User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
B-cell level may affect COVID booster efficacy in MS
Patients with multiple sclerosis (MS) treated with the B-cell-depleting medication rituximab who have not yet been vaccinated against COVID-19 should get the initial vaccination as soon as possible but wait to get a booster shot until B-cell levels increase, new research suggests.
In a prospective cohort study, 90% of patients taking rituximab whose B-cell level was at least 40 cells/mcL had a sufficient antibody response to the Pfizer vaccine, whereas among those with lower levels, the antibody response was significantly lower.
Results also showed a wide variation in the length of time needed for adequate B-cell restoration. Some patients needed a year or longer for levels to become adequate.
The findings led the hospital where the study was conducted to suspend rituximab therapy until patients could be vaccinated. The findings also prompted researchers to call for new guidelines on vaccine scheduling that are based on B-cell levels and not on the current criteria of length of time since last treatment.
“It’s meaningless to just go by some recommendation covering time since the last treatment,” study investigator Joachim Burman, MD, PhD, a consultant neurologist at Uppsala University Hospital and an associate professor at Uppsala University, both in Sweden, told this news organization.
“It’s misleading and potentially harmful for patients,” Dr. Burman said.
The findings were published online in JAMA Network Open.
Finding the cutoff
Drugs such as rituximab target CD20, a protein found on the surface of B cells, resulting in B-cell depletion.
Rituximab is the most common MS therapy used in Sweden. The drug is approved in the United States to treat rheumatoid arthritis and some forms of cancer, but it is not approved for treatment of MS.
Prior research showed that antibody response to COVID-19 vaccines was lower in patients receiving B-cell therapy than in the general population. That was not altogether surprising, given the fact that studies have found a similarly weakened antibody response to other vaccines.
But before now, there was no known B-cell threshold sufficient to mount an acceptable antibody response following COVID vaccination.
Researchers enrolled 67 patients in the study. Of those patients, 60 had received rituximab treatment, and seven had not.
Approximately 6 months after the last rituximab dose, the B-cell count was lower than 10/mcL for 40% of patients. In that group, rituximab treatment duration was the only factor significantly associated with slower B-cell mobilization (median duration, 4.0 years, vs. 2.1; P = .002).
Close monitoring needed
Six weeks after vaccination with tozinameran, the mRNA vaccine manufactured by Pfizer, 28% of patients failed to generate a sufficient antibody response. Among those patients, the median B-cell count was 22/mcL, versus 51/mcL for the remainder of the cohort (P < .001).
A cutoff value of 40/mcL rendered adequate levels of anti-spike immunoglobulin G antibodies in 90% of patients and a strong response in anti-RBD antibodies in 72%.
Study participants did register an adequate T-cell response to the vaccine, suggesting at least some level of protection.
Because MS patients are at increased risk for serious illness from SARS-CoV-2 infection, the investigators recommend that patients with MS receive their initial COVID vaccines as soon as possible – but that they should hold off on receiving a booster until their B-cell counts reach 40/mcL.
Regarding when a clinician should re-vaccinate, “the results from our study strongly suggest that you should not do that right away or just follow some generic guideline,” Dr. Burman said.
“You should closely monitor the B-cell values, and re-vaccinate once those B- cells hit the level of 40 cells/mcL” he added.
Dr. Burman said he would expect that their findings would hold with the other mRNA vaccine and with any other B-cell therapy.
Too soon for B-cell measures?
Commenting for this news organization, Robert J. Fox, MD, staff neurologist at the Mellen Center for MS and vice-chair for research at the Neurological Institute at Cleveland Clinic, Ohio, said the B-cell threshold identified in the study is much higher than what is typically seen in patients who undergo treatment with ocrelizumab, an anti-CD20 B-cell therapy approved in the United States for treating MS.
“Decisions about treatment interval need to balance efficacy in treating MS with safety, including response to vaccines,” said Dr. Fox, who was not involved with the research.
“Given the unknown efficacy of these extended intervals, I don’t think we’re at the point of making management recommendations based upon B-cell counts,” he added.
And yet, Uppsala University Hospital, where the study was conducted, and other centers in Sweden decided to do just that. They suspended administering rituximab to patients with MS until the patients were vaccinated. For patients newly diagnosed with MS, therapy was initiated using another disease-modifying treatment, and for those who were due for a rituximab infusion, that treatment was delayed.
Only one patient experienced a mild MS relapse during the rituximab suspension, and that case went into remission within a week, Dr. Burman reported.
“Ever since the Bar-Or report showing that the humeral response to vaccines is markedly diminished in MS patients treated with anti-CD20 therapies, clinicians have been struggling to balance those safety concerns related to anti-CD20 monoclonal antibody treatments and the clinical benefit of this treatment class,” Dr. Fox said.
“Given the uncharted waters of the COVID pandemic, clinicians made judgments and decisions as best they could, given the paucity of data,” he noted.
“At this point, we don’t know which decisions were right or wrong, but I certainly don’t think we should judge clinicians for making decisions the best they could.”
The study was funded by the Engkvist Foundation, the Marianne and Marcus Wallenberg Foundation, and the Swedish Society for Medical Research. Dr. Burman reported no relevant financial relationships. Dr. Fox has received consulting fees from Genentech/Roche, Biogen, and other companies that promote MS therapies.
A version of this article first appeared on Medscape.com.
Patients with multiple sclerosis (MS) treated with the B-cell-depleting medication rituximab who have not yet been vaccinated against COVID-19 should get the initial vaccination as soon as possible but wait to get a booster shot until B-cell levels increase, new research suggests.
In a prospective cohort study, 90% of patients taking rituximab whose B-cell level was at least 40 cells/mcL had a sufficient antibody response to the Pfizer vaccine, whereas among those with lower levels, the antibody response was significantly lower.
Results also showed a wide variation in the length of time needed for adequate B-cell restoration. Some patients needed a year or longer for levels to become adequate.
The findings led the hospital where the study was conducted to suspend rituximab therapy until patients could be vaccinated. The findings also prompted researchers to call for new guidelines on vaccine scheduling that are based on B-cell levels and not on the current criteria of length of time since last treatment.
“It’s meaningless to just go by some recommendation covering time since the last treatment,” study investigator Joachim Burman, MD, PhD, a consultant neurologist at Uppsala University Hospital and an associate professor at Uppsala University, both in Sweden, told this news organization.
“It’s misleading and potentially harmful for patients,” Dr. Burman said.
The findings were published online in JAMA Network Open.
Finding the cutoff
Drugs such as rituximab target CD20, a protein found on the surface of B cells, resulting in B-cell depletion.
Rituximab is the most common MS therapy used in Sweden. The drug is approved in the United States to treat rheumatoid arthritis and some forms of cancer, but it is not approved for treatment of MS.
Prior research showed that antibody response to COVID-19 vaccines was lower in patients receiving B-cell therapy than in the general population. That was not altogether surprising, given the fact that studies have found a similarly weakened antibody response to other vaccines.
But before now, there was no known B-cell threshold sufficient to mount an acceptable antibody response following COVID vaccination.
Researchers enrolled 67 patients in the study. Of those patients, 60 had received rituximab treatment, and seven had not.
Approximately 6 months after the last rituximab dose, the B-cell count was lower than 10/mcL for 40% of patients. In that group, rituximab treatment duration was the only factor significantly associated with slower B-cell mobilization (median duration, 4.0 years, vs. 2.1; P = .002).
Close monitoring needed
Six weeks after vaccination with tozinameran, the mRNA vaccine manufactured by Pfizer, 28% of patients failed to generate a sufficient antibody response. Among those patients, the median B-cell count was 22/mcL, versus 51/mcL for the remainder of the cohort (P < .001).
A cutoff value of 40/mcL rendered adequate levels of anti-spike immunoglobulin G antibodies in 90% of patients and a strong response in anti-RBD antibodies in 72%.
Study participants did register an adequate T-cell response to the vaccine, suggesting at least some level of protection.
Because MS patients are at increased risk for serious illness from SARS-CoV-2 infection, the investigators recommend that patients with MS receive their initial COVID vaccines as soon as possible – but that they should hold off on receiving a booster until their B-cell counts reach 40/mcL.
Regarding when a clinician should re-vaccinate, “the results from our study strongly suggest that you should not do that right away or just follow some generic guideline,” Dr. Burman said.
“You should closely monitor the B-cell values, and re-vaccinate once those B- cells hit the level of 40 cells/mcL” he added.
Dr. Burman said he would expect that their findings would hold with the other mRNA vaccine and with any other B-cell therapy.
Too soon for B-cell measures?
Commenting for this news organization, Robert J. Fox, MD, staff neurologist at the Mellen Center for MS and vice-chair for research at the Neurological Institute at Cleveland Clinic, Ohio, said the B-cell threshold identified in the study is much higher than what is typically seen in patients who undergo treatment with ocrelizumab, an anti-CD20 B-cell therapy approved in the United States for treating MS.
“Decisions about treatment interval need to balance efficacy in treating MS with safety, including response to vaccines,” said Dr. Fox, who was not involved with the research.
“Given the unknown efficacy of these extended intervals, I don’t think we’re at the point of making management recommendations based upon B-cell counts,” he added.
And yet, Uppsala University Hospital, where the study was conducted, and other centers in Sweden decided to do just that. They suspended administering rituximab to patients with MS until the patients were vaccinated. For patients newly diagnosed with MS, therapy was initiated using another disease-modifying treatment, and for those who were due for a rituximab infusion, that treatment was delayed.
Only one patient experienced a mild MS relapse during the rituximab suspension, and that case went into remission within a week, Dr. Burman reported.
“Ever since the Bar-Or report showing that the humeral response to vaccines is markedly diminished in MS patients treated with anti-CD20 therapies, clinicians have been struggling to balance those safety concerns related to anti-CD20 monoclonal antibody treatments and the clinical benefit of this treatment class,” Dr. Fox said.
“Given the uncharted waters of the COVID pandemic, clinicians made judgments and decisions as best they could, given the paucity of data,” he noted.
“At this point, we don’t know which decisions were right or wrong, but I certainly don’t think we should judge clinicians for making decisions the best they could.”
The study was funded by the Engkvist Foundation, the Marianne and Marcus Wallenberg Foundation, and the Swedish Society for Medical Research. Dr. Burman reported no relevant financial relationships. Dr. Fox has received consulting fees from Genentech/Roche, Biogen, and other companies that promote MS therapies.
A version of this article first appeared on Medscape.com.
Patients with multiple sclerosis (MS) treated with the B-cell-depleting medication rituximab who have not yet been vaccinated against COVID-19 should get the initial vaccination as soon as possible but wait to get a booster shot until B-cell levels increase, new research suggests.
In a prospective cohort study, 90% of patients taking rituximab whose B-cell level was at least 40 cells/mcL had a sufficient antibody response to the Pfizer vaccine, whereas among those with lower levels, the antibody response was significantly lower.
Results also showed a wide variation in the length of time needed for adequate B-cell restoration. Some patients needed a year or longer for levels to become adequate.
The findings led the hospital where the study was conducted to suspend rituximab therapy until patients could be vaccinated. The findings also prompted researchers to call for new guidelines on vaccine scheduling that are based on B-cell levels and not on the current criteria of length of time since last treatment.
“It’s meaningless to just go by some recommendation covering time since the last treatment,” study investigator Joachim Burman, MD, PhD, a consultant neurologist at Uppsala University Hospital and an associate professor at Uppsala University, both in Sweden, told this news organization.
“It’s misleading and potentially harmful for patients,” Dr. Burman said.
The findings were published online in JAMA Network Open.
Finding the cutoff
Drugs such as rituximab target CD20, a protein found on the surface of B cells, resulting in B-cell depletion.
Rituximab is the most common MS therapy used in Sweden. The drug is approved in the United States to treat rheumatoid arthritis and some forms of cancer, but it is not approved for treatment of MS.
Prior research showed that antibody response to COVID-19 vaccines was lower in patients receiving B-cell therapy than in the general population. That was not altogether surprising, given the fact that studies have found a similarly weakened antibody response to other vaccines.
But before now, there was no known B-cell threshold sufficient to mount an acceptable antibody response following COVID vaccination.
Researchers enrolled 67 patients in the study. Of those patients, 60 had received rituximab treatment, and seven had not.
Approximately 6 months after the last rituximab dose, the B-cell count was lower than 10/mcL for 40% of patients. In that group, rituximab treatment duration was the only factor significantly associated with slower B-cell mobilization (median duration, 4.0 years, vs. 2.1; P = .002).
Close monitoring needed
Six weeks after vaccination with tozinameran, the mRNA vaccine manufactured by Pfizer, 28% of patients failed to generate a sufficient antibody response. Among those patients, the median B-cell count was 22/mcL, versus 51/mcL for the remainder of the cohort (P < .001).
A cutoff value of 40/mcL rendered adequate levels of anti-spike immunoglobulin G antibodies in 90% of patients and a strong response in anti-RBD antibodies in 72%.
Study participants did register an adequate T-cell response to the vaccine, suggesting at least some level of protection.
Because MS patients are at increased risk for serious illness from SARS-CoV-2 infection, the investigators recommend that patients with MS receive their initial COVID vaccines as soon as possible – but that they should hold off on receiving a booster until their B-cell counts reach 40/mcL.
Regarding when a clinician should re-vaccinate, “the results from our study strongly suggest that you should not do that right away or just follow some generic guideline,” Dr. Burman said.
“You should closely monitor the B-cell values, and re-vaccinate once those B- cells hit the level of 40 cells/mcL” he added.
Dr. Burman said he would expect that their findings would hold with the other mRNA vaccine and with any other B-cell therapy.
Too soon for B-cell measures?
Commenting for this news organization, Robert J. Fox, MD, staff neurologist at the Mellen Center for MS and vice-chair for research at the Neurological Institute at Cleveland Clinic, Ohio, said the B-cell threshold identified in the study is much higher than what is typically seen in patients who undergo treatment with ocrelizumab, an anti-CD20 B-cell therapy approved in the United States for treating MS.
“Decisions about treatment interval need to balance efficacy in treating MS with safety, including response to vaccines,” said Dr. Fox, who was not involved with the research.
“Given the unknown efficacy of these extended intervals, I don’t think we’re at the point of making management recommendations based upon B-cell counts,” he added.
And yet, Uppsala University Hospital, where the study was conducted, and other centers in Sweden decided to do just that. They suspended administering rituximab to patients with MS until the patients were vaccinated. For patients newly diagnosed with MS, therapy was initiated using another disease-modifying treatment, and for those who were due for a rituximab infusion, that treatment was delayed.
Only one patient experienced a mild MS relapse during the rituximab suspension, and that case went into remission within a week, Dr. Burman reported.
“Ever since the Bar-Or report showing that the humeral response to vaccines is markedly diminished in MS patients treated with anti-CD20 therapies, clinicians have been struggling to balance those safety concerns related to anti-CD20 monoclonal antibody treatments and the clinical benefit of this treatment class,” Dr. Fox said.
“Given the uncharted waters of the COVID pandemic, clinicians made judgments and decisions as best they could, given the paucity of data,” he noted.
“At this point, we don’t know which decisions were right or wrong, but I certainly don’t think we should judge clinicians for making decisions the best they could.”
The study was funded by the Engkvist Foundation, the Marianne and Marcus Wallenberg Foundation, and the Swedish Society for Medical Research. Dr. Burman reported no relevant financial relationships. Dr. Fox has received consulting fees from Genentech/Roche, Biogen, and other companies that promote MS therapies.
A version of this article first appeared on Medscape.com.
Surgeons, who see it up close, offer ways to stop gun violence
Their strategies can work regardless of where you stand on the Second Amendment of the Constitution, said Patricia Turner, MD. “Our proposals are embraced by both gun owners and non–gun owners alike, and we are unique in that regard.”
These “implementable solutions” could prevent the next massacre, Dr. Turner, executive director of the American College of Surgeons, said during a news briefing the group sponsored on June 2.
“Our future – indeed all of our futures – depend on our ability to find durable, actionable steps that we can implement tomorrow to save lives,” she said.
Firsthand perspective
“Sadly I’m here today as a trauma surgeon who has cared for two of the largest mass shootings in modern U.S. history,” said Ronald Stewart, MD, chair of the department of surgery at University Hospital in San Antonio, Texas.
Dr. Stewart treated victims of the 2017 Sutherland Springs First Baptist Church shooting – where 27 people died, including the shooter – and the recent Uvalde school shooting, both in Texas.
“The injuries inflicted by high-velocity weapons used at both of these attacks are horrific. A high-capacity, magazine-fed automatic rifle such as the AR-15 causes extremely destructive tissue wounds,” he said.
One of the group’s proposals is to increase the regulation of high-velocity weapons, including AR-15s.
“These wounds are horribly lethal at close range, and sadly, most victims do not survive long enough to make it to a trauma center,” Dr. Stewart said.
