User login
Comparison of immunosuppressants for early diffuse systemic sclerosis yields mixed results
Placing patients who have early diffuse cutaneous systemic sclerosis (dcSSc ) on an immunosuppressant regimen can have a beneficial, but not necessarily sustainable, impact, according to findings from the European Scleroderma Observational Study.
“At present, there is no drug known to favorably influence disease course [because] randomized controlled trials have historically been confounded by disease rarity [and] strict entry criteria,” wrote the study investigators – led by Ariane L. Herrick, MD, of the University of Manchester (England). They sought to get around the lack of randomized, controlled trial data by comparing observational data on “the effectiveness of standard treatment approaches [in] the early management of patients with dcSSc.”
The patients receiving methotrexate had a target dose of 20-25 mg/week, either orally or subcutaneously. Patients on MMF were given two 500-mg doses a day for 2 weeks, then two 1-g doses daily. Cyclophosphamide regimens varied based on the centers, with some patients receiving one IV 500-mg/m2 dose monthly for 6-12 months and others receiving a daily dose of 1-2 mg/kg/day orally for 12 months, with most being transferred later to maintenance with methotrexate, MMF, or azathioprine. All patients underwent assessment at baseline and then every 3 months for the trial duration of 24 months; however, because the study occurred during 2010-2014 and some patients were recruited in 2013, those who joined after September 2013 were followed for only 12-24 months. Of the 326 subjects enrolled, 276 completed 12 months of follow-up and 234 completed 24 months (Ann Rheum Dis. 2017 Feb 10. doi: 10.1136/annrheumdis-2016-210503).
After weighting the 12-month outcomes between the groups by equalizing the distribution of confounding variables, all groups experienced a significant reduction in the study’s primary outcome measure, the modified Rodnan skin score (mRSS), which can range from 0 to 51. From a median baseline mRSS of 21 (interquartile range of 16-27), the mRSS for the methotrexate group fell 4.0 (IQR −5.2 to −2.7), for those on MMF it dropped 4.1 (IQR −5.3 to −2.9), for the cyclophosphamide group it decreased 3.3 (IQR −4.9 to −1.7), and for those on no immunosuppressants it dropped 2.2 (IQR −4.0 to −0.3). There were no significant differences between the groups.
Although none of the treatments had a significant effect on improving forced vital capacity (FVC) or carbon monoxide–diffusing capacity in the groups overall, the subgroup of patients with confirmed or suspected pulmonary fibrosis showed a significant difference in the rate of change over time for FVC in patients who were initially prescribed cyclophosphamide (7.4% absolute increase), but not for MMF (3.2% increase), methotrexate (2.0% decrease), or no immunosuppressant (4.0% increase). The investigators noted that this finding “confirms the relative effectiveness of cyclophosphamide in patients with pulmonary fibrosis.”
At 24 months, there were no significant differences in mortality between the four groups. After weighting, the predicted survival rates were 94% for methotrexate, 89% for MMF, 90% for cyclophosphamide, and 84% for those with no immunosuppressants. All three immunosuppressants also showed no significant difference in terms of tolerability. At this point in time, the rate of adherence to the initial protocol was comparable between the groups: 76% for methotrexate, 80% for MMF, 79% for cyclophosphamide, and 73% for those not taking an immunosuppressant, although 10 who started without an immunosuppressant later started one.
“An important point when interpreting our findings (and therefore a note of caution) is that the ‘no immunosuppressant’ group was not a control group,” Dr. Herrick and her coauthors wrote. “Patients in this group had a longer disease duration than the other three groups and were more likely to have renal involvement.”
Nevertheless, the authors contend that these findings carry a strong take-home message for clinicians: “There is a weak signal to support using immunosuppressants for early dcSSc (and in particular cyclophosphamide for patients with pulmonary fibrosis). However, it is clear that there remains a pressing need for the development of more effective and targeted treatments.”
The study was funded by a grant from the European League Against Rheumatism’s Orphan Disease Program, and additional support from Scleroderma and Raynaud’s UK. Dr. Herrick disclosed relationships with Actelion, Apricus, and GlaxoSmithKline; her coauthors disclosed numerous financial relationships of their own.
Placing patients who have early diffuse cutaneous systemic sclerosis (dcSSc ) on an immunosuppressant regimen can have a beneficial, but not necessarily sustainable, impact, according to findings from the European Scleroderma Observational Study.
“At present, there is no drug known to favorably influence disease course [because] randomized controlled trials have historically been confounded by disease rarity [and] strict entry criteria,” wrote the study investigators – led by Ariane L. Herrick, MD, of the University of Manchester (England). They sought to get around the lack of randomized, controlled trial data by comparing observational data on “the effectiveness of standard treatment approaches [in] the early management of patients with dcSSc.”
The patients receiving methotrexate had a target dose of 20-25 mg/week, either orally or subcutaneously. Patients on MMF were given two 500-mg doses a day for 2 weeks, then two 1-g doses daily. Cyclophosphamide regimens varied based on the centers, with some patients receiving one IV 500-mg/m2 dose monthly for 6-12 months and others receiving a daily dose of 1-2 mg/kg/day orally for 12 months, with most being transferred later to maintenance with methotrexate, MMF, or azathioprine. All patients underwent assessment at baseline and then every 3 months for the trial duration of 24 months; however, because the study occurred during 2010-2014 and some patients were recruited in 2013, those who joined after September 2013 were followed for only 12-24 months. Of the 326 subjects enrolled, 276 completed 12 months of follow-up and 234 completed 24 months (Ann Rheum Dis. 2017 Feb 10. doi: 10.1136/annrheumdis-2016-210503).
After weighting the 12-month outcomes between the groups by equalizing the distribution of confounding variables, all groups experienced a significant reduction in the study’s primary outcome measure, the modified Rodnan skin score (mRSS), which can range from 0 to 51. From a median baseline mRSS of 21 (interquartile range of 16-27), the mRSS for the methotrexate group fell 4.0 (IQR −5.2 to −2.7), for those on MMF it dropped 4.1 (IQR −5.3 to −2.9), for the cyclophosphamide group it decreased 3.3 (IQR −4.9 to −1.7), and for those on no immunosuppressants it dropped 2.2 (IQR −4.0 to −0.3). There were no significant differences between the groups.
Although none of the treatments had a significant effect on improving forced vital capacity (FVC) or carbon monoxide–diffusing capacity in the groups overall, the subgroup of patients with confirmed or suspected pulmonary fibrosis showed a significant difference in the rate of change over time for FVC in patients who were initially prescribed cyclophosphamide (7.4% absolute increase), but not for MMF (3.2% increase), methotrexate (2.0% decrease), or no immunosuppressant (4.0% increase). The investigators noted that this finding “confirms the relative effectiveness of cyclophosphamide in patients with pulmonary fibrosis.”
At 24 months, there were no significant differences in mortality between the four groups. After weighting, the predicted survival rates were 94% for methotrexate, 89% for MMF, 90% for cyclophosphamide, and 84% for those with no immunosuppressants. All three immunosuppressants also showed no significant difference in terms of tolerability. At this point in time, the rate of adherence to the initial protocol was comparable between the groups: 76% for methotrexate, 80% for MMF, 79% for cyclophosphamide, and 73% for those not taking an immunosuppressant, although 10 who started without an immunosuppressant later started one.
“An important point when interpreting our findings (and therefore a note of caution) is that the ‘no immunosuppressant’ group was not a control group,” Dr. Herrick and her coauthors wrote. “Patients in this group had a longer disease duration than the other three groups and were more likely to have renal involvement.”
Nevertheless, the authors contend that these findings carry a strong take-home message for clinicians: “There is a weak signal to support using immunosuppressants for early dcSSc (and in particular cyclophosphamide for patients with pulmonary fibrosis). However, it is clear that there remains a pressing need for the development of more effective and targeted treatments.”
The study was funded by a grant from the European League Against Rheumatism’s Orphan Disease Program, and additional support from Scleroderma and Raynaud’s UK. Dr. Herrick disclosed relationships with Actelion, Apricus, and GlaxoSmithKline; her coauthors disclosed numerous financial relationships of their own.
Placing patients who have early diffuse cutaneous systemic sclerosis (dcSSc ) on an immunosuppressant regimen can have a beneficial, but not necessarily sustainable, impact, according to findings from the European Scleroderma Observational Study.
“At present, there is no drug known to favorably influence disease course [because] randomized controlled trials have historically been confounded by disease rarity [and] strict entry criteria,” wrote the study investigators – led by Ariane L. Herrick, MD, of the University of Manchester (England). They sought to get around the lack of randomized, controlled trial data by comparing observational data on “the effectiveness of standard treatment approaches [in] the early management of patients with dcSSc.”
The patients receiving methotrexate had a target dose of 20-25 mg/week, either orally or subcutaneously. Patients on MMF were given two 500-mg doses a day for 2 weeks, then two 1-g doses daily. Cyclophosphamide regimens varied based on the centers, with some patients receiving one IV 500-mg/m2 dose monthly for 6-12 months and others receiving a daily dose of 1-2 mg/kg/day orally for 12 months, with most being transferred later to maintenance with methotrexate, MMF, or azathioprine. All patients underwent assessment at baseline and then every 3 months for the trial duration of 24 months; however, because the study occurred during 2010-2014 and some patients were recruited in 2013, those who joined after September 2013 were followed for only 12-24 months. Of the 326 subjects enrolled, 276 completed 12 months of follow-up and 234 completed 24 months (Ann Rheum Dis. 2017 Feb 10. doi: 10.1136/annrheumdis-2016-210503).
After weighting the 12-month outcomes between the groups by equalizing the distribution of confounding variables, all groups experienced a significant reduction in the study’s primary outcome measure, the modified Rodnan skin score (mRSS), which can range from 0 to 51. From a median baseline mRSS of 21 (interquartile range of 16-27), the mRSS for the methotrexate group fell 4.0 (IQR −5.2 to −2.7), for those on MMF it dropped 4.1 (IQR −5.3 to −2.9), for the cyclophosphamide group it decreased 3.3 (IQR −4.9 to −1.7), and for those on no immunosuppressants it dropped 2.2 (IQR −4.0 to −0.3). There were no significant differences between the groups.
Although none of the treatments had a significant effect on improving forced vital capacity (FVC) or carbon monoxide–diffusing capacity in the groups overall, the subgroup of patients with confirmed or suspected pulmonary fibrosis showed a significant difference in the rate of change over time for FVC in patients who were initially prescribed cyclophosphamide (7.4% absolute increase), but not for MMF (3.2% increase), methotrexate (2.0% decrease), or no immunosuppressant (4.0% increase). The investigators noted that this finding “confirms the relative effectiveness of cyclophosphamide in patients with pulmonary fibrosis.”
At 24 months, there were no significant differences in mortality between the four groups. After weighting, the predicted survival rates were 94% for methotrexate, 89% for MMF, 90% for cyclophosphamide, and 84% for those with no immunosuppressants. All three immunosuppressants also showed no significant difference in terms of tolerability. At this point in time, the rate of adherence to the initial protocol was comparable between the groups: 76% for methotrexate, 80% for MMF, 79% for cyclophosphamide, and 73% for those not taking an immunosuppressant, although 10 who started without an immunosuppressant later started one.
“An important point when interpreting our findings (and therefore a note of caution) is that the ‘no immunosuppressant’ group was not a control group,” Dr. Herrick and her coauthors wrote. “Patients in this group had a longer disease duration than the other three groups and were more likely to have renal involvement.”
Nevertheless, the authors contend that these findings carry a strong take-home message for clinicians: “There is a weak signal to support using immunosuppressants for early dcSSc (and in particular cyclophosphamide for patients with pulmonary fibrosis). However, it is clear that there remains a pressing need for the development of more effective and targeted treatments.”
