User login
The role of social media in aesthetic trends
Recently, but I had never heard it before. Not too long afterwards, patients were asking me about it in the office, using the same terminology, and I had several calls about it in one day. When I asked one trusted patient where she’d heard this term, which seemed to be trending, she told me that she had seen it on Instagram, as an ad or a “suggested for you” post.
Whether it’s a different name or term for a cosmetic procedure or laser we use that I’ve never heard before – such as “lip flip” or trap tox (also known as “Barbie Botox”) – many of these trendy terms spread like wildfire on social media. Some of the terms may be marketing tools started and spread by doctors who perform aesthetic procedures, something I don’t recommend as it only creates confusion for patients and practitioners, similar to the confusion consumers face regarding the plethora of over-the-counter skin care options and the marketing terms used for them. Other terms and trends are also started by nonphysician or non–professionally trained providers, sometimes leading to an unsafe or misleading term for an aesthetic procedure.
Over the past few years, several articles about the impact of social media in aesthetics have been published. In one recent paper, published in 2022, Boen and Jerdan noted that 72% of people in the United States use social media, up from 5% of American adults in 2005. In the United States, they note, “YouTube is the most popular platform with 73% of adult users, followed by Facebook (69%), Instagram (37%), SnapChat (24%), and Twitter (22%). Of the sites used daily, Facebook has the most activity (74%), followed by Instagram (64%), SnapChat (63%), YouTube (51%), and Twitter (42%).” They argue that the pros of social media in aesthetic medicine include its use as an educational tool by medical professionals to educate and provide accurate information about cosmetic procedures, and that “providing factual and evidence-based medical information to the public can help to counteract the abundant misinformation that is out there.” The cons include misinformation, no credentialing verification of the provider of the information – essentially anyone can be an “influencer” – as well as the addictive nature of social media for the consumer.
Along the same lines, younger patients tend to rely more on social media in choosing treatments and providers, further perpetuating any anxiety created from misinformation and unrealistic expectations from nonmedical influencers regarding procedures, filters used on photographs, photo editing, etc., in achieving an aesthetic result.
Physicians, particularly fellowship-trained aesthetic and surgical dermatologists, plastic and reconstructive surgeons, oculoplastic surgeons, and ENT facial plastic surgeons, who have the most training, knowledge, and expertise about aesthetic procedures, often have the least amount of time to devote to education via social media, compared with nonmedical influencers. Unless sponsored, they are also not being compensated for using it as an educational tool, except for potential indirect compensation from using it as a marketing tool for themselves and their practices. In contrast, nonmedical influencers often have many followers and time to create content, and in some cases, this is their full-time job.
All in all, most authors agree that social media has been associated with an increased acceptance of cosmetic surgery and procedures. Whether it be a trend seen on social media, or viewing one’s appearance in a filtered or photoediting app, or seeing an image of how another person looks (similar to how people in magazines, films and on television, were viewed in the past), social media has piqued people’s interest in aesthetics. It remains a balance for interested physicians to help keep information about cosmetic procedures presented in a healthy, interesting, professional, and accurate manner, and in a non–time-consuming way.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to her at [email protected]. She had no relevant disclosures.
References
Boen M and Jerdan K. Clin Dermatol. 2022 Jan-Feb;40(1):45-8.
Chen J et al. JAMA Facial Plast Surg. 2019 Sep 1;21(5):361-7.
Chopan M et al. Plast Reconstr Surg. 2019 Apr;143(4):1259-65.
Recently, but I had never heard it before. Not too long afterwards, patients were asking me about it in the office, using the same terminology, and I had several calls about it in one day. When I asked one trusted patient where she’d heard this term, which seemed to be trending, she told me that she had seen it on Instagram, as an ad or a “suggested for you” post.
Whether it’s a different name or term for a cosmetic procedure or laser we use that I’ve never heard before – such as “lip flip” or trap tox (also known as “Barbie Botox”) – many of these trendy terms spread like wildfire on social media. Some of the terms may be marketing tools started and spread by doctors who perform aesthetic procedures, something I don’t recommend as it only creates confusion for patients and practitioners, similar to the confusion consumers face regarding the plethora of over-the-counter skin care options and the marketing terms used for them. Other terms and trends are also started by nonphysician or non–professionally trained providers, sometimes leading to an unsafe or misleading term for an aesthetic procedure.
Over the past few years, several articles about the impact of social media in aesthetics have been published. In one recent paper, published in 2022, Boen and Jerdan noted that 72% of people in the United States use social media, up from 5% of American adults in 2005. In the United States, they note, “YouTube is the most popular platform with 73% of adult users, followed by Facebook (69%), Instagram (37%), SnapChat (24%), and Twitter (22%). Of the sites used daily, Facebook has the most activity (74%), followed by Instagram (64%), SnapChat (63%), YouTube (51%), and Twitter (42%).” They argue that the pros of social media in aesthetic medicine include its use as an educational tool by medical professionals to educate and provide accurate information about cosmetic procedures, and that “providing factual and evidence-based medical information to the public can help to counteract the abundant misinformation that is out there.” The cons include misinformation, no credentialing verification of the provider of the information – essentially anyone can be an “influencer” – as well as the addictive nature of social media for the consumer.
Along the same lines, younger patients tend to rely more on social media in choosing treatments and providers, further perpetuating any anxiety created from misinformation and unrealistic expectations from nonmedical influencers regarding procedures, filters used on photographs, photo editing, etc., in achieving an aesthetic result.
Physicians, particularly fellowship-trained aesthetic and surgical dermatologists, plastic and reconstructive surgeons, oculoplastic surgeons, and ENT facial plastic surgeons, who have the most training, knowledge, and expertise about aesthetic procedures, often have the least amount of time to devote to education via social media, compared with nonmedical influencers. Unless sponsored, they are also not being compensated for using it as an educational tool, except for potential indirect compensation from using it as a marketing tool for themselves and their practices. In contrast, nonmedical influencers often have many followers and time to create content, and in some cases, this is their full-time job.
All in all, most authors agree that social media has been associated with an increased acceptance of cosmetic surgery and procedures. Whether it be a trend seen on social media, or viewing one’s appearance in a filtered or photoediting app, or seeing an image of how another person looks (similar to how people in magazines, films and on television, were viewed in the past), social media has piqued people’s interest in aesthetics. It remains a balance for interested physicians to help keep information about cosmetic procedures presented in a healthy, interesting, professional, and accurate manner, and in a non–time-consuming way.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to her at [email protected]. She had no relevant disclosures.
References
Boen M and Jerdan K. Clin Dermatol. 2022 Jan-Feb;40(1):45-8.
Chen J et al. JAMA Facial Plast Surg. 2019 Sep 1;21(5):361-7.
Chopan M et al. Plast Reconstr Surg. 2019 Apr;143(4):1259-65.
Recently, but I had never heard it before. Not too long afterwards, patients were asking me about it in the office, using the same terminology, and I had several calls about it in one day. When I asked one trusted patient where she’d heard this term, which seemed to be trending, she told me that she had seen it on Instagram, as an ad or a “suggested for you” post.
Whether it’s a different name or term for a cosmetic procedure or laser we use that I’ve never heard before – such as “lip flip” or trap tox (also known as “Barbie Botox”) – many of these trendy terms spread like wildfire on social media. Some of the terms may be marketing tools started and spread by doctors who perform aesthetic procedures, something I don’t recommend as it only creates confusion for patients and practitioners, similar to the confusion consumers face regarding the plethora of over-the-counter skin care options and the marketing terms used for them. Other terms and trends are also started by nonphysician or non–professionally trained providers, sometimes leading to an unsafe or misleading term for an aesthetic procedure.
Over the past few years, several articles about the impact of social media in aesthetics have been published. In one recent paper, published in 2022, Boen and Jerdan noted that 72% of people in the United States use social media, up from 5% of American adults in 2005. In the United States, they note, “YouTube is the most popular platform with 73% of adult users, followed by Facebook (69%), Instagram (37%), SnapChat (24%), and Twitter (22%). Of the sites used daily, Facebook has the most activity (74%), followed by Instagram (64%), SnapChat (63%), YouTube (51%), and Twitter (42%).” They argue that the pros of social media in aesthetic medicine include its use as an educational tool by medical professionals to educate and provide accurate information about cosmetic procedures, and that “providing factual and evidence-based medical information to the public can help to counteract the abundant misinformation that is out there.” The cons include misinformation, no credentialing verification of the provider of the information – essentially anyone can be an “influencer” – as well as the addictive nature of social media for the consumer.
Along the same lines, younger patients tend to rely more on social media in choosing treatments and providers, further perpetuating any anxiety created from misinformation and unrealistic expectations from nonmedical influencers regarding procedures, filters used on photographs, photo editing, etc., in achieving an aesthetic result.
Physicians, particularly fellowship-trained aesthetic and surgical dermatologists, plastic and reconstructive surgeons, oculoplastic surgeons, and ENT facial plastic surgeons, who have the most training, knowledge, and expertise about aesthetic procedures, often have the least amount of time to devote to education via social media, compared with nonmedical influencers. Unless sponsored, they are also not being compensated for using it as an educational tool, except for potential indirect compensation from using it as a marketing tool for themselves and their practices. In contrast, nonmedical influencers often have many followers and time to create content, and in some cases, this is their full-time job.
All in all, most authors agree that social media has been associated with an increased acceptance of cosmetic surgery and procedures. Whether it be a trend seen on social media, or viewing one’s appearance in a filtered or photoediting app, or seeing an image of how another person looks (similar to how people in magazines, films and on television, were viewed in the past), social media has piqued people’s interest in aesthetics. It remains a balance for interested physicians to help keep information about cosmetic procedures presented in a healthy, interesting, professional, and accurate manner, and in a non–time-consuming way.
Dr. Wesley practices dermatology in Beverly Hills, Calif. Write to her at [email protected]. She had no relevant disclosures.
References
Boen M and Jerdan K. Clin Dermatol. 2022 Jan-Feb;40(1):45-8.
Chen J et al. JAMA Facial Plast Surg. 2019 Sep 1;21(5):361-7.
Chopan M et al. Plast Reconstr Surg. 2019 Apr;143(4):1259-65.
PCPs facing increased patient demand for knowledgeable menopause care
In 2017, a survey of 20 U.S. residency programs in family medicine, internal medicine, and ob.gyn. showed that only 6.8% of residents felt they were being adequately prepared to manage menopausal patients effectively, including how to use hormone therapy (HT).
Of the 177 residents who responded to the survey, 102 (56%) were in either family medicine or internal medicine.
“My guess is that there has been no substantial evolution in medical training to this day,” said lead survey study author Juliana Kling, MD, MPH, professor of medicine, chair of women’s health internal medicine, and dean, Mayo Clinic Alix School of Medicine, Scottsdale, Ariz.
The survey showed that overall 98% of residents thought it was important to know about menopause. However, 34% said they wouldn’t recommend HT in a severely symptomatic woman with no contraindications, and 60% said they wouldn’t recommend HT until at least the natural age of menopause in a prematurely menopausal woman. Some even recommended against it.
“Hormone therapy is effective, and for most healthy women younger than 60, the benefits are going to outweigh the risks,” said Dr. Kling. “We need to be comfortable, even in internal medicine, with prescribing hormones for the right women.”
The researchers concluded that “residual ambivalence about [hormone therapy] on the part of educators” may have played a role in curriculums that didn’t acknowledge the clinical relevance of menopause or include current evidence on the use of HT. Physicians should be taught to recognize menopausal symptoms, know the risks and benefits of HT and the alternatives, and how to select suitable candidates, they said.
Up to 80% of women in the United States are affected by menopausal vasomotor symptoms, but only one in four receive treatment, Dr. Kling pointed out. “Women will spend about a third of their lives after menopause, so being prepared to manage the consequences of menopause, such as bone health, vaginal dryness and painful intercourse, and increased cardiovascular disease risk, is critically important to all of us caring for women,” she emphasized. “These aren’t just ‘bothersome symptoms.’ ”
It is estimated that by 2060, there will be 90 million postmenopausal women in the United States. “Given the number of women who will experience symptoms of menopause and the considerable associated burden to their health and to the health care system, it is important to invest in educating future clinicians to provide evidence-based, comprehensive menopause management,” said Dr. Kling and coauthors in a February 2023 review of menopause treatments.
HT is the standard for the treatment of hot flashes and night sweats, and is highly effective for the prevention of bone loss and managing genitourinary syndrome of menopause. Among the alternatives to HT, the nonhormonal pharmacologic fezolinetant (Veozah) was approved by the U.S. Food and Drug Administration last May.
Following the early negative reports from the Women’s Health Initiative study of HT in 2002 and 2004, however, steep declines in HT prescription rates were seen among internists and family medicine practitioners. By 2009, only 18% of all HT prescriptions were written by primary care providers, and today, many remain wary about prescribing HT, despite evidence of its clinical value and safety.
“I think there’s a whole generation of family physicians who were taught that [hormone therapy] is dangerous and still feel very uncomfortable about using it to treat menopausal symptoms,” said Santina J.G. Wheat, MD, MPH, associate professor of family and community medicine at Northwestern University, Chicago. “These are the physicians educating the next generation of physicians,” said Dr. Wheat, who is program director for the McGaw Northwestern Family Medicine Residency Erie Humboldt Park.
Heather Hirsch, MD, an internist who specializes in menopause medicine in Columbus, Ohio, estimates that there are 300 internists among the 1,000 or so health care providers currently certified in menopause medicine through The Menopause Society (formerly the North American Menopause Society or NAMS). With 63 million women in the United States between the ages of 34 and 65, “that adds up to one doctor for several million patients,” she pointed out.
“In my opinion, the impact on menopausal care is profound,” said Jennifer T. Allen, MD, associate professor of obstetrics and gynecology, and director of menopause and midlife health at the Medical College of Georgia, Augusta. “If a physician was not exposed to menopause medicine in medical school or residency and does not choose to learn about menopause after training, then the opportunity to fully care for perimenopausal and postmenopausal women is extinguished.”
