User login
Postnatally acquired Zika infection in children usually mild
The clinical course of postnatally acquired Zika virus disease in children younger than 18 years is mild and rarely results in severe illness or death, reported Alyson Goodman, MD, and her associates at the Centers for Disease Control and Prevention (CDC), Atlanta.
There were a total of 158 confirmed or probable postnatally acquired Zika virus disease cases among children younger than 18 years reported to the CDC in the United States between January 2015 and July 2016, wrote researchers in a case series that described the epidemiology, clinical findings, and outcomes of the cases (MMWR. 2016 Sep 30;65:1-4).
The cases were reported in 30 d ifferent states, and the states with the highest numbers of reported cases were Florida (23%), New York (11%), and California (9%). All patients acquired Zika virus infections during travel to a location where mosquito-borne transmission had been documented, according to researchers.
The median patient age was 14 years, the majority of the patients were female (56%), and five patients were pregnant.
Of Zika’s four primary clinical signs and symptoms, 82% of the pediatric population had a rash, 55% had a fever, 29% had conjunctivitis, and 28% had arthralgia, with 70% of the children presenting with two or more of these symptoms.
Only two children were hospitalized because of their infections. No children were reported to have meningitis, encephalitis, or Guillain-Barré syndrome, and no patients with Zika virus infection died, researchers reported.
This data “corroborates previously published reports suggesting that the clinical course of Zika virus disease is typically mild in children, as it is in adults,” Dr. Goodman and her associates wrote.
Severe disease and death in children with postnatally acquired Zika virus infection are rare, the researchers pointed out, but they encouraged physicians to consider a Zika virus disease diagnosis for children with the four common symptoms and who reside in or traveled to an area with active Zika virus transmission. All Zika virus disease cases should be reported to state health departments.
On Twitter @jessnicolecraig
The clinical course of postnatally acquired Zika virus disease in children younger than 18 years is mild and rarely results in severe illness or death, reported Alyson Goodman, MD, and her associates at the Centers for Disease Control and Prevention (CDC), Atlanta.
There were a total of 158 confirmed or probable postnatally acquired Zika virus disease cases among children younger than 18 years reported to the CDC in the United States between January 2015 and July 2016, wrote researchers in a case series that described the epidemiology, clinical findings, and outcomes of the cases (MMWR. 2016 Sep 30;65:1-4).
The cases were reported in 30 d ifferent states, and the states with the highest numbers of reported cases were Florida (23%), New York (11%), and California (9%). All patients acquired Zika virus infections during travel to a location where mosquito-borne transmission had been documented, according to researchers.
The median patient age was 14 years, the majority of the patients were female (56%), and five patients were pregnant.
Of Zika’s four primary clinical signs and symptoms, 82% of the pediatric population had a rash, 55% had a fever, 29% had conjunctivitis, and 28% had arthralgia, with 70% of the children presenting with two or more of these symptoms.
Only two children were hospitalized because of their infections. No children were reported to have meningitis, encephalitis, or Guillain-Barré syndrome, and no patients with Zika virus infection died, researchers reported.
This data “corroborates previously published reports suggesting that the clinical course of Zika virus disease is typically mild in children, as it is in adults,” Dr. Goodman and her associates wrote.
Severe disease and death in children with postnatally acquired Zika virus infection are rare, the researchers pointed out, but they encouraged physicians to consider a Zika virus disease diagnosis for children with the four common symptoms and who reside in or traveled to an area with active Zika virus transmission. All Zika virus disease cases should be reported to state health departments.
On Twitter @jessnicolecraig
The clinical course of postnatally acquired Zika virus disease in children younger than 18 years is mild and rarely results in severe illness or death, reported Alyson Goodman, MD, and her associates at the Centers for Disease Control and Prevention (CDC), Atlanta.
There were a total of 158 confirmed or probable postnatally acquired Zika virus disease cases among children younger than 18 years reported to the CDC in the United States between January 2015 and July 2016, wrote researchers in a case series that described the epidemiology, clinical findings, and outcomes of the cases (MMWR. 2016 Sep 30;65:1-4).
The cases were reported in 30 d ifferent states, and the states with the highest numbers of reported cases were Florida (23%), New York (11%), and California (9%). All patients acquired Zika virus infections during travel to a location where mosquito-borne transmission had been documented, according to researchers.
The median patient age was 14 years, the majority of the patients were female (56%), and five patients were pregnant.
Of Zika’s four primary clinical signs and symptoms, 82% of the pediatric population had a rash, 55% had a fever, 29% had conjunctivitis, and 28% had arthralgia, with 70% of the children presenting with two or more of these symptoms.
Only two children were hospitalized because of their infections. No children were reported to have meningitis, encephalitis, or Guillain-Barré syndrome, and no patients with Zika virus infection died, researchers reported.
This data “corroborates previously published reports suggesting that the clinical course of Zika virus disease is typically mild in children, as it is in adults,” Dr. Goodman and her associates wrote.
Severe disease and death in children with postnatally acquired Zika virus infection are rare, the researchers pointed out, but they encouraged physicians to consider a Zika virus disease diagnosis for children with the four common symptoms and who reside in or traveled to an area with active Zika virus transmission. All Zika virus disease cases should be reported to state health departments.
On Twitter @jessnicolecraig
FROM MMWR
Key clinical point: Postnatally acquired Zika virus disease in children younger than 18 years is mild and rarely results in severe illness or death.
Major finding: Only two children were hospitalized because of their infections, and no children died.
Data source: Case series of 158 confirmed or probable postnatally acquired Zika virus disease cases among children.
Disclosures: The study was funded by the CDC. Author disclosures were not reported.
Focused Ultrasound Thalamotomy Reduces Hand Tremor
MRI-guided focused ultrasound thalamotomy reduces hand tremor in patients with essential tremor, according to data published August 25 in the New England Journal of Medicine. The technique also reduces disability and improves self-reported quality of life, said the researchers.
“We are excited to have this new noninvasive treatment option for patients who struggle every day with this debilitating neurologic disorder,” said Howard M. Eisenberg, MD, the R.K. Thompson Professor and Chair of Neurosurgery at the University of Maryland School of Medicine in Baltimore and an author of the study. “We saw an impressive reduction in tremors in hands and arms and an improvement in quality of life in patients who experienced no relief from medication.”
Dr. Eisenberg and colleagues randomized 76 patients with moderate to severe essential tremor that had not responded to at least two trials of medical therapy to unilateral focused ultrasound thalamotomy or a sham procedure. The investigators administered the Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor (QUEST) questionnaire to participants at baseline and at one, three, six, and 12 months. Videotaped tremor assessments were rated by an independent group of neurologists who were blinded to the treatment assignments. After three months, patients in the sham-procedure group were allowed to cross over to active treatment.
The study’s primary outcome was the between-group difference in the change from baseline to three months in hand tremor, rated on Parts A and B of the CRST. Secondary outcomes included functional limitations in daily activities, measured according to eight items in the disability subsection of the CRST; quality of life, assessed with the QUEST at three months; and the durability of the reduction in hand tremor at 12 months.
Hand-tremor scores improved by 8.5 points in the intervention group and by 0.2 points among controls. Improvement occurred in the hand contralateral to the thalamotomy. The between-group difference in the mean change was 8.3 points. The improvement in the thalamotomy group was maintained at 12 months (change from baseline, 7.2 points). Focused ultrasound thalamotomy also improved total disability score by 62% at three months, compared with 3% among controls, and the improvement was sustained at 12 months. Patients’ self-rated quality of life improved by 46% at three months in the intervention group and by 3% among controls.
Adverse events of thalamotomy included gait disturbance (36% of patients) and paresthesias or numbness (38% of patients). These adverse events persisted at 12 months in 9% and 14% of patients, respectively.
In an accompanying editorial, Elan D. Louis, MD, Chief of the Division of Movement Disorders at Yale University in New Haven, Connecticut, said that the study results are promising, particularly since the procedure, unlike traditional thalamotomy, does not require entering the skull with a probe. “Nevertheless,” he added, “there are several important concerns.” The first concern is the limited follow-up period. The sustained benefit beyond one year is not known. “This is particularly important because of tachyphylaxis, which is the second concern,” Dr. Louis wrote. Tremor score in the group that underwent focused ultrasound thalamotomy increased from 8.84 at one month to 10.89 at 12 months, an increase of 23%. A third concern is that the procedure did not achieve large improvements in everyone; the percentage change in tremor was less than 20% in nine of 56 patients. “Even with these concerns,” Dr. Louis said, “the procedure will take its place among other surgical procedures for medically refractory essential tremor.”
—Erik Greb and Glenn Williams
Suggested Reading
Elias WJ, Lipsman
Louis ED. Treatment of medically refractory essential tremor. N Engl J Med. 2016;375(8):792-793.
MRI-guided focused ultrasound thalamotomy reduces hand tremor in patients with essential tremor, according to data published August 25 in the New England Journal of Medicine. The technique also reduces disability and improves self-reported quality of life, said the researchers.
“We are excited to have this new noninvasive treatment option for patients who struggle every day with this debilitating neurologic disorder,” said Howard M. Eisenberg, MD, the R.K. Thompson Professor and Chair of Neurosurgery at the University of Maryland School of Medicine in Baltimore and an author of the study. “We saw an impressive reduction in tremors in hands and arms and an improvement in quality of life in patients who experienced no relief from medication.”
Dr. Eisenberg and colleagues randomized 76 patients with moderate to severe essential tremor that had not responded to at least two trials of medical therapy to unilateral focused ultrasound thalamotomy or a sham procedure. The investigators administered the Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor (QUEST) questionnaire to participants at baseline and at one, three, six, and 12 months. Videotaped tremor assessments were rated by an independent group of neurologists who were blinded to the treatment assignments. After three months, patients in the sham-procedure group were allowed to cross over to active treatment.
The study’s primary outcome was the between-group difference in the change from baseline to three months in hand tremor, rated on Parts A and B of the CRST. Secondary outcomes included functional limitations in daily activities, measured according to eight items in the disability subsection of the CRST; quality of life, assessed with the QUEST at three months; and the durability of the reduction in hand tremor at 12 months.
Hand-tremor scores improved by 8.5 points in the intervention group and by 0.2 points among controls. Improvement occurred in the hand contralateral to the thalamotomy. The between-group difference in the mean change was 8.3 points. The improvement in the thalamotomy group was maintained at 12 months (change from baseline, 7.2 points). Focused ultrasound thalamotomy also improved total disability score by 62% at three months, compared with 3% among controls, and the improvement was sustained at 12 months. Patients’ self-rated quality of life improved by 46% at three months in the intervention group and by 3% among controls.
Adverse events of thalamotomy included gait disturbance (36% of patients) and paresthesias or numbness (38% of patients). These adverse events persisted at 12 months in 9% and 14% of patients, respectively.
In an accompanying editorial, Elan D. Louis, MD, Chief of the Division of Movement Disorders at Yale University in New Haven, Connecticut, said that the study results are promising, particularly since the procedure, unlike traditional thalamotomy, does not require entering the skull with a probe. “Nevertheless,” he added, “there are several important concerns.” The first concern is the limited follow-up period. The sustained benefit beyond one year is not known. “This is particularly important because of tachyphylaxis, which is the second concern,” Dr. Louis wrote. Tremor score in the group that underwent focused ultrasound thalamotomy increased from 8.84 at one month to 10.89 at 12 months, an increase of 23%. A third concern is that the procedure did not achieve large improvements in everyone; the percentage change in tremor was less than 20% in nine of 56 patients. “Even with these concerns,” Dr. Louis said, “the procedure will take its place among other surgical procedures for medically refractory essential tremor.”
—Erik Greb and Glenn Williams
Suggested Reading
Elias WJ, Lipsman
Louis ED. Treatment of medically refractory essential tremor. N Engl J Med. 2016;375(8):792-793.
MRI-guided focused ultrasound thalamotomy reduces hand tremor in patients with essential tremor, according to data published August 25 in the New England Journal of Medicine. The technique also reduces disability and improves self-reported quality of life, said the researchers.
“We are excited to have this new noninvasive treatment option for patients who struggle every day with this debilitating neurologic disorder,” said Howard M. Eisenberg, MD, the R.K. Thompson Professor and Chair of Neurosurgery at the University of Maryland School of Medicine in Baltimore and an author of the study. “We saw an impressive reduction in tremors in hands and arms and an improvement in quality of life in patients who experienced no relief from medication.”
Dr. Eisenberg and colleagues randomized 76 patients with moderate to severe essential tremor that had not responded to at least two trials of medical therapy to unilateral focused ultrasound thalamotomy or a sham procedure. The investigators administered the Clinical Rating Scale for Tremor (CRST) and the Quality of Life in Essential Tremor (QUEST) questionnaire to participants at baseline and at one, three, six, and 12 months. Videotaped tremor assessments were rated by an independent group of neurologists who were blinded to the treatment assignments. After three months, patients in the sham-procedure group were allowed to cross over to active treatment.
The study’s primary outcome was the between-group difference in the change from baseline to three months in hand tremor, rated on Parts A and B of the CRST. Secondary outcomes included functional limitations in daily activities, measured according to eight items in the disability subsection of the CRST; quality of life, assessed with the QUEST at three months; and the durability of the reduction in hand tremor at 12 months.
Hand-tremor scores improved by 8.5 points in the intervention group and by 0.2 points among controls. Improvement occurred in the hand contralateral to the thalamotomy. The between-group difference in the mean change was 8.3 points. The improvement in the thalamotomy group was maintained at 12 months (change from baseline, 7.2 points). Focused ultrasound thalamotomy also improved total disability score by 62% at three months, compared with 3% among controls, and the improvement was sustained at 12 months. Patients’ self-rated quality of life improved by 46% at three months in the intervention group and by 3% among controls.
Adverse events of thalamotomy included gait disturbance (36% of patients) and paresthesias or numbness (38% of patients). These adverse events persisted at 12 months in 9% and 14% of patients, respectively.
In an accompanying editorial, Elan D. Louis, MD, Chief of the Division of Movement Disorders at Yale University in New Haven, Connecticut, said that the study results are promising, particularly since the procedure, unlike traditional thalamotomy, does not require entering the skull with a probe. “Nevertheless,” he added, “there are several important concerns.” The first concern is the limited follow-up period. The sustained benefit beyond one year is not known. “This is particularly important because of tachyphylaxis, which is the second concern,” Dr. Louis wrote. Tremor score in the group that underwent focused ultrasound thalamotomy increased from 8.84 at one month to 10.89 at 12 months, an increase of 23%. A third concern is that the procedure did not achieve large improvements in everyone; the percentage change in tremor was less than 20% in nine of 56 patients. “Even with these concerns,” Dr. Louis said, “the procedure will take its place among other surgical procedures for medically refractory essential tremor.”
—Erik Greb and Glenn Williams
Suggested Reading
Elias WJ, Lipsman
Louis ED. Treatment of medically refractory essential tremor. N Engl J Med. 2016;375(8):792-793.
Guide to Recognizing and Treating Sleep Disturbances in the Nursing Home
From the School of Aging Studies, University of South Florida, Tampa, FL (Dr. AA Gamaldo) and the Department of Neurology, Johns Hopkins Medicine, Baltimore, MD (Drs. Sloane, CE Gamaldo and Salas).
Abstract
- Objective: To provide guidance on identifying and treating sleep disturbances commonly encountered in older nursing home residents.
- Methods: Review of the literature in the context of 5 clinical cases.
- Results: Sleep disturbances continue to be a growing global epidemic, and public health initiatives have been aimed at improving sleep health across all ages. In older adults, sleep disturbances are often associated with the development and/or worsening of health conditions. Common sleep disturbances observed in older nursing home residents include obstructive sleep apnea, restless legs syndrome/Willis-Ekbom disease, circadian rhythm sleep-wake disorders, insomnia, and parasomnias. The symptoms and recommended treatment plans vary across the sleep disturbances. For many sleep disturbances, modification of residents’ daily activities and/or nursing home environment can be helpful.
- Conclusion: As the number of people residing in nursing homes increases, it is important for health care providers to be knowledgable about sleep disturbances in this population.
By 2030, almost 20% of the US population (approximately 72.1 million people) will be age 65 and older [1]. As many as 63% of older adults in the general population report sleep disturbances [2]. Specifically, older adults demonstrate difficulty with decreased total sleep duration, an increase in sleep fragmentation (ie, interruptions in nighttime sleep), and reduced total sleep time spent in rapid eye movement (REM) and slow wave sleep [3–5]. Poor sleep, either because of not getting enough sleep or having an undiagnosed and thus untreated sleep disorder, is associated with physical illness, impaired cognition, poor physical function, and mortality risk [6,7]. In fact, over 50% of individuals older than 65 years meet the diagnostic criteria for a sleep disorder, many of which are undiagnosed [6,7].
It is forecasted that we will see substantial increases in the rate of nursing home residence among the elderly [8]. The prevalence and severity of disturbed sleep is reportedly higher in NH residents [6,7]. Generally, NH residents tend to be on several medications for various medical disorders that may negatively impact sleep [7]. Reciprocally, sleep disruption may put NH residents at an increased risk for behavioral issues (eg, agitation) [9,10] as well as developing and/or exacerbating health conditions (eg, mood disorders, dementia, cardiovascular disease) [8]. Furthermore, NH residents exhibiting disturbed sleep, behavioral issues, and/or mood disorders are at an increased risk for being prescribed antipsychotic drugs [11], which are associated with adverse side effects and poorer quality of life [12]. Thus, the identification and management of sleep disturbances in the NH setting has become progressively more vital in efforts to optimize medical management of this population. This review identifies common sleep disturbances frequently underdiagnosed and undertreated among residents of NH facilities.
Case 1
A 73-year-old woman with a history of type 2 diabetes mellitus reports poor sleep quality with frequent awakenings during the night and excessive daytime sleepiness. She states that she can fall asleep within 5 minutes, but often is awoken throughout the night with a sensation of breathlessness. She has snored for many years, but the nursing staff at her NH facility has recently commented that her snoring has gone from intermittent to constant. She cannot remember the last time she has had restful sleep. She consumes 3 to 4 cups of caffeinated beverages daily to counter her sleepiness. She denies smoking or illicit drug or alcohol use. Her review of systems was notable for a 30-lb weight gain over the last year, and she reports increasing fatigue, irritability, and memory and concentration issues. Her current medication list includes metformin and amlodipine. Her examination is remarkable for a BMI of 31, large neck circumference (> 16), tonsillar enlargement, a crowded oropharynx, micrognathia, lungs clear to auscultation bilaterally, heart sounds of normal S1 and S2, and legs with trace pitting edema.
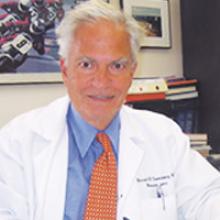
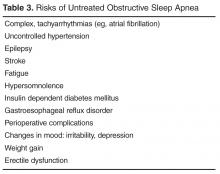
Case 1 Reflection: Sleep-Disordered Breathing
Although previous studies have observed high rates (60%–90%) of SDB in NH settings [16,17], one study observed that only 0.5% of nursing home residents carried a diagnosis with SDB, suggesting that SDB is being grossly underappreciated amongst NH residents over the age of 65 [18]. In order to evaluate for SBD, routine annual physical exams or medical chart reviews can elicit the risk factors for sleep apnea (eg, obesity [per BMI], male sex, postmenopausal women, family history of sleep apnea) as well as common comorbidities (eg, hypertension, coronary artery disease, and diabetes). Formal evaluation consists of a sleep evaluation with a sleep specialist and polysomnography (PSG; sleep study) that can be performed in the sleep center or at home depending on the patient’s history and other medical issues.
Case 1 Outcome
Case 2
An 85-year-old man with history of Alzheimer’s disease, major depression and arthritis, reports insomnia and “tingling in my legs” at bedtime. The patient cannot identify when the symptoms started but reports that his legs often jerk during sleep. He consumes a cup of coffee daily and has a previous 20 pack-year smoking history (he quit 40 years ago). On review of systems, he endorses fatigue. His current medication list includes fluoxetine, donepezil hydrochloride, ibuprofen as needed for arthritic pain, and a multivitamin. His examination was unremarkable, with a BMI of 26, neck circumference < 16, no tonsillar enlargement, normal (noncrowded) oropharynx, lungs clear to auscultation bilaterally, heart sounds demonstrating a normal S1 and S2, and legs without edema.
Case 2 Reflection: Restless Legs Syndrome/Willis-Ekbom Disease
Restless legs syndrome (RLS) also known as Willis-Ekbom disease, affects approximately 10 million adults in the United States alone [22]. RLS is a sensorimotor disorder that must satisfy the following 5 primary diagnostic criteria: (1) urge to move the legs with or without dysesthesias; (2) onset or exacerbation with rest or inactivity; (3) relief with movement; (4) symptoms are worse in the evening or at night (circadian component); (5) symptoms cannot be solely accounted for as consequence of another medical or behavioral condition. Other supporting clinical features can alert a clinician to the likelihood of a RLS diagnosis; these include positive family history, response to dopaminergic therapy, lack of profound daytime sleepiness, and presence of periodic limb movements during sleep (PLMS) [23–26]. In younger individuals, the symptoms present insidiously whereas older adults (> 50 years of age) will usually present with sudden onset [27].
Not only do patients lack the restorative sleep needed to ward off fatigue and restfulness, but patients also demonstrate higher rates of comorbidities (eg, anxiety, hypertension, depression) as well as large economic burden secondary to absenteeism and decreased on-the-job effectiveness [28,29]. As a results, patients with RLS experience significant reductions in quality of life related to this sensorimotor disorder [28].
No confirmatory laboratory test exists to diagnose RLS; however, patients suspected of having RLS should be evaluated with a basic metabolic panel, iron studies, and a thorough neurologic examination, as iron deficiency, kidney failure, uremia and peripheral neuropathy can lead to secondary RLS [30,31]. Evidence shows that RLS is common in NH residents [32] and may account for problematic behaviors, such as late night pacing [7]. Forty-five percent of community dwelling individuals over 65 years old exhibit a PLMS index (leg kicks per hour) of greater than 5 [33]. PLMS, while not a disorder in and of itself, can serve as a marker for potential disease. PLMS are characterized by intermittent episodes of stereotyped leg movements. PLMS typically do not awaken the patient from sleep and therefore do not contribute to insomnia or daytime sleepiness, representing a key clinical difference from RLS. It is important to note that PLMS are nonspecific and may be common in older adults that do not meet the diagnostic criteria for RLS.
Treatment of RLS is based on the frequency of symptoms and the level of functional impairment caused by the syndrome. RLS treatment recommendations should always espouse nonpharmacological interventions that include improving sleep practices, engagement in daily physical activity, targeted placement of sedentary activity in the morning when symptoms are less prominent, and concerted efforts to avoid the use of RLS-exacerbating medications (eg, selective serotonin reuptake inhibitor (SSRIs), neuroleptic agents, antihistamines) [28]. If there is an underlying condition contributing to RLS, such as metabolic disturbance or iron deficiency, then these conditions should be corrected before initiating RLS medications. Several medications are FDA-approved for treatment of RLS, including dopamine agonists (eg, ropinirole, rotigotine, pramipexole), dopamine precursor (eg, levodopa), glutamate-related (eg, gabapentin), benzodiazepines (eg, temazepam, clonazepam). Augmentation, the worsening of RLS symptoms, can occur in patients taking dopamine agonists. If this occurs, dopamine agents should be discontinued or switched to other agents (such as a long-acting dopamine agonist, gabapentin encarbil, as well as non-FDA approved therapies such as opioids). However, it is important to note that weaning off dopamine agents may result in mild but in most cases moderate and/or severe withdrawal from the medication, so counseling and close monitoring should be done.
Case 2 Outcome
Given the patient’s history of dementia, opioids, benzodiazepines and other delirium-inducing medications should be avoided. His antidepressive regimen, fluoxetine, should be re-evaluated as these medications have been associated with RLS exacerbation. In addition to SSRIs, medications associated with RLS are MAO inhibitors (selegeline, phenelzine), antipsychotics (risperdone, olanzapine), tricyclic antidepressants (mirtazapine), antihistamines (diphenhydramine, cimetidine), calcium channel blockers (verapamil, nifedipine, diltiazem), and phenytoin [34,35]. His treatment began with behavioral, nonpharmacological management, and blood testing for iron studies. His low iron level prompted initiation of oral supplementation, and he was asked to follow up in 3 months for reevaluation and possible initiation of low-dose dopamine agonists.
Case 3
A 73-year-old man with dementia is found to have very irregular sleep wake patterns with a variable bedtime and awakening time, often missing breakfast. He is found dozing off often during the day, particularly during times of inactivity. He has frequent awakenings during the night often calling for the staff to guide him back to bed. He has had some falls secondary to walking around his room. He has been prescribed various hypnotics without much benefit and instead, has suffered from some confusion while on these medications. His room is very dark and has no windows.
Case 3 Reflection: Circadian Rhythm Sleep-Wake Disorders
Circadian rhythm sleep-wake disorders (CRSWDs) are characterized by an individual’s natural propensity to want to go to sleep and be awake during a period that is undesirable personally and/or socially [36]. CRSWDs can be a result of the desynchronization of the 2 sleep processes: (1) homeostatic drive (regulates sleep intensity) and (2) circadian rhythm (maintains daytime alertness); [36]. CRSWDs can also be due to an individual’s naturally occurring sleep drives becoming misaligned with their social/personal sleep-wake demands (eg, employment schedule and socializing opportunities with family/friends). With increasing age, the circadian rhythm becomes less adept at functioning in a desynchronized pattern [7], which can result in daytime sleepiness and night time sleep fragmentation [7,37]. CRSWDs are highly prevalent in individuals with dementia [7,36]. As dementia progresses, the ability to maintain a balance of the 2 sleep process becomes more impaired [7]. As a result, individuals with dementia, particularly Alzheimer’s disease, are likely to experience agitation, irritability, and/or confusion during the evening and night, a behavioral problem referred to as “sundowning” [38].
There are several types of CRSWDs, including delayed sleep-phase syndrome, advanced sleep-phase syndrome, irregular sleep-wake disorder, non–24-hour sleep-wake disorder, shift work sleep disorder, and jet lag sleep disorder. However, the most common type of CRSWDs observed in older adults is advanced sleep-phase syndrome [39]. Due to excessive sleepiness in the early evening, affected individuals may report a need to shift to earlier and earlier bedtimes (~6 to 7 pm) and wake times (~3 to 4 am) [36]. For older affected adults, this can cause distress and frustration, particularly if their sleep phase prevents them from participating in evening activities (eg, socializing with family/friends) [36].
In the assessment of patients with suspected CRSWDs, sleep diaries (self-reported or caregiver) daily account of sleep and wake times over at least 1 week) and actigraphy (wrist-worn accelerometer designed to measure activity and inactivity at night) can be used, particularly in older adults with dementia [40,41].
CRSWD treatment may include behavioral modifications and/or pharmacological intervention. Behavioral modifications can consist of chronotherapy, relaxation training, and/or bright light therapy. Chronotherapy involves making gradual shifts in an individual’s sleep time to meet his/her desired sleep schedule. Relaxation training involves implementing behaviors/activities that reduce tension and enhance the smooth transition into sleep. Bright light therapy involves exposure to an appropriate intensity and duration of light, which is an important environmental cue to help the synchrony of the sleep-wake cycle [7]. Previous studies have observed that NH residents are exposed to a restricted amount of bright light during the daytime [42,43], but higher levels of artificial light at night (eg, hallway lighting) [7]. NH residents’ exposure to artificial bright light during the daytime has not only improved the residents’ sleep [44–46], but also has improved their cognitive functioning and reduced their depressive symptoms [47]. Thus, steps towards targeted light exposure in sync with the typical sleep-wake cycle (eg, mandated time in well-lit rooms during the day and during meals) for NH residents, particularly those with CRSWDs, could prove to be beneficial across several social, behavioral and neurocognitive domains. Lastly, NH residents exposed to at least 30 minutes of outdoor daylight and at least 3 occasions of low intensity physical activities for 10 to 15 minutes daily can potentially improve sleep-wake patterns [48]. Thus, it may be beneficial to have an intervention that couples bright light exposure and physical activity in the NH setting.
Pharmacological interventions can also be implemented to improve older residents’ symptoms. However, the medications prescribed should be used with caution and should not be used as part of a long-term treatment plan. Melatonin is a commonly used herbal supplement that can assist advancing the timing of the circadian rhythms in the evening but can delay the circadian rhythms in the morning [49]. Several brands of this herbal supplement can be purchased over-the-counter and are not regulated by the FDA. Since the amount of melatonin used in the herbal supplement varies by brand, caution should be used when selecting a brand [50]. Two FDA-approved drugs (modafinil and armodafinil) are currently being used to reduce daytime sleepiness and improve vigilance amongst adults, but limited research has explored the effectiveness of these medication for older adults specifically suffering with CRSWDS [36,51,52]. Other stimulants (eg, caffeine, amphetamines, and nonamphetamine-derived medications) are also currently being used to reduce daytime sleepiness in patients with CRSWDS. Stimulant use, particularly caffeine consumption, has also been associated with better cognitive functioning in older adults [53]. However, stimulants should be taken with caution, particularly in older adults, because stimulant use has been associated with potentially serious and fatal health sequalae (eg, tachycardia, heart failure, irreversible heart damage and hypertension) [36,54].
Case 3 Outcome
The patient was moved to a room with a window. An alarm clock was set for 7:30 in the morning and he was taken to breakfast, where he sat at a table near a window. Any time he appeared to be sleepy, he was encouraged to go for a walk or engage in other activities so daytime napping opportunities were limited. His environment was assessed for safety and bedrails were utilized to prevent falls.
Case 4
A 75-year-old woman with a history of anxiety and depression moved into the NH 4 months ago after suffering a stroke. She now reports difficulty falling asleep for many years, which has significantly worsened since moving to the NH. Currently, she has been getting only 3 to 4 hour of sleep per night. She reports mild but increasing daytime sleepiness and does not fall asleep until 1:00 am despite getting into bed at 10:30 pm. She occasionally reports arthritic pain that interferes with her sleep. The NH staff has mentioned that she will occasionally cry for her family when she appears to be asleep.
Case 4 Reflection: Insomnia
According to the International Classification of Sleep Disorders (ICSD-3) [39], insomnia is characterized as “a repeated difficulty with sleep initiation, duration, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep, and results in some form of daytime impairment.” Among the sleep disorders, insomnia is one of the most common sleep issues observed in sleep clinics [34]. Older adults with insomnia often have comorbid physical (eg, pulmonary disease, arthritis, chronic pain, cancer diabetes, Parkinson’s disease) and mental illness (eg, depression, panic disorder) [55]. Medications (eg, stimulants, respiratory medications, chemotherapy, decongestants, hormones, or psychotropics) may cause and exacerbate insomnia symptoms [55].
Since insomnia is a clinical diagnosis, there is no specific diagnostic tool or gold standard test to identify individuals suffering with insomnia. Insomnia screening usually involves a clinical interview, in which a health provider, preferably trained in sleep, conducts a physical examination and collects an in-depth history of a patients’ sleep problems [56]. Insomnia screening tools may also include having a patient complete a sleep diary or questionnaire, such as the insomnia severity index (ISI) [57] or Pittsburgh Sleep Quality Index (PSQI) [58].
Cognitive behavioral therapy for insomnia (CBT-I) and/or pharmacological intervention are typically used to treat insomnia in older adults. CBT-I is a combination of cognitive (eg, changing dysfunctional sleep attitudes/beliefs) and behavioral treatment (eg, adhering to a regular sleep schedule) [59]. CBT-I or a combination of CBT-I and pharmacological intervention is recommended as more effective long-term approach to insomnia treatment compared to pharmacological intervention alone [55]. CBT-I involves altering older adults’ misconceptions of their sleep and implementing behavioral techniques to their everyday life (eg, routine sleep-wake schedule, relaxation therapy). Several FDA-approved medications are available to treat insomnia; however, many commonly used medications to treat insomnia in older adults (ie, antihistamines, antidepressants, anticonvulsants, and anti-psychotics) pose more risks than benefits to their health and well-being [35,60–62]. Some of the more recent hypnotics (egm zolpidem, exzopiclone, and ramelteon) on the market have been shown to be safer and more effective pharmacological options [55]. In 2014, the FDA approved the first in class orexin receptor antagonist medication (suvorexant) to treat insomnia [63]. Unlike other medications to treat insomnia, suvorexant, via the blockade of the orexin neurotransmitter, effectively inhibits orexin (one of neurotransmitters involved in the activation pathways of the arousal system), so sleep can easily be induced and maintained [64, 65]. Furthermore, preliminary studies suggest that this medication may be associated with less severe side effects (ie, habituation) than the other approved medications on the market [64, 65]. In fact, in a recent clinical series that included both young and older insomnia patients, the most common adverse reaction to suvorexant was drowsiness [66].
Case 4 Outcome
The patient was initiated on basic CBT-I therapy strategies which included stimulus control therapy [67]; implementation of a consistent bedtime and awakening routine; reducing the use of TV, smart phone, or other electronic leisure devices 1 hour before bedtime; refraining from caffeine after lunchtime; improving the sleep environment; and relaxation techniques.
Case 5
The patient is a 65-year-old man diagnosed with Parkinson’s disease several years ago. Recently, he has often has been experiencing what appears to be very violent and terrifying dreams. While asleep, he often screams and shouts for help. In addition, he occasionally will punch, kick, and/or thrash around in bed at night, which the NH staff has noted as a concern for his safety.
Case 5 Reflection: Parasomnias
Parasomnias represent frequent arousals during sleep or in the wake-to-sleep transition due to abnormal motor movements, behaviors (eg, shouting, flailing, and leaping from bed) and/or sensory experiences (eg, “dreamlike” hallucinations) [68]. Motor movements that occur for parasomnia can be disruptive for the individual and potentially dangerous for the individual and/or bed partner. There are 3 primary types of parasomnias based on the stage of sleep that the event occurs: non-REM (NREM), REM, and other parasomnias during transitions of sleep [68]. The most commonly observed parasomnia seen in older adults is the REM-associated parasomnia or REM sleep behavior disorder (RBD), which is characterized by experiencing vivid, sometimes violent, dreams typically involving fighting an intruder or an animal to protect a loved one [69]. For RBD, disruptive behaviors typically occur during REM sleep [69]. RBD has been associated with neurodegenerative disorders (Parkinson’s disease and Lewy body disease), neurologic disorders (eg, brain tumors and stroke), other primary disorders (narcolepsy and periodic limb movement disorder), and well as some medications (eg, antidepressants and β-blockers) [68]. There is limited knowledge on the prevalence of parasomnias in NH settings. One study, however, reported that 31% of older NH residents experience parasomnias [70]. Evaluation for parasomnias generally involve a clinical evaluation by a sleep specialist and overnight sleep study (ie, polysomnography at a sleep center if there is a concern for sleep apnea or RBD [71].
Medications are not typically first-line for parasomnia. Instead education about improving sleep practices, addressing other underlying sleep disorders, and securing a safe sleep environment are first recommended. Pharmacologic treatment, particularly the use of clonazepam, is commonly used to treat RBD [72]. However, this medication should be used with caution for older adults with a dementia diagnosis, gait disorders, and OSA because the common side effects include sedation, confusion, memory dysfunction, and early morning motor incoordination [68]. Several alternative medications have also been used to treat RBD. For example, medications commonly used to Parkinson disease symptoms, such Levodopa and dopamine agonists, have also been used to treat RBD [73]. Zopiclone, a nonbenzodiazepine hypnotic agent, has also been shown to be as effective as clonazepam, but with less potential side effects [74]. Melatonin, a nutritional supplement, has also been used as a treatment and appears to alleviate some of the RBD symptoms and has fewer side effects [68]. Since melatonin is not regulated by the FDA, it has been suggested that this treatment be used with caution in the older population [73].
Case 5 Outcome
The patient was evaluated with video synchronized in lab PSG. It confirmed REM sleep without evidence of the normal atonia that should be apparent during REM. These PSG findings in combination with repeated accounts of dream enactment established the diagnosis of RBD. Patient was treated with low-dose clonazepam and closely monitored for potential side effects of daytime sedation. Bedroom environment was also carefully reconfigured for safety to avoid potential risk of injury during a dream enactment episode.
Conclusion
Sleep disturbances remain an underappreciated and undertreated health issue in NH residents. Nursing homes can help facilitate optimal sleep health and day functioning by providing mandatory natural light outlets, physical exercise opportunities, and minimal allowable time residents can spend in their bed/bedroom outside of their routine sleep period. Educating NH providers and staff on sleep medicine may benefit residents, but workload and restricted resources may hinder this. Education via mobile and internet based educational platforms and resources (Mysleep101) may be helpful in addressing education barriers [75]. Convenient and cost-effective methods to deliver sleep medicine education to NH health care providers should be part of our ongoing efforts to improve the viability, vitality and quality of life of our aging citizens.
Corresponding author: Alyssa Gamaldo, PhD, Univ. of South Florida, 13301 Bruce B. Downs Blvd, MHC 1340, Tampa, FL 33612, [email protected].
Financial disclosures: None.
1. Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key indicators of well-being. Washington, DC: U.S. Gov. Printing Office; 2012.
2. Almeida OP, Pfaff JJ. Sleep complaints among older general practice patients: association with depression. Br J Gen Pract 2005;55:864–866.
3. Wolkove N, Elkholy O, Baltzan M, et al. Sleep and aging: 1. Sleep disorders commonly found in older people. CMAJ 2007;176:1299–304.
4. Pace-Schott EF, Spencer RM. Age-related changes in the cognitive function of sleep. Prog Brain Res 2011;191:75–89.
5. Ohayon MM, Carskadon MA, Guilleminault C, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 2004;27:1255–73.
6. Jacobs D, Ancoli-Israel S, Parker L, et al. Twenty-four-hour sleep-wake patterns in a nursing home population. Psychol Aging 1989;4:352–6.
7. Neikrug AB, Ancoli-Israel S. Sleep disturbances in nursing homes. J Nutr Health Aging 2010;14:207–11.
8. Lakdawalla D, Goldman DP, Bhattacharya J, et al. Forecasting the nursing home population. Medical Care 2003;41:8-20.
9. Alessi CA, Yoon EJ, Schnelle JF, et al. A randomized trial of a combined physical activity and environmental intervention in nursing home residents: do sleep and agitation improve? J Am Geriatr Soc 1999;47:784–91.
10. Cohen-Mansfield J, Marx MS. The relationship between sleep disturbances and agitation in a nursing home. J Aging Health 1990;2:153–65.
11. Rolland Y, Andrieu S, Crochard A, et al. Psychotropic drug consumption at admission and discharge of nursing home residents. J Am Med Dir Assoc 2012;13:407 e407–412.
12. Salzman C. Antipsychotics in nursing homes. J Clin Psychopharmacol 2013;33:1–2.
13. Fleetham J, Ayas N, Bradley D, et al. Canadian Thoracic Society guidelines: diagnosis and treatment of sleep disordered breathing in adults. Can Respir J 2006;13:387–92.
14. International classification of sleep disorders: Chicago: American Academy of Sleep Medicine; 2005.
15. Gay PC. Complex sleep apnea: it really is a disease. J Clin Sleep Med 2008;4:403–5.
16. Ancoli-Israel S. Epidemiology of sleep disorders. In: Roth T, Roehrs TA, editors. Clinics in geriatric medicine. Philadelphia: WB Saunders; 1989:347–62.
17. Gehrman PR, Martin JL, Shochat T, et al. Sleep-disordered breathing and agitation in institutionalized adults with Alzheimer disease. Am J Geriatr Psychiatry 2003;11:426–33.
18. Resnick HE, Phillips B. Documentation of sleep apnea in nursing homes: United States 2004. J Am Med Dir Assoc 2008;9:260–4.
19. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc 2011;86:549–54.
20. Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 2005;353:2034–41.
21. McMillan A, Bratton DJ, Faria R, et al. Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. Lancet Resp med 2014;2:804–12.
22. Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med 2005;165:1286–92.
23. Allen RP, La Buda MC, Becker P, et al. Family history study of the restless legs syndrome. Sleep Med 2002;3 Suppl:S3–7.
24. Allen RP. Restless legs syndrome/Willis Ekbom disease: evaluation and treatment. Int Rev Psychiatry 2014;26:248–62.
25. Hening WA, Allen RP, Earley CJ, et al. An update on the dopaminergic treatment of restless legs syndrome and periodic limb movement disorder. Sleep 2004;27:560–83.
26. Gamaldo C, Benbrook AR, Allen RP, et al. Evaluating daytime alertness in individuals with Restless Legs Syndrome (RLS) compared to sleep restricted controls. Sleep Med 2009;10:134–8.
