User login
Inadvertent Perioperative Hypothermia During Orthopedic Surgery
ABSTRACT
Inadvertent perioperative hypothermia is a significant problem in patients undergoing either emergency or elective orthopedic surgery, and is associated with increased morbidity and mortality. Though in general the incidence of inadvertent perioperative hypothermia in postoperative recovery rooms has been decreasing over the last 2 decades, it still remains a significant risk in certain specialty practices, such as orthopedic surgery. This review article summarizes the currently available evidence on the incidence, risk factors, and complications of inadvertent perioperative hypothermia. Also, the effective preventive strategies in dealing with inadvertent perioperative hypothermia are reviewed and essential clinical guidelines to be followed are summarized.
Continue to: Inadvertent perioperative hypothermia...
Inadvertent perioperative hypothermia, defined as an involuntary drop in core body temperature to <35°C (95°F), is a condition associated with significant morbidity and mortality.1 This phenomenon has been reported in both emergency orthopedic admissions, such as fracture management, as well as in the elective setting such as arthroscopy, arthroplasty, and spine surgery.
In a study conducted in the United Kingdom including 781 elderly patients with a mean age of 80 years who presented with hip fractures, the 30-day mortality rate was 15.3% in patients who were admitted with a tympanic temperature of <36.5°C and only 5.1% in patients who maintained a tympanic temperature of 36.5°C to 37.5°C (odds ratio, 2.8; P > .0005).2 For an even better perspective, this analysis can be compared with the UK National Hip Fracture Database of 2013, which reported a 30-day mortality of 8.2% in patients who were admitted to the National Health Service with a diagnosis of hip fracture.3
Inadvertent perioperative hypothermia is also a common phenomenon during elective orthopedic hospital admissions. An Australian audit, which included 5050 postoperative patients, looked into the association between inadvertent perioperative hypothermia and mortality based on diagnostic criteria classifying mild hypothermia as a core temperature of <36°C and severe hypothermia as a core temperature of <35°C.4 The authors found that mild and severe hypothermia was experienced by 36% and 6% of patients, respectively. In-hospital mortality was 5.6% for normothermic patients, 8.9% for all hypothermic patients (P < .001), and 14.7% for severely hypothermic patients (P < .001). For a decrease of 1°C in core body temperature from <36°C to <35°C (but >34°C), there were higher odds of in-hospital mortality (odds ratio, 1.83; 95% confidence interval [CI], 1.20-2.60).
The physiologic response to hypothermia is to decrease heat loss by cutaneous and peripheral vasoconstriction and increase heat production by increasing the metabolic rate (eg, shivering and shifting to anaerobic metabolism). This response is blunted to a variable extent in perioperative patients for several reasons, including the effect of anesthetic drugs and old age.5
Maintenance of core body temperature >36°C is now a measured standard of perioperative care. A performance measure for perioperative temperature management was developed by the American Medical Association Physician Consortium for Performance Improvement (AMA-PCPI).6 To achieve this performance measure, mandatory documentation of use of active warming intraoperatively or a record of at least 1 body temperature ≥96.8°F (36°C) within 30 minutes immediately prior to and 15 minutes immediately after anesthesia end time is necessary. This performance measure is also endorsed by the Surgical Care Improvement Project (SCIP-Inf-10) and National Quality Forum (NQF).6
Continue to: Overall, in the last 2 decades...
Overall, in the last 2 decades, the incidence of inadvertent perioperative hypothermia has decreased, mainly due to aggressive intraoperative management.7 In spite of this, studies have shown that perioperative hypothermia remains a significant problem in patients undergoing orthopedic procedures. In a recent community hospital study conducted by the National Association for Healthcare Quality that included 4124 orthopedic patients undergoing elective surgery, it was shown that, in spite of 99% compliance to the AMA-PCPI recommendation, 7.7% of orthopedic patients were found to be hypothermic.6
Management of hypothermia has long been an integral component of “damage control surgery” and resuscitation during polytrauma, which aims to aggressively minimize hypovolemic shock and limit the development of the lethal triad of hypothermia, coagulopathy, and acidosis.8 However, critical references to prevention and management of inadvertent perioperative hypothermia are lacking in the orthopedic literature on elective surgical procedures. This review aims to bridge this knowledge gap.
Unless otherwise specified, inadvertent perioperative hypothermia in this article refers to the core body temperature. In contrast, peripheral/limb hypothermia refers primarily to the effect of tourniquet application to the involved limb and the effect after deflation of the tourniquet on core body temperature.
RISK FACTORS
There are several measurable risk factors that can contribute to inadvertent perioperative hypothermia, which can be subdivided into 3 groups: patient-related risk factors, anesthesia-related risk factors, and procedure-related risk factors (Table 1).5,9-11 It is important to note that in any given patient a combination of 2 or more risk factors predisposes them to developing inadvertent perioperative hypothermia. Conceptualizing the etiology of inadvertent perioperative hypothermia in this way helps to plan a multipronged strategy to prevent it from occurring in the first place. Some of the important risk factors for inadvertent perioperative hypothermia are discussed below.
Table 1. Risk Factors for Perioperative Hypothermia
Patient-Related Risk Factors | Anesthesia-Related Risk Factors | Procedure-Specific Risk Factors |
|
|
|
To identify patient-related risk factors, researchers from the University of Louisville conducted a study including 2138 operative patients who became hypothermic after admission, of whom 27% underwent orthopedic and spine procedures.9 The patient-related risk factors identified were a high severity of illness on admission (odds ratio, 2.81; 95% CI, 2.28-3.47), presence of a neurological disorder such as Alzheimer’s disease (odds ratio, 1.71; 95% CI,1.06-2.78), male sex (odds ratio, 1.65; 95% CI, 1.36-2.01), age >65 years (odds ratio, 1.61; 95% CI, 1.33-1.96), recent weight loss (odds ratio, 1.60; 95% CI, 1.04-2.48), anemia (odds ratio, 1.49; 95% CI, 1.12-1.98), and chronic renal failure (odds ratio, 1.43; 95% CI, 1.07-1.92). Interestingly, diabetes mellitus without end-stage organ failure was not found to be a significant risk factor (odds ratio, 0.58; 95% CI, 0.44-0.75). It is also important to note that some of these risk factors identified to contribute to perioperative hypothermia are dependent on each other and others are independent of each other. For example, chronic renal failure and anemia are dependent risk factors. In contrast, age >65 years and low body mass index as risk factors of perioperative hypothermia are independent of each other.
Continue to: The second subgroup of risk factors...
The second subgroup of risk factors for perioperative hypothermia is related to anesthesia. The effect of general and regional anesthesia on perioperative core temperature is significantly different, both in terms of intraoperative thermoregulation and postoperative recovery.12 Intraoperatively, the core body temperature during the first 2 hours of general anesthesia decreases at a rate of 1.3°C per hour due to loss of thermoregulatory cutaneous and peripheral vasoconstrictive responses resulting in heat loss exceeding metabolic heat production. However, the core temperature remains virtually constant during the subsequent 3 hours due to the return of the thermoregulatory response, which causes cutaneous and peripheral vasoconstriction and increased metabolic heat production. Postoperative recovery from the hypothermia induced by general anesthesia is significantly faster than from that induced by regional anesthesia.13
The effect of regional hypothermia on core body temperature is more complex because it must be considered in addition to the effect of an associated procedure-related variable (ie, tourniquet application). If a tourniquet is not used during a surgery with regional anesthesia, a linear decrease in core temperature follows until recovery, due to increased blood flow from the loss of sympathetic peripheral vasoconstrictive response with resultant core-to-peripheral heat redistribution to the exposed operating limb. If a tourniquet is used during surgery with regional anesthesia, there will be no significant effect of the exposed operating limb on core temperature, as there is no blood flow between them. However, once the tourniquet is deflated, the core body temperature will be affected significantly as a result of core-to-peripheral distribution of heat to the operated limb with the return of blood flow. This fall in core body temperature after tourniquet deflation can be prevented by active forced-air warming initiated from the beginning of surgery.10 The extent and rate of development of peripheral/limb hypothermia during surgery (and its subsequent effect on core body temperature) depends on several factors, including the operating room ambient temperature, duration of tourniquet application, and temperature of the irrigation fluid. Postoperative recovery from the hypothermia induced by regional anesthesia takes longer than from that induced by general anesthesia because of the prolonged period of loss of vasoconstrictive response.
The third subgroup of risk factors associated with perioperative hypothermia is procedure related. Several procedure-specific risk factors for inadvertent perioperative hypothermia during arthroscopic surgery are identified, including prolonged operating time, low blood pressure during the procedure, and low temperature of the irrigation fluid.11 It is logical to extrapolate the importance of these risk factors to other orthopedic procedures which also require prolonged operating times, are performed under hypotension, or expose the patient to irrigation fluid that is at a low temperature. Understanding the importance of each of these procedure-related risk factors is the most important from the perspective of the orthopedic surgeon when compared to the rest of the subgroups of risk factors for inadvertent perioperative hypothermia as he/she is directly responsible for them.
The ambient operating room temperature has traditionally been considered a risk factor for inadvertent hypothermia in perioperative patients, but evidence is available to the contrary. The recommended ambient room temperature as per the clinical guideline published by the American Society of PeriAnesthesia Nurses (ASPAN) is 20°C to 24°C (68°F-75°F).14 The ambient temperature can have a significant effect on peripheral/limb hypothermia when operating on a limb with a tourniquet inflated, as the limb has no blood supply to distribute heat from the core to the periphery. However, the direct effect of ambient room temperature on the patient’s core body temperature is unlikely to be clinically significant if standard active warming interventions are implemented.15
COMPLICATIONS
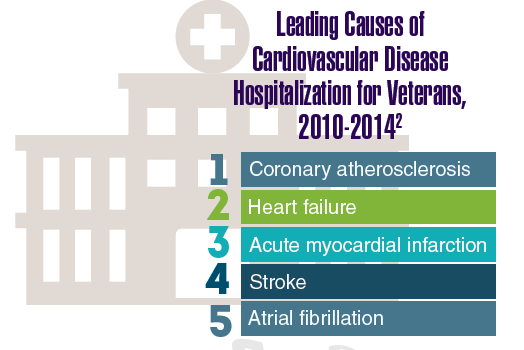
The increased incidence of mortality due to inadvertent hypothermia in the perioperative period has already been discussed. Several other complications of inadvertent perioperative hypothermia include increased incidence of coagulopathy, acidosis, stroke, sepsis, pneumonia, myocardial infarction, surgical site infections, altered drug metabolism, and longer hospital stays.8,9,16-18 Hypothermia, coagulopathy, and acidosis have long been recognized as a lethal triad more commonly seen in polytrauma patients than in elective orthopedic surgery, as this occurs at extremes of temperature, usually <32°C. When compared with patients who did not develop perioperative hypothermia, patients who developed hypothermia during elective operations were shown to experience an overall doubled complication rate (13.9% vs 26.3%; P < .001) of which the incidence of stroke (1.0% vs 6.5%; P < .001), pneumonia (1.3% vs 5.1%; P < .001), and sepsis (2.6% vs 7.5%; P < .001) were much more likely than myocardial infarction (1.1% vs 3.3%; P = .01) and wound infection (3.3% vs 5.0%; P = .14).9
Continue to: Prevention...
PREVENTION
Prevention of perioperative hypothermia is a core measure to improve the outcome after ambulatory and fast-track orthopedic surgery and rehabilitation. Preventive strategies for perioperative hypothermia can be grouped into passive heat retention methods and active external warming methods (Table 2). Passive methods aim to maintain body temperature by decreasing the heat loss by radiation (eg, reflective blanket), conduction (eg, layered cotton blankets and padding the operating table), or convection (eg, heat and humidity exchanger in the breathing circuits) to the surrounding environment. Active patient heating methods aim to bring in heat from the source to the patient’s body using conduction (eg, Hot Dog® [Eden Augustine Temperature Management]) or convection (eg, Bair Hugger® [Arizant Healthcare]) techniques.
Table 2. Methods to Prevent Inadvertent Perioperative Hypothermia
Passive Heat-Retention Methods | Active External Warming Methods |
| Conduction techniques:
Convection techniques:
|
Active patient warming is superior to passive heat retention methods. A recent Cochrane study assessed the effects of standard care (ie, use of layered clothing and warm blankets, etc.) and addition of extra thermal insulation by reflective blankets or active forced air warming to standard care on the perioperative core body temperature.19 They concluded that there is no clear benefit of addition of extra thermal insulation by reflective blankets compared with standard care alone. Also, forced-air warming in addition to standard care appeared to maintain core temperature better than standard care alone, by between 0.5°C and 1°C, but the clinical importance of this difference could not be inferred, as none of the included studies in this meta-analysis documented major cardiovascular outcomes.
Several clinical guidelines have been developed by not-for-profit, government, and professional organizations aimed at prevention of perioperative hypothermia as primary or secondary outcome. A clinical guideline was published by ASPAN in 2001 for assessment, prevention, and intervention in unplanned perioperative hypothermia.14 Cost and time effectiveness of the ASPAN Hypothermia Guideline was published in 2008.20 The assessment guideline includes identification of risk factors, repeated pre-/intra-/postoperative temperature measurement, and repeated clinical evaluation of the patient’s status. The preventive guideline is to maintain an ambient temperature of 20°C to 24°C (68°F-75°F) and use appropriate passive patient warming methods pre-, intra-, and postoperatively. Intervention in the form of active patient heating is advised only if the patient develops hypothermia in spite of the above-mentioned standard preventive measures. But many orthopedic ambulatory surgery centers currently use active patient warming as both a preventive and an intervention strategy.
Active patient warming by conduction devices occurs by direct physical contact with the device, which is set at a higher temperature, whereas heat transfer from the convection device to the patient occurs by a physical medium such as forced air or circulating water that moves in between the device and the patient. Any recommendation for use of a specific technique of active patient warming (ie, by the use of a conduction device or a convection device) should only be given after comparing evidence on 3 critical aspects: efficacy, safety, and cost effectiveness.
The heating efficacy and core rewarming rates of conduction and convection devices have been compared in the literature. Full-body forced-air heating with the Bair Hugger® and full-body resistive polymer heating with the Hot Dog® in healthy volunteers were found to be similar.21 Also, in a randomized study conducted on 80 orthopedic patients undergoing surgery, resistive polymer warming performed as efficiently as forced-air warming in patients undergoing orthopedic surgery.22
Continue to: Secondly, the safety of convection...
Secondly, the safety of convection devices such as the Bair Hugger® has been under intense scrutiny based on the evidence that it disrupts the laminar airflow in the operating theater.23-26 This disruption in laminar air flow has been shown to cause emission of significant levels of airborne contaminants of size >0.3 μm (germ size).27 Isolates of Staphylococcus aureus, coagulase-negative Staphylococcus species, and methicillin-resistant Staphylococcus aureus were detected in 13.5%, 3.9%, and 1.9% of forced-air blowers, respectively.28 However, the clinical effect on the rate of deep joint infection due to the disruption of laminar air flow has been examined in only 1 study. McGovern and colleagues29 reported a significant increase in deep joint infection during a period when forced air warming was used compared to a period when conductive fabric warming was used (odds ratio, 3.8; P = .024) and recommended air-free warming by a conduction device over forced-air warming for orthopedic procedures. Unfortunately, the prophylactic antibiotic regimen was not kept constant during their study period. During an overlapping time frame during which they shifted from the use of a convection device (Bair Hugger®) to a conduction device (Hot Dog®), they also changed their antibiotic regimen from gentamicin 4.5 mg/kg intravenous (IV) to gentamicin 3 mg/kg IV plus teicoplanin 400 mg IV. This change in antibiotic regimen is a major confounding factor that calls into question the validity of the conclusions drawn by the authors.
Finally, the cost effectiveness of conduction and convection devices has never been studied. Hence, based on the current evidence, it is not possible to recommend a particular type of active patient-warming device.
CONCLUSION
Orthopedic surgeons should be aware that inadvertent perioperative hypothermia is a common phenomenon in perioperative patients. It must be recognized that the maintenance of perioperative normothermia during all major orthopedic surgical procedures is desirable, as inadvertent perioperative hypothermia is shown to be associated with increased mortality and systemic morbidity, such as stroke and sepsis. Compliance with the current clinical guidelines for assessment, prevention, and treatment of inadvertent perioperative hypothermia will minimize, if not eliminate, such risk. We recommend the following essential clinical guidelines to prevent inadvertent perioperative hypothermia (Table 3). Identification of patient-, anesthesia-, and procedure-related risk factors is an integral component of assessment of the risk of inadvertent perioperative hypothermia. In order to achieve full compliance with implementation of active patient warming during surgery, it is prudent to make active warming information a part of the surgical timeout checklist. Irrespective of the presence of risk factors, passive heat retention methods should be part of perioperative management of patients undergoing elective orthopedic surgery to prevent inadvertent perioperative hypothermia. In addition, there should be a minimum threshold to utilize active patient-warming techniques, especially in patients with inherent risk factors and surgeries that take >30 minutes of operating time, either under regional or general anesthesia. As there are concerns about safety issues with the use of convection devices, we believe a multicenter randomized controlled trial is warranted.