Not everyone agrees. “There’s no question that women’s health in general and menopausal issues specifically are a critical part of health care that is typically covered in most family medicine curriculums,” said Neil S. Skolnik, MD, professor of family and community medicine at the Sidney Kimmel Medical College in Philadelphia. “In family medicine, we really do attend to women’s health – particularly women’s health around menopause – as an important part of resident physician training,” emphasized Dr. Skolnik who is also and also associate director of the family medicine residency program at Abington Jefferson Health in Jenkintown, Penn.
"Family physicians are in a unique position to offer female patients effective care at perimenopause and beyond," added Karen L. Smith, MD, a family physician from Raeford, N.C., who is a board member of the American Academy of Family Physicians.*
Even so, many primary care physicians remain unsure about the use of HT, according to William E. Golden, MD, an internist and geriatrician, and professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock.
“On the whole area of hot flashes and vasomotor instability, I think we’re in a state of significant flux and confusion,” Dr. Golden said in an interview. “For a long time, a lot of doctors told patients, ‘It’s okay, you’ll age out of it.’ Then the data started showing that the vasomotor symptoms continued for years so physicians began to reevaluate how to manage them. Now, the pendulum has swung back to giving estrogen.”
Many family physicians have been left to their own devices to figure out how to manage menopausal patients, said Dr. Wheat. “When there are significant changes to clinical management – or in the case of HT, a real reversal in how menopausal symptoms are managed – getting information out to physicians can be challenging.”
Meanwhile, patient demand for answers to their questions about menopause and the use of HT is changing the conversation, where it’s taking place, and with whom.
Some media-savvy doctors have taken to TikTok, where a lot of women started educating themselves about menopause during the pandemic. Dr. Hirsch is one of them. She uses the social media platform to talk about menopause and FDA-approved HT, but warned that for every clinician who is certified in menopause medicine “there are five more selling snake oil.”
Mainstream media has also jumped on the menopause bandwagon. The New York Times was one of the first, declaring that “menopause is having a moment.” On Feb. 1, the newspaper stormed the gates of the medical establishment with an article asking why more doctors weren’t offering HT to women experiencing hot flashes, sleeplessness, and pain during sex. The headline: “Women have been misled about menopause.”
On April 5, “The Menopause Talk” was posted to Oprah Daily, along with a menopause curriculum to give viewers “the tools to stay firmly in the driver’s seat as you navigate perimenopause and then menopause.” Popular topics included how to get your sex life back, premature menopause survival, and ways to work with insurers so that treatment is affordable.
“There’s been a sea-change in the culture that’s being driven by patient demand,” said Dr. Kling. “The conversation, colloquially, in the media, and with our patients, is evolving. Menopause is no longer such a taboo topic, and our patients are really demanding that we have answers for them. Clinicians are recognizing that they need better training in menopause and seeking that out.”
Last June, “Transforming Women’s Health” – the Mayo Clinic’s annual CME program held in partnership with The Menopause Society – had record physician attendance. “We’re going to make sure that our trainees are learning the up-to-date recommendations, not the ones from 20 years ago when the initial WHI reports made everyone fearful of hormones,” said Dr. Kling.
Dr. Kling disclosed that she is a medical editor for Everyday Health, and has a relationship with Evolve Medical Education. Dr. Skolnik reported relationships with numerous pharmaceutical companies. He is an MDedge Family Medicine board member. Dr. Golden is an MDedge Internal Medicine board member, and Dr. Wheat is an MDedge Family Medicine board member. Dr. Allen reported having no potential conflicts of interest.
* This story was updated on Sept 18, 2023. The quotation is attributable to Dr. Smith, not Dr. Skolnik.
In 2017, a survey of 20 U.S. residency programs in family medicine, internal medicine, and ob.gyn. showed that only 6.8% of residents felt they were being adequately prepared to manage menopausal patients effectively, including how to use hormone therapy (HT).
Of the 177 residents who responded to the survey, 102 (56%) were in either family medicine or internal medicine.
“My guess is that there has been no substantial evolution in medical training to this day,” said lead survey study author Juliana Kling, MD, MPH, professor of medicine, chair of women’s health internal medicine, and dean, Mayo Clinic Alix School of Medicine, Scottsdale, Ariz.
The survey showed that overall 98% of residents thought it was important to know about menopause. However, 34% said they wouldn’t recommend HT in a severely symptomatic woman with no contraindications, and 60% said they wouldn’t recommend HT until at least the natural age of menopause in a prematurely menopausal woman. Some even recommended against it.
“Hormone therapy is effective, and for most healthy women younger than 60, the benefits are going to outweigh the risks,” said Dr. Kling. “We need to be comfortable, even in internal medicine, with prescribing hormones for the right women.”
The researchers concluded that “residual ambivalence about [hormone therapy] on the part of educators” may have played a role in curriculums that didn’t acknowledge the clinical relevance of menopause or include current evidence on the use of HT. Physicians should be taught to recognize menopausal symptoms, know the risks and benefits of HT and the alternatives, and how to select suitable candidates, they said.
Up to 80% of women in the United States are affected by menopausal vasomotor symptoms, but only one in four receive treatment, Dr. Kling pointed out. “Women will spend about a third of their lives after menopause, so being prepared to manage the consequences of menopause, such as bone health, vaginal dryness and painful intercourse, and increased cardiovascular disease risk, is critically important to all of us caring for women,” she emphasized. “These aren’t just ‘bothersome symptoms.’ ”
It is estimated that by 2060, there will be 90 million postmenopausal women in the United States. “Given the number of women who will experience symptoms of menopause and the considerable associated burden to their health and to the health care system, it is important to invest in educating future clinicians to provide evidence-based, comprehensive menopause management,” said Dr. Kling and coauthors in a February 2023 review of menopause treatments.
HT is the standard for the treatment of hot flashes and night sweats, and is highly effective for the prevention of bone loss and managing genitourinary syndrome of menopause. Among the alternatives to HT, the nonhormonal pharmacologic fezolinetant (Veozah) was approved by the U.S. Food and Drug Administration last May.
Following the early negative reports from the Women’s Health Initiative study of HT in 2002 and 2004, however, steep declines in HT prescription rates were seen among internists and family medicine practitioners. By 2009, only 18% of all HT prescriptions were written by primary care providers, and today, many remain wary about prescribing HT, despite evidence of its clinical value and safety.
“I think there’s a whole generation of family physicians who were taught that [hormone therapy] is dangerous and still feel very uncomfortable about using it to treat menopausal symptoms,” said Santina J.G. Wheat, MD, MPH, associate professor of family and community medicine at Northwestern University, Chicago. “These are the physicians educating the next generation of physicians,” said Dr. Wheat, who is program director for the McGaw Northwestern Family Medicine Residency Erie Humboldt Park.
Heather Hirsch, MD, an internist who specializes in menopause medicine in Columbus, Ohio, estimates that there are 300 internists among the 1,000 or so health care providers currently certified in menopause medicine through The Menopause Society (formerly the North American Menopause Society or NAMS). With 63 million women in the United States between the ages of 34 and 65, “that adds up to one doctor for several million patients,” she pointed out.
“In my opinion, the impact on menopausal care is profound,” said Jennifer T. Allen, MD, associate professor of obstetrics and gynecology, and director of menopause and midlife health at the Medical College of Georgia, Augusta. “If a physician was not exposed to menopause medicine in medical school or residency and does not choose to learn about menopause after training, then the opportunity to fully care for perimenopausal and postmenopausal women is extinguished.”
Not everyone agrees. “There’s no question that women’s health in general and menopausal issues specifically are a critical part of health care that is typically covered in most family medicine curriculums,” said Neil S. Skolnik, MD, professor of family and community medicine at the Sidney Kimmel Medical College in Philadelphia. “In family medicine, we really do attend to women’s health – particularly women’s health around menopause – as an important part of resident physician training,” emphasized Dr. Skolnik who is also and also associate director of the family medicine residency program at Abington Jefferson Health in Jenkintown, Penn.
"Family physicians are in a unique position to offer female patients effective care at perimenopause and beyond," added Karen L. Smith, MD, a family physician from Raeford, N.C., who is a board member of the American Academy of Family Physicians.*
Even so, many primary care physicians remain unsure about the use of HT, according to William E. Golden, MD, an internist and geriatrician, and professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock.
“On the whole area of hot flashes and vasomotor instability, I think we’re in a state of significant flux and confusion,” Dr. Golden said in an interview. “For a long time, a lot of doctors told patients, ‘It’s okay, you’ll age out of it.’ Then the data started showing that the vasomotor symptoms continued for years so physicians began to reevaluate how to manage them. Now, the pendulum has swung back to giving estrogen.”
Many family physicians have been left to their own devices to figure out how to manage menopausal patients, said Dr. Wheat. “When there are significant changes to clinical management – or in the case of HT, a real reversal in how menopausal symptoms are managed – getting information out to physicians can be challenging.”
Meanwhile, patient demand for answers to their questions about menopause and the use of HT is changing the conversation, where it’s taking place, and with whom.
Some media-savvy doctors have taken to TikTok, where a lot of women started educating themselves about menopause during the pandemic. Dr. Hirsch is one of them. She uses the social media platform to talk about menopause and FDA-approved HT, but warned that for every clinician who is certified in menopause medicine “there are five more selling snake oil.”
Mainstream media has also jumped on the menopause bandwagon. The New York Times was one of the first, declaring that “menopause is having a moment.” On Feb. 1, the newspaper stormed the gates of the medical establishment with an article asking why more doctors weren’t offering HT to women experiencing hot flashes, sleeplessness, and pain during sex. The headline: “Women have been misled about menopause.”
On April 5, “The Menopause Talk” was posted to Oprah Daily, along with a menopause curriculum to give viewers “the tools to stay firmly in the driver’s seat as you navigate perimenopause and then menopause.” Popular topics included how to get your sex life back, premature menopause survival, and ways to work with insurers so that treatment is affordable.
“There’s been a sea-change in the culture that’s being driven by patient demand,” said Dr. Kling. “The conversation, colloquially, in the media, and with our patients, is evolving. Menopause is no longer such a taboo topic, and our patients are really demanding that we have answers for them. Clinicians are recognizing that they need better training in menopause and seeking that out.”
Last June, “Transforming Women’s Health” – the Mayo Clinic’s annual CME program held in partnership with The Menopause Society – had record physician attendance. “We’re going to make sure that our trainees are learning the up-to-date recommendations, not the ones from 20 years ago when the initial WHI reports made everyone fearful of hormones,” said Dr. Kling.
Dr. Kling disclosed that she is a medical editor for Everyday Health, and has a relationship with Evolve Medical Education. Dr. Skolnik reported relationships with numerous pharmaceutical companies. He is an MDedge Family Medicine board member. Dr. Golden is an MDedge Internal Medicine board member, and Dr. Wheat is an MDedge Family Medicine board member. Dr. Allen reported having no potential conflicts of interest.
* This story was updated on Sept 18, 2023. The quotation is attributable to Dr. Smith, not Dr. Skolnik.
In 2017, a survey of 20 U.S. residency programs in family medicine, internal medicine, and ob.gyn. showed that only 6.8% of residents felt they were being adequately prepared to manage menopausal patients effectively, including how to use hormone therapy (HT).
Of the 177 residents who responded to the survey, 102 (56%) were in either family medicine or internal medicine.
“My guess is that there has been no substantial evolution in medical training to this day,” said lead survey study author Juliana Kling, MD, MPH, professor of medicine, chair of women’s health internal medicine, and dean, Mayo Clinic Alix School of Medicine, Scottsdale, Ariz.
The survey showed that overall 98% of residents thought it was important to know about menopause. However, 34% said they wouldn’t recommend HT in a severely symptomatic woman with no contraindications, and 60% said they wouldn’t recommend HT until at least the natural age of menopause in a prematurely menopausal woman. Some even recommended against it.
“Hormone therapy is effective, and for most healthy women younger than 60, the benefits are going to outweigh the risks,” said Dr. Kling. “We need to be comfortable, even in internal medicine, with prescribing hormones for the right women.”
The researchers concluded that “residual ambivalence about [hormone therapy] on the part of educators” may have played a role in curriculums that didn’t acknowledge the clinical relevance of menopause or include current evidence on the use of HT. Physicians should be taught to recognize menopausal symptoms, know the risks and benefits of HT and the alternatives, and how to select suitable candidates, they said.
Up to 80% of women in the United States are affected by menopausal vasomotor symptoms, but only one in four receive treatment, Dr. Kling pointed out. “Women will spend about a third of their lives after menopause, so being prepared to manage the consequences of menopause, such as bone health, vaginal dryness and painful intercourse, and increased cardiovascular disease risk, is critically important to all of us caring for women,” she emphasized. “These aren’t just ‘bothersome symptoms.’ ”
It is estimated that by 2060, there will be 90 million postmenopausal women in the United States. “Given the number of women who will experience symptoms of menopause and the considerable associated burden to their health and to the health care system, it is important to invest in educating future clinicians to provide evidence-based, comprehensive menopause management,” said Dr. Kling and coauthors in a February 2023 review of menopause treatments.
HT is the standard for the treatment of hot flashes and night sweats, and is highly effective for the prevention of bone loss and managing genitourinary syndrome of menopause. Among the alternatives to HT, the nonhormonal pharmacologic fezolinetant (Veozah) was approved by the U.S. Food and Drug Administration last May.
Following the early negative reports from the Women’s Health Initiative study of HT in 2002 and 2004, however, steep declines in HT prescription rates were seen among internists and family medicine practitioners. By 2009, only 18% of all HT prescriptions were written by primary care providers, and today, many remain wary about prescribing HT, despite evidence of its clinical value and safety.
“I think there’s a whole generation of family physicians who were taught that [hormone therapy] is dangerous and still feel very uncomfortable about using it to treat menopausal symptoms,” said Santina J.G. Wheat, MD, MPH, associate professor of family and community medicine at Northwestern University, Chicago. “These are the physicians educating the next generation of physicians,” said Dr. Wheat, who is program director for the McGaw Northwestern Family Medicine Residency Erie Humboldt Park.