27. Allen RP, Earley CJ. Defining the phenotype of the restless legs syndrome (RLS) using age-of-symptom-onset. Sleep Med 2000;1:11–9.
28. Salas RE, Kwan AB. The real burden of restless legs syndrome: clinical and economic outcomes. Am J Manag Care 2012;18(9 Suppl):S207–212.
29. Silber MH, Ehrenberg BL, Allen RP, et al. An algorithm for the management of restless legs syndrome. Mayo Clin Proc 2004;79:916–22.
30. Hattan E, Chalk C, Postuma RB. Is there a higher risk of restless legs syndrome in peripheral neuropathy? Neurology 2009;72:955–60.
31. Winkelman JW, Chertow GM, Lazarus JM. Restless legs syndrome in end-stage renal disease. Am J Kidney Dis 1996;28:372–8.
32. Hornyak M, Trenkwalder C. Restless legs syndrome and periodic limb movement disorder in the elderly. J Psychosom Res 2004;56:543–8.
33. Ancoli-Israel S, Kripke DF, Klauber MR, et al. Periodic limb movements in sleep in community-dwelling elderly. Sleep 1991;14:496–500.
34. Ahmed QA. Effects of common medications used for sleep disorders. Crit Care Clin 2008;24:493–515, vi.
35. Rye DB, Trotti LM. Restless legs syndrome and periodic leg movements of sleep. Neurol clin 2012;30:1137–66.
36. Gamaldo CE, Chung Y, Kang YM, et al. Tick-tock-tick-tock: the impact of circadian rhythm disorders on cardiovascular health and wellness. J Am Soc Hypertens 2014;8:921–9.
37. Myers BL, Badia P. Changes in circadian rhythms and sleep quality with aging: mechanisms and interventions. Neurosci Biobehav Rev 1995;19:553–71.
38. National Institute on Aging. Alzheimer’s caregiving tips: sundowning. June 2013.
39. International classification of sleep disorders. 3rd ed. Darien, IL: AASD; 2014.
40. Barion A, Zee PC. A clinical approach to circadian rhythm sleep disorders. Sleep Med 2007;8:566–77.
41. Morgenthaler TI, Lee-Chiong T, Alessi C, et al. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep 2007;30:1445–59.
42. Shochat T, Martin J, Marler M, et al. Illumination levels in nursing home patients: effects on sleep and activity rhythms. J Sleep Res 2000;9:373–9.
43. Ancoli-Israel S, Klauber MR, Jones DW, et al. Variations in circadian rhythms of activity, sleep, and light exposure related to dementia in nursing-home patients. Sleep 1997;20:18–23.
44. Satlin A, Volicer L, Ross V, et al. Bright light treatment of behavioral and sleep disturbances in patients with Alzheimer’s disease. Am J Psychiatry 1992;149:1028–32.
45. Koyama E, Matsubara H, Nakano T. Bright light treatment for sleep-wake disturbances in aged individuals with dementia. Psychiatry Clin Neurosci 1999;53:227–9.
46. Burns A, Allen H, Tomenson B, et al. Bright light therapy for agitation in dementia: a randomized controlled trial. Int Psychogeriatr 2009;21:711–21.
47. Riemersma-van der Lek RF, Swaab DF, Twisk J, et al. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 2008;299:2642–55.
48. Martin JL, Marler MR, Harker JO, et al. A multicomponent nonpharmacological intervention improves activity rhythms among nursing home residents with disrupted sleep/wake patterns. J Gerontol Series A Biol Sci Med Sci 2007;62:67–72.
49. Lewy AJ, Ahmed S, Jackson JM, et al. Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiol Int 1992;9:380–92.
50. Williamson BL, Tomlinson AJ, Mishra PK, et al. Structural characterization of contaminants found in commercial preparations of melatonin: similarities to case-related compounds from L-tryptophan associated with eosinophilia-myalgia syndrome. Chem Res Toxicol 1998;11:234-40.
51. Czeisler CA, Walsh JK, Roth T, et al. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med 2005;353:476-86.
52. Howard R, Roth T, Drake CL. The effects of armodafinil on objective sleepiness and performance in a shift work disorder sample unselected for objective sleepiness. J Clin Psychopharmacol 2014;34:369–73.
53. Beydoun MA, Gamaldo AA, Beydoun HA, et al. Caffeine and alcohol intakes and overall nutrient adequacy are associated with longitudinal cognitive performance among U.S. adults. J Nutr 2014;144:890–901.
54. Pentel P. Toxicity of over-the-counter stimulants. JAMA 1984;252:1898–903.
55. Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult - a mini-review. Gerontology 2010;56:181–9.
56. Chesson A Jr, Hartse K, Anderson WM, et al. Practice parameters for the evaluation of chronic insomnia. An American Academy of Sleep Medicine report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep 2000;23:237–41.
57. Bastien CH, Vallieres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001;2:297–307.
58. Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213.
59. Trauer JM, Qian MY, Doyle JS, et al. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med 2015;163:191–204.
60. National Institutes of Health State of the Science Conference statement on manifestations and management of chronic insomnia in adults, June 13-15, 2005. Sleep 2005;28:1049–57.
61. Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med 2008;4:487–504.
62. Bain KT. Management of chronic insomnia in elderly persons. Am J Geriatr Pharmacother 2006;4:168–92.
63. FDA approves new type of sleep drug, Belsomra. 13 Aug 2014. Available at fda.gov.
64. Dubey AK, Handu SS, Mediratta PK. Suvorexant: The first orexin receptor antagonist to treat insomnia. J Pharmacol Pharmacother 2015;6:118–21.
65. Patel KV, Aspesi AV, Evoy KE. Suvorexant: a dual orexin receptor antagonist for the treatment of sleep onset and sleep maintenance insomnia. Ann Pharmacother 2015;49:477–83.
66. Michelson D, Snyder E, Paradis E, et al. Safety and efficacy of suvorexant during 1-year treatment of insomnia with subsequent abrupt treatment discontinuation: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet Neurol 2014;13:461–71.
67. Bootzin RR, Epstein D, Wood JM. Stimulus control instructions. Case studies in insomnia. New York: Springer; 1991:19–28.
68. Gulyani S, Salas RE, Gamaldo CE. Sleep medicine pharmacotherapeutics overview: today, tomorrow, and the future (part 2: hypersomnia, parasomnia, and movement disorders). Chest 2013;143:242–51.
69. Boeve BF, Silber MH, Saper CB, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain 2007;130(Pt 11):2770–88.
70. Middelkoop HA, Kerkhof GA, Smilde-van den Doel DA, et al. Sleep and ageing: the effect of institutionalization on subjective and objective characteristics of sleep. Age Ageing 1994;23:411–7.
71. Tinuper P, Provini F, Bisulli F, et al. Movement disorders in sleep: guidelines for differentiating epileptic from non-epileptic motor phenomena arising from sleep. Sleep Med Rev 2007;11:255–67.
72. Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med 2010;6:85–95.
73. Bloom HG, Ahmed I, Alessi CA, et al. Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc 2009;57:761–89.
74. Anderson KN, Shneerson JM. Drug treatment of REM sleep behavior disorder: the use of drug therapies other than clonazepam. J Clin Sleep Med 2009;5:235–9.
75. Doshi A, Gamaldo C, Kalloo A, et al. Implementing a clinical iPad application to detect sleep disorders is feasible across multiple non-sleep outpatient clinics (P7. 321). Neurology 2015;84(14 Suppl):P7.321.
From the School of Aging Studies, University of South Florida, Tampa, FL (Dr. AA Gamaldo) and the Department of Neurology, Johns Hopkins Medicine, Baltimore, MD (Drs. Sloane, CE Gamaldo and Salas).
Abstract
- Objective: To provide guidance on identifying and treating sleep disturbances commonly encountered in older nursing home residents.
- Methods: Review of the literature in the context of 5 clinical cases.
- Results: Sleep disturbances continue to be a growing global epidemic, and public health initiatives have been aimed at improving sleep health across all ages. In older adults, sleep disturbances are often associated with the development and/or worsening of health conditions. Common sleep disturbances observed in older nursing home residents include obstructive sleep apnea, restless legs syndrome/Willis-Ekbom disease, circadian rhythm sleep-wake disorders, insomnia, and parasomnias. The symptoms and recommended treatment plans vary across the sleep disturbances. For many sleep disturbances, modification of residents’ daily activities and/or nursing home environment can be helpful.
- Conclusion: As the number of people residing in nursing homes increases, it is important for health care providers to be knowledgable about sleep disturbances in this population.
By 2030, almost 20% of the US population (approximately 72.1 million people) will be age 65 and older [1]. As many as 63% of older adults in the general population report sleep disturbances [2]. Specifically, older adults demonstrate difficulty with decreased total sleep duration, an increase in sleep fragmentation (ie, interruptions in nighttime sleep), and reduced total sleep time spent in rapid eye movement (REM) and slow wave sleep [3–5]. Poor sleep, either because of not getting enough sleep or having an undiagnosed and thus untreated sleep disorder, is associated with physical illness, impaired cognition, poor physical function, and mortality risk [6,7]. In fact, over 50% of individuals older than 65 years meet the diagnostic criteria for a sleep disorder, many of which are undiagnosed [6,7].
It is forecasted that we will see substantial increases in the rate of nursing home residence among the elderly [8]. The prevalence and severity of disturbed sleep is reportedly higher in NH residents [6,7]. Generally, NH residents tend to be on several medications for various medical disorders that may negatively impact sleep [7]. Reciprocally, sleep disruption may put NH residents at an increased risk for behavioral issues (eg, agitation) [9,10] as well as developing and/or exacerbating health conditions (eg, mood disorders, dementia, cardiovascular disease) [8]. Furthermore, NH residents exhibiting disturbed sleep, behavioral issues, and/or mood disorders are at an increased risk for being prescribed antipsychotic drugs [11], which are associated with adverse side effects and poorer quality of life [12]. Thus, the identification and management of sleep disturbances in the NH setting has become progressively more vital in efforts to optimize medical management of this population. This review identifies common sleep disturbances frequently underdiagnosed and undertreated among residents of NH facilities.
Case 1
A 73-year-old woman with a history of type 2 diabetes mellitus reports poor sleep quality with frequent awakenings during the night and excessive daytime sleepiness. She states that she can fall asleep within 5 minutes, but often is awoken throughout the night with a sensation of breathlessness. She has snored for many years, but the nursing staff at her NH facility has recently commented that her snoring has gone from intermittent to constant. She cannot remember the last time she has had restful sleep. She consumes 3 to 4 cups of caffeinated beverages daily to counter her sleepiness. She denies smoking or illicit drug or alcohol use. Her review of systems was notable for a 30-lb weight gain over the last year, and she reports increasing fatigue, irritability, and memory and concentration issues. Her current medication list includes metformin and amlodipine. Her examination is remarkable for a BMI of 31, large neck circumference (> 16), tonsillar enlargement, a crowded oropharynx, micrognathia, lungs clear to auscultation bilaterally, heart sounds of normal S1 and S2, and legs with trace pitting edema.
Case 1 Reflection: Sleep-Disordered Breathing
Although previous studies have observed high rates (60%–90%) of SDB in NH settings [16,17], one study observed that only 0.5% of nursing home residents carried a diagnosis with SDB, suggesting that SDB is being grossly underappreciated amongst NH residents over the age of 65 [18]. In order to evaluate for SBD, routine annual physical exams or medical chart reviews can elicit the risk factors for sleep apnea (eg, obesity [per BMI], male sex, postmenopausal women, family history of sleep apnea) as well as common comorbidities (eg, hypertension, coronary artery disease, and diabetes). Formal evaluation consists of a sleep evaluation with a sleep specialist and polysomnography (PSG; sleep study) that can be performed in the sleep center or at home depending on the patient’s history and other medical issues.
Case 1 Outcome
Case 2
An 85-year-old man with history of Alzheimer’s disease, major depression and arthritis, reports insomnia and “tingling in my legs” at bedtime. The patient cannot identify when the symptoms started but reports that his legs often jerk during sleep. He consumes a cup of coffee daily and has a previous 20 pack-year smoking history (he quit 40 years ago). On review of systems, he endorses fatigue. His current medication list includes fluoxetine, donepezil hydrochloride, ibuprofen as needed for arthritic pain, and a multivitamin. His examination was unremarkable, with a BMI of 26, neck circumference < 16, no tonsillar enlargement, normal (noncrowded) oropharynx, lungs clear to auscultation bilaterally, heart sounds demonstrating a normal S1 and S2, and legs without edema.
Case 2 Reflection: Restless Legs Syndrome/Willis-Ekbom Disease
Restless legs syndrome (RLS) also known as Willis-Ekbom disease, affects approximately 10 million adults in the United States alone [22]. RLS is a sensorimotor disorder that must satisfy the following 5 primary diagnostic criteria: (1) urge to move the legs with or without dysesthesias; (2) onset or exacerbation with rest or inactivity; (3) relief with movement; (4) symptoms are worse in the evening or at night (circadian component); (5) symptoms cannot be solely accounted for as consequence of another medical or behavioral condition. Other supporting clinical features can alert a clinician to the likelihood of a RLS diagnosis; these include positive family history, response to dopaminergic therapy, lack of profound daytime sleepiness, and presence of periodic limb movements during sleep (PLMS) [23–26]. In younger individuals, the symptoms present insidiously whereas older adults (> 50 years of age) will usually present with sudden onset [27].
Not only do patients lack the restorative sleep needed to ward off fatigue and restfulness, but patients also demonstrate higher rates of comorbidities (eg, anxiety, hypertension, depression) as well as large economic burden secondary to absenteeism and decreased on-the-job effectiveness [28,29]. As a results, patients with RLS experience significant reductions in quality of life related to this sensorimotor disorder [28].
No confirmatory laboratory test exists to diagnose RLS; however, patients suspected of having RLS should be evaluated with a basic metabolic panel, iron studies, and a thorough neurologic examination, as iron deficiency, kidney failure, uremia and peripheral neuropathy can lead to secondary RLS [30,31]. Evidence shows that RLS is common in NH residents [32] and may account for problematic behaviors, such as late night pacing [7]. Forty-five percent of community dwelling individuals over 65 years old exhibit a PLMS index (leg kicks per hour) of greater than 5 [33]. PLMS, while not a disorder in and of itself, can serve as a marker for potential disease. PLMS are characterized by intermittent episodes of stereotyped leg movements. PLMS typically do not awaken the patient from sleep and therefore do not contribute to insomnia or daytime sleepiness, representing a key clinical difference from RLS. It is important to note that PLMS are nonspecific and may be common in older adults that do not meet the diagnostic criteria for RLS.
Treatment of RLS is based on the frequency of symptoms and the level of functional impairment caused by the syndrome. RLS treatment recommendations should always espouse nonpharmacological interventions that include improving sleep practices, engagement in daily physical activity, targeted placement of sedentary activity in the morning when symptoms are less prominent, and concerted efforts to avoid the use of RLS-exacerbating medications (eg, selective serotonin reuptake inhibitor (SSRIs), neuroleptic agents, antihistamines) [28]. If there is an underlying condition contributing to RLS, such as metabolic disturbance or iron deficiency, then these conditions should be corrected before initiating RLS medications. Several medications are FDA-approved for treatment of RLS, including dopamine agonists (eg, ropinirole, rotigotine, pramipexole), dopamine precursor (eg, levodopa), glutamate-related (eg, gabapentin), benzodiazepines (eg, temazepam, clonazepam). Augmentation, the worsening of RLS symptoms, can occur in patients taking dopamine agonists. If this occurs, dopamine agents should be discontinued or switched to other agents (such as a long-acting dopamine agonist, gabapentin encarbil, as well as non-FDA approved therapies such as opioids). However, it is important to note that weaning off dopamine agents may result in mild but in most cases moderate and/or severe withdrawal from the medication, so counseling and close monitoring should be done.
Case 2 Outcome
Given the patient’s history of dementia, opioids, benzodiazepines and other delirium-inducing medications should be avoided. His antidepressive regimen, fluoxetine, should be re-evaluated as these medications have been associated with RLS exacerbation. In addition to SSRIs, medications associated with RLS are MAO inhibitors (selegeline, phenelzine), antipsychotics (risperdone, olanzapine), tricyclic antidepressants (mirtazapine), antihistamines (diphenhydramine, cimetidine), calcium channel blockers (verapamil, nifedipine, diltiazem), and phenytoin [34,35]. His treatment began with behavioral, nonpharmacological management, and blood testing for iron studies. His low iron level prompted initiation of oral supplementation, and he was asked to follow up in 3 months for reevaluation and possible initiation of low-dose dopamine agonists.
Case 3
A 73-year-old man with dementia is found to have very irregular sleep wake patterns with a variable bedtime and awakening time, often missing breakfast. He is found dozing off often during the day, particularly during times of inactivity. He has frequent awakenings during the night often calling for the staff to guide him back to bed. He has had some falls secondary to walking around his room. He has been prescribed various hypnotics without much benefit and instead, has suffered from some confusion while on these medications. His room is very dark and has no windows.
Case 3 Reflection: Circadian Rhythm Sleep-Wake Disorders
Circadian rhythm sleep-wake disorders (CRSWDs) are characterized by an individual’s natural propensity to want to go to sleep and be awake during a period that is undesirable personally and/or socially [36]. CRSWDs can be a result of the desynchronization of the 2 sleep processes: (1) homeostatic drive (regulates sleep intensity) and (2) circadian rhythm (maintains daytime alertness); [36]. CRSWDs can also be due to an individual’s naturally occurring sleep drives becoming misaligned with their social/personal sleep-wake demands (eg, employment schedule and socializing opportunities with family/friends). With increasing age, the circadian rhythm becomes less adept at functioning in a desynchronized pattern [7], which can result in daytime sleepiness and night time sleep fragmentation [7,37]. CRSWDs are highly prevalent in individuals with dementia [7,36]. As dementia progresses, the ability to maintain a balance of the 2 sleep process becomes more impaired [7]. As a result, individuals with dementia, particularly Alzheimer’s disease, are likely to experience agitation, irritability, and/or confusion during the evening and night, a behavioral problem referred to as “sundowning” [38].
There are several types of CRSWDs, including delayed sleep-phase syndrome, advanced sleep-phase syndrome, irregular sleep-wake disorder, non–24-hour sleep-wake disorder, shift work sleep disorder, and jet lag sleep disorder. However, the most common type of CRSWDs observed in older adults is advanced sleep-phase syndrome [39]. Due to excessive sleepiness in the early evening, affected individuals may report a need to shift to earlier and earlier bedtimes (~6 to 7 pm) and wake times (~3 to 4 am) [36]. For older affected adults, this can cause distress and frustration, particularly if their sleep phase prevents them from participating in evening activities (eg, socializing with family/friends) [36].
In the assessment of patients with suspected CRSWDs, sleep diaries (self-reported or caregiver) daily account of sleep and wake times over at least 1 week) and actigraphy (wrist-worn accelerometer designed to measure activity and inactivity at night) can be used, particularly in older adults with dementia [40,41].
CRSWD treatment may include behavioral modifications and/or pharmacological intervention. Behavioral modifications can consist of chronotherapy, relaxation training, and/or bright light therapy. Chronotherapy involves making gradual shifts in an individual’s sleep time to meet his/her desired sleep schedule. Relaxation training involves implementing behaviors/activities that reduce tension and enhance the smooth transition into sleep. Bright light therapy involves exposure to an appropriate intensity and duration of light, which is an important environmental cue to help the synchrony of the sleep-wake cycle [7]. Previous studies have observed that NH residents are exposed to a restricted amount of bright light during the daytime [42,43], but higher levels of artificial light at night (eg, hallway lighting) [7]. NH residents’ exposure to artificial bright light during the daytime has not only improved the residents’ sleep [44–46], but also has improved their cognitive functioning and reduced their depressive symptoms [47]. Thus, steps towards targeted light exposure in sync with the typical sleep-wake cycle (eg, mandated time in well-lit rooms during the day and during meals) for NH residents, particularly those with CRSWDs, could prove to be beneficial across several social, behavioral and neurocognitive domains. Lastly, NH residents exposed to at least 30 minutes of outdoor daylight and at least 3 occasions of low intensity physical activities for 10 to 15 minutes daily can potentially improve sleep-wake patterns [48]. Thus, it may be beneficial to have an intervention that couples bright light exposure and physical activity in the NH setting.
Pharmacological interventions can also be implemented to improve older residents’ symptoms. However, the medications prescribed should be used with caution and should not be used as part of a long-term treatment plan. Melatonin is a commonly used herbal supplement that can assist advancing the timing of the circadian rhythms in the evening but can delay the circadian rhythms in the morning [49]. Several brands of this herbal supplement can be purchased over-the-counter and are not regulated by the FDA. Since the amount of melatonin used in the herbal supplement varies by brand, caution should be used when selecting a brand [50]. Two FDA-approved drugs (modafinil and armodafinil) are currently being used to reduce daytime sleepiness and improve vigilance amongst adults, but limited research has explored the effectiveness of these medication for older adults specifically suffering with CRSWDS [36,51,52]. Other stimulants (eg, caffeine, amphetamines, and nonamphetamine-derived medications) are also currently being used to reduce daytime sleepiness in patients with CRSWDS. Stimulant use, particularly caffeine consumption, has also been associated with better cognitive functioning in older adults [53]. However, stimulants should be taken with caution, particularly in older adults, because stimulant use has been associated with potentially serious and fatal health sequalae (eg, tachycardia, heart failure, irreversible heart damage and hypertension) [36,54].
Case 3 Outcome
The patient was moved to a room with a window. An alarm clock was set for 7:30 in the morning and he was taken to breakfast, where he sat at a table near a window. Any time he appeared to be sleepy, he was encouraged to go for a walk or engage in other activities so daytime napping opportunities were limited. His environment was assessed for safety and bedrails were utilized to prevent falls.
Case 4
A 75-year-old woman with a history of anxiety and depression moved into the NH 4 months ago after suffering a stroke. She now reports difficulty falling asleep for many years, which has significantly worsened since moving to the NH. Currently, she has been getting only 3 to 4 hour of sleep per night. She reports mild but increasing daytime sleepiness and does not fall asleep until 1:00 am despite getting into bed at 10:30 pm. She occasionally reports arthritic pain that interferes with her sleep. The NH staff has mentioned that she will occasionally cry for her family when she appears to be asleep.
Case 4 Reflection: Insomnia
According to the International Classification of Sleep Disorders (ICSD-3) [39], insomnia is characterized as “a repeated difficulty with sleep initiation, duration, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep, and results in some form of daytime impairment.” Among the sleep disorders, insomnia is one of the most common sleep issues observed in sleep clinics [34]. Older adults with insomnia often have comorbid physical (eg, pulmonary disease, arthritis, chronic pain, cancer diabetes, Parkinson’s disease) and mental illness (eg, depression, panic disorder) [55]. Medications (eg, stimulants, respiratory medications, chemotherapy, decongestants, hormones, or psychotropics) may cause and exacerbate insomnia symptoms [55].
Since insomnia is a clinical diagnosis, there is no specific diagnostic tool or gold standard test to identify individuals suffering with insomnia. Insomnia screening usually involves a clinical interview, in which a health provider, preferably trained in sleep, conducts a physical examination and collects an in-depth history of a patients’ sleep problems [56]. Insomnia screening tools may also include having a patient complete a sleep diary or questionnaire, such as the insomnia severity index (ISI) [57] or Pittsburgh Sleep Quality Index (PSQI) [58].
Cognitive behavioral therapy for insomnia (CBT-I) and/or pharmacological intervention are typically used to treat insomnia in older adults. CBT-I is a combination of cognitive (eg, changing dysfunctional sleep attitudes/beliefs) and behavioral treatment (eg, adhering to a regular sleep schedule) [59]. CBT-I or a combination of CBT-I and pharmacological intervention is recommended as more effective long-term approach to insomnia treatment compared to pharmacological intervention alone [55]. CBT-I involves altering older adults’ misconceptions of their sleep and implementing behavioral techniques to their everyday life (eg, routine sleep-wake schedule, relaxation therapy). Several FDA-approved medications are available to treat insomnia; however, many commonly used medications to treat insomnia in older adults (ie, antihistamines, antidepressants, anticonvulsants, and anti-psychotics) pose more risks than benefits to their health and well-being [35,60–62]. Some of the more recent hypnotics (egm zolpidem, exzopiclone, and ramelteon) on the market have been shown to be safer and more effective pharmacological options [55]. In 2014, the FDA approved the first in class orexin receptor antagonist medication (suvorexant) to treat insomnia [63]. Unlike other medications to treat insomnia, suvorexant, via the blockade of the orexin neurotransmitter, effectively inhibits orexin (one of neurotransmitters involved in the activation pathways of the arousal system), so sleep can easily be induced and maintained [64, 65]. Furthermore, preliminary studies suggest that this medication may be associated with less severe side effects (ie, habituation) than the other approved medications on the market [64, 65]. In fact, in a recent clinical series that included both young and older insomnia patients, the most common adverse reaction to suvorexant was drowsiness [66].
Case 4 Outcome
The patient was initiated on basic CBT-I therapy strategies which included stimulus control therapy [67]; implementation of a consistent bedtime and awakening routine; reducing the use of TV, smart phone, or other electronic leisure devices 1 hour before bedtime; refraining from caffeine after lunchtime; improving the sleep environment; and relaxation techniques.
Case 5
The patient is a 65-year-old man diagnosed with Parkinson’s disease several years ago. Recently, he has often has been experiencing what appears to be very violent and terrifying dreams. While asleep, he often screams and shouts for help. In addition, he occasionally will punch, kick, and/or thrash around in bed at night, which the NH staff has noted as a concern for his safety.
Case 5 Reflection: Parasomnias
Parasomnias represent frequent arousals during sleep or in the wake-to-sleep transition due to abnormal motor movements, behaviors (eg, shouting, flailing, and leaping from bed) and/or sensory experiences (eg, “dreamlike” hallucinations) [68]. Motor movements that occur for parasomnia can be disruptive for the individual and potentially dangerous for the individual and/or bed partner. There are 3 primary types of parasomnias based on the stage of sleep that the event occurs: non-REM (NREM), REM, and other parasomnias during transitions of sleep [68]. The most commonly observed parasomnia seen in older adults is the REM-associated parasomnia or REM sleep behavior disorder (RBD), which is characterized by experiencing vivid, sometimes violent, dreams typically involving fighting an intruder or an animal to protect a loved one [69]. For RBD, disruptive behaviors typically occur during REM sleep [69]. RBD has been associated with neurodegenerative disorders (Parkinson’s disease and Lewy body disease), neurologic disorders (eg, brain tumors and stroke), other primary disorders (narcolepsy and periodic limb movement disorder), and well as some medications (eg, antidepressants and β-blockers) [68]. There is limited knowledge on the prevalence of parasomnias in NH settings. One study, however, reported that 31% of older NH residents experience parasomnias [70]. Evaluation for parasomnias generally involve a clinical evaluation by a sleep specialist and overnight sleep study (ie, polysomnography at a sleep center if there is a concern for sleep apnea or RBD [71].
Medications are not typically first-line for parasomnia. Instead education about improving sleep practices, addressing other underlying sleep disorders, and securing a safe sleep environment are first recommended. Pharmacologic treatment, particularly the use of clonazepam, is commonly used to treat RBD [72]. However, this medication should be used with caution for older adults with a dementia diagnosis, gait disorders, and OSA because the common side effects include sedation, confusion, memory dysfunction, and early morning motor incoordination [68]. Several alternative medications have also been used to treat RBD. For example, medications commonly used to Parkinson disease symptoms, such Levodopa and dopamine agonists, have also been used to treat RBD [73]. Zopiclone, a nonbenzodiazepine hypnotic agent, has also been shown to be as effective as clonazepam, but with less potential side effects [74]. Melatonin, a nutritional supplement, has also been used as a treatment and appears to alleviate some of the RBD symptoms and has fewer side effects [68]. Since melatonin is not regulated by the FDA, it has been suggested that this treatment be used with caution in the older population [73].
Case 5 Outcome
The patient was evaluated with video synchronized in lab PSG. It confirmed REM sleep without evidence of the normal atonia that should be apparent during REM. These PSG findings in combination with repeated accounts of dream enactment established the diagnosis of RBD. Patient was treated with low-dose clonazepam and closely monitored for potential side effects of daytime sedation. Bedroom environment was also carefully reconfigured for safety to avoid potential risk of injury during a dream enactment episode.
Conclusion
Sleep disturbances remain an underappreciated and undertreated health issue in NH residents. Nursing homes can help facilitate optimal sleep health and day functioning by providing mandatory natural light outlets, physical exercise opportunities, and minimal allowable time residents can spend in their bed/bedroom outside of their routine sleep period. Educating NH providers and staff on sleep medicine may benefit residents, but workload and restricted resources may hinder this. Education via mobile and internet based educational platforms and resources (Mysleep101) may be helpful in addressing education barriers [75]. Convenient and cost-effective methods to deliver sleep medicine education to NH health care providers should be part of our ongoing efforts to improve the viability, vitality and quality of life of our aging citizens.
Corresponding author: Alyssa Gamaldo, PhD, Univ. of South Florida, 13301 Bruce B. Downs Blvd, MHC 1340, Tampa, FL 33612, [email protected].
Financial disclosures: None.
From the School of Aging Studies, University of South Florida, Tampa, FL (Dr. AA Gamaldo) and the Department of Neurology, Johns Hopkins Medicine, Baltimore, MD (Drs. Sloane, CE Gamaldo and Salas).
Abstract
- Objective: To provide guidance on identifying and treating sleep disturbances commonly encountered in older nursing home residents.
- Methods: Review of the literature in the context of 5 clinical cases.
- Results: Sleep disturbances continue to be a growing global epidemic, and public health initiatives have been aimed at improving sleep health across all ages. In older adults, sleep disturbances are often associated with the development and/or worsening of health conditions. Common sleep disturbances observed in older nursing home residents include obstructive sleep apnea, restless legs syndrome/Willis-Ekbom disease, circadian rhythm sleep-wake disorders, insomnia, and parasomnias. The symptoms and recommended treatment plans vary across the sleep disturbances. For many sleep disturbances, modification of residents’ daily activities and/or nursing home environment can be helpful.
- Conclusion: As the number of people residing in nursing homes increases, it is important for health care providers to be knowledgable about sleep disturbances in this population.
By 2030, almost 20% of the US population (approximately 72.1 million people) will be age 65 and older [1]. As many as 63% of older adults in the general population report sleep disturbances [2]. Specifically, older adults demonstrate difficulty with decreased total sleep duration, an increase in sleep fragmentation (ie, interruptions in nighttime sleep), and reduced total sleep time spent in rapid eye movement (REM) and slow wave sleep [3–5]. Poor sleep, either because of not getting enough sleep or having an undiagnosed and thus untreated sleep disorder, is associated with physical illness, impaired cognition, poor physical function, and mortality risk [6,7]. In fact, over 50% of individuals older than 65 years meet the diagnostic criteria for a sleep disorder, many of which are undiagnosed [6,7].
It is forecasted that we will see substantial increases in the rate of nursing home residence among the elderly [8]. The prevalence and severity of disturbed sleep is reportedly higher in NH residents [6,7]. Generally, NH residents tend to be on several medications for various medical disorders that may negatively impact sleep [7]. Reciprocally, sleep disruption may put NH residents at an increased risk for behavioral issues (eg, agitation) [9,10] as well as developing and/or exacerbating health conditions (eg, mood disorders, dementia, cardiovascular disease) [8]. Furthermore, NH residents exhibiting disturbed sleep, behavioral issues, and/or mood disorders are at an increased risk for being prescribed antipsychotic drugs [11], which are associated with adverse side effects and poorer quality of life [12]. Thus, the identification and management of sleep disturbances in the NH setting has become progressively more vital in efforts to optimize medical management of this population. This review identifies common sleep disturbances frequently underdiagnosed and undertreated among residents of NH facilities.
Case 1
A 73-year-old woman with a history of type 2 diabetes mellitus reports poor sleep quality with frequent awakenings during the night and excessive daytime sleepiness. She states that she can fall asleep within 5 minutes, but often is awoken throughout the night with a sensation of breathlessness. She has snored for many years, but the nursing staff at her NH facility has recently commented that her snoring has gone from intermittent to constant. She cannot remember the last time she has had restful sleep. She consumes 3 to 4 cups of caffeinated beverages daily to counter her sleepiness. She denies smoking or illicit drug or alcohol use. Her review of systems was notable for a 30-lb weight gain over the last year, and she reports increasing fatigue, irritability, and memory and concentration issues. Her current medication list includes metformin and amlodipine. Her examination is remarkable for a BMI of 31, large neck circumference (> 16), tonsillar enlargement, a crowded oropharynx, micrognathia, lungs clear to auscultation bilaterally, heart sounds of normal S1 and S2, and legs with trace pitting edema.
Case 1 Reflection: Sleep-Disordered Breathing
Although previous studies have observed high rates (60%–90%) of SDB in NH settings [16,17], one study observed that only 0.5% of nursing home residents carried a diagnosis with SDB, suggesting that SDB is being grossly underappreciated amongst NH residents over the age of 65 [18]. In order to evaluate for SBD, routine annual physical exams or medical chart reviews can elicit the risk factors for sleep apnea (eg, obesity [per BMI], male sex, postmenopausal women, family history of sleep apnea) as well as common comorbidities (eg, hypertension, coronary artery disease, and diabetes). Formal evaluation consists of a sleep evaluation with a sleep specialist and polysomnography (PSG; sleep study) that can be performed in the sleep center or at home depending on the patient’s history and other medical issues.
Case 1 Outcome
Case 2
An 85-year-old man with history of Alzheimer’s disease, major depression and arthritis, reports insomnia and “tingling in my legs” at bedtime. The patient cannot identify when the symptoms started but reports that his legs often jerk during sleep. He consumes a cup of coffee daily and has a previous 20 pack-year smoking history (he quit 40 years ago). On review of systems, he endorses fatigue. His current medication list includes fluoxetine, donepezil hydrochloride, ibuprofen as needed for arthritic pain, and a multivitamin. His examination was unremarkable, with a BMI of 26, neck circumference < 16, no tonsillar enlargement, normal (noncrowded) oropharynx, lungs clear to auscultation bilaterally, heart sounds demonstrating a normal S1 and S2, and legs without edema.
Case 2 Reflection: Restless Legs Syndrome/Willis-Ekbom Disease
Restless legs syndrome (RLS) also known as Willis-Ekbom disease, affects approximately 10 million adults in the United States alone [22]. RLS is a sensorimotor disorder that must satisfy the following 5 primary diagnostic criteria: (1) urge to move the legs with or without dysesthesias; (2) onset or exacerbation with rest or inactivity; (3) relief with movement; (4) symptoms are worse in the evening or at night (circadian component); (5) symptoms cannot be solely accounted for as consequence of another medical or behavioral condition. Other supporting clinical features can alert a clinician to the likelihood of a RLS diagnosis; these include positive family history, response to dopaminergic therapy, lack of profound daytime sleepiness, and presence of periodic limb movements during sleep (PLMS) [23–26]. In younger individuals, the symptoms present insidiously whereas older adults (> 50 years of age) will usually present with sudden onset [27].
Not only do patients lack the restorative sleep needed to ward off fatigue and restfulness, but patients also demonstrate higher rates of comorbidities (eg, anxiety, hypertension, depression) as well as large economic burden secondary to absenteeism and decreased on-the-job effectiveness [28,29]. As a results, patients with RLS experience significant reductions in quality of life related to this sensorimotor disorder [28].
No confirmatory laboratory test exists to diagnose RLS; however, patients suspected of having RLS should be evaluated with a basic metabolic panel, iron studies, and a thorough neurologic examination, as iron deficiency, kidney failure, uremia and peripheral neuropathy can lead to secondary RLS [30,31]. Evidence shows that RLS is common in NH residents [32] and may account for problematic behaviors, such as late night pacing [7]. Forty-five percent of community dwelling individuals over 65 years old exhibit a PLMS index (leg kicks per hour) of greater than 5 [33]. PLMS, while not a disorder in and of itself, can serve as a marker for potential disease. PLMS are characterized by intermittent episodes of stereotyped leg movements. PLMS typically do not awaken the patient from sleep and therefore do not contribute to insomnia or daytime sleepiness, representing a key clinical difference from RLS. It is important to note that PLMS are nonspecific and may be common in older adults that do not meet the diagnostic criteria for RLS.
Treatment of RLS is based on the frequency of symptoms and the level of functional impairment caused by the syndrome. RLS treatment recommendations should always espouse nonpharmacological interventions that include improving sleep practices, engagement in daily physical activity, targeted placement of sedentary activity in the morning when symptoms are less prominent, and concerted efforts to avoid the use of RLS-exacerbating medications (eg, selective serotonin reuptake inhibitor (SSRIs), neuroleptic agents, antihistamines) [28]. If there is an underlying condition contributing to RLS, such as metabolic disturbance or iron deficiency, then these conditions should be corrected before initiating RLS medications. Several medications are FDA-approved for treatment of RLS, including dopamine agonists (eg, ropinirole, rotigotine, pramipexole), dopamine precursor (eg, levodopa), glutamate-related (eg, gabapentin), benzodiazepines (eg, temazepam, clonazepam). Augmentation, the worsening of RLS symptoms, can occur in patients taking dopamine agonists. If this occurs, dopamine agents should be discontinued or switched to other agents (such as a long-acting dopamine agonist, gabapentin encarbil, as well as non-FDA approved therapies such as opioids). However, it is important to note that weaning off dopamine agents may result in mild but in most cases moderate and/or severe withdrawal from the medication, so counseling and close monitoring should be done.
Case 2 Outcome
Given the patient’s history of dementia, opioids, benzodiazepines and other delirium-inducing medications should be avoided. His antidepressive regimen, fluoxetine, should be re-evaluated as these medications have been associated with RLS exacerbation. In addition to SSRIs, medications associated with RLS are MAO inhibitors (selegeline, phenelzine), antipsychotics (risperdone, olanzapine), tricyclic antidepressants (mirtazapine), antihistamines (diphenhydramine, cimetidine), calcium channel blockers (verapamil, nifedipine, diltiazem), and phenytoin [34,35]. His treatment began with behavioral, nonpharmacological management, and blood testing for iron studies. His low iron level prompted initiation of oral supplementation, and he was asked to follow up in 3 months for reevaluation and possible initiation of low-dose dopamine agonists.
Case 3
A 73-year-old man with dementia is found to have very irregular sleep wake patterns with a variable bedtime and awakening time, often missing breakfast. He is found dozing off often during the day, particularly during times of inactivity. He has frequent awakenings during the night often calling for the staff to guide him back to bed. He has had some falls secondary to walking around his room. He has been prescribed various hypnotics without much benefit and instead, has suffered from some confusion while on these medications. His room is very dark and has no windows.
Case 3 Reflection: Circadian Rhythm Sleep-Wake Disorders
Circadian rhythm sleep-wake disorders (CRSWDs) are characterized by an individual’s natural propensity to want to go to sleep and be awake during a period that is undesirable personally and/or socially [36]. CRSWDs can be a result of the desynchronization of the 2 sleep processes: (1) homeostatic drive (regulates sleep intensity) and (2) circadian rhythm (maintains daytime alertness); [36]. CRSWDs can also be due to an individual’s naturally occurring sleep drives becoming misaligned with their social/personal sleep-wake demands (eg, employment schedule and socializing opportunities with family/friends). With increasing age, the circadian rhythm becomes less adept at functioning in a desynchronized pattern [7], which can result in daytime sleepiness and night time sleep fragmentation [7,37]. CRSWDs are highly prevalent in individuals with dementia [7,36]. As dementia progresses, the ability to maintain a balance of the 2 sleep process becomes more impaired [7]. As a result, individuals with dementia, particularly Alzheimer’s disease, are likely to experience agitation, irritability, and/or confusion during the evening and night, a behavioral problem referred to as “sundowning” [38].
There are several types of CRSWDs, including delayed sleep-phase syndrome, advanced sleep-phase syndrome, irregular sleep-wake disorder, non–24-hour sleep-wake disorder, shift work sleep disorder, and jet lag sleep disorder. However, the most common type of CRSWDs observed in older adults is advanced sleep-phase syndrome [39]. Due to excessive sleepiness in the early evening, affected individuals may report a need to shift to earlier and earlier bedtimes (~6 to 7 pm) and wake times (~3 to 4 am) [36]. For older affected adults, this can cause distress and frustration, particularly if their sleep phase prevents them from participating in evening activities (eg, socializing with family/friends) [36].
