User login
Official news magazine of the Society of Hospital Medicine
Copyright by Society of Hospital Medicine or related companies. All rights reserved. ISSN 1553-085X
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
div[contains(@class, 'pane-pub-article-hospitalist')]


Zika virus infection: Novel assay extends diagnostic window
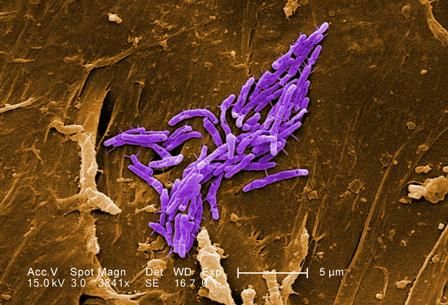
ATLANTA – A novel pyrosequencing (PSQ)–based reverse-transcription polymerase chain reaction (RT-PCR) assay improves and expands diagnostic capabilities for Zika virus infection, according to findings in 60 patients diagnosed with the virus in 2016 and 2017.
The PSQ assay provides rapid, specific, and cost-effective detection of the virus in tissues of congenital and pregnancy-associated infections, and, compared with serum-based assays, extends the time frame for Zika virus detection, Julu Bhatnagar, PhD, reported in a presentation at the International Conference on Emerging Infectious Diseases.
Dr. Bhatnagar and her colleagues from the Centers for Disease Control and Prevention in Atlanta developed the assay and evaluated it using RNA extracted from formalin-fixed, paraffin-embedded placental/fetal tissues from 53 women with varying pregnancy outcomes, and brain tissues from seven infants with microcephaly who died. In all of the tissue samples, which were received between January 2016 and August 2017, Zika virus was previously identified by conventional RT-PCR and Sanger sequencing.
The PSQ assay detected and sequence confirmed Zika virus in tissues from all 60 patients, whereas 40 negative control samples, including tissues from dengue- and chikungunya virus–confirmed cases, all tested negative.
In addition, the PSQ assay detected Zika virus in placental tissues from three other cases that were previously negative by the conventional tissue-based RT-PCR, thereby demonstrating better sensitivity of the PSQ assay in comparison to conventional tissue RT-PCR, said Dr. Bhatnagar, who is molecular pathology team leader in the Infectious Diseases Pathology Branch, Division of High-Consequence Pathogens and Pathology at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
“Importantly, PSQ results can be obtained in 1 day and at half the cost of Sanger sequencing,” she said.
The findings are important because Zika virus infection during pregnancy can cause microcephaly and is associated with pregnancy loss. Laboratory diagnosis of the virus is challenging for pregnancy-associated infections because of the short duration of viremia, she explained.
However, prolonged detection of Zika virus RNA in placental, fetal, and neonatal brain tissue has been reported.
Dr. Bhatnagar was the first author on a 2016 study published in Emerging Infectious Diseases that provided confirmation of the linkage of Zika virus with microcephaly and that suggested its association with adverse pregnancy outcomes and provided evidence of Zika virus replication and persistence in fetal brain and placenta.
“This article highlights the value of tissue analysis to expand opportunities to diagnose Zika virus congenital and pregnancy-associated infections and to enhance the understanding of mechanism of Zika virus intrauterine transmission and pathogenesis,” she and her colleagues wrote in that article. “In addition, the tissue-based RT-PCRs extend the time frame for Zika virus detection and particularly help to establish a diagnosis retrospectively, enabling pregnant women and their health care providers to identify the cause of severe microcephaly or fetal loss.”
Those findings led to the hypothesis that the PSQ assay evaluated in the current study would provide better opportunities for detection, particularly in cases where serum RT-PCR or serologic testing is negative because of testing performed outside the optimal testing window, she said.
Indeed, the novel assay not only allows for an extended time frame for Zika virus detection, it also provides insights into viral tissue tropism and persistence, she noted.
According to the CDC, no local mosquito-borne Zika virus transmissions have been reported in the continental United States in 2018, but transmission is still a threat internationally, and those traveling outside of the continental United States should find out if they are traveling to an area with risk of Zika.
Dr. Bhatnagar reported having no disclosures.
SOURCE: Bhatnagar J et al. ICEID 2018, Abstract O1.
ATLANTA – A novel pyrosequencing (PSQ)–based reverse-transcription polymerase chain reaction (RT-PCR) assay improves and expands diagnostic capabilities for Zika virus infection, according to findings in 60 patients diagnosed with the virus in 2016 and 2017.
The PSQ assay provides rapid, specific, and cost-effective detection of the virus in tissues of congenital and pregnancy-associated infections, and, compared with serum-based assays, extends the time frame for Zika virus detection, Julu Bhatnagar, PhD, reported in a presentation at the International Conference on Emerging Infectious Diseases.
Dr. Bhatnagar and her colleagues from the Centers for Disease Control and Prevention in Atlanta developed the assay and evaluated it using RNA extracted from formalin-fixed, paraffin-embedded placental/fetal tissues from 53 women with varying pregnancy outcomes, and brain tissues from seven infants with microcephaly who died. In all of the tissue samples, which were received between January 2016 and August 2017, Zika virus was previously identified by conventional RT-PCR and Sanger sequencing.
The PSQ assay detected and sequence confirmed Zika virus in tissues from all 60 patients, whereas 40 negative control samples, including tissues from dengue- and chikungunya virus–confirmed cases, all tested negative.
In addition, the PSQ assay detected Zika virus in placental tissues from three other cases that were previously negative by the conventional tissue-based RT-PCR, thereby demonstrating better sensitivity of the PSQ assay in comparison to conventional tissue RT-PCR, said Dr. Bhatnagar, who is molecular pathology team leader in the Infectious Diseases Pathology Branch, Division of High-Consequence Pathogens and Pathology at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
“Importantly, PSQ results can be obtained in 1 day and at half the cost of Sanger sequencing,” she said.
The findings are important because Zika virus infection during pregnancy can cause microcephaly and is associated with pregnancy loss. Laboratory diagnosis of the virus is challenging for pregnancy-associated infections because of the short duration of viremia, she explained.
However, prolonged detection of Zika virus RNA in placental, fetal, and neonatal brain tissue has been reported.
Dr. Bhatnagar was the first author on a 2016 study published in Emerging Infectious Diseases that provided confirmation of the linkage of Zika virus with microcephaly and that suggested its association with adverse pregnancy outcomes and provided evidence of Zika virus replication and persistence in fetal brain and placenta.
“This article highlights the value of tissue analysis to expand opportunities to diagnose Zika virus congenital and pregnancy-associated infections and to enhance the understanding of mechanism of Zika virus intrauterine transmission and pathogenesis,” she and her colleagues wrote in that article. “In addition, the tissue-based RT-PCRs extend the time frame for Zika virus detection and particularly help to establish a diagnosis retrospectively, enabling pregnant women and their health care providers to identify the cause of severe microcephaly or fetal loss.”
Those findings led to the hypothesis that the PSQ assay evaluated in the current study would provide better opportunities for detection, particularly in cases where serum RT-PCR or serologic testing is negative because of testing performed outside the optimal testing window, she said.
Indeed, the novel assay not only allows for an extended time frame for Zika virus detection, it also provides insights into viral tissue tropism and persistence, she noted.
According to the CDC, no local mosquito-borne Zika virus transmissions have been reported in the continental United States in 2018, but transmission is still a threat internationally, and those traveling outside of the continental United States should find out if they are traveling to an area with risk of Zika.
Dr. Bhatnagar reported having no disclosures.
SOURCE: Bhatnagar J et al. ICEID 2018, Abstract O1.
ATLANTA – A novel pyrosequencing (PSQ)–based reverse-transcription polymerase chain reaction (RT-PCR) assay improves and expands diagnostic capabilities for Zika virus infection, according to findings in 60 patients diagnosed with the virus in 2016 and 2017.
The PSQ assay provides rapid, specific, and cost-effective detection of the virus in tissues of congenital and pregnancy-associated infections, and, compared with serum-based assays, extends the time frame for Zika virus detection, Julu Bhatnagar, PhD, reported in a presentation at the International Conference on Emerging Infectious Diseases.
Dr. Bhatnagar and her colleagues from the Centers for Disease Control and Prevention in Atlanta developed the assay and evaluated it using RNA extracted from formalin-fixed, paraffin-embedded placental/fetal tissues from 53 women with varying pregnancy outcomes, and brain tissues from seven infants with microcephaly who died. In all of the tissue samples, which were received between January 2016 and August 2017, Zika virus was previously identified by conventional RT-PCR and Sanger sequencing.
The PSQ assay detected and sequence confirmed Zika virus in tissues from all 60 patients, whereas 40 negative control samples, including tissues from dengue- and chikungunya virus–confirmed cases, all tested negative.
In addition, the PSQ assay detected Zika virus in placental tissues from three other cases that were previously negative by the conventional tissue-based RT-PCR, thereby demonstrating better sensitivity of the PSQ assay in comparison to conventional tissue RT-PCR, said Dr. Bhatnagar, who is molecular pathology team leader in the Infectious Diseases Pathology Branch, Division of High-Consequence Pathogens and Pathology at the CDC’s National Center for Emerging and Zoonotic Infectious Diseases.
“Importantly, PSQ results can be obtained in 1 day and at half the cost of Sanger sequencing,” she said.
The findings are important because Zika virus infection during pregnancy can cause microcephaly and is associated with pregnancy loss. Laboratory diagnosis of the virus is challenging for pregnancy-associated infections because of the short duration of viremia, she explained.
However, prolonged detection of Zika virus RNA in placental, fetal, and neonatal brain tissue has been reported.
Dr. Bhatnagar was the first author on a 2016 study published in Emerging Infectious Diseases that provided confirmation of the linkage of Zika virus with microcephaly and that suggested its association with adverse pregnancy outcomes and provided evidence of Zika virus replication and persistence in fetal brain and placenta.
“This article highlights the value of tissue analysis to expand opportunities to diagnose Zika virus congenital and pregnancy-associated infections and to enhance the understanding of mechanism of Zika virus intrauterine transmission and pathogenesis,” she and her colleagues wrote in that article. “In addition, the tissue-based RT-PCRs extend the time frame for Zika virus detection and particularly help to establish a diagnosis retrospectively, enabling pregnant women and their health care providers to identify the cause of severe microcephaly or fetal loss.”
Those findings led to the hypothesis that the PSQ assay evaluated in the current study would provide better opportunities for detection, particularly in cases where serum RT-PCR or serologic testing is negative because of testing performed outside the optimal testing window, she said.
Indeed, the novel assay not only allows for an extended time frame for Zika virus detection, it also provides insights into viral tissue tropism and persistence, she noted.
According to the CDC, no local mosquito-borne Zika virus transmissions have been reported in the continental United States in 2018, but transmission is still a threat internationally, and those traveling outside of the continental United States should find out if they are traveling to an area with risk of Zika.
Dr. Bhatnagar reported having no disclosures.
SOURCE: Bhatnagar J et al. ICEID 2018, Abstract O1.
REPORTING FROM ICEID 2018
Key clinical point: A novel assay extends the time frame for diagnosing Zika virus infection.
Major finding: The PSQ assay detected and sequence confirmed Zika virus in all 60 samples; 40 negative control samples all tested negative.
Study details: An analysis of 60 tissue samples using a novel assay.
Disclosures: Dr. Bhatnagar reported having no disclosures.
Source: Bhatnagar J et al. ICEID 2018, Abstract O1.
Does nurse-physician rounding matter?
Advancing the Quadruple Aim
Inadequate and fragmented communication between physicians and nurses can lead to unwelcome events for the hospitalized patient and clinicians. Missing orders, medication errors, patient misidentification, and lack of physician awareness of significant changes in patient status are just some examples of how deficits in formal communication can affect health outcomes during acute stays.
A 2000 Institute of Medicine report showed that bad systems, not bad people, account for the majority of errors and injuries caused by complexity, professional fragmentation, and barriers in communication. Their recommendation was to train physicians, nurses, and other professionals in teamwork.1,2 However, as Milisa Manojlovich, PhD, RN, found, there are significant differences in how physicians and nurses perceive collaboration and communication.3
Nurse-physician rounding was historically standard for patient care during hospitalization. When physicians split time between inpatient and outpatient care, nurses had to maximize their time to collaborate and communicate with physicians whenever the physicians left their outpatient offices to come and round on their patients. Today most inpatient care is delivered by hospitalists on a 24-hour basis. This continuous availability of physicians reduces the perceived need to have joint rounds.
However, health care teams in acute care facilities now face higher and sicker patient volumes, different productivity models and demands, new compliance standards, changing work flows, and increased complexity of treatment and management of patients. This has led to gaps in timely communication and partnership.4-6 Erosion of the traditional nurse-physician relationships affects the quality of patient care, the patient’s experience, and patient safety.8-10 Poor communication among health care team members is one of the most common causes of patient care errors.4 Poor nurse-physician communication can also lead to medical errors, poor outcomes caused by lack of coordination within the treatment team, increased use of unnecessary resources with inefficiency, and increases in the complexity of communication among team members, and time wastage.5,7,11 All these lead to poor work flows and directly affect patient safety.7
At Lee Health System in Lee County, Fla., we saw an opportunity in this changing health care environment to promote nurse-physician rounding. We created a structured, standardized process for morning rounding and engaged unit clerks, nursing leadership, and hospitalist service line leaders. We envisioned improvement of the patient experience, nurse-physician relationship, quality of care, the discharge planning process, and efficiency, as well as decreasing length of stay, improving communication, and bringing the patient and the treatment team closer, as demonstrated by Bradley Monash, MD, et al.12
Some data suggest that patient-centered bedside rounds on hospitalized patients have no effect on patient perceptions or their satisfaction with care.13 However, we felt that collaboration among a multidisciplinary team would help us achieve better outcomes. For example, our patients would perceive the care team (MD-RN) as a cohesive unit, and in turn gain trust in the members of the treatment team, as found by Nathalie McIntosh, PhD, et al and by Jason Ramirez, MD.7,16 Our vision was to empower nurses to be advocates for patients and their family members as they navigated their acute care admission. Nurses could also support physicians by communicating the physicians’ care plans to families and patients. After rounding with the physician, the nurse would be part of the decision-making process and care planning.17
Every rounding session had discharge planning and hospital stay expectations that were shared with the patient and nurse, who could then partner with case managers and social workers, which would streamline and reduce length of stay.14 We hoped rounding would also decrease the number of nurse pages to clarify or question orders. This would, in turn, improve daily work flow for the physicians and the nursing team with improvements in employee satisfaction scores.15 A study also has demonstrated a reduction in readmission rates from nurse-physician rounding.19
A disconnect in communication and trust between physicians and the nursing staff was reflected in low patient experience scores and perceived quality of care received during in-hospital stay. Gwendolyn Lancaster, EdD, MSN, RN, CCRN, et al, as well as a Joint Commission report, demonstrated how a lack of communication and poor team dynamics can translate to poor patient experience and be a major cause for sentinel events.6,20 Artificial, forced hierarchies and role perception among health care team members led to frustration, hostility, and distrust, which compromises quality and patient safety.1
One of our biggest challenges when we started this project was explaining the “Why” to the hospitalist group and nursing staff. Physicians were used to being the dominant partner in the team. Partnering with and engaging nurses in shared decision making and care planning was a seismic shift in culture and work flow within the care team. Early gains helped skeptical team members begin to understand the value in nurse-physician rounding. Near universal adoption of the rounding process at Lee Health has caused improvements in the working relationship and trust among the health care professionals. We have seen improvements in utilization management, as well as appropriateness and timeliness of resource use, because of better communication and understanding of care plans by nursing and physicians. Collaboration with specialists and alignment in care planning are other gains. Hospitalists and nurses are both very satisfied with the decrease in the number of pages during the day, and this has lowered stressors on health care teams.
How we did it
Nurse-physician rounding is a proven method to improve collaboration, communication, and relationships among health care team members in acute care facilities. In the complex health care challenges faced today, this improved work flow for taking care of patients can help advance the Quadruple Aim of high quality, low cost, improved patient experience, physician, and staff satisfaction.21
Lee Health System includes four facilities in Lee County, with a total of 1,216 licensed adult acute care beds. The pilot project was started in 2014.
Initially the vice president of nursing and the hospitalist medical director met to create an education plan for nurses and physicians. We chose one adult medicine unit to pilot the project because there already existed a closely knit nursing and hospitalist team. In our facility there is no strict geographical rounding; each hospitalist carries between three and six patients in the unit. As a first step, a nurse floor assignment sheet was faxed in the morning to the hospitalist office with the direct phone numbers of the nurses. The unit clerk, using physician assignments in the EHR, teamed up the physician and nurses for rounding. Once the physician arrived at the unit, he or she checked in with the unit clerk, who alerted nurses that the hospitalist was available on the floor to commence rounding. If the primary nurse was unavailable because of other duties or breaks, the charge nurse rounded with the physician.