Table 3. Recommended Essential Clinical Guidelines for Prevention of Inadvertent Perioperative Hypothermia
|
- Brown DJ, Brugger H, Boyd J, Paal P. Accidental Hypothermia. N Engl J Med. 2012;367(20):1930-1938. doi:10.1056/NEJMra1114208.
- Uzoigwe CE, Khan A, Smith RP, et al. Hypothermia and low body temperature are common and associated with high mortality in hip fracture patients. Hip Int. 2014; 24(3):237-242. doi:10.5301/hipint.5000124.
- Johansen A, Wakeman R, Boulton C, Plant F, Roberts J, Williams A. National Hip Fracture Database: National Report 2013. London, UK: National Hip Fracture Database, Royal College of Physicians; 2013.
- Karalapillai D, Story DA, Calzavacca, Licari E, Liu YL, Hart GK. Inadvertent hypothermia and mortality in postoperative intensive care patients: retrospective audit of 5050 patients. Anaesthesia. 2009;64(9):968-972. doi:10.1111/j.1365-2044.2009.05989.x.
- Horosz B, Malec-Milewska M. Inadvertent intraoperative hypothermia. Anaesthesiol Intensive Ther. 2013;45(1):38-43. doi:10.5603/AIT.2013.0009.
- Steelman VM, Perkhounkova YS, Lemke JH. The gap between compliance with the quality performance measure "perioperative temperature management” and normothermia. J Healthc Qual. 2014;37(6):333-341. doi:10.1111/jhq.12063.
- National Institute for Health and Clinical Excellence. Inadvertent Perioperative Hypothermia: The Management of Inadvertent Perioperative Hypothermia in Adults. London, UK: National Institute for Health and Clinical Excellence; 2008.
- Carlino W. Damage control resuscitation from major haemorrhage in polytrauma. Eur J Orthop Surg Traumatol. 2014;24(2):137-141. doi:10.1007/s00590-013-1172-7.
- Billeter AT, Hohmann SF, Druen D, Cannon R, Polk HC Jr. Unintentional perioperative hypothermia is associated with severe complications and high mortality in elective operations. Surgery. 2014;156(5):1245-1252. doi:10.1016/j.surg.2014.04.024.
- Kim YS, Jeon YS, Lee JA, et al. Intra-operative warming with a forced-air warmer in preventing hypothermia after tourniquet deflation in elderly patients. J Int Med Res. 2009;37(5):1457-1464. doi:10.1177/147323000903700521.
- Parodi D, Tobar C, Valderrama J, et al. Hip arthroscopy and hypothermia. Arthroscopy. 2012;28(7):924-928. doi:10.1016/j.arthro.2011.12.012.
- Kurz A, Sessler DI, Christensen R, Dechert M. Heat balance and distribution during the core-temperature plateau in anesthetized humans. Anesthesiology. 1995;83(3):491-499.
- Vaughan MS, Vaughan RW, Cork RC. Postoperative hypothermia in adults: relationship of age, anesthesia, and shivering to rewarming. Anesth Analg. 1981;60(10):746-751.
- American Society of PeriAnesthesia Nurses. Clinical guideline for the prevention of unplanned perioperative hypothermia. J Perianesth Nurs. 2001;16(5):305-314.
- Inaba K, Berg R, Barmparas G, et al. Prospective evaluation of ambient operating room temperature on the core temperature of injured patients undergoing emergent surgery. J Trauma Acute Care Surg. 2012;73(6):1478-1483. doi:10.1097/TA.0b013e3182781db3.
- Barie PS. Surgical site infections: epidemiology and prevention. Surg Infect (Larchmt). 2002;3 Suppl 1:S9-S21. doi:10.1089/sur.2002.3.s1-9.
- Jeran L. Patient temperature: an introduction to the clinical guideline for the prevention of unplanned perioperative hypothermia. J Perianesth Nurs. 2001;16(5):303-304.
- Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209-1215.
- Alderson P, Campbell G, Smith AF, Warttig S, Nicholson A, Lewis SR. Thermal insulation for preventing inadvertent perioperative hypothermia. Cochrane Database Syst Rev. 2014;6:CD009908. doi:10.1002/14651858.CD009908.pub2.
- Berry D, Wick C, Magons P. A clinical evaluation of the cost and time effectiveness of the ASPAN Hypothermia Guideline. J Perianesth Nurs. 2008;23(1):24-35. doi:10.1016/j.jopan.2007.09.010.
- Kimberger O, Held C, Stadelmann K et al. Resistive polymer versus forced-air warming: comparable heat transfer and core rewarming rates in volunteers. Anesth Analg. 2008;107(5):1621-1626. doi:10.1213/ane.0b013e3181845502.
- Brandt S, Oguz R, Hüttner H, et al. Resistive-polymer versus forced-air warming: comparable efficacy in orthopedic patients. Anesth Analg. 2010;110(3):834-838. doi:10.1213/ANE.0b013e3181cb3f5f.
- Legg AJ, Hammer AJ. Forced-air patient warming blankets disrupt unidirectional airflow. Bone Joint J. 2013;95-B(3):407-410. doi:10.1302/0301-620X.95B3.29121.
- Dasari KB, Albrecht M, Harper M. Effect of forced-air warming on the performance of operating theatre laminar flow ventilation. Anaesthesia. 2012;67(3):244-249. doi:10.1111/j.1365-2044.2011.06983.x.
- Belani KG, Albrecht M, McGovern PD, Reed M, Nachtsheim C. Patient warming excess heat: the effects on orthopedic operating room ventilation performance. Anesth Analg. 2013;117(2):406-411. doi:10.1213/ANE.0b013e31825f81e2.
- Legg AJ, Cannon T, Hammer AJ. Do forced air patient-warming devices disrupt unidirectional downward airflow? J Bone Joint Surg Br. 2012;94(2):254-256. doi:10.1302/0301-620X.94B2.27562.
- Albrecht M, Gaithier RL, Belani K, Litchy M, Leaper D. Forced-air warming blowers: An evaluation of filtration adequacy and airborne contamination emissions in the operating room. Am J Infect Control. 2011;39(4):321-328. doi:10.1016/j.ajic.2010.06.011.
- Reed M, Kimberger O, McGovern PD, Albrecht MC. Forced-air warming design: evaluation of intake filtration, internal microbial buildup, and airborne-contamination emissions. AANA J. 2013;81(4):275-280.
- McGovern PD, Albercht M, Belani KG, et al. Forced-air warming and ultra-clean ventilation do not mix: an investigation of theatre ventilation, patient warming and joint replacement infection in orthopaedics. J Bone Joint Surg Br.2011;93(11):1537-1544. doi:10.1302/0301-620X.93B11.27124.
ABSTRACT
Inadvertent perioperative hypothermia is a significant problem in patients undergoing either emergency or elective orthopedic surgery, and is associated with increased morbidity and mortality. Though in general the incidence of inadvertent perioperative hypothermia in postoperative recovery rooms has been decreasing over the last 2 decades, it still remains a significant risk in certain specialty practices, such as orthopedic surgery. This review article summarizes the currently available evidence on the incidence, risk factors, and complications of inadvertent perioperative hypothermia. Also, the effective preventive strategies in dealing with inadvertent perioperative hypothermia are reviewed and essential clinical guidelines to be followed are summarized.
Continue to: Inadvertent perioperative hypothermia...
Inadvertent perioperative hypothermia, defined as an involuntary drop in core body temperature to <35°C (95°F), is a condition associated with significant morbidity and mortality.1 This phenomenon has been reported in both emergency orthopedic admissions, such as fracture management, as well as in the elective setting such as arthroscopy, arthroplasty, and spine surgery.
In a study conducted in the United Kingdom including 781 elderly patients with a mean age of 80 years who presented with hip fractures, the 30-day mortality rate was 15.3% in patients who were admitted with a tympanic temperature of <36.5°C and only 5.1% in patients who maintained a tympanic temperature of 36.5°C to 37.5°C (odds ratio, 2.8; P > .0005).2 For an even better perspective, this analysis can be compared with the UK National Hip Fracture Database of 2013, which reported a 30-day mortality of 8.2% in patients who were admitted to the National Health Service with a diagnosis of hip fracture.3
Inadvertent perioperative hypothermia is also a common phenomenon during elective orthopedic hospital admissions. An Australian audit, which included 5050 postoperative patients, looked into the association between inadvertent perioperative hypothermia and mortality based on diagnostic criteria classifying mild hypothermia as a core temperature of <36°C and severe hypothermia as a core temperature of <35°C.4 The authors found that mild and severe hypothermia was experienced by 36% and 6% of patients, respectively. In-hospital mortality was 5.6% for normothermic patients, 8.9% for all hypothermic patients (P < .001), and 14.7% for severely hypothermic patients (P < .001). For a decrease of 1°C in core body temperature from <36°C to <35°C (but >34°C), there were higher odds of in-hospital mortality (odds ratio, 1.83; 95% confidence interval [CI], 1.20-2.60).
The physiologic response to hypothermia is to decrease heat loss by cutaneous and peripheral vasoconstriction and increase heat production by increasing the metabolic rate (eg, shivering and shifting to anaerobic metabolism). This response is blunted to a variable extent in perioperative patients for several reasons, including the effect of anesthetic drugs and old age.5
Maintenance of core body temperature >36°C is now a measured standard of perioperative care. A performance measure for perioperative temperature management was developed by the American Medical Association Physician Consortium for Performance Improvement (AMA-PCPI).6 To achieve this performance measure, mandatory documentation of use of active warming intraoperatively or a record of at least 1 body temperature ≥96.8°F (36°C) within 30 minutes immediately prior to and 15 minutes immediately after anesthesia end time is necessary. This performance measure is also endorsed by the Surgical Care Improvement Project (SCIP-Inf-10) and National Quality Forum (NQF).6
Continue to: Overall, in the last 2 decades...
Overall, in the last 2 decades, the incidence of inadvertent perioperative hypothermia has decreased, mainly due to aggressive intraoperative management.7 In spite of this, studies have shown that perioperative hypothermia remains a significant problem in patients undergoing orthopedic procedures. In a recent community hospital study conducted by the National Association for Healthcare Quality that included 4124 orthopedic patients undergoing elective surgery, it was shown that, in spite of 99% compliance to the AMA-PCPI recommendation, 7.7% of orthopedic patients were found to be hypothermic.6
Management of hypothermia has long been an integral component of “damage control surgery” and resuscitation during polytrauma, which aims to aggressively minimize hypovolemic shock and limit the development of the lethal triad of hypothermia, coagulopathy, and acidosis.8 However, critical references to prevention and management of inadvertent perioperative hypothermia are lacking in the orthopedic literature on elective surgical procedures. This review aims to bridge this knowledge gap.
Unless otherwise specified, inadvertent perioperative hypothermia in this article refers to the core body temperature. In contrast, peripheral/limb hypothermia refers primarily to the effect of tourniquet application to the involved limb and the effect after deflation of the tourniquet on core body temperature.
RISK FACTORS
There are several measurable risk factors that can contribute to inadvertent perioperative hypothermia, which can be subdivided into 3 groups: patient-related risk factors, anesthesia-related risk factors, and procedure-related risk factors (Table 1).5,9-11 It is important to note that in any given patient a combination of 2 or more risk factors predisposes them to developing inadvertent perioperative hypothermia. Conceptualizing the etiology of inadvertent perioperative hypothermia in this way helps to plan a multipronged strategy to prevent it from occurring in the first place. Some of the important risk factors for inadvertent perioperative hypothermia are discussed below.
Table 1. Risk Factors for Perioperative Hypothermia
Patient-Related Risk Factors | Anesthesia-Related Risk Factors | Procedure-Specific Risk Factors |
|
|
|
To identify patient-related risk factors, researchers from the University of Louisville conducted a study including 2138 operative patients who became hypothermic after admission, of whom 27% underwent orthopedic and spine procedures.9 The patient-related risk factors identified were a high severity of illness on admission (odds ratio, 2.81; 95% CI, 2.28-3.47), presence of a neurological disorder such as Alzheimer’s disease (odds ratio, 1.71; 95% CI,1.06-2.78), male sex (odds ratio, 1.65; 95% CI, 1.36-2.01), age >65 years (odds ratio, 1.61; 95% CI, 1.33-1.96), recent weight loss (odds ratio, 1.60; 95% CI, 1.04-2.48), anemia (odds ratio, 1.49; 95% CI, 1.12-1.98), and chronic renal failure (odds ratio, 1.43; 95% CI, 1.07-1.92). Interestingly, diabetes mellitus without end-stage organ failure was not found to be a significant risk factor (odds ratio, 0.58; 95% CI, 0.44-0.75). It is also important to note that some of these risk factors identified to contribute to perioperative hypothermia are dependent on each other and others are independent of each other. For example, chronic renal failure and anemia are dependent risk factors. In contrast, age >65 years and low body mass index as risk factors of perioperative hypothermia are independent of each other.
Continue to: The second subgroup of risk factors...
The second subgroup of risk factors for perioperative hypothermia is related to anesthesia. The effect of general and regional anesthesia on perioperative core temperature is significantly different, both in terms of intraoperative thermoregulation and postoperative recovery.12 Intraoperatively, the core body temperature during the first 2 hours of general anesthesia decreases at a rate of 1.3°C per hour due to loss of thermoregulatory cutaneous and peripheral vasoconstrictive responses resulting in heat loss exceeding metabolic heat production. However, the core temperature remains virtually constant during the subsequent 3 hours due to the return of the thermoregulatory response, which causes cutaneous and peripheral vasoconstriction and increased metabolic heat production. Postoperative recovery from the hypothermia induced by general anesthesia is significantly faster than from that induced by regional anesthesia.13
The effect of regional hypothermia on core body temperature is more complex because it must be considered in addition to the effect of an associated procedure-related variable (ie, tourniquet application). If a tourniquet is not used during a surgery with regional anesthesia, a linear decrease in core temperature follows until recovery, due to increased blood flow from the loss of sympathetic peripheral vasoconstrictive response with resultant core-to-peripheral heat redistribution to the exposed operating limb. If a tourniquet is used during surgery with regional anesthesia, there will be no significant effect of the exposed operating limb on core temperature, as there is no blood flow between them. However, once the tourniquet is deflated, the core body temperature will be affected significantly as a result of core-to-peripheral distribution of heat to the operated limb with the return of blood flow. This fall in core body temperature after tourniquet deflation can be prevented by active forced-air warming initiated from the beginning of surgery.10 The extent and rate of development of peripheral/limb hypothermia during surgery (and its subsequent effect on core body temperature) depends on several factors, including the operating room ambient temperature, duration of tourniquet application, and temperature of the irrigation fluid. Postoperative recovery from the hypothermia induced by regional anesthesia takes longer than from that induced by general anesthesia because of the prolonged period of loss of vasoconstrictive response.
The third subgroup of risk factors associated with perioperative hypothermia is procedure related. Several procedure-specific risk factors for inadvertent perioperative hypothermia during arthroscopic surgery are identified, including prolonged operating time, low blood pressure during the procedure, and low temperature of the irrigation fluid.11 It is logical to extrapolate the importance of these risk factors to other orthopedic procedures which also require prolonged operating times, are performed under hypotension, or expose the patient to irrigation fluid that is at a low temperature. Understanding the importance of each of these procedure-related risk factors is the most important from the perspective of the orthopedic surgeon when compared to the rest of the subgroups of risk factors for inadvertent perioperative hypothermia as he/she is directly responsible for them.
The ambient operating room temperature has traditionally been considered a risk factor for inadvertent hypothermia in perioperative patients, but evidence is available to the contrary. The recommended ambient room temperature as per the clinical guideline published by the American Society of PeriAnesthesia Nurses (ASPAN) is 20°C to 24°C (68°F-75°F).14 The ambient temperature can have a significant effect on peripheral/limb hypothermia when operating on a limb with a tourniquet inflated, as the limb has no blood supply to distribute heat from the core to the periphery. However, the direct effect of ambient room temperature on the patient’s core body temperature is unlikely to be clinically significant if standard active warming interventions are implemented.15
COMPLICATIONS
The increased incidence of mortality due to inadvertent hypothermia in the perioperative period has already been discussed. Several other complications of inadvertent perioperative hypothermia include increased incidence of coagulopathy, acidosis, stroke, sepsis, pneumonia, myocardial infarction, surgical site infections, altered drug metabolism, and longer hospital stays.8,9,16-18 Hypothermia, coagulopathy, and acidosis have long been recognized as a lethal triad more commonly seen in polytrauma patients than in elective orthopedic surgery, as this occurs at extremes of temperature, usually <32°C. When compared with patients who did not develop perioperative hypothermia, patients who developed hypothermia during elective operations were shown to experience an overall doubled complication rate (13.9% vs 26.3%; P < .001) of which the incidence of stroke (1.0% vs 6.5%; P < .001), pneumonia (1.3% vs 5.1%; P < .001), and sepsis (2.6% vs 7.5%; P < .001) were much more likely than myocardial infarction (1.1% vs 3.3%; P = .01) and wound infection (3.3% vs 5.0%; P = .14).9
Continue to: Prevention...
