User login
FDA approves rituximab biosimilar for lymphoma
(NHL).
Celltrion’s Truxima (rituximab-abbs) is a biosimilar of Genentech’s Rituxan (rituximab) and the first biosimilar approved in the United States to treat NHL.
Truxima (formerly CT-P10) is approved to treat adults with CD20-positive, B-cell NHL, either as a single agent or in combination with chemotherapy. Truxima is approved as a single agent to treat relapsed or refractory, low grade or follicular, CD20-positive, B-cell NHL. Truxima is approved in combination with first-line chemotherapy to treat previously untreated follicular, CD20-positive, B-cell NHL.
Truxima is approved as single-agent maintenance therapy in patients with follicular, CD20-positive, B-cell NHL who achieve a complete or partial response to a rituximab product in combination with chemotherapy. Truxima also is approved as a single agent to treat nonprogressing, low-grade, CD20-positive, B-cell NHL after first-line treatment with cyclophosphamide, vincristine, and prednisone.The label for Truxima contains a boxed warning detailing the risk of fatal infusion reactions, severe skin and mouth reactions (some with fatal outcomes), hepatitis B virus reactivation that may cause serious liver problems (including liver failure and death), and progressive multifocal leukoencephalopathy.
The FDA said its approval of Truxima is “based on a review of evidence that included extensive structural and functional characterization, animal study data, human pharmacokinetic data, clinical immunogenicity data, and other clinical data that demonstrates Truxima is biosimilar to Rituxan.”
Findings from a phase 3 trial suggested that Truxima is equivalent to the reference product in patients with low-tumor-burden follicular lymphoma (Lancet Haematol. 2018 Nov;5[11]:e543-53).
(NHL).
Celltrion’s Truxima (rituximab-abbs) is a biosimilar of Genentech’s Rituxan (rituximab) and the first biosimilar approved in the United States to treat NHL.
Truxima (formerly CT-P10) is approved to treat adults with CD20-positive, B-cell NHL, either as a single agent or in combination with chemotherapy. Truxima is approved as a single agent to treat relapsed or refractory, low grade or follicular, CD20-positive, B-cell NHL. Truxima is approved in combination with first-line chemotherapy to treat previously untreated follicular, CD20-positive, B-cell NHL.
Truxima is approved as single-agent maintenance therapy in patients with follicular, CD20-positive, B-cell NHL who achieve a complete or partial response to a rituximab product in combination with chemotherapy. Truxima also is approved as a single agent to treat nonprogressing, low-grade, CD20-positive, B-cell NHL after first-line treatment with cyclophosphamide, vincristine, and prednisone.The label for Truxima contains a boxed warning detailing the risk of fatal infusion reactions, severe skin and mouth reactions (some with fatal outcomes), hepatitis B virus reactivation that may cause serious liver problems (including liver failure and death), and progressive multifocal leukoencephalopathy.
The FDA said its approval of Truxima is “based on a review of evidence that included extensive structural and functional characterization, animal study data, human pharmacokinetic data, clinical immunogenicity data, and other clinical data that demonstrates Truxima is biosimilar to Rituxan.”
Findings from a phase 3 trial suggested that Truxima is equivalent to the reference product in patients with low-tumor-burden follicular lymphoma (Lancet Haematol. 2018 Nov;5[11]:e543-53).
(NHL).
Celltrion’s Truxima (rituximab-abbs) is a biosimilar of Genentech’s Rituxan (rituximab) and the first biosimilar approved in the United States to treat NHL.
Truxima (formerly CT-P10) is approved to treat adults with CD20-positive, B-cell NHL, either as a single agent or in combination with chemotherapy. Truxima is approved as a single agent to treat relapsed or refractory, low grade or follicular, CD20-positive, B-cell NHL. Truxima is approved in combination with first-line chemotherapy to treat previously untreated follicular, CD20-positive, B-cell NHL.
Truxima is approved as single-agent maintenance therapy in patients with follicular, CD20-positive, B-cell NHL who achieve a complete or partial response to a rituximab product in combination with chemotherapy. Truxima also is approved as a single agent to treat nonprogressing, low-grade, CD20-positive, B-cell NHL after first-line treatment with cyclophosphamide, vincristine, and prednisone.The label for Truxima contains a boxed warning detailing the risk of fatal infusion reactions, severe skin and mouth reactions (some with fatal outcomes), hepatitis B virus reactivation that may cause serious liver problems (including liver failure and death), and progressive multifocal leukoencephalopathy.
The FDA said its approval of Truxima is “based on a review of evidence that included extensive structural and functional characterization, animal study data, human pharmacokinetic data, clinical immunogenicity data, and other clinical data that demonstrates Truxima is biosimilar to Rituxan.”
Findings from a phase 3 trial suggested that Truxima is equivalent to the reference product in patients with low-tumor-burden follicular lymphoma (Lancet Haematol. 2018 Nov;5[11]:e543-53).
Evidence coming on best preeclampsia treatment threshold
CHICAGO – It’s clear that there’s a dose-dependent relationship between hypertension in pregnancy and poor outcomes, but, even so, treatment usually doesn’t begin until women hit 160/105 mm Hg or higher, according to Mark Santillan, MD, PhD, an assistant professor of obstetrics and gynecology – maternal fetal medicine at the University of Iowa, Iowa City.
That might soon change. The National Institutes of Health–funded CHAPS (Chronic Hypertension and Pregnancy) trial is testing whether earlier intervention improves outcomes, and it hopes to define proper treatment targets, which are uncertain at this point. Results are expected as soon as 2020.
What’s already changed is that the old treatment standby – methyldopa – has fallen out of favor for labetalol and nifedipine, which have been shown to work better. “Sometimes, we will throw on hydrochlorothiazide after we max out our beta- and calcium channel blockers,” Dr. Santillan said at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension (Cochrane Database Syst Rev. 2018 Oct 1;10:CD002252).
For severe hypertension, “most of the time we start off with IV hydralazine or IV labetalol” in the hospital. “You give a dose and check blood pressure in 10 or 20 minutes,” he said. If it hasn’t dropped, “give another dose until you reach your max dose.” When intravenous access is an issue, oral nifedipine is a good option (Obstet Gynecol. 2017 Apr;129[4]:e90-e95).
Delivery date is key; babies exposed to chronic hypertension are more likely to be stillborn. For hypertension without symptoms, delivery is at around 38 weeks. For mild preeclampsia – hypertension with only minor symptoms – it’s at 37 weeks.
In more severe cases – hypertension with pulmonary edema, renal insufficiency, and other problems – “the general gestalt is to stabilize and deliver when you can. See if you can get up to at least 34 weeks,” Dr. Santillan said. However, when women “have full-on HELLP syndrome [hemolysis, elevated liver enzymes, low platelet count], we often just deliver [immediately] because there’s not a lot of stabilization” that can be done. “We give magnesium after delivery to help decrease the risk of seizure,” he added.
Guidelines still use 140/90 mm Hg to define hypertension in pregnancy. When that level is reached, “you don’t need proteinuria anymore to diagnose preeclampsia. You need to have hypertension and something that looks like HELLP,” such as impaired liver function or neurologic symptoms, he said. Onset before 34 weeks portends more severe disease.
Daily baby aspirin 81 mg is known to help prevent preeclampsia, if only a little bit, so anyone with a history of preeclampsia or twin pregnancy, chronic hypertension, diabetes, renal disease, or autoimmune disease should automatically be put on aspirin prophylaxis. Women with two or more moderate risk factors – first pregnancy, obesity, preeclamptic family history, or aged 35 years or older – also should also get baby aspirin. Vitamin C, bed rest, and other preventative measures haven’t panned out in trials.
Investigators are looking for better predictors of preeclampsia; uterine artery blood flow is among the promising markers. However, it and other options are “expensive ventures” if you’re just going to end up in the same place, giving baby aspirin, Dr. Santillan said.
Dr. Santillan reported that he holds three patents; two on copeptin to predict preeclampsia and one on vasopressin receptor antagonists to treat it.
CHICAGO – It’s clear that there’s a dose-dependent relationship between hypertension in pregnancy and poor outcomes, but, even so, treatment usually doesn’t begin until women hit 160/105 mm Hg or higher, according to Mark Santillan, MD, PhD, an assistant professor of obstetrics and gynecology – maternal fetal medicine at the University of Iowa, Iowa City.
That might soon change. The National Institutes of Health–funded CHAPS (Chronic Hypertension and Pregnancy) trial is testing whether earlier intervention improves outcomes, and it hopes to define proper treatment targets, which are uncertain at this point. Results are expected as soon as 2020.
What’s already changed is that the old treatment standby – methyldopa – has fallen out of favor for labetalol and nifedipine, which have been shown to work better. “Sometimes, we will throw on hydrochlorothiazide after we max out our beta- and calcium channel blockers,” Dr. Santillan said at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension (Cochrane Database Syst Rev. 2018 Oct 1;10:CD002252).
For severe hypertension, “most of the time we start off with IV hydralazine or IV labetalol” in the hospital. “You give a dose and check blood pressure in 10 or 20 minutes,” he said. If it hasn’t dropped, “give another dose until you reach your max dose.” When intravenous access is an issue, oral nifedipine is a good option (Obstet Gynecol. 2017 Apr;129[4]:e90-e95).
Delivery date is key; babies exposed to chronic hypertension are more likely to be stillborn. For hypertension without symptoms, delivery is at around 38 weeks. For mild preeclampsia – hypertension with only minor symptoms – it’s at 37 weeks.
In more severe cases – hypertension with pulmonary edema, renal insufficiency, and other problems – “the general gestalt is to stabilize and deliver when you can. See if you can get up to at least 34 weeks,” Dr. Santillan said. However, when women “have full-on HELLP syndrome [hemolysis, elevated liver enzymes, low platelet count], we often just deliver [immediately] because there’s not a lot of stabilization” that can be done. “We give magnesium after delivery to help decrease the risk of seizure,” he added.
Guidelines still use 140/90 mm Hg to define hypertension in pregnancy. When that level is reached, “you don’t need proteinuria anymore to diagnose preeclampsia. You need to have hypertension and something that looks like HELLP,” such as impaired liver function or neurologic symptoms, he said. Onset before 34 weeks portends more severe disease.
Daily baby aspirin 81 mg is known to help prevent preeclampsia, if only a little bit, so anyone with a history of preeclampsia or twin pregnancy, chronic hypertension, diabetes, renal disease, or autoimmune disease should automatically be put on aspirin prophylaxis. Women with two or more moderate risk factors – first pregnancy, obesity, preeclamptic family history, or aged 35 years or older – also should also get baby aspirin. Vitamin C, bed rest, and other preventative measures haven’t panned out in trials.
Investigators are looking for better predictors of preeclampsia; uterine artery blood flow is among the promising markers. However, it and other options are “expensive ventures” if you’re just going to end up in the same place, giving baby aspirin, Dr. Santillan said.
Dr. Santillan reported that he holds three patents; two on copeptin to predict preeclampsia and one on vasopressin receptor antagonists to treat it.
CHICAGO – It’s clear that there’s a dose-dependent relationship between hypertension in pregnancy and poor outcomes, but, even so, treatment usually doesn’t begin until women hit 160/105 mm Hg or higher, according to Mark Santillan, MD, PhD, an assistant professor of obstetrics and gynecology – maternal fetal medicine at the University of Iowa, Iowa City.
