User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Children and COVID: New cases fell as the old year ended
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
The end of 2022 saw a drop in new COVID-19 cases in children, even as rates of emergency department visits continued upward trends that began in late October.
New cases for the week of Dec. 23-29 fell for the first time since late November, according to the American Academy of Pediatrics and the Children’s Hospital Association.
The AAP/CHA analysis of publicly available state data differs somewhat from figures reported by the Centers for Disease Control and Prevention, which has new cases for the latest available week, Dec.18-24, at just over 27,000 after 3 straight weeks of declines from a count of almost 63,000 for the week ending Nov. 26. The CDC, however, updates previously reported data on a regular basis, so that 27,000 is likely to increase in the coming weeks.
The CDC line on the graph also shows a peak for the week of Oct. 30 to Nov. 5 when new cases reached almost 50,000, compared with almost 30,000 reported for the week of Oct. 28 to Nov. 3 by the AAP and CHA in their report of state-level data. The AAP and CHA put the total number of child COVID cases since the start of the pandemic at 15.2 million as of Dec. 29, while the CDC reports 16.2 million cases as of Dec. 28.
There have been 1,975 deaths from COVID-19 in children aged 0-17 years, according to the CDC, which amounts to just over 0.2% of all COVID deaths for which age group data were available.
CDC data on emergency department visits involving diagnosed COVID-19 have been rising since late October. In children aged 0-11 years, for example, COVID was involved in 1.0% of ED visits (7-day average) as late as Nov. 4, but by Dec. 27 that rate was 2.6%. Children aged 12-15 years went from 0.6% on Oct. 28 to 1.5% on Dec. 27, while 16- to 17-year-olds had ED visit rates of 0.6% on Oct. 19 and 1.7% on Dec. 27, the CDC said on its COVID Data Tracker.
New hospital admissions with diagnosed COVID, which had been following the same upward trend as ED visits since late October, halted that rise in children aged 0-17 years and have gone no higher than 0.29 per 100,000 population since Dec. 9, the CDC data show.
STEMI times to treatment usually miss established goals
Therapy initiated within national treatment-time goals set a decade ago for patients with ST-segment elevation myocardial infarction (STEMI) remains associated with improved survival in recent years. But for many such patients, time from first symptoms to initiation of reperfusion therapy still fails to meet those goals, suggests a cross-sectional registry analysis.
For example, patients initially transported to centers with percutaneous coronary intervention (PCI) capability had a median treatment time of 148 minutes, in the analysis spanning the second quarter (Q2) of 2018 to the third quarter (Q3) of 2021. But the goal for centers called for treatment initiation within 90 minutes for at least 75% of such STEMI patients.
Moreover, overall STEMI treatment times and in-hospital mortality rose in tandem significantly from Q2 2018 through the first quarter (Q1) of 2021, which included the first year of the COVID-19 pandemic. Median time to treatment went from 86 minutes to 91 minutes during that period. Meanwhile, in-hospital mortality went from 5.6% to 8.7%, report the study authors led by James G. Jollis, MD, Duke University, Durham, N.C.
Their report, based on 114,871 STEMI patients at 601 US hospitals contributing to the Get With The Guidelines – Coronary Artery Disease registry, was published online in JAMA.
Of those patients, 25,085 had been transferred from non-PCI hospitals, 32,483 were walk-ins, and 57,303 arrived via emergency medical services (EMS). Their median times from symptom onset to PCI were 240, 195, and 148 minutes, respectively.
In-hospital mortality was significantly reduced in an adjusted analysis for patients treated within target times, compared with those whose treatment missed the time goals, regardless of whether they were transported by EMS, walked into a hospital with on-site PCI, or were transferred from a non-PCI center (Table 1).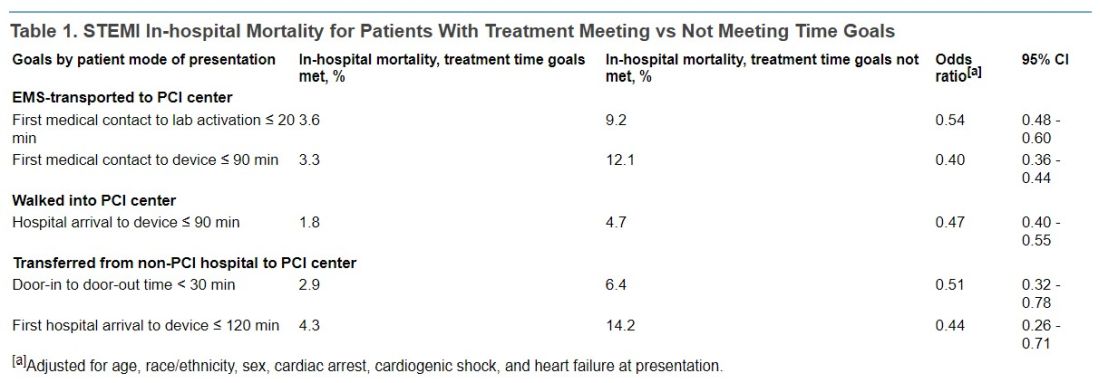
Regardless of mode of patient presentation, treatment time goals were not met most of the time, the group reports. Patients who required interhospital transfer experienced the longest system delays; only 17% were treated within 120 minutes.
Among patients who received primary PCI, 20% had a registry-defined hospital-specified reason for delay, including cardiac arrest and/or need for intubation in 6.8%, “difficulty crossing the culprit lesion” in 3.8%, and “other reasons” in 5.8%, the group reports.
“In 2020, a new reason for delay was added to the registry, ‘need for additional personal protective equipment for suspected/confirmed infectious disease.’ This reason was most commonly used in the second quarter of 2020 (6%) and then declined over time to 1% in the final 2 quarters,” they write.
“Thus, active SARS-CoV-2 infection appeared to have a smaller direct role in longer treatment times or worse outcomes.” Rather, they continue, “the pandemic potentially had a significant indirect role as hospitals were overwhelmed with patients, EMS and hospitals were challenged in maintaining paramedic and nurse staffing and intensive care bed availability, and patients experienced delayed care due to barriers to access or perceived fear of becoming entangled in an overwhelmed medical system.”
Still an important quality metric
STEMI treatment times remain an important quality metric to which hospitals should continue to pay attention because shorter times improve patient care, Deepak Bhatt, MD, MPH, told this news organization.
“Having said that, as with all metrics, one needs to be thoughtful and realize that a difference of a couple of minutes is probably not a crucial thing,” said Dr. Bhatt, Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved with the current study.
Interhospital transfers indeed involve longer delays, he observed, suggesting that regional integrated health systems should develop methods for optimizing STEMI care – even, for example, if they involve bypassing non-PCI centers or stopping patients briefly for stabilization followed by rapid transport to a PCI-capable facility.
“That, of course, requires cooperation among hospitals. Sometimes that requires hospitals putting aside economic considerations and just focusing on doing the right thing for that individual patient,” Dr. Bhatt said.
Transfer delays are common for patients presenting with STEMI at hospitals without PCI capability, he noted. “Having clear protocols in place that expedite that type of transfer, I think, could go a long way in reducing the time to treatment in patients that are presenting to the hospital without cath labs. That’s an important message that these data provide.”
The onset of COVID-19 led to widespread delays in STEMI time to treatment early in the pandemic. There were concerns about exposing cath lab personnel to SARS-CoV-2 and potential adverse consequences of sick personnel being unable to provide patient care in the subsequent weeks and months, Dr. Bhatt observed.
However, “All of that seems to have quieted down, and I don’t think COVID is impacting time to treatment right now.”
‘Suboptimal compliance’ with standards
The current findings of “suboptimal compliance with national targets underscore why reassessing quality metrics, in light of changing practice patterns and other secular trends, is critical,” write Andrew S. Oseran, MD, MBA, and Robert W. Yeh, MD, both of Harvard Medical School, in an accompanying editorial.
“While the importance of coordinated and expeditious care for this high-risk patient population is undeniable, the specific actions that hospitals can – or should – take to further improve overall STEMI outcomes are less clear,” they say.
“As physicians contemplate the optimal path forward in managing the care of STEMI patients, they must recognize the clinical and operational nuance that exists in caring for this diverse population and acknowledge the trade-offs associated with uniform quality metrics,” write the editorialists.
“Global reductions in time to treatment for STEMI patients has been one of health care’s great success stories. As we move forward, it may be time to consider whether efforts to achieve additional improvement in target treatment times will result in substantive benefits, or whether we have reached the point of diminishing returns.”
A version of this article first appeared on Medscape.com.
Therapy initiated within national treatment-time goals set a decade ago for patients with ST-segment elevation myocardial infarction (STEMI) remains associated with improved survival in recent years. But for many such patients, time from first symptoms to initiation of reperfusion therapy still fails to meet those goals, suggests a cross-sectional registry analysis.
For example, patients initially transported to centers with percutaneous coronary intervention (PCI) capability had a median treatment time of 148 minutes, in the analysis spanning the second quarter (Q2) of 2018 to the third quarter (Q3) of 2021. But the goal for centers called for treatment initiation within 90 minutes for at least 75% of such STEMI patients.
Moreover, overall STEMI treatment times and in-hospital mortality rose in tandem significantly from Q2 2018 through the first quarter (Q1) of 2021, which included the first year of the COVID-19 pandemic. Median time to treatment went from 86 minutes to 91 minutes during that period. Meanwhile, in-hospital mortality went from 5.6% to 8.7%, report the study authors led by James G. Jollis, MD, Duke University, Durham, N.C.
Their report, based on 114,871 STEMI patients at 601 US hospitals contributing to the Get With The Guidelines – Coronary Artery Disease registry, was published online in JAMA.
Of those patients, 25,085 had been transferred from non-PCI hospitals, 32,483 were walk-ins, and 57,303 arrived via emergency medical services (EMS). Their median times from symptom onset to PCI were 240, 195, and 148 minutes, respectively.
In-hospital mortality was significantly reduced in an adjusted analysis for patients treated within target times, compared with those whose treatment missed the time goals, regardless of whether they were transported by EMS, walked into a hospital with on-site PCI, or were transferred from a non-PCI center (Table 1).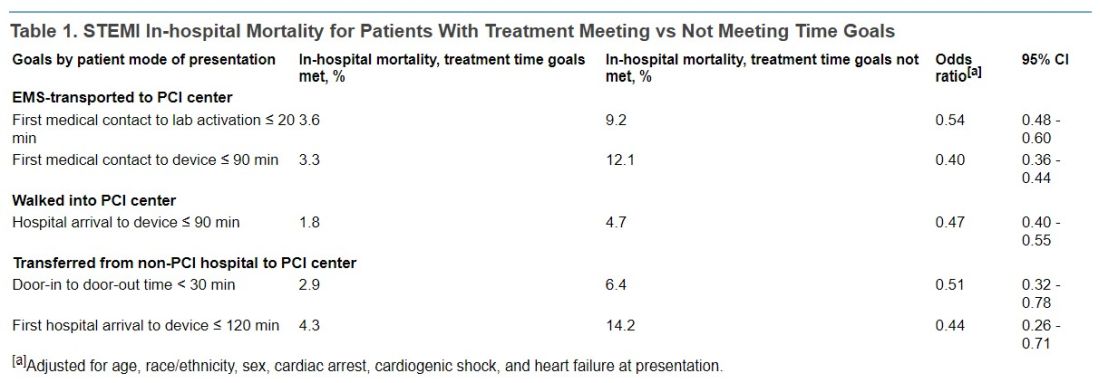
Regardless of mode of patient presentation, treatment time goals were not met most of the time, the group reports. Patients who required interhospital transfer experienced the longest system delays; only 17% were treated within 120 minutes.
Among patients who received primary PCI, 20% had a registry-defined hospital-specified reason for delay, including cardiac arrest and/or need for intubation in 6.8%, “difficulty crossing the culprit lesion” in 3.8%, and “other reasons” in 5.8%, the group reports.
“In 2020, a new reason for delay was added to the registry, ‘need for additional personal protective equipment for suspected/confirmed infectious disease.’ This reason was most commonly used in the second quarter of 2020 (6%) and then declined over time to 1% in the final 2 quarters,” they write.
“Thus, active SARS-CoV-2 infection appeared to have a smaller direct role in longer treatment times or worse outcomes.” Rather, they continue, “the pandemic potentially had a significant indirect role as hospitals were overwhelmed with patients, EMS and hospitals were challenged in maintaining paramedic and nurse staffing and intensive care bed availability, and patients experienced delayed care due to barriers to access or perceived fear of becoming entangled in an overwhelmed medical system.”
Still an important quality metric
STEMI treatment times remain an important quality metric to which hospitals should continue to pay attention because shorter times improve patient care, Deepak Bhatt, MD, MPH, told this news organization.
“Having said that, as with all metrics, one needs to be thoughtful and realize that a difference of a couple of minutes is probably not a crucial thing,” said Dr. Bhatt, Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved with the current study.
Interhospital transfers indeed involve longer delays, he observed, suggesting that regional integrated health systems should develop methods for optimizing STEMI care – even, for example, if they involve bypassing non-PCI centers or stopping patients briefly for stabilization followed by rapid transport to a PCI-capable facility.
“That, of course, requires cooperation among hospitals. Sometimes that requires hospitals putting aside economic considerations and just focusing on doing the right thing for that individual patient,” Dr. Bhatt said.
Transfer delays are common for patients presenting with STEMI at hospitals without PCI capability, he noted. “Having clear protocols in place that expedite that type of transfer, I think, could go a long way in reducing the time to treatment in patients that are presenting to the hospital without cath labs. That’s an important message that these data provide.”
The onset of COVID-19 led to widespread delays in STEMI time to treatment early in the pandemic. There were concerns about exposing cath lab personnel to SARS-CoV-2 and potential adverse consequences of sick personnel being unable to provide patient care in the subsequent weeks and months, Dr. Bhatt observed.
However, “All of that seems to have quieted down, and I don’t think COVID is impacting time to treatment right now.”
‘Suboptimal compliance’ with standards
The current findings of “suboptimal compliance with national targets underscore why reassessing quality metrics, in light of changing practice patterns and other secular trends, is critical,” write Andrew S. Oseran, MD, MBA, and Robert W. Yeh, MD, both of Harvard Medical School, in an accompanying editorial.
“While the importance of coordinated and expeditious care for this high-risk patient population is undeniable, the specific actions that hospitals can – or should – take to further improve overall STEMI outcomes are less clear,” they say.
“As physicians contemplate the optimal path forward in managing the care of STEMI patients, they must recognize the clinical and operational nuance that exists in caring for this diverse population and acknowledge the trade-offs associated with uniform quality metrics,” write the editorialists.