In the assessment of patients with suspected CRSWDs, sleep diaries (self-reported or caregiver) daily account of sleep and wake times over at least 1 week) and actigraphy (wrist-worn accelerometer designed to measure activity and inactivity at night) can be used, particularly in older adults with dementia [40,41].
CRSWD treatment may include behavioral modifications and/or pharmacological intervention. Behavioral modifications can consist of chronotherapy, relaxation training, and/or bright light therapy. Chronotherapy involves making gradual shifts in an individual’s sleep time to meet his/her desired sleep schedule. Relaxation training involves implementing behaviors/activities that reduce tension and enhance the smooth transition into sleep. Bright light therapy involves exposure to an appropriate intensity and duration of light, which is an important environmental cue to help the synchrony of the sleep-wake cycle [7]. Previous studies have observed that NH residents are exposed to a restricted amount of bright light during the daytime [42,43], but higher levels of artificial light at night (eg, hallway lighting) [7]. NH residents’ exposure to artificial bright light during the daytime has not only improved the residents’ sleep [44–46], but also has improved their cognitive functioning and reduced their depressive symptoms [47]. Thus, steps towards targeted light exposure in sync with the typical sleep-wake cycle (eg, mandated time in well-lit rooms during the day and during meals) for NH residents, particularly those with CRSWDs, could prove to be beneficial across several social, behavioral and neurocognitive domains. Lastly, NH residents exposed to at least 30 minutes of outdoor daylight and at least 3 occasions of low intensity physical activities for 10 to 15 minutes daily can potentially improve sleep-wake patterns [48]. Thus, it may be beneficial to have an intervention that couples bright light exposure and physical activity in the NH setting.
Pharmacological interventions can also be implemented to improve older residents’ symptoms. However, the medications prescribed should be used with caution and should not be used as part of a long-term treatment plan. Melatonin is a commonly used herbal supplement that can assist advancing the timing of the circadian rhythms in the evening but can delay the circadian rhythms in the morning [49]. Several brands of this herbal supplement can be purchased over-the-counter and are not regulated by the FDA. Since the amount of melatonin used in the herbal supplement varies by brand, caution should be used when selecting a brand [50]. Two FDA-approved drugs (modafinil and armodafinil) are currently being used to reduce daytime sleepiness and improve vigilance amongst adults, but limited research has explored the effectiveness of these medication for older adults specifically suffering with CRSWDS [36,51,52]. Other stimulants (eg, caffeine, amphetamines, and nonamphetamine-derived medications) are also currently being used to reduce daytime sleepiness in patients with CRSWDS. Stimulant use, particularly caffeine consumption, has also been associated with better cognitive functioning in older adults [53]. However, stimulants should be taken with caution, particularly in older adults, because stimulant use has been associated with potentially serious and fatal health sequalae (eg, tachycardia, heart failure, irreversible heart damage and hypertension) [36,54].
Case 3 Outcome
The patient was moved to a room with a window. An alarm clock was set for 7:30 in the morning and he was taken to breakfast, where he sat at a table near a window. Any time he appeared to be sleepy, he was encouraged to go for a walk or engage in other activities so daytime napping opportunities were limited. His environment was assessed for safety and bedrails were utilized to prevent falls.
Case 4
A 75-year-old woman with a history of anxiety and depression moved into the NH 4 months ago after suffering a stroke. She now reports difficulty falling asleep for many years, which has significantly worsened since moving to the NH. Currently, she has been getting only 3 to 4 hour of sleep per night. She reports mild but increasing daytime sleepiness and does not fall asleep until 1:00 am despite getting into bed at 10:30 pm. She occasionally reports arthritic pain that interferes with her sleep. The NH staff has mentioned that she will occasionally cry for her family when she appears to be asleep.
Case 4 Reflection: Insomnia
According to the International Classification of Sleep Disorders (ICSD-3) [39], insomnia is characterized as “a repeated difficulty with sleep initiation, duration, consolidation, or quality that occurs despite adequate opportunity and circumstances for sleep, and results in some form of daytime impairment.” Among the sleep disorders, insomnia is one of the most common sleep issues observed in sleep clinics [34]. Older adults with insomnia often have comorbid physical (eg, pulmonary disease, arthritis, chronic pain, cancer diabetes, Parkinson’s disease) and mental illness (eg, depression, panic disorder) [55]. Medications (eg, stimulants, respiratory medications, chemotherapy, decongestants, hormones, or psychotropics) may cause and exacerbate insomnia symptoms [55].
Since insomnia is a clinical diagnosis, there is no specific diagnostic tool or gold standard test to identify individuals suffering with insomnia. Insomnia screening usually involves a clinical interview, in which a health provider, preferably trained in sleep, conducts a physical examination and collects an in-depth history of a patients’ sleep problems [56]. Insomnia screening tools may also include having a patient complete a sleep diary or questionnaire, such as the insomnia severity index (ISI) [57] or Pittsburgh Sleep Quality Index (PSQI) [58].
Cognitive behavioral therapy for insomnia (CBT-I) and/or pharmacological intervention are typically used to treat insomnia in older adults. CBT-I is a combination of cognitive (eg, changing dysfunctional sleep attitudes/beliefs) and behavioral treatment (eg, adhering to a regular sleep schedule) [59]. CBT-I or a combination of CBT-I and pharmacological intervention is recommended as more effective long-term approach to insomnia treatment compared to pharmacological intervention alone [55]. CBT-I involves altering older adults’ misconceptions of their sleep and implementing behavioral techniques to their everyday life (eg, routine sleep-wake schedule, relaxation therapy). Several FDA-approved medications are available to treat insomnia; however, many commonly used medications to treat insomnia in older adults (ie, antihistamines, antidepressants, anticonvulsants, and anti-psychotics) pose more risks than benefits to their health and well-being [35,60–62]. Some of the more recent hypnotics (egm zolpidem, exzopiclone, and ramelteon) on the market have been shown to be safer and more effective pharmacological options [55]. In 2014, the FDA approved the first in class orexin receptor antagonist medication (suvorexant) to treat insomnia [63]. Unlike other medications to treat insomnia, suvorexant, via the blockade of the orexin neurotransmitter, effectively inhibits orexin (one of neurotransmitters involved in the activation pathways of the arousal system), so sleep can easily be induced and maintained [64, 65]. Furthermore, preliminary studies suggest that this medication may be associated with less severe side effects (ie, habituation) than the other approved medications on the market [64, 65]. In fact, in a recent clinical series that included both young and older insomnia patients, the most common adverse reaction to suvorexant was drowsiness [66].
Case 4 Outcome
The patient was initiated on basic CBT-I therapy strategies which included stimulus control therapy [67]; implementation of a consistent bedtime and awakening routine; reducing the use of TV, smart phone, or other electronic leisure devices 1 hour before bedtime; refraining from caffeine after lunchtime; improving the sleep environment; and relaxation techniques.
Case 5
The patient is a 65-year-old man diagnosed with Parkinson’s disease several years ago. Recently, he has often has been experiencing what appears to be very violent and terrifying dreams. While asleep, he often screams and shouts for help. In addition, he occasionally will punch, kick, and/or thrash around in bed at night, which the NH staff has noted as a concern for his safety.
Case 5 Reflection: Parasomnias
Parasomnias represent frequent arousals during sleep or in the wake-to-sleep transition due to abnormal motor movements, behaviors (eg, shouting, flailing, and leaping from bed) and/or sensory experiences (eg, “dreamlike” hallucinations) [68]. Motor movements that occur for parasomnia can be disruptive for the individual and potentially dangerous for the individual and/or bed partner. There are 3 primary types of parasomnias based on the stage of sleep that the event occurs: non-REM (NREM), REM, and other parasomnias during transitions of sleep [68]. The most commonly observed parasomnia seen in older adults is the REM-associated parasomnia or REM sleep behavior disorder (RBD), which is characterized by experiencing vivid, sometimes violent, dreams typically involving fighting an intruder or an animal to protect a loved one [69]. For RBD, disruptive behaviors typically occur during REM sleep [69]. RBD has been associated with neurodegenerative disorders (Parkinson’s disease and Lewy body disease), neurologic disorders (eg, brain tumors and stroke), other primary disorders (narcolepsy and periodic limb movement disorder), and well as some medications (eg, antidepressants and β-blockers) [68]. There is limited knowledge on the prevalence of parasomnias in NH settings. One study, however, reported that 31% of older NH residents experience parasomnias [70]. Evaluation for parasomnias generally involve a clinical evaluation by a sleep specialist and overnight sleep study (ie, polysomnography at a sleep center if there is a concern for sleep apnea or RBD [71].
Medications are not typically first-line for parasomnia. Instead education about improving sleep practices, addressing other underlying sleep disorders, and securing a safe sleep environment are first recommended. Pharmacologic treatment, particularly the use of clonazepam, is commonly used to treat RBD [72]. However, this medication should be used with caution for older adults with a dementia diagnosis, gait disorders, and OSA because the common side effects include sedation, confusion, memory dysfunction, and early morning motor incoordination [68]. Several alternative medications have also been used to treat RBD. For example, medications commonly used to Parkinson disease symptoms, such Levodopa and dopamine agonists, have also been used to treat RBD [73]. Zopiclone, a nonbenzodiazepine hypnotic agent, has also been shown to be as effective as clonazepam, but with less potential side effects [74]. Melatonin, a nutritional supplement, has also been used as a treatment and appears to alleviate some of the RBD symptoms and has fewer side effects [68]. Since melatonin is not regulated by the FDA, it has been suggested that this treatment be used with caution in the older population [73].
Case 5 Outcome
The patient was evaluated with video synchronized in lab PSG. It confirmed REM sleep without evidence of the normal atonia that should be apparent during REM. These PSG findings in combination with repeated accounts of dream enactment established the diagnosis of RBD. Patient was treated with low-dose clonazepam and closely monitored for potential side effects of daytime sedation. Bedroom environment was also carefully reconfigured for safety to avoid potential risk of injury during a dream enactment episode.
Conclusion
Sleep disturbances remain an underappreciated and undertreated health issue in NH residents. Nursing homes can help facilitate optimal sleep health and day functioning by providing mandatory natural light outlets, physical exercise opportunities, and minimal allowable time residents can spend in their bed/bedroom outside of their routine sleep period. Educating NH providers and staff on sleep medicine may benefit residents, but workload and restricted resources may hinder this. Education via mobile and internet based educational platforms and resources (Mysleep101) may be helpful in addressing education barriers [75]. Convenient and cost-effective methods to deliver sleep medicine education to NH health care providers should be part of our ongoing efforts to improve the viability, vitality and quality of life of our aging citizens.
Corresponding author: Alyssa Gamaldo, PhD, Univ. of South Florida, 13301 Bruce B. Downs Blvd, MHC 1340, Tampa, FL 33612, [email protected].
Financial disclosures: None.
1. Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key indicators of well-being. Washington, DC: U.S. Gov. Printing Office; 2012.
2. Almeida OP, Pfaff JJ. Sleep complaints among older general practice patients: association with depression. Br J Gen Pract 2005;55:864–866.
3. Wolkove N, Elkholy O, Baltzan M, et al. Sleep and aging: 1. Sleep disorders commonly found in older people. CMAJ 2007;176:1299–304.
4. Pace-Schott EF, Spencer RM. Age-related changes in the cognitive function of sleep. Prog Brain Res 2011;191:75–89.
5. Ohayon MM, Carskadon MA, Guilleminault C, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 2004;27:1255–73.
6. Jacobs D, Ancoli-Israel S, Parker L, et al. Twenty-four-hour sleep-wake patterns in a nursing home population. Psychol Aging 1989;4:352–6.
7. Neikrug AB, Ancoli-Israel S. Sleep disturbances in nursing homes. J Nutr Health Aging 2010;14:207–11.
8. Lakdawalla D, Goldman DP, Bhattacharya J, et al. Forecasting the nursing home population. Medical Care 2003;41:8-20.
9. Alessi CA, Yoon EJ, Schnelle JF, et al. A randomized trial of a combined physical activity and environmental intervention in nursing home residents: do sleep and agitation improve? J Am Geriatr Soc 1999;47:784–91.
10. Cohen-Mansfield J, Marx MS. The relationship between sleep disturbances and agitation in a nursing home. J Aging Health 1990;2:153–65.
11. Rolland Y, Andrieu S, Crochard A, et al. Psychotropic drug consumption at admission and discharge of nursing home residents. J Am Med Dir Assoc 2012;13:407 e407–412.
12. Salzman C. Antipsychotics in nursing homes. J Clin Psychopharmacol 2013;33:1–2.
13. Fleetham J, Ayas N, Bradley D, et al. Canadian Thoracic Society guidelines: diagnosis and treatment of sleep disordered breathing in adults. Can Respir J 2006;13:387–92.
14. International classification of sleep disorders: Chicago: American Academy of Sleep Medicine; 2005.
15. Gay PC. Complex sleep apnea: it really is a disease. J Clin Sleep Med 2008;4:403–5.
16. Ancoli-Israel S. Epidemiology of sleep disorders. In: Roth T, Roehrs TA, editors. Clinics in geriatric medicine. Philadelphia: WB Saunders; 1989:347–62.
17. Gehrman PR, Martin JL, Shochat T, et al. Sleep-disordered breathing and agitation in institutionalized adults with Alzheimer disease. Am J Geriatr Psychiatry 2003;11:426–33.
18. Resnick HE, Phillips B. Documentation of sleep apnea in nursing homes: United States 2004. J Am Med Dir Assoc 2008;9:260–4.
19. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc 2011;86:549–54.
20. Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 2005;353:2034–41.
21. McMillan A, Bratton DJ, Faria R, et al. Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. Lancet Resp med 2014;2:804–12.
22. Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med 2005;165:1286–92.
23. Allen RP, La Buda MC, Becker P, et al. Family history study of the restless legs syndrome. Sleep Med 2002;3 Suppl:S3–7.
24. Allen RP. Restless legs syndrome/Willis Ekbom disease: evaluation and treatment. Int Rev Psychiatry 2014;26:248–62.
25. Hening WA, Allen RP, Earley CJ, et al. An update on the dopaminergic treatment of restless legs syndrome and periodic limb movement disorder. Sleep 2004;27:560–83.
26. Gamaldo C, Benbrook AR, Allen RP, et al. Evaluating daytime alertness in individuals with Restless Legs Syndrome (RLS) compared to sleep restricted controls. Sleep Med 2009;10:134–8.
27. Allen RP, Earley CJ. Defining the phenotype of the restless legs syndrome (RLS) using age-of-symptom-onset. Sleep Med 2000;1:11–9.
28. Salas RE, Kwan AB. The real burden of restless legs syndrome: clinical and economic outcomes. Am J Manag Care 2012;18(9 Suppl):S207–212.
29. Silber MH, Ehrenberg BL, Allen RP, et al. An algorithm for the management of restless legs syndrome. Mayo Clin Proc 2004;79:916–22.
30. Hattan E, Chalk C, Postuma RB. Is there a higher risk of restless legs syndrome in peripheral neuropathy? Neurology 2009;72:955–60.
31. Winkelman JW, Chertow GM, Lazarus JM. Restless legs syndrome in end-stage renal disease. Am J Kidney Dis 1996;28:372–8.
32. Hornyak M, Trenkwalder C. Restless legs syndrome and periodic limb movement disorder in the elderly. J Psychosom Res 2004;56:543–8.
33. Ancoli-Israel S, Kripke DF, Klauber MR, et al. Periodic limb movements in sleep in community-dwelling elderly. Sleep 1991;14:496–500.
34. Ahmed QA. Effects of common medications used for sleep disorders. Crit Care Clin 2008;24:493–515, vi.
35. Rye DB, Trotti LM. Restless legs syndrome and periodic leg movements of sleep. Neurol clin 2012;30:1137–66.
36. Gamaldo CE, Chung Y, Kang YM, et al. Tick-tock-tick-tock: the impact of circadian rhythm disorders on cardiovascular health and wellness. J Am Soc Hypertens 2014;8:921–9.
37. Myers BL, Badia P. Changes in circadian rhythms and sleep quality with aging: mechanisms and interventions. Neurosci Biobehav Rev 1995;19:553–71.
38. National Institute on Aging. Alzheimer’s caregiving tips: sundowning. June 2013.
39. International classification of sleep disorders. 3rd ed. Darien, IL: AASD; 2014.
40. Barion A, Zee PC. A clinical approach to circadian rhythm sleep disorders. Sleep Med 2007;8:566–77.
41. Morgenthaler TI, Lee-Chiong T, Alessi C, et al. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep 2007;30:1445–59.
42. Shochat T, Martin J, Marler M, et al. Illumination levels in nursing home patients: effects on sleep and activity rhythms. J Sleep Res 2000;9:373–9.
43. Ancoli-Israel S, Klauber MR, Jones DW, et al. Variations in circadian rhythms of activity, sleep, and light exposure related to dementia in nursing-home patients. Sleep 1997;20:18–23.
44. Satlin A, Volicer L, Ross V, et al. Bright light treatment of behavioral and sleep disturbances in patients with Alzheimer’s disease. Am J Psychiatry 1992;149:1028–32.
45. Koyama E, Matsubara H, Nakano T. Bright light treatment for sleep-wake disturbances in aged individuals with dementia. Psychiatry Clin Neurosci 1999;53:227–9.
46. Burns A, Allen H, Tomenson B, et al. Bright light therapy for agitation in dementia: a randomized controlled trial. Int Psychogeriatr 2009;21:711–21.
47. Riemersma-van der Lek RF, Swaab DF, Twisk J, et al. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 2008;299:2642–55.
48. Martin JL, Marler MR, Harker JO, et al. A multicomponent nonpharmacological intervention improves activity rhythms among nursing home residents with disrupted sleep/wake patterns. J Gerontol Series A Biol Sci Med Sci 2007;62:67–72.
49. Lewy AJ, Ahmed S, Jackson JM, et al. Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiol Int 1992;9:380–92.
50. Williamson BL, Tomlinson AJ, Mishra PK, et al. Structural characterization of contaminants found in commercial preparations of melatonin: similarities to case-related compounds from L-tryptophan associated with eosinophilia-myalgia syndrome. Chem Res Toxicol 1998;11:234-40.
51. Czeisler CA, Walsh JK, Roth T, et al. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med 2005;353:476-86.
52. Howard R, Roth T, Drake CL. The effects of armodafinil on objective sleepiness and performance in a shift work disorder sample unselected for objective sleepiness. J Clin Psychopharmacol 2014;34:369–73.
53. Beydoun MA, Gamaldo AA, Beydoun HA, et al. Caffeine and alcohol intakes and overall nutrient adequacy are associated with longitudinal cognitive performance among U.S. adults. J Nutr 2014;144:890–901.
54. Pentel P. Toxicity of over-the-counter stimulants. JAMA 1984;252:1898–903.
55. Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult - a mini-review. Gerontology 2010;56:181–9.
56. Chesson A Jr, Hartse K, Anderson WM, et al. Practice parameters for the evaluation of chronic insomnia. An American Academy of Sleep Medicine report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep 2000;23:237–41.
57. Bastien CH, Vallieres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001;2:297–307.
58. Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213.
59. Trauer JM, Qian MY, Doyle JS, et al. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med 2015;163:191–204.
60. National Institutes of Health State of the Science Conference statement on manifestations and management of chronic insomnia in adults, June 13-15, 2005. Sleep 2005;28:1049–57.
61. Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med 2008;4:487–504.
62. Bain KT. Management of chronic insomnia in elderly persons. Am J Geriatr Pharmacother 2006;4:168–92.
63. FDA approves new type of sleep drug, Belsomra. 13 Aug 2014. Available at fda.gov.
64. Dubey AK, Handu SS, Mediratta PK. Suvorexant: The first orexin receptor antagonist to treat insomnia. J Pharmacol Pharmacother 2015;6:118–21.
65. Patel KV, Aspesi AV, Evoy KE. Suvorexant: a dual orexin receptor antagonist for the treatment of sleep onset and sleep maintenance insomnia. Ann Pharmacother 2015;49:477–83.
66. Michelson D, Snyder E, Paradis E, et al. Safety and efficacy of suvorexant during 1-year treatment of insomnia with subsequent abrupt treatment discontinuation: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet Neurol 2014;13:461–71.
67. Bootzin RR, Epstein D, Wood JM. Stimulus control instructions. Case studies in insomnia. New York: Springer; 1991:19–28.
68. Gulyani S, Salas RE, Gamaldo CE. Sleep medicine pharmacotherapeutics overview: today, tomorrow, and the future (part 2: hypersomnia, parasomnia, and movement disorders). Chest 2013;143:242–51.
69. Boeve BF, Silber MH, Saper CB, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain 2007;130(Pt 11):2770–88.
70. Middelkoop HA, Kerkhof GA, Smilde-van den Doel DA, et al. Sleep and ageing: the effect of institutionalization on subjective and objective characteristics of sleep. Age Ageing 1994;23:411–7.
71. Tinuper P, Provini F, Bisulli F, et al. Movement disorders in sleep: guidelines for differentiating epileptic from non-epileptic motor phenomena arising from sleep. Sleep Med Rev 2007;11:255–67.
72. Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med 2010;6:85–95.
73. Bloom HG, Ahmed I, Alessi CA, et al. Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc 2009;57:761–89.
74. Anderson KN, Shneerson JM. Drug treatment of REM sleep behavior disorder: the use of drug therapies other than clonazepam. J Clin Sleep Med 2009;5:235–9.
75. Doshi A, Gamaldo C, Kalloo A, et al. Implementing a clinical iPad application to detect sleep disorders is feasible across multiple non-sleep outpatient clinics (P7. 321). Neurology 2015;84(14 Suppl):P7.321.
1. Federal Interagency Forum on Aging-Related Statistics. Older Americans 2012: Key indicators of well-being. Washington, DC: U.S. Gov. Printing Office; 2012.
2. Almeida OP, Pfaff JJ. Sleep complaints among older general practice patients: association with depression. Br J Gen Pract 2005;55:864–866.
3. Wolkove N, Elkholy O, Baltzan M, et al. Sleep and aging: 1. Sleep disorders commonly found in older people. CMAJ 2007;176:1299–304.
4. Pace-Schott EF, Spencer RM. Age-related changes in the cognitive function of sleep. Prog Brain Res 2011;191:75–89.
5. Ohayon MM, Carskadon MA, Guilleminault C, et al. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 2004;27:1255–73.
6. Jacobs D, Ancoli-Israel S, Parker L, et al. Twenty-four-hour sleep-wake patterns in a nursing home population. Psychol Aging 1989;4:352–6.
7. Neikrug AB, Ancoli-Israel S. Sleep disturbances in nursing homes. J Nutr Health Aging 2010;14:207–11.
8. Lakdawalla D, Goldman DP, Bhattacharya J, et al. Forecasting the nursing home population. Medical Care 2003;41:8-20.
9. Alessi CA, Yoon EJ, Schnelle JF, et al. A randomized trial of a combined physical activity and environmental intervention in nursing home residents: do sleep and agitation improve? J Am Geriatr Soc 1999;47:784–91.
10. Cohen-Mansfield J, Marx MS. The relationship between sleep disturbances and agitation in a nursing home. J Aging Health 1990;2:153–65.
11. Rolland Y, Andrieu S, Crochard A, et al. Psychotropic drug consumption at admission and discharge of nursing home residents. J Am Med Dir Assoc 2012;13:407 e407–412.
12. Salzman C. Antipsychotics in nursing homes. J Clin Psychopharmacol 2013;33:1–2.
13. Fleetham J, Ayas N, Bradley D, et al. Canadian Thoracic Society guidelines: diagnosis and treatment of sleep disordered breathing in adults. Can Respir J 2006;13:387–92.
14. International classification of sleep disorders: Chicago: American Academy of Sleep Medicine; 2005.
15. Gay PC. Complex sleep apnea: it really is a disease. J Clin Sleep Med 2008;4:403–5.
16. Ancoli-Israel S. Epidemiology of sleep disorders. In: Roth T, Roehrs TA, editors. Clinics in geriatric medicine. Philadelphia: WB Saunders; 1989:347–62.
17. Gehrman PR, Martin JL, Shochat T, et al. Sleep-disordered breathing and agitation in institutionalized adults with Alzheimer disease. Am J Geriatr Psychiatry 2003;11:426–33.
18. Resnick HE, Phillips B. Documentation of sleep apnea in nursing homes: United States 2004. J Am Med Dir Assoc 2008;9:260–4.
19. Park JG, Ramar K, Olson EJ. Updates on definition, consequences, and management of obstructive sleep apnea. Mayo Clin Proc 2011;86:549–54.
20. Yaggi HK, Concato J, Kernan WN, et al. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med 2005;353:2034–41.
21. McMillan A, Bratton DJ, Faria R, et al. Continuous positive airway pressure in older people with obstructive sleep apnoea syndrome (PREDICT): a 12-month, multicentre, randomised trial. Lancet Resp med 2014;2:804–12.
22. Allen RP, Walters AS, Montplaisir J, et al. Restless legs syndrome prevalence and impact: REST general population study. Arch Intern Med 2005;165:1286–92.
23. Allen RP, La Buda MC, Becker P, et al. Family history study of the restless legs syndrome. Sleep Med 2002;3 Suppl:S3–7.
24. Allen RP. Restless legs syndrome/Willis Ekbom disease: evaluation and treatment. Int Rev Psychiatry 2014;26:248–62.
25. Hening WA, Allen RP, Earley CJ, et al. An update on the dopaminergic treatment of restless legs syndrome and periodic limb movement disorder. Sleep 2004;27:560–83.
26. Gamaldo C, Benbrook AR, Allen RP, et al. Evaluating daytime alertness in individuals with Restless Legs Syndrome (RLS) compared to sleep restricted controls. Sleep Med 2009;10:134–8.
27. Allen RP, Earley CJ. Defining the phenotype of the restless legs syndrome (RLS) using age-of-symptom-onset. Sleep Med 2000;1:11–9.
28. Salas RE, Kwan AB. The real burden of restless legs syndrome: clinical and economic outcomes. Am J Manag Care 2012;18(9 Suppl):S207–212.
29. Silber MH, Ehrenberg BL, Allen RP, et al. An algorithm for the management of restless legs syndrome. Mayo Clin Proc 2004;79:916–22.
30. Hattan E, Chalk C, Postuma RB. Is there a higher risk of restless legs syndrome in peripheral neuropathy? Neurology 2009;72:955–60.
31. Winkelman JW, Chertow GM, Lazarus JM. Restless legs syndrome in end-stage renal disease. Am J Kidney Dis 1996;28:372–8.
32. Hornyak M, Trenkwalder C. Restless legs syndrome and periodic limb movement disorder in the elderly. J Psychosom Res 2004;56:543–8.
33. Ancoli-Israel S, Kripke DF, Klauber MR, et al. Periodic limb movements in sleep in community-dwelling elderly. Sleep 1991;14:496–500.
34. Ahmed QA. Effects of common medications used for sleep disorders. Crit Care Clin 2008;24:493–515, vi.
35. Rye DB, Trotti LM. Restless legs syndrome and periodic leg movements of sleep. Neurol clin 2012;30:1137–66.
36. Gamaldo CE, Chung Y, Kang YM, et al. Tick-tock-tick-tock: the impact of circadian rhythm disorders on cardiovascular health and wellness. J Am Soc Hypertens 2014;8:921–9.
37. Myers BL, Badia P. Changes in circadian rhythms and sleep quality with aging: mechanisms and interventions. Neurosci Biobehav Rev 1995;19:553–71.
38. National Institute on Aging. Alzheimer’s caregiving tips: sundowning. June 2013.
39. International classification of sleep disorders. 3rd ed. Darien, IL: AASD; 2014.
40. Barion A, Zee PC. A clinical approach to circadian rhythm sleep disorders. Sleep Med 2007;8:566–77.
41. Morgenthaler TI, Lee-Chiong T, Alessi C, et al. Practice parameters for the clinical evaluation and treatment of circadian rhythm sleep disorders. An American Academy of Sleep Medicine report. Sleep 2007;30:1445–59.
42. Shochat T, Martin J, Marler M, et al. Illumination levels in nursing home patients: effects on sleep and activity rhythms. J Sleep Res 2000;9:373–9.
43. Ancoli-Israel S, Klauber MR, Jones DW, et al. Variations in circadian rhythms of activity, sleep, and light exposure related to dementia in nursing-home patients. Sleep 1997;20:18–23.
44. Satlin A, Volicer L, Ross V, et al. Bright light treatment of behavioral and sleep disturbances in patients with Alzheimer’s disease. Am J Psychiatry 1992;149:1028–32.
45. Koyama E, Matsubara H, Nakano T. Bright light treatment for sleep-wake disturbances in aged individuals with dementia. Psychiatry Clin Neurosci 1999;53:227–9.
46. Burns A, Allen H, Tomenson B, et al. Bright light therapy for agitation in dementia: a randomized controlled trial. Int Psychogeriatr 2009;21:711–21.
47. Riemersma-van der Lek RF, Swaab DF, Twisk J, et al. Effect of bright light and melatonin on cognitive and noncognitive function in elderly residents of group care facilities: a randomized controlled trial. JAMA 2008;299:2642–55.
48. Martin JL, Marler MR, Harker JO, et al. A multicomponent nonpharmacological intervention improves activity rhythms among nursing home residents with disrupted sleep/wake patterns. J Gerontol Series A Biol Sci Med Sci 2007;62:67–72.
49. Lewy AJ, Ahmed S, Jackson JM, et al. Melatonin shifts human circadian rhythms according to a phase-response curve. Chronobiol Int 1992;9:380–92.
50. Williamson BL, Tomlinson AJ, Mishra PK, et al. Structural characterization of contaminants found in commercial preparations of melatonin: similarities to case-related compounds from L-tryptophan associated with eosinophilia-myalgia syndrome. Chem Res Toxicol 1998;11:234-40.
51. Czeisler CA, Walsh JK, Roth T, et al. Modafinil for excessive sleepiness associated with shift-work sleep disorder. N Engl J Med 2005;353:476-86.
52. Howard R, Roth T, Drake CL. The effects of armodafinil on objective sleepiness and performance in a shift work disorder sample unselected for objective sleepiness. J Clin Psychopharmacol 2014;34:369–73.
53. Beydoun MA, Gamaldo AA, Beydoun HA, et al. Caffeine and alcohol intakes and overall nutrient adequacy are associated with longitudinal cognitive performance among U.S. adults. J Nutr 2014;144:890–901.
54. Pentel P. Toxicity of over-the-counter stimulants. JAMA 1984;252:1898–903.
55. Neikrug AB, Ancoli-Israel S. Sleep disorders in the older adult - a mini-review. Gerontology 2010;56:181–9.
56. Chesson A Jr, Hartse K, Anderson WM, et al. Practice parameters for the evaluation of chronic insomnia. An American Academy of Sleep Medicine report. Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep 2000;23:237–41.
57. Bastien CH, Vallieres A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001;2:297–307.
58. Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213.
59. Trauer JM, Qian MY, Doyle JS, et al. Cognitive behavioral therapy for chronic insomnia: a systematic review and meta-analysis. Ann Intern Med 2015;163:191–204.
60. National Institutes of Health State of the Science Conference statement on manifestations and management of chronic insomnia in adults, June 13-15, 2005. Sleep 2005;28:1049–57.
61. Schutte-Rodin S, Broch L, Buysse D, et al. Clinical guideline for the evaluation and management of chronic insomnia in adults. J Clin Sleep Med 2008;4:487–504.
62. Bain KT. Management of chronic insomnia in elderly persons. Am J Geriatr Pharmacother 2006;4:168–92.
63. FDA approves new type of sleep drug, Belsomra. 13 Aug 2014. Available at fda.gov.
64. Dubey AK, Handu SS, Mediratta PK. Suvorexant: The first orexin receptor antagonist to treat insomnia. J Pharmacol Pharmacother 2015;6:118–21.
65. Patel KV, Aspesi AV, Evoy KE. Suvorexant: a dual orexin receptor antagonist for the treatment of sleep onset and sleep maintenance insomnia. Ann Pharmacother 2015;49:477–83.
66. Michelson D, Snyder E, Paradis E, et al. Safety and efficacy of suvorexant during 1-year treatment of insomnia with subsequent abrupt treatment discontinuation: a phase 3 randomised, double-blind, placebo-controlled trial. Lancet Neurol 2014;13:461–71.
67. Bootzin RR, Epstein D, Wood JM. Stimulus control instructions. Case studies in insomnia. New York: Springer; 1991:19–28.
68. Gulyani S, Salas RE, Gamaldo CE. Sleep medicine pharmacotherapeutics overview: today, tomorrow, and the future (part 2: hypersomnia, parasomnia, and movement disorders). Chest 2013;143:242–51.
69. Boeve BF, Silber MH, Saper CB, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain 2007;130(Pt 11):2770–88.
70. Middelkoop HA, Kerkhof GA, Smilde-van den Doel DA, et al. Sleep and ageing: the effect of institutionalization on subjective and objective characteristics of sleep. Age Ageing 1994;23:411–7.
71. Tinuper P, Provini F, Bisulli F, et al. Movement disorders in sleep: guidelines for differentiating epileptic from non-epileptic motor phenomena arising from sleep. Sleep Med Rev 2007;11:255–67.
72. Aurora RN, Zak RS, Maganti RK, et al. Best practice guide for the treatment of REM sleep behavior disorder (RBD). J Clin Sleep Med 2010;6:85–95.
73. Bloom HG, Ahmed I, Alessi CA, et al. Evidence-based recommendations for the assessment and management of sleep disorders in older persons. J Am Geriatr Soc 2009;57:761–89.
74. Anderson KN, Shneerson JM. Drug treatment of REM sleep behavior disorder: the use of drug therapies other than clonazepam. J Clin Sleep Med 2009;5:235–9.
75. Doshi A, Gamaldo C, Kalloo A, et al. Implementing a clinical iPad application to detect sleep disorders is feasible across multiple non-sleep outpatient clinics (P7. 321). Neurology 2015;84(14 Suppl):P7.321.
Diagnosis and Management of Vestibular Migraine
From the Department of Neurootology, National Hospital of Neurology and Neurosurgery, London (Dr. Tsang, Miss Anwer) and the Ear Institute, University College London, and Guy’s and St Thomas’ NHS Foundation Trust, London, UK (Dr. Murdin).
Abstract
- Objective: To review the clinical manifestations, diagnosis, and management of vestibular migraine (VM).
- Methods: Review of the literature.
- Results: Apart from headache, other symptoms of VM include unsteadiness, imbalance, and spontaneous as well as visual vertigo. Acute vestibular symptoms that qualify for VM must be of at least moderate or severe intensity which lasts within a time window of 5 minutes to 72 hours. The interindividual temporal association of headache and vertigo is highly variable in VM patients Grossly normal peripheral vestibular function and audiometry both during and between attacks distinguishes VM from its mimics. Treatment options for VM are mainly based on expert opinion and include lifestyle modifications, acute and prophylactic migraine pharmacotherapy, and vestibular rehabilitation therapy.
- Conclusion: Despite a lack of diagnostic biomarkers for VM, a meticulous workup is important to exclude alternative mimics. More longitudinal and treatment studies are required to help elucidate the prognosis and optimal management of this condition.
The coexistence of migraine and vestibular symptoms has been mentioned in the headache literature for many years [1–3]. It was first addressed by Kayan and Hood in 1984, who found that dizziness and vertigo occurred in 54% of migraine patients compared with 30% of patients with tension-type headache [1]. The frequent coexistence of migraine and vertigo led researchers to hypothesize that their co-occurence could be due to more than mere chance. As per Lempert and Neuhauser’s evaluation, there is a lifetime prevalence of 16% for migraine and 7% for vertigo, with a 1.1 % chance of vertigo and migraine occurring together by chance alone [4]. In a study looking at the point prevalence of vertigo or dizziness among those presenting for a routine appointment at a headache center, an astounding 72.8% of those with severe headaches had vestibular symptoms [5].
Most epidemiologic studies of what we call vestibular migraine (VM) were based on presentations to specialist clinics and were performed in an era during which no established diagnostic criteria existed. Despite this, most neurootologists would consider VM to be one of the most common causes of spontaneous recurrent vertigo [6]. Neuhauser et al reported that VM was diagnosed in 7% of a group of 200 specialist clinic patients with dizziness and 9% of a group of 200 clinic patients who had migraine [2]. In a population-based study in Germany, the lifetime prevalence of VM according to the Neuhauser criteria was estimated to be 0.98% and the 12-month prevalence 0.89% [7]. The condition has a 3:1 female predilection [8].
VM has only recently been recognised as a separate migraine entity by the International Headache Society (IHS), appearing in the appendix of their International Classification of Headache Disorders (ICHD)–3 beta. The previous ICHD recognised vertigo as a migrainous symptom only within the framework of basilar migraine. The nomenclature used in the literature to describe this entity has been inconsistent and therefore confusing, including terms such as migraine-associated vertigo [9], migraine-related dizziness [3] or vertigo [10],migrainous vertigo [2], benign recurrent vertigo [11], and migraine-related vestibulopathy [12]. For the most part, these terms refer to the co-experience of migraine and vertigo or dizziness, with only a few terms having a more specific meaning of how the 2 symptoms relate temporally. Neuhauser and colleagues developed criteria in 2001 to classify migraineurs for whom vestibular symptoms are an integral part of migraine symptomatology, using the term migrainous vertigo [2]. Others preferred the terms migraine-associated dizziness or migraine-related dizziness [3] over migrainous vertigo because they felt the symptoms of vestibular dysfunction related to migraine are varied and may include gait instability and spatial disorientation but not necessarily with vertigo. To best avoid confounding nonvestibular dizziness or motion sickness associated with migraine, VM has been the preferred term because it emphasises the particular vestibular manifestation of migraine.
The lack of a universally accepted definition for this complex entity has contributed to delayed diagnosis and and treatment for those with this disorder. In this article, we will review the clinical manifestation, diagnosis and management of VM, with a focus on assisting in the differentiation between other potential diagnoses.
Pathophysiology of VM
A clear pathophysiology of VM has not been elucidated. Although predominantly a sporadic disease, there have been reported cases of familial occurrence with an auto-somal dominant inheritance [11,13]. Bahmad and colleagues mapped the first locus for familial VM to 5q35 within a 4-generation family [13]. On the contrary, a larger study conducted by Lee et al found VM to be to genetically heterogeneous with a subset linking to chromosome 22q12 [14]. Genetic defects of voltage-gated calcium channels are identified as causal factors for familial hemiplegic migraine and episodic ataxia type 2. Both these disease entities present with vertigo and migraine headaches suggesting a defective gene within the same chromosomal region could indicate a direct genetic link to VM. However, no such gene has been identified.
General consensus is that the action of spreading cortical depression as it reaches the somatosensory cortex in the posterior insula and temporoparietal junction elucidates migraine aura in patients with short attacks. However, due to the heterogeneity of VM, canal paresis and complex conditional nystagmus during acute stages are not explained through cortical spreading. Eggers et al suggests that vertigo symptoms occur as ictal sensation rather than the spreading of sensory or motor cortical depression [15]. However, due to discrepancies within the literature it is apparent that further research needs to be conducted to fully understand the pathophysiology of VM.
Clinical Manifestations of VM
Symptoms
As many as 80% to 90% of patients with VM report unsteadiness or balance problems, of which 50% to 60% typically report episodic spontaneous vertigo [16], either internal vertigo (a false sensation of self-motion) or external vertigo (a false sensation that the visual surround is spinning or flowing) [17]. The duration of episodes is highly variable, whereby approximately 30% of patients have episodes lasting minutes, 30% have attacks lasting hours, 30% have attacks over several days, while the remaining 10% have attacks lasting seconds only [18]. It may be difficult to distinguish if vestibular symptoms lasting seconds are related to their head motion intolerance, also known as head motion–induced vertigo [17], which is another frequent symptom in VM. Head motion–induced vertigo bears many similarities to motion sickness.
The interindividual temporal association of headache and vertigo is highly variable in VM patients and is a reason many patients find this diagnostic construct difficult to accept. Approximately 30% of adult patients eventually diagnosed with VM initially present without headaches [8]. Vertigo is only regularly associated with headache in 25% to 50% of VM patients [2,7]. A minority of patients report headache and vertigo never occurring together [2]. A temporal pattern, presenting as aura, occurs only in approximately 10% of cases [19]; therefore, vestibular episodes of VM should not be regarded as migraine auras [18]. Patients typically have migraine manifesting earlier in life with the vestibular symptoms following [13,20], whereby the mean age at onset of migraine and diagnosis of VM are approximately 22 and 35 years, respectively [2]. Consistently across studies that measure quality of life scores, VM patients report higher subjective levels of disability compared to patients with other vestibular illnesses, despite having less objective abnormalities [21]. Approximately 85% of VM patients experienced vestibular symptoms for at least 1 year before consulting neurootology services [21]. It could be argued that hypersensitivity of percept to vestibular symptoms reflect the general finding of augmented perceptions to various external stimuli underlying migraine [22,23].
