User login
Hospitalist‐Run Acute Care for Elderly
For the frail older patient, hospitalization marks a period of high risk of poor outcomes and adverse events including functional decline, delirium, pressure ulcers, adverse drug events, nosocomial infections, and falls.1, 2 Physician recognition of elderly patients at risk for adverse outcomes is poor, making it difficult to intervene to prevent them.3, 4 Among frail, elderly inpatients at an urban academic medical center, doctors documented cognitive assessments in only 5% of patients. Functional assessments are appropriately documented in 40%80% of inpatients.3, 5
The Acute Care for Elders (ACE) unit is one of several models of comprehensive inpatient geriatric care that have been developed by geriatrician researchers to address the adverse events and functional decline that often accompany hospitalization.6 The ACE unit model generally incorporates: 1) a modified hospital environment, 2) early assessment and intensive management to minimize the adverse effects of hospital care, 3) early discharge planning, 4) patient centered care protocols, and 5) a consistent nursing staff.7 Two randomized, controlled trials have shown the ACE unit model to be successful in reducing functional decline among frail older inpatients during and after hospitalization.7, 8 While meta‐analyses data also suggests the ACE unit model reduces functional decline and future institutionalization, significant impact on other outcomes is not proven.9, 10
Several barriers have prevented the successful dissemination of the ACE unit model. The chief limitations are the upfront resources required to create and maintain a modified, dedicated unit, as well as the lack of a geriatrics trained workforce.7, 1113 The rapid growth of hospital medicine presents opportunities for innovation in the care of older patients. Still, a 2006 census demonstrated that few hospitalist groups had identified geriatric care as a priority.14
In response to these challenges, the University of Colorado Hospital Medicine Group created a hospitalist‐run inpatient medical service designed for the care of the frail older patient. This Hospitalist‐Acute Care for the Elderly (Hospitalist‐ACE) unit is a hybrid of a general medical service and an inpatient geriatrics unit.7 The goals of the Hospitalist‐ACE service are to provide high quality care tailored to older inpatients, thus minimizing the risks of functional decline and adverse events associate with hospitalization, and to provide a clinical geriatrics teaching experience for Hospitalist Training Track Residents within the Internal Medicine Residency Training Program and medical students at the University of Colorado Denver School of Medicine. The Hospitalist‐ACE unit is staffed with a core group of hospitalist attendings who have, at a minimum, attended an intensive mini‐course in inpatient geriatrics. The service employs interdisciplinary rounds; a brief, standardized geriatric assessment including screens of function, cognition, and mood; a clinical focus on mitigating the hazards of hospitalization, early discharge planning; and a novel geriatric educational curriculum for medicine residents and medical students.
This article will: 1) describe the creation of the Hospitalist‐ACE service at the University of Colorado Hospital; and 2) summarize the evaluation of the Hospitalist‐ACE service in a quasi‐randomized, controlled manner during its first year. We hypothesized that, when compared to patients receiving usual care, patients cared for on the Hospitalist‐ACE service would have increased recognition of abnormal functional status; recognition of abnormal cognitive status and delirium; equivalent lengths of stay and hospital charges; and decreased falls, 30‐day readmissions, and restraint use.
METHODS
Design
We performed a quasi‐randomized, controlled study of the Hospitalist‐ACE service.
Setting
The study setting was the inpatient general medical services of the Anschutz Inpatient Pavilion (AIP) of the University of Colorado Hospital (UCH). The AIP is a 425‐bed tertiary care hospital that is the major teaching affiliate of the University of Colorado School of Medicine and a regional referral center. The control services, hereafter referred to as usual care, were comprised of the four inpatient general medicine teaching services that take admissions on a four‐day rotation (in general, two were staffed by outpatient general internists and medical subspecialists, and two were staffed by academic hospitalists). The Hospitalist‐ACE service was a novel hospitalist teaching service that began in July 2007. Hospitalist‐ACE patients were admitted to a single 12‐bed medical unit (12 West) when beds were available; 12 West is similar to the other medical/surgical units at UCH and did not have any modifications to the rooms, equipment, or common areas for the intervention. The nursing staff on this unit had no formal geriatric nursing training. The Hospitalist‐ACE team admitted patients daily (between 7 AM and 3 PM MondayFriday; between 7 AM and 12 noon Saturday and Sunday). Patients assigned to the Hospitalist‐ACE service after hours were admitted by the internal medicine resident on call for the usual care services and handed off to the Hospitalist‐ACE team at 7 AM the next morning.
Study Subjects
Eligible subjects were inpatients age 70 years admitted to the usual care or Hospitalist‐ACE services at the AIP from November 2, 2007 to April 15, 2008. All patients age 70 years were randomized to the Hospitalist‐ACE service or usual care on a general internal medicine service by the last digit of the medical record number (odd numbers admitted to the Hospitalist‐ACE service and even numbers admitted to usual care). Patients followed by the Hospitalist‐ACE service but not admitted to 12 West were included in the study. To isolate the impact of the intervention, patients admitted to a medicine subspecialty service (such as cardiology, pulmonary, or oncology), or transferred to or from the Hospitalist‐ACE or control services to another service (eg, intensive care unit [ICU] or orthopedic surgery service) were excluded from the study.
Intervention
The Hospitalist‐ACE unit implemented an interdisciplinary team approach to identify and address geriatric syndromes in patients aged 70 and over. The Hospitalist‐ACE model of care consisted of clinical care provided by a hospitalist attending with additional training in geriatric medicine, administration of standardized geriatric screens assessing function, cognition, and mood, 15 minute daily (MondayFriday) interdisciplinary rounds focusing on recognition and management of geriatric syndromes and early discharge planning, and a standardized educational curriculum for medical residents and medical students addressing hazards of hospitalization.
The Hospitalist‐ACE service was a unique rotation within the Hospitalist Training Track of the Internal Medicine Residency that was developed with the support of the University of Colorado Hospital and the Internal Medicine Residency Training Program, and input from the Geriatrics Division at the University of Colorado Denver. The director received additional training from the Donald W. Reynolds FoundationUCLA Faculty Development to Advance Geriatric Education Mini‐Fellowship for hospitalist faculty. The mission of the service was to excel at educating the next generation of hospitalists while providing a model for excellence of care for hospitalized elderly patients. Important stakeholders were identified, and a leadership teamincluding representatives from nursing, physical and occupational therapy, pharmacy, social work, case management, and later, volunteer servicescreated the model daily interdisciplinary rounds. As geographic concentration was essential for the viability of interdisciplinary rounds, one unit (12 West) within the hospital was designated as the preferred location for patients admitted to the Hospitalist‐ACE service.
The Hospitalist‐ACE unit team consisted of one attending hospitalist, one resident, one intern, and medical students. The attending was one of five hospitalists, with additional training in geriatric medicine, who rotated attending responsibilities on the service. One of the hospitalists was board certified in geriatric medicine. Each of the other four hospitalists attended the Reynolds FoundationUCLA mini‐fellowship in geriatric medicine. Hospitalist‐ACE attendings rotated on a variety of other hospitalist services throughout the academic year, including the usual care services.
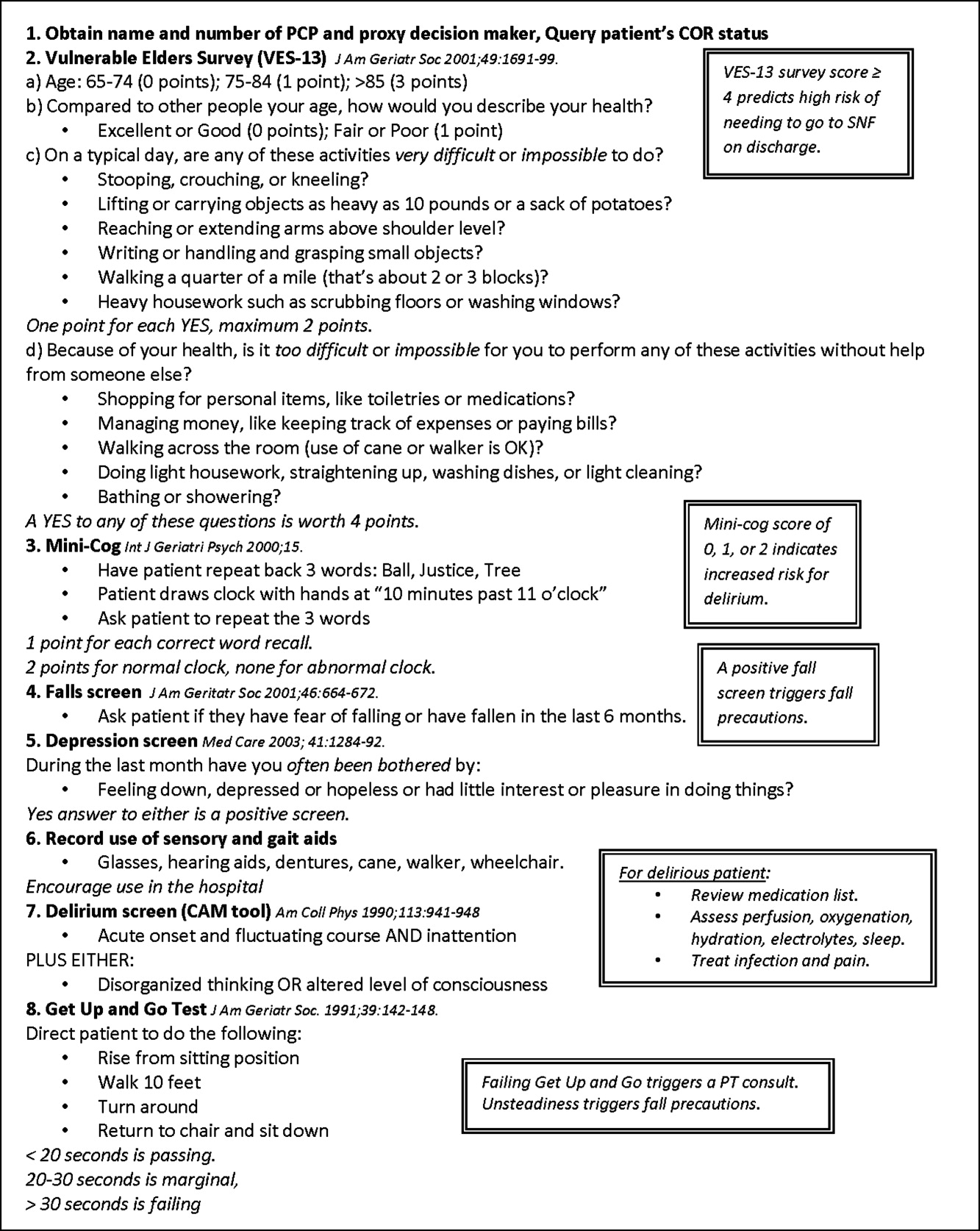
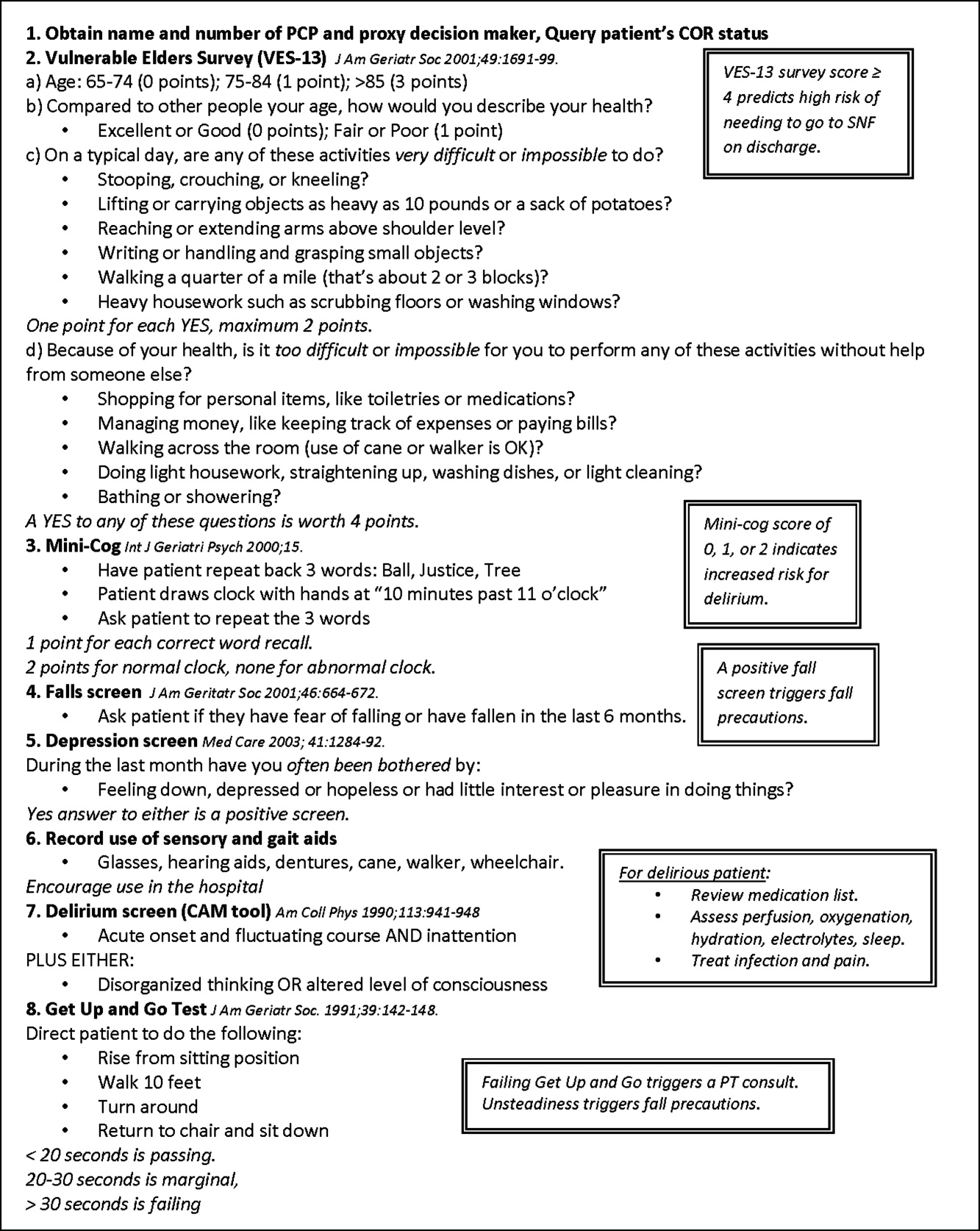
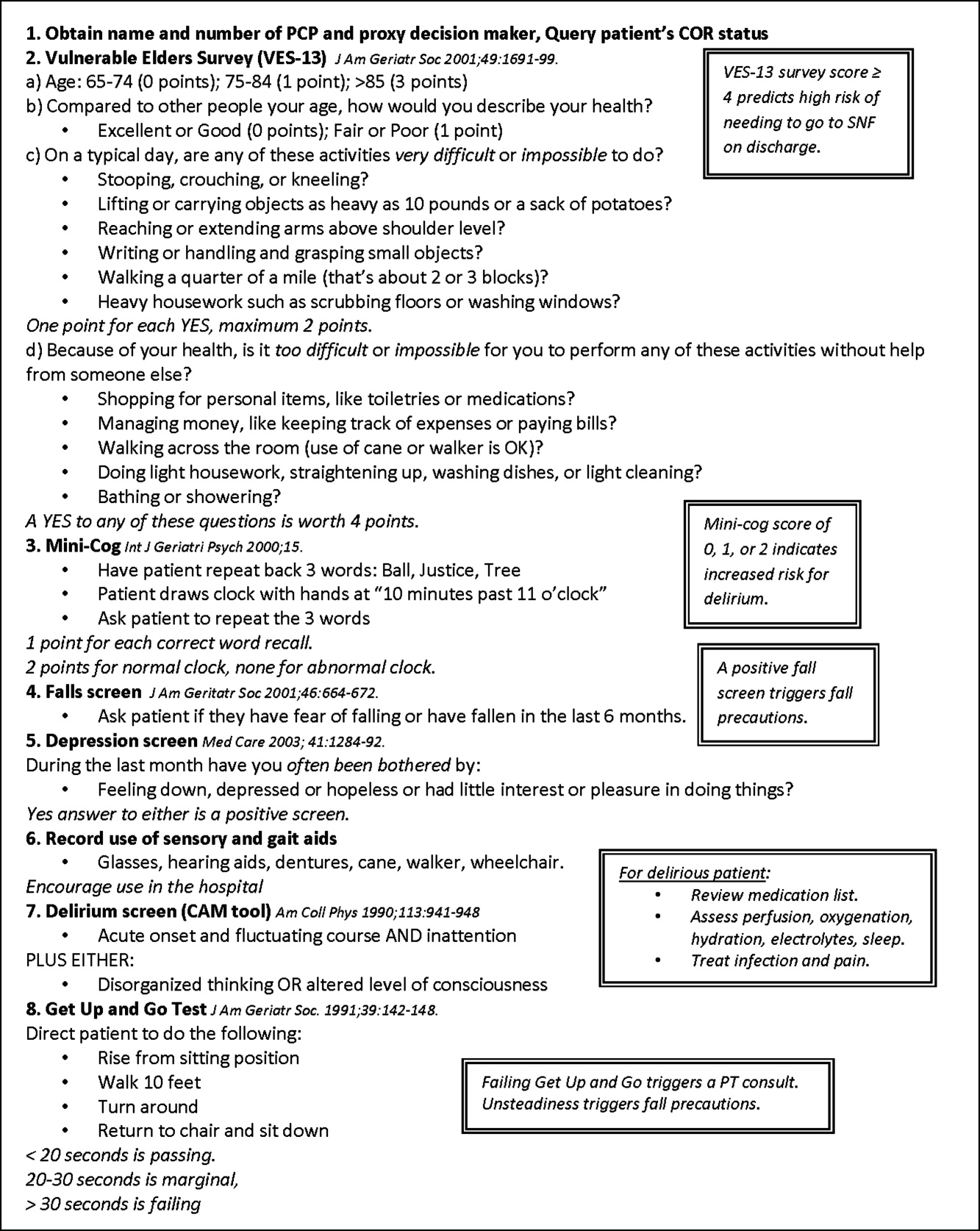
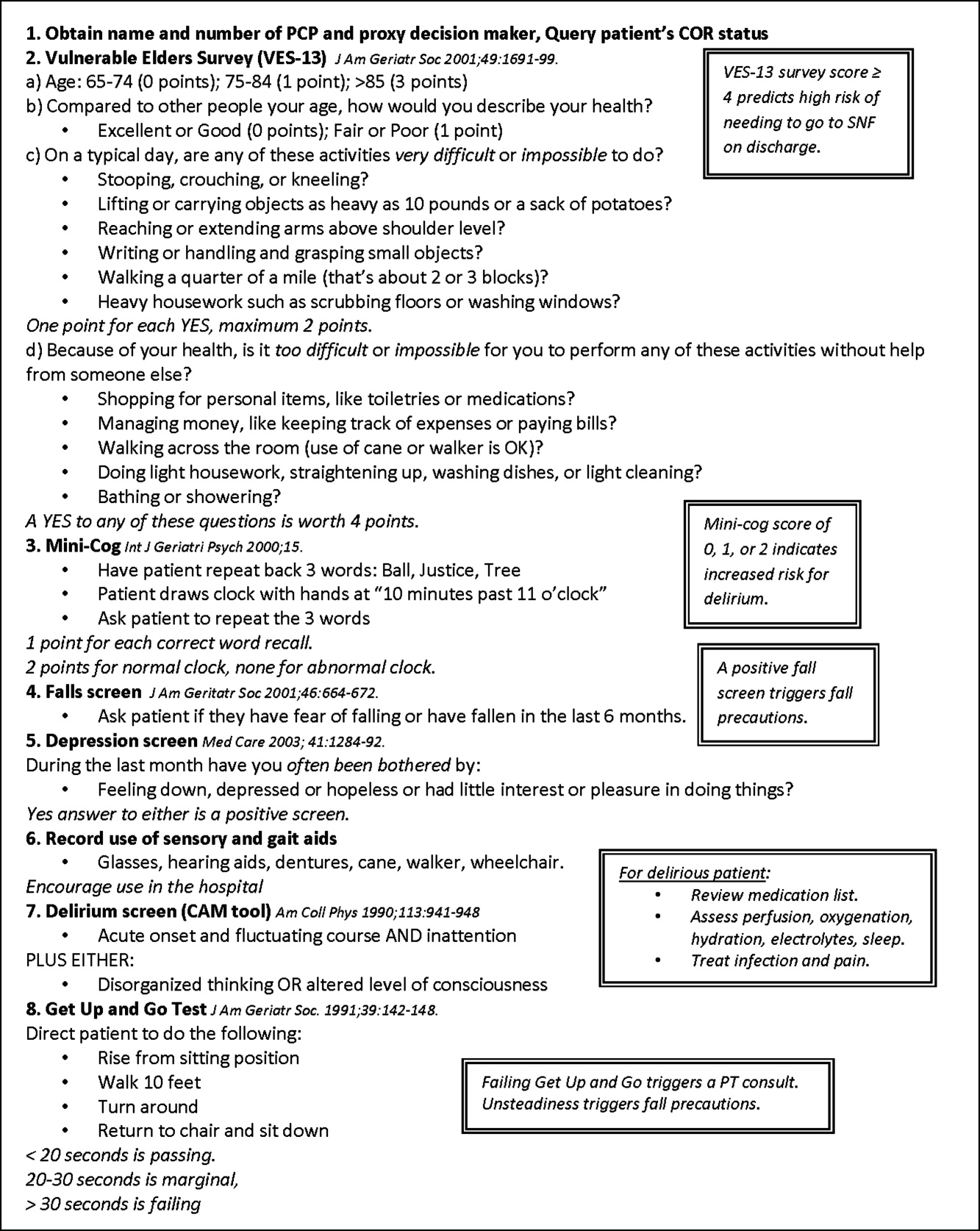
The brief standardized geriatric assessment consisted of six validated instruments, and was completed by house staff or medical students on admission, following instruction by the attending physician. The complete assessment tool is shown in Figure 1. The cognitive items included the Mini‐Cog,15 a two‐item depression screen,16 and the Confusion Assessment Method.17 The functional items included the Vulnerable Elders Survey (VES‐13),18 the Timed Get Up and Go test,19 and a two‐question falls screen.20 The elements of the assessment tool were selected by the Hospitalist‐ACE attendings for brevity and the potential to inform clinical management. To standardize the clinical and educational approach, the Hospitalist‐ACE attendings regularly discussed appropriate orders recommended in response to each positive screen, but no templated order sets were used during the study period.
Interdisciplinary rounds were attended by Hospitalist‐ACE physicians, nurses, case managers, social workers, physical or occupational therapists, pharmacists, and volunteers. Rounds were led by the attending or medical resident.
The educational curriculum encompassed 13 modules created by the attending faculty that cover delirium, falls, dementia, pressure ulcers, physiology of aging, movement disorders, medication safety, end of life care, advance directives, care transitions, financing of health care for the elderly, and ethical conundrums in the care of the elderly. A full table of contents appears in online Appendix 1. Additionally, portions of the curriculum have been published online.21, 22 Topic selection was guided by the Accreditation Council for Graduate Medical Education (ACGME) core geriatrics topics determined most relevant for the inpatient setting. Formal instruction of 3045 minutes duration occurred three to four days a week and was presented in addition to routine internal medicine educational conferences. Attendings coordinated teaching to ensure that each trainee was exposed to all of the content during the course of their four‐week rotation.
In contrast to the Hospitalist‐ACE service, usual care on the control general medical services consisted of either a hospitalist, a general internist, or an internal medicine subspecialist attending physician, with one medical resident, one intern, and medical students admitting every fourth day. The general medical teams attended daily discharge planning rounds with a discharge planner and social worker focused exclusively on discharge planning. The content of teaching rounds on the general medical services was largely left to the discretion of the attending physician.
This program evaluation of the Hospitalist‐ACE service was granted a waiver of consent and Health Insurance Portability and Accountability Act (HIPAA) by the Colorado Multiple Institutional Review Board.
Measures
Primary Outcome
The primary outcome for the study was the recognition of abnormal functional status by the primary team. Recognition of abnormal functional status was determined from chart review and consisted of both the physician's detection of abnormal functional status and evidence of a corresponding treatment plan identified in the notes or orders of a physician member of the primary team (Table 1).
| Measure | Criterion | Source | Content Examples |
|---|---|---|---|
| |||
| Recognition of abnormal functional status* | 1) Detection | MD's documentation of history | Presentation with change in function (new gait instability); use of gait aides (wheelchair) |
| OR | |||
| MD's documentation of physical exam | Observation of abnormal gait (eg, unsteady, wide‐based, shuffling) and/or balance Abnormal Get Up and Go test | ||
| AND | |||
| 2) Treatment | MD's order | PT/OT consult; home safety evaluation | |
| OR | |||
| MD's documentation assessment/plan | Inclusion of functional status (rehabilitation, PT/OT needs) on the MD's problem list | ||
| Recognition of abnormal cognitive status | Any of the following: | ||
| Delirium | 1) Detection | MD's history | Presentation of confusion or altered mental status |
| OR | |||
| MD's physical exam | Abnormal confusion assessment method | ||
| AND | |||
| 2) Treatment | MD's order | Sitter, reorienting communication, new halperidol order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of delirium on the problem list | ||
| OR | |||
| Dementia | 1) Detection | MD's history | Dementia in medical history |
| OR | OR | ||
| MD's physical exam | Abnormal Folstein Mini‐Mental Status Exam or Mini‐Cog | ||
| AND | |||
| 2) Treatment | MD's order | Cholinesterase inhibitor ordered | |
| OR | OR | ||
| MD's documentation of assessment/plan | Inclusion of dementia on the problem list | ||
| OR | |||
| Depression | 1) Detection | MD's history | Depression in medical history |
| OR | OR | ||
| MD's physical exam | Positive depression screen | ||
| AND | |||
| 2) Treatment | MD's order | New antidepressant order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of depression on the problem list | ||
Secondary Outcomes
Recognition of abnormal cognitive status was determined from chart review and consisted of both the physician's detection of dementia, depression, or delirium, and evidence of a corresponding treatment plan for any of the documented conditions identified in the notes or orders of a physician member of the primary team (Table 1). Additionally, we measured recognition and treatment of delirium alone.
Falls were determined from mandatory event reporting collected by the hospital on the University Hospitals Consortium Patient Safety Net web‐based reporting system and based on clinical assessment as reported by the nursing staff. The reports are validated by the appropriate clinical managers within 45 days of the event according to standard procedure.
Physical restraint use (type of restraint and duration) was determined from query of mandatory clinical documentation in the electronic medical record. Use of sleep aids was determined from review of the physician's order sheets in the medical record. The chart review captured any of 39 commonly prescribed hypnotic medications ordered at hour of sleep or for insomnia. The sleep medication list was compiled with the assistance of a pharmacist for an earlier chart review and included non‐benzodiazepine hypnotics, benzodiazepines, antidepressants, antihistamines, and antipsychotics.23
Length of stay, hospital charges, 30‐day readmissions to UCH (calculated from date of discharge), and discharge location were determined from administrative data.
Additional Descriptive Variables
Name, medical record number, gender, date of birth, date of admission and discharge, and primary diagnosis were obtained from the medical record. The Case Mix Index for each group of patients was determined from the average Medicare Severity‐adjusted Diagnosis Related Group (MS‐DRG) weight obtained from administrative data.
Data Collection
A two‐step, retrospective chart abstraction was employed. A professional research assistant (P.R.A.) hand‐abstracted process measures from the paper medical chart onto a data collection form designed for this study. A physician investigator performed a secondary review (H.L.W.). Discrepancies were resolved by the physician reviewer.
Data Analysis
Descriptive statistics were performed on intervention and control subjects. Means and standard deviations (age) or frequencies (gender, primary diagnoses) were calculated as appropriate. T tests were used for continuous variables, chi‐square tests for gender, and the Wilcoxon rank sum test for categorical variables.
Outcomes were reported as means and standard deviations for continuous variables (length of stay and charges) and frequencies for categorical variables (all other outcomes). T tests were used for continuous variables, Fisher's exact test for restraint use, and chi‐square tests were used for categorical variable to compare the impact of the intervention between intervention and control patients. For falls, confidence intervals were calculated for the incidence rate differences based on Poisson approximations.
Sample Size Considerations
An a priori sample size calculation was performed. A 2001 study showed that functional status is poorly documented in at least 60% of hospital charts of elderly patients.5 Given an estimated sample size of 120 per group and a power of 80%, this study was powered to be able to detect an absolute difference in the documentation of functional status of as little as 18%.
RESULTS
Two hundred seventeen patients met the study entry criteria (Table 2): 122 were admitted to the Hospitalist‐ACE service, and 95 were admitted to usual care on the general medical services. The average age of the study patients was 80.5 years, 55.3% were female. Twenty‐eight percent of subjects were admitted for pulmonary diagnoses. The two groups of patients were similar with respect to age, gender, and distribution of primary diagnoses. The Hospitalist‐ACE patients had a mean MS‐DRG weight of 1.15, which was slightly higher than that of usual care patients at 1.05 (P = 0.06). Typically, 70% of Hospitalist‐ACE patients are admitted to the designated ACE medical unit (12 West).
| Characteristic | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Age (years), mean (SD) | 80.5 (6.5) | 80.7 (7.0) | 0.86 |
| Gender (% female) | 52.5 | 59 | 0.34 |
| Case Mix Index (mean MS‐DRG weight [SD]) | 1.15 (0.43) | 1.05 (0.31) | 0.06 |
| Primary ICD‐9 diagnosis (%) | 0.59 | ||
| Pulmonary | 27.9 | 28.4 | |
| General medicine | 15.6 | 11.6 | |
| Surgery | 13.9 | 11.6 | |
| Cardiology | 9.8 | 6.3 | |
| Nephrology | 8.2 | 7.4 | |
Processes of Care
Processes of care for older patients are displayed in Table 3. Patients on the Hospitalist‐ACE service had recognition and treatment of abnormal functional status at a rate that was nearly double that of patients on the usual care services (68.9% vs 35.8%, P < 0.0001). In addition, patients on the Hospitalist‐ACE service were significantly more likely to have had recognition and treatment of any abnormal cognitive status (55.7% vs 40.0%, P = 0.02). When delirium was evaluated alone, the Hospitalist‐ACE patients were also more likely to have had recognition and treatment of delirium (27.1% vs 17.0%, P = 0.08), although this finding did not reach statistical significance.
| Measure | Percent of Hospitalist‐ACE Patients | Percent of Usual Care Patients | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Recognition and treatment of abnormal functional status | 68.9 | 35.8 | <0.0001 |
| Recognition and treatment of abnormal cognitive status* | 55.7 | 40.0 | 0.02 |
| Recognition and treatment of delirium | 27.1 | 17.0 | 0.08 |
| Documentation of resuscitation preferences | 95.1 | 91.6 | 0.3 |
| Do Not Attempt Resuscitation orders | 39.3 | 26.3 | 0.04 |
| Use of sleep medications | 28.1 | 27.4 | 0.91 |
| Use of physical restraints | 2.5 | 0 | 0.26 |
While patients on the Hospitalist‐ACE and usual care services had similar percentages of documentation of resuscitation preferences (95.1% vs 91.6%, P = 0.3), the percentage of Hospitalist‐ACE patients who had Do Not Attempt Resuscitation (DNAR) orders was significantly greater than that of the usual care patients (39.3% vs 26.3%, P = 0.04).
There were no differences in the use of physical restraints or sleep medications for Hospitalist‐ACE patients as compared to usual care patients, although the types of sleep mediations used on each service were markedly different: trazadone was employed as the first‐line sleep agent on the Hospitalist‐ACE service (77.7%), and non‐benzodiazepine hypnotics (primarily zolpidem) were employed most commonly on the usual care services (35%). There were no differences noted in the percentage of patients with benzodiazepines prescribed as sleep aids.
Outcomes
Resource utilization outcomes are reported in Table 4. Of note, there were no significant differences between Hospitalist‐ACE discharges and usual care discharges in mean length of stay (3.4 2.7 days vs 3.1 2.7 days, P = 0.52), mean charges ($24,617 15,828 vs $21,488 13,407, P = 0.12), or 30‐day readmissions to UCH (12.3% vs 9.5%, P = 0.51). Hospitalist‐ACE discharges and usual care patients were equally likely to be discharged to home (68.6% vs 67.4%, P = 0.84), with a similar proportion of Hospitalist‐ACE discharges receiving home health care or home hospice services (14.1% vs 7.4%, P = 12).
| Measure | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Length of stay in days (mean [SD]) | 3.4 (2.7) | 3.1 (2.7) | 0.52 |
| Charges in dollars (mean [SD]) | 24,617 (15,828) | 21,488 (13,407) | 0.12 |
| 30‐Day readmissions to UCH (%) | 12.3 | 9.5 | 0.51 |
| Discharges to home (%) | 68.8* | 67.4 | 0.84 |
| Discharges to home with services (%) | 14%* | 7.4% | 0.12 |
In addition, the fall rate for Hospitalist‐ACE patients was not significantly different from the fall rate for usual care patients (4.8 falls/1000 patient days vs 6.7 falls/1000 patient days, 95% confidence interval 9.613.3).
DISCUSSION
We report the implementation and evaluation of a medical service tailored to the care of the acutely ill older patient that draws from elements of the hospitalist model and the ACE unit model.7, 14, 24 For this Hospitalist‐ACE service, we developed a specialized hospitalist workforce, assembled a brief geriatric assessment tailored to the inpatient setting, instituted an interdisciplinary rounding model, and created a novel inpatient geriatrics curriculum.
During the study period, we improved performance of important processes of care for hospitalized elders, including recognition of abnormal cognitive and functional status; maintained comparable resource use; and implemented a novel, inpatient‐focused geriatric medicine educational experience. We were unable to demonstrate an impact on key clinical outcomes such as falls, physical restraint use, and readmissions. Nonetheless, there is evidence that the performance of selected processes of care is associated with improved three‐year survival status in the community‐dwelling vulnerable older patient, and may also be associated with a mortality benefit in the hospitalized vulnerable older patient.25, 26 Therefore, methods to improve the performance of these processes of care may be of clinical importance.
The finding of increased use of DNAR orders in the face of equivalent documentation of code status is of interest and generates hypotheses for further study. It is possible that the educational experience and use of geriatric assessment provides a more complete context for the code status discussion (one that incorporates the patient's social, physical, and cognitive function). However, we do not know if the patients on the ACE service had improved concordance between their code status and their goals of care.
We believe that there was no difference in key clinical outcomes between Hospitalist‐ACE and control patients because the population in this study was relatively low acuity and, therefore, the occurrence of falls and the use of physical restraints were quite low in the study population. In particular, the readmission rate was much lower than is typical for the Medicare population at our hospital, making it challenging to draw conclusions about the impact of the intervention on readmissions, however, we cannot rule out the possibility that our early discharge planning did not address the determinants of readmission for this population.
The ACE unit paradigmcharacterized by 1) closed, modified hospital units; 2) staffing by geriatricians and nurses with geriatrics training; 3) employing geriatric nursing care protocolsrequires significant resources and is not feasible for all settings.6 There is a need for alternative models of comprehensive care for hospitalized elders that require fewer resources in the form of dedicated units and specialist personnel, and can be more responsive to institutional needs. For example, in a 2005 report, one institution reported the creation of a geriatric medicine service that utilized a geriatrician and hospitalist co‐attending model.14 More recently, a large geriatrics program replaced its inpatient geriatrics unit with a mobile inpatient geriatrics service staffed by an attending geriatricianhospitalist, a geriatrics fellow, and a nurse practitioner.27 While these innovative models have eliminated the dedicated unit, they rely on board certified geriatricians, a group in short supply nationally.28 Hospitalists are a rapidly growing provider group that, with appropriate training and building on the work of geriatricians, is poised to provide leadership in acute geriatric care.29, 30
In contrast to the comprehensive inpatient geriatric care models described above, the Hospitalist‐ACE service uses a specialized hospitalist workforce and is not dependent on continuous staffing by geriatricians. Although geographic concentration is important for the success of interdisciplinary rounds, the Hospitalist‐ACE service does not require a closed or modified unit. The nursing staff caring for Hospitalist‐ACE patients have generalist nursing training and, at the time of the study, did not utilize geriatric‐care protocols. Our results need to be interpreted in the light of these differences from the ACE unit model which is a significantly more intensive intervention than the Hospitalist‐ACE service. In addition, the current practice environment is quite different from the mid‐1990s when ACE units were developed and studied. Development and maintenance of models of comprehensive inpatient geriatric care require demonstration of both value as well as return on investment. The alignment of financial and regulatory incentives for programs that provide comprehensive care to complex patients, such as those anticipated by the Affordable Care Act, may encourage the growth of such models.
These data represent findings from a six‐month evaluation of a novel inpatient service in the middle of its first year. There are several limitations related to our study design. First, the results of this small study at a single academic medical center may be of limited generalizability to other settings. Second, the program was evaluated only three months after its inception; we did not capture further improvements in methods, training, and outcomes expected as the program matured. Third, most of the Hospitalist‐ACE service attendings and residents rotate on the UCH general medical services throughout the year. Consequently, we were unable to eliminate the possibility of contamination of the control group, and we were unable to blind the physicians to the study. Fourth, the study population had a relatively low severity of illnessthe average MS‐DRG weight was near 1and low rates of important adverse events such falls and restraint use. This may have occurred because we excluded patients transferred from the ICUs and other services. It is possible that the Hospitalist‐ACE intervention might have demonstrated a larger benefit in a sicker population that would have presented greater opportunities for reductions in length of stay, costs, and adverse events. Fifth, given the retrospective nature of the data collection, we were not able to prospectively assess the incidence of important geriatric outcomes such as delirium and functional decline, nor can we make conclusions about changes in function during the hospitalization.
While the outcome measures we used are conceptually similar to several measures developed by RAND's Assessing Care of Vulnerable Elders (ACOVE) project, this study did not explicitly rely on those constructs.31 To do so would have required prospective screening by clinical staff independent from the care team for vulnerability that was beyond the scope of this project. In addition, the ACOVE measures of interest for functional and cognitive decline are limited to documentation of cognitive or functional assessments in the medical record. The ACE service's adoption of a brief standardized geriatric assessment was almost certain to meet that documentation requirement. While documentation is important, it is not clear that documentation, in and of itself, improves outcomes. Therefore, we expanded upon the ACOVE constructs to include the need for the additional evidence of a treatment plan when abnormal physical or cognitive function was documented. These constructs are important process of care for vulnerable elders. While we demonstrated improvements in several of these important processes of care for elderly patients, we are unable to draw conclusions about the impact of these differences in care on important clinical outcomes such as development of delirium, long‐term institutionalization, or mortality.
CONCLUSIONS
The risks of hospitalization for older persons are numerous, and present challenges and opportunities for inpatient physicians. As the hospitalized population agesmirroring national demographic trends and trends in use of acute care hospitalsthe challenge of avoiding harm in the older hospitalized patient will intensify. Innovations in care to improve the experience and outcomes of hospitalization for older patients are needed in the face of limited geriatrics‐trained workforce and few discretionary funds for unit redesign. The Hospitalist‐ACE service is a promising strategy for hospitalist programs with sufficient numbers of older patients and hospitalists with interest in improving clinical care for older adults. It provides a model for hospitalists to employ geriatrics principles targeted at reducing harm to their most vulnerable patients. Hospitalist‐run geriatric care models offer great promise for improving the care of acutely ill elderly patients. Future investigation should focus on demonstrating the impact of such care on important clinical outcomes between admission and discharge; on model refinement and adaptation, such as determining what components of comprehensive geriatric care are essential to success; and on how complementary interventions, such as the use of templated orders for the hospitalized elderly, impact outcomes. Additional research is needed, with a focus on demonstrating value with regard to an array of outcomes including cost, readmissions, and preventable harms of care.