“Global reductions in time to treatment for STEMI patients has been one of health care’s great success stories. As we move forward, it may be time to consider whether efforts to achieve additional improvement in target treatment times will result in substantive benefits, or whether we have reached the point of diminishing returns.”
A version of this article first appeared on Medscape.com.
Therapy initiated within national treatment-time goals set a decade ago for patients with ST-segment elevation myocardial infarction (STEMI) remains associated with improved survival in recent years. But for many such patients, time from first symptoms to initiation of reperfusion therapy still fails to meet those goals, suggests a cross-sectional registry analysis.
For example, patients initially transported to centers with percutaneous coronary intervention (PCI) capability had a median treatment time of 148 minutes, in the analysis spanning the second quarter (Q2) of 2018 to the third quarter (Q3) of 2021. But the goal for centers called for treatment initiation within 90 minutes for at least 75% of such STEMI patients.
Moreover, overall STEMI treatment times and in-hospital mortality rose in tandem significantly from Q2 2018 through the first quarter (Q1) of 2021, which included the first year of the COVID-19 pandemic. Median time to treatment went from 86 minutes to 91 minutes during that period. Meanwhile, in-hospital mortality went from 5.6% to 8.7%, report the study authors led by James G. Jollis, MD, Duke University, Durham, N.C.
Their report, based on 114,871 STEMI patients at 601 US hospitals contributing to the Get With The Guidelines – Coronary Artery Disease registry, was published online in JAMA.
Of those patients, 25,085 had been transferred from non-PCI hospitals, 32,483 were walk-ins, and 57,303 arrived via emergency medical services (EMS). Their median times from symptom onset to PCI were 240, 195, and 148 minutes, respectively.
In-hospital mortality was significantly reduced in an adjusted analysis for patients treated within target times, compared with those whose treatment missed the time goals, regardless of whether they were transported by EMS, walked into a hospital with on-site PCI, or were transferred from a non-PCI center (Table 1).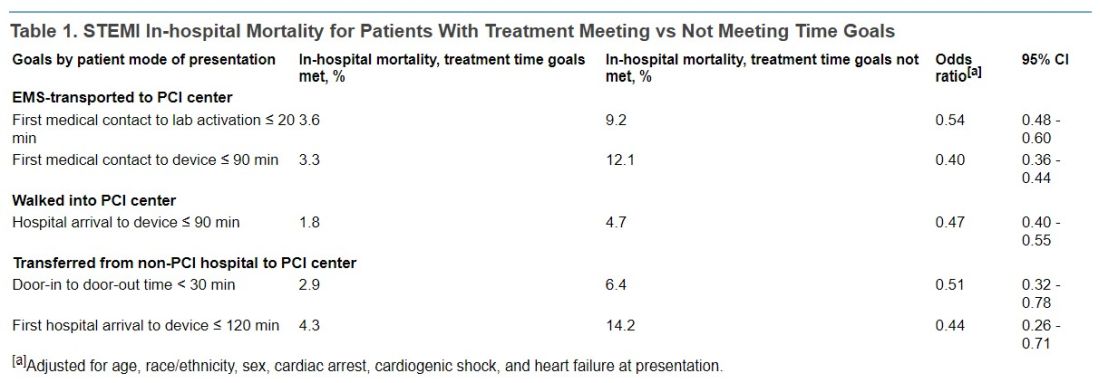
Regardless of mode of patient presentation, treatment time goals were not met most of the time, the group reports. Patients who required interhospital transfer experienced the longest system delays; only 17% were treated within 120 minutes.
Among patients who received primary PCI, 20% had a registry-defined hospital-specified reason for delay, including cardiac arrest and/or need for intubation in 6.8%, “difficulty crossing the culprit lesion” in 3.8%, and “other reasons” in 5.8%, the group reports.
“In 2020, a new reason for delay was added to the registry, ‘need for additional personal protective equipment for suspected/confirmed infectious disease.’ This reason was most commonly used in the second quarter of 2020 (6%) and then declined over time to 1% in the final 2 quarters,” they write.
“Thus, active SARS-CoV-2 infection appeared to have a smaller direct role in longer treatment times or worse outcomes.” Rather, they continue, “the pandemic potentially had a significant indirect role as hospitals were overwhelmed with patients, EMS and hospitals were challenged in maintaining paramedic and nurse staffing and intensive care bed availability, and patients experienced delayed care due to barriers to access or perceived fear of becoming entangled in an overwhelmed medical system.”
Still an important quality metric
STEMI treatment times remain an important quality metric to which hospitals should continue to pay attention because shorter times improve patient care, Deepak Bhatt, MD, MPH, told this news organization.
“Having said that, as with all metrics, one needs to be thoughtful and realize that a difference of a couple of minutes is probably not a crucial thing,” said Dr. Bhatt, Brigham and Women’s Hospital and Harvard Medical School, Boston, who was not involved with the current study.
Interhospital transfers indeed involve longer delays, he observed, suggesting that regional integrated health systems should develop methods for optimizing STEMI care – even, for example, if they involve bypassing non-PCI centers or stopping patients briefly for stabilization followed by rapid transport to a PCI-capable facility.
“That, of course, requires cooperation among hospitals. Sometimes that requires hospitals putting aside economic considerations and just focusing on doing the right thing for that individual patient,” Dr. Bhatt said.
Transfer delays are common for patients presenting with STEMI at hospitals without PCI capability, he noted. “Having clear protocols in place that expedite that type of transfer, I think, could go a long way in reducing the time to treatment in patients that are presenting to the hospital without cath labs. That’s an important message that these data provide.”
The onset of COVID-19 led to widespread delays in STEMI time to treatment early in the pandemic. There were concerns about exposing cath lab personnel to SARS-CoV-2 and potential adverse consequences of sick personnel being unable to provide patient care in the subsequent weeks and months, Dr. Bhatt observed.
However, “All of that seems to have quieted down, and I don’t think COVID is impacting time to treatment right now.”
‘Suboptimal compliance’ with standards
The current findings of “suboptimal compliance with national targets underscore why reassessing quality metrics, in light of changing practice patterns and other secular trends, is critical,” write Andrew S. Oseran, MD, MBA, and Robert W. Yeh, MD, both of Harvard Medical School, in an accompanying editorial.
“While the importance of coordinated and expeditious care for this high-risk patient population is undeniable, the specific actions that hospitals can – or should – take to further improve overall STEMI outcomes are less clear,” they say.
“As physicians contemplate the optimal path forward in managing the care of STEMI patients, they must recognize the clinical and operational nuance that exists in caring for this diverse population and acknowledge the trade-offs associated with uniform quality metrics,” write the editorialists.
“Global reductions in time to treatment for STEMI patients has been one of health care’s great success stories. As we move forward, it may be time to consider whether efforts to achieve additional improvement in target treatment times will result in substantive benefits, or whether we have reached the point of diminishing returns.”
A version of this article first appeared on Medscape.com.
FROM JAMA
Diabetes surge expected in young people
according to a new study published in Diabetes Care.
It is expected that as many as 526,000 people younger than 20 years in the United States will have diabetes by 2060, researchers from the Centers for Disease Control and Prevention report. Their projections found that the number of young people with diabetes will increase 12%, from 213,000 in 2017 to 239,000 in 2060.
The estimates include a 673% rise in the number of youth with type 2 diabetes and a 65% increase in cases of type 1 diabetes over the next 4 decades.
Most of the new cases are projected to occur among non-Hispanic Blacks, exacerbating the already significant racial disparities in type 2 diabetes in particular, the study found.
“This study’s startling projections of type 2 diabetes increases show why it is crucial to advance health equity and reduce the widespread disparities that already take a toll on people’s health,” Christopher Holliday, PhD, MPH, FACHE, director of CDC’s Division of Diabetes Translation, said in a press release about the new estimates.
Even if trends remain the same in coming decades, researchers said diagnoses of type 2 diabetes will rise almost 70% and that diagnoses of type 1 diabetes will increase by 3%.
The researchers attribute the increase in diabetes cases among youth to a variety of factors, including the growing prevalence of childhood obesity and the presence of diabetes in women of childbearing age, which is linked to obesity in their offspring.
Debra Houry, MD, MPH, acting principal director of the CDC, said the focus should be on prevention.
“This new research should serve as a wake-up call for all of us. It’s vital that we focus our efforts to ensure all Americans, especially our young people, are the healthiest they can be,” she said in a press release.
The findings come from the SEARCH for Diabetes in Youth study, funded by the CDC and the National Institutes of Health. Dr. Houry and Dr. Holliday report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study published in Diabetes Care.
It is expected that as many as 526,000 people younger than 20 years in the United States will have diabetes by 2060, researchers from the Centers for Disease Control and Prevention report. Their projections found that the number of young people with diabetes will increase 12%, from 213,000 in 2017 to 239,000 in 2060.
The estimates include a 673% rise in the number of youth with type 2 diabetes and a 65% increase in cases of type 1 diabetes over the next 4 decades.
Most of the new cases are projected to occur among non-Hispanic Blacks, exacerbating the already significant racial disparities in type 2 diabetes in particular, the study found.
“This study’s startling projections of type 2 diabetes increases show why it is crucial to advance health equity and reduce the widespread disparities that already take a toll on people’s health,” Christopher Holliday, PhD, MPH, FACHE, director of CDC’s Division of Diabetes Translation, said in a press release about the new estimates.
Even if trends remain the same in coming decades, researchers said diagnoses of type 2 diabetes will rise almost 70% and that diagnoses of type 1 diabetes will increase by 3%.
The researchers attribute the increase in diabetes cases among youth to a variety of factors, including the growing prevalence of childhood obesity and the presence of diabetes in women of childbearing age, which is linked to obesity in their offspring.
Debra Houry, MD, MPH, acting principal director of the CDC, said the focus should be on prevention.
“This new research should serve as a wake-up call for all of us. It’s vital that we focus our efforts to ensure all Americans, especially our young people, are the healthiest they can be,” she said in a press release.
The findings come from the SEARCH for Diabetes in Youth study, funded by the CDC and the National Institutes of Health. Dr. Houry and Dr. Holliday report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new study published in Diabetes Care.
It is expected that as many as 526,000 people younger than 20 years in the United States will have diabetes by 2060, researchers from the Centers for Disease Control and Prevention report. Their projections found that the number of young people with diabetes will increase 12%, from 213,000 in 2017 to 239,000 in 2060.
The estimates include a 673% rise in the number of youth with type 2 diabetes and a 65% increase in cases of type 1 diabetes over the next 4 decades.
Most of the new cases are projected to occur among non-Hispanic Blacks, exacerbating the already significant racial disparities in type 2 diabetes in particular, the study found.
“This study’s startling projections of type 2 diabetes increases show why it is crucial to advance health equity and reduce the widespread disparities that already take a toll on people’s health,” Christopher Holliday, PhD, MPH, FACHE, director of CDC’s Division of Diabetes Translation, said in a press release about the new estimates.
Even if trends remain the same in coming decades, researchers said diagnoses of type 2 diabetes will rise almost 70% and that diagnoses of type 1 diabetes will increase by 3%.
The researchers attribute the increase in diabetes cases among youth to a variety of factors, including the growing prevalence of childhood obesity and the presence of diabetes in women of childbearing age, which is linked to obesity in their offspring.
Debra Houry, MD, MPH, acting principal director of the CDC, said the focus should be on prevention.
“This new research should serve as a wake-up call for all of us. It’s vital that we focus our efforts to ensure all Americans, especially our young people, are the healthiest they can be,” she said in a press release.
The findings come from the SEARCH for Diabetes in Youth study, funded by the CDC and the National Institutes of Health. Dr. Houry and Dr. Holliday report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM DIABETES CARE
Heart benefits begin at well under 10,000 daily steps
– and the benefits accrue at well below the widely promoted threshold of 10,000 steps per day, new research shows.
Among adults aged 60 and older, those who took roughly 6,000 to 9,000 steps per day had a 40% to 50% lower risk of CVD, compared with peers logging just 2,000 steps per day.
“We hope this study will contribute evidence to future public health and clinical guidance on how many steps we need for health,” Amanda Paluch, PhD, with University of Massachusetts Amherst, told this news organization.
Getting in more steps per day can lower an individual’s risk for heart disease – but it’s not an “all or nothing” situation, Dr. Paluch said.
“The heart health benefits begin at lower than 10,000 steps per day. So, for the many adults that may find 10,000 steps a bit out of reach, it is important to promote that even small increases in steps can be beneficial for health,” Dr. Paluch said.
The study was published online in Circulation.
Attainable step goals
As part of the Steps for Health Collaborative, Dr. Paluch and colleagues examined the dose-response relationship between steps per day and CVD in a meta-analysis of eight prospective studies involving 20,152 adults (mean age 63, 52% women).
Steps were measured in each study using one of five different commercially available step-measuring devices. Adults aged 60 years and older took a median of 4,323 steps per day (interquartile range, 2,760-6,924), while younger adults walked a bit more (median 6,911 daily steps; IQR, 4,783-9,794).
During follow-up lasting an average of 6.2 years, a total of 1,523 CVD events were reported.
In the final adjusted model, for older adults, compared with those in quartile 1 who got the fewest steps per day (median 1,811), the risk of CVD was 20% lower in those in quartile 2, who got a median of 3,823 steps per day (hazard ratio, 0.80; 95% confidence interval, 0.69-0.93).
CVD risk was 38% lower in older adults in quartile 3 who got a median of 5,520 steps per day (HR, 0.62; 95% CI, 0.52-0.74) and 49% lower in those in quartile 4 who walked the most (a median of 9,259 steps per day; HR, 0.51; 95% CI, 0.41-0.63).
Restricting the analysis to individuals without known CVD at baseline showed similar results.
Among six studies that excluded adults with a history of CVD at baseline, compared with the lowest quartile, the HR for incident CVD events was 0.74 (95% CI, 0.60-0.91) in the second quartile, 0.60 (95% CI, 0.47-0.77) in the third quartile, and 0.55 (95% CI, 0.40-0.76) in the fourth quartile.
Despite the inverse association of steps with CVD in older adults, there was no association in younger adults. The researchers caution, however, that CVD is a disease of aging, and the follow-up period in these studies may not have been long enough to capture CVD incidence in younger adults.
Stepping rate (pace or cadence) was not associated with CVD risk beyond that of total steps per day. However, only four of the eight studies reported data on stepping rate, so this finding should be viewed as preliminary, Dr. Paluch and colleagues say.
Start small and go from there
Dr. Paluch said the take-home message from this study and numerous others is simple.
