base as outlined in the manuscript,” they added.
The guideline authors recognized three basic models of care in use in the United States:
The integrated care, comprehensive care, or HTC model, which generally assumes that all aspects of care will be delivered in a specialized center.
Specialist-based care, under which a hematologist may or may not have training in the management of patients with hemophilia, is provided in a hospital or medical office, but not in a specialized center.
Non-specialist care, delivered in an emergency department or primary care practitioners office.
“We believe that the ‘No Care’ model, theoretically indicating complete absence of care, does not currently operate in the U.S. Yet, this is likely the de facto model of care for many individuals with hemophilia who do not have access to care due to profound resource constraints, particularly in developing countries or underserved minorities,” the authors wrote.
The guideline’s main recommendation – that the integrated-care model is preferable to the non-integrated care model – is conditional, with moderate certainty in the evidence.
For persons with hemophilia with inhibitors to clotting factors, however, the integrated-care model recommendation is considered to be strong, with moderate certainty.
The guideline development panel found that there were significant gaps in evidence for the benefits of integrated care for specific populations such as older patients and populations with poor access to care, and called for additional studies to clarify these questions.
Additionally, the panelists call for study into which specific interventions or aspects of care should be included in the integrated model, and for more in-depth studies into the effects on patient-important outcomes.
“This collaborative project constitutes an important milestone on a critical component of evidence-based guideline methodology,” Alfonso Iorio, MD, PhD, from the Department of Clinical Epidemiology and Biostatistics at McMaster University, said in a press statement. “It demonstrates how a patient advocacy organization can promote and support a guideline process, in the true spirit of patient involvement in research and care process, without compromising a rigorous and transparent conflict of interest management process.”
The guidelines were funded by the National Hemophilia Foundation. Several guideline panelists reported financial relationships with companies that make clotting factors and other products for persons with hemophilia.
ORLANDO – An integrated care model that includes a hematologist, a specialized hematology nurse, a physical therapist, a social worker, and 24/7 access to a specialized coagulation laboratory is recommended in a new hemophilia care guideline jointly developed by the National Hemophilia Foundation and McMaster University in Hamilton, Ontario.
The guideline has been formally accepted for inclusion in the National Guideline Clearinghouse (NGC), the National Hemophilia Foundation announced at its annual meeting, held immediately before the World Hemophilia Foundation World Congress here.
“The integrated care model, as is utilized within the U.S. federally funded network of hemophilia treatment centers (HTCs), should be advocated for optimal care of persons with hemophilia,” wrote guideline coauthors Steven W. Pipe, MD, from the University of Michigan School of Medicine in Ann Arbor, and Craig M. Kessler, MD, from Georgetown University in Washington, in an introduction to the guideline, published in the journal Hemophilia.
Developed according to evidence-based principles, the guideline is hoped to “promote harmonization of care delivery and reduce practice variations within the U.S. HTC network. This guideline will inform the HTC network how best to prioritize additional ‘high-value’ research to fill data gaps or strengthen the evidence base as outlined in the manuscript,” they added.
The guideline authors recognized three basic models of care in use in the United States:
The integrated care, comprehensive care, or HTC model, which generally assumes that all aspects of care will be delivered in a specialized center.
Specialist-based care, under which a hematologist may or may not have training in the management of patients with hemophilia, is provided in a hospital or medical office, but not in a specialized center.
Non-specialist care, delivered in an emergency department or primary care practitioners office.
“We believe that the ‘No Care’ model, theoretically indicating complete absence of care, does not currently operate in the U.S. Yet, this is likely the de facto model of care for many individuals with hemophilia who do not have access to care due to profound resource constraints, particularly in developing countries or underserved minorities,” the authors wrote.
The guideline’s main recommendation – that the integrated-care model is preferable to the non-integrated care model – is conditional, with moderate certainty in the evidence.
For persons with hemophilia with inhibitors to clotting factors, however, the integrated-care model recommendation is considered to be strong, with moderate certainty.
The guideline development panel found that there were significant gaps in evidence for the benefits of integrated care for specific populations such as older patients and populations with poor access to care, and called for additional studies to clarify these questions.
Additionally, the panelists call for study into which specific interventions or aspects of care should be included in the integrated model, and for more in-depth studies into the effects on patient-important outcomes.
“This collaborative project constitutes an important milestone on a critical component of evidence-based guideline methodology,” Alfonso Iorio, MD, PhD, from the Department of Clinical Epidemiology and Biostatistics at McMaster University, said in a press statement. “It demonstrates how a patient advocacy organization can promote and support a guideline process, in the true spirit of patient involvement in research and care process, without compromising a rigorous and transparent conflict of interest management process.”
The guidelines were funded by the National Hemophilia Foundation. Several guideline panelists reported financial relationships with companies that make clotting factors and other products for persons with hemophilia.
ORLANDO – An integrated care model that includes a hematologist, a specialized hematology nurse, a physical therapist, a social worker, and 24/7 access to a specialized coagulation laboratory is recommended in a new hemophilia care guideline jointly developed by the National Hemophilia Foundation and McMaster University in Hamilton, Ontario.
The guideline has been formally accepted for inclusion in the National Guideline Clearinghouse (NGC), the National Hemophilia Foundation announced at its annual meeting, held immediately before the World Hemophilia Foundation World Congress here.
“The integrated care model, as is utilized within the U.S. federally funded network of hemophilia treatment centers (HTCs), should be advocated for optimal care of persons with hemophilia,” wrote guideline coauthors Steven W. Pipe, MD, from the University of Michigan School of Medicine in Ann Arbor, and Craig M. Kessler, MD, from Georgetown University in Washington, in an introduction to the guideline, published in the journal Hemophilia.
Developed according to evidence-based principles, the guideline is hoped to “promote harmonization of care delivery and reduce practice variations within the U.S. HTC network. This guideline will inform the HTC network how best to prioritize additional ‘high-value’ research to fill data gaps or strengthen the evidence base as outlined in the manuscript,” they added.
The guideline authors recognized three basic models of care in use in the United States:
The integrated care, comprehensive care, or HTC model, which generally assumes that all aspects of care will be delivered in a specialized center.
Specialist-based care, under which a hematologist may or may not have training in the management of patients with hemophilia, is provided in a hospital or medical office, but not in a specialized center.
Non-specialist care, delivered in an emergency department or primary care practitioners office.
“We believe that the ‘No Care’ model, theoretically indicating complete absence of care, does not currently operate in the U.S. Yet, this is likely the de facto model of care for many individuals with hemophilia who do not have access to care due to profound resource constraints, particularly in developing countries or underserved minorities,” the authors wrote.
The guideline’s main recommendation – that the integrated-care model is preferable to the non-integrated care model – is conditional, with moderate certainty in the evidence.
For persons with hemophilia with inhibitors to clotting factors, however, the integrated-care model recommendation is considered to be strong, with moderate certainty.
The guideline development panel found that there were significant gaps in evidence for the benefits of integrated care for specific populations such as older patients and populations with poor access to care, and called for additional studies to clarify these questions.
Additionally, the panelists call for study into which specific interventions or aspects of care should be included in the integrated model, and for more in-depth studies into the effects on patient-important outcomes.
“This collaborative project constitutes an important milestone on a critical component of evidence-based guideline methodology,” Alfonso Iorio, MD, PhD, from the Department of Clinical Epidemiology and Biostatistics at McMaster University, said in a press statement. “It demonstrates how a patient advocacy organization can promote and support a guideline process, in the true spirit of patient involvement in research and care process, without compromising a rigorous and transparent conflict of interest management process.”