Acknowledgements
Jean Kutner, MD, MSPH; Daniel Sandy, MPH; Shelly Limon, RN; nurses of 12 West; the UCH staff on the interdisciplinary team; and ACE patients and their families.
- ,,, et al.Functional outcomes of acute medical illness and hospitalization in older persons.Arch Intern Med.1996;156:645–652.
- ,,.Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care.Am J Med.1999;106:565–573.
- ,,, et al.Using assessing care of vulnerable elders quality indicators to measure quality of hospital care for vulnerable elders.J Am Geriatr Soc.2007;55(11):1705–1711.
- ,,, et al.Impact and recognition of cognitive impairment among hospitalized elders.J Hosp Med.2010;5:69–75.
- ,,,,.What does the medical record reveal about functional status? A comparison of medical record and interview data.J Gen Intern Med.2001;16(11):728–736.
- ,,,,,.Successful models of comprehensive care for older adults with chronic conditions: evidence for the Institute of Medicine's “Retooling for an Aging America” report.J Am Geriatr Soc.2009;57(12):2328–2337.
- ,,,,.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1344.
- ,,, et al.Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older adults: a randomized controlled trial of Acute Care for Elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1581.
- ,,, et al.The effectiveness of inpatient geriatric evaluation and management units: a systematic review and meta‐analysis.J Am Geriatr Soc.2010;58:83–92.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.A randomized, controlled clinical trial of a geriatrics consultation team: compliance with recommendations.JAMA.1986;255:2617–2621.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,.Dissemination and characteristics of Acute Care of Elders (ACE) units in the United States.Int J Technol Assess Health Care.2003;19:220–227.
- ,,.Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1:29–35.
- ,,,,.The Mini‐Cog: a cognitive “vital signs” measure for dementia screening in multi‐lingual elderly.Int J Geriatr Psychiatry.2000;15(11):1021–1027.
- ,,.The Patient Health Questionnaire‐2: validity of a two‐item depression screener.Med Care.2003;41:1284–1292.
- ,,,,,.Clarifying confusion: the Confusion Assessment Method.Ann Intern Med.1990;113(12):941–948.
- ,,, et al.The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community.J Am Geriatr Soc.2001;49:1691–1699.
- ,.The timed “Up and Go”: a test of basic functional mobility for frail elderly persons.J Am Geriatr Soc.1991;39:142–148.
- American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopedic Surgeons Panel on Falls Prevention.Guideline for the prevention of falls in older persons.J Am Geriatr Soc.2001;49:664–672.
- . Falls for the inpatient physician. Translating knowledge into action. The Portal of Online Geriatric Education (POGOe). 6–19‐2008. Available at: http://www.pogoe.org/productid/20212.
- ,,,. Incontinence and urinary catheters for the inpatient physician. The Portal of Online Geriatric Education (POGOe). 11–27‐0008. Available at: http://www.pogoe.org/productid/20296.
- ,,,.Use of medications for insomnia in the hospitalized geriatric population.J Am Geriatr Soc.2008;56(3):579–581.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130(4 pt 2):343–349.
- ,,, et al.Quality of care associated with survival in vulnerable older patients.Ann Intern Med.2005;143:274–281.
- ,,, et al.Higher quality of care for hosptialized frail older adults is associated with improved survival one year after discharge.J Hosp Med.2009;4(S1):24.
- ,,,.Operational and quality outcomes of a novel mobile acute care for the elderly service.J Am Geriatr Soc.2009;57:S1.
- Institute of Medicine (IOM).Retooling for an Aging America: Building the Health Care Workforce.Washington, DC:The National Academies Press;2008.
- ,,.Alternative solutions to the geriatric workforce deficit.Am J Med.2008;121:e23.
- ,,,,.Fulfilling the promise of hospital medicine: tailoring internal medicine training to address hospitalists' needs.J Gen Intern Med.2008;23(7):1110–1115.
- ,.Assessing care of vulnerable elders: ACOVE project overview.Ann Intern Med.2001;135(8 pt 2):642–646.
For the frail older patient, hospitalization marks a period of high risk of poor outcomes and adverse events including functional decline, delirium, pressure ulcers, adverse drug events, nosocomial infections, and falls.1, 2 Physician recognition of elderly patients at risk for adverse outcomes is poor, making it difficult to intervene to prevent them.3, 4 Among frail, elderly inpatients at an urban academic medical center, doctors documented cognitive assessments in only 5% of patients. Functional assessments are appropriately documented in 40%80% of inpatients.3, 5
The Acute Care for Elders (ACE) unit is one of several models of comprehensive inpatient geriatric care that have been developed by geriatrician researchers to address the adverse events and functional decline that often accompany hospitalization.6 The ACE unit model generally incorporates: 1) a modified hospital environment, 2) early assessment and intensive management to minimize the adverse effects of hospital care, 3) early discharge planning, 4) patient centered care protocols, and 5) a consistent nursing staff.7 Two randomized, controlled trials have shown the ACE unit model to be successful in reducing functional decline among frail older inpatients during and after hospitalization.7, 8 While meta‐analyses data also suggests the ACE unit model reduces functional decline and future institutionalization, significant impact on other outcomes is not proven.9, 10
Several barriers have prevented the successful dissemination of the ACE unit model. The chief limitations are the upfront resources required to create and maintain a modified, dedicated unit, as well as the lack of a geriatrics trained workforce.7, 1113 The rapid growth of hospital medicine presents opportunities for innovation in the care of older patients. Still, a 2006 census demonstrated that few hospitalist groups had identified geriatric care as a priority.14
In response to these challenges, the University of Colorado Hospital Medicine Group created a hospitalist‐run inpatient medical service designed for the care of the frail older patient. This Hospitalist‐Acute Care for the Elderly (Hospitalist‐ACE) unit is a hybrid of a general medical service and an inpatient geriatrics unit.7 The goals of the Hospitalist‐ACE service are to provide high quality care tailored to older inpatients, thus minimizing the risks of functional decline and adverse events associate with hospitalization, and to provide a clinical geriatrics teaching experience for Hospitalist Training Track Residents within the Internal Medicine Residency Training Program and medical students at the University of Colorado Denver School of Medicine. The Hospitalist‐ACE unit is staffed with a core group of hospitalist attendings who have, at a minimum, attended an intensive mini‐course in inpatient geriatrics. The service employs interdisciplinary rounds; a brief, standardized geriatric assessment including screens of function, cognition, and mood; a clinical focus on mitigating the hazards of hospitalization, early discharge planning; and a novel geriatric educational curriculum for medicine residents and medical students.
This article will: 1) describe the creation of the Hospitalist‐ACE service at the University of Colorado Hospital; and 2) summarize the evaluation of the Hospitalist‐ACE service in a quasi‐randomized, controlled manner during its first year. We hypothesized that, when compared to patients receiving usual care, patients cared for on the Hospitalist‐ACE service would have increased recognition of abnormal functional status; recognition of abnormal cognitive status and delirium; equivalent lengths of stay and hospital charges; and decreased falls, 30‐day readmissions, and restraint use.
METHODS
Design
We performed a quasi‐randomized, controlled study of the Hospitalist‐ACE service.
Setting
The study setting was the inpatient general medical services of the Anschutz Inpatient Pavilion (AIP) of the University of Colorado Hospital (UCH). The AIP is a 425‐bed tertiary care hospital that is the major teaching affiliate of the University of Colorado School of Medicine and a regional referral center. The control services, hereafter referred to as usual care, were comprised of the four inpatient general medicine teaching services that take admissions on a four‐day rotation (in general, two were staffed by outpatient general internists and medical subspecialists, and two were staffed by academic hospitalists). The Hospitalist‐ACE service was a novel hospitalist teaching service that began in July 2007. Hospitalist‐ACE patients were admitted to a single 12‐bed medical unit (12 West) when beds were available; 12 West is similar to the other medical/surgical units at UCH and did not have any modifications to the rooms, equipment, or common areas for the intervention. The nursing staff on this unit had no formal geriatric nursing training. The Hospitalist‐ACE team admitted patients daily (between 7 AM and 3 PM MondayFriday; between 7 AM and 12 noon Saturday and Sunday). Patients assigned to the Hospitalist‐ACE service after hours were admitted by the internal medicine resident on call for the usual care services and handed off to the Hospitalist‐ACE team at 7 AM the next morning.
Study Subjects
Eligible subjects were inpatients age 70 years admitted to the usual care or Hospitalist‐ACE services at the AIP from November 2, 2007 to April 15, 2008. All patients age 70 years were randomized to the Hospitalist‐ACE service or usual care on a general internal medicine service by the last digit of the medical record number (odd numbers admitted to the Hospitalist‐ACE service and even numbers admitted to usual care). Patients followed by the Hospitalist‐ACE service but not admitted to 12 West were included in the study. To isolate the impact of the intervention, patients admitted to a medicine subspecialty service (such as cardiology, pulmonary, or oncology), or transferred to or from the Hospitalist‐ACE or control services to another service (eg, intensive care unit [ICU] or orthopedic surgery service) were excluded from the study.
Intervention
The Hospitalist‐ACE unit implemented an interdisciplinary team approach to identify and address geriatric syndromes in patients aged 70 and over. The Hospitalist‐ACE model of care consisted of clinical care provided by a hospitalist attending with additional training in geriatric medicine, administration of standardized geriatric screens assessing function, cognition, and mood, 15 minute daily (MondayFriday) interdisciplinary rounds focusing on recognition and management of geriatric syndromes and early discharge planning, and a standardized educational curriculum for medical residents and medical students addressing hazards of hospitalization.
The Hospitalist‐ACE service was a unique rotation within the Hospitalist Training Track of the Internal Medicine Residency that was developed with the support of the University of Colorado Hospital and the Internal Medicine Residency Training Program, and input from the Geriatrics Division at the University of Colorado Denver. The director received additional training from the Donald W. Reynolds FoundationUCLA Faculty Development to Advance Geriatric Education Mini‐Fellowship for hospitalist faculty. The mission of the service was to excel at educating the next generation of hospitalists while providing a model for excellence of care for hospitalized elderly patients. Important stakeholders were identified, and a leadership teamincluding representatives from nursing, physical and occupational therapy, pharmacy, social work, case management, and later, volunteer servicescreated the model daily interdisciplinary rounds. As geographic concentration was essential for the viability of interdisciplinary rounds, one unit (12 West) within the hospital was designated as the preferred location for patients admitted to the Hospitalist‐ACE service.
The Hospitalist‐ACE unit team consisted of one attending hospitalist, one resident, one intern, and medical students. The attending was one of five hospitalists, with additional training in geriatric medicine, who rotated attending responsibilities on the service. One of the hospitalists was board certified in geriatric medicine. Each of the other four hospitalists attended the Reynolds FoundationUCLA mini‐fellowship in geriatric medicine. Hospitalist‐ACE attendings rotated on a variety of other hospitalist services throughout the academic year, including the usual care services.
The brief standardized geriatric assessment consisted of six validated instruments, and was completed by house staff or medical students on admission, following instruction by the attending physician. The complete assessment tool is shown in Figure 1. The cognitive items included the Mini‐Cog,15 a two‐item depression screen,16 and the Confusion Assessment Method.17 The functional items included the Vulnerable Elders Survey (VES‐13),18 the Timed Get Up and Go test,19 and a two‐question falls screen.20 The elements of the assessment tool were selected by the Hospitalist‐ACE attendings for brevity and the potential to inform clinical management. To standardize the clinical and educational approach, the Hospitalist‐ACE attendings regularly discussed appropriate orders recommended in response to each positive screen, but no templated order sets were used during the study period.
Interdisciplinary rounds were attended by Hospitalist‐ACE physicians, nurses, case managers, social workers, physical or occupational therapists, pharmacists, and volunteers. Rounds were led by the attending or medical resident.
The educational curriculum encompassed 13 modules created by the attending faculty that cover delirium, falls, dementia, pressure ulcers, physiology of aging, movement disorders, medication safety, end of life care, advance directives, care transitions, financing of health care for the elderly, and ethical conundrums in the care of the elderly. A full table of contents appears in online Appendix 1. Additionally, portions of the curriculum have been published online.21, 22 Topic selection was guided by the Accreditation Council for Graduate Medical Education (ACGME) core geriatrics topics determined most relevant for the inpatient setting. Formal instruction of 3045 minutes duration occurred three to four days a week and was presented in addition to routine internal medicine educational conferences. Attendings coordinated teaching to ensure that each trainee was exposed to all of the content during the course of their four‐week rotation.
In contrast to the Hospitalist‐ACE service, usual care on the control general medical services consisted of either a hospitalist, a general internist, or an internal medicine subspecialist attending physician, with one medical resident, one intern, and medical students admitting every fourth day. The general medical teams attended daily discharge planning rounds with a discharge planner and social worker focused exclusively on discharge planning. The content of teaching rounds on the general medical services was largely left to the discretion of the attending physician.
This program evaluation of the Hospitalist‐ACE service was granted a waiver of consent and Health Insurance Portability and Accountability Act (HIPAA) by the Colorado Multiple Institutional Review Board.
Measures
Primary Outcome
The primary outcome for the study was the recognition of abnormal functional status by the primary team. Recognition of abnormal functional status was determined from chart review and consisted of both the physician's detection of abnormal functional status and evidence of a corresponding treatment plan identified in the notes or orders of a physician member of the primary team (Table 1).
| Measure | Criterion | Source | Content Examples |
|---|---|---|---|
| |||
| Recognition of abnormal functional status* | 1) Detection | MD's documentation of history | Presentation with change in function (new gait instability); use of gait aides (wheelchair) |
| OR | |||
| MD's documentation of physical exam | Observation of abnormal gait (eg, unsteady, wide‐based, shuffling) and/or balance Abnormal Get Up and Go test | ||
| AND | |||
| 2) Treatment | MD's order | PT/OT consult; home safety evaluation | |
| OR | |||
| MD's documentation assessment/plan | Inclusion of functional status (rehabilitation, PT/OT needs) on the MD's problem list | ||
| Recognition of abnormal cognitive status | Any of the following: | ||
| Delirium | 1) Detection | MD's history | Presentation of confusion or altered mental status |
| OR | |||
| MD's physical exam | Abnormal confusion assessment method | ||
| AND | |||
| 2) Treatment | MD's order | Sitter, reorienting communication, new halperidol order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of delirium on the problem list | ||
| OR | |||
| Dementia | 1) Detection | MD's history | Dementia in medical history |
| OR | OR | ||
| MD's physical exam | Abnormal Folstein Mini‐Mental Status Exam or Mini‐Cog | ||
| AND | |||
| 2) Treatment | MD's order | Cholinesterase inhibitor ordered | |
| OR | OR | ||
| MD's documentation of assessment/plan | Inclusion of dementia on the problem list | ||
| OR | |||
| Depression | 1) Detection | MD's history | Depression in medical history |
| OR | OR | ||
| MD's physical exam | Positive depression screen | ||
| AND | |||
| 2) Treatment | MD's order | New antidepressant order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of depression on the problem list | ||
Secondary Outcomes
Recognition of abnormal cognitive status was determined from chart review and consisted of both the physician's detection of dementia, depression, or delirium, and evidence of a corresponding treatment plan for any of the documented conditions identified in the notes or orders of a physician member of the primary team (Table 1). Additionally, we measured recognition and treatment of delirium alone.
Falls were determined from mandatory event reporting collected by the hospital on the University Hospitals Consortium Patient Safety Net web‐based reporting system and based on clinical assessment as reported by the nursing staff. The reports are validated by the appropriate clinical managers within 45 days of the event according to standard procedure.
Physical restraint use (type of restraint and duration) was determined from query of mandatory clinical documentation in the electronic medical record. Use of sleep aids was determined from review of the physician's order sheets in the medical record. The chart review captured any of 39 commonly prescribed hypnotic medications ordered at hour of sleep or for insomnia. The sleep medication list was compiled with the assistance of a pharmacist for an earlier chart review and included non‐benzodiazepine hypnotics, benzodiazepines, antidepressants, antihistamines, and antipsychotics.23
Length of stay, hospital charges, 30‐day readmissions to UCH (calculated from date of discharge), and discharge location were determined from administrative data.
Additional Descriptive Variables
Name, medical record number, gender, date of birth, date of admission and discharge, and primary diagnosis were obtained from the medical record. The Case Mix Index for each group of patients was determined from the average Medicare Severity‐adjusted Diagnosis Related Group (MS‐DRG) weight obtained from administrative data.
Data Collection
A two‐step, retrospective chart abstraction was employed. A professional research assistant (P.R.A.) hand‐abstracted process measures from the paper medical chart onto a data collection form designed for this study. A physician investigator performed a secondary review (H.L.W.). Discrepancies were resolved by the physician reviewer.
Data Analysis
Descriptive statistics were performed on intervention and control subjects. Means and standard deviations (age) or frequencies (gender, primary diagnoses) were calculated as appropriate. T tests were used for continuous variables, chi‐square tests for gender, and the Wilcoxon rank sum test for categorical variables.
Outcomes were reported as means and standard deviations for continuous variables (length of stay and charges) and frequencies for categorical variables (all other outcomes). T tests were used for continuous variables, Fisher's exact test for restraint use, and chi‐square tests were used for categorical variable to compare the impact of the intervention between intervention and control patients. For falls, confidence intervals were calculated for the incidence rate differences based on Poisson approximations.
Sample Size Considerations
An a priori sample size calculation was performed. A 2001 study showed that functional status is poorly documented in at least 60% of hospital charts of elderly patients.5 Given an estimated sample size of 120 per group and a power of 80%, this study was powered to be able to detect an absolute difference in the documentation of functional status of as little as 18%.
RESULTS
Two hundred seventeen patients met the study entry criteria (Table 2): 122 were admitted to the Hospitalist‐ACE service, and 95 were admitted to usual care on the general medical services. The average age of the study patients was 80.5 years, 55.3% were female. Twenty‐eight percent of subjects were admitted for pulmonary diagnoses. The two groups of patients were similar with respect to age, gender, and distribution of primary diagnoses. The Hospitalist‐ACE patients had a mean MS‐DRG weight of 1.15, which was slightly higher than that of usual care patients at 1.05 (P = 0.06). Typically, 70% of Hospitalist‐ACE patients are admitted to the designated ACE medical unit (12 West).
| Characteristic | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Age (years), mean (SD) | 80.5 (6.5) | 80.7 (7.0) | 0.86 |
| Gender (% female) | 52.5 | 59 | 0.34 |
| Case Mix Index (mean MS‐DRG weight [SD]) | 1.15 (0.43) | 1.05 (0.31) | 0.06 |
| Primary ICD‐9 diagnosis (%) | 0.59 | ||
| Pulmonary | 27.9 | 28.4 | |
| General medicine | 15.6 | 11.6 | |
| Surgery | 13.9 | 11.6 | |
| Cardiology | 9.8 | 6.3 | |
| Nephrology | 8.2 | 7.4 | |
Processes of Care
Processes of care for older patients are displayed in Table 3. Patients on the Hospitalist‐ACE service had recognition and treatment of abnormal functional status at a rate that was nearly double that of patients on the usual care services (68.9% vs 35.8%, P < 0.0001). In addition, patients on the Hospitalist‐ACE service were significantly more likely to have had recognition and treatment of any abnormal cognitive status (55.7% vs 40.0%, P = 0.02). When delirium was evaluated alone, the Hospitalist‐ACE patients were also more likely to have had recognition and treatment of delirium (27.1% vs 17.0%, P = 0.08), although this finding did not reach statistical significance.
| Measure | Percent of Hospitalist‐ACE Patients | Percent of Usual Care Patients | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Recognition and treatment of abnormal functional status | 68.9 | 35.8 | <0.0001 |
| Recognition and treatment of abnormal cognitive status* | 55.7 | 40.0 | 0.02 |
| Recognition and treatment of delirium | 27.1 | 17.0 | 0.08 |
| Documentation of resuscitation preferences | 95.1 | 91.6 | 0.3 |
| Do Not Attempt Resuscitation orders | 39.3 | 26.3 | 0.04 |
| Use of sleep medications | 28.1 | 27.4 | 0.91 |
| Use of physical restraints | 2.5 | 0 | 0.26 |
While patients on the Hospitalist‐ACE and usual care services had similar percentages of documentation of resuscitation preferences (95.1% vs 91.6%, P = 0.3), the percentage of Hospitalist‐ACE patients who had Do Not Attempt Resuscitation (DNAR) orders was significantly greater than that of the usual care patients (39.3% vs 26.3%, P = 0.04).
There were no differences in the use of physical restraints or sleep medications for Hospitalist‐ACE patients as compared to usual care patients, although the types of sleep mediations used on each service were markedly different: trazadone was employed as the first‐line sleep agent on the Hospitalist‐ACE service (77.7%), and non‐benzodiazepine hypnotics (primarily zolpidem) were employed most commonly on the usual care services (35%). There were no differences noted in the percentage of patients with benzodiazepines prescribed as sleep aids.
Outcomes
Resource utilization outcomes are reported in Table 4. Of note, there were no significant differences between Hospitalist‐ACE discharges and usual care discharges in mean length of stay (3.4 2.7 days vs 3.1 2.7 days, P = 0.52), mean charges ($24,617 15,828 vs $21,488 13,407, P = 0.12), or 30‐day readmissions to UCH (12.3% vs 9.5%, P = 0.51). Hospitalist‐ACE discharges and usual care patients were equally likely to be discharged to home (68.6% vs 67.4%, P = 0.84), with a similar proportion of Hospitalist‐ACE discharges receiving home health care or home hospice services (14.1% vs 7.4%, P = 12).
| Measure | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Length of stay in days (mean [SD]) | 3.4 (2.7) | 3.1 (2.7) | 0.52 |
| Charges in dollars (mean [SD]) | 24,617 (15,828) | 21,488 (13,407) | 0.12 |
| 30‐Day readmissions to UCH (%) | 12.3 | 9.5 | 0.51 |
| Discharges to home (%) | 68.8* | 67.4 | 0.84 |
| Discharges to home with services (%) | 14%* | 7.4% | 0.12 |
In addition, the fall rate for Hospitalist‐ACE patients was not significantly different from the fall rate for usual care patients (4.8 falls/1000 patient days vs 6.7 falls/1000 patient days, 95% confidence interval 9.613.3).
DISCUSSION
We report the implementation and evaluation of a medical service tailored to the care of the acutely ill older patient that draws from elements of the hospitalist model and the ACE unit model.7, 14, 24 For this Hospitalist‐ACE service, we developed a specialized hospitalist workforce, assembled a brief geriatric assessment tailored to the inpatient setting, instituted an interdisciplinary rounding model, and created a novel inpatient geriatrics curriculum.
During the study period, we improved performance of important processes of care for hospitalized elders, including recognition of abnormal cognitive and functional status; maintained comparable resource use; and implemented a novel, inpatient‐focused geriatric medicine educational experience. We were unable to demonstrate an impact on key clinical outcomes such as falls, physical restraint use, and readmissions. Nonetheless, there is evidence that the performance of selected processes of care is associated with improved three‐year survival status in the community‐dwelling vulnerable older patient, and may also be associated with a mortality benefit in the hospitalized vulnerable older patient.25, 26 Therefore, methods to improve the performance of these processes of care may be of clinical importance.
The finding of increased use of DNAR orders in the face of equivalent documentation of code status is of interest and generates hypotheses for further study. It is possible that the educational experience and use of geriatric assessment provides a more complete context for the code status discussion (one that incorporates the patient's social, physical, and cognitive function). However, we do not know if the patients on the ACE service had improved concordance between their code status and their goals of care.
We believe that there was no difference in key clinical outcomes between Hospitalist‐ACE and control patients because the population in this study was relatively low acuity and, therefore, the occurrence of falls and the use of physical restraints were quite low in the study population. In particular, the readmission rate was much lower than is typical for the Medicare population at our hospital, making it challenging to draw conclusions about the impact of the intervention on readmissions, however, we cannot rule out the possibility that our early discharge planning did not address the determinants of readmission for this population.
The ACE unit paradigmcharacterized by 1) closed, modified hospital units; 2) staffing by geriatricians and nurses with geriatrics training; 3) employing geriatric nursing care protocolsrequires significant resources and is not feasible for all settings.6 There is a need for alternative models of comprehensive care for hospitalized elders that require fewer resources in the form of dedicated units and specialist personnel, and can be more responsive to institutional needs. For example, in a 2005 report, one institution reported the creation of a geriatric medicine service that utilized a geriatrician and hospitalist co‐attending model.14 More recently, a large geriatrics program replaced its inpatient geriatrics unit with a mobile inpatient geriatrics service staffed by an attending geriatricianhospitalist, a geriatrics fellow, and a nurse practitioner.27 While these innovative models have eliminated the dedicated unit, they rely on board certified geriatricians, a group in short supply nationally.28 Hospitalists are a rapidly growing provider group that, with appropriate training and building on the work of geriatricians, is poised to provide leadership in acute geriatric care.29, 30
In contrast to the comprehensive inpatient geriatric care models described above, the Hospitalist‐ACE service uses a specialized hospitalist workforce and is not dependent on continuous staffing by geriatricians. Although geographic concentration is important for the success of interdisciplinary rounds, the Hospitalist‐ACE service does not require a closed or modified unit. The nursing staff caring for Hospitalist‐ACE patients have generalist nursing training and, at the time of the study, did not utilize geriatric‐care protocols. Our results need to be interpreted in the light of these differences from the ACE unit model which is a significantly more intensive intervention than the Hospitalist‐ACE service. In addition, the current practice environment is quite different from the mid‐1990s when ACE units were developed and studied. Development and maintenance of models of comprehensive inpatient geriatric care require demonstration of both value as well as return on investment. The alignment of financial and regulatory incentives for programs that provide comprehensive care to complex patients, such as those anticipated by the Affordable Care Act, may encourage the growth of such models.
These data represent findings from a six‐month evaluation of a novel inpatient service in the middle of its first year. There are several limitations related to our study design. First, the results of this small study at a single academic medical center may be of limited generalizability to other settings. Second, the program was evaluated only three months after its inception; we did not capture further improvements in methods, training, and outcomes expected as the program matured. Third, most of the Hospitalist‐ACE service attendings and residents rotate on the UCH general medical services throughout the year. Consequently, we were unable to eliminate the possibility of contamination of the control group, and we were unable to blind the physicians to the study. Fourth, the study population had a relatively low severity of illnessthe average MS‐DRG weight was near 1and low rates of important adverse events such falls and restraint use. This may have occurred because we excluded patients transferred from the ICUs and other services. It is possible that the Hospitalist‐ACE intervention might have demonstrated a larger benefit in a sicker population that would have presented greater opportunities for reductions in length of stay, costs, and adverse events. Fifth, given the retrospective nature of the data collection, we were not able to prospectively assess the incidence of important geriatric outcomes such as delirium and functional decline, nor can we make conclusions about changes in function during the hospitalization.
While the outcome measures we used are conceptually similar to several measures developed by RAND's Assessing Care of Vulnerable Elders (ACOVE) project, this study did not explicitly rely on those constructs.31 To do so would have required prospective screening by clinical staff independent from the care team for vulnerability that was beyond the scope of this project. In addition, the ACOVE measures of interest for functional and cognitive decline are limited to documentation of cognitive or functional assessments in the medical record. The ACE service's adoption of a brief standardized geriatric assessment was almost certain to meet that documentation requirement. While documentation is important, it is not clear that documentation, in and of itself, improves outcomes. Therefore, we expanded upon the ACOVE constructs to include the need for the additional evidence of a treatment plan when abnormal physical or cognitive function was documented. These constructs are important process of care for vulnerable elders. While we demonstrated improvements in several of these important processes of care for elderly patients, we are unable to draw conclusions about the impact of these differences in care on important clinical outcomes such as development of delirium, long‐term institutionalization, or mortality.
CONCLUSIONS
The risks of hospitalization for older persons are numerous, and present challenges and opportunities for inpatient physicians. As the hospitalized population agesmirroring national demographic trends and trends in use of acute care hospitalsthe challenge of avoiding harm in the older hospitalized patient will intensify. Innovations in care to improve the experience and outcomes of hospitalization for older patients are needed in the face of limited geriatrics‐trained workforce and few discretionary funds for unit redesign. The Hospitalist‐ACE service is a promising strategy for hospitalist programs with sufficient numbers of older patients and hospitalists with interest in improving clinical care for older adults. It provides a model for hospitalists to employ geriatrics principles targeted at reducing harm to their most vulnerable patients. Hospitalist‐run geriatric care models offer great promise for improving the care of acutely ill elderly patients. Future investigation should focus on demonstrating the impact of such care on important clinical outcomes between admission and discharge; on model refinement and adaptation, such as determining what components of comprehensive geriatric care are essential to success; and on how complementary interventions, such as the use of templated orders for the hospitalized elderly, impact outcomes. Additional research is needed, with a focus on demonstrating value with regard to an array of outcomes including cost, readmissions, and preventable harms of care.
Acknowledgements
Jean Kutner, MD, MSPH; Daniel Sandy, MPH; Shelly Limon, RN; nurses of 12 West; the UCH staff on the interdisciplinary team; and ACE patients and their families.
For the frail older patient, hospitalization marks a period of high risk of poor outcomes and adverse events including functional decline, delirium, pressure ulcers, adverse drug events, nosocomial infections, and falls.1, 2 Physician recognition of elderly patients at risk for adverse outcomes is poor, making it difficult to intervene to prevent them.3, 4 Among frail, elderly inpatients at an urban academic medical center, doctors documented cognitive assessments in only 5% of patients. Functional assessments are appropriately documented in 40%80% of inpatients.3, 5
The Acute Care for Elders (ACE) unit is one of several models of comprehensive inpatient geriatric care that have been developed by geriatrician researchers to address the adverse events and functional decline that often accompany hospitalization.6 The ACE unit model generally incorporates: 1) a modified hospital environment, 2) early assessment and intensive management to minimize the adverse effects of hospital care, 3) early discharge planning, 4) patient centered care protocols, and 5) a consistent nursing staff.7 Two randomized, controlled trials have shown the ACE unit model to be successful in reducing functional decline among frail older inpatients during and after hospitalization.7, 8 While meta‐analyses data also suggests the ACE unit model reduces functional decline and future institutionalization, significant impact on other outcomes is not proven.9, 10
Several barriers have prevented the successful dissemination of the ACE unit model. The chief limitations are the upfront resources required to create and maintain a modified, dedicated unit, as well as the lack of a geriatrics trained workforce.7, 1113 The rapid growth of hospital medicine presents opportunities for innovation in the care of older patients. Still, a 2006 census demonstrated that few hospitalist groups had identified geriatric care as a priority.14
In response to these challenges, the University of Colorado Hospital Medicine Group created a hospitalist‐run inpatient medical service designed for the care of the frail older patient. This Hospitalist‐Acute Care for the Elderly (Hospitalist‐ACE) unit is a hybrid of a general medical service and an inpatient geriatrics unit.7 The goals of the Hospitalist‐ACE service are to provide high quality care tailored to older inpatients, thus minimizing the risks of functional decline and adverse events associate with hospitalization, and to provide a clinical geriatrics teaching experience for Hospitalist Training Track Residents within the Internal Medicine Residency Training Program and medical students at the University of Colorado Denver School of Medicine. The Hospitalist‐ACE unit is staffed with a core group of hospitalist attendings who have, at a minimum, attended an intensive mini‐course in inpatient geriatrics. The service employs interdisciplinary rounds; a brief, standardized geriatric assessment including screens of function, cognition, and mood; a clinical focus on mitigating the hazards of hospitalization, early discharge planning; and a novel geriatric educational curriculum for medicine residents and medical students.
This article will: 1) describe the creation of the Hospitalist‐ACE service at the University of Colorado Hospital; and 2) summarize the evaluation of the Hospitalist‐ACE service in a quasi‐randomized, controlled manner during its first year. We hypothesized that, when compared to patients receiving usual care, patients cared for on the Hospitalist‐ACE service would have increased recognition of abnormal functional status; recognition of abnormal cognitive status and delirium; equivalent lengths of stay and hospital charges; and decreased falls, 30‐day readmissions, and restraint use.
METHODS
Design
We performed a quasi‐randomized, controlled study of the Hospitalist‐ACE service.
Setting
The study setting was the inpatient general medical services of the Anschutz Inpatient Pavilion (AIP) of the University of Colorado Hospital (UCH). The AIP is a 425‐bed tertiary care hospital that is the major teaching affiliate of the University of Colorado School of Medicine and a regional referral center. The control services, hereafter referred to as usual care, were comprised of the four inpatient general medicine teaching services that take admissions on a four‐day rotation (in general, two were staffed by outpatient general internists and medical subspecialists, and two were staffed by academic hospitalists). The Hospitalist‐ACE service was a novel hospitalist teaching service that began in July 2007. Hospitalist‐ACE patients were admitted to a single 12‐bed medical unit (12 West) when beds were available; 12 West is similar to the other medical/surgical units at UCH and did not have any modifications to the rooms, equipment, or common areas for the intervention. The nursing staff on this unit had no formal geriatric nursing training. The Hospitalist‐ACE team admitted patients daily (between 7 AM and 3 PM MondayFriday; between 7 AM and 12 noon Saturday and Sunday). Patients assigned to the Hospitalist‐ACE service after hours were admitted by the internal medicine resident on call for the usual care services and handed off to the Hospitalist‐ACE team at 7 AM the next morning.
Study Subjects
Eligible subjects were inpatients age 70 years admitted to the usual care or Hospitalist‐ACE services at the AIP from November 2, 2007 to April 15, 2008. All patients age 70 years were randomized to the Hospitalist‐ACE service or usual care on a general internal medicine service by the last digit of the medical record number (odd numbers admitted to the Hospitalist‐ACE service and even numbers admitted to usual care). Patients followed by the Hospitalist‐ACE service but not admitted to 12 West were included in the study. To isolate the impact of the intervention, patients admitted to a medicine subspecialty service (such as cardiology, pulmonary, or oncology), or transferred to or from the Hospitalist‐ACE or control services to another service (eg, intensive care unit [ICU] or orthopedic surgery service) were excluded from the study.
Intervention
The Hospitalist‐ACE unit implemented an interdisciplinary team approach to identify and address geriatric syndromes in patients aged 70 and over. The Hospitalist‐ACE model of care consisted of clinical care provided by a hospitalist attending with additional training in geriatric medicine, administration of standardized geriatric screens assessing function, cognition, and mood, 15 minute daily (MondayFriday) interdisciplinary rounds focusing on recognition and management of geriatric syndromes and early discharge planning, and a standardized educational curriculum for medical residents and medical students addressing hazards of hospitalization.
The Hospitalist‐ACE service was a unique rotation within the Hospitalist Training Track of the Internal Medicine Residency that was developed with the support of the University of Colorado Hospital and the Internal Medicine Residency Training Program, and input from the Geriatrics Division at the University of Colorado Denver. The director received additional training from the Donald W. Reynolds FoundationUCLA Faculty Development to Advance Geriatric Education Mini‐Fellowship for hospitalist faculty. The mission of the service was to excel at educating the next generation of hospitalists while providing a model for excellence of care for hospitalized elderly patients. Important stakeholders were identified, and a leadership teamincluding representatives from nursing, physical and occupational therapy, pharmacy, social work, case management, and later, volunteer servicescreated the model daily interdisciplinary rounds. As geographic concentration was essential for the viability of interdisciplinary rounds, one unit (12 West) within the hospital was designated as the preferred location for patients admitted to the Hospitalist‐ACE service.
The Hospitalist‐ACE unit team consisted of one attending hospitalist, one resident, one intern, and medical students. The attending was one of five hospitalists, with additional training in geriatric medicine, who rotated attending responsibilities on the service. One of the hospitalists was board certified in geriatric medicine. Each of the other four hospitalists attended the Reynolds FoundationUCLA mini‐fellowship in geriatric medicine. Hospitalist‐ACE attendings rotated on a variety of other hospitalist services throughout the academic year, including the usual care services.
The brief standardized geriatric assessment consisted of six validated instruments, and was completed by house staff or medical students on admission, following instruction by the attending physician. The complete assessment tool is shown in Figure 1. The cognitive items included the Mini‐Cog,15 a two‐item depression screen,16 and the Confusion Assessment Method.17 The functional items included the Vulnerable Elders Survey (VES‐13),18 the Timed Get Up and Go test,19 and a two‐question falls screen.20 The elements of the assessment tool were selected by the Hospitalist‐ACE attendings for brevity and the potential to inform clinical management. To standardize the clinical and educational approach, the Hospitalist‐ACE attendings regularly discussed appropriate orders recommended in response to each positive screen, but no templated order sets were used during the study period.
Interdisciplinary rounds were attended by Hospitalist‐ACE physicians, nurses, case managers, social workers, physical or occupational therapists, pharmacists, and volunteers. Rounds were led by the attending or medical resident.
The educational curriculum encompassed 13 modules created by the attending faculty that cover delirium, falls, dementia, pressure ulcers, physiology of aging, movement disorders, medication safety, end of life care, advance directives, care transitions, financing of health care for the elderly, and ethical conundrums in the care of the elderly. A full table of contents appears in online Appendix 1. Additionally, portions of the curriculum have been published online.21, 22 Topic selection was guided by the Accreditation Council for Graduate Medical Education (ACGME) core geriatrics topics determined most relevant for the inpatient setting. Formal instruction of 3045 minutes duration occurred three to four days a week and was presented in addition to routine internal medicine educational conferences. Attendings coordinated teaching to ensure that each trainee was exposed to all of the content during the course of their four‐week rotation.
In contrast to the Hospitalist‐ACE service, usual care on the control general medical services consisted of either a hospitalist, a general internist, or an internal medicine subspecialist attending physician, with one medical resident, one intern, and medical students admitting every fourth day. The general medical teams attended daily discharge planning rounds with a discharge planner and social worker focused exclusively on discharge planning. The content of teaching rounds on the general medical services was largely left to the discretion of the attending physician.
This program evaluation of the Hospitalist‐ACE service was granted a waiver of consent and Health Insurance Portability and Accountability Act (HIPAA) by the Colorado Multiple Institutional Review Board.
Measures
Primary Outcome
The primary outcome for the study was the recognition of abnormal functional status by the primary team. Recognition of abnormal functional status was determined from chart review and consisted of both the physician's detection of abnormal functional status and evidence of a corresponding treatment plan identified in the notes or orders of a physician member of the primary team (Table 1).
| Measure | Criterion | Source | Content Examples |
|---|---|---|---|
| |||
| Recognition of abnormal functional status* | 1) Detection | MD's documentation of history | Presentation with change in function (new gait instability); use of gait aides (wheelchair) |
| OR | |||
| MD's documentation of physical exam | Observation of abnormal gait (eg, unsteady, wide‐based, shuffling) and/or balance Abnormal Get Up and Go test | ||
| AND | |||
| 2) Treatment | MD's order | PT/OT consult; home safety evaluation | |
| OR | |||
| MD's documentation assessment/plan | Inclusion of functional status (rehabilitation, PT/OT needs) on the MD's problem list | ||
| Recognition of abnormal cognitive status | Any of the following: | ||
| Delirium | 1) Detection | MD's history | Presentation of confusion or altered mental status |
| OR | |||
| MD's physical exam | Abnormal confusion assessment method | ||
| AND | |||
| 2) Treatment | MD's order | Sitter, reorienting communication, new halperidol order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of delirium on the problem list | ||
| OR | |||
| Dementia | 1) Detection | MD's history | Dementia in medical history |
| OR | OR | ||
| MD's physical exam | Abnormal Folstein Mini‐Mental Status Exam or Mini‐Cog | ||
| AND | |||
| 2) Treatment | MD's order | Cholinesterase inhibitor ordered | |
| OR | OR | ||
| MD's documentation of assessment/plan | Inclusion of dementia on the problem list | ||
| OR | |||
| Depression | 1) Detection | MD's history | Depression in medical history |
| OR | OR | ||
| MD's physical exam | Positive depression screen | ||
| AND | |||
| 2) Treatment | MD's order | New antidepressant order | |
| OR | |||
| MD's documentation of assessment/plan | Inclusion of depression on the problem list | ||
Secondary Outcomes
Recognition of abnormal cognitive status was determined from chart review and consisted of both the physician's detection of dementia, depression, or delirium, and evidence of a corresponding treatment plan for any of the documented conditions identified in the notes or orders of a physician member of the primary team (Table 1). Additionally, we measured recognition and treatment of delirium alone.