On a positive note, “all of our current [Uvalde] patients are improving, which really brings us joy in this dark time,” he said. “But all of them have a long road to deal with recovery with both the physical and emotional impact of their injuries.”
Jeffrey Kerby, MD, agreed.
“Trauma surgeons see the short-term physical effects of these injuries and watch patients struggle with the long-term impact of these wounds,” said Dr. Kerby, director of trauma and acute care surgery at the University of Alabama at Birmingham.
Surgeons feel ‘profound impact’ of shootings
“Firearm violence has a profound impact on surgeons, and we are the undisputed subject matter experts in treating the tragic results,” said Patrick Bailey, MD, medical director for advocacy at the American College of Surgeons.
“This impacts surgeons as well,” said Dr. Kerby, chair of the Committee on Trauma for the surgeons’ group. “We are human, and we can’t help but share in the grief, the pain, and the suffering that our patients endure.
“As a pediatric surgeon ... I have too often witnessed the impact of firearm violence, and obviously, the devastation extends beyond the victims to their families,” he said. “To put it succinctly, in our culture, parents are not supposed to be put in a position of burying their children.”
A public health crisis
“It’s important to recognize that we’ve been talking about a public health approach,” said Eileen Bulger, MD, acting chief of the trauma division at the University of Washington in Seattle. That strategy is important for engaging both firearm owners and communities that have a higher risk for firearm violence, she said.
A committee of the American College of Surgeons developed specific recommendations in 2018, which are still valid today. The group brought together surgeons from across the U.S. including “passionate firearm owners and experts in firearm safety,” Dr. Bulger said.
The committee, for example, agreed on 10 specific recommendations “that we believe are bipartisan and could have an immediate impact in saving lives.”
“I’m a lifelong gun owner,” Dr. Bailey said, emphasizing that the team’s process included participation and perspective from other surgeons “who, like me, are also gun owners, but gun owners who also seek to reduce the impact of firearm violence in our country.”
The recommendations address these areas:
- Gun ownership
- Firearm registration
- Licensure
- Education and training
- Ownership responsibilities
- Mandatory reporting and risk reduction
- Safety innovation and technology
- Research
- The culture of violence
- Social isolation and mental health
For example, “we currently have certain classes of weapons with significant offensive capability,” Dr. Bulger said, “that are appropriately restricted and regulated under the National Firearms Act as Class 3 weapons.”
This group includes fully automatic machine guns, explosive devices, and short-barrel shotguns.
“We recommend a formal reassessment of the firearms designated within each of these national firearms classifications,” Dr. Bulger said.
For example, high-capacity, magazine-fed semiautomatic rifles, such as the AR-15, should be considered for reclassification as NFA Class 3 firearms, or they should get a new designation with tighter regulation.
The ACS endorses formal firearm safety training for all new gun owners. Also, owners who do not provide reasonably safe firearm storage should be held responsible for events related to the discharge of their firearms, Dr. Bulger said. And people who are deemed an imminent threat to themselves or others through firearm ownership should be temporarily or permanently restricted, with due process.
Research and reporting reforms
The ACS is also calling for research on firearm injuries and firearm injury prevention to be federally funded, Dr. Bulger said. The research should be done in a nonpartisan manner, she said.
“We have concerns that the manner and tone in which information is released to the public may lead to copycat mass killers,” she said. “The ACS recommends that law enforcement officials and the press take steps to eliminate the notoriety of the shooter, for example.”
Dr. Bulger also addressed the mental health angle. “We encourage recognition of mental health warning signs and social isolation by teachers, counselors, peers, and parents.” When identified, immediate referral to professionals is needed.
In addition to these recommendations, another team from the American College of Surgeons has published an overview of ways to address the inequities that contribute to violence. “We advocate for federal funding to support the development of hospital-based and community programs for violence intervention and prevention,” Dr. Bulger said.
Dr. Bailey said that as a gun owner himself, he thinks other gun owners would support these recommendations.
“I do not believe that the steps recommended ... pose undue burden on the rights of individual gun owners,” he said.
The time is now
Most firearm injuries are not from mass shooting events, Dr. Kerby said.
“My own trauma center has seen a 40% increase in the number of firearm injuries just in the last 2 years,” he added, “and these numbers continue to grow.”
A version of this article first appeared on WebMD.com.
Their strategies can work regardless of where you stand on the Second Amendment of the Constitution, said Patricia Turner, MD. “Our proposals are embraced by both gun owners and non–gun owners alike, and we are unique in that regard.”
These “implementable solutions” could prevent the next massacre, Dr. Turner, executive director of the American College of Surgeons, said during a news briefing the group sponsored on June 2.
“Our future – indeed all of our futures – depend on our ability to find durable, actionable steps that we can implement tomorrow to save lives,” she said.
Firsthand perspective
“Sadly I’m here today as a trauma surgeon who has cared for two of the largest mass shootings in modern U.S. history,” said Ronald Stewart, MD, chair of the department of surgery at University Hospital in San Antonio, Texas.
Dr. Stewart treated victims of the 2017 Sutherland Springs First Baptist Church shooting – where 27 people died, including the shooter – and the recent Uvalde school shooting, both in Texas.
“The injuries inflicted by high-velocity weapons used at both of these attacks are horrific. A high-capacity, magazine-fed automatic rifle such as the AR-15 causes extremely destructive tissue wounds,” he said.
One of the group’s proposals is to increase the regulation of high-velocity weapons, including AR-15s.
“These wounds are horribly lethal at close range, and sadly, most victims do not survive long enough to make it to a trauma center,” Dr. Stewart said.
On a positive note, “all of our current [Uvalde] patients are improving, which really brings us joy in this dark time,” he said. “But all of them have a long road to deal with recovery with both the physical and emotional impact of their injuries.”
Jeffrey Kerby, MD, agreed.
“Trauma surgeons see the short-term physical effects of these injuries and watch patients struggle with the long-term impact of these wounds,” said Dr. Kerby, director of trauma and acute care surgery at the University of Alabama at Birmingham.
Surgeons feel ‘profound impact’ of shootings
“Firearm violence has a profound impact on surgeons, and we are the undisputed subject matter experts in treating the tragic results,” said Patrick Bailey, MD, medical director for advocacy at the American College of Surgeons.
“This impacts surgeons as well,” said Dr. Kerby, chair of the Committee on Trauma for the surgeons’ group. “We are human, and we can’t help but share in the grief, the pain, and the suffering that our patients endure.
“As a pediatric surgeon ... I have too often witnessed the impact of firearm violence, and obviously, the devastation extends beyond the victims to their families,” he said. “To put it succinctly, in our culture, parents are not supposed to be put in a position of burying their children.”
A public health crisis
“It’s important to recognize that we’ve been talking about a public health approach,” said Eileen Bulger, MD, acting chief of the trauma division at the University of Washington in Seattle. That strategy is important for engaging both firearm owners and communities that have a higher risk for firearm violence, she said.
A committee of the American College of Surgeons developed specific recommendations in 2018, which are still valid today. The group brought together surgeons from across the U.S. including “passionate firearm owners and experts in firearm safety,” Dr. Bulger said.
The committee, for example, agreed on 10 specific recommendations “that we believe are bipartisan and could have an immediate impact in saving lives.”
“I’m a lifelong gun owner,” Dr. Bailey said, emphasizing that the team’s process included participation and perspective from other surgeons “who, like me, are also gun owners, but gun owners who also seek to reduce the impact of firearm violence in our country.”
The recommendations address these areas:
- Gun ownership
- Firearm registration
- Licensure
- Education and training
- Ownership responsibilities
- Mandatory reporting and risk reduction
- Safety innovation and technology
- Research
- The culture of violence
- Social isolation and mental health
For example, “we currently have certain classes of weapons with significant offensive capability,” Dr. Bulger said, “that are appropriately restricted and regulated under the National Firearms Act as Class 3 weapons.”
This group includes fully automatic machine guns, explosive devices, and short-barrel shotguns.
“We recommend a formal reassessment of the firearms designated within each of these national firearms classifications,” Dr. Bulger said.
For example, high-capacity, magazine-fed semiautomatic rifles, such as the AR-15, should be considered for reclassification as NFA Class 3 firearms, or they should get a new designation with tighter regulation.
The ACS endorses formal firearm safety training for all new gun owners. Also, owners who do not provide reasonably safe firearm storage should be held responsible for events related to the discharge of their firearms, Dr. Bulger said. And people who are deemed an imminent threat to themselves or others through firearm ownership should be temporarily or permanently restricted, with due process.
Research and reporting reforms
The ACS is also calling for research on firearm injuries and firearm injury prevention to be federally funded, Dr. Bulger said. The research should be done in a nonpartisan manner, she said.
“We have concerns that the manner and tone in which information is released to the public may lead to copycat mass killers,” she said. “The ACS recommends that law enforcement officials and the press take steps to eliminate the notoriety of the shooter, for example.”
Dr. Bulger also addressed the mental health angle. “We encourage recognition of mental health warning signs and social isolation by teachers, counselors, peers, and parents.” When identified, immediate referral to professionals is needed.
In addition to these recommendations, another team from the American College of Surgeons has published an overview of ways to address the inequities that contribute to violence. “We advocate for federal funding to support the development of hospital-based and community programs for violence intervention and prevention,” Dr. Bulger said.
Dr. Bailey said that as a gun owner himself, he thinks other gun owners would support these recommendations.
“I do not believe that the steps recommended ... pose undue burden on the rights of individual gun owners,” he said.
The time is now
Most firearm injuries are not from mass shooting events, Dr. Kerby said.
“My own trauma center has seen a 40% increase in the number of firearm injuries just in the last 2 years,” he added, “and these numbers continue to grow.”
A version of this article first appeared on WebMD.com.
Their strategies can work regardless of where you stand on the Second Amendment of the Constitution, said Patricia Turner, MD. “Our proposals are embraced by both gun owners and non–gun owners alike, and we are unique in that regard.”
These “implementable solutions” could prevent the next massacre, Dr. Turner, executive director of the American College of Surgeons, said during a news briefing the group sponsored on June 2.
“Our future – indeed all of our futures – depend on our ability to find durable, actionable steps that we can implement tomorrow to save lives,” she said.
Firsthand perspective
“Sadly I’m here today as a trauma surgeon who has cared for two of the largest mass shootings in modern U.S. history,” said Ronald Stewart, MD, chair of the department of surgery at University Hospital in San Antonio, Texas.
Dr. Stewart treated victims of the 2017 Sutherland Springs First Baptist Church shooting – where 27 people died, including the shooter – and the recent Uvalde school shooting, both in Texas.
“The injuries inflicted by high-velocity weapons used at both of these attacks are horrific. A high-capacity, magazine-fed automatic rifle such as the AR-15 causes extremely destructive tissue wounds,” he said.
One of the group’s proposals is to increase the regulation of high-velocity weapons, including AR-15s.
“These wounds are horribly lethal at close range, and sadly, most victims do not survive long enough to make it to a trauma center,” Dr. Stewart said.
On a positive note, “all of our current [Uvalde] patients are improving, which really brings us joy in this dark time,” he said. “But all of them have a long road to deal with recovery with both the physical and emotional impact of their injuries.”
Jeffrey Kerby, MD, agreed.
“Trauma surgeons see the short-term physical effects of these injuries and watch patients struggle with the long-term impact of these wounds,” said Dr. Kerby, director of trauma and acute care surgery at the University of Alabama at Birmingham.
Surgeons feel ‘profound impact’ of shootings
“Firearm violence has a profound impact on surgeons, and we are the undisputed subject matter experts in treating the tragic results,” said Patrick Bailey, MD, medical director for advocacy at the American College of Surgeons.
“This impacts surgeons as well,” said Dr. Kerby, chair of the Committee on Trauma for the surgeons’ group. “We are human, and we can’t help but share in the grief, the pain, and the suffering that our patients endure.
“As a pediatric surgeon ... I have too often witnessed the impact of firearm violence, and obviously, the devastation extends beyond the victims to their families,” he said. “To put it succinctly, in our culture, parents are not supposed to be put in a position of burying their children.”
A public health crisis
“It’s important to recognize that we’ve been talking about a public health approach,” said Eileen Bulger, MD, acting chief of the trauma division at the University of Washington in Seattle. That strategy is important for engaging both firearm owners and communities that have a higher risk for firearm violence, she said.
A committee of the American College of Surgeons developed specific recommendations in 2018, which are still valid today. The group brought together surgeons from across the U.S. including “passionate firearm owners and experts in firearm safety,” Dr. Bulger said.
The committee, for example, agreed on 10 specific recommendations “that we believe are bipartisan and could have an immediate impact in saving lives.”
“I’m a lifelong gun owner,” Dr. Bailey said, emphasizing that the team’s process included participation and perspective from other surgeons “who, like me, are also gun owners, but gun owners who also seek to reduce the impact of firearm violence in our country.”
The recommendations address these areas:
- Gun ownership
- Firearm registration
- Licensure
- Education and training
- Ownership responsibilities
- Mandatory reporting and risk reduction
- Safety innovation and technology
- Research
- The culture of violence
- Social isolation and mental health
For example, “we currently have certain classes of weapons with significant offensive capability,” Dr. Bulger said, “that are appropriately restricted and regulated under the National Firearms Act as Class 3 weapons.”
This group includes fully automatic machine guns, explosive devices, and short-barrel shotguns.
“We recommend a formal reassessment of the firearms designated within each of these national firearms classifications,” Dr. Bulger said.
For example, high-capacity, magazine-fed semiautomatic rifles, such as the AR-15, should be considered for reclassification as NFA Class 3 firearms, or they should get a new designation with tighter regulation.
The ACS endorses formal firearm safety training for all new gun owners. Also, owners who do not provide reasonably safe firearm storage should be held responsible for events related to the discharge of their firearms, Dr. Bulger said. And people who are deemed an imminent threat to themselves or others through firearm ownership should be temporarily or permanently restricted, with due process.
Research and reporting reforms
The ACS is also calling for research on firearm injuries and firearm injury prevention to be federally funded, Dr. Bulger said. The research should be done in a nonpartisan manner, she said.
“We have concerns that the manner and tone in which information is released to the public may lead to copycat mass killers,” she said. “The ACS recommends that law enforcement officials and the press take steps to eliminate the notoriety of the shooter, for example.”
Dr. Bulger also addressed the mental health angle. “We encourage recognition of mental health warning signs and social isolation by teachers, counselors, peers, and parents.” When identified, immediate referral to professionals is needed.
In addition to these recommendations, another team from the American College of Surgeons has published an overview of ways to address the inequities that contribute to violence. “We advocate for federal funding to support the development of hospital-based and community programs for violence intervention and prevention,” Dr. Bulger said.
Dr. Bailey said that as a gun owner himself, he thinks other gun owners would support these recommendations.
“I do not believe that the steps recommended ... pose undue burden on the rights of individual gun owners,” he said.
The time is now
Most firearm injuries are not from mass shooting events, Dr. Kerby said.
“My own trauma center has seen a 40% increase in the number of firearm injuries just in the last 2 years,” he added, “and these numbers continue to grow.”
A version of this article first appeared on WebMD.com.
Woman who faked cancer gets 5 years in prison
A California woman who pretended to have cancer and received more than $100,000 in charitable donations from hundreds of people has been sentenced to 5 years in prison.
Amanda Christine Riley pleaded guilty to one count of wire fraud for soliciting donations from people through various social media sites to help pay for cancer treatments that she never received or needed, according to the U.S. Department of Justice.
In total, the government identified 349 individuals and entities who made contributions totaling $105,513. Ms. Riley was sentenced to 60 months in prison on May 3.
Ms. Riley is hardly the first person to fake a cancer diagnosis for money. In fact, the phenomenon of faking illness online now occurs so often that researchers have given it a name: “Munchausen by internet.” However, few appear to be penalized with prison time.
In this case, the scam began in 2012, when Ms. Riley falsely claimed to have been diagnosed with Hodgkin’s lymphoma. She used Facebook, Instagram, Twitter, and a blog to document her imaginary condition and “aggressively” solicit donations to cover her supposed medical expenses, the DOJ said.
Instead, Ms. Riley used the donations to pay living expenses.
According to the DOJ, Ms. Riley went to “great lengths to maintain her deception.” She shaved her head to appear to be undergoing chemotherapy, faked her medical records, forged physicians’ letters and medical certifications, and convinced family members to back up her false claims.
Ms. Riley’s scheme continued for 7 years, until 2019, when her deception was uncovered by an investigation of the Internal Revenue Service and the San Jose Police Department.
Ms. Riley was charged in July 2020 and pleaded guilty in October 2021.
In addition to serving 5 years in prison, Ms. Riley must pay back the $105,513 and undergo 3 years of supervision after her release.
A version of this article first appeared on Medscape.com.