“Move more and sit less! Being physically active, by getting in your steps, is an important part of keeping your heart healthy,” she said in an interview.
For adults who are currently inactive, Dr. Paluch suggests finding small ways to get in a few more steps per day. “It does not need to be drastic changes. Consider a brief 5- to 10-minute walking break at lunch, taking the stairs, or playing a game of hide and seek with the grandchildren,” Dr. Paluch advised.
“For adults starting at 3,000 steps a day, set a goal of 4,000, and then 5,000. Each improvement can lead to better heart health,” Dr. Paluch said. “And for those who are already active, keep it up, as there are benefits with higher volumes of steps per day as well.”
Support for this research was provided by the Intergovernmental Personnel Act Agreement through the Centers for Disease Control and Prevention. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
– and the benefits accrue at well below the widely promoted threshold of 10,000 steps per day, new research shows.
Among adults aged 60 and older, those who took roughly 6,000 to 9,000 steps per day had a 40% to 50% lower risk of CVD, compared with peers logging just 2,000 steps per day.
“We hope this study will contribute evidence to future public health and clinical guidance on how many steps we need for health,” Amanda Paluch, PhD, with University of Massachusetts Amherst, told this news organization.
Getting in more steps per day can lower an individual’s risk for heart disease – but it’s not an “all or nothing” situation, Dr. Paluch said.
“The heart health benefits begin at lower than 10,000 steps per day. So, for the many adults that may find 10,000 steps a bit out of reach, it is important to promote that even small increases in steps can be beneficial for health,” Dr. Paluch said.
The study was published online in Circulation.
Attainable step goals
As part of the Steps for Health Collaborative, Dr. Paluch and colleagues examined the dose-response relationship between steps per day and CVD in a meta-analysis of eight prospective studies involving 20,152 adults (mean age 63, 52% women).
Steps were measured in each study using one of five different commercially available step-measuring devices. Adults aged 60 years and older took a median of 4,323 steps per day (interquartile range, 2,760-6,924), while younger adults walked a bit more (median 6,911 daily steps; IQR, 4,783-9,794).
During follow-up lasting an average of 6.2 years, a total of 1,523 CVD events were reported.
In the final adjusted model, for older adults, compared with those in quartile 1 who got the fewest steps per day (median 1,811), the risk of CVD was 20% lower in those in quartile 2, who got a median of 3,823 steps per day (hazard ratio, 0.80; 95% confidence interval, 0.69-0.93).
CVD risk was 38% lower in older adults in quartile 3 who got a median of 5,520 steps per day (HR, 0.62; 95% CI, 0.52-0.74) and 49% lower in those in quartile 4 who walked the most (a median of 9,259 steps per day; HR, 0.51; 95% CI, 0.41-0.63).
Restricting the analysis to individuals without known CVD at baseline showed similar results.
Among six studies that excluded adults with a history of CVD at baseline, compared with the lowest quartile, the HR for incident CVD events was 0.74 (95% CI, 0.60-0.91) in the second quartile, 0.60 (95% CI, 0.47-0.77) in the third quartile, and 0.55 (95% CI, 0.40-0.76) in the fourth quartile.
Despite the inverse association of steps with CVD in older adults, there was no association in younger adults. The researchers caution, however, that CVD is a disease of aging, and the follow-up period in these studies may not have been long enough to capture CVD incidence in younger adults.
Stepping rate (pace or cadence) was not associated with CVD risk beyond that of total steps per day. However, only four of the eight studies reported data on stepping rate, so this finding should be viewed as preliminary, Dr. Paluch and colleagues say.
Start small and go from there
Dr. Paluch said the take-home message from this study and numerous others is simple.
“Move more and sit less! Being physically active, by getting in your steps, is an important part of keeping your heart healthy,” she said in an interview.
For adults who are currently inactive, Dr. Paluch suggests finding small ways to get in a few more steps per day. “It does not need to be drastic changes. Consider a brief 5- to 10-minute walking break at lunch, taking the stairs, or playing a game of hide and seek with the grandchildren,” Dr. Paluch advised.
“For adults starting at 3,000 steps a day, set a goal of 4,000, and then 5,000. Each improvement can lead to better heart health,” Dr. Paluch said. “And for those who are already active, keep it up, as there are benefits with higher volumes of steps per day as well.”
Support for this research was provided by the Intergovernmental Personnel Act Agreement through the Centers for Disease Control and Prevention. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
– and the benefits accrue at well below the widely promoted threshold of 10,000 steps per day, new research shows.
Among adults aged 60 and older, those who took roughly 6,000 to 9,000 steps per day had a 40% to 50% lower risk of CVD, compared with peers logging just 2,000 steps per day.
“We hope this study will contribute evidence to future public health and clinical guidance on how many steps we need for health,” Amanda Paluch, PhD, with University of Massachusetts Amherst, told this news organization.
Getting in more steps per day can lower an individual’s risk for heart disease – but it’s not an “all or nothing” situation, Dr. Paluch said.
“The heart health benefits begin at lower than 10,000 steps per day. So, for the many adults that may find 10,000 steps a bit out of reach, it is important to promote that even small increases in steps can be beneficial for health,” Dr. Paluch said.
The study was published online in Circulation.
Attainable step goals
As part of the Steps for Health Collaborative, Dr. Paluch and colleagues examined the dose-response relationship between steps per day and CVD in a meta-analysis of eight prospective studies involving 20,152 adults (mean age 63, 52% women).
Steps were measured in each study using one of five different commercially available step-measuring devices. Adults aged 60 years and older took a median of 4,323 steps per day (interquartile range, 2,760-6,924), while younger adults walked a bit more (median 6,911 daily steps; IQR, 4,783-9,794).
During follow-up lasting an average of 6.2 years, a total of 1,523 CVD events were reported.
In the final adjusted model, for older adults, compared with those in quartile 1 who got the fewest steps per day (median 1,811), the risk of CVD was 20% lower in those in quartile 2, who got a median of 3,823 steps per day (hazard ratio, 0.80; 95% confidence interval, 0.69-0.93).
CVD risk was 38% lower in older adults in quartile 3 who got a median of 5,520 steps per day (HR, 0.62; 95% CI, 0.52-0.74) and 49% lower in those in quartile 4 who walked the most (a median of 9,259 steps per day; HR, 0.51; 95% CI, 0.41-0.63).
Restricting the analysis to individuals without known CVD at baseline showed similar results.
Among six studies that excluded adults with a history of CVD at baseline, compared with the lowest quartile, the HR for incident CVD events was 0.74 (95% CI, 0.60-0.91) in the second quartile, 0.60 (95% CI, 0.47-0.77) in the third quartile, and 0.55 (95% CI, 0.40-0.76) in the fourth quartile.
Despite the inverse association of steps with CVD in older adults, there was no association in younger adults. The researchers caution, however, that CVD is a disease of aging, and the follow-up period in these studies may not have been long enough to capture CVD incidence in younger adults.
Stepping rate (pace or cadence) was not associated with CVD risk beyond that of total steps per day. However, only four of the eight studies reported data on stepping rate, so this finding should be viewed as preliminary, Dr. Paluch and colleagues say.
Start small and go from there
Dr. Paluch said the take-home message from this study and numerous others is simple.
“Move more and sit less! Being physically active, by getting in your steps, is an important part of keeping your heart healthy,” she said in an interview.
For adults who are currently inactive, Dr. Paluch suggests finding small ways to get in a few more steps per day. “It does not need to be drastic changes. Consider a brief 5- to 10-minute walking break at lunch, taking the stairs, or playing a game of hide and seek with the grandchildren,” Dr. Paluch advised.
“For adults starting at 3,000 steps a day, set a goal of 4,000, and then 5,000. Each improvement can lead to better heart health,” Dr. Paluch said. “And for those who are already active, keep it up, as there are benefits with higher volumes of steps per day as well.”
Support for this research was provided by the Intergovernmental Personnel Act Agreement through the Centers for Disease Control and Prevention. The authors have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CIRCULATION
Nearly 1,400% rise in young children ingesting cannabis edibles
according to a new analysis of data from poison control centers.
In 2017, centers received 207 reports of children aged 5 years and younger who ingested edible cannabis. In 2021, 3,054 such cases were reported, according to the study, which was published online in Pediatrics.
Many of the children experienced clinical effects, such as depression of the central nervous system, impaired coordination, confusion, agitation, an increase in heart rate, or dilated pupils. No deaths were reported.
“These exposures can cause significant toxicity and are responsible for an increasing number of hospitalizations,” study coauthor Marit S. Tweet, MD, of Southern Illinois University, Springfield, and colleagues wrote.
About 97% of the exposures occurred in residences – 90% at the child’s own home – and about half of the cases involved 2- and 3-year-olds, they noted.
Examining national trends
Twenty-one states have approved recreational cannabis for people aged 21 years and older.
Prior research has shown that calls to poison centers and visits to emergency departments for pediatric cannabis consumption increased in certain states after the drug became legal in those jurisdictions.
To assess national trends, Dr. Tweet’s group analyzed cases in the National Poison Data System, which tracks potentially toxic exposures reported to poison control centers in the United States.
During the 5-year period, they identified 7,043 exposures to edible cannabis by children younger than age 6. In 2.2% of the cases, the drug had a major effect, defined as being either life-threatening or causing residual disability. In 21.9% of cases, the effect was considered to be moderate, with symptoms that were more pronounced, prolonged, or systemic than minor effects.
About 8% of the children were admitted to critical care units; 14.6% were admitted to non–critical care units.
Of 4,827 cases for which there was information about the clinical effects of the exposure and therapies used, 70% involved CNS depression, including 1.9% with “more severe CNS effects, including major CNS depression or coma,” according to the report.
Patients also experienced ataxia (7.4%), agitation (7.1%), confusion (6.1%), tremor (2%), and seizures (1.6%). Other common symptoms included tachycardia (11.4%), vomiting (9.5%), mydriasis (5.9%), and respiratory depression (3.1%).
Treatments for the exposures included intravenous fluids (20.7%), food or snacks (10.3%), and oxygen therapy (4%). Some patients also received naloxone (1.4%) or charcoal (2.1%).
“The total number of children requiring intubation during the study period was 35, or approximately 1 in 140,” the researchers reported. “Although this was a relatively rare occurrence, it is important for clinicians to be aware that life-threatening sequelae can develop and may necessitate invasive supportive care measures.”
Tempting and toxic
For toddlers, edible cannabis may be especially tempting and toxic. Edibles can “resemble common treats such as candies, chocolates, cookies, or other baked goods,” the researchers wrote. Children would not recognize, for example, that one chocolate bar might contain multiple 10-mg servings of tetrahydrocannabinol intended for adults.
Poison centers have been fielding more calls about edible cannabis use by older children, as well.
Adrienne Hughes, MD, assistant professor of emergency medicine at Oregon Health and Science University, Portland, recently found that many cases of intentional misuse and abuse by adolescents involve edible forms of cannabis.
“While marijuana carries a low risk for severe toxicity, it can be inebriating to the point of poor judgment, risk of falls or other injury, and occasionally a panic reaction in the novice user and unsuspecting children who accidentally ingest these products,” Dr. Hughes said in an interview.
Measures to keep edibles away from children could include changing how the products are packaged, limiting the maximum dose of drug per package, and educating the public about the risks to children, Dr. Tweet’s group wrote. They highlighted a 2019 position statement from the American College of Medical Toxicology that includes recommendations for responsible storage habits.
Dr. Hughes echoed one suggestion that is mentioned in the position statement: Parents should consider keeping their cannabis products locked up.
The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new analysis of data from poison control centers.
In 2017, centers received 207 reports of children aged 5 years and younger who ingested edible cannabis. In 2021, 3,054 such cases were reported, according to the study, which was published online in Pediatrics.
Many of the children experienced clinical effects, such as depression of the central nervous system, impaired coordination, confusion, agitation, an increase in heart rate, or dilated pupils. No deaths were reported.
“These exposures can cause significant toxicity and are responsible for an increasing number of hospitalizations,” study coauthor Marit S. Tweet, MD, of Southern Illinois University, Springfield, and colleagues wrote.
About 97% of the exposures occurred in residences – 90% at the child’s own home – and about half of the cases involved 2- and 3-year-olds, they noted.
Examining national trends
Twenty-one states have approved recreational cannabis for people aged 21 years and older.
Prior research has shown that calls to poison centers and visits to emergency departments for pediatric cannabis consumption increased in certain states after the drug became legal in those jurisdictions.
To assess national trends, Dr. Tweet’s group analyzed cases in the National Poison Data System, which tracks potentially toxic exposures reported to poison control centers in the United States.
During the 5-year period, they identified 7,043 exposures to edible cannabis by children younger than age 6. In 2.2% of the cases, the drug had a major effect, defined as being either life-threatening or causing residual disability. In 21.9% of cases, the effect was considered to be moderate, with symptoms that were more pronounced, prolonged, or systemic than minor effects.
About 8% of the children were admitted to critical care units; 14.6% were admitted to non–critical care units.
Of 4,827 cases for which there was information about the clinical effects of the exposure and therapies used, 70% involved CNS depression, including 1.9% with “more severe CNS effects, including major CNS depression or coma,” according to the report.
Patients also experienced ataxia (7.4%), agitation (7.1%), confusion (6.1%), tremor (2%), and seizures (1.6%). Other common symptoms included tachycardia (11.4%), vomiting (9.5%), mydriasis (5.9%), and respiratory depression (3.1%).
Treatments for the exposures included intravenous fluids (20.7%), food or snacks (10.3%), and oxygen therapy (4%). Some patients also received naloxone (1.4%) or charcoal (2.1%).
“The total number of children requiring intubation during the study period was 35, or approximately 1 in 140,” the researchers reported. “Although this was a relatively rare occurrence, it is important for clinicians to be aware that life-threatening sequelae can develop and may necessitate invasive supportive care measures.”
Tempting and toxic
For toddlers, edible cannabis may be especially tempting and toxic. Edibles can “resemble common treats such as candies, chocolates, cookies, or other baked goods,” the researchers wrote. Children would not recognize, for example, that one chocolate bar might contain multiple 10-mg servings of tetrahydrocannabinol intended for adults.
Poison centers have been fielding more calls about edible cannabis use by older children, as well.
Adrienne Hughes, MD, assistant professor of emergency medicine at Oregon Health and Science University, Portland, recently found that many cases of intentional misuse and abuse by adolescents involve edible forms of cannabis.
“While marijuana carries a low risk for severe toxicity, it can be inebriating to the point of poor judgment, risk of falls or other injury, and occasionally a panic reaction in the novice user and unsuspecting children who accidentally ingest these products,” Dr. Hughes said in an interview.