PREVENTION
Prevention of perioperative hypothermia is a core measure to improve the outcome after ambulatory and fast-track orthopedic surgery and rehabilitation. Preventive strategies for perioperative hypothermia can be grouped into passive heat retention methods and active external warming methods (Table 2). Passive methods aim to maintain body temperature by decreasing the heat loss by radiation (eg, reflective blanket), conduction (eg, layered cotton blankets and padding the operating table), or convection (eg, heat and humidity exchanger in the breathing circuits) to the surrounding environment. Active patient heating methods aim to bring in heat from the source to the patient’s body using conduction (eg, Hot Dog® [Eden Augustine Temperature Management]) or convection (eg, Bair Hugger® [Arizant Healthcare]) techniques.
Table 2. Methods to Prevent Inadvertent Perioperative Hypothermia
Passive Heat-Retention Methods | Active External Warming Methods |
| Conduction techniques:
Convection techniques:
|
Active patient warming is superior to passive heat retention methods. A recent Cochrane study assessed the effects of standard care (ie, use of layered clothing and warm blankets, etc.) and addition of extra thermal insulation by reflective blankets or active forced air warming to standard care on the perioperative core body temperature.19 They concluded that there is no clear benefit of addition of extra thermal insulation by reflective blankets compared with standard care alone. Also, forced-air warming in addition to standard care appeared to maintain core temperature better than standard care alone, by between 0.5°C and 1°C, but the clinical importance of this difference could not be inferred, as none of the included studies in this meta-analysis documented major cardiovascular outcomes.
Several clinical guidelines have been developed by not-for-profit, government, and professional organizations aimed at prevention of perioperative hypothermia as primary or secondary outcome. A clinical guideline was published by ASPAN in 2001 for assessment, prevention, and intervention in unplanned perioperative hypothermia.14 Cost and time effectiveness of the ASPAN Hypothermia Guideline was published in 2008.20 The assessment guideline includes identification of risk factors, repeated pre-/intra-/postoperative temperature measurement, and repeated clinical evaluation of the patient’s status. The preventive guideline is to maintain an ambient temperature of 20°C to 24°C (68°F-75°F) and use appropriate passive patient warming methods pre-, intra-, and postoperatively. Intervention in the form of active patient heating is advised only if the patient develops hypothermia in spite of the above-mentioned standard preventive measures. But many orthopedic ambulatory surgery centers currently use active patient warming as both a preventive and an intervention strategy.
Active patient warming by conduction devices occurs by direct physical contact with the device, which is set at a higher temperature, whereas heat transfer from the convection device to the patient occurs by a physical medium such as forced air or circulating water that moves in between the device and the patient. Any recommendation for use of a specific technique of active patient warming (ie, by the use of a conduction device or a convection device) should only be given after comparing evidence on 3 critical aspects: efficacy, safety, and cost effectiveness.
The heating efficacy and core rewarming rates of conduction and convection devices have been compared in the literature. Full-body forced-air heating with the Bair Hugger® and full-body resistive polymer heating with the Hot Dog® in healthy volunteers were found to be similar.21 Also, in a randomized study conducted on 80 orthopedic patients undergoing surgery, resistive polymer warming performed as efficiently as forced-air warming in patients undergoing orthopedic surgery.22
Continue to: Secondly, the safety of convection...
Secondly, the safety of convection devices such as the Bair Hugger® has been under intense scrutiny based on the evidence that it disrupts the laminar airflow in the operating theater.23-26 This disruption in laminar air flow has been shown to cause emission of significant levels of airborne contaminants of size >0.3 μm (germ size).27 Isolates of Staphylococcus aureus, coagulase-negative Staphylococcus species, and methicillin-resistant Staphylococcus aureus were detected in 13.5%, 3.9%, and 1.9% of forced-air blowers, respectively.28 However, the clinical effect on the rate of deep joint infection due to the disruption of laminar air flow has been examined in only 1 study. McGovern and colleagues29 reported a significant increase in deep joint infection during a period when forced air warming was used compared to a period when conductive fabric warming was used (odds ratio, 3.8; P = .024) and recommended air-free warming by a conduction device over forced-air warming for orthopedic procedures. Unfortunately, the prophylactic antibiotic regimen was not kept constant during their study period. During an overlapping time frame during which they shifted from the use of a convection device (Bair Hugger®) to a conduction device (Hot Dog®), they also changed their antibiotic regimen from gentamicin 4.5 mg/kg intravenous (IV) to gentamicin 3 mg/kg IV plus teicoplanin 400 mg IV. This change in antibiotic regimen is a major confounding factor that calls into question the validity of the conclusions drawn by the authors.
Finally, the cost effectiveness of conduction and convection devices has never been studied. Hence, based on the current evidence, it is not possible to recommend a particular type of active patient-warming device.
CONCLUSION
Orthopedic surgeons should be aware that inadvertent perioperative hypothermia is a common phenomenon in perioperative patients. It must be recognized that the maintenance of perioperative normothermia during all major orthopedic surgical procedures is desirable, as inadvertent perioperative hypothermia is shown to be associated with increased mortality and systemic morbidity, such as stroke and sepsis. Compliance with the current clinical guidelines for assessment, prevention, and treatment of inadvertent perioperative hypothermia will minimize, if not eliminate, such risk. We recommend the following essential clinical guidelines to prevent inadvertent perioperative hypothermia (Table 3). Identification of patient-, anesthesia-, and procedure-related risk factors is an integral component of assessment of the risk of inadvertent perioperative hypothermia. In order to achieve full compliance with implementation of active patient warming during surgery, it is prudent to make active warming information a part of the surgical timeout checklist. Irrespective of the presence of risk factors, passive heat retention methods should be part of perioperative management of patients undergoing elective orthopedic surgery to prevent inadvertent perioperative hypothermia. In addition, there should be a minimum threshold to utilize active patient-warming techniques, especially in patients with inherent risk factors and surgeries that take >30 minutes of operating time, either under regional or general anesthesia. As there are concerns about safety issues with the use of convection devices, we believe a multicenter randomized controlled trial is warranted.
Table 3. Recommended Essential Clinical Guidelines for Prevention of Inadvertent Perioperative Hypothermia
|
ABSTRACT
Inadvertent perioperative hypothermia is a significant problem in patients undergoing either emergency or elective orthopedic surgery, and is associated with increased morbidity and mortality. Though in general the incidence of inadvertent perioperative hypothermia in postoperative recovery rooms has been decreasing over the last 2 decades, it still remains a significant risk in certain specialty practices, such as orthopedic surgery. This review article summarizes the currently available evidence on the incidence, risk factors, and complications of inadvertent perioperative hypothermia. Also, the effective preventive strategies in dealing with inadvertent perioperative hypothermia are reviewed and essential clinical guidelines to be followed are summarized.
Continue to: Inadvertent perioperative hypothermia...
Inadvertent perioperative hypothermia, defined as an involuntary drop in core body temperature to <35°C (95°F), is a condition associated with significant morbidity and mortality.1 This phenomenon has been reported in both emergency orthopedic admissions, such as fracture management, as well as in the elective setting such as arthroscopy, arthroplasty, and spine surgery.
In a study conducted in the United Kingdom including 781 elderly patients with a mean age of 80 years who presented with hip fractures, the 30-day mortality rate was 15.3% in patients who were admitted with a tympanic temperature of <36.5°C and only 5.1% in patients who maintained a tympanic temperature of 36.5°C to 37.5°C (odds ratio, 2.8; P > .0005).2 For an even better perspective, this analysis can be compared with the UK National Hip Fracture Database of 2013, which reported a 30-day mortality of 8.2% in patients who were admitted to the National Health Service with a diagnosis of hip fracture.3
Inadvertent perioperative hypothermia is also a common phenomenon during elective orthopedic hospital admissions. An Australian audit, which included 5050 postoperative patients, looked into the association between inadvertent perioperative hypothermia and mortality based on diagnostic criteria classifying mild hypothermia as a core temperature of <36°C and severe hypothermia as a core temperature of <35°C.4 The authors found that mild and severe hypothermia was experienced by 36% and 6% of patients, respectively. In-hospital mortality was 5.6% for normothermic patients, 8.9% for all hypothermic patients (P < .001), and 14.7% for severely hypothermic patients (P < .001). For a decrease of 1°C in core body temperature from <36°C to <35°C (but >34°C), there were higher odds of in-hospital mortality (odds ratio, 1.83; 95% confidence interval [CI], 1.20-2.60).
The physiologic response to hypothermia is to decrease heat loss by cutaneous and peripheral vasoconstriction and increase heat production by increasing the metabolic rate (eg, shivering and shifting to anaerobic metabolism). This response is blunted to a variable extent in perioperative patients for several reasons, including the effect of anesthetic drugs and old age.5
Maintenance of core body temperature >36°C is now a measured standard of perioperative care. A performance measure for perioperative temperature management was developed by the American Medical Association Physician Consortium for Performance Improvement (AMA-PCPI).6 To achieve this performance measure, mandatory documentation of use of active warming intraoperatively or a record of at least 1 body temperature ≥96.8°F (36°C) within 30 minutes immediately prior to and 15 minutes immediately after anesthesia end time is necessary. This performance measure is also endorsed by the Surgical Care Improvement Project (SCIP-Inf-10) and National Quality Forum (NQF).6
Continue to: Overall, in the last 2 decades...
Overall, in the last 2 decades, the incidence of inadvertent perioperative hypothermia has decreased, mainly due to aggressive intraoperative management.7 In spite of this, studies have shown that perioperative hypothermia remains a significant problem in patients undergoing orthopedic procedures. In a recent community hospital study conducted by the National Association for Healthcare Quality that included 4124 orthopedic patients undergoing elective surgery, it was shown that, in spite of 99% compliance to the AMA-PCPI recommendation, 7.7% of orthopedic patients were found to be hypothermic.6
Management of hypothermia has long been an integral component of “damage control surgery” and resuscitation during polytrauma, which aims to aggressively minimize hypovolemic shock and limit the development of the lethal triad of hypothermia, coagulopathy, and acidosis.8 However, critical references to prevention and management of inadvertent perioperative hypothermia are lacking in the orthopedic literature on elective surgical procedures. This review aims to bridge this knowledge gap.
Unless otherwise specified, inadvertent perioperative hypothermia in this article refers to the core body temperature. In contrast, peripheral/limb hypothermia refers primarily to the effect of tourniquet application to the involved limb and the effect after deflation of the tourniquet on core body temperature.
RISK FACTORS
There are several measurable risk factors that can contribute to inadvertent perioperative hypothermia, which can be subdivided into 3 groups: patient-related risk factors, anesthesia-related risk factors, and procedure-related risk factors (Table 1).5,9-11 It is important to note that in any given patient a combination of 2 or more risk factors predisposes them to developing inadvertent perioperative hypothermia. Conceptualizing the etiology of inadvertent perioperative hypothermia in this way helps to plan a multipronged strategy to prevent it from occurring in the first place. Some of the important risk factors for inadvertent perioperative hypothermia are discussed below.
Table 1. Risk Factors for Perioperative Hypothermia
Patient-Related Risk Factors | Anesthesia-Related Risk Factors | Procedure-Specific Risk Factors |
|
|
|
To identify patient-related risk factors, researchers from the University of Louisville conducted a study including 2138 operative patients who became hypothermic after admission, of whom 27% underwent orthopedic and spine procedures.9 The patient-related risk factors identified were a high severity of illness on admission (odds ratio, 2.81; 95% CI, 2.28-3.47), presence of a neurological disorder such as Alzheimer’s disease (odds ratio, 1.71; 95% CI,1.06-2.78), male sex (odds ratio, 1.65; 95% CI, 1.36-2.01), age >65 years (odds ratio, 1.61; 95% CI, 1.33-1.96), recent weight loss (odds ratio, 1.60; 95% CI, 1.04-2.48), anemia (odds ratio, 1.49; 95% CI, 1.12-1.98), and chronic renal failure (odds ratio, 1.43; 95% CI, 1.07-1.92). Interestingly, diabetes mellitus without end-stage organ failure was not found to be a significant risk factor (odds ratio, 0.58; 95% CI, 0.44-0.75). It is also important to note that some of these risk factors identified to contribute to perioperative hypothermia are dependent on each other and others are independent of each other. For example, chronic renal failure and anemia are dependent risk factors. In contrast, age >65 years and low body mass index as risk factors of perioperative hypothermia are independent of each other.
Continue to: The second subgroup of risk factors...
The second subgroup of risk factors for perioperative hypothermia is related to anesthesia. The effect of general and regional anesthesia on perioperative core temperature is significantly different, both in terms of intraoperative thermoregulation and postoperative recovery.12 Intraoperatively, the core body temperature during the first 2 hours of general anesthesia decreases at a rate of 1.3°C per hour due to loss of thermoregulatory cutaneous and peripheral vasoconstrictive responses resulting in heat loss exceeding metabolic heat production. However, the core temperature remains virtually constant during the subsequent 3 hours due to the return of the thermoregulatory response, which causes cutaneous and peripheral vasoconstriction and increased metabolic heat production. Postoperative recovery from the hypothermia induced by general anesthesia is significantly faster than from that induced by regional anesthesia.13
The effect of regional hypothermia on core body temperature is more complex because it must be considered in addition to the effect of an associated procedure-related variable (ie, tourniquet application). If a tourniquet is not used during a surgery with regional anesthesia, a linear decrease in core temperature follows until recovery, due to increased blood flow from the loss of sympathetic peripheral vasoconstrictive response with resultant core-to-peripheral heat redistribution to the exposed operating limb. If a tourniquet is used during surgery with regional anesthesia, there will be no significant effect of the exposed operating limb on core temperature, as there is no blood flow between them. However, once the tourniquet is deflated, the core body temperature will be affected significantly as a result of core-to-peripheral distribution of heat to the operated limb with the return of blood flow. This fall in core body temperature after tourniquet deflation can be prevented by active forced-air warming initiated from the beginning of surgery.10 The extent and rate of development of peripheral/limb hypothermia during surgery (and its subsequent effect on core body temperature) depends on several factors, including the operating room ambient temperature, duration of tourniquet application, and temperature of the irrigation fluid. Postoperative recovery from the hypothermia induced by regional anesthesia takes longer than from that induced by general anesthesia because of the prolonged period of loss of vasoconstrictive response.
The third subgroup of risk factors associated with perioperative hypothermia is procedure related. Several procedure-specific risk factors for inadvertent perioperative hypothermia during arthroscopic surgery are identified, including prolonged operating time, low blood pressure during the procedure, and low temperature of the irrigation fluid.11 It is logical to extrapolate the importance of these risk factors to other orthopedic procedures which also require prolonged operating times, are performed under hypotension, or expose the patient to irrigation fluid that is at a low temperature. Understanding the importance of each of these procedure-related risk factors is the most important from the perspective of the orthopedic surgeon when compared to the rest of the subgroups of risk factors for inadvertent perioperative hypothermia as he/she is directly responsible for them.
The ambient operating room temperature has traditionally been considered a risk factor for inadvertent hypothermia in perioperative patients, but evidence is available to the contrary. The recommended ambient room temperature as per the clinical guideline published by the American Society of PeriAnesthesia Nurses (ASPAN) is 20°C to 24°C (68°F-75°F).14 The ambient temperature can have a significant effect on peripheral/limb hypothermia when operating on a limb with a tourniquet inflated, as the limb has no blood supply to distribute heat from the core to the periphery. However, the direct effect of ambient room temperature on the patient’s core body temperature is unlikely to be clinically significant if standard active warming interventions are implemented.15
COMPLICATIONS
The increased incidence of mortality due to inadvertent hypothermia in the perioperative period has already been discussed. Several other complications of inadvertent perioperative hypothermia include increased incidence of coagulopathy, acidosis, stroke, sepsis, pneumonia, myocardial infarction, surgical site infections, altered drug metabolism, and longer hospital stays.8,9,16-18 Hypothermia, coagulopathy, and acidosis have long been recognized as a lethal triad more commonly seen in polytrauma patients than in elective orthopedic surgery, as this occurs at extremes of temperature, usually <32°C. When compared with patients who did not develop perioperative hypothermia, patients who developed hypothermia during elective operations were shown to experience an overall doubled complication rate (13.9% vs 26.3%; P < .001) of which the incidence of stroke (1.0% vs 6.5%; P < .001), pneumonia (1.3% vs 5.1%; P < .001), and sepsis (2.6% vs 7.5%; P < .001) were much more likely than myocardial infarction (1.1% vs 3.3%; P = .01) and wound infection (3.3% vs 5.0%; P = .14).9
Continue to: Prevention...