That might soon change. The National Institutes of Health–funded CHAPS (Chronic Hypertension and Pregnancy) trial is testing whether earlier intervention improves outcomes, and it hopes to define proper treatment targets, which are uncertain at this point. Results are expected as soon as 2020.
What’s already changed is that the old treatment standby – methyldopa – has fallen out of favor for labetalol and nifedipine, which have been shown to work better. “Sometimes, we will throw on hydrochlorothiazide after we max out our beta- and calcium channel blockers,” Dr. Santillan said at the joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension (Cochrane Database Syst Rev. 2018 Oct 1;10:CD002252).
For severe hypertension, “most of the time we start off with IV hydralazine or IV labetalol” in the hospital. “You give a dose and check blood pressure in 10 or 20 minutes,” he said. If it hasn’t dropped, “give another dose until you reach your max dose.” When intravenous access is an issue, oral nifedipine is a good option (Obstet Gynecol. 2017 Apr;129[4]:e90-e95).
Delivery date is key; babies exposed to chronic hypertension are more likely to be stillborn. For hypertension without symptoms, delivery is at around 38 weeks. For mild preeclampsia – hypertension with only minor symptoms – it’s at 37 weeks.
In more severe cases – hypertension with pulmonary edema, renal insufficiency, and other problems – “the general gestalt is to stabilize and deliver when you can. See if you can get up to at least 34 weeks,” Dr. Santillan said. However, when women “have full-on HELLP syndrome [hemolysis, elevated liver enzymes, low platelet count], we often just deliver [immediately] because there’s not a lot of stabilization” that can be done. “We give magnesium after delivery to help decrease the risk of seizure,” he added.
Guidelines still use 140/90 mm Hg to define hypertension in pregnancy. When that level is reached, “you don’t need proteinuria anymore to diagnose preeclampsia. You need to have hypertension and something that looks like HELLP,” such as impaired liver function or neurologic symptoms, he said. Onset before 34 weeks portends more severe disease.
Daily baby aspirin 81 mg is known to help prevent preeclampsia, if only a little bit, so anyone with a history of preeclampsia or twin pregnancy, chronic hypertension, diabetes, renal disease, or autoimmune disease should automatically be put on aspirin prophylaxis. Women with two or more moderate risk factors – first pregnancy, obesity, preeclamptic family history, or aged 35 years or older – also should also get baby aspirin. Vitamin C, bed rest, and other preventative measures haven’t panned out in trials.
Investigators are looking for better predictors of preeclampsia; uterine artery blood flow is among the promising markers. However, it and other options are “expensive ventures” if you’re just going to end up in the same place, giving baby aspirin, Dr. Santillan said.
Dr. Santillan reported that he holds three patents; two on copeptin to predict preeclampsia and one on vasopressin receptor antagonists to treat it.
EXPERT ANALYSIS FROM JOINT HYPERTENSION 2018
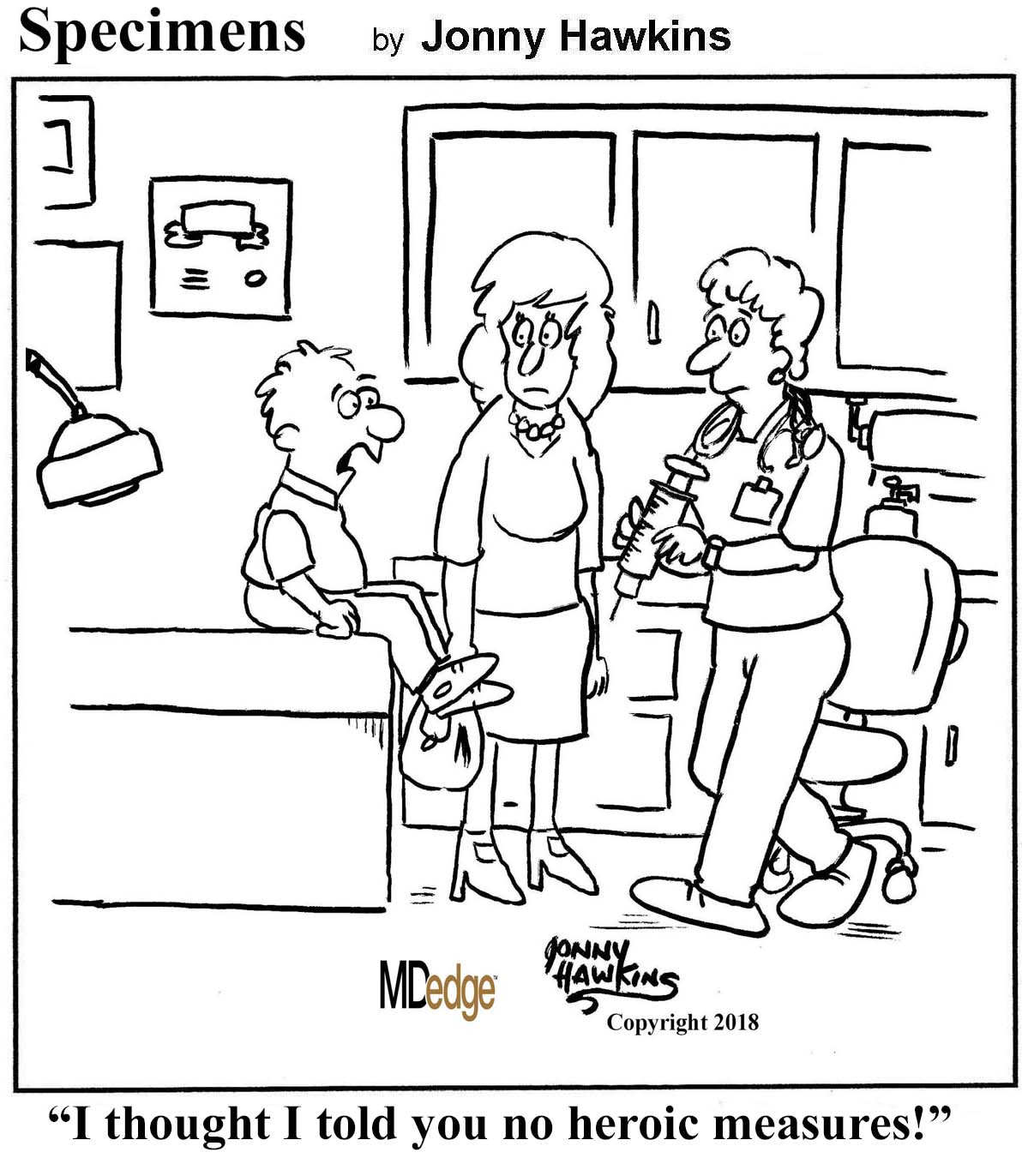
Legos for lunch, saliva-sterilized pacifiers, and a healthy personality
Legos for lunch
As any parent, teacher, or teenage babysitter knows, children try to eat everything. Six intrepid researchers from Australia and the United Kingdom decided to put their lives – or, at least, their intestines – on the line by swallowing Lego pieces to determine “typical transit times” for the commonly ingested toy. The things people do in the name of science.
The study participants first measured their bowel habits by the Stool Hardness and Transit (SHAT) score, and then measured the Found and Retrieved Time (FART) score once the Lego was ... expelled. The researchers found that the average FART score was 1.71 days.
At this point, all involved stopped to have a hearty laugh and a round of high-fives. Parents can rest assured that their little progeny who swallow Legos are safe. Everything is awesome.
Don’t wash that pacifier!
If you want to clean your child’s pacifier, you should consider passing on the sink and pop it into your own mouth instead. That’s the story from research presented at the annual scientific meeting of the American College of Allergy, Asthma, and Immunology.
In a survey of 128 mothers over an 18-month period, 41% of those whose child was currently using a pacifier reported cleaning by sterilization, and 72% reported hand washing their child’s pacifier. (We will henceforth refer to these mothers as “normal people.”) Just over 10% of mothers reported cleaning through parental pacifier sucking.
Before you cringe too much, the children of these mothers had significantly lower IgE levels than the children of normal people, indicating they were at a lower risk of developing allergies or asthma.
The study authors hypothesized that exposure to adult saliva may transfer healthy microorganisms to their children, and they advocated for further study into the subject. We suggest getting the pediatricians from the Lego study involved – they’ll eat anything for science.
One camel latte, please
An unlikely partnership between a Saudi entrepreneur and Amish farmers might lead to a brand-new dairy market in the United States. Walid Abdul-Wahub is on a mission to put camel milk on the shelves of every grocery store in America.
Middle Eastern residents have been drinking camel milk for centuries, so it’s only a matter of time until some hipster coffee shop co-opts it and starts selling camel milk lattes for $9. On the plus side, camel milk has a different protein than cow milk, making it more similar to human milk than bovine milk. This could be a godsend for people with milk allergies and need alternatives to that god-awful almond milk. One camel milkshake, coming right up.
How healthy is your personality?
It’s a question bipedal hominins have pondered since our days scrounging for snacks in the Olduvai Gorge: Is my personality why no one wants to hunt and gather with me?
Homo sapiens researchers from the University of California, Davis, and elsewhere believe they have the answer. In fact, it is your personality that leaves you scavenging for baobab alone.
What’s a healthy personality? The Scientia sapiens split personality into five factors: agreeableness, conscientiousness, extroversion, neuroticism, and openness to experience. They then surveyed scientists and college students to construct the consensus Dream Date – er, healthy personality: low levels of neuroticism, sprinkled with lots of agreeable straightforwardness, openness to feelings, positive emotions, and warmth. It wouldn’t hurt to ease up on the Old Spice, either.
The taste of deprivation
At one time or another, you’ve probably seen someone who was pretty much physically attached to his or her phone and wondered about the owner’s personal priorities and where the phone fit into them.
Wonder no more.
In a study conducted at the University at Buffalo (N.Y.), 76 students were deprived of food for 3 hours and their smartphones for 2 hours, and then given a computer task that would earn them a serving of their favorite snack or use of their phone. To make things more interesting, the amount of work needed to earn food or phone time increased as the subjects completed their tasks.
“We knew that students would be motivated to gain access to their phones, but we were surprised that, despite modest food deprivation, smartphone reinforcement far exceeded food reinforcement,” lead investigator Sara O’Donnell said in a written statement.
Recruiting subjects for the next step in this line of research – choosing between phones and breathing – could get a little tricky. But we have to admire the creative solution that got one participant disqualified from the current study: He tried to eat his phone.
Legos for lunch
As any parent, teacher, or teenage babysitter knows, children try to eat everything. Six intrepid researchers from Australia and the United Kingdom decided to put their lives – or, at least, their intestines – on the line by swallowing Lego pieces to determine “typical transit times” for the commonly ingested toy. The things people do in the name of science.
The study participants first measured their bowel habits by the Stool Hardness and Transit (SHAT) score, and then measured the Found and Retrieved Time (FART) score once the Lego was ... expelled. The researchers found that the average FART score was 1.71 days.
At this point, all involved stopped to have a hearty laugh and a round of high-fives. Parents can rest assured that their little progeny who swallow Legos are safe. Everything is awesome.
Don’t wash that pacifier!
