User login
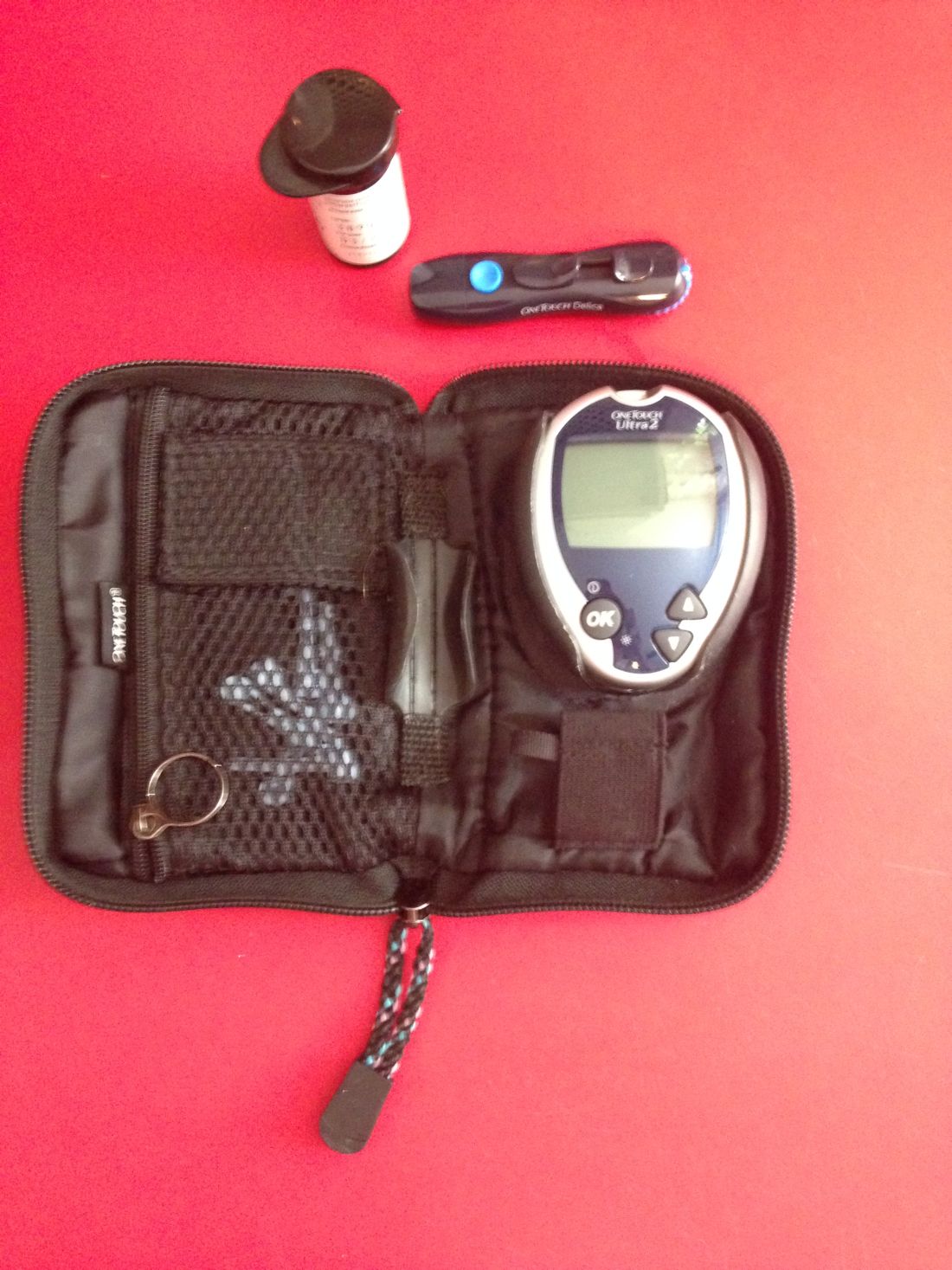
Routine blood glucose monitoring does not improve control or QOL
Self-monitoring of blood glucose in patients with non–insulin-treated type 2 diabetes mellitus (T2DM) does not appear to make any difference to blood glucose control or quality of life, a new study has found.
The researchers report the results of the Monitor Trial in which 418 patients with non–insulin-treated T2DM were randomized either to once-daily self-monitoring of blood glucose with automatic tailored messages, once-daily monitoring with no messages, and no monitoring. Their report appears in the June 10 online edition of JAMA Internal Medicine, timed to appear simultaneously with the data’s presentation at the annual meeting of the American Diabetes Association
2017.1233).
Researchers also saw no significant differences in rates of insulin initiation, the incidence of hypoglycemia, or health care utilization.
“This null result occurred despite training participants and primary care clinicians on the use and interpretation of the meter results,” wrote Laura A. Young, MD, of the University of North Carolina at Chapel Hill.
While the findings reflect data from earlier studies suggesting limited usefulness of self-monitoring of blood glucose in these patients, the authors commented that self-monitoring has persisted as a cornerstone of clinical management of non–insulin-treated T2DM.
“As the first large pragmatic U.S. trial of SMBG [self-monitoring of blood glucose], our findings provide evidence to guide patients and clinicians making important clinical decisions about routine blood glucose monitoring,” they wrote. “Based on these findings, patients and clinicians should engage in dialogue regarding SMBG with the current evidence suggesting that SMBG should not be routine for most patients with non– insulin-treated T2DM.”
The main difference seen between the three groups was in the Summary of Diabetes Self-Care Activities, which the authors said reflected the intervention itself.
Patients taking a GLP-1 agonist at baseline were significantly more likely to increase their dose of the drug if they were in one of the self-monitoring groups, compared with the no-monitoring group, but the authors noted that the numbers were small.
Researchers also saw that African Americans in the self-monitoring with messaging group had significantly lower health-related quality of life scores, compared with the no-monitoring group, although this difference was not seen with the self-monitoring without messaging.
The participants in the trial, which was conducted at 15 primary care practices in central North Carolina, were all older than 30 years and had HbA1c levels between 6.5% and 9.5% in the 6 months before screening.
Compliance rates were similar between the two self-monitoring groups and declined at a similar rate.
The authors cautioned that their study was not powered to examine the effectiveness of self-monitoring versus no monitoring in certain clinical situations, such as the initiation of a new medication or a change in medication dose.
“Proponents of routine SMBG have cited evidence that this testing approach is useful for patients with newly diagnosed diabetes or patients with poorer glycemic control,” they said.” Although disease duration, experience using SMBG, baseline glycemic control, antihyperglycemic treatment, age, race, health literacy, and number of comorbidities made no discernible difference in glycemic control at 52 weeks, absence of evidence is not evidence of absence.”
They also commented on the potential influence of more tailored interventions such as the messaging, saying that while earlier smaller studies had suggested this could be of benefit, this was not shown in their study.
The study was supported by a Patient-Centered Outcomes Research Institute Award and the National Center for Advancing Translational Sciences, National Institutes of Health. Two authors declared grants and nonfinancial support from a range of pharmaceutical companies, and the University of North Carolina licensed its interest in copyright works to Telcare for a glucose messaging and treatment algorithm for the purposes of commercialization.
In most care settings, the statement “you have diabetes” still triggers prescription of a glucometer and instruction on how to perform self-monitoring of blood glucose. Every 3 months thereafter, patients’ glucose logs are reviewed and routine self-monitoring of blood glucose is encouraged, regardless of patients’ risk of hypoglycemia or severe hyperglycemia, because common sense tells us that patients who proactively manage and monitor their diabetes should achieve better outcomes.
The surprising finding of this study make us question the current seemingly common sense–based strategy to encourage routine self-monitoring of blood glucose, and support the Choosing Wisely recommendations of the Society of General Internal Medicine and Endocrine Society that discourage frequent blood glucose monitoring among patients with type 2 diabetes. Routine self-monitoring of blood glucose merits a “less is more” designation because there were no clear benefits accrued, which leaves only possible harms.
Elaine C. Khoong, MD, is from the department of medicine, University of California, San Francisco, and Joseph S. Ross, MD, is from the section of general internal medicine, Yale University School of Medicine and associate editor of JAMA Internal Medicine. These comments are adapted from an accompanying editorial (JAMA Intern Med. 2017. Jun 10. doi: 10.1001/jamainternmed.2017.1233 ). Dr. Ross receives research funding through Yale University from Medtronic and the Food and Drug Administration, from Johnson & Johnson, the Centers for Medicare and Medicaid Services, the Blue Cross Blue Shield Association, and from the Laura and John Arnold Foundation. No other disclosures were declared.
In most care settings, the statement “you have diabetes” still triggers prescription of a glucometer and instruction on how to perform self-monitoring of blood glucose. Every 3 months thereafter, patients’ glucose logs are reviewed and routine self-monitoring of blood glucose is encouraged, regardless of patients’ risk of hypoglycemia or severe hyperglycemia, because common sense tells us that patients who proactively manage and monitor their diabetes should achieve better outcomes.
The surprising finding of this study make us question the current seemingly common sense–based strategy to encourage routine self-monitoring of blood glucose, and support the Choosing Wisely recommendations of the Society of General Internal Medicine and Endocrine Society that discourage frequent blood glucose monitoring among patients with type 2 diabetes. Routine self-monitoring of blood glucose merits a “less is more” designation because there were no clear benefits accrued, which leaves only possible harms.
Elaine C. Khoong, MD, is from the department of medicine, University of California, San Francisco, and Joseph S. Ross, MD, is from the section of general internal medicine, Yale University School of Medicine and associate editor of JAMA Internal Medicine. These comments are adapted from an accompanying editorial (JAMA Intern Med. 2017. Jun 10. doi: 10.1001/jamainternmed.2017.1233 ). Dr. Ross receives research funding through Yale University from Medtronic and the Food and Drug Administration, from Johnson & Johnson, the Centers for Medicare and Medicaid Services, the Blue Cross Blue Shield Association, and from the Laura and John Arnold Foundation. No other disclosures were declared.
In most care settings, the statement “you have diabetes” still triggers prescription of a glucometer and instruction on how to perform self-monitoring of blood glucose. Every 3 months thereafter, patients’ glucose logs are reviewed and routine self-monitoring of blood glucose is encouraged, regardless of patients’ risk of hypoglycemia or severe hyperglycemia, because common sense tells us that patients who proactively manage and monitor their diabetes should achieve better outcomes.
The surprising finding of this study make us question the current seemingly common sense–based strategy to encourage routine self-monitoring of blood glucose, and support the Choosing Wisely recommendations of the Society of General Internal Medicine and Endocrine Society that discourage frequent blood glucose monitoring among patients with type 2 diabetes. Routine self-monitoring of blood glucose merits a “less is more” designation because there were no clear benefits accrued, which leaves only possible harms.
Elaine C. Khoong, MD, is from the department of medicine, University of California, San Francisco, and Joseph S. Ross, MD, is from the section of general internal medicine, Yale University School of Medicine and associate editor of JAMA Internal Medicine. These comments are adapted from an accompanying editorial (JAMA Intern Med. 2017. Jun 10. doi: 10.1001/jamainternmed.2017.1233 ). Dr. Ross receives research funding through Yale University from Medtronic and the Food and Drug Administration, from Johnson & Johnson, the Centers for Medicare and Medicaid Services, the Blue Cross Blue Shield Association, and from the Laura and John Arnold Foundation. No other disclosures were declared.
Self-monitoring of blood glucose in patients with non–insulin-treated type 2 diabetes mellitus (T2DM) does not appear to make any difference to blood glucose control or quality of life, a new study has found.
The researchers report the results of the Monitor Trial in which 418 patients with non–insulin-treated T2DM were randomized either to once-daily self-monitoring of blood glucose with automatic tailored messages, once-daily monitoring with no messages, and no monitoring. Their report appears in the June 10 online edition of JAMA Internal Medicine, timed to appear simultaneously with the data’s presentation at the annual meeting of the American Diabetes Association
2017.1233).