The study was funded by a grant from the European League Against Rheumatism’s Orphan Disease Program, and additional support from Scleroderma and Raynaud’s UK. Dr. Herrick disclosed relationships with Actelion, Apricus, and GlaxoSmithKline; her coauthors disclosed numerous financial relationships of their own.
FROM ANNALS OF THE RHEUMATIC DISEASES
Key clinical point:
Major finding: Subjects taking no immunosuppressants showed significant reduction in mRSS over 12 months (2.2; IQR, −4.0 to −0.3), but no significant difference in survival rates over 24 months.
Data source: A prospective, observational cohort study of 326 dcSSc patients recruited in 2010-2014.
Disclosures: Funded by EULAR and Scleroderma and Raynaud’s UK. Authors reported numerous financial relationships.
Infections boost postop wound dehiscence risk
SAN DIEGO – Pre- and postsurgical infections top the list of factors in putting patients at risk of wound dehiscence after laparotomy, a database study has found.
Before surgery, a contaminated or dirty wound and sepsis doubled the risk of a post-laparotomy dehiscence, Anam Pal*, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
After surgery, a deep wound infection raised the risk by more than four times, and a superficial wound infection almost tripled the risk, said Dr. Pal, a second-year surgical resident at Hofstra Northwell School of Medicine at Staten Island University Hospital Program, New York.*
“Since infections are the strongest predictors, we need more aggressive efforts to prevent surgical site infections in these patients,” she said. Any patient who displays these risk factors should have retention sutures placed during closing as an extra measure of precaution against the potentially devastating complication.
Dr. Pal said the time is right for a new risk model of wound dehiscence after abdominal laparotomy. The existing predictive tool is almost 20 years old and was validated in the Veterans Affairs Surgical Quality Improvement Program database.
“This risk score was created using patient data gathered from 1996 to 1998 on the VA population. We know that this group is older and sicker than the general population,” she said. In fact, she ran that calculation on her own dataset and found that it “grossly overestimated” the risk of wound dehiscence in a general population. “This raises questions about the generalizability of that score.”
Among the 18,306 exploratory laparotomies in Dr. Pal’s dataset, there were 275 cases of wound dehiscence, for a rate of 1.5%.
There were striking baseline differences between the patient groups, she noted. Generally, patients with wound dehiscence were sicker and frailer than those without. “There was significantly more smoking, chronic obstructive pulmonary disease, diabetes, pneumonia and ventilator placement, obesity, and disseminated malignancy.”
She also noted significantly higher rates of wound infection and steroid use. Patients with dehiscence were significantly less likely to have lost weight during the 6 months before their laparotomy as well.
They were more likely to have sepsis or septic shock, to present emergently, and to have had a surgery within the 30 days prior. Functionally, they were significantly more likely to be rated as “totally dependent.”
A multivariate analysis identified six preoperative and four postoperative risk factors:
Preoperative
• Contaminated/dirty wound – odds ratio 2.00.
• Sepsis/septic shock – OR 1.85.
• Totally dependent status – OR 1.8.
• Male gender – OR 1.6.
• ASA class 3 or greater – OR 1.4.
• Smoking – OR 1.3.
• Weight loss protective – OR 0.44.
Postoperative
• Deep wound infection – OR 4.25.
• Superficial wound infection – OR 2.76.
• Reintubation – OR 2.38.
• Deep space infection – OR 1.67.
The investigators then split the data randomly into a 75% training cohort and 25% validation cohort. A receiver operator curve analysis determined that both cohorts had an AUC of around 0.70, meaning that the model was a moderate-good predictor of wound dehiscence.
“Our predictive model is just as good as the one that was developed 20 years ago,” and potentially, more appropriate for a general population, Dr. Pal concluded.
She had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
*An earlier version of this article misstated Dr. Pal's name and affiliation.
SAN DIEGO – Pre- and postsurgical infections top the list of factors in putting patients at risk of wound dehiscence after laparotomy, a database study has found.
Before surgery, a contaminated or dirty wound and sepsis doubled the risk of a post-laparotomy dehiscence, Anam Pal*, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
After surgery, a deep wound infection raised the risk by more than four times, and a superficial wound infection almost tripled the risk, said Dr. Pal, a second-year surgical resident at Hofstra Northwell School of Medicine at Staten Island University Hospital Program, New York.*
“Since infections are the strongest predictors, we need more aggressive efforts to prevent surgical site infections in these patients,” she said. Any patient who displays these risk factors should have retention sutures placed during closing as an extra measure of precaution against the potentially devastating complication.
Dr. Pal said the time is right for a new risk model of wound dehiscence after abdominal laparotomy. The existing predictive tool is almost 20 years old and was validated in the Veterans Affairs Surgical Quality Improvement Program database.
“This risk score was created using patient data gathered from 1996 to 1998 on the VA population. We know that this group is older and sicker than the general population,” she said. In fact, she ran that calculation on her own dataset and found that it “grossly overestimated” the risk of wound dehiscence in a general population. “This raises questions about the generalizability of that score.”
Among the 18,306 exploratory laparotomies in Dr. Pal’s dataset, there were 275 cases of wound dehiscence, for a rate of 1.5%.
There were striking baseline differences between the patient groups, she noted. Generally, patients with wound dehiscence were sicker and frailer than those without. “There was significantly more smoking, chronic obstructive pulmonary disease, diabetes, pneumonia and ventilator placement, obesity, and disseminated malignancy.”
She also noted significantly higher rates of wound infection and steroid use. Patients with dehiscence were significantly less likely to have lost weight during the 6 months before their laparotomy as well.
They were more likely to have sepsis or septic shock, to present emergently, and to have had a surgery within the 30 days prior. Functionally, they were significantly more likely to be rated as “totally dependent.”
A multivariate analysis identified six preoperative and four postoperative risk factors:
Preoperative
• Contaminated/dirty wound – odds ratio 2.00.
• Sepsis/septic shock – OR 1.85.
• Totally dependent status – OR 1.8.
• Male gender – OR 1.6.
• ASA class 3 or greater – OR 1.4.
• Smoking – OR 1.3.
• Weight loss protective – OR 0.44.
Postoperative
• Deep wound infection – OR 4.25.
• Superficial wound infection – OR 2.76.
• Reintubation – OR 2.38.
• Deep space infection – OR 1.67.
The investigators then split the data randomly into a 75% training cohort and 25% validation cohort. A receiver operator curve analysis determined that both cohorts had an AUC of around 0.70, meaning that the model was a moderate-good predictor of wound dehiscence.
“Our predictive model is just as good as the one that was developed 20 years ago,” and potentially, more appropriate for a general population, Dr. Pal concluded.
She had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
*An earlier version of this article misstated Dr. Pal's name and affiliation.
SAN DIEGO – Pre- and postsurgical infections top the list of factors in putting patients at risk of wound dehiscence after laparotomy, a database study has found.
Before surgery, a contaminated or dirty wound and sepsis doubled the risk of a post-laparotomy dehiscence, Anam Pal*, MD, said at the Association for Academic Surgery/Society of University Surgeons Academic Surgical Congress.
After surgery, a deep wound infection raised the risk by more than four times, and a superficial wound infection almost tripled the risk, said Dr. Pal, a second-year surgical resident at Hofstra Northwell School of Medicine at Staten Island University Hospital Program, New York.*
“Since infections are the strongest predictors, we need more aggressive efforts to prevent surgical site infections in these patients,” she said. Any patient who displays these risk factors should have retention sutures placed during closing as an extra measure of precaution against the potentially devastating complication.
Dr. Pal said the time is right for a new risk model of wound dehiscence after abdominal laparotomy. The existing predictive tool is almost 20 years old and was validated in the Veterans Affairs Surgical Quality Improvement Program database.
“This risk score was created using patient data gathered from 1996 to 1998 on the VA population. We know that this group is older and sicker than the general population,” she said. In fact, she ran that calculation on her own dataset and found that it “grossly overestimated” the risk of wound dehiscence in a general population. “This raises questions about the generalizability of that score.”
Among the 18,306 exploratory laparotomies in Dr. Pal’s dataset, there were 275 cases of wound dehiscence, for a rate of 1.5%.
There were striking baseline differences between the patient groups, she noted. Generally, patients with wound dehiscence were sicker and frailer than those without. “There was significantly more smoking, chronic obstructive pulmonary disease, diabetes, pneumonia and ventilator placement, obesity, and disseminated malignancy.”
She also noted significantly higher rates of wound infection and steroid use. Patients with dehiscence were significantly less likely to have lost weight during the 6 months before their laparotomy as well.
They were more likely to have sepsis or septic shock, to present emergently, and to have had a surgery within the 30 days prior. Functionally, they were significantly more likely to be rated as “totally dependent.”
A multivariate analysis identified six preoperative and four postoperative risk factors:
Preoperative
• Contaminated/dirty wound – odds ratio 2.00.
• Sepsis/septic shock – OR 1.85.
• Totally dependent status – OR 1.8.
• Male gender – OR 1.6.
• ASA class 3 or greater – OR 1.4.
• Smoking – OR 1.3.
• Weight loss protective – OR 0.44.
Postoperative
• Deep wound infection – OR 4.25.
• Superficial wound infection – OR 2.76.
• Reintubation – OR 2.38.
• Deep space infection – OR 1.67.
The investigators then split the data randomly into a 75% training cohort and 25% validation cohort. A receiver operator curve analysis determined that both cohorts had an AUC of around 0.70, meaning that the model was a moderate-good predictor of wound dehiscence.
“Our predictive model is just as good as the one that was developed 20 years ago,” and potentially, more appropriate for a general population, Dr. Pal concluded.
She had no financial disclosures.
[email protected]
On Twitter @Alz_Gal
*An earlier version of this article misstated Dr. Pal's name and affiliation.
AT THE ACADEMIC SURGICAL CONGRESS
Key clinical point:
Major finding: Deep wound infection quadrupled the risk of wound dehiscence and superficial wound infection almost tripled it.
Data source: The ACS NSQIP review comprised more than 18,000 operations.
Disclosures: Dr. Pal had no financial disclosures.
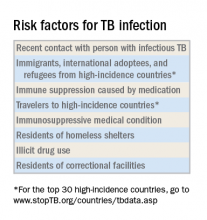
Mycobacterium tuberculosis: Overcoming one obstacle on the road to elimination
March 24 is World TB Day. It was on this date in 1882 that physician Robert Koch announced the discovery of Mycobacterium tuberculosis, the causative agent of tuberculosis. Worldwide, activities are planned to raise awareness of TB and to support initiatives for prevention, better control, and ultimately the elimination of this disease.
Globally in 2015, the World Health Organization estimated there were 10.4 million new cases of TB, including 1 million in children. Data from the United States reveal that after 20 years of annual decline, the incidence of TB has plateaued. In 2015, 9,563 cases of TB disease were reported, including 440 cases in children less than 15 years of age. While the overall incidence was 3 cases per 100,000, the incidence among foreign-born persons was 15.1 cases per 100,000. There were 3,201 cases (33.5%) among U.S.-born individuals. Foreign-born persons accounted for 66.2% of cases; however, the majority of those cases were diagnosed several years after their arrival in the United States. The top five countries of origin of these individuals were China, India, Mexico, the Philippines, and Vietnam. In contrast, only one-quarter of all pediatric cases occurred in foreign-born children. Four states (California, Florida, New York, and Texas) reported more than 500 cases each in 2015, as they have for the last 7 consecutive years. In 2015, these states accounted for slightly more than half (4,839) of all cases (MMWR 2016 Mar 25;65[11]:273-8).
