User login
Study finds inflammatory bowel disease risk higher in children, adults with atopic dermatitis
The published recently in JAMA Dermatology.
The study also found an increased risk for Crohn’s disease (CD) in adults and children with AD, as well as an increased risk for ulcerative colitis (UC) in adults with AD and in children with severe AD, researchers reported.
“It is imperative for clinicians to understand atopic dermatitis and the trajectory of our patients with it in order to provide the best standard of care,” senior author Joel M. Gelfand, MD, MSCE, professor in clinical investigation with the department of dermatology at the University of Pennsylvania, Philadelphia, said in a news release.
“There are new and better treatments for AD today, and there will likely continue to be more,” continued Dr. Gelfand. “But providers have to understand how those treatments could impact other autoimmune diseases. For patients with AD and another autoimmune disease, some currently available medications can exacerbate symptoms of their other disease or can help treat two immune diseases at the same time.”
The study results support the idea that AD and IBD may have some common underlying causes, said Sheilagh Maguiness, MD, pediatric dermatologist and associate professor in the department of dermatology at the University of Minnesota, Minneapolis, who was asked to comment on the findings.
“As the pathogenesis of AD is becoming better understood, we are recognizing that, rather than simply a cutaneous disease, the underlying inflammation and immune dysregulation that leads to AD best categorizes it as a systemic inflammatory disease with significant comorbidities,” she told this news organization. “I will be more likely to ask patients and families about GI symptoms, and if positive, may plan to refer to GI more readily than in the past,” added Dr. Maguiness, who was not involved in the study.
UK general practice cohort
AD has been associated with an increasing number of comorbidities, including IBD, but studies linking AD with IBD, including UC, have had mixed results, the authors wrote. And few studies have separately examined how AD or AD severity may be linked with UC or CD risk.
To examine the risk for new-onset IBD, UC, and CD in children and adults with atopic dermatitis, the researchers conducted a population-based cohort study using the THIN (The Health Improvement Network) electronic medical record database of patients registered with United Kingdom general practices. They used 21 years of data collected from January 1994 to February 2015.
The researchers matched each patient who had AD with up to five controls based on age, practice, and index date. Because THIN does not capture AD severity, they used treatment exposure assessed by dermatologic referrals and treatments patients received as proxy for severity. The authors used logistic regression to examine the risks for IBD, UC, and CD in children (aged 1-10) with AD, and in adults (aged 30-68) with AD, and they compared their outcomes with the outcomes for controls.
In the pediatric cohort, the team compared 409,431 children who had AD with 1.8 million children without AD. Slightly more than half were boys. In the adult cohort, they compared 625,083 people who had AD with 2.68 million controls, and slightly more than half were women. Data on race or ethnicity were not available, the authors wrote, but the THIN database is considered to be representative of the UK population.
AD severity linked with IBD risk
The risk for new-onset inflammatory bowel disease appears to be higher in children and adults with AD, and the risk varies based on age, AD severity, and subtype of inflammatory bowel disease, the authors reported.
Overall, AD in children was associated with a 44% increased risk for IBD (adjusted hazard ratio (HR), 1.44; 95% confidence interval [CI], 1.31-1.58) compared with controls, the authors reported. They found a 74% increased risk for CD in children with AD compared with controls (HR, 1.74; 95% CI, 1.54-1.97). More severe AD was linked with increased risk for both IBD and CD.
AD did not appear to increase risk for UC in children, except those with severe AD (HR, 1.65; 95% CI, 1.02-2.67).
Overall, adults with AD had a 34% (HR, 1.34; 95% CI, 1.27-1.40) increased risk for IBD, a 36% (HR, 1.36; 95% CI, 1.26-1.47) increased risk for CD, and a 32% (HR, 1.32; 95% CI, 1.24-1.41) increased risk for UC, with risk increasing with increased AD severity.
Robust data with cautionary note
“This study provides the most robust data to date on the association between IBD and AD. It provides clear evidence for an association that most dermatologists or primary care providers are not typically taught in training,” Kelly Scarberry, MD, assistant professor of dermatology at Case Western Reserve University in Cleveland, told this news organization. “I will be much more likely to pursue diagnostic workup in my AD patients who have GI complaints.”
However, AD severity was measured by proxy, added Dr. Scarberry, who was not involved in the study, and the study lacked important racial and ethnic data.
Lindsay C. Strowd, MD, associate professor of dermatology at Wake Forest University, Winston-Salem, N.C., also not involved in the study, said in an interview that she found the size of the cohort and the longitudinal data to be strengths of the study.
But, she added, the “lack of family IBD history, race and ethnicity, and comorbidities, are limitations, as is treatment exposure used as a proxy for disease severity, given that physician treatment practices differ.”
For Steven R. Feldman, MD, PhD, professor of dermatology at Wake Forest, “the most important conclusion, and it is a definitive finding, [is] that IBD is uncommon, even in patients with AD.
“The findings could be misinterpreted,” cautioned Dr. Feldman, who was not involved in the study. “While there is an increased relative risk, the absolute risk is small.” The study found that “the highest relative risk group is children with severe AD, who have a roughly fivefold increased risk for CD.” However, he added, the incidence rates of CD were 0.68 per 1,000 person-years in children with severe AD and 0.08 per 1,000 person-years in controls.
“Basically, because Crohn’s disease and IBD don’t happen very often, the modest increase in relative risk the investigators found doesn’t amount to much we’d have to worry about,” he said. “The findings do not show any need to screen patients with atopic dermatitis for IBD any more than we’d need to screen patients without atopic dermatitis.”
The increased relative risk “could be a clue to possible genetic connections between diseases,” he added. “But when we’re making clinical decisions, those decisions should be based on the absolute risk that some event may occur.”
Susan Massick, MD, dermatologist and associate professor at The Ohio State University in Columbus, who was not involved with the study, said in an interview, “We are still scratching the surface of the complexity of the immune and inflammatory pathways in AD and IBD.
“It is important to remember that correlation does not mean causation,” Dr. Massick said. “It would be premature to draw direct conclusions based on this study alone.”
The authors recommend future related studies in more diverse populations.
Dr. Gelfand and two coauthors reported ties with Pfizer, which supported the study. Dr. Gelfand and three coauthors reported ties with other pharmaceutical companies. Dr. Maguiness, Dr. Scarberry, Dr. Strowd, and Dr. Massick reported having no relevant disclosures. Dr. Feldman reported ties with Pfizer and other pharmaceutical companies.
A version of this article appeared on Medscape.com.
The published recently in JAMA Dermatology.
The study also found an increased risk for Crohn’s disease (CD) in adults and children with AD, as well as an increased risk for ulcerative colitis (UC) in adults with AD and in children with severe AD, researchers reported.
“It is imperative for clinicians to understand atopic dermatitis and the trajectory of our patients with it in order to provide the best standard of care,” senior author Joel M. Gelfand, MD, MSCE, professor in clinical investigation with the department of dermatology at the University of Pennsylvania, Philadelphia, said in a news release.
“There are new and better treatments for AD today, and there will likely continue to be more,” continued Dr. Gelfand. “But providers have to understand how those treatments could impact other autoimmune diseases. For patients with AD and another autoimmune disease, some currently available medications can exacerbate symptoms of their other disease or can help treat two immune diseases at the same time.”
The study results support the idea that AD and IBD may have some common underlying causes, said Sheilagh Maguiness, MD, pediatric dermatologist and associate professor in the department of dermatology at the University of Minnesota, Minneapolis, who was asked to comment on the findings.
“As the pathogenesis of AD is becoming better understood, we are recognizing that, rather than simply a cutaneous disease, the underlying inflammation and immune dysregulation that leads to AD best categorizes it as a systemic inflammatory disease with significant comorbidities,” she told this news organization. “I will be more likely to ask patients and families about GI symptoms, and if positive, may plan to refer to GI more readily than in the past,” added Dr. Maguiness, who was not involved in the study.
UK general practice cohort
AD has been associated with an increasing number of comorbidities, including IBD, but studies linking AD with IBD, including UC, have had mixed results, the authors wrote. And few studies have separately examined how AD or AD severity may be linked with UC or CD risk.
To examine the risk for new-onset IBD, UC, and CD in children and adults with atopic dermatitis, the researchers conducted a population-based cohort study using the THIN (The Health Improvement Network) electronic medical record database of patients registered with United Kingdom general practices. They used 21 years of data collected from January 1994 to February 2015.
The researchers matched each patient who had AD with up to five controls based on age, practice, and index date. Because THIN does not capture AD severity, they used treatment exposure assessed by dermatologic referrals and treatments patients received as proxy for severity. The authors used logistic regression to examine the risks for IBD, UC, and CD in children (aged 1-10) with AD, and in adults (aged 30-68) with AD, and they compared their outcomes with the outcomes for controls.
In the pediatric cohort, the team compared 409,431 children who had AD with 1.8 million children without AD. Slightly more than half were boys. In the adult cohort, they compared 625,083 people who had AD with 2.68 million controls, and slightly more than half were women. Data on race or ethnicity were not available, the authors wrote, but the THIN database is considered to be representative of the UK population.
AD severity linked with IBD risk
The risk for new-onset inflammatory bowel disease appears to be higher in children and adults with AD, and the risk varies based on age, AD severity, and subtype of inflammatory bowel disease, the authors reported.
Overall, AD in children was associated with a 44% increased risk for IBD (adjusted hazard ratio (HR), 1.44; 95% confidence interval [CI], 1.31-1.58) compared with controls, the authors reported. They found a 74% increased risk for CD in children with AD compared with controls (HR, 1.74; 95% CI, 1.54-1.97). More severe AD was linked with increased risk for both IBD and CD.
AD did not appear to increase risk for UC in children, except those with severe AD (HR, 1.65; 95% CI, 1.02-2.67).
Overall, adults with AD had a 34% (HR, 1.34; 95% CI, 1.27-1.40) increased risk for IBD, a 36% (HR, 1.36; 95% CI, 1.26-1.47) increased risk for CD, and a 32% (HR, 1.32; 95% CI, 1.24-1.41) increased risk for UC, with risk increasing with increased AD severity.
Robust data with cautionary note
“This study provides the most robust data to date on the association between IBD and AD. It provides clear evidence for an association that most dermatologists or primary care providers are not typically taught in training,” Kelly Scarberry, MD, assistant professor of dermatology at Case Western Reserve University in Cleveland, told this news organization. “I will be much more likely to pursue diagnostic workup in my AD patients who have GI complaints.”
However, AD severity was measured by proxy, added Dr. Scarberry, who was not involved in the study, and the study lacked important racial and ethnic data.
Lindsay C. Strowd, MD, associate professor of dermatology at Wake Forest University, Winston-Salem, N.C., also not involved in the study, said in an interview that she found the size of the cohort and the longitudinal data to be strengths of the study.
But, she added, the “lack of family IBD history, race and ethnicity, and comorbidities, are limitations, as is treatment exposure used as a proxy for disease severity, given that physician treatment practices differ.”
For Steven R. Feldman, MD, PhD, professor of dermatology at Wake Forest, “the most important conclusion, and it is a definitive finding, [is] that IBD is uncommon, even in patients with AD.
“The findings could be misinterpreted,” cautioned Dr. Feldman, who was not involved in the study. “While there is an increased relative risk, the absolute risk is small.” The study found that “the highest relative risk group is children with severe AD, who have a roughly fivefold increased risk for CD.” However, he added, the incidence rates of CD were 0.68 per 1,000 person-years in children with severe AD and 0.08 per 1,000 person-years in controls.
“Basically, because Crohn’s disease and IBD don’t happen very often, the modest increase in relative risk the investigators found doesn’t amount to much we’d have to worry about,” he said. “The findings do not show any need to screen patients with atopic dermatitis for IBD any more than we’d need to screen patients without atopic dermatitis.”
The increased relative risk “could be a clue to possible genetic connections between diseases,” he added. “But when we’re making clinical decisions, those decisions should be based on the absolute risk that some event may occur.”
Susan Massick, MD, dermatologist and associate professor at The Ohio State University in Columbus, who was not involved with the study, said in an interview, “We are still scratching the surface of the complexity of the immune and inflammatory pathways in AD and IBD.
“It is important to remember that correlation does not mean causation,” Dr. Massick said. “It would be premature to draw direct conclusions based on this study alone.”
The authors recommend future related studies in more diverse populations.
Dr. Gelfand and two coauthors reported ties with Pfizer, which supported the study. Dr. Gelfand and three coauthors reported ties with other pharmaceutical companies. Dr. Maguiness, Dr. Scarberry, Dr. Strowd, and Dr. Massick reported having no relevant disclosures. Dr. Feldman reported ties with Pfizer and other pharmaceutical companies.
A version of this article appeared on Medscape.com.
The published recently in JAMA Dermatology.
The study also found an increased risk for Crohn’s disease (CD) in adults and children with AD, as well as an increased risk for ulcerative colitis (UC) in adults with AD and in children with severe AD, researchers reported.
“It is imperative for clinicians to understand atopic dermatitis and the trajectory of our patients with it in order to provide the best standard of care,” senior author Joel M. Gelfand, MD, MSCE, professor in clinical investigation with the department of dermatology at the University of Pennsylvania, Philadelphia, said in a news release.
“There are new and better treatments for AD today, and there will likely continue to be more,” continued Dr. Gelfand. “But providers have to understand how those treatments could impact other autoimmune diseases. For patients with AD and another autoimmune disease, some currently available medications can exacerbate symptoms of their other disease or can help treat two immune diseases at the same time.”
The study results support the idea that AD and IBD may have some common underlying causes, said Sheilagh Maguiness, MD, pediatric dermatologist and associate professor in the department of dermatology at the University of Minnesota, Minneapolis, who was asked to comment on the findings.
