User login
Low-normal thyroid function tied to advanced fibrosis
Advanced fibrosis affected 5.9% of adults with low-normal thyroid function or subclinical hypothyroidism – more than double the prevalence among adults with strict-normal thyroid function (2.8%; P less than .001), according to the results of a large survey study.
Based on these findings, therapy to improve low thyroid function might help prevent advanced fibrosis secondary to nonalcoholic fatty liver disease, wrote Donghee Kim, MD, PhD, of Stanford University (Calif.), together with his associates in Clinical Gastroenterology and Hepatology.
Prior research has linked low-normal thyroid function with obesity, cardiometabolic diseases, and fractures. For this study, Dr. Kim and his coinvestigators analyzed data from 7,259 adults who lacked major etiologies of chronic liver disease and were included in the National Health and Nutrition Examination Survey between 2007 and 2012.
After accounting for demographic, socioeconomic, and clinical variables, the odds of biopsy-confirmed advanced fibrosis were 100% higher in adults with low-normal thyroid function or subclinical hypothyroidism, compared with adults with strict-normal thyroid function (odds ratio, 2.0; 95% confidence interval, 1.2-3.3). The prevalence and odds of advanced fibrosis was similar in each of these two subgroups. Furthermore, low thyroid function remained strongly linked with advanced fibrosis after accounting for insulin resistance using data from fasting subjects (OR, 2.3; 95% CI, 1.2-4.4).
Previously, Dr. Kim and his coinvestigators found a strong link between biopsy-proven advanced fibrosis and low-normal thyroid function or subclinical hypothyroidism among adults in Korea. “These [new] results are consistent with our previous observations in [an] Asian population, and show their generalizability to the Western world across all ethnicities.”
The researchers did not acknowledge external funding sources. They reported having no conflicts of interest.
SOURCE: Kim D et al. Clin Gastroenterol Hepatol. 2018 Nov 17. doi: 10.1016/j.cgh.2018.11.024.
Advanced fibrosis affected 5.9% of adults with low-normal thyroid function or subclinical hypothyroidism – more than double the prevalence among adults with strict-normal thyroid function (2.8%; P less than .001), according to the results of a large survey study.
Based on these findings, therapy to improve low thyroid function might help prevent advanced fibrosis secondary to nonalcoholic fatty liver disease, wrote Donghee Kim, MD, PhD, of Stanford University (Calif.), together with his associates in Clinical Gastroenterology and Hepatology.
Prior research has linked low-normal thyroid function with obesity, cardiometabolic diseases, and fractures. For this study, Dr. Kim and his coinvestigators analyzed data from 7,259 adults who lacked major etiologies of chronic liver disease and were included in the National Health and Nutrition Examination Survey between 2007 and 2012.
After accounting for demographic, socioeconomic, and clinical variables, the odds of biopsy-confirmed advanced fibrosis were 100% higher in adults with low-normal thyroid function or subclinical hypothyroidism, compared with adults with strict-normal thyroid function (odds ratio, 2.0; 95% confidence interval, 1.2-3.3). The prevalence and odds of advanced fibrosis was similar in each of these two subgroups. Furthermore, low thyroid function remained strongly linked with advanced fibrosis after accounting for insulin resistance using data from fasting subjects (OR, 2.3; 95% CI, 1.2-4.4).
Previously, Dr. Kim and his coinvestigators found a strong link between biopsy-proven advanced fibrosis and low-normal thyroid function or subclinical hypothyroidism among adults in Korea. “These [new] results are consistent with our previous observations in [an] Asian population, and show their generalizability to the Western world across all ethnicities.”
The researchers did not acknowledge external funding sources. They reported having no conflicts of interest.
SOURCE: Kim D et al. Clin Gastroenterol Hepatol. 2018 Nov 17. doi: 10.1016/j.cgh.2018.11.024.
Advanced fibrosis affected 5.9% of adults with low-normal thyroid function or subclinical hypothyroidism – more than double the prevalence among adults with strict-normal thyroid function (2.8%; P less than .001), according to the results of a large survey study.
Based on these findings, therapy to improve low thyroid function might help prevent advanced fibrosis secondary to nonalcoholic fatty liver disease, wrote Donghee Kim, MD, PhD, of Stanford University (Calif.), together with his associates in Clinical Gastroenterology and Hepatology.
Prior research has linked low-normal thyroid function with obesity, cardiometabolic diseases, and fractures. For this study, Dr. Kim and his coinvestigators analyzed data from 7,259 adults who lacked major etiologies of chronic liver disease and were included in the National Health and Nutrition Examination Survey between 2007 and 2012.
After accounting for demographic, socioeconomic, and clinical variables, the odds of biopsy-confirmed advanced fibrosis were 100% higher in adults with low-normal thyroid function or subclinical hypothyroidism, compared with adults with strict-normal thyroid function (odds ratio, 2.0; 95% confidence interval, 1.2-3.3). The prevalence and odds of advanced fibrosis was similar in each of these two subgroups. Furthermore, low thyroid function remained strongly linked with advanced fibrosis after accounting for insulin resistance using data from fasting subjects (OR, 2.3; 95% CI, 1.2-4.4).
Previously, Dr. Kim and his coinvestigators found a strong link between biopsy-proven advanced fibrosis and low-normal thyroid function or subclinical hypothyroidism among adults in Korea. “These [new] results are consistent with our previous observations in [an] Asian population, and show their generalizability to the Western world across all ethnicities.”
The researchers did not acknowledge external funding sources. They reported having no conflicts of interest.
SOURCE: Kim D et al. Clin Gastroenterol Hepatol. 2018 Nov 17. doi: 10.1016/j.cgh.2018.11.024.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Key clinical point: Low-normal thyroid function correlates significantly with advanced fibrosis.
Major finding: In all, 5.9% of adults with low-normal thyroid function had advanced fibrosis, compared with 2.8% of individuals with strict-normal thyroid function (P less than .001).
Study details: A study of 7,259 adults from the National Health and Nutrition Examination Survey (2007-2012).
Disclosures: The investigators did not acknowledge funding sources. They reported having no conflicts of interest.
Source: Kim D et al. Clin Gastroenterol Hepatol. 2018 Nov 17. doi: 10.1016/j.cgh.2018.11.024.
ICYMI: Caplacizumab benefits patients with acquired TTP
and were 1.55 times more likely to achieve platelet normalization, compared with placebo, according to results of the double-blind, controlled HERCULES trial published in the New England Journal of Medicine (2019 Jan 9. doi: 10.1056/NEJMoa1806311).
Patients taking caplacizumab also had a 74% lower incidence of a composite outcome that included TTP-related deaths, recurrence of TTP, or a major thromboembolic event.
We covered this story at the annual meeting of the American Society of Hematology before it was published in the journal. Find our coverage at the link below.
and were 1.55 times more likely to achieve platelet normalization, compared with placebo, according to results of the double-blind, controlled HERCULES trial published in the New England Journal of Medicine (2019 Jan 9. doi: 10.1056/NEJMoa1806311).
Patients taking caplacizumab also had a 74% lower incidence of a composite outcome that included TTP-related deaths, recurrence of TTP, or a major thromboembolic event.
We covered this story at the annual meeting of the American Society of Hematology before it was published in the journal. Find our coverage at the link below.
and were 1.55 times more likely to achieve platelet normalization, compared with placebo, according to results of the double-blind, controlled HERCULES trial published in the New England Journal of Medicine (2019 Jan 9. doi: 10.1056/NEJMoa1806311).
Patients taking caplacizumab also had a 74% lower incidence of a composite outcome that included TTP-related deaths, recurrence of TTP, or a major thromboembolic event.
We covered this story at the annual meeting of the American Society of Hematology before it was published in the journal. Find our coverage at the link below.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Secondhand vaping aerosols linked to childhood asthma exacerbations
Just like exposure to secondhand smoke, , according to a review of the 11,830 kids with asthma in the 2016 Florida Youth Tobacco survey.
Every year, the Florida Department of Health surveys public school children aged 11-17 years about various tobacco issues. In 2016, almost 12% of the asthmatic children in the survey said they vaped. Almost half were exposed to secondhand smoke, and a third reported exposure to secondhand vaping aerosols within the past 30 days. Overall, 21% reported an asthma attack in the past 12 months.
Using data from the Florida survey, the investigators crunched the numbers and found that secondhand aerosol exposure increased the odds of an asthma attack by 27%, independent of exposure to secondhand smoke and whether children smoked or vaped themselves (adjusted odds ratio, 1.27; 95% confidence interval, 1.11-1.47).
“Health professionals may wish to counsel asthmatic youth and their families regarding the potential risks of ENDS [electronic nicotine delivery system] use and exposure to ENDS aerosols.” Providers “may also consider including ENDS aerosol exposure as a possible trigger in asthma self-management/action plans and updating asthma home environment assessments to include exposure to ENDS aerosols,” said investigators led by medical student Jennifer Bayly, a research fellow at the National Institute on Minority Health and Health Disparities in Bethesda, Md.
About 4% of adults in the United States and 11% of high school students vape, and almost 10% of U.S. adolescents reported living with an ENDS user in 2014. Given the data, “it is likely that a substantial number of asthmatic youth are exposed,” the investigators said.
The study adds to a growing body of evidence linking e-cigarettes to asthma. There’s moderate evidence for increased cough and wheezing in adolescents who use e-cigarettes, plus an association with e-cigarette use and increased asthma exacerbations. The new study, however, is likely the first to look specifically at secondhand exposure among asthmatic children. Ingredients in vaping aerosols, including flavorings, propylene glycol, and vegetable glycerin, are physiologically active in the lungs, and may be lung irritants.
Overall, about half of the respondents were female, and two-thirds were 11-13 years old. About a third identified as Hispanic, a third as white, and just over a fifth as black. Three-quarters of the sample lived in large or midsized metropolitan areas, and close to two-thirds in stand-alone homes. Participants were considered exposed to secondhand aerosols if they reported that in the past month they were in a room or car with someone who was vaping.
The work was funded by the National Institutes of Health. The investigators had no disclosures.
SOURCE: Bayly JE et al. CHEST®. 2018 Oct 22. doi: 10.1016/j.chest.2018.10.005.
Just like exposure to secondhand smoke, , according to a review of the 11,830 kids with asthma in the 2016 Florida Youth Tobacco survey.
Every year, the Florida Department of Health surveys public school children aged 11-17 years about various tobacco issues. In 2016, almost 12% of the asthmatic children in the survey said they vaped. Almost half were exposed to secondhand smoke, and a third reported exposure to secondhand vaping aerosols within the past 30 days. Overall, 21% reported an asthma attack in the past 12 months.
Using data from the Florida survey, the investigators crunched the numbers and found that secondhand aerosol exposure increased the odds of an asthma attack by 27%, independent of exposure to secondhand smoke and whether children smoked or vaped themselves (adjusted odds ratio, 1.27; 95% confidence interval, 1.11-1.47).
“Health professionals may wish to counsel asthmatic youth and their families regarding the potential risks of ENDS [electronic nicotine delivery system] use and exposure to ENDS aerosols.” Providers “may also consider including ENDS aerosol exposure as a possible trigger in asthma self-management/action plans and updating asthma home environment assessments to include exposure to ENDS aerosols,” said investigators led by medical student Jennifer Bayly, a research fellow at the National Institute on Minority Health and Health Disparities in Bethesda, Md.
About 4% of adults in the United States and 11% of high school students vape, and almost 10% of U.S. adolescents reported living with an ENDS user in 2014. Given the data, “it is likely that a substantial number of asthmatic youth are exposed,” the investigators said.
The study adds to a growing body of evidence linking e-cigarettes to asthma. There’s moderate evidence for increased cough and wheezing in adolescents who use e-cigarettes, plus an association with e-cigarette use and increased asthma exacerbations. The new study, however, is likely the first to look specifically at secondhand exposure among asthmatic children. Ingredients in vaping aerosols, including flavorings, propylene glycol, and vegetable glycerin, are physiologically active in the lungs, and may be lung irritants.
Overall, about half of the respondents were female, and two-thirds were 11-13 years old. About a third identified as Hispanic, a third as white, and just over a fifth as black. Three-quarters of the sample lived in large or midsized metropolitan areas, and close to two-thirds in stand-alone homes. Participants were considered exposed to secondhand aerosols if they reported that in the past month they were in a room or car with someone who was vaping.
The work was funded by the National Institutes of Health. The investigators had no disclosures.
SOURCE: Bayly JE et al. CHEST®. 2018 Oct 22. doi: 10.1016/j.chest.2018.10.005.
Just like exposure to secondhand smoke, , according to a review of the 11,830 kids with asthma in the 2016 Florida Youth Tobacco survey.
Every year, the Florida Department of Health surveys public school children aged 11-17 years about various tobacco issues. In 2016, almost 12% of the asthmatic children in the survey said they vaped. Almost half were exposed to secondhand smoke, and a third reported exposure to secondhand vaping aerosols within the past 30 days. Overall, 21% reported an asthma attack in the past 12 months.
Using data from the Florida survey, the investigators crunched the numbers and found that secondhand aerosol exposure increased the odds of an asthma attack by 27%, independent of exposure to secondhand smoke and whether children smoked or vaped themselves (adjusted odds ratio, 1.27; 95% confidence interval, 1.11-1.47).
“Health professionals may wish to counsel asthmatic youth and their families regarding the potential risks of ENDS [electronic nicotine delivery system] use and exposure to ENDS aerosols.” Providers “may also consider including ENDS aerosol exposure as a possible trigger in asthma self-management/action plans and updating asthma home environment assessments to include exposure to ENDS aerosols,” said investigators led by medical student Jennifer Bayly, a research fellow at the National Institute on Minority Health and Health Disparities in Bethesda, Md.
About 4% of adults in the United States and 11% of high school students vape, and almost 10% of U.S. adolescents reported living with an ENDS user in 2014. Given the data, “it is likely that a substantial number of asthmatic youth are exposed,” the investigators said.
The study adds to a growing body of evidence linking e-cigarettes to asthma. There’s moderate evidence for increased cough and wheezing in adolescents who use e-cigarettes, plus an association with e-cigarette use and increased asthma exacerbations. The new study, however, is likely the first to look specifically at secondhand exposure among asthmatic children. Ingredients in vaping aerosols, including flavorings, propylene glycol, and vegetable glycerin, are physiologically active in the lungs, and may be lung irritants.
Overall, about half of the respondents were female, and two-thirds were 11-13 years old. About a third identified as Hispanic, a third as white, and just over a fifth as black. Three-quarters of the sample lived in large or midsized metropolitan areas, and close to two-thirds in stand-alone homes. Participants were considered exposed to secondhand aerosols if they reported that in the past month they were in a room or car with someone who was vaping.
The work was funded by the National Institutes of Health. The investigators had no disclosures.
SOURCE: Bayly JE et al. CHEST®. 2018 Oct 22. doi: 10.1016/j.chest.2018.10.005.
FROM CHEST®
Key clinical point: It’s important to screen asthmatic children for exposure to secondhand vaping aerosols, and minimize exposure.
Major finding: Secondhand aerosols increased the odds of an asthma attack 27%, independent of exposure to secondhand smoke and whether children smoked or vaped themselves.
Study details: Analysis of 11,830 children with asthma in the 2016 Florida Youth Tobacco survey.
Disclosures: The work was funded by the National Institutes of Health. The investigators had no disclosures.
Source: Bayly JE et al. CHEST®. 2018 Oct 22. doi: 10.1016/j.chest.2018.10.005.
Health and Economic Burden of Nonalcoholic Fatty Liver Disease in the United States and Its Impact on Veterans
Nonalcoholic fatty liver disease (NAFLD) is the hepatic manifestation of the metabolic syndrome. NAFLD also is an independent risk factor for cardiovascular disease, type 2 diabetes mellitus (T2DM), chronic kidney disease, cirrhosis, liver cancer, and all-cause mortality.1-3 As the leading cause of liver disease in the US and globally, NAFLD is strongly associated with obesity and metabolic syndrome, with the rising prevalence of NAFLD closely mirroring the epidemic of obesity and T2DM.4,5 The unrelenting increase of NAFLD prevalence has led to a significant rise in associated health care and economic burdens, compounded by the boom in childhood obesity and an aging population. In this review, we will discuss the epidemiology and economic burden of NAFLD in the US and how it affects veteran health.
NAFLD Definition
NAFLD is defined as the presence of > 5% of hepatic steatosis in the absence of excessive alcohol use, steatosis-inducing medication, or other concurrent chronic liver diseases.