A California woman who pretended to have cancer and received more than $100,000 in charitable donations from hundreds of people has been sentenced to 5 years in prison.
Amanda Christine Riley pleaded guilty to one count of wire fraud for soliciting donations from people through various social media sites to help pay for cancer treatments that she never received or needed, according to the U.S. Department of Justice.
In total, the government identified 349 individuals and entities who made contributions totaling $105,513. Ms. Riley was sentenced to 60 months in prison on May 3.
Ms. Riley is hardly the first person to fake a cancer diagnosis for money. In fact, the phenomenon of faking illness online now occurs so often that researchers have given it a name: “Munchausen by internet.” However, few appear to be penalized with prison time.
In this case, the scam began in 2012, when Ms. Riley falsely claimed to have been diagnosed with Hodgkin’s lymphoma. She used Facebook, Instagram, Twitter, and a blog to document her imaginary condition and “aggressively” solicit donations to cover her supposed medical expenses, the DOJ said.
Instead, Ms. Riley used the donations to pay living expenses.
According to the DOJ, Ms. Riley went to “great lengths to maintain her deception.” She shaved her head to appear to be undergoing chemotherapy, faked her medical records, forged physicians’ letters and medical certifications, and convinced family members to back up her false claims.
Ms. Riley’s scheme continued for 7 years, until 2019, when her deception was uncovered by an investigation of the Internal Revenue Service and the San Jose Police Department.
Ms. Riley was charged in July 2020 and pleaded guilty in October 2021.
In addition to serving 5 years in prison, Ms. Riley must pay back the $105,513 and undergo 3 years of supervision after her release.
A version of this article first appeared on Medscape.com.
A California woman who pretended to have cancer and received more than $100,000 in charitable donations from hundreds of people has been sentenced to 5 years in prison.
Amanda Christine Riley pleaded guilty to one count of wire fraud for soliciting donations from people through various social media sites to help pay for cancer treatments that she never received or needed, according to the U.S. Department of Justice.
In total, the government identified 349 individuals and entities who made contributions totaling $105,513. Ms. Riley was sentenced to 60 months in prison on May 3.
Ms. Riley is hardly the first person to fake a cancer diagnosis for money. In fact, the phenomenon of faking illness online now occurs so often that researchers have given it a name: “Munchausen by internet.” However, few appear to be penalized with prison time.
In this case, the scam began in 2012, when Ms. Riley falsely claimed to have been diagnosed with Hodgkin’s lymphoma. She used Facebook, Instagram, Twitter, and a blog to document her imaginary condition and “aggressively” solicit donations to cover her supposed medical expenses, the DOJ said.
Instead, Ms. Riley used the donations to pay living expenses.
According to the DOJ, Ms. Riley went to “great lengths to maintain her deception.” She shaved her head to appear to be undergoing chemotherapy, faked her medical records, forged physicians’ letters and medical certifications, and convinced family members to back up her false claims.
Ms. Riley’s scheme continued for 7 years, until 2019, when her deception was uncovered by an investigation of the Internal Revenue Service and the San Jose Police Department.
Ms. Riley was charged in July 2020 and pleaded guilty in October 2021.
In addition to serving 5 years in prison, Ms. Riley must pay back the $105,513 and undergo 3 years of supervision after her release.
A version of this article first appeared on Medscape.com.
High rates of med student burnout during COVID
NEW ORLEANS –
Researchers surveyed 613 medical students representing all years of a medical program during the last week of the Spring semester of 2021.
Based on the Maslach Burnout Inventory-Student Survey (MBI-SS), more than half (54%) of the students had symptoms of burnout.
Eighty percent of students scored high on emotional exhaustion, 57% scored high on cynicism, and 36% scored low on academic effectiveness.
Compared with male medical students, female medical students were more apt to exhibit signs of burnout (60% vs. 44%), emotional exhaustion (80% vs. 73%), and cynicism (62% vs. 49%).
After adjusting for associated factors, female medical students were significantly more likely to suffer from burnout than male students (odds ratio, 1.90; 95% confidence interval, 1.34-2.70; P < .001).
Smoking was also linked to higher likelihood of burnout among medical students (OR, 2.12; 95% CI, 1.18-3.81; P < .05). The death of a family member from COVID-19 also put medical students at heightened risk for burnout (OR, 1.60; 95% CI, 1.08-2.36; P < .05).
The survey results were presented at the American Psychiatric Association (APA) Annual Meeting.
The findings point to the need to study burnout prevalence in universities and develop strategies to promote the mental health of future physicians, presenter Sofia Jezzini-Martínez, fourth-year medical student, Autonomous University of Nuevo Leon, Monterrey, Mexico, wrote in her conference abstract.
In related research presented at the APA meeting, researchers surveyed second-, third-, and fourth-year medical students from California during the pandemic.
Roughly 80% exhibited symptoms of anxiety and 68% exhibited depressive symptoms, of whom about 18% also reported having thoughts of suicide.
Yet only about half of the medical students exhibiting anxiety or depressive symptoms sought help from a mental health professional, and 20% reported using substances to cope with stress.
“Given that the pandemic is ongoing, we hope to draw attention to mental health needs of medical students and influence medical schools to direct appropriate and timely resources to this group,” presenter Sarthak Angal, MD, psychiatry resident, Kaiser Permanente San Jose Medical Center, California, wrote in his conference abstract.
Managing expectations
Weighing in on medical student burnout, Ihuoma Njoku, MD, department of psychiatry and neurobehavioral sciences, University of Virginia, Charlottesville, noted that, “particularly for women in multiple fields, including medicine, there’s a lot of burden placed on them.”
“Women are pulled in a lot of different directions and have increased demands, which may help explain their higher rate of burnout,” Dr. Njoku commented.
She noted that these surveys were conducted during the COVID-19 pandemic, “a period when students’ education experience was a lot different than what they expected and maybe what they wanted.”
Dr. Njoku noted that the challenges of the pandemic are particularly hard on fourth-year medical students.
“A big part of fourth year is applying to residency, and many were doing virtual interviews for residency. That makes it hard to really get an appreciation of the place you will spend the next three to eight years of your life,” she told this news organization.
A version of this article first appeared on Medscape.com.
NEW ORLEANS –
Researchers surveyed 613 medical students representing all years of a medical program during the last week of the Spring semester of 2021.
Based on the Maslach Burnout Inventory-Student Survey (MBI-SS), more than half (54%) of the students had symptoms of burnout.
Eighty percent of students scored high on emotional exhaustion, 57% scored high on cynicism, and 36% scored low on academic effectiveness.
Compared with male medical students, female medical students were more apt to exhibit signs of burnout (60% vs. 44%), emotional exhaustion (80% vs. 73%), and cynicism (62% vs. 49%).
After adjusting for associated factors, female medical students were significantly more likely to suffer from burnout than male students (odds ratio, 1.90; 95% confidence interval, 1.34-2.70; P < .001).
Smoking was also linked to higher likelihood of burnout among medical students (OR, 2.12; 95% CI, 1.18-3.81; P < .05). The death of a family member from COVID-19 also put medical students at heightened risk for burnout (OR, 1.60; 95% CI, 1.08-2.36; P < .05).
The survey results were presented at the American Psychiatric Association (APA) Annual Meeting.
The findings point to the need to study burnout prevalence in universities and develop strategies to promote the mental health of future physicians, presenter Sofia Jezzini-Martínez, fourth-year medical student, Autonomous University of Nuevo Leon, Monterrey, Mexico, wrote in her conference abstract.
In related research presented at the APA meeting, researchers surveyed second-, third-, and fourth-year medical students from California during the pandemic.
Roughly 80% exhibited symptoms of anxiety and 68% exhibited depressive symptoms, of whom about 18% also reported having thoughts of suicide.
Yet only about half of the medical students exhibiting anxiety or depressive symptoms sought help from a mental health professional, and 20% reported using substances to cope with stress.
“Given that the pandemic is ongoing, we hope to draw attention to mental health needs of medical students and influence medical schools to direct appropriate and timely resources to this group,” presenter Sarthak Angal, MD, psychiatry resident, Kaiser Permanente San Jose Medical Center, California, wrote in his conference abstract.
Managing expectations
Weighing in on medical student burnout, Ihuoma Njoku, MD, department of psychiatry and neurobehavioral sciences, University of Virginia, Charlottesville, noted that, “particularly for women in multiple fields, including medicine, there’s a lot of burden placed on them.”
“Women are pulled in a lot of different directions and have increased demands, which may help explain their higher rate of burnout,” Dr. Njoku commented.
She noted that these surveys were conducted during the COVID-19 pandemic, “a period when students’ education experience was a lot different than what they expected and maybe what they wanted.”
Dr. Njoku noted that the challenges of the pandemic are particularly hard on fourth-year medical students.
“A big part of fourth year is applying to residency, and many were doing virtual interviews for residency. That makes it hard to really get an appreciation of the place you will spend the next three to eight years of your life,” she told this news organization.
A version of this article first appeared on Medscape.com.
NEW ORLEANS –
Researchers surveyed 613 medical students representing all years of a medical program during the last week of the Spring semester of 2021.
Based on the Maslach Burnout Inventory-Student Survey (MBI-SS), more than half (54%) of the students had symptoms of burnout.
Eighty percent of students scored high on emotional exhaustion, 57% scored high on cynicism, and 36% scored low on academic effectiveness.
Compared with male medical students, female medical students were more apt to exhibit signs of burnout (60% vs. 44%), emotional exhaustion (80% vs. 73%), and cynicism (62% vs. 49%).
After adjusting for associated factors, female medical students were significantly more likely to suffer from burnout than male students (odds ratio, 1.90; 95% confidence interval, 1.34-2.70; P < .001).
Smoking was also linked to higher likelihood of burnout among medical students (OR, 2.12; 95% CI, 1.18-3.81; P < .05). The death of a family member from COVID-19 also put medical students at heightened risk for burnout (OR, 1.60; 95% CI, 1.08-2.36; P < .05).
The survey results were presented at the American Psychiatric Association (APA) Annual Meeting.
The findings point to the need to study burnout prevalence in universities and develop strategies to promote the mental health of future physicians, presenter Sofia Jezzini-Martínez, fourth-year medical student, Autonomous University of Nuevo Leon, Monterrey, Mexico, wrote in her conference abstract.
In related research presented at the APA meeting, researchers surveyed second-, third-, and fourth-year medical students from California during the pandemic.
Roughly 80% exhibited symptoms of anxiety and 68% exhibited depressive symptoms, of whom about 18% also reported having thoughts of suicide.
Yet only about half of the medical students exhibiting anxiety or depressive symptoms sought help from a mental health professional, and 20% reported using substances to cope with stress.
“Given that the pandemic is ongoing, we hope to draw attention to mental health needs of medical students and influence medical schools to direct appropriate and timely resources to this group,” presenter Sarthak Angal, MD, psychiatry resident, Kaiser Permanente San Jose Medical Center, California, wrote in his conference abstract.
Managing expectations
Weighing in on medical student burnout, Ihuoma Njoku, MD, department of psychiatry and neurobehavioral sciences, University of Virginia, Charlottesville, noted that, “particularly for women in multiple fields, including medicine, there’s a lot of burden placed on them.”
“Women are pulled in a lot of different directions and have increased demands, which may help explain their higher rate of burnout,” Dr. Njoku commented.
She noted that these surveys were conducted during the COVID-19 pandemic, “a period when students’ education experience was a lot different than what they expected and maybe what they wanted.”
Dr. Njoku noted that the challenges of the pandemic are particularly hard on fourth-year medical students.
“A big part of fourth year is applying to residency, and many were doing virtual interviews for residency. That makes it hard to really get an appreciation of the place you will spend the next three to eight years of your life,” she told this news organization.
A version of this article first appeared on Medscape.com.
FROM APA 2022
Can lasers be used to measure nerve sensitivity in the skin?
SAN DIEGO – In a 2006 report of complications from laser dermatologic surgery, one of the authors, Dieter Manstein, MD, PhD, who had subjected his forearm to treatment with a fractional laser skin resurfacing prototype device, was included as 1 of the 19 featured cases.
Dr. Manstein, of the Cutaneous Biology Research Center in the department of dermatology at Massachusetts General Hospital, Boston, was exposed to three test spots in the evaluation of the effects of different microscopic thermal zone densities for the prototype device, emitting at 1,450 nm and an energy per MTZ of 3 mJ.
Two years later, hypopigmentation persisted at the test site treated with the highest MTZ density, while two other sites treated with the lower MTZ densities did not show any dyspigmentation. But he noticed something else during the experiment: He felt minimal to no pain as each test site was being treated.
“It took 7 minutes without any cooling or anesthesia,” Dr. Manstein recalled at the annual meeting of the American Society for Laser Medicine and Surgery. “It was not completely painless, but each time the laser was applied, sometimes I felt a little prick, sometimes I felt nothing.” Essentially, he added, “we created cell injury with a focused laser beam without anesthesia,” but this could also indicate that if skin is treated with a fractional laser very slowly, anesthesia is not needed. “Current devices are meant to treat very quickly, but if we [treat] slowly, maybe you could remove lesions painlessly without anesthesia.”
The observation from that experiment also led Dr. Manstein and colleagues to wonder: Could a focused laser beam pattern be used to assess cutaneous innervation? If so, they postulated, perhaps it could be used to not only assess nerve sensitivity of candidates for dermatologic surgery, but as a tool to help diagnose small fiber neuropathies such as diabetic neuropathy, and neuropathies in patients with HIV and sarcoidosis.
The current gold standard for making these diagnoses involves a skin biopsy, immunohistochemical analysis, and nerve fiber quantification, which is not widely available. It also requires strict histologic processing and nerve counting rules. Confocal microscopy of nerve fibers in the cornea is another approach, but is very difficult to perform, “so it would be nice if there was a simple way” to determine nerve fiber density in the skin using a focused laser beam, Dr. Manstein said.
With help from Payal Patel, MD, a dermatology research fellow at MGH, records each subject’s perception of a stimulus, and maps the areas of stimulus response. Current diameters being studied range from 0.076-1.15 mm and depths less than 0.71 mm. “We can focus the laser beam, preset the beam diameter, and very slowly, in a controlled manner, make a rectangular pattern, and after each time, inquire if the subject felt the pulse or not,” Dr. Manstein explained.
“This laser could become a new method for diagnosing nerve fiber neuropathies. If this works well, I think we can miniaturize the device,” he added.
Dr. Manstein disclosed that he is a consultant for Blossom Innovations, R2 Dermatology, and AVAVA. He is also a member of the advisory board for Blossom Innovations.
SAN DIEGO – In a 2006 report of complications from laser dermatologic surgery, one of the authors, Dieter Manstein, MD, PhD, who had subjected his forearm to treatment with a fractional laser skin resurfacing prototype device, was included as 1 of the 19 featured cases.
Dr. Manstein, of the Cutaneous Biology Research Center in the department of dermatology at Massachusetts General Hospital, Boston, was exposed to three test spots in the evaluation of the effects of different microscopic thermal zone densities for the prototype device, emitting at 1,450 nm and an energy per MTZ of 3 mJ.
Two years later, hypopigmentation persisted at the test site treated with the highest MTZ density, while two other sites treated with the lower MTZ densities did not show any dyspigmentation. But he noticed something else during the experiment: He felt minimal to no pain as each test site was being treated.
“It took 7 minutes without any cooling or anesthesia,” Dr. Manstein recalled at the annual meeting of the American Society for Laser Medicine and Surgery. “It was not completely painless, but each time the laser was applied, sometimes I felt a little prick, sometimes I felt nothing.” Essentially, he added, “we created cell injury with a focused laser beam without anesthesia,” but this could also indicate that if skin is treated with a fractional laser very slowly, anesthesia is not needed. “Current devices are meant to treat very quickly, but if we [treat] slowly, maybe you could remove lesions painlessly without anesthesia.”
The observation from that experiment also led Dr. Manstein and colleagues to wonder: Could a focused laser beam pattern be used to assess cutaneous innervation? If so, they postulated, perhaps it could be used to not only assess nerve sensitivity of candidates for dermatologic surgery, but as a tool to help diagnose small fiber neuropathies such as diabetic neuropathy, and neuropathies in patients with HIV and sarcoidosis.
The current gold standard for making these diagnoses involves a skin biopsy, immunohistochemical analysis, and nerve fiber quantification, which is not widely available. It also requires strict histologic processing and nerve counting rules. Confocal microscopy of nerve fibers in the cornea is another approach, but is very difficult to perform, “so it would be nice if there was a simple way” to determine nerve fiber density in the skin using a focused laser beam, Dr. Manstein said.