Falls were determined from mandatory event reporting collected by the hospital on the University Hospitals Consortium Patient Safety Net web‐based reporting system and based on clinical assessment as reported by the nursing staff. The reports are validated by the appropriate clinical managers within 45 days of the event according to standard procedure.
Physical restraint use (type of restraint and duration) was determined from query of mandatory clinical documentation in the electronic medical record. Use of sleep aids was determined from review of the physician's order sheets in the medical record. The chart review captured any of 39 commonly prescribed hypnotic medications ordered at hour of sleep or for insomnia. The sleep medication list was compiled with the assistance of a pharmacist for an earlier chart review and included non‐benzodiazepine hypnotics, benzodiazepines, antidepressants, antihistamines, and antipsychotics.23
Length of stay, hospital charges, 30‐day readmissions to UCH (calculated from date of discharge), and discharge location were determined from administrative data.
Additional Descriptive Variables
Name, medical record number, gender, date of birth, date of admission and discharge, and primary diagnosis were obtained from the medical record. The Case Mix Index for each group of patients was determined from the average Medicare Severity‐adjusted Diagnosis Related Group (MS‐DRG) weight obtained from administrative data.
Data Collection
A two‐step, retrospective chart abstraction was employed. A professional research assistant (P.R.A.) hand‐abstracted process measures from the paper medical chart onto a data collection form designed for this study. A physician investigator performed a secondary review (H.L.W.). Discrepancies were resolved by the physician reviewer.
Data Analysis
Descriptive statistics were performed on intervention and control subjects. Means and standard deviations (age) or frequencies (gender, primary diagnoses) were calculated as appropriate. T tests were used for continuous variables, chi‐square tests for gender, and the Wilcoxon rank sum test for categorical variables.
Outcomes were reported as means and standard deviations for continuous variables (length of stay and charges) and frequencies for categorical variables (all other outcomes). T tests were used for continuous variables, Fisher's exact test for restraint use, and chi‐square tests were used for categorical variable to compare the impact of the intervention between intervention and control patients. For falls, confidence intervals were calculated for the incidence rate differences based on Poisson approximations.
Sample Size Considerations
An a priori sample size calculation was performed. A 2001 study showed that functional status is poorly documented in at least 60% of hospital charts of elderly patients.5 Given an estimated sample size of 120 per group and a power of 80%, this study was powered to be able to detect an absolute difference in the documentation of functional status of as little as 18%.
RESULTS
Two hundred seventeen patients met the study entry criteria (Table 2): 122 were admitted to the Hospitalist‐ACE service, and 95 were admitted to usual care on the general medical services. The average age of the study patients was 80.5 years, 55.3% were female. Twenty‐eight percent of subjects were admitted for pulmonary diagnoses. The two groups of patients were similar with respect to age, gender, and distribution of primary diagnoses. The Hospitalist‐ACE patients had a mean MS‐DRG weight of 1.15, which was slightly higher than that of usual care patients at 1.05 (P = 0.06). Typically, 70% of Hospitalist‐ACE patients are admitted to the designated ACE medical unit (12 West).
| Characteristic | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Age (years), mean (SD) | 80.5 (6.5) | 80.7 (7.0) | 0.86 |
| Gender (% female) | 52.5 | 59 | 0.34 |
| Case Mix Index (mean MS‐DRG weight [SD]) | 1.15 (0.43) | 1.05 (0.31) | 0.06 |
| Primary ICD‐9 diagnosis (%) | 0.59 | ||
| Pulmonary | 27.9 | 28.4 | |
| General medicine | 15.6 | 11.6 | |
| Surgery | 13.9 | 11.6 | |
| Cardiology | 9.8 | 6.3 | |
| Nephrology | 8.2 | 7.4 | |
Processes of Care
Processes of care for older patients are displayed in Table 3. Patients on the Hospitalist‐ACE service had recognition and treatment of abnormal functional status at a rate that was nearly double that of patients on the usual care services (68.9% vs 35.8%, P < 0.0001). In addition, patients on the Hospitalist‐ACE service were significantly more likely to have had recognition and treatment of any abnormal cognitive status (55.7% vs 40.0%, P = 0.02). When delirium was evaluated alone, the Hospitalist‐ACE patients were also more likely to have had recognition and treatment of delirium (27.1% vs 17.0%, P = 0.08), although this finding did not reach statistical significance.
| Measure | Percent of Hospitalist‐ACE Patients | Percent of Usual Care Patients | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Recognition and treatment of abnormal functional status | 68.9 | 35.8 | <0.0001 |
| Recognition and treatment of abnormal cognitive status* | 55.7 | 40.0 | 0.02 |
| Recognition and treatment of delirium | 27.1 | 17.0 | 0.08 |
| Documentation of resuscitation preferences | 95.1 | 91.6 | 0.3 |
| Do Not Attempt Resuscitation orders | 39.3 | 26.3 | 0.04 |
| Use of sleep medications | 28.1 | 27.4 | 0.91 |
| Use of physical restraints | 2.5 | 0 | 0.26 |
While patients on the Hospitalist‐ACE and usual care services had similar percentages of documentation of resuscitation preferences (95.1% vs 91.6%, P = 0.3), the percentage of Hospitalist‐ACE patients who had Do Not Attempt Resuscitation (DNAR) orders was significantly greater than that of the usual care patients (39.3% vs 26.3%, P = 0.04).
There were no differences in the use of physical restraints or sleep medications for Hospitalist‐ACE patients as compared to usual care patients, although the types of sleep mediations used on each service were markedly different: trazadone was employed as the first‐line sleep agent on the Hospitalist‐ACE service (77.7%), and non‐benzodiazepine hypnotics (primarily zolpidem) were employed most commonly on the usual care services (35%). There were no differences noted in the percentage of patients with benzodiazepines prescribed as sleep aids.
Outcomes
Resource utilization outcomes are reported in Table 4. Of note, there were no significant differences between Hospitalist‐ACE discharges and usual care discharges in mean length of stay (3.4 2.7 days vs 3.1 2.7 days, P = 0.52), mean charges ($24,617 15,828 vs $21,488 13,407, P = 0.12), or 30‐day readmissions to UCH (12.3% vs 9.5%, P = 0.51). Hospitalist‐ACE discharges and usual care patients were equally likely to be discharged to home (68.6% vs 67.4%, P = 0.84), with a similar proportion of Hospitalist‐ACE discharges receiving home health care or home hospice services (14.1% vs 7.4%, P = 12).
| Measure | Hospitalist‐ACE | Usual Care | P Value |
|---|---|---|---|
| N = 122 | N = 95 | ||
| |||
| Length of stay in days (mean [SD]) | 3.4 (2.7) | 3.1 (2.7) | 0.52 |
| Charges in dollars (mean [SD]) | 24,617 (15,828) | 21,488 (13,407) | 0.12 |
| 30‐Day readmissions to UCH (%) | 12.3 | 9.5 | 0.51 |
| Discharges to home (%) | 68.8* | 67.4 | 0.84 |
| Discharges to home with services (%) | 14%* | 7.4% | 0.12 |
In addition, the fall rate for Hospitalist‐ACE patients was not significantly different from the fall rate for usual care patients (4.8 falls/1000 patient days vs 6.7 falls/1000 patient days, 95% confidence interval 9.613.3).
DISCUSSION
We report the implementation and evaluation of a medical service tailored to the care of the acutely ill older patient that draws from elements of the hospitalist model and the ACE unit model.7, 14, 24 For this Hospitalist‐ACE service, we developed a specialized hospitalist workforce, assembled a brief geriatric assessment tailored to the inpatient setting, instituted an interdisciplinary rounding model, and created a novel inpatient geriatrics curriculum.
During the study period, we improved performance of important processes of care for hospitalized elders, including recognition of abnormal cognitive and functional status; maintained comparable resource use; and implemented a novel, inpatient‐focused geriatric medicine educational experience. We were unable to demonstrate an impact on key clinical outcomes such as falls, physical restraint use, and readmissions. Nonetheless, there is evidence that the performance of selected processes of care is associated with improved three‐year survival status in the community‐dwelling vulnerable older patient, and may also be associated with a mortality benefit in the hospitalized vulnerable older patient.25, 26 Therefore, methods to improve the performance of these processes of care may be of clinical importance.
The finding of increased use of DNAR orders in the face of equivalent documentation of code status is of interest and generates hypotheses for further study. It is possible that the educational experience and use of geriatric assessment provides a more complete context for the code status discussion (one that incorporates the patient's social, physical, and cognitive function). However, we do not know if the patients on the ACE service had improved concordance between their code status and their goals of care.
We believe that there was no difference in key clinical outcomes between Hospitalist‐ACE and control patients because the population in this study was relatively low acuity and, therefore, the occurrence of falls and the use of physical restraints were quite low in the study population. In particular, the readmission rate was much lower than is typical for the Medicare population at our hospital, making it challenging to draw conclusions about the impact of the intervention on readmissions, however, we cannot rule out the possibility that our early discharge planning did not address the determinants of readmission for this population.
The ACE unit paradigmcharacterized by 1) closed, modified hospital units; 2) staffing by geriatricians and nurses with geriatrics training; 3) employing geriatric nursing care protocolsrequires significant resources and is not feasible for all settings.6 There is a need for alternative models of comprehensive care for hospitalized elders that require fewer resources in the form of dedicated units and specialist personnel, and can be more responsive to institutional needs. For example, in a 2005 report, one institution reported the creation of a geriatric medicine service that utilized a geriatrician and hospitalist co‐attending model.14 More recently, a large geriatrics program replaced its inpatient geriatrics unit with a mobile inpatient geriatrics service staffed by an attending geriatricianhospitalist, a geriatrics fellow, and a nurse practitioner.27 While these innovative models have eliminated the dedicated unit, they rely on board certified geriatricians, a group in short supply nationally.28 Hospitalists are a rapidly growing provider group that, with appropriate training and building on the work of geriatricians, is poised to provide leadership in acute geriatric care.29, 30
In contrast to the comprehensive inpatient geriatric care models described above, the Hospitalist‐ACE service uses a specialized hospitalist workforce and is not dependent on continuous staffing by geriatricians. Although geographic concentration is important for the success of interdisciplinary rounds, the Hospitalist‐ACE service does not require a closed or modified unit. The nursing staff caring for Hospitalist‐ACE patients have generalist nursing training and, at the time of the study, did not utilize geriatric‐care protocols. Our results need to be interpreted in the light of these differences from the ACE unit model which is a significantly more intensive intervention than the Hospitalist‐ACE service. In addition, the current practice environment is quite different from the mid‐1990s when ACE units were developed and studied. Development and maintenance of models of comprehensive inpatient geriatric care require demonstration of both value as well as return on investment. The alignment of financial and regulatory incentives for programs that provide comprehensive care to complex patients, such as those anticipated by the Affordable Care Act, may encourage the growth of such models.
These data represent findings from a six‐month evaluation of a novel inpatient service in the middle of its first year. There are several limitations related to our study design. First, the results of this small study at a single academic medical center may be of limited generalizability to other settings. Second, the program was evaluated only three months after its inception; we did not capture further improvements in methods, training, and outcomes expected as the program matured. Third, most of the Hospitalist‐ACE service attendings and residents rotate on the UCH general medical services throughout the year. Consequently, we were unable to eliminate the possibility of contamination of the control group, and we were unable to blind the physicians to the study. Fourth, the study population had a relatively low severity of illnessthe average MS‐DRG weight was near 1and low rates of important adverse events such falls and restraint use. This may have occurred because we excluded patients transferred from the ICUs and other services. It is possible that the Hospitalist‐ACE intervention might have demonstrated a larger benefit in a sicker population that would have presented greater opportunities for reductions in length of stay, costs, and adverse events. Fifth, given the retrospective nature of the data collection, we were not able to prospectively assess the incidence of important geriatric outcomes such as delirium and functional decline, nor can we make conclusions about changes in function during the hospitalization.
While the outcome measures we used are conceptually similar to several measures developed by RAND's Assessing Care of Vulnerable Elders (ACOVE) project, this study did not explicitly rely on those constructs.31 To do so would have required prospective screening by clinical staff independent from the care team for vulnerability that was beyond the scope of this project. In addition, the ACOVE measures of interest for functional and cognitive decline are limited to documentation of cognitive or functional assessments in the medical record. The ACE service's adoption of a brief standardized geriatric assessment was almost certain to meet that documentation requirement. While documentation is important, it is not clear that documentation, in and of itself, improves outcomes. Therefore, we expanded upon the ACOVE constructs to include the need for the additional evidence of a treatment plan when abnormal physical or cognitive function was documented. These constructs are important process of care for vulnerable elders. While we demonstrated improvements in several of these important processes of care for elderly patients, we are unable to draw conclusions about the impact of these differences in care on important clinical outcomes such as development of delirium, long‐term institutionalization, or mortality.
CONCLUSIONS
The risks of hospitalization for older persons are numerous, and present challenges and opportunities for inpatient physicians. As the hospitalized population agesmirroring national demographic trends and trends in use of acute care hospitalsthe challenge of avoiding harm in the older hospitalized patient will intensify. Innovations in care to improve the experience and outcomes of hospitalization for older patients are needed in the face of limited geriatrics‐trained workforce and few discretionary funds for unit redesign. The Hospitalist‐ACE service is a promising strategy for hospitalist programs with sufficient numbers of older patients and hospitalists with interest in improving clinical care for older adults. It provides a model for hospitalists to employ geriatrics principles targeted at reducing harm to their most vulnerable patients. Hospitalist‐run geriatric care models offer great promise for improving the care of acutely ill elderly patients. Future investigation should focus on demonstrating the impact of such care on important clinical outcomes between admission and discharge; on model refinement and adaptation, such as determining what components of comprehensive geriatric care are essential to success; and on how complementary interventions, such as the use of templated orders for the hospitalized elderly, impact outcomes. Additional research is needed, with a focus on demonstrating value with regard to an array of outcomes including cost, readmissions, and preventable harms of care.
Acknowledgements
Jean Kutner, MD, MSPH; Daniel Sandy, MPH; Shelly Limon, RN; nurses of 12 West; the UCH staff on the interdisciplinary team; and ACE patients and their families.
- ,,, et al.Functional outcomes of acute medical illness and hospitalization in older persons.Arch Intern Med.1996;156:645–652.
- ,,.Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care.Am J Med.1999;106:565–573.
- ,,, et al.Using assessing care of vulnerable elders quality indicators to measure quality of hospital care for vulnerable elders.J Am Geriatr Soc.2007;55(11):1705–1711.
- ,,, et al.Impact and recognition of cognitive impairment among hospitalized elders.J Hosp Med.2010;5:69–75.
- ,,,,.What does the medical record reveal about functional status? A comparison of medical record and interview data.J Gen Intern Med.2001;16(11):728–736.
- ,,,,,.Successful models of comprehensive care for older adults with chronic conditions: evidence for the Institute of Medicine's “Retooling for an Aging America” report.J Am Geriatr Soc.2009;57(12):2328–2337.
- ,,,,.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1344.
- ,,, et al.Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older adults: a randomized controlled trial of Acute Care for Elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1581.
- ,,, et al.The effectiveness of inpatient geriatric evaluation and management units: a systematic review and meta‐analysis.J Am Geriatr Soc.2010;58:83–92.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.A randomized, controlled clinical trial of a geriatrics consultation team: compliance with recommendations.JAMA.1986;255:2617–2621.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,.Dissemination and characteristics of Acute Care of Elders (ACE) units in the United States.Int J Technol Assess Health Care.2003;19:220–227.
- ,,.Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1:29–35.
- ,,,,.The Mini‐Cog: a cognitive “vital signs” measure for dementia screening in multi‐lingual elderly.Int J Geriatr Psychiatry.2000;15(11):1021–1027.
- ,,.The Patient Health Questionnaire‐2: validity of a two‐item depression screener.Med Care.2003;41:1284–1292.
- ,,,,,.Clarifying confusion: the Confusion Assessment Method.Ann Intern Med.1990;113(12):941–948.
- ,,, et al.The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community.J Am Geriatr Soc.2001;49:1691–1699.
- ,.The timed “Up and Go”: a test of basic functional mobility for frail elderly persons.J Am Geriatr Soc.1991;39:142–148.
- American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopedic Surgeons Panel on Falls Prevention.Guideline for the prevention of falls in older persons.J Am Geriatr Soc.2001;49:664–672.
- . Falls for the inpatient physician. Translating knowledge into action. The Portal of Online Geriatric Education (POGOe). 6–19‐2008. Available at: http://www.pogoe.org/productid/20212.
- ,,,. Incontinence and urinary catheters for the inpatient physician. The Portal of Online Geriatric Education (POGOe). 11–27‐0008. Available at: http://www.pogoe.org/productid/20296.
- ,,,.Use of medications for insomnia in the hospitalized geriatric population.J Am Geriatr Soc.2008;56(3):579–581.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130(4 pt 2):343–349.
- ,,, et al.Quality of care associated with survival in vulnerable older patients.Ann Intern Med.2005;143:274–281.
- ,,, et al.Higher quality of care for hosptialized frail older adults is associated with improved survival one year after discharge.J Hosp Med.2009;4(S1):24.
- ,,,.Operational and quality outcomes of a novel mobile acute care for the elderly service.J Am Geriatr Soc.2009;57:S1.
- Institute of Medicine (IOM).Retooling for an Aging America: Building the Health Care Workforce.Washington, DC:The National Academies Press;2008.
- ,,.Alternative solutions to the geriatric workforce deficit.Am J Med.2008;121:e23.
- ,,,,.Fulfilling the promise of hospital medicine: tailoring internal medicine training to address hospitalists' needs.J Gen Intern Med.2008;23(7):1110–1115.
- ,.Assessing care of vulnerable elders: ACOVE project overview.Ann Intern Med.2001;135(8 pt 2):642–646.
- ,,, et al.Functional outcomes of acute medical illness and hospitalization in older persons.Arch Intern Med.1996;156:645–652.
- ,,.Delirium: a symptom of how hospital care is failing older persons and a window to improve quality of hospital care.Am J Med.1999;106:565–573.
- ,,, et al.Using assessing care of vulnerable elders quality indicators to measure quality of hospital care for vulnerable elders.J Am Geriatr Soc.2007;55(11):1705–1711.
- ,,, et al.Impact and recognition of cognitive impairment among hospitalized elders.J Hosp Med.2010;5:69–75.
- ,,,,.What does the medical record reveal about functional status? A comparison of medical record and interview data.J Gen Intern Med.2001;16(11):728–736.
- ,,,,,.Successful models of comprehensive care for older adults with chronic conditions: evidence for the Institute of Medicine's “Retooling for an Aging America” report.J Am Geriatr Soc.2009;57(12):2328–2337.
- ,,,,.A randomized trial of care in a hospital medical unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1344.
- ,,, et al.Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older adults: a randomized controlled trial of Acute Care for Elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1581.
- ,,, et al.The effectiveness of inpatient geriatric evaluation and management units: a systematic review and meta‐analysis.J Am Geriatr Soc.2010;58:83–92.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.A randomized, controlled clinical trial of a geriatrics consultation team: compliance with recommendations.JAMA.1986;255:2617–2621.
- ,,, et al.A multicomponent intervention to prevent delirium in hospitalized older patients.N Engl J Med.1999;340:669–676.
- ,,,.Dissemination and characteristics of Acute Care of Elders (ACE) units in the United States.Int J Technol Assess Health Care.2003;19:220–227.
- ,,.Is there a geriatrician in the house? Geriatric care approaches in hospitalist programs.J Hosp Med.2006;1:29–35.
- ,,,,.The Mini‐Cog: a cognitive “vital signs” measure for dementia screening in multi‐lingual elderly.Int J Geriatr Psychiatry.2000;15(11):1021–1027.
- ,,.The Patient Health Questionnaire‐2: validity of a two‐item depression screener.Med Care.2003;41:1284–1292.
- ,,,,,.Clarifying confusion: the Confusion Assessment Method.Ann Intern Med.1990;113(12):941–948.
- ,,, et al.The Vulnerable Elders Survey: a tool for identifying vulnerable older people in the community.J Am Geriatr Soc.2001;49:1691–1699.
- ,.The timed “Up and Go”: a test of basic functional mobility for frail elderly persons.J Am Geriatr Soc.1991;39:142–148.
- American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopedic Surgeons Panel on Falls Prevention.Guideline for the prevention of falls in older persons.J Am Geriatr Soc.2001;49:664–672.
- . Falls for the inpatient physician. Translating knowledge into action. The Portal of Online Geriatric Education (POGOe). 6–19‐2008. Available at: http://www.pogoe.org/productid/20212.
- ,,,. Incontinence and urinary catheters for the inpatient physician. The Portal of Online Geriatric Education (POGOe). 11–27‐0008. Available at: http://www.pogoe.org/productid/20296.
- ,,,.Use of medications for insomnia in the hospitalized geriatric population.J Am Geriatr Soc.2008;56(3):579–581.
- ,,,.Hospitalists and the practice of inpatient medicine: results of a survey of the National Association of Inpatient Physicians.Ann Intern Med.1999;130(4 pt 2):343–349.
- ,,, et al.Quality of care associated with survival in vulnerable older patients.Ann Intern Med.2005;143:274–281.
- ,,, et al.Higher quality of care for hosptialized frail older adults is associated with improved survival one year after discharge.J Hosp Med.2009;4(S1):24.
- ,,,.Operational and quality outcomes of a novel mobile acute care for the elderly service.J Am Geriatr Soc.2009;57:S1.
- Institute of Medicine (IOM).Retooling for an Aging America: Building the Health Care Workforce.Washington, DC:The National Academies Press;2008.
- ,,.Alternative solutions to the geriatric workforce deficit.Am J Med.2008;121:e23.
- ,,,,.Fulfilling the promise of hospital medicine: tailoring internal medicine training to address hospitalists' needs.J Gen Intern Med.2008;23(7):1110–1115.
- ,.Assessing care of vulnerable elders: ACOVE project overview.Ann Intern Med.2001;135(8 pt 2):642–646.
Copyright © 2011 Society of Hospital Medicine
“Better Late than Never”
A 59‐year‐old man presented to the emergency department with the acute onset of right‐sided abdominal and flank pain. The pain had begun the previous night, was constant and progressively worsening, and radiated to his right groin. He denied fever, nausea, emesis, or change in his bowel habits, but he did notice mild right lower quadrant discomfort with micturition. Upon further questioning, he also complained of mild dyspnea on climbing stairs and an unspecified recent weight loss.
The most common cause of acute severe right‐sided flank and abdominal pain radiating to the groin and associated with dysuria in a middle‐aged man is ureteral colic. Other etiologies important to consider include retrocecal appendicitis, pyelonephritis, and, rarely, a dissecting abdominal aortic aneurysm. This patient's seemingly recent onset exertional dyspnea and weight loss do not neatly fit any of the above, however.
His past medical history was significant for diabetes mellitus and pemphigus vulgaris diagnosed 7 months previously. He had been treated with prednisone, and the dose decreased from 100 to 60 mg daily, 1 month previously, due to poor glycemic control as well as steroid‐induced neuropathy and myopathy. His other medications included naproxen sodium and ibuprofen for back pain, azathioprine, insulin, pioglitazone, and glimiperide. He had no past surgical history. He had lived in the United States since his emigration from Thailand in 1971. His last trip to Thailand was 5 years previously. He was a taxi cab driver. He had a ten‐pack year history of tobacco use, but had quit 20 years prior. He denied history of alcohol or intravenous drug use.
Pemphigus vulgaris is unlikely to be directly related to this patient's presentation, but in light of his poorly controlled diabetes, his azathioprine use, and particularly his high‐dose corticosteroids, he is certainly immunocompromised. Accordingly, a disseminated infection, either newly acquired or reactivated, merits consideration. His history of residence in, and subsequent travel to, Southeast Asia raises the possibility of several diseases, each of which may be protean in their manifestations; these include tuberculosis, melioidosis, and penicilliosis (infection with Penicillium marneffei). The first two may reactivate long after initial exposure, particularly with insults to the immune system. The same is probably true of penicilliosis, although I am not certain of this. On a slightly less exotic note, domestically acquired infection with histoplasmosis or other endemic fungi is possible.
On examination he was afebrile, had a pulse of 130 beats per minute and a blood pressure of 65/46 mmHg. His oxygen saturation was 92%. He appeared markedly cushingoid, and had mild pallor and generalized weakness. Cardiopulmonary examination was unremarkable. His abdominal exam was notable for distention and hypoactive bowel sounds, with tenderness and firmness to palpation on the right side. Peripheral pulses were normal. Examination of the skin demonstrated ecchymoses over the bilateral forearms, and several healed pemphigus lesions on the abdomen and upper extremities.
The patient's severely deranged hemodynamic parameters indicate either current or impending shock, and resuscitative measures should proceed in tandem with diagnostic efforts. The cause of his shock seems most likely to be either hypovolemic (abdominal wall or intra‐abdominal hemorrhage, or conceivably massive third spacing from an intra‐abdominal catastrophe), or distributive (sepsis, or acute adrenal insufficiency if he has missed recent steroid doses). His ecchymoses may simply reflect chronic glucocorticoid use, but also raise suspicion for a coagulopathy. Provided the patient can be stabilized to allow this, I would urgently obtain a computed tomography (CT) scan of the abdomen and pelvis.
Initial laboratory studies demonstrated a hemoglobin of 9.1 g/dL, white blood cell count 8000/L with 33% bands, 48% segmented neutrophils, 18% lymphocytes, and 0.7% eosinophils, platelet count 356,000/L, sodium 128 mmol/L, BUN 52 mg/dL, creatinine 2.3 mg/dL, and glucose of 232 mg/dL. Coagulation studies were normal, and lactic acid was 1.8 mmol/L (normal range, 0.7‐2.1). Fibrinogen was normal at 591 and LDH was mildly elevated at 654 (normal range, 313‐618 U/L). Total protein and albumin were 3.6 and 1.9 g/dL, respectively. Total bilirubin was 0.6 mg/dL. Random serum cortisol was 20.2 g/dL. Liver enzymes, amylase, lipase, iron stores, B12, folate, and stool for occult blood were normal. Initial cardiac biomarkers were negative, but subsequent troponin‐I was 3.81 ng/mL (elevated, >1.00). Urinalysis showed 0‐4 white blood cells per high powered field.
The laboratory studies provide a variety of useful, albeit nonspecific, information. The high percentage of band forms on white blood cell differential further raises concern for an infectious process, although severe noninfectious stress can also cause this. While we do not know whether the patient's renal failure is acute, I suspect that it is, and may result from a variety of insults including sepsis, hypotension, and volume depletion. His moderately elevated troponin‐I likely reflects supplydemand mismatch or sepsis. I would like to see an electrocardiogram, and I remain very interested in obtaining abdominal imaging.
Chest radiography showed pulmonary vascular congestion without evidence of pneumothorax. Computed tomography scan of the abdomen and pelvis showed retroperitoneal fluid bilaterally (Figure 1). This was described as suspicious for ascites versus hemorrhage, but no obvious source of bleeding was identified. There was also a small amount of right perinephric fluid, but no evidence of a renal mass. The abdominal aorta was normal; there was no lymphadenopathy.

The CT image appears to speak against simple ascites, and seems most consistent with either blood or an infectious process. Consequently, the loculated right retroperitoneal collection should be aspirated, and fluid sent for fungal, acid‐fast, and modified acid‐fast (i.e., for Nocardia) stains and culture, in addition to Gram stain and routine aerobic and anaerobic cultures.
The patient was admitted to the intensive care unit. Stress‐dose steroids were administered, and he improved after resuscitation with fluid and blood. His renal function normalized. Urine and blood cultures returned negative. His hematocrit and multiple repeat CT scans of the abdomen remained stable. A retroperitoneal hemorrhage was diagnosed, and surgical intervention was deemed unnecessary. Both adenosine thallium stress test and echocardiogram were normal. He was continued on 60 mg prednisone daily and discharged home with outpatient follow‐up.
This degree of improvement with volume expansion (and steroids) suggests the patient was markedly volume depleted upon presentation. Although a formal adrenocorticotropic hormone (ACTH) stimulation test was apparently not performed, the random cortisol level suggests adrenal insufficiency was unlikely to have been primarily responsible. While retroperitoneal hemorrhage is possible, the loculated appearance of the collection suggests infection is more likely.
Three weeks later, he was readmitted with recurrent right‐sided abdominal and flank pain. His temperature was 101.3F, and he was tachycardic and hypotensive. His examination was similar to that at the time of his previous presentation. Laboratory data revealed white blood cell count of 13,100/L with 43% bands, hemoglobin of 9.2 g/dL, glucose of 343 mg/dL, bicarbonate 25 mmol/L, normal anion gap and renal function, and lactic acid of 4.5 mmol/L. Liver function tests were normal except for an albumin of 3.0 g/dL. CT scan of the abdomen revealed loculated retroperitoneal fluid collections, increased in size since the prior scan.
The patient is once again evidencing at least early shock, manifested in his deranged hemodynamics and elevated lactate level. I remain puzzled by the fact that he appeared to respond to fluids alone at the time of his initial hospital stay, unless adrenal insufficiency played a greater role than I suspected. Of note, acute adrenal insufficiency could explain much of the current picture, including fever, and bland (uninfected) hematomas are an underappreciated cause of both fever and leukocytosis. Having said this, I remain concerned that his retroperitoneal fluid collections represent abscesses. The most accessible of these should be sampled.
Aspiration of the retroperitoneal fluid yielded purulent material which grew Klebsiella pneumoniae. The cultures were negative for mycobacteria and fungus. Blood and urine cultures were negative. Drains were placed, and he was followed as an outpatient. His fever and leukocytosis subsided, and he completed a 6‐week course of trimethoprim‐sulfamethoxazole. CT imaging confirmed complete evacuation of the fluid.
Retroperitoneal abscesses frequently present in smoldering fashion, although patients may be quite ill by the time of presentation. Most of these are secondary, i.e., they arise from another abnormality in the retroperitoneum. Most commonly this is in the large bowel, kidney, pancreas, or spine. I would carefully scour his follow‐up imaging for additional clues and, if unrevealing, proceed to colonoscopy.
He returned 1 month after drain removal, with 2‐3 days of nausea and abdominal pain. His abdomen was moderately distended but nontender, and multiple persistent petechial and purpuric lesions were present on the upper back, chest, torso, and arms. Abdominal CT scan revealed small bowel obstruction and a collection of fluid in the left paracolic gutter extending into the left retrorenal space.
The patient does not appear to have obvious risk factors for developing a small bowel obstruction. No mention is made of the presence or absence of a transition point on the CT scan, and this should be ascertained. His left‐sided abdominal fluid collection is probably infectious in nature, and I continue to be suspicious of a large bowel (or distal small bowel) source, via either gut perforation or bacterial translocation. The collection needs to be percutaneously drained for both diagnostic and therapeutic reasons, and broadly cultured. Finally, we need to account for the described dermatologic manifestations. The purpuric/petechial lesions sound vasculitic rather than thrombocytopenic in origin based on location; conversely, they may simply reflect a corticosteroid‐related adverse effect. I would like to know whether the purpura was palpable, and to repeat a complete blood count with peripheral smear.
Laboratory data showed hemoglobin of 9.3 g/dL, a platelet count of 444,000/L, and normal coagulation studies. The purpura was nonpalpable (Figure 2). The patient had a nasogastric tube placed for decompression, with bilious drainage. His left retroperitoneal fluid was drained, with cultures yielding Enterococcus faecalis and Enterobacter cloacae. The patient was treated with a course of broad‐spectrum antibiotics. His obstruction improved and the retroperitoneal collection resolved on follow‐up imaging. However, 2 days later, he had recurrent pain; abdominal CT showed a recurrence of small bowel obstruction with an unequivocal transition point in the distal jejunum. A small fluid collection was noted in the left retroperitoneum with a trace of gas in it. He improved with nasogastric suction, his prednisone was tapered to 30 mg daily, and he was discharged home.
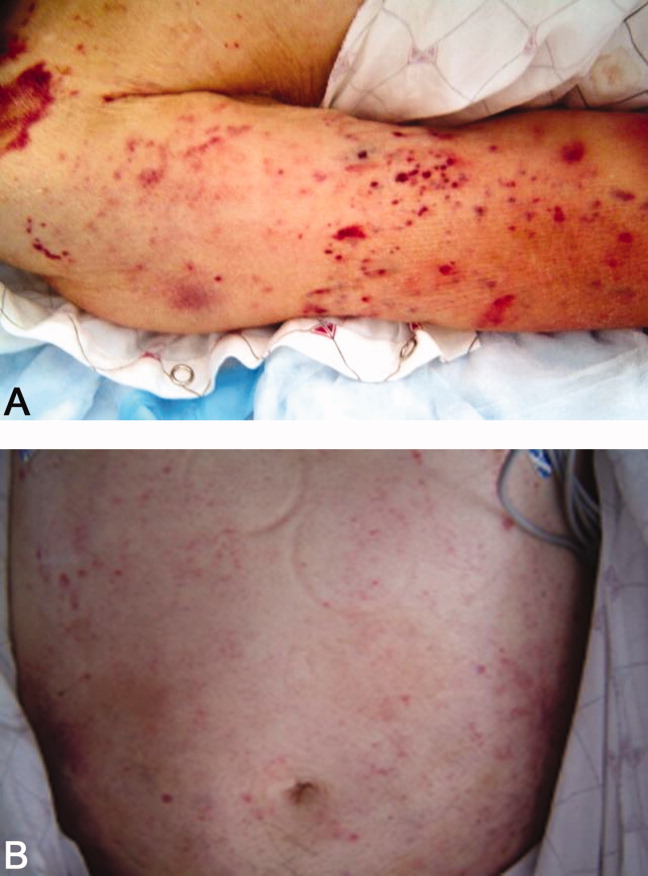
The isolation of both Enterococcus and Enterobacter species from his fluid collection, along with the previous isolation of Klebsiella, strongly suggest a bowel source for his recurrent abscesses. Based on this CT report, the patient has clear evidence of at least partial small bowel obstruction. He lacks a history of prior abdominal surgery or other more typical reasons for obstruction caused by extrinsic compression, such as hernia, although it is possible his recurrent abdominal infections may have led to obstruction due to scarring and adhesions. An intraluminal cause of obstruction also needs to be considered, with causes including malignancy (lymphoma, carcinoid, and adenocarcinoma), Crohn's disease, and infections including tuberculosis as well as parasites such as Taenia and Strongyloides. While the purpura is concerning, given the nonpalpable character along with a normal platelet count and coagulation studies, it may be reasonable to provisionally attribute it to high‐dose corticosteroid use.
He was admitted a fourth time a week after being discharged, with nausea, generalized weakness, and weight loss. At presentation, he had a blood pressure of 95/65 mmHg. His white blood cell count was 5,900/L, with 79% neutrophils and 20% bands. An AM cortisol was 18.8 /dL. He was thought to have adrenal insufficiency from steroid withdrawal, was treated with intravenous fluids and steroids, and discharged on a higher dose of prednisone at 60 mg daily. One week later, he again returned to the hospital with watery diarrhea, emesis, and generalized weakness. His blood pressure was 82/50 mmHg, and his abdomen appeared benign. He also had an erythematous rash over his mid‐abdomen. Laboratory data was significant for a sodium of 127 mmol/L, potassium of 3.0 mmol/L, chloride of 98 mmol/L, bicarbonate of 26 mmol/L, glucose of 40 mg/dL, lactate of 14 mmol/L, and albumin of 1.0 g/dL. Stool assay for Clostridium difficile was negative. A CT scan of the abdomen and pelvis showed small bilateral pleural effusions and small bowel fluid consistent with gastroenteritis, but without signs of obstruction. Esophagogastroduodenoscopy (EGD) showed bile backwash into the stomach, as well as inflammatory changes in the proximal and mid‐stomach, and inflammatory reaction and edema in the proximal duodenum. Colonoscopy showed normal appearing ileum and colon.
The patient's latest laboratory values appear to reflect his chronic illness and superimposed diarrhea. I am perplexed by his markedly elevated serum lactate value in association with a normal bicarbonate and low anion gap, and would repeat the lactate level to ensure this is not spurious. His hypoglycemia probably reflects a failure to adjust or discontinue his diabetic medications, although both hypoglycemia and type B lactic acidosis are occasionally manifestations of a paraneoplastic syndrome. The normal colonoscopy findings are helpful in exonerating the colon, provided the preparation was adequate. Presumably, the abnormal areas of the stomach and duodenum were biopsied; I remain suspicious that the answer may lie in the jejunum.
The patient was treated with intravenous fluids and stress‐dose steroids, and electrolyte abnormalities were corrected. Biopsies from the EGD and colonoscopy demonstrated numerous larvae within the mucosa of the body and antrum of the stomach, as well as duodenum. There were also rare detached larvae seen in the esophagus, and a few larvae within the ileal mucosa.
The patient appears to have Strongyloides hyperinfection, something he is at clear risk for, given his country of origin and his high‐dose corticosteroids. In retrospect, I was dissuaded from seriously considering a diagnosis of parasitic infection in large part because of the absence of peripheral eosinophilia, but this may not be seen in cases of hyperinfection. Additional clues, again in retrospect, were the repeated abscesses with bowel flora and the seemingly nonspecific abdominal rash. I would treat with a course of ivermectin, and carefully monitor his response.
The characteristics of the larvae were suggestive of Strongyloides species (Figure 3). A subsequent stool test for ova and parasites was positive for Strongyloides larvae. The patient was given a single dose of ivermectin. An endocrinology consultant felt that he did not have adrenal insufficiency, and it was recommended that his steroids be tapered off. He was discharged home once he clinically improved.
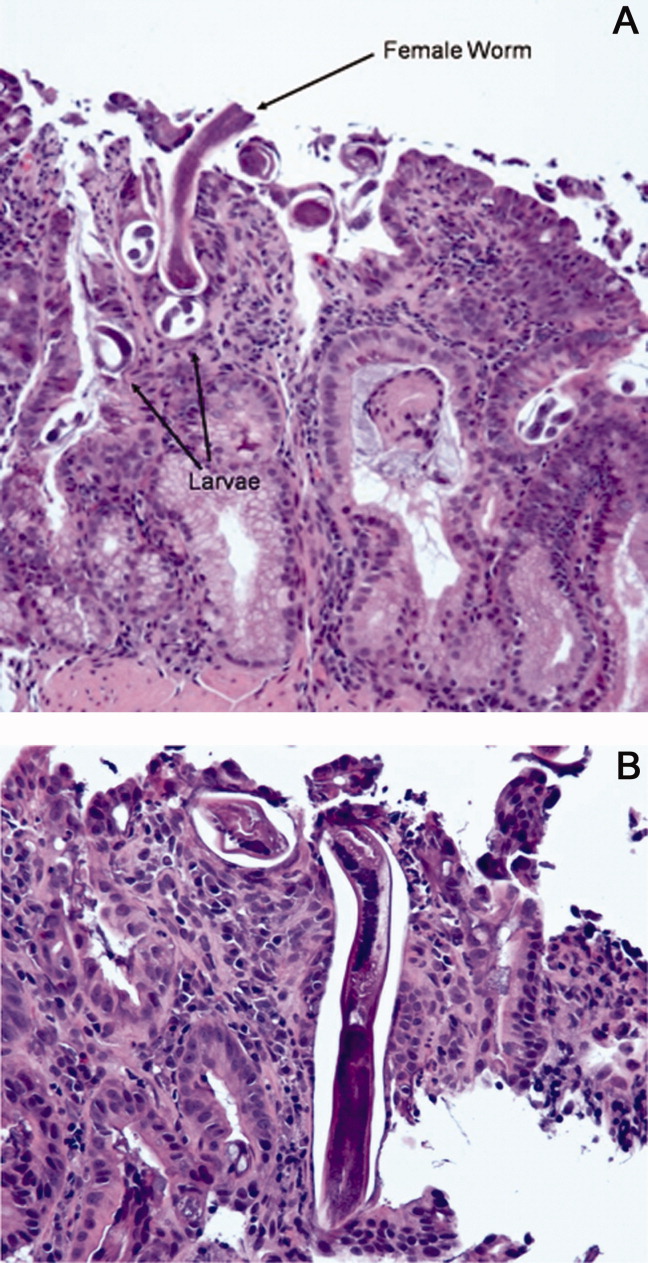
Although one or two doses of ivermectin typically suffices for uncomplicated strongyloidiasis, the risk of failure in hyperinfection mandates a longer treatment course. I don't believe this patient has been adequately treated, although the removal of his steroids will be helpful.
