User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Saddled with med school debt, yet left out of loan forgiveness plans
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.

The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.

The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
In a recently obtained plan by Politico, the Biden administration is zeroing in on a broad student loan forgiveness plan to be released imminently. The plan would broadly forgive $10,000 in federal student loans, including graduate and PLUS loans. However, there’s a rub: The plan restricts the forgiveness to those with incomes below $150,000.
This would unfairly exclude many in health care from receiving this forgiveness, an egregious oversight given how much health care providers have sacrificed during the pandemic.
What was proposed?
Previously, it was reported that the Biden administration was considering this same amount of forgiveness, but with plans to exclude borrowers by either career or income. Student loan payments have been on an extended CARES Act forbearance since March 2020, with payment resumption planned for Aug. 31. The administration has said that they would deliver a plan for further extensions before this date and have repeatedly teased including forgiveness.
Forgiveness for some ...
Forgiving $10,000 of federal student loans would relieve some 15 million borrowers of student debt, roughly one-third of the 45 million borrowers with debt.
This would provide a massive boost to these borrowers (who disproportionately are female, low-income, and non-White), many of whom were targeted by predatory institutions whose education didn’t offer any actual tangible benefit to their earnings. While this is a group that absolutely ought to have their loans forgiven, drawing an income line inappropriately restricts those in health care from receiving any forgiveness.
... But not for others
Someone making an annual gross income of $150,000 is in the 80th percentile of earners in the United States (for comparison, the top 1% took home more than $505,000 in 2021). What student loan borrowers make up the remaining 20%? Overwhelmingly, health care providers occupy that tier: physicians, dentists, veterinarians, and advanced-practice nurses.
These schools leave their graduates with some of the highest student loan burdens, with veterinarians, dentists, and physicians having the highest debt-to-income ratios of any professional careers.
Flat forgiveness is regressive
Forgiving any student debt is the right direction. Too may have fallen victim to an industry without quality control, appropriate regulation, or price control. Quite the opposite, the blank-check model of student loan financing has led to an arms race as it comes to capital improvements in university spending.

The price of medical schools has risen more than four times as fast as inflation over the past 30 years, with dental and veterinary schools and nursing education showing similarly exaggerated price increases. Trainees in these fields are more likely to have taken on six-figure debt, with average debt loads at graduation in the table below. While $10,000 will move the proverbial needle less for these borrowers, does that mean they should be excluded?
Health care workers’ income declines during the pandemic
Now, over 2½ years since the start of the COVID pandemic, multiple reports have demonstrated that health care workers have suffered a loss in income. This loss in income was never compensated for, as the Paycheck Protection Program and the individual economic stimuli typically excluded doctors and high earners.
COVID and the hazard tax
As a provider during the COVID-19 pandemic, I didn’t ask for hazard pay. I supported those who did but recognized their requests were more ceremonial than they were likely to be successful.
However, I flatly reject the idea that my fellow health care practitioners are not deserving of student loan forgiveness simply based on an arbitrary income threshold. Health care providers are saddled with high debt burden, have suffered lost income, and have given of themselves during a devastating pandemic, where more than 1 million perished in the United States.
Bottom line
Health care workers should not be excluded from student loan forgiveness. Sadly, the Biden administration has signaled that they are dropping career-based exclusions in favor of more broadly harmful income-based forgiveness restrictions. This will disproportionately harm physicians and other health care workers.
These practitioners have suffered financially as a result of working through the COVID pandemic; should they also be forced to shoulder another financial injury by being excluded from student loan forgiveness?
Dr. Palmer is the chief operating officer and cofounder of Panacea Financial. He is also a practicing pediatric hospitalist at Boston Children’s Hospital and is on faculty at Harvard Medical School, also in Boston.
A version of this article first appeared on Medscape.com.
Long COVID’s grip will likely tighten as infections continue
COVID-19 is far from done in the United States, with more than 111,000 new cases being recorded a day in the second week of August, according to Johns Hopkins University, and 625 deaths being reported every day. , a condition that already has affected between 7.7 million and 23 million Americans, according to U.S. government estimates.
“It is evident that long COVID is real, that it already impacts a substantial number of people, and that this number may continue to grow as new infections occur,” the U.S. Department of Health and Human Services (HHS) said in a research action plan released Aug. 4.
“We are heading towards a big problem on our hands,” says Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs Hospital in St. Louis. “It’s like if we are falling in a plane, hurtling towards the ground. It doesn’t matter at what speed we are falling; what matters is that we are all falling, and falling fast. It’s a real problem. We needed to bring attention to this, yesterday,” he said.
Bryan Lau, PhD, professor of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and co-lead of a long COVID study there, says whether it’s 5% of the 92 million officially recorded U.S. COVID-19 cases, or 30% – on the higher end of estimates – that means anywhere between 4.5 million and 27 million Americans will have the effects of long COVID.
Other experts put the estimates even higher.
“If we conservatively assume 100 million working-age adults have been infected, that implies 10 to 33 million may have long COVID,” Alice Burns, PhD, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, wrote in an analysis.
And even the Centers for Disease Control and Prevention says only a fraction of cases have been recorded.
That, in turn, means tens of millions of people who struggle to work, to get to school, and to take care of their families – and who will be making demands on an already stressed U.S. health care system.
The HHS said in its Aug. 4 report that long COVID could keep 1 million people a day out of work, with a loss of $50 billion in annual pay.
Dr. Lau said health workers and policymakers are woefully unprepared.
“If you have a family unit, and the mom or dad can’t work, or has trouble taking their child to activities, where does the question of support come into play? Where is there potential for food issues, or housing issues?” he asked. “I see the potential for the burden to be extremely large in that capacity.”
Dr. Lau said he has yet to see any strong estimates of how many cases of long COVID might develop. Because a person has to get COVID-19 to ultimately get long COVID, the two are linked. In other words, as COVID-19 cases rise, so will cases of long COVID, and vice versa.
Evidence from the Kaiser Family Foundation analysis suggests a significant impact on employment: Surveys showed more than half of adults with long COVID who worked before becoming infected are either out of work or working fewer hours. Conditions associated with long COVID – such as fatigue, malaise, or problems concentrating – limit people’s ability to work, even if they have jobs that allow for accommodations.
Two surveys of people with long COVID who had worked before becoming infected showed that between 22% and 27% of them were out of work after getting long COVID. In comparison, among all working-age adults in 2019, only 7% were out of work. Given the sheer number of working-age adults with long COVID, the effects on employment may be profound and are likely to involve more people over time. One study estimates that long COVID already accounts for 15% of unfilled jobs.
The most severe symptoms of long COVID include brain fog and heart complications, known to persist for weeks for months after a COVID-19 infection.
A study from the University of Norway published in Open Forum Infectious Diseases found 53% of people tested had at least one symptom of thinking problems 13 months after infection with COVID-19. According to the HHS’ latest report on long COVID, people with thinking problems, heart conditions, mobility issues, and other symptoms are going to need a considerable amount of care. Many will need lengthy periods of rehabilitation.
Dr. Al-Aly worries that long COVID has already severely affected the labor force and the job market, all while burdening the country’s health care system.
“While there are variations in how individuals respond and cope with long COVID, the unifying thread is that with the level of disability it causes, more people will be struggling to keep up with the demands of the workforce and more people will be out on disability than ever before,” he said.
Studies from Johns Hopkins and the University of Washington estimate that 5%-30% of people could get long COVID in the future. Projections beyond that are hazy.
“So far, all the studies we have done on long COVID have been reactionary. Much of the activism around long COVID has been patient led. We are seeing more and more people with lasting symptoms. We need our research to catch up,” Dr. Lau said.
Theo Vos, MD, PhD, professor of health sciences at University of Washington, Seattle, said the main reasons for the huge range of predictions are the variety of methods used, as well as differences in sample size. Also, much long COVID data is self-reported, making it difficult for epidemiologists to track.
“With self-reported data, you can’t plug people into a machine and say this is what they have or this is what they don’t have. At the population level, the only thing you can do is ask questions. There is no systematic way to define long COVID,” he said.
Dr. Vos’s most recent study, which is being peer-reviewed and revised, found that most people with long COVID have symptoms similar to those seen in other autoimmune diseases. But sometimes the immune system can overreact, causing the more severe symptoms, such as brain fog and heart problems, associated with long COVID.
One reason that researchers struggle to come up with numbers, said Dr. Al-Aly, is the rapid rise of new variants. These variants appear to sometimes cause less severe disease than previous ones, but it’s not clear whether that means different risks for long COVID.
“There’s a wide diversity in severity. Someone can have long COVID and be fully functional, while others are not functional at all. We still have a long way to go before we figure out why,” Dr. Lau said.
A version of this article first appeared on WebMD.com.
COVID-19 is far from done in the United States, with more than 111,000 new cases being recorded a day in the second week of August, according to Johns Hopkins University, and 625 deaths being reported every day. , a condition that already has affected between 7.7 million and 23 million Americans, according to U.S. government estimates.
“It is evident that long COVID is real, that it already impacts a substantial number of people, and that this number may continue to grow as new infections occur,” the U.S. Department of Health and Human Services (HHS) said in a research action plan released Aug. 4.
“We are heading towards a big problem on our hands,” says Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs Hospital in St. Louis. “It’s like if we are falling in a plane, hurtling towards the ground. It doesn’t matter at what speed we are falling; what matters is that we are all falling, and falling fast. It’s a real problem. We needed to bring attention to this, yesterday,” he said.
Bryan Lau, PhD, professor of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and co-lead of a long COVID study there, says whether it’s 5% of the 92 million officially recorded U.S. COVID-19 cases, or 30% – on the higher end of estimates – that means anywhere between 4.5 million and 27 million Americans will have the effects of long COVID.
Other experts put the estimates even higher.
“If we conservatively assume 100 million working-age adults have been infected, that implies 10 to 33 million may have long COVID,” Alice Burns, PhD, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, wrote in an analysis.
And even the Centers for Disease Control and Prevention says only a fraction of cases have been recorded.
That, in turn, means tens of millions of people who struggle to work, to get to school, and to take care of their families – and who will be making demands on an already stressed U.S. health care system.
The HHS said in its Aug. 4 report that long COVID could keep 1 million people a day out of work, with a loss of $50 billion in annual pay.
Dr. Lau said health workers and policymakers are woefully unprepared.
“If you have a family unit, and the mom or dad can’t work, or has trouble taking their child to activities, where does the question of support come into play? Where is there potential for food issues, or housing issues?” he asked. “I see the potential for the burden to be extremely large in that capacity.”
Dr. Lau said he has yet to see any strong estimates of how many cases of long COVID might develop. Because a person has to get COVID-19 to ultimately get long COVID, the two are linked. In other words, as COVID-19 cases rise, so will cases of long COVID, and vice versa.
Evidence from the Kaiser Family Foundation analysis suggests a significant impact on employment: Surveys showed more than half of adults with long COVID who worked before becoming infected are either out of work or working fewer hours. Conditions associated with long COVID – such as fatigue, malaise, or problems concentrating – limit people’s ability to work, even if they have jobs that allow for accommodations.
Two surveys of people with long COVID who had worked before becoming infected showed that between 22% and 27% of them were out of work after getting long COVID. In comparison, among all working-age adults in 2019, only 7% were out of work. Given the sheer number of working-age adults with long COVID, the effects on employment may be profound and are likely to involve more people over time. One study estimates that long COVID already accounts for 15% of unfilled jobs.
The most severe symptoms of long COVID include brain fog and heart complications, known to persist for weeks for months after a COVID-19 infection.
A study from the University of Norway published in Open Forum Infectious Diseases found 53% of people tested had at least one symptom of thinking problems 13 months after infection with COVID-19. According to the HHS’ latest report on long COVID, people with thinking problems, heart conditions, mobility issues, and other symptoms are going to need a considerable amount of care. Many will need lengthy periods of rehabilitation.
Dr. Al-Aly worries that long COVID has already severely affected the labor force and the job market, all while burdening the country’s health care system.
“While there are variations in how individuals respond and cope with long COVID, the unifying thread is that with the level of disability it causes, more people will be struggling to keep up with the demands of the workforce and more people will be out on disability than ever before,” he said.
Studies from Johns Hopkins and the University of Washington estimate that 5%-30% of people could get long COVID in the future. Projections beyond that are hazy.
“So far, all the studies we have done on long COVID have been reactionary. Much of the activism around long COVID has been patient led. We are seeing more and more people with lasting symptoms. We need our research to catch up,” Dr. Lau said.
Theo Vos, MD, PhD, professor of health sciences at University of Washington, Seattle, said the main reasons for the huge range of predictions are the variety of methods used, as well as differences in sample size. Also, much long COVID data is self-reported, making it difficult for epidemiologists to track.
“With self-reported data, you can’t plug people into a machine and say this is what they have or this is what they don’t have. At the population level, the only thing you can do is ask questions. There is no systematic way to define long COVID,” he said.
Dr. Vos’s most recent study, which is being peer-reviewed and revised, found that most people with long COVID have symptoms similar to those seen in other autoimmune diseases. But sometimes the immune system can overreact, causing the more severe symptoms, such as brain fog and heart problems, associated with long COVID.
One reason that researchers struggle to come up with numbers, said Dr. Al-Aly, is the rapid rise of new variants. These variants appear to sometimes cause less severe disease than previous ones, but it’s not clear whether that means different risks for long COVID.
“There’s a wide diversity in severity. Someone can have long COVID and be fully functional, while others are not functional at all. We still have a long way to go before we figure out why,” Dr. Lau said.
A version of this article first appeared on WebMD.com.
COVID-19 is far from done in the United States, with more than 111,000 new cases being recorded a day in the second week of August, according to Johns Hopkins University, and 625 deaths being reported every day. , a condition that already has affected between 7.7 million and 23 million Americans, according to U.S. government estimates.
“It is evident that long COVID is real, that it already impacts a substantial number of people, and that this number may continue to grow as new infections occur,” the U.S. Department of Health and Human Services (HHS) said in a research action plan released Aug. 4.
“We are heading towards a big problem on our hands,” says Ziyad Al-Aly, MD, chief of research and development at the Veterans Affairs Hospital in St. Louis. “It’s like if we are falling in a plane, hurtling towards the ground. It doesn’t matter at what speed we are falling; what matters is that we are all falling, and falling fast. It’s a real problem. We needed to bring attention to this, yesterday,” he said.
Bryan Lau, PhD, professor of epidemiology at Johns Hopkins Bloomberg School of Public Health, Baltimore, and co-lead of a long COVID study there, says whether it’s 5% of the 92 million officially recorded U.S. COVID-19 cases, or 30% – on the higher end of estimates – that means anywhere between 4.5 million and 27 million Americans will have the effects of long COVID.
Other experts put the estimates even higher.
“If we conservatively assume 100 million working-age adults have been infected, that implies 10 to 33 million may have long COVID,” Alice Burns, PhD, associate director for the Kaiser Family Foundation’s Program on Medicaid and the Uninsured, wrote in an analysis.
And even the Centers for Disease Control and Prevention says only a fraction of cases have been recorded.
That, in turn, means tens of millions of people who struggle to work, to get to school, and to take care of their families – and who will be making demands on an already stressed U.S. health care system.
The HHS said in its Aug. 4 report that long COVID could keep 1 million people a day out of work, with a loss of $50 billion in annual pay.
Dr. Lau said health workers and policymakers are woefully unprepared.
“If you have a family unit, and the mom or dad can’t work, or has trouble taking their child to activities, where does the question of support come into play? Where is there potential for food issues, or housing issues?” he asked. “I see the potential for the burden to be extremely large in that capacity.”
Dr. Lau said he has yet to see any strong estimates of how many cases of long COVID might develop. Because a person has to get COVID-19 to ultimately get long COVID, the two are linked. In other words, as COVID-19 cases rise, so will cases of long COVID, and vice versa.
Evidence from the Kaiser Family Foundation analysis suggests a significant impact on employment: Surveys showed more than half of adults with long COVID who worked before becoming infected are either out of work or working fewer hours. Conditions associated with long COVID – such as fatigue, malaise, or problems concentrating – limit people’s ability to work, even if they have jobs that allow for accommodations.
Two surveys of people with long COVID who had worked before becoming infected showed that between 22% and 27% of them were out of work after getting long COVID. In comparison, among all working-age adults in 2019, only 7% were out of work. Given the sheer number of working-age adults with long COVID, the effects on employment may be profound and are likely to involve more people over time. One study estimates that long COVID already accounts for 15% of unfilled jobs.
The most severe symptoms of long COVID include brain fog and heart complications, known to persist for weeks for months after a COVID-19 infection.
A study from the University of Norway published in Open Forum Infectious Diseases found 53% of people tested had at least one symptom of thinking problems 13 months after infection with COVID-19. According to the HHS’ latest report on long COVID, people with thinking problems, heart conditions, mobility issues, and other symptoms are going to need a considerable amount of care. Many will need lengthy periods of rehabilitation.
Dr. Al-Aly worries that long COVID has already severely affected the labor force and the job market, all while burdening the country’s health care system.
“While there are variations in how individuals respond and cope with long COVID, the unifying thread is that with the level of disability it causes, more people will be struggling to keep up with the demands of the workforce and more people will be out on disability than ever before,” he said.
Studies from Johns Hopkins and the University of Washington estimate that 5%-30% of people could get long COVID in the future. Projections beyond that are hazy.
“So far, all the studies we have done on long COVID have been reactionary. Much of the activism around long COVID has been patient led. We are seeing more and more people with lasting symptoms. We need our research to catch up,” Dr. Lau said.
Theo Vos, MD, PhD, professor of health sciences at University of Washington, Seattle, said the main reasons for the huge range of predictions are the variety of methods used, as well as differences in sample size. Also, much long COVID data is self-reported, making it difficult for epidemiologists to track.
