User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
nav[contains(@class, 'nav-ce-stack nav-ce-stack__large-screen')]
header[@id='header']
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
Amniotic fluid embolism: Management using a checklist
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
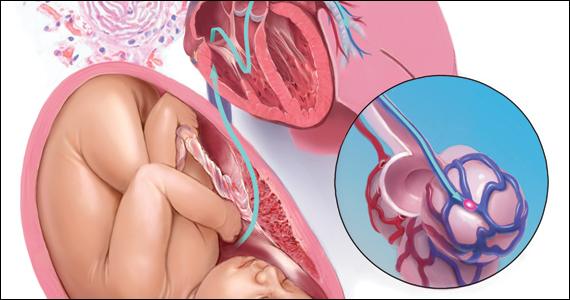
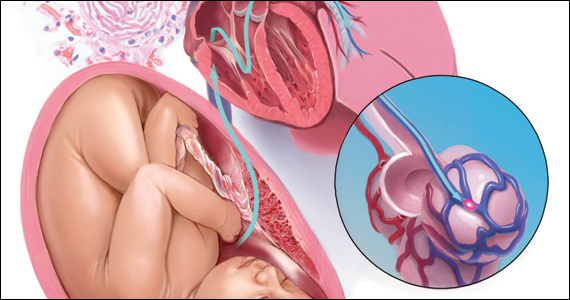
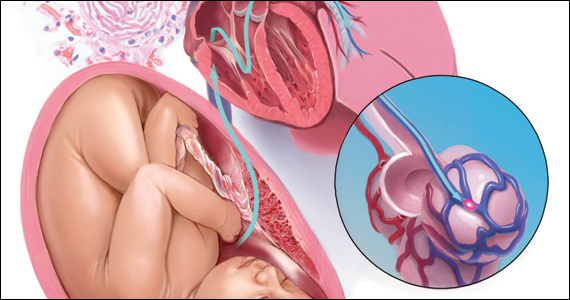
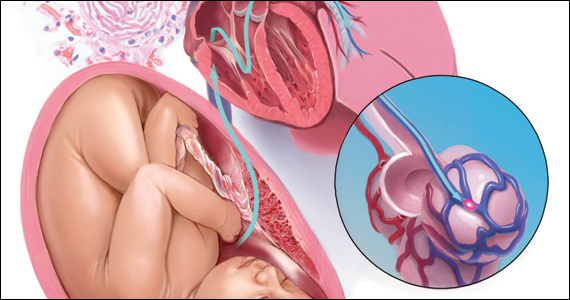
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
CASE Part 1: CPR initiated during induction of labor
A 32-year-old gravida 4 para 3-0-0-3 is undergoing induction of labor with intravenous (IV) oxytocin at 39 weeks of gestation. She has no significant medical or obstetric history. Fifteen minutes after reaching complete cervical dilation, she says “I don’t feel right,” then suddenly loses consciousness. The nurse finds no detectable pulse, calls a “code blue,” and initiates cardiopulmonary resuscitation (CPR). The obstetrician is notified, appears promptly, assesses the situation, and delivers a 3.6-kg baby via vacuum extraction. Apgar score is 2/10 at 1 minute and 6/10 at 5 minutes. After delivery of the placenta, there is uterine atony and brisk hemorrhage with 2 L of blood loss.
Management of AFE: A rare complication
This case demonstrates a classic presentation of amniotic fluid embolism (AFE) syndrome—a patient in labor or within 30 minutes after delivery has sudden onset of cardiorespiratory collapse followed by disseminated intravascular coagulation (DIC). AFE is rare, affecting only about 2 to 6 per 100,000 births, but classic cases have a reported maternal mortality rate that exceeds 50%.1 It is thought to reflect a complex, systemic proinflammatory response to maternal intravasation of pregnancy material, such as trophoblast, thromboplastins, fetal cells, or amniotic fluid. Because the syndrome is not necessarily directly caused by emboli or by amniotic fluid per se,2 it has been proposed that AFE be called “anaphylactoid syndrome of pregnancy,” but this terminology has not yet been widely adopted.3
Guidelines from the Society for Maternal-Fetal Medicine (SMFM) recommend several time-critical steps for the initial stabilization and management of patients with AFE.4 However, because AFE is rare, most obstetric providers may not encounter a case for many years or even decades after they have received training, so it is unrealistic to expect that they will remember these guidelines when they are needed. For this reason, when AFE occurs, it is important to have a readily accessible cognitive aid, such as a checklist that summarizes the key management steps. The SMFM provides a checklist for initial management of AFE that can be used at your institution; it is presented in the FIGURE and provides the outline for this discussion.5

Provide CPR immediately
Most AFE cases are accompanied by cardiorespiratory arrest. If the patient has no pulse, call a “code” to mobilize additional help and immediately start CPR. Use a backboard to make cardiac compressions most effective and manually displace the uterus or tilt the patient to avoid supine hypotension. Designate a timekeeper to call out 1-minute intervals and record critical data, such as medication administration and laboratory orders/results.
Expedite delivery
Immediate delivery is needed if maternal cardiac activity is not restored within 4 minutes of starting CPR, with a target to have delivery completed within 5 minutes. Operative vaginal delivery may be an option if delivery is imminent, as in the case presented, but cesarean delivery (CD) will be needed in most cases. This was previously called “perimortem cesarean” delivery, but the term “resuscitative hysterotomy” has been proposed because the primary goal is to improve the effectiveness of CPR6 and prevent both maternal and perinatal death. CPR is less effective in pregnant women because the pregnant uterus takes a substantial fraction of the maternal cardiac output, as well as compresses the vena cava. Some experts suggest that, rather than waiting 4 minutes, CD should be started as soon as an obstetrician or other surgeon is present, unless there is an immediate response to electrical cardioversion.6,7
In most cases, immediate CD should be performed wherever the patient is located rather than using precious minutes to move the patient to an operating room. Antiseptic preparation is expedited by simply pouring povidone-iodine or chlorhexidine over the lower abdomen if readily available; if not available, skip this step. Enter the abdomen and uterus as rapidly as possible using only a scalpel to make generous midline incisions.
If CPR is not required, proceed with cesarean or operative vaginal delivery as soon as the mother has been stabilized. These procedures should be performed using standard safety precautions outlined in the SMFM patient safety checklists for cesarean or operative vaginal delivery.8,9
Continue to: Anticipate hemorrhage...
Anticipate hemorrhage
Be prepared for uterine atony, coagulopathy, and catastrophic hemorrhage. Initiate IV oxytocin prophylaxis as soon as the infant is delivered. Have a low threshold for giving other uterotonic agents such as methylergonovine, carboprost, or misoprostol. If hemorrhage or DIC occurs, give tranexamic acid. Have the anesthesiologist or trauma team (if available) insert an intraosseous line for fluid resuscitation if peripheral IV access is inadequate.
Massive transfusion is often needed to treat DIC, which occurs in most AFE cases. Anticipate—do not wait—for DIC to occur. We propose activating your hospital’s massive transfusion protocol (MTP) as soon as you diagnose AFE so that blood products will be available as soon as possible. A typical MTP provides several units of red blood cells, a pheresis pack of platelets, and fresh/frozen plasma (FFP). If clinically indicated, administer cryoprecipitate instead of FFP to minimize volume overload, which may occur with FFP.
CASE Part 2: MTP initiated to treat DIC
The MTP is initiated. Laboratory results immediately pre-transfusion include hemoglobin 11.3 g/dL, platelet count 46,000 per mm3, fibrinogen 87 mg/dL, and an elevated prothrombin time international normalized ratio.
Expect heart failure
The initial hemodynamic picture in AFE is right heart failure, which should optimally be managed by a specialist from anesthesiology, cardiology, or critical care as soon as they are available. An emergency department physician may manage the hemodynamics until a specialist arrives. Avoidance of fluid overload is one important principle. If fluid challenges are needed for hypovolemic shock, boluses should be restricted to 500 mL rather than the traditional 1000 mL.
Pharmacologic treatment may include vasopressors, inotropic agents, and pulmonary vasodilators. Example medications and dosages recommended by SMFM are summarized in the checklist (FIGURE).5
After the initial phase of recovery, the hemodynamic picture often changes from right heart failure to left heart failure. Management of left heart failure is not covered in the SMFM checklist because, by the time it appears, the patient will usually be in the intensive care unit, managed by the critical care team. Management of left heart failure generally includes diuresis as needed for cardiogenic pulmonary edema, optimization of cardiac preload, and inotropic agents or vasopressors if needed to maintain cardiac output or perfusion pressure.4
Debrief, learning opportunities
Complex emergencies such as AFE are rarely handled 100% perfectly, even those with a good outcome, so they present opportunities for team learning and improvement. The team should conduct a 10- to 15-minute debrief soon after the patient is stabilized. Make an explicit statement that the main goal of the debrief is to gather suggestions as to how systems and processes could be improved for next time, not to find fault or lay blame on individuals. Encourage all personnel involved in the initial management to attend and discuss what went well and what did not. Another goal is to provide support for individuals who may feel traumatized by the dramatic, frightening events surrounding an AFE and by the poor patient outcome or guarded prognosis that frequently follows. Another goal is to discuss the plan for providing support and disclosure to the patient and family.
The vast majority of AFE cases meet criteria to be designated as “sentinel events,” because of patient transfer to the intensive care unit, multi-unit blood transfusion, other severe maternal morbidities, or maternal death. Therefore, most AFE cases will trigger a root cause analysis (RCA) or other formal sentinel event analysis conducted by the hospital’s Safety or Quality Department. As with the immediate post-event debrief, the first goal of the RCA is to identify systems issues that may have resulted in suboptimal care and that can be modified to improve future care. Specific issues regarding the checklist should also be addressed:
- Was the checklist used?
- Was the checklist available?
- Are there items on the checklist that need to be modified, added, or deleted?
The RCA concludes with the development of a performance improvement plan.
Ultimately, we encourage all AFE cases be reported to the registry maintained by the Amniotic Fluid Embolism Foundation at https://www.afesupport.org/, regardless of whether the outcome was favorable for the mother and newborn. The registry includes over 130 AFE cases since 2013 from around the world. Researchers periodically report on the registry findings.10 If providers report cases with both good and bad outcomes, the registry may provide future insights regarding which adjunctive or empiric treatments may or may not be promising.
Continue to: Empiric treatments...
Empiric treatments
From time-to-time, new regimens for empiric treatment of AFE are reported. It is important to recognize that these reports are generally uncontrolled case reports of favorable outcomes and that, without a control group, it is impossible to determine to what extent the treatment contributed to the outcome or was merely incidental. Given the rarity of AFE, it seems unlikely that there will ever be a randomized clinical trial or even a controlled prospective study comparing treatment regimens.
The “A-OK” regimen is an empiric treatment that has garnered some interest after an initial case report.11 It consists of an anticholinergic agent (atropine 0.2 mg IV), a selective 5-HT3 receptor antagonist (ondansetron 8 mg IV), and a nonsteroidal anti-inflammatory drug (ketorolac 15 mg IV). We have some reservations about this regimen, however, because atropine is relatively contraindicated if the patient has tachycardia (which is common in patients with hemorrhage) and ketorolac may suppress platelet function, which might be harmful for patients with DIC or thrombocytopenia.
Another empiric treatment is the “50-50-500” regimen, which includes an H1 antihistamine (diphenhydramine 50 mg IV), an H2 antihistamine (famotidine 50 mg IV), and a corticosteroid (hydrocortisone 500 mg IV). This regimen aims to suppress histamine-mediated and cell-mediated inflammatory responses, based on the notion that proinflammatory responses likely mediate much of the underlying pathophysiology of the AFE syndrome.
We would emphasize that these empiric regimens are not clinically validated, US Food and Drug Administration approved for treatment of AFE, or considered standard of care. Future reports of these and other regimens will be needed to evaluate their efficacy, limitations, and risks. Again, we encourage providers to report all AFE cases to the AFE Foundation registry, regardless of whether the treatments are successful.
CASE Conclusion
The hemorrhage stops after administration of oxytocin, carboprost, 6 units of cryoprecipitate, and a 6-unit platelet pheresis pack. The patient is transferred to the intensive care unit where she eventually requires a total of 10 units of red cells, 8 more units of cryoprecipitate, and another platelet pheresis pack. She is discharged to home in stable condition on postpartum day 4.
Be prepared, have the checklist ready
Because AFE is rare, most members of the health care team will have no prior experience managing a real case. It may have been years or decades since they had any education on AFE or they last read a review article such as this one. It is even possible the anesthesiologist, cardiologist, or critical care specialist has never heard of AFE. Thus if they rely on memory alone, there is substantial risk of forgetting items, getting dosages wrong, or other errors. With this in mind, what is the best way to prepare the team to expeditiously employ the management steps outlined here?
Use of a checklist that summarizes these key steps for early management, such as the SMFM checklist in the FIGURE, will help ensure that all relevant steps are performed in every AFE case. It is designed to be printed on a single sheet of letter-sized paper, and we propose that every labor and delivery (L&D) unit keep laminated copies of this checklist in several places where they will be immediately available should an AFE occur. Copies can be kept on the anesthesia carts in the L&D operating rooms, in an emergency procedures binder on the unit, and on the “crash carts” and hemorrhage supply carts in the L&D unit. Effective implementation of an AFE checklist requires all personnel know where to readily find it and have some familiarity with its contents.
An interdisciplinary team comprising representatives from nursing, obstetrics, and anesthesia should meet to discuss whether the checklist needs to be modified to fit the local hospital formulary or other unique local circumstances. The team should develop an implementation plan that includes where to keep checklist copies, a process to periodically ensure that the copies are still present and readable, a roll-out plan to inform all personnel about the checklist process, and most importantly a training plan that includes incorporating AFE cases into the schedule of multidisciplinary simulations and drills for obstetric emergencies. Other implementation strategies are outlined in the SMFM document.5
Ultimately an organized, systematic approach is recommended for management of AFE. There is no single best treatment of AFE; it is supportive and directed toward the underlying pathophysiology, which may vary from patient to patient. Therefore, although a checklist, in conjunction with regular education and simulation activities, may help optimize care and improve outcomes, there is still a high risk of maternal morbidity and mortality from AFE. ●
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
- Clark SL. Amniotic fluid embolism. Obstet Gynecol. 2014;123(2 Pt 1):337-348. doi:10.1097/AOG.0000000000000107.
- Funk M, Damron A, Bandi V, et al. Pulmonary vascular obstruction by squamous cells is not involved in amniotic fluid embolism. Am J Obstet Gynecol. 2018;218:460-461. doi:10.1016/j.ajog.2017.12.225.
- Gilmore DA, Wakim J, Secrest J, et al. Anaphylactoid syndrome of pregnancy: a review of the literature with latest management and outcome data. AANA J. 2003;71:120-126.
- Society for Maternal-Fetal Medicine, Pacheco LD, Saade G, et al. Amniotic fluid embolism: diagnosis and management. Am J Obstet Gynecol. 2016;215:B16-24. doi:10.1016/j.ajog.2016.03.012.
- Patient Safety and Quality Committee, Society for Maternal-Fetal Medicine; Combs CA, Montgomery DM, et al. Society for Maternal-Fetal Medicine Special Statement: checklist for initial management of amniotic fluid embolism. Am J Obstet Gynecol. 2021;224:B29-B32. doi:10.1016/j.ajog.2021.01.001.
- Rose CH, Faksh A, Traynor KD, et al. Challenging the 4- to 5-minute rule: from perimortem cesarean to resuscitative hysterotomy. Am J Obstet Gynecol. 2015;213:653-6, 653.e1. doi:10.1016/j.ajog.2015.07.019.
- Pacheco LD, Clark SL, Klassen M, et al. Amniotic fluid embolism: principles of early clinical management. Am J Obstet Gynecol. 2020;222:48-52. doi:10.1016/j.ajog.2019.07.036.
- Combs CA, Einerson BD, Toner LE, SMFM Patient Safety and Quality Committee. SMFM Special Statement: surgical safety checklists for cesarean delivery. Am J Obstet Gynecol. 2021;225:B43-B49. doi:10.1016/j.ajog.2021.07.011.
- SMFM Patient Safety and Quality Committee, Staat B, Combs CA. SMFM Special Statement: operative vaginal delivery: checklists for performance and documentation. Am J Obstet Gynecol. 2020;222:B15-B21. doi:10.1016/j.ajog.2020.02.011.
- Stafford IA, Moaddab A, Dildy GA, et al. Amniotic fluid embolism syndrome: analysis of the United States international registry. Am J Obstet Gynecol MFM. 2020;2:100083. doi:10.1016/j.ajogmf.2019.100083.
- Rezai S, Hughes AZC, Larsen TB, et al. Atypical amniotic f luid embolism managed with a novel therapeutic regimen. Case Rep Obstet Gynecol. 2017; 2017:8458375. doi:10.1155/2017/8458375.
Physicians urged to write indications on drug scripts as methotrexate users face new barriers with SCOTUS decision
.
The Court’s 5-4 decision in Dobbs v. Jackson Women’s Health Organization, which halted abortion procedures across the country, also appears to be affecting certain drug regimens. Reports have emerged that pharmacies are denying access to methotrexate (MTX), a drug often used in patients with arthritis or cancer, as well as psoriasis and other skin diseases. In very high doses, MTX it is used to terminate an ectopic pregnancy after miscarriage. The drug can also lead to birth defects.
“It’s happening all over,” Donald Miller, PharmD, professor of pharmacy practice at North Dakota State University, Fargo, said in an interview. “Pharmacists are reluctant to dispense it, and rheumatologists are reluctant to prescribe it because they’re afraid of going to jail.”
Becky Schwartz, a patient who takes MTX for lupus, recently tweeted that her physician’s office stopped prescribing the drug because it is considered an abortifacient. “I had care that made my disabled life easier, and [the Supreme Court] took that from me,” Ms. Schwartz wrote.
Prior to the Supreme Court’s ruling, physicians were concerned about the impact an overturning of the 1973 law would have on patient access to MTX and other prescription medications with abortifacient properties. Doctors in general are becoming afraid of prescribing anything that’s a teratogen, said Dr. Miller.
MTX is used far more often for autoimmune disease than as an abortifacient, said rheumatologist Kristen Young, MD, clinical assistant professor at the University of Arizona College of Medicine, Phoenix. It’s a slippery slope if states reacting to the Supreme Court ruling start regulating oral abortifacients, she added. Specifically, this will have a significant impact on patients with rheumatic disease.
Texas pharmacies target two drugs
MTX denials have caught the attention of health care organizations. “Uncertainty in financial and criminal liability for health care professionals in certain state laws and regulations are possibly compromising continuity of care and access [to] medications proven to be safe and effective by the Food and Drug Administration for these indications,” warned the American Pharmacists Association (APhA) in a statement to this news organization.
The APhA said that it was monitoring this situation to assess the effect on patients and pharmacists.
The Arthritis Foundation was made aware of challenges from patients in accessing their MTX prescription for managing their arthritis and shared a statement on the Foundation’s website.
In Texas, pharmacists can refuse to fill scripts for misoprostol and MTX, a combination used for medical abortions. According to the foundation, “Already there are reports that people in Texas who miscarry or take methotrexate for arthritis [are] having trouble getting their prescriptions filled.”
MTX, approved by the FDA in 1985, “is the absolute cornerstone of rheumatoid arthritis. We cannot deny our patients this incredibly valuable drug,” said John Reveille, MD, vice-chair for the department of medicine at the University of Texas McGovern School of Medicine and a member of the Arthritis Foundation expert panel, in an interview.
“While it’s true that methotrexate can be lethal to the fetus, misoprostol is much more likely to cause a spontaneous abortion, and the combination is especially effective,” he said.
“If you look at Cochrane clinical studies, the dose of misoprostol contained in certain combinations with NSAIDs [nonsteroidal anti-inflammatory drugs] can induce spontaneous abortions. It’s surprising that pharmacists are targeting methotrexate, an essential drug in arthritis treatment, when there are medications available that do not have this benefit that can by themselves cause loss of the fetus, such as mifepristone,” added Dr. Reveille.
The Dobbs ruling could also affect the ability of oncologists to provide lifesaving cancer care, according to Jason Westin, MD, an oncologist at the University of Texas MD Anderson Cancer Center in the department of lymphoma and myeloma.
“We have heard of medications with multiple indications, such as methotrexate, not being dispensed by pharmacies due to confusion regarding the intended use and potential consequences for the health care team,” he said in an interview.
Conflicting laws pose challenges for physicians
In North Dakota, inconsistencies in several laws are making it difficult for physicians and pharmacists to make decisions. “Lots of confusion can result when people pass laws against abortion. There’s sometimes no insight into the ramifications of those laws,” said Dr. Miller.
North Dakota approved a trigger law several years ago that makes abortion illegal 30 days after an overturning of Roe. However, another law that regulates abortion conflicts with the trigger law. “Some of the language will need clarification in the next legislative session,” he said.
APhA and other pharmacy associations strongly favor not interfering with the doctor- or pharmacist-patient relationship. The law needs to defer to appropriate care between doctor and patient, said Dr. Miller. State pharmacy associations in North Dakota are working with legislatures to clarify any exceptions in the law, he added.
Arizona lawmakers are trying to reconcile two abortion laws on the books. One, based on an 1864 territorial law, deems abortion illegal. In addition, a newly approved law bans abortions after 15 weeks. The latter will go into effect in September 2022. In both laws, a risk to the mother’s life is the only exception for abortion, said Dr. Young.
Denials aren’t widespread
Not all doctors are seeing MTX denials, but they’re worried about the future. “To date, we have not encountered difficulty in obtaining methotrexate based upon state abortion restrictions but are concerned that this could occur and result in dangerous delays in care,” said Dr. Westin.
Dr. Reveille, who practices rheumatology in Houston, has not yet received any complaints from patients. Things may be different in more rural parts of Texas, where pharmacists could be denying prescriptions based on religious issues, he offered.
It’s a little soon to see what repercussions may result from the Supreme Court ruling and state actions, said Dr. Reveille. “In Texas, we’re a bit ahead of the tidal wave.”
Access problems also haven’t shown up at the university clinic where Dr. Young practices. “In Arizona, it’s unclear if there would be a legal basis to refuse a person methotrexate on the basis that it can be used as an abortifacient,” she said.
Specificity is key in writing Rx scripts
Physicians can make things easier for patients by writing the indication and dose for the drug on the prescription slip. For example, a 10-mg script for MTX is not going to be used for an abortion, said Dr. Miller.
Rheumatologists in Texas have been doing this for some time, even before the Supreme Court ruling, said Fehmida Zahabi, MD, FACR, president of the Society of Texas Association of Rheumatology. For MTX prescriptions in premenopausal women, “patients are told their doctor needs to call the pharmacist. In the small print, we are asked to give a diagnosis to make sure we aren’t using it to terminate pregnancies,” said Dr. Zahabi.
She further noted that if the diagnosis is already indicated on the script, pharmacies generally won’t give patients a hard time.
Patients can also ask their physicians for a letter of medical necessity that confirms a drug’s use for a specific medical condition.
Mail order is another option if a local pharmacy won’t fill a prescription, said Dr. Miller. “This is legal unless a state makes it illegal to send an abortifacient across state lines,” he added.
