User login
Management of Acute Opioid Toxicity in the Outpatient Setting
Dermatologists’ offices are not immune from potentially fatal medical events. As a result, it is imperative that dermatologists are well versed in how to manage emergency situations in an outpatient setting. We discuss signs, symptoms, and management of opioid toxicity with an instructive case from our outpatient, hospital-based dermatology clinic.
A 55-year-old woman presented for Mohs micrographic surgery for a large recurrent basal cell carcinoma on the right medial cheek. After informed consent was obtained and the procedure was discussed with the patient, she took one 0.5-mg tablet of clonazepam for perioperative anxiety, which was part of her standard home medication regimen and preoperative administration of clonazepam had been discussed with the treating physician prior to her appointment. During tissue processing, the patient waited alone in the procedure room, with nursing checks every 10 to 15 minutes. Roughly 30 minutes after the initial stage was taken and clear margins were confirmed, the patient was found to be somnolent and unresponsive to voice, light, or touch. Physical examination revealed pupillary constriction, labored breathing, and absent blink reflex. Subsequent examination of the arms, which initially were covered by sleeves, revealed track marks. She was only aroused by a deep sternal rub, which caused her to moan and open her eyes. Her vital signs remained stable, with oxygen saturation greater than 90% and respiratory rate greater than 12 breaths per minute, and a registered nurse remained at her bedside to monitor her clinical status and vitals. Because this event took place in a hospital setting and the patient adequately maintained her airway, respiratory rate, and oxygenation status, the decision was made to closely observe the patient in our clinic. Without additional intervention, the patient gradually regained full awareness, orientation, and mental capacity over the course of 90 minutes. She was ambulatory and conversant at the completion of the procedure, and she declined additional screening for drug abuse or transfer to an acute care facility. She elected for discharge and was accompanied by a family member to drive her home. Later, a search of the state’s prescription monitoring service revealed she had multiple prescriptions from numerous providers for benzodiazepines and opioids. We suspect that her intoxication was the result of ingestion or injection of an opioid medication when she left to visit the restroom unaccompanied, which occurred on at least one known occasion while awaiting tissue processing.
Patients may experience several side effects when using opioid analgesics, most commonly nausea and constipation. When opioids are used long-term, patients are at increased risk for developing fractures, as opioids may decrease bone mineral density by impairing the production of exogenous sex steroid hormones.1 Respiratory depression also can occur, especially when combined with alcohol and other medications such as benzodiazepines. Lastly, opioid dependence can develop in 1 week of regular use.1,2
If opioid overdose is suspected in the office setting, early intervention is critical. Rapid serum glucose should be obtained if a glucometer is available, as hypoglycemia can be confused with opioid toxicity and is easily correctable. If serum glucose is normal, the provider should notify emergency services. In a hospital setting, a rapid response or code can be initiated. In the office setting, dial 911. If not already in place, noninvasive continuous monitoring of the patient’s pulse, oxygen saturation, and blood pressure is needed.1
The provider’s primary concern should be ensuring the patient is adequately ventilated and oxygenated. If the patient’s respiratory rate is greater than 12 breaths per minute and oxygen saturation is greater than 90% on room air, as was the case with our patient, observe and reassess the patient frequently. If the oxygen saturation drops to less than 90% but the patient is breathing spontaneously, administer supplemental oxygen followed by naloxone. If the patient is breathing fewer than 12 breaths per minute, the airway can be maintained with the head tilt–chin lift technique while ventilating using a bag valve mask with supplemental oxygen, followed by administration of naloxone.1
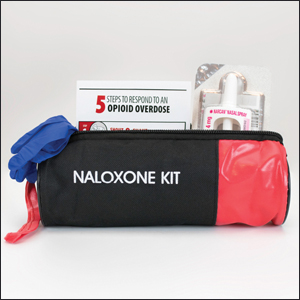
Naloxone is a short-acting opioid antagonist used to treat potentially fatal respiratory depression associated with opioid overdose. It is available in intramuscular (IM), intravenous (IV), and intranasal forms. Intramuscular and IV administration are preferred due to a more rapid onset compared to intranasal. The dosage is 0.04 to 2 mg for IM or IV formulations and 4 mg for the intranasal formulation.1,3 The anterolateral thigh is the preferred IM injection site. Lower initial doses for the IM and IV forms generally are advisable because of the possibility of naloxone precipitating opioid withdrawal in opioid-dependent patients. Naloxone may be administered every 2 to 3 minutes until emergency personnel arrive. Repeat dosing of naloxone should be given until ventilation is greater than 12 breaths per minute while ensuring oxygen saturation is greater than 90%. If there is an inadequate response after 5 to 10 mg of naloxone administration, reconsider the diagnosis. If there is no response after naloxone administration, continue to provide respiratory support with the bag valve mask and supplemental oxygen. After the administration of naloxone, the patient should be transported to the nearest emergency department regardless of the clinical appearance, as naloxone’s half-life may be shorter than the ingested opioid, requiring further observation in a monitored setting.1,3
We recommend that dermatologists consider keeping naloxone in their offices. The medication is easily administered and has a relatively long shelf-life of 1 to 2 years, with a 10-mL vial of 0.4 mg/mL solution costing less than $200 in most cases.3 Increasing cases of opioid abuse could lead to more clinical scenarios similar to what we experienced. Proper identification and management of opioid overdose is within the purview of the dermatologist and can be lifesaving.
- Stolbach A, Hoffman RS. Acute opioid intoxication in adults. UpToDate website. https://www.uptodate.com/contents/acute-opioid-intoxication-in-adults?search=acute%20opioid%20intoxication%20in%20adults&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1. Updated October 1, 2019. Accessed July 23, 2020.
- Glass JS, Hardy CL, Meeks NM, et al. Acute pain management in dermatology: risk assessment and treatment. J Am Acad Dermatol. 2015;73:543-560.
- Pruyn S, Frey J, Baker B, et al. Quality assessment of expired naloxone products from first-responders’ supplies. Prehosp Emerg Care. 2018;23:647-653.
Dermatologists’ offices are not immune from potentially fatal medical events. As a result, it is imperative that dermatologists are well versed in how to manage emergency situations in an outpatient setting. We discuss signs, symptoms, and management of opioid toxicity with an instructive case from our outpatient, hospital-based dermatology clinic.
A 55-year-old woman presented for Mohs micrographic surgery for a large recurrent basal cell carcinoma on the right medial cheek. After informed consent was obtained and the procedure was discussed with the patient, she took one 0.5-mg tablet of clonazepam for perioperative anxiety, which was part of her standard home medication regimen and preoperative administration of clonazepam had been discussed with the treating physician prior to her appointment. During tissue processing, the patient waited alone in the procedure room, with nursing checks every 10 to 15 minutes. Roughly 30 minutes after the initial stage was taken and clear margins were confirmed, the patient was found to be somnolent and unresponsive to voice, light, or touch. Physical examination revealed pupillary constriction, labored breathing, and absent blink reflex. Subsequent examination of the arms, which initially were covered by sleeves, revealed track marks. She was only aroused by a deep sternal rub, which caused her to moan and open her eyes. Her vital signs remained stable, with oxygen saturation greater than 90% and respiratory rate greater than 12 breaths per minute, and a registered nurse remained at her bedside to monitor her clinical status and vitals. Because this event took place in a hospital setting and the patient adequately maintained her airway, respiratory rate, and oxygenation status, the decision was made to closely observe the patient in our clinic. Without additional intervention, the patient gradually regained full awareness, orientation, and mental capacity over the course of 90 minutes. She was ambulatory and conversant at the completion of the procedure, and she declined additional screening for drug abuse or transfer to an acute care facility. She elected for discharge and was accompanied by a family member to drive her home. Later, a search of the state’s prescription monitoring service revealed she had multiple prescriptions from numerous providers for benzodiazepines and opioids. We suspect that her intoxication was the result of ingestion or injection of an opioid medication when she left to visit the restroom unaccompanied, which occurred on at least one known occasion while awaiting tissue processing.
Patients may experience several side effects when using opioid analgesics, most commonly nausea and constipation. When opioids are used long-term, patients are at increased risk for developing fractures, as opioids may decrease bone mineral density by impairing the production of exogenous sex steroid hormones.1 Respiratory depression also can occur, especially when combined with alcohol and other medications such as benzodiazepines. Lastly, opioid dependence can develop in 1 week of regular use.1,2
If opioid overdose is suspected in the office setting, early intervention is critical. Rapid serum glucose should be obtained if a glucometer is available, as hypoglycemia can be confused with opioid toxicity and is easily correctable. If serum glucose is normal, the provider should notify emergency services. In a hospital setting, a rapid response or code can be initiated. In the office setting, dial 911. If not already in place, noninvasive continuous monitoring of the patient’s pulse, oxygen saturation, and blood pressure is needed.1
The provider’s primary concern should be ensuring the patient is adequately ventilated and oxygenated. If the patient’s respiratory rate is greater than 12 breaths per minute and oxygen saturation is greater than 90% on room air, as was the case with our patient, observe and reassess the patient frequently. If the oxygen saturation drops to less than 90% but the patient is breathing spontaneously, administer supplemental oxygen followed by naloxone. If the patient is breathing fewer than 12 breaths per minute, the airway can be maintained with the head tilt–chin lift technique while ventilating using a bag valve mask with supplemental oxygen, followed by administration of naloxone.1
Naloxone is a short-acting opioid antagonist used to treat potentially fatal respiratory depression associated with opioid overdose. It is available in intramuscular (IM), intravenous (IV), and intranasal forms. Intramuscular and IV administration are preferred due to a more rapid onset compared to intranasal. The dosage is 0.04 to 2 mg for IM or IV formulations and 4 mg for the intranasal formulation.1,3 The anterolateral thigh is the preferred IM injection site. Lower initial doses for the IM and IV forms generally are advisable because of the possibility of naloxone precipitating opioid withdrawal in opioid-dependent patients. Naloxone may be administered every 2 to 3 minutes until emergency personnel arrive. Repeat dosing of naloxone should be given until ventilation is greater than 12 breaths per minute while ensuring oxygen saturation is greater than 90%. If there is an inadequate response after 5 to 10 mg of naloxone administration, reconsider the diagnosis. If there is no response after naloxone administration, continue to provide respiratory support with the bag valve mask and supplemental oxygen. After the administration of naloxone, the patient should be transported to the nearest emergency department regardless of the clinical appearance, as naloxone’s half-life may be shorter than the ingested opioid, requiring further observation in a monitored setting.1,3
We recommend that dermatologists consider keeping naloxone in their offices. The medication is easily administered and has a relatively long shelf-life of 1 to 2 years, with a 10-mL vial of 0.4 mg/mL solution costing less than $200 in most cases.3 Increasing cases of opioid abuse could lead to more clinical scenarios similar to what we experienced. Proper identification and management of opioid overdose is within the purview of the dermatologist and can be lifesaving.
Dermatologists’ offices are not immune from potentially fatal medical events. As a result, it is imperative that dermatologists are well versed in how to manage emergency situations in an outpatient setting. We discuss signs, symptoms, and management of opioid toxicity with an instructive case from our outpatient, hospital-based dermatology clinic.
A 55-year-old woman presented for Mohs micrographic surgery for a large recurrent basal cell carcinoma on the right medial cheek. After informed consent was obtained and the procedure was discussed with the patient, she took one 0.5-mg tablet of clonazepam for perioperative anxiety, which was part of her standard home medication regimen and preoperative administration of clonazepam had been discussed with the treating physician prior to her appointment. During tissue processing, the patient waited alone in the procedure room, with nursing checks every 10 to 15 minutes. Roughly 30 minutes after the initial stage was taken and clear margins were confirmed, the patient was found to be somnolent and unresponsive to voice, light, or touch. Physical examination revealed pupillary constriction, labored breathing, and absent blink reflex. Subsequent examination of the arms, which initially were covered by sleeves, revealed track marks. She was only aroused by a deep sternal rub, which caused her to moan and open her eyes. Her vital signs remained stable, with oxygen saturation greater than 90% and respiratory rate greater than 12 breaths per minute, and a registered nurse remained at her bedside to monitor her clinical status and vitals. Because this event took place in a hospital setting and the patient adequately maintained her airway, respiratory rate, and oxygenation status, the decision was made to closely observe the patient in our clinic. Without additional intervention, the patient gradually regained full awareness, orientation, and mental capacity over the course of 90 minutes. She was ambulatory and conversant at the completion of the procedure, and she declined additional screening for drug abuse or transfer to an acute care facility. She elected for discharge and was accompanied by a family member to drive her home. Later, a search of the state’s prescription monitoring service revealed she had multiple prescriptions from numerous providers for benzodiazepines and opioids. We suspect that her intoxication was the result of ingestion or injection of an opioid medication when she left to visit the restroom unaccompanied, which occurred on at least one known occasion while awaiting tissue processing.
Patients may experience several side effects when using opioid analgesics, most commonly nausea and constipation. When opioids are used long-term, patients are at increased risk for developing fractures, as opioids may decrease bone mineral density by impairing the production of exogenous sex steroid hormones.1 Respiratory depression also can occur, especially when combined with alcohol and other medications such as benzodiazepines. Lastly, opioid dependence can develop in 1 week of regular use.1,2
If opioid overdose is suspected in the office setting, early intervention is critical. Rapid serum glucose should be obtained if a glucometer is available, as hypoglycemia can be confused with opioid toxicity and is easily correctable. If serum glucose is normal, the provider should notify emergency services. In a hospital setting, a rapid response or code can be initiated. In the office setting, dial 911. If not already in place, noninvasive continuous monitoring of the patient’s pulse, oxygen saturation, and blood pressure is needed.1
The provider’s primary concern should be ensuring the patient is adequately ventilated and oxygenated. If the patient’s respiratory rate is greater than 12 breaths per minute and oxygen saturation is greater than 90% on room air, as was the case with our patient, observe and reassess the patient frequently. If the oxygen saturation drops to less than 90% but the patient is breathing spontaneously, administer supplemental oxygen followed by naloxone. If the patient is breathing fewer than 12 breaths per minute, the airway can be maintained with the head tilt–chin lift technique while ventilating using a bag valve mask with supplemental oxygen, followed by administration of naloxone.1
Naloxone is a short-acting opioid antagonist used to treat potentially fatal respiratory depression associated with opioid overdose. It is available in intramuscular (IM), intravenous (IV), and intranasal forms. Intramuscular and IV administration are preferred due to a more rapid onset compared to intranasal. The dosage is 0.04 to 2 mg for IM or IV formulations and 4 mg for the intranasal formulation.1,3 The anterolateral thigh is the preferred IM injection site. Lower initial doses for the IM and IV forms generally are advisable because of the possibility of naloxone precipitating opioid withdrawal in opioid-dependent patients. Naloxone may be administered every 2 to 3 minutes until emergency personnel arrive. Repeat dosing of naloxone should be given until ventilation is greater than 12 breaths per minute while ensuring oxygen saturation is greater than 90%. If there is an inadequate response after 5 to 10 mg of naloxone administration, reconsider the diagnosis. If there is no response after naloxone administration, continue to provide respiratory support with the bag valve mask and supplemental oxygen. After the administration of naloxone, the patient should be transported to the nearest emergency department regardless of the clinical appearance, as naloxone’s half-life may be shorter than the ingested opioid, requiring further observation in a monitored setting.1,3
We recommend that dermatologists consider keeping naloxone in their offices. The medication is easily administered and has a relatively long shelf-life of 1 to 2 years, with a 10-mL vial of 0.4 mg/mL solution costing less than $200 in most cases.3 Increasing cases of opioid abuse could lead to more clinical scenarios similar to what we experienced. Proper identification and management of opioid overdose is within the purview of the dermatologist and can be lifesaving.
- Stolbach A, Hoffman RS. Acute opioid intoxication in adults. UpToDate website. https://www.uptodate.com/contents/acute-opioid-intoxication-in-adults?search=acute%20opioid%20intoxication%20in%20adults&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1. Updated October 1, 2019. Accessed July 23, 2020.
- Glass JS, Hardy CL, Meeks NM, et al. Acute pain management in dermatology: risk assessment and treatment. J Am Acad Dermatol. 2015;73:543-560.
- Pruyn S, Frey J, Baker B, et al. Quality assessment of expired naloxone products from first-responders’ supplies. Prehosp Emerg Care. 2018;23:647-653.
- Stolbach A, Hoffman RS. Acute opioid intoxication in adults. UpToDate website. https://www.uptodate.com/contents/acute-opioid-intoxication-in-adults?search=acute%20opioid%20intoxication%20in%20adults&source=search_result&selectedTitle=1~150&usage_type=default&display_rank=1. Updated October 1, 2019. Accessed July 23, 2020.
- Glass JS, Hardy CL, Meeks NM, et al. Acute pain management in dermatology: risk assessment and treatment. J Am Acad Dermatol. 2015;73:543-560.
- Pruyn S, Frey J, Baker B, et al. Quality assessment of expired naloxone products from first-responders’ supplies. Prehosp Emerg Care. 2018;23:647-653.
Practice Points
- Opioid overdose continues to be a major public health concern. Dermatologists may encounter opioid toxicity in their practice, and prompt recognition and treatment are crucial.
- Naloxone is a quick-acting, easy-to-use, and relatively inexpensive medication that can easily be stored and administered in dermatologists’ offices
Tattoo Hypersensitivity Reactions: Inky Business
Sometimes regrettable yet increasingly common, tattoos are an ancient art form used in modern times as a mark of artistic and cultural expression. Allergic contact dermatitis (ACD) to tattoo ink is rare, but the popularity of tattoos makes ACD an increasingly recognized occurrence. In a retrospective study of 38,543 patch-tested patients, only 29 (0.08%) had tattoo-related ACD, with the majority of patients being female and young adults. The most common contact allergy was to paraphenylenediamine (PPD), which occurred in 22 (76%) patients.1 In this article, we will walk you through the rainbow of tattoo ACD, covering hypersensitivity reactions to both temporary and permanent tattoo inks.
Temporary Tattoo Inks
Henna is the most common temporary tattoo ink. Derived from the plant Lawsonia inermis, henna is an orange dye that has been used in many parts of the world, particularly in Islamic and Hindu cultures, to dye skin, hair, and fabrics. Application of henna tattoos is common for weddings and other celebrations, and brides may wear elaborate henna patterns. To create these tattoos, henna powder is mixed with water and sometimes essential oils and is then applied to the skin for several hours. After application, the henna pigment lawsone (2-hydroxy-1,4-naphthoquinone) interacts with keratin and leaves a red-orange stain on the skin2; longer application time leads to a deeper color. Most traditional cutaneous henna designs fade in 2 to 6 weeks, but some last longer. Red henna generally is considered safe with low incidence of contact allergy. What is referred to as black henna usually is red henna mixed with PPD, a black dye, which is added to deepen the color. Paraphenylenediamine is highly sensitizing; patients can become sensitized to the PPD in the tattoo itself.2 One study confirmed the presence of PPD in black henna tattoos, with chemical analysis of common preparations revealing concentrations ranging from less than 1% to 30%.2 Patients who undergo patch testing for tattoo reactions often are strongly positive to PPD and have concomitant reactions to azo dyes, black rubber, and anesthetics. Other aromatic amines including aminophenols have been identified in black henna tattoo ink, and these chemicals also may contribute to ACD.3 Less common sources of contact allergy from temporary black henna tattoos include resorcinol,4 para-tertiary butylphenol formaldehyde resin,5 and fragrance.6
Clinically, ACD to PPD in temporary tattoos presents 1 to 3 days after application if the patient is already sensitized or 4 to 14 days if the patient is sensitized by the tattoo ink.2 Most patients notice erythema, edema, vesicles, papules, and/or bullae, but other less common reactions including generalized dermatitis, systemic symptoms, urticaria, and pustules have been described.2 Postinflammatory hypopigmentation or hyperpigmentation also can occur.
Because of the sensitizing nature of black henna tattoos, consumers are turning to natural temporary tattoos. Jagua temporary tattoos, with pigment derived from the sap of fruit from the Genipa americana tree, have been associated with ACD.7 This black dye is applied and washed off in a similar fashion to henna tattoos. Importantly, a recent analysis of jagua dye identified no PPD. In one case, a patient who developed ACD to a jagua tattoo was patch tested to components of the dye and had a positive reaction to genipin, a component of the fruit extract.7 Thus, jagua tattoos often are marketed as safe but are an emerging source of contact dermatitis to temporary tattoos.