Once in the room with the patient, the duo introduced themselves as members of the treatment team and acknowledged the patient’s needs. During the visit, care plans and treatment were reviewed, the patient’s questions were answered, a physical exam was completed, and lab and imaging results were discussed; the nurse also helped raise questions he or she had received from family members so answers could be communicated to the family later. Patients appreciated knowing that their physicians and nurses were working together as a team for their safety and recovery. During the visit, care was taken to focus specially on the course of hospitalization and discharge planning.
We tracked the rounding with a manual paper process maintained by the charge nurse. Our initial rounding rates were 30%-40%, and we continued to promote this initiative to the team, and eventually the importance and value of these rounds caught on with both nurses and physicians, and now our current average rounding rate is 90%. We then decided to scale this to all units in the hospital.
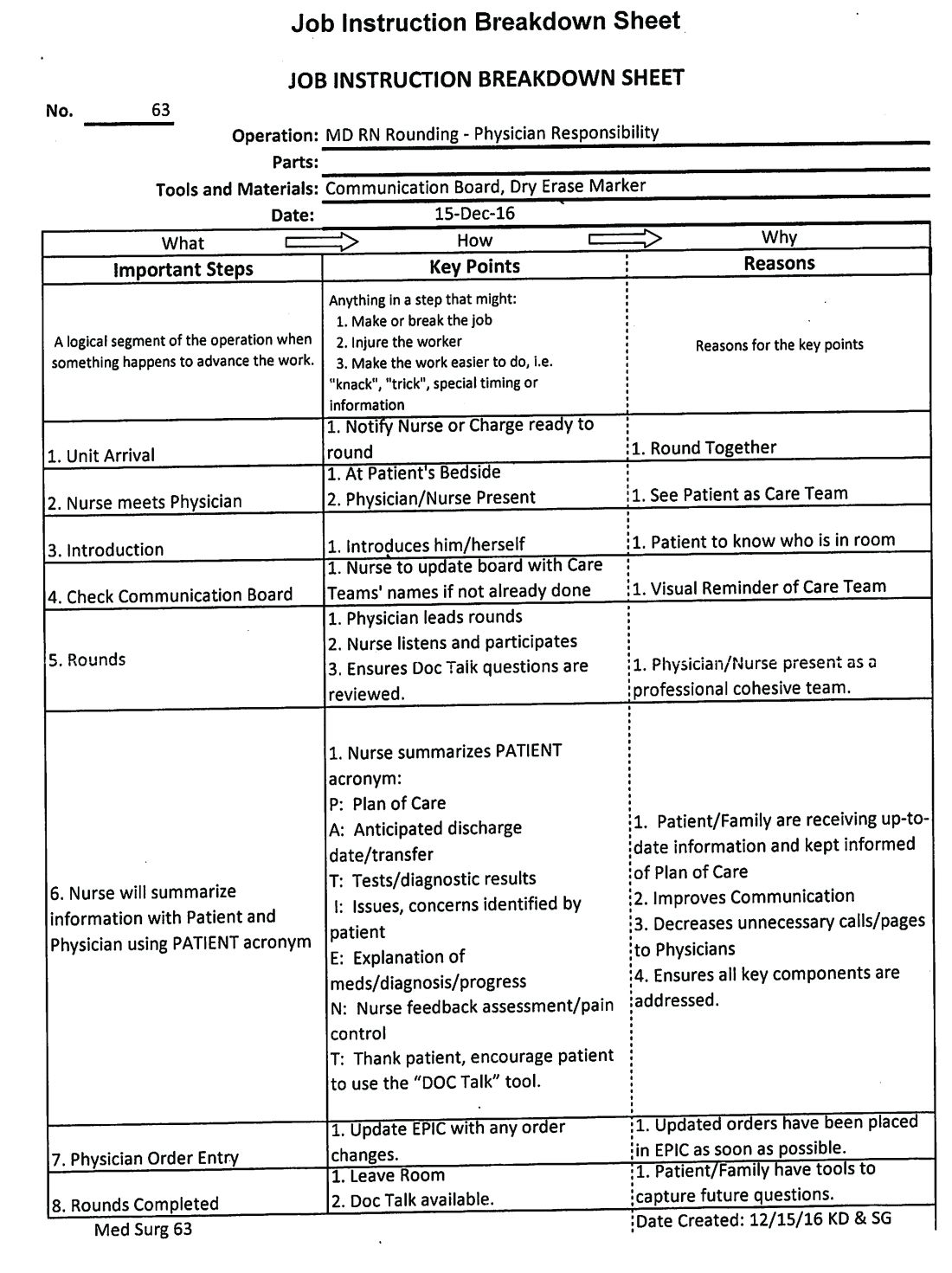
This process was repeated at other hospitals in the system once a standardized work flow was created (See Image 1). This initiative was next presented to the health system board of directors, who agreed that nurse-physician rounding should be the standard of care across our health system. Through partnership and collaboration with the IT department, we developed a tool to track nurse-physician rounding through our EHR system, which gave accountability to both physicians and nurses.
In conclusion, improved communication by timely nurse-physician rounding can lead to better outcomes for patients and also reduce costs and improve patient and staff experience, advancing the Quadruple Aim. Moving forward to build and sustain this work flow, we plan to continue nurse-physician collaboration across the health system consistently and for all areas of acute care operations.
Explaining the “Why,” sharing data on the benefits of the model, and reinforcing documentation of the rounding in our EHR are some steps we have put into action at leadership and staff meetings to sustain the activity. We are soliciting feedback, as well as monitoring and identifying any unaddressed barriers during rounding. Addition of this process measure to our quality improvement bonus opportunity also has helped to sustain performance from our teams.
Dr. Laufer is system medical director of hospital medicine and transitional care at Lee Health in Ft. Myers, Fla. Dr. Prasad is chief medical officer of Lee Physician Group, Ft. Myers, Fla.
References
1. Leape LL et al. Five years after to err is human: What we have learned? JAMA. 2005;293(19):2384-90.
2. Sutcliffe KM et al. Communication failures: An insidious contributor to medical mishaps. Acad Med. 2004;79(2):186-94.
3. Manojlovich M. Reframing communication with physicians as sensemaking. J Nurs Care Qual. 2013 Oct-Dec;28(4):295-303.
4. Siegele P. Enhancing outcomes in a surgical intensive care unit by implementing daily goals. Crit Care Nurse. 2009 Dec;29(6):58-69.
5. Asthon J et al. Qualitative evaluation of regular morning meeting aimed at improving interdisciplinary communication and patient outcomes. Int J Nurs Pract. 2005 Oct;11(5):206-13.
6. Lancaster G et al. Interdisciplinary Communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015 May;47(3):275-84.
7. McIntosh N et al. Impact of provider coordination on nurse and physician perception of patient care quality. J Nurs Care Qual. 2014 Jul-Sep;29(3):269-79.
8. Jo M et al. An organizational assessment of disruptive clinical behavior. J Nurs Care Qual. 2013 Apr-Jun;28(2):110-21.
9. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, 2010.
10. O’Connor P et al. A mixed-methods study of the causes and impact of poor teamwork between junior doctors and nurses. Int J Qual Health Care. 2016 Jun;28(3):339-45.
11. Manojlovich M. Nurse/Physician communication through a sense making lens. Med Care. 2010 Nov;48(11):941-6.
12. Monash B et al. Standardized attending rounds to improve the patient experience: A pragmatic cluster randomized controlled trial. J Hosp Med. 2017 Mar;12(3):143-9.
13. O’Leary KJ et al. Effect of patient-centered bedside rounds on hospitalized patients decision control, activation and satisfaction with care. BMJ Qual Saf. 2016 Dec;25(12):921-8.
14. Dutton RP et al. Daily multidisciplinary rounds shorten length of stay for trauma patients. J Trauma. 2003 Nov;55(5):913-9.
15. Manojlovich M et al. Healthy work environments, nurse-physician communication, and patients’ outcomes. Am J Crit Care. 2007 Nov;16(6):536-43.
16. Ramirez J et al. Patient satisfaction with bedside teaching rounds compared with nonbedside rounds. South Med J. 2016 Feb;109(2):112-5.
17. Sollami A et al. Nurse-Physician collaboration: A meta-analytical investigation of survey scores. J Interprof Care. 2015 May;29(3):223-9.
18. House S et al. Nurses and physicians perceptions of nurse-physician collaboration. J Nurs Adm. 2017 Mar;47(3):165-71.
19. Townsend-Gervis M et al. Interdisciplinary rounds and structured communications reduce re-admissions and improve some patients’ outcomes. West J Nurs Res. 2014 Aug;36(7):917-28.
20. The Joint Commission. Sentinel Events. http://www.jointcommission.org/sentinel_event.aspx. Accessed Oct 2017.
21. Bodenheimer T et al. From Triple to Quadruple Aim: Care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6.
Advancing the Quadruple Aim
Advancing the Quadruple Aim
Inadequate and fragmented communication between physicians and nurses can lead to unwelcome events for the hospitalized patient and clinicians. Missing orders, medication errors, patient misidentification, and lack of physician awareness of significant changes in patient status are just some examples of how deficits in formal communication can affect health outcomes during acute stays.
A 2000 Institute of Medicine report showed that bad systems, not bad people, account for the majority of errors and injuries caused by complexity, professional fragmentation, and barriers in communication. Their recommendation was to train physicians, nurses, and other professionals in teamwork.1,2 However, as Milisa Manojlovich, PhD, RN, found, there are significant differences in how physicians and nurses perceive collaboration and communication.3
Nurse-physician rounding was historically standard for patient care during hospitalization. When physicians split time between inpatient and outpatient care, nurses had to maximize their time to collaborate and communicate with physicians whenever the physicians left their outpatient offices to come and round on their patients. Today most inpatient care is delivered by hospitalists on a 24-hour basis. This continuous availability of physicians reduces the perceived need to have joint rounds.
However, health care teams in acute care facilities now face higher and sicker patient volumes, different productivity models and demands, new compliance standards, changing work flows, and increased complexity of treatment and management of patients. This has led to gaps in timely communication and partnership.4-6 Erosion of the traditional nurse-physician relationships affects the quality of patient care, the patient’s experience, and patient safety.8-10 Poor communication among health care team members is one of the most common causes of patient care errors.4 Poor nurse-physician communication can also lead to medical errors, poor outcomes caused by lack of coordination within the treatment team, increased use of unnecessary resources with inefficiency, and increases in the complexity of communication among team members, and time wastage.5,7,11 All these lead to poor work flows and directly affect patient safety.7
At Lee Health System in Lee County, Fla., we saw an opportunity in this changing health care environment to promote nurse-physician rounding. We created a structured, standardized process for morning rounding and engaged unit clerks, nursing leadership, and hospitalist service line leaders. We envisioned improvement of the patient experience, nurse-physician relationship, quality of care, the discharge planning process, and efficiency, as well as decreasing length of stay, improving communication, and bringing the patient and the treatment team closer, as demonstrated by Bradley Monash, MD, et al.12
Some data suggest that patient-centered bedside rounds on hospitalized patients have no effect on patient perceptions or their satisfaction with care.13 However, we felt that collaboration among a multidisciplinary team would help us achieve better outcomes. For example, our patients would perceive the care team (MD-RN) as a cohesive unit, and in turn gain trust in the members of the treatment team, as found by Nathalie McIntosh, PhD, et al and by Jason Ramirez, MD.7,16 Our vision was to empower nurses to be advocates for patients and their family members as they navigated their acute care admission. Nurses could also support physicians by communicating the physicians’ care plans to families and patients. After rounding with the physician, the nurse would be part of the decision-making process and care planning.17
Every rounding session had discharge planning and hospital stay expectations that were shared with the patient and nurse, who could then partner with case managers and social workers, which would streamline and reduce length of stay.14 We hoped rounding would also decrease the number of nurse pages to clarify or question orders. This would, in turn, improve daily work flow for the physicians and the nursing team with improvements in employee satisfaction scores.15 A study also has demonstrated a reduction in readmission rates from nurse-physician rounding.19
A disconnect in communication and trust between physicians and the nursing staff was reflected in low patient experience scores and perceived quality of care received during in-hospital stay. Gwendolyn Lancaster, EdD, MSN, RN, CCRN, et al, as well as a Joint Commission report, demonstrated how a lack of communication and poor team dynamics can translate to poor patient experience and be a major cause for sentinel events.6,20 Artificial, forced hierarchies and role perception among health care team members led to frustration, hostility, and distrust, which compromises quality and patient safety.1
One of our biggest challenges when we started this project was explaining the “Why” to the hospitalist group and nursing staff. Physicians were used to being the dominant partner in the team. Partnering with and engaging nurses in shared decision making and care planning was a seismic shift in culture and work flow within the care team. Early gains helped skeptical team members begin to understand the value in nurse-physician rounding. Near universal adoption of the rounding process at Lee Health has caused improvements in the working relationship and trust among the health care professionals. We have seen improvements in utilization management, as well as appropriateness and timeliness of resource use, because of better communication and understanding of care plans by nursing and physicians. Collaboration with specialists and alignment in care planning are other gains. Hospitalists and nurses are both very satisfied with the decrease in the number of pages during the day, and this has lowered stressors on health care teams.
How we did it
Nurse-physician rounding is a proven method to improve collaboration, communication, and relationships among health care team members in acute care facilities. In the complex health care challenges faced today, this improved work flow for taking care of patients can help advance the Quadruple Aim of high quality, low cost, improved patient experience, physician, and staff satisfaction.21
Lee Health System includes four facilities in Lee County, with a total of 1,216 licensed adult acute care beds. The pilot project was started in 2014.
Initially the vice president of nursing and the hospitalist medical director met to create an education plan for nurses and physicians. We chose one adult medicine unit to pilot the project because there already existed a closely knit nursing and hospitalist team. In our facility there is no strict geographical rounding; each hospitalist carries between three and six patients in the unit. As a first step, a nurse floor assignment sheet was faxed in the morning to the hospitalist office with the direct phone numbers of the nurses. The unit clerk, using physician assignments in the EHR, teamed up the physician and nurses for rounding. Once the physician arrived at the unit, he or she checked in with the unit clerk, who alerted nurses that the hospitalist was available on the floor to commence rounding. If the primary nurse was unavailable because of other duties or breaks, the charge nurse rounded with the physician.
Once in the room with the patient, the duo introduced themselves as members of the treatment team and acknowledged the patient’s needs. During the visit, care plans and treatment were reviewed, the patient’s questions were answered, a physical exam was completed, and lab and imaging results were discussed; the nurse also helped raise questions he or she had received from family members so answers could be communicated to the family later. Patients appreciated knowing that their physicians and nurses were working together as a team for their safety and recovery. During the visit, care was taken to focus specially on the course of hospitalization and discharge planning.
We tracked the rounding with a manual paper process maintained by the charge nurse. Our initial rounding rates were 30%-40%, and we continued to promote this initiative to the team, and eventually the importance and value of these rounds caught on with both nurses and physicians, and now our current average rounding rate is 90%. We then decided to scale this to all units in the hospital.
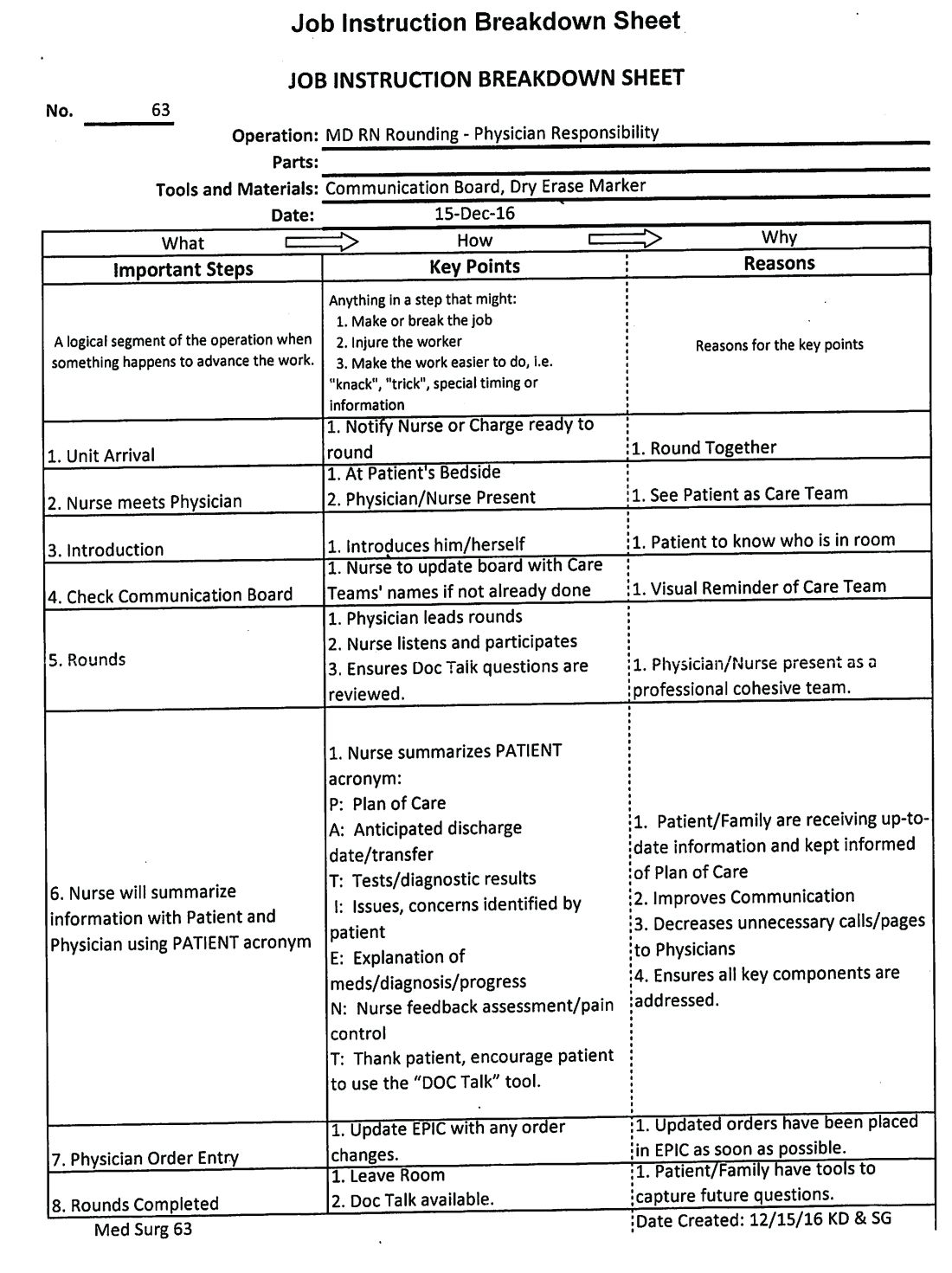
This process was repeated at other hospitals in the system once a standardized work flow was created (See Image 1). This initiative was next presented to the health system board of directors, who agreed that nurse-physician rounding should be the standard of care across our health system. Through partnership and collaboration with the IT department, we developed a tool to track nurse-physician rounding through our EHR system, which gave accountability to both physicians and nurses.
In conclusion, improved communication by timely nurse-physician rounding can lead to better outcomes for patients and also reduce costs and improve patient and staff experience, advancing the Quadruple Aim. Moving forward to build and sustain this work flow, we plan to continue nurse-physician collaboration across the health system consistently and for all areas of acute care operations.
Explaining the “Why,” sharing data on the benefits of the model, and reinforcing documentation of the rounding in our EHR are some steps we have put into action at leadership and staff meetings to sustain the activity. We are soliciting feedback, as well as monitoring and identifying any unaddressed barriers during rounding. Addition of this process measure to our quality improvement bonus opportunity also has helped to sustain performance from our teams.
Dr. Laufer is system medical director of hospital medicine and transitional care at Lee Health in Ft. Myers, Fla. Dr. Prasad is chief medical officer of Lee Physician Group, Ft. Myers, Fla.
References
1. Leape LL et al. Five years after to err is human: What we have learned? JAMA. 2005;293(19):2384-90.
2. Sutcliffe KM et al. Communication failures: An insidious contributor to medical mishaps. Acad Med. 2004;79(2):186-94.
3. Manojlovich M. Reframing communication with physicians as sensemaking. J Nurs Care Qual. 2013 Oct-Dec;28(4):295-303.
4. Siegele P. Enhancing outcomes in a surgical intensive care unit by implementing daily goals. Crit Care Nurse. 2009 Dec;29(6):58-69.
5. Asthon J et al. Qualitative evaluation of regular morning meeting aimed at improving interdisciplinary communication and patient outcomes. Int J Nurs Pract. 2005 Oct;11(5):206-13.
6. Lancaster G et al. Interdisciplinary Communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015 May;47(3):275-84.
7. McIntosh N et al. Impact of provider coordination on nurse and physician perception of patient care quality. J Nurs Care Qual. 2014 Jul-Sep;29(3):269-79.
8. Jo M et al. An organizational assessment of disruptive clinical behavior. J Nurs Care Qual. 2013 Apr-Jun;28(2):110-21.
9. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, 2010.
10. O’Connor P et al. A mixed-methods study of the causes and impact of poor teamwork between junior doctors and nurses. Int J Qual Health Care. 2016 Jun;28(3):339-45.
11. Manojlovich M. Nurse/Physician communication through a sense making lens. Med Care. 2010 Nov;48(11):941-6.
12. Monash B et al. Standardized attending rounds to improve the patient experience: A pragmatic cluster randomized controlled trial. J Hosp Med. 2017 Mar;12(3):143-9.
13. O’Leary KJ et al. Effect of patient-centered bedside rounds on hospitalized patients decision control, activation and satisfaction with care. BMJ Qual Saf. 2016 Dec;25(12):921-8.
14. Dutton RP et al. Daily multidisciplinary rounds shorten length of stay for trauma patients. J Trauma. 2003 Nov;55(5):913-9.
15. Manojlovich M et al. Healthy work environments, nurse-physician communication, and patients’ outcomes. Am J Crit Care. 2007 Nov;16(6):536-43.
16. Ramirez J et al. Patient satisfaction with bedside teaching rounds compared with nonbedside rounds. South Med J. 2016 Feb;109(2):112-5.
17. Sollami A et al. Nurse-Physician collaboration: A meta-analytical investigation of survey scores. J Interprof Care. 2015 May;29(3):223-9.
18. House S et al. Nurses and physicians perceptions of nurse-physician collaboration. J Nurs Adm. 2017 Mar;47(3):165-71.
19. Townsend-Gervis M et al. Interdisciplinary rounds and structured communications reduce re-admissions and improve some patients’ outcomes. West J Nurs Res. 2014 Aug;36(7):917-28.
20. The Joint Commission. Sentinel Events. http://www.jointcommission.org/sentinel_event.aspx. Accessed Oct 2017.
21. Bodenheimer T et al. From Triple to Quadruple Aim: Care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6.
Inadequate and fragmented communication between physicians and nurses can lead to unwelcome events for the hospitalized patient and clinicians. Missing orders, medication errors, patient misidentification, and lack of physician awareness of significant changes in patient status are just some examples of how deficits in formal communication can affect health outcomes during acute stays.
A 2000 Institute of Medicine report showed that bad systems, not bad people, account for the majority of errors and injuries caused by complexity, professional fragmentation, and barriers in communication. Their recommendation was to train physicians, nurses, and other professionals in teamwork.1,2 However, as Milisa Manojlovich, PhD, RN, found, there are significant differences in how physicians and nurses perceive collaboration and communication.3
Nurse-physician rounding was historically standard for patient care during hospitalization. When physicians split time between inpatient and outpatient care, nurses had to maximize their time to collaborate and communicate with physicians whenever the physicians left their outpatient offices to come and round on their patients. Today most inpatient care is delivered by hospitalists on a 24-hour basis. This continuous availability of physicians reduces the perceived need to have joint rounds.
However, health care teams in acute care facilities now face higher and sicker patient volumes, different productivity models and demands, new compliance standards, changing work flows, and increased complexity of treatment and management of patients. This has led to gaps in timely communication and partnership.4-6 Erosion of the traditional nurse-physician relationships affects the quality of patient care, the patient’s experience, and patient safety.8-10 Poor communication among health care team members is one of the most common causes of patient care errors.4 Poor nurse-physician communication can also lead to medical errors, poor outcomes caused by lack of coordination within the treatment team, increased use of unnecessary resources with inefficiency, and increases in the complexity of communication among team members, and time wastage.5,7,11 All these lead to poor work flows and directly affect patient safety.7
At Lee Health System in Lee County, Fla., we saw an opportunity in this changing health care environment to promote nurse-physician rounding. We created a structured, standardized process for morning rounding and engaged unit clerks, nursing leadership, and hospitalist service line leaders. We envisioned improvement of the patient experience, nurse-physician relationship, quality of care, the discharge planning process, and efficiency, as well as decreasing length of stay, improving communication, and bringing the patient and the treatment team closer, as demonstrated by Bradley Monash, MD, et al.12
Some data suggest that patient-centered bedside rounds on hospitalized patients have no effect on patient perceptions or their satisfaction with care.13 However, we felt that collaboration among a multidisciplinary team would help us achieve better outcomes. For example, our patients would perceive the care team (MD-RN) as a cohesive unit, and in turn gain trust in the members of the treatment team, as found by Nathalie McIntosh, PhD, et al and by Jason Ramirez, MD.7,16 Our vision was to empower nurses to be advocates for patients and their family members as they navigated their acute care admission. Nurses could also support physicians by communicating the physicians’ care plans to families and patients. After rounding with the physician, the nurse would be part of the decision-making process and care planning.17
Every rounding session had discharge planning and hospital stay expectations that were shared with the patient and nurse, who could then partner with case managers and social workers, which would streamline and reduce length of stay.14 We hoped rounding would also decrease the number of nurse pages to clarify or question orders. This would, in turn, improve daily work flow for the physicians and the nursing team with improvements in employee satisfaction scores.15 A study also has demonstrated a reduction in readmission rates from nurse-physician rounding.19
A disconnect in communication and trust between physicians and the nursing staff was reflected in low patient experience scores and perceived quality of care received during in-hospital stay. Gwendolyn Lancaster, EdD, MSN, RN, CCRN, et al, as well as a Joint Commission report, demonstrated how a lack of communication and poor team dynamics can translate to poor patient experience and be a major cause for sentinel events.6,20 Artificial, forced hierarchies and role perception among health care team members led to frustration, hostility, and distrust, which compromises quality and patient safety.1
One of our biggest challenges when we started this project was explaining the “Why” to the hospitalist group and nursing staff. Physicians were used to being the dominant partner in the team. Partnering with and engaging nurses in shared decision making and care planning was a seismic shift in culture and work flow within the care team. Early gains helped skeptical team members begin to understand the value in nurse-physician rounding. Near universal adoption of the rounding process at Lee Health has caused improvements in the working relationship and trust among the health care professionals. We have seen improvements in utilization management, as well as appropriateness and timeliness of resource use, because of better communication and understanding of care plans by nursing and physicians. Collaboration with specialists and alignment in care planning are other gains. Hospitalists and nurses are both very satisfied with the decrease in the number of pages during the day, and this has lowered stressors on health care teams.
How we did it
Nurse-physician rounding is a proven method to improve collaboration, communication, and relationships among health care team members in acute care facilities. In the complex health care challenges faced today, this improved work flow for taking care of patients can help advance the Quadruple Aim of high quality, low cost, improved patient experience, physician, and staff satisfaction.21
Lee Health System includes four facilities in Lee County, with a total of 1,216 licensed adult acute care beds. The pilot project was started in 2014.
Initially the vice president of nursing and the hospitalist medical director met to create an education plan for nurses and physicians. We chose one adult medicine unit to pilot the project because there already existed a closely knit nursing and hospitalist team. In our facility there is no strict geographical rounding; each hospitalist carries between three and six patients in the unit. As a first step, a nurse floor assignment sheet was faxed in the morning to the hospitalist office with the direct phone numbers of the nurses. The unit clerk, using physician assignments in the EHR, teamed up the physician and nurses for rounding. Once the physician arrived at the unit, he or she checked in with the unit clerk, who alerted nurses that the hospitalist was available on the floor to commence rounding. If the primary nurse was unavailable because of other duties or breaks, the charge nurse rounded with the physician.
Once in the room with the patient, the duo introduced themselves as members of the treatment team and acknowledged the patient’s needs. During the visit, care plans and treatment were reviewed, the patient’s questions were answered, a physical exam was completed, and lab and imaging results were discussed; the nurse also helped raise questions he or she had received from family members so answers could be communicated to the family later. Patients appreciated knowing that their physicians and nurses were working together as a team for their safety and recovery. During the visit, care was taken to focus specially on the course of hospitalization and discharge planning.
We tracked the rounding with a manual paper process maintained by the charge nurse. Our initial rounding rates were 30%-40%, and we continued to promote this initiative to the team, and eventually the importance and value of these rounds caught on with both nurses and physicians, and now our current average rounding rate is 90%. We then decided to scale this to all units in the hospital.
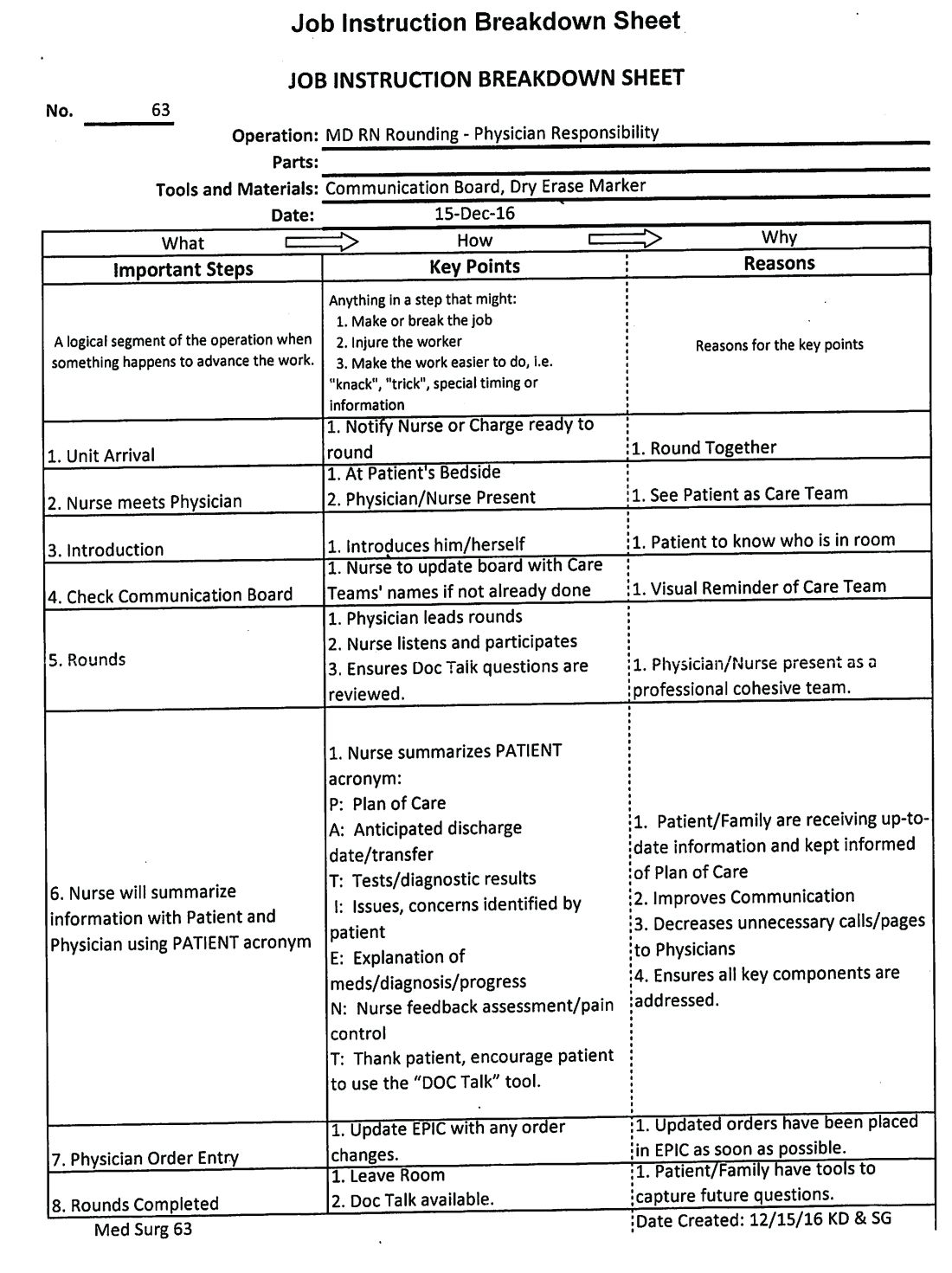
This process was repeated at other hospitals in the system once a standardized work flow was created (See Image 1). This initiative was next presented to the health system board of directors, who agreed that nurse-physician rounding should be the standard of care across our health system. Through partnership and collaboration with the IT department, we developed a tool to track nurse-physician rounding through our EHR system, which gave accountability to both physicians and nurses.