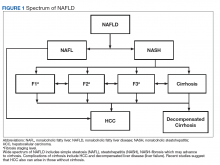
Compared with patients with NAFL, patients with NASH are at a much higher risk of developing fibrosis (scarring of the liver) and cirrhosis (significant scarring with distorted liver architecture). Patients with either NAFL or NASH, with or without advanced fibrosis, also can develop hepatocellular carcinoma (HCC). Severity of liver fibrosis (ie, fibrosis stage) is the most important predictor of liver-associated mortality and all-cause mortality; those with significant fibrosis (≥ F2 stage of fibrosis) are more likely to die of liver disease or to undergo a liver transplant compared with those with earlier stages of disease (ie, stages 0 to F1). Those with advanced scarring or cirrhosis (≥ F3 stage of fibrosis) exhibit an even higher risk of death or liver transplantation.6
NAFLD is a slow and often progressive disease. Time to progression between each stage of fibrosis is about 7 years; however, there has been a documented subset of patients with rapid progression to advanced fibrosis.7 The risk factors associated with this increased risk of fibrosis progression remain poorly understood.
Prevalence
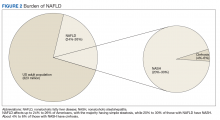
The prevalence of NAFLD in the US is about 24% to 26%—about 85 million Americans. Up to 20% to 30% of these cases (about 17-25 million Americans) are thought to have NASH (Figure 2).
Although liver biopsy remains the current gold standard for diagnosis and histopathologic staging of NAFLD, alternatives to liver biopsy include elastography techniques (ie, transient elastography using Fibroscan[Paris, France], shear wave elastography using Supersonic Image Aixplorer [Weston, FL], and magnetic resonance elastography), magnetic resonance spectroscopy, liver enzymes, and noninvasive simple and complex (serologic) scoring systems such as the Fatty Liver Index. Among these, liver enzymes and serologic scores are most likely to underestimate NAFLD disease burden. Transient elastographyis widely used because the test is easy to perform, noninvasive, and reliably estimates the degree of liver fibrosis in patients with NAFLD by measuring the speed of a mechanically induced shear wave using pulse-echo ultrasonic acquisitions in a much larger portion of the tissue (about 100 times more than a liver biopsy core). Transient elastography also can objectively quantify the amount of liver fat by measuring a 3.5 MHz ultrasound coefficient of attenuation or controlled attenuation parameter (CAP). This correlates with the degree of liver fat, and a higher CAP level reflects a greater degree of steatosis.
The largest study of US veterans utilized abnormal (ie, elevated) liver enzymes as the diagnostic criteria and reviewed nearly 10 million veterans who were followed between 2003 and 2011. Investigators reported a NAFLD prevalence of 13.6% in this population and noted an overall increase in NAFLD prevalence from 6.3% in 2003 to 17.6% in 2011, which highlights the continued growth in NAFLD clinical burden.10 This study, however, is likely to have underestimated the prevalence of NAFLD among veterans because liver enzymes are often normal among those with NAFLD (ie, low sensitivity), and the prevalence of obesity and T2DM are significantly higher in the veteran population vs the general population.
Incidence
There are limited studies on NAFLD incidence. The largest study of US veterans to date used liver enzymes as its diagnostic criteria and reported an annual NAFLD incidence of 2 to 3 per 100 persons (over 9 years from 2003 to 2011).10 There are a few studies from Asia and Europe, and a recent pooled meta-analysis of these studies reported the incidence of NAFLD in Asia to be 52.3 per 1,000 person-years; the incidence in Western countries was 28 per 1,000 person-years.5 These variances may be explained, in part, to disparities in race/background. For example, Hispanics and South Asians (ie, people from Bangladesh, India, or Pakistan) are at higher risk for NAFLD/NASH.11 These findings reinforce the need for further studies to better estimate the true incidence of NAFLD among veterans.
Chronic Liver Disease, Cirrhosis, and Hepatocellular Carcinoma
The prevalence of NASH cirrhosis also has been evaluated using serologic scores, such as aspartate aminotransferase to platelet ratio index (APRI). The National Health and Nutrition Examination Survey (NHANES) database was reviewed, and data for adults in 2 separate periods were analyzed (1999-2002 and 2009-2012) and the prevalence of NASH cirrhosis was noted to have increased 2.5-fold over the period (0.072% vs 0.178%, P < .05).11 Based on data from the HealthCore Integrated Research Database from 2006 to 2014, about 15% of cirrhosis cases were attributed to NAFLD, and about 24% each were attributed to hepatitis C virus (HCV) and alcoholic liver disease.12 A review of about 60,000 veterans with cirrhosis between 2001 and 2013 revealed a prevalence of NAFLD-related cirrhosis of about 15%, while 48% were attributed to HCV.13 In contrast to the continued increase in NAFLD prevalence, the number of patients with HCV-associated liver disease has been in gradual decline since the advent of direct acting antiviral medications in 2011.12
Based on data from the United Network for Organ Sharing (UNOS), the number of patients awaiting liver transplant due to NAFLD nearly tripled from 2004 to 2013, and in 2013 NAFLD became the second leading disease among waitlisted patients for liver transplantation.14 Dynamic Markov modeling predicts that cases of decompensated NASH cirrhosis (ie, liver failure) will rise by 161%, from about 144,000 to 376,000 cases over the next 15 years.8 These projections predict that NAFLD will overtake HCV as the leading cause of chronic liver disease among patients awaiting a liver transplant and will pose a significant clinical and economic burden in the coming years.
Aside from cirrhosis due to NAFLD, NAFLD-related HCC has been on the rise and has overtaken HCV-related HCC. UNOS data from 2003 to 2015 have shown a 2-fold decline in liver transplantation for HCV-associated HCC; however, the same period saw a 10-fold increase in liver transplantation for NAFLD-associated HCC.15,16 This trend in NAFLD-related HCC is expected to grow from 5,000 to 6,000 cases in 2005 to 45,000 cases by 2025.9 More surprisingly, studies from the US veteran population have reported that patients with NAFLD-related HCC are less likely to have cirrhosis compared with patients with HCV- or alcohol-related HCC.17 Among all US veterans who developed HCC in the absence of cirrhosis between 2005 and 2010, NAFLD and metabolic syndrome seemed to be the leading risk factors for development of HCC.18 These trends raise concern for the rise in noncirrhotic HCC in the NAFLD population and highlight the need to improve current screening guidelines for this subset of patients.
Economic Burden
With such a heavy clinical burden and a projected increase in volume over the next decade, NAFLD is expected to have a similarly exponential impact on the economic burden. A review of 976 Medicare beneficiaries with NAFLD who were hospitalized from January 1, 2010 to December 31, 2010, noted a median annual total payment of about $11,000, with significantly lower payment for patients without cirrhosis compared with those with cirrhosis ($10,146 vs $18,804, P < .01).19 Another review of 29,528 Medicare beneficiaries with NAFLD who sought outpatient care between 2005 and 2010 saw a rise in mean yearly charges in 2005 of $2,624 ± 3,308 to $3,608 ± 5,132 in 2010 (P < .05).20
To place these costs in perspective, Allen and colleagues reviewed a large national claims database of individuals enrolled with private and Medicare advantage health plans.21 Comparing patients with NAFLD with a control matched group with similar metabolic comorbidities the study revealed annual median outpatient care costs of $5,363 for the patients with NAFLD with Medicare advantage plans, which was significantly higher than $4,111 for the control group. Projection models based on similar Medicare beneficiaries estimate a rise in annual US economic burden to $103 billion from direct medical care costs alone and another $188 billion in societal costs related to NAFLD.22 New NASH/antifibrotic therapies are being evaluated in clinical trials and are expected to lead to even higher costs. Given the similarities in the trends of NAFLD prevalence between veterans and the general population, it is anticipated that a similar growth and burden in health care utilization cost will affect the VHA.
Association With Other Chronic Medical Conditions
NAFLD is closely associated with metabolic syndrome (Figure 3). Concurrent diagnosis of NAFLD in patients with existing T2DM is associated with poor glycemic control, progressive diabetic retinopathy, diabetic nephropathy, increased risk of cardiovascular complications, and a 2-fold increase in all-cause mortality.1-3
Similar associations have been described between NAFLD and other metabolic conditions such as obesity, hypertension, hypothyroidism, polycystic ovarian syndrome, and chronic kidney disease.31 Identifying patients with NAFLD may help with screening for the above metabolic diseases because patients with NAFLD (by comparison with patients with non-NAFLD) are at higher risk for diabetic, cardiovascular, and pulmonary complications and may warrant a more intensive treatment approach.
Conclusion
A leading cause of chronic liver disease and cirrhosis in the US, NAFLD is independently associated with metabolic syndrome and all-cause mortality. The number of veterans with NAFLD is expected to grow significantly over the coming years given the ongoing epidemic of adult and childhood obesity and T2DM. It is associated with many other medical conditions, including cardiovascular disease and complications, incident metabolic diseases, and may progress to liver cirrhosis and cirrhosis associated complications like HCC and liver failure. The current lack of any approved drug treatment for NASH/fibrosis and the shortage of organs for liver transplant emphasize the need for comprehensive primary prevention measures to reduce the future health and economic costs associated with NAFLD.
There is a growing need to address the epidemic of metabolic syndrome, as heralded by the World Health Organization in its 2013 global action plan. To address this multifaceted disease, initial approach should be to improve NAFLD education among veterans, beginning with the primary care teams and extending to specialty care, including hepatologists. Future steps also should include the development of a comprehensive metabolic/NAFLD clinic in all US Department of Veterans Affairs medical centers that integrates multidisciplinary care, point-of-care evaluation (eg, elastography staging of disease), and access to clinical trials, and have NAFLD care/outcome as a key performance target for all providers.
1. Targher G, Bertolini L, Padovani R, et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;30(5):1212-1218.
2. Targher G, Bertolini L, Rodella S, et al. Non-alcoholic fatty liver disease is independently associated with an increased prevalence of chronic kidney disease and proliferative/laser-treated retinopathy in type 2 diabetic patients. Diabetologia. 2008;51(3):444-450.
3. Adams LA, Harmsen S, St Sauver JL, et al. Nonalcoholic fatty liver disease increases risk of death among patients with diabetes: a community-based cohort study. Am J Gastroenterol. 2010. 105(7):1567-1573.
4. Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10(11):686-690.
5. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73-84.
6. Angulo P, Machado MV, Diehl AM. Fibrosis in nonalcoholic fatty liver disease: mechanisms and clinical implications. Semin Liver Dis. 2015;35(2):132-145.
7. Satapathy SK, Sanyal AJ. Epidemiology and natural history of nonalcoholic fatty liver disease. Semin Liver Dis. 2015;35(3):221-235.
8. Estes C, Anstee QM, Arias-Loste MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J Hepatol. 2018;69(4):896-904.
9. Ahmed O, Liu L, Gayed A, et al. The changing face of hepatocellular carcinoma: forecasting prevalence of nonalcoholic steatohepatitis and hepatitis C cirrhosis. J Clin Exp Hepatol. 2018. In press.
10. Kanwal F, Kramer JR, Duan Z, Yu X, White D, El-Serag HB. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin Gastroenterol Hepatol. 2016;14(2):301-308.
11. Kabbany MN, Conjeevaram Selvakumar PK, Watt K, et al. Prevalence of nonalcoholic steatohepatitis-associated cirrhosis in the United States: an analysis of national health and nutrition examination survey data. Am J Gastroenterol. 2017;112(4):581-587.
12. Goldberg D, Ditah IC, Saeian K, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation. Gastroenterology. 2017;152(5):1090-1099.
13. Beste LA, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001-2013. Gastroenterology. 2015;149(6):1471-1482.
14. Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547-555.
15. Belli LS, Perricone G, Adam R, et al; all the contributing centers (www.eltr.org) and the European Liver and Intestine Transplant Association (ELITA). Impact of DAAs on liver transplantation: major effects on the evolution of indications and results. An ELITA study based on the ELTR registry. J Hepatol. 2018;69(4):810-817.
16. Flemming JA, Kim WR, Brosgart CL, Terrault NA. Reduction in liver transplant wait-listing in the era of direct-acting antiviral therapy. Hepatology. 2017;65(3):804-812.
17. Mittal S, Sada YH, El-Serag HB, et al. Temporal trends of nonalcoholic fatty liver disease-related hepatocellular carcinoma in the Veteran Affairs population. Clin Gastroenterol Hepatol. 2015;13(3):594-601.
18. Mittal S, El-Serag HB, Sada YH, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14(1):124-131.e1.
19. Sayiner M, Otgonsuren M, Cable R. Variables associated with inpatient and outpatient resource utilization among medicare beneficiaries with nonalcoholic fatty liver disease with or without cirrhosis. J Clin Gastroenterol. 2017;51(3):254-260.
20. Younossi ZM, Zheng L, Stepanova M, Henry L, Venkatesan C, Mishra A. Trends in outpatient resource utilizations and outcomes for Medicare beneficiaries with nonalcoholic fatty liver disease. J Clin Gastroenterol. 2015;49(3):222-227.
21. Allen AM, Van Houten HK, Sangaralingham LR, Talwalkar JA, McCoy RG. Healthcare cost and utilization in nonalcoholic fatty liver disease: real-world data from a large US claims database. Hepatology. 2018;68(6):2230-2238.
22. Younossi ZM, Blissett D, Blissett R, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64(5):1577-1586.
23. Armstrong MJ, Hazlehurst JM, Parker R, et al. Severe asymptomatic non-alcoholic fatty liver disease in routine diabetes care; a multi-disciplinary team approach to diagnosis and management. QJM. 2014;107(1):33-41.
24. Ekstedt M, Franzén LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44(4):865-873.
25. Kim D, Choi SY, Park EH, et al. Nonalcoholic fatty liver disease is associated with coronary artery calcification. Hepatology. 2012;56(2):605-613.
26. Stepanova M, Younossi ZM. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin Gastroenterol Hepatol. 2012;10(6):646-650.
27. Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363(14):1341-1350.
28. Mir HM, Stepanova M, Afendy H, Cable R, Younossi ZM. Association of sleep disorders with nonalcoholic fatty liver disease (NAFLD): a population-based study. J Clin Exp Hepatol. 2013;3(3):181-185.
29. Agrawal S, Duseja A, Aggarwal A, et al. Obstructive sleep apnea is an important predictor of hepatic fibrosis in patients with nonalcoholic fatty liver disease in a tertiary care center. Hepatol Int. 2015;9(2):283-291.
30. Sookoian S, Pirola CJ. Obstructive sleep apnea is associated with fatty liver and abnormal liver enzymes: a meta-analysis. Obes Surg. 2013;23(11):1815-1825.
31. Armstrong MJ, Adams LA, Canbay A, Syn WK. Extrahepatic complications of nonalcoholic fatty liver disease. Hepatology. 2014;59(3):1174-1197.
Nonalcoholic fatty liver disease (NAFLD) is the hepatic manifestation of the metabolic syndrome. NAFLD also is an independent risk factor for cardiovascular disease, type 2 diabetes mellitus (T2DM), chronic kidney disease, cirrhosis, liver cancer, and all-cause mortality.1-3 As the leading cause of liver disease in the US and globally, NAFLD is strongly associated with obesity and metabolic syndrome, with the rising prevalence of NAFLD closely mirroring the epidemic of obesity and T2DM.4,5 The unrelenting increase of NAFLD prevalence has led to a significant rise in associated health care and economic burdens, compounded by the boom in childhood obesity and an aging population. In this review, we will discuss the epidemiology and economic burden of NAFLD in the US and how it affects veteran health.
NAFLD Definition
NAFLD is defined as the presence of > 5% of hepatic steatosis in the absence of excessive alcohol use, steatosis-inducing medication, or other concurrent chronic liver diseases.
Compared with patients with NAFL, patients with NASH are at a much higher risk of developing fibrosis (scarring of the liver) and cirrhosis (significant scarring with distorted liver architecture). Patients with either NAFL or NASH, with or without advanced fibrosis, also can develop hepatocellular carcinoma (HCC). Severity of liver fibrosis (ie, fibrosis stage) is the most important predictor of liver-associated mortality and all-cause mortality; those with significant fibrosis (≥ F2 stage of fibrosis) are more likely to die of liver disease or to undergo a liver transplant compared with those with earlier stages of disease (ie, stages 0 to F1). Those with advanced scarring or cirrhosis (≥ F3 stage of fibrosis) exhibit an even higher risk of death or liver transplantation.6
NAFLD is a slow and often progressive disease. Time to progression between each stage of fibrosis is about 7 years; however, there has been a documented subset of patients with rapid progression to advanced fibrosis.7 The risk factors associated with this increased risk of fibrosis progression remain poorly understood.