“With self-reported data, you can’t plug people into a machine and say this is what they have or this is what they don’t have. At the population level, the only thing you can do is ask questions. There is no systematic way to define long COVID,” he said.
Dr. Vos’s most recent study, which is being peer-reviewed and revised, found that most people with long COVID have symptoms similar to those seen in other autoimmune diseases. But sometimes the immune system can overreact, causing the more severe symptoms, such as brain fog and heart problems, associated with long COVID.
One reason that researchers struggle to come up with numbers, said Dr. Al-Aly, is the rapid rise of new variants. These variants appear to sometimes cause less severe disease than previous ones, but it’s not clear whether that means different risks for long COVID.
“There’s a wide diversity in severity. Someone can have long COVID and be fully functional, while others are not functional at all. We still have a long way to go before we figure out why,” Dr. Lau said.
A version of this article first appeared on WebMD.com.
Pro-life ob.gyns. say Dobbs not end of abortion struggle
After 49 years of labor, abortion foes received the ultimate victory in June when the United States Supreme Court struck down a federal right to terminate pregnancy. Among those most heartened by the ruling was a small organization of doctors who specialize in women’s reproductive health. The group’s leader, while grateful for the win, isn’t ready for a curtain call. Instead, she sees her task as moving from a national stage to 50 regional ones.
The decision in Dobbs v. Jackson, which overturned a woman’s constitutional right to obtain an abortion, was the biggest but not final quarry for the American Association of Pro-Life Obstetricians and Gynecologists (AAPLOG). “It actually doesn’t change anything except to turn the whole discussion on abortion back to the states, which in our opinion is where it should have been 50 years ago,” Donna Harrison, MD, the group’s chief executive officer, said in a recent interview.
Dr. Harrison, an obstetrician-gynecologist and adjunct professor of bioethics at Trinity International University in Deerfield, Ind., said she was proud of “our small role in bringing science” to the top court’s attention, noting that the ruling incorporated some of AAPLOG’s medical arguments in reversing Roe v. Wade, the 1973 decision that created a right to abortion – and prompted her group’s founding. The ruling, for instance, agreed – in a departure from the generally accepted science – that a fetus is viable at 15 weeks, and the procedure is risky for mothers thereafter. “You could congratulate us for perseverance and for bringing that information, which has been in the peer-reviewed literature for a long time, to the justices’ attention,” she said.
Dr. Harrison said she was pleased that the Supreme Court agreed with the “science” that guided its decision to overturn Roe. That the court was willing to embrace that evidence troubles the American College of Obstetricians and Gynecologists (ACOG), the nation’s leading professional group for reproductive health experts.
Defending the ‘second patient’
AAPLOG operates under the belief that life begins at the moment of fertilization, at which point “we defend the life of our second patient, the human being in the womb,” Dr. Harrison said. “For a very long time, ob.gyns. who valued both patients were not given a voice, and I think now we’re finding our voice.” The group will continue supporting abortion restrictions at the state level.
AAPLOG, with 6,000 members, was considered a “special interest” group within ACOG until the college discontinued such subgroups in 2013. ACOG, numbering 60,000 members, calls the Dobbs ruling “a huge step back for women and everyone who is seeking access to ob.gyn. care,” said Molly Meegan, JD, ACOG’s chief legal officer. Ms. Meegan expressed concern over the newfound influence of AAPLOG, which she called “a single-issue, single-topic, single-advocacy organization.”
Pro-choice groups, including ACOG, worry that the reversal of Roe has provided AAPLOG with an undeserved veneer of medical expertise. The decision also allowed judges and legislators to “insert themselves into nuanced and complex situations” they know little about and will rely on groups like AAPLOG to exert influence, Ms. Meegan said.
In turn, Dr. Harrison described ACOG as engaging in “rabid, pro-abortion activism.”
The number of abortions in the United States had steadily declined from a peak of 1.4 million per year in 1990 until 2017, after which it has risen slightly. In 2019, according to the U.S. Centers for Disease Control and Prevention, 625,000 abortions occurred nationally. Of those, 42.3% were medication abortions performed in the first 9 weeks, using a combination of the drugs mifepristone and misoprostol. Medication abortions now account for more than half of all pregnancy terminations in the United States, according to the Guttmacher Institute.
Dr. Harrison said that medication abortions put women at an elevated risk of serious, sometimes deadly bleeding, while ACOG points to evidence that the risk of childbirth to women is significantly higher. She also is no fan of Plan B, the “morning after” pill, which is available to women without having to consult a doctor. She described abortifacients as “a huge danger to women being harmed” by medications available over the counter.
In Dr. Harrison’s view, the 10-year-old Ohio girl who traveled to Indiana to obtain an abortion after she became pregnant as the result of rape should have continued her pregnancy. So, too, should young girls who are the victims of incest. “Incest is a horrific crime,” she said, “but aborting a girl because of incest doesn’t make her un-raped. It just adds another trauma.”
When told of Dr. Harrison’s comment, Ms. Meegan paused for 5 seconds before saying, “I think that statement speaks for itself.”
Louise Perkins King, MD, JD, an ob.gyn. and director of reproductive bioethics at Harvard Medical School, Boston, said she had the “horrific” experience of delivering a baby to an 11-year-old girl.
“Children are not fully developed, and they should not be having children,” Dr. King said.
Anne-Marie E. Amies Oelschlager, MD, vice chair of ACOG’s Clinical Consensus Committee and an ob.gyn. at Seattle Children’s in Washington, said in a statement that adolescents who are sexually assaulted are at extremely high risk of depression and posttraumatic stress disorder. “Do we expect a fourth-grader to carry a pregnancy to term, deliver, and expect that child to carry on after this horror?,” she asked.
Dr. Harrison dismissed such concerns. “Somehow abortion is a mental health treatment? Abortion doesn’t treat mental health problems,” she said. “Is there any proof that aborting in those circumstances improves their mental health? I would tell you there is very little research about it. …There are human beings involved, and this child who was raped, who also had a child, who was a human being, who is no longer.”
Dr. Harrison said the Dobbs decision would have no effect on up to 93% of ob.gyns. who don’t perform abortions. Dr. King said the reason that most don’t perform the procedure is the “stigma” attached to abortion. “It’s still frowned upon,” she said. “We don’t talk about it as health care.”
Ms. Meegan added that ob.gyns. are fearful in the wake of the Dobbs decision because “they might find themselves subject to civil and criminal penalties.”
Dr. Harrison said that Roe was always a political decision and the science was always behind AAPLOG – something both Ms. Meegan and Dr. King dispute. Ms. Meegan and Dr. King said they are concerned about the chilling effects on both women and their clinicians, especially with laws that prevent referrals and travel to other states.
“You can’t compel me to give blood or bone marrow,” Dr. King said. “You can’t even compel me to give my hair for somebody, and you can’t compel me to give an organ. And all of a sudden when I’m pregnant, all my rights are out the window?”
A version of this article first appeared on Medscape.com.
After 49 years of labor, abortion foes received the ultimate victory in June when the United States Supreme Court struck down a federal right to terminate pregnancy. Among those most heartened by the ruling was a small organization of doctors who specialize in women’s reproductive health. The group’s leader, while grateful for the win, isn’t ready for a curtain call. Instead, she sees her task as moving from a national stage to 50 regional ones.
The decision in Dobbs v. Jackson, which overturned a woman’s constitutional right to obtain an abortion, was the biggest but not final quarry for the American Association of Pro-Life Obstetricians and Gynecologists (AAPLOG). “It actually doesn’t change anything except to turn the whole discussion on abortion back to the states, which in our opinion is where it should have been 50 years ago,” Donna Harrison, MD, the group’s chief executive officer, said in a recent interview.
Dr. Harrison, an obstetrician-gynecologist and adjunct professor of bioethics at Trinity International University in Deerfield, Ind., said she was proud of “our small role in bringing science” to the top court’s attention, noting that the ruling incorporated some of AAPLOG’s medical arguments in reversing Roe v. Wade, the 1973 decision that created a right to abortion – and prompted her group’s founding. The ruling, for instance, agreed – in a departure from the generally accepted science – that a fetus is viable at 15 weeks, and the procedure is risky for mothers thereafter. “You could congratulate us for perseverance and for bringing that information, which has been in the peer-reviewed literature for a long time, to the justices’ attention,” she said.
Dr. Harrison said she was pleased that the Supreme Court agreed with the “science” that guided its decision to overturn Roe. That the court was willing to embrace that evidence troubles the American College of Obstetricians and Gynecologists (ACOG), the nation’s leading professional group for reproductive health experts.
Defending the ‘second patient’
AAPLOG operates under the belief that life begins at the moment of fertilization, at which point “we defend the life of our second patient, the human being in the womb,” Dr. Harrison said. “For a very long time, ob.gyns. who valued both patients were not given a voice, and I think now we’re finding our voice.” The group will continue supporting abortion restrictions at the state level.
AAPLOG, with 6,000 members, was considered a “special interest” group within ACOG until the college discontinued such subgroups in 2013. ACOG, numbering 60,000 members, calls the Dobbs ruling “a huge step back for women and everyone who is seeking access to ob.gyn. care,” said Molly Meegan, JD, ACOG’s chief legal officer. Ms. Meegan expressed concern over the newfound influence of AAPLOG, which she called “a single-issue, single-topic, single-advocacy organization.”
Pro-choice groups, including ACOG, worry that the reversal of Roe has provided AAPLOG with an undeserved veneer of medical expertise. The decision also allowed judges and legislators to “insert themselves into nuanced and complex situations” they know little about and will rely on groups like AAPLOG to exert influence, Ms. Meegan said.
In turn, Dr. Harrison described ACOG as engaging in “rabid, pro-abortion activism.”
The number of abortions in the United States had steadily declined from a peak of 1.4 million per year in 1990 until 2017, after which it has risen slightly. In 2019, according to the U.S. Centers for Disease Control and Prevention, 625,000 abortions occurred nationally. Of those, 42.3% were medication abortions performed in the first 9 weeks, using a combination of the drugs mifepristone and misoprostol. Medication abortions now account for more than half of all pregnancy terminations in the United States, according to the Guttmacher Institute.
Dr. Harrison said that medication abortions put women at an elevated risk of serious, sometimes deadly bleeding, while ACOG points to evidence that the risk of childbirth to women is significantly higher. She also is no fan of Plan B, the “morning after” pill, which is available to women without having to consult a doctor. She described abortifacients as “a huge danger to women being harmed” by medications available over the counter.
In Dr. Harrison’s view, the 10-year-old Ohio girl who traveled to Indiana to obtain an abortion after she became pregnant as the result of rape should have continued her pregnancy. So, too, should young girls who are the victims of incest. “Incest is a horrific crime,” she said, “but aborting a girl because of incest doesn’t make her un-raped. It just adds another trauma.”
When told of Dr. Harrison’s comment, Ms. Meegan paused for 5 seconds before saying, “I think that statement speaks for itself.”
Louise Perkins King, MD, JD, an ob.gyn. and director of reproductive bioethics at Harvard Medical School, Boston, said she had the “horrific” experience of delivering a baby to an 11-year-old girl.
“Children are not fully developed, and they should not be having children,” Dr. King said.
Anne-Marie E. Amies Oelschlager, MD, vice chair of ACOG’s Clinical Consensus Committee and an ob.gyn. at Seattle Children’s in Washington, said in a statement that adolescents who are sexually assaulted are at extremely high risk of depression and posttraumatic stress disorder. “Do we expect a fourth-grader to carry a pregnancy to term, deliver, and expect that child to carry on after this horror?,” she asked.
Dr. Harrison dismissed such concerns. “Somehow abortion is a mental health treatment? Abortion doesn’t treat mental health problems,” she said. “Is there any proof that aborting in those circumstances improves their mental health? I would tell you there is very little research about it. …There are human beings involved, and this child who was raped, who also had a child, who was a human being, who is no longer.”
Dr. Harrison said the Dobbs decision would have no effect on up to 93% of ob.gyns. who don’t perform abortions. Dr. King said the reason that most don’t perform the procedure is the “stigma” attached to abortion. “It’s still frowned upon,” she said. “We don’t talk about it as health care.”
Ms. Meegan added that ob.gyns. are fearful in the wake of the Dobbs decision because “they might find themselves subject to civil and criminal penalties.”
Dr. Harrison said that Roe was always a political decision and the science was always behind AAPLOG – something both Ms. Meegan and Dr. King dispute. Ms. Meegan and Dr. King said they are concerned about the chilling effects on both women and their clinicians, especially with laws that prevent referrals and travel to other states.
“You can’t compel me to give blood or bone marrow,” Dr. King said. “You can’t even compel me to give my hair for somebody, and you can’t compel me to give an organ. And all of a sudden when I’m pregnant, all my rights are out the window?”
A version of this article first appeared on Medscape.com.
After 49 years of labor, abortion foes received the ultimate victory in June when the United States Supreme Court struck down a federal right to terminate pregnancy. Among those most heartened by the ruling was a small organization of doctors who specialize in women’s reproductive health. The group’s leader, while grateful for the win, isn’t ready for a curtain call. Instead, she sees her task as moving from a national stage to 50 regional ones.
The decision in Dobbs v. Jackson, which overturned a woman’s constitutional right to obtain an abortion, was the biggest but not final quarry for the American Association of Pro-Life Obstetricians and Gynecologists (AAPLOG). “It actually doesn’t change anything except to turn the whole discussion on abortion back to the states, which in our opinion is where it should have been 50 years ago,” Donna Harrison, MD, the group’s chief executive officer, said in a recent interview.
Dr. Harrison, an obstetrician-gynecologist and adjunct professor of bioethics at Trinity International University in Deerfield, Ind., said she was proud of “our small role in bringing science” to the top court’s attention, noting that the ruling incorporated some of AAPLOG’s medical arguments in reversing Roe v. Wade, the 1973 decision that created a right to abortion – and prompted her group’s founding. The ruling, for instance, agreed – in a departure from the generally accepted science – that a fetus is viable at 15 weeks, and the procedure is risky for mothers thereafter. “You could congratulate us for perseverance and for bringing that information, which has been in the peer-reviewed literature for a long time, to the justices’ attention,” she said.
Dr. Harrison said she was pleased that the Supreme Court agreed with the “science” that guided its decision to overturn Roe. That the court was willing to embrace that evidence troubles the American College of Obstetricians and Gynecologists (ACOG), the nation’s leading professional group for reproductive health experts.
Defending the ‘second patient’
AAPLOG operates under the belief that life begins at the moment of fertilization, at which point “we defend the life of our second patient, the human being in the womb,” Dr. Harrison said. “For a very long time, ob.gyns. who valued both patients were not given a voice, and I think now we’re finding our voice.” The group will continue supporting abortion restrictions at the state level.
AAPLOG, with 6,000 members, was considered a “special interest” group within ACOG until the college discontinued such subgroups in 2013. ACOG, numbering 60,000 members, calls the Dobbs ruling “a huge step back for women and everyone who is seeking access to ob.gyn. care,” said Molly Meegan, JD, ACOG’s chief legal officer. Ms. Meegan expressed concern over the newfound influence of AAPLOG, which she called “a single-issue, single-topic, single-advocacy organization.”
Pro-choice groups, including ACOG, worry that the reversal of Roe has provided AAPLOG with an undeserved veneer of medical expertise. The decision also allowed judges and legislators to “insert themselves into nuanced and complex situations” they know little about and will rely on groups like AAPLOG to exert influence, Ms. Meegan said.
In turn, Dr. Harrison described ACOG as engaging in “rabid, pro-abortion activism.”
The number of abortions in the United States had steadily declined from a peak of 1.4 million per year in 1990 until 2017, after which it has risen slightly. In 2019, according to the U.S. Centers for Disease Control and Prevention, 625,000 abortions occurred nationally. Of those, 42.3% were medication abortions performed in the first 9 weeks, using a combination of the drugs mifepristone and misoprostol. Medication abortions now account for more than half of all pregnancy terminations in the United States, according to the Guttmacher Institute.
Dr. Harrison said that medication abortions put women at an elevated risk of serious, sometimes deadly bleeding, while ACOG points to evidence that the risk of childbirth to women is significantly higher. She also is no fan of Plan B, the “morning after” pill, which is available to women without having to consult a doctor. She described abortifacients as “a huge danger to women being harmed” by medications available over the counter.
In Dr. Harrison’s view, the 10-year-old Ohio girl who traveled to Indiana to obtain an abortion after she became pregnant as the result of rape should have continued her pregnancy. So, too, should young girls who are the victims of incest. “Incest is a horrific crime,” she said, “but aborting a girl because of incest doesn’t make her un-raped. It just adds another trauma.”
When told of Dr. Harrison’s comment, Ms. Meegan paused for 5 seconds before saying, “I think that statement speaks for itself.”
Louise Perkins King, MD, JD, an ob.gyn. and director of reproductive bioethics at Harvard Medical School, Boston, said she had the “horrific” experience of delivering a baby to an 11-year-old girl.
“Children are not fully developed, and they should not be having children,” Dr. King said.
Anne-Marie E. Amies Oelschlager, MD, vice chair of ACOG’s Clinical Consensus Committee and an ob.gyn. at Seattle Children’s in Washington, said in a statement that adolescents who are sexually assaulted are at extremely high risk of depression and posttraumatic stress disorder. “Do we expect a fourth-grader to carry a pregnancy to term, deliver, and expect that child to carry on after this horror?,” she asked.
Dr. Harrison dismissed such concerns. “Somehow abortion is a mental health treatment? Abortion doesn’t treat mental health problems,” she said. “Is there any proof that aborting in those circumstances improves their mental health? I would tell you there is very little research about it. …There are human beings involved, and this child who was raped, who also had a child, who was a human being, who is no longer.”
Dr. Harrison said the Dobbs decision would have no effect on up to 93% of ob.gyns. who don’t perform abortions. Dr. King said the reason that most don’t perform the procedure is the “stigma” attached to abortion. “It’s still frowned upon,” she said. “We don’t talk about it as health care.”