Permanent Tattoo Inks
Permanent tattoos are created by injecting small amounts of ink into the dermis. As the name suggests, these tattoos are permanent. Tattoos are common; nearly one-third of Americans have at least 1 tattoo.1 Historically, tattoos were created using black pigment composed of amorphous carbon or black iron oxides.8,9 Metallic pigments (eg, mercury, chromium, cobalt, cadmium) were once used to add color to tattoos, but these metals are now only rarely used; in fact, a 2019 study of tattoo ink components identified 44 distinct pigments in 1416 permanent inks, with an average of 3 pigments per ink.8 Of the 44 pigments, 10 had metallic components including iron, barium, zinc, copper, molybdenum, and titanium. The remaining 34 pigments contained carbon, azo, diketopyrrolopyrrole, quinacridone, anthraquinone, dioxazine (purple), or quinophthalone (yellow) dyes. The authors noted that nearly one-quarter of the tattoo pigments identified in their study had been reported as contact allergens.8
Typically, reactions to permanent tattoo inks manifest as an eczematous dermatitis occurring weeks to years after tattoo application.9,10 The dermatitis usually is locally confined to the tattoo and may be limited to particular colors; occasionally, a new tattoo reaction may trigger concurrent inflammation in older tattoos. Many tattoo reactions occur as a response to red pigment but also have occurred with other tattoo ink components.9 Many researchers have speculated as to whether the reaction is related to the ink component itself or from the photochemical breakdown of the ink by exposure to UV radiation and/or laser therapy.9
Red Pigment
Red ink is the most common color reported to cause tattoo hypersensitivity reactions. Historically, red tattoo pigments include mercuric sulfide (vermilion, cinnabar), scarlet lake, cadmium red, carmine, and cochineal,11 but today’s tattoo inks primarily are composed of other pigments, such as quinacridone and azo dyes.12 Several cases of red tattoo ink hypersensitivity reactions exist in the literature, many without completion of patch tests or without positive patch tests to relevant red pigments.11-15
Black Pigment
In general, reactions to permanent black tattoo ink are rare; however, a few case reports exist. Black pigment can be created with India ink (carbon), logwood (chrome), iron oxide, and titanium.16,17 Shellac can be used as a binding agent in tattoo ink; there is at least one report of a reaction to black tattoo ink with a positive patch test to shellac and the original black ink.18
Metals
When utilized in tattoos, metals can create a variety of colors; several have been reported to cause ACD. There has been at least one reported case of a tattoo hypersensitivity reaction to a gold tattoo, with positive patch testing for gold sodium thiosulfate.19 Green tattoo inks also have been confirmed to contain metal. One case of nickel allergy from a green tattoo has been reported, with a positive patch test for nickel sulfate and tissue confirmation of the presence of nickel with micro X-ray fluorescence and laser ablation inductively coupled plasma mass spectrometry.20 Another case series described 3 patients with pruritus and chronic dermatitis associated with green tattoos who had positive patch tests to potassium dichromate, and the green tattoo pigment flared during patch testing. Chromium oxide was presumed to be present in the green tattoo pigment, and potassium dichromate avoidance in products and food improved both the pruritus and dermatitis.21
Azo Pigments
Azo pigments frequently are used in modern tattoos due to their vibrant colors. One case of hypersensitivity to azo pigment involved an eczematous ulcerated plaque overlying yellow, red, and green ink in a recently applied tattoo. Patch testing with the inks originally used in the tattoo was negative. The authors noted that the 3 problematic ink colors all contained pigment yellow 65—an azo pigment—and attributed the reaction to this dye.22 In another azo reaction, a patient had erythema and pruritus overlying a tattoo applied 1 month prior. Patch testing was positive for aminoazobenzene, an azo pigment that was present in the orange ink of the tattoo.23
Management of Tattoo Hypersensitivity Reactions
Hypersensitivity reactions to temporary tattoos are just that—temporary. Topical steroids and time generally will allow these reactions to resolve. In the setting of vigorous reactions, patients may develop postinflammatory hypopigmentation or hyperpigmentation that may last for months. Unfortunately, bullous tattoo reactions can lead to scarring and keloid formation, requiring more aggressive therapy.
Management of reactions to permanent tattoos is more challenging. High-potency topical steroids under occlusion or intralesional corticosteroid injections may aid in treating pruritus or discomfort. For severe reactions, oral corticosteroids may be required. Patients also may consider laser tattoo removal; however, providers should be aware that there have been rare reports of systemic urticarial reactions from this procedure.24,25 Obviously limited by location and size, excision also may be offered.
Patch Testing for Tattoo Ink Contact Allergy
When patients present for evaluation and management of tattoo ACD, it is important to also consider other causes, including granulomatous tattoo reaction, pseudolymphoma, and lichenoid tattoo reaction. A biopsy can be helpful if the diagnosis is in question.
Patch testing for contact allergy to temporary tattoo inks should include PPD, fragrance, aminophenols, resorcinol, para-tertiary butylphenol formaldehyde, and essential oils. Jagua currently is not available for commercial purchase but also should be considered if the patient has the original product or in research settings. If the individual tattoo ingredients can be identified, they also should be tested. In this scenario, recall reactions may occur; testing with the tattoo paste should be avoided if the prior reaction was severe. Importantly, patients with a PPD allergy should be counseled to avoid hair dyes that contain PPD. Many patients who are sensitized to PPD have strong reactions on patch testing and are at risk for severe reactions if PPD or PPD-related compounds are encountered in hair dye.
Patch testing for ACD to permanent tattoos is complex. In most cases, patch testing is of limited utility because many of the chemicals that have been reported to cause ACD are not commercially available. Additionally, a 2014 study of 90 patients with chronic tattoo reactions found that the majority had negative patch testing to the European baseline series (66%), disperse dyes (87%), and tattoo inks (87%–92%). The investigators theorized that the allergens causing tattoo reactions are formed by haptenization of “parent” chemicals in the dermis, meaning application of chemicals present in the original tattoo ink may not identify the relevant allergen.26 If patch testing is performed, it is most ideal if individual pigment ingredients can be identified. Allergens to be considered for testing include azo dyes, aromatic amines, iron oxide, barium, zinc, copper, molybdenum, titanium, gold sodium thiosulfate, nickel sulfate, carbon, shellac, diketopyrrolopyrrole, quinacridone, anthraquinone, dioxazine (purple), quinophthalone (yellow) dyes, mercuric sulfide (vermilion, cinnabar), scarlet lake, cadmium red, carmine, and cochineal, many of which are not commercially available for purchase.
Final Interpretation
As tattoos become increasingly trendy, tattoo ACD should be recognized by the astute dermatologist. The most common allergen associated with tattoo ACD is PPD, but other potential allergens include azo dyes and newer pigments. Unlike tattoos of the past, today’s inks are unlikely to contain toxic metals. Diagnosing ACD caused by permanent tattoo inks requires a high degree of suspicion, as patch testing may be of limited utility.
- Warshaw EM, Schlarbaum JP, Taylor JS, et al. Allergic reactions to tattoos: retrospective analysis of North American Contact Dermatitis Group data, 2001-2016. J Am Acad Dermatol. 2020;82:E61-E62.
- de Groot AC. Side-effects of henna and semi-permanent ‘black henna’ tattoos: a full review. Contact Dermatitis. 2013;69:1-25.
- Romita P, Foti C, Mascia P, et al. Eyebrow allergic contact dermatitis caused by m-aminophenol and toluene-2,5-diamine secondary to a temporary black henna tattoo. Contact Dermatitis. 2018;79:51-52.
- Ormerod E, Hughes TM, Stone N. Allergic contact dermatitis caused by resorcinol following a temporary black henna tattoo. Contact Dermatitis. 2017;77:187-188.
- Rodrigo-Nicolás B, de la Cuadra J, Sierra C, et al. Contact dermatitis from a temporary tattoo in a boy with contact allergy to p-tert butyl phenol formaldehyde resin. Dermatitis. 2014;25:37-38.
- Temesvári E, Podányi B, Pónyai G, et al. Fragrance sensitization caused by temporary henna tattoo. Contact Dermatitis. 2002;47:240.
- Bircher AJ, Scherer Hofmeier K, Schlegel U, et al. Genipin in temporary jagua tattoos—black dye causing severe allergic dermatitis. Dermatitis. 2019;30:375-376.
- Liszewski W, Warshaw EM. Pigments in American tattoo inks and their propensity to elicit allergic contact dermatitis. J Am Acad Dermatol. 2019;81:379-385.
- Serup J, Hutton Carlsen K, Dommershausen N, et al. Identification of pigments related to allergic tattoo reactions in 104 human skin biopsies. Contact Dermatitis. 2020;82:73-82.
- Bjerre RD, Ulrich NH, Linneberg A, et al. Adverse reactions to tattoos in the general population of Denmark. J Am Acad Dermatol. 2018;79:770-772.
- Bhardwaj SS, Brodell RT, Taylor JS. Red tattoo reactions. Contact Dermatitis. 2003;48:236-237.
- Gaudron S, Ferrier-Le Bouëdec MC, Franck F, et al. Azo pigments and quinacridones induce delayed hypersensitivity in red tattoos. Contact Dermatitis. 2015;72:97-105.
- de Winter RW, van der Bent SAS, van Esch M, et al. Allergic reaction to red cosmetic lip tattoo treated with hydroxychloroquine. Dermatitis. 2019;30:82-83.
- Greve B, Chytry R, Raulin C. Contact dermatitis from red tattoo pigment (quinacridone) with secondary spread. Contact Dermatitis. 2003;49:265-266.
- Ruiz-Villaverde R, Fernandez-Crehuet P, Aguayo-Carreras P, et al. Inflammatory reactions to red tattoo inks: three cases highlighting an emerging problem. Sultan Qaboos Univ Med J. 2018;18:E215-E218.
- Gallo R, Parodi A, Cozzani E, et al. Allergic reaction to India ink in a black tattoo. Contact Dermatitis. 1998;38:346-347.
- de Cuyper C, Lodewick E, Schreiver I, et al. Are metals involved in tattoo-related hypersensitivity reactions? a case report. Contact Dermatitis. 2017;77:397-405.
- González-Villanueva I, Hispán Ocete P, Silvestre Salvador JF. Allergic contact dermatitis caused by a black tattoo ink in a patient allergic to shellac. Contact Dermatitis. 2016;75:247-248.
- Tammaro A, Tuchinda P, Persechino S, et al. Contact allergic dermatitis to gold in a tattoo: a case report. Int J Immunopathol Pharmacol. 2011;24:1111-1113.
- van der Bent SAS, Berg T, Karst U, et al. Allergic reaction to a green tattoo with nickel as a possible allergen. Contact Dermatitis. 2019;81:64-66.
- Jacob SE, Castanedo-Tardan MP, Blyumin ML. Inflammation in green (chromium) tattoos during patch testing. Dermatitis. 2008;19:E33-E34.
- González-Villanueva I, Álvarez-Chinchilla P, Silvestre JF. Allergic reaction to 3 tattoo inks containing pigment yellow 65. Contact Dermatitis. 2018;79:107-108.
- Tammaro A, De Marco G, D’Arino A, et al. Aminoazobenzene in tattoo: another case of allergic contact dermatitis. Int J Dermatol. 2017;56:E79-E81.
- Willardson HB, Kobayashi TT, Arnold JG, et al. Diffuse urticarial reaction associated with titanium dioxide following laser tattoo removal treatments. Photomed Laser Surg. 2017;35:176‐180.
- England RW, Vogel P, Hagan L. Immediate cutaneous hypersensitivity after treatment of tattoo with Nd:YAG laser: a case report and review of the literature. Ann Allergy Asthma Immunol. 2002;89:215‐217.
- Serup J, Carlsen KH. Patch test study of 90 patients with tattoo reactions: negative outcome of allergy patch test to baseline batteries and culprit inks suggests allergen(s) are generated in the skin through haptenization. Contact Dermatitis. 2014;71:255-263.
Sometimes regrettable yet increasingly common, tattoos are an ancient art form used in modern times as a mark of artistic and cultural expression. Allergic contact dermatitis (ACD) to tattoo ink is rare, but the popularity of tattoos makes ACD an increasingly recognized occurrence. In a retrospective study of 38,543 patch-tested patients, only 29 (0.08%) had tattoo-related ACD, with the majority of patients being female and young adults. The most common contact allergy was to paraphenylenediamine (PPD), which occurred in 22 (76%) patients.1 In this article, we will walk you through the rainbow of tattoo ACD, covering hypersensitivity reactions to both temporary and permanent tattoo inks.
Temporary Tattoo Inks
Henna is the most common temporary tattoo ink. Derived from the plant Lawsonia inermis, henna is an orange dye that has been used in many parts of the world, particularly in Islamic and Hindu cultures, to dye skin, hair, and fabrics. Application of henna tattoos is common for weddings and other celebrations, and brides may wear elaborate henna patterns. To create these tattoos, henna powder is mixed with water and sometimes essential oils and is then applied to the skin for several hours. After application, the henna pigment lawsone (2-hydroxy-1,4-naphthoquinone) interacts with keratin and leaves a red-orange stain on the skin2; longer application time leads to a deeper color. Most traditional cutaneous henna designs fade in 2 to 6 weeks, but some last longer. Red henna generally is considered safe with low incidence of contact allergy. What is referred to as black henna usually is red henna mixed with PPD, a black dye, which is added to deepen the color. Paraphenylenediamine is highly sensitizing; patients can become sensitized to the PPD in the tattoo itself.2 One study confirmed the presence of PPD in black henna tattoos, with chemical analysis of common preparations revealing concentrations ranging from less than 1% to 30%.2 Patients who undergo patch testing for tattoo reactions often are strongly positive to PPD and have concomitant reactions to azo dyes, black rubber, and anesthetics. Other aromatic amines including aminophenols have been identified in black henna tattoo ink, and these chemicals also may contribute to ACD.3 Less common sources of contact allergy from temporary black henna tattoos include resorcinol,4 para-tertiary butylphenol formaldehyde resin,5 and fragrance.6
Clinically, ACD to PPD in temporary tattoos presents 1 to 3 days after application if the patient is already sensitized or 4 to 14 days if the patient is sensitized by the tattoo ink.2 Most patients notice erythema, edema, vesicles, papules, and/or bullae, but other less common reactions including generalized dermatitis, systemic symptoms, urticaria, and pustules have been described.2 Postinflammatory hypopigmentation or hyperpigmentation also can occur.
Because of the sensitizing nature of black henna tattoos, consumers are turning to natural temporary tattoos. Jagua temporary tattoos, with pigment derived from the sap of fruit from the Genipa americana tree, have been associated with ACD.7 This black dye is applied and washed off in a similar fashion to henna tattoos. Importantly, a recent analysis of jagua dye identified no PPD. In one case, a patient who developed ACD to a jagua tattoo was patch tested to components of the dye and had a positive reaction to genipin, a component of the fruit extract.7 Thus, jagua tattoos often are marketed as safe but are an emerging source of contact dermatitis to temporary tattoos.
Permanent Tattoo Inks
Permanent tattoos are created by injecting small amounts of ink into the dermis. As the name suggests, these tattoos are permanent. Tattoos are common; nearly one-third of Americans have at least 1 tattoo.1 Historically, tattoos were created using black pigment composed of amorphous carbon or black iron oxides.8,9 Metallic pigments (eg, mercury, chromium, cobalt, cadmium) were once used to add color to tattoos, but these metals are now only rarely used; in fact, a 2019 study of tattoo ink components identified 44 distinct pigments in 1416 permanent inks, with an average of 3 pigments per ink.8 Of the 44 pigments, 10 had metallic components including iron, barium, zinc, copper, molybdenum, and titanium. The remaining 34 pigments contained carbon, azo, diketopyrrolopyrrole, quinacridone, anthraquinone, dioxazine (purple), or quinophthalone (yellow) dyes. The authors noted that nearly one-quarter of the tattoo pigments identified in their study had been reported as contact allergens.8
Typically, reactions to permanent tattoo inks manifest as an eczematous dermatitis occurring weeks to years after tattoo application.9,10 The dermatitis usually is locally confined to the tattoo and may be limited to particular colors; occasionally, a new tattoo reaction may trigger concurrent inflammation in older tattoos. Many tattoo reactions occur as a response to red pigment but also have occurred with other tattoo ink components.9 Many researchers have speculated as to whether the reaction is related to the ink component itself or from the photochemical breakdown of the ink by exposure to UV radiation and/or laser therapy.9
Red Pigment
Red ink is the most common color reported to cause tattoo hypersensitivity reactions. Historically, red tattoo pigments include mercuric sulfide (vermilion, cinnabar), scarlet lake, cadmium red, carmine, and cochineal,11 but today’s tattoo inks primarily are composed of other pigments, such as quinacridone and azo dyes.12 Several cases of red tattoo ink hypersensitivity reactions exist in the literature, many without completion of patch tests or without positive patch tests to relevant red pigments.11-15
Black Pigment
In general, reactions to permanent black tattoo ink are rare; however, a few case reports exist. Black pigment can be created with India ink (carbon), logwood (chrome), iron oxide, and titanium.16,17 Shellac can be used as a binding agent in tattoo ink; there is at least one report of a reaction to black tattoo ink with a positive patch test to shellac and the original black ink.18
Metals
When utilized in tattoos, metals can create a variety of colors; several have been reported to cause ACD. There has been at least one reported case of a tattoo hypersensitivity reaction to a gold tattoo, with positive patch testing for gold sodium thiosulfate.19 Green tattoo inks also have been confirmed to contain metal. One case of nickel allergy from a green tattoo has been reported, with a positive patch test for nickel sulfate and tissue confirmation of the presence of nickel with micro X-ray fluorescence and laser ablation inductively coupled plasma mass spectrometry.20 Another case series described 3 patients with pruritus and chronic dermatitis associated with green tattoos who had positive patch tests to potassium dichromate, and the green tattoo pigment flared during patch testing. Chromium oxide was presumed to be present in the green tattoo pigment, and potassium dichromate avoidance in products and food improved both the pruritus and dermatitis.21
Azo Pigments
Azo pigments frequently are used in modern tattoos due to their vibrant colors. One case of hypersensitivity to azo pigment involved an eczematous ulcerated plaque overlying yellow, red, and green ink in a recently applied tattoo. Patch testing with the inks originally used in the tattoo was negative. The authors noted that the 3 problematic ink colors all contained pigment yellow 65—an azo pigment—and attributed the reaction to this dye.22 In another azo reaction, a patient had erythema and pruritus overlying a tattoo applied 1 month prior. Patch testing was positive for aminoazobenzene, an azo pigment that was present in the orange ink of the tattoo.23
Management of Tattoo Hypersensitivity Reactions
Hypersensitivity reactions to temporary tattoos are just that—temporary. Topical steroids and time generally will allow these reactions to resolve. In the setting of vigorous reactions, patients may develop postinflammatory hypopigmentation or hyperpigmentation that may last for months. Unfortunately, bullous tattoo reactions can lead to scarring and keloid formation, requiring more aggressive therapy.
Management of reactions to permanent tattoos is more challenging. High-potency topical steroids under occlusion or intralesional corticosteroid injections may aid in treating pruritus or discomfort. For severe reactions, oral corticosteroids may be required. Patients also may consider laser tattoo removal; however, providers should be aware that there have been rare reports of systemic urticarial reactions from this procedure.24,25 Obviously limited by location and size, excision also may be offered.
Patch Testing for Tattoo Ink Contact Allergy
When patients present for evaluation and management of tattoo ACD, it is important to also consider other causes, including granulomatous tattoo reaction, pseudolymphoma, and lichenoid tattoo reaction. A biopsy can be helpful if the diagnosis is in question.
Patch testing for contact allergy to temporary tattoo inks should include PPD, fragrance, aminophenols, resorcinol, para-tertiary butylphenol formaldehyde, and essential oils. Jagua currently is not available for commercial purchase but also should be considered if the patient has the original product or in research settings. If the individual tattoo ingredients can be identified, they also should be tested. In this scenario, recall reactions may occur; testing with the tattoo paste should be avoided if the prior reaction was severe. Importantly, patients with a PPD allergy should be counseled to avoid hair dyes that contain PPD. Many patients who are sensitized to PPD have strong reactions on patch testing and are at risk for severe reactions if PPD or PPD-related compounds are encountered in hair dye.
Patch testing for ACD to permanent tattoos is complex. In most cases, patch testing is of limited utility because many of the chemicals that have been reported to cause ACD are not commercially available. Additionally, a 2014 study of 90 patients with chronic tattoo reactions found that the majority had negative patch testing to the European baseline series (66%), disperse dyes (87%), and tattoo inks (87%–92%). The investigators theorized that the allergens causing tattoo reactions are formed by haptenization of “parent” chemicals in the dermis, meaning application of chemicals present in the original tattoo ink may not identify the relevant allergen.26 If patch testing is performed, it is most ideal if individual pigment ingredients can be identified. Allergens to be considered for testing include azo dyes, aromatic amines, iron oxide, barium, zinc, copper, molybdenum, titanium, gold sodium thiosulfate, nickel sulfate, carbon, shellac, diketopyrrolopyrrole, quinacridone, anthraquinone, dioxazine (purple), quinophthalone (yellow) dyes, mercuric sulfide (vermilion, cinnabar), scarlet lake, cadmium red, carmine, and cochineal, many of which are not commercially available for purchase.
Final Interpretation
As tattoos become increasingly trendy, tattoo ACD should be recognized by the astute dermatologist. The most common allergen associated with tattoo ACD is PPD, but other potential allergens include azo dyes and newer pigments. Unlike tattoos of the past, today’s inks are unlikely to contain toxic metals. Diagnosing ACD caused by permanent tattoo inks requires a high degree of suspicion, as patch testing may be of limited utility.
Sometimes regrettable yet increasingly common, tattoos are an ancient art form used in modern times as a mark of artistic and cultural expression. Allergic contact dermatitis (ACD) to tattoo ink is rare, but the popularity of tattoos makes ACD an increasingly recognized occurrence. In a retrospective study of 38,543 patch-tested patients, only 29 (0.08%) had tattoo-related ACD, with the majority of patients being female and young adults. The most common contact allergy was to paraphenylenediamine (PPD), which occurred in 22 (76%) patients.1 In this article, we will walk you through the rainbow of tattoo ACD, covering hypersensitivity reactions to both temporary and permanent tattoo inks.
Temporary Tattoo Inks
Henna is the most common temporary tattoo ink. Derived from the plant Lawsonia inermis, henna is an orange dye that has been used in many parts of the world, particularly in Islamic and Hindu cultures, to dye skin, hair, and fabrics. Application of henna tattoos is common for weddings and other celebrations, and brides may wear elaborate henna patterns. To create these tattoos, henna powder is mixed with water and sometimes essential oils and is then applied to the skin for several hours. After application, the henna pigment lawsone (2-hydroxy-1,4-naphthoquinone) interacts with keratin and leaves a red-orange stain on the skin2; longer application time leads to a deeper color. Most traditional cutaneous henna designs fade in 2 to 6 weeks, but some last longer. Red henna generally is considered safe with low incidence of contact allergy. What is referred to as black henna usually is red henna mixed with PPD, a black dye, which is added to deepen the color. Paraphenylenediamine is highly sensitizing; patients can become sensitized to the PPD in the tattoo itself.2 One study confirmed the presence of PPD in black henna tattoos, with chemical analysis of common preparations revealing concentrations ranging from less than 1% to 30%.2 Patients who undergo patch testing for tattoo reactions often are strongly positive to PPD and have concomitant reactions to azo dyes, black rubber, and anesthetics. Other aromatic amines including aminophenols have been identified in black henna tattoo ink, and these chemicals also may contribute to ACD.3 Less common sources of contact allergy from temporary black henna tattoos include resorcinol,4 para-tertiary butylphenol formaldehyde resin,5 and fragrance.6
Clinically, ACD to PPD in temporary tattoos presents 1 to 3 days after application if the patient is already sensitized or 4 to 14 days if the patient is sensitized by the tattoo ink.2 Most patients notice erythema, edema, vesicles, papules, and/or bullae, but other less common reactions including generalized dermatitis, systemic symptoms, urticaria, and pustules have been described.2 Postinflammatory hypopigmentation or hyperpigmentation also can occur.