Heather Hirsch, MD, an internist who specializes in menopause medicine in Columbus, Ohio, estimates that there are 300 internists among the 1,000 or so health care providers currently certified in menopause medicine through The Menopause Society (formerly the North American Menopause Society or NAMS). With 63 million women in the United States between the ages of 34 and 65, “that adds up to one doctor for several million patients,” she pointed out.
“In my opinion, the impact on menopausal care is profound,” said Jennifer T. Allen, MD, associate professor of obstetrics and gynecology, and director of menopause and midlife health at the Medical College of Georgia, Augusta. “If a physician was not exposed to menopause medicine in medical school or residency and does not choose to learn about menopause after training, then the opportunity to fully care for perimenopausal and postmenopausal women is extinguished.”
Not everyone agrees. “There’s no question that women’s health in general and menopausal issues specifically are a critical part of health care that is typically covered in most family medicine curriculums,” said Neil S. Skolnik, MD, professor of family and community medicine at the Sidney Kimmel Medical College in Philadelphia. “In family medicine, we really do attend to women’s health – particularly women’s health around menopause – as an important part of resident physician training,” emphasized Dr. Skolnik who is also and also associate director of the family medicine residency program at Abington Jefferson Health in Jenkintown, Penn.
"Family physicians are in a unique position to offer female patients effective care at perimenopause and beyond," added Karen L. Smith, MD, a family physician from Raeford, N.C., who is a board member of the American Academy of Family Physicians.*
Even so, many primary care physicians remain unsure about the use of HT, according to William E. Golden, MD, an internist and geriatrician, and professor of medicine and public health at the University of Arkansas for Medical Sciences, Little Rock.
“On the whole area of hot flashes and vasomotor instability, I think we’re in a state of significant flux and confusion,” Dr. Golden said in an interview. “For a long time, a lot of doctors told patients, ‘It’s okay, you’ll age out of it.’ Then the data started showing that the vasomotor symptoms continued for years so physicians began to reevaluate how to manage them. Now, the pendulum has swung back to giving estrogen.”
Many family physicians have been left to their own devices to figure out how to manage menopausal patients, said Dr. Wheat. “When there are significant changes to clinical management – or in the case of HT, a real reversal in how menopausal symptoms are managed – getting information out to physicians can be challenging.”
Meanwhile, patient demand for answers to their questions about menopause and the use of HT is changing the conversation, where it’s taking place, and with whom.
Some media-savvy doctors have taken to TikTok, where a lot of women started educating themselves about menopause during the pandemic. Dr. Hirsch is one of them. She uses the social media platform to talk about menopause and FDA-approved HT, but warned that for every clinician who is certified in menopause medicine “there are five more selling snake oil.”
Mainstream media has also jumped on the menopause bandwagon. The New York Times was one of the first, declaring that “menopause is having a moment.” On Feb. 1, the newspaper stormed the gates of the medical establishment with an article asking why more doctors weren’t offering HT to women experiencing hot flashes, sleeplessness, and pain during sex. The headline: “Women have been misled about menopause.”
On April 5, “The Menopause Talk” was posted to Oprah Daily, along with a menopause curriculum to give viewers “the tools to stay firmly in the driver’s seat as you navigate perimenopause and then menopause.” Popular topics included how to get your sex life back, premature menopause survival, and ways to work with insurers so that treatment is affordable.
“There’s been a sea-change in the culture that’s being driven by patient demand,” said Dr. Kling. “The conversation, colloquially, in the media, and with our patients, is evolving. Menopause is no longer such a taboo topic, and our patients are really demanding that we have answers for them. Clinicians are recognizing that they need better training in menopause and seeking that out.”
Last June, “Transforming Women’s Health” – the Mayo Clinic’s annual CME program held in partnership with The Menopause Society – had record physician attendance. “We’re going to make sure that our trainees are learning the up-to-date recommendations, not the ones from 20 years ago when the initial WHI reports made everyone fearful of hormones,” said Dr. Kling.
Dr. Kling disclosed that she is a medical editor for Everyday Health, and has a relationship with Evolve Medical Education. Dr. Skolnik reported relationships with numerous pharmaceutical companies. He is an MDedge Family Medicine board member. Dr. Golden is an MDedge Internal Medicine board member, and Dr. Wheat is an MDedge Family Medicine board member. Dr. Allen reported having no potential conflicts of interest.
* This story was updated on Sept 18, 2023. The quotation is attributable to Dr. Smith, not Dr. Skolnik.
COVID booster may transiently raise glucose levels in T1D
TOPLINE:
METHODOLOGY:
- In a single-center prospective cohort study of 21 adults with type 1 diabetes, patients were given a blinded Dexcom G6 Pro continuous glucose monitor (CGM) at the first research clinic visit.
- After 3-4 days, participants received a COVID-19 booster vaccine.
- They returned to the clinic 10 days after the initial visit (5-6 days after booster vaccination) to have the CGM removed and glycemia assessed.
TAKEAWAY:
- Compared with baseline, the mean daily glucose level was significantly increased at day 2 (162.9 mg/dL vs. 172.8 mg/dL; P = .04) and day 3 (173.1 mg/dL; P = .02) post vaccination.
- Glucose excursions at day 0 (173.2 mg/dL; P = .058) and day 1 (173.1 mg/dL; P = .078) didn’t quite reach statistical significance.
- One participant experienced increases in glucose of 36%, 69%, 35%, 26%, 22%, and 19% on days 0-5, respectively, compared with baseline.
- Glucose excursions of at least 25% above baseline occurred in four participants on day 0 and day 1 and in three participants on days 2 and 5.
- Insulin resistance, as measured by Total Daily Insulin Resistance (a metric that integrates daily mean glucose concentration with total daily insulin dose), was also significantly increased from baseline to day 2 post vaccination (7,171 mg/dL vs. 8,070 mg/dL units; P = .03).
- No other measures of glycemia differed significantly, compared with baseline.
- Outcomes didn’t differ significantly by sex, age, or vaccine manufacturer.
IN PRACTICE:
- “To our knowledge this is the first study investigating the effect of the COVID-19 booster vaccine on glycemia specifically in people with type 1 diabetes,” say the authors.
- “Clinicians, pharmacists, and other health care providers may need to counsel people with T1D to be more vigilant with glucose testing and insulin dosing for the first 5 days after vaccination. Most importantly, insulin, required to control glycemia, may need to be transiently increased.”
- “Further studies are warranted to investigate whether other vaccines have similar glycemic effects, and which individuals are at highest risk for profound glucose perturbations post vaccination.”
SOURCE:
The study was conducted by Mihail Zilbermint, MD, of the division of hospital medicine, Johns Hopkins Medicine, Bethesda, Md., and colleagues. It was published in Diabetes Research and Clinical Practice.
LIMITATIONS:
- The sample size was small.
- There were no measurements of inflammatory markers, dietary intake, physical activity, or survey patient symptomatology to adjust for variables that may have influenced glycemic control.
- In the study cohort, glycemia was moderately well controlled at baseline.
DISCLOSURES:
The study was supported by an investigator-initiated study grant from DexCom Inc. Dr. Zilbermint has consulted for EMD Serono.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- In a single-center prospective cohort study of 21 adults with type 1 diabetes, patients were given a blinded Dexcom G6 Pro continuous glucose monitor (CGM) at the first research clinic visit.
- After 3-4 days, participants received a COVID-19 booster vaccine.
- They returned to the clinic 10 days after the initial visit (5-6 days after booster vaccination) to have the CGM removed and glycemia assessed.
TAKEAWAY:
- Compared with baseline, the mean daily glucose level was significantly increased at day 2 (162.9 mg/dL vs. 172.8 mg/dL; P = .04) and day 3 (173.1 mg/dL; P = .02) post vaccination.
- Glucose excursions at day 0 (173.2 mg/dL; P = .058) and day 1 (173.1 mg/dL; P = .078) didn’t quite reach statistical significance.
- One participant experienced increases in glucose of 36%, 69%, 35%, 26%, 22%, and 19% on days 0-5, respectively, compared with baseline.
- Glucose excursions of at least 25% above baseline occurred in four participants on day 0 and day 1 and in three participants on days 2 and 5.
- Insulin resistance, as measured by Total Daily Insulin Resistance (a metric that integrates daily mean glucose concentration with total daily insulin dose), was also significantly increased from baseline to day 2 post vaccination (7,171 mg/dL vs. 8,070 mg/dL units; P = .03).
- No other measures of glycemia differed significantly, compared with baseline.
- Outcomes didn’t differ significantly by sex, age, or vaccine manufacturer.
IN PRACTICE:
- “To our knowledge this is the first study investigating the effect of the COVID-19 booster vaccine on glycemia specifically in people with type 1 diabetes,” say the authors.
- “Clinicians, pharmacists, and other health care providers may need to counsel people with T1D to be more vigilant with glucose testing and insulin dosing for the first 5 days after vaccination. Most importantly, insulin, required to control glycemia, may need to be transiently increased.”
- “Further studies are warranted to investigate whether other vaccines have similar glycemic effects, and which individuals are at highest risk for profound glucose perturbations post vaccination.”
SOURCE:
The study was conducted by Mihail Zilbermint, MD, of the division of hospital medicine, Johns Hopkins Medicine, Bethesda, Md., and colleagues. It was published in Diabetes Research and Clinical Practice.
LIMITATIONS:
- The sample size was small.
- There were no measurements of inflammatory markers, dietary intake, physical activity, or survey patient symptomatology to adjust for variables that may have influenced glycemic control.
- In the study cohort, glycemia was moderately well controlled at baseline.
DISCLOSURES:
The study was supported by an investigator-initiated study grant from DexCom Inc. Dr. Zilbermint has consulted for EMD Serono.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- In a single-center prospective cohort study of 21 adults with type 1 diabetes, patients were given a blinded Dexcom G6 Pro continuous glucose monitor (CGM) at the first research clinic visit.
- After 3-4 days, participants received a COVID-19 booster vaccine.
- They returned to the clinic 10 days after the initial visit (5-6 days after booster vaccination) to have the CGM removed and glycemia assessed.
TAKEAWAY:
- Compared with baseline, the mean daily glucose level was significantly increased at day 2 (162.9 mg/dL vs. 172.8 mg/dL; P = .04) and day 3 (173.1 mg/dL; P = .02) post vaccination.
- Glucose excursions at day 0 (173.2 mg/dL; P = .058) and day 1 (173.1 mg/dL; P = .078) didn’t quite reach statistical significance.
- One participant experienced increases in glucose of 36%, 69%, 35%, 26%, 22%, and 19% on days 0-5, respectively, compared with baseline.
- Glucose excursions of at least 25% above baseline occurred in four participants on day 0 and day 1 and in three participants on days 2 and 5.
- Insulin resistance, as measured by Total Daily Insulin Resistance (a metric that integrates daily mean glucose concentration with total daily insulin dose), was also significantly increased from baseline to day 2 post vaccination (7,171 mg/dL vs. 8,070 mg/dL units; P = .03).
- No other measures of glycemia differed significantly, compared with baseline.
- Outcomes didn’t differ significantly by sex, age, or vaccine manufacturer.
IN PRACTICE:
- “To our knowledge this is the first study investigating the effect of the COVID-19 booster vaccine on glycemia specifically in people with type 1 diabetes,” say the authors.
- “Clinicians, pharmacists, and other health care providers may need to counsel people with T1D to be more vigilant with glucose testing and insulin dosing for the first 5 days after vaccination. Most importantly, insulin, required to control glycemia, may need to be transiently increased.”
- “Further studies are warranted to investigate whether other vaccines have similar glycemic effects, and which individuals are at highest risk for profound glucose perturbations post vaccination.”
SOURCE:
The study was conducted by Mihail Zilbermint, MD, of the division of hospital medicine, Johns Hopkins Medicine, Bethesda, Md., and colleagues. It was published in Diabetes Research and Clinical Practice.
LIMITATIONS:
- The sample size was small.
- There were no measurements of inflammatory markers, dietary intake, physical activity, or survey patient symptomatology to adjust for variables that may have influenced glycemic control.
- In the study cohort, glycemia was moderately well controlled at baseline.
DISCLOSURES:
The study was supported by an investigator-initiated study grant from DexCom Inc. Dr. Zilbermint has consulted for EMD Serono.
A version of this article first appeared on Medscape.com.
FROM DIABETES RESEARCH AND CLINICAL PRACTICE
Proposed TNM update could shift staging for lung cancers
The updates for the 9th edition of the TNM Classification of Malignant Tumors: Lung Cancer were presented at the annual World Conference on Lung Cancer. The final version will be published Jan. 1, 2024.
The core proposed change, according to Hisao Asamura, MD, chair of the IASLC Staging and Prognostic Factors Committee, is to divide N2 and M1c disease into two subcategories, while leaving the T descriptors unchanged.
This update is based on large survival differences among patients with these tumor characteristics, following an analysis of outcomes in more than 87,000 individuals diagnosed with lung cancer.
Session cochair Ramón Rami-Porta, MD, PhD, explained that previous editions of the classification were based on “pathologic stage, not clinical stage” but ultimately “we could not validate those findings” clinically.
“This is the first time that some sort of very simple quantification” of lung tumors “could be validated at the clinical stage as well,” which means that clinical staging can improve all over the world, said Dr. Rami-Porta, medical oncologist at Hospital Universitari Mútua Terrassa (Spain).
Session cochair Paul Van Schil, MD, PhD, of Antwerp (the Netherlands) University Hospital explained that the proposed changes reflect what clinicians already see in their daily practice.
The latest TNM classification included data submitted on 124,581 patients diagnosed with lung cancer between 2011 and 2019, 56% of whom were from Asia/Australia, 25% from Europe, and 16% from North America.
