User login
Most perpetrators in school shootings brought guns from home
SEATTLE – A new analysis of all school shootings, including those with four or fewer victims, reinforces the need for prevention in the home by preventing guns from falling into unauthorized use.
The researchers examined 223 shootings in the United States that occurred during 2005-2012 and found that in more than a third of the 60 cases for which information was available, the perpetrator obtained the gun from the home and was aged 17 years or younger. Furthermore, evidence of mental illness in the shooter was rare.
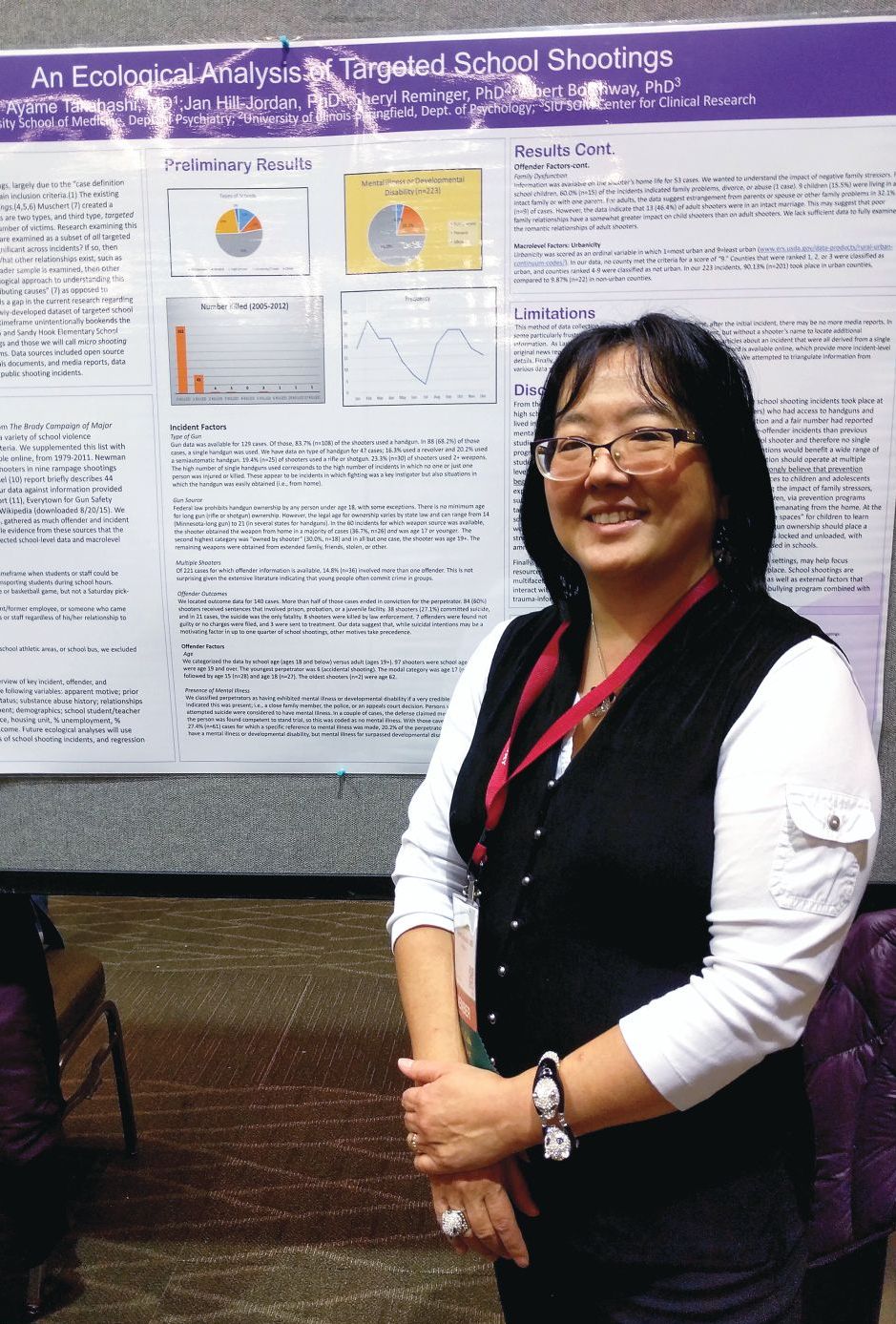
The finding complements studies of “mass shootings,” which tend to garner headlines and more research attention, according to Ayame Takahashi, MD, who presented the findings at a poster session at the annual meeting of the American Academy of Child and Adolescent Psychiatry. “What we see in the news are the big rampage shootings, with multiple victims, where the target may be anyone they can get. You hear in little bits and pieces about the single-shooter incidents, which are way more common.
“We wanted to look at as many of these cases as we could find to look at the overall variables that might be behind these smaller school shootings, which are way more common,” said Dr. Takahashi, who is an assistant professor of psychiatry at Southern Illinois University Medicine, Springfield.
The researchers identified shootings using the data from the Brady Campaign to Prevent Gun Violence during 1997-2012, and supplemented it with listings found in “The Bully Society: School shootings and the crisis of bullying in America’s schools” (New York: NYU Press, 2013). Other sources included a study on rampage shootings in U.S. high school and college settings during 2002-2008; the Virginia Tech Review Panel report, a 2014 FBI report, the Everytown for Gun Safety website, and the list of school shootings on Wikipedia.
The analysis included incidents that had occurred on a school property, including school buses, at a time when students or staff would have been at risk. The offender could have been a current or former student or employee, or anyone who came onto the school property with the intent to harm students or staff.
The sample included 223 shootings. In 60 cases, the researchers found information about how guns were obtained, and in 37% of those cases, the source was the offender’s home and the offender was 17 years old or younger. In 30% of the cases, the shooter owned the gun, but in almost all these cases, the shooter was aged 19 years or older.
Sixty-one cases had information available about the presence or absence of mental illness in the offender. In 20% of these cases, the shooter was determined to have a mental illness or, rarely, a developmental disability.
The results suggest that mental illness might be rare among school shooters, and therefore, call into question efforts to limit gun ownership among people with mental illness. “It may be barking up the wrong tree,” Dr. Takahashi said.
Instead, she advocates more messaging of gun safety in the home, to prevent unauthorized use. Psychiatrists can help by discussing these issues with patients, but she also called for more community involvement and education about the issue.
“The people who come to you, they’re kind of in your court already. so that the message gets out there beyond the folks that we see in our offices,” she said.
Dr. Takahashi has no relevant disclosures.
SEATTLE – A new analysis of all school shootings, including those with four or fewer victims, reinforces the need for prevention in the home by preventing guns from falling into unauthorized use.
The researchers examined 223 shootings in the United States that occurred during 2005-2012 and found that in more than a third of the 60 cases for which information was available, the perpetrator obtained the gun from the home and was aged 17 years or younger. Furthermore, evidence of mental illness in the shooter was rare.
The finding complements studies of “mass shootings,” which tend to garner headlines and more research attention, according to Ayame Takahashi, MD, who presented the findings at a poster session at the annual meeting of the American Academy of Child and Adolescent Psychiatry. “What we see in the news are the big rampage shootings, with multiple victims, where the target may be anyone they can get. You hear in little bits and pieces about the single-shooter incidents, which are way more common.
“We wanted to look at as many of these cases as we could find to look at the overall variables that might be behind these smaller school shootings, which are way more common,” said Dr. Takahashi, who is an assistant professor of psychiatry at Southern Illinois University Medicine, Springfield.
The researchers identified shootings using the data from the Brady Campaign to Prevent Gun Violence during 1997-2012, and supplemented it with listings found in “The Bully Society: School shootings and the crisis of bullying in America’s schools” (New York: NYU Press, 2013). Other sources included a study on rampage shootings in U.S. high school and college settings during 2002-2008; the Virginia Tech Review Panel report, a 2014 FBI report, the Everytown for Gun Safety website, and the list of school shootings on Wikipedia.
The analysis included incidents that had occurred on a school property, including school buses, at a time when students or staff would have been at risk. The offender could have been a current or former student or employee, or anyone who came onto the school property with the intent to harm students or staff.
The sample included 223 shootings. In 60 cases, the researchers found information about how guns were obtained, and in 37% of those cases, the source was the offender’s home and the offender was 17 years old or younger. In 30% of the cases, the shooter owned the gun, but in almost all these cases, the shooter was aged 19 years or older.
Sixty-one cases had information available about the presence or absence of mental illness in the offender. In 20% of these cases, the shooter was determined to have a mental illness or, rarely, a developmental disability.
The results suggest that mental illness might be rare among school shooters, and therefore, call into question efforts to limit gun ownership among people with mental illness. “It may be barking up the wrong tree,” Dr. Takahashi said.
Instead, she advocates more messaging of gun safety in the home, to prevent unauthorized use. Psychiatrists can help by discussing these issues with patients, but she also called for more community involvement and education about the issue.
“The people who come to you, they’re kind of in your court already. so that the message gets out there beyond the folks that we see in our offices,” she said.
Dr. Takahashi has no relevant disclosures.
SEATTLE – A new analysis of all school shootings, including those with four or fewer victims, reinforces the need for prevention in the home by preventing guns from falling into unauthorized use.
The researchers examined 223 shootings in the United States that occurred during 2005-2012 and found that in more than a third of the 60 cases for which information was available, the perpetrator obtained the gun from the home and was aged 17 years or younger. Furthermore, evidence of mental illness in the shooter was rare.
The finding complements studies of “mass shootings,” which tend to garner headlines and more research attention, according to Ayame Takahashi, MD, who presented the findings at a poster session at the annual meeting of the American Academy of Child and Adolescent Psychiatry. “What we see in the news are the big rampage shootings, with multiple victims, where the target may be anyone they can get. You hear in little bits and pieces about the single-shooter incidents, which are way more common.
“We wanted to look at as many of these cases as we could find to look at the overall variables that might be behind these smaller school shootings, which are way more common,” said Dr. Takahashi, who is an assistant professor of psychiatry at Southern Illinois University Medicine, Springfield.