PREVENTION
Prevention of perioperative hypothermia is a core measure to improve the outcome after ambulatory and fast-track orthopedic surgery and rehabilitation. Preventive strategies for perioperative hypothermia can be grouped into passive heat retention methods and active external warming methods (Table 2). Passive methods aim to maintain body temperature by decreasing the heat loss by radiation (eg, reflective blanket), conduction (eg, layered cotton blankets and padding the operating table), or convection (eg, heat and humidity exchanger in the breathing circuits) to the surrounding environment. Active patient heating methods aim to bring in heat from the source to the patient’s body using conduction (eg, Hot Dog® [Eden Augustine Temperature Management]) or convection (eg, Bair Hugger® [Arizant Healthcare]) techniques.
Table 2. Methods to Prevent Inadvertent Perioperative Hypothermia
Passive Heat-Retention Methods | Active External Warming Methods |
| Conduction techniques:
Convection techniques:
|
Active patient warming is superior to passive heat retention methods. A recent Cochrane study assessed the effects of standard care (ie, use of layered clothing and warm blankets, etc.) and addition of extra thermal insulation by reflective blankets or active forced air warming to standard care on the perioperative core body temperature.19 They concluded that there is no clear benefit of addition of extra thermal insulation by reflective blankets compared with standard care alone. Also, forced-air warming in addition to standard care appeared to maintain core temperature better than standard care alone, by between 0.5°C and 1°C, but the clinical importance of this difference could not be inferred, as none of the included studies in this meta-analysis documented major cardiovascular outcomes.
Several clinical guidelines have been developed by not-for-profit, government, and professional organizations aimed at prevention of perioperative hypothermia as primary or secondary outcome. A clinical guideline was published by ASPAN in 2001 for assessment, prevention, and intervention in unplanned perioperative hypothermia.14 Cost and time effectiveness of the ASPAN Hypothermia Guideline was published in 2008.20 The assessment guideline includes identification of risk factors, repeated pre-/intra-/postoperative temperature measurement, and repeated clinical evaluation of the patient’s status. The preventive guideline is to maintain an ambient temperature of 20°C to 24°C (68°F-75°F) and use appropriate passive patient warming methods pre-, intra-, and postoperatively. Intervention in the form of active patient heating is advised only if the patient develops hypothermia in spite of the above-mentioned standard preventive measures. But many orthopedic ambulatory surgery centers currently use active patient warming as both a preventive and an intervention strategy.
Active patient warming by conduction devices occurs by direct physical contact with the device, which is set at a higher temperature, whereas heat transfer from the convection device to the patient occurs by a physical medium such as forced air or circulating water that moves in between the device and the patient. Any recommendation for use of a specific technique of active patient warming (ie, by the use of a conduction device or a convection device) should only be given after comparing evidence on 3 critical aspects: efficacy, safety, and cost effectiveness.
The heating efficacy and core rewarming rates of conduction and convection devices have been compared in the literature. Full-body forced-air heating with the Bair Hugger® and full-body resistive polymer heating with the Hot Dog® in healthy volunteers were found to be similar.21 Also, in a randomized study conducted on 80 orthopedic patients undergoing surgery, resistive polymer warming performed as efficiently as forced-air warming in patients undergoing orthopedic surgery.22
Continue to: Secondly, the safety of convection...
Secondly, the safety of convection devices such as the Bair Hugger® has been under intense scrutiny based on the evidence that it disrupts the laminar airflow in the operating theater.23-26 This disruption in laminar air flow has been shown to cause emission of significant levels of airborne contaminants of size >0.3 μm (germ size).27 Isolates of Staphylococcus aureus, coagulase-negative Staphylococcus species, and methicillin-resistant Staphylococcus aureus were detected in 13.5%, 3.9%, and 1.9% of forced-air blowers, respectively.28 However, the clinical effect on the rate of deep joint infection due to the disruption of laminar air flow has been examined in only 1 study. McGovern and colleagues29 reported a significant increase in deep joint infection during a period when forced air warming was used compared to a period when conductive fabric warming was used (odds ratio, 3.8; P = .024) and recommended air-free warming by a conduction device over forced-air warming for orthopedic procedures. Unfortunately, the prophylactic antibiotic regimen was not kept constant during their study period. During an overlapping time frame during which they shifted from the use of a convection device (Bair Hugger®) to a conduction device (Hot Dog®), they also changed their antibiotic regimen from gentamicin 4.5 mg/kg intravenous (IV) to gentamicin 3 mg/kg IV plus teicoplanin 400 mg IV. This change in antibiotic regimen is a major confounding factor that calls into question the validity of the conclusions drawn by the authors.
Finally, the cost effectiveness of conduction and convection devices has never been studied. Hence, based on the current evidence, it is not possible to recommend a particular type of active patient-warming device.
CONCLUSION
Orthopedic surgeons should be aware that inadvertent perioperative hypothermia is a common phenomenon in perioperative patients. It must be recognized that the maintenance of perioperative normothermia during all major orthopedic surgical procedures is desirable, as inadvertent perioperative hypothermia is shown to be associated with increased mortality and systemic morbidity, such as stroke and sepsis. Compliance with the current clinical guidelines for assessment, prevention, and treatment of inadvertent perioperative hypothermia will minimize, if not eliminate, such risk. We recommend the following essential clinical guidelines to prevent inadvertent perioperative hypothermia (Table 3). Identification of patient-, anesthesia-, and procedure-related risk factors is an integral component of assessment of the risk of inadvertent perioperative hypothermia. In order to achieve full compliance with implementation of active patient warming during surgery, it is prudent to make active warming information a part of the surgical timeout checklist. Irrespective of the presence of risk factors, passive heat retention methods should be part of perioperative management of patients undergoing elective orthopedic surgery to prevent inadvertent perioperative hypothermia. In addition, there should be a minimum threshold to utilize active patient-warming techniques, especially in patients with inherent risk factors and surgeries that take >30 minutes of operating time, either under regional or general anesthesia. As there are concerns about safety issues with the use of convection devices, we believe a multicenter randomized controlled trial is warranted.
Table 3. Recommended Essential Clinical Guidelines for Prevention of Inadvertent Perioperative Hypothermia
|
- Brown DJ, Brugger H, Boyd J, Paal P. Accidental Hypothermia. N Engl J Med. 2012;367(20):1930-1938. doi:10.1056/NEJMra1114208.
- Uzoigwe CE, Khan A, Smith RP, et al. Hypothermia and low body temperature are common and associated with high mortality in hip fracture patients. Hip Int. 2014; 24(3):237-242. doi:10.5301/hipint.5000124.
- Johansen A, Wakeman R, Boulton C, Plant F, Roberts J, Williams A. National Hip Fracture Database: National Report 2013. London, UK: National Hip Fracture Database, Royal College of Physicians; 2013.
- Karalapillai D, Story DA, Calzavacca, Licari E, Liu YL, Hart GK. Inadvertent hypothermia and mortality in postoperative intensive care patients: retrospective audit of 5050 patients. Anaesthesia. 2009;64(9):968-972. doi:10.1111/j.1365-2044.2009.05989.x.
- Horosz B, Malec-Milewska M. Inadvertent intraoperative hypothermia. Anaesthesiol Intensive Ther. 2013;45(1):38-43. doi:10.5603/AIT.2013.0009.
- Steelman VM, Perkhounkova YS, Lemke JH. The gap between compliance with the quality performance measure "perioperative temperature management” and normothermia. J Healthc Qual. 2014;37(6):333-341. doi:10.1111/jhq.12063.
- National Institute for Health and Clinical Excellence. Inadvertent Perioperative Hypothermia: The Management of Inadvertent Perioperative Hypothermia in Adults. London, UK: National Institute for Health and Clinical Excellence; 2008.
- Carlino W. Damage control resuscitation from major haemorrhage in polytrauma. Eur J Orthop Surg Traumatol. 2014;24(2):137-141. doi:10.1007/s00590-013-1172-7.
- Billeter AT, Hohmann SF, Druen D, Cannon R, Polk HC Jr. Unintentional perioperative hypothermia is associated with severe complications and high mortality in elective operations. Surgery. 2014;156(5):1245-1252. doi:10.1016/j.surg.2014.04.024.
- Kim YS, Jeon YS, Lee JA, et al. Intra-operative warming with a forced-air warmer in preventing hypothermia after tourniquet deflation in elderly patients. J Int Med Res. 2009;37(5):1457-1464. doi:10.1177/147323000903700521.
- Parodi D, Tobar C, Valderrama J, et al. Hip arthroscopy and hypothermia. Arthroscopy. 2012;28(7):924-928. doi:10.1016/j.arthro.2011.12.012.
- Kurz A, Sessler DI, Christensen R, Dechert M. Heat balance and distribution during the core-temperature plateau in anesthetized humans. Anesthesiology. 1995;83(3):491-499.
- Vaughan MS, Vaughan RW, Cork RC. Postoperative hypothermia in adults: relationship of age, anesthesia, and shivering to rewarming. Anesth Analg. 1981;60(10):746-751.
- American Society of PeriAnesthesia Nurses. Clinical guideline for the prevention of unplanned perioperative hypothermia. J Perianesth Nurs. 2001;16(5):305-314.
- Inaba K, Berg R, Barmparas G, et al. Prospective evaluation of ambient operating room temperature on the core temperature of injured patients undergoing emergent surgery. J Trauma Acute Care Surg. 2012;73(6):1478-1483. doi:10.1097/TA.0b013e3182781db3.
- Barie PS. Surgical site infections: epidemiology and prevention. Surg Infect (Larchmt). 2002;3 Suppl 1:S9-S21. doi:10.1089/sur.2002.3.s1-9.
- Jeran L. Patient temperature: an introduction to the clinical guideline for the prevention of unplanned perioperative hypothermia. J Perianesth Nurs. 2001;16(5):303-304.
- Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209-1215.
- Alderson P, Campbell G, Smith AF, Warttig S, Nicholson A, Lewis SR. Thermal insulation for preventing inadvertent perioperative hypothermia. Cochrane Database Syst Rev. 2014;6:CD009908. doi:10.1002/14651858.CD009908.pub2.
- Berry D, Wick C, Magons P. A clinical evaluation of the cost and time effectiveness of the ASPAN Hypothermia Guideline. J Perianesth Nurs. 2008;23(1):24-35. doi:10.1016/j.jopan.2007.09.010.
- Kimberger O, Held C, Stadelmann K et al. Resistive polymer versus forced-air warming: comparable heat transfer and core rewarming rates in volunteers. Anesth Analg. 2008;107(5):1621-1626. doi:10.1213/ane.0b013e3181845502.
- Brandt S, Oguz R, Hüttner H, et al. Resistive-polymer versus forced-air warming: comparable efficacy in orthopedic patients. Anesth Analg. 2010;110(3):834-838. doi:10.1213/ANE.0b013e3181cb3f5f.
- Legg AJ, Hammer AJ. Forced-air patient warming blankets disrupt unidirectional airflow. Bone Joint J. 2013;95-B(3):407-410. doi:10.1302/0301-620X.95B3.29121.
- Dasari KB, Albrecht M, Harper M. Effect of forced-air warming on the performance of operating theatre laminar flow ventilation. Anaesthesia. 2012;67(3):244-249. doi:10.1111/j.1365-2044.2011.06983.x.
- Belani KG, Albrecht M, McGovern PD, Reed M, Nachtsheim C. Patient warming excess heat: the effects on orthopedic operating room ventilation performance. Anesth Analg. 2013;117(2):406-411. doi:10.1213/ANE.0b013e31825f81e2.
- Legg AJ, Cannon T, Hammer AJ. Do forced air patient-warming devices disrupt unidirectional downward airflow? J Bone Joint Surg Br. 2012;94(2):254-256. doi:10.1302/0301-620X.94B2.27562.
- Albrecht M, Gaithier RL, Belani K, Litchy M, Leaper D. Forced-air warming blowers: An evaluation of filtration adequacy and airborne contamination emissions in the operating room. Am J Infect Control. 2011;39(4):321-328. doi:10.1016/j.ajic.2010.06.011.
- Reed M, Kimberger O, McGovern PD, Albrecht MC. Forced-air warming design: evaluation of intake filtration, internal microbial buildup, and airborne-contamination emissions. AANA J. 2013;81(4):275-280.
- McGovern PD, Albercht M, Belani KG, et al. Forced-air warming and ultra-clean ventilation do not mix: an investigation of theatre ventilation, patient warming and joint replacement infection in orthopaedics. J Bone Joint Surg Br.2011;93(11):1537-1544. doi:10.1302/0301-620X.93B11.27124.
- Brown DJ, Brugger H, Boyd J, Paal P. Accidental Hypothermia. N Engl J Med. 2012;367(20):1930-1938. doi:10.1056/NEJMra1114208.
- Uzoigwe CE, Khan A, Smith RP, et al. Hypothermia and low body temperature are common and associated with high mortality in hip fracture patients. Hip Int. 2014; 24(3):237-242. doi:10.5301/hipint.5000124.
- Johansen A, Wakeman R, Boulton C, Plant F, Roberts J, Williams A. National Hip Fracture Database: National Report 2013. London, UK: National Hip Fracture Database, Royal College of Physicians; 2013.
- Karalapillai D, Story DA, Calzavacca, Licari E, Liu YL, Hart GK. Inadvertent hypothermia and mortality in postoperative intensive care patients: retrospective audit of 5050 patients. Anaesthesia. 2009;64(9):968-972. doi:10.1111/j.1365-2044.2009.05989.x.
- Horosz B, Malec-Milewska M. Inadvertent intraoperative hypothermia. Anaesthesiol Intensive Ther. 2013;45(1):38-43. doi:10.5603/AIT.2013.0009.
- Steelman VM, Perkhounkova YS, Lemke JH. The gap between compliance with the quality performance measure "perioperative temperature management” and normothermia. J Healthc Qual. 2014;37(6):333-341. doi:10.1111/jhq.12063.
- National Institute for Health and Clinical Excellence. Inadvertent Perioperative Hypothermia: The Management of Inadvertent Perioperative Hypothermia in Adults. London, UK: National Institute for Health and Clinical Excellence; 2008.
- Carlino W. Damage control resuscitation from major haemorrhage in polytrauma. Eur J Orthop Surg Traumatol. 2014;24(2):137-141. doi:10.1007/s00590-013-1172-7.
- Billeter AT, Hohmann SF, Druen D, Cannon R, Polk HC Jr. Unintentional perioperative hypothermia is associated with severe complications and high mortality in elective operations. Surgery. 2014;156(5):1245-1252. doi:10.1016/j.surg.2014.04.024.
- Kim YS, Jeon YS, Lee JA, et al. Intra-operative warming with a forced-air warmer in preventing hypothermia after tourniquet deflation in elderly patients. J Int Med Res. 2009;37(5):1457-1464. doi:10.1177/147323000903700521.
- Parodi D, Tobar C, Valderrama J, et al. Hip arthroscopy and hypothermia. Arthroscopy. 2012;28(7):924-928. doi:10.1016/j.arthro.2011.12.012.
- Kurz A, Sessler DI, Christensen R, Dechert M. Heat balance and distribution during the core-temperature plateau in anesthetized humans. Anesthesiology. 1995;83(3):491-499.
- Vaughan MS, Vaughan RW, Cork RC. Postoperative hypothermia in adults: relationship of age, anesthesia, and shivering to rewarming. Anesth Analg. 1981;60(10):746-751.
- American Society of PeriAnesthesia Nurses. Clinical guideline for the prevention of unplanned perioperative hypothermia. J Perianesth Nurs. 2001;16(5):305-314.
- Inaba K, Berg R, Barmparas G, et al. Prospective evaluation of ambient operating room temperature on the core temperature of injured patients undergoing emergent surgery. J Trauma Acute Care Surg. 2012;73(6):1478-1483. doi:10.1097/TA.0b013e3182781db3.
- Barie PS. Surgical site infections: epidemiology and prevention. Surg Infect (Larchmt). 2002;3 Suppl 1:S9-S21. doi:10.1089/sur.2002.3.s1-9.
- Jeran L. Patient temperature: an introduction to the clinical guideline for the prevention of unplanned perioperative hypothermia. J Perianesth Nurs. 2001;16(5):303-304.
- Kurz A, Sessler DI, Lenhardt R. Perioperative normothermia to reduce the incidence of surgical-wound infection and shorten hospitalization. Study of Wound Infection and Temperature Group. N Engl J Med. 1996;334(19):1209-1215.