Many medications used in rheumatic diseases are harmful in pregnancy, and it’s important to routinely discuss pregnancy risk and planning in the rheumatology clinic, said Dr. Young. This should include a thorough discussion and referral for long-acting reversible contraception in most cases, she suggested.
Actions at the federal, state level
President Joe Biden recently signed an executive order prompting federal regulators to protect access to medication abortions, among other steps to safeguard access to reproductive services.
In a statement on Twitter, the American College of Rheumatology (ACR) said that it was “ ... following this issue closely to determine if rheumatology providers and patients are experiencing any widespread difficulty accessing methotrexate or if any initial disruptions are potentially temporary and due to the independent actions of pharmacists trying to figure out what is and isn’t allowed where they practice.”
ACR has assembled a task force of medical and policy experts to determine the best course of action for patients.
The Arthritis Foundation also continues to monitor the situation, encouraging patients to call its hotline, said Steven Schultz, director of state legislative affairs, in an interview.
“We are analyzing how medication abortion could cause confusion on the part of providers or pharmacists dispensing the medication and what this means for specific patients,” said Mr. Schultz. Through a survey, the foundation hopes to get a better idea of what’s going on in the states at a macro level.
This may take some time, as states go through a process of lawsuits, injunctions, or coming into session to do something that may affect access to MTX, said Mr. Schultz.
Being involved in local advocacy is more important than ever, stressed Dr. Young. “Additionally, being plugged into what the ACR and other advocacy groups are doing on the national level is helpful as well to know the status of these medication access issues.”
Rheumatologists have a unique voice in this discussion, she added. “We guide our patients to stability for a safe pregnancy, and even with careful planning, we see patients who become critically ill during pregnancy and require lifesaving treatment, which at times can mean an abortion is necessary.”
Oncologists also advocate for their patients on a regular basis to make sure they have access to the care they need, said Dr. Westin. This situation with Roe is no different, he added. “We will continue to use our unique expertise to advocate for policies that assure access to high-quality, evidence-based care – and to help our patients overcome barriers that may interfere.”
Dr. Reveille participated on an advisory board with Eli Lilly in October 2021.
A version of this article first appeared on Medscape.com.
.
The Court’s 5-4 decision in Dobbs v. Jackson Women’s Health Organization, which halted abortion procedures across the country, also appears to be affecting certain drug regimens. Reports have emerged that pharmacies are denying access to methotrexate (MTX), a drug often used in patients with arthritis or cancer, as well as psoriasis and other skin diseases. In very high doses, MTX it is used to terminate an ectopic pregnancy after miscarriage. The drug can also lead to birth defects.
“It’s happening all over,” Donald Miller, PharmD, professor of pharmacy practice at North Dakota State University, Fargo, said in an interview. “Pharmacists are reluctant to dispense it, and rheumatologists are reluctant to prescribe it because they’re afraid of going to jail.”
Becky Schwartz, a patient who takes MTX for lupus, recently tweeted that her physician’s office stopped prescribing the drug because it is considered an abortifacient. “I had care that made my disabled life easier, and [the Supreme Court] took that from me,” Ms. Schwartz wrote.
Prior to the Supreme Court’s ruling, physicians were concerned about the impact an overturning of the 1973 law would have on patient access to MTX and other prescription medications with abortifacient properties. Doctors in general are becoming afraid of prescribing anything that’s a teratogen, said Dr. Miller.
MTX is used far more often for autoimmune disease than as an abortifacient, said rheumatologist Kristen Young, MD, clinical assistant professor at the University of Arizona College of Medicine, Phoenix. It’s a slippery slope if states reacting to the Supreme Court ruling start regulating oral abortifacients, she added. Specifically, this will have a significant impact on patients with rheumatic disease.
Texas pharmacies target two drugs
MTX denials have caught the attention of health care organizations. “Uncertainty in financial and criminal liability for health care professionals in certain state laws and regulations are possibly compromising continuity of care and access [to] medications proven to be safe and effective by the Food and Drug Administration for these indications,” warned the American Pharmacists Association (APhA) in a statement to this news organization.
The APhA said that it was monitoring this situation to assess the effect on patients and pharmacists.
The Arthritis Foundation was made aware of challenges from patients in accessing their MTX prescription for managing their arthritis and shared a statement on the Foundation’s website.
In Texas, pharmacists can refuse to fill scripts for misoprostol and MTX, a combination used for medical abortions. According to the foundation, “Already there are reports that people in Texas who miscarry or take methotrexate for arthritis [are] having trouble getting their prescriptions filled.”
MTX, approved by the FDA in 1985, “is the absolute cornerstone of rheumatoid arthritis. We cannot deny our patients this incredibly valuable drug,” said John Reveille, MD, vice-chair for the department of medicine at the University of Texas McGovern School of Medicine and a member of the Arthritis Foundation expert panel, in an interview.
“While it’s true that methotrexate can be lethal to the fetus, misoprostol is much more likely to cause a spontaneous abortion, and the combination is especially effective,” he said.
“If you look at Cochrane clinical studies, the dose of misoprostol contained in certain combinations with NSAIDs [nonsteroidal anti-inflammatory drugs] can induce spontaneous abortions. It’s surprising that pharmacists are targeting methotrexate, an essential drug in arthritis treatment, when there are medications available that do not have this benefit that can by themselves cause loss of the fetus, such as mifepristone,” added Dr. Reveille.
The Dobbs ruling could also affect the ability of oncologists to provide lifesaving cancer care, according to Jason Westin, MD, an oncologist at the University of Texas MD Anderson Cancer Center in the department of lymphoma and myeloma.
“We have heard of medications with multiple indications, such as methotrexate, not being dispensed by pharmacies due to confusion regarding the intended use and potential consequences for the health care team,” he said in an interview.
Conflicting laws pose challenges for physicians
In North Dakota, inconsistencies in several laws are making it difficult for physicians and pharmacists to make decisions. “Lots of confusion can result when people pass laws against abortion. There’s sometimes no insight into the ramifications of those laws,” said Dr. Miller.
North Dakota approved a trigger law several years ago that makes abortion illegal 30 days after an overturning of Roe. However, another law that regulates abortion conflicts with the trigger law. “Some of the language will need clarification in the next legislative session,” he said.
APhA and other pharmacy associations strongly favor not interfering with the doctor- or pharmacist-patient relationship. The law needs to defer to appropriate care between doctor and patient, said Dr. Miller. State pharmacy associations in North Dakota are working with legislatures to clarify any exceptions in the law, he added.
Arizona lawmakers are trying to reconcile two abortion laws on the books. One, based on an 1864 territorial law, deems abortion illegal. In addition, a newly approved law bans abortions after 15 weeks. The latter will go into effect in September 2022. In both laws, a risk to the mother’s life is the only exception for abortion, said Dr. Young.
Denials aren’t widespread
Not all doctors are seeing MTX denials, but they’re worried about the future. “To date, we have not encountered difficulty in obtaining methotrexate based upon state abortion restrictions but are concerned that this could occur and result in dangerous delays in care,” said Dr. Westin.
Dr. Reveille, who practices rheumatology in Houston, has not yet received any complaints from patients. Things may be different in more rural parts of Texas, where pharmacists could be denying prescriptions based on religious issues, he offered.
It’s a little soon to see what repercussions may result from the Supreme Court ruling and state actions, said Dr. Reveille. “In Texas, we’re a bit ahead of the tidal wave.”
Access problems also haven’t shown up at the university clinic where Dr. Young practices. “In Arizona, it’s unclear if there would be a legal basis to refuse a person methotrexate on the basis that it can be used as an abortifacient,” she said.
Specificity is key in writing Rx scripts
Physicians can make things easier for patients by writing the indication and dose for the drug on the prescription slip. For example, a 10-mg script for MTX is not going to be used for an abortion, said Dr. Miller.
Rheumatologists in Texas have been doing this for some time, even before the Supreme Court ruling, said Fehmida Zahabi, MD, FACR, president of the Society of Texas Association of Rheumatology. For MTX prescriptions in premenopausal women, “patients are told their doctor needs to call the pharmacist. In the small print, we are asked to give a diagnosis to make sure we aren’t using it to terminate pregnancies,” said Dr. Zahabi.
She further noted that if the diagnosis is already indicated on the script, pharmacies generally won’t give patients a hard time.
Patients can also ask their physicians for a letter of medical necessity that confirms a drug’s use for a specific medical condition.
Mail order is another option if a local pharmacy won’t fill a prescription, said Dr. Miller. “This is legal unless a state makes it illegal to send an abortifacient across state lines,” he added.
Many medications used in rheumatic diseases are harmful in pregnancy, and it’s important to routinely discuss pregnancy risk and planning in the rheumatology clinic, said Dr. Young. This should include a thorough discussion and referral for long-acting reversible contraception in most cases, she suggested.
Actions at the federal, state level
President Joe Biden recently signed an executive order prompting federal regulators to protect access to medication abortions, among other steps to safeguard access to reproductive services.
In a statement on Twitter, the American College of Rheumatology (ACR) said that it was “ ... following this issue closely to determine if rheumatology providers and patients are experiencing any widespread difficulty accessing methotrexate or if any initial disruptions are potentially temporary and due to the independent actions of pharmacists trying to figure out what is and isn’t allowed where they practice.”
ACR has assembled a task force of medical and policy experts to determine the best course of action for patients.
The Arthritis Foundation also continues to monitor the situation, encouraging patients to call its hotline, said Steven Schultz, director of state legislative affairs, in an interview.
“We are analyzing how medication abortion could cause confusion on the part of providers or pharmacists dispensing the medication and what this means for specific patients,” said Mr. Schultz. Through a survey, the foundation hopes to get a better idea of what’s going on in the states at a macro level.
This may take some time, as states go through a process of lawsuits, injunctions, or coming into session to do something that may affect access to MTX, said Mr. Schultz.
Being involved in local advocacy is more important than ever, stressed Dr. Young. “Additionally, being plugged into what the ACR and other advocacy groups are doing on the national level is helpful as well to know the status of these medication access issues.”
Rheumatologists have a unique voice in this discussion, she added. “We guide our patients to stability for a safe pregnancy, and even with careful planning, we see patients who become critically ill during pregnancy and require lifesaving treatment, which at times can mean an abortion is necessary.”
Oncologists also advocate for their patients on a regular basis to make sure they have access to the care they need, said Dr. Westin. This situation with Roe is no different, he added. “We will continue to use our unique expertise to advocate for policies that assure access to high-quality, evidence-based care – and to help our patients overcome barriers that may interfere.”
Dr. Reveille participated on an advisory board with Eli Lilly in October 2021.
A version of this article first appeared on Medscape.com.
.
The Court’s 5-4 decision in Dobbs v. Jackson Women’s Health Organization, which halted abortion procedures across the country, also appears to be affecting certain drug regimens. Reports have emerged that pharmacies are denying access to methotrexate (MTX), a drug often used in patients with arthritis or cancer, as well as psoriasis and other skin diseases. In very high doses, MTX it is used to terminate an ectopic pregnancy after miscarriage. The drug can also lead to birth defects.
“It’s happening all over,” Donald Miller, PharmD, professor of pharmacy practice at North Dakota State University, Fargo, said in an interview. “Pharmacists are reluctant to dispense it, and rheumatologists are reluctant to prescribe it because they’re afraid of going to jail.”
Becky Schwartz, a patient who takes MTX for lupus, recently tweeted that her physician’s office stopped prescribing the drug because it is considered an abortifacient. “I had care that made my disabled life easier, and [the Supreme Court] took that from me,” Ms. Schwartz wrote.
Prior to the Supreme Court’s ruling, physicians were concerned about the impact an overturning of the 1973 law would have on patient access to MTX and other prescription medications with abortifacient properties. Doctors in general are becoming afraid of prescribing anything that’s a teratogen, said Dr. Miller.
MTX is used far more often for autoimmune disease than as an abortifacient, said rheumatologist Kristen Young, MD, clinical assistant professor at the University of Arizona College of Medicine, Phoenix. It’s a slippery slope if states reacting to the Supreme Court ruling start regulating oral abortifacients, she added. Specifically, this will have a significant impact on patients with rheumatic disease.
Texas pharmacies target two drugs
MTX denials have caught the attention of health care organizations. “Uncertainty in financial and criminal liability for health care professionals in certain state laws and regulations are possibly compromising continuity of care and access [to] medications proven to be safe and effective by the Food and Drug Administration for these indications,” warned the American Pharmacists Association (APhA) in a statement to this news organization.
The APhA said that it was monitoring this situation to assess the effect on patients and pharmacists.
The Arthritis Foundation was made aware of challenges from patients in accessing their MTX prescription for managing their arthritis and shared a statement on the Foundation’s website.
In Texas, pharmacists can refuse to fill scripts for misoprostol and MTX, a combination used for medical abortions. According to the foundation, “Already there are reports that people in Texas who miscarry or take methotrexate for arthritis [are] having trouble getting their prescriptions filled.”
MTX, approved by the FDA in 1985, “is the absolute cornerstone of rheumatoid arthritis. We cannot deny our patients this incredibly valuable drug,” said John Reveille, MD, vice-chair for the department of medicine at the University of Texas McGovern School of Medicine and a member of the Arthritis Foundation expert panel, in an interview.
“While it’s true that methotrexate can be lethal to the fetus, misoprostol is much more likely to cause a spontaneous abortion, and the combination is especially effective,” he said.
“If you look at Cochrane clinical studies, the dose of misoprostol contained in certain combinations with NSAIDs [nonsteroidal anti-inflammatory drugs] can induce spontaneous abortions. It’s surprising that pharmacists are targeting methotrexate, an essential drug in arthritis treatment, when there are medications available that do not have this benefit that can by themselves cause loss of the fetus, such as mifepristone,” added Dr. Reveille.
The Dobbs ruling could also affect the ability of oncologists to provide lifesaving cancer care, according to Jason Westin, MD, an oncologist at the University of Texas MD Anderson Cancer Center in the department of lymphoma and myeloma.
“We have heard of medications with multiple indications, such as methotrexate, not being dispensed by pharmacies due to confusion regarding the intended use and potential consequences for the health care team,” he said in an interview.
Conflicting laws pose challenges for physicians
In North Dakota, inconsistencies in several laws are making it difficult for physicians and pharmacists to make decisions. “Lots of confusion can result when people pass laws against abortion. There’s sometimes no insight into the ramifications of those laws,” said Dr. Miller.
North Dakota approved a trigger law several years ago that makes abortion illegal 30 days after an overturning of Roe. However, another law that regulates abortion conflicts with the trigger law. “Some of the language will need clarification in the next legislative session,” he said.
APhA and other pharmacy associations strongly favor not interfering with the doctor- or pharmacist-patient relationship. The law needs to defer to appropriate care between doctor and patient, said Dr. Miller. State pharmacy associations in North Dakota are working with legislatures to clarify any exceptions in the law, he added.
Arizona lawmakers are trying to reconcile two abortion laws on the books. One, based on an 1864 territorial law, deems abortion illegal. In addition, a newly approved law bans abortions after 15 weeks. The latter will go into effect in September 2022. In both laws, a risk to the mother’s life is the only exception for abortion, said Dr. Young.
Denials aren’t widespread
Not all doctors are seeing MTX denials, but they’re worried about the future. “To date, we have not encountered difficulty in obtaining methotrexate based upon state abortion restrictions but are concerned that this could occur and result in dangerous delays in care,” said Dr. Westin.
Dr. Reveille, who practices rheumatology in Houston, has not yet received any complaints from patients. Things may be different in more rural parts of Texas, where pharmacists could be denying prescriptions based on religious issues, he offered.
It’s a little soon to see what repercussions may result from the Supreme Court ruling and state actions, said Dr. Reveille. “In Texas, we’re a bit ahead of the tidal wave.”
Access problems also haven’t shown up at the university clinic where Dr. Young practices. “In Arizona, it’s unclear if there would be a legal basis to refuse a person methotrexate on the basis that it can be used as an abortifacient,” she said.
Specificity is key in writing Rx scripts
Physicians can make things easier for patients by writing the indication and dose for the drug on the prescription slip. For example, a 10-mg script for MTX is not going to be used for an abortion, said Dr. Miller.
Rheumatologists in Texas have been doing this for some time, even before the Supreme Court ruling, said Fehmida Zahabi, MD, FACR, president of the Society of Texas Association of Rheumatology. For MTX prescriptions in premenopausal women, “patients are told their doctor needs to call the pharmacist. In the small print, we are asked to give a diagnosis to make sure we aren’t using it to terminate pregnancies,” said Dr. Zahabi.
She further noted that if the diagnosis is already indicated on the script, pharmacies generally won’t give patients a hard time.
Patients can also ask their physicians for a letter of medical necessity that confirms a drug’s use for a specific medical condition.
Mail order is another option if a local pharmacy won’t fill a prescription, said Dr. Miller. “This is legal unless a state makes it illegal to send an abortifacient across state lines,” he added.
Many medications used in rheumatic diseases are harmful in pregnancy, and it’s important to routinely discuss pregnancy risk and planning in the rheumatology clinic, said Dr. Young. This should include a thorough discussion and referral for long-acting reversible contraception in most cases, she suggested.
Actions at the federal, state level
President Joe Biden recently signed an executive order prompting federal regulators to protect access to medication abortions, among other steps to safeguard access to reproductive services.
In a statement on Twitter, the American College of Rheumatology (ACR) said that it was “ ... following this issue closely to determine if rheumatology providers and patients are experiencing any widespread difficulty accessing methotrexate or if any initial disruptions are potentially temporary and due to the independent actions of pharmacists trying to figure out what is and isn’t allowed where they practice.”
ACR has assembled a task force of medical and policy experts to determine the best course of action for patients.
The Arthritis Foundation also continues to monitor the situation, encouraging patients to call its hotline, said Steven Schultz, director of state legislative affairs, in an interview.
“We are analyzing how medication abortion could cause confusion on the part of providers or pharmacists dispensing the medication and what this means for specific patients,” said Mr. Schultz. Through a survey, the foundation hopes to get a better idea of what’s going on in the states at a macro level.
This may take some time, as states go through a process of lawsuits, injunctions, or coming into session to do something that may affect access to MTX, said Mr. Schultz.
Being involved in local advocacy is more important than ever, stressed Dr. Young. “Additionally, being plugged into what the ACR and other advocacy groups are doing on the national level is helpful as well to know the status of these medication access issues.”
Rheumatologists have a unique voice in this discussion, she added. “We guide our patients to stability for a safe pregnancy, and even with careful planning, we see patients who become critically ill during pregnancy and require lifesaving treatment, which at times can mean an abortion is necessary.”
Oncologists also advocate for their patients on a regular basis to make sure they have access to the care they need, said Dr. Westin. This situation with Roe is no different, he added. “We will continue to use our unique expertise to advocate for policies that assure access to high-quality, evidence-based care – and to help our patients overcome barriers that may interfere.”
Dr. Reveille participated on an advisory board with Eli Lilly in October 2021.
A version of this article first appeared on Medscape.com.
Pregnancy, breastfeeding, and more linked to lower CRC risk
Estrogen exposure helps protect against colorectal cancer (CRC), and in some instances, the protection is site specific, a new analysis finds.
In a 17-year study involving almost 5,000 women, researchers from Germany found that hormone replacement therapy, oral contraceptive use, pregnancy, breastfeeding, and menopause at age 50 or older were all significantly associated with reductions in CRC risk.
Interestingly, the reduced risk of CRC observed for pregnancy and breastfeeding only applied to proximal colon cancer, while the association with oral contraceptive use was confined to the distal colon and rectum.
The results were published online in JNCI Cancer Spectrum.
CRC is the second most common cause of cancer death. It is responsible for more than one million deaths globally, according to the latest figures from the Global Burden of Disease 2019 Cancer Collaboration.
And sex seems to make a difference. The Global Burden analysis, echoing previous data, found that CRC is less common among women and that fewer women die from the disease.
Little, however, is known about the mechanisms of estrogen signaling in CRC or the impact of reproductive factors on CRC, despite a large amount of literature linking CRC risk to exogenous estrogens, such as hormone replacement therapy and oral contraceptives.
In the current analysis, the team recruited 2,650 patients with CRC from 20 German cancer centers between 2003 and 2020. Researchers used standardized questionnaires to garner the women’s reproductive histories.
A matched control group of 2,175 participants who did not have a history of CRC was randomly selected from population registries. All analyses were adjusted for known CRC risk factors, such as age; body mass index; education level; family history; having previously undergone large-bowel endoscopy; diabetes; and smoking status.
The researchers found that each pregnancy was associated with a small but significant 9% reduction in CRC risk (odds ratio, 0.91), specifically in the proximal colon (OR, 0.86).
Overall, breastfeeding for a year or longer was associated with a significantly lower CRC risk, compared with never breastfeeding (OR, 0.74), but the results were only significant for the proximal colon (OR, 0.58).
Oral contraceptive use for 9 years or longer was associated with a lower CRC risk (OR, 0.75) but was only significant for the distal colon (OR, 0.63). Hormone replacement therapy was associated with a lower risk of CRC irrespective of tumor location (OR, 0.76). And using both was linked to a 42% CRC risk reduction (OR, 0.58).
Although age at menarche was not associated with CRC risk, menopause at age 50 or older was associated with a significant 17% lower risk of CRC.
In an email interview, lead author Tobias Niedermaier, PhD, expressed surprise at two of the findings. The first was the small association between pregnancies and CRC risk, “despite the strong increase in estrogen levels during pregnancy,” he said. He speculated that pregnancy-related increases in insulin levels may have “largely offset the protection effects of estrogen exposure during pregnancy.”
The second surprise was that the age at menarche did not have a bearing on CRC risk, which could be because “exposure to estrogen levels in younger ages [is] less relevant with respect to CRC risk, because CRC typically develops at comparably old age.”
John Marshall, MD, who was not involved in the research, commented that such studies “put a lot of pressure on people to perform in a certain way to modify their personal risk of something.” However, “we would not recommend people alter their life choices for reproduction for this,” said Dr. Marshall, chief of the Division of Hematology/Oncology at Georgetown University, Washington, D.C.
Dr. Niedermaier agreed that “while this knowledge will certainly not change a woman’s decision on family planning,” he noted that the findings “could influence current CRC screening strategies, for example, by risk-adapted screening intervals [and] start and stop ages of screening.”
Dr. Niedermaier and colleagues’ work was funded by the German Research Council, the German Federal Ministry of Education and Research, and the Interdisciplinary Research Program of the National Center for Tumor Diseases. Dr. Niedermaier has disclosed no relevant financial relationships. Dr. Marshall writes a column that appears regularly on Medscape: Marshall on Oncology. He has served as speaker or member of a speakers’ bureau for Genentech, Amgen, Bayer, Celgene Corporation, and Caris Life Sciences.
A version of this article first appeared on Medscape.com.
Estrogen exposure helps protect against colorectal cancer (CRC), and in some instances, the protection is site specific, a new analysis finds.
In a 17-year study involving almost 5,000 women, researchers from Germany found that hormone replacement therapy, oral contraceptive use, pregnancy, breastfeeding, and menopause at age 50 or older were all significantly associated with reductions in CRC risk.