He was readmitted 3 days later with recrudescent symptoms, and his stool remained positive for Strongyloides. He received 2 weeks of ivermectin and albendazole, and was ultimately discharged to a rehabilitation facility after a complicated hospital stay. Nine months later, the patient was reported to be doing well.
COMMENTARY
This patient's immigration status from the developing world, high‐dose corticosteroid use, and complex clinical course all suggested the possibility of an underlying chronic infectious process. Although the discussant recognized this early on and later briefly mentioned strongyloidiasis as a potential cause of intestinal obstruction, the diagnosis of Strongyloides hyperinfection was not suspected until incontrovertible evidence for it was obtained on EGD. Failure to make the diagnosis earlier by both the involved clinicians and the discussant probably stemmed largely from two factors: the absence of eosinophilia; and lack of recognition that purpura may be seen in cases of hyperinfection, presumably reflecting larval infiltration of the dermis.1 Although eosinophilia accompanies most cases of stronglyloidiasis and may be very pronounced, patients with hyperinfection syndrome frequently fail to mount an eosinophilic response due to underlying immunosuppression, with eosinophilia absent in 70% of such patients in a study from Taiwan.2
Strongyloides stercoralis is an intestinal nematode that causes strongyloidiasis. It affects as many as 100 million people globally,3 mainly in tropical and subtropical areas, but is also endemic in the Southeastern United States, Europe, and Japan. Risk factors include male sex, White race, alcoholism, working in contact with soil (farmers, coal mine workers, etc.), chronic care institutionalization, and low socioeconomic status. In nonendemic regions, it more commonly affects travelers, immigrants, or military personnel.4, 5
The life cycle of S. stercoralis is complex. Infective larvae penetrate the skin through contact with contaminated soil, enter the venous system via lymphatics, and travel to the lung.4, 6 Here, they ascend the tracheobronchial tree and migrate to the gut. In the intestine, larvae develop into adult female worms that burrow into the intestinal mucosa. These worms lay eggs that develop into noninfective rhabditiform larvae, which are then expelled in the stool. Some of the rhabditiform larvae, however, develop into infective filariform larvae, which may penetrate colonic mucosa or perianal skin, enter the bloodstream, and lead to the cycle of autoinfection and chronic strongyloidiasis (carrier state). Autoinfection typically involves a low parasite burden, and is controlled by both host immune factors as well as parasitic factors.7 The mechanism of autoinfection can lead to the persistence of strongyloidiasis for decades after the initial infection, as has been documented in former World War II prisoners of war.8
Factors leading to the impairment of cell‐mediated immunity predispose chronically infected individuals to hyperinfection, as occurred in this patient. The most important of these are corticosteroid administration and Human T‐lymphotropic virus Type‐1 (HTLV‐1) infection, both of which cause significant derangement in TH1/TH2 immune system balance.5, 9 In the hyperinfection syndrome, the burden of parasites increases dramatically, leading to a variety of clinical manifestations. Gastrointestinal phenomena frequently predominate, including watery diarrhea, anorexia, weight loss, nausea/vomiting, gastrointestinal bleeding, and occasionally small bowel obstruction. Pulmonary manifestations are likewise common, and include cough, dyspnea, and wheezing. Cutaneous findings are not uncommon, classically pruritic linear lesions of the abdomen, buttocks, and lower extremities which may be rapidly migratory (larva currens), although purpura and petechiae as displayed by our patient appear to be under‐recognized findings in hyperinfection.2, 5 Gram‐negative bacillary meningitis has been well reported as a complication of migrating larvae, and a wide variety of other organs may rarely be involved.5, 10
The presence of chronic strongyloidiasis should be suspected in patients with ongoing gastrointestinal and/or pulmonary symptoms, or unexplained eosinophilia with a potential exposure history, such as immigrants from Southeast Asia. Diagnosis in these individuals is currently most often made serologically, although stool exam provides a somewhat higher specificity for active infection, at the expense of lower sensitivity.3, 11 In the setting of hyperinfection, stool studies are almost uniformly positive for S. stercoralis, and sputum may be diagnostic as well. Consequently, failure to reach the diagnosis usually reflects a lack of clinical suspicion.5
The therapy of choice for strongyloidiasis is currently ivermectin, with a single dose repeated once, 2 weeks later, highly efficacious in eradicating chronic infection. Treatment of hyperinfection is more challenging and less well studied, but clearly necessitates a more prolonged course of treatment. Many experts advocate treating until worms are no longer present in the stool; some have suggested the combination of ivermectin and albendazole as this patient received, although this has not been examined in controlled fashion.
The diagnosis of Strongyloides hyperinfection is typically delayed or missed because of the failure to consider it, with reported mortality rates as high as 50% in hyperinfection and 87% in disseminated disease.3, 12, 13 This patient fortunately was diagnosed, albeit in delayed fashion, proving the maxim better late than never. His case highlights the need for increased clinical awareness of strongyloidiasis, and specifically the need to consider the possibility of chronic Strongyloides infection prior to administering immunosuppressive medications. In particular, serologic screening of individuals from highly endemic areas for strongyloidiasis, when initiating extended courses of corticosteroids, seems prudent.13
Teaching Points
-
Chronic strongyloidiasis is common in the developing world (particularly Southeast Asia), and places infected individuals at significant risk of life‐threatening hyperinfection if not recognized and treated prior to the initiation of immunosuppressive medication, especially corticosteroids.
-
Strongyloides hyperinfection syndrome may be protean in its manifestations, but most commonly includes gastrointestinal, pulmonary, and cutaneous signs and symptoms.
- ,,, et al.Disseminated strongyloidiasis in immunocompromised patients—report of three cases.Int J Dermatol.2009;48(9):975–978.
- ,,, et al.Clinical manifestations of strongyloidiasis in southern Taiwan.J Microbiol Immunol Infect.2002;35(1):29–36.
- ,.Diagnosis of Strongyloides stercoralis infection.Clin Infect Dis.2001;33(7):1040–1047.
- ,,.Intestinal strongyloidiasis and hyperinfection syndrome.Clin Mol Allergy.2006;4:8.
- ,.Strongyloides stercoralis in the immunocompromised population.Clin Microbiol Rev.2004;17(1):208–217.
- ,,.Intestinal strongyloidiasis: recognition, management and determinants of outcome.J Clin Gastroenterol2005;39(3):203–211.
- .Dysregulation of strongyloidiasis: a new hypothesis.Clin Microbiol Rev.1992;5(4):345–355.
- ,,,.Consequences of captivity: health effects of Far East imprisonment in World War II.Q J Med.2009;102:87–96.
- ,,,.Strongyloides hyperinfection syndrome: an emerging global infectious disease.Trans R Soc Trop Med Hyg.2008;102(4):314–318.
- ,,,,,.Strongyloides hyperinfection presenting as acute respiratory failure and Gram‐negative sepsis.Chest.2005;128(5):3681–3684.
- ,,, et al.Use of enzyme‐linked immunosorbent assay and dipstick assay for detection of Strongyloides stercoralis infection in humans.J Clin Microbiol.2007;45:438–442.
- ,,,,,.Complicated and fatal Strongyloides infection in Canadians: risk factors, diagnosis and management.Can Med Assoc J.2004;171:479–484.
- ,,, et al.Maltreatment of Strongyloides infection: case series and worldwide physicians‐in‐training survey.Am J Med.2007;120(6):545.e1–545.e8.
A 59‐year‐old man presented to the emergency department with the acute onset of right‐sided abdominal and flank pain. The pain had begun the previous night, was constant and progressively worsening, and radiated to his right groin. He denied fever, nausea, emesis, or change in his bowel habits, but he did notice mild right lower quadrant discomfort with micturition. Upon further questioning, he also complained of mild dyspnea on climbing stairs and an unspecified recent weight loss.
The most common cause of acute severe right‐sided flank and abdominal pain radiating to the groin and associated with dysuria in a middle‐aged man is ureteral colic. Other etiologies important to consider include retrocecal appendicitis, pyelonephritis, and, rarely, a dissecting abdominal aortic aneurysm. This patient's seemingly recent onset exertional dyspnea and weight loss do not neatly fit any of the above, however.
His past medical history was significant for diabetes mellitus and pemphigus vulgaris diagnosed 7 months previously. He had been treated with prednisone, and the dose decreased from 100 to 60 mg daily, 1 month previously, due to poor glycemic control as well as steroid‐induced neuropathy and myopathy. His other medications included naproxen sodium and ibuprofen for back pain, azathioprine, insulin, pioglitazone, and glimiperide. He had no past surgical history. He had lived in the United States since his emigration from Thailand in 1971. His last trip to Thailand was 5 years previously. He was a taxi cab driver. He had a ten‐pack year history of tobacco use, but had quit 20 years prior. He denied history of alcohol or intravenous drug use.
Pemphigus vulgaris is unlikely to be directly related to this patient's presentation, but in light of his poorly controlled diabetes, his azathioprine use, and particularly his high‐dose corticosteroids, he is certainly immunocompromised. Accordingly, a disseminated infection, either newly acquired or reactivated, merits consideration. His history of residence in, and subsequent travel to, Southeast Asia raises the possibility of several diseases, each of which may be protean in their manifestations; these include tuberculosis, melioidosis, and penicilliosis (infection with Penicillium marneffei). The first two may reactivate long after initial exposure, particularly with insults to the immune system. The same is probably true of penicilliosis, although I am not certain of this. On a slightly less exotic note, domestically acquired infection with histoplasmosis or other endemic fungi is possible.
On examination he was afebrile, had a pulse of 130 beats per minute and a blood pressure of 65/46 mmHg. His oxygen saturation was 92%. He appeared markedly cushingoid, and had mild pallor and generalized weakness. Cardiopulmonary examination was unremarkable. His abdominal exam was notable for distention and hypoactive bowel sounds, with tenderness and firmness to palpation on the right side. Peripheral pulses were normal. Examination of the skin demonstrated ecchymoses over the bilateral forearms, and several healed pemphigus lesions on the abdomen and upper extremities.
The patient's severely deranged hemodynamic parameters indicate either current or impending shock, and resuscitative measures should proceed in tandem with diagnostic efforts. The cause of his shock seems most likely to be either hypovolemic (abdominal wall or intra‐abdominal hemorrhage, or conceivably massive third spacing from an intra‐abdominal catastrophe), or distributive (sepsis, or acute adrenal insufficiency if he has missed recent steroid doses). His ecchymoses may simply reflect chronic glucocorticoid use, but also raise suspicion for a coagulopathy. Provided the patient can be stabilized to allow this, I would urgently obtain a computed tomography (CT) scan of the abdomen and pelvis.
Initial laboratory studies demonstrated a hemoglobin of 9.1 g/dL, white blood cell count 8000/L with 33% bands, 48% segmented neutrophils, 18% lymphocytes, and 0.7% eosinophils, platelet count 356,000/L, sodium 128 mmol/L, BUN 52 mg/dL, creatinine 2.3 mg/dL, and glucose of 232 mg/dL. Coagulation studies were normal, and lactic acid was 1.8 mmol/L (normal range, 0.7‐2.1). Fibrinogen was normal at 591 and LDH was mildly elevated at 654 (normal range, 313‐618 U/L). Total protein and albumin were 3.6 and 1.9 g/dL, respectively. Total bilirubin was 0.6 mg/dL. Random serum cortisol was 20.2 g/dL. Liver enzymes, amylase, lipase, iron stores, B12, folate, and stool for occult blood were normal. Initial cardiac biomarkers were negative, but subsequent troponin‐I was 3.81 ng/mL (elevated, >1.00). Urinalysis showed 0‐4 white blood cells per high powered field.
The laboratory studies provide a variety of useful, albeit nonspecific, information. The high percentage of band forms on white blood cell differential further raises concern for an infectious process, although severe noninfectious stress can also cause this. While we do not know whether the patient's renal failure is acute, I suspect that it is, and may result from a variety of insults including sepsis, hypotension, and volume depletion. His moderately elevated troponin‐I likely reflects supplydemand mismatch or sepsis. I would like to see an electrocardiogram, and I remain very interested in obtaining abdominal imaging.
Chest radiography showed pulmonary vascular congestion without evidence of pneumothorax. Computed tomography scan of the abdomen and pelvis showed retroperitoneal fluid bilaterally (Figure 1). This was described as suspicious for ascites versus hemorrhage, but no obvious source of bleeding was identified. There was also a small amount of right perinephric fluid, but no evidence of a renal mass. The abdominal aorta was normal; there was no lymphadenopathy.

The CT image appears to speak against simple ascites, and seems most consistent with either blood or an infectious process. Consequently, the loculated right retroperitoneal collection should be aspirated, and fluid sent for fungal, acid‐fast, and modified acid‐fast (i.e., for Nocardia) stains and culture, in addition to Gram stain and routine aerobic and anaerobic cultures.
The patient was admitted to the intensive care unit. Stress‐dose steroids were administered, and he improved after resuscitation with fluid and blood. His renal function normalized. Urine and blood cultures returned negative. His hematocrit and multiple repeat CT scans of the abdomen remained stable. A retroperitoneal hemorrhage was diagnosed, and surgical intervention was deemed unnecessary. Both adenosine thallium stress test and echocardiogram were normal. He was continued on 60 mg prednisone daily and discharged home with outpatient follow‐up.
This degree of improvement with volume expansion (and steroids) suggests the patient was markedly volume depleted upon presentation. Although a formal adrenocorticotropic hormone (ACTH) stimulation test was apparently not performed, the random cortisol level suggests adrenal insufficiency was unlikely to have been primarily responsible. While retroperitoneal hemorrhage is possible, the loculated appearance of the collection suggests infection is more likely.
Three weeks later, he was readmitted with recurrent right‐sided abdominal and flank pain. His temperature was 101.3F, and he was tachycardic and hypotensive. His examination was similar to that at the time of his previous presentation. Laboratory data revealed white blood cell count of 13,100/L with 43% bands, hemoglobin of 9.2 g/dL, glucose of 343 mg/dL, bicarbonate 25 mmol/L, normal anion gap and renal function, and lactic acid of 4.5 mmol/L. Liver function tests were normal except for an albumin of 3.0 g/dL. CT scan of the abdomen revealed loculated retroperitoneal fluid collections, increased in size since the prior scan.
The patient is once again evidencing at least early shock, manifested in his deranged hemodynamics and elevated lactate level. I remain puzzled by the fact that he appeared to respond to fluids alone at the time of his initial hospital stay, unless adrenal insufficiency played a greater role than I suspected. Of note, acute adrenal insufficiency could explain much of the current picture, including fever, and bland (uninfected) hematomas are an underappreciated cause of both fever and leukocytosis. Having said this, I remain concerned that his retroperitoneal fluid collections represent abscesses. The most accessible of these should be sampled.
Aspiration of the retroperitoneal fluid yielded purulent material which grew Klebsiella pneumoniae. The cultures were negative for mycobacteria and fungus. Blood and urine cultures were negative. Drains were placed, and he was followed as an outpatient. His fever and leukocytosis subsided, and he completed a 6‐week course of trimethoprim‐sulfamethoxazole. CT imaging confirmed complete evacuation of the fluid.
Retroperitoneal abscesses frequently present in smoldering fashion, although patients may be quite ill by the time of presentation. Most of these are secondary, i.e., they arise from another abnormality in the retroperitoneum. Most commonly this is in the large bowel, kidney, pancreas, or spine. I would carefully scour his follow‐up imaging for additional clues and, if unrevealing, proceed to colonoscopy.
He returned 1 month after drain removal, with 2‐3 days of nausea and abdominal pain. His abdomen was moderately distended but nontender, and multiple persistent petechial and purpuric lesions were present on the upper back, chest, torso, and arms. Abdominal CT scan revealed small bowel obstruction and a collection of fluid in the left paracolic gutter extending into the left retrorenal space.
The patient does not appear to have obvious risk factors for developing a small bowel obstruction. No mention is made of the presence or absence of a transition point on the CT scan, and this should be ascertained. His left‐sided abdominal fluid collection is probably infectious in nature, and I continue to be suspicious of a large bowel (or distal small bowel) source, via either gut perforation or bacterial translocation. The collection needs to be percutaneously drained for both diagnostic and therapeutic reasons, and broadly cultured. Finally, we need to account for the described dermatologic manifestations. The purpuric/petechial lesions sound vasculitic rather than thrombocytopenic in origin based on location; conversely, they may simply reflect a corticosteroid‐related adverse effect. I would like to know whether the purpura was palpable, and to repeat a complete blood count with peripheral smear.
Laboratory data showed hemoglobin of 9.3 g/dL, a platelet count of 444,000/L, and normal coagulation studies. The purpura was nonpalpable (Figure 2). The patient had a nasogastric tube placed for decompression, with bilious drainage. His left retroperitoneal fluid was drained, with cultures yielding Enterococcus faecalis and Enterobacter cloacae. The patient was treated with a course of broad‐spectrum antibiotics. His obstruction improved and the retroperitoneal collection resolved on follow‐up imaging. However, 2 days later, he had recurrent pain; abdominal CT showed a recurrence of small bowel obstruction with an unequivocal transition point in the distal jejunum. A small fluid collection was noted in the left retroperitoneum with a trace of gas in it. He improved with nasogastric suction, his prednisone was tapered to 30 mg daily, and he was discharged home.
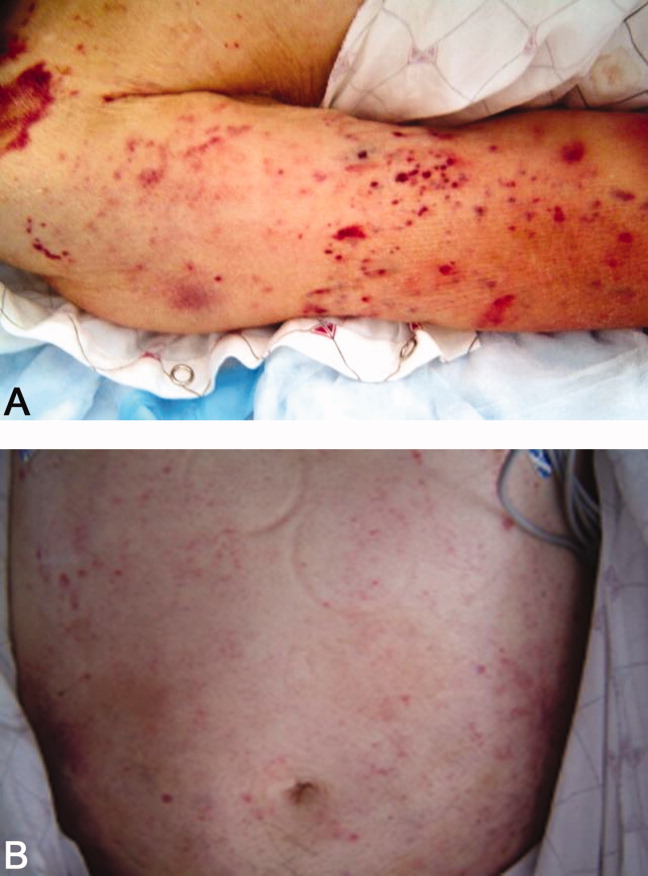
The isolation of both Enterococcus and Enterobacter species from his fluid collection, along with the previous isolation of Klebsiella, strongly suggest a bowel source for his recurrent abscesses. Based on this CT report, the patient has clear evidence of at least partial small bowel obstruction. He lacks a history of prior abdominal surgery or other more typical reasons for obstruction caused by extrinsic compression, such as hernia, although it is possible his recurrent abdominal infections may have led to obstruction due to scarring and adhesions. An intraluminal cause of obstruction also needs to be considered, with causes including malignancy (lymphoma, carcinoid, and adenocarcinoma), Crohn's disease, and infections including tuberculosis as well as parasites such as Taenia and Strongyloides. While the purpura is concerning, given the nonpalpable character along with a normal platelet count and coagulation studies, it may be reasonable to provisionally attribute it to high‐dose corticosteroid use.
He was admitted a fourth time a week after being discharged, with nausea, generalized weakness, and weight loss. At presentation, he had a blood pressure of 95/65 mmHg. His white blood cell count was 5,900/L, with 79% neutrophils and 20% bands. An AM cortisol was 18.8 /dL. He was thought to have adrenal insufficiency from steroid withdrawal, was treated with intravenous fluids and steroids, and discharged on a higher dose of prednisone at 60 mg daily. One week later, he again returned to the hospital with watery diarrhea, emesis, and generalized weakness. His blood pressure was 82/50 mmHg, and his abdomen appeared benign. He also had an erythematous rash over his mid‐abdomen. Laboratory data was significant for a sodium of 127 mmol/L, potassium of 3.0 mmol/L, chloride of 98 mmol/L, bicarbonate of 26 mmol/L, glucose of 40 mg/dL, lactate of 14 mmol/L, and albumin of 1.0 g/dL. Stool assay for Clostridium difficile was negative. A CT scan of the abdomen and pelvis showed small bilateral pleural effusions and small bowel fluid consistent with gastroenteritis, but without signs of obstruction. Esophagogastroduodenoscopy (EGD) showed bile backwash into the stomach, as well as inflammatory changes in the proximal and mid‐stomach, and inflammatory reaction and edema in the proximal duodenum. Colonoscopy showed normal appearing ileum and colon.
The patient's latest laboratory values appear to reflect his chronic illness and superimposed diarrhea. I am perplexed by his markedly elevated serum lactate value in association with a normal bicarbonate and low anion gap, and would repeat the lactate level to ensure this is not spurious. His hypoglycemia probably reflects a failure to adjust or discontinue his diabetic medications, although both hypoglycemia and type B lactic acidosis are occasionally manifestations of a paraneoplastic syndrome. The normal colonoscopy findings are helpful in exonerating the colon, provided the preparation was adequate. Presumably, the abnormal areas of the stomach and duodenum were biopsied; I remain suspicious that the answer may lie in the jejunum.
The patient was treated with intravenous fluids and stress‐dose steroids, and electrolyte abnormalities were corrected. Biopsies from the EGD and colonoscopy demonstrated numerous larvae within the mucosa of the body and antrum of the stomach, as well as duodenum. There were also rare detached larvae seen in the esophagus, and a few larvae within the ileal mucosa.
The patient appears to have Strongyloides hyperinfection, something he is at clear risk for, given his country of origin and his high‐dose corticosteroids. In retrospect, I was dissuaded from seriously considering a diagnosis of parasitic infection in large part because of the absence of peripheral eosinophilia, but this may not be seen in cases of hyperinfection. Additional clues, again in retrospect, were the repeated abscesses with bowel flora and the seemingly nonspecific abdominal rash. I would treat with a course of ivermectin, and carefully monitor his response.
The characteristics of the larvae were suggestive of Strongyloides species (Figure 3). A subsequent stool test for ova and parasites was positive for Strongyloides larvae. The patient was given a single dose of ivermectin. An endocrinology consultant felt that he did not have adrenal insufficiency, and it was recommended that his steroids be tapered off. He was discharged home once he clinically improved.
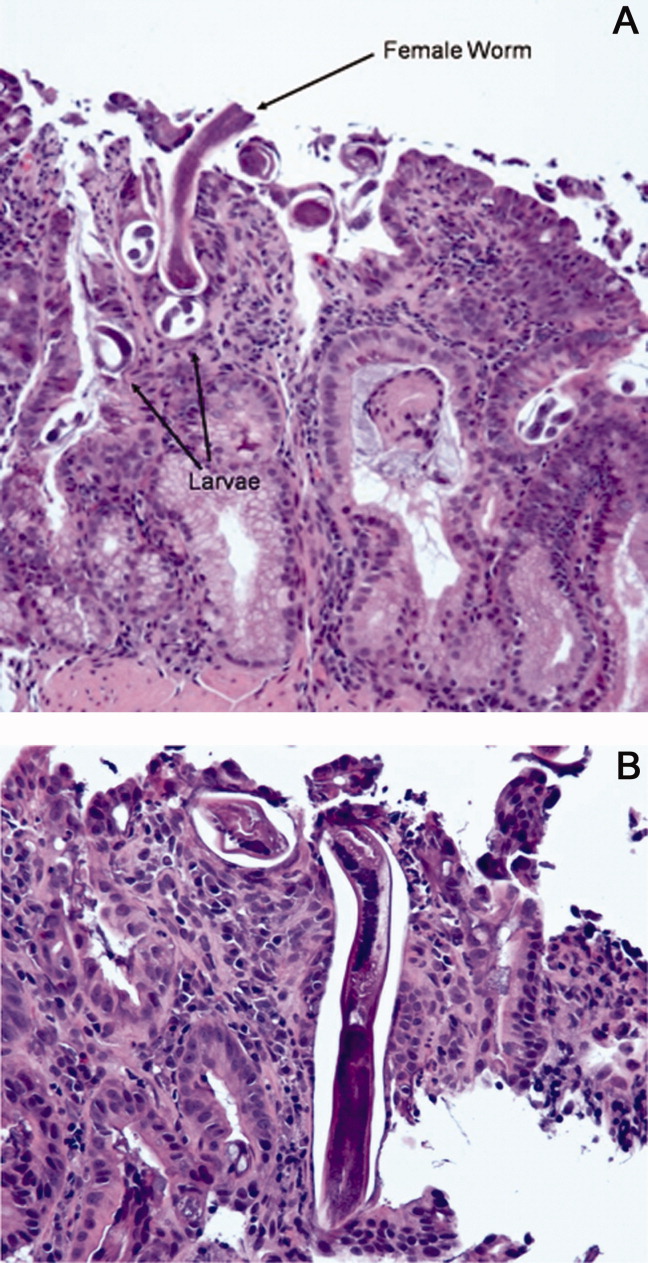
Although one or two doses of ivermectin typically suffices for uncomplicated strongyloidiasis, the risk of failure in hyperinfection mandates a longer treatment course. I don't believe this patient has been adequately treated, although the removal of his steroids will be helpful.
He was readmitted 3 days later with recrudescent symptoms, and his stool remained positive for Strongyloides. He received 2 weeks of ivermectin and albendazole, and was ultimately discharged to a rehabilitation facility after a complicated hospital stay. Nine months later, the patient was reported to be doing well.
COMMENTARY
This patient's immigration status from the developing world, high‐dose corticosteroid use, and complex clinical course all suggested the possibility of an underlying chronic infectious process. Although the discussant recognized this early on and later briefly mentioned strongyloidiasis as a potential cause of intestinal obstruction, the diagnosis of Strongyloides hyperinfection was not suspected until incontrovertible evidence for it was obtained on EGD. Failure to make the diagnosis earlier by both the involved clinicians and the discussant probably stemmed largely from two factors: the absence of eosinophilia; and lack of recognition that purpura may be seen in cases of hyperinfection, presumably reflecting larval infiltration of the dermis.1 Although eosinophilia accompanies most cases of stronglyloidiasis and may be very pronounced, patients with hyperinfection syndrome frequently fail to mount an eosinophilic response due to underlying immunosuppression, with eosinophilia absent in 70% of such patients in a study from Taiwan.2
Strongyloides stercoralis is an intestinal nematode that causes strongyloidiasis. It affects as many as 100 million people globally,3 mainly in tropical and subtropical areas, but is also endemic in the Southeastern United States, Europe, and Japan. Risk factors include male sex, White race, alcoholism, working in contact with soil (farmers, coal mine workers, etc.), chronic care institutionalization, and low socioeconomic status. In nonendemic regions, it more commonly affects travelers, immigrants, or military personnel.4, 5
The life cycle of S. stercoralis is complex. Infective larvae penetrate the skin through contact with contaminated soil, enter the venous system via lymphatics, and travel to the lung.4, 6 Here, they ascend the tracheobronchial tree and migrate to the gut. In the intestine, larvae develop into adult female worms that burrow into the intestinal mucosa. These worms lay eggs that develop into noninfective rhabditiform larvae, which are then expelled in the stool. Some of the rhabditiform larvae, however, develop into infective filariform larvae, which may penetrate colonic mucosa or perianal skin, enter the bloodstream, and lead to the cycle of autoinfection and chronic strongyloidiasis (carrier state). Autoinfection typically involves a low parasite burden, and is controlled by both host immune factors as well as parasitic factors.7 The mechanism of autoinfection can lead to the persistence of strongyloidiasis for decades after the initial infection, as has been documented in former World War II prisoners of war.8
Factors leading to the impairment of cell‐mediated immunity predispose chronically infected individuals to hyperinfection, as occurred in this patient. The most important of these are corticosteroid administration and Human T‐lymphotropic virus Type‐1 (HTLV‐1) infection, both of which cause significant derangement in TH1/TH2 immune system balance.5, 9 In the hyperinfection syndrome, the burden of parasites increases dramatically, leading to a variety of clinical manifestations. Gastrointestinal phenomena frequently predominate, including watery diarrhea, anorexia, weight loss, nausea/vomiting, gastrointestinal bleeding, and occasionally small bowel obstruction. Pulmonary manifestations are likewise common, and include cough, dyspnea, and wheezing. Cutaneous findings are not uncommon, classically pruritic linear lesions of the abdomen, buttocks, and lower extremities which may be rapidly migratory (larva currens), although purpura and petechiae as displayed by our patient appear to be under‐recognized findings in hyperinfection.2, 5 Gram‐negative bacillary meningitis has been well reported as a complication of migrating larvae, and a wide variety of other organs may rarely be involved.5, 10
The presence of chronic strongyloidiasis should be suspected in patients with ongoing gastrointestinal and/or pulmonary symptoms, or unexplained eosinophilia with a potential exposure history, such as immigrants from Southeast Asia. Diagnosis in these individuals is currently most often made serologically, although stool exam provides a somewhat higher specificity for active infection, at the expense of lower sensitivity.3, 11 In the setting of hyperinfection, stool studies are almost uniformly positive for S. stercoralis, and sputum may be diagnostic as well. Consequently, failure to reach the diagnosis usually reflects a lack of clinical suspicion.5
The therapy of choice for strongyloidiasis is currently ivermectin, with a single dose repeated once, 2 weeks later, highly efficacious in eradicating chronic infection. Treatment of hyperinfection is more challenging and less well studied, but clearly necessitates a more prolonged course of treatment. Many experts advocate treating until worms are no longer present in the stool; some have suggested the combination of ivermectin and albendazole as this patient received, although this has not been examined in controlled fashion.
The diagnosis of Strongyloides hyperinfection is typically delayed or missed because of the failure to consider it, with reported mortality rates as high as 50% in hyperinfection and 87% in disseminated disease.3, 12, 13 This patient fortunately was diagnosed, albeit in delayed fashion, proving the maxim better late than never. His case highlights the need for increased clinical awareness of strongyloidiasis, and specifically the need to consider the possibility of chronic Strongyloides infection prior to administering immunosuppressive medications. In particular, serologic screening of individuals from highly endemic areas for strongyloidiasis, when initiating extended courses of corticosteroids, seems prudent.13
Teaching Points
-
Chronic strongyloidiasis is common in the developing world (particularly Southeast Asia), and places infected individuals at significant risk of life‐threatening hyperinfection if not recognized and treated prior to the initiation of immunosuppressive medication, especially corticosteroids.
-
Strongyloides hyperinfection syndrome may be protean in its manifestations, but most commonly includes gastrointestinal, pulmonary, and cutaneous signs and symptoms.
A 59‐year‐old man presented to the emergency department with the acute onset of right‐sided abdominal and flank pain. The pain had begun the previous night, was constant and progressively worsening, and radiated to his right groin. He denied fever, nausea, emesis, or change in his bowel habits, but he did notice mild right lower quadrant discomfort with micturition. Upon further questioning, he also complained of mild dyspnea on climbing stairs and an unspecified recent weight loss.
The most common cause of acute severe right‐sided flank and abdominal pain radiating to the groin and associated with dysuria in a middle‐aged man is ureteral colic. Other etiologies important to consider include retrocecal appendicitis, pyelonephritis, and, rarely, a dissecting abdominal aortic aneurysm. This patient's seemingly recent onset exertional dyspnea and weight loss do not neatly fit any of the above, however.
His past medical history was significant for diabetes mellitus and pemphigus vulgaris diagnosed 7 months previously. He had been treated with prednisone, and the dose decreased from 100 to 60 mg daily, 1 month previously, due to poor glycemic control as well as steroid‐induced neuropathy and myopathy. His other medications included naproxen sodium and ibuprofen for back pain, azathioprine, insulin, pioglitazone, and glimiperide. He had no past surgical history. He had lived in the United States since his emigration from Thailand in 1971. His last trip to Thailand was 5 years previously. He was a taxi cab driver. He had a ten‐pack year history of tobacco use, but had quit 20 years prior. He denied history of alcohol or intravenous drug use.
Pemphigus vulgaris is unlikely to be directly related to this patient's presentation, but in light of his poorly controlled diabetes, his azathioprine use, and particularly his high‐dose corticosteroids, he is certainly immunocompromised. Accordingly, a disseminated infection, either newly acquired or reactivated, merits consideration. His history of residence in, and subsequent travel to, Southeast Asia raises the possibility of several diseases, each of which may be protean in their manifestations; these include tuberculosis, melioidosis, and penicilliosis (infection with Penicillium marneffei). The first two may reactivate long after initial exposure, particularly with insults to the immune system. The same is probably true of penicilliosis, although I am not certain of this. On a slightly less exotic note, domestically acquired infection with histoplasmosis or other endemic fungi is possible.
On examination he was afebrile, had a pulse of 130 beats per minute and a blood pressure of 65/46 mmHg. His oxygen saturation was 92%. He appeared markedly cushingoid, and had mild pallor and generalized weakness. Cardiopulmonary examination was unremarkable. His abdominal exam was notable for distention and hypoactive bowel sounds, with tenderness and firmness to palpation on the right side. Peripheral pulses were normal. Examination of the skin demonstrated ecchymoses over the bilateral forearms, and several healed pemphigus lesions on the abdomen and upper extremities.
The patient's severely deranged hemodynamic parameters indicate either current or impending shock, and resuscitative measures should proceed in tandem with diagnostic efforts. The cause of his shock seems most likely to be either hypovolemic (abdominal wall or intra‐abdominal hemorrhage, or conceivably massive third spacing from an intra‐abdominal catastrophe), or distributive (sepsis, or acute adrenal insufficiency if he has missed recent steroid doses). His ecchymoses may simply reflect chronic glucocorticoid use, but also raise suspicion for a coagulopathy. Provided the patient can be stabilized to allow this, I would urgently obtain a computed tomography (CT) scan of the abdomen and pelvis.
Initial laboratory studies demonstrated a hemoglobin of 9.1 g/dL, white blood cell count 8000/L with 33% bands, 48% segmented neutrophils, 18% lymphocytes, and 0.7% eosinophils, platelet count 356,000/L, sodium 128 mmol/L, BUN 52 mg/dL, creatinine 2.3 mg/dL, and glucose of 232 mg/dL. Coagulation studies were normal, and lactic acid was 1.8 mmol/L (normal range, 0.7‐2.1). Fibrinogen was normal at 591 and LDH was mildly elevated at 654 (normal range, 313‐618 U/L). Total protein and albumin were 3.6 and 1.9 g/dL, respectively. Total bilirubin was 0.6 mg/dL. Random serum cortisol was 20.2 g/dL. Liver enzymes, amylase, lipase, iron stores, B12, folate, and stool for occult blood were normal. Initial cardiac biomarkers were negative, but subsequent troponin‐I was 3.81 ng/mL (elevated, >1.00). Urinalysis showed 0‐4 white blood cells per high powered field.
The laboratory studies provide a variety of useful, albeit nonspecific, information. The high percentage of band forms on white blood cell differential further raises concern for an infectious process, although severe noninfectious stress can also cause this. While we do not know whether the patient's renal failure is acute, I suspect that it is, and may result from a variety of insults including sepsis, hypotension, and volume depletion. His moderately elevated troponin‐I likely reflects supplydemand mismatch or sepsis. I would like to see an electrocardiogram, and I remain very interested in obtaining abdominal imaging.
Chest radiography showed pulmonary vascular congestion without evidence of pneumothorax. Computed tomography scan of the abdomen and pelvis showed retroperitoneal fluid bilaterally (Figure 1). This was described as suspicious for ascites versus hemorrhage, but no obvious source of bleeding was identified. There was also a small amount of right perinephric fluid, but no evidence of a renal mass. The abdominal aorta was normal; there was no lymphadenopathy.

The CT image appears to speak against simple ascites, and seems most consistent with either blood or an infectious process. Consequently, the loculated right retroperitoneal collection should be aspirated, and fluid sent for fungal, acid‐fast, and modified acid‐fast (i.e., for Nocardia) stains and culture, in addition to Gram stain and routine aerobic and anaerobic cultures.
The patient was admitted to the intensive care unit. Stress‐dose steroids were administered, and he improved after resuscitation with fluid and blood. His renal function normalized. Urine and blood cultures returned negative. His hematocrit and multiple repeat CT scans of the abdomen remained stable. A retroperitoneal hemorrhage was diagnosed, and surgical intervention was deemed unnecessary. Both adenosine thallium stress test and echocardiogram were normal. He was continued on 60 mg prednisone daily and discharged home with outpatient follow‐up.
This degree of improvement with volume expansion (and steroids) suggests the patient was markedly volume depleted upon presentation. Although a formal adrenocorticotropic hormone (ACTH) stimulation test was apparently not performed, the random cortisol level suggests adrenal insufficiency was unlikely to have been primarily responsible. While retroperitoneal hemorrhage is possible, the loculated appearance of the collection suggests infection is more likely.
Three weeks later, he was readmitted with recurrent right‐sided abdominal and flank pain. His temperature was 101.3F, and he was tachycardic and hypotensive. His examination was similar to that at the time of his previous presentation. Laboratory data revealed white blood cell count of 13,100/L with 43% bands, hemoglobin of 9.2 g/dL, glucose of 343 mg/dL, bicarbonate 25 mmol/L, normal anion gap and renal function, and lactic acid of 4.5 mmol/L. Liver function tests were normal except for an albumin of 3.0 g/dL. CT scan of the abdomen revealed loculated retroperitoneal fluid collections, increased in size since the prior scan.
The patient is once again evidencing at least early shock, manifested in his deranged hemodynamics and elevated lactate level. I remain puzzled by the fact that he appeared to respond to fluids alone at the time of his initial hospital stay, unless adrenal insufficiency played a greater role than I suspected. Of note, acute adrenal insufficiency could explain much of the current picture, including fever, and bland (uninfected) hematomas are an underappreciated cause of both fever and leukocytosis. Having said this, I remain concerned that his retroperitoneal fluid collections represent abscesses. The most accessible of these should be sampled.