Another prominent feature of VM is that patients report a syndrome of visually-induced dizziness termed visual vertigo (VV). This is a heterogeneous syndrome with strabismic, peripheral, and/or central vestibular aetiologies [24]. Patients with VV complain of discomfort, postural destabilisation, dizziness, imbalance and spatial disorientation in challenging visual environments. Examples of such environments include walking down supermarket aisles, observing moving objects (eg, disco lights, people walking, moving traffic) or moving surroundings during travelling, and the movement of the eyes in general [24–26]. Most patients report more than one visual trigger [24]. Visual vertigo can often be difficult to distinguish from oscillopsia in patients with bilateral vestibular failure. What is most surprising is that patients with VV have a similar handicap level yet report much more vestibular symptoms compared with patients with bilateral vestibular failure [25]. Postural reactions triggered by external visual motion are destabilising with respect to the earth-vertical and are normally suppressed by central re-weighting of sensory postural cues [24]. Surprisingly, premorbid levels of anxiety and childhood motion sickness do not appear to have a correlation with VV [25]. Even in normal subjects, certain complex visual stimuli can induce transient motion sickness–like symptoms, as shown in experimental visually induced self-vection [27]. The Situational Characteristics Questionnaire (SVQ) is a 19-question, symptom-based questionnaire that has been shown to be useful in quantifying features of VV and may be useful in gauging improvement following physical therapies [25,26].
Early in the disease course, hearing loss should prompt an alternative diagnosis. However, late onset cochlear symptoms have been reported in VM. A study found that after 9 years of follow-up, the number of patients with cochlear symptoms more than doubled [28].
Clinical Examination Findings
The importance of the clinical examination is to rule out peripheral vestibular dysfunction and perform positional testing to look for benign paroxysmal positional vertigo (BPPV) or central positional nystagmus. Nonetheless, positional nystagmus has been reported in up to 28% of cases, including definite central-type positional nystagmus reported in as many as 18% [28].
Audiometric Findings and Auditory Brainstem Responses
Normal audiometry both during and between attacks is one of the key clinical features that distinguishes VM from Meniere’s disease [29]. Auditory brainstem response (ABR) results are typically normal in about 65% of patients [29]. Abnormal ABR results are typically nonspecific, such as mild elongation of wave I, III and V latencies and less commonly, prolongation of the inter-peak latencies.
Findings on Vestibular Function Testing
Whilst there are some reported abnormalities in vestibular function testing in VM patients, such findings need to be interpreted with caution due to the small number of subjects, as well as the variation in case definition and cut-off values. Most importantly, very few papers studied patients in the acute phase, and in some studies it was not even specified. The majority of studies report that VM patients interictally have grossly normal peripheral vestibular function with occasional minor irregularities. Profound interictal abnormalities such as complete canal paresis are usually indicative of other diagnoses. In between acute attacks, patients with VM typically have normal gaze, saccadic parameters, ocular pursuit gains and optokinetic nystagmus (OKN) gains on electronystagmography (ENG) or videonystagmography (VNG) [3]. A minority had a low amplitude (< 4 degrees per second) persistent positional nystagmus. On rotation testing of the vestibo-ocular reflex there is reduction of the mean gains compared to headache-free controls. Most reports in the literature do support that the majority of VM patients have grossly normal bithermal caloric testing, although abnormalities including higher slow phase velocities and canal paresis (usually partial) are reported [29–31]. The observation that the artificial vestibular stimulation caused by the caloric test was followed by a migraine attack within 24 hours in 49% of patients with migraine is very interesting [30], and it remains to be tested whether this phenomenon has the potential to be of assistance in the diagnosis of VM. Both VM patients and migraineurs without vertigo have similar subtle cVEMP (Cervical vestibular-evoked myogenic potentials) abnormalities, namely decreased global amplitude and absence of habituation [31]. On computerized dynamic posturography (CDP), a test of sway, VM patients typically demonstrate a surface-dependent pattern based on their SOT analysis [3], suggesting that VM patients may have a substantial vestibulo-spinal abnormality leading to difficulties integrating multiple conflicting sensory inputs [32].
Diagnostic Criteria
Separating VM into 2 diagnostic entities seems particularly useful: definite VM and the more sensitive but less specific category of probable VM. The sensitivity and specificity of the proposed criteria still need to be determined. Although some authors criticize the probable diagnostic entity for its heterogeneity, about 50% of patients initially diagnosed with probable VM ultimately progress to definite VM [12,33]. Definite vestibular migraine appears in the ICHD-3 beta but only in the appendix section for “new disorders that need further research for validation.” However, probable VM will not be included until further evidence of its utility has been accumulated.
The diagnosis is particularly challenging when headache is not a regular accompaniment of the vertiginous attacks. A patient diary may help link migrainous and vertigo symptoms. When headache is not a prominent feature of the attacks, the clinician will have to put migrainous triggers or symptoms such as photophobia or scintillating scotomas in the context of vertigo symptoms to aid with the diagnosis. One needs to be pedantic about differentiating the qualifying symptom of phonophobia, which is defined as a sound-induced discomfort that is often transient and bilateral from the uncomfortable distorted loud sound perception, which occurs with a recruiting sensorineural hearing loss, and is often persistent and unilateral [18]. Response to migraine treatment is not sufficiently specific to be included in the diagnostic criteria. High placebo response rates from migraine trials [34] suggest that placebo effects can likewise be expected in the treatment of VM. Despite these challenges, acceptance of the diagnostic entity of VM seems to be gaining momentum. In a follow-up study over 9 years, the diagnosis remained consistent in 85% of patients [33].
Benign Paroxysmal Vertigo of Childhood and Vestibular Migraine in Children
VM can present at any age, however, the ICHD specifically recognises an early vertiginous entity regarded as a precursor syndrome of migraine in otherwise healthy children called benign paroxysmal vertigo of childhood. This diagnosis requires 5 episodes of severe vertigo, occurring without warning and resolving spontaneously after minutes to hours [35]. In between episodes, neurological examination, audiometry, vestibular functions and EEG must be normal. A unilateral throbbing headache may occur during attacks but it is not a mandatory criterion. It is unclear whether these two conditions in children are the same entity, however it is important to note that the classification of VM does not involve any age limit [18].
Basilar-type Migraine
The term basilar migraine should be restricted to patients who fulfill the ICHD diagnostic criteria [35] given it is a clinically distinct entity from VM. Less than 10% of VM patients further fulfill the ICHD criteria for basilar migraine [2,18]. More than 60% of basilar-type migraine patients have vertigo and there are many overlapping clinical manifestations with VM. This diagnosis requires at least 2 symptoms from aura in the posterior circulation territory, whereas most patients with VM have vestibular symptoms only [35]. Moreover, in basilar migraine the duration of vertigo should correspond to the length of an aura, that is, between 5 and 60 minutes [35]. Further studies are required to further elucidate and delineate these 2 conditions.
Other Important Diagnostic Considerations
Meniere’s Disease
An important differential diagnosis of VM is the early presentation of Meniere’s disease (MD). Although fluctuating hearing loss, aural fullness and episodic vertigo are important symptoms in the recent updated diagnostic criteria for definite MD [36,37], these symptoms have been reported in patients with migraine [38]. Moreover, minor abnormalities in cVEMPs and arguably in caloric testing can be found in VM patients, as previously mentioned. Predominantly, the distinction can be made considering that a more sustained, albeit occasionally fluctuating, hearing loss would occur in MD, which can progress to severe hearing loss within a few years. However, the diagnosis can be difficult considering that audiometric and vestibular function abnormalities as well as the typical cochlear symptoms are often absent in the early stages of the MD. Nonetheless, preclinical labelling of patients with episodic vertigo without hearing loss as “vestibular MD” is unhelpful as this population may be overrepresented by actual migraineurs. Studies of patients with so-called benign recurrent vertigo or recurrent vestibulopathy are likely to be heterogeneous entities, with perhaps cases later evolving into VM or MD.
Coexisting migraine and MD is often challenging both in terms of diagnosis and management. Many studies have shown an increased prevalence of migraine in MD patients compared to controls [39,40], an asso-ciation suggested by Prosper Ménière himself in 1861 [41]. A study by Radtke et al found that the lifetime prevalence of migraine with and without aura was over 2 times higher in definite MD patients of both sexes compared to age-matched controls (56% versus 25%) [39]. Interestingly, 45% of the patients with MD always experienced at least 1 migrainous symptom (migrainous headache, photophobia, aura symptoms) with their Meniere attacks [39]. This may be at least partly due to the triggering effect of vestibular symptoms on migraineurs [30]. Migraine may even influence the disease course of MD as indicated by a retrospective case control study which found that definite MD patients who have concomitant ICHD criteria for migraine [35] had a significantly earlier onset of MD symptoms (mean age, 37.2 versus 49.3 years) and a much greater susceptibility to simultaneous bilateral, but not sequential, hearing loss as compared to MD patients without migraine (56% versus 4%) [42]. There were no significant differences in the severity of hearing loss between the 2 groups even when controlling for time to evaluation [42]. A family history of episodic vertigo was seen in 39% of MD patients with migraine, which is significantly higher than the 2% seen in MD patients, suggesting a possible genetic basis for this association [42]. The nature of the association between migraine and MD is not well elucidated, however, some authors propose that migraine leads to isolated microvascular ischaemic damage of the inner ear, presumably through small arterial vasospasm [40,42].
In summary, when the criteria for MD are met together with documented audiometric abnormalities, MD should be diagnosed, even if migraine symptoms occur during the vestibular attacks [18]. Only patients who experience 2 different types of attacks, one fulfilling the criteria for VM and the other for MD, should be labelled as Meniere’s disease/migraine overlap syndrome. It is hoped that future revisions of diagnostic criteria will include this overlap entity.
Migraine and Benign Paroxysmal Positional Vertigo
VM patients can experience brief positional dizziness and therefore VM may mimic BPPV. It is therefore important to perform positional testing to look for nystagmus typical for BPPV. Certainly the positional characteristics are distinct from BPPV with regard to the duration of attacks (often as long as the head position is maintained in VM rather than seconds in BPPV). BPPV may also produce attacks of vertigo that can act as triggers for migraine headaches. In these patients, treatment of the BPPV will reduce headache frequency [30].
Transient Ischemic Attacks
Transient ischemic attack (TIA) is a cerebrovascular disease with temporary neurological symptoms [43] and is differentiated from VM mainly from the characteristics of reported symptoms. Being a vascular phenomenon, one would expect TIA symptoms to have a sudden onset, with a brief duration of symptoms (typically short minutes), followed by a rapid improvement to baseline, as well as correspond to a vascular territory. The other important message is that stereotyped, frequently recurrent symptoms are less likely to be TIAs, with the exception of capsular warning syndrome [44] and limb shaking TIAs [43] described elsewhere.
Migraine and Motion Sickness
In an individual patient it may be difficult to differentiate between motion sickness and acute attacks of VM induced by motion stimuli. The distinction may be helped by observing nausea and dizziness improving after cessation of motion which points more towards motion sickness, as oppose to the persistent vertigo after the motion stimulus has ended, thus pointing more towards VM.
Episodic Ataxia Type 2
Of the various episodic ataxias, episodic ataxia type 2 would be the most important subtype in the differential diagnosis of VM given it presents with episodic vertigo and is the most frequently occurring subtype. It is a rare autosomal dominant inherited neurological disorder resulting from mutations of the calcium channel gene CACNA1A [45]. The clinical manifestations include recurrent disabling attacks of imbalance, vertigo and ataxia, which can be provoked by physical exertion or emotional stress. Patients may have downbeat nystagmus interictally. A slow progression of cerebellar signs accompanied by atrophy of midline cerebellar structures and a response to acetazolamide or 4-aminopyridine can help distinguish it from VM.
Migraine, Dizziness, and Comorbid Psychiatric Disorders
Particularly in patients with protracted symptoms, it is difficult to tease out the difference between the symptoms of migraine and dizziness from the symptoms of certain psychiatric disorders given their bidirectional associations. Migraine is a risk factor for first-onset major depression [46] and panic disorder [47]. Patients with VM have very high rates (30%–65%) of coexisting psychiatric illness, especially anxiety and depression, with frequencies higher than that associated with other migraine or vestibular disorders [48,49]. Vestibular migraine patients who have a positive history of psychiatric disorders have a comparatively higher risk of developing somatoform dizziness [48]. The unpredictability of recurrent vestibular symptoms could be a factor leading to elevated distress in VM patients. It is not uncommon to see a premature diagnosis of psychogenic dizziness to be given to patients without objective abnormalities. On the contrary, a diagnosis of psychogenic dizziness can rarely be made with certainty due to multiple reasons. Disabling vertigo leading to physical symptoms and avoidance of social activities can easily be misconstrued to have panic disorder with or without agoraphobia. Moreover, dizziness is the second most common symptom of a panic attack after palpitations [50].
Unfortunately, there are no objective tests that can reliably discriminate vestibular syndromes from psychiatric syndromes in patients with dizziness. The SVQ is not specific enough to differentiate symptoms of VV from the space and motion discomfort symptoms often found in agoraphobic patients [25]. Experimentally, agoraphobia patients may have a more surface-dependent strategy rather than a visual-dependent strategy on CDP [51]. It is unclear whether the vestibular system is causally linked to emotion processing pathways.
Chronic Subjective Dizziness
Chronic subjective dizziness is an entity characterised by chronic unsteadiness or nonvertiginous dizziness accompanied by hypersensitivity to motion stimuli and poor tolerance for complex visual stimuli lasting for 3 months or more without objective abnormalities [52]. These vestibular symptoms are often difficult to distinguish from symptoms of VM. This condition is thought to be a spatial sensory analog of allodynia experienced by some chronic migraine headache sufferers [8].
Dizziness Due to Side Effects of Migraine Prophylactic Medications
Dizziness is often listed as a side effect in the product information of various medications including those used for migraine prophylaxis. It is important to take an accurate history of the suspected offending drug in terms of its temporal relationship to vestibular symptoms. Tricyclic antidepressants (TCAs) can cause drowsiness, lightheadedness, fatigue and blurred vision [53]. Beta-blockers can cause orthostatic hypotension [53]. All the above effects could be confused with vestibular symptoms.
Treatment of Vestibular Migraine
Current treatment options for VM are mainly limited to expert opinion rather than inferred from randomized controlled trials (RCTs) [54]. Below we have offered our consensus on how VM should be managed, with concepts based on the guidelines of treatment for typical migraine [55]. Avoidance of migraine triggers should always be the first avenue of treatment. In addition, any vestibular disorder that is triggering migraine attacks should be identified and treated in its own right. Pharmacotherapy can be abortive for acute episodes and prophylactic.
Lifestyle Advice
The key first task in management is the correct diagnosis and educating the patient about the condition. A thorough explanation of the migraine origin of the attacks can address patients fear and expectations. Nonpharmaceutical approaches in the treatment of VM should not be neglected, even though only a very small proportion of patients may derive a benefit. Advice on dietary manipulation is routinely given; however, its efficacy in VM is questionable. Dietary advice includes healthy eating at regular intervals to prevent skipped meals as well as avoidance of excess caffeine and rich foods. A retrospective study found that lifestyle intervention alone resulted in 13 of 81 patients experiencing significant relief from vestibular symptoms with migraine. The remaining cohort of patients required a multifaceted approach including pharmacotherapy to achieve similar benefit [56].
Acute Abortive Treatments
Oral antiemetics are commonly prescribed for motion sickness and acute migraine, however there is no evidence supporting their effectiveness in VM (Table 2). Patients should be counselled about avoiding overuse of antiemetics given their risk of causing extrapyramidal side effects [53].
Simple analgesics, such as paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs), have been found to be helpful in acute VM attacks in observational studies. Bikhazi performed a survey of patients presenting to a headache clinic with vestibular symptoms and found that simple analgesics were valued by patients as effective symptomatic treatment, but were not considered as effective as triptans [59]. Doses of simple analgesics are listed in Table 2. Soluble formulations are preferable due to faster absorption and speed of onset. Opioids should be avoided in acute attacks of VM given the risk of developing opioid overuse headache [55].
Migraine Prophylaxis in Vestibular Migraine
TCAs remain a popular choice of migraine prophylaxis amongst neurootologists because of its additional effects on comorbid affective symptoms. We recommend that the starting dose of either amitriptyline or nortriptyline should be between 5 to 10 mg daily at night, slowly uptitrated to response over several weeks up to a maximum of 100 mg at night. Interval electrocardiography should be performed to monitor for prolongation of the QTc interval. A retrospective chart review found 46% of VM patients (by Neuhauser criteria) reported a reduction in dizziness after nortriptyline administration up to 75 mg daily [62]. However, the current evidence is limited to observational studies [59,62–64].
The evidence for beta-blockers is limited in VM but anecdotally has been useful for patients with frequent episodic migraine [59,63,64]. Recommended starting and maintenance doses are listed in Table 3. Furthermore, propranolol can be used in patients with depression [65,66]. Heart rate and electrocardiography should be monitored during dose escalation. Beta-blockers should be avoided in asthmatics. Commonly reported adverse events include cold, extremities reduced exercise tolerance and dizziness [53].
Flunarizine, a calcium channel blocker widely used in migraine [67,68] and vestibular conditions [69], was recently studied in a RCT of 12 weeks' duration for prophylaxis of migrainous vertigo (Neuhauser criteria) in 48 patients [70]. Although flunarizine 10 mg daily did not result in improved headache frequency and severity compared to the control arm, there was a significant improvement in vertigo severity. The most commonly reported side effects of flunarizine are weight gain and somnolence, both of which are minimal or infrequent. Verapamil is another calcium channel blocker that may be helpful but has major limiting adverse effects are bradycardia, constipation and peripheral edema [53].
Pizotifen, a serotonin antagonist, is one of the most well tolerated prophylaxis agents from our experience, however some patients do not adhere to treatment due to drowsiness or weight gain, as evidenced in retrospective case studies [64].
Topiramate with an average daily dose of 100 mg has reported positive results in a prospective observational study of ten patients with VM with auditory symptoms [71]. Nine of 10 patients reported no symptoms after follow-up period of up to sixteen months. The recommended dose is listed in Table 3. Common side effects include distal paresthesias, reduced ability to concentrate and drowsiness [53]. Sodium valproate has been anecdotally effective [59] and is usually well tolerated especially when starting at a low dose of 200 mg at night, slowly titrated to 1200 mg in 2 divided doses. Liver function and full blood evaluation should be monitored on a periodic basis [53].
Third-line medications have only been used anecdotally and should be reserved for extenuating cases (Table 3).
Vestibular Rehabilitation
Vestibular rehabilitation therapy (VRT) has been shown to alleviate significantly ongoing balance and dizziness symptoms in patients with various vestibular disorders [73,74] and improving confidence with balance in elderly patients [75,76]. However, the value of VRT is not as well established in VM. Anecdotally, patients with VM report persistent significant symptoms at the end of a standard VRT period, in contrast to other nonmigrainous patients who appear to be accomplishing their treatment goals faster. However, recent studies [21,73,77] are suggesting that customised VRT may play a useful role in VM, especially since it appears to target issues of anxiety, visual dependence or loss of confidence in balance. Small retrospective case series found that VRT reduced disability scores, and gait and balance function in over 85% of patients with migraine and vestibular symptoms [73,76,77]. An Australian VRT study (21) has recently assessed the efficacy of a 9-week customised VRT in 20 patients with VM compared to 16 patients with vestibular symptoms but without migraine. The customized VRT program consisted of habituation, gaze stability, static tilt, balance and gait exercises. A pictorial exercise instruction sheet for home use would describe these exercises of approximately 15 minutes duration consisting of 4 to 6 exercises to be performed 3 times a day, every day for 9 weeks. Interestingly, both groups benefitted equally from VRT. Compliance with VRT was comparable between the two groups. Commonly reported reasons for non-attendance in VM patients included a recent acute attack of VM, anxiety related to using public transport, and commitment issues related to occupation. This study also suggested that VM patients required more customized and intensive therapy as 15% of VM patients required additional appointments outside the study timeline.
Given that visual dependency has been shown to be reduced with short-term graded optokinetic stimulation exposure in healthy subjects [78], there has been interest using this intervention in conjunction with customized VRT to promote desensitization to visual stimuli as a treatment for VM patients with VV. Most promisingly is the finding that a subgroup of patients with a history of migraine improved significantly more than other vestibular patients with respect to VV symptoms.
There has been controversy surrounding whether patients should avoid medications when undergoing VRT. The protagonists of this view suggest that medications that affect the central nervous system (CNS) may modulate the rate of central compensation. In the aforementioned study by Vitkovic and colleagues [21], the same degree of improvement was seen in the VM group regardless of medication regimen. A study by Whitney and colleagues [73] found that migraine related vestibulopathy patients taking prophylaxis demonstrated better subjective and objective balance scores at baseline and after therapy. Further research is required to clarify the role of CNS-acting medication and their administration around VRT sessions.
Physical therapists dealing with VM patients may face additional challenges in encouraging exercise compliance and providing emotional support. Although more time consuming for the therapist, this is important in the face of high rates of comorbid affective disorders and head motion intolerance. Supervised VRT is believed to implicitly improve psychological status through increasing confidence, providing reassurance, and emphasizing positive effects of VRT, particularly when the patient feels their symptoms have been made worse by it.
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) has been shown to be helpful as part of the holistic treatment of various disorders including post-concussive syndrome and depression in neurology patients [79,80]. Among patients suffering from dizziness, a small study comparing explicit CBT combined with VRT versus waiting-list controls demonstrated improvements in patients’ coping ability, function, symptoms, and care satisfaction [81]. However, to our knowledge there are no studies directly evaluating the benefits of CBT specifically in VM patients. Despite this, it is our practice to request CBT for VM patients who report disabling anxiety or depressive symptoms.
Prognosis
Although migraine in general can improve in later life, this is less certain with VM given the lack of good quality longitudinal studies. Recently Radtke and colleagues published their long-term (median, 9 years) follow-up study of 61 definite VM cases (28). They found that 87% of patients had recurrent vertigo at follow-up. The frequency of vertigo was reduced in 56%, increased in 29%, and unchanged in 16% of patients. The impact of vertigo was graded as severe in 21%, moderate in 43%, and mild in 36% of patients. However, they found that concomitant cochlear symptoms with vertigo had increased from 15% at study inception to 49% at follow-up and secondly, 18% of patients had developed mild bilateral low-frequency sensorineural hearing loss. Therefore, one major criticism of the study is whether some of the patients had MD as their eventual diagnosis rather than definite VM. On the contrary, the authors conclude that these changes represent new vestibulo-cochlear dysfunction as a result of VM disease progression. Due to these reasons, the prognosis of VM patients is unclear. It is our practice to ensure patients do receive delayed follow-up to allow consideration of other neurotological diagnoses.
Conclusion
Given the large heterogeneity in presentation and objective testing, VM as a diagnostic construct has remained quite controversial, though increasingly more accepted. The more we study this common vestibular condition, the more we are realising that the complex relationship between migraine and dizziness extend beyond VM to encompass other vestibular disorders such as MD and anxiety. The lack of a physiological biomarker contributes to its diagnostic difficulties, but a meticulous workup is important to exclude alternative vestibular diagnoses. More longitudinal studies and RCTs are required to help both understand the prognosis and management of VM patients.
Corresponding author: Benjamin K-T Tsang, MBBS, FRACP, The Prince Charles Hospital, Rode Road, Chermside, Queensland 4032, Australia, [email protected].
Financial disclosures: None.
1. Kayan A, Hood JD. Neuro-otological manifestations of migraine. Brain 1984;107(Pt 4):1123–42.
2. Neuhauser H, Leopold M, von Brevern M, et al. The interrelations of migraine, vertigo, and migrainous vertigo. Neurology 2001;56:436–41.
3. Furman JM, Sparto PJ, Soso M, Marcus D. Vestibular function in migraine-related dizziness: a pilot study. J Vestib Res 2005;15:327–32.
4. Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. J Neurol 2009;256:333–8.
5. Calhoun AH, Ford S, Pruitt AP, Fisher KG. The point prevalence of dizziness or vertigo in migraine--and factors that influence presentation. Headache 2011;51:1388–92.
6. Bisdorff A. Migraine and dizziness. Curr Opin Neurol 2014;27:105–10.
7. Neuhauser HK, Radtke A, von Brevern M, et al. Migrainous vertigo: prevalence and impact on quality of life. Neurology 2006;67:1028–33.
8. Sargent EW. The challenge of vestibular migraine. Curr Opin Otolaryngol Head Neck Surg 2013;21:473–9.
9. Cha YH. Migraine-associated vertigo: diagnosis and treatment. Sem Neurol 2010;30:167–74.
10. Cherian N. Vertigo as a migraine phenomenon. Curr Neurol Neurosci Rep 2013;13:343.
11. Oh AK, Lee H, Jen JC, et al. Familial benign recurrent vertigo. Am J Med Genet 2001;100:287–91.
12. Cass SP, Furman JM, Ankerstjerne K, et al. Migraine-related vestibulopathy. Ann Otol Rhinol Laryngol 1997;106:182–9.
13. Bahmad F Jr, DePalma SR, Merchant SN, et al. Locus for familial migrainous vertigo disease maps to chromosome 5q35. Ann Otol Rhinol Laryngol 2009;118:670–6.
14. Lee H, Jen JC, Wang H, et al. A genome-wide linkage scan of familial benign recurrent vertigo: linkage to 22q12 with evidence of heterogeneity. Hum Molec Genet 2006;15:251–8.
15. Eggers SD, Neff BA, Shepard NT, Staab JP. Comorbidities in vestibular migraine. J Vestib Res 2014;24:387–95.
16. Cohen JM, Bigal ME, Newman LC. Migraine and vestibular symptoms--identifying clinical features that predict “vestibular migraine”. Headache 2011;51:1393–7.
17. Bisdorff A, Von Brevern M, Lempert T, Newman-Toker DE. Classification of vestibular symptoms: towards an international classification of vestibular disorders. J Vestib Res 2009;19:1-13.
18. Lempert T, Olesen J, Furman J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res 2012;22:167-72.
19. Dieterich M, Brandt T. Episodic vertigo related to migraine (90 cases): vestibular migraine? J Neurol 1999;246:883–92.
20. Eggers SD, Staab JP, Neff BA, et al. Investigation of the coherence of definite and probable vestibular migraine as distinct clinical entities. Otol Neurotol 2011;32:1144–51.
21. Vitkovic J, Winoto A, Rance G, et al. Vestibular rehabilitation outcomes in patients with and without vestibular migraine. J Neurol 2013;260:3039–48.
22. Kelman L. Osmophobia and taste abnormality in migraineurs: a tertiary care study. Headache 2004;44:1019–23.
23. Morrison DP. Abnormal perceptual experiences in migraine. Cephalalgia 1990;10:273–7.
24. Bronstein AM. Visual vertigo syndrome: clinical and posturography findings. J Neurol Neurosurg Psych 1995;59:472–6.
25. Guerraz M, Yardley L, Bertholon P, et al. Visual vertigo: symptom assessment, spatial orientation and postural control. Brain 2001;124(Pt 8):1646–56.
26. Pavlou M, Davies RA, Bronstein AM. The assessment of increased sensitivity to visual stimuli in patients with chronic dizziness. J Vestib Res 2006;16:223-31.
27. Dobie TG, May JG, Gutierrez C, Heller SS. The transfer of adaptation between actual and simulated rotary stimulation. Aviat Space Environ Med 1990;61:1085–91.
28. Radtke A, von Brevern M, Neuhauser H, et al. Vestibular migraine: long-term follow-up of clinical symptoms and vestibulo-cochlear findings. Neurology 2012;79:1607–14.
29. Bayazit Y, Yilmaz M, Mumbuc S, Kanlikama M. Assessment of migraine-related cochleovestibular symptoms. Revue Laryngol Otol Rhinol 2001;122:85–8.
30. Murdin L, Davies RA, Bronstein AM. Vertigo as a migraine trigger. Neurology 2009;73:638–42.
31. Roceanu A, Allena M, De Pasqua V, et al. Abnormalities of the vestibulo-collic reflex are similar in migraineurs with and without vertigo. Cephalalgia 2008;28:988–90.
32. Hong HR, Shim DB, Kim TS, et al. Results of caloric and sensory organization testing of dynamic posturography in migrainous vertigo: comparison with Meniere’s disease and vestibular neuritis. Acta Otolaryngol 2013;133:1236–41.
33. Radtke A, Neuhauser H, von Brevern M, et al. Vestibular migraine--validity of clinical diagnostic criteria. Cephalalgia 2011;31:906-13.
34. Rothner AD, Wasiewski W, Winner P, et al. Zolmitriptan oral tablet in migraine treatment: high placebo responses in adolescents. Headache 2006;46:101-9.
35. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd ed (beta version). Cephalalgia 2013;33:629–808.
36. Lopez-Escamez JA, Carey J, Chung WH, et al. Diagnostic criteria for Meniere’s disease. J Vestib Res 2015;25:1–7.
37. Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Meniere’s disease. American Academy of Otolaryngology-Head and Neck Foundation. Otolaryngol Head Neck Surg 1995;113:181–5.
38. Baloh RW. Neurotology of migraine. Headache 1997;37:615-21.
39. Radtke A, Lempert T, Gresty MA, et al. Migraine and Meniere’s disease: is there a link? Neurology 2002;59:1700–4.
40. Lee H, Lopez I, Ishiyama A, Baloh RW. Can migraine damage the inner ear? Arch Neurol 2000;57:1631–4.
41. Ménière P. Pathologie auriculaire: memoires sur une lésion de l’oreille interne donnant lieu à des symptoms de congestion cérébrale apoplectiforme. Gaz Med Paris 1861;16:597–601.
42. Cha YH, Brodsky J, Ishiyama G, et al. The relevance of migraine in patients with Meniere’s disease. Acta Otolaryngol 2007;127:1241–5.
43. Kim JS. Symptoms of transient ischemic attack. Front Neurol Neurosci 2014;33:82–102.
44. Paul NL, Simoni M, Chandratheva A, Rothwell PM. Population-based study of capsular warning syndrome and prognosis after early recurrent TIA. Neurology 2012;79:1356–62.
45. Strupp M, Zwergal A, Brandt T. Episodic ataxia type 2. Neurotherapeutics 2007;4:267–73.
46. Breslau N, Schultz LR, Stewart WF, et al. Headache and major depression: is the association specific to migraine? Neurology 2000;54:308–13.
47. Breslau N, Schultz LR, Stewart WF, et al. Headache types and panic disorder: directionality and specificity. Neurology 2001;56:350–4.
48. Best C, Eckhardt-Henn A, Tschan R, Dieterich M. Psychiatric morbidity and comorbidity in different vestibular vertigo syndromes. Results of a prospective longitudinal study over one year. J Neurol 2009;256:58–65.
49. Eckhardt-Henn A, Best C, Bense S, et al. Psychiatric comorbidity in different organic vertigo syndromes. J Neurol 2008;255:420–8.
50. Segui J, Salvador-Carulla L, Garcia L, et al. Semiology and subtyping of panic disorders. Act Psychiatr Scand 1998;97:272–7.
51. Jacob RG, Furman JM, Durrant JD, Turner SM. Surface dependence: a balance control strategy in panic disorder with agoraphobia. Psychosom Med 1997;59:323–30.
52. Ruckenstein MJ, Staab JP. Chronic subjective dizziness. Otolaryngol Clin North Am 2009;42:71–7, ix.
53. Australian medicines handbook : AMH. Adelaide, S.Aust.: Australian Medicines Handbook; 2015. p. v.
54. Maldonado Fernandez M, Birdi JS, Irving GJ, et al. Pharmacological agents for the prevention of vestibular migraine. Cochrane Database Syst Rev 2015;6:CD010600.
55. British Association for the Study of Headache. Guidelines for all healthcare professionals in the diagnosis and management of migraine, tension-type headache, cluster headache and medication overuse headache. 3rd ed. 2010.
56. Reploeg MD, Goebel JA. Migraine-associated dizziness: patient characteristics and management options. Otol Neurotol 2002;23:364–71.
57. Neuhauser H, Radtke A, von Brevern M, Lempert T. Zolmitriptan for treatment of migrainous vertigo: a pilot randomized placebo-controlled trial. Neurology 2003;60:882–3.
58. Roberto G, Raschi E, Piccinni C, et al. Adverse cardiovascular events associated with triptans and ergotamines for treatment of migraine: systematic review of observational studies. Cephalalgia 2015;35:118–31.
59. Bikhazi P, Jackson C, Ruckenstein MJ. Efficacy of antimigrainous therapy in the treatment of migraine-associated dizziness. Am J Otol 1997;18:350–4.
60. MedicinesComplete. London: Pharmaceutical Press. Available at www.medicinescomplete.com.
61. Tfelt-Hansen P, De Vries P, Saxena PR. Triptans in migraine: a comparative review of pharmacology, pharmacokinetics and efficacy. Drugs 2000;60:1259–87.
62. Mikulec AA, Faraji F, Kinsella LJ. Evaluation of the efficacy of caffeine cessation, nortriptyline, and topiramate therapy in vestibular migraine and complex dizziness of unknown etiology. Am J Otolaryngol 2012;33:121–7.
63. Maione A. Migraine-related vertigo: diagnostic criteria and prophylactic treatment. Laryngoscope 2006;116:1782–6.
64. Waterston J. Chronic migrainous vertigo. J Clin Neurosci 2004;11:384–8.
65. de Bock GH, Eelhart J, van Marwijk HW, et al. A postmarketing study of flunarizine in migraine and vertigo. Pharm World Sci 1997;19:269–74.
66. Verspeelt J, De Locht P, Amery WK. Postmarketing study of the use of flunarizine in vestibular vertigo and in migraine. Eur J Clin Pharmacol 1996;51:15–22.
67. Schmidt R, Oestreich W. Flunarizine in migraine prophylaxis: the clinical experience. J Cardiovasc Pharmacol 1991;18 Suppl 8:S21–6.
68. Lucetti C, Nuti A, Pavese N, et al. Flunarizine in migraine prophylaxis: predictive factors for a positive response. Cephalalgia 1998;18:349–52.
69. Schmidt R, Oestreich W. Flunarizine in the treatment of vestibular vertigo: experimental and clinical data. J Cardiovasc Pharmacol 1991;18 Suppl 8:S27–30.
70. Lepcha A, Amalanathan S, Augustine AM, et al. Flunarizine in the prophylaxis of migrainous vertigo: a randomized controlled trial. Eur Arch Otorhinolaryngol 2014;271:2931–6.
71. Carmona S, Settecase N. Use of topiramate (topamax) in a subgroup of migraine-vertigo patients with auditory symptoms. Ann N Y Acad Sci 2005;1039:517–20.
72. Bisdorff AR. Treatment of migraine related vertigo with lamotrigine an observational study. Bull Soc Sci Med Grand Duche Luxemb 2004:103–8.
73. Whitney SL, Rossi MM. Efficacy of vestibular rehabilitation. Otolaryngol Clin North Am 2000;33:659–72.
74. Enticott JC, Vitkovic JJ, Reid B, et al. Vestibular rehabilitation in individuals with inner-ear dysfunction: a pilot study. Audiol Neurootol 2008;13:19–28.
75. Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the activities-specific balance confidence (ABC) scale. J Gerontol Ser A Biol Sci Med Sci 1998;53:M287–94.
76. Wrisley DM, Whitney SL, Furman JM. Vestibular rehabilitation outcomes in patients with a history of migraine. Otol Neurotol 2002;23:483–7.
77. Gottshall KR, Moore RJ, Hoffer ME. Vestibular rehabilitation for migraine-associated dizziness. Int Tinnitus J 2005;11:81–4.
78. Pavlou M, Quinn C, Murray K, et al. The effect of repeated visual motion stimuli on visual dependence and postural control in normal subjects. Gait Posture 2011;33:113–8.
79. Leddy JJ, Sandhu H, Sodhi V, et al. Rehabilitation of concussion and post-concussion syndrome. Sports Health 2012;4:147–54.
80. Fernie BA, Kollmann J, Brown RG. Cognitive behavioural interventions for depression in chronic neurological conditions: a systematic review. J Psychosom Res 2015;78:411–9.
81. Andersson G, Asmundson GJ, Denev J, et al. A controlled trial of cognitive-behavior therapy combined with vestibular rehabilitation in the treatment of dizziness. Behav Res Ther 2006;44:1265–73.
From the Department of Neurootology, National Hospital of Neurology and Neurosurgery, London (Dr. Tsang, Miss Anwer) and the Ear Institute, University College London, and Guy’s and St Thomas’ NHS Foundation Trust, London, UK (Dr. Murdin).
Abstract
- Objective: To review the clinical manifestations, diagnosis, and management of vestibular migraine (VM).
- Methods: Review of the literature.
- Results: Apart from headache, other symptoms of VM include unsteadiness, imbalance, and spontaneous as well as visual vertigo. Acute vestibular symptoms that qualify for VM must be of at least moderate or severe intensity which lasts within a time window of 5 minutes to 72 hours. The interindividual temporal association of headache and vertigo is highly variable in VM patients Grossly normal peripheral vestibular function and audiometry both during and between attacks distinguishes VM from its mimics. Treatment options for VM are mainly based on expert opinion and include lifestyle modifications, acute and prophylactic migraine pharmacotherapy, and vestibular rehabilitation therapy.
- Conclusion: Despite a lack of diagnostic biomarkers for VM, a meticulous workup is important to exclude alternative mimics. More longitudinal and treatment studies are required to help elucidate the prognosis and optimal management of this condition.
The coexistence of migraine and vestibular symptoms has been mentioned in the headache literature for many years [1–3]. It was first addressed by Kayan and Hood in 1984, who found that dizziness and vertigo occurred in 54% of migraine patients compared with 30% of patients with tension-type headache [1]. The frequent coexistence of migraine and vertigo led researchers to hypothesize that their co-occurence could be due to more than mere chance. As per Lempert and Neuhauser’s evaluation, there is a lifetime prevalence of 16% for migraine and 7% for vertigo, with a 1.1 % chance of vertigo and migraine occurring together by chance alone [4]. In a study looking at the point prevalence of vertigo or dizziness among those presenting for a routine appointment at a headache center, an astounding 72.8% of those with severe headaches had vestibular symptoms [5].
Most epidemiologic studies of what we call vestibular migraine (VM) were based on presentations to specialist clinics and were performed in an era during which no established diagnostic criteria existed. Despite this, most neurootologists would consider VM to be one of the most common causes of spontaneous recurrent vertigo [6]. Neuhauser et al reported that VM was diagnosed in 7% of a group of 200 specialist clinic patients with dizziness and 9% of a group of 200 clinic patients who had migraine [2]. In a population-based study in Germany, the lifetime prevalence of VM according to the Neuhauser criteria was estimated to be 0.98% and the 12-month prevalence 0.89% [7]. The condition has a 3:1 female predilection [8].
VM has only recently been recognised as a separate migraine entity by the International Headache Society (IHS), appearing in the appendix of their International Classification of Headache Disorders (ICHD)–3 beta. The previous ICHD recognised vertigo as a migrainous symptom only within the framework of basilar migraine. The nomenclature used in the literature to describe this entity has been inconsistent and therefore confusing, including terms such as migraine-associated vertigo [9], migraine-related dizziness [3] or vertigo [10],migrainous vertigo [2], benign recurrent vertigo [11], and migraine-related vestibulopathy [12]. For the most part, these terms refer to the co-experience of migraine and vertigo or dizziness, with only a few terms having a more specific meaning of how the 2 symptoms relate temporally. Neuhauser and colleagues developed criteria in 2001 to classify migraineurs for whom vestibular symptoms are an integral part of migraine symptomatology, using the term migrainous vertigo [2]. Others preferred the terms migraine-associated dizziness or migraine-related dizziness [3] over migrainous vertigo because they felt the symptoms of vestibular dysfunction related to migraine are varied and may include gait instability and spatial disorientation but not necessarily with vertigo. To best avoid confounding nonvestibular dizziness or motion sickness associated with migraine, VM has been the preferred term because it emphasises the particular vestibular manifestation of migraine.
The lack of a universally accepted definition for this complex entity has contributed to delayed diagnosis and and treatment for those with this disorder. In this article, we will review the clinical manifestation, diagnosis and management of VM, with a focus on assisting in the differentiation between other potential diagnoses.