If you want to clean your child’s pacifier, you should consider passing on the sink and pop it into your own mouth instead. That’s the story from research presented at the annual scientific meeting of the American College of Allergy, Asthma, and Immunology.
In a survey of 128 mothers over an 18-month period, 41% of those whose child was currently using a pacifier reported cleaning by sterilization, and 72% reported hand washing their child’s pacifier. (We will henceforth refer to these mothers as “normal people.”) Just over 10% of mothers reported cleaning through parental pacifier sucking.
Before you cringe too much, the children of these mothers had significantly lower IgE levels than the children of normal people, indicating they were at a lower risk of developing allergies or asthma.
The study authors hypothesized that exposure to adult saliva may transfer healthy microorganisms to their children, and they advocated for further study into the subject. We suggest getting the pediatricians from the Lego study involved – they’ll eat anything for science.
One camel latte, please
An unlikely partnership between a Saudi entrepreneur and Amish farmers might lead to a brand-new dairy market in the United States. Walid Abdul-Wahub is on a mission to put camel milk on the shelves of every grocery store in America.
Middle Eastern residents have been drinking camel milk for centuries, so it’s only a matter of time until some hipster coffee shop co-opts it and starts selling camel milk lattes for $9. On the plus side, camel milk has a different protein than cow milk, making it more similar to human milk than bovine milk. This could be a godsend for people with milk allergies and need alternatives to that god-awful almond milk. One camel milkshake, coming right up.
How healthy is your personality?
It’s a question bipedal hominins have pondered since our days scrounging for snacks in the Olduvai Gorge: Is my personality why no one wants to hunt and gather with me?
Homo sapiens researchers from the University of California, Davis, and elsewhere believe they have the answer. In fact, it is your personality that leaves you scavenging for baobab alone.
What’s a healthy personality? The Scientia sapiens split personality into five factors: agreeableness, conscientiousness, extroversion, neuroticism, and openness to experience. They then surveyed scientists and college students to construct the consensus Dream Date – er, healthy personality: low levels of neuroticism, sprinkled with lots of agreeable straightforwardness, openness to feelings, positive emotions, and warmth. It wouldn’t hurt to ease up on the Old Spice, either.
The taste of deprivation
At one time or another, you’ve probably seen someone who was pretty much physically attached to his or her phone and wondered about the owner’s personal priorities and where the phone fit into them.
Wonder no more.
In a study conducted at the University at Buffalo (N.Y.), 76 students were deprived of food for 3 hours and their smartphones for 2 hours, and then given a computer task that would earn them a serving of their favorite snack or use of their phone. To make things more interesting, the amount of work needed to earn food or phone time increased as the subjects completed their tasks.
“We knew that students would be motivated to gain access to their phones, but we were surprised that, despite modest food deprivation, smartphone reinforcement far exceeded food reinforcement,” lead investigator Sara O’Donnell said in a written statement.
Recruiting subjects for the next step in this line of research – choosing between phones and breathing – could get a little tricky. But we have to admire the creative solution that got one participant disqualified from the current study: He tried to eat his phone.
Legos for lunch
As any parent, teacher, or teenage babysitter knows, children try to eat everything. Six intrepid researchers from Australia and the United Kingdom decided to put their lives – or, at least, their intestines – on the line by swallowing Lego pieces to determine “typical transit times” for the commonly ingested toy. The things people do in the name of science.
The study participants first measured their bowel habits by the Stool Hardness and Transit (SHAT) score, and then measured the Found and Retrieved Time (FART) score once the Lego was ... expelled. The researchers found that the average FART score was 1.71 days.
At this point, all involved stopped to have a hearty laugh and a round of high-fives. Parents can rest assured that their little progeny who swallow Legos are safe. Everything is awesome.
Don’t wash that pacifier!
If you want to clean your child’s pacifier, you should consider passing on the sink and pop it into your own mouth instead. That’s the story from research presented at the annual scientific meeting of the American College of Allergy, Asthma, and Immunology.
In a survey of 128 mothers over an 18-month period, 41% of those whose child was currently using a pacifier reported cleaning by sterilization, and 72% reported hand washing their child’s pacifier. (We will henceforth refer to these mothers as “normal people.”) Just over 10% of mothers reported cleaning through parental pacifier sucking.
Before you cringe too much, the children of these mothers had significantly lower IgE levels than the children of normal people, indicating they were at a lower risk of developing allergies or asthma.
The study authors hypothesized that exposure to adult saliva may transfer healthy microorganisms to their children, and they advocated for further study into the subject. We suggest getting the pediatricians from the Lego study involved – they’ll eat anything for science.
One camel latte, please
An unlikely partnership between a Saudi entrepreneur and Amish farmers might lead to a brand-new dairy market in the United States. Walid Abdul-Wahub is on a mission to put camel milk on the shelves of every grocery store in America.
Middle Eastern residents have been drinking camel milk for centuries, so it’s only a matter of time until some hipster coffee shop co-opts it and starts selling camel milk lattes for $9. On the plus side, camel milk has a different protein than cow milk, making it more similar to human milk than bovine milk. This could be a godsend for people with milk allergies and need alternatives to that god-awful almond milk. One camel milkshake, coming right up.
How healthy is your personality?
It’s a question bipedal hominins have pondered since our days scrounging for snacks in the Olduvai Gorge: Is my personality why no one wants to hunt and gather with me?
Homo sapiens researchers from the University of California, Davis, and elsewhere believe they have the answer. In fact, it is your personality that leaves you scavenging for baobab alone.
What’s a healthy personality? The Scientia sapiens split personality into five factors: agreeableness, conscientiousness, extroversion, neuroticism, and openness to experience. They then surveyed scientists and college students to construct the consensus Dream Date – er, healthy personality: low levels of neuroticism, sprinkled with lots of agreeable straightforwardness, openness to feelings, positive emotions, and warmth. It wouldn’t hurt to ease up on the Old Spice, either.
The taste of deprivation
At one time or another, you’ve probably seen someone who was pretty much physically attached to his or her phone and wondered about the owner’s personal priorities and where the phone fit into them.
Wonder no more.
In a study conducted at the University at Buffalo (N.Y.), 76 students were deprived of food for 3 hours and their smartphones for 2 hours, and then given a computer task that would earn them a serving of their favorite snack or use of their phone. To make things more interesting, the amount of work needed to earn food or phone time increased as the subjects completed their tasks.
“We knew that students would be motivated to gain access to their phones, but we were surprised that, despite modest food deprivation, smartphone reinforcement far exceeded food reinforcement,” lead investigator Sara O’Donnell said in a written statement.
Recruiting subjects for the next step in this line of research – choosing between phones and breathing – could get a little tricky. But we have to admire the creative solution that got one participant disqualified from the current study: He tried to eat his phone.
Study takes a look at real-world use of MBDA testing
Patients with rheumatoid arthritis and a high multibiomarker disease activity (MBDA) score were more likely than were patients with low scores to add or switch to biologics or JAK inhibitors, according to a study on the uptake and influence of MBDA testing among rheumatologists and patients.
“While we cannot provide certainty that the main reason that clinicians switched therapies was the MBDA test result, we note that the median time to add or switch to a new RA treatment was 1-2 months after testing, lending plausibility to the MBDA test being influential in this decision,” wrote Jeffrey R. Curtis, MD, of the division of clinical immunology and rheumatology at the University of Alabama at Birmingham, and his coauthors. Their report is in The Journal of Rheumatology.
The researchers analyzed Medicare data from 60,596 RA patients who had taken at least one MBDA (Vectra DA) test. Patients with high MBDA scores who were not taking biologics or a JAK inhibitor were most likely to begin one of the two treatments, at 19.7%, compared with 11.8% for a moderate MBDA score and 9.0% for a low score. For patients already receiving those treatments, the proportion adding or switching was 13.5% for high, 8.3% for moderate, and 5.2% for low MBDA scores. In addition, patients with high MBDA scores who added a new medication and saw no improvement in score were prone to see treatment fail; the likelihood of failure in that scenario was 61% higher (OR = 1.61; 95% confidence index, 1.27-2.03) than in patients whose score improved to low or moderate.
The authors acknowledged that their study did not randomize clinicians nor gather data as to why the tests were ordered, which made it “difficult to assess the incremental value of the information provided by testing above and beyond clinical measurement, or to know whether the treatment changes were appropriate.” However, they also noted the MBDA score’s value as a complement to clinical assessment and an indicator of disease activity, suggesting “ongoing clinical trials and forthcoming data (e.g., MBDA to refine the patient-specific predicted risk of future radiographic damage) will be useful to further define the optimal role for the MBDA test in clinical practice to optimize longer-term outcomes.”
The study was partly supported by Myriad Genetics, which owns Crescendo Bioscience, the company that markets the MBDA test known as Vectra DA. Dr. Curtis receives support from the National Institutes of Health and the Patient-Centered Outcomes Research Institute, along with research grants and/or consulting fees from Amgen, Bristol-Myers Squibb, Corrona, Janssen, Myriad Genetics, Pfizer, and UCB. One coauthor reported receiving support from the NIH and research grants from Pfizer.
SOURCE: Curtis JR et al. J Rheumatol. 2018 Nov 15. doi: 10.3899/jrheum.180071.
Patients with rheumatoid arthritis and a high multibiomarker disease activity (MBDA) score were more likely than were patients with low scores to add or switch to biologics or JAK inhibitors, according to a study on the uptake and influence of MBDA testing among rheumatologists and patients.
“While we cannot provide certainty that the main reason that clinicians switched therapies was the MBDA test result, we note that the median time to add or switch to a new RA treatment was 1-2 months after testing, lending plausibility to the MBDA test being influential in this decision,” wrote Jeffrey R. Curtis, MD, of the division of clinical immunology and rheumatology at the University of Alabama at Birmingham, and his coauthors. Their report is in The Journal of Rheumatology.
The researchers analyzed Medicare data from 60,596 RA patients who had taken at least one MBDA (Vectra DA) test. Patients with high MBDA scores who were not taking biologics or a JAK inhibitor were most likely to begin one of the two treatments, at 19.7%, compared with 11.8% for a moderate MBDA score and 9.0% for a low score. For patients already receiving those treatments, the proportion adding or switching was 13.5% for high, 8.3% for moderate, and 5.2% for low MBDA scores. In addition, patients with high MBDA scores who added a new medication and saw no improvement in score were prone to see treatment fail; the likelihood of failure in that scenario was 61% higher (OR = 1.61; 95% confidence index, 1.27-2.03) than in patients whose score improved to low or moderate.
The authors acknowledged that their study did not randomize clinicians nor gather data as to why the tests were ordered, which made it “difficult to assess the incremental value of the information provided by testing above and beyond clinical measurement, or to know whether the treatment changes were appropriate.” However, they also noted the MBDA score’s value as a complement to clinical assessment and an indicator of disease activity, suggesting “ongoing clinical trials and forthcoming data (e.g., MBDA to refine the patient-specific predicted risk of future radiographic damage) will be useful to further define the optimal role for the MBDA test in clinical practice to optimize longer-term outcomes.”
The study was partly supported by Myriad Genetics, which owns Crescendo Bioscience, the company that markets the MBDA test known as Vectra DA. Dr. Curtis receives support from the National Institutes of Health and the Patient-Centered Outcomes Research Institute, along with research grants and/or consulting fees from Amgen, Bristol-Myers Squibb, Corrona, Janssen, Myriad Genetics, Pfizer, and UCB. One coauthor reported receiving support from the NIH and research grants from Pfizer.
