User login
In the Literature: Research You Need to Know
In This Edition
Literature At A Glance
A guide to this month’s studies
- Screening for AAA
- Adverse events in atrial fibrillation
- Biological treatment of inflammatory bowel diseases
- Steroid treatment of inflammatory bowel diseases
- Levofloxacin for H. pylori
- Natural history of tako-tsubo cardiomyopathy
- Predicting postoperative pulmonary complications
- Code status and goals of care in the ICU
New Screening Strategy To Identify Large Abdominal Aortic Aneurysms
Clinical question: Can an effective scoring system be developed to better identify patients at risk for large abdominal aortic aneurysms (AAA)?
Background: Screening reduces AAA-related mortality by about half in men aged >65. The United States Preventive Services Task Force (USPSTF) has recommended screening for AAA in men aged 65 to 75 with a history of smoking. However, more than 50% of AAA ruptures occur in individuals outside this patient cohort, and only some AAAs detected are large enough to warrant surgery.
Study design: Retrospective, observational cohort study.
Setting: More than 20,000 screening sites across the U.S.
Synopsis: Researchers collected demographics and risk factors from 3.1 million people undergoing ultrasound screening for AAA by Life Line Screening Inc. At the screening visit, subjects completed a questionnaire about their health status and medical history. Screening data also included diameter of the infrarenal abdominal aorta. To construct and test a risk model, the screened individuals were randomly allocated into two equal groups: a data set used for model development and one for validation.
Most of the AAAs greater than 5 cm in diameter discovered were in males (84.4%) and among subjects with a smoking history (83%). Other risk factors for large AAAs included advanced age, peripheral arterial disease, and obesity. The authors estimate that there are about 121,000 people with >5.0 cm aneurysms in the general population. Current guidelines would detect only 33.7% of the existing large AAAs. Study limitations include possible selection bias, as a majority of patients were self-referred. Also, the database did not include all comorbidities that could affect the risk of AAA. The self-reported nature of health data might cause misclassification of a patient’s true health status.
Bottom line: A screening strategy based on a newly developed scoring system is an effective way to identify patients at risk of large abdominal aortic aneurysms.
Citation: Greco G, Egorova NN, Gelijns AC, et al. Development of a novel scoring tool for the identification of large >5 cm abdominal aortic aneurysms. Ann Surg. 2010;252(4):675-682.
Risk Factors for Adverse Events in Patients with Symptomatic Atrial Fibrillation
Clinical question: What are the predictors of 30-day adverse events in ED patients evaluated for symptomatic atrial fibrillation?
Background: Atrial fibrillation (AF) affects more than 2 million people in the U.S. and accounts for nearly 1% of ED visits. Physicians have little information to guide risk stratification, and they admit more than 65% of patients. A strategy to better define the ED management of patients presenting with atrial fibrillation is required.
Study design: Retrospective, observational cohort study.
Setting: Urban academic tertiary-care referral center with an adult ED.
Synopsis: A systematic review of the electronic medical records of all ED patients presenting with symptomatic atrial fibrillation over a three-year period was performed. Predefined adverse outcomes included 30-day ED return visits, unscheduled hospitalizations, cardiovascular complications, or death.
Of 832 eligible patients, 216 (25.9%) experienced at least one of the 30-day adverse events. Adverse events occurred in 181 of the 638 (28.4%) admitted patients and 35 of the 192 (18.2%) patients discharged from the ED. Increasing age, complaint of dyspnea, smoking history, inadequate ventricular rate control, and patients receiving beta-blockers were factors independently associated with higher risk for adverse events.
Study results were limited by a number of factors. This was a single-center, retrospective, observational study, with all of its inherent limitations. The predictor model did not include laboratory data, such as BNP or troponin. Patients might have experienced additional events within the 30 days that were treated at other hospitals and not recorded in the database. Patient disposition might have affected the results, as patients initially admitted from the ED had a higher rate of 30-day adverse events than patients who were discharged from the ED.
Bottom line: Patients with increased age, smoking history, complaints of dyspnea, inadequate ventricular rate control in the ED, and home beta-blocker therapy are more likely to experience an atrial-fibrillation-related adverse event within 30 days.
Citation: Barrett TW, Martin AR, Storrow AB, et al. A clinical prediction model to estimate risk for 30-day adverse events in emergency department patients with symptomatic atrial fibrillation. Ann Emerg Med. 2011;57 (1):1-12.
Biological Therapies Are Effective in Inducing Remission in Inflammatory Bowel Disease
Clinical question: Are biological therapies useful in the treatment of ulcerative colitis (UC) and Crohn’s disease (CD)?
Background: Patients with CD and UC often experience flares of disease activity, despite maintenance therapy with 5-aminosalicylic acid compounds. These flares are usually treated with corticosteroids, which carry numerous adverse side effects. The role of biological therapies in inducing remission is uncertain.
Study design: Systematic review and meta-analysis.
Setting: Twenty-seven randomized controlled trials involving 7,416 patients.
Synopsis: Anti-TNF α antibodies and natalizumab were both superior to placebo in inducing remission of luminal CD (RR of no remission 0.87 and 0.88, respectively). Anti-TNF antibodies also were superior to placebo in preventing relapse of luminal CD (RR of relapse=0.71). Infliximab was superior to placebo in inducing remission of moderate to severely active UC (RR=0.72; 95% CI, 0.57-0.91). There were no significantly increased adverse drug effects with anti-TNF α antibodies or with infliximab compared with placebo. Natalizumab caused significantly higher rates of headache.
Limitations include risk of publication bias inherent in meta-analyses. There also was evidence of moderate heterogeneity in the studies analyzed. Finally, not every study was consistent in reporting adverse drug effects.
Bottom line: Biological therapies are superior to placebo in inducing remission of active UC and CD, as well as preventing relapse of quiescent CD.
Citation: Ford AC, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011; 106(4):644-659.
Glucocorticosteroids Probably Effective in Treatment of Inflammatory Bowel Disease, Primarily in Active Ulcerative Colitis
Clinical question: Is glucocorticosteroid therapy effective in the treatment of active IBD and in preventing relapses?
Background: Crohn’s disease (CD) and ulcerative colitis (UC) are chronic inflammatory bowel diseases of unclear etiology. Use of standard glucocorticosteroids and budesonide is widespread in inflammatory bowel disease (IBD) treatment. To date, there has been no large-scale meta-analysis to examine the effectiveness of both treatments in CD and UC.
Study design: Systematic review and meta-analysis.
Setting: Twenty randomized controlled trials totaling 2,398 patients.
Synopsis: Standard glucocorticosteroids were superior to placebo for UC remission (RR of no remission=0.65; 95% CI, 0.45-0.93). Both trials of standard glucocorticosteroids in CD remission reported a statistically significant effect, but the overall effect was not significant due to heterogeneity of the studies. Budesonide was superior to placebo for CD remission (RR=0.73; 95% CI, 0.63-0.84) but not in preventing CD relapse (RR=0.93; 95% CI, 0.83-1.04). Standard glucocorticosteroids were superior to budesonide for CD remission (RR=0.82; 95% CI, 0.68-0.98) but with more adverse effects (RR=1.64; 95% CI, 1.34-2.00).
The limitations of the study include the poor overall quality of the studies included in the meta-analysis, with only one study judged as low risk of bias. There was intermediate to high heterogeneity between study results.
Bottom line: Standard glucocorticosteroids are likely effective in inducing remission in UC and, possibly, in CD. Budesonide probably is effective at inducing remission in active CD. Neither therapy was recommended in preventing relapse of UC and CD.
Citation: Ford AC, Bernstein CN, Khan KJ, et al. Glucocorticosteroid therapy in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(4):590-599.
Levofloxacin Effective in Treatment of H. Pylori in Settings of High Clarithromycin Resistance
Clinical question: In areas with high H. pylori clarithromycin resistance rates, is levofloxacin more effective in eradicating H. pylori than standard clarithromycin, based treatment regimens?
Background: The rise in antimicrobial drug resistance is a major cause for the decreasing rate of H. pylori eradication. In areas with higher than 15% H. pyloriclarithromycin-resistant strains, quadruple therapy has been suggested as first-line therapy. The efficacy of a levofloxacin-based sequential therapy in eradicating H. pylori is undetermined.
Study design: Prospective, randomized, controlled multicenter study with a parallel-group design.
Setting: Five gastroenterology clinics in Italy.
Synopsis: Researchers randomly assigned 375 patients who were infected with H. pylori and naive to treatment to one of three groups. All three treatment groups received an initial five days of omeprazole 20 mg BID and amoxicillin 1 gm BID, then five days of omeprazole 20 mg BID and tinidazole 500 mg BID. The groups also received either clarithromycin 500 mg BID, levofloxacin 250 mg BID, or levofloxacin 500 mg BID, respectively, during the second five days of treatment.
Eradication rates were 80.8% (95% CI, 72.8% to 87.3%) with clarithromycin sequential therapy, 96.0% (95% CI, 90.9% to 98.7%) with levofloxacin-250 sequential therapy, and 96.8% (95% CI, 92.0% to 99.1%) with levofloxacin-500 sequential therapy.
The clarithromycin-group eradication rate was significantly lower than both levofloxacin groups. No significant difference was observed between the levofloxacin-250 and levofloxacin-500 groups. No differences in prevalence of antimicrobial resistance or incidence of adverse events were observed between the groups. Levofloxacin-250 therapy does offer cost savings when compared with clarithromycin sequential therapy.
A potential limitation to the study is referral bias, as each of the patients first were sent by their primary physicians to a specialized GI clinic.
Bottom line: In areas with a high prevalence of clarithromycin-resistant strains of H. pylori levofloxacin-containing sequential therapy should be considered for a first-line eradication regimen.
Citation: Romano M, Cuomo A, Gravina AG, et al. Empirical levofloxacin-containing versus clarithromycin-containing sequential therapy for Helicobacter pylori eradication: a randomised trial. Gut. 2010;59(11):1465-1470.
Tako-Tsubo Cardiomyopathy Is Associated with Higher Hospital Readmission Rates and Long-Term Mortality
Clinical question: What is the natural history of patients who develop tako-tsubo cardiomyopathy?
Background: Stress-induced or tako-tsubo cardiomyopathy (TTC) is a rare acute cardiac syndrome, characterized by chest pain or dyspnea, ischemic electrocardiographic changes, transient left ventricular (LV) dysfunction, and limited release of cardiac injury markers, in the absence of epicardial coronary artery disease (CAD). The long-term outcome of this condition is unknown.
Study design: Prospective, case-control study.
Setting: Five urban-based hospitals in Italy.
Synopsis: One hundred-sixteen patients with TTC were included in the five-year study period. Patients were followed up at one and six months, then annually thereafter. Primary endpoints were death, TTC recurrence, and rehospitalization for any cause.
Mean initial LV ejection fraction (LVEF) was 36%. Two patients died of refractory heart failure during hospitalization. Of the patients who were discharged alive, all except one showed complete LV functional recovery.
At follow-up (mean two years), only 64 (55%) patients were asymptomatic. Rehospitalization rate was high (25%), with chest pain and dyspnea the most common causes. Only two patients had a recurrence of TTC. Eleven patients died (seven from cardiovascular causes). There was no significant difference in mortality or in other clinical events between patients with and without severe LV dysfunction at presentation. The standardized mortality ratio was 3.40 (95% CI, 1.83-6.34) in the TTC population, compared with the age- and sex-specific mortality of the general population.
The study is limited by a lack of patients with subclinical TTC disease and those who might have suffered from sudden cardiac death prior to enrollment, leading to a possible sampling bias, as well as the nonrandomized use of beta-blockers.
Bottom line: Tako-tsubo disease is associated with rare recurrence of the disease, common recurrence of chest pain and dyspnea, and three times the mortality rate of the general population.
Citation: Parodi G, Bellandi B, Del Pace S, et al. Natural history of tako-tsubo cardiomyopathy. Chest. 2011;139(4):887-892.
Seven Independent Risk Factors Predict Postoperative Pulmonary Complications
Clinical question: What are the clinical risk factors that predict higher rates of postoperative pulmonary complications?
Background: Postoperative pulmonary complications (PPCs) are a major cause of postoperative morbidity, mortality, and prolonged hospital stays. Previous studies looking at risk factors for PPCs were limited by sampling bias and small sample sizes.
Study design: Prospective, randomized-sample cohort study.
Setting: Fifty-nine participating Spanish hospitals (community, intermediate referral, or major tertiary-care facilities).
Synopsis: Patients undergoing surgical procedures with general, neuraxial, or regional anesthesia were selected randomly. The main outcome was the development of at least one of the following: respiratory infection, respiratory failure, bronchospasm, atelectasis, pleural effusion, pneumothorax, or aspiration pneumonitis. Of 2,464 patients enrolled, 252 events were observed in 123 patients (5%). The 30-day mortality rate was significantly higher in patients suffering a PPC than those who did not (19.5% vs. 0.5%). Additionally, regression modeling identified seven independent risk factors: low preoperative arterial oxygen saturation, acute respiratory infection within one month of surgery, advanced age, preoperative anemia, upper abdominal or intrathoracic surgery, surgical duration more than two hours, and emergency surgery.
The study was underpowered to assess the significance of all potential risk factors for PPCs. Also, given the number of centers involved in the study, variation in assessing development of PPCs is likely.
Bottom line: Postoperative pulmonary complications are a major cause of morbidity and mortality. Seven independent risk factors were identified for the development of PPCs, which could be useful in preoperative risk stratification.
Citation: Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338-1350.
Code Status Orders and Goals of Medical ICU Care
Clinical question: How familiar are patients in the medical ICU (MICU) or their surrogates regarding code-status orders and goals of care, what are their preferences, and to what extent do they and their physicians differ?
Background: Discussions about code-status orders and goals of care carry great import in the MICU. However, little data exist on patients’ code-status preferences and goals of care. More knowledge of these issues can help physicians deliver more patient-centered care.
Study design: Prospective interviews.
Setting: Twenty-six-bed MICU at a large Midwestern academic medical center.
Synopsis: Data were collected from December 2008 to December 2009 on a random sample of patients—or their surrogates—admitted to the MICU. Of 135 eligible patients/surrogates, 100 completed interviews. Patients primarily were white (95%) and from the ages of 41 to 80 (79%).
Only 28% of participants recalled having a discussion about CPR and one goal of care, while 27% recalled no discussion at all; 83% preferred full code status but had limited knowledge of CPR and its outcomes in the hospital setting. Only 4% were able to identify all components of CPR, and they estimated the mean probability of survival following in-hospital arrest with CPR to be 71.8%, although data suggest survival is closer to 18%. There was a correlation between a higher estimation of survival following CPR and preference for it. After learning about the evidence-based likelihood of a good neurologic outcome following CPR, 8% of the participants became less interested.
Discrepancies between patients’ stated code status and that in the medical record was identified 16% of the time. Additionally, 67.7% of participants differed with their physicians regarding the most important goal of care.
Bottom line: Discussions about code status and goals of care in the MICU occur less frequently than recommended, leading to widespread discrepancies between patients/surrogates and their physicians regarding the most important goal of care. This is compounded by the fact that patients and their surrogates have limited knowledge about in-hospital CPR and its likelihood of success.
Citation: Gehlbach TG, Shinkunas LA, Forman-Hoffman VL, Thomas KW, Schmidt GA, Kaldjian LC. Code status orders and goals of care in the medical ICU. Chest. 2011;139:802-809. TH
In This Edition
Literature At A Glance
A guide to this month’s studies
- Screening for AAA
- Adverse events in atrial fibrillation
- Biological treatment of inflammatory bowel diseases
- Steroid treatment of inflammatory bowel diseases
- Levofloxacin for H. pylori
- Natural history of tako-tsubo cardiomyopathy
- Predicting postoperative pulmonary complications
- Code status and goals of care in the ICU
New Screening Strategy To Identify Large Abdominal Aortic Aneurysms
Clinical question: Can an effective scoring system be developed to better identify patients at risk for large abdominal aortic aneurysms (AAA)?
Background: Screening reduces AAA-related mortality by about half in men aged >65. The United States Preventive Services Task Force (USPSTF) has recommended screening for AAA in men aged 65 to 75 with a history of smoking. However, more than 50% of AAA ruptures occur in individuals outside this patient cohort, and only some AAAs detected are large enough to warrant surgery.
Study design: Retrospective, observational cohort study.
Setting: More than 20,000 screening sites across the U.S.
Synopsis: Researchers collected demographics and risk factors from 3.1 million people undergoing ultrasound screening for AAA by Life Line Screening Inc. At the screening visit, subjects completed a questionnaire about their health status and medical history. Screening data also included diameter of the infrarenal abdominal aorta. To construct and test a risk model, the screened individuals were randomly allocated into two equal groups: a data set used for model development and one for validation.
Most of the AAAs greater than 5 cm in diameter discovered were in males (84.4%) and among subjects with a smoking history (83%). Other risk factors for large AAAs included advanced age, peripheral arterial disease, and obesity. The authors estimate that there are about 121,000 people with >5.0 cm aneurysms in the general population. Current guidelines would detect only 33.7% of the existing large AAAs. Study limitations include possible selection bias, as a majority of patients were self-referred. Also, the database did not include all comorbidities that could affect the risk of AAA. The self-reported nature of health data might cause misclassification of a patient’s true health status.
Bottom line: A screening strategy based on a newly developed scoring system is an effective way to identify patients at risk of large abdominal aortic aneurysms.
Citation: Greco G, Egorova NN, Gelijns AC, et al. Development of a novel scoring tool for the identification of large >5 cm abdominal aortic aneurysms. Ann Surg. 2010;252(4):675-682.
Risk Factors for Adverse Events in Patients with Symptomatic Atrial Fibrillation
Clinical question: What are the predictors of 30-day adverse events in ED patients evaluated for symptomatic atrial fibrillation?
Background: Atrial fibrillation (AF) affects more than 2 million people in the U.S. and accounts for nearly 1% of ED visits. Physicians have little information to guide risk stratification, and they admit more than 65% of patients. A strategy to better define the ED management of patients presenting with atrial fibrillation is required.
Study design: Retrospective, observational cohort study.
Setting: Urban academic tertiary-care referral center with an adult ED.
Synopsis: A systematic review of the electronic medical records of all ED patients presenting with symptomatic atrial fibrillation over a three-year period was performed. Predefined adverse outcomes included 30-day ED return visits, unscheduled hospitalizations, cardiovascular complications, or death.
Of 832 eligible patients, 216 (25.9%) experienced at least one of the 30-day adverse events. Adverse events occurred in 181 of the 638 (28.4%) admitted patients and 35 of the 192 (18.2%) patients discharged from the ED. Increasing age, complaint of dyspnea, smoking history, inadequate ventricular rate control, and patients receiving beta-blockers were factors independently associated with higher risk for adverse events.
Study results were limited by a number of factors. This was a single-center, retrospective, observational study, with all of its inherent limitations. The predictor model did not include laboratory data, such as BNP or troponin. Patients might have experienced additional events within the 30 days that were treated at other hospitals and not recorded in the database. Patient disposition might have affected the results, as patients initially admitted from the ED had a higher rate of 30-day adverse events than patients who were discharged from the ED.
Bottom line: Patients with increased age, smoking history, complaints of dyspnea, inadequate ventricular rate control in the ED, and home beta-blocker therapy are more likely to experience an atrial-fibrillation-related adverse event within 30 days.
Citation: Barrett TW, Martin AR, Storrow AB, et al. A clinical prediction model to estimate risk for 30-day adverse events in emergency department patients with symptomatic atrial fibrillation. Ann Emerg Med. 2011;57 (1):1-12.
Biological Therapies Are Effective in Inducing Remission in Inflammatory Bowel Disease
Clinical question: Are biological therapies useful in the treatment of ulcerative colitis (UC) and Crohn’s disease (CD)?
Background: Patients with CD and UC often experience flares of disease activity, despite maintenance therapy with 5-aminosalicylic acid compounds. These flares are usually treated with corticosteroids, which carry numerous adverse side effects. The role of biological therapies in inducing remission is uncertain.
Study design: Systematic review and meta-analysis.
Setting: Twenty-seven randomized controlled trials involving 7,416 patients.
Synopsis: Anti-TNF α antibodies and natalizumab were both superior to placebo in inducing remission of luminal CD (RR of no remission 0.87 and 0.88, respectively). Anti-TNF antibodies also were superior to placebo in preventing relapse of luminal CD (RR of relapse=0.71). Infliximab was superior to placebo in inducing remission of moderate to severely active UC (RR=0.72; 95% CI, 0.57-0.91). There were no significantly increased adverse drug effects with anti-TNF α antibodies or with infliximab compared with placebo. Natalizumab caused significantly higher rates of headache.