Ms. Meegan added that ob.gyns. are fearful in the wake of the Dobbs decision because “they might find themselves subject to civil and criminal penalties.”
Dr. Harrison said that Roe was always a political decision and the science was always behind AAPLOG – something both Ms. Meegan and Dr. King dispute. Ms. Meegan and Dr. King said they are concerned about the chilling effects on both women and their clinicians, especially with laws that prevent referrals and travel to other states.
“You can’t compel me to give blood or bone marrow,” Dr. King said. “You can’t even compel me to give my hair for somebody, and you can’t compel me to give an organ. And all of a sudden when I’m pregnant, all my rights are out the window?”
A version of this article first appeared on Medscape.com.
Does hidradenitis suppurativa worsen during pregnancy?
PORTLAND, ORE. – The recurrent boils, abscesses, and nodules of the chronic inflammatory skin condition hidradenitis suppurativa (HS) may improve during pregnancy for a subset of women, but for many, pregnancy does not change the disease course and may worsen symptoms.
In addition, HS appears to be a risk factor for adverse pregnancy and maternal outcomes.
“This is relevant, because in the United States, HS disproportionately impacts women compared with men by a ratio of about 3:1,” Jennifer Hsiao, MD, said at the annual meeting of the Pacific Dermatologic Association.
“Also, the highest prevalence of HS is among people in their 20s and 30s, so in their practice, clinicians will encounter female patients with HS who are either pregnant or actively thinking about getting pregnant,” she said.
During a wide-ranging presentation, Dr. Hsiao of the department of dermatology at the University of Southern California, Los Angeles, described the impact of pregnancy on HS, identified appropriate treatment options for this population of patients, and discussed HS comorbidities that may be exacerbated during pregnancy.
She began by noting that levels of progesterone and estrogen both rise during pregnancy. Progesterone is known to suppress development and function of Th1 and Th17 T cells, but the effect of estrogen on inflammation is less well known. At the same time, serum levels of interleukin (IL)-1 receptor antagonist and soluble TNF-alpha receptor both increase during pregnancy.
“This would lead to serum IL-1 and TNF-alpha falling, sort of like the way that we give anti–IL-1 and TNF blockers as HS treatments,” she explained. “So, presumably that might be helpful during HS in pregnancy. On the flip side, pregnancy weight gain can exacerbate HS, with increased friction between skin folds. In addition, just having more adipocytes can promote secretion of proinflammatory cytokines like TNF-alpha.”
To better understand the effect of pregnancy on patients with HS, Dr. Hsiao and colleagues conducted a systematic review and meta-analysis on the topic published in Dermatology. They included eight studies in which a total of 672 patients self-reported their HS disease course during pregnancy and 164 self-reported whether they had a postpartum HS flare or not. On pooled analyses, HS improved in 24% of patients but worsened in 20%. In addition, 60% of patients experienced a postpartum flare.
“So, at this point in time, based on the literature, it would be fair to tell your patient that during pregnancy, HS has a mixed response,” Dr. Hsiao said. “About 25% may have improvement, but for the rest, HS symptoms may be unchanged or even worsen. That’s why it’s so important to be in contact with your pregnant patients, because not only may they have to stay on treatment, but they might also have to escalate [their treatment] during pregnancy.”
Lifestyle modifications to discuss with pregnant HS patients include appropriate weight gain during pregnancy, smoking cessation, and avoidance of tight-fitting clothing, “since friction can make things worse,” she said. Topical antibiotics safe to use during pregnancy for patients with mild HS include clindamycin 1%, erythromycin 2%, and metronidazole 0.75% applied twice per day to active lesions, she continued.
As for systemic therapies, some data exist to support the use of metformin 500 mg once daily, titrating up to twice or – if needed and tolerated – three times daily for patients with mild to moderate HS, she said, referencing a paper published in the Journal of the European Academy of Dermatology and Venereology.
Zinc gluconate is another potential option. Of 22 nonpregnant HS patients with Hurley stage I-II disease who were treated with zinc gluconate 90 mg daily, 8 had a complete remission of HS and 14 had partial remission, according to a report in Dermatology.
“Zinc supplementation of up to 50 mg daily has shown no effect on neonatal or maternal outcomes at birth based on existing medical literature,” Dr. Hsiao added.
Among antibiotics, injections of intralesional Kenalog 5-10 mg/mL have been shown to decrease pain and inflammation in acute HS lesions and are unlikely to pose significant risks during pregnancy, but a course of systemic antibiotics may be warranted in moderate to severe disease, she said. These include, but are not limited to, clindamycin, erythromycin base, cephalexin, or metronidazole.
“In addition, some of my HS colleagues and I will also use other antibiotics such as Augmentin [amoxicillin/clavulanate] or cefdinir for HS and these are also generally considered safe to use in pregnancy,” she said. “Caution is advised with using rifampin, dapsone, and moxifloxacin during pregnancy.”
As for biologic agents, the first-line option is adalimumab, which is currently the only Food and Drug Administration–approved treatment for HS.
“There is also good efficacy data for infliximab,” she said. “Etanercept has less placental transfer than adalimumab or infliximab so it’s safer to use in pregnancy, but it has inconsistent data for efficacy in HS, so I would generally avoid using it to treat HS and reach for adalimumab or infliximab instead.”
Data on TNF-alpha inhibitors from the GI and rheumatology literature have demonstrated that there is minimal placental transport of maternal antibodies during the first two trimesters of pregnancy.
“It’s at the beginning of the third trimester that the placental transfer of antibodies picks up,” she said. “At that point in time, you can have a discussion with the patient: do you want to stay on treatment and treat through, or do you want to consider being taken off the medication? I think this is a discussion that needs to be had, because let’s say you peel off adalimumab or infliximab and they have severe HS flares. I’m not sure that leads to a better outcome. I usually treat through for my pregnant patients.”
To better understand clinician practice patterns on the management of HS in pregnancy, Dr. Hsiao and Erin Collier, MD, MPH, of University of California, Los Angeles, and colleagues distributed an online survey to HS specialists in North America. They reported the findings in the International Journal of Women’s Dermatology.
Of the 49 respondents, 36 (73%) directed an HS specialty clinic and 29 (59%) reported having prescribed or continued a biologic agent in a pregnant HS patient. The top three biologics prescribed were adalimumab (90%), infliximab (41%), and certolizumab pegol (34%). Dr. Hsiao noted that certolizumab pegol is a pegylated anti-TNF, so it lacks an Fc region on the medication.
“This means that it cannot be actively transported by the neonatal Fc receptor on the placenta, thus resulting in minimal placental transmission,” she said. “The main issue is that there is little data on its efficacy in HS, but it’s a reasonable option to consider in a pregnant patient, especially in a patient with severe HS who asks, ‘what’s the safest biologic that I can go on?’ But you’d have to discuss with the patient that in terms of efficacy data, there is much less in the literature compared to adalimumab or infliximab.”
Breastfeeding while on anti–TNF-alpha biologics is considered safe. “There are minimal amounts of medication in breast milk,” she said. “If any gets through, infant gastric digestion is thought to take care of the rest. Of note, babies born to mothers who are continually treated with biologic agents should not be given live vaccinations for 6 months after birth.”
In a single-center study, Dr. Hsiao and colleagues retrospectively examined pregnancy complications, pregnancy outcomes, and neonatal outcomes in patients with HS. The study population included 202 pregnancies in 127 HS patients. Of 134 babies born to mothers with HS, 74% were breastfed and 24% were bottle-fed, and presence of HS lesions on the breast was significantly associated with not breastfeeding.
“So, when we see these patients, if moms decide to breastfeed and they have lesions on the breast, it would be helpful to discuss expectations and perhaps treat HS breast lesions early, so the breastfeeding process may go more smoothly for them after they deliver,” said Dr. Hsiao, who is one of the editors of the textbook “A Comprehensive Guide to Hidradenitis Suppurativa” (Elsevier, 2021). Safety-related resources that she recommends for clinicians include Mother to Baby and the Drugs and Lactation Database (LactMed).
Dr. Hsiao concluded her presentation by spotlighting the influence of pregnancy on HS comorbidities. Patients with HS already have a higher prevalence of depression and anxiety compared to controls. “Pregnancy can exacerbate underlying mood disorders in patients,” she said. “That’s why monitoring the patient’s mood and coordinating mental health care with the patient’s primary care physician and ob.gyn. is important.”
In addition, pregnancy-related changes in body mass index, blood pressure, lipid metabolism, and glucose tolerance trend toward changes seen in metabolic syndrome, she said, and HS patients are already at higher risk of metabolic syndrome compared with the general population.
HS may also compromise a patient’s ability to have a healthy pregnancy. Dr. Hsiao worked with Amit Garg, MD, and colleagues on a study that drew from the IBM MarketScan Commercial Claims Database to evaluate adverse pregnancy and maternal outcomes in women with HS between Jan. 1, 2011, and Sept. 30, 2015.
After the researchers adjusted for age, race, smoking status, and other comorbidities, they found that HS pregnancies were independently associated with spontaneous abortion (odds ratio, 1.20), gestational diabetes (OR, 1.26), and cesarean section (OR, 1.09). The findings were published in the Journal of the American Academy of Dermatology.
A separate study that used the same database found comparable results, also published in the Journal of the American Academy of Dermatology. “What I say to patients right now is, ‘there are many women with HS who have healthy pregnancies and deliver healthy babies, but HS could be a risk factor for a higher-risk pregnancy.’ It’s important that these patients are established with an ob.gyn. and are closely monitored to make sure that we optimize their care and give them the best outcome possible for mom and baby.”
Dr. Hsiao disclosed that she is on the board of directors for the Hidradenitis Suppurativa Foundation. She has also served as an advisor for Novartis, UCB, and Boehringer Ingelheim and as a speaker and advisor for AbbVie.
PORTLAND, ORE. – The recurrent boils, abscesses, and nodules of the chronic inflammatory skin condition hidradenitis suppurativa (HS) may improve during pregnancy for a subset of women, but for many, pregnancy does not change the disease course and may worsen symptoms.
In addition, HS appears to be a risk factor for adverse pregnancy and maternal outcomes.
“This is relevant, because in the United States, HS disproportionately impacts women compared with men by a ratio of about 3:1,” Jennifer Hsiao, MD, said at the annual meeting of the Pacific Dermatologic Association.
“Also, the highest prevalence of HS is among people in their 20s and 30s, so in their practice, clinicians will encounter female patients with HS who are either pregnant or actively thinking about getting pregnant,” she said.
During a wide-ranging presentation, Dr. Hsiao of the department of dermatology at the University of Southern California, Los Angeles, described the impact of pregnancy on HS, identified appropriate treatment options for this population of patients, and discussed HS comorbidities that may be exacerbated during pregnancy.
She began by noting that levels of progesterone and estrogen both rise during pregnancy. Progesterone is known to suppress development and function of Th1 and Th17 T cells, but the effect of estrogen on inflammation is less well known. At the same time, serum levels of interleukin (IL)-1 receptor antagonist and soluble TNF-alpha receptor both increase during pregnancy.
“This would lead to serum IL-1 and TNF-alpha falling, sort of like the way that we give anti–IL-1 and TNF blockers as HS treatments,” she explained. “So, presumably that might be helpful during HS in pregnancy. On the flip side, pregnancy weight gain can exacerbate HS, with increased friction between skin folds. In addition, just having more adipocytes can promote secretion of proinflammatory cytokines like TNF-alpha.”
To better understand the effect of pregnancy on patients with HS, Dr. Hsiao and colleagues conducted a systematic review and meta-analysis on the topic published in Dermatology. They included eight studies in which a total of 672 patients self-reported their HS disease course during pregnancy and 164 self-reported whether they had a postpartum HS flare or not. On pooled analyses, HS improved in 24% of patients but worsened in 20%. In addition, 60% of patients experienced a postpartum flare.
“So, at this point in time, based on the literature, it would be fair to tell your patient that during pregnancy, HS has a mixed response,” Dr. Hsiao said. “About 25% may have improvement, but for the rest, HS symptoms may be unchanged or even worsen. That’s why it’s so important to be in contact with your pregnant patients, because not only may they have to stay on treatment, but they might also have to escalate [their treatment] during pregnancy.”
Lifestyle modifications to discuss with pregnant HS patients include appropriate weight gain during pregnancy, smoking cessation, and avoidance of tight-fitting clothing, “since friction can make things worse,” she said. Topical antibiotics safe to use during pregnancy for patients with mild HS include clindamycin 1%, erythromycin 2%, and metronidazole 0.75% applied twice per day to active lesions, she continued.
As for systemic therapies, some data exist to support the use of metformin 500 mg once daily, titrating up to twice or – if needed and tolerated – three times daily for patients with mild to moderate HS, she said, referencing a paper published in the Journal of the European Academy of Dermatology and Venereology.
Zinc gluconate is another potential option. Of 22 nonpregnant HS patients with Hurley stage I-II disease who were treated with zinc gluconate 90 mg daily, 8 had a complete remission of HS and 14 had partial remission, according to a report in Dermatology.
“Zinc supplementation of up to 50 mg daily has shown no effect on neonatal or maternal outcomes at birth based on existing medical literature,” Dr. Hsiao added.
Among antibiotics, injections of intralesional Kenalog 5-10 mg/mL have been shown to decrease pain and inflammation in acute HS lesions and are unlikely to pose significant risks during pregnancy, but a course of systemic antibiotics may be warranted in moderate to severe disease, she said. These include, but are not limited to, clindamycin, erythromycin base, cephalexin, or metronidazole.
“In addition, some of my HS colleagues and I will also use other antibiotics such as Augmentin [amoxicillin/clavulanate] or cefdinir for HS and these are also generally considered safe to use in pregnancy,” she said. “Caution is advised with using rifampin, dapsone, and moxifloxacin during pregnancy.”
As for biologic agents, the first-line option is adalimumab, which is currently the only Food and Drug Administration–approved treatment for HS.
“There is also good efficacy data for infliximab,” she said. “Etanercept has less placental transfer than adalimumab or infliximab so it’s safer to use in pregnancy, but it has inconsistent data for efficacy in HS, so I would generally avoid using it to treat HS and reach for adalimumab or infliximab instead.”
Data on TNF-alpha inhibitors from the GI and rheumatology literature have demonstrated that there is minimal placental transport of maternal antibodies during the first two trimesters of pregnancy.
“It’s at the beginning of the third trimester that the placental transfer of antibodies picks up,” she said. “At that point in time, you can have a discussion with the patient: do you want to stay on treatment and treat through, or do you want to consider being taken off the medication? I think this is a discussion that needs to be had, because let’s say you peel off adalimumab or infliximab and they have severe HS flares. I’m not sure that leads to a better outcome. I usually treat through for my pregnant patients.”
To better understand clinician practice patterns on the management of HS in pregnancy, Dr. Hsiao and Erin Collier, MD, MPH, of University of California, Los Angeles, and colleagues distributed an online survey to HS specialists in North America. They reported the findings in the International Journal of Women’s Dermatology.
Of the 49 respondents, 36 (73%) directed an HS specialty clinic and 29 (59%) reported having prescribed or continued a biologic agent in a pregnant HS patient. The top three biologics prescribed were adalimumab (90%), infliximab (41%), and certolizumab pegol (34%). Dr. Hsiao noted that certolizumab pegol is a pegylated anti-TNF, so it lacks an Fc region on the medication.
“This means that it cannot be actively transported by the neonatal Fc receptor on the placenta, thus resulting in minimal placental transmission,” she said. “The main issue is that there is little data on its efficacy in HS, but it’s a reasonable option to consider in a pregnant patient, especially in a patient with severe HS who asks, ‘what’s the safest biologic that I can go on?’ But you’d have to discuss with the patient that in terms of efficacy data, there is much less in the literature compared to adalimumab or infliximab.”
Breastfeeding while on anti–TNF-alpha biologics is considered safe. “There are minimal amounts of medication in breast milk,” she said. “If any gets through, infant gastric digestion is thought to take care of the rest. Of note, babies born to mothers who are continually treated with biologic agents should not be given live vaccinations for 6 months after birth.”
In a single-center study, Dr. Hsiao and colleagues retrospectively examined pregnancy complications, pregnancy outcomes, and neonatal outcomes in patients with HS. The study population included 202 pregnancies in 127 HS patients. Of 134 babies born to mothers with HS, 74% were breastfed and 24% were bottle-fed, and presence of HS lesions on the breast was significantly associated with not breastfeeding.
“So, when we see these patients, if moms decide to breastfeed and they have lesions on the breast, it would be helpful to discuss expectations and perhaps treat HS breast lesions early, so the breastfeeding process may go more smoothly for them after they deliver,” said Dr. Hsiao, who is one of the editors of the textbook “A Comprehensive Guide to Hidradenitis Suppurativa” (Elsevier, 2021). Safety-related resources that she recommends for clinicians include Mother to Baby and the Drugs and Lactation Database (LactMed).
Dr. Hsiao concluded her presentation by spotlighting the influence of pregnancy on HS comorbidities. Patients with HS already have a higher prevalence of depression and anxiety compared to controls. “Pregnancy can exacerbate underlying mood disorders in patients,” she said. “That’s why monitoring the patient’s mood and coordinating mental health care with the patient’s primary care physician and ob.gyn. is important.”
In addition, pregnancy-related changes in body mass index, blood pressure, lipid metabolism, and glucose tolerance trend toward changes seen in metabolic syndrome, she said, and HS patients are already at higher risk of metabolic syndrome compared with the general population.
HS may also compromise a patient’s ability to have a healthy pregnancy. Dr. Hsiao worked with Amit Garg, MD, and colleagues on a study that drew from the IBM MarketScan Commercial Claims Database to evaluate adverse pregnancy and maternal outcomes in women with HS between Jan. 1, 2011, and Sept. 30, 2015.