Interestingly, the reduced risk of CRC observed for pregnancy and breastfeeding only applied to proximal colon cancer, while the association with oral contraceptive use was confined to the distal colon and rectum.
The results were published online in JNCI Cancer Spectrum.
CRC is the second most common cause of cancer death. It is responsible for more than one million deaths globally, according to the latest figures from the Global Burden of Disease 2019 Cancer Collaboration.
And sex seems to make a difference. The Global Burden analysis, echoing previous data, found that CRC is less common among women and that fewer women die from the disease.
Little, however, is known about the mechanisms of estrogen signaling in CRC or the impact of reproductive factors on CRC, despite a large amount of literature linking CRC risk to exogenous estrogens, such as hormone replacement therapy and oral contraceptives.
In the current analysis, the team recruited 2,650 patients with CRC from 20 German cancer centers between 2003 and 2020. Researchers used standardized questionnaires to garner the women’s reproductive histories.
A matched control group of 2,175 participants who did not have a history of CRC was randomly selected from population registries. All analyses were adjusted for known CRC risk factors, such as age; body mass index; education level; family history; having previously undergone large-bowel endoscopy; diabetes; and smoking status.
The researchers found that each pregnancy was associated with a small but significant 9% reduction in CRC risk (odds ratio, 0.91), specifically in the proximal colon (OR, 0.86).
Overall, breastfeeding for a year or longer was associated with a significantly lower CRC risk, compared with never breastfeeding (OR, 0.74), but the results were only significant for the proximal colon (OR, 0.58).
Oral contraceptive use for 9 years or longer was associated with a lower CRC risk (OR, 0.75) but was only significant for the distal colon (OR, 0.63). Hormone replacement therapy was associated with a lower risk of CRC irrespective of tumor location (OR, 0.76). And using both was linked to a 42% CRC risk reduction (OR, 0.58).
Although age at menarche was not associated with CRC risk, menopause at age 50 or older was associated with a significant 17% lower risk of CRC.
In an email interview, lead author Tobias Niedermaier, PhD, expressed surprise at two of the findings. The first was the small association between pregnancies and CRC risk, “despite the strong increase in estrogen levels during pregnancy,” he said. He speculated that pregnancy-related increases in insulin levels may have “largely offset the protection effects of estrogen exposure during pregnancy.”
The second surprise was that the age at menarche did not have a bearing on CRC risk, which could be because “exposure to estrogen levels in younger ages [is] less relevant with respect to CRC risk, because CRC typically develops at comparably old age.”
John Marshall, MD, who was not involved in the research, commented that such studies “put a lot of pressure on people to perform in a certain way to modify their personal risk of something.” However, “we would not recommend people alter their life choices for reproduction for this,” said Dr. Marshall, chief of the Division of Hematology/Oncology at Georgetown University, Washington, D.C.
Dr. Niedermaier agreed that “while this knowledge will certainly not change a woman’s decision on family planning,” he noted that the findings “could influence current CRC screening strategies, for example, by risk-adapted screening intervals [and] start and stop ages of screening.”
Dr. Niedermaier and colleagues’ work was funded by the German Research Council, the German Federal Ministry of Education and Research, and the Interdisciplinary Research Program of the National Center for Tumor Diseases. Dr. Niedermaier has disclosed no relevant financial relationships. Dr. Marshall writes a column that appears regularly on Medscape: Marshall on Oncology. He has served as speaker or member of a speakers’ bureau for Genentech, Amgen, Bayer, Celgene Corporation, and Caris Life Sciences.
A version of this article first appeared on Medscape.com.
Estrogen exposure helps protect against colorectal cancer (CRC), and in some instances, the protection is site specific, a new analysis finds.
In a 17-year study involving almost 5,000 women, researchers from Germany found that hormone replacement therapy, oral contraceptive use, pregnancy, breastfeeding, and menopause at age 50 or older were all significantly associated with reductions in CRC risk.
Interestingly, the reduced risk of CRC observed for pregnancy and breastfeeding only applied to proximal colon cancer, while the association with oral contraceptive use was confined to the distal colon and rectum.
The results were published online in JNCI Cancer Spectrum.
CRC is the second most common cause of cancer death. It is responsible for more than one million deaths globally, according to the latest figures from the Global Burden of Disease 2019 Cancer Collaboration.
And sex seems to make a difference. The Global Burden analysis, echoing previous data, found that CRC is less common among women and that fewer women die from the disease.
Little, however, is known about the mechanisms of estrogen signaling in CRC or the impact of reproductive factors on CRC, despite a large amount of literature linking CRC risk to exogenous estrogens, such as hormone replacement therapy and oral contraceptives.
In the current analysis, the team recruited 2,650 patients with CRC from 20 German cancer centers between 2003 and 2020. Researchers used standardized questionnaires to garner the women’s reproductive histories.
A matched control group of 2,175 participants who did not have a history of CRC was randomly selected from population registries. All analyses were adjusted for known CRC risk factors, such as age; body mass index; education level; family history; having previously undergone large-bowel endoscopy; diabetes; and smoking status.
The researchers found that each pregnancy was associated with a small but significant 9% reduction in CRC risk (odds ratio, 0.91), specifically in the proximal colon (OR, 0.86).
Overall, breastfeeding for a year or longer was associated with a significantly lower CRC risk, compared with never breastfeeding (OR, 0.74), but the results were only significant for the proximal colon (OR, 0.58).
Oral contraceptive use for 9 years or longer was associated with a lower CRC risk (OR, 0.75) but was only significant for the distal colon (OR, 0.63). Hormone replacement therapy was associated with a lower risk of CRC irrespective of tumor location (OR, 0.76). And using both was linked to a 42% CRC risk reduction (OR, 0.58).
Although age at menarche was not associated with CRC risk, menopause at age 50 or older was associated with a significant 17% lower risk of CRC.
In an email interview, lead author Tobias Niedermaier, PhD, expressed surprise at two of the findings. The first was the small association between pregnancies and CRC risk, “despite the strong increase in estrogen levels during pregnancy,” he said. He speculated that pregnancy-related increases in insulin levels may have “largely offset the protection effects of estrogen exposure during pregnancy.”
The second surprise was that the age at menarche did not have a bearing on CRC risk, which could be because “exposure to estrogen levels in younger ages [is] less relevant with respect to CRC risk, because CRC typically develops at comparably old age.”
John Marshall, MD, who was not involved in the research, commented that such studies “put a lot of pressure on people to perform in a certain way to modify their personal risk of something.” However, “we would not recommend people alter their life choices for reproduction for this,” said Dr. Marshall, chief of the Division of Hematology/Oncology at Georgetown University, Washington, D.C.
Dr. Niedermaier agreed that “while this knowledge will certainly not change a woman’s decision on family planning,” he noted that the findings “could influence current CRC screening strategies, for example, by risk-adapted screening intervals [and] start and stop ages of screening.”
Dr. Niedermaier and colleagues’ work was funded by the German Research Council, the German Federal Ministry of Education and Research, and the Interdisciplinary Research Program of the National Center for Tumor Diseases. Dr. Niedermaier has disclosed no relevant financial relationships. Dr. Marshall writes a column that appears regularly on Medscape: Marshall on Oncology. He has served as speaker or member of a speakers’ bureau for Genentech, Amgen, Bayer, Celgene Corporation, and Caris Life Sciences.
A version of this article first appeared on Medscape.com.
Medical management of miscarriage curbs costs and maintains quality of care
Medical management of early pregnancy loss costs less and offers similar quality of life to uterine aspiration, based on data from an analytical model.
Early pregnancy loss (EPL) occurs in more than 1 million women in the United States each year, and many patients are diagnosed before they show symptoms, wrote Divyah Nagendra, MD, of Cambridge Health Alliance, Mass., and colleagues.
A 2018 study showed that medical management of EPL with mifepristone added to misoprostol increased effectiveness and reduced the need for additional medication or subsequent uterine procedures, but the cost of mifepristone is perceived as a barrier, and the cost-effectiveness of its use, compared with surgical or expectant management, has not been well studied, the researchers noted.
“We already know that adding mifepristone to the medical management of early pregnancy loss increases the effectiveness of the regimen,” coauthor Courtney A. Schreiber, MD, of the University of Pennsylvania, Philadelphia, said in an interview. “Procedural uterine aspiration is highly effective as well, so patients and providers may consider the cost when deciding on a treatment strategy,” she added.
“If medication management is preferred by many patients, decreases the need to access in-person clinical care during a pandemic, and is found to be cost-effective, clinicians and policymakers should increase efforts to improve mifepristone availability and reduce access burdens,” the researchers wrote.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers created a decision-analytic model using data from published literature and the Pregnancy Failure Regiments Trial (PreFaiR) to compare office-based uterine aspiration to medical management with mifepristone pretreatment followed by misoprostol for EPL.
The PrFaiR study randomized 300 women who experienced EPL before 12 weeks’ gestation to medication management with 800 mcg misoprostol vaginally, with or without pretreatment of 200 mg mifeprestone orally. The average age of the participants was 30.7 years, and demographics were similar between the groups.
The researchers used the PrFaiR data for medical management and patient-level data from published literature for uterine aspiration.
The primary outcome was the cost per quality-adjusted life year (QALY) gained. QALY was based on a modified utility score from the published literature. Effectiveness was based on QALY gained and the rate of complete expulsion of the gestational sac without additional intervention.
Overall, the mean costs per person were significantly higher for uterine aspiration, compared with medical management ($828 vs. $661, P = .004). Uterine aspiration was significantly more effective for complete gestational sac expulsion (97.3% vs. 83.8%, P = .0001). However, the QALYs were significantly higher for medical management, compared with uterine aspiration (0.082 vs. 0.079, P < .0001).
Cost-effectiveness was greater for medical management from a health care sector perspective, with lower costs and higher QALYs than uterine aspiration, the researchers noted.
They also evaluated the effect of mifepristone pretreatment on cost-effectiveness and found that medical management would remain cost effective, compared with uterine aspiration even if uterine aspiration procedures decreased in cost and mifepristone increased in cost, and even if medication management had a decreased completion rate and utility score, compared with uterine aspiration.
“Our analysis demonstrates that the incremental cost-effectiveness ratio (ICER) for medical management is well below the maximum willingness-to-pay threshold of approximately $100,000 per QALY gained,” the researchers wrote in their discussion of the findings.
Potential savings, uncertain access
Despite the potential savings and patient benefits, access to mifepristone remains a barrier, the researchers said.
Although the FDA lifted some restrictions on mifepristone in 2021 in the wake of the ongoing COVID-19 pandemic, the effect of new abortion-related restrictions remains to be seen.
The study findings were limited by several factors, including the use of 2018 National Medicare reimbursement rates to calculate costs, though actual costs vary by region and payer, the researchers noted. Other limitations include variations in cost of mifepristone by region and time and the differences in data sources between the uterine aspiration and medical management groups. More research is needed to assess QALYs for early pregnancy loss to establish standard measures and to assess the societal perspective of ESL as well as the health care perspective, they added.
However, the current results support medical management of EPL with mifepristone pretreatment followed by misoprostol as a “high-value care alternative” to office-based uterine aspiration, they said. “Increasing access to mifepristone and eliminating unnecessary restrictions will improve early pregnancy care,” they concluded.
“Given how effective procedural management is, we were slightly surprised that medical management remains cost effective,” Dr. Schreiber said in an interview.
Looking ahead in the wake of new restrictions on use for abortion, “patients may have difficulty accessing either medical or procedural management for early pregnancy loss,” Dr. Schreiber noted. “We support the accessibility of all evidence-based care and hope that our data will help overcome perceived financial barriers,” she said. Additional research needs include improved implementation and access to evidence-based early pregnancy loss care, she added.
Reasons to lift regulations
“Given the recent overturning of Roe v. Wade, any medications that are associated with abortion have increased scrutiny, especially mifepristone and misoprostol, even though these medications are also used for managing early pregnancy loss,” Sarah W. Prager, MD, of the University of Washington, Seattle, said in an interview. “Demonstrating that medication management of EPL with mifepristone/misoprostol is less expensive and has increased QALYs associated with it is yet another reason to deregulate mifepristone so it can also be more accessible for management of EPL,” said Dr. Prager, who was not involved in the study.
Dr. Prager said she was not surprised by the findings, as effective medication should be less expensive than a procedure. “I would caution that the increased QALYs found in this study should not be interpreted as a reason to restrict surgical management of EPL but to increase access also to medication management, even though medication has a slightly lower rate of complete gestational sac expulsion,” she noted. “Mode of management should be up to the patient, unless there is a clear medical reason for one or the other.”
Going forward, “the FDA has it in its power to remove the REMS, which would immediately make mifepristone a medication that can be prescribed through a pharmacy and therefore much more available,” said Dr. Prager. “Restrictions for both medication and surgical management of EPL will likely increase in states where abortion is illegal, and it could possibly lead to patients having less choice as to mode of management,” she explained.
“There are many studies showing that all modes of EPL management are safe and effective and should be supported with respect to patient choice,” Dr. Prager noted. “There are also substantial data supporting the overall safety of mifepristone, and there are no scientific or medical data suggesting the REMS increases safety in any way. Frankly, there are no good, evidence-based reasons to continue to keep the REMS in place,” she said.
The study was supported by the National Institute of Child Health and Human Development of the National Institutes of Health and a Society of Family Planning Research Fund Midcareer Mentor Award. The researchers had no financial conflicts to disclose. Dr. Prager had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
Medical management of early pregnancy loss costs less and offers similar quality of life to uterine aspiration, based on data from an analytical model.
Early pregnancy loss (EPL) occurs in more than 1 million women in the United States each year, and many patients are diagnosed before they show symptoms, wrote Divyah Nagendra, MD, of Cambridge Health Alliance, Mass., and colleagues.
A 2018 study showed that medical management of EPL with mifepristone added to misoprostol increased effectiveness and reduced the need for additional medication or subsequent uterine procedures, but the cost of mifepristone is perceived as a barrier, and the cost-effectiveness of its use, compared with surgical or expectant management, has not been well studied, the researchers noted.
“We already know that adding mifepristone to the medical management of early pregnancy loss increases the effectiveness of the regimen,” coauthor Courtney A. Schreiber, MD, of the University of Pennsylvania, Philadelphia, said in an interview. “Procedural uterine aspiration is highly effective as well, so patients and providers may consider the cost when deciding on a treatment strategy,” she added.
“If medication management is preferred by many patients, decreases the need to access in-person clinical care during a pandemic, and is found to be cost-effective, clinicians and policymakers should increase efforts to improve mifepristone availability and reduce access burdens,” the researchers wrote.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers created a decision-analytic model using data from published literature and the Pregnancy Failure Regiments Trial (PreFaiR) to compare office-based uterine aspiration to medical management with mifepristone pretreatment followed by misoprostol for EPL.
The PrFaiR study randomized 300 women who experienced EPL before 12 weeks’ gestation to medication management with 800 mcg misoprostol vaginally, with or without pretreatment of 200 mg mifeprestone orally. The average age of the participants was 30.7 years, and demographics were similar between the groups.
The researchers used the PrFaiR data for medical management and patient-level data from published literature for uterine aspiration.
The primary outcome was the cost per quality-adjusted life year (QALY) gained. QALY was based on a modified utility score from the published literature. Effectiveness was based on QALY gained and the rate of complete expulsion of the gestational sac without additional intervention.
Overall, the mean costs per person were significantly higher for uterine aspiration, compared with medical management ($828 vs. $661, P = .004). Uterine aspiration was significantly more effective for complete gestational sac expulsion (97.3% vs. 83.8%, P = .0001). However, the QALYs were significantly higher for medical management, compared with uterine aspiration (0.082 vs. 0.079, P < .0001).
Cost-effectiveness was greater for medical management from a health care sector perspective, with lower costs and higher QALYs than uterine aspiration, the researchers noted.
They also evaluated the effect of mifepristone pretreatment on cost-effectiveness and found that medical management would remain cost effective, compared with uterine aspiration even if uterine aspiration procedures decreased in cost and mifepristone increased in cost, and even if medication management had a decreased completion rate and utility score, compared with uterine aspiration.
“Our analysis demonstrates that the incremental cost-effectiveness ratio (ICER) for medical management is well below the maximum willingness-to-pay threshold of approximately $100,000 per QALY gained,” the researchers wrote in their discussion of the findings.
Potential savings, uncertain access
Despite the potential savings and patient benefits, access to mifepristone remains a barrier, the researchers said.
Although the FDA lifted some restrictions on mifepristone in 2021 in the wake of the ongoing COVID-19 pandemic, the effect of new abortion-related restrictions remains to be seen.
The study findings were limited by several factors, including the use of 2018 National Medicare reimbursement rates to calculate costs, though actual costs vary by region and payer, the researchers noted. Other limitations include variations in cost of mifepristone by region and time and the differences in data sources between the uterine aspiration and medical management groups. More research is needed to assess QALYs for early pregnancy loss to establish standard measures and to assess the societal perspective of ESL as well as the health care perspective, they added.
However, the current results support medical management of EPL with mifepristone pretreatment followed by misoprostol as a “high-value care alternative” to office-based uterine aspiration, they said. “Increasing access to mifepristone and eliminating unnecessary restrictions will improve early pregnancy care,” they concluded.
“Given how effective procedural management is, we were slightly surprised that medical management remains cost effective,” Dr. Schreiber said in an interview.
Looking ahead in the wake of new restrictions on use for abortion, “patients may have difficulty accessing either medical or procedural management for early pregnancy loss,” Dr. Schreiber noted. “We support the accessibility of all evidence-based care and hope that our data will help overcome perceived financial barriers,” she said. Additional research needs include improved implementation and access to evidence-based early pregnancy loss care, she added.
Reasons to lift regulations
“Given the recent overturning of Roe v. Wade, any medications that are associated with abortion have increased scrutiny, especially mifepristone and misoprostol, even though these medications are also used for managing early pregnancy loss,” Sarah W. Prager, MD, of the University of Washington, Seattle, said in an interview. “Demonstrating that medication management of EPL with mifepristone/misoprostol is less expensive and has increased QALYs associated with it is yet another reason to deregulate mifepristone so it can also be more accessible for management of EPL,” said Dr. Prager, who was not involved in the study.
Dr. Prager said she was not surprised by the findings, as effective medication should be less expensive than a procedure. “I would caution that the increased QALYs found in this study should not be interpreted as a reason to restrict surgical management of EPL but to increase access also to medication management, even though medication has a slightly lower rate of complete gestational sac expulsion,” she noted. “Mode of management should be up to the patient, unless there is a clear medical reason for one or the other.”
Going forward, “the FDA has it in its power to remove the REMS, which would immediately make mifepristone a medication that can be prescribed through a pharmacy and therefore much more available,” said Dr. Prager. “Restrictions for both medication and surgical management of EPL will likely increase in states where abortion is illegal, and it could possibly lead to patients having less choice as to mode of management,” she explained.
“There are many studies showing that all modes of EPL management are safe and effective and should be supported with respect to patient choice,” Dr. Prager noted. “There are also substantial data supporting the overall safety of mifepristone, and there are no scientific or medical data suggesting the REMS increases safety in any way. Frankly, there are no good, evidence-based reasons to continue to keep the REMS in place,” she said.
The study was supported by the National Institute of Child Health and Human Development of the National Institutes of Health and a Society of Family Planning Research Fund Midcareer Mentor Award. The researchers had no financial conflicts to disclose. Dr. Prager had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
Medical management of early pregnancy loss costs less and offers similar quality of life to uterine aspiration, based on data from an analytical model.
Early pregnancy loss (EPL) occurs in more than 1 million women in the United States each year, and many patients are diagnosed before they show symptoms, wrote Divyah Nagendra, MD, of Cambridge Health Alliance, Mass., and colleagues.
A 2018 study showed that medical management of EPL with mifepristone added to misoprostol increased effectiveness and reduced the need for additional medication or subsequent uterine procedures, but the cost of mifepristone is perceived as a barrier, and the cost-effectiveness of its use, compared with surgical or expectant management, has not been well studied, the researchers noted.
“We already know that adding mifepristone to the medical management of early pregnancy loss increases the effectiveness of the regimen,” coauthor Courtney A. Schreiber, MD, of the University of Pennsylvania, Philadelphia, said in an interview. “Procedural uterine aspiration is highly effective as well, so patients and providers may consider the cost when deciding on a treatment strategy,” she added.
“If medication management is preferred by many patients, decreases the need to access in-person clinical care during a pandemic, and is found to be cost-effective, clinicians and policymakers should increase efforts to improve mifepristone availability and reduce access burdens,” the researchers wrote.
In a study published in the American Journal of Obstetrics & Gynecology, the researchers created a decision-analytic model using data from published literature and the Pregnancy Failure Regiments Trial (PreFaiR) to compare office-based uterine aspiration to medical management with mifepristone pretreatment followed by misoprostol for EPL.
The PrFaiR study randomized 300 women who experienced EPL before 12 weeks’ gestation to medication management with 800 mcg misoprostol vaginally, with or without pretreatment of 200 mg mifeprestone orally. The average age of the participants was 30.7 years, and demographics were similar between the groups.
The researchers used the PrFaiR data for medical management and patient-level data from published literature for uterine aspiration.
The primary outcome was the cost per quality-adjusted life year (QALY) gained. QALY was based on a modified utility score from the published literature. Effectiveness was based on QALY gained and the rate of complete expulsion of the gestational sac without additional intervention.
Overall, the mean costs per person were significantly higher for uterine aspiration, compared with medical management ($828 vs. $661, P = .004). Uterine aspiration was significantly more effective for complete gestational sac expulsion (97.3% vs. 83.8%, P = .0001). However, the QALYs were significantly higher for medical management, compared with uterine aspiration (0.082 vs. 0.079, P < .0001).
Cost-effectiveness was greater for medical management from a health care sector perspective, with lower costs and higher QALYs than uterine aspiration, the researchers noted.
They also evaluated the effect of mifepristone pretreatment on cost-effectiveness and found that medical management would remain cost effective, compared with uterine aspiration even if uterine aspiration procedures decreased in cost and mifepristone increased in cost, and even if medication management had a decreased completion rate and utility score, compared with uterine aspiration.
“Our analysis demonstrates that the incremental cost-effectiveness ratio (ICER) for medical management is well below the maximum willingness-to-pay threshold of approximately $100,000 per QALY gained,” the researchers wrote in their discussion of the findings.
Potential savings, uncertain access
Despite the potential savings and patient benefits, access to mifepristone remains a barrier, the researchers said.
Although the FDA lifted some restrictions on mifepristone in 2021 in the wake of the ongoing COVID-19 pandemic, the effect of new abortion-related restrictions remains to be seen.
The study findings were limited by several factors, including the use of 2018 National Medicare reimbursement rates to calculate costs, though actual costs vary by region and payer, the researchers noted. Other limitations include variations in cost of mifepristone by region and time and the differences in data sources between the uterine aspiration and medical management groups. More research is needed to assess QALYs for early pregnancy loss to establish standard measures and to assess the societal perspective of ESL as well as the health care perspective, they added.
However, the current results support medical management of EPL with mifepristone pretreatment followed by misoprostol as a “high-value care alternative” to office-based uterine aspiration, they said. “Increasing access to mifepristone and eliminating unnecessary restrictions will improve early pregnancy care,” they concluded.