Limitations include risk of publication bias inherent in meta-analyses. There also was evidence of moderate heterogeneity in the studies analyzed. Finally, not every study was consistent in reporting adverse drug effects.
Bottom line: Biological therapies are superior to placebo in inducing remission of active UC and CD, as well as preventing relapse of quiescent CD.
Citation: Ford AC, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011; 106(4):644-659.
Glucocorticosteroids Probably Effective in Treatment of Inflammatory Bowel Disease, Primarily in Active Ulcerative Colitis
Clinical question: Is glucocorticosteroid therapy effective in the treatment of active IBD and in preventing relapses?
Background: Crohn’s disease (CD) and ulcerative colitis (UC) are chronic inflammatory bowel diseases of unclear etiology. Use of standard glucocorticosteroids and budesonide is widespread in inflammatory bowel disease (IBD) treatment. To date, there has been no large-scale meta-analysis to examine the effectiveness of both treatments in CD and UC.
Study design: Systematic review and meta-analysis.
Setting: Twenty randomized controlled trials totaling 2,398 patients.
Synopsis: Standard glucocorticosteroids were superior to placebo for UC remission (RR of no remission=0.65; 95% CI, 0.45-0.93). Both trials of standard glucocorticosteroids in CD remission reported a statistically significant effect, but the overall effect was not significant due to heterogeneity of the studies. Budesonide was superior to placebo for CD remission (RR=0.73; 95% CI, 0.63-0.84) but not in preventing CD relapse (RR=0.93; 95% CI, 0.83-1.04). Standard glucocorticosteroids were superior to budesonide for CD remission (RR=0.82; 95% CI, 0.68-0.98) but with more adverse effects (RR=1.64; 95% CI, 1.34-2.00).
The limitations of the study include the poor overall quality of the studies included in the meta-analysis, with only one study judged as low risk of bias. There was intermediate to high heterogeneity between study results.
Bottom line: Standard glucocorticosteroids are likely effective in inducing remission in UC and, possibly, in CD. Budesonide probably is effective at inducing remission in active CD. Neither therapy was recommended in preventing relapse of UC and CD.
Citation: Ford AC, Bernstein CN, Khan KJ, et al. Glucocorticosteroid therapy in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(4):590-599.
Levofloxacin Effective in Treatment of H. Pylori in Settings of High Clarithromycin Resistance
Clinical question: In areas with high H. pylori clarithromycin resistance rates, is levofloxacin more effective in eradicating H. pylori than standard clarithromycin, based treatment regimens?
Background: The rise in antimicrobial drug resistance is a major cause for the decreasing rate of H. pylori eradication. In areas with higher than 15% H. pyloriclarithromycin-resistant strains, quadruple therapy has been suggested as first-line therapy. The efficacy of a levofloxacin-based sequential therapy in eradicating H. pylori is undetermined.
Study design: Prospective, randomized, controlled multicenter study with a parallel-group design.
Setting: Five gastroenterology clinics in Italy.
Synopsis: Researchers randomly assigned 375 patients who were infected with H. pylori and naive to treatment to one of three groups. All three treatment groups received an initial five days of omeprazole 20 mg BID and amoxicillin 1 gm BID, then five days of omeprazole 20 mg BID and tinidazole 500 mg BID. The groups also received either clarithromycin 500 mg BID, levofloxacin 250 mg BID, or levofloxacin 500 mg BID, respectively, during the second five days of treatment.
Eradication rates were 80.8% (95% CI, 72.8% to 87.3%) with clarithromycin sequential therapy, 96.0% (95% CI, 90.9% to 98.7%) with levofloxacin-250 sequential therapy, and 96.8% (95% CI, 92.0% to 99.1%) with levofloxacin-500 sequential therapy.
The clarithromycin-group eradication rate was significantly lower than both levofloxacin groups. No significant difference was observed between the levofloxacin-250 and levofloxacin-500 groups. No differences in prevalence of antimicrobial resistance or incidence of adverse events were observed between the groups. Levofloxacin-250 therapy does offer cost savings when compared with clarithromycin sequential therapy.
A potential limitation to the study is referral bias, as each of the patients first were sent by their primary physicians to a specialized GI clinic.
Bottom line: In areas with a high prevalence of clarithromycin-resistant strains of H. pylori levofloxacin-containing sequential therapy should be considered for a first-line eradication regimen.
Citation: Romano M, Cuomo A, Gravina AG, et al. Empirical levofloxacin-containing versus clarithromycin-containing sequential therapy for Helicobacter pylori eradication: a randomised trial. Gut. 2010;59(11):1465-1470.
Tako-Tsubo Cardiomyopathy Is Associated with Higher Hospital Readmission Rates and Long-Term Mortality
Clinical question: What is the natural history of patients who develop tako-tsubo cardiomyopathy?
Background: Stress-induced or tako-tsubo cardiomyopathy (TTC) is a rare acute cardiac syndrome, characterized by chest pain or dyspnea, ischemic electrocardiographic changes, transient left ventricular (LV) dysfunction, and limited release of cardiac injury markers, in the absence of epicardial coronary artery disease (CAD). The long-term outcome of this condition is unknown.
Study design: Prospective, case-control study.
Setting: Five urban-based hospitals in Italy.
Synopsis: One hundred-sixteen patients with TTC were included in the five-year study period. Patients were followed up at one and six months, then annually thereafter. Primary endpoints were death, TTC recurrence, and rehospitalization for any cause.
Mean initial LV ejection fraction (LVEF) was 36%. Two patients died of refractory heart failure during hospitalization. Of the patients who were discharged alive, all except one showed complete LV functional recovery.
At follow-up (mean two years), only 64 (55%) patients were asymptomatic. Rehospitalization rate was high (25%), with chest pain and dyspnea the most common causes. Only two patients had a recurrence of TTC. Eleven patients died (seven from cardiovascular causes). There was no significant difference in mortality or in other clinical events between patients with and without severe LV dysfunction at presentation. The standardized mortality ratio was 3.40 (95% CI, 1.83-6.34) in the TTC population, compared with the age- and sex-specific mortality of the general population.
The study is limited by a lack of patients with subclinical TTC disease and those who might have suffered from sudden cardiac death prior to enrollment, leading to a possible sampling bias, as well as the nonrandomized use of beta-blockers.
Bottom line: Tako-tsubo disease is associated with rare recurrence of the disease, common recurrence of chest pain and dyspnea, and three times the mortality rate of the general population.
Citation: Parodi G, Bellandi B, Del Pace S, et al. Natural history of tako-tsubo cardiomyopathy. Chest. 2011;139(4):887-892.
Seven Independent Risk Factors Predict Postoperative Pulmonary Complications
Clinical question: What are the clinical risk factors that predict higher rates of postoperative pulmonary complications?
Background: Postoperative pulmonary complications (PPCs) are a major cause of postoperative morbidity, mortality, and prolonged hospital stays. Previous studies looking at risk factors for PPCs were limited by sampling bias and small sample sizes.
Study design: Prospective, randomized-sample cohort study.
Setting: Fifty-nine participating Spanish hospitals (community, intermediate referral, or major tertiary-care facilities).
Synopsis: Patients undergoing surgical procedures with general, neuraxial, or regional anesthesia were selected randomly. The main outcome was the development of at least one of the following: respiratory infection, respiratory failure, bronchospasm, atelectasis, pleural effusion, pneumothorax, or aspiration pneumonitis. Of 2,464 patients enrolled, 252 events were observed in 123 patients (5%). The 30-day mortality rate was significantly higher in patients suffering a PPC than those who did not (19.5% vs. 0.5%). Additionally, regression modeling identified seven independent risk factors: low preoperative arterial oxygen saturation, acute respiratory infection within one month of surgery, advanced age, preoperative anemia, upper abdominal or intrathoracic surgery, surgical duration more than two hours, and emergency surgery.
The study was underpowered to assess the significance of all potential risk factors for PPCs. Also, given the number of centers involved in the study, variation in assessing development of PPCs is likely.
Bottom line: Postoperative pulmonary complications are a major cause of morbidity and mortality. Seven independent risk factors were identified for the development of PPCs, which could be useful in preoperative risk stratification.
Citation: Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338-1350.
Code Status Orders and Goals of Medical ICU Care
Clinical question: How familiar are patients in the medical ICU (MICU) or their surrogates regarding code-status orders and goals of care, what are their preferences, and to what extent do they and their physicians differ?
Background: Discussions about code-status orders and goals of care carry great import in the MICU. However, little data exist on patients’ code-status preferences and goals of care. More knowledge of these issues can help physicians deliver more patient-centered care.
Study design: Prospective interviews.
Setting: Twenty-six-bed MICU at a large Midwestern academic medical center.
Synopsis: Data were collected from December 2008 to December 2009 on a random sample of patients—or their surrogates—admitted to the MICU. Of 135 eligible patients/surrogates, 100 completed interviews. Patients primarily were white (95%) and from the ages of 41 to 80 (79%).
Only 28% of participants recalled having a discussion about CPR and one goal of care, while 27% recalled no discussion at all; 83% preferred full code status but had limited knowledge of CPR and its outcomes in the hospital setting. Only 4% were able to identify all components of CPR, and they estimated the mean probability of survival following in-hospital arrest with CPR to be 71.8%, although data suggest survival is closer to 18%. There was a correlation between a higher estimation of survival following CPR and preference for it. After learning about the evidence-based likelihood of a good neurologic outcome following CPR, 8% of the participants became less interested.
Discrepancies between patients’ stated code status and that in the medical record was identified 16% of the time. Additionally, 67.7% of participants differed with their physicians regarding the most important goal of care.
Bottom line: Discussions about code status and goals of care in the MICU occur less frequently than recommended, leading to widespread discrepancies between patients/surrogates and their physicians regarding the most important goal of care. This is compounded by the fact that patients and their surrogates have limited knowledge about in-hospital CPR and its likelihood of success.
Citation: Gehlbach TG, Shinkunas LA, Forman-Hoffman VL, Thomas KW, Schmidt GA, Kaldjian LC. Code status orders and goals of care in the medical ICU. Chest. 2011;139:802-809. TH
In This Edition
Literature At A Glance
A guide to this month’s studies
- Screening for AAA
- Adverse events in atrial fibrillation
- Biological treatment of inflammatory bowel diseases
- Steroid treatment of inflammatory bowel diseases
- Levofloxacin for H. pylori
- Natural history of tako-tsubo cardiomyopathy
- Predicting postoperative pulmonary complications
- Code status and goals of care in the ICU
New Screening Strategy To Identify Large Abdominal Aortic Aneurysms
Clinical question: Can an effective scoring system be developed to better identify patients at risk for large abdominal aortic aneurysms (AAA)?
Background: Screening reduces AAA-related mortality by about half in men aged >65. The United States Preventive Services Task Force (USPSTF) has recommended screening for AAA in men aged 65 to 75 with a history of smoking. However, more than 50% of AAA ruptures occur in individuals outside this patient cohort, and only some AAAs detected are large enough to warrant surgery.
Study design: Retrospective, observational cohort study.
Setting: More than 20,000 screening sites across the U.S.
Synopsis: Researchers collected demographics and risk factors from 3.1 million people undergoing ultrasound screening for AAA by Life Line Screening Inc. At the screening visit, subjects completed a questionnaire about their health status and medical history. Screening data also included diameter of the infrarenal abdominal aorta. To construct and test a risk model, the screened individuals were randomly allocated into two equal groups: a data set used for model development and one for validation.
Most of the AAAs greater than 5 cm in diameter discovered were in males (84.4%) and among subjects with a smoking history (83%). Other risk factors for large AAAs included advanced age, peripheral arterial disease, and obesity. The authors estimate that there are about 121,000 people with >5.0 cm aneurysms in the general population. Current guidelines would detect only 33.7% of the existing large AAAs. Study limitations include possible selection bias, as a majority of patients were self-referred. Also, the database did not include all comorbidities that could affect the risk of AAA. The self-reported nature of health data might cause misclassification of a patient’s true health status.
Bottom line: A screening strategy based on a newly developed scoring system is an effective way to identify patients at risk of large abdominal aortic aneurysms.
Citation: Greco G, Egorova NN, Gelijns AC, et al. Development of a novel scoring tool for the identification of large >5 cm abdominal aortic aneurysms. Ann Surg. 2010;252(4):675-682.
Risk Factors for Adverse Events in Patients with Symptomatic Atrial Fibrillation
Clinical question: What are the predictors of 30-day adverse events in ED patients evaluated for symptomatic atrial fibrillation?
Background: Atrial fibrillation (AF) affects more than 2 million people in the U.S. and accounts for nearly 1% of ED visits. Physicians have little information to guide risk stratification, and they admit more than 65% of patients. A strategy to better define the ED management of patients presenting with atrial fibrillation is required.
Study design: Retrospective, observational cohort study.
Setting: Urban academic tertiary-care referral center with an adult ED.
Synopsis: A systematic review of the electronic medical records of all ED patients presenting with symptomatic atrial fibrillation over a three-year period was performed. Predefined adverse outcomes included 30-day ED return visits, unscheduled hospitalizations, cardiovascular complications, or death.
Of 832 eligible patients, 216 (25.9%) experienced at least one of the 30-day adverse events. Adverse events occurred in 181 of the 638 (28.4%) admitted patients and 35 of the 192 (18.2%) patients discharged from the ED. Increasing age, complaint of dyspnea, smoking history, inadequate ventricular rate control, and patients receiving beta-blockers were factors independently associated with higher risk for adverse events.
Study results were limited by a number of factors. This was a single-center, retrospective, observational study, with all of its inherent limitations. The predictor model did not include laboratory data, such as BNP or troponin. Patients might have experienced additional events within the 30 days that were treated at other hospitals and not recorded in the database. Patient disposition might have affected the results, as patients initially admitted from the ED had a higher rate of 30-day adverse events than patients who were discharged from the ED.
Bottom line: Patients with increased age, smoking history, complaints of dyspnea, inadequate ventricular rate control in the ED, and home beta-blocker therapy are more likely to experience an atrial-fibrillation-related adverse event within 30 days.
Citation: Barrett TW, Martin AR, Storrow AB, et al. A clinical prediction model to estimate risk for 30-day adverse events in emergency department patients with symptomatic atrial fibrillation. Ann Emerg Med. 2011;57 (1):1-12.
Biological Therapies Are Effective in Inducing Remission in Inflammatory Bowel Disease
Clinical question: Are biological therapies useful in the treatment of ulcerative colitis (UC) and Crohn’s disease (CD)?
Background: Patients with CD and UC often experience flares of disease activity, despite maintenance therapy with 5-aminosalicylic acid compounds. These flares are usually treated with corticosteroids, which carry numerous adverse side effects. The role of biological therapies in inducing remission is uncertain.
Study design: Systematic review and meta-analysis.
Setting: Twenty-seven randomized controlled trials involving 7,416 patients.
Synopsis: Anti-TNF α antibodies and natalizumab were both superior to placebo in inducing remission of luminal CD (RR of no remission 0.87 and 0.88, respectively). Anti-TNF antibodies also were superior to placebo in preventing relapse of luminal CD (RR of relapse=0.71). Infliximab was superior to placebo in inducing remission of moderate to severely active UC (RR=0.72; 95% CI, 0.57-0.91). There were no significantly increased adverse drug effects with anti-TNF α antibodies or with infliximab compared with placebo. Natalizumab caused significantly higher rates of headache.
Limitations include risk of publication bias inherent in meta-analyses. There also was evidence of moderate heterogeneity in the studies analyzed. Finally, not every study was consistent in reporting adverse drug effects.
Bottom line: Biological therapies are superior to placebo in inducing remission of active UC and CD, as well as preventing relapse of quiescent CD.
Citation: Ford AC, Sandborn WJ, Khan KJ, Hanauer SB, Talley NJ, Moayyedi P. Efficacy of biological therapies in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011; 106(4):644-659.
Glucocorticosteroids Probably Effective in Treatment of Inflammatory Bowel Disease, Primarily in Active Ulcerative Colitis
Clinical question: Is glucocorticosteroid therapy effective in the treatment of active IBD and in preventing relapses?
Background: Crohn’s disease (CD) and ulcerative colitis (UC) are chronic inflammatory bowel diseases of unclear etiology. Use of standard glucocorticosteroids and budesonide is widespread in inflammatory bowel disease (IBD) treatment. To date, there has been no large-scale meta-analysis to examine the effectiveness of both treatments in CD and UC.
Study design: Systematic review and meta-analysis.
Setting: Twenty randomized controlled trials totaling 2,398 patients.
Synopsis: Standard glucocorticosteroids were superior to placebo for UC remission (RR of no remission=0.65; 95% CI, 0.45-0.93). Both trials of standard glucocorticosteroids in CD remission reported a statistically significant effect, but the overall effect was not significant due to heterogeneity of the studies. Budesonide was superior to placebo for CD remission (RR=0.73; 95% CI, 0.63-0.84) but not in preventing CD relapse (RR=0.93; 95% CI, 0.83-1.04). Standard glucocorticosteroids were superior to budesonide for CD remission (RR=0.82; 95% CI, 0.68-0.98) but with more adverse effects (RR=1.64; 95% CI, 1.34-2.00).
The limitations of the study include the poor overall quality of the studies included in the meta-analysis, with only one study judged as low risk of bias. There was intermediate to high heterogeneity between study results.
Bottom line: Standard glucocorticosteroids are likely effective in inducing remission in UC and, possibly, in CD. Budesonide probably is effective at inducing remission in active CD. Neither therapy was recommended in preventing relapse of UC and CD.
Citation: Ford AC, Bernstein CN, Khan KJ, et al. Glucocorticosteroid therapy in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2011;106(4):590-599.
Levofloxacin Effective in Treatment of H. Pylori in Settings of High Clarithromycin Resistance
Clinical question: In areas with high H. pylori clarithromycin resistance rates, is levofloxacin more effective in eradicating H. pylori than standard clarithromycin, based treatment regimens?
Background: The rise in antimicrobial drug resistance is a major cause for the decreasing rate of H. pylori eradication. In areas with higher than 15% H. pyloriclarithromycin-resistant strains, quadruple therapy has been suggested as first-line therapy. The efficacy of a levofloxacin-based sequential therapy in eradicating H. pylori is undetermined.
Study design: Prospective, randomized, controlled multicenter study with a parallel-group design.
Setting: Five gastroenterology clinics in Italy.
Synopsis: Researchers randomly assigned 375 patients who were infected with H. pylori and naive to treatment to one of three groups. All three treatment groups received an initial five days of omeprazole 20 mg BID and amoxicillin 1 gm BID, then five days of omeprazole 20 mg BID and tinidazole 500 mg BID. The groups also received either clarithromycin 500 mg BID, levofloxacin 250 mg BID, or levofloxacin 500 mg BID, respectively, during the second five days of treatment.
Eradication rates were 80.8% (95% CI, 72.8% to 87.3%) with clarithromycin sequential therapy, 96.0% (95% CI, 90.9% to 98.7%) with levofloxacin-250 sequential therapy, and 96.8% (95% CI, 92.0% to 99.1%) with levofloxacin-500 sequential therapy.
The clarithromycin-group eradication rate was significantly lower than both levofloxacin groups. No significant difference was observed between the levofloxacin-250 and levofloxacin-500 groups. No differences in prevalence of antimicrobial resistance or incidence of adverse events were observed between the groups. Levofloxacin-250 therapy does offer cost savings when compared with clarithromycin sequential therapy.
A potential limitation to the study is referral bias, as each of the patients first were sent by their primary physicians to a specialized GI clinic.
Bottom line: In areas with a high prevalence of clarithromycin-resistant strains of H. pylori levofloxacin-containing sequential therapy should be considered for a first-line eradication regimen.
Citation: Romano M, Cuomo A, Gravina AG, et al. Empirical levofloxacin-containing versus clarithromycin-containing sequential therapy for Helicobacter pylori eradication: a randomised trial. Gut. 2010;59(11):1465-1470.
Tako-Tsubo Cardiomyopathy Is Associated with Higher Hospital Readmission Rates and Long-Term Mortality
Clinical question: What is the natural history of patients who develop tako-tsubo cardiomyopathy?
Background: Stress-induced or tako-tsubo cardiomyopathy (TTC) is a rare acute cardiac syndrome, characterized by chest pain or dyspnea, ischemic electrocardiographic changes, transient left ventricular (LV) dysfunction, and limited release of cardiac injury markers, in the absence of epicardial coronary artery disease (CAD). The long-term outcome of this condition is unknown.
Study design: Prospective, case-control study.
Setting: Five urban-based hospitals in Italy.
Synopsis: One hundred-sixteen patients with TTC were included in the five-year study period. Patients were followed up at one and six months, then annually thereafter. Primary endpoints were death, TTC recurrence, and rehospitalization for any cause.