Why as pediatricians should we be concerned? TB in a child is a sentinel event and represents recent or ongoing transmission. Young children who are infected are more likely to progress to TB disease and develop severe manifestations such as miliary TB or meningitis. Children less than 4 years old and those with certain underlying disorders, including those with an immunodeficiency or who are receiving immunosuppressive agents, also are at greater risk for progression from infection to disease. Other predictors of disease progression include diagnosis of the infection within the past 2 years, use of chemotherapy and high-dose corticosteroids, as well as certain cancers, diabetes, and chronic renal failure.
Once infected, most children and adolescents remain asymptomatic. If disease occurs, symptoms develop 1-6 months after infection and include fever, cough, weight loss or failure to thrive, night sweats, and chills. Chest radiographic findings are nonspecific. Infiltrates and intrathoracic lymph node enlargement may or may not be present. However, our goal is to diagnose at-risk children with infection, treat them, and avoid their progression to TB disease.
Screening tests
The interferon-gamma release assay is a blood test that has a greater specificity than TST and requires only one visit. A positive test is seen in both latent TB infection and TB disease. There is no cross-reaction with BCG. This is the ideal test for prior BCG recipients and others who are unlikely to return for TST readings and are at least 5 years of age.
A chest radiograph is required to differentiate latent TB infection from TB disease. Latent TB infection is diagnosed when there is an absence of parenchymal disease, opacification, or intrathoracic adenopathy.
Treatment of latent TB infection versus TB disease is beyond the scope of this article. Consultation with an infectious disease expert is recommended.
For additional information and resources, go to www.cdc.gov/tb, and for a sample TB risk assessment tool, go to www.cdc.gov/tb/publications/ltbi/appendixa.htm.
As we mark the passing of another World TB Day, we have one goal – to identify, screen, and treat children and adolescents at risk for latent TB infection and help eliminate future cases of TB disease.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
March 24 is World TB Day. It was on this date in 1882 that physician Robert Koch announced the discovery of Mycobacterium tuberculosis, the causative agent of tuberculosis. Worldwide, activities are planned to raise awareness of TB and to support initiatives for prevention, better control, and ultimately the elimination of this disease.
Globally in 2015, the World Health Organization estimated there were 10.4 million new cases of TB, including 1 million in children. Data from the United States reveal that after 20 years of annual decline, the incidence of TB has plateaued. In 2015, 9,563 cases of TB disease were reported, including 440 cases in children less than 15 years of age. While the overall incidence was 3 cases per 100,000, the incidence among foreign-born persons was 15.1 cases per 100,000. There were 3,201 cases (33.5%) among U.S.-born individuals. Foreign-born persons accounted for 66.2% of cases; however, the majority of those cases were diagnosed several years after their arrival in the United States. The top five countries of origin of these individuals were China, India, Mexico, the Philippines, and Vietnam. In contrast, only one-quarter of all pediatric cases occurred in foreign-born children. Four states (California, Florida, New York, and Texas) reported more than 500 cases each in 2015, as they have for the last 7 consecutive years. In 2015, these states accounted for slightly more than half (4,839) of all cases (MMWR 2016 Mar 25;65[11]:273-8).
Why as pediatricians should we be concerned? TB in a child is a sentinel event and represents recent or ongoing transmission. Young children who are infected are more likely to progress to TB disease and develop severe manifestations such as miliary TB or meningitis. Children less than 4 years old and those with certain underlying disorders, including those with an immunodeficiency or who are receiving immunosuppressive agents, also are at greater risk for progression from infection to disease. Other predictors of disease progression include diagnosis of the infection within the past 2 years, use of chemotherapy and high-dose corticosteroids, as well as certain cancers, diabetes, and chronic renal failure.
Once infected, most children and adolescents remain asymptomatic. If disease occurs, symptoms develop 1-6 months after infection and include fever, cough, weight loss or failure to thrive, night sweats, and chills. Chest radiographic findings are nonspecific. Infiltrates and intrathoracic lymph node enlargement may or may not be present. However, our goal is to diagnose at-risk children with infection, treat them, and avoid their progression to TB disease.
Screening tests
The interferon-gamma release assay is a blood test that has a greater specificity than TST and requires only one visit. A positive test is seen in both latent TB infection and TB disease. There is no cross-reaction with BCG. This is the ideal test for prior BCG recipients and others who are unlikely to return for TST readings and are at least 5 years of age.
A chest radiograph is required to differentiate latent TB infection from TB disease. Latent TB infection is diagnosed when there is an absence of parenchymal disease, opacification, or intrathoracic adenopathy.
Treatment of latent TB infection versus TB disease is beyond the scope of this article. Consultation with an infectious disease expert is recommended.
For additional information and resources, go to www.cdc.gov/tb, and for a sample TB risk assessment tool, go to www.cdc.gov/tb/publications/ltbi/appendixa.htm.
As we mark the passing of another World TB Day, we have one goal – to identify, screen, and treat children and adolescents at risk for latent TB infection and help eliminate future cases of TB disease.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
March 24 is World TB Day. It was on this date in 1882 that physician Robert Koch announced the discovery of Mycobacterium tuberculosis, the causative agent of tuberculosis. Worldwide, activities are planned to raise awareness of TB and to support initiatives for prevention, better control, and ultimately the elimination of this disease.
Globally in 2015, the World Health Organization estimated there were 10.4 million new cases of TB, including 1 million in children. Data from the United States reveal that after 20 years of annual decline, the incidence of TB has plateaued. In 2015, 9,563 cases of TB disease were reported, including 440 cases in children less than 15 years of age. While the overall incidence was 3 cases per 100,000, the incidence among foreign-born persons was 15.1 cases per 100,000. There were 3,201 cases (33.5%) among U.S.-born individuals. Foreign-born persons accounted for 66.2% of cases; however, the majority of those cases were diagnosed several years after their arrival in the United States. The top five countries of origin of these individuals were China, India, Mexico, the Philippines, and Vietnam. In contrast, only one-quarter of all pediatric cases occurred in foreign-born children. Four states (California, Florida, New York, and Texas) reported more than 500 cases each in 2015, as they have for the last 7 consecutive years. In 2015, these states accounted for slightly more than half (4,839) of all cases (MMWR 2016 Mar 25;65[11]:273-8).
Why as pediatricians should we be concerned? TB in a child is a sentinel event and represents recent or ongoing transmission. Young children who are infected are more likely to progress to TB disease and develop severe manifestations such as miliary TB or meningitis. Children less than 4 years old and those with certain underlying disorders, including those with an immunodeficiency or who are receiving immunosuppressive agents, also are at greater risk for progression from infection to disease. Other predictors of disease progression include diagnosis of the infection within the past 2 years, use of chemotherapy and high-dose corticosteroids, as well as certain cancers, diabetes, and chronic renal failure.
Once infected, most children and adolescents remain asymptomatic. If disease occurs, symptoms develop 1-6 months after infection and include fever, cough, weight loss or failure to thrive, night sweats, and chills. Chest radiographic findings are nonspecific. Infiltrates and intrathoracic lymph node enlargement may or may not be present. However, our goal is to diagnose at-risk children with infection, treat them, and avoid their progression to TB disease.
Screening tests
The interferon-gamma release assay is a blood test that has a greater specificity than TST and requires only one visit. A positive test is seen in both latent TB infection and TB disease. There is no cross-reaction with BCG. This is the ideal test for prior BCG recipients and others who are unlikely to return for TST readings and are at least 5 years of age.
A chest radiograph is required to differentiate latent TB infection from TB disease. Latent TB infection is diagnosed when there is an absence of parenchymal disease, opacification, or intrathoracic adenopathy.
Treatment of latent TB infection versus TB disease is beyond the scope of this article. Consultation with an infectious disease expert is recommended.
For additional information and resources, go to www.cdc.gov/tb, and for a sample TB risk assessment tool, go to www.cdc.gov/tb/publications/ltbi/appendixa.htm.
As we mark the passing of another World TB Day, we have one goal – to identify, screen, and treat children and adolescents at risk for latent TB infection and help eliminate future cases of TB disease.
Dr. Word is a pediatric infectious disease specialist and director of the Houston Travel Medicine Clinic. She said she had no relevant financial disclosures.
Hot Threads in ACS Communities
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time (communities in which the threads appear are listed in parentheses):
1. Music in the OR. (General Surgery)
2. Nephrologist to surgeon in 3 months! (General Surgery)
3. MACRA. (Advocacy)
4. Mini-fellowship – or how to “brush up” on trauma? (General Surgery)
5. Trauma/PEG for intubated polytrauma patient. (Trauma Surgery)
6. Students observing in OR. (General Surgery)
7. Pediatric appendectomy. (General Surgery)
8. Call-bladders. (General Surgery)
9. Physician rehabilitation. (General Surgery)
10. Letters to ACS Fellows, Members and Members of Congress. (Vascular Surgery)
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to [email protected].
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time (communities in which the threads appear are listed in parentheses):
1. Music in the OR. (General Surgery)
2. Nephrologist to surgeon in 3 months! (General Surgery)
3. MACRA. (Advocacy)
4. Mini-fellowship – or how to “brush up” on trauma? (General Surgery)
5. Trauma/PEG for intubated polytrauma patient. (Trauma Surgery)
6. Students observing in OR. (General Surgery)
7. Pediatric appendectomy. (General Surgery)
8. Call-bladders. (General Surgery)
9. Physician rehabilitation. (General Surgery)
10. Letters to ACS Fellows, Members and Members of Congress. (Vascular Surgery)
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to [email protected].
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time (communities in which the threads appear are listed in parentheses):
1. Music in the OR. (General Surgery)
2. Nephrologist to surgeon in 3 months! (General Surgery)
3. MACRA. (Advocacy)
4. Mini-fellowship – or how to “brush up” on trauma? (General Surgery)
5. Trauma/PEG for intubated polytrauma patient. (Trauma Surgery)
6. Students observing in OR. (General Surgery)
7. Pediatric appendectomy. (General Surgery)
8. Call-bladders. (General Surgery)
9. Physician rehabilitation. (General Surgery)
10. Letters to ACS Fellows, Members and Members of Congress. (Vascular Surgery)
To join communities, log in to ACS Communities at http://acscommunities.facs.org/home, go to “Browse All Communities” near the top of any page, and click the blue “Join” button next to the community you’d like to join. If you have any questions, please send them to [email protected].
Your colleagues already have a lot to say in 2017. Here are the top discussion threads in ACS Communities just prior to press time
FDA confirms complications from intragastric balloons
Complications from overinflation and acute pancreatitis can create problems for obesity patients treated with intragastric balloons, according to a statement from the Food and Drug Administration. In a letter to health care providers published on February 9, 2017, the FDA warned of the two specific issues that have been the subject of multiple adverse event reports.
“We recommend that you closely monitor patients with these devices for these adverse events, and to submit reports to help us better understand any complications from the use of these obesity treatment devices,” the letter said.
Most of the overinflation reports involved the Orbera Intragastric Balloon System (Apollo Endosurgery) that uses a single balloon, although some reports involved the ReShape Integrated Dual Balloon System (ReShape Medical) that uses two balloons. Neither product mentions overinflation risk in its labeling. “At this moment there is not enough information to determine what is causing the balloon to overinflate,” according to the FDA letter.
A separate set of adverse event reports noted the development of acute pancreatitis caused when the balloons compressed other gastrointestinal structures. Both the Orbera and ReShape products were associated with pancreatitis, although neither lists pancreatitis as a potential complication on their labels. Pancreatitis was reported as early as 3 days after implantation, and symptoms included severe back and abdominal pain.