The researchers identified shootings using the data from the Brady Campaign to Prevent Gun Violence during 1997-2012, and supplemented it with listings found in “The Bully Society: School shootings and the crisis of bullying in America’s schools” (New York: NYU Press, 2013). Other sources included a study on rampage shootings in U.S. high school and college settings during 2002-2008; the Virginia Tech Review Panel report, a 2014 FBI report, the Everytown for Gun Safety website, and the list of school shootings on Wikipedia.
The analysis included incidents that had occurred on a school property, including school buses, at a time when students or staff would have been at risk. The offender could have been a current or former student or employee, or anyone who came onto the school property with the intent to harm students or staff.
The sample included 223 shootings. In 60 cases, the researchers found information about how guns were obtained, and in 37% of those cases, the source was the offender’s home and the offender was 17 years old or younger. In 30% of the cases, the shooter owned the gun, but in almost all these cases, the shooter was aged 19 years or older.
Sixty-one cases had information available about the presence or absence of mental illness in the offender. In 20% of these cases, the shooter was determined to have a mental illness or, rarely, a developmental disability.
The results suggest that mental illness might be rare among school shooters, and therefore, call into question efforts to limit gun ownership among people with mental illness. “It may be barking up the wrong tree,” Dr. Takahashi said.
Instead, she advocates more messaging of gun safety in the home, to prevent unauthorized use. Psychiatrists can help by discussing these issues with patients, but she also called for more community involvement and education about the issue.
“The people who come to you, they’re kind of in your court already. so that the message gets out there beyond the folks that we see in our offices,” she said.
Dr. Takahashi has no relevant disclosures.
REPORTING FROM AACAP 2018
Key clinical point: Psychiatrists can help by discussing gun safety with patients.
Major finding: About 20% of school shooters had a confirmed mental illness or developmental disability.
Study details: Analysis of 223 school shootings in the United States between 2005 and 2012.
Disclosures: Dr. Takahashi had no relevant disclosures.
Scleroderma SCOT trial findings hold similar in lung disease
CHICAGO – Changes in quantitative lung CT scores for scleroderma-related interstitial lung disease independently validate the superiority of hematopoietic stem cell transplantation versus cyclophosphamide for severe systemic sclerosis, according to findings in a subset of patients from the SCOT (Scleroderma: Cyclophosphamide or Transplantation) trial.
The recently published findings from the SCOT trial showed that myeloablation followed by autologous hematopoietic stem cell transplant (HSCT) significantly improved event-free and overall survival of systemic sclerosis patients at 54 months, compared with 12 monthly treatments with intravenous cyclophosphamide (N Engl J Med. 2018;378:35-47).
In a subset of 75 patients from the SCOT trial, the investigators analyzed changes in lung parenchymal abnormalities on high-resolution CT scans between baseline and serial follow-up exams performed yearly for up to 5 years. Follow-up scans at 14, 26, 48, and 54 months in available patients at each time point showed that whole-lung quantitative interstitial lung disease (QILD) scores – a validated measure that combines various CT texture-based characteristics to determine disease extent – decreased significantly by 7% at 54 months in patients who underwent HSCT, compared with no change in those who received cyclophosphamide (CYC; P = .024), Keith M. Sullivan, MD, reported at the annual meeting of the American College of Rheumatology.
Additionally, whole-lung quantitative lung fibrosis (QLF) scores were stable (–1%) in the HSCT patients, but increased 3% in the CYC patients (P = .047), said Dr. Sullivan, a professor of medicine at Duke University, Durham, N.C.
Dr. Sullivan was the first author on the SCOT trial, and he reported the current study results on behalf of lead investigator Jonathan Goldin, MD, PhD, of the department of radiologic sciences at the University of California, Los Angeles.
“These are really kind of meaningful associations, especially since the worst of the [CYC] treatment group didn’t make it to month 54,” Dr. Sullivan said.
Quantitative scores of scleroderma-related interstitial lung disease were measured using computer-based quantitative image analysis of standardized, noncontrast, volumetric, thin-section, thoracic, high-resolution CT. The same CT machine was used for all time points (except for one subject) with careful attention to breath hold reproducibility and image quality. Baseline characteristics were not different between the HSCT and CYC groups, he noted, stressing the rigorous study design.
CT assessments were also compared for the most severe lobe in each patient and showed similar findings, with both QILD and QLF scores for that lobe improving in the HSCT patients relative to the CYC patients (P = .004 and P = .002, respectively), Dr. Sullivan said, adding that the direction of change in structural measures of QILD and QLF for both whole lung and most severe lobe CTs tracked with physiological pulmonary function tests, including forced vital capacity (FVC), forced expiratory volume in 1 second, and diffusing capacity of the lungs for carbon monoxide.
“The FVC improved while QILD decreased, and that’s what you would expect to see,” he said. “So for each of these ways of displaying data, there was an expected and sensible inverse correlation.”
Scleroderma-related interstitial lung disease is a major cause of morbidity and mortality in severe systemic sclerosis. In the wake of the SCOT trial findings, questions remained with respect to correlation between those findings and pulmonary function; if the improvements with HSCT are real and meaningful, they should have meaningful correlation with pulmonary function, and these findings demonstrate those correlates, he said.
“Changes in quantitative lung CT scoring of scleroderma lung disease provide an objective radiologic validation of the long-term benefits of transplant compared to cyclophosphamide in individuals with severe scleroderma and lung involvement. Improvement in imaging after transplant continues for up to 54 months after randomization, giving radiologic confirmation of a durable treatment benefit,” Dr. Sullivan concluded.
The investigators reported having no relevant disclosures.
SOURCE: Goldin J et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 901.
CHICAGO – Changes in quantitative lung CT scores for scleroderma-related interstitial lung disease independently validate the superiority of hematopoietic stem cell transplantation versus cyclophosphamide for severe systemic sclerosis, according to findings in a subset of patients from the SCOT (Scleroderma: Cyclophosphamide or Transplantation) trial.
The recently published findings from the SCOT trial showed that myeloablation followed by autologous hematopoietic stem cell transplant (HSCT) significantly improved event-free and overall survival of systemic sclerosis patients at 54 months, compared with 12 monthly treatments with intravenous cyclophosphamide (N Engl J Med. 2018;378:35-47).
In a subset of 75 patients from the SCOT trial, the investigators analyzed changes in lung parenchymal abnormalities on high-resolution CT scans between baseline and serial follow-up exams performed yearly for up to 5 years. Follow-up scans at 14, 26, 48, and 54 months in available patients at each time point showed that whole-lung quantitative interstitial lung disease (QILD) scores – a validated measure that combines various CT texture-based characteristics to determine disease extent – decreased significantly by 7% at 54 months in patients who underwent HSCT, compared with no change in those who received cyclophosphamide (CYC; P = .024), Keith M. Sullivan, MD, reported at the annual meeting of the American College of Rheumatology.
Additionally, whole-lung quantitative lung fibrosis (QLF) scores were stable (–1%) in the HSCT patients, but increased 3% in the CYC patients (P = .047), said Dr. Sullivan, a professor of medicine at Duke University, Durham, N.C.
Dr. Sullivan was the first author on the SCOT trial, and he reported the current study results on behalf of lead investigator Jonathan Goldin, MD, PhD, of the department of radiologic sciences at the University of California, Los Angeles.
“These are really kind of meaningful associations, especially since the worst of the [CYC] treatment group didn’t make it to month 54,” Dr. Sullivan said.
Quantitative scores of scleroderma-related interstitial lung disease were measured using computer-based quantitative image analysis of standardized, noncontrast, volumetric, thin-section, thoracic, high-resolution CT. The same CT machine was used for all time points (except for one subject) with careful attention to breath hold reproducibility and image quality. Baseline characteristics were not different between the HSCT and CYC groups, he noted, stressing the rigorous study design.
CT assessments were also compared for the most severe lobe in each patient and showed similar findings, with both QILD and QLF scores for that lobe improving in the HSCT patients relative to the CYC patients (P = .004 and P = .002, respectively), Dr. Sullivan said, adding that the direction of change in structural measures of QILD and QLF for both whole lung and most severe lobe CTs tracked with physiological pulmonary function tests, including forced vital capacity (FVC), forced expiratory volume in 1 second, and diffusing capacity of the lungs for carbon monoxide.
“The FVC improved while QILD decreased, and that’s what you would expect to see,” he said. “So for each of these ways of displaying data, there was an expected and sensible inverse correlation.”
Scleroderma-related interstitial lung disease is a major cause of morbidity and mortality in severe systemic sclerosis. In the wake of the SCOT trial findings, questions remained with respect to correlation between those findings and pulmonary function; if the improvements with HSCT are real and meaningful, they should have meaningful correlation with pulmonary function, and these findings demonstrate those correlates, he said.
“Changes in quantitative lung CT scoring of scleroderma lung disease provide an objective radiologic validation of the long-term benefits of transplant compared to cyclophosphamide in individuals with severe scleroderma and lung involvement. Improvement in imaging after transplant continues for up to 54 months after randomization, giving radiologic confirmation of a durable treatment benefit,” Dr. Sullivan concluded.
The investigators reported having no relevant disclosures.
SOURCE: Goldin J et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 901.
CHICAGO – Changes in quantitative lung CT scores for scleroderma-related interstitial lung disease independently validate the superiority of hematopoietic stem cell transplantation versus cyclophosphamide for severe systemic sclerosis, according to findings in a subset of patients from the SCOT (Scleroderma: Cyclophosphamide or Transplantation) trial.
The recently published findings from the SCOT trial showed that myeloablation followed by autologous hematopoietic stem cell transplant (HSCT) significantly improved event-free and overall survival of systemic sclerosis patients at 54 months, compared with 12 monthly treatments with intravenous cyclophosphamide (N Engl J Med. 2018;378:35-47).