SOURCE: Curtis JR et al. J Rheumatol. 2018 Nov 15. doi: 10.3899/jrheum.180071.
Patients with rheumatoid arthritis and a high multibiomarker disease activity (MBDA) score were more likely than were patients with low scores to add or switch to biologics or JAK inhibitors, according to a study on the uptake and influence of MBDA testing among rheumatologists and patients.
“While we cannot provide certainty that the main reason that clinicians switched therapies was the MBDA test result, we note that the median time to add or switch to a new RA treatment was 1-2 months after testing, lending plausibility to the MBDA test being influential in this decision,” wrote Jeffrey R. Curtis, MD, of the division of clinical immunology and rheumatology at the University of Alabama at Birmingham, and his coauthors. Their report is in The Journal of Rheumatology.
The researchers analyzed Medicare data from 60,596 RA patients who had taken at least one MBDA (Vectra DA) test. Patients with high MBDA scores who were not taking biologics or a JAK inhibitor were most likely to begin one of the two treatments, at 19.7%, compared with 11.8% for a moderate MBDA score and 9.0% for a low score. For patients already receiving those treatments, the proportion adding or switching was 13.5% for high, 8.3% for moderate, and 5.2% for low MBDA scores. In addition, patients with high MBDA scores who added a new medication and saw no improvement in score were prone to see treatment fail; the likelihood of failure in that scenario was 61% higher (OR = 1.61; 95% confidence index, 1.27-2.03) than in patients whose score improved to low or moderate.
The authors acknowledged that their study did not randomize clinicians nor gather data as to why the tests were ordered, which made it “difficult to assess the incremental value of the information provided by testing above and beyond clinical measurement, or to know whether the treatment changes were appropriate.” However, they also noted the MBDA score’s value as a complement to clinical assessment and an indicator of disease activity, suggesting “ongoing clinical trials and forthcoming data (e.g., MBDA to refine the patient-specific predicted risk of future radiographic damage) will be useful to further define the optimal role for the MBDA test in clinical practice to optimize longer-term outcomes.”
The study was partly supported by Myriad Genetics, which owns Crescendo Bioscience, the company that markets the MBDA test known as Vectra DA. Dr. Curtis receives support from the National Institutes of Health and the Patient-Centered Outcomes Research Institute, along with research grants and/or consulting fees from Amgen, Bristol-Myers Squibb, Corrona, Janssen, Myriad Genetics, Pfizer, and UCB. One coauthor reported receiving support from the NIH and research grants from Pfizer.
SOURCE: Curtis JR et al. J Rheumatol. 2018 Nov 15. doi: 10.3899/jrheum.180071.
FROM THE JOURNAL OF RHEUMATOLOGY
Key clinical point: Not only was a high MBDA score a likely catalyst for changing treatments, but lack of improvement in score was a strong predictor of subsequent treatment failure.
Major finding: In the study, 19.7% of rheumatoid arthritis patients with high MBDA scores who were not taking a biologic or JAK inhibitor added or switched medications.
Study details: An observational study of 60,596 Medicare-enrolled RA patients who underwent at least one MBDA test.
Disclosures: The study was partly supported by Myriad Genetics, which owns Crescendo Bioscience, the company that markets the MBDA test known as Vectra DA. Dr. Curtis receives support from the National Institutes of Health and the Patient-Centered Outcomes Research Institute, along with research grants and/or consulting fees from Amgen, Bristol-Myers Squibb, Corrona, Janssen, Myriad Genetics, Pfizer, and UCB. One coauthor reported receiving support from the NIH and research grants from Pfizer.
Source: Curtis JR et al. J Rheumatol. 2018 Nov 15. doi: 10.3899/jrheum.180071.
Despite interest, few liver transplant candidates discuss advance care planning with clinicians
SAN FRANCISCO – .
“Recent studies have shown that there have been low rates of these types of discussions in all areas of medicine, not just in liver transplantation per se,” Connie W. Wang, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “We were curious to see what it looked like in our practice setting.”
In an effort to evaluate current advanced care planning documentation practices in the liver transplantation setting, she and her colleagues reviewed the medical charts of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco, from January 2017 to June 2017. Next, to assess readiness to complete advanced care planning among liver transplant candidates, the researchers administered the Advanced Care Planning Engagement Survey to 41 adults who underwent an initial liver transplant evaluation from March 2018 to May 2018. The survey was scored on a Likert scale of 1-4, in which a score of 4 equaled “ready” or “confident,” and a score of 5 equaled “very ready” or “very confident.”
The mean age of the 168 transplant candidates was 53 years, 35% were female, and 52% were non-Hispanic white. Only 15 patients (9%) reported completing advanced care planning prior to their liver transplant evaluation and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record. Durable power of attorney for health care was discussed with 17 patients (10%). On logistic regression analysis, only white race was associated with completion of advanced care planning (OR 4.16; P = .03), but age, Child-Pugh score, and MELD-Na score were not.
The mean age of the 41 transplant candidates who completed the Advanced Care Planning Engagement Survey was 58 years, 39% were female, and 58% were non-Hispanic white. Nearly all respondents (93%) indicated that they were ready to appoint a durable power of attorney, 85% were ready to discuss end-of-life care, and 93% were ready to ask physicians questions about medical decisions. Similarly, 93% of patients felt confident to appoint a durable power of attorney, 88% felt confident to discuss end-of-life care, and 93% felt confident to ask physicians questions about medical decisions.
“It seems like from the patients’ perspective, they are very much open to having these conversations, but there hasn’t been [the right] environment or setting to have them,” said Dr. Wang, a third-year internal medicine resident at UCSF. “Or, there may be a barrier from the provider’s perspective. Clearly, there is a huge need that can be filled.” She noted that future research should focus on development of tools to facilitate discussions and documentation between transplant clinicians, patients, and their caregivers.
One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]: Abstract 771.
SAN FRANCISCO – .
“Recent studies have shown that there have been low rates of these types of discussions in all areas of medicine, not just in liver transplantation per se,” Connie W. Wang, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “We were curious to see what it looked like in our practice setting.”
In an effort to evaluate current advanced care planning documentation practices in the liver transplantation setting, she and her colleagues reviewed the medical charts of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco, from January 2017 to June 2017. Next, to assess readiness to complete advanced care planning among liver transplant candidates, the researchers administered the Advanced Care Planning Engagement Survey to 41 adults who underwent an initial liver transplant evaluation from March 2018 to May 2018. The survey was scored on a Likert scale of 1-4, in which a score of 4 equaled “ready” or “confident,” and a score of 5 equaled “very ready” or “very confident.”
The mean age of the 168 transplant candidates was 53 years, 35% were female, and 52% were non-Hispanic white. Only 15 patients (9%) reported completing advanced care planning prior to their liver transplant evaluation and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record. Durable power of attorney for health care was discussed with 17 patients (10%). On logistic regression analysis, only white race was associated with completion of advanced care planning (OR 4.16; P = .03), but age, Child-Pugh score, and MELD-Na score were not.
The mean age of the 41 transplant candidates who completed the Advanced Care Planning Engagement Survey was 58 years, 39% were female, and 58% were non-Hispanic white. Nearly all respondents (93%) indicated that they were ready to appoint a durable power of attorney, 85% were ready to discuss end-of-life care, and 93% were ready to ask physicians questions about medical decisions. Similarly, 93% of patients felt confident to appoint a durable power of attorney, 88% felt confident to discuss end-of-life care, and 93% felt confident to ask physicians questions about medical decisions.
“It seems like from the patients’ perspective, they are very much open to having these conversations, but there hasn’t been [the right] environment or setting to have them,” said Dr. Wang, a third-year internal medicine resident at UCSF. “Or, there may be a barrier from the provider’s perspective. Clearly, there is a huge need that can be filled.” She noted that future research should focus on development of tools to facilitate discussions and documentation between transplant clinicians, patients, and their caregivers.
One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]: Abstract 771.
SAN FRANCISCO – .
“Recent studies have shown that there have been low rates of these types of discussions in all areas of medicine, not just in liver transplantation per se,” Connie W. Wang, MD, said in an interview at the annual meeting of the American Association for the Study of Liver Diseases. “We were curious to see what it looked like in our practice setting.”
In an effort to evaluate current advanced care planning documentation practices in the liver transplantation setting, she and her colleagues reviewed the medical charts of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco, from January 2017 to June 2017. Next, to assess readiness to complete advanced care planning among liver transplant candidates, the researchers administered the Advanced Care Planning Engagement Survey to 41 adults who underwent an initial liver transplant evaluation from March 2018 to May 2018. The survey was scored on a Likert scale of 1-4, in which a score of 4 equaled “ready” or “confident,” and a score of 5 equaled “very ready” or “very confident.”
The mean age of the 168 transplant candidates was 53 years, 35% were female, and 52% were non-Hispanic white. Only 15 patients (9%) reported completing advanced care planning prior to their liver transplant evaluation and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record. Durable power of attorney for health care was discussed with 17 patients (10%). On logistic regression analysis, only white race was associated with completion of advanced care planning (OR 4.16; P = .03), but age, Child-Pugh score, and MELD-Na score were not.
The mean age of the 41 transplant candidates who completed the Advanced Care Planning Engagement Survey was 58 years, 39% were female, and 58% were non-Hispanic white. Nearly all respondents (93%) indicated that they were ready to appoint a durable power of attorney, 85% were ready to discuss end-of-life care, and 93% were ready to ask physicians questions about medical decisions. Similarly, 93% of patients felt confident to appoint a durable power of attorney, 88% felt confident to discuss end-of-life care, and 93% felt confident to ask physicians questions about medical decisions.
“It seems like from the patients’ perspective, they are very much open to having these conversations, but there hasn’t been [the right] environment or setting to have them,” said Dr. Wang, a third-year internal medicine resident at UCSF. “Or, there may be a barrier from the provider’s perspective. Clearly, there is a huge need that can be filled.” She noted that future research should focus on development of tools to facilitate discussions and documentation between transplant clinicians, patients, and their caregivers.
One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]: Abstract 771.
REPORTING FROM THE LIVER MEETING 2018
Key clinical point: There is a paucity of documentation of advance care planning or identification of a durable power of attorney in the medical record of liver transplant candidates.
Major finding: Only 9% of liver transplant candidates reported completing advanced care planning prior to their liver transplant evaluations and none had legal advance care planning forms scanned or end-of-life wishes documented in the medical record.
Study details: A retrospective review of 168 adults who underwent an initial liver transplant evaluation at the University of California, San Francisco.
Disclosures: One of the study authors, Jennifer C. Lai, MD, reported being a consultant for Third Rock Ventures, LLC. The other researchers reported having no financial disclosures.
Source: Hepatol. 2018;68[S1]:Abstract 771.
What is your diagnosis? - December 2018
A KOH (potassium hydroxide) test done at the visit was negative as well as a fungal culture of each toenail.
The patient was diagnosed with congenital malalignment of the great toenails (CMGTN) based on history and morphologic appearance.