The FDA letter recommends that health care providers consider overinflation and pancreatitis in their differential diagnoses of obesity patients with intragastric balloons who present with the symptoms described, and to report any type of serious adverse events associated with intragastric balloons to the FDA through the MedWatch program. For more information about reporting adverse events to the FDA, visit the MedWatch site.
Complications from overinflation and acute pancreatitis can create problems for obesity patients treated with intragastric balloons, according to a statement from the Food and Drug Administration. In a letter to health care providers published on February 9, 2017, the FDA warned of the two specific issues that have been the subject of multiple adverse event reports.
“We recommend that you closely monitor patients with these devices for these adverse events, and to submit reports to help us better understand any complications from the use of these obesity treatment devices,” the letter said.
Most of the overinflation reports involved the Orbera Intragastric Balloon System (Apollo Endosurgery) that uses a single balloon, although some reports involved the ReShape Integrated Dual Balloon System (ReShape Medical) that uses two balloons. Neither product mentions overinflation risk in its labeling. “At this moment there is not enough information to determine what is causing the balloon to overinflate,” according to the FDA letter.
A separate set of adverse event reports noted the development of acute pancreatitis caused when the balloons compressed other gastrointestinal structures. Both the Orbera and ReShape products were associated with pancreatitis, although neither lists pancreatitis as a potential complication on their labels. Pancreatitis was reported as early as 3 days after implantation, and symptoms included severe back and abdominal pain.
The FDA letter recommends that health care providers consider overinflation and pancreatitis in their differential diagnoses of obesity patients with intragastric balloons who present with the symptoms described, and to report any type of serious adverse events associated with intragastric balloons to the FDA through the MedWatch program. For more information about reporting adverse events to the FDA, visit the MedWatch site.
Complications from overinflation and acute pancreatitis can create problems for obesity patients treated with intragastric balloons, according to a statement from the Food and Drug Administration. In a letter to health care providers published on February 9, 2017, the FDA warned of the two specific issues that have been the subject of multiple adverse event reports.
“We recommend that you closely monitor patients with these devices for these adverse events, and to submit reports to help us better understand any complications from the use of these obesity treatment devices,” the letter said.
Most of the overinflation reports involved the Orbera Intragastric Balloon System (Apollo Endosurgery) that uses a single balloon, although some reports involved the ReShape Integrated Dual Balloon System (ReShape Medical) that uses two balloons. Neither product mentions overinflation risk in its labeling. “At this moment there is not enough information to determine what is causing the balloon to overinflate,” according to the FDA letter.
A separate set of adverse event reports noted the development of acute pancreatitis caused when the balloons compressed other gastrointestinal structures. Both the Orbera and ReShape products were associated with pancreatitis, although neither lists pancreatitis as a potential complication on their labels. Pancreatitis was reported as early as 3 days after implantation, and symptoms included severe back and abdominal pain.
The FDA letter recommends that health care providers consider overinflation and pancreatitis in their differential diagnoses of obesity patients with intragastric balloons who present with the symptoms described, and to report any type of serious adverse events associated with intragastric balloons to the FDA through the MedWatch program. For more information about reporting adverse events to the FDA, visit the MedWatch site.
What I wish I knew when I started my internship
In my first year of residency I faced a steep learning curve. I learned a lot about psychiatry, but I learned so much more about myself. If I had known then what I know now, my internship would have been smoother and more enjoyable.
Be organized. Create systems to remember your patients’ information and your to-do list. I have templates of progress notes, psychiatry assessments, mental status assessments, “rounds sheets” (a sheet listing every patient on my floor, including their diagnoses, laboratories, medications, and other notes). Although my system involves lots of paper, I like it. Make a system that works for you. Go out and have fun. I know you are tired, you haven’t slept, and your apartment is a mess, but you won’t remember that time you went home, did laundry, and went to bed early. You will remember the fun night when you and other interns went out and explored the city.
Unplug from medicine. Nothing is more boring than working for 12 hours, only to go out for drinks with coworkers and talk about work. Although you need to vent, life is more than medicine. Find time for something else. Read a book, play a video game, hang out with people who are not doctors. I started a monthly book club with other women around my age. Make some time for something other than your profession.
Reach out to your senior colleagues. I was so concerned about making a good first impression that I didn’t share my concerns with others. I kept my head low because I always blame myself first when something is wrong.
During an off-service rotation, I was unable to finish my shift because I had food poisoning. To make up for that uncompleted shift, the chief from that service gave me 2 extra night shifts. I found the measure extreme, but thought it was my fault for going home early. A few days later, the Psychiatry Chief Resident approached me, after he had seen my schedule and spoke with the other chief because he found the situation unfair. He was reaching out to me saying, “We’ve got your back.” I realized that it wasn’t always my fault, and I could speak up when there was an issue. I was fortunate to have seniors and chiefs who looked out for me. I always found support, good advice, and respect for my feelings.
If you have questions or concerns, are anxious, or feel something is wrong, approach a senior or the chief. They were in your shoes once and will give you their best advice.
Medicine is different in the United States. As an international medica
People understand that you are from another country. At the beginning, I used Google to search for everything, and then I realized that my 2 wonderful students didn’t think less of me because I didn’t know what BKA (below knee amputation) means. Do not be ashamed if you don’t know how things work in a different country. You will find people who are willing to help you; you will learn, and it will be a minor thing a year from now.
Keep your support system. It was 3
If you moved away from home for residency, you are surrounded by new faces and far from the people you are comfortable with. Do not lose touch with them because you never know when you might need them the most. I had a hard road getting to where I am now, and many people helped me. You have to be there for them, too; a text message takes 30 seconds, and an e-mail, 1 minute.
Remember, you need to take care of yourself before taking care of others. No matter how much the MD or DO degree makes you feel like a superhero, you are still human.
In my first year of residency I faced a steep learning curve. I learned a lot about psychiatry, but I learned so much more about myself. If I had known then what I know now, my internship would have been smoother and more enjoyable.
Be organized. Create systems to remember your patients’ information and your to-do list. I have templates of progress notes, psychiatry assessments, mental status assessments, “rounds sheets” (a sheet listing every patient on my floor, including their diagnoses, laboratories, medications, and other notes). Although my system involves lots of paper, I like it. Make a system that works for you. Go out and have fun. I know you are tired, you haven’t slept, and your apartment is a mess, but you won’t remember that time you went home, did laundry, and went to bed early. You will remember the fun night when you and other interns went out and explored the city.
Unplug from medicine. Nothing is more boring than working for 12 hours, only to go out for drinks with coworkers and talk about work. Although you need to vent, life is more than medicine. Find time for something else. Read a book, play a video game, hang out with people who are not doctors. I started a monthly book club with other women around my age. Make some time for something other than your profession.
Reach out to your senior colleagues. I was so concerned about making a good first impression that I didn’t share my concerns with others. I kept my head low because I always blame myself first when something is wrong.
During an off-service rotation, I was unable to finish my shift because I had food poisoning. To make up for that uncompleted shift, the chief from that service gave me 2 extra night shifts. I found the measure extreme, but thought it was my fault for going home early. A few days later, the Psychiatry Chief Resident approached me, after he had seen my schedule and spoke with the other chief because he found the situation unfair. He was reaching out to me saying, “We’ve got your back.” I realized that it wasn’t always my fault, and I could speak up when there was an issue. I was fortunate to have seniors and chiefs who looked out for me. I always found support, good advice, and respect for my feelings.
If you have questions or concerns, are anxious, or feel something is wrong, approach a senior or the chief. They were in your shoes once and will give you their best advice.
Medicine is different in the United States. As an international medica
People understand that you are from another country. At the beginning, I used Google to search for everything, and then I realized that my 2 wonderful students didn’t think less of me because I didn’t know what BKA (below knee amputation) means. Do not be ashamed if you don’t know how things work in a different country. You will find people who are willing to help you; you will learn, and it will be a minor thing a year from now.
Keep your support system. It was 3
If you moved away from home for residency, you are surrounded by new faces and far from the people you are comfortable with. Do not lose touch with them because you never know when you might need them the most. I had a hard road getting to where I am now, and many people helped me. You have to be there for them, too; a text message takes 30 seconds, and an e-mail, 1 minute.
Remember, you need to take care of yourself before taking care of others. No matter how much the MD or DO degree makes you feel like a superhero, you are still human.
In my first year of residency I faced a steep learning curve. I learned a lot about psychiatry, but I learned so much more about myself. If I had known then what I know now, my internship would have been smoother and more enjoyable.
Be organized. Create systems to remember your patients’ information and your to-do list. I have templates of progress notes, psychiatry assessments, mental status assessments, “rounds sheets” (a sheet listing every patient on my floor, including their diagnoses, laboratories, medications, and other notes). Although my system involves lots of paper, I like it. Make a system that works for you. Go out and have fun. I know you are tired, you haven’t slept, and your apartment is a mess, but you won’t remember that time you went home, did laundry, and went to bed early. You will remember the fun night when you and other interns went out and explored the city.
Unplug from medicine. Nothing is more boring than working for 12 hours, only to go out for drinks with coworkers and talk about work. Although you need to vent, life is more than medicine. Find time for something else. Read a book, play a video game, hang out with people who are not doctors. I started a monthly book club with other women around my age. Make some time for something other than your profession.
Reach out to your senior colleagues. I was so concerned about making a good first impression that I didn’t share my concerns with others. I kept my head low because I always blame myself first when something is wrong.
During an off-service rotation, I was unable to finish my shift because I had food poisoning. To make up for that uncompleted shift, the chief from that service gave me 2 extra night shifts. I found the measure extreme, but thought it was my fault for going home early. A few days later, the Psychiatry Chief Resident approached me, after he had seen my schedule and spoke with the other chief because he found the situation unfair. He was reaching out to me saying, “We’ve got your back.” I realized that it wasn’t always my fault, and I could speak up when there was an issue. I was fortunate to have seniors and chiefs who looked out for me. I always found support, good advice, and respect for my feelings.
If you have questions or concerns, are anxious, or feel something is wrong, approach a senior or the chief. They were in your shoes once and will give you their best advice.
Medicine is different in the United States. As an international medica
People understand that you are from another country. At the beginning, I used Google to search for everything, and then I realized that my 2 wonderful students didn’t think less of me because I didn’t know what BKA (below knee amputation) means. Do not be ashamed if you don’t know how things work in a different country. You will find people who are willing to help you; you will learn, and it will be a minor thing a year from now.
Keep your support system. It was 3
If you moved away from home for residency, you are surrounded by new faces and far from the people you are comfortable with. Do not lose touch with them because you never know when you might need them the most. I had a hard road getting to where I am now, and many people helped me. You have to be there for them, too; a text message takes 30 seconds, and an e-mail, 1 minute.
Remember, you need to take care of yourself before taking care of others. No matter how much the MD or DO degree makes you feel like a superhero, you are still human.
Watch and wait often better than resecting in ground-glass opacities
Three years of follow-up is adequate for partially solid ground-glass opacity lesions that do not progress, while pure ground-glass opacity lesions that show no progression may require further follow-up care, a study suggests.
The results of the study strengthen the argument for taking a “watch and wait” approach, and raise the question of whether patient outcomes can be improved without more precise diagnostic criteria, said study author Shigei Sawada, MD, PhD, a researcher at the Shikoku Cancer Center in Matsuyama, Japan, and his colleagues. They drew these conclusions from performing a long-term outcome investigation of 226 patients with pure or mixed ground-glass opacity lesions shown by CT imaging to be 3 cm or less in diameter.
Once established that the disease has stabilized in a pure or mixed ground-glass opacity lesion, “the frequency of CT examinations could probably be reduced or ... discontinued,” the investigators wrote. The study is published online in Chest (2017;151[2]:308-15).