Mean initial LV ejection fraction (LVEF) was 36%. Two patients died of refractory heart failure during hospitalization. Of the patients who were discharged alive, all except one showed complete LV functional recovery.
At follow-up (mean two years), only 64 (55%) patients were asymptomatic. Rehospitalization rate was high (25%), with chest pain and dyspnea the most common causes. Only two patients had a recurrence of TTC. Eleven patients died (seven from cardiovascular causes). There was no significant difference in mortality or in other clinical events between patients with and without severe LV dysfunction at presentation. The standardized mortality ratio was 3.40 (95% CI, 1.83-6.34) in the TTC population, compared with the age- and sex-specific mortality of the general population.
The study is limited by a lack of patients with subclinical TTC disease and those who might have suffered from sudden cardiac death prior to enrollment, leading to a possible sampling bias, as well as the nonrandomized use of beta-blockers.
Bottom line: Tako-tsubo disease is associated with rare recurrence of the disease, common recurrence of chest pain and dyspnea, and three times the mortality rate of the general population.
Citation: Parodi G, Bellandi B, Del Pace S, et al. Natural history of tako-tsubo cardiomyopathy. Chest. 2011;139(4):887-892.
Seven Independent Risk Factors Predict Postoperative Pulmonary Complications
Clinical question: What are the clinical risk factors that predict higher rates of postoperative pulmonary complications?
Background: Postoperative pulmonary complications (PPCs) are a major cause of postoperative morbidity, mortality, and prolonged hospital stays. Previous studies looking at risk factors for PPCs were limited by sampling bias and small sample sizes.
Study design: Prospective, randomized-sample cohort study.
Setting: Fifty-nine participating Spanish hospitals (community, intermediate referral, or major tertiary-care facilities).
Synopsis: Patients undergoing surgical procedures with general, neuraxial, or regional anesthesia were selected randomly. The main outcome was the development of at least one of the following: respiratory infection, respiratory failure, bronchospasm, atelectasis, pleural effusion, pneumothorax, or aspiration pneumonitis. Of 2,464 patients enrolled, 252 events were observed in 123 patients (5%). The 30-day mortality rate was significantly higher in patients suffering a PPC than those who did not (19.5% vs. 0.5%). Additionally, regression modeling identified seven independent risk factors: low preoperative arterial oxygen saturation, acute respiratory infection within one month of surgery, advanced age, preoperative anemia, upper abdominal or intrathoracic surgery, surgical duration more than two hours, and emergency surgery.
The study was underpowered to assess the significance of all potential risk factors for PPCs. Also, given the number of centers involved in the study, variation in assessing development of PPCs is likely.
Bottom line: Postoperative pulmonary complications are a major cause of morbidity and mortality. Seven independent risk factors were identified for the development of PPCs, which could be useful in preoperative risk stratification.
Citation: Canet J, Gallart L, Gomar C, et al. Prediction of postoperative pulmonary complications in a population-based surgical cohort. Anesthesiology. 2010;113(6):1338-1350.
Code Status Orders and Goals of Medical ICU Care
Clinical question: How familiar are patients in the medical ICU (MICU) or their surrogates regarding code-status orders and goals of care, what are their preferences, and to what extent do they and their physicians differ?
Background: Discussions about code-status orders and goals of care carry great import in the MICU. However, little data exist on patients’ code-status preferences and goals of care. More knowledge of these issues can help physicians deliver more patient-centered care.
Study design: Prospective interviews.
Setting: Twenty-six-bed MICU at a large Midwestern academic medical center.
Synopsis: Data were collected from December 2008 to December 2009 on a random sample of patients—or their surrogates—admitted to the MICU. Of 135 eligible patients/surrogates, 100 completed interviews. Patients primarily were white (95%) and from the ages of 41 to 80 (79%).
Only 28% of participants recalled having a discussion about CPR and one goal of care, while 27% recalled no discussion at all; 83% preferred full code status but had limited knowledge of CPR and its outcomes in the hospital setting. Only 4% were able to identify all components of CPR, and they estimated the mean probability of survival following in-hospital arrest with CPR to be 71.8%, although data suggest survival is closer to 18%. There was a correlation between a higher estimation of survival following CPR and preference for it. After learning about the evidence-based likelihood of a good neurologic outcome following CPR, 8% of the participants became less interested.
Discrepancies between patients’ stated code status and that in the medical record was identified 16% of the time. Additionally, 67.7% of participants differed with their physicians regarding the most important goal of care.
Bottom line: Discussions about code status and goals of care in the MICU occur less frequently than recommended, leading to widespread discrepancies between patients/surrogates and their physicians regarding the most important goal of care. This is compounded by the fact that patients and their surrogates have limited knowledge about in-hospital CPR and its likelihood of success.
Citation: Gehlbach TG, Shinkunas LA, Forman-Hoffman VL, Thomas KW, Schmidt GA, Kaldjian LC. Code status orders and goals of care in the medical ICU. Chest. 2011;139:802-809. TH
SHM’S Leadership Academy Trains Next Generation of HM Leaders
As HM programs mature, seasoned leaders begin to evaluate the leadership potential of their staff, both clinical and administrative. Although the skills that brought each staff member to their current position often are well above average, the personal tools necessary to lead teams will ultimately come to the fore.
The need to develop and enhance leadership skills within hospitalist programs has attracted nearly 1,800 participants to SHM’s Leadership Academy courses.
Hundreds more are expected to attend the next academy, Sept. 12-15 at the historic Fontainebleau Miami Beach resort. Registration is available at www.hospitalmedicine.org/leadership.
To encourage HM programs to strengthen entire teams, SHM offers a $100 discount per person for groups of three or more hospitalists. Group leaders who bring their administrators receive a 10% discount.
First-time Leadership Academy participants will participate in the "Foundations for Effective Leadership" course. Those who already have completed "Foundations" will take their leadership skills to the next level with "Advanced Leadership: Personal Leadership Excellence."
Another advanced leadership course, "Strengthening Your Organization," will be presented in February 2012 in New Orleans.
"I send every hospitalist to Leadership Academy because I believe it makes them better team members," said Eric Howell, section chief of hospital medicine and deputy director of hospital operations for the Department of Medicine at Johns Hopkins Bayview Medical Center, in a video presented at HM11. Dr. Howell, an academy faculty member, says the training makes hospitalists "better problem-solvers. I believe it makes them better doctors." TH
As HM programs mature, seasoned leaders begin to evaluate the leadership potential of their staff, both clinical and administrative. Although the skills that brought each staff member to their current position often are well above average, the personal tools necessary to lead teams will ultimately come to the fore.
The need to develop and enhance leadership skills within hospitalist programs has attracted nearly 1,800 participants to SHM’s Leadership Academy courses.
Hundreds more are expected to attend the next academy, Sept. 12-15 at the historic Fontainebleau Miami Beach resort. Registration is available at www.hospitalmedicine.org/leadership.
To encourage HM programs to strengthen entire teams, SHM offers a $100 discount per person for groups of three or more hospitalists. Group leaders who bring their administrators receive a 10% discount.
First-time Leadership Academy participants will participate in the "Foundations for Effective Leadership" course. Those who already have completed "Foundations" will take their leadership skills to the next level with "Advanced Leadership: Personal Leadership Excellence."
Another advanced leadership course, "Strengthening Your Organization," will be presented in February 2012 in New Orleans.
"I send every hospitalist to Leadership Academy because I believe it makes them better team members," said Eric Howell, section chief of hospital medicine and deputy director of hospital operations for the Department of Medicine at Johns Hopkins Bayview Medical Center, in a video presented at HM11. Dr. Howell, an academy faculty member, says the training makes hospitalists "better problem-solvers. I believe it makes them better doctors." TH
As HM programs mature, seasoned leaders begin to evaluate the leadership potential of their staff, both clinical and administrative. Although the skills that brought each staff member to their current position often are well above average, the personal tools necessary to lead teams will ultimately come to the fore.
The need to develop and enhance leadership skills within hospitalist programs has attracted nearly 1,800 participants to SHM’s Leadership Academy courses.
Hundreds more are expected to attend the next academy, Sept. 12-15 at the historic Fontainebleau Miami Beach resort. Registration is available at www.hospitalmedicine.org/leadership.
To encourage HM programs to strengthen entire teams, SHM offers a $100 discount per person for groups of three or more hospitalists. Group leaders who bring their administrators receive a 10% discount.
First-time Leadership Academy participants will participate in the "Foundations for Effective Leadership" course. Those who already have completed "Foundations" will take their leadership skills to the next level with "Advanced Leadership: Personal Leadership Excellence."
Another advanced leadership course, "Strengthening Your Organization," will be presented in February 2012 in New Orleans.
"I send every hospitalist to Leadership Academy because I believe it makes them better team members," said Eric Howell, section chief of hospital medicine and deputy director of hospital operations for the Department of Medicine at Johns Hopkins Bayview Medical Center, in a video presented at HM11. Dr. Howell, an academy faculty member, says the training makes hospitalists "better problem-solvers. I believe it makes them better doctors." TH
Policy Corner: Obama Suggests Eliminating Wasteful Regulations
The federal government is taking a hard look at many of its regulations, and hospitalists might have the chance to help identify those that no longer make sense.
On Jan. 18, President Obama issued Executive Order 13563, which calls, in part, for a comprehensive retrospective review of existing government regulations. The stated goal of this review is to improve or remove those rules that are out of date, unnecessary, excessively burdensome, or in conflict with other rules.
The Office of Information and Regulatory Affairs (OIRA), the executive-level department charged with overseeing the execution of this order, asked federal agencies to submit preliminary plans for how they will conduct their internal reviews. The agencies responded, and on May 26, the White House released 30 agency preliminary plans to the public, including those prepared by the Department of Commerce, the Department of Energy, and the Department of Health and Human Services (HHS).
When reviewing some of these publicly available preliminary plans, the easy answer for some observers is to say that most rules should be eliminated. Rules requiring the use of such technologies as film X-rays instead of digital images are obvious culprits in the out-of date category; rules defining milk as "oil" (subjecting it to the same costly environmental safeguards as real oil) are just as absurd. Both of these regulations are being lifted as a result of the review.
In contrast, many rules actually do protect public health and safety and will not be subject to review. For example, as a result of federal rulemaking, highway deaths are at the lowest level in 60 years and the risk of contracting salmonella from eggs is relatively low.
As part of HHS, the Center for Medicare & Medicaid Services (CMS) specifically stated that "the goal of the retrospective review will be to identify opportunities to improve patient care and outcomes and reduce system costs by removing obsolete or burdensome requirements." A major CMS concern will be to prevent the elimination or revision of a regulation only to find that the problem it sought to solve resurfaces, or that its removal or revision results in unanticipated and more serious outcomes.
This review could significantly impact HM in areas of quality measurement and reporting requirements:
- What quality measurements might not accomplish their intent?
- What measures might result in more harm than good?
- What reporting or process requirements could be changed to make for less duplication?
- If requirements cannot be eliminated, how can they be improved?
Due to hospitalist expertise in quality-improvement (QI) efforts and cost containment, these stated goals and the concerns that come with them are areas where hospitalists are likely to have some good answers. Hospitalists should not hesitate to provide their input to SHM Government Relations staff so that your ideas can be shared with CMS.
A complete list of agency proposals is available at www.whitehouse.gov/21stcentury gov/actions/21st-century-regulatory-system.
The federal government is taking a hard look at many of its regulations, and hospitalists might have the chance to help identify those that no longer make sense.
On Jan. 18, President Obama issued Executive Order 13563, which calls, in part, for a comprehensive retrospective review of existing government regulations. The stated goal of this review is to improve or remove those rules that are out of date, unnecessary, excessively burdensome, or in conflict with other rules.
The Office of Information and Regulatory Affairs (OIRA), the executive-level department charged with overseeing the execution of this order, asked federal agencies to submit preliminary plans for how they will conduct their internal reviews. The agencies responded, and on May 26, the White House released 30 agency preliminary plans to the public, including those prepared by the Department of Commerce, the Department of Energy, and the Department of Health and Human Services (HHS).
When reviewing some of these publicly available preliminary plans, the easy answer for some observers is to say that most rules should be eliminated. Rules requiring the use of such technologies as film X-rays instead of digital images are obvious culprits in the out-of date category; rules defining milk as "oil" (subjecting it to the same costly environmental safeguards as real oil) are just as absurd. Both of these regulations are being lifted as a result of the review.
In contrast, many rules actually do protect public health and safety and will not be subject to review. For example, as a result of federal rulemaking, highway deaths are at the lowest level in 60 years and the risk of contracting salmonella from eggs is relatively low.
As part of HHS, the Center for Medicare & Medicaid Services (CMS) specifically stated that "the goal of the retrospective review will be to identify opportunities to improve patient care and outcomes and reduce system costs by removing obsolete or burdensome requirements." A major CMS concern will be to prevent the elimination or revision of a regulation only to find that the problem it sought to solve resurfaces, or that its removal or revision results in unanticipated and more serious outcomes.
This review could significantly impact HM in areas of quality measurement and reporting requirements:
- What quality measurements might not accomplish their intent?
- What measures might result in more harm than good?
- What reporting or process requirements could be changed to make for less duplication?
- If requirements cannot be eliminated, how can they be improved?
Due to hospitalist expertise in quality-improvement (QI) efforts and cost containment, these stated goals and the concerns that come with them are areas where hospitalists are likely to have some good answers. Hospitalists should not hesitate to provide their input to SHM Government Relations staff so that your ideas can be shared with CMS.
A complete list of agency proposals is available at www.whitehouse.gov/21stcentury gov/actions/21st-century-regulatory-system.
The federal government is taking a hard look at many of its regulations, and hospitalists might have the chance to help identify those that no longer make sense.
On Jan. 18, President Obama issued Executive Order 13563, which calls, in part, for a comprehensive retrospective review of existing government regulations. The stated goal of this review is to improve or remove those rules that are out of date, unnecessary, excessively burdensome, or in conflict with other rules.
The Office of Information and Regulatory Affairs (OIRA), the executive-level department charged with overseeing the execution of this order, asked federal agencies to submit preliminary plans for how they will conduct their internal reviews. The agencies responded, and on May 26, the White House released 30 agency preliminary plans to the public, including those prepared by the Department of Commerce, the Department of Energy, and the Department of Health and Human Services (HHS).
When reviewing some of these publicly available preliminary plans, the easy answer for some observers is to say that most rules should be eliminated. Rules requiring the use of such technologies as film X-rays instead of digital images are obvious culprits in the out-of date category; rules defining milk as "oil" (subjecting it to the same costly environmental safeguards as real oil) are just as absurd. Both of these regulations are being lifted as a result of the review.
In contrast, many rules actually do protect public health and safety and will not be subject to review. For example, as a result of federal rulemaking, highway deaths are at the lowest level in 60 years and the risk of contracting salmonella from eggs is relatively low.
As part of HHS, the Center for Medicare & Medicaid Services (CMS) specifically stated that "the goal of the retrospective review will be to identify opportunities to improve patient care and outcomes and reduce system costs by removing obsolete or burdensome requirements." A major CMS concern will be to prevent the elimination or revision of a regulation only to find that the problem it sought to solve resurfaces, or that its removal or revision results in unanticipated and more serious outcomes.
This review could significantly impact HM in areas of quality measurement and reporting requirements:
- What quality measurements might not accomplish their intent?
- What measures might result in more harm than good?
- What reporting or process requirements could be changed to make for less duplication?
- If requirements cannot be eliminated, how can they be improved?
Due to hospitalist expertise in quality-improvement (QI) efforts and cost containment, these stated goals and the concerns that come with them are areas where hospitalists are likely to have some good answers. Hospitalists should not hesitate to provide their input to SHM Government Relations staff so that your ideas can be shared with CMS.
A complete list of agency proposals is available at www.whitehouse.gov/21stcentury gov/actions/21st-century-regulatory-system.
Master in HM profile
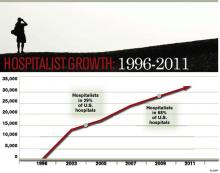
Fifteen years ago, Bob Wachter, MD, MHM, and Lee Goldman, MD, introduced hospital medicine and the term "hospitalist" to modern medicine in an article in the New England Journal of Medicine. In it, they wrote, "we anticipate the rapid growth of a new breed of physicians we call ‘hospitalists’—specialists in inpatient medicine—who will be responsible for managing the care of hospitalized patients in the same way that primary care physicians are responsible for managing the care of outpatients."
Since that introduction in 1996, the term "hospitalist" has gone from concept to cutting edge, and now to a title that describes more than 30,000 caregivers in hospitals around the world.
The evolution and growth of the hospitalist specialty owes much to Dr. Wachter. In addition to coining the term, he wrote the specialty’s first textbook, led SHM as president in 2000, and in 2010 was one of three HM pioneers honored by SHM as the first group of Masters in Hospital Medicine.
For each of the past three years, Modern Healthcare has listed him as one of healthcare’s most influential physician-executives.
Dr. Wachter used his recent presentation at HM11 to reflect on the growth of hospital medicine, where he showed how the specialty’s early focus on quality and safety puts hospitalists in positions of authority among physicians and hospitals.
Today, he is professor and associate chairman of the Department of Medicine at the University of California at San Francisco and chief of the division of hospital medicine, and chief of the medical service at UCSF Medical Center.
In July, Dr. Wachter was named chair-elect of the American Board of Internal Medicine’s (ABIM) board of directors.
Fifteen years ago, Bob Wachter, MD, MHM, and Lee Goldman, MD, introduced hospital medicine and the term "hospitalist" to modern medicine in an article in the New England Journal of Medicine. In it, they wrote, "we anticipate the rapid growth of a new breed of physicians we call ‘hospitalists’—specialists in inpatient medicine—who will be responsible for managing the care of hospitalized patients in the same way that primary care physicians are responsible for managing the care of outpatients."
Since that introduction in 1996, the term "hospitalist" has gone from concept to cutting edge, and now to a title that describes more than 30,000 caregivers in hospitals around the world.
The evolution and growth of the hospitalist specialty owes much to Dr. Wachter. In addition to coining the term, he wrote the specialty’s first textbook, led SHM as president in 2000, and in 2010 was one of three HM pioneers honored by SHM as the first group of Masters in Hospital Medicine.
For each of the past three years, Modern Healthcare has listed him as one of healthcare’s most influential physician-executives.
Dr. Wachter used his recent presentation at HM11 to reflect on the growth of hospital medicine, where he showed how the specialty’s early focus on quality and safety puts hospitalists in positions of authority among physicians and hospitals.
Today, he is professor and associate chairman of the Department of Medicine at the University of California at San Francisco and chief of the division of hospital medicine, and chief of the medical service at UCSF Medical Center.
In July, Dr. Wachter was named chair-elect of the American Board of Internal Medicine’s (ABIM) board of directors.
Fifteen years ago, Bob Wachter, MD, MHM, and Lee Goldman, MD, introduced hospital medicine and the term "hospitalist" to modern medicine in an article in the New England Journal of Medicine. In it, they wrote, "we anticipate the rapid growth of a new breed of physicians we call ‘hospitalists’—specialists in inpatient medicine—who will be responsible for managing the care of hospitalized patients in the same way that primary care physicians are responsible for managing the care of outpatients."
Since that introduction in 1996, the term "hospitalist" has gone from concept to cutting edge, and now to a title that describes more than 30,000 caregivers in hospitals around the world.
The evolution and growth of the hospitalist specialty owes much to Dr. Wachter. In addition to coining the term, he wrote the specialty’s first textbook, led SHM as president in 2000, and in 2010 was one of three HM pioneers honored by SHM as the first group of Masters in Hospital Medicine.
For each of the past three years, Modern Healthcare has listed him as one of healthcare’s most influential physician-executives.
Dr. Wachter used his recent presentation at HM11 to reflect on the growth of hospital medicine, where he showed how the specialty’s early focus on quality and safety puts hospitalists in positions of authority among physicians and hospitals.
Today, he is professor and associate chairman of the Department of Medicine at the University of California at San Francisco and chief of the division of hospital medicine, and chief of the medical service at UCSF Medical Center.
In July, Dr. Wachter was named chair-elect of the American Board of Internal Medicine’s (ABIM) board of directors.
Hospitalists on the Move
Cogent HMG has announced its new executive team and outside directors following the merger of Cogent Healthcare and Hospitalists Management Group (HMG). Gene Fleming, formerly president and CEO of Cogent Healthcare, will serve as executive chairman, assisting CEO Stephen Houff, MD, founder and CEO of Hospitalists Management Group. Ron Greeno, MD, a founder of Cogent Healthcare, will serve as chief medical officer of Cogent HMG and will steer the consulting business and serve as an advisor to the board. Antoine Agassi will serve as president and oversee day-to-day business operations. Linda Ellis will serve as COO, directing all regional and site operations.