After the researchers adjusted for age, race, smoking status, and other comorbidities, they found that HS pregnancies were independently associated with spontaneous abortion (odds ratio, 1.20), gestational diabetes (OR, 1.26), and cesarean section (OR, 1.09). The findings were published in the Journal of the American Academy of Dermatology.
A separate study that used the same database found comparable results, also published in the Journal of the American Academy of Dermatology. “What I say to patients right now is, ‘there are many women with HS who have healthy pregnancies and deliver healthy babies, but HS could be a risk factor for a higher-risk pregnancy.’ It’s important that these patients are established with an ob.gyn. and are closely monitored to make sure that we optimize their care and give them the best outcome possible for mom and baby.”
Dr. Hsiao disclosed that she is on the board of directors for the Hidradenitis Suppurativa Foundation. She has also served as an advisor for Novartis, UCB, and Boehringer Ingelheim and as a speaker and advisor for AbbVie.
PORTLAND, ORE. – The recurrent boils, abscesses, and nodules of the chronic inflammatory skin condition hidradenitis suppurativa (HS) may improve during pregnancy for a subset of women, but for many, pregnancy does not change the disease course and may worsen symptoms.
In addition, HS appears to be a risk factor for adverse pregnancy and maternal outcomes.
“This is relevant, because in the United States, HS disproportionately impacts women compared with men by a ratio of about 3:1,” Jennifer Hsiao, MD, said at the annual meeting of the Pacific Dermatologic Association.
“Also, the highest prevalence of HS is among people in their 20s and 30s, so in their practice, clinicians will encounter female patients with HS who are either pregnant or actively thinking about getting pregnant,” she said.
During a wide-ranging presentation, Dr. Hsiao of the department of dermatology at the University of Southern California, Los Angeles, described the impact of pregnancy on HS, identified appropriate treatment options for this population of patients, and discussed HS comorbidities that may be exacerbated during pregnancy.
She began by noting that levels of progesterone and estrogen both rise during pregnancy. Progesterone is known to suppress development and function of Th1 and Th17 T cells, but the effect of estrogen on inflammation is less well known. At the same time, serum levels of interleukin (IL)-1 receptor antagonist and soluble TNF-alpha receptor both increase during pregnancy.
“This would lead to serum IL-1 and TNF-alpha falling, sort of like the way that we give anti–IL-1 and TNF blockers as HS treatments,” she explained. “So, presumably that might be helpful during HS in pregnancy. On the flip side, pregnancy weight gain can exacerbate HS, with increased friction between skin folds. In addition, just having more adipocytes can promote secretion of proinflammatory cytokines like TNF-alpha.”
To better understand the effect of pregnancy on patients with HS, Dr. Hsiao and colleagues conducted a systematic review and meta-analysis on the topic published in Dermatology. They included eight studies in which a total of 672 patients self-reported their HS disease course during pregnancy and 164 self-reported whether they had a postpartum HS flare or not. On pooled analyses, HS improved in 24% of patients but worsened in 20%. In addition, 60% of patients experienced a postpartum flare.
“So, at this point in time, based on the literature, it would be fair to tell your patient that during pregnancy, HS has a mixed response,” Dr. Hsiao said. “About 25% may have improvement, but for the rest, HS symptoms may be unchanged or even worsen. That’s why it’s so important to be in contact with your pregnant patients, because not only may they have to stay on treatment, but they might also have to escalate [their treatment] during pregnancy.”
Lifestyle modifications to discuss with pregnant HS patients include appropriate weight gain during pregnancy, smoking cessation, and avoidance of tight-fitting clothing, “since friction can make things worse,” she said. Topical antibiotics safe to use during pregnancy for patients with mild HS include clindamycin 1%, erythromycin 2%, and metronidazole 0.75% applied twice per day to active lesions, she continued.
As for systemic therapies, some data exist to support the use of metformin 500 mg once daily, titrating up to twice or – if needed and tolerated – three times daily for patients with mild to moderate HS, she said, referencing a paper published in the Journal of the European Academy of Dermatology and Venereology.
Zinc gluconate is another potential option. Of 22 nonpregnant HS patients with Hurley stage I-II disease who were treated with zinc gluconate 90 mg daily, 8 had a complete remission of HS and 14 had partial remission, according to a report in Dermatology.
“Zinc supplementation of up to 50 mg daily has shown no effect on neonatal or maternal outcomes at birth based on existing medical literature,” Dr. Hsiao added.
Among antibiotics, injections of intralesional Kenalog 5-10 mg/mL have been shown to decrease pain and inflammation in acute HS lesions and are unlikely to pose significant risks during pregnancy, but a course of systemic antibiotics may be warranted in moderate to severe disease, she said. These include, but are not limited to, clindamycin, erythromycin base, cephalexin, or metronidazole.
“In addition, some of my HS colleagues and I will also use other antibiotics such as Augmentin [amoxicillin/clavulanate] or cefdinir for HS and these are also generally considered safe to use in pregnancy,” she said. “Caution is advised with using rifampin, dapsone, and moxifloxacin during pregnancy.”
As for biologic agents, the first-line option is adalimumab, which is currently the only Food and Drug Administration–approved treatment for HS.
“There is also good efficacy data for infliximab,” she said. “Etanercept has less placental transfer than adalimumab or infliximab so it’s safer to use in pregnancy, but it has inconsistent data for efficacy in HS, so I would generally avoid using it to treat HS and reach for adalimumab or infliximab instead.”
Data on TNF-alpha inhibitors from the GI and rheumatology literature have demonstrated that there is minimal placental transport of maternal antibodies during the first two trimesters of pregnancy.
“It’s at the beginning of the third trimester that the placental transfer of antibodies picks up,” she said. “At that point in time, you can have a discussion with the patient: do you want to stay on treatment and treat through, or do you want to consider being taken off the medication? I think this is a discussion that needs to be had, because let’s say you peel off adalimumab or infliximab and they have severe HS flares. I’m not sure that leads to a better outcome. I usually treat through for my pregnant patients.”
To better understand clinician practice patterns on the management of HS in pregnancy, Dr. Hsiao and Erin Collier, MD, MPH, of University of California, Los Angeles, and colleagues distributed an online survey to HS specialists in North America. They reported the findings in the International Journal of Women’s Dermatology.
Of the 49 respondents, 36 (73%) directed an HS specialty clinic and 29 (59%) reported having prescribed or continued a biologic agent in a pregnant HS patient. The top three biologics prescribed were adalimumab (90%), infliximab (41%), and certolizumab pegol (34%). Dr. Hsiao noted that certolizumab pegol is a pegylated anti-TNF, so it lacks an Fc region on the medication.
“This means that it cannot be actively transported by the neonatal Fc receptor on the placenta, thus resulting in minimal placental transmission,” she said. “The main issue is that there is little data on its efficacy in HS, but it’s a reasonable option to consider in a pregnant patient, especially in a patient with severe HS who asks, ‘what’s the safest biologic that I can go on?’ But you’d have to discuss with the patient that in terms of efficacy data, there is much less in the literature compared to adalimumab or infliximab.”
Breastfeeding while on anti–TNF-alpha biologics is considered safe. “There are minimal amounts of medication in breast milk,” she said. “If any gets through, infant gastric digestion is thought to take care of the rest. Of note, babies born to mothers who are continually treated with biologic agents should not be given live vaccinations for 6 months after birth.”
In a single-center study, Dr. Hsiao and colleagues retrospectively examined pregnancy complications, pregnancy outcomes, and neonatal outcomes in patients with HS. The study population included 202 pregnancies in 127 HS patients. Of 134 babies born to mothers with HS, 74% were breastfed and 24% were bottle-fed, and presence of HS lesions on the breast was significantly associated with not breastfeeding.
“So, when we see these patients, if moms decide to breastfeed and they have lesions on the breast, it would be helpful to discuss expectations and perhaps treat HS breast lesions early, so the breastfeeding process may go more smoothly for them after they deliver,” said Dr. Hsiao, who is one of the editors of the textbook “A Comprehensive Guide to Hidradenitis Suppurativa” (Elsevier, 2021). Safety-related resources that she recommends for clinicians include Mother to Baby and the Drugs and Lactation Database (LactMed).
Dr. Hsiao concluded her presentation by spotlighting the influence of pregnancy on HS comorbidities. Patients with HS already have a higher prevalence of depression and anxiety compared to controls. “Pregnancy can exacerbate underlying mood disorders in patients,” she said. “That’s why monitoring the patient’s mood and coordinating mental health care with the patient’s primary care physician and ob.gyn. is important.”
In addition, pregnancy-related changes in body mass index, blood pressure, lipid metabolism, and glucose tolerance trend toward changes seen in metabolic syndrome, she said, and HS patients are already at higher risk of metabolic syndrome compared with the general population.
HS may also compromise a patient’s ability to have a healthy pregnancy. Dr. Hsiao worked with Amit Garg, MD, and colleagues on a study that drew from the IBM MarketScan Commercial Claims Database to evaluate adverse pregnancy and maternal outcomes in women with HS between Jan. 1, 2011, and Sept. 30, 2015.
After the researchers adjusted for age, race, smoking status, and other comorbidities, they found that HS pregnancies were independently associated with spontaneous abortion (odds ratio, 1.20), gestational diabetes (OR, 1.26), and cesarean section (OR, 1.09). The findings were published in the Journal of the American Academy of Dermatology.
A separate study that used the same database found comparable results, also published in the Journal of the American Academy of Dermatology. “What I say to patients right now is, ‘there are many women with HS who have healthy pregnancies and deliver healthy babies, but HS could be a risk factor for a higher-risk pregnancy.’ It’s important that these patients are established with an ob.gyn. and are closely monitored to make sure that we optimize their care and give them the best outcome possible for mom and baby.”
Dr. Hsiao disclosed that she is on the board of directors for the Hidradenitis Suppurativa Foundation. She has also served as an advisor for Novartis, UCB, and Boehringer Ingelheim and as a speaker and advisor for AbbVie.
AT PDA 2022
Stressed about weight gain? Well, stress causes weight gain
Stress, meet weight gain. Weight gain, meet stress
You’re not eating differently and you’re keeping active, but your waistline is expanding. How is that happening? Since eating healthy and exercising shouldn’t make you gain weight, there may be a hidden factor getting in your way. Stress. The one thing that can have a grip on your circadian rhythm stronger than any bodybuilder.
Investigators at Weill Cornell Medicine published two mouse studies that suggest stress and other factors that throw the body’s circadian clocks out of rhythm may contribute to weight gain.
In the first study, the researchers imitated disruptive condition effects like high cortisol exposure and chronic stress by implanting pellets under the skin that released glucocorticoid at a constant rate for 21 days. Mice that received the pellets had twice as much white and brown fat, as well as much higher insulin levels, regardless of their unchanged and still-healthy diet.
In the second study, they used tagged proteins as markers to monitor the daily fluctuations of a protein that regulates fat cell production and circadian gene expression in mouse fat cell precursors. The results showed “that fat cell precursors commit to becoming fat cells only during the circadian cycle phase corresponding to evening in humans,” they said in a written statement.
“Every cell in our body has an intrinsic cell clock, just like the fat cells, and we have a master clock in our brain, which controls hormone secretion,” said senior author Mary Teruel of Cornell University. “A lot of forces are working against a healthy metabolism when we are out of circadian rhythm. The more we understand, the more likely we will be able to do something about it.”
So if you’re stressing out that the scale is or isn’t moving in the direction you want, you could be standing in your own way. Take a chill pill.
Who can smell cancer? The locust nose
If you need to smell some gas, there’s nothing better than a nose. Just ask a scientist: “Noses are still state of the art,” said Debajit Saha, PhD, of Michigan State University. “There’s really nothing like them when it comes to gas sensing.”
And when it comes to noses, dogs are best, right? After all, there’s a reason we don’t have bomb-sniffing wombats and drug-sniffing ostriches. Dogs are better. Better, but not perfect. And if they’re not perfect, then human technology can do better.
Enter the electronic nose. Which is better than dogs … except that it isn’t. “People have been working on ‘electronic noses’ for more than 15 years, but they’re still not close to achieving what biology can do seamlessly,” Dr. Saha explained in a statement from the university.
Which brings us back to dogs. If you want to detect early-stage cancer using smell, you go to the dogs, right? Nope.
Here’s Christopher Contag, PhD, also of Michigan State, who recruited Dr. Saha to the university: “I told him, ‘When you come here, we’ll detect cancer. I’m sure your locusts can do it.’ ”
Yes, locusts. Dr. Contag and his research team were looking at mouth cancers and noticed that different cell lines had different appearances. Then they discovered that those different-looking cell lines produced different metabolites, some of which were volatile.
Enter Dr. Saha’s locusts. They were able to tell the difference between normal cells and cancer cells and could even distinguish between the different cell lines. And how they were able to share this information? Not voluntarily, that’s for sure. The researchers attached electrodes to the insects’ brains and recorded their responses to gas samples from both healthy and cancer cells. Those brain signals were then used to create chemical profiles of the different cells. Piece of cake.
The whole getting-electrodes-attached-to-their-brains thing seemed at least a bit ethically ambiguous, so we contacted the locusts’ PR office, which offered some positive spin: “Humans get their early cancer detection and we get that whole swarms-that-devour-entire-countrysides thing off our backs. Win win.”
Bad news for vampires everywhere
Pop culture has been extraordinarily kind to the vampire. A few hundred years ago, vampires were demon-possessed, often-inhuman monsters. Now? They’re suave, sophisticated, beautiful, and oh-so dramatic and angst-filled about their “curse.” Drink a little human blood, live and look young forever. Such monsters they are.
It does make sense in a morbid sort of way. An old person receiving the blood of the young does seem like a good idea for rejuvenation, right? A team of Ukrainian researchers sought to find out, conducting a study in which older mice were linked with young mice via heterochronic parabiosis. For 3 months, old-young mice pairs were surgically connected and shared blood. After 3 months, the mice were disconnected from each other and the effects of the blood link were studied.
For all the vampire enthusiasts out there, we have bad news and worse news. The bad news first: The older mice received absolutely no benefit from heterochronic parabiosis. No youthfulness, no increased lifespan, nothing. The worse news is that the younger mice were adversely affected by the older blood. They aged more and experienced a shortened lifespan, even after the connection was severed. The old blood, according to the investigators, contains factors capable of inducing aging in younger mice, but the opposite is not true. Further research into aging, they added, should focus on suppressing the aging factors in older blood.
Of note, the paper was written by doctors who are currently refugees, fleeing the war in Ukraine. We don’t want to speculate on the true cause of the war, but we’re onto you, Putin. We know you wanted the vampire research for yourself, but it won’t work. Your dream of becoming Vlad “Dracula” Putin will never come to pass.
Hearing is not always believing
Have you ever heard yourself on a voice mail, or from a recording you did at work? No matter how good you sound, you still might feel like the recording sounds nothing like you. It may even cause low self-esteem for those who don’t like how their voice sounds or don’t recognize it when it’s played back to them.
Since one possible symptom of schizophrenia is not recognizing one’s own speech and having a false sense of control over actions, and those with schizophrenia may hallucinate or hear voices, not being able to recognize their own voices may be alarming.
A recent study on the sense of agency, or sense of control, involved having volunteers speak with different pitches in their voices and then having it played back to them to gauge their reactions.
“Our results demonstrate that hearing one’s own voice is a critical factor to increased self-agency over speech. In other words, we do not strongly feel that ‘I’ am generating the speech if we hear someone else’s voice as an outcome of the speech. Our study provides empirical evidence of the tight link between the sense of agency and self-voice identity,” lead author Ryu Ohata, PhD, of the University of Tokyo, said in a written statement.
As social interaction becomes more digital through platforms such as FaceTime, Zoom, and voicemail, especially since the pandemic has promoted social distancing, it makes sense that people may be more aware and more surprised by how they sound on recordings.
So, if you ever promised someone something that you don’t want to do, and they play it back to you from the recording you made, maybe you can just say you don’t recognize the voice. And if it’s not you, then you don’t have to do it.
Stress, meet weight gain. Weight gain, meet stress
You’re not eating differently and you’re keeping active, but your waistline is expanding. How is that happening? Since eating healthy and exercising shouldn’t make you gain weight, there may be a hidden factor getting in your way. Stress. The one thing that can have a grip on your circadian rhythm stronger than any bodybuilder.
Investigators at Weill Cornell Medicine published two mouse studies that suggest stress and other factors that throw the body’s circadian clocks out of rhythm may contribute to weight gain.
In the first study, the researchers imitated disruptive condition effects like high cortisol exposure and chronic stress by implanting pellets under the skin that released glucocorticoid at a constant rate for 21 days. Mice that received the pellets had twice as much white and brown fat, as well as much higher insulin levels, regardless of their unchanged and still-healthy diet.
In the second study, they used tagged proteins as markers to monitor the daily fluctuations of a protein that regulates fat cell production and circadian gene expression in mouse fat cell precursors. The results showed “that fat cell precursors commit to becoming fat cells only during the circadian cycle phase corresponding to evening in humans,” they said in a written statement.
“Every cell in our body has an intrinsic cell clock, just like the fat cells, and we have a master clock in our brain, which controls hormone secretion,” said senior author Mary Teruel of Cornell University. “A lot of forces are working against a healthy metabolism when we are out of circadian rhythm. The more we understand, the more likely we will be able to do something about it.”
So if you’re stressing out that the scale is or isn’t moving in the direction you want, you could be standing in your own way. Take a chill pill.
Who can smell cancer? The locust nose
If you need to smell some gas, there’s nothing better than a nose. Just ask a scientist: “Noses are still state of the art,” said Debajit Saha, PhD, of Michigan State University. “There’s really nothing like them when it comes to gas sensing.”
And when it comes to noses, dogs are best, right? After all, there’s a reason we don’t have bomb-sniffing wombats and drug-sniffing ostriches. Dogs are better. Better, but not perfect. And if they’re not perfect, then human technology can do better.