Because ground-glass opacities often can remain unchanged for years, reflexively choosing resection can result in a patient’s being overtreated. Meanwhile, the use of increasingly accurate imaging technology likely means detection rates of such lesions will continue to increase, leaving clinicians to wonder about optimal management protocols, particularly since several guidance documents include differing recommendations on the timing of surveillance CTs for patients with stable disease.
The study includes 10-15 years of follow-up data on the 226 patients, registered between 2000 and 2005. Across the study, there were nearly twice as many women as men, all with an average age of 61 years. About a quarter had multiple ground-glass opacities; about a quarter also had partially consolidated lesions. Of the 124 patients who’d had resections, all but one was stage IA. The most prominent histologic subtype was adenocarcinoma in situ in 63 patients, followed by 39 patients with minimally invasive adenocarcinomas, and 19 with lepidic predominant adenocarcinomas. Five patients had papillary-predominant adenocarcinomas.
Roughly one-quarter of the cohort did not receive follow-up examinations after 68 months, as their lesions either remained stable or were shown to have reduced in size. Another 45 continued to undergo follow-up examinations.
After initial detection of a pure ground-glass opacity, the CT examination schedule was every 3, 6, and 12 months, and then annually. After detection of a mixed ground-glass opacity, a CT examination was given every 3 months for the first year, then reduced to every 6 months thereafter. In patients with stable disease, the individual clinicians determined whether to obtain additional CT follow-up imaging.
A ground-glass lesion was determined to have progressed if the diameter increased, as it did in about a third of patients; or, if there was new or increased consolidation, as there was in about two-thirds of patients. The table of consolidation/tumor ratios (CTR) used included CTR zero, also referred to as a pure ground-glass lesion; CTR 1-25; CTR 26-50; and CTR equal to or greater than 51. When there were multiple lesions, the largest one detected was the target.
All cases of patients with a CTR of more than zero were identified within 3 years, while 13.6% of patients with a CTR of zero required more than 3 years to identify tumor growth. Aggressive cancer was detected in 4% of patients with a CTR of zero and in 70% of those with a CTR greater than 25% (P less than .001). Aggressive cancer was seen in 46% of those with consolidation/tumor ratios that increased during follow-up and in 8% of those whose tumors increased in diameter (P less than .007). After about 10 years of follow-up after resection, 1.6% of cancers recurred.
There were two deaths from lung cancer among the study’s patients. The first, a 54-year-old man, had an acinar-predominant adenocarcinoma, 5 mm in diameter with a consolidation/tumor ratio of 0.75 that increased during follow-up. The recurrence developed in the mediastinal lymph nodes 51 months after resection surgery. The second patient had a papillary-predominant adenocarcinoma appearing as a pure ground-glass opacity 27 mm in diameter. The consolidation/tumor ratio also increased during follow-up, with recurrences in the bone and mediastinal lymph nodes at 30 months post resectioning.
Neither patient was re-biopsied, and both were diagnosed according to CT imaging alone. There were 13 other patient deaths from non–lung cancer related causes.
Given the 3-year timespan necessary to detect tumor growth in all but the CTR zero group, and the study’s size and long-term nature, the investigators concluded that a follow-up period of 3 years for patients with part-solid lesions “should be adequate.”
By contrast, CHEST recommends CT scans be done for at least 3 years in patients with pure ground-glass lesions and between 3 and 5 years in the other CTR groups with nodules measuring 8 mm or less. The National Comprehensive Cancer Network guideline advises low-dose CT scanning until a patient is no longer eligible for definitive treatment.
Dr. Sawada and his colleagues did not use an exact criterion for tumor growth in their study, such as a precise ratio of increase in size or consolidation, in part because at the time of the study the most common form of CT evaluation was visual inspection; they reported that tumors exhibiting growth most commonly increased between 2 and 3 mm in either size or consolidation. “Evaluations based on visual inspections can be imprecise, and different physicians may arrive at different judgments,” the investigators wrote. “However, [the use of] computer-aided diagnosis systems are not yet commonly applied in clinical practice.”
Although imaging should have guided the decision to resect, according to Dr. Sawada and his coauthors, two-thirds of patients in the study were given the procedure even though their lesions were not shown by CT scans to have progressed. This was done either at the patient’s request, or per the clinical judgment of a physician.
Also becoming more specific about changing CTRs would be helpful in developing management protocols, according to Dr. Detterbeck. “In my opinion, we need to start factoring in the rate of change. A gradual 2 mm increase in size over a period of 5 years may not be an appropriate trigger for resection.”
Neither the investigators nor the editorial writer had any relevant disclosures.
[email protected]
On Twitter @whitneymcknight
Eric Gartman, MD, FCCP, comments: This study provides further support that the biology of ground-glass and part-solid nodules is different than fully solid nodules – and we should not be in a rush to resect these lesions. While the recommendations are likely to evolve over time as more information becomes available, this conservative approach toward nonsolid nodules is currently adopted in the Lung-RADS guidelines.
Eric Gartman, MD, FCCP, comments: This study provides further support that the biology of ground-glass and part-solid nodules is different than fully solid nodules – and we should not be in a rush to resect these lesions. While the recommendations are likely to evolve over time as more information becomes available, this conservative approach toward nonsolid nodules is currently adopted in the Lung-RADS guidelines.
Eric Gartman, MD, FCCP, comments: This study provides further support that the biology of ground-glass and part-solid nodules is different than fully solid nodules – and we should not be in a rush to resect these lesions. While the recommendations are likely to evolve over time as more information becomes available, this conservative approach toward nonsolid nodules is currently adopted in the Lung-RADS guidelines.
Three years of follow-up is adequate for partially solid ground-glass opacity lesions that do not progress, while pure ground-glass opacity lesions that show no progression may require further follow-up care, a study suggests.
The results of the study strengthen the argument for taking a “watch and wait” approach, and raise the question of whether patient outcomes can be improved without more precise diagnostic criteria, said study author Shigei Sawada, MD, PhD, a researcher at the Shikoku Cancer Center in Matsuyama, Japan, and his colleagues. They drew these conclusions from performing a long-term outcome investigation of 226 patients with pure or mixed ground-glass opacity lesions shown by CT imaging to be 3 cm or less in diameter.
Once established that the disease has stabilized in a pure or mixed ground-glass opacity lesion, “the frequency of CT examinations could probably be reduced or ... discontinued,” the investigators wrote. The study is published online in Chest (2017;151[2]:308-15).
Because ground-glass opacities often can remain unchanged for years, reflexively choosing resection can result in a patient’s being overtreated. Meanwhile, the use of increasingly accurate imaging technology likely means detection rates of such lesions will continue to increase, leaving clinicians to wonder about optimal management protocols, particularly since several guidance documents include differing recommendations on the timing of surveillance CTs for patients with stable disease.
The study includes 10-15 years of follow-up data on the 226 patients, registered between 2000 and 2005. Across the study, there were nearly twice as many women as men, all with an average age of 61 years. About a quarter had multiple ground-glass opacities; about a quarter also had partially consolidated lesions. Of the 124 patients who’d had resections, all but one was stage IA. The most prominent histologic subtype was adenocarcinoma in situ in 63 patients, followed by 39 patients with minimally invasive adenocarcinomas, and 19 with lepidic predominant adenocarcinomas. Five patients had papillary-predominant adenocarcinomas.
Roughly one-quarter of the cohort did not receive follow-up examinations after 68 months, as their lesions either remained stable or were shown to have reduced in size. Another 45 continued to undergo follow-up examinations.
After initial detection of a pure ground-glass opacity, the CT examination schedule was every 3, 6, and 12 months, and then annually. After detection of a mixed ground-glass opacity, a CT examination was given every 3 months for the first year, then reduced to every 6 months thereafter. In patients with stable disease, the individual clinicians determined whether to obtain additional CT follow-up imaging.
A ground-glass lesion was determined to have progressed if the diameter increased, as it did in about a third of patients; or, if there was new or increased consolidation, as there was in about two-thirds of patients. The table of consolidation/tumor ratios (CTR) used included CTR zero, also referred to as a pure ground-glass lesion; CTR 1-25; CTR 26-50; and CTR equal to or greater than 51. When there were multiple lesions, the largest one detected was the target.
All cases of patients with a CTR of more than zero were identified within 3 years, while 13.6% of patients with a CTR of zero required more than 3 years to identify tumor growth. Aggressive cancer was detected in 4% of patients with a CTR of zero and in 70% of those with a CTR greater than 25% (P less than .001). Aggressive cancer was seen in 46% of those with consolidation/tumor ratios that increased during follow-up and in 8% of those whose tumors increased in diameter (P less than .007). After about 10 years of follow-up after resection, 1.6% of cancers recurred.
There were two deaths from lung cancer among the study’s patients. The first, a 54-year-old man, had an acinar-predominant adenocarcinoma, 5 mm in diameter with a consolidation/tumor ratio of 0.75 that increased during follow-up. The recurrence developed in the mediastinal lymph nodes 51 months after resection surgery. The second patient had a papillary-predominant adenocarcinoma appearing as a pure ground-glass opacity 27 mm in diameter. The consolidation/tumor ratio also increased during follow-up, with recurrences in the bone and mediastinal lymph nodes at 30 months post resectioning.
Neither patient was re-biopsied, and both were diagnosed according to CT imaging alone. There were 13 other patient deaths from non–lung cancer related causes.
Given the 3-year timespan necessary to detect tumor growth in all but the CTR zero group, and the study’s size and long-term nature, the investigators concluded that a follow-up period of 3 years for patients with part-solid lesions “should be adequate.”
By contrast, CHEST recommends CT scans be done for at least 3 years in patients with pure ground-glass lesions and between 3 and 5 years in the other CTR groups with nodules measuring 8 mm or less. The National Comprehensive Cancer Network guideline advises low-dose CT scanning until a patient is no longer eligible for definitive treatment.
Dr. Sawada and his colleagues did not use an exact criterion for tumor growth in their study, such as a precise ratio of increase in size or consolidation, in part because at the time of the study the most common form of CT evaluation was visual inspection; they reported that tumors exhibiting growth most commonly increased between 2 and 3 mm in either size or consolidation. “Evaluations based on visual inspections can be imprecise, and different physicians may arrive at different judgments,” the investigators wrote. “However, [the use of] computer-aided diagnosis systems are not yet commonly applied in clinical practice.”
Although imaging should have guided the decision to resect, according to Dr. Sawada and his coauthors, two-thirds of patients in the study were given the procedure even though their lesions were not shown by CT scans to have progressed. This was done either at the patient’s request, or per the clinical judgment of a physician.
Also becoming more specific about changing CTRs would be helpful in developing management protocols, according to Dr. Detterbeck. “In my opinion, we need to start factoring in the rate of change. A gradual 2 mm increase in size over a period of 5 years may not be an appropriate trigger for resection.”
Neither the investigators nor the editorial writer had any relevant disclosures.
[email protected]
On Twitter @whitneymcknight
Three years of follow-up is adequate for partially solid ground-glass opacity lesions that do not progress, while pure ground-glass opacity lesions that show no progression may require further follow-up care, a study suggests.
The results of the study strengthen the argument for taking a “watch and wait” approach, and raise the question of whether patient outcomes can be improved without more precise diagnostic criteria, said study author Shigei Sawada, MD, PhD, a researcher at the Shikoku Cancer Center in Matsuyama, Japan, and his colleagues. They drew these conclusions from performing a long-term outcome investigation of 226 patients with pure or mixed ground-glass opacity lesions shown by CT imaging to be 3 cm or less in diameter.