With help from Payal Patel, MD, a dermatology research fellow at MGH, records each subject’s perception of a stimulus, and maps the areas of stimulus response. Current diameters being studied range from 0.076-1.15 mm and depths less than 0.71 mm. “We can focus the laser beam, preset the beam diameter, and very slowly, in a controlled manner, make a rectangular pattern, and after each time, inquire if the subject felt the pulse or not,” Dr. Manstein explained.
“This laser could become a new method for diagnosing nerve fiber neuropathies. If this works well, I think we can miniaturize the device,” he added.
Dr. Manstein disclosed that he is a consultant for Blossom Innovations, R2 Dermatology, and AVAVA. He is also a member of the advisory board for Blossom Innovations.
SAN DIEGO – In a 2006 report of complications from laser dermatologic surgery, one of the authors, Dieter Manstein, MD, PhD, who had subjected his forearm to treatment with a fractional laser skin resurfacing prototype device, was included as 1 of the 19 featured cases.
Dr. Manstein, of the Cutaneous Biology Research Center in the department of dermatology at Massachusetts General Hospital, Boston, was exposed to three test spots in the evaluation of the effects of different microscopic thermal zone densities for the prototype device, emitting at 1,450 nm and an energy per MTZ of 3 mJ.
Two years later, hypopigmentation persisted at the test site treated with the highest MTZ density, while two other sites treated with the lower MTZ densities did not show any dyspigmentation. But he noticed something else during the experiment: He felt minimal to no pain as each test site was being treated.
“It took 7 minutes without any cooling or anesthesia,” Dr. Manstein recalled at the annual meeting of the American Society for Laser Medicine and Surgery. “It was not completely painless, but each time the laser was applied, sometimes I felt a little prick, sometimes I felt nothing.” Essentially, he added, “we created cell injury with a focused laser beam without anesthesia,” but this could also indicate that if skin is treated with a fractional laser very slowly, anesthesia is not needed. “Current devices are meant to treat very quickly, but if we [treat] slowly, maybe you could remove lesions painlessly without anesthesia.”
The observation from that experiment also led Dr. Manstein and colleagues to wonder: Could a focused laser beam pattern be used to assess cutaneous innervation? If so, they postulated, perhaps it could be used to not only assess nerve sensitivity of candidates for dermatologic surgery, but as a tool to help diagnose small fiber neuropathies such as diabetic neuropathy, and neuropathies in patients with HIV and sarcoidosis.
The current gold standard for making these diagnoses involves a skin biopsy, immunohistochemical analysis, and nerve fiber quantification, which is not widely available. It also requires strict histologic processing and nerve counting rules. Confocal microscopy of nerve fibers in the cornea is another approach, but is very difficult to perform, “so it would be nice if there was a simple way” to determine nerve fiber density in the skin using a focused laser beam, Dr. Manstein said.
With help from Payal Patel, MD, a dermatology research fellow at MGH, records each subject’s perception of a stimulus, and maps the areas of stimulus response. Current diameters being studied range from 0.076-1.15 mm and depths less than 0.71 mm. “We can focus the laser beam, preset the beam diameter, and very slowly, in a controlled manner, make a rectangular pattern, and after each time, inquire if the subject felt the pulse or not,” Dr. Manstein explained.
“This laser could become a new method for diagnosing nerve fiber neuropathies. If this works well, I think we can miniaturize the device,” he added.
Dr. Manstein disclosed that he is a consultant for Blossom Innovations, R2 Dermatology, and AVAVA. He is also a member of the advisory board for Blossom Innovations.
AT ASLMS 2022
CDC says about 20% get long COVID. New models try to define it
As the number of people reporting persistent, and sometimes debilitating, symptoms from COVID-19 increases, researchers have struggled to pinpoint exactly how common so-called “long COVID” is, as well as how to clearly define exactly who has it or who is likely to get it.
Now, Centers for Disease Control and Prevention researchers have concluded that one in five adults aged 18 and older have at least one health condition that might be related to their previous COVID-19 illness; that number goes up to one in four among those 65 and older. Their data was published in the CDC’s Morbidity and Mortality Weekly Report.
The conditions associated with what’s been officially termed postacute sequelae of COVID-19, or PASC, include kidney failure, blood clots, other vascular issues, respiratory issues, heart problems, mental health or neurologic problems, and musculoskeletal conditions. But none of those conditions is unique to long COVID.
Another new study, published in The Lancet Digital Health, is trying to help better characterize what long COVID is, and what it isn’t.
that could help identify those likely to develop it.
CDC data
The CDC team came to its conclusions by evaluating the EHRs of more than 353,000 adults who were diagnosed with COVID-19 or got a positive test result, then comparing those records with 1.6 million patients who had a medical visit in the same month without a positive test result or a COVID-19 diagnosis.
They looked at data from March 2020 to November 2021, tagging 26 conditions often linked to post-COVID issues.
Overall, more than 38% of the COVID patients and 16% of those without COVID had at least one of these 26 conditions. They assessed the absolute risk difference between the patients and the non-COVID patients who developed one of the conditions, finding a 20.8–percentage point difference for those 18-64, yielding the one in five figure, and a 26.9–percentage point difference for those 65 and above, translating to about one in four.
“These findings suggest the need for increased awareness for post-COVID conditions so that improved post-COVID care and management of patients who survived COVID-19 can be developed and implemented,” said study author Lara Bull-Otterson, PhD, MPH, colead of data analytics at the Healthcare Data Advisory Unit of the CDC.
Pinpointing long COVID characteristics
Long COVID is difficult to identify, because many of its symptoms are similar to those of other conditions, so researchers are looking for better ways to characterize it to help improve both diagnosis and treatment.
Researchers on the Lancet study evaluated data from the National COVID Cohort Collaborative, N3C, a national NIH database that includes information from more than 8 million people. The team looked at the health records of 98,000 adult COVID patients and used that information, along with data from about nearly 600 long-COVID patients treated at three long-COVID clinics, to create three machine learning models for identifying long-COVID patients.
The models aimed to identify long-COVID patients in three groups: all patients, those hospitalized with COVID, and those with COVID but not hospitalized. The models were judged by the researchers to be accurate because those identified at risk for long COVID from the database were similar to those actually treated for long COVID at the clinics.
“Our algorithm is not intended to diagnose long COVID,” said lead author Emily Pfaff, PhD, research assistant professor of medicine at the University of North Carolina at Chapel Hill. “Rather, it is intended to identify patients in EHR data who ‘look like’ patients seen by physicians for long COVID.’’
Next, the researchers say, they will incorporate the new patterns they found with a diagnosis code for COVID and include it in the models to further test their accuracy. The models could also be used to help recruit patients for clinical trials, the researchers say.
Perspective and caveats
The figures of one in five and one in four found by the CDC researchers don’t surprise David Putrino, PT, PhD, director of rehabilitation innovation for Mount Sinai Health System in New York and director of its Abilities Research Center, which cares for long-COVID patients.
“Those numbers are high and it’s alarming,” he said. “But we’ve been sounding the alarm for quite some time, and we’ve been assuming that about one in five end up with long COVID.”
He does see a limitation to the CDC research – that some symptoms could have emerged later, and some in the control group could have had an undiagnosed COVID infection and gone on to develop long COVID.
As for machine learning, “this is something we need to approach with caution,” Dr. Putrino said. “There are a lot of variables we don’t understand about long COVID,’’ and that could result in spurious conclusions.
“Although I am supportive of this work going on, I am saying, ‘Scrutinize the tools with a grain of salt.’ Electronic records, Dr. Putrino points out, include information that the doctors enter, not what the patient says.
Dr. Pfaff responds: “It is entirely appropriate to approach both machine learning and EHR data with relevant caveats in mind. There are many clinical factors that are not recorded in the EHR, and the EHR is not representative of all persons with long COVID.” Those data can only reflect those who seek care for a condition, a natural limitation.
When it comes to algorithms, they are limited by data they have access to, such as the electronic health records in this research. However, the immense size and diversity in the data used “does allow us to make some assertations with much more confidence than if we were using data from a single or small number of health care systems,” she said.
A version of this article first appeared on Medscape.com.
As the number of people reporting persistent, and sometimes debilitating, symptoms from COVID-19 increases, researchers have struggled to pinpoint exactly how common so-called “long COVID” is, as well as how to clearly define exactly who has it or who is likely to get it.
Now, Centers for Disease Control and Prevention researchers have concluded that one in five adults aged 18 and older have at least one health condition that might be related to their previous COVID-19 illness; that number goes up to one in four among those 65 and older. Their data was published in the CDC’s Morbidity and Mortality Weekly Report.
The conditions associated with what’s been officially termed postacute sequelae of COVID-19, or PASC, include kidney failure, blood clots, other vascular issues, respiratory issues, heart problems, mental health or neurologic problems, and musculoskeletal conditions. But none of those conditions is unique to long COVID.
Another new study, published in The Lancet Digital Health, is trying to help better characterize what long COVID is, and what it isn’t.
that could help identify those likely to develop it.
CDC data
The CDC team came to its conclusions by evaluating the EHRs of more than 353,000 adults who were diagnosed with COVID-19 or got a positive test result, then comparing those records with 1.6 million patients who had a medical visit in the same month without a positive test result or a COVID-19 diagnosis.
They looked at data from March 2020 to November 2021, tagging 26 conditions often linked to post-COVID issues.
Overall, more than 38% of the COVID patients and 16% of those without COVID had at least one of these 26 conditions. They assessed the absolute risk difference between the patients and the non-COVID patients who developed one of the conditions, finding a 20.8–percentage point difference for those 18-64, yielding the one in five figure, and a 26.9–percentage point difference for those 65 and above, translating to about one in four.
“These findings suggest the need for increased awareness for post-COVID conditions so that improved post-COVID care and management of patients who survived COVID-19 can be developed and implemented,” said study author Lara Bull-Otterson, PhD, MPH, colead of data analytics at the Healthcare Data Advisory Unit of the CDC.
Pinpointing long COVID characteristics
Long COVID is difficult to identify, because many of its symptoms are similar to those of other conditions, so researchers are looking for better ways to characterize it to help improve both diagnosis and treatment.
Researchers on the Lancet study evaluated data from the National COVID Cohort Collaborative, N3C, a national NIH database that includes information from more than 8 million people. The team looked at the health records of 98,000 adult COVID patients and used that information, along with data from about nearly 600 long-COVID patients treated at three long-COVID clinics, to create three machine learning models for identifying long-COVID patients.
The models aimed to identify long-COVID patients in three groups: all patients, those hospitalized with COVID, and those with COVID but not hospitalized. The models were judged by the researchers to be accurate because those identified at risk for long COVID from the database were similar to those actually treated for long COVID at the clinics.
“Our algorithm is not intended to diagnose long COVID,” said lead author Emily Pfaff, PhD, research assistant professor of medicine at the University of North Carolina at Chapel Hill. “Rather, it is intended to identify patients in EHR data who ‘look like’ patients seen by physicians for long COVID.’’
Next, the researchers say, they will incorporate the new patterns they found with a diagnosis code for COVID and include it in the models to further test their accuracy. The models could also be used to help recruit patients for clinical trials, the researchers say.
Perspective and caveats
The figures of one in five and one in four found by the CDC researchers don’t surprise David Putrino, PT, PhD, director of rehabilitation innovation for Mount Sinai Health System in New York and director of its Abilities Research Center, which cares for long-COVID patients.
“Those numbers are high and it’s alarming,” he said. “But we’ve been sounding the alarm for quite some time, and we’ve been assuming that about one in five end up with long COVID.”
He does see a limitation to the CDC research – that some symptoms could have emerged later, and some in the control group could have had an undiagnosed COVID infection and gone on to develop long COVID.
As for machine learning, “this is something we need to approach with caution,” Dr. Putrino said. “There are a lot of variables we don’t understand about long COVID,’’ and that could result in spurious conclusions.
“Although I am supportive of this work going on, I am saying, ‘Scrutinize the tools with a grain of salt.’ Electronic records, Dr. Putrino points out, include information that the doctors enter, not what the patient says.
Dr. Pfaff responds: “It is entirely appropriate to approach both machine learning and EHR data with relevant caveats in mind. There are many clinical factors that are not recorded in the EHR, and the EHR is not representative of all persons with long COVID.” Those data can only reflect those who seek care for a condition, a natural limitation.
When it comes to algorithms, they are limited by data they have access to, such as the electronic health records in this research. However, the immense size and diversity in the data used “does allow us to make some assertations with much more confidence than if we were using data from a single or small number of health care systems,” she said.
A version of this article first appeared on Medscape.com.
As the number of people reporting persistent, and sometimes debilitating, symptoms from COVID-19 increases, researchers have struggled to pinpoint exactly how common so-called “long COVID” is, as well as how to clearly define exactly who has it or who is likely to get it.
Now, Centers for Disease Control and Prevention researchers have concluded that one in five adults aged 18 and older have at least one health condition that might be related to their previous COVID-19 illness; that number goes up to one in four among those 65 and older. Their data was published in the CDC’s Morbidity and Mortality Weekly Report.
The conditions associated with what’s been officially termed postacute sequelae of COVID-19, or PASC, include kidney failure, blood clots, other vascular issues, respiratory issues, heart problems, mental health or neurologic problems, and musculoskeletal conditions. But none of those conditions is unique to long COVID.
Another new study, published in The Lancet Digital Health, is trying to help better characterize what long COVID is, and what it isn’t.
that could help identify those likely to develop it.
CDC data
The CDC team came to its conclusions by evaluating the EHRs of more than 353,000 adults who were diagnosed with COVID-19 or got a positive test result, then comparing those records with 1.6 million patients who had a medical visit in the same month without a positive test result or a COVID-19 diagnosis.
They looked at data from March 2020 to November 2021, tagging 26 conditions often linked to post-COVID issues.
Overall, more than 38% of the COVID patients and 16% of those without COVID had at least one of these 26 conditions. They assessed the absolute risk difference between the patients and the non-COVID patients who developed one of the conditions, finding a 20.8–percentage point difference for those 18-64, yielding the one in five figure, and a 26.9–percentage point difference for those 65 and above, translating to about one in four.
“These findings suggest the need for increased awareness for post-COVID conditions so that improved post-COVID care and management of patients who survived COVID-19 can be developed and implemented,” said study author Lara Bull-Otterson, PhD, MPH, colead of data analytics at the Healthcare Data Advisory Unit of the CDC.
Pinpointing long COVID characteristics
Long COVID is difficult to identify, because many of its symptoms are similar to those of other conditions, so researchers are looking for better ways to characterize it to help improve both diagnosis and treatment.
Researchers on the Lancet study evaluated data from the National COVID Cohort Collaborative, N3C, a national NIH database that includes information from more than 8 million people. The team looked at the health records of 98,000 adult COVID patients and used that information, along with data from about nearly 600 long-COVID patients treated at three long-COVID clinics, to create three machine learning models for identifying long-COVID patients.
The models aimed to identify long-COVID patients in three groups: all patients, those hospitalized with COVID, and those with COVID but not hospitalized. The models were judged by the researchers to be accurate because those identified at risk for long COVID from the database were similar to those actually treated for long COVID at the clinics.
“Our algorithm is not intended to diagnose long COVID,” said lead author Emily Pfaff, PhD, research assistant professor of medicine at the University of North Carolina at Chapel Hill. “Rather, it is intended to identify patients in EHR data who ‘look like’ patients seen by physicians for long COVID.’’
Next, the researchers say, they will incorporate the new patterns they found with a diagnosis code for COVID and include it in the models to further test their accuracy. The models could also be used to help recruit patients for clinical trials, the researchers say.
Perspective and caveats
The figures of one in five and one in four found by the CDC researchers don’t surprise David Putrino, PT, PhD, director of rehabilitation innovation for Mount Sinai Health System in New York and director of its Abilities Research Center, which cares for long-COVID patients.
“Those numbers are high and it’s alarming,” he said. “But we’ve been sounding the alarm for quite some time, and we’ve been assuming that about one in five end up with long COVID.”
He does see a limitation to the CDC research – that some symptoms could have emerged later, and some in the control group could have had an undiagnosed COVID infection and gone on to develop long COVID.
As for machine learning, “this is something we need to approach with caution,” Dr. Putrino said. “There are a lot of variables we don’t understand about long COVID,’’ and that could result in spurious conclusions.
“Although I am supportive of this work going on, I am saying, ‘Scrutinize the tools with a grain of salt.’ Electronic records, Dr. Putrino points out, include information that the doctors enter, not what the patient says.
Dr. Pfaff responds: “It is entirely appropriate to approach both machine learning and EHR data with relevant caveats in mind. There are many clinical factors that are not recorded in the EHR, and the EHR is not representative of all persons with long COVID.” Those data can only reflect those who seek care for a condition, a natural limitation.
When it comes to algorithms, they are limited by data they have access to, such as the electronic health records in this research. However, the immense size and diversity in the data used “does allow us to make some assertations with much more confidence than if we were using data from a single or small number of health care systems,” she said.