In a subset of 75 patients from the SCOT trial, the investigators analyzed changes in lung parenchymal abnormalities on high-resolution CT scans between baseline and serial follow-up exams performed yearly for up to 5 years. Follow-up scans at 14, 26, 48, and 54 months in available patients at each time point showed that whole-lung quantitative interstitial lung disease (QILD) scores – a validated measure that combines various CT texture-based characteristics to determine disease extent – decreased significantly by 7% at 54 months in patients who underwent HSCT, compared with no change in those who received cyclophosphamide (CYC; P = .024), Keith M. Sullivan, MD, reported at the annual meeting of the American College of Rheumatology.
Additionally, whole-lung quantitative lung fibrosis (QLF) scores were stable (–1%) in the HSCT patients, but increased 3% in the CYC patients (P = .047), said Dr. Sullivan, a professor of medicine at Duke University, Durham, N.C.
Dr. Sullivan was the first author on the SCOT trial, and he reported the current study results on behalf of lead investigator Jonathan Goldin, MD, PhD, of the department of radiologic sciences at the University of California, Los Angeles.
“These are really kind of meaningful associations, especially since the worst of the [CYC] treatment group didn’t make it to month 54,” Dr. Sullivan said.
Quantitative scores of scleroderma-related interstitial lung disease were measured using computer-based quantitative image analysis of standardized, noncontrast, volumetric, thin-section, thoracic, high-resolution CT. The same CT machine was used for all time points (except for one subject) with careful attention to breath hold reproducibility and image quality. Baseline characteristics were not different between the HSCT and CYC groups, he noted, stressing the rigorous study design.
CT assessments were also compared for the most severe lobe in each patient and showed similar findings, with both QILD and QLF scores for that lobe improving in the HSCT patients relative to the CYC patients (P = .004 and P = .002, respectively), Dr. Sullivan said, adding that the direction of change in structural measures of QILD and QLF for both whole lung and most severe lobe CTs tracked with physiological pulmonary function tests, including forced vital capacity (FVC), forced expiratory volume in 1 second, and diffusing capacity of the lungs for carbon monoxide.
“The FVC improved while QILD decreased, and that’s what you would expect to see,” he said. “So for each of these ways of displaying data, there was an expected and sensible inverse correlation.”
Scleroderma-related interstitial lung disease is a major cause of morbidity and mortality in severe systemic sclerosis. In the wake of the SCOT trial findings, questions remained with respect to correlation between those findings and pulmonary function; if the improvements with HSCT are real and meaningful, they should have meaningful correlation with pulmonary function, and these findings demonstrate those correlates, he said.
“Changes in quantitative lung CT scoring of scleroderma lung disease provide an objective radiologic validation of the long-term benefits of transplant compared to cyclophosphamide in individuals with severe scleroderma and lung involvement. Improvement in imaging after transplant continues for up to 54 months after randomization, giving radiologic confirmation of a durable treatment benefit,” Dr. Sullivan concluded.
The investigators reported having no relevant disclosures.
SOURCE: Goldin J et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 901.
REPORTING FROM THE ACR ANNUAL MEETING
Key clinical point: Lung CT scores remain stable or improve following hematopoietic stem cell transplantation in patients with scleroderma-related interstitial lung disease when compared against monthly cyclophosphamide treatments.
Major finding: Quantitative interstitial lung disease scores decreased by 7% at 54 months in hematopoietic stem cell transplant patients versus no change in those who received cyclophosphamide (P = .024).
Study details: A study of 75 patients from the SCOT trial.
Disclosures: The investigators reported having no relevant disclosures.
Source: Goldin J et al. Arthritis Rheumatol. 2018;70(Suppl 10): Abstract 901.
Dr. Mary Edwards Walker Inspiring Women in Surgery Award presented to Dr. Lee
The American College of Surgeons (ACS) presented the Dr. Mary Edwards Walker Inspiring Women in Surgery Award to Yeu-Tsu Margaret Lee, MD, FACS, at the Convocation at Clinical Congress 2018 in Boston, MA. This award was established by the ACS Women in Surgery Committee (WiSC) and is presented annually at the Clinical Congress to recognize an individual’s significant contributions to the advancement of women in surgery.
Dr. Lee is from Honolulu, HI, and was born in Xian, China, in 1936. During her childhood, four of her siblings died from illness, motivating Dr. Lee to become a physician. Her family was forced to flee to Taiwan after the Chinese Civil War, and she immigrated to the U.S. in 1955, graduated from Harvard Medical School, Boston, in 1961, and has worked as a general surgeon and a surgical oncologist for more than 50 years. In the early 1980s, she was a tenured associate professor of surgery, University of Southern California (USC), Los Angeles, and head physician, Los Angeles County-USC Medical Center, but chose to pursue a different path.
In 1983, Dr. Lee moved to Hawaii, worked at Tripler Army Medical Center, Honolulu, as chief, surgical oncology section of general surgical services, and joined the U.S. Army Corps. She was deployed to Iraq during Operation Desert Storm and treated many U.S. soldiers as well as Iraqi prisoners of war. She served on a team of surgeons that performed more than 125 operations in a 400-bed hospital in northern Saudi Arabia. Dr. Lee received several accolades in the military, including an “A” Proficiency Designator from the Army Medical Department and a Certificate of Achievement. After retiring from the Army as a colonel, she became professor of surgery, University of Hawaii at Manoa, Honolulu, where she was the only woman surgeon for most of her career.
Dr. Lee has participated in medical missions to Ghana, Honduras, Cambodia, Laos, the Philippines, and other underserved countries. She has made many international trips to promote friendship and medical exchanges. Notably, in 1995, she was the leader of a Women Surgeons Delegation to Russia and Romania. The trip was a Citizen Ambassador Program sponsored by People to People International, which was established by President Dwight D. Eisenhower. From 2000 to 2017, Dr. Lee taught surgery for a month, four times a year, at the Tzu-Chi University School of Medicine, Hualien, Taiwan.
Dr. Lee was one of 21 women surgeons in attendance at a networking breakfast at the 1981 Clinical Congress—led by ACS Past-President Patricia Numann, MD, FACS—which proved to be the genesis of the Association of Women Surgeons (AWS). She has been a supporter of the association, in time and talent, since its inception, and her presence at the AWS meetings, her academic career at teaching hospitals, and her research publications provide women surgeons and medical students from around the world an example of what women can achieve in the field.
Because her home is in Hawaii, midway between the East and West, she hopes to function as a “bridge,” contributing to global understanding and promoting communication, collaboration, and goodwill, and continues to work in the areas of medical education, international health, and world peace.
Committed to improving the care of the surgical patient, Dr. Lee is an outstanding leader and role model for surgeons everywhere. Her contributions to academic medicine in surgery, in the military, and in surgical volunteerism worldwide have made a lasting impression on the surgical profession. Her passion, endless energy, and dedication to the ACS and to women in surgery are without equal.
The American College of Surgeons (ACS) presented the Dr. Mary Edwards Walker Inspiring Women in Surgery Award to Yeu-Tsu Margaret Lee, MD, FACS, at the Convocation at Clinical Congress 2018 in Boston, MA. This award was established by the ACS Women in Surgery Committee (WiSC) and is presented annually at the Clinical Congress to recognize an individual’s significant contributions to the advancement of women in surgery.
Dr. Lee is from Honolulu, HI, and was born in Xian, China, in 1936. During her childhood, four of her siblings died from illness, motivating Dr. Lee to become a physician. Her family was forced to flee to Taiwan after the Chinese Civil War, and she immigrated to the U.S. in 1955, graduated from Harvard Medical School, Boston, in 1961, and has worked as a general surgeon and a surgical oncologist for more than 50 years. In the early 1980s, she was a tenured associate professor of surgery, University of Southern California (USC), Los Angeles, and head physician, Los Angeles County-USC Medical Center, but chose to pursue a different path.
In 1983, Dr. Lee moved to Hawaii, worked at Tripler Army Medical Center, Honolulu, as chief, surgical oncology section of general surgical services, and joined the U.S. Army Corps. She was deployed to Iraq during Operation Desert Storm and treated many U.S. soldiers as well as Iraqi prisoners of war. She served on a team of surgeons that performed more than 125 operations in a 400-bed hospital in northern Saudi Arabia. Dr. Lee received several accolades in the military, including an “A” Proficiency Designator from the Army Medical Department and a Certificate of Achievement. After retiring from the Army as a colonel, she became professor of surgery, University of Hawaii at Manoa, Honolulu, where she was the only woman surgeon for most of her career.
Dr. Lee has participated in medical missions to Ghana, Honduras, Cambodia, Laos, the Philippines, and other underserved countries. She has made many international trips to promote friendship and medical exchanges. Notably, in 1995, she was the leader of a Women Surgeons Delegation to Russia and Romania. The trip was a Citizen Ambassador Program sponsored by People to People International, which was established by President Dwight D. Eisenhower. From 2000 to 2017, Dr. Lee taught surgery for a month, four times a year, at the Tzu-Chi University School of Medicine, Hualien, Taiwan.
Dr. Lee was one of 21 women surgeons in attendance at a networking breakfast at the 1981 Clinical Congress—led by ACS Past-President Patricia Numann, MD, FACS—which proved to be the genesis of the Association of Women Surgeons (AWS). She has been a supporter of the association, in time and talent, since its inception, and her presence at the AWS meetings, her academic career at teaching hospitals, and her research publications provide women surgeons and medical students from around the world an example of what women can achieve in the field.
Because her home is in Hawaii, midway between the East and West, she hopes to function as a “bridge,” contributing to global understanding and promoting communication, collaboration, and goodwill, and continues to work in the areas of medical education, international health, and world peace.
Committed to improving the care of the surgical patient, Dr. Lee is an outstanding leader and role model for surgeons everywhere. Her contributions to academic medicine in surgery, in the military, and in surgical volunteerism worldwide have made a lasting impression on the surgical profession. Her passion, endless energy, and dedication to the ACS and to women in surgery are without equal.