Congenital malalignment of the great toenails is an underrecognized and underreported nail disorder characterized by lateral deviation of the nail plate, which is not parallel to the longitudinal axis of the distal phalanx.1 The cause is unknown. Some reports suggest a genetic cause being transmitted in an autosomal dominant fashion with variable expression.2 There have been reports of CMGTN in monozygotic and dizygotic twins making this theory likely.3 Other authors consider an external cause such as amniotic bands, neonatal asphyxia, vascular malformations, and uterine pressure. This condition also has been reported in patients with Rubinstein-Taybi syndrome.4
The nail changes can occur at birth but in some cases, such as our patient, the nails become dystrophic months to years after birth. Characteristic nail changes include shorter, discolored, hyperkeratotic nails with transverse groove or ridges. In some cases, the dystrophic nails may cause inflammation and tenderness and is the most common cause of ingrown toenails in children.
The differential diagnosis includes onychomycosis, traumatic nails, nail psoriasis, pachyonychia congenital (PC), and onychomadesis. Onychomycosis can present with white or yellow discoloration of the nail that in some cases can be associated with nail breakage, hyperkeratosis, onycholysis, and subungual debris. Either fungal culture or periodic acid shift stain of nail clippings can help confirm or exclude this diagnosis. Psoriatic nails present with nail pits, oils spots, and onycholysis. Traumatic nail changes may occur from using small shoes and trauma from running or playing soccer, and presents with subungual hemorrhage and nail dystrophy of the first or second toenail. PC is a genetic disorder caused by a mutation in certain keratin proteins of the skin (k6a, k6b, K16 and K17). These patients usually have other skin findings including palmoplantar keratoderma, white plaques on the mouth, and skin cysts (steatocystoma multiplex and vellus hair cysts). Nail changes characteristic of PC includes subungual hyperkeratosis that causes a wedge shape thickening of the nail bed (pincer nails).5 Onychomadesis can be seen after viral infections such as hand-foot-mouth disease or in patients taking chemotherapy drugs that affect nail growth.
CMGTN usually resolves with time, but some patients with severe deviation and paronychia may need surgical correction.6
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Email her at [email protected].
References
1. Dermatol Online J. 2014 Jan 15;20(1):21251.
2. J Dtsch Dermatol Ges. 2012 May;10(5):326-30.
3. J Am Acad Dermatol. 2007 Oct;57(4):711-5.
4. Pediatr Dermatol. 2004 Jan-Feb;21(1):44-7.
5. Curr Opin Pediatr. 2014 Aug;26(4):440-5.
6. Skin Appendage Disord. 2018 Oct;4(4):230-5.
A KOH (potassium hydroxide) test done at the visit was negative as well as a fungal culture of each toenail.
The patient was diagnosed with congenital malalignment of the great toenails (CMGTN) based on history and morphologic appearance.
Congenital malalignment of the great toenails is an underrecognized and underreported nail disorder characterized by lateral deviation of the nail plate, which is not parallel to the longitudinal axis of the distal phalanx.1 The cause is unknown. Some reports suggest a genetic cause being transmitted in an autosomal dominant fashion with variable expression.2 There have been reports of CMGTN in monozygotic and dizygotic twins making this theory likely.3 Other authors consider an external cause such as amniotic bands, neonatal asphyxia, vascular malformations, and uterine pressure. This condition also has been reported in patients with Rubinstein-Taybi syndrome.4
The nail changes can occur at birth but in some cases, such as our patient, the nails become dystrophic months to years after birth. Characteristic nail changes include shorter, discolored, hyperkeratotic nails with transverse groove or ridges. In some cases, the dystrophic nails may cause inflammation and tenderness and is the most common cause of ingrown toenails in children.
The differential diagnosis includes onychomycosis, traumatic nails, nail psoriasis, pachyonychia congenital (PC), and onychomadesis. Onychomycosis can present with white or yellow discoloration of the nail that in some cases can be associated with nail breakage, hyperkeratosis, onycholysis, and subungual debris. Either fungal culture or periodic acid shift stain of nail clippings can help confirm or exclude this diagnosis. Psoriatic nails present with nail pits, oils spots, and onycholysis. Traumatic nail changes may occur from using small shoes and trauma from running or playing soccer, and presents with subungual hemorrhage and nail dystrophy of the first or second toenail. PC is a genetic disorder caused by a mutation in certain keratin proteins of the skin (k6a, k6b, K16 and K17). These patients usually have other skin findings including palmoplantar keratoderma, white plaques on the mouth, and skin cysts (steatocystoma multiplex and vellus hair cysts). Nail changes characteristic of PC includes subungual hyperkeratosis that causes a wedge shape thickening of the nail bed (pincer nails).5 Onychomadesis can be seen after viral infections such as hand-foot-mouth disease or in patients taking chemotherapy drugs that affect nail growth.
CMGTN usually resolves with time, but some patients with severe deviation and paronychia may need surgical correction.6
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Email her at [email protected].
References
1. Dermatol Online J. 2014 Jan 15;20(1):21251.
2. J Dtsch Dermatol Ges. 2012 May;10(5):326-30.
3. J Am Acad Dermatol. 2007 Oct;57(4):711-5.
4. Pediatr Dermatol. 2004 Jan-Feb;21(1):44-7.
5. Curr Opin Pediatr. 2014 Aug;26(4):440-5.
6. Skin Appendage Disord. 2018 Oct;4(4):230-5.
A KOH (potassium hydroxide) test done at the visit was negative as well as a fungal culture of each toenail.
The patient was diagnosed with congenital malalignment of the great toenails (CMGTN) based on history and morphologic appearance.
Congenital malalignment of the great toenails is an underrecognized and underreported nail disorder characterized by lateral deviation of the nail plate, which is not parallel to the longitudinal axis of the distal phalanx.1 The cause is unknown. Some reports suggest a genetic cause being transmitted in an autosomal dominant fashion with variable expression.2 There have been reports of CMGTN in monozygotic and dizygotic twins making this theory likely.3 Other authors consider an external cause such as amniotic bands, neonatal asphyxia, vascular malformations, and uterine pressure. This condition also has been reported in patients with Rubinstein-Taybi syndrome.4
The nail changes can occur at birth but in some cases, such as our patient, the nails become dystrophic months to years after birth. Characteristic nail changes include shorter, discolored, hyperkeratotic nails with transverse groove or ridges. In some cases, the dystrophic nails may cause inflammation and tenderness and is the most common cause of ingrown toenails in children.
The differential diagnosis includes onychomycosis, traumatic nails, nail psoriasis, pachyonychia congenital (PC), and onychomadesis. Onychomycosis can present with white or yellow discoloration of the nail that in some cases can be associated with nail breakage, hyperkeratosis, onycholysis, and subungual debris. Either fungal culture or periodic acid shift stain of nail clippings can help confirm or exclude this diagnosis. Psoriatic nails present with nail pits, oils spots, and onycholysis. Traumatic nail changes may occur from using small shoes and trauma from running or playing soccer, and presents with subungual hemorrhage and nail dystrophy of the first or second toenail. PC is a genetic disorder caused by a mutation in certain keratin proteins of the skin (k6a, k6b, K16 and K17). These patients usually have other skin findings including palmoplantar keratoderma, white plaques on the mouth, and skin cysts (steatocystoma multiplex and vellus hair cysts). Nail changes characteristic of PC includes subungual hyperkeratosis that causes a wedge shape thickening of the nail bed (pincer nails).5 Onychomadesis can be seen after viral infections such as hand-foot-mouth disease or in patients taking chemotherapy drugs that affect nail growth.
CMGTN usually resolves with time, but some patients with severe deviation and paronychia may need surgical correction.6
Dr. Matiz is a pediatric dermatologist at Southern California Permanente Medical Group, San Diego. Email her at [email protected].
References
1. Dermatol Online J. 2014 Jan 15;20(1):21251.
2. J Dtsch Dermatol Ges. 2012 May;10(5):326-30.
3. J Am Acad Dermatol. 2007 Oct;57(4):711-5.
4. Pediatr Dermatol. 2004 Jan-Feb;21(1):44-7.
5. Curr Opin Pediatr. 2014 Aug;26(4):440-5.
6. Skin Appendage Disord. 2018 Oct;4(4):230-5.
A 4-year-old boy is brought to our pediatric dermatology clinic by his mother with the concern of difficult to treat toenail fungus.
The mother reported that she started noticing the toenail changes at around 8 months of age, and it has been progressively getting worse.
He has been treated with several courses of topical antifungals and 3 months of oral terbinafine without success.
A fungal culture done 1 year prior showed slight growth of Cladosporium Sp., but the nails failed to improve after systemic therapy. He denied any associated pain or inflammation. He likes playing softball and plays soccer sometimes. The mother is very worried because the father also has a history of onychomycosis that he has not been able to clear for years.
On physical exam, he is a very pleasant young boy. His cutaneous exam is normal including hair and teeth except for thickening of the bilateral first toenails associated with transverse ridging and yellow discoloration.
Laparoscopic hysterectomy with obliterated cul-de-sac needs specialist care
LAS VEGAS – When stage IV endometriosis with obliterated posterior cul-de-sac is discovered during laparoscopic hysterectomy, or suspected beforehand, women should be referred to a minimally invasive gynecologic surgery specialist because the procedure will be much more difficult, investigators said at the meeting sponsored by AAGL.
They reviewed 333 laparoscopic hysterectomies where endometriosis was discovered in the operating room. The disease is known to increase the complexity of hysterectomy; the investigators wanted to quantify the risk by endometriosis severity. Among their subjects, 237 women (71%) had stage I, II, or III endometriosis; 96 (29%) had stage IV disease, including 55 women (57%) with obliterated posterior cul-de-sacs.
Surgery was longer among stage IV cases (137 vs. 116 minutes), and there was greater blood loss; 66% of stage IV women required laparoscopic-modified radical hysterectomy versus about a quarter of women with stage I-III endometriosis.
A total of 93% required modified radical hysterectomies versus 29% of stage IV women with intact cul-de-sacs. Additional procedures were far more likely in this population, including salpingectomy, ureterolysis, enterolysis, cystoscopy, ureteral stenting, proctoscopy, bowel oversew, and anterior resection anastomosis. The differences all were statistically significant.
Among stage IV cases, mean operating time was longer in obliterated cul-de-sac cases (159 vs. 108 minutes), with higher blood loss, 100 mL versus 50 mL.
“Patients with obliterated cul-de-sacs identified intraoperatively should be referred to minimally invasive gynecologic surgeons because of the ... extra training required to safely perform [laparoscopic hysterectomy] with limited morbidity,” said lead investigator Alexandra Melnyk, MD, a University of Pittsburgh ob.gyn resident.
There was no industry funding and the investigators reported no disclosures.
SOURCE: Melnyk A et al. 2018 AAGL Global Congress, Abstract 81.
LAS VEGAS – When stage IV endometriosis with obliterated posterior cul-de-sac is discovered during laparoscopic hysterectomy, or suspected beforehand, women should be referred to a minimally invasive gynecologic surgery specialist because the procedure will be much more difficult, investigators said at the meeting sponsored by AAGL.
They reviewed 333 laparoscopic hysterectomies where endometriosis was discovered in the operating room. The disease is known to increase the complexity of hysterectomy; the investigators wanted to quantify the risk by endometriosis severity. Among their subjects, 237 women (71%) had stage I, II, or III endometriosis; 96 (29%) had stage IV disease, including 55 women (57%) with obliterated posterior cul-de-sacs.