Aspiration of the retroperitoneal fluid yielded purulent material which grew Klebsiella pneumoniae. The cultures were negative for mycobacteria and fungus. Blood and urine cultures were negative. Drains were placed, and he was followed as an outpatient. His fever and leukocytosis subsided, and he completed a 6‐week course of trimethoprim‐sulfamethoxazole. CT imaging confirmed complete evacuation of the fluid.
Retroperitoneal abscesses frequently present in smoldering fashion, although patients may be quite ill by the time of presentation. Most of these are secondary, i.e., they arise from another abnormality in the retroperitoneum. Most commonly this is in the large bowel, kidney, pancreas, or spine. I would carefully scour his follow‐up imaging for additional clues and, if unrevealing, proceed to colonoscopy.
He returned 1 month after drain removal, with 2‐3 days of nausea and abdominal pain. His abdomen was moderately distended but nontender, and multiple persistent petechial and purpuric lesions were present on the upper back, chest, torso, and arms. Abdominal CT scan revealed small bowel obstruction and a collection of fluid in the left paracolic gutter extending into the left retrorenal space.
The patient does not appear to have obvious risk factors for developing a small bowel obstruction. No mention is made of the presence or absence of a transition point on the CT scan, and this should be ascertained. His left‐sided abdominal fluid collection is probably infectious in nature, and I continue to be suspicious of a large bowel (or distal small bowel) source, via either gut perforation or bacterial translocation. The collection needs to be percutaneously drained for both diagnostic and therapeutic reasons, and broadly cultured. Finally, we need to account for the described dermatologic manifestations. The purpuric/petechial lesions sound vasculitic rather than thrombocytopenic in origin based on location; conversely, they may simply reflect a corticosteroid‐related adverse effect. I would like to know whether the purpura was palpable, and to repeat a complete blood count with peripheral smear.
Laboratory data showed hemoglobin of 9.3 g/dL, a platelet count of 444,000/L, and normal coagulation studies. The purpura was nonpalpable (Figure 2). The patient had a nasogastric tube placed for decompression, with bilious drainage. His left retroperitoneal fluid was drained, with cultures yielding Enterococcus faecalis and Enterobacter cloacae. The patient was treated with a course of broad‐spectrum antibiotics. His obstruction improved and the retroperitoneal collection resolved on follow‐up imaging. However, 2 days later, he had recurrent pain; abdominal CT showed a recurrence of small bowel obstruction with an unequivocal transition point in the distal jejunum. A small fluid collection was noted in the left retroperitoneum with a trace of gas in it. He improved with nasogastric suction, his prednisone was tapered to 30 mg daily, and he was discharged home.
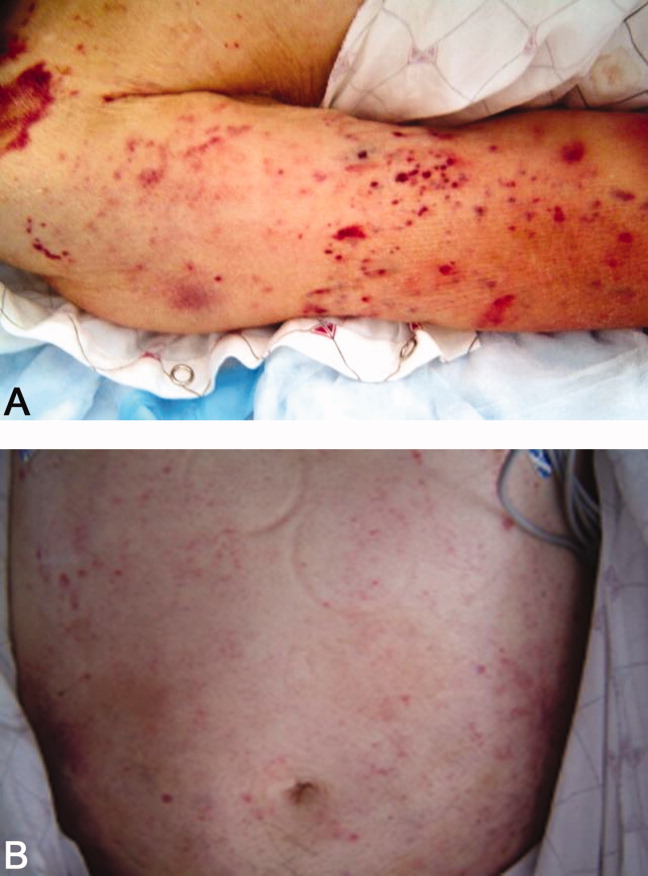
The isolation of both Enterococcus and Enterobacter species from his fluid collection, along with the previous isolation of Klebsiella, strongly suggest a bowel source for his recurrent abscesses. Based on this CT report, the patient has clear evidence of at least partial small bowel obstruction. He lacks a history of prior abdominal surgery or other more typical reasons for obstruction caused by extrinsic compression, such as hernia, although it is possible his recurrent abdominal infections may have led to obstruction due to scarring and adhesions. An intraluminal cause of obstruction also needs to be considered, with causes including malignancy (lymphoma, carcinoid, and adenocarcinoma), Crohn's disease, and infections including tuberculosis as well as parasites such as Taenia and Strongyloides. While the purpura is concerning, given the nonpalpable character along with a normal platelet count and coagulation studies, it may be reasonable to provisionally attribute it to high‐dose corticosteroid use.
He was admitted a fourth time a week after being discharged, with nausea, generalized weakness, and weight loss. At presentation, he had a blood pressure of 95/65 mmHg. His white blood cell count was 5,900/L, with 79% neutrophils and 20% bands. An AM cortisol was 18.8 /dL. He was thought to have adrenal insufficiency from steroid withdrawal, was treated with intravenous fluids and steroids, and discharged on a higher dose of prednisone at 60 mg daily. One week later, he again returned to the hospital with watery diarrhea, emesis, and generalized weakness. His blood pressure was 82/50 mmHg, and his abdomen appeared benign. He also had an erythematous rash over his mid‐abdomen. Laboratory data was significant for a sodium of 127 mmol/L, potassium of 3.0 mmol/L, chloride of 98 mmol/L, bicarbonate of 26 mmol/L, glucose of 40 mg/dL, lactate of 14 mmol/L, and albumin of 1.0 g/dL. Stool assay for Clostridium difficile was negative. A CT scan of the abdomen and pelvis showed small bilateral pleural effusions and small bowel fluid consistent with gastroenteritis, but without signs of obstruction. Esophagogastroduodenoscopy (EGD) showed bile backwash into the stomach, as well as inflammatory changes in the proximal and mid‐stomach, and inflammatory reaction and edema in the proximal duodenum. Colonoscopy showed normal appearing ileum and colon.
The patient's latest laboratory values appear to reflect his chronic illness and superimposed diarrhea. I am perplexed by his markedly elevated serum lactate value in association with a normal bicarbonate and low anion gap, and would repeat the lactate level to ensure this is not spurious. His hypoglycemia probably reflects a failure to adjust or discontinue his diabetic medications, although both hypoglycemia and type B lactic acidosis are occasionally manifestations of a paraneoplastic syndrome. The normal colonoscopy findings are helpful in exonerating the colon, provided the preparation was adequate. Presumably, the abnormal areas of the stomach and duodenum were biopsied; I remain suspicious that the answer may lie in the jejunum.
The patient was treated with intravenous fluids and stress‐dose steroids, and electrolyte abnormalities were corrected. Biopsies from the EGD and colonoscopy demonstrated numerous larvae within the mucosa of the body and antrum of the stomach, as well as duodenum. There were also rare detached larvae seen in the esophagus, and a few larvae within the ileal mucosa.
The patient appears to have Strongyloides hyperinfection, something he is at clear risk for, given his country of origin and his high‐dose corticosteroids. In retrospect, I was dissuaded from seriously considering a diagnosis of parasitic infection in large part because of the absence of peripheral eosinophilia, but this may not be seen in cases of hyperinfection. Additional clues, again in retrospect, were the repeated abscesses with bowel flora and the seemingly nonspecific abdominal rash. I would treat with a course of ivermectin, and carefully monitor his response.
The characteristics of the larvae were suggestive of Strongyloides species (Figure 3). A subsequent stool test for ova and parasites was positive for Strongyloides larvae. The patient was given a single dose of ivermectin. An endocrinology consultant felt that he did not have adrenal insufficiency, and it was recommended that his steroids be tapered off. He was discharged home once he clinically improved.
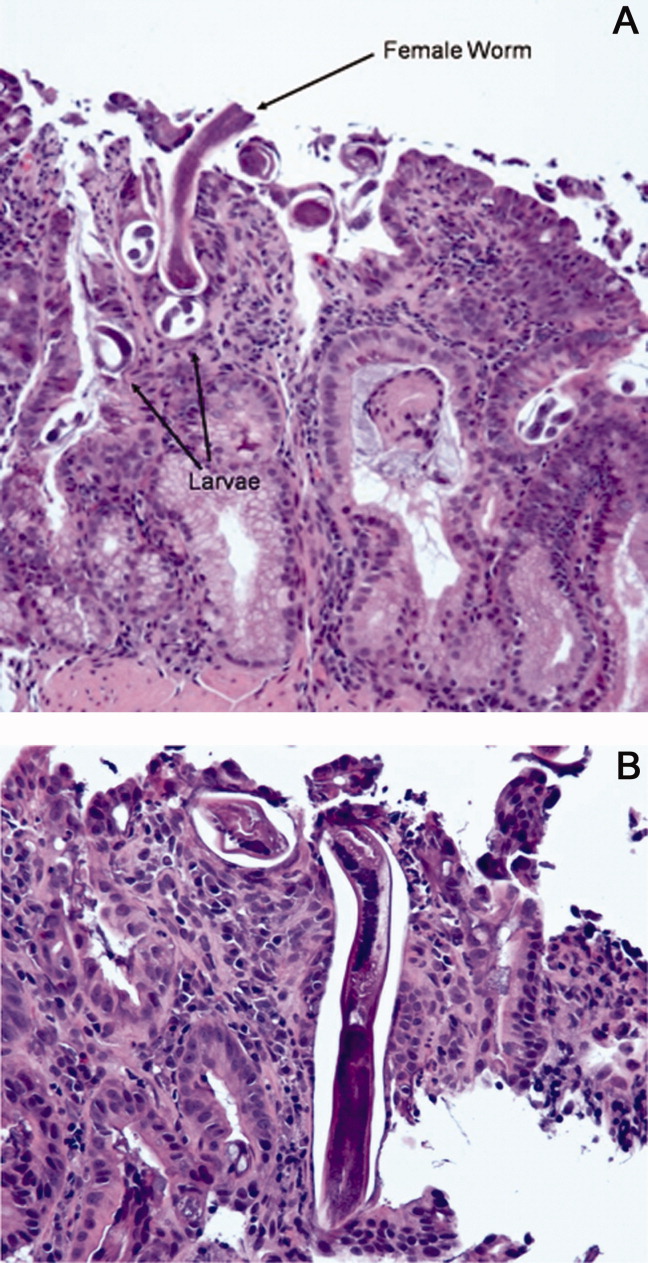
Although one or two doses of ivermectin typically suffices for uncomplicated strongyloidiasis, the risk of failure in hyperinfection mandates a longer treatment course. I don't believe this patient has been adequately treated, although the removal of his steroids will be helpful.
He was readmitted 3 days later with recrudescent symptoms, and his stool remained positive for Strongyloides. He received 2 weeks of ivermectin and albendazole, and was ultimately discharged to a rehabilitation facility after a complicated hospital stay. Nine months later, the patient was reported to be doing well.
COMMENTARY
This patient's immigration status from the developing world, high‐dose corticosteroid use, and complex clinical course all suggested the possibility of an underlying chronic infectious process. Although the discussant recognized this early on and later briefly mentioned strongyloidiasis as a potential cause of intestinal obstruction, the diagnosis of Strongyloides hyperinfection was not suspected until incontrovertible evidence for it was obtained on EGD. Failure to make the diagnosis earlier by both the involved clinicians and the discussant probably stemmed largely from two factors: the absence of eosinophilia; and lack of recognition that purpura may be seen in cases of hyperinfection, presumably reflecting larval infiltration of the dermis.1 Although eosinophilia accompanies most cases of stronglyloidiasis and may be very pronounced, patients with hyperinfection syndrome frequently fail to mount an eosinophilic response due to underlying immunosuppression, with eosinophilia absent in 70% of such patients in a study from Taiwan.2
Strongyloides stercoralis is an intestinal nematode that causes strongyloidiasis. It affects as many as 100 million people globally,3 mainly in tropical and subtropical areas, but is also endemic in the Southeastern United States, Europe, and Japan. Risk factors include male sex, White race, alcoholism, working in contact with soil (farmers, coal mine workers, etc.), chronic care institutionalization, and low socioeconomic status. In nonendemic regions, it more commonly affects travelers, immigrants, or military personnel.4, 5
The life cycle of S. stercoralis is complex. Infective larvae penetrate the skin through contact with contaminated soil, enter the venous system via lymphatics, and travel to the lung.4, 6 Here, they ascend the tracheobronchial tree and migrate to the gut. In the intestine, larvae develop into adult female worms that burrow into the intestinal mucosa. These worms lay eggs that develop into noninfective rhabditiform larvae, which are then expelled in the stool. Some of the rhabditiform larvae, however, develop into infective filariform larvae, which may penetrate colonic mucosa or perianal skin, enter the bloodstream, and lead to the cycle of autoinfection and chronic strongyloidiasis (carrier state). Autoinfection typically involves a low parasite burden, and is controlled by both host immune factors as well as parasitic factors.7 The mechanism of autoinfection can lead to the persistence of strongyloidiasis for decades after the initial infection, as has been documented in former World War II prisoners of war.8
Factors leading to the impairment of cell‐mediated immunity predispose chronically infected individuals to hyperinfection, as occurred in this patient. The most important of these are corticosteroid administration and Human T‐lymphotropic virus Type‐1 (HTLV‐1) infection, both of which cause significant derangement in TH1/TH2 immune system balance.5, 9 In the hyperinfection syndrome, the burden of parasites increases dramatically, leading to a variety of clinical manifestations. Gastrointestinal phenomena frequently predominate, including watery diarrhea, anorexia, weight loss, nausea/vomiting, gastrointestinal bleeding, and occasionally small bowel obstruction. Pulmonary manifestations are likewise common, and include cough, dyspnea, and wheezing. Cutaneous findings are not uncommon, classically pruritic linear lesions of the abdomen, buttocks, and lower extremities which may be rapidly migratory (larva currens), although purpura and petechiae as displayed by our patient appear to be under‐recognized findings in hyperinfection.2, 5 Gram‐negative bacillary meningitis has been well reported as a complication of migrating larvae, and a wide variety of other organs may rarely be involved.5, 10
The presence of chronic strongyloidiasis should be suspected in patients with ongoing gastrointestinal and/or pulmonary symptoms, or unexplained eosinophilia with a potential exposure history, such as immigrants from Southeast Asia. Diagnosis in these individuals is currently most often made serologically, although stool exam provides a somewhat higher specificity for active infection, at the expense of lower sensitivity.3, 11 In the setting of hyperinfection, stool studies are almost uniformly positive for S. stercoralis, and sputum may be diagnostic as well. Consequently, failure to reach the diagnosis usually reflects a lack of clinical suspicion.5
The therapy of choice for strongyloidiasis is currently ivermectin, with a single dose repeated once, 2 weeks later, highly efficacious in eradicating chronic infection. Treatment of hyperinfection is more challenging and less well studied, but clearly necessitates a more prolonged course of treatment. Many experts advocate treating until worms are no longer present in the stool; some have suggested the combination of ivermectin and albendazole as this patient received, although this has not been examined in controlled fashion.
The diagnosis of Strongyloides hyperinfection is typically delayed or missed because of the failure to consider it, with reported mortality rates as high as 50% in hyperinfection and 87% in disseminated disease.3, 12, 13 This patient fortunately was diagnosed, albeit in delayed fashion, proving the maxim better late than never. His case highlights the need for increased clinical awareness of strongyloidiasis, and specifically the need to consider the possibility of chronic Strongyloides infection prior to administering immunosuppressive medications. In particular, serologic screening of individuals from highly endemic areas for strongyloidiasis, when initiating extended courses of corticosteroids, seems prudent.13
Teaching Points
-
Chronic strongyloidiasis is common in the developing world (particularly Southeast Asia), and places infected individuals at significant risk of life‐threatening hyperinfection if not recognized and treated prior to the initiation of immunosuppressive medication, especially corticosteroids.
-
Strongyloides hyperinfection syndrome may be protean in its manifestations, but most commonly includes gastrointestinal, pulmonary, and cutaneous signs and symptoms.
- ,,, et al.Disseminated strongyloidiasis in immunocompromised patients—report of three cases.Int J Dermatol.2009;48(9):975–978.
- ,,, et al.Clinical manifestations of strongyloidiasis in southern Taiwan.J Microbiol Immunol Infect.2002;35(1):29–36.
- ,.Diagnosis of Strongyloides stercoralis infection.Clin Infect Dis.2001;33(7):1040–1047.
- ,,.Intestinal strongyloidiasis and hyperinfection syndrome.Clin Mol Allergy.2006;4:8.
- ,.Strongyloides stercoralis in the immunocompromised population.Clin Microbiol Rev.2004;17(1):208–217.
- ,,.Intestinal strongyloidiasis: recognition, management and determinants of outcome.J Clin Gastroenterol2005;39(3):203–211.
- .Dysregulation of strongyloidiasis: a new hypothesis.Clin Microbiol Rev.1992;5(4):345–355.
- ,,,.Consequences of captivity: health effects of Far East imprisonment in World War II.Q J Med.2009;102:87–96.
- ,,,.Strongyloides hyperinfection syndrome: an emerging global infectious disease.Trans R Soc Trop Med Hyg.2008;102(4):314–318.
- ,,,,,.Strongyloides hyperinfection presenting as acute respiratory failure and Gram‐negative sepsis.Chest.2005;128(5):3681–3684.
- ,,, et al.Use of enzyme‐linked immunosorbent assay and dipstick assay for detection of Strongyloides stercoralis infection in humans.J Clin Microbiol.2007;45:438–442.
- ,,,,,.Complicated and fatal Strongyloides infection in Canadians: risk factors, diagnosis and management.Can Med Assoc J.2004;171:479–484.
- ,,, et al.Maltreatment of Strongyloides infection: case series and worldwide physicians‐in‐training survey.Am J Med.2007;120(6):545.e1–545.e8.
- ,,, et al.Disseminated strongyloidiasis in immunocompromised patients—report of three cases.Int J Dermatol.2009;48(9):975–978.
- ,,, et al.Clinical manifestations of strongyloidiasis in southern Taiwan.J Microbiol Immunol Infect.2002;35(1):29–36.
- ,.Diagnosis of Strongyloides stercoralis infection.Clin Infect Dis.2001;33(7):1040–1047.
- ,,.Intestinal strongyloidiasis and hyperinfection syndrome.Clin Mol Allergy.2006;4:8.
- ,.Strongyloides stercoralis in the immunocompromised population.Clin Microbiol Rev.2004;17(1):208–217.
- ,,.Intestinal strongyloidiasis: recognition, management and determinants of outcome.J Clin Gastroenterol2005;39(3):203–211.
- .Dysregulation of strongyloidiasis: a new hypothesis.Clin Microbiol Rev.1992;5(4):345–355.
- ,,,.Consequences of captivity: health effects of Far East imprisonment in World War II.Q J Med.2009;102:87–96.
- ,,,.Strongyloides hyperinfection syndrome: an emerging global infectious disease.Trans R Soc Trop Med Hyg.2008;102(4):314–318.
- ,,,,,.Strongyloides hyperinfection presenting as acute respiratory failure and Gram‐negative sepsis.Chest.2005;128(5):3681–3684.
- ,,, et al.Use of enzyme‐linked immunosorbent assay and dipstick assay for detection of Strongyloides stercoralis infection in humans.J Clin Microbiol.2007;45:438–442.
- ,,,,,.Complicated and fatal Strongyloides infection in Canadians: risk factors, diagnosis and management.Can Med Assoc J.2004;171:479–484.
- ,,, et al.Maltreatment of Strongyloides infection: case series and worldwide physicians‐in‐training survey.Am J Med.2007;120(6):545.e1–545.e8.
Outcomes of a Mobile ACE Service
The traditional acute care for the elderly (ACE) unit has demonstrated improved functional outcomes without increased costs or changes in length of stay (LOS).15 It is, however, limited in scope to only those patients cared for on a fixed geographical unit. This structural limitation is of increasing relevance in times of high hospital bed occupancy rates, as during such times, many appropriate older patients are admitted elsewhere. In our experience with a traditional ACE unit‐based model, only 52% of our geriatrics practice patients were admitted to an ACE unit bed, while the remainder were admitted to various medical units throughout the hospital. We therefore abandoned our traditional unit‐based ACE service in July 2007 in favor of a mobile ACE (MACE) service, bringing the interdisciplinary, patient‐centered team approach to our hospitalized older adult patients admitted throughout the hospital.
The purpose of this study is to compare the operational and quality outcomes for patients cared for on the MACE service to those cared for on a unit‐based ACE service and matched controls cared for on other general medical services. We hypothesized that the MACE service would be associated with lower lengths of stay, reduced costs, and decreased rehospitalization rates.
METHODS
The MACE team was composed of a geriatrician‐hospitalist, geriatric medicine fellow, social worker, and nurse coordinator. The geriatric medicine attending on the MACE service was in the hospital providing patient care during regular working hours from Monday through Friday, while the weekends were covered by a rotating group of all geriatric medicine faculty. During the first and second years of MACE, there were 7 and 4 attendings, respectively; all fellowship‐trained geriatricians. Three of the 4 geriatric medicine hospitalists during year 2 had been in practice between 1 and 3 years postfellowship and also had training in palliative medicine, although were not board‐certified in the latter. The fourth hospitalist had been in practice for 5 years postfellowship. The interdisciplinary team met daily to discuss the care of all patients and used a transitional care model based on The Care Transitions Program6 adapted to our institution, with a focus on reducing the risks of hazards of hospitalization. Care coordination with the outpatient practice, early family meetings, discharge planning, patient and caregiver education, and postdischarge follow‐up phone calls were some of the key hallmarks of the service (Table 1).
| Team member(s) | Roles |
|---|---|
| |
| Team (MD, fellow, NC,SW) | Scheduled daily meetings at 8 am (or 8 am and 2 pm if needed) to discuss each patient's care and discharge plan |
| NC | Introduces the team to the patient/caregiver upon admission |
| Obtains prehospitalization information on cognitive and functional status | |
| Acts as a hospital coach educating the patient/caregiver | |
| Completes PRIs necessary for discharge to other institutions | |
| Completes medication reconciliation prior to discharge | |
| Initiates post‐discharge phone call and communicates with PCP via EMR | |
| Provides experiential one‐to‐one geriatric nursing education | |
| SW | Arranges family meeting, when indicated, with the team early in the hospitalization |
| Provides patient and family psychosocial support on an as needed basis | |
| Responsible for discharge planning | |
| MD | Attending physician of record |
| Communicates with PCP upon admission of the patient | |
| Assures discharge communiqu to PCP via EMR within 24 hours of discharge | |
We conducted a retrospective cohort study with propensity‐score matching in an urban academic medical center. Study subjects comprised 5 distinct groups. First were community‐dwelling older adults cared for at our outpatient geriatrics ambulatory practice who were discharged from our traditional ACE unit‐based acute care service at the Mount Sinai Hospital from July 1, 2006 through June 30, 2007 (N = 450). Second and third were patients from the same practice discharged from our MACE service during the first 2 years of operation (N = 556 from July 1, 2007 through June 30, 2008, and N = 501 from July 1, 2008 through June 30, 2009). Fourth and fifth were control cohorts of hospitalized older adults discharged from other medical services at the Mount Sinai Hospital during these same 2 years (N = 4863 and N = 4777, respectively). The average daily census on all services was 1012 patients.
Some patients on all 3 services are co‐managed with house staff, who are responsible for writing physician orders. Control cohort patients were cared for by a mix of private attendings (approximately 75%) or hospitalists (25%), and in contradistinction to MACE patients, their typical care did not include daily interdisciplinary team rounds, a nurse coordinator, or geriatrics fellow. Social work and case management were unit‐ as opposed to team‐based. Care on the ACE unit‐based service differed from care for matched control patients by having daily interdisciplinary team rounds, a prepared environment, and nursing‐led protocols for the patients on the ACE unit.
Because the ACE unit‐based service admitted both patients who were and were not cared for in our ambulatory practice, while the MACE service admitted only patients cared for in the ambulatory practice, we deleted from the study sample the patients who did not have a visit to our outpatient practice before the index hospitalization. This allowed us to isolate the effect of the model of care itself as opposed to the effect of simply changing the patient base for admissions. We then merged the files with the hospital's administrative database and electronic billing system to obtain demographic and claims data.
Additional demographic data were obtained through chart review of the MACE patients during year 1. The chart review process was standardized using a data abstraction instrument and by determining inter‐rater reliability of the individual data abstractors (comprised of author B.K. and 4 MACE team members).
Costs were assigned to individual admissions by the hospital's cost reporting system and include a combination of traceable costs (such as imaging, laboratory, and pharmacy) and applied costs (nursing; allocated based on geographic location in the hospital) to arrive at direct and total costs.
We made 3 distinct comparisons of operational and quality outcomes using the above 5 groups, first comparing patients cared for on our traditional ACE unit‐based service to those cared for on the MACE service, and second and third comparing patients on the MACE service to propensity score‐matched controls during the first and second year of operations. Specifically, we hypothesized that the MACE service would be associated with reduced LOS, costs, and readmission rates compared with the ACE unit‐based service and the matched control groups. We used multivariate logistic regression to estimate the association of binary quality outcomes (mortality during the hospital stay, 7‐ and 30‐day readmission rates) with the existence of MACE while adjusting for confounding variables which included patient demographic and clinical characteristics such as age, gender, race, total number of comorbidities (calculated by Elixhauser method that includes 30 categories of comorbid illnesses identified by secondary diagnosis codes and discharge diagnosis‐related groups [DRGs]).7 We considered the clustering effect due to the same attending physician into the model as well. While adjusting for the same covariates, we used generalized linear models with a gamma distribution and log link to estimate the association of continuous variables (costs and LOS) with the existence of MACE.
The same statistical methods were applied to the second and third comparisons between patients cared for on the MACE and the propensity score‐matched cohorts for the first and second year of the MACE service. First, 2 control cohorts (N = 6148 and 5803 of our hospital discharges from July 1, 2007 to June 30, 2008, and July 1, 2008 to June 30, 2009, respectively, with age > 64 and with the identical DRG and All Patient Refined DRG (APR DRG) Severity of Illness (SOI) score as those of the MACE groups were obtained from our hospital's administrative database to reduce the selection bias. Then, 4863 patients within the first cohort (N = 6148) and 4777 patients within the second cohort (N = 5,803) with the closest propensity score were matched to 545 of 556 MACE patients and 494 of 501 MACE patients, respectively, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score.
Propensity scores were determined by logistic regression on whether patients were admitted to the MACE. The covariates for the propensity model were the same as the previously stated adjusting variables. Usual care patients' data were weighted to account for the one‐to‐many propensity score‐matching algorithm.
We similarly conducted a post hoc analysis of MACE compared with a subgroup control cohort of patients cared for by medicine hospitalists in year 1 (N = 1175) and year 2 (N = 1564), with age > 64 and with the identical DRG and APR DRG SOI as those of the MACE group. We then matched 1012 of the 1175 discharges with the closest propensity score to 389 of the 411 MACE discharges who were cared for by 1 of the 4 geriatric medicine hospitalists in year 1 and 1308 of the 1564 discharges to 471 of the 501 MACE discharges in year 2, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score, using the same covariates described above.
All analyses were done using Stata software, version 9.2 (StataCorp LP, College Station, TX). This project was exempted by the Institutional Review Board at Mount Sinai School of Medicine, New York, New York.
RESULTS
Table 2 presents the characteristics of the study subjects in all 5 groups. Patients cared for on the ACE unit‐based service and the MACE service in years 1 and 2 were very similar, with a mean age of 82.6, 83.2, and 83.6 years; 74.4%, 75.9%, and 76.7% were female; and mean Elixhauser comorbidity scores were 3.4, 3.3, and 3.5, respectively. Patients in the 2 matched control groups were likewise very similar to those in the matched MACE groups with regard to all demographic variables.
| Demographics | ACE (N = 450) | Matched MACE year 1 (N = 545) | Matched controls year 1 (N = 4863) | Matched MACE year 2 (N = 494) | Matched controls year 2 (N = 4777) |
|---|---|---|---|---|---|
| |||||
| Age SD | 82.6 8.4 | 83.2 8.3 | 83.4 8.8 | 83.6 8.1 | 83.8 8.5 |
| Female, % | 74.4% | 75.9% | 74.7% | 76.7% | 77.4% |
| Race, % | |||||
| White | 35 | 37 | 36 | 43 | 42 |
| Black | 30 | 27 | 28 | 25 | 25 |
| Hispanic | 33 | 34 | 35 | 28 | 30 |
| Asian | 1 | 1 | 1 | 3 | 3 |
| Marital status, % | |||||
| Married | 20 | 20 | 21 | 23 | 23 |
| Widowed | 44 | 45 | 44 | 46 | 38 |
| Single | 25 | 22 | 27 | 21 | 28 |
| Elixhauser comorbidity index mean (SD) | 3.4 (1.8) | 3.4 (1.6) | 3.3 (1.7) | 3.5 (1.7) | 3.5 (1.7) |
| Hypertension, % | 61 | 54 | 54 | 49 | 49 |
| Heart Failure, % | 25 | 27 | 28 | 26 | 27 |
| Diabetes Mellitus, % | 26 | 25 | 25 | 24 | 25 |
| Atrial fibrillation, % | 22 | 23 | 23 | 28 | 27 |
| Chronic obstructive pulmonary disease, % | 15 | 15 | 15 | 15 | 14 |
Chart review of the year 1 MACE discharges revealed that 70% spoke English as their primary language and 46% had cognitive impairment. Most lived at home alone (49%) or with family members (41%) while receiving some paid caregiver help (59%). The remaining 10% were admitted from either an assisted living facility (5%) or subacute rehabilitation (5%). Only 12% were wheelchair or bed‐bound, while 21% ambulated without and 67% with an assistive device. Their functional status was limited, with 58% dependent for both ADLs and IADLs, 22% dependent for IADLs only, and 20% independent in both. They had relatively high prescription medication burdens, with 10% taking 05, 34% taking 610, 38% taking 1115, and 18% taking >15 medications.
Patients cared for by the MACE service had an adjusted 2.1 days shorter LOS (P 0.001) when compared with patients cared for on the ACE unit service. Additionally, there was a net savings of $2872 in total costs per hospitalization (P = 0.002), $1094 in direct costs (P = 0.016), $849 in nursing costs (P 0.001), and $237 in pharmacy costs (P = 0.002). Imaging and laboratory costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
| MACE to ACE | MACE to matched controls, year 1 | MACE to matched controls, year 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MACE (N = 556) | ACE (N = 450) | P value | MACE (N = 545) | Matched controls (N = 4863) | P value | MACE (N = 494) | Matched controls (N = 4777) | P value | |
| |||||||||
| LOS, days | 5.8 | 7.9 | 0.001 | 5.8 | 6.5 | 0.15 | 5.6 | 7.2 | 0.001 |
| Costs, $ | |||||||||
| Total | 10315 | 13187 | 0.002 | 10311 | 12764 | 0.001 | 10693 | 15636 | 0.001 |
| Direct | 4777 | 5871 | 0.016 | 4778 | 5620 | 0.03 | 4967 | 7048 | 0.001 |
| Nursing | 2361 | 3210 | 0.001 | 2356 | 2749 | 0.026 | 2143 | 3080 | 0.001 |
| Imaging | 342 | 332 | 0.61 | 344 | 349 | 0.73 | 382 | 471 | 0.06 |
| Laboratory | 206 | 243 | 0.079 | 206 | 245 | 0.029 | 213 | 281 | 0.001 |
| Pharmacy | 598 | 835 | 0.002 | 597 | 662 | 0.63 | 563 | 786 | 0.03 |
| In‐hospital mortality,% | 3.3 | 3.9 | 0.66 | 2.9 | 2.6 | 0.3 | 5.3 | 3.6 | 0.053 |
| 7‐day readmission,% | 9.3 | 10.2 | 0.55 | 9.7 | 11.8 | 0.3 | 4.8 | 5.5 | 0.71 |
| 30‐day readmission, % | 23.6 | 25.9 | 0.5 | 23.8 | 24.3 | 0.65 | 21.1 | 20.9 | 0.62 |
| 90‐day readmission, % | 40.9 | 38.7 | 0.1 | 41.3 | 38.4 | 0.005 | 38.0 | 36.5 | 0.74 |
There was no difference in LOS between the MACE patients during the first year of service compared with propensity score‐matched control patients (5.8 vs 6.5 days). There was, however, a net savings of $2453 in total costs per hospitalization (P 0.001), $842 (P = 0.03) in direct costs, $393 in nursing costs (P = 0.026), and $39 in laboratory costs (P = 0.029). Imaging and pharmacy costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day or 30‐day readmission rates between the 2 groups. However, the 90‐day readmission rate was higher in MACE patients (Table 3).
During the second year of the MACE service, however, there was a significant reduction in LOS of 1.6 days (P 0.001), a net savings of $4943 in total costs per hospitalization (P 0.001), $2081 (P 0.001) in direct costs, $937 in nursing costs (P 0.001), $68 in laboratory costs (P 0.001), and $223 in pharmacy costs (P = 0.03). There were no significant differences in imaging costs, in‐hospital mortality, and 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
A subgroup analysis of the first and second year comparisons including only those patients in the control groups cared for by medicine hospitalists demonstrated reductions in the MACE in total cost in year 1 and LOS, mortality, total, and nursing costs in year 2. However, in year 1, the 30‐day and 90‐day readmission rates were increased in the MACE compared with the control group (Table 4).
| MACE, year 1 (N = 389) | Matched controls, year 1 (N = 1012) | P Value | MACE, year 2 (N = 471) | Matched controls, year 2 (N = 1308) | P Value | |
|---|---|---|---|---|---|---|
| ||||||
| LOS, days | 6.0 | 6.0 | 0.34 | 5.7 | 6.9 | 0.001 |
| Costs, $ | ||||||
| Total | 10663 | 11599 | 0.049 | 10681 | 13493 | 0.001 |
| Direct | 4952 | 4704 | 0.98 | 4956 | 5618 | 0.055 |
| Nursing | 2394 | 2454 | 0.19 | 2124 | 2744 | 0.001 |
| Imaging | 349 | 322 | 0.63 | 387 | 390 | 0.82 |
| Laboratory | 213 | 199 | 0.49 | 212 | 225 | 0.47 |
| Pharmacy | 647 | 616 | 0.85 | 547 | 654 | 0.22 |
| In‐hospital mortality,% | 2.9 | 2.3 | 0.77 | 2.6 | 3.4 | 0.005 |
| 7‐Day readmission,% | 8.1 | 6.4 | 0.17 | 3.9 | 4.1 | 0.97 |
| 30‐Day readmission, % | 22.0 | 17.1 | 0.013 | 20.9 | 20.8 | 0.75 |
| 90‐Day readmission, % | 40.2 | 32.4 | 0.013 | 39.1 | 38.7 | 0.86 |
We found no differences in a separate post hoc subgroup analysis assessing whether a 3‐month nurse coordinator's leave of absence during year 1 affected year 1 results. The service size was unaffected by her absence, and all patients continued to receive daily visits by the attending and fellow. During this time, other team members took over many of the nurse coordinator roles, except for the postdischarge phone calls.
DISCUSSION
Older adults constitute a disproportionate share of hospital admissions and hospital days. They typically have multiple comorbid conditions, higher rates of cognitive impairment and functional dependence, and complex social situations that all increase their risk of adverse outcomes. Current efforts for national healthcare reform focus on the combined economic and quality imperatives to improve the care of hospitalized older adults. Given the increasing representation of this fastest growing segment of the population in the acute care setting, the geographical unit‐based model for care delivery is untenable in many circumstances. Therefore, we developed a mobile ACE service in an effort to provide the geriatric‐focused acute care found on ACE units to older adults admitted to any medical unit in the hospital.
Our study compared operational and quality outcomes for older patients cared for by our mobile ACE service to those cared for on the unit‐based ACE service and other general medical services. We found a significant reduction in both LOS and costs in all 3 comparisons, except for LOS during the first year of the mobile ACE service. This heightened efficiency was not associated with changes in the quality measures of in‐hospital mortality and 7‐ and 30‐day readmission rates, though the 90‐day readmission rate was slightly higher for the MACE in year 1.
The adjusted total cost savings per admission in years 1 and 2 of approximately $2400 ($12,764 vs $10,311) and $4900 ($15,636 vs $10,693), respectively, translate into an overall annual savings of roughly $1,200,000 (500 patients $2400/patient) in year 1 and $2,450,000 (500 patients $4,900/patient) in year 2. The only relevant cost of the MACE service model compared with the comparison groups is the nurse coordinator salary and benefits, which are paid for by the hospital (as job responsibilities include participation in nursing department quality improvement projects and nursing education) and would not meaningfully offset these savings. The team social worker is a re‐allocation of existing hospital resources, whose salary line is likewise paid for by the hospital.
Our study has several important limitations. First, we lack data on readmissions to other hospitals. Our readmission rates are high compared with the national 19.6% 30‐day Medicare readmission rate cited in a recent study, and we failed to show significant reductions in in‐hospital mortality or 7‐ or 30‐day readmission rates.10 This lack of benefit may be related to control group patients, some of whom receive their community care outside of our institution, being more likely to be readmitted to other hospitals compared with our MACE patients, who were all receiving their ambulatory care in our associated faculty practice. In addition, the high readmission rate on the MACE service may be driven by a relatively small number of patients who are frequently admitted. For example, of the 363 unique MACE patients from year 2, 22 had 3 and 11 had 4 or 5 admissions. We are currently evaluating these 33 patients who accounted for 22% of the admissions to better understand the causes.
A second limitation of the study is selection bias. While patients were very well‐matched through propensity scoring and had identical DRG and DRG‐SOI levels (the latter having been demonstrated in a previous study's regression analysis to be the leading correlate of LOS and cost),9 there may be unaccounted for differences between the patients cared for on the MACE and in the control group. A third limitation is the external validity of our study, which took place in a single large academic medical center in New York City. While the MACE model may very well be readily adaptable elsewhere, numerous studies have demonstrated wide variation in medical practice patterns and healthcare use which may influence the exportability of the model.11, 12 However, our LOS of 5.8 and 5.6 days in years 1 and 2 of the MACE service, respectively, are similar to national data of 5.6 days for hospitalized adults >74 years of age.13
Benefits in cost and LOS reductions may be, in part, due to the hospitalist nature of the model as hospital medicine literature has demonstrated similar reductions for Medicare patients of approximately $1000 and 0.5 days per admission.8, 9 Our findings support this hypothesis as the LOS reduction was not present during the first year of our MACE service during which the hospitalist model was not fully implemented. During this transition phase from the unit‐based ACE to the mobile ACE service, there were 4 physicians who covered more than 75% of on‐service time (10 of the 13 annual 4‐week rotations), while the remaining 25% was covered by 3 physicians (each working 1 block). The following year (July 2008 to June 2009), during which an LOS reduction was demonstrated, a full geriatric medicine hospitalist model was in effect, with patients on the MACE service cared for 100% of the time (excluding weekends) by 1 of 4 geriatric medicine hospitalists. By comparison, 22% and 29% of control group patients were cared for by medicine hospitalists during years 1 and 2, respectively. In addition to this transition to a hospitalist model, there may have been other undefined service improvements over the first year which contributed to the LOS and total cost reductions achieved in year 2 in the hospitalist subgroup analysis. Likewise, the increased 90‐day readmission rates seen in year 1 but not in year 2 in both the main and hospitalist subgroup analyses may be related to MACE service improvements over time. A more vigorous proactive intervention beyond the follow‐up phone call is likely needed to impact 90‐day readmissions.