In conclusion, improved communication by timely nurse-physician rounding can lead to better outcomes for patients and also reduce costs and improve patient and staff experience, advancing the Quadruple Aim. Moving forward to build and sustain this work flow, we plan to continue nurse-physician collaboration across the health system consistently and for all areas of acute care operations.
Explaining the “Why,” sharing data on the benefits of the model, and reinforcing documentation of the rounding in our EHR are some steps we have put into action at leadership and staff meetings to sustain the activity. We are soliciting feedback, as well as monitoring and identifying any unaddressed barriers during rounding. Addition of this process measure to our quality improvement bonus opportunity also has helped to sustain performance from our teams.
Dr. Laufer is system medical director of hospital medicine and transitional care at Lee Health in Ft. Myers, Fla. Dr. Prasad is chief medical officer of Lee Physician Group, Ft. Myers, Fla.
References
1. Leape LL et al. Five years after to err is human: What we have learned? JAMA. 2005;293(19):2384-90.
2. Sutcliffe KM et al. Communication failures: An insidious contributor to medical mishaps. Acad Med. 2004;79(2):186-94.
3. Manojlovich M. Reframing communication with physicians as sensemaking. J Nurs Care Qual. 2013 Oct-Dec;28(4):295-303.
4. Siegele P. Enhancing outcomes in a surgical intensive care unit by implementing daily goals. Crit Care Nurse. 2009 Dec;29(6):58-69.
5. Asthon J et al. Qualitative evaluation of regular morning meeting aimed at improving interdisciplinary communication and patient outcomes. Int J Nurs Pract. 2005 Oct;11(5):206-13.
6. Lancaster G et al. Interdisciplinary Communication and collaboration among physicians, nurses, and unlicensed assistive personnel. J Nurs Scholarsh. 2015 May;47(3):275-84.
7. McIntosh N et al. Impact of provider coordination on nurse and physician perception of patient care quality. J Nurs Care Qual. 2014 Jul-Sep;29(3):269-79.
8. Jo M et al. An organizational assessment of disruptive clinical behavior. J Nurs Care Qual. 2013 Apr-Jun;28(2):110-21.
9. World Health Organization. Framework for action on interprofessional education and collaborative practice. Geneva, 2010.
10. O’Connor P et al. A mixed-methods study of the causes and impact of poor teamwork between junior doctors and nurses. Int J Qual Health Care. 2016 Jun;28(3):339-45.
11. Manojlovich M. Nurse/Physician communication through a sense making lens. Med Care. 2010 Nov;48(11):941-6.
12. Monash B et al. Standardized attending rounds to improve the patient experience: A pragmatic cluster randomized controlled trial. J Hosp Med. 2017 Mar;12(3):143-9.
13. O’Leary KJ et al. Effect of patient-centered bedside rounds on hospitalized patients decision control, activation and satisfaction with care. BMJ Qual Saf. 2016 Dec;25(12):921-8.
14. Dutton RP et al. Daily multidisciplinary rounds shorten length of stay for trauma patients. J Trauma. 2003 Nov;55(5):913-9.
15. Manojlovich M et al. Healthy work environments, nurse-physician communication, and patients’ outcomes. Am J Crit Care. 2007 Nov;16(6):536-43.
16. Ramirez J et al. Patient satisfaction with bedside teaching rounds compared with nonbedside rounds. South Med J. 2016 Feb;109(2):112-5.
17. Sollami A et al. Nurse-Physician collaboration: A meta-analytical investigation of survey scores. J Interprof Care. 2015 May;29(3):223-9.
18. House S et al. Nurses and physicians perceptions of nurse-physician collaboration. J Nurs Adm. 2017 Mar;47(3):165-71.
19. Townsend-Gervis M et al. Interdisciplinary rounds and structured communications reduce re-admissions and improve some patients’ outcomes. West J Nurs Res. 2014 Aug;36(7):917-28.
20. The Joint Commission. Sentinel Events. http://www.jointcommission.org/sentinel_event.aspx. Accessed Oct 2017.
21. Bodenheimer T et al. From Triple to Quadruple Aim: Care of the patient requires care of the provider. Ann Fam Med. 2014 Nov-Dec;12(6):573-6.
Burnout may jeopardize patient care
because of depersonalization of care, according to recent research published in JAMA Internal Medicine.
“The primary conclusion of this review is that physician burnout might jeopardize patient care,” Maria Panagioti, PhD, from the National Institute for Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre at the University of Manchester (United Kingdom) and her colleagues wrote in their study. “Physician wellness and quality of patient care are critical [as are] complementary dimensions of health care organization efficiency.”
Dr. Panagioti and her colleagues performed a search of the MEDLINE, EMBASE, CINAHL, and PsycInfo databases and found 47 eligible studies on the topics of physician burnout and patient care, which altogether included data from a pooled cohort of 42,473 physicians. The physicians were median 38 years old, with 44.7% of studies looking at physicians in residency or early career (up to 5 years post residency) and 55.3% of studies examining experienced physicians. The meta-analysis also evaluated physicians in a hospital setting (63.8%), primary care (13.8%), and across various different health care settings (8.5%).
The researchers found physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85). System-reported instances of patient safety issues and low professionalism were not statistically significant, but the subgroup differences did reach statistical significance (Cohen Q, 8.14; P = .007). Among residents and physicians in their early career, there was a greater association between burnout and low professionalism (OR, 3.39; 95% CI, 2.38-4.40), compared with physicians in the middle or later in their career (OR, 1.73; 95% CI, 1.46-2.01; Cohen Q, 7.27; P = .003).
“Investments in organizational strategies to jointly monitor and improve physician wellness and patient care outcomes are needed,” Dr. Panagioti and her colleagues wrote in the study. “Interventions aimed at improving the culture of health care organizations, as well as interventions focused on individual physicians but supported and funded by health care organizations, are beneficial.”
Researchers noted the study quality was low to moderate. Variation in outcomes across studies, heterogeneity among studies, potential selection bias by excluding gray literature, and the inability to establish causal links from findings because of the cross-sectional nature of the studies analyzed were potential limitations in the study, they reported.
The study was funded by the United Kingdom NIHR School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors report no relevant conflicts of interest.
SOURCE: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
Because of a lack of funding for research into burnout and the immediate need for change based on the effect it has on patient care seen in Pangioti et al., the question of how to address physician burnout should be answered with quality improvement programs aimed at making immediate changes in health care settings, Mark Linzer, MD, wrote in a related editorial.
“Resonating with these concepts, I propose that, for the burnout prevention and wellness field, we encourage quality improvement projects of high standards: multiple sites, concurrent control groups, longitudinal design, and blinding when feasible, with assessment of outcomes and costs,” he wrote. “These studies can point us toward what we will evaluate in larger trials and allow a place for the rapidly developing information base to be viewed and thus become part of the developing science of work conditions, burnout reduction, and the anticipated result on quality and safety.”
There are research questions that have yet to be answered on this topic, he added, such as to what extent do factors like workflow redesign, use and upkeep of electronic medical records, and chaotic workplaces affect burnout. Further, regulatory environments may play a role, and it is still not known whether reducing burnout among physicians will also reduce burnout among staff. Future studies should also look at how burnout affects trainees and female physicians, he suggested.
“The link between burnout and adverse patient outcomes is stronger, thanks to the work of Panagioti and colleagues,” Dr. Linzer said. “With close to half of U.S. physicians experiencing symptoms of burnout, more work is needed to understand how to reduce it and what we can expect from doing so.”
Dr. Linzer is from the Hennepin Healthcare Systems in Minneapolis. These comments summarize his editorial regarding the findings of Pangioti et al. He reported support for Wellness Champion training by the American College of Physicians and the Association of Chiefs and Leaders in General Internal Medicine and that he has received support for American Medical Association research projects.
Because of a lack of funding for research into burnout and the immediate need for change based on the effect it has on patient care seen in Pangioti et al., the question of how to address physician burnout should be answered with quality improvement programs aimed at making immediate changes in health care settings, Mark Linzer, MD, wrote in a related editorial.
“Resonating with these concepts, I propose that, for the burnout prevention and wellness field, we encourage quality improvement projects of high standards: multiple sites, concurrent control groups, longitudinal design, and blinding when feasible, with assessment of outcomes and costs,” he wrote. “These studies can point us toward what we will evaluate in larger trials and allow a place for the rapidly developing information base to be viewed and thus become part of the developing science of work conditions, burnout reduction, and the anticipated result on quality and safety.”
There are research questions that have yet to be answered on this topic, he added, such as to what extent do factors like workflow redesign, use and upkeep of electronic medical records, and chaotic workplaces affect burnout. Further, regulatory environments may play a role, and it is still not known whether reducing burnout among physicians will also reduce burnout among staff. Future studies should also look at how burnout affects trainees and female physicians, he suggested.
“The link between burnout and adverse patient outcomes is stronger, thanks to the work of Panagioti and colleagues,” Dr. Linzer said. “With close to half of U.S. physicians experiencing symptoms of burnout, more work is needed to understand how to reduce it and what we can expect from doing so.”
Dr. Linzer is from the Hennepin Healthcare Systems in Minneapolis. These comments summarize his editorial regarding the findings of Pangioti et al. He reported support for Wellness Champion training by the American College of Physicians and the Association of Chiefs and Leaders in General Internal Medicine and that he has received support for American Medical Association research projects.
Because of a lack of funding for research into burnout and the immediate need for change based on the effect it has on patient care seen in Pangioti et al., the question of how to address physician burnout should be answered with quality improvement programs aimed at making immediate changes in health care settings, Mark Linzer, MD, wrote in a related editorial.
“Resonating with these concepts, I propose that, for the burnout prevention and wellness field, we encourage quality improvement projects of high standards: multiple sites, concurrent control groups, longitudinal design, and blinding when feasible, with assessment of outcomes and costs,” he wrote. “These studies can point us toward what we will evaluate in larger trials and allow a place for the rapidly developing information base to be viewed and thus become part of the developing science of work conditions, burnout reduction, and the anticipated result on quality and safety.”
There are research questions that have yet to be answered on this topic, he added, such as to what extent do factors like workflow redesign, use and upkeep of electronic medical records, and chaotic workplaces affect burnout. Further, regulatory environments may play a role, and it is still not known whether reducing burnout among physicians will also reduce burnout among staff. Future studies should also look at how burnout affects trainees and female physicians, he suggested.
“The link between burnout and adverse patient outcomes is stronger, thanks to the work of Panagioti and colleagues,” Dr. Linzer said. “With close to half of U.S. physicians experiencing symptoms of burnout, more work is needed to understand how to reduce it and what we can expect from doing so.”
Dr. Linzer is from the Hennepin Healthcare Systems in Minneapolis. These comments summarize his editorial regarding the findings of Pangioti et al. He reported support for Wellness Champion training by the American College of Physicians and the Association of Chiefs and Leaders in General Internal Medicine and that he has received support for American Medical Association research projects.
because of depersonalization of care, according to recent research published in JAMA Internal Medicine.
“The primary conclusion of this review is that physician burnout might jeopardize patient care,” Maria Panagioti, PhD, from the National Institute for Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre at the University of Manchester (United Kingdom) and her colleagues wrote in their study. “Physician wellness and quality of patient care are critical [as are] complementary dimensions of health care organization efficiency.”
Dr. Panagioti and her colleagues performed a search of the MEDLINE, EMBASE, CINAHL, and PsycInfo databases and found 47 eligible studies on the topics of physician burnout and patient care, which altogether included data from a pooled cohort of 42,473 physicians. The physicians were median 38 years old, with 44.7% of studies looking at physicians in residency or early career (up to 5 years post residency) and 55.3% of studies examining experienced physicians. The meta-analysis also evaluated physicians in a hospital setting (63.8%), primary care (13.8%), and across various different health care settings (8.5%).
The researchers found physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85). System-reported instances of patient safety issues and low professionalism were not statistically significant, but the subgroup differences did reach statistical significance (Cohen Q, 8.14; P = .007). Among residents and physicians in their early career, there was a greater association between burnout and low professionalism (OR, 3.39; 95% CI, 2.38-4.40), compared with physicians in the middle or later in their career (OR, 1.73; 95% CI, 1.46-2.01; Cohen Q, 7.27; P = .003).
“Investments in organizational strategies to jointly monitor and improve physician wellness and patient care outcomes are needed,” Dr. Panagioti and her colleagues wrote in the study. “Interventions aimed at improving the culture of health care organizations, as well as interventions focused on individual physicians but supported and funded by health care organizations, are beneficial.”
Researchers noted the study quality was low to moderate. Variation in outcomes across studies, heterogeneity among studies, potential selection bias by excluding gray literature, and the inability to establish causal links from findings because of the cross-sectional nature of the studies analyzed were potential limitations in the study, they reported.
The study was funded by the United Kingdom NIHR School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors report no relevant conflicts of interest.
SOURCE: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
because of depersonalization of care, according to recent research published in JAMA Internal Medicine.
“The primary conclusion of this review is that physician burnout might jeopardize patient care,” Maria Panagioti, PhD, from the National Institute for Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre at the University of Manchester (United Kingdom) and her colleagues wrote in their study. “Physician wellness and quality of patient care are critical [as are] complementary dimensions of health care organization efficiency.”
Dr. Panagioti and her colleagues performed a search of the MEDLINE, EMBASE, CINAHL, and PsycInfo databases and found 47 eligible studies on the topics of physician burnout and patient care, which altogether included data from a pooled cohort of 42,473 physicians. The physicians were median 38 years old, with 44.7% of studies looking at physicians in residency or early career (up to 5 years post residency) and 55.3% of studies examining experienced physicians. The meta-analysis also evaluated physicians in a hospital setting (63.8%), primary care (13.8%), and across various different health care settings (8.5%).
The researchers found physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85). System-reported instances of patient safety issues and low professionalism were not statistically significant, but the subgroup differences did reach statistical significance (Cohen Q, 8.14; P = .007). Among residents and physicians in their early career, there was a greater association between burnout and low professionalism (OR, 3.39; 95% CI, 2.38-4.40), compared with physicians in the middle or later in their career (OR, 1.73; 95% CI, 1.46-2.01; Cohen Q, 7.27; P = .003).
“Investments in organizational strategies to jointly monitor and improve physician wellness and patient care outcomes are needed,” Dr. Panagioti and her colleagues wrote in the study. “Interventions aimed at improving the culture of health care organizations, as well as interventions focused on individual physicians but supported and funded by health care organizations, are beneficial.”
Researchers noted the study quality was low to moderate. Variation in outcomes across studies, heterogeneity among studies, potential selection bias by excluding gray literature, and the inability to establish causal links from findings because of the cross-sectional nature of the studies analyzed were potential limitations in the study, they reported.
The study was funded by the United Kingdom NIHR School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors report no relevant conflicts of interest.
SOURCE: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Burnout among physicians was associated with lower quality of care because of unprofessionalism, reduced patient satisfaction, and an increased risk of patient safety issues.
Major finding: Physicians with burnout were significantly associated with higher rates of patient safety issues (odds ratio, 1.96; 95% confidence interval, 1.59-2.40), reduced patient satisfaction (OR, 2.28; 95% CI, 1.42-3.68), and lower quality of care (OR, 2.31; 95% CI, 1.87-2.85).
Study details: A systematic review and meta-analysis of 42,473 physicians from 47 different studies.
Disclosures: The study was funded by the United Kingdom National Institute of Health Research (NIHR) School for Primary Care Research and the NIHR Greater Manchester Patient Safety Translational Research Centre. The authors reported no relevant conflicts of interest.
Source: Panagioti M et al. JAMA Intern Med. 2018 Sept 4. doi: 10.1001/jamainternmed.2018.3713.
New stroke intervention guidelines stress volume
A consensus working group from numerous international societies has published new guidelines for standards of practice in the treatment of acute ischemic stroke (AIS). The new guidelines differ somewhat from the Joint Commission guideline, released in 2015, primarily by raising the bar for the number of mechanical thrombectomy (MT) procedures that level 1 and level 2 stroke centers should perform annually in order to maintain a minimum safety threshold.