Measures to keep edibles away from children could include changing how the products are packaged, limiting the maximum dose of drug per package, and educating the public about the risks to children, Dr. Tweet’s group wrote. They highlighted a 2019 position statement from the American College of Medical Toxicology that includes recommendations for responsible storage habits.
Dr. Hughes echoed one suggestion that is mentioned in the position statement: Parents should consider keeping their cannabis products locked up.
The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
according to a new analysis of data from poison control centers.
In 2017, centers received 207 reports of children aged 5 years and younger who ingested edible cannabis. In 2021, 3,054 such cases were reported, according to the study, which was published online in Pediatrics.
Many of the children experienced clinical effects, such as depression of the central nervous system, impaired coordination, confusion, agitation, an increase in heart rate, or dilated pupils. No deaths were reported.
“These exposures can cause significant toxicity and are responsible for an increasing number of hospitalizations,” study coauthor Marit S. Tweet, MD, of Southern Illinois University, Springfield, and colleagues wrote.
About 97% of the exposures occurred in residences – 90% at the child’s own home – and about half of the cases involved 2- and 3-year-olds, they noted.
Examining national trends
Twenty-one states have approved recreational cannabis for people aged 21 years and older.
Prior research has shown that calls to poison centers and visits to emergency departments for pediatric cannabis consumption increased in certain states after the drug became legal in those jurisdictions.
To assess national trends, Dr. Tweet’s group analyzed cases in the National Poison Data System, which tracks potentially toxic exposures reported to poison control centers in the United States.
During the 5-year period, they identified 7,043 exposures to edible cannabis by children younger than age 6. In 2.2% of the cases, the drug had a major effect, defined as being either life-threatening or causing residual disability. In 21.9% of cases, the effect was considered to be moderate, with symptoms that were more pronounced, prolonged, or systemic than minor effects.
About 8% of the children were admitted to critical care units; 14.6% were admitted to non–critical care units.
Of 4,827 cases for which there was information about the clinical effects of the exposure and therapies used, 70% involved CNS depression, including 1.9% with “more severe CNS effects, including major CNS depression or coma,” according to the report.
Patients also experienced ataxia (7.4%), agitation (7.1%), confusion (6.1%), tremor (2%), and seizures (1.6%). Other common symptoms included tachycardia (11.4%), vomiting (9.5%), mydriasis (5.9%), and respiratory depression (3.1%).
Treatments for the exposures included intravenous fluids (20.7%), food or snacks (10.3%), and oxygen therapy (4%). Some patients also received naloxone (1.4%) or charcoal (2.1%).
“The total number of children requiring intubation during the study period was 35, or approximately 1 in 140,” the researchers reported. “Although this was a relatively rare occurrence, it is important for clinicians to be aware that life-threatening sequelae can develop and may necessitate invasive supportive care measures.”
Tempting and toxic
For toddlers, edible cannabis may be especially tempting and toxic. Edibles can “resemble common treats such as candies, chocolates, cookies, or other baked goods,” the researchers wrote. Children would not recognize, for example, that one chocolate bar might contain multiple 10-mg servings of tetrahydrocannabinol intended for adults.
Poison centers have been fielding more calls about edible cannabis use by older children, as well.
Adrienne Hughes, MD, assistant professor of emergency medicine at Oregon Health and Science University, Portland, recently found that many cases of intentional misuse and abuse by adolescents involve edible forms of cannabis.
“While marijuana carries a low risk for severe toxicity, it can be inebriating to the point of poor judgment, risk of falls or other injury, and occasionally a panic reaction in the novice user and unsuspecting children who accidentally ingest these products,” Dr. Hughes said in an interview.
Measures to keep edibles away from children could include changing how the products are packaged, limiting the maximum dose of drug per package, and educating the public about the risks to children, Dr. Tweet’s group wrote. They highlighted a 2019 position statement from the American College of Medical Toxicology that includes recommendations for responsible storage habits.
Dr. Hughes echoed one suggestion that is mentioned in the position statement: Parents should consider keeping their cannabis products locked up.
The researchers disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM PEDIATRICS
Study of beliefs about what causes cancer sparks debate
The study, entitled, “Everything Causes Cancer? Beliefs and Attitudes Towards Cancer Prevention Among Anti-Vaxxers, Flat Earthers, and Reptilian Conspiracists: Online Cross Sectional Survey,” was published in the Christmas 2022 issue of The British Medical Journal (BMJ).
The authors explain that they set out to evaluate “the patterns of beliefs about cancer among people who believed in conspiracies, rejected the COVID-19 vaccine, or preferred alternative medicine.”
They sought such people on social media and online chat platforms and asked them questions about real and mythical causes of cancer.
Almost half of survey participants agreed with the statement, “It seems like everything causes cancer.”
Overall, among all participants, awareness of the actual causes of cancer was greater than awareness of the mythical causes of cancer, the authors report. However, awareness of the actual causes of cancer was lower among the unvaccinated and members of conspiracy groups than among their counterparts.
The authors are concerned that their findings suggest “a direct connection between digital misinformation and consequent potential erroneous health decisions, which may represent a further preventable fraction of cancer.”
Backlash and criticism
The study “highlights the difficulty society encounters in distinguishing the actual causes of cancer from mythical causes,” The BMJ commented on Twitter.
However, both the study and the journal received some backlash.
This is a “horrible article seeking to smear people with concerns about COVID vaccines,” commented Clare Craig, a British consultant pathologist who specializes in cancer diagnostics.
The study and its methodology were also harshly criticized on Twitter by Normal Fenton, professor of risk information management at the Queen Mary University of London.
The senior author of the study, Laura Costas, a medical epidemiologist with the Catalan Institute of Oncology, Barcelona, told this news organization that the naysayers on social media, many of whom focused their comments on the COVID-19 vaccine, prove the purpose of the study – that misinformation spreads widely on the internet.
“Most comments focused on spreading COVID-19 myths, which were not the direct subject of the study, and questioned the motivations of BMJ authors and the scientific community, assuming they had a common malevolent hidden agenda,” Ms. Costas said.
“They stated the need of having critical thinking, a trait in common with the scientific method, but dogmatically dismissed any information that comes from official sources,” she added.
Ms. Costas commented that “society encounters difficulty in differentiating actual from mythical causes of cancer owing to mass information. We therefore planned this study with a certain satire, which is in line with the essence of The BMJ Christmas issue.”
The BMJ has a long history of publishing a lighthearted Christmas edition full of original, satirical, and nontraditional studies. Previous years have seen studies that explored potential harms from holly and ivy, survival time of chocolates on hospital wards, and the question, “Were James Bond’s drinks shaken because of alcohol induced tremor?”
Study details
Ms. Costas and colleagues sought participants for their survey from online forums that included 4chan and Reddit, which are known for their controversial content posted by anonymous users. Data were also collected from ForoCoches and HispaChan, well-known Spanish online forums. These online sites were intentionally chosen because researchers thought “conspiracy beliefs would be more prevalent,” according to Ms. Costas.
Across the multiple forums, there were 1,494 participants. Of these, 209 participants were unvaccinated against COVID-19, 112 preferred alternatives rather than conventional medicine, and 62 reported that they believed the earth was flat or believed that humanoids take reptilian forms to manipulate human societies.
The team then sought to assess beliefs about actual and mythical (nonestablished) causes of cancer by presenting the participants with the closed risk factor questions on two validated scales – the Cancer Awareness Measure (CAM) and CAM–Mythical Causes Scale (CAM-MYCS).
Responses to both were recorded on a five-point scale; answers ranged from “strongly disagree” to “strongly agree.”
The CAM assesses cancer risk perceptions of 11 established risk factors for cancer: smoking actively or passively, consuming alcohol, low levels of physical activity, consuming red or processed meat, getting sunburnt as a child, family history of cancer, human papillomavirus infection, being overweight, age greater than or equal to 70 years, and low vegetable and fruit consumption.
The CAM-MYCS measure includes 12 questions on risk perceptions of mythical causes of cancer – nonestablished causes that are commonly believed to cause cancer but for which there is no supporting scientific evidence, the authors explain. These items include drinking from plastic bottles; eating food containing artificial sweeteners or additives and genetically modified food; using microwave ovens, aerosol containers, mobile phones, and cleaning products; living near power lines; feeling stressed; experiencing physical trauma; and being exposed to electromagnetic frequencies/non-ionizing radiation, such as wi-fi networks, radio, and television.
The most endorsed mythical causes of cancer were eating food containing additives (63.9%) or sweeteners (50.7%), feeling stressed (59.7%), and eating genetically modified foods (38.4%).
A version of this article first appeared on Medscape.com.
The study, entitled, “Everything Causes Cancer? Beliefs and Attitudes Towards Cancer Prevention Among Anti-Vaxxers, Flat Earthers, and Reptilian Conspiracists: Online Cross Sectional Survey,” was published in the Christmas 2022 issue of The British Medical Journal (BMJ).
The authors explain that they set out to evaluate “the patterns of beliefs about cancer among people who believed in conspiracies, rejected the COVID-19 vaccine, or preferred alternative medicine.”
They sought such people on social media and online chat platforms and asked them questions about real and mythical causes of cancer.
Almost half of survey participants agreed with the statement, “It seems like everything causes cancer.”
Overall, among all participants, awareness of the actual causes of cancer was greater than awareness of the mythical causes of cancer, the authors report. However, awareness of the actual causes of cancer was lower among the unvaccinated and members of conspiracy groups than among their counterparts.
The authors are concerned that their findings suggest “a direct connection between digital misinformation and consequent potential erroneous health decisions, which may represent a further preventable fraction of cancer.”
Backlash and criticism
The study “highlights the difficulty society encounters in distinguishing the actual causes of cancer from mythical causes,” The BMJ commented on Twitter.
However, both the study and the journal received some backlash.
This is a “horrible article seeking to smear people with concerns about COVID vaccines,” commented Clare Craig, a British consultant pathologist who specializes in cancer diagnostics.
The study and its methodology were also harshly criticized on Twitter by Normal Fenton, professor of risk information management at the Queen Mary University of London.
The senior author of the study, Laura Costas, a medical epidemiologist with the Catalan Institute of Oncology, Barcelona, told this news organization that the naysayers on social media, many of whom focused their comments on the COVID-19 vaccine, prove the purpose of the study – that misinformation spreads widely on the internet.
“Most comments focused on spreading COVID-19 myths, which were not the direct subject of the study, and questioned the motivations of BMJ authors and the scientific community, assuming they had a common malevolent hidden agenda,” Ms. Costas said.
“They stated the need of having critical thinking, a trait in common with the scientific method, but dogmatically dismissed any information that comes from official sources,” she added.
Ms. Costas commented that “society encounters difficulty in differentiating actual from mythical causes of cancer owing to mass information. We therefore planned this study with a certain satire, which is in line with the essence of The BMJ Christmas issue.”
The BMJ has a long history of publishing a lighthearted Christmas edition full of original, satirical, and nontraditional studies. Previous years have seen studies that explored potential harms from holly and ivy, survival time of chocolates on hospital wards, and the question, “Were James Bond’s drinks shaken because of alcohol induced tremor?”
Study details
Ms. Costas and colleagues sought participants for their survey from online forums that included 4chan and Reddit, which are known for their controversial content posted by anonymous users. Data were also collected from ForoCoches and HispaChan, well-known Spanish online forums. These online sites were intentionally chosen because researchers thought “conspiracy beliefs would be more prevalent,” according to Ms. Costas.
Across the multiple forums, there were 1,494 participants. Of these, 209 participants were unvaccinated against COVID-19, 112 preferred alternatives rather than conventional medicine, and 62 reported that they believed the earth was flat or believed that humanoids take reptilian forms to manipulate human societies.
The team then sought to assess beliefs about actual and mythical (nonestablished) causes of cancer by presenting the participants with the closed risk factor questions on two validated scales – the Cancer Awareness Measure (CAM) and CAM–Mythical Causes Scale (CAM-MYCS).
Responses to both were recorded on a five-point scale; answers ranged from “strongly disagree” to “strongly agree.”
The CAM assesses cancer risk perceptions of 11 established risk factors for cancer: smoking actively or passively, consuming alcohol, low levels of physical activity, consuming red or processed meat, getting sunburnt as a child, family history of cancer, human papillomavirus infection, being overweight, age greater than or equal to 70 years, and low vegetable and fruit consumption.
The CAM-MYCS measure includes 12 questions on risk perceptions of mythical causes of cancer – nonestablished causes that are commonly believed to cause cancer but for which there is no supporting scientific evidence, the authors explain. These items include drinking from plastic bottles; eating food containing artificial sweeteners or additives and genetically modified food; using microwave ovens, aerosol containers, mobile phones, and cleaning products; living near power lines; feeling stressed; experiencing physical trauma; and being exposed to electromagnetic frequencies/non-ionizing radiation, such as wi-fi networks, radio, and television.
The most endorsed mythical causes of cancer were eating food containing additives (63.9%) or sweeteners (50.7%), feeling stressed (59.7%), and eating genetically modified foods (38.4%).
A version of this article first appeared on Medscape.com.
The study, entitled, “Everything Causes Cancer? Beliefs and Attitudes Towards Cancer Prevention Among Anti-Vaxxers, Flat Earthers, and Reptilian Conspiracists: Online Cross Sectional Survey,” was published in the Christmas 2022 issue of The British Medical Journal (BMJ).
The authors explain that they set out to evaluate “the patterns of beliefs about cancer among people who believed in conspiracies, rejected the COVID-19 vaccine, or preferred alternative medicine.”
They sought such people on social media and online chat platforms and asked them questions about real and mythical causes of cancer.
Almost half of survey participants agreed with the statement, “It seems like everything causes cancer.”
Overall, among all participants, awareness of the actual causes of cancer was greater than awareness of the mythical causes of cancer, the authors report. However, awareness of the actual causes of cancer was lower among the unvaccinated and members of conspiracy groups than among their counterparts.
The authors are concerned that their findings suggest “a direct connection between digital misinformation and consequent potential erroneous health decisions, which may represent a further preventable fraction of cancer.”
Backlash and criticism
The study “highlights the difficulty society encounters in distinguishing the actual causes of cancer from mythical causes,” The BMJ commented on Twitter.
However, both the study and the journal received some backlash.
This is a “horrible article seeking to smear people with concerns about COVID vaccines,” commented Clare Craig, a British consultant pathologist who specializes in cancer diagnostics.
The study and its methodology were also harshly criticized on Twitter by Normal Fenton, professor of risk information management at the Queen Mary University of London.