The guidelines were funded by the National Hemophilia Foundation. Several guideline panelists reported financial relationships with companies that make clotting factors and other products for persons with hemophilia.
AT WFH 2016 WORLD CONGRESS
Key clinical point: An integrated care model is recommended as optimal for management of persons with hemophilia.
Major finding: The joint National Hemophilia Foundation/McMaster University guidelines have been accepted by the National Guideline Clearinghouse.
Data source: Evidence-based recommendations on models of care.
Disclosures: The guidelines were funded by the National Hemophilia Foundation. Several guideline panelists reported financial relationships with companies that make clotting factors and other products for persons with hemophilia.
Different approaches can combat negative online reviews
Like most physicians, Dr. Susan Hardwick-Smith was used to receiving the occasional negative online review about her practice. But a biting post from several years ago was so wrenching that it nearly drove the Houston ob.gyn. out of medicine for good.
The patient blasted Dr. Hardwick-Smith on a popular review site about her care during a delivery and accused the doctor of attempting to force an unnecessary C-section. The account was inaccurate, but privacy laws prevented Dr. Hardwick-Smith from defending herself online or sharing details of the actual encounter, she said.
“She wrote this very detailed account of what a terrible doctor I was, and in my version of reality, I had saved her baby’s life,” said Dr. Hardwick-Smith. “I felt extremely powerless. I lost a lot of sleep over it, and I was considering giving up delivering babies. It was a real turning point for me.”
Rather than hanging up her white coat, Dr. Hardwick-Smith began working with an online reputation company – eMerit – that works to dilute negative reviews by soliciting a greater number of reviews from patients. The offensive post is now buried under hundreds of other reviews that are primarily positive, she said.
Hiring a reputation management company is one strategy for coping with negative online reviews. But cyberlaw experts stress that removing negative posts altogether is no easy feat. The best move to take often depends on the post, the patient, and the circumstance.
By now, it’s no secret that negative online reviews can significantly impact a medical practice, from influencing patient recruitment to affecting practice revenue to ruining a reputation. A 2015 survey of 2,354 consumers by search marketing firm BrightLocal found that 92% of consumers read online reviews – up from 67% in 2010 – and 40% of consumers had formed an opinion by reading just one to three reviews. Of 2,137 patients who viewed online reviews, 35% selected a physician based on positive reviews, while 37% avoided doctors with negative reviews, according to a 2014 study in JAMA (doi:10.1001/jama.2013.283194).
Reviews have become a strong force in the health care industry, said Peter Yelkovac, an online defamation attorney in Northern Indiana.
“Online reviews have really replaced the common ‘word of mouth’ that used to be the primary source for doctors referrals,” Mr. Yelkovac said in an interview. “Now, [patients] go online. Anyone can type anything they want, whether it’s truthful, untruthful, positive, indifferent, or negative.”
Doctor vs. website
In some cases, contacting a website administrator and requesting a review be removed can end the dilemma, said Michael J. Sacopulos, a medical malpractice defense attorney based in Terre Haute, Ind.
Rating sites generally have “terms of use,” and posts that violate the terms usually will be taken down by site administrators with some nudging, Mr. Sacopulos said in an interview. Other sites have “strike policies,” where a reviewee can request that one or two negative reviews be removed.
Still other sites are not as accommodating. Amazon, for instance, has immunity against content posted on the site, Mr. Sacopulos said. Under the Communications Decency Act, interactive computer services, such as a consumer review website, cannot be liable for content independently created or developed by third-party users. Such sites are hardly motivated to remove negative comments when racy posts can drive traffic to the site, he said.
Eric M. Joseph, MD, a facial plastic surgeon in West Orange, N.J., learned this lesson firsthand when he attempted to have a video removed from YouTube. A poster had uploaded copyright-protected before and after photos from Dr. Joseph’s practice onto YouTube and made disparaging comments about the patients in a video that went viral. Dr. Joseph and the patient both flagged the video for removal, but to no avail.
“It was impossible to [talk to] a human being at Google,” Dr, Joseph said. “It almost didn’t come down, and we were in conversations about suing Google. It took months and a cyberattorney who specializes in copyright infringement.”
The video finally was removed, but not before Dr. Joseph spent $6,000 in legal fees and experienced significant distress from the incident. Although most reviews about his practice are positive, he said, it’s difficult not to be affected by negative posts.
“From a psychological standpoint, it stings,” he said. “The burn of a negative review outweighs the sweetness of a positive review 100 times.”
Reputation companies to the rescue?
Like Dr. Hardwick-Smith, Dr. Joseph has utilized the online reputation management company eMerit to improve his online presence. The company gathers reviews from patients at the point of service and posts them to dominate review sites.
The solution to pollution is dilution, which means counterbalancing negative reviews with more representative reviews,” said Jeffrey Segal, MD, a neurosurgeon and attorney, and the founder of eMerit. “The next step is to deescalate conflict if you know who the patient is – to see if the patient problem can be resolved. Typically a patient is pleasantly surprised that you took the effort to call. Because the bar is so low, it’s very easy to exceed it.”
Physicians subscribe to eMerit on a month-to-month basis, paying $100-$600 a month, depending on the practice’s needs, Dr. Segal said. He touted a greater than 90% renewal rate, and said eMerit has captured and uploaded more than 150,000 patient reviews since its inception.
For the online reputation management company Reputation.com, health care providers have become one of the its most frequent clients, said Michael Fertik, company founder. Reputation.com solicits reviews from patients after appointments and ensures their visibility on top review sites. The platform also integrates reviews from general and health care review sites to help providers address patient feedback and receive alerts when negative reviews are posted. Rates start at $50 a month.
Mr. Fertik noted that more reviews not only overtake negative posts, but they make physicians easier to find by patients.
“If you have more than 10-15 reviews, you have a higher chance of getting a new patient because the search engine is going to favor doctors that have more reviews,” he said. “Doctors that have a small number of reviews don’t exist as far as search engines are concerned.”
However, all online reputation management firms are not equal, Mr. Sacopulos warned. Some are unfamiliar with the health care space, while others are unclear on health care privacy regulations. Mr. Sacopulos learned of a company that was sending patients texts to request reviews, which was likely a privacy violation and a violation of the Telecommunications Act, he said.
““Some [companies] are much more credible, and they understand health care law more than others,” he said. “Some have the technological capabilities to do things, but don’t understand the legal environment, so you need to be very careful [about whom] you pick.”
Time to sue?
Litigation is generally the last resort to fighting unfavorable online reviews. If a doctor believes a review is unfair or defamatory, and all other efforts have been exhausted, a lawyer may be able to help, Mr. Yelkovac said.
“When someone says, ‘I want to sue,’ that’s a possibility, but that’s typically far down the road,” he said. “Lawsuits are expensive. Lawsuits have an unknown outcome, and I would say, many times when you do sue for defamation, [the poster] may or may not have a lot of money, so you may end up spending a lot of money and you don’t recover anything from the patient.”
The majority of the lawsuits Mr. Yelkovac handles related to online reviews seek to unmask the poster with the aid of subpoenas and at times computer forensics, he said. From there, doctors can decide which action to take, such as contacting the poster and asking to have the comment removed.
“Sometimes it’s a surprise,” he said. “Sometimes it’s an ex-employee. Sometimes it’s a family member, or it could potentially be a competitor. Many times it’s not even a patient, and sometimes it’s a patient [who] the doctor never thought would post a review.”