Overall, 87,339 patients were included in the analysis – 83% with non–small cell lung cancer (NSCLC) and 7% with small cell lung cancer (SCLC). Most (62%) underwent surgery, either alone (47%), alongside chemotherapy (13%), or plus radiotherapy (2%). A minority (13%) received chemotherapy alone, and 13% received all three modalities.
The committee working on the update to the TNM classification had 112 members and comprised 14 subcommittees, which focused on different aspects of diagnosing and assessing the disease.
The committee agreed there should be no changes to the T category in the upcoming 9th Edition.
Evaluating the T category, some members expressed concern that patients with T3 disease embedded in the chest wall have worse survival outcomes than those with other forms of T3 disease. But, Dr. Asamura explained, the pathological versus clinical findings were inconsistent.
On pathological assessment, patients with T3 disease in the chest wall had a worse prognosis but clinical assessment indicated no survival difference. Given the lack of consensus, “we do not recommend any changes” to the current criteria, said Dr. Asamura.
Turning to the N category, Dr. Asamura explained that N2 disease will be divided into two subcategories: N2a, categorized by single N2 station involvement, and N2b, defined as multiple N2 station involvement.
Further analysis indicated that the estimated 5-year survival was significantly worse for patients with N2b disease on clinical assessment (31% vs. 42% with N2a disease; hazard ratio for death, 1.27; P < .0001) and on pathological assessment (HR, 1.46; P < .0001).
The committee also proposed a change to the M category, dividing M1c disease into two subcategories:
- M1c1 – defined as multiple extrathoracic metastases in a single organ system
- M1c2 – defined as multiple extrathoracic metastases in multiple organ systems
This change was driven by estimates of 5-year survival among patients with M1c1 (27%) versus M1c2 disease (19%). Compared with M1b disease, M1c1 was associated with a lower risk for death than M1c2 disease (HR, 1.27 vs. 1.39).
These changes, particularly those for the N category, will have a notable impact on how patients are staged, Dr. Asamura said.
Dividing the N2 category into N2a and N2b disease will push patients with T1, N1 disease from the IIB category (8th edition) to the IIA category (9th edition). The 8th edition categorized all T1, N2 patients as IIIA but the new edition would categorize patients with T1, N2a disease as IIB overall and those with N2b disease as IIIA. And patients with T2, N2a disease will be staged as IIIA — the same category as T2, N2 disease in the 8th edition – while those with N2b disease will be staged as IIIB.
By contrast, the division of M1c into M1c1 and M1c2 disease will not affect a patient’s overall stage, which will be IVB in all cases.
Upal Basu Roy, PhD, MPH, who was not part of the committee, said the TNM classification stage of cancers is “incredibly important in cataloguing the extent of disease” and to “decide the optimal treatment option.”
TNM classification is also “used to describe the burden of disease to be eligible for a clinical trial,” said Dr. Roy, executive director of research, LUNGevity Foundation, Chicago.
The changes in N staging may require sampling more lymph nodes than the current sampling frame of six, Dr. Roy said, adding that “surgeons and pathologists may need to be educated about the need for additional sampling.”
The subcategories for M1c disease will also need to be aligned with definitions of oligometastatic disease. “This is critical,” Dr. Roy said, as this staging may affect treatment choices.
No funding was declared. Dr. Asamura declares relationships with Medtronic, Taiho Pharmaceutical, Johnson & Johnson, Lily, Astellas, and Ono Pharmaceutical. Dr. Roy declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The updates for the 9th edition of the TNM Classification of Malignant Tumors: Lung Cancer were presented at the annual World Conference on Lung Cancer. The final version will be published Jan. 1, 2024.
The core proposed change, according to Hisao Asamura, MD, chair of the IASLC Staging and Prognostic Factors Committee, is to divide N2 and M1c disease into two subcategories, while leaving the T descriptors unchanged.
This update is based on large survival differences among patients with these tumor characteristics, following an analysis of outcomes in more than 87,000 individuals diagnosed with lung cancer.
Session cochair Ramón Rami-Porta, MD, PhD, explained that previous editions of the classification were based on “pathologic stage, not clinical stage” but ultimately “we could not validate those findings” clinically.
“This is the first time that some sort of very simple quantification” of lung tumors “could be validated at the clinical stage as well,” which means that clinical staging can improve all over the world, said Dr. Rami-Porta, medical oncologist at Hospital Universitari Mútua Terrassa (Spain).
Session cochair Paul Van Schil, MD, PhD, of Antwerp (the Netherlands) University Hospital explained that the proposed changes reflect what clinicians already see in their daily practice.
The latest TNM classification included data submitted on 124,581 patients diagnosed with lung cancer between 2011 and 2019, 56% of whom were from Asia/Australia, 25% from Europe, and 16% from North America.
Overall, 87,339 patients were included in the analysis – 83% with non–small cell lung cancer (NSCLC) and 7% with small cell lung cancer (SCLC). Most (62%) underwent surgery, either alone (47%), alongside chemotherapy (13%), or plus radiotherapy (2%). A minority (13%) received chemotherapy alone, and 13% received all three modalities.
The committee working on the update to the TNM classification had 112 members and comprised 14 subcommittees, which focused on different aspects of diagnosing and assessing the disease.
The committee agreed there should be no changes to the T category in the upcoming 9th Edition.
Evaluating the T category, some members expressed concern that patients with T3 disease embedded in the chest wall have worse survival outcomes than those with other forms of T3 disease. But, Dr. Asamura explained, the pathological versus clinical findings were inconsistent.
On pathological assessment, patients with T3 disease in the chest wall had a worse prognosis but clinical assessment indicated no survival difference. Given the lack of consensus, “we do not recommend any changes” to the current criteria, said Dr. Asamura.
Turning to the N category, Dr. Asamura explained that N2 disease will be divided into two subcategories: N2a, categorized by single N2 station involvement, and N2b, defined as multiple N2 station involvement.
Further analysis indicated that the estimated 5-year survival was significantly worse for patients with N2b disease on clinical assessment (31% vs. 42% with N2a disease; hazard ratio for death, 1.27; P < .0001) and on pathological assessment (HR, 1.46; P < .0001).
The committee also proposed a change to the M category, dividing M1c disease into two subcategories:
- M1c1 – defined as multiple extrathoracic metastases in a single organ system
- M1c2 – defined as multiple extrathoracic metastases in multiple organ systems
This change was driven by estimates of 5-year survival among patients with M1c1 (27%) versus M1c2 disease (19%). Compared with M1b disease, M1c1 was associated with a lower risk for death than M1c2 disease (HR, 1.27 vs. 1.39).
These changes, particularly those for the N category, will have a notable impact on how patients are staged, Dr. Asamura said.
Dividing the N2 category into N2a and N2b disease will push patients with T1, N1 disease from the IIB category (8th edition) to the IIA category (9th edition). The 8th edition categorized all T1, N2 patients as IIIA but the new edition would categorize patients with T1, N2a disease as IIB overall and those with N2b disease as IIIA. And patients with T2, N2a disease will be staged as IIIA — the same category as T2, N2 disease in the 8th edition – while those with N2b disease will be staged as IIIB.
By contrast, the division of M1c into M1c1 and M1c2 disease will not affect a patient’s overall stage, which will be IVB in all cases.
Upal Basu Roy, PhD, MPH, who was not part of the committee, said the TNM classification stage of cancers is “incredibly important in cataloguing the extent of disease” and to “decide the optimal treatment option.”
TNM classification is also “used to describe the burden of disease to be eligible for a clinical trial,” said Dr. Roy, executive director of research, LUNGevity Foundation, Chicago.
The changes in N staging may require sampling more lymph nodes than the current sampling frame of six, Dr. Roy said, adding that “surgeons and pathologists may need to be educated about the need for additional sampling.”
The subcategories for M1c disease will also need to be aligned with definitions of oligometastatic disease. “This is critical,” Dr. Roy said, as this staging may affect treatment choices.
No funding was declared. Dr. Asamura declares relationships with Medtronic, Taiho Pharmaceutical, Johnson & Johnson, Lily, Astellas, and Ono Pharmaceutical. Dr. Roy declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The updates for the 9th edition of the TNM Classification of Malignant Tumors: Lung Cancer were presented at the annual World Conference on Lung Cancer. The final version will be published Jan. 1, 2024.
The core proposed change, according to Hisao Asamura, MD, chair of the IASLC Staging and Prognostic Factors Committee, is to divide N2 and M1c disease into two subcategories, while leaving the T descriptors unchanged.
This update is based on large survival differences among patients with these tumor characteristics, following an analysis of outcomes in more than 87,000 individuals diagnosed with lung cancer.
Session cochair Ramón Rami-Porta, MD, PhD, explained that previous editions of the classification were based on “pathologic stage, not clinical stage” but ultimately “we could not validate those findings” clinically.
“This is the first time that some sort of very simple quantification” of lung tumors “could be validated at the clinical stage as well,” which means that clinical staging can improve all over the world, said Dr. Rami-Porta, medical oncologist at Hospital Universitari Mútua Terrassa (Spain).
Session cochair Paul Van Schil, MD, PhD, of Antwerp (the Netherlands) University Hospital explained that the proposed changes reflect what clinicians already see in their daily practice.
The latest TNM classification included data submitted on 124,581 patients diagnosed with lung cancer between 2011 and 2019, 56% of whom were from Asia/Australia, 25% from Europe, and 16% from North America.
Overall, 87,339 patients were included in the analysis – 83% with non–small cell lung cancer (NSCLC) and 7% with small cell lung cancer (SCLC). Most (62%) underwent surgery, either alone (47%), alongside chemotherapy (13%), or plus radiotherapy (2%). A minority (13%) received chemotherapy alone, and 13% received all three modalities.
The committee working on the update to the TNM classification had 112 members and comprised 14 subcommittees, which focused on different aspects of diagnosing and assessing the disease.
The committee agreed there should be no changes to the T category in the upcoming 9th Edition.
Evaluating the T category, some members expressed concern that patients with T3 disease embedded in the chest wall have worse survival outcomes than those with other forms of T3 disease. But, Dr. Asamura explained, the pathological versus clinical findings were inconsistent.
On pathological assessment, patients with T3 disease in the chest wall had a worse prognosis but clinical assessment indicated no survival difference. Given the lack of consensus, “we do not recommend any changes” to the current criteria, said Dr. Asamura.
Turning to the N category, Dr. Asamura explained that N2 disease will be divided into two subcategories: N2a, categorized by single N2 station involvement, and N2b, defined as multiple N2 station involvement.
Further analysis indicated that the estimated 5-year survival was significantly worse for patients with N2b disease on clinical assessment (31% vs. 42% with N2a disease; hazard ratio for death, 1.27; P < .0001) and on pathological assessment (HR, 1.46; P < .0001).
The committee also proposed a change to the M category, dividing M1c disease into two subcategories:
- M1c1 – defined as multiple extrathoracic metastases in a single organ system
- M1c2 – defined as multiple extrathoracic metastases in multiple organ systems
This change was driven by estimates of 5-year survival among patients with M1c1 (27%) versus M1c2 disease (19%). Compared with M1b disease, M1c1 was associated with a lower risk for death than M1c2 disease (HR, 1.27 vs. 1.39).
These changes, particularly those for the N category, will have a notable impact on how patients are staged, Dr. Asamura said.
Dividing the N2 category into N2a and N2b disease will push patients with T1, N1 disease from the IIB category (8th edition) to the IIA category (9th edition). The 8th edition categorized all T1, N2 patients as IIIA but the new edition would categorize patients with T1, N2a disease as IIB overall and those with N2b disease as IIIA. And patients with T2, N2a disease will be staged as IIIA — the same category as T2, N2 disease in the 8th edition – while those with N2b disease will be staged as IIIB.
By contrast, the division of M1c into M1c1 and M1c2 disease will not affect a patient’s overall stage, which will be IVB in all cases.
Upal Basu Roy, PhD, MPH, who was not part of the committee, said the TNM classification stage of cancers is “incredibly important in cataloguing the extent of disease” and to “decide the optimal treatment option.”
TNM classification is also “used to describe the burden of disease to be eligible for a clinical trial,” said Dr. Roy, executive director of research, LUNGevity Foundation, Chicago.
The changes in N staging may require sampling more lymph nodes than the current sampling frame of six, Dr. Roy said, adding that “surgeons and pathologists may need to be educated about the need for additional sampling.”
The subcategories for M1c disease will also need to be aligned with definitions of oligometastatic disease. “This is critical,” Dr. Roy said, as this staging may affect treatment choices.
No funding was declared. Dr. Asamura declares relationships with Medtronic, Taiho Pharmaceutical, Johnson & Johnson, Lily, Astellas, and Ono Pharmaceutical. Dr. Roy declared no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM WCLC 2023
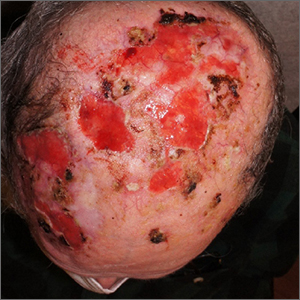
Hyperbaric oxygen therapy beneficial for calciphylaxis?
, report Daniela Kroshinsky, MD, MPH, of the department of dermatology at Massachusetts General Hospital, Boston, and colleagues.
Although intravenous sodium thiosulfate (IV STS) is considered standard care in the treatment of calciphylaxis, HBOT has been reported to have beneficial effects, they noted.
In their study, the researchers retrospectively reviewed records of 93 patients newly diagnosed with calciphylaxis, seen at Massachusetts General Hospital, between January 2006 and December 2021. They compared mortality and wound healing outcomes for 57 patients treated with IV STS only (control group) with those of 36 patients treated with HBOT plus IV STS (treatment group). Traditional survival analyses and Cox proportional hazard modeling were used to examine mortality data, and mixed effects modeling was used to analyze longitudinal wound outcomes. The study was published in the Journal of the American Academy of Dermatology.
