User login
Rio Olympics tally for U.S. athletes is 6% West Nile infections, no Zika
SAN DIEGO – When compared with pretravel blood screening, new arboviral infections were detected in 7% of U.S. athletes and support staff who attended the 2016 Olympic Games in Rio de Janeiro, according to study results revealed at an annual scientific meeting on infectious diseases.
Although the prospective screening program was largely set up and driven by concern about the risk of Zika virus infection, this was not among the arboviral infections identified, reported Krow Ampofo, MD, professor of pediatrics in the division of pediatric infectious diseases, University of Utah, Salt Lake City.
“The stories and images of children with microencephalopathy and other complications of the Zika syndrome were a major concern of athletes,” said Dr. Ampofo, who noted that many were threatening not to attend. The concern was reasonable, he said, given the scope of the epidemic and the fact that the majority of female athletes were of reproductive age.
At the time the screening program was being planned, the Zika virus epidemic in Brazil had, in fact, already peaked. Although it was not then known that the peak had been reached, the incidence rates began falling sharply beginning in about March 2016. New cases still were being reported, but the threat was greatly diminished by the time that the summer games were held.
In the screening program, blood samples were obtained prior to the games from 950 U.S. athletes and support staff. In most cases, these samples were obtained in Houston, where the Olympic team was processed just prior to departure. At that same time, the U.S. Centers for Disease Control and Prevention provided pretravel counseling about infection risk prevention.
For follow-up, the goal was to obtain blood samples within 2-12 weeks after return of all those who participated in the pretravel screening. Completion of a post-travel survey about activities in Rio de Janeiro, particularly their participation in risk prevention strategies, also was requested.
Blood samples were evaluated for four arboviral infections: Zika virus, dengue virus, chikungunya virus, and West Nile virus. The calculation of infection rates was based on the 457 (48%) of those screened prior to travel who provided blood samples after their return. Of these, 11% had antibody evidence of arboviral infections, but new infections were confirmed in only 7%.
The post-games survey was completed by 169 of those evaluated. A comparison of risk prevention behaviors in those who were and were not infected suggested that use of mosquito repellent did provide risk reduction, said Dr. Ampofo.
The substantial rate of new West Nile virus infections was “surprising,” Dr. Ampofo said. He recounted that there were no prior warnings from Brazilian authorities that West Nile virus was circulating. Infection with West Nile virus in Houston prior to departure was not considered an alternative explanation. According to Dr. Ampofo, Houston was not an endemic area for West Nile virus, and the stay in Houston for most athletes was 2 or 3 days.
SAN DIEGO – When compared with pretravel blood screening, new arboviral infections were detected in 7% of U.S. athletes and support staff who attended the 2016 Olympic Games in Rio de Janeiro, according to study results revealed at an annual scientific meeting on infectious diseases.
Although the prospective screening program was largely set up and driven by concern about the risk of Zika virus infection, this was not among the arboviral infections identified, reported Krow Ampofo, MD, professor of pediatrics in the division of pediatric infectious diseases, University of Utah, Salt Lake City.
“The stories and images of children with microencephalopathy and other complications of the Zika syndrome were a major concern of athletes,” said Dr. Ampofo, who noted that many were threatening not to attend. The concern was reasonable, he said, given the scope of the epidemic and the fact that the majority of female athletes were of reproductive age.
At the time the screening program was being planned, the Zika virus epidemic in Brazil had, in fact, already peaked. Although it was not then known that the peak had been reached, the incidence rates began falling sharply beginning in about March 2016. New cases still were being reported, but the threat was greatly diminished by the time that the summer games were held.
In the screening program, blood samples were obtained prior to the games from 950 U.S. athletes and support staff. In most cases, these samples were obtained in Houston, where the Olympic team was processed just prior to departure. At that same time, the U.S. Centers for Disease Control and Prevention provided pretravel counseling about infection risk prevention.
For follow-up, the goal was to obtain blood samples within 2-12 weeks after return of all those who participated in the pretravel screening. Completion of a post-travel survey about activities in Rio de Janeiro, particularly their participation in risk prevention strategies, also was requested.
Blood samples were evaluated for four arboviral infections: Zika virus, dengue virus, chikungunya virus, and West Nile virus. The calculation of infection rates was based on the 457 (48%) of those screened prior to travel who provided blood samples after their return. Of these, 11% had antibody evidence of arboviral infections, but new infections were confirmed in only 7%.
The post-games survey was completed by 169 of those evaluated. A comparison of risk prevention behaviors in those who were and were not infected suggested that use of mosquito repellent did provide risk reduction, said Dr. Ampofo.
The substantial rate of new West Nile virus infections was “surprising,” Dr. Ampofo said. He recounted that there were no prior warnings from Brazilian authorities that West Nile virus was circulating. Infection with West Nile virus in Houston prior to departure was not considered an alternative explanation. According to Dr. Ampofo, Houston was not an endemic area for West Nile virus, and the stay in Houston for most athletes was 2 or 3 days.
SAN DIEGO – When compared with pretravel blood screening, new arboviral infections were detected in 7% of U.S. athletes and support staff who attended the 2016 Olympic Games in Rio de Janeiro, according to study results revealed at an annual scientific meeting on infectious diseases.
Although the prospective screening program was largely set up and driven by concern about the risk of Zika virus infection, this was not among the arboviral infections identified, reported Krow Ampofo, MD, professor of pediatrics in the division of pediatric infectious diseases, University of Utah, Salt Lake City.
“The stories and images of children with microencephalopathy and other complications of the Zika syndrome were a major concern of athletes,” said Dr. Ampofo, who noted that many were threatening not to attend. The concern was reasonable, he said, given the scope of the epidemic and the fact that the majority of female athletes were of reproductive age.
At the time the screening program was being planned, the Zika virus epidemic in Brazil had, in fact, already peaked. Although it was not then known that the peak had been reached, the incidence rates began falling sharply beginning in about March 2016. New cases still were being reported, but the threat was greatly diminished by the time that the summer games were held.
In the screening program, blood samples were obtained prior to the games from 950 U.S. athletes and support staff. In most cases, these samples were obtained in Houston, where the Olympic team was processed just prior to departure. At that same time, the U.S. Centers for Disease Control and Prevention provided pretravel counseling about infection risk prevention.
For follow-up, the goal was to obtain blood samples within 2-12 weeks after return of all those who participated in the pretravel screening. Completion of a post-travel survey about activities in Rio de Janeiro, particularly their participation in risk prevention strategies, also was requested.
Blood samples were evaluated for four arboviral infections: Zika virus, dengue virus, chikungunya virus, and West Nile virus. The calculation of infection rates was based on the 457 (48%) of those screened prior to travel who provided blood samples after their return. Of these, 11% had antibody evidence of arboviral infections, but new infections were confirmed in only 7%.
The post-games survey was completed by 169 of those evaluated. A comparison of risk prevention behaviors in those who were and were not infected suggested that use of mosquito repellent did provide risk reduction, said Dr. Ampofo.
The substantial rate of new West Nile virus infections was “surprising,” Dr. Ampofo said. He recounted that there were no prior warnings from Brazilian authorities that West Nile virus was circulating. Infection with West Nile virus in Houston prior to departure was not considered an alternative explanation. According to Dr. Ampofo, Houston was not an endemic area for West Nile virus, and the stay in Houston for most athletes was 2 or 3 days.
AT ID WEEK 2017
Key clinical point: Prospective surveillance among U.S. athletes and staff attending the 2016 Olympics documented several arboviral infections, but not Zika.
Major finding: When pre- versus post-Olympics blood studies were evaluated, 6% had developed West Nile virus while no other arboviral infection incidence exceeded 1%.
Data source: Prospective and post-Olympics blood studies of 457 U.S. athletes and staff and survey results.
Disclosures: Dr. Ampofo reported no financial relationships relevant to this study.
Deep learning can assist real-time polyp detection during colonoscopies
A deep-learning algorithm for automatic polyp detection during colonoscopies showed both high sensitivity and high specificity, according to a study presented at the World Congress of Gastroenterology at ACG 2017.
The algorithm was set up using a retrospective set of 5,545 images annotated by colonoscopists, while the validation set used for the study consisted of 27,461 colonoscopy images from 1,235 patients, according to Pu Wang, MD, of the Sichuan Academy of Medical Sciences & Sichuan Provincial People’s Hospital, Chengdu, China, and his associates.
At the high-sensitivity operating point, the algorithm had a sensitivity of 94.96% and a specificity of 92.01%, and at the low–false positive rate operating point, the algorithm had a sensitivity of 92.35% and a specificity of 97.05%. The area under the curve was 0.958 in a receiver operating characteristic curve analysis.
In subgroup analyses of flat polyps, polyps less than or equal to 0.5 cm, and isochromatic polyps, the algorithm had areas under the curve of 0.943, 0.957, and 0.957 respectively.
The algorithm reported results in 60-80 ms, offering real-time assistance with polyp detection during colonoscopies, Dr. Wang and his colleagues noted.
The study was not funded by industry grants, and no disclosures were reported.
A deep-learning algorithm for automatic polyp detection during colonoscopies showed both high sensitivity and high specificity, according to a study presented at the World Congress of Gastroenterology at ACG 2017.
The algorithm was set up using a retrospective set of 5,545 images annotated by colonoscopists, while the validation set used for the study consisted of 27,461 colonoscopy images from 1,235 patients, according to Pu Wang, MD, of the Sichuan Academy of Medical Sciences & Sichuan Provincial People’s Hospital, Chengdu, China, and his associates.
At the high-sensitivity operating point, the algorithm had a sensitivity of 94.96% and a specificity of 92.01%, and at the low–false positive rate operating point, the algorithm had a sensitivity of 92.35% and a specificity of 97.05%. The area under the curve was 0.958 in a receiver operating characteristic curve analysis.
In subgroup analyses of flat polyps, polyps less than or equal to 0.5 cm, and isochromatic polyps, the algorithm had areas under the curve of 0.943, 0.957, and 0.957 respectively.
The algorithm reported results in 60-80 ms, offering real-time assistance with polyp detection during colonoscopies, Dr. Wang and his colleagues noted.
The study was not funded by industry grants, and no disclosures were reported.
A deep-learning algorithm for automatic polyp detection during colonoscopies showed both high sensitivity and high specificity, according to a study presented at the World Congress of Gastroenterology at ACG 2017.
The algorithm was set up using a retrospective set of 5,545 images annotated by colonoscopists, while the validation set used for the study consisted of 27,461 colonoscopy images from 1,235 patients, according to Pu Wang, MD, of the Sichuan Academy of Medical Sciences & Sichuan Provincial People’s Hospital, Chengdu, China, and his associates.
At the high-sensitivity operating point, the algorithm had a sensitivity of 94.96% and a specificity of 92.01%, and at the low–false positive rate operating point, the algorithm had a sensitivity of 92.35% and a specificity of 97.05%. The area under the curve was 0.958 in a receiver operating characteristic curve analysis.
In subgroup analyses of flat polyps, polyps less than or equal to 0.5 cm, and isochromatic polyps, the algorithm had areas under the curve of 0.943, 0.957, and 0.957 respectively.
The algorithm reported results in 60-80 ms, offering real-time assistance with polyp detection during colonoscopies, Dr. Wang and his colleagues noted.
The study was not funded by industry grants, and no disclosures were reported.
FROM WORLD CONGRESS OF GASTROENTEROLOGY
Key clinical point:
Major finding: The deep-learning algorithm had a sensitivity of 95% and a specificity of 92% when adjusted to the high-sensitivity operating point.
Data source: A set of 27,461 colonoscopy images from 1,235 patients.
Disclosures: The study was not funded by industry grants, and no disclosures were reported.
Better care reduces time to successful refeeding in acute pancreatitis
Enhanced recovery approaches were safe and effective at promoting earlier restoration of gut function in acute pancreatitis patients, according to a study presented at the World Congress of Gastroenterology at ACG 2017.
Patients recruited for the trial were admitted directly from an emergency department and received either enhanced care consisting of patient-directed oral intake, early ambulation, and nonopioid analgesia or received normal care consisting of opioid analgesia, physician-directed diet, and nursing parameters, Elizabeth Dong, MD, of the Kaiser Permanente Los Angeles Medical Center and her associates said.
Among the 46 patients included in the study, 61% had an etiology of gallstones, 15% had an etiology of alcohol, 13% had hyperglyceridemia, and 11% had a different etiology. Median age was 53.1 years, Dr. Dong and her associates noted.
Time to successful oral refeeding, the primary study endpoint, was significantly reduced in the enhanced treatment group, with a median time of 13.8 hours, compared with the normal treatment group, in which median time to oral refeeding was 124.8 hours. In addition, patients in the enhanced care group had a mean pancreatitis activity score of 43.5 after 48-72 hours, while patients in the control group had a mean score of 72.1.
Length of stay and frequency of 30-day readmission did not differ significantly between study groups.
The study was not funded by industry grants, and no disclosures were reported.
Enhanced recovery approaches were safe and effective at promoting earlier restoration of gut function in acute pancreatitis patients, according to a study presented at the World Congress of Gastroenterology at ACG 2017.
Patients recruited for the trial were admitted directly from an emergency department and received either enhanced care consisting of patient-directed oral intake, early ambulation, and nonopioid analgesia or received normal care consisting of opioid analgesia, physician-directed diet, and nursing parameters, Elizabeth Dong, MD, of the Kaiser Permanente Los Angeles Medical Center and her associates said.
Among the 46 patients included in the study, 61% had an etiology of gallstones, 15% had an etiology of alcohol, 13% had hyperglyceridemia, and 11% had a different etiology. Median age was 53.1 years, Dr. Dong and her associates noted.
Time to successful oral refeeding, the primary study endpoint, was significantly reduced in the enhanced treatment group, with a median time of 13.8 hours, compared with the normal treatment group, in which median time to oral refeeding was 124.8 hours. In addition, patients in the enhanced care group had a mean pancreatitis activity score of 43.5 after 48-72 hours, while patients in the control group had a mean score of 72.1.
Length of stay and frequency of 30-day readmission did not differ significantly between study groups.
The study was not funded by industry grants, and no disclosures were reported.
Enhanced recovery approaches were safe and effective at promoting earlier restoration of gut function in acute pancreatitis patients, according to a study presented at the World Congress of Gastroenterology at ACG 2017.
Patients recruited for the trial were admitted directly from an emergency department and received either enhanced care consisting of patient-directed oral intake, early ambulation, and nonopioid analgesia or received normal care consisting of opioid analgesia, physician-directed diet, and nursing parameters, Elizabeth Dong, MD, of the Kaiser Permanente Los Angeles Medical Center and her associates said.
Among the 46 patients included in the study, 61% had an etiology of gallstones, 15% had an etiology of alcohol, 13% had hyperglyceridemia, and 11% had a different etiology. Median age was 53.1 years, Dr. Dong and her associates noted.
Time to successful oral refeeding, the primary study endpoint, was significantly reduced in the enhanced treatment group, with a median time of 13.8 hours, compared with the normal treatment group, in which median time to oral refeeding was 124.8 hours. In addition, patients in the enhanced care group had a mean pancreatitis activity score of 43.5 after 48-72 hours, while patients in the control group had a mean score of 72.1.
Length of stay and frequency of 30-day readmission did not differ significantly between study groups.
The study was not funded by industry grants, and no disclosures were reported.
FROM WORLD CONGRESS OF GASTROENTEROLOGY
Key clinical point:
Major finding: Median time to successful oral refeeding was more than 4 days faster in patients who received enhanced care.
Data source: A pilot single-blind, randomized, controlled trial of 46 patients admitted from an emergency department between July 2016 and April 2017.
Disclosures: The study was not funded by industry grants, and no disclosures were reported.
Serrated polyps alone not associated with future high-risk adenomas
The presence of serrated polyps on index colonoscopies without low-risk adenomas was not associated with metachronous high-risk adenomas on surveillance exams, according to a study presented at the World Congress of Gastroenterology at ACG 2017.
Data for the study were collected from 4,616 adults who had two colonoscopies on record with the New Hampshire Colonoscopy Registry. Patients with high-risk adenomas at the index colonoscopy were excluded from the study. The median time between index and surveillance exams was 4.9 years, and median age was 61 years, according to Joseph Anderson, MD, of Geisel School of Medicine at Dartmouth, Hanover, N.H., and his associates.
Overall, the risk for metachronous high-risk adenomas in the study group was 6.3% and the risk of large serrated polyps greater than or equal to 1 cm was 1.2%. After patient age, sex, smoking, body mass index, and time between the two exams were adjusted for, low-risk adenomas at the time of the index colonoscopy were associated with an increased metachronous risk of high-risk adenomas, Dr. Anderson and his colleagues noted.
Large serrated polyps and the presence of sessile serrated polyps or traditional serrated adenomas at index exam increased the risk of metachronous serrated polyps at the surveillance colonoscopy 10-fold and 14-fold, respectively, but did not increase the risk of high-risk adenomas. The presence of both low-risk adenomas and significant serrated polyps was not associated with an increased risk of high-risk adenomas over the presence of low-risk adenomas alone.
The study was not funded by industry grants, and no disclosures were reported.
The presence of serrated polyps on index colonoscopies without low-risk adenomas was not associated with metachronous high-risk adenomas on surveillance exams, according to a study presented at the World Congress of Gastroenterology at ACG 2017.
Data for the study were collected from 4,616 adults who had two colonoscopies on record with the New Hampshire Colonoscopy Registry. Patients with high-risk adenomas at the index colonoscopy were excluded from the study. The median time between index and surveillance exams was 4.9 years, and median age was 61 years, according to Joseph Anderson, MD, of Geisel School of Medicine at Dartmouth, Hanover, N.H., and his associates.
Overall, the risk for metachronous high-risk adenomas in the study group was 6.3% and the risk of large serrated polyps greater than or equal to 1 cm was 1.2%. After patient age, sex, smoking, body mass index, and time between the two exams were adjusted for, low-risk adenomas at the time of the index colonoscopy were associated with an increased metachronous risk of high-risk adenomas, Dr. Anderson and his colleagues noted.
Large serrated polyps and the presence of sessile serrated polyps or traditional serrated adenomas at index exam increased the risk of metachronous serrated polyps at the surveillance colonoscopy 10-fold and 14-fold, respectively, but did not increase the risk of high-risk adenomas. The presence of both low-risk adenomas and significant serrated polyps was not associated with an increased risk of high-risk adenomas over the presence of low-risk adenomas alone.
The study was not funded by industry grants, and no disclosures were reported.
The presence of serrated polyps on index colonoscopies without low-risk adenomas was not associated with metachronous high-risk adenomas on surveillance exams, according to a study presented at the World Congress of Gastroenterology at ACG 2017.
Data for the study were collected from 4,616 adults who had two colonoscopies on record with the New Hampshire Colonoscopy Registry. Patients with high-risk adenomas at the index colonoscopy were excluded from the study. The median time between index and surveillance exams was 4.9 years, and median age was 61 years, according to Joseph Anderson, MD, of Geisel School of Medicine at Dartmouth, Hanover, N.H., and his associates.
Overall, the risk for metachronous high-risk adenomas in the study group was 6.3% and the risk of large serrated polyps greater than or equal to 1 cm was 1.2%. After patient age, sex, smoking, body mass index, and time between the two exams were adjusted for, low-risk adenomas at the time of the index colonoscopy were associated with an increased metachronous risk of high-risk adenomas, Dr. Anderson and his colleagues noted.
Large serrated polyps and the presence of sessile serrated polyps or traditional serrated adenomas at index exam increased the risk of metachronous serrated polyps at the surveillance colonoscopy 10-fold and 14-fold, respectively, but did not increase the risk of high-risk adenomas. The presence of both low-risk adenomas and significant serrated polyps was not associated with an increased risk of high-risk adenomas over the presence of low-risk adenomas alone.
The study was not funded by industry grants, and no disclosures were reported.
FROM THE 13TH WORLD CONGRESS OF GASTROENTEROLOGY
Key clinical point:
Major finding: After patient age, sex, smoking, body mass index, and time between index and surveillance exams were adjusted for, the presence of index serrated polyps without additional low-risk adenomas did not increase risk of high-risk adenomas at surveillance exams.
Data source: Data collected from 4,616 patients in the New Hampshire Colonoscopy Registry.
Disclosures: The study was not funded by industry grants, and no disclosures were reported.
MACRA Monday: Advance care plan
If you haven’t started reporting quality data for the Merit-Based Incentive Payment System (MIPS), there’s still time to avoid a 4% cut to your Medicare payments.
Under the Pick Your Pace approach being offered this year, the Centers for Medicare & Medicaid Services allows clinicians to test the system by reporting on one quality measure for one patient through paper-based claims. Be sure to append a Quality Data Code (QDC) to the claim form for care provided up to Dec. 31, 2017, in order to avoid a penalty in payment year 2019.
Consider this measure:
Measure #47: Care Plan
This measure is aimed at capturing the percentage of patients aged 65 years and older who have a documented advance care plan in their medical records.
What you need to do: Discuss with the patient the creation of an advance care plan or the naming of a surrogate decision maker and then document that in the medical record. If the patient does not wish to make a plan or is unable to name a decision maker, document that along with the fact that the issue of advance care planning was discussed.
Eligible cases include patients aged 65 years or older on the date of the encounter and a patient encounter during the performance period. Applicable codes include (CPT or HCPCS): 99201, 99202, 99203, 99204, 99205,99212, 99213, 99214, 99215, 99218, 99219, 99220, 99221, 99222, 99223, 99231, 99232, 99233, 99234, 99235, 99236, 99291, 99304, 99305, 99306, 99307, 99308, 99309, 99310, 99324, 99325, 99326, 99327, 99328, 99334, 99335, 99336, 99337, 99341, 99342, 99343, 99344, 99345, 99347, 99348, 99349, 99350, G0402, G0438, G0439.
To get credit under MIPS, be sure to include a Quality Data Code that shows that you successfully performed the measure or had a good reason for not doing so. For instance, CPT II 1123F indicates that advance care planning was discussed and documented, and an advance care plan or surrogate decision maker was documented in the medical record. On the other hand, CPT II 1124F should be used if advance care planning was discussed and documented in the medical record, but the patient did not wish or was not able to name a surrogate decision maker or provide an advance care plan.
CMS has a full list of measures available for claims-based reporting at qpp.cms.gov. The American Medical Association has also created a step-by-step guide for reporting on one quality measure.
Certain clinicians are exempt from reporting and do not face a penalty under MIPS:
- Those who enrolled in Medicare for the first time during a performance period.
- Those who have Medicare Part B–allowed charges of $30,000 or less.
- Those who have 100 or fewer Medicare Part B patients.
- Those who are significantly participating in an Advanced Alternative Payment Model (APM).
If you haven’t started reporting quality data for the Merit-Based Incentive Payment System (MIPS), there’s still time to avoid a 4% cut to your Medicare payments.
Under the Pick Your Pace approach being offered this year, the Centers for Medicare & Medicaid Services allows clinicians to test the system by reporting on one quality measure for one patient through paper-based claims. Be sure to append a Quality Data Code (QDC) to the claim form for care provided up to Dec. 31, 2017, in order to avoid a penalty in payment year 2019.
Consider this measure:
Measure #47: Care Plan
This measure is aimed at capturing the percentage of patients aged 65 years and older who have a documented advance care plan in their medical records.
What you need to do: Discuss with the patient the creation of an advance care plan or the naming of a surrogate decision maker and then document that in the medical record. If the patient does not wish to make a plan or is unable to name a decision maker, document that along with the fact that the issue of advance care planning was discussed.
Eligible cases include patients aged 65 years or older on the date of the encounter and a patient encounter during the performance period. Applicable codes include (CPT or HCPCS): 99201, 99202, 99203, 99204, 99205,99212, 99213, 99214, 99215, 99218, 99219, 99220, 99221, 99222, 99223, 99231, 99232, 99233, 99234, 99235, 99236, 99291, 99304, 99305, 99306, 99307, 99308, 99309, 99310, 99324, 99325, 99326, 99327, 99328, 99334, 99335, 99336, 99337, 99341, 99342, 99343, 99344, 99345, 99347, 99348, 99349, 99350, G0402, G0438, G0439.
To get credit under MIPS, be sure to include a Quality Data Code that shows that you successfully performed the measure or had a good reason for not doing so. For instance, CPT II 1123F indicates that advance care planning was discussed and documented, and an advance care plan or surrogate decision maker was documented in the medical record. On the other hand, CPT II 1124F should be used if advance care planning was discussed and documented in the medical record, but the patient did not wish or was not able to name a surrogate decision maker or provide an advance care plan.
CMS has a full list of measures available for claims-based reporting at qpp.cms.gov. The American Medical Association has also created a step-by-step guide for reporting on one quality measure.
Certain clinicians are exempt from reporting and do not face a penalty under MIPS:
- Those who enrolled in Medicare for the first time during a performance period.
- Those who have Medicare Part B–allowed charges of $30,000 or less.
- Those who have 100 or fewer Medicare Part B patients.
- Those who are significantly participating in an Advanced Alternative Payment Model (APM).
If you haven’t started reporting quality data for the Merit-Based Incentive Payment System (MIPS), there’s still time to avoid a 4% cut to your Medicare payments.
Under the Pick Your Pace approach being offered this year, the Centers for Medicare & Medicaid Services allows clinicians to test the system by reporting on one quality measure for one patient through paper-based claims. Be sure to append a Quality Data Code (QDC) to the claim form for care provided up to Dec. 31, 2017, in order to avoid a penalty in payment year 2019.
Consider this measure:
Measure #47: Care Plan
This measure is aimed at capturing the percentage of patients aged 65 years and older who have a documented advance care plan in their medical records.
What you need to do: Discuss with the patient the creation of an advance care plan or the naming of a surrogate decision maker and then document that in the medical record. If the patient does not wish to make a plan or is unable to name a decision maker, document that along with the fact that the issue of advance care planning was discussed.
Eligible cases include patients aged 65 years or older on the date of the encounter and a patient encounter during the performance period. Applicable codes include (CPT or HCPCS): 99201, 99202, 99203, 99204, 99205,99212, 99213, 99214, 99215, 99218, 99219, 99220, 99221, 99222, 99223, 99231, 99232, 99233, 99234, 99235, 99236, 99291, 99304, 99305, 99306, 99307, 99308, 99309, 99310, 99324, 99325, 99326, 99327, 99328, 99334, 99335, 99336, 99337, 99341, 99342, 99343, 99344, 99345, 99347, 99348, 99349, 99350, G0402, G0438, G0439.
To get credit under MIPS, be sure to include a Quality Data Code that shows that you successfully performed the measure or had a good reason for not doing so. For instance, CPT II 1123F indicates that advance care planning was discussed and documented, and an advance care plan or surrogate decision maker was documented in the medical record. On the other hand, CPT II 1124F should be used if advance care planning was discussed and documented in the medical record, but the patient did not wish or was not able to name a surrogate decision maker or provide an advance care plan.
CMS has a full list of measures available for claims-based reporting at qpp.cms.gov. The American Medical Association has also created a step-by-step guide for reporting on one quality measure.
Certain clinicians are exempt from reporting and do not face a penalty under MIPS:
- Those who enrolled in Medicare for the first time during a performance period.
- Those who have Medicare Part B–allowed charges of $30,000 or less.
- Those who have 100 or fewer Medicare Part B patients.
- Those who are significantly participating in an Advanced Alternative Payment Model (APM).
CBT for insomnia and hot flashes lifts mood in midlife
PHILADELPHIA – Cognitive-behavioral therapy tailored to perimenopausal and postmenopausal women who were experiencing both insomnia and vasomotor symptoms effectively improved both sleep and mood, according to a small controlled study.
When 40 women were randomized to receive either cognitive-behavioral therapy for menopausal insomnia (CBTMI) or education about menopause and sleep, those who received CBTMI had significantly reduced scores on both objective and subjective scales of depression, and their sleep also improved.
The CBTMI intervention was effective even for women with high scores on the depression scales at baseline, Sara Nowakowski, PhD, said at a top abstracts session at the annual meeting of the North American Menopause Society.
Over the 8 weeks of the study intervention, women in the CBTMI arm received four 50-minute individual sessions with either a social worker or a psychologist in a gynecology clinic outpatient setting. Counseling during the sessions focused both on hot flashes and insomnia, using evidence-based CBT techniques to address both. These included sleep restriction, changing behaviors to strengthen the association of the bed with sleep, cognitive therapy to address maladaptive beliefs about both sleep and host flashes, general sleep hygiene, hot flash coping mechanisms, and relaxation training.
Those in the menopause education control arm had a 1-hour educational session about menopausal symptoms and sleep hygiene, received written material, and were told they could make any changes desired.
Participants, whose mean age was 55 years, were included if they reported at least one nocturnal hot flash per night and met criteria for the sleep disorder of insomnia. Although patients who met criteria for major depression were not excluded, women with surgical menopause or cancer treatment–related menopause were excluded, as were those with substance use disorder, significant other psychiatric comorbidities, and those with obstructive sleep apnea or periodic limb movements/restless leg syndrome.
Dr. Nowakowski, a clinical psychologist in the department of obstetrics and gynecology, University of Texas, Galveston, and her colleagues administered the Insomnia Severity Index (ISI), the Center for Epidemiologic Studies Depression Scale (CES-D), and the Hamilton Depression Rating Scale (HDRS) both before and after the 8-week intervention.
The investigators used a mixed-models statistical analysis, finding a significant improvement over time during the study period in both patient-reported (P = .001) and clinician-assessed (P = .001) ratings of depression for the CBTMI group.
When the effect of the treatment arm was analyzed, CBTMI also offered significantly greater improvement in patient-reported (P = .009) and clinician-assessed (P = .022) depression ratings.
Patients were divided into high and low depression severity, with a score over 8 on the CES-D and 16 on the HDRS putting the participant into the high-severity category. Both groups had significant improvement on the ISI from baseline. “Treatment response for insomnia severity did not differ based on baseline depression severity,” Dr. Nowakowski said.
The efficacy of the relatively brief intervention has clinical relevance to those caring for the 39%-60% of women in midlife who have symptoms of insomnia and the 8%-40% of midlife women who report elevated depression symptoms. “Comprehensive interventions that simultaneously improve sleep and mood in midlife women are greatly needed,” she said.
The National Institutes of Health and the Hogg Foundation for Mental Health funded the study. Dr. Nowakowski reported no conflicts of interest.
[email protected]
On Twitter @karioakes
PHILADELPHIA – Cognitive-behavioral therapy tailored to perimenopausal and postmenopausal women who were experiencing both insomnia and vasomotor symptoms effectively improved both sleep and mood, according to a small controlled study.
When 40 women were randomized to receive either cognitive-behavioral therapy for menopausal insomnia (CBTMI) or education about menopause and sleep, those who received CBTMI had significantly reduced scores on both objective and subjective scales of depression, and their sleep also improved.
The CBTMI intervention was effective even for women with high scores on the depression scales at baseline, Sara Nowakowski, PhD, said at a top abstracts session at the annual meeting of the North American Menopause Society.
Over the 8 weeks of the study intervention, women in the CBTMI arm received four 50-minute individual sessions with either a social worker or a psychologist in a gynecology clinic outpatient setting. Counseling during the sessions focused both on hot flashes and insomnia, using evidence-based CBT techniques to address both. These included sleep restriction, changing behaviors to strengthen the association of the bed with sleep, cognitive therapy to address maladaptive beliefs about both sleep and host flashes, general sleep hygiene, hot flash coping mechanisms, and relaxation training.
Those in the menopause education control arm had a 1-hour educational session about menopausal symptoms and sleep hygiene, received written material, and were told they could make any changes desired.
Participants, whose mean age was 55 years, were included if they reported at least one nocturnal hot flash per night and met criteria for the sleep disorder of insomnia. Although patients who met criteria for major depression were not excluded, women with surgical menopause or cancer treatment–related menopause were excluded, as were those with substance use disorder, significant other psychiatric comorbidities, and those with obstructive sleep apnea or periodic limb movements/restless leg syndrome.
Dr. Nowakowski, a clinical psychologist in the department of obstetrics and gynecology, University of Texas, Galveston, and her colleagues administered the Insomnia Severity Index (ISI), the Center for Epidemiologic Studies Depression Scale (CES-D), and the Hamilton Depression Rating Scale (HDRS) both before and after the 8-week intervention.
The investigators used a mixed-models statistical analysis, finding a significant improvement over time during the study period in both patient-reported (P = .001) and clinician-assessed (P = .001) ratings of depression for the CBTMI group.
When the effect of the treatment arm was analyzed, CBTMI also offered significantly greater improvement in patient-reported (P = .009) and clinician-assessed (P = .022) depression ratings.
Patients were divided into high and low depression severity, with a score over 8 on the CES-D and 16 on the HDRS putting the participant into the high-severity category. Both groups had significant improvement on the ISI from baseline. “Treatment response for insomnia severity did not differ based on baseline depression severity,” Dr. Nowakowski said.
The efficacy of the relatively brief intervention has clinical relevance to those caring for the 39%-60% of women in midlife who have symptoms of insomnia and the 8%-40% of midlife women who report elevated depression symptoms. “Comprehensive interventions that simultaneously improve sleep and mood in midlife women are greatly needed,” she said.
The National Institutes of Health and the Hogg Foundation for Mental Health funded the study. Dr. Nowakowski reported no conflicts of interest.
[email protected]
On Twitter @karioakes
PHILADELPHIA – Cognitive-behavioral therapy tailored to perimenopausal and postmenopausal women who were experiencing both insomnia and vasomotor symptoms effectively improved both sleep and mood, according to a small controlled study.
When 40 women were randomized to receive either cognitive-behavioral therapy for menopausal insomnia (CBTMI) or education about menopause and sleep, those who received CBTMI had significantly reduced scores on both objective and subjective scales of depression, and their sleep also improved.
The CBTMI intervention was effective even for women with high scores on the depression scales at baseline, Sara Nowakowski, PhD, said at a top abstracts session at the annual meeting of the North American Menopause Society.
Over the 8 weeks of the study intervention, women in the CBTMI arm received four 50-minute individual sessions with either a social worker or a psychologist in a gynecology clinic outpatient setting. Counseling during the sessions focused both on hot flashes and insomnia, using evidence-based CBT techniques to address both. These included sleep restriction, changing behaviors to strengthen the association of the bed with sleep, cognitive therapy to address maladaptive beliefs about both sleep and host flashes, general sleep hygiene, hot flash coping mechanisms, and relaxation training.
Those in the menopause education control arm had a 1-hour educational session about menopausal symptoms and sleep hygiene, received written material, and were told they could make any changes desired.
Participants, whose mean age was 55 years, were included if they reported at least one nocturnal hot flash per night and met criteria for the sleep disorder of insomnia. Although patients who met criteria for major depression were not excluded, women with surgical menopause or cancer treatment–related menopause were excluded, as were those with substance use disorder, significant other psychiatric comorbidities, and those with obstructive sleep apnea or periodic limb movements/restless leg syndrome.
Dr. Nowakowski, a clinical psychologist in the department of obstetrics and gynecology, University of Texas, Galveston, and her colleagues administered the Insomnia Severity Index (ISI), the Center for Epidemiologic Studies Depression Scale (CES-D), and the Hamilton Depression Rating Scale (HDRS) both before and after the 8-week intervention.
The investigators used a mixed-models statistical analysis, finding a significant improvement over time during the study period in both patient-reported (P = .001) and clinician-assessed (P = .001) ratings of depression for the CBTMI group.
When the effect of the treatment arm was analyzed, CBTMI also offered significantly greater improvement in patient-reported (P = .009) and clinician-assessed (P = .022) depression ratings.
Patients were divided into high and low depression severity, with a score over 8 on the CES-D and 16 on the HDRS putting the participant into the high-severity category. Both groups had significant improvement on the ISI from baseline. “Treatment response for insomnia severity did not differ based on baseline depression severity,” Dr. Nowakowski said.
The efficacy of the relatively brief intervention has clinical relevance to those caring for the 39%-60% of women in midlife who have symptoms of insomnia and the 8%-40% of midlife women who report elevated depression symptoms. “Comprehensive interventions that simultaneously improve sleep and mood in midlife women are greatly needed,” she said.
The National Institutes of Health and the Hogg Foundation for Mental Health funded the study. Dr. Nowakowski reported no conflicts of interest.
[email protected]
On Twitter @karioakes
AT NAMS 2017
Key clinical point:
Major finding: Patient-reported and clinician-assessed depression scores dropped after the intervention (P = .001 for both).
Data source: Randomized controlled trial of 40 midlife women with insomnia and hot flashes.
Disclosures: The National Institutes of Health and the Hogg Foundation for Mental Health funded the study. Dr. Nowakowski reported no conflicts of interest.
Good for something, or an American tragedy
The headline in the Oct. 13, 2017, Portland (Maine) Press Herald hinted that I was about to read a sad story: “New Hampshire doctor, 85, may lose practice because she doesn’t use computer.” Anna Konopka, MD, who has a 300-patient practice in New London, doesn’t use a computer in her office, and as a consequence can’t participate in her state’s mandated prescription drug monitoring program. She has appealed to the governor, but if her appeal is denied she will be forced to close her office.
The closure will present a hardship for the residents of this small New Hampshire town, who will have to replace their obviously committed physician who has served them for more than 30 years. And I am sure that Dr. Konopka would have preferred to end her professional career on her own terms. It isn’t going to be easy to give up that positive feedback from her patients that every primary care physician enjoys even on her worst day.
I wouldn’t be surprised to learn that Dr. Konopka has listened to other physicians in her community complain about the cost and time-gobbling inefficiencies of their EHRs. She may have been put off by her own experiences as a patient whose physician spends too much time looking at his computer screen and fails to engage with her. Or she may have simply done the math and come up with the obvious answer that a computer system would be a bad investment for her small practice.
I suspect that there are days that you wish you had followed this wise older physician’s lead and never plugged into that “good-for-nothing piece of junk” sitting on the desk in your exam room. The sadness in this story is that the computer and the Internet are (or at least could be) good for some things, including the statewide prescription drug monitoring program that Dr. Konopka can’t participate in. Immunization data banks, prescribing programs that minimize physician error, and systems for storing and plotting your patient’s lab work and metrics are just a few of the things that a good computer system is good for. And, of course, there is the real-time access to the vast store of medical and research knowledge that has made textbooks obsolete.
I’m not sure where we can go from here without throwing out the baby with the bathwater and starting from scratch. We have computer scientists and physicians who I am sure could create a patient- and physician-friendly system that could cover the whole country. The trick will be keeping the politicians out of the room.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
The headline in the Oct. 13, 2017, Portland (Maine) Press Herald hinted that I was about to read a sad story: “New Hampshire doctor, 85, may lose practice because she doesn’t use computer.” Anna Konopka, MD, who has a 300-patient practice in New London, doesn’t use a computer in her office, and as a consequence can’t participate in her state’s mandated prescription drug monitoring program. She has appealed to the governor, but if her appeal is denied she will be forced to close her office.
The closure will present a hardship for the residents of this small New Hampshire town, who will have to replace their obviously committed physician who has served them for more than 30 years. And I am sure that Dr. Konopka would have preferred to end her professional career on her own terms. It isn’t going to be easy to give up that positive feedback from her patients that every primary care physician enjoys even on her worst day.
I wouldn’t be surprised to learn that Dr. Konopka has listened to other physicians in her community complain about the cost and time-gobbling inefficiencies of their EHRs. She may have been put off by her own experiences as a patient whose physician spends too much time looking at his computer screen and fails to engage with her. Or she may have simply done the math and come up with the obvious answer that a computer system would be a bad investment for her small practice.
I suspect that there are days that you wish you had followed this wise older physician’s lead and never plugged into that “good-for-nothing piece of junk” sitting on the desk in your exam room. The sadness in this story is that the computer and the Internet are (or at least could be) good for some things, including the statewide prescription drug monitoring program that Dr. Konopka can’t participate in. Immunization data banks, prescribing programs that minimize physician error, and systems for storing and plotting your patient’s lab work and metrics are just a few of the things that a good computer system is good for. And, of course, there is the real-time access to the vast store of medical and research knowledge that has made textbooks obsolete.
I’m not sure where we can go from here without throwing out the baby with the bathwater and starting from scratch. We have computer scientists and physicians who I am sure could create a patient- and physician-friendly system that could cover the whole country. The trick will be keeping the politicians out of the room.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
The headline in the Oct. 13, 2017, Portland (Maine) Press Herald hinted that I was about to read a sad story: “New Hampshire doctor, 85, may lose practice because she doesn’t use computer.” Anna Konopka, MD, who has a 300-patient practice in New London, doesn’t use a computer in her office, and as a consequence can’t participate in her state’s mandated prescription drug monitoring program. She has appealed to the governor, but if her appeal is denied she will be forced to close her office.
The closure will present a hardship for the residents of this small New Hampshire town, who will have to replace their obviously committed physician who has served them for more than 30 years. And I am sure that Dr. Konopka would have preferred to end her professional career on her own terms. It isn’t going to be easy to give up that positive feedback from her patients that every primary care physician enjoys even on her worst day.
I wouldn’t be surprised to learn that Dr. Konopka has listened to other physicians in her community complain about the cost and time-gobbling inefficiencies of their EHRs. She may have been put off by her own experiences as a patient whose physician spends too much time looking at his computer screen and fails to engage with her. Or she may have simply done the math and come up with the obvious answer that a computer system would be a bad investment for her small practice.
I suspect that there are days that you wish you had followed this wise older physician’s lead and never plugged into that “good-for-nothing piece of junk” sitting on the desk in your exam room. The sadness in this story is that the computer and the Internet are (or at least could be) good for some things, including the statewide prescription drug monitoring program that Dr. Konopka can’t participate in. Immunization data banks, prescribing programs that minimize physician error, and systems for storing and plotting your patient’s lab work and metrics are just a few of the things that a good computer system is good for. And, of course, there is the real-time access to the vast store of medical and research knowledge that has made textbooks obsolete.
I’m not sure where we can go from here without throwing out the baby with the bathwater and starting from scratch. We have computer scientists and physicians who I am sure could create a patient- and physician-friendly system that could cover the whole country. The trick will be keeping the politicians out of the room.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Restoring Function in Veterans With Complex Chronic Pain
According to the International Association for the Study of Pain (IASP), pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”1 Chronic pain (pain lasting more than 3 months) has a high prevalence in the U.S. veteran population. In a recently published article by Richard Nahin, PhD, of the National Institutes of Health, 65.5% of U.S. veterans reported pain in the previous 3 months with 9.1% classified as having severe pain (defined as “which occurs most days or every day and bothers the individual a lot”) compared with 6.4% among nonveterans.2 In addition, male veterans were more likely to report severe pain, 9%, compared with male nonveterans, 4.7%.2 Veterans make up about 6.2% of the U.S. population; therefore, the number of veterans negatively impacted by pain is substantial.3,4 Compared with individuals with other chronic diseases, such as heart disease, chronic obstructive pulmonary disease, or diabetes mellitus, a recent population-based, matched cohort study reported that only patients with Alzheimer disease have a poorer quality of life (QOL) than do those with chronic pain.5
Background
When comparing veterans to nonveterans, Nahin also reported that younger veterans aged 18 to 39 years had significantly higher rates for severe pain, compared with similarly aged nonveterans, 7.8% vs 3.2%, respectively. The prevalence of severe pain was significantly higher among veterans than it was for nonveterans experiencing the following: back pain, 21.6% vs 16.7% among nonveterans; jaw pain, 37.5% vs 22.9%, respectively; severe migraine and headaches, 26.4% vs 15.9%, respectively; and neck pain, 27.7% vs 21.9%, respectively. The veterans also were more likely than were nonveterans to have joint pain, 43.6% vs 31.5% , respectively.2
A study by Kerns and colleagues noted that almost 50% of older veterans (mean age 65.6 years) experience chronic pain regularly.6 Based on responses of 685 veterans to the Health-Risk Behavior Screening Questionnaire (HRBSQ), this study also found that the presence of pain was strongly associated with patient reports of worsening health and emotional distress. Rollin Gallagher, MD, of the Philadelphia VAMC, reported that veterans who experienced pain tended to have more personal problems due to higher rates of psychiatric and social comorbidities, such as substance abuse, depression, posttraumatic stress syndrome, and early work disabilities.7 Gallagher also has noted that the number of veterans seeking pain treatment has grown steadily over the past 2 decades due to the aging veteran population retiring and seeking VA care for chronic illness management.
In January 2017, the VA released an analysis of health care use among recent Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF), and Operation New Dawn (OND) veterans from October 2001 through June 2015.8 The VA noted that 1,965,534 veterans have become eligible for VA health care since fiscal year 2002. Of the 1,218,857 OIF/OEF/OND veterans treated during this period, 62.3% (759,850) were treated for diseases of the musculoskeletal system and connective tissue, 58.1% (708,062) were treated for mental disorders, and 58.7% (715,263) were treated for “symptoms, signs and ill-defined conditions.”
According to the VA, “the ICD-9-CM diagnostic category ‘Symptoms, Signs and Ill-Defined Conditions’ is a diverse, catch-all category that consists of 160 sub-categories and includes primarily symptoms that do not yet have an identified cause and clinical findings that are not coded elsewhere.” The most frequently reported codes in this category, in order of magnitude are General Symptoms (ICD-9-CM 780), Symptoms Involving Respiratory System and Other Chest Symptoms (ICD-9-CM 786), and Symptoms Involving Head and Neck (ICD-9-CM 784).
Musculoskeletal ailments (ie, joint and back disorders), mental health disorders and symptoms, signs, and ill-defined conditions are the 3 most frequently coded diagnoses related to medical treatment in OEF/OIF/OND veterans. This demonstrates the high rate of pain-related conditions with comorbid mental health diagnoses.
Public Health Challenge
Recognizing that pain is a public health challenge, the National Academy of Sciences published the landmark study Relieving Pain in America.9 The study reported that pain affects at least 100 million Americans, greatly reducing quality of life. In addition, annual financial costs to society are estimated at $560 to $635 billion, with federal and state costs almost $100 billion annually. Given the challenges of addressing chronic pain, especially in the U.S. veteran population, the VHA has likewise outlined 6 recommendations for transforming VA pain care:
- Educate veterans/families to promote self-efficacy and shared decision making, provide access to all relevant sources;
- Educate/train all team members to their discipline-specific competencies, including team-based care;
- Develop and integrate nonpharmacologic modalities into care plans;
- Institute evidence-based medication prescribing, use of pain procedures, and safe opioid use (universal precautions);
- Implement approaches for bringing the veteran’s whole team together, such as virtual pain consulting (SCAN-ECHO, e-consults, telehealth, clinical video teleconsultation and education) and for maintaining ongoing communication between team members; and
- Establish metrics to monitor pain care and outcomes at both the individual level and population level.10
The American Pain Society (APS) differentiates multidisciplinary care vs interdisciplinary pain care.11 Multidisciplinary pain care is provided by several disciplines that may not be coordinated. Treatment may occur with different goals and in parallel rather than with an integrated approach. The APS suggests that professional identities are clearly defined, team membership is a secondary consideration in multidisciplinary care, and the leadership is typically hierarchical with a physician in charge. In this model of care, each team member has a “clearly defined place in the overall care of the patient, contributing their expertise in relative isolation from one another.”11
In contrast, according to APS, interdisciplinary teams have complementary roles that enhance patient care. Each discipline has valuable knowledge and a set of skills that complement other team members who are collaborative partners. The interdisciplinary approach encourages complementary roles and responsibilities, conjoint problem solving, and shared accountability. Treatment decisions are consensus based.
Pain Programs
In a review of 4 interdisciplinary pain programs (Mayo Clinic Pain Rehabilitation Center, the Brooks Rehabilitation Pain Rehabilitation Program, the Rehabilitation Institute of Chicago Center for Pain Management, and the Cleveland Clinic Foundation Chronic Pain Rehabilitation Program), Stanos found that the compositions of the staff were similar.12 In general, staff consisted of pain management physicians, pain psychologists, physical and occupational therapists, and nurse coordinators. The Mayo Clinic had more personnel, including a clinical pharmacist, the Brooks program had an additional biofeedback specialist, and the Cleveland Clinic had a tai chi instructor. The programs ranged from 3 to 5 weeks of daily programming. The duration of services provided were dependent on the payers. Stanos concluded that functional status, as measured by the Pain Disability Index, improved on discharge, 6 months, and 1 year after treatment at the Cleveland Clinic.
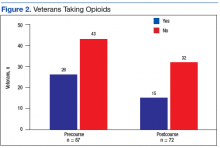
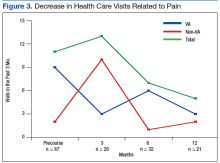
Cosio and Lin described their experience in a multidisciplinary outpatient pain clinic at Jesse Brown VAMC in Chicago.13 Their study noted that the number of veterans in their multidisciplinary pain clinic on chronic opioids significantly decreased, the degree of pain relief increased, and veterans reported improvements in mobility and ability to complete activities of daily living (ADLs). Overall veteran satisfaction with this pain program was reportedly high.
Cosio and Lin also published a study of the effect of complementary alternative medicine (CAM) utilization at a VAMC, which included a 12-week pain education school that was offered to all veterans and families.14 They noted that veterans began using at least 1 more CAM modality before the completion of the pain education program. However, it is unclear from the 2 studies whether the pain education program was incorporated into their multidisciplinary pain clinic.
Outpatient Functional Restoration Program
Given the challenges of addressing chronic pain and at the same time fostering an interdisciplinary approach to management, the VA Puget Sound Health Care System (VAPSHCS) team initiated a program development and quality improvement process for addressing pain and restoring function for veteran patients.
The VA Northwest Health Network (VISN 20) offers health care services for veterans located in the states of Alaska, Idaho, Oregon, Washington, and parts of California and Montana. VISN 20 has 8 parent facilities, which include the Seattle and American Lake divisions of the VAPSHCS. The VAPSHCS has established a comprehensive, interdisciplinary functional restoration pain program that integrates medical, psychosocial, and complementary alternative medicine.
The Outpatient Functional Restoration Program (OFRPP) pain team consists of a chief who is board certified in pain medicine and addiction medicine; a board-certified pain medicine physician; 2 physician assistants, one of whom has formal training in acupuncture and another who is trained in tai chi, qigong, hypnosis, and mindfulness; nurse care coordinators; a pain psychologist with training in acceptance and commitment therapy, cognitive behavioral therapy, yoga nidra, and hypnosis; a second pain psychologist who has a background in rehabilitation psychology; a physical therapist; and a pain clinical pharmacy specialist.
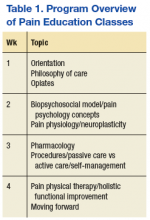
Prior to participation in OFRPP, veterans were required to attend 4 weekly pain education classes for 4 consecutive weeks. The classes educate veterans and their families on the complexity of managing chronic pain. Topics cover medical, pharmacologic and nonpharmacologic approaches to pain, including CAM and psychological modalities (Table 1). The pain orientation classes introduce veterans to available treatment options, and in some cases, veterans decide committing to a more intensive pain rehabilitation program is a good fit.
The program is based on the biopsychosocial model of pain care and Commission on Accreditation for Rehabilitation Facilities (CARF) interdisciplinary pain rehabilitation program standards. The length of the program was determined after reviewing data from existing VA outpatient pain rehabilitation programs; Pain Clinic staff availability, training and experience; and survey responses from veterans completing the 4-week education. This survey asked veterans whether they would be interested in an outpatient pain rehabilitation program and their preference for length of the program and treatment modalities.
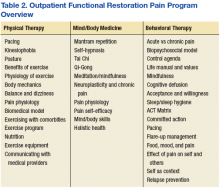
Since its inception, OFRPP has earned a 3-year CARF accreditation. Veterans participate in VAPSHCS American Lake division OFRPP education twice weekly for 4 hours for a total of 8 weeks (Table 2). Each week of programming includes 2 hours of physical therapy didactics, 2 hours of physical therapy (eg, paced cardio exercise, stretching, and core strength and conditioning), 2 hours of mind-body medicine (eg, mantram repetition and neuroplasticity education), and 2 hours of psychology education (behavioral interventions and psychological strategies for pain self-management of pain).
There is also 1 hour of pharmacotherapy education regarding commonly prescribed pain medications and how to take medications safely to avoid common adverse events. The nurse is responsible for care coordination and analysis of outcome measures, data collection, and quality improvement.
Program Effectiveness
Program effectiveness is measured using the POQ-VA (Pain Outcomes Questionnaire-VA). The POQ results and participant feedback are used to ensure ongoing program evaluation and improvement. This outcome measure was selected as the POQ-VA evaluates intervention effectiveness of all the major pain outcomes domains. This questionnaire was developed and validated by the VA.
The sample size was 957 veterans.15 The POQ-VA is reverse scored, meaning lower scores indicate improvement. Eighty-seven veterans have completed the program with 20 participants completing the 3-month outcome measures, 31 participants completing 6-month outcome measures, and 17 participants completing 12-month outcome measures.
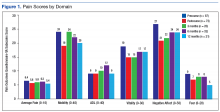
The pain score decreased close to 1 point at 12 months. The mobility gains were maintained at 12 months. The ADL did not improve much after 1 year (Figure 1).
In the other POQ-VA subscales, vitality improved somewhat.
Limitations
Only a small sample size of veterans with chronic pain participated in the functional restoration pain program. Long-term follow-up of participants who successfully completed the program also is desired.
Conclusion
Veterans experiencing complex chronic noncancer pain present a challenge for the VA health care system. Successful management of this requires cooperation among different disciplines and fostering a multimodal and interdisciplinary approach. Functional restoration pain programs have existed for a while and have shown clear evidence of their superiority over monotherapies for patients with chronic noncancer pain.
This functional restoration pain program incorporated various evidence-based medical, rehabilitative, psychological interventions with mind body medicine, mindfulness and integrative pain modalities. The authors continually meet and assess the success of the program. Although the initial outcome measures are encouraging, increased veteran participation in answering their post program completion surveys is desired. The goal is to improve veterans’ self-management of their chronic pain, leading to reductions in pain symptoms, medication, and health care provider use, as well as improve veterans’ function and overall QOL.
1. International Association for the Study of Pain. IASP taxonomy. https://www.iasp-pain.org/Taxonomy#Pain. Updated May 22, 2012. Accessed August 31, 2017.
2. Nahin RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254.
3. U.S. Census Bureau. 2011-2015 American community services 5-year estimates. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_5YRB21002&prodType=table. Accessed August 31, 2017.
4. U.S. Census Bureau, population division. Annual estimates of the resident population: April 1, 2010 to July 1, 2016. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview .xhtml?pid=PEP_2016_PEPANNRES&SPC=pt. Accessed August 31, 2017.
5. Hogan ME, Taddio A, Katz J, Shah V, Krahn M. Health utilities in people with chronic pain using a population level survey and linked health care administrative data. Pain. 2017;158(3):408-416.
6. Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans reports of pain and associations with ratings of health, health risk-behaviors, affective distress and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371-379.
7. Gallagher RM. Advancing the pain agenda in the veteran population. Anesthesiol Clin. 2016;34(2):357-378.
8. U.S. Department of Veterans Affairs. Analysis of VA health care utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans. https://www.publichealth.va.gov/docs/epidemiol ogy/healthcare-utilization-report-fy2015-qtr3.pdf. Published January 2017. Accessed August 31, 2017.
9. National Academies of Science. Institute of Medicine: Relieving pain in America: a blueprint for transforming prevention care, education, and research. https://iprcc.nih.gov/docs/032712_mtg _presentations/iom_pain_report_508comp.pdf. Published June 29, 2011. Accessed August 31, 2017.
10. U.S. Department of Veterans Affairs. Transforming VA pain care. https://www.va.gov/painmanagement/Updated August 17, 2017. Accessed August 31, 2017.
11. American Pain Society. Interdisciplinary pain management. http://americanpainsociety.org/uploads/about/position-statements/interdisciplinary-white -paper.pdf. Accessed August 31, 2017.
12. Stanos S. Focused review of interdisciplinary pain rehabilitation programs for chronic pain management. Curr Pain Headache Rep. 2012;16(2):147-152.
13. Cosio D, Lin EH. (538) Efficacy of an outpatient, multidisciplinary VA pain management clinic: findings from a one-year outcome study. Pain. 2014;15(4):S110.
14. Cosio D, Lin EH. Effects of a pain education program in complementary and alternative medicine treatment utilization at a VA medical center. Complement Ther Med. 2015;23(3):413-422.
15. Clark ME, Gironda RJ, Young RW. Development and validation of the pain outcomes questionnaire-VA. J Rehabil Res Dev. 2003;40(5)-381-395.
According to the International Association for the Study of Pain (IASP), pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”1 Chronic pain (pain lasting more than 3 months) has a high prevalence in the U.S. veteran population. In a recently published article by Richard Nahin, PhD, of the National Institutes of Health, 65.5% of U.S. veterans reported pain in the previous 3 months with 9.1% classified as having severe pain (defined as “which occurs most days or every day and bothers the individual a lot”) compared with 6.4% among nonveterans.2 In addition, male veterans were more likely to report severe pain, 9%, compared with male nonveterans, 4.7%.2 Veterans make up about 6.2% of the U.S. population; therefore, the number of veterans negatively impacted by pain is substantial.3,4 Compared with individuals with other chronic diseases, such as heart disease, chronic obstructive pulmonary disease, or diabetes mellitus, a recent population-based, matched cohort study reported that only patients with Alzheimer disease have a poorer quality of life (QOL) than do those with chronic pain.5
Background
When comparing veterans to nonveterans, Nahin also reported that younger veterans aged 18 to 39 years had significantly higher rates for severe pain, compared with similarly aged nonveterans, 7.8% vs 3.2%, respectively. The prevalence of severe pain was significantly higher among veterans than it was for nonveterans experiencing the following: back pain, 21.6% vs 16.7% among nonveterans; jaw pain, 37.5% vs 22.9%, respectively; severe migraine and headaches, 26.4% vs 15.9%, respectively; and neck pain, 27.7% vs 21.9%, respectively. The veterans also were more likely than were nonveterans to have joint pain, 43.6% vs 31.5% , respectively.2
A study by Kerns and colleagues noted that almost 50% of older veterans (mean age 65.6 years) experience chronic pain regularly.6 Based on responses of 685 veterans to the Health-Risk Behavior Screening Questionnaire (HRBSQ), this study also found that the presence of pain was strongly associated with patient reports of worsening health and emotional distress. Rollin Gallagher, MD, of the Philadelphia VAMC, reported that veterans who experienced pain tended to have more personal problems due to higher rates of psychiatric and social comorbidities, such as substance abuse, depression, posttraumatic stress syndrome, and early work disabilities.7 Gallagher also has noted that the number of veterans seeking pain treatment has grown steadily over the past 2 decades due to the aging veteran population retiring and seeking VA care for chronic illness management.
In January 2017, the VA released an analysis of health care use among recent Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF), and Operation New Dawn (OND) veterans from October 2001 through June 2015.8 The VA noted that 1,965,534 veterans have become eligible for VA health care since fiscal year 2002. Of the 1,218,857 OIF/OEF/OND veterans treated during this period, 62.3% (759,850) were treated for diseases of the musculoskeletal system and connective tissue, 58.1% (708,062) were treated for mental disorders, and 58.7% (715,263) were treated for “symptoms, signs and ill-defined conditions.”
According to the VA, “the ICD-9-CM diagnostic category ‘Symptoms, Signs and Ill-Defined Conditions’ is a diverse, catch-all category that consists of 160 sub-categories and includes primarily symptoms that do not yet have an identified cause and clinical findings that are not coded elsewhere.” The most frequently reported codes in this category, in order of magnitude are General Symptoms (ICD-9-CM 780), Symptoms Involving Respiratory System and Other Chest Symptoms (ICD-9-CM 786), and Symptoms Involving Head and Neck (ICD-9-CM 784).
Musculoskeletal ailments (ie, joint and back disorders), mental health disorders and symptoms, signs, and ill-defined conditions are the 3 most frequently coded diagnoses related to medical treatment in OEF/OIF/OND veterans. This demonstrates the high rate of pain-related conditions with comorbid mental health diagnoses.
Public Health Challenge
Recognizing that pain is a public health challenge, the National Academy of Sciences published the landmark study Relieving Pain in America.9 The study reported that pain affects at least 100 million Americans, greatly reducing quality of life. In addition, annual financial costs to society are estimated at $560 to $635 billion, with federal and state costs almost $100 billion annually. Given the challenges of addressing chronic pain, especially in the U.S. veteran population, the VHA has likewise outlined 6 recommendations for transforming VA pain care:
- Educate veterans/families to promote self-efficacy and shared decision making, provide access to all relevant sources;
- Educate/train all team members to their discipline-specific competencies, including team-based care;
- Develop and integrate nonpharmacologic modalities into care plans;
- Institute evidence-based medication prescribing, use of pain procedures, and safe opioid use (universal precautions);
- Implement approaches for bringing the veteran’s whole team together, such as virtual pain consulting (SCAN-ECHO, e-consults, telehealth, clinical video teleconsultation and education) and for maintaining ongoing communication between team members; and
- Establish metrics to monitor pain care and outcomes at both the individual level and population level.10
The American Pain Society (APS) differentiates multidisciplinary care vs interdisciplinary pain care.11 Multidisciplinary pain care is provided by several disciplines that may not be coordinated. Treatment may occur with different goals and in parallel rather than with an integrated approach. The APS suggests that professional identities are clearly defined, team membership is a secondary consideration in multidisciplinary care, and the leadership is typically hierarchical with a physician in charge. In this model of care, each team member has a “clearly defined place in the overall care of the patient, contributing their expertise in relative isolation from one another.”11
In contrast, according to APS, interdisciplinary teams have complementary roles that enhance patient care. Each discipline has valuable knowledge and a set of skills that complement other team members who are collaborative partners. The interdisciplinary approach encourages complementary roles and responsibilities, conjoint problem solving, and shared accountability. Treatment decisions are consensus based.
Pain Programs
In a review of 4 interdisciplinary pain programs (Mayo Clinic Pain Rehabilitation Center, the Brooks Rehabilitation Pain Rehabilitation Program, the Rehabilitation Institute of Chicago Center for Pain Management, and the Cleveland Clinic Foundation Chronic Pain Rehabilitation Program), Stanos found that the compositions of the staff were similar.12 In general, staff consisted of pain management physicians, pain psychologists, physical and occupational therapists, and nurse coordinators. The Mayo Clinic had more personnel, including a clinical pharmacist, the Brooks program had an additional biofeedback specialist, and the Cleveland Clinic had a tai chi instructor. The programs ranged from 3 to 5 weeks of daily programming. The duration of services provided were dependent on the payers. Stanos concluded that functional status, as measured by the Pain Disability Index, improved on discharge, 6 months, and 1 year after treatment at the Cleveland Clinic.
Cosio and Lin described their experience in a multidisciplinary outpatient pain clinic at Jesse Brown VAMC in Chicago.13 Their study noted that the number of veterans in their multidisciplinary pain clinic on chronic opioids significantly decreased, the degree of pain relief increased, and veterans reported improvements in mobility and ability to complete activities of daily living (ADLs). Overall veteran satisfaction with this pain program was reportedly high.
Cosio and Lin also published a study of the effect of complementary alternative medicine (CAM) utilization at a VAMC, which included a 12-week pain education school that was offered to all veterans and families.14 They noted that veterans began using at least 1 more CAM modality before the completion of the pain education program. However, it is unclear from the 2 studies whether the pain education program was incorporated into their multidisciplinary pain clinic.
Outpatient Functional Restoration Program
Given the challenges of addressing chronic pain and at the same time fostering an interdisciplinary approach to management, the VA Puget Sound Health Care System (VAPSHCS) team initiated a program development and quality improvement process for addressing pain and restoring function for veteran patients.
The VA Northwest Health Network (VISN 20) offers health care services for veterans located in the states of Alaska, Idaho, Oregon, Washington, and parts of California and Montana. VISN 20 has 8 parent facilities, which include the Seattle and American Lake divisions of the VAPSHCS. The VAPSHCS has established a comprehensive, interdisciplinary functional restoration pain program that integrates medical, psychosocial, and complementary alternative medicine.
The Outpatient Functional Restoration Program (OFRPP) pain team consists of a chief who is board certified in pain medicine and addiction medicine; a board-certified pain medicine physician; 2 physician assistants, one of whom has formal training in acupuncture and another who is trained in tai chi, qigong, hypnosis, and mindfulness; nurse care coordinators; a pain psychologist with training in acceptance and commitment therapy, cognitive behavioral therapy, yoga nidra, and hypnosis; a second pain psychologist who has a background in rehabilitation psychology; a physical therapist; and a pain clinical pharmacy specialist.
Prior to participation in OFRPP, veterans were required to attend 4 weekly pain education classes for 4 consecutive weeks. The classes educate veterans and their families on the complexity of managing chronic pain. Topics cover medical, pharmacologic and nonpharmacologic approaches to pain, including CAM and psychological modalities (Table 1). The pain orientation classes introduce veterans to available treatment options, and in some cases, veterans decide committing to a more intensive pain rehabilitation program is a good fit.
The program is based on the biopsychosocial model of pain care and Commission on Accreditation for Rehabilitation Facilities (CARF) interdisciplinary pain rehabilitation program standards. The length of the program was determined after reviewing data from existing VA outpatient pain rehabilitation programs; Pain Clinic staff availability, training and experience; and survey responses from veterans completing the 4-week education. This survey asked veterans whether they would be interested in an outpatient pain rehabilitation program and their preference for length of the program and treatment modalities.
Since its inception, OFRPP has earned a 3-year CARF accreditation. Veterans participate in VAPSHCS American Lake division OFRPP education twice weekly for 4 hours for a total of 8 weeks (Table 2). Each week of programming includes 2 hours of physical therapy didactics, 2 hours of physical therapy (eg, paced cardio exercise, stretching, and core strength and conditioning), 2 hours of mind-body medicine (eg, mantram repetition and neuroplasticity education), and 2 hours of psychology education (behavioral interventions and psychological strategies for pain self-management of pain).
There is also 1 hour of pharmacotherapy education regarding commonly prescribed pain medications and how to take medications safely to avoid common adverse events. The nurse is responsible for care coordination and analysis of outcome measures, data collection, and quality improvement.
Program Effectiveness
Program effectiveness is measured using the POQ-VA (Pain Outcomes Questionnaire-VA). The POQ results and participant feedback are used to ensure ongoing program evaluation and improvement. This outcome measure was selected as the POQ-VA evaluates intervention effectiveness of all the major pain outcomes domains. This questionnaire was developed and validated by the VA.
The sample size was 957 veterans.15 The POQ-VA is reverse scored, meaning lower scores indicate improvement. Eighty-seven veterans have completed the program with 20 participants completing the 3-month outcome measures, 31 participants completing 6-month outcome measures, and 17 participants completing 12-month outcome measures.
The pain score decreased close to 1 point at 12 months. The mobility gains were maintained at 12 months. The ADL did not improve much after 1 year (Figure 1).
In the other POQ-VA subscales, vitality improved somewhat.
Limitations
Only a small sample size of veterans with chronic pain participated in the functional restoration pain program. Long-term follow-up of participants who successfully completed the program also is desired.
Conclusion
Veterans experiencing complex chronic noncancer pain present a challenge for the VA health care system. Successful management of this requires cooperation among different disciplines and fostering a multimodal and interdisciplinary approach. Functional restoration pain programs have existed for a while and have shown clear evidence of their superiority over monotherapies for patients with chronic noncancer pain.
This functional restoration pain program incorporated various evidence-based medical, rehabilitative, psychological interventions with mind body medicine, mindfulness and integrative pain modalities. The authors continually meet and assess the success of the program. Although the initial outcome measures are encouraging, increased veteran participation in answering their post program completion surveys is desired. The goal is to improve veterans’ self-management of their chronic pain, leading to reductions in pain symptoms, medication, and health care provider use, as well as improve veterans’ function and overall QOL.
According to the International Association for the Study of Pain (IASP), pain is “an unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage.”1 Chronic pain (pain lasting more than 3 months) has a high prevalence in the U.S. veteran population. In a recently published article by Richard Nahin, PhD, of the National Institutes of Health, 65.5% of U.S. veterans reported pain in the previous 3 months with 9.1% classified as having severe pain (defined as “which occurs most days or every day and bothers the individual a lot”) compared with 6.4% among nonveterans.2 In addition, male veterans were more likely to report severe pain, 9%, compared with male nonveterans, 4.7%.2 Veterans make up about 6.2% of the U.S. population; therefore, the number of veterans negatively impacted by pain is substantial.3,4 Compared with individuals with other chronic diseases, such as heart disease, chronic obstructive pulmonary disease, or diabetes mellitus, a recent population-based, matched cohort study reported that only patients with Alzheimer disease have a poorer quality of life (QOL) than do those with chronic pain.5
Background
When comparing veterans to nonveterans, Nahin also reported that younger veterans aged 18 to 39 years had significantly higher rates for severe pain, compared with similarly aged nonveterans, 7.8% vs 3.2%, respectively. The prevalence of severe pain was significantly higher among veterans than it was for nonveterans experiencing the following: back pain, 21.6% vs 16.7% among nonveterans; jaw pain, 37.5% vs 22.9%, respectively; severe migraine and headaches, 26.4% vs 15.9%, respectively; and neck pain, 27.7% vs 21.9%, respectively. The veterans also were more likely than were nonveterans to have joint pain, 43.6% vs 31.5% , respectively.2
A study by Kerns and colleagues noted that almost 50% of older veterans (mean age 65.6 years) experience chronic pain regularly.6 Based on responses of 685 veterans to the Health-Risk Behavior Screening Questionnaire (HRBSQ), this study also found that the presence of pain was strongly associated with patient reports of worsening health and emotional distress. Rollin Gallagher, MD, of the Philadelphia VAMC, reported that veterans who experienced pain tended to have more personal problems due to higher rates of psychiatric and social comorbidities, such as substance abuse, depression, posttraumatic stress syndrome, and early work disabilities.7 Gallagher also has noted that the number of veterans seeking pain treatment has grown steadily over the past 2 decades due to the aging veteran population retiring and seeking VA care for chronic illness management.
In January 2017, the VA released an analysis of health care use among recent Operation Iraqi Freedom (OIF), Operation Enduring Freedom (OEF), and Operation New Dawn (OND) veterans from October 2001 through June 2015.8 The VA noted that 1,965,534 veterans have become eligible for VA health care since fiscal year 2002. Of the 1,218,857 OIF/OEF/OND veterans treated during this period, 62.3% (759,850) were treated for diseases of the musculoskeletal system and connective tissue, 58.1% (708,062) were treated for mental disorders, and 58.7% (715,263) were treated for “symptoms, signs and ill-defined conditions.”
According to the VA, “the ICD-9-CM diagnostic category ‘Symptoms, Signs and Ill-Defined Conditions’ is a diverse, catch-all category that consists of 160 sub-categories and includes primarily symptoms that do not yet have an identified cause and clinical findings that are not coded elsewhere.” The most frequently reported codes in this category, in order of magnitude are General Symptoms (ICD-9-CM 780), Symptoms Involving Respiratory System and Other Chest Symptoms (ICD-9-CM 786), and Symptoms Involving Head and Neck (ICD-9-CM 784).
Musculoskeletal ailments (ie, joint and back disorders), mental health disorders and symptoms, signs, and ill-defined conditions are the 3 most frequently coded diagnoses related to medical treatment in OEF/OIF/OND veterans. This demonstrates the high rate of pain-related conditions with comorbid mental health diagnoses.
Public Health Challenge
Recognizing that pain is a public health challenge, the National Academy of Sciences published the landmark study Relieving Pain in America.9 The study reported that pain affects at least 100 million Americans, greatly reducing quality of life. In addition, annual financial costs to society are estimated at $560 to $635 billion, with federal and state costs almost $100 billion annually. Given the challenges of addressing chronic pain, especially in the U.S. veteran population, the VHA has likewise outlined 6 recommendations for transforming VA pain care:
- Educate veterans/families to promote self-efficacy and shared decision making, provide access to all relevant sources;
- Educate/train all team members to their discipline-specific competencies, including team-based care;
- Develop and integrate nonpharmacologic modalities into care plans;
- Institute evidence-based medication prescribing, use of pain procedures, and safe opioid use (universal precautions);
- Implement approaches for bringing the veteran’s whole team together, such as virtual pain consulting (SCAN-ECHO, e-consults, telehealth, clinical video teleconsultation and education) and for maintaining ongoing communication between team members; and
- Establish metrics to monitor pain care and outcomes at both the individual level and population level.10
The American Pain Society (APS) differentiates multidisciplinary care vs interdisciplinary pain care.11 Multidisciplinary pain care is provided by several disciplines that may not be coordinated. Treatment may occur with different goals and in parallel rather than with an integrated approach. The APS suggests that professional identities are clearly defined, team membership is a secondary consideration in multidisciplinary care, and the leadership is typically hierarchical with a physician in charge. In this model of care, each team member has a “clearly defined place in the overall care of the patient, contributing their expertise in relative isolation from one another.”11
In contrast, according to APS, interdisciplinary teams have complementary roles that enhance patient care. Each discipline has valuable knowledge and a set of skills that complement other team members who are collaborative partners. The interdisciplinary approach encourages complementary roles and responsibilities, conjoint problem solving, and shared accountability. Treatment decisions are consensus based.
Pain Programs
In a review of 4 interdisciplinary pain programs (Mayo Clinic Pain Rehabilitation Center, the Brooks Rehabilitation Pain Rehabilitation Program, the Rehabilitation Institute of Chicago Center for Pain Management, and the Cleveland Clinic Foundation Chronic Pain Rehabilitation Program), Stanos found that the compositions of the staff were similar.12 In general, staff consisted of pain management physicians, pain psychologists, physical and occupational therapists, and nurse coordinators. The Mayo Clinic had more personnel, including a clinical pharmacist, the Brooks program had an additional biofeedback specialist, and the Cleveland Clinic had a tai chi instructor. The programs ranged from 3 to 5 weeks of daily programming. The duration of services provided were dependent on the payers. Stanos concluded that functional status, as measured by the Pain Disability Index, improved on discharge, 6 months, and 1 year after treatment at the Cleveland Clinic.
Cosio and Lin described their experience in a multidisciplinary outpatient pain clinic at Jesse Brown VAMC in Chicago.13 Their study noted that the number of veterans in their multidisciplinary pain clinic on chronic opioids significantly decreased, the degree of pain relief increased, and veterans reported improvements in mobility and ability to complete activities of daily living (ADLs). Overall veteran satisfaction with this pain program was reportedly high.
Cosio and Lin also published a study of the effect of complementary alternative medicine (CAM) utilization at a VAMC, which included a 12-week pain education school that was offered to all veterans and families.14 They noted that veterans began using at least 1 more CAM modality before the completion of the pain education program. However, it is unclear from the 2 studies whether the pain education program was incorporated into their multidisciplinary pain clinic.
Outpatient Functional Restoration Program
Given the challenges of addressing chronic pain and at the same time fostering an interdisciplinary approach to management, the VA Puget Sound Health Care System (VAPSHCS) team initiated a program development and quality improvement process for addressing pain and restoring function for veteran patients.
The VA Northwest Health Network (VISN 20) offers health care services for veterans located in the states of Alaska, Idaho, Oregon, Washington, and parts of California and Montana. VISN 20 has 8 parent facilities, which include the Seattle and American Lake divisions of the VAPSHCS. The VAPSHCS has established a comprehensive, interdisciplinary functional restoration pain program that integrates medical, psychosocial, and complementary alternative medicine.
The Outpatient Functional Restoration Program (OFRPP) pain team consists of a chief who is board certified in pain medicine and addiction medicine; a board-certified pain medicine physician; 2 physician assistants, one of whom has formal training in acupuncture and another who is trained in tai chi, qigong, hypnosis, and mindfulness; nurse care coordinators; a pain psychologist with training in acceptance and commitment therapy, cognitive behavioral therapy, yoga nidra, and hypnosis; a second pain psychologist who has a background in rehabilitation psychology; a physical therapist; and a pain clinical pharmacy specialist.
Prior to participation in OFRPP, veterans were required to attend 4 weekly pain education classes for 4 consecutive weeks. The classes educate veterans and their families on the complexity of managing chronic pain. Topics cover medical, pharmacologic and nonpharmacologic approaches to pain, including CAM and psychological modalities (Table 1). The pain orientation classes introduce veterans to available treatment options, and in some cases, veterans decide committing to a more intensive pain rehabilitation program is a good fit.
The program is based on the biopsychosocial model of pain care and Commission on Accreditation for Rehabilitation Facilities (CARF) interdisciplinary pain rehabilitation program standards. The length of the program was determined after reviewing data from existing VA outpatient pain rehabilitation programs; Pain Clinic staff availability, training and experience; and survey responses from veterans completing the 4-week education. This survey asked veterans whether they would be interested in an outpatient pain rehabilitation program and their preference for length of the program and treatment modalities.
Since its inception, OFRPP has earned a 3-year CARF accreditation. Veterans participate in VAPSHCS American Lake division OFRPP education twice weekly for 4 hours for a total of 8 weeks (Table 2). Each week of programming includes 2 hours of physical therapy didactics, 2 hours of physical therapy (eg, paced cardio exercise, stretching, and core strength and conditioning), 2 hours of mind-body medicine (eg, mantram repetition and neuroplasticity education), and 2 hours of psychology education (behavioral interventions and psychological strategies for pain self-management of pain).
There is also 1 hour of pharmacotherapy education regarding commonly prescribed pain medications and how to take medications safely to avoid common adverse events. The nurse is responsible for care coordination and analysis of outcome measures, data collection, and quality improvement.
Program Effectiveness
Program effectiveness is measured using the POQ-VA (Pain Outcomes Questionnaire-VA). The POQ results and participant feedback are used to ensure ongoing program evaluation and improvement. This outcome measure was selected as the POQ-VA evaluates intervention effectiveness of all the major pain outcomes domains. This questionnaire was developed and validated by the VA.
The sample size was 957 veterans.15 The POQ-VA is reverse scored, meaning lower scores indicate improvement. Eighty-seven veterans have completed the program with 20 participants completing the 3-month outcome measures, 31 participants completing 6-month outcome measures, and 17 participants completing 12-month outcome measures.
The pain score decreased close to 1 point at 12 months. The mobility gains were maintained at 12 months. The ADL did not improve much after 1 year (Figure 1).
In the other POQ-VA subscales, vitality improved somewhat.
Limitations
Only a small sample size of veterans with chronic pain participated in the functional restoration pain program. Long-term follow-up of participants who successfully completed the program also is desired.
Conclusion
Veterans experiencing complex chronic noncancer pain present a challenge for the VA health care system. Successful management of this requires cooperation among different disciplines and fostering a multimodal and interdisciplinary approach. Functional restoration pain programs have existed for a while and have shown clear evidence of their superiority over monotherapies for patients with chronic noncancer pain.
This functional restoration pain program incorporated various evidence-based medical, rehabilitative, psychological interventions with mind body medicine, mindfulness and integrative pain modalities. The authors continually meet and assess the success of the program. Although the initial outcome measures are encouraging, increased veteran participation in answering their post program completion surveys is desired. The goal is to improve veterans’ self-management of their chronic pain, leading to reductions in pain symptoms, medication, and health care provider use, as well as improve veterans’ function and overall QOL.
1. International Association for the Study of Pain. IASP taxonomy. https://www.iasp-pain.org/Taxonomy#Pain. Updated May 22, 2012. Accessed August 31, 2017.
2. Nahin RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254.
3. U.S. Census Bureau. 2011-2015 American community services 5-year estimates. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_5YRB21002&prodType=table. Accessed August 31, 2017.
4. U.S. Census Bureau, population division. Annual estimates of the resident population: April 1, 2010 to July 1, 2016. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview .xhtml?pid=PEP_2016_PEPANNRES&SPC=pt. Accessed August 31, 2017.
5. Hogan ME, Taddio A, Katz J, Shah V, Krahn M. Health utilities in people with chronic pain using a population level survey and linked health care administrative data. Pain. 2017;158(3):408-416.
6. Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans reports of pain and associations with ratings of health, health risk-behaviors, affective distress and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371-379.
7. Gallagher RM. Advancing the pain agenda in the veteran population. Anesthesiol Clin. 2016;34(2):357-378.
8. U.S. Department of Veterans Affairs. Analysis of VA health care utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans. https://www.publichealth.va.gov/docs/epidemiol ogy/healthcare-utilization-report-fy2015-qtr3.pdf. Published January 2017. Accessed August 31, 2017.
9. National Academies of Science. Institute of Medicine: Relieving pain in America: a blueprint for transforming prevention care, education, and research. https://iprcc.nih.gov/docs/032712_mtg _presentations/iom_pain_report_508comp.pdf. Published June 29, 2011. Accessed August 31, 2017.
10. U.S. Department of Veterans Affairs. Transforming VA pain care. https://www.va.gov/painmanagement/Updated August 17, 2017. Accessed August 31, 2017.
11. American Pain Society. Interdisciplinary pain management. http://americanpainsociety.org/uploads/about/position-statements/interdisciplinary-white -paper.pdf. Accessed August 31, 2017.
12. Stanos S. Focused review of interdisciplinary pain rehabilitation programs for chronic pain management. Curr Pain Headache Rep. 2012;16(2):147-152.
13. Cosio D, Lin EH. (538) Efficacy of an outpatient, multidisciplinary VA pain management clinic: findings from a one-year outcome study. Pain. 2014;15(4):S110.
14. Cosio D, Lin EH. Effects of a pain education program in complementary and alternative medicine treatment utilization at a VA medical center. Complement Ther Med. 2015;23(3):413-422.
15. Clark ME, Gironda RJ, Young RW. Development and validation of the pain outcomes questionnaire-VA. J Rehabil Res Dev. 2003;40(5)-381-395.
1. International Association for the Study of Pain. IASP taxonomy. https://www.iasp-pain.org/Taxonomy#Pain. Updated May 22, 2012. Accessed August 31, 2017.
2. Nahin RL. Severe pain in veterans: the effect of age and sex, and comparisons with the general population. J Pain. 2017;18(3):247-254.
3. U.S. Census Bureau. 2011-2015 American community services 5-year estimates. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_15_5YRB21002&prodType=table. Accessed August 31, 2017.
4. U.S. Census Bureau, population division. Annual estimates of the resident population: April 1, 2010 to July 1, 2016. https://factfinder.census.gov/faces/tableservices/jsf/pages/productview .xhtml?pid=PEP_2016_PEPANNRES&SPC=pt. Accessed August 31, 2017.
5. Hogan ME, Taddio A, Katz J, Shah V, Krahn M. Health utilities in people with chronic pain using a population level survey and linked health care administrative data. Pain. 2017;158(3):408-416.
6. Kerns RD, Otis J, Rosenberg R, Reid MC. Veterans reports of pain and associations with ratings of health, health risk-behaviors, affective distress and use of the healthcare system. J Rehabil Res Dev. 2003;40(5):371-379.
7. Gallagher RM. Advancing the pain agenda in the veteran population. Anesthesiol Clin. 2016;34(2):357-378.
8. U.S. Department of Veterans Affairs. Analysis of VA health care utilization among Operation Enduring Freedom (OEF), Operation Iraqi Freedom (OIF), and Operation New Dawn (OND) veterans. https://www.publichealth.va.gov/docs/epidemiol ogy/healthcare-utilization-report-fy2015-qtr3.pdf. Published January 2017. Accessed August 31, 2017.
9. National Academies of Science. Institute of Medicine: Relieving pain in America: a blueprint for transforming prevention care, education, and research. https://iprcc.nih.gov/docs/032712_mtg _presentations/iom_pain_report_508comp.pdf. Published June 29, 2011. Accessed August 31, 2017.
10. U.S. Department of Veterans Affairs. Transforming VA pain care. https://www.va.gov/painmanagement/Updated August 17, 2017. Accessed August 31, 2017.
11. American Pain Society. Interdisciplinary pain management. http://americanpainsociety.org/uploads/about/position-statements/interdisciplinary-white -paper.pdf. Accessed August 31, 2017.
12. Stanos S. Focused review of interdisciplinary pain rehabilitation programs for chronic pain management. Curr Pain Headache Rep. 2012;16(2):147-152.
13. Cosio D, Lin EH. (538) Efficacy of an outpatient, multidisciplinary VA pain management clinic: findings from a one-year outcome study. Pain. 2014;15(4):S110.
14. Cosio D, Lin EH. Effects of a pain education program in complementary and alternative medicine treatment utilization at a VA medical center. Complement Ther Med. 2015;23(3):413-422.
15. Clark ME, Gironda RJ, Young RW. Development and validation of the pain outcomes questionnaire-VA. J Rehabil Res Dev. 2003;40(5)-381-395.
Compound induces selective apoptosis in AML
Researchers say they have discovered a compound that can overcome resistance to apoptosis in acute myeloid leukemia (AML).
The compound, BTSA1, works by activating the BCL-2 family protein BAX.
BTSA1 prompted apoptosis in leukemia cells while sparing healthy cells. It also suppressed AML in mice without producing side effects.
Evripidis Gavathiotis, PhD, of Albert Einstein College of Medicine in Bronx, New York, and his colleagues described these results in Cancer Cell.
The team knew that apoptosis occurs when BAX is activated by pro-apoptotic proteins. However, cancer cells can avoid apoptosis by producing anti-apoptotic proteins that suppress BAX and the proteins that activate it.
“Our novel compound revives suppressed BAX molecules in cancer cells by binding with high affinity to BAX’s activation site,” Dr Gavathiotis said. “BAX can then swing into action, killing cancer cells while leaving healthy cells unscathed.”
Dr Gavathiotis was the lead author of a paper published in Nature in 2008 that first described the structure and shape of BAX’s activation site. He has since looked for small molecules that can activate BAX strongly enough to overcome cancer cells’ resistance to apoptosis.
His team initially screened more than 1 million compounds to reveal those with BAX-binding potential. The most promising 500 compounds were then evaluated in the lab.
“A compound dubbed BTSA1 (short for BAX Trigger Site Activator 1) proved to be the most potent BAX activator, causing rapid and extensive apoptosis when added to several different human AML cell lines,” said Denis Reyna, a doctoral student in Dr Gavathiotis’s lab.
The researchers also tested BTSA1 in blood samples from patients with high-risk AML. BTSA1 induced apoptosis in the patients’ AML cells but did not affect healthy hematopoietic stem cells.
Finally, the researchers generated mouse models of AML. BTSA1 was given to half the mice, while the other half served as controls.
On average, the BTSA1-treated mice survived significantly longer than the control mice—55 days and 40 days, respectively (P=0.0009). In fact, 43% of BTSA1-treated mice were still alive after 60 days and showing no signs of AML.
In addition, the mice treated with BTSA1 showed no evidence of toxicity.
“BTSA1 activates BAX and causes apoptosis in AML cells while sparing healthy cells and tissues, probably because the cancer cells are primed for apoptosis,” Dr Gavathiotis said.
He and his colleagues found that AML cells contained significantly higher BAX levels than normal blood cells from healthy subjects.
“With more BAX available in AML cells, even low BTSA1 doses will trigger enough BAX activation to cause apoptotic death, while sparing healthy cells that contain low levels of BAX or none at all,” Dr Gavathiotis said.
He and his team plan to determine if BTSA1 will elicit similar results in other cancer types. ![]()
Researchers say they have discovered a compound that can overcome resistance to apoptosis in acute myeloid leukemia (AML).
The compound, BTSA1, works by activating the BCL-2 family protein BAX.
BTSA1 prompted apoptosis in leukemia cells while sparing healthy cells. It also suppressed AML in mice without producing side effects.
Evripidis Gavathiotis, PhD, of Albert Einstein College of Medicine in Bronx, New York, and his colleagues described these results in Cancer Cell.
The team knew that apoptosis occurs when BAX is activated by pro-apoptotic proteins. However, cancer cells can avoid apoptosis by producing anti-apoptotic proteins that suppress BAX and the proteins that activate it.
“Our novel compound revives suppressed BAX molecules in cancer cells by binding with high affinity to BAX’s activation site,” Dr Gavathiotis said. “BAX can then swing into action, killing cancer cells while leaving healthy cells unscathed.”
Dr Gavathiotis was the lead author of a paper published in Nature in 2008 that first described the structure and shape of BAX’s activation site. He has since looked for small molecules that can activate BAX strongly enough to overcome cancer cells’ resistance to apoptosis.
His team initially screened more than 1 million compounds to reveal those with BAX-binding potential. The most promising 500 compounds were then evaluated in the lab.
“A compound dubbed BTSA1 (short for BAX Trigger Site Activator 1) proved to be the most potent BAX activator, causing rapid and extensive apoptosis when added to several different human AML cell lines,” said Denis Reyna, a doctoral student in Dr Gavathiotis’s lab.
The researchers also tested BTSA1 in blood samples from patients with high-risk AML. BTSA1 induced apoptosis in the patients’ AML cells but did not affect healthy hematopoietic stem cells.
Finally, the researchers generated mouse models of AML. BTSA1 was given to half the mice, while the other half served as controls.
On average, the BTSA1-treated mice survived significantly longer than the control mice—55 days and 40 days, respectively (P=0.0009). In fact, 43% of BTSA1-treated mice were still alive after 60 days and showing no signs of AML.
In addition, the mice treated with BTSA1 showed no evidence of toxicity.
“BTSA1 activates BAX and causes apoptosis in AML cells while sparing healthy cells and tissues, probably because the cancer cells are primed for apoptosis,” Dr Gavathiotis said.
He and his colleagues found that AML cells contained significantly higher BAX levels than normal blood cells from healthy subjects.
“With more BAX available in AML cells, even low BTSA1 doses will trigger enough BAX activation to cause apoptotic death, while sparing healthy cells that contain low levels of BAX or none at all,” Dr Gavathiotis said.
He and his team plan to determine if BTSA1 will elicit similar results in other cancer types. ![]()
Researchers say they have discovered a compound that can overcome resistance to apoptosis in acute myeloid leukemia (AML).
The compound, BTSA1, works by activating the BCL-2 family protein BAX.
BTSA1 prompted apoptosis in leukemia cells while sparing healthy cells. It also suppressed AML in mice without producing side effects.
Evripidis Gavathiotis, PhD, of Albert Einstein College of Medicine in Bronx, New York, and his colleagues described these results in Cancer Cell.
The team knew that apoptosis occurs when BAX is activated by pro-apoptotic proteins. However, cancer cells can avoid apoptosis by producing anti-apoptotic proteins that suppress BAX and the proteins that activate it.
“Our novel compound revives suppressed BAX molecules in cancer cells by binding with high affinity to BAX’s activation site,” Dr Gavathiotis said. “BAX can then swing into action, killing cancer cells while leaving healthy cells unscathed.”
Dr Gavathiotis was the lead author of a paper published in Nature in 2008 that first described the structure and shape of BAX’s activation site. He has since looked for small molecules that can activate BAX strongly enough to overcome cancer cells’ resistance to apoptosis.
His team initially screened more than 1 million compounds to reveal those with BAX-binding potential. The most promising 500 compounds were then evaluated in the lab.
“A compound dubbed BTSA1 (short for BAX Trigger Site Activator 1) proved to be the most potent BAX activator, causing rapid and extensive apoptosis when added to several different human AML cell lines,” said Denis Reyna, a doctoral student in Dr Gavathiotis’s lab.
The researchers also tested BTSA1 in blood samples from patients with high-risk AML. BTSA1 induced apoptosis in the patients’ AML cells but did not affect healthy hematopoietic stem cells.
Finally, the researchers generated mouse models of AML. BTSA1 was given to half the mice, while the other half served as controls.
On average, the BTSA1-treated mice survived significantly longer than the control mice—55 days and 40 days, respectively (P=0.0009). In fact, 43% of BTSA1-treated mice were still alive after 60 days and showing no signs of AML.
In addition, the mice treated with BTSA1 showed no evidence of toxicity.
“BTSA1 activates BAX and causes apoptosis in AML cells while sparing healthy cells and tissues, probably because the cancer cells are primed for apoptosis,” Dr Gavathiotis said.
He and his colleagues found that AML cells contained significantly higher BAX levels than normal blood cells from healthy subjects.
“With more BAX available in AML cells, even low BTSA1 doses will trigger enough BAX activation to cause apoptotic death, while sparing healthy cells that contain low levels of BAX or none at all,” Dr Gavathiotis said.
He and his team plan to determine if BTSA1 will elicit similar results in other cancer types. ![]()
Depression and Heart Failure? Put Down the SSRI
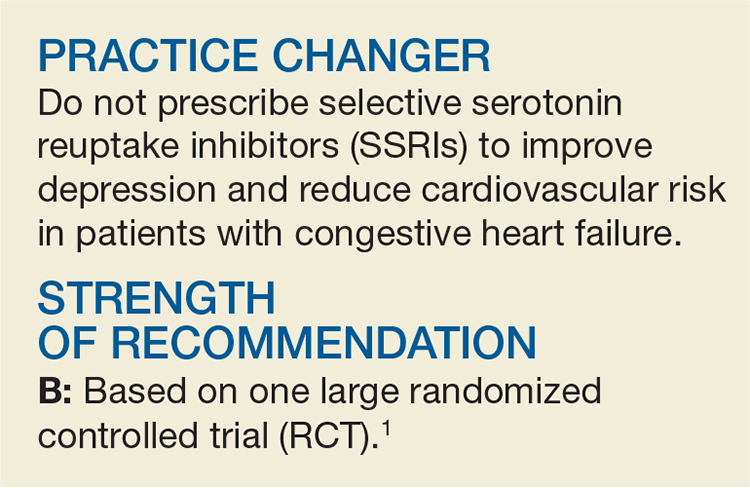
A 60-year-old man presents for a follow-up visit to talk about his congestive heart failure. He has New York Heart Association class 3 heart failure with a left ventricular ejection fraction of 30%. You notice that he is downcast, and based on his self-administered 9-item Patient Health Questionnaire (PHQ-9) score of 17, you determine that he is having a concomitant major depressive episode. Should you start him on an SSRI?
Depression is widely recognized as an independent risk factor for cardiovascular disease (CVD), as well as adverse outcomes in patients with known CVD.2-5 Previous studies have identified poor health behaviors as the primary underlying link between depression and CVD risk.2,6 Conversely, a recent systematic review found that positive constructs, mediated primarily through lifestyle behaviors, may have a protective effect on outcomes.7
Recently, researchers have focused on treating depression to simultaneously improve CVD outcomes. While some studies have shown SSRIs to be a safe and effective treatment for depression in patients with coronary disease, they have not demonstrated improvement in CVD outcomes.8,9 However, a post hoc analysis of the ENRICHD trial did suggest that SSRI treatment may improve mortality and morbidity post-MI.10
The prevalence of depression among patients with heart failure ranges from 10% to 40%, depending on disease severity.11 Depression is associated with lower quality of life (QoL), poorer treatment adherence, and higher rates of rehospitalization among patients with heart failure; it is an independent predictor of mortality in this patient population.1 Until recently, only one RCT (the SADHART-CHF study) looked at SSRI treatment in patients with heart failure and depression.12 In that 12-week trial, sertraline did not improve depression or CVD outcomes when compared with placebo—but the study period may have been too short to capture long-term outcomes.
STUDY SUMMARY
SADHART-CHF, but better
In the MOOD-HF study, investigators sought to determine whether SSRI treatment for depression in patients with heart failure could improve CVD outcomes over a longer study period (up to 24 mo).1 Specifically, this RCT assessed whether treatment with escitalopram could reduce morbidity and mortality risk in patients with comorbid chronic systolic heart failure and depression.
This double-blind, placebo-controlled trial was conducted at 16 tertiary medical centers in Germany between 2009 and 2014. Adult patients with New York Heart Association class 2 to 4 heart failure and left ventricular ejection fractions < 45% were screened for depression using the PHQ-9. Patients with PHQ-9 scores ≥ 12 underwent a structured psychiatric interview with a psychiatrist or psychosomatic specialist, and those diagnosed with major depression were invited to participate in the trial. Patients with recent SSRI use and/or psychotherapy were excluded.
Eligible participants were randomized to receive either escitalopram (10-20 mg/d) or placebo for up to 24 months, in addition to standard heart failure care. The starting dose of 5 mg was increased to 10 to 20 mg as tolerated until week 12 of the study; the dose at 12 weeks was considered the maintenance dose. Psychiatric and medical assessments were performed every six months during the study period. Depression severity was assessed using the 10-item Montgomery-Åsberg Depression Rating Scale (MADRS).
Outcomes. The study used a composite endpoint of all-cause death or hospitalization; the primary outcome was time to first event of this composite. Secondary outcomes included MADRS score at 12 weeks, anxiety as assessed by the Generalized Anxiety Disorder 7-item scale, and health-related QoL as assessed by the Kansas City Cardiomyopathy Questionnaire (KCCQ). The sample size was calculated to achieve 80% power for the primary outcome. Baseline characteristics between the intervention and placebo groups were balanced after randomization, and the modified intention-to-treat study population included participants who took at least one dose of the study medication.1
Results. Ultimately, 372 participants were included in the analysis (185 escitalopram, 187 placebo). A primary endpoint event occurred in 116 participants (63%) in the escitalopram group and in 119 participants (64%) in the placebo group (hazard ratio [HR], 0.99).1 No differences were found between treatment groups for the primary endpoints in either adjusted or unadjusted analyses.
The mean MADRS score changed from 20.2 at baseline to 11.2 at 12 weeks with escitalopram, and from 21.4 to 12.5 in the placebo group (between-group difference, –0.9).10 Overall, the two treatment groups had comparable daily medication doses and mean treatment duration (18 mo), and both groups demonstrated partial remission of depression symptoms, improved health status, and improved QoL over the study period.
Interestingly, the placebo group experienced significantly improved QoL at 12 months.1 There were no between-group differences in adverse events or safety measures.1 The trial was discontinued prematurely based on futility after a recommendation from the data and safety monitoring committee.
WHAT’S NEW
Longer study period/different SSRI
The MOOD-HF trial directly addresses the major criticism of the SADHART-CHF trial by conducting the study over a much longer duration (up to 24 mo vs 12 wk). Also, in contrast to SADHART-CHF, this trial studied escitalopram rather than sertraline, because some evidence indicates that escitalopram is superior at treating primary depression.13 Despite these differences, the results of MOOD-HF are consistent with the findings of SADHART-CHF: SSRI treatment for patients with heart failure and depression did not reduce the elevated morbidity and mortality risk seen with these comorbid conditions.
Also consistent with SADHART-CHF findings, participants in both groups in the MOOD-HF trial had partial remission of depressive symptoms over the study period, with no significant difference between those treated with escitalopram versus placebo. Given that this high-quality trial replicated the findings of SADHART-CHF with a longer treatment period and a potentially more effective SSRI, the results of MOOD-HF should put to rest the practice of initiating SSRI treatment in depressed patients with heart failure in an attempt to affect CVD outcomes.
CAVEATS
There are other SSRI fish in the sea
There are other SSRIs, besides escitalopram and sertraline, available for use. However, it is likely that this is a class effect.
Additionally, none of the patients in this trial had severe depression, as their PHQ-9 scores were all below 19. Therefore, it remains to be determined if treating severe depression has an impact on cardiovascular outcomes.
Lastly, and most importantly, this study only looked at initiating SSRIs for depression in the setting of heart failure. The trial did not include patients already taking SSRIs for pre-existing depression. Thus, the results do not imply evidence for discontinuing SSRIs in patients with heart failure.
Treating comorbid depression and CVD to mitigate the elevated risk for adverse clinical outcomes remains nuanced and elusive. The same can be said of non-CVD chronic conditions (eg, diabetes) based on recent systematic reviews.13 In sum, these studies suggest that a traditional screen-and-treat approach using SSRIs for depression treatment to affect chronic disease outcomes (that are likely lifestyle-related) may not be cost-effective or patient-centered.
A recent study showing that cognitive behavioral therapy did improve depression—but not heart failure—among patients with both conditions reaffirms that teasing out the impact of depression on lifestyle behaviors and chronic disease outcomes among multimorbid patients is more complex than previously thought.14 Nevertheless, this area of research should continue to be explored, given the worsened chronic disease outcomes in the presence of depression.
CHALLENGES TO IMPLEMENTATION
Changing the tide can be difficult
As with any behavior change, we expect that it will be a challenge to convince providers to stop initiating SSRI treatment to affect cardiovascular outcomes in patients with depression and heart failure—especially given the body of evidence denoting depression as a risk factor for increased morbidity and mortality in this population.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquires Network and The Journal of Family Practice (2017;66[9]:564-567).
1. Angermann CE, Gelbrich G, Störk S, et al; MOOD-HF Study Investigators and Committee Members. Effect of escitalopram on all-cause mortality and hospitalization in patients with heart failure and depression: the MOOD-HF randomized clinical trial. JAMA. 2016;315(24):2683-2693.
2. Sin NL, Kumar AD, Gehi AK, Whooley MA. Direction of association between depression and lifestyle behaviors in patients with coronary heart disease: the heart and soul study. Ann Behav Med. 2016;50(4):523-532.
3. Lett HS, Blumenthal JA, Babyak MA, et al. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66(3):305-315.
4. Whooley MA, Wong JM. Depression and cardiovascular disorders. Annu Rev Clin Psychol. 2013;9:327-354.
5. Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802-813.
6. Whooley MA, de Jonge P, Vittinghoff E, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300(20):2379-2388.
7. DuBois CM, Lopez OV, Beale EE, et al. Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: a systematic review. Int J Cardiol. 2015;195:265-280.
8. Glassman AH, O’Connor CM, Califf RM, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Investigators. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288(6):701-709.
9. Writing Committee for the ENRICHD Investigators. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA. 2003;289(23):3106-3116.
10. Taylor CB, Youngblood ME, Catellier D, et al, ENRICHD Investigators. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry. 2005;62(7):792-798.
11. Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48(8):1527-1537.
12. O’Connor CM, Jiang W, Kuchibhatla M, et al, SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol. 2010;56(9):692-699.
13. Health Quality Ontario. Screening and management of depression for adults with chronic diseases: an evidence-based analysis. Ont Health Technol Assess Ser. 2013;13(8):1-45.
14. Freedland KE, Carney RM, Rich MW, et al. Cognitive behavior therapy for depression and self-care in heart failure patients: a randomized clinical trial. JAMA Intern Med. 2015;175(11):1773-1782.
A 60-year-old man presents for a follow-up visit to talk about his congestive heart failure. He has New York Heart Association class 3 heart failure with a left ventricular ejection fraction of 30%. You notice that he is downcast, and based on his self-administered 9-item Patient Health Questionnaire (PHQ-9) score of 17, you determine that he is having a concomitant major depressive episode. Should you start him on an SSRI?
Depression is widely recognized as an independent risk factor for cardiovascular disease (CVD), as well as adverse outcomes in patients with known CVD.2-5 Previous studies have identified poor health behaviors as the primary underlying link between depression and CVD risk.2,6 Conversely, a recent systematic review found that positive constructs, mediated primarily through lifestyle behaviors, may have a protective effect on outcomes.7
Recently, researchers have focused on treating depression to simultaneously improve CVD outcomes. While some studies have shown SSRIs to be a safe and effective treatment for depression in patients with coronary disease, they have not demonstrated improvement in CVD outcomes.8,9 However, a post hoc analysis of the ENRICHD trial did suggest that SSRI treatment may improve mortality and morbidity post-MI.10
The prevalence of depression among patients with heart failure ranges from 10% to 40%, depending on disease severity.11 Depression is associated with lower quality of life (QoL), poorer treatment adherence, and higher rates of rehospitalization among patients with heart failure; it is an independent predictor of mortality in this patient population.1 Until recently, only one RCT (the SADHART-CHF study) looked at SSRI treatment in patients with heart failure and depression.12 In that 12-week trial, sertraline did not improve depression or CVD outcomes when compared with placebo—but the study period may have been too short to capture long-term outcomes.
STUDY SUMMARY
SADHART-CHF, but better
In the MOOD-HF study, investigators sought to determine whether SSRI treatment for depression in patients with heart failure could improve CVD outcomes over a longer study period (up to 24 mo).1 Specifically, this RCT assessed whether treatment with escitalopram could reduce morbidity and mortality risk in patients with comorbid chronic systolic heart failure and depression.
This double-blind, placebo-controlled trial was conducted at 16 tertiary medical centers in Germany between 2009 and 2014. Adult patients with New York Heart Association class 2 to 4 heart failure and left ventricular ejection fractions < 45% were screened for depression using the PHQ-9. Patients with PHQ-9 scores ≥ 12 underwent a structured psychiatric interview with a psychiatrist or psychosomatic specialist, and those diagnosed with major depression were invited to participate in the trial. Patients with recent SSRI use and/or psychotherapy were excluded.
Eligible participants were randomized to receive either escitalopram (10-20 mg/d) or placebo for up to 24 months, in addition to standard heart failure care. The starting dose of 5 mg was increased to 10 to 20 mg as tolerated until week 12 of the study; the dose at 12 weeks was considered the maintenance dose. Psychiatric and medical assessments were performed every six months during the study period. Depression severity was assessed using the 10-item Montgomery-Åsberg Depression Rating Scale (MADRS).
Outcomes. The study used a composite endpoint of all-cause death or hospitalization; the primary outcome was time to first event of this composite. Secondary outcomes included MADRS score at 12 weeks, anxiety as assessed by the Generalized Anxiety Disorder 7-item scale, and health-related QoL as assessed by the Kansas City Cardiomyopathy Questionnaire (KCCQ). The sample size was calculated to achieve 80% power for the primary outcome. Baseline characteristics between the intervention and placebo groups were balanced after randomization, and the modified intention-to-treat study population included participants who took at least one dose of the study medication.1
Results. Ultimately, 372 participants were included in the analysis (185 escitalopram, 187 placebo). A primary endpoint event occurred in 116 participants (63%) in the escitalopram group and in 119 participants (64%) in the placebo group (hazard ratio [HR], 0.99).1 No differences were found between treatment groups for the primary endpoints in either adjusted or unadjusted analyses.
The mean MADRS score changed from 20.2 at baseline to 11.2 at 12 weeks with escitalopram, and from 21.4 to 12.5 in the placebo group (between-group difference, –0.9).10 Overall, the two treatment groups had comparable daily medication doses and mean treatment duration (18 mo), and both groups demonstrated partial remission of depression symptoms, improved health status, and improved QoL over the study period.
Interestingly, the placebo group experienced significantly improved QoL at 12 months.1 There were no between-group differences in adverse events or safety measures.1 The trial was discontinued prematurely based on futility after a recommendation from the data and safety monitoring committee.
WHAT’S NEW
Longer study period/different SSRI
The MOOD-HF trial directly addresses the major criticism of the SADHART-CHF trial by conducting the study over a much longer duration (up to 24 mo vs 12 wk). Also, in contrast to SADHART-CHF, this trial studied escitalopram rather than sertraline, because some evidence indicates that escitalopram is superior at treating primary depression.13 Despite these differences, the results of MOOD-HF are consistent with the findings of SADHART-CHF: SSRI treatment for patients with heart failure and depression did not reduce the elevated morbidity and mortality risk seen with these comorbid conditions.
Also consistent with SADHART-CHF findings, participants in both groups in the MOOD-HF trial had partial remission of depressive symptoms over the study period, with no significant difference between those treated with escitalopram versus placebo. Given that this high-quality trial replicated the findings of SADHART-CHF with a longer treatment period and a potentially more effective SSRI, the results of MOOD-HF should put to rest the practice of initiating SSRI treatment in depressed patients with heart failure in an attempt to affect CVD outcomes.
CAVEATS
There are other SSRI fish in the sea
There are other SSRIs, besides escitalopram and sertraline, available for use. However, it is likely that this is a class effect.
Additionally, none of the patients in this trial had severe depression, as their PHQ-9 scores were all below 19. Therefore, it remains to be determined if treating severe depression has an impact on cardiovascular outcomes.
Lastly, and most importantly, this study only looked at initiating SSRIs for depression in the setting of heart failure. The trial did not include patients already taking SSRIs for pre-existing depression. Thus, the results do not imply evidence for discontinuing SSRIs in patients with heart failure.
Treating comorbid depression and CVD to mitigate the elevated risk for adverse clinical outcomes remains nuanced and elusive. The same can be said of non-CVD chronic conditions (eg, diabetes) based on recent systematic reviews.13 In sum, these studies suggest that a traditional screen-and-treat approach using SSRIs for depression treatment to affect chronic disease outcomes (that are likely lifestyle-related) may not be cost-effective or patient-centered.
A recent study showing that cognitive behavioral therapy did improve depression—but not heart failure—among patients with both conditions reaffirms that teasing out the impact of depression on lifestyle behaviors and chronic disease outcomes among multimorbid patients is more complex than previously thought.14 Nevertheless, this area of research should continue to be explored, given the worsened chronic disease outcomes in the presence of depression.
CHALLENGES TO IMPLEMENTATION
Changing the tide can be difficult
As with any behavior change, we expect that it will be a challenge to convince providers to stop initiating SSRI treatment to affect cardiovascular outcomes in patients with depression and heart failure—especially given the body of evidence denoting depression as a risk factor for increased morbidity and mortality in this population.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquires Network and The Journal of Family Practice (2017;66[9]:564-567).
A 60-year-old man presents for a follow-up visit to talk about his congestive heart failure. He has New York Heart Association class 3 heart failure with a left ventricular ejection fraction of 30%. You notice that he is downcast, and based on his self-administered 9-item Patient Health Questionnaire (PHQ-9) score of 17, you determine that he is having a concomitant major depressive episode. Should you start him on an SSRI?
Depression is widely recognized as an independent risk factor for cardiovascular disease (CVD), as well as adverse outcomes in patients with known CVD.2-5 Previous studies have identified poor health behaviors as the primary underlying link between depression and CVD risk.2,6 Conversely, a recent systematic review found that positive constructs, mediated primarily through lifestyle behaviors, may have a protective effect on outcomes.7
Recently, researchers have focused on treating depression to simultaneously improve CVD outcomes. While some studies have shown SSRIs to be a safe and effective treatment for depression in patients with coronary disease, they have not demonstrated improvement in CVD outcomes.8,9 However, a post hoc analysis of the ENRICHD trial did suggest that SSRI treatment may improve mortality and morbidity post-MI.10
The prevalence of depression among patients with heart failure ranges from 10% to 40%, depending on disease severity.11 Depression is associated with lower quality of life (QoL), poorer treatment adherence, and higher rates of rehospitalization among patients with heart failure; it is an independent predictor of mortality in this patient population.1 Until recently, only one RCT (the SADHART-CHF study) looked at SSRI treatment in patients with heart failure and depression.12 In that 12-week trial, sertraline did not improve depression or CVD outcomes when compared with placebo—but the study period may have been too short to capture long-term outcomes.
STUDY SUMMARY
SADHART-CHF, but better
In the MOOD-HF study, investigators sought to determine whether SSRI treatment for depression in patients with heart failure could improve CVD outcomes over a longer study period (up to 24 mo).1 Specifically, this RCT assessed whether treatment with escitalopram could reduce morbidity and mortality risk in patients with comorbid chronic systolic heart failure and depression.
This double-blind, placebo-controlled trial was conducted at 16 tertiary medical centers in Germany between 2009 and 2014. Adult patients with New York Heart Association class 2 to 4 heart failure and left ventricular ejection fractions < 45% were screened for depression using the PHQ-9. Patients with PHQ-9 scores ≥ 12 underwent a structured psychiatric interview with a psychiatrist or psychosomatic specialist, and those diagnosed with major depression were invited to participate in the trial. Patients with recent SSRI use and/or psychotherapy were excluded.
Eligible participants were randomized to receive either escitalopram (10-20 mg/d) or placebo for up to 24 months, in addition to standard heart failure care. The starting dose of 5 mg was increased to 10 to 20 mg as tolerated until week 12 of the study; the dose at 12 weeks was considered the maintenance dose. Psychiatric and medical assessments were performed every six months during the study period. Depression severity was assessed using the 10-item Montgomery-Åsberg Depression Rating Scale (MADRS).
Outcomes. The study used a composite endpoint of all-cause death or hospitalization; the primary outcome was time to first event of this composite. Secondary outcomes included MADRS score at 12 weeks, anxiety as assessed by the Generalized Anxiety Disorder 7-item scale, and health-related QoL as assessed by the Kansas City Cardiomyopathy Questionnaire (KCCQ). The sample size was calculated to achieve 80% power for the primary outcome. Baseline characteristics between the intervention and placebo groups were balanced after randomization, and the modified intention-to-treat study population included participants who took at least one dose of the study medication.1
Results. Ultimately, 372 participants were included in the analysis (185 escitalopram, 187 placebo). A primary endpoint event occurred in 116 participants (63%) in the escitalopram group and in 119 participants (64%) in the placebo group (hazard ratio [HR], 0.99).1 No differences were found between treatment groups for the primary endpoints in either adjusted or unadjusted analyses.
The mean MADRS score changed from 20.2 at baseline to 11.2 at 12 weeks with escitalopram, and from 21.4 to 12.5 in the placebo group (between-group difference, –0.9).10 Overall, the two treatment groups had comparable daily medication doses and mean treatment duration (18 mo), and both groups demonstrated partial remission of depression symptoms, improved health status, and improved QoL over the study period.
Interestingly, the placebo group experienced significantly improved QoL at 12 months.1 There were no between-group differences in adverse events or safety measures.1 The trial was discontinued prematurely based on futility after a recommendation from the data and safety monitoring committee.
WHAT’S NEW
Longer study period/different SSRI
The MOOD-HF trial directly addresses the major criticism of the SADHART-CHF trial by conducting the study over a much longer duration (up to 24 mo vs 12 wk). Also, in contrast to SADHART-CHF, this trial studied escitalopram rather than sertraline, because some evidence indicates that escitalopram is superior at treating primary depression.13 Despite these differences, the results of MOOD-HF are consistent with the findings of SADHART-CHF: SSRI treatment for patients with heart failure and depression did not reduce the elevated morbidity and mortality risk seen with these comorbid conditions.
Also consistent with SADHART-CHF findings, participants in both groups in the MOOD-HF trial had partial remission of depressive symptoms over the study period, with no significant difference between those treated with escitalopram versus placebo. Given that this high-quality trial replicated the findings of SADHART-CHF with a longer treatment period and a potentially more effective SSRI, the results of MOOD-HF should put to rest the practice of initiating SSRI treatment in depressed patients with heart failure in an attempt to affect CVD outcomes.
CAVEATS
There are other SSRI fish in the sea
There are other SSRIs, besides escitalopram and sertraline, available for use. However, it is likely that this is a class effect.
Additionally, none of the patients in this trial had severe depression, as their PHQ-9 scores were all below 19. Therefore, it remains to be determined if treating severe depression has an impact on cardiovascular outcomes.
Lastly, and most importantly, this study only looked at initiating SSRIs for depression in the setting of heart failure. The trial did not include patients already taking SSRIs for pre-existing depression. Thus, the results do not imply evidence for discontinuing SSRIs in patients with heart failure.
Treating comorbid depression and CVD to mitigate the elevated risk for adverse clinical outcomes remains nuanced and elusive. The same can be said of non-CVD chronic conditions (eg, diabetes) based on recent systematic reviews.13 In sum, these studies suggest that a traditional screen-and-treat approach using SSRIs for depression treatment to affect chronic disease outcomes (that are likely lifestyle-related) may not be cost-effective or patient-centered.
A recent study showing that cognitive behavioral therapy did improve depression—but not heart failure—among patients with both conditions reaffirms that teasing out the impact of depression on lifestyle behaviors and chronic disease outcomes among multimorbid patients is more complex than previously thought.14 Nevertheless, this area of research should continue to be explored, given the worsened chronic disease outcomes in the presence of depression.
CHALLENGES TO IMPLEMENTATION
Changing the tide can be difficult
As with any behavior change, we expect that it will be a challenge to convince providers to stop initiating SSRI treatment to affect cardiovascular outcomes in patients with depression and heart failure—especially given the body of evidence denoting depression as a risk factor for increased morbidity and mortality in this population.
ACKNOWLEDGEMENT
The PURLs Surveillance System was supported in part by Grant Number UL1RR024999 from the National Center For Research Resources, a Clinical Translational Science Award to the University of Chicago. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center For Research Resources or the National Institutes of Health.
Copyright © 2017. The Family Physicians Inquiries Network. All rights reserved.
Reprinted with permission from the Family Physicians Inquires Network and The Journal of Family Practice (2017;66[9]:564-567).
1. Angermann CE, Gelbrich G, Störk S, et al; MOOD-HF Study Investigators and Committee Members. Effect of escitalopram on all-cause mortality and hospitalization in patients with heart failure and depression: the MOOD-HF randomized clinical trial. JAMA. 2016;315(24):2683-2693.
2. Sin NL, Kumar AD, Gehi AK, Whooley MA. Direction of association between depression and lifestyle behaviors in patients with coronary heart disease: the heart and soul study. Ann Behav Med. 2016;50(4):523-532.
3. Lett HS, Blumenthal JA, Babyak MA, et al. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66(3):305-315.
4. Whooley MA, Wong JM. Depression and cardiovascular disorders. Annu Rev Clin Psychol. 2013;9:327-354.
5. Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802-813.
6. Whooley MA, de Jonge P, Vittinghoff E, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300(20):2379-2388.
7. DuBois CM, Lopez OV, Beale EE, et al. Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: a systematic review. Int J Cardiol. 2015;195:265-280.
8. Glassman AH, O’Connor CM, Califf RM, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Investigators. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288(6):701-709.
9. Writing Committee for the ENRICHD Investigators. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA. 2003;289(23):3106-3116.
10. Taylor CB, Youngblood ME, Catellier D, et al, ENRICHD Investigators. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry. 2005;62(7):792-798.
11. Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48(8):1527-1537.
12. O’Connor CM, Jiang W, Kuchibhatla M, et al, SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol. 2010;56(9):692-699.
13. Health Quality Ontario. Screening and management of depression for adults with chronic diseases: an evidence-based analysis. Ont Health Technol Assess Ser. 2013;13(8):1-45.
14. Freedland KE, Carney RM, Rich MW, et al. Cognitive behavior therapy for depression and self-care in heart failure patients: a randomized clinical trial. JAMA Intern Med. 2015;175(11):1773-1782.
1. Angermann CE, Gelbrich G, Störk S, et al; MOOD-HF Study Investigators and Committee Members. Effect of escitalopram on all-cause mortality and hospitalization in patients with heart failure and depression: the MOOD-HF randomized clinical trial. JAMA. 2016;315(24):2683-2693.
2. Sin NL, Kumar AD, Gehi AK, Whooley MA. Direction of association between depression and lifestyle behaviors in patients with coronary heart disease: the heart and soul study. Ann Behav Med. 2016;50(4):523-532.
3. Lett HS, Blumenthal JA, Babyak MA, et al. Depression as a risk factor for coronary artery disease: evidence, mechanisms, and treatment. Psychosom Med. 2004;66(3):305-315.
4. Whooley MA, Wong JM. Depression and cardiovascular disorders. Annu Rev Clin Psychol. 2013;9:327-354.
5. Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802-813.
6. Whooley MA, de Jonge P, Vittinghoff E, et al. Depressive symptoms, health behaviors, and risk of cardiovascular events in patients with coronary heart disease. JAMA. 2008;300(20):2379-2388.
7. DuBois CM, Lopez OV, Beale EE, et al. Relationships between positive psychological constructs and health outcomes in patients with cardiovascular disease: a systematic review. Int J Cardiol. 2015;195:265-280.
8. Glassman AH, O’Connor CM, Califf RM, et al; Sertraline Antidepressant Heart Attack Randomized Trial (SADHART) Investigators. Sertraline treatment of major depression in patients with acute MI or unstable angina. JAMA. 2002;288(6):701-709.
9. Writing Committee for the ENRICHD Investigators. Effects of treating depression and low perceived social support on clinical events after myocardial infarction: the Enhancing Recovery in Coronary Heart Disease Patients (ENRICHD) randomized trial. JAMA. 2003;289(23):3106-3116.
10. Taylor CB, Youngblood ME, Catellier D, et al, ENRICHD Investigators. Effects of antidepressant medication on morbidity and mortality in depressed patients after myocardial infarction. Arch Gen Psychiatry. 2005;62(7):792-798.
11. Rutledge T, Reis VA, Linke SE, et al. Depression in heart failure a meta-analytic review of prevalence, intervention effects, and associations with clinical outcomes. J Am Coll Cardiol. 2006;48(8):1527-1537.
12. O’Connor CM, Jiang W, Kuchibhatla M, et al, SADHART-CHF Investigators. Safety and efficacy of sertraline for depression in patients with heart failure: results of the SADHART-CHF (Sertraline Against Depression and Heart Disease in Chronic Heart Failure) trial. J Am Coll Cardiol. 2010;56(9):692-699.
13. Health Quality Ontario. Screening and management of depression for adults with chronic diseases: an evidence-based analysis. Ont Health Technol Assess Ser. 2013;13(8):1-45.
14. Freedland KE, Carney RM, Rich MW, et al. Cognitive behavior therapy for depression and self-care in heart failure patients: a randomized clinical trial. JAMA Intern Med. 2015;175(11):1773-1782.