The senior author of the study, Laura Costas, a medical epidemiologist with the Catalan Institute of Oncology, Barcelona, told this news organization that the naysayers on social media, many of whom focused their comments on the COVID-19 vaccine, prove the purpose of the study – that misinformation spreads widely on the internet.
“Most comments focused on spreading COVID-19 myths, which were not the direct subject of the study, and questioned the motivations of BMJ authors and the scientific community, assuming they had a common malevolent hidden agenda,” Ms. Costas said.
“They stated the need of having critical thinking, a trait in common with the scientific method, but dogmatically dismissed any information that comes from official sources,” she added.
Ms. Costas commented that “society encounters difficulty in differentiating actual from mythical causes of cancer owing to mass information. We therefore planned this study with a certain satire, which is in line with the essence of The BMJ Christmas issue.”
The BMJ has a long history of publishing a lighthearted Christmas edition full of original, satirical, and nontraditional studies. Previous years have seen studies that explored potential harms from holly and ivy, survival time of chocolates on hospital wards, and the question, “Were James Bond’s drinks shaken because of alcohol induced tremor?”
Study details
Ms. Costas and colleagues sought participants for their survey from online forums that included 4chan and Reddit, which are known for their controversial content posted by anonymous users. Data were also collected from ForoCoches and HispaChan, well-known Spanish online forums. These online sites were intentionally chosen because researchers thought “conspiracy beliefs would be more prevalent,” according to Ms. Costas.
Across the multiple forums, there were 1,494 participants. Of these, 209 participants were unvaccinated against COVID-19, 112 preferred alternatives rather than conventional medicine, and 62 reported that they believed the earth was flat or believed that humanoids take reptilian forms to manipulate human societies.
The team then sought to assess beliefs about actual and mythical (nonestablished) causes of cancer by presenting the participants with the closed risk factor questions on two validated scales – the Cancer Awareness Measure (CAM) and CAM–Mythical Causes Scale (CAM-MYCS).
Responses to both were recorded on a five-point scale; answers ranged from “strongly disagree” to “strongly agree.”
The CAM assesses cancer risk perceptions of 11 established risk factors for cancer: smoking actively or passively, consuming alcohol, low levels of physical activity, consuming red or processed meat, getting sunburnt as a child, family history of cancer, human papillomavirus infection, being overweight, age greater than or equal to 70 years, and low vegetable and fruit consumption.
The CAM-MYCS measure includes 12 questions on risk perceptions of mythical causes of cancer – nonestablished causes that are commonly believed to cause cancer but for which there is no supporting scientific evidence, the authors explain. These items include drinking from plastic bottles; eating food containing artificial sweeteners or additives and genetically modified food; using microwave ovens, aerosol containers, mobile phones, and cleaning products; living near power lines; feeling stressed; experiencing physical trauma; and being exposed to electromagnetic frequencies/non-ionizing radiation, such as wi-fi networks, radio, and television.
The most endorsed mythical causes of cancer were eating food containing additives (63.9%) or sweeteners (50.7%), feeling stressed (59.7%), and eating genetically modified foods (38.4%).
A version of this article first appeared on Medscape.com.
ED docs need a clearer path to outpatient primary care
It was 2 p.m. on a sunny and humid day, 1 hour before my 8-hour shift was over in the emergency department at the community hospital that I was rotating through. It was part of my fourth-year emergency medicine (EM) clerkship. Not that I would have noticed the weather, save for the few seconds the sliding door to the ED would open periodically, as if on its own cadence, with the sounds of stomping boots and a rolling gurney making its way through.
We were busy. At this particular hospital, I was told, EM volume is already up 35% this year compared with the previous year, and bed holds had been hitting new highs each week.
One more hour until my shift is over and a poor soul will take over my computer, seat, and the chaos.
I took a glance at the electronic health record again, seeing whether there was anything I could do to discharge any of the patients to relieve some of the strain. Knee pain, toe pain, headache/migraine, shoulder pain, elevated blood pressure. Although it’s true that any of these listed complaints could have emergent etiologies, the truth was that all of these patients were here owing to exacerbations of chronic issues. And yet most, if not all, of these patients had been here for nearly 8 hours, some even longer, waiting for treatment and exacerbating an already busy ED.
“I don’t understand. Couldn’t these patients have sought care outpatient with their PCP [primary care physician]? It would have been a lot cheaper and faster.” I asked. A seasoned ED physician, bald, graying, and whom I had just met today and hadn’t spoken to much until this very moment, turned to me and said: “We have become the dumping ground for primary care complaints.”
‘Go to the ED’
“PCPs are already too busy,” the physician continued. “It’s just easier to say: ‘Go to the ED. They’ll take care of it.’ ”
He continued: “In my 30 years of practicing, emergency medicine has changed so much. When I first started in the 1980s, I was only seeing emergencies, and it was fun. Now, 80% of my patients are primary care complaints. These days, I am more of a primary care physician than an emergency physician.”
Hmmm, I thought. Was this physician burned out and jaded? Quite possibly. Was this change the physician experienced throughout his career more likely attributed to a capitalist-run, profit-driven health care system and its cohort of underinsured and noninsured citizens? Certainly. I’m only a fourth-year medical student, so my view of the situation is no doubt limited.
But something he said definitely rang my bell: I’m more of a primary care physician than an emergency physician. That is an argument I can consider. Whether it is caused by poorly designed reimbursement schedules or the state of America’s profit-driven health care system, which effectively makes these physicians double as PCPs on a daily basis.
I let this thought ruminate on my drive home, along with how there’s a such a huge demand for PCPs, resulting in it taking up to 3 months to get an appointment with one. That’s crazy, and I understand the need to come to the ED where you’ll (hopefully) be seen the same day.
I also ruminated on how emergency physicians have the highest rate of burnout among all the specialties, with no career recourse afterward. Either you’re part of the hospital machine complex, or you’re out. Practicing EM for nearly 30 years is apparently a rarity these days. Most emergency physicians last 5 years, 10 years tops, and then are so burned out that they retire to pursue a life outside of medicine (real estate seems to be popular). But this is a shame.
Emergency docs exiting medicine
Emergency physicians have seen a ton of wildly different pathologies and have treated a variety of different conditions, including conditions usually reserved for primary care. To let knowledgeable, experienced emergency physicians just exit medicine, with no recourse to further contribute to this country’s health system outside of the hospital machine, is a travesty in its own right.
I ruminated further on the 2021 American College of Emergency Physicians 2021 report on the EM physician workforce, which stated that there is projected to be an oversupply of emergency physicians by 2030, leaving thousands of them out of work. No doubt that report has left an impact on the volume of residency applications into EM in 2021. No one wants to go through residency and be unemployed at the end of it.
And finally, I ruminated on the sheer volume of patients visiting EDs across the country. Patient volumes are up, wait times in general are up, wait times in the ED are up, and bed holds to get admitted are hitting highs across the country each week. The deluge of patients visiting the ED is not getting better, and it’s only likely to get worse as the population ages.
It’s time to offer emergency physicians a path to outpatient primary care.
Now before I get hung for this suggestion (“I went into EM precisely not to do outpatient care!”), hear me out: Such a path should be offered via a 1-year accelerated fellowship and will allow emergency physicians to practice outpatient primary care medicine independently. And although working in urgent care centers is already an option, the opportunity to own and operate their own primary care practice should also exist.
In my humble opinion, by offering such a path, the following objectives could be accomplished:
Alleviate the pressure on primary care medicine in the United States. It’s no secret that the United States needs more primary care physicians. Allowing emergency physicians who got burnt out by hospital life an alternative way to serve their community and country via outpatient primary care would greatly alleviate the pressure on the need for PCPs today.
Provide an alternative career path for emergency physicians. We would be doing a disservice if we don’t offer emergency physicians a way to revive their burnout and utilize their skill set in a post-ED life. Outpatient primary care is the perfect way to do this, and it’s a win-win-win on several fronts: We need more outpatient physicians, they need an opportunity to flex their knowledge in an alternative setting.
Solve the “ACEP” problem. The ACEP report scared medical students away from applying to residency in EM. Who wants to go through 3 years of residency only to be unemployed at the end of it? By offering a path to outpatient primary care, we can offer an important and viable path for those emergency physicians who would be unemployed to continue to practice medicine and serve the community, thereby alleviating concern about an oversupply.
For better or for worse, because of the state of health care today, ED physicians have been exposed to a myriad of primary care concerns, all of which have prepared them for a career as an outpatient PCP. By offering such a path, we can provide more flexibility for an emergency physician’s career, help alleviate the primary care shortage affecting the United States, and serve our community and country in new and helpful ways.
Dr. Gogna is a fourth-year medical student at Philadelphia College of Osteopathic Medicine Georgia, Suwanee. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
It was 2 p.m. on a sunny and humid day, 1 hour before my 8-hour shift was over in the emergency department at the community hospital that I was rotating through. It was part of my fourth-year emergency medicine (EM) clerkship. Not that I would have noticed the weather, save for the few seconds the sliding door to the ED would open periodically, as if on its own cadence, with the sounds of stomping boots and a rolling gurney making its way through.
We were busy. At this particular hospital, I was told, EM volume is already up 35% this year compared with the previous year, and bed holds had been hitting new highs each week.
One more hour until my shift is over and a poor soul will take over my computer, seat, and the chaos.
I took a glance at the electronic health record again, seeing whether there was anything I could do to discharge any of the patients to relieve some of the strain. Knee pain, toe pain, headache/migraine, shoulder pain, elevated blood pressure. Although it’s true that any of these listed complaints could have emergent etiologies, the truth was that all of these patients were here owing to exacerbations of chronic issues. And yet most, if not all, of these patients had been here for nearly 8 hours, some even longer, waiting for treatment and exacerbating an already busy ED.
“I don’t understand. Couldn’t these patients have sought care outpatient with their PCP [primary care physician]? It would have been a lot cheaper and faster.” I asked. A seasoned ED physician, bald, graying, and whom I had just met today and hadn’t spoken to much until this very moment, turned to me and said: “We have become the dumping ground for primary care complaints.”
‘Go to the ED’
“PCPs are already too busy,” the physician continued. “It’s just easier to say: ‘Go to the ED. They’ll take care of it.’ ”
He continued: “In my 30 years of practicing, emergency medicine has changed so much. When I first started in the 1980s, I was only seeing emergencies, and it was fun. Now, 80% of my patients are primary care complaints. These days, I am more of a primary care physician than an emergency physician.”
Hmmm, I thought. Was this physician burned out and jaded? Quite possibly. Was this change the physician experienced throughout his career more likely attributed to a capitalist-run, profit-driven health care system and its cohort of underinsured and noninsured citizens? Certainly. I’m only a fourth-year medical student, so my view of the situation is no doubt limited.
But something he said definitely rang my bell: I’m more of a primary care physician than an emergency physician. That is an argument I can consider. Whether it is caused by poorly designed reimbursement schedules or the state of America’s profit-driven health care system, which effectively makes these physicians double as PCPs on a daily basis.
I let this thought ruminate on my drive home, along with how there’s a such a huge demand for PCPs, resulting in it taking up to 3 months to get an appointment with one. That’s crazy, and I understand the need to come to the ED where you’ll (hopefully) be seen the same day.
I also ruminated on how emergency physicians have the highest rate of burnout among all the specialties, with no career recourse afterward. Either you’re part of the hospital machine complex, or you’re out. Practicing EM for nearly 30 years is apparently a rarity these days. Most emergency physicians last 5 years, 10 years tops, and then are so burned out that they retire to pursue a life outside of medicine (real estate seems to be popular). But this is a shame.
Emergency docs exiting medicine
Emergency physicians have seen a ton of wildly different pathologies and have treated a variety of different conditions, including conditions usually reserved for primary care. To let knowledgeable, experienced emergency physicians just exit medicine, with no recourse to further contribute to this country’s health system outside of the hospital machine, is a travesty in its own right.
I ruminated further on the 2021 American College of Emergency Physicians 2021 report on the EM physician workforce, which stated that there is projected to be an oversupply of emergency physicians by 2030, leaving thousands of them out of work. No doubt that report has left an impact on the volume of residency applications into EM in 2021. No one wants to go through residency and be unemployed at the end of it.
And finally, I ruminated on the sheer volume of patients visiting EDs across the country. Patient volumes are up, wait times in general are up, wait times in the ED are up, and bed holds to get admitted are hitting highs across the country each week. The deluge of patients visiting the ED is not getting better, and it’s only likely to get worse as the population ages.
It’s time to offer emergency physicians a path to outpatient primary care.
Now before I get hung for this suggestion (“I went into EM precisely not to do outpatient care!”), hear me out: Such a path should be offered via a 1-year accelerated fellowship and will allow emergency physicians to practice outpatient primary care medicine independently. And although working in urgent care centers is already an option, the opportunity to own and operate their own primary care practice should also exist.
In my humble opinion, by offering such a path, the following objectives could be accomplished:
Alleviate the pressure on primary care medicine in the United States. It’s no secret that the United States needs more primary care physicians. Allowing emergency physicians who got burnt out by hospital life an alternative way to serve their community and country via outpatient primary care would greatly alleviate the pressure on the need for PCPs today.
Provide an alternative career path for emergency physicians. We would be doing a disservice if we don’t offer emergency physicians a way to revive their burnout and utilize their skill set in a post-ED life. Outpatient primary care is the perfect way to do this, and it’s a win-win-win on several fronts: We need more outpatient physicians, they need an opportunity to flex their knowledge in an alternative setting.
Solve the “ACEP” problem. The ACEP report scared medical students away from applying to residency in EM. Who wants to go through 3 years of residency only to be unemployed at the end of it? By offering a path to outpatient primary care, we can offer an important and viable path for those emergency physicians who would be unemployed to continue to practice medicine and serve the community, thereby alleviating concern about an oversupply.
For better or for worse, because of the state of health care today, ED physicians have been exposed to a myriad of primary care concerns, all of which have prepared them for a career as an outpatient PCP. By offering such a path, we can provide more flexibility for an emergency physician’s career, help alleviate the primary care shortage affecting the United States, and serve our community and country in new and helpful ways.
Dr. Gogna is a fourth-year medical student at Philadelphia College of Osteopathic Medicine Georgia, Suwanee. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
It was 2 p.m. on a sunny and humid day, 1 hour before my 8-hour shift was over in the emergency department at the community hospital that I was rotating through. It was part of my fourth-year emergency medicine (EM) clerkship. Not that I would have noticed the weather, save for the few seconds the sliding door to the ED would open periodically, as if on its own cadence, with the sounds of stomping boots and a rolling gurney making its way through.