Researchers also saw no significant differences in rates of insulin initiation, the incidence of hypoglycemia, or health care utilization.
“This null result occurred despite training participants and primary care clinicians on the use and interpretation of the meter results,” wrote Laura A. Young, MD, of the University of North Carolina at Chapel Hill.
While the findings reflect data from earlier studies suggesting limited usefulness of self-monitoring of blood glucose in these patients, the authors commented that self-monitoring has persisted as a cornerstone of clinical management of non–insulin-treated T2DM.
“As the first large pragmatic U.S. trial of SMBG [self-monitoring of blood glucose], our findings provide evidence to guide patients and clinicians making important clinical decisions about routine blood glucose monitoring,” they wrote. “Based on these findings, patients and clinicians should engage in dialogue regarding SMBG with the current evidence suggesting that SMBG should not be routine for most patients with non– insulin-treated T2DM.”
The main difference seen between the three groups was in the Summary of Diabetes Self-Care Activities, which the authors said reflected the intervention itself.
Patients taking a GLP-1 agonist at baseline were significantly more likely to increase their dose of the drug if they were in one of the self-monitoring groups, compared with the no-monitoring group, but the authors noted that the numbers were small.
Researchers also saw that African Americans in the self-monitoring with messaging group had significantly lower health-related quality of life scores, compared with the no-monitoring group, although this difference was not seen with the self-monitoring without messaging.
The participants in the trial, which was conducted at 15 primary care practices in central North Carolina, were all older than 30 years and had HbA1c levels between 6.5% and 9.5% in the 6 months before screening.
Compliance rates were similar between the two self-monitoring groups and declined at a similar rate.
The authors cautioned that their study was not powered to examine the effectiveness of self-monitoring versus no monitoring in certain clinical situations, such as the initiation of a new medication or a change in medication dose.
“Proponents of routine SMBG have cited evidence that this testing approach is useful for patients with newly diagnosed diabetes or patients with poorer glycemic control,” they said.” Although disease duration, experience using SMBG, baseline glycemic control, antihyperglycemic treatment, age, race, health literacy, and number of comorbidities made no discernible difference in glycemic control at 52 weeks, absence of evidence is not evidence of absence.”
They also commented on the potential influence of more tailored interventions such as the messaging, saying that while earlier smaller studies had suggested this could be of benefit, this was not shown in their study.
The study was supported by a Patient-Centered Outcomes Research Institute Award and the National Center for Advancing Translational Sciences, National Institutes of Health. Two authors declared grants and nonfinancial support from a range of pharmaceutical companies, and the University of North Carolina licensed its interest in copyright works to Telcare for a glucose messaging and treatment algorithm for the purposes of commercialization.
Self-monitoring of blood glucose in patients with non–insulin-treated type 2 diabetes mellitus (T2DM) does not appear to make any difference to blood glucose control or quality of life, a new study has found.
The researchers report the results of the Monitor Trial in which 418 patients with non–insulin-treated T2DM were randomized either to once-daily self-monitoring of blood glucose with automatic tailored messages, once-daily monitoring with no messages, and no monitoring. Their report appears in the June 10 online edition of JAMA Internal Medicine, timed to appear simultaneously with the data’s presentation at the annual meeting of the American Diabetes Association
2017.1233).
Researchers also saw no significant differences in rates of insulin initiation, the incidence of hypoglycemia, or health care utilization.
“This null result occurred despite training participants and primary care clinicians on the use and interpretation of the meter results,” wrote Laura A. Young, MD, of the University of North Carolina at Chapel Hill.
While the findings reflect data from earlier studies suggesting limited usefulness of self-monitoring of blood glucose in these patients, the authors commented that self-monitoring has persisted as a cornerstone of clinical management of non–insulin-treated T2DM.
“As the first large pragmatic U.S. trial of SMBG [self-monitoring of blood glucose], our findings provide evidence to guide patients and clinicians making important clinical decisions about routine blood glucose monitoring,” they wrote. “Based on these findings, patients and clinicians should engage in dialogue regarding SMBG with the current evidence suggesting that SMBG should not be routine for most patients with non– insulin-treated T2DM.”
The main difference seen between the three groups was in the Summary of Diabetes Self-Care Activities, which the authors said reflected the intervention itself.
Patients taking a GLP-1 agonist at baseline were significantly more likely to increase their dose of the drug if they were in one of the self-monitoring groups, compared with the no-monitoring group, but the authors noted that the numbers were small.
Researchers also saw that African Americans in the self-monitoring with messaging group had significantly lower health-related quality of life scores, compared with the no-monitoring group, although this difference was not seen with the self-monitoring without messaging.
The participants in the trial, which was conducted at 15 primary care practices in central North Carolina, were all older than 30 years and had HbA1c levels between 6.5% and 9.5% in the 6 months before screening.
Compliance rates were similar between the two self-monitoring groups and declined at a similar rate.
The authors cautioned that their study was not powered to examine the effectiveness of self-monitoring versus no monitoring in certain clinical situations, such as the initiation of a new medication or a change in medication dose.
“Proponents of routine SMBG have cited evidence that this testing approach is useful for patients with newly diagnosed diabetes or patients with poorer glycemic control,” they said.” Although disease duration, experience using SMBG, baseline glycemic control, antihyperglycemic treatment, age, race, health literacy, and number of comorbidities made no discernible difference in glycemic control at 52 weeks, absence of evidence is not evidence of absence.”
They also commented on the potential influence of more tailored interventions such as the messaging, saying that while earlier smaller studies had suggested this could be of benefit, this was not shown in their study.
The study was supported by a Patient-Centered Outcomes Research Institute Award and the National Center for Advancing Translational Sciences, National Institutes of Health. Two authors declared grants and nonfinancial support from a range of pharmaceutical companies, and the University of North Carolina licensed its interest in copyright works to Telcare for a glucose messaging and treatment algorithm for the purposes of commercialization.
FROM JAMA INTERNAL MEDICINE
Key clinical point:
Major finding: Patients with non–insulin-treated T2DM who do not use routine self-monitoring of blood glucose show the same blood glucose control and health-related quality of life as those who do self-monitor.
Data source: A 1-year open-label randomized trial in 418 patients with T2DM.
Disclosures: The study was supported by a Patient-Centered Outcomes Research Institute Award and the National Center for Advancing Translational Sciences, National Institutes of Health. Two authors declared grants and nonfinancial support from a range of pharmaceutical companies, and the University of North Carolina licensed its interest in copyright works to Telcare for a glucose messaging and treatment algorithm for the purposes of commercialization.
When fecal transplants for C. diff. fail, try, try again
CHICAGO – The best remedy for a failed fecal microbiota transplant for recurrent Clostridium difficile infection is most likely a second – or even a third or fourth attempt, according to Monika Fischer, MD.
Fecal microbiota transplants (FMTs) cure the large majority of those with recurrent C. difficile. But for those who don’t respond or who have an early recurrence, repeating the procedure will almost always effect cure, she said at the annual Digestive Disease Week.
“My recommendation would be to repeat FMT once you make sure the diagnosis actually is recurrent C. difficile,” said Dr. Fischer of Indiana University, Indianapolis. “There are sufficient data showing that the success rate after two FMTs significantly increases independent of the delivery route. But the effectiveness rate is highest when FMT is delivered via colonoscopy, so I recommend the second FMT be delivered that way.”
Recurrent failures can also be a sign that something else is amiss clinically, she said. So before proceeding with multiple procedures, some detective work may be in order. It’s best to start with confirmatory testing for the organism, she said.
“We have seen that about 25% of patients referred for FMT don’t actually have C. difficile at all,” Dr. Fischer said. “Be thinking about an alternative diagnosis when the stool tests negative, but the patient is still symptomatic, or if, before the FMT, there was less than a 50% improvement with vancomycin or fidaxomicin therapy.”
“When evaluating a patient for FMT failure, it should be confirmed by stool testing, preferably by toxin testing. Recent studies suggest that PCR [polymerase chain reaction]–positive but toxin-negative patients may be colonized with C. difficile but that an alternative pathology is driving the symptoms. Toxin-negative patients’ outcome is similar with or without treatment, and it is very rare that toxin-negative patients develop CDI [C. difficile infection]–related complications.”
For these patients, the problem could be any of the conditions that cause chronic diarrhea: inflammatory bowel disease, irritable bowel syndrome, celiac disease, microscopic colitis, bile salt malabsorption, chronic pancreatitis, or some other kind of infection. If C. difficile is the confirmed etiology, repeated FMTs are the way to go, Dr. Fischer said.
However, it may be worth mixing up the delivery method. The ever-expanding data on FMT continue to show that colonoscopy delivery has the lowest failure rate – about 10%. Enema is the least successful, with a 40% failure rate. In between those are nasoduodenal tube delivery, which is associated with a 20% failure rate, and oral capsules, with a failure rate varying from 12% to 30%. Fresh stool is also more effective than frozen, which, in turn, is more effective than the lyophilized preparation, Dr. Fischer said.
“Options are to repeat FMT via colonoscopy, but for patients who have had several failures, consider using the upper and lower route at the same time, and give fresh stool, especially if the first transplants used frozen.”
Although the efficacy of FMT doesn’t appear to depend on donor characteristics, patient characteristics do seem to play a role. Dr. Fischer and her colleagues have created an assessment tool to predict who may be at risk for failure. The model was developed in a 300-patient FMT cohort at two centers and validated in a third academic center FMT population. Of 24 clinical variables, three were incorporated into the failure risk model: severe disease (odds ratio, 6), inpatient status (OR, 3.8), and the number of prior C. difficile–related hospitalizations (OR, 1.4 for each one). For severe disease, patients got 5 points on the scale; for inpatient status, 4 points; and for each prior hospitalization, 1 point.
“Patients in the low-risk category [0] had up to 5% chance of failing. Patients with intermediate risk [1-2] had a 15% chance of failing, and patients in the high-risk category [3 or more points] had higher than 35% chance of not responding to single FMT,” Dr. Fischer said.
She also examined this tool in an extended cohort of nearly 500 patients at four additional sites; about 5% had failed more than two FMTs. “We identified two additional risk factors for failing multiple transplants,” Dr. Fischer said. “These were immunocompromised state, which increased the risk by 4 times, and male gender, which increased the risk by 2.5 times.”
She offered some options for the rare patient who has failed repeat FMTs and doesn’t want to try again. “There are some alternative or adjunctive therapies to repeat FMTs that may be considered, in lieu of repeating FMT for the third or fourth time or even following the first FMT failure, if dictated by patient preference. We sometimes offer these for elderly or frail patients or those with a limited life expectancy. These therapy options are from small, nonrandomized trials in multiply recurrent C. difficile infections but have not been vetted in the FMT nonresponder population.”
These include a vancomycin taper, or a vancomycin taper followed by fidaxomicin. Another option, albeit with limited applicability, is suppressive low-dose vancomycin 125 mg given every day, every other day, or every third day, indefinitely. “This can be especially good for elderly, frail patients with limited life expectancy, needing ongoing antibiotic therapy for urinary tract infections,” she said.
Finally, an 8-week vancomycin taper with daily kefir ingestion has been helpful for some patients. Although probiotics have never been proven helpful in C. difficile infections or FMT success, kefir is a different sort of supplement, she said.
“Kefir is different from yogurt. It contains bacteriocins like nisin, a protein with antibacterial properties produced by Lactococcus lactis.”
[email protected]
On Twitter @alz_gal
CHICAGO – The best remedy for a failed fecal microbiota transplant for recurrent Clostridium difficile infection is most likely a second – or even a third or fourth attempt, according to Monika Fischer, MD.