Enter the electronic nose. Which is better than dogs … except that it isn’t. “People have been working on ‘electronic noses’ for more than 15 years, but they’re still not close to achieving what biology can do seamlessly,” Dr. Saha explained in a statement from the university.
Which brings us back to dogs. If you want to detect early-stage cancer using smell, you go to the dogs, right? Nope.
Here’s Christopher Contag, PhD, also of Michigan State, who recruited Dr. Saha to the university: “I told him, ‘When you come here, we’ll detect cancer. I’m sure your locusts can do it.’ ”
Yes, locusts. Dr. Contag and his research team were looking at mouth cancers and noticed that different cell lines had different appearances. Then they discovered that those different-looking cell lines produced different metabolites, some of which were volatile.
Enter Dr. Saha’s locusts. They were able to tell the difference between normal cells and cancer cells and could even distinguish between the different cell lines. And how they were able to share this information? Not voluntarily, that’s for sure. The researchers attached electrodes to the insects’ brains and recorded their responses to gas samples from both healthy and cancer cells. Those brain signals were then used to create chemical profiles of the different cells. Piece of cake.
The whole getting-electrodes-attached-to-their-brains thing seemed at least a bit ethically ambiguous, so we contacted the locusts’ PR office, which offered some positive spin: “Humans get their early cancer detection and we get that whole swarms-that-devour-entire-countrysides thing off our backs. Win win.”
Bad news for vampires everywhere
Pop culture has been extraordinarily kind to the vampire. A few hundred years ago, vampires were demon-possessed, often-inhuman monsters. Now? They’re suave, sophisticated, beautiful, and oh-so dramatic and angst-filled about their “curse.” Drink a little human blood, live and look young forever. Such monsters they are.
It does make sense in a morbid sort of way. An old person receiving the blood of the young does seem like a good idea for rejuvenation, right? A team of Ukrainian researchers sought to find out, conducting a study in which older mice were linked with young mice via heterochronic parabiosis. For 3 months, old-young mice pairs were surgically connected and shared blood. After 3 months, the mice were disconnected from each other and the effects of the blood link were studied.
For all the vampire enthusiasts out there, we have bad news and worse news. The bad news first: The older mice received absolutely no benefit from heterochronic parabiosis. No youthfulness, no increased lifespan, nothing. The worse news is that the younger mice were adversely affected by the older blood. They aged more and experienced a shortened lifespan, even after the connection was severed. The old blood, according to the investigators, contains factors capable of inducing aging in younger mice, but the opposite is not true. Further research into aging, they added, should focus on suppressing the aging factors in older blood.
Of note, the paper was written by doctors who are currently refugees, fleeing the war in Ukraine. We don’t want to speculate on the true cause of the war, but we’re onto you, Putin. We know you wanted the vampire research for yourself, but it won’t work. Your dream of becoming Vlad “Dracula” Putin will never come to pass.
Hearing is not always believing
Have you ever heard yourself on a voice mail, or from a recording you did at work? No matter how good you sound, you still might feel like the recording sounds nothing like you. It may even cause low self-esteem for those who don’t like how their voice sounds or don’t recognize it when it’s played back to them.
Since one possible symptom of schizophrenia is not recognizing one’s own speech and having a false sense of control over actions, and those with schizophrenia may hallucinate or hear voices, not being able to recognize their own voices may be alarming.
A recent study on the sense of agency, or sense of control, involved having volunteers speak with different pitches in their voices and then having it played back to them to gauge their reactions.
“Our results demonstrate that hearing one’s own voice is a critical factor to increased self-agency over speech. In other words, we do not strongly feel that ‘I’ am generating the speech if we hear someone else’s voice as an outcome of the speech. Our study provides empirical evidence of the tight link between the sense of agency and self-voice identity,” lead author Ryu Ohata, PhD, of the University of Tokyo, said in a written statement.
As social interaction becomes more digital through platforms such as FaceTime, Zoom, and voicemail, especially since the pandemic has promoted social distancing, it makes sense that people may be more aware and more surprised by how they sound on recordings.
So, if you ever promised someone something that you don’t want to do, and they play it back to you from the recording you made, maybe you can just say you don’t recognize the voice. And if it’s not you, then you don’t have to do it.
Stress, meet weight gain. Weight gain, meet stress
You’re not eating differently and you’re keeping active, but your waistline is expanding. How is that happening? Since eating healthy and exercising shouldn’t make you gain weight, there may be a hidden factor getting in your way. Stress. The one thing that can have a grip on your circadian rhythm stronger than any bodybuilder.
Investigators at Weill Cornell Medicine published two mouse studies that suggest stress and other factors that throw the body’s circadian clocks out of rhythm may contribute to weight gain.
In the first study, the researchers imitated disruptive condition effects like high cortisol exposure and chronic stress by implanting pellets under the skin that released glucocorticoid at a constant rate for 21 days. Mice that received the pellets had twice as much white and brown fat, as well as much higher insulin levels, regardless of their unchanged and still-healthy diet.
In the second study, they used tagged proteins as markers to monitor the daily fluctuations of a protein that regulates fat cell production and circadian gene expression in mouse fat cell precursors. The results showed “that fat cell precursors commit to becoming fat cells only during the circadian cycle phase corresponding to evening in humans,” they said in a written statement.
“Every cell in our body has an intrinsic cell clock, just like the fat cells, and we have a master clock in our brain, which controls hormone secretion,” said senior author Mary Teruel of Cornell University. “A lot of forces are working against a healthy metabolism when we are out of circadian rhythm. The more we understand, the more likely we will be able to do something about it.”
So if you’re stressing out that the scale is or isn’t moving in the direction you want, you could be standing in your own way. Take a chill pill.
Who can smell cancer? The locust nose
If you need to smell some gas, there’s nothing better than a nose. Just ask a scientist: “Noses are still state of the art,” said Debajit Saha, PhD, of Michigan State University. “There’s really nothing like them when it comes to gas sensing.”
And when it comes to noses, dogs are best, right? After all, there’s a reason we don’t have bomb-sniffing wombats and drug-sniffing ostriches. Dogs are better. Better, but not perfect. And if they’re not perfect, then human technology can do better.
Enter the electronic nose. Which is better than dogs … except that it isn’t. “People have been working on ‘electronic noses’ for more than 15 years, but they’re still not close to achieving what biology can do seamlessly,” Dr. Saha explained in a statement from the university.
Which brings us back to dogs. If you want to detect early-stage cancer using smell, you go to the dogs, right? Nope.
Here’s Christopher Contag, PhD, also of Michigan State, who recruited Dr. Saha to the university: “I told him, ‘When you come here, we’ll detect cancer. I’m sure your locusts can do it.’ ”
Yes, locusts. Dr. Contag and his research team were looking at mouth cancers and noticed that different cell lines had different appearances. Then they discovered that those different-looking cell lines produced different metabolites, some of which were volatile.
Enter Dr. Saha’s locusts. They were able to tell the difference between normal cells and cancer cells and could even distinguish between the different cell lines. And how they were able to share this information? Not voluntarily, that’s for sure. The researchers attached electrodes to the insects’ brains and recorded their responses to gas samples from both healthy and cancer cells. Those brain signals were then used to create chemical profiles of the different cells. Piece of cake.
The whole getting-electrodes-attached-to-their-brains thing seemed at least a bit ethically ambiguous, so we contacted the locusts’ PR office, which offered some positive spin: “Humans get their early cancer detection and we get that whole swarms-that-devour-entire-countrysides thing off our backs. Win win.”
Bad news for vampires everywhere
Pop culture has been extraordinarily kind to the vampire. A few hundred years ago, vampires were demon-possessed, often-inhuman monsters. Now? They’re suave, sophisticated, beautiful, and oh-so dramatic and angst-filled about their “curse.” Drink a little human blood, live and look young forever. Such monsters they are.
It does make sense in a morbid sort of way. An old person receiving the blood of the young does seem like a good idea for rejuvenation, right? A team of Ukrainian researchers sought to find out, conducting a study in which older mice were linked with young mice via heterochronic parabiosis. For 3 months, old-young mice pairs were surgically connected and shared blood. After 3 months, the mice were disconnected from each other and the effects of the blood link were studied.
For all the vampire enthusiasts out there, we have bad news and worse news. The bad news first: The older mice received absolutely no benefit from heterochronic parabiosis. No youthfulness, no increased lifespan, nothing. The worse news is that the younger mice were adversely affected by the older blood. They aged more and experienced a shortened lifespan, even after the connection was severed. The old blood, according to the investigators, contains factors capable of inducing aging in younger mice, but the opposite is not true. Further research into aging, they added, should focus on suppressing the aging factors in older blood.
Of note, the paper was written by doctors who are currently refugees, fleeing the war in Ukraine. We don’t want to speculate on the true cause of the war, but we’re onto you, Putin. We know you wanted the vampire research for yourself, but it won’t work. Your dream of becoming Vlad “Dracula” Putin will never come to pass.
Hearing is not always believing
Have you ever heard yourself on a voice mail, or from a recording you did at work? No matter how good you sound, you still might feel like the recording sounds nothing like you. It may even cause low self-esteem for those who don’t like how their voice sounds or don’t recognize it when it’s played back to them.
Since one possible symptom of schizophrenia is not recognizing one’s own speech and having a false sense of control over actions, and those with schizophrenia may hallucinate or hear voices, not being able to recognize their own voices may be alarming.
A recent study on the sense of agency, or sense of control, involved having volunteers speak with different pitches in their voices and then having it played back to them to gauge their reactions.
“Our results demonstrate that hearing one’s own voice is a critical factor to increased self-agency over speech. In other words, we do not strongly feel that ‘I’ am generating the speech if we hear someone else’s voice as an outcome of the speech. Our study provides empirical evidence of the tight link between the sense of agency and self-voice identity,” lead author Ryu Ohata, PhD, of the University of Tokyo, said in a written statement.
As social interaction becomes more digital through platforms such as FaceTime, Zoom, and voicemail, especially since the pandemic has promoted social distancing, it makes sense that people may be more aware and more surprised by how they sound on recordings.
So, if you ever promised someone something that you don’t want to do, and they play it back to you from the recording you made, maybe you can just say you don’t recognize the voice. And if it’s not you, then you don’t have to do it.
Hyperthyroidism rebound in pregnancy boosts adverse outcomes
Discontinuing antithyroid drugs during early pregnancy is linked to a possible rebound of hyperthyroidism and a high risk of adverse pregnancy outcomes, new research shows.
“Our study provides preliminary evidence that the risk of rebound increases in women with subnormal thyroid-stimulating hormone (TSH) and/or positive thyrotropin receptor antibody (TRAb) who stop antithyroid drugs in early pregnancy,” first author Xin Hou told this news organization.
“When discussing the pros and cons of antithyroid drug withdrawal early in pregnancy [clinicians] should consider the level of TSH and TRAb in early pregnancy,” said Hou, of the department of endocrinology and metabolism, Institute of Endocrinology, The First Affiliated Hospital of China Medical University, Shenyang.
Suvi Turunen, MD, of the University of Oulu (Finland), who has also conducted research on the issue, said the study adds important insights.
“I find this study very interesting,” Dr. Turunen said in an interview. “It is well known that medical treatment of hyperthyroidism outweighs the potential harms of antithyroid treatment.”
The new findings add to the evidence, she added. “I think that withdrawal of antithyroid drugs should be carefully considered, especially with autoantibody-positive patients,” Dr. Turunen said.
Hyperthyroidism a risk in pregnancy – with or without treatment
The potential risks of hyperthyroidism in pregnancy are well established and can range from preeclampsia to premature birth or miscarriage.
However, antithyroid drugs, including methimazole and propylthiouracil, carry their own risks. In crossing the placental barrier, the drugs can increase the risk of birth defects, particularly during 6-10 weeks of gestation, yet their discontinuation is linked to as much as a 50%-60% risk of relapse, the authors explain.
Because of the risks, the American Thyroid Association recommends that “women with a stable euthyroid state on 5-10 mg methimazole per day achieved within a few months, and a falling TRAb level, are likely candidates to withdraw from antithyroid drug therapy in early pregnancy,” the authors noted.
However, as the recommendations for women who are already pregnant are largely based on evidence from nonpregnant patients, Hou and colleagues sought to evaluate withdrawal among women who were pregnant.
For the study, published in Thyroid, they enrolled 63 women who were pregnant and part of an outpatient service of the department of endocrinology and metabolism at The First Affiliated Hospital of China Medical University, between September 2014 and March 2017, who had well-controlled hyperthyroidism in early pregnancy and discontinued the drugs.
The women were an average age of 27 years, and 28 were multigravida. Twenty-two had a history of miscarriage.
A follow-up of the patients until the end of their pregnancy showed that, overall, 20 (31.7%) had a rebound of hyperthyroidism during their pregnancy after withdrawing from the drugs.
Key factors associated with the highest risk of a rebound after discontinuation included having subnormal TSH levels (TSH < 0.35 mIU/L; odds ratio, 5.12; P = .03) or having positive TRAb (TRAb > 1.75 IU/L; OR, 3.79; P = .02) at the time of medication withdrawal, compared with those with either normal TSH levels or negative TRAb.
The combination of both subnormal TSH and positive TRAb at the time of antithyroid medication withdrawal further boosted the risk of hyperthyroidism rebound (83.3%, 5 of 6), compared with those who had both normal TSH and negative TRAb (13%, 3 of 23; OR, 33.33; P = .003).
Adverse pregnancy outcomes increased
Importantly, among the 20 patients who had a rebound, 11 (55%) had adverse pregnancy outcomes, including miscarriage, premature birth, induced labor, gestational hypertension, and gestational diabetes, compared with only 4 (9.3%) of the 43 who had no rebound (OR, 11.92; P = .0002).
Neonatal abnormalities were also higher among those experiencing a rebound (20% vs. 4.7%), however, the authors noted that “larger prospective studies are required to conclude whether antithyroid drug withdrawal affects fetal outcome.”
In the rebound group, the mean duration of antithyroid medication use was 24.7 months versus 35.1 months in the nonrebound group, however, the difference was not statistically significant (P = .07). And 40% of the rebound group had a history of miscarriage versus 32.6% in the non-rebound group, but was also not significantly different (P = .56).
The authors noted that half of those in the rebound group developed hyperthyroidism more than 4 weeks after their withdrawal from antithyroid medications, “which seemed to have circumvented the most sensitive period of teratogenesis between 6 and 10 weeks of pregnancy.”
Hou added that restarting antithyroid medication did not increase the risk of adverse outcomes for offspring.
“A low dose of antithyroid medications may be a good choice for women with subnormal TSH and/or positive TRAb in early pregnancy,” Hou concluded. “Because of the small size of our study, a larger prospective study is needed to overcome the potential selection bias and to verify the conclusions.”
Findings consistent with Finnish study
In her own recent study, which included 2,144 women in Finland who experienced hyperthyroidism during pregnancy, Dr. Turunen and colleagues found that having hyperthyroidism, with or without antithyroid drug treatment, was associated with an increased odds of pregnancy and/or prenatal complications, compared with those without thyroid disease.
“In our study, we observed an increased risk of adverse pregnancy outcomes also in mothers with previous diagnosis and/or treatment of hyperthyroidism, not only with overt hyperthyroidism treated with antithyroid drugs,” she told this news organization.
“I think that especially those patients with positive antibodies [TRAbs] are at risk even if they are euthyroid,” she noted. “Withdrawal of antithyroid drugs in these patients is a risk.”
“Probably continuing antithyroid treatment with low dose is a better option,” she said.
The authors and Dr. Turunen reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Discontinuing antithyroid drugs during early pregnancy is linked to a possible rebound of hyperthyroidism and a high risk of adverse pregnancy outcomes, new research shows.
“Our study provides preliminary evidence that the risk of rebound increases in women with subnormal thyroid-stimulating hormone (TSH) and/or positive thyrotropin receptor antibody (TRAb) who stop antithyroid drugs in early pregnancy,” first author Xin Hou told this news organization.
“When discussing the pros and cons of antithyroid drug withdrawal early in pregnancy [clinicians] should consider the level of TSH and TRAb in early pregnancy,” said Hou, of the department of endocrinology and metabolism, Institute of Endocrinology, The First Affiliated Hospital of China Medical University, Shenyang.
Suvi Turunen, MD, of the University of Oulu (Finland), who has also conducted research on the issue, said the study adds important insights.
“I find this study very interesting,” Dr. Turunen said in an interview. “It is well known that medical treatment of hyperthyroidism outweighs the potential harms of antithyroid treatment.”
The new findings add to the evidence, she added. “I think that withdrawal of antithyroid drugs should be carefully considered, especially with autoantibody-positive patients,” Dr. Turunen said.
Hyperthyroidism a risk in pregnancy – with or without treatment
The potential risks of hyperthyroidism in pregnancy are well established and can range from preeclampsia to premature birth or miscarriage.
However, antithyroid drugs, including methimazole and propylthiouracil, carry their own risks. In crossing the placental barrier, the drugs can increase the risk of birth defects, particularly during 6-10 weeks of gestation, yet their discontinuation is linked to as much as a 50%-60% risk of relapse, the authors explain.
Because of the risks, the American Thyroid Association recommends that “women with a stable euthyroid state on 5-10 mg methimazole per day achieved within a few months, and a falling TRAb level, are likely candidates to withdraw from antithyroid drug therapy in early pregnancy,” the authors noted.
However, as the recommendations for women who are already pregnant are largely based on evidence from nonpregnant patients, Hou and colleagues sought to evaluate withdrawal among women who were pregnant.
For the study, published in Thyroid, they enrolled 63 women who were pregnant and part of an outpatient service of the department of endocrinology and metabolism at The First Affiliated Hospital of China Medical University, between September 2014 and March 2017, who had well-controlled hyperthyroidism in early pregnancy and discontinued the drugs.