Previous studies have shown lower mortality in high-volume centers, but setting minimum standards can be a challenge, especially in under-served countries and localities. The authors, led by first author Laurent Pierot, MD, PhD, of University Hospital Reims (France), acknowledge that newly established level 2 centers may struggle to meet the minimum requirement for MT procedures, but that this is acceptable as long as the volume is expected to meet the minimum within 12-24 months.
The guidelines were created by a working group of delegates from 13 international societies, including the American Society of Neuroradiology, European Stroke Organization, World Stroke Organization, and the Society of NeuroInterventional Surgery.
The publication in 2015 of studies showing the efficacy of MT in anterior circulation emergent large-vessel occlusion (ELVO) stroke patients reverberated through the stroke care community, but posed a challenge in delivering this therapy to populations in diverse localities that have no access to level 1 stroke centers.
The guidelines, published online in the Journal of NeuroInterventional Surgery, aim to ensure that facilities can handle not only the MT procedure, but also the medical management before, during, and after the procedure.
According to the new guidelines, level 2 centers should handle cases when a level 1 center cannot be reached within 2 hours. Level 2 centers should care for at least 100 AIS patients per year and should also have a relationship with a level 1 center to maintain staff training, teleconsultations, referrals, and other collaborations.
Previous studies have identified 35 or 36 MT procedures annually as a threshold to be considered “high volume,” a category that led to lower mortality. The new recommendations fall below that threshold because they are intended to apply broadly, to regions that may be under-served. In highly developed countries, stroke centers should follow regional or national guidelines that have higher limits.
Level 2 centers should perform at least 50 intracranial thrombectomy procedures for ELVO, and a total of 120 diagnostic or interventional neuroendovascular procedures per year. Individual interventionists should conduct at least 15 intracranial thrombectomy and 50 interventional neuroendovascular procedures per year.
Other recommendations cover additional details about personnel, as well as community and emergency medical services outreach.
In many ways, the recommendations are in line with the Joint Commission (TJC), according to David Tirschwell, MD, who is the medical director for the UW Medicine* Comprehensive Stroke Center at Harborview Medical Center, Seattle. He was not involved in the development of the new guidelines.
Dr. Tirschwell noted one key difference with respect to the number of MT procedures required to qualify. TJC offered no minimum annual procedures for Comprehensive Stroke Centers (equivalent to level 1), and only 15 for Thrombectomy Capable Stroke Centers (level 2), versus 50 in the new guidelines. The minimum procedure numbers are also higher for individual clinicians.
The guidelines also recommend that level 2 centers have at least three interventionalists on staff available at all times, while TJC does not address this element of staffing.
“The higher minimum number of procedures in the new international recommendations is a substantial difference and would make it harder for many hospitals to qualify, compared to the TJC requirements. As such, a lower number of hospitals may qualify, and such a barrier could prevent access to mechanical thrombectomy for many patients. On the other hand, the higher minimum number may ensure a higher quality of care, which can be seen as a strong positive feature,” Dr. Tirschwell said.
A spokesman for the Joint Commission and the American Heart Association indicated that they will review the new guidelines and consider whether to make changes to their 2015 guidelines.
SOURCE: Pierot Laurent et al. J Neurointervent Surg. 2018 Aug 28. doi: 10.1136/neurintsurg-2018-014287.
*Updated Sept. 14, 2018.
A consensus working group from numerous international societies has published new guidelines for standards of practice in the treatment of acute ischemic stroke (AIS). The new guidelines differ somewhat from the Joint Commission guideline, released in 2015, primarily by raising the bar for the number of mechanical thrombectomy (MT) procedures that level 1 and level 2 stroke centers should perform annually in order to maintain a minimum safety threshold.
Previous studies have shown lower mortality in high-volume centers, but setting minimum standards can be a challenge, especially in under-served countries and localities. The authors, led by first author Laurent Pierot, MD, PhD, of University Hospital Reims (France), acknowledge that newly established level 2 centers may struggle to meet the minimum requirement for MT procedures, but that this is acceptable as long as the volume is expected to meet the minimum within 12-24 months.
The guidelines were created by a working group of delegates from 13 international societies, including the American Society of Neuroradiology, European Stroke Organization, World Stroke Organization, and the Society of NeuroInterventional Surgery.
The publication in 2015 of studies showing the efficacy of MT in anterior circulation emergent large-vessel occlusion (ELVO) stroke patients reverberated through the stroke care community, but posed a challenge in delivering this therapy to populations in diverse localities that have no access to level 1 stroke centers.
The guidelines, published online in the Journal of NeuroInterventional Surgery, aim to ensure that facilities can handle not only the MT procedure, but also the medical management before, during, and after the procedure.
According to the new guidelines, level 2 centers should handle cases when a level 1 center cannot be reached within 2 hours. Level 2 centers should care for at least 100 AIS patients per year and should also have a relationship with a level 1 center to maintain staff training, teleconsultations, referrals, and other collaborations.
Previous studies have identified 35 or 36 MT procedures annually as a threshold to be considered “high volume,” a category that led to lower mortality. The new recommendations fall below that threshold because they are intended to apply broadly, to regions that may be under-served. In highly developed countries, stroke centers should follow regional or national guidelines that have higher limits.
Level 2 centers should perform at least 50 intracranial thrombectomy procedures for ELVO, and a total of 120 diagnostic or interventional neuroendovascular procedures per year. Individual interventionists should conduct at least 15 intracranial thrombectomy and 50 interventional neuroendovascular procedures per year.
Other recommendations cover additional details about personnel, as well as community and emergency medical services outreach.
In many ways, the recommendations are in line with the Joint Commission (TJC), according to David Tirschwell, MD, who is the medical director for the UW Medicine* Comprehensive Stroke Center at Harborview Medical Center, Seattle. He was not involved in the development of the new guidelines.
Dr. Tirschwell noted one key difference with respect to the number of MT procedures required to qualify. TJC offered no minimum annual procedures for Comprehensive Stroke Centers (equivalent to level 1), and only 15 for Thrombectomy Capable Stroke Centers (level 2), versus 50 in the new guidelines. The minimum procedure numbers are also higher for individual clinicians.
The guidelines also recommend that level 2 centers have at least three interventionalists on staff available at all times, while TJC does not address this element of staffing.
“The higher minimum number of procedures in the new international recommendations is a substantial difference and would make it harder for many hospitals to qualify, compared to the TJC requirements. As such, a lower number of hospitals may qualify, and such a barrier could prevent access to mechanical thrombectomy for many patients. On the other hand, the higher minimum number may ensure a higher quality of care, which can be seen as a strong positive feature,” Dr. Tirschwell said.
A spokesman for the Joint Commission and the American Heart Association indicated that they will review the new guidelines and consider whether to make changes to their 2015 guidelines.
SOURCE: Pierot Laurent et al. J Neurointervent Surg. 2018 Aug 28. doi: 10.1136/neurintsurg-2018-014287.
*Updated Sept. 14, 2018.
A consensus working group from numerous international societies has published new guidelines for standards of practice in the treatment of acute ischemic stroke (AIS). The new guidelines differ somewhat from the Joint Commission guideline, released in 2015, primarily by raising the bar for the number of mechanical thrombectomy (MT) procedures that level 1 and level 2 stroke centers should perform annually in order to maintain a minimum safety threshold.
Previous studies have shown lower mortality in high-volume centers, but setting minimum standards can be a challenge, especially in under-served countries and localities. The authors, led by first author Laurent Pierot, MD, PhD, of University Hospital Reims (France), acknowledge that newly established level 2 centers may struggle to meet the minimum requirement for MT procedures, but that this is acceptable as long as the volume is expected to meet the minimum within 12-24 months.
The guidelines were created by a working group of delegates from 13 international societies, including the American Society of Neuroradiology, European Stroke Organization, World Stroke Organization, and the Society of NeuroInterventional Surgery.
The publication in 2015 of studies showing the efficacy of MT in anterior circulation emergent large-vessel occlusion (ELVO) stroke patients reverberated through the stroke care community, but posed a challenge in delivering this therapy to populations in diverse localities that have no access to level 1 stroke centers.
The guidelines, published online in the Journal of NeuroInterventional Surgery, aim to ensure that facilities can handle not only the MT procedure, but also the medical management before, during, and after the procedure.
According to the new guidelines, level 2 centers should handle cases when a level 1 center cannot be reached within 2 hours. Level 2 centers should care for at least 100 AIS patients per year and should also have a relationship with a level 1 center to maintain staff training, teleconsultations, referrals, and other collaborations.
Previous studies have identified 35 or 36 MT procedures annually as a threshold to be considered “high volume,” a category that led to lower mortality. The new recommendations fall below that threshold because they are intended to apply broadly, to regions that may be under-served. In highly developed countries, stroke centers should follow regional or national guidelines that have higher limits.
Level 2 centers should perform at least 50 intracranial thrombectomy procedures for ELVO, and a total of 120 diagnostic or interventional neuroendovascular procedures per year. Individual interventionists should conduct at least 15 intracranial thrombectomy and 50 interventional neuroendovascular procedures per year.
Other recommendations cover additional details about personnel, as well as community and emergency medical services outreach.
In many ways, the recommendations are in line with the Joint Commission (TJC), according to David Tirschwell, MD, who is the medical director for the UW Medicine* Comprehensive Stroke Center at Harborview Medical Center, Seattle. He was not involved in the development of the new guidelines.
Dr. Tirschwell noted one key difference with respect to the number of MT procedures required to qualify. TJC offered no minimum annual procedures for Comprehensive Stroke Centers (equivalent to level 1), and only 15 for Thrombectomy Capable Stroke Centers (level 2), versus 50 in the new guidelines. The minimum procedure numbers are also higher for individual clinicians.
The guidelines also recommend that level 2 centers have at least three interventionalists on staff available at all times, while TJC does not address this element of staffing.
“The higher minimum number of procedures in the new international recommendations is a substantial difference and would make it harder for many hospitals to qualify, compared to the TJC requirements. As such, a lower number of hospitals may qualify, and such a barrier could prevent access to mechanical thrombectomy for many patients. On the other hand, the higher minimum number may ensure a higher quality of care, which can be seen as a strong positive feature,” Dr. Tirschwell said.
A spokesman for the Joint Commission and the American Heart Association indicated that they will review the new guidelines and consider whether to make changes to their 2015 guidelines.
SOURCE: Pierot Laurent et al. J Neurointervent Surg. 2018 Aug 28. doi: 10.1136/neurintsurg-2018-014287.
*Updated Sept. 14, 2018.
FROM THE JOURNAL OF NEUROINTERVENTIONAL SURGERY
NYC outbreak of Candida auris linked to 45% mortality
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
Mortality within 90 days of infection was 45% among 51 patients diagnosed with antibiotic-resistant Candida auris infections in a multihospital outbreak in New York City from 2012 to 2017.
Transmission is ongoing in health care facilities, primarily among patients with extensive health care exposures, according to a report published in Emerging Infectious Diseases.
“Intensive infection prevention and control efforts continue; the goals are delaying endemicity, preventing outbreaks within facilities, reducing transmission and geographic spread, and blunting the effect of C. auris in New York and the rest of the United States,” Eleanor Adams, MD, of the New York Health Department, and her colleagues wrote. “Among medically fragile patients in NYC who had a history of extensive contact with health care facilities, clinicians should include C. auris in the differential diagnosis for patients with symptoms compatible with bloodstream infection.”
In the intensive case-patient analysis conducted by the New York State Health Department, 21 cases were from seven hospitals in Brooklyn, 16 were from three hospitals and one private medical office in Queens, 12 were from five hospitals and one long-term acute care hospital in Manhattan, and 1 was from a hospital in the Bronx. The remaining clinical case was identified in a western New York hospital in a patient who had recently been admitted to an involved Brooklyn hospital.
Among these patients, 31 (61%) had resided in long-term care facilities immediately before being admitted to the hospital in which their infection was diagnosed, and 19 of these 31 resided in skilled nursing facilities with ventilator beds; 1 (2%) resided in a long-term acute care hospital; 5 (10%) had been transferred from another hospital; and 4 (8%) had traveled internationally within 5 years before diagnosis, according to the investigators.
Isolates from 50 patients (98%) were resistant to fluconazole and 13 (25%) were resistant to fluconazole and amphotericin B. No initial isolates were resistant to echinocandins, although subsequent isolates obtained from 3 persons who had received an echinocandin acquired resistance to it, according to the researchers. Whole-genome sequencing performed at The Centers for Disease Control and Prevention indicated that 50 of 51 isolates belonged to a South Asia clade; the remaining isolate was the only one susceptible to fluconazole.
The work was supported by the CDC. No disclosures were reported.
SOURCE: Adams E et al. Emerg Infect Dis. 2018 Sep 12; 24(10); ID: 18-0649.
FROM EMERGING INFECTIOUS DISEASES
Pregnancy boosts cardiac disease mortality nearly 100-fold
MUNICH – Women with cardiac disease who became pregnant had a nearly 100-fold higher mortality rate, compared with pregnant women without cardiac disease, according to the outcomes of more than 5,700 pregnancies in an international registry of women with cardiac disease.
In addition to increased mortality, women with cardiac disease who become pregnant also had a greater than 100-fold higher rate of developing heart failure, compared with pregnant women without cardiac disease.
Despite these highly elevated relative risks, the absolute rate of serious complications from pregnancy for most women with heart disease was relatively modest. The worst prognosis by far was for the 1% of women in the registry who had pulmonary arterial hypertension at the time their pregnancy began. For these women, mortality during pregnancy was about 9%, and new-onset heart failure occurred in about one third. Another subgroup showing particularly poor outcomes were women classified with WHO IV maternal cardiovascular risk by the modified World Health Organization criteria, which corresponds to having an “extremely high risk of maternal mortality or severe morbidity,” according to guidelines published in the European Heart Journal (2011 Dec 1;32[24]:3147-97).These women, constituting 7% of the registry cohort, had a 2.5% mortality rate during pregnancy and a 33% incidence of heart failure.
Across all women with cardiac disease enrolled in the registry, the incidence of death during pregnancy was 0.6% and the incidence of heart failure was 11%. Women without cardiac disease have rates of 0.007% and less than 0.1%, respectively, Jolien Roos-Hesselink, MD, said at the annual congress of the European Society of Cardiology.
“The most important message of my talk is that all patients should be counseled, not just the women at high risk, for whom pregnancy is contraindicated, but also the women at low risk,” who can have a child with relative safety, she said. “Many women [with cardiac disease] can go through pregnancy at low risk.” Counseling is the key so that women know their risk before becoming pregnant, stressed Dr. Roos-Hesselink, a cardiologist at Erasmus Medical Center in Rotterdam, the Netherlands.
Based on the observed rates of mortality and other complications, pulmonary arterial hypertension and the other cardiac conditions that define a WHO IV maternal risk classification remain contraindications for pregnancy, she said. According to the 2011 guidelines from the European Society of Cardiology for managing cardiovascular disease during pregnancy, the full list of conditions that define a WHO IV classification are the following:
- Pulmonary arterial hypertension of any cause.
- Severe systemic ventricular dysfunction (a left ventricular ejection fraction of less than 30%) or New York Heart Association functional class III or IV.
- Previous peripartum cardiomyopathy with any residual impairment of left ventricular function.
- Severe mitral stenosis or severe symptomatic aortic stenosis.
- Marfan syndrome with the aorta dilated to more than 45 mm.
- Aortic dilatation greater than 50 mm in aortic disease associated with a bicuspid aortic valve.
- Native severe coarctation.
The registry data, collected during 2007-2018, showed a clear increase in the percentage of women with WHO class IV cardiovascular disease who became pregnant and entered the registry despite the contraindication designation for that classification, rising from about 1% of enrolled women in 2008 and 2009 to more than 10% of women in 2013, 2016, and 2017. “Individualization is necessary, but all these women are at very high risk and should be counseled against pregnancy,” Dr. Roos-Hesselink said.
The Registry of Pregnancy and Cardiac Disease (ROPAC) enrolled 5,739 pregnant women at any of 138 participating centers in 53 countries including the United States. Clinicians submitted WHO classification of cardiovascular risk for 5,711 of these women. The most common risk was congenital heart disease in 57% of enrolled women, followed by valvular heart disease in 29% and cardiomyopathy in 7%. Nearly 1,200 women in the registry – about 21% of the total – had a WHO I classification, which meant that they would be expected to have no detectable increase in mortality rate during pregnancy, compared with women without cardiac disease, and either no rise in morbidity or a mild effect.