“Given how effective procedural management is, we were slightly surprised that medical management remains cost effective,” Dr. Schreiber said in an interview.
Looking ahead in the wake of new restrictions on use for abortion, “patients may have difficulty accessing either medical or procedural management for early pregnancy loss,” Dr. Schreiber noted. “We support the accessibility of all evidence-based care and hope that our data will help overcome perceived financial barriers,” she said. Additional research needs include improved implementation and access to evidence-based early pregnancy loss care, she added.
Reasons to lift regulations
“Given the recent overturning of Roe v. Wade, any medications that are associated with abortion have increased scrutiny, especially mifepristone and misoprostol, even though these medications are also used for managing early pregnancy loss,” Sarah W. Prager, MD, of the University of Washington, Seattle, said in an interview. “Demonstrating that medication management of EPL with mifepristone/misoprostol is less expensive and has increased QALYs associated with it is yet another reason to deregulate mifepristone so it can also be more accessible for management of EPL,” said Dr. Prager, who was not involved in the study.
Dr. Prager said she was not surprised by the findings, as effective medication should be less expensive than a procedure. “I would caution that the increased QALYs found in this study should not be interpreted as a reason to restrict surgical management of EPL but to increase access also to medication management, even though medication has a slightly lower rate of complete gestational sac expulsion,” she noted. “Mode of management should be up to the patient, unless there is a clear medical reason for one or the other.”
Going forward, “the FDA has it in its power to remove the REMS, which would immediately make mifepristone a medication that can be prescribed through a pharmacy and therefore much more available,” said Dr. Prager. “Restrictions for both medication and surgical management of EPL will likely increase in states where abortion is illegal, and it could possibly lead to patients having less choice as to mode of management,” she explained.
“There are many studies showing that all modes of EPL management are safe and effective and should be supported with respect to patient choice,” Dr. Prager noted. “There are also substantial data supporting the overall safety of mifepristone, and there are no scientific or medical data suggesting the REMS increases safety in any way. Frankly, there are no good, evidence-based reasons to continue to keep the REMS in place,” she said.
The study was supported by the National Institute of Child Health and Human Development of the National Institutes of Health and a Society of Family Planning Research Fund Midcareer Mentor Award. The researchers had no financial conflicts to disclose. Dr. Prager had no financial conflicts to disclose and serves on the Editorial Advisory Board of Ob.Gyn. News.
FROM THE AMERICAN JOURNAL OF OBSTETRICS & GYNECOLOGY
Inflation and health care: The prognosis for doctors
Rampant inflation doesn’t just mean a spike in everyday expenses like gas and groceries. It’s also bound to have a significant impact on the cost of health care – and on your practice. A recent report from McKinsey & Company predicts that the current inflationary spiral will force health care providers to charge higher reimbursement rates, and those costs inevitably will be passed along to both employers and consumers. Bottom line: Your patients will likely have to pay more out of pocket.
How, precisely, will inflation affect your practice, and what’s the best way to minimize the damage?
Step 1: Maintain operational standards
“Based on the conversations we’ve had with our physician clients that own practices, we see the potential for cost inflation to outrun revenue inflation over the next year,” said Michael Ashley Schulman, CFA, partner and chief investment officer at Running Point Capital, El Segundo, Calif. “Staff wages, as well as office equipment and medical supply costs, are increasing faster than insurance and Medicare/Medicaid reimbursement amounts.” Even so, topflight employees are essential to keep your practice running smoothly. Prioritize excellent nursing. Instead of adding a new hire, compensate your best nurse as well as possible. The same goes for an efficient office manager: On that front, too, you should go the extra mile, even if it means trimming expenses elsewhere.
Step 2: Plan ahead for insurance challenges
Many insurers, including Medicare, set health care costs a year in advance, based on projected growth. This means insurance payouts will stay largely the same for the time being. “Almost all physicians employed by large groups won’t see costs due to inflation rise until next year,” said Mark V. Pauly, PhD, Bendheim Professor in the department of health care management at the University of Pennsylvania, Philadelphia. “For self-employed physicians, there will also be a cushion.”
“The big issue with inflation is that more patients will likely be underinsured,” said Tiffany Johnson, MBA, CFP, co-CEO and financial advisor at Piece of Wealth Planning in Atlanta. “With more out-of-pocket costs ... these patients may not seek out medical treatment or go to see a specialist if they do not believe it is necessary.” A new study from Johns Hopkins found that patients under financial pressure often delay or forgo medical treatment because of food insecurity. Compassionate care is the solution: Direct these patients to financial aid and other resources they may qualify for. That way, they can continue to receive the care they need from you, and your need to pass on costs may be lower.
Step 3: Rely on your affiliated health care organization
These are tough times when it comes to expansion. “Since we are in an environment where inflation and interest rates are both high, it will be much harder for physicians to have the capital to invest in new technology to grow or advance their practice,” Ms. Johnson said. With that in mind, keep the lines of communication between you and your affiliated hospital/health care organization more open than ever. Combining practices with another doctor is one way to increase revenue; you might ask if any affiliated doctors are seeking to team up. It’s also vital to attend meetings and pay close attention to budget cuts your organization may be making. And don’t be shy about asking your administrator for profit-boosting recommendations.
Step 4: Revisit vendor relationships
Find out if your vendors will continue to supply you with the goods you need at reasonable rates, and switch now if they won’t. Be proactive. “Test new medical suppliers,” Mr. Schulman advised. “Reread equipment leasing contracts to check if the interest rates have increased. See if buyout, prepay, or refinancing options are more economical. Also, investigate [bringing down] your rental expense by reducing square footage or moving to a lower-cost location.” In light of ongoing supply chain issues, it’s wise to consider alternative products. But stay focused on quality – you don’t want to be stuck with cheap, possibly defective equipment. Spend where it’s essential and cut the fat somewhere else.
Step 5: Don’t waste your assets
Analyze your budget in minute detail. “Now is the time to review your current inventory and overhead costs,” Ms. Johnson said. “Many physicians let their office staff handle the restocking of inventory and office supplies. While this can be efficient for their practice, it also leaves room for unnecessary business expenses.” Take a cold, hard look at your supply closet – what’s in there that you can live without? Don’t reorder it. Then seek out any revenue stream you may be overlooking. “It’s important to review billing to make sure all the services are reimbursable,” Ms. Johnson added. Small mistakes can yield dividends if you find them.
Step 6: Be poised to pivot
Get creative. “To minimize a profit decline, use video consulting – it’s more efficient and less equipment intensive,” Mr. Schulman said. “Look at how remote work and flexible hours can maximize the work your practice accomplishes while cutting office costs.”
Ms. Johnson suggests adding concierge services, noting that “concierge doctors offer personalized care and direct access for an up-front fee.” With this approach, you may see fewer patients, but your payout paperwork will decrease, and that up-front fee can be profitable. Another outside-the-box idea: Start making house calls. A Scripps study found that home health visits requested via app can result in patient care delivered by a doctor and medical assistant in less than 2 hours. House calls can be an effective and profitable solution when it comes to providing nonemergency care and preventive treatment to patients who aren’t mobile, not to mention patients who just appreciate the convenience.
Step 7: Maintain transparency
Any economic changes your practice will implement must be communicated to your staff and patients clearly and directly. Keep everyone in the loop and be ready to answer questions immediately. Show those you work with and care for that, regardless of the economy, it’s they who matter to you most. That simple reassurance will prove invaluable.
A version of this article first appeared on Medscape.com.
Rampant inflation doesn’t just mean a spike in everyday expenses like gas and groceries. It’s also bound to have a significant impact on the cost of health care – and on your practice. A recent report from McKinsey & Company predicts that the current inflationary spiral will force health care providers to charge higher reimbursement rates, and those costs inevitably will be passed along to both employers and consumers. Bottom line: Your patients will likely have to pay more out of pocket.
How, precisely, will inflation affect your practice, and what’s the best way to minimize the damage?
Step 1: Maintain operational standards
“Based on the conversations we’ve had with our physician clients that own practices, we see the potential for cost inflation to outrun revenue inflation over the next year,” said Michael Ashley Schulman, CFA, partner and chief investment officer at Running Point Capital, El Segundo, Calif. “Staff wages, as well as office equipment and medical supply costs, are increasing faster than insurance and Medicare/Medicaid reimbursement amounts.” Even so, topflight employees are essential to keep your practice running smoothly. Prioritize excellent nursing. Instead of adding a new hire, compensate your best nurse as well as possible. The same goes for an efficient office manager: On that front, too, you should go the extra mile, even if it means trimming expenses elsewhere.
Step 2: Plan ahead for insurance challenges
Many insurers, including Medicare, set health care costs a year in advance, based on projected growth. This means insurance payouts will stay largely the same for the time being. “Almost all physicians employed by large groups won’t see costs due to inflation rise until next year,” said Mark V. Pauly, PhD, Bendheim Professor in the department of health care management at the University of Pennsylvania, Philadelphia. “For self-employed physicians, there will also be a cushion.”
“The big issue with inflation is that more patients will likely be underinsured,” said Tiffany Johnson, MBA, CFP, co-CEO and financial advisor at Piece of Wealth Planning in Atlanta. “With more out-of-pocket costs ... these patients may not seek out medical treatment or go to see a specialist if they do not believe it is necessary.” A new study from Johns Hopkins found that patients under financial pressure often delay or forgo medical treatment because of food insecurity. Compassionate care is the solution: Direct these patients to financial aid and other resources they may qualify for. That way, they can continue to receive the care they need from you, and your need to pass on costs may be lower.
Step 3: Rely on your affiliated health care organization
These are tough times when it comes to expansion. “Since we are in an environment where inflation and interest rates are both high, it will be much harder for physicians to have the capital to invest in new technology to grow or advance their practice,” Ms. Johnson said. With that in mind, keep the lines of communication between you and your affiliated hospital/health care organization more open than ever. Combining practices with another doctor is one way to increase revenue; you might ask if any affiliated doctors are seeking to team up. It’s also vital to attend meetings and pay close attention to budget cuts your organization may be making. And don’t be shy about asking your administrator for profit-boosting recommendations.
Step 4: Revisit vendor relationships
Find out if your vendors will continue to supply you with the goods you need at reasonable rates, and switch now if they won’t. Be proactive. “Test new medical suppliers,” Mr. Schulman advised. “Reread equipment leasing contracts to check if the interest rates have increased. See if buyout, prepay, or refinancing options are more economical. Also, investigate [bringing down] your rental expense by reducing square footage or moving to a lower-cost location.” In light of ongoing supply chain issues, it’s wise to consider alternative products. But stay focused on quality – you don’t want to be stuck with cheap, possibly defective equipment. Spend where it’s essential and cut the fat somewhere else.
Step 5: Don’t waste your assets
Analyze your budget in minute detail. “Now is the time to review your current inventory and overhead costs,” Ms. Johnson said. “Many physicians let their office staff handle the restocking of inventory and office supplies. While this can be efficient for their practice, it also leaves room for unnecessary business expenses.” Take a cold, hard look at your supply closet – what’s in there that you can live without? Don’t reorder it. Then seek out any revenue stream you may be overlooking. “It’s important to review billing to make sure all the services are reimbursable,” Ms. Johnson added. Small mistakes can yield dividends if you find them.
Step 6: Be poised to pivot
Get creative. “To minimize a profit decline, use video consulting – it’s more efficient and less equipment intensive,” Mr. Schulman said. “Look at how remote work and flexible hours can maximize the work your practice accomplishes while cutting office costs.”
Ms. Johnson suggests adding concierge services, noting that “concierge doctors offer personalized care and direct access for an up-front fee.” With this approach, you may see fewer patients, but your payout paperwork will decrease, and that up-front fee can be profitable. Another outside-the-box idea: Start making house calls. A Scripps study found that home health visits requested via app can result in patient care delivered by a doctor and medical assistant in less than 2 hours. House calls can be an effective and profitable solution when it comes to providing nonemergency care and preventive treatment to patients who aren’t mobile, not to mention patients who just appreciate the convenience.
Step 7: Maintain transparency
Any economic changes your practice will implement must be communicated to your staff and patients clearly and directly. Keep everyone in the loop and be ready to answer questions immediately. Show those you work with and care for that, regardless of the economy, it’s they who matter to you most. That simple reassurance will prove invaluable.
A version of this article first appeared on Medscape.com.
Rampant inflation doesn’t just mean a spike in everyday expenses like gas and groceries. It’s also bound to have a significant impact on the cost of health care – and on your practice. A recent report from McKinsey & Company predicts that the current inflationary spiral will force health care providers to charge higher reimbursement rates, and those costs inevitably will be passed along to both employers and consumers. Bottom line: Your patients will likely have to pay more out of pocket.
How, precisely, will inflation affect your practice, and what’s the best way to minimize the damage?
Step 1: Maintain operational standards
“Based on the conversations we’ve had with our physician clients that own practices, we see the potential for cost inflation to outrun revenue inflation over the next year,” said Michael Ashley Schulman, CFA, partner and chief investment officer at Running Point Capital, El Segundo, Calif. “Staff wages, as well as office equipment and medical supply costs, are increasing faster than insurance and Medicare/Medicaid reimbursement amounts.” Even so, topflight employees are essential to keep your practice running smoothly. Prioritize excellent nursing. Instead of adding a new hire, compensate your best nurse as well as possible. The same goes for an efficient office manager: On that front, too, you should go the extra mile, even if it means trimming expenses elsewhere.
Step 2: Plan ahead for insurance challenges
Many insurers, including Medicare, set health care costs a year in advance, based on projected growth. This means insurance payouts will stay largely the same for the time being. “Almost all physicians employed by large groups won’t see costs due to inflation rise until next year,” said Mark V. Pauly, PhD, Bendheim Professor in the department of health care management at the University of Pennsylvania, Philadelphia. “For self-employed physicians, there will also be a cushion.”
“The big issue with inflation is that more patients will likely be underinsured,” said Tiffany Johnson, MBA, CFP, co-CEO and financial advisor at Piece of Wealth Planning in Atlanta. “With more out-of-pocket costs ... these patients may not seek out medical treatment or go to see a specialist if they do not believe it is necessary.” A new study from Johns Hopkins found that patients under financial pressure often delay or forgo medical treatment because of food insecurity. Compassionate care is the solution: Direct these patients to financial aid and other resources they may qualify for. That way, they can continue to receive the care they need from you, and your need to pass on costs may be lower.
Step 3: Rely on your affiliated health care organization
These are tough times when it comes to expansion. “Since we are in an environment where inflation and interest rates are both high, it will be much harder for physicians to have the capital to invest in new technology to grow or advance their practice,” Ms. Johnson said. With that in mind, keep the lines of communication between you and your affiliated hospital/health care organization more open than ever. Combining practices with another doctor is one way to increase revenue; you might ask if any affiliated doctors are seeking to team up. It’s also vital to attend meetings and pay close attention to budget cuts your organization may be making. And don’t be shy about asking your administrator for profit-boosting recommendations.
Step 4: Revisit vendor relationships
Find out if your vendors will continue to supply you with the goods you need at reasonable rates, and switch now if they won’t. Be proactive. “Test new medical suppliers,” Mr. Schulman advised. “Reread equipment leasing contracts to check if the interest rates have increased. See if buyout, prepay, or refinancing options are more economical. Also, investigate [bringing down] your rental expense by reducing square footage or moving to a lower-cost location.” In light of ongoing supply chain issues, it’s wise to consider alternative products. But stay focused on quality – you don’t want to be stuck with cheap, possibly defective equipment. Spend where it’s essential and cut the fat somewhere else.
Step 5: Don’t waste your assets
Analyze your budget in minute detail. “Now is the time to review your current inventory and overhead costs,” Ms. Johnson said. “Many physicians let their office staff handle the restocking of inventory and office supplies. While this can be efficient for their practice, it also leaves room for unnecessary business expenses.” Take a cold, hard look at your supply closet – what’s in there that you can live without? Don’t reorder it. Then seek out any revenue stream you may be overlooking. “It’s important to review billing to make sure all the services are reimbursable,” Ms. Johnson added. Small mistakes can yield dividends if you find them.
Step 6: Be poised to pivot
Get creative. “To minimize a profit decline, use video consulting – it’s more efficient and less equipment intensive,” Mr. Schulman said. “Look at how remote work and flexible hours can maximize the work your practice accomplishes while cutting office costs.”
Ms. Johnson suggests adding concierge services, noting that “concierge doctors offer personalized care and direct access for an up-front fee.” With this approach, you may see fewer patients, but your payout paperwork will decrease, and that up-front fee can be profitable. Another outside-the-box idea: Start making house calls. A Scripps study found that home health visits requested via app can result in patient care delivered by a doctor and medical assistant in less than 2 hours. House calls can be an effective and profitable solution when it comes to providing nonemergency care and preventive treatment to patients who aren’t mobile, not to mention patients who just appreciate the convenience.
Step 7: Maintain transparency
Any economic changes your practice will implement must be communicated to your staff and patients clearly and directly. Keep everyone in the loop and be ready to answer questions immediately. Show those you work with and care for that, regardless of the economy, it’s they who matter to you most. That simple reassurance will prove invaluable.
A version of this article first appeared on Medscape.com.
Roe v. Wade overturned: A family medicine resident reacts
I remember how small and shy she looked, curled into herself in her too-large hospital gown. I remember thinking that it was autumn, and she should have been at her first homecoming dance, not sitting in the ER staring mutely at the hospital-issued safety socks on her feet. Her mother, puffy-eyed from crying, was sitting on the bed beside her, stroking her hair.
Together, my patients and I talked about the pregnancy. She told me how scared she was, how she didn’t want to “kill her baby”, but that she also wasn’t sure she could take care of a child. She told me that she was terrified of childbirth, that she didn’t want her friends at school to know and to judge her. We talked about how she was a victim; how she was an innocent child, too. I reassured her, and her mom emphatically agreed – her body was still her own.
The man who hurt her did not take that from her. She could make any choice she wanted, and it would be the right choice.
Eventually, she was able to make a decision which was best for her. I don’t know what became of her, but I hope she is well now, and I hope she’s thriving and happy. I also hope that she doesn’t see the news about Roe v. Wade and feel stripped of her personhood, as many women did.
When I heard about the Supreme Court decision I thought of her, and how important our conversation was to the trajectory of her life. I wondered if across the country these conversations might be silenced, and patients might be left to navigate this important facet of their health alone.
Some version of the conversation I had with my young patient occurs in exam rooms across the country countless times a day. Sometimes these conversations are cut and dry. Other times, they are accompanied by heartbreak and tears.
These conversations are common – one in four women in the United States have had an abortion. I have had many friends who were faced with deciding what to do after an unexpectedly positive pregnancy test. The reasons were different for each person – one was raped at a party, another’s birth control failed, the boyfriend of a third friend wouldn’t wear a condom – but the underlying sentiments were the same for each woman. They thought: “This is a difficult choice, but it’s a choice I’m ready to make. I’m not ready to have a baby at this point in my life.”
My friends talked to their doctors, who assisted them in making an informed choice. Some of them chose abortion. Others chose to deliver their baby. All were helped along in their decision by a physician who was there to support them and assist them in making a well-considered choice for their individual circumstance.
Economic and health consequences of restricting access to abortion
The facts are clear: Nearly half of all pregnancies in American women in 2011 were unplanned, and about 4 in 10 of them ended in an elective abortion, according to the Guttmacher Institute.1 Restricting access to abortions does not stop abortions from happening; it limits the opportunity for women to seek advice from trusted friends and professionals and it reduces access to safe abortions.
The people who will be most harmed by these restrictions are the most socially and economically vulnerable. Wealthy, mobile women with the ability to travel to other states or countries will always be able to access abortion care; low-income, work-tethered women and women with other children to care for at home will struggle to do so.
Denying women abortion services puts them at increased risk for lifelong, multigenerational economic hardship. Women who sought abortions but were unable to obtain them experienced an increase in household poverty which lasted years relative to women who were able to receive an abortion, according to the authors of The Turnaway Study.2 They were less socially, geographically, and economically mobile, and were less likely to go on to receive a higher education.
In a country where citizens do not have paid maternity leave, affordable and accessible childcare services, or universal health care, raising a child is an enormous financial burden. Women who are denied abortions also are much more likely to end up as a single parent, shouldering that burden alone.
Additionally, low socioeconomic status is associated with increased all-cause mortality. People who live in poverty are disproportionately affected by diabetes and other chronic health conditions, and have lower life expectancies overall.
The reversal of Roe v. Wade is not only going to lead directly to patient death by decreasing access to safe abortion, causing women to pursue unsafe alternatives; it will also indirectly result in more women being driven into and remaining in poverty and suffering the health consequences.
In addition to risking a woman’s life medically, pregnancy also significantly increases that individual’s risk of being a victim of intimate partner violence. The number one cause of death in pregnant women is homicide, most often by their sexual partner, said an article published in Nature in 2021.3 Therefore, restricting a woman’s ability to control if and when she has children could put her at risk for death from serious pregnancy-related complications and unsafe abortion consequences and increase her likelihood of dying by domestic violence.
Patient-physicians interactions are changed
As a physician I hope that I am able to convey my intense respect for and support of a woman’s autonomy into every family planning visit I conduct. Unfortunately, this ruling will not only have an immediate impact on the lives of women across the country – it will also alter the way many of us interact with our patients on a day-to-day basis. When patients can report doctors to authorities in some states for offering terminations, and doctors can report patients for seeking them, there will be absolutely no trust in the therapeutic relationship.
With this ruling, the content of private and protected conversations between patients and their physicians will be subject to censure and potentially criminal consequences.
Regardless of where I eventually practice medicine, I should not be in the position of talking to a patient and telling them that they do not have any agency over their body unless they have the money and resources to travel to a state where abortion is legal. I should not have to tell a child that she must carry and birth another child just to appease the often-fickle whims of lawmakers.
The conversation I had with my pediatric patient was important to her health and to her future, and she deserved to have the chance to discuss her feelings with a trusted physician. Every woman has the right to make her own decisions within the sanctity of the exam room, not from the distance of a courtroom.
Dr. Persampiere is a resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at [email protected] or via [email protected].
References
1. Unintended pregnancy in the United States. Guttmacher Institute. 2019 Jan 9. https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states
2. Foster D et al. The harms of denying a woman a wanted abortion - ANSIRH. https://www.ansirh.org/sites/default/files/publications/files/the_harms_of_denying_a_woman_a_wanted_abortion_4-16-2020.pdf
3. Subbaraman N. 2021 Nov 12. Homicide is a top cause of maternal death in the United States. Nature News. https://www.nature.com/articles/d41586-021-03392-8
I remember how small and shy she looked, curled into herself in her too-large hospital gown. I remember thinking that it was autumn, and she should have been at her first homecoming dance, not sitting in the ER staring mutely at the hospital-issued safety socks on her feet. Her mother, puffy-eyed from crying, was sitting on the bed beside her, stroking her hair.
Together, my patients and I talked about the pregnancy. She told me how scared she was, how she didn’t want to “kill her baby”, but that she also wasn’t sure she could take care of a child. She told me that she was terrified of childbirth, that she didn’t want her friends at school to know and to judge her. We talked about how she was a victim; how she was an innocent child, too. I reassured her, and her mom emphatically agreed – her body was still her own.