The women were an average age of 27 years, and 28 were multigravida. Twenty-two had a history of miscarriage.
A follow-up of the patients until the end of their pregnancy showed that, overall, 20 (31.7%) had a rebound of hyperthyroidism during their pregnancy after withdrawing from the drugs.
Key factors associated with the highest risk of a rebound after discontinuation included having subnormal TSH levels (TSH < 0.35 mIU/L; odds ratio, 5.12; P = .03) or having positive TRAb (TRAb > 1.75 IU/L; OR, 3.79; P = .02) at the time of medication withdrawal, compared with those with either normal TSH levels or negative TRAb.
The combination of both subnormal TSH and positive TRAb at the time of antithyroid medication withdrawal further boosted the risk of hyperthyroidism rebound (83.3%, 5 of 6), compared with those who had both normal TSH and negative TRAb (13%, 3 of 23; OR, 33.33; P = .003).
Adverse pregnancy outcomes increased
Importantly, among the 20 patients who had a rebound, 11 (55%) had adverse pregnancy outcomes, including miscarriage, premature birth, induced labor, gestational hypertension, and gestational diabetes, compared with only 4 (9.3%) of the 43 who had no rebound (OR, 11.92; P = .0002).
Neonatal abnormalities were also higher among those experiencing a rebound (20% vs. 4.7%), however, the authors noted that “larger prospective studies are required to conclude whether antithyroid drug withdrawal affects fetal outcome.”
In the rebound group, the mean duration of antithyroid medication use was 24.7 months versus 35.1 months in the nonrebound group, however, the difference was not statistically significant (P = .07). And 40% of the rebound group had a history of miscarriage versus 32.6% in the non-rebound group, but was also not significantly different (P = .56).
The authors noted that half of those in the rebound group developed hyperthyroidism more than 4 weeks after their withdrawal from antithyroid medications, “which seemed to have circumvented the most sensitive period of teratogenesis between 6 and 10 weeks of pregnancy.”
Hou added that restarting antithyroid medication did not increase the risk of adverse outcomes for offspring.
“A low dose of antithyroid medications may be a good choice for women with subnormal TSH and/or positive TRAb in early pregnancy,” Hou concluded. “Because of the small size of our study, a larger prospective study is needed to overcome the potential selection bias and to verify the conclusions.”
Findings consistent with Finnish study
In her own recent study, which included 2,144 women in Finland who experienced hyperthyroidism during pregnancy, Dr. Turunen and colleagues found that having hyperthyroidism, with or without antithyroid drug treatment, was associated with an increased odds of pregnancy and/or prenatal complications, compared with those without thyroid disease.
“In our study, we observed an increased risk of adverse pregnancy outcomes also in mothers with previous diagnosis and/or treatment of hyperthyroidism, not only with overt hyperthyroidism treated with antithyroid drugs,” she told this news organization.
“I think that especially those patients with positive antibodies [TRAbs] are at risk even if they are euthyroid,” she noted. “Withdrawal of antithyroid drugs in these patients is a risk.”
“Probably continuing antithyroid treatment with low dose is a better option,” she said.
The authors and Dr. Turunen reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Discontinuing antithyroid drugs during early pregnancy is linked to a possible rebound of hyperthyroidism and a high risk of adverse pregnancy outcomes, new research shows.
“Our study provides preliminary evidence that the risk of rebound increases in women with subnormal thyroid-stimulating hormone (TSH) and/or positive thyrotropin receptor antibody (TRAb) who stop antithyroid drugs in early pregnancy,” first author Xin Hou told this news organization.
“When discussing the pros and cons of antithyroid drug withdrawal early in pregnancy [clinicians] should consider the level of TSH and TRAb in early pregnancy,” said Hou, of the department of endocrinology and metabolism, Institute of Endocrinology, The First Affiliated Hospital of China Medical University, Shenyang.
Suvi Turunen, MD, of the University of Oulu (Finland), who has also conducted research on the issue, said the study adds important insights.
“I find this study very interesting,” Dr. Turunen said in an interview. “It is well known that medical treatment of hyperthyroidism outweighs the potential harms of antithyroid treatment.”
The new findings add to the evidence, she added. “I think that withdrawal of antithyroid drugs should be carefully considered, especially with autoantibody-positive patients,” Dr. Turunen said.
Hyperthyroidism a risk in pregnancy – with or without treatment
The potential risks of hyperthyroidism in pregnancy are well established and can range from preeclampsia to premature birth or miscarriage.
However, antithyroid drugs, including methimazole and propylthiouracil, carry their own risks. In crossing the placental barrier, the drugs can increase the risk of birth defects, particularly during 6-10 weeks of gestation, yet their discontinuation is linked to as much as a 50%-60% risk of relapse, the authors explain.
Because of the risks, the American Thyroid Association recommends that “women with a stable euthyroid state on 5-10 mg methimazole per day achieved within a few months, and a falling TRAb level, are likely candidates to withdraw from antithyroid drug therapy in early pregnancy,” the authors noted.
However, as the recommendations for women who are already pregnant are largely based on evidence from nonpregnant patients, Hou and colleagues sought to evaluate withdrawal among women who were pregnant.
For the study, published in Thyroid, they enrolled 63 women who were pregnant and part of an outpatient service of the department of endocrinology and metabolism at The First Affiliated Hospital of China Medical University, between September 2014 and March 2017, who had well-controlled hyperthyroidism in early pregnancy and discontinued the drugs.
The women were an average age of 27 years, and 28 were multigravida. Twenty-two had a history of miscarriage.
A follow-up of the patients until the end of their pregnancy showed that, overall, 20 (31.7%) had a rebound of hyperthyroidism during their pregnancy after withdrawing from the drugs.
Key factors associated with the highest risk of a rebound after discontinuation included having subnormal TSH levels (TSH < 0.35 mIU/L; odds ratio, 5.12; P = .03) or having positive TRAb (TRAb > 1.75 IU/L; OR, 3.79; P = .02) at the time of medication withdrawal, compared with those with either normal TSH levels or negative TRAb.
The combination of both subnormal TSH and positive TRAb at the time of antithyroid medication withdrawal further boosted the risk of hyperthyroidism rebound (83.3%, 5 of 6), compared with those who had both normal TSH and negative TRAb (13%, 3 of 23; OR, 33.33; P = .003).
Adverse pregnancy outcomes increased
Importantly, among the 20 patients who had a rebound, 11 (55%) had adverse pregnancy outcomes, including miscarriage, premature birth, induced labor, gestational hypertension, and gestational diabetes, compared with only 4 (9.3%) of the 43 who had no rebound (OR, 11.92; P = .0002).
Neonatal abnormalities were also higher among those experiencing a rebound (20% vs. 4.7%), however, the authors noted that “larger prospective studies are required to conclude whether antithyroid drug withdrawal affects fetal outcome.”
In the rebound group, the mean duration of antithyroid medication use was 24.7 months versus 35.1 months in the nonrebound group, however, the difference was not statistically significant (P = .07). And 40% of the rebound group had a history of miscarriage versus 32.6% in the non-rebound group, but was also not significantly different (P = .56).
The authors noted that half of those in the rebound group developed hyperthyroidism more than 4 weeks after their withdrawal from antithyroid medications, “which seemed to have circumvented the most sensitive period of teratogenesis between 6 and 10 weeks of pregnancy.”
Hou added that restarting antithyroid medication did not increase the risk of adverse outcomes for offspring.
“A low dose of antithyroid medications may be a good choice for women with subnormal TSH and/or positive TRAb in early pregnancy,” Hou concluded. “Because of the small size of our study, a larger prospective study is needed to overcome the potential selection bias and to verify the conclusions.”
Findings consistent with Finnish study
In her own recent study, which included 2,144 women in Finland who experienced hyperthyroidism during pregnancy, Dr. Turunen and colleagues found that having hyperthyroidism, with or without antithyroid drug treatment, was associated with an increased odds of pregnancy and/or prenatal complications, compared with those without thyroid disease.
“In our study, we observed an increased risk of adverse pregnancy outcomes also in mothers with previous diagnosis and/or treatment of hyperthyroidism, not only with overt hyperthyroidism treated with antithyroid drugs,” she told this news organization.
“I think that especially those patients with positive antibodies [TRAbs] are at risk even if they are euthyroid,” she noted. “Withdrawal of antithyroid drugs in these patients is a risk.”
“Probably continuing antithyroid treatment with low dose is a better option,” she said.
The authors and Dr. Turunen reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM THYROID
Primary cesarean delivery rates in the United States
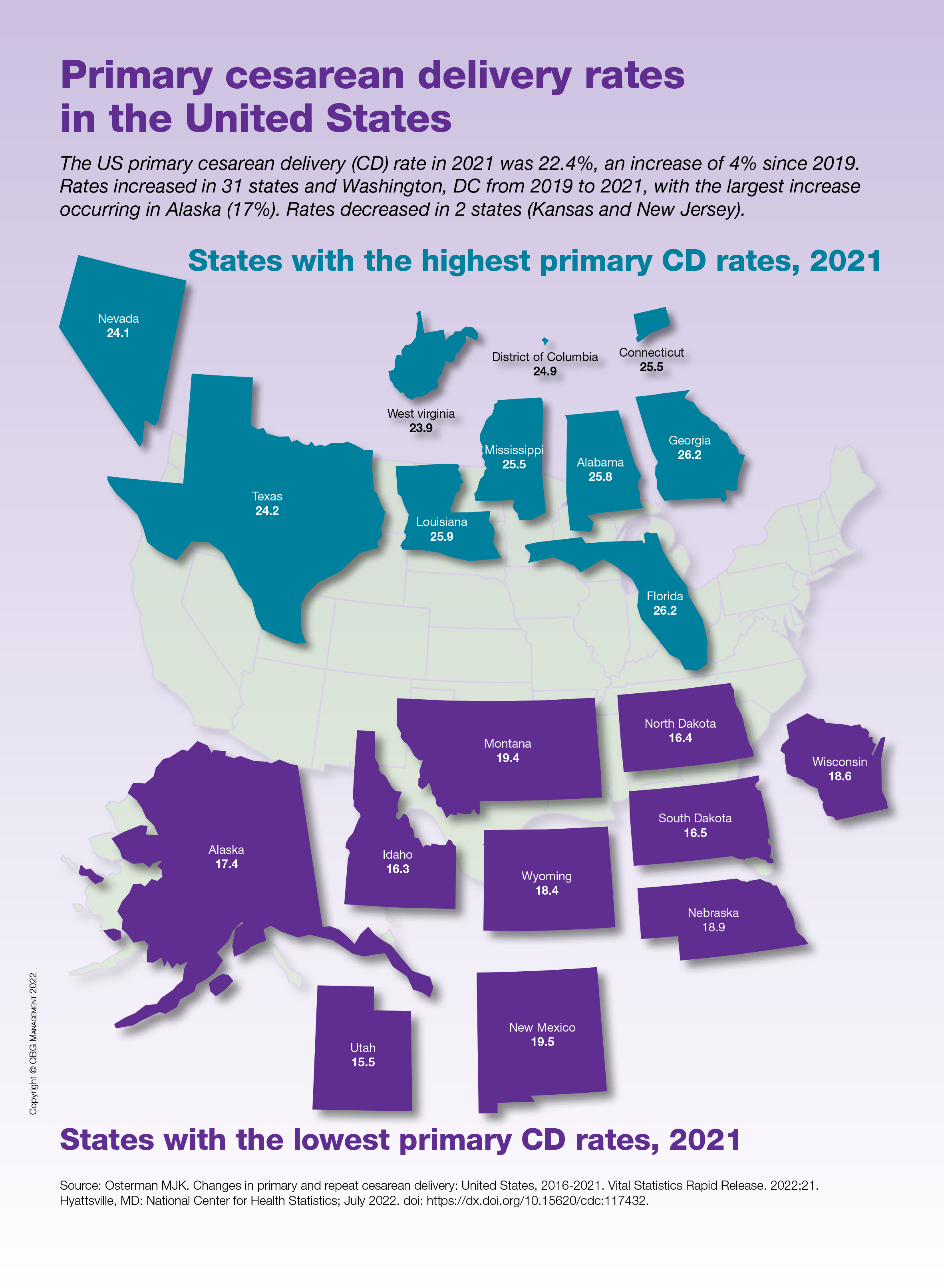
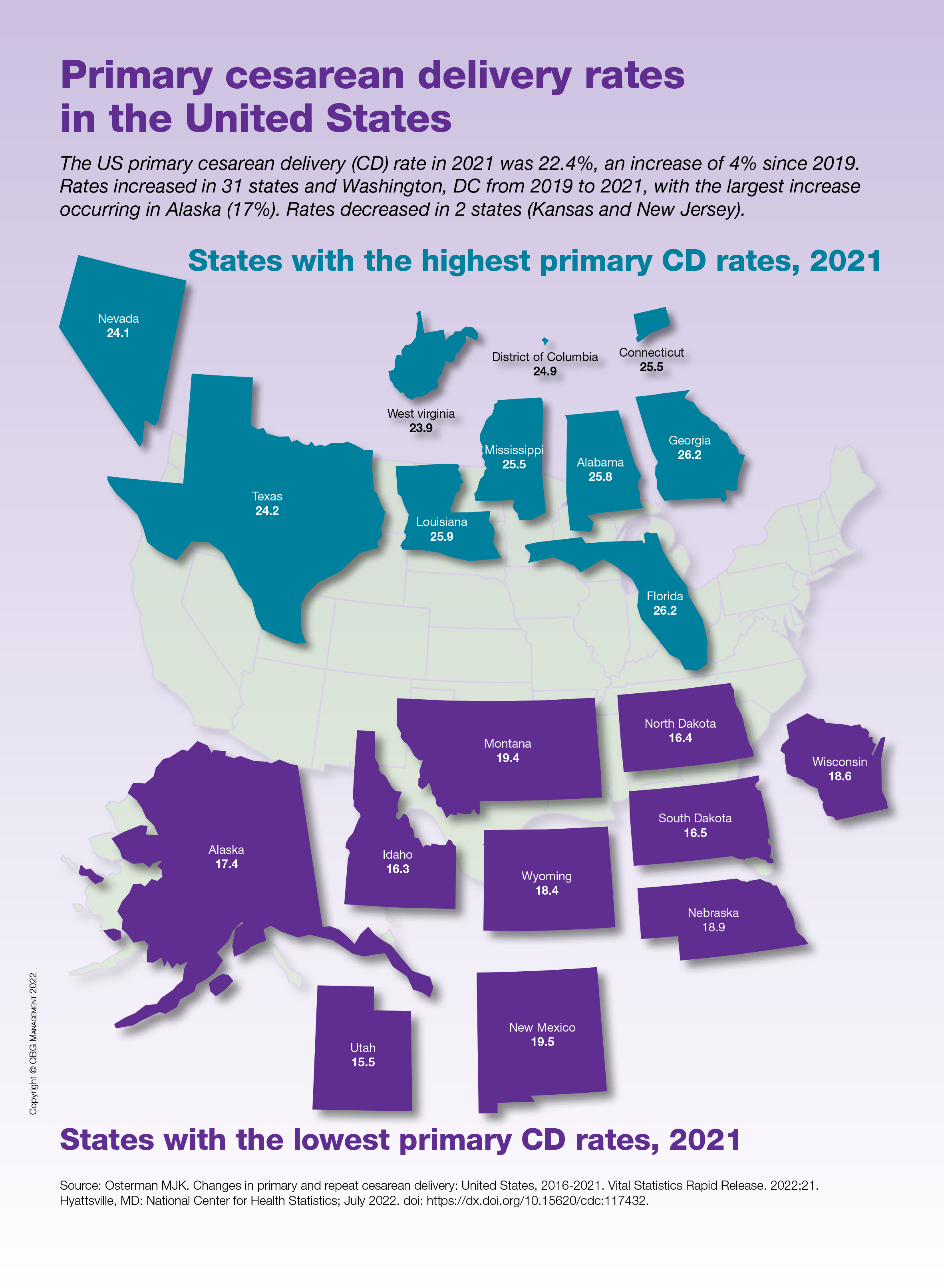
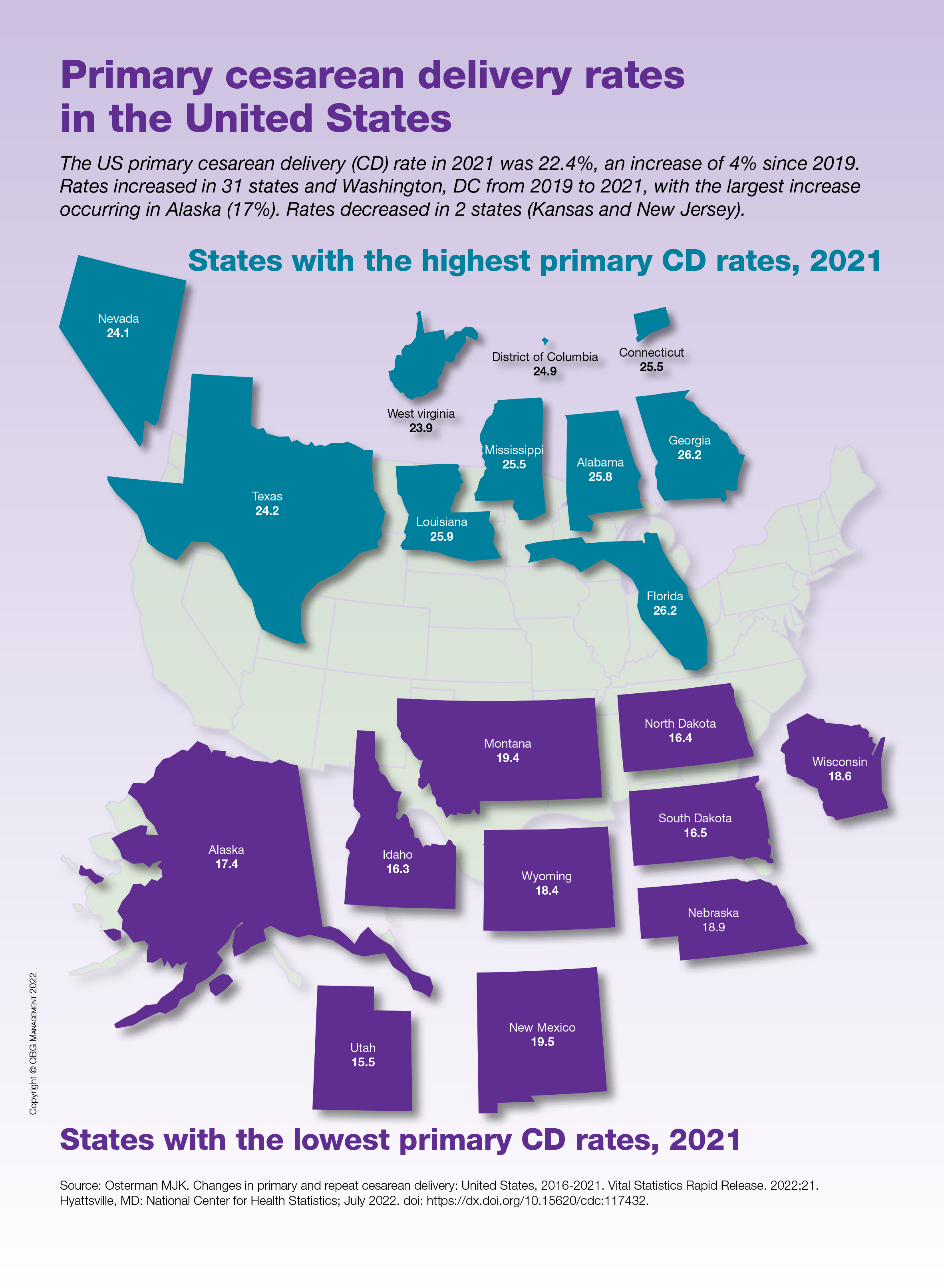
Vaginal birth possible in 50% of women with low-lying placenta
About half of women with an asymptomatic low-lying placenta in the third trimester and an internal os distance of 11-20 mm can have a vaginal birth after 35 weeks without any higher risk of severe complications than if they had undergone elective cesarean delivery, a new study indicates.