Univariate survival analyses showed that HBOT plus IV STS was associated with significantly longer survival time than IV STS alone (P = .016), particularly for those with nonnephrogenic calciphylaxis (P < .0001), they report. An increased number of HBOT sessions conferred improved mortality outcomes, with 1, 5, 10, and 20 sessions yielding decreasing hazard ratios.
There was also a significant positive association between an increasing number of HBOT sessions and increased wound score (P = .042). Increases were seen with each session.
Anxiety/claustrophobia was the most common side effect reported among those in the HBOT group (22%).
“Given the proposed benefits and seemingly low side effect profile, it is the authors’ recommendation that HBOT be offered as an additional intervention to patients with calciphylaxis, especially if they have open wounds, to improve outcomes and expedite wound healing,” the researchers concluded.
Limitations, they noted, included the small sample size, retrospective design, and the potential for not adequately capturing patients who received external care. They were also unable to match patients by disease or wound severity. Large prospective trials would help clarify the role of HBOT for calciphylaxis, they added.
The researchers reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
, report Daniela Kroshinsky, MD, MPH, of the department of dermatology at Massachusetts General Hospital, Boston, and colleagues.
Although intravenous sodium thiosulfate (IV STS) is considered standard care in the treatment of calciphylaxis, HBOT has been reported to have beneficial effects, they noted.
In their study, the researchers retrospectively reviewed records of 93 patients newly diagnosed with calciphylaxis, seen at Massachusetts General Hospital, between January 2006 and December 2021. They compared mortality and wound healing outcomes for 57 patients treated with IV STS only (control group) with those of 36 patients treated with HBOT plus IV STS (treatment group). Traditional survival analyses and Cox proportional hazard modeling were used to examine mortality data, and mixed effects modeling was used to analyze longitudinal wound outcomes. The study was published in the Journal of the American Academy of Dermatology.
Univariate survival analyses showed that HBOT plus IV STS was associated with significantly longer survival time than IV STS alone (P = .016), particularly for those with nonnephrogenic calciphylaxis (P < .0001), they report. An increased number of HBOT sessions conferred improved mortality outcomes, with 1, 5, 10, and 20 sessions yielding decreasing hazard ratios.
There was also a significant positive association between an increasing number of HBOT sessions and increased wound score (P = .042). Increases were seen with each session.
Anxiety/claustrophobia was the most common side effect reported among those in the HBOT group (22%).
“Given the proposed benefits and seemingly low side effect profile, it is the authors’ recommendation that HBOT be offered as an additional intervention to patients with calciphylaxis, especially if they have open wounds, to improve outcomes and expedite wound healing,” the researchers concluded.
Limitations, they noted, included the small sample size, retrospective design, and the potential for not adequately capturing patients who received external care. They were also unable to match patients by disease or wound severity. Large prospective trials would help clarify the role of HBOT for calciphylaxis, they added.
The researchers reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
, report Daniela Kroshinsky, MD, MPH, of the department of dermatology at Massachusetts General Hospital, Boston, and colleagues.
Although intravenous sodium thiosulfate (IV STS) is considered standard care in the treatment of calciphylaxis, HBOT has been reported to have beneficial effects, they noted.
In their study, the researchers retrospectively reviewed records of 93 patients newly diagnosed with calciphylaxis, seen at Massachusetts General Hospital, between January 2006 and December 2021. They compared mortality and wound healing outcomes for 57 patients treated with IV STS only (control group) with those of 36 patients treated with HBOT plus IV STS (treatment group). Traditional survival analyses and Cox proportional hazard modeling were used to examine mortality data, and mixed effects modeling was used to analyze longitudinal wound outcomes. The study was published in the Journal of the American Academy of Dermatology.
Univariate survival analyses showed that HBOT plus IV STS was associated with significantly longer survival time than IV STS alone (P = .016), particularly for those with nonnephrogenic calciphylaxis (P < .0001), they report. An increased number of HBOT sessions conferred improved mortality outcomes, with 1, 5, 10, and 20 sessions yielding decreasing hazard ratios.
There was also a significant positive association between an increasing number of HBOT sessions and increased wound score (P = .042). Increases were seen with each session.
Anxiety/claustrophobia was the most common side effect reported among those in the HBOT group (22%).
“Given the proposed benefits and seemingly low side effect profile, it is the authors’ recommendation that HBOT be offered as an additional intervention to patients with calciphylaxis, especially if they have open wounds, to improve outcomes and expedite wound healing,” the researchers concluded.
Limitations, they noted, included the small sample size, retrospective design, and the potential for not adequately capturing patients who received external care. They were also unable to match patients by disease or wound severity. Large prospective trials would help clarify the role of HBOT for calciphylaxis, they added.
The researchers reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
Role of Prophylactic Cranial Irradiation in Small Cell Carcinoma of Urinary Bladder: Case Report and Literature Review
INTRODUCTION
Urinary bladder is an extremely rare site of extrapulmonary small cell cancer (EPSCC). Unlike small cell lung cancer (SCLC), there is no clear guideline for prophylactic cranial irradiation (PCI) for EPSCC. In this case report and literature review, we discuss small cell cancer of urinary bladder (SCCUB) and the role of PCI in SCCUB.
CASE PRESENTATION
A 74-year-old male presented with gross hematuria and an unremarkable physical examination. CT showed 1.7 cm right anterolateral bladder wall thickening. Cystoscopy revealed a 2-3 cm high-grade bladder lesion. Pathology from transurethral resection of the tumor was consistent with T1N0M0 small cell carcinoma. MRI brain and FDG-PET showed no extravesical disease. Patient received four cycles of neoadjuvant carboplatin/etoposide per his preference as he wanted to protect his hearing due to his profession followed by radical cystoprostatectomy. Post-op pathology showed clear margins. We decided to forego PCI in favor of interval surveillance with MRI and follow- up images remain negative for distant metastases.
DISCUSSION
EPSCC accounts for 2.5-5% of all SCC, very rare in male genitourinary tract. Treatment approach is derived from SCLC, guided by extent of disease and patient’s functional status. Role of PCI in EPSCC has not been clearly described, and even less evidence is available for SCCUB. From a review of eleven studies in PubMed for the role of PCI in SCCUB or EPSCC, we found that SCCUB has lower incidence of brain metastases than SCLC. One study suggested that SCCUB arises from totipotent cells in the submucosa, unlike Kulchitsky cell origin of SCLC. This difference might explain the difference in their metastatic behavior. With this background, PCI is not routinely recommended for limited- stage SCCUB. There might still be a role for PCI in extensive SCCUB with high metastatic burden. More studies are needed to update the guidelines for the role of PCI for these tumors.
CONCLUSIONS
Per this literature review, PCI is not routinely recommended for SCCUB, likely due to different cells of origin compared to SCLC. Future studies should focus on characterizing differences in their metastatic behavior and updating guidelines for PCI for SCCUB.
INTRODUCTION
Urinary bladder is an extremely rare site of extrapulmonary small cell cancer (EPSCC). Unlike small cell lung cancer (SCLC), there is no clear guideline for prophylactic cranial irradiation (PCI) for EPSCC. In this case report and literature review, we discuss small cell cancer of urinary bladder (SCCUB) and the role of PCI in SCCUB.
CASE PRESENTATION
A 74-year-old male presented with gross hematuria and an unremarkable physical examination. CT showed 1.7 cm right anterolateral bladder wall thickening. Cystoscopy revealed a 2-3 cm high-grade bladder lesion. Pathology from transurethral resection of the tumor was consistent with T1N0M0 small cell carcinoma. MRI brain and FDG-PET showed no extravesical disease. Patient received four cycles of neoadjuvant carboplatin/etoposide per his preference as he wanted to protect his hearing due to his profession followed by radical cystoprostatectomy. Post-op pathology showed clear margins. We decided to forego PCI in favor of interval surveillance with MRI and follow- up images remain negative for distant metastases.
DISCUSSION
EPSCC accounts for 2.5-5% of all SCC, very rare in male genitourinary tract. Treatment approach is derived from SCLC, guided by extent of disease and patient’s functional status. Role of PCI in EPSCC has not been clearly described, and even less evidence is available for SCCUB. From a review of eleven studies in PubMed for the role of PCI in SCCUB or EPSCC, we found that SCCUB has lower incidence of brain metastases than SCLC. One study suggested that SCCUB arises from totipotent cells in the submucosa, unlike Kulchitsky cell origin of SCLC. This difference might explain the difference in their metastatic behavior. With this background, PCI is not routinely recommended for limited- stage SCCUB. There might still be a role for PCI in extensive SCCUB with high metastatic burden. More studies are needed to update the guidelines for the role of PCI for these tumors.
CONCLUSIONS
Per this literature review, PCI is not routinely recommended for SCCUB, likely due to different cells of origin compared to SCLC. Future studies should focus on characterizing differences in their metastatic behavior and updating guidelines for PCI for SCCUB.
INTRODUCTION
Urinary bladder is an extremely rare site of extrapulmonary small cell cancer (EPSCC). Unlike small cell lung cancer (SCLC), there is no clear guideline for prophylactic cranial irradiation (PCI) for EPSCC. In this case report and literature review, we discuss small cell cancer of urinary bladder (SCCUB) and the role of PCI in SCCUB.
CASE PRESENTATION
A 74-year-old male presented with gross hematuria and an unremarkable physical examination. CT showed 1.7 cm right anterolateral bladder wall thickening. Cystoscopy revealed a 2-3 cm high-grade bladder lesion. Pathology from transurethral resection of the tumor was consistent with T1N0M0 small cell carcinoma. MRI brain and FDG-PET showed no extravesical disease. Patient received four cycles of neoadjuvant carboplatin/etoposide per his preference as he wanted to protect his hearing due to his profession followed by radical cystoprostatectomy. Post-op pathology showed clear margins. We decided to forego PCI in favor of interval surveillance with MRI and follow- up images remain negative for distant metastases.
DISCUSSION
EPSCC accounts for 2.5-5% of all SCC, very rare in male genitourinary tract. Treatment approach is derived from SCLC, guided by extent of disease and patient’s functional status. Role of PCI in EPSCC has not been clearly described, and even less evidence is available for SCCUB. From a review of eleven studies in PubMed for the role of PCI in SCCUB or EPSCC, we found that SCCUB has lower incidence of brain metastases than SCLC. One study suggested that SCCUB arises from totipotent cells in the submucosa, unlike Kulchitsky cell origin of SCLC. This difference might explain the difference in their metastatic behavior. With this background, PCI is not routinely recommended for limited- stage SCCUB. There might still be a role for PCI in extensive SCCUB with high metastatic burden. More studies are needed to update the guidelines for the role of PCI for these tumors.
CONCLUSIONS
Per this literature review, PCI is not routinely recommended for SCCUB, likely due to different cells of origin compared to SCLC. Future studies should focus on characterizing differences in their metastatic behavior and updating guidelines for PCI for SCCUB.
Neoadjuvant durvalumab does not affect surgical outcomes in NSCLC: Study
, according to the most recent analysis of data from the phase 3 AEGEAN study.
“In terms of cancellation of surgery, surgical delay, surgically related adverse events, complications, operation time, and operation procedure, there was no difference between the durvalumab group and the placebo group. In addition, the R0 resection rate was numerically higher in the durvalumab group. These [results] indicate that adding perioperative durvalumab did not adversely affect surgical outcomes,” wrote Tetsuya Mitsudomi, MD, PhD, who presented the new results at the annual World Conference on Lung Cancer, in an email. The topline results of AEGEAN were presented earlier this year at AACR 2023, which showed that the regimen combined with adjuvant durvalumab improved event-free survival (EFS) and pathologic complete response (pCR), compared with chemotherapy plus placebo.
Dr. Mitsudomi also pointed out that AEGEAN is one of the first studies looking at immune checkpoint inhibitors (ICI) in the perioperative settings that demonstrated improved EFS and pCR with no effect on surgical outcomes. Previously, the CheckMate 816 study demonstrated efficacy of neoadjuvant ICI alone.
“The AEGEAN study showed that neoadjuvant plus adjuvant ICI is another option for these patients. However, no one knows who should receive the postoperative ICI in addition to neoadjuvant ICI, because there are no trials including ongoing ones that ask this question,” wrote Dr. Mitsudomi.
The phase 3 AEGEAN study included 740 patients who were randomized to durvalumab or placebo. The median age was 65.0 years in both groups, and 33.3% and 33.4% of patients in each group respectively had fewer than 1% of tumor cells that expressed PD-L1. Expression in 1-49% of tumor cells occurred in 36.9% and 38.0% respectively, and expression ≥ 50% occurred in 29.8% and 28.6%.
Prior to surgery, 84.7% of the durvalumab arm completed four cycles of chemotherapy, as did 87.2% in the placebo arm. The proportion of patients undergoing surgery was 80.6% and 80.7% in the two arms, respectively, and surgical completion was achieved in 77.6% and 76.7%. The durvalumab arm and placebo arm had similar median times from last neoadjuvant treatment to surgery (34.0 days for both) and median time from surgery to first adjuvant dose (50.0 versus 52.0 days).
Among patients with stage II NSCLC, 84.3% in the durvalumab arm underwent surgery, versus 88.9% in the placebo arm. Among patients with stage III disease, the numbers were 79.2% and 77.4%, respectively. There was no surgical delay in 82.7% of patients in the durvalumab arm, compared with 77.8% in the placebo arm. The most common reason for surgical delay was logistical reasons. Mediastinal lymph node dissection was completed in 86.6% of the durvalumab arm and 84.7% of the placebo arm. In both groups where surgery was completed, R0 resection rates were over 90% overall as well as in both stage I and stage II patients. Following surgery, adverse events possibly related to surgery occurred in 40.2% of the durvalumab group and 39.2% of the placebo group. The most common surgical adverse events occurred at similar frequency between groups.