Other key executives: Rusty Holman, MD, chief clinical officer; Susan Brownie, chief financial officer; Doug Mefford, chief legal officer; Anna-Gene O’Neal, senior vice president of quality; and Cheryl Slack, senior vice president of human resources. In addition to Fleming and Houff, Cogent HMG board members include Gary Chartrand, executive chairman of Acosta Sales and Marketing; Mike Leavitt, founder and chairman of Leavitt Partners and former U.S. Secretary of Health and Human Services; and Mark Neaman, president and CEO of NorthShore University HealthSystem.
The St. Anthony’s Hospital Foundation in St. Petersburg, Fla., has announced five new members of its board of directors: Emery Ellinger, CEO of the brokerage firm Aberdeen Advisors; Vitalis Unaeze, MD; Brian McNulty of USI Insurance Services; Angela Rouson, a St. Petersburg resident with a history of community service; and Dan Masi of Bright House Networks, a telecommunications company. Karim Godamunne, MD, has been promoted from medical director to vice president of clinical systems integration at Eagle Hospital Physicians in Atlanta.
Dr. Godamunne won primary stroke center designation within eight months of adding a teleneurology program to an existing Eagle hospitalist program at South Fulton Medical Center in East Point, Ga. Caitlin B. Foxley, MD, has been elected hospital medicine service chief for the Nebraska Medical Center in Omaha. Dr. Foxley is a member of Team Hospitalist.
Cynthia Roldan, MD, director of Westminster, Md.-based Carroll Hospital Center’s pediatric hospitalist program, has been selected as the hospital’s June Physician of the Month. A physician affiliated with Carroll Hospital Center for four years, Roldan was nominated for exceptional patient care and education of new and expecting mothers.
Dixon, Ill.-based Katherine Shaw Bethea Hospital has announced that hospitalist Tim Appenheimer, MD, has been promoted to vice president and CMO. The move is meant to address the growing focus on improving quality and patient safety across the country.
Cogent HMG has announced its new executive team and outside directors following the merger of Cogent Healthcare and Hospitalists Management Group (HMG). Gene Fleming, formerly president and CEO of Cogent Healthcare, will serve as executive chairman, assisting CEO Stephen Houff, MD, founder and CEO of Hospitalists Management Group. Ron Greeno, MD, a founder of Cogent Healthcare, will serve as chief medical officer of Cogent HMG and will steer the consulting business and serve as an advisor to the board. Antoine Agassi will serve as president and oversee day-to-day business operations. Linda Ellis will serve as COO, directing all regional and site operations.
Other key executives: Rusty Holman, MD, chief clinical officer; Susan Brownie, chief financial officer; Doug Mefford, chief legal officer; Anna-Gene O’Neal, senior vice president of quality; and Cheryl Slack, senior vice president of human resources. In addition to Fleming and Houff, Cogent HMG board members include Gary Chartrand, executive chairman of Acosta Sales and Marketing; Mike Leavitt, founder and chairman of Leavitt Partners and former U.S. Secretary of Health and Human Services; and Mark Neaman, president and CEO of NorthShore University HealthSystem.
The St. Anthony’s Hospital Foundation in St. Petersburg, Fla., has announced five new members of its board of directors: Emery Ellinger, CEO of the brokerage firm Aberdeen Advisors; Vitalis Unaeze, MD; Brian McNulty of USI Insurance Services; Angela Rouson, a St. Petersburg resident with a history of community service; and Dan Masi of Bright House Networks, a telecommunications company. Karim Godamunne, MD, has been promoted from medical director to vice president of clinical systems integration at Eagle Hospital Physicians in Atlanta.
Dr. Godamunne won primary stroke center designation within eight months of adding a teleneurology program to an existing Eagle hospitalist program at South Fulton Medical Center in East Point, Ga. Caitlin B. Foxley, MD, has been elected hospital medicine service chief for the Nebraska Medical Center in Omaha. Dr. Foxley is a member of Team Hospitalist.
Cynthia Roldan, MD, director of Westminster, Md.-based Carroll Hospital Center’s pediatric hospitalist program, has been selected as the hospital’s June Physician of the Month. A physician affiliated with Carroll Hospital Center for four years, Roldan was nominated for exceptional patient care and education of new and expecting mothers.
Dixon, Ill.-based Katherine Shaw Bethea Hospital has announced that hospitalist Tim Appenheimer, MD, has been promoted to vice president and CMO. The move is meant to address the growing focus on improving quality and patient safety across the country.
Cogent HMG has announced its new executive team and outside directors following the merger of Cogent Healthcare and Hospitalists Management Group (HMG). Gene Fleming, formerly president and CEO of Cogent Healthcare, will serve as executive chairman, assisting CEO Stephen Houff, MD, founder and CEO of Hospitalists Management Group. Ron Greeno, MD, a founder of Cogent Healthcare, will serve as chief medical officer of Cogent HMG and will steer the consulting business and serve as an advisor to the board. Antoine Agassi will serve as president and oversee day-to-day business operations. Linda Ellis will serve as COO, directing all regional and site operations.
Other key executives: Rusty Holman, MD, chief clinical officer; Susan Brownie, chief financial officer; Doug Mefford, chief legal officer; Anna-Gene O’Neal, senior vice president of quality; and Cheryl Slack, senior vice president of human resources. In addition to Fleming and Houff, Cogent HMG board members include Gary Chartrand, executive chairman of Acosta Sales and Marketing; Mike Leavitt, founder and chairman of Leavitt Partners and former U.S. Secretary of Health and Human Services; and Mark Neaman, president and CEO of NorthShore University HealthSystem.
The St. Anthony’s Hospital Foundation in St. Petersburg, Fla., has announced five new members of its board of directors: Emery Ellinger, CEO of the brokerage firm Aberdeen Advisors; Vitalis Unaeze, MD; Brian McNulty of USI Insurance Services; Angela Rouson, a St. Petersburg resident with a history of community service; and Dan Masi of Bright House Networks, a telecommunications company. Karim Godamunne, MD, has been promoted from medical director to vice president of clinical systems integration at Eagle Hospital Physicians in Atlanta.
Dr. Godamunne won primary stroke center designation within eight months of adding a teleneurology program to an existing Eagle hospitalist program at South Fulton Medical Center in East Point, Ga. Caitlin B. Foxley, MD, has been elected hospital medicine service chief for the Nebraska Medical Center in Omaha. Dr. Foxley is a member of Team Hospitalist.
Cynthia Roldan, MD, director of Westminster, Md.-based Carroll Hospital Center’s pediatric hospitalist program, has been selected as the hospital’s June Physician of the Month. A physician affiliated with Carroll Hospital Center for four years, Roldan was nominated for exceptional patient care and education of new and expecting mothers.
Dixon, Ill.-based Katherine Shaw Bethea Hospital has announced that hospitalist Tim Appenheimer, MD, has been promoted to vice president and CMO. The move is meant to address the growing focus on improving quality and patient safety across the country.
SQUINT Is Looking Out For You
Starting a new, hospital-based quality-improvement (QI) program can be a lonely task for hospitalists. What can begin with a rush of enthusiasm to solve a critical problem on your hospital floor quickly can lead to a single hospitalist in front of a computer screen wondering, "Has anyone else ever done this before?"
Unlike clinical knowledge, most of which comes from years of specialized formal training and volumes of peer-reviewed evidence on procedures, starting QI programs often presents a special challenge: a blank page and limited access to those who’ve taken on similar projects.
Those challenges, and the need to better understand what other hospitalists have already tried, motivated SHM’s Center for Hospital Innovation & Improvement, also known as The Center, to develop SQUINT, a new user-generated online repository of hospital-based QI programs.
"Being asked to lead a quality-improvement project is a daunting and difficult task," says Andrew Dunn, MD, FACP, professor of medicine and acting chief for Mount Sinai School of Medicine’s hospital medicine division in New York City. "Getting ideas on methods that have worked elsewhere is a great way to start. SQUINT is an easy way for hospitalists to get a head start on a project rather than start from scratch."
Access to SQUINT (SHM’s QUality Improve-ment NeTwork) is free to SHM members. Log in and gain access to summaries of QI programs from around the country. Because the summaries are searchable based on type, size, location, and specific kinds of topics, hospitalists can quickly find out whether projects similar to theirs are available through SQUINT.
For instance, a user could search for projects specifically related to transitions of care during discharge at community hospitals with 200-299 beds; a user in Oklahoma could search for all QI projects that have been uploaded from hospitals in the Sooner State. SQUINT also affords users keyword searches and browsing options.
For Hasan F. Shabbir, MD, SFHM, chief quality officer at Emory Johns Creek Hospital and assistant professor of medicine for Emory University School of Medicine’s division of hospital medicine in Atlanta, the ability to search user-generated, user-posted project files is especially important. Dr. Shabbir is no stranger to starting a QI project cold, or poring through literature and searching the Internet, worried that the materials don’t always explain the outcomes of a QI project that can be found through Google.
"You may just find a PDF on the Web and not know if it was a success," he says. "What’s unique about SQUINT is that it gives you a product, describes how it was utilized, and describes how it was—or wasn’t—effective. A lot of the work that needs to be done doesn’t always achieve the intended result."
Understanding the pitfalls and challenges of QI programs can save time and effort, he explains. "It’s equally important," he says. "Typically, only the successful stuff gets published in journals."
One of the first projects shared via SQUINT is a case study in using local resources to improve transitions of care for diabetic patients, submitted by medical director Jordan Messler, MD, SFHM, and his colleagues at Morton Plant Hospital in Clearwater, Fla.
"This was a project that we have done that we were probably not going to publish, but came up with some neat process things that we can share," says Dr. Messler, who hopes his team’s progress could help others get started. "If just one other program finds it and it saves them some time, that would be great."
Uploading descriptions of the QI programs can take as little as 15 minutes. Once project details and supporting documents are loaded into SQUINT, submissions are reviewed by members of SHM’s Health Quality and Patient Safety committee for clarity, the involvement of multidisciplinary team members, presentation of details, and the description of impacts and barriers to success.
Dr. Messler found the process of uploading simple and easy to use. He plans to add more.
"We have a variety of programs that we’ll probably upload," he says, including other recent QI programs addressing diabetes and DVT. "There’s no harm in putting them up there."
—Andrew Dunn, MD, FACP, professor, acting chief, hospital medicine division, Mount Sinai School of Medicine, New York City
Like other online user-submitted forums, submitting accepted content has added benefits: increased visibility among a community dedicated to improving the care of hospitalized patients and career advancement.
"This is a portal for you to spread what you’ve learned," Dr. Messler says. "Then, over time, this could be something that could be added to a resume or get to the point that folks will be proud of having a list of submissions to SQUINT."
For Dr. Shabbir, the utility of SQUINT extends beyond his own use.
"I have a junior colleague who is working on a new quality-improvement program. I’m going to tell her to look into SQUINT to see if others have worked on similar programs," he says. "If they have, that will put you two or three steps forward. For the novice, it also teaches the language and structure of how quality improvement happens."
Teaching and changing patient safety is a big part of SQUINT’s goal, according to Dr. Dunn.
"Hospitals should not need to start at ground zero, take months to get started and re-create every mistake made at other institutions," he says. "By sharing successful projects and learning from our errors, we can move patient safety initiatives along faster and better. … And that will, hopefully, improve outcomes across the country."
Brendon Shank is associate vice president of communications at SHM.
Starting a new, hospital-based quality-improvement (QI) program can be a lonely task for hospitalists. What can begin with a rush of enthusiasm to solve a critical problem on your hospital floor quickly can lead to a single hospitalist in front of a computer screen wondering, "Has anyone else ever done this before?"
Unlike clinical knowledge, most of which comes from years of specialized formal training and volumes of peer-reviewed evidence on procedures, starting QI programs often presents a special challenge: a blank page and limited access to those who’ve taken on similar projects.
Those challenges, and the need to better understand what other hospitalists have already tried, motivated SHM’s Center for Hospital Innovation & Improvement, also known as The Center, to develop SQUINT, a new user-generated online repository of hospital-based QI programs.
"Being asked to lead a quality-improvement project is a daunting and difficult task," says Andrew Dunn, MD, FACP, professor of medicine and acting chief for Mount Sinai School of Medicine’s hospital medicine division in New York City. "Getting ideas on methods that have worked elsewhere is a great way to start. SQUINT is an easy way for hospitalists to get a head start on a project rather than start from scratch."
Access to SQUINT (SHM’s QUality Improve-ment NeTwork) is free to SHM members. Log in and gain access to summaries of QI programs from around the country. Because the summaries are searchable based on type, size, location, and specific kinds of topics, hospitalists can quickly find out whether projects similar to theirs are available through SQUINT.
For instance, a user could search for projects specifically related to transitions of care during discharge at community hospitals with 200-299 beds; a user in Oklahoma could search for all QI projects that have been uploaded from hospitals in the Sooner State. SQUINT also affords users keyword searches and browsing options.
For Hasan F. Shabbir, MD, SFHM, chief quality officer at Emory Johns Creek Hospital and assistant professor of medicine for Emory University School of Medicine’s division of hospital medicine in Atlanta, the ability to search user-generated, user-posted project files is especially important. Dr. Shabbir is no stranger to starting a QI project cold, or poring through literature and searching the Internet, worried that the materials don’t always explain the outcomes of a QI project that can be found through Google.
"You may just find a PDF on the Web and not know if it was a success," he says. "What’s unique about SQUINT is that it gives you a product, describes how it was utilized, and describes how it was—or wasn’t—effective. A lot of the work that needs to be done doesn’t always achieve the intended result."
Understanding the pitfalls and challenges of QI programs can save time and effort, he explains. "It’s equally important," he says. "Typically, only the successful stuff gets published in journals."
One of the first projects shared via SQUINT is a case study in using local resources to improve transitions of care for diabetic patients, submitted by medical director Jordan Messler, MD, SFHM, and his colleagues at Morton Plant Hospital in Clearwater, Fla.
"This was a project that we have done that we were probably not going to publish, but came up with some neat process things that we can share," says Dr. Messler, who hopes his team’s progress could help others get started. "If just one other program finds it and it saves them some time, that would be great."
Uploading descriptions of the QI programs can take as little as 15 minutes. Once project details and supporting documents are loaded into SQUINT, submissions are reviewed by members of SHM’s Health Quality and Patient Safety committee for clarity, the involvement of multidisciplinary team members, presentation of details, and the description of impacts and barriers to success.
Dr. Messler found the process of uploading simple and easy to use. He plans to add more.
"We have a variety of programs that we’ll probably upload," he says, including other recent QI programs addressing diabetes and DVT. "There’s no harm in putting them up there."
—Andrew Dunn, MD, FACP, professor, acting chief, hospital medicine division, Mount Sinai School of Medicine, New York City
Like other online user-submitted forums, submitting accepted content has added benefits: increased visibility among a community dedicated to improving the care of hospitalized patients and career advancement.
"This is a portal for you to spread what you’ve learned," Dr. Messler says. "Then, over time, this could be something that could be added to a resume or get to the point that folks will be proud of having a list of submissions to SQUINT."
For Dr. Shabbir, the utility of SQUINT extends beyond his own use.
"I have a junior colleague who is working on a new quality-improvement program. I’m going to tell her to look into SQUINT to see if others have worked on similar programs," he says. "If they have, that will put you two or three steps forward. For the novice, it also teaches the language and structure of how quality improvement happens."
Teaching and changing patient safety is a big part of SQUINT’s goal, according to Dr. Dunn.
"Hospitals should not need to start at ground zero, take months to get started and re-create every mistake made at other institutions," he says. "By sharing successful projects and learning from our errors, we can move patient safety initiatives along faster and better. … And that will, hopefully, improve outcomes across the country."
Brendon Shank is associate vice president of communications at SHM.
Starting a new, hospital-based quality-improvement (QI) program can be a lonely task for hospitalists. What can begin with a rush of enthusiasm to solve a critical problem on your hospital floor quickly can lead to a single hospitalist in front of a computer screen wondering, "Has anyone else ever done this before?"
Unlike clinical knowledge, most of which comes from years of specialized formal training and volumes of peer-reviewed evidence on procedures, starting QI programs often presents a special challenge: a blank page and limited access to those who’ve taken on similar projects.
Those challenges, and the need to better understand what other hospitalists have already tried, motivated SHM’s Center for Hospital Innovation & Improvement, also known as The Center, to develop SQUINT, a new user-generated online repository of hospital-based QI programs.
"Being asked to lead a quality-improvement project is a daunting and difficult task," says Andrew Dunn, MD, FACP, professor of medicine and acting chief for Mount Sinai School of Medicine’s hospital medicine division in New York City. "Getting ideas on methods that have worked elsewhere is a great way to start. SQUINT is an easy way for hospitalists to get a head start on a project rather than start from scratch."
Access to SQUINT (SHM’s QUality Improve-ment NeTwork) is free to SHM members. Log in and gain access to summaries of QI programs from around the country. Because the summaries are searchable based on type, size, location, and specific kinds of topics, hospitalists can quickly find out whether projects similar to theirs are available through SQUINT.
For instance, a user could search for projects specifically related to transitions of care during discharge at community hospitals with 200-299 beds; a user in Oklahoma could search for all QI projects that have been uploaded from hospitals in the Sooner State. SQUINT also affords users keyword searches and browsing options.
For Hasan F. Shabbir, MD, SFHM, chief quality officer at Emory Johns Creek Hospital and assistant professor of medicine for Emory University School of Medicine’s division of hospital medicine in Atlanta, the ability to search user-generated, user-posted project files is especially important. Dr. Shabbir is no stranger to starting a QI project cold, or poring through literature and searching the Internet, worried that the materials don’t always explain the outcomes of a QI project that can be found through Google.
"You may just find a PDF on the Web and not know if it was a success," he says. "What’s unique about SQUINT is that it gives you a product, describes how it was utilized, and describes how it was—or wasn’t—effective. A lot of the work that needs to be done doesn’t always achieve the intended result."
Understanding the pitfalls and challenges of QI programs can save time and effort, he explains. "It’s equally important," he says. "Typically, only the successful stuff gets published in journals."
One of the first projects shared via SQUINT is a case study in using local resources to improve transitions of care for diabetic patients, submitted by medical director Jordan Messler, MD, SFHM, and his colleagues at Morton Plant Hospital in Clearwater, Fla.
"This was a project that we have done that we were probably not going to publish, but came up with some neat process things that we can share," says Dr. Messler, who hopes his team’s progress could help others get started. "If just one other program finds it and it saves them some time, that would be great."
Uploading descriptions of the QI programs can take as little as 15 minutes. Once project details and supporting documents are loaded into SQUINT, submissions are reviewed by members of SHM’s Health Quality and Patient Safety committee for clarity, the involvement of multidisciplinary team members, presentation of details, and the description of impacts and barriers to success.
Dr. Messler found the process of uploading simple and easy to use. He plans to add more.
"We have a variety of programs that we’ll probably upload," he says, including other recent QI programs addressing diabetes and DVT. "There’s no harm in putting them up there."
—Andrew Dunn, MD, FACP, professor, acting chief, hospital medicine division, Mount Sinai School of Medicine, New York City
Like other online user-submitted forums, submitting accepted content has added benefits: increased visibility among a community dedicated to improving the care of hospitalized patients and career advancement.
"This is a portal for you to spread what you’ve learned," Dr. Messler says. "Then, over time, this could be something that could be added to a resume or get to the point that folks will be proud of having a list of submissions to SQUINT."
For Dr. Shabbir, the utility of SQUINT extends beyond his own use.
"I have a junior colleague who is working on a new quality-improvement program. I’m going to tell her to look into SQUINT to see if others have worked on similar programs," he says. "If they have, that will put you two or three steps forward. For the novice, it also teaches the language and structure of how quality improvement happens."
Teaching and changing patient safety is a big part of SQUINT’s goal, according to Dr. Dunn.
"Hospitals should not need to start at ground zero, take months to get started and re-create every mistake made at other institutions," he says. "By sharing successful projects and learning from our errors, we can move patient safety initiatives along faster and better. … And that will, hopefully, improve outcomes across the country."
Brendon Shank is associate vice president of communications at SHM.
Integrated NPP systems can yield improved retention, quality of care, and patient satisfaction
Your article "NPPs to the Rescue" (May 2011, p. 24) contained one statement that is at strong variance with our experience: All your interviewees are said to agree that a 1:1 ratio of physicians to NPPs is optimally efficient and that "having one NPP work with more than one physician is not sustainable."
My group has used nonphysician providers (NPPs) for 13 years with great success and excellent retention, physician and patient satisfaction, and quality of care. We have presented nationally on the subject. We have always resisted the formation of separate "teams," and our system involves all 15 NPPs in our largest program working serially with all 35 physicians. This maximizes flexibility and helps to standardize and make uniform our practice styles and clinical methods. Also, it promotes a maximally flexible schedule, which we have found is a key to provider satisfaction.