Prevalence
The prevalence of NAFLD in the US is about 24% to 26%—about 85 million Americans. Up to 20% to 30% of these cases (about 17-25 million Americans) are thought to have NASH (Figure 2).
Although liver biopsy remains the current gold standard for diagnosis and histopathologic staging of NAFLD, alternatives to liver biopsy include elastography techniques (ie, transient elastography using Fibroscan[Paris, France], shear wave elastography using Supersonic Image Aixplorer [Weston, FL], and magnetic resonance elastography), magnetic resonance spectroscopy, liver enzymes, and noninvasive simple and complex (serologic) scoring systems such as the Fatty Liver Index. Among these, liver enzymes and serologic scores are most likely to underestimate NAFLD disease burden. Transient elastographyis widely used because the test is easy to perform, noninvasive, and reliably estimates the degree of liver fibrosis in patients with NAFLD by measuring the speed of a mechanically induced shear wave using pulse-echo ultrasonic acquisitions in a much larger portion of the tissue (about 100 times more than a liver biopsy core). Transient elastography also can objectively quantify the amount of liver fat by measuring a 3.5 MHz ultrasound coefficient of attenuation or controlled attenuation parameter (CAP). This correlates with the degree of liver fat, and a higher CAP level reflects a greater degree of steatosis.
The largest study of US veterans utilized abnormal (ie, elevated) liver enzymes as the diagnostic criteria and reviewed nearly 10 million veterans who were followed between 2003 and 2011. Investigators reported a NAFLD prevalence of 13.6% in this population and noted an overall increase in NAFLD prevalence from 6.3% in 2003 to 17.6% in 2011, which highlights the continued growth in NAFLD clinical burden.10 This study, however, is likely to have underestimated the prevalence of NAFLD among veterans because liver enzymes are often normal among those with NAFLD (ie, low sensitivity), and the prevalence of obesity and T2DM are significantly higher in the veteran population vs the general population.
Incidence
There are limited studies on NAFLD incidence. The largest study of US veterans to date used liver enzymes as its diagnostic criteria and reported an annual NAFLD incidence of 2 to 3 per 100 persons (over 9 years from 2003 to 2011).10 There are a few studies from Asia and Europe, and a recent pooled meta-analysis of these studies reported the incidence of NAFLD in Asia to be 52.3 per 1,000 person-years; the incidence in Western countries was 28 per 1,000 person-years.5 These variances may be explained, in part, to disparities in race/background. For example, Hispanics and South Asians (ie, people from Bangladesh, India, or Pakistan) are at higher risk for NAFLD/NASH.11 These findings reinforce the need for further studies to better estimate the true incidence of NAFLD among veterans.
Chronic Liver Disease, Cirrhosis, and Hepatocellular Carcinoma
The prevalence of NASH cirrhosis also has been evaluated using serologic scores, such as aspartate aminotransferase to platelet ratio index (APRI). The National Health and Nutrition Examination Survey (NHANES) database was reviewed, and data for adults in 2 separate periods were analyzed (1999-2002 and 2009-2012) and the prevalence of NASH cirrhosis was noted to have increased 2.5-fold over the period (0.072% vs 0.178%, P < .05).11 Based on data from the HealthCore Integrated Research Database from 2006 to 2014, about 15% of cirrhosis cases were attributed to NAFLD, and about 24% each were attributed to hepatitis C virus (HCV) and alcoholic liver disease.12 A review of about 60,000 veterans with cirrhosis between 2001 and 2013 revealed a prevalence of NAFLD-related cirrhosis of about 15%, while 48% were attributed to HCV.13 In contrast to the continued increase in NAFLD prevalence, the number of patients with HCV-associated liver disease has been in gradual decline since the advent of direct acting antiviral medications in 2011.12
Based on data from the United Network for Organ Sharing (UNOS), the number of patients awaiting liver transplant due to NAFLD nearly tripled from 2004 to 2013, and in 2013 NAFLD became the second leading disease among waitlisted patients for liver transplantation.14 Dynamic Markov modeling predicts that cases of decompensated NASH cirrhosis (ie, liver failure) will rise by 161%, from about 144,000 to 376,000 cases over the next 15 years.8 These projections predict that NAFLD will overtake HCV as the leading cause of chronic liver disease among patients awaiting a liver transplant and will pose a significant clinical and economic burden in the coming years.
Aside from cirrhosis due to NAFLD, NAFLD-related HCC has been on the rise and has overtaken HCV-related HCC. UNOS data from 2003 to 2015 have shown a 2-fold decline in liver transplantation for HCV-associated HCC; however, the same period saw a 10-fold increase in liver transplantation for NAFLD-associated HCC.15,16 This trend in NAFLD-related HCC is expected to grow from 5,000 to 6,000 cases in 2005 to 45,000 cases by 2025.9 More surprisingly, studies from the US veteran population have reported that patients with NAFLD-related HCC are less likely to have cirrhosis compared with patients with HCV- or alcohol-related HCC.17 Among all US veterans who developed HCC in the absence of cirrhosis between 2005 and 2010, NAFLD and metabolic syndrome seemed to be the leading risk factors for development of HCC.18 These trends raise concern for the rise in noncirrhotic HCC in the NAFLD population and highlight the need to improve current screening guidelines for this subset of patients.
Economic Burden
With such a heavy clinical burden and a projected increase in volume over the next decade, NAFLD is expected to have a similarly exponential impact on the economic burden. A review of 976 Medicare beneficiaries with NAFLD who were hospitalized from January 1, 2010 to December 31, 2010, noted a median annual total payment of about $11,000, with significantly lower payment for patients without cirrhosis compared with those with cirrhosis ($10,146 vs $18,804, P < .01).19 Another review of 29,528 Medicare beneficiaries with NAFLD who sought outpatient care between 2005 and 2010 saw a rise in mean yearly charges in 2005 of $2,624 ± 3,308 to $3,608 ± 5,132 in 2010 (P < .05).20
To place these costs in perspective, Allen and colleagues reviewed a large national claims database of individuals enrolled with private and Medicare advantage health plans.21 Comparing patients with NAFLD with a control matched group with similar metabolic comorbidities the study revealed annual median outpatient care costs of $5,363 for the patients with NAFLD with Medicare advantage plans, which was significantly higher than $4,111 for the control group. Projection models based on similar Medicare beneficiaries estimate a rise in annual US economic burden to $103 billion from direct medical care costs alone and another $188 billion in societal costs related to NAFLD.22 New NASH/antifibrotic therapies are being evaluated in clinical trials and are expected to lead to even higher costs. Given the similarities in the trends of NAFLD prevalence between veterans and the general population, it is anticipated that a similar growth and burden in health care utilization cost will affect the VHA.
Association With Other Chronic Medical Conditions
NAFLD is closely associated with metabolic syndrome (Figure 3). Concurrent diagnosis of NAFLD in patients with existing T2DM is associated with poor glycemic control, progressive diabetic retinopathy, diabetic nephropathy, increased risk of cardiovascular complications, and a 2-fold increase in all-cause mortality.1-3
Similar associations have been described between NAFLD and other metabolic conditions such as obesity, hypertension, hypothyroidism, polycystic ovarian syndrome, and chronic kidney disease.31 Identifying patients with NAFLD may help with screening for the above metabolic diseases because patients with NAFLD (by comparison with patients with non-NAFLD) are at higher risk for diabetic, cardiovascular, and pulmonary complications and may warrant a more intensive treatment approach.
Conclusion
A leading cause of chronic liver disease and cirrhosis in the US, NAFLD is independently associated with metabolic syndrome and all-cause mortality. The number of veterans with NAFLD is expected to grow significantly over the coming years given the ongoing epidemic of adult and childhood obesity and T2DM. It is associated with many other medical conditions, including cardiovascular disease and complications, incident metabolic diseases, and may progress to liver cirrhosis and cirrhosis associated complications like HCC and liver failure. The current lack of any approved drug treatment for NASH/fibrosis and the shortage of organs for liver transplant emphasize the need for comprehensive primary prevention measures to reduce the future health and economic costs associated with NAFLD.
There is a growing need to address the epidemic of metabolic syndrome, as heralded by the World Health Organization in its 2013 global action plan. To address this multifaceted disease, initial approach should be to improve NAFLD education among veterans, beginning with the primary care teams and extending to specialty care, including hepatologists. Future steps also should include the development of a comprehensive metabolic/NAFLD clinic in all US Department of Veterans Affairs medical centers that integrates multidisciplinary care, point-of-care evaluation (eg, elastography staging of disease), and access to clinical trials, and have NAFLD care/outcome as a key performance target for all providers.
Nonalcoholic fatty liver disease (NAFLD) is the hepatic manifestation of the metabolic syndrome. NAFLD also is an independent risk factor for cardiovascular disease, type 2 diabetes mellitus (T2DM), chronic kidney disease, cirrhosis, liver cancer, and all-cause mortality.1-3 As the leading cause of liver disease in the US and globally, NAFLD is strongly associated with obesity and metabolic syndrome, with the rising prevalence of NAFLD closely mirroring the epidemic of obesity and T2DM.4,5 The unrelenting increase of NAFLD prevalence has led to a significant rise in associated health care and economic burdens, compounded by the boom in childhood obesity and an aging population. In this review, we will discuss the epidemiology and economic burden of NAFLD in the US and how it affects veteran health.
NAFLD Definition
NAFLD is defined as the presence of > 5% of hepatic steatosis in the absence of excessive alcohol use, steatosis-inducing medication, or other concurrent chronic liver diseases.
Compared with patients with NAFL, patients with NASH are at a much higher risk of developing fibrosis (scarring of the liver) and cirrhosis (significant scarring with distorted liver architecture). Patients with either NAFL or NASH, with or without advanced fibrosis, also can develop hepatocellular carcinoma (HCC). Severity of liver fibrosis (ie, fibrosis stage) is the most important predictor of liver-associated mortality and all-cause mortality; those with significant fibrosis (≥ F2 stage of fibrosis) are more likely to die of liver disease or to undergo a liver transplant compared with those with earlier stages of disease (ie, stages 0 to F1). Those with advanced scarring or cirrhosis (≥ F3 stage of fibrosis) exhibit an even higher risk of death or liver transplantation.6
NAFLD is a slow and often progressive disease. Time to progression between each stage of fibrosis is about 7 years; however, there has been a documented subset of patients with rapid progression to advanced fibrosis.7 The risk factors associated with this increased risk of fibrosis progression remain poorly understood.
Prevalence
The prevalence of NAFLD in the US is about 24% to 26%—about 85 million Americans. Up to 20% to 30% of these cases (about 17-25 million Americans) are thought to have NASH (Figure 2).
Although liver biopsy remains the current gold standard for diagnosis and histopathologic staging of NAFLD, alternatives to liver biopsy include elastography techniques (ie, transient elastography using Fibroscan[Paris, France], shear wave elastography using Supersonic Image Aixplorer [Weston, FL], and magnetic resonance elastography), magnetic resonance spectroscopy, liver enzymes, and noninvasive simple and complex (serologic) scoring systems such as the Fatty Liver Index. Among these, liver enzymes and serologic scores are most likely to underestimate NAFLD disease burden. Transient elastographyis widely used because the test is easy to perform, noninvasive, and reliably estimates the degree of liver fibrosis in patients with NAFLD by measuring the speed of a mechanically induced shear wave using pulse-echo ultrasonic acquisitions in a much larger portion of the tissue (about 100 times more than a liver biopsy core). Transient elastography also can objectively quantify the amount of liver fat by measuring a 3.5 MHz ultrasound coefficient of attenuation or controlled attenuation parameter (CAP). This correlates with the degree of liver fat, and a higher CAP level reflects a greater degree of steatosis.
The largest study of US veterans utilized abnormal (ie, elevated) liver enzymes as the diagnostic criteria and reviewed nearly 10 million veterans who were followed between 2003 and 2011. Investigators reported a NAFLD prevalence of 13.6% in this population and noted an overall increase in NAFLD prevalence from 6.3% in 2003 to 17.6% in 2011, which highlights the continued growth in NAFLD clinical burden.10 This study, however, is likely to have underestimated the prevalence of NAFLD among veterans because liver enzymes are often normal among those with NAFLD (ie, low sensitivity), and the prevalence of obesity and T2DM are significantly higher in the veteran population vs the general population.
Incidence
There are limited studies on NAFLD incidence. The largest study of US veterans to date used liver enzymes as its diagnostic criteria and reported an annual NAFLD incidence of 2 to 3 per 100 persons (over 9 years from 2003 to 2011).10 There are a few studies from Asia and Europe, and a recent pooled meta-analysis of these studies reported the incidence of NAFLD in Asia to be 52.3 per 1,000 person-years; the incidence in Western countries was 28 per 1,000 person-years.5 These variances may be explained, in part, to disparities in race/background. For example, Hispanics and South Asians (ie, people from Bangladesh, India, or Pakistan) are at higher risk for NAFLD/NASH.11 These findings reinforce the need for further studies to better estimate the true incidence of NAFLD among veterans.
Chronic Liver Disease, Cirrhosis, and Hepatocellular Carcinoma
The prevalence of NASH cirrhosis also has been evaluated using serologic scores, such as aspartate aminotransferase to platelet ratio index (APRI). The National Health and Nutrition Examination Survey (NHANES) database was reviewed, and data for adults in 2 separate periods were analyzed (1999-2002 and 2009-2012) and the prevalence of NASH cirrhosis was noted to have increased 2.5-fold over the period (0.072% vs 0.178%, P < .05).11 Based on data from the HealthCore Integrated Research Database from 2006 to 2014, about 15% of cirrhosis cases were attributed to NAFLD, and about 24% each were attributed to hepatitis C virus (HCV) and alcoholic liver disease.12 A review of about 60,000 veterans with cirrhosis between 2001 and 2013 revealed a prevalence of NAFLD-related cirrhosis of about 15%, while 48% were attributed to HCV.13 In contrast to the continued increase in NAFLD prevalence, the number of patients with HCV-associated liver disease has been in gradual decline since the advent of direct acting antiviral medications in 2011.12
Based on data from the United Network for Organ Sharing (UNOS), the number of patients awaiting liver transplant due to NAFLD nearly tripled from 2004 to 2013, and in 2013 NAFLD became the second leading disease among waitlisted patients for liver transplantation.14 Dynamic Markov modeling predicts that cases of decompensated NASH cirrhosis (ie, liver failure) will rise by 161%, from about 144,000 to 376,000 cases over the next 15 years.8 These projections predict that NAFLD will overtake HCV as the leading cause of chronic liver disease among patients awaiting a liver transplant and will pose a significant clinical and economic burden in the coming years.
Aside from cirrhosis due to NAFLD, NAFLD-related HCC has been on the rise and has overtaken HCV-related HCC. UNOS data from 2003 to 2015 have shown a 2-fold decline in liver transplantation for HCV-associated HCC; however, the same period saw a 10-fold increase in liver transplantation for NAFLD-associated HCC.15,16 This trend in NAFLD-related HCC is expected to grow from 5,000 to 6,000 cases in 2005 to 45,000 cases by 2025.9 More surprisingly, studies from the US veteran population have reported that patients with NAFLD-related HCC are less likely to have cirrhosis compared with patients with HCV- or alcohol-related HCC.17 Among all US veterans who developed HCC in the absence of cirrhosis between 2005 and 2010, NAFLD and metabolic syndrome seemed to be the leading risk factors for development of HCC.18 These trends raise concern for the rise in noncirrhotic HCC in the NAFLD population and highlight the need to improve current screening guidelines for this subset of patients.
Economic Burden
With such a heavy clinical burden and a projected increase in volume over the next decade, NAFLD is expected to have a similarly exponential impact on the economic burden. A review of 976 Medicare beneficiaries with NAFLD who were hospitalized from January 1, 2010 to December 31, 2010, noted a median annual total payment of about $11,000, with significantly lower payment for patients without cirrhosis compared with those with cirrhosis ($10,146 vs $18,804, P < .01).19 Another review of 29,528 Medicare beneficiaries with NAFLD who sought outpatient care between 2005 and 2010 saw a rise in mean yearly charges in 2005 of $2,624 ± 3,308 to $3,608 ± 5,132 in 2010 (P < .05).20
To place these costs in perspective, Allen and colleagues reviewed a large national claims database of individuals enrolled with private and Medicare advantage health plans.21 Comparing patients with NAFLD with a control matched group with similar metabolic comorbidities the study revealed annual median outpatient care costs of $5,363 for the patients with NAFLD with Medicare advantage plans, which was significantly higher than $4,111 for the control group. Projection models based on similar Medicare beneficiaries estimate a rise in annual US economic burden to $103 billion from direct medical care costs alone and another $188 billion in societal costs related to NAFLD.22 New NASH/antifibrotic therapies are being evaluated in clinical trials and are expected to lead to even higher costs. Given the similarities in the trends of NAFLD prevalence between veterans and the general population, it is anticipated that a similar growth and burden in health care utilization cost will affect the VHA.