Fecal microbiota transplants (FMTs) cure the large majority of those with recurrent C. difficile. But for those who don’t respond or who have an early recurrence, repeating the procedure will almost always effect cure, she said at the annual Digestive Disease Week.
“My recommendation would be to repeat FMT once you make sure the diagnosis actually is recurrent C. difficile,” said Dr. Fischer of Indiana University, Indianapolis. “There are sufficient data showing that the success rate after two FMTs significantly increases independent of the delivery route. But the effectiveness rate is highest when FMT is delivered via colonoscopy, so I recommend the second FMT be delivered that way.”
Recurrent failures can also be a sign that something else is amiss clinically, she said. So before proceeding with multiple procedures, some detective work may be in order. It’s best to start with confirmatory testing for the organism, she said.
“We have seen that about 25% of patients referred for FMT don’t actually have C. difficile at all,” Dr. Fischer said. “Be thinking about an alternative diagnosis when the stool tests negative, but the patient is still symptomatic, or if, before the FMT, there was less than a 50% improvement with vancomycin or fidaxomicin therapy.”
“When evaluating a patient for FMT failure, it should be confirmed by stool testing, preferably by toxin testing. Recent studies suggest that PCR [polymerase chain reaction]–positive but toxin-negative patients may be colonized with C. difficile but that an alternative pathology is driving the symptoms. Toxin-negative patients’ outcome is similar with or without treatment, and it is very rare that toxin-negative patients develop CDI [C. difficile infection]–related complications.”
For these patients, the problem could be any of the conditions that cause chronic diarrhea: inflammatory bowel disease, irritable bowel syndrome, celiac disease, microscopic colitis, bile salt malabsorption, chronic pancreatitis, or some other kind of infection. If C. difficile is the confirmed etiology, repeated FMTs are the way to go, Dr. Fischer said.
However, it may be worth mixing up the delivery method. The ever-expanding data on FMT continue to show that colonoscopy delivery has the lowest failure rate – about 10%. Enema is the least successful, with a 40% failure rate. In between those are nasoduodenal tube delivery, which is associated with a 20% failure rate, and oral capsules, with a failure rate varying from 12% to 30%. Fresh stool is also more effective than frozen, which, in turn, is more effective than the lyophilized preparation, Dr. Fischer said.
“Options are to repeat FMT via colonoscopy, but for patients who have had several failures, consider using the upper and lower route at the same time, and give fresh stool, especially if the first transplants used frozen.”
Although the efficacy of FMT doesn’t appear to depend on donor characteristics, patient characteristics do seem to play a role. Dr. Fischer and her colleagues have created an assessment tool to predict who may be at risk for failure. The model was developed in a 300-patient FMT cohort at two centers and validated in a third academic center FMT population. Of 24 clinical variables, three were incorporated into the failure risk model: severe disease (odds ratio, 6), inpatient status (OR, 3.8), and the number of prior C. difficile–related hospitalizations (OR, 1.4 for each one). For severe disease, patients got 5 points on the scale; for inpatient status, 4 points; and for each prior hospitalization, 1 point.
“Patients in the low-risk category [0] had up to 5% chance of failing. Patients with intermediate risk [1-2] had a 15% chance of failing, and patients in the high-risk category [3 or more points] had higher than 35% chance of not responding to single FMT,” Dr. Fischer said.
She also examined this tool in an extended cohort of nearly 500 patients at four additional sites; about 5% had failed more than two FMTs. “We identified two additional risk factors for failing multiple transplants,” Dr. Fischer said. “These were immunocompromised state, which increased the risk by 4 times, and male gender, which increased the risk by 2.5 times.”
She offered some options for the rare patient who has failed repeat FMTs and doesn’t want to try again. “There are some alternative or adjunctive therapies to repeat FMTs that may be considered, in lieu of repeating FMT for the third or fourth time or even following the first FMT failure, if dictated by patient preference. We sometimes offer these for elderly or frail patients or those with a limited life expectancy. These therapy options are from small, nonrandomized trials in multiply recurrent C. difficile infections but have not been vetted in the FMT nonresponder population.”
These include a vancomycin taper, or a vancomycin taper followed by fidaxomicin. Another option, albeit with limited applicability, is suppressive low-dose vancomycin 125 mg given every day, every other day, or every third day, indefinitely. “This can be especially good for elderly, frail patients with limited life expectancy, needing ongoing antibiotic therapy for urinary tract infections,” she said.
Finally, an 8-week vancomycin taper with daily kefir ingestion has been helpful for some patients. Although probiotics have never been proven helpful in C. difficile infections or FMT success, kefir is a different sort of supplement, she said.
“Kefir is different from yogurt. It contains bacteriocins like nisin, a protein with antibacterial properties produced by Lactococcus lactis.”
[email protected]
On Twitter @alz_gal
CHICAGO – The best remedy for a failed fecal microbiota transplant for recurrent Clostridium difficile infection is most likely a second – or even a third or fourth attempt, according to Monika Fischer, MD.
Fecal microbiota transplants (FMTs) cure the large majority of those with recurrent C. difficile. But for those who don’t respond or who have an early recurrence, repeating the procedure will almost always effect cure, she said at the annual Digestive Disease Week.
“My recommendation would be to repeat FMT once you make sure the diagnosis actually is recurrent C. difficile,” said Dr. Fischer of Indiana University, Indianapolis. “There are sufficient data showing that the success rate after two FMTs significantly increases independent of the delivery route. But the effectiveness rate is highest when FMT is delivered via colonoscopy, so I recommend the second FMT be delivered that way.”
Recurrent failures can also be a sign that something else is amiss clinically, she said. So before proceeding with multiple procedures, some detective work may be in order. It’s best to start with confirmatory testing for the organism, she said.
“We have seen that about 25% of patients referred for FMT don’t actually have C. difficile at all,” Dr. Fischer said. “Be thinking about an alternative diagnosis when the stool tests negative, but the patient is still symptomatic, or if, before the FMT, there was less than a 50% improvement with vancomycin or fidaxomicin therapy.”
“When evaluating a patient for FMT failure, it should be confirmed by stool testing, preferably by toxin testing. Recent studies suggest that PCR [polymerase chain reaction]–positive but toxin-negative patients may be colonized with C. difficile but that an alternative pathology is driving the symptoms. Toxin-negative patients’ outcome is similar with or without treatment, and it is very rare that toxin-negative patients develop CDI [C. difficile infection]–related complications.”
For these patients, the problem could be any of the conditions that cause chronic diarrhea: inflammatory bowel disease, irritable bowel syndrome, celiac disease, microscopic colitis, bile salt malabsorption, chronic pancreatitis, or some other kind of infection. If C. difficile is the confirmed etiology, repeated FMTs are the way to go, Dr. Fischer said.
However, it may be worth mixing up the delivery method. The ever-expanding data on FMT continue to show that colonoscopy delivery has the lowest failure rate – about 10%. Enema is the least successful, with a 40% failure rate. In between those are nasoduodenal tube delivery, which is associated with a 20% failure rate, and oral capsules, with a failure rate varying from 12% to 30%. Fresh stool is also more effective than frozen, which, in turn, is more effective than the lyophilized preparation, Dr. Fischer said.
“Options are to repeat FMT via colonoscopy, but for patients who have had several failures, consider using the upper and lower route at the same time, and give fresh stool, especially if the first transplants used frozen.”
Although the efficacy of FMT doesn’t appear to depend on donor characteristics, patient characteristics do seem to play a role. Dr. Fischer and her colleagues have created an assessment tool to predict who may be at risk for failure. The model was developed in a 300-patient FMT cohort at two centers and validated in a third academic center FMT population. Of 24 clinical variables, three were incorporated into the failure risk model: severe disease (odds ratio, 6), inpatient status (OR, 3.8), and the number of prior C. difficile–related hospitalizations (OR, 1.4 for each one). For severe disease, patients got 5 points on the scale; for inpatient status, 4 points; and for each prior hospitalization, 1 point.
“Patients in the low-risk category [0] had up to 5% chance of failing. Patients with intermediate risk [1-2] had a 15% chance of failing, and patients in the high-risk category [3 or more points] had higher than 35% chance of not responding to single FMT,” Dr. Fischer said.
She also examined this tool in an extended cohort of nearly 500 patients at four additional sites; about 5% had failed more than two FMTs. “We identified two additional risk factors for failing multiple transplants,” Dr. Fischer said. “These were immunocompromised state, which increased the risk by 4 times, and male gender, which increased the risk by 2.5 times.”
She offered some options for the rare patient who has failed repeat FMTs and doesn’t want to try again. “There are some alternative or adjunctive therapies to repeat FMTs that may be considered, in lieu of repeating FMT for the third or fourth time or even following the first FMT failure, if dictated by patient preference. We sometimes offer these for elderly or frail patients or those with a limited life expectancy. These therapy options are from small, nonrandomized trials in multiply recurrent C. difficile infections but have not been vetted in the FMT nonresponder population.”
These include a vancomycin taper, or a vancomycin taper followed by fidaxomicin. Another option, albeit with limited applicability, is suppressive low-dose vancomycin 125 mg given every day, every other day, or every third day, indefinitely. “This can be especially good for elderly, frail patients with limited life expectancy, needing ongoing antibiotic therapy for urinary tract infections,” she said.
Finally, an 8-week vancomycin taper with daily kefir ingestion has been helpful for some patients. Although probiotics have never been proven helpful in C. difficile infections or FMT success, kefir is a different sort of supplement, she said.
“Kefir is different from yogurt. It contains bacteriocins like nisin, a protein with antibacterial properties produced by Lactococcus lactis.”
[email protected]
On Twitter @alz_gal
AT DDW 2017
Researchers design new, safer antiplatelet drug based on snake venom
Researchers say they have designed an antiplatelet drug based on snake venom protein that stimulates platelets to form blood clots by latching onto glycoprotein VI (GPVI), which is safer than some currently available antiplatelet drugs that target glycoproteins IIb/IIIa.
Earlier studies have shown that platelets missing GPVI do not form clots and do not lead to severe bleeding.
The researchers, therefore, designed a drug to interact with the protein glycoprotein VI.
They used trowaglerix, a protein in the venom of the Tropidolaemus wagleri snake, to block GPVI activity.
An earlier study by the team found that trowaglerix worked through GPVI antagonism.
Some currently available antiplatelet drugs are also based on protein found in snake venom but target GPIIa/IIIb instead, which leads to the side effect of bleeding.
“[W]hy that target leads to the bleeding side effect is not fully understood,” said lead co-author Tur-Fu Huang, PhD, of the National Taiwan University in Taipei.
Specifically, the team sequenced trowaglerix and found an alpha subunit that specifically targeted GPVI snaclec, which is snake venom C-type lectin protein.
They then used computational peptide design to create a series of Troα6/Troα10 peptides—a hexapeptide and decapeptide, respectively—which were derived from trowaglerix.
Mice administered this new drug, researchers report, had slower blood clot formation compared to untreated mice. In addition, the treated mice did not bleed longer than the untreated mice.
The team believes their research supports the concept that these hexa/decapeptides have therapeutic potential and can be a template for a new, safer class of antiplatelet drug with a limited bleeding side effect.
“In general, this type of molecule design does not last long in the body,” said co-author Jane Tseng, PhD, also of the National Taiwan University, “so techniques like formulation or delivery system are likely needed to extend the exposure time in the human body.”
She also indicated that the design needs to be optimized, “to ensure that the molecule only interacts with GPVI and not other proteins which can cause unintended reactions.”
The research team reported its findings in Arteriosclerosis, Thrombosis, and Vascular Biology, an American Heart Association journal.
The National Science Council of Taiwan supported the study. ![]()
Researchers say they have designed an antiplatelet drug based on snake venom protein that stimulates platelets to form blood clots by latching onto glycoprotein VI (GPVI), which is safer than some currently available antiplatelet drugs that target glycoproteins IIb/IIIa.