A version of this article first appeared on Medscape.com.
Today’s medical oxymoron: Healthy overconfidence
Doctor, doctor, gimme the news. I got a bad case of knowing better than you
Stop us if you’ve heard this before. One of your parents (let’s be honest, probably your ornery father) refuses to go to the doctor. You tell him it’s for the best, but in his words, “Doctors don’t know nothin’. I’m fine.” How many TV shows with grumpy fathers feature this exact plot in an episode as the frustrated child attempts increasingly convoluted traps to encourage the stubborn parent to get himself to the doctor?
As is so often the case, wacky sitcoms reflect reality, according to a new study from the Journal of the Economics of Aging. In a massive survey of 80,000 Europeans aged 50 years and older, the researchers found that individuals who were overconfident and rated their health as better than it actually was visited their doctor 17% less often than did those who correctly judge their own health. Fewer medical visits leaves them more vulnerable to chronic disease, since they’re not getting the preventive care they need to catch illnesses early.
Perhaps unsurprisingly, the inverse is also true: People who underestimate their health status visit the doctor 21% more often. On the one hand, regular visits to the doctor are a good thing, as is awareness of how healthy one really is. On the other hand, though, extra visits cost money and time, especially relevant in an aging society with high public health costs.
Nobody likes visiting the doctor, but it is kind of important, especially as we age and our bodies start to let us down. Confidence is fine, but don’t be overly confident. And if you do go, don’t be like a certain former president of the United States. Don’t pay a sycophant to look in your general direction and then declare that you are in very good (great!) condition on Twitter. That’s not how medicine is meant to work.
Your liver stays toddler age
Rapid cell regeneration might seem like something straight out of a sci-fi novel, but it happens to your liver all the time. So much so that the human liver is never a day over 3 years old.
How’s that possible? The liver deals with a lot of toxic substances in its job as the Brita filter of the human body, so it has a unique capacity among organs to regenerate itself after damage.
Dr. Olaf Bergmann and his team at Technical University Dresden’s (Germany) Center for Regenerative Therapies used retrospective radiocarbon birth dating to determine the age of the livers of a group of people who died at the ages of 20-84 years. The results were the same regardless of age.
This information could be a complete game changer for understanding cell regeneration. It’s important in determining cancer cell formation in the liver but also if new heart muscle cells can be generated in people with cardiovascular disease, which the researchers are looking into.
So sure, your liver may be totally capable of filtering those drinks at happy hour, but as old as it is, a juice box might be more appropriate.
To bee, or not to bee? That is the vacation
Sleeping is pretty important for humans, no doubt about that, so anything that improves sleep is worth considering, right? But how far would you go for a good night’s sleep? Would you be willing to travel to Italy to experience the ultimate white-noise generator?
For more on this exciting, yet also sleep-inducing, news story, let’s go to the village of Grottole in southern Italy, where we meet bee keeper and Airbnb host Rocco Filomeno. ”This is the first place in the world where you can sleep immersed in the distinctive sound and aroma of the bees, experiencing ‘bee-therapy’ in the most authentic and natural way,” he said in a written statement for Airbnb.
Mr. Filomeno worked with local NGO Wonder Grottole and a self-build specialist to take the next step in tiny-house evolution. The resulting structure cost just $17,000 – crowdfunded, of course, and built by 25 local bee-lievers (aka volunteers) – and consists of a single room surrounded by nine apiaries, which contain a combined total of 1 million working bees. It is now available to book on Airbnb, and guests “will receive their first lesson on bees and how to live with them,” Airbnb said.
The immersion in bee sound/scent is fully realized through the building’s most prominent interior feature, a screened box in the ceiling with a working hive that allows guests to see the bees and fall asleep to the “gently humming sound,” Airbnb explained. The sound from the hive is said to have a soothing effect that “acts as salve to day-to-day stressors,” according to the BBC.
This is just the start of a trend and we want in on it. Should our tiny house feature the sights/smells/sounds of angry rattlesnakes or a swarm of locusts?
Joysticks can make the world a better place
Someday, it might be possible for surgeons to treat a stroke or aneurysm during the “golden hour,” even if they’re not in the same hospital as the patient. MIT engineers have created a robotic system that can be controlled remotely with a modified joystick, so the patient can go to a closer, smaller hospital and be treated by a surgeon at a larger facility through live imaging.
Endovascular surgery seems difficult enough with the patient and doctor in the same hospital, “but having a robot twist with the same level of sophistication [as a surgeon] is challenging,” Yoonho Kim, lead author of a study in Science Robotics, said in a written statement. “Our system is based on a fundamentally different mechanism.”
It involves “a medical-grade robotic arm with a magnet attached to its wrist. With a joystick and live imaging, an operator can adjust the magnet’s orientation and manipulate the arm to guide a soft and thin magnetic wire through arteries and vessels,” MIT explained in the statement.
The system was tested using life-like models, and it took each surgeon about an hour of training to learn how to use the new joystick and other equipment. Another perk: No exposure to radiation from x-ray imaging.
If someone you know is obsessed with video games, stop thinking “slacker” and start thinking “neurosurgeon.”
Doctor, doctor, gimme the news. I got a bad case of knowing better than you
Stop us if you’ve heard this before. One of your parents (let’s be honest, probably your ornery father) refuses to go to the doctor. You tell him it’s for the best, but in his words, “Doctors don’t know nothin’. I’m fine.” How many TV shows with grumpy fathers feature this exact plot in an episode as the frustrated child attempts increasingly convoluted traps to encourage the stubborn parent to get himself to the doctor?
As is so often the case, wacky sitcoms reflect reality, according to a new study from the Journal of the Economics of Aging. In a massive survey of 80,000 Europeans aged 50 years and older, the researchers found that individuals who were overconfident and rated their health as better than it actually was visited their doctor 17% less often than did those who correctly judge their own health. Fewer medical visits leaves them more vulnerable to chronic disease, since they’re not getting the preventive care they need to catch illnesses early.
Perhaps unsurprisingly, the inverse is also true: People who underestimate their health status visit the doctor 21% more often. On the one hand, regular visits to the doctor are a good thing, as is awareness of how healthy one really is. On the other hand, though, extra visits cost money and time, especially relevant in an aging society with high public health costs.
Nobody likes visiting the doctor, but it is kind of important, especially as we age and our bodies start to let us down. Confidence is fine, but don’t be overly confident. And if you do go, don’t be like a certain former president of the United States. Don’t pay a sycophant to look in your general direction and then declare that you are in very good (great!) condition on Twitter. That’s not how medicine is meant to work.
Your liver stays toddler age
Rapid cell regeneration might seem like something straight out of a sci-fi novel, but it happens to your liver all the time. So much so that the human liver is never a day over 3 years old.
How’s that possible? The liver deals with a lot of toxic substances in its job as the Brita filter of the human body, so it has a unique capacity among organs to regenerate itself after damage.
Dr. Olaf Bergmann and his team at Technical University Dresden’s (Germany) Center for Regenerative Therapies used retrospective radiocarbon birth dating to determine the age of the livers of a group of people who died at the ages of 20-84 years. The results were the same regardless of age.
This information could be a complete game changer for understanding cell regeneration. It’s important in determining cancer cell formation in the liver but also if new heart muscle cells can be generated in people with cardiovascular disease, which the researchers are looking into.
So sure, your liver may be totally capable of filtering those drinks at happy hour, but as old as it is, a juice box might be more appropriate.
To bee, or not to bee? That is the vacation
Sleeping is pretty important for humans, no doubt about that, so anything that improves sleep is worth considering, right? But how far would you go for a good night’s sleep? Would you be willing to travel to Italy to experience the ultimate white-noise generator?
For more on this exciting, yet also sleep-inducing, news story, let’s go to the village of Grottole in southern Italy, where we meet bee keeper and Airbnb host Rocco Filomeno. ”This is the first place in the world where you can sleep immersed in the distinctive sound and aroma of the bees, experiencing ‘bee-therapy’ in the most authentic and natural way,” he said in a written statement for Airbnb.
Mr. Filomeno worked with local NGO Wonder Grottole and a self-build specialist to take the next step in tiny-house evolution. The resulting structure cost just $17,000 – crowdfunded, of course, and built by 25 local bee-lievers (aka volunteers) – and consists of a single room surrounded by nine apiaries, which contain a combined total of 1 million working bees. It is now available to book on Airbnb, and guests “will receive their first lesson on bees and how to live with them,” Airbnb said.
The immersion in bee sound/scent is fully realized through the building’s most prominent interior feature, a screened box in the ceiling with a working hive that allows guests to see the bees and fall asleep to the “gently humming sound,” Airbnb explained. The sound from the hive is said to have a soothing effect that “acts as salve to day-to-day stressors,” according to the BBC.
This is just the start of a trend and we want in on it. Should our tiny house feature the sights/smells/sounds of angry rattlesnakes or a swarm of locusts?
Joysticks can make the world a better place
Someday, it might be possible for surgeons to treat a stroke or aneurysm during the “golden hour,” even if they’re not in the same hospital as the patient. MIT engineers have created a robotic system that can be controlled remotely with a modified joystick, so the patient can go to a closer, smaller hospital and be treated by a surgeon at a larger facility through live imaging.
Endovascular surgery seems difficult enough with the patient and doctor in the same hospital, “but having a robot twist with the same level of sophistication [as a surgeon] is challenging,” Yoonho Kim, lead author of a study in Science Robotics, said in a written statement. “Our system is based on a fundamentally different mechanism.”
It involves “a medical-grade robotic arm with a magnet attached to its wrist. With a joystick and live imaging, an operator can adjust the magnet’s orientation and manipulate the arm to guide a soft and thin magnetic wire through arteries and vessels,” MIT explained in the statement.
The system was tested using life-like models, and it took each surgeon about an hour of training to learn how to use the new joystick and other equipment. Another perk: No exposure to radiation from x-ray imaging.
If someone you know is obsessed with video games, stop thinking “slacker” and start thinking “neurosurgeon.”
Doctor, doctor, gimme the news. I got a bad case of knowing better than you
Stop us if you’ve heard this before. One of your parents (let’s be honest, probably your ornery father) refuses to go to the doctor. You tell him it’s for the best, but in his words, “Doctors don’t know nothin’. I’m fine.” How many TV shows with grumpy fathers feature this exact plot in an episode as the frustrated child attempts increasingly convoluted traps to encourage the stubborn parent to get himself to the doctor?
As is so often the case, wacky sitcoms reflect reality, according to a new study from the Journal of the Economics of Aging. In a massive survey of 80,000 Europeans aged 50 years and older, the researchers found that individuals who were overconfident and rated their health as better than it actually was visited their doctor 17% less often than did those who correctly judge their own health. Fewer medical visits leaves them more vulnerable to chronic disease, since they’re not getting the preventive care they need to catch illnesses early.
Perhaps unsurprisingly, the inverse is also true: People who underestimate their health status visit the doctor 21% more often. On the one hand, regular visits to the doctor are a good thing, as is awareness of how healthy one really is. On the other hand, though, extra visits cost money and time, especially relevant in an aging society with high public health costs.
Nobody likes visiting the doctor, but it is kind of important, especially as we age and our bodies start to let us down. Confidence is fine, but don’t be overly confident. And if you do go, don’t be like a certain former president of the United States. Don’t pay a sycophant to look in your general direction and then declare that you are in very good (great!) condition on Twitter. That’s not how medicine is meant to work.
Your liver stays toddler age
Rapid cell regeneration might seem like something straight out of a sci-fi novel, but it happens to your liver all the time. So much so that the human liver is never a day over 3 years old.
How’s that possible? The liver deals with a lot of toxic substances in its job as the Brita filter of the human body, so it has a unique capacity among organs to regenerate itself after damage.
Dr. Olaf Bergmann and his team at Technical University Dresden’s (Germany) Center for Regenerative Therapies used retrospective radiocarbon birth dating to determine the age of the livers of a group of people who died at the ages of 20-84 years. The results were the same regardless of age.
This information could be a complete game changer for understanding cell regeneration. It’s important in determining cancer cell formation in the liver but also if new heart muscle cells can be generated in people with cardiovascular disease, which the researchers are looking into.
So sure, your liver may be totally capable of filtering those drinks at happy hour, but as old as it is, a juice box might be more appropriate.
To bee, or not to bee? That is the vacation
Sleeping is pretty important for humans, no doubt about that, so anything that improves sleep is worth considering, right? But how far would you go for a good night’s sleep? Would you be willing to travel to Italy to experience the ultimate white-noise generator?
For more on this exciting, yet also sleep-inducing, news story, let’s go to the village of Grottole in southern Italy, where we meet bee keeper and Airbnb host Rocco Filomeno. ”This is the first place in the world where you can sleep immersed in the distinctive sound and aroma of the bees, experiencing ‘bee-therapy’ in the most authentic and natural way,” he said in a written statement for Airbnb.
Mr. Filomeno worked with local NGO Wonder Grottole and a self-build specialist to take the next step in tiny-house evolution. The resulting structure cost just $17,000 – crowdfunded, of course, and built by 25 local bee-lievers (aka volunteers) – and consists of a single room surrounded by nine apiaries, which contain a combined total of 1 million working bees. It is now available to book on Airbnb, and guests “will receive their first lesson on bees and how to live with them,” Airbnb said.
The immersion in bee sound/scent is fully realized through the building’s most prominent interior feature, a screened box in the ceiling with a working hive that allows guests to see the bees and fall asleep to the “gently humming sound,” Airbnb explained. The sound from the hive is said to have a soothing effect that “acts as salve to day-to-day stressors,” according to the BBC.
This is just the start of a trend and we want in on it. Should our tiny house feature the sights/smells/sounds of angry rattlesnakes or a swarm of locusts?
Joysticks can make the world a better place
Someday, it might be possible for surgeons to treat a stroke or aneurysm during the “golden hour,” even if they’re not in the same hospital as the patient. MIT engineers have created a robotic system that can be controlled remotely with a modified joystick, so the patient can go to a closer, smaller hospital and be treated by a surgeon at a larger facility through live imaging.
Endovascular surgery seems difficult enough with the patient and doctor in the same hospital, “but having a robot twist with the same level of sophistication [as a surgeon] is challenging,” Yoonho Kim, lead author of a study in Science Robotics, said in a written statement. “Our system is based on a fundamentally different mechanism.”
It involves “a medical-grade robotic arm with a magnet attached to its wrist. With a joystick and live imaging, an operator can adjust the magnet’s orientation and manipulate the arm to guide a soft and thin magnetic wire through arteries and vessels,” MIT explained in the statement.
The system was tested using life-like models, and it took each surgeon about an hour of training to learn how to use the new joystick and other equipment. Another perk: No exposure to radiation from x-ray imaging.
If someone you know is obsessed with video games, stop thinking “slacker” and start thinking “neurosurgeon.”
How do you treat noncompliance?
Mrs. Stevens has migraines. Fortunately, they’re well controlled on nortriptyline, and she’s never had side effects from it. She’s taken it for more than 20 years now.
In that time she and I have had a strange, slow-motion, waltz.
In spite of the medicine helping her, she stops it on her own roughly twice a year, never calling my office in advance. Sometimes it’s to see if the headaches come back (they always do). Other times it’s because of something she read online, or a friend told her, or she overheard in the grocery checkout line.
Whatever the reason, her migraines always come back within a week, and then she calls my office for an urgent appointment.
I’ve never really understood this, as I know her history and am happy to just tell her to restart the medication and call it in. But, for whatever reason, the return of her migraines is something that she wants to discuss with me in person. Since it’s usually a pretty brief visit, my secretary puts her on the schedule and I get paid to tell her what could have been handled by phone. I’m not complaining. I have to make a living, too.
But still, it makes me wonder. She can’t be the only patient out there who does this. Multiply that by the number of doctors, the cost of visits, the time she takes off from work to come in ... it adds up.
So why does this happen?
Believe me, for the past 20 years I’ve spent these occasional visits reminding Mrs. Stevens about the importance of sticking with her medication and calling my office if she has questions. She agrees to, but when she’s thinking about stopping nortriptyline ... she still does it and only tells me after the fact.
I can’t change human nature, or at least not hers. And when multiplied by many like her, it creates entirely unnecessary costs on our health care system. I wish there were a way to stop it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mrs. Stevens has migraines. Fortunately, they’re well controlled on nortriptyline, and she’s never had side effects from it. She’s taken it for more than 20 years now.
In that time she and I have had a strange, slow-motion, waltz.
In spite of the medicine helping her, she stops it on her own roughly twice a year, never calling my office in advance. Sometimes it’s to see if the headaches come back (they always do). Other times it’s because of something she read online, or a friend told her, or she overheard in the grocery checkout line.
Whatever the reason, her migraines always come back within a week, and then she calls my office for an urgent appointment.