LOS reductions may also have been related to the interdisciplinary team‐based approach in which a need for family meetings to address goals of care or assess and attempt to resolve complex family/living situations was identified early in the course of hospitalization. Likewise, in New York State, the application process for discharge to a postacute care setting begins with the completion of a Patient Review Instrument (PRI), which contains detailed information on the patient's physical, medical, and cognitive status. The MACE model circumvents the traditional case manager's role of completing the PRI by having the MACE nurse coordinator trained and certified to do so. The daily or twice daily MACE team meeting may have enabled more timely initiation of this early step in the discharge process for these patients, ultimately resulting in a reduced LOS.
An important concern this study is not able to address is whether LOS reductions are achieved at a price of impaired functional status. A prospective longitudinal study on the outcomes of patients cared for by a MACE service that includes detailed assessments of functional status based upon information gathered during admission and postdischarge during follow‐up phone calls is needed to properly evaluate this possibility.
Given the lack of wide‐spread adoption of the traditional ACE unit‐based model of care and its inherent limitations in the setting of high occupancy rates, a mobile ACE service may prove useful in providing high quality clinical care with reduced LOS and costs. This team‐based, as opposed to unit‐based, approach benefits from having low entry costs, as hospital administration can re‐allocate existing resources to fit the model and avoid costly capital investments in specialized unit design and outfitting. Further research should include metrics on functional status, all‐hospital readmission rates, and patient/caregiver satisfaction to better assess the feasibility of this acute care model.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.Do acute care for elders units increase hospital costs? A cost analysis using the hospital perspective.J Am Geriatr Soc.1997;45:729–734.
- ,,, et al.Effects of multicomponent intervention of functional outcomes and process of care in hospitalized older patients: a randomized controlled trial of acute care for elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1578.
- ,,,.A medical unit for the acute care of the elderly.J Am Geriatr Soc.1994;42:545–552
- ,,, et al.A randomized trial of care in a hospital medicine unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1342.
- ,,,.The care transitions intervention.Arch Intern Med.2006;166:1822–1828.
- ,,,.Comorbidity measures for use with administrative data.Med Care.1998;36:8–27.
- ,,.The effect of full‐time faculty hospitalists on the efficiency of care at a community teaching hospital.Ann Intern Med.1998;129:197–203.
- ,,,,,.The value of a hospitalist service.Chest.2001;19:580–589.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med.2009;360:1418–1428.
- ,,.Slowing the growth of health care costs ‐ lessons from regional variation.N Engl J Med.2009;360:849–852.
- ,,, et al.Fostering accountable health care: moving forward in Medicare.Health Aff (Millwood).2009;28:w219–w231.
- Centers for Disease Control and Prevention. Health, United States, 2009. Table 102. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. Accessed June 10,2010.
The traditional acute care for the elderly (ACE) unit has demonstrated improved functional outcomes without increased costs or changes in length of stay (LOS).15 It is, however, limited in scope to only those patients cared for on a fixed geographical unit. This structural limitation is of increasing relevance in times of high hospital bed occupancy rates, as during such times, many appropriate older patients are admitted elsewhere. In our experience with a traditional ACE unit‐based model, only 52% of our geriatrics practice patients were admitted to an ACE unit bed, while the remainder were admitted to various medical units throughout the hospital. We therefore abandoned our traditional unit‐based ACE service in July 2007 in favor of a mobile ACE (MACE) service, bringing the interdisciplinary, patient‐centered team approach to our hospitalized older adult patients admitted throughout the hospital.
The purpose of this study is to compare the operational and quality outcomes for patients cared for on the MACE service to those cared for on a unit‐based ACE service and matched controls cared for on other general medical services. We hypothesized that the MACE service would be associated with lower lengths of stay, reduced costs, and decreased rehospitalization rates.
METHODS
The MACE team was composed of a geriatrician‐hospitalist, geriatric medicine fellow, social worker, and nurse coordinator. The geriatric medicine attending on the MACE service was in the hospital providing patient care during regular working hours from Monday through Friday, while the weekends were covered by a rotating group of all geriatric medicine faculty. During the first and second years of MACE, there were 7 and 4 attendings, respectively; all fellowship‐trained geriatricians. Three of the 4 geriatric medicine hospitalists during year 2 had been in practice between 1 and 3 years postfellowship and also had training in palliative medicine, although were not board‐certified in the latter. The fourth hospitalist had been in practice for 5 years postfellowship. The interdisciplinary team met daily to discuss the care of all patients and used a transitional care model based on The Care Transitions Program6 adapted to our institution, with a focus on reducing the risks of hazards of hospitalization. Care coordination with the outpatient practice, early family meetings, discharge planning, patient and caregiver education, and postdischarge follow‐up phone calls were some of the key hallmarks of the service (Table 1).
| Team member(s) | Roles |
|---|---|
| |
| Team (MD, fellow, NC,SW) | Scheduled daily meetings at 8 am (or 8 am and 2 pm if needed) to discuss each patient's care and discharge plan |
| NC | Introduces the team to the patient/caregiver upon admission |
| Obtains prehospitalization information on cognitive and functional status | |
| Acts as a hospital coach educating the patient/caregiver | |
| Completes PRIs necessary for discharge to other institutions | |
| Completes medication reconciliation prior to discharge | |
| Initiates post‐discharge phone call and communicates with PCP via EMR | |
| Provides experiential one‐to‐one geriatric nursing education | |
| SW | Arranges family meeting, when indicated, with the team early in the hospitalization |
| Provides patient and family psychosocial support on an as needed basis | |
| Responsible for discharge planning | |
| MD | Attending physician of record |
| Communicates with PCP upon admission of the patient | |
| Assures discharge communiqu to PCP via EMR within 24 hours of discharge | |
We conducted a retrospective cohort study with propensity‐score matching in an urban academic medical center. Study subjects comprised 5 distinct groups. First were community‐dwelling older adults cared for at our outpatient geriatrics ambulatory practice who were discharged from our traditional ACE unit‐based acute care service at the Mount Sinai Hospital from July 1, 2006 through June 30, 2007 (N = 450). Second and third were patients from the same practice discharged from our MACE service during the first 2 years of operation (N = 556 from July 1, 2007 through June 30, 2008, and N = 501 from July 1, 2008 through June 30, 2009). Fourth and fifth were control cohorts of hospitalized older adults discharged from other medical services at the Mount Sinai Hospital during these same 2 years (N = 4863 and N = 4777, respectively). The average daily census on all services was 1012 patients.
Some patients on all 3 services are co‐managed with house staff, who are responsible for writing physician orders. Control cohort patients were cared for by a mix of private attendings (approximately 75%) or hospitalists (25%), and in contradistinction to MACE patients, their typical care did not include daily interdisciplinary team rounds, a nurse coordinator, or geriatrics fellow. Social work and case management were unit‐ as opposed to team‐based. Care on the ACE unit‐based service differed from care for matched control patients by having daily interdisciplinary team rounds, a prepared environment, and nursing‐led protocols for the patients on the ACE unit.
Because the ACE unit‐based service admitted both patients who were and were not cared for in our ambulatory practice, while the MACE service admitted only patients cared for in the ambulatory practice, we deleted from the study sample the patients who did not have a visit to our outpatient practice before the index hospitalization. This allowed us to isolate the effect of the model of care itself as opposed to the effect of simply changing the patient base for admissions. We then merged the files with the hospital's administrative database and electronic billing system to obtain demographic and claims data.
Additional demographic data were obtained through chart review of the MACE patients during year 1. The chart review process was standardized using a data abstraction instrument and by determining inter‐rater reliability of the individual data abstractors (comprised of author B.K. and 4 MACE team members).
Costs were assigned to individual admissions by the hospital's cost reporting system and include a combination of traceable costs (such as imaging, laboratory, and pharmacy) and applied costs (nursing; allocated based on geographic location in the hospital) to arrive at direct and total costs.
We made 3 distinct comparisons of operational and quality outcomes using the above 5 groups, first comparing patients cared for on our traditional ACE unit‐based service to those cared for on the MACE service, and second and third comparing patients on the MACE service to propensity score‐matched controls during the first and second year of operations. Specifically, we hypothesized that the MACE service would be associated with reduced LOS, costs, and readmission rates compared with the ACE unit‐based service and the matched control groups. We used multivariate logistic regression to estimate the association of binary quality outcomes (mortality during the hospital stay, 7‐ and 30‐day readmission rates) with the existence of MACE while adjusting for confounding variables which included patient demographic and clinical characteristics such as age, gender, race, total number of comorbidities (calculated by Elixhauser method that includes 30 categories of comorbid illnesses identified by secondary diagnosis codes and discharge diagnosis‐related groups [DRGs]).7 We considered the clustering effect due to the same attending physician into the model as well. While adjusting for the same covariates, we used generalized linear models with a gamma distribution and log link to estimate the association of continuous variables (costs and LOS) with the existence of MACE.
The same statistical methods were applied to the second and third comparisons between patients cared for on the MACE and the propensity score‐matched cohorts for the first and second year of the MACE service. First, 2 control cohorts (N = 6148 and 5803 of our hospital discharges from July 1, 2007 to June 30, 2008, and July 1, 2008 to June 30, 2009, respectively, with age > 64 and with the identical DRG and All Patient Refined DRG (APR DRG) Severity of Illness (SOI) score as those of the MACE groups were obtained from our hospital's administrative database to reduce the selection bias. Then, 4863 patients within the first cohort (N = 6148) and 4777 patients within the second cohort (N = 5,803) with the closest propensity score were matched to 545 of 556 MACE patients and 494 of 501 MACE patients, respectively, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score.
Propensity scores were determined by logistic regression on whether patients were admitted to the MACE. The covariates for the propensity model were the same as the previously stated adjusting variables. Usual care patients' data were weighted to account for the one‐to‐many propensity score‐matching algorithm.
We similarly conducted a post hoc analysis of MACE compared with a subgroup control cohort of patients cared for by medicine hospitalists in year 1 (N = 1175) and year 2 (N = 1564), with age > 64 and with the identical DRG and APR DRG SOI as those of the MACE group. We then matched 1012 of the 1175 discharges with the closest propensity score to 389 of the 411 MACE discharges who were cared for by 1 of the 4 geriatric medicine hospitalists in year 1 and 1308 of the 1564 discharges to 471 of the 501 MACE discharges in year 2, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score, using the same covariates described above.
All analyses were done using Stata software, version 9.2 (StataCorp LP, College Station, TX). This project was exempted by the Institutional Review Board at Mount Sinai School of Medicine, New York, New York.
RESULTS
Table 2 presents the characteristics of the study subjects in all 5 groups. Patients cared for on the ACE unit‐based service and the MACE service in years 1 and 2 were very similar, with a mean age of 82.6, 83.2, and 83.6 years; 74.4%, 75.9%, and 76.7% were female; and mean Elixhauser comorbidity scores were 3.4, 3.3, and 3.5, respectively. Patients in the 2 matched control groups were likewise very similar to those in the matched MACE groups with regard to all demographic variables.
| Demographics | ACE (N = 450) | Matched MACE year 1 (N = 545) | Matched controls year 1 (N = 4863) | Matched MACE year 2 (N = 494) | Matched controls year 2 (N = 4777) |
|---|---|---|---|---|---|
| |||||
| Age SD | 82.6 8.4 | 83.2 8.3 | 83.4 8.8 | 83.6 8.1 | 83.8 8.5 |
| Female, % | 74.4% | 75.9% | 74.7% | 76.7% | 77.4% |
| Race, % | |||||
| White | 35 | 37 | 36 | 43 | 42 |
| Black | 30 | 27 | 28 | 25 | 25 |
| Hispanic | 33 | 34 | 35 | 28 | 30 |
| Asian | 1 | 1 | 1 | 3 | 3 |
| Marital status, % | |||||
| Married | 20 | 20 | 21 | 23 | 23 |
| Widowed | 44 | 45 | 44 | 46 | 38 |
| Single | 25 | 22 | 27 | 21 | 28 |
| Elixhauser comorbidity index mean (SD) | 3.4 (1.8) | 3.4 (1.6) | 3.3 (1.7) | 3.5 (1.7) | 3.5 (1.7) |
| Hypertension, % | 61 | 54 | 54 | 49 | 49 |
| Heart Failure, % | 25 | 27 | 28 | 26 | 27 |
| Diabetes Mellitus, % | 26 | 25 | 25 | 24 | 25 |
| Atrial fibrillation, % | 22 | 23 | 23 | 28 | 27 |
| Chronic obstructive pulmonary disease, % | 15 | 15 | 15 | 15 | 14 |
Chart review of the year 1 MACE discharges revealed that 70% spoke English as their primary language and 46% had cognitive impairment. Most lived at home alone (49%) or with family members (41%) while receiving some paid caregiver help (59%). The remaining 10% were admitted from either an assisted living facility (5%) or subacute rehabilitation (5%). Only 12% were wheelchair or bed‐bound, while 21% ambulated without and 67% with an assistive device. Their functional status was limited, with 58% dependent for both ADLs and IADLs, 22% dependent for IADLs only, and 20% independent in both. They had relatively high prescription medication burdens, with 10% taking 05, 34% taking 610, 38% taking 1115, and 18% taking >15 medications.
Patients cared for by the MACE service had an adjusted 2.1 days shorter LOS (P 0.001) when compared with patients cared for on the ACE unit service. Additionally, there was a net savings of $2872 in total costs per hospitalization (P = 0.002), $1094 in direct costs (P = 0.016), $849 in nursing costs (P 0.001), and $237 in pharmacy costs (P = 0.002). Imaging and laboratory costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
| MACE to ACE | MACE to matched controls, year 1 | MACE to matched controls, year 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MACE (N = 556) | ACE (N = 450) | P value | MACE (N = 545) | Matched controls (N = 4863) | P value | MACE (N = 494) | Matched controls (N = 4777) | P value | |
| |||||||||
| LOS, days | 5.8 | 7.9 | 0.001 | 5.8 | 6.5 | 0.15 | 5.6 | 7.2 | 0.001 |
| Costs, $ | |||||||||
| Total | 10315 | 13187 | 0.002 | 10311 | 12764 | 0.001 | 10693 | 15636 | 0.001 |
| Direct | 4777 | 5871 | 0.016 | 4778 | 5620 | 0.03 | 4967 | 7048 | 0.001 |
| Nursing | 2361 | 3210 | 0.001 | 2356 | 2749 | 0.026 | 2143 | 3080 | 0.001 |
| Imaging | 342 | 332 | 0.61 | 344 | 349 | 0.73 | 382 | 471 | 0.06 |
| Laboratory | 206 | 243 | 0.079 | 206 | 245 | 0.029 | 213 | 281 | 0.001 |
| Pharmacy | 598 | 835 | 0.002 | 597 | 662 | 0.63 | 563 | 786 | 0.03 |
| In‐hospital mortality,% | 3.3 | 3.9 | 0.66 | 2.9 | 2.6 | 0.3 | 5.3 | 3.6 | 0.053 |
| 7‐day readmission,% | 9.3 | 10.2 | 0.55 | 9.7 | 11.8 | 0.3 | 4.8 | 5.5 | 0.71 |
| 30‐day readmission, % | 23.6 | 25.9 | 0.5 | 23.8 | 24.3 | 0.65 | 21.1 | 20.9 | 0.62 |
| 90‐day readmission, % | 40.9 | 38.7 | 0.1 | 41.3 | 38.4 | 0.005 | 38.0 | 36.5 | 0.74 |
There was no difference in LOS between the MACE patients during the first year of service compared with propensity score‐matched control patients (5.8 vs 6.5 days). There was, however, a net savings of $2453 in total costs per hospitalization (P 0.001), $842 (P = 0.03) in direct costs, $393 in nursing costs (P = 0.026), and $39 in laboratory costs (P = 0.029). Imaging and pharmacy costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day or 30‐day readmission rates between the 2 groups. However, the 90‐day readmission rate was higher in MACE patients (Table 3).
During the second year of the MACE service, however, there was a significant reduction in LOS of 1.6 days (P 0.001), a net savings of $4943 in total costs per hospitalization (P 0.001), $2081 (P 0.001) in direct costs, $937 in nursing costs (P 0.001), $68 in laboratory costs (P 0.001), and $223 in pharmacy costs (P = 0.03). There were no significant differences in imaging costs, in‐hospital mortality, and 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
A subgroup analysis of the first and second year comparisons including only those patients in the control groups cared for by medicine hospitalists demonstrated reductions in the MACE in total cost in year 1 and LOS, mortality, total, and nursing costs in year 2. However, in year 1, the 30‐day and 90‐day readmission rates were increased in the MACE compared with the control group (Table 4).
| MACE, year 1 (N = 389) | Matched controls, year 1 (N = 1012) | P Value | MACE, year 2 (N = 471) | Matched controls, year 2 (N = 1308) | P Value | |
|---|---|---|---|---|---|---|
| ||||||
| LOS, days | 6.0 | 6.0 | 0.34 | 5.7 | 6.9 | 0.001 |
| Costs, $ | ||||||
| Total | 10663 | 11599 | 0.049 | 10681 | 13493 | 0.001 |
| Direct | 4952 | 4704 | 0.98 | 4956 | 5618 | 0.055 |
| Nursing | 2394 | 2454 | 0.19 | 2124 | 2744 | 0.001 |
| Imaging | 349 | 322 | 0.63 | 387 | 390 | 0.82 |
| Laboratory | 213 | 199 | 0.49 | 212 | 225 | 0.47 |
| Pharmacy | 647 | 616 | 0.85 | 547 | 654 | 0.22 |
| In‐hospital mortality,% | 2.9 | 2.3 | 0.77 | 2.6 | 3.4 | 0.005 |
| 7‐Day readmission,% | 8.1 | 6.4 | 0.17 | 3.9 | 4.1 | 0.97 |
| 30‐Day readmission, % | 22.0 | 17.1 | 0.013 | 20.9 | 20.8 | 0.75 |
| 90‐Day readmission, % | 40.2 | 32.4 | 0.013 | 39.1 | 38.7 | 0.86 |
We found no differences in a separate post hoc subgroup analysis assessing whether a 3‐month nurse coordinator's leave of absence during year 1 affected year 1 results. The service size was unaffected by her absence, and all patients continued to receive daily visits by the attending and fellow. During this time, other team members took over many of the nurse coordinator roles, except for the postdischarge phone calls.
DISCUSSION
Older adults constitute a disproportionate share of hospital admissions and hospital days. They typically have multiple comorbid conditions, higher rates of cognitive impairment and functional dependence, and complex social situations that all increase their risk of adverse outcomes. Current efforts for national healthcare reform focus on the combined economic and quality imperatives to improve the care of hospitalized older adults. Given the increasing representation of this fastest growing segment of the population in the acute care setting, the geographical unit‐based model for care delivery is untenable in many circumstances. Therefore, we developed a mobile ACE service in an effort to provide the geriatric‐focused acute care found on ACE units to older adults admitted to any medical unit in the hospital.
Our study compared operational and quality outcomes for older patients cared for by our mobile ACE service to those cared for on the unit‐based ACE service and other general medical services. We found a significant reduction in both LOS and costs in all 3 comparisons, except for LOS during the first year of the mobile ACE service. This heightened efficiency was not associated with changes in the quality measures of in‐hospital mortality and 7‐ and 30‐day readmission rates, though the 90‐day readmission rate was slightly higher for the MACE in year 1.
The adjusted total cost savings per admission in years 1 and 2 of approximately $2400 ($12,764 vs $10,311) and $4900 ($15,636 vs $10,693), respectively, translate into an overall annual savings of roughly $1,200,000 (500 patients $2400/patient) in year 1 and $2,450,000 (500 patients $4,900/patient) in year 2. The only relevant cost of the MACE service model compared with the comparison groups is the nurse coordinator salary and benefits, which are paid for by the hospital (as job responsibilities include participation in nursing department quality improvement projects and nursing education) and would not meaningfully offset these savings. The team social worker is a re‐allocation of existing hospital resources, whose salary line is likewise paid for by the hospital.
Our study has several important limitations. First, we lack data on readmissions to other hospitals. Our readmission rates are high compared with the national 19.6% 30‐day Medicare readmission rate cited in a recent study, and we failed to show significant reductions in in‐hospital mortality or 7‐ or 30‐day readmission rates.10 This lack of benefit may be related to control group patients, some of whom receive their community care outside of our institution, being more likely to be readmitted to other hospitals compared with our MACE patients, who were all receiving their ambulatory care in our associated faculty practice. In addition, the high readmission rate on the MACE service may be driven by a relatively small number of patients who are frequently admitted. For example, of the 363 unique MACE patients from year 2, 22 had 3 and 11 had 4 or 5 admissions. We are currently evaluating these 33 patients who accounted for 22% of the admissions to better understand the causes.
A second limitation of the study is selection bias. While patients were very well‐matched through propensity scoring and had identical DRG and DRG‐SOI levels (the latter having been demonstrated in a previous study's regression analysis to be the leading correlate of LOS and cost),9 there may be unaccounted for differences between the patients cared for on the MACE and in the control group. A third limitation is the external validity of our study, which took place in a single large academic medical center in New York City. While the MACE model may very well be readily adaptable elsewhere, numerous studies have demonstrated wide variation in medical practice patterns and healthcare use which may influence the exportability of the model.11, 12 However, our LOS of 5.8 and 5.6 days in years 1 and 2 of the MACE service, respectively, are similar to national data of 5.6 days for hospitalized adults >74 years of age.13
Benefits in cost and LOS reductions may be, in part, due to the hospitalist nature of the model as hospital medicine literature has demonstrated similar reductions for Medicare patients of approximately $1000 and 0.5 days per admission.8, 9 Our findings support this hypothesis as the LOS reduction was not present during the first year of our MACE service during which the hospitalist model was not fully implemented. During this transition phase from the unit‐based ACE to the mobile ACE service, there were 4 physicians who covered more than 75% of on‐service time (10 of the 13 annual 4‐week rotations), while the remaining 25% was covered by 3 physicians (each working 1 block). The following year (July 2008 to June 2009), during which an LOS reduction was demonstrated, a full geriatric medicine hospitalist model was in effect, with patients on the MACE service cared for 100% of the time (excluding weekends) by 1 of 4 geriatric medicine hospitalists. By comparison, 22% and 29% of control group patients were cared for by medicine hospitalists during years 1 and 2, respectively. In addition to this transition to a hospitalist model, there may have been other undefined service improvements over the first year which contributed to the LOS and total cost reductions achieved in year 2 in the hospitalist subgroup analysis. Likewise, the increased 90‐day readmission rates seen in year 1 but not in year 2 in both the main and hospitalist subgroup analyses may be related to MACE service improvements over time. A more vigorous proactive intervention beyond the follow‐up phone call is likely needed to impact 90‐day readmissions.
LOS reductions may also have been related to the interdisciplinary team‐based approach in which a need for family meetings to address goals of care or assess and attempt to resolve complex family/living situations was identified early in the course of hospitalization. Likewise, in New York State, the application process for discharge to a postacute care setting begins with the completion of a Patient Review Instrument (PRI), which contains detailed information on the patient's physical, medical, and cognitive status. The MACE model circumvents the traditional case manager's role of completing the PRI by having the MACE nurse coordinator trained and certified to do so. The daily or twice daily MACE team meeting may have enabled more timely initiation of this early step in the discharge process for these patients, ultimately resulting in a reduced LOS.
An important concern this study is not able to address is whether LOS reductions are achieved at a price of impaired functional status. A prospective longitudinal study on the outcomes of patients cared for by a MACE service that includes detailed assessments of functional status based upon information gathered during admission and postdischarge during follow‐up phone calls is needed to properly evaluate this possibility.
Given the lack of wide‐spread adoption of the traditional ACE unit‐based model of care and its inherent limitations in the setting of high occupancy rates, a mobile ACE service may prove useful in providing high quality clinical care with reduced LOS and costs. This team‐based, as opposed to unit‐based, approach benefits from having low entry costs, as hospital administration can re‐allocate existing resources to fit the model and avoid costly capital investments in specialized unit design and outfitting. Further research should include metrics on functional status, all‐hospital readmission rates, and patient/caregiver satisfaction to better assess the feasibility of this acute care model.
The traditional acute care for the elderly (ACE) unit has demonstrated improved functional outcomes without increased costs or changes in length of stay (LOS).15 It is, however, limited in scope to only those patients cared for on a fixed geographical unit. This structural limitation is of increasing relevance in times of high hospital bed occupancy rates, as during such times, many appropriate older patients are admitted elsewhere. In our experience with a traditional ACE unit‐based model, only 52% of our geriatrics practice patients were admitted to an ACE unit bed, while the remainder were admitted to various medical units throughout the hospital. We therefore abandoned our traditional unit‐based ACE service in July 2007 in favor of a mobile ACE (MACE) service, bringing the interdisciplinary, patient‐centered team approach to our hospitalized older adult patients admitted throughout the hospital.
The purpose of this study is to compare the operational and quality outcomes for patients cared for on the MACE service to those cared for on a unit‐based ACE service and matched controls cared for on other general medical services. We hypothesized that the MACE service would be associated with lower lengths of stay, reduced costs, and decreased rehospitalization rates.
METHODS
The MACE team was composed of a geriatrician‐hospitalist, geriatric medicine fellow, social worker, and nurse coordinator. The geriatric medicine attending on the MACE service was in the hospital providing patient care during regular working hours from Monday through Friday, while the weekends were covered by a rotating group of all geriatric medicine faculty. During the first and second years of MACE, there were 7 and 4 attendings, respectively; all fellowship‐trained geriatricians. Three of the 4 geriatric medicine hospitalists during year 2 had been in practice between 1 and 3 years postfellowship and also had training in palliative medicine, although were not board‐certified in the latter. The fourth hospitalist had been in practice for 5 years postfellowship. The interdisciplinary team met daily to discuss the care of all patients and used a transitional care model based on The Care Transitions Program6 adapted to our institution, with a focus on reducing the risks of hazards of hospitalization. Care coordination with the outpatient practice, early family meetings, discharge planning, patient and caregiver education, and postdischarge follow‐up phone calls were some of the key hallmarks of the service (Table 1).
| Team member(s) | Roles |
|---|---|
| |
| Team (MD, fellow, NC,SW) | Scheduled daily meetings at 8 am (or 8 am and 2 pm if needed) to discuss each patient's care and discharge plan |
| NC | Introduces the team to the patient/caregiver upon admission |
| Obtains prehospitalization information on cognitive and functional status | |
| Acts as a hospital coach educating the patient/caregiver | |
| Completes PRIs necessary for discharge to other institutions | |
| Completes medication reconciliation prior to discharge | |
| Initiates post‐discharge phone call and communicates with PCP via EMR | |
| Provides experiential one‐to‐one geriatric nursing education | |
| SW | Arranges family meeting, when indicated, with the team early in the hospitalization |
| Provides patient and family psychosocial support on an as needed basis | |
| Responsible for discharge planning | |
| MD | Attending physician of record |
| Communicates with PCP upon admission of the patient | |
| Assures discharge communiqu to PCP via EMR within 24 hours of discharge | |
We conducted a retrospective cohort study with propensity‐score matching in an urban academic medical center. Study subjects comprised 5 distinct groups. First were community‐dwelling older adults cared for at our outpatient geriatrics ambulatory practice who were discharged from our traditional ACE unit‐based acute care service at the Mount Sinai Hospital from July 1, 2006 through June 30, 2007 (N = 450). Second and third were patients from the same practice discharged from our MACE service during the first 2 years of operation (N = 556 from July 1, 2007 through June 30, 2008, and N = 501 from July 1, 2008 through June 30, 2009). Fourth and fifth were control cohorts of hospitalized older adults discharged from other medical services at the Mount Sinai Hospital during these same 2 years (N = 4863 and N = 4777, respectively). The average daily census on all services was 1012 patients.
Some patients on all 3 services are co‐managed with house staff, who are responsible for writing physician orders. Control cohort patients were cared for by a mix of private attendings (approximately 75%) or hospitalists (25%), and in contradistinction to MACE patients, their typical care did not include daily interdisciplinary team rounds, a nurse coordinator, or geriatrics fellow. Social work and case management were unit‐ as opposed to team‐based. Care on the ACE unit‐based service differed from care for matched control patients by having daily interdisciplinary team rounds, a prepared environment, and nursing‐led protocols for the patients on the ACE unit.
Because the ACE unit‐based service admitted both patients who were and were not cared for in our ambulatory practice, while the MACE service admitted only patients cared for in the ambulatory practice, we deleted from the study sample the patients who did not have a visit to our outpatient practice before the index hospitalization. This allowed us to isolate the effect of the model of care itself as opposed to the effect of simply changing the patient base for admissions. We then merged the files with the hospital's administrative database and electronic billing system to obtain demographic and claims data.
Additional demographic data were obtained through chart review of the MACE patients during year 1. The chart review process was standardized using a data abstraction instrument and by determining inter‐rater reliability of the individual data abstractors (comprised of author B.K. and 4 MACE team members).
Costs were assigned to individual admissions by the hospital's cost reporting system and include a combination of traceable costs (such as imaging, laboratory, and pharmacy) and applied costs (nursing; allocated based on geographic location in the hospital) to arrive at direct and total costs.
We made 3 distinct comparisons of operational and quality outcomes using the above 5 groups, first comparing patients cared for on our traditional ACE unit‐based service to those cared for on the MACE service, and second and third comparing patients on the MACE service to propensity score‐matched controls during the first and second year of operations. Specifically, we hypothesized that the MACE service would be associated with reduced LOS, costs, and readmission rates compared with the ACE unit‐based service and the matched control groups. We used multivariate logistic regression to estimate the association of binary quality outcomes (mortality during the hospital stay, 7‐ and 30‐day readmission rates) with the existence of MACE while adjusting for confounding variables which included patient demographic and clinical characteristics such as age, gender, race, total number of comorbidities (calculated by Elixhauser method that includes 30 categories of comorbid illnesses identified by secondary diagnosis codes and discharge diagnosis‐related groups [DRGs]).7 We considered the clustering effect due to the same attending physician into the model as well. While adjusting for the same covariates, we used generalized linear models with a gamma distribution and log link to estimate the association of continuous variables (costs and LOS) with the existence of MACE.
The same statistical methods were applied to the second and third comparisons between patients cared for on the MACE and the propensity score‐matched cohorts for the first and second year of the MACE service. First, 2 control cohorts (N = 6148 and 5803 of our hospital discharges from July 1, 2007 to June 30, 2008, and July 1, 2008 to June 30, 2009, respectively, with age > 64 and with the identical DRG and All Patient Refined DRG (APR DRG) Severity of Illness (SOI) score as those of the MACE groups were obtained from our hospital's administrative database to reduce the selection bias. Then, 4863 patients within the first cohort (N = 6148) and 4777 patients within the second cohort (N = 5,803) with the closest propensity score were matched to 545 of 556 MACE patients and 494 of 501 MACE patients, respectively, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score.
Propensity scores were determined by logistic regression on whether patients were admitted to the MACE. The covariates for the propensity model were the same as the previously stated adjusting variables. Usual care patients' data were weighted to account for the one‐to‐many propensity score‐matching algorithm.
We similarly conducted a post hoc analysis of MACE compared with a subgroup control cohort of patients cared for by medicine hospitalists in year 1 (N = 1175) and year 2 (N = 1564), with age > 64 and with the identical DRG and APR DRG SOI as those of the MACE group. We then matched 1012 of the 1175 discharges with the closest propensity score to 389 of the 411 MACE discharges who were cared for by 1 of the 4 geriatric medicine hospitalists in year 1 and 1308 of the 1564 discharges to 471 of the 501 MACE discharges in year 2, in which the logit of their propensity score was within 0.02 standard deviations of the logit of the MACE patient's score, using the same covariates described above.
All analyses were done using Stata software, version 9.2 (StataCorp LP, College Station, TX). This project was exempted by the Institutional Review Board at Mount Sinai School of Medicine, New York, New York.
RESULTS
Table 2 presents the characteristics of the study subjects in all 5 groups. Patients cared for on the ACE unit‐based service and the MACE service in years 1 and 2 were very similar, with a mean age of 82.6, 83.2, and 83.6 years; 74.4%, 75.9%, and 76.7% were female; and mean Elixhauser comorbidity scores were 3.4, 3.3, and 3.5, respectively. Patients in the 2 matched control groups were likewise very similar to those in the matched MACE groups with regard to all demographic variables.
| Demographics | ACE (N = 450) | Matched MACE year 1 (N = 545) | Matched controls year 1 (N = 4863) | Matched MACE year 2 (N = 494) | Matched controls year 2 (N = 4777) |
|---|---|---|---|---|---|
| |||||
| Age SD | 82.6 8.4 | 83.2 8.3 | 83.4 8.8 | 83.6 8.1 | 83.8 8.5 |
| Female, % | 74.4% | 75.9% | 74.7% | 76.7% | 77.4% |
| Race, % | |||||
| White | 35 | 37 | 36 | 43 | 42 |
| Black | 30 | 27 | 28 | 25 | 25 |
| Hispanic | 33 | 34 | 35 | 28 | 30 |
| Asian | 1 | 1 | 1 | 3 | 3 |
| Marital status, % | |||||
| Married | 20 | 20 | 21 | 23 | 23 |
| Widowed | 44 | 45 | 44 | 46 | 38 |
| Single | 25 | 22 | 27 | 21 | 28 |
| Elixhauser comorbidity index mean (SD) | 3.4 (1.8) | 3.4 (1.6) | 3.3 (1.7) | 3.5 (1.7) | 3.5 (1.7) |
| Hypertension, % | 61 | 54 | 54 | 49 | 49 |
| Heart Failure, % | 25 | 27 | 28 | 26 | 27 |
| Diabetes Mellitus, % | 26 | 25 | 25 | 24 | 25 |
| Atrial fibrillation, % | 22 | 23 | 23 | 28 | 27 |
| Chronic obstructive pulmonary disease, % | 15 | 15 | 15 | 15 | 14 |
Chart review of the year 1 MACE discharges revealed that 70% spoke English as their primary language and 46% had cognitive impairment. Most lived at home alone (49%) or with family members (41%) while receiving some paid caregiver help (59%). The remaining 10% were admitted from either an assisted living facility (5%) or subacute rehabilitation (5%). Only 12% were wheelchair or bed‐bound, while 21% ambulated without and 67% with an assistive device. Their functional status was limited, with 58% dependent for both ADLs and IADLs, 22% dependent for IADLs only, and 20% independent in both. They had relatively high prescription medication burdens, with 10% taking 05, 34% taking 610, 38% taking 1115, and 18% taking >15 medications.
Patients cared for by the MACE service had an adjusted 2.1 days shorter LOS (P 0.001) when compared with patients cared for on the ACE unit service. Additionally, there was a net savings of $2872 in total costs per hospitalization (P = 0.002), $1094 in direct costs (P = 0.016), $849 in nursing costs (P 0.001), and $237 in pharmacy costs (P = 0.002). Imaging and laboratory costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
| MACE to ACE | MACE to matched controls, year 1 | MACE to matched controls, year 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| MACE (N = 556) | ACE (N = 450) | P value | MACE (N = 545) | Matched controls (N = 4863) | P value | MACE (N = 494) | Matched controls (N = 4777) | P value | |
| |||||||||
| LOS, days | 5.8 | 7.9 | 0.001 | 5.8 | 6.5 | 0.15 | 5.6 | 7.2 | 0.001 |
| Costs, $ | |||||||||
| Total | 10315 | 13187 | 0.002 | 10311 | 12764 | 0.001 | 10693 | 15636 | 0.001 |
| Direct | 4777 | 5871 | 0.016 | 4778 | 5620 | 0.03 | 4967 | 7048 | 0.001 |
| Nursing | 2361 | 3210 | 0.001 | 2356 | 2749 | 0.026 | 2143 | 3080 | 0.001 |
| Imaging | 342 | 332 | 0.61 | 344 | 349 | 0.73 | 382 | 471 | 0.06 |
| Laboratory | 206 | 243 | 0.079 | 206 | 245 | 0.029 | 213 | 281 | 0.001 |
| Pharmacy | 598 | 835 | 0.002 | 597 | 662 | 0.63 | 563 | 786 | 0.03 |
| In‐hospital mortality,% | 3.3 | 3.9 | 0.66 | 2.9 | 2.6 | 0.3 | 5.3 | 3.6 | 0.053 |
| 7‐day readmission,% | 9.3 | 10.2 | 0.55 | 9.7 | 11.8 | 0.3 | 4.8 | 5.5 | 0.71 |
| 30‐day readmission, % | 23.6 | 25.9 | 0.5 | 23.8 | 24.3 | 0.65 | 21.1 | 20.9 | 0.62 |
| 90‐day readmission, % | 40.9 | 38.7 | 0.1 | 41.3 | 38.4 | 0.005 | 38.0 | 36.5 | 0.74 |
There was no difference in LOS between the MACE patients during the first year of service compared with propensity score‐matched control patients (5.8 vs 6.5 days). There was, however, a net savings of $2453 in total costs per hospitalization (P 0.001), $842 (P = 0.03) in direct costs, $393 in nursing costs (P = 0.026), and $39 in laboratory costs (P = 0.029). Imaging and pharmacy costs between the 2 groups were not statistically different. There was no significant differences in in‐hospital mortality, 7‐day or 30‐day readmission rates between the 2 groups. However, the 90‐day readmission rate was higher in MACE patients (Table 3).
During the second year of the MACE service, however, there was a significant reduction in LOS of 1.6 days (P 0.001), a net savings of $4943 in total costs per hospitalization (P 0.001), $2081 (P 0.001) in direct costs, $937 in nursing costs (P 0.001), $68 in laboratory costs (P 0.001), and $223 in pharmacy costs (P = 0.03). There were no significant differences in imaging costs, in‐hospital mortality, and 7‐day, 30‐day, or 90‐day readmission rates between the 2 groups (Table 3).
A subgroup analysis of the first and second year comparisons including only those patients in the control groups cared for by medicine hospitalists demonstrated reductions in the MACE in total cost in year 1 and LOS, mortality, total, and nursing costs in year 2. However, in year 1, the 30‐day and 90‐day readmission rates were increased in the MACE compared with the control group (Table 4).
| MACE, year 1 (N = 389) | Matched controls, year 1 (N = 1012) | P Value | MACE, year 2 (N = 471) | Matched controls, year 2 (N = 1308) | P Value | |
|---|---|---|---|---|---|---|
| ||||||
| LOS, days | 6.0 | 6.0 | 0.34 | 5.7 | 6.9 | 0.001 |
| Costs, $ | ||||||
| Total | 10663 | 11599 | 0.049 | 10681 | 13493 | 0.001 |
| Direct | 4952 | 4704 | 0.98 | 4956 | 5618 | 0.055 |
| Nursing | 2394 | 2454 | 0.19 | 2124 | 2744 | 0.001 |
| Imaging | 349 | 322 | 0.63 | 387 | 390 | 0.82 |
| Laboratory | 213 | 199 | 0.49 | 212 | 225 | 0.47 |
| Pharmacy | 647 | 616 | 0.85 | 547 | 654 | 0.22 |
| In‐hospital mortality,% | 2.9 | 2.3 | 0.77 | 2.6 | 3.4 | 0.005 |
| 7‐Day readmission,% | 8.1 | 6.4 | 0.17 | 3.9 | 4.1 | 0.97 |
| 30‐Day readmission, % | 22.0 | 17.1 | 0.013 | 20.9 | 20.8 | 0.75 |
| 90‐Day readmission, % | 40.2 | 32.4 | 0.013 | 39.1 | 38.7 | 0.86 |
We found no differences in a separate post hoc subgroup analysis assessing whether a 3‐month nurse coordinator's leave of absence during year 1 affected year 1 results. The service size was unaffected by her absence, and all patients continued to receive daily visits by the attending and fellow. During this time, other team members took over many of the nurse coordinator roles, except for the postdischarge phone calls.