Important to our system is a strong training program for new NPP hires, which allows them to function eventually with a good deal of autonomy. Also embedded in our culture is the notion that physicians and NPPs are both valued team members, and that NPPs are not asked to do work that physicians are unwilling to do. In fact, we tell providers that what physicians find satisfying and gratifying in practice are the same as those that NPPs look for, and that a strong collaborative relationship helps everyone benefit the patient. While it is clear that physicians are the clinical supervisors, NPPs and physicians are on an equal footing in many nonclinical areas of group management.
Another important piece of our system is that all billing is done by the attending physician. Thus, physicians are highly incented to work with NPPs, to seek cases on which they can collaborate, and to maintain cordial relations with their nonphysician associates.
This approach has resulted in an enormously capable clinical team and a high rate of provider retention and satisfaction.
As I heard a number of times at HM11 in Dallas in May, "If you’ve seen one hospitalist program, you’ve seen one hospitalist program." The same applies to optimal utilization of hospitalist NPPs.
Your article "NPPs to the Rescue" (May 2011, p. 24) contained one statement that is at strong variance with our experience: All your interviewees are said to agree that a 1:1 ratio of physicians to NPPs is optimally efficient and that "having one NPP work with more than one physician is not sustainable."
My group has used nonphysician providers (NPPs) for 13 years with great success and excellent retention, physician and patient satisfaction, and quality of care. We have presented nationally on the subject. We have always resisted the formation of separate "teams," and our system involves all 15 NPPs in our largest program working serially with all 35 physicians. This maximizes flexibility and helps to standardize and make uniform our practice styles and clinical methods. Also, it promotes a maximally flexible schedule, which we have found is a key to provider satisfaction.
Important to our system is a strong training program for new NPP hires, which allows them to function eventually with a good deal of autonomy. Also embedded in our culture is the notion that physicians and NPPs are both valued team members, and that NPPs are not asked to do work that physicians are unwilling to do. In fact, we tell providers that what physicians find satisfying and gratifying in practice are the same as those that NPPs look for, and that a strong collaborative relationship helps everyone benefit the patient. While it is clear that physicians are the clinical supervisors, NPPs and physicians are on an equal footing in many nonclinical areas of group management.
Another important piece of our system is that all billing is done by the attending physician. Thus, physicians are highly incented to work with NPPs, to seek cases on which they can collaborate, and to maintain cordial relations with their nonphysician associates.
This approach has resulted in an enormously capable clinical team and a high rate of provider retention and satisfaction.
As I heard a number of times at HM11 in Dallas in May, "If you’ve seen one hospitalist program, you’ve seen one hospitalist program." The same applies to optimal utilization of hospitalist NPPs.
Your article "NPPs to the Rescue" (May 2011, p. 24) contained one statement that is at strong variance with our experience: All your interviewees are said to agree that a 1:1 ratio of physicians to NPPs is optimally efficient and that "having one NPP work with more than one physician is not sustainable."
My group has used nonphysician providers (NPPs) for 13 years with great success and excellent retention, physician and patient satisfaction, and quality of care. We have presented nationally on the subject. We have always resisted the formation of separate "teams," and our system involves all 15 NPPs in our largest program working serially with all 35 physicians. This maximizes flexibility and helps to standardize and make uniform our practice styles and clinical methods. Also, it promotes a maximally flexible schedule, which we have found is a key to provider satisfaction.
Important to our system is a strong training program for new NPP hires, which allows them to function eventually with a good deal of autonomy. Also embedded in our culture is the notion that physicians and NPPs are both valued team members, and that NPPs are not asked to do work that physicians are unwilling to do. In fact, we tell providers that what physicians find satisfying and gratifying in practice are the same as those that NPPs look for, and that a strong collaborative relationship helps everyone benefit the patient. While it is clear that physicians are the clinical supervisors, NPPs and physicians are on an equal footing in many nonclinical areas of group management.
Another important piece of our system is that all billing is done by the attending physician. Thus, physicians are highly incented to work with NPPs, to seek cases on which they can collaborate, and to maintain cordial relations with their nonphysician associates.
This approach has resulted in an enormously capable clinical team and a high rate of provider retention and satisfaction.
As I heard a number of times at HM11 in Dallas in May, "If you’ve seen one hospitalist program, you’ve seen one hospitalist program." The same applies to optimal utilization of hospitalist NPPs.
Are You Delivering on the Promise of Higher Quality?
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
One hospitalist-led pilot project produced a 61% decrease in heart failure readmission rates. Another resulted in a 33% drop in all-cause readmissions. The numbers might be impressive, but what do they really say about how hospitalists have influenced healthcare quality?
When HM emerged 15 years ago, advocates pitched the fledgling physician specialty as a model of efficient inpatient care, and subsequent findings that the concept led to reductions in length of stay encouraged more hospitals to bolster their staff with the newcomers. With a rising emphasis on quality and patient safety over the past decade, and the new era of pay-for-performance, the hospitalist model of care has expanded to embrace improved quality of care as a chief selling point.
Measuring quality is no easy task, however, and researchers still debate the relative merits of metrics like 30-day readmission rates and inpatient mortality. "Without question, quality measurement is an imperfect science, and all measures will contain some level of imprecision and bias," concluded a recent commentary in Health Affairs.1
Against that backdrop, relatively few studies have looked broadly at the contributions of hospital medicine. Most interventions have been individually tailored to a hospital or instituted at only a few sites, precluding large-scale, head-to-head comparisons.
And so the question remains: Has hospital medicine lived up to its promise on quality?
The Evidence
In one of the few national surveys of HM’s impact on patient care, a yearlong comparison of more than 3,600 hospitals found that the roughly 40% that employed hospitalists scored better on multiple Hospital Quality Alliance indicators. The 2009 Archives of Internal Medicine study suggested that hospitals with hospitalists outperformed their counterparts in quality metrics for acute myocardial infarction, pneumonia, overall disease treatment and diagnosis, and counseling and prevention. Congestive heart failure was the only category of the five reviewed that lacked a statistically significant difference.2
A separate editorial, however, argued that the study’s data were not persuasive enough to support the conclusion that hospitalists bring a higher quality of care to the table.3 And even less can be said about the national impact of HM on newly elevated metrics, such as readmission rates. The obligation to gather evidence, in fact, is largely falling upon hospitalists themselves, and the multitude of research abstracts from SHM’s annual meeting in May suggests that plenty of physician scientists are taking the responsibility seriously. Among the presentations, a study led by David Boyte, MD, assistant professor of medicine at Duke University and a hospitalist at Durham Regional Hospital, found that a multidisciplinary approach greatly improved one hospital unit’s 30-day readmission rates for heart failure patients. After a three-month pilot in the cardiac nursing unit, readmission rates fell to 10.7% from 27.6%.4
Although the multidisciplinary effort has included doctors, nurses, nutritionists, pharmacists, unit managers, and other personnel, Dr. Boyte says the involvement of hospitalists has been key to the project’s success. "We feel like we were the main participants who could see the whole picture from a patient-centered perspective," he says. "We were the glue; we were the center node of all the healthcare providers." Based on that dramatic improvement, Dr. Boyte says, the same interventional protocol has been rolled out in three other medical surgical units, and the hospital is using a similar approach to address AMI readmission rates.
SHM’s Project BOOST (Better Outcomes for Older Adults through Safe Transitions; www.hospitalmedicine.org/boost )—by far the largest study of how HM is impacting readmission rates—has amassed data from more than 20 hospitals, with more expected from a growing roster of participants. So far, however, the project has only released data from six pilot sites describing the six-month periods before and after the project’s start. Among those sites, initial results suggest that readmission rates fell by an average of more than 20%, to 11.2% from 14.2%.5
Though the early numbers are encouraging, experts say rates from a larger group of participants at the one-year mark will be more telling, as will direct comparisons between BOOST units and nonparticipating counterparts at the same hospitals. Principal investigator Mark Williams, MD, FHM, professor and chief of the division of hospital medicine at the Northwestern University Feinberg School of Medicine in Chicago, says researchers still need to clean up that data before they’re ready to share it publicly.
In the meantime, some individual BOOST case studies are suggesting that hospitalist-led changes could pay big dividends. To help create cohesiveness and a sense of ownership within its HM program, St. Mary’s Health Center in St. Louis started a 20-bed hospitalist unit in 2008. Philip Vaidyan, MD, FACP, head of the hospitalist program and practice group leader for IPC: The Hospitalist Company at St. Mary’s, says one unit, 3 West, has since functioned as a lab for testing new ideas that are then introduced hospitalwide.
One early change was to bring all of the unit’s care providers together, from doctors and nurses to the unit-based case manager and social worker, for 9 a.m. handoff meetings. "We have this collective brain to find unique solutions," Dr. Vaidyan says. After seeing positive trends on length of stay, 30-day readmission rates, and patient satisfaction scores, St. Mary’s upgraded to a 32-bed hospitalist unit in early 2009. That same year, the 525-bed community teaching hospital was accepted into the BOOST program.
The hospitalist unit’s improved quality scores continued under BOOST, leading to a 33% reduction in readmission rates from 2008 to 2010 (to 10.5% from 15.7%). Rates for a nonhospitalist unit, by contrast, hovered around 17%. "For reducing readmissions, people may think that you have to have a higher length of stay," Dr. Vaidyan says. But the unit trended toward a lower length of stay, in addition to its reduced 30-day readmissions and improved patient satisfaction scores.
Flush with success, the 10 physicians and four nurse practitioners in the hospitalist program have since begun spreading their best practices to the rest of the hospital units. "Hospitalists are in the best ‘sweet spot,’ " Dr. Vaidyan says, "partnering with all of the disciplines, bringing them together, and keeping everybody on the same page."
Ironically, pinpointing the contribution of hospitalists is harder when their changes produce an ecological effect throughout an entire institution, says Siddhartha Singh, MD, MS, associate chief medical officer of Medical College Physicians, the adult practice for Medical College of Wisconsin in Milwaukee. Even so, he stresses that the impact of the two dozen hospitalists at Medical College Physicians has been felt.
"Coinciding with and following the introduction of our hospitalist program in 2004, we have noticed dramatic decreases in our length of stay throughout medicine services," he says. The same has held true for inpatient mortality. "And that, we feel, is attributable to the standardization of processes introduced by the hospitalist group." Multidisciplinary rounds; whiteboards in patient rooms; and standardized admission orders, prophylactic treatments, and discharge processes—"all of this would’ve been impossible, absolutely impossible, without the hospitalist," he says.
Over the past decade, Dr. Singh’s assessment has been echoed by several studies suggesting that individual hospitalist programs have brought significant improvements in quality measures, such as complication rates and inpatient mortality. In 2002, for example, Andrew Auerbach, MD, MPH, at the University of California San Francisco Medical Center, led a study that compared HM care with that of community physicians in a community-based teaching hospital. Patients cared for by hospitalists, the study found, had a lower risk of death during the hospitalization, as well as at 30 days and 60 days after discharge.6
A separate report by David Meltzer, MD, PhD, and colleagues at the University of Chicago found that an HM program in an academic general medicine service led to a 30% reduction in 30-day mortality rates during its second year of operation.7 And a 2004 study led by Jeanne Huddleston, MD, at the Mayo Clinic College of Medicine in Rochester, Minn., found that a hospitalist-orthopedic co-management model (versus care by orthopedic surgeons with medical consultation) led to more patients being discharged with no complications after elective hip or knee surgery.8 Hospitalist co-management also reduced the rate of minor complications, but had no effect on actual length of stay or cost.
A subsequent study by the same group, however, documented improved efficiency of care through the HM model, but no effect on the mortality of hip fracture patients up to one year after discharge.9 Multiple studies of hospitalist programs, in fact, have seen increased efficiency but little or no impact on inpatient mortality, leading researchers to broadly conclude that such programs can decrease resource use without compromising quality.
In 2007, a retrospective study of nearly 77,000 patients admitted to 45 hospitals with one of seven common diagnoses compared the care delivered by hospitalists, general internists, and family physicians.10 Although the study authors found that hospitalist care yielded a small drop in length of stay, they saw no difference in the inpatient mortality rates or 14-day readmission rates. More recently, mortality has become ensnared in controversy over its reliability as an accurate indicator of quality.

-Shai Gavi, DO, MPH, chief, section of hospital medicine, assistant professor, Stony Brook University School of Medicine, Brookhaven, N.Y.
Half of the Equation
Despite a lack of ideal metrics, another promising sign for HM might be the model’s exportability. Lee Kheng Hock, MMed, senior consultant and head of the Department of Family Medicine and Continuing Care at Singapore General Hospital, says the 1,600-bed hospital began experimenting with the hospitalist model when officials realized the existing care system wasn’t sustainable. Amid an aging population and increasingly complex and fragmented care, Hock views the hospitalist movement as a natural evolution of the healthcare system to meet the needs of a changing environment.
In a recent study, Hock and his colleagues used the hospital’s administrative database to examine the resource use and outcomes of patients cared for in 2008 by family medicine hospitalists or by specialists.11 The comparison, based on several standard metrics, found no significant improvements in quality, with similar inpatient mortality rates and 30-day, all-cause, unscheduled readmission rates regardless of the care delivery method. The study, though, revealed a significantly shorter hospital stay (4.4 days vs. 5.3 days) and lower costs per patient for those cared for by hospitalists ($2,250 vs. $2,500).11
Hock points out that, like his study, most analyses of hospitalist programs have shown an improvement in length of stay and cost of care without any increase in mortality and morbidity. If value equals quality divided by cost, he says, it stands to reason that quality must increase as overall value remains the same but costs decrease.
"The main difference is that the patients received undivided attention from a well-rounded generalist physician who is focused on providing holistic general medical care," Hock says, adding that "it is really a no-brainer that the outcome would be different."
Patients Rule
Other measures like the effectiveness of communication and seamlessness of handoffs often are assessed through their impacts on patient outcomes. But Sunil Kripalani, MD, MSc, SFHM, chief of the section of hospital medicine and an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn., says communication is now a primary focal point in Medicare’s new hospital value-based purchasing program (VBP). Within VBP’s Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) component, worth 30% of a hospital’s sum score, four of the 10 survey-based measures deal directly with communication. Patients’ overall rating and recommendation of hospitals likely will reflect their satisfaction with communication as well. Dr. Kripalani says it’s inevitable that hospitals—and hospitalists—will pay more attention to communication ratings as patients become judges of quality.
The expertise of hospitalists in handling challenging patients also leads to improved quality over time, says Shai Gavi, DO, MPH, chief of the section of hospital medicine and assistant professor of clinical medicine at Stony Brook University School of Medicine in Brookhaven, N.Y. Hospitalists, he says, excel in handling such high-stakes medical issues as gastrointestinal bleeding, pancreatitis, sepsis, and pain management that can quickly impact patient outcomes if not addressed properly and proficiently. "I think there’s significant value to having people who do this on a pretty frequent basis," he says.
And because of their broad day-to-day interactions, Dr. Gavi says, hospitalists are natural choices for committees focused on improving quality. "When we sit on committees, people often look to us for answers and directions because they know we’re on the front lines and we’ve interfaced with all of the services in the hospital," he says. "You have a good view of the whole hospital operation from A to Z, and I think that’s pretty unique to hospitalists."
The Verdict
In a recent issue brief by Lisa Sprague, principal policy analyst at the National Health Policy Forum, she asserts, "Hospitalists have the undeniable advantage of being there when a crisis occurs, when a patient is ready for discharge, and so on."12
So is "being there" the defining concept of hospital medicine, as she subsequently suggests?
Based on both scientific and anecdotal evidence, the contribution of hospitalists to healthcare quality might be better summarized as "being involved." Whether as innovators, navigators, physician champions, the "sweet spot" of interdepartmental partnerships, the "glue" of multidisciplinary teams, or the nuclei of performance committees, hospitalists are increasingly described as being in the middle of efforts to improve quality. On this basis, the discipline appears to be living up to expectations, though experts say more research is needed to better assess the impacts of HM on quality.
Dr. Vaidyan says hospitalists are particularly well positioned to understand what constitutes ideal care from the perspective of patients. "They want to be treated well: That’s patient satisfaction," he says. "They want to have their chief complaint—why they came to the hospital—properly addressed, so you need a coordinated care team. They want to go home early and don’t want come back: That’s low length of stay and a reduction in 30-day readmissions. And they don’t want any hospital-acquired complications."
Treating patients better, then, should be reflected by improved quality, even if the participation of hospitalists cannot be precisely quantified. "Being involved is something that may be difficult to measure," Dr. Gavi says, "but nonetheless, it has an important impact." TH
Bryn Nelson is a medical writer based in Seattle.
References
- Pronovost PJ, Lilford R. Analysis & commentary: A roadmap for improving the performance of performance measures. Health Aff (Millwood). 2011;30(4):569-73.
- López L, Hicks LS, Cohen AP, McKean S, Weissman JS. Hospitalists and the quality of care in hospitals. Arch Intern Med. 2009;169(15):1389-1394.
- Centor RM, Taylor BB. Do hospitalists improve quality? Arch Intern Med. 2009;169(15):1351-1352.
- Boyte D, Verma L, Wightman M. A multidisciplinary approach to reducing heart failure readmissions. J Hosp Med. 2011;6(4)Supp 2:S14.
- Williams MV, Hansen L, Greenwald J, Howell E, et al. BOOST: impact of a quality improvement project to reduce rehospitalizations. J Hosp Med. 2011;6(4) Supp 2:S88. BOOST: impact of a quality improvement project to reduce rehospitalizations.
- Auerbach AD, Wachter RM, Katz P, Showstack J, Baron RB, Goldman L. Implementation of a voluntary hospitalist service at a community teaching hospital: improved clinical efficiency and patient outcomes. Ann Intern Med. 2002;137(11):859-865.
- Meltzer D, Manning WG, Morrison J, et al. Effects of physician experience on costs and outcomes on an academic general medicine service: results of a trial of hospitalists. Ann Intern Med. 2002;137(1):866-874.
- Huddleston JM, Hall K, Naessens JM, et al. Medical and surgical comanagement after elective hip and knee arthroplasty. Ann Intern Med. 2004;141(1):28-38.
- Batsis JA, Phy MP, Melton LJ, et al. Effects of a hospitalist care model on mortality of elderly patients with hip fractures. J Hosp Med. 2007;2(4): 219–225.
- Lindenauer PK, Rothberg MB, Pekow PS, et al. Outcomes of care by hospitalists, general internists, and family physicians. N Eng J Med. 2007;357:2589-2600.
- Hock Lee K, Yang Y, Soong Yang K, Chi Ong B, Seong Ng H. Bringing generalists into the hospital: outcomes of a family medicine hospitalist model in Singapore. J Hosp Med. 2011;6(3):115-121.
- Sprague L. The hospitalist: better value in inpatient care? National Health Policy Forum website. Available at: www.nhpf.org/library/issue-briefs/IB842_Hospitalist_03-30-11.pdf. Accessed June 28, 2011.
No Easy Task
In college, while most of her fellow students were staying up late and sleeping in, Alice Marshbanks, MD, FHM, was an early riser. Now she regularly works from 4 p.m. to 2 a.m., and she sleeps in most mornings. "I’m sleeping later and living more of a teenage lifestyle," she jokes. "I’m actually getting younger."
Dr. Marshbanks might be an anomaly among established hospitalists. A physician since 1989 and a hospitalist since 1995, she actually prefers working the swing shift, and she says she’s the only one in her group at WakeMed Hospital in Raleigh, N.C., who does. Although Dr. Marshbanks is not a true nocturnist—she doesn’t work the typical 7 p.m. to 7 a.m. graveyard shift—her contracted position provides valuable transition coverage for night admissions, which have increased as the HM program at WakeMed has grown.
Surveys indicate that HM groups continue to move toward in-house coverage models to provide 24/7 hospitalist responsiveness. In the 2011 SHM-MGMA State of Hospital Medicine report, which will be released next month, 81% of responding nonteaching hospitalist practices reported providing on-site care at night. That’s up from 68% of responding HM practices that reported furnishing that service in the 2010 report. Only 53% of HM groups reported providing on-site night hospitalists in the 2007-2008 State of Hospital Medicine survey, which was produced solely by SHM.
Kenneth R. Epstein, MD, MBA, FACP, FHM, chief medical officer for Hospitalist Consultants Inc., headquartered in Traverse City, Mich., has observed this trend first-hand. In academic hospitals, due to new Accreditation Council for Graduate Medical Education (ACGME) and Resident Review Committee (RRC) regulations, "the only safety valve to handle admissions after the house staff numbers are capped is the hospitalist."