“As the pathogenesis of AD is becoming better understood, we are recognizing that, rather than simply a cutaneous disease, the underlying inflammation and immune dysregulation that leads to AD best categorizes it as a systemic inflammatory disease with significant comorbidities,” she told this news organization. “I will be more likely to ask patients and families about GI symptoms, and if positive, may plan to refer to GI more readily than in the past,” added Dr. Maguiness, who was not involved in the study.
UK general practice cohort
AD has been associated with an increasing number of comorbidities, including IBD, but studies linking AD with IBD, including UC, have had mixed results, the authors wrote. And few studies have separately examined how AD or AD severity may be linked with UC or CD risk.
To examine the risk for new-onset IBD, UC, and CD in children and adults with atopic dermatitis, the researchers conducted a population-based cohort study using the THIN (The Health Improvement Network) electronic medical record database of patients registered with United Kingdom general practices. They used 21 years of data collected from January 1994 to February 2015.
The researchers matched each patient who had AD with up to five controls based on age, practice, and index date. Because THIN does not capture AD severity, they used treatment exposure assessed by dermatologic referrals and treatments patients received as proxy for severity. The authors used logistic regression to examine the risks for IBD, UC, and CD in children (aged 1-10) with AD, and in adults (aged 30-68) with AD, and they compared their outcomes with the outcomes for controls.
In the pediatric cohort, the team compared 409,431 children who had AD with 1.8 million children without AD. Slightly more than half were boys. In the adult cohort, they compared 625,083 people who had AD with 2.68 million controls, and slightly more than half were women. Data on race or ethnicity were not available, the authors wrote, but the THIN database is considered to be representative of the UK population.
AD severity linked with IBD risk
The risk for new-onset inflammatory bowel disease appears to be higher in children and adults with AD, and the risk varies based on age, AD severity, and subtype of inflammatory bowel disease, the authors reported.
Overall, AD in children was associated with a 44% increased risk for IBD (adjusted hazard ratio (HR), 1.44; 95% confidence interval [CI], 1.31-1.58) compared with controls, the authors reported. They found a 74% increased risk for CD in children with AD compared with controls (HR, 1.74; 95% CI, 1.54-1.97). More severe AD was linked with increased risk for both IBD and CD.
AD did not appear to increase risk for UC in children, except those with severe AD (HR, 1.65; 95% CI, 1.02-2.67).
Overall, adults with AD had a 34% (HR, 1.34; 95% CI, 1.27-1.40) increased risk for IBD, a 36% (HR, 1.36; 95% CI, 1.26-1.47) increased risk for CD, and a 32% (HR, 1.32; 95% CI, 1.24-1.41) increased risk for UC, with risk increasing with increased AD severity.
Robust data with cautionary note
“This study provides the most robust data to date on the association between IBD and AD. It provides clear evidence for an association that most dermatologists or primary care providers are not typically taught in training,” Kelly Scarberry, MD, assistant professor of dermatology at Case Western Reserve University in Cleveland, told this news organization. “I will be much more likely to pursue diagnostic workup in my AD patients who have GI complaints.”
However, AD severity was measured by proxy, added Dr. Scarberry, who was not involved in the study, and the study lacked important racial and ethnic data.
Lindsay C. Strowd, MD, associate professor of dermatology at Wake Forest University, Winston-Salem, N.C., also not involved in the study, said in an interview that she found the size of the cohort and the longitudinal data to be strengths of the study.
But, she added, the “lack of family IBD history, race and ethnicity, and comorbidities, are limitations, as is treatment exposure used as a proxy for disease severity, given that physician treatment practices differ.”
For Steven R. Feldman, MD, PhD, professor of dermatology at Wake Forest, “the most important conclusion, and it is a definitive finding, [is] that IBD is uncommon, even in patients with AD.
“The findings could be misinterpreted,” cautioned Dr. Feldman, who was not involved in the study. “While there is an increased relative risk, the absolute risk is small.” The study found that “the highest relative risk group is children with severe AD, who have a roughly fivefold increased risk for CD.” However, he added, the incidence rates of CD were 0.68 per 1,000 person-years in children with severe AD and 0.08 per 1,000 person-years in controls.
“Basically, because Crohn’s disease and IBD don’t happen very often, the modest increase in relative risk the investigators found doesn’t amount to much we’d have to worry about,” he said. “The findings do not show any need to screen patients with atopic dermatitis for IBD any more than we’d need to screen patients without atopic dermatitis.”
The increased relative risk “could be a clue to possible genetic connections between diseases,” he added. “But when we’re making clinical decisions, those decisions should be based on the absolute risk that some event may occur.”
Susan Massick, MD, dermatologist and associate professor at The Ohio State University in Columbus, who was not involved with the study, said in an interview, “We are still scratching the surface of the complexity of the immune and inflammatory pathways in AD and IBD.
“It is important to remember that correlation does not mean causation,” Dr. Massick said. “It would be premature to draw direct conclusions based on this study alone.”
The authors recommend future related studies in more diverse populations.
Dr. Gelfand and two coauthors reported ties with Pfizer, which supported the study. Dr. Gelfand and three coauthors reported ties with other pharmaceutical companies. Dr. Maguiness, Dr. Scarberry, Dr. Strowd, and Dr. Massick reported having no relevant disclosures. Dr. Feldman reported ties with Pfizer and other pharmaceutical companies.
A version of this article appeared on Medscape.com.
FROM JAMA DERMATOLOGY
FDA OKs subcutaneous vedolizumab for UC maintenance therapy
The Food and Drug Administration has approved the subcutaneous administration of vedolizumab (Entyvio SC, Takeda) for maintenance therapy in adults with moderately to severely active ulcerative colitis (UC) following induction therapy with intravenous administration of vedolizumab.
The FDA approved the intravenous formulation of the biologic in 2014 for patients with moderate to severe UC and Crohn’s disease who failed or cannot tolerate other therapies.
The approval of subcutaneous (SC) vedolizumab was based on results from the phase 3, randomized, double-blind, placebo-controlled VISIBLE 1 trial.
The trial assessed the safety and efficacy of maintenance therapy with SC vedolizumab in adult patients with moderately to severely active UC who achieved clinical response at week 6 following two doses of intravenous vedolizumab.
At week 6, 162 patients were randomly allocated (2:1) to vedolizumab or placebo by subcutaneous injection every 2 weeks. The primary endpoint was clinical remission at week 52, defined as a total Mayo score of 2 or less and no individual subscore greater than 1.
At week 52, nearly half (46%) of patients who received vedolizumab SC maintenance therapy achieved clinical remission, compared with 14% of those who received placebo SC (P < .001).
The safety profile of SC vedolizumab was “generally consistent” with that of intravenous vedolizumab, with the addition of injection-site reactions, the drugmaker, Takeda, said in a news release.
The most common adverse reactions with intravenous vedolizumab are nasopharyngitis, headache, arthralgia, nausea, pyrexia (fever), upper respiratory tract infection, fatigue, cough, bronchitis, influenza, back pain, rash, pruritus, sinusitis, oropharyngeal pain, and pain in the extremities.
SC vedolizumab “can provide physicians with an additional administration option for achieving remission in their moderate to severe ulcerative colitis patients,” according to Bruce E. Sands, MD, AGAF, chief of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York. He provided a statement in the Takeda news release.
“I appreciate now having a subcutaneous administration option that provides a clinical profile consistent with Entyvio intravenous while also giving me and my appropriate UC patients a choice of how they receive their maintenance therapy,” Dr. Sands said.
The FDA is currently reviewing Takeda’s biologics license application for subcutaneous administration of vedolizumab in the treatment of adults with moderately to severely active Crohn’s disease.
Dr. Sands is a paid consultant of Takeda.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the subcutaneous administration of vedolizumab (Entyvio SC, Takeda) for maintenance therapy in adults with moderately to severely active ulcerative colitis (UC) following induction therapy with intravenous administration of vedolizumab.
The FDA approved the intravenous formulation of the biologic in 2014 for patients with moderate to severe UC and Crohn’s disease who failed or cannot tolerate other therapies.
The approval of subcutaneous (SC) vedolizumab was based on results from the phase 3, randomized, double-blind, placebo-controlled VISIBLE 1 trial.
The trial assessed the safety and efficacy of maintenance therapy with SC vedolizumab in adult patients with moderately to severely active UC who achieved clinical response at week 6 following two doses of intravenous vedolizumab.
At week 6, 162 patients were randomly allocated (2:1) to vedolizumab or placebo by subcutaneous injection every 2 weeks. The primary endpoint was clinical remission at week 52, defined as a total Mayo score of 2 or less and no individual subscore greater than 1.
At week 52, nearly half (46%) of patients who received vedolizumab SC maintenance therapy achieved clinical remission, compared with 14% of those who received placebo SC (P < .001).
The safety profile of SC vedolizumab was “generally consistent” with that of intravenous vedolizumab, with the addition of injection-site reactions, the drugmaker, Takeda, said in a news release.
The most common adverse reactions with intravenous vedolizumab are nasopharyngitis, headache, arthralgia, nausea, pyrexia (fever), upper respiratory tract infection, fatigue, cough, bronchitis, influenza, back pain, rash, pruritus, sinusitis, oropharyngeal pain, and pain in the extremities.
SC vedolizumab “can provide physicians with an additional administration option for achieving remission in their moderate to severe ulcerative colitis patients,” according to Bruce E. Sands, MD, AGAF, chief of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York. He provided a statement in the Takeda news release.
“I appreciate now having a subcutaneous administration option that provides a clinical profile consistent with Entyvio intravenous while also giving me and my appropriate UC patients a choice of how they receive their maintenance therapy,” Dr. Sands said.
The FDA is currently reviewing Takeda’s biologics license application for subcutaneous administration of vedolizumab in the treatment of adults with moderately to severely active Crohn’s disease.
Dr. Sands is a paid consultant of Takeda.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved the subcutaneous administration of vedolizumab (Entyvio SC, Takeda) for maintenance therapy in adults with moderately to severely active ulcerative colitis (UC) following induction therapy with intravenous administration of vedolizumab.
The FDA approved the intravenous formulation of the biologic in 2014 for patients with moderate to severe UC and Crohn’s disease who failed or cannot tolerate other therapies.
The approval of subcutaneous (SC) vedolizumab was based on results from the phase 3, randomized, double-blind, placebo-controlled VISIBLE 1 trial.
The trial assessed the safety and efficacy of maintenance therapy with SC vedolizumab in adult patients with moderately to severely active UC who achieved clinical response at week 6 following two doses of intravenous vedolizumab.
At week 6, 162 patients were randomly allocated (2:1) to vedolizumab or placebo by subcutaneous injection every 2 weeks. The primary endpoint was clinical remission at week 52, defined as a total Mayo score of 2 or less and no individual subscore greater than 1.
At week 52, nearly half (46%) of patients who received vedolizumab SC maintenance therapy achieved clinical remission, compared with 14% of those who received placebo SC (P < .001).
The safety profile of SC vedolizumab was “generally consistent” with that of intravenous vedolizumab, with the addition of injection-site reactions, the drugmaker, Takeda, said in a news release.
The most common adverse reactions with intravenous vedolizumab are nasopharyngitis, headache, arthralgia, nausea, pyrexia (fever), upper respiratory tract infection, fatigue, cough, bronchitis, influenza, back pain, rash, pruritus, sinusitis, oropharyngeal pain, and pain in the extremities.
SC vedolizumab “can provide physicians with an additional administration option for achieving remission in their moderate to severe ulcerative colitis patients,” according to Bruce E. Sands, MD, AGAF, chief of gastroenterology at the Icahn School of Medicine at Mount Sinai, New York. He provided a statement in the Takeda news release.
“I appreciate now having a subcutaneous administration option that provides a clinical profile consistent with Entyvio intravenous while also giving me and my appropriate UC patients a choice of how they receive their maintenance therapy,” Dr. Sands said.
The FDA is currently reviewing Takeda’s biologics license application for subcutaneous administration of vedolizumab in the treatment of adults with moderately to severely active Crohn’s disease.
Dr. Sands is a paid consultant of Takeda.
A version of this article first appeared on Medscape.com.
ChatGPT may aid decision-making in the ED for acute ulcerative colitis
(UC).
In a small study, ChatGPT version 4 (GPT-4) accurately gauged disease severity and made decisions about the need for hospitalization that were largely in line with expert gastroenterologists.
“Our findings suggest that GPT-4 has potential as a clinical decision-support tool in assessing UC severity and recommending suitable settings for further treatment,” say the authors, led by Asaf Levartovsky, MD, department of gastroenterology, Sheba Medical Center, Tel Aviv University.
The study was published online in the American Journal of Gastroenterology.
Assessing its potential
UC is a chronic inflammatory bowel disease known for episodes of flare-ups and remissions. Flare-ups often result in a trip to the ED, where staff must rapidly assess disease severity and need for hospital admission.
Dr. Levartovsky and colleagues explored how helpful GPT-4 could be in 20 distinct presentations of acute UC in the ED. They assessed the chatbot’s ability to determine the severity of disease and whether a specific presentation warranted hospital admission for further treatment.
They fed GPT-4 case summaries that included crucial data such as symptoms, vital signs, and laboratory results. For each case, they asked the chatbot to assess disease severity based on established criteria and recommend hospital admission or outpatient care.
The GPT-4 answers were compared with assessments made by gastroenterologists and the actual decision regarding hospitalization made by the physician in the ED.
Overall, ChatGPT categorized acute UC as severe in 12 patients, as moderate in 7, and as mild in 1. In each case, the chatbot provided a detailed answer depicting severity of every variable of the criteria and an overall severity classification.
ChatGPT’s assessments were consistent with gastroenterologists’ assessments 80% of the time, with a “high degree of reliability” between the two assessments, the study team reports.