The man who hurt her did not take that from her. She could make any choice she wanted, and it would be the right choice.
Eventually, she was able to make a decision which was best for her. I don’t know what became of her, but I hope she is well now, and I hope she’s thriving and happy. I also hope that she doesn’t see the news about Roe v. Wade and feel stripped of her personhood, as many women did.
When I heard about the Supreme Court decision I thought of her, and how important our conversation was to the trajectory of her life. I wondered if across the country these conversations might be silenced, and patients might be left to navigate this important facet of their health alone.
Some version of the conversation I had with my young patient occurs in exam rooms across the country countless times a day. Sometimes these conversations are cut and dry. Other times, they are accompanied by heartbreak and tears.
These conversations are common – one in four women in the United States have had an abortion. I have had many friends who were faced with deciding what to do after an unexpectedly positive pregnancy test. The reasons were different for each person – one was raped at a party, another’s birth control failed, the boyfriend of a third friend wouldn’t wear a condom – but the underlying sentiments were the same for each woman. They thought: “This is a difficult choice, but it’s a choice I’m ready to make. I’m not ready to have a baby at this point in my life.”
My friends talked to their doctors, who assisted them in making an informed choice. Some of them chose abortion. Others chose to deliver their baby. All were helped along in their decision by a physician who was there to support them and assist them in making a well-considered choice for their individual circumstance.
Economic and health consequences of restricting access to abortion
The facts are clear: Nearly half of all pregnancies in American women in 2011 were unplanned, and about 4 in 10 of them ended in an elective abortion, according to the Guttmacher Institute.1 Restricting access to abortions does not stop abortions from happening; it limits the opportunity for women to seek advice from trusted friends and professionals and it reduces access to safe abortions.
The people who will be most harmed by these restrictions are the most socially and economically vulnerable. Wealthy, mobile women with the ability to travel to other states or countries will always be able to access abortion care; low-income, work-tethered women and women with other children to care for at home will struggle to do so.
Denying women abortion services puts them at increased risk for lifelong, multigenerational economic hardship. Women who sought abortions but were unable to obtain them experienced an increase in household poverty which lasted years relative to women who were able to receive an abortion, according to the authors of The Turnaway Study.2 They were less socially, geographically, and economically mobile, and were less likely to go on to receive a higher education.
In a country where citizens do not have paid maternity leave, affordable and accessible childcare services, or universal health care, raising a child is an enormous financial burden. Women who are denied abortions also are much more likely to end up as a single parent, shouldering that burden alone.
Additionally, low socioeconomic status is associated with increased all-cause mortality. People who live in poverty are disproportionately affected by diabetes and other chronic health conditions, and have lower life expectancies overall.
The reversal of Roe v. Wade is not only going to lead directly to patient death by decreasing access to safe abortion, causing women to pursue unsafe alternatives; it will also indirectly result in more women being driven into and remaining in poverty and suffering the health consequences.
In addition to risking a woman’s life medically, pregnancy also significantly increases that individual’s risk of being a victim of intimate partner violence. The number one cause of death in pregnant women is homicide, most often by their sexual partner, said an article published in Nature in 2021.3 Therefore, restricting a woman’s ability to control if and when she has children could put her at risk for death from serious pregnancy-related complications and unsafe abortion consequences and increase her likelihood of dying by domestic violence.
Patient-physicians interactions are changed
As a physician I hope that I am able to convey my intense respect for and support of a woman’s autonomy into every family planning visit I conduct. Unfortunately, this ruling will not only have an immediate impact on the lives of women across the country – it will also alter the way many of us interact with our patients on a day-to-day basis. When patients can report doctors to authorities in some states for offering terminations, and doctors can report patients for seeking them, there will be absolutely no trust in the therapeutic relationship.
With this ruling, the content of private and protected conversations between patients and their physicians will be subject to censure and potentially criminal consequences.
Regardless of where I eventually practice medicine, I should not be in the position of talking to a patient and telling them that they do not have any agency over their body unless they have the money and resources to travel to a state where abortion is legal. I should not have to tell a child that she must carry and birth another child just to appease the often-fickle whims of lawmakers.
The conversation I had with my pediatric patient was important to her health and to her future, and she deserved to have the chance to discuss her feelings with a trusted physician. Every woman has the right to make her own decisions within the sanctity of the exam room, not from the distance of a courtroom.
Dr. Persampiere is a resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at [email protected] or via [email protected].
References
1. Unintended pregnancy in the United States. Guttmacher Institute. 2019 Jan 9. https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states
2. Foster D et al. The harms of denying a woman a wanted abortion - ANSIRH. https://www.ansirh.org/sites/default/files/publications/files/the_harms_of_denying_a_woman_a_wanted_abortion_4-16-2020.pdf
3. Subbaraman N. 2021 Nov 12. Homicide is a top cause of maternal death in the United States. Nature News. https://www.nature.com/articles/d41586-021-03392-8
I remember how small and shy she looked, curled into herself in her too-large hospital gown. I remember thinking that it was autumn, and she should have been at her first homecoming dance, not sitting in the ER staring mutely at the hospital-issued safety socks on her feet. Her mother, puffy-eyed from crying, was sitting on the bed beside her, stroking her hair.
Together, my patients and I talked about the pregnancy. She told me how scared she was, how she didn’t want to “kill her baby”, but that she also wasn’t sure she could take care of a child. She told me that she was terrified of childbirth, that she didn’t want her friends at school to know and to judge her. We talked about how she was a victim; how she was an innocent child, too. I reassured her, and her mom emphatically agreed – her body was still her own.
The man who hurt her did not take that from her. She could make any choice she wanted, and it would be the right choice.
Eventually, she was able to make a decision which was best for her. I don’t know what became of her, but I hope she is well now, and I hope she’s thriving and happy. I also hope that she doesn’t see the news about Roe v. Wade and feel stripped of her personhood, as many women did.
When I heard about the Supreme Court decision I thought of her, and how important our conversation was to the trajectory of her life. I wondered if across the country these conversations might be silenced, and patients might be left to navigate this important facet of their health alone.
Some version of the conversation I had with my young patient occurs in exam rooms across the country countless times a day. Sometimes these conversations are cut and dry. Other times, they are accompanied by heartbreak and tears.
These conversations are common – one in four women in the United States have had an abortion. I have had many friends who were faced with deciding what to do after an unexpectedly positive pregnancy test. The reasons were different for each person – one was raped at a party, another’s birth control failed, the boyfriend of a third friend wouldn’t wear a condom – but the underlying sentiments were the same for each woman. They thought: “This is a difficult choice, but it’s a choice I’m ready to make. I’m not ready to have a baby at this point in my life.”
My friends talked to their doctors, who assisted them in making an informed choice. Some of them chose abortion. Others chose to deliver their baby. All were helped along in their decision by a physician who was there to support them and assist them in making a well-considered choice for their individual circumstance.
Economic and health consequences of restricting access to abortion
The facts are clear: Nearly half of all pregnancies in American women in 2011 were unplanned, and about 4 in 10 of them ended in an elective abortion, according to the Guttmacher Institute.1 Restricting access to abortions does not stop abortions from happening; it limits the opportunity for women to seek advice from trusted friends and professionals and it reduces access to safe abortions.
The people who will be most harmed by these restrictions are the most socially and economically vulnerable. Wealthy, mobile women with the ability to travel to other states or countries will always be able to access abortion care; low-income, work-tethered women and women with other children to care for at home will struggle to do so.
Denying women abortion services puts them at increased risk for lifelong, multigenerational economic hardship. Women who sought abortions but were unable to obtain them experienced an increase in household poverty which lasted years relative to women who were able to receive an abortion, according to the authors of The Turnaway Study.2 They were less socially, geographically, and economically mobile, and were less likely to go on to receive a higher education.
In a country where citizens do not have paid maternity leave, affordable and accessible childcare services, or universal health care, raising a child is an enormous financial burden. Women who are denied abortions also are much more likely to end up as a single parent, shouldering that burden alone.
Additionally, low socioeconomic status is associated with increased all-cause mortality. People who live in poverty are disproportionately affected by diabetes and other chronic health conditions, and have lower life expectancies overall.
The reversal of Roe v. Wade is not only going to lead directly to patient death by decreasing access to safe abortion, causing women to pursue unsafe alternatives; it will also indirectly result in more women being driven into and remaining in poverty and suffering the health consequences.
In addition to risking a woman’s life medically, pregnancy also significantly increases that individual’s risk of being a victim of intimate partner violence. The number one cause of death in pregnant women is homicide, most often by their sexual partner, said an article published in Nature in 2021.3 Therefore, restricting a woman’s ability to control if and when she has children could put her at risk for death from serious pregnancy-related complications and unsafe abortion consequences and increase her likelihood of dying by domestic violence.
Patient-physicians interactions are changed
As a physician I hope that I am able to convey my intense respect for and support of a woman’s autonomy into every family planning visit I conduct. Unfortunately, this ruling will not only have an immediate impact on the lives of women across the country – it will also alter the way many of us interact with our patients on a day-to-day basis. When patients can report doctors to authorities in some states for offering terminations, and doctors can report patients for seeking them, there will be absolutely no trust in the therapeutic relationship.
With this ruling, the content of private and protected conversations between patients and their physicians will be subject to censure and potentially criminal consequences.
Regardless of where I eventually practice medicine, I should not be in the position of talking to a patient and telling them that they do not have any agency over their body unless they have the money and resources to travel to a state where abortion is legal. I should not have to tell a child that she must carry and birth another child just to appease the often-fickle whims of lawmakers.
The conversation I had with my pediatric patient was important to her health and to her future, and she deserved to have the chance to discuss her feelings with a trusted physician. Every woman has the right to make her own decisions within the sanctity of the exam room, not from the distance of a courtroom.
Dr. Persampiere is a resident in the family medicine residency program at Abington (Pa.) Jefferson Health. You can contact her directly at [email protected] or via [email protected].
References
1. Unintended pregnancy in the United States. Guttmacher Institute. 2019 Jan 9. https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states
2. Foster D et al. The harms of denying a woman a wanted abortion - ANSIRH. https://www.ansirh.org/sites/default/files/publications/files/the_harms_of_denying_a_woman_a_wanted_abortion_4-16-2020.pdf
3. Subbaraman N. 2021 Nov 12. Homicide is a top cause of maternal death in the United States. Nature News. https://www.nature.com/articles/d41586-021-03392-8
Select patients with breast cancer may skip RT after lumpectomy
The women in this trial who skipped radiotherapy, and were treated with breast-conserving surgery followed by endocrine therapy, had an overall survival rate of 97.2%. The local recurrence rate was 2.3%, which was the study’s primary endpoint.
“Women 55 and over, with low-grade luminal A-type breast cancer, following breast conserving surgery and treated with endocrine therapy alone, had a very low rate of local recurrence at 5 years,” commented lead author Timothy Joseph Whelan, MD.
“The prospective and multicenter nature of this study supports that these patients are candidates for the omission of radiotherapy,” said Dr. Whelan, oncology professor and Canada Research Chair in Breast Cancer Research at McMaster University and a radiation oncologist at the Juravinski Cancer Centre, both in Hamilton, Ont.
“Over 300,000 [people] are diagnosed with invasive breast cancer in North America annually, the majority in the United States,” said Dr. Whelan. “We estimate that these results could apply to 10%-15% of them, so about 30,000-40,000 women per year who could avoid the morbidity, the cost, and inconvenience of radiotherapy.”
The results were presented at the annual meeting of the American Society of Clinical Oncology.
Dr. Whelan explained that adjuvant radiation therapy is generally prescribed following breast conservation therapy to lower the risk of local recurrence, but the treatment is also associated with acute and late toxicity. In addition, it can incur high costs and inconvenience for the patient.
Previous studies have found that among women older than 60 with low-grade, luminal A-type breast cancer who received only breast-conserving surgery, there was a low rate of local recurrence. In women aged older than 70 years, the risk of local recurrence was about 4%-5%.
This latest study focused on patients with breast cancer with a luminal A subtype combined with clinical pathological factors (defined as estrogen receptor ≥ 1%, progesterone receptor > 20%, HER2 negative, and Ki67 ≤ 13.25%).
This was a prospective, multicenter cohort study that included 501 patients aged 55 years and older who had undergone breast-conserving surgery for grade 1-2 T1N0 cancer.
The median patient age was 67, with 442 (88%) older than 75 years. The median tumor size was 1.1 cm.
Median follow-up was 5 years. The cohort was followed every 6 months for the first 2 years and then annually.
The primary outcome was local recurrence defined as time from enrollment to any invasive or noninvasive cancer in the ipsilateral breast, and secondary endpoints included contralateral breast cancer, relapse-free survival based on any recurrence, disease free survival, second cancer or death, and overall survival.
At five years, there were 10 events of local recurrence, for a rate of 2.3%. For secondary outcomes, there were eight events of contralateral breast cancer (1.9%); 12 relapses for a recurrence-free survival rate of 97.3%; 47 disease progression (23 second nonbreast cancers) for a disease-free survival rate of 89.9%; and 13 deaths, including 1 from breast cancer, for an overall survival of 97.2%.
Confirms earlier data
Penny R. Anderson, MD, professor in the department of radiation oncology at Fox Chase Cancer Center, Philadelphia, commented that this was an “extremely well-designed and important study.
“It has identified a specific subset of patients to be appropriate candidates for consideration of omission of adjuvant breast radiation therapy after breast-conserving surgery,” she added.
Although previously published trials have helped identify certain patient groups who have a low risk of local recurrence – and therefore, for whom it may be appropriate to omit radiation – they have been based on the traditional clinical and pathologic factors of tumor size, margin status, receptor status, and patient age.
“This LUMINA trial utilizes the molecular-defined intrinsic subtype of luminal A breast cancer to provide additional prognostic information,” she said. “This finding certainly suggests that this group of patients are ideal candidates for the omission of radiation, and that this should be discussed with these patients as a potential option in their treatment management.”
Overall, this trial is a “significant addition and a very relevant contribution to the literature demonstrating that adjuvant breast radiation may safely be omitted in this particular subgroup of breast cancer patients,” she said.
Unanswered questions
Commenting on the study, Julie Gralow, MD, chief medical officer and executive vice president of ASCO, told this news organization that she thinks the take-home message is that there is “clearly a population of early-stage breast cancer [patients] who after lumpectomy do not benefit from radiation.”
“I think where there will be discussion will be what is the optimal way of identifying that group,” she said, noting that in this study the patients were screened for Ki67, a marker of proliferation.
Testing for Ki67 is not the standard of care, Dr. Gralow pointed out, and there is also a problem with reproducibility since “every lab does it somewhat differently, because it is not a standard pathology approach.”
There are now many unanswered questions, she noted. “Do we need that central testing of Ki67? Do we need to develop guidelines for how to do this? Is this better than if you’ve already run an Oncotype or a MammaPrint test to see if the patient needs chemo, then would that suffice? That is where the discussion will be. We can reduce the number of patients who need radiation without an increase in local regional recurrence.”
In terms of clinical practice, Dr. Gralow explained that there are already some data supporting the omission of radiation therapy in an older population with ER-positive small low-grade tumors, and this has become a standard clinical practice. “It’s not based on solid data, but based on an accumulation of retrospective analyses,” she said. “So we have already been doing it for an older population. This would bring down the age group, and it would better define it, and test it prospectively.”
Limitations to note
Also commenting on the study, Deborah Axelrod, MD, director of clinical breast surgery at New York University Langone’s Perlmutter Cancer Center, explained that, in the last decade, knowledge about the behavior of breast cancers based on molecular subtyping has greatly increased. “Results of studies such as this have given us information on which cancers need more treatment and for which cancers we can de-escalate treatment,” she said. “Refining this more, it’s about reducing the morbidity and improving quality of life without compromising the oncological outcome.”
She noted that a big strength of this LUMINA study is that it is prospective and multicenter. “It has been supported by other past studies as well and will define for which patients with newly treated breast cancers can we omit radiation, which has been the standard of care,” said Dr. Axelrod. “It is based on the age and biology of breast cancer in defining which patient can forgo radiation and showed a low risk of recurrence in a specific population of women with a favorable breast cancer profile”
There were limitations to the study. “There is a 5-year follow-up and local recurrence for ER-positive cancers continues to rise after 5 years, so longer-term follow-up will be important,” she said. Also, she pointed out that it is a single-arm study so there is no radiation therapy comparison arm.
Other limitations were that the patients were older with smaller tumors, and all were committed to 5 years of endocrine therapy, although compliance with that has not been reported. There may be some older patients who prefer radiation therapy, especially a week of accelerated partial breast irradiation, rather than commit to 5 years of endocrine therapy as mandated in this study.
“Overall, the takeaway message for patients is that the omission of radiation therapy should be considered an option for older women with localized breast cancer with favorable features who receive endocrine therapies,” said Dr. Axelrod.
LUMINA was sponsored by the Canadian Breast Cancer Foundation and the Canadian Cancer Society. Dr. Whelan has reported research funding from Exact Sciences (Inst). Dr. Axelrod and Dr. Anderson reported no disclosures. Dr. Gralow reported relationships with Genentech, AstraZeneca, Hexal, Puma BioTechnology, Roche, Novartis, Seagen, and Genomic Health.
A version of this article first appeared on Medscape.com.
The women in this trial who skipped radiotherapy, and were treated with breast-conserving surgery followed by endocrine therapy, had an overall survival rate of 97.2%. The local recurrence rate was 2.3%, which was the study’s primary endpoint.
“Women 55 and over, with low-grade luminal A-type breast cancer, following breast conserving surgery and treated with endocrine therapy alone, had a very low rate of local recurrence at 5 years,” commented lead author Timothy Joseph Whelan, MD.
“The prospective and multicenter nature of this study supports that these patients are candidates for the omission of radiotherapy,” said Dr. Whelan, oncology professor and Canada Research Chair in Breast Cancer Research at McMaster University and a radiation oncologist at the Juravinski Cancer Centre, both in Hamilton, Ont.
“Over 300,000 [people] are diagnosed with invasive breast cancer in North America annually, the majority in the United States,” said Dr. Whelan. “We estimate that these results could apply to 10%-15% of them, so about 30,000-40,000 women per year who could avoid the morbidity, the cost, and inconvenience of radiotherapy.”
The results were presented at the annual meeting of the American Society of Clinical Oncology.
Dr. Whelan explained that adjuvant radiation therapy is generally prescribed following breast conservation therapy to lower the risk of local recurrence, but the treatment is also associated with acute and late toxicity. In addition, it can incur high costs and inconvenience for the patient.
Previous studies have found that among women older than 60 with low-grade, luminal A-type breast cancer who received only breast-conserving surgery, there was a low rate of local recurrence. In women aged older than 70 years, the risk of local recurrence was about 4%-5%.
This latest study focused on patients with breast cancer with a luminal A subtype combined with clinical pathological factors (defined as estrogen receptor ≥ 1%, progesterone receptor > 20%, HER2 negative, and Ki67 ≤ 13.25%).
This was a prospective, multicenter cohort study that included 501 patients aged 55 years and older who had undergone breast-conserving surgery for grade 1-2 T1N0 cancer.
The median patient age was 67, with 442 (88%) older than 75 years. The median tumor size was 1.1 cm.
Median follow-up was 5 years. The cohort was followed every 6 months for the first 2 years and then annually.
The primary outcome was local recurrence defined as time from enrollment to any invasive or noninvasive cancer in the ipsilateral breast, and secondary endpoints included contralateral breast cancer, relapse-free survival based on any recurrence, disease free survival, second cancer or death, and overall survival.
At five years, there were 10 events of local recurrence, for a rate of 2.3%. For secondary outcomes, there were eight events of contralateral breast cancer (1.9%); 12 relapses for a recurrence-free survival rate of 97.3%; 47 disease progression (23 second nonbreast cancers) for a disease-free survival rate of 89.9%; and 13 deaths, including 1 from breast cancer, for an overall survival of 97.2%.
Confirms earlier data
Penny R. Anderson, MD, professor in the department of radiation oncology at Fox Chase Cancer Center, Philadelphia, commented that this was an “extremely well-designed and important study.
“It has identified a specific subset of patients to be appropriate candidates for consideration of omission of adjuvant breast radiation therapy after breast-conserving surgery,” she added.
Although previously published trials have helped identify certain patient groups who have a low risk of local recurrence – and therefore, for whom it may be appropriate to omit radiation – they have been based on the traditional clinical and pathologic factors of tumor size, margin status, receptor status, and patient age.
“This LUMINA trial utilizes the molecular-defined intrinsic subtype of luminal A breast cancer to provide additional prognostic information,” she said. “This finding certainly suggests that this group of patients are ideal candidates for the omission of radiation, and that this should be discussed with these patients as a potential option in their treatment management.”
Overall, this trial is a “significant addition and a very relevant contribution to the literature demonstrating that adjuvant breast radiation may safely be omitted in this particular subgroup of breast cancer patients,” she said.
Unanswered questions
Commenting on the study, Julie Gralow, MD, chief medical officer and executive vice president of ASCO, told this news organization that she thinks the take-home message is that there is “clearly a population of early-stage breast cancer [patients] who after lumpectomy do not benefit from radiation.”
“I think where there will be discussion will be what is the optimal way of identifying that group,” she said, noting that in this study the patients were screened for Ki67, a marker of proliferation.
Testing for Ki67 is not the standard of care, Dr. Gralow pointed out, and there is also a problem with reproducibility since “every lab does it somewhat differently, because it is not a standard pathology approach.”
There are now many unanswered questions, she noted. “Do we need that central testing of Ki67? Do we need to develop guidelines for how to do this? Is this better than if you’ve already run an Oncotype or a MammaPrint test to see if the patient needs chemo, then would that suffice? That is where the discussion will be. We can reduce the number of patients who need radiation without an increase in local regional recurrence.”
In terms of clinical practice, Dr. Gralow explained that there are already some data supporting the omission of radiation therapy in an older population with ER-positive small low-grade tumors, and this has become a standard clinical practice. “It’s not based on solid data, but based on an accumulation of retrospective analyses,” she said. “So we have already been doing it for an older population. This would bring down the age group, and it would better define it, and test it prospectively.”
Limitations to note
Also commenting on the study, Deborah Axelrod, MD, director of clinical breast surgery at New York University Langone’s Perlmutter Cancer Center, explained that, in the last decade, knowledge about the behavior of breast cancers based on molecular subtyping has greatly increased. “Results of studies such as this have given us information on which cancers need more treatment and for which cancers we can de-escalate treatment,” she said. “Refining this more, it’s about reducing the morbidity and improving quality of life without compromising the oncological outcome.”
She noted that a big strength of this LUMINA study is that it is prospective and multicenter. “It has been supported by other past studies as well and will define for which patients with newly treated breast cancers can we omit radiation, which has been the standard of care,” said Dr. Axelrod. “It is based on the age and biology of breast cancer in defining which patient can forgo radiation and showed a low risk of recurrence in a specific population of women with a favorable breast cancer profile”
There were limitations to the study. “There is a 5-year follow-up and local recurrence for ER-positive cancers continues to rise after 5 years, so longer-term follow-up will be important,” she said. Also, she pointed out that it is a single-arm study so there is no radiation therapy comparison arm.