The need for such a safety valve will increase again this summer, as new ACGME duty-hour regulations on resident hours and supervision kick in.
Nonteaching hospitals are not exempt from these pressures. To deal with increasing demands for night coverage, HM groups across the country are using a variety of practice models, such as hiring dedicated nocturnists or moonlighters to cover nights, rotating shifts among team members, or using midlevel providers (physician assistants or nurse practitioners) as night staffers. On-call or in-house coverage models are determined by a variety of factors, including the size of the HM group, patient volume and acuity, and staff availability. Sustainability continues to be a challenge for most groups; however, the in-house coverage model seems to increase nursing and ED satisfaction, most experts say, and is an added value for hospital administration, although financial returns vary.
Continuity of care is at the heart of the night-coverage issue. Some experts worry that patient outcomes will suffer if there isn’t an in-house presence, but studies looking at this issue have been inconclusive, asserts Patti VanDort, RN, MSN, NEA-BC, vice president of nursing and chief nursing officer at Holland Hospital in southwestern Michigan.
"You’ve got to have the same level and quality of care during nights and weekends that you have during the weekdays," she says. "It’s got to be the same for all."
That said, some hospitals don’t have the volume to justify in-house night staffing. Hospitalists and program directors have described the ways in which they handle night staffing, balancing demand, program size, and physician satisfaction.
Tailored to Fit
"Hospitalist programs have different scale and scope depending on the needs of the institution," says Michael R. Humphrey, MD, vice president and chief clinical officer for Emergency and Ambulatory Services at St. Rita’s Medical Center in Lima, Ohio. A 365-bed community hospital, St. Rita’s employs nocturnists as part of its 24-hour hospitalist program. Dr. Humphrey still works as an ED physician and reports that the hospitalists are invaluable for admitting, providing cross-cover, covering the ICU, and handling code blue and rapid responses. "As a Level II trauma center, we can’t have ED physicians leave the department to run upstairs and do codes," he says. "They typically don’t get back within five minutes."
Holland Hospital, a 213-bed facility, provides around-the-clock hospitalist coverage in its eight-bed ICU, according to VanDort. That change was precipitated by the nursing staff’s decision to pursue Magnet Status, which was awarded in 2007 by the American Nurses Credentialing Center (ANCC). For inpatient coverage, the hospital-owned HM group Lakeshore Health Partners, headed by Bart D. Sak, MD, MA, FHM, maintains six FTE hospitalists on a rotating block schedule. Each night, one physician works from 4 p.m. until midnight, overlapping with a nonphysician provider (NPP), a member of the hospitalist group, who works a 7 p.m. to 7 a.m. shift.
"We have two providers in-house when admissions from the ED are heating up, and then we have an NPP in-house to cover the one to three additional admissions that may come in after midnight and to field floor calls," Dr. Sak says.
The physician who worked until midnight is on call for backup support and might come back to the hospital if things get too intense in the pre-dawn hours. "This arrangement works quite well for a program of our size," Dr. Sak says. "It takes a team-oriented approach and experienced NPPs who can work independently."
The Holland approach simply wouldn’t work at Kaiser Permanente’s East Bay site in Oakland, Calif., where Tom Baudendistel, MD, FACP, is part of a 50-member hospitalist group and director of the internal-medicine residency program. "Between codes, cross-cover, ICU, and floor admissions, there is simply too much acuity and volume," he says.
The peak hours for East Bay admissions are mid-afternoon to midnight. Two overnight hospitalist shifts (one from 8 a.m. to 8 p.m., another from 7 a.m. to 7 p.m.) are supplemented with two swing shifts (one from 2 to 10 p.m., another from 4 p.m. to midnight). Four full-time nocturnists cover 10 of the 14 overnight shifts per week, which allows for vacation and some protected administrative time. The balance of the overnight shifts are covered by the rest of the hospitalist group, which has 50 members.
The contracted nocturnists are incentivized with additional compensation at the end of the year, when the chief of hospitalists allocates bonuses. They also work fewer shifts a month than the other members of the group. "One thing our group agrees on is that the night docs should get a little more," Dr. Baudendistel says. "It’s a very fair tradeoff for everyone."
A Mile in Their Shoes
Medical directors must balance a variety of factors when scheduling around-the-clock coverage. From day one, the hospitalist program at Albany Memorial Hospital in New York, where John Krisa, MD, is medical director, has been an in-house 24/7 program. Dr. Krisa’s group uses per diem physicians or fellows on their days off to cover most of the nights. The other hospitalists on the team do not escape occasional night duty, and they cover what is left after plugging in the moonlighters. This leaves from zero to five nights per month for each full-time hospitalist. Even the medical director covers night shifts, something Dr. Krisa thinks is valuable to his leadership.
"You, as the leader, still have to walk a mile in that other person’s shoes," he says. "There are different challenges associated with both day and night shifts, so you have to appreciate what your colleagues are going through on the other shifts."
Hospitalist Consultants’ Dr. Epstein agrees with that concept.
"Whenever medical directors have personal experience of how the system is working, they are better able to recommend and make changes," he says.
It’s also valuable, Dr. Krisa explains, for the group leader to interact with ED staff and hear their concerns. Working night shifts helps avoid the night team versus day team schisms, which can lead to group disunity, he says.
Different Skill Set, Different Mindset?
The fact of the matter, though, is that pulling night shifts does not appeal to most established hospitalists. Sleep researchers have found that humans’ body clocks prefer office hours. Even if night-shift hours are consistent, those who work nights never really catch up on the sleep they need during the daytime.
Even so, some physicians embrace the graveyard shift. Working the night swing shift agrees with Dr. Marshbanks’ schedule. The hours are consistent, she works fewer shifts to qualify for FTE pay, and her shift is time-limited, as opposed to work-limited. She’s also filling a niche that others in her group eschew. "It’s a shift that most people with children don’t like because the hours are very disruptive to family life," she says.
The workload at night is different. Instead of the routine rounding typical in day shifts, her work is more urgent. She does more admissions because she works the busiest ED hours, covers acute-stroke codes, and provides cross-cover. And, she says, night staff tends to be "a solid group, so we interact more on a regular basis, since there are fewer of us."
The nocturnists at St. Rita’s Hospital are not held to the same meeting schedule as their daytime hospitalist colleagues, but they’re expected to read meeting minutes and to be responsible for any changes in guidelines or operational information, Dr. Humphrey says. Also stipulated in their hospitalist contracts is the requirement that they maintain competency in procedures, such as central-line placement and airway management.
What’s Better for Patients?
Experts have raised concerns that patient care can be compromised during off-hours, when staffing levels are reduced.1 The Leapfrog Group’s ICU Physician Safety (IPS) Standard argues for high-intensity ICU staffing to reduce patient mortality.2 A number of investigators have tried to determine whether patients admitted off-hours (weekends, nights, holidays) fare worse than those admitted during weekdays. Peter Cram, MD, MBA, acting director of the division of general internal medicine and associate professor of medicine at the Carver College of Medicine at the University of Iowa in Iowa City, found in a 2004 study that patients admitted to hospitals on weekends experienced slightly higher risk-adjusted mortality than did patients admitted on weekdays.3
But here’s the problem with studies such as this, says Dr. Cram: "Patients admitted on evenings and weekends are not the same as those admitted 9 to 5 on weekdays."
During weekdays, admissions combine patients with emergent issues and those scheduled for elective procedures. On weekends, "you get only emergencies—you don’t have low-risk patients," he points out. "So, even with optimal 24/7 staffing, you would still expect those patients coming in at night, and on holidays, to have worse outcomes because they are coming in with more acute problems. It remains an open question whether 24/7 staffing will improve off-hours outcomes." More research, Dr. Cram adds, is needed to establish whether full in-house staffing is the best solution.
Dr. Epstein has compared on-call versus in-house night staffing. In a 2007 study, he found no difference when using indicators such as length of stay, readmission rates, and patient satisfaction.4 However, he noticed positives from in-house coverage. "Although there are no data supporting the value of hospitalists on these parameters, having a nocturnist in-house increases nursing satisfaction, because they are responsive to pages when there is a question about a patient," he says. "It’s also a service to hospital medical staff, because they can handle rapid responses and codes."
There is some evidence that working nights can be deleterious to physicians’ and nurses’ health. One study found that interns were more likely to be involved in collisions after leaving extended night shifts; another found an increased risk of needle-stick injury at the end of a long night shift; and data from the long-running Nurses’ Health Study indicate that long-term night work can result in increased risk of colorectal and breast cancers.5,6,7,8 The increased risks of cancer could be related to lack of exposure to light at night and the body’s decreased production of melatonin, although this remains a topic of ongoing research.
"No Easy Answers"
VanDort, the nursing director, is "passionate" about having 24/7 coverage and reports that her nursing staff is happy with the hybrid model currently used at Holland Hospital. "I do envision a day when we’ll have physicians here around the clock," she says. "Patients are sick during the middle of the night, so you can’t staff your system one way during the daytime hours and your nighttime differently. It’s not fair to those patients."
Dr. Cram, who is a hospitalist, outcomes researcher, and division director, says that in an ideal world, it would make more business sense to have the hospital operating at full capacity around the clock, seven days a week. "But we don’t live in that world," he admits. "It is hard to find ways to achieve ’round-the-clock staffing at the levels we’d like."
He also concludes that there are "no easy answers" to the night-coverage conundrum. "But it might be prudent to think about incentives," he says. "Perhaps we should pay more for staffing weekends, evenings, and holidays, or we could reduce the annual number of shifts we expect our nocturnists to do, relative to those physicians who staff days."
Dr. Krisa says he, too, is biased toward an in-house coverage model, especially when programs reach a critical volume. "There is no substitute for the immediate ability to evaluate a sick patient," he explains. "My feeling is that an in-house, 24/7 presence will become the standard." TH
Gretchen Henkel is a freelance writer based in California.
References
- Wong HJ, Morra D. Excellent hospital care for all: open and operating 24/7. J Gen Intern Med. 2011.
- Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systemic review. JAMA. 2002;288(17):2151-2162.
- Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117(3):151-157.
- Epstein KR, Juarez E, Loya K, Gorman MJ, Singer A. The effect of 24-7 hospitalist coverage on clinical metrics. Presented May 2007, annual meeting, Society of Hospital Medicine, Dallas.
- Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125-134.
- Ayas NT, Barger LK, Cade BE, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296(9):1055-1062.
- Schernhammer ES, Laden F, Speizer FE, et al. Night-shift work and risk of colorectal cancer in the nurses’ health study. J Natl Cancer Inst. 2003;95(11):825-828.
- Schernhammer ES, Laden F, Speizer FE, et al. Rotating night shifts and risk of breast cancer in women partici-pating in the nurses’ health study. J Natl Cancer Inst. 2001;93(20):1563-1568.
In college, while most of her fellow students were staying up late and sleeping in, Alice Marshbanks, MD, FHM, was an early riser. Now she regularly works from 4 p.m. to 2 a.m., and she sleeps in most mornings. "I’m sleeping later and living more of a teenage lifestyle," she jokes. "I’m actually getting younger."
Dr. Marshbanks might be an anomaly among established hospitalists. A physician since 1989 and a hospitalist since 1995, she actually prefers working the swing shift, and she says she’s the only one in her group at WakeMed Hospital in Raleigh, N.C., who does. Although Dr. Marshbanks is not a true nocturnist—she doesn’t work the typical 7 p.m. to 7 a.m. graveyard shift—her contracted position provides valuable transition coverage for night admissions, which have increased as the HM program at WakeMed has grown.
Surveys indicate that HM groups continue to move toward in-house coverage models to provide 24/7 hospitalist responsiveness. In the 2011 SHM-MGMA State of Hospital Medicine report, which will be released next month, 81% of responding nonteaching hospitalist practices reported providing on-site care at night. That’s up from 68% of responding HM practices that reported furnishing that service in the 2010 report. Only 53% of HM groups reported providing on-site night hospitalists in the 2007-2008 State of Hospital Medicine survey, which was produced solely by SHM.
Kenneth R. Epstein, MD, MBA, FACP, FHM, chief medical officer for Hospitalist Consultants Inc., headquartered in Traverse City, Mich., has observed this trend first-hand. In academic hospitals, due to new Accreditation Council for Graduate Medical Education (ACGME) and Resident Review Committee (RRC) regulations, "the only safety valve to handle admissions after the house staff numbers are capped is the hospitalist."
The need for such a safety valve will increase again this summer, as new ACGME duty-hour regulations on resident hours and supervision kick in.
Nonteaching hospitals are not exempt from these pressures. To deal with increasing demands for night coverage, HM groups across the country are using a variety of practice models, such as hiring dedicated nocturnists or moonlighters to cover nights, rotating shifts among team members, or using midlevel providers (physician assistants or nurse practitioners) as night staffers. On-call or in-house coverage models are determined by a variety of factors, including the size of the HM group, patient volume and acuity, and staff availability. Sustainability continues to be a challenge for most groups; however, the in-house coverage model seems to increase nursing and ED satisfaction, most experts say, and is an added value for hospital administration, although financial returns vary.
Continuity of care is at the heart of the night-coverage issue. Some experts worry that patient outcomes will suffer if there isn’t an in-house presence, but studies looking at this issue have been inconclusive, asserts Patti VanDort, RN, MSN, NEA-BC, vice president of nursing and chief nursing officer at Holland Hospital in southwestern Michigan.
"You’ve got to have the same level and quality of care during nights and weekends that you have during the weekdays," she says. "It’s got to be the same for all."
That said, some hospitals don’t have the volume to justify in-house night staffing. Hospitalists and program directors have described the ways in which they handle night staffing, balancing demand, program size, and physician satisfaction.
Tailored to Fit
"Hospitalist programs have different scale and scope depending on the needs of the institution," says Michael R. Humphrey, MD, vice president and chief clinical officer for Emergency and Ambulatory Services at St. Rita’s Medical Center in Lima, Ohio. A 365-bed community hospital, St. Rita’s employs nocturnists as part of its 24-hour hospitalist program. Dr. Humphrey still works as an ED physician and reports that the hospitalists are invaluable for admitting, providing cross-cover, covering the ICU, and handling code blue and rapid responses. "As a Level II trauma center, we can’t have ED physicians leave the department to run upstairs and do codes," he says. "They typically don’t get back within five minutes."
Holland Hospital, a 213-bed facility, provides around-the-clock hospitalist coverage in its eight-bed ICU, according to VanDort. That change was precipitated by the nursing staff’s decision to pursue Magnet Status, which was awarded in 2007 by the American Nurses Credentialing Center (ANCC). For inpatient coverage, the hospital-owned HM group Lakeshore Health Partners, headed by Bart D. Sak, MD, MA, FHM, maintains six FTE hospitalists on a rotating block schedule. Each night, one physician works from 4 p.m. until midnight, overlapping with a nonphysician provider (NPP), a member of the hospitalist group, who works a 7 p.m. to 7 a.m. shift.
"We have two providers in-house when admissions from the ED are heating up, and then we have an NPP in-house to cover the one to three additional admissions that may come in after midnight and to field floor calls," Dr. Sak says.
The physician who worked until midnight is on call for backup support and might come back to the hospital if things get too intense in the pre-dawn hours. "This arrangement works quite well for a program of our size," Dr. Sak says. "It takes a team-oriented approach and experienced NPPs who can work independently."
The Holland approach simply wouldn’t work at Kaiser Permanente’s East Bay site in Oakland, Calif., where Tom Baudendistel, MD, FACP, is part of a 50-member hospitalist group and director of the internal-medicine residency program. "Between codes, cross-cover, ICU, and floor admissions, there is simply too much acuity and volume," he says.
The peak hours for East Bay admissions are mid-afternoon to midnight. Two overnight hospitalist shifts (one from 8 a.m. to 8 p.m., another from 7 a.m. to 7 p.m.) are supplemented with two swing shifts (one from 2 to 10 p.m., another from 4 p.m. to midnight). Four full-time nocturnists cover 10 of the 14 overnight shifts per week, which allows for vacation and some protected administrative time. The balance of the overnight shifts are covered by the rest of the hospitalist group, which has 50 members.
The contracted nocturnists are incentivized with additional compensation at the end of the year, when the chief of hospitalists allocates bonuses. They also work fewer shifts a month than the other members of the group. "One thing our group agrees on is that the night docs should get a little more," Dr. Baudendistel says. "It’s a very fair tradeoff for everyone."
A Mile in Their Shoes
Medical directors must balance a variety of factors when scheduling around-the-clock coverage. From day one, the hospitalist program at Albany Memorial Hospital in New York, where John Krisa, MD, is medical director, has been an in-house 24/7 program. Dr. Krisa’s group uses per diem physicians or fellows on their days off to cover most of the nights. The other hospitalists on the team do not escape occasional night duty, and they cover what is left after plugging in the moonlighters. This leaves from zero to five nights per month for each full-time hospitalist. Even the medical director covers night shifts, something Dr. Krisa thinks is valuable to his leadership.
"You, as the leader, still have to walk a mile in that other person’s shoes," he says. "There are different challenges associated with both day and night shifts, so you have to appreciate what your colleagues are going through on the other shifts."
Hospitalist Consultants’ Dr. Epstein agrees with that concept.
"Whenever medical directors have personal experience of how the system is working, they are better able to recommend and make changes," he says.
It’s also valuable, Dr. Krisa explains, for the group leader to interact with ED staff and hear their concerns. Working night shifts helps avoid the night team versus day team schisms, which can lead to group disunity, he says.
Different Skill Set, Different Mindset?
The fact of the matter, though, is that pulling night shifts does not appeal to most established hospitalists. Sleep researchers have found that humans’ body clocks prefer office hours. Even if night-shift hours are consistent, those who work nights never really catch up on the sleep they need during the daytime.
Even so, some physicians embrace the graveyard shift. Working the night swing shift agrees with Dr. Marshbanks’ schedule. The hours are consistent, she works fewer shifts to qualify for FTE pay, and her shift is time-limited, as opposed to work-limited. She’s also filling a niche that others in her group eschew. "It’s a shift that most people with children don’t like because the hours are very disruptive to family life," she says.
The workload at night is different. Instead of the routine rounding typical in day shifts, her work is more urgent. She does more admissions because she works the busiest ED hours, covers acute-stroke codes, and provides cross-cover. And, she says, night staff tends to be "a solid group, so we interact more on a regular basis, since there are fewer of us."
The nocturnists at St. Rita’s Hospital are not held to the same meeting schedule as their daytime hospitalist colleagues, but they’re expected to read meeting minutes and to be responsible for any changes in guidelines or operational information, Dr. Humphrey says. Also stipulated in their hospitalist contracts is the requirement that they maintain competency in procedures, such as central-line placement and airway management.
What’s Better for Patients?
Experts have raised concerns that patient care can be compromised during off-hours, when staffing levels are reduced.1 The Leapfrog Group’s ICU Physician Safety (IPS) Standard argues for high-intensity ICU staffing to reduce patient mortality.2 A number of investigators have tried to determine whether patients admitted off-hours (weekends, nights, holidays) fare worse than those admitted during weekdays. Peter Cram, MD, MBA, acting director of the division of general internal medicine and associate professor of medicine at the Carver College of Medicine at the University of Iowa in Iowa City, found in a 2004 study that patients admitted to hospitals on weekends experienced slightly higher risk-adjusted mortality than did patients admitted on weekdays.3
But here’s the problem with studies such as this, says Dr. Cram: "Patients admitted on evenings and weekends are not the same as those admitted 9 to 5 on weekdays."
During weekdays, admissions combine patients with emergent issues and those scheduled for elective procedures. On weekends, "you get only emergencies—you don’t have low-risk patients," he points out. "So, even with optimal 24/7 staffing, you would still expect those patients coming in at night, and on holidays, to have worse outcomes because they are coming in with more acute problems. It remains an open question whether 24/7 staffing will improve off-hours outcomes." More research, Dr. Cram adds, is needed to establish whether full in-house staffing is the best solution.
Dr. Epstein has compared on-call versus in-house night staffing. In a 2007 study, he found no difference when using indicators such as length of stay, readmission rates, and patient satisfaction.4 However, he noticed positives from in-house coverage. "Although there are no data supporting the value of hospitalists on these parameters, having a nocturnist in-house increases nursing satisfaction, because they are responsive to pages when there is a question about a patient," he says. "It’s also a service to hospital medical staff, because they can handle rapid responses and codes."
There is some evidence that working nights can be deleterious to physicians’ and nurses’ health. One study found that interns were more likely to be involved in collisions after leaving extended night shifts; another found an increased risk of needle-stick injury at the end of a long night shift; and data from the long-running Nurses’ Health Study indicate that long-term night work can result in increased risk of colorectal and breast cancers.5,6,7,8 The increased risks of cancer could be related to lack of exposure to light at night and the body’s decreased production of melatonin, although this remains a topic of ongoing research.