Pathophysiology of VM
A clear pathophysiology of VM has not been elucidated. Although predominantly a sporadic disease, there have been reported cases of familial occurrence with an auto-somal dominant inheritance [11,13]. Bahmad and colleagues mapped the first locus for familial VM to 5q35 within a 4-generation family [13]. On the contrary, a larger study conducted by Lee et al found VM to be to genetically heterogeneous with a subset linking to chromosome 22q12 [14]. Genetic defects of voltage-gated calcium channels are identified as causal factors for familial hemiplegic migraine and episodic ataxia type 2. Both these disease entities present with vertigo and migraine headaches suggesting a defective gene within the same chromosomal region could indicate a direct genetic link to VM. However, no such gene has been identified.
General consensus is that the action of spreading cortical depression as it reaches the somatosensory cortex in the posterior insula and temporoparietal junction elucidates migraine aura in patients with short attacks. However, due to the heterogeneity of VM, canal paresis and complex conditional nystagmus during acute stages are not explained through cortical spreading. Eggers et al suggests that vertigo symptoms occur as ictal sensation rather than the spreading of sensory or motor cortical depression [15]. However, due to discrepancies within the literature it is apparent that further research needs to be conducted to fully understand the pathophysiology of VM.
Clinical Manifestations of VM
Symptoms
As many as 80% to 90% of patients with VM report unsteadiness or balance problems, of which 50% to 60% typically report episodic spontaneous vertigo [16], either internal vertigo (a false sensation of self-motion) or external vertigo (a false sensation that the visual surround is spinning or flowing) [17]. The duration of episodes is highly variable, whereby approximately 30% of patients have episodes lasting minutes, 30% have attacks lasting hours, 30% have attacks over several days, while the remaining 10% have attacks lasting seconds only [18]. It may be difficult to distinguish if vestibular symptoms lasting seconds are related to their head motion intolerance, also known as head motion–induced vertigo [17], which is another frequent symptom in VM. Head motion–induced vertigo bears many similarities to motion sickness.
The interindividual temporal association of headache and vertigo is highly variable in VM patients and is a reason many patients find this diagnostic construct difficult to accept. Approximately 30% of adult patients eventually diagnosed with VM initially present without headaches [8]. Vertigo is only regularly associated with headache in 25% to 50% of VM patients [2,7]. A minority of patients report headache and vertigo never occurring together [2]. A temporal pattern, presenting as aura, occurs only in approximately 10% of cases [19]; therefore, vestibular episodes of VM should not be regarded as migraine auras [18]. Patients typically have migraine manifesting earlier in life with the vestibular symptoms following [13,20], whereby the mean age at onset of migraine and diagnosis of VM are approximately 22 and 35 years, respectively [2]. Consistently across studies that measure quality of life scores, VM patients report higher subjective levels of disability compared to patients with other vestibular illnesses, despite having less objective abnormalities [21]. Approximately 85% of VM patients experienced vestibular symptoms for at least 1 year before consulting neurootology services [21]. It could be argued that hypersensitivity of percept to vestibular symptoms reflect the general finding of augmented perceptions to various external stimuli underlying migraine [22,23].
Another prominent feature of VM is that patients report a syndrome of visually-induced dizziness termed visual vertigo (VV). This is a heterogeneous syndrome with strabismic, peripheral, and/or central vestibular aetiologies [24]. Patients with VV complain of discomfort, postural destabilisation, dizziness, imbalance and spatial disorientation in challenging visual environments. Examples of such environments include walking down supermarket aisles, observing moving objects (eg, disco lights, people walking, moving traffic) or moving surroundings during travelling, and the movement of the eyes in general [24–26]. Most patients report more than one visual trigger [24]. Visual vertigo can often be difficult to distinguish from oscillopsia in patients with bilateral vestibular failure. What is most surprising is that patients with VV have a similar handicap level yet report much more vestibular symptoms compared with patients with bilateral vestibular failure [25]. Postural reactions triggered by external visual motion are destabilising with respect to the earth-vertical and are normally suppressed by central re-weighting of sensory postural cues [24]. Surprisingly, premorbid levels of anxiety and childhood motion sickness do not appear to have a correlation with VV [25]. Even in normal subjects, certain complex visual stimuli can induce transient motion sickness–like symptoms, as shown in experimental visually induced self-vection [27]. The Situational Characteristics Questionnaire (SVQ) is a 19-question, symptom-based questionnaire that has been shown to be useful in quantifying features of VV and may be useful in gauging improvement following physical therapies [25,26].
Early in the disease course, hearing loss should prompt an alternative diagnosis. However, late onset cochlear symptoms have been reported in VM. A study found that after 9 years of follow-up, the number of patients with cochlear symptoms more than doubled [28].
Clinical Examination Findings
The importance of the clinical examination is to rule out peripheral vestibular dysfunction and perform positional testing to look for benign paroxysmal positional vertigo (BPPV) or central positional nystagmus. Nonetheless, positional nystagmus has been reported in up to 28% of cases, including definite central-type positional nystagmus reported in as many as 18% [28].
Audiometric Findings and Auditory Brainstem Responses
Normal audiometry both during and between attacks is one of the key clinical features that distinguishes VM from Meniere’s disease [29]. Auditory brainstem response (ABR) results are typically normal in about 65% of patients [29]. Abnormal ABR results are typically nonspecific, such as mild elongation of wave I, III and V latencies and less commonly, prolongation of the inter-peak latencies.
Findings on Vestibular Function Testing
Whilst there are some reported abnormalities in vestibular function testing in VM patients, such findings need to be interpreted with caution due to the small number of subjects, as well as the variation in case definition and cut-off values. Most importantly, very few papers studied patients in the acute phase, and in some studies it was not even specified. The majority of studies report that VM patients interictally have grossly normal peripheral vestibular function with occasional minor irregularities. Profound interictal abnormalities such as complete canal paresis are usually indicative of other diagnoses. In between acute attacks, patients with VM typically have normal gaze, saccadic parameters, ocular pursuit gains and optokinetic nystagmus (OKN) gains on electronystagmography (ENG) or videonystagmography (VNG) [3]. A minority had a low amplitude (< 4 degrees per second) persistent positional nystagmus. On rotation testing of the vestibo-ocular reflex there is reduction of the mean gains compared to headache-free controls. Most reports in the literature do support that the majority of VM patients have grossly normal bithermal caloric testing, although abnormalities including higher slow phase velocities and canal paresis (usually partial) are reported [29–31]. The observation that the artificial vestibular stimulation caused by the caloric test was followed by a migraine attack within 24 hours in 49% of patients with migraine is very interesting [30], and it remains to be tested whether this phenomenon has the potential to be of assistance in the diagnosis of VM. Both VM patients and migraineurs without vertigo have similar subtle cVEMP (Cervical vestibular-evoked myogenic potentials) abnormalities, namely decreased global amplitude and absence of habituation [31]. On computerized dynamic posturography (CDP), a test of sway, VM patients typically demonstrate a surface-dependent pattern based on their SOT analysis [3], suggesting that VM patients may have a substantial vestibulo-spinal abnormality leading to difficulties integrating multiple conflicting sensory inputs [32].
Diagnostic Criteria
Separating VM into 2 diagnostic entities seems particularly useful: definite VM and the more sensitive but less specific category of probable VM. The sensitivity and specificity of the proposed criteria still need to be determined. Although some authors criticize the probable diagnostic entity for its heterogeneity, about 50% of patients initially diagnosed with probable VM ultimately progress to definite VM [12,33]. Definite vestibular migraine appears in the ICHD-3 beta but only in the appendix section for “new disorders that need further research for validation.” However, probable VM will not be included until further evidence of its utility has been accumulated.
The diagnosis is particularly challenging when headache is not a regular accompaniment of the vertiginous attacks. A patient diary may help link migrainous and vertigo symptoms. When headache is not a prominent feature of the attacks, the clinician will have to put migrainous triggers or symptoms such as photophobia or scintillating scotomas in the context of vertigo symptoms to aid with the diagnosis. One needs to be pedantic about differentiating the qualifying symptom of phonophobia, which is defined as a sound-induced discomfort that is often transient and bilateral from the uncomfortable distorted loud sound perception, which occurs with a recruiting sensorineural hearing loss, and is often persistent and unilateral [18]. Response to migraine treatment is not sufficiently specific to be included in the diagnostic criteria. High placebo response rates from migraine trials [34] suggest that placebo effects can likewise be expected in the treatment of VM. Despite these challenges, acceptance of the diagnostic entity of VM seems to be gaining momentum. In a follow-up study over 9 years, the diagnosis remained consistent in 85% of patients [33].
Benign Paroxysmal Vertigo of Childhood and Vestibular Migraine in Children
VM can present at any age, however, the ICHD specifically recognises an early vertiginous entity regarded as a precursor syndrome of migraine in otherwise healthy children called benign paroxysmal vertigo of childhood. This diagnosis requires 5 episodes of severe vertigo, occurring without warning and resolving spontaneously after minutes to hours [35]. In between episodes, neurological examination, audiometry, vestibular functions and EEG must be normal. A unilateral throbbing headache may occur during attacks but it is not a mandatory criterion. It is unclear whether these two conditions in children are the same entity, however it is important to note that the classification of VM does not involve any age limit [18].
Basilar-type Migraine
The term basilar migraine should be restricted to patients who fulfill the ICHD diagnostic criteria [35] given it is a clinically distinct entity from VM. Less than 10% of VM patients further fulfill the ICHD criteria for basilar migraine [2,18]. More than 60% of basilar-type migraine patients have vertigo and there are many overlapping clinical manifestations with VM. This diagnosis requires at least 2 symptoms from aura in the posterior circulation territory, whereas most patients with VM have vestibular symptoms only [35]. Moreover, in basilar migraine the duration of vertigo should correspond to the length of an aura, that is, between 5 and 60 minutes [35]. Further studies are required to further elucidate and delineate these 2 conditions.
Other Important Diagnostic Considerations
Meniere’s Disease
An important differential diagnosis of VM is the early presentation of Meniere’s disease (MD). Although fluctuating hearing loss, aural fullness and episodic vertigo are important symptoms in the recent updated diagnostic criteria for definite MD [36,37], these symptoms have been reported in patients with migraine [38]. Moreover, minor abnormalities in cVEMPs and arguably in caloric testing can be found in VM patients, as previously mentioned. Predominantly, the distinction can be made considering that a more sustained, albeit occasionally fluctuating, hearing loss would occur in MD, which can progress to severe hearing loss within a few years. However, the diagnosis can be difficult considering that audiometric and vestibular function abnormalities as well as the typical cochlear symptoms are often absent in the early stages of the MD. Nonetheless, preclinical labelling of patients with episodic vertigo without hearing loss as “vestibular MD” is unhelpful as this population may be overrepresented by actual migraineurs. Studies of patients with so-called benign recurrent vertigo or recurrent vestibulopathy are likely to be heterogeneous entities, with perhaps cases later evolving into VM or MD.
Coexisting migraine and MD is often challenging both in terms of diagnosis and management. Many studies have shown an increased prevalence of migraine in MD patients compared to controls [39,40], an asso-ciation suggested by Prosper Ménière himself in 1861 [41]. A study by Radtke et al found that the lifetime prevalence of migraine with and without aura was over 2 times higher in definite MD patients of both sexes compared to age-matched controls (56% versus 25%) [39]. Interestingly, 45% of the patients with MD always experienced at least 1 migrainous symptom (migrainous headache, photophobia, aura symptoms) with their Meniere attacks [39]. This may be at least partly due to the triggering effect of vestibular symptoms on migraineurs [30]. Migraine may even influence the disease course of MD as indicated by a retrospective case control study which found that definite MD patients who have concomitant ICHD criteria for migraine [35] had a significantly earlier onset of MD symptoms (mean age, 37.2 versus 49.3 years) and a much greater susceptibility to simultaneous bilateral, but not sequential, hearing loss as compared to MD patients without migraine (56% versus 4%) [42]. There were no significant differences in the severity of hearing loss between the 2 groups even when controlling for time to evaluation [42]. A family history of episodic vertigo was seen in 39% of MD patients with migraine, which is significantly higher than the 2% seen in MD patients, suggesting a possible genetic basis for this association [42]. The nature of the association between migraine and MD is not well elucidated, however, some authors propose that migraine leads to isolated microvascular ischaemic damage of the inner ear, presumably through small arterial vasospasm [40,42].
In summary, when the criteria for MD are met together with documented audiometric abnormalities, MD should be diagnosed, even if migraine symptoms occur during the vestibular attacks [18]. Only patients who experience 2 different types of attacks, one fulfilling the criteria for VM and the other for MD, should be labelled as Meniere’s disease/migraine overlap syndrome. It is hoped that future revisions of diagnostic criteria will include this overlap entity.
Migraine and Benign Paroxysmal Positional Vertigo
VM patients can experience brief positional dizziness and therefore VM may mimic BPPV. It is therefore important to perform positional testing to look for nystagmus typical for BPPV. Certainly the positional characteristics are distinct from BPPV with regard to the duration of attacks (often as long as the head position is maintained in VM rather than seconds in BPPV). BPPV may also produce attacks of vertigo that can act as triggers for migraine headaches. In these patients, treatment of the BPPV will reduce headache frequency [30].
Transient Ischemic Attacks
Transient ischemic attack (TIA) is a cerebrovascular disease with temporary neurological symptoms [43] and is differentiated from VM mainly from the characteristics of reported symptoms. Being a vascular phenomenon, one would expect TIA symptoms to have a sudden onset, with a brief duration of symptoms (typically short minutes), followed by a rapid improvement to baseline, as well as correspond to a vascular territory. The other important message is that stereotyped, frequently recurrent symptoms are less likely to be TIAs, with the exception of capsular warning syndrome [44] and limb shaking TIAs [43] described elsewhere.
Migraine and Motion Sickness
In an individual patient it may be difficult to differentiate between motion sickness and acute attacks of VM induced by motion stimuli. The distinction may be helped by observing nausea and dizziness improving after cessation of motion which points more towards motion sickness, as oppose to the persistent vertigo after the motion stimulus has ended, thus pointing more towards VM.
Episodic Ataxia Type 2
Of the various episodic ataxias, episodic ataxia type 2 would be the most important subtype in the differential diagnosis of VM given it presents with episodic vertigo and is the most frequently occurring subtype. It is a rare autosomal dominant inherited neurological disorder resulting from mutations of the calcium channel gene CACNA1A [45]. The clinical manifestations include recurrent disabling attacks of imbalance, vertigo and ataxia, which can be provoked by physical exertion or emotional stress. Patients may have downbeat nystagmus interictally. A slow progression of cerebellar signs accompanied by atrophy of midline cerebellar structures and a response to acetazolamide or 4-aminopyridine can help distinguish it from VM.
Migraine, Dizziness, and Comorbid Psychiatric Disorders
Particularly in patients with protracted symptoms, it is difficult to tease out the difference between the symptoms of migraine and dizziness from the symptoms of certain psychiatric disorders given their bidirectional associations. Migraine is a risk factor for first-onset major depression [46] and panic disorder [47]. Patients with VM have very high rates (30%–65%) of coexisting psychiatric illness, especially anxiety and depression, with frequencies higher than that associated with other migraine or vestibular disorders [48,49]. Vestibular migraine patients who have a positive history of psychiatric disorders have a comparatively higher risk of developing somatoform dizziness [48]. The unpredictability of recurrent vestibular symptoms could be a factor leading to elevated distress in VM patients. It is not uncommon to see a premature diagnosis of psychogenic dizziness to be given to patients without objective abnormalities. On the contrary, a diagnosis of psychogenic dizziness can rarely be made with certainty due to multiple reasons. Disabling vertigo leading to physical symptoms and avoidance of social activities can easily be misconstrued to have panic disorder with or without agoraphobia. Moreover, dizziness is the second most common symptom of a panic attack after palpitations [50].
Unfortunately, there are no objective tests that can reliably discriminate vestibular syndromes from psychiatric syndromes in patients with dizziness. The SVQ is not specific enough to differentiate symptoms of VV from the space and motion discomfort symptoms often found in agoraphobic patients [25]. Experimentally, agoraphobia patients may have a more surface-dependent strategy rather than a visual-dependent strategy on CDP [51]. It is unclear whether the vestibular system is causally linked to emotion processing pathways.
Chronic Subjective Dizziness
Chronic subjective dizziness is an entity characterised by chronic unsteadiness or nonvertiginous dizziness accompanied by hypersensitivity to motion stimuli and poor tolerance for complex visual stimuli lasting for 3 months or more without objective abnormalities [52]. These vestibular symptoms are often difficult to distinguish from symptoms of VM. This condition is thought to be a spatial sensory analog of allodynia experienced by some chronic migraine headache sufferers [8].
Dizziness Due to Side Effects of Migraine Prophylactic Medications
Dizziness is often listed as a side effect in the product information of various medications including those used for migraine prophylaxis. It is important to take an accurate history of the suspected offending drug in terms of its temporal relationship to vestibular symptoms. Tricyclic antidepressants (TCAs) can cause drowsiness, lightheadedness, fatigue and blurred vision [53]. Beta-blockers can cause orthostatic hypotension [53]. All the above effects could be confused with vestibular symptoms.
Treatment of Vestibular Migraine
Current treatment options for VM are mainly limited to expert opinion rather than inferred from randomized controlled trials (RCTs) [54]. Below we have offered our consensus on how VM should be managed, with concepts based on the guidelines of treatment for typical migraine [55]. Avoidance of migraine triggers should always be the first avenue of treatment. In addition, any vestibular disorder that is triggering migraine attacks should be identified and treated in its own right. Pharmacotherapy can be abortive for acute episodes and prophylactic.
Lifestyle Advice
The key first task in management is the correct diagnosis and educating the patient about the condition. A thorough explanation of the migraine origin of the attacks can address patients fear and expectations. Nonpharmaceutical approaches in the treatment of VM should not be neglected, even though only a very small proportion of patients may derive a benefit. Advice on dietary manipulation is routinely given; however, its efficacy in VM is questionable. Dietary advice includes healthy eating at regular intervals to prevent skipped meals as well as avoidance of excess caffeine and rich foods. A retrospective study found that lifestyle intervention alone resulted in 13 of 81 patients experiencing significant relief from vestibular symptoms with migraine. The remaining cohort of patients required a multifaceted approach including pharmacotherapy to achieve similar benefit [56].
Acute Abortive Treatments
Oral antiemetics are commonly prescribed for motion sickness and acute migraine, however there is no evidence supporting their effectiveness in VM (Table 2). Patients should be counselled about avoiding overuse of antiemetics given their risk of causing extrapyramidal side effects [53].
Simple analgesics, such as paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs), have been found to be helpful in acute VM attacks in observational studies. Bikhazi performed a survey of patients presenting to a headache clinic with vestibular symptoms and found that simple analgesics were valued by patients as effective symptomatic treatment, but were not considered as effective as triptans [59]. Doses of simple analgesics are listed in Table 2. Soluble formulations are preferable due to faster absorption and speed of onset. Opioids should be avoided in acute attacks of VM given the risk of developing opioid overuse headache [55].
Migraine Prophylaxis in Vestibular Migraine
TCAs remain a popular choice of migraine prophylaxis amongst neurootologists because of its additional effects on comorbid affective symptoms. We recommend that the starting dose of either amitriptyline or nortriptyline should be between 5 to 10 mg daily at night, slowly uptitrated to response over several weeks up to a maximum of 100 mg at night. Interval electrocardiography should be performed to monitor for prolongation of the QTc interval. A retrospective chart review found 46% of VM patients (by Neuhauser criteria) reported a reduction in dizziness after nortriptyline administration up to 75 mg daily [62]. However, the current evidence is limited to observational studies [59,62–64].
The evidence for beta-blockers is limited in VM but anecdotally has been useful for patients with frequent episodic migraine [59,63,64]. Recommended starting and maintenance doses are listed in Table 3. Furthermore, propranolol can be used in patients with depression [65,66]. Heart rate and electrocardiography should be monitored during dose escalation. Beta-blockers should be avoided in asthmatics. Commonly reported adverse events include cold, extremities reduced exercise tolerance and dizziness [53].
Flunarizine, a calcium channel blocker widely used in migraine [67,68] and vestibular conditions [69], was recently studied in a RCT of 12 weeks' duration for prophylaxis of migrainous vertigo (Neuhauser criteria) in 48 patients [70]. Although flunarizine 10 mg daily did not result in improved headache frequency and severity compared to the control arm, there was a significant improvement in vertigo severity. The most commonly reported side effects of flunarizine are weight gain and somnolence, both of which are minimal or infrequent. Verapamil is another calcium channel blocker that may be helpful but has major limiting adverse effects are bradycardia, constipation and peripheral edema [53].
Pizotifen, a serotonin antagonist, is one of the most well tolerated prophylaxis agents from our experience, however some patients do not adhere to treatment due to drowsiness or weight gain, as evidenced in retrospective case studies [64].
Topiramate with an average daily dose of 100 mg has reported positive results in a prospective observational study of ten patients with VM with auditory symptoms [71]. Nine of 10 patients reported no symptoms after follow-up period of up to sixteen months. The recommended dose is listed in Table 3. Common side effects include distal paresthesias, reduced ability to concentrate and drowsiness [53]. Sodium valproate has been anecdotally effective [59] and is usually well tolerated especially when starting at a low dose of 200 mg at night, slowly titrated to 1200 mg in 2 divided doses. Liver function and full blood evaluation should be monitored on a periodic basis [53].
Third-line medications have only been used anecdotally and should be reserved for extenuating cases (Table 3).
Vestibular Rehabilitation
Vestibular rehabilitation therapy (VRT) has been shown to alleviate significantly ongoing balance and dizziness symptoms in patients with various vestibular disorders [73,74] and improving confidence with balance in elderly patients [75,76]. However, the value of VRT is not as well established in VM. Anecdotally, patients with VM report persistent significant symptoms at the end of a standard VRT period, in contrast to other nonmigrainous patients who appear to be accomplishing their treatment goals faster. However, recent studies [21,73,77] are suggesting that customised VRT may play a useful role in VM, especially since it appears to target issues of anxiety, visual dependence or loss of confidence in balance. Small retrospective case series found that VRT reduced disability scores, and gait and balance function in over 85% of patients with migraine and vestibular symptoms [73,76,77]. An Australian VRT study (21) has recently assessed the efficacy of a 9-week customised VRT in 20 patients with VM compared to 16 patients with vestibular symptoms but without migraine. The customized VRT program consisted of habituation, gaze stability, static tilt, balance and gait exercises. A pictorial exercise instruction sheet for home use would describe these exercises of approximately 15 minutes duration consisting of 4 to 6 exercises to be performed 3 times a day, every day for 9 weeks. Interestingly, both groups benefitted equally from VRT. Compliance with VRT was comparable between the two groups. Commonly reported reasons for non-attendance in VM patients included a recent acute attack of VM, anxiety related to using public transport, and commitment issues related to occupation. This study also suggested that VM patients required more customized and intensive therapy as 15% of VM patients required additional appointments outside the study timeline.
Given that visual dependency has been shown to be reduced with short-term graded optokinetic stimulation exposure in healthy subjects [78], there has been interest using this intervention in conjunction with customized VRT to promote desensitization to visual stimuli as a treatment for VM patients with VV. Most promisingly is the finding that a subgroup of patients with a history of migraine improved significantly more than other vestibular patients with respect to VV symptoms.
There has been controversy surrounding whether patients should avoid medications when undergoing VRT. The protagonists of this view suggest that medications that affect the central nervous system (CNS) may modulate the rate of central compensation. In the aforementioned study by Vitkovic and colleagues [21], the same degree of improvement was seen in the VM group regardless of medication regimen. A study by Whitney and colleagues [73] found that migraine related vestibulopathy patients taking prophylaxis demonstrated better subjective and objective balance scores at baseline and after therapy. Further research is required to clarify the role of CNS-acting medication and their administration around VRT sessions.
Physical therapists dealing with VM patients may face additional challenges in encouraging exercise compliance and providing emotional support. Although more time consuming for the therapist, this is important in the face of high rates of comorbid affective disorders and head motion intolerance. Supervised VRT is believed to implicitly improve psychological status through increasing confidence, providing reassurance, and emphasizing positive effects of VRT, particularly when the patient feels their symptoms have been made worse by it.
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) has been shown to be helpful as part of the holistic treatment of various disorders including post-concussive syndrome and depression in neurology patients [79,80]. Among patients suffering from dizziness, a small study comparing explicit CBT combined with VRT versus waiting-list controls demonstrated improvements in patients’ coping ability, function, symptoms, and care satisfaction [81]. However, to our knowledge there are no studies directly evaluating the benefits of CBT specifically in VM patients. Despite this, it is our practice to request CBT for VM patients who report disabling anxiety or depressive symptoms.
Prognosis
Although migraine in general can improve in later life, this is less certain with VM given the lack of good quality longitudinal studies. Recently Radtke and colleagues published their long-term (median, 9 years) follow-up study of 61 definite VM cases (28). They found that 87% of patients had recurrent vertigo at follow-up. The frequency of vertigo was reduced in 56%, increased in 29%, and unchanged in 16% of patients. The impact of vertigo was graded as severe in 21%, moderate in 43%, and mild in 36% of patients. However, they found that concomitant cochlear symptoms with vertigo had increased from 15% at study inception to 49% at follow-up and secondly, 18% of patients had developed mild bilateral low-frequency sensorineural hearing loss. Therefore, one major criticism of the study is whether some of the patients had MD as their eventual diagnosis rather than definite VM. On the contrary, the authors conclude that these changes represent new vestibulo-cochlear dysfunction as a result of VM disease progression. Due to these reasons, the prognosis of VM patients is unclear. It is our practice to ensure patients do receive delayed follow-up to allow consideration of other neurotological diagnoses.
Conclusion
Given the large heterogeneity in presentation and objective testing, VM as a diagnostic construct has remained quite controversial, though increasingly more accepted. The more we study this common vestibular condition, the more we are realising that the complex relationship between migraine and dizziness extend beyond VM to encompass other vestibular disorders such as MD and anxiety. The lack of a physiological biomarker contributes to its diagnostic difficulties, but a meticulous workup is important to exclude alternative vestibular diagnoses. More longitudinal studies and RCTs are required to help both understand the prognosis and management of VM patients.
Corresponding author: Benjamin K-T Tsang, MBBS, FRACP, The Prince Charles Hospital, Rode Road, Chermside, Queensland 4032, Australia, [email protected].
Financial disclosures: None.
From the Department of Neurootology, National Hospital of Neurology and Neurosurgery, London (Dr. Tsang, Miss Anwer) and the Ear Institute, University College London, and Guy’s and St Thomas’ NHS Foundation Trust, London, UK (Dr. Murdin).
Abstract
- Objective: To review the clinical manifestations, diagnosis, and management of vestibular migraine (VM).
- Methods: Review of the literature.
- Results: Apart from headache, other symptoms of VM include unsteadiness, imbalance, and spontaneous as well as visual vertigo. Acute vestibular symptoms that qualify for VM must be of at least moderate or severe intensity which lasts within a time window of 5 minutes to 72 hours. The interindividual temporal association of headache and vertigo is highly variable in VM patients Grossly normal peripheral vestibular function and audiometry both during and between attacks distinguishes VM from its mimics. Treatment options for VM are mainly based on expert opinion and include lifestyle modifications, acute and prophylactic migraine pharmacotherapy, and vestibular rehabilitation therapy.
- Conclusion: Despite a lack of diagnostic biomarkers for VM, a meticulous workup is important to exclude alternative mimics. More longitudinal and treatment studies are required to help elucidate the prognosis and optimal management of this condition.
The coexistence of migraine and vestibular symptoms has been mentioned in the headache literature for many years [1–3]. It was first addressed by Kayan and Hood in 1984, who found that dizziness and vertigo occurred in 54% of migraine patients compared with 30% of patients with tension-type headache [1]. The frequent coexistence of migraine and vertigo led researchers to hypothesize that their co-occurence could be due to more than mere chance. As per Lempert and Neuhauser’s evaluation, there is a lifetime prevalence of 16% for migraine and 7% for vertigo, with a 1.1 % chance of vertigo and migraine occurring together by chance alone [4]. In a study looking at the point prevalence of vertigo or dizziness among those presenting for a routine appointment at a headache center, an astounding 72.8% of those with severe headaches had vestibular symptoms [5].
Most epidemiologic studies of what we call vestibular migraine (VM) were based on presentations to specialist clinics and were performed in an era during which no established diagnostic criteria existed. Despite this, most neurootologists would consider VM to be one of the most common causes of spontaneous recurrent vertigo [6]. Neuhauser et al reported that VM was diagnosed in 7% of a group of 200 specialist clinic patients with dizziness and 9% of a group of 200 clinic patients who had migraine [2]. In a population-based study in Germany, the lifetime prevalence of VM according to the Neuhauser criteria was estimated to be 0.98% and the 12-month prevalence 0.89% [7]. The condition has a 3:1 female predilection [8].
VM has only recently been recognised as a separate migraine entity by the International Headache Society (IHS), appearing in the appendix of their International Classification of Headache Disorders (ICHD)–3 beta. The previous ICHD recognised vertigo as a migrainous symptom only within the framework of basilar migraine. The nomenclature used in the literature to describe this entity has been inconsistent and therefore confusing, including terms such as migraine-associated vertigo [9], migraine-related dizziness [3] or vertigo [10],migrainous vertigo [2], benign recurrent vertigo [11], and migraine-related vestibulopathy [12]. For the most part, these terms refer to the co-experience of migraine and vertigo or dizziness, with only a few terms having a more specific meaning of how the 2 symptoms relate temporally. Neuhauser and colleagues developed criteria in 2001 to classify migraineurs for whom vestibular symptoms are an integral part of migraine symptomatology, using the term migrainous vertigo [2]. Others preferred the terms migraine-associated dizziness or migraine-related dizziness [3] over migrainous vertigo because they felt the symptoms of vestibular dysfunction related to migraine are varied and may include gait instability and spatial disorientation but not necessarily with vertigo. To best avoid confounding nonvestibular dizziness or motion sickness associated with migraine, VM has been the preferred term because it emphasises the particular vestibular manifestation of migraine.
The lack of a universally accepted definition for this complex entity has contributed to delayed diagnosis and and treatment for those with this disorder. In this article, we will review the clinical manifestation, diagnosis and management of VM, with a focus on assisting in the differentiation between other potential diagnoses.
Pathophysiology of VM
A clear pathophysiology of VM has not been elucidated. Although predominantly a sporadic disease, there have been reported cases of familial occurrence with an auto-somal dominant inheritance [11,13]. Bahmad and colleagues mapped the first locus for familial VM to 5q35 within a 4-generation family [13]. On the contrary, a larger study conducted by Lee et al found VM to be to genetically heterogeneous with a subset linking to chromosome 22q12 [14]. Genetic defects of voltage-gated calcium channels are identified as causal factors for familial hemiplegic migraine and episodic ataxia type 2. Both these disease entities present with vertigo and migraine headaches suggesting a defective gene within the same chromosomal region could indicate a direct genetic link to VM. However, no such gene has been identified.
General consensus is that the action of spreading cortical depression as it reaches the somatosensory cortex in the posterior insula and temporoparietal junction elucidates migraine aura in patients with short attacks. However, due to the heterogeneity of VM, canal paresis and complex conditional nystagmus during acute stages are not explained through cortical spreading. Eggers et al suggests that vertigo symptoms occur as ictal sensation rather than the spreading of sensory or motor cortical depression [15]. However, due to discrepancies within the literature it is apparent that further research needs to be conducted to fully understand the pathophysiology of VM.
Clinical Manifestations of VM
Symptoms
As many as 80% to 90% of patients with VM report unsteadiness or balance problems, of which 50% to 60% typically report episodic spontaneous vertigo [16], either internal vertigo (a false sensation of self-motion) or external vertigo (a false sensation that the visual surround is spinning or flowing) [17]. The duration of episodes is highly variable, whereby approximately 30% of patients have episodes lasting minutes, 30% have attacks lasting hours, 30% have attacks over several days, while the remaining 10% have attacks lasting seconds only [18]. It may be difficult to distinguish if vestibular symptoms lasting seconds are related to their head motion intolerance, also known as head motion–induced vertigo [17], which is another frequent symptom in VM. Head motion–induced vertigo bears many similarities to motion sickness.
The interindividual temporal association of headache and vertigo is highly variable in VM patients and is a reason many patients find this diagnostic construct difficult to accept. Approximately 30% of adult patients eventually diagnosed with VM initially present without headaches [8]. Vertigo is only regularly associated with headache in 25% to 50% of VM patients [2,7]. A minority of patients report headache and vertigo never occurring together [2]. A temporal pattern, presenting as aura, occurs only in approximately 10% of cases [19]; therefore, vestibular episodes of VM should not be regarded as migraine auras [18]. Patients typically have migraine manifesting earlier in life with the vestibular symptoms following [13,20], whereby the mean age at onset of migraine and diagnosis of VM are approximately 22 and 35 years, respectively [2]. Consistently across studies that measure quality of life scores, VM patients report higher subjective levels of disability compared to patients with other vestibular illnesses, despite having less objective abnormalities [21]. Approximately 85% of VM patients experienced vestibular symptoms for at least 1 year before consulting neurootology services [21]. It could be argued that hypersensitivity of percept to vestibular symptoms reflect the general finding of augmented perceptions to various external stimuli underlying migraine [22,23].
Another prominent feature of VM is that patients report a syndrome of visually-induced dizziness termed visual vertigo (VV). This is a heterogeneous syndrome with strabismic, peripheral, and/or central vestibular aetiologies [24]. Patients with VV complain of discomfort, postural destabilisation, dizziness, imbalance and spatial disorientation in challenging visual environments. Examples of such environments include walking down supermarket aisles, observing moving objects (eg, disco lights, people walking, moving traffic) or moving surroundings during travelling, and the movement of the eyes in general [24–26]. Most patients report more than one visual trigger [24]. Visual vertigo can often be difficult to distinguish from oscillopsia in patients with bilateral vestibular failure. What is most surprising is that patients with VV have a similar handicap level yet report much more vestibular symptoms compared with patients with bilateral vestibular failure [25]. Postural reactions triggered by external visual motion are destabilising with respect to the earth-vertical and are normally suppressed by central re-weighting of sensory postural cues [24]. Surprisingly, premorbid levels of anxiety and childhood motion sickness do not appear to have a correlation with VV [25]. Even in normal subjects, certain complex visual stimuli can induce transient motion sickness–like symptoms, as shown in experimental visually induced self-vection [27]. The Situational Characteristics Questionnaire (SVQ) is a 19-question, symptom-based questionnaire that has been shown to be useful in quantifying features of VV and may be useful in gauging improvement following physical therapies [25,26].
Early in the disease course, hearing loss should prompt an alternative diagnosis. However, late onset cochlear symptoms have been reported in VM. A study found that after 9 years of follow-up, the number of patients with cochlear symptoms more than doubled [28].
Clinical Examination Findings
The importance of the clinical examination is to rule out peripheral vestibular dysfunction and perform positional testing to look for benign paroxysmal positional vertigo (BPPV) or central positional nystagmus. Nonetheless, positional nystagmus has been reported in up to 28% of cases, including definite central-type positional nystagmus reported in as many as 18% [28].
Audiometric Findings and Auditory Brainstem Responses
Normal audiometry both during and between attacks is one of the key clinical features that distinguishes VM from Meniere’s disease [29]. Auditory brainstem response (ABR) results are typically normal in about 65% of patients [29]. Abnormal ABR results are typically nonspecific, such as mild elongation of wave I, III and V latencies and less commonly, prolongation of the inter-peak latencies.
Findings on Vestibular Function Testing
Whilst there are some reported abnormalities in vestibular function testing in VM patients, such findings need to be interpreted with caution due to the small number of subjects, as well as the variation in case definition and cut-off values. Most importantly, very few papers studied patients in the acute phase, and in some studies it was not even specified. The majority of studies report that VM patients interictally have grossly normal peripheral vestibular function with occasional minor irregularities. Profound interictal abnormalities such as complete canal paresis are usually indicative of other diagnoses. In between acute attacks, patients with VM typically have normal gaze, saccadic parameters, ocular pursuit gains and optokinetic nystagmus (OKN) gains on electronystagmography (ENG) or videonystagmography (VNG) [3]. A minority had a low amplitude (< 4 degrees per second) persistent positional nystagmus. On rotation testing of the vestibo-ocular reflex there is reduction of the mean gains compared to headache-free controls. Most reports in the literature do support that the majority of VM patients have grossly normal bithermal caloric testing, although abnormalities including higher slow phase velocities and canal paresis (usually partial) are reported [29–31]. The observation that the artificial vestibular stimulation caused by the caloric test was followed by a migraine attack within 24 hours in 49% of patients with migraine is very interesting [30], and it remains to be tested whether this phenomenon has the potential to be of assistance in the diagnosis of VM. Both VM patients and migraineurs without vertigo have similar subtle cVEMP (Cervical vestibular-evoked myogenic potentials) abnormalities, namely decreased global amplitude and absence of habituation [31]. On computerized dynamic posturography (CDP), a test of sway, VM patients typically demonstrate a surface-dependent pattern based on their SOT analysis [3], suggesting that VM patients may have a substantial vestibulo-spinal abnormality leading to difficulties integrating multiple conflicting sensory inputs [32].
Diagnostic Criteria
Separating VM into 2 diagnostic entities seems particularly useful: definite VM and the more sensitive but less specific category of probable VM. The sensitivity and specificity of the proposed criteria still need to be determined. Although some authors criticize the probable diagnostic entity for its heterogeneity, about 50% of patients initially diagnosed with probable VM ultimately progress to definite VM [12,33]. Definite vestibular migraine appears in the ICHD-3 beta but only in the appendix section for “new disorders that need further research for validation.” However, probable VM will not be included until further evidence of its utility has been accumulated.
The diagnosis is particularly challenging when headache is not a regular accompaniment of the vertiginous attacks. A patient diary may help link migrainous and vertigo symptoms. When headache is not a prominent feature of the attacks, the clinician will have to put migrainous triggers or symptoms such as photophobia or scintillating scotomas in the context of vertigo symptoms to aid with the diagnosis. One needs to be pedantic about differentiating the qualifying symptom of phonophobia, which is defined as a sound-induced discomfort that is often transient and bilateral from the uncomfortable distorted loud sound perception, which occurs with a recruiting sensorineural hearing loss, and is often persistent and unilateral [18]. Response to migraine treatment is not sufficiently specific to be included in the diagnostic criteria. High placebo response rates from migraine trials [34] suggest that placebo effects can likewise be expected in the treatment of VM. Despite these challenges, acceptance of the diagnostic entity of VM seems to be gaining momentum. In a follow-up study over 9 years, the diagnosis remained consistent in 85% of patients [33].
Benign Paroxysmal Vertigo of Childhood and Vestibular Migraine in Children
VM can present at any age, however, the ICHD specifically recognises an early vertiginous entity regarded as a precursor syndrome of migraine in otherwise healthy children called benign paroxysmal vertigo of childhood. This diagnosis requires 5 episodes of severe vertigo, occurring without warning and resolving spontaneously after minutes to hours [35]. In between episodes, neurological examination, audiometry, vestibular functions and EEG must be normal. A unilateral throbbing headache may occur during attacks but it is not a mandatory criterion. It is unclear whether these two conditions in children are the same entity, however it is important to note that the classification of VM does not involve any age limit [18].
Basilar-type Migraine
The term basilar migraine should be restricted to patients who fulfill the ICHD diagnostic criteria [35] given it is a clinically distinct entity from VM. Less than 10% of VM patients further fulfill the ICHD criteria for basilar migraine [2,18]. More than 60% of basilar-type migraine patients have vertigo and there are many overlapping clinical manifestations with VM. This diagnosis requires at least 2 symptoms from aura in the posterior circulation territory, whereas most patients with VM have vestibular symptoms only [35]. Moreover, in basilar migraine the duration of vertigo should correspond to the length of an aura, that is, between 5 and 60 minutes [35]. Further studies are required to further elucidate and delineate these 2 conditions.