Other limitations were that the patients were older with smaller tumors, and all were committed to 5 years of endocrine therapy, although compliance with that has not been reported. There may be some older patients who prefer radiation therapy, especially a week of accelerated partial breast irradiation, rather than commit to 5 years of endocrine therapy as mandated in this study.
“Overall, the takeaway message for patients is that the omission of radiation therapy should be considered an option for older women with localized breast cancer with favorable features who receive endocrine therapies,” said Dr. Axelrod.
LUMINA was sponsored by the Canadian Breast Cancer Foundation and the Canadian Cancer Society. Dr. Whelan has reported research funding from Exact Sciences (Inst). Dr. Axelrod and Dr. Anderson reported no disclosures. Dr. Gralow reported relationships with Genentech, AstraZeneca, Hexal, Puma BioTechnology, Roche, Novartis, Seagen, and Genomic Health.
A version of this article first appeared on Medscape.com.
The women in this trial who skipped radiotherapy, and were treated with breast-conserving surgery followed by endocrine therapy, had an overall survival rate of 97.2%. The local recurrence rate was 2.3%, which was the study’s primary endpoint.
“Women 55 and over, with low-grade luminal A-type breast cancer, following breast conserving surgery and treated with endocrine therapy alone, had a very low rate of local recurrence at 5 years,” commented lead author Timothy Joseph Whelan, MD.
“The prospective and multicenter nature of this study supports that these patients are candidates for the omission of radiotherapy,” said Dr. Whelan, oncology professor and Canada Research Chair in Breast Cancer Research at McMaster University and a radiation oncologist at the Juravinski Cancer Centre, both in Hamilton, Ont.
“Over 300,000 [people] are diagnosed with invasive breast cancer in North America annually, the majority in the United States,” said Dr. Whelan. “We estimate that these results could apply to 10%-15% of them, so about 30,000-40,000 women per year who could avoid the morbidity, the cost, and inconvenience of radiotherapy.”
The results were presented at the annual meeting of the American Society of Clinical Oncology.
Dr. Whelan explained that adjuvant radiation therapy is generally prescribed following breast conservation therapy to lower the risk of local recurrence, but the treatment is also associated with acute and late toxicity. In addition, it can incur high costs and inconvenience for the patient.
Previous studies have found that among women older than 60 with low-grade, luminal A-type breast cancer who received only breast-conserving surgery, there was a low rate of local recurrence. In women aged older than 70 years, the risk of local recurrence was about 4%-5%.
This latest study focused on patients with breast cancer with a luminal A subtype combined with clinical pathological factors (defined as estrogen receptor ≥ 1%, progesterone receptor > 20%, HER2 negative, and Ki67 ≤ 13.25%).
This was a prospective, multicenter cohort study that included 501 patients aged 55 years and older who had undergone breast-conserving surgery for grade 1-2 T1N0 cancer.
The median patient age was 67, with 442 (88%) older than 75 years. The median tumor size was 1.1 cm.
Median follow-up was 5 years. The cohort was followed every 6 months for the first 2 years and then annually.
The primary outcome was local recurrence defined as time from enrollment to any invasive or noninvasive cancer in the ipsilateral breast, and secondary endpoints included contralateral breast cancer, relapse-free survival based on any recurrence, disease free survival, second cancer or death, and overall survival.
At five years, there were 10 events of local recurrence, for a rate of 2.3%. For secondary outcomes, there were eight events of contralateral breast cancer (1.9%); 12 relapses for a recurrence-free survival rate of 97.3%; 47 disease progression (23 second nonbreast cancers) for a disease-free survival rate of 89.9%; and 13 deaths, including 1 from breast cancer, for an overall survival of 97.2%.
Confirms earlier data
Penny R. Anderson, MD, professor in the department of radiation oncology at Fox Chase Cancer Center, Philadelphia, commented that this was an “extremely well-designed and important study.
“It has identified a specific subset of patients to be appropriate candidates for consideration of omission of adjuvant breast radiation therapy after breast-conserving surgery,” she added.
Although previously published trials have helped identify certain patient groups who have a low risk of local recurrence – and therefore, for whom it may be appropriate to omit radiation – they have been based on the traditional clinical and pathologic factors of tumor size, margin status, receptor status, and patient age.
“This LUMINA trial utilizes the molecular-defined intrinsic subtype of luminal A breast cancer to provide additional prognostic information,” she said. “This finding certainly suggests that this group of patients are ideal candidates for the omission of radiation, and that this should be discussed with these patients as a potential option in their treatment management.”
Overall, this trial is a “significant addition and a very relevant contribution to the literature demonstrating that adjuvant breast radiation may safely be omitted in this particular subgroup of breast cancer patients,” she said.
Unanswered questions
Commenting on the study, Julie Gralow, MD, chief medical officer and executive vice president of ASCO, told this news organization that she thinks the take-home message is that there is “clearly a population of early-stage breast cancer [patients] who after lumpectomy do not benefit from radiation.”
“I think where there will be discussion will be what is the optimal way of identifying that group,” she said, noting that in this study the patients were screened for Ki67, a marker of proliferation.
Testing for Ki67 is not the standard of care, Dr. Gralow pointed out, and there is also a problem with reproducibility since “every lab does it somewhat differently, because it is not a standard pathology approach.”
There are now many unanswered questions, she noted. “Do we need that central testing of Ki67? Do we need to develop guidelines for how to do this? Is this better than if you’ve already run an Oncotype or a MammaPrint test to see if the patient needs chemo, then would that suffice? That is where the discussion will be. We can reduce the number of patients who need radiation without an increase in local regional recurrence.”
In terms of clinical practice, Dr. Gralow explained that there are already some data supporting the omission of radiation therapy in an older population with ER-positive small low-grade tumors, and this has become a standard clinical practice. “It’s not based on solid data, but based on an accumulation of retrospective analyses,” she said. “So we have already been doing it for an older population. This would bring down the age group, and it would better define it, and test it prospectively.”
Limitations to note
Also commenting on the study, Deborah Axelrod, MD, director of clinical breast surgery at New York University Langone’s Perlmutter Cancer Center, explained that, in the last decade, knowledge about the behavior of breast cancers based on molecular subtyping has greatly increased. “Results of studies such as this have given us information on which cancers need more treatment and for which cancers we can de-escalate treatment,” she said. “Refining this more, it’s about reducing the morbidity and improving quality of life without compromising the oncological outcome.”
She noted that a big strength of this LUMINA study is that it is prospective and multicenter. “It has been supported by other past studies as well and will define for which patients with newly treated breast cancers can we omit radiation, which has been the standard of care,” said Dr. Axelrod. “It is based on the age and biology of breast cancer in defining which patient can forgo radiation and showed a low risk of recurrence in a specific population of women with a favorable breast cancer profile”
There were limitations to the study. “There is a 5-year follow-up and local recurrence for ER-positive cancers continues to rise after 5 years, so longer-term follow-up will be important,” she said. Also, she pointed out that it is a single-arm study so there is no radiation therapy comparison arm.
Other limitations were that the patients were older with smaller tumors, and all were committed to 5 years of endocrine therapy, although compliance with that has not been reported. There may be some older patients who prefer radiation therapy, especially a week of accelerated partial breast irradiation, rather than commit to 5 years of endocrine therapy as mandated in this study.
“Overall, the takeaway message for patients is that the omission of radiation therapy should be considered an option for older women with localized breast cancer with favorable features who receive endocrine therapies,” said Dr. Axelrod.
LUMINA was sponsored by the Canadian Breast Cancer Foundation and the Canadian Cancer Society. Dr. Whelan has reported research funding from Exact Sciences (Inst). Dr. Axelrod and Dr. Anderson reported no disclosures. Dr. Gralow reported relationships with Genentech, AstraZeneca, Hexal, Puma BioTechnology, Roche, Novartis, Seagen, and Genomic Health.
A version of this article first appeared on Medscape.com.
FROM ASCO 2022
Gender surgeons on TikTok, Instagram: Appropriate or not?
A woman wearing purple surgical scrubs stares into a camera, looking frustrated, but doesn’t speak. Superimposed over her head is the text “just realized I only get to Yeet 4 Teets next week,” and a crying emoji. Rain appears to drip down over her while “Stan” by Eminem plays in the background.
That October 2020 TikTok by Sidhbh Gallagher, MD, a Miami-based plastic surgeon known as @gendersurgeon, had almost 10,000 likes and was tagged #topsurgery, #masculoplasty, #ftm, and #transman, among other hashtags.
“What health check do I have to get in preparation for teetus deletus?” is the question in another Dr. Gallagher TikTok. Dr. Gallagher is a prolific user of social media with over 268K TikTok followers and over 44K Instagram followers. Another Dr. Gallagher TikTok account, @thevagicianmd, has some 7K followers.
Another cosmetic surgeon, Tony Mangubat, MD, known as @Tikdoctony to his more than 200K followers, uses similar hashtags – like #teetusdeleetus – in his TikToks.
Clearly not medical terms, hashtags like #yeettheteet and #teetusdeletus are often used by the transgender community. The posts by Dr. Gallagher and Dr. Mangubat are part of an ever-growing wave of social media activity by medical professionals.
Plastic surgeons have never been shy about advertising their work – and many have taken to social media to do so, including showing before and after photos. A 2020 study published in Plastic and Reconstructive Surgery found that the majority of such surgeons, especially those in private practice, use social media.
especially to a younger-skewing audience.
Because of the limits on pornography and nudity of social media platforms, most social media posts by gender surgeons are about female-to-male (FTM) mastectomies, the fastest-growing transgender procedure.
The American Society of Plastic Surgeons (ASPS) started separately tracking gender-affirmation procedures in 2015. That year, members reported doing 1,360 FTM procedures.
In 2020, the ASPS further separated procedures into additional categories. That year – when many surgeries were postponed because of the COVID-19 pandemic – FTM mastectomies grew by 15%, with 8,548 procedures performed, a far greater number than for any other transgender surgery, and a sixfold increase in the number of procedures done in 2015.
‘Gimmicky,’ but building community
Surgeons interviewed for this article said they use social media primarily to connect with patients and to educate in a light-hearted way.
While Dr. Gallagher acknowledges that using #teetusdeletus is “kind of gimmicky,” she said she doesn’t view it as unprofessional because she is “using the words of the community I serve.” Many of her patients have seen a medical professional “who just didn’t understand what it is to have gender dysphoria, didn’t understand what it is to be trans, so going from that experience to somebody who uses the same language as the community uses can be quite a comfortable experience,” she said in an interview.
Dr. Mangubat, a Seattle-area plastic surgeon who has been doing mastectomies for trans male patients since 1988, said he tailors his TikToks to that group. He likes TikTok – which he started using in early 2021 – because it has rules against bullying, swearing, and pornography, he told this news organization.
“It’s really not ... advertising ... it’s a community-building platform,” said Dr. Mangubat. “If you build community, people will trust you, and if you provide good accurate information, then people will be safer,” he said.
But, “I’m not telling them to come to me,” he stressed.
He always appears in scrubs and doesn’t do music, doesn’t dance, and doesn’t post before and after photos, but he still gets thousands – or sometimes hundreds of thousands – of likes.
His mission, he said, is to answer the community’s questions. “We’re reaching patients that have had their top surgery, that are going to have their top surgery, that are looking for how to get top surgery, that are just starting on testosterone, that haven’t started on testosterone – it’s the whole spectrum of patients,” said Dr. Mangubat.
Risks downplayed?
Other surgeons have expressed concern about ethical boundaries and the tendency of social media posts to downplay risks of what are life-changing procedures.
A 2020 study of YouTube videos on top surgery, for instance, concluded that “there were no unbiased videos by board-certified plastic surgeons explaining the risks, benefits, treatment options, and alternatives to surgery.”
Alison Clayton, MBBS, an Australian psychiatrist, said that social media posts can create false expectations because they emphasize style over substance, omit risks, and can create an unwarranted sense of trust in the doctor that can spill over into the physician-patient relationship.
Dr. Clayton also believes that “the gender-affirming surgical procedures being offered to these youth have a scant empirical evidence base for benefits to psychological health and well-being.”
It is known that a number of those who transition, using either opposite sex hormones and/or surgical procedures, later have regret and “detransition,” but statistics are lacking. It is also a controversial area, with many detransitioners saying they didn’t get appropriate care and weren’t properly assessed before being given hormones or heading to surgery.
Most of the gender surgeons interviewed for this article said they see almost “zero” regret if proper mental health evaluations are performed before surgery, and they added, the procedures can relieve dysphoria.
Nevertheless, posts should not be “all fun and games,” said Josef Hadeed, MD, chair of the ASPS Patient Safety Committee and Public Education Committee and a member of its Social Media Subcommittee.
“When someone makes a decision to undergo a surgical procedure, they should be very aware there are some risks and potentially serious risks involved,” he told this news organization.
The ASPS “wants members to use social media in a judicious manner” in a way that educates the public and encourages patients to learn about a procedure and to consult with board-certified plastic surgeons, said Dr. Hadeed.
The Beverly Hills, Calif.–based surgeon does gender-affirmation procedures himself and uses Instagram, on which he has 53.4K followers, to educate patients and highlight his work using before and after photos.
“I like to think I do it in a very tasteful way,” Dr. Hadeed said. “It’s not in a way that’s sort of suggestive to patients, including minors, that this is something they need to get done, because if they are thinking about getting it done there is a lengthy process that they have to go through before they even set foot in our office.”
And he said “it may be inappropriate” to use certain hashtags or terminology, “even if it does ‘speak’ to the patients. Professionally, plastic surgeons should maintain a higher standard and maintain that even with their social media.”
Marci Bowers, MD, a gynecologic surgeon who performs gender-affirming procedures, and who is transgender herself, agreed.
“Some of the posts out there seem sensational, distasteful, and risk compromising patient confidentiality,” Dr. Bowers said in an interview.
“Much of this seemed to cross the line of good taste and appropriateness,” added Dr. Bowers, who is the incoming president of the World Professional Association for Transgender Health (WPATH). “Creating an idealized video without addressing risk is inappropriate and misleading,” she stressed.
“These surgeons would perhaps better serve their clients by focusing on and improving their clinical care,” she added.
Dr. Bowers said that although WPATH has not addressed social media use in the past, its ethics committee will be taking on the topic this year.
Social media posts about gender-affirming procedures “don’t usually talk about the barriers, they don’t talk about bad outcomes, they tend to just focus on success stories,” said Gwendolyn P. Quinn, MD, a bioethicist, and Livia S. Wan, MD, professor of obstetrics and gynecology at the NYU Grossman School of Medicine.
But she also sees some positives. The posts can help normalize gender-affirming surgery, and post-procedure photos might “help people realize that they can’t just have everything exactly the way they want it to be,” said Dr. Quinn.
Does social media influence or educate?
Studies have documented the power of social media to influence desire and decisionmaking, especially when it comes to cosmetic surgery.
“The use of social media creates a vague area between patient confidentiality and entertainment,” writes Nisha Gupta and colleagues of the UCLA David Geffen School of Medicine in a review published in the Aesthetic Surgery Journal.
While social media use is on the rise by plastic surgeons and has the potential to educate, it has also “compromised the integrity of the doctor-patient relationship,” they add.
Surgeons can use tools to place themselves higher in searches, and patients might assume that those who have hundreds of thousands of followers “are the most qualified or trusted, although this is not always the case,” they note.
Markus Rach, PhD, a researcher with the University of Applied Sciences and Arts Northwestern Switzerland, analyzed the impact of TikTok’s plastic surgery content on how adolescents perceived themselves and how it influenced their decision to have a procedure.
Most TikTok users are under age 24, and #plasticsurgery has a huge viewership with some 3.8 billion views at the time of publication, said Dr. Rach. He found that influencers tended to make adolescents feel bad and want surgery but that plastic surgeons had a moderating effect on both negative feelings and the intent to get surgery.
Dr. Bowers said that, despite her concerns, she does not “believe social media influences like TikTok and Facebook create artificial demand.”
However, Dr. Mangubat said social media can make plastic surgery seem enticing. “It can happen, and it does happen,” he said, but he added that’s true for any cosmetic procedure, not just gender-affirming surgery.
The pitfall with social media is that “patients are being sold a vision of themselves that may or may not be possible,” he observed.
Dr. Quinn worries less about people being talked into a procedure and more about those who don’t want surgery.
“There are people who identify as transgender but do not feel the need to change any parts of their body,” she said. “And that should be okay.”
Concerns about minors
New guidance from WPATH, their Standards of Care (SOC) 8 – the first update in 10 years – are due to be published this month. As reported by this news organization, and as stated in the draft of the SOC 8 published for comment in December 2021, the organization has recommended lowering the age for “top” surgery from 18 to 15 years.
Dr. Clayton has concerns about young people with gender dysphoria, who she says are “often vulnerable youth, many of whom have comorbid psychiatric and neurodevelopmental disorders.”
“This may contribute to a greater vulnerability of this population to undue influence,” added Dr. Clayton.
Sean Devitt, MD, and Jeffrey M. Kenkel, MD, of the University of Texas Southwestern Medical Center, Dallas, expressed concern that social media posts by plastic surgeons could be especially dangerous for young people.
“Given that the prefrontal cortex, which is largely responsible for impulse control, is not fully developed until the age of 25, is it ethical to allow younger patients to make life-lasting decisions under the guise of education?” they ask in a commentary on the review by Ms. Gupta and colleagues about plastic surgeons’ use of social media. The review did not focus on gender-affirmation procedures.
Many surgeons – but not all – steer clear of genital (“bottom”) surgeries in minors. However, bilateral mastectomies are being performed in those as young as age 13 based on surgeons’ risk-benefit calculus for the patient.
A study, published in May in the Annals of Plastic Surgery, showed there was a 13-fold increase in the number of bilateral mastectomies performed on under-18s between January 2013 and the end of July 2020. Of the 209 minors (age 12-17) who had the surgery, two (0.95%) expressed regret by the time of follow-up, at 3 and 7 years post-operatively, but neither had reversal surgery.
A small 2018 study, published in JAMA Pediatrics, among trans males who had top surgery found high rates of satisfaction, though one of the 68 patients reported experiencing regret “sometimes.” The mean age of patients in the surgical group was 19 years and the youngest patient was 14.
“Most of us who practice heavily in this field will make exceptions, not for genital surgery but typically for top surgery,” said Dr. Gallagher, who added that she operates on one minor [under 18] a month, while doing some 400-500 gender-affirmative surgeries a year. For some patients, “doing nothing isn’t necessarily a no-harm option,” said Dr. Gallagher.
“Arbitrarily picking the age of 18 and sentencing that patient to another year of dysphoria” might not be the best risk-benefit calculus, she said.
Dr. Mangubat agrees, especially if, for example, a trans man develops double D breasts by age 14. “You’ve sentenced them to 4 years of misery” before they can get insurance coverage, he said. His youngest top surgery patient was age 15. He said the person’s family, mental health professional, and primary care physician were all in favor of the procedure.
Dr. Mangubat also noted that some insurers, such as Kaiser Permanente, now cover bilateral mastectomy starting at age 16.
Dr. Quinn, the bioethicist, said not every minor or young adult is equipped to make the best long-term decisions.
She works with younger patients who have cancer, for example, and said her suggestions that they consider fertility preservation are often met with protestations “that they will never have children.”
The same issue arises with transgender patients. They may not want to think about having children or issues such as breast feeding while in their teens or early 20s. “But you know from your experience that they may feel differently in 10 years, but they’re just not in the mind frame to think about it,” said Dr. Quinn.
Some young people may accurately never want children, said Dr. Quinn, “but there is a lack of maturity shown when a person just shuts down a conversation and won’t even listen to infertility threats and potential preservation options.”
Concerns about regret?
Dr. Gallagher said she follows the WPATH standards, which require mental health evaluations, and as a result, “the risk of regret is incredibly low.”
However, one of Dr. Gallagher’s patients who detransitioned, Grace, who goes by @HormoneHangover on social media, said she has taken umbrage at some of the Miami surgeon’s TikToks, including one, “Why might some patients feel sad after surgery ... despite wanting it for so long??”
“This is actually not uncommon with ANY kind of surgery, but it’s temporary!” said the TikTok text. Dr. Gallagher is wearing a red dress and heels and flips her hair while the text scrolls above her.
But to Grace, the TikTok “really bothered me, because sometimes there is regret, and I think that sort of advertising paints a falsely rosy picture,” she said in an interview.
And it is emblematic of what she feels was Dr. Gallagher’s “breezy” approach to explaining the procedure to her. “The surgery itself was a shocking experience for me,” she said. “The physical experience was very jarring. It was very disturbing in a way I hadn’t anticipated or understood in advance,” said Grace.
Dr. Mangubat, who does 100 bilateral mastectomies in trans patients a year, said he goes to great lengths to ensure his patients are good candidates. Everyone – even those who self-pay – must have counseling, and if the individual seems to be considering the surgery because it’s “trendy,” he steers clear.
“If they’re not serious about it, I don’t want to operate on them,” said Dr. Mangubat. “There have been maybe two patients who have come back” to detransition, he said.
Dr. Hadeed also said he has not seen regret. He attributes this to his vetting process, which includes investigating the background of the mental health professionals who write support letters.
“We’ve turned away a lot of patients from our office either because of inadequate letters or because the person writing the letter just doesn’t really have any proper credentials,” he said.
Is social media use by plastic surgeons the new normal?
With so many plastic surgeons – including those who perform transgender procedures – using social media, it may increasingly be just part of doing business.
“Undoubtedly gender surgery teams will have a greater presence on social media in the future,” write Alireza Hamidian Jahromi, MD, and a colleague of the plastic surgery department at Rush University Medical Center, Chicago, in a letter published in Plastic and Reconstructive Surgery.
Kyle R. Latack, MD, and colleagues at the University of Southern California and the University of Michigan, have studied the use of social media by the transgender community and write that they believe “there should be an increased effort to develop high-quality and unbiased resources for patient education that can be made [available] on social media.”
Dr. Gallagher said TikTok helped her erase fear. “A bilateral mastectomy is a scary surgery for an 18-year-old or a 20-year-old,” she said, “but they have to do it for their well-being.”
“That is a criticism I’ve heard – that I seek to minimize it or that I’m flippant about it,” said Dr. Gallagher.
For “top surgery the risk profile is pretty low,” she said, “so what I try to do is educate people that it’s maybe not as scary a procedure as they think.”
Dr. Mangubat, however, is concerned about some of what he sees, especially the explosion of surgeons offering gender-affirming procedures. “Now everybody wants a piece of it,” he said.
“Let’s face it, it’s money now. You get paid for doing this surgery. Hospitals get paid a lot of money for their operating rooms for doing the surgery,” said Dr. Mangubat. “There are some surgeons who believe the transgender community is just another market.”
A version of this article first appeared on Medscape.com.
A woman wearing purple surgical scrubs stares into a camera, looking frustrated, but doesn’t speak. Superimposed over her head is the text “just realized I only get to Yeet 4 Teets next week,” and a crying emoji. Rain appears to drip down over her while “Stan” by Eminem plays in the background.
That October 2020 TikTok by Sidhbh Gallagher, MD, a Miami-based plastic surgeon known as @gendersurgeon, had almost 10,000 likes and was tagged #topsurgery, #masculoplasty, #ftm, and #transman, among other hashtags.