Reviews and malpractice risk
Remember that not all unfavorable reviews are necessarily negative for physicians, said Brant Avondet, founder of Searchlight Enterprises, a malpractice risk prediction and online physician ratings research company.
A pattern of reviews that express the same concerns or frustrations by patients can be used to address and change internal policies and problems, such as multiple complaints about long wait times or a crowded parking lot, he said. Perhaps the front desk staff is repeatedly unfriendly to patients. Taking steps to correct these concerns could help in the long run, Mr. Avondet said.
Searchlight Enterprises recently presented study findings about a suggested link between online ratings and legal risk for physicians at a national medical insurance conference. Mr. Avondet and his colleagues evaluated claims data for 4,000 Florida physicians from the Florida Healthcare Practitioner Data Portal from 2000 to 2016 and studied online physician reviews from top rating sites. Doctors were grouped into three categories: surgical, ob.gyn., and “other” specialties. Findings showed the bottom 10% of surgeons studied (those with the worst online reviews) had 150% as many claims as the average for all surgeons. Surgeons in the top 20% (doctors with the best online reviews) had roughly half of the risk of a claim, compared with the average surgeon. Similar results were found for ob.gyns. and other specialties.
“Low and behold, there’s a huge correlation,” Mr. Avondet said. “There’s no shadow of a doubt that there’s something there that predicts your malpractice risk based on how nice or mean you are in the eyes of the patient.”
Mr. Avondet said he encourages physicians to use online reviews to make improvements, thus lowering their liability.
“Look at these reviews as a lens into your practice and things you might need to correct,” he said. “Use it as [insight] for how you can improve your practice and decrease the risk of getting sued.”
On Twitter @legal_med
Like most physicians, Dr. Susan Hardwick-Smith was used to receiving the occasional negative online review about her practice. But a biting post from several years ago was so wrenching that it nearly drove the Houston ob.gyn. out of medicine for good.
The patient blasted Dr. Hardwick-Smith on a popular review site about her care during a delivery and accused the doctor of attempting to force an unnecessary C-section. The account was inaccurate, but privacy laws prevented Dr. Hardwick-Smith from defending herself online or sharing details of the actual encounter, she said.
“She wrote this very detailed account of what a terrible doctor I was, and in my version of reality, I had saved her baby’s life,” said Dr. Hardwick-Smith. “I felt extremely powerless. I lost a lot of sleep over it, and I was considering giving up delivering babies. It was a real turning point for me.”
Rather than hanging up her white coat, Dr. Hardwick-Smith began working with an online reputation company – eMerit – that works to dilute negative reviews by soliciting a greater number of reviews from patients. The offensive post is now buried under hundreds of other reviews that are primarily positive, she said.
Hiring a reputation management company is one strategy for coping with negative online reviews. But cyberlaw experts stress that removing negative posts altogether is no easy feat. The best move to take often depends on the post, the patient, and the circumstance.
By now, it’s no secret that negative online reviews can significantly impact a medical practice, from influencing patient recruitment to affecting practice revenue to ruining a reputation. A 2015 survey of 2,354 consumers by search marketing firm BrightLocal found that 92% of consumers read online reviews – up from 67% in 2010 – and 40% of consumers had formed an opinion by reading just one to three reviews. Of 2,137 patients who viewed online reviews, 35% selected a physician based on positive reviews, while 37% avoided doctors with negative reviews, according to a 2014 study in JAMA (doi:10.1001/jama.2013.283194).
Reviews have become a strong force in the health care industry, said Peter Yelkovac, an online defamation attorney in Northern Indiana.
“Online reviews have really replaced the common ‘word of mouth’ that used to be the primary source for doctors referrals,” Mr. Yelkovac said in an interview. “Now, [patients] go online. Anyone can type anything they want, whether it’s truthful, untruthful, positive, indifferent, or negative.”
Doctor vs. website
In some cases, contacting a website administrator and requesting a review be removed can end the dilemma, said Michael J. Sacopulos, a medical malpractice defense attorney based in Terre Haute, Ind.
Rating sites generally have “terms of use,” and posts that violate the terms usually will be taken down by site administrators with some nudging, Mr. Sacopulos said in an interview. Other sites have “strike policies,” where a reviewee can request that one or two negative reviews be removed.
Still other sites are not as accommodating. Amazon, for instance, has immunity against content posted on the site, Mr. Sacopulos said. Under the Communications Decency Act, interactive computer services, such as a consumer review website, cannot be liable for content independently created or developed by third-party users. Such sites are hardly motivated to remove negative comments when racy posts can drive traffic to the site, he said.
Eric M. Joseph, MD, a facial plastic surgeon in West Orange, N.J., learned this lesson firsthand when he attempted to have a video removed from YouTube. A poster had uploaded copyright-protected before and after photos from Dr. Joseph’s practice onto YouTube and made disparaging comments about the patients in a video that went viral. Dr. Joseph and the patient both flagged the video for removal, but to no avail.
“It was impossible to [talk to] a human being at Google,” Dr, Joseph said. “It almost didn’t come down, and we were in conversations about suing Google. It took months and a cyberattorney who specializes in copyright infringement.”
The video finally was removed, but not before Dr. Joseph spent $6,000 in legal fees and experienced significant distress from the incident. Although most reviews about his practice are positive, he said, it’s difficult not to be affected by negative posts.
“From a psychological standpoint, it stings,” he said. “The burn of a negative review outweighs the sweetness of a positive review 100 times.”
Reputation companies to the rescue?
Like Dr. Hardwick-Smith, Dr. Joseph has utilized the online reputation management company eMerit to improve his online presence. The company gathers reviews from patients at the point of service and posts them to dominate review sites.
The solution to pollution is dilution, which means counterbalancing negative reviews with more representative reviews,” said Jeffrey Segal, MD, a neurosurgeon and attorney, and the founder of eMerit. “The next step is to deescalate conflict if you know who the patient is – to see if the patient problem can be resolved. Typically a patient is pleasantly surprised that you took the effort to call. Because the bar is so low, it’s very easy to exceed it.”
Physicians subscribe to eMerit on a month-to-month basis, paying $100-$600 a month, depending on the practice’s needs, Dr. Segal said. He touted a greater than 90% renewal rate, and said eMerit has captured and uploaded more than 150,000 patient reviews since its inception.
For the online reputation management company Reputation.com, health care providers have become one of the its most frequent clients, said Michael Fertik, company founder. Reputation.com solicits reviews from patients after appointments and ensures their visibility on top review sites. The platform also integrates reviews from general and health care review sites to help providers address patient feedback and receive alerts when negative reviews are posted. Rates start at $50 a month.
Mr. Fertik noted that more reviews not only overtake negative posts, but they make physicians easier to find by patients.
“If you have more than 10-15 reviews, you have a higher chance of getting a new patient because the search engine is going to favor doctors that have more reviews,” he said. “Doctors that have a small number of reviews don’t exist as far as search engines are concerned.”
However, all online reputation management firms are not equal, Mr. Sacopulos warned. Some are unfamiliar with the health care space, while others are unclear on health care privacy regulations. Mr. Sacopulos learned of a company that was sending patients texts to request reviews, which was likely a privacy violation and a violation of the Telecommunications Act, he said.
““Some [companies] are much more credible, and they understand health care law more than others,” he said. “Some have the technological capabilities to do things, but don’t understand the legal environment, so you need to be very careful [about whom] you pick.”
Time to sue?
Litigation is generally the last resort to fighting unfavorable online reviews. If a doctor believes a review is unfair or defamatory, and all other efforts have been exhausted, a lawyer may be able to help, Mr. Yelkovac said.