- Alderson P, Campbell G, Smith AF, Warttig S, Nicholson A, Lewis SR. Thermal insulation for preventing inadvertent perioperative hypothermia. Cochrane Database Syst Rev. 2014;6:CD009908. doi:10.1002/14651858.CD009908.pub2.
- Berry D, Wick C, Magons P. A clinical evaluation of the cost and time effectiveness of the ASPAN Hypothermia Guideline. J Perianesth Nurs. 2008;23(1):24-35. doi:10.1016/j.jopan.2007.09.010.
- Kimberger O, Held C, Stadelmann K et al. Resistive polymer versus forced-air warming: comparable heat transfer and core rewarming rates in volunteers. Anesth Analg. 2008;107(5):1621-1626. doi:10.1213/ane.0b013e3181845502.
- Brandt S, Oguz R, Hüttner H, et al. Resistive-polymer versus forced-air warming: comparable efficacy in orthopedic patients. Anesth Analg. 2010;110(3):834-838. doi:10.1213/ANE.0b013e3181cb3f5f.
- Legg AJ, Hammer AJ. Forced-air patient warming blankets disrupt unidirectional airflow. Bone Joint J. 2013;95-B(3):407-410. doi:10.1302/0301-620X.95B3.29121.
- Dasari KB, Albrecht M, Harper M. Effect of forced-air warming on the performance of operating theatre laminar flow ventilation. Anaesthesia. 2012;67(3):244-249. doi:10.1111/j.1365-2044.2011.06983.x.
- Belani KG, Albrecht M, McGovern PD, Reed M, Nachtsheim C. Patient warming excess heat: the effects on orthopedic operating room ventilation performance. Anesth Analg. 2013;117(2):406-411. doi:10.1213/ANE.0b013e31825f81e2.
- Legg AJ, Cannon T, Hammer AJ. Do forced air patient-warming devices disrupt unidirectional downward airflow? J Bone Joint Surg Br. 2012;94(2):254-256. doi:10.1302/0301-620X.94B2.27562.
- Albrecht M, Gaithier RL, Belani K, Litchy M, Leaper D. Forced-air warming blowers: An evaluation of filtration adequacy and airborne contamination emissions in the operating room. Am J Infect Control. 2011;39(4):321-328. doi:10.1016/j.ajic.2010.06.011.
- Reed M, Kimberger O, McGovern PD, Albrecht MC. Forced-air warming design: evaluation of intake filtration, internal microbial buildup, and airborne-contamination emissions. AANA J. 2013;81(4):275-280.
- McGovern PD, Albercht M, Belani KG, et al. Forced-air warming and ultra-clean ventilation do not mix: an investigation of theatre ventilation, patient warming and joint replacement infection in orthopaedics. J Bone Joint Surg Br.2011;93(11):1537-1544. doi:10.1302/0301-620X.93B11.27124.
TAKE-HOME POINTS
- Inadvertent perioperative hypothermia, defined as an involuntary drop in core body temperature to <35°C (95°F), is a condition associated with significant morbidity and mortality.
- Maintenance of core body temperature >36°C is now a measured standard of perioperative care.
- Overall, in the last 2 decades, the incidence of inadvertent perioperative hypothermia has decreased, mainly due to aggressive intraoperative management.
- Active patient warming by conduction devices occurs by direct physical contact with the device, which is set at a higher temperature, whereas heat transfer from the convection device to the patient occurs by a physical medium such as forced air or circulating water that moves in between the device and the patient.
- Active patient warming is superior to passive heat retention methods.
SAMHSA Releases Money for Opioid Treatment
The Targeted Capacity Expansion: Medication Assisted Treatment-Prescription Drug Opioid Addiction grant program will expand access to treatment and recovery support services in states, tribes, and tribal organizations with the highest per-capita rates of primary treatment admissions for heroin and prescription opioids. The funding includes the areas with the “most dramatic increases” for heroin and prescription opioids, as identified by SAMHSA’s 2015 Treatment Episode Data Set.
“We know medication-assisted treatment is an effective, essential tool in fighting the opioid crisis,” said HHS Secretary Alex Azar, “and HHS will continue working to expand access to it.”
The Targeted Capacity Expansion: Medication Assisted Treatment-Prescription Drug Opioid Addiction grant program will expand access to treatment and recovery support services in states, tribes, and tribal organizations with the highest per-capita rates of primary treatment admissions for heroin and prescription opioids. The funding includes the areas with the “most dramatic increases” for heroin and prescription opioids, as identified by SAMHSA’s 2015 Treatment Episode Data Set.
“We know medication-assisted treatment is an effective, essential tool in fighting the opioid crisis,” said HHS Secretary Alex Azar, “and HHS will continue working to expand access to it.”
The Targeted Capacity Expansion: Medication Assisted Treatment-Prescription Drug Opioid Addiction grant program will expand access to treatment and recovery support services in states, tribes, and tribal organizations with the highest per-capita rates of primary treatment admissions for heroin and prescription opioids. The funding includes the areas with the “most dramatic increases” for heroin and prescription opioids, as identified by SAMHSA’s 2015 Treatment Episode Data Set.
“We know medication-assisted treatment is an effective, essential tool in fighting the opioid crisis,” said HHS Secretary Alex Azar, “and HHS will continue working to expand access to it.”
Federal Health Care Data Trends: Cardiovascular Diseases
Cardiovascular disease remains a significant cause of morbidity and mortality. According to the American Heart Association, in the US, every 40 seconds someone experiences a stroke, another person has a heart attack, and a third person dies of cardiovascular disease.1 More than 92 million American adults have some form of cardiovascular disease or poststroke symptoms, and the costs are well above $300 billion.1
Click here to continue reading.
Cardiovascular disease remains a significant cause of morbidity and mortality. According to the American Heart Association, in the US, every 40 seconds someone experiences a stroke, another person has a heart attack, and a third person dies of cardiovascular disease.1 More than 92 million American adults have some form of cardiovascular disease or poststroke symptoms, and the costs are well above $300 billion.1
Click here to continue reading.
Cardiovascular disease remains a significant cause of morbidity and mortality. According to the American Heart Association, in the US, every 40 seconds someone experiences a stroke, another person has a heart attack, and a third person dies of cardiovascular disease.1 More than 92 million American adults have some form of cardiovascular disease or poststroke symptoms, and the costs are well above $300 billion.1
Click here to continue reading.
Study links gut bacteria and TRALI
A new study has revealed a previously unknown link between gastrointestinal flora and transfusion-related acute lung injury (TRALI).
“We observed that the composition of the gastrointestinal flora drives the pathogenic immune response in the lungs during TRALI,” said Rick Kapur, PhD, of Lund University in Lund, Sweden.
Dr Kapur and his colleagues described this discovery in Blood Advances.
The researchers compared 2 groups of mice. One group was kept in a strictly sterile environment, allowing the gastrointestinal flora to be minimally affected by external factors. The other group was raised in a normal, less sterile environment.
“We saw that the mice kept in a more sterile environment were resistant to TRALI development, while the less sterile-raised mice developed severe TRALI,” said study author John W. Semple, PhD, of Lund University.
The composition of the gastrointestinal flora was significantly different between the 2 groups of mice, as determined by genetic sequencing of stool.
When the researchers wiped out the gastrointestinal flora with several types of antibiotics, they found that mice in the less sterile environment did not develop TRALI.
The researchers also transplanted stool from mice that developed TRALI into TRALI-resistant mice. After the stool transplant, the resistant mice were also able to develop TRALI, which confirmed the link between the composition of the gastrointestinal flora and the onset of TRALI.
The researchers still need to clarify which specific gut bacteria are directly involved, but the knowledge that intestinal bacteria may affect the lungs could facilitate diagnostics and the development of potential new drugs.
The ability to easily assess the risk for TRALI via analysis of gastrointestinal flora is equally important, according to the researchers.
“Knowing the composition of the gastrointestinal flora of people who will receive blood transfusions, an analysis which can be easily performed today, would allow you to assess who may be at increased risk for developing TRALI,” Dr Kapur said.
“The TRALI model in mice is very similar to the condition in humans, and the next step will be to validate these findings in humans,” Dr Semple said. “It’s not often that these types of findings in mice can lead directly to clinical studies in humans, but that will be our aim.”
A new study has revealed a previously unknown link between gastrointestinal flora and transfusion-related acute lung injury (TRALI).
“We observed that the composition of the gastrointestinal flora drives the pathogenic immune response in the lungs during TRALI,” said Rick Kapur, PhD, of Lund University in Lund, Sweden.
Dr Kapur and his colleagues described this discovery in Blood Advances.
The researchers compared 2 groups of mice. One group was kept in a strictly sterile environment, allowing the gastrointestinal flora to be minimally affected by external factors. The other group was raised in a normal, less sterile environment.
“We saw that the mice kept in a more sterile environment were resistant to TRALI development, while the less sterile-raised mice developed severe TRALI,” said study author John W. Semple, PhD, of Lund University.
The composition of the gastrointestinal flora was significantly different between the 2 groups of mice, as determined by genetic sequencing of stool.
When the researchers wiped out the gastrointestinal flora with several types of antibiotics, they found that mice in the less sterile environment did not develop TRALI.
The researchers also transplanted stool from mice that developed TRALI into TRALI-resistant mice. After the stool transplant, the resistant mice were also able to develop TRALI, which confirmed the link between the composition of the gastrointestinal flora and the onset of TRALI.
The researchers still need to clarify which specific gut bacteria are directly involved, but the knowledge that intestinal bacteria may affect the lungs could facilitate diagnostics and the development of potential new drugs.
The ability to easily assess the risk for TRALI via analysis of gastrointestinal flora is equally important, according to the researchers.
“Knowing the composition of the gastrointestinal flora of people who will receive blood transfusions, an analysis which can be easily performed today, would allow you to assess who may be at increased risk for developing TRALI,” Dr Kapur said.
“The TRALI model in mice is very similar to the condition in humans, and the next step will be to validate these findings in humans,” Dr Semple said. “It’s not often that these types of findings in mice can lead directly to clinical studies in humans, but that will be our aim.”
A new study has revealed a previously unknown link between gastrointestinal flora and transfusion-related acute lung injury (TRALI).
“We observed that the composition of the gastrointestinal flora drives the pathogenic immune response in the lungs during TRALI,” said Rick Kapur, PhD, of Lund University in Lund, Sweden.
Dr Kapur and his colleagues described this discovery in Blood Advances.
The researchers compared 2 groups of mice. One group was kept in a strictly sterile environment, allowing the gastrointestinal flora to be minimally affected by external factors. The other group was raised in a normal, less sterile environment.
“We saw that the mice kept in a more sterile environment were resistant to TRALI development, while the less sterile-raised mice developed severe TRALI,” said study author John W. Semple, PhD, of Lund University.
The composition of the gastrointestinal flora was significantly different between the 2 groups of mice, as determined by genetic sequencing of stool.
When the researchers wiped out the gastrointestinal flora with several types of antibiotics, they found that mice in the less sterile environment did not develop TRALI.
The researchers also transplanted stool from mice that developed TRALI into TRALI-resistant mice. After the stool transplant, the resistant mice were also able to develop TRALI, which confirmed the link between the composition of the gastrointestinal flora and the onset of TRALI.
The researchers still need to clarify which specific gut bacteria are directly involved, but the knowledge that intestinal bacteria may affect the lungs could facilitate diagnostics and the development of potential new drugs.
The ability to easily assess the risk for TRALI via analysis of gastrointestinal flora is equally important, according to the researchers.
“Knowing the composition of the gastrointestinal flora of people who will receive blood transfusions, an analysis which can be easily performed today, would allow you to assess who may be at increased risk for developing TRALI,” Dr Kapur said.
“The TRALI model in mice is very similar to the condition in humans, and the next step will be to validate these findings in humans,” Dr Semple said. “It’s not often that these types of findings in mice can lead directly to clinical studies in humans, but that will be our aim.”
Protein could be target for MLL-rearranged AML
Preclinical research has revealed a potential therapeutic target for MLL-rearranged acute myeloid leukemia (AML).
The target—F-box protein S-phase kinase-associated protein 2 (Skp2)—degrades another protein called p27Kip1 that is important to the formation of healthy blood cells.
This finding was published in the Journal of Experimental Medicine.
“Our work provides a complete mechanistic look into the function of genetic and molecular programs driving this leukemia, and it exploits these processes to identify actionable therapeutic targets,’’ said study author H. Leighton Grimes, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
For this work, Dr Grimes and his colleagues performed biochemical analyses of cells from AML patients. This gave the researchers comprehensive information about the targets and functions of the miR-196 molecular signaling pathway.
The team inserted mimics of miR-196 into MLL-AF9 leukemia cells to incorporate them into the cellular machinery. The group then lysed the cells for analyses, which revealed molecular targets of miR-196 in the leukemia cells.
Next, the researchers screened AML cells in mice for miR-196 targets. These experiments showed that certain microRNA targets are more important than others in the maintenance and spread of leukemia stem cells (LSCs).
Computer-assisted analysis of the Molecular Signature Database (a shared multi-institutional resource) allowed the researchers to identify sets of genes that show up in high numbers in MLL-AF9 leukemia.
Additional biochemical testing revealed that miR-196 directly targets and inhibits Cdkn1b/p27Kip1, which controls molecular programming in LSCs that allows them to maintain aggressive MLL-AF9 leukemia.
When miR-196 targets Cdkn1b/p27Kip1, it accelerates MLL-AF9 progression by abnormally linking stem cell activity with the growth of leukemia cells.
With the data suggesting that elevation of p27Kip1 protein levels may be therapeutic to AML patients, the researchers investigated a related molecular pathway that also regulates p27Kip1.
This investigation yielded the treatment target Skp2, which degrades the p27 protein and lowers its expression.
The researchers tested an experimental Skp2 inhibitor, SLZ P1041, on human AML cell lines and found the drug killed AML cells in a dose-dependent manner.
The team also tested SLZ P1041 in combination with other inhibitors—IBET-151, palbociclib, and MI-1. The most consistent synergies were with the combination of SLZ P1041 and MI-1, an inhibitor of the interaction between Menin and MLL.
“We still have extensive additional testing to conduct in laboratory animal models of AML before knowing if [targeting Skp2] will translate to patient care,” Dr Grimes said.
Preclinical research has revealed a potential therapeutic target for MLL-rearranged acute myeloid leukemia (AML).
The target—F-box protein S-phase kinase-associated protein 2 (Skp2)—degrades another protein called p27Kip1 that is important to the formation of healthy blood cells.
This finding was published in the Journal of Experimental Medicine.
“Our work provides a complete mechanistic look into the function of genetic and molecular programs driving this leukemia, and it exploits these processes to identify actionable therapeutic targets,’’ said study author H. Leighton Grimes, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
For this work, Dr Grimes and his colleagues performed biochemical analyses of cells from AML patients. This gave the researchers comprehensive information about the targets and functions of the miR-196 molecular signaling pathway.
The team inserted mimics of miR-196 into MLL-AF9 leukemia cells to incorporate them into the cellular machinery. The group then lysed the cells for analyses, which revealed molecular targets of miR-196 in the leukemia cells.
Next, the researchers screened AML cells in mice for miR-196 targets. These experiments showed that certain microRNA targets are more important than others in the maintenance and spread of leukemia stem cells (LSCs).
Computer-assisted analysis of the Molecular Signature Database (a shared multi-institutional resource) allowed the researchers to identify sets of genes that show up in high numbers in MLL-AF9 leukemia.
Additional biochemical testing revealed that miR-196 directly targets and inhibits Cdkn1b/p27Kip1, which controls molecular programming in LSCs that allows them to maintain aggressive MLL-AF9 leukemia.
When miR-196 targets Cdkn1b/p27Kip1, it accelerates MLL-AF9 progression by abnormally linking stem cell activity with the growth of leukemia cells.
With the data suggesting that elevation of p27Kip1 protein levels may be therapeutic to AML patients, the researchers investigated a related molecular pathway that also regulates p27Kip1.
This investigation yielded the treatment target Skp2, which degrades the p27 protein and lowers its expression.
The researchers tested an experimental Skp2 inhibitor, SLZ P1041, on human AML cell lines and found the drug killed AML cells in a dose-dependent manner.
The team also tested SLZ P1041 in combination with other inhibitors—IBET-151, palbociclib, and MI-1. The most consistent synergies were with the combination of SLZ P1041 and MI-1, an inhibitor of the interaction between Menin and MLL.
“We still have extensive additional testing to conduct in laboratory animal models of AML before knowing if [targeting Skp2] will translate to patient care,” Dr Grimes said.
Preclinical research has revealed a potential therapeutic target for MLL-rearranged acute myeloid leukemia (AML).