Surgery was longer among stage IV cases (137 vs. 116 minutes), and there was greater blood loss; 66% of stage IV women required laparoscopic-modified radical hysterectomy versus about a quarter of women with stage I-III endometriosis.
A total of 93% required modified radical hysterectomies versus 29% of stage IV women with intact cul-de-sacs. Additional procedures were far more likely in this population, including salpingectomy, ureterolysis, enterolysis, cystoscopy, ureteral stenting, proctoscopy, bowel oversew, and anterior resection anastomosis. The differences all were statistically significant.
Among stage IV cases, mean operating time was longer in obliterated cul-de-sac cases (159 vs. 108 minutes), with higher blood loss, 100 mL versus 50 mL.
“Patients with obliterated cul-de-sacs identified intraoperatively should be referred to minimally invasive gynecologic surgeons because of the ... extra training required to safely perform [laparoscopic hysterectomy] with limited morbidity,” said lead investigator Alexandra Melnyk, MD, a University of Pittsburgh ob.gyn resident.
There was no industry funding and the investigators reported no disclosures.
SOURCE: Melnyk A et al. 2018 AAGL Global Congress, Abstract 81.
LAS VEGAS – When stage IV endometriosis with obliterated posterior cul-de-sac is discovered during laparoscopic hysterectomy, or suspected beforehand, women should be referred to a minimally invasive gynecologic surgery specialist because the procedure will be much more difficult, investigators said at the meeting sponsored by AAGL.
They reviewed 333 laparoscopic hysterectomies where endometriosis was discovered in the operating room. The disease is known to increase the complexity of hysterectomy; the investigators wanted to quantify the risk by endometriosis severity. Among their subjects, 237 women (71%) had stage I, II, or III endometriosis; 96 (29%) had stage IV disease, including 55 women (57%) with obliterated posterior cul-de-sacs.
Surgery was longer among stage IV cases (137 vs. 116 minutes), and there was greater blood loss; 66% of stage IV women required laparoscopic-modified radical hysterectomy versus about a quarter of women with stage I-III endometriosis.
A total of 93% required modified radical hysterectomies versus 29% of stage IV women with intact cul-de-sacs. Additional procedures were far more likely in this population, including salpingectomy, ureterolysis, enterolysis, cystoscopy, ureteral stenting, proctoscopy, bowel oversew, and anterior resection anastomosis. The differences all were statistically significant.
Among stage IV cases, mean operating time was longer in obliterated cul-de-sac cases (159 vs. 108 minutes), with higher blood loss, 100 mL versus 50 mL.
“Patients with obliterated cul-de-sacs identified intraoperatively should be referred to minimally invasive gynecologic surgeons because of the ... extra training required to safely perform [laparoscopic hysterectomy] with limited morbidity,” said lead investigator Alexandra Melnyk, MD, a University of Pittsburgh ob.gyn resident.
There was no industry funding and the investigators reported no disclosures.
SOURCE: Melnyk A et al. 2018 AAGL Global Congress, Abstract 81.
REPORTING FROM THE AAGL GLOBAL CONGRESS
Cortactin expression aids in CLL-MCL differential
The presence or absence in tumor cells of cortactin, a cytoskeleton-remodeling adapter protein, may be a marker to help pathologists distinguish between chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL), investigators suggest.
A study of cortactin expression in tumor samples from patients with B-cell CLL, MCL, and other hematologic malignancies showed that while cortactin was present in 14 of 17 CLL samples, it was not expressed on any of 16 MCL samples, reported Marco Pizzi, MD, PhD, from the University of Padova (Italy) and his colleagues.
“In particular, cortactin may contribute to the differential diagnosis between CLL and MCL, two neoplasms with similar histological features but very different clinical outcome. Further studies are needed to clarify the molecular mechanisms of deranged cortactin expression in MCL and CLL and to investigate any possible relationship between cortactin status and the biological features of these lymphomas,” they wrote in Human Pathology.
Overexpression of cortactin has been reported in several solid tumors, and increased expression of CTTN, the gene encoding for cortactin, has been associated with aggressive, poor prognosis disease, the investigators noted.
To characterize cortactin expression in lymphoid and hematopoietic cells and detect potential associations between cortactin and virulence of hematologic malignancies, the investigators performed immunohistochemical analysis on samples from 131 patients treated at their center. The samples included 17 cases of CLL, 16 of MCL, 25 of follicular lymphoma (FL), 30 of marginal zone lymphoma (MZL), 10 of hairy cell leukemia, three of splenic diffuse red pulp small B-cell lymphomas (SDRPBL), and 30 of diffuse large B-cell lymphoma (DLBCL).
They found that cortactin was expressed in 14 of the 17 CLL samples, all 10 of the HCL samples, and 22 of the 30 DLBCL samples. In contrast, there was no cortactin expression detected in any of either 16 MCL or three SDRPBL samples. The researchers found that 13 of 30 MZL samples had low-level staining. In FL, cortactin was expressed in 2 of the samples but in the remaining 23 cases the researchers found only scattered cortactin-positive lymphoid elements of non–B-cell lineage.
The investigators also found that cortactin expression in CLL correlated with other CLL-specific markers, and found that expression of two or more of the markers had 89.1% sensitivity, 100% specificity, a 100% positive predictive value, and 90.5% negative predictive value for a diagnosis of CLL.
In addition, they saw that the immunohistochemical results were similar to those for CTTN gene expression assessed by in silico analysis.
The investigators noted that CLL and MCL are challenging to differentiate from one another because of morphologic similarities and partially overlapping immunophenotypes.
“In this context, cortactin expression would strongly sustain a diagnosis of CLL over MCL, particularly in association with other CLL markers (i.e., LEF1 and CD200),” they wrote.
The study was internally supported. The authors declared no conflicts of interest.
SOURCE: Pizzi M et al. Hum Pathol. 2018 Nov 17. doi: 10.1016/j.humpath.2018.10.038.
The presence or absence in tumor cells of cortactin, a cytoskeleton-remodeling adapter protein, may be a marker to help pathologists distinguish between chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL), investigators suggest.
A study of cortactin expression in tumor samples from patients with B-cell CLL, MCL, and other hematologic malignancies showed that while cortactin was present in 14 of 17 CLL samples, it was not expressed on any of 16 MCL samples, reported Marco Pizzi, MD, PhD, from the University of Padova (Italy) and his colleagues.
“In particular, cortactin may contribute to the differential diagnosis between CLL and MCL, two neoplasms with similar histological features but very different clinical outcome. Further studies are needed to clarify the molecular mechanisms of deranged cortactin expression in MCL and CLL and to investigate any possible relationship between cortactin status and the biological features of these lymphomas,” they wrote in Human Pathology.
Overexpression of cortactin has been reported in several solid tumors, and increased expression of CTTN, the gene encoding for cortactin, has been associated with aggressive, poor prognosis disease, the investigators noted.
To characterize cortactin expression in lymphoid and hematopoietic cells and detect potential associations between cortactin and virulence of hematologic malignancies, the investigators performed immunohistochemical analysis on samples from 131 patients treated at their center. The samples included 17 cases of CLL, 16 of MCL, 25 of follicular lymphoma (FL), 30 of marginal zone lymphoma (MZL), 10 of hairy cell leukemia, three of splenic diffuse red pulp small B-cell lymphomas (SDRPBL), and 30 of diffuse large B-cell lymphoma (DLBCL).
They found that cortactin was expressed in 14 of the 17 CLL samples, all 10 of the HCL samples, and 22 of the 30 DLBCL samples. In contrast, there was no cortactin expression detected in any of either 16 MCL or three SDRPBL samples. The researchers found that 13 of 30 MZL samples had low-level staining. In FL, cortactin was expressed in 2 of the samples but in the remaining 23 cases the researchers found only scattered cortactin-positive lymphoid elements of non–B-cell lineage.
The investigators also found that cortactin expression in CLL correlated with other CLL-specific markers, and found that expression of two or more of the markers had 89.1% sensitivity, 100% specificity, a 100% positive predictive value, and 90.5% negative predictive value for a diagnosis of CLL.
In addition, they saw that the immunohistochemical results were similar to those for CTTN gene expression assessed by in silico analysis.
The investigators noted that CLL and MCL are challenging to differentiate from one another because of morphologic similarities and partially overlapping immunophenotypes.
“In this context, cortactin expression would strongly sustain a diagnosis of CLL over MCL, particularly in association with other CLL markers (i.e., LEF1 and CD200),” they wrote.
The study was internally supported. The authors declared no conflicts of interest.
SOURCE: Pizzi M et al. Hum Pathol. 2018 Nov 17. doi: 10.1016/j.humpath.2018.10.038.
The presence or absence in tumor cells of cortactin, a cytoskeleton-remodeling adapter protein, may be a marker to help pathologists distinguish between chronic lymphocytic leukemia (CLL) and mantle cell lymphoma (MCL), investigators suggest.
A study of cortactin expression in tumor samples from patients with B-cell CLL, MCL, and other hematologic malignancies showed that while cortactin was present in 14 of 17 CLL samples, it was not expressed on any of 16 MCL samples, reported Marco Pizzi, MD, PhD, from the University of Padova (Italy) and his colleagues.
“In particular, cortactin may contribute to the differential diagnosis between CLL and MCL, two neoplasms with similar histological features but very different clinical outcome. Further studies are needed to clarify the molecular mechanisms of deranged cortactin expression in MCL and CLL and to investigate any possible relationship between cortactin status and the biological features of these lymphomas,” they wrote in Human Pathology.
Overexpression of cortactin has been reported in several solid tumors, and increased expression of CTTN, the gene encoding for cortactin, has been associated with aggressive, poor prognosis disease, the investigators noted.
To characterize cortactin expression in lymphoid and hematopoietic cells and detect potential associations between cortactin and virulence of hematologic malignancies, the investigators performed immunohistochemical analysis on samples from 131 patients treated at their center. The samples included 17 cases of CLL, 16 of MCL, 25 of follicular lymphoma (FL), 30 of marginal zone lymphoma (MZL), 10 of hairy cell leukemia, three of splenic diffuse red pulp small B-cell lymphomas (SDRPBL), and 30 of diffuse large B-cell lymphoma (DLBCL).
They found that cortactin was expressed in 14 of the 17 CLL samples, all 10 of the HCL samples, and 22 of the 30 DLBCL samples. In contrast, there was no cortactin expression detected in any of either 16 MCL or three SDRPBL samples. The researchers found that 13 of 30 MZL samples had low-level staining. In FL, cortactin was expressed in 2 of the samples but in the remaining 23 cases the researchers found only scattered cortactin-positive lymphoid elements of non–B-cell lineage.
The investigators also found that cortactin expression in CLL correlated with other CLL-specific markers, and found that expression of two or more of the markers had 89.1% sensitivity, 100% specificity, a 100% positive predictive value, and 90.5% negative predictive value for a diagnosis of CLL.
In addition, they saw that the immunohistochemical results were similar to those for CTTN gene expression assessed by in silico analysis.
The investigators noted that CLL and MCL are challenging to differentiate from one another because of morphologic similarities and partially overlapping immunophenotypes.
“In this context, cortactin expression would strongly sustain a diagnosis of CLL over MCL, particularly in association with other CLL markers (i.e., LEF1 and CD200),” they wrote.