“When someone says, ‘I want to sue,’ that’s a possibility, but that’s typically far down the road,” he said. “Lawsuits are expensive. Lawsuits have an unknown outcome, and I would say, many times when you do sue for defamation, [the poster] may or may not have a lot of money, so you may end up spending a lot of money and you don’t recover anything from the patient.”
The majority of the lawsuits Mr. Yelkovac handles related to online reviews seek to unmask the poster with the aid of subpoenas and at times computer forensics, he said. From there, doctors can decide which action to take, such as contacting the poster and asking to have the comment removed.
“Sometimes it’s a surprise,” he said. “Sometimes it’s an ex-employee. Sometimes it’s a family member, or it could potentially be a competitor. Many times it’s not even a patient, and sometimes it’s a patient [who] the doctor never thought would post a review.”
Reviews and malpractice risk
Remember that not all unfavorable reviews are necessarily negative for physicians, said Brant Avondet, founder of Searchlight Enterprises, a malpractice risk prediction and online physician ratings research company.
A pattern of reviews that express the same concerns or frustrations by patients can be used to address and change internal policies and problems, such as multiple complaints about long wait times or a crowded parking lot, he said. Perhaps the front desk staff is repeatedly unfriendly to patients. Taking steps to correct these concerns could help in the long run, Mr. Avondet said.
Searchlight Enterprises recently presented study findings about a suggested link between online ratings and legal risk for physicians at a national medical insurance conference. Mr. Avondet and his colleagues evaluated claims data for 4,000 Florida physicians from the Florida Healthcare Practitioner Data Portal from 2000 to 2016 and studied online physician reviews from top rating sites. Doctors were grouped into three categories: surgical, ob.gyn., and “other” specialties. Findings showed the bottom 10% of surgeons studied (those with the worst online reviews) had 150% as many claims as the average for all surgeons. Surgeons in the top 20% (doctors with the best online reviews) had roughly half of the risk of a claim, compared with the average surgeon. Similar results were found for ob.gyns. and other specialties.
“Low and behold, there’s a huge correlation,” Mr. Avondet said. “There’s no shadow of a doubt that there’s something there that predicts your malpractice risk based on how nice or mean you are in the eyes of the patient.”
Mr. Avondet said he encourages physicians to use online reviews to make improvements, thus lowering their liability.
“Look at these reviews as a lens into your practice and things you might need to correct,” he said. “Use it as [insight] for how you can improve your practice and decrease the risk of getting sued.”
On Twitter @legal_med
Like most physicians, Dr. Susan Hardwick-Smith was used to receiving the occasional negative online review about her practice. But a biting post from several years ago was so wrenching that it nearly drove the Houston ob.gyn. out of medicine for good.
The patient blasted Dr. Hardwick-Smith on a popular review site about her care during a delivery and accused the doctor of attempting to force an unnecessary C-section. The account was inaccurate, but privacy laws prevented Dr. Hardwick-Smith from defending herself online or sharing details of the actual encounter, she said.
“She wrote this very detailed account of what a terrible doctor I was, and in my version of reality, I had saved her baby’s life,” said Dr. Hardwick-Smith. “I felt extremely powerless. I lost a lot of sleep over it, and I was considering giving up delivering babies. It was a real turning point for me.”
Rather than hanging up her white coat, Dr. Hardwick-Smith began working with an online reputation company – eMerit – that works to dilute negative reviews by soliciting a greater number of reviews from patients. The offensive post is now buried under hundreds of other reviews that are primarily positive, she said.
Hiring a reputation management company is one strategy for coping with negative online reviews. But cyberlaw experts stress that removing negative posts altogether is no easy feat. The best move to take often depends on the post, the patient, and the circumstance.
By now, it’s no secret that negative online reviews can significantly impact a medical practice, from influencing patient recruitment to affecting practice revenue to ruining a reputation. A 2015 survey of 2,354 consumers by search marketing firm BrightLocal found that 92% of consumers read online reviews – up from 67% in 2010 – and 40% of consumers had formed an opinion by reading just one to three reviews. Of 2,137 patients who viewed online reviews, 35% selected a physician based on positive reviews, while 37% avoided doctors with negative reviews, according to a 2014 study in JAMA (doi:10.1001/jama.2013.283194).
Reviews have become a strong force in the health care industry, said Peter Yelkovac, an online defamation attorney in Northern Indiana.
“Online reviews have really replaced the common ‘word of mouth’ that used to be the primary source for doctors referrals,” Mr. Yelkovac said in an interview. “Now, [patients] go online. Anyone can type anything they want, whether it’s truthful, untruthful, positive, indifferent, or negative.”
Doctor vs. website
In some cases, contacting a website administrator and requesting a review be removed can end the dilemma, said Michael J. Sacopulos, a medical malpractice defense attorney based in Terre Haute, Ind.
Rating sites generally have “terms of use,” and posts that violate the terms usually will be taken down by site administrators with some nudging, Mr. Sacopulos said in an interview. Other sites have “strike policies,” where a reviewee can request that one or two negative reviews be removed.
Still other sites are not as accommodating. Amazon, for instance, has immunity against content posted on the site, Mr. Sacopulos said. Under the Communications Decency Act, interactive computer services, such as a consumer review website, cannot be liable for content independently created or developed by third-party users. Such sites are hardly motivated to remove negative comments when racy posts can drive traffic to the site, he said.
Eric M. Joseph, MD, a facial plastic surgeon in West Orange, N.J., learned this lesson firsthand when he attempted to have a video removed from YouTube. A poster had uploaded copyright-protected before and after photos from Dr. Joseph’s practice onto YouTube and made disparaging comments about the patients in a video that went viral. Dr. Joseph and the patient both flagged the video for removal, but to no avail.
“It was impossible to [talk to] a human being at Google,” Dr, Joseph said. “It almost didn’t come down, and we were in conversations about suing Google. It took months and a cyberattorney who specializes in copyright infringement.”
The video finally was removed, but not before Dr. Joseph spent $6,000 in legal fees and experienced significant distress from the incident. Although most reviews about his practice are positive, he said, it’s difficult not to be affected by negative posts.
“From a psychological standpoint, it stings,” he said. “The burn of a negative review outweighs the sweetness of a positive review 100 times.”
Reputation companies to the rescue?
Like Dr. Hardwick-Smith, Dr. Joseph has utilized the online reputation management company eMerit to improve his online presence. The company gathers reviews from patients at the point of service and posts them to dominate review sites.
The solution to pollution is dilution, which means counterbalancing negative reviews with more representative reviews,” said Jeffrey Segal, MD, a neurosurgeon and attorney, and the founder of eMerit. “The next step is to deescalate conflict if you know who the patient is – to see if the patient problem can be resolved. Typically a patient is pleasantly surprised that you took the effort to call. Because the bar is so low, it’s very easy to exceed it.”
Physicians subscribe to eMerit on a month-to-month basis, paying $100-$600 a month, depending on the practice’s needs, Dr. Segal said. He touted a greater than 90% renewal rate, and said eMerit has captured and uploaded more than 150,000 patient reviews since its inception.
For the online reputation management company Reputation.com, health care providers have become one of the its most frequent clients, said Michael Fertik, company founder. Reputation.com solicits reviews from patients after appointments and ensures their visibility on top review sites. The platform also integrates reviews from general and health care review sites to help providers address patient feedback and receive alerts when negative reviews are posted. Rates start at $50 a month.