I’ve never really understood this, as I know her history and am happy to just tell her to restart the medication and call it in. But, for whatever reason, the return of her migraines is something that she wants to discuss with me in person. Since it’s usually a pretty brief visit, my secretary puts her on the schedule and I get paid to tell her what could have been handled by phone. I’m not complaining. I have to make a living, too.
But still, it makes me wonder. She can’t be the only patient out there who does this. Multiply that by the number of doctors, the cost of visits, the time she takes off from work to come in ... it adds up.
So why does this happen?
Believe me, for the past 20 years I’ve spent these occasional visits reminding Mrs. Stevens about the importance of sticking with her medication and calling my office if she has questions. She agrees to, but when she’s thinking about stopping nortriptyline ... she still does it and only tells me after the fact.
I can’t change human nature, or at least not hers. And when multiplied by many like her, it creates entirely unnecessary costs on our health care system. I wish there were a way to stop it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Mrs. Stevens has migraines. Fortunately, they’re well controlled on nortriptyline, and she’s never had side effects from it. She’s taken it for more than 20 years now.
In that time she and I have had a strange, slow-motion, waltz.
In spite of the medicine helping her, she stops it on her own roughly twice a year, never calling my office in advance. Sometimes it’s to see if the headaches come back (they always do). Other times it’s because of something she read online, or a friend told her, or she overheard in the grocery checkout line.
Whatever the reason, her migraines always come back within a week, and then she calls my office for an urgent appointment.
I’ve never really understood this, as I know her history and am happy to just tell her to restart the medication and call it in. But, for whatever reason, the return of her migraines is something that she wants to discuss with me in person. Since it’s usually a pretty brief visit, my secretary puts her on the schedule and I get paid to tell her what could have been handled by phone. I’m not complaining. I have to make a living, too.
But still, it makes me wonder. She can’t be the only patient out there who does this. Multiply that by the number of doctors, the cost of visits, the time she takes off from work to come in ... it adds up.
So why does this happen?
Believe me, for the past 20 years I’ve spent these occasional visits reminding Mrs. Stevens about the importance of sticking with her medication and calling my office if she has questions. She agrees to, but when she’s thinking about stopping nortriptyline ... she still does it and only tells me after the fact.
I can’t change human nature, or at least not hers. And when multiplied by many like her, it creates entirely unnecessary costs on our health care system. I wish there were a way to stop it.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
Hearing, vision loss combo a colossal risk for cognitive decline
The combination of hearing loss and vision loss is linked to an eightfold increased risk of cognitive impairment, new research shows.
Investigators analyzed data on more than 5 million U.S. seniors. Adjusted results show that participants with hearing impairment alone had more than twice the odds of also having cognitive impairment, while those with vision impairment alone had more than triple the odds of cognitive impairment.
However, those with dual sensory impairment (DSI) had an eightfold higher risk for cognitive impairment.
In addition, half of the participants with DSI also had cognitive impairment. Of those with cognitive impairment, 16% had DSI, compared with only about 2% of their peers without cognitive impairment.
“The findings of the present study may inform interventions that can support older people with concurrent sensory impairment and cognitive impairment,” said lead author Esme Fuller-Thomson, PhD, professor, Factor-Inwentash Faculty of Social Work, University of Toronto.
“Special attention, in particular, should be given to those aged 65-74 who have serious hearing and/or vision impairment [because], if the relationship with dementia is found to be causal, such interventions can potentially mitigate the development of cognitive impairment,” said Dr. Fuller-Thomson, who is also director of the Institute for Life Course and Aging and a professor in the department of family and community medicine and faculty of nursing, all at the University of Toronto.
The findings were published online in the Journal of Alzheimer’s Disease Reports.
Sensory isolation
Hearing and vision impairment increase with age; it is estimated that one-third of U.S. adults between the ages of 65 and 74 experience hearing loss, and 4% experience vision impairment, the investigators note.
“The link between dual hearing loss and seeing loss and mental health problems such as depression and social isolation have been well researched, but we were very interested in the link between dual sensory loss and cognitive problems,” Dr. Fuller-Thomson said.
Additionally, “there have been several studies in the past decade linking hearing loss to dementia and cognitive decline, but less attention has been paid to cognitive problems among those with DSI, despite this group being particularly isolated,” she said. Existing research into DSI suggests an association with cognitive decline; the current investigators sought to expand on this previous work.
To do so, they used merged data from 10 consecutive waves from 2008 to 2017 of the American Community Survey (ACS), which was conducted by the U.S. Census Bureau. The ACS is a nationally representative sample of 3.5 million randomly selected U.S. addresses and includes community-dwelling adults and those residing in institutional settings.
Participants aged 65 or older (n = 5,405,135; 56.4% women) were asked yes/no questions regarding serious cognitive impairment, hearing impairment, and vision impairment. A proxy, such as a family member or nursing home staff member, provided answers for individuals not capable of self-report.
Potential confounding variables included age, race/ethnicity, sex, education, and household income.
Potential mechanisms
Results showed that, among those with cognitive impairment, there was a higher prevalence of hearing impairment, vision impairment, and DSI than among their peers without cognitive impairment; in addition, a lower percentage of these persons had no sensory impairment (P < .001).
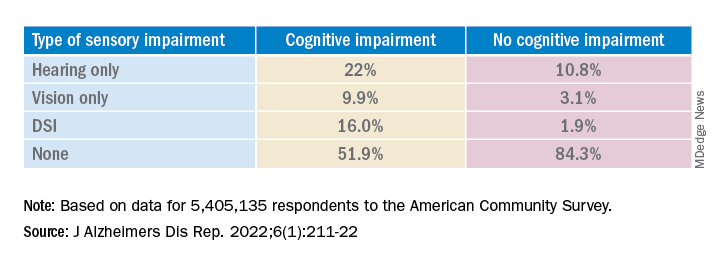
The prevalence of DSI climbed with age, from 1.5% for respondents aged 65-74 years to 2.6% for those aged 75-84 and to 10.8% in those 85 years and older.
Individuals with higher levels of poverty also had higher levels of DSI. Among those who had not completed high school, the prevalence of DSI was higher, compared with high school or university graduates (6.3% vs. 3.1% and 1.85, respectively).
After controlling for age, race, education, and income, the researchers found “substantially” higher odds of cognitive impairment in those with vs. those without sensory impairments.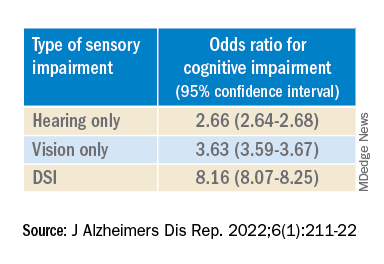
“The magnitude of the odds of cognitive impairment by sensory impairment was greatest for the youngest cohort (age 65-74) and lowest for the oldest cohort (age 85+),” the investigators wrote. Among participants in the youngest cohort, there was a “dose-response relationship” for those with hearing impairment only, visual impairment only, and DSI.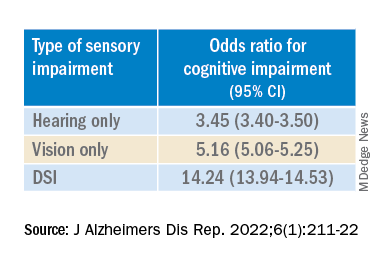
Because the study was observational, it “does not provide sufficient information to determine the reasons behind the observed link between sensory loss and cognitive problems,” Dr. Fuller-Thomson said. However, there are “several potential causal mechanisms [that] warrant future research.”
The “sensory deprivation hypothesis” suggests that DSI could cause cognitive deterioration because of decreased auditory and visual input. The “resource allocation hypothesis” posits that hearing- or vision-impaired older adults “may use more cognitive resources to accommodate for sensory deficits, allocating fewer cognitive resources for higher-order memory processes,” the researchers wrote. Hearing impairment “may also lead to social disengagement among older adults, hastening cognitive decline due to isolation and lack of stimulation,” they added.
Reverse causality is also possible. In the “cognitive load on perception” hypothesis, cognitive decline may lead to declines in hearing and vision because of “decreased resources for sensory processing.”
In addition, the association may be noncausal. “The ‘common cause hypothesis’ theorizes that sensory impairment and cognitive impairment may be due to shared age-related degeneration of the central nervous system ... or frailty,” Dr. Fuller-Thomson said.
Parallel findings
The results are similar to those from a study conducted by Phillip Hwang, PhD, of the department of anatomy and neurobiology, Boston University, and colleagues that was published online in JAMA Network Open.
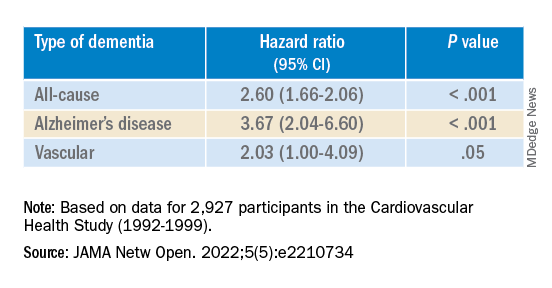
They analyzed data on 8 years of follow-up of 2,927 participants in the Cardiovascular Health Study (mean age, 74.6 years; 58.2% women).
Compared with no sensory impairment, DSI was associated with increased risk for all-cause dementia and Alzheimer’s disease, but not with vascular dementia.
“Future work in health care guidelines could consider incorporating screening of sensory impairment in older adults as part of risk assessment for dementia,” Nicholas Reed, AuD, and Esther Oh, MD, PhD, both of Johns Hopkins University, Baltimore, wrote in an accompanying editorial.
Accurate testing
Commenting on both studies, Heather Whitson, MD, professor of medicine (geriatrics) and ophthalmology and director at the Duke University Center for the Study of Aging and Human Development, Durham, N.C., said both “add further strength to the evidence base, which has really converged in the last few years to support that there is a link between sensory health and cognitive health.”
However, “we still don’t know whether hearing/vision loss causes cognitive decline, though there are plausible ways that sensory loss could affect cognitive abilities like memory, language, and executive function,” she said
Dr. Whitson, who was not involved with the research, is also codirector of the Duke/University of North Carolina Alzheimer’s Disease Research Center at Duke University, Durham, N.C., and the Durham VA Medical Center.
“The big question is whether we can improve patients’ cognitive performance by treating or accommodating their sensory impairments,” she said. “If safe and feasible things like hearing aids or cataract surgery improve cognitive health, even a little bit, it would be a huge benefit to society, because sensory loss is very common, and there are many treatment options,” Dr. Whitson added.
Dr. Fuller-Thomson emphasized that practitioners should “consider the full impact of sensory impairment on cognitive testing methods, as both auditory and visual testing methods may fail to take hearing and vision impairment into account.”
Thus, “when performing cognitive tests on older adults with sensory impairments, practitioners should ensure they are communicating audibly and/or using visual speech cues for hearing-impaired individuals, eliminating items from cognitive tests that rely on vision for those who are visually impaired, and using physical cues for individuals with hearing or dual sensory impairment, as this can help increase the accuracy of testing and prevent confounding,” she said.
The study by Fuller-Thomson et al. was funded by a donation from Janis Rotman. Its investigators have reported no relevant financial relationships. The study by Hwang et al. was funded by contracts from the National Heart, Lung, and Blood Institute, the National Institute of Neurological Disorders and Stroke, and the National Institute on Aging. Dr. Hwang reports no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Reed received grants from the National Institute on Aging during the conduct of the study and has served on the advisory board of Neosensory outside the submitted work. Dr. Oh and Dr. Whitson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The combination of hearing loss and vision loss is linked to an eightfold increased risk of cognitive impairment, new research shows.
Investigators analyzed data on more than 5 million U.S. seniors. Adjusted results show that participants with hearing impairment alone had more than twice the odds of also having cognitive impairment, while those with vision impairment alone had more than triple the odds of cognitive impairment.
However, those with dual sensory impairment (DSI) had an eightfold higher risk for cognitive impairment.
In addition, half of the participants with DSI also had cognitive impairment. Of those with cognitive impairment, 16% had DSI, compared with only about 2% of their peers without cognitive impairment.
“The findings of the present study may inform interventions that can support older people with concurrent sensory impairment and cognitive impairment,” said lead author Esme Fuller-Thomson, PhD, professor, Factor-Inwentash Faculty of Social Work, University of Toronto.
“Special attention, in particular, should be given to those aged 65-74 who have serious hearing and/or vision impairment [because], if the relationship with dementia is found to be causal, such interventions can potentially mitigate the development of cognitive impairment,” said Dr. Fuller-Thomson, who is also director of the Institute for Life Course and Aging and a professor in the department of family and community medicine and faculty of nursing, all at the University of Toronto.
The findings were published online in the Journal of Alzheimer’s Disease Reports.
Sensory isolation
Hearing and vision impairment increase with age; it is estimated that one-third of U.S. adults between the ages of 65 and 74 experience hearing loss, and 4% experience vision impairment, the investigators note.
“The link between dual hearing loss and seeing loss and mental health problems such as depression and social isolation have been well researched, but we were very interested in the link between dual sensory loss and cognitive problems,” Dr. Fuller-Thomson said.
Additionally, “there have been several studies in the past decade linking hearing loss to dementia and cognitive decline, but less attention has been paid to cognitive problems among those with DSI, despite this group being particularly isolated,” she said. Existing research into DSI suggests an association with cognitive decline; the current investigators sought to expand on this previous work.
To do so, they used merged data from 10 consecutive waves from 2008 to 2017 of the American Community Survey (ACS), which was conducted by the U.S. Census Bureau. The ACS is a nationally representative sample of 3.5 million randomly selected U.S. addresses and includes community-dwelling adults and those residing in institutional settings.
Participants aged 65 or older (n = 5,405,135; 56.4% women) were asked yes/no questions regarding serious cognitive impairment, hearing impairment, and vision impairment. A proxy, such as a family member or nursing home staff member, provided answers for individuals not capable of self-report.
Potential confounding variables included age, race/ethnicity, sex, education, and household income.
Potential mechanisms
Results showed that, among those with cognitive impairment, there was a higher prevalence of hearing impairment, vision impairment, and DSI than among their peers without cognitive impairment; in addition, a lower percentage of these persons had no sensory impairment (P < .001).
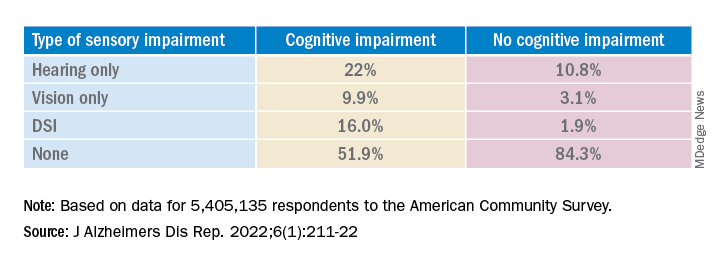
The prevalence of DSI climbed with age, from 1.5% for respondents aged 65-74 years to 2.6% for those aged 75-84 and to 10.8% in those 85 years and older.
Individuals with higher levels of poverty also had higher levels of DSI. Among those who had not completed high school, the prevalence of DSI was higher, compared with high school or university graduates (6.3% vs. 3.1% and 1.85, respectively).
After controlling for age, race, education, and income, the researchers found “substantially” higher odds of cognitive impairment in those with vs. those without sensory impairments.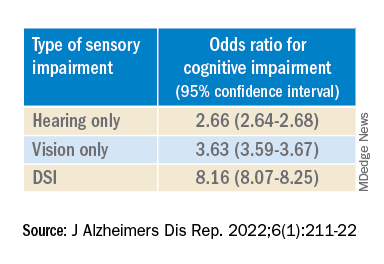
“The magnitude of the odds of cognitive impairment by sensory impairment was greatest for the youngest cohort (age 65-74) and lowest for the oldest cohort (age 85+),” the investigators wrote. Among participants in the youngest cohort, there was a “dose-response relationship” for those with hearing impairment only, visual impairment only, and DSI.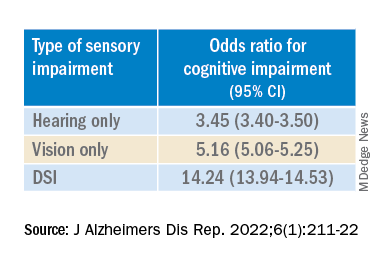
Because the study was observational, it “does not provide sufficient information to determine the reasons behind the observed link between sensory loss and cognitive problems,” Dr. Fuller-Thomson said. However, there are “several potential causal mechanisms [that] warrant future research.”
The “sensory deprivation hypothesis” suggests that DSI could cause cognitive deterioration because of decreased auditory and visual input. The “resource allocation hypothesis” posits that hearing- or vision-impaired older adults “may use more cognitive resources to accommodate for sensory deficits, allocating fewer cognitive resources for higher-order memory processes,” the researchers wrote. Hearing impairment “may also lead to social disengagement among older adults, hastening cognitive decline due to isolation and lack of stimulation,” they added.