Association With Other Chronic Medical Conditions
NAFLD is closely associated with metabolic syndrome (Figure 3). Concurrent diagnosis of NAFLD in patients with existing T2DM is associated with poor glycemic control, progressive diabetic retinopathy, diabetic nephropathy, increased risk of cardiovascular complications, and a 2-fold increase in all-cause mortality.1-3
Similar associations have been described between NAFLD and other metabolic conditions such as obesity, hypertension, hypothyroidism, polycystic ovarian syndrome, and chronic kidney disease.31 Identifying patients with NAFLD may help with screening for the above metabolic diseases because patients with NAFLD (by comparison with patients with non-NAFLD) are at higher risk for diabetic, cardiovascular, and pulmonary complications and may warrant a more intensive treatment approach.
Conclusion
A leading cause of chronic liver disease and cirrhosis in the US, NAFLD is independently associated with metabolic syndrome and all-cause mortality. The number of veterans with NAFLD is expected to grow significantly over the coming years given the ongoing epidemic of adult and childhood obesity and T2DM. It is associated with many other medical conditions, including cardiovascular disease and complications, incident metabolic diseases, and may progress to liver cirrhosis and cirrhosis associated complications like HCC and liver failure. The current lack of any approved drug treatment for NASH/fibrosis and the shortage of organs for liver transplant emphasize the need for comprehensive primary prevention measures to reduce the future health and economic costs associated with NAFLD.
There is a growing need to address the epidemic of metabolic syndrome, as heralded by the World Health Organization in its 2013 global action plan. To address this multifaceted disease, initial approach should be to improve NAFLD education among veterans, beginning with the primary care teams and extending to specialty care, including hepatologists. Future steps also should include the development of a comprehensive metabolic/NAFLD clinic in all US Department of Veterans Affairs medical centers that integrates multidisciplinary care, point-of-care evaluation (eg, elastography staging of disease), and access to clinical trials, and have NAFLD care/outcome as a key performance target for all providers.
1. Targher G, Bertolini L, Padovani R, et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;30(5):1212-1218.
2. Targher G, Bertolini L, Rodella S, et al. Non-alcoholic fatty liver disease is independently associated with an increased prevalence of chronic kidney disease and proliferative/laser-treated retinopathy in type 2 diabetic patients. Diabetologia. 2008;51(3):444-450.
3. Adams LA, Harmsen S, St Sauver JL, et al. Nonalcoholic fatty liver disease increases risk of death among patients with diabetes: a community-based cohort study. Am J Gastroenterol. 2010. 105(7):1567-1573.
4. Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10(11):686-690.
5. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73-84.
6. Angulo P, Machado MV, Diehl AM. Fibrosis in nonalcoholic fatty liver disease: mechanisms and clinical implications. Semin Liver Dis. 2015;35(2):132-145.
7. Satapathy SK, Sanyal AJ. Epidemiology and natural history of nonalcoholic fatty liver disease. Semin Liver Dis. 2015;35(3):221-235.
8. Estes C, Anstee QM, Arias-Loste MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J Hepatol. 2018;69(4):896-904.
9. Ahmed O, Liu L, Gayed A, et al. The changing face of hepatocellular carcinoma: forecasting prevalence of nonalcoholic steatohepatitis and hepatitis C cirrhosis. J Clin Exp Hepatol. 2018. In press.
10. Kanwal F, Kramer JR, Duan Z, Yu X, White D, El-Serag HB. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin Gastroenterol Hepatol. 2016;14(2):301-308.
11. Kabbany MN, Conjeevaram Selvakumar PK, Watt K, et al. Prevalence of nonalcoholic steatohepatitis-associated cirrhosis in the United States: an analysis of national health and nutrition examination survey data. Am J Gastroenterol. 2017;112(4):581-587.
12. Goldberg D, Ditah IC, Saeian K, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation. Gastroenterology. 2017;152(5):1090-1099.
13. Beste LA, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001-2013. Gastroenterology. 2015;149(6):1471-1482.
14. Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547-555.
15. Belli LS, Perricone G, Adam R, et al; all the contributing centers (www.eltr.org) and the European Liver and Intestine Transplant Association (ELITA). Impact of DAAs on liver transplantation: major effects on the evolution of indications and results. An ELITA study based on the ELTR registry. J Hepatol. 2018;69(4):810-817.
16. Flemming JA, Kim WR, Brosgart CL, Terrault NA. Reduction in liver transplant wait-listing in the era of direct-acting antiviral therapy. Hepatology. 2017;65(3):804-812.
17. Mittal S, Sada YH, El-Serag HB, et al. Temporal trends of nonalcoholic fatty liver disease-related hepatocellular carcinoma in the Veteran Affairs population. Clin Gastroenterol Hepatol. 2015;13(3):594-601.
18. Mittal S, El-Serag HB, Sada YH, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14(1):124-131.e1.
19. Sayiner M, Otgonsuren M, Cable R. Variables associated with inpatient and outpatient resource utilization among medicare beneficiaries with nonalcoholic fatty liver disease with or without cirrhosis. J Clin Gastroenterol. 2017;51(3):254-260.
20. Younossi ZM, Zheng L, Stepanova M, Henry L, Venkatesan C, Mishra A. Trends in outpatient resource utilizations and outcomes for Medicare beneficiaries with nonalcoholic fatty liver disease. J Clin Gastroenterol. 2015;49(3):222-227.
21. Allen AM, Van Houten HK, Sangaralingham LR, Talwalkar JA, McCoy RG. Healthcare cost and utilization in nonalcoholic fatty liver disease: real-world data from a large US claims database. Hepatology. 2018;68(6):2230-2238.
22. Younossi ZM, Blissett D, Blissett R, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64(5):1577-1586.
23. Armstrong MJ, Hazlehurst JM, Parker R, et al. Severe asymptomatic non-alcoholic fatty liver disease in routine diabetes care; a multi-disciplinary team approach to diagnosis and management. QJM. 2014;107(1):33-41.
24. Ekstedt M, Franzén LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44(4):865-873.
25. Kim D, Choi SY, Park EH, et al. Nonalcoholic fatty liver disease is associated with coronary artery calcification. Hepatology. 2012;56(2):605-613.
26. Stepanova M, Younossi ZM. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin Gastroenterol Hepatol. 2012;10(6):646-650.
27. Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363(14):1341-1350.
28. Mir HM, Stepanova M, Afendy H, Cable R, Younossi ZM. Association of sleep disorders with nonalcoholic fatty liver disease (NAFLD): a population-based study. J Clin Exp Hepatol. 2013;3(3):181-185.
29. Agrawal S, Duseja A, Aggarwal A, et al. Obstructive sleep apnea is an important predictor of hepatic fibrosis in patients with nonalcoholic fatty liver disease in a tertiary care center. Hepatol Int. 2015;9(2):283-291.
30. Sookoian S, Pirola CJ. Obstructive sleep apnea is associated with fatty liver and abnormal liver enzymes: a meta-analysis. Obes Surg. 2013;23(11):1815-1825.
31. Armstrong MJ, Adams LA, Canbay A, Syn WK. Extrahepatic complications of nonalcoholic fatty liver disease. Hepatology. 2014;59(3):1174-1197.
1. Targher G, Bertolini L, Padovani R, et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007;30(5):1212-1218.
2. Targher G, Bertolini L, Rodella S, et al. Non-alcoholic fatty liver disease is independently associated with an increased prevalence of chronic kidney disease and proliferative/laser-treated retinopathy in type 2 diabetic patients. Diabetologia. 2008;51(3):444-450.
3. Adams LA, Harmsen S, St Sauver JL, et al. Nonalcoholic fatty liver disease increases risk of death among patients with diabetes: a community-based cohort study. Am J Gastroenterol. 2010. 105(7):1567-1573.
4. Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013;10(11):686-690.
5. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64(1):73-84.
6. Angulo P, Machado MV, Diehl AM. Fibrosis in nonalcoholic fatty liver disease: mechanisms and clinical implications. Semin Liver Dis. 2015;35(2):132-145.
7. Satapathy SK, Sanyal AJ. Epidemiology and natural history of nonalcoholic fatty liver disease. Semin Liver Dis. 2015;35(3):221-235.
8. Estes C, Anstee QM, Arias-Loste MT, et al. Modeling NAFLD disease burden in China, France, Germany, Italy, Japan, Spain, United Kingdom, and United States for the period 2016-2030. J Hepatol. 2018;69(4):896-904.
9. Ahmed O, Liu L, Gayed A, et al. The changing face of hepatocellular carcinoma: forecasting prevalence of nonalcoholic steatohepatitis and hepatitis C cirrhosis. J Clin Exp Hepatol. 2018. In press.
10. Kanwal F, Kramer JR, Duan Z, Yu X, White D, El-Serag HB. Trends in the burden of nonalcoholic fatty liver disease in a United States cohort of veterans. Clin Gastroenterol Hepatol. 2016;14(2):301-308.
11. Kabbany MN, Conjeevaram Selvakumar PK, Watt K, et al. Prevalence of nonalcoholic steatohepatitis-associated cirrhosis in the United States: an analysis of national health and nutrition examination survey data. Am J Gastroenterol. 2017;112(4):581-587.
12. Goldberg D, Ditah IC, Saeian K, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation. Gastroenterology. 2017;152(5):1090-1099.
13. Beste LA, Leipertz SL, Green PK, Dominitz JA, Ross D, Ioannou GN. Trends in burden of cirrhosis and hepatocellular carcinoma by underlying liver disease in US veterans, 2001-2013. Gastroenterology. 2015;149(6):1471-1482.
14. Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148(3):547-555.
15. Belli LS, Perricone G, Adam R, et al; all the contributing centers (www.eltr.org) and the European Liver and Intestine Transplant Association (ELITA). Impact of DAAs on liver transplantation: major effects on the evolution of indications and results. An ELITA study based on the ELTR registry. J Hepatol. 2018;69(4):810-817.
16. Flemming JA, Kim WR, Brosgart CL, Terrault NA. Reduction in liver transplant wait-listing in the era of direct-acting antiviral therapy. Hepatology. 2017;65(3):804-812.
17. Mittal S, Sada YH, El-Serag HB, et al. Temporal trends of nonalcoholic fatty liver disease-related hepatocellular carcinoma in the Veteran Affairs population. Clin Gastroenterol Hepatol. 2015;13(3):594-601.
18. Mittal S, El-Serag HB, Sada YH, et al. Hepatocellular carcinoma in the absence of cirrhosis in United States veterans is associated with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2016;14(1):124-131.e1.
19. Sayiner M, Otgonsuren M, Cable R. Variables associated with inpatient and outpatient resource utilization among medicare beneficiaries with nonalcoholic fatty liver disease with or without cirrhosis. J Clin Gastroenterol. 2017;51(3):254-260.
20. Younossi ZM, Zheng L, Stepanova M, Henry L, Venkatesan C, Mishra A. Trends in outpatient resource utilizations and outcomes for Medicare beneficiaries with nonalcoholic fatty liver disease. J Clin Gastroenterol. 2015;49(3):222-227.
21. Allen AM, Van Houten HK, Sangaralingham LR, Talwalkar JA, McCoy RG. Healthcare cost and utilization in nonalcoholic fatty liver disease: real-world data from a large US claims database. Hepatology. 2018;68(6):2230-2238.
22. Younossi ZM, Blissett D, Blissett R, et al. The economic and clinical burden of nonalcoholic fatty liver disease in the United States and Europe. Hepatology. 2016;64(5):1577-1586.
23. Armstrong MJ, Hazlehurst JM, Parker R, et al. Severe asymptomatic non-alcoholic fatty liver disease in routine diabetes care; a multi-disciplinary team approach to diagnosis and management. QJM. 2014;107(1):33-41.
24. Ekstedt M, Franzén LE, Mathiesen UL, et al. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology. 2006;44(4):865-873.
25. Kim D, Choi SY, Park EH, et al. Nonalcoholic fatty liver disease is associated with coronary artery calcification. Hepatology. 2012;56(2):605-613.
26. Stepanova M, Younossi ZM. Independent association between nonalcoholic fatty liver disease and cardiovascular disease in the US population. Clin Gastroenterol Hepatol. 2012;10(6):646-650.
27. Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010;363(14):1341-1350.
28. Mir HM, Stepanova M, Afendy H, Cable R, Younossi ZM. Association of sleep disorders with nonalcoholic fatty liver disease (NAFLD): a population-based study. J Clin Exp Hepatol. 2013;3(3):181-185.
29. Agrawal S, Duseja A, Aggarwal A, et al. Obstructive sleep apnea is an important predictor of hepatic fibrosis in patients with nonalcoholic fatty liver disease in a tertiary care center. Hepatol Int. 2015;9(2):283-291.
30. Sookoian S, Pirola CJ. Obstructive sleep apnea is associated with fatty liver and abnormal liver enzymes: a meta-analysis. Obes Surg. 2013;23(11):1815-1825.
31. Armstrong MJ, Adams LA, Canbay A, Syn WK. Extrahepatic complications of nonalcoholic fatty liver disease. Hepatology. 2014;59(3):1174-1197.
Hospitalist movers and shakers – January 2019
The Michigan chapter of the Society of Hospital Medicine has named Peter Watson, MD, SFHM, as state Hospitalist of the Year. Dr. Watson is the vice president of care management and outcomes for Health Alliance Plan (HAP) in Detroit. The Michigan chapter cited Dr. Watson’s leadership in hospital medicine and “generosity of spirit” as reasons for his selection.
Dr. Watson oversees nurses, social workers, and support staff while also serving as HAP Midwest Health Plan’s medical director. He’s a founding member of the Michigan SHM chapter, which he formerly represented as president.
Dr. Watson spent 11 years overseeing the Henry Ford Medical Group’s hospitalist program prior to joining HAP, and still works as an attending hospitalist for Henry Ford.
Hyung (Harry) Cho, MD, was named the inaugural chief value officer for NYC Health + Hospitals, which includes 11 hospitals in New York and is the largest public health system in the United States. He will oversee systemwide initiatives in value improvement and the reduction of unnecessary testing and treatment.
Prior to this appointment, Dr. Cho served as an academic hospitalist at Mount Sinai Hospital for 7 years, leading high-value care initiatives. Currently, he is a senior fellow with the Lown Institute in Brookline, Mass., and director of quality improvement implementation for the High Value Practice Academic Alliance.
Nick Fitterman, MD, SFHM, has been promoted to executive director at Huntington (N.Y.) Hospital. Dr. Fitterman has been a long-time physician and administrator at Huntington, serving previously as vice chair of medicine as well as head of hospitalists.
Dr. Fitterman has served as president of SHM’s Long Island chapter.
Previously, Dr. Fitterman was chief resident at the State University of New York at Stony Brook, and he remains an associate professor at Hofstra University, Hempstead, N.Y.
Allen Kachalia, MD, was named director of the Armstrong Institute for Patient Safety and Quality and senior vice president of patient safety and quality for Johns Hopkins Medicine in Baltimore. Dr. Kachalia is a general internist who has been an active academic hospitalist at Brigham and Women’s Hospital in Boston.
Dr. Kachalia will oversee patient safety and quality across all of Hopkins Medicine, with a focus on ending preventable harm, improving outcomes and patient experience, and reducing waste in the system’s delivery of care. He also will guide academic efforts for the Armstrong Institute, formed recently thanks to a $10 million gift.
In addition to his hospitalist work, Dr. Kachalia comes to Hopkins after serving as chief quality officer and vice president of quality and safety at Brigham Health.
Riane Dodge, PA, has been elevated to director of clinical education in physician assistant studies at Clarkson University, Potsdam, N.Y. The veteran physician assistant previously worked as a hospitalist in the Claxton Hepburn Medical Center in Ogdensburg, N.Y. There, she cared for patients in acute rehab, mental health, and on regular medical floors.
Dodge also has a background in urgent care and family medicine, and has experience as an emergency department technician.
BUSINESS MOVES
Surgical Affiliates of Sacramento, a surgical hospitalist provider with expertise in trauma, orthopedic, neurosurgery, and general surgery for hospital systems, has added partnerships with Christus Spohn Hospital South and Christus Spohn Hospital Shoreline in Corpus Christi, Texas.
Surgical Affiliates’ hospitalist system will provide round-the-clock emergency orthopedic surgery service to adult and pediatric patients in the two hospitals. With Surgical Affiliates’ help, Christus Spohn facilities will be able to cover its own patients, as well as those requiring transfer from regional hospitals.