Earlier studies have shown that platelets missing GPVI do not form clots and do not lead to severe bleeding.
The researchers, therefore, designed a drug to interact with the protein glycoprotein VI.
They used trowaglerix, a protein in the venom of the Tropidolaemus wagleri snake, to block GPVI activity.
An earlier study by the team found that trowaglerix worked through GPVI antagonism.
Some currently available antiplatelet drugs are also based on protein found in snake venom but target GPIIa/IIIb instead, which leads to the side effect of bleeding.
“[W]hy that target leads to the bleeding side effect is not fully understood,” said lead co-author Tur-Fu Huang, PhD, of the National Taiwan University in Taipei.
Specifically, the team sequenced trowaglerix and found an alpha subunit that specifically targeted GPVI snaclec, which is snake venom C-type lectin protein.
They then used computational peptide design to create a series of Troα6/Troα10 peptides—a hexapeptide and decapeptide, respectively—which were derived from trowaglerix.
Mice administered this new drug, researchers report, had slower blood clot formation compared to untreated mice. In addition, the treated mice did not bleed longer than the untreated mice.
The team believes their research supports the concept that these hexa/decapeptides have therapeutic potential and can be a template for a new, safer class of antiplatelet drug with a limited bleeding side effect.
“In general, this type of molecule design does not last long in the body,” said co-author Jane Tseng, PhD, also of the National Taiwan University, “so techniques like formulation or delivery system are likely needed to extend the exposure time in the human body.”
She also indicated that the design needs to be optimized, “to ensure that the molecule only interacts with GPVI and not other proteins which can cause unintended reactions.”
The research team reported its findings in Arteriosclerosis, Thrombosis, and Vascular Biology, an American Heart Association journal.
The National Science Council of Taiwan supported the study. ![]()
Researchers say they have designed an antiplatelet drug based on snake venom protein that stimulates platelets to form blood clots by latching onto glycoprotein VI (GPVI), which is safer than some currently available antiplatelet drugs that target glycoproteins IIb/IIIa.
Earlier studies have shown that platelets missing GPVI do not form clots and do not lead to severe bleeding.
The researchers, therefore, designed a drug to interact with the protein glycoprotein VI.
They used trowaglerix, a protein in the venom of the Tropidolaemus wagleri snake, to block GPVI activity.
An earlier study by the team found that trowaglerix worked through GPVI antagonism.
Some currently available antiplatelet drugs are also based on protein found in snake venom but target GPIIa/IIIb instead, which leads to the side effect of bleeding.
“[W]hy that target leads to the bleeding side effect is not fully understood,” said lead co-author Tur-Fu Huang, PhD, of the National Taiwan University in Taipei.
Specifically, the team sequenced trowaglerix and found an alpha subunit that specifically targeted GPVI snaclec, which is snake venom C-type lectin protein.
They then used computational peptide design to create a series of Troα6/Troα10 peptides—a hexapeptide and decapeptide, respectively—which were derived from trowaglerix.
Mice administered this new drug, researchers report, had slower blood clot formation compared to untreated mice. In addition, the treated mice did not bleed longer than the untreated mice.
The team believes their research supports the concept that these hexa/decapeptides have therapeutic potential and can be a template for a new, safer class of antiplatelet drug with a limited bleeding side effect.
“In general, this type of molecule design does not last long in the body,” said co-author Jane Tseng, PhD, also of the National Taiwan University, “so techniques like formulation or delivery system are likely needed to extend the exposure time in the human body.”
She also indicated that the design needs to be optimized, “to ensure that the molecule only interacts with GPVI and not other proteins which can cause unintended reactions.”
The research team reported its findings in Arteriosclerosis, Thrombosis, and Vascular Biology, an American Heart Association journal.
The National Science Council of Taiwan supported the study. ![]()
Recruiting survey notes strong demand for family physicians, psychiatrists
Family medicine continues to be the most highly recruited specialty, based on nearly 3,300 permanent physician and advanced practitioner search assignments posted from April 1, 2016, to March 31, 2017, through Merritt Hawkins’ and AMN Healthcare’s physician staffing companies.
It is the 11th consecutive year that family physicians topped the search list, and the specialty’s continued dominance is “underscoring the continued urgent demand for primary care physicians in an evolving health system,” Merritt Hawkins said in its annual report on physician recruiting.
“Primary care is increasingly the province of international medical graduates,” according to the report, which notes that U.S.-based medical students continue to show low interest in primary care because of low compensation and the perceived high level of personal time commitment required.
Demand for primary care physicians continues to grow and is likely to be exacerbated by the value-based payment models that are emerging in the wake of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), the report added.
Psychiatry was the second most recruited specialty for just the second time in 24 years. The change “reflects a severe shortage of mental health professionals nationwide.”
The supply of psychiatrists is “already constrained and is soon going to diminish significantly. There currently are some 30,000 psychiatrists in active patient care in the United States, 60% of whom are 55 years or older, with many set to retire. ... With many psychiatrists aging out of the profession and with a preference among psychiatrists for outpatient practice settings, it is becoming increasingly difficult to recruit to inpatient settings.”
The top five most requested searches by medical specialty were:
- Family medicine (607), ranked first in the previous year.
- Psychiatry (256), ranked second in the previous year.
- Internal medicine (193), ranked third in the previous year.
- Nurse practitioner (137), ranked fifth in the previous year.
- Ob.gyn (109), ranked sixth in the previous year.
Family medicine continues to be the most highly recruited specialty, based on nearly 3,300 permanent physician and advanced practitioner search assignments posted from April 1, 2016, to March 31, 2017, through Merritt Hawkins’ and AMN Healthcare’s physician staffing companies.
It is the 11th consecutive year that family physicians topped the search list, and the specialty’s continued dominance is “underscoring the continued urgent demand for primary care physicians in an evolving health system,” Merritt Hawkins said in its annual report on physician recruiting.
“Primary care is increasingly the province of international medical graduates,” according to the report, which notes that U.S.-based medical students continue to show low interest in primary care because of low compensation and the perceived high level of personal time commitment required.
Demand for primary care physicians continues to grow and is likely to be exacerbated by the value-based payment models that are emerging in the wake of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), the report added.
Psychiatry was the second most recruited specialty for just the second time in 24 years. The change “reflects a severe shortage of mental health professionals nationwide.”
The supply of psychiatrists is “already constrained and is soon going to diminish significantly. There currently are some 30,000 psychiatrists in active patient care in the United States, 60% of whom are 55 years or older, with many set to retire. ... With many psychiatrists aging out of the profession and with a preference among psychiatrists for outpatient practice settings, it is becoming increasingly difficult to recruit to inpatient settings.”
The top five most requested searches by medical specialty were:
- Family medicine (607), ranked first in the previous year.
- Psychiatry (256), ranked second in the previous year.
- Internal medicine (193), ranked third in the previous year.
- Nurse practitioner (137), ranked fifth in the previous year.
- Ob.gyn (109), ranked sixth in the previous year.
Family medicine continues to be the most highly recruited specialty, based on nearly 3,300 permanent physician and advanced practitioner search assignments posted from April 1, 2016, to March 31, 2017, through Merritt Hawkins’ and AMN Healthcare’s physician staffing companies.
It is the 11th consecutive year that family physicians topped the search list, and the specialty’s continued dominance is “underscoring the continued urgent demand for primary care physicians in an evolving health system,” Merritt Hawkins said in its annual report on physician recruiting.
“Primary care is increasingly the province of international medical graduates,” according to the report, which notes that U.S.-based medical students continue to show low interest in primary care because of low compensation and the perceived high level of personal time commitment required.
Demand for primary care physicians continues to grow and is likely to be exacerbated by the value-based payment models that are emerging in the wake of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), the report added.
Psychiatry was the second most recruited specialty for just the second time in 24 years. The change “reflects a severe shortage of mental health professionals nationwide.”
The supply of psychiatrists is “already constrained and is soon going to diminish significantly. There currently are some 30,000 psychiatrists in active patient care in the United States, 60% of whom are 55 years or older, with many set to retire. ... With many psychiatrists aging out of the profession and with a preference among psychiatrists for outpatient practice settings, it is becoming increasingly difficult to recruit to inpatient settings.”
The top five most requested searches by medical specialty were:
- Family medicine (607), ranked first in the previous year.
- Psychiatry (256), ranked second in the previous year.
- Internal medicine (193), ranked third in the previous year.
- Nurse practitioner (137), ranked fifth in the previous year.
- Ob.gyn (109), ranked sixth in the previous year.
Risks of keeping controlled substances in office tilt away from benefits
I don’t stack narcotics in my office. Never have, never will.
Honestly, in this day and age, I don’t understand why anyone would.
I get the occasional patient with a bad migraine who wants to come in for “a shot.” Sorry, I don’t carry that. I suppose I could carry Ketorolac, but I try to run a simple, nonurgent practice. If you have an urgent situation, go to an emergency department or urgent care.
I couldn’t agree more. It’s better to avoid the problem altogether.
In 1998, on my very first day of work as an attending, the group I’d signed with put me in a satellite office normally used by their headache specialist. While familiarizing myself with what was where, I discovered a bottle of injectable meperidine. It wasn’t locked up, just sitting next to the zolmitriptan (Zomig) samples in an unsecured cabinet. I picked it up in shock to make sure I’d read the label correctly. I put it back down then (somewhat paranoid) picked it back up, wiped my fingerprints off, and put it down in the exact same spot it had been. Although it was obviously a serious infraction, I didn’t want to jeopardize my standing as a new hire. So, I just ignored it. But, I sure worried about what would happen if a DEA inspector showed up.
So, today, I just don’t deal with it. No controlled substances, less paperwork, fewer worries. Simplicity is bliss, and modern medicine has enough worries as it is.
This still gets me the occasional complaint of, “Well, my other neurologist did!” but, frankly, I don’t care. They can run their practice how they want, and I’ll run mine.
In a world of regulations, daily press stories on “pill mills” overusing narcotics, and my quarterly prescription tracking reports from the state board, I want to keep my involvement in them as minimal as possible. I may prescribe them, but I don’t want the potential nightmares of having them on site.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I don’t stack narcotics in my office. Never have, never will.
Honestly, in this day and age, I don’t understand why anyone would.
I get the occasional patient with a bad migraine who wants to come in for “a shot.” Sorry, I don’t carry that. I suppose I could carry Ketorolac, but I try to run a simple, nonurgent practice. If you have an urgent situation, go to an emergency department or urgent care.
I couldn’t agree more. It’s better to avoid the problem altogether.
In 1998, on my very first day of work as an attending, the group I’d signed with put me in a satellite office normally used by their headache specialist. While familiarizing myself with what was where, I discovered a bottle of injectable meperidine. It wasn’t locked up, just sitting next to the zolmitriptan (Zomig) samples in an unsecured cabinet. I picked it up in shock to make sure I’d read the label correctly. I put it back down then (somewhat paranoid) picked it back up, wiped my fingerprints off, and put it down in the exact same spot it had been. Although it was obviously a serious infraction, I didn’t want to jeopardize my standing as a new hire. So, I just ignored it. But, I sure worried about what would happen if a DEA inspector showed up.
So, today, I just don’t deal with it. No controlled substances, less paperwork, fewer worries. Simplicity is bliss, and modern medicine has enough worries as it is.
This still gets me the occasional complaint of, “Well, my other neurologist did!” but, frankly, I don’t care. They can run their practice how they want, and I’ll run mine.
In a world of regulations, daily press stories on “pill mills” overusing narcotics, and my quarterly prescription tracking reports from the state board, I want to keep my involvement in them as minimal as possible. I may prescribe them, but I don’t want the potential nightmares of having them on site.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
I don’t stack narcotics in my office. Never have, never will.