Delivery was by cesarean section in 44% of the pregnancies, roughly twice the rate in women without diagnosed cardiac disease, even though published guidelines don’t advise cesarean delivery because of cardiac disease, Dr. Roos-Hesselink said. “Cesarean sections are used too often, in my opinion,” she commented, but added that many of these women require delivery at a tertiary, specialized center.
Overall fetal mortality was 1%, nearly threefold higher than in pregnancies in women without cardiac disease, and the overall incidence of fetal and neonatal complications was especially high, at 53%, in women with pulmonary arterial hypertension. The incidence of obstetrical complications was roughly similar across the range of cardiac disease type, ranging from 16% to 24%. Premature delivery occurred in 28% of women in the high-risk WHO IV class, compared with a 13% rate among women in the WHO I class. The mortality rate was 0.2% among the WHO class I women, and their heart failure incidence was 5%.
The ROPAC registry is sponsored by the European Society of Cardiology. Dr. Roos-Hesselink had no disclosures.
MUNICH – Women with cardiac disease who became pregnant had a nearly 100-fold higher mortality rate, compared with pregnant women without cardiac disease, according to the outcomes of more than 5,700 pregnancies in an international registry of women with cardiac disease.
In addition to increased mortality, women with cardiac disease who become pregnant also had a greater than 100-fold higher rate of developing heart failure, compared with pregnant women without cardiac disease.
Despite these highly elevated relative risks, the absolute rate of serious complications from pregnancy for most women with heart disease was relatively modest. The worst prognosis by far was for the 1% of women in the registry who had pulmonary arterial hypertension at the time their pregnancy began. For these women, mortality during pregnancy was about 9%, and new-onset heart failure occurred in about one third. Another subgroup showing particularly poor outcomes were women classified with WHO IV maternal cardiovascular risk by the modified World Health Organization criteria, which corresponds to having an “extremely high risk of maternal mortality or severe morbidity,” according to guidelines published in the European Heart Journal (2011 Dec 1;32[24]:3147-97).These women, constituting 7% of the registry cohort, had a 2.5% mortality rate during pregnancy and a 33% incidence of heart failure.
Across all women with cardiac disease enrolled in the registry, the incidence of death during pregnancy was 0.6% and the incidence of heart failure was 11%. Women without cardiac disease have rates of 0.007% and less than 0.1%, respectively, Jolien Roos-Hesselink, MD, said at the annual congress of the European Society of Cardiology.
“The most important message of my talk is that all patients should be counseled, not just the women at high risk, for whom pregnancy is contraindicated, but also the women at low risk,” who can have a child with relative safety, she said. “Many women [with cardiac disease] can go through pregnancy at low risk.” Counseling is the key so that women know their risk before becoming pregnant, stressed Dr. Roos-Hesselink, a cardiologist at Erasmus Medical Center in Rotterdam, the Netherlands.
Based on the observed rates of mortality and other complications, pulmonary arterial hypertension and the other cardiac conditions that define a WHO IV maternal risk classification remain contraindications for pregnancy, she said. According to the 2011 guidelines from the European Society of Cardiology for managing cardiovascular disease during pregnancy, the full list of conditions that define a WHO IV classification are the following:
- Pulmonary arterial hypertension of any cause.
- Severe systemic ventricular dysfunction (a left ventricular ejection fraction of less than 30%) or New York Heart Association functional class III or IV.
- Previous peripartum cardiomyopathy with any residual impairment of left ventricular function.
- Severe mitral stenosis or severe symptomatic aortic stenosis.
- Marfan syndrome with the aorta dilated to more than 45 mm.
- Aortic dilatation greater than 50 mm in aortic disease associated with a bicuspid aortic valve.
- Native severe coarctation.
The registry data, collected during 2007-2018, showed a clear increase in the percentage of women with WHO class IV cardiovascular disease who became pregnant and entered the registry despite the contraindication designation for that classification, rising from about 1% of enrolled women in 2008 and 2009 to more than 10% of women in 2013, 2016, and 2017. “Individualization is necessary, but all these women are at very high risk and should be counseled against pregnancy,” Dr. Roos-Hesselink said.
The Registry of Pregnancy and Cardiac Disease (ROPAC) enrolled 5,739 pregnant women at any of 138 participating centers in 53 countries including the United States. Clinicians submitted WHO classification of cardiovascular risk for 5,711 of these women. The most common risk was congenital heart disease in 57% of enrolled women, followed by valvular heart disease in 29% and cardiomyopathy in 7%. Nearly 1,200 women in the registry – about 21% of the total – had a WHO I classification, which meant that they would be expected to have no detectable increase in mortality rate during pregnancy, compared with women without cardiac disease, and either no rise in morbidity or a mild effect.
Delivery was by cesarean section in 44% of the pregnancies, roughly twice the rate in women without diagnosed cardiac disease, even though published guidelines don’t advise cesarean delivery because of cardiac disease, Dr. Roos-Hesselink said. “Cesarean sections are used too often, in my opinion,” she commented, but added that many of these women require delivery at a tertiary, specialized center.
Overall fetal mortality was 1%, nearly threefold higher than in pregnancies in women without cardiac disease, and the overall incidence of fetal and neonatal complications was especially high, at 53%, in women with pulmonary arterial hypertension. The incidence of obstetrical complications was roughly similar across the range of cardiac disease type, ranging from 16% to 24%. Premature delivery occurred in 28% of women in the high-risk WHO IV class, compared with a 13% rate among women in the WHO I class. The mortality rate was 0.2% among the WHO class I women, and their heart failure incidence was 5%.
The ROPAC registry is sponsored by the European Society of Cardiology. Dr. Roos-Hesselink had no disclosures.
MUNICH – Women with cardiac disease who became pregnant had a nearly 100-fold higher mortality rate, compared with pregnant women without cardiac disease, according to the outcomes of more than 5,700 pregnancies in an international registry of women with cardiac disease.
In addition to increased mortality, women with cardiac disease who become pregnant also had a greater than 100-fold higher rate of developing heart failure, compared with pregnant women without cardiac disease.
Despite these highly elevated relative risks, the absolute rate of serious complications from pregnancy for most women with heart disease was relatively modest. The worst prognosis by far was for the 1% of women in the registry who had pulmonary arterial hypertension at the time their pregnancy began. For these women, mortality during pregnancy was about 9%, and new-onset heart failure occurred in about one third. Another subgroup showing particularly poor outcomes were women classified with WHO IV maternal cardiovascular risk by the modified World Health Organization criteria, which corresponds to having an “extremely high risk of maternal mortality or severe morbidity,” according to guidelines published in the European Heart Journal (2011 Dec 1;32[24]:3147-97).These women, constituting 7% of the registry cohort, had a 2.5% mortality rate during pregnancy and a 33% incidence of heart failure.
Across all women with cardiac disease enrolled in the registry, the incidence of death during pregnancy was 0.6% and the incidence of heart failure was 11%. Women without cardiac disease have rates of 0.007% and less than 0.1%, respectively, Jolien Roos-Hesselink, MD, said at the annual congress of the European Society of Cardiology.
“The most important message of my talk is that all patients should be counseled, not just the women at high risk, for whom pregnancy is contraindicated, but also the women at low risk,” who can have a child with relative safety, she said. “Many women [with cardiac disease] can go through pregnancy at low risk.” Counseling is the key so that women know their risk before becoming pregnant, stressed Dr. Roos-Hesselink, a cardiologist at Erasmus Medical Center in Rotterdam, the Netherlands.
Based on the observed rates of mortality and other complications, pulmonary arterial hypertension and the other cardiac conditions that define a WHO IV maternal risk classification remain contraindications for pregnancy, she said. According to the 2011 guidelines from the European Society of Cardiology for managing cardiovascular disease during pregnancy, the full list of conditions that define a WHO IV classification are the following:
- Pulmonary arterial hypertension of any cause.
- Severe systemic ventricular dysfunction (a left ventricular ejection fraction of less than 30%) or New York Heart Association functional class III or IV.
- Previous peripartum cardiomyopathy with any residual impairment of left ventricular function.
- Severe mitral stenosis or severe symptomatic aortic stenosis.
- Marfan syndrome with the aorta dilated to more than 45 mm.
- Aortic dilatation greater than 50 mm in aortic disease associated with a bicuspid aortic valve.
- Native severe coarctation.
The registry data, collected during 2007-2018, showed a clear increase in the percentage of women with WHO class IV cardiovascular disease who became pregnant and entered the registry despite the contraindication designation for that classification, rising from about 1% of enrolled women in 2008 and 2009 to more than 10% of women in 2013, 2016, and 2017. “Individualization is necessary, but all these women are at very high risk and should be counseled against pregnancy,” Dr. Roos-Hesselink said.
The Registry of Pregnancy and Cardiac Disease (ROPAC) enrolled 5,739 pregnant women at any of 138 participating centers in 53 countries including the United States. Clinicians submitted WHO classification of cardiovascular risk for 5,711 of these women. The most common risk was congenital heart disease in 57% of enrolled women, followed by valvular heart disease in 29% and cardiomyopathy in 7%. Nearly 1,200 women in the registry – about 21% of the total – had a WHO I classification, which meant that they would be expected to have no detectable increase in mortality rate during pregnancy, compared with women without cardiac disease, and either no rise in morbidity or a mild effect.
Delivery was by cesarean section in 44% of the pregnancies, roughly twice the rate in women without diagnosed cardiac disease, even though published guidelines don’t advise cesarean delivery because of cardiac disease, Dr. Roos-Hesselink said. “Cesarean sections are used too often, in my opinion,” she commented, but added that many of these women require delivery at a tertiary, specialized center.
Overall fetal mortality was 1%, nearly threefold higher than in pregnancies in women without cardiac disease, and the overall incidence of fetal and neonatal complications was especially high, at 53%, in women with pulmonary arterial hypertension. The incidence of obstetrical complications was roughly similar across the range of cardiac disease type, ranging from 16% to 24%. Premature delivery occurred in 28% of women in the high-risk WHO IV class, compared with a 13% rate among women in the WHO I class. The mortality rate was 0.2% among the WHO class I women, and their heart failure incidence was 5%.
The ROPAC registry is sponsored by the European Society of Cardiology. Dr. Roos-Hesselink had no disclosures.
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point: Women with cardiac disease who became pregnant had substantially increased mortality and morbidity.
Major finding: Pregnancy mortality was 0.6% in women with cardiac disease versus 0.007% in women without cardiac disorders.
Study details: The ROPAC registry, which enrolled 5,739 pregnant women at any of 138 centers in 53 countries during 2007-2018.
Disclosures: The ROPAC registry is sponsored by the European Society of Cardiology. Dr. Roos-Hesselink had no disclosures.
Review protocols, follow reprocessing guidelines to cut device-related HAIs
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
ATLANTA – Ongoing vigilance regarding the role of and transmission of antimicrobial-resistant pathogen is needed, according to Isaac Benowitz, MD, of the Centers for Disease Control and Prevention’s Division of Healthcare Quality Promotion (DHQP).
A review of records from the DHQP, which investigates and responds to infections and related adverse events in health care settings upon invitation, showed that in 2017 environmental pathogens were most often the triggers for these investigations, said Dr. Benowitz, a medical epidemiologist.
He reviewed internal records for consultations with state and local health departments involving medical devices and collected data on health care setting, pathogen, investigation findings including possible exposure or transmission, and public health actions.
Of 285 consultations, 48 involved a specific medical device or general medical device reprocessing, he said, noting that most of those 48 were in an acute care hospital (63%) or clinic (19%).
“The most frequent pathogens noted in these consultations were nontuberculous mycobacteria at 21%, Candida species ... at 10%, and Burkholderia species ... at 8%,” he said, noting that a wide variety of devices were implicated.
In the inpatient setting these devices included ventilators, dialysis machines, breast pumps, central lines, and respiratory therapy equipment. In the outpatient setting they included glucometers and opthalmic equipment.
“In many settings we saw issues with endoscopes, including duodenoscopes, but also bronchoscopes,” he added.
Actions taken as part of the investigations included medical device recalls, improved infection control and reprocessing procedures, and patient notification, education, guidance, testing, and treatment.
In some cases there was disciplinary action or oversight for health care professionals, he added.
Investigations identified medical devices contaminated in manufacturing, incorrect reprocessing of endoscopes or ventilators, and inappropriate medical device use or reuse, he said.
A number of lessons can be learned from these and other investigations, he added.
“First, devices can be reservoirs and transmission vectors for health care–associated infections. Second, health care facilities, health care facility staff, and public health partners should take opportunities to review protocols and the practices within those protocol,” he said. “These are opportunities to strengthen infection control practices even in the absence of documented transmission.”
In fact, in most of the investigations he discussed, transmission was rarely confirmed to be associated with a medical device. This was largely because of a lack of “epidemiological rigor,” but associations between health care–associated infections and medical devices “are still quite meaningful and often actionable,” he said.
Dr. Benowitz stressed the importance of engaging public health partners to discuss findings and actions, explaining that “what may look like a single-facility issue may have a very different perspective when you realize that there’s a similar issue at another facility elsewhere.”
“For all devices, it’s important to ensure adherence to the device reprocessing guidelines, “ he added, noting that these include a combination of facility protocols, manufacturer instructions for use, and guidance from organizations like the Food and Drug Administration and the CDC.
Dr. Benowitz reported having no disclosures.
[email protected]
SOURCE: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
REPORTING FROM ICEID 2018
Key clinical point: Medical devices can be reservoirs and transmission vectors for health care–associated infections.
Major finding: Of 285 consultations, 48 involved medical devices or device reprocessing.
Study details: A review of records from 285 consultations
Disclosures: Dr. Benowitz reported having no disclosures
Source: Benowitz I et al. ICEID 2018, Oral Abstract Presentation E2.
Coronary CT angiography radiation dose fell 78% from 2007-2017
MUNICH – The median radiation dosage received by patients worldwide undergoing coronary CT angiography fell by 78% from 2007 to 2017, according to a prospective study with more than 4,500 patients.
This substantial drop in radiation occurred with a steady rate of nondiagnostic CT scans, less than 2% in both 2007 and 2017.
“Given the high diagnostic accuracy and the low radiation dose, coronary CT angiography should be considered as a first-line diagnostic test,” Jörg Hausleiter, MD, said at the annual congress of the European Society of Cardiology.
The results also showed a huge disparity in the range of radiation doses used worldwide, with a 37-fold intersite variability in the median dose. This finding “underlines the need for further site-specific training and adaptation of contemporary cardiac scan protocols,” said Dr. Hausleiter, professor of medicine at the University of Munich Clinic. He suggested updated imaging guidelines on radiation levels, more educational sessions on how to perform coronary CT angiography, and actions by vendors to adjust their standard imaging protocols.
The Prospective Multicenter Registry on Radiation Dose Estimates of Cardiac CT Angiography in Daily Practice in 2017 (PROTECTION-VI) study included 4,502 patients from a total of 61 sites in 32 countries. At each participating site, investigators enrolled consecutive adults during a randomly selected month in 2017, with a median of 51 patients enrolled at each site undergoing diagnostic coronary CT angiography. Comparison data for 2007 came from a similar study run by Dr. Hausleiter and his associates at that time, with 1,965 patients undergoing coronary CT angiography (JAMA. 2009 Feb 4;301[5]:500-7). In 2007, the median dose-length product of radiation for each scan was 885 mGy x cm, which corresponds to a radiation dose of about 12.4 mSv. In 2017, the median dose-length product was 195 mGy x cm, corresponding to a dose of about 2.7 mSv. By both measures the median dose dropped by roughly 78%.
A multivariate analysis identified three changes in the way clinicians obtained most of the CT scans during the two studied time periods that seemed to explain the drop in radiation dose. First, more scan protocols in 2017 used low tube potential; second, more protocols in 2017 used prospectively ECG-triggered axial high-pitch scans; and third, 2017 had increased use of iterative image reconstruction, Dr. Hausleiter said. Patient variables that had modest but significant links with increased radiation doses were higher body weight, higher heart rate, and no sinus rhythm.
Concurrently with Dr. Hausleiter’s talk at the congress, the results appeared in an article online (Euro Heart J. 2018 Aug 25. doi: 10.1093/eurheartj/ehy546).
The results from the PROTECTION VI study show that the radiation doses used today for coronary CT angiography are very low. But the study is limited by looking only at the median doses used at 61 sites worldwide. I hope that the dose level seen in the study is what is now used at community hospitals across the United States, but for the time being we can’t be sure.
With today’s CT technology, as long as the dose-length product a patient receives is less than 200 mGy x cm, the facility is doing a good job of minimizing radiation exposure. As CT technology continues to improve, we can expect the median dose to fall even more in the future.