The American College of Surgeons (ACS) presented the Dr. Mary Edwards Walker Inspiring Women in Surgery Award to Yeu-Tsu Margaret Lee, MD, FACS, at the Convocation at Clinical Congress 2018 in Boston, MA. This award was established by the ACS Women in Surgery Committee (WiSC) and is presented annually at the Clinical Congress to recognize an individual’s significant contributions to the advancement of women in surgery.
Dr. Lee is from Honolulu, HI, and was born in Xian, China, in 1936. During her childhood, four of her siblings died from illness, motivating Dr. Lee to become a physician. Her family was forced to flee to Taiwan after the Chinese Civil War, and she immigrated to the U.S. in 1955, graduated from Harvard Medical School, Boston, in 1961, and has worked as a general surgeon and a surgical oncologist for more than 50 years. In the early 1980s, she was a tenured associate professor of surgery, University of Southern California (USC), Los Angeles, and head physician, Los Angeles County-USC Medical Center, but chose to pursue a different path.
In 1983, Dr. Lee moved to Hawaii, worked at Tripler Army Medical Center, Honolulu, as chief, surgical oncology section of general surgical services, and joined the U.S. Army Corps. She was deployed to Iraq during Operation Desert Storm and treated many U.S. soldiers as well as Iraqi prisoners of war. She served on a team of surgeons that performed more than 125 operations in a 400-bed hospital in northern Saudi Arabia. Dr. Lee received several accolades in the military, including an “A” Proficiency Designator from the Army Medical Department and a Certificate of Achievement. After retiring from the Army as a colonel, she became professor of surgery, University of Hawaii at Manoa, Honolulu, where she was the only woman surgeon for most of her career.
Dr. Lee has participated in medical missions to Ghana, Honduras, Cambodia, Laos, the Philippines, and other underserved countries. She has made many international trips to promote friendship and medical exchanges. Notably, in 1995, she was the leader of a Women Surgeons Delegation to Russia and Romania. The trip was a Citizen Ambassador Program sponsored by People to People International, which was established by President Dwight D. Eisenhower. From 2000 to 2017, Dr. Lee taught surgery for a month, four times a year, at the Tzu-Chi University School of Medicine, Hualien, Taiwan.
Dr. Lee was one of 21 women surgeons in attendance at a networking breakfast at the 1981 Clinical Congress—led by ACS Past-President Patricia Numann, MD, FACS—which proved to be the genesis of the Association of Women Surgeons (AWS). She has been a supporter of the association, in time and talent, since its inception, and her presence at the AWS meetings, her academic career at teaching hospitals, and her research publications provide women surgeons and medical students from around the world an example of what women can achieve in the field.
Because her home is in Hawaii, midway between the East and West, she hopes to function as a “bridge,” contributing to global understanding and promoting communication, collaboration, and goodwill, and continues to work in the areas of medical education, international health, and world peace.
Committed to improving the care of the surgical patient, Dr. Lee is an outstanding leader and role model for surgeons everywhere. Her contributions to academic medicine in surgery, in the military, and in surgical volunteerism worldwide have made a lasting impression on the surgical profession. Her passion, endless energy, and dedication to the ACS and to women in surgery are without equal.
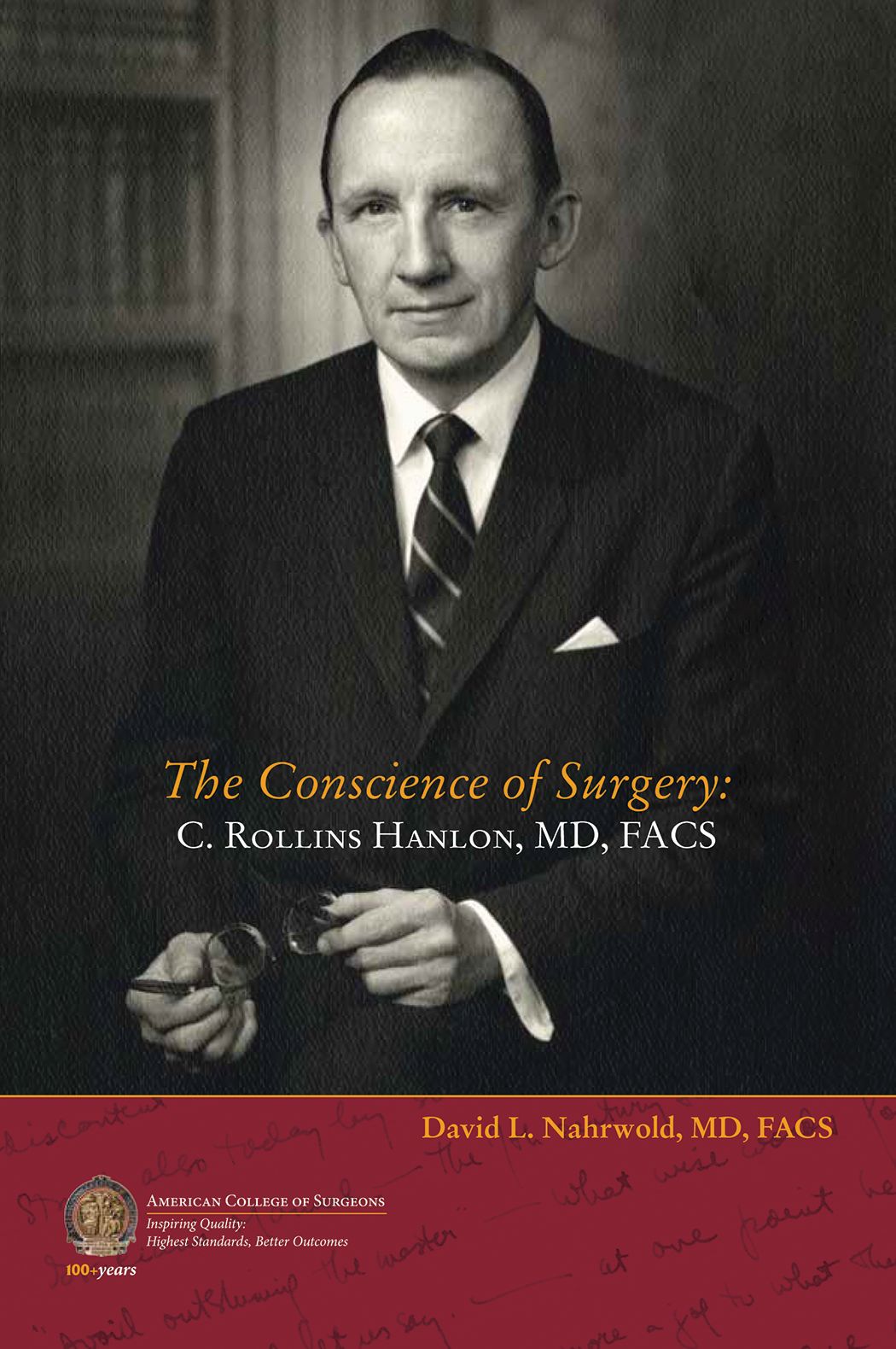
Biography of C. Rollins Hanlon, MD, FACS, Past-Director of the ACS, now available
The American College of Surgeons (ACS) recently published a new biography of C. Rollins Hanlon, MD, FACS, ACS Past-Director, a seminal figure in the history of surgery and the College, titled The Conscience of Surgery: C. Rollins Hanlon, MD, FACS. Written by David L. Nahrwold, MD, FACS, this account examines the life of the erudite, principled cardiothoracic surgeon and innovator, who co-developed the Blalock-Hanlon operation with Alfred P. Blalock, MD, FACS.
The book covers every aspect of Dr. Hanlon’s life—from his boyhood in Baltimore, MD, to his quest to be the best clinician and surgeon-scientist, to his views on the government’s increasing influence on the delivery of surgical care, and to his undying love of the written word. For many surgeons, Dr. Hanlon was the embodiment of what it means to be a Fellow of the ACS.
“I got to know [Dr. Hanlon] as a person and a professional during my stint as the Interim Director of the ACS in 1999 when he was ‘retired’ and serving as Executive Consultant,” Dr. Nahrwold writes in the book’s preface. “He insisted that the mission of the College was to advance the ethical and competent practice of surgery and not to improve the financial well-being of surgeons.”
Throughout his career, Dr. Hanlon’s mentors, colleagues, and students included many eminent surgeons at Johns Hopkins Medical School, Baltimore, MD; Cincinnati General Hospital, OH; and the University of California, San Francisco. He trained under Dean DeWitt Lewis, Walter E. Dandy, Howard C. Naffziger, Warfield “Monty” Firor, and Mont Reid (all MD, FACS). He worked alongside William P. Longmire, MD, FACS; Dr. Blalock; and Mark C. Ravitch, MD, FACS; and his residents and interns at St. Louis University, MO, included Vallee Willman, Theodore Cooper, Theodore Dubuque, and William Stoneman (all MD, FACS), among others.
Dr. Hanlon served in the U.S. Navy in World War II, and followed with a distinguished career at Johns Hopkins and at St. Louis University, where, as chair of surgery, he developed the institution’s cardiac research capabilities, which helped to pioneer early open-heart and heart transplant procedures.
Dr. Hanlon became a Fellow of the College in 1953 and served as the ACS Director for 17 years (1969–1986), making him the longest-serving Director to date. Additionally, he served on the Board of Regents and as the ACS President (1985–1986). After retirement, he stayed on as ACS Executive Consultant, offering his sage advice to his successors, including Paul A. Ebert, MD, FACS; Samuel Wells, MD, FACS; Dr. Nahrwold; Thomas R. Russell, MD, FACS; and David B. Hoyt, MD, FACS. Through these positions, Dr. Hanlon had a profound effect on the direction and philosophy of the College, including in philanthropic endeavors and the establishment of the ACS Archives. He received the first ACS Lifetime Achievement Award in 2010.