Hospitalist surgeons will handle emergency surgeries and patient surgery consultations. Clinics will be provided at each facility to care for patients after they are discharged.
The Michigan chapter of the Society of Hospital Medicine has named Peter Watson, MD, SFHM, as state Hospitalist of the Year. Dr. Watson is the vice president of care management and outcomes for Health Alliance Plan (HAP) in Detroit. The Michigan chapter cited Dr. Watson’s leadership in hospital medicine and “generosity of spirit” as reasons for his selection.
Dr. Watson oversees nurses, social workers, and support staff while also serving as HAP Midwest Health Plan’s medical director. He’s a founding member of the Michigan SHM chapter, which he formerly represented as president.
Dr. Watson spent 11 years overseeing the Henry Ford Medical Group’s hospitalist program prior to joining HAP, and still works as an attending hospitalist for Henry Ford.
Hyung (Harry) Cho, MD, was named the inaugural chief value officer for NYC Health + Hospitals, which includes 11 hospitals in New York and is the largest public health system in the United States. He will oversee systemwide initiatives in value improvement and the reduction of unnecessary testing and treatment.
Prior to this appointment, Dr. Cho served as an academic hospitalist at Mount Sinai Hospital for 7 years, leading high-value care initiatives. Currently, he is a senior fellow with the Lown Institute in Brookline, Mass., and director of quality improvement implementation for the High Value Practice Academic Alliance.
Nick Fitterman, MD, SFHM, has been promoted to executive director at Huntington (N.Y.) Hospital. Dr. Fitterman has been a long-time physician and administrator at Huntington, serving previously as vice chair of medicine as well as head of hospitalists.
Dr. Fitterman has served as president of SHM’s Long Island chapter.
Previously, Dr. Fitterman was chief resident at the State University of New York at Stony Brook, and he remains an associate professor at Hofstra University, Hempstead, N.Y.
Allen Kachalia, MD, was named director of the Armstrong Institute for Patient Safety and Quality and senior vice president of patient safety and quality for Johns Hopkins Medicine in Baltimore. Dr. Kachalia is a general internist who has been an active academic hospitalist at Brigham and Women’s Hospital in Boston.
Dr. Kachalia will oversee patient safety and quality across all of Hopkins Medicine, with a focus on ending preventable harm, improving outcomes and patient experience, and reducing waste in the system’s delivery of care. He also will guide academic efforts for the Armstrong Institute, formed recently thanks to a $10 million gift.
In addition to his hospitalist work, Dr. Kachalia comes to Hopkins after serving as chief quality officer and vice president of quality and safety at Brigham Health.
Riane Dodge, PA, has been elevated to director of clinical education in physician assistant studies at Clarkson University, Potsdam, N.Y. The veteran physician assistant previously worked as a hospitalist in the Claxton Hepburn Medical Center in Ogdensburg, N.Y. There, she cared for patients in acute rehab, mental health, and on regular medical floors.
Dodge also has a background in urgent care and family medicine, and has experience as an emergency department technician.
BUSINESS MOVES
Surgical Affiliates of Sacramento, a surgical hospitalist provider with expertise in trauma, orthopedic, neurosurgery, and general surgery for hospital systems, has added partnerships with Christus Spohn Hospital South and Christus Spohn Hospital Shoreline in Corpus Christi, Texas.
Surgical Affiliates’ hospitalist system will provide round-the-clock emergency orthopedic surgery service to adult and pediatric patients in the two hospitals. With Surgical Affiliates’ help, Christus Spohn facilities will be able to cover its own patients, as well as those requiring transfer from regional hospitals.
Hospitalist surgeons will handle emergency surgeries and patient surgery consultations. Clinics will be provided at each facility to care for patients after they are discharged.
The Michigan chapter of the Society of Hospital Medicine has named Peter Watson, MD, SFHM, as state Hospitalist of the Year. Dr. Watson is the vice president of care management and outcomes for Health Alliance Plan (HAP) in Detroit. The Michigan chapter cited Dr. Watson’s leadership in hospital medicine and “generosity of spirit” as reasons for his selection.
Dr. Watson oversees nurses, social workers, and support staff while also serving as HAP Midwest Health Plan’s medical director. He’s a founding member of the Michigan SHM chapter, which he formerly represented as president.
Dr. Watson spent 11 years overseeing the Henry Ford Medical Group’s hospitalist program prior to joining HAP, and still works as an attending hospitalist for Henry Ford.
Hyung (Harry) Cho, MD, was named the inaugural chief value officer for NYC Health + Hospitals, which includes 11 hospitals in New York and is the largest public health system in the United States. He will oversee systemwide initiatives in value improvement and the reduction of unnecessary testing and treatment.
Prior to this appointment, Dr. Cho served as an academic hospitalist at Mount Sinai Hospital for 7 years, leading high-value care initiatives. Currently, he is a senior fellow with the Lown Institute in Brookline, Mass., and director of quality improvement implementation for the High Value Practice Academic Alliance.
Nick Fitterman, MD, SFHM, has been promoted to executive director at Huntington (N.Y.) Hospital. Dr. Fitterman has been a long-time physician and administrator at Huntington, serving previously as vice chair of medicine as well as head of hospitalists.
Dr. Fitterman has served as president of SHM’s Long Island chapter.
Previously, Dr. Fitterman was chief resident at the State University of New York at Stony Brook, and he remains an associate professor at Hofstra University, Hempstead, N.Y.
Allen Kachalia, MD, was named director of the Armstrong Institute for Patient Safety and Quality and senior vice president of patient safety and quality for Johns Hopkins Medicine in Baltimore. Dr. Kachalia is a general internist who has been an active academic hospitalist at Brigham and Women’s Hospital in Boston.
Dr. Kachalia will oversee patient safety and quality across all of Hopkins Medicine, with a focus on ending preventable harm, improving outcomes and patient experience, and reducing waste in the system’s delivery of care. He also will guide academic efforts for the Armstrong Institute, formed recently thanks to a $10 million gift.
In addition to his hospitalist work, Dr. Kachalia comes to Hopkins after serving as chief quality officer and vice president of quality and safety at Brigham Health.
Riane Dodge, PA, has been elevated to director of clinical education in physician assistant studies at Clarkson University, Potsdam, N.Y. The veteran physician assistant previously worked as a hospitalist in the Claxton Hepburn Medical Center in Ogdensburg, N.Y. There, she cared for patients in acute rehab, mental health, and on regular medical floors.
Dodge also has a background in urgent care and family medicine, and has experience as an emergency department technician.
BUSINESS MOVES
Surgical Affiliates of Sacramento, a surgical hospitalist provider with expertise in trauma, orthopedic, neurosurgery, and general surgery for hospital systems, has added partnerships with Christus Spohn Hospital South and Christus Spohn Hospital Shoreline in Corpus Christi, Texas.
Surgical Affiliates’ hospitalist system will provide round-the-clock emergency orthopedic surgery service to adult and pediatric patients in the two hospitals. With Surgical Affiliates’ help, Christus Spohn facilities will be able to cover its own patients, as well as those requiring transfer from regional hospitals.
Hospitalist surgeons will handle emergency surgeries and patient surgery consultations. Clinics will be provided at each facility to care for patients after they are discharged.
Sleep disorders in children with ADHD treated with off-label medications
Sleep problems in children diagnosed with attention-deficit/hyperactivity disorder are treated with a variety of medications, many off label for sleep and unstudied for safety and effectiveness in children, a study of Medicaid prescriptions has found.
“Sleep disorders coexist with attention-deficit/hyperactivity disorder (ADHD) for many children and are associated with neuropsychiatric, physiologic, and medication-related outcomes,” wrote Tracy Klein, PhD, of Washington State University, Vancouver, and her colleagues. The report is in the Journal of Pediatric Health Care. These patients can have sleep disordered breathing and behavioral issues occurring around bedtime. Known adverse effects of the stimulant and nonstimulant medications used to treat ADHD can include sleep disturbance, delayed circadian rhythm, insomnia, and somnolence. Yet, research on both sleep problems in children with ADHD and prescribing patterns is scanty, according to the investigators.
Dr. Klein and her colleagues conducted a study aimed at identifying the off-label medications being prescribed to potentiate sleep in children with ADHD, and the characteristics of the children and their prescribers. They used 5 years of pharmacy claims for children in Oregon insured through Medicaid and had a provider diagnosis of ADHD during Jan. 1, 2012, to Dec. 31, 2016. The children were aged 3-18 years and the prescriptions measured were the number of 30-day prescriptions. Prescribers were identified by national provider identifier taxonomies (nurse, physician, other prescriber), and classified as either generalist or specialist. The medications were classified as controlled or uncontrolled as determined by Title 21 of the U.S. Controlled Substances Act.
The data yielded 14,567 prescriptions for 2,518 children for a 30-day supply of medication known to potentiate sleep but off-label for children. Children aged 3-11 years comprised about 38% of these patients. Some children were prescribed more than one of these medications. Medications specifically on label for sleep but not indicated for children were not included. Those medications indicated for comorbid conditions and those indicated for ADHD that specifically cause somnolence were excluded.
The uncontrolled medications prescribed in this sample were amitriptyline, doxepin, hydroxyzine, low-dose quetiapine, and trazodone. The controlled medications identified were clonazepam and lorazepam, and a few prescriptions for phenobarbital.
Most of the prescriptions (63.8%) went to older children aged 12-18 years and most prescriptions (66.3%) went to males. The most commonly prescribed noncontrolled medication was trazodone (5,190 prescriptions), followed by hydroxyzine (2,539), and quetiapine (2,402). The most frequently prescribed controlled medication was clonazepam (2,145), followed by lorazepam (534).
Specialist prescribers wrote most of the prescriptions for this patient group, but no differences were found in prescribing patterns between specialists and generalists.
Dr. Klein and her colleagues noted that 871 unique children were prescribed 5,190 30-day−supply prescriptions for trazodone, including 23 children under age 5. Trazodone is a serotonin modulator indicated for the treatment of major depressive disorder, but has not been studied for safety and efficacy in children and has no Food and Drug Administration indication for children. “Hydroxyzine, quetiapine, and amitriptyline also were prescribed for a large number of children, including some for children as young as 3 years, despite lack of approval for use to induce to sleep and increased potential for significant adverse reactions in children,” they wrote.
Dr. Klein suggested that prescribers receive pressure from families to “do something” for their children, who may be disruptive day and night. “Prescribers may be unaware that trazodone, which is commonly used in practice, has never been approved for treatment of insomnia in children or adults. Insurance may not adequately fund other options, such as extensive behavioral therapy,” she stated in an interview. These medications come with some risk for children, Dr. Klein noted.
especially if their reaction to it is behavioral.” There is also potential for unanticipated drug interactions between off-label medications prescribed for sleep and drugs prescribed to treat ADHD.
This study has limitations related to the absence of detailed clinical explanatory information found in claims data. Information on adherence to treatment and adverse events, for example, is not contained in claims data. The study does not address the overall rates of sleep disorders in children with ADHD nor the percentage of children with ADHD who are prescribed any medication to potentiate sleep but looks at which off-label drugs are being prescribed, to which children, and by whom.
“Most medications prescribed in this study, used to induce sleep or treat insomnia, have not been studied for safety and efficacy in children, and their use should not be extrapolated from adult studies,” the researchers concluded.
They reported having no disclosures.
SOURCE: Klein T et al. J Pediatr Health Care. 2018 Jan 8. doi: 10.1016/j.pedhc.2018.10.002.
Sleep problems in children diagnosed with attention-deficit/hyperactivity disorder are treated with a variety of medications, many off label for sleep and unstudied for safety and effectiveness in children, a study of Medicaid prescriptions has found.
“Sleep disorders coexist with attention-deficit/hyperactivity disorder (ADHD) for many children and are associated with neuropsychiatric, physiologic, and medication-related outcomes,” wrote Tracy Klein, PhD, of Washington State University, Vancouver, and her colleagues. The report is in the Journal of Pediatric Health Care. These patients can have sleep disordered breathing and behavioral issues occurring around bedtime. Known adverse effects of the stimulant and nonstimulant medications used to treat ADHD can include sleep disturbance, delayed circadian rhythm, insomnia, and somnolence. Yet, research on both sleep problems in children with ADHD and prescribing patterns is scanty, according to the investigators.
Dr. Klein and her colleagues conducted a study aimed at identifying the off-label medications being prescribed to potentiate sleep in children with ADHD, and the characteristics of the children and their prescribers. They used 5 years of pharmacy claims for children in Oregon insured through Medicaid and had a provider diagnosis of ADHD during Jan. 1, 2012, to Dec. 31, 2016. The children were aged 3-18 years and the prescriptions measured were the number of 30-day prescriptions. Prescribers were identified by national provider identifier taxonomies (nurse, physician, other prescriber), and classified as either generalist or specialist. The medications were classified as controlled or uncontrolled as determined by Title 21 of the U.S. Controlled Substances Act.
The data yielded 14,567 prescriptions for 2,518 children for a 30-day supply of medication known to potentiate sleep but off-label for children. Children aged 3-11 years comprised about 38% of these patients. Some children were prescribed more than one of these medications. Medications specifically on label for sleep but not indicated for children were not included. Those medications indicated for comorbid conditions and those indicated for ADHD that specifically cause somnolence were excluded.
The uncontrolled medications prescribed in this sample were amitriptyline, doxepin, hydroxyzine, low-dose quetiapine, and trazodone. The controlled medications identified were clonazepam and lorazepam, and a few prescriptions for phenobarbital.
Most of the prescriptions (63.8%) went to older children aged 12-18 years and most prescriptions (66.3%) went to males. The most commonly prescribed noncontrolled medication was trazodone (5,190 prescriptions), followed by hydroxyzine (2,539), and quetiapine (2,402). The most frequently prescribed controlled medication was clonazepam (2,145), followed by lorazepam (534).
Specialist prescribers wrote most of the prescriptions for this patient group, but no differences were found in prescribing patterns between specialists and generalists.
Dr. Klein and her colleagues noted that 871 unique children were prescribed 5,190 30-day−supply prescriptions for trazodone, including 23 children under age 5. Trazodone is a serotonin modulator indicated for the treatment of major depressive disorder, but has not been studied for safety and efficacy in children and has no Food and Drug Administration indication for children. “Hydroxyzine, quetiapine, and amitriptyline also were prescribed for a large number of children, including some for children as young as 3 years, despite lack of approval for use to induce to sleep and increased potential for significant adverse reactions in children,” they wrote.
Dr. Klein suggested that prescribers receive pressure from families to “do something” for their children, who may be disruptive day and night. “Prescribers may be unaware that trazodone, which is commonly used in practice, has never been approved for treatment of insomnia in children or adults. Insurance may not adequately fund other options, such as extensive behavioral therapy,” she stated in an interview. These medications come with some risk for children, Dr. Klein noted.
especially if their reaction to it is behavioral.” There is also potential for unanticipated drug interactions between off-label medications prescribed for sleep and drugs prescribed to treat ADHD.
This study has limitations related to the absence of detailed clinical explanatory information found in claims data. Information on adherence to treatment and adverse events, for example, is not contained in claims data. The study does not address the overall rates of sleep disorders in children with ADHD nor the percentage of children with ADHD who are prescribed any medication to potentiate sleep but looks at which off-label drugs are being prescribed, to which children, and by whom.
“Most medications prescribed in this study, used to induce sleep or treat insomnia, have not been studied for safety and efficacy in children, and their use should not be extrapolated from adult studies,” the researchers concluded.
They reported having no disclosures.
SOURCE: Klein T et al. J Pediatr Health Care. 2018 Jan 8. doi: 10.1016/j.pedhc.2018.10.002.
Sleep problems in children diagnosed with attention-deficit/hyperactivity disorder are treated with a variety of medications, many off label for sleep and unstudied for safety and effectiveness in children, a study of Medicaid prescriptions has found.
“Sleep disorders coexist with attention-deficit/hyperactivity disorder (ADHD) for many children and are associated with neuropsychiatric, physiologic, and medication-related outcomes,” wrote Tracy Klein, PhD, of Washington State University, Vancouver, and her colleagues. The report is in the Journal of Pediatric Health Care. These patients can have sleep disordered breathing and behavioral issues occurring around bedtime. Known adverse effects of the stimulant and nonstimulant medications used to treat ADHD can include sleep disturbance, delayed circadian rhythm, insomnia, and somnolence. Yet, research on both sleep problems in children with ADHD and prescribing patterns is scanty, according to the investigators.