Todd C. Villines, MD , a cardiologist at Georgetown University in Washington and immediate past president of the Society of Cardiovascular CT, made these comments in an interview. He had no relevant disclosures.
The results from the PROTECTION VI study show that the radiation doses used today for coronary CT angiography are very low. But the study is limited by looking only at the median doses used at 61 sites worldwide. I hope that the dose level seen in the study is what is now used at community hospitals across the United States, but for the time being we can’t be sure.
With today’s CT technology, as long as the dose-length product a patient receives is less than 200 mGy x cm, the facility is doing a good job of minimizing radiation exposure. As CT technology continues to improve, we can expect the median dose to fall even more in the future.
Todd C. Villines, MD , a cardiologist at Georgetown University in Washington and immediate past president of the Society of Cardiovascular CT, made these comments in an interview. He had no relevant disclosures.
The results from the PROTECTION VI study show that the radiation doses used today for coronary CT angiography are very low. But the study is limited by looking only at the median doses used at 61 sites worldwide. I hope that the dose level seen in the study is what is now used at community hospitals across the United States, but for the time being we can’t be sure.
With today’s CT technology, as long as the dose-length product a patient receives is less than 200 mGy x cm, the facility is doing a good job of minimizing radiation exposure. As CT technology continues to improve, we can expect the median dose to fall even more in the future.
Todd C. Villines, MD , a cardiologist at Georgetown University in Washington and immediate past president of the Society of Cardiovascular CT, made these comments in an interview. He had no relevant disclosures.
MUNICH – The median radiation dosage received by patients worldwide undergoing coronary CT angiography fell by 78% from 2007 to 2017, according to a prospective study with more than 4,500 patients.
This substantial drop in radiation occurred with a steady rate of nondiagnostic CT scans, less than 2% in both 2007 and 2017.
“Given the high diagnostic accuracy and the low radiation dose, coronary CT angiography should be considered as a first-line diagnostic test,” Jörg Hausleiter, MD, said at the annual congress of the European Society of Cardiology.
The results also showed a huge disparity in the range of radiation doses used worldwide, with a 37-fold intersite variability in the median dose. This finding “underlines the need for further site-specific training and adaptation of contemporary cardiac scan protocols,” said Dr. Hausleiter, professor of medicine at the University of Munich Clinic. He suggested updated imaging guidelines on radiation levels, more educational sessions on how to perform coronary CT angiography, and actions by vendors to adjust their standard imaging protocols.
The Prospective Multicenter Registry on Radiation Dose Estimates of Cardiac CT Angiography in Daily Practice in 2017 (PROTECTION-VI) study included 4,502 patients from a total of 61 sites in 32 countries. At each participating site, investigators enrolled consecutive adults during a randomly selected month in 2017, with a median of 51 patients enrolled at each site undergoing diagnostic coronary CT angiography. Comparison data for 2007 came from a similar study run by Dr. Hausleiter and his associates at that time, with 1,965 patients undergoing coronary CT angiography (JAMA. 2009 Feb 4;301[5]:500-7). In 2007, the median dose-length product of radiation for each scan was 885 mGy x cm, which corresponds to a radiation dose of about 12.4 mSv. In 2017, the median dose-length product was 195 mGy x cm, corresponding to a dose of about 2.7 mSv. By both measures the median dose dropped by roughly 78%.
A multivariate analysis identified three changes in the way clinicians obtained most of the CT scans during the two studied time periods that seemed to explain the drop in radiation dose. First, more scan protocols in 2017 used low tube potential; second, more protocols in 2017 used prospectively ECG-triggered axial high-pitch scans; and third, 2017 had increased use of iterative image reconstruction, Dr. Hausleiter said. Patient variables that had modest but significant links with increased radiation doses were higher body weight, higher heart rate, and no sinus rhythm.
Concurrently with Dr. Hausleiter’s talk at the congress, the results appeared in an article online (Euro Heart J. 2018 Aug 25. doi: 10.1093/eurheartj/ehy546).
MUNICH – The median radiation dosage received by patients worldwide undergoing coronary CT angiography fell by 78% from 2007 to 2017, according to a prospective study with more than 4,500 patients.
This substantial drop in radiation occurred with a steady rate of nondiagnostic CT scans, less than 2% in both 2007 and 2017.
“Given the high diagnostic accuracy and the low radiation dose, coronary CT angiography should be considered as a first-line diagnostic test,” Jörg Hausleiter, MD, said at the annual congress of the European Society of Cardiology.
The results also showed a huge disparity in the range of radiation doses used worldwide, with a 37-fold intersite variability in the median dose. This finding “underlines the need for further site-specific training and adaptation of contemporary cardiac scan protocols,” said Dr. Hausleiter, professor of medicine at the University of Munich Clinic. He suggested updated imaging guidelines on radiation levels, more educational sessions on how to perform coronary CT angiography, and actions by vendors to adjust their standard imaging protocols.
The Prospective Multicenter Registry on Radiation Dose Estimates of Cardiac CT Angiography in Daily Practice in 2017 (PROTECTION-VI) study included 4,502 patients from a total of 61 sites in 32 countries. At each participating site, investigators enrolled consecutive adults during a randomly selected month in 2017, with a median of 51 patients enrolled at each site undergoing diagnostic coronary CT angiography. Comparison data for 2007 came from a similar study run by Dr. Hausleiter and his associates at that time, with 1,965 patients undergoing coronary CT angiography (JAMA. 2009 Feb 4;301[5]:500-7). In 2007, the median dose-length product of radiation for each scan was 885 mGy x cm, which corresponds to a radiation dose of about 12.4 mSv. In 2017, the median dose-length product was 195 mGy x cm, corresponding to a dose of about 2.7 mSv. By both measures the median dose dropped by roughly 78%.
A multivariate analysis identified three changes in the way clinicians obtained most of the CT scans during the two studied time periods that seemed to explain the drop in radiation dose. First, more scan protocols in 2017 used low tube potential; second, more protocols in 2017 used prospectively ECG-triggered axial high-pitch scans; and third, 2017 had increased use of iterative image reconstruction, Dr. Hausleiter said. Patient variables that had modest but significant links with increased radiation doses were higher body weight, higher heart rate, and no sinus rhythm.
Concurrently with Dr. Hausleiter’s talk at the congress, the results appeared in an article online (Euro Heart J. 2018 Aug 25. doi: 10.1093/eurheartj/ehy546).
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point: The median radiation dose during coronary CT angiography fell from 2007 to 2017.
Major finding: The median dose-length product was 195 mGY x cm in 2017 and 885 mGy x cm in 2007.
Study details: PROTECTION VI, a prospective study run at 61 sites in 32 countries.
Disclosures: PROTECTION VI received no commercial funding. Dr. Hausleiter has received research funding from Abbott Vascular.
Cutaneous lesions? Consider C. diphtheriae in those with foreign travel
ATLANTA – Seven cases of imported Corynebacterium diphtheriae in Minnesota highlight the importance of maintaining suspicion that cutaneous lesions in individuals with recent travel to endemic countries might be associated with C. diphtheriae infection.
The cases also underscore the importance of referring C. diphtheriae isolates to state health departments for confirmatory testing, Jayne Griffith, of the Minnesota Department of Health, and her colleagues reported in a poster at the International Conference on Emerging Infectious Diseases.
“C. diphtheriae infections was not clinically suspected in any of these case-patients. All infections were initially identified solely by [matrix-assisted laser desorption/ionization time-of-flight spectrometry] testing performed at the clinical institutions,” the investigators wrote. “Confirmation and further toxigenicity testing allowed for prompt case investigation and public health response, preventing disease spread.”
Infections caused by toxigenic C. diphtheriae are rare in the United States because of widespread vaccination, but remain endemic in countries with suboptimal vaccine coverage. For this reason, infection is a concern for unvaccinated individuals traveling to diphtheria-endemic countries as well as for those who have contact with people from these areas. The investigators noted that “infections are primarily respiratory or cutaneous; respiratory infections can be life-threatening and cutaneous wounds may serve as a reservoir from which bacteria can be transmitted to susceptible contacts.”
The Minnesota cases involved patients who presented with cutaneous ulcers between 2014 and 2017. The Minnesota Department of Health confirmed C. diphtheriae status by culture after the initial identification at private institutions or providers using matrix-assisted laser desorption/ionization time-of-flight spectrometry. Isolates were sent to the Centers for Disease Control and Prevention Pertussis and Diphtheria Laboratory for biotyping and confirmation of toxigenicity.
The CDC confirmed that isolates from two patients were toxigenic C. diphtheriae biotype mitis. The remaining cases were nontoxigenic diphtheria, including C. diphtheriae mitis (three case-patients, including one who also had Staphylococcus aureus, and another who also had methicillin-resistant S. aureus) and two case-patients with C. diphtheriae belfanti.
The patients with toxigenic infection included a 35-year-old woman who developed an abdominal boil after spending months in Somalia, and a 48-year-old man who cut his leg while in Ethiopia.
The patients with nontoxigenic infection included four foreign-born individuals ranging in age from 7 to 66 years and one 24-year-old man from the United States. One of the foreign-born individuals had immigrated from a diphtheria-endemic country 3 months prior to his diagnosis, but none of the remaining four had traveled outside the United States in the 6 months prior to infection onset. One, however, lived in a home with family members who traveled frequently to eastern Africa. The vaccination status of these patients was unknown.
Contact tracing was conducted and prophylactic antibiotics were recommended as appropriate. Vaccination was recommended when a case-patient and/or contact was inadequately immunized.
Both patients with toxigenic infection experienced wound healing after appropriate antibiotic therapy.
Ms. Griffith reported having no disclosures.
ATLANTA – Seven cases of imported Corynebacterium diphtheriae in Minnesota highlight the importance of maintaining suspicion that cutaneous lesions in individuals with recent travel to endemic countries might be associated with C. diphtheriae infection.
The cases also underscore the importance of referring C. diphtheriae isolates to state health departments for confirmatory testing, Jayne Griffith, of the Minnesota Department of Health, and her colleagues reported in a poster at the International Conference on Emerging Infectious Diseases.
“C. diphtheriae infections was not clinically suspected in any of these case-patients. All infections were initially identified solely by [matrix-assisted laser desorption/ionization time-of-flight spectrometry] testing performed at the clinical institutions,” the investigators wrote. “Confirmation and further toxigenicity testing allowed for prompt case investigation and public health response, preventing disease spread.”
Infections caused by toxigenic C. diphtheriae are rare in the United States because of widespread vaccination, but remain endemic in countries with suboptimal vaccine coverage. For this reason, infection is a concern for unvaccinated individuals traveling to diphtheria-endemic countries as well as for those who have contact with people from these areas. The investigators noted that “infections are primarily respiratory or cutaneous; respiratory infections can be life-threatening and cutaneous wounds may serve as a reservoir from which bacteria can be transmitted to susceptible contacts.”
The Minnesota cases involved patients who presented with cutaneous ulcers between 2014 and 2017. The Minnesota Department of Health confirmed C. diphtheriae status by culture after the initial identification at private institutions or providers using matrix-assisted laser desorption/ionization time-of-flight spectrometry. Isolates were sent to the Centers for Disease Control and Prevention Pertussis and Diphtheria Laboratory for biotyping and confirmation of toxigenicity.
The CDC confirmed that isolates from two patients were toxigenic C. diphtheriae biotype mitis. The remaining cases were nontoxigenic diphtheria, including C. diphtheriae mitis (three case-patients, including one who also had Staphylococcus aureus, and another who also had methicillin-resistant S. aureus) and two case-patients with C. diphtheriae belfanti.
The patients with toxigenic infection included a 35-year-old woman who developed an abdominal boil after spending months in Somalia, and a 48-year-old man who cut his leg while in Ethiopia.
The patients with nontoxigenic infection included four foreign-born individuals ranging in age from 7 to 66 years and one 24-year-old man from the United States. One of the foreign-born individuals had immigrated from a diphtheria-endemic country 3 months prior to his diagnosis, but none of the remaining four had traveled outside the United States in the 6 months prior to infection onset. One, however, lived in a home with family members who traveled frequently to eastern Africa. The vaccination status of these patients was unknown.
Contact tracing was conducted and prophylactic antibiotics were recommended as appropriate. Vaccination was recommended when a case-patient and/or contact was inadequately immunized.
Both patients with toxigenic infection experienced wound healing after appropriate antibiotic therapy.
Ms. Griffith reported having no disclosures.
ATLANTA – Seven cases of imported Corynebacterium diphtheriae in Minnesota highlight the importance of maintaining suspicion that cutaneous lesions in individuals with recent travel to endemic countries might be associated with C. diphtheriae infection.
The cases also underscore the importance of referring C. diphtheriae isolates to state health departments for confirmatory testing, Jayne Griffith, of the Minnesota Department of Health, and her colleagues reported in a poster at the International Conference on Emerging Infectious Diseases.
“C. diphtheriae infections was not clinically suspected in any of these case-patients. All infections were initially identified solely by [matrix-assisted laser desorption/ionization time-of-flight spectrometry] testing performed at the clinical institutions,” the investigators wrote. “Confirmation and further toxigenicity testing allowed for prompt case investigation and public health response, preventing disease spread.”
Infections caused by toxigenic C. diphtheriae are rare in the United States because of widespread vaccination, but remain endemic in countries with suboptimal vaccine coverage. For this reason, infection is a concern for unvaccinated individuals traveling to diphtheria-endemic countries as well as for those who have contact with people from these areas. The investigators noted that “infections are primarily respiratory or cutaneous; respiratory infections can be life-threatening and cutaneous wounds may serve as a reservoir from which bacteria can be transmitted to susceptible contacts.”
The Minnesota cases involved patients who presented with cutaneous ulcers between 2014 and 2017. The Minnesota Department of Health confirmed C. diphtheriae status by culture after the initial identification at private institutions or providers using matrix-assisted laser desorption/ionization time-of-flight spectrometry. Isolates were sent to the Centers for Disease Control and Prevention Pertussis and Diphtheria Laboratory for biotyping and confirmation of toxigenicity.
The CDC confirmed that isolates from two patients were toxigenic C. diphtheriae biotype mitis. The remaining cases were nontoxigenic diphtheria, including C. diphtheriae mitis (three case-patients, including one who also had Staphylococcus aureus, and another who also had methicillin-resistant S. aureus) and two case-patients with C. diphtheriae belfanti.
The patients with toxigenic infection included a 35-year-old woman who developed an abdominal boil after spending months in Somalia, and a 48-year-old man who cut his leg while in Ethiopia.
The patients with nontoxigenic infection included four foreign-born individuals ranging in age from 7 to 66 years and one 24-year-old man from the United States. One of the foreign-born individuals had immigrated from a diphtheria-endemic country 3 months prior to his diagnosis, but none of the remaining four had traveled outside the United States in the 6 months prior to infection onset. One, however, lived in a home with family members who traveled frequently to eastern Africa. The vaccination status of these patients was unknown.
Contact tracing was conducted and prophylactic antibiotics were recommended as appropriate. Vaccination was recommended when a case-patient and/or contact was inadequately immunized.
Both patients with toxigenic infection experienced wound healing after appropriate antibiotic therapy.
Ms. Griffith reported having no disclosures.
REPORTING FROM ICEID 2018
Key clinical point: Corynebacterium diphtheriae should be considered in individuals who present with cutaneous lesions after traveling to diphtheria-endemic countries.
Major finding: Refer suspect C. diphtheriae isolates to state health departments.
Study details: A review of seven C. diphtheriae cases.
Disclosures: Ms. Griffith reported having no disclosures.
Danish endocarditis strategy halved hospital days
MUNICH – Patients with left-sided endocarditis who are clinically stable after a couple weeks of inpatient intravenous antibiotics may at that point become candidates for discharge on oral antibiotics for the remainder of their treatment course, according to the findings of the randomized, multicenter, Danish POET trial.
“Shifting to oral antibiotic treatment in stabilized patients with endocarditis was as effective and safe as continued intravenous antibiotic treatment and was given during half the antibiotic treatment period. These novel findings may have a significant impact on future clinical practice for the management of patients who are stable,” Henning Bundgård, MD, said at the annual congress of the European Society of Cardiology.
Both ESC and American Heart Association/American College of Cardiology guidelines now recommend treatment of infective endocarditis with intravenous antibiotics for up to 6 weeks. Safely cutting the duration of in-hospital intravenous antibiotics in half is likely to generate major cost savings while improving patient quality of life and avoiding prolonged exposure to the iatrogenic risks inherent to the hospital environment, noted Dr. Bundgård, a cardiologist at Copenhagen University Hospital.