The target—F-box protein S-phase kinase-associated protein 2 (Skp2)—degrades another protein called p27Kip1 that is important to the formation of healthy blood cells.
This finding was published in the Journal of Experimental Medicine.
“Our work provides a complete mechanistic look into the function of genetic and molecular programs driving this leukemia, and it exploits these processes to identify actionable therapeutic targets,’’ said study author H. Leighton Grimes, PhD, of Cincinnati Children’s Hospital Medical Center in Ohio.
For this work, Dr Grimes and his colleagues performed biochemical analyses of cells from AML patients. This gave the researchers comprehensive information about the targets and functions of the miR-196 molecular signaling pathway.
The team inserted mimics of miR-196 into MLL-AF9 leukemia cells to incorporate them into the cellular machinery. The group then lysed the cells for analyses, which revealed molecular targets of miR-196 in the leukemia cells.
Next, the researchers screened AML cells in mice for miR-196 targets. These experiments showed that certain microRNA targets are more important than others in the maintenance and spread of leukemia stem cells (LSCs).
Computer-assisted analysis of the Molecular Signature Database (a shared multi-institutional resource) allowed the researchers to identify sets of genes that show up in high numbers in MLL-AF9 leukemia.
Additional biochemical testing revealed that miR-196 directly targets and inhibits Cdkn1b/p27Kip1, which controls molecular programming in LSCs that allows them to maintain aggressive MLL-AF9 leukemia.
When miR-196 targets Cdkn1b/p27Kip1, it accelerates MLL-AF9 progression by abnormally linking stem cell activity with the growth of leukemia cells.
With the data suggesting that elevation of p27Kip1 protein levels may be therapeutic to AML patients, the researchers investigated a related molecular pathway that also regulates p27Kip1.
This investigation yielded the treatment target Skp2, which degrades the p27 protein and lowers its expression.
The researchers tested an experimental Skp2 inhibitor, SLZ P1041, on human AML cell lines and found the drug killed AML cells in a dose-dependent manner.
The team also tested SLZ P1041 in combination with other inhibitors—IBET-151, palbociclib, and MI-1. The most consistent synergies were with the combination of SLZ P1041 and MI-1, an inhibitor of the interaction between Menin and MLL.
“We still have extensive additional testing to conduct in laboratory animal models of AML before knowing if [targeting Skp2] will translate to patient care,” Dr Grimes said.
FDA releases guidance docs on gene therapy
The US Food and Drug Administration (FDA) has released several draft guidance documents on gene therapy.
Three are disease-specific guidances—for hemophilia, rare diseases, and retinal disorders—and 3 are guidances on manufacturing gene therapies.
These 6 documents are intended to serve as the building blocks of a modern, comprehensive framework for advancing the field of gene therapy, according to FDA Commissioner Scott Gottlieb, MD.
He said the documents are being issued in draft form so the FDA can solicit public input on these new policies. As with all draft guidances, all comments received will be considered before the FDA finalizes the documents.
Disease-specific guidances
The Human Gene Therapy for Rare Diseases Draft Guidance and the Human Gene Therapy for Retinal Disorders Draft Guidance include considerations for product development, preclinical research, clinical trials, expedited programs, and communication with the FDA.
The Human Gene Therapy for Hemophilia Draft Guidance covers the same topics but also includes considerations for measuring factor VIII and factor IX activity.
The draft guidance for rare diseases encompasses diseases affecting fewer than 200,000 people in the US.
Manufacturing guidances
The 3 remaining draft guidances are actually updates to existing guidances that address manufacturing issues related to gene therapy.
The first updated draft guidance, Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs), provides sponsors with recommendations on how to provide sufficient CMC information to ensure safety, identity, quality, purity, and strength/potency of investigational gene therapy products. This guidance applies to gene therapies alone and products that contain a gene therapy in combination with a drug or device.
The second draft guidance, Testing of Retroviral Vector-Based Gene Therapy Products for Replication Competent Retrovirus (RCR) during Product Manufacture and Patient Follow-up, provides recommendations regarding the proper testing for RCR during the manufacture of retroviral vector-based gene therapy products, as well as during the follow-up monitoring of patients who have received retroviral vector-based gene therapy products.
The third draft guidance, Long Term Follow-Up (LTFU) After Administration of Human Gene Therapy Products, provides recommendations regarding the design of LTFU observational studies for the collection of data on delayed adverse events after gene therapy.
Once finalized, these draft guidances will replace previous guidances issued by the FDA in April 2008 (CMC) and November 2006 (RCR and LTFU).
The US Food and Drug Administration (FDA) has released several draft guidance documents on gene therapy.
Three are disease-specific guidances—for hemophilia, rare diseases, and retinal disorders—and 3 are guidances on manufacturing gene therapies.
These 6 documents are intended to serve as the building blocks of a modern, comprehensive framework for advancing the field of gene therapy, according to FDA Commissioner Scott Gottlieb, MD.
He said the documents are being issued in draft form so the FDA can solicit public input on these new policies. As with all draft guidances, all comments received will be considered before the FDA finalizes the documents.
Disease-specific guidances
The Human Gene Therapy for Rare Diseases Draft Guidance and the Human Gene Therapy for Retinal Disorders Draft Guidance include considerations for product development, preclinical research, clinical trials, expedited programs, and communication with the FDA.
The Human Gene Therapy for Hemophilia Draft Guidance covers the same topics but also includes considerations for measuring factor VIII and factor IX activity.
The draft guidance for rare diseases encompasses diseases affecting fewer than 200,000 people in the US.
Manufacturing guidances
The 3 remaining draft guidances are actually updates to existing guidances that address manufacturing issues related to gene therapy.
The first updated draft guidance, Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs), provides sponsors with recommendations on how to provide sufficient CMC information to ensure safety, identity, quality, purity, and strength/potency of investigational gene therapy products. This guidance applies to gene therapies alone and products that contain a gene therapy in combination with a drug or device.
The second draft guidance, Testing of Retroviral Vector-Based Gene Therapy Products for Replication Competent Retrovirus (RCR) during Product Manufacture and Patient Follow-up, provides recommendations regarding the proper testing for RCR during the manufacture of retroviral vector-based gene therapy products, as well as during the follow-up monitoring of patients who have received retroviral vector-based gene therapy products.
The third draft guidance, Long Term Follow-Up (LTFU) After Administration of Human Gene Therapy Products, provides recommendations regarding the design of LTFU observational studies for the collection of data on delayed adverse events after gene therapy.
Once finalized, these draft guidances will replace previous guidances issued by the FDA in April 2008 (CMC) and November 2006 (RCR and LTFU).
The US Food and Drug Administration (FDA) has released several draft guidance documents on gene therapy.
Three are disease-specific guidances—for hemophilia, rare diseases, and retinal disorders—and 3 are guidances on manufacturing gene therapies.
These 6 documents are intended to serve as the building blocks of a modern, comprehensive framework for advancing the field of gene therapy, according to FDA Commissioner Scott Gottlieb, MD.
He said the documents are being issued in draft form so the FDA can solicit public input on these new policies. As with all draft guidances, all comments received will be considered before the FDA finalizes the documents.
Disease-specific guidances
The Human Gene Therapy for Rare Diseases Draft Guidance and the Human Gene Therapy for Retinal Disorders Draft Guidance include considerations for product development, preclinical research, clinical trials, expedited programs, and communication with the FDA.
The Human Gene Therapy for Hemophilia Draft Guidance covers the same topics but also includes considerations for measuring factor VIII and factor IX activity.
The draft guidance for rare diseases encompasses diseases affecting fewer than 200,000 people in the US.
Manufacturing guidances
The 3 remaining draft guidances are actually updates to existing guidances that address manufacturing issues related to gene therapy.
The first updated draft guidance, Chemistry, Manufacturing, and Control (CMC) Information for Human Gene Therapy Investigational New Drug Applications (INDs), provides sponsors with recommendations on how to provide sufficient CMC information to ensure safety, identity, quality, purity, and strength/potency of investigational gene therapy products. This guidance applies to gene therapies alone and products that contain a gene therapy in combination with a drug or device.
The second draft guidance, Testing of Retroviral Vector-Based Gene Therapy Products for Replication Competent Retrovirus (RCR) during Product Manufacture and Patient Follow-up, provides recommendations regarding the proper testing for RCR during the manufacture of retroviral vector-based gene therapy products, as well as during the follow-up monitoring of patients who have received retroviral vector-based gene therapy products.
The third draft guidance, Long Term Follow-Up (LTFU) After Administration of Human Gene Therapy Products, provides recommendations regarding the design of LTFU observational studies for the collection of data on delayed adverse events after gene therapy.
Once finalized, these draft guidances will replace previous guidances issued by the FDA in April 2008 (CMC) and November 2006 (RCR and LTFU).
Rash on forearm

The FP did not recognize the rash, so she decided to do a Google search. She typed the following terms into the search box: linear hypopigmented papules on the arm of a child. Almost every result described lichen striatus.
The photographs were very similar, and the description was a great fit for the patient’s condition. Clearly, this was not poison ivy and was unrelated to the camping trip. The physician learned that lichen striatus is a benign idiopathic condition that often affects children on a single extremity. The flat-topped papules tend to run parallel to the long axis of the extremity following Blaschko lines (lines related to embryogenesis). In darker-skinned patients, the papules are often hypopigmented. The papules are usually asymptomatic and resolve on their own, over time.
The mother was reassured and happy to hear that this would go away without any treatment. The physician was delighted to have been able to make a diagnosis by using her ability to describe the rash and the “intelligence” of the search engine.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.

The FP did not recognize the rash, so she decided to do a Google search. She typed the following terms into the search box: linear hypopigmented papules on the arm of a child. Almost every result described lichen striatus.
The photographs were very similar, and the description was a great fit for the patient’s condition. Clearly, this was not poison ivy and was unrelated to the camping trip. The physician learned that lichen striatus is a benign idiopathic condition that often affects children on a single extremity. The flat-topped papules tend to run parallel to the long axis of the extremity following Blaschko lines (lines related to embryogenesis). In darker-skinned patients, the papules are often hypopigmented. The papules are usually asymptomatic and resolve on their own, over time.
The mother was reassured and happy to hear that this would go away without any treatment. The physician was delighted to have been able to make a diagnosis by using her ability to describe the rash and the “intelligence” of the search engine.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.

The FP did not recognize the rash, so she decided to do a Google search. She typed the following terms into the search box: linear hypopigmented papules on the arm of a child. Almost every result described lichen striatus.
The photographs were very similar, and the description was a great fit for the patient’s condition. Clearly, this was not poison ivy and was unrelated to the camping trip. The physician learned that lichen striatus is a benign idiopathic condition that often affects children on a single extremity. The flat-topped papules tend to run parallel to the long axis of the extremity following Blaschko lines (lines related to embryogenesis). In darker-skinned patients, the papules are often hypopigmented. The papules are usually asymptomatic and resolve on their own, over time.
The mother was reassured and happy to hear that this would go away without any treatment. The physician was delighted to have been able to make a diagnosis by using her ability to describe the rash and the “intelligence” of the search engine.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Smith M. Epidermal nevus and nevus sebaceous. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:958-962.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
New hypertension guidelines would add 15.6 million new diagnoses
A new analysis estimates that adopting the 2017 ACC/AHA hypertension guidelines would add 15.6 million Americans to the ranks of the hypertensives, and half of those would be candidates for treatment.
Similar increases would occur in other countries, according to study authors, who analyzed two large datasets from the United States and China.
That happened by resetting the definition of adult hypertension from the long-standing threshold of 140/90 mm Hg to a blood pressure at or above 130/80 mm Hg, meaning more than half of people aged 45-75 years in both countries would be classified as having hypertension, according to the researchers, led by Harlan M. Krumholz, MD, of the Center for Outcomes Research and Evaluation at Yale–New Haven (Conn.) Hospital and the section of cardiovascular medicine at Yale
An additional 7.5 million Americans would be recommended for treatment under the new lower treatment thresholds, with a correspondingly large increase in the Chinese population, according to results published in the BMJ.
The guideline changes are “not firmly rooted in evidence” and could have health policy implications that include strain on public health programs, Dr. Krumholz and his colleagues said in their report on the study.
“The change occurs at a time when both countries have substantial numbers of people who are not aware of having hypertension, and who have hypertension that is not controlled, even according to the previous standards,” they wrote.
The analysis by Dr. Krumholz and his colleagues was based on the two most recent cycles of the U.S. National Health and Nutrition Examination Survey (NHANES), representing 2013-2014 and 2015-2016 periods, as well as the China Health and Retirement Longitudinal Study (CHARLS) in 2011-2012.
Under the new ACC/AHA guidelines, they found, 70.1 million Americans aged 45-65 years would be classified as hypertensive, representing 63% of that age group. That’s a 27% relative increase over the 55.3 million individuals, or 49.7%, with hypertension as defined in the JNC-8 guidelines.
In addition, 15.6 million persons would be classified as eligible for treatment but not receiving it, up from 8.1 million under the JNC-8 guidance.
Previous estimates projected a far greater jump in new hypertension classifications, including one that used data from the National Health and Nutrition Examination Survey, antihypertensive clinical trials, and population-based cohort studies. That study estimated that 31 million people would newly carry the label (JAMA Cardiol. 2018 May 23; doi: 10.1001/jamacardio.2018.1240.)
In the current analysis, in China, 267 million aged 45-65 years (55% of that age group) would be classified with hypertension under the ACC/AHA guidelines, a relative increase of 45% over the JNC-8 guidelines, while the number of candidates for treatment would be 129 million, up from 74.5 million under the earlier guidelines.
Dr. Krumholz noted that the ACC/AHA guideline changes were prompted by results from the SPRINT trial. However, the improvements in outcomes seen in SPRINT, which included patients at high risk for cardiovascular events but without diabetes, have not been observed in individuals at low or intermediate risk, or in those with diabetes, they said.
“Expanding the pool of patients who merit treatment to include those at low risk could potentially render public health programs less efficient and viable,” they wrote in a discussion of health policy implications.
The new guidelines also put millions at risk of the “psychological morbidity” that comes with the label of a chronic disease, and at risk for more adverse events caused by inappropriate use of drug therapy, they added.
Dr. Krumholz reported research agreements from Medtronic and from Johnson and Johnson (Janssen) through Yale University, and a grant from the Food and Drug Administration and Medtronic. He reported other disclosures related to UnitedHealth, the IBM Watson Health Life Sciences Board, Element Science, Aetna, and Hugo, a personal health information platform he founded. First author Rohan Khera, MD, reported support from the National Institutes of Health.
SOURCE: Khera R et al. BMJ. 2018 Jul 11;362:k2357
This article was updated 7/19/18.
This study addressing hypertension guideline changes is unique because it was initially published on a public preprint server.
Preprints are common in some scientific areas, but uncommon in major medical journals. They allow investigators to share research, quickly and openly, for critique and feedback before standard peer review and publication.
In the case of this study, researchers analyzed the public health implications of the anticipated changes to the 2017 ACC/AHA hypertension guidelines in two nationally representative data sets from the United States and China.
The authors quickly finalized their manuscript right after the revised hypertension guidelines were released. They chose the preprint approach because they realized their research would be immediately relevant to the discussion that followed, first author Rohan Khera, MD, recounted on BMJ Blogs.
“The traditional approach of submitting to a medical journal would mean being out of the public eye for several months,” Dr. Khera said in his post. “The preprint platform offered us an excellent opportunity of ensuring early dissemination of our research study in its entirety, while we sought its evaluation by peer reviewers and the refinement by a medical journal.”
The manuscript was submitted via a Web-based system and was publicly available 2 hours later on the same day the guidelines were published. The researchers received comments and suggestions on the preprint, some of which were incorporated into the final manuscript they submitted for peer review.
Then the manuscript went through the usual iterative peer review process; however, the preprint was still available online to guide other investigators and limit duplication of effort, Dr. Khera said in his blog post.
That contrasts with another recent experience in which Dr. Khera and his colleagues performed work that “failed to inform” ongoing policy discussions, and other research efforts, while they waited for eventual publication.
“We hope that more journals will accept the benefits of science that is publicly available while journal editors and peer reviewers carry out their critical role of improving both the quality and the impact of these scientific contributions,” Dr. Khera wrote.
Rohan Khera, MD, a cardiology fellow at the University of Texas (Dallas) Southwestern Medical Center in, wrote about his experience with preprints for BMJ Blogs . Dr. Khera had no conflicts of interest to disclose.
This study addressing hypertension guideline changes is unique because it was initially published on a public preprint server.
Preprints are common in some scientific areas, but uncommon in major medical journals. They allow investigators to share research, quickly and openly, for critique and feedback before standard peer review and publication.
In the case of this study, researchers analyzed the public health implications of the anticipated changes to the 2017 ACC/AHA hypertension guidelines in two nationally representative data sets from the United States and China.