“Hanlon’s integrity, faith, hard work, and service to others led him to become a role model for physicians and laypersons alike. These attributes also drove his brilliant career as an innovative surgeon, leadership in academic and organized medicine, and reputation as a humanist and ethicist,” Dr. Narhwold concludes in the preface. “Before he died I knew that I must write his biography to expose his principled life, his goodness, and his devotion to surgery and to surgeons, especially young surgeons, with the hope that they and others will find his life worthy of study and emulation.”
Dr. Nahrwold is Emeritus Professor of Surgery at Northwestern University Feinberg School of Medicine, Chicago, IL, where he was the Loyal and Edith Davis Professor and Chairman, department of surgery, and surgeon-in-chief, Northwestern Memorial Hospital. He is a recipient of the College’s highest honor—the Distinguished Service Award.
Dr. Nahrwold is author of A Mirror Reflecting Surgery, Surgeons, and their College: The Bulletin of the American College of Surgeons, and co-author, with Peter J. Kernahan, MD, PhD, FACS, of A Century of Surgeons and Surgery: The American College of Surgeons 1913–2012.
The Conscience of Surgery: C. Rollins Hanlon, MD, FACS, is available for $15.95 on the ACS E-Store at web4.facs.org/eBusiness/ProductCatalog/Product.aspx?ID=1060 and on amazon.com.
The American College of Surgeons (ACS) recently published a new biography of C. Rollins Hanlon, MD, FACS, ACS Past-Director, a seminal figure in the history of surgery and the College, titled The Conscience of Surgery: C. Rollins Hanlon, MD, FACS. Written by David L. Nahrwold, MD, FACS, this account examines the life of the erudite, principled cardiothoracic surgeon and innovator, who co-developed the Blalock-Hanlon operation with Alfred P. Blalock, MD, FACS.
The book covers every aspect of Dr. Hanlon’s life—from his boyhood in Baltimore, MD, to his quest to be the best clinician and surgeon-scientist, to his views on the government’s increasing influence on the delivery of surgical care, and to his undying love of the written word. For many surgeons, Dr. Hanlon was the embodiment of what it means to be a Fellow of the ACS.
“I got to know [Dr. Hanlon] as a person and a professional during my stint as the Interim Director of the ACS in 1999 when he was ‘retired’ and serving as Executive Consultant,” Dr. Nahrwold writes in the book’s preface. “He insisted that the mission of the College was to advance the ethical and competent practice of surgery and not to improve the financial well-being of surgeons.”
Throughout his career, Dr. Hanlon’s mentors, colleagues, and students included many eminent surgeons at Johns Hopkins Medical School, Baltimore, MD; Cincinnati General Hospital, OH; and the University of California, San Francisco. He trained under Dean DeWitt Lewis, Walter E. Dandy, Howard C. Naffziger, Warfield “Monty” Firor, and Mont Reid (all MD, FACS). He worked alongside William P. Longmire, MD, FACS; Dr. Blalock; and Mark C. Ravitch, MD, FACS; and his residents and interns at St. Louis University, MO, included Vallee Willman, Theodore Cooper, Theodore Dubuque, and William Stoneman (all MD, FACS), among others.
Dr. Hanlon served in the U.S. Navy in World War II, and followed with a distinguished career at Johns Hopkins and at St. Louis University, where, as chair of surgery, he developed the institution’s cardiac research capabilities, which helped to pioneer early open-heart and heart transplant procedures.
Dr. Hanlon became a Fellow of the College in 1953 and served as the ACS Director for 17 years (1969–1986), making him the longest-serving Director to date. Additionally, he served on the Board of Regents and as the ACS President (1985–1986). After retirement, he stayed on as ACS Executive Consultant, offering his sage advice to his successors, including Paul A. Ebert, MD, FACS; Samuel Wells, MD, FACS; Dr. Nahrwold; Thomas R. Russell, MD, FACS; and David B. Hoyt, MD, FACS. Through these positions, Dr. Hanlon had a profound effect on the direction and philosophy of the College, including in philanthropic endeavors and the establishment of the ACS Archives. He received the first ACS Lifetime Achievement Award in 2010.
“Hanlon’s integrity, faith, hard work, and service to others led him to become a role model for physicians and laypersons alike. These attributes also drove his brilliant career as an innovative surgeon, leadership in academic and organized medicine, and reputation as a humanist and ethicist,” Dr. Narhwold concludes in the preface. “Before he died I knew that I must write his biography to expose his principled life, his goodness, and his devotion to surgery and to surgeons, especially young surgeons, with the hope that they and others will find his life worthy of study and emulation.”
Dr. Nahrwold is Emeritus Professor of Surgery at Northwestern University Feinberg School of Medicine, Chicago, IL, where he was the Loyal and Edith Davis Professor and Chairman, department of surgery, and surgeon-in-chief, Northwestern Memorial Hospital. He is a recipient of the College’s highest honor—the Distinguished Service Award.
Dr. Nahrwold is author of A Mirror Reflecting Surgery, Surgeons, and their College: The Bulletin of the American College of Surgeons, and co-author, with Peter J. Kernahan, MD, PhD, FACS, of A Century of Surgeons and Surgery: The American College of Surgeons 1913–2012.
The Conscience of Surgery: C. Rollins Hanlon, MD, FACS, is available for $15.95 on the ACS E-Store at web4.facs.org/eBusiness/ProductCatalog/Product.aspx?ID=1060 and on amazon.com.
The American College of Surgeons (ACS) recently published a new biography of C. Rollins Hanlon, MD, FACS, ACS Past-Director, a seminal figure in the history of surgery and the College, titled The Conscience of Surgery: C. Rollins Hanlon, MD, FACS. Written by David L. Nahrwold, MD, FACS, this account examines the life of the erudite, principled cardiothoracic surgeon and innovator, who co-developed the Blalock-Hanlon operation with Alfred P. Blalock, MD, FACS.
The book covers every aspect of Dr. Hanlon’s life—from his boyhood in Baltimore, MD, to his quest to be the best clinician and surgeon-scientist, to his views on the government’s increasing influence on the delivery of surgical care, and to his undying love of the written word. For many surgeons, Dr. Hanlon was the embodiment of what it means to be a Fellow of the ACS.
“I got to know [Dr. Hanlon] as a person and a professional during my stint as the Interim Director of the ACS in 1999 when he was ‘retired’ and serving as Executive Consultant,” Dr. Nahrwold writes in the book’s preface. “He insisted that the mission of the College was to advance the ethical and competent practice of surgery and not to improve the financial well-being of surgeons.”
Throughout his career, Dr. Hanlon’s mentors, colleagues, and students included many eminent surgeons at Johns Hopkins Medical School, Baltimore, MD; Cincinnati General Hospital, OH; and the University of California, San Francisco. He trained under Dean DeWitt Lewis, Walter E. Dandy, Howard C. Naffziger, Warfield “Monty” Firor, and Mont Reid (all MD, FACS). He worked alongside William P. Longmire, MD, FACS; Dr. Blalock; and Mark C. Ravitch, MD, FACS; and his residents and interns at St. Louis University, MO, included Vallee Willman, Theodore Cooper, Theodore Dubuque, and William Stoneman (all MD, FACS), among others.
Dr. Hanlon served in the U.S. Navy in World War II, and followed with a distinguished career at Johns Hopkins and at St. Louis University, where, as chair of surgery, he developed the institution’s cardiac research capabilities, which helped to pioneer early open-heart and heart transplant procedures.
Dr. Hanlon became a Fellow of the College in 1953 and served as the ACS Director for 17 years (1969–1986), making him the longest-serving Director to date. Additionally, he served on the Board of Regents and as the ACS President (1985–1986). After retirement, he stayed on as ACS Executive Consultant, offering his sage advice to his successors, including Paul A. Ebert, MD, FACS; Samuel Wells, MD, FACS; Dr. Nahrwold; Thomas R. Russell, MD, FACS; and David B. Hoyt, MD, FACS. Through these positions, Dr. Hanlon had a profound effect on the direction and philosophy of the College, including in philanthropic endeavors and the establishment of the ACS Archives. He received the first ACS Lifetime Achievement Award in 2010.
“Hanlon’s integrity, faith, hard work, and service to others led him to become a role model for physicians and laypersons alike. These attributes also drove his brilliant career as an innovative surgeon, leadership in academic and organized medicine, and reputation as a humanist and ethicist,” Dr. Narhwold concludes in the preface. “Before he died I knew that I must write his biography to expose his principled life, his goodness, and his devotion to surgery and to surgeons, especially young surgeons, with the hope that they and others will find his life worthy of study and emulation.”
Dr. Nahrwold is Emeritus Professor of Surgery at Northwestern University Feinberg School of Medicine, Chicago, IL, where he was the Loyal and Edith Davis Professor and Chairman, department of surgery, and surgeon-in-chief, Northwestern Memorial Hospital. He is a recipient of the College’s highest honor—the Distinguished Service Award.
Dr. Nahrwold is author of A Mirror Reflecting Surgery, Surgeons, and their College: The Bulletin of the American College of Surgeons, and co-author, with Peter J. Kernahan, MD, PhD, FACS, of A Century of Surgeons and Surgery: The American College of Surgeons 1913–2012.
The Conscience of Surgery: C. Rollins Hanlon, MD, FACS, is available for $15.95 on the ACS E-Store at web4.facs.org/eBusiness/ProductCatalog/Product.aspx?ID=1060 and on amazon.com.
Heidi Nelson, MD, FACS, named Medical Director of ACS Cancer Programs
The American College of Surgeons (ACS) recently announced that Heidi Nelson, MD, FACS, a colorectal surgeon from Rochester, MN, will be joining the ACS Division of Research and Optimal Patient Care (DROPC) as Medical Director, Cancer Programs, succeeding David P. Winchester, MD, FACS, as he transitions from the position he has served in for more than 30 years. Dr. Nelson comes to the ACS from her position as chair, and vice-chair for research, department of surgery, Mayo Clinic, as well as professor of surgery, Mayo Clinic College of Medicine and Science, Rochester. She has master’s faculty privileges in clinical and translation science at the Mayo Clinic Graduate School of Biomedical Sciences and the Mayo Clinic College of Medicine and Science.