Because of the sensitizing nature of black henna tattoos, consumers are turning to natural temporary tattoos. Jagua temporary tattoos, with pigment derived from the sap of fruit from the Genipa americana tree, have been associated with ACD.7 This black dye is applied and washed off in a similar fashion to henna tattoos. Importantly, a recent analysis of jagua dye identified no PPD. In one case, a patient who developed ACD to a jagua tattoo was patch tested to components of the dye and had a positive reaction to genipin, a component of the fruit extract.7 Thus, jagua tattoos often are marketed as safe but are an emerging source of contact dermatitis to temporary tattoos.
Permanent Tattoo Inks
Permanent tattoos are created by injecting small amounts of ink into the dermis. As the name suggests, these tattoos are permanent. Tattoos are common; nearly one-third of Americans have at least 1 tattoo.1 Historically, tattoos were created using black pigment composed of amorphous carbon or black iron oxides.8,9 Metallic pigments (eg, mercury, chromium, cobalt, cadmium) were once used to add color to tattoos, but these metals are now only rarely used; in fact, a 2019 study of tattoo ink components identified 44 distinct pigments in 1416 permanent inks, with an average of 3 pigments per ink.8 Of the 44 pigments, 10 had metallic components including iron, barium, zinc, copper, molybdenum, and titanium. The remaining 34 pigments contained carbon, azo, diketopyrrolopyrrole, quinacridone, anthraquinone, dioxazine (purple), or quinophthalone (yellow) dyes. The authors noted that nearly one-quarter of the tattoo pigments identified in their study had been reported as contact allergens.8
Typically, reactions to permanent tattoo inks manifest as an eczematous dermatitis occurring weeks to years after tattoo application.9,10 The dermatitis usually is locally confined to the tattoo and may be limited to particular colors; occasionally, a new tattoo reaction may trigger concurrent inflammation in older tattoos. Many tattoo reactions occur as a response to red pigment but also have occurred with other tattoo ink components.9 Many researchers have speculated as to whether the reaction is related to the ink component itself or from the photochemical breakdown of the ink by exposure to UV radiation and/or laser therapy.9
Red Pigment
Red ink is the most common color reported to cause tattoo hypersensitivity reactions. Historically, red tattoo pigments include mercuric sulfide (vermilion, cinnabar), scarlet lake, cadmium red, carmine, and cochineal,11 but today’s tattoo inks primarily are composed of other pigments, such as quinacridone and azo dyes.12 Several cases of red tattoo ink hypersensitivity reactions exist in the literature, many without completion of patch tests or without positive patch tests to relevant red pigments.11-15
Black Pigment
In general, reactions to permanent black tattoo ink are rare; however, a few case reports exist. Black pigment can be created with India ink (carbon), logwood (chrome), iron oxide, and titanium.16,17 Shellac can be used as a binding agent in tattoo ink; there is at least one report of a reaction to black tattoo ink with a positive patch test to shellac and the original black ink.18
Metals
When utilized in tattoos, metals can create a variety of colors; several have been reported to cause ACD. There has been at least one reported case of a tattoo hypersensitivity reaction to a gold tattoo, with positive patch testing for gold sodium thiosulfate.19 Green tattoo inks also have been confirmed to contain metal. One case of nickel allergy from a green tattoo has been reported, with a positive patch test for nickel sulfate and tissue confirmation of the presence of nickel with micro X-ray fluorescence and laser ablation inductively coupled plasma mass spectrometry.20 Another case series described 3 patients with pruritus and chronic dermatitis associated with green tattoos who had positive patch tests to potassium dichromate, and the green tattoo pigment flared during patch testing. Chromium oxide was presumed to be present in the green tattoo pigment, and potassium dichromate avoidance in products and food improved both the pruritus and dermatitis.21
Azo Pigments
Azo pigments frequently are used in modern tattoos due to their vibrant colors. One case of hypersensitivity to azo pigment involved an eczematous ulcerated plaque overlying yellow, red, and green ink in a recently applied tattoo. Patch testing with the inks originally used in the tattoo was negative. The authors noted that the 3 problematic ink colors all contained pigment yellow 65—an azo pigment—and attributed the reaction to this dye.22 In another azo reaction, a patient had erythema and pruritus overlying a tattoo applied 1 month prior. Patch testing was positive for aminoazobenzene, an azo pigment that was present in the orange ink of the tattoo.23
Management of Tattoo Hypersensitivity Reactions
Hypersensitivity reactions to temporary tattoos are just that—temporary. Topical steroids and time generally will allow these reactions to resolve. In the setting of vigorous reactions, patients may develop postinflammatory hypopigmentation or hyperpigmentation that may last for months. Unfortunately, bullous tattoo reactions can lead to scarring and keloid formation, requiring more aggressive therapy.
Management of reactions to permanent tattoos is more challenging. High-potency topical steroids under occlusion or intralesional corticosteroid injections may aid in treating pruritus or discomfort. For severe reactions, oral corticosteroids may be required. Patients also may consider laser tattoo removal; however, providers should be aware that there have been rare reports of systemic urticarial reactions from this procedure.24,25 Obviously limited by location and size, excision also may be offered.
Patch Testing for Tattoo Ink Contact Allergy
When patients present for evaluation and management of tattoo ACD, it is important to also consider other causes, including granulomatous tattoo reaction, pseudolymphoma, and lichenoid tattoo reaction. A biopsy can be helpful if the diagnosis is in question.
Patch testing for contact allergy to temporary tattoo inks should include PPD, fragrance, aminophenols, resorcinol, para-tertiary butylphenol formaldehyde, and essential oils. Jagua currently is not available for commercial purchase but also should be considered if the patient has the original product or in research settings. If the individual tattoo ingredients can be identified, they also should be tested. In this scenario, recall reactions may occur; testing with the tattoo paste should be avoided if the prior reaction was severe. Importantly, patients with a PPD allergy should be counseled to avoid hair dyes that contain PPD. Many patients who are sensitized to PPD have strong reactions on patch testing and are at risk for severe reactions if PPD or PPD-related compounds are encountered in hair dye.
Patch testing for ACD to permanent tattoos is complex. In most cases, patch testing is of limited utility because many of the chemicals that have been reported to cause ACD are not commercially available. Additionally, a 2014 study of 90 patients with chronic tattoo reactions found that the majority had negative patch testing to the European baseline series (66%), disperse dyes (87%), and tattoo inks (87%–92%). The investigators theorized that the allergens causing tattoo reactions are formed by haptenization of “parent” chemicals in the dermis, meaning application of chemicals present in the original tattoo ink may not identify the relevant allergen.26 If patch testing is performed, it is most ideal if individual pigment ingredients can be identified. Allergens to be considered for testing include azo dyes, aromatic amines, iron oxide, barium, zinc, copper, molybdenum, titanium, gold sodium thiosulfate, nickel sulfate, carbon, shellac, diketopyrrolopyrrole, quinacridone, anthraquinone, dioxazine (purple), quinophthalone (yellow) dyes, mercuric sulfide (vermilion, cinnabar), scarlet lake, cadmium red, carmine, and cochineal, many of which are not commercially available for purchase.
Final Interpretation
As tattoos become increasingly trendy, tattoo ACD should be recognized by the astute dermatologist. The most common allergen associated with tattoo ACD is PPD, but other potential allergens include azo dyes and newer pigments. Unlike tattoos of the past, today’s inks are unlikely to contain toxic metals. Diagnosing ACD caused by permanent tattoo inks requires a high degree of suspicion, as patch testing may be of limited utility.
- Warshaw EM, Schlarbaum JP, Taylor JS, et al. Allergic reactions to tattoos: retrospective analysis of North American Contact Dermatitis Group data, 2001-2016. J Am Acad Dermatol. 2020;82:E61-E62.
- de Groot AC. Side-effects of henna and semi-permanent ‘black henna’ tattoos: a full review. Contact Dermatitis. 2013;69:1-25.
- Romita P, Foti C, Mascia P, et al. Eyebrow allergic contact dermatitis caused by m-aminophenol and toluene-2,5-diamine secondary to a temporary black henna tattoo. Contact Dermatitis. 2018;79:51-52.
- Ormerod E, Hughes TM, Stone N. Allergic contact dermatitis caused by resorcinol following a temporary black henna tattoo. Contact Dermatitis. 2017;77:187-188.
- Rodrigo-Nicolás B, de la Cuadra J, Sierra C, et al. Contact dermatitis from a temporary tattoo in a boy with contact allergy to p-tert butyl phenol formaldehyde resin. Dermatitis. 2014;25:37-38.
- Temesvári E, Podányi B, Pónyai G, et al. Fragrance sensitization caused by temporary henna tattoo. Contact Dermatitis. 2002;47:240.
- Bircher AJ, Scherer Hofmeier K, Schlegel U, et al. Genipin in temporary jagua tattoos—black dye causing severe allergic dermatitis. Dermatitis. 2019;30:375-376.
- Liszewski W, Warshaw EM. Pigments in American tattoo inks and their propensity to elicit allergic contact dermatitis. J Am Acad Dermatol. 2019;81:379-385.
- Serup J, Hutton Carlsen K, Dommershausen N, et al. Identification of pigments related to allergic tattoo reactions in 104 human skin biopsies. Contact Dermatitis. 2020;82:73-82.
- Bjerre RD, Ulrich NH, Linneberg A, et al. Adverse reactions to tattoos in the general population of Denmark. J Am Acad Dermatol. 2018;79:770-772.
- Bhardwaj SS, Brodell RT, Taylor JS. Red tattoo reactions. Contact Dermatitis. 2003;48:236-237.
- Gaudron S, Ferrier-Le Bouëdec MC, Franck F, et al. Azo pigments and quinacridones induce delayed hypersensitivity in red tattoos. Contact Dermatitis. 2015;72:97-105.
- de Winter RW, van der Bent SAS, van Esch M, et al. Allergic reaction to red cosmetic lip tattoo treated with hydroxychloroquine. Dermatitis. 2019;30:82-83.
- Greve B, Chytry R, Raulin C. Contact dermatitis from red tattoo pigment (quinacridone) with secondary spread. Contact Dermatitis. 2003;49:265-266.
- Ruiz-Villaverde R, Fernandez-Crehuet P, Aguayo-Carreras P, et al. Inflammatory reactions to red tattoo inks: three cases highlighting an emerging problem. Sultan Qaboos Univ Med J. 2018;18:E215-E218.
- Gallo R, Parodi A, Cozzani E, et al. Allergic reaction to India ink in a black tattoo. Contact Dermatitis. 1998;38:346-347.
- de Cuyper C, Lodewick E, Schreiver I, et al. Are metals involved in tattoo-related hypersensitivity reactions? a case report. Contact Dermatitis. 2017;77:397-405.
- González-Villanueva I, Hispán Ocete P, Silvestre Salvador JF. Allergic contact dermatitis caused by a black tattoo ink in a patient allergic to shellac. Contact Dermatitis. 2016;75:247-248.
- Tammaro A, Tuchinda P, Persechino S, et al. Contact allergic dermatitis to gold in a tattoo: a case report. Int J Immunopathol Pharmacol. 2011;24:1111-1113.
- van der Bent SAS, Berg T, Karst U, et al. Allergic reaction to a green tattoo with nickel as a possible allergen. Contact Dermatitis. 2019;81:64-66.
- Jacob SE, Castanedo-Tardan MP, Blyumin ML. Inflammation in green (chromium) tattoos during patch testing. Dermatitis. 2008;19:E33-E34.
- González-Villanueva I, Álvarez-Chinchilla P, Silvestre JF. Allergic reaction to 3 tattoo inks containing pigment yellow 65. Contact Dermatitis. 2018;79:107-108.
- Tammaro A, De Marco G, D’Arino A, et al. Aminoazobenzene in tattoo: another case of allergic contact dermatitis. Int J Dermatol. 2017;56:E79-E81.
- Willardson HB, Kobayashi TT, Arnold JG, et al. Diffuse urticarial reaction associated with titanium dioxide following laser tattoo removal treatments. Photomed Laser Surg. 2017;35:176‐180.
- England RW, Vogel P, Hagan L. Immediate cutaneous hypersensitivity after treatment of tattoo with Nd:YAG laser: a case report and review of the literature. Ann Allergy Asthma Immunol. 2002;89:215‐217.
- Serup J, Carlsen KH. Patch test study of 90 patients with tattoo reactions: negative outcome of allergy patch test to baseline batteries and culprit inks suggests allergen(s) are generated in the skin through haptenization. Contact Dermatitis. 2014;71:255-263.
- Warshaw EM, Schlarbaum JP, Taylor JS, et al. Allergic reactions to tattoos: retrospective analysis of North American Contact Dermatitis Group data, 2001-2016. J Am Acad Dermatol. 2020;82:E61-E62.
- de Groot AC. Side-effects of henna and semi-permanent ‘black henna’ tattoos: a full review. Contact Dermatitis. 2013;69:1-25.
- Romita P, Foti C, Mascia P, et al. Eyebrow allergic contact dermatitis caused by m-aminophenol and toluene-2,5-diamine secondary to a temporary black henna tattoo. Contact Dermatitis. 2018;79:51-52.
- Ormerod E, Hughes TM, Stone N. Allergic contact dermatitis caused by resorcinol following a temporary black henna tattoo. Contact Dermatitis. 2017;77:187-188.
- Rodrigo-Nicolás B, de la Cuadra J, Sierra C, et al. Contact dermatitis from a temporary tattoo in a boy with contact allergy to p-tert butyl phenol formaldehyde resin. Dermatitis. 2014;25:37-38.
- Temesvári E, Podányi B, Pónyai G, et al. Fragrance sensitization caused by temporary henna tattoo. Contact Dermatitis. 2002;47:240.
- Bircher AJ, Scherer Hofmeier K, Schlegel U, et al. Genipin in temporary jagua tattoos—black dye causing severe allergic dermatitis. Dermatitis. 2019;30:375-376.
- Liszewski W, Warshaw EM. Pigments in American tattoo inks and their propensity to elicit allergic contact dermatitis. J Am Acad Dermatol. 2019;81:379-385.
- Serup J, Hutton Carlsen K, Dommershausen N, et al. Identification of pigments related to allergic tattoo reactions in 104 human skin biopsies. Contact Dermatitis. 2020;82:73-82.
- Bjerre RD, Ulrich NH, Linneberg A, et al. Adverse reactions to tattoos in the general population of Denmark. J Am Acad Dermatol. 2018;79:770-772.
- Bhardwaj SS, Brodell RT, Taylor JS. Red tattoo reactions. Contact Dermatitis. 2003;48:236-237.
- Gaudron S, Ferrier-Le Bouëdec MC, Franck F, et al. Azo pigments and quinacridones induce delayed hypersensitivity in red tattoos. Contact Dermatitis. 2015;72:97-105.
- de Winter RW, van der Bent SAS, van Esch M, et al. Allergic reaction to red cosmetic lip tattoo treated with hydroxychloroquine. Dermatitis. 2019;30:82-83.
- Greve B, Chytry R, Raulin C. Contact dermatitis from red tattoo pigment (quinacridone) with secondary spread. Contact Dermatitis. 2003;49:265-266.
- Ruiz-Villaverde R, Fernandez-Crehuet P, Aguayo-Carreras P, et al. Inflammatory reactions to red tattoo inks: three cases highlighting an emerging problem. Sultan Qaboos Univ Med J. 2018;18:E215-E218.
- Gallo R, Parodi A, Cozzani E, et al. Allergic reaction to India ink in a black tattoo. Contact Dermatitis. 1998;38:346-347.
- de Cuyper C, Lodewick E, Schreiver I, et al. Are metals involved in tattoo-related hypersensitivity reactions? a case report. Contact Dermatitis. 2017;77:397-405.
- González-Villanueva I, Hispán Ocete P, Silvestre Salvador JF. Allergic contact dermatitis caused by a black tattoo ink in a patient allergic to shellac. Contact Dermatitis. 2016;75:247-248.
- Tammaro A, Tuchinda P, Persechino S, et al. Contact allergic dermatitis to gold in a tattoo: a case report. Int J Immunopathol Pharmacol. 2011;24:1111-1113.
- van der Bent SAS, Berg T, Karst U, et al. Allergic reaction to a green tattoo with nickel as a possible allergen. Contact Dermatitis. 2019;81:64-66.
- Jacob SE, Castanedo-Tardan MP, Blyumin ML. Inflammation in green (chromium) tattoos during patch testing. Dermatitis. 2008;19:E33-E34.
- González-Villanueva I, Álvarez-Chinchilla P, Silvestre JF. Allergic reaction to 3 tattoo inks containing pigment yellow 65. Contact Dermatitis. 2018;79:107-108.
- Tammaro A, De Marco G, D’Arino A, et al. Aminoazobenzene in tattoo: another case of allergic contact dermatitis. Int J Dermatol. 2017;56:E79-E81.
- Willardson HB, Kobayashi TT, Arnold JG, et al. Diffuse urticarial reaction associated with titanium dioxide following laser tattoo removal treatments. Photomed Laser Surg. 2017;35:176‐180.
- England RW, Vogel P, Hagan L. Immediate cutaneous hypersensitivity after treatment of tattoo with Nd:YAG laser: a case report and review of the literature. Ann Allergy Asthma Immunol. 2002;89:215‐217.
- Serup J, Carlsen KH. Patch test study of 90 patients with tattoo reactions: negative outcome of allergy patch test to baseline batteries and culprit inks suggests allergen(s) are generated in the skin through haptenization. Contact Dermatitis. 2014;71:255-263.
Practice Points
- Temporary tattoo pigments include red henna, black henna, and jagua.
- Black henna tattoos contain paraphenylenediamine, the most common allergen in temporary tattoos.
- Modern permanent tattoo ink components include metals, carbon, azo, diketopyrrolopyrrole, quinacridone, anthraquinone, dioxazine (purple), or quinophthalone (yellow) dyes.
- Patch testing for tattoo contact allergy is complex and challenging.
Are You Up-to-date on Dermal Fillers?
The popularity of injectable fillers for aesthetic use continues to rise, and cosmetic injectors must select from an increasing range of options to achieve optimal outcomes. In addition to formulating a treatment plan and having an intimate knowledge of the facial anatomy, filler selection is critical along with an appreciation of both approved and off-label indications for these products. Appropriate patient selection and treatment technique can minimize adverse events (AEs) and allow for the best outcomes.
The US Food and Drug Administration (FDA) approved the first injectable hyaluronic acid (HA) filler in 2003, the first addition since the approval of bovine collagen in 1981. To date, there are now 4 groups of approved fillers: (1) HA (Belotero Balance [Merz North America, Inc], Juvèderm products [Allergan], Restylane products [Galderma Laboratories, LP], Resilient HA products [Revance Therapeutics Inc and Teoxane SA]), (2) calcium hydroxylapatite (Radiesse [Merz North America, Inc]), (3) poly-L-lactic acid (Sculptra Aesthetic [Galderma Laboratories, LP]), and (4) polymethylmethacrylate (Bellafill [Suneva Medical, Inc]).1-3 Given the versatility of this wide portfolio of products, which often are used in combination with one another, we have advanced from the early goals of filling isolated lines or wrinkles on the face to the 3-dimensional restructuring of an entire treatment area. The increasing diversity of products, particularly the range of rheologic properties of HA fillers, allows the injector to strategically select the type of filler and depth of injection to achieve the desired treatment outcome. The duration of the treatment effects also is related to the properties of the filler.4,5
Advancements in injectable fillers also have led to new applications both on and off the face. Many pivotal clinical trials of fillers were performed in isolated anatomic areas, most commonly the nasolabial folds, leading to FDA approval of this indication. Other FDA-approved indications for fillers include lip augmentation (Juvèderm Ultra, Juvèderm Volbella, Restylane, Restylane Silk, Restylane Kysse), human immunodeficiency virus–associated lipoatrophy (Sculptra Aesthetic, Radiesse), volumization of the dorsal hands (Radiesse, Restylane Lyft), acne scarring (Bellafill), and age-related volume loss of the midface (Juvèderm Voluma, Restylane Lyft). Although it is considered off label, treatment of the temples, brows, tear troughs, jawline, horizontal neck lines, and etched-in radial cheek lines has been reported.6-9 It is legal to use fillers to treat these areas, but data have not yet been evaluated by the FDA to officially grant their approval, which likely will change with the conclusion of many ongoing industry-sponsored trials.