The average correlation between ChatGPT and physician ratings was 0.839 (P < .001). Inconsistencies in four cases stemmed largely from inaccurate cut-off values for systemic variables (such as hemoglobin and tachycardia).
Following severity assessment, ChatGPT leaned toward hospital admission for 16 patients, whereas in actual clinical practice, only 12 patients were hospitalized. In one patient with moderate UC who was discharged, ChatGPT was in favor of hospitalization, based on the patient’s age and comorbid conditions. For two moderate UC cases, the chatbot recommended consultation with a health care professional for further evaluation and management, which the researchers deemed to be an indecisive response.
Based on their findings, the researchers say ChatGPT could serve as a real-time decision support tool – one that is not meant to replace physicians but rather enhance human decision-making.
They note that the small sample size is a limitation and that ChatGPT’s accuracy rate requires further validation across larger samples and diverse clinical scenarios.
The study had no specific funding. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(UC).
In a small study, ChatGPT version 4 (GPT-4) accurately gauged disease severity and made decisions about the need for hospitalization that were largely in line with expert gastroenterologists.
“Our findings suggest that GPT-4 has potential as a clinical decision-support tool in assessing UC severity and recommending suitable settings for further treatment,” say the authors, led by Asaf Levartovsky, MD, department of gastroenterology, Sheba Medical Center, Tel Aviv University.
The study was published online in the American Journal of Gastroenterology.
Assessing its potential
UC is a chronic inflammatory bowel disease known for episodes of flare-ups and remissions. Flare-ups often result in a trip to the ED, where staff must rapidly assess disease severity and need for hospital admission.
Dr. Levartovsky and colleagues explored how helpful GPT-4 could be in 20 distinct presentations of acute UC in the ED. They assessed the chatbot’s ability to determine the severity of disease and whether a specific presentation warranted hospital admission for further treatment.
They fed GPT-4 case summaries that included crucial data such as symptoms, vital signs, and laboratory results. For each case, they asked the chatbot to assess disease severity based on established criteria and recommend hospital admission or outpatient care.
The GPT-4 answers were compared with assessments made by gastroenterologists and the actual decision regarding hospitalization made by the physician in the ED.
Overall, ChatGPT categorized acute UC as severe in 12 patients, as moderate in 7, and as mild in 1. In each case, the chatbot provided a detailed answer depicting severity of every variable of the criteria and an overall severity classification.
ChatGPT’s assessments were consistent with gastroenterologists’ assessments 80% of the time, with a “high degree of reliability” between the two assessments, the study team reports.
The average correlation between ChatGPT and physician ratings was 0.839 (P < .001). Inconsistencies in four cases stemmed largely from inaccurate cut-off values for systemic variables (such as hemoglobin and tachycardia).
Following severity assessment, ChatGPT leaned toward hospital admission for 16 patients, whereas in actual clinical practice, only 12 patients were hospitalized. In one patient with moderate UC who was discharged, ChatGPT was in favor of hospitalization, based on the patient’s age and comorbid conditions. For two moderate UC cases, the chatbot recommended consultation with a health care professional for further evaluation and management, which the researchers deemed to be an indecisive response.
Based on their findings, the researchers say ChatGPT could serve as a real-time decision support tool – one that is not meant to replace physicians but rather enhance human decision-making.
They note that the small sample size is a limitation and that ChatGPT’s accuracy rate requires further validation across larger samples and diverse clinical scenarios.
The study had no specific funding. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
(UC).
In a small study, ChatGPT version 4 (GPT-4) accurately gauged disease severity and made decisions about the need for hospitalization that were largely in line with expert gastroenterologists.
“Our findings suggest that GPT-4 has potential as a clinical decision-support tool in assessing UC severity and recommending suitable settings for further treatment,” say the authors, led by Asaf Levartovsky, MD, department of gastroenterology, Sheba Medical Center, Tel Aviv University.
The study was published online in the American Journal of Gastroenterology.
Assessing its potential
UC is a chronic inflammatory bowel disease known for episodes of flare-ups and remissions. Flare-ups often result in a trip to the ED, where staff must rapidly assess disease severity and need for hospital admission.
Dr. Levartovsky and colleagues explored how helpful GPT-4 could be in 20 distinct presentations of acute UC in the ED. They assessed the chatbot’s ability to determine the severity of disease and whether a specific presentation warranted hospital admission for further treatment.
They fed GPT-4 case summaries that included crucial data such as symptoms, vital signs, and laboratory results. For each case, they asked the chatbot to assess disease severity based on established criteria and recommend hospital admission or outpatient care.
The GPT-4 answers were compared with assessments made by gastroenterologists and the actual decision regarding hospitalization made by the physician in the ED.
Overall, ChatGPT categorized acute UC as severe in 12 patients, as moderate in 7, and as mild in 1. In each case, the chatbot provided a detailed answer depicting severity of every variable of the criteria and an overall severity classification.
ChatGPT’s assessments were consistent with gastroenterologists’ assessments 80% of the time, with a “high degree of reliability” between the two assessments, the study team reports.
The average correlation between ChatGPT and physician ratings was 0.839 (P < .001). Inconsistencies in four cases stemmed largely from inaccurate cut-off values for systemic variables (such as hemoglobin and tachycardia).
Following severity assessment, ChatGPT leaned toward hospital admission for 16 patients, whereas in actual clinical practice, only 12 patients were hospitalized. In one patient with moderate UC who was discharged, ChatGPT was in favor of hospitalization, based on the patient’s age and comorbid conditions. For two moderate UC cases, the chatbot recommended consultation with a health care professional for further evaluation and management, which the researchers deemed to be an indecisive response.
Based on their findings, the researchers say ChatGPT could serve as a real-time decision support tool – one that is not meant to replace physicians but rather enhance human decision-making.
They note that the small sample size is a limitation and that ChatGPT’s accuracy rate requires further validation across larger samples and diverse clinical scenarios.
The study had no specific funding. The authors report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF GASTROENTEROLOGY
Real-world data confirm efficacy of dupilumab in severe EoE
TOPLINE:
Dupilumab provides histologic, endoscopic, and symptomatic improvement in patients with severe, treatment-refractory, fibrostenotic eosinophilic esophagitis (EoE), new research shows.
METHODOLOGY:
- The researchers conducted a retrospective cohort study of 46 patients with severe, treatment-refractory fibrostenotic EoE who were prescribed dupilumab 300 mg subcutaneously every other week or weekly.
- Histologic response, endoscopic severity, and symptom improvement were assessed using the results of esophagogastroduodenoscopy (EGD) conducted before and after dupilumab therapy.
TAKEAWAY:
- Most patients demonstrated endoscopic, histologic, and symptomatic improvement on dupilumab, compared with predupilumab EGD results.
- The average peak eosinophil count improved from 70 eosinophils/high-power field to 9 eosinophils/HPF while on dupilumab, and 80% of patients achieved histologic remission (< 15 eosinophils/HPF), compared with 11% before dupilumab.
- Endoscopic features also improved on dupilumab, with a significant reduction in exudates, rings, edema, and furrows. The total EoE Endoscopic Reference Score decreased from 4.62 to 1.89 (P < .001).
- With dupilumab, a significant increase in predilation esophageal diameter (from 13.9 to 16 mm; P < .001) was observed, with no change in the proportion of strictures.
- Global symptom improvement was reported in 91% of patients while on dupilumab versus 2% before dupilumab.
IN PRACTICE:
“These results echo the results from the prior phase 3 study, but in a population where most subjects would likely have been excluded due to stricture severity and need for dilation,” the authors wrote. “ Further studies are needed to determine not only long-term efficacy of dupilumab for this group of EoE patients, but whether dupilumab could be moved earlier in the treatment algorithm for this severe subgroup.”
SOURCE:
The study, by Christopher Lee, MD, and Evan Dellon, MD, MPH, with the Center for Esophageal Diseases and Swallowing, University of North Carolina at Chapel Hill, was published online in Clinical Gastroenterology and Hepatology.
LIMITATIONS:
The study involved a single tertiary care center, which could limit the generalizability of the findings. The patients were primarily adults, so the results may not be able to be extended to younger children.
DISCLOSURES:
The study had no specific funding. Dr. Dellon has received research funding and consulting fees from multiple pharmaceutical companies. Dr. Lee has no relevant disclosures.
A version of this article first appeared on Medscape.com.
TOPLINE:
Dupilumab provides histologic, endoscopic, and symptomatic improvement in patients with severe, treatment-refractory, fibrostenotic eosinophilic esophagitis (EoE), new research shows.
METHODOLOGY:
- The researchers conducted a retrospective cohort study of 46 patients with severe, treatment-refractory fibrostenotic EoE who were prescribed dupilumab 300 mg subcutaneously every other week or weekly.
- Histologic response, endoscopic severity, and symptom improvement were assessed using the results of esophagogastroduodenoscopy (EGD) conducted before and after dupilumab therapy.
TAKEAWAY:
- Most patients demonstrated endoscopic, histologic, and symptomatic improvement on dupilumab, compared with predupilumab EGD results.
- The average peak eosinophil count improved from 70 eosinophils/high-power field to 9 eosinophils/HPF while on dupilumab, and 80% of patients achieved histologic remission (< 15 eosinophils/HPF), compared with 11% before dupilumab.
- Endoscopic features also improved on dupilumab, with a significant reduction in exudates, rings, edema, and furrows. The total EoE Endoscopic Reference Score decreased from 4.62 to 1.89 (P < .001).
- With dupilumab, a significant increase in predilation esophageal diameter (from 13.9 to 16 mm; P < .001) was observed, with no change in the proportion of strictures.
- Global symptom improvement was reported in 91% of patients while on dupilumab versus 2% before dupilumab.
IN PRACTICE:
“These results echo the results from the prior phase 3 study, but in a population where most subjects would likely have been excluded due to stricture severity and need for dilation,” the authors wrote. “ Further studies are needed to determine not only long-term efficacy of dupilumab for this group of EoE patients, but whether dupilumab could be moved earlier in the treatment algorithm for this severe subgroup.”
SOURCE:
The study, by Christopher Lee, MD, and Evan Dellon, MD, MPH, with the Center for Esophageal Diseases and Swallowing, University of North Carolina at Chapel Hill, was published online in Clinical Gastroenterology and Hepatology.
LIMITATIONS:
The study involved a single tertiary care center, which could limit the generalizability of the findings. The patients were primarily adults, so the results may not be able to be extended to younger children.
DISCLOSURES:
The study had no specific funding. Dr. Dellon has received research funding and consulting fees from multiple pharmaceutical companies. Dr. Lee has no relevant disclosures.
A version of this article first appeared on Medscape.com.
TOPLINE:
Dupilumab provides histologic, endoscopic, and symptomatic improvement in patients with severe, treatment-refractory, fibrostenotic eosinophilic esophagitis (EoE), new research shows.
METHODOLOGY:
- The researchers conducted a retrospective cohort study of 46 patients with severe, treatment-refractory fibrostenotic EoE who were prescribed dupilumab 300 mg subcutaneously every other week or weekly.
- Histologic response, endoscopic severity, and symptom improvement were assessed using the results of esophagogastroduodenoscopy (EGD) conducted before and after dupilumab therapy.
TAKEAWAY:
- Most patients demonstrated endoscopic, histologic, and symptomatic improvement on dupilumab, compared with predupilumab EGD results.
- The average peak eosinophil count improved from 70 eosinophils/high-power field to 9 eosinophils/HPF while on dupilumab, and 80% of patients achieved histologic remission (< 15 eosinophils/HPF), compared with 11% before dupilumab.
- Endoscopic features also improved on dupilumab, with a significant reduction in exudates, rings, edema, and furrows. The total EoE Endoscopic Reference Score decreased from 4.62 to 1.89 (P < .001).
- With dupilumab, a significant increase in predilation esophageal diameter (from 13.9 to 16 mm; P < .001) was observed, with no change in the proportion of strictures.
- Global symptom improvement was reported in 91% of patients while on dupilumab versus 2% before dupilumab.
IN PRACTICE:
“These results echo the results from the prior phase 3 study, but in a population where most subjects would likely have been excluded due to stricture severity and need for dilation,” the authors wrote. “ Further studies are needed to determine not only long-term efficacy of dupilumab for this group of EoE patients, but whether dupilumab could be moved earlier in the treatment algorithm for this severe subgroup.”
SOURCE:
The study, by Christopher Lee, MD, and Evan Dellon, MD, MPH, with the Center for Esophageal Diseases and Swallowing, University of North Carolina at Chapel Hill, was published online in Clinical Gastroenterology and Hepatology.
LIMITATIONS:
The study involved a single tertiary care center, which could limit the generalizability of the findings. The patients were primarily adults, so the results may not be able to be extended to younger children.