Dr. Nelson received a bachelor’s degree from Western Washington University, Bellingham, and her medical degree from the University of Washington School of Medicine, Seattle. She completed an internship and residency in general surgery at Oregon Health & Science University, Portland, where she also served as an American Cancer Society Fellow. She then went to the Mayo Clinic College of Medicine and Science, where she was a colon and rectal surgery fellow and completed a research fellowship. Dr. Nelson returned to the University of Washington, where she was a Leo Hirsch Traveling Fellow.
Dr. Nelson has received numerous awards and held membership in many professional organizations, including the American Society of Colon and Rectal Surgeons (ASCRS), the Mayo Clinic Board of Governors, the Society of Surgical Oncology, and the Association of Women Surgeons, among others.
Research activities
As the Fred C. Andersen Professor for the Mayo Foundation and a consultant for Mayo Clinic’s division of colon and rectal surgery, Dr. Nelson is internationally renowned for her research in the field of colon and rectal cancer. The goal of her research activities has been to improve the duration and quality of life for these patients. These efforts have helped to reduce the impact of surgery on patients with early-stage disease through the safe introduction of laparoscopic and minimally invasive surgical approaches. Her work also has helped to reduce the cancer burden in patients with locally advanced and recurrent rectal cancer through studies examining the role of complex operations and intraoperative radiation therapy. Dr. Nelson’s work has been funded by the National Institutes of Health, the American Cancer Society, the ASCRS, and many other organizations. In addition to her clinical activities, she has led the Center for Individualized Medicine Microbiome Program at the Mayo Clinic, where she conducts, presents, and publishes research on the human microbiome and its connection to health and disease.
Leadership
Dr. Nelson brings a wealth of experience from leading others and establishing results-oriented teams. She has mentored trainees and investigators and has served as an editor and publisher for high-impact journals. She also has been extensively involved with the ACS throughout her career—Dr. Nelson became an ACS Fellow in 1993 and has served as former Director, ACS Clinical Research Program; former co-chair, ACS Oncology Group; and as a member, Commission on Cancer Executive Committee.
Dr. Nelson started working with the ACS in September on an initial part-time basis, overlapping with Dr. Winchester to ensure a smooth transition and continuity of leadership.
“The American College of Surgeons is excited about Dr. Nelson joining our Executive Leadership Team. Her research acumen and leadership in the cancer care community are well known and widely respected. Her addition to our team will benefit our members, our relationships with cancer care organizations, and the patients whom we serve,” said ACS Executive Director David B. Hoyt, MD, FACS.
The American College of Surgeons (ACS) recently announced that Heidi Nelson, MD, FACS, a colorectal surgeon from Rochester, MN, will be joining the ACS Division of Research and Optimal Patient Care (DROPC) as Medical Director, Cancer Programs, succeeding David P. Winchester, MD, FACS, as he transitions from the position he has served in for more than 30 years. Dr. Nelson comes to the ACS from her position as chair, and vice-chair for research, department of surgery, Mayo Clinic, as well as professor of surgery, Mayo Clinic College of Medicine and Science, Rochester. She has master’s faculty privileges in clinical and translation science at the Mayo Clinic Graduate School of Biomedical Sciences and the Mayo Clinic College of Medicine and Science.
Dr. Nelson received a bachelor’s degree from Western Washington University, Bellingham, and her medical degree from the University of Washington School of Medicine, Seattle. She completed an internship and residency in general surgery at Oregon Health & Science University, Portland, where she also served as an American Cancer Society Fellow. She then went to the Mayo Clinic College of Medicine and Science, where she was a colon and rectal surgery fellow and completed a research fellowship. Dr. Nelson returned to the University of Washington, where she was a Leo Hirsch Traveling Fellow.
Dr. Nelson has received numerous awards and held membership in many professional organizations, including the American Society of Colon and Rectal Surgeons (ASCRS), the Mayo Clinic Board of Governors, the Society of Surgical Oncology, and the Association of Women Surgeons, among others.
Research activities
As the Fred C. Andersen Professor for the Mayo Foundation and a consultant for Mayo Clinic’s division of colon and rectal surgery, Dr. Nelson is internationally renowned for her research in the field of colon and rectal cancer. The goal of her research activities has been to improve the duration and quality of life for these patients. These efforts have helped to reduce the impact of surgery on patients with early-stage disease through the safe introduction of laparoscopic and minimally invasive surgical approaches. Her work also has helped to reduce the cancer burden in patients with locally advanced and recurrent rectal cancer through studies examining the role of complex operations and intraoperative radiation therapy. Dr. Nelson’s work has been funded by the National Institutes of Health, the American Cancer Society, the ASCRS, and many other organizations. In addition to her clinical activities, she has led the Center for Individualized Medicine Microbiome Program at the Mayo Clinic, where she conducts, presents, and publishes research on the human microbiome and its connection to health and disease.
Leadership
Dr. Nelson brings a wealth of experience from leading others and establishing results-oriented teams. She has mentored trainees and investigators and has served as an editor and publisher for high-impact journals. She also has been extensively involved with the ACS throughout her career—Dr. Nelson became an ACS Fellow in 1993 and has served as former Director, ACS Clinical Research Program; former co-chair, ACS Oncology Group; and as a member, Commission on Cancer Executive Committee.
Dr. Nelson started working with the ACS in September on an initial part-time basis, overlapping with Dr. Winchester to ensure a smooth transition and continuity of leadership.
“The American College of Surgeons is excited about Dr. Nelson joining our Executive Leadership Team. Her research acumen and leadership in the cancer care community are well known and widely respected. Her addition to our team will benefit our members, our relationships with cancer care organizations, and the patients whom we serve,” said ACS Executive Director David B. Hoyt, MD, FACS.
The American College of Surgeons (ACS) recently announced that Heidi Nelson, MD, FACS, a colorectal surgeon from Rochester, MN, will be joining the ACS Division of Research and Optimal Patient Care (DROPC) as Medical Director, Cancer Programs, succeeding David P. Winchester, MD, FACS, as he transitions from the position he has served in for more than 30 years. Dr. Nelson comes to the ACS from her position as chair, and vice-chair for research, department of surgery, Mayo Clinic, as well as professor of surgery, Mayo Clinic College of Medicine and Science, Rochester. She has master’s faculty privileges in clinical and translation science at the Mayo Clinic Graduate School of Biomedical Sciences and the Mayo Clinic College of Medicine and Science.
Dr. Nelson received a bachelor’s degree from Western Washington University, Bellingham, and her medical degree from the University of Washington School of Medicine, Seattle. She completed an internship and residency in general surgery at Oregon Health & Science University, Portland, where she also served as an American Cancer Society Fellow. She then went to the Mayo Clinic College of Medicine and Science, where she was a colon and rectal surgery fellow and completed a research fellowship. Dr. Nelson returned to the University of Washington, where she was a Leo Hirsch Traveling Fellow.
Dr. Nelson has received numerous awards and held membership in many professional organizations, including the American Society of Colon and Rectal Surgeons (ASCRS), the Mayo Clinic Board of Governors, the Society of Surgical Oncology, and the Association of Women Surgeons, among others.
Research activities
As the Fred C. Andersen Professor for the Mayo Foundation and a consultant for Mayo Clinic’s division of colon and rectal surgery, Dr. Nelson is internationally renowned for her research in the field of colon and rectal cancer. The goal of her research activities has been to improve the duration and quality of life for these patients. These efforts have helped to reduce the impact of surgery on patients with early-stage disease through the safe introduction of laparoscopic and minimally invasive surgical approaches. Her work also has helped to reduce the cancer burden in patients with locally advanced and recurrent rectal cancer through studies examining the role of complex operations and intraoperative radiation therapy. Dr. Nelson’s work has been funded by the National Institutes of Health, the American Cancer Society, the ASCRS, and many other organizations. In addition to her clinical activities, she has led the Center for Individualized Medicine Microbiome Program at the Mayo Clinic, where she conducts, presents, and publishes research on the human microbiome and its connection to health and disease.
Leadership
Dr. Nelson brings a wealth of experience from leading others and establishing results-oriented teams. She has mentored trainees and investigators and has served as an editor and publisher for high-impact journals. She also has been extensively involved with the ACS throughout her career—Dr. Nelson became an ACS Fellow in 1993 and has served as former Director, ACS Clinical Research Program; former co-chair, ACS Oncology Group; and as a member, Commission on Cancer Executive Committee.
Dr. Nelson started working with the ACS in September on an initial part-time basis, overlapping with Dr. Winchester to ensure a smooth transition and continuity of leadership.
“The American College of Surgeons is excited about Dr. Nelson joining our Executive Leadership Team. Her research acumen and leadership in the cancer care community are well known and widely respected. Her addition to our team will benefit our members, our relationships with cancer care organizations, and the patients whom we serve,” said ACS Executive Director David B. Hoyt, MD, FACS.
Ronald V. Maier, MD, FACS, FRCSEd(Hon), FCSHK(Hon) installed as 2018–2019
Ronald. V. Maier, MD, FACS, FRCSEd(Hon), FCSHK(Hon), the Jane and Donald D. Trunkey Endowed Chair in Trauma Surgery; vice-chairman, department of surgery; and professor of surgery, University of Washington School of Medicine, Seattle, was installed as the 99th President of the American College of Surgeons (ACS) at Convocation, October 21, at Clinical Congress 2018 in Boston, MA.
Dr. Maier is highly esteemed for his contributions to trauma surgery, surgical research, and surgical education. In addition to his positions at the University of Washington, he is director, Northwest Regional Trauma Center; and surgeon-in-chief and co-director, surgical intensive care unit (SICU), Harborview Medical Center, Seattle. He also is associate medical staff, University of Washington Medical Center and Seattle Cancer Care Alliance. A Fellow of the College since 1984, Dr. Maier served as First Vice-President of the ACS (2015−2016) and has played an active role on several key committees, most notably the Committee on Trauma (COT).