DISCUSSION
Older adults constitute a disproportionate share of hospital admissions and hospital days. They typically have multiple comorbid conditions, higher rates of cognitive impairment and functional dependence, and complex social situations that all increase their risk of adverse outcomes. Current efforts for national healthcare reform focus on the combined economic and quality imperatives to improve the care of hospitalized older adults. Given the increasing representation of this fastest growing segment of the population in the acute care setting, the geographical unit‐based model for care delivery is untenable in many circumstances. Therefore, we developed a mobile ACE service in an effort to provide the geriatric‐focused acute care found on ACE units to older adults admitted to any medical unit in the hospital.
Our study compared operational and quality outcomes for older patients cared for by our mobile ACE service to those cared for on the unit‐based ACE service and other general medical services. We found a significant reduction in both LOS and costs in all 3 comparisons, except for LOS during the first year of the mobile ACE service. This heightened efficiency was not associated with changes in the quality measures of in‐hospital mortality and 7‐ and 30‐day readmission rates, though the 90‐day readmission rate was slightly higher for the MACE in year 1.
The adjusted total cost savings per admission in years 1 and 2 of approximately $2400 ($12,764 vs $10,311) and $4900 ($15,636 vs $10,693), respectively, translate into an overall annual savings of roughly $1,200,000 (500 patients $2400/patient) in year 1 and $2,450,000 (500 patients $4,900/patient) in year 2. The only relevant cost of the MACE service model compared with the comparison groups is the nurse coordinator salary and benefits, which are paid for by the hospital (as job responsibilities include participation in nursing department quality improvement projects and nursing education) and would not meaningfully offset these savings. The team social worker is a re‐allocation of existing hospital resources, whose salary line is likewise paid for by the hospital.
Our study has several important limitations. First, we lack data on readmissions to other hospitals. Our readmission rates are high compared with the national 19.6% 30‐day Medicare readmission rate cited in a recent study, and we failed to show significant reductions in in‐hospital mortality or 7‐ or 30‐day readmission rates.10 This lack of benefit may be related to control group patients, some of whom receive their community care outside of our institution, being more likely to be readmitted to other hospitals compared with our MACE patients, who were all receiving their ambulatory care in our associated faculty practice. In addition, the high readmission rate on the MACE service may be driven by a relatively small number of patients who are frequently admitted. For example, of the 363 unique MACE patients from year 2, 22 had 3 and 11 had 4 or 5 admissions. We are currently evaluating these 33 patients who accounted for 22% of the admissions to better understand the causes.
A second limitation of the study is selection bias. While patients were very well‐matched through propensity scoring and had identical DRG and DRG‐SOI levels (the latter having been demonstrated in a previous study's regression analysis to be the leading correlate of LOS and cost),9 there may be unaccounted for differences between the patients cared for on the MACE and in the control group. A third limitation is the external validity of our study, which took place in a single large academic medical center in New York City. While the MACE model may very well be readily adaptable elsewhere, numerous studies have demonstrated wide variation in medical practice patterns and healthcare use which may influence the exportability of the model.11, 12 However, our LOS of 5.8 and 5.6 days in years 1 and 2 of the MACE service, respectively, are similar to national data of 5.6 days for hospitalized adults >74 years of age.13
Benefits in cost and LOS reductions may be, in part, due to the hospitalist nature of the model as hospital medicine literature has demonstrated similar reductions for Medicare patients of approximately $1000 and 0.5 days per admission.8, 9 Our findings support this hypothesis as the LOS reduction was not present during the first year of our MACE service during which the hospitalist model was not fully implemented. During this transition phase from the unit‐based ACE to the mobile ACE service, there were 4 physicians who covered more than 75% of on‐service time (10 of the 13 annual 4‐week rotations), while the remaining 25% was covered by 3 physicians (each working 1 block). The following year (July 2008 to June 2009), during which an LOS reduction was demonstrated, a full geriatric medicine hospitalist model was in effect, with patients on the MACE service cared for 100% of the time (excluding weekends) by 1 of 4 geriatric medicine hospitalists. By comparison, 22% and 29% of control group patients were cared for by medicine hospitalists during years 1 and 2, respectively. In addition to this transition to a hospitalist model, there may have been other undefined service improvements over the first year which contributed to the LOS and total cost reductions achieved in year 2 in the hospitalist subgroup analysis. Likewise, the increased 90‐day readmission rates seen in year 1 but not in year 2 in both the main and hospitalist subgroup analyses may be related to MACE service improvements over time. A more vigorous proactive intervention beyond the follow‐up phone call is likely needed to impact 90‐day readmissions.
LOS reductions may also have been related to the interdisciplinary team‐based approach in which a need for family meetings to address goals of care or assess and attempt to resolve complex family/living situations was identified early in the course of hospitalization. Likewise, in New York State, the application process for discharge to a postacute care setting begins with the completion of a Patient Review Instrument (PRI), which contains detailed information on the patient's physical, medical, and cognitive status. The MACE model circumvents the traditional case manager's role of completing the PRI by having the MACE nurse coordinator trained and certified to do so. The daily or twice daily MACE team meeting may have enabled more timely initiation of this early step in the discharge process for these patients, ultimately resulting in a reduced LOS.
An important concern this study is not able to address is whether LOS reductions are achieved at a price of impaired functional status. A prospective longitudinal study on the outcomes of patients cared for by a MACE service that includes detailed assessments of functional status based upon information gathered during admission and postdischarge during follow‐up phone calls is needed to properly evaluate this possibility.
Given the lack of wide‐spread adoption of the traditional ACE unit‐based model of care and its inherent limitations in the setting of high occupancy rates, a mobile ACE service may prove useful in providing high quality clinical care with reduced LOS and costs. This team‐based, as opposed to unit‐based, approach benefits from having low entry costs, as hospital administration can re‐allocate existing resources to fit the model and avoid costly capital investments in specialized unit design and outfitting. Further research should include metrics on functional status, all‐hospital readmission rates, and patient/caregiver satisfaction to better assess the feasibility of this acute care model.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.Do acute care for elders units increase hospital costs? A cost analysis using the hospital perspective.J Am Geriatr Soc.1997;45:729–734.
- ,,, et al.Effects of multicomponent intervention of functional outcomes and process of care in hospitalized older patients: a randomized controlled trial of acute care for elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1578.
- ,,,.A medical unit for the acute care of the elderly.J Am Geriatr Soc.1994;42:545–552
- ,,, et al.A randomized trial of care in a hospital medicine unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1342.
- ,,,.The care transitions intervention.Arch Intern Med.2006;166:1822–1828.
- ,,,.Comorbidity measures for use with administrative data.Med Care.1998;36:8–27.
- ,,.The effect of full‐time faculty hospitalists on the efficiency of care at a community teaching hospital.Ann Intern Med.1998;129:197–203.
- ,,,,,.The value of a hospitalist service.Chest.2001;19:580–589.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med.2009;360:1418–1428.
- ,,.Slowing the growth of health care costs ‐ lessons from regional variation.N Engl J Med.2009;360:849–852.
- ,,, et al.Fostering accountable health care: moving forward in Medicare.Health Aff (Millwood).2009;28:w219–w231.
- Centers for Disease Control and Prevention. Health, United States, 2009. Table 102. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. Accessed June 10,2010.
- ,,,,.Effectiveness of acute geriatric units on functional decline, living at home, and case fatality among older patients admitted to hospital for acute medical disorders: meta‐analysis.BMJ.2009;338:b50.
- ,,, et al.Do acute care for elders units increase hospital costs? A cost analysis using the hospital perspective.J Am Geriatr Soc.1997;45:729–734.
- ,,, et al.Effects of multicomponent intervention of functional outcomes and process of care in hospitalized older patients: a randomized controlled trial of acute care for elders (ACE) in a community hospital.J Am Geriatr Soc.2000;48:1572–1578.
- ,,,.A medical unit for the acute care of the elderly.J Am Geriatr Soc.1994;42:545–552
- ,,, et al.A randomized trial of care in a hospital medicine unit especially designed to improve the functional outcomes of acutely ill older patients.N Engl J Med.1995;332:1338–1342.
- ,,,.The care transitions intervention.Arch Intern Med.2006;166:1822–1828.
- ,,,.Comorbidity measures for use with administrative data.Med Care.1998;36:8–27.
- ,,.The effect of full‐time faculty hospitalists on the efficiency of care at a community teaching hospital.Ann Intern Med.1998;129:197–203.
- ,,,,,.The value of a hospitalist service.Chest.2001;19:580–589.
- ,,.Rehospitalizations among patients in the Medicare fee‐for‐service program.N Engl J Med.2009;360:1418–1428.
- ,,.Slowing the growth of health care costs ‐ lessons from regional variation.N Engl J Med.2009;360:849–852.
- ,,, et al.Fostering accountable health care: moving forward in Medicare.Health Aff (Millwood).2009;28:w219–w231.
- Centers for Disease Control and Prevention. Health, United States, 2009. Table 102. Available at: http://www.cdc.gov/nchs/data/hus/hus09.pdf. Accessed June 10,2010.
Platinum-Based Chemotherapy Benefits Elderly Lung Cancer Patients
Chemotherapy with a platinum-based doublet was associated with a highly significant 36% reduction in mortality, compared with monotherapy, among elderly patients with non–small cell lung cancer in a study published online Aug. 9 by the Lancet.
The combination of carboplatin and paclitaxel was associated with more toxicity than was single-drug vinorelbine or gemcitabine regimens in the phase III trial, but the investigators contended that this was outweighed by the survival benefit.
Median overall survival for patients receiving carboplatin plus paclitaxel was 10.3 months, compared with 6.2 months in those randomized to monotherapy (hazard ratio, 0.64; P less than .0001).
Although several guidelines currently recommend monotherapy for elderly patients, the current finding is "of such magnitude that we believe the treatment paradigm for elderly patients with advanced NSCLC should be reconsidered," wrote Dr. Elisabeth Quoix of the Hôpitaux Universitaires de Strasbourg (France) and colleagues (Lancet 2011 Aug. 9 [doi:10.1016/S0140-6736(11)60780-0]).
The investigators from the IFCT (Intergroupe Francophone de Cancérologie Thoracique) looked at 451 patients aged 70-89 years (median age, 77 years) with unresectable stage IV NSCLC or stage III disease that was "unsuitable" for radical radiation therapy. Patients were followed for a median of 30.3 months. To be included in the study, patients’ scores on the World Health Organization’s performance status scale had to be 2 or lower (indicating severe disease), and patients had to have a life expectancy of at least 12 weeks.
The 225 patients who were randomized to the doublet chemotherapy group received intravenous carboplatin (AUC [area under the curve] = 6) on day 1, plus 90 mg/m² of paclitaxel on days 1, 8, and 15 of 28-day cycles.
The 226-patient monotherapy cohort received 25 mg/m² vinorelbine (62 patients) on days 1 and 8 – or 1,150 mg/m² gemcitabine (164 patients) on days 1 and 8 – of 21-day cycles, with the choice of either vinorelbine or gemcitabine being made by the institution conducting the therapy.
In the doublet group, cycles were repeated every 4 weeks, such that patients received 3 weeks of treatment plus 1 week without, for doublet chemotherapy. For monotherapy, the cycle lasted 3 weeks (2 weeks of treatment plus 1 week without), with a maximum of four cycles for doublet therapy and five cycles for monotherapy.
Survival Rates for Chemotherapy Study Patients
By 1 year, the survival rate was 25.4% in the monotherapy group vs. 44.5% in the doublet therapy group (HR, 0.64; P less than .0001). The trend persisted at 2 years, with the probability of survival being 11.7% in monotherapy recipients and 22.4% in those receiving doublet therapy, wrote the authors.
Median progression-free survival also was significantly longer with the doublet (6 months vs. 2.8 months; P less than .0001).
In 2009, an independent data-monitoring committee recommended stopping recruitment based on the second interim analysis.
"Grade 3-4 neutropenia, febrile neutropenia, thrombopenia, and anemia were significantly more frequent among patients in the doublet chemotherapy group than among those in the monotherapy group, as was grade 3-4 sensory neuropathy," wrote the authors. The protocol did not allow growth factor support in the first cycle, but it was authorized as secondary prophylaxis in patients who developed grade 3 or 4 neutropenia.
In all, 10 deaths in the doublet therapy group (4.4%) and 3 in the monotherapy group (1.3%) were related to treatment: Culprit diagnoses included sepsis, respiratory distress, and diarrhea related to renal insufficiency. But the percentage of deaths in the first 3 months after the start of therapy was "markedly lower" in patients who received carboplatin plus paclitaxel.
Although quality of life scores at week 18 were similar between groups, the authors pointed out that "role functioning and fatigue were worse in the doublet chemotherapy group than in the monotherapy group" (P = .026 and .039, respectively). Full quality of life data will be published separately, they said.
The 2009 American Society of Clinical Oncology guidelines (J. Clin. Oncol. 2009;27:6251-66) recommend that age "not be used as a criterion in the decision-making process about whether to treat a patient" and call for further research devoted to elderly patients, according to Dr. Quoix and colleagues. "Conversely," they noted, "the European Organisation for Research and Treatment of Cancer Elderly Task Force and Lung Cancer Group and International Society of Geriatric Oncology highlighted in 2010 that monotherapy should be given to elderly patients with advanced NSCLC."
"We believe that monthly carboplatin and weekly paclitaxel is a feasible option for first-line therapy of advanced NSCLC in patients older than 70 years with performance status scores of 0-2," the authors wrote.
The study was funded by the IFCT and the French National Cancer Institute, with support by grants from Bristol-Myers Squibb, Roche, and Pierre Fabre. Several authors, including Dr. Quoix, disclosed financial relationships with the makers of chemotherapy drugs, including carboplatin (Bristol-Myers Squibb, Roche, and Lilly). Dr. Reckamp disclosed consulting for Amgen, Genentech, and Tragara Pharmaceuticals, as well as serving on speakers bureaus for Lilly Oncology and Genentech.
In an editorial accompanying the study, Dr. Karen L. Reckamp wrote that although older patients dominate the lung cancer population, they nevertheless continue to be underrepresented in clinical trials. Accounting for 47% of the U.S. adults with cancer, patients aged 70 years or older constitute just 13% of patients who are enrolled in clinical trials, according to the Southern Italy Cooperative Oncology Group (SICOG).
Nevertheless, there are some studies that provide guidance, she wrote.
A study by the SICOG compared vinorelbine alone with vinorelbine plus gemcitabine in patients aged 70 years and older (J. Clin. Oncol. 2000;18:2529-36). "Combination chemotherapy resulted in a significantly lower risk of death," she wrote. "Adverse events were greater in the combination group, but patients had a delay" in quality of life deterioration.
A second investigation, MILES (Multicenter Italian Lung Cancer in the Elderly Study), compared vinorelbine or gemcitabine alone or in combination. "Combination therapy did not improve overall survival and was more toxic than was either single-agent regimen," wrote Dr. Reckamp.
A third study from Japan was stopped because of futility when the interim analysis showed inferior survival with increased toxic effects in patients who were treated with weekly cisplatin and docetaxel vs. docetaxel every 3 weeks (J. Clin. Oncol. 2011;29:abstract 7509).
"The appropriate assessment to predict efficacy and toxic effects of therapy has not yet been identified," said Dr. Reckamp. As previous trials assessed multiple regimens with fractionated doses and non–platinum-based doublets, "the optimum chemotherapy regimen remains unknown, she added, concluding that "additional studies are needed that enroll adequate numbers of older adults, and include a comprehensive geriatric assessment to provide the knowledge required to properly assess the risk-benefit ratio in treatment decisions, so that a personalized approach can be taken."
Dr. Reckamp is at the City of Hope Comprehensive Cancer Center in Duarte, Calif. She disclosed consulting for Amgen, Genentech, and Tragara Pharmaceuticals, as well as serving on speakers bureaus for Lilly Oncology and Genentech. These remarks were adapted from an editorial that accompanied the study (Lancet 2011 Aug. 9 [doi:10.1016/S0140-6736(11)61259-2]).
In an editorial accompanying the study, Dr. Karen L. Reckamp wrote that although older patients dominate the lung cancer population, they nevertheless continue to be underrepresented in clinical trials. Accounting for 47% of the U.S. adults with cancer, patients aged 70 years or older constitute just 13% of patients who are enrolled in clinical trials, according to the Southern Italy Cooperative Oncology Group (SICOG).
Nevertheless, there are some studies that provide guidance, she wrote.
A study by the SICOG compared vinorelbine alone with vinorelbine plus gemcitabine in patients aged 70 years and older (J. Clin. Oncol. 2000;18:2529-36). "Combination chemotherapy resulted in a significantly lower risk of death," she wrote. "Adverse events were greater in the combination group, but patients had a delay" in quality of life deterioration.
A second investigation, MILES (Multicenter Italian Lung Cancer in the Elderly Study), compared vinorelbine or gemcitabine alone or in combination. "Combination therapy did not improve overall survival and was more toxic than was either single-agent regimen," wrote Dr. Reckamp.
A third study from Japan was stopped because of futility when the interim analysis showed inferior survival with increased toxic effects in patients who were treated with weekly cisplatin and docetaxel vs. docetaxel every 3 weeks (J. Clin. Oncol. 2011;29:abstract 7509).
"The appropriate assessment to predict efficacy and toxic effects of therapy has not yet been identified," said Dr. Reckamp. As previous trials assessed multiple regimens with fractionated doses and non–platinum-based doublets, "the optimum chemotherapy regimen remains unknown, she added, concluding that "additional studies are needed that enroll adequate numbers of older adults, and include a comprehensive geriatric assessment to provide the knowledge required to properly assess the risk-benefit ratio in treatment decisions, so that a personalized approach can be taken."
Dr. Reckamp is at the City of Hope Comprehensive Cancer Center in Duarte, Calif. She disclosed consulting for Amgen, Genentech, and Tragara Pharmaceuticals, as well as serving on speakers bureaus for Lilly Oncology and Genentech. These remarks were adapted from an editorial that accompanied the study (Lancet 2011 Aug. 9 [doi:10.1016/S0140-6736(11)61259-2]).
In an editorial accompanying the study, Dr. Karen L. Reckamp wrote that although older patients dominate the lung cancer population, they nevertheless continue to be underrepresented in clinical trials. Accounting for 47% of the U.S. adults with cancer, patients aged 70 years or older constitute just 13% of patients who are enrolled in clinical trials, according to the Southern Italy Cooperative Oncology Group (SICOG).
Nevertheless, there are some studies that provide guidance, she wrote.
A study by the SICOG compared vinorelbine alone with vinorelbine plus gemcitabine in patients aged 70 years and older (J. Clin. Oncol. 2000;18:2529-36). "Combination chemotherapy resulted in a significantly lower risk of death," she wrote. "Adverse events were greater in the combination group, but patients had a delay" in quality of life deterioration.
A second investigation, MILES (Multicenter Italian Lung Cancer in the Elderly Study), compared vinorelbine or gemcitabine alone or in combination. "Combination therapy did not improve overall survival and was more toxic than was either single-agent regimen," wrote Dr. Reckamp.
A third study from Japan was stopped because of futility when the interim analysis showed inferior survival with increased toxic effects in patients who were treated with weekly cisplatin and docetaxel vs. docetaxel every 3 weeks (J. Clin. Oncol. 2011;29:abstract 7509).
"The appropriate assessment to predict efficacy and toxic effects of therapy has not yet been identified," said Dr. Reckamp. As previous trials assessed multiple regimens with fractionated doses and non–platinum-based doublets, "the optimum chemotherapy regimen remains unknown, she added, concluding that "additional studies are needed that enroll adequate numbers of older adults, and include a comprehensive geriatric assessment to provide the knowledge required to properly assess the risk-benefit ratio in treatment decisions, so that a personalized approach can be taken."
Dr. Reckamp is at the City of Hope Comprehensive Cancer Center in Duarte, Calif. She disclosed consulting for Amgen, Genentech, and Tragara Pharmaceuticals, as well as serving on speakers bureaus for Lilly Oncology and Genentech. These remarks were adapted from an editorial that accompanied the study (Lancet 2011 Aug. 9 [doi:10.1016/S0140-6736(11)61259-2]).
Chemotherapy with a platinum-based doublet was associated with a highly significant 36% reduction in mortality, compared with monotherapy, among elderly patients with non–small cell lung cancer in a study published online Aug. 9 by the Lancet.
The combination of carboplatin and paclitaxel was associated with more toxicity than was single-drug vinorelbine or gemcitabine regimens in the phase III trial, but the investigators contended that this was outweighed by the survival benefit.
Median overall survival for patients receiving carboplatin plus paclitaxel was 10.3 months, compared with 6.2 months in those randomized to monotherapy (hazard ratio, 0.64; P less than .0001).
Although several guidelines currently recommend monotherapy for elderly patients, the current finding is "of such magnitude that we believe the treatment paradigm for elderly patients with advanced NSCLC should be reconsidered," wrote Dr. Elisabeth Quoix of the Hôpitaux Universitaires de Strasbourg (France) and colleagues (Lancet 2011 Aug. 9 [doi:10.1016/S0140-6736(11)60780-0]).
The investigators from the IFCT (Intergroupe Francophone de Cancérologie Thoracique) looked at 451 patients aged 70-89 years (median age, 77 years) with unresectable stage IV NSCLC or stage III disease that was "unsuitable" for radical radiation therapy. Patients were followed for a median of 30.3 months. To be included in the study, patients’ scores on the World Health Organization’s performance status scale had to be 2 or lower (indicating severe disease), and patients had to have a life expectancy of at least 12 weeks.
The 225 patients who were randomized to the doublet chemotherapy group received intravenous carboplatin (AUC [area under the curve] = 6) on day 1, plus 90 mg/m² of paclitaxel on days 1, 8, and 15 of 28-day cycles.
The 226-patient monotherapy cohort received 25 mg/m² vinorelbine (62 patients) on days 1 and 8 – or 1,150 mg/m² gemcitabine (164 patients) on days 1 and 8 – of 21-day cycles, with the choice of either vinorelbine or gemcitabine being made by the institution conducting the therapy.
In the doublet group, cycles were repeated every 4 weeks, such that patients received 3 weeks of treatment plus 1 week without, for doublet chemotherapy. For monotherapy, the cycle lasted 3 weeks (2 weeks of treatment plus 1 week without), with a maximum of four cycles for doublet therapy and five cycles for monotherapy.
Survival Rates for Chemotherapy Study Patients
By 1 year, the survival rate was 25.4% in the monotherapy group vs. 44.5% in the doublet therapy group (HR, 0.64; P less than .0001). The trend persisted at 2 years, with the probability of survival being 11.7% in monotherapy recipients and 22.4% in those receiving doublet therapy, wrote the authors.
Median progression-free survival also was significantly longer with the doublet (6 months vs. 2.8 months; P less than .0001).
In 2009, an independent data-monitoring committee recommended stopping recruitment based on the second interim analysis.
"Grade 3-4 neutropenia, febrile neutropenia, thrombopenia, and anemia were significantly more frequent among patients in the doublet chemotherapy group than among those in the monotherapy group, as was grade 3-4 sensory neuropathy," wrote the authors. The protocol did not allow growth factor support in the first cycle, but it was authorized as secondary prophylaxis in patients who developed grade 3 or 4 neutropenia.
In all, 10 deaths in the doublet therapy group (4.4%) and 3 in the monotherapy group (1.3%) were related to treatment: Culprit diagnoses included sepsis, respiratory distress, and diarrhea related to renal insufficiency. But the percentage of deaths in the first 3 months after the start of therapy was "markedly lower" in patients who received carboplatin plus paclitaxel.
Although quality of life scores at week 18 were similar between groups, the authors pointed out that "role functioning and fatigue were worse in the doublet chemotherapy group than in the monotherapy group" (P = .026 and .039, respectively). Full quality of life data will be published separately, they said.
The 2009 American Society of Clinical Oncology guidelines (J. Clin. Oncol. 2009;27:6251-66) recommend that age "not be used as a criterion in the decision-making process about whether to treat a patient" and call for further research devoted to elderly patients, according to Dr. Quoix and colleagues. "Conversely," they noted, "the European Organisation for Research and Treatment of Cancer Elderly Task Force and Lung Cancer Group and International Society of Geriatric Oncology highlighted in 2010 that monotherapy should be given to elderly patients with advanced NSCLC."
"We believe that monthly carboplatin and weekly paclitaxel is a feasible option for first-line therapy of advanced NSCLC in patients older than 70 years with performance status scores of 0-2," the authors wrote.
The study was funded by the IFCT and the French National Cancer Institute, with support by grants from Bristol-Myers Squibb, Roche, and Pierre Fabre. Several authors, including Dr. Quoix, disclosed financial relationships with the makers of chemotherapy drugs, including carboplatin (Bristol-Myers Squibb, Roche, and Lilly). Dr. Reckamp disclosed consulting for Amgen, Genentech, and Tragara Pharmaceuticals, as well as serving on speakers bureaus for Lilly Oncology and Genentech.
Chemotherapy with a platinum-based doublet was associated with a highly significant 36% reduction in mortality, compared with monotherapy, among elderly patients with non–small cell lung cancer in a study published online Aug. 9 by the Lancet.
The combination of carboplatin and paclitaxel was associated with more toxicity than was single-drug vinorelbine or gemcitabine regimens in the phase III trial, but the investigators contended that this was outweighed by the survival benefit.
Median overall survival for patients receiving carboplatin plus paclitaxel was 10.3 months, compared with 6.2 months in those randomized to monotherapy (hazard ratio, 0.64; P less than .0001).
Although several guidelines currently recommend monotherapy for elderly patients, the current finding is "of such magnitude that we believe the treatment paradigm for elderly patients with advanced NSCLC should be reconsidered," wrote Dr. Elisabeth Quoix of the Hôpitaux Universitaires de Strasbourg (France) and colleagues (Lancet 2011 Aug. 9 [doi:10.1016/S0140-6736(11)60780-0]).
The investigators from the IFCT (Intergroupe Francophone de Cancérologie Thoracique) looked at 451 patients aged 70-89 years (median age, 77 years) with unresectable stage IV NSCLC or stage III disease that was "unsuitable" for radical radiation therapy. Patients were followed for a median of 30.3 months. To be included in the study, patients’ scores on the World Health Organization’s performance status scale had to be 2 or lower (indicating severe disease), and patients had to have a life expectancy of at least 12 weeks.
The 225 patients who were randomized to the doublet chemotherapy group received intravenous carboplatin (AUC [area under the curve] = 6) on day 1, plus 90 mg/m² of paclitaxel on days 1, 8, and 15 of 28-day cycles.
The 226-patient monotherapy cohort received 25 mg/m² vinorelbine (62 patients) on days 1 and 8 – or 1,150 mg/m² gemcitabine (164 patients) on days 1 and 8 – of 21-day cycles, with the choice of either vinorelbine or gemcitabine being made by the institution conducting the therapy.
In the doublet group, cycles were repeated every 4 weeks, such that patients received 3 weeks of treatment plus 1 week without, for doublet chemotherapy. For monotherapy, the cycle lasted 3 weeks (2 weeks of treatment plus 1 week without), with a maximum of four cycles for doublet therapy and five cycles for monotherapy.
Survival Rates for Chemotherapy Study Patients
By 1 year, the survival rate was 25.4% in the monotherapy group vs. 44.5% in the doublet therapy group (HR, 0.64; P less than .0001). The trend persisted at 2 years, with the probability of survival being 11.7% in monotherapy recipients and 22.4% in those receiving doublet therapy, wrote the authors.
Median progression-free survival also was significantly longer with the doublet (6 months vs. 2.8 months; P less than .0001).
In 2009, an independent data-monitoring committee recommended stopping recruitment based on the second interim analysis.
"Grade 3-4 neutropenia, febrile neutropenia, thrombopenia, and anemia were significantly more frequent among patients in the doublet chemotherapy group than among those in the monotherapy group, as was grade 3-4 sensory neuropathy," wrote the authors. The protocol did not allow growth factor support in the first cycle, but it was authorized as secondary prophylaxis in patients who developed grade 3 or 4 neutropenia.
In all, 10 deaths in the doublet therapy group (4.4%) and 3 in the monotherapy group (1.3%) were related to treatment: Culprit diagnoses included sepsis, respiratory distress, and diarrhea related to renal insufficiency. But the percentage of deaths in the first 3 months after the start of therapy was "markedly lower" in patients who received carboplatin plus paclitaxel.
Although quality of life scores at week 18 were similar between groups, the authors pointed out that "role functioning and fatigue were worse in the doublet chemotherapy group than in the monotherapy group" (P = .026 and .039, respectively). Full quality of life data will be published separately, they said.
The 2009 American Society of Clinical Oncology guidelines (J. Clin. Oncol. 2009;27:6251-66) recommend that age "not be used as a criterion in the decision-making process about whether to treat a patient" and call for further research devoted to elderly patients, according to Dr. Quoix and colleagues. "Conversely," they noted, "the European Organisation for Research and Treatment of Cancer Elderly Task Force and Lung Cancer Group and International Society of Geriatric Oncology highlighted in 2010 that monotherapy should be given to elderly patients with advanced NSCLC."
"We believe that monthly carboplatin and weekly paclitaxel is a feasible option for first-line therapy of advanced NSCLC in patients older than 70 years with performance status scores of 0-2," the authors wrote.
The study was funded by the IFCT and the French National Cancer Institute, with support by grants from Bristol-Myers Squibb, Roche, and Pierre Fabre. Several authors, including Dr. Quoix, disclosed financial relationships with the makers of chemotherapy drugs, including carboplatin (Bristol-Myers Squibb, Roche, and Lilly). Dr. Reckamp disclosed consulting for Amgen, Genentech, and Tragara Pharmaceuticals, as well as serving on speakers bureaus for Lilly Oncology and Genentech.
FROM THE LANCET
Major Finding: By 1 year, median overall survival was 25.4% with monotherapy, vs. 44.5% with a carboplatin and paclitaxel doublet.
Data Source: A multicenter, open-label, phase III, randomized trial in NSCLC patients aged 70-89 years.
Disclosures: The study was funded by the IFCT and the French National Cancer Institute, with support by grants from Bristol-Myers Squibb, Roche, and Pierre Fabre. Several authors, including Dr. Quoix, disclosed financial relationships with the makers of chemotherapy drugs, including carboplatin (Bristol-Myers Squibb, Roche, and Lilly).
Endosonography Bests Surgical Lung Cancer Staging
AMSTERDAM – Initial endosonographic assessment of mediastinal lymph node metastases in patients with resectable non–small cell lung cancer surpassed initial surgical staging not just in clinical outcomes but also with lower cost and better quality of life in a controlled, head-to-head comparison of the two staging approaches.
"Given that assessment of lymph nodes by the endoscopic approach was more effective [and] better tolerated by patients, and seems cheaper than the surgical approach, we recommend that endoscopic tests be used, reserving surgical tests as a backup if endoscopy does not show evidence of cancer," Dr. Robert C. Rintoul said in presenting the results of a follow-up analysis at the World Conference on Lung Cancer.
"We think this is the way forward, and that this will change practice globally," said Dr. Rintoul, lead physician for thoracic oncology at Papworth Hospital in Cambridge, England.
He reported new data and addressed implications of the totality of evidence now available from ASTER (Assessment of Surgical Staging vs. Endoscopic Ultrasound in Lung Cancer: A Randomized Clinical Trial) that was conducted in patients with potentially resectable NSCLC.
Although the overall weight of evidence now in from ASTER uniformly favors endosonography first, perhaps the most noteworthy findings from the study were those included in a report in JAMA last November: Endosonography first cut the rate of unnecessary thoracotomies to 7% compared with an 18% rate in patients assessed by mediastinoscopy first (P = .02). In addition, 45% of patients evaluated by endosonography first had positive lymph nodes and so avoided mediastinoscopy (JAMA 2010;304:2245-52).
"A few years ago, people said all these patients need mediastinoscopy. What we’ve learned [from ASTER] is that about half never need mediastinoscopy. That is practice changing," commented Dr. Richard Gralla, chief of hematology oncology at North Shore–Long Island Jewish Health System in New Hyde Park, N.Y. "As a rule, patients find EBUS [endobronchial ultrasound–guided transbronchial needle aspiration] and EUS [transesophageal ultrasound-guided fine-needle aspiration] much simpler procedures," compared with mediastinoscopy, he noted at the meeting, which was sponsored by the International Association for the Study of Lung Cancer.
The ASTER results that were published last year proved so compelling that many surgeons and thoracic oncologists have already switched to endosonography first, noted Dr. Jouke T. Annema, a thoracic surgeon at Leiden (the Netherlands) University and lead ASTER investigator.
"EBUS is the new standard," he said in an interview, noting that earlier this year the Dutch agency responsible for setting medical policy adopted endosonography as the preferred initial method for lymph node assessment in patients with resectable NSCLC. The National Institute for Health and Clinical Excellence (NICE), which sets U.K. health policies, did not name endosonography as the preferred initial staging method for lung cancer in its revised guidelines last April because the cost-effectiveness findings reported at the meeting had not yet been published, Dr. Rintoul said.
ASTER randomized 118 patients to initial mediastinoscopy staging and 123 to initial endosonographic staging at four medical centers in the United Kingdom, the Netherlands, and Belgium. The initial results reported last November also showed that initial endosonography followed by surgical staging in patients who were initially found to be node negative produced 94% sensitivity for finding positive lymph nodes, which was significantly better than the 79% sensitivity rate using mediastinoscopy first (P = .02).
The additional analyses reported by Dr. Rintoul used patient quality of life assessment by the EQ-5D (EuroQol five-domain) instrument at baseline, immediately after staging, and again at 2 and 6 months after staging. Researchers ran EQ-5D assessments on 144 of the study’s 241 patients at baseline, and on 124 patients after 6 months. The results showed similar, average EQ-5D levels at baseline and after 2 and 6 months in the two arms of the trial; however, immediately after staging, the endosonography-first patients had a statistically significant edge in average quality of life of 0.117 EQ-5D units, compared with patients who were staged by mediastinoscopy first (P = .003).
Average medical costs rung up by patients over the 6 months of treatment after baseline were about £746 (about $1,200) less per patient using endosonography first, a difference that was not statistically significant but suggested that initial endosonographic staging produced better cost-effectiveness, Dr. Rintoul said. He also reported that initial endosonography led to an average gain per patient of 0.015 quality-adjusted life-years, an advantage over initial surgical staging that just missed statistical significance (P = .052).
ASTER received no commercial support, and Dr. Rintoul said that he had no disclosures. He said that Papworth Hospital has received unrestricted educational grants and equipment loans from Olympus. Dr. Gralla and Dr. Annema had no disclosures.
AMSTERDAM – Initial endosonographic assessment of mediastinal lymph node metastases in patients with resectable non–small cell lung cancer surpassed initial surgical staging not just in clinical outcomes but also with lower cost and better quality of life in a controlled, head-to-head comparison of the two staging approaches.
"Given that assessment of lymph nodes by the endoscopic approach was more effective [and] better tolerated by patients, and seems cheaper than the surgical approach, we recommend that endoscopic tests be used, reserving surgical tests as a backup if endoscopy does not show evidence of cancer," Dr. Robert C. Rintoul said in presenting the results of a follow-up analysis at the World Conference on Lung Cancer.
"We think this is the way forward, and that this will change practice globally," said Dr. Rintoul, lead physician for thoracic oncology at Papworth Hospital in Cambridge, England.
He reported new data and addressed implications of the totality of evidence now available from ASTER (Assessment of Surgical Staging vs. Endoscopic Ultrasound in Lung Cancer: A Randomized Clinical Trial) that was conducted in patients with potentially resectable NSCLC.
Although the overall weight of evidence now in from ASTER uniformly favors endosonography first, perhaps the most noteworthy findings from the study were those included in a report in JAMA last November: Endosonography first cut the rate of unnecessary thoracotomies to 7% compared with an 18% rate in patients assessed by mediastinoscopy first (P = .02). In addition, 45% of patients evaluated by endosonography first had positive lymph nodes and so avoided mediastinoscopy (JAMA 2010;304:2245-52).
"A few years ago, people said all these patients need mediastinoscopy. What we’ve learned [from ASTER] is that about half never need mediastinoscopy. That is practice changing," commented Dr. Richard Gralla, chief of hematology oncology at North Shore–Long Island Jewish Health System in New Hyde Park, N.Y. "As a rule, patients find EBUS [endobronchial ultrasound–guided transbronchial needle aspiration] and EUS [transesophageal ultrasound-guided fine-needle aspiration] much simpler procedures," compared with mediastinoscopy, he noted at the meeting, which was sponsored by the International Association for the Study of Lung Cancer.
The ASTER results that were published last year proved so compelling that many surgeons and thoracic oncologists have already switched to endosonography first, noted Dr. Jouke T. Annema, a thoracic surgeon at Leiden (the Netherlands) University and lead ASTER investigator.
"EBUS is the new standard," he said in an interview, noting that earlier this year the Dutch agency responsible for setting medical policy adopted endosonography as the preferred initial method for lymph node assessment in patients with resectable NSCLC. The National Institute for Health and Clinical Excellence (NICE), which sets U.K. health policies, did not name endosonography as the preferred initial staging method for lung cancer in its revised guidelines last April because the cost-effectiveness findings reported at the meeting had not yet been published, Dr. Rintoul said.
ASTER randomized 118 patients to initial mediastinoscopy staging and 123 to initial endosonographic staging at four medical centers in the United Kingdom, the Netherlands, and Belgium. The initial results reported last November also showed that initial endosonography followed by surgical staging in patients who were initially found to be node negative produced 94% sensitivity for finding positive lymph nodes, which was significantly better than the 79% sensitivity rate using mediastinoscopy first (P = .02).
The additional analyses reported by Dr. Rintoul used patient quality of life assessment by the EQ-5D (EuroQol five-domain) instrument at baseline, immediately after staging, and again at 2 and 6 months after staging. Researchers ran EQ-5D assessments on 144 of the study’s 241 patients at baseline, and on 124 patients after 6 months. The results showed similar, average EQ-5D levels at baseline and after 2 and 6 months in the two arms of the trial; however, immediately after staging, the endosonography-first patients had a statistically significant edge in average quality of life of 0.117 EQ-5D units, compared with patients who were staged by mediastinoscopy first (P = .003).
Average medical costs rung up by patients over the 6 months of treatment after baseline were about £746 (about $1,200) less per patient using endosonography first, a difference that was not statistically significant but suggested that initial endosonographic staging produced better cost-effectiveness, Dr. Rintoul said. He also reported that initial endosonography led to an average gain per patient of 0.015 quality-adjusted life-years, an advantage over initial surgical staging that just missed statistical significance (P = .052).
ASTER received no commercial support, and Dr. Rintoul said that he had no disclosures. He said that Papworth Hospital has received unrestricted educational grants and equipment loans from Olympus. Dr. Gralla and Dr. Annema had no disclosures.
AMSTERDAM – Initial endosonographic assessment of mediastinal lymph node metastases in patients with resectable non–small cell lung cancer surpassed initial surgical staging not just in clinical outcomes but also with lower cost and better quality of life in a controlled, head-to-head comparison of the two staging approaches.
"Given that assessment of lymph nodes by the endoscopic approach was more effective [and] better tolerated by patients, and seems cheaper than the surgical approach, we recommend that endoscopic tests be used, reserving surgical tests as a backup if endoscopy does not show evidence of cancer," Dr. Robert C. Rintoul said in presenting the results of a follow-up analysis at the World Conference on Lung Cancer.
"We think this is the way forward, and that this will change practice globally," said Dr. Rintoul, lead physician for thoracic oncology at Papworth Hospital in Cambridge, England.
He reported new data and addressed implications of the totality of evidence now available from ASTER (Assessment of Surgical Staging vs. Endoscopic Ultrasound in Lung Cancer: A Randomized Clinical Trial) that was conducted in patients with potentially resectable NSCLC.