DISCLOSURES:
The study had no specific funding. Dr. Dellon has received research funding and consulting fees from multiple pharmaceutical companies. Dr. Lee has no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM CLINICAL GASTROENTEROLOGY AND HEPATOLOGY
Palpable mass on exam
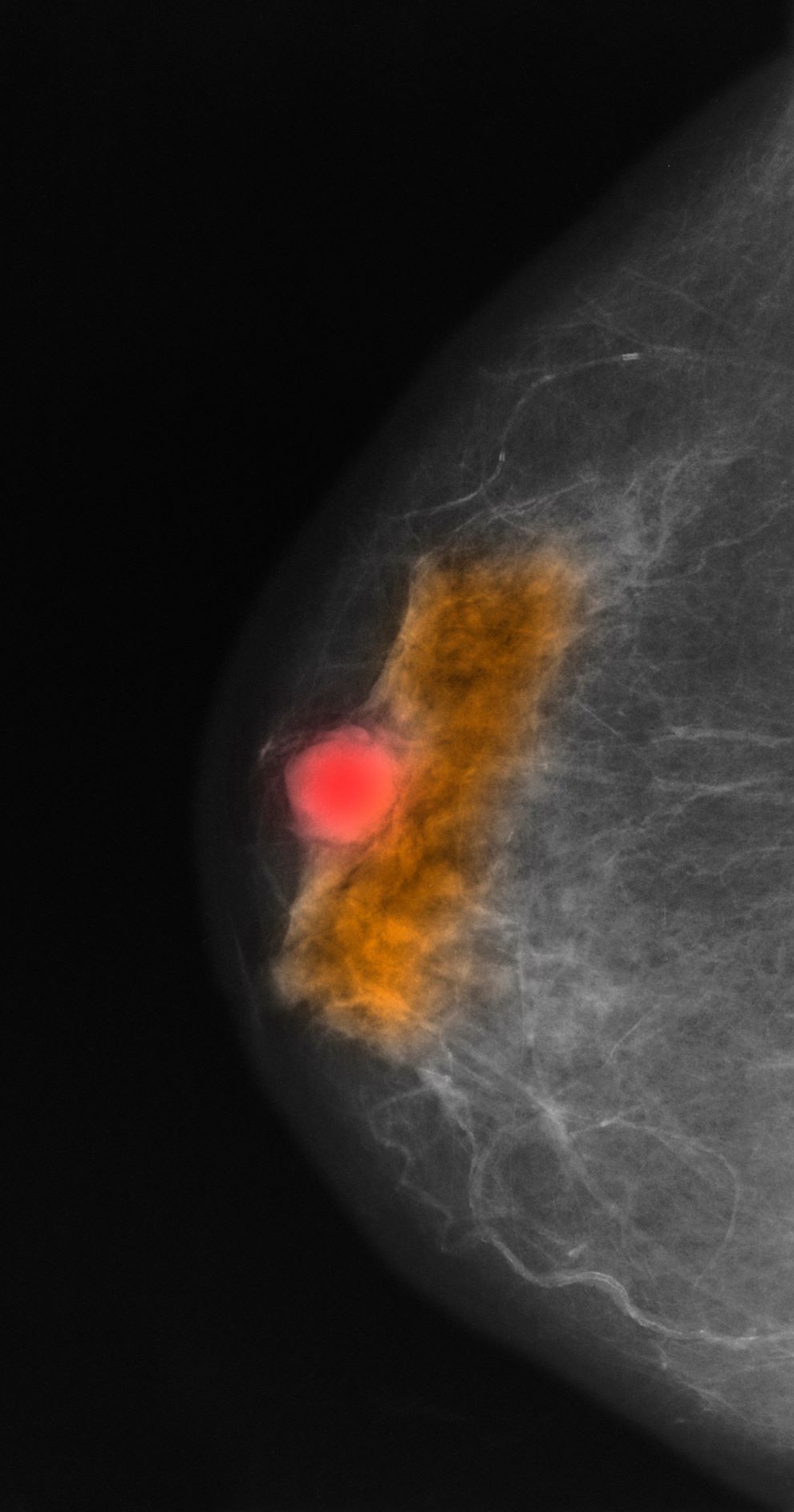
Given the age of the patient and the results of imaging, histology, and immunohistochemistry, the diagnosis is mucinous (colloid) carcinoma. The patient and oncologist discuss prognosis and discuss treatment options, such as breast-conserving surgery, local radiation, and possible adjuvant endocrine therapy.
Mucinous (colloid) carcinoma is a rare histologic subtype of invasive breast cancer that occurs in < 5% of patients and generally develops in those who are ≥ 60 years old. Patients with mucinous (colloid) carcinoma generally present with a palpable mass or, on imaging, a poorly defined tumor with rare calcifications. The histologic hallmark of mucinous (colloid) carcinoma is mucin production. There are two subtypes of mucinous breast carcinoma: pure and mixed. A pure mucinous tumor is defined as a carcinoma consisting of ≥ 90% intracellular or extracellular mucin. This pure subtype occurs more frequently than mixed mucinous breast carcinoma and is also less likely to metastasize to the lymph nodes.
Differential diagnosis can be challenging because mucinous (colloid) carcinoma can mimic a benign tumor on imaging, which is why it is important to include multiple factors when diagnosing in daily practice. According to the National Comprehensive Cancer Network (NCCN), diagnosing nonmetastatic invasive breast cancer like mucinous (colloid) carcinoma involves patient history and physical exam, diagnostic bilateral mammography (ultrasound and breast MRI, as needed), pathology review, tumor estrogen/progesterone receptor status, HER2 status, and genetic counseling for those with a family history. In most cases of mucinous (colloid) carcinoma, tumors are ER- and PR-positive and HER2-negative.
A pure mucinous histologic subtype is generally associated with a favorable prognosis; 10-year survival rates of mucinous (colloid) carcinoma are > 80%. The tumor is generally not high grade and is most often classified on surgical excision. Two main types of lesions exist — A and B — as does a combination of AB. Type A has larger quantities of extracellular mucin and is considered the classic form of mucinous carcinoma. Type B is a distinct variant with endocrine differentiation. In addition, glycoproteins MUC2 and MUC6 are predominantly expressed in mucinous (colloid) carcinoma; ductal carcinoma in situ is not often found in this setting.
NCCN recommends multidisciplinary care and development of a personalized survivorship treatment plan, which includes a customized summary of possible long-term treatment toxicities. In addition, multidisciplinary care coordination encourages close follow-up that helps patients adhere to their medications and stay current with ongoing screening.
Breast-conserving surgery and local radiation therapy are often the two modalities used to treat mucinous (colloid) carcinoma, especially because prognosis is so favorable. NCCN recommends the consideration of adjuvant endocrine treatment for patients with pure mucinous tumors that are HER2-negative and ER-positive and/or PR-positive; staged at pT1, pT2, or pT3, and pN0 or pN1mi; and ≤ 2.9 cm. Adjuvant endocrine therapy is recommended for patients with the same disease characteristics whose tumor is ≥ 3 cm.
Avan J. Armaghani, MD, Assistant Member, Department of Breast Oncology, Moffitt Cancer Center, University of South Florida, Tampa, FL.
Avan J. Armaghani, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Given the age of the patient and the results of imaging, histology, and immunohistochemistry, the diagnosis is mucinous (colloid) carcinoma. The patient and oncologist discuss prognosis and discuss treatment options, such as breast-conserving surgery, local radiation, and possible adjuvant endocrine therapy.
Mucinous (colloid) carcinoma is a rare histologic subtype of invasive breast cancer that occurs in < 5% of patients and generally develops in those who are ≥ 60 years old. Patients with mucinous (colloid) carcinoma generally present with a palpable mass or, on imaging, a poorly defined tumor with rare calcifications. The histologic hallmark of mucinous (colloid) carcinoma is mucin production. There are two subtypes of mucinous breast carcinoma: pure and mixed. A pure mucinous tumor is defined as a carcinoma consisting of ≥ 90% intracellular or extracellular mucin. This pure subtype occurs more frequently than mixed mucinous breast carcinoma and is also less likely to metastasize to the lymph nodes.
Differential diagnosis can be challenging because mucinous (colloid) carcinoma can mimic a benign tumor on imaging, which is why it is important to include multiple factors when diagnosing in daily practice. According to the National Comprehensive Cancer Network (NCCN), diagnosing nonmetastatic invasive breast cancer like mucinous (colloid) carcinoma involves patient history and physical exam, diagnostic bilateral mammography (ultrasound and breast MRI, as needed), pathology review, tumor estrogen/progesterone receptor status, HER2 status, and genetic counseling for those with a family history. In most cases of mucinous (colloid) carcinoma, tumors are ER- and PR-positive and HER2-negative.
A pure mucinous histologic subtype is generally associated with a favorable prognosis; 10-year survival rates of mucinous (colloid) carcinoma are > 80%. The tumor is generally not high grade and is most often classified on surgical excision. Two main types of lesions exist — A and B — as does a combination of AB. Type A has larger quantities of extracellular mucin and is considered the classic form of mucinous carcinoma. Type B is a distinct variant with endocrine differentiation. In addition, glycoproteins MUC2 and MUC6 are predominantly expressed in mucinous (colloid) carcinoma; ductal carcinoma in situ is not often found in this setting.
NCCN recommends multidisciplinary care and development of a personalized survivorship treatment plan, which includes a customized summary of possible long-term treatment toxicities. In addition, multidisciplinary care coordination encourages close follow-up that helps patients adhere to their medications and stay current with ongoing screening.
Breast-conserving surgery and local radiation therapy are often the two modalities used to treat mucinous (colloid) carcinoma, especially because prognosis is so favorable. NCCN recommends the consideration of adjuvant endocrine treatment for patients with pure mucinous tumors that are HER2-negative and ER-positive and/or PR-positive; staged at pT1, pT2, or pT3, and pN0 or pN1mi; and ≤ 2.9 cm. Adjuvant endocrine therapy is recommended for patients with the same disease characteristics whose tumor is ≥ 3 cm.
Avan J. Armaghani, MD, Assistant Member, Department of Breast Oncology, Moffitt Cancer Center, University of South Florida, Tampa, FL.
Avan J. Armaghani, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
Given the age of the patient and the results of imaging, histology, and immunohistochemistry, the diagnosis is mucinous (colloid) carcinoma. The patient and oncologist discuss prognosis and discuss treatment options, such as breast-conserving surgery, local radiation, and possible adjuvant endocrine therapy.
Mucinous (colloid) carcinoma is a rare histologic subtype of invasive breast cancer that occurs in < 5% of patients and generally develops in those who are ≥ 60 years old. Patients with mucinous (colloid) carcinoma generally present with a palpable mass or, on imaging, a poorly defined tumor with rare calcifications. The histologic hallmark of mucinous (colloid) carcinoma is mucin production. There are two subtypes of mucinous breast carcinoma: pure and mixed. A pure mucinous tumor is defined as a carcinoma consisting of ≥ 90% intracellular or extracellular mucin. This pure subtype occurs more frequently than mixed mucinous breast carcinoma and is also less likely to metastasize to the lymph nodes.
Differential diagnosis can be challenging because mucinous (colloid) carcinoma can mimic a benign tumor on imaging, which is why it is important to include multiple factors when diagnosing in daily practice. According to the National Comprehensive Cancer Network (NCCN), diagnosing nonmetastatic invasive breast cancer like mucinous (colloid) carcinoma involves patient history and physical exam, diagnostic bilateral mammography (ultrasound and breast MRI, as needed), pathology review, tumor estrogen/progesterone receptor status, HER2 status, and genetic counseling for those with a family history. In most cases of mucinous (colloid) carcinoma, tumors are ER- and PR-positive and HER2-negative.
A pure mucinous histologic subtype is generally associated with a favorable prognosis; 10-year survival rates of mucinous (colloid) carcinoma are > 80%. The tumor is generally not high grade and is most often classified on surgical excision. Two main types of lesions exist — A and B — as does a combination of AB. Type A has larger quantities of extracellular mucin and is considered the classic form of mucinous carcinoma. Type B is a distinct variant with endocrine differentiation. In addition, glycoproteins MUC2 and MUC6 are predominantly expressed in mucinous (colloid) carcinoma; ductal carcinoma in situ is not often found in this setting.
NCCN recommends multidisciplinary care and development of a personalized survivorship treatment plan, which includes a customized summary of possible long-term treatment toxicities. In addition, multidisciplinary care coordination encourages close follow-up that helps patients adhere to their medications and stay current with ongoing screening.
Breast-conserving surgery and local radiation therapy are often the two modalities used to treat mucinous (colloid) carcinoma, especially because prognosis is so favorable. NCCN recommends the consideration of adjuvant endocrine treatment for patients with pure mucinous tumors that are HER2-negative and ER-positive and/or PR-positive; staged at pT1, pT2, or pT3, and pN0 or pN1mi; and ≤ 2.9 cm. Adjuvant endocrine therapy is recommended for patients with the same disease characteristics whose tumor is ≥ 3 cm.
Avan J. Armaghani, MD, Assistant Member, Department of Breast Oncology, Moffitt Cancer Center, University of South Florida, Tampa, FL.
Avan J. Armaghani, MD, has disclosed no relevant financial relationships.
Image Quizzes are fictional or fictionalized clinical scenarios intended to provide evidence-based educational takeaways.
A 64-year-old woman with no prior history of cancer presents to an oncologist after referral from her primary care physician (PCP). The referral came after the patient reported feeling a lump in her left breast during self-examination. She made an appointment with her PCP, who confirmed a palpable mass on physical examination and ordered mammography. Bilateral mammography revealed a poorly defined tumor with rare calcifications in the left breast. Size of the tumor was 1.8 cm. Now, the oncologist orders a percutaneous vacuum-assisted large-gauge core-needle biopsy with image guidance. Results show the tumor is pure mucinous, ER-positive and PR-positive, and HER2-negative; staging is pT2/pN0. Immunohistochemistry reveals that the predominantly expressed glycoproteins are MUC2 and MUC6.
AMA funds standardized BP training for medical, PA, and nursing schools
according to the American Medical Association. Hypertension affects about half of U.S. adults and is a leading contributor to cardiovascular disease.
First-year medical students typically read about BP measurement in a textbook and possibly attend a lecture before practicing using a manual cuff a few times on classmates, said Martha Gulati, MD, professor and director of preventive cardiology at Cedars-Sinai Medical Center, Los Angeles.
The dearth of BP instruction is alarming because inaccurate readings contribute to under- and overtreatment of hypertension, she said in an interview.
The AMA hopes $100,000 in grants to five health education schools will help improve BP instruction. The group recently announced it would give $20,000 each to five schools that train health professionals, expanding on a 2021 program to improve BP measurement training.