Adverse events from filler injections range from the anticipated transient tenderness, swelling, and bruising, which are likely to resolve in a matter of days, to the most severe complications—intravascular occlusion with permanent sequelae, namely tissue necrosis, blindness or visual compromise, and stroke. It is critical to obtain written informed consent prior to proceeding with dermal filler injections. Masterful knowledge of the facial anatomy, in particular the location and depth of key vascular structures, is critical in minimizing these severe AEs. Injection technique, including use of a microcannula, can reduce the risk, in addition to administration of small volumes of filler at a time, aspiration prior to injection, and use of a retrograde injection technique. There also are variations in the predicted courses of vascular structures, as demonstrated in a cadaveric study showing 4 variants of the course of the angular artery.10
Hyaluronic acid fillers are the most commonly used of the available products, and hyaluronidase, which can dissolve the filler, can be utilized to manage emergent and nonemergent AEs.11 Physical examination findings related to impending necrosis include blanching of the skin in the distribution of a key vessel with a mottled or reticulated purple discoloration. Hyaluronidase, on the order of hundreds of units, may be injected into the area of vascular compromise until reperfusion is achieved, in addition to administering aspirin and applying warm compresses to the area.11,12 The most severe AEs are blindness and/or stroke, associated with findings such as immediate vision loss, pain, nausea, vomiting, and neurologic compromise. Although the glabella, nose, nasolabial folds, and forehead are the most common anatomic areas associated with these AEs (in order of frequency), injections in all areas of the face have been associated with blindness.13,14 Retrobulbar and/or peribulbar injection of hyaluronidase for management of vision changes has been reported, but in most cases vision loss associated with dermal filler injections is not reversible.14,15
Nonemergent uses of enzyme reversal of filler placement include correcting undesirable aesthetic outcomes, such as asymmetry, misplaced filler, or even delayed granulomatous reactions. Hyaluronidase dosage should be determined by the amount and type of filler that was delivered to the patient. All HA fillers are not created equally, and evidence from dosing studies indicates that higher cross-linked and more cohesive fillers require higher doses of hyaluronidase.11 For example, Juvèderm Voluma, created as a mixture of low- and high-molecular-weight HA, has a higher cross-linking ratio. Approximately 30 U of hyaluronidase are suggested to dissolve 0.1 cc of Juvèderm Voluma as compared to 10 U of hyaluronidase for 0.1 cc of Juvèderm Ultra and 5 U for 0.1 cc of Restylane.11
Treatment with dermal fillers generally is safe and effective, and as new fillers come to the market, we must identify how they will help further our goal of improving patient outcomes. The effects of coronavirus disease 19 on aesthetic medicine are still unclear, yet this uncertainty should not deflect treating clinicians from overlooking the fundamentals of dermal fillers. In addition to considering the appropriate use of each filler based on its unique characteristics and indications, we must be sure that we are prepared with the tools to manage any and all possible complications.
- Jiang B, Ramirez M, Ranjit-Reeves R, et al. Noncollagen dermal fillers: a summary of the clinical trials used for their FDA approval. Dermatol Surg. 2019;45:1585-1596.
- Monheit G, Kaufman-Janette J, Joseph J, et al. Efficacy and safety of two resilient hyaluronic acid fillers in the treatment of moderate-to-severe nasolabial folds [published online March 24, 2020]. Dermatol Surg. doi:10.1097/DSS0000000000002391.
- Kaufman-Janette J, Taylor SC, Cox SE, et al. Efficacy and safety of a new resilient hyaluronic acid dermal filler, in the correction of moderate-to-severe nasolabial folds: a 64-week, prospective, multicenter, controlled, randomized, double-blind and within-subject study. J Cosmet Dermatol. 2019;18:1244-1253.
- Jones D, Murphy D. Volumizing hyaluronic acid filler for midface volume deficit: 2 year results from a pivotal single-blind randomized controlled study. Dermatol Surg. 2013;39:1602-1611.
- Hausauer AK, Jones DH. Long-term correction of iatrogenic lipoatrophy with volumizing hyaluronic acid filler. Dermatol Surg. 2018;44(suppl 1):S60-S62.
- Black J, Jones D. Cohesive polydensified matrix hyaluronic acid for the treatment of etched-in fine facial lines: a 6-month, open-label clinical trial. Dermatol Surg. 2018;44:1002-1011.
- Breithaupt A, Jones D, Braz A, et al. Anatomic basis for safe and effective volumization of the temple. Dermatol Surg. 2015;41:S278-S283.
- Dallara JM, Baspeyras M, Bui P, et al. Calcium hydroxylapatite for jawline rejuvenation: consensus recommendations. J Cosmet Dermatol. 2014;13:3-14.
- Minokadeh A, Black J, Jones D. Effacement of transverse neck lines with VYC-15L and a cohesive polydensified matrix hyaluronic acid. Dermatol Surg. 2019;45:941-948.
- Kim YS, Choi DY, Gil YC, et al. The anatomical origin and course of the angular artery regarding its clinical implications. Dermatol Surg. 2014;40:1070-1076.
- Jones DH. Update on emergency and nonemergency use of hyaluronidase in aesthetic dermatology. JAMA Dermatol. 2018;154:763-764.
- Cohen JL, Biesman BS, Dayan SH, et al. Treatment of hyaluronic acid filler-induced impending necrosis with hyaluronidase: consensus recommendations. Aesthet Surg J. 2015;35:844-849.
- Beleznay K, Carruthers J, Humphrey S, et al. Avoiding and treating blindness from fillers: a review of the world literature. Dermatol Surg. 2015;41:1097-1117.
- Beleznay K, Carruthers J, Humphrey S, et al. Update on avoiding and treating blindness from fillers: a recent review of the world literature. Aesthet Surg J. 2019;39:662-674.
- Chestnut C. Restoration of visual loss with retrobulblar hyaluronidase injection after hyaluronic acid filler. Dermatol Surg. 2018;44:435-437.
The popularity of injectable fillers for aesthetic use continues to rise, and cosmetic injectors must select from an increasing range of options to achieve optimal outcomes. In addition to formulating a treatment plan and having an intimate knowledge of the facial anatomy, filler selection is critical along with an appreciation of both approved and off-label indications for these products. Appropriate patient selection and treatment technique can minimize adverse events (AEs) and allow for the best outcomes.
The US Food and Drug Administration (FDA) approved the first injectable hyaluronic acid (HA) filler in 2003, the first addition since the approval of bovine collagen in 1981. To date, there are now 4 groups of approved fillers: (1) HA (Belotero Balance [Merz North America, Inc], Juvèderm products [Allergan], Restylane products [Galderma Laboratories, LP], Resilient HA products [Revance Therapeutics Inc and Teoxane SA]), (2) calcium hydroxylapatite (Radiesse [Merz North America, Inc]), (3) poly-L-lactic acid (Sculptra Aesthetic [Galderma Laboratories, LP]), and (4) polymethylmethacrylate (Bellafill [Suneva Medical, Inc]).1-3 Given the versatility of this wide portfolio of products, which often are used in combination with one another, we have advanced from the early goals of filling isolated lines or wrinkles on the face to the 3-dimensional restructuring of an entire treatment area. The increasing diversity of products, particularly the range of rheologic properties of HA fillers, allows the injector to strategically select the type of filler and depth of injection to achieve the desired treatment outcome. The duration of the treatment effects also is related to the properties of the filler.4,5
Advancements in injectable fillers also have led to new applications both on and off the face. Many pivotal clinical trials of fillers were performed in isolated anatomic areas, most commonly the nasolabial folds, leading to FDA approval of this indication. Other FDA-approved indications for fillers include lip augmentation (Juvèderm Ultra, Juvèderm Volbella, Restylane, Restylane Silk, Restylane Kysse), human immunodeficiency virus–associated lipoatrophy (Sculptra Aesthetic, Radiesse), volumization of the dorsal hands (Radiesse, Restylane Lyft), acne scarring (Bellafill), and age-related volume loss of the midface (Juvèderm Voluma, Restylane Lyft). Although it is considered off label, treatment of the temples, brows, tear troughs, jawline, horizontal neck lines, and etched-in radial cheek lines has been reported.6-9 It is legal to use fillers to treat these areas, but data have not yet been evaluated by the FDA to officially grant their approval, which likely will change with the conclusion of many ongoing industry-sponsored trials.
Adverse events from filler injections range from the anticipated transient tenderness, swelling, and bruising, which are likely to resolve in a matter of days, to the most severe complications—intravascular occlusion with permanent sequelae, namely tissue necrosis, blindness or visual compromise, and stroke. It is critical to obtain written informed consent prior to proceeding with dermal filler injections. Masterful knowledge of the facial anatomy, in particular the location and depth of key vascular structures, is critical in minimizing these severe AEs. Injection technique, including use of a microcannula, can reduce the risk, in addition to administration of small volumes of filler at a time, aspiration prior to injection, and use of a retrograde injection technique. There also are variations in the predicted courses of vascular structures, as demonstrated in a cadaveric study showing 4 variants of the course of the angular artery.10
Hyaluronic acid fillers are the most commonly used of the available products, and hyaluronidase, which can dissolve the filler, can be utilized to manage emergent and nonemergent AEs.11 Physical examination findings related to impending necrosis include blanching of the skin in the distribution of a key vessel with a mottled or reticulated purple discoloration. Hyaluronidase, on the order of hundreds of units, may be injected into the area of vascular compromise until reperfusion is achieved, in addition to administering aspirin and applying warm compresses to the area.11,12 The most severe AEs are blindness and/or stroke, associated with findings such as immediate vision loss, pain, nausea, vomiting, and neurologic compromise. Although the glabella, nose, nasolabial folds, and forehead are the most common anatomic areas associated with these AEs (in order of frequency), injections in all areas of the face have been associated with blindness.13,14 Retrobulbar and/or peribulbar injection of hyaluronidase for management of vision changes has been reported, but in most cases vision loss associated with dermal filler injections is not reversible.14,15
Nonemergent uses of enzyme reversal of filler placement include correcting undesirable aesthetic outcomes, such as asymmetry, misplaced filler, or even delayed granulomatous reactions. Hyaluronidase dosage should be determined by the amount and type of filler that was delivered to the patient. All HA fillers are not created equally, and evidence from dosing studies indicates that higher cross-linked and more cohesive fillers require higher doses of hyaluronidase.11 For example, Juvèderm Voluma, created as a mixture of low- and high-molecular-weight HA, has a higher cross-linking ratio. Approximately 30 U of hyaluronidase are suggested to dissolve 0.1 cc of Juvèderm Voluma as compared to 10 U of hyaluronidase for 0.1 cc of Juvèderm Ultra and 5 U for 0.1 cc of Restylane.11
Treatment with dermal fillers generally is safe and effective, and as new fillers come to the market, we must identify how they will help further our goal of improving patient outcomes. The effects of coronavirus disease 19 on aesthetic medicine are still unclear, yet this uncertainty should not deflect treating clinicians from overlooking the fundamentals of dermal fillers. In addition to considering the appropriate use of each filler based on its unique characteristics and indications, we must be sure that we are prepared with the tools to manage any and all possible complications.
The popularity of injectable fillers for aesthetic use continues to rise, and cosmetic injectors must select from an increasing range of options to achieve optimal outcomes. In addition to formulating a treatment plan and having an intimate knowledge of the facial anatomy, filler selection is critical along with an appreciation of both approved and off-label indications for these products. Appropriate patient selection and treatment technique can minimize adverse events (AEs) and allow for the best outcomes.
The US Food and Drug Administration (FDA) approved the first injectable hyaluronic acid (HA) filler in 2003, the first addition since the approval of bovine collagen in 1981. To date, there are now 4 groups of approved fillers: (1) HA (Belotero Balance [Merz North America, Inc], Juvèderm products [Allergan], Restylane products [Galderma Laboratories, LP], Resilient HA products [Revance Therapeutics Inc and Teoxane SA]), (2) calcium hydroxylapatite (Radiesse [Merz North America, Inc]), (3) poly-L-lactic acid (Sculptra Aesthetic [Galderma Laboratories, LP]), and (4) polymethylmethacrylate (Bellafill [Suneva Medical, Inc]).1-3 Given the versatility of this wide portfolio of products, which often are used in combination with one another, we have advanced from the early goals of filling isolated lines or wrinkles on the face to the 3-dimensional restructuring of an entire treatment area. The increasing diversity of products, particularly the range of rheologic properties of HA fillers, allows the injector to strategically select the type of filler and depth of injection to achieve the desired treatment outcome. The duration of the treatment effects also is related to the properties of the filler.4,5
Advancements in injectable fillers also have led to new applications both on and off the face. Many pivotal clinical trials of fillers were performed in isolated anatomic areas, most commonly the nasolabial folds, leading to FDA approval of this indication. Other FDA-approved indications for fillers include lip augmentation (Juvèderm Ultra, Juvèderm Volbella, Restylane, Restylane Silk, Restylane Kysse), human immunodeficiency virus–associated lipoatrophy (Sculptra Aesthetic, Radiesse), volumization of the dorsal hands (Radiesse, Restylane Lyft), acne scarring (Bellafill), and age-related volume loss of the midface (Juvèderm Voluma, Restylane Lyft). Although it is considered off label, treatment of the temples, brows, tear troughs, jawline, horizontal neck lines, and etched-in radial cheek lines has been reported.6-9 It is legal to use fillers to treat these areas, but data have not yet been evaluated by the FDA to officially grant their approval, which likely will change with the conclusion of many ongoing industry-sponsored trials.
Adverse events from filler injections range from the anticipated transient tenderness, swelling, and bruising, which are likely to resolve in a matter of days, to the most severe complications—intravascular occlusion with permanent sequelae, namely tissue necrosis, blindness or visual compromise, and stroke. It is critical to obtain written informed consent prior to proceeding with dermal filler injections. Masterful knowledge of the facial anatomy, in particular the location and depth of key vascular structures, is critical in minimizing these severe AEs. Injection technique, including use of a microcannula, can reduce the risk, in addition to administration of small volumes of filler at a time, aspiration prior to injection, and use of a retrograde injection technique. There also are variations in the predicted courses of vascular structures, as demonstrated in a cadaveric study showing 4 variants of the course of the angular artery.10
Hyaluronic acid fillers are the most commonly used of the available products, and hyaluronidase, which can dissolve the filler, can be utilized to manage emergent and nonemergent AEs.11 Physical examination findings related to impending necrosis include blanching of the skin in the distribution of a key vessel with a mottled or reticulated purple discoloration. Hyaluronidase, on the order of hundreds of units, may be injected into the area of vascular compromise until reperfusion is achieved, in addition to administering aspirin and applying warm compresses to the area.11,12 The most severe AEs are blindness and/or stroke, associated with findings such as immediate vision loss, pain, nausea, vomiting, and neurologic compromise. Although the glabella, nose, nasolabial folds, and forehead are the most common anatomic areas associated with these AEs (in order of frequency), injections in all areas of the face have been associated with blindness.13,14 Retrobulbar and/or peribulbar injection of hyaluronidase for management of vision changes has been reported, but in most cases vision loss associated with dermal filler injections is not reversible.14,15
Nonemergent uses of enzyme reversal of filler placement include correcting undesirable aesthetic outcomes, such as asymmetry, misplaced filler, or even delayed granulomatous reactions. Hyaluronidase dosage should be determined by the amount and type of filler that was delivered to the patient. All HA fillers are not created equally, and evidence from dosing studies indicates that higher cross-linked and more cohesive fillers require higher doses of hyaluronidase.11 For example, Juvèderm Voluma, created as a mixture of low- and high-molecular-weight HA, has a higher cross-linking ratio. Approximately 30 U of hyaluronidase are suggested to dissolve 0.1 cc of Juvèderm Voluma as compared to 10 U of hyaluronidase for 0.1 cc of Juvèderm Ultra and 5 U for 0.1 cc of Restylane.11
Treatment with dermal fillers generally is safe and effective, and as new fillers come to the market, we must identify how they will help further our goal of improving patient outcomes. The effects of coronavirus disease 19 on aesthetic medicine are still unclear, yet this uncertainty should not deflect treating clinicians from overlooking the fundamentals of dermal fillers. In addition to considering the appropriate use of each filler based on its unique characteristics and indications, we must be sure that we are prepared with the tools to manage any and all possible complications.
- Jiang B, Ramirez M, Ranjit-Reeves R, et al. Noncollagen dermal fillers: a summary of the clinical trials used for their FDA approval. Dermatol Surg. 2019;45:1585-1596.
- Monheit G, Kaufman-Janette J, Joseph J, et al. Efficacy and safety of two resilient hyaluronic acid fillers in the treatment of moderate-to-severe nasolabial folds [published online March 24, 2020]. Dermatol Surg. doi:10.1097/DSS0000000000002391.
- Kaufman-Janette J, Taylor SC, Cox SE, et al. Efficacy and safety of a new resilient hyaluronic acid dermal filler, in the correction of moderate-to-severe nasolabial folds: a 64-week, prospective, multicenter, controlled, randomized, double-blind and within-subject study. J Cosmet Dermatol. 2019;18:1244-1253.
- Jones D, Murphy D. Volumizing hyaluronic acid filler for midface volume deficit: 2 year results from a pivotal single-blind randomized controlled study. Dermatol Surg. 2013;39:1602-1611.
- Hausauer AK, Jones DH. Long-term correction of iatrogenic lipoatrophy with volumizing hyaluronic acid filler. Dermatol Surg. 2018;44(suppl 1):S60-S62.
- Black J, Jones D. Cohesive polydensified matrix hyaluronic acid for the treatment of etched-in fine facial lines: a 6-month, open-label clinical trial. Dermatol Surg. 2018;44:1002-1011.
- Breithaupt A, Jones D, Braz A, et al. Anatomic basis for safe and effective volumization of the temple. Dermatol Surg. 2015;41:S278-S283.
- Dallara JM, Baspeyras M, Bui P, et al. Calcium hydroxylapatite for jawline rejuvenation: consensus recommendations. J Cosmet Dermatol. 2014;13:3-14.
- Minokadeh A, Black J, Jones D. Effacement of transverse neck lines with VYC-15L and a cohesive polydensified matrix hyaluronic acid. Dermatol Surg. 2019;45:941-948.
- Kim YS, Choi DY, Gil YC, et al. The anatomical origin and course of the angular artery regarding its clinical implications. Dermatol Surg. 2014;40:1070-1076.
- Jones DH. Update on emergency and nonemergency use of hyaluronidase in aesthetic dermatology. JAMA Dermatol. 2018;154:763-764.
- Cohen JL, Biesman BS, Dayan SH, et al. Treatment of hyaluronic acid filler-induced impending necrosis with hyaluronidase: consensus recommendations. Aesthet Surg J. 2015;35:844-849.
- Beleznay K, Carruthers J, Humphrey S, et al. Avoiding and treating blindness from fillers: a review of the world literature. Dermatol Surg. 2015;41:1097-1117.
- Beleznay K, Carruthers J, Humphrey S, et al. Update on avoiding and treating blindness from fillers: a recent review of the world literature. Aesthet Surg J. 2019;39:662-674.
- Chestnut C. Restoration of visual loss with retrobulblar hyaluronidase injection after hyaluronic acid filler. Dermatol Surg. 2018;44:435-437.
- Jiang B, Ramirez M, Ranjit-Reeves R, et al. Noncollagen dermal fillers: a summary of the clinical trials used for their FDA approval. Dermatol Surg. 2019;45:1585-1596.
- Monheit G, Kaufman-Janette J, Joseph J, et al. Efficacy and safety of two resilient hyaluronic acid fillers in the treatment of moderate-to-severe nasolabial folds [published online March 24, 2020]. Dermatol Surg. doi:10.1097/DSS0000000000002391.
- Kaufman-Janette J, Taylor SC, Cox SE, et al. Efficacy and safety of a new resilient hyaluronic acid dermal filler, in the correction of moderate-to-severe nasolabial folds: a 64-week, prospective, multicenter, controlled, randomized, double-blind and within-subject study. J Cosmet Dermatol. 2019;18:1244-1253.
- Jones D, Murphy D. Volumizing hyaluronic acid filler for midface volume deficit: 2 year results from a pivotal single-blind randomized controlled study. Dermatol Surg. 2013;39:1602-1611.
- Hausauer AK, Jones DH. Long-term correction of iatrogenic lipoatrophy with volumizing hyaluronic acid filler. Dermatol Surg. 2018;44(suppl 1):S60-S62.
- Black J, Jones D. Cohesive polydensified matrix hyaluronic acid for the treatment of etched-in fine facial lines: a 6-month, open-label clinical trial. Dermatol Surg. 2018;44:1002-1011.
- Breithaupt A, Jones D, Braz A, et al. Anatomic basis for safe and effective volumization of the temple. Dermatol Surg. 2015;41:S278-S283.
- Dallara JM, Baspeyras M, Bui P, et al. Calcium hydroxylapatite for jawline rejuvenation: consensus recommendations. J Cosmet Dermatol. 2014;13:3-14.
- Minokadeh A, Black J, Jones D. Effacement of transverse neck lines with VYC-15L and a cohesive polydensified matrix hyaluronic acid. Dermatol Surg. 2019;45:941-948.
- Kim YS, Choi DY, Gil YC, et al. The anatomical origin and course of the angular artery regarding its clinical implications. Dermatol Surg. 2014;40:1070-1076.
- Jones DH. Update on emergency and nonemergency use of hyaluronidase in aesthetic dermatology. JAMA Dermatol. 2018;154:763-764.
- Cohen JL, Biesman BS, Dayan SH, et al. Treatment of hyaluronic acid filler-induced impending necrosis with hyaluronidase: consensus recommendations. Aesthet Surg J. 2015;35:844-849.
- Beleznay K, Carruthers J, Humphrey S, et al. Avoiding and treating blindness from fillers: a review of the world literature. Dermatol Surg. 2015;41:1097-1117.
- Beleznay K, Carruthers J, Humphrey S, et al. Update on avoiding and treating blindness from fillers: a recent review of the world literature. Aesthet Surg J. 2019;39:662-674.
- Chestnut C. Restoration of visual loss with retrobulblar hyaluronidase injection after hyaluronic acid filler. Dermatol Surg. 2018;44:435-437.
Developing COVID-19 hospital protocols during the pandemic
As hospitalists and other physicians at the University of Texas at Austin considered how to treat COVID-19 patients in the early weeks of the pandemic, one question they had to consider was: What about convalescent plasma?
All they had to go on were small case series in Ebola, SARS, and MERS and a few small, nonrandomized COVID-19 studies showing a possible benefit and minimal risk, but the evidence was only “toward the middle or bottom” of the evidence pyramid, said Johanna Busch, MD, of the department of internal medicine at Dell Medical Center at the university.