Other Important Diagnostic Considerations
Meniere’s Disease
An important differential diagnosis of VM is the early presentation of Meniere’s disease (MD). Although fluctuating hearing loss, aural fullness and episodic vertigo are important symptoms in the recent updated diagnostic criteria for definite MD [36,37], these symptoms have been reported in patients with migraine [38]. Moreover, minor abnormalities in cVEMPs and arguably in caloric testing can be found in VM patients, as previously mentioned. Predominantly, the distinction can be made considering that a more sustained, albeit occasionally fluctuating, hearing loss would occur in MD, which can progress to severe hearing loss within a few years. However, the diagnosis can be difficult considering that audiometric and vestibular function abnormalities as well as the typical cochlear symptoms are often absent in the early stages of the MD. Nonetheless, preclinical labelling of patients with episodic vertigo without hearing loss as “vestibular MD” is unhelpful as this population may be overrepresented by actual migraineurs. Studies of patients with so-called benign recurrent vertigo or recurrent vestibulopathy are likely to be heterogeneous entities, with perhaps cases later evolving into VM or MD.
Coexisting migraine and MD is often challenging both in terms of diagnosis and management. Many studies have shown an increased prevalence of migraine in MD patients compared to controls [39,40], an asso-ciation suggested by Prosper Ménière himself in 1861 [41]. A study by Radtke et al found that the lifetime prevalence of migraine with and without aura was over 2 times higher in definite MD patients of both sexes compared to age-matched controls (56% versus 25%) [39]. Interestingly, 45% of the patients with MD always experienced at least 1 migrainous symptom (migrainous headache, photophobia, aura symptoms) with their Meniere attacks [39]. This may be at least partly due to the triggering effect of vestibular symptoms on migraineurs [30]. Migraine may even influence the disease course of MD as indicated by a retrospective case control study which found that definite MD patients who have concomitant ICHD criteria for migraine [35] had a significantly earlier onset of MD symptoms (mean age, 37.2 versus 49.3 years) and a much greater susceptibility to simultaneous bilateral, but not sequential, hearing loss as compared to MD patients without migraine (56% versus 4%) [42]. There were no significant differences in the severity of hearing loss between the 2 groups even when controlling for time to evaluation [42]. A family history of episodic vertigo was seen in 39% of MD patients with migraine, which is significantly higher than the 2% seen in MD patients, suggesting a possible genetic basis for this association [42]. The nature of the association between migraine and MD is not well elucidated, however, some authors propose that migraine leads to isolated microvascular ischaemic damage of the inner ear, presumably through small arterial vasospasm [40,42].
In summary, when the criteria for MD are met together with documented audiometric abnormalities, MD should be diagnosed, even if migraine symptoms occur during the vestibular attacks [18]. Only patients who experience 2 different types of attacks, one fulfilling the criteria for VM and the other for MD, should be labelled as Meniere’s disease/migraine overlap syndrome. It is hoped that future revisions of diagnostic criteria will include this overlap entity.
Migraine and Benign Paroxysmal Positional Vertigo
VM patients can experience brief positional dizziness and therefore VM may mimic BPPV. It is therefore important to perform positional testing to look for nystagmus typical for BPPV. Certainly the positional characteristics are distinct from BPPV with regard to the duration of attacks (often as long as the head position is maintained in VM rather than seconds in BPPV). BPPV may also produce attacks of vertigo that can act as triggers for migraine headaches. In these patients, treatment of the BPPV will reduce headache frequency [30].
Transient Ischemic Attacks
Transient ischemic attack (TIA) is a cerebrovascular disease with temporary neurological symptoms [43] and is differentiated from VM mainly from the characteristics of reported symptoms. Being a vascular phenomenon, one would expect TIA symptoms to have a sudden onset, with a brief duration of symptoms (typically short minutes), followed by a rapid improvement to baseline, as well as correspond to a vascular territory. The other important message is that stereotyped, frequently recurrent symptoms are less likely to be TIAs, with the exception of capsular warning syndrome [44] and limb shaking TIAs [43] described elsewhere.
Migraine and Motion Sickness
In an individual patient it may be difficult to differentiate between motion sickness and acute attacks of VM induced by motion stimuli. The distinction may be helped by observing nausea and dizziness improving after cessation of motion which points more towards motion sickness, as oppose to the persistent vertigo after the motion stimulus has ended, thus pointing more towards VM.
Episodic Ataxia Type 2
Of the various episodic ataxias, episodic ataxia type 2 would be the most important subtype in the differential diagnosis of VM given it presents with episodic vertigo and is the most frequently occurring subtype. It is a rare autosomal dominant inherited neurological disorder resulting from mutations of the calcium channel gene CACNA1A [45]. The clinical manifestations include recurrent disabling attacks of imbalance, vertigo and ataxia, which can be provoked by physical exertion or emotional stress. Patients may have downbeat nystagmus interictally. A slow progression of cerebellar signs accompanied by atrophy of midline cerebellar structures and a response to acetazolamide or 4-aminopyridine can help distinguish it from VM.
Migraine, Dizziness, and Comorbid Psychiatric Disorders
Particularly in patients with protracted symptoms, it is difficult to tease out the difference between the symptoms of migraine and dizziness from the symptoms of certain psychiatric disorders given their bidirectional associations. Migraine is a risk factor for first-onset major depression [46] and panic disorder [47]. Patients with VM have very high rates (30%–65%) of coexisting psychiatric illness, especially anxiety and depression, with frequencies higher than that associated with other migraine or vestibular disorders [48,49]. Vestibular migraine patients who have a positive history of psychiatric disorders have a comparatively higher risk of developing somatoform dizziness [48]. The unpredictability of recurrent vestibular symptoms could be a factor leading to elevated distress in VM patients. It is not uncommon to see a premature diagnosis of psychogenic dizziness to be given to patients without objective abnormalities. On the contrary, a diagnosis of psychogenic dizziness can rarely be made with certainty due to multiple reasons. Disabling vertigo leading to physical symptoms and avoidance of social activities can easily be misconstrued to have panic disorder with or without agoraphobia. Moreover, dizziness is the second most common symptom of a panic attack after palpitations [50].
Unfortunately, there are no objective tests that can reliably discriminate vestibular syndromes from psychiatric syndromes in patients with dizziness. The SVQ is not specific enough to differentiate symptoms of VV from the space and motion discomfort symptoms often found in agoraphobic patients [25]. Experimentally, agoraphobia patients may have a more surface-dependent strategy rather than a visual-dependent strategy on CDP [51]. It is unclear whether the vestibular system is causally linked to emotion processing pathways.
Chronic Subjective Dizziness
Chronic subjective dizziness is an entity characterised by chronic unsteadiness or nonvertiginous dizziness accompanied by hypersensitivity to motion stimuli and poor tolerance for complex visual stimuli lasting for 3 months or more without objective abnormalities [52]. These vestibular symptoms are often difficult to distinguish from symptoms of VM. This condition is thought to be a spatial sensory analog of allodynia experienced by some chronic migraine headache sufferers [8].
Dizziness Due to Side Effects of Migraine Prophylactic Medications
Dizziness is often listed as a side effect in the product information of various medications including those used for migraine prophylaxis. It is important to take an accurate history of the suspected offending drug in terms of its temporal relationship to vestibular symptoms. Tricyclic antidepressants (TCAs) can cause drowsiness, lightheadedness, fatigue and blurred vision [53]. Beta-blockers can cause orthostatic hypotension [53]. All the above effects could be confused with vestibular symptoms.
Treatment of Vestibular Migraine
Current treatment options for VM are mainly limited to expert opinion rather than inferred from randomized controlled trials (RCTs) [54]. Below we have offered our consensus on how VM should be managed, with concepts based on the guidelines of treatment for typical migraine [55]. Avoidance of migraine triggers should always be the first avenue of treatment. In addition, any vestibular disorder that is triggering migraine attacks should be identified and treated in its own right. Pharmacotherapy can be abortive for acute episodes and prophylactic.
Lifestyle Advice
The key first task in management is the correct diagnosis and educating the patient about the condition. A thorough explanation of the migraine origin of the attacks can address patients fear and expectations. Nonpharmaceutical approaches in the treatment of VM should not be neglected, even though only a very small proportion of patients may derive a benefit. Advice on dietary manipulation is routinely given; however, its efficacy in VM is questionable. Dietary advice includes healthy eating at regular intervals to prevent skipped meals as well as avoidance of excess caffeine and rich foods. A retrospective study found that lifestyle intervention alone resulted in 13 of 81 patients experiencing significant relief from vestibular symptoms with migraine. The remaining cohort of patients required a multifaceted approach including pharmacotherapy to achieve similar benefit [56].
Acute Abortive Treatments
Oral antiemetics are commonly prescribed for motion sickness and acute migraine, however there is no evidence supporting their effectiveness in VM (Table 2). Patients should be counselled about avoiding overuse of antiemetics given their risk of causing extrapyramidal side effects [53].
Simple analgesics, such as paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs), have been found to be helpful in acute VM attacks in observational studies. Bikhazi performed a survey of patients presenting to a headache clinic with vestibular symptoms and found that simple analgesics were valued by patients as effective symptomatic treatment, but were not considered as effective as triptans [59]. Doses of simple analgesics are listed in Table 2. Soluble formulations are preferable due to faster absorption and speed of onset. Opioids should be avoided in acute attacks of VM given the risk of developing opioid overuse headache [55].
Migraine Prophylaxis in Vestibular Migraine
TCAs remain a popular choice of migraine prophylaxis amongst neurootologists because of its additional effects on comorbid affective symptoms. We recommend that the starting dose of either amitriptyline or nortriptyline should be between 5 to 10 mg daily at night, slowly uptitrated to response over several weeks up to a maximum of 100 mg at night. Interval electrocardiography should be performed to monitor for prolongation of the QTc interval. A retrospective chart review found 46% of VM patients (by Neuhauser criteria) reported a reduction in dizziness after nortriptyline administration up to 75 mg daily [62]. However, the current evidence is limited to observational studies [59,62–64].
The evidence for beta-blockers is limited in VM but anecdotally has been useful for patients with frequent episodic migraine [59,63,64]. Recommended starting and maintenance doses are listed in Table 3. Furthermore, propranolol can be used in patients with depression [65,66]. Heart rate and electrocardiography should be monitored during dose escalation. Beta-blockers should be avoided in asthmatics. Commonly reported adverse events include cold, extremities reduced exercise tolerance and dizziness [53].
Flunarizine, a calcium channel blocker widely used in migraine [67,68] and vestibular conditions [69], was recently studied in a RCT of 12 weeks' duration for prophylaxis of migrainous vertigo (Neuhauser criteria) in 48 patients [70]. Although flunarizine 10 mg daily did not result in improved headache frequency and severity compared to the control arm, there was a significant improvement in vertigo severity. The most commonly reported side effects of flunarizine are weight gain and somnolence, both of which are minimal or infrequent. Verapamil is another calcium channel blocker that may be helpful but has major limiting adverse effects are bradycardia, constipation and peripheral edema [53].
Pizotifen, a serotonin antagonist, is one of the most well tolerated prophylaxis agents from our experience, however some patients do not adhere to treatment due to drowsiness or weight gain, as evidenced in retrospective case studies [64].
Topiramate with an average daily dose of 100 mg has reported positive results in a prospective observational study of ten patients with VM with auditory symptoms [71]. Nine of 10 patients reported no symptoms after follow-up period of up to sixteen months. The recommended dose is listed in Table 3. Common side effects include distal paresthesias, reduced ability to concentrate and drowsiness [53]. Sodium valproate has been anecdotally effective [59] and is usually well tolerated especially when starting at a low dose of 200 mg at night, slowly titrated to 1200 mg in 2 divided doses. Liver function and full blood evaluation should be monitored on a periodic basis [53].
Third-line medications have only been used anecdotally and should be reserved for extenuating cases (Table 3).
Vestibular Rehabilitation
Vestibular rehabilitation therapy (VRT) has been shown to alleviate significantly ongoing balance and dizziness symptoms in patients with various vestibular disorders [73,74] and improving confidence with balance in elderly patients [75,76]. However, the value of VRT is not as well established in VM. Anecdotally, patients with VM report persistent significant symptoms at the end of a standard VRT period, in contrast to other nonmigrainous patients who appear to be accomplishing their treatment goals faster. However, recent studies [21,73,77] are suggesting that customised VRT may play a useful role in VM, especially since it appears to target issues of anxiety, visual dependence or loss of confidence in balance. Small retrospective case series found that VRT reduced disability scores, and gait and balance function in over 85% of patients with migraine and vestibular symptoms [73,76,77]. An Australian VRT study (21) has recently assessed the efficacy of a 9-week customised VRT in 20 patients with VM compared to 16 patients with vestibular symptoms but without migraine. The customized VRT program consisted of habituation, gaze stability, static tilt, balance and gait exercises. A pictorial exercise instruction sheet for home use would describe these exercises of approximately 15 minutes duration consisting of 4 to 6 exercises to be performed 3 times a day, every day for 9 weeks. Interestingly, both groups benefitted equally from VRT. Compliance with VRT was comparable between the two groups. Commonly reported reasons for non-attendance in VM patients included a recent acute attack of VM, anxiety related to using public transport, and commitment issues related to occupation. This study also suggested that VM patients required more customized and intensive therapy as 15% of VM patients required additional appointments outside the study timeline.
Given that visual dependency has been shown to be reduced with short-term graded optokinetic stimulation exposure in healthy subjects [78], there has been interest using this intervention in conjunction with customized VRT to promote desensitization to visual stimuli as a treatment for VM patients with VV. Most promisingly is the finding that a subgroup of patients with a history of migraine improved significantly more than other vestibular patients with respect to VV symptoms.
There has been controversy surrounding whether patients should avoid medications when undergoing VRT. The protagonists of this view suggest that medications that affect the central nervous system (CNS) may modulate the rate of central compensation. In the aforementioned study by Vitkovic and colleagues [21], the same degree of improvement was seen in the VM group regardless of medication regimen. A study by Whitney and colleagues [73] found that migraine related vestibulopathy patients taking prophylaxis demonstrated better subjective and objective balance scores at baseline and after therapy. Further research is required to clarify the role of CNS-acting medication and their administration around VRT sessions.
Physical therapists dealing with VM patients may face additional challenges in encouraging exercise compliance and providing emotional support. Although more time consuming for the therapist, this is important in the face of high rates of comorbid affective disorders and head motion intolerance. Supervised VRT is believed to implicitly improve psychological status through increasing confidence, providing reassurance, and emphasizing positive effects of VRT, particularly when the patient feels their symptoms have been made worse by it.
Cognitive Behavioral Therapy
Cognitive behavioral therapy (CBT) has been shown to be helpful as part of the holistic treatment of various disorders including post-concussive syndrome and depression in neurology patients [79,80]. Among patients suffering from dizziness, a small study comparing explicit CBT combined with VRT versus waiting-list controls demonstrated improvements in patients’ coping ability, function, symptoms, and care satisfaction [81]. However, to our knowledge there are no studies directly evaluating the benefits of CBT specifically in VM patients. Despite this, it is our practice to request CBT for VM patients who report disabling anxiety or depressive symptoms.
Prognosis
Although migraine in general can improve in later life, this is less certain with VM given the lack of good quality longitudinal studies. Recently Radtke and colleagues published their long-term (median, 9 years) follow-up study of 61 definite VM cases (28). They found that 87% of patients had recurrent vertigo at follow-up. The frequency of vertigo was reduced in 56%, increased in 29%, and unchanged in 16% of patients. The impact of vertigo was graded as severe in 21%, moderate in 43%, and mild in 36% of patients. However, they found that concomitant cochlear symptoms with vertigo had increased from 15% at study inception to 49% at follow-up and secondly, 18% of patients had developed mild bilateral low-frequency sensorineural hearing loss. Therefore, one major criticism of the study is whether some of the patients had MD as their eventual diagnosis rather than definite VM. On the contrary, the authors conclude that these changes represent new vestibulo-cochlear dysfunction as a result of VM disease progression. Due to these reasons, the prognosis of VM patients is unclear. It is our practice to ensure patients do receive delayed follow-up to allow consideration of other neurotological diagnoses.
Conclusion
Given the large heterogeneity in presentation and objective testing, VM as a diagnostic construct has remained quite controversial, though increasingly more accepted. The more we study this common vestibular condition, the more we are realising that the complex relationship between migraine and dizziness extend beyond VM to encompass other vestibular disorders such as MD and anxiety. The lack of a physiological biomarker contributes to its diagnostic difficulties, but a meticulous workup is important to exclude alternative vestibular diagnoses. More longitudinal studies and RCTs are required to help both understand the prognosis and management of VM patients.
Corresponding author: Benjamin K-T Tsang, MBBS, FRACP, The Prince Charles Hospital, Rode Road, Chermside, Queensland 4032, Australia, [email protected].
Financial disclosures: None.
1. Kayan A, Hood JD. Neuro-otological manifestations of migraine. Brain 1984;107(Pt 4):1123–42.
2. Neuhauser H, Leopold M, von Brevern M, et al. The interrelations of migraine, vertigo, and migrainous vertigo. Neurology 2001;56:436–41.
3. Furman JM, Sparto PJ, Soso M, Marcus D. Vestibular function in migraine-related dizziness: a pilot study. J Vestib Res 2005;15:327–32.
4. Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. J Neurol 2009;256:333–8.
5. Calhoun AH, Ford S, Pruitt AP, Fisher KG. The point prevalence of dizziness or vertigo in migraine--and factors that influence presentation. Headache 2011;51:1388–92.
6. Bisdorff A. Migraine and dizziness. Curr Opin Neurol 2014;27:105–10.
7. Neuhauser HK, Radtke A, von Brevern M, et al. Migrainous vertigo: prevalence and impact on quality of life. Neurology 2006;67:1028–33.
8. Sargent EW. The challenge of vestibular migraine. Curr Opin Otolaryngol Head Neck Surg 2013;21:473–9.
9. Cha YH. Migraine-associated vertigo: diagnosis and treatment. Sem Neurol 2010;30:167–74.
10. Cherian N. Vertigo as a migraine phenomenon. Curr Neurol Neurosci Rep 2013;13:343.
11. Oh AK, Lee H, Jen JC, et al. Familial benign recurrent vertigo. Am J Med Genet 2001;100:287–91.
12. Cass SP, Furman JM, Ankerstjerne K, et al. Migraine-related vestibulopathy. Ann Otol Rhinol Laryngol 1997;106:182–9.
13. Bahmad F Jr, DePalma SR, Merchant SN, et al. Locus for familial migrainous vertigo disease maps to chromosome 5q35. Ann Otol Rhinol Laryngol 2009;118:670–6.
14. Lee H, Jen JC, Wang H, et al. A genome-wide linkage scan of familial benign recurrent vertigo: linkage to 22q12 with evidence of heterogeneity. Hum Molec Genet 2006;15:251–8.
15. Eggers SD, Neff BA, Shepard NT, Staab JP. Comorbidities in vestibular migraine. J Vestib Res 2014;24:387–95.
16. Cohen JM, Bigal ME, Newman LC. Migraine and vestibular symptoms--identifying clinical features that predict “vestibular migraine”. Headache 2011;51:1393–7.
17. Bisdorff A, Von Brevern M, Lempert T, Newman-Toker DE. Classification of vestibular symptoms: towards an international classification of vestibular disorders. J Vestib Res 2009;19:1-13.
18. Lempert T, Olesen J, Furman J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res 2012;22:167-72.
19. Dieterich M, Brandt T. Episodic vertigo related to migraine (90 cases): vestibular migraine? J Neurol 1999;246:883–92.
20. Eggers SD, Staab JP, Neff BA, et al. Investigation of the coherence of definite and probable vestibular migraine as distinct clinical entities. Otol Neurotol 2011;32:1144–51.
21. Vitkovic J, Winoto A, Rance G, et al. Vestibular rehabilitation outcomes in patients with and without vestibular migraine. J Neurol 2013;260:3039–48.
22. Kelman L. Osmophobia and taste abnormality in migraineurs: a tertiary care study. Headache 2004;44:1019–23.
23. Morrison DP. Abnormal perceptual experiences in migraine. Cephalalgia 1990;10:273–7.
24. Bronstein AM. Visual vertigo syndrome: clinical and posturography findings. J Neurol Neurosurg Psych 1995;59:472–6.
25. Guerraz M, Yardley L, Bertholon P, et al. Visual vertigo: symptom assessment, spatial orientation and postural control. Brain 2001;124(Pt 8):1646–56.
26. Pavlou M, Davies RA, Bronstein AM. The assessment of increased sensitivity to visual stimuli in patients with chronic dizziness. J Vestib Res 2006;16:223-31.
27. Dobie TG, May JG, Gutierrez C, Heller SS. The transfer of adaptation between actual and simulated rotary stimulation. Aviat Space Environ Med 1990;61:1085–91.
28. Radtke A, von Brevern M, Neuhauser H, et al. Vestibular migraine: long-term follow-up of clinical symptoms and vestibulo-cochlear findings. Neurology 2012;79:1607–14.
29. Bayazit Y, Yilmaz M, Mumbuc S, Kanlikama M. Assessment of migraine-related cochleovestibular symptoms. Revue Laryngol Otol Rhinol 2001;122:85–8.
30. Murdin L, Davies RA, Bronstein AM. Vertigo as a migraine trigger. Neurology 2009;73:638–42.
31. Roceanu A, Allena M, De Pasqua V, et al. Abnormalities of the vestibulo-collic reflex are similar in migraineurs with and without vertigo. Cephalalgia 2008;28:988–90.
32. Hong HR, Shim DB, Kim TS, et al. Results of caloric and sensory organization testing of dynamic posturography in migrainous vertigo: comparison with Meniere’s disease and vestibular neuritis. Acta Otolaryngol 2013;133:1236–41.
33. Radtke A, Neuhauser H, von Brevern M, et al. Vestibular migraine--validity of clinical diagnostic criteria. Cephalalgia 2011;31:906-13.
34. Rothner AD, Wasiewski W, Winner P, et al. Zolmitriptan oral tablet in migraine treatment: high placebo responses in adolescents. Headache 2006;46:101-9.
35. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd ed (beta version). Cephalalgia 2013;33:629–808.
36. Lopez-Escamez JA, Carey J, Chung WH, et al. Diagnostic criteria for Meniere’s disease. J Vestib Res 2015;25:1–7.
37. Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Meniere’s disease. American Academy of Otolaryngology-Head and Neck Foundation. Otolaryngol Head Neck Surg 1995;113:181–5.
38. Baloh RW. Neurotology of migraine. Headache 1997;37:615-21.
39. Radtke A, Lempert T, Gresty MA, et al. Migraine and Meniere’s disease: is there a link? Neurology 2002;59:1700–4.
40. Lee H, Lopez I, Ishiyama A, Baloh RW. Can migraine damage the inner ear? Arch Neurol 2000;57:1631–4.
41. Ménière P. Pathologie auriculaire: memoires sur une lésion de l’oreille interne donnant lieu à des symptoms de congestion cérébrale apoplectiforme. Gaz Med Paris 1861;16:597–601.
42. Cha YH, Brodsky J, Ishiyama G, et al. The relevance of migraine in patients with Meniere’s disease. Acta Otolaryngol 2007;127:1241–5.
43. Kim JS. Symptoms of transient ischemic attack. Front Neurol Neurosci 2014;33:82–102.
44. Paul NL, Simoni M, Chandratheva A, Rothwell PM. Population-based study of capsular warning syndrome and prognosis after early recurrent TIA. Neurology 2012;79:1356–62.
45. Strupp M, Zwergal A, Brandt T. Episodic ataxia type 2. Neurotherapeutics 2007;4:267–73.
46. Breslau N, Schultz LR, Stewart WF, et al. Headache and major depression: is the association specific to migraine? Neurology 2000;54:308–13.
47. Breslau N, Schultz LR, Stewart WF, et al. Headache types and panic disorder: directionality and specificity. Neurology 2001;56:350–4.
48. Best C, Eckhardt-Henn A, Tschan R, Dieterich M. Psychiatric morbidity and comorbidity in different vestibular vertigo syndromes. Results of a prospective longitudinal study over one year. J Neurol 2009;256:58–65.
49. Eckhardt-Henn A, Best C, Bense S, et al. Psychiatric comorbidity in different organic vertigo syndromes. J Neurol 2008;255:420–8.
50. Segui J, Salvador-Carulla L, Garcia L, et al. Semiology and subtyping of panic disorders. Act Psychiatr Scand 1998;97:272–7.
51. Jacob RG, Furman JM, Durrant JD, Turner SM. Surface dependence: a balance control strategy in panic disorder with agoraphobia. Psychosom Med 1997;59:323–30.
52. Ruckenstein MJ, Staab JP. Chronic subjective dizziness. Otolaryngol Clin North Am 2009;42:71–7, ix.
53. Australian medicines handbook : AMH. Adelaide, S.Aust.: Australian Medicines Handbook; 2015. p. v.
54. Maldonado Fernandez M, Birdi JS, Irving GJ, et al. Pharmacological agents for the prevention of vestibular migraine. Cochrane Database Syst Rev 2015;6:CD010600.
55. British Association for the Study of Headache. Guidelines for all healthcare professionals in the diagnosis and management of migraine, tension-type headache, cluster headache and medication overuse headache. 3rd ed. 2010.
56. Reploeg MD, Goebel JA. Migraine-associated dizziness: patient characteristics and management options. Otol Neurotol 2002;23:364–71.
57. Neuhauser H, Radtke A, von Brevern M, Lempert T. Zolmitriptan for treatment of migrainous vertigo: a pilot randomized placebo-controlled trial. Neurology 2003;60:882–3.
58. Roberto G, Raschi E, Piccinni C, et al. Adverse cardiovascular events associated with triptans and ergotamines for treatment of migraine: systematic review of observational studies. Cephalalgia 2015;35:118–31.
59. Bikhazi P, Jackson C, Ruckenstein MJ. Efficacy of antimigrainous therapy in the treatment of migraine-associated dizziness. Am J Otol 1997;18:350–4.
60. MedicinesComplete. London: Pharmaceutical Press. Available at www.medicinescomplete.com.
61. Tfelt-Hansen P, De Vries P, Saxena PR. Triptans in migraine: a comparative review of pharmacology, pharmacokinetics and efficacy. Drugs 2000;60:1259–87.
62. Mikulec AA, Faraji F, Kinsella LJ. Evaluation of the efficacy of caffeine cessation, nortriptyline, and topiramate therapy in vestibular migraine and complex dizziness of unknown etiology. Am J Otolaryngol 2012;33:121–7.
63. Maione A. Migraine-related vertigo: diagnostic criteria and prophylactic treatment. Laryngoscope 2006;116:1782–6.
64. Waterston J. Chronic migrainous vertigo. J Clin Neurosci 2004;11:384–8.
65. de Bock GH, Eelhart J, van Marwijk HW, et al. A postmarketing study of flunarizine in migraine and vertigo. Pharm World Sci 1997;19:269–74.
66. Verspeelt J, De Locht P, Amery WK. Postmarketing study of the use of flunarizine in vestibular vertigo and in migraine. Eur J Clin Pharmacol 1996;51:15–22.
67. Schmidt R, Oestreich W. Flunarizine in migraine prophylaxis: the clinical experience. J Cardiovasc Pharmacol 1991;18 Suppl 8:S21–6.
68. Lucetti C, Nuti A, Pavese N, et al. Flunarizine in migraine prophylaxis: predictive factors for a positive response. Cephalalgia 1998;18:349–52.
69. Schmidt R, Oestreich W. Flunarizine in the treatment of vestibular vertigo: experimental and clinical data. J Cardiovasc Pharmacol 1991;18 Suppl 8:S27–30.
70. Lepcha A, Amalanathan S, Augustine AM, et al. Flunarizine in the prophylaxis of migrainous vertigo: a randomized controlled trial. Eur Arch Otorhinolaryngol 2014;271:2931–6.
71. Carmona S, Settecase N. Use of topiramate (topamax) in a subgroup of migraine-vertigo patients with auditory symptoms. Ann N Y Acad Sci 2005;1039:517–20.
72. Bisdorff AR. Treatment of migraine related vertigo with lamotrigine an observational study. Bull Soc Sci Med Grand Duche Luxemb 2004:103–8.
73. Whitney SL, Rossi MM. Efficacy of vestibular rehabilitation. Otolaryngol Clin North Am 2000;33:659–72.
74. Enticott JC, Vitkovic JJ, Reid B, et al. Vestibular rehabilitation in individuals with inner-ear dysfunction: a pilot study. Audiol Neurootol 2008;13:19–28.
75. Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the activities-specific balance confidence (ABC) scale. J Gerontol Ser A Biol Sci Med Sci 1998;53:M287–94.
76. Wrisley DM, Whitney SL, Furman JM. Vestibular rehabilitation outcomes in patients with a history of migraine. Otol Neurotol 2002;23:483–7.
77. Gottshall KR, Moore RJ, Hoffer ME. Vestibular rehabilitation for migraine-associated dizziness. Int Tinnitus J 2005;11:81–4.
78. Pavlou M, Quinn C, Murray K, et al. The effect of repeated visual motion stimuli on visual dependence and postural control in normal subjects. Gait Posture 2011;33:113–8.
79. Leddy JJ, Sandhu H, Sodhi V, et al. Rehabilitation of concussion and post-concussion syndrome. Sports Health 2012;4:147–54.
80. Fernie BA, Kollmann J, Brown RG. Cognitive behavioural interventions for depression in chronic neurological conditions: a systematic review. J Psychosom Res 2015;78:411–9.
81. Andersson G, Asmundson GJ, Denev J, et al. A controlled trial of cognitive-behavior therapy combined with vestibular rehabilitation in the treatment of dizziness. Behav Res Ther 2006;44:1265–73.
1. Kayan A, Hood JD. Neuro-otological manifestations of migraine. Brain 1984;107(Pt 4):1123–42.
2. Neuhauser H, Leopold M, von Brevern M, et al. The interrelations of migraine, vertigo, and migrainous vertigo. Neurology 2001;56:436–41.
3. Furman JM, Sparto PJ, Soso M, Marcus D. Vestibular function in migraine-related dizziness: a pilot study. J Vestib Res 2005;15:327–32.
4. Lempert T, Neuhauser H. Epidemiology of vertigo, migraine and vestibular migraine. J Neurol 2009;256:333–8.
5. Calhoun AH, Ford S, Pruitt AP, Fisher KG. The point prevalence of dizziness or vertigo in migraine--and factors that influence presentation. Headache 2011;51:1388–92.
6. Bisdorff A. Migraine and dizziness. Curr Opin Neurol 2014;27:105–10.
7. Neuhauser HK, Radtke A, von Brevern M, et al. Migrainous vertigo: prevalence and impact on quality of life. Neurology 2006;67:1028–33.
8. Sargent EW. The challenge of vestibular migraine. Curr Opin Otolaryngol Head Neck Surg 2013;21:473–9.
9. Cha YH. Migraine-associated vertigo: diagnosis and treatment. Sem Neurol 2010;30:167–74.
10. Cherian N. Vertigo as a migraine phenomenon. Curr Neurol Neurosci Rep 2013;13:343.
11. Oh AK, Lee H, Jen JC, et al. Familial benign recurrent vertigo. Am J Med Genet 2001;100:287–91.
12. Cass SP, Furman JM, Ankerstjerne K, et al. Migraine-related vestibulopathy. Ann Otol Rhinol Laryngol 1997;106:182–9.
13. Bahmad F Jr, DePalma SR, Merchant SN, et al. Locus for familial migrainous vertigo disease maps to chromosome 5q35. Ann Otol Rhinol Laryngol 2009;118:670–6.
14. Lee H, Jen JC, Wang H, et al. A genome-wide linkage scan of familial benign recurrent vertigo: linkage to 22q12 with evidence of heterogeneity. Hum Molec Genet 2006;15:251–8.
15. Eggers SD, Neff BA, Shepard NT, Staab JP. Comorbidities in vestibular migraine. J Vestib Res 2014;24:387–95.
16. Cohen JM, Bigal ME, Newman LC. Migraine and vestibular symptoms--identifying clinical features that predict “vestibular migraine”. Headache 2011;51:1393–7.
17. Bisdorff A, Von Brevern M, Lempert T, Newman-Toker DE. Classification of vestibular symptoms: towards an international classification of vestibular disorders. J Vestib Res 2009;19:1-13.
18. Lempert T, Olesen J, Furman J, et al. Vestibular migraine: diagnostic criteria. J Vestib Res 2012;22:167-72.
19. Dieterich M, Brandt T. Episodic vertigo related to migraine (90 cases): vestibular migraine? J Neurol 1999;246:883–92.
20. Eggers SD, Staab JP, Neff BA, et al. Investigation of the coherence of definite and probable vestibular migraine as distinct clinical entities. Otol Neurotol 2011;32:1144–51.
21. Vitkovic J, Winoto A, Rance G, et al. Vestibular rehabilitation outcomes in patients with and without vestibular migraine. J Neurol 2013;260:3039–48.
22. Kelman L. Osmophobia and taste abnormality in migraineurs: a tertiary care study. Headache 2004;44:1019–23.
23. Morrison DP. Abnormal perceptual experiences in migraine. Cephalalgia 1990;10:273–7.
24. Bronstein AM. Visual vertigo syndrome: clinical and posturography findings. J Neurol Neurosurg Psych 1995;59:472–6.
25. Guerraz M, Yardley L, Bertholon P, et al. Visual vertigo: symptom assessment, spatial orientation and postural control. Brain 2001;124(Pt 8):1646–56.
26. Pavlou M, Davies RA, Bronstein AM. The assessment of increased sensitivity to visual stimuli in patients with chronic dizziness. J Vestib Res 2006;16:223-31.
27. Dobie TG, May JG, Gutierrez C, Heller SS. The transfer of adaptation between actual and simulated rotary stimulation. Aviat Space Environ Med 1990;61:1085–91.
28. Radtke A, von Brevern M, Neuhauser H, et al. Vestibular migraine: long-term follow-up of clinical symptoms and vestibulo-cochlear findings. Neurology 2012;79:1607–14.
29. Bayazit Y, Yilmaz M, Mumbuc S, Kanlikama M. Assessment of migraine-related cochleovestibular symptoms. Revue Laryngol Otol Rhinol 2001;122:85–8.
30. Murdin L, Davies RA, Bronstein AM. Vertigo as a migraine trigger. Neurology 2009;73:638–42.
31. Roceanu A, Allena M, De Pasqua V, et al. Abnormalities of the vestibulo-collic reflex are similar in migraineurs with and without vertigo. Cephalalgia 2008;28:988–90.
32. Hong HR, Shim DB, Kim TS, et al. Results of caloric and sensory organization testing of dynamic posturography in migrainous vertigo: comparison with Meniere’s disease and vestibular neuritis. Acta Otolaryngol 2013;133:1236–41.
33. Radtke A, Neuhauser H, von Brevern M, et al. Vestibular migraine--validity of clinical diagnostic criteria. Cephalalgia 2011;31:906-13.
34. Rothner AD, Wasiewski W, Winner P, et al. Zolmitriptan oral tablet in migraine treatment: high placebo responses in adolescents. Headache 2006;46:101-9.
35. Headache Classification Committee of the International Headache Society. The International Classification of Headache Disorders, 3rd ed (beta version). Cephalalgia 2013;33:629–808.
36. Lopez-Escamez JA, Carey J, Chung WH, et al. Diagnostic criteria for Meniere’s disease. J Vestib Res 2015;25:1–7.
37. Committee on Hearing and Equilibrium guidelines for the diagnosis and evaluation of therapy in Meniere’s disease. American Academy of Otolaryngology-Head and Neck Foundation. Otolaryngol Head Neck Surg 1995;113:181–5.
38. Baloh RW. Neurotology of migraine. Headache 1997;37:615-21.
39. Radtke A, Lempert T, Gresty MA, et al. Migraine and Meniere’s disease: is there a link? Neurology 2002;59:1700–4.
40. Lee H, Lopez I, Ishiyama A, Baloh RW. Can migraine damage the inner ear? Arch Neurol 2000;57:1631–4.
41. Ménière P. Pathologie auriculaire: memoires sur une lésion de l’oreille interne donnant lieu à des symptoms de congestion cérébrale apoplectiforme. Gaz Med Paris 1861;16:597–601.
42. Cha YH, Brodsky J, Ishiyama G, et al. The relevance of migraine in patients with Meniere’s disease. Acta Otolaryngol 2007;127:1241–5.
43. Kim JS. Symptoms of transient ischemic attack. Front Neurol Neurosci 2014;33:82–102.
44. Paul NL, Simoni M, Chandratheva A, Rothwell PM. Population-based study of capsular warning syndrome and prognosis after early recurrent TIA. Neurology 2012;79:1356–62.
45. Strupp M, Zwergal A, Brandt T. Episodic ataxia type 2. Neurotherapeutics 2007;4:267–73.
46. Breslau N, Schultz LR, Stewart WF, et al. Headache and major depression: is the association specific to migraine? Neurology 2000;54:308–13.
47. Breslau N, Schultz LR, Stewart WF, et al. Headache types and panic disorder: directionality and specificity. Neurology 2001;56:350–4.
48. Best C, Eckhardt-Henn A, Tschan R, Dieterich M. Psychiatric morbidity and comorbidity in different vestibular vertigo syndromes. Results of a prospective longitudinal study over one year. J Neurol 2009;256:58–65.
49. Eckhardt-Henn A, Best C, Bense S, et al. Psychiatric comorbidity in different organic vertigo syndromes. J Neurol 2008;255:420–8.
50. Segui J, Salvador-Carulla L, Garcia L, et al. Semiology and subtyping of panic disorders. Act Psychiatr Scand 1998;97:272–7.
51. Jacob RG, Furman JM, Durrant JD, Turner SM. Surface dependence: a balance control strategy in panic disorder with agoraphobia. Psychosom Med 1997;59:323–30.
52. Ruckenstein MJ, Staab JP. Chronic subjective dizziness. Otolaryngol Clin North Am 2009;42:71–7, ix.
53. Australian medicines handbook : AMH. Adelaide, S.Aust.: Australian Medicines Handbook; 2015. p. v.
54. Maldonado Fernandez M, Birdi JS, Irving GJ, et al. Pharmacological agents for the prevention of vestibular migraine. Cochrane Database Syst Rev 2015;6:CD010600.
55. British Association for the Study of Headache. Guidelines for all healthcare professionals in the diagnosis and management of migraine, tension-type headache, cluster headache and medication overuse headache. 3rd ed. 2010.
56. Reploeg MD, Goebel JA. Migraine-associated dizziness: patient characteristics and management options. Otol Neurotol 2002;23:364–71.
57. Neuhauser H, Radtke A, von Brevern M, Lempert T. Zolmitriptan for treatment of migrainous vertigo: a pilot randomized placebo-controlled trial. Neurology 2003;60:882–3.
58. Roberto G, Raschi E, Piccinni C, et al. Adverse cardiovascular events associated with triptans and ergotamines for treatment of migraine: systematic review of observational studies. Cephalalgia 2015;35:118–31.
59. Bikhazi P, Jackson C, Ruckenstein MJ. Efficacy of antimigrainous therapy in the treatment of migraine-associated dizziness. Am J Otol 1997;18:350–4.
60. MedicinesComplete. London: Pharmaceutical Press. Available at www.medicinescomplete.com.
61. Tfelt-Hansen P, De Vries P, Saxena PR. Triptans in migraine: a comparative review of pharmacology, pharmacokinetics and efficacy. Drugs 2000;60:1259–87.
62. Mikulec AA, Faraji F, Kinsella LJ. Evaluation of the efficacy of caffeine cessation, nortriptyline, and topiramate therapy in vestibular migraine and complex dizziness of unknown etiology. Am J Otolaryngol 2012;33:121–7.
63. Maione A. Migraine-related vertigo: diagnostic criteria and prophylactic treatment. Laryngoscope 2006;116:1782–6.
64. Waterston J. Chronic migrainous vertigo. J Clin Neurosci 2004;11:384–8.
65. de Bock GH, Eelhart J, van Marwijk HW, et al. A postmarketing study of flunarizine in migraine and vertigo. Pharm World Sci 1997;19:269–74.
66. Verspeelt J, De Locht P, Amery WK. Postmarketing study of the use of flunarizine in vestibular vertigo and in migraine. Eur J Clin Pharmacol 1996;51:15–22.
67. Schmidt R, Oestreich W. Flunarizine in migraine prophylaxis: the clinical experience. J Cardiovasc Pharmacol 1991;18 Suppl 8:S21–6.
68. Lucetti C, Nuti A, Pavese N, et al. Flunarizine in migraine prophylaxis: predictive factors for a positive response. Cephalalgia 1998;18:349–52.
69. Schmidt R, Oestreich W. Flunarizine in the treatment of vestibular vertigo: experimental and clinical data. J Cardiovasc Pharmacol 1991;18 Suppl 8:S27–30.