The new grants for interactive lessons will benefit nearly 5,000 students from Johns Hopkins University, Baltimore; Nova Southeastern University, Fort Lauderdale, Fla.; University of Washington, Seattle; Stony Brook (N.Y.) University; and the University of Pittsburgh.
In a 2021 survey of 571 clinicians, most of whom were cardiologists, Dr. Gulati found that only 23% performed accurate BP measurements despite the majority saying they trusted BP readings taken in their clinic. Accurate readings were defined as routinely checking BP in both arms, checking BP at least twice each visit, and waiting 5 minutes before taking the reading.
Med students fare no better when it comes to BP skills. In a 2017 study of 159 students from medical schools in 37 states, only one student demonstrated proficiency in all 11 elements necessary to measure BP accurately. Students, on average, performed just four of them correctly.
The elements of proper BP measurement include patients resting for 5 minutes before the measurement with legs uncrossed, feet on floor, and arm supported, not talking, reading, or using cell phone; BP taken in both arms with correct size of cuff placed over bare arm; and identifying BP from the arm with the higher reading as clinically more important and as the one to use for future readings.
Manual BP readings require an appropriately sized BP cuff, a sphygmomanometer, and a clinician skilled in using a stethoscope and auscultatory method. Meanwhile, automated readings require a clinician to place the cuff, but a digital device collects the measurement. Though preference depends on the setting and clinician, automated readings are more common. In Dr. Gulati’s study, automated BP assessment was used by 58% of respondents.
Depending on the BP device and technique, significant variations in readings can occur. In a 2021 study, Current Hypertension Reports found that automated readings may more closely reflect the patient’s baseline BP and produce results similar to ambulatory monitoring by a medical professional. An earlier JAMA Internal Medicine analysis found that clinicians’ manual readings reflect higher BP measurements than automated readings.
Though the AMA offers a free online series on BP measurement for students, making the training available to more health care team members can help prevent hypertension, said Kate Kirley, MD, director of the AMA’s chronic disease prevention and programs.
Concern over the lack of standardized BP techniques isn’t new. In 2019, the American Heart Association and the AMA created an online BP course for health care workers. Two years later, the AMA offered grants to five medical schools for training courses.
Most of the new training sessions already on the AMA website take students about 15 minutes to complete. Dr. Kirley says because equipment varies across settings, participants will learn how to conduct manual, semi-automated, and automated office BP readings and identify workarounds for less-than-ideal room setups that can skew results. They will also explore how to guide patients in performing BP readings at home.
A version of this article first appeared on Medscape.com.
according to the American Medical Association. Hypertension affects about half of U.S. adults and is a leading contributor to cardiovascular disease.
First-year medical students typically read about BP measurement in a textbook and possibly attend a lecture before practicing using a manual cuff a few times on classmates, said Martha Gulati, MD, professor and director of preventive cardiology at Cedars-Sinai Medical Center, Los Angeles.
The dearth of BP instruction is alarming because inaccurate readings contribute to under- and overtreatment of hypertension, she said in an interview.
The AMA hopes $100,000 in grants to five health education schools will help improve BP instruction. The group recently announced it would give $20,000 each to five schools that train health professionals, expanding on a 2021 program to improve BP measurement training.
The new grants for interactive lessons will benefit nearly 5,000 students from Johns Hopkins University, Baltimore; Nova Southeastern University, Fort Lauderdale, Fla.; University of Washington, Seattle; Stony Brook (N.Y.) University; and the University of Pittsburgh.
In a 2021 survey of 571 clinicians, most of whom were cardiologists, Dr. Gulati found that only 23% performed accurate BP measurements despite the majority saying they trusted BP readings taken in their clinic. Accurate readings were defined as routinely checking BP in both arms, checking BP at least twice each visit, and waiting 5 minutes before taking the reading.
Med students fare no better when it comes to BP skills. In a 2017 study of 159 students from medical schools in 37 states, only one student demonstrated proficiency in all 11 elements necessary to measure BP accurately. Students, on average, performed just four of them correctly.
The elements of proper BP measurement include patients resting for 5 minutes before the measurement with legs uncrossed, feet on floor, and arm supported, not talking, reading, or using cell phone; BP taken in both arms with correct size of cuff placed over bare arm; and identifying BP from the arm with the higher reading as clinically more important and as the one to use for future readings.
Manual BP readings require an appropriately sized BP cuff, a sphygmomanometer, and a clinician skilled in using a stethoscope and auscultatory method. Meanwhile, automated readings require a clinician to place the cuff, but a digital device collects the measurement. Though preference depends on the setting and clinician, automated readings are more common. In Dr. Gulati’s study, automated BP assessment was used by 58% of respondents.
Depending on the BP device and technique, significant variations in readings can occur. In a 2021 study, Current Hypertension Reports found that automated readings may more closely reflect the patient’s baseline BP and produce results similar to ambulatory monitoring by a medical professional. An earlier JAMA Internal Medicine analysis found that clinicians’ manual readings reflect higher BP measurements than automated readings.
Though the AMA offers a free online series on BP measurement for students, making the training available to more health care team members can help prevent hypertension, said Kate Kirley, MD, director of the AMA’s chronic disease prevention and programs.
Concern over the lack of standardized BP techniques isn’t new. In 2019, the American Heart Association and the AMA created an online BP course for health care workers. Two years later, the AMA offered grants to five medical schools for training courses.
Most of the new training sessions already on the AMA website take students about 15 minutes to complete. Dr. Kirley says because equipment varies across settings, participants will learn how to conduct manual, semi-automated, and automated office BP readings and identify workarounds for less-than-ideal room setups that can skew results. They will also explore how to guide patients in performing BP readings at home.
A version of this article first appeared on Medscape.com.
according to the American Medical Association. Hypertension affects about half of U.S. adults and is a leading contributor to cardiovascular disease.
First-year medical students typically read about BP measurement in a textbook and possibly attend a lecture before practicing using a manual cuff a few times on classmates, said Martha Gulati, MD, professor and director of preventive cardiology at Cedars-Sinai Medical Center, Los Angeles.
The dearth of BP instruction is alarming because inaccurate readings contribute to under- and overtreatment of hypertension, she said in an interview.
The AMA hopes $100,000 in grants to five health education schools will help improve BP instruction. The group recently announced it would give $20,000 each to five schools that train health professionals, expanding on a 2021 program to improve BP measurement training.
The new grants for interactive lessons will benefit nearly 5,000 students from Johns Hopkins University, Baltimore; Nova Southeastern University, Fort Lauderdale, Fla.; University of Washington, Seattle; Stony Brook (N.Y.) University; and the University of Pittsburgh.
In a 2021 survey of 571 clinicians, most of whom were cardiologists, Dr. Gulati found that only 23% performed accurate BP measurements despite the majority saying they trusted BP readings taken in their clinic. Accurate readings were defined as routinely checking BP in both arms, checking BP at least twice each visit, and waiting 5 minutes before taking the reading.
Med students fare no better when it comes to BP skills. In a 2017 study of 159 students from medical schools in 37 states, only one student demonstrated proficiency in all 11 elements necessary to measure BP accurately. Students, on average, performed just four of them correctly.
The elements of proper BP measurement include patients resting for 5 minutes before the measurement with legs uncrossed, feet on floor, and arm supported, not talking, reading, or using cell phone; BP taken in both arms with correct size of cuff placed over bare arm; and identifying BP from the arm with the higher reading as clinically more important and as the one to use for future readings.
Manual BP readings require an appropriately sized BP cuff, a sphygmomanometer, and a clinician skilled in using a stethoscope and auscultatory method. Meanwhile, automated readings require a clinician to place the cuff, but a digital device collects the measurement. Though preference depends on the setting and clinician, automated readings are more common. In Dr. Gulati’s study, automated BP assessment was used by 58% of respondents.
Depending on the BP device and technique, significant variations in readings can occur. In a 2021 study, Current Hypertension Reports found that automated readings may more closely reflect the patient’s baseline BP and produce results similar to ambulatory monitoring by a medical professional. An earlier JAMA Internal Medicine analysis found that clinicians’ manual readings reflect higher BP measurements than automated readings.
Though the AMA offers a free online series on BP measurement for students, making the training available to more health care team members can help prevent hypertension, said Kate Kirley, MD, director of the AMA’s chronic disease prevention and programs.
Concern over the lack of standardized BP techniques isn’t new. In 2019, the American Heart Association and the AMA created an online BP course for health care workers. Two years later, the AMA offered grants to five medical schools for training courses.
Most of the new training sessions already on the AMA website take students about 15 minutes to complete. Dr. Kirley says because equipment varies across settings, participants will learn how to conduct manual, semi-automated, and automated office BP readings and identify workarounds for less-than-ideal room setups that can skew results. They will also explore how to guide patients in performing BP readings at home.
A version of this article first appeared on Medscape.com.
FDA gives semaglutide two drug safety–related label changes
The FDA added a warning to the drug-interaction section of the Ozempiclabel that reiterates a warning that is already in place in other label sections, reinforcing the message that the glucagon-like peptide-1 (GLP-1) receptor agonist Ozempiccan potentially interact with the action of certain other agents to increase a person’s risk for hypoglycemia.
The added text says: “Ozempic stimulates insulin release in the presence of elevated blood glucose concentrations. Patients receiving Ozempic in combination with an insulin secretagogue (for instance, sulfonylurea) or insulin may have an increased risk of hypoglycemia, including severe hypoglycemia.”
This text was already included in both the “Warning and Precautions” and the “Adverse Reactions” sections of the label. The warning also advises, “The risk of hypoglycemia may be lowered by a reduction in the dose of sulfonylurea (or other concomitantly administered insulin secretagogue) or insulin. Inform patients using these concomitant medications of the risk of hypoglycemia and educate them on the signs and symptoms of hypoglycemia.”
Reports of ileus episodes after approval
The second addition concerns a new adverse reaction that was identified during the postmarketing experience.
The FDA has received more than 8,500 reports of gastrointestinal issues among patients prescribed glucagon-like peptide-1 (GLP-1) receptor agonists. Ileus is mentioned in 33 cases, including two deaths, associated with semaglutide. The FDA stopped short of saying there is a direct link between the drug and intestinal blockages.
“Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure,” the FDA stated in its approval of the label update.
The same warning for the risk of intestinal blockages is already listed on the labels for tirzepatide (Mounjaro, Lilly) and semaglutide injection 2.4 mg (Wegovy, Novo Nordisk).
The label change comes after a Louisiana woman filed a lawsuit in August that claims she was “severely injured” after using Mounjaro and Ozempic. She claimed the drug makers failed to disclose risks of vomiting and diarrhea due to inflammation of the stomach lining, as well as the risk of gastroparesis.
*Correction, 10/3/23: An earlier version of this article misstated the semaglutide formulation that received the updates.
A version of this article first appeared on Medscape.com.
The FDA added a warning to the drug-interaction section of the Ozempiclabel that reiterates a warning that is already in place in other label sections, reinforcing the message that the glucagon-like peptide-1 (GLP-1) receptor agonist Ozempiccan potentially interact with the action of certain other agents to increase a person’s risk for hypoglycemia.
The added text says: “Ozempic stimulates insulin release in the presence of elevated blood glucose concentrations. Patients receiving Ozempic in combination with an insulin secretagogue (for instance, sulfonylurea) or insulin may have an increased risk of hypoglycemia, including severe hypoglycemia.”
This text was already included in both the “Warning and Precautions” and the “Adverse Reactions” sections of the label. The warning also advises, “The risk of hypoglycemia may be lowered by a reduction in the dose of sulfonylurea (or other concomitantly administered insulin secretagogue) or insulin. Inform patients using these concomitant medications of the risk of hypoglycemia and educate them on the signs and symptoms of hypoglycemia.”
Reports of ileus episodes after approval
The second addition concerns a new adverse reaction that was identified during the postmarketing experience.
The FDA has received more than 8,500 reports of gastrointestinal issues among patients prescribed glucagon-like peptide-1 (GLP-1) receptor agonists. Ileus is mentioned in 33 cases, including two deaths, associated with semaglutide. The FDA stopped short of saying there is a direct link between the drug and intestinal blockages.
“Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure,” the FDA stated in its approval of the label update.
The same warning for the risk of intestinal blockages is already listed on the labels for tirzepatide (Mounjaro, Lilly) and semaglutide injection 2.4 mg (Wegovy, Novo Nordisk).
The label change comes after a Louisiana woman filed a lawsuit in August that claims she was “severely injured” after using Mounjaro and Ozempic. She claimed the drug makers failed to disclose risks of vomiting and diarrhea due to inflammation of the stomach lining, as well as the risk of gastroparesis.
*Correction, 10/3/23: An earlier version of this article misstated the semaglutide formulation that received the updates.
A version of this article first appeared on Medscape.com.
The FDA added a warning to the drug-interaction section of the Ozempiclabel that reiterates a warning that is already in place in other label sections, reinforcing the message that the glucagon-like peptide-1 (GLP-1) receptor agonist Ozempiccan potentially interact with the action of certain other agents to increase a person’s risk for hypoglycemia.
The added text says: “Ozempic stimulates insulin release in the presence of elevated blood glucose concentrations. Patients receiving Ozempic in combination with an insulin secretagogue (for instance, sulfonylurea) or insulin may have an increased risk of hypoglycemia, including severe hypoglycemia.”
This text was already included in both the “Warning and Precautions” and the “Adverse Reactions” sections of the label. The warning also advises, “The risk of hypoglycemia may be lowered by a reduction in the dose of sulfonylurea (or other concomitantly administered insulin secretagogue) or insulin. Inform patients using these concomitant medications of the risk of hypoglycemia and educate them on the signs and symptoms of hypoglycemia.”