Once established that the disease has stabilized in a pure or mixed ground-glass opacity lesion, “the frequency of CT examinations could probably be reduced or ... discontinued,” the investigators wrote. The study is published online in Chest (2017;151[2]:308-15).
Because ground-glass opacities often can remain unchanged for years, reflexively choosing resection can result in a patient’s being overtreated. Meanwhile, the use of increasingly accurate imaging technology likely means detection rates of such lesions will continue to increase, leaving clinicians to wonder about optimal management protocols, particularly since several guidance documents include differing recommendations on the timing of surveillance CTs for patients with stable disease.
The study includes 10-15 years of follow-up data on the 226 patients, registered between 2000 and 2005. Across the study, there were nearly twice as many women as men, all with an average age of 61 years. About a quarter had multiple ground-glass opacities; about a quarter also had partially consolidated lesions. Of the 124 patients who’d had resections, all but one was stage IA. The most prominent histologic subtype was adenocarcinoma in situ in 63 patients, followed by 39 patients with minimally invasive adenocarcinomas, and 19 with lepidic predominant adenocarcinomas. Five patients had papillary-predominant adenocarcinomas.
Roughly one-quarter of the cohort did not receive follow-up examinations after 68 months, as their lesions either remained stable or were shown to have reduced in size. Another 45 continued to undergo follow-up examinations.
After initial detection of a pure ground-glass opacity, the CT examination schedule was every 3, 6, and 12 months, and then annually. After detection of a mixed ground-glass opacity, a CT examination was given every 3 months for the first year, then reduced to every 6 months thereafter. In patients with stable disease, the individual clinicians determined whether to obtain additional CT follow-up imaging.
A ground-glass lesion was determined to have progressed if the diameter increased, as it did in about a third of patients; or, if there was new or increased consolidation, as there was in about two-thirds of patients. The table of consolidation/tumor ratios (CTR) used included CTR zero, also referred to as a pure ground-glass lesion; CTR 1-25; CTR 26-50; and CTR equal to or greater than 51. When there were multiple lesions, the largest one detected was the target.
All cases of patients with a CTR of more than zero were identified within 3 years, while 13.6% of patients with a CTR of zero required more than 3 years to identify tumor growth. Aggressive cancer was detected in 4% of patients with a CTR of zero and in 70% of those with a CTR greater than 25% (P less than .001). Aggressive cancer was seen in 46% of those with consolidation/tumor ratios that increased during follow-up and in 8% of those whose tumors increased in diameter (P less than .007). After about 10 years of follow-up after resection, 1.6% of cancers recurred.
There were two deaths from lung cancer among the study’s patients. The first, a 54-year-old man, had an acinar-predominant adenocarcinoma, 5 mm in diameter with a consolidation/tumor ratio of 0.75 that increased during follow-up. The recurrence developed in the mediastinal lymph nodes 51 months after resection surgery. The second patient had a papillary-predominant adenocarcinoma appearing as a pure ground-glass opacity 27 mm in diameter. The consolidation/tumor ratio also increased during follow-up, with recurrences in the bone and mediastinal lymph nodes at 30 months post resectioning.
Neither patient was re-biopsied, and both were diagnosed according to CT imaging alone. There were 13 other patient deaths from non–lung cancer related causes.
Given the 3-year timespan necessary to detect tumor growth in all but the CTR zero group, and the study’s size and long-term nature, the investigators concluded that a follow-up period of 3 years for patients with part-solid lesions “should be adequate.”
By contrast, CHEST recommends CT scans be done for at least 3 years in patients with pure ground-glass lesions and between 3 and 5 years in the other CTR groups with nodules measuring 8 mm or less. The National Comprehensive Cancer Network guideline advises low-dose CT scanning until a patient is no longer eligible for definitive treatment.
Dr. Sawada and his colleagues did not use an exact criterion for tumor growth in their study, such as a precise ratio of increase in size or consolidation, in part because at the time of the study the most common form of CT evaluation was visual inspection; they reported that tumors exhibiting growth most commonly increased between 2 and 3 mm in either size or consolidation. “Evaluations based on visual inspections can be imprecise, and different physicians may arrive at different judgments,” the investigators wrote. “However, [the use of] computer-aided diagnosis systems are not yet commonly applied in clinical practice.”
Although imaging should have guided the decision to resect, according to Dr. Sawada and his coauthors, two-thirds of patients in the study were given the procedure even though their lesions were not shown by CT scans to have progressed. This was done either at the patient’s request, or per the clinical judgment of a physician.
Also becoming more specific about changing CTRs would be helpful in developing management protocols, according to Dr. Detterbeck. “In my opinion, we need to start factoring in the rate of change. A gradual 2 mm increase in size over a period of 5 years may not be an appropriate trigger for resection.”
Neither the investigators nor the editorial writer had any relevant disclosures.
[email protected]
On Twitter @whitneymcknight
FROM CHEST
Key clinical point:
Major finding: Of 226 patients with ground-glass opacity lesions 3 cm or less in size, 124 had resection, 57 required no further follow-up, and 45 continue to receive follow-up.
Data source: Long-term study of 226 patients with pure or mixed ground-glass opacities of 3 cm or less given regular CT imaging between 2000 and 2005.
Disclosures: Neither the investigators nor the editorial writer had any relevant disclosures.
Pregnancy medical home reduces hospital visits, overall costs
LAS VEGAS – Women and their newborns who received care through a pregnancy medical home model used the emergency department less and had fewer inpatient stays, resulting in significant cost savings to a state health insurance plan.
In the single-center, retrospective cohort study, women who had at least one medical home visit had 897 emergency department visits per 1,000 member months, compared with 1,969/1,000 member months for patients who had no medical home visits (P less than .01). Newborns in the medical home group had fewer inpatient days per 1,000 member months as well, compared with non–medical home infants (698 vs. 1,799 days/member month, P less than .01). Inpatient stays for pregnant women receiving medical home care were also reduced (4,279 vs. 2,939 inpatient days, P less than .01).
The pregnancy medical home project was conducted jointly by the Texas Children’s Health Plan and Baylor College of Medicine. The care delivery model, offered from the Baylor Center for Children and Women, gave pregnant women enhanced access, used evidence-based protocols for treatment, and emphasized both quality care and the patient experience, said Dr. Suhag, professor of ob.gyn. at Baylor College of Medicine, Houston.
The pregnancy medical home includes extended hours, walk-in appointments, 24-hour nurse availability for triage, and a laborist model for hospital coverage.
From a payment perspective, the medical home is a fully capitated, full-risk model. “Our center is paid on a monthly basis to provide care to members of our panel,” Dr. Suhag said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The primary outcomes measured by the study were the number of inpatient days and the rate of emergency department usage among pregnancy medical home participants, compared with nonparticipating pregnant women and newborns seen at the Center for Children and Women. Annualized cost savings for the pregnancy medical home model was a secondary outcome measure.
Over a 1-year period, the study examined claims data for pregnant women and newborns who were enrolled in the Texas Children’s Health Plan and were assigned to the pregnancy medical home panel. In total, 27,912 member months (including care for both women and newborns) were examined; of these, about 37% (10,402) were for women and newborns who had at least one medical home visit, and 63% (17,510) of the member months accrued to patients who had no medical home visits. Women and their infants were excluded from the cohort if they received care billed to another health plan.
Participation in the medical home group resulted in lower costs, with annualized estimated emergency department cost savings of $330,161 and $30,739 for pregnant women and newborns, respectively. The reduced number of inpatient days in the medical home group resulted in a total savings of $494,313 for pregnant women and $1,606,392 for newborns in this cohort.
The integrated care model, which used a care coordinator and provided care from multiple specialties at a single site, was likely the key to success, Dr. Suhag said. “With this access, 40% of our pregnant moms were able to access prenatal care in the first trimester, which likely improved outcomes and contributed to the cost savings,” she said.
The control group in the study was made up of individuals who had been randomized to the medical home, but who had chosen care from another provider instead. Because the researchers were relying on health claims data, they were not able to perform a detailed comparison between the two groups, leaving open the possibility that patient characteristics may have accounted for part of the differences in outcomes. Women “could self-select to receive care at the Center for Children and Women,” Dr. Suhag said in an interview. “It is possible that they are different than the women who did not choose care in our clinic.”
A strength of the study, Dr. Suhag said, is that it evaluated outcomes from the medical home model by comparing it to several other medical practices caring for a similar demographic in the same geographic area.
The study was conducted by the Texas Children’s Health Plan and Baylor College of Medicine. Dr. Suhag reported having no other outside sources of funding or conflicts of interest.
Dr. Suhag reported having no outside sources of funding beyond the study’s two sponsoring organizations and no conflicts of interest.
[email protected]
On Twitter @karioakes
LAS VEGAS – Women and their newborns who received care through a pregnancy medical home model used the emergency department less and had fewer inpatient stays, resulting in significant cost savings to a state health insurance plan.
In the single-center, retrospective cohort study, women who had at least one medical home visit had 897 emergency department visits per 1,000 member months, compared with 1,969/1,000 member months for patients who had no medical home visits (P less than .01). Newborns in the medical home group had fewer inpatient days per 1,000 member months as well, compared with non–medical home infants (698 vs. 1,799 days/member month, P less than .01). Inpatient stays for pregnant women receiving medical home care were also reduced (4,279 vs. 2,939 inpatient days, P less than .01).
The pregnancy medical home project was conducted jointly by the Texas Children’s Health Plan and Baylor College of Medicine. The care delivery model, offered from the Baylor Center for Children and Women, gave pregnant women enhanced access, used evidence-based protocols for treatment, and emphasized both quality care and the patient experience, said Dr. Suhag, professor of ob.gyn. at Baylor College of Medicine, Houston.
The pregnancy medical home includes extended hours, walk-in appointments, 24-hour nurse availability for triage, and a laborist model for hospital coverage.
From a payment perspective, the medical home is a fully capitated, full-risk model. “Our center is paid on a monthly basis to provide care to members of our panel,” Dr. Suhag said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The primary outcomes measured by the study were the number of inpatient days and the rate of emergency department usage among pregnancy medical home participants, compared with nonparticipating pregnant women and newborns seen at the Center for Children and Women. Annualized cost savings for the pregnancy medical home model was a secondary outcome measure.
Over a 1-year period, the study examined claims data for pregnant women and newborns who were enrolled in the Texas Children’s Health Plan and were assigned to the pregnancy medical home panel. In total, 27,912 member months (including care for both women and newborns) were examined; of these, about 37% (10,402) were for women and newborns who had at least one medical home visit, and 63% (17,510) of the member months accrued to patients who had no medical home visits. Women and their infants were excluded from the cohort if they received care billed to another health plan.
Participation in the medical home group resulted in lower costs, with annualized estimated emergency department cost savings of $330,161 and $30,739 for pregnant women and newborns, respectively. The reduced number of inpatient days in the medical home group resulted in a total savings of $494,313 for pregnant women and $1,606,392 for newborns in this cohort.
The integrated care model, which used a care coordinator and provided care from multiple specialties at a single site, was likely the key to success, Dr. Suhag said. “With this access, 40% of our pregnant moms were able to access prenatal care in the first trimester, which likely improved outcomes and contributed to the cost savings,” she said.
The control group in the study was made up of individuals who had been randomized to the medical home, but who had chosen care from another provider instead. Because the researchers were relying on health claims data, they were not able to perform a detailed comparison between the two groups, leaving open the possibility that patient characteristics may have accounted for part of the differences in outcomes. Women “could self-select to receive care at the Center for Children and Women,” Dr. Suhag said in an interview. “It is possible that they are different than the women who did not choose care in our clinic.”