The retrospective analysis of 128,233 births between 2007 and 2012 at six hospitals in France showed that of the 171 women (0.13%) with low-lying placenta, 70 underwent a trial of labor, and 101 had an elective cesarean delivery. The vaginal delivery rate was 50.0% in the group of 38 women with an internal os distance of 11-20 mm, and 18.5% among 27 women with an internal os distance of 1-10 mm.
Similar rates of severe postpartum hemorrhage (PPH) were observed whether the patient opted for a trial of labor or for elective cesarean delivery (22.9% vs. 23.0%), regardless of maternal age, prepregnancy body mass index, nulliparity, and previous cesarean delivery. Rates of severe maternal and neonatal morbidity were 2.9% vs. 2.0%, and 12.9% vs. 9.9%, respectively, both nonsignificantly different, the study showed.
These findings confirm results from an earlier study and could reduce the incidence of unnecessary cesarean deliveries in women with low-lying placenta, said researchers led by Loïc Sentilhes, MD, PhD, of the department of obstetrics and gynecology at Bordeaux (France) University Hospital Center.
“Our results support a policy of offering a trial of labor to women with low-lying placenta at or after 35 weeks of gestation and a distance of 11-20 mm between the placental edge and the internal os on ultrasonography,” they wrote in Obstetrics & Gynecology.
Although an internal os distance of 1-10 mm did not increase the incidence of severe PPH or other severe maternal morbidity, 80% of these patients went on to have an emergency cesarean section. For this reason, the high risk of emergency cesarean should be discussed during shared decision-making, the study authors said.
Avoiding unnecessary cesarean deliveries is crucial to limiting the occurrence of low-lying placenta, placenta previa, vasa previa, and placenta accreta spectrum in subsequent pregnancies, Dr. Sentilhes told this news organization. “We hope that our results will help caregivers to objectively advise their patients with low-lying placenta regarding the choice of their mode of delivery.”
“This is further evidence to reassure clinicians that managing such patients with labor is a reasonable approach,” said Aaron B. Caughey, MD, MPH, PhD, professor and chair of the department of obstetrics and gynecology at Oregon Health & Science University, Portland. He was not involved in the study.
Many obstetricians have practiced this for decades, noted Dr. Caughey, associate dean for women’s health research and policy at Oregon Health. “We manage these patients expectantly with a plan for a trial of labor.”
“I am absolutely in agreement,” said Sarah L. Pachtman, MD, an obstetrician-gynecologist at Long Island Jewish Medical Center in New York, who is an independent expert. Dr. Pachtman noted that since she works at a hospital equipped for emergency cesarean deliveries, “I can get a baby out in 5 minutes if necessary.”
Dr. Pachtman’s practice consists of “a very large population of women who strongly desire vaginal delivery.
“It’s a better recovery for them, avoids the risks of abdominal surgery, gives them quicker skin-to-skin contact with their newborn and they can start breastfeeding sooner,” she said in an interview. “And the risk of bleeding is actually lower compared to elective cesarean delivery.”
Deciding on the mode of delivery should be based on patient preference and physician comfort, shared decision-making, and where the patient delivers, Dr. Pachtman said. “If the placental edge is between 1 mm and 10 mm or abutting the internal os, I explain to the patient that there is a risk of bleeding even before labor starts, and they would most likely want to choose an elective cesarean delivery.”
Although low-lying placenta can be associated with significant maternal and neonatal morbidity and mortality, particularly when diagnosed at delivery, universal cervical length screening during routine anatomic ultrasound is identifying the presence of low-lying placenta much earlier in pregnancy.
“We’re identifying it more, following it more, and reporting it more,” Dr. Pachtman said. And in the vast majority of patients, she emphasized, the 28-week follow-up transvaginal ultrasound shows that the low-lying placenta has resolved.
Dr. Sentilhes reported a relationship with Ferring Laboratories. No other study authors disclosed having conflicts of interest. Dr. Caughey and Dr. Pachtman reported having no conflicts of interest.
About half of women with an asymptomatic low-lying placenta in the third trimester and an internal os distance of 11-20 mm can have a vaginal birth after 35 weeks without any higher risk of severe complications than if they had undergone elective cesarean delivery, a new study indicates.
The retrospective analysis of 128,233 births between 2007 and 2012 at six hospitals in France showed that of the 171 women (0.13%) with low-lying placenta, 70 underwent a trial of labor, and 101 had an elective cesarean delivery. The vaginal delivery rate was 50.0% in the group of 38 women with an internal os distance of 11-20 mm, and 18.5% among 27 women with an internal os distance of 1-10 mm.
Similar rates of severe postpartum hemorrhage (PPH) were observed whether the patient opted for a trial of labor or for elective cesarean delivery (22.9% vs. 23.0%), regardless of maternal age, prepregnancy body mass index, nulliparity, and previous cesarean delivery. Rates of severe maternal and neonatal morbidity were 2.9% vs. 2.0%, and 12.9% vs. 9.9%, respectively, both nonsignificantly different, the study showed.
These findings confirm results from an earlier study and could reduce the incidence of unnecessary cesarean deliveries in women with low-lying placenta, said researchers led by Loïc Sentilhes, MD, PhD, of the department of obstetrics and gynecology at Bordeaux (France) University Hospital Center.
“Our results support a policy of offering a trial of labor to women with low-lying placenta at or after 35 weeks of gestation and a distance of 11-20 mm between the placental edge and the internal os on ultrasonography,” they wrote in Obstetrics & Gynecology.
Although an internal os distance of 1-10 mm did not increase the incidence of severe PPH or other severe maternal morbidity, 80% of these patients went on to have an emergency cesarean section. For this reason, the high risk of emergency cesarean should be discussed during shared decision-making, the study authors said.
Avoiding unnecessary cesarean deliveries is crucial to limiting the occurrence of low-lying placenta, placenta previa, vasa previa, and placenta accreta spectrum in subsequent pregnancies, Dr. Sentilhes told this news organization. “We hope that our results will help caregivers to objectively advise their patients with low-lying placenta regarding the choice of their mode of delivery.”
“This is further evidence to reassure clinicians that managing such patients with labor is a reasonable approach,” said Aaron B. Caughey, MD, MPH, PhD, professor and chair of the department of obstetrics and gynecology at Oregon Health & Science University, Portland. He was not involved in the study.
Many obstetricians have practiced this for decades, noted Dr. Caughey, associate dean for women’s health research and policy at Oregon Health. “We manage these patients expectantly with a plan for a trial of labor.”
“I am absolutely in agreement,” said Sarah L. Pachtman, MD, an obstetrician-gynecologist at Long Island Jewish Medical Center in New York, who is an independent expert. Dr. Pachtman noted that since she works at a hospital equipped for emergency cesarean deliveries, “I can get a baby out in 5 minutes if necessary.”
Dr. Pachtman’s practice consists of “a very large population of women who strongly desire vaginal delivery.
“It’s a better recovery for them, avoids the risks of abdominal surgery, gives them quicker skin-to-skin contact with their newborn and they can start breastfeeding sooner,” she said in an interview. “And the risk of bleeding is actually lower compared to elective cesarean delivery.”
Deciding on the mode of delivery should be based on patient preference and physician comfort, shared decision-making, and where the patient delivers, Dr. Pachtman said. “If the placental edge is between 1 mm and 10 mm or abutting the internal os, I explain to the patient that there is a risk of bleeding even before labor starts, and they would most likely want to choose an elective cesarean delivery.”
Although low-lying placenta can be associated with significant maternal and neonatal morbidity and mortality, particularly when diagnosed at delivery, universal cervical length screening during routine anatomic ultrasound is identifying the presence of low-lying placenta much earlier in pregnancy.
“We’re identifying it more, following it more, and reporting it more,” Dr. Pachtman said. And in the vast majority of patients, she emphasized, the 28-week follow-up transvaginal ultrasound shows that the low-lying placenta has resolved.
Dr. Sentilhes reported a relationship with Ferring Laboratories. No other study authors disclosed having conflicts of interest. Dr. Caughey and Dr. Pachtman reported having no conflicts of interest.
About half of women with an asymptomatic low-lying placenta in the third trimester and an internal os distance of 11-20 mm can have a vaginal birth after 35 weeks without any higher risk of severe complications than if they had undergone elective cesarean delivery, a new study indicates.
The retrospective analysis of 128,233 births between 2007 and 2012 at six hospitals in France showed that of the 171 women (0.13%) with low-lying placenta, 70 underwent a trial of labor, and 101 had an elective cesarean delivery. The vaginal delivery rate was 50.0% in the group of 38 women with an internal os distance of 11-20 mm, and 18.5% among 27 women with an internal os distance of 1-10 mm.
Similar rates of severe postpartum hemorrhage (PPH) were observed whether the patient opted for a trial of labor or for elective cesarean delivery (22.9% vs. 23.0%), regardless of maternal age, prepregnancy body mass index, nulliparity, and previous cesarean delivery. Rates of severe maternal and neonatal morbidity were 2.9% vs. 2.0%, and 12.9% vs. 9.9%, respectively, both nonsignificantly different, the study showed.
These findings confirm results from an earlier study and could reduce the incidence of unnecessary cesarean deliveries in women with low-lying placenta, said researchers led by Loïc Sentilhes, MD, PhD, of the department of obstetrics and gynecology at Bordeaux (France) University Hospital Center.
“Our results support a policy of offering a trial of labor to women with low-lying placenta at or after 35 weeks of gestation and a distance of 11-20 mm between the placental edge and the internal os on ultrasonography,” they wrote in Obstetrics & Gynecology.
Although an internal os distance of 1-10 mm did not increase the incidence of severe PPH or other severe maternal morbidity, 80% of these patients went on to have an emergency cesarean section. For this reason, the high risk of emergency cesarean should be discussed during shared decision-making, the study authors said.
Avoiding unnecessary cesarean deliveries is crucial to limiting the occurrence of low-lying placenta, placenta previa, vasa previa, and placenta accreta spectrum in subsequent pregnancies, Dr. Sentilhes told this news organization. “We hope that our results will help caregivers to objectively advise their patients with low-lying placenta regarding the choice of their mode of delivery.”
“This is further evidence to reassure clinicians that managing such patients with labor is a reasonable approach,” said Aaron B. Caughey, MD, MPH, PhD, professor and chair of the department of obstetrics and gynecology at Oregon Health & Science University, Portland. He was not involved in the study.
Many obstetricians have practiced this for decades, noted Dr. Caughey, associate dean for women’s health research and policy at Oregon Health. “We manage these patients expectantly with a plan for a trial of labor.”
“I am absolutely in agreement,” said Sarah L. Pachtman, MD, an obstetrician-gynecologist at Long Island Jewish Medical Center in New York, who is an independent expert. Dr. Pachtman noted that since she works at a hospital equipped for emergency cesarean deliveries, “I can get a baby out in 5 minutes if necessary.”
Dr. Pachtman’s practice consists of “a very large population of women who strongly desire vaginal delivery.
“It’s a better recovery for them, avoids the risks of abdominal surgery, gives them quicker skin-to-skin contact with their newborn and they can start breastfeeding sooner,” she said in an interview. “And the risk of bleeding is actually lower compared to elective cesarean delivery.”
Deciding on the mode of delivery should be based on patient preference and physician comfort, shared decision-making, and where the patient delivers, Dr. Pachtman said. “If the placental edge is between 1 mm and 10 mm or abutting the internal os, I explain to the patient that there is a risk of bleeding even before labor starts, and they would most likely want to choose an elective cesarean delivery.”
Although low-lying placenta can be associated with significant maternal and neonatal morbidity and mortality, particularly when diagnosed at delivery, universal cervical length screening during routine anatomic ultrasound is identifying the presence of low-lying placenta much earlier in pregnancy.
“We’re identifying it more, following it more, and reporting it more,” Dr. Pachtman said. And in the vast majority of patients, she emphasized, the 28-week follow-up transvaginal ultrasound shows that the low-lying placenta has resolved.
Dr. Sentilhes reported a relationship with Ferring Laboratories. No other study authors disclosed having conflicts of interest. Dr. Caughey and Dr. Pachtman reported having no conflicts of interest.
FROM OBSTETRICS & GYNECOLOGY
Genetic counseling for cancer often costs patients nothing
But even among those who do, the cost is $16 or less, a cohort study shows.
“The findings highlight the relatively low financial costs of genetic counseling, a form of care with potentially substantial implications for cancer treatment,” lead author Mya Roberson, PhD, Vanderbilt University, Nashville, Tenn., and colleagues explained.
The study was published online in JAMA Health Forum.
Genetic counseling is an important feature of cancer care that can affect treatment decisions and surveillance. But coverage of genetic counseling services varies across insurance types.
To understand the costs to patients, the investigators used data from IBM Watson Health MarketScan to create a cohort of privately insured patients with breast, prostate, endometrial, ovarian, colorectal, and pancreatic cancer who had at least one genetic counseling session from 2013 to the end of 2019.
Dr. Roberson and colleagues then calculated out-of-pocket costs – including coinsurance, copayments, and deductibles – and total costs paid on claims for genetic counseling encounters. The cohort included 16,791 patients, the majority of whom had breast cancer.
Although the median insurance payment for genetic counseling encounters was $118 ($58-$211), most patients paid nothing out of pocket for these services. Among the 31% of patients with an out-of-pocket expense, the cost was $16 or less.
Compared with breast cancer patients, men with prostate cancer were 28% more likely to have out-of-pocket costs for genetic counseling, which may “reflect a lack of awareness about the medical necessity of genetic counseling,” the authors suggested.
Overall, the study highlights the value of genetic counseling in cancer care.
“Cancer genetic counseling not only promotes informed decision-making about genetic testing and cancer treatment in the era of precision medicine, but it also is a form of low-cost, high-value care,” the authors wrote.
The study was funded by a grant from the National Cancer Institute. Dr. Roberson disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
But even among those who do, the cost is $16 or less, a cohort study shows.
“The findings highlight the relatively low financial costs of genetic counseling, a form of care with potentially substantial implications for cancer treatment,” lead author Mya Roberson, PhD, Vanderbilt University, Nashville, Tenn., and colleagues explained.
The study was published online in JAMA Health Forum.
Genetic counseling is an important feature of cancer care that can affect treatment decisions and surveillance. But coverage of genetic counseling services varies across insurance types.
To understand the costs to patients, the investigators used data from IBM Watson Health MarketScan to create a cohort of privately insured patients with breast, prostate, endometrial, ovarian, colorectal, and pancreatic cancer who had at least one genetic counseling session from 2013 to the end of 2019.
Dr. Roberson and colleagues then calculated out-of-pocket costs – including coinsurance, copayments, and deductibles – and total costs paid on claims for genetic counseling encounters. The cohort included 16,791 patients, the majority of whom had breast cancer.
Although the median insurance payment for genetic counseling encounters was $118 ($58-$211), most patients paid nothing out of pocket for these services. Among the 31% of patients with an out-of-pocket expense, the cost was $16 or less.
Compared with breast cancer patients, men with prostate cancer were 28% more likely to have out-of-pocket costs for genetic counseling, which may “reflect a lack of awareness about the medical necessity of genetic counseling,” the authors suggested.
Overall, the study highlights the value of genetic counseling in cancer care.
“Cancer genetic counseling not only promotes informed decision-making about genetic testing and cancer treatment in the era of precision medicine, but it also is a form of low-cost, high-value care,” the authors wrote.
The study was funded by a grant from the National Cancer Institute. Dr. Roberson disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
But even among those who do, the cost is $16 or less, a cohort study shows.