70. Lepcha A, Amalanathan S, Augustine AM, et al. Flunarizine in the prophylaxis of migrainous vertigo: a randomized controlled trial. Eur Arch Otorhinolaryngol 2014;271:2931–6.
71. Carmona S, Settecase N. Use of topiramate (topamax) in a subgroup of migraine-vertigo patients with auditory symptoms. Ann N Y Acad Sci 2005;1039:517–20.
72. Bisdorff AR. Treatment of migraine related vertigo with lamotrigine an observational study. Bull Soc Sci Med Grand Duche Luxemb 2004:103–8.
73. Whitney SL, Rossi MM. Efficacy of vestibular rehabilitation. Otolaryngol Clin North Am 2000;33:659–72.
74. Enticott JC, Vitkovic JJ, Reid B, et al. Vestibular rehabilitation in individuals with inner-ear dysfunction: a pilot study. Audiol Neurootol 2008;13:19–28.
75. Myers AM, Fletcher PC, Myers AH, Sherk W. Discriminative and evaluative properties of the activities-specific balance confidence (ABC) scale. J Gerontol Ser A Biol Sci Med Sci 1998;53:M287–94.
76. Wrisley DM, Whitney SL, Furman JM. Vestibular rehabilitation outcomes in patients with a history of migraine. Otol Neurotol 2002;23:483–7.
77. Gottshall KR, Moore RJ, Hoffer ME. Vestibular rehabilitation for migraine-associated dizziness. Int Tinnitus J 2005;11:81–4.
78. Pavlou M, Quinn C, Murray K, et al. The effect of repeated visual motion stimuli on visual dependence and postural control in normal subjects. Gait Posture 2011;33:113–8.
79. Leddy JJ, Sandhu H, Sodhi V, et al. Rehabilitation of concussion and post-concussion syndrome. Sports Health 2012;4:147–54.
80. Fernie BA, Kollmann J, Brown RG. Cognitive behavioural interventions for depression in chronic neurological conditions: a systematic review. J Psychosom Res 2015;78:411–9.
81. Andersson G, Asmundson GJ, Denev J, et al. A controlled trial of cognitive-behavior therapy combined with vestibular rehabilitation in the treatment of dizziness. Behav Res Ther 2006;44:1265–73.
Nurse-Managed Protocols Offer Benefits in the Outpatient Management of Adults with Chronic Illness
Study Overview
Objective. To determine whether nurse-managed protocols are effective for the outpatient management of adults with diabetes, hypertension, and hyperlipidemia.
Study design. Systematic review and meta-analysis.
Data sources. The authors searched MEDLINE, Cochrane Central Register of Controlled Trials, EMBASE, and CINAHL for English-language peer-reviewed studies published between January 1980 and January 2014 that evaluated interventions that compared nurse-managed protocols with usual care in investigations targeting adults with chronic conditions. Two reviewers used eligibility criteria to assess titles, abstracts, and full texts, and resolved their disagreements by discussion or by consulting a third reviewer. Eligibility criteria included the involvement of an RN or LPN functioning beyond the usual scope of practice, such as adjusting medications, and conducting interventions based on a written protocol.
Main outcome measures. The effects of nurse-managed protocols on biophysical markers, patient treatment adherence, nurse protocol adherence, adverse effects, and resource use. When quantitative synthesis was feasible, dichotomous outcomes were combined using odds ratios and continuous outcomes were combined using mean differences in random-effects models. When quantitative synthesis was not feasible, the authors annualized data qualitatively, giving more weight to evidence from higher-quality studies. They evaluated overall strength of evidence (SOE) by assessing risk of bias, consistency, directness, and precision, and assigned a rating of high, moderate, or low SOE, or insufficient evidence.
Main results. Of the 2954 studies in the search results, 18 were ultimately eligible and included in the review, 16 randomized controlled trials and 2 before and after diabetes studies. Eleven were done in Western Europe and 7 in the United States. An RN or non-US equivalent was the interventionist in all studies (none used an LPN). In only 11 of the 18 studies were nurses independently allowed to initiate new medications. The meta-analysis found that hemoglobin A1c (HbA1c) level decreased by 0.4% (moderate SOE) (95% confidence interval {CI}, 0.1% to 0.7%) (n = 8), systolic and diastolic blood pressure decreased by 3.68 mm Hg (CI, 1.05 to 6.31) and 1.56 mm Hg (CI, 0.36 to 2.76), respectively (moderate SOE) (n = 12); total cholesterol level decreased by 9.37 mg/dL (20.77-mg/dL decrease to 2.02-mg/dL increase) (n = 9); and low-density-lipoprotein cholesterol level decreased by 12.07 mg/dL (CI, 28.27-mg/dL decrease to 4.13-mg/dL increase) (low SOE) (n = 6). The SOE was insufficient to estimate a treatment effect for all other outcomes.
Conclusion. A team approach that uses nurse-managed protocols may have positive effects on the outpatient management of adults with chronic conditions such as diabetes, hypertension, and hyperlipidemia.
Commentary
Hypertension, diabetes, and hyperlipidemia are major causes of morbidity and mortality worldwide and are widely prevalent in the United States. These chronic illnesses require long-term medical management, often requiring management of multiple medications and patient lifestyle changes and self-monitoring [1]. The patient-centered medical home, which involves a team approach, is increasingly being recognized as a promising model for delivering effective chronic disease care. Likewise, expanding the role of nurses as part of team care is increasingly being explored to help achieve high quality patient outcomes. The use of nurse-managed protocols can be an appropriate strategy in this scenario.
In this study, the researchers aimed to determine whether nurse-managed protocols are effective for outpatient management of adults with diabetes, hypertension, and hyperlipidemia and performed a systematic review and meta-analysis. Researchers followed a standardized procedure to conduct their search and carefully reviewed the studies, including contacting authors for missing data or clarification. They followed the approach recommended by the Agency for Healthcare Research and Quality (AHRQ) to evaluate the overall strength of the body of evidence [2].
However, some limitations must be taken into account. They acknowledge that they may have missed studies in which nurses had autonomy to practice in capacities beyond their scope of practice. In addition, the literature lacked details about the interventions and protocols used. Also, the researchers searched for studies across a 34-year range (1980–2014). Changes occurring in the nursing profession over these years may have impacted the findings.
Applications for Clinical Practice
Team-based care that includes nurse-managed protocols for titrating medications can be beneficial in the management of chronic conditions in primary care patients. With physician shortages predicted, which will impact primary care more than other specialties, team approaches using nurse-managed protocols have the potential to help lighten physician workloads and ensure quality care.
—Paloma Cesar de Sales, BN, RN, MS
1. Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009;28:75–85.
2. Agency for Healthcare Research and Quality. Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
Study Overview
Objective. To determine whether nurse-managed protocols are effective for the outpatient management of adults with diabetes, hypertension, and hyperlipidemia.
Study design. Systematic review and meta-analysis.
Data sources. The authors searched MEDLINE, Cochrane Central Register of Controlled Trials, EMBASE, and CINAHL for English-language peer-reviewed studies published between January 1980 and January 2014 that evaluated interventions that compared nurse-managed protocols with usual care in investigations targeting adults with chronic conditions. Two reviewers used eligibility criteria to assess titles, abstracts, and full texts, and resolved their disagreements by discussion or by consulting a third reviewer. Eligibility criteria included the involvement of an RN or LPN functioning beyond the usual scope of practice, such as adjusting medications, and conducting interventions based on a written protocol.
Main outcome measures. The effects of nurse-managed protocols on biophysical markers, patient treatment adherence, nurse protocol adherence, adverse effects, and resource use. When quantitative synthesis was feasible, dichotomous outcomes were combined using odds ratios and continuous outcomes were combined using mean differences in random-effects models. When quantitative synthesis was not feasible, the authors annualized data qualitatively, giving more weight to evidence from higher-quality studies. They evaluated overall strength of evidence (SOE) by assessing risk of bias, consistency, directness, and precision, and assigned a rating of high, moderate, or low SOE, or insufficient evidence.
Main results. Of the 2954 studies in the search results, 18 were ultimately eligible and included in the review, 16 randomized controlled trials and 2 before and after diabetes studies. Eleven were done in Western Europe and 7 in the United States. An RN or non-US equivalent was the interventionist in all studies (none used an LPN). In only 11 of the 18 studies were nurses independently allowed to initiate new medications. The meta-analysis found that hemoglobin A1c (HbA1c) level decreased by 0.4% (moderate SOE) (95% confidence interval {CI}, 0.1% to 0.7%) (n = 8), systolic and diastolic blood pressure decreased by 3.68 mm Hg (CI, 1.05 to 6.31) and 1.56 mm Hg (CI, 0.36 to 2.76), respectively (moderate SOE) (n = 12); total cholesterol level decreased by 9.37 mg/dL (20.77-mg/dL decrease to 2.02-mg/dL increase) (n = 9); and low-density-lipoprotein cholesterol level decreased by 12.07 mg/dL (CI, 28.27-mg/dL decrease to 4.13-mg/dL increase) (low SOE) (n = 6). The SOE was insufficient to estimate a treatment effect for all other outcomes.
Conclusion. A team approach that uses nurse-managed protocols may have positive effects on the outpatient management of adults with chronic conditions such as diabetes, hypertension, and hyperlipidemia.
Commentary
Hypertension, diabetes, and hyperlipidemia are major causes of morbidity and mortality worldwide and are widely prevalent in the United States. These chronic illnesses require long-term medical management, often requiring management of multiple medications and patient lifestyle changes and self-monitoring [1]. The patient-centered medical home, which involves a team approach, is increasingly being recognized as a promising model for delivering effective chronic disease care. Likewise, expanding the role of nurses as part of team care is increasingly being explored to help achieve high quality patient outcomes. The use of nurse-managed protocols can be an appropriate strategy in this scenario.
In this study, the researchers aimed to determine whether nurse-managed protocols are effective for outpatient management of adults with diabetes, hypertension, and hyperlipidemia and performed a systematic review and meta-analysis. Researchers followed a standardized procedure to conduct their search and carefully reviewed the studies, including contacting authors for missing data or clarification. They followed the approach recommended by the Agency for Healthcare Research and Quality (AHRQ) to evaluate the overall strength of the body of evidence [2].
However, some limitations must be taken into account. They acknowledge that they may have missed studies in which nurses had autonomy to practice in capacities beyond their scope of practice. In addition, the literature lacked details about the interventions and protocols used. Also, the researchers searched for studies across a 34-year range (1980–2014). Changes occurring in the nursing profession over these years may have impacted the findings.
Applications for Clinical Practice
Team-based care that includes nurse-managed protocols for titrating medications can be beneficial in the management of chronic conditions in primary care patients. With physician shortages predicted, which will impact primary care more than other specialties, team approaches using nurse-managed protocols have the potential to help lighten physician workloads and ensure quality care.
—Paloma Cesar de Sales, BN, RN, MS
Study Overview
Objective. To determine whether nurse-managed protocols are effective for the outpatient management of adults with diabetes, hypertension, and hyperlipidemia.
Study design. Systematic review and meta-analysis.
Data sources. The authors searched MEDLINE, Cochrane Central Register of Controlled Trials, EMBASE, and CINAHL for English-language peer-reviewed studies published between January 1980 and January 2014 that evaluated interventions that compared nurse-managed protocols with usual care in investigations targeting adults with chronic conditions. Two reviewers used eligibility criteria to assess titles, abstracts, and full texts, and resolved their disagreements by discussion or by consulting a third reviewer. Eligibility criteria included the involvement of an RN or LPN functioning beyond the usual scope of practice, such as adjusting medications, and conducting interventions based on a written protocol.
Main outcome measures. The effects of nurse-managed protocols on biophysical markers, patient treatment adherence, nurse protocol adherence, adverse effects, and resource use. When quantitative synthesis was feasible, dichotomous outcomes were combined using odds ratios and continuous outcomes were combined using mean differences in random-effects models. When quantitative synthesis was not feasible, the authors annualized data qualitatively, giving more weight to evidence from higher-quality studies. They evaluated overall strength of evidence (SOE) by assessing risk of bias, consistency, directness, and precision, and assigned a rating of high, moderate, or low SOE, or insufficient evidence.
Main results. Of the 2954 studies in the search results, 18 were ultimately eligible and included in the review, 16 randomized controlled trials and 2 before and after diabetes studies. Eleven were done in Western Europe and 7 in the United States. An RN or non-US equivalent was the interventionist in all studies (none used an LPN). In only 11 of the 18 studies were nurses independently allowed to initiate new medications. The meta-analysis found that hemoglobin A1c (HbA1c) level decreased by 0.4% (moderate SOE) (95% confidence interval {CI}, 0.1% to 0.7%) (n = 8), systolic and diastolic blood pressure decreased by 3.68 mm Hg (CI, 1.05 to 6.31) and 1.56 mm Hg (CI, 0.36 to 2.76), respectively (moderate SOE) (n = 12); total cholesterol level decreased by 9.37 mg/dL (20.77-mg/dL decrease to 2.02-mg/dL increase) (n = 9); and low-density-lipoprotein cholesterol level decreased by 12.07 mg/dL (CI, 28.27-mg/dL decrease to 4.13-mg/dL increase) (low SOE) (n = 6). The SOE was insufficient to estimate a treatment effect for all other outcomes.
Conclusion. A team approach that uses nurse-managed protocols may have positive effects on the outpatient management of adults with chronic conditions such as diabetes, hypertension, and hyperlipidemia.
Commentary
Hypertension, diabetes, and hyperlipidemia are major causes of morbidity and mortality worldwide and are widely prevalent in the United States. These chronic illnesses require long-term medical management, often requiring management of multiple medications and patient lifestyle changes and self-monitoring [1]. The patient-centered medical home, which involves a team approach, is increasingly being recognized as a promising model for delivering effective chronic disease care. Likewise, expanding the role of nurses as part of team care is increasingly being explored to help achieve high quality patient outcomes. The use of nurse-managed protocols can be an appropriate strategy in this scenario.
In this study, the researchers aimed to determine whether nurse-managed protocols are effective for outpatient management of adults with diabetes, hypertension, and hyperlipidemia and performed a systematic review and meta-analysis. Researchers followed a standardized procedure to conduct their search and carefully reviewed the studies, including contacting authors for missing data or clarification. They followed the approach recommended by the Agency for Healthcare Research and Quality (AHRQ) to evaluate the overall strength of the body of evidence [2].
However, some limitations must be taken into account. They acknowledge that they may have missed studies in which nurses had autonomy to practice in capacities beyond their scope of practice. In addition, the literature lacked details about the interventions and protocols used. Also, the researchers searched for studies across a 34-year range (1980–2014). Changes occurring in the nursing profession over these years may have impacted the findings.
Applications for Clinical Practice
Team-based care that includes nurse-managed protocols for titrating medications can be beneficial in the management of chronic conditions in primary care patients. With physician shortages predicted, which will impact primary care more than other specialties, team approaches using nurse-managed protocols have the potential to help lighten physician workloads and ensure quality care.
—Paloma Cesar de Sales, BN, RN, MS
1. Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009;28:75–85.
2. Agency for Healthcare Research and Quality. Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
1. Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the Chronic Care Model in the new millennium. Health Aff (Millwood) 2009;28:75–85.
2. Agency for Healthcare Research and Quality. Methods guide for effectiveness and comparative effectiveness reviews. Rockville, MD: Agency for Healthcare Research and Quality; 2008.
Increased Dementia Risk Among Men and Women With Posttraumatic Stress Disorder
TORONTO—Posttraumatic stress disorder (PTSD) is a risk factor for dementia in men and women. Among men, PTSD is associated with a 90% increased risk of incident dementia, according to research presented at the Alzheimer’s Association International Conference.
Women and PTSD
Previous studies indicate that women are at a higher risk of PTSD, but little research is available concerning the risk of dementia in women diagnosed with PTSD. “They are more likely to experience trauma, maybe from domestic abuse, violence, [and] rape … so I think this is a huge area that needs research,” said Jason Flatt, PhD, MPH, Assistant Professor of Health and Aging at the University of California, San Francisco. To analyze the link between PTSD and dementia in both genders, Dr. Flatt and colleagues examined data from a diverse population.
“The objectives of the study were to look at the effect of PTSD on the risk of dementia over 13 years among older men and women and see if the association is explained by medical comorbidities like depression and traumatic brain injury,” said Dr. Flatt.
Diverse Population Sample
Participants were selected from the Kaiser Permanente Northern California healthcare system and were age 60 or older in January 2002. Women made up 54.7% of the population, 68% of the population was white, 5.5% was black, 6.5% was Hispanic, and 9% was Asian. Mean age at baseline was 71. The dementia diagnoses were collected from medical records for January 1, 2002 through December 31, 2014. Mean follow-up was approximately eight years.
Investigators evaluated the association between PTSD and dementia using gender-modified models adjusted for age, race, diabetes, and stroke, with censoring for death and gaps in health coverage of greater than 90 days. In all, 1,147 patients were diagnosed with PTSD. In addition, researchers found that during the 13-year follow-up period, 11.8% of subjects received a diagnosis of dementia.
People with PTSD were more likely to experience traumatic brain injuries and depression. Patients with PTSD also had a 56% increased risk of developing dementia, compared with controls without PTSD. Men with PTSD had a 90% increase in dementia risk, and women with PTSD had a 41% increase in dementia risk, compared with controls.
“This is the first large study of PTSD and risk of dementia in women, and results suggest that PTSD is a risk factor in both genders,” said Dr. Flatt.
Strengths of this study include its longitudinal design, diverse sample, and 13-year follow-up period. Dementia was diagnosed by physicians, however, and as a result, researchers were unable to observe dementia subtypes.
“Future research should think about these mechanisms and how to link and better understand how PTSD may be involved in dementia risk,” said Dr. Flatt.
Suggested Reading
Wang TY, Wei HT, Liou YJ et al. Risk for developing dementia among patients with posttraumatic stress disorder: A nationwide longitudinal study. J Affect Disord. 2016 Aug 16 [Epub ahead of print].
McCartney JR, Severson K. Sexual violence, post-traumatic stress disorder and dementia. J Am Geriatr Soc. 1997; 45(1):76-78.
TORONTO—Posttraumatic stress disorder (PTSD) is a risk factor for dementia in men and women. Among men, PTSD is associated with a 90% increased risk of incident dementia, according to research presented at the Alzheimer’s Association International Conference.
Women and PTSD
Previous studies indicate that women are at a higher risk of PTSD, but little research is available concerning the risk of dementia in women diagnosed with PTSD. “They are more likely to experience trauma, maybe from domestic abuse, violence, [and] rape … so I think this is a huge area that needs research,” said Jason Flatt, PhD, MPH, Assistant Professor of Health and Aging at the University of California, San Francisco. To analyze the link between PTSD and dementia in both genders, Dr. Flatt and colleagues examined data from a diverse population.
“The objectives of the study were to look at the effect of PTSD on the risk of dementia over 13 years among older men and women and see if the association is explained by medical comorbidities like depression and traumatic brain injury,” said Dr. Flatt.
Diverse Population Sample
Participants were selected from the Kaiser Permanente Northern California healthcare system and were age 60 or older in January 2002. Women made up 54.7% of the population, 68% of the population was white, 5.5% was black, 6.5% was Hispanic, and 9% was Asian. Mean age at baseline was 71. The dementia diagnoses were collected from medical records for January 1, 2002 through December 31, 2014. Mean follow-up was approximately eight years.
Investigators evaluated the association between PTSD and dementia using gender-modified models adjusted for age, race, diabetes, and stroke, with censoring for death and gaps in health coverage of greater than 90 days. In all, 1,147 patients were diagnosed with PTSD. In addition, researchers found that during the 13-year follow-up period, 11.8% of subjects received a diagnosis of dementia.
People with PTSD were more likely to experience traumatic brain injuries and depression. Patients with PTSD also had a 56% increased risk of developing dementia, compared with controls without PTSD. Men with PTSD had a 90% increase in dementia risk, and women with PTSD had a 41% increase in dementia risk, compared with controls.
“This is the first large study of PTSD and risk of dementia in women, and results suggest that PTSD is a risk factor in both genders,” said Dr. Flatt.
Strengths of this study include its longitudinal design, diverse sample, and 13-year follow-up period. Dementia was diagnosed by physicians, however, and as a result, researchers were unable to observe dementia subtypes.
“Future research should think about these mechanisms and how to link and better understand how PTSD may be involved in dementia risk,” said Dr. Flatt.
Suggested Reading
Wang TY, Wei HT, Liou YJ et al. Risk for developing dementia among patients with posttraumatic stress disorder: A nationwide longitudinal study. J Affect Disord. 2016 Aug 16 [Epub ahead of print].
McCartney JR, Severson K. Sexual violence, post-traumatic stress disorder and dementia. J Am Geriatr Soc. 1997; 45(1):76-78.
TORONTO—Posttraumatic stress disorder (PTSD) is a risk factor for dementia in men and women. Among men, PTSD is associated with a 90% increased risk of incident dementia, according to research presented at the Alzheimer’s Association International Conference.
Women and PTSD
Previous studies indicate that women are at a higher risk of PTSD, but little research is available concerning the risk of dementia in women diagnosed with PTSD. “They are more likely to experience trauma, maybe from domestic abuse, violence, [and] rape … so I think this is a huge area that needs research,” said Jason Flatt, PhD, MPH, Assistant Professor of Health and Aging at the University of California, San Francisco. To analyze the link between PTSD and dementia in both genders, Dr. Flatt and colleagues examined data from a diverse population.
“The objectives of the study were to look at the effect of PTSD on the risk of dementia over 13 years among older men and women and see if the association is explained by medical comorbidities like depression and traumatic brain injury,” said Dr. Flatt.
Diverse Population Sample
Participants were selected from the Kaiser Permanente Northern California healthcare system and were age 60 or older in January 2002. Women made up 54.7% of the population, 68% of the population was white, 5.5% was black, 6.5% was Hispanic, and 9% was Asian. Mean age at baseline was 71. The dementia diagnoses were collected from medical records for January 1, 2002 through December 31, 2014. Mean follow-up was approximately eight years.
Investigators evaluated the association between PTSD and dementia using gender-modified models adjusted for age, race, diabetes, and stroke, with censoring for death and gaps in health coverage of greater than 90 days. In all, 1,147 patients were diagnosed with PTSD. In addition, researchers found that during the 13-year follow-up period, 11.8% of subjects received a diagnosis of dementia.
People with PTSD were more likely to experience traumatic brain injuries and depression. Patients with PTSD also had a 56% increased risk of developing dementia, compared with controls without PTSD. Men with PTSD had a 90% increase in dementia risk, and women with PTSD had a 41% increase in dementia risk, compared with controls.
“This is the first large study of PTSD and risk of dementia in women, and results suggest that PTSD is a risk factor in both genders,” said Dr. Flatt.
Strengths of this study include its longitudinal design, diverse sample, and 13-year follow-up period. Dementia was diagnosed by physicians, however, and as a result, researchers were unable to observe dementia subtypes.
“Future research should think about these mechanisms and how to link and better understand how PTSD may be involved in dementia risk,” said Dr. Flatt.
Suggested Reading
Wang TY, Wei HT, Liou YJ et al. Risk for developing dementia among patients with posttraumatic stress disorder: A nationwide longitudinal study. J Affect Disord. 2016 Aug 16 [Epub ahead of print].
McCartney JR, Severson K. Sexual violence, post-traumatic stress disorder and dementia. J Am Geriatr Soc. 1997; 45(1):76-78.
Glymphatic System May Play Key Role in Removing Brain Waste
SAN DIEGO—A recently discovered system known as the glymphatic system clears waste from the brain. It is most active during sleep and may have implications in headache and in neurodegenerative diseases associated with pathologic protein aggregation, including Parkinson’s disease and Alzheimer’s disease, said Helene Benveniste, MD, PhD, Professor of Anesthesiology and Vice Chair for Research at Stony Brook School of Medicine in New York. Data suggest that sleep, posture, and brain injury may affect this waste removal system.
“We look at the glymphatic pathway as a bit of an overlooked compartment of the vasculature or the perivascular space that is … facilitating solute and waste removal,” Dr. Benveniste said at the 58th Annual Scientific Meeting of the American Headache Society. Although most studies of the glymphatic system so far have been performed in rodents, “data are starting to come out showing that this system is also present in humans,” she said.
A Brainwide Pathway
The glymphatic system, which gets its name from the glial cells and lymphatic system that it mimics, may explain how the brain—one of the most metabolically active organs—clears excess fluids, solutes, and waste products without authentic lymph vessels, Dr. Benveniste said. The system consists of a brainwide pathway that facilitates the exchange of CSF with interstitial fluid to clear interstitial waste from the brain parenchyma. The waste is moved into perivenous pathways and ultimately cleared via cervical lymphatic vessels.
Researchers first described the concept of the glymphatic system in Science Translational Medicine in 2012. They injected fluorescent tracers into the cisterna magna and fluorescent-tagged amyloid beta into brain parenchyma of mice and observed distribution of the tracers along the glymphatic pathway using two-photon imaging. The paper’s senior author, Maiken Nedergaard, MD, DMSc, Professor of Neurosurgery and Translational Neuromedicine at the University of Rochester in New York, contacted Dr. Benveniste to develop a way to visualize the system using MRI, which they accomplished using a 9.4-T system and small molecular weight contrast dye injected via an intrathecal catheter inserted in the cisterna magna.
In 2015, researchers in Norway published a case report in Acta Radiologica Open supporting the existence of a glymphatic system in humans. They administered intrathecal gadobutrol to diagnose a CSF leak in a patient. The patient underwent 3D T1-weighted imaging at one hour and 4.5 hours. The distribution of gadobutrol into the brain was consistent with that observed in rodents and supports the concept of a glymphatic pathway in the human brain, the authors concluded.
Researchers still are evaluating the glymphatic system’s role in maintaining brain health and how it differs in humans and rodents. Aquaporin channels, which are crucial in facilitating CSF transport from the periarterial space and into the interstitial space to drive waste removal via the glymphatic pathway, may be positioned differently in rodents and humans, Dr. Benveniste said. In addition, waste clearance may be orders of magnitude slower in humans due to brain size and complexity, she said.
Factors Affecting Glymphatic Flow
In mice genetically modified to lack aquaporin channels, convective flow and waste removal via the glymphatic pathway are slowed down immensely.
After traumatic brain injury, glymphatic pathway function was reduced by approximately 60% in mice for at least one month, Iliff et al reported in the Journal of Neuroscience in 2014. In mice without aquaporin channels, however, glymphatic pathway dysfunction was further exacerbated, and those animals developed neurofibrillary pathology and neurodegeneration.
One of the most important factors affecting glymphatic flow is interstitial space volume, which increases by 40% to 60% during sleep, Dr. Benveniste said. Natural sleep and certain types of anesthetics dramatically increase interstitial space volume, Xie et al reported in Science in 2013. Likewise, awaking sleeping mice sharply reduces glymphatic flow. The authors concluded, “the restorative function of sleep may be a consequence of the enhanced removal of potentially neurotoxic waste products that accumulate in the awake CNS.”
Injecting a norepinephrine receptor antagonist intrathecally can stimulate intense glymphatic transport in animals in the awake state, indicating that noradrenergic tone may be responsible for the process, Dr. Benveniste said.
She and her colleagues studied glymphatic clearance in mice anesthetized with dexmedetomidine, which induces a state similar to stage 2 sleep, versus the inhalational anesthetic isoflurane. Glymphatic processing was much greater in rodents that received dexmedetomidine.
Sleep Position
Hedok Lee, PhD, Clinical Assistant Professor of Anesthesiology at Stony Brook School of Medicine, Dr. Benveniste, and colleagues studied the effect of body posture on brain glymphatic transport in rats. They found that glymphatic transport and amyloid beta clearance were most efficient in the lateral and supine positions, while the prone position (ie, most upright and mimicking awake posture) resulted in slower clearance.
“Right lateral seems to be the position where you have got the best efflux and influx,” Dr. Benveniste said. The findings suggest that sleep position’s effect on the glymphatic system may be relevant for imaging the system in humans, and ultimately for patient care.
—Jake Remaly
Suggested Reading
Eide PK, Ringstad G. MRI with intrathecal MRI gadolinium contrast medium administration: a possible method to assess glymphatic function in human brain. Acta Radiol Open. 2015;4(11):2058460115609635.
Iliff JJ, Chen MJ, Plog BA, et al. Impairment of glymphatic pathway function promotes tau pathology after traumatic brain injury. J Neurosci. 2014;34(49):16180-16193.
Iliff JJ, Wang M, Liao Y, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4(147):147ra111.
Lee H, Xie L, Yu M, et al. The effect of body posture on brain glymphatic transport. J Neurosci. 2015;35(31):11034-11044.
Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373-377.
SAN DIEGO—A recently discovered system known as the glymphatic system clears waste from the brain. It is most active during sleep and may have implications in headache and in neurodegenerative diseases associated with pathologic protein aggregation, including Parkinson’s disease and Alzheimer’s disease, said Helene Benveniste, MD, PhD, Professor of Anesthesiology and Vice Chair for Research at Stony Brook School of Medicine in New York. Data suggest that sleep, posture, and brain injury may affect this waste removal system.
“We look at the glymphatic pathway as a bit of an overlooked compartment of the vasculature or the perivascular space that is … facilitating solute and waste removal,” Dr. Benveniste said at the 58th Annual Scientific Meeting of the American Headache Society. Although most studies of the glymphatic system so far have been performed in rodents, “data are starting to come out showing that this system is also present in humans,” she said.
A Brainwide Pathway
The glymphatic system, which gets its name from the glial cells and lymphatic system that it mimics, may explain how the brain—one of the most metabolically active organs—clears excess fluids, solutes, and waste products without authentic lymph vessels, Dr. Benveniste said. The system consists of a brainwide pathway that facilitates the exchange of CSF with interstitial fluid to clear interstitial waste from the brain parenchyma. The waste is moved into perivenous pathways and ultimately cleared via cervical lymphatic vessels.
Researchers first described the concept of the glymphatic system in Science Translational Medicine in 2012. They injected fluorescent tracers into the cisterna magna and fluorescent-tagged amyloid beta into brain parenchyma of mice and observed distribution of the tracers along the glymphatic pathway using two-photon imaging. The paper’s senior author, Maiken Nedergaard, MD, DMSc, Professor of Neurosurgery and Translational Neuromedicine at the University of Rochester in New York, contacted Dr. Benveniste to develop a way to visualize the system using MRI, which they accomplished using a 9.4-T system and small molecular weight contrast dye injected via an intrathecal catheter inserted in the cisterna magna.
In 2015, researchers in Norway published a case report in Acta Radiologica Open supporting the existence of a glymphatic system in humans. They administered intrathecal gadobutrol to diagnose a CSF leak in a patient. The patient underwent 3D T1-weighted imaging at one hour and 4.5 hours. The distribution of gadobutrol into the brain was consistent with that observed in rodents and supports the concept of a glymphatic pathway in the human brain, the authors concluded.
Researchers still are evaluating the glymphatic system’s role in maintaining brain health and how it differs in humans and rodents. Aquaporin channels, which are crucial in facilitating CSF transport from the periarterial space and into the interstitial space to drive waste removal via the glymphatic pathway, may be positioned differently in rodents and humans, Dr. Benveniste said. In addition, waste clearance may be orders of magnitude slower in humans due to brain size and complexity, she said.
Factors Affecting Glymphatic Flow
In mice genetically modified to lack aquaporin channels, convective flow and waste removal via the glymphatic pathway are slowed down immensely.
After traumatic brain injury, glymphatic pathway function was reduced by approximately 60% in mice for at least one month, Iliff et al reported in the Journal of Neuroscience in 2014. In mice without aquaporin channels, however, glymphatic pathway dysfunction was further exacerbated, and those animals developed neurofibrillary pathology and neurodegeneration.
One of the most important factors affecting glymphatic flow is interstitial space volume, which increases by 40% to 60% during sleep, Dr. Benveniste said. Natural sleep and certain types of anesthetics dramatically increase interstitial space volume, Xie et al reported in Science in 2013. Likewise, awaking sleeping mice sharply reduces glymphatic flow. The authors concluded, “the restorative function of sleep may be a consequence of the enhanced removal of potentially neurotoxic waste products that accumulate in the awake CNS.”
Injecting a norepinephrine receptor antagonist intrathecally can stimulate intense glymphatic transport in animals in the awake state, indicating that noradrenergic tone may be responsible for the process, Dr. Benveniste said.
She and her colleagues studied glymphatic clearance in mice anesthetized with dexmedetomidine, which induces a state similar to stage 2 sleep, versus the inhalational anesthetic isoflurane. Glymphatic processing was much greater in rodents that received dexmedetomidine.
Sleep Position
Hedok Lee, PhD, Clinical Assistant Professor of Anesthesiology at Stony Brook School of Medicine, Dr. Benveniste, and colleagues studied the effect of body posture on brain glymphatic transport in rats. They found that glymphatic transport and amyloid beta clearance were most efficient in the lateral and supine positions, while the prone position (ie, most upright and mimicking awake posture) resulted in slower clearance.
“Right lateral seems to be the position where you have got the best efflux and influx,” Dr. Benveniste said. The findings suggest that sleep position’s effect on the glymphatic system may be relevant for imaging the system in humans, and ultimately for patient care.
—Jake Remaly
Suggested Reading
Eide PK, Ringstad G. MRI with intrathecal MRI gadolinium contrast medium administration: a possible method to assess glymphatic function in human brain. Acta Radiol Open. 2015;4(11):2058460115609635.
Iliff JJ, Chen MJ, Plog BA, et al. Impairment of glymphatic pathway function promotes tau pathology after traumatic brain injury. J Neurosci. 2014;34(49):16180-16193.
Iliff JJ, Wang M, Liao Y, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4(147):147ra111.
Lee H, Xie L, Yu M, et al. The effect of body posture on brain glymphatic transport. J Neurosci. 2015;35(31):11034-11044.
Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373-377.
SAN DIEGO—A recently discovered system known as the glymphatic system clears waste from the brain. It is most active during sleep and may have implications in headache and in neurodegenerative diseases associated with pathologic protein aggregation, including Parkinson’s disease and Alzheimer’s disease, said Helene Benveniste, MD, PhD, Professor of Anesthesiology and Vice Chair for Research at Stony Brook School of Medicine in New York. Data suggest that sleep, posture, and brain injury may affect this waste removal system.
“We look at the glymphatic pathway as a bit of an overlooked compartment of the vasculature or the perivascular space that is … facilitating solute and waste removal,” Dr. Benveniste said at the 58th Annual Scientific Meeting of the American Headache Society. Although most studies of the glymphatic system so far have been performed in rodents, “data are starting to come out showing that this system is also present in humans,” she said.
A Brainwide Pathway
The glymphatic system, which gets its name from the glial cells and lymphatic system that it mimics, may explain how the brain—one of the most metabolically active organs—clears excess fluids, solutes, and waste products without authentic lymph vessels, Dr. Benveniste said. The system consists of a brainwide pathway that facilitates the exchange of CSF with interstitial fluid to clear interstitial waste from the brain parenchyma. The waste is moved into perivenous pathways and ultimately cleared via cervical lymphatic vessels.
Researchers first described the concept of the glymphatic system in Science Translational Medicine in 2012. They injected fluorescent tracers into the cisterna magna and fluorescent-tagged amyloid beta into brain parenchyma of mice and observed distribution of the tracers along the glymphatic pathway using two-photon imaging. The paper’s senior author, Maiken Nedergaard, MD, DMSc, Professor of Neurosurgery and Translational Neuromedicine at the University of Rochester in New York, contacted Dr. Benveniste to develop a way to visualize the system using MRI, which they accomplished using a 9.4-T system and small molecular weight contrast dye injected via an intrathecal catheter inserted in the cisterna magna.
In 2015, researchers in Norway published a case report in Acta Radiologica Open supporting the existence of a glymphatic system in humans. They administered intrathecal gadobutrol to diagnose a CSF leak in a patient. The patient underwent 3D T1-weighted imaging at one hour and 4.5 hours. The distribution of gadobutrol into the brain was consistent with that observed in rodents and supports the concept of a glymphatic pathway in the human brain, the authors concluded.
Researchers still are evaluating the glymphatic system’s role in maintaining brain health and how it differs in humans and rodents. Aquaporin channels, which are crucial in facilitating CSF transport from the periarterial space and into the interstitial space to drive waste removal via the glymphatic pathway, may be positioned differently in rodents and humans, Dr. Benveniste said. In addition, waste clearance may be orders of magnitude slower in humans due to brain size and complexity, she said.
Factors Affecting Glymphatic Flow
In mice genetically modified to lack aquaporin channels, convective flow and waste removal via the glymphatic pathway are slowed down immensely.
After traumatic brain injury, glymphatic pathway function was reduced by approximately 60% in mice for at least one month, Iliff et al reported in the Journal of Neuroscience in 2014. In mice without aquaporin channels, however, glymphatic pathway dysfunction was further exacerbated, and those animals developed neurofibrillary pathology and neurodegeneration.
One of the most important factors affecting glymphatic flow is interstitial space volume, which increases by 40% to 60% during sleep, Dr. Benveniste said. Natural sleep and certain types of anesthetics dramatically increase interstitial space volume, Xie et al reported in Science in 2013. Likewise, awaking sleeping mice sharply reduces glymphatic flow. The authors concluded, “the restorative function of sleep may be a consequence of the enhanced removal of potentially neurotoxic waste products that accumulate in the awake CNS.”
Injecting a norepinephrine receptor antagonist intrathecally can stimulate intense glymphatic transport in animals in the awake state, indicating that noradrenergic tone may be responsible for the process, Dr. Benveniste said.
She and her colleagues studied glymphatic clearance in mice anesthetized with dexmedetomidine, which induces a state similar to stage 2 sleep, versus the inhalational anesthetic isoflurane. Glymphatic processing was much greater in rodents that received dexmedetomidine.
Sleep Position
Hedok Lee, PhD, Clinical Assistant Professor of Anesthesiology at Stony Brook School of Medicine, Dr. Benveniste, and colleagues studied the effect of body posture on brain glymphatic transport in rats. They found that glymphatic transport and amyloid beta clearance were most efficient in the lateral and supine positions, while the prone position (ie, most upright and mimicking awake posture) resulted in slower clearance.
“Right lateral seems to be the position where you have got the best efflux and influx,” Dr. Benveniste said. The findings suggest that sleep position’s effect on the glymphatic system may be relevant for imaging the system in humans, and ultimately for patient care.
—Jake Remaly
Suggested Reading
Eide PK, Ringstad G. MRI with intrathecal MRI gadolinium contrast medium administration: a possible method to assess glymphatic function in human brain. Acta Radiol Open. 2015;4(11):2058460115609635.
Iliff JJ, Chen MJ, Plog BA, et al. Impairment of glymphatic pathway function promotes tau pathology after traumatic brain injury. J Neurosci. 2014;34(49):16180-16193.
Iliff JJ, Wang M, Liao Y, et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid β. Sci Transl Med. 2012;4(147):147ra111.
Lee H, Xie L, Yu M, et al. The effect of body posture on brain glymphatic transport. J Neurosci. 2015;35(31):11034-11044.
Xie L, Kang H, Xu Q, et al. Sleep drives metabolite clearance from the adult brain. Science. 2013;342(6156):373-377.
Clinical Considerations of New and Pending MS Treatments
HILTON HEAD, SC—Managing patient expectations is important when discussing new and pending treatments for multiple sclerosis (MS), according to a lecture given at the 39th Annual Contemporary Clinical Neurology Symposium. The FDA’s recent approval of daclizumab and ongoing priority review of ocrelizumab mean that neurologists likely will be discussing these therapies with patients in their clinics. Conversations may revolve around efficacy, laboratory monitoring, and risk of adverse events.
In the case of daclizumab (Zinbryta), which was approved in May 2016, patient counseling may focus on monthly laboratory monitoring requirements that are part of the drug’s risk evaluation and mitigation strategy (REMS) program and the potential for adverse events at any time during treatment, said Harold Moses Jr, MD, Associate Professor of Neurology at Vanderbilt University in Nashville.
Ocrelizumab (Ocrevus) could be the first drug approved for primary progressive MS and a new treatment option for patients with relapsing MS. Neurologists may need to temper patients’ expectations regarding the drug’s efficacy in patients with more advanced progressive disease.
“If this drug gets approved for progressive MS, you are going to have a number of patients coming to your clinics to ask for this drug,” he said. It is unclear, however, how beneficial the treatment might be for patients with advanced disease, based on the clinical trial conducted in primary progressive MS. “In my opinion, if someone is 65 to 70 years old and has had primary progressive MS for 15 to 20 years and has been wheelchair-confined for five or more years, it is unlikely that this drug is going to be very meaningful for them. Although, I do not know that for a fact. Therefore, my plan is to offer this [treatment], probably for approximately a year, and see what happens. We will continue to follow them and make a decision together about continuing therapy or stopping.”