After the presentation, Solange Peters, MD, PhD, served as a discussant. She pointed out other studies that have examined ICI therapy for NSCLC in both the neoadjuvant and adjuvant setting, including Keynote-671 (pembrolizumab), Neotorch (toripalimab), CheckMate 77T (nivolumab), and Impower030 (atezolizumab). She pointed out that AEGEAN, Keynote-671, CheckMate 816, and NeoTorch all had similar trial designs and showed similar magnitude of benefit. “We have a growing paradigm [for combining neoadjuvant and adjuvant ICI therapy]. We are quite all convinced in the community that there is a biological rationale to use neoadjuvant immunotherapy because of the fit immune system, because of the presence of the neoantigens within the tumor at the time of the start of neoadjuvant treatment, [leading to] better priming of immune cells,” said Dr. Peters, who is a professor of medical oncology at University Hospital of Lausanne, Switzerland.
About one in five patients across the trials who would be eligible for surgery never undergo it, but there is promising data from CheckMate 816 that neoadjuvant ICB may improve the odds of surgery, according to Dr. Solange. The AEGEAN data produced some “quite interesting” data about the reasons that patients don’t make it to surgery, as it showed that 8%-10% of patients don’t reach surgery because of progression, but 10%-15% may fall out because they turned out not to be a good candidate for surgery. “I think we probably have to blame the enthusiasm we have to add all these patients into the trial, hoping for the best for the patient but maybe making a wrong selection,” said Dr. Peters.
The study was funded by AstraZeneca. Dr. Mitsudomi has received speaker fees, honoraria, or research funding from AstraZeneca, Chugai, Ono, Bristol Myers Squibb, and MSD. Dr. Peters has financial relationships with AstraZeneca as well as a wide range of other pharmaceutical companies.
, according to the most recent analysis of data from the phase 3 AEGEAN study.
“In terms of cancellation of surgery, surgical delay, surgically related adverse events, complications, operation time, and operation procedure, there was no difference between the durvalumab group and the placebo group. In addition, the R0 resection rate was numerically higher in the durvalumab group. These [results] indicate that adding perioperative durvalumab did not adversely affect surgical outcomes,” wrote Tetsuya Mitsudomi, MD, PhD, who presented the new results at the annual World Conference on Lung Cancer, in an email. The topline results of AEGEAN were presented earlier this year at AACR 2023, which showed that the regimen combined with adjuvant durvalumab improved event-free survival (EFS) and pathologic complete response (pCR), compared with chemotherapy plus placebo.
Dr. Mitsudomi also pointed out that AEGEAN is one of the first studies looking at immune checkpoint inhibitors (ICI) in the perioperative settings that demonstrated improved EFS and pCR with no effect on surgical outcomes. Previously, the CheckMate 816 study demonstrated efficacy of neoadjuvant ICI alone.
“The AEGEAN study showed that neoadjuvant plus adjuvant ICI is another option for these patients. However, no one knows who should receive the postoperative ICI in addition to neoadjuvant ICI, because there are no trials including ongoing ones that ask this question,” wrote Dr. Mitsudomi.
The phase 3 AEGEAN study included 740 patients who were randomized to durvalumab or placebo. The median age was 65.0 years in both groups, and 33.3% and 33.4% of patients in each group respectively had fewer than 1% of tumor cells that expressed PD-L1. Expression in 1-49% of tumor cells occurred in 36.9% and 38.0% respectively, and expression ≥ 50% occurred in 29.8% and 28.6%.
Prior to surgery, 84.7% of the durvalumab arm completed four cycles of chemotherapy, as did 87.2% in the placebo arm. The proportion of patients undergoing surgery was 80.6% and 80.7% in the two arms, respectively, and surgical completion was achieved in 77.6% and 76.7%. The durvalumab arm and placebo arm had similar median times from last neoadjuvant treatment to surgery (34.0 days for both) and median time from surgery to first adjuvant dose (50.0 versus 52.0 days).
Among patients with stage II NSCLC, 84.3% in the durvalumab arm underwent surgery, versus 88.9% in the placebo arm. Among patients with stage III disease, the numbers were 79.2% and 77.4%, respectively. There was no surgical delay in 82.7% of patients in the durvalumab arm, compared with 77.8% in the placebo arm. The most common reason for surgical delay was logistical reasons. Mediastinal lymph node dissection was completed in 86.6% of the durvalumab arm and 84.7% of the placebo arm. In both groups where surgery was completed, R0 resection rates were over 90% overall as well as in both stage I and stage II patients. Following surgery, adverse events possibly related to surgery occurred in 40.2% of the durvalumab group and 39.2% of the placebo group. The most common surgical adverse events occurred at similar frequency between groups.
After the presentation, Solange Peters, MD, PhD, served as a discussant. She pointed out other studies that have examined ICI therapy for NSCLC in both the neoadjuvant and adjuvant setting, including Keynote-671 (pembrolizumab), Neotorch (toripalimab), CheckMate 77T (nivolumab), and Impower030 (atezolizumab). She pointed out that AEGEAN, Keynote-671, CheckMate 816, and NeoTorch all had similar trial designs and showed similar magnitude of benefit. “We have a growing paradigm [for combining neoadjuvant and adjuvant ICI therapy]. We are quite all convinced in the community that there is a biological rationale to use neoadjuvant immunotherapy because of the fit immune system, because of the presence of the neoantigens within the tumor at the time of the start of neoadjuvant treatment, [leading to] better priming of immune cells,” said Dr. Peters, who is a professor of medical oncology at University Hospital of Lausanne, Switzerland.
About one in five patients across the trials who would be eligible for surgery never undergo it, but there is promising data from CheckMate 816 that neoadjuvant ICB may improve the odds of surgery, according to Dr. Solange. The AEGEAN data produced some “quite interesting” data about the reasons that patients don’t make it to surgery, as it showed that 8%-10% of patients don’t reach surgery because of progression, but 10%-15% may fall out because they turned out not to be a good candidate for surgery. “I think we probably have to blame the enthusiasm we have to add all these patients into the trial, hoping for the best for the patient but maybe making a wrong selection,” said Dr. Peters.
The study was funded by AstraZeneca. Dr. Mitsudomi has received speaker fees, honoraria, or research funding from AstraZeneca, Chugai, Ono, Bristol Myers Squibb, and MSD. Dr. Peters has financial relationships with AstraZeneca as well as a wide range of other pharmaceutical companies.
, according to the most recent analysis of data from the phase 3 AEGEAN study.
“In terms of cancellation of surgery, surgical delay, surgically related adverse events, complications, operation time, and operation procedure, there was no difference between the durvalumab group and the placebo group. In addition, the R0 resection rate was numerically higher in the durvalumab group. These [results] indicate that adding perioperative durvalumab did not adversely affect surgical outcomes,” wrote Tetsuya Mitsudomi, MD, PhD, who presented the new results at the annual World Conference on Lung Cancer, in an email. The topline results of AEGEAN were presented earlier this year at AACR 2023, which showed that the regimen combined with adjuvant durvalumab improved event-free survival (EFS) and pathologic complete response (pCR), compared with chemotherapy plus placebo.
Dr. Mitsudomi also pointed out that AEGEAN is one of the first studies looking at immune checkpoint inhibitors (ICI) in the perioperative settings that demonstrated improved EFS and pCR with no effect on surgical outcomes. Previously, the CheckMate 816 study demonstrated efficacy of neoadjuvant ICI alone.
“The AEGEAN study showed that neoadjuvant plus adjuvant ICI is another option for these patients. However, no one knows who should receive the postoperative ICI in addition to neoadjuvant ICI, because there are no trials including ongoing ones that ask this question,” wrote Dr. Mitsudomi.
The phase 3 AEGEAN study included 740 patients who were randomized to durvalumab or placebo. The median age was 65.0 years in both groups, and 33.3% and 33.4% of patients in each group respectively had fewer than 1% of tumor cells that expressed PD-L1. Expression in 1-49% of tumor cells occurred in 36.9% and 38.0% respectively, and expression ≥ 50% occurred in 29.8% and 28.6%.
Prior to surgery, 84.7% of the durvalumab arm completed four cycles of chemotherapy, as did 87.2% in the placebo arm. The proportion of patients undergoing surgery was 80.6% and 80.7% in the two arms, respectively, and surgical completion was achieved in 77.6% and 76.7%. The durvalumab arm and placebo arm had similar median times from last neoadjuvant treatment to surgery (34.0 days for both) and median time from surgery to first adjuvant dose (50.0 versus 52.0 days).
Among patients with stage II NSCLC, 84.3% in the durvalumab arm underwent surgery, versus 88.9% in the placebo arm. Among patients with stage III disease, the numbers were 79.2% and 77.4%, respectively. There was no surgical delay in 82.7% of patients in the durvalumab arm, compared with 77.8% in the placebo arm. The most common reason for surgical delay was logistical reasons. Mediastinal lymph node dissection was completed in 86.6% of the durvalumab arm and 84.7% of the placebo arm. In both groups where surgery was completed, R0 resection rates were over 90% overall as well as in both stage I and stage II patients. Following surgery, adverse events possibly related to surgery occurred in 40.2% of the durvalumab group and 39.2% of the placebo group. The most common surgical adverse events occurred at similar frequency between groups.
After the presentation, Solange Peters, MD, PhD, served as a discussant. She pointed out other studies that have examined ICI therapy for NSCLC in both the neoadjuvant and adjuvant setting, including Keynote-671 (pembrolizumab), Neotorch (toripalimab), CheckMate 77T (nivolumab), and Impower030 (atezolizumab). She pointed out that AEGEAN, Keynote-671, CheckMate 816, and NeoTorch all had similar trial designs and showed similar magnitude of benefit. “We have a growing paradigm [for combining neoadjuvant and adjuvant ICI therapy]. We are quite all convinced in the community that there is a biological rationale to use neoadjuvant immunotherapy because of the fit immune system, because of the presence of the neoantigens within the tumor at the time of the start of neoadjuvant treatment, [leading to] better priming of immune cells,” said Dr. Peters, who is a professor of medical oncology at University Hospital of Lausanne, Switzerland.
About one in five patients across the trials who would be eligible for surgery never undergo it, but there is promising data from CheckMate 816 that neoadjuvant ICB may improve the odds of surgery, according to Dr. Solange. The AEGEAN data produced some “quite interesting” data about the reasons that patients don’t make it to surgery, as it showed that 8%-10% of patients don’t reach surgery because of progression, but 10%-15% may fall out because they turned out not to be a good candidate for surgery. “I think we probably have to blame the enthusiasm we have to add all these patients into the trial, hoping for the best for the patient but maybe making a wrong selection,” said Dr. Peters.
The study was funded by AstraZeneca. Dr. Mitsudomi has received speaker fees, honoraria, or research funding from AstraZeneca, Chugai, Ono, Bristol Myers Squibb, and MSD. Dr. Peters has financial relationships with AstraZeneca as well as a wide range of other pharmaceutical companies.
FROM WCLC 2023
Debate: Should smoldering myeloma be treated?
Hematologist Sagar Lonial, MD, a multiple myeloma specialist and researcher at Emory University, Atlanta, argued for treatment. Hematologist Angela Dispenzieri, MD, also a myeloma researcher and specialist at the Mayo Clinic in Rochester, Minn., took the opposing side, arguing for watchful waiting.
The two experts based their arguments largely on the same two studies, the only randomized trials to tackle the issue to date. While Dr. Dispenzieri focused on their shortcomings, Dr. Lonial focused on their strengths.
In a poll after the debate, about a third of audience members agreed that watchful waiting is the way to go, but about two-thirds favored a personalized approach to smoldering myeloma treatment based on patient risk.
“I’m taking this as a win,” Dr. Lonial said.
Different interpretations of two trials
The first of the two trials recruited from 2007 to 2010 and was conducted in Spain and Portugal. Fifty-seven high-risk patients were randomized to lenalidomide plus dexamethasone (Len-Dex) for up to 2 years; 62 others were randomized to observation.
At 3 years, 70% of observed patients had progressed to multiple myeloma versus only 20% in the Len-Dex group; 82% of Len-Dex patients were alive at data cut-off in 2015 versus 64% of observation patients.
The second, more recent trial, which was led by Dr. Lonial, randomized 92 intermediate or high-risk smoldering myeloma patients to lenalidomide alone for a median of 2 years and 90 others to observation. Three-year progression-free survival (PFS) was 91% in the treatment arm versus 66% with observation. Overall survival data have not yet been reported.
Dr. Dispenzieri acknowledged that the results from Spain and Portugal are impressive. “Treating with Len-Dex gives you a far superior freedom from progression. ... Overall survival was better too.” Results for Len-Dex were “fantastic,” she said.
However, the trial was done before myeloma-defining event criteria existed, so it’s very likely that the treatment arm in the Spanish study included actual myeloma cases, she said.
About 46% of treated patients in Dr. Lonial’s study met the current definition for high risk for progression based on the 2-20-20 rule, which Dr. Dispenzieri helped develop. Although there was an improvement in PFS in the high-risk group, there was no significant improvement for intermediate- and low-risk subjects. Also, more than 80% of observed patients hadn’t progressed by 2 years, and overall survival data are missing.
Meanwhile, treated patients in both trials had more adverse events, including secondary malignancies, and there’s the possibility that early treatment may make patients resistant to treatment later on when they progress to multiple myeloma, although that didn’t seem to happen in the Spanish trial.
“Of course, we want to prevent morbidity, of course we would love to cure the disease,” but “should we treat high-risk smoldering myeloma patients based on overall survival data from a trial of” just 119 “patients that may have been contaminated with actual myeloma” cases? Is it ethical to treat low- and intermediate-risk patients who have only a 50% chance of developing myeloma after 10 years?”
Her answer to both questions was “no and no. ... There’s just a lot of work to be done” to better understand the condition and when and how to intervene. In the meantime, “don’t treat smoldering melanoma patients” outside of a trial, she said.
“First, do no harm,” Dr. Dispenzieri cautioned in her final slide.
Dr. Lonial said he agreed with many of Dr. Dispenzieri’s points, but disagreed with her conclusion not to treat.