Mr. Fertik noted that more reviews not only overtake negative posts, but they make physicians easier to find by patients.
“If you have more than 10-15 reviews, you have a higher chance of getting a new patient because the search engine is going to favor doctors that have more reviews,” he said. “Doctors that have a small number of reviews don’t exist as far as search engines are concerned.”
However, all online reputation management firms are not equal, Mr. Sacopulos warned. Some are unfamiliar with the health care space, while others are unclear on health care privacy regulations. Mr. Sacopulos learned of a company that was sending patients texts to request reviews, which was likely a privacy violation and a violation of the Telecommunications Act, he said.
““Some [companies] are much more credible, and they understand health care law more than others,” he said. “Some have the technological capabilities to do things, but don’t understand the legal environment, so you need to be very careful [about whom] you pick.”
Time to sue?
Litigation is generally the last resort to fighting unfavorable online reviews. If a doctor believes a review is unfair or defamatory, and all other efforts have been exhausted, a lawyer may be able to help, Mr. Yelkovac said.
“When someone says, ‘I want to sue,’ that’s a possibility, but that’s typically far down the road,” he said. “Lawsuits are expensive. Lawsuits have an unknown outcome, and I would say, many times when you do sue for defamation, [the poster] may or may not have a lot of money, so you may end up spending a lot of money and you don’t recover anything from the patient.”
The majority of the lawsuits Mr. Yelkovac handles related to online reviews seek to unmask the poster with the aid of subpoenas and at times computer forensics, he said. From there, doctors can decide which action to take, such as contacting the poster and asking to have the comment removed.
“Sometimes it’s a surprise,” he said. “Sometimes it’s an ex-employee. Sometimes it’s a family member, or it could potentially be a competitor. Many times it’s not even a patient, and sometimes it’s a patient [who] the doctor never thought would post a review.”
Reviews and malpractice risk
Remember that not all unfavorable reviews are necessarily negative for physicians, said Brant Avondet, founder of Searchlight Enterprises, a malpractice risk prediction and online physician ratings research company.
A pattern of reviews that express the same concerns or frustrations by patients can be used to address and change internal policies and problems, such as multiple complaints about long wait times or a crowded parking lot, he said. Perhaps the front desk staff is repeatedly unfriendly to patients. Taking steps to correct these concerns could help in the long run, Mr. Avondet said.
Searchlight Enterprises recently presented study findings about a suggested link between online ratings and legal risk for physicians at a national medical insurance conference. Mr. Avondet and his colleagues evaluated claims data for 4,000 Florida physicians from the Florida Healthcare Practitioner Data Portal from 2000 to 2016 and studied online physician reviews from top rating sites. Doctors were grouped into three categories: surgical, ob.gyn., and “other” specialties. Findings showed the bottom 10% of surgeons studied (those with the worst online reviews) had 150% as many claims as the average for all surgeons. Surgeons in the top 20% (doctors with the best online reviews) had roughly half of the risk of a claim, compared with the average surgeon. Similar results were found for ob.gyns. and other specialties.
“Low and behold, there’s a huge correlation,” Mr. Avondet said. “There’s no shadow of a doubt that there’s something there that predicts your malpractice risk based on how nice or mean you are in the eyes of the patient.”
Mr. Avondet said he encourages physicians to use online reviews to make improvements, thus lowering their liability.
“Look at these reviews as a lens into your practice and things you might need to correct,” he said. “Use it as [insight] for how you can improve your practice and decrease the risk of getting sued.”
On Twitter @legal_med
No one-size-fits-all approach for reducing hospital readmissions
SAN DIEGO – Despite advances in the way surgeons practice their craft and measure outcomes in a meaningful way, the rate of hospital readmissions remains unacceptably high, according to an Emory University surgeon who has studied the readmission patterns.
“Readmission is a problem, not only from a cost and penalties standpoint but also from the rates of readmission affecting patients’ lives and expectations,” Jyotirmay Sharma, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Sharma, director of thyroid and endocrine surgery at Emory University Hospital, Atlanta, cited recent federal data estimating that among Medicare patients discharged from a hospital, 20% are rehospitalized within 30 days, and 34% are rehospitalized within 90 days. In 2013 alone, the Centers for Medicare & Medicaid Services levied readmission penalties against 2,213 hospitals to the tune of $280 million. “So clearly it’s a major issue,” he said.
In a study conducted by one of Dr. Sharma’s associates, researchers evaluated the risk factors for 30-day hospital readmission among general surgery patients treated at Emory University Hospital (J Am Coll Surg. 2012 Sep;215[3]:322-30). Pancreatectomy accounted for 18% of readmissions, followed by colectomy/colostomy (13%), small bowel resection (12%), and gastrectomy and ventral hernia repair (both 11%).
An unrelated analysis of a 498,875 operations found that lower extremity vascular bypass procedures accounted for 16% of readmissions, followed by colectomy or proctectomy (11%), bariatric surgery (5%), and ventral hernia repair (4%). In addition, the readmission rates were 6% among patients with no complications, 16% among those with one complications such as surgical site infections (SSIs), bleeding, and ileus, 37% among those with two or more complications, and 29% among those with three or more complications (JAMA 2015;313[3]:483-95). The most common complication overall was SSI (20%), followed by ileus (10%).
When the Emory study researchers drilled down on their data, they found that the following preexisting conditions were associated with readmissions among colectomy patients: steroid use, hypertension, readmission, cancer, COPD, smoking, poor functional status, and diabetes. At the same time, preexisting conditions associated with readmissions among vascular patients were diabetes and renal failure. The only preexisting condition associated with readmissions among thyroidectomy was renal failure. When the researchers evaluated the association between readmission risk and system-wide complications, they found that vascular surgery and urinary surgery conferred the highest risks (sixfold and fivefold, respectively).
“Just looking at your semiannual report quickly can give you a sense of which complications are associated with that readmission,” Dr. Sharma said. “There are many areas of potential intervention.” Preoperatively, he recommends screening surgery patients for obstructive sleep apnea, hypertension, and diabetes. “Looking at preexisting comorbid dyspnea, cancer, and renal failure can give you those target populations very quickly,” he said.
Intraoperatively, “it’s all about reduction of complications,” he said. These include using the WHO checklist, employing SSI prevention practices and considering certain anesthesia techniques such as low tidal volume ventilation and fluid limitation, control of hyperglycemia, and enhanced recovery after surgery protocols (ERAS).
Postoperative strategies to reduce readmission risk include ERAS for multimodal analgesia, fluid restriction, oral intake, and ambulation, and being aggressive about follow-up with high-risk populations and discharge planning. “The strategies for readmission reduction should be based on the preoperative assessment and the ability to identify high-risk populations,” Dr. Sharma said. “At Emory, we found that ileostomy patients had the highest risk of readmission. This made sense from a dehydration standpoint. So a colorectal surgeon led the creation of an Emory-wide protocol for teaching patients and their families, giving them signs of dehydration, what to look for, direct access to a dedicated nurse for follow-up, and an arrangement with the infusion center for rehydration as needed.”
He concluded by noting that there is no one-size-fits-all approach to reducing hospital readmissions. “I think an overarching readmission improvement process is not the way to go, unless you’re talking about a preoperative assessment area,” he said. “Identifying high-risk patients and giving them a lifeline where they can call so you can intervene and avoid that readmission, is better.”
Dr. Sharma reported having no relevant disclosures.
SAN DIEGO – Despite advances in the way surgeons practice their craft and measure outcomes in a meaningful way, the rate of hospital readmissions remains unacceptably high, according to an Emory University surgeon who has studied the readmission patterns.