The study was internally supported. The authors declared no conflicts of interest.
SOURCE: Pizzi M et al. Hum Pathol. 2018 Nov 17. doi: 10.1016/j.humpath.2018.10.038.
FROM HUMAN PATHOLOGY
Key clinical point:
Major finding: Cortactin was expressed on 14 of 17 CLL samples vs. none of 16 MCL samples.
Study details: Immunohistochemistry analysis of samples from 131 patients with B-cell lineage non-Hodgkin lymphomas.
Disclosures: The study was internally supported. The authors reported having no conflicts of interest.
Source: Pizzi M et al. Hum Pathol. 2018 Nov 17. doi: 10.1016/j.humpath.2018.10.038.
New brain circuitry found with Parkinson’s disease gene therapy
A gene therapy for Parkinson’s disease, focusing on the subthalamic nucleus, appears to lead to the formation of unique brain circuitry that correlates with clinical improvement.
In a paper published online Nov. 28 in Science Translational Medicine, researchers describe the findings of a metabolic imaging study to explore the mechanism underlying benefits seen in a phase 2, blinded, sham-controlled clinical trial of the gene therapy.
The therapy in question used an adeno-associated viral vector to deliver the gene for glutamic acid decarboxylase into the subthalamic nucleus – a region of the brain known to be overactivated in Parkinson’s disease – which was intended to have an inhibitory effect on the neurons in that region.
Martin Niethammer, MD, PhD, of the Center for Neurosciences at The Feinstein Institute for Medical Research in New York, and his coauthors used 18F-fluorodeoxyglucose positron emission tomography at baseline, 6, and 12 months in 15 gene-therapy patients and 21 sham-treated patients, which revealed the development of new brain circuits in patients treated with the gene therapy.
The circuits, which researchers called the glutamic acid decarboxylase-related pattern, or GADRP, presented with increased metabolism in the premotor region – which also extended into the adjacent motor cortex – and in the supramarginal gyrus. There was also decreased metabolic activity in the caudate, anterior putamen, and adjacent globus pallidus; the ventral anterior and medial dorsal thalamic nuclei; and in the inferior frontal gyrus.
All 15 patients who received the gene therapy showed significant trends in GADRP expression after the treatment, compared with patients who underwent the sham procedure. Furthermore, these correlated significantly with improved clinical outcomes.
The imaging also revealed increased connectivity between regions in the GADRP space among patients who received the gene therapy, with researchers noting five new intrahemispheric node-to-node connections in these patients that were not seen in the sham procedure group.
These included connection linking the left caudate nucleus to the left superior frontal node, the right superior frontal node to the right supramarginal gyrus, and linking the left anterior putamen and globus pallidus with the ipsilateral thalamic node.
The authors also found that overall connectivity in the network rose to “abnormal” levels in the 12 months after gene therapy, while no similar increases were seen in the sham group.
Given that deep brain stimulation for Parkinson’s disease also targets the subthalamic nucleus, researchers looked at changes to the GADRP network in these patients, compared with those who received sham therapy and those who received gene therapy.
They saw that changes in GADRP expression were significantly different between the gene therapy-treated patients and those treated with deep brain stimulation and sham surgery. However, the differences between deep brain stimulation and sham surgery were not significant.
“The current study indicates that customized networks can be characterized using functional imaging data acquired in randomized, controlled phase 2 clinical trials and, if validated, could be used as quantitative outcome measures in more definitive, later-stage clinical trials,” the authors wrote.
The study was supported by Neurologix. Two authors were consultants and stockholders of MeiraGTx.
SOURCE: Niethammer N et al. Sci Transl Med. 2018 Nov 28. doi: 10.1126/scitranslmed.aau0713.
A gene therapy for Parkinson’s disease, focusing on the subthalamic nucleus, appears to lead to the formation of unique brain circuitry that correlates with clinical improvement.
In a paper published online Nov. 28 in Science Translational Medicine, researchers describe the findings of a metabolic imaging study to explore the mechanism underlying benefits seen in a phase 2, blinded, sham-controlled clinical trial of the gene therapy.
The therapy in question used an adeno-associated viral vector to deliver the gene for glutamic acid decarboxylase into the subthalamic nucleus – a region of the brain known to be overactivated in Parkinson’s disease – which was intended to have an inhibitory effect on the neurons in that region.
Martin Niethammer, MD, PhD, of the Center for Neurosciences at The Feinstein Institute for Medical Research in New York, and his coauthors used 18F-fluorodeoxyglucose positron emission tomography at baseline, 6, and 12 months in 15 gene-therapy patients and 21 sham-treated patients, which revealed the development of new brain circuits in patients treated with the gene therapy.
The circuits, which researchers called the glutamic acid decarboxylase-related pattern, or GADRP, presented with increased metabolism in the premotor region – which also extended into the adjacent motor cortex – and in the supramarginal gyrus. There was also decreased metabolic activity in the caudate, anterior putamen, and adjacent globus pallidus; the ventral anterior and medial dorsal thalamic nuclei; and in the inferior frontal gyrus.
All 15 patients who received the gene therapy showed significant trends in GADRP expression after the treatment, compared with patients who underwent the sham procedure. Furthermore, these correlated significantly with improved clinical outcomes.
The imaging also revealed increased connectivity between regions in the GADRP space among patients who received the gene therapy, with researchers noting five new intrahemispheric node-to-node connections in these patients that were not seen in the sham procedure group.
These included connection linking the left caudate nucleus to the left superior frontal node, the right superior frontal node to the right supramarginal gyrus, and linking the left anterior putamen and globus pallidus with the ipsilateral thalamic node.
The authors also found that overall connectivity in the network rose to “abnormal” levels in the 12 months after gene therapy, while no similar increases were seen in the sham group.
Given that deep brain stimulation for Parkinson’s disease also targets the subthalamic nucleus, researchers looked at changes to the GADRP network in these patients, compared with those who received sham therapy and those who received gene therapy.
They saw that changes in GADRP expression were significantly different between the gene therapy-treated patients and those treated with deep brain stimulation and sham surgery. However, the differences between deep brain stimulation and sham surgery were not significant.
“The current study indicates that customized networks can be characterized using functional imaging data acquired in randomized, controlled phase 2 clinical trials and, if validated, could be used as quantitative outcome measures in more definitive, later-stage clinical trials,” the authors wrote.
The study was supported by Neurologix. Two authors were consultants and stockholders of MeiraGTx.
SOURCE: Niethammer N et al. Sci Transl Med. 2018 Nov 28. doi: 10.1126/scitranslmed.aau0713.
A gene therapy for Parkinson’s disease, focusing on the subthalamic nucleus, appears to lead to the formation of unique brain circuitry that correlates with clinical improvement.
In a paper published online Nov. 28 in Science Translational Medicine, researchers describe the findings of a metabolic imaging study to explore the mechanism underlying benefits seen in a phase 2, blinded, sham-controlled clinical trial of the gene therapy.
The therapy in question used an adeno-associated viral vector to deliver the gene for glutamic acid decarboxylase into the subthalamic nucleus – a region of the brain known to be overactivated in Parkinson’s disease – which was intended to have an inhibitory effect on the neurons in that region.
Martin Niethammer, MD, PhD, of the Center for Neurosciences at The Feinstein Institute for Medical Research in New York, and his coauthors used 18F-fluorodeoxyglucose positron emission tomography at baseline, 6, and 12 months in 15 gene-therapy patients and 21 sham-treated patients, which revealed the development of new brain circuits in patients treated with the gene therapy.
The circuits, which researchers called the glutamic acid decarboxylase-related pattern, or GADRP, presented with increased metabolism in the premotor region – which also extended into the adjacent motor cortex – and in the supramarginal gyrus. There was also decreased metabolic activity in the caudate, anterior putamen, and adjacent globus pallidus; the ventral anterior and medial dorsal thalamic nuclei; and in the inferior frontal gyrus.
All 15 patients who received the gene therapy showed significant trends in GADRP expression after the treatment, compared with patients who underwent the sham procedure. Furthermore, these correlated significantly with improved clinical outcomes.
The imaging also revealed increased connectivity between regions in the GADRP space among patients who received the gene therapy, with researchers noting five new intrahemispheric node-to-node connections in these patients that were not seen in the sham procedure group.
These included connection linking the left caudate nucleus to the left superior frontal node, the right superior frontal node to the right supramarginal gyrus, and linking the left anterior putamen and globus pallidus with the ipsilateral thalamic node.
The authors also found that overall connectivity in the network rose to “abnormal” levels in the 12 months after gene therapy, while no similar increases were seen in the sham group.
Given that deep brain stimulation for Parkinson’s disease also targets the subthalamic nucleus, researchers looked at changes to the GADRP network in these patients, compared with those who received sham therapy and those who received gene therapy.
They saw that changes in GADRP expression were significantly different between the gene therapy-treated patients and those treated with deep brain stimulation and sham surgery. However, the differences between deep brain stimulation and sham surgery were not significant.
“The current study indicates that customized networks can be characterized using functional imaging data acquired in randomized, controlled phase 2 clinical trials and, if validated, could be used as quantitative outcome measures in more definitive, later-stage clinical trials,” the authors wrote.
The study was supported by Neurologix. Two authors were consultants and stockholders of MeiraGTx.
SOURCE: Niethammer N et al. Sci Transl Med. 2018 Nov 28. doi: 10.1126/scitranslmed.aau0713.
FROM SCIENCE TRANSLATIONAL MEDICINE
Key clinical point:
Major finding: Gene therapy for Parkinson’s disease was associated with increased brain connectivity.
Study details: A phase 2, blinded, sham-controlled study of 36 patients with Parkinson’s disease.
Disclosures: The study was supported by Neurologix. Two authors were consultants and stockholders of MeiraGTx.
Source: Niethammer N et al. Sci Transl Med. 2018 Nov 28. doi: 10.1126/scitranslmed.aau0713.
What is the ‘meta’ in ‘metaleadership’?
The knowns and the unknowns
Over the course of a career, it is not uncommon for people to become narrower and more focused in their work purview and interests. Competence in select procedures and practices imparts confidence and reliability in performance and results. One develops a reputation for those skills and capabilities, and others call upon them.
Rewards and incentives encourage advancement and promotion along established career paths, further accelerating specialization and concentration. At the top of your game, you advocate for and ease into your comfort zone. That zone is defined by the knowns of practice and the certainties they provide.
For those who prefer to practice in the confines of a narrow clinical sphere, that strategy could be the pathway to career success.
However, for those promoted to leadership positions, the inward and insulated focus today is counterproductive and even dangerous. Many times, physicians advance to a senior position because it is the next step in a preset career ladder, the reward for acumen in clinical skills, or simply out of boredom, with hope for a new landscape and a higher wage. But just because one has a high rank or impressive title does not mean that one is fulfilling the mandates of leadership. It takes more than that. You must be attuned to what is known and unknown in building stability and progress for those you lead.
A brief historic angle: For years, medicine occupied a sweet spot within the health care system. The profession protected its perks and privileges deriving from its untouchable status. With it came superiority, dominance, and protectionism. It was an inward, parochial focus of thinking, status, and reward. The problem was: This insulated mindset prompted a blind spot. The profession missed changes and transformation that were occurring just beyond the comfort zone. Those changes were unknowns in planning and perspective.