Dr. Klein and her colleagues conducted a study aimed at identifying the off-label medications being prescribed to potentiate sleep in children with ADHD, and the characteristics of the children and their prescribers. They used 5 years of pharmacy claims for children in Oregon insured through Medicaid and had a provider diagnosis of ADHD during Jan. 1, 2012, to Dec. 31, 2016. The children were aged 3-18 years and the prescriptions measured were the number of 30-day prescriptions. Prescribers were identified by national provider identifier taxonomies (nurse, physician, other prescriber), and classified as either generalist or specialist. The medications were classified as controlled or uncontrolled as determined by Title 21 of the U.S. Controlled Substances Act.
The data yielded 14,567 prescriptions for 2,518 children for a 30-day supply of medication known to potentiate sleep but off-label for children. Children aged 3-11 years comprised about 38% of these patients. Some children were prescribed more than one of these medications. Medications specifically on label for sleep but not indicated for children were not included. Those medications indicated for comorbid conditions and those indicated for ADHD that specifically cause somnolence were excluded.
The uncontrolled medications prescribed in this sample were amitriptyline, doxepin, hydroxyzine, low-dose quetiapine, and trazodone. The controlled medications identified were clonazepam and lorazepam, and a few prescriptions for phenobarbital.
Most of the prescriptions (63.8%) went to older children aged 12-18 years and most prescriptions (66.3%) went to males. The most commonly prescribed noncontrolled medication was trazodone (5,190 prescriptions), followed by hydroxyzine (2,539), and quetiapine (2,402). The most frequently prescribed controlled medication was clonazepam (2,145), followed by lorazepam (534).
Specialist prescribers wrote most of the prescriptions for this patient group, but no differences were found in prescribing patterns between specialists and generalists.
Dr. Klein and her colleagues noted that 871 unique children were prescribed 5,190 30-day−supply prescriptions for trazodone, including 23 children under age 5. Trazodone is a serotonin modulator indicated for the treatment of major depressive disorder, but has not been studied for safety and efficacy in children and has no Food and Drug Administration indication for children. “Hydroxyzine, quetiapine, and amitriptyline also were prescribed for a large number of children, including some for children as young as 3 years, despite lack of approval for use to induce to sleep and increased potential for significant adverse reactions in children,” they wrote.
Dr. Klein suggested that prescribers receive pressure from families to “do something” for their children, who may be disruptive day and night. “Prescribers may be unaware that trazodone, which is commonly used in practice, has never been approved for treatment of insomnia in children or adults. Insurance may not adequately fund other options, such as extensive behavioral therapy,” she stated in an interview. These medications come with some risk for children, Dr. Klein noted.
especially if their reaction to it is behavioral.” There is also potential for unanticipated drug interactions between off-label medications prescribed for sleep and drugs prescribed to treat ADHD.
This study has limitations related to the absence of detailed clinical explanatory information found in claims data. Information on adherence to treatment and adverse events, for example, is not contained in claims data. The study does not address the overall rates of sleep disorders in children with ADHD nor the percentage of children with ADHD who are prescribed any medication to potentiate sleep but looks at which off-label drugs are being prescribed, to which children, and by whom.
“Most medications prescribed in this study, used to induce sleep or treat insomnia, have not been studied for safety and efficacy in children, and their use should not be extrapolated from adult studies,” the researchers concluded.
They reported having no disclosures.
SOURCE: Klein T et al. J Pediatr Health Care. 2018 Jan 8. doi: 10.1016/j.pedhc.2018.10.002.
FROM THE JOURNAL OF PEDIATRIC HEALTH CARE
Key clinical point: The most commonly prescribed off-label medications prescribed to children were trazodone (5,190), hydroxyzine (2,539), quetiapine (2,402), and clonazepam (2,145).
Major finding: Most of the prescriptions (63.8%) went to older children aged 12-18 years, and most prescriptions (66.3%) went to males.
Study details: Medicaid claims data for Jan. 1, 2012, to Dec. 31, 2016, yielding 14,567 prescriptions of off-label medications for 2,518 children.
Disclosures: The investigators reported no disclosures.
Source: Klein T et al. J Pediatr Health Care. 2018 Jan 8. doi: 10.1016/j.pedhc.2018.10.002.
Treprostinil improves function for complex PAH patients
Treatment with , a study based on data from 105 adults has shown.
Data on the treatment of chronic thromboembolic pulmonary hypertension (CTEPH) with treprostinil are limited, although alternatives to surgery are needed for many patients with the condition, wrote Roela Sadushi-Koliçi, MD, of the Medical University of Vienna, and her colleagues.
The researchers conducted a phase 3 randomized, controlled trial of the safety and efficacy of subcutaneous treprostinil for nonoperable CTEPH or persistent or recurrent pulmonary hypertension after pulmonary endarterectomy; the findings were published online in the Lancet Respiratory Medicine. The patients received continuous subcutaneous treprostinil at either 30 ng/kg per min (high dose) or 3 ng/kg per min (low dose) and all patients were assessed at weeks 6, 12, 18, and 24.
Overall, 6-minute walk distance, hemodynamics, and functional status significantly improved in the high-dose patients, compared with the low-dose patients.
The primary outcome of 6-minute walk distance increased by 44.98 m from baseline in the high-dose group, compared with an increase of 4.29 m from baseline in the low-dose group.
In addition, “changes in pulmonary vascular resistance, one of the most important prognostic indicators of CTEPH, were significant in favour of high-dose subcutaneous treprostinil, as were improvements of WHO functional class and N-terminal probrain natriuretic peptide,” the researchers noted.
Rates of serious adverse events were similar between the groups; a total of 12 serious adverse events were reported in 10 of 52 patients in the low-dose group (19%) and 16 serious adverse events were reported in 9 of 53 patients in the high-dose group (17%). In both groups, the most common treatment-related adverse events were infusion site pain and other infusion site reactions.
The findings were limited by the small sample size and the possibility that the 6-minute walk test might not translate to long-term outcomes for PAH and CTEPH, the researchers wrote. However, the data support the safety and efficacy of subcutaneous treprostinil for CTEPH patients who do not tolerate riociguat, the other approved option for nonoperable CTEPH, or those who need combination therapy, they said.
The study was supported in part by SciPharm Sàrl and United Therapeutics, which provided the medication for part of the study. Dr. Sadushi-Koliçi disclosed relationships with Actelion, AOP Orphan Pharmaceuticals, Bayer Schering Pharma, GlaxoSmithKline, and SciPharm Sàrl, among others.
SOURCE: Sadushi-Koliçi R et al. Lancet Respir Med. 2018 Nov 23. doi: 10.1016/S2213-2600(18)30367-9.
Treatment with , a study based on data from 105 adults has shown.
Data on the treatment of chronic thromboembolic pulmonary hypertension (CTEPH) with treprostinil are limited, although alternatives to surgery are needed for many patients with the condition, wrote Roela Sadushi-Koliçi, MD, of the Medical University of Vienna, and her colleagues.
The researchers conducted a phase 3 randomized, controlled trial of the safety and efficacy of subcutaneous treprostinil for nonoperable CTEPH or persistent or recurrent pulmonary hypertension after pulmonary endarterectomy; the findings were published online in the Lancet Respiratory Medicine. The patients received continuous subcutaneous treprostinil at either 30 ng/kg per min (high dose) or 3 ng/kg per min (low dose) and all patients were assessed at weeks 6, 12, 18, and 24.
Overall, 6-minute walk distance, hemodynamics, and functional status significantly improved in the high-dose patients, compared with the low-dose patients.
The primary outcome of 6-minute walk distance increased by 44.98 m from baseline in the high-dose group, compared with an increase of 4.29 m from baseline in the low-dose group.
In addition, “changes in pulmonary vascular resistance, one of the most important prognostic indicators of CTEPH, were significant in favour of high-dose subcutaneous treprostinil, as were improvements of WHO functional class and N-terminal probrain natriuretic peptide,” the researchers noted.
Rates of serious adverse events were similar between the groups; a total of 12 serious adverse events were reported in 10 of 52 patients in the low-dose group (19%) and 16 serious adverse events were reported in 9 of 53 patients in the high-dose group (17%). In both groups, the most common treatment-related adverse events were infusion site pain and other infusion site reactions.
The findings were limited by the small sample size and the possibility that the 6-minute walk test might not translate to long-term outcomes for PAH and CTEPH, the researchers wrote. However, the data support the safety and efficacy of subcutaneous treprostinil for CTEPH patients who do not tolerate riociguat, the other approved option for nonoperable CTEPH, or those who need combination therapy, they said.
The study was supported in part by SciPharm Sàrl and United Therapeutics, which provided the medication for part of the study. Dr. Sadushi-Koliçi disclosed relationships with Actelion, AOP Orphan Pharmaceuticals, Bayer Schering Pharma, GlaxoSmithKline, and SciPharm Sàrl, among others.
SOURCE: Sadushi-Koliçi R et al. Lancet Respir Med. 2018 Nov 23. doi: 10.1016/S2213-2600(18)30367-9.
Treatment with , a study based on data from 105 adults has shown.
Data on the treatment of chronic thromboembolic pulmonary hypertension (CTEPH) with treprostinil are limited, although alternatives to surgery are needed for many patients with the condition, wrote Roela Sadushi-Koliçi, MD, of the Medical University of Vienna, and her colleagues.
The researchers conducted a phase 3 randomized, controlled trial of the safety and efficacy of subcutaneous treprostinil for nonoperable CTEPH or persistent or recurrent pulmonary hypertension after pulmonary endarterectomy; the findings were published online in the Lancet Respiratory Medicine. The patients received continuous subcutaneous treprostinil at either 30 ng/kg per min (high dose) or 3 ng/kg per min (low dose) and all patients were assessed at weeks 6, 12, 18, and 24.
Overall, 6-minute walk distance, hemodynamics, and functional status significantly improved in the high-dose patients, compared with the low-dose patients.
The primary outcome of 6-minute walk distance increased by 44.98 m from baseline in the high-dose group, compared with an increase of 4.29 m from baseline in the low-dose group.
In addition, “changes in pulmonary vascular resistance, one of the most important prognostic indicators of CTEPH, were significant in favour of high-dose subcutaneous treprostinil, as were improvements of WHO functional class and N-terminal probrain natriuretic peptide,” the researchers noted.
Rates of serious adverse events were similar between the groups; a total of 12 serious adverse events were reported in 10 of 52 patients in the low-dose group (19%) and 16 serious adverse events were reported in 9 of 53 patients in the high-dose group (17%). In both groups, the most common treatment-related adverse events were infusion site pain and other infusion site reactions.
The findings were limited by the small sample size and the possibility that the 6-minute walk test might not translate to long-term outcomes for PAH and CTEPH, the researchers wrote. However, the data support the safety and efficacy of subcutaneous treprostinil for CTEPH patients who do not tolerate riociguat, the other approved option for nonoperable CTEPH, or those who need combination therapy, they said.
The study was supported in part by SciPharm Sàrl and United Therapeutics, which provided the medication for part of the study. Dr. Sadushi-Koliçi disclosed relationships with Actelion, AOP Orphan Pharmaceuticals, Bayer Schering Pharma, GlaxoSmithKline, and SciPharm Sàrl, among others.
SOURCE: Sadushi-Koliçi R et al. Lancet Respir Med. 2018 Nov 23. doi: 10.1016/S2213-2600(18)30367-9.
FROM THE LANCET RESPIRATORY MEDICINE
Key clinical point: Treprostinil is a safe and effective nonsurgical treatment option for severe CTEPH patients.
Major finding: After 24 weeks, 6-minute walk distance improved by 44.98 m from baseline in the high-dose group compared with an increase of 4.29 m from baseline in the low-dose group.
Study details: The data come from a randomized trial of 105 adults with confirmed CTEPH.
Disclosures: The study was supported in part by SciPharm Sàrl and United Therapeutics, which provided the medication for part of the study. Dr. Sadushi-Koliçi disclosed relationships with Actelion, AOP Orphan Pharmaceuticals, Bayer Schering Pharma, GlaxoSmithKline, and SciPharm Sàrl, among others.
Source: Sadushi-Koliçi R et al. Lancet Respir Med. 2018 Nov 23. doi: 10.1016/S2213-2600(18)30367-9.
A prescription for ‘deprescribing’: A case report
In 2016, Swapnil Gupta, MD, and John Daniel Cahill, MD, PhD, challenged the field of psychiatry to reexamine our prescribing patterns. They warned against our use of polypharmacy when not attached to improvement in functioning for our patients.1 They were concerned about the lack of evidence for those treatment regimens and for our diagnostic criteria. In their inspiring article, they described how psychiatrists might proceed in the process of “deprescribing” – which they define as a process of pharmacologic regimen optimization through reducing or ending medications for which “benefits no longer outweigh risks.”1
In my practice, I routinely confront medication regimens that I have never encountered in the literature. The evidence for two psychotropics is limited but certainly available, in particular adjunct treatment of antidepressants2 and mood stabilizers.3 The evidence supporting the use of more than two psychotropics, however, is quite sparse. Yet, patients often enter my office on more than five psychotropics. I am also confronted with poorly defined diagnostic labels – which present more as means to justify polypharmacy than a thorough review of the patient’s current state.
Dr. Gupta and Dr. Cahill recommend a series of steps aimed at attempting the deprescription of psychotropics. Those steps include timeliness, knowledge of the patient’s current regimen, discussion about the risk of prescriptions, discussion about deprescribing, choosing the right medications to stop, a plan for describing, and monitoring. In the case presented below, I used some of those steps in an effort to provide the best care for the patient. Key details of the case have been changed, including the name, to protect the patient’s confidentiality.
Overview of the case
Rosalie Bertin is a 54-year-old female who has been treated for depression by a variety of primary care physicians for the better part of the last 30 years. She had tried an array of antidepressants, including sertraline, citalopram, duloxetine, and mirtazapine, over that time. Each seemed to provide some benefit when reviewing the notes, but there is no mention of why she was continued on those medications despite the absence of continuing symptoms. Occasionally, Rosalie would present to her clinician tearful and endorsing sadness, though the record did not comment on reports of energy, concentration, sleep, appetite, and interest.
In 2014, Rosalie’s husband passed away from lung cancer. His death was fairly quick, and initially, Rosalie did not mention any significant emotional complaints. However, when visiting her primary care physician 4 months later, she was noted to experience auditory hallucinations. “Sometimes I hear my husband when I am alone in my home,” she said. Rosalie was referred to a psychiatrist with a diagnosis of “psychosis not otherwise specified.”
When discussing her condition with the psychiatrist, Rosalie mentioned experiencing low mood, and having diminished interest in engaging in activities. “I miss Marc when I go places; I used to do everything with him.” She reported hearing him often but only when at her home. He would say things like, “I miss you,” or ask her about her day. She was diagnosed with “major depressive disorder with psychotic features.” Risperidone was added to the escitalopram, buspirone, and gabapentin that had been started by her primary care physician.
After several months of psychotropic management, the dose of risperidone was titrated to 8 mg per day. Her mood symptoms were unchanged, but she now was complaining of poor concentration and memory. The psychiatrist performed a Mini-Mental State Examination (MMSE). It was noted that taking the MMSE engendered significant anxiety for the patient. Rosalie received a score suggesting mild cognitive impairment. She was started on donepezil for the memory complaint, quetiapine for the continued voices, and recommended for disability.
Once on short-term disability, the patient relocated to live closer to her mother in San Diego and subsequently contacted me about continuing psychiatric care.
Initial visit
Rosalie is a petite white woman, raised in the Midwest, who married her high school sweetheart, and subsequently became an administrative assistant. Rosalie and Marc were unable to have children. Marc was an engineer, and a longtime smoker. She describes their lives as simple – “few friends, few vacations, few problems, few regrets.” She states she misses her husband and often cries when thinking about him.
When asked about psychiatric diagnoses, she answered: “I have psychosis. … My doctor said maybe schizophrenia, but he is not sure yet.” She described schizophrenia as hearing voices. Rosalie also mentioned having memory problems: “They cannot tell if it is Alzheimer’s disease until I die and they look at my brain, but the medication should delay the progression.”
She reported no significant effect from her prior antidepressant trials: “I am not sure if or how they helped.” Rosalie could not explain the role of the medication. “I take medications as prescribed by my doctor,” she said.
When discussing her antipsychotics, she mentioned: “Those are strong medications; it is hard for me to stay awake with them.” She declared having had no changes in the voices while on the risperidone but said they went away since also being on the quetiapine: “I wonder if the combination of the two really fixed my brain imbalance.”
Assessment
I admit that I have a critical bias against the overuse of psychotropics, and this might have painted how I interpreted Rosalie’s story. Nonetheless, I was honest with her and told her of my concerns. I informed her that her diagnosis was not consistent with my understanding of mood and thought disorders. Her initial reports of depression neither met the DSM criteria for depression nor felt consistent with my conceptualization of the illness. She had retained appropriate functioning and seemed to be responding with the sadness expected when facing difficult challenges like grief.