A strength of the study, Dr. Suhag said, is that it evaluated outcomes from the medical home model by comparing it to several other medical practices caring for a similar demographic in the same geographic area.
The study was conducted by the Texas Children’s Health Plan and Baylor College of Medicine. Dr. Suhag reported having no other outside sources of funding or conflicts of interest.
Dr. Suhag reported having no outside sources of funding beyond the study’s two sponsoring organizations and no conflicts of interest.
[email protected]
On Twitter @karioakes
LAS VEGAS – Women and their newborns who received care through a pregnancy medical home model used the emergency department less and had fewer inpatient stays, resulting in significant cost savings to a state health insurance plan.
In the single-center, retrospective cohort study, women who had at least one medical home visit had 897 emergency department visits per 1,000 member months, compared with 1,969/1,000 member months for patients who had no medical home visits (P less than .01). Newborns in the medical home group had fewer inpatient days per 1,000 member months as well, compared with non–medical home infants (698 vs. 1,799 days/member month, P less than .01). Inpatient stays for pregnant women receiving medical home care were also reduced (4,279 vs. 2,939 inpatient days, P less than .01).
The pregnancy medical home project was conducted jointly by the Texas Children’s Health Plan and Baylor College of Medicine. The care delivery model, offered from the Baylor Center for Children and Women, gave pregnant women enhanced access, used evidence-based protocols for treatment, and emphasized both quality care and the patient experience, said Dr. Suhag, professor of ob.gyn. at Baylor College of Medicine, Houston.
The pregnancy medical home includes extended hours, walk-in appointments, 24-hour nurse availability for triage, and a laborist model for hospital coverage.
From a payment perspective, the medical home is a fully capitated, full-risk model. “Our center is paid on a monthly basis to provide care to members of our panel,” Dr. Suhag said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
The primary outcomes measured by the study were the number of inpatient days and the rate of emergency department usage among pregnancy medical home participants, compared with nonparticipating pregnant women and newborns seen at the Center for Children and Women. Annualized cost savings for the pregnancy medical home model was a secondary outcome measure.
Over a 1-year period, the study examined claims data for pregnant women and newborns who were enrolled in the Texas Children’s Health Plan and were assigned to the pregnancy medical home panel. In total, 27,912 member months (including care for both women and newborns) were examined; of these, about 37% (10,402) were for women and newborns who had at least one medical home visit, and 63% (17,510) of the member months accrued to patients who had no medical home visits. Women and their infants were excluded from the cohort if they received care billed to another health plan.
Participation in the medical home group resulted in lower costs, with annualized estimated emergency department cost savings of $330,161 and $30,739 for pregnant women and newborns, respectively. The reduced number of inpatient days in the medical home group resulted in a total savings of $494,313 for pregnant women and $1,606,392 for newborns in this cohort.
The integrated care model, which used a care coordinator and provided care from multiple specialties at a single site, was likely the key to success, Dr. Suhag said. “With this access, 40% of our pregnant moms were able to access prenatal care in the first trimester, which likely improved outcomes and contributed to the cost savings,” she said.
The control group in the study was made up of individuals who had been randomized to the medical home, but who had chosen care from another provider instead. Because the researchers were relying on health claims data, they were not able to perform a detailed comparison between the two groups, leaving open the possibility that patient characteristics may have accounted for part of the differences in outcomes. Women “could self-select to receive care at the Center for Children and Women,” Dr. Suhag said in an interview. “It is possible that they are different than the women who did not choose care in our clinic.”
A strength of the study, Dr. Suhag said, is that it evaluated outcomes from the medical home model by comparing it to several other medical practices caring for a similar demographic in the same geographic area.
The study was conducted by the Texas Children’s Health Plan and Baylor College of Medicine. Dr. Suhag reported having no other outside sources of funding or conflicts of interest.
Dr. Suhag reported having no outside sources of funding beyond the study’s two sponsoring organizations and no conflicts of interest.
[email protected]
On Twitter @karioakes
AT THE PREGNANCY MEETING
Key clinical point:
Major finding: Medical home patients had 897 emergency department visits, compared with 1,969 per 1,000 member months for non–medical home patients (P less than .01).
Data source: A retrospective cohort study of 27,912 patient member months comparing pregnancy medical home patients with non–medical home patients.
Disclosures: The study was conducted by the Texas Children’s Health Plan and Baylor College of Medicine. Dr. Suhag reported having no other outside sources of funding or conflicts of interest.
Weekend births linked to higher maternal-fetal mortality
LAS VEGAS – Weekend deliveries were associated with a significantly increased risk of maternal-fetal morbidity and death, according to a review of all U.S. deliveries over the past decade.
“Maternal morbidity and mortality were increased on weekends, compared to weekdays, and stillbirth and neonatal morbidity were also increased in infants delivered on weekends. Both of these findings occur against a background of lower intrinsic risk among weekend deliveries,” Amirhossein Moaddab, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Study objectives included measuring both maternal and fetal mortality ratios by the day and month of death or delivery; the study also tracked maternal and neonatal morbidities according to the day of the week the delivery occurred.
Using publicly available data sets (the National Vital Statistics System and the Centers for Disease Control and Prevention WONDER online database), Dr. Moaddab and his colleagues examined all live births and all maternal and fetal deaths in all 50 states and the District of Columbia for the period from 2004 to 2014.
In total, there were 45,036,622 live births, 7,551 maternal deaths, and 275,914 stillbirths during this period.
On weekdays, the maternal mortality rate was 15.3/100,000 live births; the rate rose to 22.8 maternal deaths per 100,000 live births on the weekends (P less than .001). Fetal mortality followed a similar pattern: The weekday fetal mortality rate was 5.85/1,000 live births, compared with 7.21/1,000 live births on the weekends (P less than .001).
A wide range of maternal and fetal morbidities were also more common when deliveries happened on the weekend. For mothers, the adjusted relative risk (aRR) ranged from 1.41 for maternal transfusion to 1.166 for perineal lacerations with Saturday or Sunday deliveries. Unplanned hysterectomy, however, was less likely on the weekend (aRR, 0.810).
Neonatal morbidities with a higher adjusted relative risk included gestational age less than 28 weeks (aRR, 1.481), a 5-minute Apgar score less than 7 (aRR, 1.251), and being placed on a ventilator or admitted to the neonatal intensive care unit (aRRs, 1.219 and 1.199, respectively). The odds of having a chromosomal abnormality were lower for infants delivered on weekends (aRR, 0.864), a result consistent with the increased likelihood of planned delivery for fetuses whose chromosomal status was known, said Dr. Moaddab, a postdoctoral fellow in obstetrics and gynecology at the Baylor College of Medicine, Houston .
Examining maternal characteristics, Dr. Moaddab and his colleagues did find some significant differences between those delivering on weekdays and weekends. However, because the weekend group was healthier overall than the weekday group, these differences were not likely to account for the worse weekend outcomes.
“We were able to control for pregnancy complications, and found that most women with pregnancy complications known to lead to death actually deliver on weekdays, suggesting that the total problem with weekend deliveries is even greater,” said Dr. Clark, professor of ob.gyn. at Baylor College of Medicine.
For example, women delivering on weekends were less likely to be smokers, have diabetes or gestational diabetes, or have chronic or gestational hypertension; they were also less likely to have had a previous cesarean delivery (all P equal to or less than .0001). They were, however, more likely to be nulliparous and to have eclampsia (P equal to or less than .0001).
Dr. Moaddab said that his group’s examination of monthly variations in maternal and fetal morbidity and mortality showed no sign of the “July phenomenon,” the worsening in outcomes seen in some specialties when new interns take to the wards and clinics.
The “weekend effect,” said Dr. Moaddab, has been documented elsewhere as well. In the United Kingdom, a recent observational study of obstetric outcomes found “increases in the rates of death and other complications for both women and babies born at weekends,” he said (BMJ. 2015;351:h5774).
Though Dr. Moaddab’s descriptive study couldn’t get at underlying causes, he said that there are many possible culprits. These can include the divided physician attention and reduced provider availability that can come with weekend staffing, as well as the possibility that the experience level of both physician and nurse staff drops on weekends. Long work hours that come with call may also contribute, he said.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
LAS VEGAS – Weekend deliveries were associated with a significantly increased risk of maternal-fetal morbidity and death, according to a review of all U.S. deliveries over the past decade.
“Maternal morbidity and mortality were increased on weekends, compared to weekdays, and stillbirth and neonatal morbidity were also increased in infants delivered on weekends. Both of these findings occur against a background of lower intrinsic risk among weekend deliveries,” Amirhossein Moaddab, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Study objectives included measuring both maternal and fetal mortality ratios by the day and month of death or delivery; the study also tracked maternal and neonatal morbidities according to the day of the week the delivery occurred.
Using publicly available data sets (the National Vital Statistics System and the Centers for Disease Control and Prevention WONDER online database), Dr. Moaddab and his colleagues examined all live births and all maternal and fetal deaths in all 50 states and the District of Columbia for the period from 2004 to 2014.
In total, there were 45,036,622 live births, 7,551 maternal deaths, and 275,914 stillbirths during this period.
On weekdays, the maternal mortality rate was 15.3/100,000 live births; the rate rose to 22.8 maternal deaths per 100,000 live births on the weekends (P less than .001). Fetal mortality followed a similar pattern: The weekday fetal mortality rate was 5.85/1,000 live births, compared with 7.21/1,000 live births on the weekends (P less than .001).
A wide range of maternal and fetal morbidities were also more common when deliveries happened on the weekend. For mothers, the adjusted relative risk (aRR) ranged from 1.41 for maternal transfusion to 1.166 for perineal lacerations with Saturday or Sunday deliveries. Unplanned hysterectomy, however, was less likely on the weekend (aRR, 0.810).
Neonatal morbidities with a higher adjusted relative risk included gestational age less than 28 weeks (aRR, 1.481), a 5-minute Apgar score less than 7 (aRR, 1.251), and being placed on a ventilator or admitted to the neonatal intensive care unit (aRRs, 1.219 and 1.199, respectively). The odds of having a chromosomal abnormality were lower for infants delivered on weekends (aRR, 0.864), a result consistent with the increased likelihood of planned delivery for fetuses whose chromosomal status was known, said Dr. Moaddab, a postdoctoral fellow in obstetrics and gynecology at the Baylor College of Medicine, Houston .
Examining maternal characteristics, Dr. Moaddab and his colleagues did find some significant differences between those delivering on weekdays and weekends. However, because the weekend group was healthier overall than the weekday group, these differences were not likely to account for the worse weekend outcomes.
“We were able to control for pregnancy complications, and found that most women with pregnancy complications known to lead to death actually deliver on weekdays, suggesting that the total problem with weekend deliveries is even greater,” said Dr. Clark, professor of ob.gyn. at Baylor College of Medicine.
For example, women delivering on weekends were less likely to be smokers, have diabetes or gestational diabetes, or have chronic or gestational hypertension; they were also less likely to have had a previous cesarean delivery (all P equal to or less than .0001). They were, however, more likely to be nulliparous and to have eclampsia (P equal to or less than .0001).
Dr. Moaddab said that his group’s examination of monthly variations in maternal and fetal morbidity and mortality showed no sign of the “July phenomenon,” the worsening in outcomes seen in some specialties when new interns take to the wards and clinics.
The “weekend effect,” said Dr. Moaddab, has been documented elsewhere as well. In the United Kingdom, a recent observational study of obstetric outcomes found “increases in the rates of death and other complications for both women and babies born at weekends,” he said (BMJ. 2015;351:h5774).