We were busy. At this particular hospital, I was told, EM volume is already up 35% this year compared with the previous year, and bed holds had been hitting new highs each week.
One more hour until my shift is over and a poor soul will take over my computer, seat, and the chaos.
I took a glance at the electronic health record again, seeing whether there was anything I could do to discharge any of the patients to relieve some of the strain. Knee pain, toe pain, headache/migraine, shoulder pain, elevated blood pressure. Although it’s true that any of these listed complaints could have emergent etiologies, the truth was that all of these patients were here owing to exacerbations of chronic issues. And yet most, if not all, of these patients had been here for nearly 8 hours, some even longer, waiting for treatment and exacerbating an already busy ED.
“I don’t understand. Couldn’t these patients have sought care outpatient with their PCP [primary care physician]? It would have been a lot cheaper and faster.” I asked. A seasoned ED physician, bald, graying, and whom I had just met today and hadn’t spoken to much until this very moment, turned to me and said: “We have become the dumping ground for primary care complaints.”
‘Go to the ED’
“PCPs are already too busy,” the physician continued. “It’s just easier to say: ‘Go to the ED. They’ll take care of it.’ ”
He continued: “In my 30 years of practicing, emergency medicine has changed so much. When I first started in the 1980s, I was only seeing emergencies, and it was fun. Now, 80% of my patients are primary care complaints. These days, I am more of a primary care physician than an emergency physician.”
Hmmm, I thought. Was this physician burned out and jaded? Quite possibly. Was this change the physician experienced throughout his career more likely attributed to a capitalist-run, profit-driven health care system and its cohort of underinsured and noninsured citizens? Certainly. I’m only a fourth-year medical student, so my view of the situation is no doubt limited.
But something he said definitely rang my bell: I’m more of a primary care physician than an emergency physician. That is an argument I can consider. Whether it is caused by poorly designed reimbursement schedules or the state of America’s profit-driven health care system, which effectively makes these physicians double as PCPs on a daily basis.
I let this thought ruminate on my drive home, along with how there’s a such a huge demand for PCPs, resulting in it taking up to 3 months to get an appointment with one. That’s crazy, and I understand the need to come to the ED where you’ll (hopefully) be seen the same day.
I also ruminated on how emergency physicians have the highest rate of burnout among all the specialties, with no career recourse afterward. Either you’re part of the hospital machine complex, or you’re out. Practicing EM for nearly 30 years is apparently a rarity these days. Most emergency physicians last 5 years, 10 years tops, and then are so burned out that they retire to pursue a life outside of medicine (real estate seems to be popular). But this is a shame.
Emergency docs exiting medicine
Emergency physicians have seen a ton of wildly different pathologies and have treated a variety of different conditions, including conditions usually reserved for primary care. To let knowledgeable, experienced emergency physicians just exit medicine, with no recourse to further contribute to this country’s health system outside of the hospital machine, is a travesty in its own right.
I ruminated further on the 2021 American College of Emergency Physicians 2021 report on the EM physician workforce, which stated that there is projected to be an oversupply of emergency physicians by 2030, leaving thousands of them out of work. No doubt that report has left an impact on the volume of residency applications into EM in 2021. No one wants to go through residency and be unemployed at the end of it.
And finally, I ruminated on the sheer volume of patients visiting EDs across the country. Patient volumes are up, wait times in general are up, wait times in the ED are up, and bed holds to get admitted are hitting highs across the country each week. The deluge of patients visiting the ED is not getting better, and it’s only likely to get worse as the population ages.
It’s time to offer emergency physicians a path to outpatient primary care.
Now before I get hung for this suggestion (“I went into EM precisely not to do outpatient care!”), hear me out: Such a path should be offered via a 1-year accelerated fellowship and will allow emergency physicians to practice outpatient primary care medicine independently. And although working in urgent care centers is already an option, the opportunity to own and operate their own primary care practice should also exist.
In my humble opinion, by offering such a path, the following objectives could be accomplished:
Alleviate the pressure on primary care medicine in the United States. It’s no secret that the United States needs more primary care physicians. Allowing emergency physicians who got burnt out by hospital life an alternative way to serve their community and country via outpatient primary care would greatly alleviate the pressure on the need for PCPs today.
Provide an alternative career path for emergency physicians. We would be doing a disservice if we don’t offer emergency physicians a way to revive their burnout and utilize their skill set in a post-ED life. Outpatient primary care is the perfect way to do this, and it’s a win-win-win on several fronts: We need more outpatient physicians, they need an opportunity to flex their knowledge in an alternative setting.
Solve the “ACEP” problem. The ACEP report scared medical students away from applying to residency in EM. Who wants to go through 3 years of residency only to be unemployed at the end of it? By offering a path to outpatient primary care, we can offer an important and viable path for those emergency physicians who would be unemployed to continue to practice medicine and serve the community, thereby alleviating concern about an oversupply.
For better or for worse, because of the state of health care today, ED physicians have been exposed to a myriad of primary care concerns, all of which have prepared them for a career as an outpatient PCP. By offering such a path, we can provide more flexibility for an emergency physician’s career, help alleviate the primary care shortage affecting the United States, and serve our community and country in new and helpful ways.
Dr. Gogna is a fourth-year medical student at Philadelphia College of Osteopathic Medicine Georgia, Suwanee. He reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Vonoprazan triple therapy most cost-effective for H. pylori: Study
A new analysis finds that vonoprazan triple therapy (Voquezna) is the most cost-effective first-line regimen to eradicate Helicobacter pylori infection in the United States.
Rifabutin triple therapy (Talicia) is the second most cost-effective strategy for H. pylori eradication, followed in order of decreasing cost-effectiveness by vonoprazan dual therapy, bismuth quadruple therapy, and clarithromycin triple therapy.
The analysis is believed to be the first to report on the cost-effectiveness of vonoprazan- and rifabutin-based regimens as first-line treatments for H. pylori infection from the perspective of U.S. health care payers.
for U.S. payers, reported Ismaeel Yunusa, PharmD, PhD, of the University of South Carolina College of Pharmacy in Columbia, and colleagues.
The study was published online in the American Journal of Gastroenterology.
It’s estimated that more than 114 million people in the United States have H. pylori infection. Clinical practice guidelines recommend H. pylori eradication in all patients with a positive test of active infection.
Using a Markov model, Dr. Yunusa and colleagues estimated the cost-effectiveness of five prepackaged or co-formulated H. pylori eradication regimens: clarithromycin triple therapy, bismuth quadruple therapy, vonoprazan dual therapy, vonoprazan triple therapy, and rifabutin triple therapy.
The model estimated the expected costs in 2022 U.S. dollars, expected quality-adjusted life years (QALYs), incremental cost-effectiveness ratio (ICERs), and expected net monetary benefit over 20 years.
Among their key findings and conclusions:
- Bismuth quadruple therapy had the highest expected cost ($1,439) and rifabutin triple regimen had the lowest expected cost ($1,048).
- Because rifabutin triple therapy was predicted to cost less and was more effective than clarithromycin triple therapy, bismuth quadruple therapy, and vonoprazan dual therapy, it dominated all treatment strategies – except for vonoprazan triple therapy.
- Compared with rifabutin triple therapy, vonoprazan triple therapy had a higher expected cost ($1,172 vs. $1,048) and expected QALY (14.262 vs. 14.256), yielding an ICER of $22,573 per QALY.
- Vonoprazan triple therapy had the highest expected net monetary benefit and was the most cost-effective at willingness to pay thresholds between $50,000 and $150,000 per QALY, followed by rifabutin triple therapy.
- Vonoprazan triple therapy would result on average in an incremental net benefit of $1,655 per patient than clarithromycin triple therapy.
- Because the rifabutin-based regimen was more cost-effective than all but vonoprazan triple therapy, it has a potential role as an alternative first-line treatment.
- Rifabutin triple therapy and vonoprazan dual therapy would need to be considerably discounted (by 15%-43% and by 44%-85%, respectively), to be cost-effective at commonly used cost-effectiveness thresholds.
- Vonoprazan dual therapy demonstrated limited value relative to other available options; thus, its widespread adoption as a first-line strategy seems unlikely.
- Based on the results, it would be hard to justify the use of bismuth quadruple therapy or clarithromycin triple therapy since they provide the lowest net monetary benefit and have lower eradication rates.
The investigators noted that their analysis considered only direct costs of therapy, not other costs such as appointments, travel, and time away from work.
They also assumed medical costs, including endoscopy and H. pylori testing, would not change regardless of treatment regimen. Therefore, total health care costs may be underestimated.
The study did not receive any funding. The authors have declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new analysis finds that vonoprazan triple therapy (Voquezna) is the most cost-effective first-line regimen to eradicate Helicobacter pylori infection in the United States.
Rifabutin triple therapy (Talicia) is the second most cost-effective strategy for H. pylori eradication, followed in order of decreasing cost-effectiveness by vonoprazan dual therapy, bismuth quadruple therapy, and clarithromycin triple therapy.
The analysis is believed to be the first to report on the cost-effectiveness of vonoprazan- and rifabutin-based regimens as first-line treatments for H. pylori infection from the perspective of U.S. health care payers.
for U.S. payers, reported Ismaeel Yunusa, PharmD, PhD, of the University of South Carolina College of Pharmacy in Columbia, and colleagues.
The study was published online in the American Journal of Gastroenterology.
It’s estimated that more than 114 million people in the United States have H. pylori infection. Clinical practice guidelines recommend H. pylori eradication in all patients with a positive test of active infection.
Using a Markov model, Dr. Yunusa and colleagues estimated the cost-effectiveness of five prepackaged or co-formulated H. pylori eradication regimens: clarithromycin triple therapy, bismuth quadruple therapy, vonoprazan dual therapy, vonoprazan triple therapy, and rifabutin triple therapy.
The model estimated the expected costs in 2022 U.S. dollars, expected quality-adjusted life years (QALYs), incremental cost-effectiveness ratio (ICERs), and expected net monetary benefit over 20 years.
Among their key findings and conclusions:
- Bismuth quadruple therapy had the highest expected cost ($1,439) and rifabutin triple regimen had the lowest expected cost ($1,048).
- Because rifabutin triple therapy was predicted to cost less and was more effective than clarithromycin triple therapy, bismuth quadruple therapy, and vonoprazan dual therapy, it dominated all treatment strategies – except for vonoprazan triple therapy.
- Compared with rifabutin triple therapy, vonoprazan triple therapy had a higher expected cost ($1,172 vs. $1,048) and expected QALY (14.262 vs. 14.256), yielding an ICER of $22,573 per QALY.
- Vonoprazan triple therapy had the highest expected net monetary benefit and was the most cost-effective at willingness to pay thresholds between $50,000 and $150,000 per QALY, followed by rifabutin triple therapy.
- Vonoprazan triple therapy would result on average in an incremental net benefit of $1,655 per patient than clarithromycin triple therapy.
- Because the rifabutin-based regimen was more cost-effective than all but vonoprazan triple therapy, it has a potential role as an alternative first-line treatment.
- Rifabutin triple therapy and vonoprazan dual therapy would need to be considerably discounted (by 15%-43% and by 44%-85%, respectively), to be cost-effective at commonly used cost-effectiveness thresholds.
- Vonoprazan dual therapy demonstrated limited value relative to other available options; thus, its widespread adoption as a first-line strategy seems unlikely.
- Based on the results, it would be hard to justify the use of bismuth quadruple therapy or clarithromycin triple therapy since they provide the lowest net monetary benefit and have lower eradication rates.
The investigators noted that their analysis considered only direct costs of therapy, not other costs such as appointments, travel, and time away from work.
They also assumed medical costs, including endoscopy and H. pylori testing, would not change regardless of treatment regimen. Therefore, total health care costs may be underestimated.
The study did not receive any funding. The authors have declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new analysis finds that vonoprazan triple therapy (Voquezna) is the most cost-effective first-line regimen to eradicate Helicobacter pylori infection in the United States.
Rifabutin triple therapy (Talicia) is the second most cost-effective strategy for H. pylori eradication, followed in order of decreasing cost-effectiveness by vonoprazan dual therapy, bismuth quadruple therapy, and clarithromycin triple therapy.
The analysis is believed to be the first to report on the cost-effectiveness of vonoprazan- and rifabutin-based regimens as first-line treatments for H. pylori infection from the perspective of U.S. health care payers.
for U.S. payers, reported Ismaeel Yunusa, PharmD, PhD, of the University of South Carolina College of Pharmacy in Columbia, and colleagues.
The study was published online in the American Journal of Gastroenterology.
It’s estimated that more than 114 million people in the United States have H. pylori infection. Clinical practice guidelines recommend H. pylori eradication in all patients with a positive test of active infection.
Using a Markov model, Dr. Yunusa and colleagues estimated the cost-effectiveness of five prepackaged or co-formulated H. pylori eradication regimens: clarithromycin triple therapy, bismuth quadruple therapy, vonoprazan dual therapy, vonoprazan triple therapy, and rifabutin triple therapy.
The model estimated the expected costs in 2022 U.S. dollars, expected quality-adjusted life years (QALYs), incremental cost-effectiveness ratio (ICERs), and expected net monetary benefit over 20 years.
Among their key findings and conclusions:
- Bismuth quadruple therapy had the highest expected cost ($1,439) and rifabutin triple regimen had the lowest expected cost ($1,048).
- Because rifabutin triple therapy was predicted to cost less and was more effective than clarithromycin triple therapy, bismuth quadruple therapy, and vonoprazan dual therapy, it dominated all treatment strategies – except for vonoprazan triple therapy.
- Compared with rifabutin triple therapy, vonoprazan triple therapy had a higher expected cost ($1,172 vs. $1,048) and expected QALY (14.262 vs. 14.256), yielding an ICER of $22,573 per QALY.
- Vonoprazan triple therapy had the highest expected net monetary benefit and was the most cost-effective at willingness to pay thresholds between $50,000 and $150,000 per QALY, followed by rifabutin triple therapy.
- Vonoprazan triple therapy would result on average in an incremental net benefit of $1,655 per patient than clarithromycin triple therapy.
- Because the rifabutin-based regimen was more cost-effective than all but vonoprazan triple therapy, it has a potential role as an alternative first-line treatment.
- Rifabutin triple therapy and vonoprazan dual therapy would need to be considerably discounted (by 15%-43% and by 44%-85%, respectively), to be cost-effective at commonly used cost-effectiveness thresholds.
- Vonoprazan dual therapy demonstrated limited value relative to other available options; thus, its widespread adoption as a first-line strategy seems unlikely.