Although the overall weight of evidence now in from ASTER uniformly favors endosonography first, perhaps the most noteworthy findings from the study were those included in a report in JAMA last November: Endosonography first cut the rate of unnecessary thoracotomies to 7% compared with an 18% rate in patients assessed by mediastinoscopy first (P = .02). In addition, 45% of patients evaluated by endosonography first had positive lymph nodes and so avoided mediastinoscopy (JAMA 2010;304:2245-52).
"A few years ago, people said all these patients need mediastinoscopy. What we’ve learned [from ASTER] is that about half never need mediastinoscopy. That is practice changing," commented Dr. Richard Gralla, chief of hematology oncology at North Shore–Long Island Jewish Health System in New Hyde Park, N.Y. "As a rule, patients find EBUS [endobronchial ultrasound–guided transbronchial needle aspiration] and EUS [transesophageal ultrasound-guided fine-needle aspiration] much simpler procedures," compared with mediastinoscopy, he noted at the meeting, which was sponsored by the International Association for the Study of Lung Cancer.
The ASTER results that were published last year proved so compelling that many surgeons and thoracic oncologists have already switched to endosonography first, noted Dr. Jouke T. Annema, a thoracic surgeon at Leiden (the Netherlands) University and lead ASTER investigator.
"EBUS is the new standard," he said in an interview, noting that earlier this year the Dutch agency responsible for setting medical policy adopted endosonography as the preferred initial method for lymph node assessment in patients with resectable NSCLC. The National Institute for Health and Clinical Excellence (NICE), which sets U.K. health policies, did not name endosonography as the preferred initial staging method for lung cancer in its revised guidelines last April because the cost-effectiveness findings reported at the meeting had not yet been published, Dr. Rintoul said.
ASTER randomized 118 patients to initial mediastinoscopy staging and 123 to initial endosonographic staging at four medical centers in the United Kingdom, the Netherlands, and Belgium. The initial results reported last November also showed that initial endosonography followed by surgical staging in patients who were initially found to be node negative produced 94% sensitivity for finding positive lymph nodes, which was significantly better than the 79% sensitivity rate using mediastinoscopy first (P = .02).
The additional analyses reported by Dr. Rintoul used patient quality of life assessment by the EQ-5D (EuroQol five-domain) instrument at baseline, immediately after staging, and again at 2 and 6 months after staging. Researchers ran EQ-5D assessments on 144 of the study’s 241 patients at baseline, and on 124 patients after 6 months. The results showed similar, average EQ-5D levels at baseline and after 2 and 6 months in the two arms of the trial; however, immediately after staging, the endosonography-first patients had a statistically significant edge in average quality of life of 0.117 EQ-5D units, compared with patients who were staged by mediastinoscopy first (P = .003).
Average medical costs rung up by patients over the 6 months of treatment after baseline were about £746 (about $1,200) less per patient using endosonography first, a difference that was not statistically significant but suggested that initial endosonographic staging produced better cost-effectiveness, Dr. Rintoul said. He also reported that initial endosonography led to an average gain per patient of 0.015 quality-adjusted life-years, an advantage over initial surgical staging that just missed statistical significance (P = .052).
ASTER received no commercial support, and Dr. Rintoul said that he had no disclosures. He said that Papworth Hospital has received unrestricted educational grants and equipment loans from Olympus. Dr. Gralla and Dr. Annema had no disclosures.
FROM THE WORLD CONFERENCE ON LUNG CANCER
Major Finding: For patients staged with initial endosonographic assessment of lymph node metastases, quality of life on the EQ-5D surpassed that in patients initially staged surgically by 0.117 units (P = 0.003), and saved an average of £746 (about $1,200) per patient.
Data Source: ASTER, which randomized 241 patients with potentially resectable lung cancer.
Disclosures: ASTER received no commercial support, and Dr. Rintoul said that he had no disclosures. He said that Papworth Hospital received unrestricted educational grants and equipment loans from Olympus. Dr. Gralla and Dr. Annema had no disclosures.
Brd4: Potential new target in AML

Researchers at Cold Spring Harbor Laboratory (CSHL) and 5 other laboratories may have identified a new drug target for the treatment of acute myeloid leukemia (AML).
They pinpointed a protein called Brd4, which contains a distinct region known as bromodomain and is a member of the BET protein family, known for regulating gene expression.
A new drug candidate that inhibits Brd4 was able to suppress AML in experimental models.
“The drug candidate not only displays remarkable anti-leukemia activity in aggressive disease models and against cells derived from patients with diverse, genetic subtypes of AML, but is also minimally toxic to non-cancerous cells,” said Chris Vakoc, MD, PhD, leader of the study at CSHL.
“The drug is currently being developed for therapeutic use for cancer patients by Tensha Therapeutics and is expected to enter clinical trials within 2 years.”
The team used RNAi screening in an AML murine model. The RNAi screen introduced small hairpin-shaped pieces of RNA (shRNA) that encode epigenetic proteins into mice that harbor leukemia-causing mutations.
The mice in this study carried the oncogene Nras and rearranged forms of the MLL gene, both of which are mutations often found in patients whose leukemia is resistant to standard chemotherapy.
The drinking water for the mice was also supplemented with doxycyline.
“Inducing shRNA that shuts down a gene required for the survival of leukemic cells can lead to complete disease remission,” said Johannes Zuber, MD, former postdoctoral researcher at CSHL. “This ability to use shRNA to simulate the effect of an anti-cancer drug illustrates the power of this approach.”
The team also identified another potential target in AML called Myb. The team found that suppressing the activity of Myb also eliminated AML in mice. The team screened more than 1000 shRNAs targeting 243 known epigenetic regulators of chromatin.
They homed in on Brd4 as a target and found that suppressing the protein led to the most dramatic changes in AML. The cell cycle was arrested, the leukemic cells died, leukemia progression was delayed, and the mice survived longer.
Previously, James Bradner, MD, at Dana-Farber Cancer Institute in Boston, and his research team had developed a small molecule inhibitor of Brd4 called JQ1. The two groups collaborated, reproducing the antileukemic effects in the Brd4 shRNA experiments. They consider JQ1 to be an ideal drug candidate.
Their findings were published online in Nature.![]()

Researchers at Cold Spring Harbor Laboratory (CSHL) and 5 other laboratories may have identified a new drug target for the treatment of acute myeloid leukemia (AML).
They pinpointed a protein called Brd4, which contains a distinct region known as bromodomain and is a member of the BET protein family, known for regulating gene expression.
A new drug candidate that inhibits Brd4 was able to suppress AML in experimental models.
“The drug candidate not only displays remarkable anti-leukemia activity in aggressive disease models and against cells derived from patients with diverse, genetic subtypes of AML, but is also minimally toxic to non-cancerous cells,” said Chris Vakoc, MD, PhD, leader of the study at CSHL.
“The drug is currently being developed for therapeutic use for cancer patients by Tensha Therapeutics and is expected to enter clinical trials within 2 years.”
The team used RNAi screening in an AML murine model. The RNAi screen introduced small hairpin-shaped pieces of RNA (shRNA) that encode epigenetic proteins into mice that harbor leukemia-causing mutations.
The mice in this study carried the oncogene Nras and rearranged forms of the MLL gene, both of which are mutations often found in patients whose leukemia is resistant to standard chemotherapy.
The drinking water for the mice was also supplemented with doxycyline.
“Inducing shRNA that shuts down a gene required for the survival of leukemic cells can lead to complete disease remission,” said Johannes Zuber, MD, former postdoctoral researcher at CSHL. “This ability to use shRNA to simulate the effect of an anti-cancer drug illustrates the power of this approach.”
The team also identified another potential target in AML called Myb. The team found that suppressing the activity of Myb also eliminated AML in mice. The team screened more than 1000 shRNAs targeting 243 known epigenetic regulators of chromatin.
They homed in on Brd4 as a target and found that suppressing the protein led to the most dramatic changes in AML. The cell cycle was arrested, the leukemic cells died, leukemia progression was delayed, and the mice survived longer.
Previously, James Bradner, MD, at Dana-Farber Cancer Institute in Boston, and his research team had developed a small molecule inhibitor of Brd4 called JQ1. The two groups collaborated, reproducing the antileukemic effects in the Brd4 shRNA experiments. They consider JQ1 to be an ideal drug candidate.
Their findings were published online in Nature.![]()

Researchers at Cold Spring Harbor Laboratory (CSHL) and 5 other laboratories may have identified a new drug target for the treatment of acute myeloid leukemia (AML).
They pinpointed a protein called Brd4, which contains a distinct region known as bromodomain and is a member of the BET protein family, known for regulating gene expression.
A new drug candidate that inhibits Brd4 was able to suppress AML in experimental models.
“The drug candidate not only displays remarkable anti-leukemia activity in aggressive disease models and against cells derived from patients with diverse, genetic subtypes of AML, but is also minimally toxic to non-cancerous cells,” said Chris Vakoc, MD, PhD, leader of the study at CSHL.
“The drug is currently being developed for therapeutic use for cancer patients by Tensha Therapeutics and is expected to enter clinical trials within 2 years.”
The team used RNAi screening in an AML murine model. The RNAi screen introduced small hairpin-shaped pieces of RNA (shRNA) that encode epigenetic proteins into mice that harbor leukemia-causing mutations.
The mice in this study carried the oncogene Nras and rearranged forms of the MLL gene, both of which are mutations often found in patients whose leukemia is resistant to standard chemotherapy.
The drinking water for the mice was also supplemented with doxycyline.
“Inducing shRNA that shuts down a gene required for the survival of leukemic cells can lead to complete disease remission,” said Johannes Zuber, MD, former postdoctoral researcher at CSHL. “This ability to use shRNA to simulate the effect of an anti-cancer drug illustrates the power of this approach.”
The team also identified another potential target in AML called Myb. The team found that suppressing the activity of Myb also eliminated AML in mice. The team screened more than 1000 shRNAs targeting 243 known epigenetic regulators of chromatin.
They homed in on Brd4 as a target and found that suppressing the protein led to the most dramatic changes in AML. The cell cycle was arrested, the leukemic cells died, leukemia progression was delayed, and the mice survived longer.
Previously, James Bradner, MD, at Dana-Farber Cancer Institute in Boston, and his research team had developed a small molecule inhibitor of Brd4 called JQ1. The two groups collaborated, reproducing the antileukemic effects in the Brd4 shRNA experiments. They consider JQ1 to be an ideal drug candidate.
Their findings were published online in Nature.![]()
Power Through Afternoon Energy Slumps
Late-afternoon slowdowns are natural, explains Susan Swadener, PhD, RD, dietetic internship director and lecturer in the Food Science and Nutrition Department at California State University San Luis Obispo. "Your enzyme levels go down, which is part of your diurnal pattern to slow down the body's processes to get ready for the evening and sleep," she says.
Common-Sense Nutrition
To fight afternoon fatigue, adopt good nutritional habits throughout your day. It's essential to have a healthy breakfast in the morning, advises Dr. Swadener, who's also a registered dietitian in private practice. Make sure you eat lunch, too, with a balance of protein, carbohydrates, and fats.
Afternoon snacks are a good idea, especially if they incorporate some protein. Foods high in protein can increase norepinephrine and epinephrine production, which helps you stay alert. Some examples of quick and nutritious snacks: string cheese and an apple; sliced cheese or peanut butter on whole-wheat crackers; yogurt; a handful of almonds or walnuts; or trail mix.
And don't forget one of the most common directives to your patients: "Push the fluids." Have a glass of water or nonfat milk with your lunch, and make sure you keep your water bottle handy at your desk.
As for coffee, "you don't want to be drinking it constantly to keep your energy level up, because you'll just crash afterwards," Dr. Swadener says. If you don't abuse caffeine, one cup of coffee in the morning and one in the afternoon is found to be most effective in increasing your alertness.
Change It Up
Desk tasks can make you drowsy. Daniel Markovitz is president of TimeBack Management, which specializes in applying Lean manufacturing principles to increase personal productivity for healthcare workers. He's found—and research such as a 2003 study in Ergonomics and a 2007 National Institute for Occupational Safety and Health study in the American Journal of Industrial Medicine supports these conclusions—that taking mini-breaks and then returning to the task at hand can refresh you and make you more productive.
You also get energy by using it, so a brisk walk around the hospital or walking up and down a couple of flights of stairs can increase circulation and blood flow to the brain. "You don't even have to get up from your desk," Markovitz says. "Just by changing the nature of the work you're doing, it's refreshing to your brain." That might mean switching from dictation to administrative work, or from scheduling to research.
And remember the value of play, Markovitz advises. "We tend to discourage going on Facebook or playing a video game at work. But if you take a 15-minute break to do something that's pleasurable, that causes your brain to fire in different ways, that can be another helpful adaptation."
Gretchen Henkel is a freelance writer based in California.
Interactions are Engaging
You've just finished a brain-numbing administrative report, and you've got 10 minutes before your next task. Don't just fill that time with checking your email.
Corporate consultant Daniel Markovitz advises another tack: Walk down the hall to touch base with colleagues. "You don't have to get into an involved conversation about their QI project. Just ask them how it's going for them," he advises.
Breaking up a busy day with exercise or a social call can get you over the doldrums hump, he says, because "you're getting up and interacting with someone. At the same time, you're doing something that's really important for the hospital: You're strengthening those bonds and interrelationships with people.—GH
Late-afternoon slowdowns are natural, explains Susan Swadener, PhD, RD, dietetic internship director and lecturer in the Food Science and Nutrition Department at California State University San Luis Obispo. "Your enzyme levels go down, which is part of your diurnal pattern to slow down the body's processes to get ready for the evening and sleep," she says.
Common-Sense Nutrition
To fight afternoon fatigue, adopt good nutritional habits throughout your day. It's essential to have a healthy breakfast in the morning, advises Dr. Swadener, who's also a registered dietitian in private practice. Make sure you eat lunch, too, with a balance of protein, carbohydrates, and fats.
Afternoon snacks are a good idea, especially if they incorporate some protein. Foods high in protein can increase norepinephrine and epinephrine production, which helps you stay alert. Some examples of quick and nutritious snacks: string cheese and an apple; sliced cheese or peanut butter on whole-wheat crackers; yogurt; a handful of almonds or walnuts; or trail mix.
And don't forget one of the most common directives to your patients: "Push the fluids." Have a glass of water or nonfat milk with your lunch, and make sure you keep your water bottle handy at your desk.
As for coffee, "you don't want to be drinking it constantly to keep your energy level up, because you'll just crash afterwards," Dr. Swadener says. If you don't abuse caffeine, one cup of coffee in the morning and one in the afternoon is found to be most effective in increasing your alertness.
Change It Up
Desk tasks can make you drowsy. Daniel Markovitz is president of TimeBack Management, which specializes in applying Lean manufacturing principles to increase personal productivity for healthcare workers. He's found—and research such as a 2003 study in Ergonomics and a 2007 National Institute for Occupational Safety and Health study in the American Journal of Industrial Medicine supports these conclusions—that taking mini-breaks and then returning to the task at hand can refresh you and make you more productive.
You also get energy by using it, so a brisk walk around the hospital or walking up and down a couple of flights of stairs can increase circulation and blood flow to the brain. "You don't even have to get up from your desk," Markovitz says. "Just by changing the nature of the work you're doing, it's refreshing to your brain." That might mean switching from dictation to administrative work, or from scheduling to research.
And remember the value of play, Markovitz advises. "We tend to discourage going on Facebook or playing a video game at work. But if you take a 15-minute break to do something that's pleasurable, that causes your brain to fire in different ways, that can be another helpful adaptation."
Gretchen Henkel is a freelance writer based in California.
Interactions are Engaging
You've just finished a brain-numbing administrative report, and you've got 10 minutes before your next task. Don't just fill that time with checking your email.
Corporate consultant Daniel Markovitz advises another tack: Walk down the hall to touch base with colleagues. "You don't have to get into an involved conversation about their QI project. Just ask them how it's going for them," he advises.
Breaking up a busy day with exercise or a social call can get you over the doldrums hump, he says, because "you're getting up and interacting with someone. At the same time, you're doing something that's really important for the hospital: You're strengthening those bonds and interrelationships with people.—GH
Late-afternoon slowdowns are natural, explains Susan Swadener, PhD, RD, dietetic internship director and lecturer in the Food Science and Nutrition Department at California State University San Luis Obispo. "Your enzyme levels go down, which is part of your diurnal pattern to slow down the body's processes to get ready for the evening and sleep," she says.
Common-Sense Nutrition
To fight afternoon fatigue, adopt good nutritional habits throughout your day. It's essential to have a healthy breakfast in the morning, advises Dr. Swadener, who's also a registered dietitian in private practice. Make sure you eat lunch, too, with a balance of protein, carbohydrates, and fats.
Afternoon snacks are a good idea, especially if they incorporate some protein. Foods high in protein can increase norepinephrine and epinephrine production, which helps you stay alert. Some examples of quick and nutritious snacks: string cheese and an apple; sliced cheese or peanut butter on whole-wheat crackers; yogurt; a handful of almonds or walnuts; or trail mix.
And don't forget one of the most common directives to your patients: "Push the fluids." Have a glass of water or nonfat milk with your lunch, and make sure you keep your water bottle handy at your desk.
As for coffee, "you don't want to be drinking it constantly to keep your energy level up, because you'll just crash afterwards," Dr. Swadener says. If you don't abuse caffeine, one cup of coffee in the morning and one in the afternoon is found to be most effective in increasing your alertness.
Change It Up
Desk tasks can make you drowsy. Daniel Markovitz is president of TimeBack Management, which specializes in applying Lean manufacturing principles to increase personal productivity for healthcare workers. He's found—and research such as a 2003 study in Ergonomics and a 2007 National Institute for Occupational Safety and Health study in the American Journal of Industrial Medicine supports these conclusions—that taking mini-breaks and then returning to the task at hand can refresh you and make you more productive.
You also get energy by using it, so a brisk walk around the hospital or walking up and down a couple of flights of stairs can increase circulation and blood flow to the brain. "You don't even have to get up from your desk," Markovitz says. "Just by changing the nature of the work you're doing, it's refreshing to your brain." That might mean switching from dictation to administrative work, or from scheduling to research.
And remember the value of play, Markovitz advises. "We tend to discourage going on Facebook or playing a video game at work. But if you take a 15-minute break to do something that's pleasurable, that causes your brain to fire in different ways, that can be another helpful adaptation."
Gretchen Henkel is a freelance writer based in California.
Interactions are Engaging
You've just finished a brain-numbing administrative report, and you've got 10 minutes before your next task. Don't just fill that time with checking your email.
Corporate consultant Daniel Markovitz advises another tack: Walk down the hall to touch base with colleagues. "You don't have to get into an involved conversation about their QI project. Just ask them how it's going for them," he advises.
Breaking up a busy day with exercise or a social call can get you over the doldrums hump, he says, because "you're getting up and interacting with someone. At the same time, you're doing something that's really important for the hospital: You're strengthening those bonds and interrelationships with people.—GH
Paraneoplastic Autoimmune Multiorgan Syndrome Proves Rapidly Fatal
The skin may hold the key to differentiating classic pemphigus from the heterogenous autoimmune syndrome known as paraneoplastic autoimmune multiorgan syndrome.
It is a distinction of critical prognostic importance, because paraneoplastic autoimmune multiorgan syndrome (PAMS) typically is rapidly fatal, according to Dr. Sergei A. Grando, professor of dermatology and biologic chemistry at the University of California, Irvine. "The vast majority of patients die within several months of diagnosis, usually due to infections or respiratory failure, often taking the form of multiorgan system failure."
Two-thirds of patients with PAMS have a known internal malignancy at the time of their first mucocutaneous eruption. The most common of these neoplasms are non-Hodgkin’s lymphoma, which is present in more than 40% of PAMS patients; chronic lymphocytic leukemia, present in 30%; Castleman disease, present in 10%; and thymoma, present in 6%.
When a patient meets the diagnostic criteria for PAMS without having a known cancer, it is appropriate to launch a search for hidden malignancy, said Dr. Grando.
A key distinction between the skin lesions of PAMS and classic pemphigus is that PAMS involves inflammatory macules, papules, plaques, and blisters occurring on an inflammatory background over the trunk and extremities, including the palms and soles, but sparing the scalp.
In contrast, the generally more vesicular blisters and crusted erosions of pemphigus vulgaris display little erythema and usually occur on a noninflammatory background on the scalp, trunk, and extremities (but sparing the palms and soles). The most common location for skin lesions in PAMS is the palms; in pemphigus vulgaris, it is the scalp.
Also, Nikolsky's sign is positive in pemphigus vulgaris, but negative in PAMS, added Dr. Grando, who was among the investigators who first described PAMS a decade ago (Arch. Dermatol. 2001;137:193-206).
PAMS is characterized by severe and diffuse oral mucous membrane involvement, with persistent painful stomatitis because of blisters and erosions, and frequent involvement of other mucous membranes, including the eyes and genitalia. Cicatrizing conjunctivitis is particularly common in PAMS. In contrast, oral mucous membrane involvement in pemphigus is more discrete, with the eyes or other nonoral mucosa rarely involved.
Another key in the differential diagnosis: PAMS is associated with the HLA-DRB1*03 allele, whereas pemphigus vulgaris and foliaceous are strongly associated with the -04 and -14 alleles, respectively.
A hallmark of PAMS is respiratory involvement, with the sloughing of bronchial epithelial cells contributing to small airway occlusion and bronchiolitis obliterans. Classic pemphigus is free of respiratory involvement.
Both the esophagus and colon may be involved in PAMS, whereas only the esophagus is affected in pemphigus vulgaris.
In a published series of 28 PAMS patients, painful and generalized oral stomatitis was present in all 28, respiratory involvement was in 26, death from respiratory failure occurred in 22, and lichenoid skin involvement was present in 19. Only seven patients had no skin lesions (Br. J. Dermatol. 2003;149:1143-51).
At least five different subtypes of PAMS can be distinguished on the basis of the skin disease manifestations they most resemble. These subtypes of pemphiguslike PAMS include paraneoplastic pemphigus, bullous pemphigoid–like, erythema multiforme–like, lichen planus–like, and graft-vs.-host-disease–like versions of PAMS.
Dr. Grando eschews the term "paraneoplastic pemphigus" as too restrictive. After all, true pemphigus doesn’t usually affect the lungs, he noted.
Whereas most patients with classic pemphigus respond well to high-dose corticosteroids and recalcitrant disease can be effectively treated with cytotoxic agents, cyclosporine, intravenous gamma globulin, and other second-line agents, PAMS is resistant to all conventional forms of therapy.
"What can we offer? Really not much," Dr. Grando said during his presentation at the World Congress of Dermatology in Seoul, South Korea.
The preferred treatment regimen is a combination of prednisone and cyclosporine, with or without cyclophosphamide. Monthly courses of IVIG can buy patients a few extra months, he added.
Dr. Grando declared having no relevant financial interests.
The skin may hold the key to differentiating classic pemphigus from the heterogenous autoimmune syndrome known as paraneoplastic autoimmune multiorgan syndrome.
It is a distinction of critical prognostic importance, because paraneoplastic autoimmune multiorgan syndrome (PAMS) typically is rapidly fatal, according to Dr. Sergei A. Grando, professor of dermatology and biologic chemistry at the University of California, Irvine. "The vast majority of patients die within several months of diagnosis, usually due to infections or respiratory failure, often taking the form of multiorgan system failure."
Two-thirds of patients with PAMS have a known internal malignancy at the time of their first mucocutaneous eruption. The most common of these neoplasms are non-Hodgkin’s lymphoma, which is present in more than 40% of PAMS patients; chronic lymphocytic leukemia, present in 30%; Castleman disease, present in 10%; and thymoma, present in 6%.
When a patient meets the diagnostic criteria for PAMS without having a known cancer, it is appropriate to launch a search for hidden malignancy, said Dr. Grando.
A key distinction between the skin lesions of PAMS and classic pemphigus is that PAMS involves inflammatory macules, papules, plaques, and blisters occurring on an inflammatory background over the trunk and extremities, including the palms and soles, but sparing the scalp.
In contrast, the generally more vesicular blisters and crusted erosions of pemphigus vulgaris display little erythema and usually occur on a noninflammatory background on the scalp, trunk, and extremities (but sparing the palms and soles). The most common location for skin lesions in PAMS is the palms; in pemphigus vulgaris, it is the scalp.
Also, Nikolsky's sign is positive in pemphigus vulgaris, but negative in PAMS, added Dr. Grando, who was among the investigators who first described PAMS a decade ago (Arch. Dermatol. 2001;137:193-206).
PAMS is characterized by severe and diffuse oral mucous membrane involvement, with persistent painful stomatitis because of blisters and erosions, and frequent involvement of other mucous membranes, including the eyes and genitalia. Cicatrizing conjunctivitis is particularly common in PAMS. In contrast, oral mucous membrane involvement in pemphigus is more discrete, with the eyes or other nonoral mucosa rarely involved.
Another key in the differential diagnosis: PAMS is associated with the HLA-DRB1*03 allele, whereas pemphigus vulgaris and foliaceous are strongly associated with the -04 and -14 alleles, respectively.
A hallmark of PAMS is respiratory involvement, with the sloughing of bronchial epithelial cells contributing to small airway occlusion and bronchiolitis obliterans. Classic pemphigus is free of respiratory involvement.
Both the esophagus and colon may be involved in PAMS, whereas only the esophagus is affected in pemphigus vulgaris.
In a published series of 28 PAMS patients, painful and generalized oral stomatitis was present in all 28, respiratory involvement was in 26, death from respiratory failure occurred in 22, and lichenoid skin involvement was present in 19. Only seven patients had no skin lesions (Br. J. Dermatol. 2003;149:1143-51).
At least five different subtypes of PAMS can be distinguished on the basis of the skin disease manifestations they most resemble. These subtypes of pemphiguslike PAMS include paraneoplastic pemphigus, bullous pemphigoid–like, erythema multiforme–like, lichen planus–like, and graft-vs.-host-disease–like versions of PAMS.
Dr. Grando eschews the term "paraneoplastic pemphigus" as too restrictive. After all, true pemphigus doesn’t usually affect the lungs, he noted.
Whereas most patients with classic pemphigus respond well to high-dose corticosteroids and recalcitrant disease can be effectively treated with cytotoxic agents, cyclosporine, intravenous gamma globulin, and other second-line agents, PAMS is resistant to all conventional forms of therapy.
"What can we offer? Really not much," Dr. Grando said during his presentation at the World Congress of Dermatology in Seoul, South Korea.
The preferred treatment regimen is a combination of prednisone and cyclosporine, with or without cyclophosphamide. Monthly courses of IVIG can buy patients a few extra months, he added.
Dr. Grando declared having no relevant financial interests.
The skin may hold the key to differentiating classic pemphigus from the heterogenous autoimmune syndrome known as paraneoplastic autoimmune multiorgan syndrome.
It is a distinction of critical prognostic importance, because paraneoplastic autoimmune multiorgan syndrome (PAMS) typically is rapidly fatal, according to Dr. Sergei A. Grando, professor of dermatology and biologic chemistry at the University of California, Irvine. "The vast majority of patients die within several months of diagnosis, usually due to infections or respiratory failure, often taking the form of multiorgan system failure."
Two-thirds of patients with PAMS have a known internal malignancy at the time of their first mucocutaneous eruption. The most common of these neoplasms are non-Hodgkin’s lymphoma, which is present in more than 40% of PAMS patients; chronic lymphocytic leukemia, present in 30%; Castleman disease, present in 10%; and thymoma, present in 6%.
When a patient meets the diagnostic criteria for PAMS without having a known cancer, it is appropriate to launch a search for hidden malignancy, said Dr. Grando.
A key distinction between the skin lesions of PAMS and classic pemphigus is that PAMS involves inflammatory macules, papules, plaques, and blisters occurring on an inflammatory background over the trunk and extremities, including the palms and soles, but sparing the scalp.
In contrast, the generally more vesicular blisters and crusted erosions of pemphigus vulgaris display little erythema and usually occur on a noninflammatory background on the scalp, trunk, and extremities (but sparing the palms and soles). The most common location for skin lesions in PAMS is the palms; in pemphigus vulgaris, it is the scalp.
Also, Nikolsky's sign is positive in pemphigus vulgaris, but negative in PAMS, added Dr. Grando, who was among the investigators who first described PAMS a decade ago (Arch. Dermatol. 2001;137:193-206).
PAMS is characterized by severe and diffuse oral mucous membrane involvement, with persistent painful stomatitis because of blisters and erosions, and frequent involvement of other mucous membranes, including the eyes and genitalia. Cicatrizing conjunctivitis is particularly common in PAMS. In contrast, oral mucous membrane involvement in pemphigus is more discrete, with the eyes or other nonoral mucosa rarely involved.
Another key in the differential diagnosis: PAMS is associated with the HLA-DRB1*03 allele, whereas pemphigus vulgaris and foliaceous are strongly associated with the -04 and -14 alleles, respectively.
A hallmark of PAMS is respiratory involvement, with the sloughing of bronchial epithelial cells contributing to small airway occlusion and bronchiolitis obliterans. Classic pemphigus is free of respiratory involvement.
Both the esophagus and colon may be involved in PAMS, whereas only the esophagus is affected in pemphigus vulgaris.
In a published series of 28 PAMS patients, painful and generalized oral stomatitis was present in all 28, respiratory involvement was in 26, death from respiratory failure occurred in 22, and lichenoid skin involvement was present in 19. Only seven patients had no skin lesions (Br. J. Dermatol. 2003;149:1143-51).
At least five different subtypes of PAMS can be distinguished on the basis of the skin disease manifestations they most resemble. These subtypes of pemphiguslike PAMS include paraneoplastic pemphigus, bullous pemphigoid–like, erythema multiforme–like, lichen planus–like, and graft-vs.-host-disease–like versions of PAMS.
Dr. Grando eschews the term "paraneoplastic pemphigus" as too restrictive. After all, true pemphigus doesn’t usually affect the lungs, he noted.
Whereas most patients with classic pemphigus respond well to high-dose corticosteroids and recalcitrant disease can be effectively treated with cytotoxic agents, cyclosporine, intravenous gamma globulin, and other second-line agents, PAMS is resistant to all conventional forms of therapy.
"What can we offer? Really not much," Dr. Grando said during his presentation at the World Congress of Dermatology in Seoul, South Korea.
The preferred treatment regimen is a combination of prednisone and cyclosporine, with or without cyclophosphamide. Monthly courses of IVIG can buy patients a few extra months, he added.
Dr. Grando declared having no relevant financial interests.
Study: Post-Discharge Costs Negate HM's In-Hospital Savings
A new report that suggests the lower costs and reduced length of stay (LOS) associated with hospitalist care of hospitalized Medicare beneficiaries is offset by higher costs post-discharge highlights progress and opportunities for hospitalists, SHM's president says.
The federally-funded study published Monday in Annals of Internal Medicine showed that while hospitalists clearly reduced LOS and cut in-hospital spending (by $282 per hospital visit), Medicare costs in the 30 days post-discharge were $332 higher than those followed up by primary care physicians. Patients discharged by hospitalists were less likely to be sent straight home and more likely to be admitted to a nursing home.
SHM President Joseph Li, MD, SFHM, associate professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, says the data underscores the need for programs like SHM's Project BOOST, which helps hospitals improve discharge and reduce readmissions.
Dr. Li notes two limitations to the research. First, the patients reviewed were all from 2001-2006, long before the current healthcare debate surrounding cost containment and patient safety. Second, the review does not account for the quality of medical care.
“The study was done at a time which was early in the hospitalist movement,” Dr. Li says. “It’s fair to say at that point we weren’t talking as a field as much about trying to prevent unnecessary readmissions. ... When I look at this study, I think it’s an opportunity for hospitalists to think how we can improve on communications with post-discharge facilities. How we can improve transitions.”
An accompanying editorial agreed, noting that while hospitalists and outpatient care might be viewed in different silos, “patients regularly move back and forth across that divide.”
“It is important to better understand the association between hospitalist care and costs,” editorial co-author Lena Chen, MD, MS, Division of General Medicine, University of Michigan, writes in an email to The Hospitalist. “This paper takes a big step towards addressing this subject with a large study, and will hopefully spur additional related research. That would be a good thing for hospital medicine.”
A new report that suggests the lower costs and reduced length of stay (LOS) associated with hospitalist care of hospitalized Medicare beneficiaries is offset by higher costs post-discharge highlights progress and opportunities for hospitalists, SHM's president says.
The federally-funded study published Monday in Annals of Internal Medicine showed that while hospitalists clearly reduced LOS and cut in-hospital spending (by $282 per hospital visit), Medicare costs in the 30 days post-discharge were $332 higher than those followed up by primary care physicians. Patients discharged by hospitalists were less likely to be sent straight home and more likely to be admitted to a nursing home.
SHM President Joseph Li, MD, SFHM, associate professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, says the data underscores the need for programs like SHM's Project BOOST, which helps hospitals improve discharge and reduce readmissions.
Dr. Li notes two limitations to the research. First, the patients reviewed were all from 2001-2006, long before the current healthcare debate surrounding cost containment and patient safety. Second, the review does not account for the quality of medical care.
“The study was done at a time which was early in the hospitalist movement,” Dr. Li says. “It’s fair to say at that point we weren’t talking as a field as much about trying to prevent unnecessary readmissions. ... When I look at this study, I think it’s an opportunity for hospitalists to think how we can improve on communications with post-discharge facilities. How we can improve transitions.”
An accompanying editorial agreed, noting that while hospitalists and outpatient care might be viewed in different silos, “patients regularly move back and forth across that divide.”
“It is important to better understand the association between hospitalist care and costs,” editorial co-author Lena Chen, MD, MS, Division of General Medicine, University of Michigan, writes in an email to The Hospitalist. “This paper takes a big step towards addressing this subject with a large study, and will hopefully spur additional related research. That would be a good thing for hospital medicine.”
A new report that suggests the lower costs and reduced length of stay (LOS) associated with hospitalist care of hospitalized Medicare beneficiaries is offset by higher costs post-discharge highlights progress and opportunities for hospitalists, SHM's president says.
The federally-funded study published Monday in Annals of Internal Medicine showed that while hospitalists clearly reduced LOS and cut in-hospital spending (by $282 per hospital visit), Medicare costs in the 30 days post-discharge were $332 higher than those followed up by primary care physicians. Patients discharged by hospitalists were less likely to be sent straight home and more likely to be admitted to a nursing home.
SHM President Joseph Li, MD, SFHM, associate professor of medicine at Harvard Medical School and director of the hospital medicine division at Beth Israel Deaconess Medical Center in Boston, says the data underscores the need for programs like SHM's Project BOOST, which helps hospitals improve discharge and reduce readmissions.
Dr. Li notes two limitations to the research. First, the patients reviewed were all from 2001-2006, long before the current healthcare debate surrounding cost containment and patient safety. Second, the review does not account for the quality of medical care.
“The study was done at a time which was early in the hospitalist movement,” Dr. Li says. “It’s fair to say at that point we weren’t talking as a field as much about trying to prevent unnecessary readmissions. ... When I look at this study, I think it’s an opportunity for hospitalists to think how we can improve on communications with post-discharge facilities. How we can improve transitions.”
An accompanying editorial agreed, noting that while hospitalists and outpatient care might be viewed in different silos, “patients regularly move back and forth across that divide.”
“It is important to better understand the association between hospitalist care and costs,” editorial co-author Lena Chen, MD, MS, Division of General Medicine, University of Michigan, writes in an email to The Hospitalist. “This paper takes a big step towards addressing this subject with a large study, and will hopefully spur additional related research. That would be a good thing for hospital medicine.”
CMS Ups the Stakes for Coordinated Care
Health organizations and providers experienced in providing care across multiple settings have until Aug. 19 to apply for a new accountable care organizations (ACO) program through the Centers for Medicare & Medicaid Services (CMS) that promises to offer a higher level of savings than that offered through a previous initiative.
“Hospital medicine groups in and of themselves won’t be applying for it,” says Ron Greeno, MD, MHM, chief medical officer of Brentwood, Tenn.-based Cogent HMG, and chair of SHM's Public Policy Committee. “But the groups that are looking to participate will have hospitalists working for them.”
The new program, tiled the Pioneer ACO Model, was created to offer potentially higher payments to providers and organizations who have already worked under contracts tied to shared savings or care coordination. A related model, the Medicare Shared Savings Program, does not require any previous experience with such contracts. The latter program has completed accepting public comments, but no application deadline has yet been set. (updated Aug. 15, 2011)
Just how many groups apply for the Pioneer program will be interesting: Initially, CMS will enter participation agreements with up to 30 organizations, and each must serve at least 15,000 beneficiaries (5,000 in rural areas). The capped cohort size didn’t seem to spur additional interest, as CMS originally set an application deadline for July, but pushed it back a month after providers questioned whether they were given enough time.
Still, Dr. Greeno, for one, is anxious to see the first round of applications. “It won’t interest me in terms of who jumps in,” he says. “The robustness of the response is what I’m interested in…It’s not going to do (CMS) any good to build a program nobody participates in.”
Health organizations and providers experienced in providing care across multiple settings have until Aug. 19 to apply for a new accountable care organizations (ACO) program through the Centers for Medicare & Medicaid Services (CMS) that promises to offer a higher level of savings than that offered through a previous initiative.
“Hospital medicine groups in and of themselves won’t be applying for it,” says Ron Greeno, MD, MHM, chief medical officer of Brentwood, Tenn.-based Cogent HMG, and chair of SHM's Public Policy Committee. “But the groups that are looking to participate will have hospitalists working for them.”
The new program, tiled the Pioneer ACO Model, was created to offer potentially higher payments to providers and organizations who have already worked under contracts tied to shared savings or care coordination. A related model, the Medicare Shared Savings Program, does not require any previous experience with such contracts. The latter program has completed accepting public comments, but no application deadline has yet been set. (updated Aug. 15, 2011)
Just how many groups apply for the Pioneer program will be interesting: Initially, CMS will enter participation agreements with up to 30 organizations, and each must serve at least 15,000 beneficiaries (5,000 in rural areas). The capped cohort size didn’t seem to spur additional interest, as CMS originally set an application deadline for July, but pushed it back a month after providers questioned whether they were given enough time.
Still, Dr. Greeno, for one, is anxious to see the first round of applications. “It won’t interest me in terms of who jumps in,” he says. “The robustness of the response is what I’m interested in…It’s not going to do (CMS) any good to build a program nobody participates in.”
Health organizations and providers experienced in providing care across multiple settings have until Aug. 19 to apply for a new accountable care organizations (ACO) program through the Centers for Medicare & Medicaid Services (CMS) that promises to offer a higher level of savings than that offered through a previous initiative.
“Hospital medicine groups in and of themselves won’t be applying for it,” says Ron Greeno, MD, MHM, chief medical officer of Brentwood, Tenn.-based Cogent HMG, and chair of SHM's Public Policy Committee. “But the groups that are looking to participate will have hospitalists working for them.”
The new program, tiled the Pioneer ACO Model, was created to offer potentially higher payments to providers and organizations who have already worked under contracts tied to shared savings or care coordination. A related model, the Medicare Shared Savings Program, does not require any previous experience with such contracts. The latter program has completed accepting public comments, but no application deadline has yet been set. (updated Aug. 15, 2011)
Just how many groups apply for the Pioneer program will be interesting: Initially, CMS will enter participation agreements with up to 30 organizations, and each must serve at least 15,000 beneficiaries (5,000 in rural areas). The capped cohort size didn’t seem to spur additional interest, as CMS originally set an application deadline for July, but pushed it back a month after providers questioned whether they were given enough time.
Still, Dr. Greeno, for one, is anxious to see the first round of applications. “It won’t interest me in terms of who jumps in,” he says. “The robustness of the response is what I’m interested in…It’s not going to do (CMS) any good to build a program nobody participates in.”