In the 1990s, medicine as a whole woke up to calls for change and a new order. The rise of the hospitalist was in part an outgrowth of that wake-up call. It reshaped power structures, status, and lucrative business arrangements within the profession. For many, the sweet spot soured.
The problem with collapsing into a sweet spot today is that so much is changing: all that is known and much that is unknown. Finances, technology, and demand are all in flux. The health care system finds itself in a quantity/quality/cost paradox. Volume accelerates, but at what cost to quality and morale? If someone or something can accomplish similar outcomes at less cost, why not go with the cheaper option? These questions can best be addressed by seeing them in the context of larger changes happening in the health system.
A new view for leaders
The “meta” in metaleadership hopes to provide a broader, disciplined slant on this phenomenon. That prefix – used to modify many concepts and terms – refers to a wider, more expansive view or a more comprehensive and transcendent perch on a topic. A “meta-” prefix invites a critical analysis of the original topic with the addition of new perspectives and insights, as with a meta-analysis.
Why then the need now for a “meta” view among health care leaders? It is easy in the course of career progression to lose track of the bigger picture of what you are doing and how it fits into changes occurring in society and for the profession. Even if your focus is on a particular clinical procedure, how does what you are doing fit into larger metatrends and changes? How might you tangibly contribute to the evolution of those trends? If you are in a leadership position, how do you fit your practice or department into the bigger picture? How might this enterprise perspective speak to your career trajectory?
To inform these questions, build your platform for knowns and unknowns. There are four combinations in the “known-unknown” equation. They are each important and provocative for leaders. Your awareness of them prompts curiosity about “meta” problems and problem solving.
- There are the “known-knowns”: what you know and you know you know it. The problem here is that you may assume that you know something that you don’t.
- There are the “known-unknowns”: Clear and curious about what you need to learn, you develop pathways to find out.
- There are the “unknown-knowns”: what others know and you don’t; a point of vulnerability if you are not careful to discover and figure this out.
- And finally, the “unknown-unknowns”: the mysteries of what could lie ahead that no one yet fully comprehends.
The task for the “metaleader”? Be clear on what you know, and seek always to learn and discover those unknowns. The better you factor them into your assessments, the better you are able to shape trends and the less likely you are to be overrun by them.
Just as you become more specialized with time, as a leader, you can leverage your experience to widen your lens and see more, understand it better, and – with that knowledge – chart a pathway that corresponds with where the health system is going. With this wider mindset, you fashion a fresh and innovative perspective on what is happening with health care and the options for constructively addressing new constraints and opportunities. You think big, reach far, and with this broader understanding, foment a lively set of perspectives and options that would otherwise not be available for those you lead. And when seen as a puzzle to learn and solve, the “meta” perch provides an engaging angle on the game of health care change. You too can be a player.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution at Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
The knowns and the unknowns
The knowns and the unknowns
Over the course of a career, it is not uncommon for people to become narrower and more focused in their work purview and interests. Competence in select procedures and practices imparts confidence and reliability in performance and results. One develops a reputation for those skills and capabilities, and others call upon them.
Rewards and incentives encourage advancement and promotion along established career paths, further accelerating specialization and concentration. At the top of your game, you advocate for and ease into your comfort zone. That zone is defined by the knowns of practice and the certainties they provide.
For those who prefer to practice in the confines of a narrow clinical sphere, that strategy could be the pathway to career success.
However, for those promoted to leadership positions, the inward and insulated focus today is counterproductive and even dangerous. Many times, physicians advance to a senior position because it is the next step in a preset career ladder, the reward for acumen in clinical skills, or simply out of boredom, with hope for a new landscape and a higher wage. But just because one has a high rank or impressive title does not mean that one is fulfilling the mandates of leadership. It takes more than that. You must be attuned to what is known and unknown in building stability and progress for those you lead.
A brief historic angle: For years, medicine occupied a sweet spot within the health care system. The profession protected its perks and privileges deriving from its untouchable status. With it came superiority, dominance, and protectionism. It was an inward, parochial focus of thinking, status, and reward. The problem was: This insulated mindset prompted a blind spot. The profession missed changes and transformation that were occurring just beyond the comfort zone. Those changes were unknowns in planning and perspective.
In the 1990s, medicine as a whole woke up to calls for change and a new order. The rise of the hospitalist was in part an outgrowth of that wake-up call. It reshaped power structures, status, and lucrative business arrangements within the profession. For many, the sweet spot soured.
The problem with collapsing into a sweet spot today is that so much is changing: all that is known and much that is unknown. Finances, technology, and demand are all in flux. The health care system finds itself in a quantity/quality/cost paradox. Volume accelerates, but at what cost to quality and morale? If someone or something can accomplish similar outcomes at less cost, why not go with the cheaper option? These questions can best be addressed by seeing them in the context of larger changes happening in the health system.
A new view for leaders
The “meta” in metaleadership hopes to provide a broader, disciplined slant on this phenomenon. That prefix – used to modify many concepts and terms – refers to a wider, more expansive view or a more comprehensive and transcendent perch on a topic. A “meta-” prefix invites a critical analysis of the original topic with the addition of new perspectives and insights, as with a meta-analysis.
Why then the need now for a “meta” view among health care leaders? It is easy in the course of career progression to lose track of the bigger picture of what you are doing and how it fits into changes occurring in society and for the profession. Even if your focus is on a particular clinical procedure, how does what you are doing fit into larger metatrends and changes? How might you tangibly contribute to the evolution of those trends? If you are in a leadership position, how do you fit your practice or department into the bigger picture? How might this enterprise perspective speak to your career trajectory?
To inform these questions, build your platform for knowns and unknowns. There are four combinations in the “known-unknown” equation. They are each important and provocative for leaders. Your awareness of them prompts curiosity about “meta” problems and problem solving.
- There are the “known-knowns”: what you know and you know you know it. The problem here is that you may assume that you know something that you don’t.
- There are the “known-unknowns”: Clear and curious about what you need to learn, you develop pathways to find out.
- There are the “unknown-knowns”: what others know and you don’t; a point of vulnerability if you are not careful to discover and figure this out.
- And finally, the “unknown-unknowns”: the mysteries of what could lie ahead that no one yet fully comprehends.
The task for the “metaleader”? Be clear on what you know, and seek always to learn and discover those unknowns. The better you factor them into your assessments, the better you are able to shape trends and the less likely you are to be overrun by them.
Just as you become more specialized with time, as a leader, you can leverage your experience to widen your lens and see more, understand it better, and – with that knowledge – chart a pathway that corresponds with where the health system is going. With this wider mindset, you fashion a fresh and innovative perspective on what is happening with health care and the options for constructively addressing new constraints and opportunities. You think big, reach far, and with this broader understanding, foment a lively set of perspectives and options that would otherwise not be available for those you lead. And when seen as a puzzle to learn and solve, the “meta” perch provides an engaging angle on the game of health care change. You too can be a player.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution at Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].
Over the course of a career, it is not uncommon for people to become narrower and more focused in their work purview and interests. Competence in select procedures and practices imparts confidence and reliability in performance and results. One develops a reputation for those skills and capabilities, and others call upon them.
Rewards and incentives encourage advancement and promotion along established career paths, further accelerating specialization and concentration. At the top of your game, you advocate for and ease into your comfort zone. That zone is defined by the knowns of practice and the certainties they provide.
For those who prefer to practice in the confines of a narrow clinical sphere, that strategy could be the pathway to career success.
However, for those promoted to leadership positions, the inward and insulated focus today is counterproductive and even dangerous. Many times, physicians advance to a senior position because it is the next step in a preset career ladder, the reward for acumen in clinical skills, or simply out of boredom, with hope for a new landscape and a higher wage. But just because one has a high rank or impressive title does not mean that one is fulfilling the mandates of leadership. It takes more than that. You must be attuned to what is known and unknown in building stability and progress for those you lead.
A brief historic angle: For years, medicine occupied a sweet spot within the health care system. The profession protected its perks and privileges deriving from its untouchable status. With it came superiority, dominance, and protectionism. It was an inward, parochial focus of thinking, status, and reward. The problem was: This insulated mindset prompted a blind spot. The profession missed changes and transformation that were occurring just beyond the comfort zone. Those changes were unknowns in planning and perspective.
In the 1990s, medicine as a whole woke up to calls for change and a new order. The rise of the hospitalist was in part an outgrowth of that wake-up call. It reshaped power structures, status, and lucrative business arrangements within the profession. For many, the sweet spot soured.
The problem with collapsing into a sweet spot today is that so much is changing: all that is known and much that is unknown. Finances, technology, and demand are all in flux. The health care system finds itself in a quantity/quality/cost paradox. Volume accelerates, but at what cost to quality and morale? If someone or something can accomplish similar outcomes at less cost, why not go with the cheaper option? These questions can best be addressed by seeing them in the context of larger changes happening in the health system.
A new view for leaders
The “meta” in metaleadership hopes to provide a broader, disciplined slant on this phenomenon. That prefix – used to modify many concepts and terms – refers to a wider, more expansive view or a more comprehensive and transcendent perch on a topic. A “meta-” prefix invites a critical analysis of the original topic with the addition of new perspectives and insights, as with a meta-analysis.
Why then the need now for a “meta” view among health care leaders? It is easy in the course of career progression to lose track of the bigger picture of what you are doing and how it fits into changes occurring in society and for the profession. Even if your focus is on a particular clinical procedure, how does what you are doing fit into larger metatrends and changes? How might you tangibly contribute to the evolution of those trends? If you are in a leadership position, how do you fit your practice or department into the bigger picture? How might this enterprise perspective speak to your career trajectory?
To inform these questions, build your platform for knowns and unknowns. There are four combinations in the “known-unknown” equation. They are each important and provocative for leaders. Your awareness of them prompts curiosity about “meta” problems and problem solving.
- There are the “known-knowns”: what you know and you know you know it. The problem here is that you may assume that you know something that you don’t.
- There are the “known-unknowns”: Clear and curious about what you need to learn, you develop pathways to find out.
- There are the “unknown-knowns”: what others know and you don’t; a point of vulnerability if you are not careful to discover and figure this out.
- And finally, the “unknown-unknowns”: the mysteries of what could lie ahead that no one yet fully comprehends.
The task for the “metaleader”? Be clear on what you know, and seek always to learn and discover those unknowns. The better you factor them into your assessments, the better you are able to shape trends and the less likely you are to be overrun by them.
Just as you become more specialized with time, as a leader, you can leverage your experience to widen your lens and see more, understand it better, and – with that knowledge – chart a pathway that corresponds with where the health system is going. With this wider mindset, you fashion a fresh and innovative perspective on what is happening with health care and the options for constructively addressing new constraints and opportunities. You think big, reach far, and with this broader understanding, foment a lively set of perspectives and options that would otherwise not be available for those you lead. And when seen as a puzzle to learn and solve, the “meta” perch provides an engaging angle on the game of health care change. You too can be a player.
Dr. Marcus is coauthor of “Renegotiating Health Care: Resolving Conflict to Build Collaboration,” 2nd ed. (San Francisco: Jossey-Bass Publishers, 2011) and is director of the program for health care negotiation and conflict resolution at Harvard T.H. Chan School of Public Health, Boston. Dr. Marcus teaches regularly in the SHM Leadership Academy. He can be reached at [email protected].