- Based on the results, it would be hard to justify the use of bismuth quadruple therapy or clarithromycin triple therapy since they provide the lowest net monetary benefit and have lower eradication rates.
The investigators noted that their analysis considered only direct costs of therapy, not other costs such as appointments, travel, and time away from work.
They also assumed medical costs, including endoscopy and H. pylori testing, would not change regardless of treatment regimen. Therefore, total health care costs may be underestimated.
The study did not receive any funding. The authors have declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Topical psoriasis treatments
LAS VEGAS – ,” said Linda Stein Gold, MD, in a presentation at Medscape Live’s annual Las Vegas Dermatology Seminar.
However, when using topical treatments, combination therapy is generally more effective than monotherapy for psoriasis, especially for plaque psoriasis, said Dr. Stein Gold, director of clinical research and division head of dermatology at the Henry Ford Health System, Detroit.
Two combination products, calcipotriene/betamethasone (CAL/BDP) and tazarotene/halobetasol lotion, each offer a complimentary mechanism of action that minimizes side effects, with decreased irritation and less atrophy, she said. Calcipotriene/betamethasone (CAL/BDP) is available as a cream or foam, Dr. Stein Gold noted. The cream is engineered for rapid onset, as well as enhanced penetration, she said. CAL/BDP foam also is designed for enhanced penetration, and has been shown to have long-term maintenance efficacy, she said.
The currently available CAL/BDP cream is made using a patented technology known as “PAD,” in which the internal oil of the cream vehicle is stabilized by encapsulation in “a robust aqueous film,” Dr. Stein Gold said, noting that the greater solubility enhances skin penetration. The creation of “a robust oil droplet” addresses the problems associated with the surfactants present in many cream vehicles, namely irritation and impedance of skin penetration of the cream, she said.
In an 8-week study published in 2021, researchers compared CAL/BDP cream with PAD technology to CAL/BDP topical suspension in adults with mild to moderate psoriasis.
Patients randomized to treatment with CAL/BDP cream were significantly more likely to achieve the primary endpoint of Physician Global Assessment (PGA) treatment success than those randomized to the topical solution or vehicle (37.4%, 22.8%, and 3.7%, respectively).
Get proactive to maintain results
With topical psoriasis treatment, a proactive strategy helps maintain results over time, Dr. Stein Gold said. As an example, she cited a study published in 2021. In that study, known as PSO-LONG, which evaluated topical CAL/BDP foam, proactive management with the CAL/BDP foam formulation, “reduced the risk of experiencing relapse by 43%,” compared with reactive management (treatment with the vehicle foam), she said. Patients in the proactive-management group experienced an average of 41 more days in remission, compared with those in the reactive management group over a 1-year period.
Dr. Stein Gold also highlighted the value of tazarotene/halobetasol lotion for psoriasis, which she described as having synergistic efficacy,
She shared data presented at the 2021 Maui Dermatology meeting showing treatment success by 8 weeks with halobetasol/tazarotene with significantly reduced mean scores on measures of itching, dryness, and burning/stinging, compared with those on vehicle.
What’s new and approved
Joining the current topical treatment options for psoriasis is tapinarof, a small molecule that works by down-regulating Th17 cytokines, said Dr. Stein Gold. Tapinarof is Food and Drug Administration approved for treating psoriasis and is being studied in clinical trials for atopic dermatitis, she noted.
Dr. Stein Gold reviewed data from the PSOARING program published in the New England Journal of Medicine that served as a foundation for the FDA approval of tapinarof 1% cream. In the PSOARING 1 and 2 studies, patients with PSORIASIS showed significant improvement compared with vehicle over 12 weeks for the primary endpoint of Physicians’ Global Assessment scores of 0 or 1 (clear or almost clear). In the two studies, 60.7% and 56.9% of patients randomized to tapinarof met the patient-reported outcome of a minimum 4-point improvement in peak pruritus on the numerical rating scale (NRS) from baseline vs. 43.2% and 29.7% of placebo patients in the two studies, respectively.
In PSOARING 1 and 2, folliculitis (mostly mild or moderate), contact dermatitis, headache, pruritus, and dermatitis were the most common treatment-emergent adverse events, occurring in 1% or more of patients. Adverse event profiles for tapinarof are similar to those seen in previous studies, and a long-term extension showed a consistent safety profile, Dr. Stein Gold said.
Another recently approved topical treatment for psoriasis, a cream formulation of roflumilast, a phosphodiesterase (PDE)-4 inhibitor, has shown efficacy for treating plaque psoriasis, she said.
Patients with psoriasis in the DERMIS 1 and DERMIS 2 phase 3 studies randomized to 0.3% roflumilast cream showed significant improvement compared with those randomized to vehicle in terms of Investigator Global Assessment scores of clear or almost clear with an improvement of at least 2 grades from baseline.
Roflumilast foam also has shown success in improving scalp and body psoriasis, but this vehicle and indication has not yet been approved, Dr. Stein Gold said.
Dr. Stein Gold disclosed serving as a consultant or adviser for companies including AbbVie, Amgen, Arcutis, Bristol Myers Squibb, Dermavant, EPI Health, Galderma, Janssen, Incyte, Ortho Dermatologics, Pfizer, Regeneron, Sanofi; UCB, and serving as a speaker or member of speakers’ bureau for Amgen, AbbVie, Incyte, Pfizer, Regeneron, Sanofi, and Sun Research. She also disclosed receiving funding from AbbVie Amgen, Arcutis, Dermata, Dermavant, Galderma, Incyte, Ortho Dermatologics, Pfizer, and UCB.
MedscapeLive and this news organization are owned by the same parent company.
LAS VEGAS – ,” said Linda Stein Gold, MD, in a presentation at Medscape Live’s annual Las Vegas Dermatology Seminar.
However, when using topical treatments, combination therapy is generally more effective than monotherapy for psoriasis, especially for plaque psoriasis, said Dr. Stein Gold, director of clinical research and division head of dermatology at the Henry Ford Health System, Detroit.
Two combination products, calcipotriene/betamethasone (CAL/BDP) and tazarotene/halobetasol lotion, each offer a complimentary mechanism of action that minimizes side effects, with decreased irritation and less atrophy, she said. Calcipotriene/betamethasone (CAL/BDP) is available as a cream or foam, Dr. Stein Gold noted. The cream is engineered for rapid onset, as well as enhanced penetration, she said. CAL/BDP foam also is designed for enhanced penetration, and has been shown to have long-term maintenance efficacy, she said.
The currently available CAL/BDP cream is made using a patented technology known as “PAD,” in which the internal oil of the cream vehicle is stabilized by encapsulation in “a robust aqueous film,” Dr. Stein Gold said, noting that the greater solubility enhances skin penetration. The creation of “a robust oil droplet” addresses the problems associated with the surfactants present in many cream vehicles, namely irritation and impedance of skin penetration of the cream, she said.
In an 8-week study published in 2021, researchers compared CAL/BDP cream with PAD technology to CAL/BDP topical suspension in adults with mild to moderate psoriasis.
Patients randomized to treatment with CAL/BDP cream were significantly more likely to achieve the primary endpoint of Physician Global Assessment (PGA) treatment success than those randomized to the topical solution or vehicle (37.4%, 22.8%, and 3.7%, respectively).
Get proactive to maintain results
With topical psoriasis treatment, a proactive strategy helps maintain results over time, Dr. Stein Gold said. As an example, she cited a study published in 2021. In that study, known as PSO-LONG, which evaluated topical CAL/BDP foam, proactive management with the CAL/BDP foam formulation, “reduced the risk of experiencing relapse by 43%,” compared with reactive management (treatment with the vehicle foam), she said. Patients in the proactive-management group experienced an average of 41 more days in remission, compared with those in the reactive management group over a 1-year period.
Dr. Stein Gold also highlighted the value of tazarotene/halobetasol lotion for psoriasis, which she described as having synergistic efficacy,
She shared data presented at the 2021 Maui Dermatology meeting showing treatment success by 8 weeks with halobetasol/tazarotene with significantly reduced mean scores on measures of itching, dryness, and burning/stinging, compared with those on vehicle.
What’s new and approved
Joining the current topical treatment options for psoriasis is tapinarof, a small molecule that works by down-regulating Th17 cytokines, said Dr. Stein Gold. Tapinarof is Food and Drug Administration approved for treating psoriasis and is being studied in clinical trials for atopic dermatitis, she noted.
Dr. Stein Gold reviewed data from the PSOARING program published in the New England Journal of Medicine that served as a foundation for the FDA approval of tapinarof 1% cream. In the PSOARING 1 and 2 studies, patients with PSORIASIS showed significant improvement compared with vehicle over 12 weeks for the primary endpoint of Physicians’ Global Assessment scores of 0 or 1 (clear or almost clear). In the two studies, 60.7% and 56.9% of patients randomized to tapinarof met the patient-reported outcome of a minimum 4-point improvement in peak pruritus on the numerical rating scale (NRS) from baseline vs. 43.2% and 29.7% of placebo patients in the two studies, respectively.
In PSOARING 1 and 2, folliculitis (mostly mild or moderate), contact dermatitis, headache, pruritus, and dermatitis were the most common treatment-emergent adverse events, occurring in 1% or more of patients. Adverse event profiles for tapinarof are similar to those seen in previous studies, and a long-term extension showed a consistent safety profile, Dr. Stein Gold said.
Another recently approved topical treatment for psoriasis, a cream formulation of roflumilast, a phosphodiesterase (PDE)-4 inhibitor, has shown efficacy for treating plaque psoriasis, she said.
Patients with psoriasis in the DERMIS 1 and DERMIS 2 phase 3 studies randomized to 0.3% roflumilast cream showed significant improvement compared with those randomized to vehicle in terms of Investigator Global Assessment scores of clear or almost clear with an improvement of at least 2 grades from baseline.
Roflumilast foam also has shown success in improving scalp and body psoriasis, but this vehicle and indication has not yet been approved, Dr. Stein Gold said.
Dr. Stein Gold disclosed serving as a consultant or adviser for companies including AbbVie, Amgen, Arcutis, Bristol Myers Squibb, Dermavant, EPI Health, Galderma, Janssen, Incyte, Ortho Dermatologics, Pfizer, Regeneron, Sanofi; UCB, and serving as a speaker or member of speakers’ bureau for Amgen, AbbVie, Incyte, Pfizer, Regeneron, Sanofi, and Sun Research. She also disclosed receiving funding from AbbVie Amgen, Arcutis, Dermata, Dermavant, Galderma, Incyte, Ortho Dermatologics, Pfizer, and UCB.
MedscapeLive and this news organization are owned by the same parent company.
LAS VEGAS – ,” said Linda Stein Gold, MD, in a presentation at Medscape Live’s annual Las Vegas Dermatology Seminar.
However, when using topical treatments, combination therapy is generally more effective than monotherapy for psoriasis, especially for plaque psoriasis, said Dr. Stein Gold, director of clinical research and division head of dermatology at the Henry Ford Health System, Detroit.
Two combination products, calcipotriene/betamethasone (CAL/BDP) and tazarotene/halobetasol lotion, each offer a complimentary mechanism of action that minimizes side effects, with decreased irritation and less atrophy, she said. Calcipotriene/betamethasone (CAL/BDP) is available as a cream or foam, Dr. Stein Gold noted. The cream is engineered for rapid onset, as well as enhanced penetration, she said. CAL/BDP foam also is designed for enhanced penetration, and has been shown to have long-term maintenance efficacy, she said.
The currently available CAL/BDP cream is made using a patented technology known as “PAD,” in which the internal oil of the cream vehicle is stabilized by encapsulation in “a robust aqueous film,” Dr. Stein Gold said, noting that the greater solubility enhances skin penetration. The creation of “a robust oil droplet” addresses the problems associated with the surfactants present in many cream vehicles, namely irritation and impedance of skin penetration of the cream, she said.
In an 8-week study published in 2021, researchers compared CAL/BDP cream with PAD technology to CAL/BDP topical suspension in adults with mild to moderate psoriasis.
Patients randomized to treatment with CAL/BDP cream were significantly more likely to achieve the primary endpoint of Physician Global Assessment (PGA) treatment success than those randomized to the topical solution or vehicle (37.4%, 22.8%, and 3.7%, respectively).
Get proactive to maintain results
With topical psoriasis treatment, a proactive strategy helps maintain results over time, Dr. Stein Gold said. As an example, she cited a study published in 2021. In that study, known as PSO-LONG, which evaluated topical CAL/BDP foam, proactive management with the CAL/BDP foam formulation, “reduced the risk of experiencing relapse by 43%,” compared with reactive management (treatment with the vehicle foam), she said. Patients in the proactive-management group experienced an average of 41 more days in remission, compared with those in the reactive management group over a 1-year period.
Dr. Stein Gold also highlighted the value of tazarotene/halobetasol lotion for psoriasis, which she described as having synergistic efficacy,
She shared data presented at the 2021 Maui Dermatology meeting showing treatment success by 8 weeks with halobetasol/tazarotene with significantly reduced mean scores on measures of itching, dryness, and burning/stinging, compared with those on vehicle.
What’s new and approved
Joining the current topical treatment options for psoriasis is tapinarof, a small molecule that works by down-regulating Th17 cytokines, said Dr. Stein Gold. Tapinarof is Food and Drug Administration approved for treating psoriasis and is being studied in clinical trials for atopic dermatitis, she noted.
Dr. Stein Gold reviewed data from the PSOARING program published in the New England Journal of Medicine that served as a foundation for the FDA approval of tapinarof 1% cream. In the PSOARING 1 and 2 studies, patients with PSORIASIS showed significant improvement compared with vehicle over 12 weeks for the primary endpoint of Physicians’ Global Assessment scores of 0 or 1 (clear or almost clear). In the two studies, 60.7% and 56.9% of patients randomized to tapinarof met the patient-reported outcome of a minimum 4-point improvement in peak pruritus on the numerical rating scale (NRS) from baseline vs. 43.2% and 29.7% of placebo patients in the two studies, respectively.
In PSOARING 1 and 2, folliculitis (mostly mild or moderate), contact dermatitis, headache, pruritus, and dermatitis were the most common treatment-emergent adverse events, occurring in 1% or more of patients. Adverse event profiles for tapinarof are similar to those seen in previous studies, and a long-term extension showed a consistent safety profile, Dr. Stein Gold said.
Another recently approved topical treatment for psoriasis, a cream formulation of roflumilast, a phosphodiesterase (PDE)-4 inhibitor, has shown efficacy for treating plaque psoriasis, she said.