Reverse causality is also possible. In the “cognitive load on perception” hypothesis, cognitive decline may lead to declines in hearing and vision because of “decreased resources for sensory processing.”
In addition, the association may be noncausal. “The ‘common cause hypothesis’ theorizes that sensory impairment and cognitive impairment may be due to shared age-related degeneration of the central nervous system ... or frailty,” Dr. Fuller-Thomson said.
Parallel findings
The results are similar to those from a study conducted by Phillip Hwang, PhD, of the department of anatomy and neurobiology, Boston University, and colleagues that was published online in JAMA Network Open.
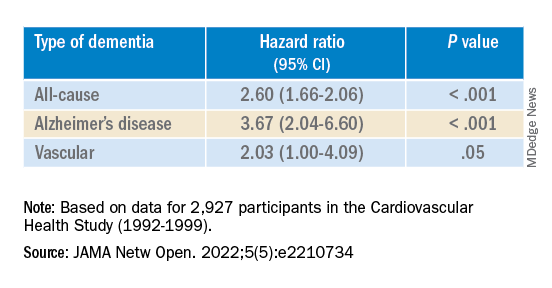
They analyzed data on 8 years of follow-up of 2,927 participants in the Cardiovascular Health Study (mean age, 74.6 years; 58.2% women).
Compared with no sensory impairment, DSI was associated with increased risk for all-cause dementia and Alzheimer’s disease, but not with vascular dementia.
“Future work in health care guidelines could consider incorporating screening of sensory impairment in older adults as part of risk assessment for dementia,” Nicholas Reed, AuD, and Esther Oh, MD, PhD, both of Johns Hopkins University, Baltimore, wrote in an accompanying editorial.
Accurate testing
Commenting on both studies, Heather Whitson, MD, professor of medicine (geriatrics) and ophthalmology and director at the Duke University Center for the Study of Aging and Human Development, Durham, N.C., said both “add further strength to the evidence base, which has really converged in the last few years to support that there is a link between sensory health and cognitive health.”
However, “we still don’t know whether hearing/vision loss causes cognitive decline, though there are plausible ways that sensory loss could affect cognitive abilities like memory, language, and executive function,” she said
Dr. Whitson, who was not involved with the research, is also codirector of the Duke/University of North Carolina Alzheimer’s Disease Research Center at Duke University, Durham, N.C., and the Durham VA Medical Center.
“The big question is whether we can improve patients’ cognitive performance by treating or accommodating their sensory impairments,” she said. “If safe and feasible things like hearing aids or cataract surgery improve cognitive health, even a little bit, it would be a huge benefit to society, because sensory loss is very common, and there are many treatment options,” Dr. Whitson added.
Dr. Fuller-Thomson emphasized that practitioners should “consider the full impact of sensory impairment on cognitive testing methods, as both auditory and visual testing methods may fail to take hearing and vision impairment into account.”
Thus, “when performing cognitive tests on older adults with sensory impairments, practitioners should ensure they are communicating audibly and/or using visual speech cues for hearing-impaired individuals, eliminating items from cognitive tests that rely on vision for those who are visually impaired, and using physical cues for individuals with hearing or dual sensory impairment, as this can help increase the accuracy of testing and prevent confounding,” she said.
The study by Fuller-Thomson et al. was funded by a donation from Janis Rotman. Its investigators have reported no relevant financial relationships. The study by Hwang et al. was funded by contracts from the National Heart, Lung, and Blood Institute, the National Institute of Neurological Disorders and Stroke, and the National Institute on Aging. Dr. Hwang reports no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Reed received grants from the National Institute on Aging during the conduct of the study and has served on the advisory board of Neosensory outside the submitted work. Dr. Oh and Dr. Whitson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The combination of hearing loss and vision loss is linked to an eightfold increased risk of cognitive impairment, new research shows.
Investigators analyzed data on more than 5 million U.S. seniors. Adjusted results show that participants with hearing impairment alone had more than twice the odds of also having cognitive impairment, while those with vision impairment alone had more than triple the odds of cognitive impairment.
However, those with dual sensory impairment (DSI) had an eightfold higher risk for cognitive impairment.
In addition, half of the participants with DSI also had cognitive impairment. Of those with cognitive impairment, 16% had DSI, compared with only about 2% of their peers without cognitive impairment.
“The findings of the present study may inform interventions that can support older people with concurrent sensory impairment and cognitive impairment,” said lead author Esme Fuller-Thomson, PhD, professor, Factor-Inwentash Faculty of Social Work, University of Toronto.
“Special attention, in particular, should be given to those aged 65-74 who have serious hearing and/or vision impairment [because], if the relationship with dementia is found to be causal, such interventions can potentially mitigate the development of cognitive impairment,” said Dr. Fuller-Thomson, who is also director of the Institute for Life Course and Aging and a professor in the department of family and community medicine and faculty of nursing, all at the University of Toronto.
The findings were published online in the Journal of Alzheimer’s Disease Reports.
Sensory isolation
Hearing and vision impairment increase with age; it is estimated that one-third of U.S. adults between the ages of 65 and 74 experience hearing loss, and 4% experience vision impairment, the investigators note.
“The link between dual hearing loss and seeing loss and mental health problems such as depression and social isolation have been well researched, but we were very interested in the link between dual sensory loss and cognitive problems,” Dr. Fuller-Thomson said.
Additionally, “there have been several studies in the past decade linking hearing loss to dementia and cognitive decline, but less attention has been paid to cognitive problems among those with DSI, despite this group being particularly isolated,” she said. Existing research into DSI suggests an association with cognitive decline; the current investigators sought to expand on this previous work.
To do so, they used merged data from 10 consecutive waves from 2008 to 2017 of the American Community Survey (ACS), which was conducted by the U.S. Census Bureau. The ACS is a nationally representative sample of 3.5 million randomly selected U.S. addresses and includes community-dwelling adults and those residing in institutional settings.
Participants aged 65 or older (n = 5,405,135; 56.4% women) were asked yes/no questions regarding serious cognitive impairment, hearing impairment, and vision impairment. A proxy, such as a family member or nursing home staff member, provided answers for individuals not capable of self-report.
Potential confounding variables included age, race/ethnicity, sex, education, and household income.
Potential mechanisms
Results showed that, among those with cognitive impairment, there was a higher prevalence of hearing impairment, vision impairment, and DSI than among their peers without cognitive impairment; in addition, a lower percentage of these persons had no sensory impairment (P < .001).
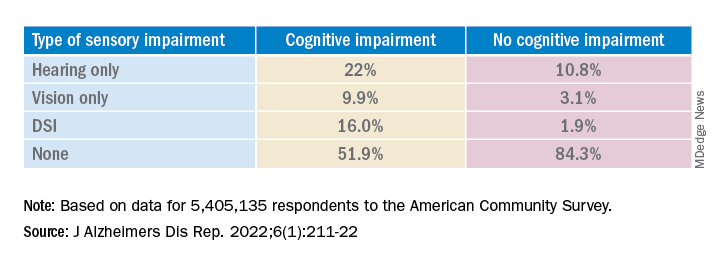
The prevalence of DSI climbed with age, from 1.5% for respondents aged 65-74 years to 2.6% for those aged 75-84 and to 10.8% in those 85 years and older.
Individuals with higher levels of poverty also had higher levels of DSI. Among those who had not completed high school, the prevalence of DSI was higher, compared with high school or university graduates (6.3% vs. 3.1% and 1.85, respectively).
After controlling for age, race, education, and income, the researchers found “substantially” higher odds of cognitive impairment in those with vs. those without sensory impairments.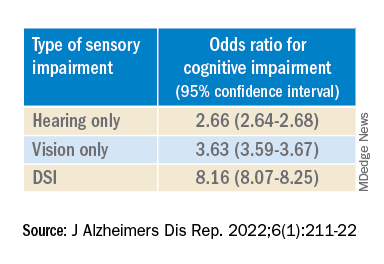
“The magnitude of the odds of cognitive impairment by sensory impairment was greatest for the youngest cohort (age 65-74) and lowest for the oldest cohort (age 85+),” the investigators wrote. Among participants in the youngest cohort, there was a “dose-response relationship” for those with hearing impairment only, visual impairment only, and DSI.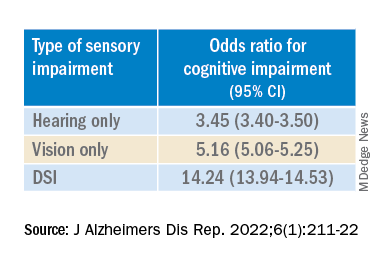
Because the study was observational, it “does not provide sufficient information to determine the reasons behind the observed link between sensory loss and cognitive problems,” Dr. Fuller-Thomson said. However, there are “several potential causal mechanisms [that] warrant future research.”
The “sensory deprivation hypothesis” suggests that DSI could cause cognitive deterioration because of decreased auditory and visual input. The “resource allocation hypothesis” posits that hearing- or vision-impaired older adults “may use more cognitive resources to accommodate for sensory deficits, allocating fewer cognitive resources for higher-order memory processes,” the researchers wrote. Hearing impairment “may also lead to social disengagement among older adults, hastening cognitive decline due to isolation and lack of stimulation,” they added.
Reverse causality is also possible. In the “cognitive load on perception” hypothesis, cognitive decline may lead to declines in hearing and vision because of “decreased resources for sensory processing.”
In addition, the association may be noncausal. “The ‘common cause hypothesis’ theorizes that sensory impairment and cognitive impairment may be due to shared age-related degeneration of the central nervous system ... or frailty,” Dr. Fuller-Thomson said.
Parallel findings
The results are similar to those from a study conducted by Phillip Hwang, PhD, of the department of anatomy and neurobiology, Boston University, and colleagues that was published online in JAMA Network Open.
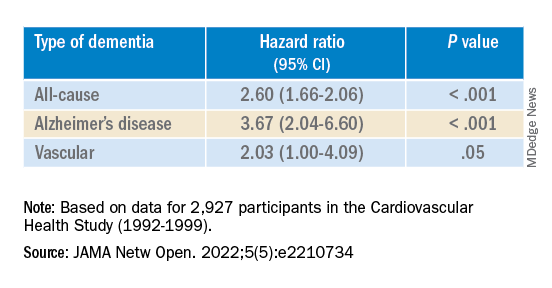
They analyzed data on 8 years of follow-up of 2,927 participants in the Cardiovascular Health Study (mean age, 74.6 years; 58.2% women).
Compared with no sensory impairment, DSI was associated with increased risk for all-cause dementia and Alzheimer’s disease, but not with vascular dementia.
“Future work in health care guidelines could consider incorporating screening of sensory impairment in older adults as part of risk assessment for dementia,” Nicholas Reed, AuD, and Esther Oh, MD, PhD, both of Johns Hopkins University, Baltimore, wrote in an accompanying editorial.
Accurate testing
Commenting on both studies, Heather Whitson, MD, professor of medicine (geriatrics) and ophthalmology and director at the Duke University Center for the Study of Aging and Human Development, Durham, N.C., said both “add further strength to the evidence base, which has really converged in the last few years to support that there is a link between sensory health and cognitive health.”
However, “we still don’t know whether hearing/vision loss causes cognitive decline, though there are plausible ways that sensory loss could affect cognitive abilities like memory, language, and executive function,” she said
Dr. Whitson, who was not involved with the research, is also codirector of the Duke/University of North Carolina Alzheimer’s Disease Research Center at Duke University, Durham, N.C., and the Durham VA Medical Center.
“The big question is whether we can improve patients’ cognitive performance by treating or accommodating their sensory impairments,” she said. “If safe and feasible things like hearing aids or cataract surgery improve cognitive health, even a little bit, it would be a huge benefit to society, because sensory loss is very common, and there are many treatment options,” Dr. Whitson added.
Dr. Fuller-Thomson emphasized that practitioners should “consider the full impact of sensory impairment on cognitive testing methods, as both auditory and visual testing methods may fail to take hearing and vision impairment into account.”
Thus, “when performing cognitive tests on older adults with sensory impairments, practitioners should ensure they are communicating audibly and/or using visual speech cues for hearing-impaired individuals, eliminating items from cognitive tests that rely on vision for those who are visually impaired, and using physical cues for individuals with hearing or dual sensory impairment, as this can help increase the accuracy of testing and prevent confounding,” she said.
The study by Fuller-Thomson et al. was funded by a donation from Janis Rotman. Its investigators have reported no relevant financial relationships. The study by Hwang et al. was funded by contracts from the National Heart, Lung, and Blood Institute, the National Institute of Neurological Disorders and Stroke, and the National Institute on Aging. Dr. Hwang reports no relevant financial relationships. The other investigators’ disclosures are listed in the original article. Dr. Reed received grants from the National Institute on Aging during the conduct of the study and has served on the advisory board of Neosensory outside the submitted work. Dr. Oh and Dr. Whitson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF ALZHEIMER’S DISEASE REPORTS
Long COVID neuropsychiatric deficits greater than expected
NEW ORLEANS – , adding to mounting evidence of the significant toll the chronic condition can have on mental health.
“Many clinicians have observed the symptoms we describe in this study, however this report is among the first which identify the specific deficits using neuropsychological testing to better characterize the syndrome,” Sean T. Lynch, MD, first author of a study on the issue presented at the annual meeting of the American Psychiatric Association, said in an interview.
Dr. Lynch, of the department of psychiatry, Westchester Medical Center Health System, Valhalla, N.Y., and his colleagues enrolled 60 participants who had experienced acute COVID-19 disease 6-8 months earlier and had undergone neuropsychological, psychiatric, medical, functional, and quality-of-life assessments. Results from the study were published online in the Journal of the Academy of Consultation–Liaison Psychiatry (2022 Jan 25. doi: 10.1016/j.jaclp.2022.01.003).
Among the study participants, 32 were seeking treatment for brain fog in a clinical program for survivors of COVID-19, while the remaining 28 were part of an ongoing longitudinal investigation of neuropsychological, medical, and psychiatric sequelae of COVID-19, but were not seeking care for the persistent symptoms.
Assessments for neurocognitive impairment included a battery of tests used in infectious and other diseases, including the Test of Premorbid Function, the Patient Assessment of Own Function, the Trail Making Test parts A and B, the Stroop Color and Word Test, and others.
Overall, the battery of assessments showed that 37 (62%) of participants had neuropsychological test impairment, with results below the 16th percentile in two tests, while 16 (27%) showed scores indicative of severe impairment (below the second percentile in at least one test and below the 16th percentile in one test).
Those reporting brain fog had scores that were even lower than expected on tests of attention, processing speed, memory, and executive function. And among those reporting brain fog, significantly more had scores reflecting severe impairment compared with the controls (38% vs. 14%; P < .04).
“Based on what we’ve observed in our patients and what others have previously reported, we did expect to find some impairment in this study sample,” Dr. Lynch noted.
“However, we were surprised to find that 27% of the study sample had extremely low neuropsychological test scores, meaning that they scored at least two standard deviations below the expected score on at least one neuropsychological test based on their age and level of education.”
The brain fog group also reported significantly higher levels of depression, fatigue, PTSD, and functional difficulties, and lower quality of life.
Severe impairment on the neuropsychological tests correlated with the extent of acute COVID-19 symptoms, as well as depression scores, number of medical comorbidities, and subjective cognitive complaints.
An analysis of serum levels of the inflammatory markers among 50 of the 60 participants showed that 45% of the patients had an elevated IL-6, 20% had elevated TNF-alpha, and 41% had elevated CRP, compared with reference ranges.
IL-6 levels were found to correlate with acute COVID-19 symptoms, the number of medical comorbidities, fatigue, and measures of executive function, while C-reactive protein (CRP) correlated with current COVID-19 symptoms and depression scores.
In terms of clinical factors that might predict low neuropsychological test scores, Dr. Lynch noted that the “markers that we found to be significant included severity of acute COVID-19 illness, current post-COVID-19 symptoms, measures of depression and anxiety, level of fatigue, and number of medical comorbidities.”
Dr. Lynch noted that the ongoing study will include up to 18-month follow-ups that are currently underway. “The [follow-ups] will examine if symptoms improve over time and evaluate if any intervention that took place was successful,” he said.
Survey supports findings
The detrimental effects of mental health symptoms in long COVID were further supported in another study at the APA meeting, an online survey of 787 survivors of acute COVID-19.
In the community survey, presented by Michael Van Ameringen, MD, a professor in the department of psychiatry and behavioral neurosciences at McMaster University, in Hamilton, Ont., all respondents (100%) reported having persistent symptoms of the virus, and as many as 68% indicated that they had not returned to normal functioning, despite only 15% of the respondents having been hospitalized with COVID-19.