Her subsequent reports of auditory hallucinations were not associated with delusions or forms of disorganization that I would expect in someone with a thought disorder. Furthermore, the context of the onset gave me the impression that this was part of her process of grief. Her poor result in the dementia screen was most surprising and inconsistent with my evaluation. I told her that I suspected that she was not suffering from Alzheimer’s but from being overmedicated and from anxiety at the time of the testing.
She was excited and hesitant about my report. She was surprised by the length of our visit and interested in hearing more from me. Strangely, I wished she had challenged my different approach. I think that I was hoping she would question my conceptualization, the way I hoped she would have done with her prior clinicians. Nonetheless, she agreed to make a plan with me.
Treatment plan
We decided to review each of her medications and discuss their benefits and risks over a couple of visits. She was most eager to discontinue the donepezil, which had caused diarrhea. She was concerned when I informed her of the potential side effects of antipsychotics. “My doctor asked me if I had any side effects at each visit; I answered that I felt nothing wrong; I had not realized that side effects could appear later.”
She was adamant about staying on buspirone, as she felt it helped her the most with her anxiety at social events. She voiced concern about discontinuing the antipsychotics despite being unsettled by my review of their risks. She asked that we taper them slowly.
In regard to receiving psychosocial support throughout this period of deprescribing, Rosalie declined weekly psychotherapy. She reported having a good social network in San Diego that she wanted to rely on.
Outcome
I often worry about consequences of stopping a medication, especially when I was not present at the time of its initiation. I agonize that the patient might relapse from my need to carry out my agenda on deprescribing. I try to remind myself that the evidence supports my decision making. The risks of psychotropics often are slow to show up, making the benefit of deprescribing less tangible. However, this case was straightforward.
Rosalie quickly improved. Tapering the antipsychotics was astonishing to her: “I can think clearly again.” Within 6 months, she was on buspirone only – though willing to discuss its discontinuation. She had a lead for a job and was hoping to return to work soon. Rosalie continued to miss her husband but had not heard him in some time. She has not had symptoms of psychosis or depression. Her cognition and mood were intact on my clinical assessment.
Discussion
Sadly and shockingly, cases like that of Rosalie are common. In my practice, I routinely see patients on multiple psychotropics – often on more than one antipsychotic. Their diagnoses are vague and dubious, and include diagnoses such as “unspecified psychosis” and “cognitive impairments.” Clinicians occasionally worry about relapse and promote a narrative that treatment must be not only long term but lifelong.4 There is some evidence for this perspective in a research context, but the clinical world also is filled with patients like Rosalie.
Her reports of auditory hallucinations were better explained by her grief than by a psychotic process.5 Her memory complaints were better explained by anxiety at the time of her testing while suffering from the side effects from her numerous psychotropics.6 Her depressive complaints were better explained by appropriate sadness in response to stressors. Several months later with fewer diagnoses and far fewer psychotropics, she is functioning better.
Take-home points
- Polypharmacy can lead to psychiatric symptoms and functional impairment.
- Patients often are unaware of the complete risks of psychotropics.
- Psychiatric symptoms are not always associated with a psychiatric disorder.
- Deprescribing can be performed safely and effectively.
- Deprescribing can be performed with the patient’s informed consent and agreement.
References
1. Psychiatr Serv. 2016 Aug 1;67(8):904-7.
2. Focus. 2016 Apr 13; doi: 10.1176/appi.focus.20150041.
3. Bipolar Disord. 2016 Dec;18(8):684-91.
4. Am J Psychiatry. 2017 Sep 1;174(9):840-9.
5. World Psychiatry. 2009 Jun;8(2):67-74.
6. Hosp Community Psychiatry. 1983 Sep;34(9):830-5.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings is chapter 7 in the new book “Critical Psychiatry: Controversies and Clinical Implications” (Springer, 2019).
*This column was updated 1/11/2019.
In 2016, Swapnil Gupta, MD, and John Daniel Cahill, MD, PhD, challenged the field of psychiatry to reexamine our prescribing patterns. They warned against our use of polypharmacy when not attached to improvement in functioning for our patients.1 They were concerned about the lack of evidence for those treatment regimens and for our diagnostic criteria. In their inspiring article, they described how psychiatrists might proceed in the process of “deprescribing” – which they define as a process of pharmacologic regimen optimization through reducing or ending medications for which “benefits no longer outweigh risks.”1
In my practice, I routinely confront medication regimens that I have never encountered in the literature. The evidence for two psychotropics is limited but certainly available, in particular adjunct treatment of antidepressants2 and mood stabilizers.3 The evidence supporting the use of more than two psychotropics, however, is quite sparse. Yet, patients often enter my office on more than five psychotropics. I am also confronted with poorly defined diagnostic labels – which present more as means to justify polypharmacy than a thorough review of the patient’s current state.
Dr. Gupta and Dr. Cahill recommend a series of steps aimed at attempting the deprescription of psychotropics. Those steps include timeliness, knowledge of the patient’s current regimen, discussion about the risk of prescriptions, discussion about deprescribing, choosing the right medications to stop, a plan for describing, and monitoring. In the case presented below, I used some of those steps in an effort to provide the best care for the patient. Key details of the case have been changed, including the name, to protect the patient’s confidentiality.
Overview of the case
Rosalie Bertin is a 54-year-old female who has been treated for depression by a variety of primary care physicians for the better part of the last 30 years. She had tried an array of antidepressants, including sertraline, citalopram, duloxetine, and mirtazapine, over that time. Each seemed to provide some benefit when reviewing the notes, but there is no mention of why she was continued on those medications despite the absence of continuing symptoms. Occasionally, Rosalie would present to her clinician tearful and endorsing sadness, though the record did not comment on reports of energy, concentration, sleep, appetite, and interest.
In 2014, Rosalie’s husband passed away from lung cancer. His death was fairly quick, and initially, Rosalie did not mention any significant emotional complaints. However, when visiting her primary care physician 4 months later, she was noted to experience auditory hallucinations. “Sometimes I hear my husband when I am alone in my home,” she said. Rosalie was referred to a psychiatrist with a diagnosis of “psychosis not otherwise specified.”
When discussing her condition with the psychiatrist, Rosalie mentioned experiencing low mood, and having diminished interest in engaging in activities. “I miss Marc when I go places; I used to do everything with him.” She reported hearing him often but only when at her home. He would say things like, “I miss you,” or ask her about her day. She was diagnosed with “major depressive disorder with psychotic features.” Risperidone was added to the escitalopram, buspirone, and gabapentin that had been started by her primary care physician.
After several months of psychotropic management, the dose of risperidone was titrated to 8 mg per day. Her mood symptoms were unchanged, but she now was complaining of poor concentration and memory. The psychiatrist performed a Mini-Mental State Examination (MMSE). It was noted that taking the MMSE engendered significant anxiety for the patient. Rosalie received a score suggesting mild cognitive impairment. She was started on donepezil for the memory complaint, quetiapine for the continued voices, and recommended for disability.
Once on short-term disability, the patient relocated to live closer to her mother in San Diego and subsequently contacted me about continuing psychiatric care.
Initial visit
Rosalie is a petite white woman, raised in the Midwest, who married her high school sweetheart, and subsequently became an administrative assistant. Rosalie and Marc were unable to have children. Marc was an engineer, and a longtime smoker. She describes their lives as simple – “few friends, few vacations, few problems, few regrets.” She states she misses her husband and often cries when thinking about him.
When asked about psychiatric diagnoses, she answered: “I have psychosis. … My doctor said maybe schizophrenia, but he is not sure yet.” She described schizophrenia as hearing voices. Rosalie also mentioned having memory problems: “They cannot tell if it is Alzheimer’s disease until I die and they look at my brain, but the medication should delay the progression.”
She reported no significant effect from her prior antidepressant trials: “I am not sure if or how they helped.” Rosalie could not explain the role of the medication. “I take medications as prescribed by my doctor,” she said.
When discussing her antipsychotics, she mentioned: “Those are strong medications; it is hard for me to stay awake with them.” She declared having had no changes in the voices while on the risperidone but said they went away since also being on the quetiapine: “I wonder if the combination of the two really fixed my brain imbalance.”
Assessment
I admit that I have a critical bias against the overuse of psychotropics, and this might have painted how I interpreted Rosalie’s story. Nonetheless, I was honest with her and told her of my concerns. I informed her that her diagnosis was not consistent with my understanding of mood and thought disorders. Her initial reports of depression neither met the DSM criteria for depression nor felt consistent with my conceptualization of the illness. She had retained appropriate functioning and seemed to be responding with the sadness expected when facing difficult challenges like grief.
Her subsequent reports of auditory hallucinations were not associated with delusions or forms of disorganization that I would expect in someone with a thought disorder. Furthermore, the context of the onset gave me the impression that this was part of her process of grief. Her poor result in the dementia screen was most surprising and inconsistent with my evaluation. I told her that I suspected that she was not suffering from Alzheimer’s but from being overmedicated and from anxiety at the time of the testing.
She was excited and hesitant about my report. She was surprised by the length of our visit and interested in hearing more from me. Strangely, I wished she had challenged my different approach. I think that I was hoping she would question my conceptualization, the way I hoped she would have done with her prior clinicians. Nonetheless, she agreed to make a plan with me.
Treatment plan
We decided to review each of her medications and discuss their benefits and risks over a couple of visits. She was most eager to discontinue the donepezil, which had caused diarrhea. She was concerned when I informed her of the potential side effects of antipsychotics. “My doctor asked me if I had any side effects at each visit; I answered that I felt nothing wrong; I had not realized that side effects could appear later.”
She was adamant about staying on buspirone, as she felt it helped her the most with her anxiety at social events. She voiced concern about discontinuing the antipsychotics despite being unsettled by my review of their risks. She asked that we taper them slowly.
In regard to receiving psychosocial support throughout this period of deprescribing, Rosalie declined weekly psychotherapy. She reported having a good social network in San Diego that she wanted to rely on.
Outcome
I often worry about consequences of stopping a medication, especially when I was not present at the time of its initiation. I agonize that the patient might relapse from my need to carry out my agenda on deprescribing. I try to remind myself that the evidence supports my decision making. The risks of psychotropics often are slow to show up, making the benefit of deprescribing less tangible. However, this case was straightforward.
Rosalie quickly improved. Tapering the antipsychotics was astonishing to her: “I can think clearly again.” Within 6 months, she was on buspirone only – though willing to discuss its discontinuation. She had a lead for a job and was hoping to return to work soon. Rosalie continued to miss her husband but had not heard him in some time. She has not had symptoms of psychosis or depression. Her cognition and mood were intact on my clinical assessment.
Discussion
Sadly and shockingly, cases like that of Rosalie are common. In my practice, I routinely see patients on multiple psychotropics – often on more than one antipsychotic. Their diagnoses are vague and dubious, and include diagnoses such as “unspecified psychosis” and “cognitive impairments.” Clinicians occasionally worry about relapse and promote a narrative that treatment must be not only long term but lifelong.4 There is some evidence for this perspective in a research context, but the clinical world also is filled with patients like Rosalie.
Her reports of auditory hallucinations were better explained by her grief than by a psychotic process.5 Her memory complaints were better explained by anxiety at the time of her testing while suffering from the side effects from her numerous psychotropics.6 Her depressive complaints were better explained by appropriate sadness in response to stressors. Several months later with fewer diagnoses and far fewer psychotropics, she is functioning better.
Take-home points
- Polypharmacy can lead to psychiatric symptoms and functional impairment.
- Patients often are unaware of the complete risks of psychotropics.
- Psychiatric symptoms are not always associated with a psychiatric disorder.
- Deprescribing can be performed safely and effectively.
- Deprescribing can be performed with the patient’s informed consent and agreement.
References
1. Psychiatr Serv. 2016 Aug 1;67(8):904-7.
2. Focus. 2016 Apr 13; doi: 10.1176/appi.focus.20150041.
3. Bipolar Disord. 2016 Dec;18(8):684-91.
4. Am J Psychiatry. 2017 Sep 1;174(9):840-9.
5. World Psychiatry. 2009 Jun;8(2):67-74.
6. Hosp Community Psychiatry. 1983 Sep;34(9):830-5.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings is chapter 7 in the new book “Critical Psychiatry: Controversies and Clinical Implications” (Springer, 2019).
*This column was updated 1/11/2019.
In 2016, Swapnil Gupta, MD, and John Daniel Cahill, MD, PhD, challenged the field of psychiatry to reexamine our prescribing patterns. They warned against our use of polypharmacy when not attached to improvement in functioning for our patients.1 They were concerned about the lack of evidence for those treatment regimens and for our diagnostic criteria. In their inspiring article, they described how psychiatrists might proceed in the process of “deprescribing” – which they define as a process of pharmacologic regimen optimization through reducing or ending medications for which “benefits no longer outweigh risks.”1
In my practice, I routinely confront medication regimens that I have never encountered in the literature. The evidence for two psychotropics is limited but certainly available, in particular adjunct treatment of antidepressants2 and mood stabilizers.3 The evidence supporting the use of more than two psychotropics, however, is quite sparse. Yet, patients often enter my office on more than five psychotropics. I am also confronted with poorly defined diagnostic labels – which present more as means to justify polypharmacy than a thorough review of the patient’s current state.
Dr. Gupta and Dr. Cahill recommend a series of steps aimed at attempting the deprescription of psychotropics. Those steps include timeliness, knowledge of the patient’s current regimen, discussion about the risk of prescriptions, discussion about deprescribing, choosing the right medications to stop, a plan for describing, and monitoring. In the case presented below, I used some of those steps in an effort to provide the best care for the patient. Key details of the case have been changed, including the name, to protect the patient’s confidentiality.
Overview of the case
Rosalie Bertin is a 54-year-old female who has been treated for depression by a variety of primary care physicians for the better part of the last 30 years. She had tried an array of antidepressants, including sertraline, citalopram, duloxetine, and mirtazapine, over that time. Each seemed to provide some benefit when reviewing the notes, but there is no mention of why she was continued on those medications despite the absence of continuing symptoms. Occasionally, Rosalie would present to her clinician tearful and endorsing sadness, though the record did not comment on reports of energy, concentration, sleep, appetite, and interest.
In 2014, Rosalie’s husband passed away from lung cancer. His death was fairly quick, and initially, Rosalie did not mention any significant emotional complaints. However, when visiting her primary care physician 4 months later, she was noted to experience auditory hallucinations. “Sometimes I hear my husband when I am alone in my home,” she said. Rosalie was referred to a psychiatrist with a diagnosis of “psychosis not otherwise specified.”
When discussing her condition with the psychiatrist, Rosalie mentioned experiencing low mood, and having diminished interest in engaging in activities. “I miss Marc when I go places; I used to do everything with him.” She reported hearing him often but only when at her home. He would say things like, “I miss you,” or ask her about her day. She was diagnosed with “major depressive disorder with psychotic features.” Risperidone was added to the escitalopram, buspirone, and gabapentin that had been started by her primary care physician.
After several months of psychotropic management, the dose of risperidone was titrated to 8 mg per day. Her mood symptoms were unchanged, but she now was complaining of poor concentration and memory. The psychiatrist performed a Mini-Mental State Examination (MMSE). It was noted that taking the MMSE engendered significant anxiety for the patient. Rosalie received a score suggesting mild cognitive impairment. She was started on donepezil for the memory complaint, quetiapine for the continued voices, and recommended for disability.
Once on short-term disability, the patient relocated to live closer to her mother in San Diego and subsequently contacted me about continuing psychiatric care.
Initial visit
Rosalie is a petite white woman, raised in the Midwest, who married her high school sweetheart, and subsequently became an administrative assistant. Rosalie and Marc were unable to have children. Marc was an engineer, and a longtime smoker. She describes their lives as simple – “few friends, few vacations, few problems, few regrets.” She states she misses her husband and often cries when thinking about him.
When asked about psychiatric diagnoses, she answered: “I have psychosis. … My doctor said maybe schizophrenia, but he is not sure yet.” She described schizophrenia as hearing voices. Rosalie also mentioned having memory problems: “They cannot tell if it is Alzheimer’s disease until I die and they look at my brain, but the medication should delay the progression.”
She reported no significant effect from her prior antidepressant trials: “I am not sure if or how they helped.” Rosalie could not explain the role of the medication. “I take medications as prescribed by my doctor,” she said.
When discussing her antipsychotics, she mentioned: “Those are strong medications; it is hard for me to stay awake with them.” She declared having had no changes in the voices while on the risperidone but said they went away since also being on the quetiapine: “I wonder if the combination of the two really fixed my brain imbalance.”