Patients with psoriasis in the DERMIS 1 and DERMIS 2 phase 3 studies randomized to 0.3% roflumilast cream showed significant improvement compared with those randomized to vehicle in terms of Investigator Global Assessment scores of clear or almost clear with an improvement of at least 2 grades from baseline.
Roflumilast foam also has shown success in improving scalp and body psoriasis, but this vehicle and indication has not yet been approved, Dr. Stein Gold said.
Dr. Stein Gold disclosed serving as a consultant or adviser for companies including AbbVie, Amgen, Arcutis, Bristol Myers Squibb, Dermavant, EPI Health, Galderma, Janssen, Incyte, Ortho Dermatologics, Pfizer, Regeneron, Sanofi; UCB, and serving as a speaker or member of speakers’ bureau for Amgen, AbbVie, Incyte, Pfizer, Regeneron, Sanofi, and Sun Research. She also disclosed receiving funding from AbbVie Amgen, Arcutis, Dermata, Dermavant, Galderma, Incyte, Ortho Dermatologics, Pfizer, and UCB.
MedscapeLive and this news organization are owned by the same parent company.
AT INNOVATIONS IN DERMATOLOGY
Bad breath? Mouthwash is out. Yogurt is in.
Leave the mouthwash. Take the yogurt
Most of us have experienced some sort of bad breath. It’s common in the morning right after waking up, but it also may be a sign for underlying medical issues like dental problems or acid reflux. Wherever it comes from, we always want to get rid of it. A recent meta-analysis in BMJ Open may have found the answer in some common foods.
For those with halitosis, the basic problem is that the bacteria in their mouths are not happy about where they are. The researchers looked at 130 studies and found seven that suggested fermented food has some effect in combating bad breath.
Now when we say fermented food, we’re not talking about that science project waiting to happen in the back of the refrigerator. Think yogurt, sourdough bread, or miso soup. Anything that contains probiotic bacteria.
Matthew J. Messina, DDS, assistant professor of dentistry at Ohio State University, who was not involved with the study, told Healthline that “the whole idea behind probiotics is [bacteria replacement]. Supplant the ‘bad guys’ with the ‘good guys,’ then we’ll end up with a better result.” Essentially balancing the scales in your mouth.
It may not be a long-term solution, Dr. Messina said, but the short-term data are positive. So if you experience bad breath from time to time, try a little bowl of yogurt instead of chewing gum. If nothing else, the bacteria in your mouth will thank you.
You can talk the silly talk, but can you walk the silly walk?
The Ministry of Silly Walks sketch from Monty Python is an enduring comedy classic, and one of surprising relevance for doctors. After all, this isn’t the first time a study has analyzed the unusual strides of Mr. Putey and Mr. Teabag.
The BMJ Christmas edition truly is the gift that keeps on giving. For this plunge into the Flying Circus, the study authors recruited a small group of fairly average adults and had them walk normally around a track for 5 minutes, monitoring their oxygen intake and energy expenditure. After that, the study participants imitated Mr. Putey’s walk and then Mr. Teabag’s.
In the sketch, Mr. Teabag notes that Mr. Putey’s walk is “not particularly silly,” which is borne out in the research. When imitating Mr. Putey’s walk, oxygen intake and energy expenditure were barely higher than a normal walk, not enough to achieve a meaningful difference. Hopefully he’ll get that government grant to further develop his silly walk, because right now Mr. Putey’s walk simply doesn’t cut it.
Mr. Teabag’s walk is a different story and the very image of inefficiency. Oxygen intake was 2.5 times higher than during the normal walk, and energy expenditure was noticeably higher (8 kcal in men and 5.2 kcal in women). In fact, the walk was so inefficient and its effect so drastic it actually reached the level of vigorous exercise. Thanks to this, the study authors noted that just 11 minutes a day of walking like Mr. Teabag would be enough to reach the general goal of 75 minutes of vigorous exercise per week. Boosting that to 12-19 minutes would increase daily energy expenditure by 100 kcal.
The study authors wrote, “Had an initiative to promote inefficient movement been adopted in the early 1970s, we might now be living among a healthier society. Efforts to promote higher energy – and perhaps more joyful – walking should ensure inclusivity and inefficiency for all.” We think they just advocated for a real-life Ministry of Silly Walks. Well, there have been worse ideas. Just look at Twitter.
When efficient gut microbes go bad
With the latest news from the Ministry of Silly Walks, is it time for humans to embrace all things inefficient? Maybe.
Turns out that individuals with more efficient digestive systems – those that extract more energy from the fuel supplied to them by the busy mouths above – tend to gain more weight than those with less efficient guts, even when they eat the same food, according to a recent study published in Microbiome.
The researchers took a look at the composition of gut microbes in a group of 85 volunteers and found that about 40% had microbiomes dominated by Bacteroides bacteria, which are more effective at extracting nutrients from food. That group also weighed 10% more on average, amounting to an extra 9 kg.
In a rather blatant demonstration of efficiency, the investigators also measured the speed of the participants’ digestion, as they had hypothesized that those with the longest digestive travel times would be the ones who harvested the most nutrition from their food. That was not the case.
The study subjects with the most efficient gut bacteria “also have the fastest passage through the gastrointestinal system, which has given us something to think about,” senior author Henrik Roager of the University of Copenhagen said in a written statement.
You know what gives us something to think about? Stool energy density and intestinal transit time and faecal bacterial cell counts, that’s what. Ick. Sometimes science is gross.
Here’s another thought, though: Seeing faecal instead of fecal is kind of funny to our American eyes, but adding that extra letter is also inefficient, which could mean that it’s good. So, in the spirit of embracing the inefficient as a new year begins, we’re resolving to wrap our editorial arms around faecal and the faeces it represents. Well, not literally, of course. More like we’re embracing the spirit of faeces.
Leave the mouthwash. Take the yogurt
Most of us have experienced some sort of bad breath. It’s common in the morning right after waking up, but it also may be a sign for underlying medical issues like dental problems or acid reflux. Wherever it comes from, we always want to get rid of it. A recent meta-analysis in BMJ Open may have found the answer in some common foods.
For those with halitosis, the basic problem is that the bacteria in their mouths are not happy about where they are. The researchers looked at 130 studies and found seven that suggested fermented food has some effect in combating bad breath.
Now when we say fermented food, we’re not talking about that science project waiting to happen in the back of the refrigerator. Think yogurt, sourdough bread, or miso soup. Anything that contains probiotic bacteria.
Matthew J. Messina, DDS, assistant professor of dentistry at Ohio State University, who was not involved with the study, told Healthline that “the whole idea behind probiotics is [bacteria replacement]. Supplant the ‘bad guys’ with the ‘good guys,’ then we’ll end up with a better result.” Essentially balancing the scales in your mouth.
It may not be a long-term solution, Dr. Messina said, but the short-term data are positive. So if you experience bad breath from time to time, try a little bowl of yogurt instead of chewing gum. If nothing else, the bacteria in your mouth will thank you.
You can talk the silly talk, but can you walk the silly walk?
The Ministry of Silly Walks sketch from Monty Python is an enduring comedy classic, and one of surprising relevance for doctors. After all, this isn’t the first time a study has analyzed the unusual strides of Mr. Putey and Mr. Teabag.
The BMJ Christmas edition truly is the gift that keeps on giving. For this plunge into the Flying Circus, the study authors recruited a small group of fairly average adults and had them walk normally around a track for 5 minutes, monitoring their oxygen intake and energy expenditure. After that, the study participants imitated Mr. Putey’s walk and then Mr. Teabag’s.
In the sketch, Mr. Teabag notes that Mr. Putey’s walk is “not particularly silly,” which is borne out in the research. When imitating Mr. Putey’s walk, oxygen intake and energy expenditure were barely higher than a normal walk, not enough to achieve a meaningful difference. Hopefully he’ll get that government grant to further develop his silly walk, because right now Mr. Putey’s walk simply doesn’t cut it.
Mr. Teabag’s walk is a different story and the very image of inefficiency. Oxygen intake was 2.5 times higher than during the normal walk, and energy expenditure was noticeably higher (8 kcal in men and 5.2 kcal in women). In fact, the walk was so inefficient and its effect so drastic it actually reached the level of vigorous exercise. Thanks to this, the study authors noted that just 11 minutes a day of walking like Mr. Teabag would be enough to reach the general goal of 75 minutes of vigorous exercise per week. Boosting that to 12-19 minutes would increase daily energy expenditure by 100 kcal.
The study authors wrote, “Had an initiative to promote inefficient movement been adopted in the early 1970s, we might now be living among a healthier society. Efforts to promote higher energy – and perhaps more joyful – walking should ensure inclusivity and inefficiency for all.” We think they just advocated for a real-life Ministry of Silly Walks. Well, there have been worse ideas. Just look at Twitter.
When efficient gut microbes go bad
With the latest news from the Ministry of Silly Walks, is it time for humans to embrace all things inefficient? Maybe.
Turns out that individuals with more efficient digestive systems – those that extract more energy from the fuel supplied to them by the busy mouths above – tend to gain more weight than those with less efficient guts, even when they eat the same food, according to a recent study published in Microbiome.
The researchers took a look at the composition of gut microbes in a group of 85 volunteers and found that about 40% had microbiomes dominated by Bacteroides bacteria, which are more effective at extracting nutrients from food. That group also weighed 10% more on average, amounting to an extra 9 kg.
In a rather blatant demonstration of efficiency, the investigators also measured the speed of the participants’ digestion, as they had hypothesized that those with the longest digestive travel times would be the ones who harvested the most nutrition from their food. That was not the case.
The study subjects with the most efficient gut bacteria “also have the fastest passage through the gastrointestinal system, which has given us something to think about,” senior author Henrik Roager of the University of Copenhagen said in a written statement.
You know what gives us something to think about? Stool energy density and intestinal transit time and faecal bacterial cell counts, that’s what. Ick. Sometimes science is gross.
Here’s another thought, though: Seeing faecal instead of fecal is kind of funny to our American eyes, but adding that extra letter is also inefficient, which could mean that it’s good. So, in the spirit of embracing the inefficient as a new year begins, we’re resolving to wrap our editorial arms around faecal and the faeces it represents. Well, not literally, of course. More like we’re embracing the spirit of faeces.
Leave the mouthwash. Take the yogurt
Most of us have experienced some sort of bad breath. It’s common in the morning right after waking up, but it also may be a sign for underlying medical issues like dental problems or acid reflux. Wherever it comes from, we always want to get rid of it. A recent meta-analysis in BMJ Open may have found the answer in some common foods.
For those with halitosis, the basic problem is that the bacteria in their mouths are not happy about where they are. The researchers looked at 130 studies and found seven that suggested fermented food has some effect in combating bad breath.
Now when we say fermented food, we’re not talking about that science project waiting to happen in the back of the refrigerator. Think yogurt, sourdough bread, or miso soup. Anything that contains probiotic bacteria.
Matthew J. Messina, DDS, assistant professor of dentistry at Ohio State University, who was not involved with the study, told Healthline that “the whole idea behind probiotics is [bacteria replacement]. Supplant the ‘bad guys’ with the ‘good guys,’ then we’ll end up with a better result.” Essentially balancing the scales in your mouth.
It may not be a long-term solution, Dr. Messina said, but the short-term data are positive. So if you experience bad breath from time to time, try a little bowl of yogurt instead of chewing gum. If nothing else, the bacteria in your mouth will thank you.
You can talk the silly talk, but can you walk the silly walk?
The Ministry of Silly Walks sketch from Monty Python is an enduring comedy classic, and one of surprising relevance for doctors. After all, this isn’t the first time a study has analyzed the unusual strides of Mr. Putey and Mr. Teabag.
The BMJ Christmas edition truly is the gift that keeps on giving. For this plunge into the Flying Circus, the study authors recruited a small group of fairly average adults and had them walk normally around a track for 5 minutes, monitoring their oxygen intake and energy expenditure. After that, the study participants imitated Mr. Putey’s walk and then Mr. Teabag’s.
In the sketch, Mr. Teabag notes that Mr. Putey’s walk is “not particularly silly,” which is borne out in the research. When imitating Mr. Putey’s walk, oxygen intake and energy expenditure were barely higher than a normal walk, not enough to achieve a meaningful difference. Hopefully he’ll get that government grant to further develop his silly walk, because right now Mr. Putey’s walk simply doesn’t cut it.
Mr. Teabag’s walk is a different story and the very image of inefficiency. Oxygen intake was 2.5 times higher than during the normal walk, and energy expenditure was noticeably higher (8 kcal in men and 5.2 kcal in women). In fact, the walk was so inefficient and its effect so drastic it actually reached the level of vigorous exercise. Thanks to this, the study authors noted that just 11 minutes a day of walking like Mr. Teabag would be enough to reach the general goal of 75 minutes of vigorous exercise per week. Boosting that to 12-19 minutes would increase daily energy expenditure by 100 kcal.
The study authors wrote, “Had an initiative to promote inefficient movement been adopted in the early 1970s, we might now be living among a healthier society. Efforts to promote higher energy – and perhaps more joyful – walking should ensure inclusivity and inefficiency for all.” We think they just advocated for a real-life Ministry of Silly Walks. Well, there have been worse ideas. Just look at Twitter.
When efficient gut microbes go bad
With the latest news from the Ministry of Silly Walks, is it time for humans to embrace all things inefficient? Maybe.
Turns out that individuals with more efficient digestive systems – those that extract more energy from the fuel supplied to them by the busy mouths above – tend to gain more weight than those with less efficient guts, even when they eat the same food, according to a recent study published in Microbiome.
The researchers took a look at the composition of gut microbes in a group of 85 volunteers and found that about 40% had microbiomes dominated by Bacteroides bacteria, which are more effective at extracting nutrients from food. That group also weighed 10% more on average, amounting to an extra 9 kg.
In a rather blatant demonstration of efficiency, the investigators also measured the speed of the participants’ digestion, as they had hypothesized that those with the longest digestive travel times would be the ones who harvested the most nutrition from their food. That was not the case.
The study subjects with the most efficient gut bacteria “also have the fastest passage through the gastrointestinal system, which has given us something to think about,” senior author Henrik Roager of the University of Copenhagen said in a written statement.
You know what gives us something to think about? Stool energy density and intestinal transit time and faecal bacterial cell counts, that’s what. Ick. Sometimes science is gross.
Here’s another thought, though: Seeing faecal instead of fecal is kind of funny to our American eyes, but adding that extra letter is also inefficient, which could mean that it’s good. So, in the spirit of embracing the inefficient as a new year begins, we’re resolving to wrap our editorial arms around faecal and the faeces it represents. Well, not literally, of course. More like we’re embracing the spirit of faeces.