"No Easy Answers"
VanDort, the nursing director, is "passionate" about having 24/7 coverage and reports that her nursing staff is happy with the hybrid model currently used at Holland Hospital. "I do envision a day when we’ll have physicians here around the clock," she says. "Patients are sick during the middle of the night, so you can’t staff your system one way during the daytime hours and your nighttime differently. It’s not fair to those patients."
Dr. Cram, who is a hospitalist, outcomes researcher, and division director, says that in an ideal world, it would make more business sense to have the hospital operating at full capacity around the clock, seven days a week. "But we don’t live in that world," he admits. "It is hard to find ways to achieve ’round-the-clock staffing at the levels we’d like."
He also concludes that there are "no easy answers" to the night-coverage conundrum. "But it might be prudent to think about incentives," he says. "Perhaps we should pay more for staffing weekends, evenings, and holidays, or we could reduce the annual number of shifts we expect our nocturnists to do, relative to those physicians who staff days."
Dr. Krisa says he, too, is biased toward an in-house coverage model, especially when programs reach a critical volume. "There is no substitute for the immediate ability to evaluate a sick patient," he explains. "My feeling is that an in-house, 24/7 presence will become the standard." TH
Gretchen Henkel is a freelance writer based in California.
References
- Wong HJ, Morra D. Excellent hospital care for all: open and operating 24/7. J Gen Intern Med. 2011.
- Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systemic review. JAMA. 2002;288(17):2151-2162.
- Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117(3):151-157.
- Epstein KR, Juarez E, Loya K, Gorman MJ, Singer A. The effect of 24-7 hospitalist coverage on clinical metrics. Presented May 2007, annual meeting, Society of Hospital Medicine, Dallas.
- Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125-134.
- Ayas NT, Barger LK, Cade BE, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296(9):1055-1062.
- Schernhammer ES, Laden F, Speizer FE, et al. Night-shift work and risk of colorectal cancer in the nurses’ health study. J Natl Cancer Inst. 2003;95(11):825-828.
- Schernhammer ES, Laden F, Speizer FE, et al. Rotating night shifts and risk of breast cancer in women partici-pating in the nurses’ health study. J Natl Cancer Inst. 2001;93(20):1563-1568.
In college, while most of her fellow students were staying up late and sleeping in, Alice Marshbanks, MD, FHM, was an early riser. Now she regularly works from 4 p.m. to 2 a.m., and she sleeps in most mornings. "I’m sleeping later and living more of a teenage lifestyle," she jokes. "I’m actually getting younger."
Dr. Marshbanks might be an anomaly among established hospitalists. A physician since 1989 and a hospitalist since 1995, she actually prefers working the swing shift, and she says she’s the only one in her group at WakeMed Hospital in Raleigh, N.C., who does. Although Dr. Marshbanks is not a true nocturnist—she doesn’t work the typical 7 p.m. to 7 a.m. graveyard shift—her contracted position provides valuable transition coverage for night admissions, which have increased as the HM program at WakeMed has grown.
Surveys indicate that HM groups continue to move toward in-house coverage models to provide 24/7 hospitalist responsiveness. In the 2011 SHM-MGMA State of Hospital Medicine report, which will be released next month, 81% of responding nonteaching hospitalist practices reported providing on-site care at night. That’s up from 68% of responding HM practices that reported furnishing that service in the 2010 report. Only 53% of HM groups reported providing on-site night hospitalists in the 2007-2008 State of Hospital Medicine survey, which was produced solely by SHM.
Kenneth R. Epstein, MD, MBA, FACP, FHM, chief medical officer for Hospitalist Consultants Inc., headquartered in Traverse City, Mich., has observed this trend first-hand. In academic hospitals, due to new Accreditation Council for Graduate Medical Education (ACGME) and Resident Review Committee (RRC) regulations, "the only safety valve to handle admissions after the house staff numbers are capped is the hospitalist."
The need for such a safety valve will increase again this summer, as new ACGME duty-hour regulations on resident hours and supervision kick in.
Nonteaching hospitals are not exempt from these pressures. To deal with increasing demands for night coverage, HM groups across the country are using a variety of practice models, such as hiring dedicated nocturnists or moonlighters to cover nights, rotating shifts among team members, or using midlevel providers (physician assistants or nurse practitioners) as night staffers. On-call or in-house coverage models are determined by a variety of factors, including the size of the HM group, patient volume and acuity, and staff availability. Sustainability continues to be a challenge for most groups; however, the in-house coverage model seems to increase nursing and ED satisfaction, most experts say, and is an added value for hospital administration, although financial returns vary.
Continuity of care is at the heart of the night-coverage issue. Some experts worry that patient outcomes will suffer if there isn’t an in-house presence, but studies looking at this issue have been inconclusive, asserts Patti VanDort, RN, MSN, NEA-BC, vice president of nursing and chief nursing officer at Holland Hospital in southwestern Michigan.
"You’ve got to have the same level and quality of care during nights and weekends that you have during the weekdays," she says. "It’s got to be the same for all."
That said, some hospitals don’t have the volume to justify in-house night staffing. Hospitalists and program directors have described the ways in which they handle night staffing, balancing demand, program size, and physician satisfaction.
Tailored to Fit
"Hospitalist programs have different scale and scope depending on the needs of the institution," says Michael R. Humphrey, MD, vice president and chief clinical officer for Emergency and Ambulatory Services at St. Rita’s Medical Center in Lima, Ohio. A 365-bed community hospital, St. Rita’s employs nocturnists as part of its 24-hour hospitalist program. Dr. Humphrey still works as an ED physician and reports that the hospitalists are invaluable for admitting, providing cross-cover, covering the ICU, and handling code blue and rapid responses. "As a Level II trauma center, we can’t have ED physicians leave the department to run upstairs and do codes," he says. "They typically don’t get back within five minutes."
Holland Hospital, a 213-bed facility, provides around-the-clock hospitalist coverage in its eight-bed ICU, according to VanDort. That change was precipitated by the nursing staff’s decision to pursue Magnet Status, which was awarded in 2007 by the American Nurses Credentialing Center (ANCC). For inpatient coverage, the hospital-owned HM group Lakeshore Health Partners, headed by Bart D. Sak, MD, MA, FHM, maintains six FTE hospitalists on a rotating block schedule. Each night, one physician works from 4 p.m. until midnight, overlapping with a nonphysician provider (NPP), a member of the hospitalist group, who works a 7 p.m. to 7 a.m. shift.
"We have two providers in-house when admissions from the ED are heating up, and then we have an NPP in-house to cover the one to three additional admissions that may come in after midnight and to field floor calls," Dr. Sak says.
The physician who worked until midnight is on call for backup support and might come back to the hospital if things get too intense in the pre-dawn hours. "This arrangement works quite well for a program of our size," Dr. Sak says. "It takes a team-oriented approach and experienced NPPs who can work independently."
The Holland approach simply wouldn’t work at Kaiser Permanente’s East Bay site in Oakland, Calif., where Tom Baudendistel, MD, FACP, is part of a 50-member hospitalist group and director of the internal-medicine residency program. "Between codes, cross-cover, ICU, and floor admissions, there is simply too much acuity and volume," he says.
The peak hours for East Bay admissions are mid-afternoon to midnight. Two overnight hospitalist shifts (one from 8 a.m. to 8 p.m., another from 7 a.m. to 7 p.m.) are supplemented with two swing shifts (one from 2 to 10 p.m., another from 4 p.m. to midnight). Four full-time nocturnists cover 10 of the 14 overnight shifts per week, which allows for vacation and some protected administrative time. The balance of the overnight shifts are covered by the rest of the hospitalist group, which has 50 members.
The contracted nocturnists are incentivized with additional compensation at the end of the year, when the chief of hospitalists allocates bonuses. They also work fewer shifts a month than the other members of the group. "One thing our group agrees on is that the night docs should get a little more," Dr. Baudendistel says. "It’s a very fair tradeoff for everyone."
A Mile in Their Shoes
Medical directors must balance a variety of factors when scheduling around-the-clock coverage. From day one, the hospitalist program at Albany Memorial Hospital in New York, where John Krisa, MD, is medical director, has been an in-house 24/7 program. Dr. Krisa’s group uses per diem physicians or fellows on their days off to cover most of the nights. The other hospitalists on the team do not escape occasional night duty, and they cover what is left after plugging in the moonlighters. This leaves from zero to five nights per month for each full-time hospitalist. Even the medical director covers night shifts, something Dr. Krisa thinks is valuable to his leadership.
"You, as the leader, still have to walk a mile in that other person’s shoes," he says. "There are different challenges associated with both day and night shifts, so you have to appreciate what your colleagues are going through on the other shifts."
Hospitalist Consultants’ Dr. Epstein agrees with that concept.
"Whenever medical directors have personal experience of how the system is working, they are better able to recommend and make changes," he says.
It’s also valuable, Dr. Krisa explains, for the group leader to interact with ED staff and hear their concerns. Working night shifts helps avoid the night team versus day team schisms, which can lead to group disunity, he says.
Different Skill Set, Different Mindset?
The fact of the matter, though, is that pulling night shifts does not appeal to most established hospitalists. Sleep researchers have found that humans’ body clocks prefer office hours. Even if night-shift hours are consistent, those who work nights never really catch up on the sleep they need during the daytime.
Even so, some physicians embrace the graveyard shift. Working the night swing shift agrees with Dr. Marshbanks’ schedule. The hours are consistent, she works fewer shifts to qualify for FTE pay, and her shift is time-limited, as opposed to work-limited. She’s also filling a niche that others in her group eschew. "It’s a shift that most people with children don’t like because the hours are very disruptive to family life," she says.
The workload at night is different. Instead of the routine rounding typical in day shifts, her work is more urgent. She does more admissions because she works the busiest ED hours, covers acute-stroke codes, and provides cross-cover. And, she says, night staff tends to be "a solid group, so we interact more on a regular basis, since there are fewer of us."
The nocturnists at St. Rita’s Hospital are not held to the same meeting schedule as their daytime hospitalist colleagues, but they’re expected to read meeting minutes and to be responsible for any changes in guidelines or operational information, Dr. Humphrey says. Also stipulated in their hospitalist contracts is the requirement that they maintain competency in procedures, such as central-line placement and airway management.
What’s Better for Patients?
Experts have raised concerns that patient care can be compromised during off-hours, when staffing levels are reduced.1 The Leapfrog Group’s ICU Physician Safety (IPS) Standard argues for high-intensity ICU staffing to reduce patient mortality.2 A number of investigators have tried to determine whether patients admitted off-hours (weekends, nights, holidays) fare worse than those admitted during weekdays. Peter Cram, MD, MBA, acting director of the division of general internal medicine and associate professor of medicine at the Carver College of Medicine at the University of Iowa in Iowa City, found in a 2004 study that patients admitted to hospitals on weekends experienced slightly higher risk-adjusted mortality than did patients admitted on weekdays.3
But here’s the problem with studies such as this, says Dr. Cram: "Patients admitted on evenings and weekends are not the same as those admitted 9 to 5 on weekdays."
During weekdays, admissions combine patients with emergent issues and those scheduled for elective procedures. On weekends, "you get only emergencies—you don’t have low-risk patients," he points out. "So, even with optimal 24/7 staffing, you would still expect those patients coming in at night, and on holidays, to have worse outcomes because they are coming in with more acute problems. It remains an open question whether 24/7 staffing will improve off-hours outcomes." More research, Dr. Cram adds, is needed to establish whether full in-house staffing is the best solution.
Dr. Epstein has compared on-call versus in-house night staffing. In a 2007 study, he found no difference when using indicators such as length of stay, readmission rates, and patient satisfaction.4 However, he noticed positives from in-house coverage. "Although there are no data supporting the value of hospitalists on these parameters, having a nocturnist in-house increases nursing satisfaction, because they are responsive to pages when there is a question about a patient," he says. "It’s also a service to hospital medical staff, because they can handle rapid responses and codes."
There is some evidence that working nights can be deleterious to physicians’ and nurses’ health. One study found that interns were more likely to be involved in collisions after leaving extended night shifts; another found an increased risk of needle-stick injury at the end of a long night shift; and data from the long-running Nurses’ Health Study indicate that long-term night work can result in increased risk of colorectal and breast cancers.5,6,7,8 The increased risks of cancer could be related to lack of exposure to light at night and the body’s decreased production of melatonin, although this remains a topic of ongoing research.
"No Easy Answers"
VanDort, the nursing director, is "passionate" about having 24/7 coverage and reports that her nursing staff is happy with the hybrid model currently used at Holland Hospital. "I do envision a day when we’ll have physicians here around the clock," she says. "Patients are sick during the middle of the night, so you can’t staff your system one way during the daytime hours and your nighttime differently. It’s not fair to those patients."
Dr. Cram, who is a hospitalist, outcomes researcher, and division director, says that in an ideal world, it would make more business sense to have the hospital operating at full capacity around the clock, seven days a week. "But we don’t live in that world," he admits. "It is hard to find ways to achieve ’round-the-clock staffing at the levels we’d like."
He also concludes that there are "no easy answers" to the night-coverage conundrum. "But it might be prudent to think about incentives," he says. "Perhaps we should pay more for staffing weekends, evenings, and holidays, or we could reduce the annual number of shifts we expect our nocturnists to do, relative to those physicians who staff days."
Dr. Krisa says he, too, is biased toward an in-house coverage model, especially when programs reach a critical volume. "There is no substitute for the immediate ability to evaluate a sick patient," he explains. "My feeling is that an in-house, 24/7 presence will become the standard." TH
Gretchen Henkel is a freelance writer based in California.
References
- Wong HJ, Morra D. Excellent hospital care for all: open and operating 24/7. J Gen Intern Med. 2011.
- Pronovost PJ, Angus DC, Dorman T, Robinson KA, Dremsizov TT, Young TL. Physician staffing patterns and clinical outcomes in critically ill patients: a systemic review. JAMA. 2002;288(17):2151-2162.
- Cram P, Hillis SL, Barnett M, Rosenthal GE. Effects of weekend admission and hospital teaching status on in-hospital mortality. Am J Med. 2004;117(3):151-157.
- Epstein KR, Juarez E, Loya K, Gorman MJ, Singer A. The effect of 24-7 hospitalist coverage on clinical metrics. Presented May 2007, annual meeting, Society of Hospital Medicine, Dallas.
- Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125-134.
- Ayas NT, Barger LK, Cade BE, et al. Extended work duration and the risk of self-reported percutaneous injuries in interns. JAMA. 2006;296(9):1055-1062.
- Schernhammer ES, Laden F, Speizer FE, et al. Night-shift work and risk of colorectal cancer in the nurses’ health study. J Natl Cancer Inst. 2003;95(11):825-828.
- Schernhammer ES, Laden F, Speizer FE, et al. Rotating night shifts and risk of breast cancer in women partici-pating in the nurses’ health study. J Natl Cancer Inst. 2001;93(20):1563-1568.
What’s Next for Hospital Medicine?
At the Medical University of South Carolina (MUSC) in Charleston, a familiar scene plays out in the hospitalist program. New hospitalists express an interest in a certain area and the university tries to accommodate them, making time for them to pursue additional training as they juggle the daily demands of treating patients, says Patrick Cawley, MD, MBA, SFHM, associate professor at the university and a former SHM president.
"We try to have a personal growth plan for each hospitalist that aligns with their interest," Dr. Cawley says. "So if we have a hospitalist that’s very, very interested in quality improvement, we’ll seek out opportunities to get that hospitalist experience, and start with smaller projects and then bigger projects."
As the field of HM hits a notable mark in its history—it’s been 15 years since the term "hospitalist" was coined—more advanced training will continue to emerge as a key issue and obstacle in the field, say experts who were asked to take a look into HM’s crystal ball.
They also predict continued growth of the field, with tens of thousands of new hospitalists emerging in the next decade or so. They also say that hospitalists will emerge as leaders in the application and use of new technology, and that there will be more demands placed on hospitalists to show their worth in hard data.
There also promises to be a growing presence of private management firms providing hospitalists to hospitals, which doctors both inside and outside of those firms say could have a beneficial effect on the overall quality of patient care.

-Patrick Cawley, MD, MBA, SFHM, associate professor, Medical University of South Carolina, Charleston, former SHM president
Father Time
For now, Dr. Cawley says, at MUSC and elsewhere, hospitalist programs are scrambling for time to enhance the skills needed to tend to increased demands.
"You have to carve out time. That’s literally what you have to do," he explains. "That’s expensive to take a doctor away from clinical service for a week, or an even an hour or two a week. I mean, somebody’s got to pay for that."
Training on hospitalist-specific management topics, he says, needs to evolve further. "I think there’s a recognition that this stuff is important and that hospitals and hospitalists need to get better aligned," he says. "This is something that will continue to mature over the next 10 years."
The range of tasks is growing ever broader for the hospitalist, and so the need for enhanced training is greater, says Larry Wellikson, MD, SFHM, CEO of SHM.
"They’re being asked to do bedside patient care, but they’re being asked to do more. They’re asked to be systems engineers, they’re asked to be safety experts, they’re asked to be the information manager, if you will, the IT guys," he says. "These skills they have not been trained to do and they need … either to say, ‘No, I can’t do that because I haven’t been trained,’ or they need to go and look where they can get that expertise.
"That’s what we try to do at SHM, with our Leadership Academy and our Practice Management Academy."
Frank Michota, MD, FHM, director of academic affairs in the Department of Hospital Medicine at The Cleveland Clinic, says that one of the biggest challenges the field needs to tackle over the next several years is to better standardize the education of hospitalists, saying there is "incredible inconsistency from hospitalist to hospitalist in terms of knowledge base, experience and … understanding the scope of practice."
"We continue to have significant variation in hospital practice models and the types of measurements that are available to those hospitalists for practice improvement," he says. "We continue to see significant turnover in the field with kind of a lack of maturity"—and not the kind of experience base that "you would like to see 15 years in."
"There is really no confidence that everyone at the base of that iceberg will ever make it to the tip because it’s still not viewed by many who entered the field as being a long-term career choice," Dr. Michota says. For many, he said, it is "a look-and-see proposition."
All of this, he says, points to the need for a full certification process by an HM board.
"I don’t want to make it sound like it has not been an impressive evolution to this point, but I think if we are going to meet the expectations, we do have to do more than we’re doing now," Dr. Michota says.
Some of the gaps in training might be able to be filled by private hospital management groups, which have training programs for their doctors that are made possible by their scale and whose presence is predicted to grow over the next 15 years.
Robert Bessler, MD, who in 2001 founded Tacoma, Wash.-based Sound Physicians, which has become one of the largest private hospitalist organizations in the country, says private companies are able to conduct training that is impossible for many hospitals to conduct themselves.
"You’re going to get good people who are all of good training and good knowledge, but they’re not all going to have experience," he says, "and so what are the hospitals that are employing 50% of the hospitalists in this country going to do about that? It’s pretty much nothing. They’re going to occasionally send some people to conferences and hope—because they don’t have that infrastructure."
At teaching institutes like those at private firms, the process is sped up, Dr. Bessler adds.
"That’s why we built our hospitalists’ institute at Sound—to turn really good, quality doctors into effective hospitalists in a much more rapid fashion," he says. "Because before we built this, it was just get them involved and hope after a couple of years they’ve really become efficient. Our hospital partners and the patients can’t wait that long."
Robert Reynolds, MD, founder of PrimeDoc, an Asheville, N.C.-based company that provides doctors for 12 hospitalist programs and employs about 100 doctors, says there needs to be more focus on teaching the "realistic side of the business of medicine," as well as on quality outcomes and patient satisfaction. But he also doubts there will be much change in training.
"[From] my cynical side and the voice of experience, I don’t see any change in the near future," he says. "What we’re seeing now is physicians come out of residency with a good clinical base, but really having no idea of how the healthcare system works in a bigger picture, how it works as an industry. So we’re having to spend a lot of time and effort training physicians to start thinking like practicing physicians."
The experts all agree that there will be an increase in hospitalists being provided by private corporations. Dr. Reynolds says that trend will continue in part due to healthcare reform’s emphasis on outcomes for reimbursement and a corporation’s ability to assist with physician training, as well as data and reporting needs.
"More and more hospital compensation and physician compensation is going to be based on actual data, performance data," he says. "And in order to really do a good job of capturing and reporting that kind of data, you need enough size to support an IT system and training systems that will produce and capture the kind of data that will be necessary."
Erin Fisher, MD, MHM, a pediatric hospitalist at Rady Children’s Hospital in San Diego, says a major goal of the future should be to change the reimbursement structure "so that you have something that is reasonable and encourages appropriate testing, treatments, and coordination of our healthcare system in a systematic way, rather than pieces." In such a system, hospitalists might see something to prompt them to intervene in a preventive way.
"The bigger question is, can our healthcare system, in five to 10 years, change itself enough that it uses every episode of care as an opportunity to do preventive care and coordinate care in the best way?" says Dr. Fisher, an SHM board member.
Continued Growth?
There is agreement that the field will continue to expand, with SHM predicting that the number of hospitalists in the U.S. will reach 40,000 in the next several years, up from today’s 30,000 figure.
Dr. Wellikson says that the figure could rise to as many as 70,000 or more if specialty hospitalists—such as surgical hospitalists, neuro-hospitalists, and laborists—are included. Those hospital-based specialties are now only in their infancy.
"Everything you can see shows that people are still flocking into hospital medicine," Dr. Wellikson adds.
Hospitalists numbered in the hundreds just 15 years ago, so growth has been explosive the past decade. Dr. Cawley, however, says the pace of growth might be starting to slow already, shifting to undeveloped or underserved areas. "Hospitalist programs are at almost all the large [hospitals] and really the growth has been at the smaller hospitals in the last several years," he says.
With the projected rise of Medicare beneficiaries due to the aging of the baby-boom generation, use of hospitals is expected to skyrocket, meaning more hospitalists will be needed, Dr. Bessler says. He also cites data from the National Rural Health Association noting that 25% of the U.S. population lives in areas considered rural, but that only 10% of the physicians live in those areas, indicating a potential growth area for hospitalists.
"That would tell me that demand will continue to outpace supply," he says.
Mike Tarwater, a member of the board of the American Hospital Association and CEO of Carolinas Medical Center in Charlotte, N.C., agrees with Dr. Bessler. Even with the move toward more outpatient care, Tarwater says, the aging of the population will mean a higher demand for hospitalists.

-Mike Tarwater, board member, American Hospital Association, CEO, Carolinas Medical Center, Charlotte, N.C.
"I think that the primary-care physicians—either because of their love for it or their belief that it’s the better way to go with the treatment of their patients—are going to be really stretched to keep that ambulatory practice going and to get to round on patients in the hospitals," he says. "I think there’s going to be a continued growth of the trend that we’ve seen over the last 15 years."
That growth also will mean a greater emphasis on technology use, whether it’s technology used for quick diagnostics like portable ultrasound or more widely used and refined electronic health records (EHR)—or, as Tarwater describes, "probably things we don’t imagine today."
"Our doctors, more than any other doctors, are tech-savvy; they’re early adopters," Dr. Wellikson says.
Hospitalists likely will emerge as leaders in the adoption of new technology, several experts predict.
Without a doubt, I think that hospitalists are going to be a driving force in the adaptation of the electronic [health] record to the clinical care within their hospitals," Dr. Michota says.
As the needs of HM grow, and the field grows more complex, there will inevitably be more divisions and departments of hospital medicine in places where it is now only a section, Dr. Cawley says.
"When you’re a division or a department, you have more autonomy over your own future, so I see this happening," he says. "I think more and more will carve themselves out of general internal medicine, and a lot of that will come because of a demand for more independence and greater autonomy." TH
Thomas R. Collins is a medical writer based in Florida.
At the Medical University of South Carolina (MUSC) in Charleston, a familiar scene plays out in the hospitalist program. New hospitalists express an interest in a certain area and the university tries to accommodate them, making time for them to pursue additional training as they juggle the daily demands of treating patients, says Patrick Cawley, MD, MBA, SFHM, associate professor at the university and a former SHM president.
"We try to have a personal growth plan for each hospitalist that aligns with their interest," Dr. Cawley says. "So if we have a hospitalist that’s very, very interested in quality improvement, we’ll seek out opportunities to get that hospitalist experience, and start with smaller projects and then bigger projects."
As the field of HM hits a notable mark in its history—it’s been 15 years since the term "hospitalist" was coined—more advanced training will continue to emerge as a key issue and obstacle in the field, say experts who were asked to take a look into HM’s crystal ball.
They also predict continued growth of the field, with tens of thousands of new hospitalists emerging in the next decade or so. They also say that hospitalists will emerge as leaders in the application and use of new technology, and that there will be more demands placed on hospitalists to show their worth in hard data.
There also promises to be a growing presence of private management firms providing hospitalists to hospitals, which doctors both inside and outside of those firms say could have a beneficial effect on the overall quality of patient care.

-Patrick Cawley, MD, MBA, SFHM, associate professor, Medical University of South Carolina, Charleston, former SHM president
Father Time
For now, Dr. Cawley says, at MUSC and elsewhere, hospitalist programs are scrambling for time to enhance the skills needed to tend to increased demands.
"You have to carve out time. That’s literally what you have to do," he explains. "That’s expensive to take a doctor away from clinical service for a week, or an even an hour or two a week. I mean, somebody’s got to pay for that."
Training on hospitalist-specific management topics, he says, needs to evolve further. "I think there’s a recognition that this stuff is important and that hospitals and hospitalists need to get better aligned," he says. "This is something that will continue to mature over the next 10 years."
The range of tasks is growing ever broader for the hospitalist, and so the need for enhanced training is greater, says Larry Wellikson, MD, SFHM, CEO of SHM.
"They’re being asked to do bedside patient care, but they’re being asked to do more. They’re asked to be systems engineers, they’re asked to be safety experts, they’re asked to be the information manager, if you will, the IT guys," he says. "These skills they have not been trained to do and they need … either to say, ‘No, I can’t do that because I haven’t been trained,’ or they need to go and look where they can get that expertise.
"That’s what we try to do at SHM, with our Leadership Academy and our Practice Management Academy."
Frank Michota, MD, FHM, director of academic affairs in the Department of Hospital Medicine at The Cleveland Clinic, says that one of the biggest challenges the field needs to tackle over the next several years is to better standardize the education of hospitalists, saying there is "incredible inconsistency from hospitalist to hospitalist in terms of knowledge base, experience and … understanding the scope of practice."
"We continue to have significant variation in hospital practice models and the types of measurements that are available to those hospitalists for practice improvement," he says. "We continue to see significant turnover in the field with kind of a lack of maturity"—and not the kind of experience base that "you would like to see 15 years in."
"There is really no confidence that everyone at the base of that iceberg will ever make it to the tip because it’s still not viewed by many who entered the field as being a long-term career choice," Dr. Michota says. For many, he said, it is "a look-and-see proposition."
All of this, he says, points to the need for a full certification process by an HM board.
"I don’t want to make it sound like it has not been an impressive evolution to this point, but I think if we are going to meet the expectations, we do have to do more than we’re doing now," Dr. Michota says.
Some of the gaps in training might be able to be filled by private hospital management groups, which have training programs for their doctors that are made possible by their scale and whose presence is predicted to grow over the next 15 years.
Robert Bessler, MD, who in 2001 founded Tacoma, Wash.-based Sound Physicians, which has become one of the largest private hospitalist organizations in the country, says private companies are able to conduct training that is impossible for many hospitals to conduct themselves.
"You’re going to get good people who are all of good training and good knowledge, but they’re not all going to have experience," he says, "and so what are the hospitals that are employing 50% of the hospitalists in this country going to do about that? It’s pretty much nothing. They’re going to occasionally send some people to conferences and hope—because they don’t have that infrastructure."
At teaching institutes like those at private firms, the process is sped up, Dr. Bessler adds.
"That’s why we built our hospitalists’ institute at Sound—to turn really good, quality doctors into effective hospitalists in a much more rapid fashion," he says. "Because before we built this, it was just get them involved and hope after a couple of years they’ve really become efficient. Our hospital partners and the patients can’t wait that long."
Robert Reynolds, MD, founder of PrimeDoc, an Asheville, N.C.-based company that provides doctors for 12 hospitalist programs and employs about 100 doctors, says there needs to be more focus on teaching the "realistic side of the business of medicine," as well as on quality outcomes and patient satisfaction. But he also doubts there will be much change in training.
"[From] my cynical side and the voice of experience, I don’t see any change in the near future," he says. "What we’re seeing now is physicians come out of residency with a good clinical base, but really having no idea of how the healthcare system works in a bigger picture, how it works as an industry. So we’re having to spend a lot of time and effort training physicians to start thinking like practicing physicians."
The experts all agree that there will be an increase in hospitalists being provided by private corporations. Dr. Reynolds says that trend will continue in part due to healthcare reform’s emphasis on outcomes for reimbursement and a corporation’s ability to assist with physician training, as well as data and reporting needs.
"More and more hospital compensation and physician compensation is going to be based on actual data, performance data," he says. "And in order to really do a good job of capturing and reporting that kind of data, you need enough size to support an IT system and training systems that will produce and capture the kind of data that will be necessary."
Erin Fisher, MD, MHM, a pediatric hospitalist at Rady Children’s Hospital in San Diego, says a major goal of the future should be to change the reimbursement structure "so that you have something that is reasonable and encourages appropriate testing, treatments, and coordination of our healthcare system in a systematic way, rather than pieces." In such a system, hospitalists might see something to prompt them to intervene in a preventive way.
"The bigger question is, can our healthcare system, in five to 10 years, change itself enough that it uses every episode of care as an opportunity to do preventive care and coordinate care in the best way?" says Dr. Fisher, an SHM board member.
Continued Growth?
There is agreement that the field will continue to expand, with SHM predicting that the number of hospitalists in the U.S. will reach 40,000 in the next several years, up from today’s 30,000 figure.
Dr. Wellikson says that the figure could rise to as many as 70,000 or more if specialty hospitalists—such as surgical hospitalists, neuro-hospitalists, and laborists—are included. Those hospital-based specialties are now only in their infancy.
"Everything you can see shows that people are still flocking into hospital medicine," Dr. Wellikson adds.
Hospitalists numbered in the hundreds just 15 years ago, so growth has been explosive the past decade. Dr. Cawley, however, says the pace of growth might be starting to slow already, shifting to undeveloped or underserved areas. "Hospitalist programs are at almost all the large [hospitals] and really the growth has been at the smaller hospitals in the last several years," he says.
With the projected rise of Medicare beneficiaries due to the aging of the baby-boom generation, use of hospitals is expected to skyrocket, meaning more hospitalists will be needed, Dr. Bessler says. He also cites data from the National Rural Health Association noting that 25% of the U.S. population lives in areas considered rural, but that only 10% of the physicians live in those areas, indicating a potential growth area for hospitalists.
"That would tell me that demand will continue to outpace supply," he says.
Mike Tarwater, a member of the board of the American Hospital Association and CEO of Carolinas Medical Center in Charlotte, N.C., agrees with Dr. Bessler. Even with the move toward more outpatient care, Tarwater says, the aging of the population will mean a higher demand for hospitalists.

-Mike Tarwater, board member, American Hospital Association, CEO, Carolinas Medical Center, Charlotte, N.C.
"I think that the primary-care physicians—either because of their love for it or their belief that it’s the better way to go with the treatment of their patients—are going to be really stretched to keep that ambulatory practice going and to get to round on patients in the hospitals," he says. "I think there’s going to be a continued growth of the trend that we’ve seen over the last 15 years."
That growth also will mean a greater emphasis on technology use, whether it’s technology used for quick diagnostics like portable ultrasound or more widely used and refined electronic health records (EHR)—or, as Tarwater describes, "probably things we don’t imagine today."
"Our doctors, more than any other doctors, are tech-savvy; they’re early adopters," Dr. Wellikson says.
Hospitalists likely will emerge as leaders in the adoption of new technology, several experts predict.
Without a doubt, I think that hospitalists are going to be a driving force in the adaptation of the electronic [health] record to the clinical care within their hospitals," Dr. Michota says.
As the needs of HM grow, and the field grows more complex, there will inevitably be more divisions and departments of hospital medicine in places where it is now only a section, Dr. Cawley says.
"When you’re a division or a department, you have more autonomy over your own future, so I see this happening," he says. "I think more and more will carve themselves out of general internal medicine, and a lot of that will come because of a demand for more independence and greater autonomy." TH
Thomas R. Collins is a medical writer based in Florida.
At the Medical University of South Carolina (MUSC) in Charleston, a familiar scene plays out in the hospitalist program. New hospitalists express an interest in a certain area and the university tries to accommodate them, making time for them to pursue additional training as they juggle the daily demands of treating patients, says Patrick Cawley, MD, MBA, SFHM, associate professor at the university and a former SHM president.
"We try to have a personal growth plan for each hospitalist that aligns with their interest," Dr. Cawley says. "So if we have a hospitalist that’s very, very interested in quality improvement, we’ll seek out opportunities to get that hospitalist experience, and start with smaller projects and then bigger projects."
As the field of HM hits a notable mark in its history—it’s been 15 years since the term "hospitalist" was coined—more advanced training will continue to emerge as a key issue and obstacle in the field, say experts who were asked to take a look into HM’s crystal ball.
They also predict continued growth of the field, with tens of thousands of new hospitalists emerging in the next decade or so. They also say that hospitalists will emerge as leaders in the application and use of new technology, and that there will be more demands placed on hospitalists to show their worth in hard data.
There also promises to be a growing presence of private management firms providing hospitalists to hospitals, which doctors both inside and outside of those firms say could have a beneficial effect on the overall quality of patient care.

-Patrick Cawley, MD, MBA, SFHM, associate professor, Medical University of South Carolina, Charleston, former SHM president
Father Time
For now, Dr. Cawley says, at MUSC and elsewhere, hospitalist programs are scrambling for time to enhance the skills needed to tend to increased demands.
"You have to carve out time. That’s literally what you have to do," he explains. "That’s expensive to take a doctor away from clinical service for a week, or an even an hour or two a week. I mean, somebody’s got to pay for that."
Training on hospitalist-specific management topics, he says, needs to evolve further. "I think there’s a recognition that this stuff is important and that hospitals and hospitalists need to get better aligned," he says. "This is something that will continue to mature over the next 10 years."
The range of tasks is growing ever broader for the hospitalist, and so the need for enhanced training is greater, says Larry Wellikson, MD, SFHM, CEO of SHM.
"They’re being asked to do bedside patient care, but they’re being asked to do more. They’re asked to be systems engineers, they’re asked to be safety experts, they’re asked to be the information manager, if you will, the IT guys," he says. "These skills they have not been trained to do and they need … either to say, ‘No, I can’t do that because I haven’t been trained,’ or they need to go and look where they can get that expertise.
"That’s what we try to do at SHM, with our Leadership Academy and our Practice Management Academy."
Frank Michota, MD, FHM, director of academic affairs in the Department of Hospital Medicine at The Cleveland Clinic, says that one of the biggest challenges the field needs to tackle over the next several years is to better standardize the education of hospitalists, saying there is "incredible inconsistency from hospitalist to hospitalist in terms of knowledge base, experience and … understanding the scope of practice."
"We continue to have significant variation in hospital practice models and the types of measurements that are available to those hospitalists for practice improvement," he says. "We continue to see significant turnover in the field with kind of a lack of maturity"—and not the kind of experience base that "you would like to see 15 years in."
"There is really no confidence that everyone at the base of that iceberg will ever make it to the tip because it’s still not viewed by many who entered the field as being a long-term career choice," Dr. Michota says. For many, he said, it is "a look-and-see proposition."
All of this, he says, points to the need for a full certification process by an HM board.
"I don’t want to make it sound like it has not been an impressive evolution to this point, but I think if we are going to meet the expectations, we do have to do more than we’re doing now," Dr. Michota says.
Some of the gaps in training might be able to be filled by private hospital management groups, which have training programs for their doctors that are made possible by their scale and whose presence is predicted to grow over the next 15 years.
Robert Bessler, MD, who in 2001 founded Tacoma, Wash.-based Sound Physicians, which has become one of the largest private hospitalist organizations in the country, says private companies are able to conduct training that is impossible for many hospitals to conduct themselves.
"You’re going to get good people who are all of good training and good knowledge, but they’re not all going to have experience," he says, "and so what are the hospitals that are employing 50% of the hospitalists in this country going to do about that? It’s pretty much nothing. They’re going to occasionally send some people to conferences and hope—because they don’t have that infrastructure."
At teaching institutes like those at private firms, the process is sped up, Dr. Bessler adds.
"That’s why we built our hospitalists’ institute at Sound—to turn really good, quality doctors into effective hospitalists in a much more rapid fashion," he says. "Because before we built this, it was just get them involved and hope after a couple of years they’ve really become efficient. Our hospital partners and the patients can’t wait that long."
Robert Reynolds, MD, founder of PrimeDoc, an Asheville, N.C.-based company that provides doctors for 12 hospitalist programs and employs about 100 doctors, says there needs to be more focus on teaching the "realistic side of the business of medicine," as well as on quality outcomes and patient satisfaction. But he also doubts there will be much change in training.
"[From] my cynical side and the voice of experience, I don’t see any change in the near future," he says. "What we’re seeing now is physicians come out of residency with a good clinical base, but really having no idea of how the healthcare system works in a bigger picture, how it works as an industry. So we’re having to spend a lot of time and effort training physicians to start thinking like practicing physicians."
The experts all agree that there will be an increase in hospitalists being provided by private corporations. Dr. Reynolds says that trend will continue in part due to healthcare reform’s emphasis on outcomes for reimbursement and a corporation’s ability to assist with physician training, as well as data and reporting needs.
"More and more hospital compensation and physician compensation is going to be based on actual data, performance data," he says. "And in order to really do a good job of capturing and reporting that kind of data, you need enough size to support an IT system and training systems that will produce and capture the kind of data that will be necessary."
Erin Fisher, MD, MHM, a pediatric hospitalist at Rady Children’s Hospital in San Diego, says a major goal of the future should be to change the reimbursement structure "so that you have something that is reasonable and encourages appropriate testing, treatments, and coordination of our healthcare system in a systematic way, rather than pieces." In such a system, hospitalists might see something to prompt them to intervene in a preventive way.
"The bigger question is, can our healthcare system, in five to 10 years, change itself enough that it uses every episode of care as an opportunity to do preventive care and coordinate care in the best way?" says Dr. Fisher, an SHM board member.
Continued Growth?
There is agreement that the field will continue to expand, with SHM predicting that the number of hospitalists in the U.S. will reach 40,000 in the next several years, up from today’s 30,000 figure.
Dr. Wellikson says that the figure could rise to as many as 70,000 or more if specialty hospitalists—such as surgical hospitalists, neuro-hospitalists, and laborists—are included. Those hospital-based specialties are now only in their infancy.
"Everything you can see shows that people are still flocking into hospital medicine," Dr. Wellikson adds.
Hospitalists numbered in the hundreds just 15 years ago, so growth has been explosive the past decade. Dr. Cawley, however, says the pace of growth might be starting to slow already, shifting to undeveloped or underserved areas. "Hospitalist programs are at almost all the large [hospitals] and really the growth has been at the smaller hospitals in the last several years," he says.
With the projected rise of Medicare beneficiaries due to the aging of the baby-boom generation, use of hospitals is expected to skyrocket, meaning more hospitalists will be needed, Dr. Bessler says. He also cites data from the National Rural Health Association noting that 25% of the U.S. population lives in areas considered rural, but that only 10% of the physicians live in those areas, indicating a potential growth area for hospitalists.
"That would tell me that demand will continue to outpace supply," he says.
Mike Tarwater, a member of the board of the American Hospital Association and CEO of Carolinas Medical Center in Charlotte, N.C., agrees with Dr. Bessler. Even with the move toward more outpatient care, Tarwater says, the aging of the population will mean a higher demand for hospitalists.

-Mike Tarwater, board member, American Hospital Association, CEO, Carolinas Medical Center, Charlotte, N.C.
"I think that the primary-care physicians—either because of their love for it or their belief that it’s the better way to go with the treatment of their patients—are going to be really stretched to keep that ambulatory practice going and to get to round on patients in the hospitals," he says. "I think there’s going to be a continued growth of the trend that we’ve seen over the last 15 years."
That growth also will mean a greater emphasis on technology use, whether it’s technology used for quick diagnostics like portable ultrasound or more widely used and refined electronic health records (EHR)—or, as Tarwater describes, "probably things we don’t imagine today."
"Our doctors, more than any other doctors, are tech-savvy; they’re early adopters," Dr. Wellikson says.
Hospitalists likely will emerge as leaders in the adoption of new technology, several experts predict.
Without a doubt, I think that hospitalists are going to be a driving force in the adaptation of the electronic [health] record to the clinical care within their hospitals," Dr. Michota says.
As the needs of HM grow, and the field grows more complex, there will inevitably be more divisions and departments of hospital medicine in places where it is now only a section, Dr. Cawley says.
"When you’re a division or a department, you have more autonomy over your own future, so I see this happening," he says. "I think more and more will carve themselves out of general internal medicine, and a lot of that will come because of a demand for more independence and greater autonomy." TH
Thomas R. Collins is a medical writer based in Florida.