“Everybody can always be critical of randomized trials, but at the end of the day, we now have two randomized phase 3 trials comparing early intervention with no intervention demonstrating a significant delay in developing myeloma. I think it’s time to end the ‘we need more data; we need more trials.’ It’s time for us to take a stand.”
He argued for 2 years of lenalidomide for patients who meet the 2-20-20 high-risk definition, based on the median time people were treated in his trial.
He said he discusses the option “with every smoldering patient [who] walks in to see me” if they aren’t eligible for a trial.
Dr. Lonial mentioned his team is currently pulling together longer-term survival data for their trial.
Hematologist Sagar Lonial, MD, a multiple myeloma specialist and researcher at Emory University, Atlanta, argued for treatment. Hematologist Angela Dispenzieri, MD, also a myeloma researcher and specialist at the Mayo Clinic in Rochester, Minn., took the opposing side, arguing for watchful waiting.
The two experts based their arguments largely on the same two studies, the only randomized trials to tackle the issue to date. While Dr. Dispenzieri focused on their shortcomings, Dr. Lonial focused on their strengths.
In a poll after the debate, about a third of audience members agreed that watchful waiting is the way to go, but about two-thirds favored a personalized approach to smoldering myeloma treatment based on patient risk.
“I’m taking this as a win,” Dr. Lonial said.
Different interpretations of two trials
The first of the two trials recruited from 2007 to 2010 and was conducted in Spain and Portugal. Fifty-seven high-risk patients were randomized to lenalidomide plus dexamethasone (Len-Dex) for up to 2 years; 62 others were randomized to observation.
At 3 years, 70% of observed patients had progressed to multiple myeloma versus only 20% in the Len-Dex group; 82% of Len-Dex patients were alive at data cut-off in 2015 versus 64% of observation patients.
The second, more recent trial, which was led by Dr. Lonial, randomized 92 intermediate or high-risk smoldering myeloma patients to lenalidomide alone for a median of 2 years and 90 others to observation. Three-year progression-free survival (PFS) was 91% in the treatment arm versus 66% with observation. Overall survival data have not yet been reported.
Dr. Dispenzieri acknowledged that the results from Spain and Portugal are impressive. “Treating with Len-Dex gives you a far superior freedom from progression. ... Overall survival was better too.” Results for Len-Dex were “fantastic,” she said.
However, the trial was done before myeloma-defining event criteria existed, so it’s very likely that the treatment arm in the Spanish study included actual myeloma cases, she said.
About 46% of treated patients in Dr. Lonial’s study met the current definition for high risk for progression based on the 2-20-20 rule, which Dr. Dispenzieri helped develop. Although there was an improvement in PFS in the high-risk group, there was no significant improvement for intermediate- and low-risk subjects. Also, more than 80% of observed patients hadn’t progressed by 2 years, and overall survival data are missing.
Meanwhile, treated patients in both trials had more adverse events, including secondary malignancies, and there’s the possibility that early treatment may make patients resistant to treatment later on when they progress to multiple myeloma, although that didn’t seem to happen in the Spanish trial.
“Of course, we want to prevent morbidity, of course we would love to cure the disease,” but “should we treat high-risk smoldering myeloma patients based on overall survival data from a trial of” just 119 “patients that may have been contaminated with actual myeloma” cases? Is it ethical to treat low- and intermediate-risk patients who have only a 50% chance of developing myeloma after 10 years?”
Her answer to both questions was “no and no. ... There’s just a lot of work to be done” to better understand the condition and when and how to intervene. In the meantime, “don’t treat smoldering melanoma patients” outside of a trial, she said.
“First, do no harm,” Dr. Dispenzieri cautioned in her final slide.
Dr. Lonial said he agreed with many of Dr. Dispenzieri’s points, but disagreed with her conclusion not to treat.
“Everybody can always be critical of randomized trials, but at the end of the day, we now have two randomized phase 3 trials comparing early intervention with no intervention demonstrating a significant delay in developing myeloma. I think it’s time to end the ‘we need more data; we need more trials.’ It’s time for us to take a stand.”
He argued for 2 years of lenalidomide for patients who meet the 2-20-20 high-risk definition, based on the median time people were treated in his trial.
He said he discusses the option “with every smoldering patient [who] walks in to see me” if they aren’t eligible for a trial.
Dr. Lonial mentioned his team is currently pulling together longer-term survival data for their trial.
Hematologist Sagar Lonial, MD, a multiple myeloma specialist and researcher at Emory University, Atlanta, argued for treatment. Hematologist Angela Dispenzieri, MD, also a myeloma researcher and specialist at the Mayo Clinic in Rochester, Minn., took the opposing side, arguing for watchful waiting.
The two experts based their arguments largely on the same two studies, the only randomized trials to tackle the issue to date. While Dr. Dispenzieri focused on their shortcomings, Dr. Lonial focused on their strengths.
In a poll after the debate, about a third of audience members agreed that watchful waiting is the way to go, but about two-thirds favored a personalized approach to smoldering myeloma treatment based on patient risk.
“I’m taking this as a win,” Dr. Lonial said.
Different interpretations of two trials
The first of the two trials recruited from 2007 to 2010 and was conducted in Spain and Portugal. Fifty-seven high-risk patients were randomized to lenalidomide plus dexamethasone (Len-Dex) for up to 2 years; 62 others were randomized to observation.
At 3 years, 70% of observed patients had progressed to multiple myeloma versus only 20% in the Len-Dex group; 82% of Len-Dex patients were alive at data cut-off in 2015 versus 64% of observation patients.
The second, more recent trial, which was led by Dr. Lonial, randomized 92 intermediate or high-risk smoldering myeloma patients to lenalidomide alone for a median of 2 years and 90 others to observation. Three-year progression-free survival (PFS) was 91% in the treatment arm versus 66% with observation. Overall survival data have not yet been reported.
Dr. Dispenzieri acknowledged that the results from Spain and Portugal are impressive. “Treating with Len-Dex gives you a far superior freedom from progression. ... Overall survival was better too.” Results for Len-Dex were “fantastic,” she said.
However, the trial was done before myeloma-defining event criteria existed, so it’s very likely that the treatment arm in the Spanish study included actual myeloma cases, she said.
About 46% of treated patients in Dr. Lonial’s study met the current definition for high risk for progression based on the 2-20-20 rule, which Dr. Dispenzieri helped develop. Although there was an improvement in PFS in the high-risk group, there was no significant improvement for intermediate- and low-risk subjects. Also, more than 80% of observed patients hadn’t progressed by 2 years, and overall survival data are missing.
Meanwhile, treated patients in both trials had more adverse events, including secondary malignancies, and there’s the possibility that early treatment may make patients resistant to treatment later on when they progress to multiple myeloma, although that didn’t seem to happen in the Spanish trial.
“Of course, we want to prevent morbidity, of course we would love to cure the disease,” but “should we treat high-risk smoldering myeloma patients based on overall survival data from a trial of” just 119 “patients that may have been contaminated with actual myeloma” cases? Is it ethical to treat low- and intermediate-risk patients who have only a 50% chance of developing myeloma after 10 years?”
Her answer to both questions was “no and no. ... There’s just a lot of work to be done” to better understand the condition and when and how to intervene. In the meantime, “don’t treat smoldering melanoma patients” outside of a trial, she said.
“First, do no harm,” Dr. Dispenzieri cautioned in her final slide.
Dr. Lonial said he agreed with many of Dr. Dispenzieri’s points, but disagreed with her conclusion not to treat.
“Everybody can always be critical of randomized trials, but at the end of the day, we now have two randomized phase 3 trials comparing early intervention with no intervention demonstrating a significant delay in developing myeloma. I think it’s time to end the ‘we need more data; we need more trials.’ It’s time for us to take a stand.”
He argued for 2 years of lenalidomide for patients who meet the 2-20-20 high-risk definition, based on the median time people were treated in his trial.
He said he discusses the option “with every smoldering patient [who] walks in to see me” if they aren’t eligible for a trial.
Dr. Lonial mentioned his team is currently pulling together longer-term survival data for their trial.
FROM SOHO 2023
Nonhealing postsurgical scalp ulcers

Two shave biopsies were taken, 1 in the center of a previous SCC site with hyperkeratosis, the other in a site not previously affected by SCC but with the physical features of a pustule. Biopsy results from both sites were consistent with erosive pustular dermatosis, an unusual inflammatory disorder that mimics SCC.
Erosive pustular dermatosis of the scalp is an uncommon dermatitis that usually affects older women but may appear in men and women of all ages. It can mimic many other conditions that can affect the scalp, including seborrheic dermatitis, psoriasis, actinic keratosis, and SCC.
The exact causative mechanism is not understood, and cases may develop spontaneously. Rough papules, pustules, crusts, and ulcers develop and (apart from the pustules) share many features of actinic keratoses, SCCs, and field cancerization. The presence of pustules helps point to the diagnosis.
Triggers include previous surgery or physical trauma, burns, skin or hair grafts, and treatment of actinic keratoses with imiquimod, 5-fluourouracil, or photodynamic therapy. Some autoimmune diseases (including Hashimoto thyroiditis, autoimmune hepatitis, and rheumatoid arthritis) have been linked to disease occurrence and severity.1
Treatment includes potent or super-potent topical steroids such as clobetasol 0.05% ointment. Topical tacrolimus 0.1% ointment and calcipotriene 0.005% cream have been reported as steroid alternatives. Paradoxically, photodynamic therapy, while associated with triggering disease, has also been used therapeutically. Systemic immunomodulators such as cyclosporine 3 mg/kg/d or prednisone 0.5 to 1 mg/kg/d may be needed in severe cases. Antibiotics including topical dapsone 5% gel, systemic dapsone from 50 mg bid to tid, and doxycycline have been helpful due, in part, to their immunomodulatory effects.1,2
This patient was told to apply topical triamcinolone 0.1% ointment around and over ulcers and pustules and to take doxycycline 100 mg twice daily. The patient cleared well after 6 weeks. He continued to apply topical triamcinolone every few days as maintenance therapy.
He had some mild recurrence after discontinuing all topical and oral therapy, so he currently is being maintained on topical clobetasol 0.05% ointment every other day. He comes in for follow-up appointments every 3 months to monitor for control of the erosive pustular dermatosis of the scalp and for skin cancer surveillance.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME
1. Karanfilian KM, Wassef C. Erosive pustular dermatosis of the scalp: causes and treatments. Int J Dermatol. 2021;60:25-32. doi: 10.1111/ijd.14955
2. Sasaki R, Asano Y, Fujimura T. A pediatric case of corticosteroid-resistant erosive pustular dermatosis of scalp-like alopecia treated successfully with oral indomethacin, doxycycline, and topical tacrolimus. J Dermatol. 2022;49: e299-e300. doi: 10.1111/1346-8138.16425

Two shave biopsies were taken, 1 in the center of a previous SCC site with hyperkeratosis, the other in a site not previously affected by SCC but with the physical features of a pustule. Biopsy results from both sites were consistent with erosive pustular dermatosis, an unusual inflammatory disorder that mimics SCC.
Erosive pustular dermatosis of the scalp is an uncommon dermatitis that usually affects older women but may appear in men and women of all ages. It can mimic many other conditions that can affect the scalp, including seborrheic dermatitis, psoriasis, actinic keratosis, and SCC.
The exact causative mechanism is not understood, and cases may develop spontaneously. Rough papules, pustules, crusts, and ulcers develop and (apart from the pustules) share many features of actinic keratoses, SCCs, and field cancerization. The presence of pustules helps point to the diagnosis.
Triggers include previous surgery or physical trauma, burns, skin or hair grafts, and treatment of actinic keratoses with imiquimod, 5-fluourouracil, or photodynamic therapy. Some autoimmune diseases (including Hashimoto thyroiditis, autoimmune hepatitis, and rheumatoid arthritis) have been linked to disease occurrence and severity.1
Treatment includes potent or super-potent topical steroids such as clobetasol 0.05% ointment. Topical tacrolimus 0.1% ointment and calcipotriene 0.005% cream have been reported as steroid alternatives. Paradoxically, photodynamic therapy, while associated with triggering disease, has also been used therapeutically. Systemic immunomodulators such as cyclosporine 3 mg/kg/d or prednisone 0.5 to 1 mg/kg/d may be needed in severe cases. Antibiotics including topical dapsone 5% gel, systemic dapsone from 50 mg bid to tid, and doxycycline have been helpful due, in part, to their immunomodulatory effects.1,2
This patient was told to apply topical triamcinolone 0.1% ointment around and over ulcers and pustules and to take doxycycline 100 mg twice daily. The patient cleared well after 6 weeks. He continued to apply topical triamcinolone every few days as maintenance therapy.
He had some mild recurrence after discontinuing all topical and oral therapy, so he currently is being maintained on topical clobetasol 0.05% ointment every other day. He comes in for follow-up appointments every 3 months to monitor for control of the erosive pustular dermatosis of the scalp and for skin cancer surveillance.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME

Two shave biopsies were taken, 1 in the center of a previous SCC site with hyperkeratosis, the other in a site not previously affected by SCC but with the physical features of a pustule. Biopsy results from both sites were consistent with erosive pustular dermatosis, an unusual inflammatory disorder that mimics SCC.
Erosive pustular dermatosis of the scalp is an uncommon dermatitis that usually affects older women but may appear in men and women of all ages. It can mimic many other conditions that can affect the scalp, including seborrheic dermatitis, psoriasis, actinic keratosis, and SCC.
The exact causative mechanism is not understood, and cases may develop spontaneously. Rough papules, pustules, crusts, and ulcers develop and (apart from the pustules) share many features of actinic keratoses, SCCs, and field cancerization. The presence of pustules helps point to the diagnosis.