Reports of ileus episodes after approval
The second addition concerns a new adverse reaction that was identified during the postmarketing experience.
The FDA has received more than 8,500 reports of gastrointestinal issues among patients prescribed glucagon-like peptide-1 (GLP-1) receptor agonists. Ileus is mentioned in 33 cases, including two deaths, associated with semaglutide. The FDA stopped short of saying there is a direct link between the drug and intestinal blockages.
“Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to reliably estimate their frequency or establish a causal relationship to drug exposure,” the FDA stated in its approval of the label update.
The same warning for the risk of intestinal blockages is already listed on the labels for tirzepatide (Mounjaro, Lilly) and semaglutide injection 2.4 mg (Wegovy, Novo Nordisk).
The label change comes after a Louisiana woman filed a lawsuit in August that claims she was “severely injured” after using Mounjaro and Ozempic. She claimed the drug makers failed to disclose risks of vomiting and diarrhea due to inflammation of the stomach lining, as well as the risk of gastroparesis.
*Correction, 10/3/23: An earlier version of this article misstated the semaglutide formulation that received the updates.
A version of this article first appeared on Medscape.com.
What potential does AI offer for endocrinology?
However, hurdles encountered with the latest AI iterations of chatbots underscore the need to proceed with caution.
“In contrast to other medical fields, endocrinology is not connected to a single organ structure; rather, it is a complicated biological system of hormones and metabolites, [intertwined with] various receptors, signaling pathways and intricate feedback mechanisms,” explained the authors of a recent article on the issue in Nature Reviews Endocrinology.
With interconnections that are “often beyond the comprehension and reasoning capabilities of the human brain, AI [is anticipated] to be exceptionally well-suited to tackle this remarkable heterogeneity and complexity,” they wrote.
Since the first regulatory approvals for AI-based technology were granted back in 2015, endocrinology has already been revolutionized by AI-based tools, most notably with AI biosensors for continuous glucose monitoring systems alerting patients of glucose levels, and automated insulin-delivery systems.
AI-based machine learning has also ushered in improved detection and analysis of thyroid nodules and potential malignancies, with algorithms in the analysis of radiological test images enabling detection through a deeper analysis than can be applied with individual specialists.
Likewise, the benefits of AI in imaging extend to osteoporosis.
“Imaging certainly is one of the most promising fields, including (but not limited to) conventional radiography, computed tomography, and magnetic resonance tomography,” explained Hans Peter Dimai, MD, a professor of medicine and endocrinology at the Medical University of Graz (Austria), and the past president of the Austrian Bone and Mineral Society.
“A typical indication is fracture detection, not in terms of replacing expert radiologists or orthopedists but rather in terms of supporting those who are in specialist training,” he said in an interview.
“Particularly the underdiagnosis of vertebral fractures has been an issue in past decades, with dramatic implications for the individual, since the first vertebral fracture would multiply the risk for any future fracture, and therefore requires immediate action from a physician’s side.”
The areas expected to further benefit from AI continue to grow as systems evolve, with advances being reported across a variety of endocrinologic conditions.
Papillary thyroid cancer (PTC): Central lymph node metastasis of papillary thyroid cancer is predictive of tumor recurrence and overall survival in PTC. However, few tests are able to diagnose the metastasis in the cancer with high accuracy. Using a convolutional neural network prediction model built with a deep-learning algorithm, researchers described high diagnostic sensitivity and specificity of a model, as reported in a study published in Feburary. The prediction model, developed using genetic mutations and clinicopathologic factors, showed high prediction efficacy, with validation in subclinical as well as clinical metastasis groups, suggesting broad applicability.
Adrenal tumors: Adrenal incidentalomas, or masses that are incidentally discovered when performing abdominal imaging for other reasons, can be a perplexing clinical challenge. Discovery of these is increasing as imaging technology advances. However, an AI-based machine learning approach utilizing CT is being developed to differentiate between subclinical pheochromocytoma and lipid-poor adenomas. As reported in a 2022 study, the prediction model scoring system used traditional radiological features on CT images to provide for a noninvasive method in assisting in the diagnosis and providing personalized care for people with adrenal tumors.
Osteoporosis – bone mineral density (BMD): In the diagnosis of osteoporosis, the measurement of BMD using dual-energy x-ray absorptiometry (DXA) is the gold standard. However, the availability of DXA devices in many countries is inadequate, leaving an unmet need for alternative approaches. But one AI-based algorithm shows promising diagnostic accuracy, compared with DXA, potentially providing a low-cost screening alternative for the early diagnosis of osteoporosis.
Osteoporosis – Fracture Risk Assessment Tool (FRAX): In fracture risk and prevention, the free FRAX tool, available online, is the gold standard and recommended in nearly all osteoporosis guidelines. However, several studies on AI-based tools show some benefit over FRAX, including one approach using longitudinal data with conventional spine radiographs, showing predictive accuracy that exceeds FRAX.
Osteoporosis – treatment: And for the often challenging process of treatment decision-making in osteoporosis, AI-based software, developed from more than 15,000 osteoporosis patients followed over 10 years, shows high accuracy in the prediction of response to treatment in terms of BMD increase, as described in another study. “Our results show that it is feasible to use a combination of electronic medical records–derived information to develop a machine-learning algorithm to predict a BMD response following osteoporosis treatment,” the authors reported. “This alternative approach can aid physicians to select an optimal therapeutic regimen in order to maximize a patient-specific treatment outcome.”
Chatbot wrinkles
The prospects of large language models (LLMs) and ChatGPT unleash the potential to understand and generate text in a similar capacity as humans. Although controversial, they could likewise be compelling.
However, such systems can be vastly more complex than earlier AI-based tools, and some studies are illustrating the kinds of stumbling blocks that need to be overcome.
For instance, in a study published in May, researchers explored the potential of ChatGPT 4.0 to synthesize clinical guidelines for diabetic ketoacidosis from three different sources to reflect the latest evidence and local context.
Such efforts are important but can be very resource-intensive when conducted without the use of AI assistance.
The study’s results showed that, although ChatGPT was able to generate a comprehensive table comparing the guidelines, there were multiple recurrent errors in misreporting and nonreporting, as well as inconsistencies, “rendering the results unreliable,” the authors wrote.
“Although ChatGPT demonstrates the potential for the synthesis of clinical guidelines, the presence of multiple recurrent errors and inconsistencies underscores the need for expert human intervention and validation,” the authors concluded.
Likewise, other research using ChatGPT for use in vitreoretinal diseases, including diabetic retinopathy, further demonstrated disappointing results, with the technology showing the chatbot provided completely accurate responses to only 8 (15.4%) of 52 questions, with some responses containing inappropriate or potentially harmful medical advice.
“For example, in response to ‘How do you get rid of epiretinal membrane?’, the platform described vitrectomy but also included incorrect options of injection therapy and laser therapy,” the authors wrote.
“The study highlights the limitations of using ChatGPT for the adaptation of clinical guidelines without expert human intervention,” they concluded.
And in research published in August that looked at the ability of ChatGPT to interpret guidelines – in this case 26 diagnosis descriptions from the National Comprehensive Cancer Network – results showed that as many as one-third of treatments recommended by the chatbot were at least partially not concordant with information stated in the NCCN guidelines, with recommendations varying based on how the question about treatment was presented.
“Clinicians should advise patients that LLM chatbots are not a reliable source of treatment information,” the authors wrote.
Diversity concerns
Among the most prominent concerns about chatbot inaccuracy has been the known lack of racial and ethnic diversity in large databases utilized in developing AI systems, potentially resulting in critical flaws in the information the systems produce.
In an editorial published with the NCCN guideline study, Atul Butte, MD, PhD, from the University of California, San Francisco, noted that the shortcomings should be weighed with the potential benefits.
“There is no doubt that AI and LLMs are not yet perfect, and they carry biases that will need to be addressed,” Dr. Butte wrote. “These algorithms will need to be carefully monitored as they are brought into health systems, [but] this does not alter the potential of how they can improve care for both the haves and have-nots of health care.”
In a comment, Dr. Butte elaborated that, once the system flaws are refined, a key benefit will be the broader application of top standards of care to more patients who may have limited resources.
“It is a privilege to get the very best level of care from the very best centers, but that privilege is not distributable to all right now,” Dr. Butte said.
“The real potential of LLMs and AI will be their ability to be trained from the patient, clinical, and outcomes data from the very best centers, and then used to deliver the best care through digital tools to all patients, especially to those without access to the best care or [those with] limited resources,” he said.
Further commenting on the issue of potential bias with chatbots, Matthew Li, MD, from the University of Alberta, Edmonton, said that awareness of the nature of the problem and need for diversity in data for training and testing AI-systems issues appears to be improving.
“Thanks to much research on this topic in recent years, I think most AI researchers in medicine are at least aware of these challenges now, which was not the case only a few years ago,” he said in an interview.
Across specialties, “the careful deployment of AI tools accounting for issues regarding AI model generalization, biases, and performance drift will be critical for ensuring safe and fair patient care,” Dr. Li noted.
On a broader level is the ongoing general concern of the potential for over-reliance on the technology by clinicians. For example, a recent study showing radiologists across all experience levels reading mammograms were prone to automation bias when being supported by an AI-based system.
“Concerns regarding over-reliance on AI remain,” said Dr. Li, who coauthored a study published in June on the issue.
“Ongoing research into and monitoring of the impact of AI systems as they are developed and deployed will be important to ensure safe patient care moving forward,” he said.
Ultimately, the clinical benefit of AI systems to patients should be the bottom line, Dr. Dimai added.
“In my opinion, the clinical relevance, i.e., the benefit for patients and/or physicians of a to-be-developed AI tool, must be clearly proven before its development starts and first clinical studies are carried out,” he said.
“This is not always the case,” Dr. Dimai said. “In other words, innovation per se should not be the only rationale and driving force for the development of such tools.”
Dr. Li, an associate editor for the journal Radiology: Artificial Intelligence, reports no relevant financial relationships. Dr. Dimai is a member of the key medical advisor team of Image Biopsy Lab.
A version of this article first appeared on Medscape.com.
However, hurdles encountered with the latest AI iterations of chatbots underscore the need to proceed with caution.
“In contrast to other medical fields, endocrinology is not connected to a single organ structure; rather, it is a complicated biological system of hormones and metabolites, [intertwined with] various receptors, signaling pathways and intricate feedback mechanisms,” explained the authors of a recent article on the issue in Nature Reviews Endocrinology.
With interconnections that are “often beyond the comprehension and reasoning capabilities of the human brain, AI [is anticipated] to be exceptionally well-suited to tackle this remarkable heterogeneity and complexity,” they wrote.
Since the first regulatory approvals for AI-based technology were granted back in 2015, endocrinology has already been revolutionized by AI-based tools, most notably with AI biosensors for continuous glucose monitoring systems alerting patients of glucose levels, and automated insulin-delivery systems.
AI-based machine learning has also ushered in improved detection and analysis of thyroid nodules and potential malignancies, with algorithms in the analysis of radiological test images enabling detection through a deeper analysis than can be applied with individual specialists.
Likewise, the benefits of AI in imaging extend to osteoporosis.
“Imaging certainly is one of the most promising fields, including (but not limited to) conventional radiography, computed tomography, and magnetic resonance tomography,” explained Hans Peter Dimai, MD, a professor of medicine and endocrinology at the Medical University of Graz (Austria), and the past president of the Austrian Bone and Mineral Society.
“A typical indication is fracture detection, not in terms of replacing expert radiologists or orthopedists but rather in terms of supporting those who are in specialist training,” he said in an interview.
“Particularly the underdiagnosis of vertebral fractures has been an issue in past decades, with dramatic implications for the individual, since the first vertebral fracture would multiply the risk for any future fracture, and therefore requires immediate action from a physician’s side.”
The areas expected to further benefit from AI continue to grow as systems evolve, with advances being reported across a variety of endocrinologic conditions.
Papillary thyroid cancer (PTC): Central lymph node metastasis of papillary thyroid cancer is predictive of tumor recurrence and overall survival in PTC. However, few tests are able to diagnose the metastasis in the cancer with high accuracy. Using a convolutional neural network prediction model built with a deep-learning algorithm, researchers described high diagnostic sensitivity and specificity of a model, as reported in a study published in Feburary. The prediction model, developed using genetic mutations and clinicopathologic factors, showed high prediction efficacy, with validation in subclinical as well as clinical metastasis groups, suggesting broad applicability.
Adrenal tumors: Adrenal incidentalomas, or masses that are incidentally discovered when performing abdominal imaging for other reasons, can be a perplexing clinical challenge. Discovery of these is increasing as imaging technology advances. However, an AI-based machine learning approach utilizing CT is being developed to differentiate between subclinical pheochromocytoma and lipid-poor adenomas. As reported in a 2022 study, the prediction model scoring system used traditional radiological features on CT images to provide for a noninvasive method in assisting in the diagnosis and providing personalized care for people with adrenal tumors.
Osteoporosis – bone mineral density (BMD): In the diagnosis of osteoporosis, the measurement of BMD using dual-energy x-ray absorptiometry (DXA) is the gold standard. However, the availability of DXA devices in many countries is inadequate, leaving an unmet need for alternative approaches. But one AI-based algorithm shows promising diagnostic accuracy, compared with DXA, potentially providing a low-cost screening alternative for the early diagnosis of osteoporosis.
Osteoporosis – Fracture Risk Assessment Tool (FRAX): In fracture risk and prevention, the free FRAX tool, available online, is the gold standard and recommended in nearly all osteoporosis guidelines. However, several studies on AI-based tools show some benefit over FRAX, including one approach using longitudinal data with conventional spine radiographs, showing predictive accuracy that exceeds FRAX.