“Readmission is a problem, not only from a cost and penalties standpoint but also from the rates of readmission affecting patients’ lives and expectations,” Jyotirmay Sharma, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Sharma, director of thyroid and endocrine surgery at Emory University Hospital, Atlanta, cited recent federal data estimating that among Medicare patients discharged from a hospital, 20% are rehospitalized within 30 days, and 34% are rehospitalized within 90 days. In 2013 alone, the Centers for Medicare & Medicaid Services levied readmission penalties against 2,213 hospitals to the tune of $280 million. “So clearly it’s a major issue,” he said.
In a study conducted by one of Dr. Sharma’s associates, researchers evaluated the risk factors for 30-day hospital readmission among general surgery patients treated at Emory University Hospital (J Am Coll Surg. 2012 Sep;215[3]:322-30). Pancreatectomy accounted for 18% of readmissions, followed by colectomy/colostomy (13%), small bowel resection (12%), and gastrectomy and ventral hernia repair (both 11%).
An unrelated analysis of a 498,875 operations found that lower extremity vascular bypass procedures accounted for 16% of readmissions, followed by colectomy or proctectomy (11%), bariatric surgery (5%), and ventral hernia repair (4%). In addition, the readmission rates were 6% among patients with no complications, 16% among those with one complications such as surgical site infections (SSIs), bleeding, and ileus, 37% among those with two or more complications, and 29% among those with three or more complications (JAMA 2015;313[3]:483-95). The most common complication overall was SSI (20%), followed by ileus (10%).
When the Emory study researchers drilled down on their data, they found that the following preexisting conditions were associated with readmissions among colectomy patients: steroid use, hypertension, readmission, cancer, COPD, smoking, poor functional status, and diabetes. At the same time, preexisting conditions associated with readmissions among vascular patients were diabetes and renal failure. The only preexisting condition associated with readmissions among thyroidectomy was renal failure. When the researchers evaluated the association between readmission risk and system-wide complications, they found that vascular surgery and urinary surgery conferred the highest risks (sixfold and fivefold, respectively).
“Just looking at your semiannual report quickly can give you a sense of which complications are associated with that readmission,” Dr. Sharma said. “There are many areas of potential intervention.” Preoperatively, he recommends screening surgery patients for obstructive sleep apnea, hypertension, and diabetes. “Looking at preexisting comorbid dyspnea, cancer, and renal failure can give you those target populations very quickly,” he said.
Intraoperatively, “it’s all about reduction of complications,” he said. These include using the WHO checklist, employing SSI prevention practices and considering certain anesthesia techniques such as low tidal volume ventilation and fluid limitation, control of hyperglycemia, and enhanced recovery after surgery protocols (ERAS).
Postoperative strategies to reduce readmission risk include ERAS for multimodal analgesia, fluid restriction, oral intake, and ambulation, and being aggressive about follow-up with high-risk populations and discharge planning. “The strategies for readmission reduction should be based on the preoperative assessment and the ability to identify high-risk populations,” Dr. Sharma said. “At Emory, we found that ileostomy patients had the highest risk of readmission. This made sense from a dehydration standpoint. So a colorectal surgeon led the creation of an Emory-wide protocol for teaching patients and their families, giving them signs of dehydration, what to look for, direct access to a dedicated nurse for follow-up, and an arrangement with the infusion center for rehydration as needed.”
He concluded by noting that there is no one-size-fits-all approach to reducing hospital readmissions. “I think an overarching readmission improvement process is not the way to go, unless you’re talking about a preoperative assessment area,” he said. “Identifying high-risk patients and giving them a lifeline where they can call so you can intervene and avoid that readmission, is better.”
Dr. Sharma reported having no relevant disclosures.
SAN DIEGO – Despite advances in the way surgeons practice their craft and measure outcomes in a meaningful way, the rate of hospital readmissions remains unacceptably high, according to an Emory University surgeon who has studied the readmission patterns.
“Readmission is a problem, not only from a cost and penalties standpoint but also from the rates of readmission affecting patients’ lives and expectations,” Jyotirmay Sharma, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference.
Dr. Sharma, director of thyroid and endocrine surgery at Emory University Hospital, Atlanta, cited recent federal data estimating that among Medicare patients discharged from a hospital, 20% are rehospitalized within 30 days, and 34% are rehospitalized within 90 days. In 2013 alone, the Centers for Medicare & Medicaid Services levied readmission penalties against 2,213 hospitals to the tune of $280 million. “So clearly it’s a major issue,” he said.
In a study conducted by one of Dr. Sharma’s associates, researchers evaluated the risk factors for 30-day hospital readmission among general surgery patients treated at Emory University Hospital (J Am Coll Surg. 2012 Sep;215[3]:322-30). Pancreatectomy accounted for 18% of readmissions, followed by colectomy/colostomy (13%), small bowel resection (12%), and gastrectomy and ventral hernia repair (both 11%).
An unrelated analysis of a 498,875 operations found that lower extremity vascular bypass procedures accounted for 16% of readmissions, followed by colectomy or proctectomy (11%), bariatric surgery (5%), and ventral hernia repair (4%). In addition, the readmission rates were 6% among patients with no complications, 16% among those with one complications such as surgical site infections (SSIs), bleeding, and ileus, 37% among those with two or more complications, and 29% among those with three or more complications (JAMA 2015;313[3]:483-95). The most common complication overall was SSI (20%), followed by ileus (10%).
When the Emory study researchers drilled down on their data, they found that the following preexisting conditions were associated with readmissions among colectomy patients: steroid use, hypertension, readmission, cancer, COPD, smoking, poor functional status, and diabetes. At the same time, preexisting conditions associated with readmissions among vascular patients were diabetes and renal failure. The only preexisting condition associated with readmissions among thyroidectomy was renal failure. When the researchers evaluated the association between readmission risk and system-wide complications, they found that vascular surgery and urinary surgery conferred the highest risks (sixfold and fivefold, respectively).
“Just looking at your semiannual report quickly can give you a sense of which complications are associated with that readmission,” Dr. Sharma said. “There are many areas of potential intervention.” Preoperatively, he recommends screening surgery patients for obstructive sleep apnea, hypertension, and diabetes. “Looking at preexisting comorbid dyspnea, cancer, and renal failure can give you those target populations very quickly,” he said.
Intraoperatively, “it’s all about reduction of complications,” he said. These include using the WHO checklist, employing SSI prevention practices and considering certain anesthesia techniques such as low tidal volume ventilation and fluid limitation, control of hyperglycemia, and enhanced recovery after surgery protocols (ERAS).
Postoperative strategies to reduce readmission risk include ERAS for multimodal analgesia, fluid restriction, oral intake, and ambulation, and being aggressive about follow-up with high-risk populations and discharge planning. “The strategies for readmission reduction should be based on the preoperative assessment and the ability to identify high-risk populations,” Dr. Sharma said. “At Emory, we found that ileostomy patients had the highest risk of readmission. This made sense from a dehydration standpoint. So a colorectal surgeon led the creation of an Emory-wide protocol for teaching patients and their families, giving them signs of dehydration, what to look for, direct access to a dedicated nurse for follow-up, and an arrangement with the infusion center for rehydration as needed.”
He concluded by noting that there is no one-size-fits-all approach to reducing hospital readmissions. “I think an overarching readmission improvement process is not the way to go, unless you’re talking about a preoperative assessment area,” he said. “Identifying high-risk patients and giving them a lifeline where they can call so you can intervene and avoid that readmission, is better.”
Dr. Sharma reported having no relevant disclosures.
EXPERT ANALYSIS AT THE ACS NSQIP NATIONAL CONFERENCE
FDA updates warning label for systemic fluoroquinolones
The Food and Drug Administration has amended the boxed warning on labels for fluoroquinolone antibiotics, taken either orally or by injection, to reflect recent findings of the drugs’ alarming potential adverse events.
“These medicines are associated with disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient,” the FDA stated in its Safety Announcement.
As a result, health care providers should reserve systemic fluoroquinolones for patients who have no other treatment options for any of the following conditions: acute bacterial sinusitis (ABS), acute bacterial exacerbation of chronic bronchitis (ABECB), and uncomplicated urinary tract infections (UTIs). The FDA also said that, for some serious bacterial infections, the benefits of fluoroquinolones outweigh the risks, and it is appropriate for them to remain available as a therapeutic option.
Patients taking fluoroquinolones must also be vigilant and let their provider know immediately if they begin suffering from any new pain in their joints, tendons, or muscles. Additionally, if patients begin feeling any numbness in their arms and legs, a prickling or “pins and needles” sensation, or confusion and hallucinations, they should contact their health care provider right away so that they may be switched onto a nonfluoroquinolone antibacterial drug for the remainder of their treatment regimen.
Avelox; Cipro, both standard and extended release; Factive; Levaquin; and ofloxacin are the fluoroquinolones currently approved by the FDA for systemic use. Their active ingredients are moxifloxacin, ciprofloxacin, gemifloxacin, levofloxacin, and ofloxacin, respectively.
Additional side effects for patients taking fluoroquinolones could include tendinitis, tendon rupture, and joint swelling. Central nervous system afflictions could include depression and thoughts of suicide. Fluoroquinolones could also bring about skin rashes, sunburn, arrhythmia, diarrhea, as well as aggravate myasthenia gravis in patients who suffer from it. Warnings regarding these conditions are already included on the drugs’ existing boxed warning.
“In addition to updating information in the Boxed Warning, we are also including information about these safety issues in the Warnings and Precautions section of the label,” the FDA stated. “The Indications and Usage section contains new limitation-of-use statements to reserve fluoroquinolones for patients who do not have other available treatment options for ABS, ABECB, and uncomplicated UTIs.”
The FDA also added that it will continue to monitor and assess safety issues associated with fluoroquinolones and will issue any further updates if necessary.
The Food and Drug Administration has amended the boxed warning on labels for fluoroquinolone antibiotics, taken either orally or by injection, to reflect recent findings of the drugs’ alarming potential adverse events.
“These medicines are associated with disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient,” the FDA stated in its Safety Announcement.
As a result, health care providers should reserve systemic fluoroquinolones for patients who have no other treatment options for any of the following conditions: acute bacterial sinusitis (ABS), acute bacterial exacerbation of chronic bronchitis (ABECB), and uncomplicated urinary tract infections (UTIs). The FDA also said that, for some serious bacterial infections, the benefits of fluoroquinolones outweigh the risks, and it is appropriate for them to remain available as a therapeutic option.
Patients taking fluoroquinolones must also be vigilant and let their provider know immediately if they begin suffering from any new pain in their joints, tendons, or muscles. Additionally, if patients begin feeling any numbness in their arms and legs, a prickling or “pins and needles” sensation, or confusion and hallucinations, they should contact their health care provider right away so that they may be switched onto a nonfluoroquinolone antibacterial drug for the remainder of their treatment regimen.
Avelox; Cipro, both standard and extended release; Factive; Levaquin; and ofloxacin are the fluoroquinolones currently approved by the FDA for systemic use. Their active ingredients are moxifloxacin, ciprofloxacin, gemifloxacin, levofloxacin, and ofloxacin, respectively.
Additional side effects for patients taking fluoroquinolones could include tendinitis, tendon rupture, and joint swelling. Central nervous system afflictions could include depression and thoughts of suicide. Fluoroquinolones could also bring about skin rashes, sunburn, arrhythmia, diarrhea, as well as aggravate myasthenia gravis in patients who suffer from it. Warnings regarding these conditions are already included on the drugs’ existing boxed warning.
“In addition to updating information in the Boxed Warning, we are also including information about these safety issues in the Warnings and Precautions section of the label,” the FDA stated. “The Indications and Usage section contains new limitation-of-use statements to reserve fluoroquinolones for patients who do not have other available treatment options for ABS, ABECB, and uncomplicated UTIs.”
The FDA also added that it will continue to monitor and assess safety issues associated with fluoroquinolones and will issue any further updates if necessary.
The Food and Drug Administration has amended the boxed warning on labels for fluoroquinolone antibiotics, taken either orally or by injection, to reflect recent findings of the drugs’ alarming potential adverse events.
“These medicines are associated with disabling and potentially permanent side effects of the tendons, muscles, joints, nerves, and central nervous system that can occur together in the same patient,” the FDA stated in its Safety Announcement.
As a result, health care providers should reserve systemic fluoroquinolones for patients who have no other treatment options for any of the following conditions: acute bacterial sinusitis (ABS), acute bacterial exacerbation of chronic bronchitis (ABECB), and uncomplicated urinary tract infections (UTIs). The FDA also said that, for some serious bacterial infections, the benefits of fluoroquinolones outweigh the risks, and it is appropriate for them to remain available as a therapeutic option.
Patients taking fluoroquinolones must also be vigilant and let their provider know immediately if they begin suffering from any new pain in their joints, tendons, or muscles. Additionally, if patients begin feeling any numbness in their arms and legs, a prickling or “pins and needles” sensation, or confusion and hallucinations, they should contact their health care provider right away so that they may be switched onto a nonfluoroquinolone antibacterial drug for the remainder of their treatment regimen.
Avelox; Cipro, both standard and extended release; Factive; Levaquin; and ofloxacin are the fluoroquinolones currently approved by the FDA for systemic use. Their active ingredients are moxifloxacin, ciprofloxacin, gemifloxacin, levofloxacin, and ofloxacin, respectively.
Additional side effects for patients taking fluoroquinolones could include tendinitis, tendon rupture, and joint swelling. Central nervous system afflictions could include depression and thoughts of suicide. Fluoroquinolones could also bring about skin rashes, sunburn, arrhythmia, diarrhea, as well as aggravate myasthenia gravis in patients who suffer from it. Warnings regarding these conditions are already included on the drugs’ existing boxed warning.
“In addition to updating information in the Boxed Warning, we are also including information about these safety issues in the Warnings and Precautions section of the label,” the FDA stated. “The Indications and Usage section contains new limitation-of-use statements to reserve fluoroquinolones for patients who do not have other available treatment options for ABS, ABECB, and uncomplicated UTIs.”
The FDA also added that it will continue to monitor and assess safety issues associated with fluoroquinolones and will issue any further updates if necessary.
VIDEO: Medicare pays billions for potentially avoidable hospital admissions in dementia patients
TORONTO – In 2013, Medicare spent $2.6 billion on potentially avoidable hospitalizations for patients with Alzheimer’s disease and other dementias.
About half of these hospital visits – each of which cost Medicare around $7,000 – were for conditions that could have been effectively managed in primary care settings, Pei-Jung Lin, PhD, said at the Alzheimer’s Association International Conference 2016.