Honestly, in this day and age, I don’t understand why anyone would.
I get the occasional patient with a bad migraine who wants to come in for “a shot.” Sorry, I don’t carry that. I suppose I could carry Ketorolac, but I try to run a simple, nonurgent practice. If you have an urgent situation, go to an emergency department or urgent care.
I couldn’t agree more. It’s better to avoid the problem altogether.
In 1998, on my very first day of work as an attending, the group I’d signed with put me in a satellite office normally used by their headache specialist. While familiarizing myself with what was where, I discovered a bottle of injectable meperidine. It wasn’t locked up, just sitting next to the zolmitriptan (Zomig) samples in an unsecured cabinet. I picked it up in shock to make sure I’d read the label correctly. I put it back down then (somewhat paranoid) picked it back up, wiped my fingerprints off, and put it down in the exact same spot it had been. Although it was obviously a serious infraction, I didn’t want to jeopardize my standing as a new hire. So, I just ignored it. But, I sure worried about what would happen if a DEA inspector showed up.
So, today, I just don’t deal with it. No controlled substances, less paperwork, fewer worries. Simplicity is bliss, and modern medicine has enough worries as it is.
This still gets me the occasional complaint of, “Well, my other neurologist did!” but, frankly, I don’t care. They can run their practice how they want, and I’ll run mine.
In a world of regulations, daily press stories on “pill mills” overusing narcotics, and my quarterly prescription tracking reports from the state board, I want to keep my involvement in them as minimal as possible. I may prescribe them, but I don’t want the potential nightmares of having them on site.
Dr. Block has a solo neurology practice in Scottsdale, Ariz.
FDA approves generic version of HIV drug Truvada
The U.S. Food and Drug Administration has approved the first generic version of emtricitabine and tenofovir disoproxil fumarate tablets, previously known by the brand name Truvada, for the treatment of HIV-1 infection.
Like Truvada, the generic version of the drug – produced by Teva Pharmaceuticals USA and approved in 200-mg/300-mg tablet form – is indicated for use in combination with other antiretrovirals for patients infected with HIV-1 and for pre-exposure prophylaxis (PrEP) to prevent sexually-acquired HIV infection in high-risk adults.
Women infected with HIV-1 should not breastfeed while taking emtricitabine and tenofovir disoproxil fumarate, the FDA said, and the drug can be used only in pediatric patients weighing more than 17 kg.
[email protected]
On Twitter @richpizzi
The U.S. Food and Drug Administration has approved the first generic version of emtricitabine and tenofovir disoproxil fumarate tablets, previously known by the brand name Truvada, for the treatment of HIV-1 infection.
Like Truvada, the generic version of the drug – produced by Teva Pharmaceuticals USA and approved in 200-mg/300-mg tablet form – is indicated for use in combination with other antiretrovirals for patients infected with HIV-1 and for pre-exposure prophylaxis (PrEP) to prevent sexually-acquired HIV infection in high-risk adults.
Women infected with HIV-1 should not breastfeed while taking emtricitabine and tenofovir disoproxil fumarate, the FDA said, and the drug can be used only in pediatric patients weighing more than 17 kg.
[email protected]
On Twitter @richpizzi
The U.S. Food and Drug Administration has approved the first generic version of emtricitabine and tenofovir disoproxil fumarate tablets, previously known by the brand name Truvada, for the treatment of HIV-1 infection.
Like Truvada, the generic version of the drug – produced by Teva Pharmaceuticals USA and approved in 200-mg/300-mg tablet form – is indicated for use in combination with other antiretrovirals for patients infected with HIV-1 and for pre-exposure prophylaxis (PrEP) to prevent sexually-acquired HIV infection in high-risk adults.
Women infected with HIV-1 should not breastfeed while taking emtricitabine and tenofovir disoproxil fumarate, the FDA said, and the drug can be used only in pediatric patients weighing more than 17 kg.
[email protected]
On Twitter @richpizzi
Revisions coming to McDonald Criteria for MS
NEW ORLEANS – Changes are coming to the current McDonald Criteria for diagnosing multiple sclerosis, primarily because of advances in the understanding of MS since the criteria were last updated in 2010.
Such advances include the availability of new data regarding the relationship between MS and other spectrum disorders and data concerning the performance of the 2010 McDonald Criteria in several patient populations, according to Jeffrey A. Cohen, MD, who cochaired the effort known as the International Panel on Diagnosis of Multiple Sclerosis. “There also were new data concerning the utility of cerebrospinal fluid evaluation and increasing recognition that the role of cerebrospinal fluid (CSF) examination perhaps needs increased emphasis,” Dr. Cohen said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “It’s been somewhat de-emphasized in previous versions of the criteria. Then, there was identification of subsets of patients that were felt to have a high likelihood of MS but in whom the diagnosis could not be made by the current criteria – patients who fell through the cracks. There was also increasing recognition of the frequency and important consequences of misdiagnosis.”
The panel emphasized that evidence supporting the McDonald criteria is predominately based on patients with a typical clinically isolated syndrome (CIS) at onset. It also acknowledged the difficulty of confirming a diagnosis of MS, the importance of addressing alternative diagnoses and absence of atypical features and red flags, and the rigor necessary for interpreting clinical, imaging, and laboratory studies. “Misdiagnosis is common,” Dr. Cohen told meeting attendees. “In some series, upwards of 50%-60% of patients referred to a specialized MS center turn out to have some other diagnosis. Our panel had discussions related to the tradeoff between sensitivity of the criteria and trying to make the diagnosis earlier and in a broader range of patients but counterbalancing that against the risk of a misdiagnosis. Our conclusion was that, although some of that might be created by the criteria, it’s mostly a problem of misapplying the criteria. One needs to remember that to make the diagnosis of MS does not merely require demonstrating that the patient has a disease process that involves potentially multiple places in the CNS and as recurrent events over time, but one has to apply the diagnostic data with rigor.”
Another emphasis expected to be included in updated McDonald criteria is the use of CSF and spinal cord imaging, as well as the notion that a history, examination, and synthesis of a patient’s overall clinical picture “needs to be made by a clinician with MS-related expertise,” Dr. Cohen said. “One cannot merely use the criteria as a checklist.”
The panelists also discussed modifying the term “possible MS,” which is already in the McDonald criteria, to include patients with CIS who do not (yet) fulfill the diagnostic criteria for MS; radiologically isolated syndrome (RIS); solitary sclerosis; and patients with clinical manifestations, imaging, and other features that are compatible with MS but not typical for those who may or may not be determined to have MS or in the future.
Dr. Cohen noted that additional data concerning the applicability of the McDonald criteria to Asian and Latin populations have been published since 2010 but are modest. “There is no indication the McDonald criteria cannot be used in these populations,” he said. “Care is needed to address alternative diagnoses, particularly neuromyelitis optica spectrum disorder (NMOSD) in both and also infectious diseases in Latin America.” Several studies also support the applicability of the McDonald criteria in children, with certain caveats. “One needs to be careful in diagnosing MS in people younger than 11 years of age,” Dr. Cohen said. “If the initial event is [acute disseminated encephalomyelitis], they also need to have a typical clinically isolated syndrome.”
Panelists also agreed that the McDonald criteria apply to older patients, with caveats that a new diagnosis of MS is rarely considered in older adults. “They are more likely to have a progressive course, either progressive from onset or following previous unrecognized relapses,” Dr. Cohen said. “There needs to be careful consideration of alternative diagnoses and, particularly, comorbidities. This represents an example of a diagnostic scenario for which CSF examination is advised.”
Panel members found that the recognized range of potential clinical manifestations of NMOSD is becoming wider and is still being defined. “Emerging data suggests a substantial proportion of AQP-4 seronegative patients with NMOSD features (about 20%) have anti–myelin oligodendrocyte glycoprotein antibodies,” he said. “Although some features of MS and NMOSD overlap, they are now understood to be distinct disorders.”
Other points under consideration for the 2017 revision of the McDonald Criteria included incorporating the revised phenotype categories (relapse-remitting, secondary progressive, primary progressive, and progressive relapsing), expanding the role of CSF to allow diagnosis of MS with CIS plus DIS plus oligoclonal bands, determining whether to accept 2016 Revised Magnetic Resonance Imaging in Multiple Sclerosis MRI criteria in aggregate or in part, and incorporating optic nerve involvement.
Dr. Cohen disclosed that he has received compensation as a consultant for Adamas, Celgene, Merck, Mallinckrodt, and Novartis.
NEW ORLEANS – Changes are coming to the current McDonald Criteria for diagnosing multiple sclerosis, primarily because of advances in the understanding of MS since the criteria were last updated in 2010.
Such advances include the availability of new data regarding the relationship between MS and other spectrum disorders and data concerning the performance of the 2010 McDonald Criteria in several patient populations, according to Jeffrey A. Cohen, MD, who cochaired the effort known as the International Panel on Diagnosis of Multiple Sclerosis. “There also were new data concerning the utility of cerebrospinal fluid evaluation and increasing recognition that the role of cerebrospinal fluid (CSF) examination perhaps needs increased emphasis,” Dr. Cohen said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “It’s been somewhat de-emphasized in previous versions of the criteria. Then, there was identification of subsets of patients that were felt to have a high likelihood of MS but in whom the diagnosis could not be made by the current criteria – patients who fell through the cracks. There was also increasing recognition of the frequency and important consequences of misdiagnosis.”
The panel emphasized that evidence supporting the McDonald criteria is predominately based on patients with a typical clinically isolated syndrome (CIS) at onset. It also acknowledged the difficulty of confirming a diagnosis of MS, the importance of addressing alternative diagnoses and absence of atypical features and red flags, and the rigor necessary for interpreting clinical, imaging, and laboratory studies. “Misdiagnosis is common,” Dr. Cohen told meeting attendees. “In some series, upwards of 50%-60% of patients referred to a specialized MS center turn out to have some other diagnosis. Our panel had discussions related to the tradeoff between sensitivity of the criteria and trying to make the diagnosis earlier and in a broader range of patients but counterbalancing that against the risk of a misdiagnosis. Our conclusion was that, although some of that might be created by the criteria, it’s mostly a problem of misapplying the criteria. One needs to remember that to make the diagnosis of MS does not merely require demonstrating that the patient has a disease process that involves potentially multiple places in the CNS and as recurrent events over time, but one has to apply the diagnostic data with rigor.”
Another emphasis expected to be included in updated McDonald criteria is the use of CSF and spinal cord imaging, as well as the notion that a history, examination, and synthesis of a patient’s overall clinical picture “needs to be made by a clinician with MS-related expertise,” Dr. Cohen said. “One cannot merely use the criteria as a checklist.”
The panelists also discussed modifying the term “possible MS,” which is already in the McDonald criteria, to include patients with CIS who do not (yet) fulfill the diagnostic criteria for MS; radiologically isolated syndrome (RIS); solitary sclerosis; and patients with clinical manifestations, imaging, and other features that are compatible with MS but not typical for those who may or may not be determined to have MS or in the future.
Dr. Cohen noted that additional data concerning the applicability of the McDonald criteria to Asian and Latin populations have been published since 2010 but are modest. “There is no indication the McDonald criteria cannot be used in these populations,” he said. “Care is needed to address alternative diagnoses, particularly neuromyelitis optica spectrum disorder (NMOSD) in both and also infectious diseases in Latin America.” Several studies also support the applicability of the McDonald criteria in children, with certain caveats. “One needs to be careful in diagnosing MS in people younger than 11 years of age,” Dr. Cohen said. “If the initial event is [acute disseminated encephalomyelitis], they also need to have a typical clinically isolated syndrome.”
Panelists also agreed that the McDonald criteria apply to older patients, with caveats that a new diagnosis of MS is rarely considered in older adults. “They are more likely to have a progressive course, either progressive from onset or following previous unrecognized relapses,” Dr. Cohen said. “There needs to be careful consideration of alternative diagnoses and, particularly, comorbidities. This represents an example of a diagnostic scenario for which CSF examination is advised.”