A large proportion showed significant depression, anxiety, and posttraumatic stress disorder (PTSD), and the most commonly reported persistent symptoms were fatigue in 75.9% of respondents, brain fog in 67.9%, concentration difficulties in 61.1%, and weakness in 51.2%.
As many as 88.2% of patients said they experienced persistent neurocognitive symptoms, with poor memory and concentration; 56% reported problems with word finding; and 54.1% had slowed thinking.
The respondents showed high rates of anxiety (41.7%) as well as depression (61.4%) as determined by scores above 9 on the Generalized Anxiety Disorder–7 (GAD-7) and Patient Health Questionnaires (PHQ-9).
As many as 40.5% of respondents showed probable PTSD, with scores above 30 on the PTSD checklist (PCL-5). Their mean resilience score on the Brief Resilient Coping Scale was 13.5, suggesting low resilience.
Among the respondents, 43.3% said they had received past treatment for mental health, while 33.5% were currently receiving mental health treatment.
Dr. Van Ameringen noted the important limitation of the study being an online survey with no control group, but said the responses nevertheless raise the question of the role of prior psychiatric disorders in long COVID.
“In our sample, 40% of respondents had a past psychiatric history, so you wonder if that also makes you vulnerable to long COVID,” he said in an interview.
“About a third were getting psychiatric help, but I think the more impaired you are, the more likely you are to seek help.”
Those who were hospitalized with COVID-19 were at a higher risk of PTSD compared with those not hospitalized (P < .001), as were those under the age of 30 (P < .05) or between 31 and 50 vs. over 50 (P < .01).
Dr. Van Ameringen noted that the survey’s high rate of subjects who had not returned to normal functioning was especially striking.
“This is not a minor issue – these are people who are no longer functioning in society,” he said.
In pandemics, the brain tends to be ‘overlooked’
Further addressing the neurological effects of COVID-19 at the APA meeting, Avindra Nath, MD, clinical director of the National Institutes of Neurologic Disorders and Stroke in Bethesda, Md., noted that the persisting cognitive and psychiatric symptoms after illness, such as brain fog and depression and anxiety, are not necessarily unique to COVID-19.
“We have seen this before,” he said. “There have been at least seven or eight human coronaviruses, and the interesting thing is each one affects the brain and causes neurological complications.”
The effects are classified differently and have slightly different receptors, “but the consequences are the same.”
Of note, however, research published in The Lancet Psychiatry (2021 May. doi: 10.1016/S2215-0366[21]00084-5) revealed that symptoms such as dementia, mood, and anxiety are significantly higher after COVID-19 compared with other respiratory infections, with the differences increasing at 180 days since the index event.
Dr. Nath noted that, over the decades, he has observed that in pandemics “the brain tends to get overlooked.” He explained that “what can be most important in the end is what happened in the brain, because those are the things that really cause the long-term consequences.”
“These patients are depressed; they have dementia, they have brain fog, and even now that we recognize these issues, we haven’t done a very good job of studying them,” he said. “There’s so much we still don’t know, and a lot of patients are left with these symptoms and nowhere to go.”
Dr. Lynch, Dr. Van Ameringen, and Dr. Nath had no disclosures to report.
NEW ORLEANS – , adding to mounting evidence of the significant toll the chronic condition can have on mental health.
“Many clinicians have observed the symptoms we describe in this study, however this report is among the first which identify the specific deficits using neuropsychological testing to better characterize the syndrome,” Sean T. Lynch, MD, first author of a study on the issue presented at the annual meeting of the American Psychiatric Association, said in an interview.
Dr. Lynch, of the department of psychiatry, Westchester Medical Center Health System, Valhalla, N.Y., and his colleagues enrolled 60 participants who had experienced acute COVID-19 disease 6-8 months earlier and had undergone neuropsychological, psychiatric, medical, functional, and quality-of-life assessments. Results from the study were published online in the Journal of the Academy of Consultation–Liaison Psychiatry (2022 Jan 25. doi: 10.1016/j.jaclp.2022.01.003).
Among the study participants, 32 were seeking treatment for brain fog in a clinical program for survivors of COVID-19, while the remaining 28 were part of an ongoing longitudinal investigation of neuropsychological, medical, and psychiatric sequelae of COVID-19, but were not seeking care for the persistent symptoms.
Assessments for neurocognitive impairment included a battery of tests used in infectious and other diseases, including the Test of Premorbid Function, the Patient Assessment of Own Function, the Trail Making Test parts A and B, the Stroop Color and Word Test, and others.
Overall, the battery of assessments showed that 37 (62%) of participants had neuropsychological test impairment, with results below the 16th percentile in two tests, while 16 (27%) showed scores indicative of severe impairment (below the second percentile in at least one test and below the 16th percentile in one test).
Those reporting brain fog had scores that were even lower than expected on tests of attention, processing speed, memory, and executive function. And among those reporting brain fog, significantly more had scores reflecting severe impairment compared with the controls (38% vs. 14%; P < .04).
“Based on what we’ve observed in our patients and what others have previously reported, we did expect to find some impairment in this study sample,” Dr. Lynch noted.
“However, we were surprised to find that 27% of the study sample had extremely low neuropsychological test scores, meaning that they scored at least two standard deviations below the expected score on at least one neuropsychological test based on their age and level of education.”
The brain fog group also reported significantly higher levels of depression, fatigue, PTSD, and functional difficulties, and lower quality of life.
Severe impairment on the neuropsychological tests correlated with the extent of acute COVID-19 symptoms, as well as depression scores, number of medical comorbidities, and subjective cognitive complaints.
An analysis of serum levels of the inflammatory markers among 50 of the 60 participants showed that 45% of the patients had an elevated IL-6, 20% had elevated TNF-alpha, and 41% had elevated CRP, compared with reference ranges.
IL-6 levels were found to correlate with acute COVID-19 symptoms, the number of medical comorbidities, fatigue, and measures of executive function, while C-reactive protein (CRP) correlated with current COVID-19 symptoms and depression scores.
In terms of clinical factors that might predict low neuropsychological test scores, Dr. Lynch noted that the “markers that we found to be significant included severity of acute COVID-19 illness, current post-COVID-19 symptoms, measures of depression and anxiety, level of fatigue, and number of medical comorbidities.”
Dr. Lynch noted that the ongoing study will include up to 18-month follow-ups that are currently underway. “The [follow-ups] will examine if symptoms improve over time and evaluate if any intervention that took place was successful,” he said.
Survey supports findings
The detrimental effects of mental health symptoms in long COVID were further supported in another study at the APA meeting, an online survey of 787 survivors of acute COVID-19.
In the community survey, presented by Michael Van Ameringen, MD, a professor in the department of psychiatry and behavioral neurosciences at McMaster University, in Hamilton, Ont., all respondents (100%) reported having persistent symptoms of the virus, and as many as 68% indicated that they had not returned to normal functioning, despite only 15% of the respondents having been hospitalized with COVID-19.
A large proportion showed significant depression, anxiety, and posttraumatic stress disorder (PTSD), and the most commonly reported persistent symptoms were fatigue in 75.9% of respondents, brain fog in 67.9%, concentration difficulties in 61.1%, and weakness in 51.2%.
As many as 88.2% of patients said they experienced persistent neurocognitive symptoms, with poor memory and concentration; 56% reported problems with word finding; and 54.1% had slowed thinking.
The respondents showed high rates of anxiety (41.7%) as well as depression (61.4%) as determined by scores above 9 on the Generalized Anxiety Disorder–7 (GAD-7) and Patient Health Questionnaires (PHQ-9).
As many as 40.5% of respondents showed probable PTSD, with scores above 30 on the PTSD checklist (PCL-5). Their mean resilience score on the Brief Resilient Coping Scale was 13.5, suggesting low resilience.
Among the respondents, 43.3% said they had received past treatment for mental health, while 33.5% were currently receiving mental health treatment.
Dr. Van Ameringen noted the important limitation of the study being an online survey with no control group, but said the responses nevertheless raise the question of the role of prior psychiatric disorders in long COVID.
“In our sample, 40% of respondents had a past psychiatric history, so you wonder if that also makes you vulnerable to long COVID,” he said in an interview.
“About a third were getting psychiatric help, but I think the more impaired you are, the more likely you are to seek help.”
Those who were hospitalized with COVID-19 were at a higher risk of PTSD compared with those not hospitalized (P < .001), as were those under the age of 30 (P < .05) or between 31 and 50 vs. over 50 (P < .01).
Dr. Van Ameringen noted that the survey’s high rate of subjects who had not returned to normal functioning was especially striking.
“This is not a minor issue – these are people who are no longer functioning in society,” he said.
In pandemics, the brain tends to be ‘overlooked’
Further addressing the neurological effects of COVID-19 at the APA meeting, Avindra Nath, MD, clinical director of the National Institutes of Neurologic Disorders and Stroke in Bethesda, Md., noted that the persisting cognitive and psychiatric symptoms after illness, such as brain fog and depression and anxiety, are not necessarily unique to COVID-19.
“We have seen this before,” he said. “There have been at least seven or eight human coronaviruses, and the interesting thing is each one affects the brain and causes neurological complications.”
The effects are classified differently and have slightly different receptors, “but the consequences are the same.”
Of note, however, research published in The Lancet Psychiatry (2021 May. doi: 10.1016/S2215-0366[21]00084-5) revealed that symptoms such as dementia, mood, and anxiety are significantly higher after COVID-19 compared with other respiratory infections, with the differences increasing at 180 days since the index event.
Dr. Nath noted that, over the decades, he has observed that in pandemics “the brain tends to get overlooked.” He explained that “what can be most important in the end is what happened in the brain, because those are the things that really cause the long-term consequences.”
“These patients are depressed; they have dementia, they have brain fog, and even now that we recognize these issues, we haven’t done a very good job of studying them,” he said. “There’s so much we still don’t know, and a lot of patients are left with these symptoms and nowhere to go.”
Dr. Lynch, Dr. Van Ameringen, and Dr. Nath had no disclosures to report.
NEW ORLEANS – , adding to mounting evidence of the significant toll the chronic condition can have on mental health.
“Many clinicians have observed the symptoms we describe in this study, however this report is among the first which identify the specific deficits using neuropsychological testing to better characterize the syndrome,” Sean T. Lynch, MD, first author of a study on the issue presented at the annual meeting of the American Psychiatric Association, said in an interview.
Dr. Lynch, of the department of psychiatry, Westchester Medical Center Health System, Valhalla, N.Y., and his colleagues enrolled 60 participants who had experienced acute COVID-19 disease 6-8 months earlier and had undergone neuropsychological, psychiatric, medical, functional, and quality-of-life assessments. Results from the study were published online in the Journal of the Academy of Consultation–Liaison Psychiatry (2022 Jan 25. doi: 10.1016/j.jaclp.2022.01.003).
Among the study participants, 32 were seeking treatment for brain fog in a clinical program for survivors of COVID-19, while the remaining 28 were part of an ongoing longitudinal investigation of neuropsychological, medical, and psychiatric sequelae of COVID-19, but were not seeking care for the persistent symptoms.
Assessments for neurocognitive impairment included a battery of tests used in infectious and other diseases, including the Test of Premorbid Function, the Patient Assessment of Own Function, the Trail Making Test parts A and B, the Stroop Color and Word Test, and others.
Overall, the battery of assessments showed that 37 (62%) of participants had neuropsychological test impairment, with results below the 16th percentile in two tests, while 16 (27%) showed scores indicative of severe impairment (below the second percentile in at least one test and below the 16th percentile in one test).
Those reporting brain fog had scores that were even lower than expected on tests of attention, processing speed, memory, and executive function. And among those reporting brain fog, significantly more had scores reflecting severe impairment compared with the controls (38% vs. 14%; P < .04).
“Based on what we’ve observed in our patients and what others have previously reported, we did expect to find some impairment in this study sample,” Dr. Lynch noted.
“However, we were surprised to find that 27% of the study sample had extremely low neuropsychological test scores, meaning that they scored at least two standard deviations below the expected score on at least one neuropsychological test based on their age and level of education.”
The brain fog group also reported significantly higher levels of depression, fatigue, PTSD, and functional difficulties, and lower quality of life.
Severe impairment on the neuropsychological tests correlated with the extent of acute COVID-19 symptoms, as well as depression scores, number of medical comorbidities, and subjective cognitive complaints.
An analysis of serum levels of the inflammatory markers among 50 of the 60 participants showed that 45% of the patients had an elevated IL-6, 20% had elevated TNF-alpha, and 41% had elevated CRP, compared with reference ranges.
IL-6 levels were found to correlate with acute COVID-19 symptoms, the number of medical comorbidities, fatigue, and measures of executive function, while C-reactive protein (CRP) correlated with current COVID-19 symptoms and depression scores.
In terms of clinical factors that might predict low neuropsychological test scores, Dr. Lynch noted that the “markers that we found to be significant included severity of acute COVID-19 illness, current post-COVID-19 symptoms, measures of depression and anxiety, level of fatigue, and number of medical comorbidities.”
Dr. Lynch noted that the ongoing study will include up to 18-month follow-ups that are currently underway. “The [follow-ups] will examine if symptoms improve over time and evaluate if any intervention that took place was successful,” he said.
Survey supports findings
The detrimental effects of mental health symptoms in long COVID were further supported in another study at the APA meeting, an online survey of 787 survivors of acute COVID-19.
In the community survey, presented by Michael Van Ameringen, MD, a professor in the department of psychiatry and behavioral neurosciences at McMaster University, in Hamilton, Ont., all respondents (100%) reported having persistent symptoms of the virus, and as many as 68% indicated that they had not returned to normal functioning, despite only 15% of the respondents having been hospitalized with COVID-19.
A large proportion showed significant depression, anxiety, and posttraumatic stress disorder (PTSD), and the most commonly reported persistent symptoms were fatigue in 75.9% of respondents, brain fog in 67.9%, concentration difficulties in 61.1%, and weakness in 51.2%.
As many as 88.2% of patients said they experienced persistent neurocognitive symptoms, with poor memory and concentration; 56% reported problems with word finding; and 54.1% had slowed thinking.
The respondents showed high rates of anxiety (41.7%) as well as depression (61.4%) as determined by scores above 9 on the Generalized Anxiety Disorder–7 (GAD-7) and Patient Health Questionnaires (PHQ-9).
As many as 40.5% of respondents showed probable PTSD, with scores above 30 on the PTSD checklist (PCL-5). Their mean resilience score on the Brief Resilient Coping Scale was 13.5, suggesting low resilience.
Among the respondents, 43.3% said they had received past treatment for mental health, while 33.5% were currently receiving mental health treatment.
Dr. Van Ameringen noted the important limitation of the study being an online survey with no control group, but said the responses nevertheless raise the question of the role of prior psychiatric disorders in long COVID.
“In our sample, 40% of respondents had a past psychiatric history, so you wonder if that also makes you vulnerable to long COVID,” he said in an interview.
“About a third were getting psychiatric help, but I think the more impaired you are, the more likely you are to seek help.”
Those who were hospitalized with COVID-19 were at a higher risk of PTSD compared with those not hospitalized (P < .001), as were those under the age of 30 (P < .05) or between 31 and 50 vs. over 50 (P < .01).
Dr. Van Ameringen noted that the survey’s high rate of subjects who had not returned to normal functioning was especially striking.
“This is not a minor issue – these are people who are no longer functioning in society,” he said.
In pandemics, the brain tends to be ‘overlooked’
Further addressing the neurological effects of COVID-19 at the APA meeting, Avindra Nath, MD, clinical director of the National Institutes of Neurologic Disorders and Stroke in Bethesda, Md., noted that the persisting cognitive and psychiatric symptoms after illness, such as brain fog and depression and anxiety, are not necessarily unique to COVID-19.
“We have seen this before,” he said. “There have been at least seven or eight human coronaviruses, and the interesting thing is each one affects the brain and causes neurological complications.”
The effects are classified differently and have slightly different receptors, “but the consequences are the same.”
Of note, however, research published in The Lancet Psychiatry (2021 May. doi: 10.1016/S2215-0366[21]00084-5) revealed that symptoms such as dementia, mood, and anxiety are significantly higher after COVID-19 compared with other respiratory infections, with the differences increasing at 180 days since the index event.
Dr. Nath noted that, over the decades, he has observed that in pandemics “the brain tends to get overlooked.” He explained that “what can be most important in the end is what happened in the brain, because those are the things that really cause the long-term consequences.”
“These patients are depressed; they have dementia, they have brain fog, and even now that we recognize these issues, we haven’t done a very good job of studying them,” he said. “There’s so much we still don’t know, and a lot of patients are left with these symptoms and nowhere to go.”
Dr. Lynch, Dr. Van Ameringen, and Dr. Nath had no disclosures to report.
AT APA 2022