“The findings highlight the relatively low financial costs of genetic counseling, a form of care with potentially substantial implications for cancer treatment,” lead author Mya Roberson, PhD, Vanderbilt University, Nashville, Tenn., and colleagues explained.
The study was published online in JAMA Health Forum.
Genetic counseling is an important feature of cancer care that can affect treatment decisions and surveillance. But coverage of genetic counseling services varies across insurance types.
To understand the costs to patients, the investigators used data from IBM Watson Health MarketScan to create a cohort of privately insured patients with breast, prostate, endometrial, ovarian, colorectal, and pancreatic cancer who had at least one genetic counseling session from 2013 to the end of 2019.
Dr. Roberson and colleagues then calculated out-of-pocket costs – including coinsurance, copayments, and deductibles – and total costs paid on claims for genetic counseling encounters. The cohort included 16,791 patients, the majority of whom had breast cancer.
Although the median insurance payment for genetic counseling encounters was $118 ($58-$211), most patients paid nothing out of pocket for these services. Among the 31% of patients with an out-of-pocket expense, the cost was $16 or less.
Compared with breast cancer patients, men with prostate cancer were 28% more likely to have out-of-pocket costs for genetic counseling, which may “reflect a lack of awareness about the medical necessity of genetic counseling,” the authors suggested.
Overall, the study highlights the value of genetic counseling in cancer care.
“Cancer genetic counseling not only promotes informed decision-making about genetic testing and cancer treatment in the era of precision medicine, but it also is a form of low-cost, high-value care,” the authors wrote.
The study was funded by a grant from the National Cancer Institute. Dr. Roberson disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA HEALTH FORUM
Blood test for cancer available, but is it ready for prime time?
The Galleri blood test is being now offered by a number of United States health networks.
The company marketing the test, GRAIL, has established partnerships with the U.S. Department of Veterans Affairs, Mercy Health, Ochsner Health, Intermountain Healthcare, Community Health Network, Knight Cancer Institute at Oregon Health & Science University, Premier, and Cleveland Clinic, among others.
Cleveland Clinic’s Eric Klein, MD, emeritus chair of the Glickman Urological Kidney Institute, is enthusiastic about the test, describing it as a “game-changer” and emphasizing that it can detect many different cancers and at a very early stage.
“It completely changes the way we think about screening for cancer,” commented Jeff Venstrom, MD, chief medical officer at GRAIL. He joined the company because “there are not many things in life where you can be part of a disruptive paradigm and disruptive technology, and this really is disruptive,” he said in an interview.
‘The devil is in the details’
But there is some concern among clinicians that widespread clinical use of the test may be premature.
Having a blood test for multiple cancers is a “very good idea, and the scientific basis for this platform is sound,” commented Timothy R. Rebbeck, PhD, professor of cancer prevention, Harvard T.H. Chan School of Public Health, and Division of Population Sciences, Dana-Farber Cancer Institute, both in Boston.
“But the devil is in the details to ensure the test can accurately detect very early cancers and there is a pathway for subsequent workup (diagnosis, monitoring, treatment, etc.),” Dr. Rebbeck told this news organization.
Galleri is offering the test to individuals who are older than 50 and have a family history of cancer or those who are high risk for cancer or immunocompromised. They suggest that interested individuals get in touch with their health care professional, who then needs to register with GRAIL and order the test.
As well as needing a prescription, interested individuals will have to pay for it out of pocket, around $950. The test is not covered by medical insurance and is not approved by the U.S. Food and Drug Administration.
Falls into primary care setting
Dr. Rebbeck commented that Galleri is a screening test for individuals who don’t have cancer, so the test is intended to fall into the primary care setting. But he warned that “clinical pathways are not yet in place (but are being developed) so that primary care providers can effectively use them.”
The test uses next-generation sequencing to analyze the arrangement of methyl groups on circulating tumor (or cell-free) DNA in a blood sample.
The methylation turns genes on or off, explains Cleveland Clinic’s Dr. Klein in his post. “It’s like fingerprints and how fingerprints tell the difference between two people,” he wrote. “The methylation patterns are fingerprints that are characteristic of each kind of cancer. They look one way for lung cancer and different for colon cancer.”
The test returns one of two possible results: either “positive, cancer signal detected” or “negative, no cancer signal detected.”
According to the company, when a cancer signal is detected, the Galleri test predicts the cancer signal origin “with high accuracy, to help guide the next steps to diagnosis.”
However, one problem for clinical practice is all the follow-up tests an individual may undergo if their test comes back positive, said Sameek Roychowdhury, MD, PhD, an oncologist with Ohio State University Comprehensive Cancer Center, Columbus.
“Not everybody will have an actual cancer, but they may undergo many tests, with a lot of stress and cost and still not find anything. I can tell you every time someone undergoes a test looking for cancer, that is not an easy day,” Dr. Roychowdhury said in an interview.
In a large-scale validation study, the Galleri test had a specificity of 99.5% (false-positive rate of 0.5%), meaning in roughly 200 people tested without cancer, only one person received a false-positive result (that is, “cancer signal detected” when cancer is not present).
The overall sensitivity of the test for any stage of cancer was 51.5%, although it was higher for later-stage cancers (77% for stage III and 90.1% for stage IV) and lower for early-stage cancers (16.8% for stage I and 40.4% for stage II).
Exacerbate health disparities?
In Dr. Rebbeck’s view, the characteristics of the test are still “relatively poor for detecting very early cancers, so it will need additional tweaking before it really achieves the goal of multi-cancer EARLY detection,” he said.
Dr. Venstrom acknowledges that the test is “not perfect yet” and says the company will continue to update and improve its performance. “We have some new data coming out in September,” he said.
Clinical data are being accumulated in the United Kingdom, where the Galleri test is being investigated in a large trial run by the National Health Service (NHS). The company recently announced that the enrollment of 140,000 healthy cancer-free volunteers aged 50-77 into this trial has now been completed and claimed this the largest-ever study of a multi-cancer early detection test.
Dr. Roychowdhury said he would encourage anyone interested in the test to join a clinical trial.
Another expert approached for comment last year, when GRAIL first started marketing the test, was in agreement. This test should be viewed as one that is still under clinical investigation, commented William Grady, MD, a member of the clinical research division and public health sciences division at the Fred Hutchinson Cancer Research Center, Seattle.
“The Galleri test is still unproven in the clinical care setting and ... I am concerned that many of the results will be false-positives and will cause many unnecessary follow-up tests and imaging studies as well as anxiety in the people getting the test done,” Dr. Grady said.
Dr. Rebbeck said another issue that needs to be addressed is whether all populations will have access to and benefit from these types of blood tests to screen for cancer, given that they are expensive.
“There is a great danger – as we have seen with many other technological innovations – that the wealthy and connected benefit, but the majority of the population, and particularly those who are underserved, do not,” Dr. Rebbeck said.
“As a result, health disparities are created or exacerbated. This is something that needs to be addressed so that the future use of these tests will provide equitable benefits,” he added.
Dr. Rebbeck and Dr. Roychowdhury have reported no relevant financial relationships. Dr. Venstrom is an employee of GRAIL.
A version of this article first appeared on Medscape.com.
The Galleri blood test is being now offered by a number of United States health networks.
The company marketing the test, GRAIL, has established partnerships with the U.S. Department of Veterans Affairs, Mercy Health, Ochsner Health, Intermountain Healthcare, Community Health Network, Knight Cancer Institute at Oregon Health & Science University, Premier, and Cleveland Clinic, among others.
Cleveland Clinic’s Eric Klein, MD, emeritus chair of the Glickman Urological Kidney Institute, is enthusiastic about the test, describing it as a “game-changer” and emphasizing that it can detect many different cancers and at a very early stage.
“It completely changes the way we think about screening for cancer,” commented Jeff Venstrom, MD, chief medical officer at GRAIL. He joined the company because “there are not many things in life where you can be part of a disruptive paradigm and disruptive technology, and this really is disruptive,” he said in an interview.
‘The devil is in the details’
But there is some concern among clinicians that widespread clinical use of the test may be premature.
Having a blood test for multiple cancers is a “very good idea, and the scientific basis for this platform is sound,” commented Timothy R. Rebbeck, PhD, professor of cancer prevention, Harvard T.H. Chan School of Public Health, and Division of Population Sciences, Dana-Farber Cancer Institute, both in Boston.
“But the devil is in the details to ensure the test can accurately detect very early cancers and there is a pathway for subsequent workup (diagnosis, monitoring, treatment, etc.),” Dr. Rebbeck told this news organization.
Galleri is offering the test to individuals who are older than 50 and have a family history of cancer or those who are high risk for cancer or immunocompromised. They suggest that interested individuals get in touch with their health care professional, who then needs to register with GRAIL and order the test.
As well as needing a prescription, interested individuals will have to pay for it out of pocket, around $950. The test is not covered by medical insurance and is not approved by the U.S. Food and Drug Administration.
Falls into primary care setting
Dr. Rebbeck commented that Galleri is a screening test for individuals who don’t have cancer, so the test is intended to fall into the primary care setting. But he warned that “clinical pathways are not yet in place (but are being developed) so that primary care providers can effectively use them.”
The test uses next-generation sequencing to analyze the arrangement of methyl groups on circulating tumor (or cell-free) DNA in a blood sample.
The methylation turns genes on or off, explains Cleveland Clinic’s Dr. Klein in his post. “It’s like fingerprints and how fingerprints tell the difference between two people,” he wrote. “The methylation patterns are fingerprints that are characteristic of each kind of cancer. They look one way for lung cancer and different for colon cancer.”
The test returns one of two possible results: either “positive, cancer signal detected” or “negative, no cancer signal detected.”
According to the company, when a cancer signal is detected, the Galleri test predicts the cancer signal origin “with high accuracy, to help guide the next steps to diagnosis.”
However, one problem for clinical practice is all the follow-up tests an individual may undergo if their test comes back positive, said Sameek Roychowdhury, MD, PhD, an oncologist with Ohio State University Comprehensive Cancer Center, Columbus.
“Not everybody will have an actual cancer, but they may undergo many tests, with a lot of stress and cost and still not find anything. I can tell you every time someone undergoes a test looking for cancer, that is not an easy day,” Dr. Roychowdhury said in an interview.
In a large-scale validation study, the Galleri test had a specificity of 99.5% (false-positive rate of 0.5%), meaning in roughly 200 people tested without cancer, only one person received a false-positive result (that is, “cancer signal detected” when cancer is not present).
The overall sensitivity of the test for any stage of cancer was 51.5%, although it was higher for later-stage cancers (77% for stage III and 90.1% for stage IV) and lower for early-stage cancers (16.8% for stage I and 40.4% for stage II).
Exacerbate health disparities?
In Dr. Rebbeck’s view, the characteristics of the test are still “relatively poor for detecting very early cancers, so it will need additional tweaking before it really achieves the goal of multi-cancer EARLY detection,” he said.
Dr. Venstrom acknowledges that the test is “not perfect yet” and says the company will continue to update and improve its performance. “We have some new data coming out in September,” he said.
Clinical data are being accumulated in the United Kingdom, where the Galleri test is being investigated in a large trial run by the National Health Service (NHS). The company recently announced that the enrollment of 140,000 healthy cancer-free volunteers aged 50-77 into this trial has now been completed and claimed this the largest-ever study of a multi-cancer early detection test.
Dr. Roychowdhury said he would encourage anyone interested in the test to join a clinical trial.
Another expert approached for comment last year, when GRAIL first started marketing the test, was in agreement. This test should be viewed as one that is still under clinical investigation, commented William Grady, MD, a member of the clinical research division and public health sciences division at the Fred Hutchinson Cancer Research Center, Seattle.
“The Galleri test is still unproven in the clinical care setting and ... I am concerned that many of the results will be false-positives and will cause many unnecessary follow-up tests and imaging studies as well as anxiety in the people getting the test done,” Dr. Grady said.
Dr. Rebbeck said another issue that needs to be addressed is whether all populations will have access to and benefit from these types of blood tests to screen for cancer, given that they are expensive.
“There is a great danger – as we have seen with many other technological innovations – that the wealthy and connected benefit, but the majority of the population, and particularly those who are underserved, do not,” Dr. Rebbeck said.
“As a result, health disparities are created or exacerbated. This is something that needs to be addressed so that the future use of these tests will provide equitable benefits,” he added.
Dr. Rebbeck and Dr. Roychowdhury have reported no relevant financial relationships. Dr. Venstrom is an employee of GRAIL.
A version of this article first appeared on Medscape.com.
The Galleri blood test is being now offered by a number of United States health networks.
The company marketing the test, GRAIL, has established partnerships with the U.S. Department of Veterans Affairs, Mercy Health, Ochsner Health, Intermountain Healthcare, Community Health Network, Knight Cancer Institute at Oregon Health & Science University, Premier, and Cleveland Clinic, among others.
Cleveland Clinic’s Eric Klein, MD, emeritus chair of the Glickman Urological Kidney Institute, is enthusiastic about the test, describing it as a “game-changer” and emphasizing that it can detect many different cancers and at a very early stage.
“It completely changes the way we think about screening for cancer,” commented Jeff Venstrom, MD, chief medical officer at GRAIL. He joined the company because “there are not many things in life where you can be part of a disruptive paradigm and disruptive technology, and this really is disruptive,” he said in an interview.
‘The devil is in the details’
But there is some concern among clinicians that widespread clinical use of the test may be premature.
Having a blood test for multiple cancers is a “very good idea, and the scientific basis for this platform is sound,” commented Timothy R. Rebbeck, PhD, professor of cancer prevention, Harvard T.H. Chan School of Public Health, and Division of Population Sciences, Dana-Farber Cancer Institute, both in Boston.
“But the devil is in the details to ensure the test can accurately detect very early cancers and there is a pathway for subsequent workup (diagnosis, monitoring, treatment, etc.),” Dr. Rebbeck told this news organization.
Galleri is offering the test to individuals who are older than 50 and have a family history of cancer or those who are high risk for cancer or immunocompromised. They suggest that interested individuals get in touch with their health care professional, who then needs to register with GRAIL and order the test.
As well as needing a prescription, interested individuals will have to pay for it out of pocket, around $950. The test is not covered by medical insurance and is not approved by the U.S. Food and Drug Administration.
Falls into primary care setting
Dr. Rebbeck commented that Galleri is a screening test for individuals who don’t have cancer, so the test is intended to fall into the primary care setting. But he warned that “clinical pathways are not yet in place (but are being developed) so that primary care providers can effectively use them.”
The test uses next-generation sequencing to analyze the arrangement of methyl groups on circulating tumor (or cell-free) DNA in a blood sample.
The methylation turns genes on or off, explains Cleveland Clinic’s Dr. Klein in his post. “It’s like fingerprints and how fingerprints tell the difference between two people,” he wrote. “The methylation patterns are fingerprints that are characteristic of each kind of cancer. They look one way for lung cancer and different for colon cancer.”
The test returns one of two possible results: either “positive, cancer signal detected” or “negative, no cancer signal detected.”
According to the company, when a cancer signal is detected, the Galleri test predicts the cancer signal origin “with high accuracy, to help guide the next steps to diagnosis.”
However, one problem for clinical practice is all the follow-up tests an individual may undergo if their test comes back positive, said Sameek Roychowdhury, MD, PhD, an oncologist with Ohio State University Comprehensive Cancer Center, Columbus.
“Not everybody will have an actual cancer, but they may undergo many tests, with a lot of stress and cost and still not find anything. I can tell you every time someone undergoes a test looking for cancer, that is not an easy day,” Dr. Roychowdhury said in an interview.
In a large-scale validation study, the Galleri test had a specificity of 99.5% (false-positive rate of 0.5%), meaning in roughly 200 people tested without cancer, only one person received a false-positive result (that is, “cancer signal detected” when cancer is not present).
The overall sensitivity of the test for any stage of cancer was 51.5%, although it was higher for later-stage cancers (77% for stage III and 90.1% for stage IV) and lower for early-stage cancers (16.8% for stage I and 40.4% for stage II).
Exacerbate health disparities?
In Dr. Rebbeck’s view, the characteristics of the test are still “relatively poor for detecting very early cancers, so it will need additional tweaking before it really achieves the goal of multi-cancer EARLY detection,” he said.
Dr. Venstrom acknowledges that the test is “not perfect yet” and says the company will continue to update and improve its performance. “We have some new data coming out in September,” he said.
Clinical data are being accumulated in the United Kingdom, where the Galleri test is being investigated in a large trial run by the National Health Service (NHS). The company recently announced that the enrollment of 140,000 healthy cancer-free volunteers aged 50-77 into this trial has now been completed and claimed this the largest-ever study of a multi-cancer early detection test.
Dr. Roychowdhury said he would encourage anyone interested in the test to join a clinical trial.
Another expert approached for comment last year, when GRAIL first started marketing the test, was in agreement. This test should be viewed as one that is still under clinical investigation, commented William Grady, MD, a member of the clinical research division and public health sciences division at the Fred Hutchinson Cancer Research Center, Seattle.
“The Galleri test is still unproven in the clinical care setting and ... I am concerned that many of the results will be false-positives and will cause many unnecessary follow-up tests and imaging studies as well as anxiety in the people getting the test done,” Dr. Grady said.
Dr. Rebbeck said another issue that needs to be addressed is whether all populations will have access to and benefit from these types of blood tests to screen for cancer, given that they are expensive.
“There is a great danger – as we have seen with many other technological innovations – that the wealthy and connected benefit, but the majority of the population, and particularly those who are underserved, do not,” Dr. Rebbeck said.
“As a result, health disparities are created or exacerbated. This is something that needs to be addressed so that the future use of these tests will provide equitable benefits,” he added.
Dr. Rebbeck and Dr. Roychowdhury have reported no relevant financial relationships. Dr. Venstrom is an employee of GRAIL.
A version of this article first appeared on Medscape.com.