Panel members found that the recognized range of potential clinical manifestations of NMOSD is becoming wider and is still being defined. “Emerging data suggests a substantial proportion of AQP-4 seronegative patients with NMOSD features (about 20%) have anti–myelin oligodendrocyte glycoprotein antibodies,” he said. “Although some features of MS and NMOSD overlap, they are now understood to be distinct disorders.”
Other points under consideration for the 2017 revision of the McDonald Criteria included incorporating the revised phenotype categories (relapse-remitting, secondary progressive, primary progressive, and progressive relapsing), expanding the role of CSF to allow diagnosis of MS with CIS plus DIS plus oligoclonal bands, determining whether to accept 2016 Revised Magnetic Resonance Imaging in Multiple Sclerosis MRI criteria in aggregate or in part, and incorporating optic nerve involvement.
Dr. Cohen disclosed that he has received compensation as a consultant for Adamas, Celgene, Merck, Mallinckrodt, and Novartis.
NEW ORLEANS – Changes are coming to the current McDonald Criteria for diagnosing multiple sclerosis, primarily because of advances in the understanding of MS since the criteria were last updated in 2010.
Such advances include the availability of new data regarding the relationship between MS and other spectrum disorders and data concerning the performance of the 2010 McDonald Criteria in several patient populations, according to Jeffrey A. Cohen, MD, who cochaired the effort known as the International Panel on Diagnosis of Multiple Sclerosis. “There also were new data concerning the utility of cerebrospinal fluid evaluation and increasing recognition that the role of cerebrospinal fluid (CSF) examination perhaps needs increased emphasis,” Dr. Cohen said at the annual meeting of the Consortium of Multiple Sclerosis Centers. “It’s been somewhat de-emphasized in previous versions of the criteria. Then, there was identification of subsets of patients that were felt to have a high likelihood of MS but in whom the diagnosis could not be made by the current criteria – patients who fell through the cracks. There was also increasing recognition of the frequency and important consequences of misdiagnosis.”
The panel emphasized that evidence supporting the McDonald criteria is predominately based on patients with a typical clinically isolated syndrome (CIS) at onset. It also acknowledged the difficulty of confirming a diagnosis of MS, the importance of addressing alternative diagnoses and absence of atypical features and red flags, and the rigor necessary for interpreting clinical, imaging, and laboratory studies. “Misdiagnosis is common,” Dr. Cohen told meeting attendees. “In some series, upwards of 50%-60% of patients referred to a specialized MS center turn out to have some other diagnosis. Our panel had discussions related to the tradeoff between sensitivity of the criteria and trying to make the diagnosis earlier and in a broader range of patients but counterbalancing that against the risk of a misdiagnosis. Our conclusion was that, although some of that might be created by the criteria, it’s mostly a problem of misapplying the criteria. One needs to remember that to make the diagnosis of MS does not merely require demonstrating that the patient has a disease process that involves potentially multiple places in the CNS and as recurrent events over time, but one has to apply the diagnostic data with rigor.”
Another emphasis expected to be included in updated McDonald criteria is the use of CSF and spinal cord imaging, as well as the notion that a history, examination, and synthesis of a patient’s overall clinical picture “needs to be made by a clinician with MS-related expertise,” Dr. Cohen said. “One cannot merely use the criteria as a checklist.”
The panelists also discussed modifying the term “possible MS,” which is already in the McDonald criteria, to include patients with CIS who do not (yet) fulfill the diagnostic criteria for MS; radiologically isolated syndrome (RIS); solitary sclerosis; and patients with clinical manifestations, imaging, and other features that are compatible with MS but not typical for those who may or may not be determined to have MS or in the future.
Dr. Cohen noted that additional data concerning the applicability of the McDonald criteria to Asian and Latin populations have been published since 2010 but are modest. “There is no indication the McDonald criteria cannot be used in these populations,” he said. “Care is needed to address alternative diagnoses, particularly neuromyelitis optica spectrum disorder (NMOSD) in both and also infectious diseases in Latin America.” Several studies also support the applicability of the McDonald criteria in children, with certain caveats. “One needs to be careful in diagnosing MS in people younger than 11 years of age,” Dr. Cohen said. “If the initial event is [acute disseminated encephalomyelitis], they also need to have a typical clinically isolated syndrome.”
Panelists also agreed that the McDonald criteria apply to older patients, with caveats that a new diagnosis of MS is rarely considered in older adults. “They are more likely to have a progressive course, either progressive from onset or following previous unrecognized relapses,” Dr. Cohen said. “There needs to be careful consideration of alternative diagnoses and, particularly, comorbidities. This represents an example of a diagnostic scenario for which CSF examination is advised.”
Panel members found that the recognized range of potential clinical manifestations of NMOSD is becoming wider and is still being defined. “Emerging data suggests a substantial proportion of AQP-4 seronegative patients with NMOSD features (about 20%) have anti–myelin oligodendrocyte glycoprotein antibodies,” he said. “Although some features of MS and NMOSD overlap, they are now understood to be distinct disorders.”
Other points under consideration for the 2017 revision of the McDonald Criteria included incorporating the revised phenotype categories (relapse-remitting, secondary progressive, primary progressive, and progressive relapsing), expanding the role of CSF to allow diagnosis of MS with CIS plus DIS plus oligoclonal bands, determining whether to accept 2016 Revised Magnetic Resonance Imaging in Multiple Sclerosis MRI criteria in aggregate or in part, and incorporating optic nerve involvement.
Dr. Cohen disclosed that he has received compensation as a consultant for Adamas, Celgene, Merck, Mallinckrodt, and Novartis.
EXPERT ANALYSIS AT THE CMSC ANNUAL MEETING
Transcranial magnetic stimulation shows more promise in refractory OCD
SAN FRANCISCO – Mounting evidence suggests that transcranial magnetic stimulation is an effective noninvasive therapy for obsessive-compulsive disorder refractory to first-line medications, Eric Hollander, MD, said at the annual conference of the Anxiety and Depression Association of America.
A novel treatment for obsessive-compulsive disorder (OCD) would be most welcome. This is a disorder that’s common – affecting 2%-3% of the population – debilitating, and notoriously tough to treat. Roughly half of patients with OCD don’t respond to first-line therapy, which is selective serotonin reuptake inhibitors, cognitive-behavioral therapy, or both, according to Dr. Hollander, director of the autism and obsessive-compulsive spectrum program as well as the anxiety and depression program at Albert Einstein College of Medicine in New York.
Four companies now have FDA-cleared TMS devices indicated for treatment of major depression: Brainsway, which markets a dTMS device, and Neuronetics, MagVenture, and Magstim, which sell repetitive TMS (rTMS) devices that do not penetrate as deeply beneath the skull as dTMS and therefore target different brain structures.
TMS for OCD is, at present, off-label therapy. Yet, there is now sufficient experience derived from formal clinical trials and off-label use in clinical practice to be able to state that the standard target area for rTMS is the supplementary motor area (SMA), according to Dr. Hollander.
He was senior author of a randomized open-label pilot study involving 50 consecutive OCD patients refractory to SSRIs. Half were assigned to a popular second-line strategy: augmentation with antipsychotic agents. The other half received five 20-minute-long rTMS sessions per week for 3 weeks using low-frequency 1 Hz bilateral stimulation of the SMA.
At 3 weeks, the treatment response rate as defined by at least a 25% reduction from baseline on the Yale-Brown Obsessive-Compulsive Scale (YBOCS) was 68% in the rTMS group, compared with 24% in the control arm. Thus, rTMS was better than treatment as usual (J Psychopharmacol. 2016 Jun;30[6]:568-78).
“That’s considerable improvement after only 3 weeks of stimulation, which is a very short time, compared to other OCD treatments,” the psychiatrist noted.
In another study, Dr. Hollander and his coinvestigators used the same rTMS regimen targeting the SMA in 22 SSRI-refractory OCD patients. After 3 weeks of rTMS, 12 of the 22 were treatment responders and 3 patients were in remission.
Moreover, these effects were long-lasting. At 6 months, 13 patients were responders and 4 were in remission, and, at 12 months – nearly a year after their relatively brief course of rTMS – there were 12 responders and 3 remitters.
Participants also showed significant reductions on both the Hamilton Depression Rating Scale (HAM-D) and the Hamilton Anxiety Rating Scale (HAM-A), effects that were sustained during follow-up, although the improvement in OCD symptoms was more impressive, he said.
Other investigators also have reported positive results using rTMS for OCD, with the first publication coming from Italian investigators more than a decade ago (Int J Neuropsychopharmacol. 2006 Feb;9[1]:95-100).
Studies of dTMS for OCD are a more recent development. In 2016, investigators reported on 40 OCD patients treated double-blind with either high-stimulation dTMS at 20 Hz, low-stimulation at 1 Hz, or a sham magnetic coil daily for 5 weeks. The target areas were the medial prefrontal and anterior cingulate cortices, areas too deep to be reached using rTMS. At the 5-week mark, the patients who received high-stimulation dTMS showed a mean 26% improvement in YBOCS scores, compared with a 6% reduction in the low-stimulation and sham-treatment arms.
In this study, electroencephalogram evoked potential responses over the anterior cingulate cortex correlated with clinical response, thus providing a welcome biomarker of treatment efficacy.
How TMS works in OCD
TMS involves placing a coil on the scalp to create a magnetic pulse that passes through the skull and achieves predictable changes in neuronal activity in brain tissue, either exciting or deactivating target regions depending upon whether high- or low-frequency TMS is applied.
Brain imaging studies show that OCD is characterized by hyperactivation of the medial frontal cortex and the SMA. The dysfunctional circuitry of OCD has been worked out. It’s striatally based, involving frontal-striatal-thalamic circuits. The SMA sits right above the anterior cingulate cortex and provides access to these key pathways. Basically, increased neuronal activity in the frontal lobes of OCD patients results in miscommunication with the striatal and thalamic regions, with resultant thalamic hyperactivity. This failure of cortical inhibition leads to persistent intrusive thoughts and behaviors, Dr. Hollander explained.
The neural circuitry of OCD is distinct from that of other anxiety disorders, and it appears that TMS is not as effective in those disorders as in OCD, he added.
The anterior cingulate is one step closer than the SMA to the frontal-striatal-thalamic circuits, which are of particular therapeutic interest in OCD, and it’s accessible by dTMS. Anterior cingulate activity is decreased in OCD. When high-frequency dTMS revs up that activity, the result is symptomatic improvement. Of note, the anterior cingulate also is the target for cingulotomy, an established surgical treatment for OCD.
Dr. Hollander reported receiving research funding from the National Institute of Mental Health, the National Institute on Drug Abuse, and the National Institute of Neurological Disorders and Stroke. He serves as a consultant to a number of pharmaceutical companies.
SAN FRANCISCO – Mounting evidence suggests that transcranial magnetic stimulation is an effective noninvasive therapy for obsessive-compulsive disorder refractory to first-line medications, Eric Hollander, MD, said at the annual conference of the Anxiety and Depression Association of America.
A novel treatment for obsessive-compulsive disorder (OCD) would be most welcome. This is a disorder that’s common – affecting 2%-3% of the population – debilitating, and notoriously tough to treat. Roughly half of patients with OCD don’t respond to first-line therapy, which is selective serotonin reuptake inhibitors, cognitive-behavioral therapy, or both, according to Dr. Hollander, director of the autism and obsessive-compulsive spectrum program as well as the anxiety and depression program at Albert Einstein College of Medicine in New York.
Four companies now have FDA-cleared TMS devices indicated for treatment of major depression: Brainsway, which markets a dTMS device, and Neuronetics, MagVenture, and Magstim, which sell repetitive TMS (rTMS) devices that do not penetrate as deeply beneath the skull as dTMS and therefore target different brain structures.