Triggers include previous surgery or physical trauma, burns, skin or hair grafts, and treatment of actinic keratoses with imiquimod, 5-fluourouracil, or photodynamic therapy. Some autoimmune diseases (including Hashimoto thyroiditis, autoimmune hepatitis, and rheumatoid arthritis) have been linked to disease occurrence and severity.1
Treatment includes potent or super-potent topical steroids such as clobetasol 0.05% ointment. Topical tacrolimus 0.1% ointment and calcipotriene 0.005% cream have been reported as steroid alternatives. Paradoxically, photodynamic therapy, while associated with triggering disease, has also been used therapeutically. Systemic immunomodulators such as cyclosporine 3 mg/kg/d or prednisone 0.5 to 1 mg/kg/d may be needed in severe cases. Antibiotics including topical dapsone 5% gel, systemic dapsone from 50 mg bid to tid, and doxycycline have been helpful due, in part, to their immunomodulatory effects.1,2
This patient was told to apply topical triamcinolone 0.1% ointment around and over ulcers and pustules and to take doxycycline 100 mg twice daily. The patient cleared well after 6 weeks. He continued to apply topical triamcinolone every few days as maintenance therapy.
He had some mild recurrence after discontinuing all topical and oral therapy, so he currently is being maintained on topical clobetasol 0.05% ointment every other day. He comes in for follow-up appointments every 3 months to monitor for control of the erosive pustular dermatosis of the scalp and for skin cancer surveillance.
Photos and text for Photo Rounds Friday courtesy of Jonathan Karnes, MD (copyright retained). Dr. Karnes is the medical director of MDFMR Dermatology Services, Augusta, ME
1. Karanfilian KM, Wassef C. Erosive pustular dermatosis of the scalp: causes and treatments. Int J Dermatol. 2021;60:25-32. doi: 10.1111/ijd.14955
2. Sasaki R, Asano Y, Fujimura T. A pediatric case of corticosteroid-resistant erosive pustular dermatosis of scalp-like alopecia treated successfully with oral indomethacin, doxycycline, and topical tacrolimus. J Dermatol. 2022;49: e299-e300. doi: 10.1111/1346-8138.16425
1. Karanfilian KM, Wassef C. Erosive pustular dermatosis of the scalp: causes and treatments. Int J Dermatol. 2021;60:25-32. doi: 10.1111/ijd.14955
2. Sasaki R, Asano Y, Fujimura T. A pediatric case of corticosteroid-resistant erosive pustular dermatosis of scalp-like alopecia treated successfully with oral indomethacin, doxycycline, and topical tacrolimus. J Dermatol. 2022;49: e299-e300. doi: 10.1111/1346-8138.16425
Don’t call them ‘private parts’
This transcript has been edited for clarity.
Today, I’d like to talk about private parts. You know: the genitals, down there.
I hate all of that. I really wish that we can get to a place where we can talk about genitals and sexual health the same way we do about high blood pressure and diabetes. In fact, when a new patient comes in and they get a new diagnosis of diabetes, you spend time explaining to them how their pancreas works. I don’t remember all the details because I’m a urologist. But you explain the details of diabetes, how it works, why therapy is important, and how it’s very important for quality of life.
I say to patients, “You have to know what parts you have in order to figure out how they drive, right?” We want them to drive better.
Let me give you an example. Many men come to see me with complaints of erectile dysfunction. They refuse to take sildenafil and tadalafil (Viagra and Cialis), saying, “Oh my gosh, those are magic pills. I won’t be a man if take them.” We all know that doesn’t make any sense. I explain to them how their penis works: “Your penis is a muscle. The muscle does two things. It contracts and it relaxes, just like your bicep. It’s just that your penis muscle is smooth muscle, which means it responds to fight or flight. It’s on the autonomic nervous system.”
I explain that if the muscle of the penis is relaxed, it fills with blood and expands. It gets big and hard, and it traps the blood. But when the muscles of the penis are contracted, when they are tight, it squeezes out all the blood, like squeezing out a sponge. So the important thing to do if you want to have good erections is to get the muscles to relax. Relaxed muscle increases erections. I get them to understand that sildenafil and tadalafil are phosphodiesterase 5 inhibitors: smooth-muscle relaxants. Instead of saying, “I need to take Viagra or Cialis because I’m broken,” it’s, “Oh hey honey, I need to take my muscle relaxants because my muscles aren’t working the way that they used to.”
In the future, I’ll go into what happens in erectile dysfunction. We’ll go into what can happen with erectile dysfunction and the many reasons why it happens. It’s getting them to understand that if we get the muscles to relax, you will have better erections. This is how the penis works. It’s why the medicine works. The patients will actually try the therapy and they’ll feel so much better about it. They’ll say, “Oh my gosh, this makes so much sense.” They work on their mental muscles to get the muscles of the penis to relax. Understanding anatomy and physiology helps them understand the treatments, which leads to better outcomes.
How about the female side? If a woman comes to see me reporting that she can’t have an orgasm, part of it is education and understanding the anatomy and physiology. The clitoris and the penis are exactly the same thing. The head of the clitoris and the head of the penis are the same. The clitoris has legs that go all the way down to the butt bone. So everyone is sitting on their genitals right now. The butt bones connect to the bottom of the clitoris or the bottom of the penis. They each have legs called crura. When you get patients to understand where their anatomy is and how it functions, they will then understand how to maximize their quality of life.
The clitoris has smooth muscle just like the penis. When that smooth muscle relaxes, it gorges with blood. When you stimulate it, it can lead to orgasm for most people. But, wait a minute. The clitoris is not inside the vagina. It’s outside. It’s behind the labia majora. If you follow the labia minora up, you get to the head of the clitoris. If patients understand that, they then will understand that penetration is not the way the majority of people orgasm.
I love pictures. I show everyone pictures in my office. They help patients to understand why vibration or outside stimulation on the vulva will allow orgasm to happen. And so instead of patients coming in saying, “I’m broken, I can’t orgasm from penetration,” or, “Dr. Rubin, I’m broken because I can’t get erections,” getting them to understand the anatomy and physiology helps them understand the treatment.
As we go forward, I’ll talk more about anatomy and physiology and how to increase the sexual health of our patients. For now though, please stop calling them private parts. Please use your understanding of anatomy and physiology to educate your patients to have better sexual health and higher quality of life. You may be the only clinician to ever do so, and it will make their life so much better.
Dr. Rubin is an assistant clinical professor, department of urology, at Georgetown University, Washington. She reported conflicts of interest with Sprout, Maternal Medical, Absorption Pharmaceuticals, GlaxoSmithKline, and Endo.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Today, I’d like to talk about private parts. You know: the genitals, down there.
I hate all of that. I really wish that we can get to a place where we can talk about genitals and sexual health the same way we do about high blood pressure and diabetes. In fact, when a new patient comes in and they get a new diagnosis of diabetes, you spend time explaining to them how their pancreas works. I don’t remember all the details because I’m a urologist. But you explain the details of diabetes, how it works, why therapy is important, and how it’s very important for quality of life.
I say to patients, “You have to know what parts you have in order to figure out how they drive, right?” We want them to drive better.
Let me give you an example. Many men come to see me with complaints of erectile dysfunction. They refuse to take sildenafil and tadalafil (Viagra and Cialis), saying, “Oh my gosh, those are magic pills. I won’t be a man if take them.” We all know that doesn’t make any sense. I explain to them how their penis works: “Your penis is a muscle. The muscle does two things. It contracts and it relaxes, just like your bicep. It’s just that your penis muscle is smooth muscle, which means it responds to fight or flight. It’s on the autonomic nervous system.”
I explain that if the muscle of the penis is relaxed, it fills with blood and expands. It gets big and hard, and it traps the blood. But when the muscles of the penis are contracted, when they are tight, it squeezes out all the blood, like squeezing out a sponge. So the important thing to do if you want to have good erections is to get the muscles to relax. Relaxed muscle increases erections. I get them to understand that sildenafil and tadalafil are phosphodiesterase 5 inhibitors: smooth-muscle relaxants. Instead of saying, “I need to take Viagra or Cialis because I’m broken,” it’s, “Oh hey honey, I need to take my muscle relaxants because my muscles aren’t working the way that they used to.”
In the future, I’ll go into what happens in erectile dysfunction. We’ll go into what can happen with erectile dysfunction and the many reasons why it happens. It’s getting them to understand that if we get the muscles to relax, you will have better erections. This is how the penis works. It’s why the medicine works. The patients will actually try the therapy and they’ll feel so much better about it. They’ll say, “Oh my gosh, this makes so much sense.” They work on their mental muscles to get the muscles of the penis to relax. Understanding anatomy and physiology helps them understand the treatments, which leads to better outcomes.
How about the female side? If a woman comes to see me reporting that she can’t have an orgasm, part of it is education and understanding the anatomy and physiology. The clitoris and the penis are exactly the same thing. The head of the clitoris and the head of the penis are the same. The clitoris has legs that go all the way down to the butt bone. So everyone is sitting on their genitals right now. The butt bones connect to the bottom of the clitoris or the bottom of the penis. They each have legs called crura. When you get patients to understand where their anatomy is and how it functions, they will then understand how to maximize their quality of life.
The clitoris has smooth muscle just like the penis. When that smooth muscle relaxes, it gorges with blood. When you stimulate it, it can lead to orgasm for most people. But, wait a minute. The clitoris is not inside the vagina. It’s outside. It’s behind the labia majora. If you follow the labia minora up, you get to the head of the clitoris. If patients understand that, they then will understand that penetration is not the way the majority of people orgasm.
I love pictures. I show everyone pictures in my office. They help patients to understand why vibration or outside stimulation on the vulva will allow orgasm to happen. And so instead of patients coming in saying, “I’m broken, I can’t orgasm from penetration,” or, “Dr. Rubin, I’m broken because I can’t get erections,” getting them to understand the anatomy and physiology helps them understand the treatment.
As we go forward, I’ll talk more about anatomy and physiology and how to increase the sexual health of our patients. For now though, please stop calling them private parts. Please use your understanding of anatomy and physiology to educate your patients to have better sexual health and higher quality of life. You may be the only clinician to ever do so, and it will make their life so much better.
Dr. Rubin is an assistant clinical professor, department of urology, at Georgetown University, Washington. She reported conflicts of interest with Sprout, Maternal Medical, Absorption Pharmaceuticals, GlaxoSmithKline, and Endo.
A version of this article first appeared on Medscape.com.
This transcript has been edited for clarity.
Today, I’d like to talk about private parts. You know: the genitals, down there.
I hate all of that. I really wish that we can get to a place where we can talk about genitals and sexual health the same way we do about high blood pressure and diabetes. In fact, when a new patient comes in and they get a new diagnosis of diabetes, you spend time explaining to them how their pancreas works. I don’t remember all the details because I’m a urologist. But you explain the details of diabetes, how it works, why therapy is important, and how it’s very important for quality of life.
I say to patients, “You have to know what parts you have in order to figure out how they drive, right?” We want them to drive better.
Let me give you an example. Many men come to see me with complaints of erectile dysfunction. They refuse to take sildenafil and tadalafil (Viagra and Cialis), saying, “Oh my gosh, those are magic pills. I won’t be a man if take them.” We all know that doesn’t make any sense. I explain to them how their penis works: “Your penis is a muscle. The muscle does two things. It contracts and it relaxes, just like your bicep. It’s just that your penis muscle is smooth muscle, which means it responds to fight or flight. It’s on the autonomic nervous system.”
I explain that if the muscle of the penis is relaxed, it fills with blood and expands. It gets big and hard, and it traps the blood. But when the muscles of the penis are contracted, when they are tight, it squeezes out all the blood, like squeezing out a sponge. So the important thing to do if you want to have good erections is to get the muscles to relax. Relaxed muscle increases erections. I get them to understand that sildenafil and tadalafil are phosphodiesterase 5 inhibitors: smooth-muscle relaxants. Instead of saying, “I need to take Viagra or Cialis because I’m broken,” it’s, “Oh hey honey, I need to take my muscle relaxants because my muscles aren’t working the way that they used to.”
In the future, I’ll go into what happens in erectile dysfunction. We’ll go into what can happen with erectile dysfunction and the many reasons why it happens. It’s getting them to understand that if we get the muscles to relax, you will have better erections. This is how the penis works. It’s why the medicine works. The patients will actually try the therapy and they’ll feel so much better about it. They’ll say, “Oh my gosh, this makes so much sense.” They work on their mental muscles to get the muscles of the penis to relax. Understanding anatomy and physiology helps them understand the treatments, which leads to better outcomes.
How about the female side? If a woman comes to see me reporting that she can’t have an orgasm, part of it is education and understanding the anatomy and physiology. The clitoris and the penis are exactly the same thing. The head of the clitoris and the head of the penis are the same. The clitoris has legs that go all the way down to the butt bone. So everyone is sitting on their genitals right now. The butt bones connect to the bottom of the clitoris or the bottom of the penis. They each have legs called crura. When you get patients to understand where their anatomy is and how it functions, they will then understand how to maximize their quality of life.
The clitoris has smooth muscle just like the penis. When that smooth muscle relaxes, it gorges with blood. When you stimulate it, it can lead to orgasm for most people. But, wait a minute. The clitoris is not inside the vagina. It’s outside. It’s behind the labia majora. If you follow the labia minora up, you get to the head of the clitoris. If patients understand that, they then will understand that penetration is not the way the majority of people orgasm.
I love pictures. I show everyone pictures in my office. They help patients to understand why vibration or outside stimulation on the vulva will allow orgasm to happen. And so instead of patients coming in saying, “I’m broken, I can’t orgasm from penetration,” or, “Dr. Rubin, I’m broken because I can’t get erections,” getting them to understand the anatomy and physiology helps them understand the treatment.
As we go forward, I’ll talk more about anatomy and physiology and how to increase the sexual health of our patients. For now though, please stop calling them private parts. Please use your understanding of anatomy and physiology to educate your patients to have better sexual health and higher quality of life. You may be the only clinician to ever do so, and it will make their life so much better.
Dr. Rubin is an assistant clinical professor, department of urology, at Georgetown University, Washington. She reported conflicts of interest with Sprout, Maternal Medical, Absorption Pharmaceuticals, GlaxoSmithKline, and Endo.
A version of this article first appeared on Medscape.com.