Half of the admissions were for chronic illnesses such as diabetes, hypertension, and asthma that are often poorly controlled as dementia progresses. The other half was for acute illnesses, said Dr. Lin, director of the Center for the Evaluation of Value and Risk in Health at Tufts University, Boston. But these admissions for acute conditions involved problems that could be treated on an outpatient basis if they’d been caught early – urinary tract infections, pneumonias, and dehydration.
“In 2013, 1 in 10 Alzheimer’s disease patients had at least one potentially avoidable hospitalization, and 1 in 7 hospital admissions among these patients (14%) was for a potentially avoidable condition,” she said during a press briefing.
Although the financial finding is striking, it isn’t the whole story, Dr. Lin said. Hospitalizations put patients at increased risk for infections, confusion, and delirium – any of which can initiate a downward clinical spiral that results in more intervention, more stress, and more cost.
“Not only are these incidences expensive, they can be dangerous for our patients. Being in the hospital is stressful for someone with little grasp of reality. Patients can become even more confused and disoriented. They’re at risk for hospital-acquired infections, which increase costs and caregiver stress, and decrease patient quality of life,” she said.
Dr. Lin and her team looked for potentially avoidable hospitalizations filed in 2013 among 2.75 million patients with Alzheimer’s and other dementias. The acute conditions included in the analysis were bacterial pneumonia, urinary tract infection, and dehydration, and chronic conditions were diabetes, cardiovascular diseases, and respiratory conditions.
About half these admissions (188,870; 47%) were for acute conditions, while the rest were for chronic conditions. About half of all the admissions also occurred in patients with late-stage disease, and these were the most expensive ones. Admissions for these late-stage patients accounted for 59% of the expenditures and cost Medicare $1.53 billion in 2013.
Claims data don’t offer the kind of details that allow a case-by-case review of how the admissions could have been prevented. But one message comes through loud and clear, Dr. Lin said.
“Comorbidity management is simply not optimal among many of our patients with Alzheimer’s disease. Many of these admissions, and much of this cost, could have been prevented with better ambulatory care and early, effective treatment.”
Dr. Richard Caselli, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., commented on these issues in a video interview.
Dr. Lin had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
TORONTO – In 2013, Medicare spent $2.6 billion on potentially avoidable hospitalizations for patients with Alzheimer’s disease and other dementias.
About half of these hospital visits – each of which cost Medicare around $7,000 – were for conditions that could have been effectively managed in primary care settings, Pei-Jung Lin, PhD, said at the Alzheimer’s Association International Conference 2016.
Half of the admissions were for chronic illnesses such as diabetes, hypertension, and asthma that are often poorly controlled as dementia progresses. The other half was for acute illnesses, said Dr. Lin, director of the Center for the Evaluation of Value and Risk in Health at Tufts University, Boston. But these admissions for acute conditions involved problems that could be treated on an outpatient basis if they’d been caught early – urinary tract infections, pneumonias, and dehydration.
“In 2013, 1 in 10 Alzheimer’s disease patients had at least one potentially avoidable hospitalization, and 1 in 7 hospital admissions among these patients (14%) was for a potentially avoidable condition,” she said during a press briefing.
Although the financial finding is striking, it isn’t the whole story, Dr. Lin said. Hospitalizations put patients at increased risk for infections, confusion, and delirium – any of which can initiate a downward clinical spiral that results in more intervention, more stress, and more cost.
“Not only are these incidences expensive, they can be dangerous for our patients. Being in the hospital is stressful for someone with little grasp of reality. Patients can become even more confused and disoriented. They’re at risk for hospital-acquired infections, which increase costs and caregiver stress, and decrease patient quality of life,” she said.
Dr. Lin and her team looked for potentially avoidable hospitalizations filed in 2013 among 2.75 million patients with Alzheimer’s and other dementias. The acute conditions included in the analysis were bacterial pneumonia, urinary tract infection, and dehydration, and chronic conditions were diabetes, cardiovascular diseases, and respiratory conditions.
About half these admissions (188,870; 47%) were for acute conditions, while the rest were for chronic conditions. About half of all the admissions also occurred in patients with late-stage disease, and these were the most expensive ones. Admissions for these late-stage patients accounted for 59% of the expenditures and cost Medicare $1.53 billion in 2013.
Claims data don’t offer the kind of details that allow a case-by-case review of how the admissions could have been prevented. But one message comes through loud and clear, Dr. Lin said.
“Comorbidity management is simply not optimal among many of our patients with Alzheimer’s disease. Many of these admissions, and much of this cost, could have been prevented with better ambulatory care and early, effective treatment.”
Dr. Richard Caselli, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., commented on these issues in a video interview.
Dr. Lin had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
TORONTO – In 2013, Medicare spent $2.6 billion on potentially avoidable hospitalizations for patients with Alzheimer’s disease and other dementias.
About half of these hospital visits – each of which cost Medicare around $7,000 – were for conditions that could have been effectively managed in primary care settings, Pei-Jung Lin, PhD, said at the Alzheimer’s Association International Conference 2016.
Half of the admissions were for chronic illnesses such as diabetes, hypertension, and asthma that are often poorly controlled as dementia progresses. The other half was for acute illnesses, said Dr. Lin, director of the Center for the Evaluation of Value and Risk in Health at Tufts University, Boston. But these admissions for acute conditions involved problems that could be treated on an outpatient basis if they’d been caught early – urinary tract infections, pneumonias, and dehydration.
“In 2013, 1 in 10 Alzheimer’s disease patients had at least one potentially avoidable hospitalization, and 1 in 7 hospital admissions among these patients (14%) was for a potentially avoidable condition,” she said during a press briefing.
Although the financial finding is striking, it isn’t the whole story, Dr. Lin said. Hospitalizations put patients at increased risk for infections, confusion, and delirium – any of which can initiate a downward clinical spiral that results in more intervention, more stress, and more cost.
“Not only are these incidences expensive, they can be dangerous for our patients. Being in the hospital is stressful for someone with little grasp of reality. Patients can become even more confused and disoriented. They’re at risk for hospital-acquired infections, which increase costs and caregiver stress, and decrease patient quality of life,” she said.
Dr. Lin and her team looked for potentially avoidable hospitalizations filed in 2013 among 2.75 million patients with Alzheimer’s and other dementias. The acute conditions included in the analysis were bacterial pneumonia, urinary tract infection, and dehydration, and chronic conditions were diabetes, cardiovascular diseases, and respiratory conditions.
About half these admissions (188,870; 47%) were for acute conditions, while the rest were for chronic conditions. About half of all the admissions also occurred in patients with late-stage disease, and these were the most expensive ones. Admissions for these late-stage patients accounted for 59% of the expenditures and cost Medicare $1.53 billion in 2013.
Claims data don’t offer the kind of details that allow a case-by-case review of how the admissions could have been prevented. But one message comes through loud and clear, Dr. Lin said.
“Comorbidity management is simply not optimal among many of our patients with Alzheimer’s disease. Many of these admissions, and much of this cost, could have been prevented with better ambulatory care and early, effective treatment.”
Dr. Richard Caselli, professor of neurology at the Mayo Clinic, Scottsdale, Ariz., commented on these issues in a video interview.
Dr. Lin had no financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @alz_gal
AT AAIC 2016
Key clinical point: Billions are being spent on potentially avoidable hospitalizations for people with Alzheimer’s disease and other dementias.
Major finding: In 2013, Medicare spent $2.6 billion on possibly avoidable hospitalizations for acute and chronic illnesses that could have been prevented with better primary care.
Data source: The study included 2013 Medicare claims data on 2.75 million patients with Alzheimer’s and other dementias.
Disclosures: Dr. Lin had no financial disclosures.