TMS for OCD is, at present, off-label therapy. Yet, there is now sufficient experience derived from formal clinical trials and off-label use in clinical practice to be able to state that the standard target area for rTMS is the supplementary motor area (SMA), according to Dr. Hollander.
He was senior author of a randomized open-label pilot study involving 50 consecutive OCD patients refractory to SSRIs. Half were assigned to a popular second-line strategy: augmentation with antipsychotic agents. The other half received five 20-minute-long rTMS sessions per week for 3 weeks using low-frequency 1 Hz bilateral stimulation of the SMA.
At 3 weeks, the treatment response rate as defined by at least a 25% reduction from baseline on the Yale-Brown Obsessive-Compulsive Scale (YBOCS) was 68% in the rTMS group, compared with 24% in the control arm. Thus, rTMS was better than treatment as usual (J Psychopharmacol. 2016 Jun;30[6]:568-78).
“That’s considerable improvement after only 3 weeks of stimulation, which is a very short time, compared to other OCD treatments,” the psychiatrist noted.
In another study, Dr. Hollander and his coinvestigators used the same rTMS regimen targeting the SMA in 22 SSRI-refractory OCD patients. After 3 weeks of rTMS, 12 of the 22 were treatment responders and 3 patients were in remission.
Moreover, these effects were long-lasting. At 6 months, 13 patients were responders and 4 were in remission, and, at 12 months – nearly a year after their relatively brief course of rTMS – there were 12 responders and 3 remitters.
Participants also showed significant reductions on both the Hamilton Depression Rating Scale (HAM-D) and the Hamilton Anxiety Rating Scale (HAM-A), effects that were sustained during follow-up, although the improvement in OCD symptoms was more impressive, he said.
Other investigators also have reported positive results using rTMS for OCD, with the first publication coming from Italian investigators more than a decade ago (Int J Neuropsychopharmacol. 2006 Feb;9[1]:95-100).
Studies of dTMS for OCD are a more recent development. In 2016, investigators reported on 40 OCD patients treated double-blind with either high-stimulation dTMS at 20 Hz, low-stimulation at 1 Hz, or a sham magnetic coil daily for 5 weeks. The target areas were the medial prefrontal and anterior cingulate cortices, areas too deep to be reached using rTMS. At the 5-week mark, the patients who received high-stimulation dTMS showed a mean 26% improvement in YBOCS scores, compared with a 6% reduction in the low-stimulation and sham-treatment arms.
In this study, electroencephalogram evoked potential responses over the anterior cingulate cortex correlated with clinical response, thus providing a welcome biomarker of treatment efficacy.
How TMS works in OCD
TMS involves placing a coil on the scalp to create a magnetic pulse that passes through the skull and achieves predictable changes in neuronal activity in brain tissue, either exciting or deactivating target regions depending upon whether high- or low-frequency TMS is applied.
Brain imaging studies show that OCD is characterized by hyperactivation of the medial frontal cortex and the SMA. The dysfunctional circuitry of OCD has been worked out. It’s striatally based, involving frontal-striatal-thalamic circuits. The SMA sits right above the anterior cingulate cortex and provides access to these key pathways. Basically, increased neuronal activity in the frontal lobes of OCD patients results in miscommunication with the striatal and thalamic regions, with resultant thalamic hyperactivity. This failure of cortical inhibition leads to persistent intrusive thoughts and behaviors, Dr. Hollander explained.
The neural circuitry of OCD is distinct from that of other anxiety disorders, and it appears that TMS is not as effective in those disorders as in OCD, he added.
The anterior cingulate is one step closer than the SMA to the frontal-striatal-thalamic circuits, which are of particular therapeutic interest in OCD, and it’s accessible by dTMS. Anterior cingulate activity is decreased in OCD. When high-frequency dTMS revs up that activity, the result is symptomatic improvement. Of note, the anterior cingulate also is the target for cingulotomy, an established surgical treatment for OCD.
Dr. Hollander reported receiving research funding from the National Institute of Mental Health, the National Institute on Drug Abuse, and the National Institute of Neurological Disorders and Stroke. He serves as a consultant to a number of pharmaceutical companies.
SAN FRANCISCO – Mounting evidence suggests that transcranial magnetic stimulation is an effective noninvasive therapy for obsessive-compulsive disorder refractory to first-line medications, Eric Hollander, MD, said at the annual conference of the Anxiety and Depression Association of America.
A novel treatment for obsessive-compulsive disorder (OCD) would be most welcome. This is a disorder that’s common – affecting 2%-3% of the population – debilitating, and notoriously tough to treat. Roughly half of patients with OCD don’t respond to first-line therapy, which is selective serotonin reuptake inhibitors, cognitive-behavioral therapy, or both, according to Dr. Hollander, director of the autism and obsessive-compulsive spectrum program as well as the anxiety and depression program at Albert Einstein College of Medicine in New York.
Four companies now have FDA-cleared TMS devices indicated for treatment of major depression: Brainsway, which markets a dTMS device, and Neuronetics, MagVenture, and Magstim, which sell repetitive TMS (rTMS) devices that do not penetrate as deeply beneath the skull as dTMS and therefore target different brain structures.
TMS for OCD is, at present, off-label therapy. Yet, there is now sufficient experience derived from formal clinical trials and off-label use in clinical practice to be able to state that the standard target area for rTMS is the supplementary motor area (SMA), according to Dr. Hollander.
He was senior author of a randomized open-label pilot study involving 50 consecutive OCD patients refractory to SSRIs. Half were assigned to a popular second-line strategy: augmentation with antipsychotic agents. The other half received five 20-minute-long rTMS sessions per week for 3 weeks using low-frequency 1 Hz bilateral stimulation of the SMA.
At 3 weeks, the treatment response rate as defined by at least a 25% reduction from baseline on the Yale-Brown Obsessive-Compulsive Scale (YBOCS) was 68% in the rTMS group, compared with 24% in the control arm. Thus, rTMS was better than treatment as usual (J Psychopharmacol. 2016 Jun;30[6]:568-78).
“That’s considerable improvement after only 3 weeks of stimulation, which is a very short time, compared to other OCD treatments,” the psychiatrist noted.
In another study, Dr. Hollander and his coinvestigators used the same rTMS regimen targeting the SMA in 22 SSRI-refractory OCD patients. After 3 weeks of rTMS, 12 of the 22 were treatment responders and 3 patients were in remission.
Moreover, these effects were long-lasting. At 6 months, 13 patients were responders and 4 were in remission, and, at 12 months – nearly a year after their relatively brief course of rTMS – there were 12 responders and 3 remitters.
Participants also showed significant reductions on both the Hamilton Depression Rating Scale (HAM-D) and the Hamilton Anxiety Rating Scale (HAM-A), effects that were sustained during follow-up, although the improvement in OCD symptoms was more impressive, he said.
Other investigators also have reported positive results using rTMS for OCD, with the first publication coming from Italian investigators more than a decade ago (Int J Neuropsychopharmacol. 2006 Feb;9[1]:95-100).
Studies of dTMS for OCD are a more recent development. In 2016, investigators reported on 40 OCD patients treated double-blind with either high-stimulation dTMS at 20 Hz, low-stimulation at 1 Hz, or a sham magnetic coil daily for 5 weeks. The target areas were the medial prefrontal and anterior cingulate cortices, areas too deep to be reached using rTMS. At the 5-week mark, the patients who received high-stimulation dTMS showed a mean 26% improvement in YBOCS scores, compared with a 6% reduction in the low-stimulation and sham-treatment arms.
In this study, electroencephalogram evoked potential responses over the anterior cingulate cortex correlated with clinical response, thus providing a welcome biomarker of treatment efficacy.
How TMS works in OCD
TMS involves placing a coil on the scalp to create a magnetic pulse that passes through the skull and achieves predictable changes in neuronal activity in brain tissue, either exciting or deactivating target regions depending upon whether high- or low-frequency TMS is applied.
Brain imaging studies show that OCD is characterized by hyperactivation of the medial frontal cortex and the SMA. The dysfunctional circuitry of OCD has been worked out. It’s striatally based, involving frontal-striatal-thalamic circuits. The SMA sits right above the anterior cingulate cortex and provides access to these key pathways. Basically, increased neuronal activity in the frontal lobes of OCD patients results in miscommunication with the striatal and thalamic regions, with resultant thalamic hyperactivity. This failure of cortical inhibition leads to persistent intrusive thoughts and behaviors, Dr. Hollander explained.
The neural circuitry of OCD is distinct from that of other anxiety disorders, and it appears that TMS is not as effective in those disorders as in OCD, he added.
The anterior cingulate is one step closer than the SMA to the frontal-striatal-thalamic circuits, which are of particular therapeutic interest in OCD, and it’s accessible by dTMS. Anterior cingulate activity is decreased in OCD. When high-frequency dTMS revs up that activity, the result is symptomatic improvement. Of note, the anterior cingulate also is the target for cingulotomy, an established surgical treatment for OCD.
Dr. Hollander reported receiving research funding from the National Institute of Mental Health, the National Institute on Drug Abuse, and the National Institute of Neurological Disorders and Stroke. He serves as a consultant to a number of pharmaceutical companies.
EXPERT ANALYSIS FROM THE ANXIETY AND DEPRESSION CONFERENCE 2017
Sacroiliac structural changes show on MRI in nonradiographic axial SpA despite no inflammation
Structural lesions of the sacroiliac joints (SIJ) may be present on MRI in patients with nonradiographic axial spondyloarthritis (nr-axSpA), even when radiographs are normal or inconclusive for such lesions and there is no evidence of inflammation on MRI, according to findings from a cohort of patients in a randomized trial.
In the study, the patients who exhibited such lesions, especially erosions, were more likely to have more severe disease and greater spinal inflammation than were patients who did not have the structural lesions on MRI.
The presence of MRI structural lesions appeared to reflect more severe disease with greater spinal inflammation, the investigators said, based on higher mean SPARCC spinal scores in 23 discovertebral units. The mean number of discovertebral units involved was significantly greater overall among patients with structural lesions (6.5), compared with those without (3.3). Both Bath Ankylosing Spondylitis Activity Index and Bath Ankylosing Spondylitis Functional Index scores were also significantly higher for patients with BME but no MRI structural lesions (a mean of 6.4 cm and 4.6 cm, respectively), when compared with patients who had both (a mean of 5.7 cm and 3.7 cm, respectively).
Age, sex, and HLA-B27 status also appeared to play a role in the frequency with which MRI structural lesions coexisted with BME. The group of patients with both BME and structural lesions in the sacroiliac joint were significantly more often male (83% vs. 48%), younger (mean age of 30 vs. 34 years), and HLA-B27 positive (87% vs. 63%) than in those with only BME.
“These data support the concept that nr-axSpA is an early stage of axSpA and that structural lesions in the SIJ are associated with a more severe phenotype characterized by more active spinal inflammation,” the investigators wrote.
The presence of structural lesions might also identify patients who would benefit the most from early treatment with biologics, they suggested. “It has been suggested that there is a window of opportunity for disease modification with anti-inflammatory agents by treating acute inflammatory lesions before bone formation pathways are triggered in more complex inflammatory lesions. Consequently, the presence of structural lesions in the SIJ may help select patients for intervention with anti-TNF agents early in the disease course.”
The study was funded by Pfizer. Three of the authors are employees of Pfizer. Two authors have received consulting fees and/or research funding/grants from a variety of companies that make drugs for the treatment of ankylosing spondylitis, including Pfizer.
Structural lesions of the sacroiliac joints (SIJ) may be present on MRI in patients with nonradiographic axial spondyloarthritis (nr-axSpA), even when radiographs are normal or inconclusive for such lesions and there is no evidence of inflammation on MRI, according to findings from a cohort of patients in a randomized trial.