Mark C. Weissler, MD, FACS, Past-Chair of the ACS Board of Regents (2014−2015) was installed as the First Vice-President. An otolaryngologist-head and neck surgeon, Dr. Weissler is the Joseph P. Riddle Distinguished Professor, department of otolaryngology–head and neck surgery, and chief, division of head and neck surgery, University of North Carolina (UNC) School of Medicine, Chapel Hill. An ACS Fellow since 1989, Dr. Weissler is a former ACS Regent, serving as Vice-Chair of the Board of Regents for two years (2012–2014) and Chair for one year (2014−2015). He has served on the ACS Board of Governors and in other leadership capacities for the College, including the Committee on Ethics, Central Judiciary Committee, Advisory Council for Otolaryngology−Head and Neck Surgery; and President, North Carolina Chapter of the ACS.
The Second Vice-President is Phillip R. Caropreso, MD, FACS, a general surgeon from Keokuk, IA. A committed rural surgeon, Dr. Caropreso has practiced in Mason City, IA; Keokuk, IA; and Carthage, IL. Academic positions have included serving on the teaching faculty, family practice residency, North Iowa Medical Center, Mason City; adjunct clinical professor of surgery, University of Iowa, Iowa City; and director, general surgery rotation, North Iowa Medical Center. A Fellow of the ACS since 1979, Dr. Caropreso has been active at the local and national level. He was Chair, Iowa State COT; President of the Iowa Chapter; and ACS Governor, serving on the Board of Governors Committee on Surgical Practices.
Read more about Dr. Maier, Dr. Weissler, and Dr. Caropreso in the November Bulletin at www.bulletin.facs.org.
Ronald. V. Maier, MD, FACS, FRCSEd(Hon), FCSHK(Hon), the Jane and Donald D. Trunkey Endowed Chair in Trauma Surgery; vice-chairman, department of surgery; and professor of surgery, University of Washington School of Medicine, Seattle, was installed as the 99th President of the American College of Surgeons (ACS) at Convocation, October 21, at Clinical Congress 2018 in Boston, MA.
Dr. Maier is highly esteemed for his contributions to trauma surgery, surgical research, and surgical education. In addition to his positions at the University of Washington, he is director, Northwest Regional Trauma Center; and surgeon-in-chief and co-director, surgical intensive care unit (SICU), Harborview Medical Center, Seattle. He also is associate medical staff, University of Washington Medical Center and Seattle Cancer Care Alliance. A Fellow of the College since 1984, Dr. Maier served as First Vice-President of the ACS (2015−2016) and has played an active role on several key committees, most notably the Committee on Trauma (COT).
Mark C. Weissler, MD, FACS, Past-Chair of the ACS Board of Regents (2014−2015) was installed as the First Vice-President. An otolaryngologist-head and neck surgeon, Dr. Weissler is the Joseph P. Riddle Distinguished Professor, department of otolaryngology–head and neck surgery, and chief, division of head and neck surgery, University of North Carolina (UNC) School of Medicine, Chapel Hill. An ACS Fellow since 1989, Dr. Weissler is a former ACS Regent, serving as Vice-Chair of the Board of Regents for two years (2012–2014) and Chair for one year (2014−2015). He has served on the ACS Board of Governors and in other leadership capacities for the College, including the Committee on Ethics, Central Judiciary Committee, Advisory Council for Otolaryngology−Head and Neck Surgery; and President, North Carolina Chapter of the ACS.
The Second Vice-President is Phillip R. Caropreso, MD, FACS, a general surgeon from Keokuk, IA. A committed rural surgeon, Dr. Caropreso has practiced in Mason City, IA; Keokuk, IA; and Carthage, IL. Academic positions have included serving on the teaching faculty, family practice residency, North Iowa Medical Center, Mason City; adjunct clinical professor of surgery, University of Iowa, Iowa City; and director, general surgery rotation, North Iowa Medical Center. A Fellow of the ACS since 1979, Dr. Caropreso has been active at the local and national level. He was Chair, Iowa State COT; President of the Iowa Chapter; and ACS Governor, serving on the Board of Governors Committee on Surgical Practices.
Read more about Dr. Maier, Dr. Weissler, and Dr. Caropreso in the November Bulletin at www.bulletin.facs.org.
Ronald. V. Maier, MD, FACS, FRCSEd(Hon), FCSHK(Hon), the Jane and Donald D. Trunkey Endowed Chair in Trauma Surgery; vice-chairman, department of surgery; and professor of surgery, University of Washington School of Medicine, Seattle, was installed as the 99th President of the American College of Surgeons (ACS) at Convocation, October 21, at Clinical Congress 2018 in Boston, MA.
Dr. Maier is highly esteemed for his contributions to trauma surgery, surgical research, and surgical education. In addition to his positions at the University of Washington, he is director, Northwest Regional Trauma Center; and surgeon-in-chief and co-director, surgical intensive care unit (SICU), Harborview Medical Center, Seattle. He also is associate medical staff, University of Washington Medical Center and Seattle Cancer Care Alliance. A Fellow of the College since 1984, Dr. Maier served as First Vice-President of the ACS (2015−2016) and has played an active role on several key committees, most notably the Committee on Trauma (COT).
Mark C. Weissler, MD, FACS, Past-Chair of the ACS Board of Regents (2014−2015) was installed as the First Vice-President. An otolaryngologist-head and neck surgeon, Dr. Weissler is the Joseph P. Riddle Distinguished Professor, department of otolaryngology–head and neck surgery, and chief, division of head and neck surgery, University of North Carolina (UNC) School of Medicine, Chapel Hill. An ACS Fellow since 1989, Dr. Weissler is a former ACS Regent, serving as Vice-Chair of the Board of Regents for two years (2012–2014) and Chair for one year (2014−2015). He has served on the ACS Board of Governors and in other leadership capacities for the College, including the Committee on Ethics, Central Judiciary Committee, Advisory Council for Otolaryngology−Head and Neck Surgery; and President, North Carolina Chapter of the ACS.
The Second Vice-President is Phillip R. Caropreso, MD, FACS, a general surgeon from Keokuk, IA. A committed rural surgeon, Dr. Caropreso has practiced in Mason City, IA; Keokuk, IA; and Carthage, IL. Academic positions have included serving on the teaching faculty, family practice residency, North Iowa Medical Center, Mason City; adjunct clinical professor of surgery, University of Iowa, Iowa City; and director, general surgery rotation, North Iowa Medical Center. A Fellow of the ACS since 1979, Dr. Caropreso has been active at the local and national level. He was Chair, Iowa State COT; President of the Iowa Chapter; and ACS Governor, serving on the Board of Governors Committee on Surgical Practices.
Read more about Dr. Maier, Dr. Weissler, and Dr. Caropreso in the November Bulletin at www.bulletin.facs.org.
Investigation Into New Antimalarial Drug Begins
In 2016, a staggering 216 million people developed malaria, and 445,000 died—primarily children in sub-Saharan Africa. But a new first-in-human study sponsored by the National Institute of Allergy and Infectious Disease may help reduce the numbers of future victims.
Enrollment has begun in a phase I trial to test the safety of DM1157, an investigational modified form of chloroquine. Many strains of Plasmodium falciparum are now resistant to chloroquine. In fact, the parasites can expel the drug before it can affect them. Like chloroquine, DM1157 interferes with the parasite’s metabolism, but it also inhibits the parasite’s ability to expel the drug.
The study will enroll up to 104 healthy volunteers aged 18-45 years. One group will fast overnight and then receive either a single dose of the experimental drug at 1 of 7 dosage levels or a placebo. A second group also will fast and receive 1 dose at 1 of 4 dosage levels and repeat the routine for 2 more consecutive days. A third group will be given either a single 300-mg dose or placebo after eating a high-fat meal.
The study is expected to be completed by June 2019.
In 2016, a staggering 216 million people developed malaria, and 445,000 died—primarily children in sub-Saharan Africa. But a new first-in-human study sponsored by the National Institute of Allergy and Infectious Disease may help reduce the numbers of future victims.
Enrollment has begun in a phase I trial to test the safety of DM1157, an investigational modified form of chloroquine. Many strains of Plasmodium falciparum are now resistant to chloroquine. In fact, the parasites can expel the drug before it can affect them. Like chloroquine, DM1157 interferes with the parasite’s metabolism, but it also inhibits the parasite’s ability to expel the drug.
The study will enroll up to 104 healthy volunteers aged 18-45 years. One group will fast overnight and then receive either a single dose of the experimental drug at 1 of 7 dosage levels or a placebo. A second group also will fast and receive 1 dose at 1 of 4 dosage levels and repeat the routine for 2 more consecutive days. A third group will be given either a single 300-mg dose or placebo after eating a high-fat meal.
The study is expected to be completed by June 2019.
In 2016, a staggering 216 million people developed malaria, and 445,000 died—primarily children in sub-Saharan Africa. But a new first-in-human study sponsored by the National Institute of Allergy and Infectious Disease may help reduce the numbers of future victims.
Enrollment has begun in a phase I trial to test the safety of DM1157, an investigational modified form of chloroquine. Many strains of Plasmodium falciparum are now resistant to chloroquine. In fact, the parasites can expel the drug before it can affect them. Like chloroquine, DM1157 interferes with the parasite’s metabolism, but it also inhibits the parasite’s ability to expel the drug.
The study will enroll up to 104 healthy volunteers aged 18-45 years. One group will fast overnight and then receive either a single dose of the experimental drug at 1 of 7 dosage levels or a placebo. A second group also will fast and receive 1 dose at 1 of 4 dosage levels and repeat the routine for 2 more consecutive days. A third group will be given either a single 300-mg dose or placebo after eating a high-fat meal.
The study is expected to be completed by June 2019.
Robin Cooper: Climate Change
In this edition of the Psychcast, Lorenzo Norris, MD, welcomes Robin Cooper, MD, to discuss the impacts of global climate change on both patients and communities.
Dr. Cooper “has been in private practice with a focus on both psychotherapy and medical management throughout her 35 years of practice.”