“What health check do I have to get in preparation for teetus deletus?” is the question in another Dr. Gallagher TikTok. Dr. Gallagher is a prolific user of social media with over 268K TikTok followers and over 44K Instagram followers. Another Dr. Gallagher TikTok account, @thevagicianmd, has some 7K followers.
Another cosmetic surgeon, Tony Mangubat, MD, known as @Tikdoctony to his more than 200K followers, uses similar hashtags – like #teetusdeleetus – in his TikToks.
Clearly not medical terms, hashtags like #yeettheteet and #teetusdeletus are often used by the transgender community. The posts by Dr. Gallagher and Dr. Mangubat are part of an ever-growing wave of social media activity by medical professionals.
Plastic surgeons have never been shy about advertising their work – and many have taken to social media to do so, including showing before and after photos. A 2020 study published in Plastic and Reconstructive Surgery found that the majority of such surgeons, especially those in private practice, use social media.
especially to a younger-skewing audience.
Because of the limits on pornography and nudity of social media platforms, most social media posts by gender surgeons are about female-to-male (FTM) mastectomies, the fastest-growing transgender procedure.
The American Society of Plastic Surgeons (ASPS) started separately tracking gender-affirmation procedures in 2015. That year, members reported doing 1,360 FTM procedures.
In 2020, the ASPS further separated procedures into additional categories. That year – when many surgeries were postponed because of the COVID-19 pandemic – FTM mastectomies grew by 15%, with 8,548 procedures performed, a far greater number than for any other transgender surgery, and a sixfold increase in the number of procedures done in 2015.
‘Gimmicky,’ but building community
Surgeons interviewed for this article said they use social media primarily to connect with patients and to educate in a light-hearted way.
While Dr. Gallagher acknowledges that using #teetusdeletus is “kind of gimmicky,” she said she doesn’t view it as unprofessional because she is “using the words of the community I serve.” Many of her patients have seen a medical professional “who just didn’t understand what it is to have gender dysphoria, didn’t understand what it is to be trans, so going from that experience to somebody who uses the same language as the community uses can be quite a comfortable experience,” she said in an interview.
Dr. Mangubat, a Seattle-area plastic surgeon who has been doing mastectomies for trans male patients since 1988, said he tailors his TikToks to that group. He likes TikTok – which he started using in early 2021 – because it has rules against bullying, swearing, and pornography, he told this news organization.
“It’s really not ... advertising ... it’s a community-building platform,” said Dr. Mangubat. “If you build community, people will trust you, and if you provide good accurate information, then people will be safer,” he said.
But, “I’m not telling them to come to me,” he stressed.
He always appears in scrubs and doesn’t do music, doesn’t dance, and doesn’t post before and after photos, but he still gets thousands – or sometimes hundreds of thousands – of likes.
His mission, he said, is to answer the community’s questions. “We’re reaching patients that have had their top surgery, that are going to have their top surgery, that are looking for how to get top surgery, that are just starting on testosterone, that haven’t started on testosterone – it’s the whole spectrum of patients,” said Dr. Mangubat.
Risks downplayed?
Other surgeons have expressed concern about ethical boundaries and the tendency of social media posts to downplay risks of what are life-changing procedures.
A 2020 study of YouTube videos on top surgery, for instance, concluded that “there were no unbiased videos by board-certified plastic surgeons explaining the risks, benefits, treatment options, and alternatives to surgery.”
Alison Clayton, MBBS, an Australian psychiatrist, said that social media posts can create false expectations because they emphasize style over substance, omit risks, and can create an unwarranted sense of trust in the doctor that can spill over into the physician-patient relationship.
Dr. Clayton also believes that “the gender-affirming surgical procedures being offered to these youth have a scant empirical evidence base for benefits to psychological health and well-being.”
It is known that a number of those who transition, using either opposite sex hormones and/or surgical procedures, later have regret and “detransition,” but statistics are lacking. It is also a controversial area, with many detransitioners saying they didn’t get appropriate care and weren’t properly assessed before being given hormones or heading to surgery.
Most of the gender surgeons interviewed for this article said they see almost “zero” regret if proper mental health evaluations are performed before surgery, and they added, the procedures can relieve dysphoria.
Nevertheless, posts should not be “all fun and games,” said Josef Hadeed, MD, chair of the ASPS Patient Safety Committee and Public Education Committee and a member of its Social Media Subcommittee.
“When someone makes a decision to undergo a surgical procedure, they should be very aware there are some risks and potentially serious risks involved,” he told this news organization.
The ASPS “wants members to use social media in a judicious manner” in a way that educates the public and encourages patients to learn about a procedure and to consult with board-certified plastic surgeons, said Dr. Hadeed.
The Beverly Hills, Calif.–based surgeon does gender-affirmation procedures himself and uses Instagram, on which he has 53.4K followers, to educate patients and highlight his work using before and after photos.
“I like to think I do it in a very tasteful way,” Dr. Hadeed said. “It’s not in a way that’s sort of suggestive to patients, including minors, that this is something they need to get done, because if they are thinking about getting it done there is a lengthy process that they have to go through before they even set foot in our office.”
And he said “it may be inappropriate” to use certain hashtags or terminology, “even if it does ‘speak’ to the patients. Professionally, plastic surgeons should maintain a higher standard and maintain that even with their social media.”
Marci Bowers, MD, a gynecologic surgeon who performs gender-affirming procedures, and who is transgender herself, agreed.
“Some of the posts out there seem sensational, distasteful, and risk compromising patient confidentiality,” Dr. Bowers said in an interview.
“Much of this seemed to cross the line of good taste and appropriateness,” added Dr. Bowers, who is the incoming president of the World Professional Association for Transgender Health (WPATH). “Creating an idealized video without addressing risk is inappropriate and misleading,” she stressed.
“These surgeons would perhaps better serve their clients by focusing on and improving their clinical care,” she added.
Dr. Bowers said that although WPATH has not addressed social media use in the past, its ethics committee will be taking on the topic this year.
Social media posts about gender-affirming procedures “don’t usually talk about the barriers, they don’t talk about bad outcomes, they tend to just focus on success stories,” said Gwendolyn P. Quinn, MD, a bioethicist, and Livia S. Wan, MD, professor of obstetrics and gynecology at the NYU Grossman School of Medicine.
But she also sees some positives. The posts can help normalize gender-affirming surgery, and post-procedure photos might “help people realize that they can’t just have everything exactly the way they want it to be,” said Dr. Quinn.
Does social media influence or educate?
Studies have documented the power of social media to influence desire and decisionmaking, especially when it comes to cosmetic surgery.
“The use of social media creates a vague area between patient confidentiality and entertainment,” writes Nisha Gupta and colleagues of the UCLA David Geffen School of Medicine in a review published in the Aesthetic Surgery Journal.
While social media use is on the rise by plastic surgeons and has the potential to educate, it has also “compromised the integrity of the doctor-patient relationship,” they add.
Surgeons can use tools to place themselves higher in searches, and patients might assume that those who have hundreds of thousands of followers “are the most qualified or trusted, although this is not always the case,” they note.
Markus Rach, PhD, a researcher with the University of Applied Sciences and Arts Northwestern Switzerland, analyzed the impact of TikTok’s plastic surgery content on how adolescents perceived themselves and how it influenced their decision to have a procedure.
Most TikTok users are under age 24, and #plasticsurgery has a huge viewership with some 3.8 billion views at the time of publication, said Dr. Rach. He found that influencers tended to make adolescents feel bad and want surgery but that plastic surgeons had a moderating effect on both negative feelings and the intent to get surgery.
Dr. Bowers said that, despite her concerns, she does not “believe social media influences like TikTok and Facebook create artificial demand.”
However, Dr. Mangubat said social media can make plastic surgery seem enticing. “It can happen, and it does happen,” he said, but he added that’s true for any cosmetic procedure, not just gender-affirming surgery.
The pitfall with social media is that “patients are being sold a vision of themselves that may or may not be possible,” he observed.
Dr. Quinn worries less about people being talked into a procedure and more about those who don’t want surgery.
“There are people who identify as transgender but do not feel the need to change any parts of their body,” she said. “And that should be okay.”
Concerns about minors
New guidance from WPATH, their Standards of Care (SOC) 8 – the first update in 10 years – are due to be published this month. As reported by this news organization, and as stated in the draft of the SOC 8 published for comment in December 2021, the organization has recommended lowering the age for “top” surgery from 18 to 15 years.
Dr. Clayton has concerns about young people with gender dysphoria, who she says are “often vulnerable youth, many of whom have comorbid psychiatric and neurodevelopmental disorders.”
“This may contribute to a greater vulnerability of this population to undue influence,” added Dr. Clayton.
Sean Devitt, MD, and Jeffrey M. Kenkel, MD, of the University of Texas Southwestern Medical Center, Dallas, expressed concern that social media posts by plastic surgeons could be especially dangerous for young people.
“Given that the prefrontal cortex, which is largely responsible for impulse control, is not fully developed until the age of 25, is it ethical to allow younger patients to make life-lasting decisions under the guise of education?” they ask in a commentary on the review by Ms. Gupta and colleagues about plastic surgeons’ use of social media. The review did not focus on gender-affirmation procedures.
Many surgeons – but not all – steer clear of genital (“bottom”) surgeries in minors. However, bilateral mastectomies are being performed in those as young as age 13 based on surgeons’ risk-benefit calculus for the patient.
A study, published in May in the Annals of Plastic Surgery, showed there was a 13-fold increase in the number of bilateral mastectomies performed on under-18s between January 2013 and the end of July 2020. Of the 209 minors (age 12-17) who had the surgery, two (0.95%) expressed regret by the time of follow-up, at 3 and 7 years post-operatively, but neither had reversal surgery.
A small 2018 study, published in JAMA Pediatrics, among trans males who had top surgery found high rates of satisfaction, though one of the 68 patients reported experiencing regret “sometimes.” The mean age of patients in the surgical group was 19 years and the youngest patient was 14.
“Most of us who practice heavily in this field will make exceptions, not for genital surgery but typically for top surgery,” said Dr. Gallagher, who added that she operates on one minor [under 18] a month, while doing some 400-500 gender-affirmative surgeries a year. For some patients, “doing nothing isn’t necessarily a no-harm option,” said Dr. Gallagher.
“Arbitrarily picking the age of 18 and sentencing that patient to another year of dysphoria” might not be the best risk-benefit calculus, she said.
Dr. Mangubat agrees, especially if, for example, a trans man develops double D breasts by age 14. “You’ve sentenced them to 4 years of misery” before they can get insurance coverage, he said. His youngest top surgery patient was age 15. He said the person’s family, mental health professional, and primary care physician were all in favor of the procedure.
Dr. Mangubat also noted that some insurers, such as Kaiser Permanente, now cover bilateral mastectomy starting at age 16.
Dr. Quinn, the bioethicist, said not every minor or young adult is equipped to make the best long-term decisions.
She works with younger patients who have cancer, for example, and said her suggestions that they consider fertility preservation are often met with protestations “that they will never have children.”
The same issue arises with transgender patients. They may not want to think about having children or issues such as breast feeding while in their teens or early 20s. “But you know from your experience that they may feel differently in 10 years, but they’re just not in the mind frame to think about it,” said Dr. Quinn.
Some young people may accurately never want children, said Dr. Quinn, “but there is a lack of maturity shown when a person just shuts down a conversation and won’t even listen to infertility threats and potential preservation options.”
Concerns about regret?
Dr. Gallagher said she follows the WPATH standards, which require mental health evaluations, and as a result, “the risk of regret is incredibly low.”
However, one of Dr. Gallagher’s patients who detransitioned, Grace, who goes by @HormoneHangover on social media, said she has taken umbrage at some of the Miami surgeon’s TikToks, including one, “Why might some patients feel sad after surgery ... despite wanting it for so long??”
“This is actually not uncommon with ANY kind of surgery, but it’s temporary!” said the TikTok text. Dr. Gallagher is wearing a red dress and heels and flips her hair while the text scrolls above her.
But to Grace, the TikTok “really bothered me, because sometimes there is regret, and I think that sort of advertising paints a falsely rosy picture,” she said in an interview.
And it is emblematic of what she feels was Dr. Gallagher’s “breezy” approach to explaining the procedure to her. “The surgery itself was a shocking experience for me,” she said. “The physical experience was very jarring. It was very disturbing in a way I hadn’t anticipated or understood in advance,” said Grace.
Dr. Mangubat, who does 100 bilateral mastectomies in trans patients a year, said he goes to great lengths to ensure his patients are good candidates. Everyone – even those who self-pay – must have counseling, and if the individual seems to be considering the surgery because it’s “trendy,” he steers clear.
“If they’re not serious about it, I don’t want to operate on them,” said Dr. Mangubat. “There have been maybe two patients who have come back” to detransition, he said.
Dr. Hadeed also said he has not seen regret. He attributes this to his vetting process, which includes investigating the background of the mental health professionals who write support letters.
“We’ve turned away a lot of patients from our office either because of inadequate letters or because the person writing the letter just doesn’t really have any proper credentials,” he said.
Is social media use by plastic surgeons the new normal?
With so many plastic surgeons – including those who perform transgender procedures – using social media, it may increasingly be just part of doing business.
“Undoubtedly gender surgery teams will have a greater presence on social media in the future,” write Alireza Hamidian Jahromi, MD, and a colleague of the plastic surgery department at Rush University Medical Center, Chicago, in a letter published in Plastic and Reconstructive Surgery.
Kyle R. Latack, MD, and colleagues at the University of Southern California and the University of Michigan, have studied the use of social media by the transgender community and write that they believe “there should be an increased effort to develop high-quality and unbiased resources for patient education that can be made [available] on social media.”
Dr. Gallagher said TikTok helped her erase fear. “A bilateral mastectomy is a scary surgery for an 18-year-old or a 20-year-old,” she said, “but they have to do it for their well-being.”
“That is a criticism I’ve heard – that I seek to minimize it or that I’m flippant about it,” said Dr. Gallagher.
For “top surgery the risk profile is pretty low,” she said, “so what I try to do is educate people that it’s maybe not as scary a procedure as they think.”
Dr. Mangubat, however, is concerned about some of what he sees, especially the explosion of surgeons offering gender-affirming procedures. “Now everybody wants a piece of it,” he said.
“Let’s face it, it’s money now. You get paid for doing this surgery. Hospitals get paid a lot of money for their operating rooms for doing the surgery,” said Dr. Mangubat. “There are some surgeons who believe the transgender community is just another market.”
A version of this article first appeared on Medscape.com.
A woman wearing purple surgical scrubs stares into a camera, looking frustrated, but doesn’t speak. Superimposed over her head is the text “just realized I only get to Yeet 4 Teets next week,” and a crying emoji. Rain appears to drip down over her while “Stan” by Eminem plays in the background.
That October 2020 TikTok by Sidhbh Gallagher, MD, a Miami-based plastic surgeon known as @gendersurgeon, had almost 10,000 likes and was tagged #topsurgery, #masculoplasty, #ftm, and #transman, among other hashtags.
“What health check do I have to get in preparation for teetus deletus?” is the question in another Dr. Gallagher TikTok. Dr. Gallagher is a prolific user of social media with over 268K TikTok followers and over 44K Instagram followers. Another Dr. Gallagher TikTok account, @thevagicianmd, has some 7K followers.
Another cosmetic surgeon, Tony Mangubat, MD, known as @Tikdoctony to his more than 200K followers, uses similar hashtags – like #teetusdeleetus – in his TikToks.
Clearly not medical terms, hashtags like #yeettheteet and #teetusdeletus are often used by the transgender community. The posts by Dr. Gallagher and Dr. Mangubat are part of an ever-growing wave of social media activity by medical professionals.
Plastic surgeons have never been shy about advertising their work – and many have taken to social media to do so, including showing before and after photos. A 2020 study published in Plastic and Reconstructive Surgery found that the majority of such surgeons, especially those in private practice, use social media.
especially to a younger-skewing audience.
Because of the limits on pornography and nudity of social media platforms, most social media posts by gender surgeons are about female-to-male (FTM) mastectomies, the fastest-growing transgender procedure.
The American Society of Plastic Surgeons (ASPS) started separately tracking gender-affirmation procedures in 2015. That year, members reported doing 1,360 FTM procedures.
In 2020, the ASPS further separated procedures into additional categories. That year – when many surgeries were postponed because of the COVID-19 pandemic – FTM mastectomies grew by 15%, with 8,548 procedures performed, a far greater number than for any other transgender surgery, and a sixfold increase in the number of procedures done in 2015.
‘Gimmicky,’ but building community
Surgeons interviewed for this article said they use social media primarily to connect with patients and to educate in a light-hearted way.
While Dr. Gallagher acknowledges that using #teetusdeletus is “kind of gimmicky,” she said she doesn’t view it as unprofessional because she is “using the words of the community I serve.” Many of her patients have seen a medical professional “who just didn’t understand what it is to have gender dysphoria, didn’t understand what it is to be trans, so going from that experience to somebody who uses the same language as the community uses can be quite a comfortable experience,” she said in an interview.
Dr. Mangubat, a Seattle-area plastic surgeon who has been doing mastectomies for trans male patients since 1988, said he tailors his TikToks to that group. He likes TikTok – which he started using in early 2021 – because it has rules against bullying, swearing, and pornography, he told this news organization.
“It’s really not ... advertising ... it’s a community-building platform,” said Dr. Mangubat. “If you build community, people will trust you, and if you provide good accurate information, then people will be safer,” he said.
But, “I’m not telling them to come to me,” he stressed.
He always appears in scrubs and doesn’t do music, doesn’t dance, and doesn’t post before and after photos, but he still gets thousands – or sometimes hundreds of thousands – of likes.
His mission, he said, is to answer the community’s questions. “We’re reaching patients that have had their top surgery, that are going to have their top surgery, that are looking for how to get top surgery, that are just starting on testosterone, that haven’t started on testosterone – it’s the whole spectrum of patients,” said Dr. Mangubat.
Risks downplayed?
Other surgeons have expressed concern about ethical boundaries and the tendency of social media posts to downplay risks of what are life-changing procedures.
A 2020 study of YouTube videos on top surgery, for instance, concluded that “there were no unbiased videos by board-certified plastic surgeons explaining the risks, benefits, treatment options, and alternatives to surgery.”
Alison Clayton, MBBS, an Australian psychiatrist, said that social media posts can create false expectations because they emphasize style over substance, omit risks, and can create an unwarranted sense of trust in the doctor that can spill over into the physician-patient relationship.
Dr. Clayton also believes that “the gender-affirming surgical procedures being offered to these youth have a scant empirical evidence base for benefits to psychological health and well-being.”
It is known that a number of those who transition, using either opposite sex hormones and/or surgical procedures, later have regret and “detransition,” but statistics are lacking. It is also a controversial area, with many detransitioners saying they didn’t get appropriate care and weren’t properly assessed before being given hormones or heading to surgery.
Most of the gender surgeons interviewed for this article said they see almost “zero” regret if proper mental health evaluations are performed before surgery, and they added, the procedures can relieve dysphoria.
Nevertheless, posts should not be “all fun and games,” said Josef Hadeed, MD, chair of the ASPS Patient Safety Committee and Public Education Committee and a member of its Social Media Subcommittee.
“When someone makes a decision to undergo a surgical procedure, they should be very aware there are some risks and potentially serious risks involved,” he told this news organization.
The ASPS “wants members to use social media in a judicious manner” in a way that educates the public and encourages patients to learn about a procedure and to consult with board-certified plastic surgeons, said Dr. Hadeed.
The Beverly Hills, Calif.–based surgeon does gender-affirmation procedures himself and uses Instagram, on which he has 53.4K followers, to educate patients and highlight his work using before and after photos.
“I like to think I do it in a very tasteful way,” Dr. Hadeed said. “It’s not in a way that’s sort of suggestive to patients, including minors, that this is something they need to get done, because if they are thinking about getting it done there is a lengthy process that they have to go through before they even set foot in our office.”
And he said “it may be inappropriate” to use certain hashtags or terminology, “even if it does ‘speak’ to the patients. Professionally, plastic surgeons should maintain a higher standard and maintain that even with their social media.”
Marci Bowers, MD, a gynecologic surgeon who performs gender-affirming procedures, and who is transgender herself, agreed.
“Some of the posts out there seem sensational, distasteful, and risk compromising patient confidentiality,” Dr. Bowers said in an interview.
“Much of this seemed to cross the line of good taste and appropriateness,” added Dr. Bowers, who is the incoming president of the World Professional Association for Transgender Health (WPATH). “Creating an idealized video without addressing risk is inappropriate and misleading,” she stressed.
“These surgeons would perhaps better serve their clients by focusing on and improving their clinical care,” she added.
Dr. Bowers said that although WPATH has not addressed social media use in the past, its ethics committee will be taking on the topic this year.
Social media posts about gender-affirming procedures “don’t usually talk about the barriers, they don’t talk about bad outcomes, they tend to just focus on success stories,” said Gwendolyn P. Quinn, MD, a bioethicist, and Livia S. Wan, MD, professor of obstetrics and gynecology at the NYU Grossman School of Medicine.
But she also sees some positives. The posts can help normalize gender-affirming surgery, and post-procedure photos might “help people realize that they can’t just have everything exactly the way they want it to be,” said Dr. Quinn.
Does social media influence or educate?
Studies have documented the power of social media to influence desire and decisionmaking, especially when it comes to cosmetic surgery.
“The use of social media creates a vague area between patient confidentiality and entertainment,” writes Nisha Gupta and colleagues of the UCLA David Geffen School of Medicine in a review published in the Aesthetic Surgery Journal.
While social media use is on the rise by plastic surgeons and has the potential to educate, it has also “compromised the integrity of the doctor-patient relationship,” they add.
Surgeons can use tools to place themselves higher in searches, and patients might assume that those who have hundreds of thousands of followers “are the most qualified or trusted, although this is not always the case,” they note.
Markus Rach, PhD, a researcher with the University of Applied Sciences and Arts Northwestern Switzerland, analyzed the impact of TikTok’s plastic surgery content on how adolescents perceived themselves and how it influenced their decision to have a procedure.
Most TikTok users are under age 24, and #plasticsurgery has a huge viewership with some 3.8 billion views at the time of publication, said Dr. Rach. He found that influencers tended to make adolescents feel bad and want surgery but that plastic surgeons had a moderating effect on both negative feelings and the intent to get surgery.
Dr. Bowers said that, despite her concerns, she does not “believe social media influences like TikTok and Facebook create artificial demand.”
However, Dr. Mangubat said social media can make plastic surgery seem enticing. “It can happen, and it does happen,” he said, but he added that’s true for any cosmetic procedure, not just gender-affirming surgery.
The pitfall with social media is that “patients are being sold a vision of themselves that may or may not be possible,” he observed.
Dr. Quinn worries less about people being talked into a procedure and more about those who don’t want surgery.
“There are people who identify as transgender but do not feel the need to change any parts of their body,” she said. “And that should be okay.”
Concerns about minors
New guidance from WPATH, their Standards of Care (SOC) 8 – the first update in 10 years – are due to be published this month. As reported by this news organization, and as stated in the draft of the SOC 8 published for comment in December 2021, the organization has recommended lowering the age for “top” surgery from 18 to 15 years.