The rationale for the POET (Partial Oral Treatment of Endocarditis) trial was the investigators’ recognition that, even though infectious endocarditis is a feared disease with an in-hospital mortality of 15% or more, the great majority of serious complications occur in the early critical phase of therapy; that is, during the first 10 days or so of inpatient intravenous antibiotic therapy.
“After stabilization, the main reason for staying in the hospital is just to receive IV antibiotics,” Dr. Bundgård noted.
POET included 400 patients with left-sided endocarditis hospitalized at multiple cardiac centers across Denmark, 35% of whom had at least one major comorbid condition. When this reporter observed that this was the smallest study he’d ever seen reported from Denmark, where researchers famously like to utilize interconnected national databases to conduct nationwide observational studies incorporating the country’s entire population, the cardiologist replied, “Denmark is a small country, but we like to make big trials. And this is actually the largest-ever clinical trial in endocarditis, so we are still going big.”
Important to the generalizability of the POET results was the requirement that all 400 participants had to be infected with streptococcus, Staphylococcus aureus, Enterococcus faecalis, or coagulase-negative staphylococci – the major pathogens responsible for three-quarters of all cases of infectious endocarditis.
Once participants were clinically stable after a median of 17 days of intravenous antibiotics, they were randomized to continued in-hospital intravenous antibiotic therapy for a median of another 19 days or to discharge on two oral antibiotics from different classes with different mechanisms of action administered for a median of 17 days, with selection of the oral agents being guided by the results of bacterial susceptibility testing.
The primary outcome was a composite of all-cause mortality, embolic events, unplanned cardiac surgery, and relapse of bacteremia from randomization through 6 months after completion of antibiotic therapy. This occurred in 9.0% of the orally treated group and 12.1% of patients on full-course intravenous therapy for a 28% relative risk reduction, which statistically established the noninferioritiy of the partial oral regimen. The results were similar in patients with native as compared with prosthetic valves, with or without major comorbidities, and in surgically as opposed to conservatively treated patients.
Rates of three of the four components of the composite endpoint were similar in both groups. However, all-cause mortality occurred in 3.5% of the oral therapy group, compared with 6.5% of those on intravenous therapy. Dr. Bundgård said he and his coinvestigators think the disparity in mortality was probably caused by play of chance, although he added that they were struck that four sudden deaths occurred in the intravenous group and none in patients who got oral antibiotics.
Side effects were similarly mild and low frequency in both study arms.
Audience members were eager for details on how the Danish investigators decided patients were clinically stable on intravenous antibiotics and thus ready for randomization, as well as the outpatient follow-up procedures employed in those discharged on oral therapy.
Dr. Bundgård explained that clinical stability required that a patient be afebrile, have C-reactive protein and leukocyte levels less than 35% of their peaks, and needed to have been on intravenous antibiotics for a minimum of 10 days. Moreover, patients who underwent valve surgery during their hospitalization, as did 38% of POET participants, had to wait a minimum of 7 days afterwards before they could be declared clinically stable. Lastly, just prior to randomization all participants underwent transesophageal echocardiography to rule out abscess formation or other valve abnormalities requiring surgery.
Outpatient follow-up required that patients drop in two or three times per week to be checked by a familiar physician or nurse at the hospital ward where they had stayed. Compliance was very good, although it should be noted that only five patients in the POET study were intravenous drug abusers.
Asked why investigators discharged patients on oral therapy rather than on home intravenous antibiotics, Dr. Bundgård explained that home intravenous antibiotic therapy isn’t utilized in Denmark because of the expense and logistic complexity.
Discussant Chris P. Gale, MD, urged care in generalizing the study findings.
“The ‘O’ in POET does not stand for ‘outpatient.’ Outpatients were only selected for oral therapy if they had no heart failure, no emboli, no arrhythmia, no complicating comorbidities, and they were strictly monitored – and frequently. Should we elect to adopt POET into practice, I would recommend strict adherence to the study’s patient selection and monitoring criteria,” said Dr. Gale, a cardiologist at the University of Leeds (England).
The POET results clearly swayed the full-house audience attending the late-breaking Hot Line session in the conference main arena. Immediately before Dr. Bundgård’s presentation, 66% of the audience indicated electronically that they would continue intravenous antibiotics for another 2-4 weeks in a patient with infectious endocarditis who had responded well to 2 weeks of such therapy. After seeing the study results, however, only 19% would still follow that course of action, while 59% of the audience would switch to oral antibiotics and discharge the patient.
Dr. Bundgård reported having no financial conflicts regarding the POET study, which was funded by the Danish Heart Foundation and other research foundations.
Simultaneous with Dr. Bundgård’s presentation in Munich, the POET results were published online by the New England Journal of Medicine (2018 Aug 28. doi: 10.1056/NEJMoa1808312).
MUNICH – Patients with left-sided endocarditis who are clinically stable after a couple weeks of inpatient intravenous antibiotics may at that point become candidates for discharge on oral antibiotics for the remainder of their treatment course, according to the findings of the randomized, multicenter, Danish POET trial.
“Shifting to oral antibiotic treatment in stabilized patients with endocarditis was as effective and safe as continued intravenous antibiotic treatment and was given during half the antibiotic treatment period. These novel findings may have a significant impact on future clinical practice for the management of patients who are stable,” Henning Bundgård, MD, said at the annual congress of the European Society of Cardiology.
Both ESC and American Heart Association/American College of Cardiology guidelines now recommend treatment of infective endocarditis with intravenous antibiotics for up to 6 weeks. Safely cutting the duration of in-hospital intravenous antibiotics in half is likely to generate major cost savings while improving patient quality of life and avoiding prolonged exposure to the iatrogenic risks inherent to the hospital environment, noted Dr. Bundgård, a cardiologist at Copenhagen University Hospital.
The rationale for the POET (Partial Oral Treatment of Endocarditis) trial was the investigators’ recognition that, even though infectious endocarditis is a feared disease with an in-hospital mortality of 15% or more, the great majority of serious complications occur in the early critical phase of therapy; that is, during the first 10 days or so of inpatient intravenous antibiotic therapy.
“After stabilization, the main reason for staying in the hospital is just to receive IV antibiotics,” Dr. Bundgård noted.
POET included 400 patients with left-sided endocarditis hospitalized at multiple cardiac centers across Denmark, 35% of whom had at least one major comorbid condition. When this reporter observed that this was the smallest study he’d ever seen reported from Denmark, where researchers famously like to utilize interconnected national databases to conduct nationwide observational studies incorporating the country’s entire population, the cardiologist replied, “Denmark is a small country, but we like to make big trials. And this is actually the largest-ever clinical trial in endocarditis, so we are still going big.”
Important to the generalizability of the POET results was the requirement that all 400 participants had to be infected with streptococcus, Staphylococcus aureus, Enterococcus faecalis, or coagulase-negative staphylococci – the major pathogens responsible for three-quarters of all cases of infectious endocarditis.
Once participants were clinically stable after a median of 17 days of intravenous antibiotics, they were randomized to continued in-hospital intravenous antibiotic therapy for a median of another 19 days or to discharge on two oral antibiotics from different classes with different mechanisms of action administered for a median of 17 days, with selection of the oral agents being guided by the results of bacterial susceptibility testing.
The primary outcome was a composite of all-cause mortality, embolic events, unplanned cardiac surgery, and relapse of bacteremia from randomization through 6 months after completion of antibiotic therapy. This occurred in 9.0% of the orally treated group and 12.1% of patients on full-course intravenous therapy for a 28% relative risk reduction, which statistically established the noninferioritiy of the partial oral regimen. The results were similar in patients with native as compared with prosthetic valves, with or without major comorbidities, and in surgically as opposed to conservatively treated patients.
Rates of three of the four components of the composite endpoint were similar in both groups. However, all-cause mortality occurred in 3.5% of the oral therapy group, compared with 6.5% of those on intravenous therapy. Dr. Bundgård said he and his coinvestigators think the disparity in mortality was probably caused by play of chance, although he added that they were struck that four sudden deaths occurred in the intravenous group and none in patients who got oral antibiotics.
Side effects were similarly mild and low frequency in both study arms.
Audience members were eager for details on how the Danish investigators decided patients were clinically stable on intravenous antibiotics and thus ready for randomization, as well as the outpatient follow-up procedures employed in those discharged on oral therapy.
Dr. Bundgård explained that clinical stability required that a patient be afebrile, have C-reactive protein and leukocyte levels less than 35% of their peaks, and needed to have been on intravenous antibiotics for a minimum of 10 days. Moreover, patients who underwent valve surgery during their hospitalization, as did 38% of POET participants, had to wait a minimum of 7 days afterwards before they could be declared clinically stable. Lastly, just prior to randomization all participants underwent transesophageal echocardiography to rule out abscess formation or other valve abnormalities requiring surgery.
Outpatient follow-up required that patients drop in two or three times per week to be checked by a familiar physician or nurse at the hospital ward where they had stayed. Compliance was very good, although it should be noted that only five patients in the POET study were intravenous drug abusers.
Asked why investigators discharged patients on oral therapy rather than on home intravenous antibiotics, Dr. Bundgård explained that home intravenous antibiotic therapy isn’t utilized in Denmark because of the expense and logistic complexity.
Discussant Chris P. Gale, MD, urged care in generalizing the study findings.
“The ‘O’ in POET does not stand for ‘outpatient.’ Outpatients were only selected for oral therapy if they had no heart failure, no emboli, no arrhythmia, no complicating comorbidities, and they were strictly monitored – and frequently. Should we elect to adopt POET into practice, I would recommend strict adherence to the study’s patient selection and monitoring criteria,” said Dr. Gale, a cardiologist at the University of Leeds (England).
The POET results clearly swayed the full-house audience attending the late-breaking Hot Line session in the conference main arena. Immediately before Dr. Bundgård’s presentation, 66% of the audience indicated electronically that they would continue intravenous antibiotics for another 2-4 weeks in a patient with infectious endocarditis who had responded well to 2 weeks of such therapy. After seeing the study results, however, only 19% would still follow that course of action, while 59% of the audience would switch to oral antibiotics and discharge the patient.
Dr. Bundgård reported having no financial conflicts regarding the POET study, which was funded by the Danish Heart Foundation and other research foundations.
Simultaneous with Dr. Bundgård’s presentation in Munich, the POET results were published online by the New England Journal of Medicine (2018 Aug 28. doi: 10.1056/NEJMoa1808312).
MUNICH – Patients with left-sided endocarditis who are clinically stable after a couple weeks of inpatient intravenous antibiotics may at that point become candidates for discharge on oral antibiotics for the remainder of their treatment course, according to the findings of the randomized, multicenter, Danish POET trial.
“Shifting to oral antibiotic treatment in stabilized patients with endocarditis was as effective and safe as continued intravenous antibiotic treatment and was given during half the antibiotic treatment period. These novel findings may have a significant impact on future clinical practice for the management of patients who are stable,” Henning Bundgård, MD, said at the annual congress of the European Society of Cardiology.
Both ESC and American Heart Association/American College of Cardiology guidelines now recommend treatment of infective endocarditis with intravenous antibiotics for up to 6 weeks. Safely cutting the duration of in-hospital intravenous antibiotics in half is likely to generate major cost savings while improving patient quality of life and avoiding prolonged exposure to the iatrogenic risks inherent to the hospital environment, noted Dr. Bundgård, a cardiologist at Copenhagen University Hospital.
The rationale for the POET (Partial Oral Treatment of Endocarditis) trial was the investigators’ recognition that, even though infectious endocarditis is a feared disease with an in-hospital mortality of 15% or more, the great majority of serious complications occur in the early critical phase of therapy; that is, during the first 10 days or so of inpatient intravenous antibiotic therapy.
“After stabilization, the main reason for staying in the hospital is just to receive IV antibiotics,” Dr. Bundgård noted.
POET included 400 patients with left-sided endocarditis hospitalized at multiple cardiac centers across Denmark, 35% of whom had at least one major comorbid condition. When this reporter observed that this was the smallest study he’d ever seen reported from Denmark, where researchers famously like to utilize interconnected national databases to conduct nationwide observational studies incorporating the country’s entire population, the cardiologist replied, “Denmark is a small country, but we like to make big trials. And this is actually the largest-ever clinical trial in endocarditis, so we are still going big.”
Important to the generalizability of the POET results was the requirement that all 400 participants had to be infected with streptococcus, Staphylococcus aureus, Enterococcus faecalis, or coagulase-negative staphylococci – the major pathogens responsible for three-quarters of all cases of infectious endocarditis.
Once participants were clinically stable after a median of 17 days of intravenous antibiotics, they were randomized to continued in-hospital intravenous antibiotic therapy for a median of another 19 days or to discharge on two oral antibiotics from different classes with different mechanisms of action administered for a median of 17 days, with selection of the oral agents being guided by the results of bacterial susceptibility testing.
The primary outcome was a composite of all-cause mortality, embolic events, unplanned cardiac surgery, and relapse of bacteremia from randomization through 6 months after completion of antibiotic therapy. This occurred in 9.0% of the orally treated group and 12.1% of patients on full-course intravenous therapy for a 28% relative risk reduction, which statistically established the noninferioritiy of the partial oral regimen. The results were similar in patients with native as compared with prosthetic valves, with or without major comorbidities, and in surgically as opposed to conservatively treated patients.
Rates of three of the four components of the composite endpoint were similar in both groups. However, all-cause mortality occurred in 3.5% of the oral therapy group, compared with 6.5% of those on intravenous therapy. Dr. Bundgård said he and his coinvestigators think the disparity in mortality was probably caused by play of chance, although he added that they were struck that four sudden deaths occurred in the intravenous group and none in patients who got oral antibiotics.
Side effects were similarly mild and low frequency in both study arms.
Audience members were eager for details on how the Danish investigators decided patients were clinically stable on intravenous antibiotics and thus ready for randomization, as well as the outpatient follow-up procedures employed in those discharged on oral therapy.
Dr. Bundgård explained that clinical stability required that a patient be afebrile, have C-reactive protein and leukocyte levels less than 35% of their peaks, and needed to have been on intravenous antibiotics for a minimum of 10 days. Moreover, patients who underwent valve surgery during their hospitalization, as did 38% of POET participants, had to wait a minimum of 7 days afterwards before they could be declared clinically stable. Lastly, just prior to randomization all participants underwent transesophageal echocardiography to rule out abscess formation or other valve abnormalities requiring surgery.
Outpatient follow-up required that patients drop in two or three times per week to be checked by a familiar physician or nurse at the hospital ward where they had stayed. Compliance was very good, although it should be noted that only five patients in the POET study were intravenous drug abusers.
Asked why investigators discharged patients on oral therapy rather than on home intravenous antibiotics, Dr. Bundgård explained that home intravenous antibiotic therapy isn’t utilized in Denmark because of the expense and logistic complexity.
Discussant Chris P. Gale, MD, urged care in generalizing the study findings.
“The ‘O’ in POET does not stand for ‘outpatient.’ Outpatients were only selected for oral therapy if they had no heart failure, no emboli, no arrhythmia, no complicating comorbidities, and they were strictly monitored – and frequently. Should we elect to adopt POET into practice, I would recommend strict adherence to the study’s patient selection and monitoring criteria,” said Dr. Gale, a cardiologist at the University of Leeds (England).
The POET results clearly swayed the full-house audience attending the late-breaking Hot Line session in the conference main arena. Immediately before Dr. Bundgård’s presentation, 66% of the audience indicated electronically that they would continue intravenous antibiotics for another 2-4 weeks in a patient with infectious endocarditis who had responded well to 2 weeks of such therapy. After seeing the study results, however, only 19% would still follow that course of action, while 59% of the audience would switch to oral antibiotics and discharge the patient.
Dr. Bundgård reported having no financial conflicts regarding the POET study, which was funded by the Danish Heart Foundation and other research foundations.
Simultaneous with Dr. Bundgård’s presentation in Munich, the POET results were published online by the New England Journal of Medicine (2018 Aug 28. doi: 10.1056/NEJMoa1808312).
REPORTING FROM THE ESC CONGRESS 2018
Key clinical point: Clinically stable patients with left-sided infectious endocarditis can safely and effectively be discharged on oral antibiotics after completing half of a full course of intravenous antibiotics.
Major finding: Key 6-month outcomes were similar in patients with left-sided infectious endocarditis regardless of whether they were discharged early on carefully selected oral antibiotics or remained in hospital to complete a full course of intravenous antibiotics.
Study details: This prospective, multicenter, Danish randomized trial included 400 patients with left-sided infectious endocarditis.
Disclosures: The presenter reported having no financial conflicts regarding the POET study, which was funded by the Danish Heart Foundation and other research foundations.