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
In this edition of the Psychcast, Lorenzo Norris, MD, welcomes Robin Cooper, MD, to discuss the impacts of global climate change on both patients and communities.
Dr. Cooper “has been in private practice with a focus on both psychotherapy and medical management throughout her 35 years of practice.”
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
In this edition of the Psychcast, Lorenzo Norris, MD, welcomes Robin Cooper, MD, to discuss the impacts of global climate change on both patients and communities.
Dr. Cooper “has been in private practice with a focus on both psychotherapy and medical management throughout her 35 years of practice.”
Amazon Alexa
Apple Podcasts
Google Podcasts
Spotify
Vitamin D, fish out, and primary prevention
Also today, atopic dermatitis can harm both mental health and quality of life, apixaban is the safest effective DOAC for stroke prevention in atrial fibrillation, and a program that is aimed to increase awareness by reduced fetal movement is not effective at preventing stillbirths.
Amazon Alexa
Apple Podcasts
Spotify
Also today, atopic dermatitis can harm both mental health and quality of life, apixaban is the safest effective DOAC for stroke prevention in atrial fibrillation, and a program that is aimed to increase awareness by reduced fetal movement is not effective at preventing stillbirths.
Amazon Alexa
Apple Podcasts
Spotify
Also today, atopic dermatitis can harm both mental health and quality of life, apixaban is the safest effective DOAC for stroke prevention in atrial fibrillation, and a program that is aimed to increase awareness by reduced fetal movement is not effective at preventing stillbirths.
Amazon Alexa
Apple Podcasts
Spotify
Markers associated with efficacy of malaria vaccine
New research has revealed markers associated with efficacy of the RTS,S/AS01E malaria vaccine (Mosquirix™).
The study suggests malaria protection depends on the amount and subclass of antibodies generated upon vaccination and on previous exposure levels to the malaria parasite.
Researchers believe these findings, published in BMC Medicine, could aid the development of more effective vaccines and guide efforts to improve the effectiveness of RTS,S.
The RTS,S vaccine demonstrated partial effectiveness in a phase 3 study—31% in infants ages 6 weeks to 12 weeks and 56% in children ages 5 months to 17 months.
Carlota Dobaño Lázaro, PhD, of ISGlobal in Barcelona, Spain, and her colleagues have been working to understand the reasons for this variability and identify vaccine protection correlates.
The team used a quantitative assay to investigate the levels and types of antibodies induced by RTS,S. In particular, they measured total IgM, IgG, and IgG1–4 subclass antibodies to hepatitis B surface antigen (HBsAg) and three constructs of the Plasmodium falciparum circumsporozoite protein (CSP).
The researchers analyzed serum and plasma from 195 infants and children from Kintampo, Ghana (an area with high malaria transmission) and Manhiça, Mozambique (low malaria transmission), who were vaccinated during the phase 3 trial for RTS,S.
The results confirmed that RTS,S induces significant levels of IgG antibodies against both CSP and HBsAg, which are higher in children than in infants.
The researchers found that higher HBsAg antibody levels post-vaccination were associated with protection from malaria.
However, the same could not be said for all subclasses of CSP antibodies. Higher levels of IgG1 and IgG3 antibodies were associated with protection, while higher levels of IgG2 and IgG4 were associated with a greater risk of developing malaria.
“The balance between the different subclasses seems to be more important than the total IgG levels,” said study author Itzi Ubillos Escriche, of ISGlobal.
“This could be because IgG1 and IgG3 antibodies have the capacity to stick to the parasite and give an ‘eat-me’ signal to cells of the immune system.”
The results also showed that subjects with higher pre-vaccine levels of anti-P falciparum and anti-CSP antibodies were less protected against malaria post-vaccination.
“This means that the vaccine will exert a larger benefit to infants who have not been exposed to the parasite in utero or during the first weeks of life,” Dr. Dobaño Lázaro said.
“This study . . . identifies new correlates of vaccine success and failure in African children and provides a basis for designing more efficacious vaccines.”
This research was funded by the National Institutes of Health-National Institute of Allergy and Infectious Diseases, PATH Malaria Vaccine Initiative, Ministerio de Economía y Competitividad, and EVIMalaR and AGAUR-Catalonia. ISGlobal is a member of the CERCA Program, Generalitat de Catalunya.
The authors said they have no competing interests.
The phase 3 trial of RTS,S was supported by GlaxoSmithKline Biologicals SA and the PATH Malaria Vaccine Initiative.
New research has revealed markers associated with efficacy of the RTS,S/AS01E malaria vaccine (Mosquirix™).
The study suggests malaria protection depends on the amount and subclass of antibodies generated upon vaccination and on previous exposure levels to the malaria parasite.
Researchers believe these findings, published in BMC Medicine, could aid the development of more effective vaccines and guide efforts to improve the effectiveness of RTS,S.
The RTS,S vaccine demonstrated partial effectiveness in a phase 3 study—31% in infants ages 6 weeks to 12 weeks and 56% in children ages 5 months to 17 months.
Carlota Dobaño Lázaro, PhD, of ISGlobal in Barcelona, Spain, and her colleagues have been working to understand the reasons for this variability and identify vaccine protection correlates.
The team used a quantitative assay to investigate the levels and types of antibodies induced by RTS,S. In particular, they measured total IgM, IgG, and IgG1–4 subclass antibodies to hepatitis B surface antigen (HBsAg) and three constructs of the Plasmodium falciparum circumsporozoite protein (CSP).
The researchers analyzed serum and plasma from 195 infants and children from Kintampo, Ghana (an area with high malaria transmission) and Manhiça, Mozambique (low malaria transmission), who were vaccinated during the phase 3 trial for RTS,S.
The results confirmed that RTS,S induces significant levels of IgG antibodies against both CSP and HBsAg, which are higher in children than in infants.
The researchers found that higher HBsAg antibody levels post-vaccination were associated with protection from malaria.
However, the same could not be said for all subclasses of CSP antibodies. Higher levels of IgG1 and IgG3 antibodies were associated with protection, while higher levels of IgG2 and IgG4 were associated with a greater risk of developing malaria.
“The balance between the different subclasses seems to be more important than the total IgG levels,” said study author Itzi Ubillos Escriche, of ISGlobal.
“This could be because IgG1 and IgG3 antibodies have the capacity to stick to the parasite and give an ‘eat-me’ signal to cells of the immune system.”
The results also showed that subjects with higher pre-vaccine levels of anti-P falciparum and anti-CSP antibodies were less protected against malaria post-vaccination.
“This means that the vaccine will exert a larger benefit to infants who have not been exposed to the parasite in utero or during the first weeks of life,” Dr. Dobaño Lázaro said.
“This study . . . identifies new correlates of vaccine success and failure in African children and provides a basis for designing more efficacious vaccines.”
This research was funded by the National Institutes of Health-National Institute of Allergy and Infectious Diseases, PATH Malaria Vaccine Initiative, Ministerio de Economía y Competitividad, and EVIMalaR and AGAUR-Catalonia. ISGlobal is a member of the CERCA Program, Generalitat de Catalunya.
The authors said they have no competing interests.
The phase 3 trial of RTS,S was supported by GlaxoSmithKline Biologicals SA and the PATH Malaria Vaccine Initiative.
New research has revealed markers associated with efficacy of the RTS,S/AS01E malaria vaccine (Mosquirix™).
The study suggests malaria protection depends on the amount and subclass of antibodies generated upon vaccination and on previous exposure levels to the malaria parasite.
Researchers believe these findings, published in BMC Medicine, could aid the development of more effective vaccines and guide efforts to improve the effectiveness of RTS,S.
The RTS,S vaccine demonstrated partial effectiveness in a phase 3 study—31% in infants ages 6 weeks to 12 weeks and 56% in children ages 5 months to 17 months.
Carlota Dobaño Lázaro, PhD, of ISGlobal in Barcelona, Spain, and her colleagues have been working to understand the reasons for this variability and identify vaccine protection correlates.
The team used a quantitative assay to investigate the levels and types of antibodies induced by RTS,S. In particular, they measured total IgM, IgG, and IgG1–4 subclass antibodies to hepatitis B surface antigen (HBsAg) and three constructs of the Plasmodium falciparum circumsporozoite protein (CSP).
The researchers analyzed serum and plasma from 195 infants and children from Kintampo, Ghana (an area with high malaria transmission) and Manhiça, Mozambique (low malaria transmission), who were vaccinated during the phase 3 trial for RTS,S.
The results confirmed that RTS,S induces significant levels of IgG antibodies against both CSP and HBsAg, which are higher in children than in infants.
The researchers found that higher HBsAg antibody levels post-vaccination were associated with protection from malaria.
However, the same could not be said for all subclasses of CSP antibodies. Higher levels of IgG1 and IgG3 antibodies were associated with protection, while higher levels of IgG2 and IgG4 were associated with a greater risk of developing malaria.
“The balance between the different subclasses seems to be more important than the total IgG levels,” said study author Itzi Ubillos Escriche, of ISGlobal.
“This could be because IgG1 and IgG3 antibodies have the capacity to stick to the parasite and give an ‘eat-me’ signal to cells of the immune system.”
The results also showed that subjects with higher pre-vaccine levels of anti-P falciparum and anti-CSP antibodies were less protected against malaria post-vaccination.
“This means that the vaccine will exert a larger benefit to infants who have not been exposed to the parasite in utero or during the first weeks of life,” Dr. Dobaño Lázaro said.
“This study . . . identifies new correlates of vaccine success and failure in African children and provides a basis for designing more efficacious vaccines.”
This research was funded by the National Institutes of Health-National Institute of Allergy and Infectious Diseases, PATH Malaria Vaccine Initiative, Ministerio de Economía y Competitividad, and EVIMalaR and AGAUR-Catalonia. ISGlobal is a member of the CERCA Program, Generalitat de Catalunya.
The authors said they have no competing interests.
The phase 3 trial of RTS,S was supported by GlaxoSmithKline Biologicals SA and the PATH Malaria Vaccine Initiative.