Dr. Clayton has concerns about young people with gender dysphoria, who she says are “often vulnerable youth, many of whom have comorbid psychiatric and neurodevelopmental disorders.”
“This may contribute to a greater vulnerability of this population to undue influence,” added Dr. Clayton.
Sean Devitt, MD, and Jeffrey M. Kenkel, MD, of the University of Texas Southwestern Medical Center, Dallas, expressed concern that social media posts by plastic surgeons could be especially dangerous for young people.
“Given that the prefrontal cortex, which is largely responsible for impulse control, is not fully developed until the age of 25, is it ethical to allow younger patients to make life-lasting decisions under the guise of education?” they ask in a commentary on the review by Ms. Gupta and colleagues about plastic surgeons’ use of social media. The review did not focus on gender-affirmation procedures.
Many surgeons – but not all – steer clear of genital (“bottom”) surgeries in minors. However, bilateral mastectomies are being performed in those as young as age 13 based on surgeons’ risk-benefit calculus for the patient.
A study, published in May in the Annals of Plastic Surgery, showed there was a 13-fold increase in the number of bilateral mastectomies performed on under-18s between January 2013 and the end of July 2020. Of the 209 minors (age 12-17) who had the surgery, two (0.95%) expressed regret by the time of follow-up, at 3 and 7 years post-operatively, but neither had reversal surgery.
A small 2018 study, published in JAMA Pediatrics, among trans males who had top surgery found high rates of satisfaction, though one of the 68 patients reported experiencing regret “sometimes.” The mean age of patients in the surgical group was 19 years and the youngest patient was 14.
“Most of us who practice heavily in this field will make exceptions, not for genital surgery but typically for top surgery,” said Dr. Gallagher, who added that she operates on one minor [under 18] a month, while doing some 400-500 gender-affirmative surgeries a year. For some patients, “doing nothing isn’t necessarily a no-harm option,” said Dr. Gallagher.
“Arbitrarily picking the age of 18 and sentencing that patient to another year of dysphoria” might not be the best risk-benefit calculus, she said.
Dr. Mangubat agrees, especially if, for example, a trans man develops double D breasts by age 14. “You’ve sentenced them to 4 years of misery” before they can get insurance coverage, he said. His youngest top surgery patient was age 15. He said the person’s family, mental health professional, and primary care physician were all in favor of the procedure.
Dr. Mangubat also noted that some insurers, such as Kaiser Permanente, now cover bilateral mastectomy starting at age 16.
Dr. Quinn, the bioethicist, said not every minor or young adult is equipped to make the best long-term decisions.
She works with younger patients who have cancer, for example, and said her suggestions that they consider fertility preservation are often met with protestations “that they will never have children.”
The same issue arises with transgender patients. They may not want to think about having children or issues such as breast feeding while in their teens or early 20s. “But you know from your experience that they may feel differently in 10 years, but they’re just not in the mind frame to think about it,” said Dr. Quinn.
Some young people may accurately never want children, said Dr. Quinn, “but there is a lack of maturity shown when a person just shuts down a conversation and won’t even listen to infertility threats and potential preservation options.”
Concerns about regret?
Dr. Gallagher said she follows the WPATH standards, which require mental health evaluations, and as a result, “the risk of regret is incredibly low.”
However, one of Dr. Gallagher’s patients who detransitioned, Grace, who goes by @HormoneHangover on social media, said she has taken umbrage at some of the Miami surgeon’s TikToks, including one, “Why might some patients feel sad after surgery ... despite wanting it for so long??”
“This is actually not uncommon with ANY kind of surgery, but it’s temporary!” said the TikTok text. Dr. Gallagher is wearing a red dress and heels and flips her hair while the text scrolls above her.
But to Grace, the TikTok “really bothered me, because sometimes there is regret, and I think that sort of advertising paints a falsely rosy picture,” she said in an interview.
And it is emblematic of what she feels was Dr. Gallagher’s “breezy” approach to explaining the procedure to her. “The surgery itself was a shocking experience for me,” she said. “The physical experience was very jarring. It was very disturbing in a way I hadn’t anticipated or understood in advance,” said Grace.
Dr. Mangubat, who does 100 bilateral mastectomies in trans patients a year, said he goes to great lengths to ensure his patients are good candidates. Everyone – even those who self-pay – must have counseling, and if the individual seems to be considering the surgery because it’s “trendy,” he steers clear.
“If they’re not serious about it, I don’t want to operate on them,” said Dr. Mangubat. “There have been maybe two patients who have come back” to detransition, he said.
Dr. Hadeed also said he has not seen regret. He attributes this to his vetting process, which includes investigating the background of the mental health professionals who write support letters.
“We’ve turned away a lot of patients from our office either because of inadequate letters or because the person writing the letter just doesn’t really have any proper credentials,” he said.
Is social media use by plastic surgeons the new normal?
With so many plastic surgeons – including those who perform transgender procedures – using social media, it may increasingly be just part of doing business.
“Undoubtedly gender surgery teams will have a greater presence on social media in the future,” write Alireza Hamidian Jahromi, MD, and a colleague of the plastic surgery department at Rush University Medical Center, Chicago, in a letter published in Plastic and Reconstructive Surgery.
Kyle R. Latack, MD, and colleagues at the University of Southern California and the University of Michigan, have studied the use of social media by the transgender community and write that they believe “there should be an increased effort to develop high-quality and unbiased resources for patient education that can be made [available] on social media.”
Dr. Gallagher said TikTok helped her erase fear. “A bilateral mastectomy is a scary surgery for an 18-year-old or a 20-year-old,” she said, “but they have to do it for their well-being.”
“That is a criticism I’ve heard – that I seek to minimize it or that I’m flippant about it,” said Dr. Gallagher.
For “top surgery the risk profile is pretty low,” she said, “so what I try to do is educate people that it’s maybe not as scary a procedure as they think.”
Dr. Mangubat, however, is concerned about some of what he sees, especially the explosion of surgeons offering gender-affirming procedures. “Now everybody wants a piece of it,” he said.
“Let’s face it, it’s money now. You get paid for doing this surgery. Hospitals get paid a lot of money for their operating rooms for doing the surgery,” said Dr. Mangubat. “There are some surgeons who believe the transgender community is just another market.”
A version of this article first appeared on Medscape.com.
PCOS ups risk of heart complications during delivery period
Pregnant women with polycystic ovary syndrome (PCOS) appear to be at significantly increased risk of experiencing cardiac complications while hospitalized during and after delivery.
An estimated 5 million women of childbearing age in the United States have PCOS, a hormone disorder linked to infertility. PCOS is also known to contribute to the development of cardiometabolic abnormalities like high cholesterol and high blood pressure, which are associated with acute cardiovascular complications during delivery.
But a study, published online in the Journal of the American Heart Association, found that even after accounting for pre-eclampsia, age, comorbidities, and race, PCOS was linked to a 76% increased risk for heart failure, a 79% higher risk of a weakened heart, and an 82% increased risk of having blood clots in the hours and days around giving birth in hospital settings, compared with women without PCOS.
“Perhaps women need a closer follow-up during their pregnancy,” said Erin Michos, MD, MHS, associate director of preventive cardiology at Johns Hopkins Medicine, Baltimore, and a co-author of the study. “They’re counseled about the difficulties of getting pregnant, but what about when they get pregnant?”
Hospitalizations of women with PCOS were also associated with longer stays (3 vs. 2 days) and higher costs ($4,901 vs. $3616; P < .01), compared with women without PCOS.
Over the 17-year analysis period, the number of women with PCOS rose from 569 per 100,000 deliveries to 15,349 per 100,000 deliveries. The researchers attributed the increase in part to greater awareness and diagnosis of the disorder. Dr. Michos and her colleagues used the National Inpatient Sample, managed by the Agency for Healthcare Research and Quality, to pull claims data for women who gave birth in hospitals between 2002 and 2019.
Solutions?
Dr. Michos said there may be more prevention work from og.gyns. to both educate patients about their heart risks during the delivery process and also to refer them to relevant cardiac specialists.
“These women may seek out a gynecologist because of the symptoms, perhaps irregular menses, but along with that should come counseling of the long-term cardiovascular complication,” Dr. Michos said. “And after a pregnancy there should be a good handoff to a primary care provider, so they get a cardiovascular assessment.”
Lifestyle management before, during, and after pregnancy can help prevent the onset of the long-term consequences of cardiac complications during delivery, according to Valerie Baker, MD, director of the division of reproductive endocrinology and infertility at Hopkins Medicine, and her colleagues in a viewpoint published in the journal Fertility and Sterility.
“Once women with PCOS are identified by screening to be at higher risk for [cardiovascular disease], the foundational approach should be lifestyle management followed by statin therapy,” Dr. Baker’s group wrote. “These interventions should include dietary management and physical activity, especially for those who are prediabetic.”
The current study came on the heels of a June 14 meta-analysis by Dr. Michos’ group that found that women with PCOS may be twice as likely as those without PCOS to have coronary artery calcification, a precursor to atherosclerosis and a sign of the early onset of cardiovascular disease.
“We shouldn’t assume that all women of reproductive age are low risk,” Dr. Michos said. “This is the window of time that we can reshape the trajectory early in life.”
The study was supported by the Amato Fund for Women’s Cardiovascular Health research at Johns Hopkins University and through grant support from the American Heart Association (940166). Dr. Michos reported advisory board participation for AstraZeneca, Amarin, Novartis, Novo Nordisk, Bayer, Boehringer Ingelheim, Esperion, and Pfizer. Study coauthor Michael Honigberg, MD, reported consulting fees from CRISPR Therapeutics, unrelated to the present work. The remaining authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women with polycystic ovary syndrome (PCOS) appear to be at significantly increased risk of experiencing cardiac complications while hospitalized during and after delivery.
An estimated 5 million women of childbearing age in the United States have PCOS, a hormone disorder linked to infertility. PCOS is also known to contribute to the development of cardiometabolic abnormalities like high cholesterol and high blood pressure, which are associated with acute cardiovascular complications during delivery.
But a study, published online in the Journal of the American Heart Association, found that even after accounting for pre-eclampsia, age, comorbidities, and race, PCOS was linked to a 76% increased risk for heart failure, a 79% higher risk of a weakened heart, and an 82% increased risk of having blood clots in the hours and days around giving birth in hospital settings, compared with women without PCOS.
“Perhaps women need a closer follow-up during their pregnancy,” said Erin Michos, MD, MHS, associate director of preventive cardiology at Johns Hopkins Medicine, Baltimore, and a co-author of the study. “They’re counseled about the difficulties of getting pregnant, but what about when they get pregnant?”
Hospitalizations of women with PCOS were also associated with longer stays (3 vs. 2 days) and higher costs ($4,901 vs. $3616; P < .01), compared with women without PCOS.
Over the 17-year analysis period, the number of women with PCOS rose from 569 per 100,000 deliveries to 15,349 per 100,000 deliveries. The researchers attributed the increase in part to greater awareness and diagnosis of the disorder. Dr. Michos and her colleagues used the National Inpatient Sample, managed by the Agency for Healthcare Research and Quality, to pull claims data for women who gave birth in hospitals between 2002 and 2019.
Solutions?
Dr. Michos said there may be more prevention work from og.gyns. to both educate patients about their heart risks during the delivery process and also to refer them to relevant cardiac specialists.
“These women may seek out a gynecologist because of the symptoms, perhaps irregular menses, but along with that should come counseling of the long-term cardiovascular complication,” Dr. Michos said. “And after a pregnancy there should be a good handoff to a primary care provider, so they get a cardiovascular assessment.”
Lifestyle management before, during, and after pregnancy can help prevent the onset of the long-term consequences of cardiac complications during delivery, according to Valerie Baker, MD, director of the division of reproductive endocrinology and infertility at Hopkins Medicine, and her colleagues in a viewpoint published in the journal Fertility and Sterility.
“Once women with PCOS are identified by screening to be at higher risk for [cardiovascular disease], the foundational approach should be lifestyle management followed by statin therapy,” Dr. Baker’s group wrote. “These interventions should include dietary management and physical activity, especially for those who are prediabetic.”
The current study came on the heels of a June 14 meta-analysis by Dr. Michos’ group that found that women with PCOS may be twice as likely as those without PCOS to have coronary artery calcification, a precursor to atherosclerosis and a sign of the early onset of cardiovascular disease.
“We shouldn’t assume that all women of reproductive age are low risk,” Dr. Michos said. “This is the window of time that we can reshape the trajectory early in life.”
The study was supported by the Amato Fund for Women’s Cardiovascular Health research at Johns Hopkins University and through grant support from the American Heart Association (940166). Dr. Michos reported advisory board participation for AstraZeneca, Amarin, Novartis, Novo Nordisk, Bayer, Boehringer Ingelheim, Esperion, and Pfizer. Study coauthor Michael Honigberg, MD, reported consulting fees from CRISPR Therapeutics, unrelated to the present work. The remaining authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pregnant women with polycystic ovary syndrome (PCOS) appear to be at significantly increased risk of experiencing cardiac complications while hospitalized during and after delivery.
An estimated 5 million women of childbearing age in the United States have PCOS, a hormone disorder linked to infertility. PCOS is also known to contribute to the development of cardiometabolic abnormalities like high cholesterol and high blood pressure, which are associated with acute cardiovascular complications during delivery.
But a study, published online in the Journal of the American Heart Association, found that even after accounting for pre-eclampsia, age, comorbidities, and race, PCOS was linked to a 76% increased risk for heart failure, a 79% higher risk of a weakened heart, and an 82% increased risk of having blood clots in the hours and days around giving birth in hospital settings, compared with women without PCOS.
“Perhaps women need a closer follow-up during their pregnancy,” said Erin Michos, MD, MHS, associate director of preventive cardiology at Johns Hopkins Medicine, Baltimore, and a co-author of the study. “They’re counseled about the difficulties of getting pregnant, but what about when they get pregnant?”
Hospitalizations of women with PCOS were also associated with longer stays (3 vs. 2 days) and higher costs ($4,901 vs. $3616; P < .01), compared with women without PCOS.
Over the 17-year analysis period, the number of women with PCOS rose from 569 per 100,000 deliveries to 15,349 per 100,000 deliveries. The researchers attributed the increase in part to greater awareness and diagnosis of the disorder. Dr. Michos and her colleagues used the National Inpatient Sample, managed by the Agency for Healthcare Research and Quality, to pull claims data for women who gave birth in hospitals between 2002 and 2019.
Solutions?
Dr. Michos said there may be more prevention work from og.gyns. to both educate patients about their heart risks during the delivery process and also to refer them to relevant cardiac specialists.
“These women may seek out a gynecologist because of the symptoms, perhaps irregular menses, but along with that should come counseling of the long-term cardiovascular complication,” Dr. Michos said. “And after a pregnancy there should be a good handoff to a primary care provider, so they get a cardiovascular assessment.”
Lifestyle management before, during, and after pregnancy can help prevent the onset of the long-term consequences of cardiac complications during delivery, according to Valerie Baker, MD, director of the division of reproductive endocrinology and infertility at Hopkins Medicine, and her colleagues in a viewpoint published in the journal Fertility and Sterility.
“Once women with PCOS are identified by screening to be at higher risk for [cardiovascular disease], the foundational approach should be lifestyle management followed by statin therapy,” Dr. Baker’s group wrote. “These interventions should include dietary management and physical activity, especially for those who are prediabetic.”
The current study came on the heels of a June 14 meta-analysis by Dr. Michos’ group that found that women with PCOS may be twice as likely as those without PCOS to have coronary artery calcification, a precursor to atherosclerosis and a sign of the early onset of cardiovascular disease.
“We shouldn’t assume that all women of reproductive age are low risk,” Dr. Michos said. “This is the window of time that we can reshape the trajectory early in life.”
The study was supported by the Amato Fund for Women’s Cardiovascular Health research at Johns Hopkins University and through grant support from the American Heart Association (940166). Dr. Michos reported advisory board participation for AstraZeneca, Amarin, Novartis, Novo Nordisk, Bayer, Boehringer Ingelheim, Esperion, and Pfizer. Study coauthor Michael Honigberg, MD, reported consulting fees from CRISPR Therapeutics, unrelated to the present work. The remaining authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Docs reveal perils of giving medical advice to friends and family
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.
Stephen Pribut, DPM, a sports medicine podiatrist based in Washington, has had many friends or family members ask him for medical advice. It’s a scenario every doctor will face at one point or another in their careers, and it’s never an easy one.
Dr. Pribut received a call from a friend about a sore shoulder from swimming, saying that his doctor had dismissed the potential for a rotator cuff injury. “Months later, images revealed it was a rotator cuff tear and he wanted my advice,” says Dr. Pribut.
Not being a shoulder specialist, Dr. Pribut limited his input. “I told him to consider a good physical therapist or a shoulder specialist and gave him some alternative strokes for swimming that hopefully wouldn’t aggravate the injury,” he explains.
But he admits some situations are challenging. “I had a relative asking about a third party with an ankle injury. I advised he hold off on using a balance board until things healed, and to make sure he went to see a specialist. Unfortunately, he went to his general practitioner who likely knows nothing about ankle anatomy,” says Dr. Pribut.
“I finally saw a photo, which revealed swelling higher up on the ankle and no evidence of a hematoma – much lower than we would see in an ankle ligament injury. I would like him to see a sports podiatrist or foot and ankle orthopedist, but now I have to stay calm when the advice isn’t followed,” he says.
When asked, “Do you give medical advice to your friends?” 96% of respondents answered yes.
Yazan Abou-Ismail, MD, assistant professor of medicine in the division of hematology at the University of Utah, Salt Lake City, has often faced questions from friends and family, particularly throughout the COVID-19 pandemic. “How you respond is something all physicians need to analyze carefully,” he says. “I get questions on a regular basis, but this greatly increased with COVID.”
“Sharing general information is okay, and it’s even a requirement that we educate on such topics,” says Dr. Abou-Ismail. “But if someone knows they have COVID, for instance, and wants advice on how to proceed, it’s important to send them to their primary care physician for an evaluation rather than give them instructions on care.”
Dr. Abou-Ismail says that most “curbside consulting” equates to lack of an ethical follow-up. “If you gave medical advice without having assessed them, you’re lacking the medical history, a physical exam, and you should not be giving advice,” he says. “This applies to follow-ups, too.”
Throughout the pandemic, Dr. Abou-Ismail’s requests for advice on COVID even extended to online inquiries, often from strangers. “This is not a place to do a formal assessment,” he reminds. “But there are certain types of advice you can offer appropriately.”
Dr. Abou-Ismail considers safe advice to be simple public health messages that stay far out of specifics. Things like “don’t smoke,” or “eat a healthy diet,” and “get enough sleep,” fall into this safety zone. Even, “What is XYZ disease?” or “How do COVID vaccines work?” are topics he says he answers comfortably.
“But telling someone you need a specific treatment for a condition is inappropriate,” he explains. “This is a general way of practicing medicine – your advice should never venture into the potential of doing harm.”
This approach is exactly in line with legal advice, according to Jeff Caesar Chukwuma, founder and senior partner at Chukwuma Law Group, Miami. “It doesn’t mean that doctors should never give medical advice to friends or family, but if they do, they should make sure to take several precautions to protect both themselves and their family and friends,” he says.
When the request for medical advice from an acquaintance migrates into areas in which a physician is not a specialist, sharing recommendations gets even trickier – and more ethically questionable.
Says Mr. Chukwuma, “Doctors should avoid giving advice in areas outside their area of expertise to lower the possibility of providing erroneous or harmful information,” he says.
How to stay safe when asked for advice
The American Medical Association has weighed in on the topic. In the Code of Medical Ethics Opinion 1.2.1, the AMA states that, “Treating oneself or a member of one’s own family poses several challenges for physicians, including concerns about professional objectivity, patient autonomy, and informed consent.”
What about friends or acquaintances, however?
Even so, some respondents voiced their concerns with the scenario. Responses like, “Due to ethics, I would prefer they go and get first, second, and third opinions,” and “Usually the medical advice is very basic first aid (often mental health first aid), and if it’s anything remotely more complicated, I direct them to the appropriate provider.”
The AMA places advising friends in the same basket as advising and treating family members or oneself. In an article appearing in the AMA Journal of Ethics, Horacio Hojman, MD, of Tufts University School of Medicine, Boston, weighed in: “First and foremost, patients deserve objectivity from their doctors. When a physician is emotionally involved with a patient, that physician’s objectivity can be called into question.”
Why is medical advice so thorny when dealing with friends or relatives?
In some cases, a physician might not ask a friend relevant personal questions about his or her medical history, for instance. Or the friend might not want to share details with the doctor. In either case, the lack of information exchange can lead to improper advice.
The issue of giving medical advice to friends, family, and acquaintances can also wade into legal territory. “Personally or professionally, trust is the decisive factor that puts us at ease with the people we surround ourselves with,” says Mr. Chukwuma. “Nowhere is this truer than in medicine, where we approach doctors with some of the most sensitive matters in our lives and entrust our care to them, especially when the physician in question is a close friend or family member.”
Mr. Chukwuma points out that, while there are few strict legal prohibitions against doctors providing care or advice to family and friends, the AMA’s code of ethics states that such action should be reserved for rare situations, such as emergency settings or isolated settings where there is no other qualified physician available, or for minor, not long-term problems.
This was part of the equation for Dr. Pribut when helping his mother navigate her treatment for breast cancer. “With close relatives, offering advice and help can be very hard,” he says.
“This is to protect both patients and doctors,” says Mr. Chukwuma. “Although seeking advice from a family member or friend who is a doctor may be more convenient for a patient, they run the risk of receiving inadequate care by not going in for a formal medical visit complete with tests, medical examination, and follow-up care.”
Mr. Chukwuma offers guidance on how to share medical advice ethically and legally with family, friends, and acquaintances. “First, as much as possible, speak to general medical facts and knowledge rather than comment directly on the patient’s particular situation,” he says. “In the absence of thorough examination and tests, the doctor’s knowledge of a patient’s condition is limited, therefore, you should take care not to provide seemingly definitive answers on that patient’s unique condition in situations where they can’t rely on data to back up their advice and recommendations.”
The AMA’s Journal of Ethics article shares these tips for staying on the right side of the ethical line when dealing with friends and family members:
- Politely decline.
- Offer other forms of assistance – this might help a friend find the right qualified physician – as Dr. Pribut tends to do. Maybe help in navigating the sometimes-confusing health care system.
- Don’t hesitate in an emergency – the old “is there a doctor on board,” scenario on a plane when someone is in distress is a perfectly acceptable, and recommended, time to step in, even if it is a friend or family member.
Dr. Pribut, a long-time veteran of the tricky medical waters involving friends and family, has this to offer: “Be cautious and always stay in the realm of what you know,” he says. “Always encourage people to seek an opinion from a qualified doctor. Help them find a reputable doctor if that’s useful.”
Mr. Chukwuma adds also that doctors should stand firm when pushed by a friend or family member, especially when offering advice, even if it’s in the form of general education. “The doctor should make it clear to the family member or friend that their advice in no way takes the place of actual treatment or examination by a medical professional and that, if need be, the patient should seek formal medical help from another doctor, ideally one not related to or friends with the patient,” he says.
A version of this article first appeared on Medscape.com.