Osteoporosis – treatment: And for the often challenging process of treatment decision-making in osteoporosis, AI-based software, developed from more than 15,000 osteoporosis patients followed over 10 years, shows high accuracy in the prediction of response to treatment in terms of BMD increase, as described in another study. “Our results show that it is feasible to use a combination of electronic medical records–derived information to develop a machine-learning algorithm to predict a BMD response following osteoporosis treatment,” the authors reported. “This alternative approach can aid physicians to select an optimal therapeutic regimen in order to maximize a patient-specific treatment outcome.”
Chatbot wrinkles
The prospects of large language models (LLMs) and ChatGPT unleash the potential to understand and generate text in a similar capacity as humans. Although controversial, they could likewise be compelling.
However, such systems can be vastly more complex than earlier AI-based tools, and some studies are illustrating the kinds of stumbling blocks that need to be overcome.
For instance, in a study published in May, researchers explored the potential of ChatGPT 4.0 to synthesize clinical guidelines for diabetic ketoacidosis from three different sources to reflect the latest evidence and local context.
Such efforts are important but can be very resource-intensive when conducted without the use of AI assistance.
The study’s results showed that, although ChatGPT was able to generate a comprehensive table comparing the guidelines, there were multiple recurrent errors in misreporting and nonreporting, as well as inconsistencies, “rendering the results unreliable,” the authors wrote.
“Although ChatGPT demonstrates the potential for the synthesis of clinical guidelines, the presence of multiple recurrent errors and inconsistencies underscores the need for expert human intervention and validation,” the authors concluded.
Likewise, other research using ChatGPT for use in vitreoretinal diseases, including diabetic retinopathy, further demonstrated disappointing results, with the technology showing the chatbot provided completely accurate responses to only 8 (15.4%) of 52 questions, with some responses containing inappropriate or potentially harmful medical advice.
“For example, in response to ‘How do you get rid of epiretinal membrane?’, the platform described vitrectomy but also included incorrect options of injection therapy and laser therapy,” the authors wrote.
“The study highlights the limitations of using ChatGPT for the adaptation of clinical guidelines without expert human intervention,” they concluded.
And in research published in August that looked at the ability of ChatGPT to interpret guidelines – in this case 26 diagnosis descriptions from the National Comprehensive Cancer Network – results showed that as many as one-third of treatments recommended by the chatbot were at least partially not concordant with information stated in the NCCN guidelines, with recommendations varying based on how the question about treatment was presented.
“Clinicians should advise patients that LLM chatbots are not a reliable source of treatment information,” the authors wrote.
Diversity concerns
Among the most prominent concerns about chatbot inaccuracy has been the known lack of racial and ethnic diversity in large databases utilized in developing AI systems, potentially resulting in critical flaws in the information the systems produce.
In an editorial published with the NCCN guideline study, Atul Butte, MD, PhD, from the University of California, San Francisco, noted that the shortcomings should be weighed with the potential benefits.
“There is no doubt that AI and LLMs are not yet perfect, and they carry biases that will need to be addressed,” Dr. Butte wrote. “These algorithms will need to be carefully monitored as they are brought into health systems, [but] this does not alter the potential of how they can improve care for both the haves and have-nots of health care.”
In a comment, Dr. Butte elaborated that, once the system flaws are refined, a key benefit will be the broader application of top standards of care to more patients who may have limited resources.
“It is a privilege to get the very best level of care from the very best centers, but that privilege is not distributable to all right now,” Dr. Butte said.
“The real potential of LLMs and AI will be their ability to be trained from the patient, clinical, and outcomes data from the very best centers, and then used to deliver the best care through digital tools to all patients, especially to those without access to the best care or [those with] limited resources,” he said.
Further commenting on the issue of potential bias with chatbots, Matthew Li, MD, from the University of Alberta, Edmonton, said that awareness of the nature of the problem and need for diversity in data for training and testing AI-systems issues appears to be improving.
“Thanks to much research on this topic in recent years, I think most AI researchers in medicine are at least aware of these challenges now, which was not the case only a few years ago,” he said in an interview.
Across specialties, “the careful deployment of AI tools accounting for issues regarding AI model generalization, biases, and performance drift will be critical for ensuring safe and fair patient care,” Dr. Li noted.
On a broader level is the ongoing general concern of the potential for over-reliance on the technology by clinicians. For example, a recent study showing radiologists across all experience levels reading mammograms were prone to automation bias when being supported by an AI-based system.
“Concerns regarding over-reliance on AI remain,” said Dr. Li, who coauthored a study published in June on the issue.
“Ongoing research into and monitoring of the impact of AI systems as they are developed and deployed will be important to ensure safe patient care moving forward,” he said.
Ultimately, the clinical benefit of AI systems to patients should be the bottom line, Dr. Dimai added.
“In my opinion, the clinical relevance, i.e., the benefit for patients and/or physicians of a to-be-developed AI tool, must be clearly proven before its development starts and first clinical studies are carried out,” he said.
“This is not always the case,” Dr. Dimai said. “In other words, innovation per se should not be the only rationale and driving force for the development of such tools.”
Dr. Li, an associate editor for the journal Radiology: Artificial Intelligence, reports no relevant financial relationships. Dr. Dimai is a member of the key medical advisor team of Image Biopsy Lab.
A version of this article first appeared on Medscape.com.
However, hurdles encountered with the latest AI iterations of chatbots underscore the need to proceed with caution.
“In contrast to other medical fields, endocrinology is not connected to a single organ structure; rather, it is a complicated biological system of hormones and metabolites, [intertwined with] various receptors, signaling pathways and intricate feedback mechanisms,” explained the authors of a recent article on the issue in Nature Reviews Endocrinology.
With interconnections that are “often beyond the comprehension and reasoning capabilities of the human brain, AI [is anticipated] to be exceptionally well-suited to tackle this remarkable heterogeneity and complexity,” they wrote.
Since the first regulatory approvals for AI-based technology were granted back in 2015, endocrinology has already been revolutionized by AI-based tools, most notably with AI biosensors for continuous glucose monitoring systems alerting patients of glucose levels, and automated insulin-delivery systems.
AI-based machine learning has also ushered in improved detection and analysis of thyroid nodules and potential malignancies, with algorithms in the analysis of radiological test images enabling detection through a deeper analysis than can be applied with individual specialists.
Likewise, the benefits of AI in imaging extend to osteoporosis.
“Imaging certainly is one of the most promising fields, including (but not limited to) conventional radiography, computed tomography, and magnetic resonance tomography,” explained Hans Peter Dimai, MD, a professor of medicine and endocrinology at the Medical University of Graz (Austria), and the past president of the Austrian Bone and Mineral Society.
“A typical indication is fracture detection, not in terms of replacing expert radiologists or orthopedists but rather in terms of supporting those who are in specialist training,” he said in an interview.
“Particularly the underdiagnosis of vertebral fractures has been an issue in past decades, with dramatic implications for the individual, since the first vertebral fracture would multiply the risk for any future fracture, and therefore requires immediate action from a physician’s side.”
The areas expected to further benefit from AI continue to grow as systems evolve, with advances being reported across a variety of endocrinologic conditions.
Papillary thyroid cancer (PTC): Central lymph node metastasis of papillary thyroid cancer is predictive of tumor recurrence and overall survival in PTC. However, few tests are able to diagnose the metastasis in the cancer with high accuracy. Using a convolutional neural network prediction model built with a deep-learning algorithm, researchers described high diagnostic sensitivity and specificity of a model, as reported in a study published in Feburary. The prediction model, developed using genetic mutations and clinicopathologic factors, showed high prediction efficacy, with validation in subclinical as well as clinical metastasis groups, suggesting broad applicability.
Adrenal tumors: Adrenal incidentalomas, or masses that are incidentally discovered when performing abdominal imaging for other reasons, can be a perplexing clinical challenge. Discovery of these is increasing as imaging technology advances. However, an AI-based machine learning approach utilizing CT is being developed to differentiate between subclinical pheochromocytoma and lipid-poor adenomas. As reported in a 2022 study, the prediction model scoring system used traditional radiological features on CT images to provide for a noninvasive method in assisting in the diagnosis and providing personalized care for people with adrenal tumors.
Osteoporosis – bone mineral density (BMD): In the diagnosis of osteoporosis, the measurement of BMD using dual-energy x-ray absorptiometry (DXA) is the gold standard. However, the availability of DXA devices in many countries is inadequate, leaving an unmet need for alternative approaches. But one AI-based algorithm shows promising diagnostic accuracy, compared with DXA, potentially providing a low-cost screening alternative for the early diagnosis of osteoporosis.
Osteoporosis – Fracture Risk Assessment Tool (FRAX): In fracture risk and prevention, the free FRAX tool, available online, is the gold standard and recommended in nearly all osteoporosis guidelines. However, several studies on AI-based tools show some benefit over FRAX, including one approach using longitudinal data with conventional spine radiographs, showing predictive accuracy that exceeds FRAX.
Osteoporosis – treatment: And for the often challenging process of treatment decision-making in osteoporosis, AI-based software, developed from more than 15,000 osteoporosis patients followed over 10 years, shows high accuracy in the prediction of response to treatment in terms of BMD increase, as described in another study. “Our results show that it is feasible to use a combination of electronic medical records–derived information to develop a machine-learning algorithm to predict a BMD response following osteoporosis treatment,” the authors reported. “This alternative approach can aid physicians to select an optimal therapeutic regimen in order to maximize a patient-specific treatment outcome.”
Chatbot wrinkles
The prospects of large language models (LLMs) and ChatGPT unleash the potential to understand and generate text in a similar capacity as humans. Although controversial, they could likewise be compelling.
However, such systems can be vastly more complex than earlier AI-based tools, and some studies are illustrating the kinds of stumbling blocks that need to be overcome.
For instance, in a study published in May, researchers explored the potential of ChatGPT 4.0 to synthesize clinical guidelines for diabetic ketoacidosis from three different sources to reflect the latest evidence and local context.
Such efforts are important but can be very resource-intensive when conducted without the use of AI assistance.
The study’s results showed that, although ChatGPT was able to generate a comprehensive table comparing the guidelines, there were multiple recurrent errors in misreporting and nonreporting, as well as inconsistencies, “rendering the results unreliable,” the authors wrote.
“Although ChatGPT demonstrates the potential for the synthesis of clinical guidelines, the presence of multiple recurrent errors and inconsistencies underscores the need for expert human intervention and validation,” the authors concluded.
Likewise, other research using ChatGPT for use in vitreoretinal diseases, including diabetic retinopathy, further demonstrated disappointing results, with the technology showing the chatbot provided completely accurate responses to only 8 (15.4%) of 52 questions, with some responses containing inappropriate or potentially harmful medical advice.
“For example, in response to ‘How do you get rid of epiretinal membrane?’, the platform described vitrectomy but also included incorrect options of injection therapy and laser therapy,” the authors wrote.
“The study highlights the limitations of using ChatGPT for the adaptation of clinical guidelines without expert human intervention,” they concluded.
And in research published in August that looked at the ability of ChatGPT to interpret guidelines – in this case 26 diagnosis descriptions from the National Comprehensive Cancer Network – results showed that as many as one-third of treatments recommended by the chatbot were at least partially not concordant with information stated in the NCCN guidelines, with recommendations varying based on how the question about treatment was presented.
“Clinicians should advise patients that LLM chatbots are not a reliable source of treatment information,” the authors wrote.
Diversity concerns
Among the most prominent concerns about chatbot inaccuracy has been the known lack of racial and ethnic diversity in large databases utilized in developing AI systems, potentially resulting in critical flaws in the information the systems produce.
In an editorial published with the NCCN guideline study, Atul Butte, MD, PhD, from the University of California, San Francisco, noted that the shortcomings should be weighed with the potential benefits.
“There is no doubt that AI and LLMs are not yet perfect, and they carry biases that will need to be addressed,” Dr. Butte wrote. “These algorithms will need to be carefully monitored as they are brought into health systems, [but] this does not alter the potential of how they can improve care for both the haves and have-nots of health care.”
In a comment, Dr. Butte elaborated that, once the system flaws are refined, a key benefit will be the broader application of top standards of care to more patients who may have limited resources.
“It is a privilege to get the very best level of care from the very best centers, but that privilege is not distributable to all right now,” Dr. Butte said.
“The real potential of LLMs and AI will be their ability to be trained from the patient, clinical, and outcomes data from the very best centers, and then used to deliver the best care through digital tools to all patients, especially to those without access to the best care or [those with] limited resources,” he said.
Further commenting on the issue of potential bias with chatbots, Matthew Li, MD, from the University of Alberta, Edmonton, said that awareness of the nature of the problem and need for diversity in data for training and testing AI-systems issues appears to be improving.
“Thanks to much research on this topic in recent years, I think most AI researchers in medicine are at least aware of these challenges now, which was not the case only a few years ago,” he said in an interview.
Across specialties, “the careful deployment of AI tools accounting for issues regarding AI model generalization, biases, and performance drift will be critical for ensuring safe and fair patient care,” Dr. Li noted.
On a broader level is the ongoing general concern of the potential for over-reliance on the technology by clinicians. For example, a recent study showing radiologists across all experience levels reading mammograms were prone to automation bias when being supported by an AI-based system.
“Concerns regarding over-reliance on AI remain,” said Dr. Li, who coauthored a study published in June on the issue.
“Ongoing research into and monitoring of the impact of AI systems as they are developed and deployed will be important to ensure safe patient care moving forward,” he said.
Ultimately, the clinical benefit of AI systems to patients should be the bottom line, Dr. Dimai added.
“In my opinion, the clinical relevance, i.e., the benefit for patients and/or physicians of a to-be-developed AI tool, must be clearly proven before its development starts and first clinical studies are carried out,” he said.