The center’s COVID-19 committee asked a few of its members – infectious disease and internal medicine physicians – to analyze the literature and other factors. In the end, the committee – which meets regularly and also includes pulmonology–critical care experts, nursing experts, and others – recommended using convalescent plasma because of the evidence and the available supply. But in subsequent meetings, as the pandemic surged in the South and the supply dwindled, the committee changed its recommendation for convalescent plasma to more limited use, she said during the virtual annual meeting of the Society of Hospital Medicine.
“It’s all about teamwork,” said W. Michael Brode, MD, of the department of internal medicine at Dell. “The interprofessional team members know their roles and have shared expectations because they have a common understanding of the protocol.” It’s okay to deviate from the protocol, he said, as long as the language exists to communicate these deviations.
“Maybe the approach is more important than the actual content,” he said.
What Dr. Brode and Dr. Busch described was in large part a fine-tuning of communication – being available to communicate in real time and being aware of when certain specialists should be contacted – for instance, to determine at what oxygenation level internal medicine staff should get in touch with the pulmonary–critical care team.
Dr. Brode said that the groundwork is laid for productive meetings, with agendas announced ahead of time and readings assigned and presenters ready with near-finished products at meeting time, “with a clear path for operationalizing it.”
“We don’t want people kind of riffing off the top of their heads,” he said.
Committee members are encouraged to be as specific as possible when giving input into COVID-19 care decisions, he said.
“We’re so used to dealing with uncertainty, but that doesn’t really help when we’re trying to make tough decisions,” Dr. Brode said. They might be asked, “What are you going to write in your consult note template?” or “It’s 1:00 a.m. and your intern’s panicked and calling you – what are you going to tell them to do over the phone?”
The recommendations have to go into writing and are incorporated into the electronic medical record, a process that required some workarounds, he said. He also noted that the committee learned early on that they should assume that no one reads the e-mails – especially after being off for a period of time – so they likely won’t digest updates on an email-by-email basis.
“We quickly learned,” Dr. Brode said, “that this information needs to live on a Web site or [be] linked to the most up-to-date version in a cloud-sharing platform.”
In a question-and-answer discussion, session viewers expressed enthusiasm for the presenters’ one-page summary of protocols – much more, they said, and it could feel overwhelming.
Dr. Busch and Dr. Brode were asked how standardized order sets for COVID patients could be justified without comparison to a control group that didn’t use the standard order set.
Dr. Busch responded that, while there was no controlled trial, the order sets they use have evolved based on experience.
“At the beginning, we were following every inflammatory marker known to mankind, and then we realized as we gained more experience with COVID and COVID patients that some of those markers were not really informing any of our clinical decisions,” she said. “Obviously, as literature comes out we may reevaluate what goes into that standard order set and how frequently we follow labs.”
Dr. Brode said the context – a pandemic – has to be considered.
“In an ideal world, we could show that the intervention is superior through a randomized fashion with a control group, but really our thought process behind it is just, what is the default?” he said. “I looked at the order sets [as] not that they’re going to be dictating care, but it’s really like the guardrails of what’s reasonable. And when you’re in the middle of a surge, what is usually reasonable and easiest is what is going to be done.”
Dr. Busch and Dr. Brode reported no relevant financial relationships.
As hospitalists and other physicians at the University of Texas at Austin considered how to treat COVID-19 patients in the early weeks of the pandemic, one question they had to consider was: What about convalescent plasma?
All they had to go on were small case series in Ebola, SARS, and MERS and a few small, nonrandomized COVID-19 studies showing a possible benefit and minimal risk, but the evidence was only “toward the middle or bottom” of the evidence pyramid, said Johanna Busch, MD, of the department of internal medicine at Dell Medical Center at the university.
The center’s COVID-19 committee asked a few of its members – infectious disease and internal medicine physicians – to analyze the literature and other factors. In the end, the committee – which meets regularly and also includes pulmonology–critical care experts, nursing experts, and others – recommended using convalescent plasma because of the evidence and the available supply. But in subsequent meetings, as the pandemic surged in the South and the supply dwindled, the committee changed its recommendation for convalescent plasma to more limited use, she said during the virtual annual meeting of the Society of Hospital Medicine.
“It’s all about teamwork,” said W. Michael Brode, MD, of the department of internal medicine at Dell. “The interprofessional team members know their roles and have shared expectations because they have a common understanding of the protocol.” It’s okay to deviate from the protocol, he said, as long as the language exists to communicate these deviations.
“Maybe the approach is more important than the actual content,” he said.
What Dr. Brode and Dr. Busch described was in large part a fine-tuning of communication – being available to communicate in real time and being aware of when certain specialists should be contacted – for instance, to determine at what oxygenation level internal medicine staff should get in touch with the pulmonary–critical care team.
Dr. Brode said that the groundwork is laid for productive meetings, with agendas announced ahead of time and readings assigned and presenters ready with near-finished products at meeting time, “with a clear path for operationalizing it.”
“We don’t want people kind of riffing off the top of their heads,” he said.
Committee members are encouraged to be as specific as possible when giving input into COVID-19 care decisions, he said.
“We’re so used to dealing with uncertainty, but that doesn’t really help when we’re trying to make tough decisions,” Dr. Brode said. They might be asked, “What are you going to write in your consult note template?” or “It’s 1:00 a.m. and your intern’s panicked and calling you – what are you going to tell them to do over the phone?”
The recommendations have to go into writing and are incorporated into the electronic medical record, a process that required some workarounds, he said. He also noted that the committee learned early on that they should assume that no one reads the e-mails – especially after being off for a period of time – so they likely won’t digest updates on an email-by-email basis.
“We quickly learned,” Dr. Brode said, “that this information needs to live on a Web site or [be] linked to the most up-to-date version in a cloud-sharing platform.”
In a question-and-answer discussion, session viewers expressed enthusiasm for the presenters’ one-page summary of protocols – much more, they said, and it could feel overwhelming.
Dr. Busch and Dr. Brode were asked how standardized order sets for COVID patients could be justified without comparison to a control group that didn’t use the standard order set.
Dr. Busch responded that, while there was no controlled trial, the order sets they use have evolved based on experience.
“At the beginning, we were following every inflammatory marker known to mankind, and then we realized as we gained more experience with COVID and COVID patients that some of those markers were not really informing any of our clinical decisions,” she said. “Obviously, as literature comes out we may reevaluate what goes into that standard order set and how frequently we follow labs.”
Dr. Brode said the context – a pandemic – has to be considered.
“In an ideal world, we could show that the intervention is superior through a randomized fashion with a control group, but really our thought process behind it is just, what is the default?” he said. “I looked at the order sets [as] not that they’re going to be dictating care, but it’s really like the guardrails of what’s reasonable. And when you’re in the middle of a surge, what is usually reasonable and easiest is what is going to be done.”
Dr. Busch and Dr. Brode reported no relevant financial relationships.
As hospitalists and other physicians at the University of Texas at Austin considered how to treat COVID-19 patients in the early weeks of the pandemic, one question they had to consider was: What about convalescent plasma?
All they had to go on were small case series in Ebola, SARS, and MERS and a few small, nonrandomized COVID-19 studies showing a possible benefit and minimal risk, but the evidence was only “toward the middle or bottom” of the evidence pyramid, said Johanna Busch, MD, of the department of internal medicine at Dell Medical Center at the university.
The center’s COVID-19 committee asked a few of its members – infectious disease and internal medicine physicians – to analyze the literature and other factors. In the end, the committee – which meets regularly and also includes pulmonology–critical care experts, nursing experts, and others – recommended using convalescent plasma because of the evidence and the available supply. But in subsequent meetings, as the pandemic surged in the South and the supply dwindled, the committee changed its recommendation for convalescent plasma to more limited use, she said during the virtual annual meeting of the Society of Hospital Medicine.
“It’s all about teamwork,” said W. Michael Brode, MD, of the department of internal medicine at Dell. “The interprofessional team members know their roles and have shared expectations because they have a common understanding of the protocol.” It’s okay to deviate from the protocol, he said, as long as the language exists to communicate these deviations.
“Maybe the approach is more important than the actual content,” he said.
What Dr. Brode and Dr. Busch described was in large part a fine-tuning of communication – being available to communicate in real time and being aware of when certain specialists should be contacted – for instance, to determine at what oxygenation level internal medicine staff should get in touch with the pulmonary–critical care team.
Dr. Brode said that the groundwork is laid for productive meetings, with agendas announced ahead of time and readings assigned and presenters ready with near-finished products at meeting time, “with a clear path for operationalizing it.”
“We don’t want people kind of riffing off the top of their heads,” he said.
Committee members are encouraged to be as specific as possible when giving input into COVID-19 care decisions, he said.
“We’re so used to dealing with uncertainty, but that doesn’t really help when we’re trying to make tough decisions,” Dr. Brode said. They might be asked, “What are you going to write in your consult note template?” or “It’s 1:00 a.m. and your intern’s panicked and calling you – what are you going to tell them to do over the phone?”
The recommendations have to go into writing and are incorporated into the electronic medical record, a process that required some workarounds, he said. He also noted that the committee learned early on that they should assume that no one reads the e-mails – especially after being off for a period of time – so they likely won’t digest updates on an email-by-email basis.
“We quickly learned,” Dr. Brode said, “that this information needs to live on a Web site or [be] linked to the most up-to-date version in a cloud-sharing platform.”
In a question-and-answer discussion, session viewers expressed enthusiasm for the presenters’ one-page summary of protocols – much more, they said, and it could feel overwhelming.
Dr. Busch and Dr. Brode were asked how standardized order sets for COVID patients could be justified without comparison to a control group that didn’t use the standard order set.
Dr. Busch responded that, while there was no controlled trial, the order sets they use have evolved based on experience.
“At the beginning, we were following every inflammatory marker known to mankind, and then we realized as we gained more experience with COVID and COVID patients that some of those markers were not really informing any of our clinical decisions,” she said. “Obviously, as literature comes out we may reevaluate what goes into that standard order set and how frequently we follow labs.”
Dr. Brode said the context – a pandemic – has to be considered.
“In an ideal world, we could show that the intervention is superior through a randomized fashion with a control group, but really our thought process behind it is just, what is the default?” he said. “I looked at the order sets [as] not that they’re going to be dictating care, but it’s really like the guardrails of what’s reasonable. And when you’re in the middle of a surge, what is usually reasonable and easiest is what is going to be done.”
Dr. Busch and Dr. Brode reported no relevant financial relationships.
FROM HM20 VIRTUAL
Elotuzumab-based therapy may benefit post-transplant response in multiple myeloma
Elotuzumab-based maintenance therapy may improve the posttransplant response for multiple myeloma (MM), according to the results of a small retrospective study at a single institution.
In addition, the therapies appear to be safely administered even to older patients because of the low rate of adverse effects, as indicated in a report published online in Blood Cells, Molecules and Diseases.
The researchers retrospectively evaluated the outcomes of seven MM patients who were started on elotuzumab-based maintenance (elotuzumab/lenalidomide/dexamethasone, elotuzumab/bortezomib/dexamethasone, or elotuzumab/bortezomib/methylprednisolone) following transplant, according to Xin Wang, MD, of the UMass Memorial Medical Center, Worcester, and colleagues.
The median age was 68 years (ranging from 56 years to 81 years) at the time of transplant, and median lines of induction therapy was 2; three patients (42.9%) had high-risk cytogenetics and five (71.4%) had stage II or greater disease at diagnosis.
Promising elotuzumab results
At a median follow-up of 24 months, five patients (71.4%) had improvement in their quality of response. Among all patients, there was a combined complete response (CR) or very good partial response (VGPR) rate increase from 57.1% to 100% (CR = 3, VGPR = 4). VGPR was defined by the researchers as an absence of abnormal immunofixation and soft tissue plasmacytoma without bone marrow biopsy.
All patients were alive without relapse or progression at the time of the final analysis. In terms of adverse effects, grade 3-4 events were observed in three (42.9%) of the patients. None of the patients discontinued the treatment because of intolerance, according to the researchers.
“Our study demonstrates that elotuzumab-based maintenance may deepen response post transplant in MM and can be safely administered even in older patients. Given its unique action and rare side effects, further studies of elotuzumab in the post-transplant setting are warranted,” the researchers concluded.
The study had no outside funding and the researchers reported that they had no disclosures.
SOURCE: Wang X et al. Blood Cells Mol Dis. 2020 Jul 28. doi: 10.1016/j.bcmd.2020.102482.
Elotuzumab-based maintenance therapy may improve the posttransplant response for multiple myeloma (MM), according to the results of a small retrospective study at a single institution.
In addition, the therapies appear to be safely administered even to older patients because of the low rate of adverse effects, as indicated in a report published online in Blood Cells, Molecules and Diseases.
The researchers retrospectively evaluated the outcomes of seven MM patients who were started on elotuzumab-based maintenance (elotuzumab/lenalidomide/dexamethasone, elotuzumab/bortezomib/dexamethasone, or elotuzumab/bortezomib/methylprednisolone) following transplant, according to Xin Wang, MD, of the UMass Memorial Medical Center, Worcester, and colleagues.
The median age was 68 years (ranging from 56 years to 81 years) at the time of transplant, and median lines of induction therapy was 2; three patients (42.9%) had high-risk cytogenetics and five (71.4%) had stage II or greater disease at diagnosis.
Promising elotuzumab results
At a median follow-up of 24 months, five patients (71.4%) had improvement in their quality of response. Among all patients, there was a combined complete response (CR) or very good partial response (VGPR) rate increase from 57.1% to 100% (CR = 3, VGPR = 4). VGPR was defined by the researchers as an absence of abnormal immunofixation and soft tissue plasmacytoma without bone marrow biopsy.
All patients were alive without relapse or progression at the time of the final analysis. In terms of adverse effects, grade 3-4 events were observed in three (42.9%) of the patients. None of the patients discontinued the treatment because of intolerance, according to the researchers.
“Our study demonstrates that elotuzumab-based maintenance may deepen response post transplant in MM and can be safely administered even in older patients. Given its unique action and rare side effects, further studies of elotuzumab in the post-transplant setting are warranted,” the researchers concluded.
The study had no outside funding and the researchers reported that they had no disclosures.
SOURCE: Wang X et al. Blood Cells Mol Dis. 2020 Jul 28. doi: 10.1016/j.bcmd.2020.102482.
Elotuzumab-based maintenance therapy may improve the posttransplant response for multiple myeloma (MM), according to the results of a small retrospective study at a single institution.
In addition, the therapies appear to be safely administered even to older patients because of the low rate of adverse effects, as indicated in a report published online in Blood Cells, Molecules and Diseases.
The researchers retrospectively evaluated the outcomes of seven MM patients who were started on elotuzumab-based maintenance (elotuzumab/lenalidomide/dexamethasone, elotuzumab/bortezomib/dexamethasone, or elotuzumab/bortezomib/methylprednisolone) following transplant, according to Xin Wang, MD, of the UMass Memorial Medical Center, Worcester, and colleagues.
The median age was 68 years (ranging from 56 years to 81 years) at the time of transplant, and median lines of induction therapy was 2; three patients (42.9%) had high-risk cytogenetics and five (71.4%) had stage II or greater disease at diagnosis.
Promising elotuzumab results
At a median follow-up of 24 months, five patients (71.4%) had improvement in their quality of response. Among all patients, there was a combined complete response (CR) or very good partial response (VGPR) rate increase from 57.1% to 100% (CR = 3, VGPR = 4). VGPR was defined by the researchers as an absence of abnormal immunofixation and soft tissue plasmacytoma without bone marrow biopsy.
All patients were alive without relapse or progression at the time of the final analysis. In terms of adverse effects, grade 3-4 events were observed in three (42.9%) of the patients. None of the patients discontinued the treatment because of intolerance, according to the researchers.
“Our study demonstrates that elotuzumab-based maintenance may deepen response post transplant in MM and can be safely administered even in older patients. Given its unique action and rare side effects, further studies of elotuzumab in the post-transplant setting are warranted,” the researchers concluded.
The study had no outside funding and the researchers reported that they had no disclosures.
SOURCE: Wang X et al. Blood Cells Mol Dis. 2020 Jul 28. doi: 10.1016/j.bcmd.2020.102482.
FROM BLOOD CELLS, MOLECULES AND DISEASES
‘Doubling down’ on hydroxychloroquine QT prolongation in COVID-19
A new analysis from Michigan’s largest health system provides sobering verification of the risks for QT interval prolongation in COVID-19 patients treated with hydroxychloroquine and azithromycin (HCQ/AZM).
One in five patients (21%) had a corrected QT (QTc) interval of at least 500 msec, a value that increases the risk for torsade de pointes in the general population and at which cardiovascular leaders have suggested withholding HCQ/AZM in COVID-19 patients.
“One of the most striking findings was when we looked at the other drugs being administered to these patients; 61% were being administered drugs that had QT-prolonging effects concomitantly with the HCQ and AZM therapy. So they were inadvertently doubling down on the QT-prolonging effects of these drugs,” senior author David E. Haines, MD, director of the Heart Rhythm Center at William Beaumont Hospital, Royal Oak, Mich., said in an interview.
A total of 34 medications overlapped with HCQ/AZM therapy are known or suspected to increase the risk for torsade de pointes, a potentially life-threatening ventricular tachycardia. The most common of these were propofol coadministered in 123 patients, ondansetron in 114, dexmedetomidine in 54, haloperidol in 44, amiodarone in 43, and tramadol in 26.
“This speaks to the medical complexity of this patient population, but also suggests inadequate awareness of the QT-prolonging effects of many common medications,” the researchers say.
The study was published Aug. 5 in JACC Clinical Electrophysiology.
Both hydroxychloroquine and azithromycin increase the risk for QTc-interval prolongation by blocking the KCHN2-encoded hERG potassium channel. Several reports have linked the drugs to a triggering of QT prolongation in patients with COVID-19.
For the present study, Dr. Haines and colleagues examined data from 586 consecutive patients admitted with COVID-19 to the Beaumont Hospitals in Royal Oak and Troy, Mich., between March 13 and April 6. A baseline QTc interval was measured with 12-lead ECG prior to treatment initiation with hydroxychloroquine 400 mg twice daily for two doses, then 200 mg twice daily for 4 days, and azithromycin 500 mg once followed by 250 mg daily for 4 days.
Because of limited availability at the time, lead II ECG telemetry monitoring over the 5-day course of HCQ/AZM was recommended only in patients with baseline QTc intervals of at least 440 msec.
Patients without an interpretable baseline ECG or available telemetry/ECG monitoring for at least 1 day were also excluded, leaving 415 patients (mean age, 64 years; 45% female) in the study population. More than half (52%) were Black, 52% had hypertension, 30% had diabetes, and 14% had cancer.
As seen in previous studies, the QTc interval increased progressively and significantly after the administration of HCQ/AZM, from 443 msec to 473 msec.
The average time to maximum QTc was 2.9 days in a subset of 135 patients with QTc measurements prior to starting therapy and on days 1 through 5.
In multivariate analysis, independent predictors of a potentially hazardous QTc interval of at least 500 msec were:
- Age older than 65 years (odds ratio, 3.0; 95% confidence interval, 1.62-5.54).
- History of (OR, 4.65; 95% CI, 2.01-10.74).
- Admission of at least 1.5 mg/dL (OR, 2.22; 95% CI, 1.28-3.84).
- Peak troponin I level above 0.04 mg/mL (OR, 3.89; 95% CI, 2.22-6.83).
- Body mass index below 30 kg/m2 (OR for a BMI of 30 kg/m2 or higher, 0.45; 95% CI, 0.26-0.78).
Concomitant use of drugs with known risk for torsade de pointes was a significant risk factor in univariate analysis (OR, 1.73; P = .036), but fell out in the multivariate model.
No patients experienced high-grade arrhythmias during the study. In all, 112 of the 586 patients died during hospitalization, including 85 (21%) of the 415 study patients.
The change in QTc interval from baseline was greater in patients who died. Despite this, the only independent predictor of mortality was older age. One possible explanation is that the decision to monitor patients with baseline QTc intervals of at least 440 msec may have skewed the study population toward people with moderate or slightly long QTc intervals prior to the initiation of HCQ/AZM, Dr. Haines suggested. Monitoring and treatment duration were short, and clinicians also likely adjusted medications when excess QTc prolongation was observed.
Although it’s been months since data collection was completed in April, and the paper was written in record-breaking time, the study “is still very relevant because the drug is still out there,” observed Dr. Haines. “Even though it may not be used in as widespread a fashion as it had been when we first submitted the paper, it is still being used routinely by many hospitals and many practitioners.”
The use of hydroxychloroquine is “going through the roof” because of COVID-19, commented Dhanunjaya Lakkireddy, MD, medical director for the Kansas City Heart Rhythm Institute, HCA Midwest Health, Overland Park, Kan., who was not involved in the study.
“This study is very relevant, and I’m glad they shared their experience, and it’s pretty consistent with the data presented by other people. The question of whether hydroxychloroquine helps people with COVID is up for debate, but there is more evidence today that it is not as helpful as it was 3 months ago,” said Dr. Lakkireddy, who is also chair of the American College of Cardiology Electrophysiology Council.
He expressed concern for patients who may be taking HCQ with other medications that have QT-prolonging effects, and for the lack of long-term protocols in place for the drug.
In the coming weeks, however, the ACC and rheumatology leaders will be publishing an expert consensus statement that addresses key issues, such as how to best to use HCQ, maintenance HCQ, electrolyte monitoring, the optimal timing of electrocardiography and cardiac magnetic imaging, and symptoms to look for if cardiac involvement is suspected, Dr. Lakkireddy said.
Asked whether HCQ and AZM should be used in COVID-19 patients, Dr. Haines said in an interview that the “QT-prolonging effects are real, the arrhythmogenic potential is real, and the benefit to patients is nil or marginal. So I think that use of these drugs is appropriate and reasonable if it is done in a setting of a controlled trial, and I support that. But the routine use of these drugs probably is not warranted based on the data that we have available.”
Still, hydroxychloroquine continues to be dragged into the spotlight in recent days as an effective treatment for COVID-19, despite discredited research and the U.S. Food and Drug Administration’s June 15 revocation of its emergency-use authorization to allow use of HCQ and chloroquine to treat certain hospitalized COVID-19 patients.
“The unfortunate politicization of this issue has really muddied the waters because the general public doesn’t know what to believe or who to believe. The fact that treatment for a disease as serious as COVID should be modulated by political affiliation is just crazy to me,” said Dr. Haines. “We should be using the best science and taking careful observations, and whatever the recommendations derived from that should be uniformly adopted by everybody, irrespective of your political affiliation.”
Dr. Haines has received honoraria from Biosense Webster, Farapulse, and Sagentia, and is a consultant for Affera, Boston Scientific, Integer, Medtronic, Philips Healthcare, and Zoll. Dr. Lakkireddy has served as a consultant to Abbott, Biosense Webster, Biotronik, Boston Scientific, and Medtronic.
A version of this article originally appeared on Medscape.com.
A new analysis from Michigan’s largest health system provides sobering verification of the risks for QT interval prolongation in COVID-19 patients treated with hydroxychloroquine and azithromycin (HCQ/AZM).
One in five patients (21%) had a corrected QT (QTc) interval of at least 500 msec, a value that increases the risk for torsade de pointes in the general population and at which cardiovascular leaders have suggested withholding HCQ/AZM in COVID-19 patients.
“One of the most striking findings was when we looked at the other drugs being administered to these patients; 61% were being administered drugs that had QT-prolonging effects concomitantly with the HCQ and AZM therapy. So they were inadvertently doubling down on the QT-prolonging effects of these drugs,” senior author David E. Haines, MD, director of the Heart Rhythm Center at William Beaumont Hospital, Royal Oak, Mich., said in an interview.
A total of 34 medications overlapped with HCQ/AZM therapy are known or suspected to increase the risk for torsade de pointes, a potentially life-threatening ventricular tachycardia. The most common of these were propofol coadministered in 123 patients, ondansetron in 114, dexmedetomidine in 54, haloperidol in 44, amiodarone in 43, and tramadol in 26.
“This speaks to the medical complexity of this patient population, but also suggests inadequate awareness of the QT-prolonging effects of many common medications,” the researchers say.
The study was published Aug. 5 in JACC Clinical Electrophysiology.
Both hydroxychloroquine and azithromycin increase the risk for QTc-interval prolongation by blocking the KCHN2-encoded hERG potassium channel. Several reports have linked the drugs to a triggering of QT prolongation in patients with COVID-19.
For the present study, Dr. Haines and colleagues examined data from 586 consecutive patients admitted with COVID-19 to the Beaumont Hospitals in Royal Oak and Troy, Mich., between March 13 and April 6. A baseline QTc interval was measured with 12-lead ECG prior to treatment initiation with hydroxychloroquine 400 mg twice daily for two doses, then 200 mg twice daily for 4 days, and azithromycin 500 mg once followed by 250 mg daily for 4 days.
Because of limited availability at the time, lead II ECG telemetry monitoring over the 5-day course of HCQ/AZM was recommended only in patients with baseline QTc intervals of at least 440 msec.
Patients without an interpretable baseline ECG or available telemetry/ECG monitoring for at least 1 day were also excluded, leaving 415 patients (mean age, 64 years; 45% female) in the study population. More than half (52%) were Black, 52% had hypertension, 30% had diabetes, and 14% had cancer.
As seen in previous studies, the QTc interval increased progressively and significantly after the administration of HCQ/AZM, from 443 msec to 473 msec.
The average time to maximum QTc was 2.9 days in a subset of 135 patients with QTc measurements prior to starting therapy and on days 1 through 5.
In multivariate analysis, independent predictors of a potentially hazardous QTc interval of at least 500 msec were:
- Age older than 65 years (odds ratio, 3.0; 95% confidence interval, 1.62-5.54).
- History of (OR, 4.65; 95% CI, 2.01-10.74).
- Admission of at least 1.5 mg/dL (OR, 2.22; 95% CI, 1.28-3.84).
- Peak troponin I level above 0.04 mg/mL (OR, 3.89; 95% CI, 2.22-6.83).
- Body mass index below 30 kg/m2 (OR for a BMI of 30 kg/m2 or higher, 0.45; 95% CI, 0.26-0.78).
Concomitant use of drugs with known risk for torsade de pointes was a significant risk factor in univariate analysis (OR, 1.73; P = .036), but fell out in the multivariate model.
No patients experienced high-grade arrhythmias during the study. In all, 112 of the 586 patients died during hospitalization, including 85 (21%) of the 415 study patients.
The change in QTc interval from baseline was greater in patients who died. Despite this, the only independent predictor of mortality was older age. One possible explanation is that the decision to monitor patients with baseline QTc intervals of at least 440 msec may have skewed the study population toward people with moderate or slightly long QTc intervals prior to the initiation of HCQ/AZM, Dr. Haines suggested. Monitoring and treatment duration were short, and clinicians also likely adjusted medications when excess QTc prolongation was observed.
Although it’s been months since data collection was completed in April, and the paper was written in record-breaking time, the study “is still very relevant because the drug is still out there,” observed Dr. Haines. “Even though it may not be used in as widespread a fashion as it had been when we first submitted the paper, it is still being used routinely by many hospitals and many practitioners.”
The use of hydroxychloroquine is “going through the roof” because of COVID-19, commented Dhanunjaya Lakkireddy, MD, medical director for the Kansas City Heart Rhythm Institute, HCA Midwest Health, Overland Park, Kan., who was not involved in the study.
“This study is very relevant, and I’m glad they shared their experience, and it’s pretty consistent with the data presented by other people. The question of whether hydroxychloroquine helps people with COVID is up for debate, but there is more evidence today that it is not as helpful as it was 3 months ago,” said Dr. Lakkireddy, who is also chair of the American College of Cardiology Electrophysiology Council.
He expressed concern for patients who may be taking HCQ with other medications that have QT-prolonging effects, and for the lack of long-term protocols in place for the drug.
In the coming weeks, however, the ACC and rheumatology leaders will be publishing an expert consensus statement that addresses key issues, such as how to best to use HCQ, maintenance HCQ, electrolyte monitoring, the optimal timing of electrocardiography and cardiac magnetic imaging, and symptoms to look for if cardiac involvement is suspected, Dr. Lakkireddy said.
Asked whether HCQ and AZM should be used in COVID-19 patients, Dr. Haines said in an interview that the “QT-prolonging effects are real, the arrhythmogenic potential is real, and the benefit to patients is nil or marginal. So I think that use of these drugs is appropriate and reasonable if it is done in a setting of a controlled trial, and I support that. But the routine use of these drugs probably is not warranted based on the data that we have available.”
Still, hydroxychloroquine continues to be dragged into the spotlight in recent days as an effective treatment for COVID-19, despite discredited research and the U.S. Food and Drug Administration’s June 15 revocation of its emergency-use authorization to allow use of HCQ and chloroquine to treat certain hospitalized COVID-19 patients.
“The unfortunate politicization of this issue has really muddied the waters because the general public doesn’t know what to believe or who to believe. The fact that treatment for a disease as serious as COVID should be modulated by political affiliation is just crazy to me,” said Dr. Haines. “We should be using the best science and taking careful observations, and whatever the recommendations derived from that should be uniformly adopted by everybody, irrespective of your political affiliation.”
Dr. Haines has received honoraria from Biosense Webster, Farapulse, and Sagentia, and is a consultant for Affera, Boston Scientific, Integer, Medtronic, Philips Healthcare, and Zoll. Dr. Lakkireddy has served as a consultant to Abbott, Biosense Webster, Biotronik, Boston Scientific, and Medtronic.
A version of this article originally appeared on Medscape.com.
A new analysis from Michigan’s largest health system provides sobering verification of the risks for QT interval prolongation in COVID-19 patients treated with hydroxychloroquine and azithromycin (HCQ/AZM).
One in five patients (21%) had a corrected QT (QTc) interval of at least 500 msec, a value that increases the risk for torsade de pointes in the general population and at which cardiovascular leaders have suggested withholding HCQ/AZM in COVID-19 patients.
“One of the most striking findings was when we looked at the other drugs being administered to these patients; 61% were being administered drugs that had QT-prolonging effects concomitantly with the HCQ and AZM therapy. So they were inadvertently doubling down on the QT-prolonging effects of these drugs,” senior author David E. Haines, MD, director of the Heart Rhythm Center at William Beaumont Hospital, Royal Oak, Mich., said in an interview.
A total of 34 medications overlapped with HCQ/AZM therapy are known or suspected to increase the risk for torsade de pointes, a potentially life-threatening ventricular tachycardia. The most common of these were propofol coadministered in 123 patients, ondansetron in 114, dexmedetomidine in 54, haloperidol in 44, amiodarone in 43, and tramadol in 26.
“This speaks to the medical complexity of this patient population, but also suggests inadequate awareness of the QT-prolonging effects of many common medications,” the researchers say.
The study was published Aug. 5 in JACC Clinical Electrophysiology.
Both hydroxychloroquine and azithromycin increase the risk for QTc-interval prolongation by blocking the KCHN2-encoded hERG potassium channel. Several reports have linked the drugs to a triggering of QT prolongation in patients with COVID-19.
For the present study, Dr. Haines and colleagues examined data from 586 consecutive patients admitted with COVID-19 to the Beaumont Hospitals in Royal Oak and Troy, Mich., between March 13 and April 6. A baseline QTc interval was measured with 12-lead ECG prior to treatment initiation with hydroxychloroquine 400 mg twice daily for two doses, then 200 mg twice daily for 4 days, and azithromycin 500 mg once followed by 250 mg daily for 4 days.
Because of limited availability at the time, lead II ECG telemetry monitoring over the 5-day course of HCQ/AZM was recommended only in patients with baseline QTc intervals of at least 440 msec.
Patients without an interpretable baseline ECG or available telemetry/ECG monitoring for at least 1 day were also excluded, leaving 415 patients (mean age, 64 years; 45% female) in the study population. More than half (52%) were Black, 52% had hypertension, 30% had diabetes, and 14% had cancer.
As seen in previous studies, the QTc interval increased progressively and significantly after the administration of HCQ/AZM, from 443 msec to 473 msec.
The average time to maximum QTc was 2.9 days in a subset of 135 patients with QTc measurements prior to starting therapy and on days 1 through 5.
In multivariate analysis, independent predictors of a potentially hazardous QTc interval of at least 500 msec were:
- Age older than 65 years (odds ratio, 3.0; 95% confidence interval, 1.62-5.54).
- History of (OR, 4.65; 95% CI, 2.01-10.74).
- Admission of at least 1.5 mg/dL (OR, 2.22; 95% CI, 1.28-3.84).
- Peak troponin I level above 0.04 mg/mL (OR, 3.89; 95% CI, 2.22-6.83).
- Body mass index below 30 kg/m2 (OR for a BMI of 30 kg/m2 or higher, 0.45; 95% CI, 0.26-0.78).
Concomitant use of drugs with known risk for torsade de pointes was a significant risk factor in univariate analysis (OR, 1.73; P = .036), but fell out in the multivariate model.
No patients experienced high-grade arrhythmias during the study. In all, 112 of the 586 patients died during hospitalization, including 85 (21%) of the 415 study patients.
The change in QTc interval from baseline was greater in patients who died. Despite this, the only independent predictor of mortality was older age. One possible explanation is that the decision to monitor patients with baseline QTc intervals of at least 440 msec may have skewed the study population toward people with moderate or slightly long QTc intervals prior to the initiation of HCQ/AZM, Dr. Haines suggested. Monitoring and treatment duration were short, and clinicians also likely adjusted medications when excess QTc prolongation was observed.
Although it’s been months since data collection was completed in April, and the paper was written in record-breaking time, the study “is still very relevant because the drug is still out there,” observed Dr. Haines. “Even though it may not be used in as widespread a fashion as it had been when we first submitted the paper, it is still being used routinely by many hospitals and many practitioners.”
The use of hydroxychloroquine is “going through the roof” because of COVID-19, commented Dhanunjaya Lakkireddy, MD, medical director for the Kansas City Heart Rhythm Institute, HCA Midwest Health, Overland Park, Kan., who was not involved in the study.
“This study is very relevant, and I’m glad they shared their experience, and it’s pretty consistent with the data presented by other people. The question of whether hydroxychloroquine helps people with COVID is up for debate, but there is more evidence today that it is not as helpful as it was 3 months ago,” said Dr. Lakkireddy, who is also chair of the American College of Cardiology Electrophysiology Council.
He expressed concern for patients who may be taking HCQ with other medications that have QT-prolonging effects, and for the lack of long-term protocols in place for the drug.
In the coming weeks, however, the ACC and rheumatology leaders will be publishing an expert consensus statement that addresses key issues, such as how to best to use HCQ, maintenance HCQ, electrolyte monitoring, the optimal timing of electrocardiography and cardiac magnetic imaging, and symptoms to look for if cardiac involvement is suspected, Dr. Lakkireddy said.
Asked whether HCQ and AZM should be used in COVID-19 patients, Dr. Haines said in an interview that the “QT-prolonging effects are real, the arrhythmogenic potential is real, and the benefit to patients is nil or marginal. So I think that use of these drugs is appropriate and reasonable if it is done in a setting of a controlled trial, and I support that. But the routine use of these drugs probably is not warranted based on the data that we have available.”
Still, hydroxychloroquine continues to be dragged into the spotlight in recent days as an effective treatment for COVID-19, despite discredited research and the U.S. Food and Drug Administration’s June 15 revocation of its emergency-use authorization to allow use of HCQ and chloroquine to treat certain hospitalized COVID-19 patients.
“The unfortunate politicization of this issue has really muddied the waters because the general public doesn’t know what to believe or who to believe. The fact that treatment for a disease as serious as COVID should be modulated by political affiliation is just crazy to me,” said Dr. Haines. “We should be using the best science and taking careful observations, and whatever the recommendations derived from that should be uniformly adopted by everybody, irrespective of your political affiliation.”
Dr. Haines has received honoraria from Biosense Webster, Farapulse, and Sagentia, and is a consultant for Affera, Boston Scientific, Integer, Medtronic, Philips Healthcare, and Zoll. Dr. Lakkireddy has served as a consultant to Abbott, Biosense Webster, Biotronik, Boston Scientific, and Medtronic.
A version of this article originally appeared on Medscape.com.
CT-FFR offers a noninvasive ‘one-stop shop’ for pre-TAVR assessment
Fractional flow reserve derived noninvasively from coronary CT angiography is a safe and accurate method for assessing the significance of coronary artery disease in patients with severe aortic stenosis who are headed for transcatheter aortic valve replacement (TAVR), according to results of the CAST-FFR prospective study.
Indeed, utilization of coronary CT angiography–derived fractional flow reserve (CT-FFR) for this purpose offers the advantage of using a single noninvasive imaging method to replace two invasive procedures: coronary angiography to assess the anatomy of coronary lesions, and conventional FFR using a pressure wire to determine the functional significance of a given coronary stenosis as a cause of ischemia, Michael Michail, MBBS, explained in reporting the results at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
“Because up to 50% of patients with severe aortic stenosis undergoing TAVR have coexisting coronary artery disease, it remains common practice to perform prior invasive coronary angiography. However, this is associated with inherent risks, particularly in an elderly cohort with comorbidities. Additionally, coronary angiography provides no information on the functional impact of coronary stenoses, which may be important in guiding revascularization decisions prior to TAVR,” noted Dr. Michail, a cardiologist at Monash University, Melbourne.
Simulating FFR: ‘A one-stop shop cardiac CT’
Dr. Michail presented the results of the prospective CAST-FFR study, the first evaluation of CT-FFR for assessment of coronary arteries in patients with severe symptomatic aortic stenosis. This method uses computational fluid dynamics to transform data obtained noninvasively from a standard coronary CT angiography acquisition into a simulated FFR. And it offers the potential to streamline patient care.
“In current practice we see elderly patients with a long pre-TAVR assessment period, with numerous appointments and invasive procedures. Our vision is a one-stop shop cardiac CT that will provide the cardiologist with a complete assessment of the annular measurements, peripheral vasculature, and the coronary arteries ahead of their procedure,” according to Dr. Michail.
“We believe the ability to perform the requisite coronary assessment using CT-FFR will translate to improved patient care in several ways,” he continued. “Firstly, this will shorten the number of tests and overall diagnostic journey for patients. It will reduce the risk from unnecessary invasive procedures, and this will also reduce discomfort for the patient. Based on emerging evidence on the adverse prognostic impact of functionally significant coronary disease in aortic stenosis, this data has the potential to improve procedural risk stratification. And finally, contingent on further data, this may improve lesion selection for upfront revascularization.”
The CAST-FFR study was a small, single-center, proof-of-concept study in which 42 patients with severe aortic stenosis underwent both coronary CT angiography and conventional FFR with a pressure wire. The CT data was sent to a core laboratory for conversion into CT-FFR by evaluators blinded to the conventional FFR values.
Of the 42 participants, 39 (93%) had usable CT-FFR data on 60 coronary vessels. Dr. Michail and coinvestigators found a strong correlation between the conventional pressure wire FFR and CT-FFR findings, with a receiver operating characteristic area under the curve of 0.83 per vessel. CT-FFR had a diagnostic sensitivity and specificity of 73.9% and 78.4%, respectively, with a positive predictive value of 68%, a negative predictive value of 82.9%, and a diagnostic accuracy of 76.7%.
He cited as study limitations the small size, the fact that patients with previous revascularization or significant left ventricular impairment were excluded, and the study cohort’s relative youth.
“With a mean age of 76.2 years, it’s unclear whether these results can be extrapolated to very elderly patients with more calcified arteries undergoing TAVR. Encouragingly, though, a subgroup analysis based on calcium score showed no effect on accuracy,” according to the cardiologist.
CT-FFR may ‘shorten the diagnostic journey’ for fragile patients
Discussant Daniele Andreini, MD, PhD, praised the investigators’ concept of integrating the functional assessment provided by CT-FFR into a one-stop shop examination by cardiac CT angiography for TAVR planning.
“I would like to underline one of Dr. Michail’s messages: It’s really important to shorten the diagnostic journey for these fragile, older patients with aortic stenosis in order to improve safety, use less contrast, and avoid complications,” said Dr. Andreini, a cardiologist at the University of Milan and director of the cardiovascular CT and radiology unit at Monzino Cardiology Center, also in Milan.
Both Dr. Michail and Dr. Andreini reported having no financial conflicts of interest.
Fractional flow reserve derived noninvasively from coronary CT angiography is a safe and accurate method for assessing the significance of coronary artery disease in patients with severe aortic stenosis who are headed for transcatheter aortic valve replacement (TAVR), according to results of the CAST-FFR prospective study.
Indeed, utilization of coronary CT angiography–derived fractional flow reserve (CT-FFR) for this purpose offers the advantage of using a single noninvasive imaging method to replace two invasive procedures: coronary angiography to assess the anatomy of coronary lesions, and conventional FFR using a pressure wire to determine the functional significance of a given coronary stenosis as a cause of ischemia, Michael Michail, MBBS, explained in reporting the results at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
“Because up to 50% of patients with severe aortic stenosis undergoing TAVR have coexisting coronary artery disease, it remains common practice to perform prior invasive coronary angiography. However, this is associated with inherent risks, particularly in an elderly cohort with comorbidities. Additionally, coronary angiography provides no information on the functional impact of coronary stenoses, which may be important in guiding revascularization decisions prior to TAVR,” noted Dr. Michail, a cardiologist at Monash University, Melbourne.
Simulating FFR: ‘A one-stop shop cardiac CT’
Dr. Michail presented the results of the prospective CAST-FFR study, the first evaluation of CT-FFR for assessment of coronary arteries in patients with severe symptomatic aortic stenosis. This method uses computational fluid dynamics to transform data obtained noninvasively from a standard coronary CT angiography acquisition into a simulated FFR. And it offers the potential to streamline patient care.
“In current practice we see elderly patients with a long pre-TAVR assessment period, with numerous appointments and invasive procedures. Our vision is a one-stop shop cardiac CT that will provide the cardiologist with a complete assessment of the annular measurements, peripheral vasculature, and the coronary arteries ahead of their procedure,” according to Dr. Michail.
“We believe the ability to perform the requisite coronary assessment using CT-FFR will translate to improved patient care in several ways,” he continued. “Firstly, this will shorten the number of tests and overall diagnostic journey for patients. It will reduce the risk from unnecessary invasive procedures, and this will also reduce discomfort for the patient. Based on emerging evidence on the adverse prognostic impact of functionally significant coronary disease in aortic stenosis, this data has the potential to improve procedural risk stratification. And finally, contingent on further data, this may improve lesion selection for upfront revascularization.”
The CAST-FFR study was a small, single-center, proof-of-concept study in which 42 patients with severe aortic stenosis underwent both coronary CT angiography and conventional FFR with a pressure wire. The CT data was sent to a core laboratory for conversion into CT-FFR by evaluators blinded to the conventional FFR values.
Of the 42 participants, 39 (93%) had usable CT-FFR data on 60 coronary vessels. Dr. Michail and coinvestigators found a strong correlation between the conventional pressure wire FFR and CT-FFR findings, with a receiver operating characteristic area under the curve of 0.83 per vessel. CT-FFR had a diagnostic sensitivity and specificity of 73.9% and 78.4%, respectively, with a positive predictive value of 68%, a negative predictive value of 82.9%, and a diagnostic accuracy of 76.7%.
He cited as study limitations the small size, the fact that patients with previous revascularization or significant left ventricular impairment were excluded, and the study cohort’s relative youth.
“With a mean age of 76.2 years, it’s unclear whether these results can be extrapolated to very elderly patients with more calcified arteries undergoing TAVR. Encouragingly, though, a subgroup analysis based on calcium score showed no effect on accuracy,” according to the cardiologist.
CT-FFR may ‘shorten the diagnostic journey’ for fragile patients
Discussant Daniele Andreini, MD, PhD, praised the investigators’ concept of integrating the functional assessment provided by CT-FFR into a one-stop shop examination by cardiac CT angiography for TAVR planning.
“I would like to underline one of Dr. Michail’s messages: It’s really important to shorten the diagnostic journey for these fragile, older patients with aortic stenosis in order to improve safety, use less contrast, and avoid complications,” said Dr. Andreini, a cardiologist at the University of Milan and director of the cardiovascular CT and radiology unit at Monzino Cardiology Center, also in Milan.
Both Dr. Michail and Dr. Andreini reported having no financial conflicts of interest.
Fractional flow reserve derived noninvasively from coronary CT angiography is a safe and accurate method for assessing the significance of coronary artery disease in patients with severe aortic stenosis who are headed for transcatheter aortic valve replacement (TAVR), according to results of the CAST-FFR prospective study.
Indeed, utilization of coronary CT angiography–derived fractional flow reserve (CT-FFR) for this purpose offers the advantage of using a single noninvasive imaging method to replace two invasive procedures: coronary angiography to assess the anatomy of coronary lesions, and conventional FFR using a pressure wire to determine the functional significance of a given coronary stenosis as a cause of ischemia, Michael Michail, MBBS, explained in reporting the results at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
“Because up to 50% of patients with severe aortic stenosis undergoing TAVR have coexisting coronary artery disease, it remains common practice to perform prior invasive coronary angiography. However, this is associated with inherent risks, particularly in an elderly cohort with comorbidities. Additionally, coronary angiography provides no information on the functional impact of coronary stenoses, which may be important in guiding revascularization decisions prior to TAVR,” noted Dr. Michail, a cardiologist at Monash University, Melbourne.
Simulating FFR: ‘A one-stop shop cardiac CT’
Dr. Michail presented the results of the prospective CAST-FFR study, the first evaluation of CT-FFR for assessment of coronary arteries in patients with severe symptomatic aortic stenosis. This method uses computational fluid dynamics to transform data obtained noninvasively from a standard coronary CT angiography acquisition into a simulated FFR. And it offers the potential to streamline patient care.
“In current practice we see elderly patients with a long pre-TAVR assessment period, with numerous appointments and invasive procedures. Our vision is a one-stop shop cardiac CT that will provide the cardiologist with a complete assessment of the annular measurements, peripheral vasculature, and the coronary arteries ahead of their procedure,” according to Dr. Michail.
“We believe the ability to perform the requisite coronary assessment using CT-FFR will translate to improved patient care in several ways,” he continued. “Firstly, this will shorten the number of tests and overall diagnostic journey for patients. It will reduce the risk from unnecessary invasive procedures, and this will also reduce discomfort for the patient. Based on emerging evidence on the adverse prognostic impact of functionally significant coronary disease in aortic stenosis, this data has the potential to improve procedural risk stratification. And finally, contingent on further data, this may improve lesion selection for upfront revascularization.”
The CAST-FFR study was a small, single-center, proof-of-concept study in which 42 patients with severe aortic stenosis underwent both coronary CT angiography and conventional FFR with a pressure wire. The CT data was sent to a core laboratory for conversion into CT-FFR by evaluators blinded to the conventional FFR values.
Of the 42 participants, 39 (93%) had usable CT-FFR data on 60 coronary vessels. Dr. Michail and coinvestigators found a strong correlation between the conventional pressure wire FFR and CT-FFR findings, with a receiver operating characteristic area under the curve of 0.83 per vessel. CT-FFR had a diagnostic sensitivity and specificity of 73.9% and 78.4%, respectively, with a positive predictive value of 68%, a negative predictive value of 82.9%, and a diagnostic accuracy of 76.7%.
He cited as study limitations the small size, the fact that patients with previous revascularization or significant left ventricular impairment were excluded, and the study cohort’s relative youth.
“With a mean age of 76.2 years, it’s unclear whether these results can be extrapolated to very elderly patients with more calcified arteries undergoing TAVR. Encouragingly, though, a subgroup analysis based on calcium score showed no effect on accuracy,” according to the cardiologist.
CT-FFR may ‘shorten the diagnostic journey’ for fragile patients
Discussant Daniele Andreini, MD, PhD, praised the investigators’ concept of integrating the functional assessment provided by CT-FFR into a one-stop shop examination by cardiac CT angiography for TAVR planning.
“I would like to underline one of Dr. Michail’s messages: It’s really important to shorten the diagnostic journey for these fragile, older patients with aortic stenosis in order to improve safety, use less contrast, and avoid complications,” said Dr. Andreini, a cardiologist at the University of Milan and director of the cardiovascular CT and radiology unit at Monzino Cardiology Center, also in Milan.
Both Dr. Michail and Dr. Andreini reported having no financial conflicts of interest.
REPORTING FROM EUROPCR 2020
HM20 Virtual product theaters: Aug. 18-20
Aug. 18, 2020. 12:00 p.m. – 1:00 p.m. ET
Selecting A First-Choice Therapy for Systolic HF: Meeting the Burden of Proof
Speaker:
Javed Butler, MD, MPH, MBA
Chairman, Department of Medicine
University of Mississippi Medical Center, Jackson
Program description:
What is the burden of proof that needs to be met before a therapy can be selected for the treatment of systolic heart failure (HF)? Hear from Dr. Javed Butler, chairman of the department of medicine at the University of Mississippi Medical Center, Jackson, to learn more about selecting a first-choice therapy for your patients with systolic heart failure.
In this program, Dr. Butler will discuss how aligning your therapy selection to pathophysiologic pathways for heart failure with reduced ejection fraction (HFrEF), it is possible to reduce mortality and morbidity while providing a proven safety and tolerability profile.
Regardless of your patients’ previous HF treatment history, following this program, you can feel confident selecting your first-choice therapy for your patients with HFrEF.
Sponsored by Novartis Pharmaceuticals Corporation, and the faculty will be compensated for his or her time.
Aug. 19, 2020. 12:00 p.m.– 1:00 p.m. ET
COVID-19 and Beyond: Integrating Mobile Messaging and Patient Records for Inpatient Care Team Collaboration
Speaker:
Christopher Maiona, MD
Chief Medical Officer
PatientKeeper
Program description:
In this stressful and unpredictable time for hospitalists (and all clinicians), focusing hospital investments where they have the most immediate impact on patient care is more vital than ever. Of all the technology capabilities a hospital might consider implementing today, none would be more valuable to hospitalists than MOBILITY ... because instant access to patient records and care team colleagues – anytime, anywhere, from their smartphones and tablets – will provide a direct and immediate benefit to providers and patients.
In this HM20 Virtual Product Theater, you’ll discover that adding mobility and instant communications in a manner that intuitively supports hospitalist workflow is not only possible, it’s a relatively easy lift. We will introduce the PatientKeeper Clinical Communications Suite and demonstrate how it lets providers:
- Immediately access patient records via native iOS and Android apps on smartphones and tablets
- Securely instant message care team members, consultants, practice administrators, and any other necessary hospital staff, with embedded patient context
- Share quick notes about patients with other providers using a simple “scratch pad” to capture the most salient points -- ideal for handing off to coverage and/or in a high-volume, high-throughput crisis care/triage environment
- Treat more patients, more expeditiously
Sponsored by PatientKeeper
Aug. 20, 2020. 12:00 p.m. – 1:00 p.m. ET
The PRODIGY Study and the PRODIGY Risk Prediction Tool: First Step Toward Improving Outcomes and Reducing Costs
Speakers:
Sabry Ayad, MD
Cleveland Clinic
Roop Kaw, MD
Cleveland Clinic
Objectives:
- Describe implementation strategy for continuous respiratory monitoring
- Discuss the challenges associated with predicting respiratory compromise postoperatively
- Recognize patients at risk for respiratory compromise
- Introduce evidence-based guidelines for monitoring patients for OIRD
- Identify methods to operationalize and integrate best risk stratification and monitoring practices into your facility
Sponsored by Medtronic
Aug. 18, 2020. 12:00 p.m. – 1:00 p.m. ET
Selecting A First-Choice Therapy for Systolic HF: Meeting the Burden of Proof
Speaker:
Javed Butler, MD, MPH, MBA
Chairman, Department of Medicine
University of Mississippi Medical Center, Jackson
Program description:
What is the burden of proof that needs to be met before a therapy can be selected for the treatment of systolic heart failure (HF)? Hear from Dr. Javed Butler, chairman of the department of medicine at the University of Mississippi Medical Center, Jackson, to learn more about selecting a first-choice therapy for your patients with systolic heart failure.
In this program, Dr. Butler will discuss how aligning your therapy selection to pathophysiologic pathways for heart failure with reduced ejection fraction (HFrEF), it is possible to reduce mortality and morbidity while providing a proven safety and tolerability profile.
Regardless of your patients’ previous HF treatment history, following this program, you can feel confident selecting your first-choice therapy for your patients with HFrEF.
Sponsored by Novartis Pharmaceuticals Corporation, and the faculty will be compensated for his or her time.
Aug. 19, 2020. 12:00 p.m.– 1:00 p.m. ET
COVID-19 and Beyond: Integrating Mobile Messaging and Patient Records for Inpatient Care Team Collaboration
Speaker:
Christopher Maiona, MD
Chief Medical Officer
PatientKeeper
Program description:
In this stressful and unpredictable time for hospitalists (and all clinicians), focusing hospital investments where they have the most immediate impact on patient care is more vital than ever. Of all the technology capabilities a hospital might consider implementing today, none would be more valuable to hospitalists than MOBILITY ... because instant access to patient records and care team colleagues – anytime, anywhere, from their smartphones and tablets – will provide a direct and immediate benefit to providers and patients.
In this HM20 Virtual Product Theater, you’ll discover that adding mobility and instant communications in a manner that intuitively supports hospitalist workflow is not only possible, it’s a relatively easy lift. We will introduce the PatientKeeper Clinical Communications Suite and demonstrate how it lets providers:
- Immediately access patient records via native iOS and Android apps on smartphones and tablets
- Securely instant message care team members, consultants, practice administrators, and any other necessary hospital staff, with embedded patient context
- Share quick notes about patients with other providers using a simple “scratch pad” to capture the most salient points -- ideal for handing off to coverage and/or in a high-volume, high-throughput crisis care/triage environment
- Treat more patients, more expeditiously
Sponsored by PatientKeeper
Aug. 20, 2020. 12:00 p.m. – 1:00 p.m. ET
The PRODIGY Study and the PRODIGY Risk Prediction Tool: First Step Toward Improving Outcomes and Reducing Costs
Speakers:
Sabry Ayad, MD
Cleveland Clinic
Roop Kaw, MD
Cleveland Clinic
Objectives:
- Describe implementation strategy for continuous respiratory monitoring
- Discuss the challenges associated with predicting respiratory compromise postoperatively
- Recognize patients at risk for respiratory compromise
- Introduce evidence-based guidelines for monitoring patients for OIRD
- Identify methods to operationalize and integrate best risk stratification and monitoring practices into your facility
Sponsored by Medtronic
Aug. 18, 2020. 12:00 p.m. – 1:00 p.m. ET
Selecting A First-Choice Therapy for Systolic HF: Meeting the Burden of Proof
Speaker:
Javed Butler, MD, MPH, MBA
Chairman, Department of Medicine
University of Mississippi Medical Center, Jackson
Program description:
What is the burden of proof that needs to be met before a therapy can be selected for the treatment of systolic heart failure (HF)? Hear from Dr. Javed Butler, chairman of the department of medicine at the University of Mississippi Medical Center, Jackson, to learn more about selecting a first-choice therapy for your patients with systolic heart failure.
In this program, Dr. Butler will discuss how aligning your therapy selection to pathophysiologic pathways for heart failure with reduced ejection fraction (HFrEF), it is possible to reduce mortality and morbidity while providing a proven safety and tolerability profile.
Regardless of your patients’ previous HF treatment history, following this program, you can feel confident selecting your first-choice therapy for your patients with HFrEF.
Sponsored by Novartis Pharmaceuticals Corporation, and the faculty will be compensated for his or her time.
Aug. 19, 2020. 12:00 p.m.– 1:00 p.m. ET
COVID-19 and Beyond: Integrating Mobile Messaging and Patient Records for Inpatient Care Team Collaboration
Speaker:
Christopher Maiona, MD
Chief Medical Officer
PatientKeeper
Program description:
In this stressful and unpredictable time for hospitalists (and all clinicians), focusing hospital investments where they have the most immediate impact on patient care is more vital than ever. Of all the technology capabilities a hospital might consider implementing today, none would be more valuable to hospitalists than MOBILITY ... because instant access to patient records and care team colleagues – anytime, anywhere, from their smartphones and tablets – will provide a direct and immediate benefit to providers and patients.
In this HM20 Virtual Product Theater, you’ll discover that adding mobility and instant communications in a manner that intuitively supports hospitalist workflow is not only possible, it’s a relatively easy lift. We will introduce the PatientKeeper Clinical Communications Suite and demonstrate how it lets providers:
- Immediately access patient records via native iOS and Android apps on smartphones and tablets
- Securely instant message care team members, consultants, practice administrators, and any other necessary hospital staff, with embedded patient context
- Share quick notes about patients with other providers using a simple “scratch pad” to capture the most salient points -- ideal for handing off to coverage and/or in a high-volume, high-throughput crisis care/triage environment
- Treat more patients, more expeditiously
Sponsored by PatientKeeper
Aug. 20, 2020. 12:00 p.m. – 1:00 p.m. ET
The PRODIGY Study and the PRODIGY Risk Prediction Tool: First Step Toward Improving Outcomes and Reducing Costs
Speakers:
Sabry Ayad, MD
Cleveland Clinic
Roop Kaw, MD
Cleveland Clinic
Objectives:
- Describe implementation strategy for continuous respiratory monitoring
- Discuss the challenges associated with predicting respiratory compromise postoperatively
- Recognize patients at risk for respiratory compromise
- Introduce evidence-based guidelines for monitoring patients for OIRD
- Identify methods to operationalize and integrate best risk stratification and monitoring practices into your facility
Sponsored by Medtronic
Stress-induced brain activity linked to chest pain in CAD patients
The brain’s reaction to stress may be an important contributor to chest pain in patients with coronary artery disease (CAD), according to results of a cohort study.
“Although more research is needed, these results may potentially shift the paradigm by which angina is evaluated by refocusing clinical evaluation and management of psychological stress as adjunct to traditional cardiac evaluations,” wrote Kasra Moazzami, MD, MPH, of Emory University in Atlanta, and his coauthors in Circulation: Cardiovascular Imaging.
To determine if an association exists between stress-induced frontal lobe activity and angina, the researchers launched a study of 148 patients with stable CAD. Their mean age was 62, 69% were male, and roughly 36% were Black. Angina symptoms were assessed at baseline and also after 2 years through the Seattle Angina Questionnaire’s angina frequency subscale.
As the patients underwent stress testing that included both speech and arithmetic stressors, they also received eight brain scans via high-resolution positron emission tomography (HR-PET) brain imaging. Two scans occurred during each of the two control and two stress conditions. Subsequent analysis of these images evaluated regional blood flow relative to total brain flow. Each patient also underwent myocardial perfusion imaging (MPI) at rest, under stress conditions, and during conventional stress testing.
At baseline, patients who reported experiencing angina monthly (35) or daily/weekly (19) had higher rates of mental stress–induced ischemia, more common symptoms of depression and anxiety, and more use of antidepressants and nitrates. Patients reporting angina during stress testing with MPI had higher inferior frontal lobe activation (1.43), compared with patients without active chest pain (1.19; P = 0.03). Patients reporting angina during stress testing also had fewer years of education, higher Beck Depression Inventory scores, and higher posttraumatic stress disorder (PTSD) checklist scores.
More angina correlates with more mental stress
At 2-year-follow-up, 28 (24%) of the 112 returning patients reported an increase in angina episodes. Those patients had a higher mean inferior frontal lobe activation with mental stress at baseline, compared with returning patients who reported a decrease in chest pain frequency (1.82 versus 0.92; P = .01).
After adjustment for sociodemographic and lifestyle variables, any doubling in inferior frontal lobe activation led to an increase in angina frequency by 13.7 units at baseline (95% confidence interval, 6.3-21.7; P = .008) and 11.6 units during follow-up (95% CI, 4.1-19.2; P = .01). After relative importance analysis, the most important correlate of angina was found to be inferior frontal lobe activation at 36.5%, followed by Beck Depression Inventory score and PTSD checklist score.
‘It shows that the heart and brain are connected’
“Previous studies have linked mental stress with ischemia using nuclear stress testing. This study is unique in that it looked at brain activity associated with mental stress and was able to correlate that activity with angina,” said cardiologist Nieca Goldberg, MD, of NYU Langone in New York City in an interview. “It shows that the heart and brain are connected.”
The authors acknowledged their study’s limitations, including using standard stress-inducing protocols that did not account for or reflect any real-life stressors. In addition, although their methods are still considered clinically relevant, retrospectively collecting angina symptoms via questionnaire rather than a prospective diary could have led to incomplete responses.
Dr. Goldberg noted that additional research should include a more diverse population – women in particular were underrepresented in this study – while focusing on how interventions for stress can play a role in angina symptoms and brain activity.
That said, she added, “until there are more studies, it is important to consider mental stress in assessing angina symptoms in patients.”
The study was supported by grants from the National Institutes of Health. The authors reported no potential conflicts of interest.
SOURCE: Moazzami K et al. Circ Cardiovasc Imaging. 2020 Aug 10. doi: 10.1161/circimaging.120.010710.
The brain’s reaction to stress may be an important contributor to chest pain in patients with coronary artery disease (CAD), according to results of a cohort study.
“Although more research is needed, these results may potentially shift the paradigm by which angina is evaluated by refocusing clinical evaluation and management of psychological stress as adjunct to traditional cardiac evaluations,” wrote Kasra Moazzami, MD, MPH, of Emory University in Atlanta, and his coauthors in Circulation: Cardiovascular Imaging.
To determine if an association exists between stress-induced frontal lobe activity and angina, the researchers launched a study of 148 patients with stable CAD. Their mean age was 62, 69% were male, and roughly 36% were Black. Angina symptoms were assessed at baseline and also after 2 years through the Seattle Angina Questionnaire’s angina frequency subscale.
As the patients underwent stress testing that included both speech and arithmetic stressors, they also received eight brain scans via high-resolution positron emission tomography (HR-PET) brain imaging. Two scans occurred during each of the two control and two stress conditions. Subsequent analysis of these images evaluated regional blood flow relative to total brain flow. Each patient also underwent myocardial perfusion imaging (MPI) at rest, under stress conditions, and during conventional stress testing.
At baseline, patients who reported experiencing angina monthly (35) or daily/weekly (19) had higher rates of mental stress–induced ischemia, more common symptoms of depression and anxiety, and more use of antidepressants and nitrates. Patients reporting angina during stress testing with MPI had higher inferior frontal lobe activation (1.43), compared with patients without active chest pain (1.19; P = 0.03). Patients reporting angina during stress testing also had fewer years of education, higher Beck Depression Inventory scores, and higher posttraumatic stress disorder (PTSD) checklist scores.
More angina correlates with more mental stress
At 2-year-follow-up, 28 (24%) of the 112 returning patients reported an increase in angina episodes. Those patients had a higher mean inferior frontal lobe activation with mental stress at baseline, compared with returning patients who reported a decrease in chest pain frequency (1.82 versus 0.92; P = .01).
After adjustment for sociodemographic and lifestyle variables, any doubling in inferior frontal lobe activation led to an increase in angina frequency by 13.7 units at baseline (95% confidence interval, 6.3-21.7; P = .008) and 11.6 units during follow-up (95% CI, 4.1-19.2; P = .01). After relative importance analysis, the most important correlate of angina was found to be inferior frontal lobe activation at 36.5%, followed by Beck Depression Inventory score and PTSD checklist score.
‘It shows that the heart and brain are connected’
“Previous studies have linked mental stress with ischemia using nuclear stress testing. This study is unique in that it looked at brain activity associated with mental stress and was able to correlate that activity with angina,” said cardiologist Nieca Goldberg, MD, of NYU Langone in New York City in an interview. “It shows that the heart and brain are connected.”
The authors acknowledged their study’s limitations, including using standard stress-inducing protocols that did not account for or reflect any real-life stressors. In addition, although their methods are still considered clinically relevant, retrospectively collecting angina symptoms via questionnaire rather than a prospective diary could have led to incomplete responses.
Dr. Goldberg noted that additional research should include a more diverse population – women in particular were underrepresented in this study – while focusing on how interventions for stress can play a role in angina symptoms and brain activity.
That said, she added, “until there are more studies, it is important to consider mental stress in assessing angina symptoms in patients.”
The study was supported by grants from the National Institutes of Health. The authors reported no potential conflicts of interest.
SOURCE: Moazzami K et al. Circ Cardiovasc Imaging. 2020 Aug 10. doi: 10.1161/circimaging.120.010710.
The brain’s reaction to stress may be an important contributor to chest pain in patients with coronary artery disease (CAD), according to results of a cohort study.
“Although more research is needed, these results may potentially shift the paradigm by which angina is evaluated by refocusing clinical evaluation and management of psychological stress as adjunct to traditional cardiac evaluations,” wrote Kasra Moazzami, MD, MPH, of Emory University in Atlanta, and his coauthors in Circulation: Cardiovascular Imaging.
To determine if an association exists between stress-induced frontal lobe activity and angina, the researchers launched a study of 148 patients with stable CAD. Their mean age was 62, 69% were male, and roughly 36% were Black. Angina symptoms were assessed at baseline and also after 2 years through the Seattle Angina Questionnaire’s angina frequency subscale.
As the patients underwent stress testing that included both speech and arithmetic stressors, they also received eight brain scans via high-resolution positron emission tomography (HR-PET) brain imaging. Two scans occurred during each of the two control and two stress conditions. Subsequent analysis of these images evaluated regional blood flow relative to total brain flow. Each patient also underwent myocardial perfusion imaging (MPI) at rest, under stress conditions, and during conventional stress testing.