The authors quickly finalized their manuscript right after the revised hypertension guidelines were released. They chose the preprint approach because they realized their research would be immediately relevant to the discussion that followed, first author Rohan Khera, MD, recounted on BMJ Blogs.
“The traditional approach of submitting to a medical journal would mean being out of the public eye for several months,” Dr. Khera said in his post. “The preprint platform offered us an excellent opportunity of ensuring early dissemination of our research study in its entirety, while we sought its evaluation by peer reviewers and the refinement by a medical journal.”
The manuscript was submitted via a Web-based system and was publicly available 2 hours later on the same day the guidelines were published. The researchers received comments and suggestions on the preprint, some of which were incorporated into the final manuscript they submitted for peer review.
Then the manuscript went through the usual iterative peer review process; however, the preprint was still available online to guide other investigators and limit duplication of effort, Dr. Khera said in his blog post.
That contrasts with another recent experience in which Dr. Khera and his colleagues performed work that “failed to inform” ongoing policy discussions, and other research efforts, while they waited for eventual publication.
“We hope that more journals will accept the benefits of science that is publicly available while journal editors and peer reviewers carry out their critical role of improving both the quality and the impact of these scientific contributions,” Dr. Khera wrote.
Rohan Khera, MD, a cardiology fellow at the University of Texas (Dallas) Southwestern Medical Center in, wrote about his experience with preprints for BMJ Blogs . Dr. Khera had no conflicts of interest to disclose.
This study addressing hypertension guideline changes is unique because it was initially published on a public preprint server.
Preprints are common in some scientific areas, but uncommon in major medical journals. They allow investigators to share research, quickly and openly, for critique and feedback before standard peer review and publication.
In the case of this study, researchers analyzed the public health implications of the anticipated changes to the 2017 ACC/AHA hypertension guidelines in two nationally representative data sets from the United States and China.
The authors quickly finalized their manuscript right after the revised hypertension guidelines were released. They chose the preprint approach because they realized their research would be immediately relevant to the discussion that followed, first author Rohan Khera, MD, recounted on BMJ Blogs.
“The traditional approach of submitting to a medical journal would mean being out of the public eye for several months,” Dr. Khera said in his post. “The preprint platform offered us an excellent opportunity of ensuring early dissemination of our research study in its entirety, while we sought its evaluation by peer reviewers and the refinement by a medical journal.”
The manuscript was submitted via a Web-based system and was publicly available 2 hours later on the same day the guidelines were published. The researchers received comments and suggestions on the preprint, some of which were incorporated into the final manuscript they submitted for peer review.
Then the manuscript went through the usual iterative peer review process; however, the preprint was still available online to guide other investigators and limit duplication of effort, Dr. Khera said in his blog post.
That contrasts with another recent experience in which Dr. Khera and his colleagues performed work that “failed to inform” ongoing policy discussions, and other research efforts, while they waited for eventual publication.
“We hope that more journals will accept the benefits of science that is publicly available while journal editors and peer reviewers carry out their critical role of improving both the quality and the impact of these scientific contributions,” Dr. Khera wrote.
Rohan Khera, MD, a cardiology fellow at the University of Texas (Dallas) Southwestern Medical Center in, wrote about his experience with preprints for BMJ Blogs . Dr. Khera had no conflicts of interest to disclose.
A new analysis estimates that adopting the 2017 ACC/AHA hypertension guidelines would add 15.6 million Americans to the ranks of the hypertensives, and half of those would be candidates for treatment.
Similar increases would occur in other countries, according to study authors, who analyzed two large datasets from the United States and China.
That happened by resetting the definition of adult hypertension from the long-standing threshold of 140/90 mm Hg to a blood pressure at or above 130/80 mm Hg, meaning more than half of people aged 45-75 years in both countries would be classified as having hypertension, according to the researchers, led by Harlan M. Krumholz, MD, of the Center for Outcomes Research and Evaluation at Yale–New Haven (Conn.) Hospital and the section of cardiovascular medicine at Yale
An additional 7.5 million Americans would be recommended for treatment under the new lower treatment thresholds, with a correspondingly large increase in the Chinese population, according to results published in the BMJ.
The guideline changes are “not firmly rooted in evidence” and could have health policy implications that include strain on public health programs, Dr. Krumholz and his colleagues said in their report on the study.
“The change occurs at a time when both countries have substantial numbers of people who are not aware of having hypertension, and who have hypertension that is not controlled, even according to the previous standards,” they wrote.
The analysis by Dr. Krumholz and his colleagues was based on the two most recent cycles of the U.S. National Health and Nutrition Examination Survey (NHANES), representing 2013-2014 and 2015-2016 periods, as well as the China Health and Retirement Longitudinal Study (CHARLS) in 2011-2012.
Under the new ACC/AHA guidelines, they found, 70.1 million Americans aged 45-65 years would be classified as hypertensive, representing 63% of that age group. That’s a 27% relative increase over the 55.3 million individuals, or 49.7%, with hypertension as defined in the JNC-8 guidelines.
In addition, 15.6 million persons would be classified as eligible for treatment but not receiving it, up from 8.1 million under the JNC-8 guidance.
Previous estimates projected a far greater jump in new hypertension classifications, including one that used data from the National Health and Nutrition Examination Survey, antihypertensive clinical trials, and population-based cohort studies. That study estimated that 31 million people would newly carry the label (JAMA Cardiol. 2018 May 23; doi: 10.1001/jamacardio.2018.1240.)
In the current analysis, in China, 267 million aged 45-65 years (55% of that age group) would be classified with hypertension under the ACC/AHA guidelines, a relative increase of 45% over the JNC-8 guidelines, while the number of candidates for treatment would be 129 million, up from 74.5 million under the earlier guidelines.
Dr. Krumholz noted that the ACC/AHA guideline changes were prompted by results from the SPRINT trial. However, the improvements in outcomes seen in SPRINT, which included patients at high risk for cardiovascular events but without diabetes, have not been observed in individuals at low or intermediate risk, or in those with diabetes, they said.
“Expanding the pool of patients who merit treatment to include those at low risk could potentially render public health programs less efficient and viable,” they wrote in a discussion of health policy implications.
The new guidelines also put millions at risk of the “psychological morbidity” that comes with the label of a chronic disease, and at risk for more adverse events caused by inappropriate use of drug therapy, they added.
Dr. Krumholz reported research agreements from Medtronic and from Johnson and Johnson (Janssen) through Yale University, and a grant from the Food and Drug Administration and Medtronic. He reported other disclosures related to UnitedHealth, the IBM Watson Health Life Sciences Board, Element Science, Aetna, and Hugo, a personal health information platform he founded. First author Rohan Khera, MD, reported support from the National Institutes of Health.
SOURCE: Khera R et al. BMJ. 2018 Jul 11;362:k2357
This article was updated 7/19/18.
A new analysis estimates that adopting the 2017 ACC/AHA hypertension guidelines would add 15.6 million Americans to the ranks of the hypertensives, and half of those would be candidates for treatment.
Similar increases would occur in other countries, according to study authors, who analyzed two large datasets from the United States and China.
That happened by resetting the definition of adult hypertension from the long-standing threshold of 140/90 mm Hg to a blood pressure at or above 130/80 mm Hg, meaning more than half of people aged 45-75 years in both countries would be classified as having hypertension, according to the researchers, led by Harlan M. Krumholz, MD, of the Center for Outcomes Research and Evaluation at Yale–New Haven (Conn.) Hospital and the section of cardiovascular medicine at Yale
An additional 7.5 million Americans would be recommended for treatment under the new lower treatment thresholds, with a correspondingly large increase in the Chinese population, according to results published in the BMJ.
The guideline changes are “not firmly rooted in evidence” and could have health policy implications that include strain on public health programs, Dr. Krumholz and his colleagues said in their report on the study.
“The change occurs at a time when both countries have substantial numbers of people who are not aware of having hypertension, and who have hypertension that is not controlled, even according to the previous standards,” they wrote.
The analysis by Dr. Krumholz and his colleagues was based on the two most recent cycles of the U.S. National Health and Nutrition Examination Survey (NHANES), representing 2013-2014 and 2015-2016 periods, as well as the China Health and Retirement Longitudinal Study (CHARLS) in 2011-2012.
Under the new ACC/AHA guidelines, they found, 70.1 million Americans aged 45-65 years would be classified as hypertensive, representing 63% of that age group. That’s a 27% relative increase over the 55.3 million individuals, or 49.7%, with hypertension as defined in the JNC-8 guidelines.
In addition, 15.6 million persons would be classified as eligible for treatment but not receiving it, up from 8.1 million under the JNC-8 guidance.
Previous estimates projected a far greater jump in new hypertension classifications, including one that used data from the National Health and Nutrition Examination Survey, antihypertensive clinical trials, and population-based cohort studies. That study estimated that 31 million people would newly carry the label (JAMA Cardiol. 2018 May 23; doi: 10.1001/jamacardio.2018.1240.)
In the current analysis, in China, 267 million aged 45-65 years (55% of that age group) would be classified with hypertension under the ACC/AHA guidelines, a relative increase of 45% over the JNC-8 guidelines, while the number of candidates for treatment would be 129 million, up from 74.5 million under the earlier guidelines.
Dr. Krumholz noted that the ACC/AHA guideline changes were prompted by results from the SPRINT trial. However, the improvements in outcomes seen in SPRINT, which included patients at high risk for cardiovascular events but without diabetes, have not been observed in individuals at low or intermediate risk, or in those with diabetes, they said.
“Expanding the pool of patients who merit treatment to include those at low risk could potentially render public health programs less efficient and viable,” they wrote in a discussion of health policy implications.
The new guidelines also put millions at risk of the “psychological morbidity” that comes with the label of a chronic disease, and at risk for more adverse events caused by inappropriate use of drug therapy, they added.
Dr. Krumholz reported research agreements from Medtronic and from Johnson and Johnson (Janssen) through Yale University, and a grant from the Food and Drug Administration and Medtronic. He reported other disclosures related to UnitedHealth, the IBM Watson Health Life Sciences Board, Element Science, Aetna, and Hugo, a personal health information platform he founded. First author Rohan Khera, MD, reported support from the National Institutes of Health.
SOURCE: Khera R et al. BMJ. 2018 Jul 11;362:k2357
This article was updated 7/19/18.
FROM THE BMJ
Key clinical point: The 2017 ACC/AHA hypertension guidelines could dramatically increase the number of individuals with hypertension and candidates for treatment.
Major finding: The number of individuals with untreated hypertension increased from 8.1 million to 15.6 million.
Study details: A cross-sectional study of adults in nationally representative databases in the United States (NHANES) and China (CHARLS).
Disclosures: Authors reported disclosures related to Medtronic, Johnson and Johnson (Janssen), the Food and Drug Administration, UnitedHealth, the IBM Watson Health Life Sciences Board, Element Science, Aetna, and Hugo.
Source: Khera R et al. BMJ 2018;362:k2357.
IVF linked to slight increase in risk of some cancers
A large observational study from Great Britain paints a mixed picture of cancer risks associated with assisted reproduction technologies such as in vitro fertilization (IVF).
Among nearly 256,000 women who had assisted reproduction over a 2-decade period and were followed for more than 2.25 million person-years, there was no significant increase in risk of uterine cancers or invasive breast cancers.
However, these women were at slight but significantly increased risk for in situ breast cancers and invasive or borderline ovarian cancers, although the ovarian tumors may be related more to patient factors than to the assisted reproduction technology itself, reported Alastair Sutcliffe, MD, PhD, from University College London, and his colleagues.
“We were not able to distinguish between a genuine increase in risk of borderline ovarian tumors and other explanations including surveillance bias. Further investigation of this and longer follow-up is warranted to continue monitoring these important outcomes in this ever-growing population,” they wrote in BMJ.
Women who undergo IVF and related procedures are typically exposed to high levels of estradiol, luteinizing hormone, follicle-stimulating hormone, and multiple ovarian punctures, all of which are potentially carcinogenic, the authors noted.
Previous studies of cancer risk in women who undergo assisted reproduction treatment have had conflicting or inconsistent results and lacked information on potential confounders, they pointed out.
To get a better sense of the potential risks, the investigators looked at linked data from the United Kingdom’s Human Fertilization and Embryology Authority and national cancer registries. They identified a total of 255,786 women treated from 1991 through 2010. Total follow-up was for 2,257,789 person-years.
They found that, during an average 8.8 years of follow-up, women had no significant increase in risk of tumors of the uterine corpus, with 164 cancers observed vs. 146.9 expected, for a standardized incidence ratio (SIR) of 1.12 (95% confidence interval, 0.95-1.30).
Similarly, there was no significant increase in risk of either breast cancer overall (2,578 observed vs. 2,641.2 expected; SIR, 0.98; 95% CI, 0.94-1.01) or invasive breast cancer (2,272 observed vs. 2,371.4 expected; SIR, 0.96; 95% CI, 0.92-1.00).
As noted, however, there was an increased risk of in situ breast cancer with 291 vs. 253.5 cases, respectively, translating into a SIR of 1.15 (95% CI, 1.02-1.29), for an absolute excess risk (AER) of 1.7 cases per 100,000 person-years, associated with an increasing number of treatment cycles (P = .03).
Additionally, the women in the study had an increased risk of ovarian cancer with an observed incidence of 405 vs. 291.82 expected, for an SIR of 1.39 (95% CI, 1.26-1.53) and an AER of 5.0 cases per 100,000 person-years.
There was a significantly increased risk for both invasive tumors, with 264 cases vs. 188.1 expected, for an SIR of 1.40 (95% CI, 1.24-1.58) and an AER of 3.4 cases per 100,000 person-years, and borderline ovarian cancers, with 141 vs. 103.7, for an SIR of 1.36 (95% CI, 1.15-1.60) and an AER of 1.7 cases per 100,000 person-years.
Increased risks of ovarian tumors were limited to women with endometriosis, low parity, or both. This study found no increased risk of any ovarian tumor in women treated because of only male-factor or unexplained infertility.
Women who had previously given birth and did not have a diagnosis of endometriosis had no increase in risk for ovarian cancer. Instead, increased risk appeared to be limited to women with endometriosis, few or no births (low parity), or both.
The authors emphasized that ongoing monitoring of outcomes for women who have undergone assisted reproduction is essential.
The study was funded by Cancer Research UK and the National Institute for Health Research, and supported by the NIHR Biomedical Research Centre at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London. Three authors reported personal fees or royalties from entities not involved in the study.
SOURCE: Williams CL et al. BMJ. 2018;362:k2644.
A large observational study from Great Britain paints a mixed picture of cancer risks associated with assisted reproduction technologies such as in vitro fertilization (IVF).
Among nearly 256,000 women who had assisted reproduction over a 2-decade period and were followed for more than 2.25 million person-years, there was no significant increase in risk of uterine cancers or invasive breast cancers.
However, these women were at slight but significantly increased risk for in situ breast cancers and invasive or borderline ovarian cancers, although the ovarian tumors may be related more to patient factors than to the assisted reproduction technology itself, reported Alastair Sutcliffe, MD, PhD, from University College London, and his colleagues.
“We were not able to distinguish between a genuine increase in risk of borderline ovarian tumors and other explanations including surveillance bias. Further investigation of this and longer follow-up is warranted to continue monitoring these important outcomes in this ever-growing population,” they wrote in BMJ.
Women who undergo IVF and related procedures are typically exposed to high levels of estradiol, luteinizing hormone, follicle-stimulating hormone, and multiple ovarian punctures, all of which are potentially carcinogenic, the authors noted.
Previous studies of cancer risk in women who undergo assisted reproduction treatment have had conflicting or inconsistent results and lacked information on potential confounders, they pointed out.
To get a better sense of the potential risks, the investigators looked at linked data from the United Kingdom’s Human Fertilization and Embryology Authority and national cancer registries. They identified a total of 255,786 women treated from 1991 through 2010. Total follow-up was for 2,257,789 person-years.
They found that, during an average 8.8 years of follow-up, women had no significant increase in risk of tumors of the uterine corpus, with 164 cancers observed vs. 146.9 expected, for a standardized incidence ratio (SIR) of 1.12 (95% confidence interval, 0.95-1.30).
Similarly, there was no significant increase in risk of either breast cancer overall (2,578 observed vs. 2,641.2 expected; SIR, 0.98; 95% CI, 0.94-1.01) or invasive breast cancer (2,272 observed vs. 2,371.4 expected; SIR, 0.96; 95% CI, 0.92-1.00).
As noted, however, there was an increased risk of in situ breast cancer with 291 vs. 253.5 cases, respectively, translating into a SIR of 1.15 (95% CI, 1.02-1.29), for an absolute excess risk (AER) of 1.7 cases per 100,000 person-years, associated with an increasing number of treatment cycles (P = .03).
Additionally, the women in the study had an increased risk of ovarian cancer with an observed incidence of 405 vs. 291.82 expected, for an SIR of 1.39 (95% CI, 1.26-1.53) and an AER of 5.0 cases per 100,000 person-years.
There was a significantly increased risk for both invasive tumors, with 264 cases vs. 188.1 expected, for an SIR of 1.40 (95% CI, 1.24-1.58) and an AER of 3.4 cases per 100,000 person-years, and borderline ovarian cancers, with 141 vs. 103.7, for an SIR of 1.36 (95% CI, 1.15-1.60) and an AER of 1.7 cases per 100,000 person-years.
Increased risks of ovarian tumors were limited to women with endometriosis, low parity, or both. This study found no increased risk of any ovarian tumor in women treated because of only male-factor or unexplained infertility.
Women who had previously given birth and did not have a diagnosis of endometriosis had no increase in risk for ovarian cancer. Instead, increased risk appeared to be limited to women with endometriosis, few or no births (low parity), or both.
The authors emphasized that ongoing monitoring of outcomes for women who have undergone assisted reproduction is essential.
The study was funded by Cancer Research UK and the National Institute for Health Research, and supported by the NIHR Biomedical Research Centre at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London. Three authors reported personal fees or royalties from entities not involved in the study.
SOURCE: Williams CL et al. BMJ. 2018;362:k2644.
A large observational study from Great Britain paints a mixed picture of cancer risks associated with assisted reproduction technologies such as in vitro fertilization (IVF).
Among nearly 256,000 women who had assisted reproduction over a 2-decade period and were followed for more than 2.25 million person-years, there was no significant increase in risk of uterine cancers or invasive breast cancers.
However, these women were at slight but significantly increased risk for in situ breast cancers and invasive or borderline ovarian cancers, although the ovarian tumors may be related more to patient factors than to the assisted reproduction technology itself, reported Alastair Sutcliffe, MD, PhD, from University College London, and his colleagues.
“We were not able to distinguish between a genuine increase in risk of borderline ovarian tumors and other explanations including surveillance bias. Further investigation of this and longer follow-up is warranted to continue monitoring these important outcomes in this ever-growing population,” they wrote in BMJ.
Women who undergo IVF and related procedures are typically exposed to high levels of estradiol, luteinizing hormone, follicle-stimulating hormone, and multiple ovarian punctures, all of which are potentially carcinogenic, the authors noted.
Previous studies of cancer risk in women who undergo assisted reproduction treatment have had conflicting or inconsistent results and lacked information on potential confounders, they pointed out.
To get a better sense of the potential risks, the investigators looked at linked data from the United Kingdom’s Human Fertilization and Embryology Authority and national cancer registries. They identified a total of 255,786 women treated from 1991 through 2010. Total follow-up was for 2,257,789 person-years.
They found that, during an average 8.8 years of follow-up, women had no significant increase in risk of tumors of the uterine corpus, with 164 cancers observed vs. 146.9 expected, for a standardized incidence ratio (SIR) of 1.12 (95% confidence interval, 0.95-1.30).
Similarly, there was no significant increase in risk of either breast cancer overall (2,578 observed vs. 2,641.2 expected; SIR, 0.98; 95% CI, 0.94-1.01) or invasive breast cancer (2,272 observed vs. 2,371.4 expected; SIR, 0.96; 95% CI, 0.92-1.00).
As noted, however, there was an increased risk of in situ breast cancer with 291 vs. 253.5 cases, respectively, translating into a SIR of 1.15 (95% CI, 1.02-1.29), for an absolute excess risk (AER) of 1.7 cases per 100,000 person-years, associated with an increasing number of treatment cycles (P = .03).
Additionally, the women in the study had an increased risk of ovarian cancer with an observed incidence of 405 vs. 291.82 expected, for an SIR of 1.39 (95% CI, 1.26-1.53) and an AER of 5.0 cases per 100,000 person-years.
There was a significantly increased risk for both invasive tumors, with 264 cases vs. 188.1 expected, for an SIR of 1.40 (95% CI, 1.24-1.58) and an AER of 3.4 cases per 100,000 person-years, and borderline ovarian cancers, with 141 vs. 103.7, for an SIR of 1.36 (95% CI, 1.15-1.60) and an AER of 1.7 cases per 100,000 person-years.
Increased risks of ovarian tumors were limited to women with endometriosis, low parity, or both. This study found no increased risk of any ovarian tumor in women treated because of only male-factor or unexplained infertility.
Women who had previously given birth and did not have a diagnosis of endometriosis had no increase in risk for ovarian cancer. Instead, increased risk appeared to be limited to women with endometriosis, few or no births (low parity), or both.
The authors emphasized that ongoing monitoring of outcomes for women who have undergone assisted reproduction is essential.
The study was funded by Cancer Research UK and the National Institute for Health Research, and supported by the NIHR Biomedical Research Centre at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London. Three authors reported personal fees or royalties from entities not involved in the study.
SOURCE: Williams CL et al. BMJ. 2018;362:k2644.
FROM BMJ
Key clinical point: Assisted reproductive technologies may be linked to increased risk for in situ breast and ovarian cancers.
Major finding: The standardized incidence ratios (observed vs. expected cases) for invasive and borderline ovarian tumors were 1.40 and 1.41, respectively, both statistically significant.
Study details: Observational study with linked fertility clinic and cancer registry data on 255,786 women with total follow-up of 2,257,789 person-years.
Disclosures: The study was funded by Cancer Research UK and the National Institute for Health Research, and supported by the NIHR Biomedical Research Centre at Great Ormond Street Hospital for Children NHS Foundation Trust and University College London. Three authors reported personal fees or royalties from entities not involved in the study.
Source: Williams CL et al. BMJ. 2018;362:k2644.
Abatacept loses ALLURE in lupus nephritis
AMSTERDAM – Abatacept used on top of the standard of care did not improve the primary endpoint of a complete renal response versus placebo in the ALLURE phase 3 study.
Criteria for a complete renal response (CRR) at 1 year was met by 35.1% of abatacept-treated and 33.5% of placebo-treated patients (P = .73). CRR criteria included having a urine protein to creatinine ratio (UPCR) of less than 0.5, a normal estimated glomerular filtration rate (eGFR) or an eGFR of 85% or more of baseline values, no cellular casts, and a daily corticosteroid dose of 10 mg or less.
“We also saw a more rapid decline in proteinuria in those people treated with abatacept, and that seemed to be sustained over the course of the study,” said Dr. Furie, professor of medicine at Hofstra University, Hempstead, N.Y., chief of the division of rheumatology at Northwell Health in Great Neck, N.Y., and a professor at the Center for Autoimmune, Musculoskeletal, and Hematopoietic Diseases in the Feinstein Institute for Medical Research in Manhasset, N.Y. After about 12 weeks, the adjusted mean change in UPCR from baseline was –2.5 for abatacept and –2.0 for placebo; the values at 1 year were a respective –2.95 vs. –2.68 and at 2 years were –3.13 vs. –2.72.
Renal function was not negatively impacted by treatment with abatacept, with about a 5%-8% increase in eGFR seen in both groups.
Furthermore, improvements in lupus-related biomarkers were more pronounced in patients treated with abatacept than placebo, Dr. Furie said. This included a greater decrease in anti–double-stranded DNA autoantibody titers and an increase in complement C3 and C4 levels.
Eric Morand, MD, who was not involved in the ALLURE study, commented during discussion that the main result of the study was “very sad.”
Dr. Morand of Monash University in Melbourne observed that the duration of renal disease at study entry was about 14 months and that around 38% had been previously treated with mycophenolate mofetil (MMF). So, could this have influenced the findings?
Dr. Furie was unable to answer the question but confirmed that MMF was one of two background medications given in the trial, at an oral dose of 1.5 g/day, alongside of oral prednisone up to 60-mg daily.
ALLURE was a 2-year randomized, double-blind study with an open-ended, blinded, long-term extension in 405 patients with active class III or IV lupus nephritis. The aim of the trial was to determine the efficacy and safety of abatacept versus placebo in the treatment of active proliferative lupus nephritis.
Abatacept was given intravenously, first at a dose of 30 mg/kg on days 1, 15, 29, and 57, and then at a dose of 10 mg/kg every 4 weeks.
In terms of safety, 14 deaths occurred during the course of the study and its long-term extension. Seven abatacept patients died in year 1, two of whom died more than 56 days after discontinuing the study drug. Five patients in the placebo group died in year 1, one in year 2, and one in the long-term extension. Rates of any or serious adverse events were similar among the groups, decreasing over time.
“The safety signals were really no different to what we already know about abatacept,” Dr. Furie said. As for the future, more analyses from the trial can be expected, he added.
The study was sponsored by Bristol-Myers Squibb. Dr. Furie disclosed receiving grant or research support from, and acting as a consultant to, the company. All but 3 of the study’s 12 authors had financial ties to many pharmaceutical companies, some of which included Bristol-Myers Squibb. Two authors are employees of Bristol-Myers Squibb. Dr. Monash was not involved in the ALLURE study but has received research support from Bristol-Myers Squibb, among other pharmaceutical companies.
SOURCE: Furie RA et al. EULAR 2018. Abstract OP0253.
AMSTERDAM – Abatacept used on top of the standard of care did not improve the primary endpoint of a complete renal response versus placebo in the ALLURE phase 3 study.
Criteria for a complete renal response (CRR) at 1 year was met by 35.1% of abatacept-treated and 33.5% of placebo-treated patients (P = .73). CRR criteria included having a urine protein to creatinine ratio (UPCR) of less than 0.5, a normal estimated glomerular filtration rate (eGFR) or an eGFR of 85% or more of baseline values, no cellular casts, and a daily corticosteroid dose of 10 mg or less.
“We also saw a more rapid decline in proteinuria in those people treated with abatacept, and that seemed to be sustained over the course of the study,” said Dr. Furie, professor of medicine at Hofstra University, Hempstead, N.Y., chief of the division of rheumatology at Northwell Health in Great Neck, N.Y., and a professor at the Center for Autoimmune, Musculoskeletal, and Hematopoietic Diseases in the Feinstein Institute for Medical Research in Manhasset, N.Y. After about 12 weeks, the adjusted mean change in UPCR from baseline was –2.5 for abatacept and –2.0 for placebo; the values at 1 year were a respective –2.95 vs. –2.68 and at 2 years were –3.13 vs. –2.72.
Renal function was not negatively impacted by treatment with abatacept, with about a 5%-8% increase in eGFR seen in both groups.
Furthermore, improvements in lupus-related biomarkers were more pronounced in patients treated with abatacept than placebo, Dr. Furie said. This included a greater decrease in anti–double-stranded DNA autoantibody titers and an increase in complement C3 and C4 levels.
Eric Morand, MD, who was not involved in the ALLURE study, commented during discussion that the main result of the study was “very sad.”
Dr. Morand of Monash University in Melbourne observed that the duration of renal disease at study entry was about 14 months and that around 38% had been previously treated with mycophenolate mofetil (MMF). So, could this have influenced the findings?
Dr. Furie was unable to answer the question but confirmed that MMF was one of two background medications given in the trial, at an oral dose of 1.5 g/day, alongside of oral prednisone up to 60-mg daily.
ALLURE was a 2-year randomized, double-blind study with an open-ended, blinded, long-term extension in 405 patients with active class III or IV lupus nephritis. The aim of the trial was to determine the efficacy and safety of abatacept versus placebo in the treatment of active proliferative lupus nephritis.
Abatacept was given intravenously, first at a dose of 30 mg/kg on days 1, 15, 29, and 57, and then at a dose of 10 mg/kg every 4 weeks.
In terms of safety, 14 deaths occurred during the course of the study and its long-term extension. Seven abatacept patients died in year 1, two of whom died more than 56 days after discontinuing the study drug. Five patients in the placebo group died in year 1, one in year 2, and one in the long-term extension. Rates of any or serious adverse events were similar among the groups, decreasing over time.
“The safety signals were really no different to what we already know about abatacept,” Dr. Furie said. As for the future, more analyses from the trial can be expected, he added.
The study was sponsored by Bristol-Myers Squibb. Dr. Furie disclosed receiving grant or research support from, and acting as a consultant to, the company. All but 3 of the study’s 12 authors had financial ties to many pharmaceutical companies, some of which included Bristol-Myers Squibb. Two authors are employees of Bristol-Myers Squibb. Dr. Monash was not involved in the ALLURE study but has received research support from Bristol-Myers Squibb, among other pharmaceutical companies.
SOURCE: Furie RA et al. EULAR 2018. Abstract OP0253.
AMSTERDAM – Abatacept used on top of the standard of care did not improve the primary endpoint of a complete renal response versus placebo in the ALLURE phase 3 study.
Criteria for a complete renal response (CRR) at 1 year was met by 35.1% of abatacept-treated and 33.5% of placebo-treated patients (P = .73). CRR criteria included having a urine protein to creatinine ratio (UPCR) of less than 0.5, a normal estimated glomerular filtration rate (eGFR) or an eGFR of 85% or more of baseline values, no cellular casts, and a daily corticosteroid dose of 10 mg or less.
“We also saw a more rapid decline in proteinuria in those people treated with abatacept, and that seemed to be sustained over the course of the study,” said Dr. Furie, professor of medicine at Hofstra University, Hempstead, N.Y., chief of the division of rheumatology at Northwell Health in Great Neck, N.Y., and a professor at the Center for Autoimmune, Musculoskeletal, and Hematopoietic Diseases in the Feinstein Institute for Medical Research in Manhasset, N.Y. After about 12 weeks, the adjusted mean change in UPCR from baseline was –2.5 for abatacept and –2.0 for placebo; the values at 1 year were a respective –2.95 vs. –2.68 and at 2 years were –3.13 vs. –2.72.
Renal function was not negatively impacted by treatment with abatacept, with about a 5%-8% increase in eGFR seen in both groups.
Furthermore, improvements in lupus-related biomarkers were more pronounced in patients treated with abatacept than placebo, Dr. Furie said. This included a greater decrease in anti–double-stranded DNA autoantibody titers and an increase in complement C3 and C4 levels.
Eric Morand, MD, who was not involved in the ALLURE study, commented during discussion that the main result of the study was “very sad.”
Dr. Morand of Monash University in Melbourne observed that the duration of renal disease at study entry was about 14 months and that around 38% had been previously treated with mycophenolate mofetil (MMF). So, could this have influenced the findings?
Dr. Furie was unable to answer the question but confirmed that MMF was one of two background medications given in the trial, at an oral dose of 1.5 g/day, alongside of oral prednisone up to 60-mg daily.
ALLURE was a 2-year randomized, double-blind study with an open-ended, blinded, long-term extension in 405 patients with active class III or IV lupus nephritis. The aim of the trial was to determine the efficacy and safety of abatacept versus placebo in the treatment of active proliferative lupus nephritis.
Abatacept was given intravenously, first at a dose of 30 mg/kg on days 1, 15, 29, and 57, and then at a dose of 10 mg/kg every 4 weeks.
In terms of safety, 14 deaths occurred during the course of the study and its long-term extension. Seven abatacept patients died in year 1, two of whom died more than 56 days after discontinuing the study drug. Five patients in the placebo group died in year 1, one in year 2, and one in the long-term extension. Rates of any or serious adverse events were similar among the groups, decreasing over time.
“The safety signals were really no different to what we already know about abatacept,” Dr. Furie said. As for the future, more analyses from the trial can be expected, he added.
The study was sponsored by Bristol-Myers Squibb. Dr. Furie disclosed receiving grant or research support from, and acting as a consultant to, the company. All but 3 of the study’s 12 authors had financial ties to many pharmaceutical companies, some of which included Bristol-Myers Squibb. Two authors are employees of Bristol-Myers Squibb. Dr. Monash was not involved in the ALLURE study but has received research support from Bristol-Myers Squibb, among other pharmaceutical companies.
SOURCE: Furie RA et al. EULAR 2018. Abstract OP0253.
REPORTING FROM THE EULAR 2018 CONGRESS
Key clinical point: Abatacept treatment did not improve the complete renal response rate versus placebo.
Major finding: A complete renal response rate at 1 year was seen in 35.1% of abatacept-treated and 33.5% of placebo-treated patients (P = .73).
Study details: The phase 3 ALLURE study, a 2-year, randomized, double-blind study with an open-ended, blinded, long-term extension in 405 patients with active class III or IV lupus nephritis.
Disclosures: The study was sponsored by Bristol-Myers Squibb. Dr. Furie disclosed receiving grant or research support from, and acting as a consultant to, the company. All but 3 of the study’s 12 authors had financial ties to many pharmaceutical companies, some of which included Bristol-Myers Squibb. Two authors are employees of Bristol-Myers Squibb. Dr. Monash was not involved in the ALLURE study but has received research support from Bristol-Myers Squibb, among other pharmaceutical companies.
Source: Furie RA et al. EULAR 2018. Abstract OP0253.