Though Dr. Moaddab’s descriptive study couldn’t get at underlying causes, he said that there are many possible culprits. These can include the divided physician attention and reduced provider availability that can come with weekend staffing, as well as the possibility that the experience level of both physician and nurse staff drops on weekends. Long work hours that come with call may also contribute, he said.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
LAS VEGAS – Weekend deliveries were associated with a significantly increased risk of maternal-fetal morbidity and death, according to a review of all U.S. deliveries over the past decade.
“Maternal morbidity and mortality were increased on weekends, compared to weekdays, and stillbirth and neonatal morbidity were also increased in infants delivered on weekends. Both of these findings occur against a background of lower intrinsic risk among weekend deliveries,” Amirhossein Moaddab, MD, said at the annual Pregnancy Meeting sponsored by the Society for Maternal-Fetal Medicine.
Study objectives included measuring both maternal and fetal mortality ratios by the day and month of death or delivery; the study also tracked maternal and neonatal morbidities according to the day of the week the delivery occurred.
Using publicly available data sets (the National Vital Statistics System and the Centers for Disease Control and Prevention WONDER online database), Dr. Moaddab and his colleagues examined all live births and all maternal and fetal deaths in all 50 states and the District of Columbia for the period from 2004 to 2014.
In total, there were 45,036,622 live births, 7,551 maternal deaths, and 275,914 stillbirths during this period.
On weekdays, the maternal mortality rate was 15.3/100,000 live births; the rate rose to 22.8 maternal deaths per 100,000 live births on the weekends (P less than .001). Fetal mortality followed a similar pattern: The weekday fetal mortality rate was 5.85/1,000 live births, compared with 7.21/1,000 live births on the weekends (P less than .001).
A wide range of maternal and fetal morbidities were also more common when deliveries happened on the weekend. For mothers, the adjusted relative risk (aRR) ranged from 1.41 for maternal transfusion to 1.166 for perineal lacerations with Saturday or Sunday deliveries. Unplanned hysterectomy, however, was less likely on the weekend (aRR, 0.810).
Neonatal morbidities with a higher adjusted relative risk included gestational age less than 28 weeks (aRR, 1.481), a 5-minute Apgar score less than 7 (aRR, 1.251), and being placed on a ventilator or admitted to the neonatal intensive care unit (aRRs, 1.219 and 1.199, respectively). The odds of having a chromosomal abnormality were lower for infants delivered on weekends (aRR, 0.864), a result consistent with the increased likelihood of planned delivery for fetuses whose chromosomal status was known, said Dr. Moaddab, a postdoctoral fellow in obstetrics and gynecology at the Baylor College of Medicine, Houston .
Examining maternal characteristics, Dr. Moaddab and his colleagues did find some significant differences between those delivering on weekdays and weekends. However, because the weekend group was healthier overall than the weekday group, these differences were not likely to account for the worse weekend outcomes.
“We were able to control for pregnancy complications, and found that most women with pregnancy complications known to lead to death actually deliver on weekdays, suggesting that the total problem with weekend deliveries is even greater,” said Dr. Clark, professor of ob.gyn. at Baylor College of Medicine.
For example, women delivering on weekends were less likely to be smokers, have diabetes or gestational diabetes, or have chronic or gestational hypertension; they were also less likely to have had a previous cesarean delivery (all P equal to or less than .0001). They were, however, more likely to be nulliparous and to have eclampsia (P equal to or less than .0001).
Dr. Moaddab said that his group’s examination of monthly variations in maternal and fetal morbidity and mortality showed no sign of the “July phenomenon,” the worsening in outcomes seen in some specialties when new interns take to the wards and clinics.
The “weekend effect,” said Dr. Moaddab, has been documented elsewhere as well. In the United Kingdom, a recent observational study of obstetric outcomes found “increases in the rates of death and other complications for both women and babies born at weekends,” he said (BMJ. 2015;351:h5774).
Though Dr. Moaddab’s descriptive study couldn’t get at underlying causes, he said that there are many possible culprits. These can include the divided physician attention and reduced provider availability that can come with weekend staffing, as well as the possibility that the experience level of both physician and nurse staff drops on weekends. Long work hours that come with call may also contribute, he said.
The study authors reported no outside sources of funding and no conflicts of interest.
[email protected]
On Twitter @karioakes
AT THE PREGNANCY MEETING
Key clinical point:
Major finding: On weekends, the maternal death rate was 22.8/100,000 live births, compared with a weekday rate of 15.3/100,000 (P less than .001).
Data source: A retrospective study of U.S. publicly available maternal-fetal data, including 45,036,622 live births, 7,551 maternal deaths, and 275,914 stillbirths from 2004 to 2014.
Disclosures: The study authors reported no outside sources of funding and no conflicts of interest.
Want better patient engagement? Use social media
ORLANDO – Looking for a better way to reach your patients and guide them to being more engaged in their own health care? Then expand your social media presence.
That was the message Kevin Campbell, MD, a cardiologist at the University of North Carolina, Chapel Hill, told attendees at the annual meeting of the Healthcare Information and Management Systems Society.
“Social media is where our patients, customers, and consumers, as well as our colleagues are and where we need to be,” Dr. Campbell said.
He called out three specific social media tools – Twitter, Facebook Live, and blogging – as the most effective for physicians. The first two offer a key way to connect with patients and colleagues – the ability to use video.
“The most important thing out in the digital space in terms of engagement is video and the visual,” Dr. Campbell said. “You’ll get 6,000% more engagement with a video-type point of contact. That can be a link from Twitter or it can be a Facebook Live [session] or a YouTube video.”
Video messaging also helps doctors support their peers, Dr. Campbell said.
“We can provide timely information to our colleagues,” he noted. “We have Twitter chats with fellows-in-training … I can talk to fellows who are in Germany about a technique we’re using here and then they can learn more about that technique.”
Secure social media channels also can be used to share thoughts and ideas regarding a clinical query regarding a specific test or imaging result, he said.
“The patient benefits because there are more brains thinking about their problem,” he noted.
Blogging also can be effective for reaching out to patients and colleagues as it provides a way to disseminate information on topics such as new treatments or learning about disease states.
But if the blog is set up to be interactive, doctors can get insights into their patients’ health concerns, Dr. Campbell said.
“I let patients write on my blog and I actually learn a ton about the patient experience,” he said. “I don’t even think of X, Y, and Z situation. I will be more empathetic to this because of what [they] told me.”
The caveat, of course, is that specific, protected information cannot be shared or posted.
“The attorneys will really get upset,” he noted. “So you do not develop a legal duty to that patient. But you can talk about treatments and what’s out there and what’s available. ... There may be a new treatment for leukemia that’s experimental that’s coming out of a university in Philadelphia and I can talk about that treatment.”
Dr. Campbell also said social media can be effective for doctors to promote themselves, pointing to his own career where he serves as a regular commentator on both the national and local levels. Engaging with media outlets can help turn a doctor into a key opinion leader, he said.
“If you say something important, engage about important issues, patients, consumers, industry partners and other leaders in the field are going to engage with you,” he said.
Dr. Campbell reported no conflicts of interest.
ORLANDO – Looking for a better way to reach your patients and guide them to being more engaged in their own health care? Then expand your social media presence.
That was the message Kevin Campbell, MD, a cardiologist at the University of North Carolina, Chapel Hill, told attendees at the annual meeting of the Healthcare Information and Management Systems Society.
“Social media is where our patients, customers, and consumers, as well as our colleagues are and where we need to be,” Dr. Campbell said.
He called out three specific social media tools – Twitter, Facebook Live, and blogging – as the most effective for physicians. The first two offer a key way to connect with patients and colleagues – the ability to use video.
“The most important thing out in the digital space in terms of engagement is video and the visual,” Dr. Campbell said. “You’ll get 6,000% more engagement with a video-type point of contact. That can be a link from Twitter or it can be a Facebook Live [session] or a YouTube video.”
Video messaging also helps doctors support their peers, Dr. Campbell said.
“We can provide timely information to our colleagues,” he noted. “We have Twitter chats with fellows-in-training … I can talk to fellows who are in Germany about a technique we’re using here and then they can learn more about that technique.”
Secure social media channels also can be used to share thoughts and ideas regarding a clinical query regarding a specific test or imaging result, he said.
“The patient benefits because there are more brains thinking about their problem,” he noted.
Blogging also can be effective for reaching out to patients and colleagues as it provides a way to disseminate information on topics such as new treatments or learning about disease states.
But if the blog is set up to be interactive, doctors can get insights into their patients’ health concerns, Dr. Campbell said.
“I let patients write on my blog and I actually learn a ton about the patient experience,” he said. “I don’t even think of X, Y, and Z situation. I will be more empathetic to this because of what [they] told me.”
The caveat, of course, is that specific, protected information cannot be shared or posted.
“The attorneys will really get upset,” he noted. “So you do not develop a legal duty to that patient. But you can talk about treatments and what’s out there and what’s available. ... There may be a new treatment for leukemia that’s experimental that’s coming out of a university in Philadelphia and I can talk about that treatment.”
Dr. Campbell also said social media can be effective for doctors to promote themselves, pointing to his own career where he serves as a regular commentator on both the national and local levels. Engaging with media outlets can help turn a doctor into a key opinion leader, he said.
“If you say something important, engage about important issues, patients, consumers, industry partners and other leaders in the field are going to engage with you,” he said.
Dr. Campbell reported no conflicts of interest.
ORLANDO – Looking for a better way to reach your patients and guide them to being more engaged in their own health care? Then expand your social media presence.
That was the message Kevin Campbell, MD, a cardiologist at the University of North Carolina, Chapel Hill, told attendees at the annual meeting of the Healthcare Information and Management Systems Society.
“Social media is where our patients, customers, and consumers, as well as our colleagues are and where we need to be,” Dr. Campbell said.
He called out three specific social media tools – Twitter, Facebook Live, and blogging – as the most effective for physicians. The first two offer a key way to connect with patients and colleagues – the ability to use video.
“The most important thing out in the digital space in terms of engagement is video and the visual,” Dr. Campbell said. “You’ll get 6,000% more engagement with a video-type point of contact. That can be a link from Twitter or it can be a Facebook Live [session] or a YouTube video.”
Video messaging also helps doctors support their peers, Dr. Campbell said.
“We can provide timely information to our colleagues,” he noted. “We have Twitter chats with fellows-in-training … I can talk to fellows who are in Germany about a technique we’re using here and then they can learn more about that technique.”
Secure social media channels also can be used to share thoughts and ideas regarding a clinical query regarding a specific test or imaging result, he said.
“The patient benefits because there are more brains thinking about their problem,” he noted.
Blogging also can be effective for reaching out to patients and colleagues as it provides a way to disseminate information on topics such as new treatments or learning about disease states.
But if the blog is set up to be interactive, doctors can get insights into their patients’ health concerns, Dr. Campbell said.
“I let patients write on my blog and I actually learn a ton about the patient experience,” he said. “I don’t even think of X, Y, and Z situation. I will be more empathetic to this because of what [they] told me.”
The caveat, of course, is that specific, protected information cannot be shared or posted.
“The attorneys will really get upset,” he noted. “So you do not develop a legal duty to that patient. But you can talk about treatments and what’s out there and what’s available. ... There may be a new treatment for leukemia that’s experimental that’s coming out of a university in Philadelphia and I can talk about that treatment.”
Dr. Campbell also said social media can be effective for doctors to promote themselves, pointing to his own career where he serves as a regular commentator on both the national and local levels. Engaging with media outlets can help turn a doctor into a key opinion leader, he said.
“If you say something important, engage about important issues, patients, consumers, industry partners and other leaders in the field are going to engage with you,” he said.
Dr. Campbell reported no conflicts of interest.
AT HIMSS17