At baseline, patients who reported experiencing angina monthly (35) or daily/weekly (19) had higher rates of mental stress–induced ischemia, more common symptoms of depression and anxiety, and more use of antidepressants and nitrates. Patients reporting angina during stress testing with MPI had higher inferior frontal lobe activation (1.43), compared with patients without active chest pain (1.19; P = 0.03). Patients reporting angina during stress testing also had fewer years of education, higher Beck Depression Inventory scores, and higher posttraumatic stress disorder (PTSD) checklist scores.
More angina correlates with more mental stress
At 2-year-follow-up, 28 (24%) of the 112 returning patients reported an increase in angina episodes. Those patients had a higher mean inferior frontal lobe activation with mental stress at baseline, compared with returning patients who reported a decrease in chest pain frequency (1.82 versus 0.92; P = .01).
After adjustment for sociodemographic and lifestyle variables, any doubling in inferior frontal lobe activation led to an increase in angina frequency by 13.7 units at baseline (95% confidence interval, 6.3-21.7; P = .008) and 11.6 units during follow-up (95% CI, 4.1-19.2; P = .01). After relative importance analysis, the most important correlate of angina was found to be inferior frontal lobe activation at 36.5%, followed by Beck Depression Inventory score and PTSD checklist score.
‘It shows that the heart and brain are connected’
“Previous studies have linked mental stress with ischemia using nuclear stress testing. This study is unique in that it looked at brain activity associated with mental stress and was able to correlate that activity with angina,” said cardiologist Nieca Goldberg, MD, of NYU Langone in New York City in an interview. “It shows that the heart and brain are connected.”
The authors acknowledged their study’s limitations, including using standard stress-inducing protocols that did not account for or reflect any real-life stressors. In addition, although their methods are still considered clinically relevant, retrospectively collecting angina symptoms via questionnaire rather than a prospective diary could have led to incomplete responses.
Dr. Goldberg noted that additional research should include a more diverse population – women in particular were underrepresented in this study – while focusing on how interventions for stress can play a role in angina symptoms and brain activity.
That said, she added, “until there are more studies, it is important to consider mental stress in assessing angina symptoms in patients.”
The study was supported by grants from the National Institutes of Health. The authors reported no potential conflicts of interest.
SOURCE: Moazzami K et al. Circ Cardiovasc Imaging. 2020 Aug 10. doi: 10.1161/circimaging.120.010710.
FROM CIRCULATION: CARDIOVASCULAR IMAGING
Primary care doctors look at payment overhaul after pandemic disruption
For Gabe Charbonneau, MD, a primary care doctor in Stevensville, Mont., the coronavirus pandemic is an existential threat.
Dr. Charbonneau, 43, his 2 partners and 10 staff members are struggling to keep their rural practice alive. Patient volume is slowly returning to pre–COVID-19 levels. But the large Seattle-area company that owns his practice is reassessing its operations as it adjusts to the new reality in health care.
Dr. Charbonneau has been given until September to demonstrate that his practice, Lifespan Family Medicine, is financially viable – or face possible sale or closure.
“We think we’re going to be okay,” said Dr. Charbonneau. “But it’s stressful and pushes us to cut costs and bring in more revenue. If the virus surges in the fall … well, that will significantly add to the challenge.”
Like other businesses around the country, many doctors were forced to close their offices – or at least see only emergency cases – when the pandemic struck. That led to sharp revenue losses, layoffs and pay cuts.
The primary care practice of Kevin Anderson, MD, in Cadillac, Mich., is also scrambling. The practice – like others – shifted in March to seeing many patients via telemedicine but still saw a dramatic drop in patients and revenue. Dr. Anderson, 49, and his five partners are back to about 80% of the volume of patients they had before the pandemic. But to enhance their chances of survival, they plan to overhaul the way the practice gets paid by Medicare.
Jodi Faustlin, CEO of the for-profit Center for Primary Care in Evans, Ga., manages 37 doctors at eight family medicine practices in the state. She’s confident all eight will emerge from the pandemic intact. But that is more likely if the company shifts from getting paid piecemeal for every service to a per-patient, per-month reimbursement.
One of those 37 doctors is Jacqueline Fincher, MD, the president of the American College of Physicians. Dr. Fincher said the pandemic “has laid bare the flaws in primary care” and the “misguided allocation of money and resources” in the U.S. health care system.
“It’s nuts how we get paid,” said Dr. Fincher, whose practice is in Thomson, Ga. “It doesn’t serve patients well, and it doesn’t work for doctors either – ever, let alone in a pandemic.”
The efforts also aim to address long-festering problems: a predicted widespread shortage of primary care doctors in the next decade, a rising level of physician burnout and a long-recognized underinvestment in primary care overall.
No data yet exist on how many of the nation’s primary care doctors have closed up shop permanently, hastened retirement or planned other moves following the COVID-19 outbreak. An analysis by the American Academy of Family Physicians in late April forecast furloughs, layoffs, and reduced hours that translated to 58,000 fewer primary care doctors and as many as 725,000 fewer nurses and other staff in their offices by July if the pandemic’s impact continued. In 2018, the United States had about 223,000 primary care doctors.
“The majority [of primary care doctors] are hanging in there, so we haven’t yet seen the scope of closures we forecast,” said Jack Westfall, MD, a researcher at the academy. “But the situation is still precarious, with many doctors struggling to make ends meet. We’re also hearing more anecdotal stories about older doctors retiring and others looking to sell their practices.”
Three-quarters of the more than 500 doctors contacted in an online survey by McKinsey said they expected their practices would not make a profit in 2020.
A study in the journal Health Affairs, published in June, put a hard number on that. It estimated that primary care practices would lose an average of $68,000, or 13%, in gross revenues per full-time physician in 2020. That works out to a loss of about $15 billion nationwide.
One main problem, said Dr. Westfall, is that payment for telehealth and virtual visits is still inadequate, and telehealth is not available to everyone.
Reengineering primary care payments
The remedy being most widely promoted is to change the way doctors are reimbursed – away from the predominant system today, under which doctors are paid a fee for every service they provide (commonly called “fee for service”).
Health economists and patient advocates have long advocated such a transition – primarily to eliminate or at least greatly reduce the incentive to provide excessive and unneeded care and promote better management of people with chronic conditions. Stabilizing doctors’ incomes was previously a secondary goal.
Achieving this transition has been slow for many reasons, not the least of which is that some early experiments ended up paying doctors too little to sustain their businesses or improve patient care. Instead, over the past decade doctors have sought safety in larger groups or ownership of their practices by large hospitals and health systems or other entities, including private equity firms.
A 2018 survey of 8,700 doctors by the Physicians Foundation, a nonprofit advocacy and research group found, for example, that only 31% of doctors owned or coowned their practice, down from 48.5% in 2012.
Dr. Fincher predicts the pandemic will propel more primary care doctors to consolidate and be managed collectively. “More and more know they can’t make it on their own.”
A 2018 survey by the American Medical Association found that, on average, 70% of doctor’s office revenue that year came from fee for service, with the rest from per-member, per-month payments and other methods.
The pandemic has renewed the push to get rid of fee for service – in large part because it has underscored that doctors don’t get paid at all when they can’t see patients and bill piecemeal for care.
“Primary care doctors now know how vulnerable they are, in ways they didn’t before,” said Rebecca Etz, a researcher at the Larry A. Green Center, a Richmond, Va., advocacy group for primary care doctors.
Dr. Charbonneau said he’s “absolutely ready” to leave fee for service behind. However, he’s not sure the company that owns his practice, Providence Health System – which operates 1,100 clinics and doctors’ practices in the West – is committed to moving in that direction.
Dr. Anderson is embracing a new payment model being launched next year under Medicare called Primary Care First. He’ll get a fixed monthly payment for each of his Medicare patients and be rewarded with extra revenue if he meets health goals for them and penalized if he doesn’t.
Medicare to launch new payment system
The Trump administration – following in the footsteps of the Obama administration – has been pushing for physician payment reform.
Medicare’s Primary Care First program is a main vehicle in that effort. It will launch in 26 areas in January 2021. Doctors will get a fixed per-patient monthly fee along with flat fees for each patient visit. A performance-based adjustment will allow for bonuses up to 50% when doctors hit certain quality markers, such as blood pressure and blood sugar control and colorectal cancer screening, in a majority of patients.
But doctors also face penalties up to 10% if they don’t meet those and other standards.
Some private insurers are also leveraging the pandemic to enhance payment reform. Blue Cross and Blue Shield of North Carolina, for example, is offering financial incentives starting in September 2020 to primary care practices that commit to a shift away from fee for service. Independent Health, an insurer in New York state, is giving primary care practices per-patient fixed payments during the pandemic to bolster cash flow.
Meanwhile, two of the nation’s largest primary care practice companies continue to pull back from fee for service: Central Ohio Primary Care, with 75 practices serving 450,000 patients, and Oak Street Health, which owns 50 primary care practices in eight states.
“Primary care docs would have been better off during the pandemic if they had been getting fixed payments per month,” said T. Larry Blosser, MD, the medical director for outpatient services for the Central Ohio firm.
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
For Gabe Charbonneau, MD, a primary care doctor in Stevensville, Mont., the coronavirus pandemic is an existential threat.
Dr. Charbonneau, 43, his 2 partners and 10 staff members are struggling to keep their rural practice alive. Patient volume is slowly returning to pre–COVID-19 levels. But the large Seattle-area company that owns his practice is reassessing its operations as it adjusts to the new reality in health care.
Dr. Charbonneau has been given until September to demonstrate that his practice, Lifespan Family Medicine, is financially viable – or face possible sale or closure.
“We think we’re going to be okay,” said Dr. Charbonneau. “But it’s stressful and pushes us to cut costs and bring in more revenue. If the virus surges in the fall … well, that will significantly add to the challenge.”
Like other businesses around the country, many doctors were forced to close their offices – or at least see only emergency cases – when the pandemic struck. That led to sharp revenue losses, layoffs and pay cuts.
The primary care practice of Kevin Anderson, MD, in Cadillac, Mich., is also scrambling. The practice – like others – shifted in March to seeing many patients via telemedicine but still saw a dramatic drop in patients and revenue. Dr. Anderson, 49, and his five partners are back to about 80% of the volume of patients they had before the pandemic. But to enhance their chances of survival, they plan to overhaul the way the practice gets paid by Medicare.
Jodi Faustlin, CEO of the for-profit Center for Primary Care in Evans, Ga., manages 37 doctors at eight family medicine practices in the state. She’s confident all eight will emerge from the pandemic intact. But that is more likely if the company shifts from getting paid piecemeal for every service to a per-patient, per-month reimbursement.
One of those 37 doctors is Jacqueline Fincher, MD, the president of the American College of Physicians. Dr. Fincher said the pandemic “has laid bare the flaws in primary care” and the “misguided allocation of money and resources” in the U.S. health care system.
“It’s nuts how we get paid,” said Dr. Fincher, whose practice is in Thomson, Ga. “It doesn’t serve patients well, and it doesn’t work for doctors either – ever, let alone in a pandemic.”
The efforts also aim to address long-festering problems: a predicted widespread shortage of primary care doctors in the next decade, a rising level of physician burnout and a long-recognized underinvestment in primary care overall.
No data yet exist on how many of the nation’s primary care doctors have closed up shop permanently, hastened retirement or planned other moves following the COVID-19 outbreak. An analysis by the American Academy of Family Physicians in late April forecast furloughs, layoffs, and reduced hours that translated to 58,000 fewer primary care doctors and as many as 725,000 fewer nurses and other staff in their offices by July if the pandemic’s impact continued. In 2018, the United States had about 223,000 primary care doctors.
“The majority [of primary care doctors] are hanging in there, so we haven’t yet seen the scope of closures we forecast,” said Jack Westfall, MD, a researcher at the academy. “But the situation is still precarious, with many doctors struggling to make ends meet. We’re also hearing more anecdotal stories about older doctors retiring and others looking to sell their practices.”
Three-quarters of the more than 500 doctors contacted in an online survey by McKinsey said they expected their practices would not make a profit in 2020.
A study in the journal Health Affairs, published in June, put a hard number on that. It estimated that primary care practices would lose an average of $68,000, or 13%, in gross revenues per full-time physician in 2020. That works out to a loss of about $15 billion nationwide.
One main problem, said Dr. Westfall, is that payment for telehealth and virtual visits is still inadequate, and telehealth is not available to everyone.
Reengineering primary care payments
The remedy being most widely promoted is to change the way doctors are reimbursed – away from the predominant system today, under which doctors are paid a fee for every service they provide (commonly called “fee for service”).
Health economists and patient advocates have long advocated such a transition – primarily to eliminate or at least greatly reduce the incentive to provide excessive and unneeded care and promote better management of people with chronic conditions. Stabilizing doctors’ incomes was previously a secondary goal.
Achieving this transition has been slow for many reasons, not the least of which is that some early experiments ended up paying doctors too little to sustain their businesses or improve patient care. Instead, over the past decade doctors have sought safety in larger groups or ownership of their practices by large hospitals and health systems or other entities, including private equity firms.
A 2018 survey of 8,700 doctors by the Physicians Foundation, a nonprofit advocacy and research group found, for example, that only 31% of doctors owned or coowned their practice, down from 48.5% in 2012.
Dr. Fincher predicts the pandemic will propel more primary care doctors to consolidate and be managed collectively. “More and more know they can’t make it on their own.”
A 2018 survey by the American Medical Association found that, on average, 70% of doctor’s office revenue that year came from fee for service, with the rest from per-member, per-month payments and other methods.
The pandemic has renewed the push to get rid of fee for service – in large part because it has underscored that doctors don’t get paid at all when they can’t see patients and bill piecemeal for care.
“Primary care doctors now know how vulnerable they are, in ways they didn’t before,” said Rebecca Etz, a researcher at the Larry A. Green Center, a Richmond, Va., advocacy group for primary care doctors.
Dr. Charbonneau said he’s “absolutely ready” to leave fee for service behind. However, he’s not sure the company that owns his practice, Providence Health System – which operates 1,100 clinics and doctors’ practices in the West – is committed to moving in that direction.
Dr. Anderson is embracing a new payment model being launched next year under Medicare called Primary Care First. He’ll get a fixed monthly payment for each of his Medicare patients and be rewarded with extra revenue if he meets health goals for them and penalized if he doesn’t.
Medicare to launch new payment system
The Trump administration – following in the footsteps of the Obama administration – has been pushing for physician payment reform.
Medicare’s Primary Care First program is a main vehicle in that effort. It will launch in 26 areas in January 2021. Doctors will get a fixed per-patient monthly fee along with flat fees for each patient visit. A performance-based adjustment will allow for bonuses up to 50% when doctors hit certain quality markers, such as blood pressure and blood sugar control and colorectal cancer screening, in a majority of patients.
But doctors also face penalties up to 10% if they don’t meet those and other standards.
Some private insurers are also leveraging the pandemic to enhance payment reform. Blue Cross and Blue Shield of North Carolina, for example, is offering financial incentives starting in September 2020 to primary care practices that commit to a shift away from fee for service. Independent Health, an insurer in New York state, is giving primary care practices per-patient fixed payments during the pandemic to bolster cash flow.
Meanwhile, two of the nation’s largest primary care practice companies continue to pull back from fee for service: Central Ohio Primary Care, with 75 practices serving 450,000 patients, and Oak Street Health, which owns 50 primary care practices in eight states.
“Primary care docs would have been better off during the pandemic if they had been getting fixed payments per month,” said T. Larry Blosser, MD, the medical director for outpatient services for the Central Ohio firm.
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
For Gabe Charbonneau, MD, a primary care doctor in Stevensville, Mont., the coronavirus pandemic is an existential threat.
Dr. Charbonneau, 43, his 2 partners and 10 staff members are struggling to keep their rural practice alive. Patient volume is slowly returning to pre–COVID-19 levels. But the large Seattle-area company that owns his practice is reassessing its operations as it adjusts to the new reality in health care.
Dr. Charbonneau has been given until September to demonstrate that his practice, Lifespan Family Medicine, is financially viable – or face possible sale or closure.
“We think we’re going to be okay,” said Dr. Charbonneau. “But it’s stressful and pushes us to cut costs and bring in more revenue. If the virus surges in the fall … well, that will significantly add to the challenge.”
Like other businesses around the country, many doctors were forced to close their offices – or at least see only emergency cases – when the pandemic struck. That led to sharp revenue losses, layoffs and pay cuts.
The primary care practice of Kevin Anderson, MD, in Cadillac, Mich., is also scrambling. The practice – like others – shifted in March to seeing many patients via telemedicine but still saw a dramatic drop in patients and revenue. Dr. Anderson, 49, and his five partners are back to about 80% of the volume of patients they had before the pandemic. But to enhance their chances of survival, they plan to overhaul the way the practice gets paid by Medicare.
Jodi Faustlin, CEO of the for-profit Center for Primary Care in Evans, Ga., manages 37 doctors at eight family medicine practices in the state. She’s confident all eight will emerge from the pandemic intact. But that is more likely if the company shifts from getting paid piecemeal for every service to a per-patient, per-month reimbursement.
One of those 37 doctors is Jacqueline Fincher, MD, the president of the American College of Physicians. Dr. Fincher said the pandemic “has laid bare the flaws in primary care” and the “misguided allocation of money and resources” in the U.S. health care system.
“It’s nuts how we get paid,” said Dr. Fincher, whose practice is in Thomson, Ga. “It doesn’t serve patients well, and it doesn’t work for doctors either – ever, let alone in a pandemic.”
The efforts also aim to address long-festering problems: a predicted widespread shortage of primary care doctors in the next decade, a rising level of physician burnout and a long-recognized underinvestment in primary care overall.
No data yet exist on how many of the nation’s primary care doctors have closed up shop permanently, hastened retirement or planned other moves following the COVID-19 outbreak. An analysis by the American Academy of Family Physicians in late April forecast furloughs, layoffs, and reduced hours that translated to 58,000 fewer primary care doctors and as many as 725,000 fewer nurses and other staff in their offices by July if the pandemic’s impact continued. In 2018, the United States had about 223,000 primary care doctors.
“The majority [of primary care doctors] are hanging in there, so we haven’t yet seen the scope of closures we forecast,” said Jack Westfall, MD, a researcher at the academy. “But the situation is still precarious, with many doctors struggling to make ends meet. We’re also hearing more anecdotal stories about older doctors retiring and others looking to sell their practices.”
Three-quarters of the more than 500 doctors contacted in an online survey by McKinsey said they expected their practices would not make a profit in 2020.
A study in the journal Health Affairs, published in June, put a hard number on that. It estimated that primary care practices would lose an average of $68,000, or 13%, in gross revenues per full-time physician in 2020. That works out to a loss of about $15 billion nationwide.
One main problem, said Dr. Westfall, is that payment for telehealth and virtual visits is still inadequate, and telehealth is not available to everyone.
Reengineering primary care payments
The remedy being most widely promoted is to change the way doctors are reimbursed – away from the predominant system today, under which doctors are paid a fee for every service they provide (commonly called “fee for service”).
Health economists and patient advocates have long advocated such a transition – primarily to eliminate or at least greatly reduce the incentive to provide excessive and unneeded care and promote better management of people with chronic conditions. Stabilizing doctors’ incomes was previously a secondary goal.
Achieving this transition has been slow for many reasons, not the least of which is that some early experiments ended up paying doctors too little to sustain their businesses or improve patient care. Instead, over the past decade doctors have sought safety in larger groups or ownership of their practices by large hospitals and health systems or other entities, including private equity firms.
A 2018 survey of 8,700 doctors by the Physicians Foundation, a nonprofit advocacy and research group found, for example, that only 31% of doctors owned or coowned their practice, down from 48.5% in 2012.
Dr. Fincher predicts the pandemic will propel more primary care doctors to consolidate and be managed collectively. “More and more know they can’t make it on their own.”
A 2018 survey by the American Medical Association found that, on average, 70% of doctor’s office revenue that year came from fee for service, with the rest from per-member, per-month payments and other methods.
The pandemic has renewed the push to get rid of fee for service – in large part because it has underscored that doctors don’t get paid at all when they can’t see patients and bill piecemeal for care.
“Primary care doctors now know how vulnerable they are, in ways they didn’t before,” said Rebecca Etz, a researcher at the Larry A. Green Center, a Richmond, Va., advocacy group for primary care doctors.
Dr. Charbonneau said he’s “absolutely ready” to leave fee for service behind. However, he’s not sure the company that owns his practice, Providence Health System – which operates 1,100 clinics and doctors’ practices in the West – is committed to moving in that direction.
Dr. Anderson is embracing a new payment model being launched next year under Medicare called Primary Care First. He’ll get a fixed monthly payment for each of his Medicare patients and be rewarded with extra revenue if he meets health goals for them and penalized if he doesn’t.
Medicare to launch new payment system
The Trump administration – following in the footsteps of the Obama administration – has been pushing for physician payment reform.
Medicare’s Primary Care First program is a main vehicle in that effort. It will launch in 26 areas in January 2021. Doctors will get a fixed per-patient monthly fee along with flat fees for each patient visit. A performance-based adjustment will allow for bonuses up to 50% when doctors hit certain quality markers, such as blood pressure and blood sugar control and colorectal cancer screening, in a majority of patients.
But doctors also face penalties up to 10% if they don’t meet those and other standards.
Some private insurers are also leveraging the pandemic to enhance payment reform. Blue Cross and Blue Shield of North Carolina, for example, is offering financial incentives starting in September 2020 to primary care practices that commit to a shift away from fee for service. Independent Health, an insurer in New York state, is giving primary care practices per-patient fixed payments during the pandemic to bolster cash flow.
Meanwhile, two of the nation’s largest primary care practice companies continue to pull back from fee for service: Central Ohio Primary Care, with 75 practices serving 450,000 patients, and Oak Street Health, which owns 50 primary care practices in eight states.
“Primary care docs would have been better off during the pandemic if they had been getting fixed payments per month,” said T. Larry Blosser, MD, the medical director for outpatient services for the Central Ohio firm.
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.