“Remember, half the people in the world who have MS have progressive disease,” Dr. Moses said. “They have seen more than 20 years of therapies [approved] for relapsing MS, so they have a lot of pent-up expectations about a treatment option, and rightfully so. I just think this potential treatment has to be discussed in a broader context of how the study was done.”
Daclizumab
Daclizumab is an interleukin-2 receptor blocking humanized monoclonal antibody approved for use in relapsing forms of MS. It is self-administered as a subcutaneous injection once per month at a dose of 150 mg/mL. The drug’s label notes, “Because of its safety profile, the use of Zinbryta should generally be reserved for patients who have had an inadequate response to two or more drugs indicated for the treatment of MS.” This FDA guidance is similar to that for alemtuzumab. “With more than a dozen drugs for MS, it is not too surprising we are seeing this,” Dr. Moses said.
The efficacy of the drug was demonstrated in two randomized, double-blind studies. One study compared daclizumab with interferon beta-1a. The other study compared daclizumab and placebo.
In the active comparator study, 919 patients received daclizumab and 922 received interferon beta-1a. Compared with interferon beta-1a, daclizumab had a statistically significant effect on annualized relapse rate (0.393 vs 0.216; relative reduction, 45%) and on the number of new or newly enlarging T2 hyperintense lesions. Treatment did not significantly affect 12-week confirmed disability progression.
In some patients, daclizumab has a significant impact on the liver. As a result, physicians are asked to assess transaminase levels and total bilirubin monthly during treatment and for six months after stopping therapy, Dr. Moses said.
Autoimmune hepatitis and other immune-mediated disorders, including lymphadenopathy, noninfectious colitis, and cutaneous adverse events, were seen with daclizumab treatment.
Dermatologic reactions to daclizumab can range from mild rashes to serious reactions, and can include psoriasiform nail changes, erythematous changes and swelling, and desquamation and erythema of the palms. Neurologists should advise patients that these reactions “could happen at any point while they are taking this medication,” Dr. Moses said. Some patients experienced reactions after receiving the therapy for nearly three years.Patients also experienced adverse events related to infection, including nasopharyngitis, bronchitis, and tonsillitis. “Daclizumab is the newest approved drug for relapsing MS,” Dr. Moses said. “It has a unique mechanism of action and a favorable dosing schedule. Challenges exist with monitoring requirements and potential serious adverse events.”
Ocrelizumab
Ocrelizumab is a humanized monoclonal antibody that depletes CD20+ B cells.
Two identical studies, OPERA I and II, evaluated ocrelizumab in patients with relapsing MS. Another trial, ORATORIO, assessed ocrelizumab in patients with primary progressive MS. In the trials, patients received 600 mg of ocrelizumab by IV infusion every 24 weeks.
In OPERA I and II, treatment with ocrelizumab resulted in a 46% and 47% reduction in annualized relapse rate, respectively, compared with interferon beta-1a. In addition, ocrelizumab reduced the risk of confirmed disability progression for 12 weeks by 43% and 37%, respectively. Ocrelizumab also dramatically reduced the number of T1 gadolinium-enhancing lesions and the number of new or enlarging T2 hyperintense lesions, compared with interferon beta-1a.
The ORATORIO study included 732 patients with primary progressive MS who received ocrelizumab or placebo. Patients were ages 18 to 55, had an Expanded Disability Status Scale score of 3.0 to 6.5, and had abnormal CSF. Patients were treated for at least 120 weeks. Investigators measured slowing of disability progression as the primary outcome. There was a 24% reduction in clinical disability sustained for at least 12 weeks, compared with placebo.
Ocrelizumab generally was well tolerated. In the clinical trials, a similar proportion of patients treated with ocrelizumab and controls experienced adverse events. In OPERA I and II, the most common adverse event associated with ocrelizumab was infusion-related reactions, which occurred in 34.3% of patients in the ocrelizumab arm, compared with 9.7% of patients in the interferon beta-1a arm.
In ORATORIO, more malignancies were reported in patients treated with ocrelizumab, compared with patients who received placebo (11 vs 2). The implications of that finding are unclear. “We will see how that plays out in terms of what the FDA thinks about that,” Dr. Moses said.
The FDA has granted a priority review designation to ocrelizumab, with a targeted action date of December 28, 2016. “Ocrelizumab remains on the horizon with a potential role in both relapsing and progressive MS,” Dr. Moses said.
—Jake Remaly
HILTON HEAD, SC—Managing patient expectations is important when discussing new and pending treatments for multiple sclerosis (MS), according to a lecture given at the 39th Annual Contemporary Clinical Neurology Symposium. The FDA’s recent approval of daclizumab and ongoing priority review of ocrelizumab mean that neurologists likely will be discussing these therapies with patients in their clinics. Conversations may revolve around efficacy, laboratory monitoring, and risk of adverse events.
In the case of daclizumab (Zinbryta), which was approved in May 2016, patient counseling may focus on monthly laboratory monitoring requirements that are part of the drug’s risk evaluation and mitigation strategy (REMS) program and the potential for adverse events at any time during treatment, said Harold Moses Jr, MD, Associate Professor of Neurology at Vanderbilt University in Nashville.
Ocrelizumab (Ocrevus) could be the first drug approved for primary progressive MS and a new treatment option for patients with relapsing MS. Neurologists may need to temper patients’ expectations regarding the drug’s efficacy in patients with more advanced progressive disease.
“If this drug gets approved for progressive MS, you are going to have a number of patients coming to your clinics to ask for this drug,” he said. It is unclear, however, how beneficial the treatment might be for patients with advanced disease, based on the clinical trial conducted in primary progressive MS. “In my opinion, if someone is 65 to 70 years old and has had primary progressive MS for 15 to 20 years and has been wheelchair-confined for five or more years, it is unlikely that this drug is going to be very meaningful for them. Although, I do not know that for a fact. Therefore, my plan is to offer this [treatment], probably for approximately a year, and see what happens. We will continue to follow them and make a decision together about continuing therapy or stopping.”
“Remember, half the people in the world who have MS have progressive disease,” Dr. Moses said. “They have seen more than 20 years of therapies [approved] for relapsing MS, so they have a lot of pent-up expectations about a treatment option, and rightfully so. I just think this potential treatment has to be discussed in a broader context of how the study was done.”
Daclizumab
Daclizumab is an interleukin-2 receptor blocking humanized monoclonal antibody approved for use in relapsing forms of MS. It is self-administered as a subcutaneous injection once per month at a dose of 150 mg/mL. The drug’s label notes, “Because of its safety profile, the use of Zinbryta should generally be reserved for patients who have had an inadequate response to two or more drugs indicated for the treatment of MS.” This FDA guidance is similar to that for alemtuzumab. “With more than a dozen drugs for MS, it is not too surprising we are seeing this,” Dr. Moses said.
The efficacy of the drug was demonstrated in two randomized, double-blind studies. One study compared daclizumab with interferon beta-1a. The other study compared daclizumab and placebo.
In the active comparator study, 919 patients received daclizumab and 922 received interferon beta-1a. Compared with interferon beta-1a, daclizumab had a statistically significant effect on annualized relapse rate (0.393 vs 0.216; relative reduction, 45%) and on the number of new or newly enlarging T2 hyperintense lesions. Treatment did not significantly affect 12-week confirmed disability progression.
In some patients, daclizumab has a significant impact on the liver. As a result, physicians are asked to assess transaminase levels and total bilirubin monthly during treatment and for six months after stopping therapy, Dr. Moses said.
Autoimmune hepatitis and other immune-mediated disorders, including lymphadenopathy, noninfectious colitis, and cutaneous adverse events, were seen with daclizumab treatment.
Dermatologic reactions to daclizumab can range from mild rashes to serious reactions, and can include psoriasiform nail changes, erythematous changes and swelling, and desquamation and erythema of the palms. Neurologists should advise patients that these reactions “could happen at any point while they are taking this medication,” Dr. Moses said. Some patients experienced reactions after receiving the therapy for nearly three years.Patients also experienced adverse events related to infection, including nasopharyngitis, bronchitis, and tonsillitis. “Daclizumab is the newest approved drug for relapsing MS,” Dr. Moses said. “It has a unique mechanism of action and a favorable dosing schedule. Challenges exist with monitoring requirements and potential serious adverse events.”
Ocrelizumab
Ocrelizumab is a humanized monoclonal antibody that depletes CD20+ B cells.
Two identical studies, OPERA I and II, evaluated ocrelizumab in patients with relapsing MS. Another trial, ORATORIO, assessed ocrelizumab in patients with primary progressive MS. In the trials, patients received 600 mg of ocrelizumab by IV infusion every 24 weeks.
In OPERA I and II, treatment with ocrelizumab resulted in a 46% and 47% reduction in annualized relapse rate, respectively, compared with interferon beta-1a. In addition, ocrelizumab reduced the risk of confirmed disability progression for 12 weeks by 43% and 37%, respectively. Ocrelizumab also dramatically reduced the number of T1 gadolinium-enhancing lesions and the number of new or enlarging T2 hyperintense lesions, compared with interferon beta-1a.
The ORATORIO study included 732 patients with primary progressive MS who received ocrelizumab or placebo. Patients were ages 18 to 55, had an Expanded Disability Status Scale score of 3.0 to 6.5, and had abnormal CSF. Patients were treated for at least 120 weeks. Investigators measured slowing of disability progression as the primary outcome. There was a 24% reduction in clinical disability sustained for at least 12 weeks, compared with placebo.
Ocrelizumab generally was well tolerated. In the clinical trials, a similar proportion of patients treated with ocrelizumab and controls experienced adverse events. In OPERA I and II, the most common adverse event associated with ocrelizumab was infusion-related reactions, which occurred in 34.3% of patients in the ocrelizumab arm, compared with 9.7% of patients in the interferon beta-1a arm.
In ORATORIO, more malignancies were reported in patients treated with ocrelizumab, compared with patients who received placebo (11 vs 2). The implications of that finding are unclear. “We will see how that plays out in terms of what the FDA thinks about that,” Dr. Moses said.
The FDA has granted a priority review designation to ocrelizumab, with a targeted action date of December 28, 2016. “Ocrelizumab remains on the horizon with a potential role in both relapsing and progressive MS,” Dr. Moses said.
—Jake Remaly
HILTON HEAD, SC—Managing patient expectations is important when discussing new and pending treatments for multiple sclerosis (MS), according to a lecture given at the 39th Annual Contemporary Clinical Neurology Symposium. The FDA’s recent approval of daclizumab and ongoing priority review of ocrelizumab mean that neurologists likely will be discussing these therapies with patients in their clinics. Conversations may revolve around efficacy, laboratory monitoring, and risk of adverse events.
In the case of daclizumab (Zinbryta), which was approved in May 2016, patient counseling may focus on monthly laboratory monitoring requirements that are part of the drug’s risk evaluation and mitigation strategy (REMS) program and the potential for adverse events at any time during treatment, said Harold Moses Jr, MD, Associate Professor of Neurology at Vanderbilt University in Nashville.
Ocrelizumab (Ocrevus) could be the first drug approved for primary progressive MS and a new treatment option for patients with relapsing MS. Neurologists may need to temper patients’ expectations regarding the drug’s efficacy in patients with more advanced progressive disease.
“If this drug gets approved for progressive MS, you are going to have a number of patients coming to your clinics to ask for this drug,” he said. It is unclear, however, how beneficial the treatment might be for patients with advanced disease, based on the clinical trial conducted in primary progressive MS. “In my opinion, if someone is 65 to 70 years old and has had primary progressive MS for 15 to 20 years and has been wheelchair-confined for five or more years, it is unlikely that this drug is going to be very meaningful for them. Although, I do not know that for a fact. Therefore, my plan is to offer this [treatment], probably for approximately a year, and see what happens. We will continue to follow them and make a decision together about continuing therapy or stopping.”
“Remember, half the people in the world who have MS have progressive disease,” Dr. Moses said. “They have seen more than 20 years of therapies [approved] for relapsing MS, so they have a lot of pent-up expectations about a treatment option, and rightfully so. I just think this potential treatment has to be discussed in a broader context of how the study was done.”
Daclizumab
Daclizumab is an interleukin-2 receptor blocking humanized monoclonal antibody approved for use in relapsing forms of MS. It is self-administered as a subcutaneous injection once per month at a dose of 150 mg/mL. The drug’s label notes, “Because of its safety profile, the use of Zinbryta should generally be reserved for patients who have had an inadequate response to two or more drugs indicated for the treatment of MS.” This FDA guidance is similar to that for alemtuzumab. “With more than a dozen drugs for MS, it is not too surprising we are seeing this,” Dr. Moses said.
The efficacy of the drug was demonstrated in two randomized, double-blind studies. One study compared daclizumab with interferon beta-1a. The other study compared daclizumab and placebo.
In the active comparator study, 919 patients received daclizumab and 922 received interferon beta-1a. Compared with interferon beta-1a, daclizumab had a statistically significant effect on annualized relapse rate (0.393 vs 0.216; relative reduction, 45%) and on the number of new or newly enlarging T2 hyperintense lesions. Treatment did not significantly affect 12-week confirmed disability progression.
In some patients, daclizumab has a significant impact on the liver. As a result, physicians are asked to assess transaminase levels and total bilirubin monthly during treatment and for six months after stopping therapy, Dr. Moses said.
Autoimmune hepatitis and other immune-mediated disorders, including lymphadenopathy, noninfectious colitis, and cutaneous adverse events, were seen with daclizumab treatment.
Dermatologic reactions to daclizumab can range from mild rashes to serious reactions, and can include psoriasiform nail changes, erythematous changes and swelling, and desquamation and erythema of the palms. Neurologists should advise patients that these reactions “could happen at any point while they are taking this medication,” Dr. Moses said. Some patients experienced reactions after receiving the therapy for nearly three years.Patients also experienced adverse events related to infection, including nasopharyngitis, bronchitis, and tonsillitis. “Daclizumab is the newest approved drug for relapsing MS,” Dr. Moses said. “It has a unique mechanism of action and a favorable dosing schedule. Challenges exist with monitoring requirements and potential serious adverse events.”
Ocrelizumab
Ocrelizumab is a humanized monoclonal antibody that depletes CD20+ B cells.
Two identical studies, OPERA I and II, evaluated ocrelizumab in patients with relapsing MS. Another trial, ORATORIO, assessed ocrelizumab in patients with primary progressive MS. In the trials, patients received 600 mg of ocrelizumab by IV infusion every 24 weeks.
In OPERA I and II, treatment with ocrelizumab resulted in a 46% and 47% reduction in annualized relapse rate, respectively, compared with interferon beta-1a. In addition, ocrelizumab reduced the risk of confirmed disability progression for 12 weeks by 43% and 37%, respectively. Ocrelizumab also dramatically reduced the number of T1 gadolinium-enhancing lesions and the number of new or enlarging T2 hyperintense lesions, compared with interferon beta-1a.
The ORATORIO study included 732 patients with primary progressive MS who received ocrelizumab or placebo. Patients were ages 18 to 55, had an Expanded Disability Status Scale score of 3.0 to 6.5, and had abnormal CSF. Patients were treated for at least 120 weeks. Investigators measured slowing of disability progression as the primary outcome. There was a 24% reduction in clinical disability sustained for at least 12 weeks, compared with placebo.
Ocrelizumab generally was well tolerated. In the clinical trials, a similar proportion of patients treated with ocrelizumab and controls experienced adverse events. In OPERA I and II, the most common adverse event associated with ocrelizumab was infusion-related reactions, which occurred in 34.3% of patients in the ocrelizumab arm, compared with 9.7% of patients in the interferon beta-1a arm.
In ORATORIO, more malignancies were reported in patients treated with ocrelizumab, compared with patients who received placebo (11 vs 2). The implications of that finding are unclear. “We will see how that plays out in terms of what the FDA thinks about that,” Dr. Moses said.
The FDA has granted a priority review designation to ocrelizumab, with a targeted action date of December 28, 2016. “Ocrelizumab remains on the horizon with a potential role in both relapsing and progressive MS,” Dr. Moses said.
—Jake Remaly
Take steps to relieve ataxia in patients with alcohol use disorder
Ataxia is a well-known complication of chronic alcohol abuse, which is attributed to degeneration of the cerebellar vermis. However, effective treatment approaches, as well as the timing and level of recovery, remain unclear. One cross-sectional study found that long-term abstainers from alcohol had less severe ataxia than short-term abstainers,1 suggesting that improvement is possible with continued sobriety. However, a recent longitudinal study contradicts this finding, reporting no improvement in ataxia in patients abstinent for 10 weeks to 1 year.2
CASE REPORT
Unable to walk, heavy alcohol use
Mr. G, a 59-year-old white male with a history of daily, heavy alcohol use, presents to the emergency room reporting that he has “not been able to walk right” for 3 weeks. He is in a wheelchair because of ataxia and difficulty balancing. He denies headaches, visual changes, weakness, numbness, and difficulty speaking or swallowing.
Mr. G reports drinking one 40-oz bottle of malt liquor and 2 pints of vodka per day for more than 40 years. His alcohol abuse led to homelessness, unemployment, and divorce. Despite heavy drinking, he denies signs of withdrawal, including shaking, sweating, seizures, and delirium.
Mr. G has no other medical conditions. He denies a family history of neurologic disorders or substance abuse.
His pulse is 100 beats per minute, respirations of 16 breaths per minute, temperature of 37°C, and blood pressure of 143/89 mm Hg. Physical examination reveals a wide-based gait.
Mr. G is admitted to the inpatient psychiatric unit to monitor and treat his alcohol withdrawal and to undergo further workup of the gait disturbance.
A head CT scan shows non-specific changes; an EEG also is within normal limits. Complete blood count, basic metabolic panel, liver function test, HIV test, acute hepatitis panel, thyroid function test, erythrocyte sedimentation rate, and vitamin B12 tests are within normal ranges.
A full neurologic exam reveals a wide-based gait, impaired heel-shin test, and dysmetria on finger-nose-finger test. Mr. G is given a diagnosis of ataxia due to alcoholic cerebellar degeneration. Thiamine repletion is suggested.
Treatment and outcome
Mr. G continues on thiamine, 100 mg, twice daily, and oxazepam, 15 mg, as needed, to manage withdrawal symptoms. He receives gait training 3 times per week.
Approximately 10 days after admission, Mr. G is able to ambulate with a walker. Three weeks after admission, his gait has improved and he walks with a cane. (See the video at CurrentPsychiatry.com for an illustration of this progressive recovery.)
After discharge, Mr. G is referred to an addiction psychiatrist and addiction psychotherapist for ongoing treatment of alcohol use disorder.
Making the diagnosis
In a patient complaining of balance difficulties, consider ataxia secondary to cerebellar degeneration.
- Take a complete history. Ask about the onset and progression of ataxia.
- Obtain a family history. Some types of ataxia are genetic.
- Perform a neurologic examination, which may reveal signs of cerebellar deficits, particularly characteristic wide-based gait. These patients will have difficulty when walking in tandem. Other impairments on the neurologic exam that may raise suspicion for a cerebellar disorder include: impaired heel-shin test, impaired finger-nose-finger test (dysmetria), impaired rapid alternating movements (dysdiadochokinesia), nystagmus, impaired smooth pursuits, intention tremor, or speech abnormalities.
- Perform head imaging, such as a CT scan or MRI. In patients with ataxia secondary to alcohol abuse, imaging might reveal degeneration of the cerebellar vermis.
- Perform laboratory tests, such as inflammatory markers, vitamin levels, and thyroid function testing to detect possible toxic-metabolic or inflammatory causes.
Alcohol-induced ataxia can be diagnosed in patients with a history of heavy drinking if the workup does not reveal another possible cause for the gait disturbance. Other less common deficits associated with alcohol-induced cerebellar injury include:
- dysarthria
- abnormal rate and force of movement
- limb ataxia.3
Recommendations
- Be able to recognize the characteristic gait of patients with alcohol-induced ataxia.
- Provide thiamine supplementation.
- Refer patients to physical therapy.
- Educate your patients that their gait will not improve and may worsen if they continue to drink.
- Refer patients for ongoing treatment for alcohol use disorder, including medication management and psychotherapy.
Our experience suggests that patients with alcohol use disorder with cerebellar ataxia could have a good prognosis for ambulation. Improvement could occur over several weeks; it is unclear whether further gains can be expected with months or years of abstinence.
1. Smith S, Fein G. Persistent but less severe ataxia in long-term versus short-term abstinent alcoholic men and women: a cross-sectional analysis. Alcohol Clin Exp Res. 2011;35(12):2184-2192.
2. Fein G, Greenstein D. Gait and balance deficits in chronic alcoholics: no improvement from 10 weeks through 1 year abstinence. Alcohol Clin Exp Res. 2013;37(1):86-95.
3. Fitzpatrick LE, Jackson M, Crowe SF. Characterization of cerebellar ataxia in chronic alcoholics using the International Cooperative Ataxia Rating Scale (ICARS). Alcohol Clin Exp Res. 2012;36(11):1942-1951.
Ataxia is a well-known complication of chronic alcohol abuse, which is attributed to degeneration of the cerebellar vermis. However, effective treatment approaches, as well as the timing and level of recovery, remain unclear. One cross-sectional study found that long-term abstainers from alcohol had less severe ataxia than short-term abstainers,1 suggesting that improvement is possible with continued sobriety. However, a recent longitudinal study contradicts this finding, reporting no improvement in ataxia in patients abstinent for 10 weeks to 1 year.2
CASE REPORT
Unable to walk, heavy alcohol use
Mr. G, a 59-year-old white male with a history of daily, heavy alcohol use, presents to the emergency room reporting that he has “not been able to walk right” for 3 weeks. He is in a wheelchair because of ataxia and difficulty balancing. He denies headaches, visual changes, weakness, numbness, and difficulty speaking or swallowing.
Mr. G reports drinking one 40-oz bottle of malt liquor and 2 pints of vodka per day for more than 40 years. His alcohol abuse led to homelessness, unemployment, and divorce. Despite heavy drinking, he denies signs of withdrawal, including shaking, sweating, seizures, and delirium.
Mr. G has no other medical conditions. He denies a family history of neurologic disorders or substance abuse.
His pulse is 100 beats per minute, respirations of 16 breaths per minute, temperature of 37°C, and blood pressure of 143/89 mm Hg. Physical examination reveals a wide-based gait.
Mr. G is admitted to the inpatient psychiatric unit to monitor and treat his alcohol withdrawal and to undergo further workup of the gait disturbance.
A head CT scan shows non-specific changes; an EEG also is within normal limits. Complete blood count, basic metabolic panel, liver function test, HIV test, acute hepatitis panel, thyroid function test, erythrocyte sedimentation rate, and vitamin B12 tests are within normal ranges.
A full neurologic exam reveals a wide-based gait, impaired heel-shin test, and dysmetria on finger-nose-finger test. Mr. G is given a diagnosis of ataxia due to alcoholic cerebellar degeneration. Thiamine repletion is suggested.
Treatment and outcome
Mr. G continues on thiamine, 100 mg, twice daily, and oxazepam, 15 mg, as needed, to manage withdrawal symptoms. He receives gait training 3 times per week.
Approximately 10 days after admission, Mr. G is able to ambulate with a walker. Three weeks after admission, his gait has improved and he walks with a cane. (See the video at CurrentPsychiatry.com for an illustration of this progressive recovery.)
After discharge, Mr. G is referred to an addiction psychiatrist and addiction psychotherapist for ongoing treatment of alcohol use disorder.
Making the diagnosis
In a patient complaining of balance difficulties, consider ataxia secondary to cerebellar degeneration.
- Take a complete history. Ask about the onset and progression of ataxia.
- Obtain a family history. Some types of ataxia are genetic.
- Perform a neurologic examination, which may reveal signs of cerebellar deficits, particularly characteristic wide-based gait. These patients will have difficulty when walking in tandem. Other impairments on the neurologic exam that may raise suspicion for a cerebellar disorder include: impaired heel-shin test, impaired finger-nose-finger test (dysmetria), impaired rapid alternating movements (dysdiadochokinesia), nystagmus, impaired smooth pursuits, intention tremor, or speech abnormalities.
- Perform head imaging, such as a CT scan or MRI. In patients with ataxia secondary to alcohol abuse, imaging might reveal degeneration of the cerebellar vermis.
- Perform laboratory tests, such as inflammatory markers, vitamin levels, and thyroid function testing to detect possible toxic-metabolic or inflammatory causes.
Alcohol-induced ataxia can be diagnosed in patients with a history of heavy drinking if the workup does not reveal another possible cause for the gait disturbance. Other less common deficits associated with alcohol-induced cerebellar injury include:
- dysarthria
- abnormal rate and force of movement
- limb ataxia.3
Recommendations
- Be able to recognize the characteristic gait of patients with alcohol-induced ataxia.
- Provide thiamine supplementation.
- Refer patients to physical therapy.
- Educate your patients that their gait will not improve and may worsen if they continue to drink.
- Refer patients for ongoing treatment for alcohol use disorder, including medication management and psychotherapy.
Our experience suggests that patients with alcohol use disorder with cerebellar ataxia could have a good prognosis for ambulation. Improvement could occur over several weeks; it is unclear whether further gains can be expected with months or years of abstinence.
Ataxia is a well-known complication of chronic alcohol abuse, which is attributed to degeneration of the cerebellar vermis. However, effective treatment approaches, as well as the timing and level of recovery, remain unclear. One cross-sectional study found that long-term abstainers from alcohol had less severe ataxia than short-term abstainers,1 suggesting that improvement is possible with continued sobriety. However, a recent longitudinal study contradicts this finding, reporting no improvement in ataxia in patients abstinent for 10 weeks to 1 year.2
CASE REPORT
Unable to walk, heavy alcohol use
Mr. G, a 59-year-old white male with a history of daily, heavy alcohol use, presents to the emergency room reporting that he has “not been able to walk right” for 3 weeks. He is in a wheelchair because of ataxia and difficulty balancing. He denies headaches, visual changes, weakness, numbness, and difficulty speaking or swallowing.
Mr. G reports drinking one 40-oz bottle of malt liquor and 2 pints of vodka per day for more than 40 years. His alcohol abuse led to homelessness, unemployment, and divorce. Despite heavy drinking, he denies signs of withdrawal, including shaking, sweating, seizures, and delirium.
Mr. G has no other medical conditions. He denies a family history of neurologic disorders or substance abuse.
His pulse is 100 beats per minute, respirations of 16 breaths per minute, temperature of 37°C, and blood pressure of 143/89 mm Hg. Physical examination reveals a wide-based gait.
Mr. G is admitted to the inpatient psychiatric unit to monitor and treat his alcohol withdrawal and to undergo further workup of the gait disturbance.
A head CT scan shows non-specific changes; an EEG also is within normal limits. Complete blood count, basic metabolic panel, liver function test, HIV test, acute hepatitis panel, thyroid function test, erythrocyte sedimentation rate, and vitamin B12 tests are within normal ranges.
A full neurologic exam reveals a wide-based gait, impaired heel-shin test, and dysmetria on finger-nose-finger test. Mr. G is given a diagnosis of ataxia due to alcoholic cerebellar degeneration. Thiamine repletion is suggested.
Treatment and outcome
Mr. G continues on thiamine, 100 mg, twice daily, and oxazepam, 15 mg, as needed, to manage withdrawal symptoms. He receives gait training 3 times per week.
Approximately 10 days after admission, Mr. G is able to ambulate with a walker. Three weeks after admission, his gait has improved and he walks with a cane. (See the video at CurrentPsychiatry.com for an illustration of this progressive recovery.)
After discharge, Mr. G is referred to an addiction psychiatrist and addiction psychotherapist for ongoing treatment of alcohol use disorder.
Making the diagnosis
In a patient complaining of balance difficulties, consider ataxia secondary to cerebellar degeneration.
- Take a complete history. Ask about the onset and progression of ataxia.
- Obtain a family history. Some types of ataxia are genetic.
- Perform a neurologic examination, which may reveal signs of cerebellar deficits, particularly characteristic wide-based gait. These patients will have difficulty when walking in tandem. Other impairments on the neurologic exam that may raise suspicion for a cerebellar disorder include: impaired heel-shin test, impaired finger-nose-finger test (dysmetria), impaired rapid alternating movements (dysdiadochokinesia), nystagmus, impaired smooth pursuits, intention tremor, or speech abnormalities.
- Perform head imaging, such as a CT scan or MRI. In patients with ataxia secondary to alcohol abuse, imaging might reveal degeneration of the cerebellar vermis.
- Perform laboratory tests, such as inflammatory markers, vitamin levels, and thyroid function testing to detect possible toxic-metabolic or inflammatory causes.
Alcohol-induced ataxia can be diagnosed in patients with a history of heavy drinking if the workup does not reveal another possible cause for the gait disturbance. Other less common deficits associated with alcohol-induced cerebellar injury include:
- dysarthria
- abnormal rate and force of movement
- limb ataxia.3
Recommendations
- Be able to recognize the characteristic gait of patients with alcohol-induced ataxia.
- Provide thiamine supplementation.
- Refer patients to physical therapy.
- Educate your patients that their gait will not improve and may worsen if they continue to drink.
- Refer patients for ongoing treatment for alcohol use disorder, including medication management and psychotherapy.
Our experience suggests that patients with alcohol use disorder with cerebellar ataxia could have a good prognosis for ambulation. Improvement could occur over several weeks; it is unclear whether further gains can be expected with months or years of abstinence.
1. Smith S, Fein G. Persistent but less severe ataxia in long-term versus short-term abstinent alcoholic men and women: a cross-sectional analysis. Alcohol Clin Exp Res. 2011;35(12):2184-2192.
2. Fein G, Greenstein D. Gait and balance deficits in chronic alcoholics: no improvement from 10 weeks through 1 year abstinence. Alcohol Clin Exp Res. 2013;37(1):86-95.
3. Fitzpatrick LE, Jackson M, Crowe SF. Characterization of cerebellar ataxia in chronic alcoholics using the International Cooperative Ataxia Rating Scale (ICARS). Alcohol Clin Exp Res. 2012;36(11):1942-1951.
1. Smith S, Fein G. Persistent but less severe ataxia in long-term versus short-term abstinent alcoholic men and women: a cross-sectional analysis. Alcohol Clin Exp Res. 2011;35(12):2184-2192.
2. Fein G, Greenstein D. Gait and balance deficits in chronic alcoholics: no improvement from 10 weeks through 1 year abstinence. Alcohol Clin Exp Res. 2013;37(1):86-95.
3. Fitzpatrick LE, Jackson M, Crowe SF. Characterization of cerebellar ataxia in chronic alcoholics using the International Cooperative Ataxia Rating Scale (ICARS). Alcohol Clin Exp Res. 2012;36(11):1942-1951.
No more 'stickies'!: Help your patients bring their ‘to-do’ list into the 21st century
Difficulty with time management and organization is one of the most common complaints of patients with attention-deficit/hyperactivity disorder (ADHD). Being unproductive and inefficient also is anxiety-producing and depressing, leaving patients with additional comorbidity.
Although medication can help improve a person’s focus, if the patient is focusing on a set of poorly designed systems, he (she) will see little improvement. A comprehensive approach to improving day-to-day task management, similar to the one I describe here and use with my patients, is therefore as important as medication.
Needed: An ‘organizing principle’
Imagine that supermarkets displayed food in the order it arrives from the food distributors and producers. You’d walk in to the store and see a display of food that lacks hierarchy—1 random item placed next to another. The experience would be jarring, and shopping would be a much slower chore. Furthermore, what if you had to go to 5 stores to cover all your needs?
Yet, that is how most “to-do” lists are executed: A thought comes in, a thought goes down on paper. Or on a sticky note. Or in an app. Or in a calendar. Or all of the above! Often, there is neither an organizing principle (other than perhaps chronological order) or a central repository. No wonder it’s hard to feel present and clear-minded. Add to this disorganization the volume of information coming in from the environment—e-mails, voice mails, texts, notifications, dings, beeps, buzzes, and maybe even snail mail—and the feeling of being overwhelmed grows.
Unconscious motives for maintaining poor systems also might play a role. People with a “need to please” personality type or who are more passive-aggressive in their communication are more likely to overcommit, and then forget or be late completing their tasks, rather than saying “No” from the outset or delegating the work.
Survival basics for time management
Assuming there is simply a skills deficit, you can teach basic time and project management skills to patients with ADHD (and to any patient with suboptimal executive functioning). Here are basic principles to adopt:
- If you can forget it, you will, so all tasks should go onto the to-do list.
- You should keep only 1 list. Adding on “stickies” is not allowed.
- Your list is like an extra lobe of your brain: It should be present at all times, whether you keep it in “the Cloud,” on your desktop, or on paper.
- Review your list and clean it up at least daily. This takes time, but it also saves time—in spades—when you can call upon the right task, at the right time, with energy and drive.
- The first action you should take in the daily review is to weed out or delegate tasks.
- Next, categorize remaining tasks. (Note: The free smartphone app Evernote allows you to do this with “tags.”) Categorizing allows you to process sets of tasks in buckets that can be tackled as a bundle and, therefore, more efficiently. For example, having all of your errands, items to research, and telephone calls that need to be returned in separate buckets allows for speedier processing—as opposed to veering back and forth between line items.
- Then, move remaining high-priority items to the top of the list. However, remember that, if everything is urgent, nothing is. Items that are low-hanging fruit that you can cross off the list in a matter of minutes can be prioritized even if they are not as urgent. By doing that, your list becomes more manageable and your brain can dive deeper into more complex tasks.
- Block out calendar time for each of your buckets with this formula: (1) Estimate how much time you’ll need to complete the tasks in each bucket, then add 50% for each bucket. (2) Add in commuting, set-up, or wind-down time, if you need it, to the grand total for all buckets, and then add 50% more than you’ve estimated
Set the brain free!
This process will seem like a burden at the beginning, when the synapses underneath it still need to get stronger (much like how the body responds to exercise). However, as long as these principles are put into action daily, they will become a trusted, second-nature system that frees the brain from distraction and anxiety—and, ultimately,
Difficulty with time management and organization is one of the most common complaints of patients with attention-deficit/hyperactivity disorder (ADHD). Being unproductive and inefficient also is anxiety-producing and depressing, leaving patients with additional comorbidity.
Although medication can help improve a person’s focus, if the patient is focusing on a set of poorly designed systems, he (she) will see little improvement. A comprehensive approach to improving day-to-day task management, similar to the one I describe here and use with my patients, is therefore as important as medication.
Needed: An ‘organizing principle’
Imagine that supermarkets displayed food in the order it arrives from the food distributors and producers. You’d walk in to the store and see a display of food that lacks hierarchy—1 random item placed next to another. The experience would be jarring, and shopping would be a much slower chore. Furthermore, what if you had to go to 5 stores to cover all your needs?
Yet, that is how most “to-do” lists are executed: A thought comes in, a thought goes down on paper. Or on a sticky note. Or in an app. Or in a calendar. Or all of the above! Often, there is neither an organizing principle (other than perhaps chronological order) or a central repository. No wonder it’s hard to feel present and clear-minded. Add to this disorganization the volume of information coming in from the environment—e-mails, voice mails, texts, notifications, dings, beeps, buzzes, and maybe even snail mail—and the feeling of being overwhelmed grows.
Unconscious motives for maintaining poor systems also might play a role. People with a “need to please” personality type or who are more passive-aggressive in their communication are more likely to overcommit, and then forget or be late completing their tasks, rather than saying “No” from the outset or delegating the work.
Survival basics for time management
Assuming there is simply a skills deficit, you can teach basic time and project management skills to patients with ADHD (and to any patient with suboptimal executive functioning). Here are basic principles to adopt:
- If you can forget it, you will, so all tasks should go onto the to-do list.
- You should keep only 1 list. Adding on “stickies” is not allowed.
- Your list is like an extra lobe of your brain: It should be present at all times, whether you keep it in “the Cloud,” on your desktop, or on paper.
- Review your list and clean it up at least daily. This takes time, but it also saves time—in spades—when you can call upon the right task, at the right time, with energy and drive.
- The first action you should take in the daily review is to weed out or delegate tasks.
- Next, categorize remaining tasks. (Note: The free smartphone app Evernote allows you to do this with “tags.”) Categorizing allows you to process sets of tasks in buckets that can be tackled as a bundle and, therefore, more efficiently. For example, having all of your errands, items to research, and telephone calls that need to be returned in separate buckets allows for speedier processing—as opposed to veering back and forth between line items.
- Then, move remaining high-priority items to the top of the list. However, remember that, if everything is urgent, nothing is. Items that are low-hanging fruit that you can cross off the list in a matter of minutes can be prioritized even if they are not as urgent. By doing that, your list becomes more manageable and your brain can dive deeper into more complex tasks.
- Block out calendar time for each of your buckets with this formula: (1) Estimate how much time you’ll need to complete the tasks in each bucket, then add 50% for each bucket. (2) Add in commuting, set-up, or wind-down time, if you need it, to the grand total for all buckets, and then add 50% more than you’ve estimated
Set the brain free!
This process will seem like a burden at the beginning, when the synapses underneath it still need to get stronger (much like how the body responds to exercise). However, as long as these principles are put into action daily, they will become a trusted, second-nature system that frees the brain from distraction and anxiety—and, ultimately,
Difficulty with time management and organization is one of the most common complaints of patients with attention-deficit/hyperactivity disorder (ADHD). Being unproductive and inefficient also is anxiety-producing and depressing, leaving patients with additional comorbidity.
Although medication can help improve a person’s focus, if the patient is focusing on a set of poorly designed systems, he (she) will see little improvement. A comprehensive approach to improving day-to-day task management, similar to the one I describe here and use with my patients, is therefore as important as medication.
Needed: An ‘organizing principle’
Imagine that supermarkets displayed food in the order it arrives from the food distributors and producers. You’d walk in to the store and see a display of food that lacks hierarchy—1 random item placed next to another. The experience would be jarring, and shopping would be a much slower chore. Furthermore, what if you had to go to 5 stores to cover all your needs?
Yet, that is how most “to-do” lists are executed: A thought comes in, a thought goes down on paper. Or on a sticky note. Or in an app. Or in a calendar. Or all of the above! Often, there is neither an organizing principle (other than perhaps chronological order) or a central repository. No wonder it’s hard to feel present and clear-minded. Add to this disorganization the volume of information coming in from the environment—e-mails, voice mails, texts, notifications, dings, beeps, buzzes, and maybe even snail mail—and the feeling of being overwhelmed grows.
Unconscious motives for maintaining poor systems also might play a role. People with a “need to please” personality type or who are more passive-aggressive in their communication are more likely to overcommit, and then forget or be late completing their tasks, rather than saying “No” from the outset or delegating the work.
Survival basics for time management
Assuming there is simply a skills deficit, you can teach basic time and project management skills to patients with ADHD (and to any patient with suboptimal executive functioning). Here are basic principles to adopt:
- If you can forget it, you will, so all tasks should go onto the to-do list.
- You should keep only 1 list. Adding on “stickies” is not allowed.
- Your list is like an extra lobe of your brain: It should be present at all times, whether you keep it in “the Cloud,” on your desktop, or on paper.
- Review your list and clean it up at least daily. This takes time, but it also saves time—in spades—when you can call upon the right task, at the right time, with energy and drive.
- The first action you should take in the daily review is to weed out or delegate tasks.
- Next, categorize remaining tasks. (Note: The free smartphone app Evernote allows you to do this with “tags.”) Categorizing allows you to process sets of tasks in buckets that can be tackled as a bundle and, therefore, more efficiently. For example, having all of your errands, items to research, and telephone calls that need to be returned in separate buckets allows for speedier processing—as opposed to veering back and forth between line items.
- Then, move remaining high-priority items to the top of the list. However, remember that, if everything is urgent, nothing is. Items that are low-hanging fruit that you can cross off the list in a matter of minutes can be prioritized even if they are not as urgent. By doing that, your list becomes more manageable and your brain can dive deeper into more complex tasks.
- Block out calendar time for each of your buckets with this formula: (1) Estimate how much time you’ll need to complete the tasks in each bucket, then add 50% for each bucket. (2) Add in commuting, set-up, or wind-down time, if you need it, to the grand total for all buckets, and then add 50% more than you’ve estimated
Set the brain free!
This process will seem like a burden at the beginning, when the synapses underneath it still need to get stronger (much like how the body responds to exercise). However, as long as these principles are put into action daily, they will become a trusted, second-nature system that frees the brain from distraction and anxiety—and, ultimately,