In the study, the patients who exhibited such lesions, especially erosions, were more likely to have more severe disease and greater spinal inflammation than were patients who did not have the structural lesions on MRI.
The presence of MRI structural lesions appeared to reflect more severe disease with greater spinal inflammation, the investigators said, based on higher mean SPARCC spinal scores in 23 discovertebral units. The mean number of discovertebral units involved was significantly greater overall among patients with structural lesions (6.5), compared with those without (3.3). Both Bath Ankylosing Spondylitis Activity Index and Bath Ankylosing Spondylitis Functional Index scores were also significantly higher for patients with BME but no MRI structural lesions (a mean of 6.4 cm and 4.6 cm, respectively), when compared with patients who had both (a mean of 5.7 cm and 3.7 cm, respectively).
Age, sex, and HLA-B27 status also appeared to play a role in the frequency with which MRI structural lesions coexisted with BME. The group of patients with both BME and structural lesions in the sacroiliac joint were significantly more often male (83% vs. 48%), younger (mean age of 30 vs. 34 years), and HLA-B27 positive (87% vs. 63%) than in those with only BME.
“These data support the concept that nr-axSpA is an early stage of axSpA and that structural lesions in the SIJ are associated with a more severe phenotype characterized by more active spinal inflammation,” the investigators wrote.
The presence of structural lesions might also identify patients who would benefit the most from early treatment with biologics, they suggested. “It has been suggested that there is a window of opportunity for disease modification with anti-inflammatory agents by treating acute inflammatory lesions before bone formation pathways are triggered in more complex inflammatory lesions. Consequently, the presence of structural lesions in the SIJ may help select patients for intervention with anti-TNF agents early in the disease course.”
The study was funded by Pfizer. Three of the authors are employees of Pfizer. Two authors have received consulting fees and/or research funding/grants from a variety of companies that make drugs for the treatment of ankylosing spondylitis, including Pfizer.
Structural lesions of the sacroiliac joints (SIJ) may be present on MRI in patients with nonradiographic axial spondyloarthritis (nr-axSpA), even when radiographs are normal or inconclusive for such lesions and there is no evidence of inflammation on MRI, according to findings from a cohort of patients in a randomized trial.
In the study, the patients who exhibited such lesions, especially erosions, were more likely to have more severe disease and greater spinal inflammation than were patients who did not have the structural lesions on MRI.
The presence of MRI structural lesions appeared to reflect more severe disease with greater spinal inflammation, the investigators said, based on higher mean SPARCC spinal scores in 23 discovertebral units. The mean number of discovertebral units involved was significantly greater overall among patients with structural lesions (6.5), compared with those without (3.3). Both Bath Ankylosing Spondylitis Activity Index and Bath Ankylosing Spondylitis Functional Index scores were also significantly higher for patients with BME but no MRI structural lesions (a mean of 6.4 cm and 4.6 cm, respectively), when compared with patients who had both (a mean of 5.7 cm and 3.7 cm, respectively).
Age, sex, and HLA-B27 status also appeared to play a role in the frequency with which MRI structural lesions coexisted with BME. The group of patients with both BME and structural lesions in the sacroiliac joint were significantly more often male (83% vs. 48%), younger (mean age of 30 vs. 34 years), and HLA-B27 positive (87% vs. 63%) than in those with only BME.
“These data support the concept that nr-axSpA is an early stage of axSpA and that structural lesions in the SIJ are associated with a more severe phenotype characterized by more active spinal inflammation,” the investigators wrote.
The presence of structural lesions might also identify patients who would benefit the most from early treatment with biologics, they suggested. “It has been suggested that there is a window of opportunity for disease modification with anti-inflammatory agents by treating acute inflammatory lesions before bone formation pathways are triggered in more complex inflammatory lesions. Consequently, the presence of structural lesions in the SIJ may help select patients for intervention with anti-TNF agents early in the disease course.”
The study was funded by Pfizer. Three of the authors are employees of Pfizer. Two authors have received consulting fees and/or research funding/grants from a variety of companies that make drugs for the treatment of ankylosing spondylitis, including Pfizer.
FROM ARTHRITIS RESEARCH & THERAPY
Key clinical point:
Major finding: Sacroiliac joint erosions on MRI occurred in 11% of patients who did not have bone marrow edema, which was significantly less than its occurrence in 45% of those with BME.
Data source: A study of 183 patients with nr-axSpA who had participated in a treatment trial.
Disclosures: The study was funded by Pfizer. Three of the authors are employees of Pfizer. Two authors have received consulting fees and/or research funding/grants from a variety of companies that make drugs for the treatment of ankylosing spondylitis, including Pfizer.
Who’s best suited for Internet-based CBT?
SAN FRANCISCO – Nearly 6% of patients deteriorated during Internet-based cognitive-behavioral therapy (iCBT) in an individual patient data meta-analysis totaling 2,866 participants in 29 published clinical trials, Alexander Rozental, PhD, reported at the annual conference of the Anxiety and Depression Association of America.
On the other hand, the meta-analysis also highlighted the hazards of doing nothing for patients experiencing mental distress: 17.4% of patients deteriorated while in wait-list control groups in the 29 trials, a rate of harm triple the 5.8% deterioration rate in patients during iCBT, added Dr. Rozental, a clinical psychologist at Stockholm University.
This meta-analysis is one of the very few studies to look at the negative effects of a psychologic treatment. Psychotherapy research has focused almost entirely on the positive effects. That’s at odds with the way pharmacologic research is conducted, in which reporting of adverse events is mandatory, he noted.
Of patients in the meta-analysis, 61% sought treatment for anxiety disorders, 20% for depression, and the rest for erectile dysfunction, pathological gambling, or relationship problems.
iCBT is particularly popular in Sweden, where it was developed two decades ago as a means of disseminating evidence-based, manualized therapy to a broad population in a highly cost-effective manner. This form of psychotherapy typically entails 8 to 12 weekly treatment modules, with weekly assignments, predetermined deadlines, texts and exercises, and regular, albeit relatively brief, contact with a therapist via secure email.
Dr. Rozental and his coinvestigators reviewed individual patient data in search of predictors of treatment success or deterioration. A profile emerged of the patients least likely to deteriorate while on iCBT: older age, university-educated, in a stable relationship, and with a higher level of symptoms pretreatment.
“You might interpret the findings as an indicator for matching the right type of treatment to the right patient. Perhaps those [who] are younger, have less than a university degree, and are not in a relationship might be better off in a face to face treatment, at least in terms of preventing deterioration,” he observed in an interview. “This makes sense if you think about the amount of work you have to do on your own in Internet-based psychological treatments, which include limited access to a therapist and require reading a lot of text material.”
Patients participating in iCBT who fit that profile might need extra support from a therapist in order to improve, Dr. Rozental added.
He reported having no financial conflicts regarding his study, which was funded by the Swedish Research Council for Health, Working Life, and Welfare.
SAN FRANCISCO – Nearly 6% of patients deteriorated during Internet-based cognitive-behavioral therapy (iCBT) in an individual patient data meta-analysis totaling 2,866 participants in 29 published clinical trials, Alexander Rozental, PhD, reported at the annual conference of the Anxiety and Depression Association of America.
On the other hand, the meta-analysis also highlighted the hazards of doing nothing for patients experiencing mental distress: 17.4% of patients deteriorated while in wait-list control groups in the 29 trials, a rate of harm triple the 5.8% deterioration rate in patients during iCBT, added Dr. Rozental, a clinical psychologist at Stockholm University.
This meta-analysis is one of the very few studies to look at the negative effects of a psychologic treatment. Psychotherapy research has focused almost entirely on the positive effects. That’s at odds with the way pharmacologic research is conducted, in which reporting of adverse events is mandatory, he noted.
Of patients in the meta-analysis, 61% sought treatment for anxiety disorders, 20% for depression, and the rest for erectile dysfunction, pathological gambling, or relationship problems.
iCBT is particularly popular in Sweden, where it was developed two decades ago as a means of disseminating evidence-based, manualized therapy to a broad population in a highly cost-effective manner. This form of psychotherapy typically entails 8 to 12 weekly treatment modules, with weekly assignments, predetermined deadlines, texts and exercises, and regular, albeit relatively brief, contact with a therapist via secure email.
Dr. Rozental and his coinvestigators reviewed individual patient data in search of predictors of treatment success or deterioration. A profile emerged of the patients least likely to deteriorate while on iCBT: older age, university-educated, in a stable relationship, and with a higher level of symptoms pretreatment.
“You might interpret the findings as an indicator for matching the right type of treatment to the right patient. Perhaps those [who] are younger, have less than a university degree, and are not in a relationship might be better off in a face to face treatment, at least in terms of preventing deterioration,” he observed in an interview. “This makes sense if you think about the amount of work you have to do on your own in Internet-based psychological treatments, which include limited access to a therapist and require reading a lot of text material.”
Patients participating in iCBT who fit that profile might need extra support from a therapist in order to improve, Dr. Rozental added.
He reported having no financial conflicts regarding his study, which was funded by the Swedish Research Council for Health, Working Life, and Welfare.
SAN FRANCISCO – Nearly 6% of patients deteriorated during Internet-based cognitive-behavioral therapy (iCBT) in an individual patient data meta-analysis totaling 2,866 participants in 29 published clinical trials, Alexander Rozental, PhD, reported at the annual conference of the Anxiety and Depression Association of America.
On the other hand, the meta-analysis also highlighted the hazards of doing nothing for patients experiencing mental distress: 17.4% of patients deteriorated while in wait-list control groups in the 29 trials, a rate of harm triple the 5.8% deterioration rate in patients during iCBT, added Dr. Rozental, a clinical psychologist at Stockholm University.
This meta-analysis is one of the very few studies to look at the negative effects of a psychologic treatment. Psychotherapy research has focused almost entirely on the positive effects. That’s at odds with the way pharmacologic research is conducted, in which reporting of adverse events is mandatory, he noted.
Of patients in the meta-analysis, 61% sought treatment for anxiety disorders, 20% for depression, and the rest for erectile dysfunction, pathological gambling, or relationship problems.
iCBT is particularly popular in Sweden, where it was developed two decades ago as a means of disseminating evidence-based, manualized therapy to a broad population in a highly cost-effective manner. This form of psychotherapy typically entails 8 to 12 weekly treatment modules, with weekly assignments, predetermined deadlines, texts and exercises, and regular, albeit relatively brief, contact with a therapist via secure email.
Dr. Rozental and his coinvestigators reviewed individual patient data in search of predictors of treatment success or deterioration. A profile emerged of the patients least likely to deteriorate while on iCBT: older age, university-educated, in a stable relationship, and with a higher level of symptoms pretreatment.
“You might interpret the findings as an indicator for matching the right type of treatment to the right patient. Perhaps those [who] are younger, have less than a university degree, and are not in a relationship might be better off in a face to face treatment, at least in terms of preventing deterioration,” he observed in an interview. “This makes sense if you think about the amount of work you have to do on your own in Internet-based psychological treatments, which include limited access to a therapist and require reading a lot of text material.”
Patients participating in iCBT who fit that profile might need extra support from a therapist in order to improve, Dr. Rozental added.
He reported having no financial conflicts regarding his study, which was funded by the Swedish Research Council for Health, Working Life, and Welfare.
AT THE ANXIETY AND DEPRESSION CONFERENCE 2017
Key clinical point:
Major finding: Slightly less than 6% of patients deteriorated while participating in Internet-based cognitive-behavioral therapy, mostly for anxiety disorders or depression.
Data source: This individual patient data meta-analysis involved 2,866 participants in 29 published clinical trials of internet-based cognitive-behavioral therapy.
Disclosures: The study was funded by the Swedish Research Council for Health, Working Life, and Welfare. The presenter reported having no financial conflicts.