Assessment
I admit that I have a critical bias against the overuse of psychotropics, and this might have painted how I interpreted Rosalie’s story. Nonetheless, I was honest with her and told her of my concerns. I informed her that her diagnosis was not consistent with my understanding of mood and thought disorders. Her initial reports of depression neither met the DSM criteria for depression nor felt consistent with my conceptualization of the illness. She had retained appropriate functioning and seemed to be responding with the sadness expected when facing difficult challenges like grief.
Her subsequent reports of auditory hallucinations were not associated with delusions or forms of disorganization that I would expect in someone with a thought disorder. Furthermore, the context of the onset gave me the impression that this was part of her process of grief. Her poor result in the dementia screen was most surprising and inconsistent with my evaluation. I told her that I suspected that she was not suffering from Alzheimer’s but from being overmedicated and from anxiety at the time of the testing.
She was excited and hesitant about my report. She was surprised by the length of our visit and interested in hearing more from me. Strangely, I wished she had challenged my different approach. I think that I was hoping she would question my conceptualization, the way I hoped she would have done with her prior clinicians. Nonetheless, she agreed to make a plan with me.
Treatment plan
We decided to review each of her medications and discuss their benefits and risks over a couple of visits. She was most eager to discontinue the donepezil, which had caused diarrhea. She was concerned when I informed her of the potential side effects of antipsychotics. “My doctor asked me if I had any side effects at each visit; I answered that I felt nothing wrong; I had not realized that side effects could appear later.”
She was adamant about staying on buspirone, as she felt it helped her the most with her anxiety at social events. She voiced concern about discontinuing the antipsychotics despite being unsettled by my review of their risks. She asked that we taper them slowly.
In regard to receiving psychosocial support throughout this period of deprescribing, Rosalie declined weekly psychotherapy. She reported having a good social network in San Diego that she wanted to rely on.
Outcome
I often worry about consequences of stopping a medication, especially when I was not present at the time of its initiation. I agonize that the patient might relapse from my need to carry out my agenda on deprescribing. I try to remind myself that the evidence supports my decision making. The risks of psychotropics often are slow to show up, making the benefit of deprescribing less tangible. However, this case was straightforward.
Rosalie quickly improved. Tapering the antipsychotics was astonishing to her: “I can think clearly again.” Within 6 months, she was on buspirone only – though willing to discuss its discontinuation. She had a lead for a job and was hoping to return to work soon. Rosalie continued to miss her husband but had not heard him in some time. She has not had symptoms of psychosis or depression. Her cognition and mood were intact on my clinical assessment.
Discussion
Sadly and shockingly, cases like that of Rosalie are common. In my practice, I routinely see patients on multiple psychotropics – often on more than one antipsychotic. Their diagnoses are vague and dubious, and include diagnoses such as “unspecified psychosis” and “cognitive impairments.” Clinicians occasionally worry about relapse and promote a narrative that treatment must be not only long term but lifelong.4 There is some evidence for this perspective in a research context, but the clinical world also is filled with patients like Rosalie.
Her reports of auditory hallucinations were better explained by her grief than by a psychotic process.5 Her memory complaints were better explained by anxiety at the time of her testing while suffering from the side effects from her numerous psychotropics.6 Her depressive complaints were better explained by appropriate sadness in response to stressors. Several months later with fewer diagnoses and far fewer psychotropics, she is functioning better.
Take-home points
- Polypharmacy can lead to psychiatric symptoms and functional impairment.
- Patients often are unaware of the complete risks of psychotropics.
- Psychiatric symptoms are not always associated with a psychiatric disorder.
- Deprescribing can be performed safely and effectively.
- Deprescribing can be performed with the patient’s informed consent and agreement.
References
1. Psychiatr Serv. 2016 Aug 1;67(8):904-7.
2. Focus. 2016 Apr 13; doi: 10.1176/appi.focus.20150041.
3. Bipolar Disord. 2016 Dec;18(8):684-91.
4. Am J Psychiatry. 2017 Sep 1;174(9):840-9.
5. World Psychiatry. 2009 Jun;8(2):67-74.
6. Hosp Community Psychiatry. 1983 Sep;34(9):830-5.
Dr. Badre is a forensic psychiatrist in San Diego and an expert in correctional mental health. He holds teaching positions at the University of California, San Diego, and the University of San Diego. He teaches medical education, psychopharmacology, ethics in psychiatry, and correctional care. Among his writings is chapter 7 in the new book “Critical Psychiatry: Controversies and Clinical Implications” (Springer, 2019).
*This column was updated 1/11/2019.
Dealing with difficult people
Dealing with difficult people is not a new problem. As long as there are at least two people, the potential for conflict will arise. Unfortunately, the workplace or hospital is not immune from tragedies that are born out of poor conflict resolution. Before we go further, please do not ignore the fact that more than 1 million workers are assaulted each year, and more than 60% of Americans are aware of some type of abusive conduct occurring on the job.
Who are those difficult people we may encounter? Anyone and everyone. Difficult people may include our significant others, family members, supervisors, department chairs, colleagues, competitors, trainees, patients and their families, and ancillary personnel. Looking at this list, it is amazing that we aren’t either stymied by never-ending conflict resolution seminars, or rendered completely ineffective in all aspects of life. Daily conflicts can vary in intensity and degree. At one end one can be disgruntled at the person who secured the last doughnut in the break room, and at the other extreme end one is committed to moving forward with a multimillion dollar lawsuit against the company.
Conflicts arise because of a multiplicity of reasons – work style differences, background differences, attitude difference, personality types, and competitive versus cooperative differences. To be effective, each of us must realize that we are more alike than different, and it is our differences that should fuel our passion for providing excellent patient care and customer service.
In particular, be aware of things that can accelerate the potential for conflicts – performance ratings, evaluations, recommendation for promotion, absence of role models or mentors, lack of support amongst colleagues, and failures on the part of leadership to keep promises, appreciate people, maintain personal integrity, or take responsibility for their own errors.
When conflict arises – deal with it! Identify the problem, and if it is legitimate address it as soon as possible. Always remember to document the details in writing; never forget the old adage most of us learned during training: “If it’s not written/documented it wasn’t done or didn’t happen.” More than likely you won’t need to retrieve your written documents concerning a particular conflict, but if the conflict escalates, this type of documentation will prove invaluable.
Communicate with the person or persons with whom you have the conflict – it is essential that you have the “difficult” conversation. This conversation must be done face-to-face and in private. Never communicate by email, social media, or through gossip. Remain calm, professional, and show respect even if the other person does not. At this meeting detail the problem, but also come prepared with suggestions as to how the conflict might be resolved.
Take responsibility – you can’t control situations or people – but you can choose how you will respond to every situation. This is the appropriate time to establish boundaries; avoid any behavior that might be considered bullying or harassment. Redirect negativity that emanates from the person with whom you have the conflict as well as any potentially self-imposed negativity. Make every effort to avoid statements that include “you never” and “you always,” as there are very few absolutes in life. Consider the other person’s perspective as well; try to see it from their point of view because your “personal truth” is not the only “truth.” Our individual personal life experiences form the foundation for much of our opinions and views; therefore, it should be obvious that persons from widely varied backgrounds and cultures will differ in their approaches. If at all possible, give the person another chance; even the most difficult person has good attributes.
Once you have had the “difficult” conversation and there is still no resolution in sight you should take it to management. Everyone has a boss – even the Boss! There is much to gain from involving an impartial party or mediator. This impartial individual is able to understand the viewpoint of all parties involved and frequently that person’s solution may be considered acceptable because it is coming from someone not directly affected by the conflict.
Unresolved conflicts result in many negative effects – interference with one’s career is foremost – and that alone can be a source of undue stress. Other negative effects are the development of a hostile work environment, diminished productivity, low morale, and high employee turnover. Physicians in particular are prone to experiencing an increase in medical errors, litigation claims, and poor patient care when there are unresolved conflicts on the table.
In an ideal world, there are no difficult people; there are either no conflicts or all conflicts are resolved immediately without any lasting deleterious effects. Unfortunately, the world abounds in conflict at varying stages of resolution. As a final bit of advice, in dealing with difficult persons, do not allow conflicts to obscure your goals for successful patient care and/or customer service. Focus on why you decided to join your place of employment and realize that everyone has a role in making the team work! If you are dedicated to addressing conflicts as they arise, and utilizing the strategies outlined, you will often find that foes can truly become friends.
Dr. Cole is associate section chief, gastroenterology, and chief, GI endoscopy, Michael E. DeBakey VA Medical Center; and associate professor, internal medicine, Baylor College of Medicine, Houston.
Dealing with difficult people is not a new problem. As long as there are at least two people, the potential for conflict will arise. Unfortunately, the workplace or hospital is not immune from tragedies that are born out of poor conflict resolution. Before we go further, please do not ignore the fact that more than 1 million workers are assaulted each year, and more than 60% of Americans are aware of some type of abusive conduct occurring on the job.
Who are those difficult people we may encounter? Anyone and everyone. Difficult people may include our significant others, family members, supervisors, department chairs, colleagues, competitors, trainees, patients and their families, and ancillary personnel. Looking at this list, it is amazing that we aren’t either stymied by never-ending conflict resolution seminars, or rendered completely ineffective in all aspects of life. Daily conflicts can vary in intensity and degree. At one end one can be disgruntled at the person who secured the last doughnut in the break room, and at the other extreme end one is committed to moving forward with a multimillion dollar lawsuit against the company.
Conflicts arise because of a multiplicity of reasons – work style differences, background differences, attitude difference, personality types, and competitive versus cooperative differences. To be effective, each of us must realize that we are more alike than different, and it is our differences that should fuel our passion for providing excellent patient care and customer service.
In particular, be aware of things that can accelerate the potential for conflicts – performance ratings, evaluations, recommendation for promotion, absence of role models or mentors, lack of support amongst colleagues, and failures on the part of leadership to keep promises, appreciate people, maintain personal integrity, or take responsibility for their own errors.
When conflict arises – deal with it! Identify the problem, and if it is legitimate address it as soon as possible. Always remember to document the details in writing; never forget the old adage most of us learned during training: “If it’s not written/documented it wasn’t done or didn’t happen.” More than likely you won’t need to retrieve your written documents concerning a particular conflict, but if the conflict escalates, this type of documentation will prove invaluable.
Communicate with the person or persons with whom you have the conflict – it is essential that you have the “difficult” conversation. This conversation must be done face-to-face and in private. Never communicate by email, social media, or through gossip. Remain calm, professional, and show respect even if the other person does not. At this meeting detail the problem, but also come prepared with suggestions as to how the conflict might be resolved.
Take responsibility – you can’t control situations or people – but you can choose how you will respond to every situation. This is the appropriate time to establish boundaries; avoid any behavior that might be considered bullying or harassment. Redirect negativity that emanates from the person with whom you have the conflict as well as any potentially self-imposed negativity. Make every effort to avoid statements that include “you never” and “you always,” as there are very few absolutes in life. Consider the other person’s perspective as well; try to see it from their point of view because your “personal truth” is not the only “truth.” Our individual personal life experiences form the foundation for much of our opinions and views; therefore, it should be obvious that persons from widely varied backgrounds and cultures will differ in their approaches. If at all possible, give the person another chance; even the most difficult person has good attributes.
Once you have had the “difficult” conversation and there is still no resolution in sight you should take it to management. Everyone has a boss – even the Boss! There is much to gain from involving an impartial party or mediator. This impartial individual is able to understand the viewpoint of all parties involved and frequently that person’s solution may be considered acceptable because it is coming from someone not directly affected by the conflict.
Unresolved conflicts result in many negative effects – interference with one’s career is foremost – and that alone can be a source of undue stress. Other negative effects are the development of a hostile work environment, diminished productivity, low morale, and high employee turnover. Physicians in particular are prone to experiencing an increase in medical errors, litigation claims, and poor patient care when there are unresolved conflicts on the table.
In an ideal world, there are no difficult people; there are either no conflicts or all conflicts are resolved immediately without any lasting deleterious effects. Unfortunately, the world abounds in conflict at varying stages of resolution. As a final bit of advice, in dealing with difficult persons, do not allow conflicts to obscure your goals for successful patient care and/or customer service. Focus on why you decided to join your place of employment and realize that everyone has a role in making the team work! If you are dedicated to addressing conflicts as they arise, and utilizing the strategies outlined, you will often find that foes can truly become friends.
Dr. Cole is associate section chief, gastroenterology, and chief, GI endoscopy, Michael E. DeBakey VA Medical Center; and associate professor, internal medicine, Baylor College of Medicine, Houston.
Dealing with difficult people is not a new problem. As long as there are at least two people, the potential for conflict will arise. Unfortunately, the workplace or hospital is not immune from tragedies that are born out of poor conflict resolution. Before we go further, please do not ignore the fact that more than 1 million workers are assaulted each year, and more than 60% of Americans are aware of some type of abusive conduct occurring on the job.
Who are those difficult people we may encounter? Anyone and everyone. Difficult people may include our significant others, family members, supervisors, department chairs, colleagues, competitors, trainees, patients and their families, and ancillary personnel. Looking at this list, it is amazing that we aren’t either stymied by never-ending conflict resolution seminars, or rendered completely ineffective in all aspects of life. Daily conflicts can vary in intensity and degree. At one end one can be disgruntled at the person who secured the last doughnut in the break room, and at the other extreme end one is committed to moving forward with a multimillion dollar lawsuit against the company.
Conflicts arise because of a multiplicity of reasons – work style differences, background differences, attitude difference, personality types, and competitive versus cooperative differences. To be effective, each of us must realize that we are more alike than different, and it is our differences that should fuel our passion for providing excellent patient care and customer service.
In particular, be aware of things that can accelerate the potential for conflicts – performance ratings, evaluations, recommendation for promotion, absence of role models or mentors, lack of support amongst colleagues, and failures on the part of leadership to keep promises, appreciate people, maintain personal integrity, or take responsibility for their own errors.
When conflict arises – deal with it! Identify the problem, and if it is legitimate address it as soon as possible. Always remember to document the details in writing; never forget the old adage most of us learned during training: “If it’s not written/documented it wasn’t done or didn’t happen.” More than likely you won’t need to retrieve your written documents concerning a particular conflict, but if the conflict escalates, this type of documentation will prove invaluable.
Communicate with the person or persons with whom you have the conflict – it is essential that you have the “difficult” conversation. This conversation must be done face-to-face and in private. Never communicate by email, social media, or through gossip. Remain calm, professional, and show respect even if the other person does not. At this meeting detail the problem, but also come prepared with suggestions as to how the conflict might be resolved.
Take responsibility – you can’t control situations or people – but you can choose how you will respond to every situation. This is the appropriate time to establish boundaries; avoid any behavior that might be considered bullying or harassment. Redirect negativity that emanates from the person with whom you have the conflict as well as any potentially self-imposed negativity. Make every effort to avoid statements that include “you never” and “you always,” as there are very few absolutes in life. Consider the other person’s perspective as well; try to see it from their point of view because your “personal truth” is not the only “truth.” Our individual personal life experiences form the foundation for much of our opinions and views; therefore, it should be obvious that persons from widely varied backgrounds and cultures will differ in their approaches. If at all possible, give the person another chance; even the most difficult person has good attributes.
Once you have had the “difficult” conversation and there is still no resolution in sight you should take it to management. Everyone has a boss – even the Boss! There is much to gain from involving an impartial party or mediator. This impartial individual is able to understand the viewpoint of all parties involved and frequently that person’s solution may be considered acceptable because it is coming from someone not directly affected by the conflict.
Unresolved conflicts result in many negative effects – interference with one’s career is foremost – and that alone can be a source of undue stress. Other negative effects are the development of a hostile work environment, diminished productivity, low morale, and high employee turnover. Physicians in particular are prone to experiencing an increase in medical errors, litigation claims, and poor patient care when there are unresolved conflicts on the table.
In an ideal world, there are no difficult people; there are either no conflicts or all conflicts are resolved immediately without any lasting deleterious effects. Unfortunately, the world abounds in conflict at varying stages of resolution. As a final bit of advice, in dealing with difficult persons, do not allow conflicts to obscure your goals for successful patient care and/or customer service. Focus on why you decided to join your place of employment and realize that everyone has a role in making the team work! If you are dedicated to addressing conflicts as they arise, and utilizing the strategies outlined, you will often find that foes can truly become friends.
Dr. Cole is associate section chief, gastroenterology, and chief, GI endoscopy, Michael E. DeBakey VA Medical Center; and associate professor, internal medicine, Baylor College of Medicine, Houston.