“This is not always the case,” Dr. Dimai said. “In other words, innovation per se should not be the only rationale and driving force for the development of such tools.”
Dr. Li, an associate editor for the journal Radiology: Artificial Intelligence, reports no relevant financial relationships. Dr. Dimai is a member of the key medical advisor team of Image Biopsy Lab.
A version of this article first appeared on Medscape.com.
These adverse events linked to improved cancer prognosis
TOPLINE:
.
METHODOLOGY:
- Emerging evidence suggests that the presence of cutaneous immune-related adverse events may be linked with favorable outcomes among patients with cancer who receive ICIs.
- Researchers conducted a systematic review and meta-analysis that included 23 studies and a total of 22,749 patients with cancer who received ICI treatment; studies compared outcomes among patients with and those without cutaneous immune-related adverse events.
- The major outcomes evaluated in the analysis were overall survival and progression-free survival (PFS); subgroup analyses assessed cutaneous immune-related adverse event type, cancer type, and other factors.
TAKEAWAY:
- The occurrence of cutaneous immune-related adverse events was associated with improved PFS (hazard ratio, 0.52; P < .001) and overall survival (HR, 0.61; P < .001).
- In the subgroup analysis, patients with eczematous (HR, 0.69), lichenoid or lichen planus–like skin lesions (HR, 0.51), pruritus without rash (HR, 0.70), psoriasis (HR, 0.63), or vitiligo (HR, 0.30) demonstrated a significant overall survival advantage. Vitiligo was the only adverse event associated with a PFS advantage (HR, 0.28).
- Among patients with melanoma, analyses revealed a significant association between the incidence of cutaneous immune-related adverse events and improved overall survival (HR, 0.51) and PFS (HR, 0.45). The authors highlighted similar findings among patients with non–small cell lung cancer (HR, 0.50 for overall survival and 0.61 for PFS).
IN PRACTICE:
“These data suggest that [cutaneous immune-related adverse events] may have useful prognostic value in ICI treatment,” the authors concluded.
SOURCE:
The analysis, led by Fei Wang, MD, Zhong Da Hospital, School of Medicine, Southeast University, Nanjing, China, was published online in JAMA Dermatology.
LIMITATIONS:
Most of the data came from retrospective studies, and there were limited data on specific patient subgroups. The Egger tests, used to assess potential publication bias in meta-analyses, revealed publication bias.
DISCLOSURES:
No disclosures were reported. The study was supported by a grant from the Postgraduate Research and Practice Innovation Program of Jiangsu Province.
A version of this article first appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- Emerging evidence suggests that the presence of cutaneous immune-related adverse events may be linked with favorable outcomes among patients with cancer who receive ICIs.
- Researchers conducted a systematic review and meta-analysis that included 23 studies and a total of 22,749 patients with cancer who received ICI treatment; studies compared outcomes among patients with and those without cutaneous immune-related adverse events.
- The major outcomes evaluated in the analysis were overall survival and progression-free survival (PFS); subgroup analyses assessed cutaneous immune-related adverse event type, cancer type, and other factors.
TAKEAWAY:
- The occurrence of cutaneous immune-related adverse events was associated with improved PFS (hazard ratio, 0.52; P < .001) and overall survival (HR, 0.61; P < .001).
- In the subgroup analysis, patients with eczematous (HR, 0.69), lichenoid or lichen planus–like skin lesions (HR, 0.51), pruritus without rash (HR, 0.70), psoriasis (HR, 0.63), or vitiligo (HR, 0.30) demonstrated a significant overall survival advantage. Vitiligo was the only adverse event associated with a PFS advantage (HR, 0.28).
- Among patients with melanoma, analyses revealed a significant association between the incidence of cutaneous immune-related adverse events and improved overall survival (HR, 0.51) and PFS (HR, 0.45). The authors highlighted similar findings among patients with non–small cell lung cancer (HR, 0.50 for overall survival and 0.61 for PFS).
IN PRACTICE:
“These data suggest that [cutaneous immune-related adverse events] may have useful prognostic value in ICI treatment,” the authors concluded.
SOURCE:
The analysis, led by Fei Wang, MD, Zhong Da Hospital, School of Medicine, Southeast University, Nanjing, China, was published online in JAMA Dermatology.
LIMITATIONS:
Most of the data came from retrospective studies, and there were limited data on specific patient subgroups. The Egger tests, used to assess potential publication bias in meta-analyses, revealed publication bias.
DISCLOSURES:
No disclosures were reported. The study was supported by a grant from the Postgraduate Research and Practice Innovation Program of Jiangsu Province.
A version of this article first appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- Emerging evidence suggests that the presence of cutaneous immune-related adverse events may be linked with favorable outcomes among patients with cancer who receive ICIs.
- Researchers conducted a systematic review and meta-analysis that included 23 studies and a total of 22,749 patients with cancer who received ICI treatment; studies compared outcomes among patients with and those without cutaneous immune-related adverse events.
- The major outcomes evaluated in the analysis were overall survival and progression-free survival (PFS); subgroup analyses assessed cutaneous immune-related adverse event type, cancer type, and other factors.
TAKEAWAY:
- The occurrence of cutaneous immune-related adverse events was associated with improved PFS (hazard ratio, 0.52; P < .001) and overall survival (HR, 0.61; P < .001).
- In the subgroup analysis, patients with eczematous (HR, 0.69), lichenoid or lichen planus–like skin lesions (HR, 0.51), pruritus without rash (HR, 0.70), psoriasis (HR, 0.63), or vitiligo (HR, 0.30) demonstrated a significant overall survival advantage. Vitiligo was the only adverse event associated with a PFS advantage (HR, 0.28).
- Among patients with melanoma, analyses revealed a significant association between the incidence of cutaneous immune-related adverse events and improved overall survival (HR, 0.51) and PFS (HR, 0.45). The authors highlighted similar findings among patients with non–small cell lung cancer (HR, 0.50 for overall survival and 0.61 for PFS).
IN PRACTICE:
“These data suggest that [cutaneous immune-related adverse events] may have useful prognostic value in ICI treatment,” the authors concluded.
SOURCE:
The analysis, led by Fei Wang, MD, Zhong Da Hospital, School of Medicine, Southeast University, Nanjing, China, was published online in JAMA Dermatology.
LIMITATIONS:
Most of the data came from retrospective studies, and there were limited data on specific patient subgroups. The Egger tests, used to assess potential publication bias in meta-analyses, revealed publication bias.
DISCLOSURES:
No disclosures were reported. The study was supported by a grant from the Postgraduate Research and Practice Innovation Program of Jiangsu Province.
A version of this article first appeared on Medscape.com.
Does the number of primary melanomas affect survival?
TOPLINE:
.
METHODOLOGY:
- The difference in outcomes between people with multiple primary melanomas (MPMs) and a single primary melanoma (SPM) has not been established.
- To compare 10-year melanoma-specific mortality and overall mortality between people with MPMs and SPM, researchers drew from the Melanoma Patterns of Care study, a population-based observational analysis of residents in the state of New South Wales, Australia, who had a melanoma reported to the state cancer registry over 12 months in 2006-2007, and were followed up until 2018, for a median of almost 12 years.
- The researchers performed logistic regression analyses to assess 10-year melanoma-specific mortality differences between the two groups.
TAKEAWAY:
- Of 3,404 people included in the analysis, 2,830 had an SPM and 574 developed MPMs during follow-up.
- On multivariable regression adjusted for pathologic characteristics of the thickest lesion in the MPM group, no significant differences were seen in 10-year melanoma-specific mortality between the two groups (odds ratio, 0.85; 95% confidence interval, 0.58-1.24; P = .40).
- Sensitivity analyses adjusted for parameters of the first primary melanoma among patients with MPMs revealed similar findings (OR, 1.34; 95% CI, 0.92-1.96; P = .12).
- On multivariable analysis using data from the thickest lesion, factors independently associated with melanoma-specific mortality were male sex, disadvantaged socioeconomic status (based on location of residence), and Breslow thickness.
- Factors independently associated with 10-year overall mortality were like those seen in other studies and included sex, Breslow thickness, ulceration status, and socioeconomic disadvantage.
IN PRACTICE:
“The results of our study suggest that the number of primary melanomas is not an independent risk factor for mortality,” the researchers concluded. “In addition, the detection of melanoma at an early stage (with a thin Breslow thickness) rather than an intrinsic biologic factor remains the biggest influence on melanoma mortality after diagnosis of one or more melanomas.”
SOURCE:
Corresponding author Serigne N. Lo, PhD, of the Melanoma Institute Australia, led the research. The study was published in the Journal of the American Academy of Dermatology.
LIMITATIONS:
No adjustments for treatment modality were made in the study, and at baseline survey, effective systemic treatments for melanoma were not available.
DISCLOSURES:
This study was supported by the Australian National Health and Medical Research Council, Cancer Institute New South Wales, and the New South Wale State Government via a grant to the New South Wales Melanoma Network. Additional support was provided by Melanoma Institute Australia and the New South Wales Melanoma Network.
A version of this article first appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- The difference in outcomes between people with multiple primary melanomas (MPMs) and a single primary melanoma (SPM) has not been established.
- To compare 10-year melanoma-specific mortality and overall mortality between people with MPMs and SPM, researchers drew from the Melanoma Patterns of Care study, a population-based observational analysis of residents in the state of New South Wales, Australia, who had a melanoma reported to the state cancer registry over 12 months in 2006-2007, and were followed up until 2018, for a median of almost 12 years.
- The researchers performed logistic regression analyses to assess 10-year melanoma-specific mortality differences between the two groups.
TAKEAWAY:
- Of 3,404 people included in the analysis, 2,830 had an SPM and 574 developed MPMs during follow-up.
- On multivariable regression adjusted for pathologic characteristics of the thickest lesion in the MPM group, no significant differences were seen in 10-year melanoma-specific mortality between the two groups (odds ratio, 0.85; 95% confidence interval, 0.58-1.24; P = .40).
- Sensitivity analyses adjusted for parameters of the first primary melanoma among patients with MPMs revealed similar findings (OR, 1.34; 95% CI, 0.92-1.96; P = .12).
- On multivariable analysis using data from the thickest lesion, factors independently associated with melanoma-specific mortality were male sex, disadvantaged socioeconomic status (based on location of residence), and Breslow thickness.
- Factors independently associated with 10-year overall mortality were like those seen in other studies and included sex, Breslow thickness, ulceration status, and socioeconomic disadvantage.
IN PRACTICE:
“The results of our study suggest that the number of primary melanomas is not an independent risk factor for mortality,” the researchers concluded. “In addition, the detection of melanoma at an early stage (with a thin Breslow thickness) rather than an intrinsic biologic factor remains the biggest influence on melanoma mortality after diagnosis of one or more melanomas.”
SOURCE:
Corresponding author Serigne N. Lo, PhD, of the Melanoma Institute Australia, led the research. The study was published in the Journal of the American Academy of Dermatology.
LIMITATIONS:
No adjustments for treatment modality were made in the study, and at baseline survey, effective systemic treatments for melanoma were not available.
DISCLOSURES:
This study was supported by the Australian National Health and Medical Research Council, Cancer Institute New South Wales, and the New South Wale State Government via a grant to the New South Wales Melanoma Network. Additional support was provided by Melanoma Institute Australia and the New South Wales Melanoma Network.
A version of this article first appeared on Medscape.com.
TOPLINE:
.
METHODOLOGY:
- The difference in outcomes between people with multiple primary melanomas (MPMs) and a single primary melanoma (SPM) has not been established.
- To compare 10-year melanoma-specific mortality and overall mortality between people with MPMs and SPM, researchers drew from the Melanoma Patterns of Care study, a population-based observational analysis of residents in the state of New South Wales, Australia, who had a melanoma reported to the state cancer registry over 12 months in 2006-2007, and were followed up until 2018, for a median of almost 12 years.
- The researchers performed logistic regression analyses to assess 10-year melanoma-specific mortality differences between the two groups.
TAKEAWAY:
- Of 3,404 people included in the analysis, 2,830 had an SPM and 574 developed MPMs during follow-up.
- On multivariable regression adjusted for pathologic characteristics of the thickest lesion in the MPM group, no significant differences were seen in 10-year melanoma-specific mortality between the two groups (odds ratio, 0.85; 95% confidence interval, 0.58-1.24; P = .40).
- Sensitivity analyses adjusted for parameters of the first primary melanoma among patients with MPMs revealed similar findings (OR, 1.34; 95% CI, 0.92-1.96; P = .12).
- On multivariable analysis using data from the thickest lesion, factors independently associated with melanoma-specific mortality were male sex, disadvantaged socioeconomic status (based on location of residence), and Breslow thickness.
- Factors independently associated with 10-year overall mortality were like those seen in other studies and included sex, Breslow thickness, ulceration status, and socioeconomic disadvantage.
IN PRACTICE:
“The results of our study suggest that the number of primary melanomas is not an independent risk factor for mortality,” the researchers concluded. “In addition, the detection of melanoma at an early stage (with a thin Breslow thickness) rather than an intrinsic biologic factor remains the biggest influence on melanoma mortality after diagnosis of one or more melanomas.”
SOURCE:
Corresponding author Serigne N. Lo, PhD, of the Melanoma Institute Australia, led the research. The study was published in the Journal of the American Academy of Dermatology.
LIMITATIONS:
No adjustments for treatment modality were made in the study, and at baseline survey, effective systemic treatments for melanoma were not available.
DISCLOSURES:
This study was supported by the Australian National Health and Medical Research Council, Cancer Institute New South Wales, and the New South Wale State Government via a grant to the New South Wales Melanoma Network. Additional support was provided by Melanoma Institute Australia and the New South Wales Melanoma Network.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY