User login
In the Know
Since the late 1960s, a growing body of evidence has suggested the chances that patients truly understand what they are consenting to in informed consent documents are not only unlikely but “remote.”1 A review of 70 studies conducted in a variety of clinical settings demonstrated that, although consent and refusals were legally and institutionally valid, they failed to result in “genuinely autonomous decision making.”
Factors associated with such outcomes included low socioeconomic status, poor education, old age, lengthy hospital stay, stress, language barriers, and misinterpretation of probabilistic data. Accompanying disclosure practices were also found inadequate, though perfectly legal.
Research by the National Quality Forum (NQF) revealed that, despite having signed a consent form, 18% to 45% of patients are unable to recall even the major risks associated with their surgeries. Many cannot answer basic questions about the services or procedures they agreed to receive, while 44% do not know the exact nature of their operation, and most (60% to 69%) do not understand or read the information contained in generic hospital consent forms.2 Treating patients such as these can lead to compromised care and safety and increased medical malpractice risk.
Many bioethicists endorse the position that “striving for fully informed consent is generally unfeasible and perhaps even undesirable.”-- Others argue that the concept of fully informed consent should at least serve as an ideal. For that to be achieved, patients would need to understand fully their conditions and treatment. At a minimum, then, and as law, patients have the right to be given information that will optimize their autonomy.3-6 That information includes:
- The nature of the procedure or treatment being offered, including whether it is diagnostic or therapeutic;
- The risks and potential complications of a procedure or medical treatment;
- The benefits of the procedure; and
- Treatment alternatives, along with their risks and benefits.7
The ideal is far from reality. Frequently cited factors interfering with full comprehension, in addition to those already mentioned, include personal or cultural beliefs and low health literacy rates.1,2 Providers’ inability to communicate clearly in a rushed environment is also a factor, as is a tendency for providers who see the act of acquiring informed consent as a legal formality to delegate to a junior colleague.
But “the patient’s consent happens during the process of dialogue with the surgeon,” wrote Bernat and Peterson in the January 2006 Archives of Surgery:8 “The signature on a surgical consent form is merely the culmination and formalization of this preceding consent discussion and agreement.”
A signed consent form represents evidence of the patient’s consent—not of his or her understanding. That signed form may not be sufficient to protect providers in cases of liability. According to Jury Verdict Research, informed consent issues are among the top 10 most common reasons patients file malpractice claims.2
The low health literacy of almost half of adults in the United States limits their ability to understand the basic health information and services that are needed to make appropriate health decisions. In fact, articles in two of the July 2006 issues of the New England Journal of Medicine, as well as the entire August 2006 issue of the Journal of General Internal Medicine, are devoted to the subject of health literacy.9-11
Given that surgeons and other specialists are often responsible for securing informed consent, what are the areas of informed consent to which hospitalists should be attuned?
Key Considerations for the Hospitalist
Ordinarily, the person whose name is at the top of the patient’s chart has full responsibility for informed consent, although sometimes a subspecialty consultant, such as a cardiologist asking for a particular study, might help. A hospitalist might be named as the responsible provider in an area in which he or she is active.
Ben Rich, JD, PhD, a professor of bioethics at the University of California-Davis School (UCD) of Medicine in Sacramento, Calif., has considered the critical problems or distinctions that the hospitalist, as opposed to other physicians, may have in the area of informed consent. One area that strikes him as potentially risky is that of advance directives. Dr. Rich, who teaches a course on medicine and law at UCD, says that for decades experts have urged primary care physicians (PCPs) to discuss advance directives with patients as part of routine care. Even so, he acknowledges, if a patient is in critical condition and is hospitalized, “it is entirely possible that their personal physician won’t even know about it. So here is the person who is supposed to have apprised herself of the patient’s values and priorities in circumstances like that, and they’re out of the picture. And the person who is trying to interpret advance directives, if there is one, is the hospitalist.”
It might be difficult for the hospitalist to interpret any ambiguities. If the hospitalist believes it is impossible to know what the patient understood at the time they drafted the directive about the circumstances they are now facing, he or she may be more likely to dismiss it as invalid and simply make a decision as to what is medically appropriate, says Dr. Rich.
The discontinuity of care imposed by the hospitalist systems raises several ethical concerns, wrote Steven Pantilat, MD, in JAMA.12 The primary care physician and patient have previously negotiated, through the process of medical decision-making, the patient’s goals and values regarding medical interventions. “Because hospitalist systems leave no formal inpatient role for the PCP,” wrote Dr. Pantilat, “ … patients can no longer rely on agreements reached in the office following them to the hospital. Nonetheless, the hospitalist shares the PCP’s obligations to respect the ethical principles that agreements about preferences for care or individual values often represent.”
Another important but somewhat controversial issue involves whether a consent discussion held preoperatively also encompasses the management of post-procedure complications.8 Although it is impossible to mention all possible serious complications beforehand, it is prudent to reference the patient’s goals and general treatment preferences and to ensure that a family member (if not the designated surrogate) is present during this conversation. Just the same, each new intervention or procedure requires a new conversation and, in some cases, a new signed form. “Because at the end of the day,” says Patrick O’Rourke, JD, an attorney in Denver who regularly represents physicians in medical malpractice cases, “physicians are the people who have the obligation to obtain informed consent; the hospital as an institution does not, because hospitals don’t practice medicine; physicians do.”
Particularly with patients who face serious illness and those confronting what may be a chronic condition going forward, says Dr. Rich, “there’s a school of thought [that maintains] that part of the informed consent process is obsessively focused on procedures and pays woefully inadequate attention to the reasonable goals of care. This is nowhere more obvious than in the ICU setting.”
Continuums of Care and Consent
Indeed, any expert on medical law will tell you that informed consent is a process—not an event.8 Though a hospitalist may not have secured the signature on a consent form, a hospitalist’s practice is as much a part of a patient’s ongoing process of “consent” as is that of the surgeon who performed the patient’s operation.
The American Academy of Family Physicians has adopted the following guideline: “During the period of hospitalization, decisions regarding care, consultation, admission, transfer, and discharge should be the sole responsibility of the inpatient care physician in consultation with the patient and, as appropriate, the patient’s family physician and/or family members.”13 The times when patients actually sign informed consent documents are junctures in the continuum of consent that covers a lifetime healthcare experience. Hospitalists, then, are involved in informed consent from patient assignment to patient discharge.
“And the manner in which the process is conducted is at least as important as substantive information given,” says Dr. Rich. “A skilled and experienced physician can give any patient two descriptions of the procedure that they’re recommending,” he says. “[After o]ne, couched in a certain way, but not inaccurate, the patient would say, ‘Well, of course, I want that.’ And if the physician gives it in the other way, still accurate, the patient would say, Well, who would want that? And it all has to do with the terms you use, your tone of voice, your body language, the setting in which you provide it. … All that can profoundly shape the informed consent process. And it is not something that physicians are routinely taught.”
Because the process of informed consent is ongoing, discussions may continue for several sessions over a length of time before a patient decides to undergo a treatment. This gives patients more time to think of questions or concerns they may have. Addressing those concerns is a crucial part of the process.
“The reason that’s important is that you always want to offer and document that you have an opportunity to address what the patient’s questions were so the consent is truly informed,” says O’Rourke. One-way delivery of information is not equivalent to the dialogue implied by the term “informed consent.” “It is vitally important to ask, ‘What other information can I give you?’” he explains, especially because informed consent cases often deal with complications that develop after surgery.
Community Standard
The risks of procedures mentioned in informed consent discussions comprise a special category, says O’Rourke, “because there are some things that are not easily foreseen.” Some complications are not within the range generally anticipated after a procedure. “And the way the law works is that you don’t have to imagine the million-to-one shot [complication]; you would review the risks in terms of what a physician should disclose … in terms of significance.”
Physicians are judged by how well they informed patients of the risks as assessed by a community standard of what reasonable practitioners in the community say the risks are, he says. Physicians need to be knowledgeable about the risks of the procedure based on the medical literature, their training, and their discussions with colleagues.14
“Oftentimes, in order to give and get full informed consent, we use the knowledge from our subspecialty consultants,” says Dennis Manning, MD, FACP, FACC, a hospitalist and director of quality in the Department of Medicine and an assistant professor at the Mayo Clinic College of Medicine, Rochester, Minn. “We ask them, ‘What do you think the risks are?’ We might have to pick their brains in order to become fully aware of the hazards in a particular patient.”
“Risk is the category where litigation pops up and where you see the most challenges,” says O’Rourke, because the patient filing a claim may say, “ ‘Well, the doctor didn’t tell me about this risk and had I known this occurred, I would have elected to forego this procedure; I would have chosen one of the other alternatives.’ ”
If a patient develops a complication and the hospitalist must initiate a new intervention, then it’s the hospitalist’s duty to get informed consent for that next intervention. “Every time a physician undertakes a particular intervention, the patient has to be informed in why that intervention is being taken and what the risks, benefits, and alternatives are,” says O’Rourke.
If a patient is incapable of giving consent, then consider whether there is a significant risk in waiting until the patient is capable of giving informed consent. If the answer is “no,” then consider whether or not to delay the intervention. “If there’s no potential harm caused by waiting until the patient hits a higher level of consciousness,” says O’Rourke, “then that’s perfectly appropriate.”
In an emergency situation, a surrogate may need to make the decision. If neither one of those alternatives is available, “the law presumes that the patient is going to do what is reasonable and necessary in order to preserve his or her health, unless there’s been some instruction otherwise,” notes O’Rourke.
Teach Back
Studies show that when patients are asked to repeat what they understood from their informed consent discussions, they have greater recall and comprehension of the risks and benefits of surgical procedures.2,15 “Teach back” is an especially valuable technique to use with low literacy patients. The NQF discovered that the providers and departments using teach back were widely recognized by their peers as having the most well-informed patients compared with departments that did not use this method.2 (See “Teach Back in Action,” above right.) A number of studies have found that when a provider asks a patient to restate information or instructions, the benefits include providing a check for lapses of recall and understanding, revealing health beliefs, reinforcing and individualizing health messages, and motivating patients by activating dialogue.15
In May 2003, the NQF published Safe Practices for Better Healthcare, which endorsed a set of consensus standards for 30 healthcare practices, one of which (Safe Practice 10) recommends that all healthcare professionals ask patients to teach back what they have been told by their providers during their informed consent discussions.2
In its 2001 report, Making Health Care Safer: A Critical Analysis of Patient Safety Practices (project director, Robert M. Wachter, MD), the Agency for Healthcare Research and Quality suggested that special attention be paid to implementing 11 particular practices, one of which was “asking that patients recall and restate what they have been told during the informed consent process.”16
Even if you are not asking for a signed form, physicians, nurses, interpreters, and any professional who communicates with patients regarding their healthcare decisions is involved in the informed consent process and should use teach back—especially with those patients who find even basic health information difficult to understand. Although the NQF found that physicians were reluctant to incorporate this technique into their communications, the providers reported anecdotally that teach back takes less than a minute to complete; research backs up the claim that the more the technique is practiced, the speedier it gets.2
The provision of this “interactive communication loop,” as it has been called,15 has also been shown to affect clinical outcomes. In a study by Schillinger and colleagues conducted at an outpatient general internal medicine clinic and at San Francisco General Hospital, physicians assessed recall and comprehension of any new concept in 12 (20%) of 61 outpatient visits by diabetic patients for 15 (12%) of 124 concepts.15 The patients whose physicians assessed their recall by means of teach back were more likely to have hemoglobin A1c levels below the mean compared with patients whose doctors did not. The two variables found to be independently associated with good glycemic control were higher health literacy levels and physicians’ application of the teach-back strategy.
Consent Forms
The informed consent process is intended to protect patients and physicians both.7 Legal doctrine, including hospital accreditation standards, ethical theories, and perspectives on the physician-patient relationship, emphasizes the importance of full patient comprehension regarding treatment. But many hospitals do not use forms that contribute to that objective. In a study by Bottrell and colleagues of 540 forms from 157 hospitals nationwide, 96% indicated the nature of the procedure for the patient; however, only 26% of forms included all four elements of informed consent: procedure, risks, benefits, and alternative treatment options. Thirty-five percent included three of four elements, 23% provided two of four elements, 14% listed only one element, and 2% contained none of the elements.
In general, the investigators concluded, the forms appear to be designed to authorize treatment or protect hospitals and caregivers from liability rather than to help patients clarify information or make decisions. Even hospitals in states that have statutes requiring institutions to include all four elements on their forms were no more likely to do so than those in other states. Fewer than 40% of forms were found to support models of shared decision making, the basis of patient autonomy and the overarching intention for informed consent.
“Generally … informed consent forms are seen as mere documentation vehicles, and perhaps as legal protection, regardless of whether the process of informed consent was successfully accomplished or of minimal quality,” this study’s authors wrote, and because patients are not blind to the intentions of these forms, this may add to their discomfort.7 Most forms, the authors concluded, are insufficient because the language used does not accommodate low health literacy or because there are no graphic features.
On the other hand, “informed consent can sometimes get very awkward and cumbersome,” says William Jacott, MD, special advisor for professional relations at the Joint Commission on Accreditation of Healthcare Organizations, St. Paul, Minn., for the past five years and liaison to SHM for the past two. Some institutions or organizations interpret Joint Commission and other legal standards excessively, he says, “and I’ve seen 10-page consent forms, which just overwhelms the patient, let alone the doctor. So an over-interpretation and overkill need to be avoided.”
Conclusion: Communication and Documentation
The ways in which hospitalists can avoid the pitfalls of faulty informed consent conversations include close communication with surgeons as well as other colleagues.
“We have a great tendency to communicate via the medical record,” says Dr. Jacott, and if a patient’s co-managers (the hospitalist and subspecialist) don’t communicate, “one might assume the other has already done [informed consent], and nobody does it.”
He has also seen instances in teaching hospitals in which both the surgeon and the hospitalist incorrectly assume that the house staff has acquired informed consent.
Nurses can also help hospitalists ensure that patients are comfortable with their treatment choices. “Nurses often have more firsthand information about when patients are confused or scared or dubious or are somehow being coerced or manipulated into consenting to something,” says Dr. Rich.
Hospitalists should also avoid making assumptions about the completeness of their colleagues’ discussions with patients and should look for clear documentation as well as record their own. “Some subspecialists play fast and loose with informed consent,” Dr. Rich says, “and [may] resent a medical staff colleague who takes it seriously and attempts to hold them accountable for really doing it right. And for the hospitalist, that’s where it is critical that their institution stand behind them.”
A hospitalist’s responsibilities with regard to informed consent also include ensuring that the patient’s consent is truly informed. Using the teach back method, allowing time for the patient to ask questions and voice concerns, and including all four elements of informed consent on the patient’s consent form are just some of the ways the hospitalist can play an essential role in the continuum that is informed consent.
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Epstein M. Why effective consent presupposes autonomous authorisation: a counterorthodox argument. J Med Ethics. 2006;32:342-345.
- National Quality Forum. Implementing a national voluntary consensus standard for informed consent: a user’s guide for healthcare professionals. September 2005. Available at: www.qualityforum.org/publications.html. Accessed September 5, 2006.
- Rizzo v Schiller, 445 SE2d 153 (Va. 1994). Available at: www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10184327&dopt=Abstract. Accessed September 11, 2006.
- Gorab v Zook, 943 P2d 423 (Colo. 1997). Available at: http://caselaw.lp.findlaw.com/scripts/getcase.pl?court=co&vol=2003app%5C3477&invol=1. Accessed September 11, 2006.
- Schuck PH. Rethinking informed consent. Yale Law J. 1994;103:899-959.
- Culbertson v Mernitz, 602 NE2d 98 (Ind. 1992).
- Bottrell MM, Alpert H, Fischbach RL, et al. Hospital informed consent for procedure forms: facilitating quality patient-physician interaction. Arch Surg. 2000 Jan;135(1):26-33.
- Bernat JL, Peterson LM. Patient-centered informed consent in surgical practice. Arch Surg. 2006 Jan;141(7):86-92.
- Marcus EN. The silent epidemic—the health effects of illiteracy. N Engl J Med. 2006;355:339-341.
- Flores G. Language barriers to health care in the United States. N Engl J Med. 2006 Jul;355:229-231.
- Carmona RH. Health literacy: a national priority. J Gen Intern Med. 2006;21:803.
- Pantilat SZ, Alpers A, Wachter RM. A new doctor in the house: ethical issues in hospitalist systems. JAMA. 1999 Jul 14;282:171-174.
- Henry LA. What the hospitalist movement means to family physicians. Fam Pract Manag. 1998 Nov-Dec;5(10):54-62.
- Rajput V, Bekes CE. Ethical issues in hospital medicine. Med Clin North Am. 2002 Jul;86(4):869-886.
- Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003 Jan 13;163(1):83-90.
- University of California at San Francisco (UCSF)-Stanford University Evidence-based Practice Center. Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment: Number 43. AHRQ Publication No. 01-E058, July 2001. Agency for Healthcare Research and Quality. Available at: www.ahrq.gov/clinic/ptsafety/. Accessed September 5, 2006.
- Baum N. Comprehension is the key: the challenge hospitals face is that many patients do not understand the fundamental information regarding their treatment plans. Patient Safety Quality Healthcare. May/June 2006:35-38.
Since the late 1960s, a growing body of evidence has suggested the chances that patients truly understand what they are consenting to in informed consent documents are not only unlikely but “remote.”1 A review of 70 studies conducted in a variety of clinical settings demonstrated that, although consent and refusals were legally and institutionally valid, they failed to result in “genuinely autonomous decision making.”
Factors associated with such outcomes included low socioeconomic status, poor education, old age, lengthy hospital stay, stress, language barriers, and misinterpretation of probabilistic data. Accompanying disclosure practices were also found inadequate, though perfectly legal.
Research by the National Quality Forum (NQF) revealed that, despite having signed a consent form, 18% to 45% of patients are unable to recall even the major risks associated with their surgeries. Many cannot answer basic questions about the services or procedures they agreed to receive, while 44% do not know the exact nature of their operation, and most (60% to 69%) do not understand or read the information contained in generic hospital consent forms.2 Treating patients such as these can lead to compromised care and safety and increased medical malpractice risk.
Many bioethicists endorse the position that “striving for fully informed consent is generally unfeasible and perhaps even undesirable.”-- Others argue that the concept of fully informed consent should at least serve as an ideal. For that to be achieved, patients would need to understand fully their conditions and treatment. At a minimum, then, and as law, patients have the right to be given information that will optimize their autonomy.3-6 That information includes:
- The nature of the procedure or treatment being offered, including whether it is diagnostic or therapeutic;
- The risks and potential complications of a procedure or medical treatment;
- The benefits of the procedure; and
- Treatment alternatives, along with their risks and benefits.7
The ideal is far from reality. Frequently cited factors interfering with full comprehension, in addition to those already mentioned, include personal or cultural beliefs and low health literacy rates.1,2 Providers’ inability to communicate clearly in a rushed environment is also a factor, as is a tendency for providers who see the act of acquiring informed consent as a legal formality to delegate to a junior colleague.
But “the patient’s consent happens during the process of dialogue with the surgeon,” wrote Bernat and Peterson in the January 2006 Archives of Surgery:8 “The signature on a surgical consent form is merely the culmination and formalization of this preceding consent discussion and agreement.”
A signed consent form represents evidence of the patient’s consent—not of his or her understanding. That signed form may not be sufficient to protect providers in cases of liability. According to Jury Verdict Research, informed consent issues are among the top 10 most common reasons patients file malpractice claims.2
The low health literacy of almost half of adults in the United States limits their ability to understand the basic health information and services that are needed to make appropriate health decisions. In fact, articles in two of the July 2006 issues of the New England Journal of Medicine, as well as the entire August 2006 issue of the Journal of General Internal Medicine, are devoted to the subject of health literacy.9-11
Given that surgeons and other specialists are often responsible for securing informed consent, what are the areas of informed consent to which hospitalists should be attuned?
Key Considerations for the Hospitalist
Ordinarily, the person whose name is at the top of the patient’s chart has full responsibility for informed consent, although sometimes a subspecialty consultant, such as a cardiologist asking for a particular study, might help. A hospitalist might be named as the responsible provider in an area in which he or she is active.
Ben Rich, JD, PhD, a professor of bioethics at the University of California-Davis School (UCD) of Medicine in Sacramento, Calif., has considered the critical problems or distinctions that the hospitalist, as opposed to other physicians, may have in the area of informed consent. One area that strikes him as potentially risky is that of advance directives. Dr. Rich, who teaches a course on medicine and law at UCD, says that for decades experts have urged primary care physicians (PCPs) to discuss advance directives with patients as part of routine care. Even so, he acknowledges, if a patient is in critical condition and is hospitalized, “it is entirely possible that their personal physician won’t even know about it. So here is the person who is supposed to have apprised herself of the patient’s values and priorities in circumstances like that, and they’re out of the picture. And the person who is trying to interpret advance directives, if there is one, is the hospitalist.”
It might be difficult for the hospitalist to interpret any ambiguities. If the hospitalist believes it is impossible to know what the patient understood at the time they drafted the directive about the circumstances they are now facing, he or she may be more likely to dismiss it as invalid and simply make a decision as to what is medically appropriate, says Dr. Rich.
The discontinuity of care imposed by the hospitalist systems raises several ethical concerns, wrote Steven Pantilat, MD, in JAMA.12 The primary care physician and patient have previously negotiated, through the process of medical decision-making, the patient’s goals and values regarding medical interventions. “Because hospitalist systems leave no formal inpatient role for the PCP,” wrote Dr. Pantilat, “ … patients can no longer rely on agreements reached in the office following them to the hospital. Nonetheless, the hospitalist shares the PCP’s obligations to respect the ethical principles that agreements about preferences for care or individual values often represent.”
Another important but somewhat controversial issue involves whether a consent discussion held preoperatively also encompasses the management of post-procedure complications.8 Although it is impossible to mention all possible serious complications beforehand, it is prudent to reference the patient’s goals and general treatment preferences and to ensure that a family member (if not the designated surrogate) is present during this conversation. Just the same, each new intervention or procedure requires a new conversation and, in some cases, a new signed form. “Because at the end of the day,” says Patrick O’Rourke, JD, an attorney in Denver who regularly represents physicians in medical malpractice cases, “physicians are the people who have the obligation to obtain informed consent; the hospital as an institution does not, because hospitals don’t practice medicine; physicians do.”
Particularly with patients who face serious illness and those confronting what may be a chronic condition going forward, says Dr. Rich, “there’s a school of thought [that maintains] that part of the informed consent process is obsessively focused on procedures and pays woefully inadequate attention to the reasonable goals of care. This is nowhere more obvious than in the ICU setting.”
Continuums of Care and Consent
Indeed, any expert on medical law will tell you that informed consent is a process—not an event.8 Though a hospitalist may not have secured the signature on a consent form, a hospitalist’s practice is as much a part of a patient’s ongoing process of “consent” as is that of the surgeon who performed the patient’s operation.
The American Academy of Family Physicians has adopted the following guideline: “During the period of hospitalization, decisions regarding care, consultation, admission, transfer, and discharge should be the sole responsibility of the inpatient care physician in consultation with the patient and, as appropriate, the patient’s family physician and/or family members.”13 The times when patients actually sign informed consent documents are junctures in the continuum of consent that covers a lifetime healthcare experience. Hospitalists, then, are involved in informed consent from patient assignment to patient discharge.
“And the manner in which the process is conducted is at least as important as substantive information given,” says Dr. Rich. “A skilled and experienced physician can give any patient two descriptions of the procedure that they’re recommending,” he says. “[After o]ne, couched in a certain way, but not inaccurate, the patient would say, ‘Well, of course, I want that.’ And if the physician gives it in the other way, still accurate, the patient would say, Well, who would want that? And it all has to do with the terms you use, your tone of voice, your body language, the setting in which you provide it. … All that can profoundly shape the informed consent process. And it is not something that physicians are routinely taught.”
Because the process of informed consent is ongoing, discussions may continue for several sessions over a length of time before a patient decides to undergo a treatment. This gives patients more time to think of questions or concerns they may have. Addressing those concerns is a crucial part of the process.
“The reason that’s important is that you always want to offer and document that you have an opportunity to address what the patient’s questions were so the consent is truly informed,” says O’Rourke. One-way delivery of information is not equivalent to the dialogue implied by the term “informed consent.” “It is vitally important to ask, ‘What other information can I give you?’” he explains, especially because informed consent cases often deal with complications that develop after surgery.
Community Standard
The risks of procedures mentioned in informed consent discussions comprise a special category, says O’Rourke, “because there are some things that are not easily foreseen.” Some complications are not within the range generally anticipated after a procedure. “And the way the law works is that you don’t have to imagine the million-to-one shot [complication]; you would review the risks in terms of what a physician should disclose … in terms of significance.”
Physicians are judged by how well they informed patients of the risks as assessed by a community standard of what reasonable practitioners in the community say the risks are, he says. Physicians need to be knowledgeable about the risks of the procedure based on the medical literature, their training, and their discussions with colleagues.14
“Oftentimes, in order to give and get full informed consent, we use the knowledge from our subspecialty consultants,” says Dennis Manning, MD, FACP, FACC, a hospitalist and director of quality in the Department of Medicine and an assistant professor at the Mayo Clinic College of Medicine, Rochester, Minn. “We ask them, ‘What do you think the risks are?’ We might have to pick their brains in order to become fully aware of the hazards in a particular patient.”
“Risk is the category where litigation pops up and where you see the most challenges,” says O’Rourke, because the patient filing a claim may say, “ ‘Well, the doctor didn’t tell me about this risk and had I known this occurred, I would have elected to forego this procedure; I would have chosen one of the other alternatives.’ ”
If a patient develops a complication and the hospitalist must initiate a new intervention, then it’s the hospitalist’s duty to get informed consent for that next intervention. “Every time a physician undertakes a particular intervention, the patient has to be informed in why that intervention is being taken and what the risks, benefits, and alternatives are,” says O’Rourke.
If a patient is incapable of giving consent, then consider whether there is a significant risk in waiting until the patient is capable of giving informed consent. If the answer is “no,” then consider whether or not to delay the intervention. “If there’s no potential harm caused by waiting until the patient hits a higher level of consciousness,” says O’Rourke, “then that’s perfectly appropriate.”
In an emergency situation, a surrogate may need to make the decision. If neither one of those alternatives is available, “the law presumes that the patient is going to do what is reasonable and necessary in order to preserve his or her health, unless there’s been some instruction otherwise,” notes O’Rourke.
Teach Back
Studies show that when patients are asked to repeat what they understood from their informed consent discussions, they have greater recall and comprehension of the risks and benefits of surgical procedures.2,15 “Teach back” is an especially valuable technique to use with low literacy patients. The NQF discovered that the providers and departments using teach back were widely recognized by their peers as having the most well-informed patients compared with departments that did not use this method.2 (See “Teach Back in Action,” above right.) A number of studies have found that when a provider asks a patient to restate information or instructions, the benefits include providing a check for lapses of recall and understanding, revealing health beliefs, reinforcing and individualizing health messages, and motivating patients by activating dialogue.15
In May 2003, the NQF published Safe Practices for Better Healthcare, which endorsed a set of consensus standards for 30 healthcare practices, one of which (Safe Practice 10) recommends that all healthcare professionals ask patients to teach back what they have been told by their providers during their informed consent discussions.2
In its 2001 report, Making Health Care Safer: A Critical Analysis of Patient Safety Practices (project director, Robert M. Wachter, MD), the Agency for Healthcare Research and Quality suggested that special attention be paid to implementing 11 particular practices, one of which was “asking that patients recall and restate what they have been told during the informed consent process.”16
Even if you are not asking for a signed form, physicians, nurses, interpreters, and any professional who communicates with patients regarding their healthcare decisions is involved in the informed consent process and should use teach back—especially with those patients who find even basic health information difficult to understand. Although the NQF found that physicians were reluctant to incorporate this technique into their communications, the providers reported anecdotally that teach back takes less than a minute to complete; research backs up the claim that the more the technique is practiced, the speedier it gets.2
The provision of this “interactive communication loop,” as it has been called,15 has also been shown to affect clinical outcomes. In a study by Schillinger and colleagues conducted at an outpatient general internal medicine clinic and at San Francisco General Hospital, physicians assessed recall and comprehension of any new concept in 12 (20%) of 61 outpatient visits by diabetic patients for 15 (12%) of 124 concepts.15 The patients whose physicians assessed their recall by means of teach back were more likely to have hemoglobin A1c levels below the mean compared with patients whose doctors did not. The two variables found to be independently associated with good glycemic control were higher health literacy levels and physicians’ application of the teach-back strategy.
Consent Forms
The informed consent process is intended to protect patients and physicians both.7 Legal doctrine, including hospital accreditation standards, ethical theories, and perspectives on the physician-patient relationship, emphasizes the importance of full patient comprehension regarding treatment. But many hospitals do not use forms that contribute to that objective. In a study by Bottrell and colleagues of 540 forms from 157 hospitals nationwide, 96% indicated the nature of the procedure for the patient; however, only 26% of forms included all four elements of informed consent: procedure, risks, benefits, and alternative treatment options. Thirty-five percent included three of four elements, 23% provided two of four elements, 14% listed only one element, and 2% contained none of the elements.
In general, the investigators concluded, the forms appear to be designed to authorize treatment or protect hospitals and caregivers from liability rather than to help patients clarify information or make decisions. Even hospitals in states that have statutes requiring institutions to include all four elements on their forms were no more likely to do so than those in other states. Fewer than 40% of forms were found to support models of shared decision making, the basis of patient autonomy and the overarching intention for informed consent.
“Generally … informed consent forms are seen as mere documentation vehicles, and perhaps as legal protection, regardless of whether the process of informed consent was successfully accomplished or of minimal quality,” this study’s authors wrote, and because patients are not blind to the intentions of these forms, this may add to their discomfort.7 Most forms, the authors concluded, are insufficient because the language used does not accommodate low health literacy or because there are no graphic features.
On the other hand, “informed consent can sometimes get very awkward and cumbersome,” says William Jacott, MD, special advisor for professional relations at the Joint Commission on Accreditation of Healthcare Organizations, St. Paul, Minn., for the past five years and liaison to SHM for the past two. Some institutions or organizations interpret Joint Commission and other legal standards excessively, he says, “and I’ve seen 10-page consent forms, which just overwhelms the patient, let alone the doctor. So an over-interpretation and overkill need to be avoided.”
Conclusion: Communication and Documentation
The ways in which hospitalists can avoid the pitfalls of faulty informed consent conversations include close communication with surgeons as well as other colleagues.
“We have a great tendency to communicate via the medical record,” says Dr. Jacott, and if a patient’s co-managers (the hospitalist and subspecialist) don’t communicate, “one might assume the other has already done [informed consent], and nobody does it.”
He has also seen instances in teaching hospitals in which both the surgeon and the hospitalist incorrectly assume that the house staff has acquired informed consent.
Nurses can also help hospitalists ensure that patients are comfortable with their treatment choices. “Nurses often have more firsthand information about when patients are confused or scared or dubious or are somehow being coerced or manipulated into consenting to something,” says Dr. Rich.
Hospitalists should also avoid making assumptions about the completeness of their colleagues’ discussions with patients and should look for clear documentation as well as record their own. “Some subspecialists play fast and loose with informed consent,” Dr. Rich says, “and [may] resent a medical staff colleague who takes it seriously and attempts to hold them accountable for really doing it right. And for the hospitalist, that’s where it is critical that their institution stand behind them.”
A hospitalist’s responsibilities with regard to informed consent also include ensuring that the patient’s consent is truly informed. Using the teach back method, allowing time for the patient to ask questions and voice concerns, and including all four elements of informed consent on the patient’s consent form are just some of the ways the hospitalist can play an essential role in the continuum that is informed consent.
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Epstein M. Why effective consent presupposes autonomous authorisation: a counterorthodox argument. J Med Ethics. 2006;32:342-345.
- National Quality Forum. Implementing a national voluntary consensus standard for informed consent: a user’s guide for healthcare professionals. September 2005. Available at: www.qualityforum.org/publications.html. Accessed September 5, 2006.
- Rizzo v Schiller, 445 SE2d 153 (Va. 1994). Available at: www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10184327&dopt=Abstract. Accessed September 11, 2006.
- Gorab v Zook, 943 P2d 423 (Colo. 1997). Available at: http://caselaw.lp.findlaw.com/scripts/getcase.pl?court=co&vol=2003app%5C3477&invol=1. Accessed September 11, 2006.
- Schuck PH. Rethinking informed consent. Yale Law J. 1994;103:899-959.
- Culbertson v Mernitz, 602 NE2d 98 (Ind. 1992).
- Bottrell MM, Alpert H, Fischbach RL, et al. Hospital informed consent for procedure forms: facilitating quality patient-physician interaction. Arch Surg. 2000 Jan;135(1):26-33.
- Bernat JL, Peterson LM. Patient-centered informed consent in surgical practice. Arch Surg. 2006 Jan;141(7):86-92.
- Marcus EN. The silent epidemic—the health effects of illiteracy. N Engl J Med. 2006;355:339-341.
- Flores G. Language barriers to health care in the United States. N Engl J Med. 2006 Jul;355:229-231.
- Carmona RH. Health literacy: a national priority. J Gen Intern Med. 2006;21:803.
- Pantilat SZ, Alpers A, Wachter RM. A new doctor in the house: ethical issues in hospitalist systems. JAMA. 1999 Jul 14;282:171-174.
- Henry LA. What the hospitalist movement means to family physicians. Fam Pract Manag. 1998 Nov-Dec;5(10):54-62.
- Rajput V, Bekes CE. Ethical issues in hospital medicine. Med Clin North Am. 2002 Jul;86(4):869-886.
- Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003 Jan 13;163(1):83-90.
- University of California at San Francisco (UCSF)-Stanford University Evidence-based Practice Center. Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment: Number 43. AHRQ Publication No. 01-E058, July 2001. Agency for Healthcare Research and Quality. Available at: www.ahrq.gov/clinic/ptsafety/. Accessed September 5, 2006.
- Baum N. Comprehension is the key: the challenge hospitals face is that many patients do not understand the fundamental information regarding their treatment plans. Patient Safety Quality Healthcare. May/June 2006:35-38.
Since the late 1960s, a growing body of evidence has suggested the chances that patients truly understand what they are consenting to in informed consent documents are not only unlikely but “remote.”1 A review of 70 studies conducted in a variety of clinical settings demonstrated that, although consent and refusals were legally and institutionally valid, they failed to result in “genuinely autonomous decision making.”
Factors associated with such outcomes included low socioeconomic status, poor education, old age, lengthy hospital stay, stress, language barriers, and misinterpretation of probabilistic data. Accompanying disclosure practices were also found inadequate, though perfectly legal.
Research by the National Quality Forum (NQF) revealed that, despite having signed a consent form, 18% to 45% of patients are unable to recall even the major risks associated with their surgeries. Many cannot answer basic questions about the services or procedures they agreed to receive, while 44% do not know the exact nature of their operation, and most (60% to 69%) do not understand or read the information contained in generic hospital consent forms.2 Treating patients such as these can lead to compromised care and safety and increased medical malpractice risk.
Many bioethicists endorse the position that “striving for fully informed consent is generally unfeasible and perhaps even undesirable.”-- Others argue that the concept of fully informed consent should at least serve as an ideal. For that to be achieved, patients would need to understand fully their conditions and treatment. At a minimum, then, and as law, patients have the right to be given information that will optimize their autonomy.3-6 That information includes:
- The nature of the procedure or treatment being offered, including whether it is diagnostic or therapeutic;
- The risks and potential complications of a procedure or medical treatment;
- The benefits of the procedure; and
- Treatment alternatives, along with their risks and benefits.7
The ideal is far from reality. Frequently cited factors interfering with full comprehension, in addition to those already mentioned, include personal or cultural beliefs and low health literacy rates.1,2 Providers’ inability to communicate clearly in a rushed environment is also a factor, as is a tendency for providers who see the act of acquiring informed consent as a legal formality to delegate to a junior colleague.
But “the patient’s consent happens during the process of dialogue with the surgeon,” wrote Bernat and Peterson in the January 2006 Archives of Surgery:8 “The signature on a surgical consent form is merely the culmination and formalization of this preceding consent discussion and agreement.”
A signed consent form represents evidence of the patient’s consent—not of his or her understanding. That signed form may not be sufficient to protect providers in cases of liability. According to Jury Verdict Research, informed consent issues are among the top 10 most common reasons patients file malpractice claims.2
The low health literacy of almost half of adults in the United States limits their ability to understand the basic health information and services that are needed to make appropriate health decisions. In fact, articles in two of the July 2006 issues of the New England Journal of Medicine, as well as the entire August 2006 issue of the Journal of General Internal Medicine, are devoted to the subject of health literacy.9-11
Given that surgeons and other specialists are often responsible for securing informed consent, what are the areas of informed consent to which hospitalists should be attuned?
Key Considerations for the Hospitalist
Ordinarily, the person whose name is at the top of the patient’s chart has full responsibility for informed consent, although sometimes a subspecialty consultant, such as a cardiologist asking for a particular study, might help. A hospitalist might be named as the responsible provider in an area in which he or she is active.
Ben Rich, JD, PhD, a professor of bioethics at the University of California-Davis School (UCD) of Medicine in Sacramento, Calif., has considered the critical problems or distinctions that the hospitalist, as opposed to other physicians, may have in the area of informed consent. One area that strikes him as potentially risky is that of advance directives. Dr. Rich, who teaches a course on medicine and law at UCD, says that for decades experts have urged primary care physicians (PCPs) to discuss advance directives with patients as part of routine care. Even so, he acknowledges, if a patient is in critical condition and is hospitalized, “it is entirely possible that their personal physician won’t even know about it. So here is the person who is supposed to have apprised herself of the patient’s values and priorities in circumstances like that, and they’re out of the picture. And the person who is trying to interpret advance directives, if there is one, is the hospitalist.”
It might be difficult for the hospitalist to interpret any ambiguities. If the hospitalist believes it is impossible to know what the patient understood at the time they drafted the directive about the circumstances they are now facing, he or she may be more likely to dismiss it as invalid and simply make a decision as to what is medically appropriate, says Dr. Rich.
The discontinuity of care imposed by the hospitalist systems raises several ethical concerns, wrote Steven Pantilat, MD, in JAMA.12 The primary care physician and patient have previously negotiated, through the process of medical decision-making, the patient’s goals and values regarding medical interventions. “Because hospitalist systems leave no formal inpatient role for the PCP,” wrote Dr. Pantilat, “ … patients can no longer rely on agreements reached in the office following them to the hospital. Nonetheless, the hospitalist shares the PCP’s obligations to respect the ethical principles that agreements about preferences for care or individual values often represent.”
Another important but somewhat controversial issue involves whether a consent discussion held preoperatively also encompasses the management of post-procedure complications.8 Although it is impossible to mention all possible serious complications beforehand, it is prudent to reference the patient’s goals and general treatment preferences and to ensure that a family member (if not the designated surrogate) is present during this conversation. Just the same, each new intervention or procedure requires a new conversation and, in some cases, a new signed form. “Because at the end of the day,” says Patrick O’Rourke, JD, an attorney in Denver who regularly represents physicians in medical malpractice cases, “physicians are the people who have the obligation to obtain informed consent; the hospital as an institution does not, because hospitals don’t practice medicine; physicians do.”
Particularly with patients who face serious illness and those confronting what may be a chronic condition going forward, says Dr. Rich, “there’s a school of thought [that maintains] that part of the informed consent process is obsessively focused on procedures and pays woefully inadequate attention to the reasonable goals of care. This is nowhere more obvious than in the ICU setting.”
Continuums of Care and Consent
Indeed, any expert on medical law will tell you that informed consent is a process—not an event.8 Though a hospitalist may not have secured the signature on a consent form, a hospitalist’s practice is as much a part of a patient’s ongoing process of “consent” as is that of the surgeon who performed the patient’s operation.
The American Academy of Family Physicians has adopted the following guideline: “During the period of hospitalization, decisions regarding care, consultation, admission, transfer, and discharge should be the sole responsibility of the inpatient care physician in consultation with the patient and, as appropriate, the patient’s family physician and/or family members.”13 The times when patients actually sign informed consent documents are junctures in the continuum of consent that covers a lifetime healthcare experience. Hospitalists, then, are involved in informed consent from patient assignment to patient discharge.
“And the manner in which the process is conducted is at least as important as substantive information given,” says Dr. Rich. “A skilled and experienced physician can give any patient two descriptions of the procedure that they’re recommending,” he says. “[After o]ne, couched in a certain way, but not inaccurate, the patient would say, ‘Well, of course, I want that.’ And if the physician gives it in the other way, still accurate, the patient would say, Well, who would want that? And it all has to do with the terms you use, your tone of voice, your body language, the setting in which you provide it. … All that can profoundly shape the informed consent process. And it is not something that physicians are routinely taught.”
Because the process of informed consent is ongoing, discussions may continue for several sessions over a length of time before a patient decides to undergo a treatment. This gives patients more time to think of questions or concerns they may have. Addressing those concerns is a crucial part of the process.
“The reason that’s important is that you always want to offer and document that you have an opportunity to address what the patient’s questions were so the consent is truly informed,” says O’Rourke. One-way delivery of information is not equivalent to the dialogue implied by the term “informed consent.” “It is vitally important to ask, ‘What other information can I give you?’” he explains, especially because informed consent cases often deal with complications that develop after surgery.
Community Standard
The risks of procedures mentioned in informed consent discussions comprise a special category, says O’Rourke, “because there are some things that are not easily foreseen.” Some complications are not within the range generally anticipated after a procedure. “And the way the law works is that you don’t have to imagine the million-to-one shot [complication]; you would review the risks in terms of what a physician should disclose … in terms of significance.”
Physicians are judged by how well they informed patients of the risks as assessed by a community standard of what reasonable practitioners in the community say the risks are, he says. Physicians need to be knowledgeable about the risks of the procedure based on the medical literature, their training, and their discussions with colleagues.14
“Oftentimes, in order to give and get full informed consent, we use the knowledge from our subspecialty consultants,” says Dennis Manning, MD, FACP, FACC, a hospitalist and director of quality in the Department of Medicine and an assistant professor at the Mayo Clinic College of Medicine, Rochester, Minn. “We ask them, ‘What do you think the risks are?’ We might have to pick their brains in order to become fully aware of the hazards in a particular patient.”
“Risk is the category where litigation pops up and where you see the most challenges,” says O’Rourke, because the patient filing a claim may say, “ ‘Well, the doctor didn’t tell me about this risk and had I known this occurred, I would have elected to forego this procedure; I would have chosen one of the other alternatives.’ ”
If a patient develops a complication and the hospitalist must initiate a new intervention, then it’s the hospitalist’s duty to get informed consent for that next intervention. “Every time a physician undertakes a particular intervention, the patient has to be informed in why that intervention is being taken and what the risks, benefits, and alternatives are,” says O’Rourke.
If a patient is incapable of giving consent, then consider whether there is a significant risk in waiting until the patient is capable of giving informed consent. If the answer is “no,” then consider whether or not to delay the intervention. “If there’s no potential harm caused by waiting until the patient hits a higher level of consciousness,” says O’Rourke, “then that’s perfectly appropriate.”
In an emergency situation, a surrogate may need to make the decision. If neither one of those alternatives is available, “the law presumes that the patient is going to do what is reasonable and necessary in order to preserve his or her health, unless there’s been some instruction otherwise,” notes O’Rourke.
Teach Back
Studies show that when patients are asked to repeat what they understood from their informed consent discussions, they have greater recall and comprehension of the risks and benefits of surgical procedures.2,15 “Teach back” is an especially valuable technique to use with low literacy patients. The NQF discovered that the providers and departments using teach back were widely recognized by their peers as having the most well-informed patients compared with departments that did not use this method.2 (See “Teach Back in Action,” above right.) A number of studies have found that when a provider asks a patient to restate information or instructions, the benefits include providing a check for lapses of recall and understanding, revealing health beliefs, reinforcing and individualizing health messages, and motivating patients by activating dialogue.15
In May 2003, the NQF published Safe Practices for Better Healthcare, which endorsed a set of consensus standards for 30 healthcare practices, one of which (Safe Practice 10) recommends that all healthcare professionals ask patients to teach back what they have been told by their providers during their informed consent discussions.2
In its 2001 report, Making Health Care Safer: A Critical Analysis of Patient Safety Practices (project director, Robert M. Wachter, MD), the Agency for Healthcare Research and Quality suggested that special attention be paid to implementing 11 particular practices, one of which was “asking that patients recall and restate what they have been told during the informed consent process.”16
Even if you are not asking for a signed form, physicians, nurses, interpreters, and any professional who communicates with patients regarding their healthcare decisions is involved in the informed consent process and should use teach back—especially with those patients who find even basic health information difficult to understand. Although the NQF found that physicians were reluctant to incorporate this technique into their communications, the providers reported anecdotally that teach back takes less than a minute to complete; research backs up the claim that the more the technique is practiced, the speedier it gets.2
The provision of this “interactive communication loop,” as it has been called,15 has also been shown to affect clinical outcomes. In a study by Schillinger and colleagues conducted at an outpatient general internal medicine clinic and at San Francisco General Hospital, physicians assessed recall and comprehension of any new concept in 12 (20%) of 61 outpatient visits by diabetic patients for 15 (12%) of 124 concepts.15 The patients whose physicians assessed their recall by means of teach back were more likely to have hemoglobin A1c levels below the mean compared with patients whose doctors did not. The two variables found to be independently associated with good glycemic control were higher health literacy levels and physicians’ application of the teach-back strategy.
Consent Forms
The informed consent process is intended to protect patients and physicians both.7 Legal doctrine, including hospital accreditation standards, ethical theories, and perspectives on the physician-patient relationship, emphasizes the importance of full patient comprehension regarding treatment. But many hospitals do not use forms that contribute to that objective. In a study by Bottrell and colleagues of 540 forms from 157 hospitals nationwide, 96% indicated the nature of the procedure for the patient; however, only 26% of forms included all four elements of informed consent: procedure, risks, benefits, and alternative treatment options. Thirty-five percent included three of four elements, 23% provided two of four elements, 14% listed only one element, and 2% contained none of the elements.
In general, the investigators concluded, the forms appear to be designed to authorize treatment or protect hospitals and caregivers from liability rather than to help patients clarify information or make decisions. Even hospitals in states that have statutes requiring institutions to include all four elements on their forms were no more likely to do so than those in other states. Fewer than 40% of forms were found to support models of shared decision making, the basis of patient autonomy and the overarching intention for informed consent.
“Generally … informed consent forms are seen as mere documentation vehicles, and perhaps as legal protection, regardless of whether the process of informed consent was successfully accomplished or of minimal quality,” this study’s authors wrote, and because patients are not blind to the intentions of these forms, this may add to their discomfort.7 Most forms, the authors concluded, are insufficient because the language used does not accommodate low health literacy or because there are no graphic features.
On the other hand, “informed consent can sometimes get very awkward and cumbersome,” says William Jacott, MD, special advisor for professional relations at the Joint Commission on Accreditation of Healthcare Organizations, St. Paul, Minn., for the past five years and liaison to SHM for the past two. Some institutions or organizations interpret Joint Commission and other legal standards excessively, he says, “and I’ve seen 10-page consent forms, which just overwhelms the patient, let alone the doctor. So an over-interpretation and overkill need to be avoided.”
Conclusion: Communication and Documentation
The ways in which hospitalists can avoid the pitfalls of faulty informed consent conversations include close communication with surgeons as well as other colleagues.
“We have a great tendency to communicate via the medical record,” says Dr. Jacott, and if a patient’s co-managers (the hospitalist and subspecialist) don’t communicate, “one might assume the other has already done [informed consent], and nobody does it.”
He has also seen instances in teaching hospitals in which both the surgeon and the hospitalist incorrectly assume that the house staff has acquired informed consent.
Nurses can also help hospitalists ensure that patients are comfortable with their treatment choices. “Nurses often have more firsthand information about when patients are confused or scared or dubious or are somehow being coerced or manipulated into consenting to something,” says Dr. Rich.
Hospitalists should also avoid making assumptions about the completeness of their colleagues’ discussions with patients and should look for clear documentation as well as record their own. “Some subspecialists play fast and loose with informed consent,” Dr. Rich says, “and [may] resent a medical staff colleague who takes it seriously and attempts to hold them accountable for really doing it right. And for the hospitalist, that’s where it is critical that their institution stand behind them.”
A hospitalist’s responsibilities with regard to informed consent also include ensuring that the patient’s consent is truly informed. Using the teach back method, allowing time for the patient to ask questions and voice concerns, and including all four elements of informed consent on the patient’s consent form are just some of the ways the hospitalist can play an essential role in the continuum that is informed consent.
Andrea Sattinger is a frequent contributor to The Hospitalist.
References
- Epstein M. Why effective consent presupposes autonomous authorisation: a counterorthodox argument. J Med Ethics. 2006;32:342-345.
- National Quality Forum. Implementing a national voluntary consensus standard for informed consent: a user’s guide for healthcare professionals. September 2005. Available at: www.qualityforum.org/publications.html. Accessed September 5, 2006.
- Rizzo v Schiller, 445 SE2d 153 (Va. 1994). Available at: www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&list_uids=10184327&dopt=Abstract. Accessed September 11, 2006.
- Gorab v Zook, 943 P2d 423 (Colo. 1997). Available at: http://caselaw.lp.findlaw.com/scripts/getcase.pl?court=co&vol=2003app%5C3477&invol=1. Accessed September 11, 2006.
- Schuck PH. Rethinking informed consent. Yale Law J. 1994;103:899-959.
- Culbertson v Mernitz, 602 NE2d 98 (Ind. 1992).
- Bottrell MM, Alpert H, Fischbach RL, et al. Hospital informed consent for procedure forms: facilitating quality patient-physician interaction. Arch Surg. 2000 Jan;135(1):26-33.
- Bernat JL, Peterson LM. Patient-centered informed consent in surgical practice. Arch Surg. 2006 Jan;141(7):86-92.
- Marcus EN. The silent epidemic—the health effects of illiteracy. N Engl J Med. 2006;355:339-341.
- Flores G. Language barriers to health care in the United States. N Engl J Med. 2006 Jul;355:229-231.
- Carmona RH. Health literacy: a national priority. J Gen Intern Med. 2006;21:803.
- Pantilat SZ, Alpers A, Wachter RM. A new doctor in the house: ethical issues in hospitalist systems. JAMA. 1999 Jul 14;282:171-174.
- Henry LA. What the hospitalist movement means to family physicians. Fam Pract Manag. 1998 Nov-Dec;5(10):54-62.
- Rajput V, Bekes CE. Ethical issues in hospital medicine. Med Clin North Am. 2002 Jul;86(4):869-886.
- Schillinger D, Piette J, Grumbach K, et al. Closing the loop: physician communication with diabetic patients who have low health literacy. Arch Intern Med. 2003 Jan 13;163(1):83-90.
- University of California at San Francisco (UCSF)-Stanford University Evidence-based Practice Center. Making health care safer: a critical analysis of patient safety practices. Evidence Report/Technology Assessment: Number 43. AHRQ Publication No. 01-E058, July 2001. Agency for Healthcare Research and Quality. Available at: www.ahrq.gov/clinic/ptsafety/. Accessed September 5, 2006.
- Baum N. Comprehension is the key: the challenge hospitals face is that many patients do not understand the fundamental information regarding their treatment plans. Patient Safety Quality Healthcare. May/June 2006:35-38.
Calculating the Future of CMS Payments
Hospitalists and other physicians with Medicare patients are awaiting final word on proposed changes to the Medicare Physician Fee Schedule, due to take effect next year.
How, exactly, will the fee changes affect you? What will your revenue look like in 2007? You can find answers to these questions by understanding what the changes will be and by using a new online tool developed by the American College of Physicians (ACP).
A Look at the Proposed Payment Changes
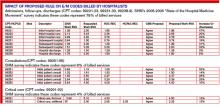
The Centers for Medicare and Medicaid Services (CMS) has proposed specific changes to the Medicare Physician Fee Schedule that would significantly increase payments for Medicare beneficiaries’ hospital visits, office visits, consultations, and other evaluation and management (E/M) services. If the proposed changes are enacted, Medicare payments would substantially increase for these services. How substantial are the increases? The work relative value unit (RVU) for initial hospital care (CPT code 99221) would increase by 47%, and the work RVU for subsequent hospital care (CPT code 99232) would increase by 31%. (For a detailed breakdown of the “Impact of the Proposed Rule on E/M Codes Billed by Hospitalists,” see p. 38.)
How will these proposed increases affect your income? The dollar amount is difficult to calculate, partly because, due to legislative restrictions, Medicare payments won’t increase by the same percentage as the E/M relative values. CMS can make only budget-neutral changes. This means it can’t increase payments by more than $20 million per year. Because the proposed 2007 changes exceed this amount—they come close to $4 billion—CMS has proposed an additional adjustment that reduces payment equally for all physician services in order to maintain 2007 expenditures at roughly their 2006 level. This adjustment means that payment for some low-level E/M services will decrease.
An Online Calculator Can Help
The ACP has developed an interactive revenue calculator to enable its members to estimate their reimbursements under the proposed changes. Available for members only on the ACP Web site (www.acponline.org/private/pmc/emimpact.html), the calculator estimates the potential revenue change for E/M services only.
“We thought [the calculator] would be helpful to our members,” explains Brian Whitman, senior analyst for Regulatory and Insurer Affairs, ACP. “The RVU changes are technical and complex, and it’s hard for a practicing physician to translate the changes. Doctors see dollars, not RVUs. Also, the changes all depend on the volume of Medicare patients they have and how they code.”
Physicians who use the ACP reimbursement calculator enter the number of visits they provide to Medicare beneficiaries in a typical week, categorized under individual CPT codes. The calculator then determines their Medicare revenue for 2006 and their projected Medicare revenue for 2007. Finally, it estimates how much their 2007 revenue will change in a typical week and in the upcoming year.
Of course, the Medicare payment received for many non-E/M services will decrease because, as stated earlier, the Medicare statute requires CMS to keep 2007 expenditures at roughly the same level as those generated in 2006.
After using the online calculator to determine their payments from the affected E/M codes, ACP members can then estimate their projected net revenue change. The ACP recommends that physicians estimate their 2006 Medicare revenue for all services not specifically listed in the calculator and then multiply that figure by 0.95 to account for the budget neutrality adjustment. They can then subtract that number from the total payment found in the online calculator to get an estimate of their net Medicare payment change in 2007.
The ACP’s reimbursement calculator is not designed to be precise; that would be impossible. “The calculator itself is an estimate,” warns Whitman. For one thing, the payments per RVU will not be certain until CMS publishes its final 2007 relative values. In addition, E/M service payments by private health plans that use the Medicare-approved RVUs for determining their own fee schedules are likely to increase.
What Happens Next?
CMS proposed the changes in June. According to the law, CMS must solicit comments from the public for 60 days. Some time after considering these comments, CMS will announce its final decision on the payment changes for E/M and other services. “They usually release their final rule in October or November,” says Whitman. CMS has proposed using the revised RVUs beginning January 1, 2007.
For the latest news on the proposed payment changes, check the SHM Web site at www.hospitalmedicine.org. If you’re a member of the ACP, check out the online reimbursement calculator at www.acponline.org/private/pmc/emimpact.html. TH
Hospitalists and other physicians with Medicare patients are awaiting final word on proposed changes to the Medicare Physician Fee Schedule, due to take effect next year.
How, exactly, will the fee changes affect you? What will your revenue look like in 2007? You can find answers to these questions by understanding what the changes will be and by using a new online tool developed by the American College of Physicians (ACP).
A Look at the Proposed Payment Changes
The Centers for Medicare and Medicaid Services (CMS) has proposed specific changes to the Medicare Physician Fee Schedule that would significantly increase payments for Medicare beneficiaries’ hospital visits, office visits, consultations, and other evaluation and management (E/M) services. If the proposed changes are enacted, Medicare payments would substantially increase for these services. How substantial are the increases? The work relative value unit (RVU) for initial hospital care (CPT code 99221) would increase by 47%, and the work RVU for subsequent hospital care (CPT code 99232) would increase by 31%. (For a detailed breakdown of the “Impact of the Proposed Rule on E/M Codes Billed by Hospitalists,” see p. 38.)
How will these proposed increases affect your income? The dollar amount is difficult to calculate, partly because, due to legislative restrictions, Medicare payments won’t increase by the same percentage as the E/M relative values. CMS can make only budget-neutral changes. This means it can’t increase payments by more than $20 million per year. Because the proposed 2007 changes exceed this amount—they come close to $4 billion—CMS has proposed an additional adjustment that reduces payment equally for all physician services in order to maintain 2007 expenditures at roughly their 2006 level. This adjustment means that payment for some low-level E/M services will decrease.
An Online Calculator Can Help
The ACP has developed an interactive revenue calculator to enable its members to estimate their reimbursements under the proposed changes. Available for members only on the ACP Web site (www.acponline.org/private/pmc/emimpact.html), the calculator estimates the potential revenue change for E/M services only.
“We thought [the calculator] would be helpful to our members,” explains Brian Whitman, senior analyst for Regulatory and Insurer Affairs, ACP. “The RVU changes are technical and complex, and it’s hard for a practicing physician to translate the changes. Doctors see dollars, not RVUs. Also, the changes all depend on the volume of Medicare patients they have and how they code.”
Physicians who use the ACP reimbursement calculator enter the number of visits they provide to Medicare beneficiaries in a typical week, categorized under individual CPT codes. The calculator then determines their Medicare revenue for 2006 and their projected Medicare revenue for 2007. Finally, it estimates how much their 2007 revenue will change in a typical week and in the upcoming year.
Of course, the Medicare payment received for many non-E/M services will decrease because, as stated earlier, the Medicare statute requires CMS to keep 2007 expenditures at roughly the same level as those generated in 2006.
After using the online calculator to determine their payments from the affected E/M codes, ACP members can then estimate their projected net revenue change. The ACP recommends that physicians estimate their 2006 Medicare revenue for all services not specifically listed in the calculator and then multiply that figure by 0.95 to account for the budget neutrality adjustment. They can then subtract that number from the total payment found in the online calculator to get an estimate of their net Medicare payment change in 2007.
The ACP’s reimbursement calculator is not designed to be precise; that would be impossible. “The calculator itself is an estimate,” warns Whitman. For one thing, the payments per RVU will not be certain until CMS publishes its final 2007 relative values. In addition, E/M service payments by private health plans that use the Medicare-approved RVUs for determining their own fee schedules are likely to increase.
What Happens Next?
CMS proposed the changes in June. According to the law, CMS must solicit comments from the public for 60 days. Some time after considering these comments, CMS will announce its final decision on the payment changes for E/M and other services. “They usually release their final rule in October or November,” says Whitman. CMS has proposed using the revised RVUs beginning January 1, 2007.
For the latest news on the proposed payment changes, check the SHM Web site at www.hospitalmedicine.org. If you’re a member of the ACP, check out the online reimbursement calculator at www.acponline.org/private/pmc/emimpact.html. TH
Hospitalists and other physicians with Medicare patients are awaiting final word on proposed changes to the Medicare Physician Fee Schedule, due to take effect next year.
How, exactly, will the fee changes affect you? What will your revenue look like in 2007? You can find answers to these questions by understanding what the changes will be and by using a new online tool developed by the American College of Physicians (ACP).
A Look at the Proposed Payment Changes
The Centers for Medicare and Medicaid Services (CMS) has proposed specific changes to the Medicare Physician Fee Schedule that would significantly increase payments for Medicare beneficiaries’ hospital visits, office visits, consultations, and other evaluation and management (E/M) services. If the proposed changes are enacted, Medicare payments would substantially increase for these services. How substantial are the increases? The work relative value unit (RVU) for initial hospital care (CPT code 99221) would increase by 47%, and the work RVU for subsequent hospital care (CPT code 99232) would increase by 31%. (For a detailed breakdown of the “Impact of the Proposed Rule on E/M Codes Billed by Hospitalists,” see p. 38.)
How will these proposed increases affect your income? The dollar amount is difficult to calculate, partly because, due to legislative restrictions, Medicare payments won’t increase by the same percentage as the E/M relative values. CMS can make only budget-neutral changes. This means it can’t increase payments by more than $20 million per year. Because the proposed 2007 changes exceed this amount—they come close to $4 billion—CMS has proposed an additional adjustment that reduces payment equally for all physician services in order to maintain 2007 expenditures at roughly their 2006 level. This adjustment means that payment for some low-level E/M services will decrease.
An Online Calculator Can Help
The ACP has developed an interactive revenue calculator to enable its members to estimate their reimbursements under the proposed changes. Available for members only on the ACP Web site (www.acponline.org/private/pmc/emimpact.html), the calculator estimates the potential revenue change for E/M services only.
“We thought [the calculator] would be helpful to our members,” explains Brian Whitman, senior analyst for Regulatory and Insurer Affairs, ACP. “The RVU changes are technical and complex, and it’s hard for a practicing physician to translate the changes. Doctors see dollars, not RVUs. Also, the changes all depend on the volume of Medicare patients they have and how they code.”
Physicians who use the ACP reimbursement calculator enter the number of visits they provide to Medicare beneficiaries in a typical week, categorized under individual CPT codes. The calculator then determines their Medicare revenue for 2006 and their projected Medicare revenue for 2007. Finally, it estimates how much their 2007 revenue will change in a typical week and in the upcoming year.
Of course, the Medicare payment received for many non-E/M services will decrease because, as stated earlier, the Medicare statute requires CMS to keep 2007 expenditures at roughly the same level as those generated in 2006.
After using the online calculator to determine their payments from the affected E/M codes, ACP members can then estimate their projected net revenue change. The ACP recommends that physicians estimate their 2006 Medicare revenue for all services not specifically listed in the calculator and then multiply that figure by 0.95 to account for the budget neutrality adjustment. They can then subtract that number from the total payment found in the online calculator to get an estimate of their net Medicare payment change in 2007.
The ACP’s reimbursement calculator is not designed to be precise; that would be impossible. “The calculator itself is an estimate,” warns Whitman. For one thing, the payments per RVU will not be certain until CMS publishes its final 2007 relative values. In addition, E/M service payments by private health plans that use the Medicare-approved RVUs for determining their own fee schedules are likely to increase.
What Happens Next?
CMS proposed the changes in June. According to the law, CMS must solicit comments from the public for 60 days. Some time after considering these comments, CMS will announce its final decision on the payment changes for E/M and other services. “They usually release their final rule in October or November,” says Whitman. CMS has proposed using the revised RVUs beginning January 1, 2007.
For the latest news on the proposed payment changes, check the SHM Web site at www.hospitalmedicine.org. If you’re a member of the ACP, check out the online reimbursement calculator at www.acponline.org/private/pmc/emimpact.html. TH
Peripheral Arterial Disease
Supplement Editors:
Amjad AlMahameed, MD, and John R. Bartholomew, MD
Contents
The magnitude of the problem of peripheral arterial disease: Epidemiology and clinical significance
Mary McGrae McDermott, MD
Pathophysiology of peripheral arterial disease and risk factors for its development
John R. Bartholomew, MD, and Jeffrey W. Olin, DO
The clinical presentation of peripheral arterial disease and guidance for early recognition
Sean P. Lyden, MD, and Douglas Joseph, DO
Noninvasive diagnostic strategies for peripheral arterial disease
Susan M. Begelman, MD, and Michael R. Jaff, DO
Contemporary management of peripheral arterial disease: I. Cardiovascular risk-factor modification
Heather L. Gornik, MD, MHS, and Mark A. Creager, MD
Contemporary management of peripheral arterial disease: II. Improving walking distance and quality of life
Teresa L. Carman, MD, and Bernardo B. Fernandez, Jr., MD
Contemporary management of peripheral arterial disease: III. Endovascular and surgical management
Amjad AlMahameed, MD, MPH, FACP, and Deepak L. Bhatt, MD, FACC, FSCAI, FESC, FACP
Supplement Editors:
Amjad AlMahameed, MD, and John R. Bartholomew, MD
Contents
The magnitude of the problem of peripheral arterial disease: Epidemiology and clinical significance
Mary McGrae McDermott, MD
Pathophysiology of peripheral arterial disease and risk factors for its development
John R. Bartholomew, MD, and Jeffrey W. Olin, DO
The clinical presentation of peripheral arterial disease and guidance for early recognition
Sean P. Lyden, MD, and Douglas Joseph, DO
Noninvasive diagnostic strategies for peripheral arterial disease
Susan M. Begelman, MD, and Michael R. Jaff, DO
Contemporary management of peripheral arterial disease: I. Cardiovascular risk-factor modification
Heather L. Gornik, MD, MHS, and Mark A. Creager, MD
Contemporary management of peripheral arterial disease: II. Improving walking distance and quality of life
Teresa L. Carman, MD, and Bernardo B. Fernandez, Jr., MD
Contemporary management of peripheral arterial disease: III. Endovascular and surgical management
Amjad AlMahameed, MD, MPH, FACP, and Deepak L. Bhatt, MD, FACC, FSCAI, FESC, FACP
Supplement Editors:
Amjad AlMahameed, MD, and John R. Bartholomew, MD
Contents
The magnitude of the problem of peripheral arterial disease: Epidemiology and clinical significance
Mary McGrae McDermott, MD
Pathophysiology of peripheral arterial disease and risk factors for its development
John R. Bartholomew, MD, and Jeffrey W. Olin, DO
The clinical presentation of peripheral arterial disease and guidance for early recognition
Sean P. Lyden, MD, and Douglas Joseph, DO
Noninvasive diagnostic strategies for peripheral arterial disease
Susan M. Begelman, MD, and Michael R. Jaff, DO
Contemporary management of peripheral arterial disease: I. Cardiovascular risk-factor modification
Heather L. Gornik, MD, MHS, and Mark A. Creager, MD
Contemporary management of peripheral arterial disease: II. Improving walking distance and quality of life
Teresa L. Carman, MD, and Bernardo B. Fernandez, Jr., MD
Contemporary management of peripheral arterial disease: III. Endovascular and surgical management
Amjad AlMahameed, MD, MPH, FACP, and Deepak L. Bhatt, MD, FACC, FSCAI, FESC, FACP